Attached files
| file | filename |
|---|---|
| EX-99.2 - EX-99.2 - Innoviva, Inc. | a16-17822_1ex99d2.htm |
| 8-K - 8-K - Innoviva, Inc. | a16-17822_18k.htm |
Exhibit 99.1
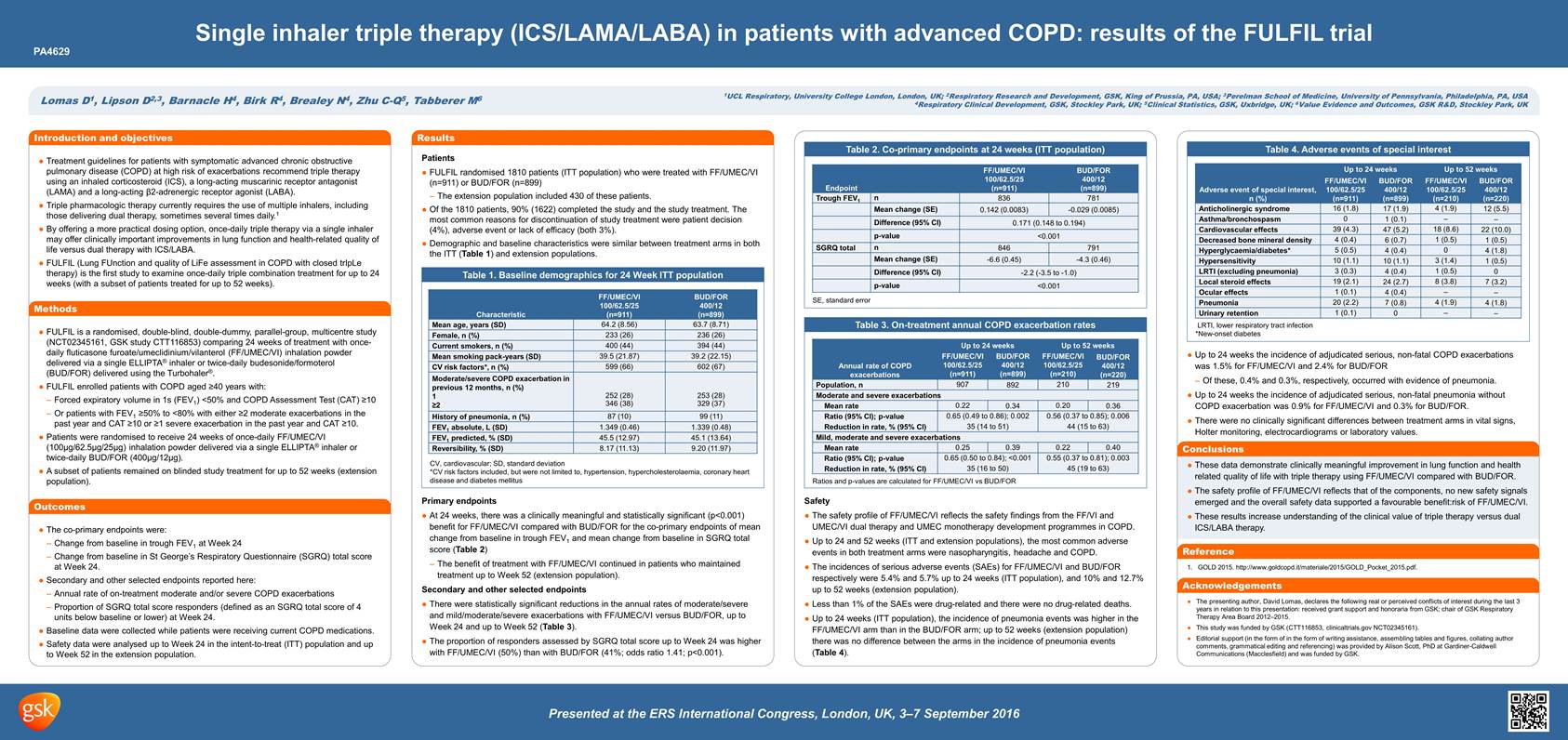
PA4629 Single inhaler triple therapy (ICS/LAMA/LABA) in patients with advanced COPD: results of the FULFIL trial Lomas D1, Lipson D2,3, Barnacle H4, Birk R4, Brealey N4, Zhu C-Q5, Tabberer M6 1UCL Respiratory, University College London, London, UK; 2Respiratory Research and Development, GSK, King of Prussia, PA, USA; 3Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA 4Respiratory Clinical Development, GSK, Stockley Park, UK; 5Clinical Statistics, GSK, Uxbridge, UK; 6Value Evidence and Outcomes, GSK R&D, Stockley Park, UK Introduction and objectivesTreatment guidelines for patients with symptomatic advanced chronic obstructive pulmonary disease (COPD) at high risk of exacerbations recommend triple therapy using an inhaled corticosteroid (ICS), a long-acting muscarinic receptor antagonist (LAMA) and a long-acting β2-adrenergic receptor agonist (LABA). Triple pharmacologic therapy currently requires the use of multiple inhalers, including those delivering dual therapy, sometimes several times daily.1 By offering a more practical dosing option, once-daily triple therapy via a single inhaler may offer clinically important improvements in lung function and health-related quality of life versus dual therapy with ICS/LABA. FULFIL (Lung FUnction and quality of LiFe assessment in COPD with closed trIpLe therapy) is the first study to examine once-daily triple combination treatment for up to 24 weeks (with a subset of patients treated for up to 52 weeks). Methods FULFIL is a randomised, double-blind, double-dummy, parallel-group, multicentre study (NCT02345161, GSK study CTT116853) comparing 24 weeks of treatment with once-daily fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) inhalation powder delivered via a single ELLIPTA® inhaler or twice-daily budesonide/formoterol (BUD/FOR) delivered using the Turbohaler®. FULFIL enrolled patients with COPD aged ≥40 years with: Forced expiratory volume in 1s (FEV1) <50% and COPD Assessment Test (CAT) ≥10 Or patients with FEV1 ≥50% to <80% with either ≥2 moderate exacerbations in the past year and CAT ≥10 or ≥1 severe exacerbation in the past year and CAT ≥10. Patients were randomised to receive 24 weeks of once-daily FF/UMEC/VI (100μg/62.5μg/25μg) inhalation powder delivered via a single ELLIPTA® inhaler or twice-daily BUD/FOR (400μg/12μg). A subset of patients remained on blinded study treatment for up to 52 weeks (extension population). Outcomes The co-primary endpoints were: Change from baseline in trough FEV1 at Week 24 Change from baseline in St George’s Respiratory Questionnaire (SGRQ) total score at Week 24. Secondary and other selected endpoints reported here: Annual rate of on-treatment moderate and/or severe COPD exacerbations Proportion of SGRQ total score responders (defined as an SGRQ total score of 4 units below baseline or lower) at Week 24. Baseline data were collected while patients were receiving current COPD medications. Safety data were analysed up to Week 24 in the intent-to-treat (ITT) population and up to Week 52 in the extension population. Results Patients FULFIL randomised 1810 patients (ITT population) who were treated with FF/UMEC/VI (n=911) or BUD/FOR (n=899) The extension population included 430 of these patients. Of the 1810 patients, 90% (1622) completed the study and the study treatment. The most common reasons for discontinuation of study treatment were patient decision (4%), adverse event or lack of efficacy (both 3%). Demographic and baseline characteristics were similar between treatment arms in both the ITT (Table 1) and extension populations. Table 1. Baseline demographics for 24 Week ITT population Characteristic FF/UMEC/VI 100/62.5/25 (n=911) BUD/FOR 400/12 (n=899) Mean age, years (SD) 64.2 (8.56) 63.7 (8.71) Female, n (%) 233 (26) 236 (26) Current smokers, n (%) 400 (44) 394 (44) Mean smoking pack-years (SD) 39.5 (21.87) 39.2 (22.15) CV risk factors*, n (%) 599 (66) 602 (67) Moderate/severe COPD exacerbation in previous 12 months, n (%) 1≥2 252 (28) 346 (38) 253 (28) 329 (37) History of pneumonia, n (%) 87 (10) 99 (11) FEV1 absolute, L (SD) 1.349 (0.46) 1.339 (0.48) FEV1 predicted, % (SD) 45.5 (12.97) 45.1 (13.64) Reversibility, % (SD) 8.17 (11.13) 9.20 (11.97) CV, cardiovascular; SD, standard deviation *CV risk factors included, but were not limited to, hypertension, hypercholesterolaemia, coronary heart disease and diabetes mellitus Primary endpoints At 24 weeks, there was a clinically meaningful and statistically significant (p<0.001) benefit for FF/UMEC/VI compared with BUD/FOR for the co-primary endpoints of mean change from baseline in trough FEV1 and mean change from baseline in SGRQ total score (Table 2) The benefit of treatment with FF/UMEC/VI continued in patients who maintained treatment up to Week 52 (extension population). Secondary and other selected endpoints There were statistically significant reductions in the annual rates of moderate/severe and mild/moderate/severe exacerbations with FF/UMEC/VI versus BUD/FOR, up to Week 24 and up to Week 52 (Table 3). The proportion of responders assessed by SGRQ total score up to Week 24 was higher with FF/UMEC/VI (50%) than with BUD/FOR (41%; odds ratio 1.41; p<0.001). Table 2. Co-primary endpoints at 24 weeks (ITT population) Endpoint FF/UMEC/VI 100/62.5/25 (n=911) BUD/FOR 400/12 (n=899) Trough FEV1 n 836 781 Mean change (SE) 0.142 (0.0083) -0.029 (0.0085) Difference (95% CI) 0.171 (0.148 to 0.194) p-value <0.001 SGRQ total n 846 791 Mean change (SE) -6.6 (0.45) -4.3 (0.46) Difference (95% CI) -2.2 (-3.5 to -1.0) p-value <0.001 SE, standard error Table 3. On-treatment annual COPD exacerbation rates Annual rate of COPD exacerbations Up to 24 weeks Up to 52 weeks FF/UMEC/VI 100/62.5/25 (n=911) BUD/FOR 400/12 (n=899) FF/UMEC/VI 100/62.5/25 (n=210) BUD/FOR 400/12 (n=220) Population, n 907 892 210 219 Moderate and severe exacerbations Mean rate 0.22 0.34 0.20 0.36 Ratio (95% CI); p-value 0.65 (0.49 to 0.86); 0.002 0.56 (0.37 to 0.85); 0.006 Reduction in rate, % (95% CI) 35 (14 to 51) 44 (15 to 63) Mild, moderate and severe exacerbations Mean rate 0.25 0.39 0.22 0.40 Ratio (95% CI); p-value 0.65 (0.50 to 0.84); <0.001 0.55 (0.37 to 0.81); 0.003 Reduction in rate, % (95% CI) 35 (16 to 50) 45 (19 to 63) Ratios and p-values are calculated for FF/UMEC/VI vs BUD/FOR Safety The safety profile of FF/UMEC/VI reflects the safety findings from the FF/VI and UMEC/VI dual therapy and UMEC monotherapy development programmes in COPD. Up to 24 and 52 weeks (ITT and extension populations), the most common adverse events in both treatment arms were nasopharyngitis, headache and COPD. The incidences of serious adverse events (SAEs) for FF/UMEC/VI and BUD/FOR respectively were 5.4% and 5.7% up to 24 weeks (ITT population), and 10% and 12.7% up to 52 weeks (extension population). Less than 1% of the SAEs were drug-related and there were no drug-related deaths. Up to 24 weeks (ITT population), the incidence of pneumonia events was higher in the FF/UMEC/VI arm than in the BUD/FOR arm; up to 52 weeks (extension population) there was no difference between the arms in the incidence of pneumonia events (Table 4). Table 4. Adverse events of special interest Adverse event of special interest, n (%) FF/UMEC/VI 100/62.5/25 (n=911) BUD/FOR 400/12 (n=899) FF/UMEC/VI 100/62.5/25 (n=210) BUD/FOR 400/12 (n=220) Anticholinergic syndrome 16 (1.8) 17 (1.9) 4 (1.9) 12 (5.5) Asthma/bronchospasm 0 1 (0.1) – – Cardiovascular effects 39 (4.3) 47 (5.2) 18 (8.6) 22 (10.0) Decreased bone mineral density 4 (0.4) 6 (0.7) 1 (0.5) 1 (0.5) Hyperglycaemia/diabetes* 5 (0.5) 4 (0.4) 0 4 (1.8) Hypersensitivity 10 (1.1) 10 (1.1) 3 (1.4) 1 (0.5) LRTI (excluding pneumonia) 3 (0.3) 4 (0.4) 1 (0.5) 0 Local steroid effects 19 (2.1) 24 (2.7) 8 (3.8) 7 (3.2) Ocular effects 1 (0.1) 4 (0.4) – – Pneumonia 20 (2.2) 7 (0.8) 4 (1.9) 4 (1.8) Urinary retention 1 (0.1) 0 – – LRTI, lower respiratory tract infection *New-onset diabetes • Up to 24 weeks the incidence of adjudicated serious, non-fatal COPD exacerbations was 1.5% for FF/UMEC/VI and 2.4% for BUD/FOR Of these, 0.4% and 0.3%, respectively, occurred with evidence of pneumonia. Up to 24 weeks the incidence of adjudicated serious, non-fatal pneumonia without COPD exacerbation was 0.9% for FF/UMEC/VI and 0.3% for BUD/FOR. There were no clinically significant differences between treatment arms in vital signs, Holter monitoring, electrocardiograms or laboratory values. Conclusions These data demonstrate clinically meaningful improvement in lung function and health related quality of life with triple therapy using FF/UMEC/VI compared with BUD/FOR. The safety profile of FF/UMEC/VI reflects that of the components, no new safety signals emerged and the overall safety data supported a favourable benefit:risk of FF/UMEC/VI. These results increase understanding of the clinical value of triple therapy versus dual ICS/LABA therapy. Reference 1. GOLD 2015. http://www.goldcopd.it/materiale/2015/GOLD_Pocket_2015.pdf. Acknowledgements The presenting author, David Lomas, declares the following real or perceived conflicts of interest during the last 3 years in relation to this presentation: received grant support and honoraria from GSK; chair of GSK Respiratory Therapy Area Board 2012–2015. This study was funded by GSK (CTT116853, clinicaltrials.gov NCT02345161). Editorial support (in the form of in the form of writing assistance, assembling tables and figures, collating author comments, grammatical editing and referencing) was provided by Alison Scott, PhD at Gardiner-Caldwell Communications (Macclesfield) and was funded by GSK.