Attached files
| file | filename |
|---|---|
| EX-10.53 - EX-10.53 - VIVUS INC | vvus-20151231ex10535b1d3.htm |
| EX-31.2 - EX-31.2 - VIVUS INC | vvus-20151231ex31285d0ab.htm |
| EX-31.1 - EX-31.1 - VIVUS INC | vvus-20151231ex31179e490.htm |
| EX-23.1 - EX-23.1 - VIVUS INC | vvus-20151231ex231137c38.htm |
| EX-32.1 - EX-32.1 - VIVUS INC | vvus-20151231ex321a2508e.htm |
| EX-21.1 - EX-21.1 - VIVUS INC | vvus-20151231ex21137aae1.htm |
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10‑K
|
☒ |
ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
|
For the fiscal year ended December 31, 2015 |
|
|
OR |
|
|
☐ |
TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
|
For the transition period from to |
|
Commission File Number 001‑33389
VIVUS, INC.
(Exact name of Registrant as specified in its charter)
|
Delaware |
94‑3136179 |
|
351 E. Evelyn Avenue |
94041 |
Registrant’s telephone number, including area code: (650) 934‑5200
Securities registered pursuant to Section 12(b) of the Act:
|
Title of Each Class |
Name of Each Exchange on Which Registered |
|
Common Stock, $.001 Par Value |
The NASDAQ Global Select Market |
|
Preferred Share Purchase Rights |
|
Securities registered pursuant to Section 12(g) of the Act:
None
Indicate by check mark if the registrant is a well‑known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☒ No ☐
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ☐ No ☒
Indicate by check mark whether the Registrant: (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the Registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ☒ No ☐
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S‑T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ☒ No ☐
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S‑K (§229.405) is not contained herein, and will not be contained, to the best of Registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10‑K or any amendment to this Form 10‑K. ☒
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non‑accelerated filer, or a smaller reporting company. See the definitions of “large accelerated filer,” “accelerated filer” and “smaller reporting company” in Rule 12b‑2 of the Exchange Act. (Check one):
|
Large accelerated filer ☐ |
Accelerated filer ☒ |
Non‑accelerated filer ☐ |
Smaller reporting company ☐ |
Indicate by check mark whether the Registrant is a shell company (as defined in Rule 12b‑2 of the Act). Yes ☐ No ☒
The aggregate market value of the common equity held by non‑affiliates of the Registrant as of June 30, 2015, totaled approximately $238,937,273 based on the closing stock price as reported by the NASDAQ Global Market.
As of February 29, 2016, there were 104,075,642 shares of the Registrant’s common stock, $0.001 par value per share, outstanding.
DOCUMENTS INCORPORATED BY REFERENCE
|
Document Description |
10‑K |
|
Portions of the Registrant’s notice of annual meeting of stockholders and proxy statement to be filed pursuant to Regulation 14A within 120 days after Registrant’s fiscal year end of December 31, 2015, are incorporated by reference into Part III of this report. |
Part III - ITEMS 10, 11, 12, 13, 14 |
VIVUS, INC.
FISCAL 2015 FORM 10‑K
|
|
|
|
|
|
|
|
|
|
|
|
5 |
||
|
|
32 |
||
|
|
68 |
||
|
|
68 |
||
|
|
68 |
||
|
|
70 |
||
|
|
|
|
|
|
|
71 |
||
|
|
72 |
||
|
Management’s Discussion and Analysis of Financial Condition and Results of Operations |
|
73 |
|
|
|
94 |
||
|
|
95 |
||
|
Changes in and Disagreements with Accountants on Accounting and Financial Disclosure |
|
134 |
|
|
|
134 |
||
|
|
135 |
||
|
|
|
|
|
|
|
136 |
||
|
|
136 |
||
|
Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
|
136 |
|
|
Certain Relationships and Related Transactions, and Director Independence |
|
137 |
|
|
|
137 |
||
|
|
|
|
|
|
|
138 |
||
|
|
139 |
||
|
|
140 |
||
|
|
141 |
||
|
Certification of Chief Executive Officer |
|
|
|
|
Certification of Chief Financial Officer |
|
|
|
|
Certification of Chief Executive Officer and Chief Financial Officer |
|
|
|
2
FORWARD‑LOOKING STATEMENTS
This Form 10-K contains “forward looking” statements that involve risks and uncertainties. These statements typically may be identified by the use of forward-looking words or phrases such as “may,” “believe,” “expect,” “forecast,” “intend,” “anticipate,” “predict,” “should,” “planned,” “likely,” “opportunity,” “estimated,” and “potential,” the negative use of these words or other similar words. All forward-looking statements included in this document are based on our current expectations, and we assume no obligation to update any such forward-looking statements. The Private Securities Litigation Reform Act of 1995 provides a “safe harbor” for such forward-looking statements. In order to comply with the terms of the safe harbor, we note that a variety of factors could cause actual results and experiences to differ materially from the anticipated results or other expectations expressed in such forward-looking statements. The risks and uncertainties that may affect the operations, performance, development, and results of our business include but are not limited to:
|
· |
our limited commercial experience with Qsymia® in the United States, or U.S.; |
|
· |
the timing of initiation and completion of the post-approval clinical studies required as part of the approval of Qsymia by the U.S. Food and Drug Administration, or FDA; |
|
· |
the response from the FDA to the data that we will submit relating to post-approval clinical studies; |
|
· |
the impact of the indicated uses and contraindications contained in the Qsymia label and the Risk Evaluation and Mitigation Strategy requirements; |
|
· |
our ability to continue to certify and add to the Qsymia retail pharmacy network and sell Qsymia through this network; |
|
· |
whether the Qsymia retail pharmacy network will simplify and reduce the prescribing burden for physicians, improve access and reduce waiting times for patients seeking to initiate therapy with Qsymia; |
|
· |
that we may be required to provide further analysis of previously submitted clinical trial data; |
|
· |
our ability to work with leading cardiovascular outcome trial experts in planning substantial revisions to the original design and execution of the clinical post-marketing cardiovascular outcomes trial, or CVOT, with the goal of reducing trial costs and obtaining FDA agreement that the revised CVOT would fulfill the requirement of demonstrating the long-term cardiovascular safety of Qsymia; |
|
· |
our ongoing dialog with the European Medicines Agency, or EMA, relating to our CVOT, and the resubmission of an application for the grant of a marketing authorization to the EMA, the timing of such resubmission, if any, the results of the CVOT, assessment by the EMA of the application for marketing authorization, and their agreement with the data from the CVOT; |
|
· |
our ability to successfully seek approval for Qsymia in other territories outside the U.S. and EU; |
|
· |
whether healthcare providers, payors and public policy makers will recognize the significance of the American Medical Association officially recognizing obesity as a disease, or the new American Association of Clinical Endocrinologists guidelines; |
|
· |
our ability to successfully commercialize Qsymia including risks and uncertainties related to expansion to retail distribution, the broadening of payor reimbursement, the expansion of Qsymia’s primary care presence, and the outcomes of our discussions with pharmaceutical companies and our strategic and franchise-specific pathways for Qsymia; |
|
· |
our ability to focus our promotional efforts on health-care providers and on patient education that, along with increased access to Qsymia and ongoing improvements in reimbursement, will result in the accelerated adoption of Qsymia; |
|
· |
our ability to eliminate expenses that are not essential to expanding the use of Qsymia and fully realize the anticipated benefits from our cost reduction and corporate restructuring plans, including the timing thereof; |
|
· |
the impact of lower annual net cost savings than currently expected; |
|
· |
the impact of our cost reduction and corporate restructuring plans on our business and unanticipated charges not currently contemplated that may occur as a result of such cost reduction and corporate restructuring plans; |
3
|
· |
our ability to ensure that the entire supply chain for Qsymia efficiently and consistently delivers Qsymia to our customers; |
|
· |
risks and uncertainties related to the timing, strategy, tactics and success of the launches and commercialization of STENDRA® (avanafil) or SPEDRA™ (avanafil) by our sublicensees in the EU, Australia, New Zealand, Africa, the Middle East, Turkey, and the Commonwealth of Independent States, including Russia; |
|
· |
our ability to successfully complete on acceptable terms, and on a timely basis, avanafil partnering discussions for territories under our license with Mitsubishi Tanabe Pharma Corporation in which we do not have or will be ending a commercial collaboration, including the U.S., Canada and Latin America; |
|
· |
our ability, either by ourselves or through a third party, to successfully commercialize STENDRA in the U.S. and Canada; |
|
· |
the impact of the return of the U.S. and Canadian rights for the commercialization of STENDRA; |
|
· |
Sanofi Chimie’s ability to undertake manufacturing of the avanafil active pharmaceutical ingredient and Sanofi Winthrop Industrie’s ability to undertake manufacturing of the tablets for avanafil; |
|
· |
the ability of our partners to maintain regulatory approvals to manufacture and adequately supply our products to meet demand; |
|
· |
our ability to accurately forecast Qsymia demand; |
|
· |
our ability to commercialize Qsymia efficiently in 2016; |
|
· |
the number of Qsymia prescriptions dispensed through the mail order system and through certified retail pharmacies; |
|
· |
the impact of promotional programs for Qsymia on our net product revenue and net income (loss) in future periods; |
|
· |
our history of losses and variable quarterly results; |
|
· |
substantial competition; |
|
· |
risks related to the failure to protect our intellectual property and litigation in which we are involved or may become involved; |
|
· |
uncertainties of government or third-party payor reimbursement; |
|
· |
our reliance on sole-source suppliers, third parties and our collaborative partners; |
|
· |
our failure to continue to develop innovative investigational drug candidates and drugs; |
|
· |
risks related to the failure to obtain FDA or foreign authority clearances or approvals and noncompliance with FDA or foreign authority regulations; |
|
· |
our ability to demonstrate through clinical testing the quality, safety, and efficacy of our investigational drug candidates; |
|
· |
the timing of initiation and completion of clinical trials and submissions to foreign authorities; |
|
· |
the results of post-marketing studies are not favorable; |
|
· |
compliance with post-marketing regulatory standards, post-marketing obligations or pharmacovigilance rules is not maintained; |
|
· |
the volatility and liquidity of the financial markets; |
|
· |
our liquidity and capital resources; |
|
· |
our expected future revenues, operations and expenditures; |
|
· |
potential change in our business strategy to enhance long-term stockholder value; |
|
· |
the impact, if any, of changes to our Board of Directors or management team; and |
|
· |
other factors that are described from time to time in our periodic filings with the Securities and Exchange Commission, or the SEC, including those set forth in this filing as “Item 1A. Risk Factors.” |
4
When we refer to “we,” “our,” “us,” the “Company” or “VIVUS” in this document, we mean the current Delaware corporation, or VIVUS, Inc., and its California predecessor, as well as all of our consolidated subsidiaries.
Overview
VIVUS is a biopharmaceutical company with two therapies approved by the FDA: Qsymia® (phentermine and topiramate extended‑release) for chronic weight management and STENDRA® (Avanafil) for erectile dysfunction, or ED. STENDRA is also approved by the European Commission, or EC, under the trade name, SPEDRA, for the treatment of ED in the EU.
Qsymia was approved by the FDA in July 2012 as an adjunct to a reduced‑calorie diet and increased physical activity for chronic weight management in adult patients with an initial body mass index, or BMI, of 30 or greater, or obese patients, or a BMI of 27 or greater, or overweight patients, in the presence of at least one weight‑related comorbidity, such as hypertension, type 2 diabetes mellitus or high cholesterol, or dyslipidemia. Qsymia incorporates a proprietary formulation combining low doses of active ingredients from two previously approved drugs, phentermine and topiramate. Although the exact mechanism of action is unknown, Qsymia is believed to suppress appetite and increase satiety, or the feeling of being full, the two main mechanisms that impact eating behavior. In September 2012, Qsymia became available in the U.S. market through a limited number of certified home delivery networks. In July 2013, Qsymia became available in retail pharmacies nationwide. As of the date of this report, Qsymia is available in over 40,000 certified retail pharmacies nationwide. We intend to continue to certify and add new pharmacies to the Qsymia retail pharmacy network, including national and regional chains as well as independent pharmacies.
Challenges continue within the obesity pharmacotherapy market, in particular with respect to the tendency on the part of healthcare providers to treat the co-morbid conditions of obesity rather than the obesity disease itself. In addition, there is a narrow focus on certain patient types for treatment, historically low third-party insurance coverage, and the continued exclusion of anti-obesity medications from Medicare Part D.
We continue to develop efficient ways to address the obesity market. We completed a realignment of our field sales territories during April 2015 and July 2015, reducing the number of territories from 150 to approximately 50. Each of these adjustments was accompanied by a parallel streamlining of corporate headquarters headcount as we have sought to right-size the organization to match the market opportunity as it currently exists.
Prior to August 2015, we commercialized Qsymia in the U.S. primarily through a dedicated contract sales force, supported by an internal commercial team. In August 2015, we directly hired approximately 50 former contract sales representatives to continue promoting Qsymia to physicians. Our efforts to expand the appropriate use of Qsymia include scientific publications, participation and presentations at medical conferences, and development and implementation of patient-directed support programs. We have rolled out marketing programs to encourage targeted prescribers to gain more experience with Qsymia, including a partnership with Kadmon Corporation to focus on liver disease specialists. In 2015, we increased our investment in digital media in order to amplify our messaging to information-seeking consumers. The digital messaging encourages those consumers most likely to take action to speak with their physicians about obesity treatment options. We believe our enhanced web-based strategies will deliver clear and compelling communications to potential patients. We launched the “Smart Changes Program” in which we partner Qsymia with the Mayo Clinic diet to help on-line patients make the behavioral changes needed for sustained weight-loss. We have also employed a physician referral service to help patients identify prescribers in their area.
We defined and identified the healthcare provider, or HCP, audience of anti-obesity prescribers as numbering approximately 8,000 to 10,000. Of these, we believe the most highly productive writers are adequately covered by the newly-configured VIVUS sales force. We are focused on maintaining a commercial presence with important Qsymia prescribers, and we have capacity to cover new potential prescribers, who are those physicians that begin prescribing branded obesity products. We are constantly monitoring prescribing activity in the market, and we have seen new
5
prescriptions being written by HCPs on whom we have not previously dedicated field sales resources. We believe that part of the current realignment addresses this new prescriber group, and we look forward to initiating and maintaining dialog with these HCPs.
In October 2012, we received a negative opinion from the European Medicines Agency, or EMA, Committee for Medicinal Products for Human Use, or CHMP, recommending refusal of the marketing authorization for the medicinal product QsivaTM, the intended trade name for Qsymia in the EU, due to concerns over the potential cardiovascular and central nervous system effects associated with long-term use, potential for interfering with the development of a fetus and use by patients for whom Qsiva would not have been indicated. We requested that this opinion be re-examined by the CHMP. After re-examination of the CHMP opinion, in February 2013, the CHMP adopted a final opinion that reaffirmed the Committee’s earlier negative opinion to refuse the marketing authorization for Qsiva in the EU. In May 2013, the EC issued a decision refusing the grant of marketing authorization for Qsiva in the EU.
In September 2013, we submitted a request to the EMA for Scientific Advice, a procedure similar to the U.S. Special Protocol Assessment process, regarding use of a pre-specified interim analysis from the CVOT, known as AQCLAIM, to assess the long-term treatment effect of Qsymia on the incidence of major adverse cardiovascular events in overweight and obese subjects with confirmed cardiovascular disease. Our request was to allow this interim analysis to support the resubmission of an application for a marketing authorization for Qsiva for treatment of obesity in accordance with the EU centralized marketing authorization procedure. We received feedback in 2014 from the EMA and the various competent authorities of the EU Member States associated with review of the AQCLAIM CVOT protocol, and we received feedback from the FDA in late 2014 regarding the amended protocol. As a part of addressing the FDA comments from a May 2015 meeting to discuss alternatives to completion of a CVOT, we are now working with cardiovascular and epidemiology experts in exploring alternate solutions to demonstrate the long-term cardiovascular safety of Qsymia. After reviewing a summary of Phase 3 data relevant to cardiovascular, or CV, risk and post-marketing safety data, the cardiology experts noted that they believe there was an absence of an overt CV risk signal and indicated that they did not believe a randomized placebo controlled CVOT would provide additional information regarding the CV risk of Qsymia. The epidemiology experts maintained that a well-conducted retrospective observational study could provide data to further inform on potential CV risk. We are working with the expert group to develop a protocol for the retrospective observational study and feasibility assessment. Although we and the consulted experts believe there is no overt signal for CV risk to justify the AQCLAIM CVOT, VIVUS is committed to working with the FDA to reach a resolution. As for the EU, even if the FDA were to accept a retrospective observational study in lieu of a CVOT, there would be no assurance that the EMA would accept the same.
In addition, we are evaluating Qsymia for a new indication in obstructive sleep apnea, or OSA. We do not anticipate further development of Qsymia for OSA prior to resolving the Qsymia CVOT requirement with the FDA. We also intend to seek regulatory approval for Qsymia in territories outside the United States and the EU and, if approved, to commercialize the product through collaboration agreements with third parties.
STENDRA is an oral phosphodiesterase type 5, or PDE5, inhibitor that we have licensed from Mitsubishi Tanabe Pharma Corporation, or MTPC. STENDRA was approved by the FDA in April 2012 for the treatment of ED in the United States. In June 2013, the EC adopted a decision granting marketing authorization for SPEDRA, the approved trade name for avanafil in the EU, for the treatment of ED in the EU. In July 2013, we entered into an agreement with the Menarini Group, through its subsidiary Berlin Chemie AG, or Menarini, under which Menarini received an exclusive license to commercialize and promote SPEDRA for the treatment of ED in over 40 European countries, including the EU, as well as Australia and New Zealand. Menarini commenced its commercialization launch of the product in the EU in early 2014. As of the date of this filing, SPEDRA is commercially available in 25 countries within the territory granted to Menarini pursuant to the license and commercialization agreement.
In October 2013, we entered into an agreement with Auxilium Pharmaceuticals, Inc., or Auxilium, under which Auxilium received an exclusive license to commercialize and promote STENDRA in the United States and Canada. On the same date, we also entered into a supply agreement with Auxilium, whereby we would supply Auxilium with STENDRA for commercialization. Auxilium began commercializing STENDRA in the U.S. market in December 2013. In January 2015, Auxilium was acquired by Endo International, plc, or Endo. In December 2015, Auxilium notified us of
6
its intention to return the U.S. and Canadian commercial rights for STENDRA to us. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016.
In December 2013, we entered into an agreement with Sanofi under which Sanofi received an exclusive license to commercialize and promote avanafil for therapeutic use in humans in Africa, the Middle East, Turkey, and the Commonwealth of Independent States, or CIS, including Russia. Sanofi will be responsible for obtaining regulatory approval in its territories. Sanofi intends to market avanafil under the trade name SPEDRA or STENDRA. Effective as of December 11, 2013, we also entered into a supply agreement, or the Sanofi Supply Agreement, with Sanofi Winthrop Industrie, a wholly owned subsidiary of Sanofi.
Under the license agreements with Menarini, Auxilium and Sanofi, avanafil is expected to be commercialized in over 100 countries worldwide. Under our agreement with Auxilium, we have received approximately $45.0 million in license and milestone payments out of a potential of $300.0 million, as well as royalty payments. We do not anticipate any additional milestone revenue from the Auxilium agreement. Under the Menarini agreement, we have received approximately $63.0 million in license and milestone payments out of a potential of approximately $100.0 million, as well as royalty payments. Under the Sanofi agreement, we have received approximately $10.0 million in license and milestone payments out of a potential of $61.0 million. In addition, we are currently in discussions with potential collaboration partners to market and sell STENDRA in territories in which we do not currently have a commercial collaboration, including Latin America and India. We have engaged a strategic advisor to assist us in the evaluation of our alternatives not only for STENDRA, but also for our overall business strategy.
On September 18, 2014, the FDA approved a supplemental new drug application (sNDA) for STENDRA. STENDRA is now indicated to be taken as early as approximately 15 minutes before sexual activity. Additionally, on January 23, 2015, the EC adopted a commission implementing decision amending the marketing authorization for SPEDRA. SPEDRA is now indicated to be taken as needed approximately 15 to 30 minutes before sexual activity.
Foreign regulatory approvals, including EC marketing authorization to market Qsiva in the EU, may not be obtained on a timely basis, or at all, and the failure to receive regulatory approvals in a foreign country would prevent us from marketing our products that have failed to receive such approval in that market, which could have a material adverse effect on our business, financial condition and results of operations.
VIVUS was incorporated in California in 1991 and reincorporated in Delaware in 1996. Our corporate headquarters is located at 351 E. Evelyn Avenue, Mountain View, California and our telephone number is (650) 934‑5200.
7
Products and Development Programs
Our approved drugs and investigational drug candidates are summarized as follows:
|
Drug |
|
Indication |
|
Status |
|
Commercial rights |
|
Qsymia (phentermine and topiramate extended‑release) |
|
Obesity |
|
United States |
|
Worldwide |
|
|
|
|
New Drug Application, or NDA, approved July 2012; First commercial sale September 2012; |
|
|
|
|
|
|
|
|
Expansion to retail pharmacies July 2013 |
|
|
|
|
|
|
|
EU |
|
|
|
|
|
|
|
Marketing Authorization Application, or MAA, denied in 2014. |
|
|
|
Qsymia (phentermine and topiramate extended‑release) |
|
Obstructive Sleep Apnea |
|
Phase 2 study completed. |
|
Worldwide |
|
Qsymia (phentermine and topiramate extended‑release) |
|
Diabetes |
|
Phase 2 study completed. |
|
Worldwide |
|
|
|
|
|
|
|
|
|
STENDRA (avanafil) |
|
Erectile dysfunction |
|
United States |
|
Worldwide license from MTPC (excluding certain Asian markets). U.S. and Canada commercial rights licensed to Auxilium. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016. |
|
|
|
|
|
NDA approved April 2012 |
|
EU, Australia and New Zealand commercial rights licensed to Menarini Group |
|
|
|
|
|
sNDA: Label expansion for 15 minute onset claim approved Sep 2014. |
|
Middle East, Africa, Turkey and the Commonwealth of Independent States commercial rights licensed to Sanofi |
|
|
|
|
|
EU |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Marketing Authorization, or MA, granted in June 2013. |
|
|
|
|
|
|
|
Label expansion for 15 minute onset claim approved Jan 2015. |
|
|
Qsymia for the Treatment of Obesity
Many factors contribute to excess weight gain. These include environmental factors, genetics, health conditions, certain medications, emotional factors and other behaviors. All this contributes to more than 110 million Americans being obese or overweight with at least one weight‑related comorbidity. Excess weight increases the risk of cardiometabolic and other conditions including type 2 diabetes, high cholesterol, high blood pressure, heart disease,
8
sleep apnea, stroke and osteoarthritis. According to the National Institutes of Health, or NIH, losing just 10% of body weight may help obese patients reduce the risk of developing other weight‑related medical conditions, while making a meaningful difference in health and well‑being.
Qsymia for the treatment of obesity was approved as an adjunct to a reduced‑calorie diet and increased physical activity for chronic weight management in adult patients with an initial BMI of 30 or greater, or obese patients, or 27 or greater, or overweight patients, in the presence of at least one weight‑related comorbidity, such as hypertension, type 2 diabetes mellitus or high cholesterol, or dyslipidemia. Qsymia incorporates low doses of active ingredients from two previously approved drugs, phentermine and topiramate. Although the exact mechanism of action is unknown, Qsymia is believed to target appetite and satiety, or the feeling of being full, the two main mechanisms that impact eating behavior.
Qsymia was approved with a Risk Evaluation and Mitigation Strategy, or REMS, with a goal of informing prescribers and patients of reproductive potential regarding an increased risk of orofacial clefts in infants exposed to Qsymia during the first trimester of pregnancy, the importance of pregnancy prevention for females of reproductive potential receiving Qsymia and the need to discontinue Qsymia immediately if pregnancy occurs. The Qsymia REMS program includes a medication guide, patient brochure, voluntary healthcare provider training, distribution through certified home delivery and retail pharmacies, an implementation system and a time‑table for assessments.
As part of the approval of Qsymia, we are required to conduct post‑marketing studies. In September 2013, we submitted a request to the EMA for Scientific Advice, a procedure similar to the U.S. Special Protocol Assessment process, regarding use of a pre-specified interim analysis from the CVOT, known as AQCLAIM, to assess the long-term treatment effect of Qsymia on the incidence of major adverse cardiovascular events in overweight and obese subjects with confirmed cardiovascular disease. Our request was to allow this interim analysis to support the resubmission of an application for a marketing authorization for Qsiva for treatment of obesity in accordance with the EU centralized marketing authorization procedure. We received feedback in 2014 from the EMA and the various competent authorities of the EU Member States associated with review of the AQCLAIM CVOT protocol, and we received feedback from the FDA in late 2014 regarding the amended protocol. As a part of addressing the FDA comments from a May 2015 meeting to discuss alternatives to completion of a CVOT, we are now working with cardiovascular and epidemiology experts in exploring alternate solutions to demonstrate the long-term cardiovascular safety of Qsymia. After reviewing a summary of Phase 3 data relevant to CV risk and post-marketing safety data, the cardiology experts noted that they believe there was an absence of an overt CV risk signal and indicated that they did not believe a randomized placebo controlled CVOT would provide additional information regarding the CV risk of Qsymia. The epidemiology experts maintained that a well-conducted retrospective observational study could provide data to further inform on potential CV risk. We are working with the expert group to develop a protocol for the retrospective observational study and feasibility assessment. Although we and the consulted experts believe there is no overt signal for CV risk to justify the AQCLAIM CVOT, VIVUS is committed to working with the FDA to reach a resolution. As for the EU, even if the FDA were to accept a retrospective observational study in lieu of a CVOT, there would be no assurance that the EMA would accept the same.
Qsymia in Development for Obstructive Sleep Apnea
Obstructive sleep apnea, or OSA, is a chronic and potentially serious sleep disorder in which breathing is abnormally shallow, or hypopnea, or stops altogether, or apnea, for at least 10 seconds. These repetitive events are associated with collapse of the upper airway during sleep, and may occur five to thirty or more times per hour. Although many cases are unrecognized, symptoms may include snoring, fatigue or sleepiness during the day.
OSA afflicts approximately 3% to 7% of the U.S. population. Data from the Wisconsin Cohort Study indicate that the prevalence of OSA in people 30‑60 years of age is 9‑24% for men and 4‑9% for women. OSA is associated with an increased risk of hypertension, cardiovascular disease, myocardial infarction, stroke and increased mortality.
The current standard of care treatment for OSA is continuous positive airway pressure, or CPAP, in which the upper airway is kept open by increased air pressure, but CPAP provides benefits only when used consistently. Many patients find CPAP to be inconvenient or uncomfortable, and compliance with CPAP treatment limits its effectiveness.
9
We believe a safe and effective pharmacologic treatment for OSA could be useful and more acceptable to some patients than CPAP, but no drug is currently approved to treat OSA.
In January 2010, we announced positive results from a Phase 2 study evaluating the safety and efficacy of Qsymia for the treatment of moderate to severe OSA. This Phase 2 study (OB‑204) was a single‑center, randomized, double‑blind, placebo‑controlled parallel group trial including 45 obese men and women (BMI 30 to 40 kg/m2 inclusive), 30 to 65 years of age with OSA (apnea‑hypopnea index, or AHI, greater than or equal to 15 at baseline) who had not been treated with, or who were not compliant with CPAP, within three months of screening. Patients were randomized to placebo or top dose Qsymia. We are currently contemplating development of Qsymia for OSA, but expect no future development until the CVOT issue is resolved with the FDA.
Qsymia in Development for Diabetes
Diabetes is a disease in which the body does not produce or properly use insulin. Insulin is a hormone that is needed to convert sugar and starches into energy needed for daily life. Type 2 diabetes is characterized by inadequate response to insulin and/or inadequate secretion of insulin as blood glucose levels rise. Currently approved therapies for type 2 diabetes are directed toward correcting the body’s inadequate response with oral or injectable medications, or directly modifying insulin levels through injection of insulin or insulin analogs. The cause of diabetes continues to be a mystery, although both genetics and environmental factors such as obesity and lack of exercise appear to play roles.
In 2012, there were an estimated 29.1 million children and adults in the U.S., or 9.3% of the population, who have diabetes. While an estimated 21.0 million Americans have been diagnosed with diabetes, unfortunately, another 8.1 million Americans (or over one quarter) are unaware that they have the disease. It is estimated that there are nearly 350 million diabetics worldwide.
According to the American Diabetes Association, or ADA, an estimated 86 million Americans aged 20 or older have prediabetes and 1.4 million Americans are diagnosed with diabetes each year. Millions more are known to have metabolic syndrome, a cluster of symptoms that includes high blood pressure, large waist size, high levels of fats in the blood, and the body’s inability to handle glucose, which collectively increase a person’s chances of developing cardiovascular disease. Qsymia is not currently indicated for the treatment of hypertension, type 2 diabetes mellitus, prediabetes, stroke or heart disease.
In May 2013, the American Association of Clinical Endocrinologists introduced a new algorithm for the comprehensive management of weight in persons with prediabetes or type 2 diabetes in order to provide clinicians with a practical guide that considers the whole patient, the spectrum of risks and complications for the patient, and evidence‑based approaches to treatment. In addition to advocating for glycemic control, the treatment algorithm focuses on obesity and prediabetes as the underlying risk factors for diabetes and associated complications, and specifically includes pharmacotherapy as part of the recommended treatment paradigm for managing weight.
The currently approved oral medications for type 2 diabetes include insulin releasers such as glyburide, insulin sensitizers such as Actos® and Avandia®, inhibitors of glucose production by the liver such as metformin, DPP‑IV inhibitors like Januvia®, as well as Precose® and Glyset, which slow the uptake of glucose from the intestine. Approved injectable medications for type 2 diabetes treatment include glucagon‑like peptide‑1, or GLP‑1, analogs such as liraglutide, marketed under the brand name Victoza®, developed by Novo Nordisk and exenatide, marketed under the brand name Byetta®, and a long‑acting version of exenatide marketed under the brand name Bydureon®, developed by Amylin Pharmaceuticals and Eli Lilly and Company. Studies to date suggest GLP‑1s improve control of blood glucose by increasing insulin secretion, delaying gastric emptying, and suppressing prandial glucagon secretion. Clinical studies have reported that patients treated with GLP‑1s experienced weight loss of approximately six to eight pounds. Newer agents recently approved for type 2 diabetes include Invokana® (canaglifozin) from Johnson & Johnson’s Janssen Pharmaceuticals, a sodium glucose co‑transporter 2, or SGLT2, inhibitor that has demonstrated modest, single‑digit weight loss in clinical studies.
It is estimated that a significant portion of type 2 diabetics fail oral medications and require injected insulin therapy. Current oral medications for type 2 diabetes have a number of common drug‑related side effects, including
10
hypoglycemia, weight gain and edema. Numerous pharmaceutical and biotechnology companies are seeking to develop insulin sensitizers, novel insulin formulations and other therapeutics to improve the treatment of diabetes. Previous clinical studies of topiramate, a component of Qsymia, in type 2 diabetics resulted in a clinically meaningful reduction of hemoglobin A1c, or HbA1c, a measure used to determine treatment efficacy of anti‑diabetic agents.
In December 2008, we announced the results of our DM‑230 diabetes study. The DM‑230 Phase 2 study enrolled 130 patients, who had completed our Phase 2 study for the treatment of obesity (OB‑202), at 10 study sites in the U.S., to continue in a blinded fashion as previously randomized for an additional 28 weeks. The results of the DM‑230 study included assessments from the start of the OB‑202 study through the end of the DM‑230 study in this population, for a total treatment period of 56 weeks.
Patients treated with Qsymia had a reduction in HbA1c of 1.6%, from 8.8% to 7.2%, as compared to 1.1% from 8.5% to 7.4% in the placebo‑treated standard of care group (Intent to Treat population Using the Last Observation Carried Forward Method, or ITT LOCF, p=0.0381) at 56 weeks. All patients in the study were actively managed according to the ADA standards of care with respect to diabetes medications and lifestyle modification. For patients treated with placebo, increases in the number and doses of concurrent anti‑diabetic medications were required to bring about the observed reduction in HbA1c. By contrast, concurrent anti‑diabetic medications were reduced over the course of the trial in patients treated with Qsymia (p<0.05).
Over 56 weeks, patients treated with Qsymia also lost 9.4% of their baseline body weight, or 20.5 pounds, as compared to 2.7%, or 6.1 pounds, for the placebo group (p<0.0001). Sixty‑five percent of the Qsymia patients lost at least 5% of their body weight, as compared to 24% in the placebo group (p<0.001), and 37% of the Qsymia patients lost at least 10% of their body weight, as compared to 9% of patients in the placebo group (p<0.001). Patients treated with Qsymia had reductions in blood pressure, triglycerides and waist circumference. Both treatment groups had a study completion rate of greater than 90%.
The most common drug‑related side effects reported were tingling, constipation and nausea. Patients on antidepressants such as selective serotonin reuptake inhibitors, or SSRIs, or serotonin and norepinephrine reuptake inhibitors, or SNRIs, were allowed to participate in the studies. Patients were monitored for depression and suicidality using the Patient Health Questionnaire‑9, or PHQ‑9, a validated mental health assessment tool agreed to by the FDA for use in our studies. Patients treated with Qsymia demonstrated greater improvements in PHQ‑9 scores from baseline to the end of the study than patients in the placebo group.
Despite a mean baseline HbA1c level of 8.8%, 53% of the patients treated with Qsymia were able to achieve the ADA recommended goal of 7% or lower, versus 40% of the patients in the placebo arm (p<0.05). The incidence of hypoglycemia in the treatment and placebo arms was similar (12% and 9%, respectively). Patients in the Qsymia arm experienced no treatment‑related serious adverse events.
We also studied the effect of Qsymia on well‑controlled diabetics as part of our Phase 3 obesity study, CONQUER (OB‑303). The results were consistent and supportive of the Phase 2 results.
Data from the EQUATE trial (OB‑301) Phase 3 demonstrated that weight loss with Qsymia stops the progression of type 2 diabetes in obese, non‑diabetic patients. The results of DM‑230 demonstrated that weight loss with Qsymia can significantly lower blood sugar in type 2 diabetics. Results from both of these studies were presented at the ADA’s annual scientific session in June 2009.
In October 2013, we announced new data published online in Diabetes Care demonstrating the effects of Qsymia on the progression to type 2 diabetes. In the study, high‑risk overweight or obese patients with prediabetes and/or metabolic syndrome who were taking Qsymia over a two‑year period experienced reductions of up to 78.7% in the annualized incidence rate of type 2 diabetes, in addition to losing weight. The American Association of Clinical Endocrinologists recognizes obesity and prediabetes as significant risk factors for progression to diabetes and associated complications.
11
The publication analyzed 475 high‑risk overweight or obese patients with prediabetes and/or metabolic syndrome at baseline from the two‑year SEQUEL study, for their progression to type 2 diabetes and their changes in cardiometabolic parameters. After 108 weeks, it was observed that patients receiving Qsymia, in conjunction with lifestyle modifications, experienced significant weight loss along with markedly reduced progression to type 2 diabetes and improvements in multiple cardiometabolic disease risk factors.
Subjects in the Qsymia recommended dose (7.5mg/46mg) and top dose (15mg/92mg) treatment groups experienced reductions of 70.5% and 78.7% in the annualized incidence rate of type 2 diabetes, respectively, versus placebo, which was related to degree of weight lost (10.9% and 12.1%, respectively, versus 2.5% with placebo; ITT‑MI; P < 0.0001). Qsymia therapy was well tolerated by this subgroup over two years.
Among patients in the study taking Qsymia, common adverse events included paraesthesia, or tingling in the fingers or feet, sinusitis, dry mouth, constipation, headache, and dysgeusia, or change in perception of taste. The types and severity of adverse events seen in this subgroup analysis were similar to those seen in the overall SEQUEL patient population and in other clinical trials.
We are currently contemplating further development of Qsymia for the treatment of diabetes, but expect no future development until the CVOT issue is resolved with the FDA.
Qsymia in Development for Other Indications
We believe Qsymia may be helpful in treating other obesity‑related diseases, including nonalcoholic steatohepatitis, or NASH, or its precursor, nonalcoholic fatty liver disease, or NAFLD, also known as fatty liver disease. We believe Qsymia may also be helpful in treating hyperlipidemia, or an elevation of lipids, or fats, in the bloodstream. These lipids include cholesterol, cholesterol esters, or compounds, phospholipids and triglycerides. In addition, we believe Qsymia may be helpful in patients with hypertension who do not respond well to antihypertensive medication. We are currently contemplating whether to pursue these other indications, but expect no future development until the CVOT issue is resolved with the FDA.
STENDRA for the Treatment of Erectile Dysfunction
ED affects an estimated 52% of men between the ages of 40 and 70. Prevalence increases with age and can be caused by a variety of factors, including medications (anti‑hypertensives, histamine receptor antagonists); lifestyle (tobacco, alcohol use); diseases (diabetes, cardiovascular conditions, prostate cancer); and spinal cord injuries. Left untreated, ED can negatively impact relationships and self‑esteem, causing feelings of embarrassment and guilt. About half of men being treated with currently available phosphodiesterase 5, or PDE5, inhibitors are dissatisfied with treatment. The market opportunity for ED medical treatments continues to grow, with worldwide sales of PDE5 inhibitors exceeding $5 billion in 2012.
STENDRA is an oral PDE5 inhibitor we have licensed from MTPC. STENDRA was approved in the U.S. by the FDA on April 27, 2012, for the treatment of ED. As part of the approval of STENDRA, we were committed to conduct two post‑approval clinical studies. The first was a randomized, double‑blind, placebo‑controlled, parallel group multicenter clinical trial on the effect of STENDRA on spermatogenesis in healthy adult males and males with mild ED. The other study was a double‑blind, randomized, placebo‑controlled, single‑dose clinical trial to assess the effects of STENDRA on multiple parameters of vision, including, but not limited to, visual acuity, intraocular pressure, pupillometry, and color vision discrimination in healthy male subjects. These studies are completed.
On June 19, 2013, we announced clinical study results showing avanafil is effective for sexual activity within 15 minutes in men with ED. In the 440‑patient study conducted at 30 sites in the U.S., STENDRA patients achieved statistically significant improvement versus placebo in the mean proportion of attempts that resulted in erections sufficient for successful intercourse as early as 10 minutes for the 200‑mg dose and 12 minutes for the 100‑mg dose following administration. On September 18, 2014, the FDA approved an sNDA for STENDRA. STENDRA is now indicated to be taken as early as approximately 15 minutes before sexual activity. On January 23, 2015, the EC adopted
12
the commission implementing decision amending the marketing authorization for SPEDRA. SPEDRA is now approved in the EU to be taken as needed approximately 15 to 30 minutes before sexual activity.
We have granted an exclusive license to Menarini to commercialize and promote SPEDRA for the treatment of ED in over 40 European countries, including the EU, plus Australia and New Zealand. In addition, we had granted an exclusive license to Auxilium to market STENDRA in the United States and Canada. Auxilium was purchased by Endo in January 2015. In December 2015, Auxilium notified us of its intention to return the U.S. and Canadian commercial rights for STENDRA to us. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016. We have also granted an exclusive license to Sanofi to commercialize avanafil in Africa, the Middle East, Turkey, and the CIS, including Russia. We are currently in discussions with potential partners to commercialize STENDRA in other territories under our license with MTPC in which we do not currently have a commercial collaboration. We have engaged a strategic advisor to assist us in the evaluation of our alternatives not only for STENDRA, but also for our overall business strategy.
Other Programs
We have licensed and intend to continue to license from third parties the rights to other investigational drug candidates to treat various diseases and medical conditions. We also sponsor early‑stage clinical trials at various research institutions and intend to conduct early‑stage proof of concept studies on our own. We expect to continue to use our expertise in designing and conducting clinical trials, formulation and investigational drug candidate development to commercialize pharmaceuticals for unmet medical needs or for disease states that are underserved by currently approved drugs. We intend to develop products with a proprietary position or that complement our other products currently under development, although there can be no assurance that any of these investigational product candidates will be successfully developed and approved by regulatory authorities.
Government Regulations
FDA Regulation
Prescription pharmaceutical products are subject to extensive pre‑ and post‑marketing regulation by the FDA. The Federal Food, Drug, and Cosmetic Act, and its implementing regulations govern, among other things, requirements for the testing, development, manufacturing, quality control, safety, efficacy, approval, labeling, storage, recordkeeping, reporting, distribution, import, export, advertising and promotion of drug products.
The activities required before a pharmaceutical agent may be marketed in the U.S. begin with pre‑clinical testing. Pre‑clinical tests generally include laboratory evaluation of potential products and animal studies to assess the potential safety and efficacy of the product and its formulations. The results of these studies and other information must be submitted to the FDA as part of an investigational new drug application, or IND, which must be reviewed by the FDA before proposed clinical testing in human volunteers can begin. Clinical trials involve the administration of the investigational new drug to healthy volunteers or to patients under the supervision of a qualified principal investigator. Clinical trials must be conducted in accordance with good clinical practices, or GCP, which establishes standards for conducting, recording data from, and reporting results of, clinical trials, and are intended to assure that the data and reported results are credible, accurate, and that the rights, safety and well‑being of study participants are protected. Clinical trials must be under protocols that detail the objectives of the study, the parameters to be used to monitor safety and the efficacy criteria to be evaluated. Each protocol must be submitted to the FDA as part of the IND. Further, each clinical study must be conducted under the auspices of an independent institutional review board, or IRB. The IRB will consider, among other things, regulations and guidelines for obtaining informed consent from study subjects, as well as other ethical factors and the safety of human patients. The sponsoring company, the FDA, or the IRB may suspend or terminate a clinical trial at any time on various grounds, including a finding that the subjects or patients are being exposed to an unacceptable health risk.
Typically, human clinical trials are conducted in three phases that may overlap. In Phase 1, clinical trials are conducted with a small number of patients to determine the early safety profile and pharmacology of the new therapy. In
13
Phase 2, clinical trials are conducted with groups of patients afflicted with a specific disease or medical condition in order to determine preliminary efficacy, optimal dosages and expanded evidence of safety. In Phase 3, large‑scale, multicenter clinical trials are conducted with patients afflicted with a target disease or medical condition in order to provide substantial evidence of efficacy and safety required by the FDA and others.
The results of the pre‑clinical and clinical testing, together with chemistry and manufacturing information, are submitted to the FDA in the form of a New Drug Application, or NDA, for a pharmaceutical product in order to obtain approval to commence commercial sales. In responding to an NDA, the FDA may grant marketing approvals, may request additional information or further research or studies, or may deny the application if it determines that the application does not satisfy its regulatory approval criteria. FDA approval for a pharmaceutical product may not be granted on a timely basis, if at all. Under the goals and policies agreed to by the FDA under the Prescription Drug User Fee Act, or PDUFA, the FDA has twelve months in which to complete its initial review of a standard NDA and respond to the applicant, and eight months for a priority NDA. The FDA does not always meet its PDUFA goal dates and in certain circumstances, the review process and the PDUFA goal date may be extended. A subsequent application for approval of an additional indication must also be reviewed by the FDA under the same criteria as apply to original applications, and may be denied as well. In addition, even if FDA approval is granted, it may not cover all the clinical indications for which approval is sought or may contain significant limitations in the form of warnings, precautions or contraindications with respect to conditions of use. In addition, the FDA may require the development and implementation of a Risk Evaluation and Mitigation Strategy, or REMS, to address specific safety issues at the time of approval or after marketing of the product. A REMS may, for instance, restrict distribution and impose burdensome implementation requirements. Our approved product Qsymia is subject to a REMS program.
Satisfaction of FDA premarket approval requirements for new drugs typically takes several years and the actual time required may vary substantially based upon the type, complexity and novelty of the product or targeted disease. Government regulation may delay or prevent marketing of potential products for a considerable period of time and may impose costly procedures upon our activities. Success in early‑stage clinical trials or with prior versions of products does not assure success in later stage clinical trials. Data obtained from clinical activities are not always conclusive and may be susceptible to varying interpretations that could delay, limit or prevent regulatory approval.
Once approved, products are subject to continuing regulation by the FDA. The FDA may withdraw the product approval if compliance with post‑marketing regulatory standards is not maintained or if problems occur after the product reaches the marketplace. In addition, the FDA may require post‑marketing studies or trials, referred to as PMRs, to evaluate safety issues related to the approved product, and may withdraw approval or impose marketing restrictions based on the results of post‑market studies or trials or other relevant data. The FDA has required us to perform PMR studies and trials for both of our approved products, Qsymia and STENDRA. The FDA has broad post‑market regulatory and enforcement powers, including the ability to levy fines and civil penalties, suspend or delay issuance of approvals, seize or recall products, or withdraw approvals. Additionally, the Food and Drug Administration Amendments Act of 2007 requires all clinical trials we conduct for our investigational drug candidates, both before and after approval, and the results of those trials when available, to be included in a clinical trials registry database that is available and accessible to the public via the Internet. Our failure to properly participate in the clinical trial database registry may subject us to significant civil penalties.
Facilities used to manufacture drugs are subject to periodic inspection by the FDA, and other authorities where applicable, and must comply with the FDA’s current Good Manufacturing Practice, or cGMP regulations. Compliance with cGMP includes adhering to requirements relating to organization of personnel, buildings and facilities, equipment, control of components and drug product containers and closures, production and process controls, packaging and labeling controls, holding and distribution, laboratory controls, and records and reports. Failure to comply with the statutory and regulatory requirements subjects the manufacturer to possible legal or regulatory action, such as suspension of manufacturing, seizure of product or voluntary recall of a product.
The FDA imposes a number of complex regulations on entities that advertise and promote pharmaceuticals, which include, among other things, standards and regulations relating to direct‑to‑consumer advertising, off‑label promotion, industry‑sponsored scientific and educational activities, and promotional activities involving the Internet. A product cannot be commercially promoted before it is approved. After approval, product promotion can include only
14
those claims relating to safety and effectiveness that are consistent with the labeling approved by the FDA. The FDA has very broad enforcement authority. Failure to abide by these regulations can result in adverse publicity, and/or enforcement actions, including the issuance of a warning letter directing the entity to correct deviations from FDA standards, and state and federal civil and criminal investigations and prosecutions. This could subject a company to a range of penalties that could have a significant commercial impact, including civil and criminal fines and agreements that materially restrict the manner in which a company promotes or distributes drug products.
Companies that manufacture or distribute drug products or that hold approved NDAs must comply with other regulatory requirements, including submitting annual reports, reporting information about adverse drug experiences, and maintaining certain records. In addition, we are subject to various laws and regulations regarding the use and disposal of hazardous or potentially hazardous substances in connection with our manufacture and research. In each of these areas, as noted above, the government has broad regulatory and enforcement powers, including the ability to levy fines and civil penalties, suspend or delay issuance of approvals, seize or recall products, and withdraw approvals, any one or more of which could have a material adverse effect upon us.
Other Government Regulations
In addition to laws and regulations enforced by the FDA, we are also subject to regulation under National Institutes of Health guidelines as well as under the Controlled Substances Act, the Occupational Safety and Health Act, the Environmental Protection Act, the Toxic Substances Control Act, the Resource Conservation and Recovery Act and other present and potential future federal, state or local laws and regulations, as our research and development may involve the controlled use of hazardous materials, chemicals, viruses and various radioactive compounds.
In addition to regulations in the U.S., we are subject to a variety of foreign regulations governing clinical trials, commercial sales, and distribution of our investigational drug candidates. We must obtain separate approvals by the comparable regulatory authorities of foreign countries before we can commence marketing of the product in those countries. For example, in the EU, the conduct of clinical trials is governed by Directive 2001/20/EC which imposes obligations and procedures that are similar to those provided in applicable US laws. The European Union Good Clinical Practice rules, or GCP, and EU Good Laboratory Practice, or GLP, obligations must also be respected during conduct of the trials. Clinical trials must be approved by the competent authorities and the competent Ethics Committees in the EU Member States in which the clinical trials take place. A clinical trial application, or CTA, must be submitted to each EU Member State’s national health authority. Moreover, an application for a positive opinion must be submitted to the competent Ethics Committee prior to commencement of clinical trials of a medicinal product. The competent authorities of the EU Member States in which the clinical trial is conducted must authorize the conduct of the trial and the competent Ethics Committees must grant their positive opinion prior to commencement of a clinical trial in an EU Member State. The approval process varies from country to country, and the time may be longer or shorter than that required for FDA approval. The requirements governing the conduct of clinical trials, product licensing, pricing and reimbursement vary greatly from country to country.
To obtain marketing approval of a medicinal product in the EU, we would be required to submit marketing authorization applications based on the ICH Common Technical Document to the competent authorities, and must demonstrate the quality, safety and efficacy of our medicinal products. This would require us to conduct human clinical trials to generate the necessary clinical data. Moreover, we would be required to demonstrate in our application that studies have been conducted with the medicinal product in the pediatric population as provided by a Pediatric Investigation Plan, or PIP, approved by the Pediatric Committee of the EMA. Alternatively, confirmation that we have been granted a waiver or deferral from the conduct of these studies must be provided.
Medicinal products are authorized in the EU in one of two ways, either by the competent authorities of the EU Member States through the decentralized procedure or mutual recognition procedure, or through the centralized procedure by the European Commission following a positive opinion by the EMA. The authorization process is essentially the same irrespective of which route is used.
The centralized procedure provides for the grant of a single marketing authorization that is valid for all EU Member States. The centralized procedure is compulsory for medicinal products produced by certain biotechnological
15
processes, products designated as orphan medicinal products, and products with a new active substance indicated for the treatment of certain diseases. It is optional for those products that are highly innovative or for which a centralized process is in the interest of patients. Under the centralized procedure in the EU, the maximum timeframe for the evaluation of a marketing authorization application is 210 days (excluding clock stops, when additional written or oral information is to be provided by the applicant in response to questions asked by the CHMP). Accelerated evaluation may be granted by the CHMP in exceptional cases. These are defined as circumstances in which a medicinal product is expected to be of a “major public health interest.” Three cumulative criteria must be fulfilled in such circumstances: the seriousness of the disease, such as heavy disabling or life‑threatening diseases, to be treated; the absence or insufficiency of an appropriate alternative therapeutic approach; and anticipation of high therapeutic benefit. In these circumstances, the EMA ensures that the opinion of the CHMP is given within 150 days.
The decentralized procedure provides for approval by one or more other (“concerned”) EU Member States of an assessment of an application for marketing authorization conducted by one EU Member State, known as the reference EU Member State. In accordance with this procedure, an applicant submits an application for marketing authorization to the reference EU Member State and the concerned EU Member States. This application is identical to the application that would be submitted to the EMA for authorization through the centralized procedure. The reference EU Member State prepares a draft assessment and drafts of the related materials within 120 days after receipt of a valid application. The resulting assessment report is submitted to the concerned EU Member States who, within 90 days of receipt must decide whether to approve the assessment report and related materials. If a concerned EU Member State cannot approve the assessment report and related materials due to concerns relating to a potential serious risk to public health, disputed elements may be referred to the European Commission, whose decision is binding on all EU Member States. In accordance with the mutual recognition procedure, the sponsor applies for national marketing authorization in one EU Member State. Upon receipt of this authorization the sponsor can then seek the recognition of this authorization by other EU Member States. Authorization in accordance with either of these procedures will result in authorization of the medicinal product only in the reference EU Member State and in the other concerned EU Member States.
Innovative medicinal products authorized in the EU on the basis of a full marketing authorization application (as opposed to an application for marketing authorization that relies on data available in the marketing authorization dossier for another, previously approved, medicinal product) are entitled to eight years’ data exclusivity. During this period, applicants for authorization of generics or biosimilars of these innovative products cannot rely on data contained in the marketing authorization dossier submitted for the innovative medicinal product. Innovative medicinal products are also entitled to ten years’ market exclusivity. During this ten year period no generic or biosimilar of this medicinal product can be placed on the EU market. The ten‑year period of market exclusivity can be extended to a maximum of 11 years if, during the first eight years of those ten years, the Marketing Authorization Holder for the innovative product obtains an authorization for one or more new therapeutic indications which, during the scientific evaluation prior to their authorization, are held to bring a significant clinical benefit in comparison with existing therapies.
Similarly to the U.S., marketing authorization holders and manufacturers of medicinal products are subject to comprehensive regulatory oversight by the EMA and/or the competent authorities of the EU Member States. This oversight applies both before and after grant of manufacturing and marketing authorizations. It includes control of compliance with EU GMP rules and pharmacovigilance rules. We cannot guarantee that we would be able to comply with the post‑marketing obligations imposed as part of the marketing authorization for SPEDRA. Failure to comply with these requirements may lead to the suspension, variation or withdrawal of the marketing authorization for SPEDRA in the EU.
In the EU, the advertising and promotion of our products will also be subject to EU Member States’ laws concerning promotion of medicinal products, interactions with physicians, misleading and comparative advertising and unfair commercial practices, as well as other EU Member State legislation that may apply to the advertising and promotion of medicinal products. These laws require that promotional materials and advertising in relation to medicinal products comply with the product’s Summary of Product Characteristics, or SmPC, as approved by the competent authorities. The SmPC is the document that provides information to physicians concerning the safe and effective use of the medicinal product. It forms an intrinsic and integral part of the marketing authorization granted for the medicinal product. Promotion of a medicinal product that does not comply with the SmPC is considered to constitute off‑label promotion. The off‑label promotion of medicinal products is prohibited in the EU. The applicable laws at the EU level
16
and in the individual EU Member States also prohibit the direct‑to‑consumer advertising of prescription‑only medicinal products. Violations of the rules governing the promotion of medicinal products in the EU could be penalized by administrative measures, fines and imprisonment. These laws may further limit or restrict communications concerning the advertising and promotion of our products to the general public and may also impose limitations on our promotional activities with healthcare professionals.
Failure to comply with the EU Member State laws implementing the Community Code on medicinal products, and EU rules governing the promotion of medicinal products, interactions with physicians, misleading and comparative advertising and unfair commercial practices, with the EU Member State laws that apply to the promotion of medicinal products, statutory health insurance, bribery and anti‑corruption or with other applicable regulatory requirements can result in enforcement action by the EU Member State authorities, which may include any of the following: fines, imprisonment, orders forfeiting products or prohibiting or suspending their supply to the market, or requiring the manufacturer to issue public warnings, or to conduct a product recall.
Interactions between pharmaceutical companies and physicians are also governed by strict laws, regulations, industry self‑regulation codes of conduct and physicians’ codes of professional conduct in the individual EU Member States. The provision of benefits or advantages to physicians to induce or encourage the prescription, recommendation, endorsement, purchase, supply, order or use of medicinal products is prohibited in the EU. The provision of benefits or advantages to physicians is also governed by the national anti‑bribery laws of the EU Member States. One example is the UK Bribery Act 2010. This Act applies to any company incorporated in or “carrying on business” in the UK, irrespective of where in the world the alleged bribery activity occurs. This Act could have implications for our interactions with physicians in and outside the UK. Violation of these laws could result in substantial fines and imprisonment.
Payments made to physicians in certain EU Member States must be publically disclosed. Moreover, agreements with physicians must often be the subject of prior notification and approval by the physician’s employer, his/her competent professional organization, and/or the competent authorities of the individual EU Member States. These requirements are provided in the national laws, industry codes, or professional codes of conduct, applicable in the EU Member States. Failure to comply with these requirements could result in reputational risk, public reprimands, administrative penalties, fines or imprisonment.
United States Healthcare Reform
In March 2010, the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010, collectively referred to in this report as the Affordable Care Act was adopted in the United States. This law substantially changed the way healthcare is financed by both governmental and private insurers and significantly impacted the pharmaceutical industry. The Affordable Care Act contains a number of provisions that are expected to impact our business and operations. Changes that may affect our business include those governing enrollment in federal healthcare programs, reimbursement changes, rules regarding prescription drug benefits under the health insurance exchanges, expansion of the 340B program, and fraud and abuse and enforcement. These changes will impact existing government healthcare programs and will result in the development of new programs, including Medicare payment for performance initiatives and improvements to the physician quality reporting system and feedback program.
The Affordable Care Act made significant changes to the Medicaid Drug Rebate program. Effective March 23, 2010, rebate liability expanded from fee‑for‑service Medicaid utilization to include the utilization of Medicaid managed care organizations as well. With regard to the amount of the rebates owed, the Affordable Care Act increased the minimum Medicaid rebate from 15.1% to 23.1% of the average manufacturer price for most innovator products and from 11% to 13% for non‑innovator products; changed the calculation of the rebate for certain innovator products that qualify as line extensions of existing drugs; and capped the total rebate amount for innovator drugs at 100% of the average manufacturer price. In addition, the Affordable Care Act and subsequent legislation changed the definition of average manufacturer price. In February 2016,, the Centers for Medicare and Medicaid Services, or CMS, the federal agency that administers Medicare and the Medicaid Drug Rebate program, issued final regulations to implement the changes to the Medicaid Drug Rebate program under the Affordable Care Act. These regulations become effective on April 1, 2016. We are evaluating the impact of these regulations on our business and operations. In addition, the Affordable Care Act
17
requires pharmaceutical manufacturers of branded prescription drugs to pay a branded prescription drug fee to the federal government beginning in 2011. Each individual pharmaceutical manufacturer pays a prorated share of the branded prescription drug fee of $3.0 billion in 2016, based on the dollar value of its branded prescription drug sales to certain federal programs identified in the law.
Additional provisions of the Affordable Care Act may negatively affect our revenues in the future. For example, as part of the Affordable Care Act’s provisions closing a coverage gap that currently exists in the Medicare Part D prescription drug program, or the donut hole, manufacturers are required to provide a 50% discount on branded prescription drugs dispensed to beneficiaries within this donut hole. We currently do not have coverage under Medicare Part D for our drugs, but this could change in the future.
The Affordable Care Act also expanded the Public Health Service’s 340B drug pricing discount program. The 340B pricing program requires participating manufacturers to agree to charge statutorily defined covered entities no more than the 340B “ceiling price” for the manufacturer’s covered outpatient drugs. The Affordable Care Act expanded the 340B program to include additional types of covered entities: certain free‑standing cancer hospitals, critical access hospitals, rural referral centers and sole community hospitals, each as defined by the Affordable Care Act. The Affordable Care Act also obligates the Secretary of the Department of Health and Human Services to create regulations and processes to improve the integrity of the 340B program and to ensure the agreement that manufacturers must sign to participate in the 340B program obligates a manufacturer to offer the 340B price to covered entities if the manufacturer makes the drug available to any other purchaser at any price and to report to the government the ceiling prices for its drugs. The Health Resources and Services Administration, or HRSA, the agency that administers the 340B program, recently issued a proposed regulation regarding the calculation of the 340B ceiling price and the imposition of civil monetary penalties on manufacturers that knowingly and intentionally overcharge covered entities, as well as proposed omnibus guidance that addresses many aspects of the 340B program. HRSA is currently expected to issue additional proposed regulations in 2016. When such regulations and guidance are finalized, they could affect our obligations under the 340B program in ways we cannot anticipate. In addition, legislation may be introduced that, if passed, would further expand the 340B program to additional covered entities or would require participating manufacturers to agree to provide 340B discounted pricing on drugs used in the inpatient setting.
Some states have elected not to expand their Medicaid programs by raising the income limit to 133% of the federal poverty level as permitted under the Affordable Care Act. For each state that does not choose to expand its Medicaid program, there may be fewer insured patients overall, which could impact our sales, business and financial condition.
Coverage and Reimbursement
In both U.S. and foreign markets, our ability to commercialize our products successfully and to attract commercialization partners for our products, depends in significant part on the availability of adequate financial coverage and reimbursement from third‑party payors, including, in the United States, governmental payors such as Medicare and Medicaid, as well as managed care organizations, private health insurers and other organizations. Third‑party payors decide which drugs they will pay for and establish reimbursement and co‑pay levels. Third‑party payors are increasingly challenging the prices charged for medicines and examining their cost‑effectiveness, in addition to their safety and efficacy. We may need to conduct expensive pharmacoeconomic studies in order to demonstrate the cost‑effectiveness of our products. Even with studies, our products may be considered less safe, less effective or less cost‑effective than existing products, and third‑party payors may not provide coverage and reimbursement for our product candidates, in whole or in part.
Political, economic and regulatory influences are subjecting the healthcare industry in the United States to fundamental changes. There have been, and we expect there will continue to be, legislative and regulatory proposals to change the healthcare system in ways that could impact our ability to sell our products profitably. We anticipate that the United States Congress, state legislatures and the private sector will continue to consider and may adopt healthcare policies intended to curb rising healthcare costs. These cost‑containment measures include: controls on government funded reimbursement for drugs; new or increased requirements to pay prescription drug rebates to government healthcare programs; controls on healthcare providers; challenges to the pricing of drugs or limits or prohibitions on
18
reimbursement for specific products through other means; requirements to try less expensive products or generics before a more expensive branded product; changes in drug importation laws; expansion of use of managed care systems in which healthcare providers contract to provide comprehensive healthcare for a fixed cost per person; and public funding for cost‑effectiveness research, which may be used by government and private third‑party payors to make coverage and payment decisions. Further, federal budgetary concerns could result in the implementation of significant federal spending cuts, including cuts in Medicare and other health related spending in the near‑term. For example, beginning April 2013, Medicare payments were reduced by up to 2% under sequestration and, through subsequent legislation, those reductions will continue to 2025.
Payors also are increasingly considering new metrics as the basis for reimbursement rates, such as average sales price, average manufacturer price and Actual Acquisition Cost. The existing data for reimbursement based on these metrics is relatively limited, although certain states have begun to survey acquisition cost data for the purpose of setting Medicaid reimbursement rates. CMS surveys and publishes retail community pharmacy acquisition cost information in the form of National Average Drug Acquisition Cost, or NADAC, files to provide state Medicaid agencies with a basis of comparison for their own reimbursement and pricing methodologies and rates. It may be difficult to project the impact of these evolving reimbursement mechanics on the willingness of payors to cover our products.
We participate in the Medicaid Drug Rebate program, established by the Omnibus Budget Reconciliation Act of 1990 and amended by the Veterans Health Care Act of 1992 as well as subsequent legislation. Under the Medicaid Drug Rebate program, we are required to pay a rebate to each state Medicaid program for our covered outpatient drugs that are dispensed to Medicaid beneficiaries and paid for by a state Medicaid program as a condition of having federal funds being made available to the states for our drugs under Medicaid and Medicare Part B. Those rebates are based on pricing data reported by us on a monthly and quarterly basis to CMS. These data include the average manufacturer price and, in the case of innovator products, the best price for each drug.
Federal law requires that any company that participates in the Medicaid Drug Rebate program also participate in the Public Health Service’s 340B drug pricing discount program in order for federal funds to be available for the manufacturer’s drugs under Medicaid and Medicare Part B. The 340B pricing program requires participating manufacturers to agree to charge statutorily defined covered entities no more than the 340B “ceiling price” for the manufacturer’s covered outpatient drugs. These 340B covered entities include a variety of community health clinics and other entities that receive health services grants from the Public Health Service, as well as hospitals that serve a disproportionate share of low‑income patients. The 340B ceiling price is calculated using a statutory formula, which is based on the average manufacturer price and rebate amount for the covered outpatient drug as calculated under the Medicaid Drug Rebate program. Changes to the definition of average manufacturer price and the Medicaid Drug Rebate amount under the Affordable Care Act and CMS’s issuance of final regulations implementing those changes also could affect our 340B ceiling price calculations and negatively impact our results of operations.
In order to be eligible to have our products paid for with federal funds under the Medicaid and Medicare Part B programs and purchased by certain federal agencies and certain federal grantees, we participate in the Department of Veterans Affairs, or VA, Federal Supply Schedule, or FSS, pricing program, established by Section 603 of the Veterans Health Care Act of 1992. Under this program, we are obligated to make our product available for procurement on an FSS contract and charge a price to four federal agencies—VA, Department of Defense, Public Health Service, and Coast Guard—that is no higher than the statutory Federal Ceiling Price, or FCP. The FCP is based on the non‑federal average manufacturer price, or Non‑FAMP, which we calculate and report to the VA on a quarterly and annual basis. We also participate in the Tricare Retail Pharmacy program, established by Section 703 of the National Defense Authorization Act for FY 2008, and related regulations, under which we pay quarterly rebates on utilization of innovator products that are dispensed to Tricare beneficiaries. The rebates are calculated as the difference between Annual Non‑FAMP and FCP.
We expect to experience pricing pressures in the United States in connection with the sale of our products due to the trend toward managed healthcare, the increasing influence of health maintenance organizations and additional legislative proposals. In various EU countries, we expect to be subject to continuous cost‑cutting measures, such as lower maximum prices, lower or lack of reimbursement coverage and incentives to use cheaper, usually generic, products as an alternative.
19
We are unable to predict what additional legislation, regulations or policies, if any, relating to the healthcare industry or third‑party coverage and reimbursement may be enacted in the future or what effect such legislation, regulations or policies would have on our business. Any cost‑containment measures, including those listed above, or other healthcare system reforms that are adopted, could have a material adverse effect on our ability to operate profitably.
Once an applicant receives marketing authorization in an EU Member State, through any application route, the applicant is then required to engage in pricing discussions and negotiations with a separate pricing authority in that country. The legislators, policymakers and healthcare insurance funds in the EU Member States continue to propose and implement cost‑containing measures to keep healthcare costs down, due in part to the attention being paid to healthcare cost‑containment and other austerity measures in the EU. Certain of these changes could impose limitations on the prices pharmaceutical companies are able to charge for their products. The amounts of reimbursement available from governmental agencies or third‑party payors for these products may increase the tax obligations on pharmaceutical companies such as ours, or may facilitate the introduction of generic competition with respect to our products. Furthermore, an increasing number of EU Member States and other foreign countries use prices for medicinal products established in other countries as “reference prices” to help determine the price of the product in their own territory. Consequently, a downward trend in prices of medicinal products in some countries could contribute to similar downward trends elsewhere. In addition, the ongoing budgetary difficulties faced by a number of EU Member States, including Greece and Spain, have led and may continue to lead to substantial delays in payment and payment partially with government bonds rather than cash for medicinal products, which could negatively impact our revenues and profitability. Moreover, in order to obtain reimbursement of our medicinal products in some countries, including some EU Member States, we may be required to conduct Health Technology Assessments, or HTAs, that compare the cost‑effectiveness of our products to other available therapies. There can be no assurance that our medicinal products will obtain favorable reimbursement status in any country.
In the EU, the sole legal instrument at the EU level governing the pricing and reimbursement of medicinal products is Council Directive 89/105/EEC, or the Price Transparency Directive. The aim of this Directive is to ensure that pricing and reimbursement mechanisms established in the EU Member States are transparent and objective, do not hinder the free movement and trade of medicinal products in the EU and do not hinder, prevent or distort competition on the market. The Price Transparency Directive does not provide any guidance concerning the specific criteria on the basis of which pricing and reimbursement decisions are to be made in individual EU Member States. Neither does it have any direct consequence for pricing nor reimbursement levels in individual EU Member States. The EU Member States are free to restrict the range of medicinal products for which their national health insurance systems provide reimbursement and to control the prices and/or reimbursement levels of medicinal products for human use. An EU Member State may approve a specific price or level of reimbursement for the medicinal product, or alternatively adopt a system of direct or indirect controls on the profitability of the company responsible for placing the medicinal product on the market, including volume‑based arrangements and reference pricing mechanisms.
Health Technology Assessment, or HTA, of medicinal products is becoming an increasingly common part of the pricing and reimbursement procedures in some EU Member States. These EU Member States include the United Kingdom, France, Germany and Sweden. The HTA process in the EEA Member States is governed by the national laws of these countries. HTA is the procedure according to which the assessment of the public health impact, therapeutic impact and the economic and societal impact of use of a given medicinal product in the national healthcare systems of the individual country is conducted. HTA generally focuses on the clinical efficacy and effectiveness, safety, cost, and cost‑effectiveness of individual medicinal products as well as their potential implications for the healthcare system. Those elements of medicinal products are compared with other treatment options available on the market.
The outcome of HTA regarding specific medicinal products will often influence the pricing and reimbursement status granted to these medicinal products by the competent authorities of individual EU Member States. The extent to which pricing and reimbursement decisions are influenced by the HTA of the specific medicinal product vary between EU Member States.
In 2011, Directive 2011/24/EU was adopted at the EU level. This Directive concerns the application of patients’ rights in cross‑border healthcare. The Directive is intended to establish rules for facilitating access to safe and
20
high‑quality cross‑border healthcare in the EU. It also provides for the establishment of a voluntary network of national authorities or bodies responsible for HTA in the individual EU Member States. The purpose of the network is to facilitate and support the exchange of scientific information concerning HTAs. This could lead to harmonization between EU Member States of the criteria taken into account in the conduct of HTA and their impact on pricing and reimbursement decisions.
Fraud and Abuse and Privacy and Data Security Laws and Regulations
The healthcare industry, and thus our business, is subject to extensive federal, state, local and foreign regulation. Some of the pertinent laws have not been definitively interpreted by the regulatory authorities or the courts, and their provisions are open to a variety of interpretations. In addition, these laws and their interpretations are subject to change. Both federal and state governmental agencies continue to subject the healthcare industry to intense regulatory scrutiny, including heightened civil and criminal enforcement efforts.
The restrictions under applicable federal and state healthcare fraud and abuse and privacy and data security laws and regulations that may affect our ability to operate include, but are not limited to:
|
· |
the federal Anti‑Kickback Law, which prohibits, among other things, knowingly or willingly offering, paying, soliciting or receiving remuneration, directly or indirectly, in cash or in kind, to induce or reward the purchasing, leasing, ordering or arranging for or recommending the purchase, lease or order of any healthcare items or service for which payment may be made, in whole or in part, by federal healthcare programs such as Medicare and Medicaid. This statute has been interpreted to apply to arrangements between pharmaceutical companies on one hand and prescribers, purchasers and formulary managers on the other. Further, the Affordable Care Act, among other things, clarified that liability may be established under the federal Anti‑Kickback Law without proving actual knowledge of the federal Anti‑Kickback statute or specific intent to violate it. In addition, the Affordable Care Act amended the Social Security Act to provide that the government may assert that a claim including items or services resulting from a violation of the federal Anti‑Kickback Law constitutes a false or fraudulent claim for purposes of the federal civil False Claims Act. Although there are a number of statutory exemptions and regulatory safe harbors to the federal Anti‑Kickback Law protecting certain common business arrangements and activities from prosecution or regulatory sanctions, the exemptions and safe harbors are drawn narrowly, and practices that do not fit squarely within an exemption or safe harbor may be subject to scrutiny. We seek to comply with the exemptions and safe harbors whenever possible, but our practices may not in all cases meet all of the criteria for safe harbor protection from anti‑kickback liability; |
|
· |
the federal civil False Claims Act, which prohibits, among other things, individuals or entities from knowingly presenting, or causing to be presented, a false or fraudulent claim for payment of government funds or knowingly making, using or causing to be made or used, a false record or statement material to an obligation to pay money to the government or knowingly concealing or knowingly and improperly avoiding, decreasing, or concealing an obligation to pay money to the federal government. Many pharmaceutical and other healthcare companies have been investigated and have reached substantial financial settlements with the federal government under the civil False Claims Act for a variety of alleged improper marketing activities, including providing free product to customers with the expectation that the customers would bill federal programs for the product; providing consulting fees, grants, free travel, and other benefits to physicians to induce them to prescribe the company’s products; and inflating prices reported to private price publication services, which are used to set drug payment rates under government healthcare programs. In addition, in recent years the government has pursued civil False Claims Act cases against a number of pharmaceutical companies for causing false claims to be submitted as a result of the marketing of their products for unapproved, and thus non‑reimbursable, uses. Pharmaceutical and other healthcare companies also are subject to other federal false claim laws, including, among others, federal criminal healthcare fraud and false statement statutes that extend to non‑government health benefit programs; |
21
|
· |
numerous U.S. federal and state laws and regulations, including state data breach notification laws, state health information privacy laws and federal and state consumer protection laws, govern the collection, use, disclosure, and protection of personal information. Other countries also have, or are developing, laws governing the collection, use, disclosure, and protection of personal information. In addition, most healthcare providers who prescribe our products and from whom we obtain patient health information are subject to privacy and security requirements under the Health Insurance Portability and Accountability Act of 1996, as amended by the Health Information Technology for Economic and Clinical Health Act, or HIPAA. We are not a HIPAA‑covered entity and we do not operate as a business associate to any covered entities. Therefore, the HIPAA privacy and security requirements do not apply to us (other than potentially with respect to providing certain employee benefits). However, we could be subject to criminal penalties if we knowingly obtain individually identifiable health information from a covered entity in a manner that is not authorized or permitted by HIPAA or for aiding and abetting and/or conspiring to commit a violation of HIPAA. We are unable to predict whether our actions could be subject to prosecution in the event of an impermissible disclosure of health information to us. The legislative and regulatory landscape for privacy and data security continues to evolve, and there has been an increasing amount of focus on privacy and data security issues with the potential to affect our business. These privacy and data security laws and regulations could increase our cost of doing business, and failure to comply with these laws and regulations could result in government enforcement actions (which could include civil or criminal penalties), private litigation and/or adverse publicity and could negatively affect our operating results and business; |
|
· |
analogous state laws and regulations, such as state anti‑kickback and false claims laws, may apply to items or services reimbursed under Medicaid and other state programs or, in several states, apply regardless of the payor. Some state laws also require pharmaceutical companies to report expenses relating to the marketing and promotion of pharmaceutical products and to report gifts and payments to certain health care providers in the states. Other states prohibit providing meals to prescribers or other marketing‑related activities. In addition, California, Connecticut, Nevada, and Massachusetts require pharmaceutical companies to implement compliance programs or marketing codes of conduct. Foreign governments often have similar regulations, which we also will be subject to in those countries where we market and sell products; |
|
· |
the federal Physician Payment Sunshine Act, being implemented as the Open Payments Program, requires certain pharmaceutical manufacturers to engage in extensive tracking of payments and other transfers of value to physicians and teaching hospitals, and to submit such data to CMS, which will then make all of this data publicly available on the CMS website. Pharmaceutical manufacturers with products for which payment is available under Medicare, Medicaid or the State Children’s Health Insurance Program are required to have started tracking reportable payments on August 1, 2013, and must submit a report to CMS on or before the 90th day of each calendar year disclosing reportable payments made in the previous calendar year. Failure to comply with the reporting obligations may result in civil monetary penalties; and |
|
· |
the federal Foreign Corrupt Practices Act of 1977 and other similar anti‑bribery laws in other jurisdictions generally prohibit companies and their intermediaries from providing money or anything of value to officials of foreign governments, foreign political parties, or international organizations with the intent to obtain or retain business or seek a business advantage. Recently, there has been a substantial increase in anti‑bribery law enforcement activity by U.S. regulators, with more frequent and aggressive investigations and enforcement proceedings by both the Department of Justice and the U.S. Securities and Exchange Commission. A determination that our operations or activities are not, or were not, in compliance with United States or foreign laws or regulations could result in the imposition of substantial fines, interruptions of business, loss of supplier, vendor or other third‑party relationships, termination of necessary licenses and permits, and other legal or equitable sanctions. Other internal or government investigations or legal or regulatory proceedings, including lawsuits brought by private litigants, may also follow as a consequence. |
If our operations are found to be in violation of any of the laws or regulations described above or any other governmental regulations that apply to us, we may be subject to significant civil, criminal and administrative penalties, damages, fines, exclusion from government‑funded healthcare programs, like Medicare and Medicaid, and the
22
curtailment or restructuring of our operations. Any penalties, damages, fines, curtailment or restructuring of our operations could adversely affect our ability to operate our business and our financial results. Although compliance programs can mitigate the risk of investigation and prosecution for violations of these laws and regulations, the risks cannot be entirely eliminated. Any action against us for violation of these laws or regulations, even if we successfully defend against it, could cause us to incur significant legal expenses and divert our management’s attention from the operation of our business. Moreover, achieving and sustaining compliance with applicable federal and state privacy, data security and fraud laws and regulations may prove costly.
Collaboration Agreements
Mitsubishi Tanabe Pharma Corporation
In January 2001, we entered into an exclusive development, license and clinical trial and commercial supply agreement with Tanabe Seiyaku Co., Ltd., now Mitsubishi Tanabe Pharma Corporation, or MTPC, for the development and commercialization of avanafil, a PDE5 inhibitor compound for the oral and local treatment of male and female sexual dysfunction. Under the terms of the agreement, MTPC agreed to grant an exclusive license to us for products containing avanafil outside of Japan, North Korea, South Korea, China, Taiwan, Singapore, Indonesia, Malaysia, Thailand, Vietnam and the Philippines. We agreed to grant MTPC an exclusive, royalty‑free license within those countries for oral products that we develop containing avanafil. In addition, we agreed to grant MTPC an exclusive option to obtain an exclusive, royalty‑bearing license within those countries for non‑oral products that we develop containing avanafil. MTPC agreed to manufacture and supply us with avanafil for use in clinical trials, which were our primary responsibility. The MTPC agreement contains a number of milestone payments to be made by us based on various triggering events.
The term of the MTPC agreement is based on a country‑by‑country and on a product‑by‑product basis. The term shall continue until the later of (i) 10 years after the date of the first sale for a particular product or (ii) the expiration of the last‑to‑expire patents within the MTPC patents covering such product in such country. In the event that our product is deemed to be (i) insufficiently effective or insufficiently safe relative to other PDE5 inhibitor compounds based on published information or (ii) not economically feasible to develop due to unforeseen regulatory hurdles or costs as measured by standards common in the pharmaceutical industry for this type of product, we have the right to terminate the agreement with MTPC with respect to such product.
In August 2012, we entered into an amendment to our agreement with MTPC that permits us to manufacture the active pharmaceutical ingredient, or API, and tablets for STENDRA ourselves or through third parties. In 2015, we transferred the manufacturing of the API and tablets for STENDRA to Sanofi.
On February 21, 2013, we entered into the third amendment to our agreement with MTPC which, among other things, expands our rights, or those of our sublicensees, to enforce the patents licensed under the MTPC agreement against alleged infringement, and clarifies the rights and duties of the parties and our sublicensees upon termination of the MTPC agreement. In addition, we were obligated to use our best commercial efforts to market STENDRA in the U.S. by December 31, 2013, which was achieved by our commercialization partner, Auxilium.
On July 23, 2013, we entered into the fourth amendment to our agreement with MTPC which, among other things, changes the definition of net sales used to calculate royalties owed by us to MTPC.
Menarini Group
On July 5, 2013, we entered into a license and commercialization agreement, or the Menarini License Agreement, and a supply agreement, or the Menarini Supply Agreement, with the Menarini Group through its subsidiary Berlin‑Chemie AG, or Menarini.
Under the terms of the Menarini License Agreement, Menarini received an exclusive license to commercialize and promote our drug SPEDRA for the treatment of ED in over 40 countries, including the EU, plus Australia and New Zealand. Additionally, we agreed to transfer to Menarini ownership of the marketing authorization for SPEDRA in the
23
EU for the treatment of ED, which was granted by the EC in June 2013. Each party agreed not to develop, commercialize, or in‑license any other product that operates as phosphodiesterase type‑5 inhibitor for the treatment of ED for a limited time period, subject to certain exceptions.
Under the Menarini License Agreement, we have received payments of $63.0 million relating to license and milestone payments and royalty prepayments through December 31, 2015. Additionally, we are entitled to receive potential milestone payments based on certain net sales targets, plus royalties on SPEDRA sales. Menarini will also reimburse us for payments made to cover various obligations to MTPC during the term of the Menarini License Agreement. The Menarini License Agreement will terminate on a country‑by‑country basis in the relevant territories upon the latest to occur of the following: (i) the expiration of the last‑to‑expire valid VIVUS patent covering SPEDRA; (ii) the expiration of data protection covering SPEDRA; or (iii) 10 years after the SPEDRA product launch. In addition, Menarini may terminate the Menarini License Agreement if certain additional regulatory obligations are imposed on SPEDRA, and we may terminate the Menarini License Agreement if Menarini challenges our patents covering SPEDRA or if Menarini commits certain legal violations. Either party may terminate the Menarini License Agreement for the other party’s uncured material breach or bankruptcy.
Under the terms of the Menarini Supply Agreement, we will supply Menarini with STENDRA drug product until December 31, 2018. Menarini also has the right to manufacture STENDRA independently, provided that it continues to satisfy certain minimum purchase obligations to us. Following the expiration of the Menarini Supply Agreement, Menarini will be responsible for its own supply of STENDRA. Either party may terminate the Menarini Supply Agreement for the other party’s uncured material breach or bankruptcy, or upon the termination of the Menarini License Agreement.
Auxilium Pharmaceuticals, Inc.
On October 10, 2013, we entered into a license and commercialization agreement, or the Auxilium License Agreement, and a commercial supply agreement, or the Auxilium Supply Agreement, with Auxilium Pharmaceuticals, Inc., or Auxilium. On January 29, 2015, Auxilium was purchased by Endo International, plc.
Under the terms of the Auxilium License Agreement, Auxilium received an exclusive license to commercialize and promote our drug STENDRA for the treatment of ED in the United States and Canada and their respective territories, or the Auxilium Territory. Additionally, following the completion of certain events, we have agreed to transfer to Auxilium ownership of the product marketing authorization for STENDRA for the treatment of ED, which was granted by the FDA in April 2012. Each party agreed not to develop, commercialize, or in‑license any other product that operates as a PDE‑5 inhibitor for the treatment of ED in the Auxilium Territory for a limited time period, subject to certain exceptions. A PDE‑5 inhibitor means any product that operates as a phosphodiesterase type‑5 inhibitor.
We received an upfront license fee of $30.0 million in October 2013 and a regulatory milestone payment of $15.0 million in 2014 upon approval by the FDA of a specific time of onset claim for STENDRA in the Auxilium Territory. We receive royalty payments based on tiered percentages of the aggregate annual net sales of STENDRA in the Auxilium Territory on a quarterly basis. The percentage of Auxilium’s aggregate annual net sales to be paid to VIVUS increases in accordance with the achievement of specific thresholds of aggregate annual net sales of STENDRA in the Auxilium Territory. If Auxilium’s net sales of STENDRA in a country are reduced by certain amounts following the entry of a generic product to the market, royalty payments will be reduced by certain percentages based on such reductions. Auxilium will also reimburse VIVUS for payments made to cover various obligations to MTPC during the term of the Auxilium License Agreement.
Auxilium received an exclusive license, with a right to sublicense, subject to certain limitations, under certain of our trademarks, including STENDRA, to market, sell and distribute STENDRA for the treatment of ED in the Auxilium Territory. In addition, Auxilium received an exclusive license, with a right to sublicense, subject to certain limitations, under certain of our patents and know‑how (i) to use, distribute, import, promote, market, sell, offer for sale and otherwise commercialize STENDRA for the treatment of erectile dysfunction in the Auxilium Territory; (ii) to make and have made STENDRA anywhere in the world, with certain exceptions, where STENDRA is solely for use or sale for the treatment of erectile dysfunction in the Auxilium Territory; and (iii) to conduct certain development activities on
24
STENDRA for the treatment of erectile dysfunction in support of obtaining regulatory approval in the Auxilium Territory.
Auxilium obtains STENDRA exclusively from us for a mutually agreed term pursuant to the Auxilium Supply Agreement, as further described below. Auxilium may elect to transfer the control of the supply chain for STENDRA for the Auxilium Territory to itself or its designee by assigning to Auxilium our agreements with the contract manufacturer, which is referred to below as the Supply Chain Transfer.
At our sole cost and expense, we were responsible for preparing and filing with the FDA the appropriate documents to obtain a label expansion for STENDRA referencing a specific time‑to‑onset claim. Further, we were responsible for conducting any post‑regulatory studies of STENDRA that were required by the FDA in the Auxilium Territory. Such costs were split equally between the parties. These studies have been completed.
Under the terms of the Auxilium Supply Agreement, we were to supply Auxilium with STENDRA drug product until December 31, 2018, at the latest. For 2015, and each subsequent year during the term of the Auxilium Supply Agreement, if Auxilium fails to purchase an agreed minimum purchase amount of STENDRA from us, it will reimburse us for the shortfall as it relates to our out‑of‑ pocket costs to acquire certain raw materials needed to manufacture STENDRA. Either party may terminate the Auxilium Supply Agreement for the other party’s uncured material breach or bankruptcy, or upon the termination of the License Agreement. The Auxilium Supply Agreement will automatically terminate upon completion of the Supply Chain Transfer, as described above.
In December 2015, we were notified by Auxilium of Auxilium's intention to return the U.S. and Canadian commercial rights for STENDRA to us. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016.
Sanofi
On December 11, 2013, we entered into a license and commercialization agreement, or the Sanofi License Agreement, with Sanofi. Effective as of December 11, 2013, we entered into a supply agreement, or the Sanofi Supply Agreement, with Sanofi Winthrop Industrie, a wholly owned subsidiary of Sanofi.
Under the terms of the Sanofi License Agreement, Sanofi received an exclusive license to commercialize and promote avanafil for therapeutic use in humans in Africa, the Middle East—Turkey and Commonwealth of Independent States, or the Sanofi Territory. During the term of the License Agreement, each party agreed not to develop, commercialize, or in‑license any other product that operates as a phosphodiesterase type‑5 inhibitor for therapeutic use in humans in the Sanofi Territory for a limited time period, subject to certain exceptions. Sanofi will reimburse us for a portion of any sales milestone paid by us to MTPC based on the share of Sanofi’s net sales in the total worldwide net sales amount triggering the payment of such sales milestone.
In December 2013, we received an upfront license fee of $5.0 million and a $1.5 million manufacturing milestone payment, and in February 2014, we received an additional $3.5 million in manufacturing milestone payments. We are also eligible to receive up to $6.0 million in regulatory milestone payments, and up to $45.0 million in sales milestone payments, plus royalties on avanafil sales based on tiered percentages of the aggregate annual net sales in the Sanofi Territory. Sanofi will also reimburse us for a portion of any sales milestone paid by us to MTPC based on the share of Sanofi’s net sales in the total worldwide net sales amount triggering the payment of such sales milestone.
Royalty payment obligations under the Sanofi License Agreement will be payable for avanafil in each country in the Sanofi Territory until the later to occur of (i) the expiration of the last‑to‑expire valid claim within the VIVUS patents that, absent the licenses granted to Sanofi under the Sanofi License Agreement, would be infringed by the sale of avanafil in such country and (ii) December 11, 2029, or the Sanofi Royalty Payment Term. The Sanofi License Agreement will terminate as follows: (i) as to avanafil in each country in the Sanofi Territory, upon the expiration of the Sanofi Royalty Payment Term with respect to avanafil in such country, provided however, that Sanofi’s obligation to reimburse us for Sanofi’s pro‑rata share of any sales milestone paid by us to MTPC will survive if such sales milestone
25
has not yet come due; and (ii) in its entirety, upon the expiration of all royalty payment obligations arising under the Sanofi License Agreement in all countries in the Sanofi Territory.
In addition, we may terminate the Sanofi License Agreement immediately upon written notice to Sanofi on a country‑by‑country basis if Sanofi becomes subject to certain regulatory actions or legal restrictions. We may also terminate the Sanofi License Agreement in its entirety upon written notice to Sanofi if Sanofi or any affiliate commences any action or proceeding that challenges the validity, enforceability or scope of any VIVUS patent in the Sanofi Territory or any country outside of the Sanofi Territory, or if a similar action is instituted by a sublicensee and Sanofi does not terminate the sublicense after being aware of such action for a specified period. Further, Sanofi may terminate the Sanofi License Agreement in whole or on a country‑by‑country basis for convenience at any time upon advance notice to us. Either party may terminate the Sanofi License Agreement for the other party’s uncured material breach, or bankruptcy or related actions or proceedings. In the event of an uncured material breach by us, Sanofi may, in lieu of terminating the Sanofi License Agreement in its entirety, elect to continue the Sanofi License Agreement in full force and effect except (i) we will have no further rights to receive certain commercialization reports and (ii) Sanofi may set off any payments or amounts due by Sanofi but not yet paid to us against all direct and undisputed damages suffered by Sanofi as a result of the breach.
Under the terms of the Sanofi Supply Agreement, we supplied Sanofi Winthrop Industrie with avanafil tablets until June 30, 2015. The Sanofi Supply Agreement will automatically terminate upon the termination of the Sanofi License Agreement.
On July 31, 2013, we entered into a Commercial Supply Agreement with Sanofi Chimie to manufacture and supply the API for our drug avanafil on an exclusive basis in the United States and other territories and on a semi‑exclusive basis in Europe, including the EU, Latin America and other territories. On November 18, 2013, we entered into a Manufacturing and Supply Agreement with Sanofi Winthrop Industrie to manufacture and supply the avanafil tablets on an exclusive basis in the United States and other territories and on a semi‑exclusive basis in Europe, including the EU, Latin America and other territories. We have obtained approval from the FDA and the European Medicines Agency, or EMA, of Sanofi Chimie as a qualified supplier of avanafil API and of Sanofi Winthrop Industrie as a qualified supplier of the avanafil tablets. We have minimum annual purchase commitments under these agreements for at least the initial five‑year terms.
Other
In October 2001, we entered into an assignment agreement, or the Assignment Agreement, with Thomas Najarian, M.D., for a combination of pharmaceutical agents for the treatment of obesity and other disorders, or the Combination Therapy, that has since been the focus of our investigational drug candidate development program for Qsymia for the treatment of obesity, obstructive sleep apnea and diabetes. The Combination Therapy and all related patent applications, or the Patents, were transferred to us with worldwide rights to develop and commercialize the Combination Therapy and exploit the Patents. In addition, the Assignment Agreement requires us to pay royalties on worldwide net sales of a product for the treatment of obesity that is based upon the Combination Therapy and Patents until the last‑to‑expire of the assigned Patents. To the extent that we decide not to commercially exploit the Patents, the Assignment Agreement will terminate and the Combination Therapy and Patents will be assigned back to Dr. Najarian. In 2006, Dr. Najarian joined the Company as a part‑time employee and served as a Principal Scientist. In November 2013, Dr. Najarian’s employment with the Company ended, and he continues to be available as a consultant.
26
Patents, Proprietary Technology and Data Exclusivity
We own or are the exclusive licensee of more than 30 patents and numerous published patent applications in the U.S. and Canada. We intend to develop, maintain and secure intellectual property rights and to aggressively defend and pursue new patents to expand upon our current patent base. Our portfolio of patents as it primarily relates to Qsymia, our FDA‑approved drug for the treatment of obesity, and STENDRA, our FDA‑approved drug for the treatment of ED, is summarized as follows:
|
QSYMIA |
|
|
|
|
U.S. Patent No. 7,056,890 |
|
Expiring 06/14/2020 |
|
|
U.S. Patent No. 7,553,818 |
|
Expiring 06/14/2020 |
|
|
U.S. Patent No. 7,659,256 |
|
Expiring 06/14/2020 |
|
|
U.S. Patent No. 7,674,776 |
|
Expiring 06/14/2020 |
|
|
U.S. Patent No. 8,802,636 |
|
Expiring 06/14/2020 |
|
|
U.S. Patent No. 8,580,299 |
|
Expiring 06/14/2029* |
|
|
U.S. Patent No. 8,895,058 |
|
Expiring 06/09/2028 |
|
|
U.S. Patent No. 9,011,905 |
|
Expiring 06/09/2028 |
|
|
U.S. Patent Publication No. 2014/0308346 A1 |
|
Pending |
|
|
U.S. Patent Publication No. 2015/0025134 A1 |
|
Pending |
|
|
U.S. Patent No. 8,580,298 |
|
Expiring 05/15/2029* |
|
|
U.S. Patent No. 8,895,057 |
|
Expiring 06/09/2028 |
|
|
U.S. Patent No. 9,011,906 |
|
Expiring 06/09/2028 |
|
|
U.S. Patent No. 6,071,537 |
|
Expiring 06/23/2017 |
|
|
U.S. Patent Publication No. 2015/0313870 A1 |
|
Pending |
|
|
U.S. Patent Publication No. 2016/0022630 A1 |
|
Pending |
|
|
Canadian Patent No. 2,377,330 |
|
Expiring 06/14/2020 |
|
|
Canadian Patent No. 2,727,313 |
|
Expiring 06/09/2029 |
|
|
Canadian Patent Publication No. 2,727,319 A1 |
|
Pending |
|
|
STENDRA |
|
|
|
|
U.S. Patent No. 6,656,935 |
|
Expiring 04/26/2025 |
|
|
U.S. Patent No. 7,501,409 |
|
Expiring 05/05/2023 |
|
|
Canadian Patent No. 2,383,466 |
|
Expiring 09/13/2020 |
|
|
ERECTILE DYSFUNCTION |
|
|
|
|
U.S. Patent No. 5,922,341 |
|
Expiring 10/28/2017 |
|
|
U.S. Patent No. 5,925,629 |
|
Expiring 10/28/2017 |
|
|
U.S. Patent No. 6,037,346 |
|
Expiring 10/28/2017 |
|
|
U.S. Patent No. 6,093,181 |
|
Expiring 07/25/2017 |
|
|
U.S. Patent No. 6,127,363 |
|
Expiring 10/28/2017 |
|
|
U.S. Patent No. 6,156,753 |
|
Expiring 10/28/2017 |
|
|
U.S. Patent No. 6,403,597 |
|
Expiring 10/28/2017 |
|
|
U.S. Patent No. 6,495,154 |
|
Expiring 11/21/2020 |
|
|
U.S. Patent No. 6,548,490 |
|
Expiring 10/28/2017 |
|
|
U.S. Patent No. 6,946,141 |
|
Expiring 11/21/2020 |
|
|
Canadian Patent No. 2,305,394 |
|
Expiring 10/28/2018 |
|
*These expiration dates are based on the number of days of patent term adjustment, or PTA, calculated by the U.S. Patent and Trademark Office, or USPTO. An independent calculation of PTA suggested that the patents may be entitled to fewer days of PTA than determined by the USPTO.
The EU has adopted a harmonized approach to data and marketing exclusivity under Regulation (EC) No. 726/2004 and Directive 2001/83/EC. The exclusivity scheme applies to products that have been authorized in the EU by either the European Commission, through the centralized procedure, or the competent authorities of the Member States of the European Economic Area, or EEA, under the Decentralized or Mutual Recognition procedures. The approach (known as the 8+2+1 formula) permits eight years of data exclusivity and 10 years of marketing exclusivity.
27
Within the first eight years of the 10 years, a generic applicant is not permitted to cross refer to the preclinical and clinical trial data relating to the reference product. Even if the generic product is authorized after expiry of the eight years of data exclusivity, it cannot be placed on the market until the full 10‑year market exclusivity has expired. This 10‑year market exclusivity may be extended cumulatively to a maximum period of 11 years if during the first eight years of those 10 years, the marketing authorization holder obtains an authorization for a new (second) therapeutic indication which, during the scientific evaluation prior to its authorization, is held to bring a significant clinical benefit in comparison with existing therapies.
In addition to the Canadian patents and applications identified in the table, we also hold foreign counterparts, patents and patent applications in major foreign jurisdictions related to our U.S. patents. We have developed and acquired exclusive rights to patented technology in support of our development and commercialization of our approved drugs and investigational drug candidates, and we rely on trade secrets and proprietary technologies in developing potential drugs. We continue to place significant emphasis on securing global intellectual property rights and are aggressively pursuing new patents to expand upon our strong foundation for commercializing investigational drug candidates in development.
Manufacturing
Our commercial products, Qsymia and STENDRA, together with their respective APIs and finished products, as well as our clinical supplies, are manufactured on a contract basis. In addition, packaging for the commercial distribution of the Qsymia product capsules and the STENDRA product tablets is performed by contract packaging companies. We expect to continue to contract with other third‑party providers for manufacturing services, including APIs, finished products, and packaging operations as needed. We believe that our current agreements and purchase orders with third‑party manufacturers provide for sufficient operating capacity to support the anticipated commercial demand for Qsymia and STENDRA and our clinical supplies. However, if we are unable to obtain a sufficient supply of Qsymia or STENDRA for our commercial sales, or the clinical supplies to support our clinical trials, or if we should encounter delays or difficulties in our relationships with our manufacturers or packagers, we may lose potential sales, have difficulty entering into collaboration agreements for the commercialization of STENDRA for territories in which we do not have a commercial collaboration or our clinical trials may be delayed.
The API and the tablets for STENDRA were manufactured by MTPC into 2015. In August 2012, we entered into an amendment to our agreement with MTPC that permits us to manufacture the API and tablets for STENDRA ourselves or through third‑party suppliers at any time. Beginning in 2015, the API and the tablets for STENDRA are manufactured by Sanofi.
As indicated above, on July 31, 2013, we entered into a Commercial Supply Agreement with Sanofi Chimie, a wholly owned subsidiary of Sanofi, pursuant to which Sanofi Chimie will manufacture and supply the API for STENDRA. Further, as indicated above, on November 18, 2013, we entered into a Manufacturing and Supply Agreement with Sanofi Winthrop Industrie, a wholly owned subsidiary of Sanofi, pursuant to which Sanofi Winthrop Industrie will manufacture and supply the tablets for our drug avanafil. We have obtained approval from the FDA and the European Medicines Agency, or EMA, of Sanofi Chimie as a qualified supplier of avanafil API and of Sanofi Winthrop Industrie as a qualified supplier of the avanafil tablets.
We currently do not have any manufacturing facilities and intend to continue to rely on third parties for the supply of the starting materials, API and finished dosage forms (tablets and capsules). However, we cannot be certain that we will be successful in entering into additional supplier agreements or that we will be able to obtain the necessary regulatory approvals for any suppliers in a timely manner or at all.
Catalent manufactures our clinical and commercial supplies for Qsymia. Catalent has been successful in validating the commercial manufacturing process for Qsymia at a scale that has been able to support the launch of Qsymia in the U.S. market.
We attempt to prevent disruption of supplies through supply agreements, purchase orders, appropriate forecasting, maintaining stock levels and other strategies. In the event we are unable to manufacture our products, either
28
directly or indirectly through others or on commercially acceptable terms, if at all, we may not be able to commercialize our products as planned. Although we are taking these actions to avoid a disruption in supply, we cannot provide assurance that we may not experience a disruption in the future.
Marketing and Sales
Prior to August 2015, we commercialized Qsymia in the U.S. primarily through a dedicated contract sales force, supported by an internal commercial team. In August 2015, we directly hired approximately 50 former contract sales representatives to continue promoting Qsymia to physicians. Our efforts to expand the appropriate use of Qsymia include scientific publications, participation and presentations at medical conferences, and development and implementation of patient-directed support programs. We have rolled out marketing programs to encourage targeted prescribers to gain more experience with Qsymia, including a partnership with Kadmon Corporation to focus on liver disease specialists. In 2015, we increased our investment in digital media in order to amplify our messaging to information-seeking consumers. The digital messaging encourages those consumers most likely to take action to speak with their physicians about obesity treatment options. We believe our enhanced web-based strategies will deliver clear and compelling communications to potential patients. We launched the “Smart Changes Program” in which we partner Qsymia with the Mayo Clinic diet to help on-line patients make the behavioral changes needed for sustained weight-loss. We have also employed a physician referral service to help patients identify prescribers in their area.
Qsymia Distribution and REMS
We rely on Cardinal Health 105, Inc., or Cardinal Health, a third‑party distribution and supply‑chain management company, to warehouse Qsymia and distribute it to the certified home delivery pharmacies and wholesalers that then distribute Qsymia directly to patients and certified retail pharmacies. Cardinal Health provides billing, collection and returns services. Cardinal Health is our exclusive supplier of distribution logistics services, and accordingly we depend on Cardinal Health to satisfactorily perform its obligations under our agreement with them.
Pursuant to the REMS program applicable to Qsymia, our distribution network is through a broader network of certified retail pharmacies and through a small number of certified home delivery pharmacies and wholesalers. We have contracted through a third‑party vendor to certify the retail pharmacies and collect required data to support the Qsymia REMS program. In addition to providing services to support the distribution and use of Qsymia, each of the certified pharmacies has agreed to comply with the REMS program requirements and, through our third‑party data collection vendor, will provide us with the necessary patient and prescribing healthcare provider, or HCP, data. In addition, we have contracted with third‑party data warehouses to store this patient and HCP data and report it to us. We rely on this third‑party data in order to recognize revenue and comply with the REMS requirements for Qsymia, such as data analysis. This distribution and data collection network requires significant coordination with our sales and marketing, finance, regulatory and medical affairs teams, in light of the REMS requirements applicable to Qsymia.
Competition
Competition in the pharmaceutical and medical products industries is intense and is characterized by costly and extensive research efforts and rapid technological progress. We are aware of several pharmaceutical companies also actively engaged in the development of therapies for the treatment of obesity, diabetes and sexual health and medical device companies engaged in the development of therapies for the treatment of sleep apnea. Many of these companies have substantially greater research and development capabilities as well as substantially greater marketing, financial and human resources than VIVUS. Our competitors may develop technologies and products that are more effective than those we are currently marketing or researching and developing. Some of the drugs that may compete with Qsymia may not have a REMS requirement and the accompanying complexities such a requirement presents. Such developments could render Qsymia and STENDRA less competitive or possibly obsolete. We are also competing with respect to marketing capabilities and manufacturing efficiency, areas in which we have limited experience.
Qsymia for the treatment of chronic weight management competes with several approved anti‑obesity drugs including, Belviq® (lorcaserin), Arena Pharmaceutical’s anti‑obesity compound being marketed by Eisai Inc., Eisai Co., Ltd.’s U.S. subsidiary; Contrave® (naltrexone/bupropion), Orexigen Therapeutics’ anti‑obesity product being
29
marketed by Takeda Pharmaceutical Company Limited; Xenical® (orlistat), marketed by Roche; alli®, the over‑the‑counter version of orlistat, marketed by GlaxoSmithKline; and Suprenza™ (phentermine hydrochloride), marketed by Akrimax Pharmaceuticals, LLC. Also, in 2015, Novo Nordisk A/S launched Saxenda® (liraglutide) 3.0 mg which was approved by the FDA for obesity.
Agents approved for type 2 diabetes that have demonstrated weight loss in clinical studies may also compete with Qsymia. These agents include Victoza® (liraglutide; approved for diabetes at 1.2mg and 1.8mg dosage strengths) from Novo Nordisk A/S, a GLP‑1 receptor agonist approved January 25, 2010, Invokana® (canaglifozin) from Johnson & Johnson’s Janssen Pharmaceuticals, an SGLT2 inhibitor, approved March 29, 2013; Farxiga™ (dapagliflozin) from AstraZeneca and Bristol‑Myers Squibb, an SGLT2 inhibitor, approved January 8, 2014; Jardiance® (empagliflozin) from Boehringer Ingelheim, an SGLT2 inhibitor, approved August 1, 2014; and Glyxambi® (empagliflozin/linagliptin) from Boehringer Ingelheim and Eli Lilly, an SGLT2 inhibitor and DPP‑4 inhibitor combination product, approved January 30, 2015. Also, on January 14, 2015, the FDA approved the Maestro Rechargeable System for certain obese adults, the first weight loss treatment device that targets the nerve pathway between the brain and the stomach that controls feelings of hunger and fullness. The Maestro Rechargeable System is approved to treat patients aged 18 and older who have not been able to lose weight with a weight loss program, and who have a body mass index of 35 to 45 with at least one other obesity‑related condition, such as type 2 diabetes.
In addition, there are several other investigational drug candidates in Phase 2 clinical trials. Zafgen’s beloranib, currently in Phase 2 for severe obesity, is a methionine aminopeptidase 2 (MetAP2) inhibitor, which is believed to work by re‑establishing balance to the ways the body packages and metabolizes fat. In January 2013, Rhythm Pharmaceuticals, or Rhythm, announced the initiation of a Phase 2 clinical trial with RM‑493, a small‑peptide melanocortin 4 receptor, or MC4R, agonist, for the treatment of obesity. Rhythm announced in September 2013, that RM‑493 is being studied in Phase 1B for the treatment of obesity in individuals with a genetic deficiency in the MC4R pathway. There are a number of generic pharmaceutical drugs that are prescribed for obesity, predominantly phentermine, which is sold at much lower prices than we charge for Qsymia and is also widely available in retail pharmacies. The availability of branded prescription drugs, generic drugs and over‑the‑counter drugs could limit the demand and the price we are able to charge for Qsymia.
We may also face competition from the off‑label use of the generic components in our drugs. In particular, it is possible that patients will seek to acquire phentermine and topiramate, the generic components of Qsymia. Neither of these generic components has a REMS program. Although these products have not been approved by the FDA for use in the treatment of chronic obesity, the off‑label use of the generic components in the U.S. or the importation of the generic components from foreign markets could adversely affect the commercial potential for our drugs and adversely affect our overall business, financial condition and results of operations.
Qsymia and STENDRA may also face challenges and competition from newly developed generic products. Under the U.S. Drug Price Competition and Patent Term Restoration Act of 1984, known as the Hatch‑Waxman Act, newly approved drugs and indications may benefit from a statutory period of non‑patent marketing exclusivity. The Hatch‑Waxman Act stimulates competition by providing incentives to generic pharmaceutical manufacturers to introduce non‑infringing forms of patented pharmaceutical products and to challenge patents on branded pharmaceutical products. If we are unsuccessful in challenging an Abbreviated New Drug Application, or ANDA, filed pursuant to the Hatch‑Waxman Act, a generic version of Qsymia or STENDRA may be launched, which would harm our business.
There are also surgical approaches to treat severe obesity that are becoming increasingly accepted. Two of the most well‑established surgical procedures are gastric bypass surgery and adjustable gastric banding, or lap bands. In February 2011, the FDA approved the use of a lap band in patients with a BMI of 30 (reduced from 35) with comorbidities. The lowering of the BMI requirement will make more obese patients eligible for lap band surgery. In addition, other potential approaches that utilize various implantable devices or surgical tools are in development. Some of these approaches are in late‑stage development and may be approved for marketing.
We anticipate that STENDRA for the treatment of ED will compete with PDE5 inhibitors in the form of oral medications including Viagra® (sildenafil citrate), marketed by Pfizer, Inc.; Cialis® (tadalafil), marketed by Eli Lilly and Company; Levitra® (vardenafil), co‑marketed by GlaxoSmithKline plc and Schering‑Plough Corporation in the U.S.; and
30
STAXYN® (vardenafil in an oral disintegrating tablet, or ODT), co‑promoted by GlaxoSmithKline plc and Merck & Co., Inc.
We anticipate that generic PDE5 inhibitors will enter the market in the U.S. in late 2017. Generic PDE5 inhibitors would likely be sold at lower prices than current prescriptions and thus may impact the demand for STENDRA. In addition, PDE5 inhibitors are in various stages of development by other companies. Warner‑Chilcott plc, which was acquired by Actavis, Inc. and changed its name to Actavis plc, has licensed the U.S. rights to udenafil, a PDE5 inhibitor from Dong‑A Pharmaceutical, now known as Mezzion Pharma Co. Ltd. Warner‑Chilcott continues Phase 3 development of this compound. Actavis, Inc. acquired Allergan, changed its name to Allergan, plc and has announced that it is being acquired by Pfizer. Other treatments for ED exist, such as needle injection therapies, vacuum constriction devices and penile implants, and the manufacturers of these products will most likely continue to develop or improve these therapies.
New developments, including the development of other drug technologies and methods of preventing the incidence of disease, occur in the pharmaceutical and medical technology industries at a rapid pace. These developments may render our drugs and future investigational drug candidates obsolete or noncompetitive. Compared to us, many of our potential competitors have substantially greater:
|
· |
research and development resources, including personnel and technology; |
|
· |
regulatory experience; |
|
· |
investigational drug candidate development and clinical trial experience; |
|
· |
experience and expertise in exploitation of intellectual property rights; and |
|
· |
access to strategic partners and capital resources. |
As a result of these factors, our competitors may obtain regulatory approval of their products more rapidly than we or may obtain patent protection or other intellectual property rights that limit our ability to develop or commercialize our investigational drug candidates. Our competitors may also develop drugs or surgical approaches that are more effective, more useful and less costly than ours and may also be more successful in manufacturing and marketing their products. In addition, our competitors may be more effective in commercializing their products. We currently outsource our manufacturing and therefore rely on third parties for that competitive expertise. There can be no assurance that we will be able to develop or contract for these capabilities on acceptable economic terms, or at all.
Avanafil qualifies as an innovative medicinal product in the EU. Innovative medicinal products authorized in the EU on the basis of a full marketing authorization application (as opposed to an application for marketing authorization that relies on data in the marketing authorization dossier for another, previously approved medicinal product) are entitled to eight years’ data exclusivity. During this period, applicants for approval of generics of these innovative products cannot rely on data contained in the marketing authorization dossier submitted for the innovative medicinal product. Innovative medicinal products are also entitled to 10 years’ market exclusivity. During this 10‑year period no generic medicinal product can be placed on the EU market. The 10‑year period of market exclusivity can be extended to a maximum of 11 years if, during the first eight years of those 10 years, the Marketing Authorization Holder for the innovative product obtains an authorization for one or more new therapeutic indications which, during the scientific evaluation prior to their authorization, are held to bring a significant clinical benefit in comparison with existing therapies. If we do not obtain extended patent protection and data exclusivity for our product candidates, our business may be materially harmed.
Research and Development
We incurred $10.1 million, $13.8 million and $29.7 million in 2015, 2014 and 2013, respectively, in research and development expenses, primarily to support the approval efforts, post‑marketing requirements, and clinical programs for Qsymia and STENDRA/SPEDRA.
31
Employees
As of February 29, 2016, we had 82 employees located at our corporate headquarters in Mountain View, California and in the field. None of our current employees are represented by a labor union or are the subject of a collective bargaining agreement. We believe that our relations with our employees are good, and we have never experienced a work stoppage at any of our facilities.
Insurance
We maintain product liability insurance for our clinical trials and commercial sales and general liability and directors’ and officers’ liability insurance for our operations. Insurance coverage is becoming increasingly expensive and no assurance can be given that we will be able to maintain insurance coverage at a reasonable cost or in sufficient amounts to protect us against losses due to liability. Although we have obtained product liability insurance coverage, we may be unable to maintain this product liability coverage for our approved drugs in amounts or scope sufficient to provide us with adequate coverage against all potential risks.
Geographic Area Financial Information
For financial information concerning the geographic areas in which we operate, see Note 18: “Segment Information and Concentration of Customers and Suppliers—Geographic Information” to our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K.
Available Information
Our Annual Report on Form 10‑K, Quarterly Reports on Form 10‑Q, Current Reports on Form 8‑K and amendments to reports filed pursuant to Section 13(a) and 15(d) of the Securities Exchange Act of 1934, as amended, are available on our website at www.vivus.com, when such reports are available on the SEC website. Copies of our Annual Report will be made available, free of charge, upon written request.
The public may read and copy any materials filed by VIVUS with the SEC at the SEC’s Public Reference Room at 100 F Street, NE, Washington, DC 20549. The public may obtain information on the operation of the Public Reference Room by calling the SEC at 1‑800‑SEC‑0330. The SEC maintains an Internet site that contains reports, proxy and information statements and other information regarding issuers that file electronically with the SEC at http://www.sec.gov. The contents of these websites are not incorporated into this filing. Further, VIVUS’s references to the URLs for these websites are intended to be inactive textual references only.
In addition, information regarding our code of ethics and the charters of our Audit, Compensation, and Nominating and Governance Committees are available free of charge on our website listed above.
Set forth below and elsewhere in this Annual Report on Form 10‑K and in other documents we file with the Securities and Exchange Commission, or the SEC, are risks and uncertainties that could cause actual results to differ materially from the results contemplated by the forward‑looking statements contained in this Annual Report on Form 10‑K. These are not the only risks and uncertainties facing VIVUS. Additional risks and uncertainties not presently known to us or that we currently deem immaterial may also impair our business operations.
Risks Relating to our Business
Changes to our management and strategic business plan may cause uncertainty regarding the future of our business, and may adversely impact employee hiring and retention, our stock price, and our revenue, operating results, and financial condition.
Since 2013, there have been significant changes in our management. For example, several members of
32
management have departed the Company, including our President in September 2013, our Chief Financial Officer in December 2013, our Vice President, U.S. Operations and General Manager in May 2014, our Chief Financial Officer and Chief Accounting Officer in September 2015 and our Vice President, Clinical Development in December 2015. In addition, we commenced corporate restructuring plans in November 2013 and July 2015 that resulted in significant reductions in our workforce. These changes, and the potential for additional changes to our management, organizational structure and strategic business plan, may cause speculation and uncertainty regarding our future business strategy and direction. These changes may cause or result in:
|
· |
disruption of our business or distraction of our employees and management; |
|
· |
difficulty in recruiting, hiring, motivating and retaining talented and skilled personnel; |
|
· |
stock price volatility; and |
|
· |
difficulty in negotiating, maintaining or consummating business or strategic relationships or transactions. |
If we are unable to mitigate these or other potential risks, our revenue, operating results and financial condition may be adversely impacted.
Our success will depend on our ability to effectively and profitably commercialize Qsymia® and avanafil.
Our success will depend on our ability to effectively and profitably commercialize Qsymia and avanafil, which will include our ability to:
|
· |
expand the use of Qsymia through targeted patient and physician education; |
|
· |
obtain marketing authorization by the EC for Qsiva™ in the EU through the centralized marketing authorization procedure; |
|
· |
our ability, either by ourselves or through a third party, to successfully commercialize STENDRA in the U.S. and Canada; |
|
· |
manage our alliances with Menarini, MTPC and Sanofi, to help ensure the commercial success of avanafil; |
|
· |
manage costs; |
|
· |
continue to certify and add to the Qsymia retail pharmacy network nationwide and sell Qsymia through this network; |
|
· |
improve third-party payor coverage, lower out-of-pocket costs to patients with discount programs, and obtain coverage for obesity under Medicare Part D; |
|
· |
create market demand for Qsymia through patient and physician education, marketing and sales activities; |
|
· |
achieve market acceptance and generate product sales; |
|
· |
comply with the post-marketing requirements established by the FDA, including Qsymia’s Risk Evaluation and Mitigation Strategy, or REMS, any future changes to the REMS, and any other requirements established by the FDA in the future; |
|
· |
conduct the post-marketing studies required by the FDA; |
|
· |
comply with other healthcare regulatory requirements; |
33
|
· |
maintain and defend our patents, if challenged; |
|
· |
ensure that the active pharmaceutical ingredients, or APIs, for Qsymia and avanafil and the finished products are manufactured in sufficient quantities and in compliance with requirements of the FDA and similar foreign regulatory agencies and with an acceptable quality and pricing level in order to meet commercial demand; |
|
· |
ensure that the entire supply chain for Qsymia and avanafil, from APIs to finished products, efficiently and consistently delivers Qsymia and avanafil to customers; and |
|
· |
manage our internal sales force and internal commercial team in their commercialization efforts for Qsymia. |
Prior to the commercialization of Qsymia, we have not had any commercial products since the divestiture of MUSE® in November 2010. While our management and key personnel have significant experience developing, launching and commercializing drugs at VIVUS and at other companies, we cannot be certain that we will be successful. If we are unable to successfully commercialize Qsymia, our ability to generate product sales will be severely limited, which will have a material adverse impact on our business, financial condition, and results of operations.
We may not fully realize the anticipated benefits from a corporate restructuring plan we announced in July 2015.
On July 30, 2015, we announced a corporate restructuring plan that reduced our headcount and expenses, with an objective of achieving neutral or positive operating cash flows by the end of 2016. We reduced our Qsymia sales territories to 50 and further streamlined our headquarters headcount resulting in the elimination of approximately 60 job positions. Consequently, our future sales forecast for Qsymia was reduced and has resulted in excess inventory as disclosed in Note 4 to the financial statements. In addition, we incurred charges for severance of approximately $2.5 million in 2015 related to this corporate restructuring plan. We expect annual savings of approximately $14.4 million in operating expenses beginning in fiscal year 2016. We may not fully realize the anticipated benefits from this corporate restructuring plan.
We depend on our collaboration partners to gain or maintain approval, market, and sell avanafil in their respective licensed territories.
In July 2013, we entered into a license and commercialization agreement with Menarini under which Menarini received an exclusive license to commercialize and promote SPEDRA for the treatment of ED in over 40 countries, including the EU, plus Australia and New Zealand. In October 2013, we entered into a license and commercialization agreement with Auxilium under which Auxilium received an exclusive license to commercialize and promote STENDRA for the treatment of erectile dysfunction, or ED, in the United States and Canada. In January 2015, Auxilium was acquired by Endo International, plc. In December 2015, Auxilium notified us of its intention to return the U.S. and Canadian commercial rights for STENDRA to us. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016. In December 2013, we entered into a license and commercialization agreement with Sanofi under which Sanofi received an exclusive license to commercialize and promote avanafil for therapeutic use in humans in Africa, the Middle East, Turkey, and CIS, including Russia. Sanofi will be responsible for obtaining regulatory approval in its territories. Sanofi intends to market avanafil under the trade name SPEDRA or STENDRA.
We are relying on our collaboration partners to successfully commercialize STENDRA or SPEDRA in their respective territories, inclusive of obtaining any necessary approvals. There can be no assurances that these collaboration partners will be successful in doing so. In general, we cannot control the amount and timing of resources that our collaboration partners devote to the commercialization of our drugs. If any of our collaboration partners fails to successfully commercialize our drug products, our business may be negatively affected. For example, if our collaboration partners do not successfully commercialize STENDRA or SPEDRA, we may receive limited or no
34
revenues under our agreements with them. As noted above, Auxillium has notified us of their intention to terminate the license and commercialization agreement with us. If we are unable to or decide not to commercialize STENDRA or SPEDRA in the U.S. and Canada ourselves, we will have to enter into a collaborative arrangement or strategic alliance to commercialize STENDRA or SPEDRA in these territories. We may be unable to enter into agreements with third parties for STENDRA or SPEDRA for these territories on favorable terms or at all, which could delay, impair, or preclude our ability to commercialize STENDRA or SPEDRA in these territories.
Under our license agreement with MTPC, we are obligated to ensure that Sanofi, Auxilium and Menarini, as sublicensees, comply with its terms and conditions. MTPC has the right to terminate our license rights to avanafil in the event of any uncured material breach of the license agreement. Consequently, failure by Sanofi, Auxilium or Menarini to comply with these terms and conditions could result in termination of our license rights to avanafil on a worldwide basis, which could delay, impair, or preclude our ability to commercialize avanafil.
We depend on collaborative arrangements or strategic alliances for the commercialization of STENDRA or SPEDRA.
Our dependence on collaborative arrangements or strategic alliances for the commercialization of STENDRA or SPEDRA, including our license agreements with MTPC, Sanofi, Auxilium and Menarini, will subject us to a number of risks, including the following:
|
· |
We may not be able to control the commercialization of our drug products in the relevant territories, including amount, timing and quality of resources that our collaborators may devote to our drug products; |
|
· |
our collaborators may experience financial, regulatory or operational difficulties, which may impair their ability to commercialize our drug products; |
|
· |
our collaborators may be required under the laws of the relevant territory to disclose our confidential information or may fail to protect our confidential information; |
|
· |
as a requirement of the collaborative arrangement, we may be required to relinquish important rights with respect to our drug products, such as marketing and distribution rights; |
|
· |
business combinations or significant changes in a collaborator’s business strategy may adversely affect a collaborator’s willingness or ability to satisfactorily complete its commercialization or other obligations under any collaborative arrangement; |
|
· |
legal disputes or disagreements may occur with one or more of our collaborators; |
|
· |
a collaborator could independently move forward with a competing investigational drug candidate developed either independently or in collaboration with others, including with one of our competitors; and |
|
· |
a collaborator could terminate the collaborative arrangement, which could negatively impact the continued commercialization of our drug products. For example, in December 2015, Auxilium notified us of its intention to return the U.S. and Canadian commercial rights for STENDRA to us. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016. If we are unable, either by ourselves or through a third party, to successfully commercialize STENDRA in the U.S. and Canada, it could have a significant negative impact on our financial position. |
We currently rely on reports from our commercialization partners in determining our royalty revenues, and these reports may be subject to adjustment or restatement, which may materially affect our financial results.
We have license and commercialization agreements for STENDRA or SPEDRA with Menarini, Auxilium and
35
Sanofi. In determining our royalty revenue from such agreements, we rely on our collaboration partners to provide accounting estimates and reports for various discounts and allowances, including product returns. As a result of fluctuations in inventory, allowances and buying patterns, actual sales and product returns of STENDRA or SPEDRA in particular reporting periods may be affected, resulting in the need for our commercialization partners to adjust or restate their accounting estimates set forth in the reports provided to us. For example, in April 2015, we were informed by Endo upon their purchase of Auxilium that Endo had revised its accounting estimate for STENDRA return reserve related to sales made in 2014. Under the terms of our license and commercialization agreement, adjustments to the return reserve can be deducted from reported net revenue. As a result, in the year ended December 31, 2015, we recorded an adjustment of $1.2 million to reduce our royalty revenue on net sales of STENDRA. The reduction in royalty revenue resulted in an increase to net loss of $1.2 million, or $0.01 per share, for the year ended December 31, 2015. Such adjustments or restatements may materially and negatively affect our financial position and results of operations.
If we are unable to enter into agreements with collaborators for the territories that are not covered by our existing commercialization agreements, our ability to commercialize STENDRA in these territories may be impaired.
We intend to enter into collaborative arrangements or a strategic alliance with one or more pharmaceutical partners or others to commercialize STENDRA in territories that are not covered by our current commercial collaboration agreements. In addition, in December 2015, Auxilium notified us of its intention to return the U.S. and Canadian commercial rights for STENDRA to us. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016. If we are unable to or decide not to commercialize STENDRA in the U.S. or Canada ourselves, we will have to enter into a collaborative arrangement or strategic alliance to commercialize STENDRA in these territories. We may be unable to enter into agreements with third parties for STENDRA for these territories on favorable terms or at all, which could delay, impair, or preclude our ability to commercialize STENDRA in these territories.
Failure to obtain regulatory approval in foreign jurisdictions will prevent us from marketing our products abroad.
In order to market products in many foreign jurisdictions, we must obtain separate regulatory approvals. Approval by the FDA in the U.S. does not ensure approval by regulatory authorities in other countries, and approval by one foreign regulatory authority does not ensure approval by regulatory authorities in other foreign countries. For example, while our drug STENDRA has been approved in both the U.S. and the EU, our drug Qsymia has been approved in the U.S. but Qsiva (the intended trade name for Qsymia in the EU) was denied a marketing authorization by the EC due to concerns over the potential cardiovascular and central nervous system effects associated with long-term use, teratogenic potential and use by patients for whom Qsiva would not have been indicated. We intend to seek approval, either directly or through our collaboration partners, for Qsymia and STENDRA in other territories outside the U.S. and the EU. However, we have had limited interactions with foreign regulatory authorities, and the approval procedures vary among countries and can involve additional testing. Foreign regulatory approvals may not be obtained, by us or our collaboration partners responsible for obtaining approval, on a timely basis, or at all, for any of our products. The failure to receive regulatory approvals in a foreign country would prevent us from marketing and commercializing our products in that country, which could have a material adverse effect on our business, financial condition and results of operations.
We, together with Sanofi, Menarini and potential future collaborators in certain territories, intend to market STENDRA or SPEDRA outside the U.S., which will subject us to risks related to conducting business internationally.
We, through Sanofi, Menarini and potential future collaborators in certain territories, intend to manufacture, market, and distribute STENDRA or SPEDRA outside the U.S. We expect that we will be subject to additional risks related to conducting business internationally, including:
|
· |
different regulatory requirements for drug approvals in foreign countries; |
|
· |
differing U.S. and foreign drug import and export rules; |
36
|
· |
reduced protection for intellectual property rights in some foreign countries; |
|
· |
unexpected changes in tariffs, trade barriers and regulatory requirements; |
|
· |
different reimbursement systems; |
|
· |
economic weakness, including inflation, or political instability in particular foreign economies and markets; |
|
· |
compliance with tax, employment, immigration and labor laws for employees living or traveling abroad; |
|
· |
foreign taxes, including withholding of payroll taxes; |
|
· |
foreign currency fluctuations, which could result in increased operating expenses and reduced revenues, and other obligations incidental to doing business in another country; |
|
· |
workforce uncertainty in countries where labor unrest is more common than in the U.S.; |
|
· |
production shortages resulting from events affecting raw material supply or manufacturing capabilities abroad; |
|
· |
potential liability resulting from development work conducted by these distributors; and |
|
· |
business interruptions resulting from geopolitical actions, including war and terrorism, or natural disasters. |
We have significant inventories on hand and, for the years ended December 31, 2015, 2014 and 2013, we recorded inventory impairment and commitment fees totaling $29.5 million, $2.2 million and $10.2 million, respectively, primarily to write off excess inventory related to Qsymia.
We maintain significant inventories and evaluate these inventories on a periodic basis for potential excess and obsolescence. During the years ended December 31, 2015, 2014 and 2013, we recognized total charges of $29.5 million, $2.2 million and $10.2 million, respectively, primarily for Qsymia inventories on hand in excess of demand. The inventory impairment charges were based on our analysis of current Qsymia inventory on hand and remaining shelf life, in relation to our projected demand for the product. The current FDA-approved commercial product shelf life for Qsymia is 36 months. STENDRA is approved in the U.S. and SPEDRA is approved in the EU for 48 months of commercial product shelf life.
Our write-down for excess and obsolete inventory is subjective and requires forecasting of the future market demand for our products. Forecasting demand for Qsymia, a drug in the obesity market in which there had been no new FDA-approved medications in over a decade prior to 2012, and for which reimbursement from third-party payors had previously been non-existent, has been difficult. Forecasting demand for STENDRA or SPEDRA, a drug that is new to a crowded and competitive market and has limited sales history, is also difficult. We will continue to evaluate our inventories on a periodic basis. The value of our inventories could be impacted if actual sales differ significantly from our estimates of future demand or if any significant unanticipated changes in future product demand or market conditions occur. Any of these events, or a combination thereof, could result in additional inventory write-downs in future periods, which could be material.
Our failure to manage and maintain our distribution network for Qsymia or compliance with certain requirements of the Qsymia REMS program could compromise the commercialization of this product.
We rely on Cardinal Health 105, Inc., or Cardinal Health, a third-party distribution and supply-chain management company, to warehouse Qsymia and distribute it to the certified home delivery pharmacies and wholesalers that then distribute Qsymia directly to patients and certified retail pharmacies. Cardinal Health provides billing, collection and returns services. Cardinal Health is our exclusive supplier of distribution logistics services, and accordingly we depend on Cardinal Health to satisfactorily perform its obligations under our agreement with them.
37
Pursuant to the REMS program applicable to Qsymia, our distribution network is through a small number of certified home delivery pharmacies and wholesalers and through a broader network of certified retail pharmacies. We have contracted through a third-party vendor to certify the retail pharmacies and collect required data to support the Qsymia REMS program. In addition to providing services to support the distribution and use of Qsymia, each of the certified pharmacies has agreed to comply with the REMS program requirements and, through our third-party data collection vendor, will provide us with the necessary patient and prescribing healthcare provider, or HCP, data. In addition, we have contracted with third-party data warehouses to store this patient and HCP data and report it to us. We rely on this third-party data in order to recognize revenue and comply with the REMS requirements for Qsymia, such as data analysis. This distribution and data collection network requires significant coordination with our sales and marketing, finance, regulatory and medical affairs teams, in light of the REMS requirements applicable to Qsymia.
We rely on the certified pharmacies to implement a number of safety procedures and report certain information to our third-party REMS data collection vendor. Failure to maintain our contracts with Cardinal Health, our third-party REMS data collection vendor, or with the third-party data warehouses, or the inability or failure of any of them to adequately perform under our contracts with them, could negatively impact the distribution of Qsymia, or adversely affect our ability to comply with the REMS applicable to Qsymia. Failure to comply with a requirement of an approved REMS can result in, among other things, civil penalties, imposition of additional burdensome REMS requirements, suspension or revocation of regulatory approval and criminal prosecution. Failure to coordinate financial systems could also negatively impact our ability to accurately report and forecast product revenue. If we are unable to effectively manage the distribution and data collection process, sales of Qsymia could be severely compromised and our business, financial condition and results of operations would be harmed.
If we are unable to enter into agreements with suppliers or our suppliers fail to supply us with the APIs for our products or finished products or if we rely on sole-source suppliers, we may experience delays in commercializing our products.
We currently do not have supply agreements for topiramate or phentermine, which are APIs used in Qsymia. We cannot guarantee that we will be successful in entering into supply agreements on reasonable terms or at all or that we will be able to obtain or maintain the necessary regulatory approvals for potential future suppliers in a timely manner or at all.
We anticipate that we will continue to rely on single-source suppliers for phentermine and topiramate for the foreseeable future. Any production shortfall on the part of our suppliers that impairs the supply of phentermine or topiramate could have a material adverse effect on our business, financial condition and results of operations. If we are unable to obtain a sufficient quantity of these compounds, there could be a substantial delay in successfully developing a second source supplier. An inability to continue to source product from any of these suppliers, which could be due to regulatory actions or requirements affecting the supplier, adverse financial or other strategic developments experienced by a supplier, labor disputes or shortages, unexpected demands or quality issues, could adversely affect our ability to satisfy demand for Qsymia, which could adversely affect our product sales and operating results materially, which could significantly harm our business.
We currently do not have any manufacturing facilities and intend to continue to rely on third parties for the supply of the API and tablets, as well as for the supply of starting materials. However, we cannot be certain that we will be able to obtain or maintain the necessary regulatory approvals for these suppliers in a timely manner or at all. In August 2012, we entered into an amendment to our license agreement with MTPC that permits us to manufacture the API and tablets for STENDRA ourselves or through third-parties. In 2015, we transferred the manufacturing of the API and tables for STENDRA to Sanofi.
In July 2013, we entered into a Commercial Supply Agreement with Sanofi Chimie to manufacture and supply the API for avanafil on an exclusive basis in the United States and other territories and on a semi-exclusive basis in Europe, including the EU, Latin America and other territories. In November 2013, we entered into a Manufacturing and Supply Agreement with Sanofi Winthrop Industrie to manufacture and supply the avanafil tablets on an exclusive basis in the United States and other territories and on a semi-exclusive basis in Europe, including the EU, Latin America and
38
other territories. We have obtained approval from the FDA and the European Medicines Agency, or EMA, of Sanofi Chimie as a qualified supplier of avanafil API and of Sanofi Winthrop Industrie as a qualified supplier of the avanafil tablets. We have entered into supply agreements with Menarini and Auxilium under which we are obligated to supply them with avanafil tablets. If we are unable to maintain a reliable supply of avanafil API or tablets from Sanofi Chimie and/or Sanofi Winthrop Industrie, we may be unable to satisfy our obligations under these supply agreements in a timely manner or at all, and we may, as a result, be in breach of one or both of these agreements.
We have in-licensed all or a portion of the rights to Qsymia and STENDRA from third parties. If we default on any of our material obligations under those licenses, we could lose rights to these drugs.
We have in-licensed and otherwise contracted for rights to Qsymia and STENDRA, and we may enter into similar licenses in the future. Under the relevant agreements, we are subject to commercialization, development, supply, sublicensing, royalty, insurance and other obligations. If we fail to comply with any of these requirements, or otherwise breach these license agreements, the licensor may have the right to terminate the license in whole or to terminate the exclusive nature of the license. Loss of any of these licenses or the exclusive rights provided therein could harm our financial condition and operating results.
In particular, we license the rights to avanafil from MTPC, and we have certain obligations to MTPC in connection with that license. We license the rights to Qsymia from Dr. Najarian. We believe we are in compliance with the material terms of our license agreements with MTPC and Dr. Najarian. However, there can be no assurance that this compliance will continue or that the licensors will not have a differing interpretation of the material terms of the agreements. If the license agreements were terminated early or if the terms of the licenses were contested for any reason, it would have a material adverse impact on our ability to commercialize products subject to these agreements, our ability to raise funds to finance our operations, our stock price and our overall financial condition. The monetary and disruption costs of any disputes involving our agreements could be significant despite rulings in our favor.
Our ability to gain market acceptance and generate revenues will be subject to a variety of risks, many of which are out of our control.
Qsymia and STENDRA may not gain market acceptance among physicians, patients, healthcare payors or the medical community. We believe that the degree of market acceptance and our ability to generate revenues from such drugs will depend on a number of factors, including:
|
· |
our ability to expand the use of Qsymia through targeted patient and physician education; |
|
· |
our ability to find the right partner for expanded Qsymia commercial promotion to a broader primary care physician audience; |
|
· |
our ability to obtain marketing authorization by the EC for Qsiva in the EU through the centralized procedure; |
|
· |
our ability to successfully expand the certified retail pharmacy distribution channel in the United States; |
|
· |
contraindications for Qsymia and STENDRA; |
|
· |
competition and timing of market introduction of competitive drugs; |
|
· |
quality, safety and efficacy in the approved setting; |
|
· |
prevalence and severity of any side effects, including those of the generic components of our drugs; |
|
· |
emergence of previously unknown side effects, including those of the generic components of our drugs; |
|
· |
results of any post-approval studies; |
39
|
· |
potential or perceived advantages or disadvantages over alternative treatments, including generics; |
|
· |
the relative convenience and ease of administration and dosing schedule; |
|
· |
the convenience and ease of purchasing the drug, as perceived by potential patients; |
|
· |
strength of sales, marketing and distribution support; |
|
· |
price, both in absolute terms and relative to alternative treatments; |
|
· |
the effectiveness of our or any future collaborators’ sales and marketing strategies; |
|
· |
the effect of current and future healthcare laws; |
|
· |
availability of coverage and reimbursement from government and other third-party payors; |
|
· |
the level of mandatory discounts required under federal and state healthcare programs and the volume of sales subject to those discounts; |
|
· |
recommendations for prescribing physicians to complete certain educational programs for prescribing drugs; |
|
· |
the willingness of patients to pay out-of-pocket in the absence of government or third-party coverage; and |
|
· |
product labeling, product insert, or new REMS requirements of the FDA or other regulatory authorities. |
Our drugs may fail to achieve market acceptance or generate significant revenue to achieve or sustain profitability. In addition, our efforts to educate the medical community and third-party payors on the safety and benefits of our drugs may require significant resources and may not be successful.
We are required to complete post-approval studies and trials mandated by the FDA for Qsymia, and such studies and trials are expected to be costly and time consuming. If the results of these studies and trials reveal unacceptable safety risks, Qsymia may be required to be withdrawn from the market.
As part of the approval of Qsymia, we are required to conduct several post-marketing studies and trials, including a clinical trial to assess the long-term treatment effect of Qsymia on the incidence of major adverse cardiovascular events in overweight and obese subjects with confirmed cardiovascular disease, or AQCLAIM, studies to assess the safety and efficacy of Qsymia for weight management in obese pediatric and adolescent subjects, studies to assess drug utilization and pregnancy exposure and a study to assess renal function. We estimate the AQCLAIM trial as currently designed will cost between $180 million and $220 million and the trial could take as long as five to six years to complete. In September 2013, we submitted a request to the EMA for Scientific Advice, a procedure similar to the U.S. Special Protocol Assessment process, regarding use of a pre-specified interim analysis from the CVOT, known as AQCLAIM, to assess the long-term treatment effect of Qsymia on the incidence of major adverse cardiovascular events in overweight and obese subjects with confirmed cardiovascular disease. Our request was to allow this interim analysis to support the resubmission of an application for a marketing authorization for Qsiva for treatment of obesity in accordance with the EU centralized marketing authorization procedure. We received feedback in 2014 from the EMA and the various competent authorities of the EU Member States associated with review of the AQCLAIM CVOT protocol, and we received feedback from the FDA in late 2014 regarding the amended protocol. As a part of addressing the FDA comments from a May 2015 meeting to discuss alternatives to completion of a CVOT, we are now working with cardiovascular and epidemiology experts in exploring alternate solutions to demonstrate the long-term cardiovascular safety of Qsymia. After reviewing a summary of Phase 3 data relevant to CV risk and post-marketing safety data, the cardiology experts noted that they believe there was an absence of an overt CV risk signal and indicated that they did not see a justification for a randomized placebo controlled CVOT trial. The epidemiology experts
40
maintained that a well-conducted retrospective observational study could provide data to further inform on potential CV risk. We are working with the expert group to develop a protocol for the retrospective observational study and feasibility assessment. Although we and the consulted experts believe there is no overt signal for CV risk to justify the AQCLAIM CVOT, VIVUS is committed to working with the FDA to reach a resolution. As for the EU, even if the FDA were to accept a retrospective observational study in lieu of a CVOT, there would be no assurance that the EMA would accept the same. There can be no assurance that we will be successful in developing a further revised protocol or that any such revised protocol will reduce the costs of the study or obtain FDA or EMA agreement that it will fulfill the requirement of demonstrating the long-term cardiovascular safety of Qsymia. Furthermore, there can be no assurance that the FDA or EMA will not request or require us to provide additional information or undertake additional preclinical studies and clinical trials or retrospective observational studies.
In addition to these studies, the FDA may also require us to perform other lengthy post-approval studies or trials, for which we would have to expend significant additional resources, which could have an adverse effect on our operating results, financial condition and stock price. Failure to comply with the applicable regulatory requirements, including the completion of post-marketing studies and trials, can result in, among other things, civil monetary penalties, suspensions of regulatory approvals, operating restrictions and criminal prosecution. The restriction, suspension or revocation of regulatory approvals or any other failure to comply with regulatory requirements could have a material adverse effect on our business, financial condition, results of operations and stock price. We have not complied with all the regulatory timelines for the required post-marketing trials and studies, and this may be considered a violation of the statute if the FDA does not find good cause.
We depend upon consultants and outside contractors extensively in important roles within our company.
We outsource many key functions of our business and therefore rely on a substantial number of consultants, and we will need to be able to effectively manage these consultants to ensure that they successfully carry out their contractual obligations and meet expected deadlines. However, if we are unable to effectively manage our outsourced activities or if the quality or accuracy of the services provided by consultants is compromised for any reason, our clinical trials or other development activities may be extended, delayed or terminated, and we may not be able to complete our post-approval clinical trials for Qsymia and STENDRA, obtain regulatory approval for our future investigational drug candidates, successfully commercialize our approved drugs or otherwise advance our business. There can be no assurance that we will be able to manage our existing consultants or find other competent outside contractors and consultants on commercially reasonable terms, or at all.
Qsymia is a combination of two active ingredient drug products approved individually by the FDA that are commercially available and marketed by other companies, although the specific dose strengths differ. As a result, Qsymia may be subject to substitution by prescribing physicians, or by pharmacists, with individual drugs contained in the Qsymia formulation, which would adversely affect our business.
Although Qsymia is a once-a-day, proprietary extended-release formulation, both of the approved APIs (phentermine and topiramate) that are combined to produce Qsymia are commercially available as drug products at prices that together are lower than the price at which we sell Qsymia. In addition, the distribution and sale of these drug products is not limited under a REMS program, as is the case with Qsymia. Further, the individual drugs contained in the Qsymia formulation are available in retail pharmacies and phentermine has a Pregnancy Category X, which is used to indicate that the risks involved in the use of the drug in pregnant women clearly outweigh potential benefits. We cannot be sure that physicians will view Qsymia as sufficiently superior to a treatment regimen of Qsymia’s individual APIs to justify the significantly higher cost for Qsymia, and they may prescribe the individual generic drugs already approved and marketed by other companies instead of our combination drug. Although our U.S. and European patents contain composition, product formulation and method-of-use claims that we believe protect Qsymia, these patents may be ineffective or impractical to prevent physicians from prescribing, or pharmacists from dispensing, the individual generic constituents marketed by other companies instead of our combination drug. Phentermine and topiramate are currently available in generic form, although the doses used in Qsymia are currently not available. In the third quarter of 2013, Supernus Pharmaceuticals, Inc. launched Trokendi XR™ and in the second quarter of 2014, Upsher-Smith Laboratories, Inc. launched Qudexy™. Both products provide an extended-release formulation of the generic drug topiramate that is indicated for certain types of seizures and migraines. Topiramate is not approved for obesity treatment,
41
and phentermine is only approved for short-term treatment of obesity. However, because the price of Qsymia is significantly higher than the prices of the individual components as marketed by other companies, physicians may have a greater incentive to write prescriptions for the individual components outside of their approved indication, instead of for our combination drug, and this may limit how we price or market Qsymia. Similar concerns could also limit the reimbursement amounts private health insurers or government agencies in the U.S. are prepared to pay for Qsymia, which could also limit market and patient acceptance of our drug and could negatively impact our revenues.
In many regions and countries where we may plan to market Qsymia, the pricing of reimbursed prescription drugs is controlled by the government or regulatory agencies. The government or regulatory agencies in these countries could determine that the pricing for Qsymia should be based on prices for its APIs when sold separately, rather than allowing us to market Qsymia at a premium as a new drug, which could limit our pricing of Qsymia and negatively impact our revenues.
Once an applicant receives authorization to market a medicinal product in an EU Member State, through any application route, the applicant is required to engage in pricing discussions and negotiations with a separate pricing authority in that country. The legislators, policymakers and healthcare insurance funds in the EU Member States continue to propose and implement cost-containing measures to keep healthcare costs down, due in part to the attention being paid to healthcare cost containment and other austerity measures in the EU. Certain of these changes could impose limitations on the prices pharmaceutical companies are able to charge for their products. The amounts of reimbursement available from governmental agencies or third-party payors for these products may increase the tax obligations on pharmaceutical companies such as ours, or may facilitate the introduction of generic competition with respect to our products. Furthermore, an increasing number of EU Member States and other foreign countries use prices for medicinal products established in other countries as “reference prices” to help determine the price of the product in their own territory. Consequently, a downward trend in the price of medicinal products in some countries could contribute to similar downward trends elsewhere. In addition, the ongoing budgetary difficulties faced by a number of EU Member States, including Greece and Spain, have led and may continue to lead to substantial delays in payment and payment partially with government bonds rather than cash for medicinal products, which could negatively impact our revenues and profitability. Moreover, in order to obtain reimbursement of our medicinal products in some countries, including some EU Member States, we may be required to conduct clinical trials that compare the cost-effectiveness of our products to other available therapies. There can be no assurance that our medicinal products will obtain favorable reimbursement status in any country.
If we become subject to product liability claims, we may be required to pay damages that exceed our insurance coverage.
Qsymia and STENDRA, like all pharmaceutical products, are subject to heightened risk for product liability claims due to inherent potential side effects. For example, because topiramate, a component of Qsymia, may increase the risk of congenital malformation in infants exposed to topiramate during the first trimester of pregnancy and also may increase the risk of suicidal thoughts and behavior, such risks may be associated with Qsymia as well. Other potential risks involving Qsymia may include, but are not limited to, an increase in resting heart rate, acute angle closure glaucoma, cognitive and psychiatric adverse events, metabolic acidosis, an increase in serum creatinine, hypoglycemia in patients with type 2 diabetes, kidney stone formation, decreased sweating and hypokalemia, or lower-than-normal amount of potassium in the blood.
Although we have obtained product liability insurance coverage for Qsymia, we may be unable to maintain this product liability coverage for Qsymia or any other of our approved drugs in amounts or scope sufficient to provide us with adequate coverage against all potential risks. A product liability claim in excess of, or excluded from, our insurance coverage would have to be paid out of cash reserves and could have a material adverse effect upon our business, financial condition and results of operations. Product liability insurance is expensive even with large self-insured retentions or deductibles, difficult to maintain, and current or increased coverage may not be available on acceptable terms, if at all.
In addition, we develop, test, and manufacture through third parties, approved drugs and future investigational drug candidates that are used by humans. We face an inherent risk of product liability exposure related to the testing of
42
our approved drugs and investigational drug candidates in clinical trials. An individual may bring a liability claim against us if one of our approved drugs or future investigational drug candidates causes, or merely appears to have caused, an injury.
If we cannot successfully defend ourselves against a product liability claim, whether involving Qsymia, STENDRA or a future investigational drug candidate or product, we may incur substantial liabilities. Regardless of merit or eventual outcome, liability claims may result in:
|
· |
injury to our reputation; |
|
· |
withdrawal of clinical trial patients; |
|
· |
costs of defending the claim and/or related litigation; |
|
· |
cost of any potential adverse verdict; |
|
· |
substantial monetary awards to patients or other claimants; and |
|
· |
the inability to commercialize our drugs. |
Damages awarded in a product liability action could be substantial and could have a negative impact on our financial condition. Whether or not we were ultimately successful in product liability litigation, such litigation would consume substantial amounts of our financial and managerial resources, and might result in adverse publicity, all of which would impair our business. In addition, product liability claims could result in an FDA investigation of the safety or efficacy of our product, our third-party manufacturing processes and facilities, or our marketing programs. An FDA investigation could also potentially lead to a recall of our products or more serious enforcement actions, limitations on the indications for which they may be used, or suspension or withdrawal of approval.
The markets in which we operate are highly competitive and we may be unable to compete successfully against new entrants or established companies.
Competition in the pharmaceutical and medical products industries is intense and is characterized by costly and extensive research efforts and rapid technological progress. We are aware of several pharmaceutical companies also actively engaged in the development of therapies for the treatment of obesity and erectile dysfunction. Many of these companies have substantially greater research and development capabilities as well as substantially greater marketing, financial and human resources than we do. Some of the drugs that may compete with Qsymia may not have a REMS requirement and the accompanying complexities such a requirement presents. Our competitors may develop technologies and products that are more effective than those we are currently marketing or researching and developing. Such developments could render Qsymia and STENDRA less competitive or possibly obsolete. We are also competing with respect to marketing capabilities and manufacturing efficiency, areas in which we have limited experience.
Qsymia for the treatment of chronic weight management competes with several approved anti-obesity drugs including, Belviq® (lorcaserin), Arena Pharmaceutical’s approved anti-obesity compound marketed by Eisai Inc., Eisai Co., Ltd.’s U.S. subsidiary; Xenical® (orlistat), marketed by Roche; alli®, the over-the-counter version of orlistat, marketed by GlaxoSmithKline; Suprenza™, an orally disintegrating tablet (phentermine hydrochloride), marketed by Akrimax Pharmaceuticals, LCL; Contrave® (naltrexone/bupropion), Orexigen Therapeutics, Inc.’s anti-obesity compound marketed by Takeda Pharmaceutical Company Limited; and Saxenda® (liraglutide), an anti-obesity compound marketed by Novo Nordisk A/S. Agents that have been approved for type 2 diabetes that have demonstrated weight loss in clinical studies may also compete with Qsymia. These include Farxiga™ (dapagliflozin) from AstraZeneca and Bristol-Myers Squibb, an SGLT2 inhibitor, approved January 8, 2014; Jardiance® (empagliflozin) from Boehringer Ingelheim, an SGLT2 inhibitor, approved August 1, 2014; Victoza® (liraglutide) from Novo Nordisk A/S, a GLP-1 receptor agonist approved January 25, 2010; Invokana® (canaglifozin) from Johnson & Johnson’s Janssen Pharmaceuticals, an SGLT2 inhibitor, approved March 29, 2013 and Glyxambi® (empagliflozin/linagliptin) from Boehringer Ingelheim and Eli Lilly, an SGLT2 inhibitor and DPP-4 inhibitor combination product, approved January 30,
43
2015. Also, on January 14, 2015, FDA approved the Maestro Rechargeable System for certain obese adults, the first weight loss treatment device that targets the nerve pathway between the brain and the stomach that controls feelings of hunger and fullness. The Maestro Rechargeable System is approved to treat patients aged 18 and older who have not been able to lose weight with a weight loss program, and who have a body mass index of 35 to 45 with at least one other obesity-related condition, such as type 2 diabetes.
There are also several other investigational drug candidates in Phase 2 clinical trials for the treatment of obesity. There are also a number of generic pharmaceutical drugs that are prescribed for obesity, predominantly phentermine. Phentermine is sold at much lower prices than we charge for Qsymia. The availability of branded prescription drugs, generic drugs and over-the-counter drugs could limit the demand for, and the price we are able to charge for, Qsymia.
We also may face competition from the off-label use of the generic components in our drugs. In particular, it is possible that patients will seek to acquire phentermine and topiramate, the generic components of Qsymia. Neither of these generic components has a REMS program and both are available at retail pharmacies. Although the dose strength of these generic components has not been approved by the FDA for use in the treatment of obesity, the off-label use of the generic components in the U.S. or the importation of the generic components from foreign markets could adversely affect the commercial potential for our drugs and adversely affect our overall business, financial condition and results of operations.
There are also surgical approaches to treat severe obesity that are becoming increasingly accepted. Two of the most well established surgical procedures are gastric bypass surgery and adjustable gastric banding, or lap bands. In February 2011, the FDA approved the use of a lap band in patients with a BMI of 30 (reduced from 35) with comorbidities. The lowering of the BMI requirement will make more obese patients eligible for lap band surgery. In addition, other potential approaches that utilize various implantable devices or surgical tools are in development. Some of these approaches are in late-stage development and may be approved for marketing.
We anticipate that STENDRA for the treatment of erectile dysfunction will compete with PDE5 inhibitors in the form of oral medications, including Viagra® (sildenafil citrate), marketed by Pfizer, Inc.; Cialis® (tadalafil), marketed by Eli Lilly and Company; Levitra® (vardenafil), co-marketed by GlaxoSmithKline plc and Schering-Plough Corporation in the U.S.; and STAXYN® (vardenafil in an oral disintegrating tablet, or ODT), co-marketed by GlaxoSmithKline plc and Merck & Co., Inc.
We anticipate that generic PDE5 inhibitors will enter the market in the U.S. in late 2017. Generic PDE5 inhibitors would likely be sold at lower prices and may reduce the demand for STENDRA, especially at the prices we would be required to charge for STENDRA to cover our manufacturing and other costs. In addition, PDE5 inhibitors are in various stages of development by other companies. Warner-Chilcott plc, which was acquired by Actavis, Inc. and changed its name to Actavis plc, has licensed the U.S. rights to udenafil, a PDE5 inhibitor, from Dong-A Pharmaceutical, now known as Mezzion Pharma Co. Ltd. Actavis, Inc. acquired Allergan, changed its name to Allergan, plc and has announced that it is being acquired by Pfizer. Other treatments for ED exist, such as needle injection therapies, vacuum constriction devices and penile implants, and the manufacturers of these products will most likely continue to develop or improve these therapies.
Qsymia and STENDRA may also face challenges and competition from newly developed generic products. Under the U.S. Drug Price Competition and Patent Term Restoration Act of 1984, known as the Hatch-Waxman Act, newly approved drugs and indications may benefit from a statutory period of non-patent marketing exclusivity. The Hatch-Waxman Act stimulates competition by providing incentives to generic pharmaceutical manufacturers to introduce non-infringing forms of patented pharmaceutical products and to challenge patents on branded pharmaceutical products. If we are unsuccessful at challenging an Abbreviated New Drug Application, or ANDA, filed pursuant to the Hatch-Waxman Act, a generic version of Qsymia or STENDRA may be launched, which would harm our business.
The FDCA provides that an ANDA and an innovator drug with a REMS with Elements to Assure Safe use, like Qsymia, must use a single shared REMS system to assure safe use unless FDA waives this requirement and permits the ANDA holder to implement a separate but comparable REMS. We cannot predict the outcome or impact on our business of any future action that we may take with regard to sharing our REMS program or if the FDA grants a waiver allowing
44
the generic competitor to market a generic drug with a separate but compatible REMS.
New developments, including the development of other drug technologies and methods of preventing the incidence of disease, occur in the pharmaceutical and medical technology industries at a rapid pace. These developments may render our drugs and future investigational drug candidates obsolete or noncompetitive. Compared to us, many of our potential competitors have substantially greater:
|
· |
research and development resources, including personnel and technology; |
|
· |
regulatory experience; |
|
· |
investigational drug candidate development and clinical trial experience; |
|
· |
experience and expertise in exploitation of intellectual property rights; and |
|
· |
access to strategic partners and capital resources. |
As a result of these factors, our competitors may obtain regulatory approval of their products more rapidly than we or may obtain patent protection or other intellectual property rights that limit our ability to develop or commercialize our future investigational drug candidates. Our competitors may also develop drugs or surgical approaches that are more effective, more useful and less costly than ours and may also be more successful in manufacturing and marketing their products. In addition, our competitors may be more effective in commercializing their products. We currently outsource our manufacturing and therefore rely on third parties for that competitive expertise. There can be no assurance that we will be able to develop or contract for these capabilities on acceptable economic terms, or at all.
We may participate in new partnerships and other strategic transactions that could impact our liquidity, increase our expenses and present significant distractions to our management.
From time to time, we consider strategic transactions, such as out-licensing or in-licensing of compounds or technologies, acquisitions of companies and asset purchases. Additional potential transactions we may consider include a variety of different business arrangements, including strategic partnerships, joint ventures, spin-offs, restructurings, divestitures, business combinations and investments. In addition, another entity may pursue us as an acquisition target. Any such transactions may require us to incur non-recurring or other charges, may increase our near- and long-term expenditures and may pose significant integration challenges, require additional expertise or disrupt our management or business, any of which could harm our operations and financial results.
As part of an effort to enter into significant transactions, we conduct business, legal and financial due diligence with the goal of identifying and evaluating material risks involved in the transaction. Despite our efforts, we ultimately may be unsuccessful in ascertaining or evaluating all such risks and, as a result, might not realize the expected benefits of the transaction. If we fail to realize the expected benefits from any transaction we may consummate, whether as a result of unidentified risks, integration difficulties, regulatory setbacks or other events, our business, results of operations and financial condition could be adversely affected.
Our failure to successfully acquire, develop and market additional investigational drug candidates or approved drugs would impair our ability to grow.
As part of our growth strategy, we may acquire, in-license, develop and/or market additional products and investigational drug candidates. We have not in-licensed any new product candidates in several years. Because our internal research capabilities are limited, we may be dependent upon pharmaceutical and biotechnology companies, academic scientists and other researchers to sell or license products or technology to us. The success of this strategy depends partly upon our ability to identify, select and acquire promising pharmaceutical investigational drug candidates and products.
The process of proposing, negotiating and implementing a license or acquisition of an investigational drug
45
candidate or approved product is lengthy and complex. Other companies, including some with substantially greater financial, marketing and sales resources, may compete with us for the license or acquisition of investigational drug candidates and approved products. We have limited resources to identify and execute the acquisition or in-licensing of third-party products, businesses and technologies and integrate them into our current infrastructure. Moreover, we may devote resources to potential acquisitions or in-licensing opportunities that are never completed, or we may fail to realize the anticipated benefits of such efforts. We may not be able to acquire the rights to additional investigational drug candidates on terms that we find acceptable, or at all.
In addition, future acquisitions may entail numerous operational and financial risks, including:
|
· |
exposure to unknown liabilities; |
|
· |
disruption of our business and diversion of our management’s time and attention to develop acquired products or technologies; |
|
· |
incurrence of substantial debt or dilutive issuances of securities to pay for acquisitions; |
|
· |
higher than expected acquisition, integration and maintenance costs; |
|
· |
increased amortization expenses; |
|
· |
difficulty and cost in combining the operations and personnel of any acquired businesses with our operations and personnel; |
|
· |
impairment of relationships with key suppliers or customers of any acquired businesses due to changes in management and ownership; and |
|
· |
inability to retain key employees of any acquired businesses. |
Further, any investigational drug candidate that we acquire may require additional development efforts prior to commercial sale, including extensive clinical testing and obtaining approval by the FDA and applicable foreign regulatory authorities. All investigational drug candidates are prone to certain failures that are relatively common in the field of drug development, including the possibility that an investigational drug candidate will not be shown to be sufficiently safe and effective for approval by regulatory authorities. In addition, we cannot be certain that any drugs that we develop or approved products that we may acquire will be commercialized profitably or achieve market acceptance.
If we fail to retain our key personnel and hire, train and retain qualified employees, we may not be able to compete effectively, which could result in reduced revenues or delays in the development of our investigational drug candidates or commercialization of our approved drugs.
Our success is highly dependent upon the skills of a limited number of key management personnel. To reach our business objectives, we will need to retain and hire qualified personnel in the areas of manufacturing, commercial operations, research and development, regulatory and legal affairs, business development, clinical trial design, execution and analysis, and pre-clinical testing. There can be no assurance that we will be able to retain or hire such personnel, as we must compete with other companies, academic institutions, government entities and other agencies. The loss of any of our key personnel or the failure to attract or retain necessary new employees could have an adverse effect on our research programs, investigational drug candidate development, approved drug commercialization efforts and business operations.
We rely on third parties and collaborative partners to manufacture sufficient quantities of compounds within product specifications as required by regulatory agencies for use in our pre-clinical and clinical trials and commercial operations and an interruption to this service may harm our business.
We do not have the ability to manufacture the materials we use in our pre-clinical and clinical trials and commercial operations. Rather, we rely on various third parties to manufacture these materials and there may be long
46
lead times to obtain materials. There can be no assurance that we will be able to identify, contract with, qualify and obtain prior regulatory approval for additional sources of clinical materials. If interruptions in this supply occur for any reason, including a decision by the third parties to discontinue manufacturing, technical difficulties, labor disputes, natural or other disasters, or a failure of the third parties to follow regulations, we may not be able to obtain regulatory approvals for our investigational drug candidates and may not be able to successfully commercialize these investigational drug candidates or our approved drugs.
Our third-party manufacturers and collaborative partners may encounter delays and problems in manufacturing our approved drugs or investigational drug candidates for a variety of reasons, including accidents during operation, failure of equipment, delays in receiving materials, natural or other disasters, political or governmental changes, or other factors inherent in operating complex manufacturing facilities. Supply-chain management is difficult. Commercially available starting materials, reagents, excipients, and other materials may become scarce, more expensive to procure, or not meet quality standards, and we may not be able to obtain favorable terms in agreements with subcontractors. Our third-party manufacturers may not be able to operate manufacturing facilities in a cost-effective manner or in a time frame that is consistent with our expected future manufacturing needs. If our third-party manufacturers, cease or interrupt production or if our third-party manufacturers and other service providers fail to supply materials, products or services to us for any reason, such interruption could delay progress on our programs, or interrupt the commercial supply, with the potential for additional costs and lost revenues. If this were to occur, we may also need to seek alternative means to fulfill our manufacturing needs.
For example, Catalent Pharma Solutions, LLC, or Catalent, supplied the product for the Phase 3 program for Qsymia and is our sole source of clinical and commercial supplies for Qsymia. Catalent has been successful in validating the commercial manufacturing process for Qsymia at an initial scale, which has been able to support the launch of Qsymia in the U.S. market. While Catalent has significant experience in commercial scale manufacturing, there is no assurance that Catalent will be successful in increasing the scale of the initial Qsymia manufacturing process, should the market demand for Qsymia expand beyond the level supportable by the current validated manufacturing process. Such a failure by Catalent to further scale up the commercial manufacturing process for Qsymia could have a material adverse impact on our ability to realize commercial success with Qsymia in the U.S. market, and have a material adverse impact on our plan, market price of our common stock and financial condition.
In the case of avanafil, we currently rely on Sanofi to supply the API and tablets for STENDRA and SPEDRA. Sanofi is responsible for all aspects of manufacture, including obtaining the starting materials for the production of API. If Sanofi is unable to manufacture the API or tablets in sufficient quantities to meet projected demand, future sales could be adversely affected, which in turn could have a detrimental impact on our financial results, our license, commercialization, and supply agreements with our collaboration partners, and our ability to enter into a collaboration agreement for the commercialization in other territories.
In July 2013, we entered into a Commercial Supply Agreement with Sanofi Chimie to manufacture and supply the API for avanafil on an exclusive basis in the United States and other territories and on a semi-exclusive basis in Europe, including the EU, Latin America and other territories. On November 18, 2013, we entered into a Manufacturing and Supply Agreement with Sanofi Winthrop Industrie to manufacture and supply the avanafil tablets on an exclusive basis in the United States and other territories and on a semi-exclusive basis in Europe, including the EU, Latin America and other territories. Sanofi received FDA and EMA approval in 2015 and began manufacturing API and tablets for avanafil in 2015.
Any failure of current or future manufacturing sites, including those of Sanofi Chimie and Sanofi Winthrop Industrie, to receive or maintain approval from FDA or foreign authorities, obtain and maintain ongoing FDA or foreign regulatory compliance, or manufacture avanafil API or tablets in expected quantities could have a detrimental impact on our ability to commercialize STENDRA under our agreements with Sanofi, Auxilium and Menarini and our ability to enter into a collaboration agreement for the commercialization of STENDRA in our other territories not covered by our agreements with Sanofi, Auxilium and Menarini.
47
We rely on third parties to maintain appropriate levels of confidentiality of the data compiled during clinical, pre-clinical and retrospective observational studies and trials.
We seek to maintain the confidential nature of our confidential information through contractual provisions in our agreements with third parties, including our agreements with clinical research organizations, or CROs, that manage our clinical studies for our investigational drug candidates. These CROs may fail to comply with their obligations of confidentiality or may be required as a matter of law to disclose our confidential information. As the success of our clinical studies depends in large part on our confidential information remaining confidential prior to, during and after a clinical study, any disclosure or breach affecting that information could have a material adverse effect on the outcome of a clinical study, our business, financial condition and results of operations.
The collection and use of personal health data and other personal data in the EU is governed by the provisions of the Data Protection Directive as implemented into national laws by the EU Member States. This Directive imposes restrictions on the processing (e.g., collection, use, disclosure) of personal data, including a number of requirements relating to the consent of the individuals to whom the personal data relates, the information provided to the individuals prior to processing their personal data, notification of data processing obligations to the competent national data protection authorities and the security and confidentiality of the personal data. The Data Protection Directive also imposes strict restrictions on the transfer of personal data out of the EU to the United States. Failure to comply with the requirements of the Data Protection Directive and the related national data protection laws of the EU Member States may result in fines and other administrative penalties. On December 15, 2015, a proposal for an EU Data Protection Regulation, intended to replace the current EU Data Protection Directive, was agreed to by the European Parliament, the Council of the European Union and the European Commission. The EU Data Protection Regulation, which will be officially adopted in early 2016, will introduce new data protection requirements in the EU and substantial fines for violations of the data protection rules. The EU Data Protection Regulation, which will be applicable two years after the date of its publication in the Official Journal for the European Union, will increase our responsibility and liability in relation to EU personal data that we process and we may be required to put in place additional mechanisms ensuring compliance with the new EU data protection rules. This may be onerous and increase our cost of doing business.
If we fail to comply with applicable healthcare and privacy and data security laws and regulations, we could face substantial penalties, liability and adverse publicity and our business, operations and financial condition could be adversely affected.
Our arrangements with third-party payors and customers expose us to broadly applicable federal and state healthcare laws and regulations pertaining to fraud and abuse. In addition, our operations expose us to privacy and data security laws and regulations. The restrictions under applicable federal and state healthcare laws and regulations, and privacy and data security laws and regulations, that may affect our ability to operate include, but are not limited to:
|
· |
the federal Anti-Kickback Law, which prohibits, among other things, knowingly or willingly offering, paying, soliciting or receiving remuneration, directly or indirectly, in cash or in kind, to induce or reward the purchasing, leasing, ordering or arranging for or recommending the purchase, lease or order of any healthcare items or service for which payment may be made, in whole or in part, by federal healthcare programs such as Medicare and Medicaid. This statute has been interpreted to apply to arrangements between pharmaceutical companies on one hand and prescribers, purchasers and formulary managers on the other. Further, the Affordable Care Act, among other things, clarified that liability may be established under the federal Anti-Kickback Law without proving actual knowledge of the federal Anti-Kickback statute or specific intent to violate it. In addition, the Affordable Care Act amended the Social Security Act to provide that the government may assert that a claim including items or services resulting from a violation of the federal Anti-Kickback Law constitutes a false or fraudulent claim for purposes of the federal civil False Claims Act. Although there are a number of statutory exemptions and regulatory safe harbors to the federal Anti-Kickback Law protecting certain common business arrangements and activities from prosecution or regulatory sanctions, the exemptions and safe harbors are drawn narrowly, and practices that do not fit squarely within an exemption or safe harbor may be subject to scrutiny. We seek to comply with the exemptions and safe harbors whenever possible, but our practices may not in all cases meet all of the criteria for safe harbor protection from anti-kickback liability; |
48
|
· |
the federal civil False Claims Act, which prohibits, among other things, individuals or entities from knowingly presenting, or causing to be presented, a false or fraudulent claim for payment of government funds or knowingly making, using, or causing to be made or used, a false record or statement material to an obligation to pay money to the government or knowingly concealing, or knowingly and improperly avoiding, decreasing, or concealing an obligation to pay money to the federal government. Many pharmaceutical and other healthcare companies have been investigated and have reached substantial financial settlements with the federal government under the civil False Claims Act for a variety of alleged improper marketing activities, including providing free product to customers with the expectation that the customers would bill federal programs for the product; providing consulting fees, grants, free travel, and other benefits to physicians to induce them to prescribe the company’s products; and inflating prices reported to private price publication services, which are used to set drug payment rates under government healthcare programs. In addition, in recent years the government has pursued civil False Claims Act cases against a number of pharmaceutical companies for causing false claims to be submitted as a result of the marketing of their products for unapproved, and thus non-reimbursable, uses. Pharmaceutical and other healthcare companies also are subject to other federal false claim laws, including, among others, federal criminal healthcare fraud and false statement statutes that extend to non-government health benefit programs; |
|
· |
numerous U.S. federal and state laws and regulations, including state data breach notification laws, state health information privacy laws and federal and state consumer protection laws, govern the collection, use, disclosure and protection of personal information. Other countries also have, or are developing, laws governing the collection, use, disclosure and protection of personal information. In addition, most healthcare providers who prescribe our products and from whom we obtain patient health information are subject to privacy and security requirements under the Health Insurance Portability and Accountability Act of 1996, as amended by the Health Information Technology for Economic and Clinical Health Act, or HIPAA. We are not a HIPAA-covered entity and we do not operate as a business associate to any covered entities. Therefore, the HIPAA privacy and security requirements do not apply to us (other than potentially with respect to providing certain employee benefits). However, we could be subject to criminal penalties if we knowingly obtain individually identifiable health information from a covered entity in a manner that is not authorized or permitted by HIPAA or for aiding and abetting and/or conspiring to commit a violation of HIPAA. We are unable to predict whether our actions could be subject to prosecution in the event of an impermissible disclosure of health information to us. The legislative and regulatory landscape for privacy and data security continues to evolve, and there has been an increasing amount of focus on privacy and data security issues with the potential to affect our business. These privacy and data security laws and regulations could increase our cost of doing business, and failure to comply with these laws and regulations could result in government enforcement actions (which could include civil or criminal penalties), private litigation and/or adverse publicity and could negatively affect our operating results and business; |
|
· |
analogous state laws and regulations, such as state anti-kickback and false claims laws, may apply to items or services reimbursed under Medicaid and other state programs or, in several states, apply regardless of the payor. Some state laws also require pharmaceutical companies to report expenses relating to the marketing and promotion of pharmaceutical products and to report gifts and payments to certain health care providers in the states. Other states prohibit providing meals to prescribers or other marketing-related activities. In addition, California, Connecticut, Nevada, and Massachusetts require pharmaceutical companies to implement compliance programs or marketing codes of conduct. Foreign governments often have similar regulations, which we also will be subject to in those countries where we market and sell products; |
|
· |
the federal Physician Payment Sunshine Act, being implemented as the Open Payments Program, requires certain pharmaceutical manufacturers to engage in extensive tracking of payments and other transfers of value to physicians and teaching hospitals, and to submit such data to CMS, which will then make all of this data publicly available on the CMS website. Pharmaceutical manufacturers with products for which |
49
payment is available under Medicare, Medicaid or the State Children’s Health Insurance Program were required to have started tracking reportable payments on August 1, 2013, and must submit a report to CMS on or before the 90th day of each calendar year disclosing reportable payments made in the previous calendar year. Failure to comply with the reporting obligations may result in civil monetary penalties; and |
|
· |
the federal Foreign Corrupt Practices Act of 1977 and other similar anti-bribery laws in other jurisdictions generally prohibit companies and their intermediaries from providing money or anything of value to officials of foreign governments, foreign political parties, or international organizations with the intent to obtain or retain business or seek a business advantage. Recently, there has been a substantial increase in anti-bribery law enforcement activity by U.S. regulators, with more frequent and aggressive investigations and enforcement proceedings by both the Department of Justice and the SEC. A determination that our operations or activities are not, or were not, in compliance with United States or foreign laws or regulations could result in the imposition of substantial fines, interruptions of business, loss of supplier, vendor or other third-party relationships, termination of necessary licenses and permits, and other legal or equitable sanctions. Other internal or government investigations or legal or regulatory proceedings, including lawsuits brought by private litigants, may also follow as a consequence. |
If our operations are found to be in violation of any of the laws and regulations described above or any other governmental regulations that apply to us, we may be subject to significant civil, criminal and administrative penalties, damages, fines, exclusion from government-funded healthcare programs, like Medicare and Medicaid, and the curtailment or restructuring of our operations. Any penalties, damages, fines, curtailment or restructuring of our operations could adversely affect our ability to operate our business and our financial results. Although compliance programs can mitigate the risk of investigation and prosecution for violations of these laws and regulations, the risks cannot be entirely eliminated. Any action against us for violation of these laws or regulations, even if we successfully defend against it, could cause us to incur significant legal expenses and divert our management’s attention from the operation of our business. Moreover, achieving and sustaining compliance with applicable federal and state privacy data, security and fraud laws and regulations may prove costly.
In the EU, the advertising and promotion of our products will also be subject to EU Member States’ laws concerning promotion of medicinal products, interactions with physicians, misleading and comparative advertising and unfair commercial practices, as well as other EU Member State legislation governing statutory health insurance, bribery and anti-corruption. Failure to comply with these rules can result in enforcement action by the EU Member State authorities, which may include any of the following: fines, imprisonment, orders forfeiting products or prohibiting or suspending their supply to the market, or requiring the manufacturer to issue public warnings, or to conduct a product recall.
Significant disruptions of information technology systems or security breaches could adversely affect our business.
We are increasingly dependent upon information technology systems, infrastructure and data to operate our business. In the ordinary course of business, we collect, store and transmit large amounts of confidential information (including but not limited to trade secrets or other intellectual property, proprietary business information and personal information). It is critical that we do so in a secure manner to maintain the confidentiality and integrity of such confidential information. We also have outsourced elements of our operations to third parties, and as a result we manage a number of third party vendors who may or could have access to our confidential information. The size and complexity of our information technology systems, and those of third party vendors with whom we contract, and the large amounts of confidential information stored on those systems, make such systems potentially vulnerable to service interruptions or to security breaches from inadvertent or intentional actions by our employees, third party vendors, and/or business partners, or from cyber-attacks by malicious third parties. Cyber-attacks are increasing in their frequency, sophistication, and intensity, and have become increasingly difficult to detect. Cyber-attacks could include the deployment of harmful malware, denial-of-service attacks, social engineering and other means to affect service reliability and threaten the confidentiality, integrity and availability of information.
Significant disruptions of our information technology systems or security breaches could adversely affect our business operations and/or result in the loss, misappropriation and/or unauthorized access, use or disclosure of, or the
50
prevention of access to, confidential information (including but not limited to trade secrets or other intellectual property, proprietary business information and personal information), and could result in financial, legal, business and reputational harm to us. For example, any such event that leads to unauthorized access, use or disclosure of personal information, including personal information regarding patients or employees, could harm our reputation, require us to comply with federal and/or state breach notification laws and foreign law equivalents, and otherwise subject us to liability under laws and regulations that protect the privacy and security of personal information. Security breaches and other inappropriate access can be difficult to detect, and any delay in identifying them may lead to increased harm of the type described above. While we have implemented security measures to protect our information technology systems and infrastructure, there can be no assurance that such measures will prevent service interruptions or security breaches that could adversely affect our business.
Marketing activities for our approved drugs are subject to continued governmental regulation.
The FDA, and third-country authorities, including the competent authorities of the EU Member States, have the authority to impose significant restrictions, including REMS requirements, on approved products through regulations on advertising, promotional and distribution activities. After approval, if products are marketed in contradiction with FDA laws and regulations, the FDA may issue warning letters that require specific remedial measures to be taken, as well as an immediate cessation of the impermissible conduct, resulting in adverse publicity. The FDA may also require that all future promotional materials receive prior agency review and approval before use. Certain states have also adopted regulations and reporting requirements surrounding the promotion of pharmaceuticals. Qsymia and STENDRA are subject to these regulations. Failure to comply with state requirements may affect our ability to promote or sell pharmaceutical drugs in certain states. This, in turn, could have a material adverse impact on our financial results and financial condition and could subject us to significant liability, including civil and administrative remedies as well as criminal sanctions.
We are subject to ongoing regulatory obligations and restrictions, which may result in significant expense and limit our ability to commercialize our drugs.
We are required to comply with extensive regulations for drug manufacturing, labeling, packaging, adverse event reporting, storage, distribution, advertising, promotion and record keeping in connection with the marketing of Qsymia and STENDRA. Regulatory approvals may also be subject to significant limitations on the indicated uses or marketing of the investigational drug candidates or to whom and how we may distribute our products. Even after FDA approval is obtained, the FDA may still impose significant restrictions on a drug’s indicated uses or marketing or impose ongoing requirements for REMS or potentially costly post-approval studies. For example, the labeling approved for Qsymia includes restrictions on use, including recommendations for pregnancy testing, level of obesity and duration of treatment. We are subject to ongoing regulatory obligations and restrictions that may result in significant expense and limit our ability to commercialize Qsymia. The FDA has also required the distribution of a Medication Guide to Qsymia patients outlining the increased risk of teratogenicity with fetal exposure and the possibility of suicidal thinking or behavior. In addition, the FDA has required a REMS that may act to limit access to the drug, reduce our revenues and/or increase our costs. The FDA may modify the Qsymia REMS in the future to be more or less restrictive.
Even if we maintain FDA approval, or receive a marketing authorization from the EC, and other regulatory approvals, if we or others identify adverse side effects after any of our products are on the market, or if manufacturing problems occur, regulatory approval or EU marketing authorization may be varied, suspended or withdrawn and reformulation of our products, additional clinical trials, changes in labeling and additional marketing applications may be required, any of which could harm our business and cause our stock price to decline.
We and our contract manufacturers are subject to significant regulation with respect to manufacturing of our products.
All of those involved in the preparation of a therapeutic drug for clinical trials or commercial sale, including our existing supply contract manufacturers, and clinical trial investigators, are subject to extensive regulation. Components of a finished drug product approved for commercial sale or used in late-stage clinical trials must be manufactured in accordance with current Good Manufacturing Practices, or cGMP. These regulations govern quality control of the
51
manufacturing processes and documentation policies and procedures, and the implementation and operation of quality systems to control and assure the quality of investigational products and products approved for sale. Our facilities and quality systems and the facilities and quality systems of our third-party contractors must be inspected routinely for compliance. If any such inspection or audit identifies a failure to comply with applicable regulations or if a violation of our product specifications or applicable regulation occurs independent of such an inspection or audit, we or the FDA may require remedial measures that may be costly and/or time consuming for us or a third party to implement and that may include the issuance of a warning letter, temporary or permanent suspension of a clinical trial or commercial sales, recalls, market withdrawals, seizures, or the temporary or permanent closure of a facility. Any such remedial measures would be imposed upon us or third parties with whom we contract until satisfactory cGMP compliance is achieved. The FDA could also impose civil penalties. We must also comply with similar regulatory requirements of foreign regulatory agencies.
We obtain the necessary raw materials and components for the manufacture of Qsymia and STENDRA as well as certain services, such as analytical testing packaging and labeling, from third parties. In particular, we rely on Catalent to supply Qsymia capsules and Packaging Coordinators, Inc., or PCI, for Qsymia packaging services. We rely on Sanofi Chimie and Sanofi Winthrop to supply avanafil API and tablets. We and these suppliers and service providers are required to follow cGMP requirements and are subject to routine and unannounced inspections by the FDA and by state and foreign regulatory agencies for compliance with cGMP requirements and other applicable regulations. Upon inspection of these facilities, the FDA or foreign regulatory agencies may find the manufacturing process or facilities are not in compliance with cGMP requirements and other regulations. Because manufacturing processes are highly complex and are subject to a lengthy regulatory approval process, alternative qualified supply may not be available on a timely basis or at all.
Difficulties, problems or delays in our suppliers and service providers’ manufacturing and supply of raw materials, components and services could delay our clinical trials, increase our costs, damage our reputation and cause us to lose revenue or market share if we are unable to timely meet market demands.
If we fail to comply with our reporting and payment obligations under the Medicaid Drug Rebate program or other governmental pricing programs, we could be subject to additional reimbursement requirements, penalties, sanctions and fines, which could have a material adverse effect on our business, financial condition, results of operations and growth prospects.
We participate in the Medicaid Drug Rebate program, established by the Omnibus Budget Reconciliation Act of 1990 and amended by the Veterans Health Care Act of 1992 as well as subsequent legislation. Under the Medicaid Drug Rebate program, we are required to pay a rebate to each state Medicaid program for our covered outpatient drugs that are dispensed to Medicaid beneficiaries and paid for by a state Medicaid program as a condition of having federal funds being made available to the states for our drugs under Medicaid and Medicare Part B. Those rebates are based on pricing data reported by us on a monthly and quarterly basis to CMS, the federal agency that administers the Medicaid Drug Rebate program. These data include the average manufacturer price and, in the case of innovator products, the best price for each drug.
The Affordable Care Act made significant changes to the Medicaid Drug Rebate program. Effective in March 2010, rebate liability expanded from fee-for-service Medicaid utilization to include the utilization of Medicaid managed care organizations as well. With regard to the amount of the rebates owed, the Affordable Care Act increased the minimum Medicaid rebate from 15.1% to 23.1% of the average manufacturer price for most innovator products and from 11% to 13% for non-innovator products; changed the calculation of the rebate for certain innovator products that qualify as line extensions of existing drugs; and capped the total rebate amount for innovator drugs at 100% of the average manufacturer price. In addition, the Affordable Care Act and subsequent legislation changed the definition of average manufacturer price. Finally, the Affordable Care Act requires pharmaceutical manufacturers of branded prescription drugs to pay a branded prescription drug fee to the federal government beginning in 2011. Each individual pharmaceutical manufacturer pays a prorated share of the branded prescription drug fee of $3.0 billion in 2015, based on the dollar value of its branded prescription drug sales to certain federal programs identified in the law.
In February 2016, CMS issued final regulations to implement the changes to the Medicaid Drug Rebate
52
program under the Affordable Care Act These regulations become effective on April 1, 2016. We are evaluating the impact of these regulations on our business and operations. Moreover, in the future, Congress could enact legislation that further increases Medicaid drug rebates or other costs and charges associated with participating in the Medicaid Drug Rebate program. The issuance of regulations and coverage expansion by various governmental agencies relating to the Medicaid Drug Rebate program has and will continue to increase our costs and the complexity of compliance, has been and will be time consuming, and could have a material adverse effect on our results of operations.
Federal law requires that any company that participates in the Medicaid Drug Rebate program also participate in the Public Health Service’s 340B drug pricing discount program in order for federal funds to be available for the manufacturer’s drugs under Medicaid and Medicare Part B. The 340B pricing program requires participating manufacturers to agree to charge statutorily defined covered entities no more than the 340B “ceiling price” for the manufacturer’s covered outpatient drugs. These 340B covered entities include a variety of community health clinics and other entities that receive health services grants from the Public Health Service, as well as hospitals that serve a disproportionate share of low-income patients. The 340B ceiling price is calculated using a statutory formula, which is based on the average manufacturer price and rebate amount for the covered outpatient drug as calculated under the Medicaid Drug Rebate program. Changes to the definition of average manufacturer price and the Medicaid rebate amount under the Affordable Care Act and CMS’s issuance of final regulations implementing those changes also could affect our 340B ceiling price calculations and negatively impact our results of operations.
The Affordable Care Act expanded the 340B program to include additional entity types: certain free-standing cancer hospitals, critical access hospitals, rural referral centers and sole community hospitals, each as defined by the Affordable Care Act. The Affordable Care Act also obligates the Secretary of the U.S. Department of Health and Human Services, or HHS, to create regulations and processes to improve the integrity of the 340B program and to update the agreement that manufacturers must sign to participate in the 340B program to obligate a manufacturer to offer the 340B price to covered entities if the manufacturer makes the drug available to any other purchaser at any price and to report to the government the ceiling prices for its drugs. The Health Resources and Services Administration, or HRSA, the agency that administers the 340B program, recently issued a proposed regulation regarding the calculation of the 340B ceiling price and the imposition of civil monetary penalties on manufacturers that knowingly and intentionally overcharge covered entities, as well as proposed omnibus guidance that addresses many aspects of the 340B program. HRSA is currently expected to issue additional proposed regulations in 2016. When such regulations and guidance are finalized, they could affect our obligations under the 340B program in ways we cannot anticipate. In addition, legislation may be introduced that, if passed, would further expand the 340B program to additional covered entities or would require participating manufacturers to agree to provide 340B discounted pricing on drugs used in the inpatient setting.
Pricing and rebate calculations vary among products and programs. The calculations are complex and are often subject to interpretation by us, governmental or regulatory agencies and the courts. The Medicaid rebate amount is computed each quarter based on our submission to CMS of our current average manufacturer prices and best prices for the quarter. If we become aware that our reporting for a prior quarter was incorrect, or has changed as a result of recalculation of the pricing data, we are obligated to resubmit the corrected data for a period not to exceed 12 quarters from the quarter in which the data originally were due. Such restatements and recalculations increase our costs for complying with the laws and regulations governing the Medicaid Drug Rebate program. Any corrections to our rebate calculations could result in an overage or underage in our rebate liability for past quarters, depending on the nature of the correction. Price recalculations also may affect the ceiling price at which we are required to offer our products to certain covered entities, such as safety-net providers, under the 340B drug discount program.
We are liable for errors associated with our submission of pricing data. In addition to retroactive rebates and the potential for 340B program refunds, if we are found to have knowingly submitted false average manufacturer price or best price information to the government, we may be liable for civil monetary penalties in the amount of $100,000 per item of false information. Our failure to submit monthly/quarterly average manufacturer price and best price data on a timely basis could result in a civil monetary penalty of $10,000 per day for each day the information is late beyond the due date. Such failure also could be grounds for CMS to terminate our Medicaid drug rebate agreement, pursuant to which we participate in the Medicaid program. In the event that CMS terminates our rebate agreement, no federal payments would be available under Medicaid or Medicare Part B for our covered outpatient drugs.
53
In September 2010, CMS and the Office of the Inspector General indicated that they intend to pursue more aggressively companies that fail to report these data to the government in a timely manner. Governmental agencies may also make changes in program interpretations, requirements or conditions of participation, some of which may have implications for amounts previously estimated or paid. We cannot assure you that our submissions will not be found by CMS to be incomplete or incorrect.
If we misstate Non-FAMPs or FCPs, we must restate these figures. Additionally, pursuant to the VHCA, knowing provision of false information in connection with a Non-FAMP filing can subject us to penalties of $100,000 for each item of false information. If we overcharge the government in connection with our FSS contract or the Tricare Retail Pharmacy Program, whether due to a misstated FCP or otherwise, we are required to refund the difference to the government. Failure to make necessary disclosures and/or to identify contract overcharges can result in allegations against us under the False Claims Act and other laws and regulations. Unexpected refunds to the government, and responding to a government investigation or enforcement action, would be expensive and time-consuming, and could have a material adverse effect on our business, financial condition, results of operations and growth prospects.
Changes in reimbursement procedures by government and other third-party payors, including changes in healthcare law and implementing regulations, may limit our ability to market and sell our approved drugs, or any future drugs, if approved, may limit our product revenues and delay profitability, and may impact our business in ways that we cannot currently predict. These changes could have a material adverse effect on our business and financial condition.
In the U.S. and abroad, sales of pharmaceutical drugs are dependent, in part, on the availability of reimbursement to the consumer from third-party payors, such as government and private insurance plans. Third-party payors are increasingly challenging the prices charged for medical products and services. Some third-party payor benefit packages restrict reimbursement, charge co-pays to patients, or do not provide coverage for specific drugs or drug classes.
In addition, certain healthcare providers are moving towards a managed care system in which such providers contract to provide comprehensive healthcare services, including prescription drugs, for a fixed cost per person. We are unable to predict the reimbursement policies employed by third-party healthcare payors.
Payors also are increasingly considering new metrics as the basis for reimbursement rates, such as average sales price, average manufacturer price and Actual Acquisition Cost. The existing data for reimbursement based on these metrics is relatively limited, although certain states have begun to survey acquisition cost data for the purpose of setting Medicaid reimbursement rates. CMS, the federal agency that administers Medicare and the Medicaid Drug Rebate program, surveys and publishes retail community pharmacy acquisition cost information in the form of National Average Drug Acquisition Cost, or NADAC, files to provide state Medicaid agencies with a basis of comparison for their own reimbursement and pricing methodologies and rates. It may be difficult to project the impact of these evolving reimbursement mechanics on the willingness of payors to cover our products.
The healthcare industry in the U.S. and abroad is undergoing fundamental changes that are the result of political, economic and regulatory influences. The levels of revenue and profitability of pharmaceutical companies may be affected by the continuing efforts of governmental and third-party payors to contain or reduce healthcare costs through various means. Reforms that have been and may be considered include mandated basic healthcare benefits, controls on healthcare spending through limitations on the increase in private health insurance premiums and the types of drugs eligible for reimbursement and Medicare and Medicaid spending, the creation of large insurance purchasing groups, and fundamental changes to the healthcare delivery system. These proposals include measures that would limit or prohibit payments for some medical treatments or subject the pricing of drugs to government control and regulations changing the rebates we are required to provide. Further, federal budgetary concerns could result in the implementation of significant federal spending cuts, including cuts in Medicare and other health related spending in the near-term. For example, recent legislative enactments have resulted in Medicare payments being subject to a two percent reduction, referred to as sequestration, until 2025. These changes could impact our ability to maximize revenues in the federal marketplace.
In March 2010, the President signed the Patient Protection and Affordable Care Act, as amended by the Health
54
Care and Education Reconciliation Act of 2010, collectively referred to in this report as the Affordable Care Act. The Affordable Care Act substantially changed the way healthcare is financed by both governmental and private insurers, and could have a material adverse effect on our future business, cash flows, financial condition and results of operations, including by operation of the following provisions:
|
· |
Effective in March 2010, rebate liability expanded from fee-for-service Medicaid utilization to include the utilization of Medicaid managed care organizations as well. This expanded eligibility affects rebate liability for that utilization. |
|
· |
With regard to the amount of the rebates owed, the Affordable Care Act increased the minimum Medicaid rebate from 15.1% to 23.1% of the average manufacturer price for most innovator products and from 11% to 13% for non-innovator products; changed the calculation of the rebate for certain innovator products that qualify as line extensions of existing drugs; and capped the total rebate amount for innovator drugs at 100% of the average manufacturer price. |
|
· |
Effective in January 2011, pharmaceutical companies must provide a 50% discount on branded prescription drugs dispensed to beneficiaries within the Medicare Part D coverage gap or “donut hole,” which is a coverage gap that currently exists in the Medicare Part D prescription drug program. We currently do not have coverage under Medicare Part D for our drugs, but this could change in the future. |
|
· |
Effective in January 2011, the Affordable Care Act requires pharmaceutical manufacturers of branded prescription drugs to pay a branded prescription drug fee to the federal government. Each individual pharmaceutical manufacturer pays a prorated share of the branded prescription drug fee of $3.0 billion in 2016, based on the dollar value of its branded prescription drug sales to certain federal programs identified in the law. |
|
· |
Some states have elected to expand their Medicaid programs by raising the income limit to 133% of the federal poverty level. For each state that does not choose to expand its Medicaid program, there may be fewer insured patients overall, which could impact our sales, business and financial condition. We expect any Medicaid expansion to impact the number of adults in Medicaid more than children because many states have already set their eligibility criteria for children at or above the level designated in the Affordable Care Act. An increase in the proportion of patients who receive our drugs and who are covered by Medicaid could adversely affect our net sales. |
In February 2016, CMS issued final regulations to implement the changes to the Medicaid Drug Rebate Program under the Affordable Care Act. These regulations become effective on April 1, 2016. We are evaluating the impact of these regulations on our business and operations. At this time, we cannot predict the full impact of the Affordable Care Act, or the timing and impact of any future rules or regulations promulgated to implement the Affordable Care Act.
The Affordable Care Act also expanded the Public Health Service’s 340B drug pricing discount program. The 340B pricing program requires participating manufacturers to agree to charge statutorily defined covered entities no more than the 340B “ceiling price” for the manufacturer’s covered outpatient drugs. The Affordable Care Act expanded the 340B program to include additional types of covered entities: certain free-standing cancer hospitals, critical access hospitals, rural referral centers and sole community hospitals, each as defined by the Affordable Care Act. The Affordable Care Act also obligates the Secretary of the Department of Health and Human Services to create regulations and processes to improve the integrity of the 340B program and to ensure the agreement that manufacturers must sign to participate in the 340B program obligates a manufacturer to offer the 340B price to covered entities if the manufacturer makes the drug available to any other purchaser at any price and to report to the government the ceiling prices for its drugs. The Health Resources and Services Administration, or HRSA, the agency that administers the 340B program, recently issued a proposed regulation regarding the calculation of the 340B ceiling price and the imposition of civil monetary penalties on manufacturers that knowingly and intentionally overcharge covered entities, as well as proposed omnibus guidance that addresses many aspects of the 340B program. HRSA is currently expected to issue additional proposed regulations in 2016. When such regulations and guidance are finalized, they could affect our obligations under
55
the 340B program in ways we cannot anticipate. In addition, legislation may be introduced that, if passed, would further expand the 340B program to additional covered entities or would require participating manufacturers to agree to provide 340B discounted pricing on drugs used in the inpatient setting.
There can be no assurance that future healthcare legislation or other changes in the administration or interpretation of government healthcare or third-party reimbursement programs will not have a material adverse effect on us. Healthcare reform is also under consideration in other countries where we intend to market Qsymia.
We expect to experience pricing and reimbursement pressures in connection with the sale of Qsymia, STENDRA and our investigational drug candidates, if approved, due to the trend toward managed healthcare, the increasing influence of health maintenance organizations and additional legislative proposals. In addition, we may confront limitations in insurance coverage for Qsymia, STENDRA and our investigational drug candidates. For example, the Medicare program generally does not provide coverage for drugs used to treat erectile dysfunction or drugs used to treat obesity. Similarly, other insurers may determine that such products are not covered under their programs. If we fail to successfully secure and maintain reimbursement coverage for our approved drugs and investigational drug candidates or are significantly delayed in doing so, we will have difficulty achieving market acceptance of our approved drugs and investigational drug candidates and our business will be harmed. Congress has enacted healthcare reform and may enact further reform, which could adversely affect the pharmaceutical industry as a whole, and therefore could have a material adverse effect on our business.
Both of the active pharmaceutical ingredients in Qsymia, phentermine and topiramate, are available as generics and do not have a REMS requirement. The exact doses of the active ingredients in Qsymia are different than those currently available for the generic components. State pharmacy laws prohibit pharmacists from substituting drugs with differing doses and formulations. The safety and efficacy of Qsymia is dependent on the titration, dosing and formulation, which we believe could not be easily duplicated, if at all, with the use of generic substitutes. However, there can be no assurance that we will be able to provide for optimal reimbursement of Qsymia as a treatment for obesity or, if approved, for any other indication, from third-party payors or the U.S. government. Furthermore, there can be no assurance that healthcare providers would not actively seek to provide patients with generic versions of the active ingredients in Qsymia in order to treat obesity at a potential lower cost and outside of the REMS requirements.
An increasing number of EU Member States and other foreign countries use prices for medicinal products established in other countries as “reference prices” to help determine the price of the product in their own territory. Consequently, a downward trend in prices of medicinal products in some countries could contribute to similar downward trends elsewhere. In addition, the ongoing budgetary difficulties faced by a number of EU Member States, including Greece and Spain, have led and may continue to lead to substantial delays in payment and payment partially with government bonds rather than cash for medicinal products, which could negatively impact our revenues and profitability. Moreover, in order to obtain reimbursement of our medicinal products in some countries, including some EU Member States, we may be required to conduct clinical trials that compare the cost effectiveness of our products to other available therapies. There can be no assurance that our medicinal products will obtain favorable reimbursement status in any country.
Setbacks and consolidation in the pharmaceutical and biotechnology industries, and our, or our collaborators’, inability to obtain third-party coverage and adequate reimbursement, could make partnering more difficult and diminish our revenues.
Setbacks in the pharmaceutical and biotechnology industries, such as those caused by safety concerns relating to high-profile drugs like Avandia®, Vioxx® and Celebrex®, or investigational drug candidates, as well as competition from generic drugs, litigation, and industry consolidation, may have an adverse effect on us. For example, pharmaceutical companies may be less willing to enter into new collaborations or continue existing collaborations if they are integrating a new operation as a result of a merger or acquisition or if their therapeutic areas of focus change following a merger. Moreover, our and our collaborators’ ability to commercialize any of our approved drugs or future investigational drug candidates will depend in part on government regulation and the availability of coverage and adequate reimbursement from third-party payors, including private health insurers and government payors, such as the Medicaid and Medicare programs, increases in government-run, single-payor health insurance plans and compulsory licenses of drugs.
56
Government and third-party payors are increasingly attempting to contain healthcare costs by limiting coverage and reimbursement levels for new drugs. Given the continuing discussion regarding the cost of healthcare, managed care, universal healthcare coverage and other healthcare issues, we cannot predict with certainty what additional healthcare initiatives, if any, will be implemented or the effect any future legislation or regulation will have on our business. These efforts may limit our commercial opportunities by reducing the amount a potential collaborator is willing to pay to license our programs or investigational drug candidates in the future due to a reduction in the potential revenues from drug sales. Adoption of legislation and regulations could limit pricing approvals for, and reimbursement of, drugs. A government or third-party payor decision not to approve pricing for, or provide adequate coverage and reimbursements of, our drugs could limit market acceptance of these drugs.
Our business and operations would suffer in the event of system failures.
Despite the implementation of security measures, our internal computer systems and those of our contract sales organization, or CSO, CROs, safety monitoring company and other contractors and consultants are vulnerable to damage from computer viruses, unauthorized access, natural disasters, accidents, terrorism, war and telecommunication and electrical failures. While we have not experienced any such system failure, accident or security breach to date, if such an event were to occur and cause interruptions in our operations, it could result in a material disruption of our investigational drug candidate development programs and drug manufacturing operations. For example, the loss of clinical trial data from completed or ongoing clinical trials for our investigational drug candidates could result in delays in our regulatory approval efforts with the FDA, the EC, or the competent authorities of the EU Member States, and significantly increase our costs to recover or reproduce the data. To the extent that any disruption or security breach was to result in a loss of or damage to our data or applications, or inappropriate disclosure of confidential or proprietary information, we could incur liability and the further development of our investigational drug candidates, or commercialization of our approved drugs, could be delayed. If we are unable to restore our information systems in the event of a systems failure, our communications, daily operations and the ability to develop our investigational drug candidates and approved drug commercialization efforts would be severely affected.
Natural disasters or resource shortages could disrupt our investigational drug candidate development and approved drug commercialization efforts and adversely affect results.
Our ongoing or planned clinical trials and approved drug commercialization efforts could be delayed or disrupted indefinitely upon the occurrence of a natural disaster. For example, Hurricane Sandy in October 2012, hindered our Qsymia sales efforts. In 2005, our clinical trials in the New Orleans area were interrupted by Hurricane Katrina. In addition, our offices are located in the San Francisco Bay Area near known earthquake fault zones and are therefore vulnerable to damage from earthquakes. In October 1989, a major earthquake in our area caused significant property damage and a number of fatalities. We are also vulnerable to damage from other disasters, such as power loss, fire, floods and similar events. If a significant disaster occurs, our ability to continue our operations could be seriously impaired and we may not have adequate insurance to cover any resulting losses. Any significant unrecoverable losses could seriously impair our operations and financial condition.
Risks Relating to our Intellectual Property
Obtaining intellectual property rights is a complex process, and we may be unable to adequately protect our proprietary technologies.
We hold various patents and patent applications in the U.S. and abroad targeting obesity and morbidities related to obesity, including sleep apnea and diabetes, and sexual health, among other indications. The procedures for obtaining a patent in the U.S. and in most foreign countries are complex. These procedures require an analysis of the scientific technology related to the invention and many sophisticated legal issues. Consequently, the process for having our pending patent applications issue as patents will be difficult, complex and time consuming. We do not know when, or if, we will obtain additional patents for our technologies, or if the scope of the patents obtained will be sufficient to protect our investigational drug candidates or products, or be considered sufficient by parties reviewing our patent positions pursuant to a potential licensing or financing transaction.
57
In addition, we cannot make assurances as to how much protection, if any, will be provided by our issued patents. Our existing patents and any future patents we obtain may not be sufficiently broad to prevent others from practicing our technologies or from developing competing products. Others may independently develop similar or alternative technologies or design around our patented technologies or products. These companies would then be able to develop, manufacture and sell products that compete directly with our products. In that case, our revenues and operating results could decline.
Other entities may also challenge the validity or enforceability of our patents and patent applications in litigation or administrative proceedings. The sponsor of a generic application seeking to rely on one of our approved drug products as the reference listed drug must make one of several certifications regarding each listed patent. A “Paragraph III” certification is the sponsor’s statement that it will wait for the patent to expire before obtaining approval for its product. A “Paragraph IV” certification is a challenge to the patent; it is an assertion that the patent does not block approval of the later product, either because the patent is invalid or unenforceable or because the patent, even if valid, is not infringed by the new product. Once the FDA accepts for filing a generic application containing a Paragraph IV certification, the applicant must within 20 days provide notice to the reference listed drug, or RLD, NDA holder and patent owner that the application with patent challenge has been submitted, and provide the factual and legal basis for the applicant’s assertion that the patent is invalid or not infringed. If the NDA holder or patent owner file suit against the generic applicant for patent infringement within 45 days of receiving the Paragraph IV notice, the FDA is prohibited from approving the generic application for a period of 30 months from the date of receipt of the notice. If the RLD has new chemical entity exclusivity and the notice is given and suit filed during the fifth year of exclusivity, the 30-month stay does not begin until five years after the RLD approval. The FDA may approve the proposed product before the expiration of the 30-month stay if a court finds the patent invalid or not infringed or if the court shortens the period because the parties have failed to cooperate in expediting the litigation. If a competitor or a generic pharmaceutical provider successfully challenges our patents, the protection provided by these patents could be reduced or eliminated and our ability to commercialize any approved drugs would be at risk. In addition, if a competitor or generic manufacturer were to receive approval to sell a generic or follow-on version of one of our products, our approved product would become subject to increased competition and our revenues for that product would be adversely affected.
We also may rely on trade secrets and other unpatented confidential information to protect our technology, especially where we do not believe patent protection is appropriate or obtainable. However, trade secrets are difficult to protect. We seek to protect our trade secrets and other confidential information by entering into confidentiality agreements with employees, collaborators, vendors (including CROs and our CSO), consultants and, at times, potential investors. Nevertheless, employees, collaborators, vendors, consultants or potential investors may still disclose or misuse our trade secrets and other confidential information, and we may not be able to meaningfully protect our trade secrets. In addition, others may independently develop substantially equivalent information or techniques or otherwise gain access to our trade secrets. Disclosure or misuse of our confidential information would harm our competitive position and could cause our revenues and operating results to decline.
If we believe that others have infringed or misappropriated our proprietary rights, we may need to institute legal action to protect our intellectual property rights. Such legal action may be expensive, and we may not be able to afford the costs of enforcing or defending our intellectual property rights against others.
We have received notices of ANDA filings for Qsymia submitted by generic drug companies. These ANDA filings assert that a generic form of Qsymia would not infringe on our issued patents. As a result of these filings, we have commenced litigation to defend our patent rights, which is expected to be costly and time-consuming and, depending on the outcome of the litigation, we may face competition from lower cost generic or follow-on products in the near term.
Qsymia is approved under the provisions of the Federal Food, Drug and Cosmetic Act, or FDCA, which renders it susceptible to potential competition from generic manufacturers via the Hatch-Waxman Act and ANDA process. Generic manufacturers pursuing ANDA approval are not required to conduct costly and time-consuming clinical trials to establish the safety and efficacy of their products; rather, they are permitted to rely on the FDA’s finding that the innovator’s product is safe and effective. Additionally, generic drug companies generally do not expend significant sums on sales and marketing activities, instead relying on physicians or payors to substitute the generic form of a drug for the
58
branded form. Thus, generic manufacturers can sell their products at prices much lower than those charged by the innovative pharmaceutical or biotechnology companies who have incurred substantial expenses associated with the research and development of the drug product and who must spend significant sums marketing a new drug.
The ANDA procedure includes provisions allowing generic manufacturers to challenge the innovator’s patent protection by submitting “Paragraph IV” certifications to the FDA in which the generic manufacturer claims that the innovator’s patent is invalid, unenforceable and/or will not be infringed by the manufacture, use, or sale of the generic product. A patent owner who receives a Paragraph IV certification may choose to sue the generic applicant for patent infringement.
We have received a Paragraph IV certification notice from Actavis Laboratories FL, Inc., or Actavis, contending that our patents listed in the Orange Book for Qsymia (U.S. Patents 7,056,890, 7,553,818, 7,659,256, 7,674,776, 8,580,298, and 8,580,299) are invalid, unenforceable and/or will not be infringed by the manufacture, use, or sale of a generic form of Qsymia. In response to this notice, we have filed suit to defend our patent rights. We have received a second Paragraph IV certification notice from Actavis contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 8,895,057 and 8,895,058) are invalid, unenforceable and/or will not be infringed by the manufacture, use, or sale of a generic form of Qsymia. In response to this second notice, we have filed a second lawsuit against Actavis. We have received a third Paragraph IV certification notice from Actavis contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 9,011,905 and 9,011,906) are invalid, unenforceable and/or will not be infringed by the manufacture, use, or sale of a generic form of Qsymia. In response to this third notice, we have filed a third lawsuit against Actavis. The lawsuits have been consolidated into a single suit.
In accordance with the Hatch-Waxman Act, as a result of having filed a timely lawsuit against Actavis, FDA approval of Actavis’ ANDA will be stayed until the earlier of (i) up to 30 months from our May 7, 2014 receipt of Actavis’ Paragraph IV certification notice (i.e. November 7, 2016) or (ii) a District Court decision finding that the identified patents are invalid, unenforceable or not infringed.
We have also received a Paragraph IV certification notice from Teva Pharmaceutical USA, Inc. and Teva Pharmaceutical Industries, Ltd. (collectively, Teva) contending that eight of our patents listed in the Orange Book for Qsymia (U.S. Patents 7,056,890, 7,533,818, 7,659,256, 7,674,776, 8,580,298, 8,580,299, 8,895,057, and 8,895,058) are invalid, unenforceable and/or will not be infringed by the manufacture, use or sale of a generic form of Qsymia. In response to this notice, we have filed suit against Teva to defend our patent rights. We have received a second Paragraph IV certification notice from Teva contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 9,011,905 and 9,011,906) are invalid, unenforceable and/or will not be infringed by the manufacture, use, or sale of a generic form of Qsymia. In response to this second notice, we have filed a second lawsuit against Teva. The lawsuits have been consolidated into a single suit.
In accordance with the Hatch-Waxman Act, as a result of having filed a timely lawsuit against Teva, FDA approval of Teva’s ANDA will be stayed until the earlier of (i) up to 30 months from our March 5, 2015 receipt of Teva’s Paragraph IV certification notice (i.e. September 5, 2017) or (ii) a District Court decision finding that the identified patents are invalid, unenforceable or not infringed.
Although we intend to vigorously enforce our intellectual property rights relating to Qsymia, there can be no assurance that we will prevail in our defense of our patent rights. Our existing patents could be invalidated, found unenforceable or found not to cover a generic form of Qsymia. If an ANDA filer were to receive approval to sell a generic version of Qsymia and/or prevail in any patent litigation, Qsymia would become subject to increased competition and our revenue would be adversely affected.
We may be sued for infringing the intellectual property rights of others, which could be costly and result in delays or termination of our future research, development, manufacturing and sales activities.
Our commercial success also depends, in part, upon our ability to develop future investigational drug candidates, market and sell approved drugs and conduct our other research, development and commercialization activities without infringing or misappropriating the patents and other proprietary rights of others. There are many
59
patents and patent applications owned by others that could be relevant to our business. For example, there are numerous U.S. and foreign issued patents and pending patent applications owned by others that are related to the therapeutic areas in which we have approved drugs or future investigational drug candidates as well as the therapeutic targets to which these drugs and candidates are directed. There are also numerous issued patents and patent applications covering chemical compounds or synthetic processes that may be necessary or useful to use in our research, development, manufacturing or commercialization activities. Because patent applications can take many years to issue, there may be currently pending applications, unknown to us, which may later result in issued patents that our approved drugs, future investigational drug candidates or technologies may infringe. There also may be existing patents, of which we are not aware, that our approved drugs, investigational drug candidates or technologies may infringe. Further, it is not always clear to industry participants, including us, which patents cover various types of products or methods. The coverage of patents is subject to interpretation by the courts, and the interpretation is not always uniform. We cannot assure you that others holding any of these patents or patent applications will not assert infringement claims against us for damages or seek to enjoin our activities. If we are sued for patent infringement, we would need to demonstrate that our products or methods do not infringe the patent claims of the relevant patent and/or that the patent claims are invalid or unenforceable, and we may not be able to do this.
There can be no assurance that approved drugs or future investigational drug candidates do not or will not infringe on the patents or proprietary rights of others. In addition, third parties may already own or may obtain patents in the future and claim that use of our technologies infringes these patents.
If a person or entity files a legal action or administrative action against us, or our collaborators, claiming that our drug discovery, development, manufacturing or commercialization activities infringe a patent owned by the person or entity, we could incur substantial costs and diversion of the time and attention of management and technical personnel in defending ourselves against any such claims. Furthermore, parties making claims against us may be able to obtain injunctive or other equitable relief that could effectively block our ability to further develop, commercialize and sell any current or future approved drugs, and such claims could result in the award of substantial damages against us. In the event of a successful claim of infringement against us, we may be required to pay damages and obtain one or more licenses from third parties. We may not be able to obtain these licenses at a reasonable cost, if at all. In that case, we could encounter delays in product introductions while we attempt to develop alternative investigational drug candidates or be required to cease commercializing any affected current or future approved drugs and our operating results would be harmed.
Furthermore, because of the substantial amount of pre-trial document and witness discovery required in connection with intellectual property litigation, there is a risk that some of our confidential information could be compromised by disclosure during this type of litigation. In addition, during the course of this kind of litigation, there could be public announcements of the results of hearings, motions or other interim proceedings or developments. If securities analysts or investors perceive these results to be negative, it could have a substantial adverse effect on the trading price of our common stock.
We may face additional competition outside of the U.S. as a result of a lack of patent coverage in some territories and differences in patent prosecution and enforcement laws in foreign countries.
Filing, prosecuting, defending and enforcing patents on all of our drug discovery technologies and all of our approved drugs and potential investigational drug candidates throughout the world would be prohibitively expensive. While we have filed patent applications in many countries outside the U.S., and have obtained some patent coverage for approved drugs in certain foreign countries, we do not currently have widespread patent protection for these drugs outside the U.S. and have no protection in many foreign jurisdictions. Competitors may use our technologies to develop their own drugs in jurisdictions where we have not obtained patent protection. These drugs may compete with our approved drugs or future investigational drug candidates and may not be covered by any of our patent claims or other intellectual property rights.
Even if international patent applications ultimately issue or receive approval, it is likely that the scope of protection provided by such patents will be different from, and possibly less than, the scope provided by our corresponding U.S. patents. The success of our international market opportunity is dependent upon the enforcement of
60
patent rights in various other countries. A number of countries in which we have filed or intend to file patent applications have a history of weak enforcement and/or compulsory licensing of intellectual property rights. Moreover, the legal systems of certain countries, particularly certain developing countries, do not favor the aggressive enforcement of patents and other intellectual property protection, particularly those relating to biotechnology and/or pharmaceuticals, which make it difficult for us to stop the infringement of our patents. Even if we have patents issued in these jurisdictions, there can be no assurance that our patent rights will be sufficient to prevent generic competition or unauthorized use.
Attempting to enforce our patent rights in foreign jurisdictions could result in substantial cost and divert our efforts and attention from other aspects of our business.
Risks Relating to our Financial Position and Need for Financing
We may require additional capital for our future operating plans, and we may not be able to secure the requisite additional funding on acceptable terms, or at all, which would force us to delay, reduce or eliminate commercialization or development efforts.
We expect that our existing capital resources combined with future anticipated cash flows will be sufficient to support our operating activities at least through the next twelve months. However, we anticipate that we will be required to obtain additional financing to fund our commercialization efforts, additional clinical studies for approved products and the development of our research and development pipeline in future periods. Our future capital requirements will depend upon numerous factors, including:
|
· |
our ability to expand the use of Qsymia through targeted patient and physician education; |
|
· |
our ability to find the right partner for expanded Qsymia commercial promotion to a broader primary care physician audience on a timely basis; |
|
· |
our ability to obtain marketing authorization by the EC for Qsiva in the EU through the centralized marketing authorization procedure; |
|
· |
our ability to manage costs; |
|
· |
the substantial cost to expand into certified retail pharmacy locations and the cost required to maintain the REMS program for Qsymia; |
|
· |
the cost, timing and outcome of the post-approval clinical studies the FDA has required us to perform as part of the approval for STENDRA and Qsymia; |
|
· |
our ability, along with our collaboration partners, to successfully commercialize STENDRA in the EU, Australia, New Zealand, Africa, the Middle East, Turkey, and the CIS, including Russia; |
|
· |
our ability, either by ourselves or through a third party, to successfully commercialize STENDRA in the U.S. and Canada; |
|
· |
the impact of the return of the U.S. and Canadian rights for the commercialization of STENDRA; |
|
· |
our ability to successfully commercialize STENDRA in other territories in which we do not currently have a commercial collaboration; |
|
· |
the progress and costs of our research and development programs; |
|
· |
the scope, timing, costs and results of pre-clinical, clinical and retrospective observational studies and trials; |
61
|
· |
the cost of access to electronic records and databases that allow for retrospective observational studies; |
|
· |
patient recruitment and enrollment in future clinical trials; |
|
· |
the costs involved in seeking regulatory approvals for future drug candidates; |
|
· |
the costs involved in filing and pursuing patent applications, defending and enforcing patent claims; |
|
· |
the establishment of collaborations, sublicenses and strategic alliances and the related costs, including milestone payments; |
|
· |
the cost of manufacturing and commercialization activities and arrangements; |
|
· |
the level of resources devoted to our future sales and marketing capabilities; |
|
· |
the cost, timing and outcome of litigation, if any; |
|
· |
the impact of healthcare reform, if any, imposed by the federal government; and |
|
· |
the activities of competitors. |
Future capital requirements will also depend on the extent to which we acquire or invest in additional complementary businesses, products and technologies. We currently have no commitments or agreements relating to any of these types of transactions.
To obtain additional capital when needed, we will evaluate alternative financing sources, including, but not limited to, the issuance of equity or debt securities, corporate alliances, joint ventures and licensing agreements. However, there can be no assurance that funding will be available on favorable terms, if at all. We are continually evaluating our existing portfolio and we may choose to divest, sell or spin-off one or more of our drugs and/or investigational drug candidates at any time. We cannot assure you that our drugs will generate revenues sufficient to enable us to earn a profit. If we are unable to obtain additional capital, management may be required to explore alternatives to reduce cash used by operating activities, including the termination of research and development efforts that may appear to be promising to us, the sale of certain assets and the reduction in overall operating activities. If adequate funds are not available, we may be required to delay, reduce the scope of or eliminate one or more of our development programs or our commercialization efforts.
Raising additional funds by issuing securities will cause dilution to existing stockholders and raising funds through lending and licensing arrangements may restrict our operations or require us to relinquish proprietary rights.
To the extent that we raise additional capital by issuing equity securities, our existing stockholders’ ownership will be diluted. We have financed our operations, and we expect to continue to finance our operations, primarily by issuing equity and debt securities. Moreover, any issuances by us of equity securities may be at or below the prevailing market price of our common stock and in any event may have a dilutive impact on your ownership interest, which could cause the market price of our common stock to decline. To raise additional capital, we may choose to issue additional securities at any time and at any price.
As of December 31, 2015, we have $250.0 million in 4.5% Convertible Senior Notes due May 1, 2020, which we refer to as the Convertible Notes. The Convertible Notes are convertible into approximately 16,826,000 shares of our common stock under certain circumstances prior to maturity at a conversion rate of 67.3038 shares per $1,000 principal amount of Convertible Notes, which represents a conversion price of approximately $14.858 per share, subject to adjustment under certain conditions. On October 8, 2015, IEH Biopharma LLC, a subsidiary of Icahn Enterprises L.P., announced that it had received tenders for $170,165,000 of the aggregate principal amount of our Convertible Notes in its previously announced cash tender offer for any and all of the outstanding Convertible Notes. The Convertible Notes
62
are convertible at the option of the holders under certain conditions at any time prior to the close of business on the business day immediately preceding November 1, 2019. Investors in our common stock will be diluted to the extent the Convertible Notes are converted into shares of our common stock, rather than being settled in cash.
We may also raise additional capital through the incurrence of debt, and the holders of any debt we may issue would have rights superior to our stockholders’ rights in the event we are not successful and are forced to seek the protection of bankruptcy laws.
In addition, debt financing typically contains covenants that restrict operating activities. For example, on March 25, 2013, we entered into the Purchase and Sale Agreement with BioPharma Secured Investments III Holdings Cayman LP, or BioPharma, which provides for the purchase of a debt-like instrument. Under the BioPharma Agreement, we may not (i) incur indebtedness greater than a specified amount, (ii) pay a dividend or other cash distribution on our capital stock, unless we have cash and cash equivalents in excess of a specified amount, (iii) amend or restate our certificate of incorporation or bylaws unless such amendments or restatements do not affect BioPharma’s interests under the BioPharma Agreement, (iv) encumber the collateral, or (v) abandon certain patent rights, in each case without the consent of BioPharma. Any future debt financing we enter into may involve similar or more onerous covenants that restrict our operations.
If we raise additional capital through collaboration, licensing or other similar arrangements, it may be necessary to relinquish potentially valuable rights to our drugs or future investigational drug candidates, potential products or proprietary technologies, or grant licenses on terms that are not favorable to us. If adequate funds are not available, our ability to achieve profitability or to respond to competitive pressures would be significantly limited and we may be required to delay, significantly curtail or eliminate the commercialization of one or more of our approved drugs or the development of one or more of our future investigational drug candidates.
The investment of our cash balance and our available-for-sale securities are subject to risks that may cause losses and affect the liquidity of these investments.
At December 31, 2015, we had $95.4 million in cash and cash equivalents and $146.2 million in available-for-sale securities. While at December 31, 2015, our excess cash balances were invested in money market, U.S. Treasury securities and corporate debt securities, our investment policy as approved by our Board of Directors, also provides for investments in debt securities of U.S. government agencies, corporate debt securities and asset-backed securities. Our investment policy has the primary investment objectives of preservation of principal. However, there may be times when certain of the securities in our portfolio will fall below the credit ratings required in the policy. Although the U.S. Congress was able to resolve the debt ceiling issue in time to avoid default, the major credit rating agencies have expressed their ongoing concern about the high levels of debt that the U.S. government has taken on. Standard & Poor’s announced that it had revised its outlook on the long-term credit rating of the U.S. to negative, which could affect the trading market for U.S. government securities. These factors could impact the liquidity or valuation of our available-for-sale securities, all of which were invested in U.S. Treasury securities or corporate debt securities as of December 31, 2015. If those securities are downgraded or impaired we would experience losses in the value of our portfolio which would have an adverse effect on our results of operations, liquidity and financial condition. An investment in money market mutual funds is not insured or guaranteed by the Federal Deposit Insurance Corporation or any other government agency. Although money market mutual funds seek to preserve the value of the investment at $1 per share, it is possible to lose money by investing in money market mutual funds.
Our involvement in securities-related class action and shareholder litigation could divert our resources and management’s attention and harm our business.
The stock markets have from time to time experienced significant price and volume fluctuations that have affected the market prices for the common stock of pharmaceutical companies. These broad market fluctuations may cause the market price of our common stock to decline. In the past, securities-related class action litigation has often been brought against a company following a decline in the market price of its securities. This risk is especially relevant for us because biotechnology and biopharmaceutical companies often experience significant stock price volatility in connection with their investigational drug candidate development programs, the review of marketing applications by
63
regulatory authorities and the commercial launch of newly approved drugs. We were a defendant in federal and consolidated state shareholder derivative lawsuits. These securities-related class action lawsuits generally alleged that we and our officers misled the investing public regarding the safety and efficacy of Qsymia and the prospects for the FDA’s approval of the Qsymia NDA as a treatment for obesity. Securities-related class action litigation often is expensive and diverts management’s attention and our financial resources, which could adversely affect our business.
For example, on March 27, 2014, Mary Jane and Thomas Jasin, who purport to be purchasers of VIVUS common stock, filed an Amended Complaint in Santa Clara County Superior Court alleging securities fraud against the Company and three of its former officers and directors. In that complaint, captioned Jasin v. VIVUS, Inc., Case No. 114-cv-261427, plaintiffs asserted claims under California’s securities and consumer protection securities statutes. Plaintiffs alleged generally that defendants misrepresented the prospects for the Company’s success, including with respect to the launch of Qsymia, while purportedly selling VIVUS stock for personal profit. Plaintiffs alleged losses of “at least” $2.8 million, and sought damages and other relief. On June 5, 2014, the Company and the other defendants filed a demurrer to the Amended Complaint seeking its dismissal. With the demurrer pending, on July 18, 2014, the same plaintiffs filed a complaint in the United States District Court for the Northern District of California, captioned Jasin v. VIVUS, Inc., Case No. 5:14-cv-03263. The Jasins’ federal complaint alleges violations of Sections 10(b) and 20(a) of the Securities Exchange Act of 1934, as amended, based on facts substantially similar to those alleged in their state court action. On September 15, 2014, pursuant to an agreement between the parties, plaintiffs moved to voluntarily dismiss, with prejudice, the state court action. In the federal action, defendants filed a motion to dismiss on November 12, 2014. On December 3, 2014, plaintiffs filed a First Amended Complaint in the federal action. On January 21, 2015, defendants filed a motion to dismiss the First Amended Complaint. The court ruled on that motion on June 18, 2015, dismissing the seven California claims with prejudice and dismissing the two federal claims with leave to amend. Plaintiffs filed a second amended complaint on August 17, 2015. Defendants moved to dismiss the complaint on October 2, 2015. On September 10, 2015, plaintiffs moved for entry of judgment on their state claims. Briefing on both defendants’ motion to dismiss and plaintiffs’ motion for entry of judgment was completed on December 15, 2015. The court heard oral argument on both motions on January 14, 2016. The court has not yet issued a ruling on either motion. The Company and the defendant former officers and directors cannot predict the outcome of the motions or the lawsuit generally, but believe that the lawsuit is without merit and intend to continue vigorously to defend against the claims.
The Company maintains directors’ and officers’ liability insurance that it believes affords coverage for much of the anticipated cost of the remaining Jasin action, subject to the use of our financial resources to pay for our self-insured retention and the policies’ terms and conditions.
We have an accumulated deficit of $836.4 million as of December 31, 2015, and we may continue to incur substantial operating losses for the future.
We have generated a cumulative net loss of $836.4 million for the period from our inception through December 31, 2015, and we anticipate losses in future years due to continued investment in our research and development programs. There can be no assurance that we will be able to achieve or maintain profitability or that we will be successful in the future.
Our ability to utilize our net operating loss carryforwards and other tax attributes to offset future taxable income may be limited.
As of December 31, 2015, we had approximately $675.6 million and $301.5 million of net operating loss, or NOL, carryforwards with which to offset our future taxable income for federal and state income tax reporting purposes, respectively. Utilization of our net operating loss and tax credit carryforwards, or tax attributes, may be subject to substantial annual limitations provided by the Internal Revenue Code and similar state provisions to the extent certain ownership changes are deemed to occur. Such an annual limitation could result in the expiration of the tax attributes before utilization. The tax attributes reflected above have not been reduced by any limitations. To the extent it is determined upon completion of the analysis that such limitations do apply, we will adjust the tax attributes accordingly. We face the risk that our ability to use our tax attributes will be substantially restricted if we undergo an “ownership change” as defined in Section 382 of the U.S. Internal Revenue Code, or Section 382. An ownership change under Section 382 would occur if “5-percent shareholders,” within the meaning of Section 382, collectively increased their
64
ownership in the Company by more than 50 percentage points over a rolling three-year period. We have not completed a recent study to assess whether any change of control has occurred or whether there have been multiple changes of control since the Company’s formation, due to the significant complexity and cost associated with the study. We have completed studies through December 31, 2015 and concluded no adjustments were required. If we have experienced a change of control at any time since our formation, our NOL carryforwards and tax credits may not be available, or their utilization could be subject to an annual limitation under Section 382. A full valuation allowance has been provided against our NOL carryforwards, and if an adjustment is required, this adjustment would be offset by an adjustment to the valuation allowance. Accordingly, there would be no impact on the consolidated balance sheet or statement of operations.
We may have exposure to additional tax liabilities that could negatively impact our income tax provision, net income, and cash flow.
We are subject to income taxes and other taxes in both the U.S. and the foreign jurisdictions in which we currently operate or have historically operated. The determination of our worldwide provision for income taxes and current and deferred tax assets and liabilities requires judgment and estimation. In the ordinary course of our business, there are many transactions and calculations where the ultimate tax determination is uncertain. We are subject to regular review and audit by U.S. tax authorities as well as subject to the prospective and retrospective effects of changing tax regulations and legislation. Although we believe our tax estimates are reasonable, the ultimate tax outcome may materially differ from the tax amounts recorded in our consolidated financial statements and may materially affect our income tax provision, net income, or cash flows in the period or periods for which such determination and settlement is made.
Risks Relating to an Investment in our Common Stock
Our stock price has been and may continue to be volatile.
The market price of our common stock has been volatile and is likely to continue to be so. The market price of our common stock may fluctuate due to factors including, but not limited to:
|
· |
our ability to meet the expectations of investors related to the commercialization of Qsymia and STENDRA; |
|
· |
the impact of the return of the U.S. and Canadian rights for the commercialization of STENDRA; |
|
· |
our ability, either by ourselves or through a third party, to successfully commercialize STENDRA in the U.S. and Canada; |
|
· |
our ability to find the right partner for expanded Qsymia commercial promotion to a broader primary care physician audience; |
|
· |
our ability to obtain marketing authorization for our products in foreign jurisdictions, including authorization from the EC for Qsiva in the EU through the centralized marketing authorization procedure; |
|
· |
the costs, timing and outcome of post-approval clinical studies which the FDA has required us to perform as part of the approval for Qsymia and STENDRA; |
|
· |
the substantial cost to expand into certified retail pharmacy locations and the cost required to maintain the REMS program for Qsymia; |
|
· |
results within the clinical trial programs for Qsymia and STENDRA or other results or decisions affecting the development of our investigational drug candidates; |
65
|
· |
announcements of technological innovations or new products by us or our competitors; |
|
· |
approval of, or announcements of, other anti-obesity compounds in development; |
|
· |
publication of generic drug combination weight loss data by outside individuals or companies; |
|
· |
actual or anticipated fluctuations in our financial results; |
|
· |
our ability to obtain needed financing; |
|
· |
sales by insiders or major stockholders; |
|
· |
economic conditions in the U.S. and abroad; |
|
· |
the volatility and liquidity of the financial markets; |
|
· |
comments by or changes in assessments of us or financial estimates by security analysts; |
|
· |
negative reports by the media or industry analysts on various aspects of our products, our performance and our future operations; |
|
· |
adverse regulatory actions or decisions; |
|
· |
any loss of key management; |
|
· |
deviations in our operating results from the estimates of securities analysts or other analyst comments; |
|
· |
discussions about us or our stock price by the financial and scientific press and in online investor communities; |
|
· |
investment activities employed by short sellers of our common stock; |
|
· |
developments or disputes concerning patents or other proprietary rights; |
|
· |
reports of prescription data by us or from independent third parties for our products; |
|
· |
licensing, product, patent or securities litigation; and |
|
· |
public concern as to the safety and efficacy of our drugs or future investigational drug candidates developed by us. |
These factors and fluctuations, as well as political and other market conditions, may adversely affect the market price of our common stock. Additionally, volatility or a lack of positive performance in our stock price may adversely affect our ability to retain or recruit key employees, all of whom have been or will be granted equity awards as an important part of their compensation packages.
Our operating results are unpredictable and may fluctuate. If our operating results are below the expectations of securities analysts or investors, the trading price of our stock could decline.
Our operating results will likely fluctuate from fiscal quarter to fiscal quarter, and from year to year, and are difficult to predict. Although we have commenced sales of Qsymia, we may never increase these sales or become profitable. If we are unable to or decide not to commercialize STENDRA in the U.S. and Canada ourselves, we will have to enter into a collaborative arrangement or strategic alliance to commercialize STENDRA. We may be unable to enter
66
into agreements with third parties for STENDRA for these territories on favorable terms or at all, which could delay, impair, or preclude our ability to commercialize STENDRA in these territories. In addition, although we have entered into license and commercialization agreements with Sanofi and Menarini, to commercialize avanafil for the treatment of ED on an exclusive basis in Africa, the Middle East, Turkey, and the CIS, including Russia, to commercialize and promote SPEDRA for the treatment of ED in over 40 countries, including the EU, plus Australia and New Zealand, respectively, we may not be successful in commercializing avanafil in these territories. Our operating expenses are largely independent of sales in any particular period. We believe that our quarterly and annual results of operations may be negatively affected by a variety of factors. These factors include, but are not limited to, the level of patient demand for Qsymia and STENDRA, the ability of our distribution partners to process and ship product on a timely basis, the success of our third-party’s manufacturing efforts to meet customer demand, fluctuations in foreign exchange rates, investments in sales and marketing efforts to support the sales of Qsymia and STENDRA, investments in the research and development efforts, and expenditures we may incur to acquire additional products.
Future sales of our common stock may depress our stock price.
Sales of our stock by our executive officers and directors, or the perception that such sales may occur, could adversely affect the market price of our stock. We have also registered all common stock that we may issue under our employee benefits plans. As a result, these shares can be freely sold in the public market upon issuance, subject to restrictions under the securities laws. Any of our executive officers or directors may adopt trading plans under SEC Rule 10b5-1 to dispose of a portion of their stock. If any of these events cause a large number of our shares to be sold in the public market, the sales could reduce the trading price of our common stock and impede our ability to raise future capital.
Our charter documents and Delaware law could make an acquisition of our company difficult, even if an acquisition may benefit our stockholders.
Our Board of Directors has adopted a Preferred Shares Rights Plan which, if not earlier triggered, expires on April 13, 2017. The Preferred Shares Rights Plan has the effect of causing substantial dilution to a person or group that attempts to acquire us on terms not approved by our Board of Directors. The existence of the Preferred Shares Rights Plan could limit the price that certain investors might be willing to pay in the future for shares of our common stock and could discourage, delay or prevent a merger or acquisition that a stockholder may consider favorable.
Some provisions of our Amended and Restated Certificate of Incorporation and Amended and Restated Bylaws could delay or prevent a change in control of our Company. Some of these provisions:
|
· |
authorize the issuance of preferred stock by the Board without prior stockholder approval, commonly referred to as “blank check” preferred stock, with rights senior to those of common stock; |
|
· |
prohibit stockholder actions by written consent; |
|
· |
specify procedures for director nominations by stockholders and submission of other proposals for consideration at stockholder meetings; and |
|
· |
eliminate cumulative voting in the election of directors. |
In addition, we are governed by the provisions of Section 203 of Delaware General Corporation Law. These provisions may prohibit large stockholders, in particular those owning 15% or more of our outstanding voting stock, from merging or combining with us. These and other provisions in our charter documents could reduce the price that investors might be willing to pay for shares of our common stock in the future and result in the market price being lower than it would be without these provisions.
67
Item 1B. Unresolved Staff Comments
None.
We have a lease on 4,914 square feet of office space located at 1174 Castro Street, Mountain View, California, or the Castro Facility. The lease for the Castro Facility has a term of 60 months commencing March 15, 2012, with an option to extend the term for one year from the expiration of the new lease. The Castro Facility has been subleased commencing on September 1, 2014 for a period of 31 months.
We entered into a lease effective as of December 11, 2012, for our current principal executive offices, consisting of an approximately 45,240 square foot building, located at 351 East Evelyn Avenue, Mountain View, California, or the Evelyn Lease. The Evelyn Lease has an initial term of approximately 84 months, commencing on May 11, 2013. We have one option to renew the Evelyn Lease for a term of three years at the prevailing market rate. As part of a cost reduction plan, approximately 14,105 square feet of the Evelyn Lease has been subleased commencing on May 1, 2014 for a period of 36 months.
In general, our existing facilities are in good condition and adequate for all present and near‑term uses.
For additional information regarding obligations under operating leases, see Note 16: “Commitments” to our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K.
Securities Related Class Action and Shareholder Derivative Lawsuits
The Company, a current officer and a former officer were defendants in a putative class action captioned Kovtun v. VIVUS, Inc., et al., Case No. 4:10‑CV‑04957‑PJH, in the U.S. District Court, Northern District of California. The action, filed in November 2010, alleged violations of Section 10(b) and 20(a) of the federal Securities Exchange Act of 1934 based on allegedly false or misleading statements made by the defendants in connection with the Company’s clinical trials and New Drug Application, or NDA, for Qsymia as a treatment for obesity. The Court granted defendants’ motions to dismiss both plaintiff’s Amended Class Action Complaint and Second Amended Class Action Complaint; by order dated September 27, 2012, the latter dismissal was with prejudice and final judgment was entered for defendants the same day. On October 26, 2012, plaintiff filed a Notice of Appeal to the U.S. Court of Appeals for the Ninth Circuit. Following briefing of the appeal, the Court of Appeals held oral argument on January 16, 2015. On January 29, 2015, the Court of Appeals issued a Memorandum decision affirming the District Court’s ruling. On February 12, 2015, plaintiff asked the Court of Appeals’ panel to rehear the case or for the Court to rehear the case en banc. The Court of Appeals denied that petition on March 16, 2015, and the matter is now concluded.
Additionally, certain of the Company’s former officers and directors and a current director are defendants in a shareholder derivative lawsuit captioned Turberg v. Logan, et al., Case No. CV‑10‑05271‑PJH, pending in the same federal court. In the plaintiff’s Verified Amended Shareholder Derivative Complaint filed June 3, 2011, the plaintiff largely restated the allegations of the Kovtun action and alleged that the directors breached fiduciary duties to the Company by purportedly permitting the Company to violate the federal securities laws as alleged in the Kovtun action. The same individuals are also named defendants in consolidated shareholder derivative suits pending in the California Superior Court, Santa Clara County, under the caption In re VIVUS, Inc. Derivative Litigation, Master File No. 11 0 CV188439. The allegations in the state court derivative suits are substantially similar to the other lawsuits. The Company is named as a nominal defendant in these actions, neither of which seeks any recovery from the Company. The parties agreed to stay the derivative lawsuits pending the outcome of the appeal of the securities class action. Following the resolution of the class action in the Company’s favor, discussed above, the Turberg plaintiff dismissed the derivative litigation.
68
On March 27, 2014, Mary Jane and Thomas Jasin, who purport to be purchasers of VIVUS common stock, filed an Amended Complaint in Santa Clara County Superior Court alleging securities fraud against the Company and three of its former officers and directors. In that complaint, captioned Jasin v. VIVUS, Inc., Case No. 114‑cv‑261427, plaintiffs asserted claims under California’s securities and consumer protection securities statutes. Plaintiffs alleged generally that defendants misrepresented the prospects for the Company’s success, including with respect to the launch of Qsymia, while purportedly selling VIVUS stock for personal profit. Plaintiffs alleged losses of “at least” $2.8 million, and sought damages and other relief. On June 5, 2014, the Company and the other defendants filed a demurrer to the Amended Complaint seeking its dismissal. With the demurrer pending, on July 18, 2014, the same plaintiffs filed a complaint in the United States District Court for the Northern District of California, captioned Jasin v. VIVUS, Inc., Case No. 5:14‑cv‑03263. The Jasins’ federal complaint alleges violations of Sections 10(b) and 20(a) of the Securities Exchange Act of 1934, based on facts substantially similar to those alleged in their state court action. On September 15, 2014, pursuant to an agreement between the parties, plaintiffs moved to voluntarily dismiss, with prejudice, the state court action. In the federal action, defendants filed a motion to dismiss on November 12, 2014. On December 3, 2014, plaintiffs filed a First Amended Complaint in the federal action. On January 21, 2015, defendants filed a motion to dismiss the First Amended Complaint. The court ruled on that motion on June 18, 2015, dismissing the seven California claims with prejudice and dismissing the two federal claims with leave to amend. Plaintiffs filed a second amended complaint on August 17, 2015. Defendants moved to dismiss that complaint on October 2, 2015. On September 10, 2015, plaintiffs moved for entry of judgment on their state claims. Briefing on both defendants’ motion to dismiss and plaintiffs’ motion for entry of judgment was completed on December 15, 2015. The court heard oral argument on both motions on January 14, 2016. The court has not yet issued a ruling on either motion. The Company maintains directors’ and officers’ liability insurance that it believes affords coverage for much of the anticipated cost of the remaining Jasin action, subject to the use of our financial resources to pay for our self‑insured retention and the policies’ terms and conditions.
The Company and the defendant officers and directors cannot predict the outcome of the various shareholder lawsuits, but they believe the various shareholder lawsuits are without merit and intend to continue vigorously defending them.
Qsymia ANDA Litigation
On May 7, 2014, the Company received a Paragraph IV certification notice from Actavis Laboratories FL indicating that it filed an abbreviated new drug application, or ANDA, with the U.S. Food and Drug Administration, or FDA, requesting approval to market a generic version of Qsymia and contending that the patents listed for Qsymia in the FDA Orange Book at the time the notice was received (U.S. Patents 7,056,890, 7,553,818, 7,659,256, 7,674,776, 8,580,298, and 8,580,299 (collectively “patents‑in‑suit”)) are invalid, unenforceable and/or will not be infringed by the manufacture, use, sale or offer for sale of a generic form of Qsymia as described in their ANDA. On June 12, 2014, the Company filed a lawsuit in the U.S. District Court for the District of New Jersey against Actavis Laboratories FL, Inc., Actavis, Inc., and Actavis PLC, collectively referred to as Actavis. The lawsuit (Case No. 14‑3786 (SRC)(CLW)) was filed on the basis that Actavis’ submission of their ANDA to obtain approval to manufacture, use, sell or offer for sale generic versions of Qsymia prior to the expiration of the patents‑in‑suit constitutes infringement of one or more claims of those patents.
In accordance with the Hatch‑Waxman Act, as a result of having filed a timely lawsuit against Actavis, FDA approval of Actavis’ ANDA will be stayed until the earlier of (i) up to 30 months from the Company’s May 7, 2014 receipt of Actavis’ Paragraph IV certification notice (i.e. November 7, 2016) or (ii) a District Court decision finding that the identified patents are invalid, unenforceable or not infringed.
On January 21, 2015, the Company received a second Paragraph IV certification notice from Actavis contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 8,895,057 and 8,895,058) are invalid, unenforceable and/or will not be infringed by the manufacture, use, sale, or offer for sale of a generic form of Qsymia. On March 4, 2015, the Company filed a second lawsuit in the U.S. District Court for the District of New Jersey against Actavis (Case No. 15-1636 (SRC)(CLW)) in response to the second Paragraph IV certification notice on the basis that Actavis’ submission of their ANDA constitutes infringement of one or more claims of the patents-in-suit.
69
On July 7, 2015, the Company received a third Paragraph IV certification notice from Actavis contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 9,011,905 and 9,011,906) are invalid, unenforceable and/or will not be infringed by the manufacture, use, sale, or offer for sale of a generic form of Qsymia. On August 17, 2015, the Company filed a third lawsuit in the U.S. District Court for the District of New Jersey against Actavis (Case No. 15-6256 (SRC)(CLW)) in response to the third Paragraph IV certification notice on the basis that Actavis’ submission of their ANDA constitutes infringement of one or more claims of the patents-in-suit. The three lawsuits against Actavis have been consolidated into a single suit (Case No. 14-3786 (SRC)(CLW)).
On March 5, 2015, the Company received a Paragraph IV certification notice from Teva Pharmaceuticals USA, Inc. indicating that it filed an ANDA with the FDA, requesting approval to market a generic version of Qsymia and contending that eight patents listed for Qsymia in the Orange Book at the time of the notice (U.S. Patents 7,056,890, 7,553,818, 7,659,256, 7,674,776, 8,580,298, 8,580,299, 8,895,057 and 8,895,058) (collectively “patents-in-suit”) are invalid, unenforceable and/or will not be infringed by the manufacture, use or sale of a generic form of Qsymia as described in their ANDA. On April 15, 2015, the Company filed a lawsuit in the U.S. District Court for the District of New Jersey against Teva Pharmaceutical USA, Inc. and Teva Pharmaceutical Industries, Ltd., collectively referred to as Teva. The lawsuit (Case No. 15-2693 (SRC)(CLW)) was filed on the basis that Teva’s submission of their ANDA to obtain approval to manufacture, use, sell, or offer for sale generic versions of Qsymia prior to the expiration of the patents-in-suit constitutes infringement of one or more claims of those patents.
In accordance with the Hatch-Waxman Act, as a result of having filed a timely lawsuit against Teva, FDA approval of Teva’s ANDA will be stayed until the earlier of (i) up to 30 months from our March 5, 2015 receipt of Teva’s Paragraph IV certification notice (i.e. September 5, 2017) or (ii) a District Court decision finding that the identified patents are invalid, unenforceable or not infringed.
On August 5, 2015, the Company received a second Paragraph IV certification notice from Teva contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 9,011,905 and 9,011,906) are invalid, unenforceable and/or will not be infringed by the manufacture, use, sale, or offer for sale of a generic form of Qsymia. On September 18, 2015, the Company filed a second lawsuit in the U.S. District Court for the District of New Jersey against Teva (Case No. 15-6957(SRC)(CLW)) in response to the second Paragraph IV certification notice on the basis that Teva’s submission of their ANDA constitutes infringement of one or more claims of the patents-in-suit. The two lawsuits against Teva have been consolidated into a single suit (Case No. 15-2693 (SRC)(CLW)).
The Company intends to vigorously enforce its intellectual property rights relating to Qsymia, but the Company cannot predict the outcome of these matters.
The Company is not aware of any other asserted or unasserted claims against it where it believes that an unfavorable resolution would have an adverse material impact on the operations or financial position of the Company.
Item 4. Mine Safety Disclosures.
None.
70
Item 5. Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities.
VIVUS’s common stock trades publicly on the NASDAQ Global Select Market under the symbol “VVUS.” The following table sets forth for the periods indicated the quarterly high and low sales prices of our common stock as reported on the NASDAQ Global Select Market.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Three Months Ended |
|
||||||||||
|
|
|
March 31 |
|
June 30 |
|
September 30 |
|
December 31 |
|
||||
|
2015 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
High |
|
$ |
3.40 |
|
$ |
2.65 |
|
$ |
2.39 |
|
$ |
2.25 |
|
|
Low |
|
|
2.41 |
|
|
2.22 |
|
|
0.94 |
|
|
0.95 |
|
|
2014 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
High |
|
$ |
9.80 |
|
$ |
6.28 |
|
$ |
5.45 |
|
$ |
3.89 |
|
|
Low |
|
|
5.50 |
|
|
4.56 |
|
|
3.32 |
|
|
2.72 |
|
Stockholders
As of February 29, 2016, there were 107,075,642 shares of outstanding common stock that were held by 2,889 stockholders of record and no outstanding shares of preferred stock. On February 29, 2016, the last reported sales price of our common stock on the NASDAQ Global Select Market was $1.04 per share.
Dividends
We have not paid any dividends since our inception and we do not intend to declare or pay any dividends on our common stock in the foreseeable future. Declaration or payment of future dividends, if any, will be at the discretion of our Board of Directors after taking into account various factors, including VIVUS’s financial condition, operating results and current and anticipated cash needs.
Stock Performance Graph
The following graph shows a comparison of total stockholder return for holders of our common stock from December 31, 2010 through December 31, 2015 compared with the NASDAQ Composite Index and the RDG SmallCap Pharmaceutical Index. Total stockholder return assumes $100 invested at the beginning of the period in our common stock, the stock represented in the NASDAQ Composite Index and the stock represented by the RDG SmallCap Pharmaceutical Index, respectively. This graph is presented pursuant to SEC rules. We believe that while total stockholder return can be an important indicator of corporate performance, the stock prices of small cap pharmaceutical stocks like VIVUS are subject to a number of market‑related factors other than company performance, such as competitive announcements, mergers and acquisitions in the industry, the general state of the economy, and the performance of other medical technology stocks.
71
COMPARISON OF 5‑YEAR CUMULATIVE TOTAL RETURN*
Among VIVUS, Inc., the NASDAQ Composite Index, and the RDG SmallCap
Pharmaceutical Index
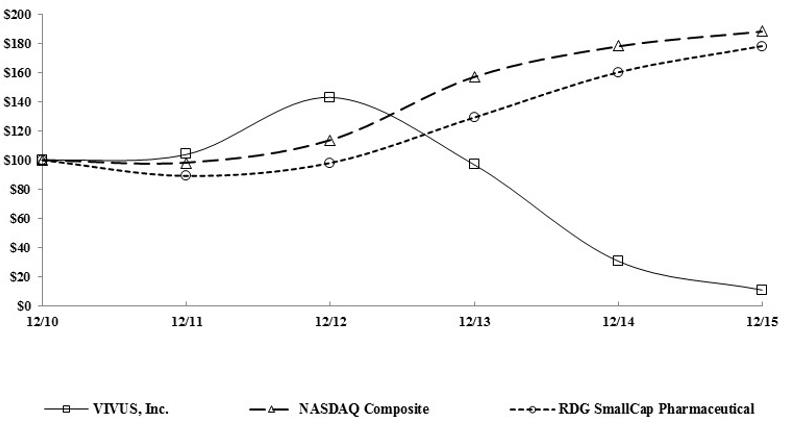
*$100 invested on 12/31/2010 in stock or index, including reinvestment of dividends. Fiscal year ending December 31.
Item 6. Selected Financial Data
The following selected financial data have been derived from our audited financial statements. The information set forth below is not necessarily indicative of the results of future operations and should be read in conjunction with “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the financial statements and notes thereto included elsewhere in this Annual Report on Form 10‑K. The selected data is not intended to replace the financial statements.
72
Selected Financial Data
(In thousands, except per share data)
Selected Annual Financial Data
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Year Ended December 31, |
|
|||||||||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
2012 |
|
2011 |
|
|||||
|
Income Statement Data: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total revenue |
|
$ |
95,430 |
|
$ |
114,181 |
|
$ |
81,082 |
|
$ |
2,012 |
|
$ |
— |
|
|
Total operating expenses |
|
$ |
155,707 |
|
$ |
164,892 |
|
$ |
235,696 |
|
$ |
141,917 |
|
$ |
47,076 |
|
|
Loss from operations |
|
$ |
(60,277) |
|
$ |
(50,711) |
|
$ |
(154,614) |
|
$ |
(139,905) |
|
$ |
(47,076) |
|
|
Loss from continuing operations |
|
$ |
(93,107) |
|
$ |
(82,647) |
|
$ |
(174,946) |
|
$ |
(139,733) |
|
$ |
(47,026) |
|
|
Net loss |
|
$ |
(93,107) |
|
$ |
(82,647) |
|
$ |
(174,456) |
|
$ |
(139,881) |
|
$ |
(46,140) |
|
|
Basic and diluted net loss per share—Continuing operations |
|
$ |
(0.90) |
|
$ |
(0.80) |
|
$ |
(1.72) |
|
$ |
(1.42) |
|
$ |
(0.56) |
|
|
Balance Sheet Data: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Working capital |
|
$ |
214,143 |
|
$ |
301,789 |
|
$ |
371,934 |
|
$ |
220,671 |
|
$ |
140,764 |
|
|
Total assets |
|
$ |
280,581 |
|
$ |
366,938 |
|
$ |
431,796 |
|
$ |
264,114 |
|
$ |
152,056 |
|
|
Long-term debt |
|
$ |
234,769 |
|
$ |
227,783 |
|
$ |
213,106 |
|
$ |
— |
|
$ |
— |
|
|
Accumulated deficit |
|
$ |
(836,356) |
|
$ |
(743,249) |
|
$ |
(660,602) |
|
$ |
(486,146) |
|
$ |
(346,265) |
|
|
Stockholders’ (deficit) equity |
|
$ |
(7,085) |
|
$ |
82,518 |
|
$ |
153,369 |
|
$ |
222,909 |
|
$ |
141,084 |
|
Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations
All percentage amounts and ratios were calculated using the underlying data in thousands. Operating results for the year ended December 31, 2015, are not necessarily indicative of the results that may be expected for future fiscal years. The following discussion and analysis should be read in conjunction with our historical financial statements and the notes to those financial statements that are included in Item 8 of Part II of this Form 10‑K.
Overview
VIVUS is a biopharmaceutical company with two therapies approved by the FDA: Qsymia® (phentermine and topiramate extended‑release) for chronic weight management and STENDRA® (avanafil) for erectile dysfunction, or ED. STENDRA is also approved by the European Commission, or EC, under the trade name, SPEDRA, for the treatment of ED in the EU.
Qsymia was approved by the FDA in July 2012, as an adjunct to a reduced‑calorie diet and increased physical activity for chronic weight management in adult patients with an initial body mass index, or BMI, of 30 or greater, or obese patients, or 27 or greater, or overweight patients, in the presence of at least one weight‑related comorbidity, such as hypertension, type 2 diabetes mellitus or high cholesterol, or dyslipidemia. Qsymia incorporates a proprietary formulation combining low doses of active ingredients from two previously approved drugs, phentermine and topiramate. Although the exact mechanism of action is unknown, Qsymia is believed to suppress appetite and increase satiety, or the feeling of being full, the two main mechanisms that impact eating behavior. In September 2012, Qsymia became available in the U.S. market through a limited number of certified home delivery networks. In July 2013, Qsymia became available in retail pharmacies nationwide. As of the date of this report, Qsymia is available in over 40,000 certified retail pharmacies nationwide, including all of the major pharmacy chains in the country. We intend to continue to certify and add new pharmacies to the Qsymia retail pharmacy network, including national and regional chains as well as independent pharmacies.
Prior to August 2015, we commercialized Qsymia in the U.S. primarily through a dedicated contract sales force, supported by an internal commercial team. In August 2015, we directly hired approximately 50 former contract sales representatives to continue promoting Qsymia to physicians. Our efforts to expand the appropriate use of Qsymia include scientific publications, participation and presentations at medical conferences, and development and implementation of patient-directed support programs. Most recently, we have rolled out unique marketing programs to encourage targeted prescribers to gain more experience with Qsymia with their obese patient population. In 2015, we increased our investment in digital media in order to amplify our messaging to information-seeking consumers. The digital messaging encourages those consumers most likely to take action to speak with their physicians about obesity
73
treatment options. We believe our enhanced web-based strategies will deliver clear and compelling communications to potential patients. We have also employed a physician referral service to help patients identify prescribers in their area.
Challenges continue within the obesity pharmacotherapy market, in particular with respect to the tendency on the part of healthcare providers to treat the co-morbid conditions of obesity rather than the obesity disease itself. In addition, there is a narrow focus on certain patient types for treatment, historically low third-party insurance coverage, and the continued exclusion of anti-obesity medications from Medicare Part D.
We continue to develop efficient ways to address the obesity market. We completed a realignment of our field sales territories during April 2015 and July 2015, reducing the number of territories from 150 to approximately 50. Each of these adjustments was accompanied by a parallel streamlining of corporate headquarters headcount as we have sought to right-size the organization to match the market opportunity as it currently exists.
We defined and identified the healthcare provider, or HCP, audience of anti-obesity prescribers as numbering approximately 8,000 to 10,000. Of these, we believe the most highly productive writers are adequately covered by the newly-configured VIVUS sales force. We are focused on maintaining a commercial presence with important Qsymia prescribers, and we have capacity to cover new potential prescribers, who are those physicians that begin prescribing branded obesity products. We are constantly monitoring prescribing activity in the market, and we have seen new prescriptions being written by HCPs on whom we have not previously dedicated field sales resources. We believe that part of the current realignment addresses this new prescriber group, and we look forward to initiating and maintaining dialog with these HCPs.
Qsymia is approved for the treatment of obesity in the U.S. In October 2012, we received a negative opinion from the European Medicines Agency, or EMA, Committee for Medicinal Products for Human Use, or CHMP, recommending refusal of the marketing authorization for the medicinal product QsivaTM, the intended trade name for Qsymia in the EU, due to concerns over the potential cardiovascular and central nervous system effects associated with long-term use, potential for interfering with the development of a fetus and use by patients for whom Qsiva would not have been indicated. We requested that this opinion be re-examined by the CHMP. After re-examination of the CHMP opinion, in February 2013, the CHMP adopted a final opinion that reaffirmed the Committee’s earlier negative opinion to refuse the marketing authorization for Qsiva in the EU. In May 2013, the EC issued a decision refusing the grant of marketing authorization for Qsiva in the EU.
In September 2013, we submitted a request to the EMA for Scientific Advice, a procedure similar to the U.S. Special Protocol Assessment process, regarding use of a pre-specified interim analysis from the CVOT, known as AQCLAIM, to assess the long-term treatment effect of Qsymia on the incidence of major adverse cardiovascular events in overweight and obese subjects with confirmed cardiovascular disease. Our request was to allow this interim analysis to support the resubmission of an application for a marketing authorization for Qsiva for treatment of obesity in accordance with the EU centralized marketing authorization procedure. We received feedback in 2014 from the EMA and the various competent authorities of the EU Member States associated with review of the AQCLAIM CVOT protocol, and we received feedback from the FDA in late 2014 regarding the amended protocol. As a part of addressing the FDA comments from a May 2015 meeting to discuss alternatives to completion of a CVOT, we are now working with cardiovascular and epidemiology experts in exploring alternate solutions to demonstrate the long-term cardiovascular safety of Qsymia. After reviewing a summary of Phase 3 data relevant to cardiovascular, or CV, risk and post-marketing safety data, the cardiology experts noted that they believe there was an absence of an overt CV risk signal and indicated that they did not believe a randomized placebo controlled CVOT would provide additional information regarding the CV risk of Qsymia. The epidemiology experts maintained that a well-conducted retrospective observational study could provide data to further inform on potential CV risk. We are working with the expert group to develop a protocol for the retrospective observational study and feasibility assessment. Although we and the consulted experts believe there is no overt signal for CV risk to justify the AQCLAIM CVOT, VIVUS is committed to working with the FDA to reach a resolution. As for the EU, even if the FDA were to accept a retrospective observational study in lieu of a CVOT, there would be no assurance that the EMA would accept the same.
In addition, we are in the process of pursuing a new indication for Qsymia in obstructive sleep apnea, or OSA. We also intend to seek regulatory approval for Qsymia in territories outside the U.S. and the EU and, if approved, to
74
commercialize the product through collaboration agreements with third parties. We plan to optimize spending while pursuing these potential objectives.
STENDRA is an oral phosphodiesterase type 5, or PDE5, inhibitor that we have licensed from Mitsubishi Tanabe Pharma Corporation, or MTPC. STENDRA was approved by the FDA in April 2012 for the treatment of ED in the United States. In June 2013, the EC adopted a decision granting marketing authorization for SPEDRA, the approved trade name for avanafil in the EU, for the treatment of ED in the EU. In July 2013, we entered into an agreement with the Menarini Group, through its subsidiary Berlin Chemie AG, or Menarini, under which Menarini received an exclusive license to commercialize and promote SPEDRA for the treatment of ED in over 40 European countries, including the EU, as well as Australia and New Zealand. Menarini commenced its commercialization launch of the product in the EU in early 2014. As of the date of this filing, SPEDRA is commercially available in 25 countries within the territory granted to Menarini pursuant to the license and commercialization agreement.
In October 2013, we entered into an agreement with Auxilium Pharmaceuticals, Inc., or Auxilium, under which Auxilium received an exclusive license to commercialize and promote STENDRA in the United States and Canada. On the same date, we also entered into a supply agreement with Auxilium, whereby we would supply Auxilium with STENDRA for commercialization. Auxilium began commercializing STENDRA in the U.S. market in December 2013. In January 2015, Auxilium was acquired by Endo International, plc, or Endo. In December 2015, Auxilium notified us of its intention to return the U.S. and Canadian commercial rights for STENDRA to us. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016.
In December 2013, we entered into an agreement with Sanofi under which Sanofi received an exclusive license to commercialize and promote avanafil for therapeutic use in humans in Africa, the Middle East, Turkey, and the Commonwealth of Independent States, or CIS, including Russia. Sanofi will be responsible for obtaining regulatory approval in its territories. Sanofi intends to market avanafil under the trade name SPEDRA or STENDRA. Effective as of December 11, 2013, we also entered into a supply agreement, or the Sanofi Supply Agreement, with Sanofi Winthrop Industrie, a wholly owned subsidiary of Sanofi.
Under the license agreements with Menarini, Auxilium and Sanofi, avanafil is expected to be commercialized in over 100 countries worldwide. Under our agreement with Auxilium, we have received approximately $45.0 million in license and milestone payments out of a potential of $300.0 million, as well as royalty payments. We do not anticipate any additional milestone revenue from the Auxilium agreement. Under the Menarini agreement, we have received approximately $63.0 million in license and milestone payments out of a potential of approximately $100.0 million, as well as royalty payments. Under the Sanofi agreement, we have received approximately $10.0 million in license and milestone payments out of a potential of $61.0 million. In addition, we are currently in discussions with potential collaboration partners to market and sell STENDRA for our other territories, including Latin America, in which we do not currently have a commercial collaboration. We have engaged a strategic advisor to assist us in the evaluation of our alternatives not only for STENDRA, but also for our overall business strategy.
On September 18, 2014, the FDA approved a supplemental new drug application (sNDA) for STENDRA. STENDRA is now indicated to be taken as early as approximately 15 minutes before sexual activity. Additionally, on January 23, 2015, the EC adopted a commission implementing decision amending the marketing authorization for SPEDRA. SPEDRA is now indicated to be taken as needed approximately 15 to 30 minutes before sexual activity.
Foreign regulatory approvals, including EC marketing authorization to market Qsiva in the EU, may not be obtained on a timely basis, or at all, and the failure to receive regulatory approvals in a foreign country would prevent us from marketing our products that have failed to receive such approval in that market, which could have a material adverse effect on our business, financial condition and results of operations.
Critical Accounting Policies and Estimates
The discussion and analysis of our financial condition and results of operations are based upon our consolidated financial statements, which have been prepared in accordance with accounting principles generally accepted in the U.S.
75
The preparation of these financial statements requires us to make estimates and judgments that affect the reported amounts of assets, liabilities, revenues, expenses and related disclosures. On an ongoing basis, we evaluate our estimates, including those related to available‑for‑sale securities, research and development expenses, income taxes, inventories, revenues, including revenues from multiple‑element arrangements, contingencies and litigation and share‑based compensation. We base our estimates on historical experience, information received from third parties and on various market specific and other relevant assumptions that are believed to be reasonable under the circumstances, the results of which form the basis for making judgments about the carrying values of assets and liabilities that are not readily apparent from other sources. Actual results may differ significantly from these estimates under different assumptions or conditions. Our significant accounting policies are more fully described in Note 1 to our Consolidated Financial Statements included elsewhere in this report.
We believe the following critical accounting policies affect our more significant judgments and estimates used in the preparation of our consolidated financial statements:
Revenue Recognition
Product Revenue
We recognize product revenue from the sales of Qsymia when: (i) persuasive evidence that an arrangement exists, (ii) delivery has occurred and title has passed, (iii) the price is fixed or determinable, and (iv) collectability is reasonably assured. Revenue from sales transactions where the customer has the right to return the product is recognized at the time of sale only if: (i) our price to the customer is substantially fixed or determinable at the date of sale, (ii) the customer has paid us, or the customer is obligated to pay us and the obligation is not contingent on resale of the product, (iii) the customer’s obligation to us would not be changed in the event of theft or physical destruction or damage of the product, (iv) the customer acquiring the product for resale has economic substance apart from that provided by us, (v) we do not have significant obligations for future performance to directly bring about resale of the product by the customer, and (vi) the amount of future returns can be reasonably estimated.
Product Revenue Allowances
Product revenue is recognized net of consideration paid to our customers, wholesalers and certified pharmacies, for services rendered by the wholesalers and pharmacies in accordance with the wholesalers and certified pharmacy services network agreements, and include a fixed rate per prescription shipped and monthly program management and data fees. These services are not deemed sufficiently separable from the customers’ purchase of the product; therefore, they are recorded as a reduction of revenue at the time of revenue recognition.
Other product revenue allowances include certain prompt pay discounts and allowances offered to our customers, program rebates and chargebacks. These product revenue allowances are recognized as a reduction of revenue or as a selling expense at the later of the date at which the related revenue is recognized or the date at which the allowance is offered. We also offer discount programs to patients. Calculating certain of these items involves estimates and judgments based on sales or invoice data, contractual terms, utilization rates, new information regarding changes in these programs’ regulations and guidelines that would impact the amount of the actual rebates or chargebacks. We review the adequacy of product revenue allowances on a quarterly basis. Amounts accrued for product revenue allowances are adjusted when trends or significant events indicate that adjustment is appropriate and to reflect actual experience.
76
The following table summarizes the activity in the accounts related to Qsymia product revenue allowances (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Wholesaler/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Discount |
|
Pharmacy |
|
Cash |
|
Rebates/ |
|
|
|
|
||||
|
|
|
programs |
|
fees |
|
discounts |
|
Chargebacks |
|
Total |
|
|||||
|
Balance at January 1, 2013 |
|
$ |
— |
|
$ |
(143) |
|
$ |
(57) |
|
$ |
— |
|
$ |
(200) |
|
|
Current provision related to sales made during current period* |
|
|
(8,801) |
|
|
(5,070) |
|
|
(1,050) |
|
|
(280) |
|
|
(15,201) |
|
|
Payments |
|
|
8,099 |
|
|
3,789 |
|
|
973 |
|
|
201 |
|
|
13,062 |
|
|
Balance at December 31, 2013 |
|
|
(702) |
|
|
(1,424) |
|
|
(134) |
|
|
(79) |
|
|
(2,339) |
|
|
Current provision related to sales made during current period* |
|
|
(17,579) |
|
|
(6,973) |
|
|
(1,712) |
|
|
(2,110) |
|
|
(28,374) |
|
|
Payments |
|
|
17,418 |
|
|
7,393 |
|
|
1,696 |
|
|
1,752 |
|
|
28,259 |
|
|
Balance at December 31, 2014 |
|
|
(863) |
|
|
(1,004) |
|
|
(150) |
|
|
(437) |
|
|
(2,454) |
|
|
Current provision related to sales made during current period* |
|
|
(19,044) |
|
|
(6,958) |
|
|
(1,934) |
|
|
(2,706) |
|
|
(30,642) |
|
|
Payments |
|
|
18,935 |
|
|
6,802 |
|
|
1,920 |
|
|
2,663 |
|
|
30,320 |
|
|
Balance at December 31, 2015 |
|
$ |
(972) |
|
$ |
(1,160) |
|
$ |
(164) |
|
$ |
(480) |
|
$ |
(2,776) |
|
*Current provision related to sales made during current period includes $28.7 million, $24.6 million and $14.2 million for product revenue allowances related to revenue recognized during the years ended December 31, 2015, 2014 and 2013, respectively. The remaining amounts for the respective years were recorded on the consolidated balance sheets as deferred revenue at the end of each period.
Qsymia was approved by the FDA in July 2012. We sell Qsymia product in the U.S. to wholesalers and select certified pharmacies through their home delivery pharmacy services networks, which are collectively, our customers. Under this arrangement, title and risk of loss transfer to our customers upon delivery of the product to their distribution facilities. Wholesalers, in turn, sell product to certified retail pharmacies. Both mail order and retail certified pharmacies in turn, sell and dispense directly to patients, either at their retail pharmacies or through their mail order home delivery service.
We shipped initial orders of Qsymia to our customers in September 2012, and in July 2013, we expanded our distribution network to include certified retail pharmacies in accordance with the FDA‑approved amendment to our NDA for Qsymia. Qsymia has a 36‑month shelf life and we grant rights to our customers to return unsold product six months prior to and up to 12 months after product expiration and issue credits that may be applied against existing or future invoices. Given our limited history of selling Qsymia and the duration of the return period, we do not have sufficient information to reliably estimate expected returns of Qsymia at the time of shipment, and therefore we recognize revenue when units are dispensed to patients through prescriptions, at which point, the product is not subject to return. We obtain prescription shipment data from the pharmacies to determine the amount of revenue to recognize.
We will continue to recognize revenue for Qsymia based upon prescription sell‑through until we have sufficient historical information to reliably estimate returns. As of December 31, 2015, we have deferred revenue of $19.3 million related to shipments of Qsymia, which represents product shipped to our customers, but not yet dispensed to patients through prescriptions. A corresponding accounts receivable is also recorded for this amount, as the payments from customers are not contingent upon the sale of product to patients.
Supply Revenue
We recognize supply revenue from the sales of STENDRA or SPEDRA when the four basic revenue recognition criteria described above are met. We produce STENDRA or SPEDRA through a contract manufacturing partner and then sell it to our commercialization partners. As the primary responsible party in the commercial supply arrangements, we bear significant risk in the fulfillment of the obligations, including risks associated with manufacturing, regulatory compliance and quality assurance, as well as inventory, financial, and credit loss. As such, we
77
recognize supply revenue on a gross basis as principal party in the arrangements. Our commercialization partners for STENDRA or SPEDRA sell the product through their distribution channels to patients. Under our product supply agreements, as long as product meets specified product dating criteria at the time of shipment to the partner, our commercialization partners do not have a right of return or credit for expired product. As such, we recognize revenue for products that meet the dating criteria at the time of shipment.
Revenue from Multiple‑Element Arrangements
We account for multiple‑element arrangements, such as license and commercialization agreements in which a customer may purchase several deliverables, in accordance with ASC Topic 605‑25, Revenue Recognition—Multiple‑Element Arrangements, or ASC 605‑25. We evaluate if the deliverables in the arrangement represent separate units of accounting. In determining the units of accounting, we evaluate certain criteria, including whether the deliverables have value to our customers on a stand‑alone basis. Factors considered in this determination include whether the deliverable is proprietary to us, whether the customer can use the license or other deliverables for their intended purpose without the receipt of the remaining elements, whether the value of the deliverable is dependent on the undelivered items, and whether there are other vendors that can provide the undelivered items. Deliverables that meet these criteria are considered a separate unit of accounting. Deliverables that do not meet these criteria are combined and accounted for as a single unit of accounting.
When deliverables are separable, we allocate non‑contingent consideration to each separate unit of accounting based upon the relative selling price of each element. When applying the relative selling price method, we determine the selling price for each deliverable using vendor‑specific objective evidence, or VSOE, of selling price, if it exists, or third‑party evidence, or TPE, of selling price, if it exists. If neither VSOE nor TPE of selling price exists for a deliverable, we use best estimated selling price, or BESP, for that deliverable. Significant management judgment may be required to determine the relative selling price of each element. Revenue allocated to each element is then recognized based on when the following four basic revenue recognition criteria are met for each element: (i) persuasive evidence of an arrangement exists; (ii) delivery has occurred or services have been rendered; (iii) the price is fixed or determinable; and (iv) collectability is reasonably assured.
Determining whether and when some of these criteria have been satisfied often involves assumptions and judgments that can have a significant impact on the timing and amount of revenue we report. Changes in assumptions or judgments, or changes to the elements in an arrangement, could cause a material increase or decrease in the amount of revenue that we report in a particular period.
ASC Topic 605‑28, Revenue Recognition—Milestone Method, or ASC 605‑28, established the milestone method as an acceptable method of revenue recognition for certain contingent, event‑based payments under research and development arrangements. Under the milestone method, a payment that is contingent upon the achievement of a substantive milestone is recognized in its entirety in the period in which the milestone is achieved. A milestone is an event: (i) that can be achieved based in whole or in part on either our performance or on the occurrence of a specific outcome resulting from our performance, (ii) for which there is substantive uncertainty at the date the arrangement is entered into that the event will be achieved, and (iii) that would result in additional payments being due to us. The determination that a milestone is substantive requires judgment and is made at the inception of the arrangement. Milestones are considered substantive when the consideration earned from the achievement of the milestone is: (i) commensurate with either our performance to achieve the milestone or the enhancement of value of the item delivered as a result of a specific outcome resulting from our performance to achieve the milestone, (ii) relates solely to past performance, and (iii) is reasonable relative to all deliverables and payment terms in the arrangement.
Other contingent, event‑based payments received for which payment is either contingent solely upon the passage of time or the results of a collaborative partner’s performance are not considered milestones under ASC 605‑28. In accordance with ASC 605, such payments will be recognized as revenue when all of the four basic revenue recognition criteria are met.
Revenues recognized for royalty payments are recognized as earned when the four basic revenue recognition criteria described above are met.
78
Inventories
Inventories are valued at the lower of cost or market. Cost is determined using the first‑in, first‑out method for all inventories, which are valued using a weighted average cost method calculated for each production batch. Inventory includes the cost of active pharmaceutical ingredients, or APIs, raw materials and third‑party contract manufacturing and packaging services. Indirect overhead costs associated with production and distribution are allocated to the appropriate cost pool and then absorbed into inventory based on the units produced or distributed, assuming normal capacity, in the applicable period.
Inventory costs of product shipped to customers, but not yet recognized as revenue, are recorded as deferred costs within inventories on the consolidated balance sheets and are subsequently recognized to cost of goods sold when revenue recognition criteria have been met.
Our policy is to write down inventory that has become obsolete, inventory that has a cost basis in excess of its expected net realizable value and inventory in excess of expected requirements. The estimate of excess quantities is subjective and primarily dependent on our estimates of future demand for a particular product. If the estimate of future demand is inaccurate based on actual sales, we may increase the write down for excess inventory for that product and record a charge to inventory impairment and commitment fee in the consolidated statements of operations. We periodically evaluate the carrying value of inventory on hand for potential excess amount over demand using the same lower of cost or market approach as that used to value the inventory.
Research and Development Expenses
Research and development, or R&D, expenses include license fees, related compensation, consultants’ fees, facilities costs, accrued milestones, administrative expenses related to R&D activities and clinical trial costs incurred by clinical research organizations, or CROs, and research institutions under agreements that are generally cancelable, among other related R&D costs. We also record accruals for estimated ongoing clinical trial costs. Clinical trial costs represent costs incurred by CROs and clinical sites and include advertising for clinical trials and patient recruitment costs. These costs are recorded as a component of R&D expenses and are expensed as incurred. Under our agreements, progress payments are typically made to investigators, clinical sites and CROs. We analyze the progress of the clinical trials, including levels of patient enrollment, invoices received and contracted costs when evaluating the adequacy of accrued liabilities. Significant judgments and estimates must be made and used in determining the accrued balance in any accounting period. Actual results could differ from those estimates under different assumptions. Revisions are charged to expense in the period in which the facts that give rise to the revision become known.
In addition, we have obtained rights to patented intellectual properties under several licensing agreements for use in research and development activities. Non‑refundable licensing payments made for intellectual properties that have no alternative future use are expensed to research and development as incurred.
Share‑Based Payments
We follow the fair value method of accounting for share‑based compensation arrangements in accordance with the Financial Accounting Standards Board, or FASB, Accounting Standards Codification, or ASC, topic 718, Compensation—Stock Compensation, or ASC 718. Under ASC 718, the estimated fair value of share‑based compensation, including stock options and restricted stock units granted under our stock option plans and purchases of common stock by employees at a discount to market price under our Employee Stock Purchase Plan, or the ESPP, is recognized as compensation expense. Compensation expense for purchases under the ESPP is recognized based on the estimated fair value of the common stock purchase rights during each offering period and the percentage of the purchase discount.
We use the Black‑Scholes option pricing model to estimate the fair value of the share‑based awards as of the grant date. The Black‑Scholes model, by its design, is highly complex, and dependent upon key data inputs estimated by management. The primary data inputs with the greatest degree of judgment are the estimated lives of the share‑based awards and the estimated volatility of our stock price. The Black‑Scholes model is highly sensitive to changes in these
79
two data inputs. The expected term of the options represents the period of time that options granted are expected to be outstanding and is derived by analyzing the historical experience of similar awards, giving consideration to the contractual terms of the share‑based awards, vesting schedules and expectations of future employee behavior. We determine expected volatility using the historical method, which is based on the daily historical trading data of our common stock over the expected term of the option. Management selected the historical method primarily because we have not identified a more reliable or appropriate method to predict future volatility. For more information about our share‑based payments, see Note 15: “Stock Option and Purchase Plans” to our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K.
Share‑based compensation expense is allocated among cost of goods sold, research and development and selling, general and administrative expenses, or included in the inventory carrying value and absorbed into inventory, based on the function of the related employee.
Fair Value Measurements
The authoritative literature for fair value measurements established a three‑tier fair value hierarchy, which prioritizes the inputs in measuring fair value. These tiers are as follows: Level 1, defined as observable inputs such as quoted market prices in active markets; Level 2, defined as inputs other than the quoted prices in active markets that are either directly or indirectly observable; and Level 3, defined as significant unobservable inputs (entity developed assumptions) in which little or no market data exists.
Financial instruments include cash equivalents, available‑for‑sale securities, accounts receivable, accounts payable and accrued liabilities. Available‑for‑sale securities are carried at estimated fair value. The carrying value of cash equivalents, accounts payable and accrued liabilities approximate their estimated fair value due to the relatively short nature of these instruments. As of December 31, 2015, our cash, cash equivalents and available‑for‑sale securities measured at fair value on a recurring basis totaled $241.6 million.
All of our cash, cash equivalents and available‑for‑sale securities are in cash, money market instruments, U.S. Treasury securities and corporate debt securities at December 31, 2015. The valuation techniques used to measure the fair values of these financial instruments were derived from quoted market prices, as substantially all of these instruments have maturity dates, if any, within one year from the date of purchase and active markets for these instruments exist.
In May 2013, we closed on an offering totaling $250.0 million in Convertible Notes. The fair value of the liability component of the Convertible Notes, excluding the conversion feature, was derived using a binomial lattice model, or Level 3 inputs. To arrive at the appropriate risk adjusted rate, or market yield, for the Convertible Notes, we performed (i) a synthetic credit rating analysis estimating the issuer level credit rating of the Company using a regression model, (ii) research on appropriate market yields using option adjusted spread indications for similar credit ratings, and (iii) considered the market yield implied for the Convertible Notes from a binomial lattice model. Using these inputs, the initial fair value of the liability component of the Convertible Notes was estimated at $154.7 million. The Convertible Notes are described further below and in Note 13: “Long‑Term Debt” to our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K.
Debt instruments are initially recorded at fair value, with coupon interest and amortization of debt issuance discounts recognized in the statements of operations as interest expense at each period end while such instruments are outstanding. If we issue shares to discharge the liability, the debt obligation is derecognized and common stock and additional paid‑in capital are recognized on the issuance of those shares.
Our Convertible Notes contain a conversion option that is classified as equity. The fair value of the liability component of the debt instrument was deducted from the initial proceeds to determine the proceeds to be allocated to the conversion option. The excess of the proceeds received from the Convertible Notes over the initial amount allocated to the liability component, is allocated to the equity component. This excess is reported as a debt discount and subsequently amortized as non‑cash interest expense, using the interest method, over the expected life of the Convertible Notes.
80
Issuance costs related to the equity component of the Convertible Notes were charged to additional paid‑in capital. The remaining portion related to the debt component has been capitalized as a deferred charge and included in non‑current assets in the consolidated balance sheets, and is being amortized and recorded as additional interest expense over the expected life of the Convertible Notes. In connection with the issuance of the Convertible Notes, we entered into capped call transactions with certain counterparties affiliated with the underwriters. The fair value of the purchased capped calls was recorded to stockholders’ equity.
Concentration of Credit Risk
Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cash, cash equivalents, available‑for‑sale‑securities, and accounts receivable. We have established guidelines to limit our exposure to credit risk by placing investments with a number of high credit quality institutions, in U.S. Treasury securities, in corporate debt securities, diversifying our investment portfolio and placing investments with maturities that maintain safety and liquidity within our liquidity needs.
Accounts Receivable, Allowances for Doubtful Accounts and Cash Discounts
We extend credit to our customers for product sales resulting in accounts receivable. Customer accounts are monitored for past due amounts. Past due accounts receivable, determined to be uncollectible, are written off against the allowance for doubtful accounts. Allowances for doubtful accounts are estimated based upon past due amounts, historical losses and existing economic factors, and are adjusted periodically. Historically, we have not had any significant uncollected accounts. We offer cash discounts to our customers, generally 2% of the sales price, as an incentive for prompt payment. The estimate of cash discounts is recorded at the time of sale. We account for the cash discounts by reducing revenue and accounts receivable by the amount of the discounts we expect our customers to take. The accounts receivable are reported in the consolidated balance sheets, net of the allowances for doubtful accounts and cash discounts. There is no allowance for doubtful accounts at December 31, 2015 or 2014.
Inventory Impairment and Other Non‑Recurring Charges
Our inventory impairment and other non‑recurring charges consist of inventory impairment charges, proxy contest expenses and charges from cost reduction plans, including employee severance, one‑time termination benefits and ongoing benefits related to the reduction of our workforce, facilities and other exit costs. We periodically evaluate the carrying value of our inventory on hand for potential excess amount over demand using the lower of cost or market price. Any excess amount is written off. Liabilities for costs associated with a cost reduction activity are recognized when the liability is incurred, as opposed to when management commits to a cost reduction plan. In addition, liabilities associated with cost reduction activities are measured at fair value. One‑time termination benefits are expensed at the date we notify the employee, unless the employee must provide future service, in which case the benefits are expensed ratably over the future service period. Ongoing benefits are expensed when cost reduction activities are probable and the benefit amounts are estimable. Other costs primarily consist of legal, consulting, and other costs related to employee terminations and are expensed when incurred. Expenses related to termination benefits are calculated in accordance with the various agreements with certain of our employees.
Income Taxes
We make certain estimates and judgments in determining income tax expense for financial statement purposes. These estimates and judgments occur in the calculation of certain tax assets and liabilities, which arise from differences in the timing of recognition of revenue and expense for tax and financial statement purposes.
We are required to estimate our income taxes in each of the jurisdictions in which we operate. This process involves estimating our current tax exposure under the most recent tax laws and assessing temporary differences resulting from differing treatment of items for tax and accounting purposes. These differences result in deferred tax assets and liabilities, which are included in our consolidated balance sheets.
81
We assess the likelihood that we will be able to recover our deferred tax assets. We consider all available evidence, both positive and negative, including historical levels of income, expectations and risks associated with estimates of future taxable income and ongoing prudent and feasible tax planning strategies in assessing the need for a valuation allowance. If it is not more likely than not that we will recover our deferred tax assets, we will increase our provision for taxes by recording a valuation allowance against the deferred tax assets that we estimate will not ultimately be recoverable. As a result of our analysis of all available evidence, both positive and negative, as of December 31, 2015, it was considered more likely than not that our deferred tax assets would not be realized. However, should there be a change in our ability to recover our deferred tax assets, we would recognize a benefit to our tax provision in the period in which we determine that it is more likely than not that we will recover our deferred tax assets.
Contingencies and Litigation
We are periodically involved in disputes and litigation related to a variety of matters. When it is probable that we will experience a loss, and that loss is quantifiable, we record appropriate reserves. We record legal fees and costs as an expense when incurred.
RESULTS OF OPERATIONS
Revenues
|
Year Ended December 31, |
|||||||||
|
2015 |
2014 |
2013 |
|||||||
|
Net Qsymia product revenue |
$ |
54,622 |
$ |
45,277 |
$ |
23,718 | |||
|
License and milestone revenue |
11,574 | 38,614 | 55,838 | ||||||
|
Supply revenue |
26,674 | 26,519 | 1,526 | ||||||
|
Royalty revenue |
2,560 | 3,771 |
-- |
||||||
|
Basic and diluted net loss per share |
$ |
95,430 |
$ |
114,181 |
$ |
81,082 | |||
Net Qsymia product revenue
We recognize net product revenue for Qsymia based on prescription sell‑through by the certified retail pharmacies and home delivery pharmacy services networks to patients as we do not have sufficient historical information to reliably estimate returns. Currently, Qsymia is only approved for sale in the U.S.; therefore, all net product revenue for Qsymia to date has been earned in the U.S.
The following table reconciles gross Qsymia product revenue to net Qsymia product revenue (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Gross Qsymia product revenue |
|
$ |
83,338 |
|
$ |
69,870 |
|
$ |
37,897 |
|
|
Discount programs |
|
|
(18,441) |
|
|
(16,140) |
|
|
(8,801) |
|
|
Wholesaler/Pharmacy fees |
|
|
(5,913) |
|
|
(4,970) |
|
|
(4,348) |
|
|
Cash discounts |
|
|
(1,656) |
|
|
(1,373) |
|
|
(750) |
|
|
Rebates/Chargebacks |
|
|
(2,706) |
|
|
(2,110) |
|
|
(280) |
|
|
Net product revenue |
|
$ |
54,622 |
|
$ |
45,277 |
|
$ |
23,718 |
|
For the years ended December 31, 2015, 2014 and 2013, approximately 566,000, 534,000 and 373,000 Qsymia prescriptions were dispensed, respectively. Approximately 63% of our total prescriptions for the year ended December 31, 2015 included either a free good or discount offer, with approximately 99,000 of those prescriptions dispensed as free goods. In comparison, for the year ended December 31, 2014, approximately 60% of our total prescriptions included either a free good or discount offer, with approximately 109,000 of those prescriptions dispensed
82
as free goods, and for the year ended December 31, 2013, approximately 102,000, or 52%, of our total prescriptions were dispensed as free goods.
At December 31, 2015, we had Qsymia deferred gross revenue of $19.3 million, which represents Qsymia product shipped to wholesalers and certified retail pharmacies, but not yet dispensed to patients through prescriptions, net of prompt‑payment discounts. We expect Qsymia net product revenue in 2016 to decrease from 2015 levels due to market conditions.
License and milestone revenue
During 2013, we entered into license and commercialization agreements and commercial supply agreements with the Menarini Group, through its subsidiary Berlin‑Chemie AG, or Menarini, Auxilium Pharmaceuticals, Inc., or Auxilium, and Sanofi and its affiliate, or Sanofi, to commercialize and promote STENDRA or SPEDRA in their respective territories. Menarini’s territory consists of over 40 countries, including the EU, as well as Australia and New Zealand. Auxilium’s territory consists of the United States and Canada and their respective territories. In December 2015, Auxilium notified us of its intention to return the U.S. and Canadian commercial rights for STENDRA to us. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016. Sanofi’s territory consists of Africa, the Middle East, Turkey and Eurasia.
For the year ended December 31, 2015, we recognized $11.6 million in license and milestone revenue primarily attributable to milestone payments related to the approval of the Time‑to‑Onset Claim in the EU. For the year ended December 31, 2014, we recognized $38.6 million in license and milestone revenue primarily attributable to milestone payments related to product launches in certain EU countries, the approval of the Time-to-Onset Claim in the U.S. and the delivery of the license rights and know-how under our agreement with Sanofi. For the year ended December 31, 2013, we recognized $55.8 million in license and milestone revenue, primarily due to the delivery of license rights and related know‑how under the license agreements with Auxilium and Menarini, and the achievement of a regulatory milestone in Europe. License and milestone revenue is dependent upon the timing of the achievement of certain milestones and the timing of entering into collaborative agreements. As a result, our license and milestone revenue could fluctuate materially between periods.
For further discussion on the revenue from our above‑mentioned license and commercialization agreements, refer to Note 12: “License, Commercialization and Supply Agreements” to our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K.
For geographic information with respect to license and milestone revenue, see Note 18: “Segment Information and Concentration of Customers and Suppliers—Geographic Information” to our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K.
Net STENDRA/SPEDRA supply revenue
We began distributing STENDRA or SPEDRA tablets to our commercialization partners in December 2013. Auxilium launched the commercialization of STENDRA in the U.S. and Canada in December 2013. Menarini launched the commercialization of SPEDRA in the EU‑5 (France, Germany, Italy, Spain and the United Kingdom) in the first half of 2014, and the product is available in retail in 25 countries in the Menarini territory. In addition, we began selling avanafil API to Sanofi in December 2013, to support their technology transfer to qualify as a second supplier for avanafil API and tablets.
We recognize supply revenue upon shipment to our commercialization partners. As a result, supply revenue may or may not represent our commercialization partners’ sales to end users. The timing of purchases by our commercialization partners will be affected by, among other items, their minimum purchase commitments, end user demand, and distributor inventory levels. As a result, supply revenue may fluctuate materially between reporting periods. In 2016, we anticipate that our supply revenue will be affected by our decision to commercialize STENDRA in the U.S. and Canada ourselves or to license the U.S. and Canadian rights to a third party, end user demand for
83
STENDRA/SPEDRA, the timing of entering into additional commercialization partnerships in territories not currently licensed, and the timing of our partners receiving approvals to commercialize STENDRA/SPEDRA in additional countries.
For geographic information with respect to STENDRA/SPEDRA supply revenue, see Note 18: “Segment Information and Concentration of Customers and Suppliers—Geographic Information” to our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K.
Royalty revenue
Royalty revenue for the years ended December 31, 2015 and 2014 was primarily attributable to commercialization agreements with Menarini and Auxilium that we entered into during the second half of 2013, for which we earn royalties based upon a certain percentage of net sales reported by commercialization partners. In April 2015, we were informed by Endo upon their purchase of Auxilium that Endo had revised its accounting estimate for return reserve for STENDRA sold in 2014. Under the terms of the license and commercialization agreement, adjustments to the return reserve can be deducted from the reported net revenue. As a result, in 2015, we recorded an adjustment of $1.2 million to reduce our royalty revenue. We did not record royalty revenue in 2013 as there were no net sales reported by our commercialization partners. In 2016, we anticipate that our royalty revenue levels will be significantly impacted by our decision to commercialize STENDRA in the U.S. and Canada ourselves or to license the U.S. and Canadian rights to a third party and, if we license the U.S. and Canadian rights to a third party, the timing of entering into such an agreement.
Cost of goods sold
|
Year Ended December 31, |
|||||||||
|
2015 |
2014 |
2013 |
|||||||
|
Qsymia cost of goods sold |
$ |
8,720 |
$ |
7,155 |
$ |
2,755 | |||
|
STENDRA/SPEDRA cost of goods sold |
25,437 | 26,232 | 2,113 | ||||||
|
Cost of goods sold |
$ |
34,157 |
$ |
33,387 |
$ |
4,868 | |||
Cost of goods sold for Qsymia dispensed to patients includes the inventory costs of APIs, third‑party contract manufacturing and packaging and distribution costs, royalties, cargo insurance, freight, shipping, handling and storage costs, and overhead costs of the employees involved with production. Cost of goods sold for STENDRA or SPEDRA shipped to our commercialization partners includes the inventory costs of purchased tablets, freight, shipping and handling costs. The cost of goods sold associated with deferred revenue on Qsymia and STENDRA or SPEDRA product shipments is recorded as deferred costs, which are included in inventories in the consolidated balance sheets, until such time as the deferred revenue is recognized.
Selling, general and administrative
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
% Change |
|
||
|
|
|
Years Ended December 31, |
|
Increase/(Decrease) |
|
|||||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
2015 vs 2014 |
|
2014 vs 2013 |
|
|||
|
|
|
(In thousands, except percentages) |
|
|||||||||||
|
Selling and marketing |
|
$ |
52,988 |
|
$ |
72,330 |
|
$ |
94,841 |
|
(27) |
% |
(24) |
% |
|
General and administrative |
|
|
26,399 |
|
|
39,209 |
|
|
63,394 |
|
(33) |
% |
(38) |
% |
|
Total selling, general and administrative expenses |
|
$ |
79,387 |
|
$ |
111,539 |
|
$ |
158,235 |
|
(29) |
% |
(30) |
% |
The decrease in selling and marketing expenses in 2015 as compared to 2014 was primarily due to lower promotional activities for Qsymia, driven by a lower workforce and more targeted spending. The decrease in 2014 as compared to 2013 was primarily due to lower selling and marketing activities for Qsymia, as a result of our more targeted and focused spending on marketing and promotional activities in 2014.
84
The decrease in general and administrative expenses in 2015 as compared to 2014 was primarily due to our cost control initiatives, including a reduction in headcount and other employee costs. The decrease in 2014 as compared to 2013 was primarily due to factors attributable to our cost control initiatives, including reduction in headcount and other employee costs, including share‑based compensation expense, and lower spending on professional fees and other corporate activities.
We expect both selling and marketing expenses and general and administrative expenses to decrease in 2016 from 2015 as a result of the cost reduction efforts implemented in 2015. However, if we commercialize STENDRA in the U.S. and Canada in 2016, our selling and marketing expenses and general and administrative expenses could increase over 2015 levels.
Research and development
|
|
|
|
|
|
|
|
|
|
|
|
% Change |
|
|
||
|
|
|
Years Ended December 31, |
|
Increase/(Decrease) |
|
|
|||||||||
|
Drug Indication/Description |
|
2015 |
|
2014 |
|
2013 |
|
2015 vs 2014 |
|
2014 vs 2013 |
|
|
|||
|
|
|
(In thousands, except percentages) |
|
|
|||||||||||
|
Qsymia for obesity |
|
$ |
3,328 |
|
$ |
4,457 |
|
$ |
10,520 |
|
(25) |
% |
(58) |
% |
|
|
STENDRA for ED |
|
|
840 |
|
|
2,356 |
|
|
8,391 |
|
(64) |
% |
(72) |
% |
|
|
Other projects |
|
|
— |
|
|
30 |
|
|
314 |
|
(100) |
% |
(90) |
% |
|
|
Share-based compensation |
|
|
398 |
|
|
1,177 |
|
|
2,361 |
|
(66) |
% |
(50) |
% |
|
|
Overhead costs* |
|
|
5,536 |
|
|
5,773 |
|
|
8,091 |
|
(4) |
% |
(29) |
% |
|
|
Total research and development expenses |
|
$ |
10,102 |
|
$ |
13,793 |
|
$ |
29,677 |
|
(27) |
% |
(54) |
% |
|
*Overhead costs include compensation and related expenses, consulting, legal and other professional services fees relating to research and development activities, which we do not allocate to specific projects.
The decrease in total research and development expenses in 2015 as compared to 2014 was due primarily to the timing of clinical activity, the impact of our cost reduction efforts implemented during 2015 and lower share-based compensation expense, as a result of our lower share price and decrease in headcount. The decrease in total research and development expenses in 2014, as compared to 2013, was due primarily to the completion of various product studies, including the STENDRA 15‑minute and spermatogenesis studies. Other factors that favorably impacted research and development expenses include (i) a decrease due to the timing of Qsymia study activities, known as the AQCLAIM study, and (ii) decreases in employee costs (including share‑based compensation expense), external staffing and consulting fees, other project costs and overhead costs, most of which were attributable to a cost reduction plan.
We anticipate that there will be additional research and development expenses for post‑approval studies related to Qsymia, specifically a retrospective cohort study and an adolescent pharmacokinetics study. We expect that our research and development expenses will fluctuate from period to period due to the timing and scope of our development activities and the results of clinical and pre‑clinical studies.
85
Inventory impairment and other non‑recurring charges
Inventory impairment and other non‑recurring charges consist of (in thousands):
|
|
|
Years Ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Inventory impairment |
|
$ |
29,522 |
|
$ |
2,170 |
|
$ |
10,225 |
|
|
Employee severance and related costs |
|
|
2,503 |
|
|
1,711 |
|
|
8,546 |
|
|
Patent settlement |
|
|
— |
|
|
1,949 |
|
|
— |
|
|
Share-based compensation |
|
|
36 |
|
|
343 |
|
|
14,072 |
|
|
Proxy contest expenses |
|
|
— |
|
|
— |
|
|
8,863 |
|
|
Operating lease termination costs |
|
|
— |
|
|
— |
|
|
1,210 |
|
|
Total inventory impairment and other non-recurring expense |
|
$ |
32,061 |
|
$ |
6,173 |
|
$ |
42,916 |
|
Inventories are stated at the lower of cost or market. Cost is determined using the first in, first out method for all inventories, which are valued using a weighted average cost method calculated for each production batch. We periodically evaluate the carrying value of inventory on hand for potential excess amount over demand using the same lower of cost or market approach as that used to value the inventory. In 2015, we recorded inventory impairment charges primarily for Qsymia API inventory in excess of expected demand. In 2014, we recorded inventory impairment charges for finished goods and certain non-API raw materials on hand in excess of demand and, in 2013, we recorded inventory impairment charges for inventories on hand in excess of demand, plus a purchase commitment fee.
In 2015, we recorded employee severance and related costs and share-based compensation related to the July 2015 corporate restructuring plan, which reduced our workforce by approximately 60 job positions. In 2014 and 2013, we recorded employee severance and related costs, share-based compensation and operating lease termination costs related to the 2013 cost reduction plan that reduced our workforce by approximately 20 employees.
In 2014, we paid $5.0 million in connection with the transfer and assignment of certain patents from Janssen Pharmaceuticals, Inc. Of the $5.0 million, approximately $1.9 million was recognized as a non-recurring expense for the year ended December 31, 2014 as it related to a legal settlement. The remaining balance of approximately $3.1 million was recorded as an intangible asset and is being amortized as cost of goods sold through their expiration dates.
In 2013, we entered into a settlement agreement with First Manhattan in connection with a proxy contest related to our 2013 Annual Meeting of Stockholders. According to the terms of the settlement agreement, more than a majority of the members of our Board of Directors resigned and new members were appointed. The change in the majority of the members of our Board of Directors, effective July 19, 2013, triggered certain “change of control” benefits in accordance with the terms of various agreements with certain of our employees. Under these agreements, all unvested stock options held by these employees automatically vested in full and became immediately exercisable. In addition, the resignations of both our Chief Executive Officer and President resulted in severance charges under these agreements. As part of the settlement agreement with First Manhattan, we paid the reasonable and documented expenses incurred by First Manhattan in connection with its proxy contest.
Interest and other expense (income)
Interest and other expense (income) consists primarily of interest expense and the amortization of issuance costs from our Convertible Notes and Senior Secured Notes and the amortization of the debt discount on the Convertible Notes. Interest expense (income) was $33.3 million, $32.5 million and $19.5 million for the years ended December 31, 2015, 2014 and 2013, respectively. The increase in interest expense (income) for the year ended December 31, 2014, compared with the same period in 2013, was primarily due to the timing of the issuance of our Convertible Senior Notes of $250.0 million, which closed in May 2013, and the issuance of our Senior Secured Notes of $50.0 million, which closed in April 2013, which consequently impacted 2014 for a full year but for only a partial year in 2013. Other expense
86
and income were not significant. We expect interest and other expense (income) in 2016 to remain relatively consistent with 2015 levels.
Provision for (Benefit from) income taxes
We recorded a net provision for income taxes of $3,000 for the year ended December 31, 2015, as compared to a net benefit from income taxes for the year ended December 31, 2014 of $629,000 and a provision for income taxes of $97,000 for the year ended December 31, 2013. The tax provision in 2015 is the result of certain state tax liabilities. The reduction in tax expense in 2014 as compared to 2013 primarily relates to favorable settlements with state tax authorities, as discussed below, partially offset by tax liabilities in some states.
The tax provision for the year ended December 31, 2015 primarily relates to tax liabilities in certain states. The tax benefit for the year ended December 31, 2014 primarily relates to tax liabilities in certain states, offset by a tax refund received from the State of New Jersey as a result of a settlement of an audit and acceptance of a refund claim for the tax year ended December 31, 2007 amounting to $462,000 (including interest) and a reduction of the Company’s unrecognized tax benefits as a result of the California Franchise Tax Board audit that was favorably settled amounting to approximately $208,000. The tax provision for the year ended December 31, 2013 relates to state tax liabilities.
Discontinued operations
On November 5, 2010, we completed the sale of the MUSE product to Meda AB. For the year ended December 31, 2013, we recorded some minor adjustments related to the MUSE disposition, primarily adjustments to our sales reserves for accrued product returns.
LIQUIDITY AND CAPITAL RESOURCES
Continuing Operations
Cash. Cash, cash equivalents and available‑for‑sale securities totaled $241.6 million at December 31, 2015, as compared to $299.6 million at December 31, 2014. The decrease is primarily due to cash used in the funding of our operations. In 2015, we received payments for license and milestone revenue of $11.6 million. In 2014, we received payments for license and milestone revenue of $35.3 million. In April 2013, we received a net amount of $48.4 million through the sale of a debt‑like instrument, or the Senior Secured Notes, to BioPharma Secured Investments III Holdings Cayman LP, or BioPharma. On May 21, 2013, we closed an offering of $220.0 million in 4.5% Convertible Senior Notes due May 1, 2020, or the Convertible Notes. On May 29, 2013, we closed on an additional $30.0 million of Convertible Notes upon the exercise of an option by the initial purchasers of the Convertible Notes. Total net proceeds from the Convertible Notes were approximately $241.8 million. In addition, in 2013, we received upfront payments totaling $26.6 million, net of withholding taxes, under the license agreement with Menarini, $30.0 million under the license agreement with Auxilium and $5.0 million under the license agreement with Sanofi.
Since inception, we have financed operations primarily from the issuance of equity, debt and debt‑like securities. Through December 31, 2015, we have raised approximately $931.1 million from financing activities, received $150 million from the sale of Evamist, received a total of $118.0 million in license and milestone payments related to the STENDRA or SPEDRA license and commercialization agreements, and had an accumulated deficit of $836.4 million at December 31, 2015.
At December 31, 2015, we had $95.4 million in cash and cash equivalents and $146.2 million in available‑for‑sale securities. We invest our excess cash balances in money market, U.S. government securities and corporate debt securities in accordance with our investment policy. Our investment policy has the primary investment objectives of preservation of principal; however, there may be times when certain of the securities in our portfolio will fall below the credit ratings required in the policy. If those securities are downgraded or impaired, we would experience realized or unrealized losses in the value of our portfolio, which would have an adverse effect on our results of operations, liquidity and financial condition.
87
Investment securities are exposed to various risks, such as interest rate, market and credit. Due to the level of risk associated with certain investment securities and the level of uncertainty related to changes in the value of investment securities, it is possible that changes in these risk factors in the near term could have an adverse material impact on our results of operations or stockholders’ equity.
Accounts Receivable. We extend credit to our customers for product sales resulting in accounts receivable. Customer accounts are monitored for past due amounts. Past due accounts receivable, determined to be uncollectible, are written off against the allowance for doubtful accounts. Allowances for doubtful accounts are estimated based upon past due amounts, historical losses and existing economic factors, and are adjusted periodically. Historically, we have had no significant uncollectable accounts receivable. We offer cash discounts to our customers, generally 2% of the sales price as an incentive for prompt payment.
Accounts receivable (net of allowance for cash discounts) at December 31, 2015, was $9.0 million, as compared to $11.6 million at December 31, 2014. Currently, we do not have any significant concerns related to accounts receivable or collections. As of February 29, 2016, we had collected 95% of the accounts receivable outstanding at December 31, 2015.
Liabilities. Total liabilities were $287.7 million at December 31, 2015, compared to $284.4 million at December 31, 2014. The increase in total liabilities was primarily due to timing differences in our various liability accounts.
Summary Cash Flows
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Years Ended December 31, |
|
|||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
|
|
(in thousands) |
|
|||||||
|
Cash provided by (used for): |
|
|
|
|
|
|
|
|
|
|
|
Operating activities |
|
$ |
(46,332) |
|
$ |
(38,105) |
|
$ |
(135,325) |
|
|
Investing activities |
|
|
67,404 |
|
|
15,893 |
|
|
(90,121) |
|
|
Financing activities |
|
|
(8,851) |
|
|
2,124 |
|
|
270,103 |
|
Operating Activities.
The increase in cash used from operating activities in 2015 as compared to 2014 was primarily due to the reduction in total revenue, due to a reduction in license and milestone receipts, and spending on inventory for contractually-mandated purchases, partially offset by lower operating expenses, primarily attributable to our cost reduction plan in 2015. The decrease in cash used from operating activities in 2014, compared to 2013, was primarily due to higher net product revenue from sales of Qsymia, royalty and supply revenue from sales of STENDRA, partially offset by lower license and milestone revenue from the license and commercialization agreements for STENDRA or SPEDRA, and lower operating expenses, primarily attributable to a cost reduction plan initiated in the fourth quarter of 2013, conclusion of various clinical studies, and more targeted and focused spending on marketing and promotional activities. These factors were partially offset by changes in assets and liabilities for the year ended December 31, 2014, compared with the same period in 2013.
During the year ended December 31, 2015, our loss from continuing operations of $93.1 million was offset by non-cash charges of $29.5 million due to an inventory impairment charge, $17.2 million in amortization of debt issuance costs and discounts and $3.6 million in share-based compensation expense. Additional cash used in operating activities was due to increases in inventory and decreases in accounts payable due to timing of payments made, partially offset by decreases in accounts receivable and prepaid expenses.
During the year ended December 31, 2014, our loss from continuing operations of $82.6 million was offset by $15.9 million in amortization of debt issuance costs and discounts, $9.8 million in non‑cash share‑based compensation expense and $2.2 million due to an inventory impairment charge for Qsymia. Additional cash used in operating activities
88
was due to decreases in deferred revenue due to recognition of revenue for Qsymia and STENDRA, partially offset by decreases in inventories due to increased shipments of Qsymia and STENDRA and prepaid expenses and other assets due mainly to a withholding tax receivable in the prior year which was collected in 2014.
During the year ended December 31, 2013, our loss from continuing operations of $174.9 million was offset by $32.4 million in non‑cash share‑based compensation expense due to increased headcount and the automatic acceleration of vesting of unvested stock options held by certain employees as a result of the settlement agreement we entered into with First Manhattan Company and the termination benefits plan, $8.4 million in amortization of debt issuance costs and discounts, and $7.5 million due to an inventory impairment charge for Qsymia. Additional cash used in operating activities resulted from changes in assets and liabilities during the period, including a net $30.2 million increase in inventories, primarily for Qsymia and STENDRA, an increase of $26.5 million in deferred revenue mainly due to the license and commercialization agreements with Menarini and Sanofi for SPEDRA, as well as Qsymia deferred product revenue, and a decrease in accounts payable of $14.8 million during the year ended December 31, 2013, due to the timing of activities and vendor payments.
Investing Activities. Cash used or provided by investing activities primarily relates to the purchases and maturities of investment securities. The fluctuations from period to period are due primarily to the timing of purchases, sales and maturities of these investment securities.
Financing Activities. Cash used in financing activities for the year ended December 31, 2015 consist primarily of our repayments of $9.0 million under our Senior Secured Notes. Cash provided by financing activities for the year ended December 31, 2014 consisted of cash received for the exercise of stock options and purchases of stock under the employee stock purchase plan. For the year ended December 31, 2013, net cash provided by financing activities included $290.2 million in net proceeds from debt issuances, partially offset by $34.7 million in payments for capped call transactions.
On May 21, 2013, we closed an offering of $220.0 million in 4.5% Convertible Senior Notes due May 1, 2020. On May 29, 2013, we closed an additional $30.0 million of Convertible Notes upon the exercise of an option by the initial purchasers of the Convertible Notes. Total net proceeds from the Convertible Notes were approximately $241.8 million. For a further discussion of the Convertible Notes, see “Contractual Obligations—Notes Payable and Interest Payable” below.
On March 25, 2013, we entered into the Purchase and Sale Agreement with BioPharma providing for the purchase of a debt‑like instrument, or the Senior Secured Notes. Under the BioPharma agreement, we received a net amount of approximately $48.4 million, at the closing on April 9, 2013. For a further discussion of the Senior Secured Notes, see “Contractual Obligations—Notes Payable and Interest Payable” below.
The funding necessary to execute our business strategies is subject to numerous uncertainties, which may adversely affect our liquidity and capital resources. Commercialization of Qsymia may be more costly than we planned. In addition, completion of clinical trials and approval by the FDA of investigational drug candidates may take several years or more, but the length of time generally varies substantially according to the type, complexity, novelty and intended use of an investigational drug candidate. It is also important to note that if an investigational drug candidate is identified, the further development of that candidate can be halted or abandoned at any time due to a number of factors. These factors include, but are not limited to, funding constraints, lack of efficacy or safety or change in market demand.
We anticipate that our existing capital resources combined with anticipated future cash flows will be sufficient to support our operating needs at least for the next twelve months. However, we anticipate that we may require additional funding to expand the use of Qsymia through targeted patient and physician education, find the right partner for expanded Qsymia commercial promotion to a broader primary care physician audience, create a pathway for centralized approval of the marketing authorization application for Qsiva in the EU, continue the expansion of our distribution of Qsymia through certified retail pharmacy locations, conduct post‑approval clinical studies for Qsymia, conduct non‑clinical and clinical research and development work to support regulatory submissions and applications for our future investigational drug candidates, finance the costs involved in filing and prosecuting patent applications and enforcing or defending our patent claims, if any, to fund operating expenses, establish additional or new manufacturing
89
and marketing capabilities, and manufacture quantities of our drugs and investigational drug candidates and to make payments under our existing license and supply agreements for STENDRA.
If we require additional capital, we may seek any required additional funding through collaborations, public and private equity or debt financings, capital lease transactions or other available financing sources. Additional financing may not be available on acceptable terms, or at all. If additional funds are raised by issuing equity securities, substantial dilution to existing stockholders may result. If adequate funds are not available, we may be required to delay, reduce the scope of or eliminate one or more of our commercialization or development programs or obtain funds through collaborations with others that are on unfavorable terms or that may require us to relinquish rights to certain of our technologies, product candidates or products that we would otherwise seek to develop on our own.
Contractual Obligations
The following table summarizes our contractual obligations at December 31, 2015, excluding amounts already recorded on our consolidated balance sheet as accounts payable or accrued liabilities, and the effect such obligations are expected to have on our liquidity and cash flow in future fiscal years. This table includes our enforceable, non‑cancelable, and legally binding obligations and future commitments as of December 31, 2015. The amounts below do not include contingent milestone payments or royalties, and assume the agreements and commitments will run through the end of terms, as such no early termination fees or penalties are included herein:
|
|
|
Payments Due by Period |
|
|||||||||||||
|
Contractual obligations |
|
Total |
|
2016 |
|
2017 - 2019 |
|
2020 - 2021 |
|
Thereafter |
|
|||||
|
|
|
(in thousands) |
|
|||||||||||||
|
Operating leases |
|
$ |
8,869 |
|
$ |
2,164 |
|
$ |
6,020 |
|
$ |
685 |
|
$ |
— |
|
|
Purchase obligations |
|
|
34,358 |
|
|
11,579 |
|
|
22,779 |
|
|
— |
|
|
— |
|
|
Notes payable |
|
|
291,002 |
|
|
15,550 |
|
|
275,452 |
|
|
— |
|
|
— |
|
|
Interest payable |
|
|
41,601 |
|
|
15,700 |
|
|
25,901 |
|
|
— |
|
|
— |
|
|
Total contractual obligations |
|
$ |
375,830 |
|
$ |
44,993 |
|
$ |
330,152 |
|
$ |
685 |
|
$ |
— |
|
Operating Leases
We have a lease on 4,914 square feet of office space located at 1174 Castro Street, Mountain View, California, or the Castro Facility. The average base rent for the Castro Facility is approximately $2.87 per square foot or $14,124 per month. The lease for the Castro Facility has a term of 60 months commencing March 15, 2012, with an option to extend the term for one year from the expiration of the new lease. Commencing on September 1, 2014, we subleased the Castro Facility for a term of 31 months at a starting monthly rental rate of $4.42 per square feet (subject to agreed increases). The sublessee is entitled to abatement of the first monthly installment.
We entered into a lease effective as of December 11, 2012, for new principal executive offices, consisting of an approximately 45,240 square foot building, located at 351 East Evelyn Avenue, Mountain View, California, or the Evelyn Lease. The Evelyn Lease has an initial term of approximately 84 months, commencing on May 11, 2013, at a starting annual rental rate of $31.20 per rentable square foot (subject to agreed increases). We received an abatement of the monthly installments of rent for months seven through 12 of the initial term subject to the conditions detailed in the Evelyn Lease. We have one option to renew the Evelyn Lease for a term of three years at the prevailing market rate as detailed in the Evelyn Lease. In addition, we have a one‑time right to accelerate the termination date of the Evelyn Lease from the expiration of the 84th full calendar month of the term to the expiration of the 60th full calendar month of the term, subject to the conditions detailed in the Evelyn Lease. If this acceleration of the termination date is exercised, the following will be payable to the landlord: (i) six months of the monthly installments of rent and our proportionate share of expenses and taxes subject to the fifth lease year; and (ii) the unamortized portion of all of the leasing commissions and legal fees, the initial alterations, and the landlord’s allowance towards the cost of performing the initial alterations. Commencing on May 1, 2014, we subleased a portion of our Evelyn Lease consisting of approximately 14,105 square feet of space for a term of 36 months at a starting annual rental rate of $42 per square feet (subject to agreed increases). The sublessee received an abatement of monthly installments of rents for months one through four. Upon the completion
90
of the sublease for this space, the Company expects to either find usage or to locate a suitable sublessee for the duration of the Company’s Evelyn Lease.
For additional information regarding obligations under operating leases, see Note 16: “Commitments” to our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K.
Purchase Obligations
Purchase obligations consist of agreements to purchase goods or services that are enforceable and legally binding on us and that specify all significant terms, including fixed or minimum quantities to be purchased; fixed, minimum or variable price provisions; and the approximate timing of the transaction.
The API and the tablets for STENDRA/SPEDRA (avanafil) are currently manufactured by Sanofi. We have minimum purchase commitments with Sanofi to purchase API materials and tablets through 2018. Our minimum purchase commitments with Sanofi totaled approximately $34.2 million as of December 31, 2015. We have no purchase commitments for raw material supplies for Qsymia at December 31, 2015, but have open purchase orders totaling $190,000.
Notes Payable and Interest Payable
Convertible Senior Notes Due 2020
On May 21, 2013, we closed an offering of $220.0 million in 4.5% Convertible Senior Notes due May 1, 2020, or the Convertible Notes. The Convertible Notes are governed by an indenture, dated as of May 21, 2013, between the Company and Deutsche Bank National Trust Company, as trustee. On May 29, 2013, we closed on an additional $30.0 million of Convertible Notes upon exercise of an option by the initial purchasers of the Convertible Notes. Total net proceeds from the Convertible Notes were approximately $241.8 million. The Convertible Notes are convertible at the option of the holders at any time prior to the close of business on the business day immediately preceding November 1, 2019, only under certain conditions. On or after November 1, 2019, holders may convert all or any portion of their Convertible Notes at any time at their option at the conversion rate then in effect, regardless of these conditions. Subject to certain limitations, we will settle conversions of the Convertible Notes by paying or delivering, as the case may be, cash, shares of our common stock or a combination of cash and shares of our common stock, at our election. The current conversion rate of the Convertible Notes is $14.86 per share. For the year ended December 31, 2015, total interest expense related to the Convertible Notes was $27.2 million, including amortization of $16.0 million of the debt discount and $848,000 of deferred financing costs. For the year ended December 31, 2014, total interest expense related to the Convertible Notes was $25.0 million, including amortization of $14.7 million of the debt discount and $784,000 of deferred financing costs.
Senior Secured Notes Due 2018
On March 25, 2013, we entered into a Purchase and Sale Agreement with BioPharma providing for the purchase of a debt‑like instrument, or the Senior Secured Notes. Under the agreement, we received $50 million, less $500,000 in funding and facility payments, at the initial closing on April 9, 2013. We had the option, but elected not to exercise it, to receive an additional $60 million, less $600,000 in a funding payment, at a secondary closing no later than January 15, 2014. The scheduled quarterly payments on the Senior Secured Notes are subject to the net sales of (i) Qsymia and (ii) any other obesity agent developed or marketed by us or our affiliates or licensees. The scheduled quarterly payments, other than the payment(s) scheduled to be made in the second quarter of 2018, are capped at the lower of the scheduled payment amounts or 25% of the net sales of (i) and (ii) above. Accordingly, if 25% of the net sales is less than the scheduled quarterly payment, then 25% of the net sales is due for that quarter, with the exception of the payment(s) scheduled to be made in the second quarter of 2018, when any unpaid scheduled quarterly payments plus any accrued and unpaid make whole premiums must be paid. Any quarterly payment less than the scheduled quarterly payment amount will be subject to a make whole premium equal to the applicable scheduled quarterly payment of the preceding quarter less the actual payment made to BioPharma for the preceding quarter multiplied by 1.03. We may elect to pay full scheduled quarterly payments if we choose. For the year ended December 31, 2015, the interest expense
91
related to the Senior Secured Notes was $6.3 million, including amortization of deferred financing costs amounting to $393,000. For the year ended December 31, 2014, the interest expense related to the Senior Secured Notes was $7.5 million, including amortization of deferred financing costs amounting to $468,000.
Additional Contingent Payments
We have entered into development, license and supply agreements that contain provisions for payments upon completion of certain development, regulatory and sales milestones. Due to the uncertainty concerning when and if these milestones may be completed or other payments are due, we have not included these potential future obligations in the above table.
Mitsubishi Tanabe Pharma Corporation
In January 2001, we entered into an exclusive development, license and clinical trial and commercial supply agreement with Tanabe Seiyaku Co., Ltd., now Mitsubishi Tanabe Pharma Corporation, or MTPC, for the development and commercialization of avanafil, a PDE5 inhibitor compound for the oral and local treatment of male and female sexual dysfunction. Under the terms of the agreement, MTPC agreed to grant an exclusive license to us for products containing avanafil outside of Japan, North Korea, South Korea, China, Taiwan, Singapore, Indonesia, Malaysia, Thailand, Vietnam and the Philippines. We agreed to grant MTPC an exclusive, royalty‑free license within those countries for oral products that we develop containing avanafil. In addition, we agreed to grant MTPC an exclusive option to obtain an exclusive, royalty‑bearing license within those countries for non‑oral products that we develop containing avanafil. MTPC agreed to manufacture and supply us with avanafil for use in clinical trials, which were our primary responsibility. The MTPC agreement contains a number of milestone payments to be made by us based on various triggering events.
We have made and expect to make substantial milestone payments to MTPC in accordance with this agreement as we continue to develop avanafil in our territories outside of the United States and, if approved for sale, commercialize avanafil for the oral treatment of male sexual dysfunction in those territories. Potential future milestone payments include $6.0 million upon achievement of $250.0 million or more in worldwide net sales during any calendar year.
The term of the MTPC agreement is based on a country‑by‑country and on a product‑by‑product basis. The term shall continue until the later of (i) 10 years after the date of the first sale for a particular product or (ii) the expiration of the last‑to‑expire patents within the MTPC patents covering such product in such country. In the event that our product is deemed to be (i) insufficiently effective or insufficiently safe relative to other PDE5 inhibitor compounds based on published information or (ii) not economically feasible to develop due to unforeseen regulatory hurdles or costs as measured by standards common in the pharmaceutical industry for this type of product, we have the right to terminate the agreement with MTPC with respect to such product.
In August 2012, we entered into an amendment to our agreement with MTPC that permits us to manufacture the API and tablets for STENDRA ourselves or through third parties. As mentioned above, on July 31, 2013, we entered into a Commercial Supply Agreement with Sanofi Chimie to manufacture and supply the API for avanafil on an exclusive basis in the United States and other territories and on a semi‑exclusive basis in Europe, including the EU, Latin America and other territories. Further, as mentioned above, on November 18, 2013, we entered into a Manufacturing and Supply Agreement with Sanofi Winthrop Industrie to manufacture and supply the avanafil tablets on an exclusive basis in the United States and other territories and on a semi‑exclusive basis in Europe, including the EU, Latin America and other territories. Sanofi began producing API and tablets in 2015.
On February 21, 2013, we entered into the third amendment to our agreement with MTPC which, among other things, expands our rights, or those of our sublicensees, to enforce the patents licensed under the MTPC agreement against alleged infringement, and clarifies the rights and duties of the parties and our sublicensees upon termination of the MTPC agreement. In addition, we were obligated to use our best commercial efforts to market STENDRA in the U.S. by December 31, 2013, which was achieved by our commercialization partner, Auxilium.
92
On July 23, 2013, we entered into the fourth amendment to our agreement with MTPC which, among other things, changes the definition of net sales used to calculate royalties owed by us to MTPC.
Other
In October 2001, we entered into an assignment agreement, or the Assignment Agreement, with Thomas Najarian, M.D., for a combination of pharmaceutical agents for the treatment of obesity and other disorders, or the Combination Therapy, that has since been the focus of our investigational drug candidate development program for Qsymia for the treatment of obesity, obstructive sleep apnea and diabetes. The Combination Therapy and all related patent applications, or the Patents, were transferred to us with worldwide rights to develop and commercialize the Combination Therapy and exploit the Patents. The Assignment Agreement requires us to pay royalties on worldwide net sales of a product for the treatment of obesity that is based upon the Combination Therapy and Patents until the last‑to‑expire of the assigned Patents. To the extent that we decide not to commercially exploit the Patents, the Assignment Agreement will terminate and the Combination Therapy and Patents will be assigned back to Dr. Najarian.
Off‑Balance Sheet Arrangements
We have not entered into any off‑balance sheet financing arrangements and have not established any special purpose entities. We have not guaranteed any debt or commitments of other entities or entered into any options on non‑financial assets.
Indemnifications
In the normal course of business, we provide indemnifications of varying scope to certain customers against claims of intellectual property infringement made by third parties arising from the use of its products and to its clinical research organizations and investigator sites against liabilities incurred in connection with any third‑party claim arising from the work performed on behalf of the Company, among others. Historically, costs related to these indemnification provisions have not been significant and we are unable to estimate the maximum potential impact of these indemnification provisions on our future results of operations.
On May 15, 2007, we closed a transaction with K‑V Pharmaceutical Company, or K‑V, for the sale of its investigational drug candidate, Evamist. At the time of the sale, Evamist was an investigational drug candidate and was not yet approved by the FDA for marketing. Pursuant to the terms of the Asset Purchase Agreement for the sale of Evamist, we made certain representations and warranties concerning our rights and assets related to Evamist and our authority to enter into and consummate the transaction. We also made certain covenants that survived the closing date of the transaction, including a covenant not to operate a business that competes, in the U.S. and its territories and protectorates, with the Evamist product.
To the extent permitted under Delaware law, we have agreements whereby we indemnify our officers and directors for certain events or occurrences while the officer or director is, or was, serving at our request in such capacity. The indemnification period covers all pertinent events and occurrences during the officer’s or director’s lifetime. The maximum potential amount of future payments we could be required to make under these indemnification agreements is unlimited; however, we maintain director and officer insurance coverage that reduces our exposure and enables us to recover a portion of any future amounts paid. We believe the estimated fair value of these indemnification agreements in excess of applicable insurance coverage is minimal.
93
Recent Accounting Pronouncements
The information on recent account pronouncements in incorporated by reference to Note 1 to our Consolidated Financial Statements included elsewhere in this report.
Dividend Policy
We have not paid any dividends since our inception and do not intend to declare or pay any dividends on our common stock in the foreseeable future. Declaration or payment of future dividends, if any, will be at the discretion of our Board of Directors after taking into account various factors, including our financial condition, operating results and current and anticipated cash needs.
Item 7A. Quantitative and Qualitative Disclosures about Market Risk
The Securities and Exchange Commission’s rule related to market risk disclosure requires that we describe and quantify our potential losses from market risk sensitive instruments attributable to reasonably possible market changes. Market risk sensitive instruments include all financial or commodity instruments and other financial instruments that are sensitive to future changes in interest rates, currency exchange rates, commodity prices or other market factors.
Market and Interest Rate Risk
Our cash, cash equivalents and available‑for‑sale securities as of December 31, 2015, consisted primarily of money market funds and U.S. Treasury securities. Our cash is invested in accordance with an investment policy approved by our Board of Directors that specifies the categories (money market funds, U.S. Treasury securities and debt securities of U.S. government agencies, corporate bonds, asset‑backed securities, and other securities), allocations, and ratings of securities we may consider for investment. Currently, we have focused on investing in U.S. Treasuries until market conditions improve.
Our primary exposure to market risk is interest income sensitivity, which is affected by changes in the general level of U.S. interest rates, particularly because the majority of our investments are in short‑term marketable debt securities. The primary objective of our investment activities is to preserve principal. Some of the securities that we invest in may be subject to market risk. This means that a change in prevailing interest rates may cause the value of the investment to fluctuate. For example, if we purchase a security that was issued with a fixed interest rate and the prevailing interest rate later rises, the value of our investment may decline. A hypothetical 100 basis point increase in interest rates would reduce the fair value of our available‑for‑sale securities at December 31, 2015, by approximately $1.1 million. In general, money market funds are not subject to market risk because the interest paid on such funds fluctuates with the prevailing interest rate.
94
Item 8. Financial Statements and Supplementary Data
VIVUS, INC.
1.Index to Consolidated Financial Statements
The following financial statements are filed as part of this Report:
95
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
The Board of Directors and Stockholders of
VIVUS, Inc.
We have audited the accompanying consolidated balance sheets of VIVUS, Inc. as of December 31, 2015 and 2014, and the related consolidated statements of operations, comprehensive loss, stockholders’ (deficit) equity and cash flows for each of the three years in the period ended December 31, 2015. In connection with our audits of the financial statements, we have also audited the financial statement schedule listed in the accompanying index. These financial statements and schedule are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements and schedule based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit also includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements and schedule. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the consolidated financial statements referred to above present fairly, in all material respects, the financial position of VIVUS, Inc. at December 31, 2015 and 2014, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2015, in conformity with accounting principles generally accepted in the United States of America.
As discussed in Note 17 to the consolidated financial statements, in 2015 the Company changed the manner in which it accounts for the classification of deferred taxes in the consolidated balance sheets due to the adoption of ASU 2015-17, Balance Sheet Classification of Deferred Taxes.
Also, in our opinion, the financial statement schedule, when considered in relation to the basic consolidated financial statements taken as a whole, presents fairly, in all material respects, the information set forth therein.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), VIVUS, Inc.’s internal control over financial reporting as of December 31, 2015, based on criteria established in Internal Control—Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission and our report dated March 9, 2016 expressed an unqualified opinion thereon.
/s/ OUM & Co. LLP
San Francisco, California
March 9, 2016
96
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
The Board of Directors and Stockholders of
VIVUS, Inc.
We have audited VIVUS, Inc.’s internal control over financial reporting as of December 31, 2015, based on criteria established in Internal Control—Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission (the COSO criteria). VIVUS, Inc.’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Annual Report on Internal Control Over Financial Reporting included in Item 9A. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, and testing and evaluating the design and operating effectiveness of internal control based on the assessed risk. Our audit also included performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
In our opinion, VIVUS, Inc. maintained, in all material respects, effective internal control over financial reporting as of December 31, 2015, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated balance sheets of VIVUS, Inc. as of December 31, 2015 and 2014, and the related consolidated statements of operations, comprehensive loss, stockholders’ (deficit) equity, and cash flows for each of the three years in the period ended December 31, 2015 and our report dated March 9, 2016 expressed an unqualified opinion thereon.
/s/ OUM & Co. LLP
San Francisco, California
March 9, 2016
97
VIVUS, INC.
(In thousands, except par value)
|
|
|
|
|
|
|
|
|
|
|
|
December 31, |
|
||||
|
|
|
2015 |
|
2014 |
|
||
|
ASSETS |
|
|
|
|
|
|
|
|
Current assets: |
|
|
|
|
|
|
|
|
Cash and cash equivalents |
|
$ |
95,395 |
|
$ |
83,174 |
|
|
Available-for-sale securities |
|
|
146,168 |
|
|
216,397 |
|
|
Accounts receivable, net |
|
|
8,997 |
|
|
11,595 |
|
|
Inventories |
|
|
13,602 |
|
|
34,447 |
|
|
Prepaid expenses and other current assets |
|
|
10,624 |
|
|
12,824 |
|
|
Total current assets |
|
|
274,786 |
|
|
358,437 |
|
|
Property and equipment, net |
|
|
994 |
|
|
1,346 |
|
|
Non-current assets |
|
|
4,801 |
|
|
7,155 |
|
|
Total assets |
|
$ |
280,581 |
|
$ |
366,938 |
|
|
LIABILITIES AND STOCKHOLDERS’ (DEFICIT) EQUITY |
|
|
|
|
|
|
|
|
Current liabilities: |
|
|
|
|
|
|
|
|
Accounts payable |
|
$ |
7,060 |
|
$ |
10,430 |
|
|
Accrued and other liabilities |
|
|
15,891 |
|
|
16,314 |
|
|
Deferred revenue |
|
|
22,142 |
|
|
19,445 |
|
|
Current portion of long-term debt |
|
|
15,550 |
|
|
10,459 |
|
|
Total current liabilities |
|
|
60,643 |
|
|
56,648 |
|
|
Long-term debt, net of current portion |
|
|
219,219 |
|
|
217,324 |
|
|
Deferred revenue, net of current portion |
|
|
6,508 |
|
|
8,876 |
|
|
Non-current accrued and other liabilities |
|
|
1,296 |
|
|
1,572 |
|
|
Total liabilities |
|
|
287,666 |
|
|
284,420 |
|
|
Commitments and contingencies |
|
|
|
|
|
|
|
|
Stockholders’ (deficit) equity: |
|
|
|
|
|
|
|
|
Preferred stock; $1.00 par value; 5,000 shares authorized; no shares issued and outstanding at December 31, 2015 and 2014 |
|
|
— |
|
|
— |
|
|
Common stock; $.001 par value; 200,000 shares authorized; 104,055 and 103,729 shares issued and outstanding at December 31, 2015 and 2014, respectively |
|
|
104 |
|
|
104 |
|
|
Additional paid-in capital |
|
|
829,428 |
|
|
825,691 |
|
|
Accumulated other comprehensive loss |
|
|
(261) |
|
|
(28) |
|
|
Accumulated deficit |
|
|
(836,356) |
|
|
(743,249) |
|
|
Total stockholders’ (deficit) equity |
|
|
(7,085) |
|
|
82,518 |
|
|
Total liabilities and stockholders’ (deficit) equity |
|
$ |
280,581 |
|
$ |
366,938 |
|
See accompanying notes to consolidated financial statements.
98
VIVUS, INC.
CONSOLIDATED STATEMENTS OF OPERATIONS
(In thousands, except per share data)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Year Ended December 31, |
|
|||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Revenue: |
|
|
|
|
|
|
|
|
|
|
|
Net product revenue |
|
$ |
54,622 |
|
$ |
45,277 |
|
$ |
23,718 |
|
|
License and milestone revenue |
|
|
11,574 |
|
|
38,614 |
|
|
55,838 |
|
|
Supply revenue |
|
|
26,674 |
|
|
26,519 |
|
|
1,526 |
|
|
Royalty revenue |
|
|
2,560 |
|
|
3,771 |
|
|
— |
|
|
Total revenue |
|
|
95,430 |
|
|
114,181 |
|
|
81,082 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Operating expenses: |
|
|
|
|
|
|
|
|
|
|
|
Cost of goods sold |
|
|
34,157 |
|
|
33,387 |
|
|
4,868 |
|
|
Selling, general and administrative |
|
|
79,387 |
|
|
111,539 |
|
|
158,235 |
|
|
Research and development |
|
|
10,102 |
|
|
13,793 |
|
|
29,677 |
|
|
Inventory impairment and other non-recurring charges |
|
|
32,061 |
|
|
6,173 |
|
|
42,916 |
|
|
Total operating expenses |
|
|
155,707 |
|
|
164,892 |
|
|
235,696 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Loss from operations |
|
|
(60,277) |
|
|
(50,711) |
|
|
(154,614) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Interest and other expense: |
|
|
|
|
|
|
|
|
|
|
|
Interest expense |
|
|
33,317 |
|
|
32,535 |
|
|
19,532 |
|
|
Other expense (income), net |
|
|
(490) |
|
|
30 |
|
|
703 |
|
|
Total interest and other expense |
|
|
32,827 |
|
|
32,565 |
|
|
20,235 |
|
|
Loss from continuing operations before income taxes |
|
|
(93,104) |
|
|
(83,276) |
|
|
(174,849) |
|
|
Provision for (benefit from) income taxes |
|
|
3 |
|
|
(629) |
|
|
97 |
|
|
Loss from continuing operations |
|
|
(93,107) |
|
|
(82,647) |
|
|
(174,946) |
|
|
Income from discontinued operations, net of tax |
|
|
— |
|
|
— |
|
|
490 |
|
|
Net loss |
|
$ |
(93,107) |
|
$ |
(82,647) |
|
$ |
(174,456) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Basic and diluted net loss per share: |
|
|
|
|
|
|
|
|
|
|
|
Continuing operations |
|
$ |
(0.90) |
|
$ |
(0.80) |
|
$ |
(1.72) |
|
|
Discontinued operations |
|
|
- |
|
|
- |
|
|
- |
|
|
Basic and diluted net loss per share |
|
$ |
(0.90) |
|
$ |
(0.80) |
|
$ |
(1.72) |
|
|
Shares used in per share computation: |
|
|
|
|
|
|
|
|
|
|
|
Basic and diluted |
|
|
103,926 |
|
|
103,456 |
|
|
101,174 |
|
VIVUS, INC.
CONSOLIDATED STATEMENTS OF COMPREHENSIVE LOSS
(In thousands)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Year Ended December 31, |
|
|||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Net loss |
|
$ |
(93,107) |
|
$ |
(82,647) |
|
$ |
(174,456) |
|
|
Unrealized (loss) gain on securities, net of taxes |
|
|
(233) |
|
|
(94) |
|
|
33 |
|
|
Comprehensive loss |
|
$ |
(93,340) |
|
$ |
(82,741) |
|
$ |
(174,423) |
|
See accompanying notes to consolidated financial statements.
99
VIVUS, INC.
CONSOLIDATED STATEMENTS OF STOCKHOLDERS’ (DEFICIT) EQUITY
(In thousands)
|
|
|
|
|
|
|
|
|
|
|
Accumulated |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Additional |
|
Other |
|
|
|
|
|
|
|
||
|
|
|
Common Stock |
|
Paid-In |
|
Comprehensive |
|
Accumulated |
|
|
|
|
||||||
|
|
|
Shares |
|
Amount |
|
Capital |
|
Income (Loss) |
|
Deficit |
|
Total |
|
|||||
|
Balances, December 31, 2012 |
|
100,659 |
|
$ |
101 |
|
$ |
708,921 |
|
$ |
33 |
|
$ |
(486,146) |
|
$ |
222,909 |
|
|
Sale of common stock through employee stock purchase plan |
|
103 |
|
|
— |
|
|
860 |
|
|
— |
|
|
— |
|
|
860 |
|
|
Exercise of common stock options for cash |
|
2,366 |
|
|
2 |
|
|
13,704 |
|
|
— |
|
|
— |
|
|
13,706 |
|
|
Vesting of restricted stock units |
|
33 |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
Share-based compensation expense |
|
— |
|
|
— |
|
|
32,877 |
|
|
— |
|
|
— |
|
|
32,877 |
|
|
Equity component of convertible debt |
|
— |
|
|
— |
|
|
95,262 |
|
|
— |
|
|
— |
|
|
95,262 |
|
|
Offering cost allocated to equity |
|
— |
|
|
— |
|
|
(3,113) |
|
|
— |
|
|
— |
|
|
(3,113) |
|
|
Purchase of capped call transaction |
|
— |
|
|
— |
|
|
(34,709) |
|
|
— |
|
|
— |
|
|
(34,709) |
|
|
Net unrealized gain on securities |
|
— |
|
|
— |
|
|
— |
|
|
33 |
|
|
— |
|
|
33 |
|
|
Net loss |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
(174,456) |
|
|
(174,456) |
|
|
Balances, December 31, 2013 |
|
103,161 |
|
|
103 |
|
|
813,802 |
|
|
66 |
|
|
(660,602) |
|
|
153,369 |
|
|
Sale of common stock through employee stock purchase plan |
|
113 |
|
|
— |
|
|
405 |
|
|
— |
|
|
— |
|
|
405 |
|
|
Exercise of common stock options for cash |
|
385 |
|
|
1 |
|
|
1,718 |
|
|
— |
|
|
— |
|
|
1,719 |
|
|
Vesting of restricted stock units |
|
70 |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
Share-based compensation expense |
|
— |
|
|
— |
|
|
9,766 |
|
|
— |
|
|
— |
|
|
9,766 |
|
|
Net unrealized loss on securities |
|
— |
|
|
— |
|
|
— |
|
|
(94) |
|
|
— |
|
|
(94) |
|
|
Net loss |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
(82,647) |
|
|
(82,647) |
|
|
Balances, December 31, 2014 |
|
103,729 |
|
|
104 |
|
|
825,691 |
|
|
(28) |
|
|
(743,249) |
|
|
82,518 |
|
|
Sale of common stock through employee stock purchase plan |
|
77 |
|
|
— |
|
|
147 |
|
|
— |
|
|
— |
|
|
147 |
|
|
Vesting of restricted stock units |
|
249 |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
Share-based compensation expense |
|
— |
|
|
— |
|
|
3,590 |
|
|
— |
|
|
— |
|
|
3,590 |
|
|
Net unrealized loss on securities |
|
— |
|
|
— |
|
|
— |
|
|
(233) |
|
|
— |
|
|
(233) |
|
|
Net loss |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
(93,107) |
|
|
(93,107) |
|
|
Balances, December 31, 2015 |
|
104,055 |
|
$ |
104 |
|
$ |
829,428 |
|
$ |
(261) |
|
$ |
(836,356) |
|
$ |
(7,085) |
|
See accompanying notes to consolidated financial statements.
100
VIVUS, INC.
CONSOLIDATED STATEMENTS OF CASH FLOWS
(In thousands)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Year Ended December 31, |
|
|||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Cash flows from operating activities: |
|
|
|
|
|
|
|
|
|
|
|
Net loss |
|
$ |
(93,107) |
|
$ |
(82,647) |
|
$ |
(174,946) |
|
|
Adjustments to reconcile net loss to net cash used for operating activities: |
|
|
|
|
|
|
|
|
|
|
|
Depreciation and amortization |
|
|
1,387 |
|
|
1,112 |
|
|
973 |
|
|
Amortization of debt issuance costs and discounts |
|
|
17,174 |
|
|
15,923 |
|
|
8,369 |
|
|
Amortization of discount or premium on available-for-sale securities |
|
|
2,282 |
|
|
4,016 |
|
|
2,635 |
|
|
Share-based compensation expense |
|
|
3,590 |
|
|
9,766 |
|
|
32,397 |
|
|
Unrealized foreign currency remeasurement gain |
|
|
— |
|
|
— |
|
|
(235) |
|
|
Loss on disposal and impairment of property and equipment |
|
|
— |
|
|
— |
|
|
896 |
|
|
Inventory impairment charge |
|
|
29,522 |
|
|
2,170 |
|
|
7,525 |
|
|
Changes in assets and liabilities: |
|
|
|
|
|
|
|
|
|
|
|
Accounts receivable |
|
|
2,598 |
|
|
619 |
|
|
(9,436) |
|
|
Inventories |
|
|
(8,487) |
|
|
11,886 |
|
|
(30,195) |
|
|
Prepaid expenses and other assets |
|
|
2,639 |
|
|
7,734 |
|
|
2,086 |
|
|
Accounts payable |
|
|
(3,370) |
|
|
(329) |
|
|
(14,821) |
|
|
Accrued and other liabilities |
|
|
(889) |
|
|
(9,061) |
|
|
13,170 |
|
|
Deferred revenue |
|
|
329 |
|
|
706 |
|
|
26,465 |
|
|
Net cash used for operating activities from continuing operations |
|
|
(46,332) |
|
|
(38,105) |
|
|
(135,117) |
|
|
Net cash used for operating activities from discontinued operations |
|
|
— |
|
|
— |
|
|
(208) |
|
|
Net cash used for operating activities |
|
|
(46,332) |
|
|
(38,105) |
|
|
(135,325) |
|
|
Cash flows from investing activities: |
|
|
|
|
|
|
|
|
|
|
|
Property and equipment purchases |
|
|
(310) |
|
|
(262) |
|
|
(1,795) |
|
|
Purchases of available-for-sale securities |
|
|
(213,536) |
|
|
(240,983) |
|
|
(329,145) |
|
|
Proceeds from maturity of available-for-sale securities |
|
|
281,250 |
|
|
260,500 |
|
|
242,500 |
|
|
Non-current assets |
|
|
— |
|
|
(3,362) |
|
|
(1,681) |
|
|
Net cash provided by (used for) investing activities |
|
|
67,404 |
|
|
15,893 |
|
|
(90,121) |
|
|
Cash flows from financing activities: |
|
|
|
|
|
|
|
|
|
|
|
Net proceeds from debt issuance |
|
|
— |
|
|
— |
|
|
290,247 |
|
|
Payments of notes payable |
|
|
(8,998) |
|
|
— |
|
|
— |
|
|
Payments for capped call transaction |
|
|
— |
|
|
— |
|
|
(34,709) |
|
|
Net proceeds from exercise of common stock options |
|
|
— |
|
|
1,719 |
|
|
13,706 |
|
|
Sale of common stock through employee stock purchase plan |
|
|
147 |
|
|
405 |
|
|
859 |
|
|
Net cash (used for) provided by financing activities |
|
|
(8,851) |
|
|
2,124 |
|
|
270,103 |
|
|
Net decrease in cash and cash equivalents |
|
|
12,221 |
|
|
(20,088) |
|
|
44,657 |
|
|
Cash and cash equivalents: |
|
|
|
|
|
|
|
|
|
|
|
Beginning of year |
|
|
83,174 |
|
|
103,262 |
|
|
58,605 |
|
|
End of period |
|
$ |
95,395 |
|
$ |
83,174 |
|
$ |
103,262 |
|
|
Supplemental cash flow disclosure: |
|
|
|
|
|
|
|
|
|
|
|
Interest paid |
|
$ |
18,756 |
|
$ |
20,251 |
|
$ |
5,000 |
|
|
Income taxes paid |
|
$ |
58 |
|
$ |
94 |
|
$ |
32 |
|
|
Non-cash investing activities: |
|
|
|
|
|
|
|
|
|
|
|
Unrealized (loss) gain on securities |
|
$ |
(233) |
|
$ |
(94) |
|
$ |
33 |
|
See accompanying notes to consolidated financial statements.
101
Note 1. Business and Significant Accounting Policies
Business
VIVUS, Inc. is a biopharmaceutical company with two therapies approved by the U.S. Food and Drug Administration, or FDA: Qsymia® for chronic weight management and STENDRA® for erectile dysfunction. STENDRA is also approved by the European Commission, or EC, under the trade name, SPEDRA™, for the treatment of erectile dysfunction in the EU.
Qsymia, or phentermine and topiramate extended-release, was approved by the FDA in July 2012, as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adult patients with an initial body mass index, or BMI, of 30 or greater, or obese patients, or 27 or greater, or overweight patients, in the presence of at least one weight‑related comorbidity, such as hypertension, type 2 diabetes mellitus or high cholesterol, or dyslipidemia. In September 2012, Qsymia became available in the U.S. market through a limited number of certified home delivery networks and, in July 2013, Qsymia became available in retail pharmacies.
Prior to August 2015, the Company commercialized Qsymia in the U.S. primarily through a dedicated contract sales force, supported by an internal commercial team. In August 2015, the Company directly hired approximately 50 former contract sales representatives to continue promoting Qsymia to physicians.
STENDRA, or avanafil, is an oral phosphodiesterase type 5, or PDE5, inhibitor that the Company has licensed from Mitsubishi Tanabe Pharma Corporation, or MTPC. In July 2013, the Company entered into an agreement with the Menarini Group, through its subsidiary Berlin-Chemie AG, or Menarini, under which Menarini received an exclusive license to commercialize and promote SPEDRA for the treatment of ED in over 40 European countries, including the EU, as well as Australia and New Zealand. Menarini commenced its commercialization launch of the product in the EU in early 2014.
In October 2013, the Company entered into an agreement with Auxilium Pharmaceuticals, Inc., or Auxilium, under which Auxilium received an exclusive license to commercialize and promote STENDRA in the United States and Canada. On the same date, we also entered into a supply agreement with Auxilium, whereby VIVUS will supply Auxilium with STENDRA drug product for commercialization. Auxilium began commercializing STENDRA in the U.S. market in December 2013. In January 2015, Auxilium was purchased by Endo International, plc. In December 2015, Auxilium notified the Company of its intention to return the U.S. and Canadian commercial rights for STENDRA. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and the Company for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016.
In December 2013, the Company entered into an agreement with Sanofi under which Sanofi received an exclusive license to commercialize and promote avanafil for therapeutic use in humans in Africa, the Middle East, Turkey, and the Commonwealth of Independent States, or CIS, including Russia. Sanofi will be responsible for obtaining regulatory approval in its territories. Sanofi intends to market avanafil under the trade name SPEDRA or STENDRA. Effective as of December 2013, the Company also entered into a supply agreement, or the Sanofi Supply Agreement, with Sanofi Winthrop Industrie, a wholly-owned subsidiary of Sanofi.
Under the license agreements with Menarini, Auxilium and Sanofi, avanafil is expected to be commercialized in over 100 countries worldwide. Under the Auxilium agreement, the Company has received approximately $45.0 million in license and milestone payments out of a potential of $300.0 million, as well as royalty payments. The Company does not anticipate any additional milestone revenue from the Auxilium agreement. Under the Menarini agreement, the Company has received approximately $63.0 million in license and milestone payments out of a potential of approximately $100.0 million, as well as royalty payments. Under the Sanofi agreement, the Company has received
102
approximately $10.0 million in license and milestone payments out of a potential of $61.0 million. In addition, the Company is currently in discussions with potential collaboration partners to market and sell STENDRA for other territories in which it does not currently have a commercial collaboration.
At December 31, 2015, the Company’s accumulated deficit was approximately $836.4 million. Based on current plans, management expects to incur further losses for the foreseeable future. Management believes that the Company’s existing capital resources combined with anticipated future cash flows will be sufficient to support its operating needs at least for the next twelve months. However, the Company anticipates that it may require additional funding to expand the use of Qsymia through targeted patient and physician education, find the right partner for expanded Qsymia commercial promotion to a broader primary care physician audience, create a pathway for centralized approval of the marketing authorization application for Qsiva in the EU, continue the expansion of our distribution of Qsymia through certified retail pharmacy locations, conduct post-approval clinical studies for Qsymia, conduct non-clinical and clinical research and development work to support regulatory submissions and applications for our future investigational drug candidates, finance the costs involved in filing and prosecuting patent applications and enforcing or defending our patent claims, if any, to fund operating expenses, establish additional or new manufacturing and marketing capabilities, and manufacture quantities of its drugs and investigational drug candidates and to make payments under its existing license agreement and supply agreements for STENDRA.
If the Company requires additional capital, it may seek any required additional funding through collaborations, public and private equity or debt financings, capital lease transactions or other available financing sources. Additional financing may not be available on acceptable terms, or at all. If additional funds are raised by issuing equity securities, substantial dilution to existing stockholders may result. If adequate funds are not available, the Company may be required to delay, reduce the scope of or eliminate one or more of its commercialization or development programs or obtain funds through collaborations with others that are on unfavorable terms or that may require the Company to relinquish rights to certain of its technologies, product candidates or products that it would otherwise seek to develop on its own. Management has evaluated all events and transactions that occurred after December 31, 2015, through the date these consolidated financial statements were filed. There were no events or transactions occurring during this period that require recognition or disclosure in these consolidated financial statements. The Company operates in a single segment, the development and commercialization of novel therapeutic products.
Significant Accounting Policies
Reclassifications
Certain prior year amounts in the consolidated financial statements have been reclassified to conform to the current year’s presentation. In the prior year, certain amounts related to the long-term portion of deferred rent were included in current liabilities as they were considered immaterial. In the current year, the Company has presented these in non-current accrued and other liabilities on the balance sheet and reclassified the amounts from the prior year accordingly.
Principles of Consolidation
The consolidated financial statements include the accounts of VIVUS, Inc., and its wholly owned subsidiaries. All significant intercompany transactions and balances have been eliminated in consolidation.
Use of Estimates
The preparation of financial statements in conformity with U.S. generally accepted accounting principles requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosures of contingent assets and liabilities at the date of the financial statements and the reported amounts of revenues and expenses during the reporting period. On an ongoing basis, the Company evaluates its estimates, including critical accounting policies or estimates related to available‑for‑sale securities, debt instruments, research and development expenses, income taxes, inventories, contingencies and litigation and share‑based compensation. The Company bases its estimates on historical experience, information received from third parties and on various market
103
specific and other relevant assumptions that it believes to be reasonable under the circumstances, the results of which form the basis for making judgments about the carrying values of assets and liabilities that are not readily apparent from other sources. Actual results could differ significantly from those estimates under different assumptions or conditions.
Cash and Cash Equivalents
The Company considers highly liquid investments with maturities from the date of purchase of three months or less to be cash equivalents. At December 31, 2015 and 2014, all cash equivalents were invested in money market funds and U.S. Treasury securities. These investments are recorded at fair value.
Available‑for‑Sale Securities
The Company determines the appropriate classification of marketable securities at the time of purchase and reevaluates such designation at each balance sheet date. Marketable securities have been classified and accounted for as available‑for‑sale. The Company may or may not hold securities with stated maturities greater than 12 months until maturity. In response to changes in the availability of and the yield on alternative investments as well as liquidity requirements, the Company may sell these securities prior to their stated maturities. As these securities are viewed by the Company as available to support current operations, securities with maturities beyond 12 months are classified as current assets.
Securities are carried at fair value, with the unrealized gains and losses, net of taxes, reported as a component of stockholders’ (deficit) equity, unless the decline in value is deemed to be other‑than‑temporary, in which case such securities are written down to fair value and the loss is charged to other‑than‑temporary loss on impaired securities. The Company periodically evaluates its investment securities for other‑than‑temporary declines based on quantitative and qualitative factors. Any losses that are deemed other-than-temporary are recognized as a non-operating loss. To date, the Company has not had any other-than-temporary declines in the value of any of its investment portfolio. Any realized gains or losses on the sale of marketable securities are determined on a specific identification method, and such gains and losses are reflected as a component of interest and other income (expense).
Fair Value Measurements
Financial instruments include cash equivalents, available‑for‑sale securities, accounts receivable, accounts payable and accrued liabilities. Available‑for‑sale securities are carried at fair value. The carrying value of cash equivalents, accounts payable and accrued liabilities approximate their fair value due to the relatively short‑term nature of these instruments.
Debt instruments are initially recorded at face value, with coupon interest and amortization of debt issuance discounts and costs recognized as interest expense.
The Company’s Convertible Notes contain a conversion option that is classified as equity. The Company determined the fair value of the liability component of the debt instrument and allocated the excess amount of $95.3 million from the initial proceeds to the conversion option in additional paid-in capital. The fair value of the debt component was determined by estimating a risk adjusted interest rate, or market yield, at the time of issuance for similar notes that do not include the conversion feature. This excess is reported as a debt discount and is amortized as non‑cash interest expense, using the effective-interest method, over the expected life of the Convertible Notes. The Convertible Notes are recorded in the balance sheet as a component of long-term debt.
Issuance costs related to the conversion feature of the Convertible Notes were charged to additional paid‑in capital. The portion of the issuance costs related to the debt component is being amortized and recorded as additional interest expense over the expected life of the Convertible Notes. In connection with the issuance of the Convertible Notes, the Company entered into capped call transactions with certain counterparties affiliated with the underwriters. The fair value of the purchased capped calls of $34.7 million was recorded to additional paid-in capital.
104
Concentration of Credit Risk
Financial instruments that potentially subject the Company to concentrations of credit risk consist primarily of cash, cash equivalents, available‑for‑sale‑securities, and accounts receivable. The Company has established guidelines to limit its exposure to credit risk by placing investments in high credit quality money market funds, U.S. Treasury securities or corporate debt securities and by placing investments with maturities that maintain safety and liquidity within the Company’s liquidity needs. The Company has also established guidelines for the issuance of credit to existing and potential customers.
Accounts Receivable, Allowances for Doubtful Accounts and Cash Discounts
The Company extends credit to its customers for product sales resulting in accounts receivable. Customer accounts are monitored for past due amounts. Past due accounts receivable that are determined to be uncollectible are written off against the allowance for doubtful accounts. Allowances for doubtful accounts are estimated based upon past due amounts, historical losses and existing economic factors, and are adjusted periodically. Historically, the Company has not had any significant uncollected accounts. The Company offers cash discounts to its customers, generally 2% of the sales price, as an incentive for prompt payment. The estimate of cash discounts is recorded at the time of sale. The Company accounts for the cash discounts by reducing revenue and accounts receivable by the amount of the discounts it expects the customers to take. The accounts receivable are reported in the consolidated balance sheets, net of the allowances for doubtful accounts and cash discounts. There is no allowance for doubtful accounts at December 31, 2015 or 2014. The allowance for cash discounts is $164,000 and $150,000 at December 31, 2015 and 2014, respectively.
Inventories
Inventories are valued at the lower of cost or market. Cost is determined using the first‑in, first‑out method using a weighted average cost method calculated for each production batch. Inventory includes the cost of the active pharmaceutical ingredients, or APIs, raw materials and third‑party contract manufacturing and packaging services. Indirect overhead costs associated with production and distribution are allocated to the appropriate cost pool and then absorbed into inventory based on the units produced or distributed, assuming normal capacity, in the applicable period.
Inventory costs of product shipped to customers, but not yet recognized as revenue, are recorded within inventories on the consolidated balance sheets and are subsequently recognized to cost of goods sold when revenue recognition criteria have been met.
The Company’s policy is to write down inventory that has become obsolete, inventory that has a cost basis in excess of its expected net realizable value and inventory in excess of expected requirements. The estimate of excess quantities is subjective and primarily dependent on the Company’s estimates of future demand for a particular product. If the estimate of future demand is inaccurate based on lower actual sales, the Company may increase the write down for excess inventory for that product and record a charge to inventory impairment in the accompanying consolidated statements of operations. The Company periodically evaluates the carrying value of inventory on hand for potential excess amount over demand using the same lower of cost or market approach as that used to value the inventory. As a result of this evaluation, for the year ended December 31, 2015, the Company recognized an impairment charge of $29.5 million for Qsymia API inventory in excess of projected demand. For the year ended December 31, 2014, the Company recognized a total charge of $2.2 million for Qsymia inventories on hand in excess of projected demand. For the year ended December 31, 2013, the Company recognized a total charge of $10.2 million for Qsymia inventories on hand in excess of demand, plus a purchase commitment fee.
Property and Equipment
Property and equipment is stated at cost and includes leasehold improvements, computers and software and furniture and fixtures. Depreciation is computed using the straight‑line method over the estimated useful lives of two to seven years for computers, software, furniture and fixtures. Leasehold improvements are amortized using the straight‑line method over the shorter of the remaining lease term or the estimated useful lives. Expenditures for repairs and maintenance, which do not extend the useful life of the property and equipment, are expensed as incurred. Gains and
105
losses associated with dispositions are reflected as a non-operating gain or loss in the accompanying consolidated statements of operations.
Long‑lived assets, such as property and equipment, are reviewed for impairment whenever events or changes in circumstances indicate that the carrying amount of an asset may not be recoverable. Recoverability of assets to be held and used is measured by a comparison of the carrying amount of an asset to an estimate of undiscounted future cash flows expected to be generated by the asset. If the carrying amount of the asset exceeds its estimated future cash flows, an impairment charge is recognized for the amount by which the carrying amount of the asset exceeds the fair value of the asset.
Debt Issuance Costs
Debt issuance costs, which are included in other assets, are amortized as interest expense using the effective-interest method over the expected term of the debt.
Revenue Recognition
Product Revenue:
The Company recognizes product revenue from the sales of Qsymia, when: (i) persuasive evidence that an arrangement exists, (ii) delivery has occurred and title has passed, (iii) the price is fixed or determinable and (iv) collectability is reasonably assured. Revenue from sales transactions where the customer has the right to return the product is recognized at the time of sale only if: (i) the Company’s price to the customer is substantially fixed or determinable at the date of sale, (ii) the customer has paid the Company, or the customer is obligated to pay the Company and the obligation is not contingent on resale of the product, (iii) the customer’s obligation to the Company would not be changed in the event of theft or physical destruction or damage of the product, (iv) the customer acquiring the product for resale has economic substance apart from that provided by the Company, (v) the Company does not have significant obligations for future performance to directly bring about resale of the product by the customer, and (vi) the amount of future returns can be reasonably estimated.
Product Revenue Allowances:
Product revenue is recognized net of consideration paid to the Company’s customers, wholesalers and certified pharmacies, for services rendered by the wholesalers and pharmacies in accordance with the wholesalers and certified pharmacy services network agreements, and include a fixed rate per prescription shipped and monthly program management and data fees. These services are not deemed sufficiently separable from the customers’ purchase of the product; therefore, they are recorded as a reduction of revenue at the time of revenue recognition.
Other product revenue allowances include certain prompt pay discounts and allowances offered to the Company’s customers, program rebates and chargebacks. These product revenue allowances are recognized as a reduction of revenue at the later of the date at which the related revenue is recognized or the date at which the allowance is offered. The Company also offers discount programs to patients. Calculating certain of these items involves estimates and judgments based on sales or invoice data, contractual terms, utilization rates, new information regarding changes in these programs’ regulations and guidelines that would impact the amount of the actual rebates or chargebacks. The Company reviews the adequacy of product revenue allowances on a quarterly basis. Amounts accrued for product revenue allowances are adjusted when trends or significant events indicate that adjustment is appropriate and to reflect actual experience.
The Company ships units of Qsymia through a distribution network that includes certified retail pharmacies. Qsymia has a 36–month shelf life and the Company grants rights to its customers to return unsold product six months prior to and up to 12 months after product expiration and issue credits that may be applied against existing or future invoices. Given the Company’s limited history of selling Qsymia and the duration of the return period, the Company has not had sufficient information to reliably estimate expected returns of Qsymia at the time of shipment, and therefore revenue is recognized when units are dispensed to patients through prescriptions, at which point, the product is not
106
subject to return. The Company obtains prescription shipment data from the pharmacies to determine the amount of revenue to recognize.
The Company will continue to recognize revenue for Qsymia based upon prescription sell‑through until it has sufficient historical information to reliably estimate returns. As of December 31, 2015, the Company had deferred revenue of $19.3 million related to shipments of Qsymia, which represents product shipped to its customers, but not yet dispensed to patients through prescriptions. A corresponding accounts receivable is also recorded for this amount, as the payments from customers are not contingent upon the sale of product to patients.
Supply Revenue:
The Company recognizes supply revenue from the sales of STENDRA or SPEDRA when the four basic revenue recognition criteria described above are met. The Company produces STENDRA or SPEDRA through a contract manufacturing partner and then sells it to its commercialization partners. The Company is the primary responsible party in the commercial supply arrangements and bears significant risk in the fulfillment of the obligations, including risks associated with manufacturing, regulatory compliance and quality assurance, as well as inventory, financial and credit loss. As such, the Company recognizes supply revenue on a gross basis as the principal party in the arrangements. Under the Company’s product supply agreements, as long as the product meets specified product dating criteria at the time of shipment to the partner, the Company’s commercialization partners do not have a right of return or credit for expired product. As such, the Company recognizes revenue for products that meet the dating criteria at the time of shipment.
Revenue from Multiple‑Element Arrangements:
The Company accounts for multiple‑element arrangements, such as license and commercialization agreements in which a customer may purchase several deliverables, in accordance with ASC Topic 605‑25, Revenue Recognition —Multiple‑Element Arrangements, or ASC 605‑25. The Company evaluates if the deliverables in the arrangement represent separate units of accounting. In determining the units of accounting, management evaluates certain criteria, including whether the deliverables have value to its customers on a stand‑alone basis. Factors considered in this determination include whether the deliverable is proprietary to the Company, whether the customer can use the license or other deliverables for their intended purpose without the receipt of the remaining elements, whether the value of the deliverable is dependent on the undelivered items, and whether there are other vendors that can provide the undelivered items. Deliverables that meet these criteria are considered a separate unit of accounting. Deliverables that do not meet these criteria are combined and accounted for as a single unit of accounting.
When deliverables are separable, the Company allocates non‑contingent consideration to each separate unit of accounting based upon the relative selling price of each element. When applying the relative selling price method, the Company determines the selling price for each deliverable using vendor‑specific objective evidence, or VSOE, of selling price, if it exists, or third‑party evidence, or TPE, of selling price, if it exists. If neither VSOE nor TPE of selling price exists for a deliverable, the Company uses best estimated selling price, or BESP, for that deliverable. Significant management judgment may be required to determine the relative selling price of each element. Revenue allocated to each element is then recognized based on when the following four basic revenue recognition criteria are met for each element: (i) persuasive evidence of an arrangement exists; (ii) delivery has occurred or services have been rendered; (iii) the price is fixed or determinable; and (iv) collectability is reasonably assured.
Determining whether and when some of these criteria have been satisfied often involves assumptions and judgments that can have a significant impact on the timing and amount of revenue the Company reports. Changes in assumptions or judgments, or changes to the elements in an arrangement, could cause a material increase or decrease in the amount of revenue reported in a particular period.
ASC Topic 605‑28, Revenue Recognition — Milestone Method or (ASC 605‑28), established the milestone method as an acceptable method of revenue recognition for certain contingent, event‑based payments under research and development arrangements. Under the milestone method, a payment that is contingent upon the achievement of a substantive milestone is recognized in its entirety in the period in which the milestone is achieved. A milestone is an event: (i) that can be achieved based in whole or in part on either the Company’s performance or on the occurrence of a specific outcome resulting from the Company’s performance, (ii) for which there is substantive uncertainty at the date
107
the arrangement is entered into that the event will be achieved, and (iii) that would result in additional payments being due to the Company. The determination that a milestone is substantive requires judgment and is made at the inception of the arrangement. Milestones are considered substantive when the consideration earned from the achievement of the milestone is: (i) commensurate with either the Company’s performance to achieve the milestone or the enhancement of value of the item delivered as a result of a specific outcome resulting from the Company’s performance to achieve the milestone, (ii) relates solely to past performance, and (iii) is reasonable relative to all deliverables and payment terms in the arrangement.
Other contingent, event‑based payments received for which payment is either contingent solely upon the passage of time or the results of a collaborative partner’s performance are not considered milestones under ASC 605‑28. In accordance with ASC 605, such payments will be recognized as revenue when all of the four basic revenue recognition criteria are met.
Revenues recognized for royalty payments are recognized when the four basic revenue recognition criteria described above are met.
Cost of Goods Sold
Cost of goods sold for units dispensed to patients through prescriptions, or shipped to customers without a right of return or credit, includes the inventory costs of APIs, third‑party contract manufacturing costs, packaging and distribution costs, royalties, cargo insurance, freight, shipping, handling and storage costs, and overhead costs of the employees involved with production. Specifically, cost of goods sold for Qsymia dispensed to patients includes the inventory costs of the APIs, third‑party contract manufacturing and packaging and distribution costs, royalties, cargo insurance, freight, shipping, handling and storage costs, and overhead costs of the employees involved with production; cost of goods sold for STENDRA shipped to partners includes the inventory costs of purchased tablets, freight, shipping and handling costs. The cost of goods sold associated with deferred revenue on Qsymia and STENDRA product shipments is recorded as deferred costs, which are included in inventories in the consolidated balance sheets, until such time as the deferred revenue is recognized.
Research and Development Expenses
Research and development, or R&D, expenses include license fees, related compensation, consultants’ fees, facilities costs, administrative expenses related to R&D activities and clinical trial costs incurred by clinical research organizations or CROs, and research institutions under agreements that are generally cancelable, among other related R&D costs. The Company also records accruals for estimated ongoing clinical trial costs. Clinical trial costs represent costs incurred by CRO and clinical sites and include advertising for clinical trials and patient recruitment costs. These costs are recorded as a component of R&D expenses and are expensed as incurred. Under the Company’s agreements, progress payments are typically made to investigators, clinical sites and CROs. The Company analyzes the progress of the clinical trials, including levels of patient enrollment, invoices received and contracted costs when evaluating the adequacy of accrued liabilities. Significant judgments and estimates must be made and used in determining the accrued balance in any accounting period. Actual results could differ from those estimates under different assumptions. Revisions are charged to expense in the period in which the facts that give rise to the revision become known.
In addition, the Company has obtained rights to patented intellectual properties under several licensing agreements for use in research and development activities. Non‑refundable licensing payments made for intellectual properties that have no alternative future uses are expensed to research and development as incurred.
Advertising Expenses
Advertising expenses are expensed as incurred. The Company incurred advertising and sales promotion costs related to its marketing of Qsymia of $12.6 million, $10.1 million and $26.1 million in 2015, 2014 and 2013, respectively.
Share‑Based Compensation
The Company follows the fair value method of accounting for share‑based compensation arrangements in accordance with FASB ASC topic 718, Compensation—Stock Compensation, or ASC 718. Compensation expense is
108
recognized, using a fair‑value based method, for all costs related to share‑based payments including stock options and restricted stock units and stock issued under the employee stock purchase plan. The Company estimates the fair value of share‑based payment awards on the date of the grant using the Black‑Scholes option‑pricing model. The fair value of each option award is estimated on the grant date using a Black‑Scholes option‑pricing model. The expected term, which represents the period of time that options granted are expected to be outstanding, is derived by analyzing the historical experience of similar awards, giving consideration to the contractual terms of the share‑based awards, vesting schedules and expectations of future employee behavior. Expected volatilities are estimated using the historical share price performance over the expected term of the option. The Company also considers other factors such as its planned clinical trials and other company activities that may affect the volatility of VIVUS’s stock in the future but determined that, at this time, the historical volatility was more indicative of expected future stock price volatility. The risk‑free interest rate for the period matching the expected term of the option is based on the U.S. Treasury yield curve in effect at the time of the grant. The Black‑Scholes Model also requires a single expected dividend yield as an input. The Company does not anticipate paying any dividends in the near future. The Company develops pre‑vesting forfeiture assumptions based on an analysis of historical data.
Inventory Impairment and Other Non‑Recurring Charges
The Company’s inventory impairment and other non-recurring charges consist of inventory impairment charges, proxy contest expenses and charges from cost reduction plans, including employee severance, one time termination benefits and ongoing benefits related to the reduction of our workforce, facilities and other facility exit costs. Liabilities for costs associated with the cost reduction plan are recognized when the liability is incurred. In addition, liabilities associated with cost reduction activities are measured at fair value. One-time termination benefits are expensed at the date the entity notifies the employee, unless the employee must provide future service, in which case the benefits are expensed ratably over the future service period. Ongoing benefits are expensed when cost reduction activities are probable and the benefit amounts are estimable. Other costs primarily consist of legal, consulting, and other costs related to employee terminations and are expensed when incurred. Termination benefits are calculated in accordance with the various agreements with certain of the Company’s employees.
Income Taxes
The Company makes certain estimates and judgments in determining income tax expense for financial statement purposes. These estimates and judgments occur in the calculation of certain tax assets and liabilities, which arise from differences in the timing of recognition of revenue and expense for tax and financial statement purposes.
As part of the process of preparing the Company’s consolidated financial statements, the Company is required to estimate its income taxes in each of the jurisdictions in which the Company operates. This process involves the Company estimating its current tax exposure under the most recent tax laws and assessing temporary differences resulting from differing treatment of items for tax and accounting purposes. These differences result in deferred tax assets and liabilities, which are included in the Company’s consolidated balance sheets.
The Company assesses the likelihood that it will be able to recover its deferred tax assets. The Company considers all available evidence, both positive and negative, including historical levels of income, expectations and risks associated with estimates of future taxable income and ongoing prudent and feasible tax planning strategies in assessing the need for a valuation allowance. If it is not more likely than not that the Company will recover its deferred tax assets, the Company will increase its provision for taxes by recording a valuation allowance against the deferred tax assets that the Company estimates will not ultimately be recoverable. As a result of the Company’s analysis of all available evidence, both positive and negative, as of December 31, 2015, it was considered more likely than not that the Company’s deferred tax assets would not be realized. However, should there be a change in the Company’s ability to recover its deferred tax assets, the Company would recognize a benefit to its tax provision in the period in which the Company determines that it is more likely than not that it will recover its deferred tax assets.
The Company recognizes interest and penalties accrued on any unrecognized tax benefits as a component of its provision for income taxes.
109
FASB ASC topic 740, Income Taxes, or ASC 740, prescribes a recognition threshold and measurement attribute for the financial statement recognition and measurement of uncertain tax positions taken or expected to be taken in a company’s income tax return, and also provides guidance on derecognition, classification, interest and penalties, accounting in interim periods, disclosure, and transition. ASC 740‑10 utilizes a two‑step approach for evaluating uncertain tax positions. Step one, Recognition, requires a company to determine if the weight of available evidence indicates that a tax position is more likely than not to be sustained upon audit, including resolution of related appeals or litigation processes, if any. Step two, Measurement, is based on the largest amount of benefit, which is more likely than not to be realized on ultimate settlement. The Company also recognizes interest and penalties accrued on any unrecognized tax benefits as a component of its provision for income taxes. As of December 31, 2015, the Company does not have any unrecognized tax positions.
Discontinued operations
On November 5, 2010, the Company completed the sale of the MUSE product to Meda AB. For the year ended December 31, 2013, the Company recorded some minor adjustments related to the MUSE disposition, primarily adjustments to its sales reserves for accrued product returns.
Foreign Currency Transactions
Transactions in foreign currencies are initially recorded at the rates of exchange prevailing on the dates of the transactions. Monetary assets and liabilities denominated in foreign currencies are retranslated into the Company’s functional currency at the rates prevailing on the balance sheet date.
Non‑monetary items carried at fair value that are denominated in foreign currencies are retranslated at the rates prevailing on the initial transaction dates.
Exchange differences arising on the settlement of monetary items, and on the retranslation of monetary items, are included in the profit and loss account for the period. Exchange differences arising on the retranslation of non‑monetary items carried at fair value are included in other expense in the accompanying consolidated statements of operations for the period.
Contingencies and Litigation
The Company is periodically involved in disputes and litigation related to a variety of matters. When it is probable that the Company will experience a loss, and that loss is quantifiable, the Company records appropriate reserves. The Company records legal fees and costs as an expense when incurred.
Intangible Assets
The Company records acquired intangible assets at cost and amortizes them over the estimated useful life of the asset. When events or changes in circumstances indicate that the carrying value of intangible assets may not be recoverable, the Company evaluates such impairment if the net book value of such assets exceeds the future undiscounted cash flows attributable to such assets. Should an impairment exist, the impairment loss would be measured based on the excess carrying value of the asset over the asset’s fair value or discounted estimates of future cash flows attributable to the assets. To date, the Company has recorded no impairment losses on its intangible assets.
Net Loss Per Share
The Company computes basic net loss per share applicable to common stockholders based on the weighted average number of common shares outstanding during the period. Diluted net loss per share is based on the weighted average number of common and common equivalent shares, which represent shares that may be issued in the future upon the exercise of outstanding stock options or upon a net share settlement of the Company’s Convertible Notes. Common share equivalents are excluded from the computation in periods in which they have an anti‑dilutive effect. Stock options for which the price exceeds the average market price over the period have an anti‑dilutive effect on net income per share
110
and, accordingly, are excluded from the calculation. As discussed in Note 13, the triggering conversion conditions that allow holders of the Convertible Notes to convert have not been met. If such conditions are met and the note holders opt to convert, the Company may choose to pay in cash, common stock, or a combination thereof. However, if this occurs, the Company has the intent and ability to net share settle this debt security; thus the Company uses the treasury stock method for earnings per share purposes. Due to the effect of the capped call instrument purchased in relation to the Convertible Notes, there would be no net shares issued until the market value of the Company’s stock exceeds $20 per share, and thus no impact on diluted net income per share. Further, when there is a net loss, other potentially dilutive common equivalent shares are not included in the calculation of net loss per share since their inclusion would be anti‑dilutive.
As the Company recognized a net loss from continuing operations for the years ended December 31, 2015, 2014 and 2013, 7,167,000, 8,096,000 and 7,027,000 potentially dilutive outstanding stock options were not included in the computation of diluted net loss per share, respectively, because the effect would have been anti‑dilutive.
Recent Accounting Pronouncements
In May 2014, the Financial Accounting Standards Board, or FASB, issued Accounting Standards Update No. 2014-09, Revenue from Contracts with Customers, which provides a single comprehensive model for entities to use in accounting for revenue arising from contracts with customers and will supersede most current revenue recognition guidance. As originally issued, the standard would be effective for the Company’s fiscal year beginning January 1, 2017, with early adoption not permitted. In July 2015, the FASB voted to delay the effective date of the standard by one year to the first quarter of 2018 to provide companies sufficient time to implement the standard. Early adoption will be permitted, but not before the first quarter of 2017. Adoption can occur using one of two prescribed transition methods. The Company is currently evaluating the method by which it will implement this standard and the impact of the adoption of this standard on the Company’s consolidated financial statements.
In April 2015, the FASB issued Accounting Standards Update No. 2015-03, Interest - Imputation of Interest (Subtopic 835-30): Simplifying the Presentation of Debt Issuance Costs. The standard requires that debt issuance costs related to a recognized debt liability be presented in the balance sheet as a direct deduction from the carrying amount of that debt liability, consistent with debt discounts. The standard is effective for annual and interim periods beginning on or after December 15, 2015. As of December 31, 2015, the Company has $3.4 million of net deferred financing costs that would be reclassified from a current and long-term asset to a reduction in the carrying amount of its debt.
In July 2015, the FASB issued Accounting Standards Update 2015-11, Simplifying the Measurement of Inventory - Inventory (Topic 330), which changes the measurement principle for inventory from the lower of cost or market to lower of cost and net realizable value. Net realizable value is defined as the “estimated selling prices in the ordinary course of business, less reasonably predictable costs of completion, disposal and transportation.” The standard eliminates the guidance that entities consider replacement cost or net realizable value less an approximately normal profit margin in the subsequent measurement of inventory when cost is determined on a first-in, first-out or average cost basis. The standard is effective for public entities with fiscal years beginning after December 15, 2016. The Company is currently evaluating the impact of the adoption of this standard on the Company's consolidated financial statements.
In February 2016, the FASB issued Accounting Standards Update 2016-02, Leases (Topic 842), which modifies the accounting by lessees for all leases with a term greater than 12 months. The standard will require lessees to recognize on the balance sheet the assets and liabilities for the rights and obligations created by those leases. For public companies, the standard is effective for annual and interim periods beginning on or after December 15, 2018. Early adoption is permitted. The Company is currently evaluating the impact of the adoption of this standard on the Company’s consolidated financial statements.
111
Note 2. Cash, Cash Equivalents and Available‑for‑Sale Securities
The fair value and the amortized cost of cash, cash equivalents, and available-for-sale securities by major security type consist of the following (in thousands):
|
|
|
As of December 31, 2015 |
|
||||||||||
|
|
|
|
|
|
Gross |
|
Gross |
|
|
|
|
||
|
Cash and cash equivalents and available-for-sale |
|
Amortized |
|
Unrealized |
|
Unrealized |
|
Estimated |
|
||||
|
securities |
|
Cost |
|
Gains |
|
Losses |
|
Fair Value |
|
||||
|
Cash and money market funds |
|
$ |
95,395 |
|
$ |
— |
|
$ |
— |
|
$ |
95,395 |
|
|
U.S. Treasury securities |
|
|
84,734 |
|
|
— |
|
|
(107) |
|
|
84,627 |
|
|
Corporate debt securities |
|
|
61,696 |
|
|
20 |
|
|
(175) |
|
|
61,541 |
|
|
Total |
|
|
241,825 |
|
|
20 |
|
|
(282) |
|
|
241,563 |
|
|
Less amounts classified as cash and cash equivalents |
|
|
(95,395) |
|
|
— |
|
|
— |
|
|
(95,395) |
|
|
Total available-for-sale securities |
|
$ |
146,430 |
|
$ |
20 |
|
$ |
(282) |
|
$ |
146,168 |
|
|
|
|
As of December 31, 2014 |
|
||||||||||
|
|
|
|
|
|
Gross |
|
Gross |
|
|
|
|
||
|
Cash and cash equivalents and available-for-sale |
|
Amortized |
|
Unrealized |
|
Unrealized |
|
Estimated |
|
||||
|
securities |
|
Cost |
|
Gains |
|
Losses |
|
Fair Value |
|
||||
|
Cash and money market funds |
|
$ |
83,174 |
|
$ |
— |
|
$ |
— |
|
$ |
83,174 |
|
|
U.S. Treasury securities |
|
|
216,425 |
|
|
35 |
|
|
(63) |
|
|
216,397 |
|
|
Total |
|
|
299,599 |
|
|
35 |
|
|
(63) |
|
|
299,571 |
|
|
Less amounts classified as cash and cash equivalents |
|
|
(83,174) |
|
|
— |
|
|
— |
|
|
(83,174) |
|
|
Total available-for-sale securities |
|
$ |
216,425 |
|
$ |
35 |
|
$ |
(63) |
|
$ |
216,397 |
|
As of December 31, 2015, the Company’s available‑for‑sale securities have original contractual maturities up to 36 months. In response to changes in the availability of and the yield on alternative investments as well as liquidity requirements, the Company may sell securities prior to their stated maturities. As these securities are viewed by the Company as available to support current operations, securities with maturities beyond 12 months are classified as current assets. Due to their short‑term maturities, the Company believes that the fair value of its bank deposits, accounts payable and accrued expenses approximate their carrying value.
Fair Value Measurements
Fair value is defined as the exchange price that would be received for an asset or paid to transfer a liability in the principal or most advantageous market for the asset or liability in an orderly transaction between market participants on the measurement date. Valuation techniques used to measure fair value must maximize the use of observable inputs and minimize the use of unobservable inputs. Three levels of inputs, of which the first two are considered observable and the last unobservable, may be used to measure fair value. The three levels are:
|
· |
Level 1 — Quoted prices in active markets for identical assets or liabilities. |
|
· |
Level 2 — Inputs other than Level 1 that are observable, either directly or indirectly, such as quoted prices for similar assets or liabilities; quoted prices in markets that are not active; or other inputs that are observable or can be corroborated by observable market data for substantially the full term of the assets or liabilities. |
|
· |
Level 3 — Unobservable inputs that are supported by little or no market activity and that are significant to the fair value of the assets or liabilities. |
112
The following table represents the fair value hierarchy for our cash equivalents and available-for-sale securities by major security type (in thousands):
|
|
|
As of December 31, 2015 |
||||||||||
|
|
|
Level 1 |
|
Level 2 |
|
Level 3 |
|
Total |
||||
|
Cash and money market funds |
|
$ |
95,395 |
|
$ |
— |
|
$ |
— |
|
$ |
95,395 |
|
U.S. Treasury securities |
|
|
84,627 |
|
|
— |
|
|
— |
|
|
84,627 |
|
Corporate debt securities |
|
|
— |
|
|
61,541 |
|
|
— |
|
|
61,541 |
|
Total |
|
$ |
180,022 |
|
$ |
61,541 |
|
$ |
— |
|
$ |
241,563 |
|
|
|
As of December 31, 2014 |
||||||||||
|
|
|
Level 1 |
|
Level 2 |
|
Level 3 |
|
Total |
||||
|
Cash and money market funds |
|
$ |
83,174 |
|
$ |
— |
|
$ |
— |
|
$ |
83,174 |
|
U.S. Treasury securities |
|
|
216,397 |
|
|
— |
|
|
— |
|
|
216,397 |
|
Total |
$ |
299,571 |
$ |
— |
$ |
— |
$ |
299,571 | ||||
Note 3. Accounts Receivable
Accounts receivable consist of the following (in thousands):
|
|
|
Balance as of |
|
||||
|
|
|
December 31, |
|
December 31, |
|
||
|
|
|
2015 |
|
2014 |
|
||
|
Qsymia |
|
$ |
8,508 |
|
$ |
6,874 |
|
|
STENDRA/SPEDRA |
|
|
652 |
|
|
4,871 |
|
|
|
|
|
9,160 |
|
|
11,745 |
|
|
Qsymia allowance for cash discounts |
|
|
(163) |
|
|
(150) |
|
|
Net |
|
$ |
8,997 |
|
|
11,595 |
|
There was no allowance for doubtful accounts at December 31, 2015 or 2014.
Note 4. Inventories
Inventories consist of the following (in thousands):
|
Balance as of |
||||||
|
December 31, |
December 31, |
|||||
|
2015 |
2014 |
|||||
|
Raw materials |
$ |
8,645 |
$ |
29,765 | ||
|
Work-in-process |
247 | 889 | ||||
|
Finished goods |
4,282 | 1,544 | ||||
|
Deferred costs |
428 | 2,249 | ||||
|
Inventories |
$ |
13,602 |
$ |
34,447 | ||
Raw materials inventories as of December 31, 2015 consist primarily of the active pharmaceutical ingredients, or API, for Qsymia and STENDRA/SPEDRA. Raw materials inventories as of December 31, 2014 consisted primarily of API for Qsymia. Deferred costs inventories consist primarily of Qsymia and represents Qsymia product shipped to the Company’s wholesalers and certified retail pharmacies, but not yet dispensed to patients through prescriptions, net of prompt payment discounts, and for which recognition of revenue has been deferred.
113
Note 5. Prepaid Expenses and Other Current Assets
Prepaid expenses and other current assets consist of the following (in thousands):
|
|
|
Balance as of |
|
||||
|
|
|
December 31, |
|
December 31, |
|
||
|
|
|
2015 |
|
2014 |
|
||
|
Prepaid sales and marketing expenses |
|
$ |
3,434 |
|
$ |
4,123 |
|
|
Debt issuance costs |
|
|
1,194 |
|
|
1,246 |
|
|
Prepaid insurance |
|
|
1,124 |
|
|
1,612 |
|
|
Other prepaid expenses and assets |
|
|
4,872 |
|
|
5,843 |
|
|
Total |
|
$ |
10,624 |
|
$ |
12,824 |
|
The amounts included in prepaid expenses and other assets consist primarily of prepayments for future services, a receivable from a supplier, prepaid interest and interest income receivable. These costs have been deferred as prepaid expenses and other current assets on the consolidated balance sheets and will be either (i) charged to expense accordingly when the related prepaid services are rendered to the Company, or (ii) converted to cash when the receivable is collected by the Company.
Note 6. Property and Equipment
Property and equipment consist of the following (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
Balance as of |
|
||||
|
|
|
December 31, |
|
December 31, |
|
||
|
|
|
2015 |
|
2014 |
|
||
|
Computers and software |
|
$ |
2,300 |
|
$ |
2,404 |
|
|
Furniture and fixtures |
|
|
943 |
|
|
937 |
|
|
Manufacturing equipment |
|
|
213 |
|
|
213 |
|
|
Leasehold improvements |
|
|
876 |
|
|
876 |
|
|
|
|
|
4,332 |
|
|
4,430 |
|
|
Accumulated depreciation |
|
|
(3,338) |
|
|
(3,084) |
|
|
Property and equipment, net |
|
$ |
994 |
|
$ |
1,346 |
|
Note 7. Non‑Current Assets
Non‑current assets consist of the following (in thousands):
|
|
|
Balance as of |
|
||||
|
|
|
December 31, |
|
December 31, |
|
||
|
|
|
2015 |
|
2014 |
|
||
|
Debt issuance costs |
|
$ |
2,185 |
|
$ |
3,375 |
|
|
Other non-current assets |
|
|
2,616 |
|
|
3,780 |
|
|
Total |
|
$ |
4,801 |
|
$ |
7,155 |
|
The amounts included in other non-current assets primarily consist of patent acquisition and assignment costs (see Note 10).
114
Note 8. Accrued and Other Liabilities
Accrued and other liabilities consist of the following (in thousands):
|
|
|
Balance as of |
|
||||
|
|
|
December 31, |
|
December 31, |
|
||
|
|
|
2015 |
|
2014 |
|
||
|
Accrued employee compensation and benefits |
|
$ |
3,621 |
|
$ |
4,230 |
|
|
Accrued non-recurring charges (see Note 10) |
|
|
503 |
|
|
3,284 |
|
|
Accrued interest on debt (see Note 13) |
|
|
1,293 |
|
|
2,921 |
|
|
Accrued manufacturing costs |
|
|
5,408 |
|
|
400 |
|
|
Other accrued liabilities |
|
|
5,066 |
|
|
5,479 |
|
|
Total |
|
$ |
15,891 |
|
$ |
16,314 |
|
The amounts included in other accrued liabilities consist of obligations primarily related to sales, marketing, research, clinical development, corporate activities and royalties, including a payable to Endo related to the royalty revenue adjustment.
Note 9. Non‑Current Accrued and Other Liabilities
Non‑current accrued and other liabilities were $1.3 million and $1.6 million at December 31, 2015 and 2014, respectively, and were primarily comprised of deferred rent and costs associated with the exit of certain operating leases and security deposits relating to the sublease agreements (see Note 10).
Note 10. Inventory Impairment and Other Non-Recurring Charges
Inventory impairment and other non-recurring charges consist of the following (in thousands):
|
|
|
Year Ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Inventory impairment (see Note 4) |
|
$ |
29,522 |
|
$ |
2,170 |
|
$ |
10,225 |
|
|
Employee severance and related costs |
|
|
2,503 |
|
|
1,711 |
|
|
8,546 |
|
|
Patent settlement |
|
|
— |
|
|
1,949 |
|
|
— |
|
|
Share-based compensation (see Note 15) |
|
|
36 |
|
|
343 |
|
|
14,072 |
|
|
Proxy contest expenses |
|
|
— |
|
|
— |
|
|
8,863 |
|
|
Operating lease termination costs |
|
|
— |
|
|
— |
|
|
1,210 |
|
|
Total inventory impairment and other non-recurring expense |
|
$ |
32,061 |
|
$ |
6,173 |
|
$ |
42,916 |
|
As discussed in Note 4, in 2015 the Company recorded inventory impairment charges primarily for Qsymia API inventory in excess of expected demand. In 2014, the Company recorded inventory impairment charges for finished goods and certain non-API raw materials on hand in excess of demand and, in 2013, the Company recorded inventory impairment charges for inventories on hand in excess of demand, plus a purchase commitment fee.
In 2015, the Company recorded employee severance and related costs and share-based compensation related to the July 2015 corporate restructuring plan, which reduced the Company’s workforce by approximately 60 job positions. In 2014 and 2013, the Company recorded employee severance and related costs, share-based compensation and operating lease termination costs related to the 2013 cost reduction plan that reduced the Company’s workforce by approximately 20 employees.
115
In 2014, the Company paid $5.0 million in connection with the transfer and assignment of certain patents from Janssen Pharmaceuticals, Inc. Of the $5.0 million, approximately $1.9 million was recognized as a non-recurring expense for the year ended December 31, 2014 as it related to a legal settlement. The remaining balance of approximately $3.1 million was recorded as an intangible asset and is being amortized as cost of goods sold through their expiration dates.
In 2013, the Company entered into a settlement agreement with First Manhattan in connection with a proxy contest related to the Company’s 2013 Annual Meeting of Stockholders. According to the terms of the settlement agreement, more than a majority of the members of the Company’s Board of Directors resigned and new members were appointed. The change in the majority of the members of the Company’s Board of Directors, effective July 19, 2013, triggered certain “change of control” benefits in accordance with the terms of various agreements with certain of the Company’s employees. Under these agreements, all unvested stock options held by these employees automatically vested in full and became immediately exercisable. In addition, the resignations of both the Company’s Chief Executive Officer and President resulted in severance charges under these agreements. As part of the settlement agreement with First Manhattan, the Company paid the reasonable and documented expenses incurred by First Manhattan in connection with its proxy contest.
The following table sets forth activity for the proxy contest and cost reduction plans, the balance of which is primarily comprised of employee severance costs (in thousands):
|
|
|
Proxy |
|
|
|
Facilities- |
|
|
|
||||
|
|
|
contest |
|
Severance |
|
related |
|
|
|
||||
|
|
|
costs |
|
obligations |
|
obligations |
|
Total |
|
||||
|
Balance of accrued costs at December 31, 2012 |
|
$ |
— |
|
$ |
— |
|
$ |
— |
|
$ |
— |
|
|
Charges |
|
|
8,863 |
|
|
8,546 |
|
|
1,210 |
|
|
18,619 |
|
|
Payments |
|
|
(8,863) |
|
|
(2,037) |
|
|
(188) |
|
|
(11,088) |
|
|
Balance of accrued costs at December 31, 2013 |
|
|
— |
|
|
6,509 |
|
|
1,022 |
|
|
7,531 |
|
|
Charges |
|
|
— |
|
|
1,711 |
|
|
— |
|
|
1,711 |
|
|
Payments |
|
|
— |
|
|
(4,940) |
|
|
(450) |
|
|
(5,390) |
|
|
Balance of accrued costs at December 31, 2014 |
|
|
— |
|
|
3,280 |
|
|
572 |
|
|
3,852 |
|
|
Charges |
|
|
— |
|
|
2,474 |
|
|
— |
|
|
2,474 |
|
|
Payments |
|
|
— |
|
|
(5,344) |
|
|
(101) |
|
|
(5,445) |
|
|
Balance of accrued costs at December 31, 2015 |
|
$ |
— |
|
$ |
410 |
|
$ |
471 |
|
$ |
881 |
|
|
(1) |
The accrued facilities-related costs at December 31, 2015 represent estimated losses, net of expected subleases, on space vacated as part of the Company’s cost reduction plan. The noncancelable operating leases and scheduled payments against the amounts accrued extend through May 2020, unless the Company is able to negotiate earlier terminations. |
|
(2) |
In addition to the above non-recurring charges, the Company incurred non-cash share-based compensation expense of $0.3 million and $14.1 million for the years ended December 31, 2014 and 2013, respectively (see Note 15). |
Commencing in May 2014, the Company subleased a portion of its Evelyn Lease consisting of approximately 14,105 square feet of space for a term of 36 months at a starting annual rental rate of $42 per square feet (subject to agreed increases). The sublessee received an abatement of monthly installments of rents for months one through four. Minimum rents expected to be received under this sublease as of December 31, 2015 are $626,000 and $212,000 in fiscal years 2016 and 2017, respectively. Upon the completion of the sublease for this space, the Company expects to either find usage or to locate a suitable sublessee for the remaining duration of the Company’s Evelyn Lease.
Commencing in September 2014, the Company subleased the expansion space relating to the Castro Lease. The sublease consists of approximately 4,914 square feet of space for a term of 31 months at a starting annual rental rate of $53 per square feet (subject to agreed increases). The sublessee received an abatement of the first monthly installment. Minimum rents expected to be received under this sublease as of December 31, 2015 are $274,000 and $69,000 in fiscal years 2016 and 2017, respectively.
116
Of the total accrued employee severance and facilities-related costs as of December 31, 2015, $0.5 million is included under current liabilities in “Accrued and other liabilities" and $0.4 million is included in “Non‑current accrued and other liabilities.”
The balance of the accrued employee severance and facilities-related costs at December 31, 2015 is anticipated to be paid out as follows (in thousands):
|
2016 |
|
$ |
503 |
|
|
2017 |
|
|
351 |
|
|
2018 |
|
|
11 |
|
|
Thereafter |
|
|
16 |
|
|
|
|
$ |
881 |
|
Note 11. Deferred Revenue
Deferred revenue consists of the following (in thousands):
|
Balance as of |
||||||
|
December 31, |
December 31, |
|||||
|
2015 |
2014 |
|||||
|
Qsymia deferred revenue - current |
$ |
19,275 |
$ |
16,433 | ||
|
SPEDRA deferred revenue - current |
2,867 | 3,012 | ||||
|
Deferred revenue - current |
$ |
22,142 |
$ |
19,445 | ||
|
SPEDRA deferred revenue - non-current |
$ |
6,508 |
$ |
8,876 | ||
Qsymia deferred revenue consists of product shipped to the Company’s wholesalers, certified retail pharmacies and certified home delivery pharmacy services networks, but not yet dispensed to patients through prescriptions, net of prompt payment discounts. SPEDRA deferred revenue relates to a prepayment for future royalties on sales of SPEDRA.
Note 12. License, Commercialization and Supply Agreements
During 2013, the Company entered into license and commercialization agreements and commercial supply agreements with the Menarini Group, through its subsidiary Berlin Chemie AG, or Menarini, Auxilium Pharmaceuticals, Inc., or Auxilium, and Sanofi and its affiliate, or Sanofi, to commercialize and promote STENDRA or SPEDRA in their respective territories. Menarini’s territory consists of over 40 European countries, including the EU, plus Australia and New Zealand. Auxilium’s territory consists of the United States and Canada and their respective territories. In January 2015, Auxilium was purchased by Endo International, plc. In December 2015, Auxilium notified the Company of Auxilium’s intention to return the U.S. and Canadian commercial rights for STENDRA to the Company. Auxilium has provided its contractually required six-month notice of termination which, absent an agreement between Auxilium and us for an earlier termination date, will result in the termination of the license agreement and supply agreement on June 30, 2016. Sanofi’s territory consists of Africa, the Middle East, Turkey and Eurasia.
Note 13. Long‑Term Debt
Convertible Senior Notes Due 2020
In May 2013, the Company closed an offering of $220.0 million in 4.5% Convertible Senior Notes due May 2020, or the Convertible Notes. The Convertible Notes are governed by an indenture, dated May 2013 between the
117
Company and Deutsche Bank National Trust Company, as trustee. In May 2013, the Company closed on an additional $30.0 million of Convertible Notes upon exercise of an option by the initial purchasers of the Convertible Notes at a conversion rate of approximately $14.86 per share. Total net proceeds from the Convertible Notes were approximately $241.8 million. The Convertible Notes are convertible at the option of the holders under certain conditions at any time prior to the close of business on the business day immediately preceding November 1, 2019. On or after November 1, 2019, holders may convert all or any portion of their Convertible Notes at any time at their option at the conversion rate then in effect, regardless of these conditions. Subject to certain limitations, the Company will settle conversions of the Convertible Notes by paying or delivering, as the case may be, cash, shares of its common stock or a combination of cash and shares of our common stock, at the Company’s election. Interest payments are made quarterly.
For the year ended December 31, 2015, total interest expense related to the Convertible Notes was $27.2 million, including amortization of $16.0 million of the debt discount and $848,000 of deferred financing costs. For the year ended December 31, 2014, total interest expense related to the Convertible Notes was $25.0 million, including amortization of $14.7 million of the debt discount and $784,000 of deferred financing costs.
Senior Secured Notes Due 2018
In March 2013, the Company entered into the Purchase and Sale Agreement between the Company and BioPharma Secured Investments III Holdings Cayman LP, a Cayman Islands exempted limited partnership, providing for the purchase of a debt‑like instrument, or the Senior Secured Notes. Under the agreement, the Company received $50 million, less $500,000 in funding and facility payments, at the initial closing in April 2013. The Company had the option, but elected not to exercise it, to receive an additional $60 million, less $600,000 in a funding payment, at a secondary closing no later than January 15, 2014. The scheduled quarterly payments on the Senior Secured Notes are subject to the net sales of (i) Qsymia and (ii) any other obesity agent developed or marketed by us or our affiliates or licensees. The scheduled quarterly payments, other than the payment(s) scheduled to be made in the second quarter of 2018, are capped at the lower of the scheduled payment amounts or 25% of the net sales of (i) and (ii) above. Accordingly, if 25% of the net sales is less than the scheduled quarterly payment, then 25% of the net sales is due for that quarter, with the exception of the payment(s) scheduled to be made in the second quarter of 2018, when any unpaid scheduled quarterly payments plus any accrued and unpaid make whole premiums must be paid. Any quarterly payment less than the scheduled quarterly payment amount will be subject to a make whole premium equal to the applicable scheduled quarterly payment of the preceding quarter less the actual payment made to BioPharma for the preceding quarter multiplied by 1.03. The Company may elect to pay full scheduled quarterly payments if it chooses.
For the year ended December 31, 2015, the interest expense related to the Senior Secured Notes was $6.3 million, including amortization of deferred financing costs amounting to $393,000. For the year ended December 31, 2014, the interest expense related to the Senior Secured Notes was $7.5 million, including amortization of deferred financing costs amounting to $468,000.
118
The following table summarizes information on the debt (in thousands) as of December 31, 2015:
|
|
|
December 31, |
|
|
|
|
|
2015 |
|
|
|
|
|
|
|
|
|
Convertible Senior Notes due 2020 |
|
$ |
250,000 |
|
|
Senior Secured Notes due 2018 |
|
|
41,002 |
|
|
|
|
|
291,002 |
|
|
Less: Discount on convertible senior notes |
|
|
(56,233) |
|
|
|
|
|
234,769 |
|
|
Less: Current portion |
|
|
(15,550) |
|
|
Long-term debt, net of current portion |
|
$ |
219,219 |
|
|
|
|
|
|
|
|
Future estimated payments on debt as of December 31, 2015 are as follows: |
|
|
|
|
|
|
|
|
|
|
|
2016 |
|
|
31,250 |
|
|
2017 |
|
|
31,250 |
|
|
2018 |
|
|
20,103 |
|
|
Total |
|
|
82,603 |
|
|
Less: Interest portion |
|
|
(41,601) |
|
|
Senior Secured Notes |
|
$ |
41,002 |
|
Note 14. Stockholders’ Equity
Common Stock
The Company is authorized to issue 200,000,000 shares of common stock. As of December 31, 2015 and 2014, there were 104,055,000 and 103,729,000 shares, respectively, issued and outstanding.
Preferred Stock
The Company is authorized to issue 5,000,000 shares of undesignated preferred stock with a par value of $1.00 per share. As of December 31, 2015 and 2014, there were no preferred shares issued or outstanding. The Company may issue shares of preferred stock in the future, without stockholder approval, upon such terms as the Company’s management and Board of Directors may determine.
Stockholder Rights Plan
On March 26, 2007, the Board of Directors of the Company adopted a Stockholder Rights Plan, or the Rights Plan, and amended its bylaws. Under the Rights Plan, the Company will issue a dividend of one right for each share of its common stock held by stockholders of record as of the close of business on April 13, 2007.
The Rights Plan is designed to guard against partial tender offers and other coercive tactics to gain control of the Company without offering a fair and adequate price and terms to all of the Company’s stockholders. The Rights Plan is intended to provide the Board of Directors with sufficient time to consider any and all alternatives to such an action and is similar to plans adopted by many other publicly traded companies. The Rights Plan was not adopted in response to any efforts to acquire the Company and the Company is not aware of any such efforts.
Each right will initially entitle stockholders to purchase a fractional share of the Company’s preferred stock for $26.00. However, the rights are not immediately exercisable and will become exercisable only upon the occurrence of certain events. If a person or group acquires, or announces a tender or exchange offer that would result in the acquisition of 15% or more of the Company’s common stock while the Stockholder Rights Plan remains in place, then, unless the rights are redeemed by the Company for $.001 per right, the rights will become exercisable by all rights holders except the acquiring person or group for the Company’s shares or shares of the third‑party acquirer having a value of twice the
119
right’s then‑current exercise price. The Rights will expire on the earliest of (i) April 13, 2017 (the final expiration date), or (ii) redemption or exchange of the Rights.
Note 15. Stock Option and Purchase Plans
Stock Option Plan
On March 29, 2010, the Company’s Board of Directors terminated the 2001 Stock Option Plan and adopted and approved a new 2010 Equity Incentive Plan, or the 2010 Plan, with 32,000 shares remaining reserved and unissued under the 2001 Plan, subject to the approval of the Company’s stockholders. The 2001 Plan, however, continues to govern awards previously granted under it. On June 25, 2010, the Company’s stockholders approved the 2010 Plan at the Company’s 2010 Annual Meeting of Stockholders. The 2010 Plan provides for the grant of stock options, stock appreciation rights, restricted stock, restricted stock units, performance shares and performance units to employees, directors and consultants, to be granted from time to time as determined by the Board of Directors, the Compensation Committee of the Board of Directors, or its designees. The term of the option is determined by the Board of Directors on the date of grant but shall not be longer than 10 years. Options under this plan generally vest over four years. The 2010 Plan’s share reserve, which the stockholders approved, is 8,400,000 shares, plus any shares reserved but not issued pursuant to awards under the 2001 Plan as of the date of stockholder approval, or 99,975 shares, plus any shares subject to outstanding awards under the 2001 Plan that expire or otherwise terminate without having been exercised in full, or are forfeited to or repurchased by the Company, up to a maximum of 8,111,273 shares (which was the number of shares subject to outstanding options under the 2001 Plan as of March 11, 2010). In September 2014, the Company’s stockholders approved an increase to the total number of shares reserved under the 2010 Plan by 5,950,000 for a total of 14,350,000 shares.
Restricted Stock Units
Beginning in 2012, the Company began issuing restricted units under the 2010 Plan on a limited basis. A summary of restricted stock unit award activity under the 2010 Plan is as follows:
|
|
|
|
|
|
|
|
|
|
|
|
|
Weighted |
|
|
|
|
|
Number of |
|
Average |
|
|
|
|
|
Restricted |
|
Grant Date |
|
|
|
|
|
Stock Units |
|
Fair Value |
|
|
|
Restricted stock units outstanding January 1, 2013 |
|
35,000 |
|
$ |
24.88 |
|
|
Granted |
|
144,500 |
|
|
12.63 |
|
|
Vested |
|
(33,296) |
|
|
14.15 |
|
|
Forfeited |
|
(146,204) |
|
|
13.83 |
|
|
Restricted stock units outstanding, December 31, 2012 |
|
— |
|
|
— |
|
|
Granted |
|
521,900 |
|
|
8.20 |
|
|
Vested |
|
(70,500) |
|
|
8.37 |
|
|
Forfeited |
|
(117,900) |
|
|
8.17 |
|
|
Restricted stock units outstanding December 31, 2014 |
|
333,500 |
|
|
8.17 |
|
|
Granted |
|
1,954,000 |
|
|
1.85 |
|
|
Vested |
|
(248,688) |
|
|
2.73 |
|
|
Forfeited |
|
(628,937) |
|
|
7.99 |
|
|
Restricted stock units outstanding, December 31, 2015 |
|
1,409,875 |
|
$ |
1.87 |
|
120
Stock Options
A summary of stock option award activity under these plans is as follows:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Years Ended December 31, |
|
|||||||||||||
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||||||||
|
|
|
|
|
Weighted- |
|
|
|
Weighted- |
|
|
|
Weighted- |
|
|||
|
|
|
|
|
Average |
|
|
|
Average |
|
|
|
Average |
|
|||
|
|
|
Number of |
|
Exercise |
|
Number of |
|
Exercise |
|
Number of |
|
Exercise |
|
|||
|
|
|
Shares |
|
Price |
|
Shares |
|
Price |
|
Shares |
|
Price |
|
|||
|
Balance at beginning of year |
|
5,956,459 |
|
$ |
12.09 |
|
8,906,451 |
|
$ |
12.06 |
|
8,510,917 |
|
$ |
10.33 |
|
|
Options: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Granted |
|
3,499,200 |
|
$ |
2.46 |
|
935,800 |
|
$ |
6.89 |
|
4,166,292 |
|
$ |
12.86 |
|
|
Exercised |
|
— |
|
$ |
— |
|
(374,530) |
|
$ |
4.48 |
|
(2,375,688) |
|
$ |
5.79 |
|
|
Cancelled |
|
(3,733,554) |
|
$ |
9.38 |
|
(3,511,262) |
|
$ |
11.45 |
|
(1,395,070) |
|
$ |
14.54 |
|
|
Balance at end of year |
|
5,722,105 |
|
$ |
7.97 |
|
5,956,459 |
|
$ |
12.09 |
|
8,906,451 |
|
$ |
12.06 |
|
|
Exercisable at end of year |
|
3,042,888 |
|
$ |
11.48 |
|
4,053,329 |
|
$ |
12.34 |
|
6,616,555 |
|
$ |
11.00 |
|
|
Weighted average grant-date fair value of options granted during the year |
|
|
|
$ |
1.44 |
|
|
|
$ |
4.34 |
|
|
|
$ |
8.32 |
|
At December 31, 2015, stock options were outstanding and exercisable as follows:
|
|
|
|
|
|
|
Options Outstanding |
|
Options Exercisable |
|
||||||||
|
|
|
|
|
|
|
|
|
Weighted- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Number |
|
Average |
|
Weighted- |
|
Number |
|
Weighted- |
|
||
|
|
|
|
|
|
|
Outstanding at |
|
Remaining |
|
Average |
|
Exercisable |
|
Average |
|
||
|
|
|
|
|
|
|
December 31, |
|
Contractual |
|
Exercise |
|
December 31, |
|
Exercise |
|
||
|
Range of Exercise Prices |
|
2015 |
|
Life |
|
Price |
|
2015 |
|
Price |
|
||||||
|
$ |
1.26 |
— |
$ |
2.53 |
|
700,500 |
|
6.45 |
years |
$ |
1.44 |
|
118,747 |
|
$ |
2.33 |
|
|
$ |
2.74 |
— |
$ |
2.74 |
|
1,550,800 |
|
6.06 |
years |
$ |
2.74 |
|
— |
|
$ |
— |
|
|
$ |
2.79 |
— |
$ |
12.04 |
|
1,524,513 |
|
3.62 |
years |
$ |
7.56 |
|
1,291,467 |
|
$ |
7.79 |
|
|
$ |
12.39 |
— |
$ |
25.74 |
|
1,946,292 |
|
4.90 |
years |
$ |
14.80 |
|
1,632,674 |
|
$ |
15.06 |
|
|
$ |
1.26 |
— |
$ |
25.74 |
|
5,722,105 |
|
5.06 |
years |
$ |
7.97 |
|
3,042,888 |
|
$ |
11.48 |
|
The aggregate intrinsic value of outstanding options as of December 31, 2015 was zero as all of the outstanding stock options had an exercise price greater than the share price of common stock as of that date.
At December 31, 2015, 8,585,900 options remained available for grant.
Valuation Assumptions
The fair value of each option is estimated on the date of grant using the Black‑Scholes option pricing model, assuming no expected dividends and the following weighted average assumptions:
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
2013 |
|
|
Expected life (in years) |
|
4.69 |
|
4.84 |
|
4.88 |
|
|
Volatility |
|
70.8 |
% |
79.1 |
% |
83.4 |
% |
|
Risk-free interest rate |
|
1.28 |
% |
1.74 |
% |
1.12 |
% |
|
Dividend yield |
|
— |
|
— |
|
— |
|
Employee Stock Purchase Plan
Under the 1994 Employee Stock Purchase Plan, or the ESPP, the Company reserved 800,000 shares of common stock for issuance to employees pursuant to the ESPP, under which eligible employees may authorize payroll deductions
121
of up to 10% of their base compensation (as defined) to purchase common stock at a price equal to 85% of the lower of the fair market value as of the beginning or the end of the offering period.
At the annual meeting held on June 4, 2003, the stockholders approved amendments to the ESPP to (i) extend the original term of the ESPP by an additional 10 years such that the ESPP would expire in April 2014 (subject to earlier termination as described in the ESPP) and (ii) increase the number of shares of common stock reserved for issuance under the ESPP by 600,000 shares to a new total of 1,400,000.
In June 2011, the Company’s stockholders approved amendments to the Company’s ESPP to increase the number of shares reserved for issuance under the ESPP by 600,000 shares to a new total of 2,000,000, to remove the Plan’s 20–year term, and to include certain changes consistent with Treasury Regulations relating to employee stock purchase plans under Section 423 of the Internal Revenue Code of 1986, as amended, and other applicable law.
As of December 31, 2015, 1,691,809 shares have been issued to employees and there are 308,191 shares available for issuance under the ESPP. The weighted average fair value of shares issued under the ESPP in 2015, 2014 and 2013 was $0.69, $1.05 and $3.53 per share, respectively.
Valuation Assumptions
The fair value of shares issued under the ESPP is estimated using the Black‑Scholes option pricing model, assuming no expected dividends and the following weighted average assumptions:
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
2013 |
|
|
Expected life (in years) |
|
0.5 |
|
0.5 |
|
0.5 |
|
|
Volatility |
|
63.4 |
% |
44.9 |
% |
54.2 |
% |
|
Risk-free interest rate |
|
0.2 |
% |
0.1 |
% |
0.1 |
% |
|
Dividend yield |
|
— |
|
— |
|
— |
|
Share‑Based Compensation Expense
Total estimated share‑based compensation expense, related to all of the Company’s share‑based awards, was comprised as follows (in thousands):
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Cost of goods sold |
|
$ |
132 |
|
$ |
118 |
|
$ |
— |
|
|
Selling, general and administrative |
|
|
2,862 |
|
|
1,177 |
|
|
2,361 |
|
|
Research and development |
|
|
398 |
|
|
8,128 |
|
|
15,964 |
|
|
Non-recurring charges |
|
|
198 |
|
|
343 |
|
|
14,072 |
|
|
Total share-based compensation expense |
|
$ |
3,590 |
|
$ |
9,766 |
|
$ |
32,397 |
|
On July 18, 2013, the Company entered into a settlement agreement with First Manhattan Company, or First Manhattan, in connection with a proxy contest related to the Company’s 2013 Annual Meeting of Stockholders. According to the terms of the settlement agreement, more than a majority of the members of the Company’s Board of Directors resigned and new members were appointed. The change in the majority of the members of the Company’s Board of Directors, effective July 19, 2013, triggered certain “change of control” benefits in accordance with the various agreements with certain of the Company’s employees; specifically, all unvested stock options held by these employees automatically vested in full and became immediately exercisable. In accordance with ASC 718, all unamortized expense for options that were expected to vest on the date of grant and the modified fair value of the options that were not expected to vest on the date of grant (due to expected forfeitures) were immediately expensed. As a result, for the year ended December 31, 2013, the Company recognized approximately $12.9 million in additional share‑based compensation expense related to this event.
As part of the Company’s ongoing efforts to reduce costs by eliminating expenses that are not essential to expanding the use of Qsymia, the Company implemented a cost reduction plan that reduced the Company’s workforce
122
by approximately 20 employees, or 17% of its workforce, excluding the sales force, for the year ended December 31, 2013. As a result, the Company incurred $1.2 million in additional share‑based compensation expense for the year ended December 31, 2013, related to the automatic acceleration of vesting of unvested stock options held by the terminated employees.
Total share‑based compensation cost capitalized as part of the cost of inventory was $23,000, $0 and $480,000 for the years ended December 31, 2015, 2014 and 2013, respectively.
The following table summarizes share‑based compensation, net of estimated forfeitures associated with each type of award (in thousands):
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Restricted stock units |
|
$ |
1,409 |
|
$ |
1,334 |
|
$ |
471 |
|
|
Stock options |
|
|
2,143 |
|
|
8,305 |
|
|
31,610 |
|
|
Employee stock purchase plan |
|
|
38 |
|
|
127 |
|
|
316 |
|
|
|
|
$ |
3,590 |
|
$ |
9,766 |
|
$ |
32,397 |
|
As of December 31, 2015, unrecognized estimated compensation expense totaled $6.1 million related to non‑vested stock options and restricted stock units and $10,000 related to the ESPP. The weighted average remaining requisite service period for the non‑vested stock options was 2.6 years and for the ESPP was less than 6 months.
Note 16. Commitments
Lease Commitments
In November 2006, the Company entered into a 30-month lease for its former corporate headquarters located in Mountain View, California, or Castro Lease. On February 14, 2012, the Company entered into the most current, fourth amendment to the Castro Lease. Under the fourth amendment to the Castro Lease, the lease term for the headquarters’ premises terminated July 31, 2013. The fourth amendment also included a new lease on an additional 4,914 square feet of office space located at 1174 Castro Street, Mountain View, California, or the Expansion Space, which is adjacent to the Company’s former corporate headquarters. The average base rent for the Expansion Space is approximately $2.87 per square foot or $14,124 per month. The new lease for the Expansion Space has a term of 60 months commencing March 15, 2012, with an option to extend the term for one year from the expiration of the new lease. Commencing on September 1, 2014, the Company subleased the expansion space for a term of 31 months at a starting monthly rental rate of $4.42 per square feet (subject to agreed increases). The sublessee is entitled to abatement of the first monthly installment. Minimum rents expected to be received under this sublease are $274,000 and $69,000 for the years ending December 31, 2016 and 2017, respectively.
The Company entered into a lease effective as of December 11, 2012, with SFERS Real Estate Corp. U, or the Landlord, for new principal executive offices, consisting of an approximately 45,240 square foot building, located at 351 East Evelyn Avenue, Mountain View, California, or the Evelyn Lease. The Evelyn Lease has an initial term of approximately 84 months, commencing on May 11, 2013, and at a starting annual rental rate of $31.20 per rentable square foot (subject to agreed increases). The Company is entitled to an abatement of the monthly installments of rent for months seven through 12 of the initial term subject to the conditions detailed in the Evelyn Lease. The Company has one option to renew the Evelyn Lease for a term of three years at the prevailing market rate as detailed in the Evelyn Lease. In addition, the Company has a one–time right to accelerate the termination date of the Evelyn Lease from the expiration of the 84th full calendar month of the term to the expiration of the 60th full calendar month of the term subject to the conditions detailed in the Evelyn Lease. If this acceleration of the termination date is exercised, the following will be payable to the Landlord: (i) six months of the monthly installments of rent and the Company’s proportionate share of expenses and taxes subject to the fifth lease year and (ii) the unamortized portion of all of the following: (a) any leasing commissions and legal fees, (b) the initial alterations as detailed in the Evelyn Lease, and (c) Landlord’s allowance towards the cost of performing the initial alterations, which is $7.00 per rentable square foot; provided that the amount payable to the Landlord will be increased by the unamortized portion of any leasing commissions, tenant improvements
123
and allowances, or other concessions incurred by the Landlord in connection with any additional space other than the premises leased by the Company and that is subject to acceleration under the Evelyn Lease.
Commencing on May 1, 2014, the Company subleased a portion of its Evelyn Lease consisting of approximately 14,105 square feet of space for a term of 36 months at a starting annual rental rate of $42 per square feet (subject to agreed increases). The sublessee is entitled to abatement of monthly installments of rents for months one through four. Minimum rents expected to be received under this sublease are $626,000 and $212,000 for the years ending December 31, 2016 and 2017, respectively. Upon the completion of the sublease for this space, the Company expects to either find usage or to locate a suitable sublessee for the remaining duration of the Company’s Evelyn Lease.
Future minimum lease payments under operating leases at December 31, 2015, were as follows (in thousands):
|
2016 |
|
$ |
2,164 |
|
|
2017 |
|
|
1,989 |
|
|
2018 |
|
|
1,991 |
|
|
2019 |
|
|
2,040 |
|
|
2020 |
|
|
685 |
|
|
|
|
$ |
8,869 |
|
Included in the operating lease commitments above are obligations under leases for which the Company has vacated the underlying facilities as part of a cost reduction plan. These leases expire at various dates through 2020 and represent an aggregate obligation of $3.6 million through 2020. The Company has cost reduction accruals of $0.5 million at December 31, 2015, which represents the difference between this aggregate future obligation and expected future sublease income under estimated potential sublease agreements, as well as other facilities‑related obligations (see Note 10). Rent expense under operating leases was $2.1 million, $1.6 million and $2.9 million for the years ended December 31, 2015, 2014 and 2013, respectively.
As a condition of the FDA granting approval to commercialize Qsymia in the U.S., the Company agreed to complete certain post-marketing requirements (“PMRs”). One requirement was to perform a cardiovascular outcomes trial (“CVOT”), on Qsymia. The cost of a CVOT is estimated to be between $180 million and $220 million incurred over a period of approximately five years. The Company is working with the FDA to determine a pathway to provide the FDA with information to support the safety of Qsymia in a more cost effective manner. To date, the Company has not incurred expenses related to the CVOT.
.
124
Note 17. Income Taxes
Deferred income taxes result from differences in the recognition of expenses for tax and financial reporting purposes, as well as operating loss and tax credit carryforwards. Significant components of the Company’s deferred income tax assets as of December 31, 2015 and 2014, are as follows (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
||
|
Deferred tax assets: |
|
|
|
|
|
|
|
|
Net operating loss carry forwards |
|
$ |
235,714 |
|
$ |
219,786 |
|
|
Research and development credit carry forwards |
|
|
16,562 |
|
|
16,464 |
|
|
Share-based compensation |
|
|
7,939 |
|
|
10,298 |
|
|
Accruals and other |
|
|
20,589 |
|
|
9,502 |
|
|
Depreciation |
|
|
104 |
|
|
128 |
|
|
Deferred revenue |
|
|
3,492 |
|
|
4,146 |
|
|
|
|
|
284,400 |
|
|
260,324 |
|
|
Valuation allowance |
|
|
(284,400) |
|
|
(260,324) |
|
|
Total |
|
$ |
— |
|
$ |
— |
|
The net increase in the valuation allowance for the years ended December 31, 2015 and 2014, was $24.1 million, and $2.7 million respectively. As of December 31, 2015, the Company had no significant deferred tax liabilities.
As of December 31, 2015, the Company had approximately $675.6 million and $301.5 million of net operating loss, or NOL, carryforwards with which to offset its future taxable income for federal and state income tax reporting purposes, respectively. The federal and state NOL carryforwards will begin expiring in 2022 and 2028, respectively, unless previously utilized.
As of December 31, 2015, the Company has federal and state research credit carryforwards of approximately $13.2 million, and $5.2 million, respectively. The federal research credit carryforwards will begin expiring in 2018, unless previously utilized. The state research credit carryforwards do not expire.
Utilization of the Company’s NOL and tax credit carryforwards, or Tax Attributes, may be subject to substantial annual limitations provided by the Internal Revenue Code and similar state provisions to the extent certain ownership changes are deemed to occur. Such an annual limitation could result in the expiration of the Tax Attributes before utilization. The Tax Attributes reflected above have not been reduced by any limitations. To the extent it is determined upon completion of the analysis that such limitations do apply, the Company will adjust the Tax Attributes accordingly. The Company faces the risk that its ability to use its Tax Attributes will be substantially restricted if it undergoes an “ownership change” as defined in Section 382 of the U.S. Internal Revenue Code, or Section 382.
An ownership change under Section 382 would occur if “5-percent shareholders,” within the meaning of Section 382, collectively increased their ownership in the Company by more than 50 percentage points over a rolling three-year period. The Company has completed studies through December 31, 2015 and concluded that no adjustments were required. If the Company has experienced a change of control at any time since its formation, its NOL carryforwards and tax credits may not be available, or their utilization could be subject to an annual limitation under Section 382. A full valuation allowance has been provided against the Company’s NOL carryforwards, and if an adjustment is required, this adjustment would be offset by an adjustment to the valuation allowance. Accordingly, there would be no impact on the consolidated financial statements.
The Company uses the with-and-without approach described in guidance which has been incorporated into ASC 740 Income Taxes to determine the recognition and measurement of excess tax benefits. Accordingly, the Company has elected to recognize excess income tax benefits from stock option exercises in additional paid-in capital only if an incremental income tax benefit would be realized after considering all other tax attributes presently available to the Company. As of December 31, 2015, the amount of excess tax benefits from stock options included in federal and state net operating losses is $48.4 million and $9.9 million, respectively. The impact of this excess tax benefit is recognized as additional paid-in capital when it reduces taxes payable. In addition, the Company has elected to account for the
125
indirect effects of stock-based awards on other tax attributes, such as the research and alternative minimum tax credits, through the consolidated statement of operations.
The provision (benefit) for income taxes is based upon the loss from continuing operations before income taxes as follows (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Loss before income taxes: |
|
|
|
|
|
|
|
|
|
|
|
Domestic |
|
$ |
(92,967) |
|
$ |
(83,151) |
|
$ |
(174,083) |
|
|
International |
|
|
(137) |
|
|
(125) |
|
|
(766) |
|
|
Loss before taxes |
|
$ |
(93,104) |
|
$ |
(83,276) |
|
$ |
(174,849) |
|
The provision (benefit) for income taxes consists of the following (in thousands):
Continuing Operations:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Current: |
|
|
|
|
|
|
|
|
|
|
|
Federal |
|
$ |
— |
|
$ |
— |
|
$ |
— |
|
|
State |
|
|
3 |
|
|
(629) |
|
|
97 |
|
|
Foreign |
|
|
— |
|
|
— |
|
|
— |
|
|
Total current provision (benefit) for income taxes |
|
$ |
3 |
|
$ |
(629) |
|
$ |
97 |
|
|
Deferred: |
|
|
|
|
|
|
|
|
|
|
|
Federal |
|
$ |
— |
|
$ |
— |
|
$ |
— |
|
|
State |
|
|
— |
|
|
— |
|
|
— |
|
|
Foreign |
|
|
— |
|
|
— |
|
|
— |
|
|
Total deferred provision for income taxes |
|
$ |
— |
|
$ |
— |
|
$ |
— |
|
|
Total provision (benefit) for income taxes from continuing operations |
|
$ |
3 |
|
$ |
(629) |
|
$ |
97 |
|
The effective tax rate differs from the amount computed by applying the statutory federal income tax rates as follows:
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
2013 |
|
|
Tax at U.S. federal statutory rate |
|
(35) |
% |
(35) |
% |
(35) |
% |
|
Change in valuation allowance |
|
31 |
|
29 |
|
35 |
|
|
Permanent items |
|
6 |
|
7 |
|
2 |
|
|
Tax credits |
|
— |
|
— |
|
(1) |
|
|
Other |
|
(2) |
|
(2) |
|
(1) |
|
|
Effective tax rate |
|
— |
% |
(1) |
% |
— |
% |
126
The reconciliation of the beginning and ending amount of unrecognized tax benefits is as follows (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
2013 |
|
|||
|
Unrecognized tax benefits as of January 1 |
|
$ |
— |
|
$ |
1,662 |
|
$ |
1,215 |
|
|
Gross increase/(decrease) for tax positions of prior years |
|
|
— |
|
|
— |
|
|
447 |
|
|
Gross increase/(decrease) for tax positions of current year |
|
|
38 |
|
|
— |
|
|
— |
|
|
Settlements |
|
|
— |
|
|
(1,662) |
|
|
— |
|
|
Lapse of statute of limitations |
|
|
— |
|
|
— |
|
|
— |
|
|
Unrecognized tax benefits balance at December 31 |
|
$ |
38 |
|
$ |
— |
|
$ |
1,662 |
|
The remaining balance recorded on the Company’s consolidated balance sheets is as follows (in thousands):
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
||
|
Total unrecognized tax benefits |
|
$ |
38 |
|
$ |
— |
|
|
Amounts netted against deferred tax assets |
|
|
(38) |
|
|
— |
|
|
Unrecognized tax benefits recorded on consolidated balance sheets |
|
$ |
— |
|
$ |
— |
|
As the Company is not currently under examination, it is reasonable to assume that the balance of gross unrecognized tax benefits will likely not change in the next twelve months. The Company currently does not recognize interest and penalties relating to uncertain tax positions in income tax expense.
On December 18, 2015, The Consolidated Appropriations Act of 2014 was signed into law, which retroactively reinstated and made permanent the federal research tax credit provisions from January 1, 2015 through December 31, 2015.
In November 2015, the FASB issued ASU 2015-17, Balance Sheet Classification of Deferred Taxes, related to balance sheet classification of deferred taxes. The ASU requires that deferred tax assets and liabilities be classified as noncurrent in the statement of financial position, thereby simplifying the current guidance that requires an entity to separate deferred assets and liabilities into current and noncurrent amounts. The ASU will be effective for the Company beginning in the first quarter of fiscal year 2018 though early adoption is permitted. The Company early-adopted the ASU as of December 31, 2015 and its statement of financial position as of this date reflects the revised classification of current deferred tax assets and liabilities as noncurrent. There was no impact to the adoption of this ASU on the Company as its deferred tax assets are entirely reserved.
Note 18. Segment Information and Concentration of Customers and Suppliers
The Company operates in one business segment — the development and commercialization of novel therapeutic products. Therefore, results of operations are reported on a consolidated basis for purposes of segment reporting, consistent with internal management reporting. Disclosures about product revenues by geographic area, revenues and accounts receivable from major customers, and major suppliers are presented below.
Geographic Information
Outside the United States, the Company sells products principally in the EU. The geographic classification of product sales was based on the location of the customer. The geographic classification of all other revenues was based on the domicile of the entity from which the revenues were earned.
127
Product revenue by geographic region is as follows (in thousands):
|
|
|
Years Ended December 31, |
|
|
|
|
|||||||||||||
|
|
|
2015 |
|
|
|
|
2014 |
|
|
|
|
||||||||
|
|
|
U.S. |
|
ROW |
|
Total |
|
U.S. |
|
ROW |
|
Total |
|
||||||
|
Qsymia—Net product revenue |
|
$ |
54,622 |
|
$ |
— |
|
$ |
54,622 |
|
$ |
45,277 |
|
$ |
— |
|
$ |
45,277 |
|
|
STENDRA/SPEDRA—License and milestone revenue |
|
|
— |
|
|
11,574 |
|
|
11,574 |
|
|
15,406 |
|
|
23,208 |
|
|
38,614 |
|
|
STENDRA/SPEDRA—Supply revenue |
|
|
16,602 |
|
|
10,072 |
|
|
26,674 |
|
|
9,059 |
|
|
17,460 |
|
|
26,519 |
|
|
STENDRA/SPEDRA —Royalty revenue |
|
|
418 |
|
|
2,142 |
|
|
2,560 |
|
|
2,176 |
|
|
1,595 |
|
|
3,771 |
|
|
Total revenue |
|
$ |
71,642 |
|
$ |
23,788 |
(1) |
$ |
95,430 |
|
$ |
71,918 |
|
$ |
42,263 |
(2) |
$ |
114,181 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2013 |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
U.S. |
|
ROW |
|
Total |
|
|
|
|
|
|
|
|
|
|
|||
|
Qsymia—Net product revenue |
|
$ |
23,718 |
|
$ |
— |
|
$ |
23,718 |
|
|
|
|
|
|
|
|
|
|
|
STENDRA/SPEDRA—License and milestone revenue |
|
|
30,393 |
|
|
25,445 |
|
|
55,838 |
|
|
|
|
|
|
|
|
|
|
|
STENDRA/SPEDRA—Supply revenue |
|
|
1,080 |
|
|
446 |
|
|
1,526 |
|
|
|
|
|
|
|
|
|
|
|
STENDRA/SPEDRA —Royalty revenue |
|
|
— |
|
|
— |
|
|
— |
|
|
|
|
|
|
|
|
|
|
|
Total revenue |
|
$ |
55,191 |
|
$ |
25,891 |
(3) |
$ |
81,082 |
|
|
|
|
|
|
|
|
|
|
|
(1) |
$23.7 million of which is attributable to Germany. |
|
(2) |
$37.2 million of which is attributable to Germany. |
|
(3) |
$21.0 million of which is attributable to Germany. |
Major customers
Revenues from significant customers as a percentage of total revenues is as follows:
|
|
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
2013 |
|
|
Menarini |
|
25 |
% |
32 |
% |
26 |
% |
|
McKesson |
|
21 |
% |
13 |
% |
2 |
% |
|
Auxilium |
|
18 |
% |
23 |
% |
39 |
% |
|
Amerisource Bergen |
|
18 |
% |
14 |
% |
— |
% |
|
Cardinal Health, Inc. |
|
17 |
% |
11 |
% |
4 |
% |
|
Express Scripts, Inc. |
|
— |
% |
1 |
% |
3 |
% |
|
CVS |
|
— |
% |
— |
% |
9 |
% |
|
Walgreens |
|
— |
% |
— |
% |
6 |
% |
Accounts receivable by significant customer as a percentage of the total gross accounts receivable balance are as follows:
|
|
|
|
|
|
|
|
|
|
2015 |
|
2014 |
|
|
McKesson |
|
33 |
% |
18 |
% |
|
Amerisource Bergen |
|
32 |
% |
19 |
% |
|
Cardinal Health, Inc. |
|
25 |
% |
20 |
% |
|
Auxilium |
|
4 |
% |
16 |
% |
|
Menarini |
|
3 |
% |
25 |
% |
Major suppliers
The Company relies on third‑party sole‑source manufacturers to produce its clinical trial materials, raw materials and finished goods. Catalent Pharma Solutions, LLC, or Catalent, which supplied the product for the
128
Phase 3b/4 program for Qsymia, is the Company’s sole source of clinical and commercial supplies for Qsymia. Until 2015, MTPC was the Company’s sole‑source supplier for the API and the tablets for STENDRA (avanafil). In 2015, the Company transitioned to Sanofi as it sole-source supply for STENDRA API and tablets. The Company does not have any manufacturing facilities and intends to continue to rely on third parties for the supply of the starting materials, API and tablets. Third‑party manufacturers may not be able to meet the Company’s needs with respect to timing, quantity or quality. In July 2013, the Company entered into a Commercial Supply Agreement with Sanofi Chimie to manufacture and supply the API for our drug avanafil on an exclusive basis in the United States and other territories and on a semi-exclusive basis in Europe, including the EU, Latin America and other territories. In November 2013, the Company entered into a Manufacturing and Supply Agreement with Sanofi Winthrop Industrie to manufacture and supply the avanafil tablets on an exclusive basis in the United States and other territories and on a semi-exclusive basis in Europe, including the EU, Latin America and other territories.
During the years ended December 31, 2015, 2014 and 2013, the Company incurred expenses for work performed by a third‑party clinical research organization, or CRO, for Qsymia and STENDRA post‑approval studies that accounted for 11%, 27% and 29%, respectively, of total research and development expenses.
Note 19. 401(k) Plan
All of the Company’s full‑time employees are eligible to participate in the VIVUS 401(k) Plan. Employer‑matching contributions for the years ended December 31, 2015, 2014 and 2013 were $406,000, $467,000 and $565,000, respectively.
Note 20. Legal Matters
Securities Related Class Action and Shareholder Derivative Lawsuits
The Company, a current officer and a former officer were defendants in a putative class action captioned Kovtun v. VIVUS, Inc., et al., Case No. 4:10-CV-04957-PJH, in the U.S. District Court, Northern District of California. The action, filed in November 2010, alleged violations of Section 10(b) and 20(a) of the federal Securities Exchange Act of 1934 based on allegedly false or misleading statements made by the defendants in connection with the Company’s clinical trials and New Drug Application, or NDA, for Qsymia as a treatment for obesity. The Court granted defendants’ motions to dismiss both plaintiff’s Amended Class Action Complaint and Second Amended Class Action Complaint; by order dated September 27, 2012, the latter dismissal was with prejudice and final judgment was entered for defendants the same day. On October 26, 2012, plaintiff filed a Notice of Appeal to the U.S. Court of Appeals for the Ninth Circuit. Following briefing of the appeal, the Court of Appeals held oral argument on January 16, 2015. On January 29, 2015, the Court of Appeals issued a Memorandum decision affirming the District Court’s ruling. On February 12, 2015, plaintiff asked the Court of Appeals’ panel to rehear the case or for the Court to rehear the case en banc. The Court of Appeals denied that petition on March 16, 2015, and the matter is now concluded.
Additionally, certain of the Company’s former officers and directors and a current director are defendants in a shareholder derivative lawsuit captioned Turberg v. Logan, et al., Case No. CV-10-05271-PJH, pending in the same federal court. In the plaintiff’s Verified Amended Shareholder Derivative Complaint filed June 3, 2011, the plaintiff largely restated the allegations of the Kovtun action and alleged that the directors breached fiduciary duties to the Company by purportedly permitting the Company to violate the federal securities laws as alleged in the Kovtun action. The same individuals are also named defendants in consolidated shareholder derivative suits pending in the California Superior Court, Santa Clara County, under the caption In re VIVUS, Inc. Derivative Litigation, Master File No. 11 0 CV188439. The allegations in the state court derivative suits are substantially similar to the other lawsuits. The Company is named as a nominal defendant in these actions, neither of which seeks any recovery from the Company. The parties agreed to stay the derivative lawsuits pending the outcome of the appeal of the securities class action. Following the resolution of the class action in the Company’s favor, discussed above, the Turberg plaintiff dismissed the derivative litigation.
On March 27, 2014, Mary Jane and Thomas Jasin, who purport to be purchasers of VIVUS common stock, filed an Amended Complaint in Santa Clara County Superior Court alleging securities fraud against the Company and three of
129
its former officers and directors. In that complaint, captioned Jasin v. VIVUS, Inc., Case No. 114-cv-261427, plaintiffs asserted claims under California’s securities and consumer protection securities statutes. Plaintiffs alleged generally that defendants misrepresented the prospects for the Company’s success, including with respect to the launch of Qsymia, while purportedly selling VIVUS stock for personal profit. Plaintiffs alleged losses of “at least” $2.8 million, and sought damages and other relief. On June 5, 2014, the Company and the other defendants filed a demurrer to the Amended Complaint seeking its dismissal. With the demurrer pending, on July 18, 2014, the same plaintiffs filed a complaint in the United States District Court for the Northern District of California, captioned Jasin v. VIVUS, Inc., Case No. 5:14-cv-03263. The Jasins’ federal complaint alleges violations of Sections 10(b) and 20(a) of the Securities Exchange Act of 1934, based on facts substantially similar to those alleged in their state court action. On September 15, 2014, pursuant to an agreement between the parties, plaintiffs moved to voluntarily dismiss, with prejudice, the state court action. In the federal action, defendants filed a motion to dismiss on November 12, 2014. On December 3, 2014, plaintiffs filed a First Amended Complaint in the federal action. On January 21, 2015, defendants filed a motion to dismiss the First Amended Complaint. The court ruled on that motion on June 18, 2015, dismissing the seven California claims with prejudice and dismissing the two federal claims with leave to amend. Plaintiffs filed a second amended complaint on August 17, 2015. Defendants moved to dismiss that complaint on October 2, 2015. On September 10, 2015, plaintiffs moved for entry of judgment on their state claims. Briefing on both defendants’ motion to dismiss and plaintiffs’ motion for entry of judgment was completed on December 15, 2015. The court heard oral argument on both motions on January 14, 2016. The court has not yet issued a ruling on either motion. The Company maintains directors’ and officers’ liability insurance that it believes affords coverage for much of the anticipated cost of the remaining Jasin action, subject to the use of the Company’s financial resources to pay for its self-insured retention and the policies’ terms and conditions.
The Company and the defendant officers and directors cannot predict the outcome of the various shareholder lawsuits, but they believe the various shareholder lawsuits are without merit and intend to continue vigorously defending them.
Qsymia ANDA Litigation
On May 7, 2014, the Company received a Paragraph IV certification notice from Actavis Laboratories FL indicating that it filed an abbreviated new drug application, or ANDA, with the U.S. Food and Drug Administration, or FDA, requesting approval to market a generic version of Qsymia and contending that the patents listed for Qsymia in the FDA Orange Book at the time the notice was received (U.S. Patents 7,056,890, 7,553,818, 7,659,256, 7,674,776, 8,580,298, and 8,580,299 (collectively “patents-in-suit”)) are invalid, unenforceable and/or will not be infringed by the manufacture, use, sale or offer for sale of a generic form of Qsymia as described in their ANDA. On June 12, 2014, the Company filed a lawsuit in the U.S. District Court for the District of New Jersey against Actavis Laboratories FL, Inc., Actavis, Inc., and Actavis PLC, collectively referred to as Actavis. The lawsuit (Case No. 14-3786 (SRC)(CLW)) was filed on the basis that Actavis’ submission of their ANDA to obtain approval to manufacture, use, sell or offer for sale generic versions of Qsymia prior to the expiration of the patents-in-suit constitutes infringement of one or more claims of those patents.
In accordance with the Hatch-Waxman Act, as a result of having filed a timely lawsuit against Actavis, FDA approval of Actavis’ ANDA will be stayed until the earlier of (i) up to 30 months from the Company’s May 7, 2014 receipt of Actavis’ Paragraph IV certification notice (i.e. November 7, 2016) or (ii) a District Court decision finding that the identified patents are invalid, unenforceable or not infringed.
On January 21, 2015, the Company received a second Paragraph IV certification notice from Actavis contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 8,895,057 and 8,895,058) are invalid, unenforceable and/or will not be infringed by the manufacture, use, sale, or offer for sale of a generic form of Qsymia. On March 4, 2015, the Company filed a second lawsuit in the U.S. District Court for the District of New Jersey against Actavis (Case No. 15-1636 (SRC)(CLW)) in response to the second Paragraph IV certification notice on the basis that Actavis’ submission of their ANDA constitutes infringement of one or more claims of the patents-in-suit.
On July 7, 2015, the Company received a third Paragraph IV certification notice from Actavis contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 9,011,905 and 9,011,906) are invalid, unenforceable and/or will not be infringed by the manufacture, use, sale, or offer for sale of a generic form of Qsymia.
130
On August 17, 2015, the Company filed a third lawsuit in the U.S. District Court for the District of New Jersey against Actavis (Case No. 15-6256 (SRC)(CLW)) in response to the third Paragraph IV certification notice on the basis that Actavis’ submission of their ANDA constitutes infringement of one or more claims of the patents-in-suit. The three lawsuits against Actavis have been consolidated into a single suit (Case No. 14-3786 (SRC)(CLW)).
On March 5, 2015, the Company received a Paragraph IV certification notice from Teva Pharmaceuticals USA, Inc. indicating that it filed an ANDA with the FDA, requesting approval to market a generic version of Qsymia and contending that eight patents listed for Qsymia in the Orange Book at the time of the notice (U.S. Patents 7,056,890, 7,553,818, 7,659,256, 7,674,776, 8,580,298, 8,580,299, 8,895,057 and 8,895,058) (collectively “patents-in-suit”) are invalid, unenforceable and/or will not be infringed by the manufacture, use or sale of a generic form of Qsymia as described in their ANDA. On April 15, 2015, the Company filed a lawsuit in the U.S. District Court for the District of New Jersey against Teva Pharmaceutical USA, Inc. and Teva Pharmaceutical Industries, Ltd., collectively referred to as Teva. The lawsuit (Case No. 15-2693 (SRC)(CLW)) was filed on the basis that Teva’s submission of their ANDA to obtain approval to manufacture, use, sell, or offer for sale generic versions of Qsymia prior to the expiration of the patents-in-suit constitutes infringement of one or more claims of those patents.
In accordance with the Hatch-Waxman Act, as a result of having filed a timely lawsuit against Teva, FDA approval of Teva’s ANDA will be stayed until the earlier of (i) up to 30 months from our March 5, 2015 receipt of Teva’s Paragraph IV certification notice (i.e. September 5, 2017) or (ii) a District Court decision finding that the identified patents are invalid, unenforceable or not infringed.
On August 5, 2015, the Company received a second Paragraph IV certification notice from Teva contending that two additional patents listed in the Orange Book for Qsymia (U.S. Patents 9,011,905 and 9,011,906) are invalid, unenforceable and/or will not be infringed by the manufacture, use, sale, or offer for sale of a generic form of Qsymia. On September 18, 2015, the Company filed a second lawsuit in the U.S. District Court for the District of New Jersey against Teva (Case No. 15-6957(SRC)(CLW)) in response to the second Paragraph IV certification notice on the basis that Teva’s submission of their ANDA constitutes infringement of one or more claims of the patents-in-suit. The two lawsuits against Teva have been consolidated into a single suit (Case No. 15-2693 (SRC)(CLW)).
The Company intends to vigorously enforce its intellectual property rights relating to Qsymia, but the Company cannot predict the outcome of these matters.
The Company is not aware of any other asserted or unasserted claims against it where it believes that an unfavorable resolution would have an adverse material impact on the operations or financial position of the Company.
131
Note 21. Selected Financial Data (Unaudited)
Selected Quarterly Financial Data (in thousands except per share data)
|
|
|
Quarter Ended, |
|
||||||||||
|
|
|
March 31 |
|
June 30 |
|
September 30 |
|
December 31 |
|
||||
|
2015 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total revenue |
|
$ |
32,166 |
|
$ |
22,985 |
|
$ |
24,936 |
|
$ |
15,343 |
|
|
Total gross profit |
|
|
22,270 |
|
|
13,115 |
|
|
13,171 |
|
|
12,717 |
|
|
Operating expenses |
|
|
38,990 |
|
|
64,192 |
|
|
32,965 |
|
|
19,560 |
|
|
Net loss |
|
|
(15,466) |
|
|
(49,352) |
|
|
(16,106) |
|
|
(12,183) |
|
|
Basic and diluted net loss per share |
|
$ |
(0.15) |
|
$ |
(0.48) |
|
$ |
(0.15) |
|
$ |
(0.12) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2014 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total revenue |
|
$ |
36,691 |
|
$ |
21,881 |
|
$ |
33,877 |
|
$ |
21,732 |
|
|
Total gross profit |
|
|
27,158 |
|
|
14,866 |
|
|
26,609 |
|
|
12,161 |
|
|
Operating expenses |
|
|
44,619 |
|
|
39,367 |
|
|
41,789 |
|
|
39,117 |
|
|
Net loss |
|
|
(15,550) |
|
|
(25,825) |
|
|
(15,825) |
|
|
(25,447) |
|
|
Basic and diluted net loss per share |
|
$ |
(0.15) |
|
$ |
(0.25) |
|
$ |
(0.15) |
|
$ |
(0.25) |
|
132
FINANCIAL STATEMENT SCHEDULE
The financial statement Schedule II—VALUATION AND QUALIFYING ACCOUNTS is filed as part of the Form 10‑K.
VIVUS, Inc.
SCHEDULE II—VALUATION AND QUALIFYING ACCOUNTS
(in thousands)
Each of the following valuation and qualifying accounts are reported as assets and liabilities of continuing and discontinued operations in the consolidated balance sheets for all periods presented.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Balance at |
|
Charged |
|
|
|
|
Balance at |
|
|||
|
|
|
Beginning of |
|
to |
|
Charges |
|
End of |
|
||||
|
|
|
Period |
|
Operations* |
|
Utilized |
|
Period |
|
||||
|
Allowance for Cash Discounts |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Fiscal year ended December 31, 2013 |
|
$ |
57 |
|
$ |
1,050 |
|
$ |
(973) |
|
$ |
134 |
|
|
Fiscal year ended December 31, 2014 |
|
$ |
134 |
|
$ |
1,712 |
|
$ |
(1,696) |
|
$ |
150 |
|
|
Fiscal year ended December 31, 2015 |
|
$ |
150 |
|
$ |
1,933 |
|
$ |
(1,919) |
|
$ |
164 |
|
*Amount charged to operations during fiscal years ended December 31, 2015, 2014 and 2013, includes $1,656,000, $1,373,000 and $750,000, respectively, for cash discount allowances related to revenue recognized during each fiscal year. The remaining amounts were recorded on the consolidated balance sheets as deferred revenue at the end of each period, respectively.
133
Item 9. Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
None.
Item 9A. Controls and Procedures
Evaluation of Disclosure Controls and Procedures.
We maintain disclosure controls and procedures that are designed to ensure that information required to be disclosed in our Exchange Act reports is recorded, processed, summarized and reported within the timelines specified in the Securities and Exchange Commission’s rules and forms, and that such information is accumulated and communicated to our management, including our Chief Executive Officer and Chief Financial Officer, as appropriate, to allow timely decisions regarding required disclosure. In designing and evaluating the disclosure controls and procedures, management recognized that any controls and procedures, no matter how well designed and operated, can only provide reasonable assurance of achieving the desired control objectives, and in reaching a reasonable level of assurance, management necessarily was required to apply its judgment in evaluating the cost‑benefit relationship of possible controls and procedures.
As required by SEC Rule 13a‑15(b), the Company carried out an evaluation, under the supervision and with the participation of the Company’s management, including the Company’s Chief Executive Officer and the Company’s Chief Financial Officer, of the effectiveness of the design and operation of the Company’s disclosure controls and procedures as of the end of the year covered by this report. Based on the foregoing, our Chief Executive Officer and Chief Financial Officer concluded that the design and operation of our disclosure controls and procedures were effective at the reasonable assurance level.
Management’s Annual Report on Internal Control Over Financial Reporting
Internal control over financial reporting refers to the process designed by, or under the supervision of, our Chief Executive Officer and Chief Financial Officer, and effected by our Board of Directors, management and other personnel, to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles, and includes those policies and procedures that:
|
(1) |
Pertain to the maintenance of records that in reasonable detail accurately and fairly reflect the transactions and dispositions of our assets; |
|
(2) |
Provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that our receipts and expenditures are being made only in accordance with authorization of our management and directors; and |
|
(3) |
Provide reasonable assurance regarding prevention or timely detection of unauthorized acquisitions, use or disposition of our assets that could have a material effect on the financial statements. |
Internal control over financial reporting cannot provide absolute assurance of achieving financial reporting objectives because of its inherent limitations. Internal control over financial reporting is a process that involves human diligence and compliance and is subject to lapses in judgment and breakdowns resulting from human failures. Internal control over financial reporting also can be circumvented by collusion or improper management override. Because of such limitations, there is a risk that material misstatements may not be prevented or detected on a timely basis by internal control over financial reporting. However, these inherent limitations are known features of the financial reporting process. Therefore, it is possible to design into the process safeguards to reduce, though not eliminate, this risk. Our management is responsible for establishing and maintaining adequate internal control over financial reporting for the company, as such term is defined in Rules 13a-15(f) and 15d-15(f) of the Exchange Act.
134
Our management has used the framework set forth in the report entitled Internal Control—Integrated Framework published by the Committee of Sponsoring Organizations of the Treadway Commission (2013), known as COSO Framework, to evaluate the effectiveness of the Company’s internal control over financial reporting. Based on this assessment, management has concluded that our internal control over financial reporting was effective as of December 31, 2015.
Attestation Report of the Registered Public Accounting Firm
OUM & Co. LLP, the independent registered public accounting firm that audited our Consolidated Financial Statements included elsewhere in this Annual Report on Form 10‑K, has issued an attestation report on the effectiveness of our internal control over financial reporting as of December 31, 2015. This report, which expresses an unqualified opinion on the effectiveness of our internal controls over financial reporting as of December 31, 2015, is included herein.
Changes in Internal Controls Over Financial Reporting
There has been no change in our internal controls over financial reporting during our most recent fiscal quarter that has materially affected, or is reasonably likely to materially affect, our internal controls over financial reporting.
None.
135
Item 10. Directors, Executive Officers and Corporate Governance
The information required by this item is hereby incorporated by reference from the information under the captions “Election of Directors,” “Corporate Governance—Board Committees,” “Executive Officers” and “Section 16(a) Beneficial Ownership Reporting Compliance” contained in the Company’s definitive Proxy Statement, to be filed with the Securities and Exchange Commission no later than 120 days from the end of the Company’s last fiscal year in connection with the solicitation of proxies for its 2016 Annual Meeting of Stockholders.
The Company has adopted a code of ethics that applies to its Chief Executive Officer, Chief Financial Officer, and to all of its other officers, directors, employees and agents. The code of ethics is available at the Corporate Governance section of the Investor Relations page on the Company’s website at www.vivus.com. The Company intends to disclose future amendments to, or waivers from, certain provisions of its code of ethics on the above website within four business days following the date of such amendment or waiver.
Item 11. Executive Compensation
The information required by this item is incorporated by reference from the information under the caption “Corporate Governance—Compensation Committee Interlocks and Insider Participation,” “Executive Compensation” and “Executive and Director Compensation Tables” in the Company’s Proxy Statement referred to in Item 10 above.
Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
Equity Compensation Plan Information
Information about our equity compensation plans at December 31, 2015, that were approved by our stockholders was as follows:
|
|
|
|
|
|
|
|
|
|
|
|
|
Number of Shares |
|
Weighted Average |
|
Number of Shares |
|
|
|
|
|
to be issued Upon |
|
Exercise Price of |
|
Remaining |
|
|
|
|
|
Exercise of Outstanding |
|
Outstanding |
|
Available for |
|
|
|
Plan Category |
|
Options and Rights |
|
Options |
|
Future Issuance(c) |
|
|
|
Equity compensation plans approved by stockholders(a) |
|
7,162,536 |
|
$ |
6.38 |
|
8,569,091 |
|
|
Equity compensation plans not approved by stockholders(b) |
|
— |
|
$ |
N/A |
|
325,000 |
|
|
Total |
|
7,162,536 |
|
$ |
6.38 |
|
8,894,091 |
|
|
(a) |
Consists of two plans: our 2001 Stock Option Plan and our 2010 Equity Incentive Plan. |
|
(b) |
On April 30, 2010, the Company’s Board of Directors granted an option to purchase 400,000 shares of the Company’s common stock, or the Inducement Grant, to Michael P. Miller, the Company’s former Senior Vice President and Chief Commercial Officer. The Inducement Grant was granted outside of the Company’s 2010 Equity Incentive Plan and without stockholder approval pursuant to NASDAQ Listing Rule 5635(c)(4) and is subject to the terms and conditions of the Stand‑Alone Stock Option Agreement between the Company and Michael P. Miller. |
|
(c) |
Includes 8,585,900 shares for the 2010 Equity Incentive Plan and 308,191 shares for the 1994 Employee Stock Purchase Plan. |
The remaining information required by this item is incorporated by reference from the information under the caption “Security Ownership of Certain Beneficial Owners and Management” in the Company’s Proxy Statement referred to in Item 10 above.
136
Item 13. Certain Relationships and Related Transactions, and Director Independence
The information required by this item is incorporated by reference from the information under the caption “Certain Relationships and Related Transactions” and “Corporate Governance—Board Independence” in the Company’s Proxy Statement referred to in Item 10 above.
Item 14. Principal Accounting Fees and Services
The information required by this item is incorporated by reference from the information under the caption “Ratification of Appointment of Independent Registered Public Accounting Firm” in the Company’s Proxy Statement referred to in Item 10 above.
137
Item 15. Exhibits and Financial Statement Schedules
(a)Documents filed as part of this report
1. Financial Statements
Reference is made to the financial statements included under Item 8 of Part II hereof.
2. Financial Statement Schedules
Reference is made to the financial statement schedules included under Item 8 of Part II hereof. All other schedules are omitted because they are not applicable or the required information is shown in the financial statements or the notes thereto.
3. Exhibits Refer to Item 15(b) immediately below.
(b)The exhibits required by Item 601 of Regulation S‑K are listed in the Exhibit Index attached hereto and are incorporated herein by reference.
138
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized:
|
|
VIVUS, INC., |
|
|
|
a Delaware Corporation |
|
|
|
|
|
|
|
By: |
/s/ Seth H. Z. Fischer |
|
|
|
Seth H. Z. Fischer |
|
|
|
Chief Executive Officer |
|
|
|
(Principal Executive Officer) |
|
|
|
|
|
Date: March 9, 2016 |
|
|
139
KNOW ALL PERSONS BY THESE PRESENTS, that each person whose signature appears below constitutes and appoints each of Seth H. Z. Fischer and Mark K. Oki as his attorney‑in‑fact for him, in any and all capacities, to sign each amendment to this Report on Form 10‑K, and to file the same, with exhibits thereto and other documents in connection therewith, with the Securities and Exchange Commission, hereby ratifying and confirming all that said attorney‑in‑fact or his substitute or substitutes may lawfully do or cause to be done by virtue hereof.
Pursuant to the requirements of the Securities Exchange Act of 1934, this Report has been signed below by the following persons on behalf of the Registrant and in the capacities and on the dates indicated:
|
Signature |
|
Title |
|
Date |
|
|
|
|
|
|
|
/s/ Seth H. Z. Fischer |
|
Chief Executive Officer (Principal Executive Officer) and Director |
|
March 9, 2016 |
|
Seth H. Z. Fischer |
||||
|
|
|
|
|
|
|
/s/ David Y. Norton |
|
Chairman of the Board of Directors and Director |
|
March 9, 2016 |
|
David Y. Norton |
||||
|
|
|
|
|
|
|
/s/ Mark K. Oki |
Chief Financial Officer and Chief Accounting Officer (Principal Financial and Accounting Officer) |
March 9, 2016 |
||
|
Mark K. Oki |
||||
|
|
|
|
|
|
|
/s/ Jorge Plutzky, M.D. |
|
Director |
|
March 9, 2016 |
|
Jorge Plutzky, M.D. |
||||
|
|
|
|
|
|
|
/s/ Eric W. Roberts |
|
Director |
|
March 9, 2016 |
|
Eric W. Roberts |
|
|||
|
|
|
|
|
|
|
/s/ Herman Rosenman |
|
Director |
|
March 9, 2016 |
|
Herman Rosenman |
||||
|
|
|
|
|
|
|
/s/ Allan L. Shaw |
|
Director |
|
March 9, 2016 |
|
Allan L. Shaw |
||||
|
|
|
|
|
|
|
/s/ Mayuran Sriskandarajah |
|
Director |
|
March 9, 2016 |
|
Mayuran Sriskandarajah |
140
VIVUS, INC.
REPORT ON FORM 10‑K FOR
THE YEAR ENDED DECEMBER 31, 2015
|
Exhibit |
|
Description |
|
2.1(1)† |
|
Asset Purchase Agreement between the Registrant and K‑V Pharmaceutical Company dated as of March 30, 2007 |
|
2.2(2)† |
|
Asset Purchase Agreement dated October 1, 2010, between the Registrant, MEDA AB and Vivus Real Estate, LLC |
|
3.1(3) |
|
Amended and Restated Certificate of Incorporation of the Registrant |
|
3.2(4) |
|
Amended and Restated Bylaws of the Registrant |
|
3.3(5) |
|
Amendment No. 1 to the Amended and Restated Bylaws of the Registrant |
|
3.4(6) |
|
Amendment No. 2 to the Amended and Restated Bylaws of the Registrant |
|
3.5(7) |
|
Amendment No. 3 to the Amended and Restated Bylaws of the Registrant |
|
3.6(8) |
|
Amendment No. 4 to the Amended and Restated Bylaws of the Registrant |
|
3.7(9) |
|
Amendment No. 5 to the Amended and Restated Bylaws of the Registrant |
|
3.8(10) |
|
Amended and Restated Certificate of Designation of Rights, Preferences and Privileges of Series A Participating Preferred Stock of the Registrant |
|
4.1(11) |
|
Specimen Common Stock Certificate of the Registrant |
|
4.2(12) |
|
Preferred Stock Rights Agreement dated as of March 27, 2007, between the Registrant and Computershare Investor Services, LLC |
|
4.3(13) |
|
Indenture dated as of May 21, 2013, by and between the Registrant and Deutsche Bank Trust Company Americas, as trustee |
|
4.4(14) |
|
Form of 4.50% Convertible Senior Note due May 1, 2020 |
|
10.1(15)* |
|
Form of Indemnification Agreement by and among the Registrant and the Officers of the Registrant |
|
10.2(16)* |
|
Form of Indemnification Agreement by and among the Registrant and the Directors of the Registrant |
|
10.3(17)* |
|
1994 Employee Stock Purchase Plan, as amended, Form of Subscription Agreement and Form of Notice of Withdrawal |
|
10.4(18)* |
|
2001 Stock Option Plan and Form of Agreement thereunder |
|
10.5(19)* |
|
2001 Stock Option Plan, as amended on July 12, 2006 |
|
10.6(20)* |
|
Form of Notice of Grant and Restricted Stock Unit Agreement under the VIVUS, Inc. 2001 Stock Option Plan |
|
10.7(21)* |
|
2010 Equity Incentive Plan and Form of Agreement thereunder |
|
10.8(22)* |
|
2010 Equity Incentive Plan, as amended on September 12, 2014 |
|
10.9(23)* |
|
Stand‑Alone Stock Option Agreement with Michael P. Miller dated as of April 30, 2010 |
|
10.10(24)* |
|
Employment Agreement dated December 20, 2007, between the Registrant and Leland F. Wilson |
|
10.11(25)* |
|
First Amendment dated January 23, 2009, to the Employment Agreement dated December 20, 2007, by and between the Registrant and Leland F. Wilson |
|
10.12(26)* |
|
Second Amendment dated January 21, 2011, to the Employment Agreement dated December 20, 2007, by and between the Registrant and Leland F. Wilson |
|
10.13(27)* |
|
Third Amendment dated January 27, 2012, to the Employment Agreement dated December 20, 2007, by and between the Registrant and Leland F. Wilson |
|
10.14(28)* |
|
Fourth Amendment dated January 25, 2013, to the Employment Agreement dated December 20, 2007, by and between the Registrant and Leland F. Wilson |
|
10.15(29)† |
|
Agreement effective as of December 28, 2000, between the Registrant and Tanabe Seiyaku Co., Ltd. |
|
10.16(30) |
|
Amendment No. 1 effective as of January 9, 2004, to the Agreement effective as of December 28, 2000, between the Registrant and Tanabe Seiyaku Co., Ltd. |
|
10.17(31) |
|
Termination and Release executed by Tanabe Holding America, Inc. dated May 1, 2007 |
141
|
Exhibit |
|
Description |
|
10.18(32)† |
|
Second Amendment effective as of August 1, 2012, to the Agreement dated as of December 28, 2000, between the Registrant and Mitsubishi Tanabe Pharma Corporation (formerly Tanabe Seiyaku Co., Ltd.) |
|
10.19(33)† |
|
Third Amendment effective as of February 21, 2013, to the Agreement dated as of December 28, 2000, between the Registrant and Mitsubishi Tanabe Pharma Corporation (formerly Tanabe Seiyaku Co., Ltd.) |
|
10.20(34)† |
|
Settlement and Modification Agreement dated July 12, 2001, between ASIVI, LLC, AndroSolutions, Inc., Gary W. Neal and the Registrant |
|
10.21(35)† |
|
Assignment Agreement between Thomas Najarian, M.D. and the Registrant dated October 16, 2001 |
|
10.22(36)† |
|
Master Services Agreement dated as of September 12, 2007, between the Registrant and Medpace, Inc. |
|
10.23(37)† |
|
Exhibit A: Medpace Task Order Number: 06 dated as of December 15, 2008, pursuant to that certain Master Services Agreement, between the Registrant and Medpace, Inc., dated as of September 12, 2007 |
|
10.24(38)† |
|
Transition Services Agreement dated November 5, 2010, between the Registrant and MEDA AB |
|
10.25(39)† |
|
Commercial Manufacturing and Packaging Agreement by and between the Registrant and Catalent Pharma Solutions, LLC dated as of July 17, 2012 |
|
10.26(40) |
|
Lease Agreement effective November 1, 2006, by and between the Registrant and Castro Mountain View, LLC, Thomas A. Lynch, Trudy Molina Flores, Trustee of the Jolen Flores and Trudy Molina Flores Joint Living Trust dated April 3, 2001, E William and Charlotte Duerkson, The Duerkson Family Trust dated February 16, 1999, The Dutton Family Trust dated September 16, 1993, The Noel S. Schuurman Trust, The Duarte Family Partners, L.P., The Marie Antoinette Clough Revocable Living Trust dated January 11, 1989, Blue Oak Properties, Inc., and CP6CC, LLC |
|
10.27(41) |
|
First Amendment to Lease dated November 18, 2008, between Castro Mountain View, LLC, CP6CC, LLC and the Registrant |
|
10.28(42) |
|
Second Amendment to Lease effective November 12, 2009, between Castro Mountain View, LLC, CP6CC, LLC and the Registrant |
|
10.29(43) |
|
Third Amendment to Lease effective December 3, 2010, between Castro Mountain View, LLC, CP6CC, LLC and the Registrant |
|
10.30(44) |
|
Fourth Amendment to Lease effective February 14, 2012, between Castro Mountain View, LLC, CP6CC, LLC and the Registrant |
|
10.31(45) |
|
Lease Agreement effective December 11, 2012, by and between the Registrant and SFERS Real Estate Corp. U |
|
10.32(46)† |
|
Purchase and Sale Agreement effective as of March 25, 2013, between the Registrant and BioPharma Secured Investments III Holdings Cayman LP |
|
10.33(47) |
|
Capped Call Confirmation dated May 15, 2013, by and between the Registrant and Deutsche Bank AG, London Branch |
|
10.34(48)* |
|
Form of Amended and Restated Change of Control and Severance Agreement |
|
10.35(49)† |
|
License and Commercialization Agreement dated July 5, 2013, between the Registrant and Berlin‑Chemie AG |
|
10.36(50)† |
|
Commercial Supply Agreement dated as of July 5, 2013, between the Registrant and Berlin‑Chemie AG |
|
10.37(51) |
|
Agreement dated July 18, 2013, by and between the Registrant and First Manhattan Co. |
|
10.38(52)* |
|
Letter Agreement dated July 18, 2013, by and among the Registrant, First Manhattan Co. and Peter Y. Tam |
|
10.39(53) |
|
Fourth Amendment to the Agreement dated as of December 28, 2000, between the Registrant and Mitsubishi Tanabe Pharma Corporation (formerly Tanabe Seiyaku Co., Ltd.), effective as of July 1, 2013 |
|
10.40(54)† |
|
Commercial Supply Agreement dated July 31, 2013, by and between the Registrant and Sanofi Chimie |
|
10.41(55)* |
|
Employment Agreement dated September 3, 2013, by and between the Registrant and Seth H. Z. Fischer |
|
10.42(56)† |
|
License and Commercialization Agreement dated as of October 10, 2013, by and between the Registrant and Auxilium Pharmaceuticals, Inc. |
142
|
Exhibit |
|
Description |
|
10.43(57)† |
|
Commercial Supply Agreement dated as of October 10, 2013, by and between the Registrant and Auxilium Pharmaceuticals, Inc. |
|
10.44(58)* |
|
Letter Agreement dated November 4, 2013, by and between the Registrant and Timothy E. Morris |
|
10.45(59)† |
|
Manufacturing and Supply Agreement dated November 18, 2013, by and between the Registrant and Sanofi Winthrop Industrie |
|
10.46(60)† |
|
License and Commercialization Agreement dated December 11, 2013, by and between the Registrant and Sanofi |
|
10.47(61)† |
|
Supply Agreement effective as of December 11, 2013, by and between the Registrant and Sanofi Winthrop Industrie |
|
10.48(62)† |
|
Patent Assignment Agreement, dated August 24, 2014, by and between the Registrant and Janssen Pharmaceuticals, Inc. |
|
10.49(63)* |
|
Letter Agreement dated April 13, 2015, by and between the Registrant and Guy P. Marsh |
|
10.50(64)* |
|
Form of Second Amended and Restated Change of Control and Severance Agreement |
|
10.51(65)* |
|
Letter Agreement dated July 20, 2015, by and between the Registrant and Wesley W. Day, Ph.D. |
|
10.52(66)* |
|
Letter Agreement dated August 17, 2015, by and between the Registrant and Svai S. Sanford |
| 10.53 |
|
Letter Regarding Termination Notice dated December 30, 2015, from Auxilium Pharmaceuticals, Inc. and Endo Ventures Limited to the Registrant |
| 21.1 |
|
List of Subsidiaries |
| 23.1 |
|
Consent of Independent Registered Public Accounting Firm |
| 24.1 |
|
Power of Attorney (See signature page) |
| 31.1 |
|
Certification of Chief Executive Officer pursuant to Rules 13a‑14 and 15d‑14 promulgated under the Securities Exchange Act of 1934, as amended |
| 31.2 |
|
Certification of Chief Financial Officer pursuant to Rules 13a‑14 and 15d‑14 promulgated under the Securities Exchange Act of 1934, as amended |
| 32.1 |
|
Certification of Chief Executive Officer and Chief Financial Officer pursuant to Section 18 U.S.C. 1350, as adopted pursuant to Section 906 of the Sarbanes‑Oxley Act of 2002 |
| 101 |
|
The following materials from the Registrant’s Annual Report on Form 10‑K for the year ended December 31, 2015, formatted in Extensible Business Reporting Language (XBRL), include: (i) the Consolidated Balance Sheets, (ii) the Consolidated Statements of Operations, (iii) the Consolidated Statements of Comprehensive Loss, (iv) the Consolidated Statements of Cash Flows, and (v) related notes |
†Confidential treatment granted.
*Indicates management contract or compensatory plan or arrangement.
|
(1) |
Incorporated by reference to Exhibit 2.1 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2012, filed with the SEC on February 26, 2013. |
|
(2) |
Incorporated by reference to Exhibit 2.2 filed with the Registrant’s Annual Report on Form 10‑K/A for the fiscal year ended December 31, 2012, filed with the SEC on June 12, 2013. |
|
(3) |
Incorporated by reference to Exhibit 3.2 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 1996, filed with the SEC on March 28, 1997. |
|
(4) |
Incorporated by reference to Exhibit 3.2 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on April 20, 2012. |
|
(5) |
Incorporated by reference to Exhibit 3.3 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended March 31, 2013, filed with the SEC on May 8, 2013. |
|
(6) |
Incorporated by reference to Exhibit 3.4 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended March 31, 2013, filed with the SEC on May 8, 2013. |
143
|
(7) |
Incorporated by reference to Exhibit 3.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on May 13, 2013. |
|
(8) |
Incorporated by reference to Exhibit 3.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 24, 2013. |
|
(9) |
Incorporated by reference to Exhibit 3.1 filed with the Registrant’s Current Report on Form 8-K filed with the SEC on September 18, 2015. |
|
(10) |
Incorporated by reference to Exhibit 3.3 filed with the Registrant’s Registration Statement on Form 8‑A filed with the SEC on March 28, 2007. |
|
(11) |
Incorporated by reference to Exhibit 4.1 filed with the Registrant’s Annual Report on Form 10‑K/A for the fiscal year ended December 31, 1996, filed with the SEC on April 16, 1997. |
|
(12) |
Incorporated by reference to Exhibit 4.1 filed with the Registrant’s Registration Statement on Form 8‑A filed with the SEC on March 28, 2007. |
|
(13) |
Incorporated by reference to Exhibit 4.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on May 21, 2013. |
|
(14) |
Incorporated by reference to Exhibit 4.2 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on May 21, 2013. |
|
(15) |
Incorporated by reference to Exhibit 10.11 filed with the Registrant’s Form 8‑B filed with the SEC on June 25, 1996. |
|
(16) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on August 12, 2014. |
|
(17) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 29, 2011. |
|
(18) |
Incorporated by reference to Exhibit 10.44 filed with the Registrant’s Registration Statement on Form S‑8 filed with the SEC on November 15, 2001. |
|
(19) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 13, 2006. |
|
(20) |
Incorporated by reference to Exhibit 10.2 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 13, 2006. |
|
(21) |
Incorporated by reference to Exhibit 10.7 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2010, filed with the SEC on March 1, 2011. |
|
(22) |
Incorporated by reference to Exhibit 4.1 filed with the Registrant’s Registration Statement on Form S‑8 filed with the SEC on November 5, 2014. |
|
(23) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on May 6, 2010. |
|
(24) |
Incorporated by reference to Exhibit 10.63 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on December 24, 2007. |
|
(25) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on January 29, 2009. |
|
(26) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on January 26, 2011. |
|
(27) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on January 27, 2012. |
144
|
(28) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on January 30, 2013. |
|
(29) |
Incorporated by reference to Exhibit 10.15 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2012, filed with the SEC on February 26, 2013. |
|
(30) |
Incorporated by reference to Exhibit 10.42A filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended March 31, 2004, filed with the SEC on May 7, 2004. |
|
(31) |
Incorporated by reference to Exhibit 10.61 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on May 4, 2007. |
|
(32) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on August 10, 2012. |
|
(33) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on February 25, 2013. |
|
(34) |
Incorporated by reference to Exhibit 10.20 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2012, filed with the SEC on February 26, 2013. |
|
(35) |
Incorporated by reference to Exhibit 10.79 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2009, filed with the SEC on March 10, 2010. |
|
(36) |
Incorporated by reference to Exhibit 10.2 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended March 31, 2013, filed with the SEC on May 8, 2013. |
|
(37) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K/A filed with the SEC on July 15, 2009. |
|
(38) |
Incorporated by reference to Exhibit 10.27 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2012, filed with the SEC on February 26, 2013. |
|
(39) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 23, 2012. |
|
(40) |
Incorporated by reference to Exhibit 10.60 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on November 7, 2006. |
|
(41) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on December 18, 2008. |
|
(42) |
Incorporated by reference to Exhibit 10.78 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2009, filed with the SEC on March 10, 2010. |
|
(43) |
Incorporated by reference to Exhibit 10.28 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2010, filed with the SEC on March 1, 2011. |
|
(44) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on February 16, 2012. |
|
(45) |
Incorporated by reference to Exhibit 10.34 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2012, filed with the SEC on February 26, 2013. |
|
(46) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended March 31, 2013, filed with the SEC on May 8, 2013. |
|
(47) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on May 16, 2013. |
|
(48) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 5, 2013. |
145
|
(49) |
Incorporated by reference to Exhibit 10.3 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended June 30, 2013, filed with the SEC on August 8, 2013. |
|
(50) |
Incorporated by reference to Exhibit 10.4 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended June 30, 2013, filed with the SEC on August 8, 2013. |
|
(51) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 19, 2013. |
|
(52) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 24, 2013. |
|
(53) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on July 29, 2013. |
|
(54) |
Incorporated by reference to Exhibit 10.8 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended June 30, 2013, filed with the SEC on August 8, 2013. |
|
(55) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on September 4, 2013. |
|
(56) |
Incorporated by reference to Exhibit 10.9 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended September 30, 2013, filed with the SEC on November 7, 2013. |
|
(57) |
Incorporated by reference to Exhibit 10.10 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended September 30, 2013, filed with the SEC on November 7, 2013. |
|
(58) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8‑K filed with the SEC on November 5, 2013. |
|
(59) |
Incorporated by reference to Exhibit 10.45 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2013, filed with the SEC on February 28, 2014. |
|
(60) |
Incorporated by reference to Exhibit 10.46 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2013, filed with the SEC on February 28, 2014. |
|
(61) |
Incorporated by reference to Exhibit 10.47 filed with the Registrant’s Annual Report on Form 10‑K for the fiscal year ended December 31, 2013, filed with the SEC on February 28, 2014. |
|
(62) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Quarterly Report on Form 10‑Q for the fiscal quarter ended September 30, 2014, filed with the SEC on November 5, 2014. |
|
(63) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Quarterly Report on Form 10-Q for the fiscal quarter ended June 30, 2015, filed with the SEC on August 3, 2015. |
|
(64) |
Incorporated by reference to Exhibit 10.1 filed with the Registrant’s Current Report on Form 8-K filed with the SEC on June 24, 2015. |
|
(65) |
Incorporated by reference to Exhibit 10.3 filed with the Registrant’s Quarterly Report on Form 10-Q for the fiscal quarter ended June 30, 2015, filed with the SEC on August 3, 2015. |
|
(66) |
Incorporated by reference to Exhibit 10.3 filed with the Registrant’s Quarterly Report on Form 10-Q for the fiscal quarter ended September 30, 2015, filed with the SEC on November 4, 2015. |
146
