Attached files
| file | filename |
|---|---|
| EX-32.2 - EX-32.2 - ALMOST FAMILY INC | afam-20171229ex322099b18.htm |
| EX-32.1 - EX-32.1 - ALMOST FAMILY INC | afam-20171229ex32125562b.htm |
| EX-31.2 - EX-31.2 - ALMOST FAMILY INC | afam-20171229ex312838567.htm |
| EX-31.1 - EX-31.1 - ALMOST FAMILY INC | afam-20171229ex311fc6b6e.htm |
| EX-23.1 - EX-23.1 - ALMOST FAMILY INC | afam-20171229ex231aff02f.htm |
| EX-21 - EX-21 - ALMOST FAMILY INC | afam-20171229ex2106b5269.htm |
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
☒ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
For the fiscal year ended December 29, 2017
OR
☐TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
For the transition period from to
Commission file number 001-09848

ALMOST FAMILY, INC.
(Exact name of Registrant as specified in its charter)
|
Delaware |
|
06-1153720 |
|
(State or other jurisdiction of incorporation or organization) |
|
(I.R.S. Employer Identification Number) |
9510 Ormsby Station Road, Suite 300, Louisville, Kentucky 40223
(Address of principal executive offices)
(502) 891-1000
(Registrant’s telephone number, including area code)
Not Applicable
(Former name, former address and former fiscal year, if changed since last report)
Securities registered pursuant to Section 12(b) of the Act
|
Title of each class |
|
Name of each exchange on which registered |
|
Common Stock, par value $0.10 per share |
|
NASDAQ Global Select Market |
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☐ No ☒
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Exchange Act. Yes ☐ No ☒
Indicate by check mark whether the Registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ☒ No ☐
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ☒ No ☐
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of the Registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. ☐
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer”, “smaller reporting company” and “emerging growth company” in Rule 12b-2 of the Exchange Act. (Check one):
|
Large accelerated filer ☒ |
|
Accelerated filer ☐ |
|
Non-accelerated filer ☐ |
|
Smaller reporting company ☐ |
|
(Do not check if a smaller reporting company) |
|
Emerging growth company ☐ |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act) Yes☐ No ☒
The aggregate market value of the registrant’s common stock held by non-affiliates of the registrant as of the last day of the second fiscal quarter ended June 30, 2017 was $789,578,553 based on the last sale price of a share of the common stock as of June 30, 2017 ($61.65), as reported by the NASDAQ Global Market.
Indicate the number of shares outstanding of each of the issuer’s classes of common stock, as of the latest practicable date.
|
Class |
|
Outstanding at February 23 2018 |
|
Common Stock, $0.10 par value per share |
|
13,992,729 Shares |
|
|
|
|
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the 2017 definitive proxy statement relating to the registrant’s Annual Meeting of Stockholders are incorporated by reference in Part III to the extent described therein.
2
In this report, the terms “Company,” “we,” “us” or “our” mean Almost Family, Inc. and all subsidiaries included in our consolidated financial statements.
Special Caution Regarding Forward-Looking Statements
Certain statements contained in this annual report on Form 10-K, including, without limitation, statements containing the words “believes,” “anticipates,” “intends,” “expects,” “assumes,” “trends” and similar expressions, constitute “forward-looking statements” within the meaning of the Private Securities Litigation Reform Act of 1995. Forward-looking statements are based upon the Company’s current plans, expectations and projections about future events. However, such statements involve known and unknown risks, uncertainties and other factors that may cause the actual results, performance or achievements of the Company to be materially different from any future results, performance or achievements expressed or implied by such forward-looking statements. These factors include, among others, the following:
|
· |
general economic and business conditions; |
|
· |
demographic changes; |
|
· |
changes in, or failure to comply with, existing governmental regulations; |
|
· |
legislative proposals for healthcare reform; |
|
· |
changes in Medicare and Medicaid reimbursement levels; |
|
· |
changes in laws and regulations with respect to Accountable Care Organizations; |
|
· |
effects of competition in the markets in which the Company operates; |
|
· |
liability and other claims asserted against the Company; |
|
· |
potential audits and investigations by government and regulatory agencies, including the impact of any negative publicity or litigation; |
|
· |
ability to attract and retain qualified personnel; |
|
· |
availability and terms of capital; |
|
· |
loss of significant contracts or reduction in revenues associated with major payor sources; |
|
· |
ability of customers to pay for services; |
|
· |
business disruption due to natural disasters or terrorist acts; |
|
· |
ability to successfully integrate the operations of acquired businesses and achieve expected synergies and operating efficiencies from the acquisition, in each case within expected time-frames or at all; |
|
· |
ability to successfully develop investments made by our healthcare innovations segment, in light of the highly speculative nature of these early stage investments; |
|
· |
significant deterioration in economic conditions and significant market volatility; |
|
· |
effect on liquidity of the Company’s financing arrangements; |
|
· |
changes in estimates and judgments associated with critical accounting policies and estimates; |
|
· |
the risk that the merger with LHC Group, Inc. (“LHC Group”) may be delayed or not completed; and |
|
· |
the risk that the anticipated benefits of the merger with LHC Group may not be fully realized, |
For a detailed discussion of these and other factors that could cause the Company’s actual results to differ materially from the results contemplated by the forward-looking statements, please refer to Item 1A. “Risk Factors” and Item 7 “Management’s Discussion and Analysis of Financial Condition and Results of Operations” elsewhere in this report. The reader should not place undue reliance on forward-looking statements, which speak only as of the date of this report. Except as required by law, the Company does not intend to publicly release any revisions to forward-looking statements to reflect unforeseen or other events after the date of this report. The Company has provided a detailed discussion of risk factors within this annual report on Form 10-K and various filings with the Securities and Exchange Commission (“SEC”). The reader is encouraged to review these risk factors and filings.
3
Introduction
Almost Family, Inc. TM and subsidiaries (collectively “Almost Family” or the “Company”) is a leading provider of cost efficient, high quality home healthcare services and related innovations to drive savings for payors and improve patient outcomes and experience. Our Company, founded in 1976, operates over 330 locations across 26 states.
LHC Group, Inc. and Almost Family, Inc. Merger
On November 15, 2017, our Company entered into an Agreement and Plan of Merger (the “Merger Agreement”) with LHC Group, Inc., a Delaware corporation (“LHC Group”), and Hammer Merger Sub, Inc., a newly-formed Delaware corporation and a wholly owned subsidiary of LHC Group (“Merger Sub”), providing for a “merger of equals” business combination of our Company and LHC Group. The Merger Agreement provides that, if the conditions to the Merger are satisfied or waived and the Merger is consummated, stockholders of our Company will receive 0.9150 shares of LHC Group common stock for each share of our Company’s common stock, plus the cash equivalent of any fractional share. The Merger Agreement provides that, upon the terms and subject to the conditions set forth therein, at the closing Merger Sub will be merged with and into our Company (the “Merger”), with our Company continuing as the surviving corporation and as a wholly owned subsidiary of LHC Group. The parties’ obligations to complete the Merger are subject to several conditions, including, among others, (i) the adoption of the Merger Agreement by the affirmative vote of the holders of at least a majority of the outstanding shares of the Company’s common stock; (ii) the approval of the issuance of shares of LHC Group’s common stock to be issued to our stockholders in the merger by the affirmative vote of a majority of the shares of LHC Group’s common stock present in person or represented by proxy at LHC Group’s special meeting; (iii) the expiration or termination of the required waiting periods under the Hart-Scott Rodino Act (which occurred on February 21, 2018); (iv) the absence of any order or law prohibiting the Merger or the other transactions contemplated by the Merger Agreement; (v) the receipt of certain tax opinions; and (vi) the absence of a material adverse effect with respect to either LHC Group or our Company (as defined in the Merger Agreement).
The Merger Agreement contains certain termination rights for both our Company and LHC Group, including if the Merger is not consummated on or before July 1, 2018 (subject to extension to October 1, 2018 in certain circumstances) and if the required approval of the stockholders of either our Company or LHC Group is not obtained. The Merger Agreement further provides that, upon termination of the Merger Agreement under specified circumstances, including the termination of the Merger Agreement by our Company or LHC Group as a result of an adverse change in the recommendation of the other party’s board of directors, our Company may be required to pay to LHC Group, or LHC Group may be required to pay to our Company, as applicable, a termination fee of $30 million. Further, if the Merger Agreement is terminated as a result of the stockholders of either our Company or LHC Group failing to approve the transaction, our Company may be required to reimburse to LHC Group, or LHC Group may be required to reimburse to our Company, the other party’s expenses in connection with the proposed transaction, up to a maximum of $5 million.
In the absence of a completed merger, we will continue to operate on a stand-alone basis. All references within this Form 10-K assumes Almost Family, Inc. operating on a stand-alone basis.
Our Business Plan
Our future success depends on our ability to execute our business plan. Over the next three to five years we will try to accomplish the following:
|
· |
Generate meaningful same store sales growth through the focused provision of high quality services and attending to the needs of our patients; |
4
|
· |
Drive our costs down, while continuing to provide high quality patient care, by improving the productivity of our work force through improved monitoring, tighter controls, workflow automation, use of technology and other opportunities for efficiency gains; |
|
· |
Expand the significance of our home health services by selectively acquiring other quality providers, through the startup of new agencies and potentially by providing new services in patients’ homes consistent with our Senior Advocacy mission; |
|
· |
Make additional strategic investments which expand our Healthcare Innovation segment in its mission to find solutions for more effective, efficient and appropriate delivery of homecare; and |
|
· |
Expand our capital base through both earnings performance and by seeking additional capital investments in our Company. |
Website Access to Our Reports
Our annual reports on Form 10-K, quarterly reports on Form 10-Q, current reports on Form 8-K, and all amendments to those reports are available free of charge on our website at www.almostfamily.com as soon as reasonably practicable after such material is electronically filed with or furnished to the SEC. Information contained on Almost Family’s website is not part of this annual report on Form 10-K and is not incorporated by reference in this document.
How We Are Currently Organized and Operate
The Company has three reportable segments: a) Home Health (“HH”), b) Other Home-Based Services (“OHBS”) which includes all other home care services outside of Home Health services and c) the Healthcare Innovations (“HCI”) segment. Reportable segments have been identified based upon how management has organized the business by services provided to customers and the criteria in Accounting Standards Codification (“ASC”) Topic 280, Segment Reporting.
Our HH segment provides a comprehensive range of Medicare-certified home health nursing services to patients in need of recuperative care, typically following a period of hospitalization or care in another type of inpatient facility. Our services are often provided to patients in lieu of additional care in other settings, such as long term acute care hospitals, inpatient rehabilitation hospitals or skilled nursing facilities. Our nurses, therapists, medical social workers and home health aides work closely with patients and their families to design and implement an individualized treatment response to a physician-prescribed plan of care. Under the umbrella of our “Senior Advocacy” mission, we offer special clinically-based protocols customized to meet the needs of the increasingly medically complex, chronic and co-morbid patient populations we serve. Examples include Optimum Balance, Silver Steps, Cardiocare, Orthopedic and Congestive Heart Failure in the Home. HH Medicare revenues are generated on a per episode basis rather than a fee per visit or hourly basis. Approximately 95% of the HH segment revenues are generated from the Medicare program while the balance is generated from Medicaid and private insurance programs.
Our OHBS segment includes traditional personal care (“PC”) services (generally provided by paraprofessional staff such as home health aides) which are generally of a custodial rather than skilled nature, as well as hospice services. PC provides services in patients’ homes primarily on an as-needed, hourly basis. These services include personal care, medication management, meal preparation, caregiver respite and homemaking. Our services are often provided to patients who would otherwise be admitted to skilled nursing facilities for long term custodial care. PC revenues are generated on an hourly basis. PC segment revenues are generated from Medicaid and other government programs while the balance is generated from insurance programs and private pay patients (approximately 80% of personal care revenues). Hospice services are largely provided in patients’ homes and generally require specialized hospice nursing skills. Hospice revenues are generated on a per diem basis and are primarily from Medicare (approximately 93% of hospice revenues).
Our HCI business segment is used to report on our developmental activities outside our HH and OHBS businesses. The HCI segment includes: a) an ACO enablement company; b) an in-home assessment company serving the long-term care insurance industry and managed care organizations; and c) an investment in a population-health analytics company.
5
Additional financial information about our segments can be found in Part II, Item 8, “Notes to Consolidated Financial Statements” and related notes included elsewhere in this Form 10-K.
Our View on Reimbursement and Diversification of Risk
Our Company is highly dependent on government reimbursement programs which pay for the majority of the services we provide to our patients and customers. Reimbursement under these programs, primarily Medicare and Medicaid, is subject to frequent changes as policy makers balance constituents’ needs for health care services within the constraints of the specific government’s fiscal budget. Medicare and Medicaid, respectively, are consuming a greater percentage of federal and states’ budgets, which is exacerbated in times of economic downturn. We believe that these financial issues are cyclical in nature rather than indicative of the long-term prospect for Medicare and Medicaid funding of health care services. Additionally, we believe our services offer the lowest cost alternative to institutional care and are a part of the solution to the federal government’s Medicare and states’ Medicaid financing problems.
We believe that an important key to our historical success and to our future success is our ability to adapt our operations to meet changes in reimbursement as they occur. One important way in which we have achieved this adaptability in the past, and in which we plan to achieve it in the future, is to maintain some level of diversification in our business mix.
The execution of our business plan will place primary emphasis on the development of our home health operations. As our business grows, we may evaluate opportunities for the provision of other health care services in patients’ homes that would be consistent with our Senior Advocacy mission.
6
Overview of Our Services
Home Health Division Services
Operating Locations
Our current operating locations for our Home Health and Other Home-based Services segments as of our last two fiscal years were as follows:
|
|
|
2017 |
|
2016 |
|
||||
|
|
|
Branches |
|
Branches |
|
||||
|
|
|
Home |
|
Other Home- |
|
Home |
|
Other Home- |
|
|
States |
|
Health |
|
Based Services |
|
Health |
|
Based Services |
|
|
Alabama |
|
6 |
|
— |
|
1 |
|
— |
|
|
Alaska |
|
1 |
|
1 |
|
— |
|
— |
|
|
Arizona |
|
1 |
|
— |
|
— |
|
— |
|
|
Arkansas |
|
5 |
|
— |
|
— |
|
— |
|
|
Connecticut |
|
6 |
|
14 |
|
5 |
|
16 |
|
|
Florida |
|
56 |
|
9 |
|
48 |
|
8 |
|
|
Georgia |
|
11 |
|
1 |
|
9 |
|
— |
|
|
Illinois |
|
9 |
|
1 |
|
3 |
|
— |
|
|
Indiana |
|
12 |
|
— |
|
9 |
|
— |
|
|
Kentucky |
|
24 |
|
4 |
|
21 |
|
4 |
|
|
Massachusetts |
|
6 |
|
— |
|
6 |
|
— |
|
|
Mississippi |
|
3 |
|
— |
|
2 |
|
— |
|
|
Missouri |
|
4 |
|
— |
|
4 |
|
— |
|
|
New Jersey |
|
7 |
|
— |
|
7 |
|
— |
|
|
New Mexico |
|
1 |
|
— |
|
— |
|
— |
|
|
New York |
|
6 |
|
7 |
|
5 |
|
7 |
|
|
North Carolina |
|
1 |
|
— |
|
— |
|
— |
|
|
Ohio |
|
15 |
|
21 |
|
14 |
|
22 |
|
|
Oklahoma |
|
5 |
|
— |
|
— |
|
— |
|
|
Pennsylvania |
|
17 |
|
9 |
|
6 |
|
3 |
|
|
South Carolina |
|
3 |
|
2 |
|
— |
|
— |
|
|
Tennessee |
|
30 |
|
10 |
|
22 |
|
6 |
|
|
Texas |
|
4 |
|
— |
|
— |
|
— |
|
|
Virginia |
|
3 |
|
— |
|
— |
|
— |
|
|
Washington |
|
2 |
|
1 |
|
— |
|
— |
|
|
West Virginia |
|
1 |
|
— |
|
— |
|
— |
|
|
Wisconsin |
|
3 |
|
11 |
|
6 |
|
11 |
|
|
|
|
|
|
|
|
|
|
|
|
|
Total |
|
242 |
|
91 |
|
168 |
|
77 |
|
The increase in branch locations in 2017 was largely the result of the acquisition of an 80% controlling interest in the entity holding the home health and hospice assets of Community Health Systems, Inc. (NYSE: CYH) (referred to herein as “CHS Home Health”). CHS Home Health, a provider of skilled home health and hospice services, operated 74 home health and 15 hospice branch locations in 22 states.
Home Health Services Segment
Our HH segment provides a comprehensive range of Medicare-certified home health nursing services to patients in need of recuperative health care, typically following a period of hospitalization or care in another type of inpatient facility. Our patients are referred to us by their physicians or upon discharge from a hospital or other type of in-patient facility.
7
Our HH segment operates 242 Medicare-certified home health agencies. This segment generated 74% of our revenues for 2017, of which approximately 95% were derived from the Medicare program.
We receive payment from Medicare, Medicaid and private insurance companies. Our professional staff includes registered nurses, licensed practical nurses, physical, speech and occupational therapists, and medical social workers. They fulfill medical treatment plans prescribed by physicians. Our professional staff are subject to state licensing requirements in the particular states in which they practice. Para-professional staff members (primarily home health aides) also provide care to these patients.
Our HH segment operations located in Florida normally experience higher admissions during the first quarter and lower admissions during the third quarter than in the other quarters due to seasonal population fluctuations. HH segment operations located in Florida generated approximately 20% of our revenue for 2017.
Other Home-Based Services Segment
Personal care services are also provided in patients’ homes on an as needed hourly basis, including personal care, medication management, meal preparation, caregiver respite and homemaking. These services (generally provided by para-professional staff such as home health aides) are generally of a custodial rather than skilled nature. Generally, PC revenues are generated on an hourly basis, of which approximately 80% were derived from the Medicaid program. We currently operate 75 Personal Care locations. Hospice services are largely provided in patients’ homes and generally require specialized hospice nursing skills. Hospice revenues are generated on a per diem basis and are primarily from Medicare (approximately 93% of hospice revenues). We operate 16 Hospice locations. Our OHBS segment generated 23% of our revenues for 2017.
Healthcare Innovations Segment
Our HCI business segment was created to house and separately report on our developmental activities outside our traditional home health business platform. These activities are intended ultimately, whether directly or indirectly, to benefit our patients and payers through the enhanced provision of home health services. HCI activities all share a common goal of improving patient experiences and quality outcomes, while lowering costs. These include, but are not limited to: technology, information, population health management, risk-sharing, assessments, care coordination and transitions, clinical advancements, enhanced patient engagement and informed clinical decision making. We believe these activities help us discover valuable insight and experiences that would not otherwise be gained in the routine operation of our core home health business segments. Further, we believe these innovation activities will play an important role in collaborating with policy makers, payers, providers, and anyone who assumes financial risk for managing patient populations, to seek to reduce costs, and improve quality by providing increasingly more care for more patients in their homes than ever before. This segment generated approximately 3% of our revenue for 2017.
As discussed further below, the HCI segment currently includes: a) Imperium Health Management, LLC ("Imperium"), an ACO enablement company, b) Long Term Solutions, Inc. ("LTS"), an in-home assessment company serving the long-term care insurance industry, c) Ingenios Health Co. ("Ingenios"), a Nurse-Practitioner-oriented and mobile technology-enabled health risk assessment company primarily serving managed care organizations; and d) an investment in Care Journey (formerly NavHealth, Inc.), a population-health analytics company,
Some of these initiatives are highly speculative and have been made in development stage enterprises. There can be no assurance that we will receive any return on, or of, the capital we invest in these ventures. However, we believe these activities already have, and will continue to help us, discover valuable insights and experiences we would not otherwise gain in the routine operation of our core home health business segments. These endeavors are part of a growing number of care-related innovations and reforms. We expect more will be attempted over the next several years.
Imperium
Imperium's purpose is to assist health care systems and independent primary care physician practices in establishing and successfully operating Accountable Care Organizations ("ACOs") first made possible by 2010's Affordable Care Act.
8
Through improved care management, in a coordinated effort led by primary care physicians, with nurses and home health agencies using evidence-based clinical standards, we seek to reduce avoidable hospitalizations, emergent care, and non-impactful health care services. We seek to work together with primary care physicians to manage high-cost patients in lower-cost settings, with a goal of generating, and sharing in, savings to the Medicare program. By linking physicians with home health care through the ACO vehicle we seek to deliver meaningful savings to the healthcare system and participate in a share of those savings under the Medicare Shared Savings Program ("MSSP") and such other similar models as may evolve in the future.
Imperium has rapidly expanded its customer base growing from 3 ACOs under contract in 2013, to 7 in 2014, 11 in 2015, 14 in 2016, 15 in 2017 and 30 in 2018. In terms of covered Medicare beneficiaries, Imperium has grown from 23,000 in 2013, to 45,000 in 2014 and 85,000 in 2015, 124,000 in 2016, 142,000 in 2017 and 405,000 in 2018. While we intend to work together toward the development of additional ACO relationships in markets in which Almost Family also provides home health services, Imperium also currently has, and will continue to seek, ACO customers in other service territories. We own 72% of Imperium and consolidate its result in our financial statements. We report a provision for noncontrolling interests (“NCI”) to reflect the income or losses attributable to the 28% interest that we do not own.
CMS announced the first year financial reconciliation and quality performance results for ACOs in September of 2014, in which, fifty-three ACOs generated shared savings during their first performance year ended December 31, 2013. ACOs that generated savings earned a performance payment, if they met the quality standard. CMS announced the fourth year results in August of 2017. Imperium serviced ACOs have received an MSSP payments in the first, second, third and fourth CMS results. Imperium received its share of $2.3 million in 2017 for 2016 services, $4.3 million in 2016 for 2015 services, $1.4 million in 2015 for 2014 services and $1.6 million in 2014 for 2013 services. There can be no assurance that future payments will be made by CMS, the structure of MSSP payments will remain as currently deployed, or that an MSSP payment will be received in 2018 related to our 2017 services or any future period.
Long Term Solutions
LTS performs in-home nursing assessments for the long-term care insurance industry. LTS also provides a suite of planning and support services to insurance companies, employers and direct to individuals and families throughout the United States. LTS, through its network of thousands of assessment service partners provides assessments in all 50 U.S. states and a number of foreign countries. LTS estimates that the majority of its assessments result in the patient ultimately receiving home health, assisted living or skilled nursing care in accordance with their long-term care insurance benefits.
Ingenios Health Co.
Ingenios is a provider of technology enabled in-home clinical assessments for Medicare Advantage, Managed Medicaid and Commercial Exchange lives. We believe health assessment capabilities provide the key element in the evolution of improved care planning and delivery as healthcare delivery and reimbursement models evolve.
Care Journey (formerly NavHealth)
Care Journey is a development-stage enterprise whose business plan is focused on the development of technology-based tools designed to help health systems anticipate and inform a patient’s journey through the health care system. Among its other objectives, Care Journey seeks to develop and market a software platform designed to assist health care providers, managed care organizations and insurers in their efforts to aggregate patient data from various sources, improve patient engagement, satisfaction and outcomes and lower the overall cost of healthcare delivery. We are co-invested with founders Aneesh Chopra and Hunch Analytics which Chopra co-founded with Sanju Bansal. Mr. Bansal is the co-founder and former COO of MicroStrategy (MSTR), a worldwide provider of enterprise software for cloud business intelligence and big data services. We made an initial $1 million noncontrolling investment in Care Journey on January 29, 2015 and may, at our option, invest another $1 million. We account for this non-controlling investment under the cost method.
9
Compensation for Home Health Services
We are compensated for our home health services by (i) Medicare, (ii) Medicaid, (iii) other third party payors (e.g., insurance companies and other sources), and (iv) private pay (paid by personal funds). The rates of reimbursement we receive from Medicare, Medicaid and other government programs are generally dictated by those programs. In determining charge rates for goods and services provided to our other customers, we evaluate several factors including cost and market competition. We sometimes negotiate contract rates with third party providers such as insurance companies.
Our reliance on government sponsored reimbursement programs makes us vulnerable to possible legislative and administrative regulation changes and budget cut-backs that could adversely affect the number of persons eligible for such programs, the amount of allowed reimbursements or other aspects of the programs, any of which could materially affect us. In addition, loss of certification or qualification under Medicare or Medicaid programs could materially affect our ability to effectively market our services.
The following table sets forth our revenues from operations derived from each major payor class during the indicated periods (by percentage of net revenues) for the following years:
|
Payor Group |
|
2017 |
|
2016 |
|
2015 |
|
|
Medicare |
|
75.1 |
% |
68.2 |
% |
71.4 |
% |
|
Medicaid and Other Government Programs |
|
19.8 |
% |
23.2 |
% |
22.5 |
% |
|
Insurance and private pay |
|
5.1 |
% |
8.6 |
% |
6.1 |
% |
Medicare revenues account for 95% of HH segment revenues. Historical changes in payment sources are primarily a result of changes in the types of customers we attract.
See “Government Regulation” and “Risk Factors.” We will monitor the effects of such items and may consider modifications to our expansion and development strategy when and if necessary.
Acquisitions
The Company has completed several acquisitions over the past few years and will continue to seek to acquire other quality providers of Medicare-certified home health and/or personal care services, along with making investments in healthcare innovators through our Healthcare Innovations segment.
Factors which may affect future acquisition decisions include, but are not limited to, the quality and potential profitability of the business under consideration, and our profitability and ability to finance the transaction.
2017 Acquisitions
On November 20, 2017, our CHS-JV purchased assets of a Medicare-certified home health agency in Fort Myers, Florida. Post-acquisition operating results are reported in our HH segment.
On July 14, 2017, our CHS-JV purchased assets of a Medicare-certified home health agency and related private duty company in Key West, Florida. Post-acquisition operating results are reported in our HH and OHBS segments.
On December 31, 2016, the first day of our 2017 fiscal year, we acquired an 80% controlling interest in the entity holding the home health and hospice assets of Community Health Systems, Inc. (NYSE: CYH) (referred to herein as “CHS Home Health”). CHS Home Health, a provider of skilled home health and hospice services, operated 74 home health and 15 hospice branch locations in 22 states. The purchase price of $128 million was funded through borrowings on the Company’s revolving credit facility.
2016 Acquisitions
During the third quarter of 2016, one of our HCI subsidiaries redeemed certain outstanding shares increasing our ownership percentage to 72.04% from 61.50%.
10
On June 18, 2016, we acquired certain home health agency assets primarily in Wisconsin, but also in Connecticut and Kentucky (collectively, the Wisconsin acquisition) for a purchase price of $6.1 million, funded through borrowings on the Company’s bank credit facility. The post-acquisition operating results of these agencies are primarily reported in our PC segment.
On January 5, 2016, we acquired 100% of the equity of LTS for a purchase price of $37 million, funded through borrowings on the Company's bank credit facility, seller notes and issuance of the Company's common stock. LTS's post acquisition operating results are reported in our HCI segment.
On January 5, 2016, we purchased the assets of a Medicare-certified home health agency owned by Bayonne Visiting Nurse Association (“Bayonne”) located in New Jersey. Bayonne’s post acquisition operating results are reported in our HH segment.
2015 Acquisitions
On November 5, 2015, we acquired the stock of Black Stone Operations, LLC (“Black Stone”). Black Stone is a provider of in-home personal care and skilled home health services in western Ohio and operates under the name “Home Care by Black Stone.” The purchase price of $40 million was funded through borrowings on the Company’s bank credit facility, seller notes and issuance of the Company’s common stock. Black Stone’s post acquisition operating results are reported in our HH and PC segments.
On July 22, 2015, we acquired 100% of the equity of Ingenios for approximately $11.4 million of the Company’s common stock plus $2 million in cash. Ingenios is a leading provider of technology enabled in-home clinical assessments for Medicare Advantage, Managed Medicaid and Commercial Exchange lives in four states and Washington, D.C. The post acquisition operating results of Ingenios are reported in our HCI segment.
On August 29, 2015, we acquired 100% of the equity of Bracor, Inc. (dba “WillCare”). WillCare, based in Buffalo, NY, owned and operated HH and PC branch locations in New York (12) and Connecticut (1). The purchase price was approximately $50.8 million. The transaction was funded by borrowings under the Company’s bank credit facility. WillCare’s New York and Connecticut post acquisition operating results are reported in our HH and PC segments.
On March 1, 2015, we acquired the stock of WillCare’s Ohio operations for $3.0 million. WillCare’s Ohio post acquisition operating results are reported in our HH and PC segments.
On January 29, 2015, we acquired a noncontrolling interest in a development stage analytics and software company, Care Journey. The investment is an asset of our Healthcare Innovations segment.
Competition, Marketing and Customers
The home health industry is highly competitive and fragmented. Competitors include larger publicly held companies such as Amedisys, Inc. (NasdaqGS: AMED), Kindred Healthcare, Inc. (NYSE: KND), and LHC Group, Inc. (NasdaqGS: LHCG), and numerous privately held multi-site home care companies, privately held single-site agencies and a significant number of hospital-based agencies. Competition for customers at the local market level is very fragmented and market specific. Generally, each local market has its own competitive profile and no one competitor has significant market share across all our markets. To the best of our knowledge, no individual provider has more than 7% share of the national Medicare home health market.
We believe the primary competitive factors are quality of service and reputation among referral sources. We market our services through our site managers and marketing staff. These individuals contact referral sources in their areas to market our services. Major referral sources include: physicians, hospital discharge planners, Offices on Aging, social workers, and group living facilities. We also utilize, to a lesser degree, consumer-direct sales, marketing and advertising programs designed to attract customers.
11
The personal care and hospice industries are likewise highly competitive and fragmented. Competitors include home health providers, senior adult associations, and the private hiring of caregivers. We market our services primarily through our site managers, and we compete by offering a high quality of care and by helping families identify and access solutions for care. Major referral sources include case managers, physicians and hospital discharge planners.
Our HCI segment competes in new industries, some of which were created by the Patient Protection and Affordable Care Act (the “ACA”), signed into law in 2010. In certain cases, we operate in relatively new and unproven markets which include new competitors that are identified regularly and which range in size from start-up companies to larger publicly held companies like Universal American Corp., now owned by WellCare Health Plans, Inc. (NYSE: WCG). We market our services directly to our customers.
Government Regulation
Medicare Home Health Program
Payment Methodology
As shown in “Compensation for Home Health Services” above, approximately 75% of our 2017 consolidated net service revenues were derived from the Medicare Home Health Program. Medicare reimburses home health care providers under the Prospective Payment System (“PPS”), which pays a fixed, predetermined rate for services and supplies under an episode of care. An episode of home health care spans a 60-day period, starting with the first day a billable visit is furnished to a Medicare beneficiary and ending 60 days later. If a patient is still in treatment on the 60th day, a new episode begins on the 61st day, commonly referred to as a recertification episode, regardless of whether a billable visit is rendered on that day and ends 60 days later.
Payment rates are subject to adjustment based on certain variables including, but not limited to: (a) a case-mix adjustment, which drives the home health resource group (“HHRG”) to which the Medicare patient is assigned based on such factors as the patient’s clinical, functional, and services utilization characteristics; (b) geographic wage adjustment, including rural rate add-ons, if any; (c) a payment adjustment based upon the level of therapy services required (thresholds set at 6, 14 and 20 visits); (d) a low utilization payment adjustment (“LUPA”) if the number of visits was fewer than five; (e) an outlier payment if our patient’s care was unusually costly (capped at 10% of total reimbursement at the agency level); (f) a partial payment if our patient transferred to another provider or we received a patient from another provider before completing the episode; (g) the number of episodes of care provided to a patient; and (h) sequestration, a 2% legislated reduction pursuant to the Budget Control Act (“BCA”) signed into law on August 2, 2011, which was effective for episodes ended after March 31, 2013.
In establishing payment rates for the last three years, the Medicare Program recalibrated the national average case-mix levels and maintained budget neutrality by making a corresponding adjustment to the National, Standardized 60-Day Episode Payment Rate (“Base Episode Payment Rate”). These nominal case-mix and payment rate recalibrations result in a lower case mix and higher base rates and are intended to have no effect on payments actually made. We have presented the Base Episode Payment Rate established by the Medicare Program for all episodes of care ended on or after the applicable time periods, along with the Base Episode Payment Rate for each period as if the case-mix resets were in effect for all prior periods below:
|
|
|
|
|
Base Episode Payment Rate |
|
||
|
|
|
Base Episode |
|
Adjusted for Case-mix |
|
||
|
Period |
|
Payment Rate (1) |
|
Recalibrations (2) |
|
||
|
January 1, 2018 through December 31, 2018 |
|
$ |
3,040 |
|
$ |
3,040 |
|
|
January 1, 2017 through December 31, 2017 |
|
|
2,990 |
|
|
3,038 |
|
|
January 1, 2016 through December 31, 2016 |
|
|
2,965 |
|
|
3,077 |
|
|
January 1, 2015 through December 31, 2015 |
|
|
2,961 |
|
|
3,130 |
|
|
(1) |
Reflects the payment rates as published by the Medicare Program. |
12
|
(2) |
Presents the payment rates on a consistent basis as if the case-mix recalibrations had been in effect for all periods presented. As applicable, adjusted payment rates for each of the years 2015-2017 were calculated by multiplying the actual Base Episode Payment by 1.0187 (2015 Final Rule), then by 1.0214 (2016 Final Rule) and then by 1.0160 (2017 Final Rule). |
After determining the appropriate PPS payment rate, we record net revenues as services are rendered to patients over the 60-day episode period. At the end of each month, a portion of our revenue is estimated for episodes that have not yet been completed, which are generally referred to as episodes in progress. As a result, net service revenues recorded for an episode in progress is subject to change if the actual number of visits differs from the number anticipated at the start of care. Our revenue recognition under the Medicare reimbursement program is discussed in greater detail in Part II, Item 7 “Critical Accounting Policies” and Item 8, “Notes to Consolidated Financial Statements”.
2018 CMS Related Updates
The Bipartisan Budget Act of 2018, enacted in February 2018 has the following provisions impacting health care services provided at home:
|
· |
Restores the 3% home health rate add-on for patients who reside in rural geographies, effective January 1, 2018. The add-on rate will be phased downward over a five year period following a formula specified in the legislation. |
|
· |
Mandates the development of a new case mix model for home health services using a 30 day payment period, through a transparent process including the home health industry and Congressional committees of Medicare jurisdiction. The law requires any new case mix model to be implemented in 2020 in a budget neutral manner. |
|
· |
Face-to-face documentation improvements allowing the home health medical record in its entirety to be used to support the physician’s attestation of medical necessity. |
|
· |
A study to be conducted by the GAO (Government Accounting Office) on Medicare improvements to address the needs of the chronically ill including the provision of services provided at home, including interdisciplinary care management, tele-health and tele-monitoring for managed care plans, requiring states to better integrate Medicare and Medicaid services for the dually eligible and extension of the Independence at Home Demonstration Program. |
|
· |
A specific home health market basket annual inflationary update percentage of 1.5% for FY2020, leaving intact the full market basket update (generally expected to be between 2% and 3%) for FY2019. |
On November 1, 2017, the Centers for Medicare and Medicaid Services (“CMS”) released the final rule for FY2018 home health reimbursement, which includes a 0.4% rate cut consisting of a 1.0% market basket update, a 0.97% case mix adjustment and sunset of the rural add-on provision. Among other things, the rule finalizes proposals for the Home Health Value Based Purchasing (“HHVBP”) Model and the Home Health Quality Reporting Program (“HH QRP”). CMS did not finalize the Home Health Groupings Model but instead elected to “further engage with stakeholders to move towards a system that shifts the focus from volume of services to a more patient –centered model”. On September 25, 2017, the Company submitted a comment letter to CMS which provides an alternative course of action that we believe better protects Medicare beneficiaries and their right to access appropriate and necessary home health service. The comment letter to CMS entitled “CY 2018 Home Health Prospective Payment System Rate Update – September 2017” can be found on the Company’s website, along with a series of responses to various other stakeholder requests from the Senate Finance Committee, the House Ways and Means Committee and CMS dating to 2013 and including the Company’s executive testimony before the Congress.
In January of 2017, CMS released a final rule revising the conditions of participation (“CoPs”) for home health agencies to participate in the Medicare and Medicaid programs. The rule, originally effective July 13, 2017, and deferred through the end of 2017, focuses on, among other things, care delivered to patients, an interdisciplinary view of patient care, greater flexibility in meeting quality of care standards and the elimination of certain unneeded procedural burdens on providers. This new rule is not expected to have a significant impact on our result of operations or financial position.
On June 8, 2016, CMS announced the “Pre-Claim Review Demonstration of Home Health Services” which seeks to demonstrate that a review of selected documentation prior to payment of claims can decrease “improper payments
13
because of insufficient documentation.” According to CMS, the pre-claim review demonstration was designed to help educate Home Health Agencies on what documentation is required and encourage them to submit the correct documentation, while still allowing the HHA to begin providing services and receive initial payments prior to the pre-claim review decision. The pre-claim review demonstration began in Illinois in 2016, but currently has been suspended. Further expansion to Florida, Texas, Michigan and Massachusetts has also been delayed. Currently, it is unclear as to when this demonstration program will be resumed, if ever.
Potential Future Developments in Medicare Home Health
While there have been many changes enacted over the past several years, the Congress and/or CMS may take future actions which could have an adverse impact on our business, including possible:
|
· |
Extension of the rebasing period to a period longer than the currently legislated 2014-2017 four-year phase in; |
|
· |
Changes in cost sharing between the Medicare program (“Program”) and beneficiaries (i.e., co-pays); |
|
· |
Removal of or changes to codes in the case-mix system or recalibration of the case-mix system including further case-mix creep coding adjustments, all of which could result in changes to rates under the national standardized 60-day episodic payment; |
|
· |
Post-acute care bundling; |
|
· |
Removal or reductions to established statutory reductions to the annual inflationary rate adjustments we would have otherwise received; |
|
· |
“Productivity” payment reductions to reimbursement rates we would have otherwise received; |
|
· |
Changes that put providers “at risk” for patient outcomes; |
|
· |
Addition of new pre-authorization requirements for home health services; |
|
· |
Implementation and/or expansion of Value-based pricing programs could result in reduction of reimbursement rates we would otherwise receive or could impact our reimbursement in ways we do not currently anticipate, and |
|
· |
Other types of changes of which we may not currently be aware. |
We are unable to predict when or whether any of these types of changes may be enacted or what impact, if any, they may have on our business.
Medicaid Reimbursement
As shown in “Compensation for Home Health Services” above, approximately 20% of our 2017 consolidated net service revenues were derived from state Medicaid and Other Government Programs, with approximately 7.5%, 3.4%, 3.1%, 1.9% and 1.1% generated from Medicaid reimbursement programs in the states of Ohio, Connecticut, New York, Tennessee and Kentucky, respectively. Net service revenues under such state programs are derived from services provided under a per visit, per hour or unit basis (as opposed to episodic). Revenues are calculated and recorded using payor-specific or patient-specific fee schedules based on the contracted rates.
The financial condition of the Medicaid programs in each of the states in which we operate is cyclical with some currently facing significant budget issues. States may be expected from time to time to take actions or evaluate taking actions to control the rate of growth of Medicaid expenditures. Among these actions are the following:
|
· |
redefining eligibility standards for Medicaid coverage, |
|
· |
redefining coverage criteria for home and community based care services, |
|
· |
slowing payments to providers by increasing the minimum time in which payments are made, |
|
· |
limiting reimbursement rate increases or implementing rate cuts, |
|
· |
increased utilization of self-directed care alternatives, |
|
· |
shifting beneficiaries from traditional coverage to Medicaid managed care providers, and |
|
· |
changing regulations under which providers must operate. |
14
Medicaid programs, while partially federally funded, are administered by the individual states under the broad supervision of CMS. Accordingly, developments typically occur on a state-by-state basis. Specific programs and changes are enacted regularly. Any such changes, if enacted, could adversely impact our operations.
Medicare and Medicaid Reimbursement Summary
The health care industry has experienced, and is expected to continue to experience, extensive and dynamic periods of change. In addition to economic forces and regulatory influences, continuing political debate subjects the health care industry to significant reform. Health care reforms have been enacted as discussed elsewhere in this document and proposals for additional changes are continuously formulated by departments of the federal government, Congress, and state legislatures. Such governmental payors provide for approximately 95% of our consolidated net service revenues, including Medicare Advantage plans run by private insurers which are also dependent on federal funding.
We expect legislators and government officials to continuously review and assess alternative health care delivery systems and payment methodologies. Changes in the law or new interpretations of existing laws may have a dramatic effect on the definition of permissible or impermissible activities, the relative cost of doing business, and the methods and amounts of payments for medical care by both governmental and other payors. We expect legislative changes intended to “balance the budget” and slow the annual rate of growth of Medicare and Medicaid to continue. Such future changes may further impact reimbursement for our services. There can be no assurance that future legislation or regulatory changes will not have a material adverse effect on our results of operations.
Governments might take or consider taking further actions because the number of Medicare and Medicaid beneficiaries and their related expenditures are growing at a faster rate than the governments’ revenue. Medicare and Medicaid are consuming increasing percentages of budgets and may expand further driven by state based exchanges resulting from the ACA and implementing regulations. Health care financing issues are exacerbated when revenues slow in a down economy. We believe that these financing issues are cyclical in nature rather than indicative of the long-term prospect for Medicare and Medicaid funding of health care services for the populations we serve. Additionally, we believe our services offer the lowest cost alternative to institutional care and are a critical part of the solution to our nation’s health care financing problems.
Given the broad and far reaching implications of all the changes in the rapidly evolving environment in which we operate, the incomplete nature of these changes, the pace at which the changes are taking place and the prospects for future changes to be made, we cannot predict the ultimate impact, which may be material and adverse, that health care reform efforts and resulting Medicare and Medicaid reimbursement rates will have on our liquidity, our results of operations, the realizability of the carrying amounts of our intangible assets, including goodwill, or our financial condition. Further, we are unable to predict what effect, if any, such material adverse effect, if it were to occur, might have on our ability to continue to comply with the financial covenants of our revolving credit facility and our ability to continue to access debt capital through that facility.
Permits and Licensure
Many states require companies providing certain health care services to be licensed as home health agencies. In addition, certain health care practitioners employed by us require state licensure and/or registration and must comply with laws and regulations governing standards of practice. The failure to obtain, renew or maintain any of the required regulatory approvals or licenses could adversely affect our business. We believe we are currently licensed appropriately where required by the laws of the states in which we operate. There can be no assurance that either the states or the federal government will not impose additional regulations upon our activities which might adversely affect our results of operations, financial condition, or liquidity.
Certificates of Need
Certain states require companies providing health care services to obtain a certificate of need issued by a state health-planning agency. Where required by law, we have obtained certificates of need from those states. There can be no assurance that we will be able to obtain any certificates of need which may be required in the future, if we expand the
15
scope of our services or if state laws change to impose additional certificate of need requirements, and any attempt to obtain additional certificates of need will cause us to incur certain expenses.
Medicare and Medicaid Participation
Effective March 25, 2011, CMS implemented new enrollment regulations which were a response to aspects of the ACA designed to enhance enrollment procedures to protect against fraud. The regulations authorize the establishment of risk categories with risk level dictating the enrollment screening activities, i.e., more rigorous screening as the perceived risk increases. For Medicare, there are three categories of providers i.e., “limited,” “moderate,” or “high” risk, and CMS has placed newly enrolling home health agencies in the “high risk” category, with existing enrolled home health agencies categorized as “moderate risk.” In addition to the low risk provider screening procedures, providers in the moderate risk category will be subject to unannounced site visits. For high risk providers, any individual with a 5% or more ownership interest will be subject to fingerprint-based criminal history record checks. Additionally, the new regulations authorize Medicare and state Medicaid agencies to impose temporary enrollment moratoria for a particular type of provider if determined to be necessary to combat fraud, waste, or abuse. To the extent that home health agencies are subject to a moratorium, any newly enrolling home health agency, including any change of ownership subject to the 36 month rule, and any expansion to add a branch would be affected by the moratorium.
Other Regulations
A series of laws and regulations dating back to the Omnibus Budget Reconciliation Act of 1987 (“OBRA 1987”) and through the ACA and related subsequent legislation have been enacted and apply to us. Changes in applicable laws and regulations have occurred from time to time since OBRA 1987 including reimbursement reductions and changes to payment rules. Changes are also expected to occur continuously for the foreseeable future.
As a provider of services under Medicare and Medicaid programs, we are subject to the Medicare and Medicaid anti-kickback statute and other “fraud and abuse laws.” The anti-kickback statute prohibits any bribe, kickback, rebate or remuneration of any kind in return for, or as an inducement for, the referral of Medicare or Medicaid patients. We may also be affected by the federal physician self-referral prohibition, known as the “Stark” law, which, with certain exceptions, prohibits physicians from referring patients to entities in which they have a financial interest or from which they receive financial benefit. Penalties for violations of the federal Stark law include payment sanctions, civil monetary penalties, and/or program exclusion. Many states in which we operate have adopted similar self-referral laws, as well as laws that prohibit certain direct or indirect payments or fee-splitting arrangements between health care providers, if such arrangements are designed to induce or to encourage the referral of patients to a particular provider.
As a result of the Health Insurance Portability and Accountability Act of 1996 and other legislative and administrative initiatives, federal and state enforcement efforts against the health care industry have increased dramatically, subjecting all health care providers to increased risk of scrutiny and increased compliance costs.
We are subject to routine and periodic surveys, audits and investigations by various governmental agencies. In addition to surveys to determine compliance with the conditions of participation, CMS has engaged a number of contractors (including Fiscal Intermediaries, Recovery Audit Contractors, Program Safeguard Contractors, Zone Program Integrity Contractors, and Medicaid Integrity Contributors) to conduct audits to evaluate billing practices and identify overpayments. In addition to audits by CMS contractors, individual states are implementing similar programs such as using Medicaid Recovery Audit Contractors. We believe that we are in material compliance with applicable laws. However, we are unable to predict what additional government regulations, if any, affecting our business may be enacted in the future, how existing or future laws and regulations might be interpreted or whether we will be able to comply with such laws and regulations either in the markets in which we presently conduct, or wish to commence, business.
Medicare Accountable Care Organizations (ACOs)
The ACA also established ACOs as a tool to improve quality and lower costs through increased care coordination in the Medicare fee-for-service (“FFS”) program, also known as “Original Medicare.” The Medicare FFS program covers approximately 70% of the Medicare recipients or approximately 36 million eligible Medicare beneficiaries. ACOs are
16
groups of doctors and other healthcare providers working together to provide high quality services and care for their patients. Provider and beneficiary participation in an ACO is purely voluntary and Medicare beneficiaries retain their current ability to seek treatment from any provider they wish. ACOs are legal entities that contract with CMS for three-year periods. Beneficiaries are assigned to ACOs using an “attribution” model based on a plurality of services provided by the primary care physician. Beneficiaries still have the right to use any doctor or hospital who accepts Medicare, at any time. In order to receive revenues from CMS under the MSSP, the ACO must meet certain minimum savings rates (i.e. save the federal government money) and meet certain quality measures. More specifically, the ACOs costs of medical expenses for its members during a relevant measurement year must be below the ACO’s benchmark by a minimum amount as established by CMS for such ACO.
CMS established the MSSP to facilitate coordination and cooperation among providers to improve the quality of care for Medicare FFS beneficiaries and reduce unnecessary costs. Eligible providers, hospitals, and suppliers may participate in the MSSP by creating, participating in or contracting with an ACO. The MSSP is designed to improve beneficiary outcomes and increase value of care by (1) promoting accountability for the care of Medicare FFS beneficiaries; (2) requiring coordinated care for all services provided under Medicare FFS; and (3) encouraging investment in infrastructure and redesigned care processes. The MSSP will reward ACOs that reduce health care costs below their benchmark while also meeting performance standards on quality of care. Under the final MSSP rules, Medicare will continue to pay individual providers and suppliers for specific items and services as it currently does under the FFS payment methodologies. MSSP rules require CMS to develop a benchmark for savings to be achieved by each ACO, if the ACO is to receive shared savings or for ACOs that have elected to accept responsibility for losses. An ACO that meets the program’s quality performance standards will be eligible to receive a share of the savings to the extent its assigned beneficiary medical expenditures are below its own medical expenditure benchmark provided by CMS.
Insurance Programs and Costs
We bear significant risk under our large-deductible workers’ compensation insurance program and our self-insured employee health program. Under the workers’ compensation insurance program, we bear risk up to $400,000 per incident.
We purchase stop-loss insurance for the employee health plan that places a specific limit, generally $300,000, on our exposure for any individual covered life. The ACA also includes regulatory changes related to employer sponsored health insurance benefit plans, the most significant of which was initially effective for the Company January 1, 2015. However, certain components continue to evolve, be delayed or have additional developments. Management has implemented portions of its procedures and is currently working to evaluate the implications of these changes and to develop appropriate courses of action for the Company. At this time, we are unable to predict the full impact of such changes on our health insurance benefit programs or the costs of such programs to the Company.
Malpractice and general patient liability claims for incidents which may give rise to litigation have been asserted against us by various claimants. The claims are in various stages of processing and some may ultimately be brought to trial. We are aware of incidents that have occurred through December 29, 2017, that may result in the assertion of additional claims. We currently carry professional and general liability insurance coverage (on a claims made basis) for this exposure with no deductible.
We also carry D&O coverage for potential claims against our directors and officers, including securities actions, with deductibles ranging from $175,000 to $500,000 per claim.
Total premiums, excluding estimated exposure to claims and deductibles, for all our non-health insurance programs were approximately $2.5 million for the contract year ended May 31, 2017.
We record estimated liabilities for our insurance programs based on information provided by the third-party plan administrators, historical claims experience, the life cycle of claims, expected costs of claims incurred but not paid, and expected costs to settle unpaid claims. We monitor our estimated insurance-related liabilities and related insurance recoveries on a monthly basis and have recorded amounts due under insurance policies in other current assets, while
17
recording the estimated carrier liability in other current liabilities in our consolidated balance sheets. As facts change, it may become necessary to make adjustments that could be material to our results of operations and financial condition.
We believe that our present insurance coverage is adequate. As part of our on-going risk management, regulatory compliance and cost control efforts, we continually seek alternatives that might provide a different balance of cost and risk, including potentially accepting additional self-insurance risk in lieu of higher premium costs.
Executive Officers of the Registrant
See Part III, Item 10 of this Form 10-K for information about the Company’s executive officers.
Employees and Labor Relations
As of December 29, 2017, we had approximately 17,100 employees. None of our employees are represented by a labor organization. We believe our relationship with our employees is satisfactory.
Described below and elsewhere in this report are risks, uncertainties and other factors that can adversely affect our business, results of operations, cash flow, liquidity or financial condition. Investing in our common stock involves a degree of risk. You should consider carefully the following risks, as well as other information in this filing and the incorporated documents before investing in our common stock.
Risk Factors Relating to the Merger with LHC Group
The consummation of the Merger is contingent upon the satisfaction of a number of conditions, including stockholder and regulatory approvals, that are outside of the Company’s control and that the Company and LHC Group may be unable to satisfy or obtain or which may delay the consummation of the Merger or result in the imposition of conditions that could reduce the anticipated benefits from the Merger or cause the parties to abandon the Merger.
Consummation of the Merger (as described in Item 7 “Management’s Discussion and Analysis of Financial Condition and Results of Operations”) is contingent upon the satisfaction of a number of conditions, some of which are beyond the Company’s control, including, among others: (i) the adoption of the Merger Agreement by the affirmative vote of the holders of at least a majority of the outstanding shares of the Company’s common stock; (ii) the approval of the issuance of shares of LHC Group’s common stock to be issued to the Company’s stockholders in the merger by the affirmative vote of a majority of the shares of LHC Group’s common stock present in person or represented by proxy at LHC Group’s special meeting; (iii) the expiration or termination of the required waiting periods under the Hart-Scott Rodino Act (which occurred on February 21, 2018); (iv) the absence of any order or law prohibiting the Merger or the other transactions contemplated by the Merger Agreement; (v) the receipt of certain tax opinions; and (vi) the absence of a material adverse effect with respect to either LHC Group or the Company (as defined in the Merger Agreement). The Company and LHC Group may be unable to obtain the regulatory approvals required for the Merger or the required regulatory approvals may delay the Merger or result in the imposition of conditions, possibly including imposition of conditions that may require certain operations to be divested, that could reduce the anticipated benefits from the Merger or cause the parties to abandon the Merger. Any delay in completing the Merger could cause the combined company not to realize, or to be delayed in realizing, some or all of the benefits that we expect to achieve if the Merger is successfully completed within its expected time frame.
The Merger Agreement also requires that the Company and LHC Group use reasonable best efforts to obtain all necessary or advisable approvals from governmental authorities, including those from a number of the federal, state and municipal authorities that regulate the businesses of the Company and LHC Group, including in New York state, which accounts for approximately 7% of the Company’s annual revenues. There can be no assurances that these regulatory approvals will be obtained or what conditions may be imposed on the companies in order to obtain such approvals. While these regulatory approvals are not a condition to closing the Merger, the failure to obtain any of these regulatory
18
approvals could impose additional material costs on or materially limit the revenue of the combined company following the Merger, including ceasing operations or divesting assets in certain jurisdictions, including New York State.
While the Merger is pending, the Company will be subject to business uncertainties that could adversely affect its businesses and operations.
Uncertainty about the effect of the Merger on employees, joint venture partners, third party payors, customers and other persons with whom the Company has a business relationship may have an adverse effect on the Company’s business, operations and stock price. In connection with the pendency of the Merger, existing customers or partners could decide to no longer do business with the Company. In addition, certain projects may be delayed or ceased and business decisions could be deferred. Persons with whom the Company has a business relationship, such as joint venture partners and third party payors, could also decide to terminate, modify or renegotiate their relationships with the Company or take other actions as a result of the Merger that could negatively affect the Company’s revenue, earnings and cash flows. Employee retention may be challenging during the pendency of the Merger, as certain employees may experience uncertainty about their future roles. If key employees depart, the businesses of the Company and LHC Group before the Merger, and the business of the combined company following the merger, could be materially harmed. In addition, stockholders and market analysts could also have a negative perception of the merger, which could cause a material reduction in the Company’s and LHC Group’s stock prices and could also result in (i) LHC Group not achieving the requisite vote to approve the issuance of LHC Group’s shares in the merger and/or (ii) the Company not achieving the requisite vote to adopt the Merger.
Legal proceedings in connection with the merger could delay or prevent the completion of the merger.
If either the Company or LHC Group is the subject of litigation that is related to the Merger, it could cause either company to incur substantial expenditures, generate adverse publicity and could delay or prevent the Merger. As described in Part I, Item 3 “Legal Proceedings,” several lawsuits have been filed against LHC Group, Merger Sub, the Company and/or the Company’s board of directors challenging the adequacy of public disclosures related to the Merger and an adverse ruling may prevent the Merger from being completed. LHC Group, Merger Sub, the Company and/or the members of the Company’s board of directors were named as defendants in three lawsuits brought by alleged stockholders of the Company challenging the adequacy of public disclosures related to the Merger and seeking, among other things, injunctive relief to enjoin the defendants from completing the Merger pursuant to these disclosures. Additional lawsuits may be filed against LHC Group, Merger Sub, the Company and/or their respective directors or officers in connection with the Merger. Defense of these or any other lawsuit, even if successful, could require substantial time and attention of the Company’s management and could require the expenditure of significant amounts for legal fees and other related costs, which could have a material adverse effect on the business, financial condition and results of operations of the Company or the combined company.
Failure to complete the Merger could negatively impact the stock prices and the future business and financial results of the Company.
Completion of the Merger is not assured. If the Merger is not completed, the ongoing businesses and financial results of the Company may be adversely affected and the Company will be subject to several risks, including the following:
|
|
• |
|
the price of the Company’s common stock may decline to the extent that its current market prices reflect a market assumption that the Merger will be completed; |
|
|
• |
|
having to pay significant costs relating to the merger without receiving the benefits of the merger, including, in certain circumstances, a termination fee of $30 million or an expense reimbursement of up to $5 million; |
|
|
• |
|
negative reactions from customers, stockholders and market analysts; |
|
|
• |
|
the possible loss of employees necessary to operate the Company’s business; |
|
|
• |
|
the Company will have been subject to certain restrictions on the conduct of its business, which may have prevented us from making certain acquisitions or dispositions or pursuing certain business opportunities while the Merger was pending; and |
19
|
|
• |
|
the diversion of the focus of the Company’s management to the merger instead of on pursuing other opportunities that could have been beneficial to the Company. |
If the Merger is not completed, the Company cannot assure you that these risks will not materialize and will not materially adversely affect the Company’s business, financial results and stock price.
The Company expects to incur substantial transaction-related costs in connection with the Merger.
The Company has incurred and expects to incur significant costs, expenses and fees for professional services and other transaction costs in connection with the Merger. In addition, the Merger could result in additional costs and expenses that were not expected or anticipated, and such costs and expenses could have a material adverse effect on the Company’s financial condition and results of operation before the Merger and of the combined company thereafter.
Risks Related to Our Industry
The Trump administration, recent changes in members and leadership of the US Congress and related changes in leadership and key individuals in federal regulatory agencies could have a material adverse impact on our results of operations or financial condition in ways not currently anticipated by us.
Future actions by the Trump Administration and the U.S. Congress including, but not limited to, repeal or replacement of the Affordable Care Act (ACA, see below) could have a material adverse impact on our results of operations or financial condition. Additionally, all or a portion of the ACA and related subsequent legislation may be modified, repealed or otherwise invalidated through judicial challenge. Our Imperium subsidiary, an ACO-enablement company, generates substantially all its revenues from the Medicare Shared Savings Program which was enacted with the ACA, and any legislative and regulatory changes could adversely affect its operations. We can provide you with no assurance that the ultimate outcome of the ACA, health care reform efforts and/or the federal budget and resulting Medicare reimbursement rates will not have a material adverse effect on our liquidity, our results of operation, the realizability of the carrying amounts of our intangible assets, including goodwill, or our financial condition. Further, we are unable to predict what effect, if any, such material adverse effect, if it were to occur, might have on our ability to continue to comply with the financial covenants of our revolving credit facility and our ability to continue to access debt capital through that facility.
Complying with health care reform legislation and the implementing regulations and programmatic guidelines could have a material adverse impact on our results of operations or financial condition in ways not currently anticipated by us.
The health care industry has experienced, and is expected to continue to experience, extensive and dynamic periods of change. In addition to economic forces and regulatory influences, continuing political debate subjects the health care industry to significant reform. Very often, sweeping new legislation is followed by subsequent legislation to address previously unanticipated consequences, or to further define provisions that were too vague to implement based on the language of the original legislation and by legal actions to challenge its constitutionality. In our view, it is reasonable to expect this to occur over the next few years. The Patient Protection and Affordable Care Act (the “ACA”), signed into law in March 2010, has adversely impacted our business and it is reasonable to expect this law and future health care reform law to have an impact on our business in the future. As a result of the broad scope of the ACA and related legislation, the significant changes it will effect in the healthcare industry and society generally, and the complexity of the technical issues it addresses, we are unable to predict, at this time, all the ramifications the ACA, its implementing regulations and future health care reform legislation may have on our business as a health care provider or a sponsor of an employee health insurance benefit plan. The ACA, its implementing regulations and programmatic guidelines and future health care reform legislation could have a material adverse impact on our results of operations or financial condition in ways not currently anticipated by us.
Additionally, we may be unable to take actions to mitigate any or all of the negative implications of the ACA, its implementing regulations or programmatic guidelines and future health care regulation which may result in unfavorable earnings, losses, or impairment charges.
20
The current status of federal and state budgets may have a material adverse effect on our future results of operations and financial condition, as well as our ability to access credit and capital.
There can be no assurance that federal and state governments will be able to operate balanced budgets. While the ultimate outcome of these events cannot be predicted, they may have a material adverse effect on the Company. Historic economic conditions, stimulus efforts by the federal government and costly new programs created by the ACA have placed significant strain on federal and state budgets, many of which are in a deficit position. Efforts to reduce spending at the federal and/or state levels may result in reductions in reimbursement by Medicare, Medicaid and other third-party payors along with tax increases, which may in turn result in decreased revenue growth and a decrease in our profitability. Our contractors and suppliers may also be negatively impacted by these conditions and our ability to provide patient care at a lower cost may diminish and reduce our profitability. Future disruptions in the credit and capital markets, if any, may restrict our access to capital. As a result, our ability to incur additional indebtedness to fund acquisitions and operations may be constrained. If the federal and state budgets’ conditions deteriorate or do not improve, our results of operations or financial condition could be materially and adversely affected.
Our profitability depends principally on the level of government-mandated payment rates. Reductions in rates, or rate increases that do not cover cost increases, may adversely affect our business.
We generally receive fixed payments from Medicare and Medicaid for our services based on the level of care that we provide patients. Consequently, our profitability largely depends upon our ability to manage the cost of providing services. Although current Medicare legislation provides for an annual adjustment of the payment rates based on the increase or decrease of the medical care expenditure category of the Consumer Price Index, these Medicare payment rate increases may be less than actual inflation or could be eliminated or reduced in any given year. Since April 1, 2013, Medicare reimbursement has been reduced an additional 2% through sequestration as mandated by federal legislation. Consequently, if our cost of providing services, which consists primarily of labor costs, is greater than the respective Medicare or Medicaid payment rate, our profitability would be negatively impacted. Based on our analysis of Medicare’s final regulations for the home health prospective payment system, we expect our Medicare reimbursement rates for home health services provided in 2018 to be about 1% lower than in 2017.
Any changes to the laws and regulations governing our business, or the interpretation and enforcement of those laws or regulations, could cause us to modify our operations and could negatively impact our operating results.
The federal government and the states in which we operate regulate our industry extensively, including payment, coding and billing for services; financial relationships with physicians and referral sources; certification of agencies; licensure and certificates of need; and maintenance and protection of patient health information. The laws and regulations governing our operations, along with the terms of participation in various government programs, regulate how we do business, the services we offer, and our interactions with patients and the public. These laws and regulations, and their interpretations, are subject to frequent change. Changes in existing laws and regulations, or their interpretations, or the enactment of new laws or regulations could reduce our profitability by:
|
· |
increasing our liability; |
|
· |
increasing our administrative and other costs; |
|
· |
increasing or decreasing mandated services; |
|
· |
forcing us to restructure our relationships with referral sources, providers or joint venture partners; or |
|
· |
requiring us to implement additional or different programs and systems. |
Violation of the laws governing our operations, or changes in interpretations of those laws, could result in the imposition of fines, civil or criminal penalties, the termination of our rights to participate in federal and state-sponsored programs, the suspension or revocation of our licenses, or claims for damages. If we become subject to material fines or if other sanctions or other corrective actions are imposed on us, we might suffer a substantial reduction in profitability.
21
We have been, and could become, the subject of governmental investigations, claims and litigation that could have a material adverse effect on our financial position, results of operation and liquidity.
Over the years, we have been the subject of civil investigations, and qui tam or “whistleblower” suits relating to our Medicare-reimbursed operations. We may become, or unknown to us may already be, the subject of investigations, qui tams, or lawsuits that could have a material adverse effect on our financial position, results of operation and liquidity.
Governmental agencies and their agents, such as the Medicare Administrative Contractors (“MACs”), fiscal intermediaries and carriers, as well as the US Office of Inspector General (“OIG”), CMS and state Medicaid programs, conduct audits, reviews and investigations of our health care operations. These include audits conducted through recovery audit contractor programs and zone program integrity contractor programs, in which third party firms engaged by CMS conduct extensive reviews of claims data and records to identify potential improper payments under the Medicare program. In addition, in 2016 CMS initiated the Pre-Claim Review Demonstration for Home Health Services, which requires home health agencies in certain states to submit a request for pre-claim review for each episode of care, along with documentation that supports the medical necessity of the care. This Demonstration was put on hold with no clear resumption date. In recent years, federal and state civil and criminal enforcement agencies have heighted and coordinated their oversight efforts related to the healthcare industry, including with respect to referral practices, cost reporting, billing practices, joint ventures and other financial relationships among health care providers. Depending on the nature of the conduct found in such audits, reviews and investigation and whether the underlying conduct could be considered systemic, the resolution of these matters could have a material adverse effect on our financial position, results of operation and liquidity.
For example, home health providers, including the Company, have received pre-pay Additional Development Requests (“ADR”) in addition to Recovery Audit Contractor audits (“RAC”) from the Palmetto Government Benefits Administration (“PGBA”) as a result of additional CMS funding allocations to MACs to conduct pre-payment reviews. ADR and RAC audits are both general and focused in nature. The PGBA acts as one of our four fiscal intermediaries, but processes the majority of our claims. We would expect ADR and RAC audits to continue in the future. If such ADR or RAC audits result in reimbursement adjustments, we may suffer reduced profitability. Further, our appeal rights related to such audits may lead to cash flow delays due to significant backlog at the Administrative Law Judge level.
If we are unable to maintain relationships with existing patient referral sources, including but not limited to the hospitals of CHS, or to establish new referral sources, our growth and profitability could be adversely affected.
Our success depends significantly on referrals from physicians, hospitals, case managers and other patient referral sources in the communities that our home care agencies serve, as well as on our ability to maintain good relationships with these referral sources. Our referral sources are not contractually obligated to refer home care patients to us and may refer their patients to other providers. Our growth and profitability depend on our ability to establish and maintain close working relationships with these patient referral sources and to increase awareness and acceptance of the benefits of home care by our referral sources and their patients. We cannot assure you that we will be able to maintain our existing referral source relationships or that we will be able to develop and maintain new relationships in existing or new markets. Our loss of, or failure to maintain, existing relationships or our failure to develop new relationships could adversely affect our ability to expand our operations and operate profitably. As described further below, our relationships with referral sources are heavily regulated and failure to comply with applicable regulations could have a material adverse effect on our financial position or results of operation.
We are subject to federal and state laws that govern our operations and financial relationships with physicians, hospitals and other healthcare providers and entities, potential or current referral sources, including specifically the hospitals of CHS.
Our operations are subject to extensive federal, state and local government laws and regulations, all of which are subject to change, including those relating to billing practices, healthcare fraud and abuse, and financial relationships with physicians, hospitals and other healthcare providers and entities. These government laws and regulations currently include, among others, the federal Anti-Kickback Statute, the Physician Self-Referral Law, also known as the Stark Law, the federal False Claims Act (“FCA”), the Civil Monetary Penalties Law, and similar state laws. Significant areas of
22
regulations include:
|
· |
the federal Anti-Kickback Statute, which prohibits persons from knowingly and willfully soliciting, receiving, offering or providing remuneration, directly or indirectly, in cash or in kind, in exchange for or to induce either the referral of an individual for, or the purchase, order or recommendation of, any goods or service for which payment may be made under governmental payor programs such as Medicare and Medicaid; |
We currently have contractual relationships with current and potential referral sources, including certain physicians who provide medical director and consulting services to our Company and joint ventures with hospitals. Many of these physicians and hospitals are current or potential referral sources. Although we believe our arrangements currently comply with state and federal anti-kickback and Stark laws, we cannot assure you that courts or regulatory agencies will not interpret these laws in ways that will implicate our arrangements. Violations of any existing or future laws and regulations could lead to fines, civil or criminal penalties, or sanctions, including under the False Claims Act, the termination of our rights to participate in federal and state-sponsored programs that may have a material adverse effect on our operations.
If our joint ventures, particularly our relationship with CHS violate the law, our business could be adversely affected.
The structures and operations of our joint ventures and our arrangements with hospitals, including CHS, and physicians are required to comply with government laws and regulations, including federal and state anti-kickback and referral laws. While we have structured our joint ventures to comply with many of the criteria for safe harbor protection under the Federal Anti-Kickback Statute, our investments in these joint venture arrangements may not satisfy all elements of the safe harbor requirements. If any of our joint ventures were found to be in violation of federal or state anti-kickback or referral laws, we could be required to restructure or terminate them. We also could be required to repay damages to Medicare and Medicaid based on the amounts we have received pursuant to any prohibited referrals, and we could suffer civil or criminal fines and penalties, including the loss of our licenses to operate and our ability to participate in federal and state health care programs. The imposition of any of these penalties could have a material adverse effect on our business, financial condition and results of operations.
If any of our agencies fail to comply with the conditions of participation in the Medicare program, that agency could be terminated from the Medicare program, which would adversely affect our net service revenue and profitability.
Each of our home care and hospice agencies must comply with the extensive conditions of participation in the Medicare program. If any of our agencies fail to meet any of the Medicare conditions of participation, that agency may receive a notice of deficiency from the applicable state surveyor. If that agency then fails to institute a plan of correction to correct the deficiency within the correction period provided by the state surveyor, that agency could be terminated from the Medicare program. Additionally, failure to comply with the conditions of participation related to enrollment could result in a deactivation or revocation of billing privileges. To the extent that billing privileges are revoked, there is a mandated
23
one to three-year bar to re-enrollment. The failure to pass a site verification visit, for example, could result in a revocation of billing privileges with a mandated two-year bar to re-enrollment. Although the revocation would only immediately affect the particular enrollment subject to the revocation, the Centers for Medicare and Medicaid Services (“CMS”) has indicated that following a revocation it will review the enrollment files for providers under common ownership or control to determine if a similar sanction is warranted for any of the other related providers. Similarly, we could face liability under the False Claims Act if we submit claims to Medicare or Medicaid while not in compliance with certain conditions of participation that would cause the government to refuse payment. Any termination of one or more of our home care agencies from the Medicare program for failure to satisfy the program’s conditions of participation, including proposed and future amendments could adversely affect our net service revenue and profitability.
We may be subject to substantial malpractice or other similar claims.
The services we offer involve an inherent risk of professional liability and related substantial damage awards. On any given day, we have thousands of nurses, therapists and other direct care personnel driving to and from patients’ homes where they deliver medical and other care. Due to the nature of our business, we and the caregivers who provide services on our behalf may be the subject of medical malpractice claims. These caregivers could be considered our agents, and, as a result, we could be held liable for their medical negligence. We are also subject to claims against us for negligence and intentional misconduct and violations of applicable law, and claims alleging personal injury, assault, abuse, wrongful death, and other charges. Regulatory agencies may initiate administrative proceedings alleging that our services, employees or agents violate applicable laws and seek to impose monetary penalties on us or ask for recoupment of amounts paid. We could be required to incur significant costs to respond to regulatory investigations or defend against lawsuits and, if we do not prevail, we could be required to pay substantial amounts of money in damages, settlement amounts or penalties arising from these legal proceedings. We cannot predict the effect that any claims of this nature, regardless of their ultimate outcome, could have on our business, reputation, or on our ability to attract and retain patients and employees. We maintain malpractice and various other liability insurance or re-insurance policies and are responsible for deductibles and, as applicable, amounts in excess of the limits of our coverage. Although we contract with highly rated carriers, we cannot guarantee collection of amounts expected to be recovered under various insurance or reinsurance policies.
Delays in reimbursement may cause liquidity problems.
Our business is characterized by delays in reimbursement from the time we provide services to the time we receive reimbursement or payment for these services. Data submission requirements change from time to time for payors, payments to us may be delayed pending additional data or documentation requests by the fiscal intermediary, or our ability to effectively respond to such requirements may delay our payment cycle. If we have information system problems or issues that arise with Medicare or Medicaid, we may encounter delays in our payment cycle. Such a timing delay may cause working capital shortages. Working capital management, including prompt and diligent billing and collection, is an important factor in our results of operations and liquidity. System problems, Medicare or Medicaid issues or industry trends may extend our collection period, adversely impact our working capital. Our working capital management procedures may not successfully negate this risk. There are often timing delays when attempting to collect funds from Medicaid programs. Delays in receiving reimbursement or payments from these programs may adversely impact our working capital.
On June 8, 2016, CMS announced the “Pre-Claim Review Demonstration of Home Health Services” which seeks to demonstrate that a review of selected documentation prior to payment of claims can decrease “improper payments because of insufficient documentation.” According to the CMS announcement, the pre-claim review demonstration will help educate Home Health Agencies (HHA) on what documentation is required and encourage them to submit the correct documentation, while still allowing the HHA to begin providing services and receive initial payments prior to the pre-claim review decision. The pre-claim review demonstration began in Illinois in late 2016 and was put on indefinite hold. The Company is currently unable to predict if or when the demonstration program may be resumed or what impact, if any, this program may have on its result of operations or financial position when and if resumed.
24
The home health care and hospice industry is highly competitive.
Our agencies compete with local and regional home health care and hospice companies, hospitals, nursing homes, and other businesses that provide home nursing services, some of which are large established companies that have significantly greater resources than we do. Our primary competition comes from local companies in each of our markets, and these privately-owned or hospital-owned health care providers vary by region and market. We compete based on the availability of personnel; the quality, expertise, and value of our services; and in select instances, on the price of our services. Increased competition in the future from existing competitors or new entrants may limit our ability to maintain or increase our market share. We cannot assure you that we will be able to compete successfully against current or future competitors or that competitive pressures will not have a material adverse impact on our business, financial condition, or results of operations.
Some of our existing and potential new competitors may enjoy greater name recognition and greater financial, technical, and marketing resources than we do. This may permit our competitors to devote greater resources than we can to the development and promotion of services. These competitors may undertake more far-reaching and effective marketing campaigns and may offer more attractive opportunities to existing and potential employees and services to referral sources.
We expect our competitors to develop new strategic relationships with providers, referral sources, and payors, which could result in increased competition. The introduction of new and enhanced service offerings, in combination with industry consolidation and the development of strategic relationships by our competitors, could cause a decline in revenue or loss of market acceptance of our services or make our services less attractive. Additionally, we compete with a number of non-profit organizations that can finance acquisitions and capital expenditures on a tax-exempt basis or receive charitable contributions that are unavailable to us.
We expect that industry forces will continue to have an impact on our business and that of our competitors. In recent years, the health care industry has undergone significant changes driven by efforts to reduce costs, and we expect these cost containment measures to continue in the future. Frequent regulatory changes in our industry, including reductions in reimbursement rates and changes in services covered, have increased competition among home health care providers. If we are unable to react competitively to new developments, our operating results may suffer.
Portions of our Healthcare Innovations segment compete in relatively new and developing markets, face larger more well-capitalized competitors and rely on small numbers of relatively large customers.
Portions of our Healthcare Innovations segment compete in new and developing markets with new competitors or solutions developed and introduced to the market regularly. Such new products may capture market share more quickly or may have access to more capital than the capital we have allocated for such projects. Our efforts to bring new solutions to the market may prove unsuccessful, may prove to be unprofitable or may prove to be costlier to bring to market than anticipated. Our investments in these activities are highly speculative in nature and subject to loss. Specifically, our Ingenios assessment subsidiary competes with larger, better capitalized competitors and our LTS assessment subsidiary is particularly reliant on a small number of large customers, the loss of which could significantly and adversely impact its results.
A shortage of qualified registered nursing staff, physical therapists, occupational therapists and other caregivers could adversely affect our ability to attract, train and retain qualified personnel and could increase operating costs.
We rely significantly on our ability to attract and retain caregivers who possess the skills, experience, and licenses necessary to meet the requirements of our patients. We compete for personnel with other providers of health care services. Our ability to attract and retain caregivers depends on several factors, including our ability to provide these caregivers with attractive assignments and competitive benefits and salaries. We cannot assure you that we will succeed in any of these areas. In addition, there are occasional shortages of qualified healthcare personnel in some of the markets in which we operate. As a result, we may face higher costs of attracting caregivers and providing them with attractive benefit packages than we originally anticipated, and if that occurs, our profitability could decline. Finally, although this is currently not a significant factor in our existing markets, if we expand our operations into geographic areas where
25
healthcare providers have historically unionized, we cannot assure you that the negotiation of collective bargaining agreements will not have a negative effect on our ability to timely and successfully recruit qualified personnel. Generally, if we are unable to attract and retain caregivers, the quality of our services may decline, and we could lose patients and referral sources.
Risks Related to Our Business
We depend on government sponsored reimbursement programs with Medicare accounting for the largest portion of our revenues.
For the years ended December 29, 2017, December 30, 2016 and January 1, 2016, we received 75%, 68% and 71%, respectively, of our revenue from Medicare. Reductions in Medicare reimbursement have historically and may continue to adversely impact our profitability. Such reductions in payments to us could be caused by:
|
· |
administrative or legislative changes to the base episode rate; |
|
· |
the elimination or reduction of annual rate increases based on medical inflation; |
|
· |
the imposition by Medicare of co-payments or other mechanisms shifting responsibility for a portion of payment to beneficiaries; |
|
· |
adjustments to the relative components of the wage index; |
|
· |
changes to or imposition of regulations impacting our case-mix or therapy thresholds; or |
|
· |
other adverse changes to the way we are paid for delivering our services. |
Our non-Medicare revenues and profitability also are affected by the continuing efforts of third-party payors to contain or reduce the costs of health care by lowering reimbursement rates, narrowing the scope of covered services, increasing case management review of services, and negotiating reduced contract pricing. Any changes in reimbursement levels from these third-party payor sources and any changes in applicable government regulations could have a material adverse effect on our revenues and profitability. We can provide no assurance that we will continue to maintain the current payor or revenue mix.
Our reliance on government sponsored reimbursement programs such as Medicare and Medicaid makes us vulnerable to possible legislative and administrative regulations and budget cut-backs that could adversely affect the number of persons eligible for such programs, the amount of allowed reimbursements or other aspects of the programs, any of which could materially affect us. In addition, loss of certification or qualification under Medicare or Medicaid programs could materially affect our ability to effectively market our services.
We have a significant dependence on state Medicaid reimbursement programs.
Approximately 20%, 23% and 23% of our 2017, 2016 and 2015 revenues, respectively, were derived from state Medicaid and other government programs, many of which currently face significant budget issues. Further, the acquisitions completed by us in 2016, 2015 and 2013 increased our dependence on Medicaid reimbursement. Our largest Medicaid reimbursement is concentrated in the states of Ohio, Connecticut, New York, Tennessee and Kentucky. See Part II, Item 8, Note 1, “Summary of Significant Accounting Policies,” elsewhere in this Form 10-K for further details.
The financial condition of the Medicaid programs in each of the states in which we operate is cyclical and many may be expected from time to time to take actions or evaluate taking actions to control the rate of growth of Medicaid expenditures. Among these actions are the following:
|
· |
redefining eligibility standards for Medicaid coverage, |
|
· |
redefining coverage criteria for home and community based care services, |
|
· |
slowing payments to providers by increasing the minimum time in which payments are made, |
|
· |
limiting reimbursement rate increases, |
|
· |
increasing utilization of self-directed care alternatives, |
|
· |
shifting beneficiaries from traditional coverage to Medicaid managed care providers, and |
|
· |
changing regulations under which providers must operate. |
26
States may be expected to address these issues because the number of Medicaid beneficiaries and their related expenditures are growing at a faster rate than the government’s revenue. Medicaid is consuming a greater percentage of states’ budgets. This issue is exacerbated when revenues slow in a slowing economy. It is possible that the actions taken by the federal government or state Medicaid programs in the future could have a significant unfavorable impact on our results of operations, financial condition and liquidity.
Migration of our Medicare beneficiary patients to Medicare managed care providers could negatively impact our operating results.
Historically, we have generated a substantial portion of our revenue from the Medicare fee-for-service market. The Congress continues to allocate significant additional funds and other incentives to Medicare managed care providers in order to promote greater participation in those plans by Medicare beneficiaries. If these increased funding levels have the intended result, the size of the potential Medicare fee-for-service market could decline, thereby reducing the size of our potential patient population, which could cause our operating results to suffer.
Our growth strategy depends on our ability to manage growing and changing operations.
Our business plan calls for significant growth in our business over the next several years. This growth will place significant demands on our management and information technology systems, internal controls, and financial and professional resources. In addition, we will need to further develop our financial controls and reporting systems to accommodate future growth. This could require us to incur expenses for hiring additional qualified personnel, retaining professionals to assist in developing the appropriate control systems, and expanding our information technology infrastructure. Our inability to manage growth effectively could have a material adverse effect on our financial results.
Our home health growth strategy depends on our ability to develop and to acquire additional agencies on favorable terms and to integrate and operate these agencies effectively. If we are unable to do so, our future growth and operating results could be negatively impacted.
With regard to development, we expect to continue to open agencies in our existing and new markets. Our new agency growth, however, will depend on several factors, including our ability to:
|
· |
obtain locations for agencies in markets where need exists; |
|
· |
identify and hire a sufficient number of sales personnel and appropriately trained home care and other health care professionals; |
|
· |
obtain adequate financing to fund growth; and |
|
· |
operate successfully under applicable government regulations. |
With regard to acquisitions, we are focusing significant time and resources on the acquisition of home healthcare providers, or of certain of their assets, in targeted markets. We may be unable to identify, negotiate, and complete suitable acquisition opportunities on reasonable terms. We may incur future liabilities related to acquisitions. Should any of the following problems, or others, occur as a result of our acquisition strategy, the impact could be material:
|
· |
difficulties integrating personnel from acquired entities and other corporate cultures into our business; |
|
· |
difficulties integrating information systems; |
|
· |
the potential loss of key employees or referral sources of acquired companies or a reduction in patient referrals by hospitals from which we have acquired home health care agencies; |
|
· |
the assumption of liabilities and exposure to undisclosed liabilities of acquired companies; |
|
· |
the acquisition of an agency with undisclosed compliance problems; |
|
· |
the diversion of management attention from existing operations; |
|
· |
difficulties in recouping partial episode payments and other types of misdirected payments for services from the previous owners; or |
|
· |
an unsuccessful claim for indemnification rights from previous owners for acts or omissions arising prior to the date of acquisition. |
CMS has placed certain limitations on the sale or transfer of the Medicare Provider Agreement for any Medicare-
27
certified home health agency that has been in existence for less than 36 months or that has undergone a change of ownership in the last 36 months. This limitation may reduce the number of home health agencies that otherwise would have been available for acquisition and may limit our ability to successfully pursue our acquisition strategy.
We have invested in development stage companies which may require further funding to support their respective business plans, which may ultimately prove unsuccessful.
Our HCI segment provides strategic health management services to ACOs that have been approved to participate in the Medicare Shared Savings Program (“MSSP”). In addition to our ownership interests in ACOs, we also have service agreements with ACOs that provide for sharing of MSSPs received by the ACO, if any. During 2013, we invested $5.8 million in our Imperium acquisition of which $3 million went to fund operations in pursuit of its business plan. In 2015, we also invested $1.0 million for a noncontrolling interest in Care Journey (formerly NavHealth, Inc.), a development stage analytics and software company, and $13.1 million in Ingenios Health Co. a provider of in-home technology enabled in-home clinical assessments. On January 5, 2016, we acquired Long Term Solutions, Inc. (“LTS”), a provider of in-home nursing assessments for the long-term care insurance industry for a purchase price of $37 million. These investments are highly speculative and are at risk and we may choose to make further investments, all of which may ultimately provide no return and could lead to a total loss of our investment.
ACOs, created with the Affordable Care Act, are entities that contract with CMS to serve the Medicare fee-for-service population with the goal of better care for individuals, improved health for populations and lower costs. ACOs share savings with CMS to the extent that the actual costs of serving assigned beneficiaries are below certain trended benchmarks of such beneficiaries and certain quality performance measures are achieved.
Notwithstanding our efforts, our ACOs may be unable to meet the required savings rates or may not satisfy the quality measures and efforts to drive other revenue may not cover operating costs of these investments. In addition, as the MSSP is a new program, it presents challenges and risks associated with the timeliness and accuracy of data and interpretation of complex rules, which may have a material adverse effect on our ability to recoup any of our investments. Further, there can be no assurance that we will maintain positive relations with our ACO partners or significant customers, which could result in a loss of our investment.
In addition, CMS, the OIG, the Internal Revenue Service, the Federal Trade Commission, US Department of Justice, and various states have adopted or are considering adopting new legislation, rules, regulations and guidance relating to formation and operation of ACOs. Such laws may, among other things, require ACOs to become subject to financial regulation such as maintaining deposits of assets with the states in which they operate, the filing of periodic reports with the insurance department and/or department of health, or holding certain licenses or certifications in the jurisdictions in which the ACOs operate. Failure to comply with legal or regulatory restrictions may result in CMS terminating the ACOs agreement with CMS and/or subjecting the ACO to loss of the right to engage in some or all business in a state, payments fines or penalties, or may implicate federal and state fraud and abuse laws relating to anti-trust, physician fee-sharing arrangements, anti-kickback prohibitions, prohibited referrals, any of which may adversely affect our operations and/or profitability.
We may require additional capital to pursue our acquisition strategy.
We cannot assure you that cash flows from operations combined with borrowings available under our revolving credit facility will be sufficient, nor continue to be fully available, to support our current growth strategies. We cannot readily predict the timing, size, and success of our acquisition efforts and the associated capital commitments. If we do not have sufficient cash resources, our growth could be limited unless we obtain additional equity or debt financing.
At some future point, we may elect to issue additional equity or debt securities in conjunction with raising capital or completing an acquisition. We cannot assure you that such issuances will not be dilutive to existing shareholders. Conversely, our board may approve stock repurchase programs in the future, which may use funds previously otherwise available for the pursuit of growth. We cannot predict the effect that future sales of our common stock, or the perception that these sales may occur, or other equity-related securities would have on the market price of our common stock.
28
Our business depends on our information systems. Our inability to effectively integrate, manage, and keep secure our information systems could disrupt our operations.
Our business depends on effective and secure information systems that assist us in, among other things, monitoring utilization and other cost factors, processing claims, reporting financial results, measuring outcomes and quality of care, managing regulatory compliance controls, and maintaining operational efficiencies. These systems include software developed in-house and systems provided by external contractors and other service providers. To the extent that these external contractors or other service providers become insolvent or fail to support the software or systems, our operations could be negatively affected. Our agencies also depend upon our information systems for accounting, billing, collections, risk management, quality assurance, payroll, learning management and other information. If we experience a reduction in the performance, reliability, or availability of our information systems, our operations and ability to process transactions and produce timely and accurate reports could be adversely affected.
Our information systems and applications require continual maintenance, upgrading, and enhancement to meet our operational needs. Our acquisitions require transitions and integration of various information systems. We regularly upgrade and expand our information systems’ capabilities. If we experience difficulties with the transition and integration of information systems or are unable to implement, maintain, or expand our systems properly, we could suffer from, among other things, operational disruptions, regulatory problems, working capital disruptions and increases in administrative expenses.
Our business requires the secure transmission of confidential information over public networks. Advances in computer capabilities, new discoveries in the field of cryptography or other events or developments could result in compromises or breaches of our security systems and patient data stored in our information systems. Anyone who circumvents our security measures could misappropriate our confidential information or cause interruptions in our services or operations. The Internet is a public network, and data is sent over this network from many sources. In the past, computer viruses or software programs that disable or impair computers have been distributed and have rapidly spread over the Internet. Computer viruses could be introduced into our systems, or those of our providers or regulators, which could disrupt our operations or make our systems inaccessible to our providers or regulators. We may be required to expend significant capital and other resources, to implement physical, technical and administrative safeguards to protect against the threat of security breaches or to alleviate problems caused by breaches. Our security measures may be inadequate to prevent security breaches, and our business operations would be negatively impacted by cancellation of contracts and loss of patients if security breaches are not prevented.
Further, our information systems are vulnerable to damage or interruption from fire, flood, natural disaster, power loss, telecommunications failure, break-ins and similar events. A failure to implement our disaster recovery plans or ultimately restore our information systems after the occurrence of any of these events could have a material adverse effect on our business, financial condition and results of operations.
Because of the confidential health information we store and transmit, loss or theft of patient health information for any reason could expose us to a risk of regulatory action, litigation, reputation damage, possible liability and loss.
We face additional federal and state requirements in the transmission and retention and protection of health information.
The Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) was enacted to ensure that employees can retain and at times transfer their health insurance when they change jobs and to simplify healthcare administrative processes. The enactment of HIPAA expanded protection of the privacy and security of personal medical data and required the adoption of standards for the exchange of electronic health information. Among the standards that the Secretary of the U.S. Department of Health and Human Services has adopted pursuant to HIPAA are standards for electronic transactions and code sets, unique identifiers for providers, employers, health plans and individuals, security and electronic signatures, privacy and enforcement. We are subject to HIPAA as a covered entity.
HIPAA was amended by the Health Information Technology for Economic and Clinical Health Act of 2009 (“HITECH Act”), which set forth health information security breach notification requirements. The HITECH Act requires patient
29
notification for all breaches related to Protected Health Information, media notification of breaches of over 500 patients and at least annual reporting of all breaches to the Secretary of HHS. The HITECH Act, as amended by the Federal Civil Penalties Inflation Adjustment Improvements Act of 2015, provides for sanctions for violations of HIPAA and HITECH of up to $1,650,300 per year for each violation. A single breach incident can result in violation of multiple standards, resulting in maximum possible penalties in excess of $1,650,300. HIPAA mandates that the Secretary of HHS conduct periodic compliance audits, which could result in penalties if we become subject to an audit and are found not to be in compliance with our obligations. Failure to comply with HIPAA, HITECH, and state privacy and security laws could result in fines and penalties or civil liability that could have a material adverse effect on us.
We develop portions of our clinical software system in-house. Failure of, or problems with, our system could harm our business and operating results.
We develop and utilize a proprietary clinical software system to collect assessment data, log patient visits, generate medical orders, and monitor treatments and outcomes in accordance with established medical standards. The system integrates billing and collections functionality as well as accounting, human resource, payroll, and employee benefits programs provided by third parties. Problems with, or the failure of, our technology and systems could negatively impact data capture, billing, collections, and management and reporting capabilities. Any such problems or failures could adversely affect our operations and reputation, result in significant costs to us, and impair our ability to provide our services in the future. The costs incurred in correcting any errors or problems may be substantial and could adversely affect our profitability.
We depend on outside software providers.
In operating our business, we depend on the proper functioning and availability of our information systems, some of which are provided and/or hosted by outside software providers. These information systems and applications require continual maintenance, upgrading, and enhancement to meet our operational needs. If our providers are unable to maintain or expand our information systems properly, we could suffer from operational disruptions and an increase in administrative expenses, among other things. The regulatory environment related to information security and privacy is evolving and increasingly demanding. Furthermore, we also rely on cloud computing and other similar hosted technologies that result in third parties holding significant amounts of customer or employee information on our behalf. If our security and information systems, or those of outsourced third party providers, we use to store or process such information are compromised or if we, or such third parties, otherwise fail to comply with applicable laws and regulations, we could face litigation and the imposition of penalties that could adversely affect our financial performance. Our reputation as a brand or as an employer could also be adversely affected from security breaches or regulatory violations, which could impair our sales or ability to attract and keep qualified employees.
Our insurance coverage may not be sufficient for our business needs and/or the cost of such coverage may adversely impact our results of operations.
We bear significant insurance risk under our large-deductible workers’ compensation insurance program and our self-insured employee health program. We also carry D&O coverage for potential claims against our directors and officers, including securities actions. Claims made to date or in the future may exceed the limits of such insurance, if any. Such claims, if successful and in excess of such limits, could have a material adverse effect on our ability to conduct business or on our assets. Benefits provided by our employer sponsored health insurance plan may require changes as a result of the ACA or other regulatory action. Such changes may have an adverse impact on our operating results.
Our insurance coverage also includes fire, property damage, and general liability with varying limits. Although we maintain insurance consistent with industry practice, we cannot assure you that the insurance we maintain will satisfy claims made against us. In addition, as a result of operating in the home healthcare industry, our business entails an inherent risk of claims, losses, and potential lawsuits alleging employee accidents that may occur in a patient’s home. Finally, insurance coverage may not continue to be available to us at commercially reasonable rates, in adequate amounts or on satisfactory terms. Any claims made against us, regardless of their merit or eventual outcome, could damage our reputation and business.
30
We estimate Medicare and Medicaid liabilities that may be payable by us in the future. These liabilities may be subject to audit or further review, and we may owe additional amounts beyond what we expect and have reserved.
The Company is paid for its services primarily by federal and state third-party reimbursement programs, commercial insurance companies, and patients. Revenues are recorded at established rates in the period during which the services are rendered. Appropriate allowances are recorded when the services are rendered, if necessary, to give recognition to third party payment arrangements.
Laws and regulations governing the Medicare and Medicaid programs are extremely complex and subject to interpretation. It is common for issues to arise related to: (1) medical coding, particularly with respect to Medicare, (2) patient eligibility, particularly related to Medicaid, and (3) other reasons unrelated to credit risk, all of which may result in adjustments to recorded revenue amounts. Management continuously evaluates the potential for revenue adjustments and when appropriate provides allowances for losses based upon the best available information. There is at least a reasonable possibility that recorded estimates could change by material amounts in the near term.
We depend on the services of our executive officers and other key employees.
Our success depends upon the continued employment of certain members of our senior management team, including our Chairman and Chief Executive Officer, William B. Yarmuth, and our other named executive officers. We also depend upon the continued employment of the individuals that manage several of our key functional areas, including operations, business development, accounting, finance, human resources, marketing, information systems, contracting and compliance. The departure of any member of our senior management team or our inability to appropriately implement succession plans may materially affect our operations.
Our operations could be affected by natural disasters.
A substantial number of our agencies are located in Florida or coastal regions in the northeast, increasing our exposure to hurricanes and other natural disasters. The occurrence of natural disasters in the markets in which we operate could not only affect the day-to-day operations of our agencies but also could disrupt our relationships with patients, employees and referral sources located in the affected areas. In addition, any episode of care that is not completed due to the impact of a natural disaster will generally result in lower revenue for the episode. We cannot assure you that hurricanes or other natural disasters will not have a material adverse impact on our business, financial condition or results of operations in the future.
Risks Related to Ownership of Our Common Stock
The price of our common stock may be volatile and this may adversely affect our stockholders.
The price at which our common stock trades may be volatile. The stock market has from time to time experienced significant price and volume fluctuations that have affected the market prices of securities, particularly securities of health care companies. The market price of our common stock may be influenced by many factors, including:
|
· |
our operating and financial performance; |
|
· |
variances in our quarterly financial results compared to expectations; |
|
· |
the depth and liquidity of the market for our common stock; |
|
· |
future sales of common stock or the perception that sales could occur; |
|
· |
investor perception of our business and our prospects; |
|
· |
developments relating to litigation or governmental investigations; |
|
· |
changes or proposed changes in health care laws or regulations or enforcement of these laws and regulations, or announcements relating to these matters; or |
|
· |
general industry, economic and stock market conditions. |
In addition, the stock market in general has experienced price and volume fluctuations that have often been unrelated or disproportionate to the operating performance of health care provider companies. These broad market and industry
31
factors may materially reduce the market price of our common stock, regardless of our operating performance. In the past, securities class-action litigation has often been brought against companies following periods of volatility in the market price of their respective securities. We may become involved in this type of litigation in the future. Litigation of this type is often expensive to defend and may divert our management team’s attention as well as resources from the operation of our business.
Sales of substantial amounts of our common stock, or the availability of those shares for future sale, could adversely affect our stock price and limit our ability to raise capital.
At December 29, 2017, outstanding shares of our common stock totaled 13,991,414. In 2017, we established the 2017 Stock and Incentive Compensation Plan for the benefit of employees and directors providing for the issuance of up to 997,465 shares of common stock. As of December 29, 2017, shares of our common stock remained reserved for issuance pursuant to our incentive compensation plans totaled 983,965 and shares of our common stock reserved for issuance pursuant to our employee stock purchase plan totaled 300,000. The market price of our common stock could decline as a result of sales of substantial amounts of our common stock to the public or the perception that substantial sales could occur. These sales also may make it more difficult for us to sell common stock in the future to raise capital.
We do not regularly pay dividends on our common stock and you should not expect to receive dividends on shares of our common stock.
We do not regularly pay dividends and intend to retain all future earnings to finance the continued growth and development of our business. In addition, we do not anticipate paying any cash dividends on our common stock in the foreseeable future. Any future payment of cash dividends will depend upon our financial condition, capital requirements, earnings, and other factors deemed relevant by our board of directors
Our Board of Directors may use anti-takeover provisions or issue stock to discourage control contests.
We have implemented anti-takeover provisions or provisions that could have an anti-takeover effect, including advance notice requirements for director nominations and stockholder proposals. These provisions, and others that the Board of Directors may adopt hereafter, may discourage offers to acquire us and may permit our Board of Directors to choose not to entertain offers to purchase us, even if such offers include a substantial premium to the market price of our stock. Therefore, our stockholders may be deprived of opportunities to profit from a sale of control.
ITEM 1B. UNRESOLVED STAFF COMMENTS
NONE.
Our executive offices are located in Louisville, Kentucky, in approximately 54,000 square feet of space leased from an unaffiliated party.
As of December 29, 2017, we had 367 real estate location leases ranging from approximately 100 to 54,000 square feet of space in their respective locations. We also own the land and buildings for two properties located in Tennessee and Florida. See Part I, Item 1, “Business - Operating Segments” and Part II, Item 8, “Notes to Consolidated Financial Statements.” We believe that our facilities are adequate to meet our current needs, and that additional or substitute facilities will be available if needed.
On January 18, 2018, Jordan Rosenblatt, a purported stockholder of our Company, filed a class action complaint alleging violations of the Securities Exchange Act of 1934 in the United States District Court for the Western District of Kentucky, styled Rosenblatt v. Almost Family, Inc., et al., Case No. 3:18-cv-40-TBR (the “Rosenblatt Class Action”),
32
against our Company, our board of directors, LHC Group and Merger Sub. The complaint in the Rosenblatt Class Action alleges that the Form S-4 Registration Statement filed on December 21, 2017 omitted material information with respect to the proposed transaction, rendering the Registration Statement false and misleading. The complaint in the Rosenblatt Action asserts claims against our Company and our board of directors for violations of Section 14(a) of the 1934 Act in connection with the dissemination of the Registration Statement, and asserts claims against the our board of directors and LHC Group for violations of Section 20(a) of the 1934 Act as controlling persons of our Company. The Rosenblatt Class Action seeks, among other things, an injunction enjoining the proposed transaction from closing, and an award of attorneys’ fees and costs.
On January 23, 2018, Leonard Stein, a purported stockholder of our Company, filed a class action complaint alleging violations of Sections 14(a) and 20(a) of the Securities Exchange Act of 1934 in the United States District Court for the District of Delaware, styled Stein v. Almost Family, Inc., et al., Case No. 1:18-cv-00126-UNA(the “Stein Class Action”), against our Company and our board of directors. The complaint in the Stein Class Action alleges that the Form S-4 Registration Statement filed on December 21, 2017 omitted material information with respect to the proposed transaction, rendering the Registration Statement false and misleading. The complaint in the Stein Class Action asserts claims against our Company and our board of directors for violations of Section 14(a) of the 1934 Act, SEC Regulation G, and SEC Rule 14a-9, and asserts claims against our board of directors for violations of Section 20(a) of the 1934 Act as controlling persons of our Company. The Stein Class Action seeks, among other things, an injunction enjoining both the shareholder vote and the proposed transaction from closing, monetary damages to a class of shareholders, and an award of attorneys’ fees and costs.
On January 23, 2018, Shiva Stein, a purported stockholder of our Company, filed a complaint alleging violations of Sections 14(a) and 20(a) of the Securities Exchange Act of 1934 in the United States District Court for the District of Delaware, styled Stein v. Almost Family, Inc., et al., Case No. 1:18-cv-000127-UNA (the “Stein Individual Action”), against our Company and our board of directors. The complaint in the Stein Individual Action alleges that the Form S-4 Registration Statement filed on December 21, 2017 contained materially incomplete and misleading statements with respect to the proposed transaction. The complaint in the Stein Individual Action asserts claims against our Company and our board of directors for violations of Section 14(a) of the 1934 Act, and asserts claims against our board of directors for violations of Section 20(a) of the 1934 Act as controlling persons of our Company. The Stein Individual Action seeks, among other things, an injunction enjoining the proposed transaction from closing, monetary damages suffered by Plaintiff, and an award of attorneys’ fees and costs.
We, our board of directors, LHC Group and Merger Sub believe that the claims in the complaints are without merit and intend to defend these actions vigorously.
From time to time, we are subject to various other legal actions arising in the ordinary course of our business, including claims for damages for personal injuries. In our opinion, after discussion with legal counsel, the ultimate resolution of any of these pending ordinary course claims and legal proceedings will not have a material effect on our financial position or results of operations.
ITEM 4. MINE SAFETY DISCLOSURES
Not applicable.
33
ITEM 5. MARKET FOR THE REGISTRANT’S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
Our common stock is traded on the NASDAQ Global Select market under the symbol “AFAM” Set forth below are the high and low close prices for the common stock for the periods indicated as reported by NASDAQ:
|
Closing Common Stock Prices |
|
|
|
|
|
|
Quarter Ended: |
|
High |
|
Low |
|
|
December 29, 2017 |
$ |
64.35 |
$ |
40.40 |
|
|
September 29, 2017 |
|
62.45 |
|
45.90 |
|
|
June 30, 2017 |
|
62.25 |
|
46.20 |
|
|
March 31, 2017 |
|
50.00 |
|
45.30 |
|
|
December 30, 2016 |
|
44.85 |
|
36.21 |
|
|
September 30, 2016 |
|
44.39 |
|
35.41 |
|
|
July 1, 2016 |
|
44.01 |
|
36.75 |
|
|
April 1, 2016 |
|
40.78 |
|
34.62 |
|
On February 26, 2018, the last reported sale price for the common stock reported by NASDAQ was $59.20 and there were approximately 243 holders of record of our common stock. We did not pay dividends in 2017 or 2016. We do not intend to pay additional dividends on our common stock and will retain our earnings for future operations and the growth of our business.
|
|
|
|
|
|
|
|
|
|
(d) Maximum Number |
|
|
|
(a) Total |
|
|
|
|
(c) Total Number of |
|
(or Approximate Dollar |
|
|
|
Number of |
|
(b) Average |
|
Shares (or Units) |
|
Value) of Shares (or |
|
|
|
|
Shares (or |
|
Price Paid |
|
Purchased as Part of |
|
Units) that May Yet Be |
|
|
|
|
Units) |
|
per Share |
|
Publicly Announced |
|
Purchased Under the |
|
|
Period |
|
Purchased (1) |
|
(or Unit) |
|
Plans or Programs |
|
Plans or Programs |
|
|
September 20, 2017 – October 27, 2017 |
|
— |
|
$ |
- |
|
— |
|
— |
|
October 28, 2017 – November 24, 2017 |
|
— |
|
|
- |
|
— |
|
— |
|
November 25, 2017 – December 29, 2017 |
|
82,767 |
|
|
56.60 |
|
— |
|
— |
|
Total |
|
82,767 |
|
$ |
56.60 |
|
— |
|
— |
|
|
|
|
|
|
|
|
|
|
|
|
(1) Shares were submitted by employees in lieu of tax withholding that would have otherwise been due on exercise of |
|||||||||
|
stock options or vesting of restricted shares approved by the Company's Board of Directors. |
|||||||||
Except as previously reported, there were no securities sold by the Company during the period covered by this annual report on Form 10-K that were not registered under the Securities Act of 1933, as amended.
34
STOCK PERFORMANCE GRAPH
The following stock performance graph does not constitute soliciting material and should not be deemed filed or incorporated by reference into any other Company filing under the Securities Act of 1933 or the Securities Exchange Act of 1934, except to the extent the Company specifically incorporates the performance graph by reference therein.
The Performance Graph below compares the cumulative total stockholder return on our common stock, $0.10 par value per share, for the five-year period ended December 29, 2017, with the cumulative total return on the Russell 2000 index and an industry peer group over the same period (assuming the investment of $100 in each on December 31, 2012 and the reinvestment of dividends, if any). The peer group we selected is comprised of: Amedisys, Inc. (AMED) and LHC Group, Inc. (LHCG). The cumulative total stockholder return on the following graph is historical and is not necessarily indicative of future stock price performance.
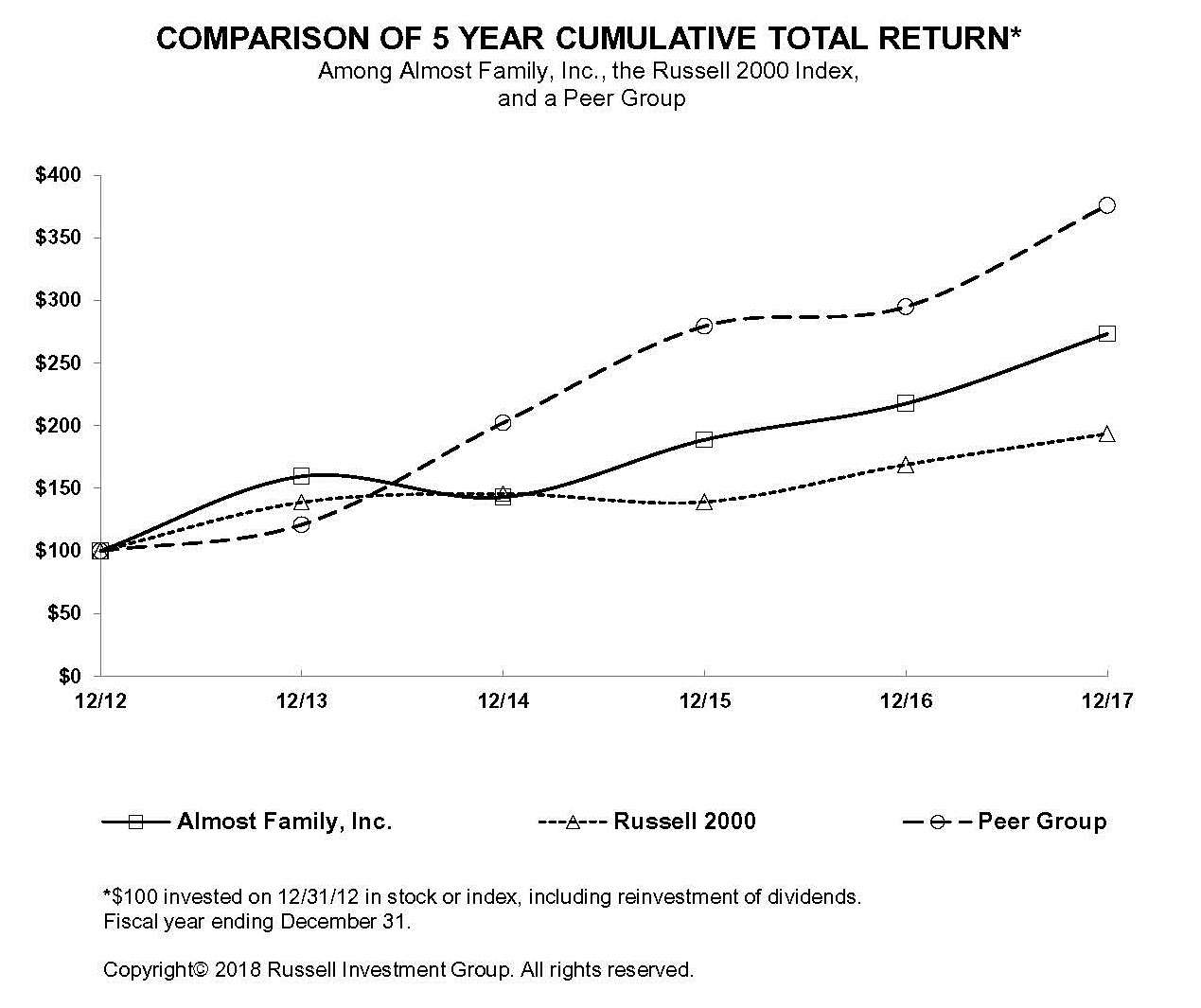
|
|
|
12/12 |
|
12/13 |
|
12/14 |
|
12/15 |
|
12/16 |
|
12/17 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Almost Family, Inc. |
|
100 |
|
159.58 |
|
142.89 |
|
188.70 |
|
217.67 |
|
273.20 |
|
|
Russell 2000 |
|
100 |
|
138.82 |
|
145.62 |
|
139.19 |
|
168.85 |
|
193.58 |
|
|
Peer Group |
|
100 |
|
121.02 |
|
202.35 |
|
279.34 |
|
294.87 |
|
375.84 |
|
35
ITEM 6. SELECTED FINANCIAL DATA
The following table sets forth selected financial information derived from the consolidated financial statements of the Company for the periods and at the dates indicated. The information should be read in conjunction with the consolidated financial statements and related notes included elsewhere in this and prior year Form 10-Ks.
|
|
|
Fiscal Year(1) |
|
Calendar Year |
|||||||||||
|
(In thousands except per share data) |
|
2017 |
|
2016 |
|
2015 |
|
2014 |
|
2013 |
|||||
|
Results of operations data: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Net service revenues |
|
$ |
796,965 |
|
$ |
623,541 |
|
$ |
532,214 |
|
$ |
495,829 |
|
$ |
356,912 |
|
Net income attributable to Almost Family, Inc. |
|
$ |
20,414 |
|
$ |
17,653 |
|
$ |
20,009 |
|
$ |
13,763 |
|
$ |
8,226 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Per share: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Basic: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Number of shares |
|
|
13,539 |
|
|
10,153 |
|
|
9,505 |
|
|
9,333 |
|
|
9,279 |
|
Net income attributable to Almost Family, Inc. |
|
$ |
1.51 |
|
$ |
1.74 |
|
$ |
2.11 |
|
$ |
1.47 |
|
$ |
0.89 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diluted: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Number of shares |
|
|
13,757 |
|
|
10,346 |
|
|
9,745 |
|
|
9,462 |
|
|
9,374 |
|
Net income attributable to Almost Family, Inc. |
|
$ |
1.48 |
|
$ |
1.71 |
|
$ |
2.05 |
|
$ |
1.45 |
|
$ |
0.88 |
|
(1) |
See page 39 for discussion regarding the Company’s change to a 52-53 week reporting calendar in 2015. |
|
|
|
2017 |
|
2016 |
|
2015 |
|
2014 |
|
2013 |
|
|||||
|
Balance sheet data |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Working capital |
|
$ |
74,492 |
|
$ |
68,904 |
|
$ |
54,643 |
|
$ |
40,274 |
|
$ |
44,148 |
|
|
Total assets |
|
|
717,818 |
|
|
658,712 |
|
|
464,769 |
|
|
345,258 |
|
|
354,362 |
|
|
Long-term liabilities |
|
|
134,073 |
|
|
302,682 |
|
|
136,048 |
|
|
60,432 |
|
|
83,436 |
|
|
Total liabilities |
|
|
211,265 |
|
|
354,532 |
|
|
190,869 |
|
|
112,066 |
|
|
136,669 |
|
|
Noncontrolling interest-redeemable - Healthcare Innovations |
|
|
2,256 |
|
|
2,256 |
|
|
3,639 |
|
|
3,639 |
|
|
3,639 |
|
|
Stockholders’ equity |
|
|
504,297 |
|
|
301,924 |
|
|
270,261 |
|
|
229,553 |
|
|
214,054 |
|
36
ITEM 7. MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
OVERVIEW
The Company has three reportable segments: a) Home Health (“HH”), b) Other Home-Based Services (“OHBS”) which includes all other home care services outside of Home Health services and c) the Healthcare Innovations (“HCI”) segment. Reportable segments have been identified based upon how management has organized the business by services provided to customers and the criteria in Accounting Standards Codification (“ASC”) Topic 280, Segment Reporting. Consistent with information given to our chief operating decision maker, we do not allocate certain expenses to the reportable segments. We evaluate the performance of our business segments based on operating income.
Our HH segment provides skilled medical services in patients’ homes largely to enable recipients to reduce or avoid periods of hospitalization and/or nursing home care. Approximately 95% of our HH segment revenues were generated from the Medicare program, while the balance was generated from Medicaid and private insurance programs.
Our OHBS segment includes traditional personal care services (“PC”) (generally provided by paraprofessional staff such as home health aides) which are generally of a custodial rather than skilled nature, as well as hospice services. Personal care revenues are generated on an hourly basis and are primarily from Medicaid (approximately 80% of personal care revenues). Hospice services are largely provided in patients’ homes and generally require specialized hospice nursing skills. Hospice revenues are generated on a per diem basis and are primarily from Medicare (approximately 93% of hospice revenues).
Our HCI business segment is used to report on our developmental activities outside our HH and OHBS businesses. The HCI segment includes: a) an ACO enablement company; b) an in-home assessment company serving the long-term care insurance industry and managed care organizations; and c) an investment in a population-health analytics company.
LHC Group and Almost Family Merger of Equals
On November 15, 2017, our Company entered into an Agreement and Plan of Merger (the “Merger Agreement”) with LHC Group, Inc., a Delaware corporation (“LHC Group”), and Hammer Merger Sub, Inc., a newly-formed Delaware corporation and a wholly owned subsidiary of LHC Group (“Merger Sub”), providing for a “merger of equals” business combination of our Company and LHC Group. The Merger Agreement provides that, if the conditions to the Merger are satisfied or waived and the Merger is consummated, stockholders of our Company will receive 0.9150 shares of LHC Group common stock for each share of our Company’s common stock, plus the cash equivalent of any fractional share. The Merger Agreement provides that, upon the terms and subject to the conditions set forth therein, at the closing Merger Sub will be merged with and into our Company (the “Merger”), with our Company continuing as the surviving corporation and as a wholly owned subsidiary of LHC Group. The parties’ obligations to complete the Merger are subject to several conditions, including, among others, (i) the adoption of the Merger Agreement by the affirmative vote of the holders of at least a majority of the outstanding shares of the Company’s common stock; (ii) the approval of the issuance of shares of LHC Group’s common stock to be issued to our stockholders in the merger by the affirmative vote of a majority of the shares of LHC Group’s common stock present in person or represented by proxy at LHC Group’s special meeting; (iii) the expiration or termination of the required waiting periods under the Hart-Scott Rodino Act (which occurred on February 21, 2018); (iv) the absence of any order or law prohibiting the Merger or the other transactions contemplated by the Merger Agreement; (v) the receipt of certain tax opinions; and (vi) the absence of a material adverse effect with respect to either LHC Group or our Company (as defined in the Merger Agreement).
The Merger Agreement contains certain termination rights for both our Company and LHC Group, including if the Merger is not consummated on or before July 1, 2018 (subject to extension to October 1, 2018 in certain circumstances) and if the required approval of the stockholders of either our Company or LHC Group is not obtained. The Merger Agreement further provides that, upon termination of the Merger Agreement under specified circumstances, including the termination of the Merger Agreement by our Company or LHC Group as a result of an adverse change in the recommendation of the other party’s board of directors, our Company may be required to pay to LHC Group, or LHC Group may be required to pay to our Company, as applicable, a termination fee of $30 million. Further, if the Merger
37
Agreement is terminated as a result of the stockholders of either our Company or LHC Group failing to approve the transaction, our Company may be required to reimburse to LHC Group, or LHC Group may be required to reimburse to our Company, the other party’s expenses in connection with the proposed transaction, up to a maximum of $5 million.
In the absence of required stockholder approvals, we will continue to operate on a stand-alone basis. All references within this Form 10-K assumes Almost Family, Inc. operating on a stand-alone basis.
2017 Acquisitions
On November 20, 2017, our CHS-JV purchased assets of a Medicare-certified home health agency in Fort Myers, Florida. The purchase price was $0.5 million. Post-acquisition operating results are reported in our HH segments.
On July 14, 2017, our CHS-JV purchased assets of a Medicare-certified home health agency and related private duty company in Key West, Florida. The purchase price was $1.2 million. Post-acquisition operating results are reported in our HH and OHBS segments.
On December 31, 2016, the first day of our 2017 fiscal year end, we acquired an 80% controlling interest in the entity holding the home health and hospice assets of Community Health Systems, Inc. (NYSE: CYH) (referred to herein as “CHS Home Health”). CHS Home Health, a provider of skilled home health and hospice services, operated 74 home health and 15 hospice branch locations in 22 states. The purchase price of $128 million was funded through borrowings on the Company's Revolving Credit Facility. Post-acquisition results are reported in our HH and OHBS segments.
2017 Common Stock Offering
On January 25, 2017, we sold 3,450 shares of common stock at $44.50 per share for gross proceeds of approximately $153.5 million. Total net proceeds, after underwriting discounts and commissions and our offering expenses, were approximately $143.9 million. These proceeds were used to repay obligations under the revolving credit facility.
2015 and 2016 Acquisitions
During 2016, we completed three acquisitions and increased our ownership of one of our HCI subsidiaries. In the third quarter, one of our HCI subsidiaries redeemed certain outstanding shares increasing our ownership percentage to 72.0% from 61.5%. On June 18, 2016, we acquired certain home health agency assets primarily in Wisconsin, but also in Connecticut and Kentucky (collectively, the “Wisconsin Acquisition”). On January 5, 2016, we acquired 100% of the equity of LTS for a purchase price of $37 million. On January 5, 2016, we also purchased the assets of a Medicare-certified home health agency owned by Bayonne Visiting Nurse Association (“Bayonne”) located in New Jersey.
During 2015, we completed four acquisitions and made a cost based investment. On November 5, 2015, we completed the acquisition of Black Stone Operations, LLC (“Black Stone”). Black Stone owned and operated personal care and skilled home health services in western Ohio. On August 29, 2015, we completed the acquisition of Bracor, Inc. (dba “WillCare”). WillCare owned and operated HH and PC branch locations in New York (12) and Connecticut (1). On March 1, 2015 we acquired the stock of WillCare’s Ohio operations. On July 22, 2015, we acquired Ingenios Health Co. Ingenios is a leading provider of technology enabled in-home clinical assessments for Medicare Advantage, Managed Medicaid and Commercial Exchange lives in 7 states and Washington, D.C. The results of the Black Stone and WillCare acquisitions are reported in our HH and OHBS segments, while our Ingenios acquisition results are included in the Healthcare Innovations segment.
On January 29, 2015, we acquired a noncontrolling interest in a development stage analytics and software company, Care Journey. The investment is an asset of our Healthcare Innovations segment.
Our View on Reimbursement and Diversification of Risk
Our Company is highly dependent on government reimbursement programs which pay for the majority of the services we provide to our patients. Reimbursement under these programs, primarily Medicare and Medicaid, is subject to
38
frequent changes as policy makers balance their own needs to meet the health care needs of constituents while also meeting their fiscal objectives. Medicare and Medicaid are consuming a greater percentage of federal and states’ budgets, respectively, which is exacerbated in times of economic downturn. We believe that these financial issues are cyclical in nature rather than indicative of the long-term prospect for Medicare and Medicaid funding of health care services. Additionally, we believe our services offer the lowest cost alternative to institutional care and is a part of the solution to both balancing the federal budget and the states’ Medicaid financing problems.
We believe that an important key to our historical success and to our future success is our ability to adapt our operations to meet changes in reimbursement as they occur. One important way in which we have achieved this adaptability in the past, and in which we plan to achieve it in the future, is to maintain some level of diversification in our business mix.
The execution of our business plan will place primary emphasis on the development of our home health operations. As our business grows, we may evaluate opportunities for the provision of other health care services in patients’ homes that would be consistent with our Senior Advocacy mission.
Our Business Plan
Our future success depends on our ability to execute our business plan. Over the next three to five years we will try to accomplish the following:
|
· |
Generate meaningful same store sales growth through the focused provision of high quality services and attending to the needs of our patients; |
|
· |
Drive our costs down, while continuing to provide high-quality patient care, by improving the productivity of our work force through improved monitoring, tighter controls, workflow automation, use of technology and other opportunities for efficiency gains; |
|
· |
Expand the significance of our home health services by selectively acquiring other quality providers, through the startup of new agencies and potentially by providing new services in patients’ homes consistent with our Senior Advocacy mission; |
|
· |
Make additional strategic investments which expand our Healthcare Innovation segment in its mission to find solutions for more effective, efficient and appropriate delivery of homecare; and |
|
· |
Expand our capital base through both earnings performance and by seeking additional capital investments in our Company. |
Health Care Reform Legislation and Medicare Regulations
The Federal Government has been pursuing a comprehensive reform of the US healthcare system since early 2009. Numerous changes have been enacted, proposed and continue to be debated, which are discussed in more detail in Part I, Item 1, “Government Regulation” and Part I, Item 1A, “Risk Factors.” Many of the change provisions do not take effect for an extended period of time and most will require the publication of implementing regulations and/or the issuance of programmatic guidelines.
It is reasonable to expect that recent and potential changes described in Part I, Item 1, Government Regulation, might have a more immediate and negative impact on those providers generating lower margins than us, with more leverage relative to earnings than us, with less capital resources than us, or with less ability to adapt their operations. We believe this may result in a contraction of the number of home health providers. In the event of such a contraction in the number of providers, we believe the surviving providers may benefit from a higher rate of admissions growth than would have otherwise occurred. Those surviving providers may earn incremental margins on those higher admissions that may serve to offset a portion of the rate reduction from the Medicare program. However, there can be no assurance that we will be successful in attracting such higher admissions.
39
It is also reasonable to expect that future rate cuts will present additional opportunities for us to make acquisitions of other providers at valuations and on terms that are attractive to us and enable us to spread our segment and unallocated corporate overhead expenses across a larger business base. However, there can be no assurance that we will be successful in making such acquisitions or that such opportunities will present themselves.
As a result of the broad scope of health care reform, the significant changes it will effect in the healthcare industry and society generally, and the complexity of the technical issues it addresses, we are unable to predict, at this time, all the ramifications health care reform may have on our business as a health care provider or a sponsor of an employee health insurance benefit plan. These matters could have a material adverse impact on our results of operations or financial condition in ways not currently anticipated by us. This may increase our costs, decrease our revenues, expose us to expanded liability or require us to revise the ways in which we conduct our business. Refer to the results of operations for the impact of these items on revenue, operating and net income for the years ended December 29, 2017, December 30, 2016 and January 1, 2016.
Management is continuing its work to evaluate the implications of these changes and to develop appropriate courses of action for the Company. Additionally, we may be unable to take actions to mitigate any, or all, of the negative implications of these matters.
We contemplate formulating and taking actions intended to mitigate or otherwise offset some of the negative effects of reimbursement changes. These actions may include any or all of the following:
|
· |
Attempting to increase our revenues by: investing more resources in sales and marketing activities, development of diagnosis related specialty programs and increasing our educational programs regarding the value of home health to drive admission growth, establishing startup branch operations to expand our service territories, and acquisitions of underperforming providers with strong referral relationships, |
|
· |
Attempting to reduce our costs by: developing a more efficient delivery model, increasing the productivity standards for our staff, optimizing the appropriate use of different levels of professional staff, limiting or eliminating the growth in wage rates, limiting or reducing the size of our work force, closing unprofitable branch operations and accelerating our efforts to evaluate the use of various technological approaches to the delivery of patient care to improve patient outcomes and/or improve the productivity of our workforce, |
|
· |
Evaluating the potential implications of health care reform on our employee benefit plans, and possible changes we may need to make to our plans, and |
|
· |
Potentially other actions we deem appropriate including evaluation of potential additional service offerings in patients’ homes consistent with our Senior Advocacy mission or changing the mix of the types of services we provide. |
Although we will attempt to mitigate or otherwise offset the negative effect of health care reform on our revenue and our employee benefit plans, our actions may not ultimately be cost effective or prove successful.
Seasonality
Our HH segment operations in Florida normally experience higher admissions during the first quarter and lower admissions during the third quarter than in the other quarters due to seasonal population fluctuations. Florida operations generated approximately 20% of our 2017 revenue.
In our HCI segment, first quarter assessment revenues are traditionally lower than the other quarters due to the seasonal nature of our Medicare Advantage plan customers, while the majority of our ACO Management revenues have historically been generated in the third quarter.
Fiscal Year End
Effective with the first quarter of 2015, the Company adopted a 52-53 week fiscal reporting calendar under which it will report its annual results going forward in four equal 13-week quarters. Every fifth year, one quarter will include 14 weeks and that year will include 53 weeks of operating results. This approach minimizes the impact of calendar
40
differences when comparing different historical periods. All references herein for the years 2017, 2016 and 2015 represent the fiscal years ended December 29, 2017 and December 30, 2016 and the calendar year ended January 1, 2016, respectively.
Critical Accounting Policies
The accompanying consolidated financial statements have been prepared in conformity with accounting principles generally accepted in the United States. When more than one accounting principle, or the method of its application, is generally accepted, we select the principle or method that is appropriate in the specific circumstances. Application of these accounting principles requires us to make estimates about the future resolution of existing uncertainties; actual results could differ from these estimates. We evaluate our estimates, including those related to revenue recognition, collectability of accounts receivable, insurance reserves, goodwill, intangibles, income taxes, stock-based compensation, litigation, and contingencies on an on-going basis. We base these estimates on our historical experience and other assumptions that we believe are appropriate under the circumstances. In preparing these consolidated financial statements, we have made our best estimates and judgments of the amounts and disclosures included in the consolidated financial statements.
Revenue Recognition
We recognize revenues when patient services are provided, primarily in our patients’ homes. Net service revenues are stated at amounts estimated by us to be their net realizable values. We are paid for our services primarily by federal and state third-party reimbursement programs and, to a lesser degree, commercial insurance companies and patients.
Medicare Episodic Revenues
Approximately 75% of our consolidated net service revenues are derived from the Medicare program. Net service revenues are recorded under the Medicare prospective payment program (“PPS”) based on a 60-day episode payment rate that is subject to adjustment based on certain variables including, but not limited to: (a) changes in the base episode payments established by the Medicare program; (b) adjustments to the base episode payments for case-mix and geographic wages; (c) a low utilization payment adjustment (“LUPA”) if the number of visits was fewer than five; (d) a partial payment if our patient transferred to another provider or we received a patient from another provider before completing the episode; (e) a payment adjustment based upon the level of therapy services required (thresholds set at 6, 14 and 20 visits); (f) an outlier payment if our patient’s care was unusually costly (capped at 10% of total reimbursement at the agency level); (g) the number of episodes of care provided to a patient; and (h) 2% sequestration reduction.
At the beginning of each Medicare episode, we calculate an estimate of the amount of expected reimbursement based on the variables outlined above and recognize Medicare revenue on an episode-by-episode basis during the course of each episode over its expected number of visits. Over the course of each episode, as changes in the variables become known, we calculate and record adjustments as needed to reflect changes in expectations for that episode from those established at the start of the 60 day period until its ultimate outcome at the end of the 60 day period is known.
Non-Medicare Revenues
Substantially all remaining revenues are derived from services provided under a per visit, per hour or unit basis (as opposed to episodic) for which revenues are calculated and recorded using payor-specific or patient-specific fee schedules based on the contracted rates in each third party payor agreement.
Contingent Service Revenues
Our Healthcare Innovations segment provides strategic health management services to ACOs that have been approved to participate in the “MSSP.” In addition to having ownership interests in a few ACOs, we also have service agreements with ACOs that provide for sharing of MSSP payments received by the ACO, if any. ACOs are entities that contract with Centers for Medicare and Medicaid Services (CMS) to serve the Medicare fee-for-service population with the goal of better care for individuals, improved health for populations and lower costs. ACOs share savings with CMS to the
41
extent that the actual costs of serving assigned beneficiaries are below certain trended benchmarks of such beneficiaries and certain quality performance measures are achieved. The MSSP is relatively new and therefore has limited historical experience, which impacts the Company’s ability to accurately accumulate and interpret the data available for calculating an ACOs’ shared savings, if any. MSSP payments are not recognized in revenue until persuasive evidence of an arrangement exists, services have been rendered, the payment is fixed and determinable and collectability is assured, which generally is satisfied only upon cash receipt. Under such agreements, we recognized $2.4 million and $4.3 million in MSSP payments for cash received during 2017 and 2016 related to savings generated for the program period ended December 31, 2016 and December 31, 2015, respectively, which accounted for 9% and 17%, respectively of our HCI segment revenues. No revenue has been recognized related to potential MSSP payments for savings generated for the program period ended December 31, 2017, if any.
Revenue Adjustments
Laws and regulations governing the Medicare and Medicaid programs are extremely complex and subject to interpretation. As a result, we may adjust previously recorded revenue amounts due to issues related to: a) medical coding, particularly with respect to Medicare, b) patient eligibility, particularly with respect to Medicaid, and c) other reasons unrelated to credit risk. Revenue adjustments, if any, to reflect actual payment amounts for completed episodes or services provided under per visit, per hour or unit basis which differ from our estimates or audit adjustments are recorded when known and estimable. Historically, revenue adjustments have not been significant and as such, we believe that net service revenues and accounts receivable - net reflect their net realizable value. Changes in estimates related to prior periods (increased) decreased revenues by approximately ($780,000), ($608,000) and ($365,000) in the years ended December 29, 2017, December 30, 2016 and January 1, 2016, respectively.
Accounts Receivable
Accounts receivable are reported at their estimated net realizable value and are net of estimated allowances for uncollectible accounts and adjustments. Accounts receivable consist primarily of amounts due from third-party payors and patients. We evaluate the collectability of our accounts receivable based on certain factors, such as payor types, historical collection trends and aging categories. We calculate our reserve for uncollectible accounts based on the length of time that the receivables are past due. The percentage applied to the receivable balances for each payor’s various aging categories is based on historical collection experience, business and economic conditions and reimbursement trends.
New Revenue Recognition Guidance
In May 2014, the FASB issued ASU 2014-09, Revenue from Contracts with Customers (“Topic 606”). Topic 606 affects virtually all aspects of an entity’s revenue recognition, including determining the measurement of revenue and the timing of when it is recognized for the transfer of goods or services to customers. We adopted Topic 606 effective for our next fiscal year beginning December 30, 2017 using a modified retrospective approach. Based on our assessment of the guidance, no opening balance sheet adjustment to retained earnings was identified. We do, however, anticipate the reclassification of all bad debt expense to net patient service revenue on a go-forward basis, as the standard largely limits bad debt expense to bankruptcies or changes in credit risk.
A significant element of implementing Topic 606 is reviewing sources of revenue and evaluating the characteristics of the patient population to develop the appropriate portfolio distribution with similar characteristics that when evaluated under the new revenue standard, will result in a materially consistent revenue amount for such portfolios as if each patient account was evaluated on a “contract-by-contract” basis. Our review supports an allocation of patients to portfolios that is consistent with our current MD&A, segment and footnote disclosures. Additionally, we believe the adoption will have minimal impact on our financial statement disclosures.
Application of this guidance by the healthcare industry is continuing to develop, and changes could arise that are inconsistent with our year-end assessment. We will continue to monitor the application Topic 606 by peer organizations.
42
Insurance Programs
We bear significant risk under our large-deductible workers’ compensation insurance program and our self-insured employee health program. Under the workers’ compensation insurance program, we bear risk up to $400,000 per incident. We purchase stop-loss insurance for the employee health plan that places a specific limit, generally $300,000, on our exposure for any individual covered life.
Malpractice and general patient liability claims for incidents which may give rise to litigation have been asserted against us by various claimants. The claims are in various stages of processing and some may ultimately be brought to trial. We are aware of incidents that have occurred through year-end that may result in the assertion of additional claims. We currently carry professional and general liability insurance coverage (on a claims made basis) for this exposure with no deductible. We also carry D&O coverage (also on a claims made basis) for potential claims against our directors and officers, including securities actions, with deductibles ranging from $175,000 to $500,000 per claim.
We record estimated liabilities for our insurance programs based on information provided by the third-party plan administrators, historical claims experience, the life cycle of claims, expected costs of claims incurred but not paid, and expected costs to settle unpaid claims. We monitor our estimated insurance-related liabilities and recoveries, if any, on a monthly basis and as required by ASU 2010-24, Health Care Entities (Topic 954): Presentation of Insurance Claims and Related Insurance Recoveries, record amounts due under insurance policies in other current assets, while recording the estimated carrier liability in other current liabilities in the consolidated balance sheets. As facts change, it may become necessary to make adjustments that could be material to our results of operations and financial condition.
Goodwill and Other Intangible Assets
Intangible assets are stated at fair value at the time of acquisition and goodwill represents the excess cost over the fair value of net assets acquired and liabilities assumed. Finite lived intangible assets are amortized on a straight-line basis over the estimated useful life of the asset. Goodwill and indefinite-lived assets are not amortized. We perform impairment analysis of goodwill and indefinite lived assets as required by ASC Topic 350, Intangibles - Goodwill and Other on at least an annual basis. In 2017 we performed qualitative assessments to determine whether any goodwill or indefinite lived assets were impaired. We evaluated the relevant events and circumstances, such as the market conditions, financial performance, and share price to determine if any impairment is indicated. Based on our 2017 analysis, an impairment of goodwill or indefinite lived assets was not indicated. Had our 2017 assessments indicated impairment, we would perform a quantitative test similar to 2016 and 2015 as follows.
Our 2016 and 2015 quantitative impairment analysis required numerous subjective assumptions and estimates to determine fair value of the respective reporting units. We estimated the fair value of the related reporting units using a combined market approach (guideline company and similar transaction method) and income approach (discounted cash flow analysis). These models were based on our projections of future revenues and operating costs and were reconciled to our consolidated market capitalization. Discounted cash flow models are highly reliant on various assumptions. Significant assumptions we utilized in these models included: projected business results and future industry direction, long-term growth factor of 3% and weighted-average cost of capital of 15%. We used assumptions that we deemed to be reasonable estimates of likely future events and compared the total fair values of each reporting unit to our overall market capitalization, and implied control premium, to determine if the fair values were reasonable compared to external market indicators. Subsequent changes in these key assumptions could affect the results of future qualitative impairment reviews.
Important to our overall impairment conclusion was the comparison of the aggregate fair values of the reporting units to our overall market capitalization at the annual assessment date, including the implied control premium, to determine if the fair values are reasonable compared to external market indicators. The aggregate fair value for each reporting unit did not exceed our market value as of the annual impairment testing date. A negative control premium indicated conservatism built into our fair value models.
Because the fair value results for each reporting unit did not indicate a potential impairment existed, we did not recognize any goodwill or intangible asset impairment during 2016 and 2015. Specifically, each of our 2016 and 2015
43
reporting unit fair values were significantly over their carrying value. Based on the sensitivity analysis performed on two key assumptions in the discounted cash flow models of each reporting unit, a 100 basis point change in either assumption (either individually or in the aggregate) would not result in any impairment of our goodwill or intangible assets within any reporting unit.
Assuming no changes in the key assumptions identified and projected results, we currently anticipate the future fair value of our reporting units to increase over time; however, future declines in the operating results of either reporting unit could indicate a need to reevaluate the fair value of these businesses under U.S. GAAP requirements and may ultimately result in an impairment to goodwill. We will continue to monitor for any potential indicators of impairment.
Accounting for Income Taxes
We account for taxes in accordance with ASC Topic 740, Income Taxes. As of December 29, 2017, we have net deferred tax liabilities of approximately $18.6 million. The net deferred tax liability is composed of approximately $15.3 million of deferred tax assets and approximately $33.9 million of deferred tax liabilities. We have provided a valuation allowance against certain deferred tax assets based upon our estimates of realizability of those assets through future taxable income. This valuation allowance was based in large part on our history of generating operating income or losses in individual tax locales and expectations for the future. Our ability to generate the expected amounts of taxable income from future operations is dependent upon general economic conditions, competitive pressures on revenues and margins and legislation and regulation at all levels of government. Further, we have book goodwill of $105.1 million which is not deductible for tax purposes. The remaining deductible goodwill provides an annual tax deduction approximating $15.1 million through 2022. We have considered the above factors in reaching our conclusion that it is more likely than not that future taxable income will be sufficient to fully utilize the deferred tax assets (net of the valuation allowance) as of December 29, 2017.
The Tax Cuts and Jobs Act (Tax Act) was enacted on December 22, 2017 and introduces significant changes to the U.S. income tax law. Effective in 2018, the Tax Act reduces U.S. statutory tax rates from 35% to 21%. Accordingly, we remeasured our deferred taxes as of December 29, 2017 to reflect the reduced rate that will apply in future periods when these deferred taxes are settled or realized, resulting in a one-time $9.5 million net tax benefit in 2017.
Due to the timing of the enactment and the complexity involved in applying the provisions of the Tax Act, we have made reasonable estimates of the effects and recorded provisional amounts in our financial statements as of December 29, 2017. As we collect and prepare necessary data, and interpret the Tax Act and any additional guidance issued by the Internal Revenue Service, and other standard-setting bodies, we may make adjustments to the provisional amounts. Those adjustments may materially impact our provision for income taxes and effective tax rate in the period in which adjustments are made. The accounting for the tax effects of the Tax Act will be completed in 2018.
44
RESULTS OF OPERATIONS
Year Ended December 29, 2017 Compared with Year Ended December 30, 2016
(In thousands)
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
2017 |
|
2016 |
|
Change |
|
|||||||||
|
Consolidated |
|
Amount |
|
% Rev |
|
Amount |
|
% Rev |
|
Amount |
|
% |
|
|||
|
Net service revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
586,070 |
|
73.5 |
% |
$ |
434,968 |
|
69.8 |
% |
$ |
151,102 |
|
34.7 |
% |
|
Other Home-Based Services |
|
|
184,752 |
|
23.2 |
% |
|
162,546 |
|
26.1 |
% |
|
22,206 |
|
13.7 |
% |
|
Healthcare Innovations |
|
|
26,143 |
|
3.3 |
% |
|
26,027 |
|
4.2 |
% |
|
116 |
|
0.4 |
% |
|
|
|
|
796,965 |
|
100.0 |
% |
|
623,541 |
|
100.0 |
% |
|
173,424 |
|
27.8 |
% |
|
Operating income before corporate expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
|
75,587 |
|
12.9 |
% |
|
56,564 |
|
13.0 |
% |
|
19,023 |
|
33.6 |
% |
|
Other Home-Based Services |
|
|
14,555 |
|
7.9 |
% |
|
13,519 |
|
8.3 |
% |
|
1,036 |
|
7.7 |
% |
|
Healthcare Innovations |
|
|
4,046 |
|
15.5 |
% |
|
5,657 |
|
21.7 |
% |
|
(1,611) |
|
(28.5) |
% |
|
|
|
|
94,188 |
|
11.8 |
% |
|
75,740 |
|
12.1 |
% |
|
18,448 |
|
24.4 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Corporate expenses |
|
|
35,565 |
|
4.5 |
% |
|
28,457 |
|
4.6 |
% |
|
7,108 |
|
25.0 |
% |
|
Deal, transition and other costs |
|
|
29,405 |
|
3.7 |
% |
|
11,842 |
|
1.9 |
% |
|
17,563 |
|
148.3 |
% |
|
Operating income |
|
|
29,218 |
|
3.7 |
% |
|
35,441 |
|
5.7 |
% |
|
(6,223) |
|
(17.6) |
% |
|
Interest expense, net |
|
|
7,391 |
|
0.9 |
% |
|
6,285 |
|
1.0 |
% |
|
1,106 |
|
17.6 |
% |
|
Net income - noncontrolling interests |
|
|
3,523 |
|
0.4 |
% |
|
519 |
|
0.1 |
% |
|
3,004 |
|
578.8 |
% |
|
Net income before income taxes |
|
$ |
18,304 |
|
2.3 |
% |
$ |
28,637 |
|
4.6 |
% |
$ |
(10,333) |
|
(36.1) |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Adjusted EBITDA (1) |
|
$ |
67,965 |
|
8.5 |
% |
$ |
54,552 |
|
8.7 |
% |
$ |
13,413 |
|
24.6 |
% |
|
Adjusted net income (1) |
|
$ |
28,864 |
|
3.6 |
% |
$ |
24,640 |
|
4.0 |
% |
$ |
4,224 |
|
17.1 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(1) |
See page 52 for GAAP reconciliation of Adjusted EBITDA and Adjusted net income attributable to Almost Family, Inc. |
Home Health segment net revenues increased 34.7% or $151.1 million to $586.1 million from $435.0 million in the prior year, and episodic admissions grew by 40.4% to 118,115 from 84,401, primarily due to the CHS-JV acquisition. Revenues from the Home Health facilities acquired in the CHS-JV acquisition were $167.7 million for 2017.
Other Home-Based Services segment net revenues increased year over year by $22.2 million or 13.7% to $184.8 million from $162.5 million primarily as a result of the CHS-JV acquisition’s 15 hospice facilities. Hospice revenues were $29.8 million for 2017.
Healthcare Innovations segment net revenues and operating income were $26.1 million and $4.0 million in 2017 as compared to $26.0 million and $5.7 million in 2016, respectively.
Each of our operating segments experienced prolonged disruption during the third quarter of 2017 as a result of Hurricanes Irma and Harvey (the “Hurricanes”), with our Home Health segment operations in Florida the most severely affected. The Hurricanes reduced operating income by approximately $3.3 million, largely on lost volume.
Refer to the individual segment discussions for further operating performance details.
Corporate expenses as a percentage of revenue decreased 0.1% to 4.5% in 2017. Deal, transition and other costs were $29.4 million, largely driven by transaction costs of the pending LHC Group merger and the CHS-JV acquisition, in addition to the conversion of the Home Health segment to the Homecare Homebase information system. Unused fees associated with our larger credit facility and higher amortization of loan costs increased interest expense to $7.4 million from $6.3 million in the prior year.
45
We recorded a net tax benefit of $2.1 million in our fiscal 2017 due to a favorable $9.5 million impact from the 2017 Tax Cuts and Jobs Act (Tax Act); excluding Tax Act impact our tax expense and effective tax rate would have been $7.4 million and 40.5%, respectively, for the full year. The 2016 effective tax rate was 38.4%. The increase was largely due to an increase in the ratio of permanent current year non-deductible items to pre-tax income driven largely by merger related differences.
The Tax Act was signed into law on December 22, 2017, is effective for our fiscal 2018 and will reduce our U.S. corporate tax rate from 35% to 21% in 2018. We expect our effective tax rate will approximate 26.5% in 2018. See Part II, Item 8, “Note 6 – Income Taxes” for further discussion of the Tax Act.
Home Health Segment
Approximately 95% of the HH segment revenues were generated from the Medicare program while the balance was generated from Medicaid and private insurance programs. In addition to our focus on operating income from the Home
46
Health segment, we also measure this segment’s performance in terms of admissions, episodes, visits, patient months of care, revenue per episode and visits per episode. (In thousands, except statistical information)
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
2017 |
|
2016 |
|
Change |
|
|||||||||
|
|
Amount |
|
% Rev |
|
Amount |
|
% Rev |
|
Amount |
|
% |
|
|||
|
Net service revenues |
$ |
586,070 |
|
100.0 |
% |
$ |
434,968 |
|
100.0 |
% |
$ |
151,102 |
|
34.7 |
% |
|
Cost of service revenues |
|
287,270 |
|
49.0 |
% |
|
212,744 |
|
48.9 |
% |
|
74,526 |
|
35.0 |
% |
|
Gross margin |
|
298,800 |
|
51.0 |
% |
|
222,224 |
|
51.1 |
% |
|
76,576 |
|
34.5 |
% |
|
General and administrative expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Salaries and benefits |
|
164,015 |
|
28.0 |
% |
|
121,972 |
|
28.0 |
% |
|
42,043 |
|
34.5 |
% |
|
Other |
|
59,198 |
|
10.1 |
% |
|
43,688 |
|
10.0 |
% |
|
15,510 |
|
35.5 |
% |
|
Total general and administrative expenses |
|
223,213 |
|
38.1 |
% |
|
165,660 |
|
38.1 |
% |
|
57,553 |
|
34.7 |
% |
|
Operating income before corporate expenses |
$ |
75,587 |
|
12.9 |
% |
$ |
56,564 |
|
13.0 |
% |
$ |
19,023 |
|
33.6 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Average number of locations |
|
242 |
|
|
|
|
168 |
|
|
|
|
74 |
|
44.0 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
All payors: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Admissions |
|
159,079 |
|
|
|
|
107,576 |
|
|
|
|
51,503 |
|
47.9 |
% |
|
Census |
|
31,224 |
|
|
|
|
22,980 |
|
|
|
|
8,244 |
|
35.9 |
% |
|
Visits |
|
3,729,562 |
|
|
|
|
2,870,277 |
|
|
|
|
859,285 |
|
29.9 |
% |
|
Cost per visit |
$ |
77 |
|
|
|
$ |
74 |
|
|
|
$ |
3 |
|
3.9 |
% |
|
G&A expense per census |
$ |
7,149 |
|
|
|
$ |
7,209 |
|
|
|
$ |
(60) |
|
(0.8) |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Episodic: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Admissions |
|
118,535 |
|
|
|
|
84,401 |
|
|
|
|
34,134 |
|
40.4 |
% |
|
Census |
|
23,874 |
|
|
|
|
17,894 |
|
|
|
|
5,980 |
|
33.4 |
% |
|
Episodes |
|
178,540 |
|
|
|
|
130,003 |
|
|
|
|
48,537 |
|
37.3 |
% |
|
Visits |
|
2,933,044 |
|
|
|
|
2,317,540 |
|
|
|
|
615,504 |
|
26.6 |
% |
|
Revenue (in thousands) |
$ |
498,075 |
|
85.0 |
% |
$ |
379,701 |
|
87.3 |
% |
$ |
118,374 |
|
31.2 |
% |
|
Revenue per episode |
$ |
2,790 |
|
|
|
$ |
2,921 |
|
|
|
$ |
(131) |
|
(4.5) |
% |
|
Visits per episode |
|
16.4 |
|
|
|
|
17.8 |
|
|
|
|
(1.4) |
|
(7.8) |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Non-episodic: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Admissions |
|
40,544 |
|
|
|
|
23,175 |
|
|
|
|
17,369 |
|
74.9 |
% |
|
Census |
|
7,350 |
|
|
|
|
5,086 |
|
|
|
|
2,264 |
|
44.5 |
% |
|
Visits |
|
796,518 |
|
|
|
|
552,737 |
|
|
|
|
243,781 |
|
44.1 |
% |
|
Revenue (in thousands) |
$ |
87,995 |
|
15.0 |
% |
$ |
55,267 |
|
12.7 |
% |
$ |
32,728 |
|
59.2 |
% |
|
Revenue per visit |
$ |
110 |
|
|
|
$ |
100 |
|
|
|
$ |
10 |
|
10.5 |
% |
|
Visits per admission |
|
19.6 |
|
|
|
|
23.9 |
|
|
|
|
(4.2) |
|
(17.6) |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(1) |
Percentages pertain to percentage of total admissions or total billable visits, as applicable. |
Home Health segment net service revenues increased by $151.1 million or 34.7% to $586.1 million from $435.0 million in the prior year and episodic admissions grew by 40.4% to 118,535 from 84,401 primarily due to the CHS-JV acquisition. Excluding the CHS-JV acquisition, episodic admissions grew by approximately 2%, which was reduced by the impact of the Hurricanes. Volume growth was partially offset by a net effective 1% Medicare rate cut and the impact of the Hurricanes.
Gross margin as a percent of revenue declined 0.1% from prior year due to the combined impact of a 1.0% Medicare rate cut and an annual cost of living wage rate adjustment of 2%, both effective January 1, 2017, that slightly outpaced cost side improvements. Cost per visit increased 3.9% due to a combination of increased wage rates, lower visit utilization and costs associated with the Homecare Homebase implementation.
47
Total general and administrative expenses remained consistent at 38.1%, as a percent of revenue.
Home Health segment contribution increased $19.0 million, or 33.6%, to $75.6 million, from $56.6 million in the prior year.
48
Other Home-Based Services
Approximately 80% of the OHBS segment revenues were generated from Medicaid and other government programs while the balance is generated from insurance programs and private pay patients. (In thousands, except statistical information)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2017 |
|
2016 |
|
Change |
|
|||||||||
|
|
|
Amount |
|
% Rev |
|
Amount |
|
% Rev |
|
Amount |
|
% |
|
|||
|
Net service revenues |
|
$ |
184,752 |
|
100.0 |
% |
$ |
162,546 |
|
100.0 |
% |
$ |
22,206 |
|
13.7 |
% |
|
Cost of service revenues |
|
|
121,946 |
|
66.0 |
% |
|
111,973 |
|
68.9 |
% |
|
9,973 |
|
8.9 |
% |
|
Gross margin |
|
|
62,806 |
|
34.0 |
% |
|
50,573 |
|
31.1 |
% |
|
12,233 |
|
24.2 |
% |
|
General and administrative expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Salaries and benefits |
|
|
31,743 |
|
17.2 |
% |
|
24,592 |
|
15.1 |
% |
|
7,151 |
|
29.1 |
% |
|
Other |
|
|
16,508 |
|
8.9 |
% |
|
12,462 |
|
7.7 |
% |
|
4,046 |
|
32.5 |
% |
|
Total general and administrative expenses |
|
|
48,251 |
|
26.1 |
% |
|
37,054 |
|
22.8 |
% |
|
11,197 |
|
30.2 |
% |
|
Operating income before corporate expenses |
|
$ |
14,555 |
|
7.9 |
% |
$ |
13,519 |
|
8.3 |
% |
$ |
1,036 |
|
7.7 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Personal Care: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Locations |
|
|
75 |
|
|
|
|
76 |
|
|
|
|
(1) |
|
(1.3) |
% |
|
Admissions |
|
|
9,420 |
|
|
|
|
9,671 |
|
|
|
|
(251) |
|
(2.6) |
% |
|
Census |
|
|
12,603 |
|
|
|
|
13,216 |
|
|
|
|
(613) |
|
(4.6) |
% |
|
Hours of service |
|
|
7,197,211 |
|
|
|
|
7,538,223 |
|
|
|
|
(341,012) |
|
(4.5) |
% |
|
Hours per patient per week |
|
|
11.0 |
|
|
|
|
11.0 |
|
|
|
|
0.0 |
|
0.1 |
% |
|
Revenue |
|
$ |
154,937 |
|
83.9 |
% |
$ |
161,367 |
|
99.3 |
% |
$ |
(6,430) |
|
(4.0) |
% |
|
Operating income |
|
$ |
10,102 |
|
|
|
$ |
13,509 |
|
|
|
$ |
(3,407) |
|
(25.2) |
% |
|
Revenue per hour |
|
$ |
21.53 |
|
|
|
$ |
21.41 |
|
|
|
$ |
0.12 |
|
0.6 |
% |
|
Cost per hour |
|
$ |
13.19 |
|
|
|
$ |
13.15 |
|
|
|
$ |
0.04 |
|
0.3 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hospice: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Locations |
|
|
16 |
|
|
|
|
1 |
|
|
|
|
15 |
|
NM |
|
|
Admissions |
|
|
2,879 |
|
|
|
|
97 |
|
|
|
|
2,782 |
|
NM |
|
|
Census |
|
|
482 |
|
|
|
|
23 |
|
|
|
|
459 |
|
NM |
|
|
Length of stay |
|
|
61 |
|
|
|
|
42 |
|
|
|
|
19 |
|
51.7 |
% |
|
Revenue |
|
$ |
29,815 |
|
16.1 |
% |
$ |
1,179 |
|
0.7 |
% |
$ |
28,636 |
|
NM |
|
|
Operating income |
|
$ |
4,453 |
|
|
|
$ |
10 |
|
|
|
$ |
4,443 |
|
NM |
|
|
Revenue per day |
|
$ |
170 |
|
|
|
$ |
141 |
|
|
|
$ |
29 |
|
20.3 |
% |
OHBS segment net service revenues increased $22.2 million or 13.7% to $184.8 million from $162.6 million, primarily as a result of the 15 hospice facilities acquired in the CHS-JV transaction. Hospice revenues were $29.8 million. Personal care revenues were down $6.4 million or 4.0% from prior year on lower volumes. Additionally, mix changes combined with rate cuts and increases in wages influenced by increases in statutory minimum wage rates in certain states negatively impacted personal care margins. Overall OHBS segment contribution before corporate expenses increased $1.0 million or 7.7%, as compared to the same period of last year.
49
Healthcare Innovations Segment
(In thousands, except statistical information)
|
|
|
2017 |
|
2016 |
|
Change |
|
|||||||||
|
|
|
Amount |
|
% Rev |
|
Amount |
|
% Rev |
|
Amount |
|
% |
|
|||
|
Net service revenues |
|
$ |
26,143 |
|
100.0 |
% |
$ |
26,027 |
|
100.0 |
% |
$ |
116 |
|
0.4 |
% |
|
Cost of service revenues |
|
|
10,069 |
|
38.5 |
% |
|
10,733 |
|
41.2 |
% |
|
(664) |
|
(6.2) |
% |
|
Gross margin |
|
|
16,074 |
|
61.5 |
% |
|
15,294 |
|
58.8 |
% |
|
780 |
|
5.1 |
% |
|
General and administrative expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Salaries and benefits |
|
|
7,014 |
|
26.8 |
% |
|
5,915 |
|
22.7 |
% |
|
1,099 |
|
18.6 |
% |
|
Other |
|
|
5,014 |
|
19.2 |
% |
|
3,722 |
|
14.3 |
% |
|
1,292 |
|
34.7 |
% |
|
Total general and administrative expenses |
|
|
12,028 |
|
46.0 |
% |
|
9,637 |
|
37.0 |
% |
|
2,391 |
|
24.8 |
% |
|
Operating income before corporate expenses |
|
$ |
4,046 |
|
15.5 |
% |
$ |
5,657 |
|
21.7 |
% |
$ |
(1,611) |
|
(28.5) |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ACO Management |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medicare ACO enrollees under management |
|
|
141,556 |
|
|
|
|
121,881 |
|
|
|
|
19,675 |
|
16.1 |
% |
|
ACOs under contract |
|
|
15 |
|
|
|
|
14 |
|
|
|
|
1 |
|
7.1 |
% |
|
Revenue |
|
$ |
5,076 |
|
19.4 |
% |
$ |
5,294 |
|
20.3 |
% |
$ |
(218) |
|
(4.1) |
% |
|
Operating income |
|
$ |
479 |
|
|
|
$ |
2,714 |
|
|
|
$ |
(2,235) |
|
82.4 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Assessment Services |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Assessments |
|
|
87,948 |
|
|
|
|
75,814 |
|
|
|
|
12,134 |
|
16.0 |
% |
|
Revenue |
|
$ |
21,067 |
|
80.6 |
% |
$ |
20,733 |
|
79.7 |
% |
$ |
334 |
|
1.6 |
% |
|
Operating income |
|
$ |
3,567 |
|
|
|
$ |
2,943 |
|
|
|
$ |
624 |
|
21.2 |
% |
HCI segment net revenues increased slightly to $26.1 million in 2017 from $26.0 million in 2016. Increases in both ACO Management membership fees and Assessment Services revenue largely offset a $1.9 million reduction in ACO shared savings payments revenue in 2017 versus the prior year. As such, HCI operating income before corporate expenses decreased $1.6 million to $4.0 million in 2017.
50
Year Ended December 30, 2016 Compared with Year Ended January 1, 2016
(in thousands)
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
2016 |
|
2015 |
|
Change |
|
|||||||||
|
Consolidated |
|
Amount |
|
% Rev |
|
Amount |
|
% Rev |
|
Amount |
|
% |
|
|||
|
Net service revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
434,968 |
|
69.8 |
% |
$ |
400,133 |
|
75.2 |
% |
$ |
34,835 |
|
8.7 |
% |
|
Other Home-Based Services |
|
|
162,546 |
|
26.1 |
% |
|
128,630 |
|
24.2 |
% |
|
33,916 |
|
26.4 |
% |
|
Healthcare Innovations |
|
|
26,027 |
|
4.2 |
% |
|
3,451 |
|
0.6 |
% |
|
22,576 |
|
654.2 |
% |
|
|
|
|
623,541 |
|
100.0 |
% |
|
532,214 |
|
100.0 |
% |
|
91,327 |
|
17.2 |
% |
|
Operating income before corporate expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
|
56,564 |
|
13.0 |
% |
|
49,608 |
|
12.4 |
% |
|
6,956 |
|
14.0 |
% |
|
Other Home-Based Services |
|
|
13,519 |
|
8.3 |
% |
|
14,434 |
|
11.2 |
% |
|
(915) |
|
(6.3) |
% |
|
Healthcare Innovations |
|
|
5,657 |
|
21.7 |
% |
|
(1,217) |
|
(35.3) |
% |
|
6,874 |
|
(564.8) |
% |
|
|
|
|
75,740 |
|
12.1 |
% |
|
62,825 |
|
11.8 |
% |
|
12,915 |
|
20.6 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Corporate expenses |
|
|
28,457 |
|
4.6 |
% |
|
25,737 |
|
4.8 |
% |
|
2,720 |
|
10.6 |
% |
|
Deal, transition and other costs |
|
|
11,842 |
|
1.9 |
% |
|
4,139 |
|
0.8 |
% |
|
7,703 |
|
186.1 |
% |
|
Operating income |
|
|
35,441 |
|
5.7 |
% |
|
32,949 |
|
6.2 |
% |
|
2,492 |
|
7.6 |
% |
|
Interest expense, net |
|
|
6,285 |
|
1.0 |
% |
|
2,852 |
|
0.5 |
% |
|
3,433 |
|
120.4 |
% |
|
Net income - noncontrolling interests |
|
|
519 |
|
0.1 |
% |
|
(468) |
|
(0.1) |
% |
|
987 |
|
(210.9) |
% |
|
Net income before income taxes |
|
|
28,637 |
|
4.6 |
% |
|
30,565 |
|
5.7 |
% |
$ |
(1,928) |
|
(6.3) |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Adjusted EBITDA (1) |
|
$ |
54,552 |
|
8.7 |
% |
$ |
43,745 |
|
8.2 |
% |
$ |
10,807 |
|
24.7 |
% |
|
Adjusted net income (1) |
|
$ |
24,640 |
|
4.0 |
% |
$ |
20,746 |
|
3.9 |
% |
$ |
3,894 |
|
18.8 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(1) |
See page 52 for GAAP reconciliation of Adjusted EBITDA and Adjusted net income attributable to Almost Family, Inc. |
Home Health segment and Other Home-Based Services net service revenues in 2016 increased $34.8 million and $33.9 million, respectively from prior year primarily due to acquisitions occurring late in 2015 (WillCare and Black Stone) and in 2016 (Bayonne and Wisconsin). Refer to HH and OHBS segment discussions for further operating performance details.
HCI segment net service revenues increased $22.6 million to $26.0 million in 2016 versus $3.5 million in 2015, as acquired assessment service revenues were $20.7 million and shared-savings revenues from our ACO business in 2016 increased to $4.3 million in 2016, as compared to $1.4 million in 2015. Overall HCI segment contribution improved $6.9 million to $5.7 million in 2016 versus a $1.2 million net loss in 2015.
Corporate expenses as a percentage of revenue declined to 4.6% from 4.9% in the prior year period due to the expansion of the size and scope of our operations. Deal, transition and other costs were $11.8 million for 2016, primarily as a result of costs related to acquisitions, while the prior year included a one-time $4.2 million benefit related to legal settlements.
51
Borrowings related to acquisitions, fees associated with our credit facility and higher amortization of loan costs increased interest expense to $6.3 million, from $2.9 million in 2015. Further, in the fourth quarter of 2016, we commenced our HH Segment’s company-wide clinical system conversion to the Homecare Homebase information platform. Such implementation, training and related costs began in the fourth quarter of 2016 and continued throughout 2017.
Our effective tax rate for 2016 was 38.4% compared to 34.5% for 2015, respectively. The lower effective tax rate for 2015 was primarily related to the tax treatment of a legal settlement. Excluding the non-taxable settlement and other nondeductible deal costs, our effective tax rate for 2015 would have been 40.5%.
52
Home Health Segment
Approximately 95% of the HH segment revenues were generated from the Medicare program while the balance was generated from Medicaid and private insurance programs. (In thousands, except statistical information)
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
2016 |
|
2015 |
|
Change |
|
|||||||||
|
|
Amount |
|
% Rev |
|
Amount |
|
% Rev |
|
Amount |
|
% |
|
|||
|
Net service revenues |
$ |
434,968 |
|
100.0 |
% |
$ |
400,133 |
|
100.0 |
% |
$ |
34,835 |
|
8.7 |
% |
|
Cost of service revenues |
|
212,744 |
|
48.9 |
% |
|
193,674 |
|
48.4 |
% |
|
19,070 |
|
9.8 |
% |
|
Gross margin |
|
222,224 |
|
51.1 |
% |
|
206,459 |
|
51.6 |
% |
|
15,765 |
|
7.6 |
% |
|
General and administrative expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Salaries and benefits |
|
121,972 |
|
28.0 |
% |
|
114,781 |
|
28.7 |
% |
|
7,191 |
|
6.3 |
% |
|
Other |
|
43,688 |
|
10.0 |
% |
|
42,070 |
|
10.5 |
% |
|
1,618 |
|
3.8 |
% |
|
Total general and administrative expenses |
|
165,660 |
|
38.1 |
% |
|
156,851 |
|
39.2 |
% |
|
8,809 |
|
5.6 |
% |
|
Operating income before corporate expenses |
$ |
56,564 |
|
13.0 |
% |
$ |
49,608 |
|
12.4 |
% |
$ |
6,956 |
|
14.0 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Average number of locations |
|
168 |
|
|
|
|
164 |
|
|
|
|
4 |
|
2.4 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
All payors: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Admissions |
|
107,576 |
|
|
|
|
102,381 |
|
|
|
|
5,195 |
|
5.1 |
% |
|
Census |
|
22,980 |
|
|
|
|
83,703 |
|
|
|
|
(60,723) |
|
(72.5) |
% |
|
Visits |
|
2,870,277 |
|
|
|
|
2,621,443 |
|
|
|
|
248,834 |
|
9.5 |
% |
|
Cost per visit |
$ |
74 |
|
|
|
$ |
74 |
|
|
|
$ |
0 |
|
0.3 |
% |
|
G&A expense per census |
$ |
7,209 |
|
|
|
$ |
1,874 |
|
|
|
$ |
5,335 |
|
284.7 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Episodic: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Admissions |
|
84,401 |
|
|
|
|
80,341 |
|
|
|
|
4,060 |
|
5.1 |
% |
|
Census |
|
17,894 |
|
|
|
|
68,127 |
|
|
|
|
(50,233) |
|
(73.7) |
% |
|
Episodes |
|
130,003 |
|
|
|
|
124,205 |
|
|
|
|
5,798 |
|
4.7 |
% |
|
Visits |
|
2,317,540 |
|
|
|
|
2,198,927 |
|
|
|
|
118,613 |
|
5.4 |
% |
|
Revenue (in thousands) |
$ |
379,701 |
|
87.3 |
% |
$ |
356,739 |
|
89.2 |
% |
$ |
22,962 |
|
6.4 |
% |
|
Revenue per episode |
$ |
2,921 |
|
|
|
$ |
2,872 |
|
|
|
$ |
49 |
|
1.7 |
% |
|
Visits per episode |
|
17.8 |
|
|
|
|
17.7 |
|
|
|
|
0.1 |
|
0.7 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Non-episodic: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Admissions |
|
23,175 |
|
|
|
|
22,040 |
|
|
|
|
1,135 |
|
5.1 |
% |
|
Census |
|
5,086 |
|
|
|
|
15,576 |
|
|
|
|
(10,490) |
|
(67.3) |
% |
|
Visits |
|
552,737 |
|
|
|
|
422,516 |
|
|
|
|
130,221 |
|
30.8 |
% |
|
Revenue (in thousands) |
$ |
55,267 |
|
12.7 |
% |
$ |
43,394 |
|
10.8 |
% |
$ |
11,873 |
|
27.4 |
% |
|
Revenue per visit |
$ |
100 |
|
|
|
$ |
103 |
|
|
|
$ |
(3) |
|
(2.6) |
% |
|
Visits per admission |
|
23.9 |
|
|
|
|
19.2 |
|
|
|
|
4.7 |
|
24.4 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(1) |
Percentages pertain to percentage of total admissions or total billable visits, as applicable. |
HH segment net service revenues increased $34.8 million or 8.7% to $435.0 million in 2016 primarily due to acquisitions occurring late in 2015 (WillCare and Black Stone) and in 2016 (Bayonne). Acquisitions drove increases in episodic admissions, which increased 5.1% to 84,401 in 2016.
53
Substantially all of the changes in cost of service revenues, general and administrative expenses and payor information were due to acquisitions.
Gross margin as a percentage of revenue decreased to 51.1% from 51.6% primarily due to higher labor costs per visit from acquired agencies and higher insurance claims experience. Total general and administrative expenses declined slightly as a percentage of revenue to 38.1% from 39.2% in 2015 primarily from the effect of acquired operations plus the closure of selected underperforming branches in late 2015.
As a result, HH segment operating income before corporate expenses improved $7.0 million to $56.6 million from $49.6 million in the prior year, while HH segment operating income as a percentage of revenue increased to 13.0% from 12.4% in the prior year.
54
Other Home-Based Services
Approximately 83% of the OHBS segment revenues were generated from Medicaid and other government programs while the balance is generated from insurance programs and private pay patients. (In thousands, except statistical information)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2016 |
|
2015 |
|
Change |
|
|||||||||
|
|
|
Amount |
|
% Rev |
|
Amount |
|
% Rev |
|
Amount |
|
% |
|
|||
|
Net service revenues |
|
$ |
162,546 |
|
100.0 |
% |
$ |
128,630 |
|
100.0 |
% |
$ |
33,916 |
|
26.4 |
% |
|
Cost of service revenues |
|
|
111,973 |
|
68.9 |
% |
|
87,066 |
|
67.7 |
% |
|
24,907 |
|
28.6 |
% |
|
Gross margin |
|
|
50,573 |
|
31.1 |
% |
|
41,564 |
|
32.3 |
% |
|
9,009 |
|
21.7 |
% |
|
General and administrative expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Salaries and benefits |
|
|
24,592 |
|
15.1 |
% |
|
17,594 |
|
13.7 |
% |
|
6,998 |
|
39.8 |
% |
|
Other |
|
|
12,462 |
|
7.7 |
% |
|
9,536 |
|
7.4 |
% |
|
2,926 |
|
30.7 |
% |
|
Total general and administrative expenses |
|
|
37,054 |
|
22.8 |
% |
|
27,130 |
|
21.1 |
% |
|
9,924 |
|
36.6 |
% |
|
Operating income before corporate expenses |
|
$ |
13,519 |
|
8.3 |
% |
$ |
14,434 |
|
11.2 |
% |
$ |
(915) |
|
(6.3) |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Personal Care: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Locations |
|
|
76 |
|
|
|
|
73 |
|
|
|
|
3 |
|
4.1 |
% |
|
Admissions |
|
|
9,671 |
|
|
|
|
6,879 |
|
|
|
|
2,792 |
|
40.6 |
% |
|
Census |
|
|
13,216 |
|
|
|
|
34,843 |
|
|
|
|
(21,627) |
|
(62.1) |
% |
|
Hours of service |
|
|
7,538,223 |
|
|
|
|
5,863,888 |
|
|
|
|
1,674,335 |
|
28.6 |
% |
|
Hours per patient per week |
|
|
11.0 |
|
|
|
|
12.9 |
|
|
|
|
(1.9) |
|
(15.0) |
% |
|
Revenue |
|
$ |
161,367 |
|
99.3 |
% |
$ |
127,712 |
|
99.3 |
% |
$ |
33,655 |
|
26.4 |
% |
|
Operating income |
|
$ |
13,509 |
|
|
|
$ |
14,170 |
|
|
|
$ |
(661) |
|
(4.7) |
% |
|
Revenue per hour |
|
$ |
21.41 |
|
|
|
$ |
21.78 |
|
|
|
$ |
(0.37) |
|
(1.7) |
% |
|
Cost per hour |
|
$ |
13.15 |
|
|
|
$ |
13.09 |
|
|
|
$ |
0.06 |
|
0.5 |
% |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hospice: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Locations |
|
|
1 |
|
|
|
|
1 |
|
|
|
|
— |
|
NM |
|
|
Admissions |
|
|
97 |
|
|
|
|
69 |
|
|
|
|
28 |
|
NM |
|
|
Census |
|
|
23 |
|
|
|
|
18 |
|
|
|
|
5 |
|
NM |
|
|
Length of stay |
|
|
42 |
|
|
|
|
33 |
|
|
|
|
9 |
|
51.7 |
% |
|
Revenue |
|
$ |
1,179 |
|
0.7 |
% |
$ |
918 |
|
0.7 |
% |
$ |
261 |
|
NM |
|
|
Operating income |
|
$ |
10 |
|
|
|
$ |
264 |
|
|
|
$ |
(254) |
|
NM |
|
|
Revenue per day |
|
$ |
141 |
|
|
|
$ |
141 |
|
|
|
$ |
0 |
|
0.2 |
% |
PC segment net service revenues increased $33.7 million or 26.4% to $161.4 million due to acquisitions in the second half of 2015 (WillCare and Black Stone) and in mid-2016 (Wisconsin). Cost of service revenues as a percentage of net service revenues increased slightly to 68.9% in 2016 from 67.7% in 2015 due to the mix of acquired operations and rate reductions in certain skilled elements of the Connecticut and Ohio Medicaid programs.
Total general and administrative expenses increased as a percent of net service revenues to 22.8% from 21.1% in 2015, largely due to higher insurance claims experience in 2016 as compared to 2015.
As a result, OHBS segment operating income before corporate expenses as a percentage of revenue decreased 6.3%, or $0.9 million.
55
Healthcare Innovations Segment
(In thousands, except statistical information)
|
|
|
2016 |
|
2015 |
|
Change |
|
|||||||||
|
|
|
Amount |
|
% Rev |
|
Amount |
|
% Rev |
|
Amount |
|
% |
|
|||
|
Net service revenues |
|
$ |
26,027 |
|
100.0 |
% |
$ |
3,451 |
|
100.0 |
% |
$ |
22,576 |
|
NM |
|
|
Cost of service revenues |
|
|
10,733 |
|
41.2 |
% |
|
1,102 |
|
31.9 |
% |
|
9,631 |
|
NM |
|
|
Gross margin |
|
|
15,294 |
|
58.8 |
% |
|
2,349 |
|
68.1 |
% |
|
12,945 |
|
NM |
|
|
General and administrative expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Salaries and benefits |
|
|
5,915 |
|
22.7 |
% |
|
2,434 |
|
70.5 |
% |
|
3,481 |
|
NM |
|
|
Other |
|
|
3,722 |
|
14.3 |
% |
|
1,132 |
|
32.8 |
% |
|
2,590 |
|
NM |
|
|
Total general and administrative expenses |
|
|
9,637 |
|
37.0 |
% |
|
3,566 |
|
103.3 |
% |
|
6,071 |
|
NM |
|
|
Operating income before corporate expenses |
|
$ |
5,657 |
|
21.7 |
% |
$ |
(1,217) |
|
(35.3) |
% |
$ |
6,874 |
|
NM |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ACO Management |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medicare ACO enrollees under management |
|
|
121,881 |
|
|
|
|
83,133 |
|
|
|
|
38,748 |
|
NM |
|
|
ACOs under contract |
|
|
14 |
|
|
|
|
11 |
|
|
|
|
3 |
|
NM |
|
|
Revenue |
|
$ |
5,294 |
|
20.3 |
% |
$ |
1,758 |
|
50.9 |
% |
$ |
3,536 |
|
NM |
|
|
Operating income (loss) |
|
$ |
2,714 |
|
|
|
$ |
(257) |
|
|
|
$ |
2,971 |
|
NM |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Assessment Services |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Assessments |
|
|
75,814 |
|
|
|
|
5,394 |
|
|
|
|
70,420 |
|
NM |
|
|
Revenue |
|
$ |
20,733 |
|
79.7 |
% |
$ |
1,693 |
|
49.1 |
% |
$ |
19,040 |
|
NM |
|
|
Operating income (loss) |
|
$ |
2,943 |
|
|
|
$ |
(959) |
|
|
|
$ |
3,902 |
|
NM |
|
HCI segment net service revenues increased $22.6 million to $26.0 million in 2016 versus $3.5 million, as acquired assessment services revenues were $20.6 million and shared-savings revenue from our ACO business in 2016 increased to $4.3 million in 2016, as compared to $1.4 million in 2015. Overall HCI segment contribution improved $6.9 million to $5.7 million in 2016 versus a $1.2 million net loss in 2015.
Liquidity and Capital Resources
We believe that a certain amount of debt has an appropriate place in our overall capital structure, when reimbursement visibility permits, and it is not our strategy to eliminate all debt financing. We believe that our cash flow from operations, cash on hand, and borrowing capacity on our bank credit facility, described below, will be sufficient to cover operating needs, future capital expenditure requirements and scheduled debt payments of miscellaneous small borrowing arrangements. In addition, it is likely that we will pursue growth from acquisitions, partnerships and other ventures that would be funded from excess cash from operations, cash on hand, credit available under the bank credit agreement and other financing arrangements that are normally available in the marketplace. Further, our board may pursue a stock repurchase program or may decide to pay special dividends in the future.
56
2017 Common Stock Offering
On January 25, 2017, we sold 3,450 shares of common stock at $44.50 per share for gross proceeds of approximately $153.5 million. Total net proceeds, after underwriting discounts and commissions and our offering expenses, were approximately $143.9 million. These proceeds were used to repay obligations under the revolving credit facility.
Revolving Credit Facility
We have a senior secured revolving credit facility with JPMorgan Chase Bank, N.A., as Administrative Agent, and certain other lenders (the “Facility”). The Facility provides a credit line of up to $350 million with a maturity date of December 3, 2021, and an “accordion” feature providing for potential future expansion of the Facility up to $150 million of additional borrowings upon our further request and approval by a lender or lenders willing to extend such borrowings. Daily borrowings bear interest at a varying rate equal to prime plus 1.25%, while short term borrowings bear interest at a varying rate equal to the London Interbank Offered Rate (“LIBOR”) plus a margin which varies from 1.50% to 2.75%, depending on the Company’s leverage ratio. Interest expense also includes unused commitment fees related to total borrowing capacity, as well as letters of credit related fees. The Facility is secured by substantially all our assets and the assets and stock of our subsidiaries. Debt issuance costs of $4.7 million were capitalized in the fourth quarter of 2016 with the Facility and are being amortized to interest expense through December 2021.
Borrowings under the Facility are subject to various covenants, including a maximum leverage ratio for all calculation dates ending on or before December 31, 2017, of 4.0 times earnings before interest, taxes, depreciation and amortization, as adjusted (“EBITDA”) plus “Acquired EBITDA” from pro-forma acquisitions as defined. The maximum leverage ratio steps down, to a maximum leverage ratio of 3.75 times EBITDA plus Acquired EBITDA for calculation dates after December 31, 2017, and on or before June 30, 2018, and to a maximum leverage ratio of 3.5 times EBITDA plus Acquired EBITDA for calculation dates on and after September 30, 2018. Borrowings under the revolving credit facility may be used for general corporate purposes, including acquisitions. A portion of the proceeds were used to repay all the outstanding obligations of our prior credit agreement.
On December 30, 2016, we borrowed approximately $128.9 million from the Facility to finance the CHS-JV transaction, which was classified as a Transaction deposit and was included in revolving credit facility in the December 30, 2016 Consolidated Balance Sheet. On December 31, 2016, the first day of the Company’s 2017 fiscal year, the Transaction deposit converted to purchase price with the closing of the CHS-JV acquisition. On January 25, 2017, we sold 3,450 shares of common stock for net proceeds of $143.9 million, after deducting the underwriting discounts and commissions and our offering expenses, which were used to repay obligations under the Facility.
As of December 29, 2017, we were in compliance with the various financial covenants. Application of the Facility’s borrowing formula as of December 29, 2017, would have permitted approximately $221.3 million to be used. We had irrevocable letters of credit totaling $15.7 million in connection with our self-insurance programs.
The effective interest rates on our borrowings under the revolving credit facilities for 2017 and 2016 were 3.7% and 3.6%, respectively.
We believe the Facility will be sufficient to fund our operating needs and expansion plans for at least the next year. We will continue to evaluate additional capital, including possible debt and equity investments in the Company, to support a more rapid development of the business than would be possible with internal funds.
57
Cash Flows
Key elements to the Consolidated Statements of Cash Flows were as follows for the fiscal years: (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Net Change in Cash and Cash Equivalents (in thousands) |
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Provided by (used in): |
|
|
|
|
|
|
|
|
|
|
|
|
Operating activities |
|
|
$ |
30,530 |
|
$ |
24,443 |
|
$ |
21,206 |
|
|
Investing activities |
|
|
|
(7,990) |
|
|
(166,622) |
|
|
(86,695) |
|
|
Financing activities |
|
|
|
(21,340) |
|
|
144,767 |
|
|
66,125 |
|
|
Net increase (decrease) in cash and cash equivalents |
|
|
$ |
1,200 |
|
$ |
2,588 |
|
$ |
636 |
|
2017 Compared to 2016
Net cash provided by operating activities of $30.5 million resulted from current period net income of $20.4 million plus certain non-cash items, net of changes in accounts receivables and accounts payable and accrued expenses. Accounts receivable days sales outstanding were 57 at December 29, 2017, as compared to 60 days at December 30, 2016. The decline in days outstanding from the prior year were largely driven by the prior year including a temporary backlog related to an acquisition.
Cash used in investing activities was driven by capital expenditures largely related to our implementation of the Homecare Homebase information system. Cash used for the acquisition of the CHS-JV was offset by the reduction of the December 2016 transaction deposit.
Cash provided by financing activities from the sale of common stock of $143.9 million was used to repay obligations under the revolving credit facility.
2016 Compared to 2015
Net cash provided by operating activities of $24.4 million resulted primarily from current year net income of $17.7 million and the net impact of non-cash and other working capital changes. As a result of not acquiring accounts receivable in conjunction with our Wisconsin acquisition in June 2016 and normal delays from obtaining applicable licensure approvals, accounts receivable increased $10.2 million without which cash flows from operating activities would have been $34.6 million. Excluding the acquisition related build, accounts receivable days sales outstanding declined 5 days to 53 at December 30, 2016 from 58 at January 1, 2016. The decline was due to improved collections throughout the home health division, particularly related to previously disclosed backlogs of accounts receivable in Tennessee.
Cash used in investing activities was largely driven by acquisition related activity including the $128.9 million transaction deposit for CHS JV Transaction, $19.7 million for LTS, $6.1 million for Wisconsin, and $4.1 million for Bayonne. Capital expenditures were $6.2 million, up $3.1 million from 2015, primarily related to information systems investments related to our HH segment’s conversion to Homecare Homebase which began in the fourth quarter of 2016.
Cash provided by financing activities was driven by borrowings on the revolving credit facility, net of repayments from operating cash flows, primarily for acquisitions, along with $3.9 million for debt issuance costs incurred with the new credit facility.
Acquisitions
The Company completed several acquisitions over the past three years and will continue to actively seek to acquire other quality providers of home health services like our current operations.
Factors which may affect future acquisition decisions include, but are not limited to, the quality and potential profitability of the business under consideration, potential regulatory limitations and our profitability and ability to
58
finance the transaction. See Part II, Item 8, Notes 11 and 13 to the accompanying Notes to Consolidated Financial Statements for details regarding these acquisitions.
Contractual Obligations
The following table provides information about the payment dates of our contractual obligations at December 29, 2017, excluding current liabilities except for the current portion of long-term debt and additional consideration related to acquisitions (in thousands):
|
|
|
2018 |
|
2019 |
|
2020 |
|
2021 |
|
2022 |
|
Thereafter |
|
Total |
|
|||||||
|
Revolving credit facility |
|
$ |
— |
|
$ |
— |
|
$ |
— |
|
$ |
100,254 |
|
$ |
— |
|
$ |
— |
|
$ |
100,254 |
|
|
Notes payable |
|
|
4,961 |
|
|
7,650 |
|
|
150 |
|
|
— |
|
|
— |
|
|
— |
|
|
12,761 |
|
|
Operating leases |
|
|
9,683 |
|
|
6,283 |
|
|
4,141 |
|
|
2,837 |
|
|
1,607 |
|
|
5,560 |
|
|
30,111 |
|
|
Total |
|
$ |
14,644 |
|
$ |
13,933 |
|
$ |
4,291 |
|
$ |
103,091 |
|
$ |
1,607 |
|
$ |
5,560 |
|
$ |
143,126 |
|
Letters of Credit
We have outstanding letters of credit totaling $15.7 million at December 29, 2017, which benefit our third-party insurer/administrators for our self-insurance programs. The amount of such insurance program letters of credit is subject to negotiation annually upon renewal and may vary in the future based upon such negotiation, our historical claims experience and expected future claims. It is reasonable to expect that the amount of the letter of credit will increase in the future, however, we are unable to predict to what degree.
We currently have no contingent obligations related to acquisition agreements.
Our commitments and contingencies are also impacted by our general and professional liabilities, pending litigation and investigations, and health care reform discussed elsewhere in this form 10-K. Please refer to Part I, Item 1, “Government Regulation”, Part I, Item 1A, “Risk Factors”, Part I, Item 3 “Legal Proceedings”, Part II, Item 7, “Management’s Discussion and Analysis of Financial Condition and Results of Operations — Overview” and Part II, Item 8, “Notes to Consolidated Financial Statements”.
Impact of Inflation
We do not believe that inflation has had a material effect on income during the past several years.
Effective with the start of fiscal year 2018 the Company implemented a 2% cost of living wage increase for eligible employees.
Non-GAAP Financial Measures
The information provided in this annual report on Form 10-K includes certain non-GAAP financial measures as defined under SEC rules. In accordance with SEC rules, the Company has provided, in the supplemental information and the footnotes to the tables, a reconciliation of those measures to the most directly comparable GAAP measures.
Adjusted Net Income
Adjusted net income attributable to Almost Family, Inc. (“Adjusted Net Income”) is not a measure of financial performance under accounting principles generally accepted in the United States of America (“US GAAP”). It should not be considered in isolation or as a substitute for net income, operating income, cash flows from operating, investing or financing activities, or any other measure calculated in accordance with generally accepted accounting principles. We believe the use of non-GAAP measures on a consolidated and business segment basis assists investors in understanding the ongoing operating performance by presenting comparable financial results between periods. The non-GAAP
59
information provided is used by us and may not be determined in a manner consistent with the methodologies used by other companies.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(in thousands) |
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Net income attributable to Almost Family, Inc. |
|
|
$ |
20,414 |
|
$ |
17,653 |
|
$ |
20,009 |
|
|
Addbacks: |
|
|
|
|
|
|
|
|
|
|
|
|
Deal, transition and other costs |
|
|
|
29,405 |
|
|
11,842 |
|
|
4,139 |
|
|
Taxes |
|
|
|
(20,955) |
|
|
(4,855) |
|
|
(3,402) |
|
|
Deal, transition and other costs, net of tax |
|
|
|
8,450 |
|
|
6,987 |
|
|
737 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Adjusted net income attributable to Almost Family, Inc. |
|
|
$ |
28,864 |
|
$ |
24,640 |
|
$ |
20,746 |
|
|
Per share amounts-basic: |
|
|
|
|
|
|
|
|
|
|
|
|
Average shares outstanding |
|
|
|
13,539 |
|
|
10,153 |
|
|
9,505 |
|
|
Net income attributable to Almost Family, Inc. |
|
|
$ |
1.51 |
|
$ |
1.74 |
|
$ |
2.11 |
|
|
Addbacks: |
|
|
|
|
|
|
|
|
|
|
|
|
Deal, transition and other costs, net of tax |
|
|
|
0.62 |
|
|
0.69 |
|
|
0.08 |
|
|
Adjusted net income attributable to Almost Family, Inc. |
|
|
$ |
2.13 |
|
$ |
2.43 |
|
$ |
2.18 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Per share amounts-diluted: |
|
|
|
|
|
|
|
|
|
|
|
|
Average shares outstanding |
|
|
|
13,757 |
|
|
10,346 |
|
|
9,745 |
|
|
Merger transaction related |
|
|
|
38 |
|
|
— |
|
|
— |
|
|
Adjusted average shares outstanding |
|
|
|
13,719 |
|
|
10,346 |
|
|
9,745 |
|
|
Net income attributable to Almost Family, Inc. |
|
|
$ |
1.49 |
|
$ |
1.71 |
|
$ |
2.05 |
|
|
Addbacks: |
|
|
|
|
|
|
|
|
|
|
|
|
Deal, transition and other costs, net of tax |
|
|
|
0.62 |
|
|
0.68 |
|
|
0.08 |
|
|
Adjusted net income attributable to Almost Family, Inc. |
|
|
$ |
2.10 |
|
$ |
2.38 |
|
$ |
2.13 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Adjusted EBITDA
Adjusted earnings before interest, income tax, depreciation, amortization, amortization of stock-based compensation, and deal, transition and other (“Adjusted EBITDA”) is not a measure of financial performance under U.S. GAAP. It should not be considered in isolation or as a substitute for net income, operating income, cash flows from operating, investing or financing activities, or any other measure calculated in accordance with generally accepted accounting principles. The items excluded from Adjusted EBITDA are significant components in understanding and evaluating financial performance and liquidity. Management routinely calculates and communicates Adjusted EBITDA and believes that it is useful to investors because it is commonly used as an analytical indicator within our industry to evaluate performance, measure leverage capacity and debt service ability, and to estimate current or prospective enterprise value. Adjusted EBITDA is used in certain covenants contained in our revolving credit facility.
60
The following table sets forth a reconciliation of net income to Adjusted EBITDA for the year (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(in thousands) |
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Net income attributable to Almost Family, Inc. |
|
|
$ |
20,414 |
|
$ |
17,653 |
|
$ |
20,009 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Add back: |
|
|
|
|
|
|
|
|
|
|
|
|
Net income attributable to noncontrolling interests |
|
|
|
3,523 |
|
|
519 |
|
|
(468) |
|
|
Interest expense, net |
|
|
|
7,391 |
|
|
6,285 |
|
|
2,852 |
|
|
Income tax (benefit) expense |
|
|
|
(2,110) |
|
|
10,984 |
|
|
10,556 |
|
|
Franchise taxes |
|
|
|
954 |
|
|
625 |
|
|
609 |
|
|
Depreciation and amortization |
|
|
|
5,438 |
|
|
3,909 |
|
|
3,927 |
|
|
Stock-based compensation |
|
|
|
2,950 |
|
|
2,735 |
|
|
2,121 |
|
|
Deal, transition and other costs |
|
|
|
29,405 |
|
|
11,842 |
|
|
4,139 |
|
|
Adjusted EBITDA |
|
|
$ |
67,965 |
|
$ |
54,552 |
|
$ |
43,745 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ITEM 7A. Quantitative and Qualitative Disclosures About Market Risk
Derivative Instruments
We do not use derivative instruments.
Market Risk of Financial Instruments
Our primary market risk exposure with regard to financial instruments is to changes in interest rates.
At December 29, 2017, a hypothetical 100 basis point increase in short-term interest rates would result in a reduction of approximately $1.0 million in our annual pre-tax earnings.
61
ITEM 8. FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
ALMOST FAMILY, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF INCOME
(In thousands, except per share data)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Net service revenues |
|
|
$ |
796,965 |
|
$ |
623,541 |
|
$ |
532,214 |
|
|
Cost of service revenues (excluding depreciation and amortization) |
|
|
|
419,394 |
|
|
335,472 |
|
|
281,842 |
|
|
Gross margin |
|
|
|
377,571 |
|
|
288,069 |
|
|
250,372 |
|
|
General and administrative expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
Salaries and benefits |
|
|
|
223,016 |
|
|
168,356 |
|
|
147,849 |
|
|
Other |
|
|
|
95,932 |
|
|
72,430 |
|
|
65,435 |
|
|
Deal, transition and other costs |
|
|
|
29,405 |
|
|
11,842 |
|
|
4,139 |
|
|
Total general and administrative expenses |
|
|
|
348,353 |
|
|
252,628 |
|
|
217,423 |
|
|
Operating income |
|
|
|
29,218 |
|
|
35,441 |
|
|
32,949 |
|
|
Interest expense, net |
|
|
|
7,391 |
|
|
6,285 |
|
|
2,852 |
|
|
Income before noncontrolling interests and income taxes |
|
|
|
21,827 |
|
|
29,156 |
|
|
30,097 |
|
|
Net income attributable to noncontrolling interests |
|
|
|
3,523 |
|
|
519 |
|
|
(468) |
|
|
Net income before income taxes |
|
|
|
18,304 |
|
|
28,637 |
|
|
30,565 |
|
|
Income tax (benefit) expense |
|
|
|
(2,110) |
|
|
10,984 |
|
|
10,556 |
|
|
Net income attributable to Almost Family, Inc. |
|
|
$ |
20,414 |
|
$ |
17,653 |
|
$ |
20,009 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Per share amounts-basic: |
|
|
|
|
|
|
|
|
|
|
|
|
Average shares outstanding |
|
|
|
13,539 |
|
|
10,153 |
|
|
9,505 |
|
|
Net income attributable to Almost Family, Inc. |
|
|
$ |
1.51 |
|
$ |
1.74 |
|
$ |
2.11 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Per share amounts-diluted: |
|
|
|
|
|
|
|
|
|
|
|
|
Average shares outstanding |
|
|
|
13,757 |
|
|
10,346 |
|
|
9,745 |
|
|
Net income attributable to Almost Family, Inc. |
|
|
$ |
1.48 |
|
$ |
1.71 |
|
$ |
2.05 |
|
The accompanying notes to consolidated financial statements are an integral part of these financial statements.
62
ALMOST FAMILY, INC. AND SUBSIDIARIES
(In thousands)
|
|
|
|
|
|
|
|
|
|
|
|
December 29, 2017 |
|
December 30, 2016 |
|
||
|
ASSETS |
|
|
|
|
|
|
|
|
CURRENT ASSETS: |
|
|
|
|
|
|
|
|
Cash and cash equivalents |
|
$ |
11,310 |
|
$ |
10,110 |
|
|
Accounts receivable - net |
|
|
125,860 |
|
|
99,212 |
|
|
Prepaid expenses and other current assets |
|
|
14,514 |
|
|
11,432 |
|
|
TOTAL CURRENT ASSETS |
|
|
151,684 |
|
|
120,754 |
|
|
PROPERTY AND EQUIPMENT - NET |
|
|
15,246 |
|
|
10,732 |
|
|
GOODWILL |
|
|
390,754 |
|
|
305,476 |
|
|
OTHER INTANGIBLE ASSETS - NET |
|
|
145,522 |
|
|
85,063 |
|
|
TRANSACTION DEPOSIT |
|
|
— |
|
|
128,930 |
|
|
ASSETS HELD FOR SALE |
|
|
3,800 |
|
|
— |
|
|
OTHER ASSETS |
|
|
10,812 |
|
|
7,757 |
|
|
TOTAL ASSETS |
|
$ |
717,818 |
|
$ |
658,712 |
|
|
|
|
|
|
|
|
|
|
|
LIABILITIES AND STOCKHOLDERS’ EQUITY |
|
|
|
|
|
|
|
|
CURRENT LIABILITIES: |
|
|
|
|
|
|
|
|
Accounts payable |
|
$ |
22,049 |
|
$ |
12,122 |
|
|
Accrued other liabilities |
|
|
50,182 |
|
|
39,728 |
|
|
Current portion - Seller Notes |
|
|
4,961 |
|
|
— |
|
|
TOTAL CURRENT LIABILITIES |
|
|
77,192 |
|
|
51,850 |
|
|
|
|
|
|
|
|
|
|
|
LONG-TERM LIABILITIES: |
|
|
|
|
|
|
|
|
Revolving credit facility |
|
|
100,254 |
|
|
262,456 |
|
|
Deferred tax liabilities |
|
|
18,595 |
|
|
21,145 |
|
|
Seller notes, net of current portion |
|
|
7,800 |
|
|
12,500 |
|
|
Other liabilities |
|
|
7,424 |
|
|
6,581 |
|
|
TOTAL LONG-TERM LIABILITIES |
|
|
134,073 |
|
|
302,682 |
|
|
TOTAL LIABILITIES |
|
|
211,265 |
|
|
354,532 |
|
|
|
|
|
|
|
|
|
|
|
NONCONTROLLING INTEREST - REDEEMABLE - |
|
|
|
|
|
|
|
|
HEALTHCARE INNOVATIONS |
|
|
2,256 |
|
|
2,256 |
|
|
|
|
|
|
|
|
|
|
|
STOCKHOLDERS’ EQUITY: |
|
|
|
|
|
|
|
|
Preferred stock, par value $0.05; authorized 2,000 shares; none issued or outstanding |
|
|
— |
|
|
— |
|
|
Common stock, par value $0.10; authorized 25,000; 14,243 and 10,504 issued and outstanding |
|
|
1,425 |
|
|
1,051 |
|
|
Treasury stock, at cost, 251 and 117 shares |
|
|
(10,453) |
|
|
(3,258) |
|
|
Additional paid-in capital |
|
|
294,448 |
|
|
141,233 |
|
|
Retained earnings |
|
|
184,309 |
|
|
163,763 |
|
|
Almost Family, Inc. stockholders' equity |
|
|
469,729 |
|
|
302,789 |
|
|
Noncontrolling interests - nonredeemable |
|
|
34,568 |
|
|
(865) |
|
|
TOTAL STOCKHOLDERS’ EQUITY |
|
|
504,297 |
|
|
301,924 |
|
|
TOTAL LIABILITIES AND STOCKHOLDERS’ EQUITY |
|
$ |
717,818 |
|
$ |
658,712 |
|
The accompanying notes to consolidated financial statements are an integral part of these financial statements.
63
ALMOST FAMILY, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF STOCKHOLDERS’ EQUITY
(In thousands)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Non- |
|
|
|
|
|
Non- |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
Additional |
|
|
|
|
controlling |
|
Total |
|
|
controlling |
|
||||
|
|
|
Common Stock |
|
Treasury Stock |
|
Paid-in |
|
Retained |
|
Interest - Non- |
|
Stockholders’ |
|
|
Interest - |
|
|||||||||||
|
|
|
Shares |
|
Amount |
|
Shares |
|
Amount |
|
Capital |
|
Earnings |
|
redeemable |
|
Equity |
|
|
Redeemable |
|
|||||||
|
Balance, December 31, 2014 |
|
9,574 |
|
$ |
957 |
|
(94) |
|
$ |
(2,392) |
|
$ |
105,862 |
|
$ |
125,546 |
|
$ |
(420) |
|
$ |
229,553 |
|
|
$ |
3,639 |
|
|
Share award maturities, net of shares surrendered or withheld |
|
10 |
|
|
1 |
|
(9) |
|
|
(339) |
|
|
128 |
|
|
— |
|
|
— |
|
|
(210) |
|
|
|
— |
|
|
Share awards and related compensation |
|
100 |
|
|
11 |
|
— |
|
|
— |
|
|
2,110 |
|
|
— |
|
|
— |
|
|
2,121 |
|
|
|
— |
|
|
Tax gain from stock-based compensation |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
215 |
|
|
— |
|
|
— |
|
|
215 |
|
|
|
— |
|
|
Stock provided in acquisitions |
|
441 |
|
|
44 |
|
— |
|
|
— |
|
|
18,938 |
|
|
— |
|
|
— |
|
|
18,982 |
|
|
|
— |
|
|
Net loss noncontrolling interests - redeemable |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
|
(99) |
|
|
Noncontrolling interests - redeemable fair value accretion |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
(99) |
|
|
— |
|
|
(99) |
|
|
|
99 |
|
|
Net loss noncontrolling interests - nonredeemable |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
(310) |
|
|
(310) |
|
|
|
— |
|
|
Net income attributable to Almost Family, Inc. |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
20,009 |
|
|
— |
|
|
20,009 |
|
|
|
— |
|
|
Balance, January 1, 2016 |
|
10,125 |
|
|
1,013 |
|
(103) |
|
|
(2,731) |
|
|
127,253 |
|
|
145,456 |
|
|
(730) |
|
|
270,261 |
|
|
|
3,639 |
|
|
Share award maturities, net of shares surrendered or withheld |
|
1 |
|
|
— |
|
(14) |
|
|
(527) |
|
|
230 |
|
|
— |
|
|
— |
|
|
(297) |
|
|
|
— |
|
|
Share awards and related compensation |
|
98 |
|
|
10 |
|
— |
|
|
— |
|
|
2,750 |
|
|
— |
|
|
— |
|
|
2,760 |
|
|
|
— |
|
|
Tax gain from stock-based compensation |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
353 |
|
|
— |
|
|
— |
|
|
353 |
|
|
|
— |
|
|
Stock provided in acquisitions |
|
280 |
|
|
28 |
|
— |
|
|
— |
|
|
10,647 |
|
|
— |
|
|
— |
|
|
10,675 |
|
|
|
— |
|
|
Acquired noncontrolling interest |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
|
(1,383) |
|
|
Net gain noncontrolling interests - redeemable |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
|
654 |
|
|
Noncontrolling interests - redeemable fair value accretion |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
654 |
|
|
— |
|
|
654 |
|
|
|
(654) |
|
|
Net loss noncontrolling interests - nonredeemable |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
(135) |
|
|
(135) |
|
|
|
— |
|
|
Net income attributable to Almost Family, Inc. |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
17,653 |
|
|
— |
|
|
17,653 |
|
|
|
— |
|
|
Balance, December 30, 2016 |
|
10,504 |
|
|
1,051 |
|
(117) |
|
|
(3,258) |
|
|
141,233 |
|
|
163,763 |
|
|
(865) |
|
|
301,924 |
|
|
|
2,256 |
|
|
Share award maturities, net of shares surrendered or withheld |
|
201 |
|
|
20 |
|
(134) |
|
|
(7,195) |
|
|
4,324 |
|
|
— |
|
|
— |
|
|
(2,851) |
|
|
|
— |
|
|
Share awards and related compensation |
|
88 |
|
|
9 |
|
— |
|
|
— |
|
|
5,459 |
|
|
— |
|
|
— |
|
|
5,468 |
|
|
|
— |
|
|
Distribution of capital |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
(128) |
|
|
— |
|
|
— |
|
|
(128) |
|
|
|
— |
|
|
Equity offering |
|
3,450 |
|
|
345 |
|
— |
|
|
— |
|
|
143,560 |
|
|
— |
|
|
— |
|
|
143,905 |
|
|
|
— |
|
|
Acquired noncontrolling interests |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
32,042 |
|
|
32,042 |
|
|
|
— |
|
|
Net gain noncontrolling interests - redeemable |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
|
132 |
|
|
Noncontrolling interests - redeemable fair value accretion |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
132 |
|
|
— |
|
|
132 |
|
|
|
(132) |
|
|
Net loss noncontrolling interests - nonredeemable |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
3,391 |
|
|
3,391 |
|
|
|
— |
|
|
Net income attributable to Almost Family, Inc. |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
20,414 |
|
|
— |
|
|
20,414 |
|
|
|
— |
|
|
Balance, December 29, 2017 |
|
14,243 |
|
$ |
1,425 |
|
(251) |
|
$ |
(10,453) |
|
$ |
294,448 |
|
$ |
184,309 |
|
$ |
34,568 |
|
$ |
504,297 |
|
|
$ |
2,256 |
|
The accompanying notes to consolidated financial statements are an integral part of these financial statements.
64
ALMOST FAMILY, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS
(in thousands)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Cash flows from operating activities: |
|
|
|
|
|
|
|
|
|
|
|
Net income attributable to Almost Family, Inc. |
|
$ |
20,414 |
|
$ |
17,653 |
|
$ |
20,009 |
|
|
Net income attributable to noncontrolling interests |
|
|
3,523 |
|
|
519 |
|
|
(468) |
|
|
Consolidated net income |
|
|
23,937 |
|
|
18,172 |
|
|
19,541 |
|
|
Adjustments to reconcile net income to net cash provided by operating activities: |
|
|
|
|
|
|
|
|
|
|
|
Depreciation and amortization |
|
|
5,916 |
|
|
4,445 |
|
|
3,927 |
|
|
Provision for uncollectible accounts |
|
|
14,526 |
|
|
11,708 |
|
|
12,743 |
|
|
Stock-based compensation |
|
|
5,468 |
|
|
2,760 |
|
|
2,121 |
|
|
Loan cost amortization |
|
|
954 |
|
|
336 |
|
|
281 |
|
|
Deferred income taxes |
|
|
(2,550) |
|
|
8,725 |
|
|
3,914 |
|
|
|
|
|
48,251 |
|
|
46,146 |
|
|
42,527 |
|
|
Change in certain net assets and liabilities, net of the effects of acquisitions: |
|
|
|
|
|
|
|
|
|
|
|
Accounts receivable |
|
|
(19,664) |
|
|
(18,701) |
|
|
(17,393) |
|
|
Prepaid expenses and other current assets |
|
|
(2,242) |
|
|
(377) |
|
|
2,402 |
|
|
Other assets |
|
|
(3,966) |
|
|
(1,215) |
|
|
(585) |
|
|
Accounts payable and accrued expenses |
|
|
8,151 |
|
|
(1,410) |
|
|
(5,745) |
|
|
Net cash provided by operating activities |
|
|
30,530 |
|
|
24,443 |
|
|
21,206 |
|
|
Cash flows from investing activities: |
|
|
|
|
|
|
|
|
|
|
|
Capital expenditures |
|
|
(6,112) |
|
|
(6,206) |
|
|
(3,117) |
|
|
Cost basis investment |
|
|
— |
|
|
— |
|
|
(1,000) |
|
|
Transaction deposit |
|
|
128,930 |
|
|
(128,930) |
|
|
— |
|
|
Acquisitions, net of cash acquired |
|
|
(130,808) |
|
|
(31,486) |
|
|
(82,578) |
|
|
Net cash used in investing activities |
|
|
(7,990) |
|
|
(166,622) |
|
|
(86,695) |
|
|
Cash flows from financing activities: |
|
|
|
|
|
|
|
|
|
|
|
Credit facility borrowings |
|
|
245,471 |
|
|
389,328 |
|
|
233,425 |
|
|
Credit facility repayments, net |
|
|
(407,673) |
|
|
(240,662) |
|
|
(166,082) |
|
|
Debt issuance fees |
|
|
(25) |
|
|
(3,900) |
|
|
(1,161) |
|
|
Distribution of capital |
|
|
(128) |
|
|
— |
|
|
— |
|
|
Proceeds from stock offering, net |
|
|
143,905 |
|
|
— |
|
|
— |
|
|
Proceeds from stock option exercises |
|
|
4,344 |
|
|
230 |
|
|
128 |
|
|
Purchase of common stock in connection with share awards |
|
|
(7,195) |
|
|
(527) |
|
|
(338) |
|
|
Tax impact of share awards |
|
|
— |
|
|
353 |
|
|
215 |
|
|
Payment of special dividend |
|
|
— |
|
|
— |
|
|
(50) |
|
|
Principal payments on notes payable and capital leases |
|
|
(39) |
|
|
(55) |
|
|
(12) |
|
|
Net cash (used in) provided by financing activities |
|
|
(21,340) |
|
|
144,767 |
|
|
66,125 |
|
|
Net increase (decrease) in cash and cash equivalents |
|
|
1,200 |
|
|
2,588 |
|
|
636 |
|
|
Cash and cash equivalents at beginning of period |
|
|
10,110 |
|
|
7,522 |
|
|
6,886 |
|
|
Cash and cash equivalents at end of period |
|
$ |
11,310 |
|
$ |
10,110 |
|
$ |
7,522 |
|
|
Supplemental disclosures of cash flow information: |
|
|
|
|
|
|
|
|
|
|
|
Cash payment of interest, net of amounts capitalized |
|
$ |
6,471 |
|
$ |
5,980 |
|
$ |
1,890 |
|
|
Cash payment of taxes |
|
$ |
576 |
|
$ |
2,549 |
|
$ |
4,651 |
|
|
Summary of non-cash investing and financing activities: |
|
|
|
|
|
|
|
|
|
|
|
Acquisitions funded by notes payable |
|
$ |
300 |
|
$ |
6,000 |
|
$ |
5,000 |
|
|
Acquisitions funded by stock |
|
$ |
— |
|
$ |
10,675 |
|
$ |
18,982 |
|
The accompanying notes to consolidated financial statements are an integral part of these financial statements.
65
ALMOST FAMILY, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
(Unless otherwise indicated all dollar and share amounts are in thousands)
NOTE 1 - SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
Basis of Consolidation and Description of Business
The consolidated financial statements include the accounts of Almost Family, Inc. (a Delaware corporation) and its wholly-owned subsidiaries (collectively “Almost Family” or the “Company”). The Company is a leading provider of cost efficient, high quality home healthcare care services and related innovations to drive savings for payors and improve patient outcomes and experience.
On the first day of fiscal 2017, the Company acquired an 80% controlling interest in the entity holding the home health and hospice assets of Community Health Systems, Inc. (NYSE: CYH) (“CHS-JV”). Community Health Systems, Inc. ("CHS") is one of the largest publicly-traded hospital companies in the United States and a leading operator of general acute care hospitals in communities across the country. CHS retained the remaining 20%. The purchase price of $128.9 million was funded through borrowings on the Company's revolving credit facility, which resulted in a deposit in the December 30, 2016 balance sheet. The deposit was converted to purchase consideration at closing. The borrowing was subsequently repaid with proceeds from the Company’s stock offering on January 25, 2017. The final purchase price is subject to a working capital adjustment. At acquisition, the CHS-JV operated 74 home health and 15 hospice branch locations in 22 states.
On June 18, 2016, the Company acquired certain home health agency assets primarily in Wisconsin, but also in Connecticut and Kentucky (collectively, the “Wisconsin Acquisition”). On January 5, 2016, the Company acquired 100% of the equity of Long Term Solutions, Inc. (“LTS”) for a purchase price of $37 million. On January 5, 2016, the Company purchased the assets of a Medicare-certified home health agency owned by Bayonne Visiting Nurse Association (“Bayonne”) located in New Jersey. On November 5, 2015, the Company completed the acquisition of Black Stone Operations, LLC (“Black Stone”). Black Stone owned and operated personal care and skilled home health services in western Ohio. On August 29, 2015, the Company completed the acquisition of Bracor, Inc. (dba “WillCare”). WillCare owned and operated Home Health (“HH”) and Personal Care (“PC”) branch locations in New York (12), and Connecticut (1). On July 22, 2015, the Company acquired Ingenios Health (“Ingenios”). Ingenios is a leading provider of technology enabled in-house clinical assessments for Medicare Advantage, Managed Medicaid and Commercial Exchange lives in four states and Washington, D.C. On March 2, 2015, the Company acquired the stock of WillCare’s Ohio operations. On January 29, 2015, the Company acquired a noncontrolling interest in a development stage analytics and software company, Care Journey (formerly NavHealth, Inc.). The acquisitions are more fully described in Note 11, “Acquisitions.”
The Company’s consolidated financial statements are prepared in accordance with U.S. generally accepted accounting principles (“US GAAP”). All intercompany balances and transactions have been eliminated. The Company does not have other comprehensive income or losses, therefore net income is equivalent to comprehensive income for all periods presented.
Reclassifications
Consistent with the terms of the Company’s revolving credit facility, the Company now classifies unused commitment (“Unused”) and Letter of Credit (“LOC”) fees as a part of interest expense. Historically, such costs were included in General and administrative – Other. Unused and LOC fees for prior periods were reclassified to interest expense for consistency. Unused and LOC fees included in Interest expense for the year ended 2017 were $0.7 million and $0.4 million, respectively, while 2016 amounts were $0.1 million and $0.4 million, respectively, and 2015 amounts were $0.3 million and $0.2 million, respectively.
66
Fiscal Year End
The Company uses a 52-53 week fiscal reporting calendar under which annual results are reported in four equal 13-week quarters. Every fifth year, one quarter will include 14 weeks and that year will include 53 weeks of operating results. All references herein for the years 2017, 2016 and 2015 represent the fiscal years ended December 29, 2017, December 30, 2016, and January 1, 2016, respectively.
Recently Adopted Accounting Pronouncements
In the first quarter of 2017, the Company adopted Financial Accounting Standards Board (“FASB”) Accounting Standards Update (“ASU”) ASU 2016-09, Compensation – Stock Compensation (“ASU 2016-09”). Under the new guidance, the Company recognizes all excess tax benefits or losses, if applicable, related to stock-based compensation as a component of income taxes in its consolidated statement of income and as operating cash flow in its consolidated statement of cash flows (with other income tax cash flows). Previous guidance required recognition as additional paid-in capital and classified those amounts as financing activity in the statement of cash flows. As a result, net income and operating cash flows for the year-ended 2017 include excess tax benefits of approximately $2.1 million. Prior financial statements did not require adjustment under the new guidance. The future impact of adopting this new standard on the Company’s financial statements will be dependent on the timing and intrinsic value of future share-based compensation award exercises. The adoption of this standard will increase the volatility of the income tax provision in the Company’s results of operations.
Recently Issued Accounting Pronouncements Not Yet Adopted
In January 2017, the FASB issued ASU 2017-01, Business Combinations (“Topic 805”), Clarifying the Definition of a Business (“ASU 2017-01”). ASU 2017-01 changes the definition of a business in an effort to assist entities with evaluating whether a set of transferred assets and activities is a business when accounting for acquisitions, disposals, goodwill, impairment and consolidations. The guidance will require an entity to evaluate whether substantially all of the fair value of the gross assets acquired is concentrated in a single identifiable asset or a group of similar identifiable assets, and thus is not a business combination. The guidance is effective for annual and interim impairment tests performed for periods beginning after December 15, 2019. The Company is currently evaluating the impact of ASU 2017-01.
In January 2017, the FASB issued ASU 2017-04, Intangible – Goodwill and Other, Simplifying the Test for Goodwill Impairment, (“ASU 2017-04”) that simplifies the measurement for goodwill impairment into a single step. The guidance eliminates Step 2 of the goodwill impairment test that required a hypothetical purchase price allocation of an implied fair value of goodwill to measure a goodwill impairment charge. Under the new guidance, entities failing Step 1 of the goodwill impairment test will always record an impairment charge based on the excess of a reporting unit’s carrying amount over it fair value. ASU 2017-04 does not change Step 1 guidance. The guidance is effective for annual reporting periods beginning after December 15, 2017, including interim periods in those years. Early adoption is permitted for annual and interim goodwill impairment testing dates after January 1, 2017. The Company is currently evaluating the impact of ASU 2017-04.
In August 2016, the FASB issued ASU 2016-15, Statement of Cash Flows, Classification of Certain Cash Receipts and Cash Payments (“ASU 2016-15”). ASU 2016-15 clarifies how entities should classify eight categories of cash receipts and cash payments on the statement of cash flows including debt prepayment or extinguishment costs, maturity of a zero coupon bond, settlement of contingent consideration liabilities of a business combination, proceeds from insurance settlement and distribution from certain equity method investees. It also clarifies how the predominance principle should be applied when cash receipts and cash payments have aspects of more than one class of cash flows. ASU 2016-15 is effective for annual reporting periods beginning after December 15, 2017, and interim periods within those years. Early adoption is permitted. The Company is currently evaluating the impact ASU 2016-15 will have on its consolidated financial statements.
In February 2016, the FASB issued ASU 2016-02, Leases (“ASU 2016-02”). ASU 2016-02 requires lessees to recognize assets and liabilities on their balance sheet related to the rights and obligations created by most leases, while continuing to recognize expenses on their income statements over the lease term. The ASU further requires disclosures
67
designed to give financial statement users information regarding the amount, timing, and uncertainty of cash flows arising from leases. The guidance is effective for annual reporting periods beginning after December 15, 2018, and interim periods within those years. Early adoption is permitted for all entities. The Company is currently evaluating the impact ASU 2016-02 will have on its consolidated financial statements and associated disclosures.
In May 2014, the FASB issued ASU 2014-09, Revenue from Contracts with Customers (“Topic 606”). Topic 606 affects virtually all aspects of an entity’s revenue recognition, including determining the measurement of revenue and the timing of when it is recognized for the transfer of goods or services to customers. The Company adopted Topic 606 effective for the next fiscal year beginning after December 29, 2017 using a modified retrospective approach.
Based on the assessment of the guidance, no opening balance sheet adjustment to retained earnings was identified; however, a reclassification of all bad debt expense to net patient service revenue on a go-forward basis will occur, as the standard largely limits bad debt expense to bankruptcies or changes in credit risk.
A significant element of implementing Topic 606 is reviewing sources of revenue and evaluating the characteristics of the patient population to develop the appropriate portfolio distribution with similar characteristics that when evaluated under the new revenue standard, will result in a materially consistent revenue amount for such portfolios as if each patient account was evaluated on a “contract-by-contract” basis. The Company’s review supports an allocation of patients to portfolios that is consistent with our current MD&A, segment and footnote disclosures. Additionally, the Company believes the adoption will have minimal impact on our financial statement disclosures.
Application of this guidance by the healthcare industry is continuing to develop, and changes could arise that are inconsistent with the Company’s year-end assessment. The Company will continue to monitor the application of Topic 606 by peer organizations.
Cash and Cash Equivalents
The Company considers all highly liquid debt instruments purchased with an original maturity of three months or less to be cash equivalents.
Uninsured deposits at December 29, 2017 and December 30, 2016 were approximately $7,524 and $7,845, respectively. These amounts have been deposited with national financial institutions.
Property and Equipment
Property and equipment are stated at cost. Depreciation is computed using the straight-line method over the estimated useful lives (generally two to ten years for medical and office equipment and three years for internally developed software). Leasehold improvements are depreciated over the terms of the respective leases (generally three to ten years). Buildings are depreciated over the estimated life of the 39 years. Such costs are periodically reviewed for recoverability when impairment indicators are present. Such indicators include, among other factors, operating losses, unused capacity, market value declines and technological obsolescence. Recorded values of asset groups of property, plant and equipment that are not expected to be recovered through undiscounted future net cash flows are written down to current fair value, which generally is determined from estimated discounted future net cash flows (assets held for use) or net realizable value (assets held for sale).
Goodwill and Other Intangible Assets
Goodwill and indefinite lived intangible assets acquired are stated at fair value at the date of acquisition. Subsequent to acquisition, the Company conducts annual reviews for impairment, or more frequently if circumstances indicate impairment may have occurred. In 2017 the Company performed qualitative assessments to determine whether any goodwill or indefinite lived assets were impaired. Specifically the Company evaluated the relevant events and circumstances, such as the market conditions, financial performance, and share price to determine if any impairment is indicated. Based on our 2017 analysis, an impairment of goodwill or indefinite lived assets was not indicated. Had the qualitative assessment indicated impairment, the Company would perform the following quantitative tests as performed in 2016 and 2015 as follows:
68
The Company’s quantitative test of goodwill is based on its identified reporting units, which are the same as its reportable segments. The quantitative test for goodwill compares the carrying value to the estimated fair value of its reporting units, determined using a combination of the market approach (guideline company and similar transaction method) and income approach (discounted cash flow analysis). The Company’s quantitative test of indefinite-lived intangible assets, principally trade names, certificates of need, provider numbers and licenses, uses a “relief-from-royalty” valuation method compared to the carrying value. Significant assumptions inherent in the valuation methodologies for goodwill and other intangibles are employed and include, but are not limited to, such estimates as future projected business results, growth rates, legislated changes in payment rates, weighted-average cost of capital for a market participant, royalty and discount rates.
Finite-lived intangible assets are amortized on a straight-line basis over their estimated useful lives, such as the cost of non-compete agreements for which their estimated useful life is usually 3 years, beginning after the earn-out period, if any.
The following table summarizes the activity related to the Company’s goodwill and other intangible assets:
|
|
|
|
|
|
Other Intangible Assets |
|
|||||||||||||
|
|
|
|
|
Certificates |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
of Need and |
|
Trade |
|
Non-compete |
|
Customer |
|
|
|
|
|||||
|
|
|
Goodwill |
|
Licenses |
|
Names |
|
Agreements |
|
Relationships |
|
Total |
|
||||||
|
Balances at January 1, 2016 |
|
$ |
277,061 |
|
$ |
46,044 |
|
$ |
18,401 |
|
$ |
184 |
|
$ |
— |
|
$ |
64,629 |
|
|
Acquisitions |
|
|
28,415 |
|
|
5,388 |
|
|
4,930 |
|
|
600 |
|
|
10,190 |
|
|
21,108 |
|
|
Amortization |
|
|
— |
|
|
— |
|
|
(8) |
|
|
(164) |
|
|
(502) |
|
|
(674) |
|
|
Balances at December 30, 2016 |
|
|
305,476 |
|
|
51,432 |
|
|
23,323 |
|
|
620 |
|
|
9,688 |
|
|
85,063 |
|
|
Acquisitions |
|
|
85,278 |
|
|
52,103 |
|
|
9,880 |
|
|
490 |
|
|
— |
|
|
62,473 |
|
|
Assets held for sale |
|
|
— |
|
|
(1,290) |
|
|
— |
|
|
— |
|
|
— |
|
|
(1,290) |
|
|
Amortization |
|
|
— |
|
|
— |
|
|
— |
|
|
(216) |
|
|
(508) |
|
|
(724) |
|
|
Balances at December 29, 2017 |
|
$ |
390,754 |
|
$ |
102,245 |
|
$ |
33,203 |
|
$ |
894 |
|
$ |
9,180 |
|
$ |
145,522 |
|
See Note 11 for further discussion of acquisitions.
The following table summarizes the Company’s goodwill and other intangible assets by segment:
|
|
|
|
|
Other Intangible Assets |
|
||||||||||||||
|
|
|
|
|
Certificates |
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
of Need and |
|
Trade |
|
Non-compete |
|
Customer |
|
|
|
||||||
|
|
|
Goodwill |
|
Licenses |
|
Names |
|
Agreements |
|
Relationships |
|
Total |
|
||||||
|
Home Health |
|
$ |
193,824 |
|
$ |
47,252 |
|
$ |
13,198 |
|
$ |
69 |
|
$ |
— |
|
$ |
60,519 |
|
|
Other Home-Based Services |
|
|
75,003 |
|
|
4,180 |
|
|
5,195 |
|
|
69 |
|
|
— |
|
|
9,444 |
|
|
Healthcare Innovations |
|
|
36,649 |
|
|
— |
|
|
4,930 |
|
|
482 |
|
|
9,688 |
|
|
15,100 |
|
|
December 30, 2016 balances |
|
$ |
305,476 |
|
$ |
51,432 |
|
$ |
23,323 |
|
$ |
620 |
|
$ |
9,688 |
|
$ |
85,063 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
272,306 |
|
$ |
92,585 |
|
$ |
21,668 |
|
$ |
420 |
|
$ |
— |
|
$ |
114,673 |
|
|
Other Home-Based Services |
|
|
81,799 |
|
|
9,660 |
|
|
6,605 |
|
|
112 |
|
|
— |
|
|
16,377 |
|
|
Healthcare Innovations |
|
|
36,649 |
|
|
— |
|
|
4,930 |
|
|
362 |
|
|
9,180 |
|
|
14,472 |
|
|
December 29, 2017 balances |
|
$ |
390,754 |
|
$ |
102,245 |
|
$ |
33,203 |
|
$ |
894 |
|
$ |
9,180 |
|
$ |
145,522 |
|
Capitalization Policies
Maintenance, repairs and minor replacements are charged to expense as incurred. Major renovations and replacements are capitalized to appropriate property and equipment accounts. Upon sale or retirement of property, the cost and related
69
accumulated depreciation are eliminated from the accounts and the related gain or loss is recognized in the consolidated statement of income.
The Company capitalizes the cost of internally developed computer software for the Company’s own use. Software development costs of approximately $951, $1,279 and $788 were capitalized in 2017, 2016 and 2015, respectively.
Assets Held for Sale
As of December 29, 2017, Assets Held for Sale includes the land, building, CON licenses and all related equipment and fixtures of one hospice facility that the Company is actively marketing and intends to sale.
Insurance Programs
The Company bears significant risk under its large-deductible workers’ compensation insurance program and its self-insured employee health program. Under the workers’ compensation insurance program, the Company bears risk up to $400 per incident, after which stop-loss coverage is maintained. The Company purchases stop-loss insurance for the employee health plan that places a specific limit, generally $300, on its exposure for any individual covered life.
Malpractice and general patient liability claims for incidents which may give rise to litigation have been asserted against the Company by various claimants. The claims are in various stages of processing and some may ultimately be brought to trial. The Company currently carries professional and general liability insurance coverage (on a claims made basis) for this exposure with no deductible. The Company also carries D&O coverage (also on a claims made basis) for potential claims against the Company’s directors and officers, including securities actions, with deductibles ranging from $175 to $500 per claim.
The Company records estimated liabilities for its insurance programs based on information provided by the third-party plan administrators, historical claims experience, the life cycle of claims, expected costs of claims incurred but not paid, and expected costs to settle unpaid claims. The Company monitors its estimated insurance-related liabilities and recoveries, if any, on a monthly basis and records amounts due under insurance policies in other current assets, while recording the estimated carrier liability in other current liabilities. As facts change, it may become necessary to make adjustments that could be material to the Company’s results of operations and financial condition.
Accounting for Income Taxes
The Company recognizes deferred tax assets and liabilities for the expected future tax consequences of events that have been included in the financial statements or tax returns. Under this method, deferred tax assets and liabilities are determined based on the difference between the Company’s book and tax bases of assets and liabilities and tax carry-forwards using enacted tax rates in effect for the year in which the differences are expected to reverse. The effect of changes in tax rates on deferred taxes is recognized in the period in which the enactment dates change. Valuation allowances are established when necessary on a jurisdictional basis to reduce deferred tax assets to the amounts expected to be realized.
70
Noncontrolling Interest
Noncontrolling interest represents the ownership interests of minority shareholders in the operating results of the period. The following details the minority shareholders’ interest that is excluded from the Consolidated Statements of Income.
|
|
|
2017 |
|
2016 |
|
2015 |
|||
|
CHS-JV |
|
$ |
3,506 |
|
$ |
— |
|
$ |
— |
|
Other |
|
|
(115) |
|
|
(135) |
|
|
(369) |
|
Noncontrolling interest - nonredeemable |
|
|
3,391 |
|
|
(135) |
|
|
(369) |
|
Noncontrolling interest - redeemable - Imperium |
|
|
132 |
|
|
654 |
|
|
(99) |
|
Net income attributable to noncontrolling interests |
|
$ |
3,523 |
|
$ |
519 |
|
$ |
(468) |
The Company currently owns a 72% controlling interest in Imperium. The Company is party to a put and call arrangement with respect to the remaining 28% non-controlling interest in Imperium. The redemption value for both the put and the call arrangement is equal to fair value. Due to the existing put and call arrangements, the noncontrolling interest is considered to be redeemable and is recorded on the balance sheet as a redeemable noncontrolling interest outside of permanent equity. The redeemable noncontrolling interest is recognized at the higher of 1) the accumulated earnings associated with the noncontrolling interest or 2) the redemption value as of the balance sheet date.
Seasonality
Our HH segment operations located in Florida normally experience higher admissions during the first quarter and lower admissions during the third quarter than in the other quarters due to seasonal population fluctuations. Florida operations generated approximately 20% of our 2017 revenue.
In our HCI segment, first quarter assessment revenues are traditionally lower than the other quarters due to the seasonal nature of our Medicare Advantage plan customers, while the majority of our ACO Management revenues have historically been generated in the third quarter.
Further, our third quarter falls within the “Hurricane season” including the peak months of August and September. Our operations may thus be subject to periods of unexpected disruption, which lower volumes and increase costs. The impact of lost admissions, visits, assessments and revenue on operating income was approximately $3.25 million in the third quarter of 2017.
Net Service Revenues
The Company is paid for its services primarily by federal and state third-party reimbursement programs, commercial insurance companies, and patients. Revenues are recorded at established rates in the period during which the services are rendered. Appropriate allowances to give recognition to third party payment arrangements are recorded when the services are rendered.
Approximately 75% of the Company’s consolidated net service revenues are derived from the Medicare program. Net service revenues are recorded under the Medicare prospective payment program (PPS) based on a 60-day episode payment rate that is subject to adjustment based on certain variables including, but not limited to: (a) changes in the base episode payments established by the Medicare program; (b) adjustments to the base episode payments for case-mix and geographic wages; (c) a low utilization payment adjustment (LUPA) if the number of visits was fewer than five; (d) a partial payment if a patient is transferred to another provider or if a patient is received from another provider before completing the episode; (e) a payment adjustment based upon the level of therapy services required (thresholds set at 6, 14 and 20 visits); (f) an outlier payment if the patient’s care was unusually costly (capped at 10% of total reimbursement); (g) the number of episodes of care provided to a patient; and (h) a 2% reduction for sequestration.
At the beginning of each Medicare episode the Company calculates an estimate of the amount of expected reimbursement based on the variables outlined above and recognizes Medicare revenue on an episode-by-episode basis during the course of each episode over its expected number of visits. Over the course of each episode, as changes in the
71
variables become known, adjustments are calculated and recorded as needed to reflect changes in expectations for that episode from those established at the start of the 60 day period until its ultimate outcome at the end of the 60 day period is known.
Substantially all remaining revenues are earned on a per visit, hour or unit basis (as opposed to episodic). For all services provided, the Company uses either payor-specific or patient-specific fee schedules for the recording of revenues at the amounts actually expected to be received.
Laws and regulations governing the Medicare and Medicaid programs are extremely complex and subject to interpretation. It is common for issues to arise related to: 1) medical coding, particularly with respect to Medicare, 2) patient eligibility, particularly related to Medicaid, and 3) other reasons unrelated to credit risk, all of which may result in adjustments to recorded revenue amounts. The Company continuously evaluates the potential for revenue adjustments and when appropriate provides allowances for losses based upon the best available information. There is at least a reasonable possibility that recorded estimates could change by material amounts in the near term. Changes in estimates related to prior periods (increased) decreased revenues by approximately ($780), ($608), and ($365) in 2017, 2016 and 2015, respectively.
Revenue and Receivable Concentrations
The following table sets forth the percent of the Company’s revenues generated from Medicare, state Medicaid programs and other payors for the year ended:
|
|
|
2017 |
2016 |
2015 |
|||
|
Medicare |
|
75.1 |
% |
68.2 |
% |
71.4 |
% |
|
Medicaid & other government programs: |
|
|
|
|
|
|
|
|
Ohio |
|
7.5 |
% |
9.6 |
% |
9.1 |
% |
|
Connecticut |
|
3.4 |
% |
5.0 |
% |
5.5 |
% |
|
New York |
|
3.1 |
% |
4.0 |
% |
1.7 |
% |
|
Tennessee |
|
1.9 |
% |
2.3 |
% |
3.2 |
% |
|
Kentucky |
|
1.1 |
% |
1.0 |
% |
1.7 |
% |
|
Wisconsin |
|
1.4 |
% |
0.9 |
% |
— |
% |
|
Florida |
|
0.6 |
% |
0.3 |
% |
0.9 |
% |
|
Others |
|
0.8 |
% |
0.1 |
% |
0.4 |
% |
|
Subtotal |
|
19.8 |
% |
23.2 |
% |
22.5 |
% |
|
All other payors |
|
5.1 |
% |
8.6 |
% |
6.1 |
% |
|
Total |
|
100.0 |
% |
100.0 |
% |
100.0 |
% |
72
Concentrations in the Company’s accounts receivable were as follows:
|
|
|
2017 |
|
2016 |
|
||||||
|
|
|
Amount |
|
Percent |
|
Amount |
|
Percent |
|
||
|
Medicare |
|
$ |
96,464 |
|
62.6 |
% |
$ |
64,128 |
|
53.2 |
% |
|
Medicaid & other government programs: |
|
|
|
|
|
|
|
|
|
|
|
|
Ohio |
|
|
9,341 |
|
6.1 |
% |
|
10,937 |
|
9.1 |
% |
|
Connecticut |
|
|
5,638 |
|
3.7 |
% |
|
6,735 |
|
5.6 |
% |
|
Kentucky |
|
|
4,135 |
|
2.7 |
% |
|
3,741 |
|
3.1 |
% |
|
Tennessee |
|
|
3,549 |
|
2.3 |
% |
|
5,756 |
|
4.8 |
% |
|
New York |
|
|
3,444 |
|
2.2 |
% |
|
3,216 |
|
2.7 |
% |
|
Wisconsin |
|
|
3,416 |
|
2.2 |
% |
|
4,451 |
|
3.7 |
% |
|
Florida |
|
|
3,229 |
|
2.1 |
% |
|
3,338 |
|
2.8 |
% |
|
Others |
|
|
2,423 |
|
1.6 |
% |
|
651 |
|
0.5 |
% |
|
Subtotal |
|
|
35,175 |
|
22.8 |
% |
|
38,825 |
|
32.2 |
% |
|
All other payors |
|
|
22,402 |
|
14.5 |
% |
|
17,561 |
|
14.6 |
% |
|
Subtotal |
|
|
154,041 |
|
100.0 |
% |
|
120,514 |
|
100.0 |
% |
|
Allowances |
|
|
(28,181) |
|
|
|
|
(21,302) |
|
|
|
|
Total |
|
$ |
125,860 |
|
|
|
$ |
99,212 |
|
|
|
The ability of payors to meet their obligations depends upon their financial stability, future legislation and regulatory actions. The Company does not believe there are any significant credit risks associated with receivables from federal and state third-party reimbursement programs. The allowance for uncollectible accounts principally consists of management’s estimate of amounts that may prove uncollectible for coverage, eligibility and other technical reasons.
Payor Mix Concentrations and Related Aging of Accounts Receivable
The approximate breakdown by payor classification as a percent of total accounts receivable, net of contractual allowances, if any, were as follows:
|
|
|
2017 |
|
||||||||
|
Payor |
|
0-90 |
|
91-180 |
|
181-365 |
|
>1 yr. |
|
Total |
|
|
Medicare |
|
31 |
% |
13 |
% |
13 |
% |
5 |
% |
62 |
% |
|
Medicaid & Government |
|
11 |
% |
3 |
% |
4 |
% |
6 |
% |
24 |
% |
|
Self Pay |
|
1 |
% |
— |
% |
1 |
% |
— |
% |
2 |
% |
|
Insurance |
|
5 |
% |
1 |
% |
2 |
% |
4 |
% |
12 |
% |
|
Total |
|
48 |
% |
17 |
% |
20 |
% |
15 |
% |
100 |
% |
|
|
|
2016 |
|
||||||||
|
Payor |
|
0-90 |
|
91-180 |
|
181-365 |
|
>1 yr. |
|
Total |
|
|
Medicare |
|
27 |
% |
13 |
% |
8 |
% |
5 |
% |
53 |
% |
|
Medicaid & Government |
|
15 |
% |
5 |
% |
4 |
% |
8 |
% |
32 |
% |
|
Self Pay |
|
1 |
% |
— |
% |
— |
% |
— |
% |
1 |
% |
|
Insurance |
|
6 |
% |
2 |
% |
2 |
% |
4 |
% |
14 |
% |
|
Total |
|
49 |
% |
20 |
% |
14 |
% |
17 |
% |
100 |
% |
Variations between years are largely attributable to acquisitions and systems conversions.
Allowance for Uncollectible Accounts by Payor Mix and Related Aging
The Company records an estimated allowance for uncollectible accounts by applying estimated bad debt percentages to its accounts receivable aging. The percentages to be applied by payor type are based on the Company’s historical collection and loss experience. The Company’s effective allowances for uncollectible accounts as a percent of accounts receivable were as follows:
73
|
|
|
2017 |
|
||||||||
|
Payor |
|
0-90 |
|
91-180 |
|
181-365 |
|
>1 yr. |
|
>2 yrs. |
|
|
Medicare |
|
1 |
% |
2 |
% |
20 |
% |
77 |
% |
100 |
% |
|
Medicaid & Government |
|
1 |
% |
3 |
% |
15 |
% |
81 |
% |
100 |
% |
|
Self Pay |
|
0 |
% |
5 |
% |
24 |
% |
70 |
% |
100 |
% |
|
Insurance |
|
1 |
% |
3 |
% |
18 |
% |
79 |
% |
100 |
% |
|
Total |
|
1 |
% |
2 |
% |
19 |
% |
78 |
% |
100 |
% |
|
|
|
2016 |
|
||||||||
|
Payor |
|
0-90 |
|
91-180 |
|
181-365 |
|
>1 yr. |
|
>2 yrs. |
|
|
Medicare |
|
1 |
% |
3 |
% |
16 |
% |
73 |
% |
100 |
% |
|
Medicaid & Government |
|
1 |
% |
3 |
% |
16 |
% |
81 |
% |
100 |
% |
|
Self Pay |
|
1 |
% |
6 |
% |
28 |
% |
100 |
% |
100 |
% |
|
Insurance |
|
2 |
% |
4 |
% |
20 |
% |
75 |
% |
100 |
% |
|
Total |
|
1 |
% |
3 |
% |
17 |
% |
77 |
% |
100 |
% |
Variations between years are largely attributable to collection results for specific payors.
The Company’s allowance for uncollectible accounts at December 29, 2017 and December 30, 2016 was approximately $27,047 and $21,302, respectively.
Contingent Service Revenues
The Company, through its Imperium acquisition, provides strategic health management services to ACOs that have been approved to participate in the Medicare Shared Savings Program (“MSSP”). In some cases, the Company also had ownership interests in ACOs beginning January 1, 2015.
ACOs are entities that contract with CMS to serve the Medicare fee-for-service population with the goal of better care for individuals, improved health for populations and lower costs. ACOs share savings with CMS to the extent that the actual costs of serving assigned beneficiaries are below certain trended benchmarks of such beneficiaries and certain quality performance measures are achieved. The MSSP is relatively new and therefore has limited historical experience, which impacts the Company’s ability to accurately accumulate and interpret the data available for calculating an ACO’s shared savings, if any. MSSP payments are not recognized in revenue until persuasive evidence of an agreement exists, services have been rendered, the payment is fixed and determinable and collectability is insured, which is generally satisfied upon cash receipt. Under such agreements, the Company recognized $2.3 million and $4.3 million in MSSP payments for cash received during 2017 and 2016 related to savings generated for the program periods ended 2016 and 2015, respectively, which are included in the Company’s Healthcare Innovations segment revenues. The Company has yet to recognize potential MSSP payments, if any, for savings generated for the 2017 program period.
Weighted Average Shares
Net income per share is presented as a unit of basic shares outstanding and diluted shares outstanding. Diluted shares outstanding is computed based on the weighted average number of common shares and common equivalent shares outstanding. Common equivalent shares result from dilutive stock options and unvested restricted shares. The following table is a reconciliation of basic to diluted shares used in the earnings per share calculation for the fiscal year ended:
|
|
|
2017 |
|
2016 |
|
2015 |
|
|
Basic weighted average outstanding shares |
|
13,539 |
|
10,153 |
|
9,505 |
|
|
Dilutive effect of outstanding compensation awards |
|
218 |
|
193 |
|
240 |
|
|
Diluted weighted average outstanding shares |
|
13,757 |
|
10,346 |
|
9,745 |
|
The assumed conversions to common stock of 58, 76 and 20 of the Company’s outstanding stock options and unmet performance shares were excluded from the diluted EPS computation in 2017, 2016 and 2015, respectively, because these items, on an individual basis, have an anti-dilutive effect on diluted EPS.
74
Use of Estimates
The preparation of financial statements in conformity with accounting principles generally accepted in the United States requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements and reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates.
Stock-Based Compensation
Stock options and restricted stock are granted under various stock compensation programs to employees and independent directors. The Company accounts for such grants in accordance with ASC Topic 718, Compensation — Stock Compensation and amortizes the fair value of awards, after estimated forfeiture, on a straight-line basis over the requisite service periods.
Accounting for Leases
The Company accounts for operating leases using the straight-line rents method, which amortizes contracted total rents due evenly over the lease term.
Advertising Costs
The Company expenses the costs of advertising, as incurred. Advertising expense was $643, $403 and $393 for 2017, 2016 and 2015, respectively.
NOTE 2 - ACCRUED LIABILITIES
Accrued liabilities consist of the following as of the fiscal year ended:
|
|
|
2017 |
|
2016 |
|
||
|
Wages and employee benefits |
|
$ |
28,424 |
|
$ |
17,792 |
|
|
Insurance accruals |
|
|
14,894 |
|
|
14,535 |
|
|
Accrued taxes |
|
|
642 |
|
|
633 |
|
|
Accrued professional fees and other |
|
|
6,222 |
|
|
6,768 |
|
|
|
|
$ |
50,182 |
|
$ |
39,728 |
|
NOTE 3 - PROPERTY AND EQUIPMENT, NET
Property and equipment, net, consist of the following as of the fiscal year ended:
|
|
|
2017 |
|
2016 |
|
||
|
Leasehold improvements |
|
$ |
3,739 |
|
$ |
2,856 |
|
|
Land and buildings |
|
|
2,240 |
|
|
— |
|
|
Medical equipment |
|
|
1,507 |
|
|
1,518 |
|
|
Computer equipment |
|
|
18,049 |
|
|
12,414 |
|
|
Internally developed software |
|
|
2,541 |
|
|
4,158 |
|
|
Office and other equipment |
|
|
7,438 |
|
|
6,717 |
|
|
Vehicles |
|
|
130 |
|
|
146 |
|
|
|
|
|
35,644 |
|
|
27,809 |
|
|
Less accumulated depreciation |
|
|
(20,398) |
|
|
(17,077) |
|
|
|
|
$ |
15,246 |
|
$ |
10,732 |
|
Depreciation and amortization expense related to property, plant and equipment is recorded in general and administrative expenses - other and was $5,192, $3,768 and $3,321 in 2017, 2016 and 2015, respectively.
75
NOTE 4 - REVOLVING CREDIT FACILITY
The Company has a senior secured revolving credit facility with JPMorgan Chase Bank, N.A., as Administrative Agent, and certain other lenders (the “Facility”). The Facility provides a credit line up to $350 million with a maturity date of December 3, 2021 and an “accordion” feature providing for potential future expansion of the Facility up to $150 million of additional borrowings upon further request and approval by a lender or lenders willing to extend such borrowings. The Facility allows for daily and short term (generally one month to one year) borrowings. Daily borrowings bear interest at a varying rate equal to prime plus 1.25%, while short term borrowings bear interest at a varying rate equal to the London Interbank Offered Rate (“LIBOR”) plus a margin which varies from 1.50% to 2.75%, depending on the Company’s leverage ratio. Interest expense also includes unused commitment fees related to total borrowing capacity, as well as letters of credit related fees. The Facility is secured by substantially all assets and the assets and stock of the Company’s subsidiaries. The subsidiaries have also guaranteed the Facility. Our subsidiaries have also guaranteed the Facility. Debt issuance costs of $4.7 million were capitalized with the Facility and are being amortized to interest expense through December, 2021.
Borrowings under the Facility are subject to various covenants, including a maximum leverage ratio for all calculation dates ending on or before December 31, 2017, of 4.0 times earnings before interest, taxes, depreciation and amortization, as adjusted (“EBITDA”) plus “Acquired EBITDA” from pro-forma acquisitions as defined. The maximum leverage ratio steps down, to a maximum leverage ratio of 3.75 times EBITDA plus Acquired EBITDA for calculation dates after December 31, 2017, and on or before June 30, 2018, and to a maximum leverage ratio of 3.5 times EBITDA plus Acquired EBITDA for calculation dates on and after September 30, 2018. Borrowings under the revolving credit facility may be used for general corporate purposes, including acquisitions.
On December 30, 2016 the Company borrowed approximately $128.9 million from the Facility to finance the CHS Home Health transaction, which was classified as a Transaction Deposit and included in Revolving credit facility in the Consolidated Balance Sheets. On December 31, 2016, the first day of the Company’s 2017 fiscal year, the Transaction deposit converted to purchase price with the closing of the CHS-JV acquisition. On January 25, 2017, the Company sold 3,450 shares of common stock for net proceeds of $143.9 million, after deducting the estimated underwriting discounts and commissions and our offering expenses, which were used to repay obligations under the Facility.
As of December 29, 2017, the Company was in compliance with the various financial covenants. Application of the Facility’s borrowing formula as of December 29, 2017, would have permitted approximately $221.3 million to be used. We had irrevocable letters of credit totaling $15.7 million in connection with our self-insurance programs.
The effective interest rates on our borrowings were 3.7% and 3.6% for 2017 and 2016, respectively.
NOTE 5 - FAIR VALUE MEASUREMENTS
The Company’s financial instruments consist of cash, accounts receivable, payables and debt instruments. Due to their short-term nature, the book values of cash, accounts receivable and payables are considered representative of their respective fair values. The fair value of the Company’s debt instruments approximates their carrying values as substantially all of such debt instruments have rates which fluctuate with changes in market rates.
As of December 29, 2017, the Company does not have any assets or liabilities carried at fair value that are measured on a recurring basis.
76
NOTE 6 - INCOME TAXES
The provision for income taxes consists of the following as of the fiscal year ended:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Federal - current |
|
$ |
(82) |
|
$ |
1,329 |
|
$ |
5,283 |
|
|
State and local - current |
|
|
522 |
|
|
930 |
|
|
1,359 |
|
|
Deferred |
|
|
(2,550) |
|
|
8,725 |
|
|
3,914 |
|
|
Tax (benefit) expense |
|
$ |
(2,110) |
|
$ |
10,984 |
|
$ |
10,556 |
|
A reconciliation of the statutory to the effective rate of the Company is as follows as of the fiscal year ended:
|
|
|
2017 |
|
2016 |
|
2015 |
|
|
Tax provision using statutory rate |
|
35.0 |
% |
35.0 |
% |
35.0 |
% |
|
State and local taxes, net of Federal benefit |
|
5.7 |
% |
4.3 |
% |
4.4 |
% |
|
Valuation allowance |
|
0.1 |
% |
(0.4) |
% |
0.2 |
% |
|
Permanent differences |
|
0.3 |
% |
(0.5) |
% |
0.3 |
% |
|
Legal settlement related |
|
— |
% |
— |
% |
(5.4) |
% |
|
|
|
41.1 |
% |
38.4 |
% |
34.5 |
% |
|
Stock-based compensation and merger related |
|
(0.6) |
% |
— |
% |
— |
% |
|
Impact of the Tax Act |
|
(52.0) |
% |
— |
% |
— |
% |
|
Tax provision |
|
(11.5) |
% |
38.4 |
% |
34.5 |
% |
|
|
|
|
|
|
|
|
|
The Tax Cuts and Jobs Act (Tax Act) was enacted on December 22, 2017 and introduces significant changes to the U.S. income tax law. Effective in 2018, the Tax Act reduces U.S. statutory tax rates from 35% to 21%. Accordingly, the Company remeasured its deferred taxes as of December 29, 2017 to reflect the reduced rate that will apply in future periods when these deferred taxes are settled or realized, resulting in a one-time $9.5 million net tax benefit in 2017.
Due to the timing of the enactment and the complexity involved in applying the provisions of the Tax Act, the Company has made reasonable estimates of the effects and recorded provisional amounts in our financial statements as of December 29, 2017. As the Company collects and prepares necessary data, and interprets the Tax Act and any additional guidance issued by the Internal Revenue Service and other standard-setting bodies, it may make adjustments to the provisional amounts. Those adjustments may materially impact our provision for income taxes and effective tax rate in the period in which adjustments are made. The accounting for the tax effects of the Tax Act will be completed in 2018.
The favorable impact of Stock-based compensation and merger related includes a favorable $2.1 million impact from the adoption of ASU 2016-09 as discussed in Note 1 which was largely offset by the unfavorable impact of the federal and state tax limits on executive compensation related to the merger.
77
The principal tax carry-forwards and temporary differences were as follows as of the fiscal year ended:
|
|
|
2017 |
|
2016 |
|
||
|
Deferred tax assets |
|
|
|
|
|
|
|
|
Non-deductible reserves and allowances |
|
$ |
10,912 |
|
$ |
12,688 |
|
|
Insurance accruals |
|
|
2,227 |
|
|
3,506 |
|
|
Net operating loss carryforwards |
|
|
5,062 |
|
|
5,229 |
|
|
|
|
|
18,201 |
|
|
21,423 |
|
|
Valuation allowance |
|
|
(2,893) |
|
|
(2,487) |
|
|
Total deferred tax assets |
|
|
15,308 |
|
|
18,936 |
|
|
|
|
|
|
|
|
|
|
|
Deferred tax liabilities |
|
|
|
|
|
|
|
|
Goodwill & intangibles |
|
|
(30,993) |
|
|
(38,706) |
|
|
Joint venture interests |
|
|
(1,911) |
|
|
— |
|
|
Accelerated depreciation |
|
|
(999) |
|
|
(1,375) |
|
|
Total deferred tax liabilities |
|
|
(33,903) |
|
|
(40,081) |
|
|
Net deferred tax liabilities |
|
$ |
(18,595) |
|
$ |
(21,145) |
|
|
|
|
|
|
|
|
|
|
|
Total net deferred tax liabilities are reflected in the accompanying balance sheet as long-term liabilities. |
|
||||||
As of December 29, 2017, the Company has U.S. operating loss carry forwards of $8.1 million that are available to reduce future taxable income. If not used to offset taxable income, the losses will expire between 2028 and 2034. Due to U.S. limitations on acquired operating losses, a valuation allowance has been established on $0.8 million of these losses.
State operating loss carryforwards totaling $46.3 million at December 29, 2017 are being carried forward in jurisdictions where the Company is permitted to use tax losses from prior periods to reduce future taxable income. If not used to offset future taxable income, these losses will expire between 2018 and 2037. Due to uncertainty regarding the Company’s ability to use some of the carryforwards, a valuation allowance has been established on $37.6 million of state net operating loss carryforwards. Based on the Company’s historical record of producing taxable income and expectations for the future, the Company has concluded that future operating income will be sufficient to give rise to taxable income sufficient to utilize the remaining state net operating loss carryforwards.
The Company has provided a valuation allowance against certain net deferred tax assets based upon management’s estimation of realizability of those assets through future taxable income. This valuation allowance was based in large part on the Company’s history of generating operating income or losses in individual tax locales and expectations for the future. The Company’s ability to generate the expected amounts of taxable income from future operations to realize its recorded net deferred tax assets is dependent upon general economic conditions, competitive pressures on revenues and margins and legislation and regulation at all levels of government. There can be no assurances that the Company will meet its expectations of future taxable income. However, management has considered the above factors in reaching its conclusion that it is more likely than not that future taxable income will be sufficient to realize the deferred tax assets (net of valuation allowance) as of December 29, 2017. During 2017, the valuation allowance increased by $0.4 million due to a change in expected realizability of deferred tax assets.
The Company had book goodwill of $105.1 million at December 29, 2017, which was not deductible for tax purposes.
US GAAP prescribes a recognition threshold and measurement attribute for the accounting and financial statement disclosure of tax positions taken or expected to be taken in a tax return. The evaluation of a tax position is a two-step process. The first step requires the Company to determine whether it is more likely than not that a tax position will be sustained upon examination based on the technical merits of the position. The second step requires the Company to recognize in the financial statements each tax position that meets the more likely than not criteria, measured at the amount of benefit that has a greater than 50% likelihood of being realized. The Company’s unrecognized tax benefits would affect the tax rate, if recognized. The Company includes the full amount of unrecognized tax benefits in other noncurrent liabilities in the consolidated balance sheets. The Company anticipates it is reasonably possible an increase
78
or decrease in the amount of unrecognized tax benefits could be made in the next twelve months. However, the Company does not presently anticipate that any increase or decrease in unrecognized tax benefits will be material to the consolidated financial statements. Changes in unrecognized tax benefits were as follows.
|
|
|
|
2017 |
|
2016 |
|
2015 |
|||
|
Beginning of fiscal year |
|
$ |
3,558 |
|
$ |
2,470 |
|
$ |
1,186 |
|
|
Increases related to positions taken on items from prior years |
|
|
— |
|
|
— |
|
|
— |
|
|
Decreases related to positions taken on items from prior years |
|
|
— |
|
|
(94) |
|
|
— |
|
|
Increases related to positions taken in the current year |
|
|
269 |
|
|
1,182 |
|
|
1,284 |
|
|
Lapse of statute of limitations |
|
|
(99) |
|
|
— |
|
|
— |
|
|
Settlement of uncertain tax positions with tax authorities |
|
|
— |
|
|
— |
|
|
— |
|
|
Balance at end of fiscal year |
|
$ |
3,728 |
|
$ |
3,558 |
|
$ |
2,470 |
|
For federal tax purposes, the Company is currently subject to examinations for tax years after 2013, while for state purposes, tax years after 2010 are subject to examination, depending on the specific state rules and regulations. The Internal Revenue Service completed an examination of the Company’s December 31, 2011 tax year as well as an examination of Omni Home Health Holdings, Inc.’s federal tax returns for the year ended December 31, 2012 and the period ended December 6, 2013.
The Company may from time to time be assessed interest and penalties by major tax jurisdictions, although any such assessments historically have been minimal and immaterial to its financial results. Assessments for interest and/or penalties are classified in the Consolidated Statement of Income as General and administrative - other.
NOTE 7 - STOCKHOLDERS’ EQUITY
2017 Common Stock Offering
On January 25, 2017, the Company sold 3.5 million shares of common stock at $44.50 per share for gross proceeds of approximately $153.5 million. Total net proceeds, after underwriting discounts and commissions and offering expenses, were approximately $143.9 million. These proceeds were used to repay obligations under the revolving credit facility.
Employee Stock Incentive Plans
The Company has a 2007 Stock and Incentive Compensation Plan that provides for stock awards up to 500 shares of the Company’s common stock to employees, non-employee directors or independent contractors, with a maximum number of full value restricted share awards up to 200. As of December 29, 2017, options for 120 shares were outstanding under this plan, while 162 restricted shares had been awarded. There are no shares available for future grant.
The 2013 Stock and Incentive Compensation Plan provides for stock awards up to 700 shares of the Company’s common stock to employees, non-employee directors or independent contractors. As of December 29, 2017, options awarded and outstanding under this plan were 232 and 188, respectively, and restricted shares awarded and outstanding were 361 and 157, respectively. There are 97 shares available for future grant.
The 2017 Stock and Incentive Compensation Plan provides for stock awards up to 900 shares of the Company’s common stock to employees, non-employee directors or independent contractors. As of December 29, 2017, restricted shares awarded and outstanding were 14. There are 886 shares available for future grant.
Historically, the Company has issued restricted share and/or option awards to employees and non-employee directors. The Board of Directors determines the amount and terms of the options, which cannot exceed ten years. Under both the 2017 and 2013 Stock and Incentive Compensation Plans, restricted share awards cliff vest on the third anniversary, while option share awards vest annually in 25% increments over four years.
79
The Company has granted 97 performance-based, restricted share awards (“performance shares”) under the 2013 Stock and Incentive Compensation Plans to key executives. These performance shares entitle certain executives to receive a number of shares of our common stock based upon the Company’s satisfaction of certain performance criteria approved by the Board of Directors. The awards cliff-vest at the end of three years and were valued at the market price of a share of the Company’s stock on the date of grant assuming 100% achievement. Under the plan, achievement ranges from 0% to 200%. The Company recorded $2.6 million of stock compensation expense for these performance shares in 2017 and no compensation expense for these performance shares in 2016.
Changes in award shares outstanding are summarized as follows:
|
|
|
Performance shares |
|
Restricted shares |
|
Options |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Wtd. Avg. |
|
|
|
Wtd. Avg. |
|
|
|
Wtd. Avg. |
|||
|
|
|
Shares |
|
Grant Price |
|
Shares |
|
Grant Price |
|
Shares |
|
Ex. Price |
|||
|
December 30, 2016 |
|
55 |
|
|
36.03 |
|
158 |
|
|
34.93 |
|
501 |
|
|
27.69 |
|
Granted |
|
42 |
|
|
49.05 |
|
46 |
|
|
50.35 |
|
42 |
|
|
49.05 |
|
Vested or Exercised |
|
(38) |
|
|
41.62 |
|
(85) |
|
|
32.53 |
|
(219) |
|
|
23.99 |
|
Forfeited |
|
(1) |
|
|
(36.03) |
|
(6) |
|
|
(38.70) |
|
(16) |
|
|
(33.20) |
|
December 29, 2017 |
|
58 |
|
$ |
43.35 |
|
113 |
|
$ |
41.80 |
|
308 |
|
$ |
32.93 |
Aggregate intrinsic value represents the estimated value of the Company’s common stock at end of the period in excess of the weighted average exercise price multiplied by the number of options outstanding or exercisable. The aggregate intrinsic value of options outstanding and exercisable at December 29, 2017 is $6,905 and $4,868, respectively. The total intrinsic value of stock options exercised during 2017, 2016 and 2015 was $6,868, $442 and $171, respectively.
The following table summarizes information about stock options at December 29, 2017:
|
|
|
Options Outstanding |
|
Options Exercisable |
|
||||||||||
|
|
|
|
|
Wtd. Avg. |
|
|
|
|
|
Wtd. Avg. |
|
|
|
||
|
Range of |
|
|
|
Remaining |
|
Wtd. Avg. |
|
|
|
Remaining |
|
Wtd. Avg. |
|
||
|
Exercise |
|
|
|
Contractual |
|
Exercise |
|
|
|
Contractual |
|
Exercise |
|
||
|
Price |
|
Shares |
|
Life |
|
Price |
|
Shares |
|
Life |
|
Price |
|
||
|
$0.00-20.00 |
|
9 |
|
5.36 |
|
$ |
19.52 |
|
9 |
|
5.36 |
|
$ |
19.52 |
|
|
$20.01-30.00 |
|
99 |
|
5.31 |
|
$ |
21.67 |
|
93 |
|
4.55 |
|
$ |
23.10 |
|
|
Over $30.00 |
|
200 |
|
5.96 |
|
$ |
39.15 |
|
81 |
|
3.57 |
|
$ |
36.26 |
|
|
|
|
308 |
|
5.73 |
|
$ |
32.93 |
|
183 |
|
4.16 |
|
$ |
28.75 |
|
The following table details exercisable options and related information for year end:
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Exercisable at end of year |
|
|
183 |
|
|
352 |
|
|
312 |
|
|
Weighted average price |
|
$ |
28.75 |
|
$ |
25.91 |
|
$ |
25.49 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Weighted average fair value of options granted during the year |
|
$ |
25.18 |
|
$ |
18.80 |
|
$ |
12.35 |
|
The following table details unvested option activity for the year ended December 29, 2017:
|
|
|
|
|
Wtd. Avg. |
|
|
|
|
|
Shares |
|
Ex. Price |
|
|
|
December 30, 2016 |
|
149 |
|
$ |
31.91 |
|
|
Vested |
|
61 |
|
|
28.94 |
|
|
Granted |
|
42 |
|
|
49.05 |
|
|
Forfeited |
|
(5) |
|
|
(32.50) |
|
|
December 29, 2017 |
|
125 |
|
$ |
39.09 |
|
80
The fair value of each option award is estimated on the date of grant using the Monte Carlo option valuation model with suboptimal exercise behavior. The Monte Carlo model places greater emphasis on market evidence and predicts more realistic results because it considers open form information including volatility, employee exercise behaviors and turnover. Stock options have a contractual term of 10 years. The following assumptions were used in determining the fair value of option awards:
|
|
|
Equivalent |
|
Expected |
|
Implied |
|
Grant date |
|
interest rate |
|
volatility |
|
expected lives |
|
March 10, 2017 |
|
2.36 |
% |
46.00 |
% |
7.74 |
|
March 4, 2016 |
|
1.68 |
% |
49.00 |
% |
8.35 |
|
March 2, 2015 |
|
2.07 |
% |
32.50 |
% |
6.86 |
Expected volatility is based on an analysis that looks at the unbiased standard deviation of the Company’s common stock over the option term. The expected life of the options represents the period of time that the Company expects the options granted to be outstanding. The risk-free rate is based on the U.S. Treasury yield curve in effect at the time of the grant of the option for the expected term of the instrument. A 0% dividend yield was assumed as no dividend payout over the term of the award is expected.
As of December 29, 2017, there was $3,385 of total unrecognized compensation cost, including performance restricted shares at 100% of target, after estimated forfeitures, related to unvested share-based compensation granted under the plans. That cost is expected to be recognized over a weighted-average period of 2.05 years. The total fair value of option shares vested during 2017 and 2016 was $568 and $697, respectively.
Employee Stock Purchase Plan
The Company has an Employee Stock Purchase Plan (“2009 ESPP”) which, if implemented, could provide employees of the Company and its subsidiaries with an opportunity to participate in the growth of the Company and to further align the interest of the employees with the interests of the Company through the purchase of shares of the Company’s Common Stock. Under the 2009 ESPP, 300 shares of the Company’s Common Stock have been authorized for issuance. As of December 29, 2017, all 300 shares remain available for issuance.
NOTE 8 - RETIREMENT PLAN
The Company administers a 401(k) defined contribution retirement plan for the benefit of the majority of its employees. Employees may participate in the plan immediately upon employment. The Company matches contributions in an amount equal to one-quarter of the first 5% of each participant’s contribution to the plan after completion of one year of service with the Company. 401(k) assets are held by an independent trustee, are not assets of the Company, and accordingly are not reflected in the Company’s balance sheets. The Company’s retirement plan expense was approximately $1,393, $1,054 and $1,080 in 2017, 2016 and 2015, respectively.
NOTE 9 - COMMITMENTS AND CONTINGENCIES
Operating Leases
The Company leases certain real estate, office space, and equipment under non-cancelable operating leases expiring at various dates through 2025 and which contain various renewal and escalation clauses. Rent expense amounted to
81
approximately $18,460, $13,969 and $11,356 for 2017, 2016 and 2015, respectively. At December 29, 2017, minimum rental payments under these leases were as follows:
|
2018 |
|
$ |
9,683 |
|
|
2019 |
|
|
6,283 |
|
|
2020 |
|
|
4,141 |
|
|
2021 |
|
|
2,837 |
|
|
2022 |
|
|
1,607 |
|
|
Thereafter |
|
|
5,560 |
|
|
Total |
|
$ |
30,111 |
|
Legal Proceedings
On January 18, 2018, Jordan Rosenblatt, a purported stockholder of the Company, filed a class action complaint alleging violations of the Securities Exchange Act of 1934 in the United States District Court for the Western District of Kentucky, styled Rosenblatt v. Almost Family, Inc., et al., Case No. 3:18-cv-40-TBR (the “Rosenblatt Class Action”), against the Company, the Company’s board of directors, LHC Group and Merger Sub. The complaint in the Rosenblatt Class Action alleges that the Form S-4 Registration Statement filed on December 21, 2017 omitted material information with respect to the proposed transaction, rendering the Registration Statement false and misleading. The complaint in the Rosenblatt Class Action asserts claims against the Company and the Company’s board of directors for violations of Section 14(a) of the 1934 Act in connection with the dissemination of the Registration Statement, and asserts claims against the Company’s board of directors and LHC Group for violations of Section 20(a) of the 1934 Act as controlling persons of the Company. The Rosenblatt Class Action seeks, among other things, an injunction enjoining the proposed transaction from closing, and an award of attorneys’ fees and costs.
On January 23, 2018, Leonard Stein, a purported stockholder of our Company, filed a Class Action Complaint alleging violations of Sections 14(a) and 20(a) of the Securities Exchange Act of 1934 in the United States District Court for the District of Delaware, styled Stein v. Almost Family, Inc., et al., Case No. 1:18-cv-00126-UNA(the “Stein Class Action”), against the Company and the Company’s board of directors. The complaint in the Stein Class Action alleges that the Form S-4 Registration Statement filed on December 21, 2017 omitted material information with respect to the proposed transaction, rendering the Registration Statement false and misleading. The complaint in the Stein Class Action asserts claims against the Company and the Company’s board of directors for violations of Section 14(a) of the 1934 Act, SEC Regulation G, and SEC Rule 14a-9, and asserts claims against the Company’s board of directors for violations of Section 20(a) of the 1934 Act as controlling persons of the Company. The Stein Class Action seeks, among other things, an injunction enjoining both the shareholder vote and the proposed transaction from closing, monetary damages to a class of shareholders, and an award of attorneys’ fees and costs.
On January 23, 2018, Shiva Stein, a purported stockholder of our Company, filed a Complaint for violations of Sections 14(a) and 20(a) of the Securities Exchange Act of 1934 in the United States District Court for the District of Delaware, styled Stein v. Almost Family, Inc., et al., Case No. 1:18-cv-000127-UNA (the “Stein Individual Action”), against the Company and the Company’s board of directors. The complaint in the Stein Individual Action alleges that the Form S-4 Registration Statement filed on December 21, 2017 contained materially incomplete and misleading statements with respect to the proposed transaction. The complaint in the Stein Individual Action asserts claims against the Company and the Company’s board of directors for violations of Section 14(a) of the 1934 Act, and asserts claims against the Company’s board of directors for violations of Section 20(a) of the 1934 Act as controlling persons of our Company. The Stein Individual Action seeks, among other things, an injunction enjoining the proposed transaction from closing, monetary damages suffered by Plaintiff, and an award of attorneys’ fees and costs.
The Company, the Company’s board of directors, LHC Group and Merger Sub believe that the claims in the complaints are without merit and intend to defend these actions vigorously.
From time to time, the Company is subject to various other legal actions arising in the ordinary course of the Company’s business, including claims for damages for personal injuries. In the Company’s opinion, after discussion with legal
82
counsel, the ultimate resolution of any of these pending ordinary course claims and legal proceedings will not have a material effect on the Company’s financial position or results of operations.
NOTE 10 - SEGMENT DATA
The Company has three reportable segments: a) Home Health (“HH”), b) Other Home-Based Services (“OHBS”) which includes all other home care services outside of Home Health services and c) the Healthcare Innovations (“HCI”) segment. Reportable segments have been identified based upon how management has organized the business by services provided to customers and the criteria in Accounting Standards Codification (“ASC”) Topic 280, Segment Reporting. Consistent with information given to the chief operating decision maker, the Company does not allocate certain expenses to the reportable segments. The Company evaluates the performance of its business segments based on operating income. Intercompany and intersegment transactions have been eliminated.
The HH segment provides skilled medical services in patients’ homes largely to enable recipients to reduce or avoid periods of hospitalization and/or nursing home care. Approximately 95% of the HH segment revenues were generated from the Medicare program, while the balance is generated from Medicaid and private insurance programs.
The OHBS segment includes traditional personal care services (“PC”) (generally provided by paraprofessional staff such as home health aides) which are generally of a custodial rather than skilled nature, as well as hospice services. Personal care revenues are generated on an hourly basis and are primarily from Medicaid (approximately 80% of personal care revenues). Hospice services are largely provided in patients’ homes and generally require specialized hospice nursing skills. Hospice revenues are generated on a per diem basis and are primarily from Medicare (approximately 93% of hospice revenues).
The Company’s HCI business segment is used to report on the Company’s developmental activities outside its HH and OHBS businesses. The HCI segment includes: a) an ACO enablement company; b) an in-home assessment company serving the long-term care insurance industry and managed care organizations; and c) an investment in a population-health analytics company.
83
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Net service revenues |
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
586,070 |
|
$ |
434,968 |
|
$ |
400,133 |
|
|
Other Home-based Services |
|
|
184,752 |
|
|
162,546 |
|
|
128,630 |
|
|
Healthcare Innovations |
|
|
26,143 |
|
|
26,027 |
|
|
3,451 |
|
|
|
|
$ |
796,965 |
|
$ |
623,541 |
|
$ |
532,214 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Operating income (loss) |
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
75,587 |
|
$ |
56,564 |
|
$ |
49,608 |
|
|
Other Home-based Services |
|
|
14,555 |
|
|
13,519 |
|
|
14,434 |
|
|
Healthcare Innovations |
|
|
4,046 |
|
|
5,657 |
|
|
(1,217) |
|
|
Unallocated |
|
|
(64,970) |
|
|
(40,299) |
|
|
(29,876) |
|
|
|
|
$ |
29,218 |
|
$ |
35,441 |
|
$ |
32,949 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Identifiable assets |
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
496,146 |
|
$ |
456,841 |
|
|
|
|
|
Other Home-based Services |
|
|
136,661 |
|
|
116,085 |
|
|
|
|
|
Healthcare Innovations |
|
|
58,814 |
|
|
60,159 |
|
|
|
|
|
Unallocated |
|
|
26,197 |
|
|
25,627 |
|
|
|
|
|
|
|
$ |
717,818 |
|
$ |
658,712 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Identifiable liabilities |
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
57,783 |
|
$ |
31,792 |
|
|
|
|
|
Other Home-based Services |
|
|
31,872 |
|
|
25,241 |
|
|
|
|
|
Healthcare Innovations |
|
|
4,293 |
|
|
5,076 |
|
|
|
|
|
Unallocated |
|
|
117,317 |
|
|
292,423 |
|
|
|
|
|
|
|
$ |
211,265 |
|
$ |
354,532 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Noncontrolling Interest - Redeemable |
|
|
|
|
|
|
|
|
|
|
|
Healthcare Innovations |
|
$ |
2,256 |
|
$ |
2,256 |
|
|
3,639 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Capital expenditures |
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
4,193 |
|
$ |
1,099 |
|
$ |
1,388 |
|
|
Other Home-based Services |
|
|
376 |
|
|
294 |
|
|
203 |
|
|
Healthcare Innovations |
|
|
327 |
|
|
908 |
|
|
108 |
|
|
Unallocated |
|
|
1,216 |
|
|
3,905 |
|
|
1,418 |
|
|
|
|
$ |
6,112 |
|
$ |
6,206 |
|
$ |
3,117 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Depreciation and amortization |
|
|
|
|
|
|
|
|
|
|
|
Home Health |
|
$ |
1,371 |
|
$ |
1,124 |
|
$ |
1,210 |
|
|
Other Home-based Services |
|
|
460 |
|
|
301 |
|
|
264 |
|
|
Healthcare Innovations |
|
|
1,395 |
|
|
1,200 |
|
|
97 |
|
|
Unallocated |
|
|
2,690 |
|
|
1,820 |
|
|
2,356 |
|
|
|
|
$ |
5,916 |
|
$ |
4,445 |
|
$ |
3,927 |
|
NOTE 11 - ACQUISITIONS
The Company completed each of the following acquisitions in pursuit of its strategy for operational expansion in the eastern United States through an expanded service base and enhanced position in certain geographic areas. The purchase price of each acquisition was determined based on the Company’s analysis of comparable acquisitions, expected cash flows and arm’s length negotiation with the sellers. Each acquisition was included in the Company’s consolidated financial statements from the respective acquisition date.
84
Goodwill recognized from the acquisitions primarily relates to expected contributions of each entity to the overall corporate strategy in addition to synergies and acquired workforce, which are not separable from goodwill. Goodwill and other intangible assets generated in asset purchase transactions are expected to be amortizable for tax purposes on a straight-line basis over 15 years, unless otherwise noted. Goodwill and other intangible assets generated in stock purchase transactions are not amortizable, unless otherwise noted.
CHS-JV Acquisition
The acquisition of the CHS-JV closed on the Company’s first day of 2017 fiscal year. As a result, the Company’s twelve months ended December 29, 2017 included four full quarters of revenue, operating income and non-controlling interest of approximately $198 million, $26.4 million and $3.5 million, respectively.
The following table summarizes the fair values estimates of the assets acquired and liabilities assumed in the CHS-JV acquisition:
|
|
|
|
Purchase |
|
|
|
|
|
|
Price Allocation |
|
|
|
Accounts receivable, net |
|
|
$ |
21,444 |
|
|
Prepaids and other assets |
|
|
|
854 |
|
|
Property, plant & equipment |
|
|
|
6,104 |
|
|
Goodwill |
|
|
|
84,016 |
|
|
Intangibles |
|
|
|
61,570 |
|
|
Assets acquired |
|
|
|
173,988 |
|
|
Liabilities assumed |
|
|
|
(13,016) |
|
|
Non-controlling interest |
|
|
|
(32,042) |
|
|
Net assets acquired |
|
|
$ |
128,930 |
|
Goodwill arising from the CHS-JV transaction is based upon expected contributions to the overall corporate strategy in addition to synergies and acquired workforce, which are not separable from goodwill. Revenues and goodwill associated with this transaction are assigned to the Home Health and Other Home-Based Services segments. The Company expects the goodwill and intangibles from this transaction to be deductible for tax purposes.
Other Acquisitions
On November 20, 2017, the Company’s CHS-JV purchased assets of a Medicare-certified home health agency in Fort Myers, Florida. Post-acquisition operating results are reported in the Company’s HH segment.
On July 14, 2017, the Company’s CHS-JV purchased assets of a Medicare-certified home health agency and related private duty company in Key West, Florida. Post-acquisition operating results are reported in the Company’s HH and OHBS segments.
During the third quarter of 2016, one of the Company’s HCI subsidiaries redeemed certain outstanding shares increasing the Company's ownership percentage to 72.0% from 61.5%.
On June 18, 2016, the Company acquired certain home health agency assets primarily in Wisconsin, but also in Connecticut and Kentucky (collectively, the “Wisconsin acquisition”). The purchase price was $6.1 million, funded through borrowings on the Company’s bank credit facility. The post-acquisition operating results of these agencies are primarily reported in the Company’s PC segment. No accounts receivable were acquired. Thus, accounts receivable need to accumulate to normal levels post close.
On January 5, 2016, the Company acquired 100% of the equity of LTS, a provider of in-home nursing assessments for the long-term care insurance industry. LTS provides assessments in all 50 U.S. states and a number of foreign countries. The purchase price of $37 million was funded through borrowings on the Company’s bank credit facility, seller notes and issuance of the Company’s common stock. The Company expects goodwill from this transaction to be deductible
85
for tax purposes. Approximately 74.4% of LTS’s 2016 revenue was from two customers. LTS’s post acquisition operating results are reported in the Healthcare Innovations business segment.
On January 5, 2016, the Company purchased the assets of a Medicare-certified home health agency owned by Bayonne located in New Jersey. Bayonne’s post acquisition operating results are reported in the HH segment.
NOTE 12 - QUARTERLY FINANCIAL DATA— (UNAUDITED)
Summarized quarterly financial data are as follows for 2017 and 2016:
|
|
|
Q4 |
|
Q3 |
|
Q2 |
|
Q1 |
|
Q4 |
|
Q3 |
|
Q2 |
|
Q1 |
|
||||||||
|
|
|
2017 |
|
2017 |
|
2017 |
|
2017 |
|
2016 |
|
2016 |
|
2016 |
|
2016 |
|
||||||||
|
Net service revenues |
|
$ |
200,618 |
|
$ |
194,302 |
|
|
200,733 |
|
|
201,312 |
|
$ |
153,427 |
|
$ |
160,421 |
|
$ |
155,996 |
|
$ |
153,698 |
|
|
Gross margin |
|
|
95,321 |
|
|
90,525 |
|
|
96,681 |
|
|
95,044 |
|
|
69,952 |
|
|
74,347 |
|
|
72,304 |
|
|
71,466 |
|
|
Net income attributable to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Almost Family, Inc. |
|
$ |
8,835 |
|
$ |
3,170 |
|
$ |
4,776 |
|
$ |
3,633 |
|
$ |
3,593 |
|
$ |
5,366 |
|
$ |
4,777 |
|
$ |
3,917 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Average shares outstanding |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Basic |
|
|
13,809 |
|
|
13,731 |
|
|
13,717 |
|
|
12,695 |
|
|
10,162 |
|
|
10,172 |
|
|
10,158 |
|
|
10,089 |
|
|
Diluted |
|
|
14,014 |
|
|
13,941 |
|
|
13,954 |
|
|
12,937 |
|
|
10,330 |
|
|
10,310 |
|
|
10,322 |
|
|
10,260 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Net income attributable to Almost Family, Inc. per share |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Basic |
|
$ |
0.64 |
|
$ |
0.23 |
|
$ |
0.35 |
|
$ |
0.29 |
|
$ |
0.35 |
|
$ |
0.53 |
|
$ |
0.47 |
|
$ |
0.39 |
|
|
Diluted |
|
$ |
0.63 |
|
$ |
0.23 |
|
$ |
0.34 |
|
$ |
0.28 |
|
$ |
0.35 |
|
$ |
0.52 |
|
$ |
0.46 |
|
$ |
0.38 |
|
NOTE 13 - SUBSEQUENT EVENTS
Management has evaluated all events and transactions that occurred after December 29, 2017. During this period, the Company had no material subsequent events requiring recognition in the consolidated financial statements.
On January 8, 2018, the Company purchased substantially all of the assets of MD2U Management LLC (“MD2U”) out of bankruptcy, legally free and clear of liens or encumbrances and interests. MD2U provides primary medical care for home-bound or home-limited patients with chronic and acute illnesses who have difficulty traveling to a doctor’s office. The purchase price was $3.6 million with post-acquisition operating results to be reported in the Company’s HCI segment in the first quarter of 2018.
86
Report of Independent Registered Public Accounting Firm
To the Shareholders and the Board of Directors of Almost Family, Inc. and Subsidiaries
Opinion on Internal Control over Financial Reporting
We have audited Almost Family, Inc. and Subsidiaries’ internal control over financial reporting as of December 29, 2017, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) (the COSO criteria). In our opinion, Almost Family, Inc. and Subsidiaries (the Company) maintained, in all material respects, effective internal control over financial reporting as of December 29, 2017, based on the COSO criteria.
As indicated in the accompanying Management’s Report on Internal Control over Financial Reporting, management’s assessment of and conclusion on the effectiveness of internal control over financial reporting did not include the internal controls of Community Health United Home Care, LLC, which is included in the 2017 consolidated financial statements of the Company and constituted 8% of total assets as of December 29, 2017 and 25% of revenues for the year then ended. Our audit of internal control over financial reporting of the Company also did not include an evaluation of the internal control over financial reporting of Community Health United Home Care, LLC.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the consolidated balance sheets of the Company as of December 29, 2017 and December 30, 2016, the related consolidated statements of income, stockholders’ equity and cash flows for each of the three years in the period ended December 29, 2017, and the related notes and financial statement schedule listed in the Index at Item 15(a) and our report dated February 27, 2018 expressed an unqualified opinion thereon.
Basis for Opinion
The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying “Management’s Report on Internal Control over Financial Reporting.” Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects.
Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
Definition and Limitations of Internal Control over Financial Reporting
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
87
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/s/ Ernst & Young LLP
Louisville, Kentucky
February 27, 2018
88
Management’s Report on Internal Control over Financial Reporting
The consolidated financial statements appearing in this Annual Report have been prepared by management that is responsible for their preparation, integrity and fair presentation. The statements have been prepared in accordance with U.S. generally accepted accounting principles, which requires management to make estimates and assumptions that affect the amounts reported in the consolidated financial statements and accompanying notes.
Our management is responsible for establishing and maintaining adequate internal control over financial reporting (as defined in Rules 13a-15(f) and 15d-15(f) of the Securities Exchange Act of 1934, as amended). Our internal control system was designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles.
All internal control systems, no matter how well designed, have inherent limitations. Therefore, even those systems determined to be effective can provide only reasonable assurance with respect to financial statement preparation and presentation. Further, because of changes in conditions, the effectiveness of an internal control system may vary over time.
Under the supervision and with the participation of our management, including our Chief Executive Officer (CEO) and Principal Financial Officer (PFO), we conducted an evaluation of the effectiveness of our internal control over financial reporting as of December 29, 2017 based on the framework in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) (COSO) with the exception of the operations of Community Health United Home Care, LLC, which constituted 8% of total assets as of December 29, 2017 and 25% of net service revenues for the fiscal year then ended. Based on that evaluation, our management concluded our internal control over financial reporting was effective based on the criteria described above as of December 29, 2017.
Ernst & Young LLP, an independent registered public accounting firm, has audited and reported on the effectiveness of our internal control over financial reporting. The report of Ernst & Young LLP is contained in this Annual Report.
|
/s/ William B. Yarmuth |
|
/s/ C. Steven Guenthner |
|
William B. Yarmuth |
|
C. Steven Guenthner |
|
Chairman and Chief Executive Officer |
|
President & Principal Financial Officer |
|
|
|
|
|
Date: February 27, 2018 |
|
February 27, 2018 |
89
Report of Independent Registered Public Accounting Firm
To the Shareholders and the Board of Directors of Almost Family, Inc. and Subsidiaries
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of Almost Family, Inc. and Subsidiaries (the Company) as of December 29, 2017 and December 30, 2016, the related consolidated statements of income, stockholders' equity and cash flows for each of the three years in the period ended December 29, 2017, and the related notes and financial statement schedule listed in the Index at Item 15(a) (collectively referred to as the “financial statements”). In our opinion, the financial statements present fairly, in all material respects, the consolidated financial position of the Company at December 29, 2017 and December 30, 2016, and the consolidated results of its operations and its cash flows for each of the three years in the period ended December 29, 2017, in conformity with U.S. generally accepted accounting principles.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the Company’s internal control over financial reporting as of December 29, 2017, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) and our report dated February 27, 2018 expressed an unqualified opinion thereon.
Basis for Opinion
These financial statements are the responsibility of the Company's management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
/s/ Ernst & Young LLP
We have served as the Company’s auditor since 2002.
Louisville, Kentucky
February 27, 2018
90
ITEM 9. CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE
None.
ITEM 9A. CONTROLS AND PROCEDURES
Disclosure Controls and Procedures — As of December 29, 2017, the Company’s management, with participation of the Company’s Chief Executive Officer and Principal Financial Officer, evaluated the effectiveness of the Company’s disclosure controls and procedures as defined in Exchange Act Rules 13a-15(e) and 15d-15(e). Based on that evaluation, the Chief Executive Officer and Principal Financial Officer concluded that the Company’s disclosure controls and procedures were effective as of December 29, 2017.
Internal Control — Pursuant to Section 404 of the Sarbanes-Oxley Act of 2002, we have included a report that provides management’s assessment of our internal control over financial reporting as part of this annual report on Form 10-K for the year ended December 29, 2017. Management’s report is included in Item 8 of this report under the caption entitled “Management’s Report on Internal Control Over Financial Reporting,” and is incorporated herein by reference. Our independent registered public accounting firm has issued an attestation report on the effectiveness of our internal control over financial reporting. This attestation report is included in Item 8 of this report under the caption entitled “Report of Independent Registered Public Accounting Firm” and is incorporated herein by reference.
Changes in Internal Control Over Financial Reporting - There were no changes in the Company’s internal control over financial reporting during the fourth quarter of 2017, that have materially affected, or are reasonably likely to materially affect, Almost Family, Inc.’s internal control over financial reporting.
None.
ITEM 10. DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE
The information required by this Item is set forth in the Registrant’s definitive proxy statement to be filed with the Commission no later than 120 days after December 29, 2017, except for the information regarding executive officers of the Company. The information required by this Item contained in such definitive proxy statement is incorporated herein by reference.
The following table sets forth certain information with respect to the Company’s executive officers.
|
Name |
|
Age |
|
Position with the Company |
|
William B. Yarmuth (1) |
|
65 |
|
Chairman of the Board and Chief Executive Officer |
|
C. Steven Guenthner (2) |
|
57 |
|
President and Principal Financial Officer |
|
P. Todd Lyles (3) |
|
56 |
|
Senior Vice President — Administration |
|
Daniel J. Schwartz (4) |
|
51 |
|
Senior Vice President and Chief Operating Officer |
|
Jeffrey T. Reibel (5) |
|
46 |
|
Vice President and Chief Accounting Officer |
|
John Sherymen (6) |
|
64 |
|
Senior Vice President - Healthcare Innovations |
|
Sandra Hogston (7) |
|
60 |
|
Senior Vice President - Hospital JV Operations |
Executive officers of the Company are elected by the Board of Directors and serve at the pleasure of the Board of Directors with the exception of William B. Yarmuth who has an employment agreement with the Company. There are no family relationships between any director or executive officer.
91
|
(1) |
William B. Yarmuth has been a director and officer of the Company since 1991. Mr. Yarmuth became Chairman and Chief Executive Officer in 1992; he also served as President until the appointment of Steve Guenthner as President in 2012. Mr. Yarmuth has served as a member of the board of directors of Industrial Services of America, Inc. since June 2014. |
|
(2) |
C. Steven Guenthner has been President and Principal Financial Officer since June of 2012. Prior to which, Mr. Guenthner served as Senior Vice President and Chief Financial Officer of the Company for twenty years. From 1983 through 1992, Mr. Guenthner was employed as a C.P.A. with Arthur Andersen LLP. |
|
(3) |
P. Todd Lyles joined the Company as Senior Vice President Planning and Development in 1997 and now serves as Senior Vice President — Administration. Prior to joining the Company Mr. Lyles was Vice President Development for the Kentucky Division of Columbia/HCA, a position he had held since 1993. Mr. Lyles’ experience also includes 8 years with Humana Inc. in various financial and hospital management positions. |
|
(4) |
Daniel J. Schwartz joined the Company as Senior Vice President - Operations in April 2013, becoming Senior Vice President and Chief Operating Officer in December 2013. Mr. Schwartz’s healthcare operations management experience includes previously serving as Chief Operating Officer of Addus Healthcare, Inc. from January 2011 until November 2012; owner of New Paradigm Senior Services, LLC from April 2010 until January 2011; and Senior Vice President — North American Operations for Sunrise Senior Living, Inc. from 2006 until April 2010. Mr. Schwartz served Sunrise Senior Living, Inc. a total of 15 years. Mr. Schwartz also served as chief operating officer of New Perspective Senior Living from November 2012 until joining the Company. |
|
(5) |
Jeffrey T. Reibel, a C.P.A., joined the Company in September of 2010 as Vice President of Finance and became Vice President and Chief Accounting Officer in 2012. Prior to joining the Company, Mr. Reibel served as Chief Executive Officer of a private compliance company he founded in 2006. Mr. Reibel’s experience also includes three years as Controller and Principal Accounting Officer for a publicly traded company in addition to twelve years with Ernst & Young LLP, specializing in audits of public companies and various clients in the healthcare industry, including home health. |
|
(6) |
John Shermyen joined the Company as Senior Vice President – Healthcare Innovations in July 2015. Mr. Shermyen’s experience in technology-enabled healthcare service management includes previously serving as founder and CEO of Ingenios Health, September 2013 – present, as well as, founder and CEO of LogistiCare Solutions from September 1995 to July 2009. |
|
(7) |
Sandra Hogston joined the Company as Senior Vice President – Hospital Partnership Division in 2017. Ms. Hogston’s healthcare management experience includes previously serving as Division President – Homecare Division with Community Health Systems, Inc. from 2014 to 2016; Senior Director, Home Health Division with Lifepoint Health from 2009 to 2014; owner of Preferred Home Health from 1998 to 2009; President of Legacy Hospice from 2004 to 2014 and 20 years’ experience with Clinch Valley Medical Center. |
Code of Ethics
The Company has adopted a Code of Ethics for Senior Financial Officers that applies to its chief executive officer, principal financial officer, chief accounting officer and any person performing similar functions. The Company has made the Code of Ethics available on its website at www.almostfamily.com and will post any waivers to the Code of Ethics on the website.
ITEMS 11, 12, 13 and 14. EXECUTIVE COMPENSATION; SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS; CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS AND DIRECTOR INDEPENDENCE; AND PRINCIPAL ACCOUNTANT FEES AND SERVICES
The Registrant intends to file a definitive proxy statement with the Commission pursuant to Regulation 14A (17 CFR 240.14a) not later than 120 days after the close of the fiscal year covered by this report. In accordance with General
92
Instruction G(3) to Form 10-K, the information called for by Items 11, 12, 13 and 14 is incorporated herein by reference to portions of the definitive proxy statement.
Equity Compensation Plans
As of December 29, 2017, shares of common stock authorized for issuance under our equity compensation plans are summarized in the following table. See Note 7 to the consolidated financial statements for a description of the plans. The table below is furnished pursuant to Item 12.
|
|
|
Shares to be |
|
Weighted |
|
Shares |
|
|
|
|
|
Issued Upon |
|
Average Option |
|
Available for |
|
|
|
Plan Category |
|
Exercise |
|
Exercise Price |
|
Future Grants |
|
|
|
|
|
|
|
|
|
|
|
|
|
Plans approved by shareholders |
|
308 |
|
$ |
32.93 |
|
984 |
|
|
Plans not approved by shareholders |
|
— |
|
|
— |
|
— |
|
|
Total |
|
308 |
|
$ |
32.93 |
|
984 |
|
93
ITEM 15. EXHIBITS AND FINANCIAL STATEMENT SCHEDULES
|
|
|
|
Page Number |
|
(a) |
The following items are filed as part of this report: |
|
|
|
|
|
|
|
|
|
1. |
Index to Consolidated Financial Statements |
|
|
|
|
|
|
|
|
|
62 |
|
|
|
|
|
|
|
|
|
Consolidated Balance Sheets as of December 29, 2017 and December 30, 2016 |
63 |
|
|
|
|
|
|
|
|
64 |
|
|
|
|
|
|
|
|
|
65 |
|
|
|
|
|
|
|
|
|
66 |
|
|
|
|
|
|
|
|
|
87 |
|
|
|
|
|
|
|
|
2. |
Index to Financial Statement Schedule |
|
|
|
|
|
|
|
|
|
101 |
|
|
|
|
|
|
|
|
|
All other Schedules have been omitted because they are either not required, not applicable, or the information has otherwise been supplied in the financial statements or notes thereto. |
|
|
|
|
|
|
|
(b) |
Exhibits required to be filed by Item 601 of Regulation S-K are set forth below: |
|
|
94
|
Number |
|
Description of Exhibit |
|
|
|
|
|
2.1 |
|
|
|
|
|
|
|
2.2 |
|
|
|
|
|
|
|
2.3 |
|
|
|
|
|
|
|
2.4 |
|
|
|
|
|
|
|
2.5 |
|
|
|
|
|
|
95
|
2.6 |
|
Attachment ALLC Agreement Attachment BPurchaser Required Consents (2) Attachment CRequired Actions (2) Attachment DSeller Required Consents (2) Attachment EServices Agreement Attachment FCompany Indebtedness (2) Attachment GNoncompetition Agreement Attachment HAffiliation Agreement
(1) Schedules have been omitted pursuant to Item 601(b)(2) of Regulation S-K. Almost Family hereby undertakes to furnish supplementally copies of any of the omitted schedules upon request by the U.S. Securities and Exchange Commission.
(2) The information scheduled at this Attachment has been omitted pursuant to Item 601(b)(2) of Regulation S-K. Almost Family hereby undertakes to furnish supplementally copies of any of the omitted schedules upon request by the U.S. Securities and Exchange Commission.(incorporated by reference to Exhibit 2.1 to Registrant’s Quarterly Report on Form 10-Q for the quarterly period ended September 30, 2016) (SEC File No. 001-09848). |
|
|
|
|
|
2.7 |
|
|
|
|
|
|
|
3.1 |
|
|
|
|
|
|
|
3.2 |
|
|
|
|
|
|
|
4.1 |
|
|
|
|
|
|
|
4.2 |
|
|
|
|
|
|
|
4.3 |
|
Other Debt Instruments — copies of other debt instruments for which the total debt is less than 10% of assets will be furnished to the Commission upon request. |
|
|
|
|
96
|
10.1+ |
|
|
|
|
|
|
|
10.2+ |
|
|
|
|
|
|
|
10.3+ |
|
|
|
|
|
|
|
10.4+ |
|
|
|
|
|
|
|
10.5+ |
|
|
|
|
|
|
|
10.6+ |
|
|
|
|
|
|
|
10.7+ |
|
|
|
|
|
|
|
10.8+ |
|
|
|
|
|
|
|
10.9 |
|
|
|
|
|
|
|
10.10 |
|
|
|
|
|
|
|
10.11 |
|
|
|
|
|
|
|
10.12 |
|
97
|
|
|
|
|
10.13 |
|
|
|
|
|
|
|
10.14 |
|
|
|
|
|
|
|
10.15 |
|
|
|
|
|
|
|
10.16+ |
|
|
|
|
|
|
|
10.17+ |
|
|
|
|
|
|
|
10.18+ |
|
|
|
|
|
|
|
21* |
|
|
|
|
|
|
|
23.1* |
|
|
|
|
|
|
|
31.1* |
|
|
|
|
|
|
|
31.2* |
|
|
|
|
|
|
|
32.1* |
|
|
|
|
|
|
|
32.2* |
|
|
|
|
|
|
|
101* |
|
Financial statements from the Annual Report on Form 10-K of Almost Family, Inc. for the fiscal year ended December 29, 2017, filed on February 27, 2018, formatted in XBRL: (i) Consolidated Balance Sheets, (ii) Consolidated Statements of Income, (iii) Consolidated Statements of Cash Flows, (iv) Consolidated Statements of Stockholders’ Equity, and (v) the Notes to Consolidated Financial Statements. |
98
*Denotes filed herein.
+Denotes compensatory plan or management contract.
Not applicable.
99
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
ALMOST FAMILY, INC.
|
By: |
/s/ William B. Yarmuth |
February 27, 2018 |
|
|
William B. Yarmuth |
|
||
|
Chairman, Chief Executive Officer |
|
||
|
|
|
|
|
|
By: |
/s/ C. Steven Guenthner |
February 27, 2018 |
|
|
C. Steven Guenthner |
|
||
|
President and Principal Financial Officer |
|
||
Pursuant to the requirements of the Securities Exchange Act of 1934, as amended, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
|
Signature |
|
Title |
|
Date |
|
|
|
|
|
|
|
|
|
By: |
/s/ William B. Yarmuth |
|
Director, Chief Executive Officer |
|
February 27, 2018 |
|
|
William B. Yarmuth |
|
(principal executive officer) |
|
|
|
|
|
|
|
|
|
|
By: |
/s/ C. Steven Guenthner |
|
President and Principal Financial Officer |
|
February 27, 2018 |
|
|
C. Steven Guenthner |
|
|
|
|
|
|
|
|
|
|
|
|
By: |
/s/ Jeffrey T. Reibel |
|
Vice President of Finance and Chief Accounting Officer |
|
February 27, 2018 |
|
|
Jeffrey T. Reibel |
|
|
|
|
|
|
|
|
|
|
|
|
By: |
/s/ Steven B. Bing |
|
Director |
|
February 27, 2018 |
|
|
Steven B. Bing |
|
|
|
|
|
|
|
|
|
|
|
|
By: |
/s/ Donald G. McClinton |
|
Director |
|
February 27, 2018 |
|
|
Donald G. McClinton |
|
|
|
|
|
|
|
|
|
|
|
|
By: |
/s/ Tyree G. Wilburn |
|
Director |
|
February 27, 2018 |
|
|
Tyree G. Wilburn |
|
|
|
|
|
|
|
|
|
|
|
|
By: |
/s/ Jonathan D. Goldberg |
|
Director |
|
February 27, 2018 |
|
|
Jonathan D. Goldberg |
|
|
|
|
|
|
|
|
|
|
|
|
By: |
/s/ W. Earl Reed, III |
|
Director |
|
February 27, 2018 |
|
|
W. Earl Reed, III |
|
|
|
|
|
|
|
|
|
|
|
|
By: |
/s/ Henry M. Altman, Jr. |
|
Director |
|
February 27, 2018 |
|
|
Henry M. Altman, Jr. |
|
|
|
|
|
|
|
|
|
|
|
|
By: |
/s/ Clifford S. Holtz |
|
Director |
|
February 27, 2018 |
|
|
Clifford S. Holtz |
|
|
|
|
100
ALMOST FAMILY, INC. AND SUBSIDIARIES
VALUATION AND QUALIFYING ACCOUNTS
(In thousands)
|
|
|
Col. A |
|
Col. B |
|
Col. C |
|
Col. D |
|
Col. E |
|
|||||
|
|
|
|
|
|
Additions/(Deductions) |
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
(1) |
|
(2) |
|
|
|
|
|
|
|
||
|
|
|
Balance at |
|
Charged to |
|
Charged to |
|
|
|
|
Balance at |
|
||||
|
|
|
Beginning |
|
Costs and |
|
Other |
|
(3) |
|
End of |
|
|||||
|
Description |
|
of Period |
|
Expenses |
|
Accounts |
|
Deductions |
|
Period |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Allowances: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Year Ended December 29, 2017 |
|
$ |
21,302 |
|
$ |
14,526 |
|
$ |
193 |
|
$ |
(8,974) |
|
$ |
27,047 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Year Ended December 30, 2016 |
|
$ |
17,514 |
|
$ |
11,708 |
|
$ |
25 |
|
$ |
(7,945) |
|
$ |
21,302 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Year Ended January 1, 2016 |
|
$ |
8,880 |
|
$ |
12,743 |
|
$ |
1,891 |
|
$ |
(6,000) |
|
$ |
17,514 |
|
|
(1) |
Charged to bad debt expense. |
|
(2) |
Acquired uncollectible accounts reserves. |
|
(3) |
Write-off of accounts. |
101
