Attached files
| file | filename |
|---|---|
| 8-K - FORM 8-K - HEALTH NET INC | d8k.htm |
| EX-99.2 - PRESS RELEASE - HEALTH NET INC | dex992.htm |
 Health Net, Inc.
Health Net, Inc.
2011 Investor Day
2011 Investor Day
February 17, 2011
Exhibit 99.1 |
 Cautionary Statement
2
All statements in this presentation, other than statements of
historical information provided herein, including but not limited
to the guidance for future periods included herein and the assumptions
and underlying such projections, may be deemed to be
forward-looking statements and as such are subject to a number of risks and uncertainties. These statements are based on
management’s analysis, judgment, belief and expectation only as of
the date hereof, and are subject to uncertainty and changes in
circumstances. Without limiting the foregoing, the guidance as to expected future period results and statements
including the words “believes,” “anticipates,”
“plans,” “expects,” “may,” “should,” “could,” “estimate,” “intend” and other
similar expressions are intended to identify forward-looking
statements. Actual results could differ materially due to, among
other things, health care reform, including the ultimate impact of the
Affordable Care Act, which could materially adversely affect the
company’s financial condition, results of operations and cash flows through, among other things, reduced
revenues, new taxes, expanded liability, and increased costs (including
medical, administrative, technology or other costs), or require
changes to the ways in which the company does business; rising health care costs; continued slow economic
growth or a further decline in the economy; negative prior period
claims reserve developments; trends in medical care ratios;
membership declines; unexpected utilization patterns or unexpectedly severe or widespread illnesses; rate cuts
affecting the company’s Medicare or Medicaid businesses; costs,
fees and expenses related to the post-closing administrative
services provided under the administrative services agreements entered into in connection with the sale of the
company’s Northeast business; potential termination of the
administrative services agreements by the service recipients
should the company breach such agreements or fail to perform all or a
material part of the services required thereunder; any
liabilities of the Northeast business that were incurred prior to the
closing of its sale as well as those liabilities incurred
through the winding-up and running-out period of the Northeast
business; litigation costs; regulatory issues with agencies such
as the California Department of Managed Health Care, the Centers for Medicare and Medicaid Services and state
departments of insurance, including the continued suspension of the
marketing of and enrollment into the company’s Medicare
products for a significant period of time, which could have a material adverse impact on the company’s Medicare
business; operational issues; investment portfolio impairment charges;
volatility in the financial markets; and general business and
market conditions. Additional factors that could cause actual results to differ materially from those reflected in
the forward-looking statements include, but are not limited to, the
risks discussed in the “Risk Factors” section included
within the company's most recent Annual Report on Form 10-K
and subsequent Quarterly Reports on Form 10-Q filed with
the Securities and Exchange Commission (“SEC”), and the risks
discussed in the company’s other filings with the SEC.
Readers are cautioned not to place undue reliance on these
forward-looking statements. The company undertakes no
obligation to publicly revise its guidance, the assessment of the
underlying assumptions or any of its forward-looking
statements to reflect events or circumstances that arise after the date
of this presentation. |
 3
Non-GAAP Measures
These presentations include quarterly and full year
income statement measurements that are not calculated
and presented in accordance with Generally Accepted
Accounting Principles. Audience participants should refer
to the financial table included in the Appendix to the
presentations, which also is available on the company’s
website at www.healthnet.com, and reconciles certain
non-GAAP financial information to GAAP financial
information. |
 4
Agenda
8.30 a.m. –
9.00 a.m.
Welcoming Remarks
Angie McCabe, Vice President, Investor Relations
Introduction and Strategic Overview
Jay Gellert, President and Chief Executive Officer
9.00 a.m. –
10.00 a.m.
Commercial Growth and Margin Expansion
Steven Sell, President, Western Region Health Plan
Underwriting and Actuarial Review
Richard Hall, FSA, MAAA, Chief Actuarial Officer
10.00 a.m. –
10.15 a.m.
BREAK
10.15 a.m. –
11.15 a.m.
Medicare and State Programs
Scott Kelly, Chief Government Programs Officer
Federal Services
Steven Tough, President, Government Programs
11.15 a.m. –
12.15 p.m.
Operations Review
Juanell
Hefner, Chief Customer Services Officer
Jay Gellert, President and Chief Executive Officer
Financial Review
Joseph Capezza, Chief Financial Officer
12.15 p.m. –
12.30 p.m.
Closing Remarks
Jay Gellert, President and Chief Executive Officer
Note: Presentation times subject to change. |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
 Strategic
Overview Strategic Overview
Jay Gellert
President and
Chief Executive Officer |
 7
Emerging Environment
Emerging Environment
•
Economy is driving change
•
Federal and state budget pressures
will affect health care
•
Future implementation of Affordable Care Act
remains to be defined
•
Diverse book of businesses where value
differentiation is key |
 8
Our Strategy To Date
Our Strategy To Date
•
Build value-based products
•
Diverse book of businesses
–
Risk and fee
–
Medicaid, Medicare, TRICARE and commercial
•
Deemphasize volatile segments
–
e.g., individual
•
Invest in G&A efficiencies
•
Dispose of weak assets
•
Strengthen balance sheet |
 9
2011 Key Milestones
2011 Key Milestones
•
Stronger risk membership
•
TRICARE to ASO
•
Maintain low G&A ratio
•
Expand commercial margins
•
Continue to add new products
•
Use cash for benefit of shareholders |
 10
Future Opportunities
Future Opportunities
•
Broadening commercial business
•
Rebound in Medicare
•
Medicaid expansion
•
Department of Defense options
•
G&A leverage
•
Balance sheet flexibility |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
 Commercial
Growth Commercial Growth
and Margin Expansion
and Margin Expansion
Steven Sell
President, Western Region Health Plan |
 Commercial: Positioned for Growth
Commercial: Positioned for Growth
•
Economy is driving HMO demand
•
Health Net has a strong and sustainable
HMO market position
•
Tailored products and networks drive growth
•
Margin expansion opportunities
13 |
 Economy Driving Demand
•
Market research shows customers looking for:
–
Affordable solutions
–
Convenient access
–
Clear and simple choices
•
Consumer-directed health plans (CDHP)
show some stress
–
Among highest premium increases
•
HMO value proposition: “back to the future”
–
Affordable premiums
–
Primary care leadership
–
Comprehensive benefits / low copays
14 |
 Health Care Reform
Health Care Reform
Favors Managed Care
Favors Managed Care
•
PPO benefit advantages being reduced
–
Elimination of annual and lifetime limits in 2011
–
Zero copay
preventive care in 2011
–
Deductible caps coming in 2014
•
Traditional ASO vs. risk
–
Risk still best value in California –
even for large,
national employers
•
Providers will play more prominent role
–
Incentives in law to create managed care
infrastructure (e.g., accountable care organizations)
–
Seeking to balance Medicare and Medicaid revenue
pressures with commercial growth
15 |
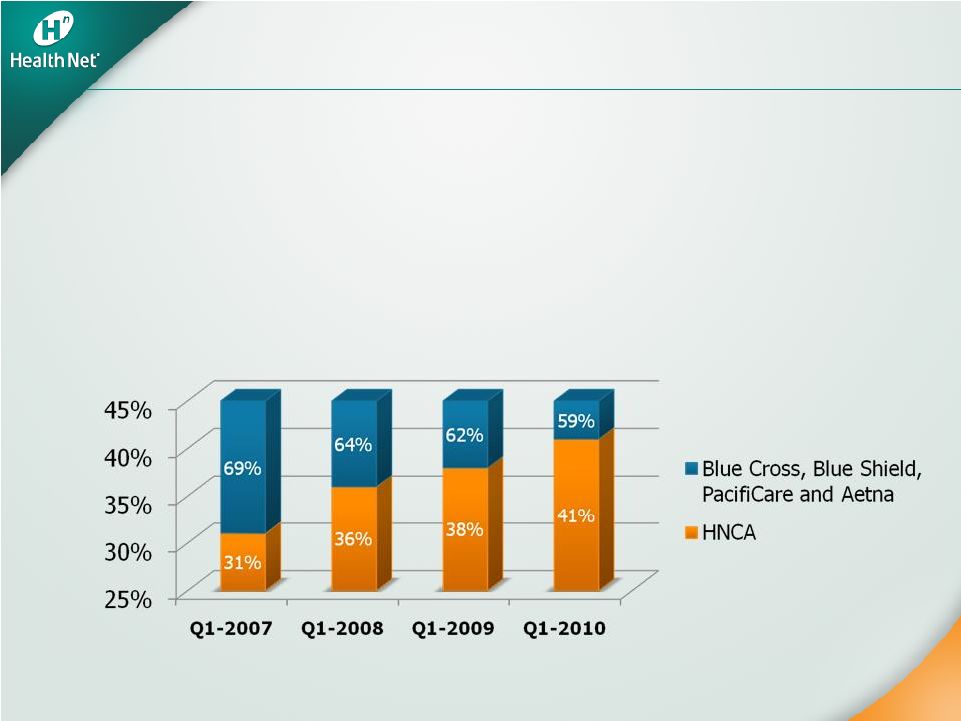 16
Health Net:
Health Net:
Strong HMO Market Share
Strong HMO Market Share
•
Dominant network HMO player in California market
•
Steady market share growth over the last four years
•
Small group market share increase: 31 percent
to 41 percent in the past four years
Source: Data from Department of Managed Health Care and excludes Kaiser and all PPO
data. Percent share reflects percent share of top statewide competitors.
Small Group Network Model HMO Market Share |
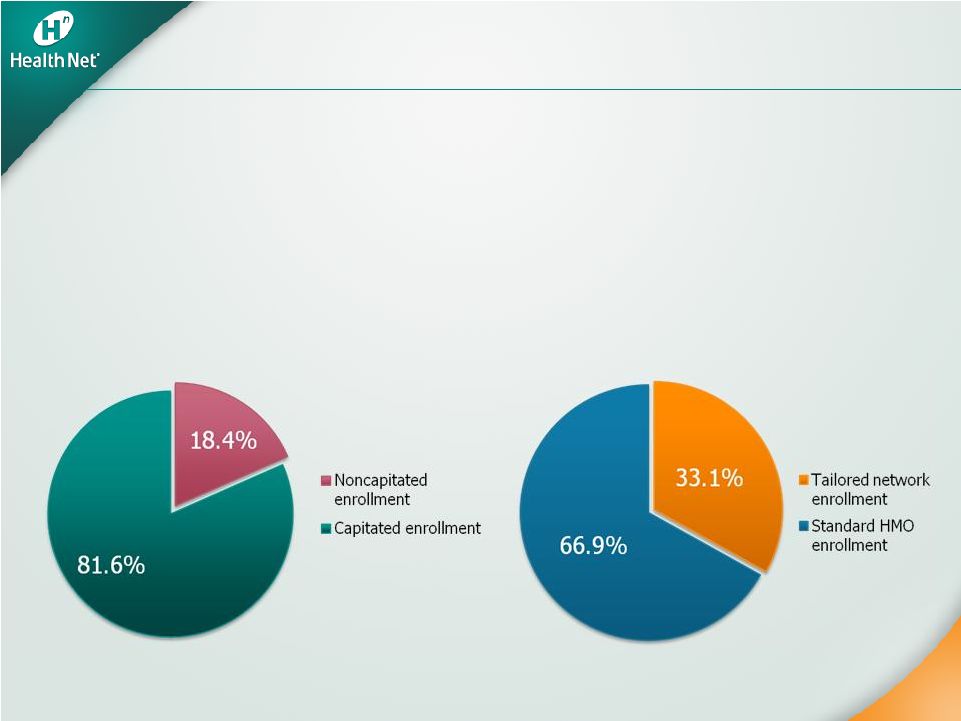 The Power of
Capitation The Power of Capitation
•
Focuses providers on cost management and commercial growth
•
Stabilizes trends and makes them more predictable
•
Reduces administrative costs as claims processing is delegated
Source: Based on Health Net internal data as of December 31, 2010.
More than 80 percent of HNCA’s
commercial membership is enrolled
in capitated
medical groups
More than 30 percent of HNCA’s
commercial capitated
membership is
enrolled in tailored network plans
17 |
 •
Drives volume to “high value”
providers (low cost/high quality)
•
Employer premiums up to 30 percent lower
•
Offers comprehensive coverage
•
Increased interest in new geographies and segments
Strong and Evolving Tailored Networks
Strong and Evolving Tailored Networks
18
Source: Based on Health Net internal data
HNT Tailored Network Membership |
 How
Tailored Network Products Work How Tailored Network Products Work
•
Foundation is traditional HMO capitated
networks
–
Broad physician panel in group or IPA
–
Includes wide range of institutional options
–
Comprehensive benefits with low copays
•
Tailored networks
–
Include cost-effective provider groups
•
Stronger partnerships built on higher volume
and joint marketing
–
Includes select institutional options that optimize
cost and quality
•
Substantial savings accrue to customer by excluding
high cost, geographically remote institutions
–
Comprehensive benefits with low copays
19 |
 Growth with Margin Expansion
Growth with Margin Expansion
•
Strategically changing mix
–
Segment: small group and mid-market
–
Product: tailored network products
–
Geographic: Southern California vs.
Northern California
•
Targeted sales and improved retention
•
Disciplined underwriting and pricing
•
Continued focus on health care cost containment
–
Stronger provider partnerships
20 |
 Well Positioned for Growth
Well Positioned for Growth
•
Growing market share in California
•
Product solutions meeting market demand
–
Opportunities to apply solutions to
Arizona and Oregon
•
Margin expansion driven by:
–
Improved product and segment mix
–
Consistent underwriting and pricing discipline
•
Provider-payor
relationships evolving
21 |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
 Underwriting
and Underwriting and
Actuarial Review
Actuarial Review
Richard T. Hall, FSA, MAAA
Chief Actuarial Officer |
 A
New Commercial Environment A New Commercial Environment
•
Underwriting and pricing discipline
•
Return to HMO plans / pressure on
less managed plans
•
Regulatory pressure and individual
market issues
•
Providers seeking commercial share to
offset growing cost shift
•
2011 pricing assumptions and outlook
24 |
 Underwriting and Pricing Discipline
Underwriting and Pricing Discipline
•
Rigorous planning process
–
Analyze membership
–
Identify best gross margin opportunities
–
Sensitivity analyses
•
Targeted geographies, segments and
products where we have a clear
competitive advantage
•
Enhanced sales and underwriting process to
optimize profitable membership growth
25 |
 26
2010 Results Affirm Strategy
2010 Results Affirm Strategy
•
Targeted pricing to improve mix in large group
–
MCR of renewing groups in California was better
than canceled groups by 100 basis points in 2010
–
Implemented processes to achieve an improved
retention rate
•
From 81 percent in 2010 to 91 percent in
January 2011
•
Industry standard is approximately 82 percent
•
Membership and margin opportunities in small group segment
–
MCR of renewing groups was better than canceled groups by
210 basis points in 2010 |
 Return to HMO
Return to HMO
•
Demonstrable premium differential for
equivalent benefits
•
ASO vs. risk: California experience
•
Growing out-of-pocket limits not sustainable
for members and providers
•
Health care reform and economy limit ability
to shift costs to employees
27 |
 Premium Differentials
Premium Differentials
•
Traditional HMO vs. PPO –
HMO is 30 percent less
–
Example: Los Angeles County
–
HMO –
$30 copay
/ $2,000 out-of-pocket maximum
–
PPO –
$30 copay
in-network / $500 deductible /
$2,000 out-of-pocket maximum
•
Tailored network 10 percent to 25 percent less than
traditional HMO
–
Targeted to specific, cost-effective provider groups
–
Better performing MCR than traditional HMO
–
Less expensive than Kaiser in many cases
28 |
 Regulatory Pressure
Regulatory Pressure
and Individual Market Issues
and Individual Market Issues
•
Cautious approach to individual market
•
Emerging regulatory environment
•
External focus on rate increases
•
Preparing for implementation of exchanges
29 |
 Changing the Provider-Payor
Changing the Provider-Payor
Paradigm
Paradigm
30
•
Market driving to integrated approach
•
Health Net offers value to providers
–
People and relationships
–
True local presence
–
Business model
–
All segment focus
–
Providers seeking to retain and build
commercial market share
•
Joint efforts in cost and quality management |
 2011 Commercial Pricing Assumptions
2011 Commercial Pricing Assumptions
•
2010 physician and institutional utilization
moderated from 2009
•
2011 pricing assumes upward pressure on
physician and institutional utilization
•
2011 unit cost trends expected to be lower
than 2010 trends
•
2011 pharmacy cost increases expected to
be similar to 2010
31 |
 Beyond 2011
Beyond 2011
•
Sectoral
–
not cyclical –
changes in market
–
Driven by health care reform and economy
•
Trends remain moderate by historical standards
–
Growing impact of tailored network plans
and focus on affordability
•
Steadily growing influence of capitated
systems
•
Institutional providers seek new partnerships to
achieve cost effectiveness and enhance
competitive position
32 |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
 Medicare
and Medicare and
State Programs
State Programs
Scott Kelly
Chief Government
Programs Officer |
 Solid Medicare Outlook
Solid Medicare Outlook
•
Balance Medicare Advantage revenue,
benefits/premiums and costs to ensure:
–
Stable margins
–
Continued competitive product offerings
•
Continued focus on capitated
networks
•
Enhance strategic provider partnerships in
coordination with commercial business
•
Position Part D book for 2012 growth
•
Strengthening operations and controls to
respond to CMS sanction issues
35 |
 Medicare Advantage: 2011
Medicare Advantage: 2011
•
Building from solid 2010
•
January enrollment results better than
initial expectations
•
Total revenues PMPM expected to be up 1.5 percent
–
Member premiums up 3.4 percent PMPM
•
Expect MCR to be flat year-over-year
–
Health care cost stability
–
Benefit changes: hospital and outpatient
copays, deductibles
•
Preparing for 2012 bidding process
36 |
 Medicare Part D
Medicare Part D
•
2010 margins maintained by favorable
prescription drug performance and unit costs
•
2011 enrollment expected to decline
14 percent to 16 percent compared with 2010
•
Guiding to breakeven 2011 performance due to
effects of CMS sanctions
37 |
 CMS
Sanctions CMS Sanctions
What Happened?
•
CMS identified issues in HNT’s
Part D program
What’s Next?
•
Corrective actions are in process
•
Plan to review corrective actions with CMS in
second quarter of 2011
•
Broader compliance initiatives in place to
ensure appropriate administration of
government business overall
38 |
 Medicare Advantage
Medicare Advantage
Provider Networks
Provider Networks
•
Nearly 40 percent of health care costs capitated
–
Over 50 percent in California market
–
More than 135 provider groups in 21 counties
•
Mostly percent of premium contracts
•
Collaboration with organized health systems to
reduce total costs to achieve margin stability
•
Working closely on risk adjuster capture and
accuracy with key groups
39 |
 State Health
Programs State Health Programs
•
Potential for growth
–
Health care reform
–
Seniors and Persons
with Disabilities (SPD)
–
New counties
40
Total State Program Revenues |
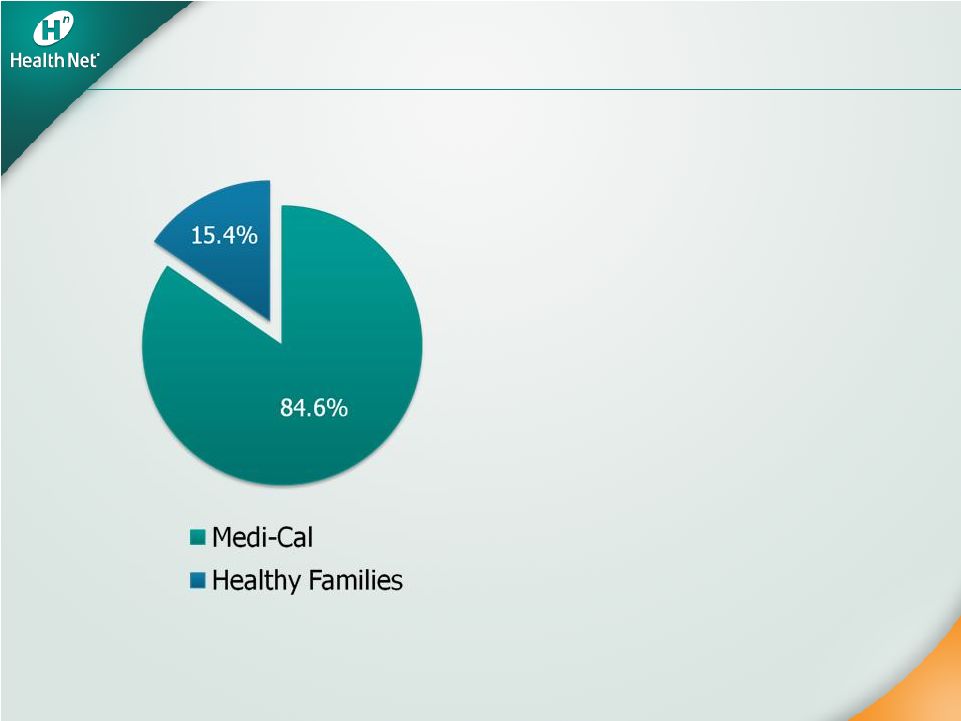
 Medi-Cal Position
Medi-Cal Position
•
753,700 members at year-end 2010, an
increase of 7 percent year-over-year
•
Second largest Medi-Cal plan in California
–
58 percent of membership in
Los Angeles County
–
34 percent in Central Valley
•
Market share stable at over 24 percent
•
Remain the highest ranking Medi-Cal HMO plan
in California by U.S. News and World Report
41 |
 2011 Medi-Cal Outlook
2011 Medi-Cal Outlook
•
Expect 6 percent membership growth
•
Maintain stable financial performance
–
Rate environment understood
•
Key strategic position for health care reform
•
SPD program offers potential significant
growth opportunity
42 |
 Healthy Families
Healthy Families
•
145,800 members at year-end 2010, a
decrease of 4.7 percent year-over-year
–
Market share remains flat as general
statewide enrollment declines
•
2011 program outlook
–
Expect 6 percent membership decline
–
Margin stable
43 |
 State Programs Provider Networks
State Programs Provider Networks
•
80 percent of State Programs enrollment
linked to capitated
provider groups
•
Over 45 percent of health care costs under
capitated
arrangements
–
75 percent of physician costs
–
27 percent of hospital costs
•
Noncapitated
hospital rates on Medicaid
fee schedule
44 |
 Stable Government Programs
Stable Government Programs
•
Margin stability in long-standing Medicare
Advantage network-model markets
–
Predictable cost structure
–
Solid membership retention
•
Medi-Cal: prepare for growth of SPDs
and
health care reform expansion
•
2011 focus on strong operational and
regulatory performance and preparations
for 2012 open enrollment
45 |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
 Federal
Services Federal Services
Steve Tough
President,
Government Programs |
 Government Contracts Highlights
Government Contracts Highlights
•
New TRICARE contract begins April 1, 2011
•
ASO, fee-based, five-year contract
•
Improves company balance between risk
and fee-based businesses
•
Opens door to new opportunities as
Department of Defense (DoD) faces
budget pressures
48 |
 2011: A Transition Year
2011: A Transition Year
•
Contract financial structure changes from cost
plus risk sharing to cost plus incentive
–
New contract accounted for as ASO
•
2011 includes ¼
year of current contract,
¾
year of new contract, plus current contract
phase-out revenues and expenses
–
Expect 2011 pretax contribution from
Government Contracts to decline by
approximately $25 million from 2010
49 |
 Current Contract to New Contract:
Current Contract to New Contract:
Incentive and Risk Changes
Incentive and Risk Changes
•
Fixed-dollar underwriting fee
•
Administrative efficiencies under a fixed
administrative budget
•
Underwriting incentives –
network discount, network
usage and national cost trend
–
National cost trend incentive based on our PMPM
health care cost trend for contractor enrollees vs.
national health care expenditure per capita trend
•
Performance guarantees and incentives
•
Award fee calculated twice yearly (Q2 and Q4) under
new contract vs. quarterly under current contract
50 |
 Growth Opportunities
Growth Opportunities
•
Military & Family Life Consultant (MFLC)
program success
–
Apply MFLC model to other federal customers
•
DoD
efforts under way –
budget challenges create
potential opportunities
–
Extend services to National Guard and Reservists
–
Managed solutions for TRICARE for Life
•
Behavioral health outreach requirements continue to
grow as needs escalate
•
Veterans Affairs (VA) seeks expansion of its rural
behavioral health support program
•
Existing services and products have application to other
government programs
51 |
 Key
Takeaways Key Takeaways
•
Well positioned to continue leadership role
with DoD
and VA
•
Transition to new contract on track
•
Wide range of behavioral health opportunities
–
Build on MFLC success
•
Continue to expand VA and state
administrative footprint
52 |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
 Operations
Review Operations Review
Jay Gellert
President and
Chief Executive Officer
Juanell Hefner
Chief Customer Services Officer |
 Operations
Strategy Operations Strategy
and Stranded Costs
and Stranded Costs
•
Announced a three-year effort to restructure
operations in 2007
•
Built around these goals:
Optimize outsourcing
Eliminate operations and system inefficiencies
Enhance scalability
Improve competitive platform
•
Reduce “stranded costs”
associated with sale of
Northeast and new TRICARE contract
•
Goal: support sustained long-term margin improvement
55 |
 G&A Expense
Reductions G&A Expense Reductions
•
Invested $145 million after tax in G&A expense
reduction activities over the last three years
(i.e., severance, asset impairment, etc.)
•
Without these investments, Western Region G&A
would have been higher by approximately
$100 million pretax in 2010
•
Achieved additional savings in the Northeast and
Government Contracts division
•
Targeting an additional $100 million in pretax
savings in 2011 and 2012 to compensate for
Northeast stranded costs and TRICARE gap
–
Savings primarily from headcount reductions
56 |
 Northeast
Wind-down and Overhead Reductions
Northeast Wind-down and
Overhead Reductions
Operations Strategy
Operations Strategy
•
Infrastructure outsourcing
•
Application outsourcing
•
Business process outsourcing
•
Management restructuring
•
Operational efficiencies
•
Vendor management
•
Wind-down of NE operations
•
Finance outsourcing
•
Additional operations outsourcing
•
Managerial restructuring
•
Arizona systems migration
•
Print and fulfillment
•
Real estate cost improvements
•
Operational efficiencies
Areas of Savings
Areas of Savings
57 |
 Improved
Operations Improved Operations
•
Operations are better integrated
–
More consistent procedures
–
Greater flexibility to use staff and
resources efficiently
–
Improved performance management
•
Have realized benefits from business process
outsourcing of noncustomer facing functions
–
Scalability
–
Cost improvements
–
High levels of quality and performance
58 |
 Improved
Operational Performance Improved Operational Performance
•
Claims
–
Accuracy
–
Claims turnaround time
•
Call center performance
–
First call resolution
•
Enrollment and eligibility performance
–
Enrollment accuracy
–
Enrollment timeliness
–
Eligibility accuracy
All key operational metrics have improved or
All key operational metrics have improved or
stabilized over the past three years
stabilized over the past three years
59 |
 Positioned for
the Future •
Improved speed to market
–
Outsourcing allows for rapid capacity
ramp-up to support growth
–
Can leverage vendor expertise and
resources to create new and expanded
operational capabilities
•
Technology infrastructure now positioned to
support future performance and growth
–
New equipment and software upgrades
–
Network upgrades
–
Investment in strategic applications
60 |
 Key
Takeaways Key Takeaways
•
Further G&A reductions will contribute
to margin improvement
•
Operations positioned to support
long-term growth
•
G&A positioned to offset minimum
MCR requirements
•
Eliminating stranded costs associated with
Northeast business and new TRICARE contract
•
Improved operations enhance capacity to deliver
new products and services
61 |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
 Financial
Review Financial Review
Joseph C. Capezza
Chief Financial Officer |
 64
Original Guidance
Actual
Year-end membership
•
Commercial: -1% to -2%
•
Medicaid: +5% to +6%
•
Medicare Advantage: -2% to -3%
•
PDP: +1% to +2%
-4.4%
+5.1%
-2.2%
-7.2%
Consolidated revenues
$13 billion to $13.5 billion
$13.6 billion
Commercial premium yields
(a)
~ 8.3% to 8.8%
(Western Region 2009: ~$316 PMPM)
7.9%
Commercial health care cost
trends
(a)
~ 20-40 bps < premium yields
(Western Region 2009: ~$274 PMPM)
Government Contracts ratio
~ 94.5% to 95%
94.7%
G&A Expense ratio
~ 8.8% to 9%
8.9%
Weighted-average fully
diluted shares outstanding
103 million to 104 million
GAAP EPS
Combined Western Region
Operations and Government
Contracts EPS
$1.92 to $2.02
$2.32 to $2.42
$2.06
(a)
Commercial premium yields and commercial health care cost comparisons are on a same-store
basis for the company’s Western Region Operations only for both 2009 and
2010. 80 bps
80 bps
99.2 M
99.2 M
$2.60
$2.60
2010 Results
2010 Results |
 65
A Solid 2010 Sets Stage for 2011
A Solid 2010 Sets Stage for 2011
•
Strong year: met or exceeded key commitments
•
Commercial margin expansion
–
2010 gross margin increased 13 percent to
$47 per member per month (PMPM)
•
Commercial enrollment stabilized in the second half
of 2010
•
Strong cash: operating cash flow of $271 million, or
1.3 times net income
•
Repurchased 9 percent of 2009 shares outstanding
•
Further margin improvement opportunities |
 Stronger Balance
Sheet Stronger Balance Sheet
66
2010
2009
Current ratio
1.70
1.68
Adjusted days claims payable
*
57.2
54.2
Debt-to-total capital ratio
19%
26%
Tangible net equity per share
$11
$10
Risk-based capital
>400%
>400%
*See Appendix for a reconciliation of this metric to the comparable GAAP financial
measure |
 Northeast
Transaction Net Cash Northeast Transaction Net Cash
67
2009
$377 million
2010
$63 million
2011
$80 million to $100 million
Total
$520 million to $540 million
Original
Guidance
$490 million to $610 million |
 68
2011 Earnings Guidance
2011 Earnings Guidance
Year-end membership
(a)
•
Medicaid: +6% to +7%
•
Medicare Advantage
(d)
: -15% to -17%
•
Total Western Region Operations
medical membership: +2% to +3%
•
PDP
(d)
: -14% to -16%
Consolidated revenues
(b)(d)
$12.0 to $12.5 billion
Commercial premium yields
(a)
~ 7.8% to 8.3%
Commercial health care cost trends
(a)
G&A expense ratio
(a)
~ 8.7% to 8.9%
Weighted-average fully
diluted shares outstanding
(c)
96 million to 97 million
GAAP EPS
(c)(d)
Combined Western Region Operations and
Government Contracts segments EPS
(c)(d)
At least $2.05
Commercial: +1% to +2%
Commercial: +1% to +2%
~
~
40
40
to
to
60
60
bps
bps
<
<
Premium
Premium
Yields
Yields
(a)
For the company’s Western Region Operations segment
(b)
For the combined Western Region Operations and Government Contracts segments
(c)
The company’s guidance does not include the impact of share repurchases other than to
counter dilution. (d)
Includes
the
impact
of
the
CMS
sanctions
previously
announced
on
November
19,
2010
At least $2.75
At least $2.75 |
 69
2011 Cash at Parent
2011 Cash at Parent
Beginning cash (12/31/10)
$204
Sources of cash
Net cash flow from subsidiaries
NE proceeds
$225 -
$235
$80 -
$100
Uses of cash
Share repurchases through 1/31/11
Other corporate uses
$34
~$85
Ending cash*
(12/31/11)
~$390 -
$420
*Excludes the impact of any future share repurchases
$ in millions |
 70
HNT: On Track
HNT: On Track
•
Continued commercial gross margin expansion
•
Commercial membership growth
•
Seamless transition to new TRICARE contract
•
Continued strong cash flow performance
–
Opportunities for further capital deployment |
 Appendix
Appendix |
 Disclosures
Regarding Disclosures Regarding
Non-GAAP Financial Information
Non-GAAP Financial Information
72
Q4 2010
Q3 2010
Q4 2009
FY 2010
FY 2009
(1)Reserve for Claims and Other Settlements
$942.0
$904.4
$951.7
$942.0
$951.7
Less: Reserve for Claims and Other Settlements for Divested Businesses
-
-
-
-
-
Less: Capitation Payable, Provider and Other Claim Settlements and Medicare Part D
(108.7)
(130.0)
(162.8)
(108.7)
(162.8)
(2)Reserve
for
Claims
and
Other
Settlements -
Adjusted
$833.3
$774.4
$788.9
$833.3
$788.9
(3)Health Plan Services Cost
$2,100.0
$2,134.7
$2,557.1
$8,609.1
$10,732.0
Less: Health Plan Services Cost for Divested Businesses
-
-
(460.7)
-
(2,123.0)
Less: Capitation Payable, Provider and Other Claim Settlements and Medicare Part D
(762.6)
(804.4)
(818.4)
(3,291.1)
(3,296.0)
(4)Health Plan Services Cost -
Adjusted
$1,337.4
$1,330.3
$1,278.0
$5,318.0
$5,313.0
(5)Number of Days in Period
92
92
92
365
365
=
(1)
/
(3)
*
(5)
Days
Claims
Payable
-
(using
end
of
period
reserve
amount)
41.3
39.0
34.2
39.9
32.4
=
(2)
/
(4)
*
(5)
Days
Claims
Payable
-
Adjusted
(using
end
of
period
reserve
amount)
57.3
53.6
56.8
57.2
54.2
Management believes that adjusted days claims payable (adjusted for divested businesses,
capitation, provider and other claim settlements and
Medicare
Part
D),
a
non-GAAP
financial
measure,
provides
useful
information
to
investors
because
the
adjusted
days
claims
payable
calculation excludes amounts related to divested businesses and health care costs for which no
or minimal reserves are maintained. Therefore,
management
believes
that
adjusted
days
claims
payable
may
present
a
more
accurate
reflection
of
days
claims
payable
calculated
from claims-based reserves than does GAAP days claims payable, which includes such costs.
This non-GAAP financial information should be considered in addition to, not as a
substitute for, financial information prepared in accordance with GAAP. The following table provides a
reconciliation of the differences between adjusted days claims payable and days claims payable,
the most directly comparable GAAP financial measure. You are encouraged to evaluate
these adjustments and the reasons we consider them appropriate for supplemental analysis. In
evaluating the adjusted amounts, you should be aware that we have incurred expenses that are
the same as or similar to some of the adjustments in the current presentation and we may
incur them again in the future. Our
presentation
of
the
adjusted
amounts
should
not
be
construed
as
an
inference
that
our
future
results
will
be
unaffected
by
unusual
or
non-recurring items.
$ in millions |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
 Closing
Remarks Closing Remarks
Jay Gellert
President and
Chief Executive Officer |
 75
HNT: Building Shareholder Value
HNT: Building Shareholder Value
•
Strategic response to changing environment
•
Diverse book of stable businesses
•
Opportunities for growth and further
gross margin and G&A improvements
•
Financial flexibility |
 Health Net,
Inc. Health Net, Inc.
2011 Investor Day
2011 Investor Day |
