Attached files
|
UNITED STATES
|
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, D.C. 20549
FORM 10-K
|
ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
|
For the fiscal year ended December 31, 2010
OR
|
TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
For the transition period from to
|
Commission file number 001-33245
EMPLOYERS HOLDINGS, INC.
(Exact name of registrant as specified in its charter)
|
NEVADA
(State or other jurisdiction of
incorporation or organization)
|
04-3850065
(IRS Employer
Identification No.)
|
10375 Professional Circle, Reno, Nevada 89521
(Address of principal executive offices and zip code)
(888) 682-6671
(Registrant’s telephone number, including area code)
Securities registered pursuant to Section 12(b) of the Act:
|
Title of each class
Common Stock, $0.01 par value per share
|
Name of each exchange on which registered
New York Stock Exchange
|
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes x No o
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Exchange Act. Yes o No x
Indicate by check mark whether the registrant: (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No o
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes xNo o
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. o
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a small reporting company. See definitions of “large accelerated filer,” “accelerated filer,” “non-accelerated filer,” and “smaller reporting company” in Rule 12b-2 of the Exchange Act. (Check one):
The aggregate market value of the voting and non-voting common equity held by non-affiliates of the registrant as of June 30, 2010 was $613,703,664
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). Yes o No x
|
Class
Common Stock, $0.01 par value per share
|
February 18, 2011
38,467,790 shares outstanding
|
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the registrant’s Definitive Proxy Statement relating to the 2011 Annual Meeting of Stockholders are incorporated by reference in Items 10, 11, 12, 13 and 14 of Part III of this report.
|
TABLE OF CONTENTS
|
|||
|
Page
|
|||
|
No.
|
|||
|
Forward-Looking Statements
|
3
|
||
|
PART I
|
|||
|
Item 1
|
Business
|
4
|
|
|
Item 1A
|
Risk Factors
|
21
|
|
|
Item 1B
|
Unresolved Staff Comments
|
30
|
|
|
Item 2
|
Properties
|
30
|
|
|
Item 3
|
Legal Proceedings
|
30
|
|
|
Item 4
|
(Removed and Reserved)
|
30
|
|
|
PART II
|
|||
|
Item 5
|
Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities
|
31
|
|
|
Item 6
|
Selected Financial Data
|
34
|
|
|
Item 7
|
Management’s Discussion and Analysis of Financial Condition and Results of Operations
|
37
|
|
|
Item 7A
|
Quantitative and Qualitative Disclosures About Market Risk
|
58
|
|
|
Item 8
|
Financial Statements and Supplementary Data
|
60
|
|
|
Item 9
|
Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
|
97
|
|
|
Item 9A
|
Controls and Procedures
|
97
|
|
|
Item 9B
|
Other Information
|
97
|
|
|
PART III
|
|||
|
Item 10
|
Directors, Executive Officers and Corporate Governance
|
98
|
|
|
Item 11
|
Executive Compensation
|
98
|
|
|
Item 12
|
Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
|
98
|
|
|
Item 13
|
Certain Relationships and Related Transactions, and Director Independence
|
98
|
|
|
Item 14
|
Principal Accountant Fees and Services
|
98
|
|
|
PART IV
|
|||
|
Item 15
|
Exhibits and Financial Statement Schedules
|
99
|
|
2
Forward-Looking Statements
The Private Securities Litigation Reform Act of 1995 provides a safe harbor for forward-looking statements if accompanied by meaningful cautionary statements identifying important factors that could cause actual results to differ materially from those discussed. You should not place undue reliance on these statements, which speak only as of the date of this report. Forward-looking statements include those related to our expected financial position, business, financing plans, litigation, future premiums, revenues, earnings, pricing, investments, business relationships, expected losses, loss reserves, acquisitions, competition, and rate increases with respect to our business and the insurance industry in general. Statements including words such as “expect,” “intend,” “plan,” “believe,” “estimate,” “may,” “anticipate,” “will” or similar statements of a future or forward-looking nature identify forward-looking statements.
We undertake no obligation to publicly update or revise any forward-looking statements, whether as a result of new information, future events or otherwise, except as required by law. All forward-looking statements address matters that involve risks and uncertainties that could cause actual results to differ materially from historical or anticipated results, depending on a number of factors. These risks and uncertainties include, but are not limited to, those set forth in Item 1A. “Risk Factors.”
Note Regarding Reliance on Statements in Our Contracts
The agreements included or incorporated by reference as exhibits to this Annual Report on Form 10-K contain representations and warranties by each of the parties to the applicable agreement. These representations and warranties were made solely for the benefit of the other parties to the applicable agreement and:
|
|
·
|
were not intended to be treated as categorical statements of fact, but rather as a way of allocating the risk to one of the parties if those statements prove to be inaccurate;
|
|
|
·
|
may have been qualified in such agreement by disclosures that were made to the other party in connection with the negotiation of the applicable agreement;
|
|
|
·
|
may apply contract standards of “materiality” that are different from “materiality” under the applicable securities laws; and
|
|
|
·
|
were made only as of the date of the applicable agreement or such other date or dates as may be specified in the agreement.
|
Notwithstanding the inclusion of the foregoing cautionary statements, the Company acknowledges that it is responsible for considering whether additional specific disclosures of material information regarding material contractual provisions are required to make the statements in this report not misleading.
3
PART I
Item 1. Business
General
Employers Holdings, Inc. (EHI) is a Nevada holding company and is the successor to EIG Mutual Holding Company (EIG), which was incorporated in Nevada in 2005. Unless otherwise indicated, all references to “we,” “us,” “our,” the “Company” or similar terms refer to EHI together with its subsidiaries. We had 699 full-time employees at December 31, 2010 and our principal executive offices are located at 10375 Professional Circle, in Reno, Nevada.
Our insurance subsidiaries have each been assigned an A.M. Best Company (A.M. Best) rating of “A-” (Excellent), with a “stable” financial outlook.
Our Annual Report on Form 10-K, Quarterly Reports on Form 10-Q, current reports on Form 8-K, and amendments to those reports, and Proxy Statement for our Annual Meeting of Stockholders are available free of charge on our website at www.employers.com as soon as reasonably practicable after they are electronically filed with or furnished to the Securities and Exchange Commission (SEC). Our website also provides access to reports filed by our Directors, executive officers and certain significant stockholders pursuant to Section 16 of the Securities Exchange Act of 1934. In addition, our Corporate Governance Guidelines, Code of Business Conduct and Ethics, Code of Ethics for Senior Financial Officers, and charters for the standing committees of our Board of Directors are available on our website. Copies of these documents may also be obtained free of charge by written request to Investor Relations, 10375 Professional Circle, Reno, Nevada 89521-4802. The SEC also maintains a website at www.sec.gov that contains this material and other information that we file electronically with the SEC.
Description of Business
We are a specialty provider of workers' compensation insurance focused on select small businesses engaged in low to medium hazard industries. We employ a disciplined, conservative underwriting approach designed to individually select specific types of businesses, predominantly those in the lowest four of the seven workers' compensation insurance industry-defined hazard groups, that we believe will have fewer and less costly claims relative to other businesses in the same hazard groups. Workers' compensation is a statutory system that generally requires an employer to provide coverage for its employees' medical, disability, vocational rehabilitation, and death benefit costs for work-related injuries or illnesses. We market and sell our products primarily through independent agents and brokers and through our strategic partnerships and alliances, including our principal strategic partners, ADP, Inc. (ADP) and Anthem Blue Cross of California (Anthem). We operate as a single reportable segment and conduct operations in 30 states and the District of Columbia, with approximately half of our business in California.
In July 2010, we announced the reorganization of our operations to eliminate duplicative services and better align resources with business activity and growth opportunities. We combined our four regional operating units into two units, Eastern and Western, with the Strategic Partnerships and Alliances unit remaining structurally unchanged. In connection with these efforts and with general cost control efforts, we eliminated approximately 160 positions. These changes to our workforce were substantially completed during the third quarter of 2010.
In the first quarter of 2010, we restructured our operations to reduce staffing levels to reflect activity levels in our insurance operations at that time.
On October 31, 2008, we acquired 100% of the outstanding common stock of AmCOMP Incorporated (the Acquisition). The Acquisition included two insurance subsidiaries and three other subsidiaries: EIG Services, Inc. (formerly Pinnacle Administrative Company), Pinnacle Benefits, Inc. and AmSERV, Inc. The acquired insurance subsidiaries, Employers Preferred Insurance Company and Employers Assurance Company (formerly AmCOMP Preferred Insurance Company and AmCOMP Assurance Corporation, respectively), are mono-line workers’ compensation insurance companies focused on small sized businesses engaged in low to medium hazard industries.
We had net premiums written of $313.1 million and $368.3 million, total revenues of $415.6 million and $495.9 million and net income of $62.8 million and $83.0 million for the years ended December 31, 2010 and 2009, respectively. At December 31, 2010, we had total assets of $3.48 billion. Our combined ratio on a statutory basis, a measurement of underwriting profitability, was 109.8% for the year ended December 31, 2010 (elsewhere in this report, unless otherwise
4
stated, the term “combined ratio” refers to a calculation based on U.S. generally accepted accounting principles (GAAP)). Our combined ratio on a statutory basis for the five years ended December 31, 2009 was 86.3%, compared to the industry composite statutory combined ratio of 108.1% for the same five-year period (calculated by A.M. Best for individual companies that have more than 50% of their business in workers' compensation). Companies with lower combined ratios than their peers generally experience greater profitability.
Our insurance subsidiaries are domiciled in the following states:
|
State of Domicile
|
|
|
Employers Insurance Company of Nevada (EICN)
|
Nevada
|
|
Employers Compensation Insurance Company (ECIC)
|
California
|
|
Employers Preferred Insurance Company (EPIC)
|
Florida
|
|
Employers Assurance Company (EAC)
|
Florida
|
Products and Services
Workers’ compensation provides insurance coverage for the statutorily prescribed benefits that employers are required to provide to their employees who may be injured or suffer illness in the course of employment. The level of benefits varies by state, the nature and severity of the injury or disease, and the wages of the injured worker. Each state has a statutory, regulatory, and adjudicatory system that sets the amount of wage replacement to be paid, determines the level of medical care required to be provided, establishes the degree of permanent impairment, and specifies the options in selecting healthcare providers. These state laws generally require two types of benefits for injured employees: (a) medical benefits, including expenses related to the diagnosis and treatment of an injury, disease, or both, as well as any required rehabilitation and (b) indemnity payments, which consist of temporary wage replacement, permanent disability payments, and death benefits to surviving family members.
Total direct premiums written for the workers’ compensation industry (excluding governmental writers) were approximately $35.0 billion and $39.0 billion in 2009 and 2008, respectively, according to A.M. Best. A.M. Best reported that we were the seventeenth largest writer of non-governmental workers’ compensation insurance in the United States in 2009.
Disciplined Underwriting
Our underwriting guidelines are designed to minimize underwriting of classes and subclasses of business which have historically demonstrated claims severity that do not meet our target risk profiles. We price our policies based on the specific risks associated with each potential insured rather than solely on the industry class in which a potential insured is classified. Our disciplined underwriting approach is a critical element of our culture and has allowed us to offer competitive prices, diversify our risks, and achieve profitable growth.
The following table compares our statutory losses and loss adjustment expenses (LAE) ratio, a measure which relates inversely to our underwriting profitability, to the statutory industry composite losses and LAE ratio reported by A.M. Best (calculated for U.S. insurance companies having more than 50% of their premiums generated by workers' compensation insurance products) for the past five years as of December 31, 2009 (the most recent information available):
|
Statutory Losses and LAE Ratio
|
||||||||
|
Year
|
EMPLOYERS
|
A.M. Best
|
||||||
|
2005
|
58.3 | % | 79.7 | % | ||||
|
2006
|
37.9 | 77.1 | ||||||
|
2007
|
46.5 | 77.7 | ||||||
|
2008
|
47.1 | 78.6 | ||||||
|
2009
|
57.5 | 86.1 | ||||||
|
2010
|
66.2 | N/A | ||||||
Our underwriting strategy is to focus on disciplined underwriting and continue to pursue profitable growth opportunities across market cycles. We carefully monitor market trends to assess new business opportunities that we expect will meet our pricing and risk standards.
5
We execute our underwriting processes through automated systems and experienced underwriters with specific knowledge of local markets. We have developed automated underwriting templates for specific classes of business that produce faster quotes when certain underwriting criteria are met. Our underwriting guidelines consider many factors, such as type of business, nature of operations and risk exposures, and are designed to minimize or prevent underwriting of certain undesirable classes and subclasses of business while increasing the number of policies underwritten to targeted small businesses in low to medium hazard industries.
Loss Control
Our loss control professionals provide consultation to policyholders to assist them in preventing losses and containing costs once claims occur. They also assist our underwriting personnel in evaluating potential and current policyholders and are an important part of our underwriting and loss control strategies.
Premium Audit
We conduct premium audits on our policyholders annually upon the policy expiration. Audits allow us to comply with applicable state and reporting bureau requirements and to verify that policyholders have accurately reported their payroll and employee job classifications. We also selectively perform interim audits on certain classes of business if unusual claims are filed or concerns are raised regarding projected annual payrolls, which could result in substantial variances at final audit.
Claims and Medical Case Management
The role of our claims department is to actively and efficiently investigate, evaluate, and pay claims, and to aid injured workers in returning to work in accordance with applicable laws and regulations. We have implemented rigorous claims guidelines and control procedures in our claims units and have claims operations throughout the markets we serve. We also provide medical case management services for those claims that we determine will benefit from such involvement.
Our claims department also provides claims management services for those claims incurred by the Nevada State Industrial Insurance System (the Fund) and assumed by EICN and subject to a 100% retroactive reinsurance agreement (the LPT Agreement) with dates of injury prior to July 1, 1995. Additional information regarding the LPT Agreement is set forth under “—Reinsurance—LPT Agreement.” We receive a management fee from the third party reinsurers equal to 7% of the loss payments on these claims.
We maintain an exclusive medical provider network in Nevada. We make every appropriate effort to direct injured workers into this network for medical treatments. We utilize networks affiliated with Anthem and Coventry Health Care, Inc. in other states. In addition to our medical networks, we work closely with local vendors, including attorneys, medical professionals, and investigators, to bring local expertise to our reported claims. We pay special attention to reducing costs in each region and have established discounting arrangements with the aforementioned service providers. We use preferred provider organizations, bill review services, and utilization management to closely monitor medical costs.
We actively pursue fraud and subrogation recoveries to mitigate claims costs. Subrogation rights are based upon state and federal laws, as well as the insurance policies issued to insureds. Our fraud and subrogation efforts are handled through dedicated units.
Information Technology
Core Operating Systems
We have an efficient, cost-effective and scalable infrastructure that complements our geographic reach and business model. We have developed a highly automated underwriting system. This technology allows for the electronic submission, review, and quoting of insurance applications applying our underwriting standards and guidelines. This policy administration system reduces transaction costs and provides for more efficient and timely processing of applications for small policies that meet our underwriting standards. We believe this approach saves our independent agents and brokers considerable time in processing customer applications and maintains our competitiveness in our target markets. In January 2009, we implemented a new claims system that was designed to improve efficiency and enhance our ability to support claims processing. We will continue to invest in technology and systems across our business to maximize efficiency and create increased capacity that will allow us to lower our expense ratios while growing premiums. In January 2010, EPIC and EAC were successfully converted to both our policy and claims administration systems and their legacy systems were discontinued.
6
Business Continuity/Disaster Recovery
We maintain business continuity and disaster recovery plans for our critical business functions, including the restoration of information technology infrastructure and applications. We have two data centers that act as production facilities and as disaster recovery sites for each other. In addition, we utilize an offsite data storage facility.
Customers and Workers’ Compensation Premiums
The workers' compensation insurance industry classifies risks into seven hazard groups, as defined by the National Council on Compensation Insurance (NCCI), based on severity of claims with businesses in the first or lowest group having the lowest claims costs.
We target select small businesses engaged in low to medium hazard industries. Our historical loss experience has been more favorable for lower industry-defined hazard groups than for higher hazard groups. Further, we believe it is generally less costly to service and manage the risks associated with these lower hazard groups. Our underwriters use their local market expertise and disciplined underwriting to select specific types of businesses and risks that are underwritten on the basis of individual risk characteristics, as opposed to following an occupational class-based underwriting approach, that allow us to generate loss ratios that are consistently better than the industry average. For example, while we insure many physician offices, our underwriting guidelines generally exclude offices that we believe have a higher risk profile, such as psychiatrist offices and drug treatment centers.
The following table sets forth our in-force premiums by hazard group and as a percentage of our total in-force premiums as of December 31:
|
Hazard
Group
|
2010
|
Percentage
of 2010 Total
|
2009
|
Percentage
of 2009 Total
|
2008
|
Percentage
of 2008 Total
|
|||||||||||||||||||
|
(in thousands, except percentages)
|
|||||||||||||||||||||||||
| A | $ | 45,537 | 14.2 | % | $ | 45,683 | 11.9 | % | $ | 46,838 | 10.1 | % | |||||||||||||
| B | 74,435 | 23.2 | 82,086 | 21.3 | 94,080 | 20.2 | |||||||||||||||||||
| C | 120,656 | 37.6 | 137,973 | 35.8 | 157,481 | 33.8 | |||||||||||||||||||
| D | 47,906 | 14.9 | 54,582 | 14.2 | 63,206 | 13.6 | |||||||||||||||||||
| E | 24,592 | 7.7 | 43,036 | 11.2 | 61,936 | 13.3 | |||||||||||||||||||
| F | 7,531 | 2.3 | 20,131 | 5.2 | 39,410 | 8.5 | |||||||||||||||||||
| G | 480 | 0.1 | 1,534 | 0.4 | 2,657 | 0.5 | |||||||||||||||||||
|
Total
|
$ | 321,137 | 100 | % | $ | 385,025 | 100.0 | % | $ | 465,608 | 100.0 | % | |||||||||||||
The following table sets forth our in-force premiums for our top ten types of insureds and as a percentage of our total in-force premiums as of December 31, 2010:
|
Employer Classifications
|
Hazard
Group Level
|
In-force
Premiums
|
Percentage
of Total
|
|||||||||
|
(in thousands, except percentages)
|
||||||||||||
|
Restaurants
|
A | $ | 36,026 | 11.2 | % | |||||||
|
Physician and physician office clerical
|
C | 28,673 | 8.9 | |||||||||
|
Automobile service or repair center and drivers
|
D | 25,696 | 8.0 | |||||||||
|
Store: Wholesale not otherwise classified
|
B | 14,756 | 4.6 | |||||||||
|
College: Professional employees and clerical
|
B | 9,758 | 3.0 | |||||||||
|
Store: Retail not otherwise classified
|
B | 8,583 | 2.7 | |||||||||
|
Hotel: All other employees and salespersons, drivers
|
B | 6,416 | 2.0 | |||||||||
|
Machine shops not otherwise classified
|
D | 6,379 | 2.0 | |||||||||
|
Clerical office employees not otherwise classified
|
C | 5,999 | 1.9 | |||||||||
|
Stores: Groceries and provisions - retail
|
C | 5,326 | 1.7 | |||||||||
|
Total
|
$ | 147,612 | 46.0 | % | ||||||||
7
We currently write business in 30 states and the District of Columbia and are licensed to write business in seven additional states. Our business is concentrated in California, which makes the results of our operations more dependent on the trends that are unique to that state and that from time-to-time may differ from national trends. State legislation, local competition, economic and employment trends, climate and environmental changes, and workers’ compensation medical costs trends can be material to our financial results.
As of December 31, 2010, our policyholders had average annual in-force premiums of approximately $7,200. We are not dependent on any single policyholder and the loss of any single policyholder would not have a material adverse effect on our business.
Our total in-force premiums and number of policies in-force by state are shown in the table below as of December 31:
|
2010
|
2009
|
2008
|
||||||||||||||||||||||
|
State
|
Premium
In-force
|
Policies
In-force
|
Premium
In-force
|
Policies
In-force
|
Premium
In-force
|
Policies
In-force
|
||||||||||||||||||
|
(dollars in thousands)
|
||||||||||||||||||||||||
|
California
|
$ | 172,621 | 29,244 | $ | 180,474 | 27,812 | $ | 203,694 | 27,942 | |||||||||||||||
|
Illinois
|
18,617 | 932 | 19,389 | 801 | 17,885 | 689 | ||||||||||||||||||
|
Nevada
|
16,940 | 3,596 | 24,050 | 4,119 | 38,971 | 5,221 | ||||||||||||||||||
|
Florida
|
15,071 | 1,963 | 27,964 | 2,630 | 46,248 | 3,115 | ||||||||||||||||||
|
Wisconsin
|
14,573 | 764 | 24,125 | 922 | 29,040 | 892 | ||||||||||||||||||
|
Other
|
83,315 | 8,061 | 109,023 | 7,870 | 129,770 | 7,740 | ||||||||||||||||||
|
Total
|
$ | 321,137 | 44,560 | $ | 385,025 | 44,154 | $ | 465,608 | 45,599 | |||||||||||||||
The following trends affected our workers compensation business from 2008 through 2010:
|
|
•
|
The decrease in premium in-force reflects the impacts of the recession, which has particularly affected certain classes of small business, including contractors and restaurants, and declining payrolls due to reduced employment and work hours, closures of small businesses and our continued focus on profitable underwriting despite aggressive pricing in a highly competitive market; and
|
|
|
•
|
The increase in total policies in-force in 2010 reflects our efforts to continue to grow our business profitably across market cycles, partially offset by declines in certain states, including Nevada and Florida, as a result of the continuing effects of the recession and our continued focus on disciplined underwriting.
|
We cannot be certain how these trends will ultimately impact our consolidated financial position and results of operations as we continue to emphasize disciplined pricing objectives and underwriting guidelines; however, we believe we are well positioned to continue to grow profitably in the future.
Premiums for all of our policies are generally a function of the applicable premium rate, the amount of the insured’s payroll, and if applicable, a factor reflecting the insured’s historical loss experience (experience modification factor). Premium rates vary by state according to the nature of the employee’s duties and the business of the employer. The premium is computed by applying the applicable premium rate to each class of the insured’s payroll after it has been appropriately classified. Total policy premium is determined after applying an experience modification factor and a further adjustment, known as a schedule rating adjustment, which may be made in certain circumstances, to increase or decrease the policy premium. Schedule rating adjustments are made at the discretion of the underwriter based on individual risk characteristics of the insured and subject to maximum amounts as established in our premium rate filings.
Our premium rates are determined by our actuaries for each state in which we do business, except in “administered pricing” states, where premium rates are set by state insurance regulators, primarily Florida and Wisconsin. In California, where approximately half of our premiums are earned, the Workers’ Compensation Insurance Rating Bureau (WCIRB) recommends claims cost benchmarks to be used by companies in determining their premium rates. The California Commissioner of Insurance (California Commissioner) also adopts and publishes his own claims cost benchmark. The benchmark rates are advisory rates that cover expected loss costs, but do not contain an element to cover operating expenses or profit. We are not required to use these benchmark rates.
8
The WCIRB recommended a 22.8% increase in the claims cost benchmark effective January 1, 2010. This recommendation was based upon an evaluation of March 31, 2009 loss experience, which produced an indicated increase in the claims cost benchmark of 16.0%, reflecting increased medical costs. The recommendation also indicated an increase of 5.8% directly attributable to additional costs arising from several Workers’ Compensation Appeals Board decisions. The California Commissioner rejected the WCIRB recommendation and left the claims cost benchmark unchanged. In April 2010, the WCIRB submitted an analysis of premium and loss experience as of December 31, 2009, indicating a 21.1% increase in the claims cost benchmark, but did not make a recommendation to the California Commissioner. Subsequently, the WCIRB recommended a 29.6% increase in the January 1, 2011 claims cost benchmark, based on an evaluation of March 31, 2010 loss experience. The WCIRB amended its August filing in September 2010 to recommend a 27.7% increase in the claims cost benchmark in lieu of the 29.6% increase based on an analysis of June 30, 2010 loss experience. In November 2010 the California Commissioner rejected the recommendation of the WCIRB and left the claims cost benchmark unchanged.
We set our premium rates in California based upon actuarial analyses of current and anticipated loss trends with a goal of maintaining underwriting profitability. We reduced our filed premium rates in California from 2003 through 2008 due to favorable loss costs trends originating from the 2003 and 2004 legislative reforms (see “Workers’ Compensation Reform Legislation”). Due to increasing loss costs, primarily medical cost inflation, we increased our filed premium rates by a cumulative 28.3% since February 1, 2009.
The following table sets forth the percentage increases to our filed California rates effective for new and renewal policies incepting on or after the dates shown.
|
Effective Date
|
Premium Rate Change
Filed in California
|
|||
|
February 1, 2009
|
10.0 | % | ||
|
August 15, 2009
|
10.5 | |||
|
March 15, 2010
|
3.0 | |||
|
March 15, 2011
|
2.5 | |||
In October 2010, the Florida Insurance Commissioner (Florida Commissioner) approved a 7.8% increase in workers’ compensation rates to be effective January 1, 2011 for new and renewal business. The increase followed a 6.8% decrease in Florida for new and renewal policies incepting on or after January 1, 2010.
In Nevada, we filed for a 6.7% rate decrease for new and renewal policies incepting on or after March 1, 2010.
Workers’ Compensation Reform Legislation
California enacted three key pieces of workers' compensation legislation in 2003 and 2004 that reformed medical determinations of injuries or illness, established medical fee schedules, allowed for the use of medical provider panels, modified benefit levels, changed the proof needed to file claims, and reformed many additional areas of the workers' compensation benefits and delivery system. Workers' compensation insurers in California responded to these reforms, which have reduced claim costs, by reducing their rates through 2008.
In Florida, legislation was enacted effective in 2003 to reverse a trend of increasing workers’ compensation costs in the state. These reforms have reduced claim costs and resulted in subsequent rate decreases. In October 2008, a Florida Supreme Court decision materially impacted the statutory caps on attorney fees that were part of the 2003 reforms; however, during 2009, the Florida Legislature restored the statutory caps on attorney fees. Through January 2010, there was a cumulative 63.2% rate decrease since the reforms of 2003.
Losses and LAE Reserves and Loss Development
We are directly liable for losses and LAE under the terms of insurance policies our insurance subsidiaries write. Significant periods of time can elapse between the occurrence of an insured loss, the reporting of the loss to us and our payment of that loss. Loss reserves are reflected on our consolidated balance sheets under the line item caption “unpaid losses and loss adjustment expenses.” Estimating reserves is a complex process that involves a considerable degree of judgment by management and, as of any given date, is inherently uncertain. Loss reserve estimates represent a significant risk to the business, which we attempt to mitigate by continually reviewing loss cost trends and by attempting to set ourpremium rates to adequately cover anticipated costs. We minimize the estimation risk by performing a comprehensive review of our loss reserves.
9
The amount by which revised estimated losses, measured subsequently by reference to payments and additional information, differs from those originally reported for a period is known as “development.” Development is favorable when losses ultimately settle for less than the amount reserved or subsequent estimates indicate a basis for reducing loss reserves on open claims. Development is unfavorable when losses ultimately settle for more than the levels at which they were reserved or subsequent estimates indicate a basis for reserve increases on open claims. Favorable or unfavorable development of loss reserves is reflected on our consolidated statements of income under the line item “losses and LAE” in the period in which the change is made.
For a detailed description of our reserves, the judgments, key assumptions and actuarial methodologies that we use to estimate our reserves and the role of our consulting actuary, see “Item 7—Management's Discussion and Analysis of Financial Condition and Results of Operations—Critical Accounting Policies—Reserves for Losses and LAE” and Note 9 in the Notes to our Consolidated Financial Statements.
The following tables show changes in the historical loss reserves, on a gross basis and net of reinsurance, for each of the eleven years ended December 31, 2010 for EICN and ECIC, and for each of the years ended December 31, 2010, 2009, and 2008, for EPIC and EAC. These tables are presented on a GAAP basis. The paid and reserve data in the following tables is presented on a calendar year basis.
The top line of each table shows the net and gross reserves for unpaid losses and LAE recorded at each year-end. Such amount represents an estimate of unpaid losses and LAE occurring in that year as well as future payments on claims occurring in prior years. The upper portion of these tables (net and gross cumulative amounts paid, respectively) present the cumulative amounts paid during subsequent years on those losses for which reserves were carried as of each specific year. The lower portions (net and gross reserves re-estimated, respectively) show the re-estimated amounts of the previously recorded reserves based on experience as of the end of each succeeding year. The re-estimated amounts change as more information becomes known about the actual losses for which the initial reserve was carried. An adjustment to the carrying value of unpaid losses for a prior year will also be reflected in the adjustments for each subsequent year. For example, an adjustment made in the 2000 year will be reflected in the re-estimated ultimate net loss for each subsequent year. The gross cumulative redundancy, or deficiency, line represents the cumulative change in estimates since the initial reserve was established. It is equal to the difference between the initial reserve and the latest re-estimated reserve amount. A redundancy means that the original estimate was higher than the current estimate. A deficiency means that the current estimate is higher than the original estimate.
10
|
2000
|
2001
|
2002
|
2003
|
2004
|
2005
|
2006
|
2007
|
2008
|
2009
|
2010
|
|||||||||||||||||||||||
|
(in thousands)
|
|||||||||||||||||||||||||||||||||
|
Net reserves for losses
and LAE
|
|||||||||||||||||||||||||||||||||
|
Originally estimated
|
$ | 936,000 | $ | 887,000 | $ | 908,326 | $ | 962,457 | $ | 1,089,814 | $ | 1,208,481 | $ | 1,209,652 | $ | 1,217,069 | $ | 1,430,128 | $ | 1,373,153 | $ | 1,323,686 | |||||||||||
|
Net cumulative amounts paid
as of:
|
|||||||||||||||||||||||||||||||||
|
One year later
|
108,748 | 81,022 | 80,946 | 91,130 | 96,661 | 106,859 | 109,129 | 127,912 | 214,499 | 206,653 | |||||||||||||||||||||||
|
Two years later
|
161,721 | 120,616 | 130,386 | 150,391 | 161,252 | 175,531 | 186,014 | 219,496 | 342,174 | ||||||||||||||||||||||||
|
Three years later
|
191,453 | 149,701 | 165,678 | 193,766 | 207,868 | 229,911 | 249,059 | 295,646 | |||||||||||||||||||||||||
|
Four years later
|
215,015 | 173,204 | 194,400 | 226,127 | 247,217 | 279,405 | 302,863 | ||||||||||||||||||||||||||
|
Five years later
|
235,613 | 194,980 | 218,453 | 255,851 | 285,388 | 321,060 | |||||||||||||||||||||||||||
|
Six years later
|
255,772 | 215,507 | 242,143 | 288,039 | 317,489 | ||||||||||||||||||||||||||||
|
Seven years later
|
275,750 | 235,653 | 269,341 | 315,180 | |||||||||||||||||||||||||||||
|
Eight years later
|
294,760 | 260,036 | 292,791 | ||||||||||||||||||||||||||||||
|
Nine years later
|
318,262 | 280,809 | |||||||||||||||||||||||||||||||
|
Ten years later
|
338,059 | ||||||||||||||||||||||||||||||||
|
Net reserves re-estimated
as of:
|
|||||||||||||||||||||||||||||||||
|
One year later
|
896,748 | 875,522 | 847,917 | 924,878 | 1,011,759 | 1,101,352 | 1,149,641 | 1,151,246 | $ | 1,378,767 | 1,359,023 | ||||||||||||||||||||||
|
Two years later
|
885,221 | 781,142 | 805,058 | 886,711 | 975,765 | 1,049,628 | 1,085,358 | 1,100,706 | 1,352,021 | ||||||||||||||||||||||||
|
Three years later
|
800,959 | 742,272 | 779,373 | 884,426 | 954,660 | 1,004,589 | 1,035,028 | 1,079,913 | |||||||||||||||||||||||||
|
Four years later
|
766,204 | 719,912 | 788,262 | 877,151 | 927,382 | 970,671 | 1,010,407 | ||||||||||||||||||||||||||
|
Five years later
|
743,997 | 730,112 | 788,481 | 858,617 | 900,588 | 949,446 | |||||||||||||||||||||||||||
|
Six years later
|
754,447 | 730,456 | 776,329 | 839,430 | 883,388 | ||||||||||||||||||||||||||||
|
Seven years later
|
754,462 | 720,155 | 763,988 | 826,608 | |||||||||||||||||||||||||||||
|
Eight years later
|
745,665 | 712,717 | 755,793 | ||||||||||||||||||||||||||||||
|
Nine years later
|
744,085 | 707,037 | |||||||||||||||||||||||||||||||
|
Ten years later
|
739,822 | ||||||||||||||||||||||||||||||||
|
Net cumulative redundancy:
|
196,178 | 179,963 | 152,533 | 135,849 | 206,426 | 259,035 | 199,245 | 137,156 | 78,105 | 14,129 | 0 | ||||||||||||||||||||||
|
Gross reserves –
December 31
|
2,326,000 | 2,226,000 | 2,212,368 | 2,193,439 | 2,284,542 | 2,349,981 | 2,307,755 | 2,269,710 | 2,506,478 | 2,425,658 | 2,279,729 | ||||||||||||||||||||||
|
Reinsurance recoverable,
gross
|
1,390,000 | 1,339,000 | 1,304,042 | 1,230,982 | 1,194,728 | 1,141,500 | 1,098,1032 | 1,052,641 | 1,076,350 | 1,052,505 | 956,043 | ||||||||||||||||||||||
|
Net reserves – December 31
|
936,000 | 887,000 | 908,326 | 962,457 | 1,089,814 | 1,208,481 | 1,209,652 | 1,217,069 | 1,430,128 | 1,373,153 | 1,323,686 | ||||||||||||||||||||||
|
Gross re-estimated reserves
|
2,062,283 | 1,979,480 | 1,986,694 | 2,011,945 | 2,027,187 | 2,053,869 | 2,074,466 | 2,110,230 | 2,405,837 | 2,373,479 | 2,279,729 | ||||||||||||||||||||||
|
Re-estimated reinsurance
recoverables
|
1,322,461 | 1,272,442 | 1,230,901 | 1,185,337 | 1,143,799 | 1,104,422 | 1,064,059 | 1,030,317 | 1,053,816 | 1,014,456 | 956,043 | ||||||||||||||||||||||
|
Net re-estimated reserves
|
739,822 | 707,037 | 755,793 | 826,608 | 883,388 | 949,446 | 1,010,407 | 1,079,913 | 1,352,021 | 1,359,023 | 1,323,686 | ||||||||||||||||||||||
|
Gross reserves for losses
and LAE
|
|||||||||||||||||||||||||||||||||
|
Originally estimated
|
2,326,000 | 2,226,000 | 2,212,368 | 2,193,439 | 2,284,542 | 2,349,981 | 2,307,755 | 2,269,710 | 2,506,478 | 2,425,658 | 2,279,729 | ||||||||||||||||||||||
|
Gross cumulative amounts
paid as of:
|
|||||||||||||||||||||||||||||||||
|
One year later
|
160,978 | 128,066 | 128,462 | 137,968 | 142,632 | 152,006 | 152,879 | 170,626 | 258,412 | 269,771 | |||||||||||||||||||||||
|
Two years later
|
260,995 | 215,176 | 224,740 | 243,203 | 252,379 | 264,430 | 272,478 | 304,146 | 449,206 | ||||||||||||||||||||||||
|
Three years later
|
338,243 | 291,099 | 306,006 | 331,731 | 342,748 | 361,524 | 377,459 | 422,862 | |||||||||||||||||||||||||
|
Four years later
|
408,643 | 360,535 | 379,881 | 407,845 | 424,811 | 452,955 | 473,828 | ||||||||||||||||||||||||||
|
Five years later
|
475,174 | 427,307 | 447,687 | 480,283 | 504,918 | 537,175 | |||||||||||||||||||||||||||
|
Six years later
|
540,329 | 490,296 | 514,091 | 554,408 | 579,585 | ||||||||||||||||||||||||||||
|
Seven years later
|
602,371 | 553,103 | 583,226 | 624,114 | |||||||||||||||||||||||||||||
|
Eight years later
|
664,042 | 619,373 | 649,241 | ||||||||||||||||||||||||||||||
|
Nine years later
|
729,432 | 682,656 | |||||||||||||||||||||||||||||||
|
Ten years later
|
791,739 | ||||||||||||||||||||||||||||||||
|
Gross reserves re-estimated
as of:
|
|||||||||||||||||||||||||||||||||
|
One year later
|
2,280,978 | 2,211,566 | 2,121,867 | 2,148,829 | 2,178,514 | 2,233,077 | 2,233,176 | 2,200,689 | 2,470,746 | 2,373,479 | |||||||||||||||||||||||
|
Two years later
|
2,266,495 | 2,089,850 | 2,072,205 | 2,088,437 | 2,138,648 | 2,170,292 | 2,162,695 | 2,148,399 | 2,405,837 | ||||||||||||||||||||||||
|
Three years later
|
2,157,647 | 2,049,340 | 2,024,790 | 2,084,764 | 2,110,481 | 2,119,764 | 2,110,615 | 2,110,230 | |||||||||||||||||||||||||
|
Four years later
|
2,121,397 | 2,000,560 | 2,032,553 | 2,072,428 | 2,078,223 | 2,084,854 | 2,074,466 | ||||||||||||||||||||||||||
|
Five years later
|
2,072,866 | 2,009,608 | 2,028,211 | 2,050,124 | 2,050,937 | 2,053,869 | |||||||||||||||||||||||||||
|
Six years later
|
2,082,409 | 2,009,480 | 2,012,943 | 2,030,945 | 2,027,187 | ||||||||||||||||||||||||||||
|
Seven years later
|
2,082,287 | 1,997,550 | 2,000,610 | 2,011,945 | |||||||||||||||||||||||||||||
|
Eight years later
|
2,072,850 | 1,990,116 | 1,986,694 | ||||||||||||||||||||||||||||||
|
Nice years later
|
2,071,274 | 1,979,480 | |||||||||||||||||||||||||||||||
|
Ten years later
|
2,062,283 | ||||||||||||||||||||||||||||||||
|
Gross cumulative
redundancy:
|
$ | 263,717 | $ | 246,520 | $ | 225,674 | $ | 181,494 | $ | 257,355 | $ | 296,112 | $ | 233,289 | $ | 159,480 | $ | 100,640 | $ | 52,179 | $ | 0 | |||||||||||
11
Reinsurance
Reinsurance is a transaction between insurance companies in which an original insurer, or ceding company, remits a portion of its premiums to a reinsurer, or assuming company, as payment for the reinsurer assuming a portion of the risk. Reinsurance agreements may be proportional in nature, under which the assuming company shares proportionally in the premiums and losses of the ceding company. This arrangement is known as quota share reinsurance. Reinsurance agreements may also be structured so that the assuming company indemnifies the ceding company against all or a specified portion of losses on underlying insurance policies in excess of a specified amount, which is called an “attachment level” or “retention” in return for a premium, usually determined as a percentage of the ceding company's primary insurance premiums. This arrangement is known as excess of loss reinsurance. Excess of loss reinsurance may be written in layers, in which a reinsurer or group of reinsurers accepts a band of coverage up to a specified amount. Any liability exceeding the coverage limits of the reinsurance program is retained by the ceding company. The ceding company also bears the credit risk of a reinsurers' insolvency. In accordance with general industry practices, we purchase excess of loss reinsurance to protect against the impact of large individual, irregularly-occurring losses, and aggregate catastrophic losses from natural perils and terrorism. Such reinsurance reduces the magnitude of such losses on net income and the capital of our insurance subsidiaries.
Excess of Loss Reinsurance
Our current reinsurance program applies to all covered losses occurring between 12:01 a.m. July 1, 2010 and 12:01 a.m. July 1, 2011. The reinsurance program consists of one treaty covering excess of loss and catastrophic loss events in five layers of coverage. Our reinsurance coverage is $195.0 million in excess of our $5.0 million retention on a per occurrence basis, subject to a $2.0 million annual aggregate deductible and certain exclusions. We are solely responsible for any losses we suffer above $200.0 million except those covered by the Terrorism Risk Insurance Program Reauthorization Act of 2007 (TRIPRA). Covered losses which occur prior to expiration or cancellation of the agreement continue to be obligations of the subscribing reinsurers, subject to the other conditions in the agreement. The subscribing reinsurers may terminate the agreement only for our breach of the obligations of the agreement. We are responsible for the losses if the subscribing reinsurer cannot or refuses to pay.
The agreements include certain exclusions for which our subscribing reinsurers are not liable for losses, including but not limited to losses arising from the following: reinsurance assumed by us under obligatory reinsurance agreements; financial guarantee and insolvency; certain nuclear risks; liability as a member, subscriber or reinsurer of any pool, syndicate or association, but not assigned risk plans; liability arising from participation or membership in any insolvency fund; loss or damage caused by war or civil unrest other than terrorism; certain workers’ compensation business covering persons employed in Minnesota; any loss or damage caused by any act of terrorism involving biological, chemical, nuclear or radioactive pollution or contamination. Our underwriting guidelines generally require that insured risks fall within the coverage provided in the reinsurance program. Any risks written outside the reinsurance program require executive review and approval.
The agreements provide that we, or any subscribing reinsurer, may request commutation of any outstanding claim or claims 10 years after the effective date of termination or expiration of the agreements and provide a mechanism for the parties to achieve valuation for commutation. We may require a special commutation of the percentage share of any loss in the reinsurance program of any subscribing reinsurer that is in runoff.
LPT Agreement
In 1999, Nevada enacted Senate Bill 37 (SB37).That bill stated that the Fund could take retroactive credit as an asset or a reduction of liability, amounts ceded to (reinsured with) assuming insurers with security based on discounted reserves for losses related to periods beginning before July 1, 1995, at a rate not to exceed 6%.
The Fund entered into a retroactive 100% quota share reinsurance agreement through a loss portfolio transfer transaction with third party reinsurers. The LPT Agreement commenced on June 30, 1999 and will remain in effect until all claims for loss and outstanding loss under the covered policies have closed, the agreement is commuted, or terminated, upon the mutual agreement of the parties, or the reinsurer's aggregate maximum limit of liability is exhausted, whichever occurs earlier. The LPT Agreement does not provide for any additional termination terms. The LPT Agreement substantially reduced the Fund's exposure to losses for pre-July 1, 1995 Nevada insured risks. On January 1, 2000, EICN assumed all of the assets, liabilities and operations of the Fund, including the Fund's rights and obligations associated with the LPT Agreement.
12
Under the LPT Agreement, the Fund initially ceded $1.525 billion in liabilities for the incurred but unpaid losses and LAE related to claims incurred prior to July 1, 1995, for consideration of $775.0 million in cash. The LPT Agreement, which ceded to the reinsurers substantially all of the Fund's outstanding losses as of June 30, 1999 for claims with original dates of injury prior to July 1, 1995, provides coverage for losses up to $2.0 billion, excluding losses for burial and transportation expenses. The estimated remaining liabilities subject to the LPT Agreement were approximately $846.7 million, and $888.4 million, as of December 31, 2010 and 2009, respectively. Losses and LAE paid with respect to the LPT Agreement totaled approximately $530.7 million and $489.0 million through December 31, 2010 and 2009, respectively.
The reinsurers agreed to assume responsibilities for the claims at the benefit levels which existed in June 1999. The LPT Agreement required each reinsurer to place assets supporting the payment of claims by them in individual trusts that require collateral be held at a specified level. The level must not be less than the outstanding reserve for losses and a loss expense allowance equal to 7% of estimated paid losses discounted at a rate of 6%. If the assets held in trust fall below this threshold, we may require the reinsurers to contribute additional assets to maintain the required minimum level of collateral. The value of these assets as of December 31, 2010 and 2009 was $962.1 million and $883.6 million, respectively.
The reinsurers currently party to the LPT Agreement include ACE Bermuda Insurance Limited, XL Reinsurance Limited, and National Indemnity Company. The contract provides that during the term of the agreement all reinsurers need to maintain a rating of no less than “A-” as determined by A.M. Best.
We account for the LPT Agreement as retroactive reinsurance. Upon entry into the LPT Agreement, an initial deferred reinsurance gain was recorded as a liability in our consolidated balance sheet. This gain is amortized using the recovery method, whereby the amortization is determined by the proportion of actual reinsurance recoveries to total estimated recoveries, and the amortization is reflected in losses and LAE in our consolidated financial statements.
We are also entitled to receive a contingent profit commission under the LPT Agreement. The contingent profit commission is estimated based on both actual paid results to date and projections of expected paid losses under the LPT Agreement. Since the inception of the agreement, we have recognized approximately $26 million in contingent profit commission. Increases and decreases in the estimated contingent profit commission are reflected in our commission expense in the period that the estimate is revised.
Recoverability of Reinsurance
Reinsurance makes the assuming reinsurer liable to the ceding company to the extent of the reinsurance. It does not, however, discharge the ceding company from its primary liability to its policyholders in the event the reinsurer is unable to meet its obligations under such reinsurance. We monitor the financial strength of our reinsurers and we do not believe that we are currently exposed to any material credit risk through our reinsurance arrangements because our reinsurance is recoverable from generally large, well-capitalized reinsurance companies. At December 31, 2010, $962.1 million was in a trust account for reinsurance related to the LPT Agreement and an additional $11.6 million, not related to the LPT Agreement, was collateralized by cash or letter of credit.
In 2010, we re-negotiated the terms of a reinsurance agreement with Clarendon National Insurance Company (Clarendon), which resulted in the release and return of funds held by Clarendon to us in the amount of $74.6 million. We placed $47.1 million in trust for the benefit of Clarendon to support the liabilities under the reinsurance agreement.
13
The following table provides certain information regarding our ceded reinsurance recoverables as of December 31, 2010.
|
Reinsurer
|
A.M.
Best
Rating(1)
|
Total
Paid
|
Total Unpaid Losses and LAE, net
|
Total
|
|||||||||||
|
(in thousands)
|
|||||||||||||||
|
ACE Bermuda Insurance Limited
|
A | + | $ | 1,079 | $ | 84,674 | $ | 85,753 | |||||||
|
Ace Property & Casualty Insurance Company
|
A | + | — | 1,568 | 1,568 | ||||||||||
|
Alterra Bermuda Limited
|
A | 623 | 5,379 | 6,002 | |||||||||||
|
American Healthcare Indemnity Co
|
B | + | — | 2,684 | 2,684 | ||||||||||
|
Aspen Insurance UK Limited
|
A | 231 | 2,493 | 2,724 | |||||||||||
|
Continental Casualty Company
|
A | — | 180 | 180 | |||||||||||
|
Everest Reinsurance Company
|
A | + | 56 | 4,504 | 4,560 | ||||||||||
|
Finial Reinsurance
|
A | - | — | 5,204 | 5,204 | ||||||||||
|
Hannover Rueckversicherung-AG
|
A | 462 | 5,552 | 6,014 | |||||||||||
|
Munich Reinsurance America, Inc
|
A | + | 240 | 11,127 | 11,367 | ||||||||||
|
National Indemnity Company
|
A | ++ | 5,934 | 465,709 | 471,643 | ||||||||||
|
National Union Fire Insurance Company of Pittsburgh
|
A | 151 | 2,229 | 2,380 | |||||||||||
|
Odyssey America Reinsurance Corp
|
A | — | 502 | 502 | |||||||||||
|
PartnerRe Group
|
A | - | — | 1,796 | 1,796 | ||||||||||
|
ReliaStar Life Insurance Company
|
A | 199 | 2,833 | 3,032 | |||||||||||
|
St. Paul Fire & Marine Insurance Company
|
A | + | 16 | 4,151 | 4,167 | ||||||||||
|
Swiss Reinsurance America Company
|
A | 1,071 | 11,541 | 12,612 | |||||||||||
|
Tokio Marine & Nichido Fire Ins Ltd (US)
|
A | ++ | 150 | 6,077 | 6,227 | ||||||||||
|
Westport Insurance Company
|
A | 241 | 1,479 | 1,720 | |||||||||||
|
XL Re Limited
|
A | 3,776 | 296,360 | 300,136 | |||||||||||
|
Lloyds Syndicates
|
A | 5 | 24,024 | 24,029 | |||||||||||
|
All Other
|
Various
|
181 | 15,977 | 16,158 | |||||||||||
|
Total
|
$ | 14,415 | $ | 956,043 | $ | 970,458 | |||||||||
|
(1)
|
A.M. Best's highest financial strength ratings for insurance companies are “A++” and “A+” (superior) and “A” and “A−” (excellent).
|
We review the aging of our reinsurance recoverables on a quarterly basis. At December 31, 2010, 4.2% of our reinsurance recoverables on paid losses were greater than 90 days overdue.
Inter-Company Reinsurance Pooling Agreement
Our insurance subsidiaries are parties to an inter-company pooling agreement for statutory reporting purposes. Under this agreement, the results of underwriting operations of each company are transferred to and combined with those of the others and the combined results are then reapportioned. The allocations under the pooling agreement are as follows:
|
|
•
|
EICN – 53%
|
|
|
•
|
ECIC – 27%
|
|
|
•
|
EPIC – 10%
|
|
|
•
|
EAC – 10%
|
Transactions under the pooling agreement are eliminated on consolidation and have no impact on our consolidated GAAP financial statements.
Investments
As of December 31, 2010, the total amortized cost of our investment portfolio was $1.95 billion and the fair market value of the portfolio was $2.08 billion. These investments provide a source of income, although short-term changes in interest rates and our current investment strategies affect the amount of investment income we earn and the fair value of our portfolio. Our investment strategy balances consideration of duration, yield, and credit risk.
14
We seek to maximize total investment returns within the constraints of prudent portfolio management. The asset allocation is reevaluated by the Finance Committee of the Board of Directors on a quarterly basis. We employ Conning Asset Management (Conning) as our independent investment manager. Conning follows our written investment guidelines based upon strategies approved by our Board of Directors. We also utilize Conning’s investment advisory services. These services include investment accounting and company modeling using Dynamic Financial Analysis (DFA). The DFA tool is utilized in developing a tailored set of portfolio targets and objectives, which in turn, is used in constructing an optimal portfolio.
Additional information regarding our investment portfolio, including our approach to managing investment risk, is set forth under “Item 7—Management's Discussion and Analysis of Financial Condition and Results of Operations—Critical Accounting Policies—Investments” and “Item 7A—Quantitative and Qualitative Disclosures about Market Risk.”
Marketing and Distribution
We market and sell our workers' compensation insurance products through independent local, regional and national agents and brokers, and through our strategic partnerships and alliances, including our principal partners ADP and Anthem. We do not delegate underwriting authority to agents or brokers or to our strategic distribution partners that sell our insurance.
Independent Insurance Agents and Brokers
We establish and maintain strong, long-term relationships with independent agencies that actively market our products and services. We offer ease of doing business, provide responsive service, and pay competitive commissions. Our sales representatives and field underwriters work closely with independent agencies to market and underwrite our business, regularly visiting their offices and participating in presentations to customers. This results in enhanced understanding of the businesses and risks we underwrite and the needs of prospective customers.
We marketed and sold our insurance products through approximately 2,610, 2,290, and 2,350 independent insurance agencies as of December 31, 2010, 2009, and 2008, respectively. This represents an increase in our network of insurance agencies of approximately 14% in 2010 as we continue to execute our growth strategy. Those agencies produced $247.8 million, $309.5 million, and $381.9 million, or 77.1%, 80.4%, and 82.0% of our in-force premiums as of December 31, 2010, 2009, and 2008, respectively.
Our largest agency accounted for 1.2%, 0.7%, and 1.2% of our in-force premiums as of December 31, 2010, 2009, and 2008, respectively.
Strategic Partnerships and Alliances
We have developed important strategic relationships with companies that have established sales forces and common markets to expand our reach to alternative distribution channels. Since 2002, we have jointly marketed our workers’ compensation insurance products with ADP’s payroll services and with Anthem’s group health insurance plans. In 2010, we expanded our relationship with ADP to offer our products in 30 states and expanded our relationship with Anthem beyond California into Colorado. Additionally, we have entered into other strategic partnerships and alliances with payroll service providers and insurance brokerages, including the launch of a new program in conjunction with Hiscox USA to deliver our workers’ compensation insurance direct to small businesses online in 17 states. These relationships have allowed us to access new customers and to write attractive business in an efficient manner and we are actively pursuing additional strategic partnership and alliance opportunities.
Policies underwritten through our strategic partnerships and alliances generated $71.0 million, $72.3 million, and $78.9 million, or 22.1%, 18.8%, and 16.9% of our in-force premiums as of December 31, 2010, 2009, and 2008, respectively.
ADP. ADP is the largest payroll services provider in the United States servicing small and medium-sized businesses. As part of its services, ADP sells our workers' compensation insurance product along with its payroll and accounting services through their insurance agency and field sales staff primarily to small businesses in 30 states. The majority of business written is through ADP’s small business unit, which has accounts of 1 to 50 employees. We pay ADP fees that are a percentage of premiums received for services provided through the ADP program.
15
ADP utilizes innovative methods to market workers' compensation insurance including the Pay-by-Pay® (PBP) program. An advantage of ADP’s PBP program is that the policyholder is not required to pay a deposit at the inception of thepolicy. The workers' compensation premium is deducted each time ADP processes the policyholders’ payrolls along with their appropriate federal, state, and local taxes. These characteristics of the PBP program enable us to competitively price the workers' compensation insurance written as a part of that program.
Our relationship with ADP is non-exclusive; however, we believe we are a key strategic partner of ADP for our selected markets and classes of business. Our agreement with ADP may be terminated without cause upon 120 days notice.
Anthem. The Integrated MediCompSM joint marketing program is based on two agreements, a small group health insurance plan (for businesses with 1 to 50 employees) and a large group health insurance plan (for businesses with 51 to 250 employees). This exclusive relationship allows us to combine Anthem’s group health and our workers' compensation product through a single bill. In California, Anthem’s life and health agents can sell our workers’ compensation product. Integrated MediComp also offers policyholders a discount on workers’ compensation premiums. We believe that, in general, when businesses purchase this combination of coverage, their employees make fewer workers' compensation claims because those employees are insured for non-work related illnesses or injuries and thus are less likely to seek treatment for a non-work related illness or injury through their employers' workers' compensation insurance policy. Another key benefit to this program is the increased satisfaction from employees who are able to use the same medical network for occupational and non-occupational illness and injury. As the largest group health carrier in California, Anthem has negotiated favorable rates with its medical providers and associated facilities, which we benefit from through reduced claims costs. We pay Anthem fees that are a percentage of premiums received for services provided under the Integrated MediComp program.
The small group and large group agreements automatically renew for one-year periods unless terminated by either party with at least 60 days notice prior to the expiration of the current term. These agreements have automatically renewed through January 1, 2012 and July 1, 2011, respectively.
Direct Business
We write a small amount of business that comes to us directly without using an agent or broker or one of our strategic distribution relationships. This direct business is a legacy of our assumption of the assets and liabilities of the Fund. Although we do not market any direct business, we intend to maintain this book of business because it is very well known by our underwriters and is profitable. Policies underwritten directly generated $2.3 million, $3.2 million, and $4.8 million of our in-force premiums at December 31, 2010, 2009, and 2008, respectively.
Competition and Market Conditions
Competition in the workers’ compensation insurance business is based upon price and quality of services. The insurance industry is highly competitive, and there is significant competition in the national workers’ compensation industry. We compete with other specialty workers' compensation carriers, state agencies, multi-line insurance companies, professional employer organizations, third-party administrators, self-insurance funds, and state insurance pools. Many of our competitors are significantly larger, are more widely known, and/or possess considerably greater financial resources. Our three primary competitors in California are the California State Compensation Insurance Fund, Berkshire Hathaway Insurance Group, and Republic Indemnity Company of America.
Our competitive advantages include our strong reputation in the markets in which we operate, excellent claims service, experienced and professional independent agents and brokers, and our strategic partnerships and alliances. We also strive to maintain the high quality of our care management services, and to provide consultation services to our agents and insureds on loss prevention and loss reduction strategies. We also compete on price, based on our actuarial analysis of current and anticipated loss cost trends, as appropriate.
The workers' compensation sector continued to see average medical and indemnity claims costs rise as claim frequency declined in 2009, while partial year data for 2010 is indicating an increase in claim frequency.
Currently, the industry is experiencing decreasing operating margins caused primarily by a combination of increased price competition and decreasing premiums due to continued downward rate pressure and lower payrolls. We continue to have concerns related to the volatility and uncertainty in the financial markets and current economic conditions, including the high rate of unemployment. We believe that overall market conditions, while challenging, still allow for profitable operations.
16
Regulation
Holding Company Regulation
Nearly all states have enacted legislation that regulates insurance holding company systems. Each insurance company in a holding company system is required to register with the insurance regulator of its state of domicile and furnish information concerning the operations of companies within the holding company system that may materially affect the operations, management or financial condition of the insurers within the system. All transactions within a holding company system affecting an insurer must have fair and reasonable terms, charges or fees for services performed must be reasonable, the insurer's total statutory surplus following any transaction must be both reasonable in relation to its outstanding liabilities and adequate for its needs, and are subject to other standards and requirements established by law and regulation. Notice to state insurance regulators is required prior to the consummation of certain affiliated and other transactions involving our insurance subsidiaries and such transactions may be disapproved by the state insurance regulators.
Pursuant to applicable insurance holding company laws, EICN is required to register with the Nevada Division of Insurance (Nevada DOI), ECIC is required to register with the California Department of Insurance (California DOI), and EPIC and EAC are required to register with the Florida Office of Insurance Regulation (Florida OIR). Under these laws, the respective state insurance departments may examine us at any time, require disclosure of material transactions and require prior notice for, or approval of, certain transactions.
Change of Control
Under Nevada insurance law and our amended and restated articles of incorporation that became effective on February 5, 2007, for a period of five years following February 5, 2007, no person may acquire or offer to acquire beneficial ownership of five percent or more of any class of our voting securities without prior approval by the Nevada Commissioner of Insurance (Nevada Commissioner) of an application for acquisition. Under Nevada insurance law, the Nevada Commissioner may not approve an application for such acquisition unless the Commissioner finds that: (a) the acquisition will not frustrate the plan of conversion as approved by our members and the Commissioner; (b) the Board of Directors of EICN has approved the acquisition or extraordinary circumstances not contemplated in the plan of conversion have arisen which would warrant approval of the acquisition; and (c) the acquisition is consistent with the purpose of relevant Nevada insurance statutes to permit conversions on terms and conditions that are fair and equitable to the members eligible to receive consideration. Accordingly, as a practical matter, any person seeking to acquire us within five years after February 5, 2007 may only do so with the approval of our Board of Directors. In December 2007, the Nevada Commissioner approved our application to waive any beneficial ownership over 5% if the excess was caused by the 2007 stock repurchase program.
In addition, the insurance laws of California, Florida, and Nevada generally require that any person seeking to acquire control of a domestic insurance company obtain the prior approval of the insurance commissioner. Insurance laws in many states in which we are licensed contain provisions that require pre-notification to the insurance commissioner of a change in control of a non-domestic insurance company licensed in those states. “Control” is generally presumed to exist through the direct or indirect ownership of ten percent or more of the voting securities of a domestic insurance company or of any entity that controls a domestic insurance company. Generally, other states’ insurance laws require prior notification to the insurance department of those states of a change of control of a non-domiciliary insurance company licensed to transact insurance in that state. Because we have insurance subsidiaries domiciled in California, Florida, and Nevada, any future transaction that would constitute a change in control of us would generally require the party seeking to acquire control to obtain the prior approval of the California Commissioner, the Florida Commissioner, and Nevada Commissioner, and may require pre-notification of the change of control.
State Insurance Regulation
Insurance companies are subject to regulation and supervision by the insurance regulator in the state in which they are domiciled and, to a lesser extent, other states in which they conduct business. As an insurance holding company, we, as well as our insurance subsidiaries, are subject to regulation by the states in which our insurance subsidiaries are domiciled or transact business. These state agencies have broad regulatory, supervisory and administrative powers, including among other things, the power to grant and revoke licenses to transact business, license agencies, set the standards of solvency to be met and maintained, determine the nature of, and limitations on, investments and dividends,approve policy forms and rates in some states, periodically examine financial statements, determine the form and content of required financial statements, and periodically examine market conduct.
17
Detailed annual and quarterly financial statements, prepared in accordance with statutory accounting practices, and other reports are required to be filed with the insurance regulator in each of the states in which we are licensed to transact business. The California DOI, Florida OIR, and Nevada DOI periodically examine the statutory financial statements of their respective domiciliary insurance companies. In 2009, California and Nevada completed exams for ECIC and EICN, respectively. There were no material findings.
In Florida, workers’ compensation insurance companies are subject to statutes related to excessive profits. Florida excessive profits are calculated based upon a statutory formula that is applied over rolling three year periods. Workers’ compensation insurers are required to file annual excessive profit forms and to return any “Florida excessive profits” to policyholders in the form of a cash refund or credit toward the future purchase of insurance.
In addition, many states have laws and regulations that limit an insurer’s ability to withdraw from a particular market. For example, states may limit an insurer’s ability to cancel or not renew policies. Furthermore, certain states prohibit an insurer from withdrawing one or more lines of business from the state, except pursuant to a plan that is approved by the state insurance regulator. The state insurance regulator may disapprove a plan that may lead to market disruption. Laws and regulations that limit cancellation and non-renewal and that subject program withdrawals to prior approval requirements may restrict our ability to exit unprofitable markets.
Premium Rate Restrictions
State laws regulate not only the amounts and types of workers' compensation benefits that must be paid to injured workers, but in some instances the premium rates that we may charge to insure businesses for those liabilities. In administered pricing states, including Florida, Wisconsin, and Idaho, premium rates are set by state insurance regulators and are adjusted periodically. Idaho also allows insurance companies to file rates that deviate upwards or downwards from the benchmark rates set by the insurance regulators.
In the vast majority of states, workers' compensation insurers have flexibility to offer rates that reflect the risk assumed by the insurer based on each employer's profile. These states are referred to as “loss cost” states. Most states in which we currently operate, including California, are loss cost states. In loss cost states, the state first approves a set of loss costs that provide for expected loss and, in most cases, LAE payments, which are prepared by an insurance rating bureau (for example, the WCIRB in California). An insurer then selects a factor, known as a loss cost multiplier, to apply to loss costs to determine its rates. In these states, regulators permit pricing flexibility primarily through: (a) the selection of the loss cost multiplier; and (b) schedule rating modifications that allow an insurer to adjust premiums upward or downward for specific risk characteristics of the policyholder such as:
|
|
•
|
type of work;
|
|
|
•
|
on-site medical facilities;
|
|
|
•
|
level of employee safety;
|
|
|
•
|
use of safety equipment; and
|
|
|
•
|
policyholder management practices.
|
Financial, Dividend, and Investment Restrictions
State laws require insurance companies to maintain minimum levels of surplus and place limits on the amount of premiums a company may write based on the amount of that company's surplus. These limitations may restrict the rate at which our insurance operations can grow.
State laws also require insurance companies to establish reserves for payments of policyholder liabilities and impose restrictions on the kinds of assets in which insurance companies may invest. These restrictions may require us to invest in assets more conservatively than we would if we were not subject to state law restrictions and may prevent us from obtaining as high a return on our assets as we might otherwise be able to realize absent the restrictions.
The ability of EHI to pay dividends on our common stock and to pay other expenses will be dependent to a significant extent upon the ability of our Nevada domiciled insurance company, EICN, and our Florida domiciled insurance company, EPIC, to pay dividends to their immediate holding company, Employers Group, Inc. (EGI) and, in turn, the ability of EGI to pay dividends to EHI. Additional information regarding financial, dividend, and investment restrictions is set forth in Note 16 in the Notes to our Consolidated Financial Statements, included elsewhere in this report.
18
Guaranty Fund Assessments
All of the states where our insurance subsidiaries are licensed to transact business require property and casualty insurers doing business within the respective state to participate as member insurers in a guaranty association, which is organized to pay contractual benefits owed pursuant to insurance policies issued by insolvent or failed insurers. These associations levy assessments, up to prescribed limits, on all member insurers in a particular state on the basis of the proportionate share of the premium written by member insurers.
In California, unpaid workers' compensation liabilities from insolvent insurers are the responsibility of the California Insurance Guarantee Association (CIGA). We pass CIGA assessments on to our policyholders, via a surcharge based upon the estimated annual premium at the policy's inception. We have recorded an asset of $6.2 million as of December 31, 2010, for assessments paid to CIGA that includes prepaid policy surcharges to be collected in the future from policyholders. We also write workers' compensation insurance in other states with similar obligations as those in California. In these states, we are directly responsible for payment of the assessment. We recorded an estimate of $2.1 million and $4.5 million for our expected liability for guaranty fund assessments at December 31, 2010 and 2009, respectively.
Pooling Arrangements
As a condition to conduct business in some states, including California, insurance companies are required to participate in mandatory workers’ compensation shared market mechanisms, or pooling arrangements, which provide workers’ compensation insurance coverage to private businesses that are otherwise unable to obtain coverage due, for example, to their prior loss experiences.
The National Association of Insurance Commissioners (NAIC)
NAIC is a group formed by state insurance regulators to discuss issues and formulate policy with respect to regulation, reporting and accounting of and by U.S. insurance companies. Although the NAIC has no legislative authority and insurance companies are at all times subject to the laws of their respective domiciliary states and, to a lesser extent, other states in which they conduct business, the NAIC is influential in determining the form in which such laws are enacted. Model Insurance Laws, Regulations and Guidelines (Model Laws) have been promulgated by the NAIC as a minimum standard by which state regulatory systems and regulations are measured. Adoption of state laws that provide for substantially similar regulations to those described in the Model Laws is a requirement for accreditation of state insurance regulatory agencies by the NAIC.
Under the Model Laws, insurers are required to maintain minimum levels of capital based on their investments and operations. These risk-based capital (RBC) requirements provide a standard by which regulators can assess the adequacy of an insurance company’s capital and surplus relative to its operations. An insurance company must maintain capital and surplus of at least 200% of the RBC computed by the NAIC’s RBC model, known as the “Authorized Control Level” of RBC. At December 31, 2010, each of our insurance subsidiaries had total adjusted capital in excess of the minimum RBC requirements.
The key financial ratios of the NAIC’s Insurance Regulatory Information System (IRIS) were developed to assist state regulators in overseeing the financial condition of insurance companies. These ratios are reviewed by financial examiners of the NAIC and state insurance regulators for the purposes of detecting financial distress and preventing insolvency and to select those companies that merit highest priority in the allocation of the regulators’ resources. IRIS identifies 13 key financial ratios and specifies a “usual range” for each. Departure from the usual ranges on four or more of the ratios can lead to inquiries from individual state insurance commissioners as to certain aspects of an insurer’s business. None of our insurance subsidiaries are currently subject to any action by any state regulator with respect to IRIS ratios.
Statutory Accounting and Solvency Regulations
State regulation of insurance company financial transactions and financial condition are based on statutory accounting principles (SAP). SAP differs in a number of ways from GAAP, which governs the financial reporting of most other businesses. SAP financial statements are generally more conservative than GAAP financial statements, reflecting lower asset balances, higher liability balances and lower equity.
19
State insurance regulators closely monitor the financial condition of insurance companies reflected in SAP financial statements and can impose significant financial and operating restrictions on an insurance company that becomes financially impaired under SAP guidelines. State insurance regulators can generally impose restrictions or conditions on the activities of a financially impaired insurance company, including: the transfer or disposition of assets; the withdrawal of funds from bank accounts; payment of dividends or other distributions; the extension of credit or the advancement of loans; and investments of funds, including business acquisitions or combinations.
Privacy Regulations
In 1999, the United States Congress enacted the Gramm-Leach-Bliley Act, which, among other things, protects consumers from the unauthorized dissemination of certain personal non-public financial information. Subsequently, a majority of states adopted additional regulations to address privacy issues. These laws and regulations apply to all financial institutions, including insurance and finance companies, and require us to maintain appropriate procedures for managing and protecting certain personal information of our customers and to fully disclose our privacy practices to our customers. In 2000, the NAIC adopted the Privacy of Consumer Financial and Health Information Model Regulation, which assisted states in promulgating regulations to comply with the Gramm-Leach-Bliley Act. In 2002, to further facilitate the implementation of the Gramm-Leach-Bliley Act, the NAIC adopted the Standards for Safeguarding Customer Information Model Regulation. Our insurance subsidiaries have established policies and procedures to comply with the Gramm-Leach-Bliley-related state privacy requirements.
Federal Legislative Changes
The Terrorism Risk Insurance Act of 2002 (the 2002 Act) was enacted in November 2002. The principal purpose of the 2002 Act was to create a role for the Federal government in the provision of insurance for losses sustained in connection with foreign terrorism. Prior to the Act, insurance (except for workers' compensation insurance) and reinsurance for losses arising out of acts of terrorism were largely unavailable from private insurance and reinsurance companies.
The 2002 Act was extended by TRIPRA, with the inclusion of some adjustments. The workers' compensation laws of the various states generally do not permit the exclusion of coverage for losses arising from terrorism or nuclear, biological, and chemical or radiological attacks. In addition, we are not able to limit our losses arising from any one catastrophe or any one claimant. Our reinsurance policies exclude coverage for losses arising out of nuclear, biological, chemical or radiological attacks. Under TRIPRA, federal protection is currently provided to the insurance industry for events, including acts of foreign and domestic terrorism, that result in an industry loss of at least $100 million in 2007 through 2014. In the event of a qualifying industry loss (which must occur out of an act of terrorism certified as such by the Secretary of the Treasury), each insurance company is responsible for a deductible of 20% of direct earned premiums in the previous year, with the federal government responsible to reimburse each company for 85% of the insurer’s loss up to the insurer’s proportionate share of the $100 billion industry aggregate limit in any one year. Accordingly, events may not be covered by, or may result in losses exceeding the capacity of our reinsurance protection and any protection offered by the TRIPRA or any subsequent legislation.
Small businesses constitute a large portion of our policies, and we monitor the geographic concentration of our policyholders to help mitigate the risk of loss from terrorist acts. The impact of any future terrorist acts is unpredictable, and the ultimate impact on our insurance subsidiaries, if any, of losses from any future terrorist acts will depend upon their nature, extent, location and timing.
Current economic conditions have also raised the possibility of future legislative and regulatory actions, in addition to the enactment of the Emergency Economic Stabilization Act of 2008 (EESA) and the Dodd-Frank Wall Street Reform and Consumer Protection Act of 2010, which could further impact our business. We cannot predict whether or when such actions may occur, or what effect, if any, such actions could have on our business, results of operations, and financial condition.
The Patient Protection and Affordable Care Act, as amended by the Healthcare and Education Reconciliation Act (Affordable Care Act), was enacted in March 2010. We cannot predict what affect, if any, the implementation of the provisions of the Affordable Care Act, which will continue through 2014, will have on our business, results of operations, or financial condition.
20
Item 1A. Risk Factors
Investing in our common stock involves risks. In evaluating our company, you should carefully consider the risks described below, together with all the information included in this annual report. The risks facing our company include, but are not limited to, those described below. The occurrence of one or more of these events could significantly and adversely affect our business, prospects, financial condition, results of operations, cash flows and stock price and you could lose all or part of your investment.
Risks Related to Our Business
Difficult conditions in the economy and capital markets may adversely affect our profitability, financial condition and results of operations.
The significant financial market volatility experienced worldwide during 2008 and 2009 continued into 2010. Although the U.S. and other foreign governments have taken various actions to stabilize the financial markets, it is uncertain whether those actions will be effective over the long-term. Therefore, the financial market volatility could continue, resulting in a prolonged negative economic impact.
We cannot predict future market conditions or their impact on our stock price, investment portfolio, or our workers' compensation business. In addition, continuing financial market volatility and economic downturn could have a material adverse affect on our insureds, agents, claimants, reinsurers, vendors, and competitors. Depending on financial market conditions, we could incur additional realized and unrealized losses in the future in our investment portfolio, which could have an adverse effect on our results of operations and financial condition. Reduced employment and payrolls have contributed to the decline in our premium. Selection of customers is more complex as certain businesses are facing unprecedented challenges in sustaining their operations. Over time we expect that recovery from the recession will improve hiring and payroll trends, but we cannot predict when this will occur.
Our liability for losses and LAE is based on estimates and may be inadequate to cover our actual losses and expenses.
We must establish and maintain reserves for our estimated losses and LAE. We establish loss reserves in our financial statements that represent an estimate of amounts needed to pay and administer claims with respect to insured claims that have occurred, including claims that have occurred but have not yet been reported to us. Loss reserves are estimates of the ultimate cost of individual claims based on actuarial estimation techniques, are inherently uncertain, and do not represent an exact measure of liability.
Several factors contribute to the uncertainty in establishing estimated losses, including the length of time to settle long-term, severe cases, claim cost inflation (deflation) trends, and uncertainties in the long-term outcome of the 2003 and 2004 legislative reforms in California and the 2003 legislative reforms in Florida. Judgment is required in applying actuarial techniques to determine the relevance of historical payment and claim settlement patterns under current facts and circumstances. In certain states, we have a relatively short operating history and must rely on a combination of industry experience and our specific experience to establish our best estimate of reserves for losses and LAE. The interpretation of historical data can be impacted by external forces, principally legislative changes, medical cost inflation, economic fluctuations, judicial decisions, and legal trends. As we receive new information and update our assumptions over time regarding the ultimate liability, our loss reserves may prove to be inadequate to cover our actual losses. Any changes in these estimates could be material and could have an adverse effect on our results of operations and financial condition during the period the changes are made.
Our estimates of incurred losses and LAE attributable to insured events of prior years have decreased for past accident years because actual losses and LAE paid and current projections of unpaid losses and LAE were less than we originally anticipated. These estimates are established by management utilizing actuarial indications based upon our historical and industry experience regarding claims emergence and payment patterns, medical cost inflation, and claim cost trends, adjusted for future anticipated changes in claims-related and economic trends, as well as regulatory and legislative changes, to establish our best estimate of reserves for losses and LAE. While we have generally had favorable developments over the past five years, the inherent uncertainty in our liability for losses and LAE could result in favorable or unfavorable developments in the future.
21
The insurance business is subject to extensive regulation and legislative changes, which impact the manner in which we operate our business.
Our insurance business is subject to extensive regulation by the applicable state agencies in the jurisdictions in which we operate, most significantly by the insurance regulators in California, Florida, and Nevada, the states in which our insurance subsidiaries are domiciled. As of December 31, 2010, 53.8% of our in-force premiums were generated in California. Accordingly, we are particularly affected by regulation in California. The passage of any form of rate regulation in California could impair our ability to operate profitably in California, and any such impairment could have a material adverse effect on our financial condition and results of operations. Insurance regulators have broad regulatory powers designed to protect policyholders and claimants, not stockholders or other investors. Regulations vary from state to state, but typically address or include:
|
|
•
|
standards of solvency, including risk-based capital measurements;
|
|
|
•
|
restrictions on the nature, quality and concentration of investments;
|
|
|
•
|
restrictions on the types of terms that we can include in the insurance policies we offer;
|
|
|
•
|
mandates that may affect wage replacement and medical care benefits paid under the workers' compensation system;
|
|
|
•
|
requirements for the handling and reporting of claims;
|
|
|
•
|
procedures for adjusting claims, which can affect the cost of a claim;
|
|
|
•
|
restrictions on the way rates are developed and premiums are determined;
|
|
|
•
|
the manner in which agents may be appointed;
|
|
|
•
|
establishment of liabilities for unearned premiums, unpaid losses and LAE, and other purposes;
|
|
|
•
|
limitations on our ability to transact business with affiliates;
|
|
|
•
|
mergers, acquisitions, and divestitures involving our insurance subsidiaries;
|
|
|
•
|
licensing requirements and approvals that affect our ability to do business;
|
|
|
•
|
compliance with all applicable privacy laws;
|
|
|
•
|
potential assessments for the settlement of covered claims under insurance policies issued by impaired, insolvent, or failed insurance companies or other assessments imposed by regulatory agencies; and
|
|
|
•
|
the amount of dividends that our insurance subsidiaries may pay to EGI and, in turn, the ability of EGI to pay dividends to EHI.
|
In addition, workers' compensation insurance is statutorily provided for in all of the states in which we do business. State laws and regulations specify the form and content of policy coverage and the rights and benefits that are available to injured workers, their representatives, and medical providers. In “administered pricing” states, insurance rates are set by the state insurance regulators and are adjusted periodically. Rate competition is generally not permitted in these states. Of the states in which we currently operate, Florida, Wisconsin, and Idaho are administered pricing states. Additionally, we are exposed to the risk that other states in which we operate will adopt administered pricing laws.
Legislation and regulation also impact our ability to investigate fraud and other abuses of the workers' compensation system in the states in which we do business. Our relationships with medical providers are also impacted by legislation and regulation, including penalties for failure to make timely payments.
Federal legislation typically does not directly impact our workers' compensation business, but our business can be indirectly affected by changes in healthcare, occupational safety and health, and tax regulations. Since healthcare costs are the largest component of our loss costs, we may be impacted by changes in healthcare legislation, such as the Affordable Care Act. Also, the unprecedented events in the financial markets have re-opened discussions regarding the possibility of federal regulation of insurance.
This extensive regulation of our business may affect the cost or demand for our products and may limit our ability to obtain rate increases or to take other actions that we might desire to maintain our profitability. In addition, we may be unable to maintain all required approvals or comply fully with applicable laws and regulations, or the relevant governmental authority's interpretation of such laws and regulations. Further, changes in the level of regulation of the insurance industry or changes in laws or regulations or interpretations by regulatory authorities could impact our operations, require us to bear additional costs of compliance, and impact our profitability.
22
If we fail to price our insurance policies appropriately, our business competitiveness, financial condition, or results of operations could be materially adversely affected.
Premiums are based on the particular class of business and our estimates of expected losses and LAE and other expenses related to the policies we underwrite. We analyze many factors when pricing a policy, including the policyholder's prior loss history and industry classification. Inaccurate information regarding a policyholder's past claims experience could put us at risk for mispricing our policies. For example, when initiating coverage on a policyholder, we must rely on the information provided by the policyholder or the policyholder's previous insurer(s) to properly estimate future claims expense. If the claims information is not accurately stated, we may under price our policies by using claims estimates that are too low. In order to set premium rates accurately, we must utilize an appropriate pricing model which correctly assesses risks based on their individual characteristics and takes into account actual and projected industry characteristics. As a result, our business, financial condition, and results of operations could be materially adversely affected.
Our concentration in California ties our performance to the business, economic, demographic, natural perils, and regulatory conditions in that state.
Our business is concentrated in California, where we generated 53.8% of our in-force premiums as of December 31, 2010. Accordingly, unfavorable business, economic, demographic, competitive, or regulatory conditions in California could negatively impact our business.
California has been greatly affected by the overall economic downturn, tightening of the credit markets, and the resulting impacts on the residential real estate markets. California is also experiencing budget deficits. The economic condition of the state has resulted in high unemployment and decreased payrolls. In addition, many California businesses are dependent on tourism revenues, which are, in turn, dependent on a robust economy. The downturn in the national economy and the economy of California, or any other event that causes deterioration in tourism, could adversely impact small businesses, such as restaurants, that we have targeted as customers. The departure or insolvency of a significant number of small businesses could also have a material adverse effect on our financial condition or results of operations. In addition, California is exposed to climate and environmental changes, natural perils such as earthquakes, along with the possibility of pandemics or terrorist acts. Accordingly, we could suffer losses as a result of catastrophic events in this state. Because our business is concentrated in this manner, we may be exposed to economic and regulatory risks or risk from natural perils that are greater than the risks associated with greater geographic diversification.
We rely on independent insurance agents and brokers.
We market and sell our insurance products primarily through independent, non-exclusive insurance agents and brokers. These agents and brokers are not obligated to promote our products and can and do sell our competitors' products. The loss of a number of our independent agents and brokers or the failure or inability of these agents to successfully market our insurance programs could have a material adverse effect on our business, financial condition and results of operations. In addition, these agents and brokers may find it easier to promote the broader range of programs of some of our competitors than to promote our single-line workers' compensation insurance products.
We rely on our principal strategic partners.
We have agreements with two principal strategic partners, ADP and Anthem, to market and service our insurance products through their sales forces and insurance agencies. The in-force premiums for ADP and Anthem were 9.5% and 11.6%, respectively, of total in-force premiums as of December 31, 2010. Our agreement with ADP is not exclusive, and ADP may terminate the agreement without cause upon 120 days notice. Although our distribution agreements with Anthem are exclusive, Anthem may terminate its agreements with us if the A.M. Best financial strength rating of ECIC is downgraded and we are not able to provide coverage through a carrier with an A.M. Best financial strength rating of “B++” or better. Anthem may also terminate its agreements with us without cause upon 60 days notice. The termination of any of our principal strategic partnership agreements, our failure to maintain good relationships with our principal strategic partners, or their failure to successfully market our products may materially reduce our revenues and could have a material adverse effect on our results of operations. In addition, we are subject to the risk that our principal strategic partners may face financial difficulties, reputational issues, or problems with respect to their own products and services, which may lead to decreased sales of our products and services. Moreover, if either of our principal strategic partners consolidates or aligns itself with another company or changes its products that are currently offered with our workers' compensation insurance product, we may lose business or suffer decreased revenues.
23
We are also subject to credit risk with respect to ADP and Anthem, as they collect premiums on our behalf for the workers' compensation products that are marketed together with their own products. Any failure to remit such premiums to us or to remit such amounts on a timely basis could have an adverse effect on our results of operations.
A downgrade in our financial strength rating could reduce the amount of business that we are able to write or result in the termination of certain of our agreements with our strategic partners.
Rating agencies rate insurance companies based on financial strength as an indication of an ability to pay claims. Our insurance subsidiaries are currently assigned a group letter rating of “A−” (Excellent) by A.M. Best, which is the rating agency that we believe has the most influence on our business. This rating is assigned to companies that, in the opinion of A.M. Best, have demonstrated an excellent overall performance when compared to industry standards. A.M. Best considers “A−” rated companies to have an excellent ability to meet their ongoing obligations to policyholders. This rating does not refer to our ability to meet non-insurance obligations.
The financial strength ratings of A.M. Best and other rating agencies are subject to periodic review using, among other things, proprietary capital adequacy models, and are subject to revision or withdrawal at any time. Insurance financial strength ratings are directed toward the concerns of policyholders and insurance agents and are not intended for the protection of investors or as a recommendation to buy, hold, or sell securities. Our competitive position relative to other companies is determined in part by our financial strength rating. A reduction in our A.M. Best rating could adversely affect the amount of business we could write, as well as our relationships with independent agents and brokers and strategic partners.
In view of the difficulties experienced recently by many financial institutions, including our competitors in the insurance industry, we believe that it is possible that external rating agencies, such as A.M. Best, may increase their scrutiny of financial institutions, increase the frequency and scope of their reviews, request additional information from the companies that they rate, including additional information regarding the valuation of investment securities held, and may adjust upward the capital and other requirements employed in their models for maintenance of certain rating levels. We cannot predict what actions rating agencies may take, or what actions we may take in response to the actions of rating agencies.
One of our strategic partners, Anthem, requires that we offer workers’ compensation coverage through a carrier with a financial strength rating of “B++” or better by A.M. Best. We currently offer this coverage through our subsidiary, ECIC. Our inability to offer such coverage could cause a reduction in the number of policies we write. If ECIC's financial strength rating were downgraded, and we were not able to enter into an agreement to provide coverage through a carrier rated “B++” or better by A.M. Best, Anthem could terminate its distribution agreements with us. We cannot assure you that we would be able to enter such an agreement if our rating was downgraded.
If we are unable to obtain reinsurance or collect on ceded reinsurance, our ability to write new policies and to renew existing policies could be adversely affected and our financial condition and results of operations could be materially adversely affected.
At December 31, 2010, we had $970.5 million of reinsurance recoverables for paid and unpaid losses and LAE of which $14.4 million was due to us on paid claims.
We purchase reinsurance to protect us against the costs of severe claims and catastrophic events, including natural perils and acts of terrorism, excluding nuclear, biological, chemical, and radiological events. On July 1, 2010, we entered into a new reinsurance program that is effective through June 30, 2011. The reinsurance program consists of one treaty covering excess of loss and catastrophic loss events in five layers of coverage. Our reinsurance coverage is $195.0 million in excess of our $5.0 million retention on a per occurrence basis, subject to a $2.0 million annual aggregate deductible and certain exclusions.
The availability, amount, and cost of reinsurance depend on market conditions and our loss experience and may vary significantly. We cannot be certain that our reinsurance agreements will be renewed or replaced prior to their expiration upon terms satisfactory to us. If we are unable to renew or replace our reinsurance agreements upon terms satisfactory to us, our net liability on individual risks would increase and we would have greater exposure to catastrophic losses, which could have a material adverse affect on our financial condition and results of operations.
24
In addition, we are subject to credit risk with respect to our reinsurers, and they may also refuse to pay or may delay payment of losses we cede to them. We remain liable to our policyholders even if we are unable to make recoveries to which we believe we are entitled under our reinsurance contracts. Losses may not be recovered from our reinsurers until claims are paid and, in the case of long-term workers' compensation cases, the creditworthiness of our reinsurers may change before we can recover amounts to which we are entitled, see “Item 1—Business —Reinsurance.” The inability of any of our reinsurers to meet its financial obligations could have a material adverse affect on our financial condition and results of operations.
We obtained reinsurance covering the losses incurred prior to July 1, 1995, and we could be liable for all of those losses if the coverage provided by the LPT Agreement proves inadequate or we fail to collect from the reinsurers party to such transaction.
On January 1, 2000, our Nevada insurance subsidiary assumed all of the assets, liabilities and operations of the Fund, including losses incurred by the Fund prior to such date. Our Nevada insurance subsidiary also assumed the Fund's rights and obligations associated with the LPT Agreement that the Fund entered into with third party reinsurers with respect to its losses incurred prior to July 1, 1995, see “Item 1—Business —Reinsurance —LPT Agreement.” We could be liable for all of those losses if the coverage provided by the LPT Agreement proves inadequate or we fail to collect from the reinsurers party to such transaction. With the exception of certain losses assumed from the Fund, these recoverables are unsecured. If we are unable to collect on these reinsurance recoverables, our financial condition and results of operations could be materially adversely affected. As of December 31, 2010, the estimated remaining liabilities subject to the LPT Agreement were approximately $846.7 million.
The reinsurers under the LPT Agreement agreed to assume responsibilities for the claims at the benefit levels which existed in June 1999. Accordingly, if the Nevada legislature were to increase the benefits payable for the pre-July 1, 1995 claims, we would be responsible for the increased benefit costs to the extent of the legislative increase. Similarly, if the credit rating of any of the third party reinsurers that are party to the LPT Agreement were to fall below ‘‘A−’’ as determined by A.M. Best or one of the reinsurers becomes insolvent, we would be responsible for replacing any such reinsurer or would be liable for the claims that otherwise would have been transferred to such reinsurer. For example, in 2002, the rating of one of the original reinsurers under the LPT Agreement, Gerling Global International Reinsurance Company Ltd. (Gerling), dropped below the mandatory ‘‘A−’’ A.M. Best rating to ‘‘B+.’’ Accordingly, we entered into an agreement to replace Gerling with National Indemnity Company (NICO) at a cost to us of $32.8 million. We can give no assurance that circumstances requiring us to replace one or more of the current reinsurers under the LPT Agreement will not occur in the future, that we will be successful in replacing such reinsurer or reinsurers in such circumstances, or that the cost of such replacement or replacements will not have a material adverse effect on our results of operations or financial condition.
The LPT Agreement also required the reinsurers to each place assets supporting the payment of claims by them in individual trusts that require that collateral be held at a specified level. The collateralization level must not be less than the outstanding reserve for losses and a loss expense allowance equal to 7% of estimated paid losses discounted at a rate of 6%. If the assets held in trust fall below this threshold, we can require the reinsurers to contribute additional assets to maintain the required minimum level. The value of these assets at December 31, 2010 was approximately $962.1 million. If the value of the collateral in the trusts drops below the required minimum level and the reinsurers are unable to contribute additional assets, we could be responsible for substituting a new reinsurer or paying those claims without the benefit of reinsurance. One of the reinsurers has collateralized its obligations under the LPT Agreement by placing shares of stock of a publicly held corporation, with a value of $729.3 million at December 31, 2010, in a trust to secure the reinsurer's obligation of $472.6 million. The value of this collateral is subject to fluctuations in the market price of such stock. The other reinsurers have placed treasury and fixed maturity securities in trusts to collateralize their obligations.
Intense competition and the fact that we write only a single line of insurance could adversely affect our ability to sell policies at rates we deem adequate.
The market for workers' compensation insurance products is highly competitive. Competition in our business is based on many factors, including premiums charged, services provided, financial ratings assigned by independent rating agencies, speed of claims payments, reputation, policyholder dividends, perceived financial strength, and general experience. In some cases, our competitors offer lower priced products than we do. If our competitors offer more competitive premiums, dividends or payment plans, services or commissions to independent agents, brokers and other distributors,
25
we could lose market share or have to reduce our premium rates, which could adversely affect our profitability. We compete with regional and national insurance companies, professional employer organizations, third-party administrators, self-insured employers, and state insurance funds. Our main competitors in each of the states in which we currently operate vary from state to state, but are usually those companies that offer a full range of services in underwriting, loss control, and claims. We compete on the basis of the services that we offer to our policyholders and on ease of doing business rather than solely on price.
Many of our competitors are significantly larger and possess greater financial, marketing, and management resources than we do. Some of our competitors benefit financially by not being subject to federal income tax. Intense competitive pressure on prices can result from the actions of even a single large competitor. Competitors with more surplus than us have the potential to expand in our markets more quickly than we can. Greater financial resources also permit an insurer to gain market share through more competitive pricing, even if that pricing results in reduced underwriting margins or an underwriting loss.
Many of our competitors are multi-line carriers that can price the workers' compensation insurance they offer at a loss in order to obtain other lines of business at a profit. This creates a competitive disadvantage for us, as we only offer a single line of insurance. For example, a business may find it more efficient or less expensive to purchase multiple lines of commercial insurance coverage from a single carrier.
The property and casualty insurance industry is cyclical in nature and is characterized by periods of so-called “soft” market conditions in which premium rates are stable or falling, insurance is readily available, and insurers' profits decline, and by periods of so-called “hard” market conditions, in which rates rise, insurance may be more difficult to find, and insurers' profits increase. According to the Insurance Information Institute, since 1970, the property and casualty insurance industry experienced hard market conditions from 1975 to 1978, 1984 to 1987, and 2001 to 2004. Although the financial performance of an individual insurance company is dependent on its own specific business characteristics, the profitability of most workers' compensation insurance companies generally tends to follow this cyclical market pattern. We believe the workers’ compensation industry is currently experiencing increased price competition and excess underwriting capacity. This results in lower rate levels and smaller profit margins.
Because of cyclicality in the workers’ compensation market, due in large part to competition, capacity, and general economic factors, we cannot predict the timing or duration of changes in the market cycle. We have experienced significant increased price competition in our target markets since 2003. This cyclical pattern has in the past and could in the future adversely affect our financial condition and results of operations. If we are unable to compete effectively, our business and financial condition could be materially adversely affected.
We may be unable to realize our investment objectives and economic conditions in the financial markets could lead to investment losses.
Investment income is an important component of our revenue and net income. Our investment portfolio is managed by an independent asset manager that operates under investment guidelines approved by our Board of Directors. Although these guidelines stress diversification and capital preservation, our investments are subject to a variety of risks that are beyond our control, including risks related to general economic conditions, interest rate fluctuations, and market volatility. Interest rates are highly sensitive to many factors, including governmental monetary policies and domestic and international economic and political conditions. These and other factors affect the capital markets and, consequently, the value of our investment portfolio.
We are exposed to significant financial risks related to the capital markets, including the risk of potential economic loss principally arising from adverse changes in the fair value of financial instruments. The major components of market risk affecting us are interest rate risk, credit spread risk, credit risk, and equity price risk. For more information regarding market, interest rate, credit risk, or equity price risk, see Item 7A—"Quantitative and Qualitative Disclosures About Market Risk."
The outlook for our investment income is dependent on the future direction of interest rates, maturity schedules, and cash flow from operations that is available for investment. The fair values of fixed maturity securities that are “available-for-sale” fluctuate with changes in interest rates and cause fluctuations in our stockholders’ equity. Any significant decline in our investment income or the value of our investments as a result of falling interest rates, deterioration in the credit of companies in which we have invested, decreased dividend payments, general market conditions, or events that have an adverse impact on any particular industry or geographic region in which we hold significant investments could have an adverse effect on our net income and, as a result, on our stockholders’ equity and policyholders’ surplus.
26
The valuation of our investments, including the determination of the amount of impairments, include estimates and assumptions and could result in changes to investment valuations that may adversely affect our financial condition and results of operations.
Our estimates of fair value for our investments are based upon the inputs used in the valuation and give the highest priority to quoted prices in active markets and require that observable inputs be used in the valuations when available. In determining the level of the hierarchy in which the valuation is disclosed, the highest priority is given to unadjusted quoted prices in active markets and the lowest priority to unobservable inputs that reflect the Company’s significant market assumptions. The use of internally developed valuation techniques may have a material effect on the estimated fair value amounts of our investments and our financial condition.
Additionally, we regularly review our entire investment portfolio, including the identification of other-than-temporary declines in fair value. The determination of the amount of impairments taken on our investments is based on our periodic evaluation and assessment of our investments and known and inherent risks associated with the various asset classes. There can be no assurance that our management has accurately assessed the level of impairments in determining the other-than-temporary impairments reflected in our financial statements and additional impairments may need to be taken in the future. Historical trends may not be indicative of future impairments. Additional information regarding the determination impairments on our investments is set forth under “Item 7—Management’s Discussion and Analysis of Financial Condition and Results of Operations —Investments.”
We may require additional capital in the future, which may not be available to us or may be available only on unfavorable terms.
Our future capital requirements will depend on many factors, including state regulatory requirements and our ability to write new business successfully and to establish premium rates and reserves at levels sufficient to cover losses. If we have to raise additional capital, equity or debt financing may not be available on terms that are favorable to us. In the case of equity financings, dilution to our stockholders could result and the securities may have rights, preferences, and privileges senior to the common stock. In the case of debt financings, we may be subject to covenants that restrict our ability to freely operate our business. If we cannot obtain adequate capital on favorable terms or at all, we may be unable to implement our future growth or operating plans and our business, financial condition, or results of operations could be materially adversely affected.
The capital and credit markets continue to experience volatility and disruption that have negatively affected market liquidity conditions. In some cases, the markets have produced downward pressure on stock prices and limited the availability of credit for certain issuers without regard to those issuers’ underlying financial strength. As a result, we may be forced to delay raising capital or be unable to raise capital on favorable terms, or at all, which could decrease our profitability, significantly reduce our financial flexibility and cause rating agencies to reevaluate our financial strength ratings.
We have outstanding indebtedness, which could impair our financial strength ratings and adversely affect our ability to react to changes in our business and fulfill our debt obligations.
Our indebtedness could have significant consequences, including:
|
|
·
|
making it more difficult for us to satisfy our financial obligations;
|
|
|
·
|
limiting our ability to borrow additional amounts to fund working capital, capital expenditures, debt service requirements, the execution of our business strategy, acquisitions, and other purposes;
|
|
|
·
|
affecting the way we manage our business due to restrictive covenants;
|
|
|
·
|
requiring us to provide collateral which restricts our use of funds;
|
|
|
·
|
requiring us to use a portion of our cash flow from operations to pay principal and interest on our debt; and
|
|
|
·
|
making us more vulnerable to adverse changes in general economic and industry conditions, and limiting our flexibility to plan for, and react quickly to, changing conditions.
|
27
We rely on our information technology and telecommunication systems, and the failure of these systems could materially and adversely affect our business.
Our business is highly dependent upon the successful and uninterrupted functioning of our information technology and telecommunications systems. We rely on these systems to process new and renewal business, provide customer service, administer and make payments on claims, facilitate collections, and to automatically underwrite and administer the policies we write. The failure of any of our systems could interrupt our operations or materially impact our ability to evaluate and write new business. Our information technology and telecommunications systems interface with and depend on third-party systems; and we could experience service denials if demand for such services exceeds capacity or such third-party systems fail or experience interruptions.
Certain events outside of our control could render our systems inoperable such that we would be unable to service our agents, insureds, and injured workers, or meet certain regulatory requirements. If such an event were to occur and our systems were unable to be restored or secured within a reasonable timeframe, our results of operations and financial condition could be adversely affected. Additionally, a breach of security could jeopardize the privacy, confidentiality, and integrity of our data or our customers' data, which could harm our reputation and expose us to possible liability.
Acts of terrorism and catastrophes could materially adversely impact our financial condition and results of operations.
Under our workers' compensation policies and applicable laws in the states in which we operate, we are required to provide workers' compensation benefits for losses arising from acts of terrorism. The impact of any terrorist act is unpredictable, and the ultimate impact on us would depend upon the nature, extent, location, and timing of such an act. We would be particularly adversely affected by a terrorist act affecting any metropolitan area where our policyholders have a large concentration of workers.
Notwithstanding the protection provided by the reinsurance we have purchased and any protection provided by the 2002 Act, or its extension, the TRIPRA, the risk of severe losses to us from acts of terrorism has not been eliminated because our excess of loss reinsurance treaty program contains various sub-limits and exclusions limiting our reinsurers' obligation to cover losses caused by acts of terrorism. Our excess of loss reinsurance treaties do not protect against nuclear, biological, chemical, or radiological events. If such an event were to impact one or more of the businesses we insure, we would be entirely responsible for any workers' compensation claims arising out of such event, subject to the terms of the 2002 Act, and the TRIPRA (see “Item 1—Business—Regulation—Federal Legislative Changes”) and could suffer substantial losses as a result.
Our operations also expose us to claims arising out of catastrophes because we may be required to pay benefits to workers who are injured in the workplace as a result of a catastrophe. Catastrophes can be caused by various unpredictable events, either natural or man-made. Any catastrophe occurring in the states in which we operate could expose us to potentially substantial losses and, accordingly, could have a material adverse effect on our financial condition and results of operations.
We are a holding company with no direct operations. We depend on the ability of our subsidiaries to transfer funds to us to meet our obligations, and our insurance subsidiaries' ability to pay dividends to us is restricted by law.
EHI is a holding company that transacts substantially all of its business through operating subsidiaries. Its primary assets are the shares of stock of our insurance subsidiaries. The ability of EHI to meet obligations on outstanding debt, to pay stockholder dividends and to make other payments, depends on the surplus and earnings of our subsidiaries and their ability to pay dividends or to advance or repay funds, and upon the ability of our insurance subsidiaries, to pay dividends to EGI and, in turn, the ability of EGI to pay dividends to EHI.
Payments of dividends by our insurance subsidiaries are restricted by state insurance laws, including laws establishing minimum solvency and liquidity thresholds, and could be subject to contractual restrictions in the future, including those imposed by indebtedness we may incur in the future, see “Item 1—Business—Regulation—Financial, Dividend and Investment Restrictions” and Note 16 in the Notes to our Consolidated Financial Statements. As a result, we may not be able to receive dividends from these subsidiaries and we may not receive dividends in the amounts necessary to meet our obligations or to pay dividends on our common stock.
28
Administrative proceedings or legal actions involving our insurance subsidiaries could have a material adverse effect on our business, financial condition or results of operations.
Our insurance subsidiaries are involved in various administrative proceedings and legal actions in the normal course of their insurance operations. Our subsidiaries have responded to the actions and intend to defend against these claims. These claims concern issues including eligibility for workers' compensation insurance coverage or benefits, the extent of injuries, wage determinations, and disability ratings. Adverse decisions in multiple administrative proceedings or legal actions could require us to pay significant amounts in the aggregate or to change the manner in which we administer claims, which could have a material adverse effect on our financial condition and results of operations.
Our business is largely dependent on the efforts of our management because of its industry expertise, knowledge of our markets, and relationships with the independent agents and brokers that sell our products.
Our success depends in substantial part upon our ability to attract and retain qualified executive officers, experienced underwriting personnel, and other skilled employees who are knowledgeable about our business. The current success of our business is dependent in significant part on the efforts of Douglas D. Dirks, our President and Chief Executive Officer, and William E. Yocke, our Executive Vice President and Chief Financial Officer. Many of our regional and local officers are also critical to our operations because of their industry expertise, knowledge of our markets, and relationships with the independent agents and brokers who sell our products. We have entered into employment agreements with certain of our key executives. Currently, we do not maintain key man life insurance for our executives or senior management team. If we were to lose the services of members of our management team or key regional or local officers, we may be unable to find replacements satisfactory to us and our business. As a result, our operations may be disrupted and our financial performance may be adversely affected.
Assessments and other surcharges for guaranty funds, second injury funds, and other mandatory pooling arrangements may reduce our profitability.
All states require insurance companies licensed to do business in their state to bear a portion of the unfunded obligations of insolvent insurance companies. These obligations are funded by assessments that can be expected to continue in the future in the states in which we operate. Many states also have laws that established second injury funds to provide compensation to injured employees for aggravation of a prior condition or injury, which are funded by either assessments based on paid losses or premium surcharge mechanisms. In addition, as a condition to the ability to conduct business in some states, insurance companies are required to participate in mandatory workers' compensation shared market mechanisms or pooling arrangements, which provide workers' compensation insurance coverage from private insurers. The effect of these assessments and mandatory shared market mechanisms or changes in them could reduce our profitability in any given period or limit our ability to grow our business.
Insurance laws of Nevada, California, Florida, and other applicable states, certain provisions of our charter documents, and Nevada corporation law could prevent or delay a change of control that could be beneficial to us and our stockholders.
Under Nevada insurance law and our amended and restated articles of incorporation that became effective upon completion of the conversion, for a period of five years following February 5, 2007 or, if earlier, until such date as we no longer directly or indirectly own a majority of the outstanding voting stock of EICN, no person may directly or indirectly acquire or offer to acquire in any manner beneficial ownership of 5% or more of any class of our voting securities without the prior approval of the Nevada Commissioner, see “Item 1—Business—Regulation—Change of Control.”
Additionally, we have insurance subsidiaries domiciled in California and Florida. The insurance laws of California and Florida require prior approval from the California DOI and the Florida OIR for any change of control of the subsidiary domiciled in their respective states. Insurance laws in many other states also contain provisions that require pre-notification to the insurance commissioners of a change in control of a non-domestic insurance company licensed in those states. In Florida, "control" is generally presumed to exist through the direct or indirect ownership of 5% or more of the voting securities of a domestic insurance company or of any entity that controls a domestic insurance company, while in California and Nevada, "control" is presumed to exist through the direct or indirect ownership of 10% or more of the voting securities of a domestic insurance company or of any entity that controls a domestic insurance company. Because we have insurance subsidiaries domiciled in California, Florida, and Nevada, any future transaction that would constitute a change in control of us would generally require the party acquiring control to obtain the prior approval of the
29
California Commissioner, Florida Commissioner and the Nevada Commissioner and may require pre-notification in those states that have adopted pre-notification provisions upon a change of control. Obtaining these approvals may result in a material delay of, or deter, any such transaction. These laws may discourage potential acquisition proposals or tender offers, and may delay, deter, or prevent a change of control, even if the acquisition proposal or tender offer is beneficial to our stockholders.
Provisions of our amended and restated articles of incorporation and amended and restated by-laws could discourage, delay, or prevent a merger, acquisition, or other change in control of us, even if our stockholders might consider such a change in control to be in their best interests. These provisions could also discourage proxy contests and make it more difficult for you and other stockholders to elect Directors and take other corporate actions. In particular, our amended and restated articles of incorporation and amended and restated by-laws include provisions:
|
|
•
|
dividing our Board of Directors into three classes;
|
|
|
•
|
eliminating the ability of our stockholders to call special meetings of stockholders;
|
|
|
•
|
permitting our Board of Directors to issue preferred stock in one or more series;
|
|
|
•
|
imposing advance notice requirements for nominations for election to our Board of Directors or for proposing matters that can be acted upon by stockholders at the stockholder meetings;
|
|
|
•
|
prohibiting stockholder action by written consent, thereby limiting stockholder action to that taken at a meeting of our stockholders; and
|
|
|
•
|
providing our Board of Directors with exclusive authority to adopt or amend our by-laws.
|
These provisions may make it difficult for stockholders to replace Directors and could have the effect of discouraging a future takeover attempt that is not approved by our Board of Directors, but which stockholders might consider favorable. Additionally, these provisions could limit the price that investors are willing to pay in the future for shares of our common stock.
Item 1B. Unresolved Staff Comments
None.
Item 2. Properties
Our principal executive offices are 79,533 square feet located in leased premises in Reno, Nevada. In addition to serving as our corporate headquarters, it also serves as a branch office providing services in marketing, loss control, and underwriting related support. As of February 1, 2011, we leased 308,042 square feet of total office space in 13 states. We also own a 15,120 square foot building in Carson City, Nevada, which is used as a storage facility. We believe that our existing office space is adequate for our current needs and we will continue to enter into or exit lease agreements to address future space requirements, as necessary.
Item 3. Legal Proceedings
From time to time, we are involved in pending and threatened litigation in the normal course of business in which claims for monetary damages are asserted. In the opinion of management, the ultimate liability, if any, arising from such pending or threatened litigation is not expected to have a material effect on our result of operations, liquidity, or financial position.
Item 4. (Removed and Reserved)
30
PART II
Item 5. Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities
Market Information and Holders
Our common stock has been listed on the New York Stock Exchange (NYSE) under the symbol “EIG” since our IPO on January 31, 2007. Prior to that time, there was no public market for our common stock.
The table below sets forth the reported high and low sales prices for our common stock for each quarterly period as reported by the NYSE during the last two fiscal years.
|
2009
|
High
|
Low
|
||||||
|
First quarter
|
$ | 16.44 | $ | 8.25 | ||||
|
Second quarter
|
13.90 | 8.00 | ||||||
|
Third quarter
|
15.94 | 11.99 | ||||||
|
Fourth quarter
|
16.73 | 13.90 | ||||||
|
2010
|
High
|
Low
|
||||||
|
First quarter
|
$ | 15.75 | $ | 12.31 | ||||
|
Second quarter
|
17.27 | 14.09 | ||||||
|
Third quarter
|
16.87 | 13.92 | ||||||
|
Fourth quarter
|
17.75 | 15.16 | ||||||
There were 1,690 holders of record as of February 18, 2011.
Limitations on Acquisitions of Common Stock
Under Nevada insurance law and our amended and restated articles of incorporation that became effective on completion of the conversion, for a period of five years following February 5, 2007 or, if earlier, until such date as EHI no longer directly or indirectly owns a majority of the outstanding voting stock of EICN, no person may directly or indirectly acquire or offer to acquire in any manner beneficial ownership of five percent or more of any class of voting securities of EHI without the prior approval by the Nevada Commissioner of an application for acquisition under Section 693A.500 of the Nevada Revised Statutes. Under Nevada insurance law, the Nevada Commissioner may not approve an application for such acquisition unless the Commissioner finds that: (a) the acquisition will not frustrate the plan of conversion as approved by our members and the Commissioner; (b) our Board of Directors has approved the acquisition or extraordinary circumstances not contemplated in the plan of conversion have arisen which would warrant approval of the acquisition; and (c) the acquisition is consistent with the purpose of relevant Nevada insurance statutes to permit conversions on terms and conditions that are fair and equitable to the members eligible to receive consideration. Accordingly, as a practical matter, any person seeking to acquire us within five years after February 5, 2007 may only do so with the approval of the Board of Directors of EICN. Furthermore, any person or entity who individually or together with an affiliate (as defined by applicable law) seeks to directly or indirectly acquire in any manner, at any time, beneficial ownership of 5% or more of any class of our voting securities will be subject to certain requirements, including the prior approval of the proposed acquisition by certain state insurance regulators, depending upon the circumstances involved. Any such acquisition without prior satisfaction of applicable regulatory requirements may be deemed void under state law.
31
Stockholder Dividends
Our Board of Directors has authorized the payment of a quarterly dividend of $0.06 per share of common stock to our stockholders of record in every quarter since the second quarter of 2007. Any determination to pay additional or future dividends will be at the discretion of our Board of Directors and will be dependent upon:
|
|
•
|
the surplus and earnings of our subsidiaries and their ability to pay dividends and/or other statutorily permissible payments to us, in particular the ability of EICN and EPIC to pay dividends to EGI and, in turn, the ability of EGI to pay dividends to EHI;
|
|
|
•
|
our results of operations and cash flows;
|
|
|
•
|
our financial position and capital requirements;
|
|
|
•
|
general business conditions;
|
|
|
•
|
any legal, tax, regulatory, and contractual restrictions on the payment of dividends; and
|
|
|
•
|
any other factors our Board of Directors deems relevant.
|
Following is a summary of dividends paid to stockholders by EHI:
|
Dividends Declared
|
First
|
Second
|
Third
|
Fourth
|
|||||||||||
|
2009
|
$ | 0.06 | $ | 0.06 | $ | 0.06 | $ | 0.06 | |||||||
|
2010
|
$ | 0.06 | $ | 0.06 | $ | 0.06 | $ | 0.06 | |||||||
On February 23, 2011, the EHI Board of Directors (Board of Directors) declared a $0.06 dividend per share, payable March 23, 2011, to stockholders of record on March 9, 2011. It is currently expected that cash dividends will continue to be paid in the future.
Issuer Purchases of Equity Securities
The following table summarizes the repurchase of our common stock for the quarter ended December 31, 2010:
|
Period
|
Total
Number of
Shares
Purchased
|
Average
Price
Paid Per
Share (1)
|
Total Number
of Shares Purchased
as Part of Publicly
Announced
Programs
|
Approximate
Dollar Value of
Shares that May Yet be Purchased Under the Program (2)
|
|||||||||||
|
(in millions)
|
|||||||||||||||
|
October 1 – October 31, 2010
|
— | $ | — | — | $ | — | |||||||||
|
November 1 – November 30, 2010
|
429,843 | 16.10 | 429,843 | 93.1 | |||||||||||
|
December 1 – December 31, 2010
|
437,306 | 17.07 | 437,306 | 85.6 | |||||||||||
|
Total Repurchases
|
867,149 | 16.59 | 867,149 | ||||||||||||
|
(1)
|
Includes fees and commissions paid on stock repurchases.
|
|
(2)
|
On November 3, 2010, the Board of Directors authorized a share repurchase program for up to $100 million of the Company's common stock (the 2011 Program). We expect that shares may be purchased at prevailing market prices from November 8, 2010 through June 30, 2012 through a variety of methods, including open market or private transactions, in accordance with applicable laws and regulations and as determined by management. The timing and actual number of shares repurchased will depend on a variety of factors, including the share price, corporate and regulatory requirements, and other market and economic conditions. Repurchases under the 2011 Program may be commenced, modified, or suspended from time to time without prior notice, and the program may be suspended or discontinued at any time.
|
In November 2009, the Board of Directors authorized a share repurchase program for $50 million of the Company’s common stock from January 1, 2010 through December 31, 2010 (the 2010 Program). Through September 30, 2010, we repurchased a total of 3,291,709 shares of common stock under the 2010 Program at an average price of $15.19 per share, including commissions, for a total of $50.0 million.
32
Performance Graph
Our common stock has been listed on the NYSE since our intial public offering on January 31, 2007. The following graph compares the cumulative total return on $100 invested in the common stock of EHI, ticker symbol EIG, for the period commencing on January 31, 2007 and ending on December 31, 2010 with the cumulative total return on $100 invested in each of the Standard and Poor’s 500 Index (S&P 500) and the Standard and Poor’s 500 Property-Casualty Insurance Index (S&P P&C Insurance Index). The calculation of cumulative total return assumes the reinvestment of dividends. The following graph and related information shall not be deemed to be “soliciting material” or to be “filed” with the SEC, nor shall such information be incorporated by reference into any filing pursuant to the Securities Act of 1933 or the Security Exchange Act of 1934, except to the extent that we specifically incorporate it by reference into such filing.
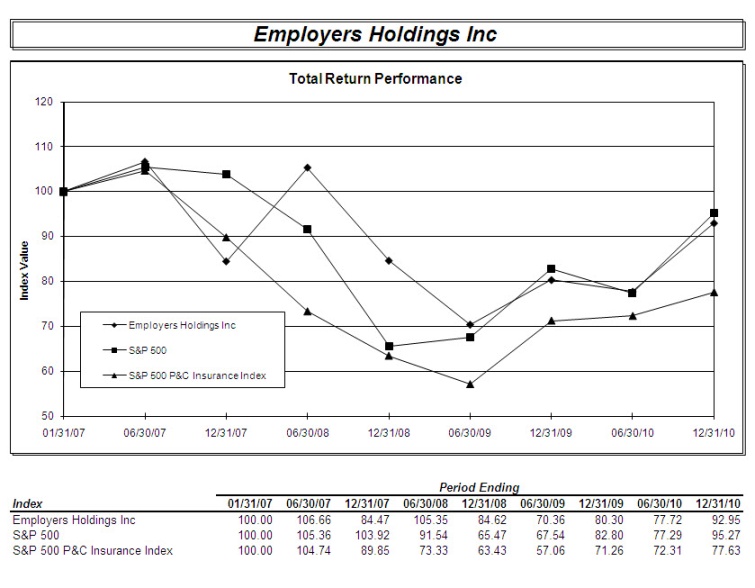 |
33
Item 6. Selected Financial Data
The following selected historical consolidated financial data should be read in conjunction with ‘‘Item 7—Management’s Discussion and Analysis of Financial Condition and Results of Operations’’ and the consolidated financial statements and related notes included elsewhere in this annual report on Form 10-K.
|
Years Ended December 31,
|
||||||||||||||||||||
|
2010
|
2009
|
2008(1)
|
2007
|
2006
|
||||||||||||||||
|
Income Statement Data
|
(in thousands, except per share amounts and ratios)
|
|||||||||||||||||||
|
Revenues:
|
||||||||||||||||||||
|
Net premiums earned
|
$ | 321,786 | $ | 404,247 | $ | 328,947 | $ | 346,884 | $ | 392,986 | ||||||||||
|
Net investment income
|
83,032 | 90,484 | 78,062 | 78,623 | 68,187 | |||||||||||||||
|
Realized gains (losses) on investments, net
|
10,137 | 791 | (11,524 | ) | 180 | 54,277 | ||||||||||||||
|
Other income
|
649 | 413 | 1,293 | 4,236 | 4,800 | |||||||||||||||
|
Total revenues
|
415,604 | 495,935 | 396,778 | 429,923 | 520,250 | |||||||||||||||
|
Net income before income taxes
|
66,322 | 92,298 | 112,051 | 150,886 | 254,292 | |||||||||||||||
|
Income tax expense
|
3,523 | 9,277 | 10,266 | 30,603 | 82,722 | |||||||||||||||
|
Net income
|
$ | 62,799 | $ | 83,021 | $ | 101,785 | $ | 120,283 | $ | 171,570 | ||||||||||
|
Earnings per common share(2)
|
||||||||||||||||||||
|
Basic
|
$ | 1.52 | $ | 1.81 | $ | 2.07 | $ | 2.19 | ||||||||||||
|
Diluted
|
1.51 | 1.80 | 2.07 | 2.19 | ||||||||||||||||
|
Pro forma earnings per common share -basic and diluted-(2)
|
2.32 | $ | 3.43 | |||||||||||||||||
|
Selected Operating Data
|
||||||||||||||||||||
|
Gross premiums written(3)
|
$ | 322,277 | $ | 379,949 | $ | 318,392 | $ | 351,847 | $ | 386,796 | ||||||||||
|
Net premiums written(4)
|
313,098 | 368,290 | 308,317 | 339,720 | 372,224 | |||||||||||||||
|
Combined ratio(5)
|
106.8 | % | 98.0 | % | 85.9 | % | 80.4 | % | 67.7 | % | ||||||||||
|
Net income before impact of the deferred reinsurance gain—
LPT Agreement(6)(7)(8)
|
$ | 44,566 | $ | 65,014 | $ | 83,364 | $ | 102,249 | $ | 152,197 | ||||||||||
|
Earnings per common share before impact of LPT(6)
|
||||||||||||||||||||
|
Basic
|
$ | 1.08 | $ | 1.42 | $ | 1.69 | ||||||||||||||
|
Diluted
|
1.07 | 1.41 | 1.69 | |||||||||||||||||
|
Pro forma earnings per common share—basic and
diluted before impact of LPT(2)(8)
|
$ | 1.98 | $ | 3.04 | ||||||||||||||||
|
Dividends declared
|
0.24 | 0.24 | 0.24 | 0.18 | — | |||||||||||||||
34
|
As of December 31,
|
|||||||||||||||||||
|
2010
|
2009
|
2008(1)
|
2007
|
2006
|
|||||||||||||||
|
Balance Sheet Data
|
(in thousands, except per share amounts and ratios)
|
||||||||||||||||||
|
Cash and cash equivalents
|
$ | 119,825 | $ | 188,883 | $ | 197,429 | $ | 144,384 | $ | 74,039 | |||||||||
|
Total investments
|
2,080,494 | 2,029,560 | 2,042,941 | 1,726,280 | 1,715,673 | ||||||||||||||
|
Reinsurance recoverable on paid and unpaid losses
|
970,458 | 1,064,843 | 1,087,738 | 1,061,551 | 1,107,900 | ||||||||||||||
|
Total assets
|
3,480,120 | 3,676,653 | 3,825,098 | 3,264,309 | 3,266,840 | ||||||||||||||
|
Unpaid losses and loss adjustment expense
|
2,279,729 | 2,425,658 | 2,506,478 | 2,269,710 | 2,307,755 | ||||||||||||||
|
Deferred reinsurance gain—LPT Agreement(6)(7)
|
370,341 | 388,574 | 406,581 | 425,002 | 443,036 | ||||||||||||||
|
Notes payable
|
132,000 | 132,000 | 182,000 | — | — | ||||||||||||||
|
Total liabilities
|
2,990,004 | 3,178,254 | 3,380,370 | 2,884,856 | 2,963,063 | ||||||||||||||
|
Total equity
|
490,116 | 498,399 | 444,728 | 379,453 | 303,777 | ||||||||||||||
|
Other Financial Data
|
|||||||||||||||||||
|
Total equity including deferred reinsurance gain —
LPT Agreement(6)(7)(9)
|
$ | 860,457 | $ | 886,973 | $ | 851,309 | $ | 804,455 | $ | 746,813 | |||||||||
|
(1)
|
The income statement data for the year ended December 31, 2008 includes the operating results of AmCOMP from November 1, 2008 through December 31, 2008. The balance sheet data as of December 31, 2008 includes the assets and liabilities acquired from AmCOMP (see Note 4 in the Notes to our Consolidated Financial Statements which are included elsewhere in this report).
|
|
(2)
|
For 2007, the pro forma earnings per common share –basic– was calculated using the net income for the 12 months ended December 31, 2007, as presented on the accompanying consolidated statements of income. The weighted average shares outstanding was calculated using those shares available to eligible members in the conversion (50,000,002) for the period prior to the IPO, and the actual weighted average shares outstanding for the period after the IPO. Earnings per common share –diluted– is based on the pro forma weighted shares outstanding – basic – adjusted by the number of additional common shares that would have been outstanding had potentially dilutive common shares been issued and reduced by the number of common shares that could have been purchased from the proceeds of the potentially dilutive shares. Outstanding options have been excluded from the diluted earnings per share for the pro forma year ended December 31, 2007, because their inclusion would be anti-dilutive. Although there were 8,665 dilutive potential common shares at December 31, 2007, they did not impact the pro forma earnings per share number as shown. (See Note 19 in the Notes to our Consolidated Financial Statements.)
|
For 2006, the pro forma earnings per common share – basic and diluted – is presented to depict the impact of our conversion described above, as prior to the conversion we did not have any outstanding common shares. The pro forma earnings per common share –basic and diluted– was computed using only the shares of the our common stock issued to eligible members in the conversion (50,000,002), and does not include any shares issued to new investors in connection with our IPO or the impact of the cash elections made by eligible members. We had no common stock equivalents outstanding for the periods presented prior to 2007 that would create a dilutive effect on pro forma earnings per share.
|
(3)
|
Gross premiums written is the sum of both direct premiums written and assumed premiums written before the effect of ceded reinsurance. Direct premiums written are the premiums on all policies our insurance subsidiaries have issued during the year. Assumed premiums written are premiums that our insurance subsidiaries have received from any authorized state-mandated pools and a previous fronting facility. (See Note 10 in the Notes to our Consolidated Financial Statements.)
|
|
(4)
|
Net premiums written is the sum of direct premiums written and assumed premiums written less ceded premiums written. Ceded premiums written is the portion of direct premiums written that we cede to our reinsurers under our reinsurance contracts. (See Note 10 in the Notes to our Consolidated Financial Statements.)
|
|
(5)
|
Combined ratio is the sum of the losses and LAE expense, the commission expense, dividends to policyholders, and the underwriting and other operating expenses, all divided by net earned premiums. Because we only have one operating segment, holding company expenses are included in the combined ratio.
|
|
(6)
|
In connection with our January 1, 2000 assumption of the assets, liabilities and operations of the Fund, our Nevada insurance subsidiary assumed the Fund’s rights and obligations associated with the LPT Agreement, a retroactive 100% quota share reinsurance agreement with third party reinsurers, which substantially reduced exposure to losses for pre-July 1, 1995 Nevada insured risks. Pursuant to the
|
35
LPT Agreement, the Fund initially ceded $1.525 billion in liabilities for incurred but unpaid losses and LAE, which represented substantially all of the Fund’s outstanding losses as of June 30, 1999 for claims with original dates of injury prior to July 1, 1995.
|
(7)
|
Deferred reinsurance gain—LPT Agreement reflects the unamortized gain from our LPT Agreement. Under GAAP, this gain is deferred and is being amortized using the recovery method, whereby the amortization is determined by the proportion of actual reinsurance recoveries to total estimated recoveries, and the amortization is reflected in losses and LAE. We periodically reevaluate the remaining direct reserves subject to the LPT Agreement. Our reevaluation results in corresponding adjustments, if needed, to reserves, ceded reserves, reinsurance recoverables and the deferred reinsurance gain, with the net effect being an increase or decrease, as the case may be, to net income.
|
|
(8)
|
We define net income before impact of the deferred reinsurance gain—LPT Agreement as net income less: (a) amortization of deferred reinsurance gain—LPT Agreement and (b) adjustments to LPT Agreement ceded reserves. For 2006, we define pro forma earnings per share –basic and diluted– before impact of the LPT Agreement as net income before impact of the deferred reinsurance gain—LPT Agreement divided by the common shares issued in our conversion (50,000,002). These are not measurements of financial performance under GAAP, but rather reflect the difference in accounting treatment between statutory and GAAP, and should not be considered in isolation or as an alternative to any other measure of performance derived in accordance with GAAP.
|
We present net income before impact of the deferred reinsurance gain—LPT Agreement because we believe that it is an important supplemental measure of operating performance to be used by analysts, investors, and other interested parties in evaluating us. We present pro forma earnings per share –basic and diluted– before impact of the deferred reinsurance gain—LPT Agreement because we believe that it is an important supplemental measure of performance by outstanding common share issued in our conversion.
The LPT Agreement was a non-recurring transaction which does not result in ongoing cash benefits and consequently we believe these presentations are useful in providing a meaningful understanding of our operating performance. In addition, we believe these non-GAAP measures, as we have defined them, are helpful to our management in identifying trends in our performance because the item excluded has limited significance in our current and ongoing operations.
The table below shows the reconciliation of net income to net income before impact of the deferred reinsurance gain – LPT Agreement for the periods presented:
|
Years Ended December 31,
|
||||||||||||||||||||
|
2010
|
2009
|
2008
|
2007
|
2006
|
||||||||||||||||
|
(in thousands)
|
||||||||||||||||||||
|
Net income
|
$ | 62,799 | $ | 83,021 | $ | 101,785 | $ | 120,283 | $ | 171,570 | ||||||||||
|
Less impact of deferred reinsurance gain – LPT Agreement
|
18,233 | 18,007 | 18,421 | 18,034 | 19,373 | |||||||||||||||
|
Net income before impact of the deferred reinsurance gain—
LPT Agreement
|
$ | 44,566 | $ | 65,014 | $ | 83,364 | $ | 102,249 | $ | 152,197 | ||||||||||
|
(9)
|
We define total equity including deferred reinsurance gain—LPT Agreement as total equity plus deferred reinsurance gain—LPT Agreement. Total equity including deferred reinsurance gain—LPT Agreement is not a measurement of financial position under GAAP and should not be considered in isolation or as an alternative to total equity or any other measure of financial health derived in accordance with GAAP.
|
We present total equity including deferred reinsurance gain—LPT Agreement because we believe that it is an important supplemental measure of financial position to be used by analysts, investors and other interested parties in evaluating us. The LPT Agreement was a non-recurring transaction and the treatment of the deferred gain does not result in ongoing cash benefits or charges to our current operations and consequently we believe this presentation is useful in providing a meaningful understanding of our financial position.
The table below shows the reconciliation of total equity to total equity including deferred reinsurance gain—LPT Agreement for the periods presented:
|
As of December 31,
|
||||||||||||||||||||
|
2010
|
2009
|
2008
|
2007
|
2006
|
||||||||||||||||
|
(in thousands)
|
||||||||||||||||||||
|
Total equity
|
$ | 490,116 | $ | 498,399 | $ | 444,728 | $ | 379,453 | $ | 303,777 | ||||||||||
|
Deferred reinsurance gain – LPT Agreement
|
370,341 | 388,574 | 406,581 | 425,002 | 443,036 | |||||||||||||||
|
Total equity including deferred reinsurance
gain – LPT Agreement
|
$ | 860,457 | $ | 886,973 | $ | 851,309 | $ | 804,455 | $ | 746,813 | ||||||||||
36
Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations
The following discussion and analysis of our financial condition and results of operations should be read in conjunction with the consolidated financial statements and the accompanying notes thereto included in Item 8 and Item 15 of this report. In addition to historical information, the following discussion contains forward-looking statements that are subject to risks and uncertainties and other factors described in Item 1A of this report. Our actual results in future periods may differ from those referred to herein due to a number of factors, including the risks described in the sections entitled “Risk Factors” and “Forward-Looking Statements” elsewhere in this report.
Overview
We are a Nevada holding company. Through our insurance subsidiaries, we provide workers’ compensation insurance coverage to select, small businesses in low to medium hazard industries. Workers’ compensation insurance is provided under a statutory system wherein most employers are required to provide coverage for their employees’ medical, disability, vocational rehabilitation, and/or death benefit costs for work-related injuries or illnesses. We provide workers’ compensation insurance in 30 states and the District of Columbia, with a concentration in California. Our revenues are primarily comprised of net premiums earned, net investment income, and net realized gains (losses) on investments.
We target small businesses, as we believe that this market is characterized by fewer competitors, more attractive pricing, and stronger persistency when compared to the U.S. workers’ compensation insurance industry in general. We believe we are able to price our policies at levels which are competitive and profitable over the long-term. Our underwriting approach is to consistently underwrite small business accounts at an appropriate and competitive price without sacrificing long-term profitability and stability for short-term top-line revenue growth.
We market and sell our workers' compensation insurance products through independent local, regional and national agents and brokers, and through our strategic partnerships and alliances, including our principal partners ADP, Inc. and Anthem Blue Cross (Anthem).
On October 31, 2008, we acquired 100% of the outstanding common stock of AmCOMP Incorporated (AmCOMP) for $188.4 million (the Acquisition). Our results of operations for 2008 include the acquired operations of AmCOMP for the period November 1, 2008 through December 31, 2008.
Results of Operations
Our goal is to maintain focus on disciplined underwriting and to continue to pursue profitable growth opportunities across market cycles; however, we continue to be affected by the impacts of the most recent economic recession. The pace of recovery remains uncertain and, although it appears to us that the declines in total employment and payroll may have leveled-off, we do not believe the situation will significantly improve in the near-term. In 2010, we reduced our expenses while maintaining and improving our ability to provide services to our customers. We believe that we will be positioned to grow our business when the economy and employment trends improve.
We measure our performance by our ability to increase stockholders’ equity, including the impact of the deferred reinsurance gain–LPT Agreement (Deferred Gain), over the long-term. Our stockholders’ equity, including the Deferred Gain, was $860.5 million, $887.0 million, and $851.3 million at December 31, 2010, 2009, and 2008, respectively. Stockholders’ equity, including the Deferred Gain, is a non-GAAP measure that is defined as total stockholders’ equity plus the deferred reinsurance gain—LPT Agreement, which we believe is an important supplemental measure of our capital position. Stockholders’ equity on a GAAP basis was $490.1 million, $498.4 million, and $444.7 million at December 31, 2010, 2009, and 2008, respectively.
Overall, net income was $62.8 million, $83.0 million, and $101.8 million in 2010, 2009, and 2008. Net income decreased primarily due to year over year reductions in net premiums earned, increasing combined ratios (decreasing underwriting income), and the impact of net investment income and realized gains (losses) on investments.
Underwriting (loss) income is determined by deducting losses and LAE, commission expenses, dividends to policyholders, and underwriting and other operating expenses from net premiums earned. Our underwriting (loss) income was $(21.8) million, $8.0 million, and $46.4 million for the years ended December 31, 2010, 2009, and 2008, respectively. Investment income and realized gains (losses) on investments, along with our interest expense and income tax expense, further contribute to our net income.
37
The comparative components of net income are set forth in the following table for the years ended December 31:
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Net premiums earned
|
$ | 321,786 | $ | 404,247 | $ | 328,947 | ||||||
|
Net investment income
|
83,032 | 90,484 | 78,062 | |||||||||
|
Realized gains (losses) on investments
|
10,137 | 791 | (11,524 | ) | ||||||||
|
Other income
|
649 | 413 | 1,293 | |||||||||
|
Total revenues
|
415,604 | 495,935 | 396,778 | |||||||||
|
Losses and LAE
|
194,779 | 214,461 | 136,515 | |||||||||
|
Commission expense
|
38,468 | 36,150 | 43,618 | |||||||||
|
Dividends to policyholders
|
4,316 | 6,930 | 1,295 | |||||||||
|
Underwriting and other operating expenses
|
106,026 | 138,687 | 101,164 | |||||||||
|
Interest expense
|
5,693 | 7,409 | 2,135 | |||||||||
|
Income tax expense
|
3,523 | 9,277 | 10,266 | |||||||||
|
Total expenses
|
352,805 | 412,914 | 294,993 | |||||||||
|
Net income
|
$ | 62,799 | 83,021 | $ | 101,785 | |||||||
|
Net income before impact of the deferred reinsurance gain— LPT Agreement(1)
|
$ | 44,566 | $ | 65,014 | $ | 83,364 | ||||||
|
(1)
|
We define net income before impact of the deferred reinsurance gain—LPT Agreement as net income less: (a) amortization of deferred reinsurance gain—LPT Agreement and (b) adjustments to LPT Agreement ceded reserves. Deferred reinsurance gain—LPT Agreement reflects the unamortized gain from our LPT Agreement. Under GAAP, this gain is deferred and is being amortized using the recovery method, whereby the amortization is determined by the proportion of actual reinsurance recoveries to total estimated recoveries, and the amortization is reflected in losses and LAE. We periodically reevaluate the remaining direct reserves subject to the LPT Agreement. Our reevaluation results in corresponding adjustments, if needed, to reserves, ceded reserves, reinsurance recoverables and the deferred reinsurance gain, with the net effect being an increase or decrease, as the case may be, to net income. Net income before impact of the deferred reinsurance gain—LPT Agreement is not a measurement of financial performance under GAAP, but rather reflects the difference in accounting treatment between statutory and GAAP, and should not be considered in isolation or as an alternative to net income before income taxes or net income or any other measure of performance derived in accordance with GAAP.
|
We present net income before impact of the deferred reinsurance gain—LPT Agreement because we believe that it is an important supplemental measure of operating performance to be used by analysts, investors and other interested parties in evaluating us. The LPT Agreement was a non-recurring transaction which does not result in ongoing cash benefits, and, consequently, we believe this presentation is useful in providing a meaningful understanding of our operating performance. In addition, we believe this non-GAAP measure, as we have defined it, is helpful to our management in identifying trends in our performance because the excluded item has limited significance in our current and ongoing operations.
The table below shows the reconciliation of net income to net income before impact of the deferred reinsurance gain—LPT Agreement for the years ended:
|
December 31,
|
|||||||||||
|
2010
|
2009
|
2008
|
|||||||||
|
(in thousands)
|
|||||||||||
|
Net income
|
$ | 62,799 | $ | 83,021 | $ | 101,785 | |||||
|
Less impact of the deferred reinsurance gain—LPT Agreement
|
18,233 | 18,007 | 18,421 | ||||||||
|
Net income before impact of the deferred reinsurance gain—LPT Agreement
|
$ | 44,566 | $ | 65,014 | $ | 83,364 | |||||
Net Premiums Earned
Net premiums earned declined $82.5 million for the year ended December 31, 2010, compared to prior year. This decrease reflects the impacts of the recession, including high unemployment and fewer hours worked, declines in our policyholders’ payroll, lower net rates, and our application of disciplined pricing objectives and underwriting guidelines in a highly competitive market. The increase in net premiums earned for the year ended December 31, 2009, compared to the same period of 2008, was primarily due to the Acquisition. This increase in 2009 was partially offset by lower premiums, primarily in California and Nevada, as a result of rate reductions, competition, and impacts of economic conditions.
38
The following table shows the percentage change in our in-force policy count, average policy size, and payroll exposure, upon which our premiums are based, and net rate as of December 31 for each of the periods presented.
|
Percentage
Increase (Decrease)
2010 Over 2009
|
Percentage (Decrease) 2009 Over 2008
|
|||||||
|
In-force policy count
|
0.9 | % | (3.2 | )% | ||||
|
Average in-force policy size
|
(17.4 | ) | (14.6 | ) | ||||
|
In-force payroll exposure
|
(12.1 | ) | (11.0 | ) | ||||
|
Net rate(1)
|
(5.1 | ) | (7.1 | ) | ||||
|
(1)
|
Net rate, defined as total premium in-force divided by total insured payroll exposure, is a function of a variety of factors, including rate changes, underwriting risk profiles and pricing, and changes in business mix related to economic and competitive pressures.
|
Approximately one-half of our business is generated in California, where we saw increased net rate on renewal business for 17 consecutive months, through August 2010. We continue to see a steady level of new business submittals and our policy count in California has increased 5.1% during the year ended December 31, 2010.
We set our own premium rates in California based upon actuarial analysis of current and anticipated loss trends with a goal of maintaining underwriting profitability. We reduced our filed premium rates in California from 2003 through 2008 due to favorable loss costs trends originating from the 2003 and 2004 legislative reforms. Due to increasing loss costs, primarily medical cost inflation, we have increased our filed premium rates by a cumulative 28.3% since February 1, 2009.
Premium revenues in 2011 will continue to reflect rate increases in California, rate changes (increases and reductions) in several of our other states, as well as competitive pressures and the continuing effects of the recession.
As we continue to execute our growth strategy, we have increased our network of independent insurance agencies by approximately 14% in 2010 and continue to deploy our technology to make it easier for agents to do business with us. While the effects of the recession have resulted in lower total in-force payroll exposure and average policy size, we increased our in-force policy count by 0.9% in 2010, including a 2.4% increase during the fourth quarter.
Net Investment Income and Realized Gains (Losses) on Investments
We invest our holding company assets, statutory surplus, and the funds supporting our insurance liabilities, including unearned premiums and unpaid losses and LAE. We invest in fixed maturity securities, equity securities, short-term investments, and cash equivalents. Net investment income includes interest and dividends earned on our invested assets and amortization of premiums and discounts on our fixed maturity securities, less bank service charges and custodial and portfolio management fees.
We have established a high quality/short duration bias in our investment portfolio with high underlying credit quality of our municipal bond holdings. The performance of our investment portfolio, with its diversified structure and quality bias, has been exceptionally strong.
Net investment income decreased $7.5 million for the year ended December 31, 2010, compared to the same period of 2009, but increased $12.4 million in 2009, compared to 2008. The decrease in 2010 was primarily related to a 1.4% decrease in average invested assets for the year. This decrease in our average invested assets was primarily due to repayment of debt and the return of capital to stockholders through share repurchases and stockholder dividends. The increase in net investment income for the year ended 2009, compared to the same period of 2008, was related to a 17.0% increase in average invested assets year-over-year. The average pre-tax book yield on invested assets was 4.2%, 4.5%, and 4.2% at December 31, 2010, 2009, and 2008, respectively. The tax-equivalent yield on invested assets was 5.3%, 5.6%, and 5.5% at December 31, 2010, 2009, and 2008, respectively.
Realized gains and losses on our investments are reported separately from our net investment income. Realized gains and losses on investments include the gain or loss on a security at the time of sale compared to its original cost (equity securities) or amortized cost (fixed maturity securities). Realized losses are recognized when securities are written down as a result of an other-than-temporary impairment.
39
Realized gains on investments increased $9.3 million, for the year ended December 31, 2010, compared to the same period of 2009. We evaluated our portfolio allocation during the fourth quarter of 2010 and elected to shift $20.0 million of our equity securities into a high dividend yield portfolio, which resulted in a $9.2 million gain. In 2008, we had realized losses on investments of $11.5 million. The realized losses for 2008 were the result of other-than-temporary impairments on equity securities and sales of impaired fixed maturity securities in our investment portfolio.
Additional information regarding our Investments is set forth under “—Liquidity and Capital Resources—Investments.”
Combined Ratio
The combined ratio, expressed as a percentage, is a key measurement of underwriting profitability. The combined ratio is the sum of the losses and LAE ratio, the commission expense ratio, dividends to policyholders’ ratio, and underwriting and other operating expenses ratio. When the combined ratio is below 100%, we have recorded underwriting income, and conversely, when the combined ratio is greater than 100%, we cannot be profitable without investment income. Because we only have one operating segment, holding company expenses are included in our calculation of the combined ratio.
The following table provides the calculation of our calendar year combined ratios for the years ended December 31:
|
2010
|
2009
|
2008
|
||||||||||
|
Losses and LAE ratio
|
60.5 | % | 53.1 | % | 41.5 | % | ||||||
|
Underwriting and other operating expenses ratio
|
33.0 | 34.3 | 30.7 | |||||||||
|
Commission expense ratio
|
12.0 | 8.9 | 13.3 | |||||||||
|
Dividends to policyholders’ ratio
|
1.3 | 1.7 | 0.4 | |||||||||
|
Combined ratio
|
106.8 | % | 98.0 | % | 85.9 | % | ||||||
Losses and LAE Ratio. Expressed as a percentage, this is the ratio of losses and LAE to net premiums earned.
We analyze our losses and LAE ratios on both a calendar year and accident year basis. A calendar year losses and LAE ratio is calculated by dividing the losses and LAE incurred during the calendar year, regardless of when the underlying insured event occurred, by the net premiums earned during that calendar year. The calendar year losses and LAE ratio includes changes made during the calendar year in reserves for losses and LAE established for insured events occurring in the current and prior years. A calendar year losses and LAE ratio is calculated using premiums and losses and LAE that are net of amounts ceded to reinsurers.
The accident year losses and LAE ratio, or losses and LAE for insured events that occurred during a particular year divided by the premiums earned for the year, is calculated by dividing the losses and LAE, regardless of when such losses and LAE are incurred, for insured events that occurred during a particular year by the net premiums earned for that year. The accident year losses and LAE ratio is calculated using premiums and losses and LAE that are net of amounts ceded to reinsurers. The accident year losses and LAE ratio for a particular year can decrease or increase when recalculated in subsequent periods as the reserves established for insured events occurring during that year develop favorably or unfavorably; and is an operating ratio based on our statutory financial statements and is not derived from our GAAP financial information. The calendar year losses and LAE ratio for a particular year will not change in future periods.
We analyze our calendar year losses and LAE ratio to measure our profitability in a particular year and to evaluate the adequacy of our premium rates charged in a particular year to cover expected losses and LAE from all periods, including development (whether favorable or unfavorable) of reserves established in prior periods. In contrast, we analyze our accident year losses and LAE ratios to evaluate our underwriting performance and the adequacy of the premium rates we charged in a particular year in relation to ultimate losses and LAE from insured events occurring during that year. The losses and LAE ratios provided in this report are calendar year losses and LAE ratios, except where they are expressly identified as accident year losses and LAE ratios.
Losses and LAE expense represents our largest expense item and includes claim payments made, amortization of the LPT deferred gain, estimates for future claim payments, and changes in those estimates for current and prior periods, and costs associated with investigating, defending and adjusting claims. The quality of our financial reporting depends in large part on accurately predicting our losses and LAE, which are inherently uncertain as they are estimates of the ultimate cost of individual claims based on actuarial estimation techniques.
40
In California, our loss data indicates an upward trend in medical costs that is reflected in our loss reserves. We are also seeing increased medical costs in many of our other states, partially offset by long-term favorable loss cost trends in Nevada. We believe our loss reserve estimates are adequate; however, the ultimate losses will not be known with any certainty for several years. We assume that increasing medical cost trends will continue and will impact our long-term claims costs and loss reserves. Additionally, the impact, if any, of the recession on our claims costs is not yet known. We will continue to evaluate our estimate of loss reserves to reflect the most current data and judgments. Additional information regarding our reserves for losses and LAE is set forth under “—Critical Accounting Policies—Reserves for Losses and LAE.”
Overall, losses and LAE decreased $19.7 million for the year ended December 31, 2010, compared to the same period of 2009, primarily due to lower payroll exposures. Favorable prior accident year loss development decreased $34.8 million to $16.6 million for the year ended December 31, 2010, compared to the same period of 2009. Additionally, a $1.6 million expense related to the commutation of certain reinsurance treaties, and a $0.9 million expense related to the write-off of certain reinsurance recoverables that had previously been accounted for as an allowance for bad debt, are included in losses and LAE for the year ended December 31, 2010.
The $77.9 million increase in losses and LAE for the year ended December 31, 2009, compared to the same period of 2008, was primarily attributable to the Acquisition, partially offset by a change in overall payroll exposures, which reduced losses and LAE by approximately $51.9 million. Our current accident year loss estimates were 70.9%, 70.2%, and 68.9% for the years ended December 31, 2010, 2009, and 2008, respectively.
The table below reflects the losses and LAE reserve adjustments for the periods presented.
|
Years Ended
|
Quarters Ended
|
||||||||||||||||||||||
|
2010
|
2009
|
2008
|
2010
|
2009
|
2008
|
||||||||||||||||||
|
(in millions)
|
|||||||||||||||||||||||
|
Prior accident year favorable development, net(1)
|
$ | 16.6 | $ | 51.4 | $ | 71.7 | $ | — | $ | 11.8 | $ | 18.4 | |||||||||||
|
LPT amortization of the deferred reinsurance gain
|
$ | 18.2 | $ | 18.0 | $ | 18.4 | $ | 4.7 | $ | 4.6 | $ | 4.5 | |||||||||||
|
(1)
|
Prior accident year favorable development, net, excludes a $1.6 million expense related to the commutation of certain reinsurance treaties and a $0.9 million expense related to the write-off of certain reinsurance recoverables, which are included in losses and LAE for the year ended December 31, 2010.
|
Excluding the impact from the LPT Agreement, losses and LAE would have been $213.0 million, $232.5 million, and $154.9 million, or 66.2%, 57.5%, and 47.1%, of net premiums earned for the year ended December 31, 2010, 2009, and 2008, respectively.
Underwriting and Other Operating Expenses Ratio. The underwriting and other operating expenses ratio is the ratio (expressed as a percentage) of underwriting and other operating expenses to net premiums earned, and measures an insurance company's operational efficiency in producing, underwriting, and administering its insurance business.
Underwriting and other operating expenses are those costs that we incur to underwrite and maintain the insurance policies we issue, excluding commission. These expenses include premium taxes and certain other general expenses that vary with, and are primarily related to, producing new or renewal business. Other underwriting expenses include changes in estimates of future write-offs of premiums receivable, general administrative expenses such as salaries and benefits, rent, office supplies, depreciation, and all other operating expenses not otherwise classified separately. Policy acquisition costs are variable based on premiums earned; however, other operating costs are more fixed in nature and become a larger percentage of net premiums earned as premiums decline.
In January 2009, we restructured our operations as a result of the Acquisition and incurred one-time pre-tax integration and restructuring charges of approximately $5.7 million, including $2.8 million of severance benefits, for the year ended December 31, 2009. As a result of the restructuring, we achieved pre-tax cost savings of approximately $12.0 million in fiscal 2009.In the first quarter of 2010, we incurred charges of $0.9 million related to staffing reductions to adjust our insurance operations to reflect activity levels at that time.
41
In July 2010, we announced the reorganization of our operations to eliminate duplicative services and better align resources with business activity and growth opportunities. We combined our four regional operating units into two units, Eastern and Western, with the Strategic Partnerships and Alliances unit remaining structurally unchanged. In connection with these efforts and with general cost control efforts, we eliminated approximately 160 positions. These changes to our workforce were substantially completed in the third quarter of 2010. Facility closures associated with this reorganization were completed in the second half of 2010. In conjunction with this reorganization, we recorded restructuring charges of $5.2 million in 2010, including $3.0 million related to workforce reductions and $2.2 million related to leases for facilities that were vacated during the year.
Beginning in 2011, we anticipate combined annualized cost savings of approximately $23.6 million, comprised of $21.0 million in salaries and benefits and $2.6 million in lease related savings, associated with restructuring activities that occurred in 2010.
Underwriting and other operating expenses decreased 23.6% for the year ended December 31, 2010, compared to the same period of 2009, including restructuring items for both years. We incurred charges of $6.1 million in the year ended December 31, 2010, including $3.9 million related to workforce reductions and $2.2 million related to leases for facilities that were vacated. This compared to integration and restructuring charges of $5.7 million for the same period of 2009 related to the Acquisition. Excluding these restructuring charges, underwriting and other operating expenses decreased $33.1 million, or 24.9%, for the year ended December 31, 2010, compared to the same period of 2009. The decrease reflects efforts to manage our expenses during a period of declining premiums. During the year ended December 31, 2010 information technology expenses declined $3.5 million and compensation expenses declined $16.5 million, compared to the same period of 2009. Additionally, there was a $5.8 million decrease in premium taxes and a $3.6 million decrease in bad debt expense.
Our underwriting and other operating expenses increased 37.1%, for the year ended December 31, 2009, as compared to the same period in 2008, including restructuring items in 2009. The increase was primarily related to the acquired operations of AmCOMP. The increase included a $19.3 million increase in compensation expense, a $5.7 million increase in premium taxes, and $3.0 million increase in bad debt expense.
Commission Expense Ratio. The commission expense ratio is the ratio (expressed as a percentage) of commission expense to net premiums earned and measures the cost of compensating agents and brokers for the business we have underwritten.
Commission expense includes direct commissions to our agents and brokers for the premiums that they produce for us, as well as incentive payments, other marketing costs, and fees. Additionally, we are entitled to receive a contingent profit commission under the LPT Agreement. The contingent profit is an amount based on the favorable difference between actual paid losses and LAE and expected paid losses and LAE under the LPT Agreement. Loss expenses are deemed to be 7% of total losses paid and are paid to us as compensation for management of the LPT claims. The calculation of actual amounts paid versus expected amounts is determined every five years beginning June 30, 2004 for the first twenty-five years of the agreement. The reinsurers pay us 30% of any favorable difference between the actual and expected amounts paid at each calculation point. Conversely, we could be required to return any previously paid contingent profit commission, plus interest, in the event of unfavorable differences.
We accrue the estimated ultimate contingent profit commission through June 30, 2024. Increases or decreases in the estimated contingent profit commission are reflected in commission expense in the period that the estimate is revised. In 2010, an increase in the estimated contingent profit commission of $0.8 million resulted in a decrease in the commission expense for the year. For the year ended December 31, 2009, we decreased commission expenses by $15.0 million as a result of an increase in contingent profit commissions and received cash payment of $10.3 million from the reinsurers. At December 31, 2010, expected amounts to be paid for losses under the LPT Agreement for the period July 1, 1999 through June 30, 2014, were $677.7 million, compared to contractually expected losses and LAE of approximately $775.0 million.
Our commission expense was $38.5 million, $36.2 million, and $43.6 million for the years ended December 31, 2010, 2009, and 2008, respectively. The increase from 2009 to 2010 was primarily due to a $15.0 million adjustment in the accrual for the LPT contingent profit commission during the year ended December 31, 2009 and re-negotiation of the terms of a separate reinsurance agreement resulting in an additional $1.8 million in commission expense in the fourth quarter of 2010. This increase was partially offset by lower net premiums earned and a $3.0 million reduction in the
42
estimate of certain administrative fees due Anthem under our joint marketing agreements, which decreased the commission expense in the fourth quarter of 2010. The decrease in 2009, compared to 2008, of $7.5 million, or 17.1%, was primarily attributable to a $15.0 million increase in the LPT contingent profit commission, partially offset by increased commission expense from our acquired subsidiaries. Excluding the impact of the LPT contingent profit commission, the re-negotiated reinsurance agreement, and the change in accrual for fees due Anthem, commission expense would have been 12.6%, 12.7%, and 13.3% of net premiums earned for the years ended December 31, 2010, 2009, and 2008, respectively.
Dividends to Policyholders Ratio. The dividends to policyholders ratio is the ratio (expressed as a percentage) of dividends to policyholders expense to net premiums earned and measures the cost of returning premium to policyholders in the form of dividends.
In administered pricing states such as Florida and Wisconsin, insurance rates are set by state insurance regulators. Rate competition generally is not permitted and policyholder dividend programs are an important competitive factor in these states. We offer dividend programs to eligible policyholders, under which a portion of the policyholders’ premium may be returned in the form of a dividend.
Florida statutes also require the return of the portion of policyholders’ premiums that are deemed to be excessive profits under Florida law. We account for these payments as dividends to policyholders.
Dividends to policyholders were $4.3 million, $6.9 million, and $1.3 million for the years ended December 31, 2010, 2009, and 2008, respectively. The decrease in dividends to policyholders from 2009 to 2010 was primarily due to lower premium levels on dividend policies in Florida and Wisconsin and fewer policies eligible for dividend payments in 2010. The increase in 2009, compared to 2008, was primarily due to the Acquisition.
Interest Expense
We incur interest expenses on notes payable. We also had an interest rate swap agreement on our credit facility with Wells Fargo Bank, National Association (Wells Fargo), which expired on September 30, 2010.
Interest expense decreased 23.2% for the year ended December 31, 2010, compared to the same period of 2009, primarily due to a $50.0 million reduction in the principal balance on our credit facility with Wells Fargo in the fourth quarter of 2009 and the expiration of the interest rate swap in the third quarter of 2010. Interest expense increased $5.3 million for the year ended December 31, 2009, compared to the same period of 2008, as we had no debt or related interest expense for the first ten months of 2008.
Income Tax Expense
Income tax expense decreased $5.8 million for the year ended December 31, 2010, compared to the same period of 2009. Similarly, income taxes decreased $1.0 million for the year ended December 31, 2009, compared to the same period of 2008. The effective tax rates for the years ended December 31, 2010, 2009, and 2008 were 5.3%, 10.1%, and 9.2%, respectively. Tax exempt income as a percentage of pre-tax income was 50.6%, 36.8%, and 27.7% for the years ended December 31, 2010, 2009, and 2008, respectively. The increase in tax exempt income in 2010, as a percentage of pre-tax income, was primarily due to a $28.9 million decrease in pre-tax income, partially offset by the $15.0 million LPT contingent profit commission in 2009, which was not subject to tax.
The increase in the effective tax rate in 2009, compared to 2008, was primarily the result of transactions that decreased 2008 income taxes related to the final reversal of the liability for previously unrecognized tax benefits in the amount of $10.6 million, including interest, and the reduction of tax-exempt reserves in the amount of $5.2 million. These comparative increases were largely offset by a $19.8 million decrease in 2009 pre-tax income, the impact of tax-exempt investment income and the LPT contingent profit commission of $15.0 million, which is not subject to tax.
Liquidity and Capital Resources
Parent Company
Operating Cash and Short-Term Investments. We are a holding company and our ability to fund our operations is contingent upon our insurance subsidiaries’ and their ability to pay dividends to the holding company. Payment of dividends by our insurance subsidiaries is restricted by state insurance laws, including laws establishing minimum solvency and liquidity thresholds. We require cash to pay stockholder dividends, repurchase common stock, make interest and principal payments on our outstanding debt obligations, fund our operating expenses, and support our growth strategy.
43
During 2010, EICN and EPIC paid dividends of $100.3 million and $14.9 million, respectively, to Employers Group, Inc. (EGI), their immediate holding company, and subsequently from EGI to EHI. These amounts represented the maximum dividends that could be paid without prior approval by the respective state insurance regulator.
Additionally, on May 27, 2010, we received approval from the Nevada Commissioner of Insurance to pay $150.0 million in extraordinary dividends from EICN special surplus. This $150.0 million extraordinary dividend was paid by EICN to EGI, and subsequently from EGI to EHI, on June 3, 2010. As a result of the payment of the extraordinary dividend from special surplus, any dividends paid by EICN through June 3, 2011 will require prior approval by the Nevada Commissioner of Insurance.
Based on reported capital, surplus, and dividends paid within the last 12 months, the maximum dividends that may be paid by EICN between June 3 and December 31, 2011, and by EPIC in 2011, without prior approval by the respective state insurance regulator are $51.9 million and $15.5 million, respectively.
As of December 31, 2010, the holding company had cash and fixed maturity securities maturing within the next 24 months of $74.9 million. Ten million dollars of our line of credit is due annually beginning on December 31, 2011 through December 31, 2014. We believe that the liquidity needs of the holding company over the next 24 months will be met with cash, maturing investments, and dividends from our insurance subsidiaries.
Share Repurchases.In November 2009, the EHI Board of Directors (Board of Directors) authorized a share repurchase program for $50 million of the Company’s common stock from January 1, 2010 through December 31, 2010 (the 2010 Program). Through September 30, 2010, we repurchased a total of 3,291,709 shares of common stock under the 2010 Program at an average price of $15.19 per share, including commissions, for a total of $50.0 million.
On November 3, 2010, the Board of Directors authorized a share repurchase program for up to $100 million of the Company’s common stock from November 8, 2010 through June 30, 2012 (the 2011 Program). Through December 31, 2010, we repurchased a total of 867,149 shares of common stock under the 2011 Program at an average price of $16.59 per share, including commissions, for a total of $14.4 million. Repurchases under this program may be commenced or suspended from time to time without prior notice, and the program may be suspended or discontinued at any time.
Outstanding Debt. We entered into the Second Amended and Restated Secured Credit Facility with Wells Fargo (Existing Credit Facility), in September 2008, under which we borrowed $150.0 million. The Existing Credit Facility provided us with: (a) $150.0 million line of credit through December 31, 2009; (b) $100.0 million line of credit from January 1, 2010 through December 31, 2010; and (c) $50.0 million line of credit from January 1, 2011 through March 26, 2011. Amounts outstanding bore interest at a rate equal to, at our option: (a) a fluctuating rate of 1.25% above prime rate or (b) a fixed rate that is 1.25% above the LIBOR rate then in effect.
In accordance with the terms of the contract, we repaid $50.0 million of the line of credit provided by the Amended Credit Facility on December 30, 2009. In connection with the borrowing, we had entered into an interest rate swap agreement for an interest rate of 4.84% on the notional amount of $100.0 million, which expired on September 30, 2010.
On December 28, 2010, we entered into the Third Amended and Restated Credit Agreement with Wells Fargo (Amended Credit Facility) under which we are provided with: (a) $100.0 million line of credit through December 31, 2011; (b) $90.0 million line of credit from January 1, 2012 through December 31, 2012; (c) $80.0 million line of credit from January 1, 2013 through December 31, 2013; (d) $70 million line of credit from January 1, 2014 through December 31, 2014; and (e) $60 million line of credit from January 1, 2015 through December 31, 2015. Amounts outstanding bear interest at a rate equal to, at our option: (a) a fluctuating rate of 1.75% above prime rate or (b) a fixed rate that is 1.75% above the LIBOR rate then in effect. The Amended Credit Facility is secured by fixed maturity securities and cash and cash equivalents that had a fair value of $129.0 million and $2.0 million of restricted cash and cash equivalents at December 31, 2010. The Amended Credit Facility contains customary non-financial covenants and requires us to maintain $5.0 million of cash and cash equivalents at all times at the holding company. We are currently in compliance with all applicable covenants.
Our total outstanding debt was $132.0 million as of December 31, 2010 and 2009. Interest and fees on debt obligations totaled $5.7 million in 2010, down $1.7 million from 2009.
44
Our capital structure is comprised of outstanding debt and stockholders’ equity. As of December 31, 2010, our capital structure consisted of $100.0 million principal balance on our Amended Credit Facility, $32.0 million in surplus notes maturing in 2034, and $860.5 million of stockholders’ equity, including the deferred reinsurance gain—LPT Agreement. Outstanding debt was 13.3% of total capitalization, including the deferred reinsurance gain—LPT Agreement, as of December 31, 2010.
Operating Subsidiaries
Operating Cash and Short-Term Investments. The primary sources of cash for our insurance operating subsidiaries are funds generated from underwriting operations, investment income, and maturities of investments. The primary uses of cash are payments of claims and operating expenses, purchases of investments, and payments of dividends to the parent holding company, which are subject to state insurance laws and regulations.
Our insurance subsidiaries had total cash and fixed maturity securities of $270.5 million maturing within the next 24 months at December 31, 2010. We believe that our subsidiaries’ liquidity needs over the next 24 months will be met with cash from operations, investment income, and maturing investments.
We purchase reinsurance to protect us against the costs of severe claims and catastrophic events. On July 1, 2010, we entered into a new reinsurance program that is effective through June 30, 2011. The reinsurance program consists of one treaty covering excess of loss and catastrophic loss events in five layers of coverage. Our reinsurance coverage is $195.0 million in excess of our $5.0 million retention on a per occurrence basis, subject to a $2.0 million annual aggregate deductible and certain exclusions. We believe that our reinsurance program meets our needs and that we are sufficiently capitalized for the above described retention.
Our insurance subsidiaries are required by law to maintain a certain minimum level of surplus on a statutory basis. Surplus is calculated by subtracting total liabilities from total admitted assets. The amount of capital in our insurance subsidiaries is maintained relative to standardized capital adequacy measures such as risk-based capital (RBC), as established by the National Association of Insurance Commissioners. The RBC standard was designed to provide a measure by which regulators can assess the adequacy of an insurance company’s capital and surplus relative to its operations. An insurance company must maintain capital and surplus of at least 200% of RBC. Each of our insurance subsidiaries had total adjusted capital in excess of the minimum RBC requirements that correspond to any level of regulatory action at December 31, 2010.
Various state regulations require us to keep securities or letters of credit on deposit with the states in which we do business in depository accounts. Securities having a fair market value of $558.6 million and $554.2 million were on deposit at December 31, 2010 and 2009, respectively. These laws and regulations govern both the amount and type of fixed maturity security that is eligible for deposit. Additionally, certain reinsurance contracts require Company funds to be held in trust for the benefit of the ceding reinsurer to secure the outstanding liabilities we assumed. The fair value of securities held in trust for reinsurance at December 31, 2010 and 2009 was $52.9 million and $6.1 million, respectively.
In the fourth quarter of 2010, we re-negotiated the terms of a reinsurance agreement with Clarendon National Insurance Company (Clarendon), resulting in the release and return of funds held by Clarendon to us in the amount of $74.6 million. We placed $47.1 million in trust for the benefit of Clarendon to support liabilities under the reinsurance agreement and invested the remaining $27.5 million.
Cash Flows
We monitor cash flows at both the consolidated and subsidiary levels. We use trend and variance analyses to project future cash needs, making adjustments to our forecasts as appropriate.
The table below shows our net cash flows for the years ended December 31:
|
2010
|
2009
|
2008
|
||||||||||
|
Cash and cash equivalents provided by (used in)
|
(in thousands)
|
|||||||||||
|
Operating activities
|
$ | 56,981 | $ | 40,751 | $ | 67,314 | ||||||
|
Investing activities
|
(51,327 | ) | 85,992 | (135,218 | ) | |||||||
|
Financing activities
|
(74,662 | ) | (135,339 | ) | 120,949 | |||||||
|
(Decrease) increase in cash and cash equivalents
|
$ | (69,008 | ) | $ | (8,596 | ) | $ | 53,045 | ||||
45
Net cash provided by operating activities increased $16.2 million for the year ended December 31, 2010, compared to the same period of 2009.
Significant items increasing net cash from operations included:
|
·
|
decreased funds held of $72.8 million, including the release of funds held by Clarendon;
|
|
·
|
decreased losses and LAE paid of $26.9 million;
|
|
·
|
decreased underwriting and other operating expenses paid of $12.0 million, including lower premium taxes paid of $5.9 million;
|
Significant items decreasing net cash from operations included:
|
·
|
decreased net premiums received of $71.6 million;
|
|
·
|
increased restricted cash and cash equivalents of $12.2 million;
|
|
·
|
increased commissions paid of $4.8 million, primarily due to $10.3 million received from the LPT contingent profit commission in 2009;
|
|
·
|
decreased investment income received of $3.6 million; and
|
|
·
|
increased income taxes paid of $7.3 million.
|
Net cash provided by operating activities decreased $26.6 million in 2009, compared to 2008. This decrease was primarily due to increased payments for losses and LAE of $103.3 million and increase payments for underwriting and other operating expenses of $39.3 million, partially offset by increased net premiums received of $62.6 million, decreased income taxes paid of $26.3 million, increased investment income of $13.3 million, and cash received on the LPT contingent commission of $10.3 million.
Net cash used in investing activities was $56.3 million in 2010, compared to cash provided of $86.0 million in 2009. In 2008, we had $135.2 million of net cash used by investing activities. The difference in 2010, compared to 2009, was primarily due to the reinvestment of funds from maturities and redemptions in 2010. The difference in 2009, compared to 2008, was primarily due to the purchase of AmCOMP for $188.4 million in 2008. We also used proceeds from maturities and redemptions of investments primarily for the repurchase of our common stock in 2009 and 2008.
Net cash used in financing activities was $74.7 million in 2010, compared to $135.3 million in 2009. In 2008, $120.9 million of net cash was provided by financing activities. The majority of cash used in financing activities in 2010 was to repurchase $64.4 million of our common stock and to pay dividends to stockholders. In 2009, the majority of cash used in financing activities was to repurchase $74.2 million of our common stock and to pay down $50 million of the line of credit provided by the Amended Credit Facility. In 2008, cash was provided by proceeds from our Amended Credit Facility, which was later used for the acquisition of AmCOMP.
Investments
The amortized cost of our investment portfolio was $1.95 billion and the fair value was $2.08 billion as of December 31, 2010.
We employ an investment strategy that emphasizes asset quality and considers the durations of fixed maturity securities against anticipated claim payments and expenditures, other liabilities, and capital needs. Our investment portfolio is structured so that investments mature periodically in reasonable relation to current expectations of future claim payments. Currently, we make claim payments from positive cash flow from operations and use excess cash to invest in operations, invest in marketable securities, return capital to our stockholders, and fund our growth strategy.
As of December 31, 2010, our investment portfolio, which is classified as available-for-sale, consisted of 96.1% fixed maturity securities whose fair values may fluctuate. We strive to limit interest rate risk by managing the duration of our fixed maturity securities. Our fixed maturity securities (excluding cash and cash equivalents) had a duration of 4.91 at December 31, 2010. To minimize interest rate risk, our portfolio is weighted toward short-term and intermediate-term bonds; however, our investment strategy balances consideration of duration, yield and credit risk. Our investment guidelines require that the minimum weighted average quality of our fixed maturity securities portfolio shall be “AA”. As of December 31, 2010, our fixed maturity securities portfolio had an average quality of “AA” using ratings assigned by Standard & Poor’s with approximately 73.3% of the market value rated “AA” or better.
We carry our portfolio of equity securities on our balance sheet at fair value. We minimize our exposure to equity price risk by investing primarily in the equity securities of mid-to-large capitalization issuers and by diversifying our equity holdings across several industry sectors. At December 31, 2010, equity securities represented 3.9% of our investment portfolio.
46
Given the economic uncertainty and continued market volatility, we believe our asset allocation best meets our strategy to preserve capital for policyholders, to provide sufficient income to support insurance operations, and to effectively grow book value over a long-term investment horizon.
We seek to maximize total investment returns within the constraints of prudent portfolio management. The asset allocation is reevaluated by the Finance Committee of the Board of Directors on a quarterly basis. We employ Conning Asset Management (Conning) to act as our independent investment manager. Conning follows our written investment guidelines based upon strategies approved by the Board of Directors. In addition to the construction and management of the portfolio, we utilize the investment advisory services of Conning. These services include investment accounting and company modeling using Dynamic Financial Analysis (DFA). The DFA tool is utilized to develop portfolio targets and objectives, which in turn are used in constructing an optimal portfolio.
The following table shows the fair value, the percentage of the fair value to total invested assets and the tax equivalent yield based on the fair value of each category of invested assets as of December 31, 2010:
|
Category
|
Fair Value
|
Percentage of
Total
|
Yield
|
|||||||||
|
(in thousands, except percentages)
|
||||||||||||
|
U.S. Treasuries
|
$ | 144,725 | 7.0 | % | 3.6 | % | ||||||
|
U.S. Agencies
|
123,802 | 5.9 | 4.0 | |||||||||
|
States and municipalities
|
966,002 | 46.4 | 5.9 | |||||||||
|
Corporate securities
|
479,424 | 23.0 | 4.9 | |||||||||
|
Residential mortgaged-backed securities
|
246,756 | 11.9 | 5.5 | |||||||||
|
Commercial mortgaged-back securities
|
25,077 | 1.2 | 5.2 | |||||||||
|
Asset-backed securities
|
14,578 | 0.7 | 4.3 | |||||||||
|
Equity securities
|
80,130 | 3.9 | 4.4 | |||||||||
|
Total investments
|
$ | 2,080,494 | 100.0 | % | ||||||||
|
Weighted average yield
|
5.3 | |||||||||||
The following table shows the percentage of total market share of our fixed maturity securities as of December 31, 2010 by credit rating category, as defined by Standard & Poor’s.
|
Rating
|
Percentage of Total
Market Value
|
||
|
“AAA”
|
37.7 | % | |
|
“AA”
|
35.6 | ||
| “A” | 19.5 | ||
|
“BBB”
|
7.0 | ||
|
Below Investment Grade
|
0.2 | ||
|
Total
|
100.0 | % |
Investments that we currently own could be subject to default by the issuer or could suffer declines in fair value that become other-than-temporary. We regularly assess individual securities as part of our ongoing portfolio management, including the identification of other-than-temporary declines in fair value. Our other-than-temporary assessment includes reviewing the extent and duration of declines in fair value of investments below amortized cost, historical and projected financial performance and near-term prospects of the issuer, the outlook for industry sectors, credit rating, and macro-economic changes. We also make a determination as to whether it is not more likely than not that we will not be required to sell the security before its fair value recovers above cost, or to maturity.
For the year ended December 31, 2010, we recognized an impairment of $46 thousand in the fair value of one of our fixed maturity holdings as a result of an anticipated sale of this security due to a strategic rebalancing in our investment portfolio and not from credit impairment. None of our equity securities were impaired in 2010. We determined that the unrealized losses on equity securities at December 31, 2010 were not considered to be other-than-temporary due to the financial condition and the near term prospects of the issuers. We also determined that the remaining unrealized losses on fixed maturity securities were primarily the result of prevailing interest rates and not the credit quality of the issuers.
47
For the year ended December 31, 2009, we recognized an impairment of $1.9 million in the fair value of equity securities in our investment portfolio. The impairment was recognized as a result of the severity and duration of the decline in the market values of these securities primarily due to market conditions. We determined that the remaining unrealized losses on equity securities were not considered to be other-than-temporary due to the financial condition and the near term prospects of the issuers. None of our fixed maturity securities were impaired in 2009. Based on our review of fixed maturity and equity securities, we believe that we have appropriately identified the declines in the fair values of our unrealized losses at December 31, 2010 and 2009.
The amortized cost, gross unrealized gains, gross unrealized losses, and estimated fair value of our investments were as follows:
|
Amortized
Cost
|
Gross
Unrealized Gains
|
Gross
Unrealized Losses
|
Estimated
Fair Value
|
||||||||||||
|
At December 31, 2010
|
(in thousands)
|
||||||||||||||
|
Fixed maturity securities
|
|||||||||||||||
|
U.S. Treasuries
|
$ | 135,265 | $ | 9,619 | $ | (159 | ) | $ | 144,725 | ||||||
|
U.S. Agencies
|
116,747 | 7,142 | (87 | ) | 123,802 | ||||||||||
|
States and municipalities
|
927,668 | 43,054 | (4,720 | ) | 966,002 | ||||||||||
|
Corporate
|
453,851 | 28,655 | (3,082 | ) | 479,424 | ||||||||||
|
Residential mortgage-backed securities
|
230,518 | 16,926 | (688 | ) | 246,756 | ||||||||||
|
Commercial mortgage-backed securities
|
23,877 | 1,201 | (1 | ) | 25,077 | ||||||||||
|
Asset-backed securities
|
13,852 | 727 | (1 | ) | 14,578 | ||||||||||
|
Total fixed maturity securities
|
1,901,778 | 107,324 | (8,738 | ) | 2,000,364 | ||||||||||
|
Equity securities
|
|||||||||||||||
|
Consumer goods
|
19,141 | 7,550 | (45 | ) | 26,646 | ||||||||||
|
Energy and utilities
|
5,106 | 5,160 | (1 | ) | 10,265 | ||||||||||
|
Financial
|
6,603 | 2,916 | (19 | ) | 9,500 | ||||||||||
|
Technology and communications
|
7,499 | 8,500 | (9 | ) | 15,990 | ||||||||||
|
Industrial and other
|
10,932 | 6,841 | (44 | ) | 17,729 | ||||||||||
|
Total equity securities
|
49,281 | 30,967 | (118 | ) | 80,130 | ||||||||||
|
Total investments
|
$ | 1,951,059 | $ | 138,291 | $ | (8,856 | ) | $ | 2,080,494 | ||||||
|
Amortized
Cost
|
Gross
Unrealized Gains
|
Gross
Unrealized Losses
|
Estimated
Fair Value
|
||||||||||||
|
At December 31, 2009
|
(in thousands)
|
||||||||||||||
|
Fixed maturity securities
|
|||||||||||||||
|
U.S. Treasuries
|
$ | 140,269 | $ | 6,366 | $ | (171 | ) | $ | 146,464 | ||||||
|
U.S. Agencies
|
117,844 | 7,125 | — | 124,969 | |||||||||||
|
States and municipalities
|
979,364 | 50,600 | (1,687 | ) | 1,028,277 | ||||||||||
|
Corporate
|
314,692 | 23,335 | (417 | ) | 337,610 | ||||||||||
|
Residential mortgage-backed securities
|
265,056 | 15,697 | (790 | ) | 279,963 | ||||||||||
|
Commercial mortgage-backed securities
|
29,407 | 391 | (24 | ) | 29,774 | ||||||||||
|
Asset-backed securities
|
12,442 | 793 | — | 13,235 | |||||||||||
|
Total fixed maturity securities
|
1,859,074 | 104,307 | (3,089 | ) | 1,960,292 | ||||||||||
|
Equity securities
|
|||||||||||||||
|
Consumer goods
|
14,421 | 8,069 | (6 | ) | 22,484 | ||||||||||
|
Energy and utilities
|
4,715 | 5,067 | — | 9,782 | |||||||||||
|
Financial
|
6,613 | 2,861 | (74 | ) | 9,400 | ||||||||||
|
Technology and communications
|
7,930 | 7,686 | (15 | ) | 15,601 | ||||||||||
|
Industrial and other
|
6,257 | 5,758 | (14 | ) | 12,001 | ||||||||||
|
Total equity securities
|
39,936 | 29,441 | (109 | ) | 69,268 | ||||||||||
|
Total investments
|
$ | 1,899,010 | $ | 133,748 | $ | (3,198 | ) | $ | 2,029,560 | ||||||
48
The scheduled maturity dates for fixed maturity securities, including the amortized cost and estimated fair value at December 31, 2010 are shown below. Actual maturities may differ from those scheduled as a result of prepayments by the issuer.
|
Amortized Cost
|
Estimated Fair Value
|
||||||
|
(in thousands)
|
|||||||
|
Due in one year or less
|
$ | 113,888 | $ | 115,532 | |||
|
Due after one year through five years
|
577,069 | 612,759 | |||||
|
Due after five years through ten years
|
576,440 | 610,784 | |||||
|
Due after ten years
|
366,134 | 374,878 | |||||
|
Mortgage and asset-backed securities
|
268,247 | 286,411 | |||||
|
Total
|
$ | 1,901,778 | $ | 2,000,364 | |||
Net realized and unrealized investment gains (losses) on fixed maturity and equity securities were as follows for the years ended December 31:
|
2010
|
2009
|
2008
|
||||||||||
|
Net realized gains (losses):
|
(in thousands)
|
|||||||||||
|
Fixed maturity securities
|
$ | 710 | $ | (855 | ) | $ | (560 | ) | ||||
|
Equity securities
|
9,427 | 1,820 | (10,964 | ) | ||||||||
|
Short-term investments and other
|
— | (174 | ) | — | ||||||||
| $ | 10,137 | $ | 791 | $ | (11,524 | ) | ||||||
|
Change in unrealized gains (losses):
|
||||||||||||
|
Fixed maturity securities
|
$ | (2,632 | ) | $ | 62,054 | $ | 14,420 | |||||
|
Equity securities
|
1,517 | 13,820 | (31,314 | ) | ||||||||
|
Short-term investments
|
— | (72 | ) | 72 | ||||||||
| $ | (1,115 | ) | $ | 75,802 | $ | (16,822 | ) | |||||
Net investment income was as follows for the years ended December 31:
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Fixed maturity securities
|
$ | 83,730 | $ | 89,522 | $ | 72,602 | ||||||
|
Equity securities
|
1,399 | 1,402 | 1,855 | |||||||||
|
Short-term investments and cash equivalents
|
327 | 1,910 | 6,017 | |||||||||
| 85,456 | 92,834 | 80,474 | ||||||||||
|
Investment expenses
|
(2,424 | ) | (2,350 | ) | (2,412 | ) | ||||||
|
Net investment income
|
$ | 83,032 | $ | 90,484 | $ | 78,062 | ||||||
49
Contractual Obligations and Commitments
The following table identifies our long-term debt and contractual obligations as of December 31, 2010.
|
Payment Due By Period
|
|||||||||||||||||||
|
Total
|
Less Than
1-Year
|
1-3 Years
|
4-5 Years
|
More Than
5-Years
|
|||||||||||||||
|
(in thousands)
|
|||||||||||||||||||
|
Operating leases
|
$ | 33,168 | $ | 6,825 | $ | 11,928 | $ | 9,034 | $ | 5,381 | |||||||||
|
Purchased liabilities
|
500 | 400 | 100 | — | — | ||||||||||||||
|
Notes payable(1)
|
172,058 | 13,007 | 25,546 | 74,912 | 58,593 | ||||||||||||||
|
Capital leases
|
2,165 | 614 | 1,551 | — | — | ||||||||||||||
|
Losses and LAE reserves(2)(3)
|
2,279,729 | 234,985 | 301,825 | 209,815 | 1,533,105 | ||||||||||||||
|
Total contractual obligations
|
$ | 2,487,621 | $ | 255,831 | $ | 340,950 | $ | 293,761 | $ | 1,597,079 | |||||||||
|
(1)
|
Notes payable obligations reflect payments for the principal and estimated interest expense based on LIBOR rates plus a margin. The estimated interest expense was based on the contractual obligations of the debt outstanding as of December 31, 2010. The interest rates range from 1.55% to 4.54%.
|
|
(2)
|
The losses and LAE reserves are presented gross of our reinsurance recoverables on unpaid losses, which were as follows for each of the periods presented above:
|
|
Recoveries Due By Period
|
||||||||||||||||||||
|
Total
|
Less Than
1 Year
|
1-3 Years
|
4-5 Years
|
More Than
5 Years
|
||||||||||||||||
|
(in thousands)
|
||||||||||||||||||||
|
Reinsurance recoverables
|
$ | (956,043 | ) | $ | (44,242 | ) | $ | (86,964 | ) | $ | (84,511 | ) | $ | (740,326 | ) | |||||
|
(3)
|
Estimated losses and LAE reserve payment patterns have been computed based on historical information. Our calculation of loss and LAE reserve payments by period is subject to the same uncertainties associated with determining the level of reserves and to the additional uncertainties arising from the difficulty of predicting when claims (including claims that have not yet been reported to us) will be paid. For a discussion of our reserving process, see ‘‘—Critical Accounting Policies—Reserves for Losses and Loss Adjustment Expenses.’’ Actual payments of losses and LAE by period will vary, perhaps materially, from the above table to the extent that current estimates of losses and LAE reserves vary from actual ultimate claims amounts due to variations between expected and actual payout patterns.
|
Off-Balance Sheet Arrangements
We have no off-balance sheet arrangements.
Critical Accounting Policies
The preparation of financial statements in accordance with GAAP requires both the use of estimates and judgment relative to the application of appropriate accounting policies. Our accounting policies are described in the Notes to our Consolidated Financial Statements, but we believe that the following matters are particularly important to an understanding of our financial statements because changes in these estimates or changes in the assumptions used to make them could have a material impact on the results of operations, financial condition, and cash flows.
Reserves for Losses and LAE
Accounting for workers’ compensation insurance requires us to estimate the liability for the expected ultimate cost of unpaid losses and LAE (loss reserves) as of a balance sheet date. Loss reserve estimates are inherently uncertain because the ultimate amount we pay for many of the claims we have incurred as of the balance sheet date will not be known for many years. Our estimate of loss reserves is intended to equal the difference between the expected ultimate losses and LAE of all claims that have occurred as of a balance sheet date and amounts already paid. We establish loss reserves based on our own analysis of emerging claims experience and environmental conditions in our markets and review of the results of various actuarial projections. Our aggregate carried reserve for unpaid losses and LAE is the sum of our reserves for each accident year (point estimate) and represents our best estimate of outstanding loss reserves.
50
The amount by which estimated losses in the aggregate, measured subsequently by reference to payments and additional estimates, differ from those previously estimated for a specific time period is known as reserve “development.” Reserve
development is unfavorable when losses ultimately settle for more than the amount reserved or subsequent estimates indicate a basis for reserve increases on open claims, causing the previously estimated loss reserves to be ‘‘deficient.’’ Reserve development is favorable when estimates of ultimate losses indicate a decrease in established reserves, causing the previously estimated loss reserves to be ‘‘redundant.’’ Development is reflected in our operating results through an adjustment to incurred losses and LAE during the period in which it is recognized.
Although claims for which reserves are established may not be paid for several years or more, we do not discount loss reserves in our financial statements for the time value of money.
The three main components of our reserves for unpaid losses and LAE are case reserves, incurred but not reported (IBNR) reserves, and LAE reserves.
When losses are reported to us, we establish, individually, estimates of the ultimate cost of the claims (case reserves). These case reserves are continually monitored and revised in response to new information and for amounts paid.
IBNR is an actuarial estimate of future payments on claims that have occurred but have not yet been reported to us. In addition to this provision for late reported claims, we also estimate, and make a provision for, the extent to which the case reserves on known claims may develop and for additional payments on closed claims, known as “reopening.” IBNR reserves apply to the entire body of claims arising from a specific time period, rather than a specific claim.
Most of our IBNR reserves relate to estimated future claim payments on recorded open claims. Workers’ compensation claims are generally reported to the employer and to the insurance company relatively quickly and relatively small amounts are paid on claims that have already been closed. Consequently, late reporting and reopening of claims are a less significant part of IBNR for our insurance subsidiaries.
LAE reserves are our estimate of the future expenses of investigating, administering, and settling claims, including legal expenses that will be paid to manage claims that have occurred. LAE reserves are established in the aggregate, rather than on a claim-by-claim basis.
A portion of our obligations for losses and LAE are ceded to unaffiliated reinsurers. The amount of reinsurance that will be recoverable on our losses and LAE reserves includes both the reinsurance recoverable from our excess of loss reinsurance policies, as well as reinsurance recoverable under the terms of the LPT Agreement.
Our reserve for unpaid losses and LAE (gross and net of reinsurance), including the main components of such reserves, were as follows as of December 31:
|
2010
|
2009
|
2008
|
|||||||||
|
(in thousands)
|
|||||||||||
|
Case reserves
|
$ | 897,401 | $ | 915,378 | $ | 886,789 | |||||
|
IBNR
|
1,089,498 | 1,198,019 | 1,293,313 | ||||||||
|
LAE
|
292,830 | 312,261 | 326,376 | ||||||||
|
Gross unpaid losses and LAE
|
2,279,729 | 2,425,658 | 2,506,478 | ||||||||
|
Less reinsurance recoverables on unpaid losses and LAE, gross
|
956,043 | 1,052,505 | 1,076,350 | ||||||||
|
Net unpaid losses and LAE
|
$ | 1,323,686 | $ | 1,373,153 | $ | 1,430,128 | |||||
Actuarial methodologies are used by workers’ compensation insurance companies, including us, to analyze and estimate the aggregate amount of unpaid losses and LAE. As mentioned above, management considers the results of various actuarial projection methods and their underlying assumptions, among other factors, in establishing reserves for unpaid losses and LAE.
Judgment is required in the actuarial estimation of loss reserves, including the selection of various actuarial methodologies to project the following: the ultimate cost of claims; the selection of projection parameters based on historical company data, industry data, and other benchmarks; the identification and quantification of potential changes in parameters from historical levels to current and future levels due to changes in future claims development expectations; and the weighting of differing reserve indications resulting from alternative methods and assumptions. The adequacy of our ultimate loss reserves is inherently uncertain and represents a significant risk to our business. We attempt to mitigate this risk through our claims management process and by monitoring and reacting to statistics relating to the cost and duration of claims.
51
We retain an independent actuarial consulting firm (Consulting Actuary) to perform comprehensive studies of our losses and LAE liability on a semi-annual basis. The role of our Consulting Actuary is to conduct sufficient analyses to produce a range of reasonable estimates, as well as a point estimate, of our unpaid losses and LAE liability, and to present those results to our actuarial staff and to management. In 2009, we changed our Consulting Actuary.
Prior to this change, the Consulting Actuary based its point estimate for EICN strictly on the basis of paid loss development methods. Beginning in 2009, our new Consulting Actuary determined its point estimate for EICN based on a combination of methodologies, similar to those utilized for our other insurance subsidiaries, as described below. While such a determination, based on a combination of methodologies is valid, this change in methodologies prevents any direct year over year comparison of the Consulting Actuaries’ point estimates. The new Consulting Actuary has provided us with a separate calculation for EICN that is based strictly on the historically utilized paid loss methods for 2010 and 2009. This calculation in combination with the new Consulting Actuary’s point estimate for our other insurance subsidiaries allows for comparability of our overall carried reserves, relative to the previous Consulting Actuary’s calculations. Management believes that using strictly paid loss methods for Nevada losses is the preferred approach given our depth of knowledge of Nevada losses and the consistency of paid data over time resulting from and related to the statutory prohibition of entering into full and final settlements of Nevada claims.
We compile and aggregate our claims data by grouping the claims according to the year or quarter in which the claim occurred (“accident year” or “accident quarter”) when analyzing claim payment and emergence patterns and trends over time. Additionally, claims data is aggregated and compiled separately for different types of claims or claimant benefits, or for different states or groups of states in which we do business, or both.
Our internal actuaries and the Consulting Actuary prepare reserve estimates for all accident years using our own historical claims data and many of the generally accepted actuarial methodologies for estimating loss reserves, such as paid loss development methods, incurred loss development methods, and Bornhuetter-Ferguson methods. These methods vary in their responsiveness to different information, characteristics and dynamics in the data, and the results assist the actuary in considering these characteristics and dynamics in the historical data. The methods employed for each segment of claims data, and the relative weight accorded to each method, vary depending on the nature of the claims segment and on the age of the claims.
Each actuarial methodology requires the selection and application of various parameters and assumptions. The key parameters and assumptions include: the pattern with which our aggregate claims data will be paid or will emerge over time; claims cost inflation rates; the effects of legislative benefit changes and/or judicial changes; and trends in the frequency of claims, both overall and by severity of claim. We believe the pattern with which our aggregate claims data will be paid or emerge over time and claims cost inflation rates are the most important parimeters and assumptions.
In Nevada, one method involves adjusting historical data for inflation. The inflation rates used in the analysis are judgmentally selected based on historical year-to-year movements in the cost of claims observed in our insurance subsidiaries’ data and industry-wide data, as well as on broader inflation indices. The results of this method would differ if different inflation rates were selected.
In projections using December 31, 2010 data, the method that uses explicit medical cost inflation assumptions included medical cost inflation assumptions ranging from 5.5% to 7.5%. The selection of medical cost inflation assumptions used has been based on observed recent and longer-term historical medical cost inflation in our claims data and in the U.S. economy more generally. The rate of medical cost inflation, as reflected in our historical medical payments per claim, has averaged approximately 5.5% over the past ten years. The rate of medical cost inflation in the general U.S. economy, as measured by the consumer price index—medical care, has averaged approximately 4.1% over the past ten years.
Management along with internal actuarial staff and the Consulting Actuary separately analyze LAE and estimate unpaid LAE. These analyses rely primarily on examining the relationship between the aggregate amounts that have been spent on LAE historically, compared with the volume of claims activity for the corresponding historical calendar periods. The portion of unpaid LAE that will be recoverable from reinsurers is estimated based on the contractual reinsurance terms.
The range of estimates of loss reserves produced by the Consulting Actuary is intended to represent the range in which it is most likely that the ultimate losses will fall. This range is narrower than the range of indications produced by the individual methods applied because it is not likely that the high or low result will emerge for every claim segment and accident year. The Consulting Actuary’s point estimate of loss reserves is based on a judgmental selection for each claim segment from within the range of results indicated by the different actuarial methods.
52
Management formally establishes loss reserves for financial statement purposes on a quarterly basis. In doing so, we make reference to the most current analyses of our Consulting Actuary, including a review of the assumptions and the results of the various actuarial methods used. Comprehensive studies are conducted as of June 30 and December 31 by both internal actuarial staff and the Consulting Actuary. On the alternate quarters, the preceding study results are updated for actual claim payment activity during the quarter.
The aggregate carried reserve calculated by management represents our best estimate of our outstanding unpaid losses and LAE. We believe that we should be conservative in our reserving practices due to the “long-tail” nature of workers’ compensation claims payouts, the susceptibility of those future payments to unpredictable external forces such as medical cost inflation and other economic conditions, and the actual variability of loss reserve adequacy that we have observed in the workers’ compensation insurance industry.
In establishing management’s best estimate of unpaid losses and LAE at December 31 for the last three years, management and internal actuarial staff reviewed and considered the following: (a) the Consulting Actuary assumptions, point estimate, and range; (b) the inherent uncertainty of workers' compensation liabilities for unpaid losses and LAE; and (c) the particular uncertainties associated with the potential for legislative and/or judicial reversal of California and Florida reforms, and the degree of movement observed in EICN's prior years' projections of losses and LAE in Nevada following premium and market share reductions. Management did not quantify a specific loss reserve increment for each uncertainty, but rather established an overall provision for loss reserves that represented management’s best estimate of unpaid losses and LAE in light of the historical data, actuarial assumptions, point estimate and range, and current facts and circumstances. Management continued to use a range and point estimate for EICN, based on paid loss methods, which our experience in Nevada indicates is more appropriate.
Management’s best estimate of unpaid losses and LAE, net of reinsurance, was $13.8 million, $54.6 million, and $16.5 million above the value calculated based on the historically utilized paid loss methods for EICN and a combination of methodologies for our other insurance subsidiaries at December 31, 2010, 2009, and 2008, respectively.
The table below provides the actuarial range of estimated liabilities for net unpaid losses and LAE and our carried reserves as of December 31:
|
2010
|
2009
|
2008
|
|||||||||
|
(in thousands)
|
|||||||||||
|
Low end of actuarial range
|
$ | 1,244,038 | $ | 1,234,222 | $ | 1,306,506 | |||||
|
Carried reserves
|
1,323,686 | 1,373,153 | 1,430,128 | ||||||||
|
High end of actuarial range
|
1,499,042 | 1,523,983 | 1,586,777 | ||||||||
Each of the actuarial methods used in the analysis and estimation of loss reserves depend in part on the selection of an expected pattern with which the aggregate claims data will be paid or will emerge over time, and the assumption that this expected pattern will prevail into the future. We select relevant patterns as part of the periodic review and projection of unpaid losses and LAE. In selecting these patterns, we examine long and short-term historical data for our insurance subsidiaries, benchmarks based on industry data, and forecasts made by industry rating bureaus regarding the effect of legislative benefit changes on these patterns.
53
The following table reconciles the beginning and ending loss reserves as of December 31:
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Unpaid losses and LAE, gross of reinsurance, at beginning of period
|
$ | 2,425,658 | $ | 2,506,478 | $ | 2,269,710 | ||||||
|
Less reinsurance recoverable, excluding bad debt allowance, on unpaid losses and LAE unpaid losses and LAE
|
1,052,505 | 1,076,350 | 1,052,641 | |||||||||
|
Net unpaid losses and LAE at beginning of period
|
1,373,153 | 1,430,128 | 1,217,069 | |||||||||
|
Losses and LAE, net of reinsurance, acquired in business combination
|
— | — | 247,006 | |||||||||
|
Losses and LAE, net of reinsurance, incurred in:
|
||||||||||||
|
Current year
|
227,143 | 283,827 | 226,643 | |||||||||
|
Prior years
|
(14,130 | ) | (51,359 | ) | (71,707 | ) | ||||||
|
Total net losses and LAE incurred during the period
|
213,013 | 232,468 | 154,936 | |||||||||
|
Deduct payments for losses and LAE, net of reinsurance, related to:
|
||||||||||||
|
Current year
|
55,827 | 74,944 | 53,397 | |||||||||
|
Prior years
|
206,653 | 214,499 | 135,486 | |||||||||
|
Total net payments for losses and LAE during the period
|
262,480 | 289,443 | 188,883 | |||||||||
|
Ending unpaid losses and LAE, net of reinsurance
|
1,323,686 | 1,373,153 | 1,430,128 | |||||||||
|
Reinsurance recoverable, excluding bad debt allowance, on unpaid losses and LAE unpaid losses and LAE
|
956,043 | 1,052,505 | 1,076,350 | |||||||||
|
Unpaid losses and LAE, gross of reinsurance, at end of period
|
$ | 2,279,729 | $ | 2,425,658 | $ | 2,506,478 | ||||||
Estimates of incurred losses and LAE attributable to insured events for prior years have decreased due to continued favorable development in such prior accident years.
The major sources of favorable development include actual paid losses that have been less than expected and the impact of new information on selected patterns of claims emergence and payment used in the projection of future loss payments. New information includes our own data regarding patterns of claims emergence, development and payment that have been observed in the most recent periods, and external information regarding the workers’ compensation environments in the states in which we operate.
As of December 31, 2010, California and Nevada represented approximately 78% of our reserves for unpaid losses and LAE on our consolidated balance sheet.
In California, where our operations began in 2002, the actuaries’ and management's initial expectations of the ultimate level of losses and patterns of loss emergence and payment were based on benchmarks derived from analyses of historical insurance industry data in California. No historical data from our California insurance subsidiary existed prior to July 1, 2002; however, some historical data was available for the prior years for some of the market segments we entered in California, but was limited as to the number of loss reserve evaluation points available. The industry-based benchmarks were judgmentally adjusted for the anticipated impact of significant environmental changes, specifically the enactment of major changes to the statutory workers' compensation benefit structure and the manner in which claims are administered and adjudicated in California. The actual emergence and payment of claims by our California insurance subsidiary has been more favorable than those initial expectations through 2009, due at least in part to the impact of enactment of the major changes in the California workers’ compensation environment, however, our recent loss experience, beginning in 2010, indicates an upward trend in medical costs that is reflected in our loss reserves. We assume that increasing medical cost trends will continue and will impact our long-term claims costs and loss reserves. At each evaluation date, the projected claim activity underlying prior loss reserves is replaced by actual claim activity, and the expectation of future emergence and payment of California claims underlying the actuarial projections is reevaluated based on our insurance subsidiaries’ emerging experience and on updating the benchmarks that are derived from observing and analyzing the insurance industry data for California workers’ compensation.
We have also seen a significant improvement in claims emergence and payment patterns in Nevada in recent years, and have given these improved patterns significant weight in establishing loss reserves for our Nevada business. If future emergence in Nevada more closely resembles long-term historical patterns of the Nevada State Industrial Insurance System (the Fund), our current loss reserves could develop unfavorably over time. Additionally, the impact, if any, of the recession on our claim costs is not yet known. We will continue to evaluate our estimate of loss reserves to reflect the most current data and judgments.
54
In Nevada, we have compiled a lengthy history of workers' compensation claims payment patterns based on the business of the Fund and EICN, but the emergence and payment of claims in recent years has been more favorable than in the long-term history in Nevada with the Fund. The expected patterns of claim payments and emergence used in the projection of our ultimate claim payments are based on both long and short-term historical data. In recent evaluations, claim patterns have continued to emerge in a manner consistent with short-term historical data. Consequently, our selection of claim projection patterns has relied more heavily on patterns observed in recent years.
Our insurance subsidiaries have been operating in a period of drastically changing environmental conditions in our major markets, entry into new markets, and operational changes. During periods characterized by such changes, at each evaluation, the actuaries and management must make judgments as to the relative weight to accord to long-term historical and recent company data, external data, evaluations of environmental and operational changes, and other factors in selecting the methods to use in projecting ultimate losses and LAE, the parameters to incorporate in those methods, and the relative weights to accord to the different projection indications. At each evaluation, management has given weight to new data, recent indications, and evaluations of environmental conditions and changes that implicitly reflect management’s expectation as to the degree to which the future will resemble the most recent information and most recent changes, compared with long-term claim payment, claims emergence, and claim cost inflation patterns.
More than 57% of our claims payments during the three years ended December 31, 2010 related to medical care for injured workers. The utilization and cost of medical services in the future is a significant source of uncertainty in the establishment of loss reserves for workers' compensation. Our loss reserves are established based on reviewing the results of actuarial methods, some of which do not contain explicit medical claim cost inflation rates, however, because medical care may be provided to an injured worker over many years, and in some cases decades, the pace of medical claim cost inflation has a significant impact on our ultimate claim payments. For example, if the rate of medical claim cost inflation increases by 1% above the inflation rate that is implicitly included in the loss reserves at December 31, 2010, we estimate that future medical costs over the lifetime of current claims would increase by approximately $79 million on a net-of-reinsurance basis.
Our reserve estimates reflect expected increases in the costs of contested claims, but do not assume any losses resulting from significant new legal liability theories. Our reserve estimates also assume that there will not be significant future changes in the regulatory and legislative environment. In the event of significant new legal liability theories or new regulation or legislation, we will attempt to quantify its impact on our business.
The range of estimates of unpaid losses and LAE produced by our actuarial reviews of medical cost inflation data provide some indication of the potential variability of future losses and LAE payments; however, the full range of potential variation is difficult to estimate because our insurance subsidiaries do not have a lengthy operating history in many of the states in which we now operate.
If the actual unpaid losses and LAE were at the high or the low end of the actuarial range, the impact on our financial results would have been as follows:
|
December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Increase (decrease) in reserves
|
(in thousands)
|
|||||||||||
|
At low end of range
|
$ | (79,648 | ) | $ | (138,931 | ) | $ | (123,622 | ) | |||
|
At high end of range
|
175,356 | 150,741 | 156,649 | |||||||||
|
Increase (decrease) in equity and net income, net of income tax effect
|
||||||||||||
|
At low end of range
|
$ | 51,771 | $ | 90,305 | $ | 80,354 | ||||||
|
At high end of range
|
(113,981 | ) | (97,982 | ) | (101,822 | ) | ||||||
Actual losses are affected by a more complex combination of forces and dynamics than any one model or actuarial methodology can represent; and each methodology is an approximation of these complex forces and dynamics. None of the methods are designed or intended to produce an indication that is systematically higher or lower than the other methods. At any given evaluation date, some of the actuarial projection methods produce indications outside the Consulting Actuary’s selected range. Accordingly, we believe that the range of potential outcomes is considerably wider than the actuarially estimated range of the most likely outcomes. We have decreased our prior years' reserves for unpaid losses and LAE $14.1 million, $51.4 million, and $71.7 million as of December 31, 2010, 2009, and 2008, respectively,
55
illustrating that changes in estimates of loss reserves can be significant from year to year. We have no basis for anticipating whether actual future payments of losses and LAE may be either greater than or less than the reserve for unpaid losses and LAE on our current balance sheet.
Reinsurance Recoverables
Reinsurance recoverables represent: (a) amounts currently due from reinsurers on paid losses and LAE; (b) amounts recoverable from reinsurers on case basis estimates of reported losses; and (c) amounts recoverable from reinsurers on actuarial estimates of IBNR for losses and LAE. These recoverables are based on our current estimates of the underlying losses and LAE, and are reported on our consolidated balance sheets separately as assets, as reinsurance does not relieve us of our legal liability to policyholders. We bear credit risk with respect to the reinsurers, which can be significant considering that some of the unpaid losses and LAE remain outstanding for an extended period of time. Reinsurers may refuse or fail to pay losses that we cede to them, or they might delay payment. We are required to pay losses even if a reinsurer refuses or fails to meet its obligations under the applicable reinsurance agreement. We continually monitor the financial condition and rating agency ratings of our reinsurers. No material amounts due from reinsurers have been written-off as uncollectible since our inception in 2000; and we believe that amounts currently reflected in our consolidated financial statements will similarly not require any material prospective adjustment.
Under the LPT Agreement, the Fund initially ceded $1.525 billion in liabilities for the incurred but unpaid losses and LAE related to claims incurred prior to July 1, 1995, for consideration of $775 million in cash. The estimated remaining liabilities subject to the LPT Agreement were $846.7 million as of December 31, 2010. Losses and LAE paid with respect to the LPT Agreement totaled $530.7 million at December 31, 2010. We account for the LPT Agreement as retroactive reinsurance. Entry into the LPT Agreement resulted in a deferred reinsurance gain that was recorded on our consolidated balance sheet as a liability. This deferred gain is being amortized using the recovery method, whereby the amortization is determined by the proportion of actual reinsurance recoveries to total estimated recoveries, and the amortization is reflected in losses and LAE. In addition, we are entitled to receive a contingent commission under the LPT Agreement. Changes in the estimated contingent commission are reflected in our commission expense in the period that the estimate is revised.
Recognition of Premium Revenue
Premium revenue is recognized over the period of the contract in proportion to the amount of insurance protection provided. At the end of the policy term, payroll-based premium audits are performed on substantially all policyholder accounts to determine net premiums earned for the policy year. Earned but unbilled premiums include estimated future audit premiums based on our historical experience. These estimates are subject to changes in policyholders' payrolls, economic conditions, and seasonality; and are continually reviewed and adjusted as experience develops or new information becomes known. Any such adjustments are included in current operations. No material adjustments have been made to our accrual for earned but unbilled premium since our inception in 2000. Although considerable variability is inherent in such estimates, we believe that amounts currently reflected in our consolidated financial statements will similarly not require any material prospective adjustment.
Income Taxes
Our accounting for income taxes considers the current and deferred tax consequences of all transactions that have been recognized in the financial statements using the provisions of enacted tax laws. Deferred tax assets and liabilities are determined based on differences between the financial reporting and tax bases of assets and liabilities and are measured using the enacted tax rates and laws that will be in effect when the differences are expected to reverse. The effect on deferred tax assets and liabilities resulting from a tax rate change affects our net income or loss in the period that includes the enactment date of the tax rate change. Our income tax returns are subject to audit by the Internal Revenue Service and various state tax authorities. Significant disputes may arise with these tax authorities involving issues of the timing and amount of deductions and allocations of income among various tax jurisdictions because of differing interpretations of tax laws and regulations. We periodically evaluate our exposures associated with tax filing positions. Although we believe our positions comply with applicable laws, we record liabilities based upon estimates of the ultimate outcomes of these matters.
56
In assessing whether our deferred tax assets will be realized, we consider whether it is more likely than not that we will generate future taxable income during the periods in which those temporary differences become deductible. We consider the scheduled reversal of deferred tax liabilities, tax planning strategies, and projected future taxable income in making this assessment. If necessary, we establish a valuation allowance to reduce the deferred tax assets to the amounts that are more likely than not to be realized.
In 2008, we reversed $10.6 million of a remaining liability for unrecognized tax benefits, including $2.3 million in interest, as certain statutory periods had expired. The reversal of the liability caused a decrease in our tax expense and effective tax rate in 2008.
Valuation of Investments
Our investments in fixed maturity and equity securities are classified as available-for-sale and are reported at fair value with unrealized gains and losses excluded from earnings and reported in a separate component of equity, net of deferred taxes, as a component of net accumulated other comprehensive income (loss). Realized gains and losses on sales of investments are recognized in operations on the specific identification basis.
Impairment of Investment Securities. Impairment of an investment security results in a reduction of the carrying value of the security and the realization of a loss when the fair value of the security declines below our cost or amortized cost, as applicable, and the impairment is deemed to be other-than-temporary. We regularly review our investment portfolio to evaluate the necessity of recording impairment losses for other-than-temporary declines in the fair value of our investments. We consider various factors in determining if a decline in the fair value of an individual security is other-than-temporary.
Some of the factors we consider include:
|
|
•
|
how long and by how much the fair value of the security has been below its cost or amortized cost;
|
|
|
•
|
the financial condition and near-term prospects of the issuer of the security, including any specific events that may affect its operations or earnings;
|
|
|
•
|
the outlook for industry sectors and macro-economic changes;
|
|
|
•
|
that it is not more likely than not that we will not be required to sell the securities until its fair value recovers above cost, or to maturity;
|
|
|
•
|
any downgrades of the security by a rating agency;
|
|
|
•
|
any reduction or elimination of dividends, or nonpayment of scheduled interest payments; and
|
|
|
•
|
our intent to hold or sell the security.
|
The amount of any write-downs is determined by the difference between cost or amortized cost of the investment and its fair value at the time the other-than-temporary decline was identified.
Goodwill and Other Intangible Assets
We prepare a valuation analysis for goodwill and other intangible assets, whereby we identify whether events have occurred that may impact the carrying value of these assets and make assumptions regarding future events, such as cash flows and profitability. Differences between the assumptions used to prepare these valuations and actual results could materially impact the carrying amount of these assets and our operating results.
New Accounting Standards
As of December 31, 2010, there was recently issued accounting guidance that we either implemented during the year or will implement in future periods. None of this guidance that has been implemented had, or is expected to have, a material effect on our consolidated financial condition or results of operation; however, we have not yet determined the effect certain pronouncements that will be implemented in future periods will have on our financial statements. See Note 2 in the Notes to our Consolidated Financial Statements.
57
Item 7A. Quantitative and Qualitative Disclosures about Market Risk
Market risk is the risk of potential economic loss principally arising from adverse changes in the fair value of financial instruments. The major components of market risk affecting us are credit risk, interest rate risk, and equity price risk.
Credit Risk
Our fixed maturity securities portfolio is exposed to credit risk, which we attempt to manage through issuer and industry diversification. Our investment guidelines include limitations on the minimum rating of fixed maturity securities in our investment portfolio, as well as restrictions on investments in fixed maturity securities of a single issuer.
We also bear credit risk with respect to the reinsurers, which can be significant considering that some of the unpaid losses and LAE remain outstanding for an extended period of time. We are required to pay losses even if a reinsurer refuses or fails to meet its obligations under the applicable reinsurance agreement. We continually monitor the financial condition and rating agency ratings of our reinsurers.
Interest Rate Risk
Investments
The fair value of our fixed maturity securities portfolio is exposed to interest rate risk, the risk of loss in fair value resulting from changes in prevailing interest rates, which we strive to limit by managing duration. Our investments (excluding cash and cash equivalents) had a duration of 4.91 at December 31, 2010. To minimize interest rate risk, our portfolio is weighted toward short-term and intermediate-term bonds; however, our investment strategy balances consideration of duration, yield and credit risk. We continually monitor the impact of interest rate changes on our liquidity obligations.
Sensitivity Analysis
The fair values or cash flows of market sensitive instruments are subject to potential losses in future earnings resulting from changes in interest rates and other market rates or prices. Our sensitivity analysis model uses a hypothetical change in market rates that reflects what we believe are reasonably possible near-term changes in those rates (covering a period of time going forward up to one year from the date of the consolidated financial statements). Actual results may differ from the hypothetical change in market rates assumed in this disclosure. This sensitivity analysis does not reflect the results of any action that we may take to mitigate such hypothetical losses in fair value.
We use fair values to measure our potential loss in this model, which includes fixed maturity securities and short-term investments. For invested assets, we use modified duration modeling to calculate changes in fair values. Durations on invested assets are adjusted for call, put, and interest rate reset features. Invested asset portfolio durations are calculated on a market value weighted basis, excluding accrued investment income, using holdings as of December 31, 2010. The estimated changes in fair values on our fixed maturity securities including short-term investments, valued at $2.08 billion as of December 31, 2010, based on specific changes in interest rates are as follows:
|
Changes in Interest Rates
|
Estimated Increase (Decrease)
in Fair Value
|
|||||||
|
(in thousands, except percentages)
|
||||||||
|
300 basis point rise
|
$ | (255,452 | ) | (12.8 | )% | |||
|
200 basis point rise
|
(178,176 | ) | (8.9 | ) | ||||
|
100 basis point rise
|
(92,955 | ) | (4.7 | ) | ||||
|
50 basis point decline
|
48,746 | 2.4 | ||||||
|
100 basis point decline
|
97,575 | 4.9 | ||||||
This model produces a predicted pre-tax loss in fair value of market-sensitive instruments of $93.0 million, or 4.7%, resulting from a 100 basis point increase in interest rates as of December 31, 2010.
The most significant assessment of the effects of hypothetical changes in interest rates on investment income would be based on FASB guidance related to “Accounting for Nonrefundable Fees and Costs Associated with Originating or Acquiring Loans and Initial Direct Costs of Leases,” which requires amortization adjustments for mortgage-backed securities. The rates at which the mortgages underlying mortgage-backed securities are prepaid, and therefore the average
58
life of mortgage-backed securities, can vary depending on changes in interest rates (for example, mortgages are prepaid faster and the average life of mortgage-backed securities falls when interest rates decline). Adjustments for changes in amortization are based on revised average life assumptions and would have an impact on investment income if a significant portion of our mortgage-backed securities were purchased at significant discounts or premiums to par value. As of December 31, 2010, the par value of our mortgage-backed securities holdings was $231.9 million. Amortized cost is 99.4% of par value. Since a majority of our mortgage-backed securities were purchased at a premium or discount that is significant as a percentage of par, an adjustment could have a significant effect on investment income; however, given the current economic conditions and prevailing interest rate environment, the rate of prepayments is unlikely to accelerate. The mortgage-backed securities portion of the portfolio totaled 11.9% of total investments as of December 31, 2010. Agency-backed mortgage pass-throughs totaled $243.3 million, or 98.6%, of the mortgage-backed securities portion of the portfolio, and 11.7% of the total portfolio as of December 31, 2010.
Equity Price Risk
Equity price risk is the risk that we may incur losses in the fair value of the equity securities we hold in our available-for-sale investment portfolio. Adverse changes in the market prices of the equity securities we hold in our investment portfolio would result in decreases in the fair value of our total assets. We minimize our exposure to equity price risk by investing primarily in the equity securities of mid-to-large capitalization issuers and by diversifying our equity holdings across several industry sectors. At December 31, 2010, equity securities had a fair value of $80.1 million, or 3.9% of our investment portfolio.
The table below shows the sensitivity of our equity securities to price changes as of December 31, 2010:
|
Cost
|
Fair Value
|
10%Fair
Value
Decrease
|
Pre-tax
Impact on
Total Equity
Securities
|
10% Fair
Value
Increase
|
Pre-tax
Impact on Total Equity
Securities
|
||||||||||||||||||
|
(in thousands)
|
|||||||||||||||||||||||
|
Total Domestic equities
|
$ | 49,281 | $ | 80,130 | $ | 72,117 | $ | (8,013 | ) | $ | 88,143 | $ | 8,013 | ||||||||||
Effects of Inflation
Inflation could impact our financial statements and results of operations. Our estimates for losses and LAE include assumptions about future payments for closure of claims and claims handling expenses, such as medical treatments and litigation costs. To the extent inflation causes these costs to increase above established reserves, we will be required to increase those reserves for losses and LAE, reducing our earnings in the period in which the deficiency is identified. We consider inflation in the reserving process by reviewing cost trends and our historical reserving results. We also consider an estimate of increased costs in determining the adequacy of our rates, particularly as it relates to medical and hospital rates where historical inflation rates have exceeded general inflation rates.
Fluctuations in rates of inflation also influence interest rates, which in turn impact the market value of our investment portfolio and yields on new investments. Operating expenses, including payrolls, are also impacted to a certain degree by inflation.
59
Item 8. Financial Statements and Supplementary Data
Audited Financial Statements as of December 31, 2010 and 2009 and for each of the three years in the period ended December 31, 2010:
|
Page
|
|
|
Management’s Report on Internal Control Over Financial Reporting
|
61
|
|
Report of Independent Registered Public Accounting Firm on Internal Control over Financial Reporting
|
62
|
|
Report of Independent Registered Public Accounting Firm
|
63
|
|
Consolidated Balance Sheets as of December 31, 2010 and 2009
|
64
|
|
Consolidated Statements of Income for each of the three years ended December 31, 2010
|
65
|
|
Consolidated Statements of Stockholders’ Equity for each of the three years ended December 31, 2010
|
66
|
|
Consolidated Statements of Cash Flows for each of the three years ended December 31, 2010
|
67
|
|
Notes to Consolidated Financial Statements
|
68
|
|
The following financial statement schedules are filed in Item 15 of Part III of this report:
|
|
|
Financial Statement Schedules:
|
|
|
Schedule II. Condensed Financial Information of Registrant
|
100
|
|
Schedule VI. Supplemental Information Concerning Property-Casualty Insurance Operations
|
104
|
|
Pursuant to Rule 7-05 of Regulation S-X, Schedules I, III, IV and V have been omitted as the information to be set forth therein is included in the notes to the audited consolidated financial statements.
|
60
Management’s Report on Internal Control Over Financial Reporting
Management of Employers Holdings, Inc. and Subsidiaries (the Company) is responsible for establishing and maintaining adequate internal control over financial reporting and for the assessment of the effectiveness of internal control over financial reporting. As defined by the Securities and Exchange Commission, internal control over financial reporting is a process designed by, or under the supervision of, the Company’s principal executive officer and principal financial officer, and effected by the Company’s Board of Directors, management and other personnel, to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements in accordance with U.S. generally accepted accounting principles (GAAP).
The Company’s internal control over financial reporting includes policies and procedures that: (a) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the Company’s assets; (b) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with GAAP, and that receipts and expenditures of the Company are being made only in accordance with authorizations of its management and Board of Directors; and (c) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use or disposition of the Company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect all misstatements. Projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Management conducted an assessment of the effectiveness of the Company’s internal control over financial reporting as of December 31, 2010 based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO Framework).
Based on this assessment, management did not identify any material weaknesses in the internal control over financial reporting and management has concluded that the Company’s internal control over financial reporting was effective as of December 31, 2010.
The Company’s independent registered public accounting firm, Ernst & Young LLP, has independently assessed the effectiveness of the Company’s internal control over financial reporting. A copy of their report is included in Item 8 of this Annual Report on Form 10-K.
February 24, 2011
61
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM ON INTERNAL CONTROL OVER FINANCIAL REPORTING
The Board of Directors and Stockholders
Employers Holdings, Inc. and Subsidiaries
We have audited Employers Holdings, Inc. and Subsidiaries’ (the Company) internal control over financial reporting as of December 31, 2010, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (the COSO criteria). The Company’s management is responsible for maintaining effective internal control over financial reporting, and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with U.S. generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
In our opinion, Employers Holdings, Inc. and Subsidiaries maintained, in all material respects, effective internal control over financial reporting as of December 31, 2010, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated balance sheet of Employers Holdings. Inc. and Subsidiaries as of December 31, 2010 and 2009, and the related consolidated statements of income, stockholders’ equity, and cash flows for each of the three years in the period ended December 31, 2010 and our report dated February 24, 2011 expressed an unqualified opinion thereon.
/s/ Ernst & Young LLP
Los Angeles, California
February 24, 2011
62
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
The Board of Directors and Stockholders
Employers Holdings, Inc. and Subsidiaries
We have audited the accompanying consolidated balance sheets of Employers Holdings, Inc. and Subsidiaries (the Company) as of December 31, 2010 and 2009, and the related consolidated statements of income, stockholders’ equity, and cash flows for each of the three years in the period ended December 31, 2010. Our audits also included the financial statement schedules listed in the Index at Item 15(a). These financial statements and schedules are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements and schedules based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated financial position of Employers Holdings, Inc. and Subsidiaries at December 31, 2010 and 2009, and the consolidated results of their operations and their cash flows for each of the three years in the period ended December 31, 2010, in conformity with U.S. generally accepted accounting principles. Also, in our opinion, the related financial statement schedules, when considered in relation to the basic financial statements taken as a whole, present fairly in all material respects the information set forth therein.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), Employers Holdings, Inc. and Subsidiaries’ internal control over financial reporting as of December 31, 2010, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission and our report dated February 24, 2011 expressed an unqualified opinion thereon.
/s/ Ernst & Young LLP
Los Angeles, California
February 24, 2011
63
|
Employers Holdings, Inc. and Subsidiaries
|
||||||||
|
Consolidated Balance Sheets
|
||||||||
|
December 31,
|
||||||||
|
2010
|
2009
|
|||||||
|
Assets
|
(in thousands, except share data)
|
|||||||
|
Available for sale:
|
||||||||
|
Fixed maturity securities at fair value (amortized cost $1,901,778 at December 31, 2010 and $1,859,074 at December 31, 2009
|
$ | 2,000,364 | $ | 1,960,292 | ||||
|
Equity securities at fair value (cost $49,281 at December 31, 2010 and $39,936 at December 31, 2009)
|
80,130 | 69,268 | ||||||
|
Total investments
|
2,080,494 | 2,029,560 | ||||||
|
Cash and cash equivalents
|
119,825 | 188,833 | ||||||
| Restricted cash and cash equivalents | 16,949 | 2,739 | ||||||
|
Accrued investment income
|
23,022 | 23,055 | ||||||
|
Premiums receivable, less bad debt allowance of $7,603 at December 31, 2010 and $9,879 at December 31, 2009
|
109,987 | 119,976 | ||||||
|
Reinsurance recoverable for:
|
||||||||
|
Paid losses
|
14,415 | 13,673 | ||||||
|
Unpaid losses, less allowance of $0 at December 31, 2010 and $1,335 at December 31, 2009
|
956,043 | 1,051,170 | ||||||
|
Funds held by or deposited with reinsureds
|
3,701 | 82,339 | ||||||
|
Deferred policy acquisition costs
|
32,239 | 33,695 | ||||||
|
Federal income taxes recoverable
|
4,048 | 4,092 | ||||||
|
Deferred income taxes, net
|
38,078 | 43,502 | ||||||
|
Property and equipment, net
|
11,712 | 13,059 | ||||||
|
Intangible assets, net
|
13,279 | 15,442 | ||||||
|
Goodwill
|
36,192 | 36,192 | ||||||
|
Other assets
|
20,136 | 19,326 | ||||||
|
Total assets
|
$ | 3,480,120 | $ | 3,676,653 | ||||
|
Liabilities and stockholders’ equity
|
||||||||
|
Claims and policy liabilities:
|
||||||||
|
Unpaid losses and loss adjustment expenses
|
$ | 2,279,729 | $ | 2,425,658 | ||||
|
Unearned premiums
|
149,485 | 158,577 | ||||||
|
Policyholders' dividends accrued
|
5,218 | 7,958 | ||||||
|
Total claims and policy liabilities
|
2,434,432 | 2,592,193 | ||||||
|
Commissions and premium taxes payable
|
17,313 | 20,763 | ||||||
|
Accounts payable and accrued expenses
|
18,601 | 19,033 | ||||||
|
Deferred reinsurance gain – LPT Agreement
|
370,341 | 388,574 | ||||||
|
Notes payable
|
132,000 | 132,000 | ||||||
|
Other liabilities
|
17,317 | 25,691 | ||||||
|
Total liabilities
|
2,990,004 | 3,178,254 | ||||||
|
Commitments and contingencies (Note 13)
|
||||||||
|
Stockholders’ equity
|
||||||||
|
Common stock, $0.01 par value; 150,000,000 shares authorized; 53,779,118 and 53,563,299 shares issued and 38,965,126 and 42,908,165 shares outstanding at December 31, 2010 and 2009 respectively
|
538 | 536 | ||||||
|
Preferred stock, $0.01 par value; 25,000,000 shares authorized; none issued
|
— | — | ||||||
|
Additional paid-in capital
|
314,212 | 311,282 | ||||||
|
Retained earnings
|
319,341 | 266,491 | ||||||
|
Accumulated other comprehensive income, net
|
84,133 | 83,812 | ||||||
|
Treasury stock, at cost (14,813,992 shares at December 31, 2010 and 10,655,134 shares at December 31, 2009)
|
(228,108 | ) | (163,722 | ) | ||||
|
Total stockholders’ equity
|
490,116 | 498,399 | ||||||
|
Total liabilities and stockholders’ equity
|
$ | 3,480,120 | $ | 3,676,653 | ||||
|
See accompanying notes.
|
||||||||
64
|
Employers Holdings, Inc. and Subsidiaries
|
||||||||||||
|
Consolidated Statements of Income
|
||||||||||||
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Revenues
|
(in thousands, except per share data)
|
|||||||||||
|
Net premiums earned
|
$ | 321,786 | $ | 404,247 | $ | 328,947 | ||||||
|
Net investment income
|
83,032 | 90,484 | 78,062 | |||||||||
|
Realized gains (losses) on investments, net
|
10,137 | 791 | (11,524 | ) | ||||||||
|
Other income
|
649 | 413 | 1,293 | |||||||||
|
Total revenues
|
415,604 | 495,935 | 396,778 | |||||||||
|
Expenses
|
||||||||||||
|
Losses and loss adjustment expenses
|
194,779 | 214,461 | 136,515 | |||||||||
|
Commission expense
|
38,468 | 36,150 | 43,618 | |||||||||
|
Dividends to policyholders
|
4,316 | 6,930 | 1,295 | |||||||||
|
Underwriting and other operating expenses
|
106,026 | 138,687 | 101,164 | |||||||||
|
Interest expense
|
5,693 | 7,409 | 2,135 | |||||||||
|
Total expenses
|
349,282 | 403,637 | 284,727 | |||||||||
|
Net income before income taxes
|
66,322 | 92,298 | 112,051 | |||||||||
|
Income tax expense
|
3,523 | 9,277 | 10,266 | |||||||||
|
Net income
|
$ | 62,799 | $ | 83,021 | $ | 101,785 | ||||||
|
Earnings per common share for the stated periods (Note 19)
|
||||||||||||
|
Basic
|
$ | 1.52 | $ | 1.81 | $ | 2.07 | ||||||
|
Diluted
|
$ | 1.51 | $ | 1.80 | $ | 2.07 | ||||||
|
Cash dividends declared per common share
|
$ | 0.24 | $ | 0.24 | $ | 0.24 | ||||||
|
Realized gains on investments, net
|
||||||||||||
|
Net realized gains on investments before credit related impairments on fixed maturity securities
|
$ | 10,182 | $ | 2,712 | ||||||||
|
Other-than-temporary impairments , credit losses recognized in earnings
|
(45 | ) | (1,921 | ) | ||||||||
|
Portion of impairment recognized in other comprehensive income
|
— | — | ||||||||||
|
Realized gains on investments, net
|
$ | 10,137 | $ | 791 | ||||||||
|
See accompanying notes.
|
||||||||||||
65
|
Employers Holdings, Inc. and Subsidiaries
|
|||||||||||||||||||||
|
Consolidated Statements of Stockholders’ Equity
|
|||||||||||||||||||||
|
Accumulated
|
|||||||||||||||||||||
|
Additional
|
Other
|
Treasury
|
Total
|
||||||||||||||||||
|
Common Stock
|
Paid In
|
Retained
|
Comprehensive
|
Stock
|
Stockholders’
|
||||||||||||||||
|
Shares
|
Amount
|
Capital
|
Earnings
|
Income, Net
|
at Cost
|
Equity
|
|||||||||||||||
|
(in thousands, except share data)
|
|||||||||||||||||||||
|
Balance, January 1, 2008
|
53,527,907 | $ | 535 | $ | 302,862 | $ | 104,536 | $ | 46,520 | $ | (75,000 | ) | $ | 379,453 | |||||||
|
Stock-based compensation (Note 15)
|
— | — | 3,161 | — | — | — | 3,161 | ||||||||||||||
|
Stock options exercised
|
300 | — | 5 | — | — | — | 5 | ||||||||||||||
|
Acquisition of treasury stock (Note 14)
|
— | — | — | — | — | (14,152 | ) | (14,152 | ) | ||||||||||||
|
Dividend to common stockholders
|
— | — | 4 | (11,812 | ) | — | — | (11,808 | ) | ||||||||||||
|
Comprehensive income:
|
|||||||||||||||||||||
|
Net income for the period
|
— | — | — | 101,785 | — | — | 101,785 | ||||||||||||||
|
Change in net unrealized gains on investments, net of taxes
|
— | — | — | — | (13,716 | ) | — | (13,716 | ) | ||||||||||||
|
Total comprehensive income, net
|
88,069 | ||||||||||||||||||||
|
Balance, December 31, 2008
|
53,528,207 | $ | 535 | $ | 306,032 | $ | 194,509 | $ | 32,804 | $ | (89,152 | ) | $ | 444,728 | |||||||
|
Balance, January 1, 2009
|
53,528,207 | $ | 535 | $ | 306,032 | $ | 194,509 | $ | 32,804 | $ | (89,152 | ) | $ | 444,728 | |||||||
|
Stock-based compensation (Note 15)
|
— | — | 5,366 | — | — | — | 5,366 | ||||||||||||||
|
Vesting of restricted stock units, net of shares withheld to
satisfy minimum tax withholding (Note 15)
|
35,092 | 1 | (124 | ) | — | — | — | (123 | ) | ||||||||||||
|
Acquisition of treasury stock (Note 14)
|
— | — | — | — | — | (74,570 | ) | (74,570 | ) | ||||||||||||
|
Dividend to common stockholders
|
— | — | 8 | (11,039 | ) | — | — | (11,031 | ) | ||||||||||||
|
Comprehensive income:
|
|||||||||||||||||||||
|
Net income for the period
|
— | — | — | 83,021 | — | — | 83,021 | ||||||||||||||
|
Change in net unrealized gains on investments,
net of taxes
|
— | — | — | — | 51,008 | — | 51,008 | ||||||||||||||
|
Total comprehensive income, net
|
134,029 | ||||||||||||||||||||
|
Balance, December 31, 2009
|
53,563,299 | $ | 536 | $ | 311,282 | $ | 266,491 | $ | 83,812 | $ | (163,722 | ) | $ | 498,399 | |||||||
|
Balance, January 1, 2010
|
53,563,299 | $ | 536 | $ | 311,282 | $ | 266,491 | $ | 83,812 | $ | (163,722 | ) | 498,399 | ||||||||
|
Stock-based compensation (Note 15)
|
— | — | 4,053 | — | — | — | 4,053 | ||||||||||||||
|
Stock options exercised
|
7,783 | — | 94 | — | — | — | 94 | ||||||||||||||
|
Vesting of restricted stock units, net of shares withheld to
satisfy minimum tax withholding (Note 15)
|
208,036 | 2 | (1,231 | ) | — | — | — | (1,229 | ) | ||||||||||||
|
Acquisition of treasury stock (Note 14)
|
— | — | — | — | — | (64,386 | ) | (64,386 | ) | ||||||||||||
|
Dividend to common stockholders
|
— | — | 14 | (9,949 | ) | — | — | (9,935 | ) | ||||||||||||
|
Comprehensive income:
|
|||||||||||||||||||||
|
Net income for the period
|
— | — | — | 62,799 | — | — | 62,799 | ||||||||||||||
|
Change in net unrealized gains on investments,
net of taxes
|
— | — | — | — | 321 | — | 321 | ||||||||||||||
|
Total comprehensive income, net
|
63,120 | ||||||||||||||||||||
|
Balance, December 31, 2010
|
53,779,118 | $ | 538 | $ | 314,212 | $ | 319,341 | $ | 84,133 | $ | (228,108 | ) | $ | 490,116 | |||||||
|
See accompanying notes.
|
|||||||||||||||||||||
66
|
Employers Holdings, Inc. and Subsidiaries
|
||||||||||||
|
Consolidated Statements of Cash Flows
|
||||||||||||
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Operating activities
|
(in thousands)
|
|||||||||||
|
Net income
|
$ | 62,799 | $ | 83,021 | $ | 101,785 | ||||||
|
Adjustments to reconcile net income to net cash provided by operating activities:
|
||||||||||||
|
Depreciation and amortization
|
7,098 | 9,899 | 7,226 | |||||||||
|
Stock-based compensation
|
4,053 | 5,366 | 3,161 | |||||||||
|
Amortization of premium on investments, net
|
6,105 | 5,047 | 6,226 | |||||||||
|
Allowance for doubtful accounts
|
(3,611 | ) | 1,968 | (678 | ) | |||||||
|
Deferred income tax expense
|
4,680 | 10,991 | 4,503 | |||||||||
|
Realized (gains) losses on investments, net
|
(10,137 | ) | (791 | ) | 11,524 | |||||||
|
Realized losses on retirement of assets
|
420 | 69 | 22 | |||||||||
|
Change in operating assets and liabilities:
|
||||||||||||
|
Accrued investment income
|
33 | 1,146 | (469 | ) | ||||||||
|
Premiums receivable
|
12,265 | 28,558 | 27,341 | |||||||||
|
Reinsurance recoverable on paid and unpaid losses
|
95,720 | 22,895 | 37,938 | |||||||||
|
Funds held by or deposited with reinsureds
|
78,638 | 5,824 | 7,721 | |||||||||
|
Federal income taxes
|
44 | 6,950 | (20,672 | ) | ||||||||
|
Unpaid losses and loss adjustment expenses
|
(145,929 | ) | (80,820 | ) | (71,980 | ) | ||||||
|
Unearned premiums
|
(9,092 | ) | (38,118 | ) | (24,476 | ) | ||||||
|
Accounts payable, accrued expenses and other liabilities
|
(10,455 | ) | (13,188 | ) | (3,660 | ) | ||||||
|
Deferred reinsurance gain–LPT Agreement
|
(18,233 | ) | (18,007 | ) | (18,421 | ) | ||||||
| Restricted cash and cash equivalents | (12,210 | ) | — | — | ||||||||
|
Other
|
(5,207 | ) | 9,941 | 223 | ||||||||
|
Net cash provided by operating activities
|
56,981 | 40,751 | 67,314 | |||||||||
|
Investing activities
|
||||||||||||
|
Purchase of fixed maturities
|
(273,833 | ) | (175,790 | ) | (113,587 | ) | ||||||
|
Purchase of equity securities
|
(17,673 | ) | (12,614 | ) | (558 | ) | ||||||
|
Proceeds from sale of fixed maturities
|
102,659 | 85,541 | 42,467 | |||||||||
|
Proceeds from sale of equity securities
|
17,753 | 20,634 | 4,010 | |||||||||
|
Proceeds from maturities and redemptions of investments
|
123,672 | 170,278 | 105,424 | |||||||||
|
Cash paid for acquisition, net of cash and cash equivalents acquired
|
— | (100 | ) | (168,903 | ) | |||||||
|
Capital expenditures and other, net
|
(1,905 | ) | (4,682 | ) | (3,926 | ) | ||||||
| Restricted cash and cash equivalents (used in) provided by investment activities | (2,000 | ) | 2,725 | (145) | ||||||||
|
Net cash (used in) provided by investing activities
|
(51,327 | ) | 85,992 | (135,218 | ) | |||||||
|
Financing activities
|
||||||||||||
|
Acquisition of treasury stock
|
(63,592 | ) | (74,185 | ) | (14,152 | ) | ||||||
|
Cash transactions related to stock-based compensation
|
(1,135 | ) | (123 | ) | — | |||||||
|
Dividend paid to stockholders
|
(9,935 | ) | (11,031 | ) | (11,808 | ) | ||||||
|
Debt issuance costs
|
— | — | (375 | ) | ||||||||
|
Payments on notes payable
|
— | (50,000 | ) | (2,678 | ) | |||||||
|
Proceeds from notes payable
|
— | — | 150,000 | |||||||||
|
Other
|
— | — | (38 | ) | ||||||||
|
Net cash (used in) provided by financing activities
|
(74,662 | ) | (135,339 | ) | 120,949 | |||||||
|
Net (decrease) increase in cash and cash equivalents
|
(69,008 | ) | (8,596 | ) | 53,045 | |||||||
|
Cash and cash equivalents at the beginning of the period
|
188,833 | 197,429 | 144,384 | |||||||||
|
Cash and cash equivalents at the end of the period
|
$ | 119,825 | $ | 188,833 | $ | 197,429 | ||||||
|
Cash paid (received) for income taxes
|
$ | 1,007 | $ | (8,581 | ) | $ | 26,277 | |||||
|
Cash paid for interest
|
$ | 6,000 | $ | 7,514 | $ | 1,782 | ||||||
|
Schedule of non-cash transactions
|
||||||||||||
|
Financed property and equipment purchases
|
$ | 2,009 | $ | 1,283 | $ | — | ||||||
|
See accompanying notes.
|
||||||||||||
67
Employers Holdings, Inc. and Subsidiaries
Notes to Consolidated Financial Statements
December 31, 2010
1. Basis of Presentation and Summary of Operations
Nature of Operations and Organization
Employers Holdings, Inc. (EHI) is a Nevada holding company. Through its wholly owned insurance subsidiaries, Employers Insurance Company of Nevada (EICN), Employers Compensation Insurance Company (ECIC), Employers Preferred Insurance Company (EPIC), and Employers Assurance Company (EAC), EHI is engaged in the commercial property and casualty insurance industry, specializing in workers’ compensation products and services. Unless otherwise indicated, all references to the “Company” refer to EHI, together with its subsidiaries.
On October 31, 2008, the Company acquired 100% of the outstanding common stock of AmCOMP Incorporated (AmCOMP), including two insurance subsidiaries, AmCOMP Preferred Insurance Company and AmCOMP Assurance Corporation (the Acquisition) (see Note 4). On December 16, 2008, the Florida Insurance Commissioner approved the name changes of AmCOMP Preferred Insurance Company and AmCOMP Assurance Corporation to EPIC and EAC, respectively.
Basis of Presentation
The accompanying consolidated financial statements have been prepared in accordance with U.S. generally accepted accounting principles (GAAP). All intercompany transactions and balances have been eliminated in consolidation. The accompanying consolidated statement of income for the year ended December 31, 2008, does not include the results of AmCOMP for the period prior to the Acquisition Date.
The Company considers an operating segment to be any component of its business whose operating results are regularly reviewed by the Company’s chief operating decision makers to make decisions about resources to be allocated to the segment and assess its performance based on discrete financial information. Currently, the Company has one operating segment, workers’ compensation insurance and related services.
Use of Estimates
The preparation of consolidated financial statements in conformity with GAAP requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements and the reported amounts of revenue and expenses during the reporting period. As a result, actual results could differ from these estimates. The most significant areas that require management judgment are the estimate of unpaid losses and loss adjustment expenses (LAE), evaluation of reinsurance recoverables, recognition of premium revenue, deferred policy acquisition costs, deferred income taxes, policyholders’ dividends, the valuation of assets acquired and liabilities assumed in its business combination and the valuation of investments.
Reclassifications
Certain prior year information has been reclassified to conform to the current period presentation.
2. Summary of Significant Accounting Policies
Cash and Cash Equivalents
The Company considers all highly liquid investments with an initial maturity of three months or less at the date of purchase to be cash equivalents.
Restricted Cash and Cash Equivalents
The Company had $16.9 million and $2.7 million of restricted cash at December 31, 2010 and 2009, respectively, primarily related to funds held in trust for Clarendon National Insurance Company (Clarendon).
68
Investments
Investments with remaining maturities of one year or less at the time of acquisition are classified as short-term investments. The Company’s investments in fixed maturity securities, equity securities, and short-term investments are classified as available-for-sale and are reported at fair value with unrealized gains and losses excluded from earnings and reported as a separate component of equity, net of deferred taxes, in accumulated other comprehensive income, net.
Investment income consists primarily of interest and dividends. Interest is recognized on an accrual basis, and dividends are recorded as earned at the ex-dividend date. Interest income on mortgage-backed and asset-backed securities is determined using the effective-yield method based on estimated principal repayments.
Realized capital gains and losses on investments are determined on a specific-identification basis.
When, in the opinion of management, a decline in the fair value of an equity security below its cost is considered to be “other-than-temporary,” the equity security’s cost is written-down to its fair value at the time the other-than-temporary decline is identified. The determination of an other-than-temporary decline for debt securities includes, in addition to other relevant factors, a presumption that if the market value is below cost by a significant amount for a period of time, a bifurcation of the write-down may be necessary. If management has the intent to sell the debt security or more likely than not will be required to sell the debt security before its anticipated recovery, the investment is written-down to its fair value and the entire impairment is recorded as a realized loss due to credit in the accompanying consolidated statements of income. If management does not have the intent to sell or will not be required to sell the debt security but does not expect to recover the amortized cost basis of the debt security, the amount of the other-than-temporary impairment is bifurcated between credit loss and other loss and recorded as a component of realized gains and losses in the consolidated statements of income and to other comprehensive income, respectively. The amount of any write-down is determined by the difference between the cost or amortized cost of the debt security and its fair value at the time the other-than-temporary decline is identified (see Note 6).
Recognition of Revenue and Expense
Revenue Recognition
Premiums are billed and collected according to policy terms, predominantly in the form of installments during the policy period. Premiums are earned pro rata over the terms of the policies. Billed premiums applicable to the unexpired terms of policies in-force are recorded in the accompanying consolidated balance sheets as a liability for unearned premiums.
Earned premiums include an estimate for earned but unbilled premiums. The Company estimates the amount of earned but unbilled premiums by analyzing the historical final premiums billed compared to the original estimated amounts billed. At December 31, 2010, premiums receivable on the consolidated balance sheet are net of $4.0 million to be returned to policyholders for final audits. At December 31, 2009, premiums receivable included $0.2 million of additional premiums expected to be received from policyholders for final audits.
The Company establishes a bad debt allowance on its premiums receivable through a charge included in underwriting and other operating expenses in the accompanying consolidated statements of income. This bad debt allowance is determined based on estimates and assumptions to project future experience. After all collection efforts have been exhausted, the Company reduces the bad debt allowance for write-offs of premiums receivable that have been deemed uncollectible. The Company had write-offs, net of recoveries of amounts previously written off, of $0.8 million, $1.2 million, and $1.0 million for the years ended December 31, 2010, 2009, and 2008, respectively.
Deferred Policy Acquisition Costs
Policy acquisition costs, consisting of commissions, premium taxes, and certain other underwriting costs that vary with, and are primarily related to, the production of new or renewal business are deferred and amortized as the related premiums are earned.
A premium deficiency is recognized if the sum of expected claims costs, claims adjustment expenses, expected dividends to policyholders, unamortized acquisition costs, and policy maintenance costs exceed the related unearned premiums and future investment income from related in-force policies. A premium deficiency would first be recognized by charging any unamortized acquisition costs to expense to the extent required to eliminate the deficiency. If the premium deficiency was greater than unamortized acquisition costs, a liability would be accrued for the excess deficiency. There was no premium deficiency at December 31, 2010 or 2009.
Deferred policy acquisition costs were $32.2 million and $33.7 million at December 31, 2010 and 2009, respectively. Amortization for the years ended December 31, 2010, 2009, and 2008, was $72.1 million, $87.6 million, and $66.4 million, respectively.
69
Unpaid Loss and Loss Adjustment Expense (LAE) Reserves
Loss and LAE reserves represent management’s best estimate of the ultimate net cost of all reported and unreported losses incurred for the applicable periods. The estimated reserves for losses and LAE include the accumulation of estimates for all claims reported prior to the balance sheet date, estimates (based on projections of relevant historical data) of claims incurred but not reported, and estimates of expenses for investigating and adjusting all incurred and unadjusted claims. Amounts reported are necessarily subject to the impact of future changes in economic, regulatory and social conditions. Management believes that, subject to the inherent variability in any such estimate, the reserves are within a reasonable and acceptable range of adequacy. Estimates for claims reported prior to the balance sheet date are continually monitored and reviewed, and as settlements are made or reserves adjusted, the differences are reported in current operations. Salvage and subrogation recoveries are estimated based on a review of the level of historical salvage and subrogation recoveries.
Commission Expense
Commission expense includes direct commissions to agents and brokers for the premiums that they produce for the Company, as well as incentive payments, other marketing costs, and fees. Additionally, the Company is entitled to receive a contingent profit commission under the LPT Agreement. The contingent profit is an amount based on the favorable difference between actual paid losses and LAE and expected paid losses and LAE under the LPT Agreement. Loss expenses are deemed to be 7% of total losses paid and are paid to the Company as compensation for management of the LPT claims. The calculation of actual amounts paid versus expected amounts is determined every five years beginning June 30, 2004 for the first twenty-five years of the agreement. The reinsurers pay the Company 30% of any favorable difference between the actual and expected amounts paid at each calculation point. Conversely, the Company could be required to return any previously paid contingent profit commission, plus interest, in the event of unfavorable differences. The Company accrues the estimated ultimate contingent profit commission through June 30, 2024. Increases or decreases in the estimated contingent profit commission are reflected in commission expense in the period that the estimate is revised.
At December 31, 2010, the Company reduced its estimate of certain administrative fees due under its joint marketing agreements (Change in Estimate), which reduced its accrual for commission expense by $3.0 million. This Change in Estimate was the result of new information that materially impacted conditions that existed as of December 31, 2010 and is reflected in the financial statements for the period ended December 31, 2010. This Change in Estimate increased net income by $3.0 million, or $0.07 per basic and diluted share, for the three and twelve months ended December 31, 2010.
Reinsurance
In the ordinary course of business and in accordance with general insurance industry practices, the Company purchases excess of loss reinsurance to protect the Company against the impact of large and/or catastrophic losses in its workers’ compensation business. Additionally, the Company is a party to a 100% quota share retroactive reinsurance agreement, (see Note 10). This reinsurance reduces the financial impact of such losses on current operations and the equity of the Company. Reinsurance makes the assuming reinsurer liable to the ceding company to the extent of the reinsurance coverage provided. It does not, however, discharge the Company from its liability to its policyholders in the event the reinsurer is unable or unwilling to meet its obligations under its reinsurance agreement with the Company.
Net premiums earned and losses and LAE incurred are stated in the accompanying consolidated statements of income after deduction of amounts ceded to reinsurers. Balances due from reinsurers on unpaid losses, including an estimate of such recoverables related to reserves for incurred but not reported losses, are reported as assets and are included in reinsurance recoverables even though amounts due on unpaid losses and LAE are not recoverable from the reinsurer until such losses are paid. Recoverables from reinsurers on unpaid losses and LAE amounted to $1.0 billion and $1.1 billion at December 31, 2010 and 2009, respectively.
Ceded losses and LAE are accounted for on a basis consistent with those used in accounting for the original policies issued and the terms of the relevant reinsurance agreement.
70
The 100% quota share retroactive reinsurance agreement was entered into in 1999 by the Nevada State Industrial Insurance System (the Fund) and assumed by EICN, which the Company refers to as the Loss Portfolio Transfer (LPT) Agreement (see Note 10). The Company accounts for this transaction as retroactive reinsurance, whereby the initial deferred gain was recorded as a liability in the accompanying consolidated balance sheets as deferred reinsurance gain – LPT Agreement. This gain is amortized using the recovery method, whereby the amortization is determined by the proportion of actual reinsurance recoveries to total estimated recoveries, and is recorded in losses and LAE incurred in the accompanying consolidated statements of income. Any adjustment to the estimated reserves ceded under the LPT Agreement is recognized in earnings in the period of change with a corresponding change to reinsurance recoverables for unpaid losses and deferred reinsurance gain. A cumulative amortization adjustment is also then recognized in earnings so that the deferred reinsurance gain reflects the balance that would have existed had the revised reserves been available at the inception of the LPT Agreement.
In addition, the Company is entitled to receive a contingent profit commission under the LPT Agreement. The contingent profit is an amount based on the favorable difference between actual paid losses and LAE and expected paid losses and LAE as established in the LPT Agreement. The calculation of actual amounts paid versus expected amounts is determined every five years beginning June 30, 2004 for the first twenty-five years of the agreement. The Company is paid 30% of the favorable difference between the actual and expected losses and LAE paid at each calculation point.
Conversely, the Company could be required to return any previously paid contingent profit commission, plus interest, in the event of unfavorable differences.
The Company accrues the estimated ultimate contingent profit commission through June 30, 2024. Increases or decreases in the estimated contingent profit commission are reflected in commission expense in the period that the estimate is revised.
Property and Equipment
Property and equipment are stated at cost less accumulated depreciation (see Note 7). Expenditures for maintenance and repairs are charged against operations as incurred.
Electronic data processing equipment, software, furniture and equipment, and automobiles are depreciated using the straight-line method over three to seven years. Leasehold improvements are carried at cost less accumulated amortization. The Company amortizes leasehold improvements using the straight-line method over the lesser of the useful life of the asset or the remaining original lease term, excluding options or renewal periods. Leasehold improvements are generally amortized over three to five years.
Obligations Held Under Capital Leases
Leased property and equipment meeting capital lease criteria are capitalized at the lower of the present value of the related lease payments or the fair value of the leased asset at the inception of the lease. Amortization is calculated using the straight-line method based on the term of the lease and is included in the depreciation expense of property and equipment. See Note 13 for additional disclosures related to capital leases.
Restructuring
The Company accounts for its restructuring plans by recording a loss when it is probable that a liability has been incurred. The amount of the loss is estimated and recorded at fair value using the Company’s incremental interest rate.
Policyholder Dividends
Certain policyholders have entered into agreements that provide the opportunity for dividends. Dividends are accrued on such policies based on specific dividend contract provisions and the policies’ earned premiums and loss ratios. Additionally, dividend agreements also allow the Company to reduce the amount to be paid at the Company’s discretion, based on the overall profitability. Should management choose to reduce the ultimate dividends to be paid, once the amount of the total dividend that will be paid for a policy year is determined, the dividend accrued would be reduced to the level determined by the Company. The reduced dividend amount would be allocated ratably to the participating policies, based on the dividend amount calculated prior to the reduction. Approximately 5.2%, 9.6%, and 2.6% of direct written premiums were subject to dividend participation during the years ended December 31, 2010, 2009, and 2008,
71
respectively. Policyholder dividends are ultimately paid at the sole discretion of the Board of Directors and must be approved by the Board prior to payment. Board-approved dividends accrued for 2010, 2009, and 2008 policies reflect the full potential amount allowed under the respective policies.
Income Taxes
Deferred tax assets, net of any applicable valuation allowance, and deferred tax liabilities are provided for the future tax consequences attributable to temporary differences between the financial statement carrying amounts of assets and liabilities and their respective tax bases. Deferred tax assets and liabilities are measured using enacted tax rates expected to apply to taxable income in the years in which those temporary differences are expected to be recovered or settled. The net deferred tax asset is recorded in the accompanying consolidated balance sheets as deferred income taxes, net.
Credit Risk
Financial instruments that potentially subject the Company to concentrations of credit risk are primarily cash and cash equivalents, investments, premiums receivable, and reinsurance recoverable balances.
Cash equivalents include investments in commercial paper of companies with high credit ratings, investments in money market securities and securities backed by the U.S. government. Investments are diversified throughout many industries and geographic regions. The Company limits the amount of credit exposure with any one financial institution and believes that no significant concentration of credit risk exists with respect to cash and cash equivalents and investments.
At December 31, 2010 and 2009, the outstanding premiums receivable balance was generally diversified due to the large number of entities composing the Company’s policyholder base and their dispersion across many different industries. To reduce credit risk, the Company performs ongoing evaluations of its policyholders’ financial condition, but does not generally require collateral. The Company also has recoverables from its reinsurers. Reinsurance contracts do not relieve the Company of its obligations to claimants or policyholders. Failure of reinsurers to honor their obligations could result in losses to the Company. The Company evaluates the financial condition of its reinsurers to minimize its exposure to significant losses from reinsurer insolvencies. The Company obtains collateral to mitigate the risks related to reinsurance insolvencies. At December 31, 2010, $11.6 million was collateralized by cash or letter of credit and an additional $962.1 million was in trust accounts for reinsurance related to the LPT Agreement.
The Company enters into securities lending agreements with financial institutions to improve investment income. Selected securities are loaned and are secured by collateral equal to at least 102% of the fair value of the securities. Collateral is in the form of cash or securities issued or guaranteed by the U.S. government, and the securities lending agent has provided counterparty indemnification in the event of borrower insolvency. The maximum amounts loaned under our securities lending program during the years ended 2010 and 2009 were $36.2 million and $36.7 million, respectively. As of December 31, 2010 and 2009, there were no outstanding securities lending transactions.
Fair Value of Financial Instruments
Estimated fair value amounts, defined as the quoted market price of a financial instrument, have been determined using available market information and other appropriate valuation methodologies. Judgment is required in developing the estimates of fair value where quoted market prices are not available. Accordingly, these estimates are not necessarily indicative of the amounts that could be realized in a current market exchange. The use of different market assumptions or estimating methodologies may have an effect on the estimated fair value amounts.
The following methods and assumptions were used by the Company in estimating the fair value disclosures for financial investments in the accompanying consolidated financial statements and in these notes for the years ended 2010 and 2009:
Cash and cash equivalents, premiums receivable, and accrued expenses and other liabilities. The carrying amounts for these financial instruments as reported in the accompanying consolidated balance sheets approximate their fair values.
Investments. The estimated fair values for available-for-sale securities generally represent quoted market prices for securities traded in the public marketplace or estimated values for securities not traded in the public marketplace. Additional data with respect to fair values of the Company’s investment securities is disclosed in Note 6. The fair values reported in the accompanying consolidated balance sheets equal the carrying amounts for these investments.
72
Derivatives. The fair value of the Company’s interest rate swap was derived by using an industry standard swap valuation model, with market based inputs for swaps having similar characteristics (see Note 12). The fair value, reported as a component of other liabilities in the accompanying consolidated balance sheets, equals the carrying amount.
Notes payable. The Company’s notes payable are composed of floating rate long-term debt. Accordingly, the carrying amount reported in the accompanying consolidated balance sheets is estimated to approximate fair value.
The estimated fair values of the Company’s financial instruments at December 31, 2010, are as follows:
|
Carrying Value
|
Estimated Fair Value
|
||||||
|
Financial assets
|
(in thousands)
|
||||||
|
Investments (Note 6)
|
$ | 2,080,494 | $ | 2,080,494 | |||
|
Cash and cash equivalents
|
119,825 | 119,825 | |||||
|
Financial liabilities
|
|||||||
|
Notes payable (Note 11)
|
132,000 | 132,000 | |||||
Other financial instruments qualify as insurance-related products and are specifically exempted from fair value disclosure requirements.
Goodwill and Other Intangible Assets
The Company tests for impairment of goodwill and non-amortizable intangible assets in the fourth quarter of each year. At the end of each quarter, management considers the results of the previous analysis as well as any recent developments that may constitute triggering events requiring the impairment analysis of goodwill and other intangible assets to be updated. The Company has assessed the continuing negative effects of the economic slowdown on the Company’s gross premiums written and changes in the Company’s stock price and determined that there were no impairments as of December 31, 2010 and 2009.
The Company acquired intangible assets in the acquisition of AmCOMP (see Note 4) comprised of state licenses, insurance relationships and other intangible assets. The intangible assets related to state licenses are not subject to amortization, and the remaining intangibles are being amortized over an eight year period.
The following table presents the gross carrying value, accumulated amortization and net carrying value for the Company’s intangible assets, by major class, as of December 31:
|
2010
|
2009
|
||||||||||||||||||||||
|
Gross
Carrying
Value
|
Accumulated
Amortization
|
Net
Carrying
Value
|
Gross
Carrying
Value
|
Accumulated
Amortization
|
Net
Carrying
Value
|
||||||||||||||||||
|
(in thousands)
|
|||||||||||||||||||||||
|
State licenses
|
$ | 7,700 | $ | — | $ | 7,700 | $ | 7,700 | $ | — | $ | 7,700 | |||||||||||
|
Insurance relationships
|
9,400 | (3,821 | ) | 5,579 | 9,400 | (1,848 | ) | 7,552 | |||||||||||||||
|
Other
|
1,700 | (1,700 | ) | — | 1,700 | (1,510 | ) | 190 | |||||||||||||||
|
Total
|
$ | 18,800 | $ | (5,521 | ) | $ | 13,279 | $ | 18,800 | $ | (3,358 | ) | $ | 15,442 | |||||||||
During the years ended December 31, 2010, 2009, and 2008, the Company recognized $2.2 million, $2.8 million, and $0.6 million in amortization expenses, respectively. These amortization expenses are included in the accompanying consolidated statements of income in underwriting and other operating expenses. Amortization expense for the next five years related to amortizable intangible assets is expected to be as follows:
|
Year
|
Amount
|
||
|
(in thousands)
|
|||
|
2011
|
$ | 1,550 | |
|
2012
|
1,170 | ||
|
2013
|
873 | ||
|
2014
|
651 | ||
|
2015
|
489 | ||
|
Thereafter
|
846 | ||
| $ | 5,579 | ||
73
Stock-Based Compensation
The Company issues stock-based payments, which are recognized in the consolidated statements of income based on their fair values over the employees’ service period (see Note 15).
3. New Accounting Standards
In January 2010, the Financial Accounting Standards Board (FASB) issued guidance on Improving Disclosures about Fair Value Measurements that requires additional disclosures regarding fair value measurements. The update changes fair value disclosures by requiring: (a) separate disclosure of the amounts of significant transfers in and out of Level 1 and Level 2 fair value measurements and a description of the reasons for the transfers; and (b) separate disclosure of information about purchases, sales, issuances, and settlements of Level 3 fair value measurements. This guidance was effective for interim and annual reporting periods beginning after December 15, 2009, except for the disclosures regarding Level 3 fair value measurements, which were effective for fiscal years beginning after December 15, 2010. The Company has included the required disclosures in the Notes to Consolidated Financial Statements.
In October 2010, the FASB issued Update Number 2010-26, Accounting for Costs Associated with Acquiring or Renewing Insurance Contracts. This update changes the definition of acquisition costs which may be capitalized to specify costs which relate directly to the successful acquisition of new or renewal insurance contracts; adds to the definition the concept of incremental costs; further restricts costs to be capitalized by identifying only those costs which may be capitalized; and requires additional granularity in the disclosures related to type of acquisition costs capitalized during the period. This guidance becomes effective for interim and annual reporting periods beginning after December 15, 2011. The Company has not yet determined if it will adopt the standard on a prospective or retrospective basis and is evaluating the impact the adoption will have on its financial statements.
4. Acquisition of AmCOMP
On October 31, 2008, EHI acquired 100% of the outstanding common stock of AmCOMP for $188.4 million. The Company believes the Acquisition has significantly advanced its strategic goals and vision of being the leader in the property and casualty insurance industry specializing in workers’ compensation.
Unaudited Pro Forma Financial Information
Net income for the years ended December 31, 2010 and 2009, presented in the accompanying consolidated statements of income, includes the results of AmCOMP for the full year. The unaudited financial information in the table below summarizes the combined results of operations of EHI and AmCOMP, on a pro forma basis, as though the companies had been combined as of the beginning of the period presented. The unaudited pro forma financial information is presented for informational purposes only and is not indicative of the results that would have been achieved if the Acquisition had taken place at the beginning of the period presented, nor is the pro forma information intended to be indicative of the Company’s future results of operations.
The unaudited pro forma financial information for the year ended December 31, 2008 combines the results for EHI for the year ended December 31, 2008, which includes the results of AmCOMP subsequent to the acquisition date, and the historical results of AmCOMP for the period January 1, 2008 through October 31, 2008, including a charge of $8.0
million for realized Florida excessive profits for accident years 2003-2006. The historical financial information has been adjusted to give effect to pro forma items that are directly attributable to the Acquisition and are expected to have a continuing impact on the consolidated results. These items include adjustments for amortization of intangible assets acquired, increases in interest expense and decreases in underwriting and other expenses for integration and restructuring savings. The following table summarizes the pro forma financial information:
|
Year Ended December 31, 2008
|
|
|
(in thousands, except per share data)
|
|
|
Net premiums earned
|
$ 495,080
|
|
Net income
|
105,770
|
|
Earnings per common share – basic
|
2.15
|
|
Earnings per common share – diluted
|
2.15
|
74
5. Fair Value of Financial Instruments
The Company’s estimates of fair value for financial assets and liabilities are based on the inputs used in the valuation and give the highest priority to quoted prices in active markets and require that observable inputs be used in the valuations when available. The disclosure of fair value estimates is based on whether the significant inputs into the valuation are observable. In determining the level of the hierarchy in which the estimate is disclosed, the highest priority is given to unadjusted quoted prices in active markets and the lowest priority to unobservable inputs that reflect the Company’s significant market assumptions.
The three levels of the hierarchy are as follows:
|
|
·
|
Level 1 – Valuations based on unadjusted quoted market prices for identical assets or liabilities in active markets. The Company uses the quoted market prices as fair value and includes these prices in the amounts disclosed in Level 1 of the hierarchy.
|
|
|
·
|
Level 2 – Valuations based on observable inputs (other than Level 1 prices), such as quoted prices for similar assets or liabilities at the measurement date; quoted prices in inactive markets; or other inputs that are observable, either directly or indirectly. When quoted market prices are unavailable, the Company estimates fair value based on objectively verifiable information, if available, and these estimates are included in the amount disclosed in Level 2 of the hierarchy.
|
|
|
·
|
Level 3 – Valuations based on inputs that are unobservable and significant to the overall fair value measurement and involve management judgment. The fair value of certain privately held or thinly traded securities is determined using internal analytical methods based on the best information available.
|
If quoted market prices and an estimate determined by using objectively verifiable information are unavailable, the Company produces an estimate of fair value based on internally developed valuation techniques, which, depending on the level of observable market inputs, will render the fair value estimate as Level 2 or Level 3. The Company bases all of its estimates of fair value for assets on the bid price as it represents what a third party market participant would be willing to pay in an arm’s length transaction. The valuation methods used by the Company, by type of investment, are described below.
Equity Securities. The Company utilizes market quotations for equity securities that have quoted prices in active markets.
Fixed Maturities, Short-Term Investments. Fair value measurements for these securities are estimated using relevant inputs, including available market information, benchmark curves, benchmarking of like securities, sector groupings, and matrix pricing. An Option Adjusted Spread model is also used to develop prepayment and interest rate scenarios. Industry standard models are used to analyze and value securities with embedded options or prepayment sensitivities.
Derivatives. The fair value of the Company’s interest rate swap, reported as a component of other liabilities in the accompanying 2009 consolidated balance sheet, was derived by using an industry standard swap valuation model, with market-based inputs for swaps having similar characteristics (see Note 12).
Each asset class is evaluated based on relevant market information, credit information, perceived market movements, and sector news. The market inputs utilized in the pricing evaluation include: benchmark yields, reported trades, broker/dealer quotes, issuer spreads, two-sided markets, benchmark securities, bids, offers, reference data, and industry and economic events. The extent of the use of each market input depends on the asset class and the market conditions.
These methods of valuation will only produce an estimate of fair value if there is objectively verifiable information to produce a valuation. If objectively verifiable information is not available, the Company would be required to produce an estimate of fair value using some of the same methodologies, making assumptions for market based inputs that are unavailable.
Most estimates of fair value for fixed maturities are based on estimates using objectively verifiable information and are included in the amount disclosed in Level 2 of the hierarchy. The fair value estimates for determining Level 3 fair value include the Company’s assumptions about risk assessments and market participant assumptions based on the best information available, including quotes from market makers and other broker/dealers recognized as market participants, using standard or trade derived inputs, new issue data, monthly payment information, cash flow generation, prepayment speeds, spread adjustments, or rating updates.
The following table presents the items in the accompanying consolidated balance sheets that are stated at fair value and the fair value measurements.
75
|
Level 1
|
Level 2
|
Level 3
|
|||||||||
|
At December 31, 2010
|
(in thousands)
|
||||||||||
|
Fixed maturity securities
|
|||||||||||
|
U.S. Treasuries
|
$ | — | $ | 144,725 | $ | — | |||||
|
U.S. Agencies
|
— | 123,802 | — | ||||||||
|
States and municipalities
|
— | 966,002 | — | ||||||||
|
Corporate
|
— | 479,424 | — | ||||||||
|
Residential mortgage-backed securities
|
— | 246,756 | — | ||||||||
|
Commercial mortgage-backed securities
|
— | 25,077 | — | ||||||||
|
Asset-backed securities
|
— | 14,578 | — | ||||||||
|
Total fixed maturity securities
|
$ | — | $ | 2,000,364 | $ | — | |||||
|
Equity securities
|
|||||||||||
|
Consumer goods
|
26,646 | — | — | ||||||||
|
Energy and utilities
|
10,265 | — | — | ||||||||
|
Financial
|
9,500 | — | — | ||||||||
|
Technology and communications
|
15,990 | — | — | ||||||||
|
Industrial and other
|
17,729 | — | — | ||||||||
|
Total equity securities
|
$ | 80,130 | $ | — | $ | — | |||||
|
Level 1
|
Level 2
|
Level 3
|
|||||||||
|
At December 31, 2009
|
(in thousands)
|
||||||||||
|
Fixed maturity securities
|
|||||||||||
|
U.S. Treasuries
|
$ | — | $ | 146,464 | $ | — | |||||
|
U.S. Agencies
|
— | 124,969 | — | ||||||||
|
States and municipalities
|
— | 1,028,277 | — | ||||||||
|
Corporate
|
— | 337,610 | — | ||||||||
|
Residential mortgage-backed securities
|
— | 279,963 | — | ||||||||
|
Commercial mortgage-backed securities
|
— | 29,774 | — | ||||||||
|
Asset-backed securities
|
— | 13,235 | — | ||||||||
|
Total fixed maturity securities
|
$ | — | $ | 1,960,292 | $ | — | |||||
|
Equity securities
|
|||||||||||
|
Consumer goods
|
$ | 22,484 | $ | — | $ | — | |||||
|
Energy and utilities
|
9,782 | — | — | ||||||||
|
Financial
|
9,400 | — | — | ||||||||
|
Technology and communications
|
15,601 | — | — | ||||||||
|
Industrial and other
|
12,001 | — | — | ||||||||
|
Total equity securities
|
$ | 69,268 | $ | — | $ | — | |||||
|
Derivatives
|
|||||||||||
|
Other liabilities
|
$ | — | $ | (2,180 | ) | $ | — | ||||
76
A reconciliation of the beginning and ending balances, for the above items, that are measured using Level 3 inputs were as follows:
|
Residential
Mortgage-backed
Securities
|
Asset-backed
Securities
|
|||||||
|
(in thousands)
|
||||||||
|
Balance January 1, 2009
|
$ | — | $ | 4,950 | ||||
|
Transfers in (out) of Level 3
|
80 | (5,449 | ) | |||||
|
Unrealized gains in other comprehensive income
|
13 | 499 | ||||||
|
Purchase, settlements and issuances, net
|
(93 | ) | — | |||||
|
Balance, December 31, 2009
|
$ | — | $ | — | ||||
The Company had no Level 3 investment activity during the year ended December 31, 2010.
6. Investments
The amortized cost, gross unrealized gains, gross unrealized losses, and estimated fair value of the Company’s investments were as follows:
|
Amortized
Cost
|
Gross Unrealized Gains
|
Gross
Unrealized Losses
|
Estimated
Fair Value
|
||||||||||||
|
At December 31, 2010
|
(in thousands)
|
||||||||||||||
|
Fixed maturity securities
|
|||||||||||||||
|
U.S. Treasuries
|
$ | 135,265 | $ | 9,619 | $ | (159 | ) | $ | 144,725 | ||||||
|
U.S. Agencies
|
116,747 | 7,142 | (87 | ) | 123,802 | ||||||||||
|
States and municipalities
|
927,668 | 43,054 | (4,720 | ) | 966,002 | ||||||||||
|
Corporate
|
453,851 | 28,655 | (3,082 | ) | 479,424 | ||||||||||
|
Residential mortgage-backed securities
|
230,518 | 16,926 | (688 | ) | 246,756 | ||||||||||
|
Commercial mortgage-backed securities
|
23,877 | 1,201 | (1 | ) | 25,077 | ||||||||||
|
Asset-backed securities
|
13,852 | 727 | (1 | ) | 14,578 | ||||||||||
|
Total fixed maturity securities
|
1,901,778 | 107,324 | (8,738 | ) | 2,000,364 | ||||||||||
|
Equity securities
|
|||||||||||||||
|
Consumer goods
|
19,141 | 7,550 | (45 | ) | 26,646 | ||||||||||
|
Energy and utilities
|
5,106 | 5,160 | (1 | ) | 10,265 | ||||||||||
|
Financial
|
6,603 | 2,916 | (19 | ) | 9,500 | ||||||||||
|
Technology and communications
|
7,499 | 8,500 | (9 | ) | 15,990 | ||||||||||
|
Industrial and other
|
10,932 | 6,841 | (44 | ) | 17,729 | ||||||||||
|
Total equity securities
|
49,281 | 30,967 | (118 | ) | 80,130 | ||||||||||
|
Total investments
|
$ | 1,951,059 | $ | 138,291 | $ | (8,856 | ) | $ | 2,080,494 | ||||||
77
|
Amortized
Cost
|
Gross Unrealized Gains
|
Gross
Unrealized Losses
|
Estimated
Fair Value
|
||||||||||||
|
At December 31, 2009
|
(in thousands)
|
||||||||||||||
|
Fixed maturity securities
|
|||||||||||||||
|
U.S. Treasuries
|
$ | 140,269 | $ | 6,366 | $ | (171 | ) | $ | 146,464 | ||||||
|
U.S. Agencies
|
117,844 | 7,125 | — | 124,969 | |||||||||||
|
States and municipalities
|
979,364 | 50,600 | (1,687 | ) | 1,028,277 | ||||||||||
|
Corporate
|
314,692 | 23,335 | (417 | ) | 337,610 | ||||||||||
|
Residential mortgage-backed securities
|
265,056 | 15,697 | (790 | ) | 279,963 | ||||||||||
|
Commercial mortgage-backed securities
|
29,407 | 391 | (24 | ) | 29,774 | ||||||||||
|
Asset-backed securities
|
12,442 | 793 | — | 13,235 | |||||||||||
|
Total fixed maturity securities
|
1,859,074 | 104,307 | (3,089 | ) | 1,960,292 | ||||||||||
|
Equity securities
|
|||||||||||||||
|
Consumer goods
|
14,421 | 8,069 | (6 | ) | 22,484 | ||||||||||
|
Energy and utilities
|
4,715 | 5,067 | — | 9,782 | |||||||||||
|
Financial
|
6,613 | 2,861 | (74 | ) | 9,400 | ||||||||||
|
Technology and communications
|
7,930 | 7,686 | (15 | ) | 15,601 | ||||||||||
|
Industrial and other
|
6,257 | 5,758 | (14 | ) | 12,001 | ||||||||||
|
Total equity securities
|
39,936 | 29,441 | (109 | ) | 69,268 | ||||||||||
|
Total investments
|
$ | 1,899,010 | $ | 133,748 | $ | (3,198 | ) | $ | 2,029,560 | ||||||
The amortized cost and estimated fair value of fixed maturity securities at December 31, 2010, by contractual maturity, are shown below. Expected maturities differ from contractual maturities because borrowers may have the right to call or prepay obligations with or without call or prepayment penalties.
|
Amortized
Cost
|
Estimated
Fair Value
|
||||||
|
(in thousands)
|
|||||||
|
Due in one year or less
|
$ | 113,888 | $ | 115,532 | |||
|
Due after one year through five years
|
577,069 | 612,759 | |||||
|
Due after five years through ten years
|
576,440 | 610,784 | |||||
|
Due after ten years
|
366,134 | 374,878 | |||||
|
Mortgage and asset backed securities
|
268,247 | 286,411 | |||||
|
Total
|
$ | 1,901,778 | $ | 2,000,364 | |||
78
The following is a summary of investments that have been in a continuous unrealized loss position for less than 12 months and those that have been in a continuous unrealized loss position for 12 months or greater, in each case as of December 31, 2010 and December 31, 2009:
|
December 31, 2010
|
||||||||||||||||||||||||
|
Less Than 12 Months
|
12 Months or Greater
|
Total
|
||||||||||||||||||||||
|
Estimated
Fair
Value
|
Gross
Unrealized
Losses
|
Estimated
Fair
Value
|
Gross
Unrealized
Losses
|
Estimated
Fair
Value
|
Gross
Unrealized
Losses
|
|||||||||||||||||||
|
Fixed maturity securities
|
(in thousands)
|
|||||||||||||||||||||||
|
U.S. Treasuries
|
$ | 4,548 | $ | (159 | ) | $ | — | $ | — | $ | 4,548 | $ | (159 | ) | ||||||||||
|
U.S. Agencies
|
14,500 | (87 | ) | — | — | 14,500 | (87 | ) | ||||||||||||||||
|
States and municipalities
|
124,245 | (4,720 | ) | — | — | 124,245 | (4,720 | ) | ||||||||||||||||
|
Corporate
|
123,216 | (3,082 | ) | — | — | 123,216 | (3,082 | ) | ||||||||||||||||
|
Residential mortgage-backed securities
|
15,161 | (304 | ) | 3,465 | (384 | ) | 18,626 | (688 | ) | |||||||||||||||
|
Commercial mortgage-backed securities
|
1,365 | (1 | ) | — | — | 1,365 | (1 | ) | ||||||||||||||||
|
Asset-backed securities
|
923 | (1 | ) | — | — | 923 | (1 | ) | ||||||||||||||||
|
Total fixed maturity securities
|
283,958 | (8,354 | ) | 3,465 | (384 | ) | 287,423 | (8,738 | ) | |||||||||||||||
|
Equity securities
|
||||||||||||||||||||||||
|
Consumer goods
|
4,993 | (45 | ) | — | — | 4,993 | (45 | ) | ||||||||||||||||
|
Energy and utilities
|
163 | (1 | ) | — | — | 163 | (1 | ) | ||||||||||||||||
|
Financial
|
1,695 | (16 | ) | 66 | (3 | ) | 1,761 | (19 | ) | |||||||||||||||
|
Technology and communications
|
801 | (9 | ) | — | — | 801 | (9 | ) | ||||||||||||||||
|
Industrial and other
|
2,999 | (44 | ) | — | — | 2,999 | (44 | ) | ||||||||||||||||
|
Total equity securities
|
10,651 | (115 | ) | 66 | (3 | ) | 10,717 | (118 | ) | |||||||||||||||
|
Total investments
|
$ | 294,609 | $ | (8,469 | ) | $ | 3,531 | $ | (387 | ) | $ | 298,140 | $ | (8,856 | ) | |||||||||
|
December 31, 2009
|
||||||||||||||||||||||||
|
Less Than 12 Months
|
12 Months or Greater
|
Total
|
||||||||||||||||||||||
|
Estimated
Fair
Value
|
Gross
Unrealized
Losses
|
Estimated
Fair
Value
|
Gross
Unrealized
Losses
|
Estimated
Fair
Value
|
Gross
Unrealized
Losses
|
|||||||||||||||||||
|
Fixed maturity securities
|
(in thousands)
|
|||||||||||||||||||||||
|
U.S. Treasuries
|
$ | 10,922 | $ | (171 | ) | $ | — | $ | — | $ | 10,922 | $ | (171 | ) | ||||||||||
|
States and municipalities
|
45,939 | (889 | ) | 15,715 | (798 | ) | 61,654 | (1,687 | ) | |||||||||||||||
|
Corporate
|
21,238 | (312 | ) | 5,506 | (105 | ) | 26,744 | (417 | ) | |||||||||||||||
|
Residential mortgage-backed securities
|
28 | — | 4,164 | (790 | ) | 4,192 | (790 | ) | ||||||||||||||||
|
Commercial mortgage-backed securities
|
1,998 | (24 | ) | — | — | 1,998 | (24 | ) | ||||||||||||||||
|
Total fixed maturity securities
|
80,125 | (1,396 | ) | 25,385 | (1,693 | ) | 105,510 | (3,089 | ) | |||||||||||||||
|
Equity securities
|
||||||||||||||||||||||||
|
Consumer goods
|
79 | (6 | ) | — | — | 79 | (6 | ) | ||||||||||||||||
|
Financial
|
1,271 | (74 | ) | — | — | 1,271 | (74 | ) | ||||||||||||||||
|
Technology and communications
|
270 | (15 | ) | — | — | 270 | (15 | ) | ||||||||||||||||
|
Industrial and other
|
214 | (14 | ) | — | — | 214 | (14 | ) | ||||||||||||||||
|
Total equity securities
|
1,834 | (109 | ) | — | — | 1,834 | (109 | ) | ||||||||||||||||
|
Total investments
|
$ | 81,959 | $ | (1,505 | ) | $ | 25,385 | $ | (1,693 | ) | $ | 107,344 | $ | (3,198 | ) | |||||||||
Based on reviews of the fixed maturity securities, the Company determined that unrealized losses as of December 31, 2010 and 2009 were primarily the result of changes in prevailing interest rates and not the credit quality of the issuers.
79
As of December 31, 2010, the Company expected to sell one fixed maturity security that was in an unrealized loss position before reaching maturity and recognized an impairment of less than $0.1 million as a realized loss on investments. All other fixed maturity securities whose fair values were less than amortized cost were not determined to be other-than-temporarily impaired given the severity and duration of the impairment, the credit quality of the issuers, the Company’s intent on not selling the securities, and a determination was made that it is not more likely than not that the Company will be required to sell the securities until fair value recovers above cost, or to maturity.
Based on reviews of the equity securities as of December 31, 2010, the Company determined that the unrealized losses as of that date were not considered to be other-than-temporary due to the financial condition and near term prospects of the issuers. Based on reviews of the equity securities as of December 31, 2009, the Company recognized total impairments of $1.9 million in the fair values of 26 equity securities as of that date because of the severity and duration of the change in fair values of those securities.
Net realized gains (losses) and the change in unrealized gains (losses) on fixed maturity and equity securities are determined on a specific-identification basis and were as follows:
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Net realized gains (losses)
|
(in thousands)
|
|||||||||||
|
Fixed maturity securities
|
$ | 710 | $ | (855 | ) | $ | (560 | ) | ||||
|
Equity securities
|
9,427 | 1,820 | (10,964 | ) | ||||||||
|
Short-term investments
|
— | (174 | ) | — | ||||||||
|
Total
|
$ | 10,137 | $ | 791 | $ | (11,524 | ) | |||||
|
Change in unrealized gains (losses)
|
||||||||||||
|
Fixed maturity securities
|
$ | (2,632 | ) | $ | 62,054 | $ | 14,420 | |||||
|
Equity securities
|
1,517 | 13,820 | (31,314 | ) | ||||||||
|
Short-term investments
|
— | (72 | ) | 72 | ||||||||
|
Total
|
$ | (1,115 | ) | $ | 75,802 | $ | (16,822 | ) | ||||
Net investment income was as follows:
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Fixed maturity securities
|
$ | 83,730 | $ | 89,522 | $ | 72,602 | ||||||
|
Equity securities
|
1,399 | 1,402 | 1,855 | |||||||||
|
Short-term investments and cash equivalents
|
327 | 1,910 | 6,017 | |||||||||
| 85,456 | 92,834 | 80,474 | ||||||||||
|
Investment expenses
|
(2,424 | ) | (2,350 | ) | (2,412 | ) | ||||||
|
Net investment income
|
$ | 83,032 | $ | 90,484 | $ | 78,062 | ||||||
The Company is required by various state laws and regulations to keep securities or letters of credit on deposit with the states in which it does business. As of December 31, 2010 and 2009, securities having a fair value of $558.6 million and $554.2 million, respectively, were on deposit. These laws and regulations govern not only the amount, but also the type of security that is eligible for deposit. Additionally, certain reinsurance contracts require Company funds to be held in trust for the benefit of the ceding reinsurer to secure the outstanding liabilities assumed by the Company. The fair value of securities held in trust for reinsurance at December 31, 2010 and 2009, was $52.9 million and $6.1 million, respectively.
80
7. Property and Equipment
Property and equipment consists of the following:
|
As of December 31,
|
||||||||
|
2010
|
2009
|
|||||||
|
(in thousands)
|
||||||||
|
Land
|
$ | 95 | $ | 95 | ||||
|
Furniture and equipment
|
3,129 | 4,006 | ||||||
|
Leasehold improvements
|
4,283 | 4,486 | ||||||
|
Computers and software
|
21,993 | 31,955 | ||||||
|
Automobiles
|
1,844 | 139 | ||||||
| 31,344 | 40,681 | |||||||
|
Accumulated amortization and depreciation
|
(19,632 | ) | (27,622 | ) | ||||
|
Property and equipment, net
|
$ | 11,712 | $ | 13,059 | ||||
Depreciation and amortization expenses related to property and equipment for the years ended December 31, 2010, 2009 and 2008, were $4.8 million, $6.9 million, and $6.5 million, respectively. Internally developed software costs of $0.1 million and $0.7 million were capitalized during the years ended December 31, 2010 and 2009, respectively.
8. Income Taxes
The Company files a consolidated federal income tax return. The insurance subsidiaries pay premium taxes on gross premiums written in lieu of some states’ income or franchise taxes.
The provision for income taxes consisted of the following:
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Current tax (benefit) expense:
|
(in thousands)
|
|||||||||||
|
Federal
|
$ | (1,228 | ) | $ | (2,061 | ) | $ | 5,591 | ||||
|
State
|
71 | 347 | 172 | |||||||||
|
Total current tax (benefit) expense:
|
(1,157 | ) | (1,714 | ) | 5,763 | |||||||
|
Deferred tax expense:
|
||||||||||||
|
Federal
|
4,680 | 10,991 | 4,561 | |||||||||
|
State
|
— | — | (58 | ) | ||||||||
|
Total deferred tax expense
|
4,680 | 10,991 | 4,503 | |||||||||
|
Income tax expense
|
$ | 3,523 | $ | 9,277 | $ | 10,266 | ||||||
The difference between the statutory federal tax rate of 35% and the Company’s effective tax rate on net income before income taxes as reflected in the consolidated statements of income was as follows:
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Expense computed at statutory rate
|
$ | 23,213 | $ | 32,304 | $ | 39,218 | ||||||
|
LPT contingent profit commission
|
(284 | ) | (5,259 | ) | — | |||||||
|
Dividends received deduction and tax-exempt interest
|
(12,039 | ) | (12,176 | ) | (11,197 | ) | ||||||
|
LPT deferred gain amortization
|
(6,381 | ) | (6,302 | ) | (6,447 | ) | ||||||
|
Pre-privatization reserve adjustments
|
(1,358 | ) | (576 | ) | (2,394 | ) | ||||||
|
Impact of previously unrecognized tax benefits
|
— | — | (10,155 | ) | ||||||||
|
Other
|
372 | 1,286 | 1,241 | |||||||||
|
Income tax expense
|
$ | 3,523 | $ | 9,277 | $ | 10,266 | ||||||
On January 1, 2000, EICN assumed the assets, liabilities, and operations of the Fund pursuant to legislation passed in the 1999 Nevada Legislature (the Privatization). Prior to the Privatization, the Fund was a part of the State of Nevada and therefore was not subject to federal income tax; accordingly, it did not take an income tax deduction with respect to the
81
establishment of its unpaid loss and LAE reserves. Due to favorable loss experience after the Privatization, it was determined that certain of the pre-Privatization unpaid loss and LAE reserves assumed by EICN as part of the Privatization were no longer necessary and the unpaid loss and LAE reserves were reduced accordingly. Such downward adjustments of pre-Privatization unpaid loss reserves increases GAAP net income, but does not increase taxable income. For the years ended December 31, 2010, 2009, and 2008 there were downward adjustments of pre-Privatization unpaid loss reserves of $3.9 million, $1.6 million, and $6.8 million, respectively.
For the years ended December 31, 2010 and 2009, the Company increased the estimated ultimate contingent profit commission related to the LPT Agreement by $0.8 million and $15.0 million, respectively. Such increases to the estimated ultimate contingent profit commission increases GAAP net income but does not increase taxable income. There was no change to the estimate during the year ended December 31, 2008.
As of December 31, 2010 and 2009, the Company had no unrecognized tax benefits. The following is a reconciliation of the beginning and ending amounts for unrecognized tax benefits and related interest for the year ended:
|
December 31, 2008
|
||||
|
(in thousands)
|
||||
|
Balance, January 1, 2008
|
$ | 10,155 | ||
|
Gross amount of interest accrued
|
406 | |||
|
Less:
|
||||
|
Recognition of tax benefits
|
(8,274 | ) | ||
|
Gross amount of related interest accrued
|
(2,287 | ) | ||
|
Balance, December 31, 2008
|
$ | — | ||
During the third quarter of the year ended December 31, 2008, the Company reversed $10.6 million of liabilities for previously unrecognized tax benefits (including $2.3 million of related accrued interest) as a result of certain statutory periods expiring. The total amount of the reversals reduced the effective tax rate during 2008.
Tax years 2007 through 2009 are subject to examination by the federal taxing authority.
The significant components of deferred income taxes, net, were as follows as of December 31:
|
2010
|
2009
|
||||||||||||||
|
Deferred Tax
|
Deferred Tax
|
||||||||||||||
|
Assets
|
Liabilities
|
Assets
|
Liabilities
|
||||||||||||
|
(in thousands)
|
|||||||||||||||
|
Unrealized capital gains, net
|
$ | — | $ | 45,302 | $ | — | $ | 44,142 | |||||||
|
Deferred policy acquisition costs
|
— | 11,430 | — | 13,216 | |||||||||||
|
Intangible assets
|
— | 4,648 | — | 6,106 | |||||||||||
|
Loss reserve discounting for tax reporting
|
65,353 | — | 75,315 | — | |||||||||||
|
Unearned premiums
|
10,257 | — | 11,988 | — | |||||||||||
|
Allowance for bad debt
|
2,661 | — | 3,925 | — | |||||||||||
|
Accrued liabilities
|
9,735 | — | 15,688 | — | |||||||||||
|
Minimum tax credit
|
13,055 | — | 2,831 | — | |||||||||||
|
Other
|
3,173 | 776 | 5,841 | 8,622 | |||||||||||
|
Total
|
$ | 104,234 | $ | 66,156 | $ | 115,588 | $ | 72,086 | |||||||
|
Deferred income taxes, net
|
$ | 38,078 | $ | 43,502 | |||||||||||
At December 31, 2010, the Company had no net operating loss carry forward.
Deferred tax assets are required to be reduced by a valuation allowance if it is more likely than not that all or some portion of the deferred tax asset will not be realized. Realization of the deferred income tax asset is dependent on the Company generating sufficient taxable income in future years as the deferred income tax charges become currently deductible for tax reporting purposes. Although realization is not assured, management believes that it is more likely than not that the net deferred income tax asset will be realized.
82
9. Liability for Unpaid Losses and Loss Adjustment Expenses
The following table represents a reconciliation of changes in the liability for unpaid losses and LAE for the years ended:
|
December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Unpaid losses and LAE, gross of reinsurance, at beginning of period
|
$ | 2,425,658 | $ | 2,506,478 | $ | 2,269,710 | ||||||
|
Less reinsurance recoverable, excluding bad debt allowance, on unpaid losses and LAE
|
1,052,505 | 1,076,350 | 1,052,641 | |||||||||
|
Net unpaid losses and LAE at beginning of period
|
1,373,153 | 1,430,128 | 1,217,069 | |||||||||
|
Losses and LAE, net of reinsurance, acquired in business combination
|
— | — | 247,006 | |||||||||
|
Losses and LAE, net of reinsurance, incurred in:
|
||||||||||||
|
Current year
|
227,143 | 283,827 | 226,643 | |||||||||
|
Prior years
|
(14,130 | ) | (51,359 | ) | (71,707 | ) | ||||||
|
Total net losses and LAE incurred during the period
|
213,013 | 232,468 | 154,936 | |||||||||
|
Deduct payments for losses and LAE, net of reinsurance, related to:
|
||||||||||||
|
Current year
|
55,827 | 74,944 | 53,397 | |||||||||
|
Prior years
|
206,653 | 214,499 | 135,486 | |||||||||
|
Total net payments for losses and LAE during the period
|
262,480 | 289,443 | 188,883 | |||||||||
|
Ending unpaid losses and LAE, net of reinsurance
|
1,323,686 | 1,373,153 | 1,430,128 | |||||||||
|
Reinsurance recoverable, excluding bad debt allowance, on unpaid losses and LAE
|
956,043 | 1,052,505 | 1,076,350 | |||||||||
|
Unpaid losses and LAE, gross of reinsurance, at end of period
|
$ | 2,279,729 | $ | 2,425,658 | $ | 2,506,478 | ||||||
Total net losses and LAE included in the above table excludes the impact of the amortization of the deferred reinsurance gain–LPT Agreement (Note 10).
Estimates of incurred losses and LAE attributable to insured events of prior years have decreased due to continued favorable development in such prior accident years.
The major sources of this favorable development in all the years presented above include actual paid losses that have been less than expected and the impact of new information on selected patterns of claims emergence and payment used in the projection of future loss payments.
In California, where the Company’s operations began on July 1, 2002, the actuaries’ and management’s initial expectations of the ultimate level of its losses and patterns of loss emergence and payment were based on benchmarks derived from analyses of historical insurance industry data in California. No historical data from the Company’s California insurance subsidiary existed prior to July 1, 2002; however, some historical data was available for the prior years for some of the market segments the Company entered in California, but was limited as to the number of loss reserve evaluation points available. The industry-based benchmarks were judgmentally adjusted for the anticipated impact of significant environmental changes, specifically the enactment of major changes to the statutory workers’ compensation benefit structure and the manner in which claims are administered and adjudicated in California. The actual emergence and payment of claims by the Company’s California insurance subsidiary has been more favorable than those initial expectations, due at least in part to the enactment of the major changes in the California workers’ compensation environment. Other insurance companies writing workers’ compensation insurance in California also have experienced claims emergence and payment patterns more favorable than anticipated following the enactment of legislative changes.
In Nevada, the Company has compiled a lengthy history of workers’ compensation claims payment patterns based on the business of the Fund and EICN, but the emergence and payment of claims in recent years has been more favorable than in the long-term history in Nevada with the Fund. The expected patterns of claim payments and emergence used in the projection of the Company’s ultimate claim payments are based on both the long and short-term historical paid data. In recent evaluations, claim patterns have continued to emerge in a manner consistent with short-term historical data. Consequently, the Company’s selection of claim projection patterns has relied more heavily on patterns observed in recent years.
83
The Company continues to develop its own loss experience and will rely more on its experience and less on historical industry data in projecting its reserve requirements as such data becomes available. As the actual experience of the Company emerges, it will continue to evaluate prior estimates, which may result in additional adjustments in reserves.
A $1.6 million expense related to the commutation of certain reinsurance treaties, and a $0.9 million expense related to the write-off of certain reinsurance recoverables that had previously been accounted for as an allowance for bad debt, increased losses and LAE incurred in prior periods for the year ended December 31, 2010, which are included in the $14.1 million prior period development.
Loss reserves shown in the consolidated balance sheets are net of $18.2 million and $19.2 million for anticipated subrogation recoveries as of December 31, 2010 and 2009, respectively.
10. Reinsurance
The Company is involved in the cession and assumption of reinsurance with non-affiliated companies. Risks are reinsured with other companies on both a quota share and excess of loss basis.
Reinsurance transactions reflected in the accompanying consolidated statements of income were as follows for the years ended December 31:
|
2010
|
2009
|
2008
|
||||||||||||||||||||||
|
Written
|
Earned
|
Written
|
Earned
|
Written
|
Earned
|
|||||||||||||||||||
|
(in thousands)
|
||||||||||||||||||||||||
|
Direct premiums
|
$ | 319,773 | $ | 328,165 | $ | 376,651 | $ | 411,897 | $ | 315,818 | $ | 335,547 | ||||||||||||
|
Assumed premiums
|
2,504 | 2,800 | 3,298 | 4,009 | 2,574 | 3,475 | ||||||||||||||||||
|
Gross premiums
|
322,277 | 330,965 | 379,949 | 415,906 | 318,392 | 339,022 | ||||||||||||||||||
|
Ceded premiums
|
(9,179 | ) | (9,179 | ) | (11,659 | ) | (11,659 | ) | (10,075 | ) | (10,075 | ) | ||||||||||||
|
Net premiums
|
$ | 313,098 | $ | 321,786 | $ | 368,290 | $ | 404,247 | $ | 308,317 | $ | 328,947 | ||||||||||||
|
Ceded losses and LAE incurred
|
$ | 15,111 | $ | 38,075 | $ | 23,558 | ||||||||||||||||||
Ceded losses and LAE incurred includes the amortization of the deferred reinsurance gain – LPT Agreement.
Excess of Loss Reinsurance
The Company maintains reinsurance for losses from a single occurrence or event in excess of $5.0 million and up to $200.0 million, subject to a $2.0 million annual aggregate deductible and certain exclusions. The reinsurance coverage includes coverage for acts of terrorism, excluding nuclear, biological, chemical, and radiological events. Any liability outside the coverage limits of the reinsurance program is retained by the Company.
LPT Agreement
Recoverables from reinsurers on unpaid losses and LAE amounted to $1.0 billion and $1.1 billion at December 31, 2010 and 2009, respectively. At December 31, 2010 and 2009, approximately $0.8 billion and $0.9 billion, respectively, of those recoverables were related to the LPT Agreement that was entered into in 1999 by the Fund and assumed by EICN. Under the LPT Agreement, substantially all of the Fund’s losses and LAE on claims incurred prior to July 1, 1995, have been ceded to three unaffiliated reinsurers on a 100% quota share basis. Investments have been placed in trust by the three reinsurers as security for payment of the reinsured claims. Under the LPT Agreement, $1.5 billion in liabilities for the incurred but unpaid losses and LAE related to claims incurred prior to July 1, 1995, were reinsured for consideration of $775 million. The LPT Agreement provides coverage up to $2.0 billion. Through December 31, 2010, the Company has paid losses and LAE claims totaling $530.8 million related to the LPT Agreement.
The initial deferred gain resulting from the LPT Agreement was recorded as a liability in the accompanying consolidated balance sheets and is being amortized using the recovery method, whereby the amortization is determined by the proportion of actual reinsurance recoveries to total estimated recoveries. The Company amortized $18.2 million, $18.0 million, and $18.4 million of the deferred gain for the years ended December 31, 2010, 2009, and 2008, respectively. There were no adjustments to the direct reserves ceded under the LPT Agreement or related adjustment to the deferred
84
gain for the years ended December 31, 2010, 2009, and 2008. The amortization of the deferred gain and adjustments due to development in the reserves are recorded in losses and LAE incurred in the accompanying consolidated statements of income. The remaining deferred gain was $370.3 million and $388.6 million as of December 31, 2010 and 2009, respectively, which is included in the accompanying consolidated balance sheets as deferred reinsurance gain – LPT Agreement.
The Company is also entitled to receive a contingent profit commission under the LPT Agreement. The Company accrues the estimated ultimate contingent profit commission to be received through June 30, 2024. The estimate was revised to increase the ultimate contingent profit commission by $0.8 million and $15.0 million, for the years ended December 31, 2010 and 2009, respectively. The Company recorded no change to the estimate for the year ended December 31, 2008. As of December 31, 2010, and 2009, the Company had a receivable of $1.7 million and a receivable of $0.9 million related to the contingent profit commission, respectively.
Funds Held
In the fourth quarter of 2010, the Company re-negotiated the terms of a reinsurance agreement with Clarendon, which resulted in the release and return of funds held by Clarendon in the amount of $74.6 million, The Company placed $47.1 million in trust, of which $35.0 million was placed in an investment trust and $12.1 million is classified as restricted cash and cash equivalents, for the benefit of Clarendon to support the liabilities under the reinsurance agreement and invested the remaining $27.5 million.
11. Notes Payable
Notes payable is comprised of the following:
|
December 31,
|
|||||||
|
2010
|
2009
|
||||||
|
(in thousands)
|
|||||||
|
Amended Credit Facility, due December 31, 2015 with variable interest, as described below
|
$ | 100,000 | $ | 100,000 | |||
|
Dekania Surplus Note, due April 30, 2034 with variable interest of 425 basis points above 90-day LIBOR
|
10,000 | 10,000 | |||||
|
ICONS Surplus Note, due May 26, 2034 with variable interest of 425 basis points above 90-day LIBOR
|
12,000 | 12,000 | |||||
|
Alesco Surplus Note, due December 15, 2034 with variable interest of 405 basis points above 90-day LIBOR
|
10,000 | 10,000 | |||||
|
Balance
|
$ | 132,000 | $ | 132,000 | |||
On December 28, 2010, the Company entered into the Third Amended and Restated Credit Agreement (Amended Credit Facility) with Wells Fargo Bank, National Association (Wells Fargo), under which the Company is provided with: (a) $100.0 million line of credit through December 31, 2011; (b) $90.0 million line of credit from January 1, 2012 through December 31, 2012; (c) $80.0 million line of credit from January 1, 2013 through December 31, 2013; (d) $70 million line of credit from January 1, 2014 through December 31, 2014; and (e) $60 million line of credit from January 1, 2015 through December 31, 2015. Amounts outstanding bear interest at a rate equal to, at the Company’s option: (a) a fluctuating rate of 1.75% above prime rate or (b) a fixed rate that is 1.75% above the LIBOR rate then in effect. The Amended Credit Facility is secured by fixed maturity securities and cash and cash equivalents that had a fair value of $131.0 million at December 31, 2010. The Amended Credit Facility contains customary non-financial covenants and requires EHI to maintain $5.0 million of cash and cash equivalents at all times. The Company is currently in compliance with all applicable covenants.
On September 30, 2008, EHI borrowed $150.0 million through the Second Amended Restated Credit Facility with Wells Fargo (Existing Credit Facility. The proceeds borrowed under the Existing Credit Facility were used to finance the acquisition of AmCOMP (see Note 4) and for general working capital purposes. Interest paid during the years ended December 31, 2010, 2009, and 2008, including the interest rate swap (see Note 12), totaled $4.4 million, $5.8 million, and $1.2 million, respectively. In accordance with the terms of the contract, a repayment of $50.0 million was made toward the Amended Credit Facility on December 30, 2009.
EPIC has a $10.0 million surplus note to Dekania CDO II, Ltd., issued as part of a pooled transaction. The note matures in 2034 and became callable by the Company in the second quarter of 2009. The terms of the note provide for quarterly interest payments at a rate 425 basis points in excess of the 90-day LIBOR. Both the payment of interest and repayment of the principal under this note and the surplus notes described in the succeeding two paragraphs are subject to the prior
85
approval of the Florida Department of Financial Services. Interest paid during the year ended December 31, 2010 and 2009 was $0.5 million and $0.6 million, respectively, and during the two months ended December 31, 2008 was $0.2 million. Interest accrued as of December 31, 2010 and 2009 was $0.1 million.
EPIC has a $12.0 million surplus note, to ICONS, Inc., issued as part of a pooled transaction. The note matures in 2034 and became callable by the Company in the second quarter of 2009. The terms of the note provide for quarterly interest payments at a rate 425 basis points in excess of the 90-day LIBOR. Interest paid during the years ended December 31, 2010 and 2009, was $0.6 million and $0.7 million, respectively, and during the two months ended December 31, 2008, was $0.2 million. Interest accrued as of December 31, 2010 and 2009 was $0.1 million.
EPIC has a $10.0 million surplus note, to Alesco Preferred Funding V, LTD, issued as part of a pooled transaction. The note matures in 2034 and became callable by the Company in the fourth quarter of 2009. The terms of the note provide for quarterly interest payments at a rate 405 basis points in excess of the 90-day LIBOR. Interest paid during the years ended December 31, 2010 and 2009, was $0.4 million and $0.5 million, respectively, and during the two months ended December 31, 2008, was $0.2 million. Interest accrued as of December 31, 2010 and 2009 was $0.1 million and less than $0.1 million, respectively.
Principal payment obligations on notes payable outstanding at December 31, 2010, were as follows:
|
Year
|
Principal Due
|
||
|
(in thousands)
|
|||
|
2011
|
$ | 10,000 | |
|
2012
|
10,000 | ||
|
2013
|
10,000 | ||
|
2014
|
10,000 | ||
|
2015
|
60,000 | ||
|
Thereafter
|
32,000 | ||
12. Derivatives
Interest Rate Swap
On September 30, 2008, the Company, in connection with the borrowings made under the Existing Credit Facility (Note 11), executed an interest rate swap with Wells Fargo with a notional amount of $100.0 million. Execution of the interest rate swap established a fixed interest rate of 4.84%, on the notional amount, which expired September 30, 2010. The Company used its interest rate swap to mitigate the risks associated with unexpected cash outflows resulting from shifts in variable interest rates. As of December 31, 2009, the interest rate swap had a negative fair value of $2.2 million, and is included in other liabilities on the accompanying consolidated balance sheets. The corresponding unrealized losses of $2.2 million for the year ended December 31, 2009 is included in accumulated other comprehensive income, net.
13. Commitments and Contingencies
Leases
The Company leases office facilities and certain equipment under operating and capital leases. Most leases have renewal options, typically with increased rental rates during the option period. Certain of these leases contain options to purchase the property at amounts that approximate fair market value; other leases contain options to purchase at a bargain purchase price. At December 31, 2010, the remaining lease terms expire over the next eight years.
86
The future lease payments for the next five years and thereafter on these non-cancelable operating and capital leases at December 31, 2010, were as follows:
|
Year
|
Operating Leases
|
Capital Leases
|
|||||
|
(in thousands)
|
|||||||
|
2011
|
$ | 6,825 | $ | 614 | |||
|
2012
|
6,549 | 1,065 | |||||
|
2013
|
5,380 | 486 | |||||
|
2014
|
5,034 | — | |||||
|
2015
|
3,998 | — | |||||
|
Thereafter
|
5,381 | — | |||||
| $ | 33,167 | $ | 2,165 | ||||
Included in the future minimum capital lease payments are future interest charges of $0.2 million. Facilities rent expense was $8.9 million, $7.4 million, and $5.9 million for the years ended December 31, 2010, 2009, and 2008, respectively.
Property held under capital leases is included in property and equipment as follows:
|
Asset Class
|
2010
|
2009
|
||||||
|
(in thousands)
|
||||||||
|
Furniture and equipment
|
$ | 100 | $ | 100 | ||||
|
Computers and software
|
1,282 | 1,758 | ||||||
|
Automobiles
|
1,880 | — | ||||||
| 3,262 | 1,858 | |||||||
|
Accumulated amortization
|
(1,076 | ) | (379 | ) | ||||
|
Total
|
$ | 2,186 | $ | 1,479 | ||||
Contingencies Surrounding Insurance Assessments
The Company writes workers’ compensation insurance in California in which unpaid workers’ compensation liabilities from insolvent insurers are the responsibility of the California Insurance Guarantee Association (CIGA). The Company passes through the CIGA assessment to its policyholders via a surcharge based upon the estimated annual premium at the policy’s inception and has received, and expects to continue to receive, these guarantee fund assessments which are paid to CIGA based on premiums written by the Company. As of December 31, 2010 and 2009, the Company recorded an asset of $6.2 million and $7.1 million, respectively, in other assets, for assessments paid to the CIGA that includes prepaid policy surcharges still to be collected in the future from policyholders.
The Company also writes workers’ compensation insurance in other states with similar obligations as those in California. In these states, the Company is directly responsible for payment of the assessment. Generally, assessments are levied by guaranty associations within the state up to prescribed limits on all insurers doing business in that state on the basis of the proportionate share of premiums written by insurers doing business in that state in the lines of business in which the impaired, insolvent or failed insurer is engaged. The Company accrues a liability for estimated assessments as direct premiums are written and defers these costs and recognizes them as an expense as the related premiums are earned. The Company is continually notified of assessments from various states relating to insolvencies in that particular state; however, the Company estimates the potential future assessment in the absence of an actual assessment. As of December 31, 2010 and 2009, the Company recorded an estimate of $2.1 million and $4.5 million, respectively, for its expected liability for guaranty fund assessments, in states other than California. The guaranty fund assessments are expected to be paid within two years of recognition.
Additionally, as of December 31, 2010 and 2009 guarantee fund receivable assets, excluding CIGA, of $0.6 million and $1.1 million, respectively, are included in other assets, as they can be used as a credit against future premium taxes owed. Maximum contributions required by law in any one state in which the Company offers insurance vary between 0.2% and 2.0% of direct premiums written.
87
14. Stockholders’ Equity
Stock Repurchase Program
On February 21, 2008, the EHI Board of Directors (Board of Directors) authorized a stock repurchase program (the 2008 Program). The 2008 Program authorized the Company to repurchase up to $100.0 million of the Company’s common stock through June 30, 2009. On February 25, 2009, the Board of Directors extended the 2008 Program through December 31, 2009. From inception of the 2008 Program through the end of the 2008 Program on December 31, 2009, the Company repurchased 6,743,862 shares at a cost of $88.7 million, or $13.16 per share, including commissions.
On November 4, 2009, the Board of Directors authorized a share repurchase program for up to $50.0 million of the Company’s common stock from January 1, 2010 through December 31, 2010 (the 2010 Program). Through September 30, 2010, the Company repurchased 3,291,709 shares of common stock under the 2010 Program at an average price of $15.19 per share, including commissions, for a total of $50.0 million.
On November 3, 2010, the Board of Directors authorized a share repurchase program for up to $100.0 million of the Company’s common stock from November 8, 2010 through June 30, 2012 (the 2011 Program). The Company expects that shares may be purchased at prevailing market prices through a variety of methods, including open market or private transactions, in accordance with applicable laws and regulations. The timing and actual number of shares repurchased
will depend on a variety of factors, including the share price, corporate and regulatory requirements, and other market and economic conditions. Repurchases under the 2011 Program may be commenced or suspended from time to time without prior notice, and the program may be suspended or discontinued at any time. Through December 31, 2010, the Company repurchased 867,149 shares of common stock under the 2011 Program at an average price per share of $16.59, including commissions, for a total of $14.4 million.
The 14,813,992 shares of common stock repurchased by the Company since its initial public offering in February 2007 under all programs are reported as treasury stock, at cost, in the accompanying consolidated balance sheets. As of December 31, 2010, the average cost of common stock repurchased through the Company’s stock repurchase programs since inception was $15.40 per share.
15. Stock-Based Compensation
The Employers Holdings, Inc. Amended and Restated Equity and Incentive Plan (the Plan) is administered by the Compensation Committee of the Board of Directors, which is authorized to grant, at its discretion, awards to officers, employees, non-employee directors, consultants, and independent contractors. The maximum number of common shares reserved for grants of awards under the Plan is 7,105,838 shares. The Plan provides for the grant of stock options (both incentive stock options and nonqualified stock options), stock appreciation rights, restricted stock, restricted stock units, stock-based performance awards, and other stock-based awards.
As of December 31, 2010, nonqualified stock options, restricted stock units, and performance share awards have been granted, but no incentive stock options, stock appreciation rights, or restricted stock have been granted under the Plan.
Net stock-based compensation expense recognized in the accompanying consolidated statements of income was as follows:
|
Years Ended
|
|||||||||||
|
2010
|
2009
|
2008
|
|||||||||
|
Stock-based compensation expense related to:
|
(in thousands)
|
||||||||||
|
Nonqualified stock options
|
$ | 2,039 | $ | 1,782 | $ | 1,254 | |||||
|
Restricted stock units
|
2,014 | 1,473 | 902 | ||||||||
|
Performance shares
|
— | 2,111 | 1,005 | ||||||||
|
Total
|
4,053 | 5,366 | 3,161 | ||||||||
|
Less: related tax benefit
|
1,419 | 1,759 | 1,096 | ||||||||
|
Net stock-based compensation expense
|
$ | 2,634 | $ | 3,607 | $ | 2,065 | |||||
88
Nonqualified Stock Options
During the year ended December 31, 2007, the Company made “founders’ grants” to employees, excluding senior officers, in the form of 186,000 nonqualified stock options and also awarded 420,916 nonqualified stock options to its officers. The founders’ grants awards vest pro rata on each of the first three anniversaries of the effective date of EHI’s IPO. The options awarded to the officers of the Company vested 25% on February 8, 2008, 2009, and 2010 and the remaining 25% vested pro rata on February 8, 2011. All options granted in 2007 have an exercise price equal to the fair market value of the Company’s common stock on the date of grant.
On May 29, 2008, the Company awarded 475,167 options to the officers of the Company. These options have a service vesting period of four years and vested 25% on May 29, 2009 and 2010, and will vest 25% on the subsequent two anniversaries of such date. The options are subject to accelerated vesting in certain limited circumstances, such as: death or disability, or in connection with a change of control of the Company. The options expire seven years from the date of grant.
On May 28, 2009, the Company awarded 531,082 options to certain officers of the Company. These options have a service vesting period of four years and vested 25% on May 28, 2010, and will vest 25% on each of the subsequent three anniversaries of such date. The options are subject to accelerated vesting in the following circumstances: death or disability of the holder, or in connection with a change of control of the Company. The options expire seven years from the date of grant.
On March 30, 2010, the Company awarded 406,020 options to certain officers of the Company. These options have a service vesting period of four years and vest 25% on March 30, 2011, and 25% on each of the subsequent three anniversaries of such date. The options are subject to accelerated vesting in the following circumstances: death or disability of the holder, or in connection with a change of control of the Company. The options expire seven years from the date of grant.
The fair value of the stock options granted is estimated using a Black-Scholes option pricing model that uses the assumptions noted in the following table. During the years ended December 31, 2010 and 2009, the expected stock price volatility used to value the options granted in 2010 and 2009 was based on the volatility of the Company’s historical stock price since February 2007. During the year ended December 31, 2008, the expected stock price volatility used to value the options granted was based on a weighted average of the Company’s historical stock price volatility since February 2007 and the historical volatility of peer companies’ stock for a period of time equal to the expected term of the options. The expected term of the options granted in 2010, 2009, and 2008 was calculated using the ‘plain-vanilla’ calculation provided in the guidance of the Securities and Exchange Commission’s Staff Accounting Bulletin No. 107. The dividend yield was calculated using amounts authorized by the Board of Directors. The risk-free interest rate is the yield on the grant date of the options of U.S. Treasury zero coupon securities with a maturity comparable to the expected term of the options.
The Company anticipates issuing new shares upon exercise of stock options.
The fair market value of the stock options granted during the years ended December 31, 2010, 2009, and 2008 were calculated using the following weighted average assumptions:
|
2010
|
2009
|
2008
|
||||||||||
|
Expected volatility
|
47.3 | % | 51.0 | % | 34.9 | % | ||||||
|
Expected life (in years)
|
4.8 | 4.8 | 4.8 | |||||||||
|
Dividend yield
|
1.6 | % | 2.0 | % | 1.3 | % | ||||||
|
Risk-free interest rate
|
2.6 | % | 2.5 | % | 3.4 | % | ||||||
|
Weighted average grant date fair values of options granted
|
$ | 5.80 | $ | 4.59 | $ | 6.01 | ||||||
89
Changes in outstanding stock options for the year ended December 31, 2010 were as follows:
|
`
|
Number of
Options
|
Weighted-
Average Exercise
Price
|
Weighted
Average
Remaining
Contractual Life
|
||||||||
|
Options outstanding at January 1, 2010:
|
1,512,706 | $ | 16.30 | 4.5 | |||||||
|
Granted
|
406,020 | 15.31 | 6.2 | ||||||||
|
Exercised
|
(7,783 | ) | 12.03 | ||||||||
|
Expired
|
(35,441 | ) | 17.94 | ||||||||
|
Forfeited
|
(112,399 | ) | 15.03 | ||||||||
|
Options outstanding at December 31, 2010
|
1,763,103 | 16.14 | 4.8 | ||||||||
|
Exercisable at December 31, 2010
|
745,295 | 17.47 | 3.5 | ||||||||
The fair value of options that vested in 2010 was $1.8 million and as of December 31, 2010, outstanding and exercisable options had intrinsic values of $3.5 million and $0.7 million, respectively. At December 31, 2010, the Company had yet to recognize $4.0 million in deferred compensation related to nonqualified stock options grants and expects to recognize these costs on a straight-line basis over the next 39 months.
Performance Share Awards
On August 8, 2007, officers of the Company were awarded, in aggregate, 140,311 performance share awards (PSAs) for a performance period that ended December 31, 2009. These PSAs were subject to certain performance targets with ultimate payouts of 150% of the target award. The fair market value of the PSAs on the date of grant was $2.6 million. In March 2010, 196,071 PSAs were vested.
Restricted Stock Units
On May 29, 2008, 23,760 restricted stock units (RSUs) awarded to the non-employee members of the Board of Directors during 2007, vested in connection with the annual stockholders meeting. The vested RSUs will be settled in common stock six months following the awardees’ termination of service from the Board of Directors. Prior to settlement, dividend equivalents are paid with respect to these vested RSUs and are credited as additional vested RSUs.
On May 29, 2009, 24,984 RSUs, awarded to the non-employee members of the Board of Directors during 2008, vested in connection with the annual stockholders meeting. 9,369 of the vested RSUs, at the awardees’ election, were settled in common stock and the remaining 15,615 RSUs were deferred until six months following the awardees’ termination of service from the Board of Directors. In the event of a deferral election, dividend equivalents are paid with respect to vested RSUs and are credited as additional vested RSUs. During the years ended December 31, 2009 and 2008, in connection with the Company’s dividends to its stockholders, an aggregate of 632 and 240 RSUs were credited to vested RSU holders, respectively.
On May 28, 2009, the Company awarded the non-employee members of the Board of Directors, in the aggregate, 40,536 RSUs. These RSUs vest on May 28, 2010, except for accelerated vesting in the case of death or disability of the Director or in connection with a change of control. Vested RSUs will be settled in common stock within 30 days after the vesting date or can be deferred until six months following the awardees’ termination of service from the Board of Directors, at the awardees’ election. In the event of a deferral election, dividend equivalents are paid with respect to vested RSUs and are credited as additional vested RSUs.
On May 27, 2010, the Company awarded the non-employee members of the Board of Directors, in the aggregate, 30,728 RSUs. These RSUs vest on May 27, 2011, except for accelerated vesting in the case of death or disability of the Director or in connection with a change of control. Vested RSUs will be settled in common stock within 30 days after the vesting date or can be deferred until six months following the awardees’ termination of service from the Board of Directors, at the awardees’ election. In the event of a deferral election, dividend equivalents are paid with respect to vested RSUs and are credited as additional vested RSUs.
On May 29, 2008, the Company awarded 152,564 RSUs to certain officers of the Company. The RSUs have a service vesting period of four years and vested 25% on May 29, 2009, and the subsequent three anniversaries of such date. On May 29, 2009, 35,874 RSUs, vested with an intrinsic value of $0.4 million. Of the 35,874 RSUs vested, 10,151 shares of
90
common stock were withheld to satisfy minimum employee tax withholding. The RSUs are subject to accelerated vesting in certain limited circumstances, such as: death or disability of the holder, or in connection with a change of control of the Company.
On May 28, 2009, the Company awarded 176,871 RSUs to certain officers of the Company. The RSUs have a service vesting period of four years and vest 25% on May 28, 2010 and 25% on each of the subsequent three anniversaries of such date. The RSUs are subject to accelerated vesting in certain limited circumstances, such as: death or disability of the holder, or in connection with a change of control of the Company.
On March 30, 2010, the Company awarded 163,660 RSUs to certain officers of the Company. The RSUs have a service vesting period of four years and vest 25% on March 30, 2011 and 25% on each of the subsequent three anniversaries of such date. The RSUs are subject to accelerated vesting in certain limited circumstances, such as: death or disability of the holder, or in connection with a change of control of the Company.
Changes in outstanding RSUs for the year ended December 31, 2010 were as follows:
|
Number of
RSUs
|
Weighted Average
Grant Date
Fair Value
|
||||||
|
RSUs outstanding at January 1, 2010
|
365,343 | $ | 14.66 | ||||
|
Granted
|
195,301 | 15.36 | |||||
|
Forfeited
|
(38,837 | ) | 14.81 | ||||
|
Vested
|
(93,292 | ) | 14.60 | ||||
|
RSUs outstanding at December 31, 2010
|
428,515 | 14.98 | |||||
|
Vested but unsettled RSUs at December 31, 2010
|
66,495 | 15.43 | |||||
As of December 31, 2010 outstanding RSUs have an intrinsic value of $7.5 million.
16. Statutory Matters
Statutory Financial Data
The combined capital stock, surplus and net income of the Company’s insurance subsidiaries (EICN, ECIC, EPIC, and EAC), prepared in accordance with the statutory accounting practices of the National Association of Insurance Commissioners (NAIC) as well as statutory accounting principles permitted by the states of California, Florida, and Nevada (SAP), were as follows:
|
December 31,
|
|||||||
|
2010
|
2009
|
||||||
|
(in thousands)
|
|||||||
|
Capital stock and unassigned surplus
|
$ | 301,590 | $ | 351,419 | |||
|
Paid in capital
|
64,900 | 64,900 | |||||
|
Special surplus funds
|
55,771 | 213,027 | |||||
|
Surplus notes
|
32,000 | 32,000 | |||||
|
Total statutory surplus
|
$ | 454,261 | $ | 661,346 | |||
Net income for the Company’s insurance subsidiaries prepared in accordance with SAP for the years ended December 31, 2010, 2009 and 2008 was $59.1 million, $89.5 million and $101.7 million, respectively. Under SAP, the statutory operating results of EPIC and EAC are combined with the operating results of EICN and ECIC for the entire year of 2008, the year of the Acquisition.
Treatment of the LPT Agreement and the surplus notes (see Notes 10 and 11) are the primary differences in the SAP-basis capital stock and total surplus of the insurance subsidiaries of $454.3 million and $661.3 million, and the GAAP-basis equity of the Company of $490.1 million and $498.4 million as of December 31, 2010 and 2009, respectively. Under SAP accounting, the retroactive reinsurance gain resulting from the LPT Agreement is recorded as a special component of surplus (special surplus funds) in the initial year of the contract, and not reported as unassigned surplus until the
91
Company has recovered amounts in excess of the original consideration paid. The special surplus funds are also reduced by the amount of extraordinary dividends as approved by the Nevada Division of Insurance. Under GAAP accounting, the gain is deferred and amortized over the period the underlying reinsured claims are paid (see Note 10). Under SAP, the surplus notes are recorded as a separate component of surplus. Under GAAP, the surplus notes are considered debt.
Insurance Company Dividends
The ability of EHI to pay dividends on the Company’s common stock and to pay other expenses will be dependent to a significant extent upon the ability of the Nevada domiciled insurance company, EICN, and the Florida domiciled insurance company, EPIC, to pay dividends to their immediate holding company, Employers Group, Inc. (EGI) and, in turn, the ability of EGI to pay dividends to EHI. ECIC and EAC have the ability to declare and pay dividends to EICN and EPIC, respectively, subject to certain restrictions. The amount of dividends each of the Company’s subsidiaries may pay to their immediate parent is limited by the laws of their respective state of domicile.
Nevada law limits the payment of cash dividends by EICN to its parent by providing that payments cannot be made except from available and accumulated surplus, otherwise unrestricted (unassigned), and derived from realized net operating profits and realized and unrealized capital gains. A stock dividend may be paid out of any available surplus. A cash or stock dividend prohibited by these restrictions may only be declared and distributed as an extraordinary dividend upon the prior approval of the Nevada Commissioner of Insurance (Nevada Commissioner). EICN may not pay such an extraordinary dividend or make an extraordinary distribution until the Nevada Commissioner either approves or does not disapprove the payment within 30 days after receiving notice of its declaration. An extraordinary dividend or distribution is defined by statute to include any dividend or distribution of cash or property whose fair market value, together with that of other dividends or distributions made within the preceding 12 months, exceeds the greater of: (a) 10% of EICN’s statutory surplus as regards to policyholders at the next preceding December 31; or (b) EICN’s statutory net income, not including realized capital gains, for the 12-month period ending at the next preceding December 31.
As of December 31, 2010, EICN had positive unassigned surplus of $243.1 million. During 2010, EICN paid dividends of $100.3 million to EGI, and subsequently from EGI to EHI. Additionally, as a result of approval by the Nevada Commissioner in 2010 and 2008, extraordinary dividends totaling $150.0 million and $355.0 million were paid to EGI, and in turn to EHI, prior to December 31, 2010 and 2008, respectively, from EICN’s special surplus. As a result of the payment of the extraordinary dividend from special surplus in 2010, any dividends paid by EICN through June 3, 2011 will require prior approval by the Nevada Commissioner. The maximum dividends that may be paid by EICN between June 3 and December 31, 2011 without prior approval is $51.9 million.
Under Florida law, without regulatory approval, EPIC may pay dividends if they do not exceed the greater of: the lesser of 10% of surplus or net income, not including realized capital gains, plus a 2-year carryforward; 10% of surplus, with dividends payable limited to unassigned funds minus 25% of unrealized capital gains; or, the lesser of 10% of surplus or net investment income plus a 3-year carryforward with dividends payable limited to unassigned funds minus 25% of unrealized capital gains. During 2010, EPIC declared and paid a dividend of $14.9 million to EGI, and in turn to EHI. The maximum dividends that may be paid in 2011 by EPIC without prior approval, is $15.5 million.
Regulatory Requirements and Restrictions
ECIC is subject to regulation by the California Department of Insurance (California DOI). The ability of ECIC to pay dividends was further limited by restrictions imposed by the California DOI in its approval of the Company’s October 1, 2008 reinsurance pooling agreement. Under that approval: (a) ECIC must initiate discussions of its business plan with the California DOI if its premium to policyholder surplus ratio exceeds 1.5 to 1; (b) ECIC will not exceed a ratio of premium to policyholder surplus of 2 to 1 without approval of the California DOI; (c) if at any time ECIC’s policyholder surplus decreases to 80% or less than the September 30, 2008 balance, ECIC shall cease issuing new policies in California but may continue to renew existing policies until it has (i) received a capital infusion to bring its surplus position to the same level as that as of September 30, 2008 and (ii) submitted a new business plan to the California DOI; (d) ECIC will maintain a risk based capital (RBC) level of at least 350%; (e) should ECIC fail to comply with any commitments listed herein, ECIC will consent to any request by the California DOI to cease issuing new policies in California, but may continue to renew existing policies until such time that as ECIC is able to achieve full compliance with each commitment; and (f) the obligations listed shall only terminate with the written consent of the California DOI.
92
EPIC and EAC are subject to regulation by the Florida Department of Financial Services (FDFS). Florida statute Section 624.408 requires EPIC and EAC to maintain minimum capital and surplus of the greater of $4.0 million or 10% of total liabilities. Florida statute Section 624.4095 requires EPIC and EAC to maintain a ratio of written premiums times 1.25 to surplus of no greater than 10-to-1 for gross written premiums and 4-to-1 for net written premiums. During the years ended December 31, 2010, 2009, and 2008, EPIC and EAC were in compliance with these statutes.
Additionally, EICN, ECIC, EPIC, and EAC are required to comply with NAIC RBC requirements. RBC is a method of measuring the amount of capital appropriate for an insurance company to support its overall business operations in light of its size and risk profile. NAIC RBC standards are used by regulators to determine appropriate regulatory actions relating to insurers that show signs of weak or deteriorating conditions. As of December 31, 2010, 2009, and 2008, EICN, ECIC, EPIC, and EAC’s total adjusted capital was above all regulatory action levels.
ECIC, EPIC, and EAC are subject to Florida statute and applicable regulations related to Florida excessive profits for workers’ compensation insurance companies. Florida excessive profits are calculated based upon a complex statutory formula which is applied over a rolling three year period. Companies are required to file annual excessive profits forms, and they are required to return so-called “Florida excessive profits” to policyholders in the form of a cash refund or credit toward the future purchase of insurance. As of December 31, 2010 and 2009, the Company had no amounts accrued for estimated additional Florida excessive profits based on its statutory underwriting results for the years ended 2007-2009.
17. Accumulated Other Comprehensive Income, Net
Accumulated other comprehensive income, net, is comprised of unrealized appreciation on investments classified as available-for-sale and unrealized depreciation on derivatives, net of deferred tax expense. The following table summarizes the components of accumulated other comprehensive income, net:
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Net unrealized gain on investments, before taxes
|
$ | 129,435 | $ | 130,550 | $ | 54,748 | ||||||
|
Net unrealized loss on derivatives, before taxes
|
— | (2,180 | ) | (3,868 | ) | |||||||
|
Deferred tax expense
|
(45,302 | ) | (44,558 | ) | (18,076 | ) | ||||||
|
Total accumulated other comprehensive income, net
|
$ | 84,133 | $ | 83,812 | $ | 32,804 | ||||||
The following table summarizes the changes in the components of total comprehensive income:
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Unrealized gains (losses) during the period, before taxes
|
$ | 11,202 | $ | 78,281 | $ | (32,214 | ) | |||||
|
Less: income tax expense (benefit)
|
4,292 | 26,759 | (11,007 | ) | ||||||||
|
Unrealized gains (losses) during the period, net of taxes
|
6,910 | 51,522 | (21,207 | ) | ||||||||
|
Less reclassification adjustment:
|
||||||||||||
|
Realized gains (losses) in net income
|
10,137 | 791 | (11,524 | ) | ||||||||
|
Income tax expense (benefit)
|
3,548 | 277 | (4,033 | ) | ||||||||
|
Reclassification adjustment for gains (losses) realized in net income
|
6,589 | 514 | (7,491 | ) | ||||||||
|
Other comprehensive income (loss)
|
321 | 51,008 | (13,716 | ) | ||||||||
|
Net income
|
62,799 | 83,021 | 101,785 | |||||||||
|
Total comprehensive income
|
$ | 63,120 | $ | 134,029 | $ | 88,069 | ||||||
18. Employee Benefit and Retirement Plans
The Company maintains two 401(k) defined contribution plans covering all eligible Company employees. One plan covers eligible employees of the Company that existed prior to the acquisition of AmCOMP (see Note 4) (the Employers 401(k) Plan). Beginning with the plan year 2007, the Company adopted a safe harbor matching contribution to the Employers 401(k) Plan. The safe harbor matching consists of a dollar-for-dollar matching contribution on salary deferrals up to 3% of compensation and then fifty-cents on the dollar matching contribution on salary deferrals from 3% to 5% of compensation. The Company’s contribution to the Employers 401(k) Plan was $1.4 million, $1.6 million, and $1.5 million for the years ended December 31, 2010, 2009, and 2008, respectively.
93
The second plan covers all eligible employees of the Company acquired in the AmCOMP acquisition (the AmCOMP 401(k) Plan). For employees covered under the AmCOMP 401(k) Plan, the Company’s discretionary match consists of a dollar-for-dollar matching contribution on salary deferrals up to 2% of compensation and then fifty-cents on the dollar matching contribution on salary deferrals for the next 4% of compensation. Expenses relating to the AmCOMP 401(k) Plan were $0.5 million and $0.7 million for the years ended December 31, 2010 and 2009, respectively, and $0.1 million for the two month period ended December 31, 2008.
19. Earnings Per Share
Basic earnings per share includes no dilution and is computed by dividing income applicable to common stockholders by the weighted average number of common shares outstanding for the period. Diluted earnings per share reflect the potential dilution of securities that could share in the earnings of equity. Diluted earnings per common share includes common shares assumed issued under the “treasury stock method,” which reflects the potential dilution that would occur if outstanding options were to be exercised.
The following table presents the net income and the weighted average shares outstanding used in the earnings per common share calculations for the years ended December 31:
|
2010
|
2009
|
2008
|
|||||||||
|
(in thousands, except share and per share data)
|
|||||||||||
|
Net income available to common stockholders – basic and diluted
|
$ | 62,799 | $ | 83,021 | $ | 101,785 | |||||
|
Weighted average number of common shares outstanding – basic
|
41,390,984 | 45,953,868 | 49,217,829 | ||||||||
|
Effect of dilutive securities:
|
|||||||||||
|
Performance share awards
|
— | 114,968 | 40,504 | ||||||||
|
Restricted stock units
|
129,335 | 21,996 | 2,895 | ||||||||
|
Dilutive potential common shares
|
129,335 | 136,964 | 43,399 | ||||||||
|
Weighted average number of common shares outstanding – diluted
|
41,520,319 | 46,090,832 | 49,261,228 | ||||||||
Diluted earnings per share exclude outstanding options and other common stock equivalents in periods where the inclusion of such potential common stock instruments would be anti-dilutive in the periods presented. For the years ended December 31, 2010, 2009, and 2008, 0.9 million, 1.0 million, and 1.0 million, respectively, of stock options were excluded from diluted earnings per share, as the options’ exercise price was greater than the average market price of the common stock during the period. During the same periods, 0.4 million, 0.7 million, and 0.2 million, respectively, of outstanding RSU’s and stock options were excluded from diluted earnings per share under the treasury method, as the potential proceeds on settlement or exercise was greater than the value of shares acquired.
20. Strategic Restructuring Plan
On July 2, 2010, the Company announced the reorganization of its operations to eliminate duplicative services and better align resources with business activity and growth opportunities. The Company combined its four regional operating units into two units, Eastern and Western, with the Strategic Partnerships and Alliances unit remaining structurally unchanged. In connection with these efforts and with general cost control efforts, the Company eliminated approximately 160 positions and announced the closure of four offices. The changes to the Company’s workforce were substantially completed in the third quarter of 2010.
During the year ended December 31, 2010, the Company recorded total restructuring charges of $6.1 million, including $3.9 million related to workforce reductions and $2.2 million related to leases for facilities that were vacated during the year. These charges are included in underwriting and other operating expense in the consolidated statements of income. As of December 31, 2010, the Company had accrued $0.2 million for personnel-related termination costs and $2.3 million related to leases for facilities that were vacated, which are included in accounts payable and accrued expenses in the accompanying consolidated balance sheets.
94
On January 23, 2009, the Company announced a strategic restructuring plan to achieve the corporate and operational objectives set forth as part of its acquisition and integration of AmCOMP, and in response to then current economic conditions.
The restructuring plan included a staff reduction of 14% of the Company’s total workforce and consolidation of corporate activities into the Company’s Reno, Nevada headquarters. During the year ended December 31, 2009, the Company incurred integration and restructuring charges of $5.7 million, including $2.8 million in personnel-related termination costs. These charges are included in underwriting and other operating expenses in the consolidated statements of income. Cash payments relating to the 2009 restructuring were $0.6 million and $5.1 million during the years ending December 31, 2010 and 2009, respectively. As of December 31, 2010 and 2009, the Company had $0.0 million and $0.6 million accrued, respectively, for the remaining 2009 restructuring costs that are included in accounts payable and accrued expenses in the accompanying consolidated balance sheets.
21. Selected Quarterly Financial Data (Unaudited)
Quarterly results for the years ended December 31, 2010 and 2009 were as follows:
|
2010 Quarters Ended
|
|||||||||||||||
|
March 31
|
June 30
|
September 30
|
December 31
|
||||||||||||
|
(in thousands except per share data)
|
|||||||||||||||
|
Net premiums earned
|
$ | 79,291 | $ | 78,235 | $ | 80,695 | $ | 83,565 | |||||||
|
Realized (losses) gains on investment, net
|
540 | 352 | 8 | 9,237 | |||||||||||
|
Losses and loss adjustment expenses
|
40,288 | 45,045 | 52,764 | 56,682 | |||||||||||
|
Commission expense (benefit)
|
9,905 | 9,176 | 9,971 | 9,416 | |||||||||||
|
Underwriting and other operating expenses
|
32,267 | 25,143 | 25,722 | 22,894 | |||||||||||
|
Income tax (benefit) expense
|
(530 | ) | 1,636 | 58 | 2,359 | ||||||||||
|
Net income
|
16,097 | 16,499 | 10,054 | 20,149 | |||||||||||
|
Earnings per common share:
|
|||||||||||||||
|
Basic
|
0.38 | 0.39 | 0.25 | 0.51 | |||||||||||
|
Diluted
|
0.38 | 0.39 | 0.25 | 0.51 | |||||||||||
|
2009 Quarters Ended
|
||||||||||||||||
|
March 31
|
June 30
|
September 30
|
December 31
|
|||||||||||||
|
(in thousands, except per share data)
|
||||||||||||||||
|
Net premiums earned
|
$ | 111,600 | $ | 104,381 | $ | 98,240 | $ | 90,026 | ||||||||
|
Realized (losses) gains on investment, net
|
(2,112 | ) | (392 | ) | 3,564 | (269 | ) | |||||||||
|
Losses and loss adjustment expenses
|
59,162 | 54,100 | 53,395 | 47,804 | ||||||||||||
|
Commission expense (benefit)
|
13,658 | 13,229 | (1,276 | ) | 10,539 | |||||||||||
|
Underwriting and other operating expenses
|
36,484 | 32,452 | 33,688 | 36,063 | ||||||||||||
|
Income tax expense (benefit)
|
(1,196 | ) | 3,300 | 4,594 | 2,579 | |||||||||||
|
Net income
|
20,855 | 20,345 | 30,557 | 11,264 | ||||||||||||
|
Earnings per common share:
|
||||||||||||||||
|
Basic
|
0.43 | 0.44 | 0.68 | 0.26 | ||||||||||||
|
Diluted
|
0.43 | 0.44 | 0.67 | 0.26 | ||||||||||||
Net Premiums Earned
The decrease in net premiums earned in 2009 and the first six months of 2010 was primarily due to the decrease in gross premium written, resulting from lower rates, competitive pressures, and changes in business conditions due to the economy and its impact on small businesses. In the third and fourth quarters of 2010 the net premiums earned increased primarily as a result of favorable adjustments in the final audit accrual.
95
Realized (Losses) Gains on Investments, Net
The Company evaluated its portfolio allocation during the fourth quarter of 2010 and elected to shift $20.0 million of equity securities into a high-yield dividend portfolio, resulting in a $9.2 million realized gain.
During the third quarter of 2009, the Company sold equity securities, the majority of which were previously impaired and realized a gain of $3.6 million.
Losses and Loss Adjustment Expenses
Favorable prior accident year reserve development was recognized in each of the first two quarters of 2010 in the amounts of $11.1 million and $5.5 million, respectively, and unfavorable loss development of $0.9 million, was recognized in the fourth quarter of 2010. The unfavorable development in the fourth quarter was related to the write-off of certain reinsurance recoverables that had previously been accounted for as an allowance for bad debt.
Favorable prior accident year reserve development was recognized in each of the quarters of 2009 in the amount of $13.5 million, $15.7 million, $10.4 million, and $11.8 million, for the first quarter through fourth quarters, respectively.
Commission Expense
During the fourth quarter of 2010 the Company reduced its estimate of certain administrative fees due under its joint marketing agreements by $3.0 million, which decreased the commission expense in the fourth quarter of 2010. The Company also re-negotiated the terms of certain reinsurance agreements, which increased commission expense by $1.8 million in the fourth quarter of 2010.
During the third and fourth quarters of 2009, the estimate on the LPT ultimate contingent profit commission was increased by $14.1 million and $0.9 million, respectively, yielding a net negative commission expense for the third quarter 2009.
Underwriting and Other Operating Expenses
Underwriting and other operating expenses declined in the first, second, and fourth quarters of 2010 as the Company managed its expenses, primarily through workforce reductions. The first quarter included charges of a $0.9 million expense related to workforce reductions. In the third quarter of 2010, the Company recorded a $4.3 million expense related to workforce reductions and leases for facilities that were vacated during the quarter. The fourth quarter included a $0.9 million expense related to leases for facilities that were vacated during that quarter.
During the first quarter of 2009, the Company announced a strategic restructuring plan (Note 20) and recognized an additional expense of $3.0 million for personnel-related termination costs. The increase in underwriting and other operating expenses in the fourth quarter 2009 was primarily attributable to an accrual of $2.3 million for management bonuses.
Income Taxes
Income tax expense (benefit) for interim periods is measured using an estimated effective tax rate for the annual period based on projected net income and tax adjustments. On an interim basis, actual results to date replace the projections and the annual effective tax rate is updated. A cumulative change is recorded in the quarter the effective tax rate changes.
The third and fourth quarters of 2009 were impacted by the favorable adjustments to the LPT contingent profit commission which is tax-exempt. The remaining quarterly variances are due to changes in the relative level of tax-exempt investment income to net income for the quarters.
22. Subsequent Events
On January 19, 2011, the Company and Martin J. Welch, the President and Chief Operating Officer of, among others, the insurance subsidiaries of the Company, mutually agreed to the separation of Mr. Welch’s employment with the Company. Effective February 1, 2011, Mr. Welch (i) ceased his employment with the Company and its subsidiaries, and (ii) resigned as a member of the Company’s Board of Directors and the Boards of Directors of all subsidiaries of the Company on which he served. Mr. Welch’s resignation was not the result of any disagreement with the Company on any matter relating to the Company’s operations, policies or practices.
The Company has negotiated a separation agreement with Mr. Welch that provided for severance pursuant to the terms of Mr. Welch’s existing employment agreement. Mr. Welch’s employment agreement is filed as Exhibit 10.4 to the Company’s Current Report on Form 8-K filed with the Securities and Exchange Commission on December 23, 2008.
96
Item 9. Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
None.
Item 9A. Controls and Procedures
Disclosure Controls and Procedures
We maintain disclosure controls and procedures (as defined in Rules 13a-15(e) and 15d-15(e) of the Securities Exchange Act of 1934, as amended (the “Exchange Act”)) designed to provide reasonable assurance that the information required to be reported in the Exchange Act filings is recorded, processed, summarized and reported within the time periods specified and pursuant to SEC regulations, including controls and procedures designed to ensure that this information is accumulated and communicated to management, including its chief executive officer and chief financial officer, as appropriate, to allow timely decisions regarding the required disclosure. It should be noted that, because of inherent limitations, our disclosure controls and procedures, however well designed and operated, can provide only reasonable, and not absolute, assurance that the objectives of the disclosure controls and procedures are met.
Our management, with the participation of our Chief Executive Officer and Chief Financial Officer, evaluated the effectiveness of our disclosure controls and procedures as of the end of the period covered by this report. Based upon that evaluation, our Chief Executive Officer and Chief Financial Officer have concluded that our disclosure controls and procedures were effective at a reasonable level of assurance as of December 31, 2010.
Management’s Report on Internal Control Over Financial Reporting
Management’s report regarding internal control over financial reporting is set forth in Item 8 of this Annual Report on Form 10-K under the caption “Management’s Report on Internal Control over Financial Reporting” and incorporated herein by reference.
Attestation Report of Independent Registered Public Accounting Firm
The attestation report of the Company’s independent registered public accounting firm regarding internal control over financial reporting is set forth in Item 8 of this Annual Report on Form 10-K under the caption “Report of Independent Registered Public Accounting Firm” and incorporated herein by reference.
Changes in Internal Control Over Financial Reporting
There have not been any changes in our internal control over financial reporting (as such term is defined in Rules 13a-15(f) in the Exchange Act) during the fourth fiscal quarter of the year to which this report relates that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
Item 9B. Other Information
None.
97
PART III
Item 10. Directors, Executive Officers, and Corporate Governance
The information required by Item 10 with respect to our executive officers and key employees is included under the caption “Executive Officers of the Registrant” in our Proxy Statement for the 2011 Annual Meeting and is incorporated herein by reference. We plan to file such Proxy Statement within 120 days after December 31, 2010, the end of our fiscal year.
The information required by Item 10 with respect to our Directors is included under the caption “Election of Directors” in our Proxy Statement for the 2011 Annual Meeting of Stockholders and is incorporated herein by reference.
The information required by Item 10 with respect to compliance with Section 16 of the Exchange Act is included under the caption “Section 16(a) Beneficial Ownership Reporting Compliance” in our Proxy Statement for the 2011 Annual Meeting of Stockholders and is incorporated herein by reference.
The information required by Item 10 with respect to our audit committee and our audit committee financial expert is included under the caption “The Board of Directors and its Committees – Audit Committee” in our Proxy Statement for the 2011 Annual Meeting of Stockholders and is incorporated herein by reference.
The information required by Item 10 with respect to our Code of Business Conduct and Ethics and our Code of Ethics for Senior Financial Officers is posted on our website at www.employers.com in the Investors section under “Governance.” We will post information regarding any amendment to, or waiver from, our Code of Business Conduct and Ethics on our website in the Investor section under Governance.
Item 11. Executive Compensation
The information required by Item 11 is included under the captions “Compensation Discussion and Analysis,” “Compensation Committee Report” and “Compensation Committee Interlocks and Insider Participation” in our Proxy Statement for the 2011 Annual Meeting of Stockholders and is incorporated herein by reference.
Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
Certain information required by Item 12 is included under the captions “Security Ownership of Certain Beneficial Owners and Management” and “Compensation Discussion and Analysis” in our Proxy Statement for the 2011 Annual Meeting of Stockholders and is incorporated herein by reference.
Equity and Incentive Plan
The following table gives information about our common stock that may be issued upon the exercise of options, warrants, and rights under all of our existing equity compensation plans as of December 31, 2010. We do not have any plans not approved by the stockholders. The plan is discussed further in Note 15 in the Notes to our Consolidated Financial Statements, which are included herein.
|
Plan Category
|
(a)
Number of securities
to be issued upon
exercise of outstanding
options, warrants, and
rights
|
(b)
Weighted-average
exercised price of
outstanding
warrants, and
rights
|
(c)
Number of securities remaining available for further issuance
under compensation plans
(excluding securities
reflected in column (a))
|
||||||||
|
Equity compensation plans approved by stockholders
|
1,763,103 | $ | 16.14 | 4,552,014 | |||||||
|
Equity compensation plans not approved by stockholders
|
— | — | — | ||||||||
|
Total
|
1,763,103 | $ | 16.14 | 4,552,014 | |||||||
Item 13. Certain Relationships and Related Transactions and Director Independence
The information required by Item 13 is included under the captions “Certain Relationships and Related Transactions” and “Director Independence” in our Proxy Statement for the 2011 Annual Meeting of Stockholders and is incorporated herein by reference.
Item 14. Principal Accountant Fees and Services
The information required by Item 14 with respect to the fees and services of Ernst & Young LLP, our independent registered public accounting firm, is included under the caption “Audit Matters” in our Proxy Statement for the 2011 Annual Meeting of Stockholders and is incorporated herein by reference.
98
PART IV
Item 15. Exhibits and Financial Statement Schedules
The following consolidated financial statements are filed in Item 8 of Part II of this report:
|
Page
|
|
|
Report of Independent Registered Public Accounting Firm
|
63
|
|
Consolidated Balance Sheets as of December 31, 2010 and 2009
|
64
|
|
Consolidated Statements of Income for each of the three years ended December 31, 2010
|
65
|
|
Consolidated Statements of Stockholders’ Equity for each of the three years ended December 31, 2010
|
66
|
|
Consolidated Statements of Cash Flows for each of the three years ended December 31, 2010
|
67
|
|
Notes to Consolidated Financial Statements
|
68
|
|
Financial Statement Schedules:
|
|
|
Schedule II. Condensed Financial Information of Registrant
|
100
|
|
Schedule VI. Supplemental Information Concerning Property-Casualty Insurance Operations
|
104
|
|
Pursuant to Rule 7-05 of Regulation S-X, Schedules I, III, IV, and V have been omitted as the information to be set forth therein is included in the notes to the audited consolidated financial statements.
|
99
Schedule II. Condensed Financial Information of Registrant
|
Employers Holdings, Inc.
|
||||||||
|
Condensed Balance Sheets
|
||||||||
|
December 31,
|
||||||||
|
2010
|
2009
|
|||||||
|
Assets
|
(in thousands, except share data)
|
|||||||
|
Investments:
|
||||||||
|
Investment in subsidiaries
|
$ | 196,714 | $ | 395,510 | ||||
|
Investment in securities available-for-sale (amortized cost $339,956 in 2010 and $131,749 in 2009)
|
345,060 | 141,973 | ||||||
|
Total investments
|
541,774 | 537,483 | ||||||
|
Cash and cash equivalents
|
27,991 | 55,176 | ||||||
| Restricted cash and cash equivalents | 2,017 | 17 | ||||||
|
Intercompany receivable
|
7,485 | 330 | ||||||
|
Federal income taxes receivable – intercompany
|
— | 8,637 | ||||||
|
Deferred income taxes, net
|
7,541 | — | ||||||
|
Other assets
|
5,739 | 2,788 | ||||||
|
Total assets
|
$ | 592,547 | $ | 604,431 | ||||
|
Liabilities and stockholders’ equity
|
||||||||
|
Accounts payable and accrued expenses
|
$ | 2,141 | $ | 2,505 | ||||
|
Income tax payable
|
256 | 1,325 | ||||||
|
Notes payable
|
100,000 | 100,000 | ||||||
|
Other liabilities
|
34 | 2,202 | ||||||
|
Total liabilities
|
102,431 | 106,032 | ||||||
|
Stockholders’ equity:
|
||||||||
|
Common stock, $0.01 par value; 150,000,000 shares authorized 53,779,118 and 53,563,299 shares issued and 38,965,126 and 42,908,165 shares outstanding at December 31, 2010 and 2009, respectively
|
538 | 536 | ||||||
|
Preferred stock, $0.01 par value; 25,000,000 shares authorized non-issued
|
— | — | ||||||
|
Additional paid-in capital
|
314,212 | 311,282 | ||||||
|
Retained earnings
|
319,341 | 266,491 | ||||||
|
Accumulated other comprehensive income, net
|
84,133 | 83,812 | ||||||
|
Treasury stock, at cost (14,813,992 shares at December 31, 2010 and 10,655,134 shares at December 31, 2009)
|
(228,108 | ) | (163,722 | ) | ||||
|
Total stockholders’ equity
|
490,116 | 498,399 | ||||||
|
Total liabilities and stockholders’ equity
|
$ | 592,547 | $ | 604,431 | ||||
|
See accompanying notes.
|
||||||||
100
|
Employers Holdings, Inc.
|
||||||||||||
|
Condensed Statements of Income
|
||||||||||||
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands, except per share data)
|
||||||||||||
|
Revenues
|
||||||||||||
|
Net investment income
|
$ | 8,740 | $ | 7,089 | $ | 7,125 | ||||||
|
Realized gains on investments
|
— | 2,682 | — | |||||||||
|
Total revenues
|
8,740 | 9,771 | 7,125 | |||||||||
|
Expenses
|
||||||||||||
|
Other operating expenses
|
10,597 | 14,036 | 12,179 | |||||||||
|
Interest expense
|
4,080 | 5,719 | 1,738 | |||||||||
|
Total expenses
|
14,677 | 19,755 | 13,917 | |||||||||
|
Loss before income taxes and equity in earnings of subsidiaries
|
(5,937 | ) | (9,984 | ) | (6,792 | ) | ||||||
|
Income tax benefit
|
(6,836 | ) | (5,990 | ) | (3,585 | ) | ||||||
|
Net income (loss) before equity in earnings of subsidiaries
|
899 | (3,994 | ) | (3,207 | ) | |||||||
|
Equity in net income of subsidiaries
|
61,900 | 87,015 | 104,992 | |||||||||
|
Net income
|
$ | 62,799 | $ | 83,021 | $ | 101,785 | ||||||
|
Earnings per common share for the stated periods (Note 19):
|
||||||||||||
|
Basic
|
$ | 1.52 | $ | 1.81 | $ | 2.07 | ||||||
|
Diluted
|
$ | 1.51 | $ | 1.80 | $ | 2.07 | ||||||
|
Cash dividends declared per common share
|
$ | 0.24 | $ | 0.24 | $ | 0.24 | ||||||
|
See accompanying notes.
|
||||||||||||
101
|
Employers Holdings, Inc.
|
||||||||||||
|
Condensed Statement of Cash Flows
|
||||||||||||
|
Years Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
(in thousands)
|
||||||||||||
|
Operating activities
|
||||||||||||
|
Net income
|
$ | 62,799 | $ | 83,021 | $ | 101,785 | ||||||
|
Adjustments to reconcile net income to net cash provided
|
||||||||||||
|
by operating activities:
|
||||||||||||
|
Equity in net income of subsidiaries
|
(61,900 | ) | (87,015 | ) | (104,992 | ) | ||||||
|
Amortization expense
|
94 | 188 | 148 | |||||||||
|
Realized gains on investments
|
— | (2,682 | ) | — | ||||||||
|
Stock-based compensation
|
4,053 | 5,366 | 3,161 | |||||||||
|
Amortization of premium or investments, net
|
3,794 | 1,428 | 849 | |||||||||
|
Deferred income tax expense
|
(9,930 | ) | (47 | ) | (907 | ) | ||||||
|
Change in operating assets and liabilities:
|
||||||||||||
|
Accounts payable, accrued expense and other liabilities
|
(1,147 | ) | (1,106 | ) | 381 | |||||||
|
Federal income taxes
|
8,637 | (5,960 | ) | (750 | ) | |||||||
|
Other assets
|
(470 | ) | 924 | (3,025 | ) | |||||||
|
Intercompany payable/receivable
|
(7,155 | ) | (718 | ) | 575 | |||||||
|
Net cash used in operating activities
|
(1,225 | ) | (6,601 | ) | (2,775 | ) | ||||||
|
Investing activities
|
||||||||||||
|
Purchase of fixed maturities
|
— | — | (1,994 | ) | ||||||||
|
Proceeds from sale of fixed maturities
|
— | 59,660 | 997 | |||||||||
|
Proceeds from maturities and redemptions of investments
|
12,319 | 10,000 | — | |||||||||
|
Cash dividends received from subsidiaries
|
38,383 | 27,700 | 152,995 | |||||||||
|
Capital contributions to subsidiary
|
— | — | (193,423 | ) | ||||||||
| Restricted cash (used in) provided by investment activities | (2,000 | ) | (17 | ) | — | |||||||
|
Net cash provided by (used in) investing activities
|
48,702 | 97,343 | (41,425 | ) | ||||||||
|
Financing activities
|
||||||||||||
|
Acquisition of treasury stock
|
(63,592 | ) | (74,185 | ) | (14,152 | ) | ||||||
|
Cash transactions related to stock-based compensation
|
(1,135 | ) | (123 | ) | — | |||||||
|
Dividends paid to stockholders
|
(9,935 | ) | (11,031 | ) | (11,808 | ) | ||||||
|
Debt issuance costs
|
— | — | (375 | ) | ||||||||
|
Payments on notes payable
|
— | (50,000 | ) | — | ||||||||
|
Proceeds from notes payable
|
— | — | 150,000 | |||||||||
|
Other
|
— | — | 5 | |||||||||
|
Net cash (used in) provided by financing activities
|
(74,662 | ) | (135,339 | ) | 123,670 | |||||||
|
Net (decrease) increase in cash and cash equivalents
|
(27,185 | ) | (44,597 | ) | 79,470 | |||||||
|
Cash and cash equivalents at the beginning of the period
|
55,176 | 99,773 | 20,303 | |||||||||
|
Cash and cash equivalents at the end of the period
|
$ | 27,991 | $ | 55,176 | $ | 99,773 | ||||||
|
Schedule of non-cash transactions
|
||||||||||||
|
Fixed maturities transferred in for dividend
|
$ | — | $ | — | $ | 200,087 | ||||||
|
See accompanying notes.
|
||||||||||||
102
1. Nature of Operations and Summary of Significant Accounting Policies
Operations and Basis of Presentation
Employers Holdings, Inc. (EHI) is a Nevada holding company. Through its wholly owned insurance subsidiaries, Employers Insurance Company of Nevada (EICN), Employers Compensation Insurance Company (ECIC), Employers Preferred Insurance Company (EPIC), and Employers Assurance Company (EAC), EHI is engaged in the commercial property and casualty insurance industry, specializing in workers’ compensation products and services. Unless otherwise indicated, all references to the “Company” refer to EHI, together with its subsidiaries.
EHI prepares its condensed financial statements in accordance with U.S. generally accepted accounting principles (GAAP), using the equity method. Under the equity method, the investment in subsidiaries is stated at cost plus equity in earnings (loss) of its subsidiaries. EHI receives dividends from its insurance subsidiaries in the form of cash and securities. The book value for these securities is stated at the fair market value at the date of transfer. These condensed financial statements should be read in conjunction with EHI’s consolidated financial statements included elsewhere in this Annual Report on Form 10-K.
Estimates and Assumptions
The preparation of the financial statements in conformity with GAAP requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities, and disclosure of contingent assets and liabilities at the date of the financial statements, and the reported amounts of revenue and expenses during the reporting period. As a result, actual results could differ from these estimates.
2. Income Taxes
EHI files a consolidated federal income tax return with its subsidiaries and has a tax allocation agreement with its subsidiaries. The equity in the undistributed earnings of subsidiaries included in the accompanying condensed statements of income is net of income taxes.
3. Investments
EHI holds fixed maturity securities at December 31, 2010 for purposes of securing the Third and Amended and Restated Secured Revolving Credit Facility (Amended Credit Facility). The amortized cost and estimated fair value of fixed maturity securities at December 31, 2010, by contractual maturity are shown below. Expected maturities differ from contractual maturities because borrowers may have the right to call or prepay obligations with or without call or prepayment penalties.
|
Amortized
Cost
|
Estimated
Fair
Value
|
||||||
|
(in thousands)
|
|||||||
|
Due in one year or less
|
$ | 27,838 | $ | 27,836 | |||
|
Due after one year through five years
|
202,103 | 211,093 | |||||
|
Due after five years through ten years
|
53,109 | 52,476 | |||||
|
Due after 10 years
|
56,906 | 53,655 | |||||
|
Total
|
$ | 339,956 | $ | 345,060 | |||
At December 31, 2010, the fixed maturity securities had unrealized gains of $5.1 million which are included in accumulated comprehensive income, net in the accompanying condensed balance sheets.
4. Notes Payable
Effective September 30, 2008, EHI and Wells Fargo Bank, National Association (Wells Fargo) entered into the Amended Credit Facility. See Note 13 of the Consolidated Financial Statements of Employers Holdings, Inc. and Subsidiaries included herein for a description of the terms of the Amended Credit Facility.
On September 30, 2008, EHI borrowed $150.0 million through the Amended Credit Facility. The proceeds borrowed under the Amended Credit Facility were used to finance the acquisition of AmCOMP Incorporated and for general working capital purposes. Interest paid during the years ended December 31, 2010, 2009, and 2008, including the interest rate swap (see Note 5), totaled $4.4 million, $5.8 million, and $1.2 million, respectively. In accordance with the terms of the contract, a repayment of $50.0 million was made toward the Amended Credit Facility on December 30, 2009. The Amended Credit Facility is secured by fixed maturity securities which had a fair value of $131.0 million at December 31, 2010.
103
5. Derivatives
Interest Rate Swap
On September 30, 2008, the Company, in connection with the borrowings made under the Amended Credit Facility (See Note 11 to the Consolidated Financial Statements), executed an interest rate swap with Wells Fargo with a notional amount of $100.0 million. Execution of the interest rate swap established a fixed interest rate of 4.84%, on the notional amount, which expired September 30, 2010. The Company used its interest rate swap to mitigate the risks associated with unexpected cash outflows resulting from shifts in variable interest rates. As of December 31, 2009, the interest rate swap had a negative fair value of $2.2 million, and is included in other liabilities on the accompanying consolidated balance sheets. The corresponding unrealized loss of $2.2 million for the year ended December 31, 2009 is included in accumulated other comprehensive income, net.
6. Stock-Based Compensation
During 2008, EHI granted 24,984 RSUs to non-employee Directors and 152,564 RSUs to officers and 475,167 non-qualified stock options to officers. During 2009, EHI granted 40,536 RSUs to non-employee Directors and 176,871 RSUs to officers and 531,082 non-qualified stock options to officers. See Note 15 of the Consolidated Financial Statements of Employers Holdings, Inc. and Subsidiaries’ included herein for a detailed description of the stock-based compensation.
During 2010, EHI granted 30,728 RSUs to non-employee Directors, 163,660 RSUs to officers, and 406,020 non-qualified stock options to officers.
|
Schedule VI. Supplemental Information Concerning Property — Casualty Insurance Operations
|
|||||||||||||||||||||||||||||||||||||||
|
Employers Holdings, Inc. and Subsidiaries
|
|||||||||||||||||||||||||||||||||||||||
|
Consolidated Supplemental Information Concerning Property and Casualty Insurance Operations
|
|||||||||||||||||||||||||||||||||||||||
|
Year
Ended
|
Deferred
Policy
Acquisition
Costs
|
Reserves For
Unpaid
Losses And
LAE
|
Unearned
Premiums
|
Earned
Premiums
|
Net Investment
Income
|
Losses and
LAE Related
to Current
Years
|
Losses and
LAE Related to Prior
Years
|
Amortization
of Deferred
Policy
Acquisition Costs
|
Paid Losses And LAE
|
Net
Premiums
Written
|
|||||||||||||||||||||||||||||
|
(in thousands)
|
|||||||||||||||||||||||||||||||||||||||
|
2010
|
$ | 32,239 | $ | 2,279,729 | $ | 149,485 | $ | 321,786 | $ | 83,032 | $ | 227,143 | $ | (14,130 | ) | $ | 72,071 | $ | 262,480 | $ | 313,098 | ||||||||||||||||||
|
2009
|
$ | 33,695 | $ | 2,425,658 | $ | 158,577 | $ | 404,247 | $ | 90,484 | $ | 283,827 | $ | (51,359 | ) | $ | 87,638 | $ | 289,443 | $ | 368,290 | ||||||||||||||||||
|
2008
|
$ | 41,521 | $ | 2,506,478 | $ | 196,695 | $ | 328,947 | $ | 78,062 | $ | 226,643 | $ | (71,707 | ) | $ | 66,415 | $ | 188,883 | $ | 308,317 | ||||||||||||||||||
Exhibits:
|
Exhibit
No.
|
Description of Exhibit
|
Included Herewith
|
Incorporated by Reference Herein
|
|||||||
|
Form
|
Exhibit
|
Filing Date
|
||||||||
|
2.1
|
Agreement and Plan of Merger by and among AmCOMP Incorporated, Employers Holdings, Inc. and Sapphire Acquisition Corporation, dated as of January 10, 2008
|
8-K
|
2.1
|
January 10, 2008
|
||||||
|
2.2
|
Amendment No. 2 to the Agreement and Plan of Merger, dated August 29, 2008, by and among AmCOMP Incorporated, Employers Holdings, Inc. and Sapphire Acquisition Corp.
|
8-K
|
2.1
|
August 29, 2008
|
||||||
| 3.1 | Amended and Restated Articles of Incorporation of Employers Holdings, Inc. | 10-K | 3.1 | March 30, 2007 | ||||||
| 3.2 | Amended and Restated Bylaws of Employers Holdings, Inc. | 10-Q | 3.1 | November 5, 2009 | ||||||
| 4.1 | Form of Common Stock Certificate | S-1/A | 4.1 | January 18, 2007 | ||||||
| 10.1 | Quota Share Reinsurance Agreement, dated as of June 30, 1999, between State Industrial Insurance System of Nevada, D.B.A.: Employers Insurance Company of Nevada and the various Reinsurers as identified by the Interests and Liabilities Agreements attached thereto (1) | S-1/A | 10.1 | January 18, 2007 | ||||||
104
|
10.2
|
Producer Agreement, dated as of May 1, 2005, between Employers Compensation Insurance Company and Automatic Data Processing Insurance Agency, Inc. (1)
|
S-1/A
|
10.2
|
January 18, 2007
|
||||||
|
10.3
|
Joint Marketing and Network Access Agreement, dated as of January 1, 2006, between Employers Insurance Company of Nevada and Blue Cross of California, BC Life & Health Insurance Company, and Comprehensive Integrated Marketing Services (1)
|
S-1/A
|
10.3
|
January 18, 2007
|
||||||
|
10.4
|
Joint Marketing and Network Access Agreement, dated as of July 1, 2006, between Employers Insurance Company of Nevada and Blue Cross of California, BC Life & Health Insurance Company, and Comprehensive Integrated Marketing Services (1)
|
S-1/A
|
10.4
|
January 18, 2007
|
||||||
|
*10.5
|
Employers Holdings, Inc. Equity and Incentive Plan Stock Option Agreement
|
8-K
|
10.1
|
August 10, 2007
|
||||||
|
*10.6
|
Employers Holdings, Inc. Equity and Incentive Plan Performance Share Agreement
|
8-K
|
10.2
|
August 10, 2007
|
||||||
|
*10.7
|
Employers Holdings, Inc. Amended and Restated Equity Incentive Plan
|
8-K
|
10.1
|
May 28, 2010
|
||||||
|
*10.8
|
Form of Restricted Stock Unit Agreement
|
8-K
|
10.1
|
June 2, 2008
|
||||||
|
*10.9
|
Employment Agreement by and between Employers Holdings, Inc. and Douglas D. Dirks, dated December 17, 2008 and effective as of January 1, 2009
|
8-K
|
10.1
|
December 23, 2008
|
||||||
|
*10.10
|
Employment Agreement by and between Employers Holdings, Inc. and Ann W. Nelson, dated December 17, 2008 and effective as of January 1, 2009
|
8-K
|
10.2
|
December 23, 2008
|
105
|
*10.11
|
Employment Agreement by and between Employers Holdings, Inc. and Lenard T. Ormsby, dated December 17, 2008 and effective as of January 1, 2009
|
8-K
|
10.3
|
December 23, 2008
|
||||||
|
*10.12
|
Employment Agreement by and between Employers Holdings, Inc. and Martin J. Welch, dated December 17, 2008 and effective as of January 1, 2009
|
8-K
|
10.4
|
December 23, 2008
|
||||||
|
*10.13
|
Employment Agreement by and between Employers Holdings, Inc. and William E. Yocke, dated December 17, 2008 and effective as of January 1, 2009
|
8-K
|
10.5
|
December 23, 2008
|
||||||
|
*10.14
|
Employment Agreement by and between Employers Holdings, Inc. and John P. Nelson, dated December 17, 2008, and effective as of January 1, 2009
|
10-Q
|
10.1
|
May 7, 2009
|
||||||
|
*10.15
|
Form of Restricted Stock Unit Agreement for Non- Employee Directors
|
10-Q
|
10.1
|
August 7, 2009
|
||||||
|
10.16
|
Third Amended and Restated Credit Agreement, dated December 30, 2010, between Employers Holdings, Inc. and Wells Fargo Bank, National Association
|
8-K
|
10.1
|
December 30, 2010
|
||||||
|
10.17
|
Third Amended and Restated Revolving Line of Credit Note, dated December 30, 2010, between Employers Holdings Inc. and Wells Fargo Bank, National Association
|
8-K
|
10.2
|
December 30, 2010
|
106
|
10.18
|
Separation and Release Agreement by and between Employers Insurance Company of Nevada and Martin J. Welch, dated January 18, 2011 and effective February 1, 2011
|
X
|
||||||||
|
21.1
|
Subsidiaries of Employers Holdings, Inc.
|
X
|
||||||||
|
23.1
|
Consent of Ernst & Young LLP, Independent Registered Public Accounting Firm
|
X
|
||||||||
|
31.1
|
Certification of Douglas D. Dirks Pursuant to Section 302
|
X
|
||||||||
|
31.2
|
Certification of William E. Yocke Pursuant to Section 302
|
X
|
||||||||
|
32.1
|
Certification of Douglas D. Dirks Pursuant to Section 906
|
X
|
||||||||
|
32.2
|
Certification of William E. Yocke Pursuant to Section 906
|
X
|
||||||||
|
**101.INS
|
XBRL Instance Document
|
X
|
||||||||
|
**101.SCH
|
XBRL Taxonomy Extension Schema Document
|
X
|
||||||||
|
**101.CAL
|
XBRL Taxonomy Extension Calculation Linkbase Document
|
X
|
||||||||
|
**101.LAB
|
XBRL Taxonomy Extension Label Linkbase Document
|
X
|
|
**101.PRE
|
XBRL Taxonomy Extension Presentation Linkbase Document
|
X
|
For purposes of the incorporation by reference of documents as Exhibits, all references to Forms S-1 and S-1/A of Employers Holdings, Inc. refer to Forms S-1 and S-1/A filed with the Commission under Registration Number 333-139092.
*Identify management contracts and compensatory plans or arrangements.
**XBRL (eXtensible Business Reporting Language) information is furnished and not filed for purposes of Sections 11 and 12 of the Securities Act of 1933 and Section 18 of the Securities Exchange Act of 1934.
|
(1)
|
Confidential treatment has been requested for certain confidential portions of this exhibit; these confidential portions have been omitted from this exhibit and filed separately with the Securities and Exchange Commission.
|
107
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Act of 1934, the Registrant has duly caused this Report to be signed on its behalf by the undersigned, thereunto duly authorized, in the City of Reno, State of Nevada on February 24, 2011.
|
|
||
|
EMPLOYERS HOLDINGS, INC.
|
||
|
By:
|
/s/ Douglas D. Dirks
|
|
|
Title: Chief Executive Officer
|
||
|
Name: Douglas D. Dirks
|
||
|
Title: Chief Executive Officer
|
||
Pursuant to the requirements of the Securities Exchange Act of 1934, this Report has been signed by the following persons in the capacities and on the dates indicated:
|
Signature
|
Title
|
Date
|
||
|
/s/ Robert J. Kolesar
Robert J. Kolesar
|
Chairman of the Board
|
February 24, 2011
|
||
|
/s/ Douglas D. Dirks
Douglas D. Dirks
|
President and Chief Executive Officer, Director (Principal Executive Officer)
|
February 24, 2011
|
||
|
/s/ William E. Yocke
William E. Yocke
|
Executive Vice President and Chief Financial Officer (Principal Financial and Accounting Officer)
|
February 24, 2011
|
||
|
/s/ Richard W. Blakey
Richard W. Blakey
|
Director
|
February 24, 2011
|
||
|
/s/ Valerie R. Glenn
Valerie R. Glenn
|
Director
|
February 24, 2011
|
||
|
/s/ Rose E. McKinney-James
Rose E. McKinney-James
|
Director
|
February 24, 2011
|
||
|
/s/ Ronald F. Mosher
Ronald F. Mosher
|
Director
|
February 24, 2011
|
||
|
/s/ Katherine W. Ong
Katherine W. Ong
|
Director
|
February 24, 2011
|
||
|
/s/ Michael D. Rumbolz
Michael D. Rumbolz
|
Director
|
February 24, 2011
|
||
|
/s/ John P. Sande III
John P. Sande III
|
Director
|
February 24, 2011
|
||
108
