Attached files
| file | filename |
|---|---|
| 8-K - 8-K - VIVUS INC | a11-15509_28k.htm |
| EX-99.1 - EX-99.1 - VIVUS INC | a11-15509_2ex99d1.htm |
| EX-99.3 - EX-99.3 - VIVUS INC | a11-15509_2ex99d3.htm |
Exhibit 99.2
Below is a reproduction of the contents of the poster entitled, “Diabetes Prevention and Normalization of Fasting Glucose in Subjects with Prediabetes Using Controlled-Release Phentermine/Topiramate in a 2-Year Weight Loss Intervention”:

Below is a reproduction of the contents of the poster entitled, “Diabetes Prevention and Normalization of Fasting Glucose in Subjects with Prediabetes Using Controlled-Release Phentermine/Topiramate in a 2-Year Weight Loss Intervention”:
Authors: Donna H. Ryan, MD(a); W. Timothy Garvey, MD(b); Barbara Troupin, MD(c); Wesley W. Day, PhD(c)
(a) Pennington Biomedical Research Center, Baton Rouge, LA; (b)University of Alabama at Birmingham; Birmingham VA Medical Center, Birmingham, AL; (c)Vivus, Inc., Mountain View, CA
Contact details: Donna H. Ryan, MD; Pennington Biomedical Research Center, 6400 Perkins Rd, Baton Rouge, LA 70808; Office: 225.763.2514; E-mail: ryandh@pbrc.edu
· Introduction
· Obesity is associated with increased mortality, which is exacerbated by weight-related comorbidities, such as type 2 diabetes mellitus (T2DM).(1)-(5)
· Prediabetes, defined as impaired fasting glucose or impaired glucose tolerance, increases the risk of developing T2DM and is also associated with obesity.(6)
· Even modest weight loss in patients with Prediabetes may delay progression to T2DM and produce improvements in glycemic parameters.(6),(7)
· When used in conjunction with lifestyle-modification counseling, phentermine/topiramate controlled release (PHEN/TPM CR), an investigational combination therapy, has previously demonstrated improvements in glycemic parameters and reduced overall rates of progression to T2DM in the 56-week Phase 3 CONQUER study.(8)
· The SEQUEL study was a 52-week, placebo-controlled extension of CONQUER.
· Objectives
· The purpose of this prespecified subgroup analysis was to assess the effects of lifestyle + PHEN/TPM CR on weight loss, glycemic parameters, and changes in diabetic status during a 108-week period in a subset of patients with Prediabetes at baseline.
· Methods
· Lifestyle + PHEN/TPM CR was evaluated during 108 weeks in 2 consecutive, double-blind, placebo-controlled clinical studies:
· CONQUER randomized 2487 overweight/obese adult subjects with >2 weight-related comorbidities to lifestyle + placebo, lifestyle + PHEN 7.5 mg/TPM CR 46 mg (lifestyle + 7.5/46), or lifestyle + PHEN 15 mg/TPM CR 92 mg (lifestyle + 15/92) for 56 weeks.(8)
· Patients completing CONQUER at sites selected for high initial enrollment and retention rates were eligible to volunteer for the SEQUEL extension study, where they remained on original randomized treatment for a further 52 weeks.
· All subjects were managed to standard of care for their respective comorbidities, including medication management as needed, and received lifestyle modification counseling, including guidance on nutrition and increased physical activity, based on the LEARN program.(9)
· Assessments
· The primary efficacy endpoint for the SEQUEL trial was percent weight loss from baseline (CONQUER Week 0) to Week 108 in the intent-to-treat (ITT) population with last observation carried forward (LOCF). The overall ITT-LOCF population included patients with normoglycemia, Prediabetes, and T2DM.
· A prespecified subgroup analysis assessed changes at Week 108 in glycemic parameters and change in Prediabetic status among subjects with Prediabetes (defined as impaired fasting glucose >100 to <125 mg/dL or impaired glucose tolerance >140 to <199 mg/dL as measured by oral glucose tolerance test [OGTT] at baseline.
· Analysis of covariance (ANCOVA) was used to evaluate changes in weight and other outcomes. The ANCOVA model used factors of treatment, gender, and diabetic status as fixed effects, with baseline weight as a covariate.
· Results
Baseline Characteristics
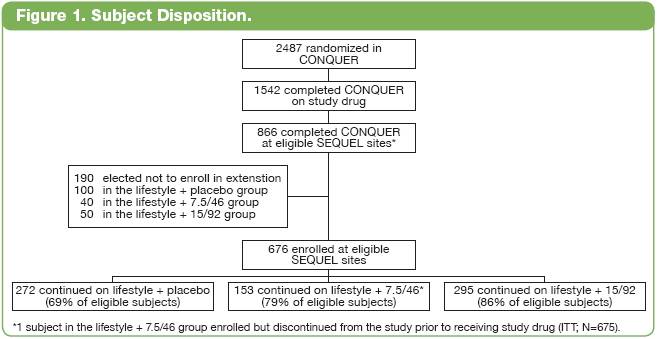
· In total, 866 subjects were eligible to participate in SEQUEL; 676 subjects (78%) were enrolled in the study, and the remainder (190 subjects) elected not to continue (Figure 1).
Effects of PHEN/TPM CR on the Overall Population
· At Week 0, subjects had a mean weight of 101.7 kg, mean body mass index of 36.1 kg/m2, mean fasting glucose of 109.2 mg/dL, and mean HbA1c of 6.0%. A total of 145 (21.5%) subjects had T2DM at Week 0.
· After 108 weeks of treatment, lifestyle + PHEN/TPM CR had significantly greater effects on weight and glycemic parameters when compared with lifestyle + placebo (Table 1).
Table 1. Effects of Lifestyle + PHEN/TPM CR on the Overall Population From Baseline to Week 108.
|
|
|
Lifestyle + Placebo |
|
Lifestyle + 7.5/46 |
|
Lifestyle + 15/92 |
|
|
|
|
|
|
|
|
|
|
|
LS mean percent weight loss |
|
-1.8 |
|
-9.3* |
|
-10.5* |
|
|
LS mean change in HbA1c (%) |
|
0.2 |
|
0.0† |
|
0.0† |
|
|
LS mean change in fasting glucose (mg/dL) |
|
3.7 |
|
0.1 |
|
-1.2† |
|
|
LS mean change in fasting insulin (µIU/mL) |
|
-2.6 |
|
-5.3† |
|
-5.2† |
|
LS=least-squares
*P<.0001 vs lifestyle + placebo; †P<.005 vs lifestyle + placebo
Weight Loss: Prediabetes Subgroup
· Of those subjects subsequently enrolling in the SEQUEL extension study, 316 (46.7%) were considered to have Prediabetes at baseline (lifestyle + placebo, n=103 [45.4%]; lifestyle + 7.5/46, n=83 [54.2%]; lifestyle + 15/92, n=130 [44.1%]).
· Least-squares (LS) mean percent weight loss in the Prediabetes subgroup was significantly greater with lifestyle + PHEN/TPM CR compared with lifestyle + placebo through 108 weeks of treatment (P<.0001 vs lifestyle + placebo for all time points; Figure 2).

Glycemic Parameters: Prediabetes Subgroup
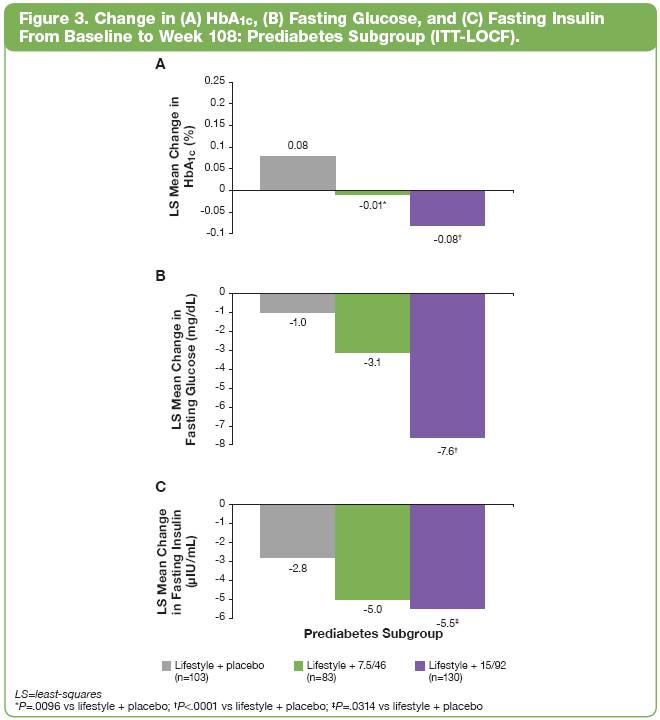
· Dose-related improvements were observed in HbA1c, fasting glucose, and fasting insulin at Week 108 with lifestyle + PHEN/TPM CR when compared with lifestyle + placebo (Figure 3).
Change in Prediabetic Status: Prediabetes Subgroup
· Among subjects with Prediabetes at Week 0, more subjects treated with lifestyle + PHEN/TPM CR achieved normoglycemia than those receiving lifestyle + placebo treatment; in contrast, progression to T2DM was more common with lifestyle + placebo than with lifestyle + PHEN/TPM CR (Figure 4).

Safety Summary: Overall Safety Population
· The most common treatment-emergent adverse events (TEAEs) are shown in Table 2. There were no new safety signals seen between Weeks 56 and 108.
· The percentage of subjects who discontinued study drug due to AEs was 3.1% in the lifestyle + placebo group, 4.6% in the lifestyle + 7.5/46 group, and 4.4% in the lifestyle + 15/92 group.
· Rates of hypoglycemia were low and comparable to placebo: 1.8%, 0.7%, and 1.7% for lifestyle + placebo, lifestyle + 7.5/46, and lifestyle + 15/92, respectively.
· In total, 47 subjects had a serious AE (SAE) between baseline and Week 108: 14 (6.2%) subjects in the lifestyle + placebo group, 9 (5.9%) in the lifestyle + 7.5/46 group, and 24 (8.1%) in the lifestyle + 15/92 group.
· There were no drug-related SAEs.
· No deaths were reported during the study.
Table 2. Most Common TEAEs Between Baseline and Week 108 (Safety Population*).
|
TEAE, % |
|
Lifestyle + Placebo |
|
Lifestyle + 7.5/46 |
|
Lifestyle + 15/92 |
|
|
Upper respiratory tract infection |
|
32.6 |
|
27.5 |
|
28.5 |
|
|
Constipation |
|
9.7 |
|
22.2 |
|
22.7 |
|
|
Paresthesia |
|
2.6 |
|
14.4 |
|
22.4 |
|
|
Sinusitis |
|
13.7 |
|
15.7 |
|
21.0 |
|
|
Dry mouth |
|
2.6 |
|
14.4 |
|
20.7 |
|
|
Nasopharyngitis |
|
22.0 |
|
19.0 |
|
17.3 |
|
|
Dysgeusia |
|
1.8 |
|
11.8 |
|
13.6 |
|
|
Headache |
|
11.5 |
|
7.2 |
|
12.9 |
|
|
Insomnia |
|
9.7 |
|
12.4 |
|
11.5 |
|
|
Back pain |
|
11.5 |
|
11.1 |
|
11.5 |
|
*The safety population was defined as all subjects who received at least 1 dose of study drug.
· Conclusions
· In subjects with Prediabetes, both doses of PHEN/TPM CR together with lifestyle intervention led to sustained weight loss and improvements in glycemic parameters over 108 weeks, and these changes were significantly greater than observed with lifestyle + placebo.
· Lifestyle + PHEN/TPM CR therapy resulted in reductions in fasting glucose, insulin, and HbA1c, and normalization of glycemia in more than one half of subjects with Prediabetes at baseline receiving lifestyle + 15/92.
· Treatment with lifestyle + 15/92 also led to significant reductions in the proportion of subjects with Prediabetes progressing to T2DM when compared with lifestyle + placebo.
· PHEN/TPM CR was generally well tolerated based on rates of enrollment into the extension study, completion rates, and overall AEs.
· These findings demonstrate the sustained effectiveness and consistent tolerability profile of PHEN/TPM CR over 108 weeks as an adjunct to lifestyle-modification in the management of obesity and prevention of diabetes.
This trial is registered at ClinicalTrials.gov, number NCT00796367.
References: (1) Reaven GM. Ann Intern Med. 2003;138(5):420-423. (2) Flegal KM, et al. JAMA. 2002;288(14):1723-1727. (3) Adams KF, et al. N Engl J Med. 2006;355(8):763-778. (4) Logue J, et al. Heart. 2011;97(7):564-568. (5) Tzotzas T, et al. Obes Rev. 2011;12(5):e282-e289. (6) American Diabetes Association. Diabetes Care. 2010;33(suppl 1):S11-S61. (7) UKPDS Group. Metabolism. 1990;39(9):905-912. (8) Gadde KM, et al. Lancet. 2011;377(9774):1341-1352. (9) Brownell KD. The LEARN Program for Weight Management. 2004.
Acknowledgments: We would like to acknowledge and thank the SEQUEL investigators and study coordinators, the Medpace team (study CRO), Michael Schwiers (for data assistance), The Lockwood Group (for poster development assistance), and VIVUS internal contributors.
