Attached files
| file | filename |
|---|---|
| EX-32 - EXHIBIT 32 - Diversicare Healthcare Services, Inc. | dvcr-ex32x33118certificati.htm |
| EX-31.1 - EXHIBIT 31.1 - Diversicare Healthcare Services, Inc. | dvcr-ex311x33118certificat.htm |
| EX-31.2 - EXHIBIT 31.2 - Diversicare Healthcare Services, Inc. | dvcr-ex312x33118certificat.htm |
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
________________________________
FORM 10-Q
________________________________
CHECK ONE:
ý | QUARTERLY REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the Quarterly Period Ended: March 31, 2018
OR
¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to .
Commission file No.: 1-12996
________________________________
Diversicare Healthcare Services, Inc.
(exact name of registrant as specified in its charter)
________________________________
Delaware | 62-1559667 | |
(State or other jurisdiction of incorporation or organization) | (IRS Employer Identification No.) | |
1621 Galleria Boulevard, Brentwood, TN 37027
(Address of principal executive offices) (Zip Code)
(615) 771-7575
(Registrant’s telephone number, including area code)
Indicate by check mark whether the registrant: (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ý No ¨
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ý No ¨
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company” and "emerging growth company" in Rule 12b-2 of the Exchange Act. (Check one):
Large accelerated filer | ¨ | Accelerated filer | ¨ | ||
Non-accelerated filer | ¨(do not check if a smaller reporting company) | Smaller reporting company | ý | ||
Emerging growth company | ¨ | ||||
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. | ¨ | ||||
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). Yes ¨ No ý
6,451,495
(Outstanding shares of the issuer’s common stock as of April 30, 2018)
Part I. FINANCIAL INFORMATION
ITEM 1 – FINANCIAL STATEMENTS
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
INTERIM CONSOLIDATED BALANCE SHEETS
(in thousands)
March 31, 2018 | December 31, 2017 | ||||||
(Unaudited) | |||||||
CURRENT ASSETS: | |||||||
Cash and cash equivalents | $ | 6,418 | $ | 3,524 | |||
Receivables, less allowance for doubtful accounts and other contractual allowances of $15,129 and $14,235, respectively | 62,212 | 64,929 | |||||
Other receivables | 1,128 | 375 | |||||
Prepaid expenses and other current assets | 3,671 | 3,248 | |||||
Income tax refundable | 569 | 537 | |||||
Current assets of discontinued operations | 20 | 45 | |||||
Total current assets | 74,018 | 72,658 | |||||
PROPERTY AND EQUIPMENT, at cost | 133,754 | 147,549 | |||||
Less accumulated depreciation and amortization | (78,548 | ) | (78,345 | ) | |||
Property and equipment, net | 55,206 | 69,204 | |||||
OTHER ASSETS: | |||||||
Deferred income taxes, net | 15,020 | 15,154 | |||||
Deferred lease and other costs, net | 125 | 137 | |||||
Acquired leasehold interest, net | 6,595 | 6,691 | |||||
Assets held for sale | 13,228 | — | |||||
Other noncurrent assets | 3,656 | 3,725 | |||||
Total other assets | 38,624 | 25,707 | |||||
$ | 167,848 | $ | 167,569 | ||||
The accompanying notes are an integral part of these interim consolidated financial statements.
2
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
INTERIM CONSOLIDATED BALANCE SHEETS
(in thousands, except per share amounts)
(continued)
March 31, 2018 | December 31, 2017 | ||||||
(Unaudited) | |||||||
CURRENT LIABILITIES: | |||||||
Current portion of long-term debt and capitalized lease obligations | $ | 12,913 | $ | 13,065 | |||
Trade accounts payable | 13,775 | 14,080 | |||||
Current liabilities of discontinued operations | 462 | 461 | |||||
Accrued expenses: | |||||||
Payroll and employee benefits | 18,890 | 20,013 | |||||
Self-insurance reserves, current portion | 9,134 | 8,792 | |||||
Other current liabilities | 8,859 | 7,856 | |||||
Total current liabilities | 64,033 | 64,267 | |||||
NONCURRENT LIABILITIES: | |||||||
Long-term debt and capitalized lease obligations, less current portion and deferred financing costs, net | 75,669 | 74,603 | |||||
Self-insurance reserves, less current portion | 13,891 | 13,458 | |||||
Other noncurrent liabilities | 7,880 | 8,779 | |||||
Total noncurrent liabilities | 97,440 | 96,840 | |||||
COMMITMENTS AND CONTINGENCIES | |||||||
SHAREHOLDERS’ EQUITY: | |||||||
Common stock, authorized 20,000 shares, $.01 par value, 6,773 and 6,687 shares issued, and 6,542 and 6,455 shares outstanding, respectively | 68 | 67 | |||||
Treasury stock at cost, 232 shares of common stock | (2,500 | ) | (2,500 | ) | |||
Paid-in capital | 22,890 | 22,720 | |||||
Accumulated deficit | (15,000 | ) | (14,534 | ) | |||
Accumulated other comprehensive income | 917 | 709 | |||||
Total shareholders’ equity | 6,375 | 6,462 | |||||
$ | 167,848 | $ | 167,569 | ||||
The accompanying notes are an integral part of these interim consolidated financial statements.
3
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
INTERIM CONSOLIDATED STATEMENTS OF OPERATIONS
(in thousands, except per share amounts, unaudited)
Three Months Ended March 31, | |||||||
2018 | 2017 | ||||||
PATIENT REVENUES, net | $ | 141,285 | $ | 141,500 | |||
EXPENSES: | |||||||
Operating | 112,278 | 110,667 | |||||
Lease and rent expense | 13,713 | 13,743 | |||||
Professional liability | 2,775 | 2,670 | |||||
General and administrative | 8,139 | 8,973 | |||||
Depreciation and amortization | 2,881 | 2,487 | |||||
Total expenses | 139,786 | 138,540 | |||||
OPERATING INCOME | 1,499 | 2,960 | |||||
OTHER INCOME (EXPENSE): | |||||||
Gain on sale of investment in unconsolidated affiliate | — | 733 | |||||
Other income | 51 | — | |||||
Interest expense, net | (1,669 | ) | (1,483 | ) | |||
Total other expense | (1,618 | ) | (750 | ) | |||
INCOME (LOSS) FROM CONTINUING OPERATIONS BEFORE INCOME TAXES | (119 | ) | 2,210 | ||||
BENEFIT (PROVISION) FOR INCOME TAXES | 38 | (862 | ) | ||||
INCOME (LOSS) FROM CONTINUING OPERATIONS | (81 | ) | 1,348 | ||||
LOSS FROM DISCONTINUED OPERATIONS: | |||||||
Operating loss, net of tax benefit of $11 and $9, respectively | (22 | ) | (15 | ) | |||
NET INCOME (LOSS) | $ | (103 | ) | $ | 1,333 | ||
NET INCOME (LOSS) PER COMMON SHARE: | |||||||
Per common share – basic | |||||||
Continuing operations | $ | (0.01 | ) | $ | 0.22 | ||
Discontinued operations | — | — | |||||
$ | (0.01 | ) | $ | 0.22 | |||
Per common share – diluted | |||||||
Continuing operations | $ | (0.01 | ) | $ | 0.21 | ||
Discontinued operations | — | — | |||||
$ | (0.01 | ) | $ | 0.21 | |||
COMMON STOCK DIVIDENDS DECLARED PER SHARE OF COMMON STOCK | $ | 0.055 | $ | 0.055 | |||
WEIGHTED AVERAGE COMMON SHARES OUTSTANDING: | |||||||
Basic | 6,314 | 6,233 | |||||
Diluted | 6,314 | 6,440 | |||||
The accompanying notes are an integral part of these interim consolidated financial statements.
4
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
INTERIM CONSOLIDATED STATEMENTS OF COMPREHENSIVE LOSS
(in thousands and unaudited)
Three Months Ended March 31, | |||||||
2018 | 2017 | ||||||
NET INCOME (LOSS) | $ | (103 | ) | $ | 1,333 | ||
OTHER COMPREHENSIVE INCOME: | |||||||
Change in fair value of cash flow hedge, net of tax | 322 | 254 | |||||
Less: reclassification adjustment for amounts recognized in net income | (114 | ) | (117 | ) | |||
Total other comprehensive income | 208 | 137 | |||||
COMPREHENSIVE INCOME | $ | 105 | $ | 1,470 | |||
The accompanying notes are an integral part of these interim consolidated financial statements.
5
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
INTERIM CONSOLIDATED STATEMENTS OF CASH FLOWS
(in thousands and unaudited)
Three Months Ended March 31, | |||||||
2018 | 2017 | ||||||
CASH FLOWS FROM OPERATING ACTIVITIES: | |||||||
Net income (loss) | $ | (103 | ) | $ | 1,333 | ||
Discontinued operations | (22 | ) | (15 | ) | |||
Income from continuing operations | (81 | ) | 1,348 | ||||
Adjustments to reconcile income (loss) from continuing operations to net cash provided by (used in) operating activities: | |||||||
Depreciation and amortization | 2,881 | 2,487 | |||||
Provision for doubtful accounts | — | 1,970 | |||||
Deferred income tax provision | — | 354 | |||||
Provision for self-insured professional liability, net of cash payments | 956 | (83 | ) | ||||
Stock-based compensation | 284 | 241 | |||||
Gain on sale of unconsolidated affiliate | — | (733 | ) | ||||
Provision for leases in excess of cash payments | (453 | ) | (91 | ) | |||
Deferred bonus | — | 500 | |||||
Other | 140 | 123 | |||||
Changes in assets and liabilities affecting operating activities: | |||||||
Receivables, net | 2,017 | (6,518 | ) | ||||
Prepaid expenses and other assets | (439 | ) | 1,081 | ||||
Trade accounts payable and accrued expenses | (86 | ) | (1,468 | ) | |||
Net cash provided by (used in) continuing operations | 5,219 | (789 | ) | ||||
Discontinued operations | (474 | ) | (67 | ) | |||
Net cash provided by (used in) operating activities | 4,745 | (856 | ) | ||||
CASH FLOWS FROM INVESTING ACTIVITIES: | |||||||
Purchases of property and equipment | (2,012 | ) | (2,237 | ) | |||
Net cash used in continuing operations | (2,012 | ) | (2,237 | ) | |||
Discontinued operations | — | — | |||||
Net cash used in investing activities | (2,012 | ) | (2,237 | ) | |||
CASH FLOWS FROM FINANCING ACTIVITIES: | |||||||
Repayment of debt obligations | (4,762 | ) | (9,193 | ) | |||
Proceeds from issuance of debt | 5,651 | 12,567 | |||||
Financing costs | (132 | ) | (10 | ) | |||
Issuance and redemption of employee equity awards | (78 | ) | (94 | ) | |||
Payment of common stock dividends | (350 | ) | (346 | ) | |||
Payment for preferred stock restructuring | (168 | ) | (163 | ) | |||
Net cash provided by financing activities | 161 | 2,761 | |||||
Discontinued operations | — | — | |||||
Net cash provided by financing activities | $ | 161 | $ | 2,761 | |||
The accompanying notes are an integral part of these interim consolidated financial statements.
6
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
INTERIM CONSOLIDATED STATEMENTS OF CASH FLOWS
(in thousands and unaudited)
(continued)
Three Months Ended March 31, | |||||||
2018 | 2017 | ||||||
NET INCREASE (DECREASE) IN CASH AND CASH EQUIVALENTS | $ | 2,894 | $ | (332 | ) | ||
CASH AND CASH EQUIVALENTS, beginning of period | 3,524 | 4,263 | |||||
CASH AND CASH EQUIVALENTS, end of period | $ | 6,418 | $ | 3,931 | |||
SUPPLEMENTAL INFORMATION: | |||||||
Cash payments of interest | $ | 1,432 | $ | 1,231 | |||
Cash payments (refunds) of income taxes | $ | (16 | ) | $ | 6 | ||
The accompanying notes are an integral part of these interim consolidated financial statements.
7
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
NOTES TO INTERIM CONSOLIDATED FINANCIAL STATEMENTS
MARCH 31, 2018 AND 2017
(Dollars and shares in thousands, except per share data)
(Unaudited)
1. | BUSINESS |
Diversicare Healthcare Services, Inc. (together with its subsidiaries, “Diversicare” or the “Company”) provides long-term care services to nursing center patients in ten states, primarily in the Southeast, Midwest, and Southwest. The Company’s centers provide a range of health care services to their patients and residents that include nursing, personal care, and social services. Additionally, the Company’s nursing centers also offer a variety of comprehensive rehabilitation services, as well as nutritional support services. The Company's continuing operations include centers in Alabama, Florida, Indiana, Kansas, Kentucky, Mississippi, Missouri, Ohio, Tennessee, and Texas.
As of March 31, 2018, the Company’s continuing operations consist of 76 nursing centers with 8,456 licensed nursing beds. The Company owns 18 and leases 58 of its nursing centers. Our nursing centers range in size from 48 to 320 licensed nursing beds. The licensed nursing bed count does not include 497 licensed assisted and residential living beds.
2. | CONSOLIDATION AND BASIS OF PRESENTATION OF FINANCIAL STATEMENTS |
The interim consolidated financial statements include the operations and accounts of Diversicare Healthcare Services and its subsidiaries, all wholly-owned. All significant intercompany accounts and transactions have been eliminated in consolidation. The Company had one equity method investee, which was sold during the fourth quarter of 2016. The sale resulted in a $1,366 gain in the fourth quarter of 2016. Subsequently, the Company recognized an additional gain of $733 for the three-month period ended March 31, 2017, related to the liquidation of remaining assets affiliated with the partnership.
The interim consolidated financial statements for the three month periods ended March 31, 2018 and 2017, included herein have been prepared by the Company, without audit, pursuant to the rules and regulations of the Securities and Exchange Commission. Certain information and footnote disclosures normally included in financial statements prepared in accordance with accounting principles generally accepted in the United States of America have been condensed or omitted pursuant to such rules and regulations. In the opinion of management of the Company, the accompanying interim consolidated financial statements reflect all normal, recurring adjustments necessary to present fairly the Company’s financial position at March 31, 2018, and the results of operations and cash flows for the three month periods ended March 31, 2018 and 2017. The Company’s balance sheet information at December 31, 2017, was derived from its audited consolidated financial statements as of December 31, 2017.
Effective January 1, 2018, we adopted the requirements of Accounting Standards Update ("ASU") No. 2014-09, Revenue from Contracts with Customers as discussed in Notes 3 and 4 to the interim consolidated financial statements. All amounts and disclosures set forth in this Form 10-Q have been updated to comply with the new standard.
The results of operations for the periods ended March 31, 2018 and 2017 are not necessarily indicative of the operating results that may be expected for a full year. These interim consolidated financial statements should be read in connection with the audited consolidated financial statements and notes thereto included in the Company’s Annual Report on Form 10-K for the fiscal year ended December 31, 2017.
3. | RECENT ACCOUNTING GUIDANCE |
Recent Accounting Standards Adopted by the Company
In May 2014, the Financial Accounting Standards Board ("FASB") issued ASU No. 2014-09, Revenue from Contracts with Customers (Topic 606), which outlines a single comprehensive model for recognizing revenue and supersedes most existing revenue recognition guidance, including guidance specific to the healthcare industry. Topic 606 is effective for annual and interim reporting periods beginning after December 15, 2017. The Company adopted the requirements of this standard effective January 1, 2018. The Company elected to apply the modified retrospective approach with the cumulative transition effect recognized in beginning retained earnings as of the date of adoption. The impact of the implementation to the consolidated financial statements for periods subsequent to adoption is not material. See Note 4, "Revenue Recognition" for a discussion regarding revenue recognition under the new standard.
In March 2016, the FASB issued ASU No. 2016-09, Compensation - Stock Compensation (Topic 718): Improvements to Employee Share-Based Payment Accounting. The ASU was issued as part of the FASB Simplification Initiative and involves several aspects of accounting for share-based payment transactions, including the income tax consequences and classification on the statement
8
of cash flows. We adopted this standard as of January 1, 2017. The adoption did not have a material impact on our financial position, results of operations or cash flows.
In August 2016, the FASB issued ASU No. 2016-15, Statement of Cash Flows (Topic 230). The ASU provides clarification regarding how certain cash receipts and cash payments are presented and classified in the statement of cash flows. The guidance addresses eight specific cash flow issues with the objective of reducing the existing diversity in practice. The ASU is effective for annual and interim periods beginning after December 15, 2017, which required the Company to adopt these provisions in the first quarter of fiscal 2018 using a retrospective approach. The adoption did not have a material impact on our financial position, results of operations or cash flows.
In November 2016, the FASB issued ASU No. 2016-18, Statement of Cash Flows (Topic 230): Restricted Cash, which requires that the Statement of Cash Flows explain the changes during the period of cash and cash equivalents inclusive of amounts categorized as Restricted Cash. As a result, amounts generally described as restricted cash and restricted cash equivalents should be included with cash and cash equivalents when reconciling the beginning-of-period and end-of-period total amounts shown on the statement of cash flows. The standard is effective for periods beginning after December 15, 2017, which required the Company to adopt these provisions in the first quarter of fiscal 2018. The adoption did not have a material impact on our financial position, results of operations or cash flows.
In January 2017, the FASB issued ASU No. 2017-01, Business Combinations (Topic 805) - Clarifying the Definition of a Business, which provides guidance to assist entities with evaluating whether transactions should be accounted for as acquisitions (or disposals) of assets or businesses. The adoption is effective for annual and interim periods beginning after December 15, 2017. The Company will evaluate future acquisitions under this guidance, which may result in future acquisitions being accounted for as asset acquisitions.
In May 2017, the FASB issued ASU No. 2017-09, Compensation - Stock Compensation (Topic 718): Scope of Modification Accounting. The amended standard specifies the modification accounting applicable to any entity which changes the terms or conditions of a share-based payment award. The new guidance is effective for all entities after December 15, 2017. The adoption did not have a material impact on our financial position, results of operations or cash flows.
Accounting Standards Recently Issued But Not Yet Adopted by the Company
In February 2016, the FASB issued ASU No. 2016-02, Leases. The new standard establishes a right-of-use (ROU) model that requires a lessee to record a ROU asset and a lease liability on the balance sheet for all leases with terms longer than 12 months. Leases will be classified as either finance or operating, with classification affecting the pattern of expense recognition in the income statement. The new standard is effective for fiscal years beginning after December 15, 2018, including interim periods within those fiscal years. A modified retrospective transition approach is required for lessees for capital and operating leases existing at, or entered into after, the beginning of the earliest comparative period presented in the financial statements, with certain practical expedients available. Disclosures will be required to meet the objective of enabling users of financial statements to assess the amount, timing, and uncertainty of cash flows arising from leases. We anticipate this standard will have a material impact on our consolidated financial position and results of operations. We have organized an implementation group of cross-functional departmental management to ensure the completeness of our lease information, analyze the appropriate classification of current leases under the new standard, and develop new processes to execute, approve and classify leases on an ongoing basis. We are continuing to evaluate the extent of this anticipated impact on our consolidated financial position and results of operations and the quantitative and qualitative factors that will impact the Company as part of the adoption.
In June 2016, the FASB issued ASU No. 2016-13, Measurement of Credit Losses on Financial Instruments. This update is intended to improve financial reporting by requiring timelier recognition of credit losses on loans and other financial instruments that are not accounted for at fair value through net income, including loans held for investment, held-to-maturity debt securities, trade and other receivables, net investment in leases and other such commitments. This update requires that financial statement assets measured at an amortized cost be presented at the net amount expected to be collected, through an allowance for credit losses that is deducted from the amortized cost basis. This standard is effective for the fiscal year beginning after December 15, 2019 with early adoption permitted. The Company is in the initial stages of evaluating the impact from the adoption of this new standard on the consolidated financial statements and related notes.
In August 2017, the FASB issued ASU No. 2017-12, Derivatives and Hedging - Targeted Improvements to Accounting for Hedging Activities, which is intended to simplify and amend the application of hedge accounting to more clearly portray the economics of an entity’s risk management strategies in its financial statements. The new guidance will make more financial and nonfinancial hedging strategies eligible for hedge accounting and reduce complexity in fair value hedges of interest rate risk. The new guidance also changes how companies assess effectiveness and amends the presentation and disclosure requirements. The new guidance eliminates the requirement to separately measure and report hedge ineffectiveness and generally the entire change in the fair value of a hedging instrument will be required to be presented in the same income statement line as the hedged item. The new guidance also eases certain documentation and assessment requirements and modifies the accounting for components excluded from the assessment of hedge effectiveness. The new guidance is effective for public entities for fiscal years beginning after December 15,
9
2018, including interim periods within those years. Early adoption is permitted in any interim period or fiscal year before the effective date. The Company is evaluating the effect this guidance will have on our consolidated financial statements and related disclosures.
In February 2018, the FASB issued ASU No. 2018-02, Income Statement- Reporting Comprehensive Income (Topic 220): Reclassification of Certain Tax Effects from Accumulated Other Comprehensive Income. The new guidance allows entities the option to reclassify stranded tax effects resulting from the Tax Cuts and Jobs Act from accumulated other comprehensive income (OCI) to retained earnings. The new guidance allows the option to apply the guidance retrospectively or in the period of adoption. The guidance is effective for fiscal years beginning after December 15, 2018, and interim periods within those fiscal years. Early adoption is permitted. The Company is evaluating the effect this guidance will have on our consolidated financial statements and related disclosures.
In March 2018, the FASB issued ASU No. 2018-05, Income Taxes (Topic 740): Amendments to SEC Paragraphs Pursuant to SEC Staff Accounting Bulletin No. 118 which allowed SEC registrants to record provisional amounts in earnings for the year ended December 31, 2017 due to the complexities involved in accounting for the enactment of the Tax Cuts and Jobs Act. The Company recognized the estimated income tax effects of the Tax Cuts and Jobs Act in its 2017 Consolidated Financial Statements in accordance with SEC Staff Accounting Bulletin No. 118 ("SAB No. 118").
4. REVENUE RECOGNITION
On January 1, 2018, the Company adopted Accounting Standards Codification ("ASC") 606 using the modified retrospective method for all contracts as of the date of adoption. The reported results for 2018 reflect the application of ASC 606 guidance while the reported results for 2017 were prepared under the guidance of ASC 605, Revenue Recognition (ASC 605), which is also referred to herein as "legacy GAAP". The adoption of ASC 606 represents a change in accounting principle that will more closely align revenue recognition with the delivery of the Company's services. The amount of revenue recognized reflects the consideration to which the Company expects to be entitled to receive in exchange for these services. ASC 606 requires companies to exercise more judgment and recognize revenue in accordance with the standard's core principle by applying the following five steps:
Step 1: Identify the contract with a customer.
Step 2: Identify the performance obligations in the contract.
Step 3: Determine the transaction price.
Step 4: Allocate the transaction price to the performance obligations in the contract.
Step 5: Recognize revenue when (or as) the entity satisfies a performance obligation.
Performance obligations are promises made in a contract to transfer a distinct good or service to the customer. A contract's transaction price is allocated to each distinct performance obligation and recognized as revenue when, or as, the performance obligation is satisfied. The Company has concluded that the contracts with patients and residents represent a bundle of distinct services that are substantially the same, with the same pattern of transfer to the customer. Accordingly, the promise to provide quality care is accounted for as a single performance obligation.
The Company performed analyses using the application of the portfolio approach as a practical expedient to group patient contracts with similar characteristics, such that revenue for a given portfolio would not be materially different than if it were evaluated on a contract-by-contract basis. These analyses incorporated consideration of reimbursements at varying rates from Medicaid, Medicare, Managed Care, Private Pay, Assisted Living, Hospice, and Veterans for services provided in each corresponding states. It was determined that the contracts are not materially different for the following groups: Medicaid, Medicare, Managed Care and Private Pay and other (Assisted Living, Hospice and Veterans).
In order to determine the transaction price, the Company estimates the amount of variable consideration at the beginning of the contract using the expected value method. The estimates consider (i) payor type, (ii) historical payment trends, (iii) the maturity of the portfolio, and (iv) geographic payment trends throughout a class of similar payors. The Company typically enters into agreements with third-party payors that provide for payments at amounts different from the established charges. These arrangement terms provide for subsequent settlement and cash flows that may occur well after the service is provided. The Company constrains (reduces) the estimates of variable consideration such that it is probable that a significant reversal of previously recognized revenue will not occur throughout the life of the contract. Changes in the Company's expectation of the amount it will receive from the patient or third-party payors will be recorded in revenue unless these is a specific event that suggests the patient or third-party payor no longer has the ability and intent to pay the amount due and , therefore, the changes in its estimate of variable consideration better represent and impairment, or bad debt. These estimates are re-assessed each reporting period, and any amounts allocated to a satisfied performance obligation are recognized as revenue or a reduction of revenue in the period in which the transaction price changes.
10
The Company satisfies its performance obligation by providing quality of care services to its patients and residents on a daily basis until termination of the contract. The performance obligation is recognized on a time elapsed basis, by day, for which the services are provided. For these contracts, the Company has the right to consideration from the customer in an amount that directly corresponds with the value to the customer of the Company's performance to date. Therefore, the Company recognizes revenue based on the amount billable to the customer in accordance with the practical expedient in ASC 606-10-55-18. Additionally, since the Company applied ASC 606 using certain practical expedients, the Company elected not to disclose the aggregate amount of the transaction price for unsatisfied, or partially unsatisfied, performance obligations for all contracts with an original expected length of one year or less.
The Company incurs costs related to patient/resident contracts, such as legal and advertising expenses. The contract costs are expensed as incurred. They are not expected to be recovered and are not chargeable to the patient/resident regardless of whether the contract is executed.
Financial Statement Impact of Adopting ASC 606
The Company adopted ASC 606 using the modified retrospective method. The cumulative effect of applying the new guidance to all contracts with customers as of January 1, 2018 was not material to the interim consolidated financial statements. As a result of applying the modified retrospective method to adopt ASC 606, the following adjustments were made to our operating results (dollar amounts in thousands):
Three Months Ended March 31, 2018 | |||||
As Reported | Increase (Decrease) | Balances as if the previous accounting guidance was in effect | |||
Patient Revenues, net | $141,285 | 3,463 (256) 3,207 | (a) (b) | $144,492 | |
Accounts Receivable, net | $62,212 | (256) | (b) | $61,956 | |
Accumulated Deficit | $(15,000) | 256 (82) 174 | (b) (c) | $(14,826) | |
(a) Adjusts for the implicit price concession of bad debt expense.
(b) Adjusts for the implementation of ASC 606.
(c) Reflects the tax adjustment for the ASC 606 adjustment of $256.
Disaggregation of Revenue
The following table summarizes revenue from contracts with customers by payor source for the periods presented (dollar amounts in thousands):
Three Months Ended March 31, | |||||||||||||||||
2018 | 2018 | 2017(1) | |||||||||||||||
As reported | As Adjusted to Legacy GAAP | As reported | |||||||||||||||
Medicaid | $ | 63,886 | 45.2 | % | $ | 73,214 | 50.7 | % | $ | 72,873 | 51.5 | % | |||||
Medicare | 29,751 | 21.1 | % | 38,139 | 26.4 | % | 38,011 | 26.9 | % | ||||||||
Managed Care | 14,212 | 10.1 | % | 12,092 | 8.4 | % | 10,806 | 7.6 | % | ||||||||
Private Pay and other | 33,436 | 23.6 | % | 21,047 | 14.5 | % | 19,810 | 14.0 | % | ||||||||
Total | $ | 141,285 | 100.0 | % | $ | 144,492 | 100.0 | % | $ | 141,500 | 100.0 | % | |||||
(1) As noted above, prior period amounts have not been adjusted under the application of the modified retrospective method.
5. | LONG-TERM DEBT AND INTEREST RATE SWAP |
11
The Company has agreements with a syndicate of banks for a mortgage term loan ("Original Mortgage Loan") and the Company’s revolving credit agreement ("Original Revolver"). On February 26, 2016, the Company executed an Amended and Restated Credit Agreement (the "Credit Agreement") which modified the terms of the Original Mortgage Loan and the Original Revolver Agreements dated April 30, 2013. The Credit Agreement increased the Company's borrowing capacity to $100,000 allocated between a $72,500 Mortgage Loan ("Amended Mortgage Loan") and a $27,500 Revolver ("Amended Revolver"). The Amended Mortgage Loan consists of a $60,000 term loan facility and a $12,500 acquisition loan facility. Loan acquisition costs associated with the Amended Mortgage Loan and the Amended Revolver were capitalized in the amount of $2,162 and are being amortized over the five-year term of the agreements.
Under the terms of the amended agreements, the syndicate of banks provided the Amended Mortgage Loan with an original principal balance of $72,500 with a five-year maturity through February 26, 2021, and a $27,500 Amended Revolver through February 26, 2021. The Amended Mortgage Loan has a term of five years, with principal and interest payable monthly based on a 25-year amortization. Interest on the term and acquisition loan facilities is based on LIBOR plus 4.0% and 4.75%, respectively. A portion of the Amended Mortgage Loan is effectively fixed at 5.79% pursuant to an interest rate swap with an initial notional amount of $30,000. The Amended Mortgage Loan balance was $73,000 as of March 31, 2018, consisting of $64,000 on the term loan facility with an interest rate of 5.75% and $9,000 on the acquisition loan facility with an interest rate of 6.5%. The Amended Mortgage Loan is secured by eighteen owned nursing centers, related equipment and a lien on the accounts receivable of these centers. The Amended Mortgage Loan and the Amended Revolver are cross-collateralized and cross-defaulted. The Company’s Amended Revolver has an interest rate of LIBOR plus 4.0% and is secured by accounts receivable and is subject to limits on the maximum amount of loans that can be outstanding under the revolver based on borrowing base restrictions.
Effective October 3, 2016, the Company entered into the Second Amendment ("Second Revolver Amendment") to amend the Amended Revolver. The Second Revolver Amendment increased the Amended Revolver capacity from the $27,500 in the Amended Revolver to $52,250; provided that the maximum revolving facility be reduced to $42,250 on August 1, 2017. Subsequently, on June 30, 2017, the Company executed a Fourth Amendment (the "Fourth Revolver Amendment") to amend the Amended Revolver, which modifies the capacity of the revolver to remain at $52,250.
On December 29, 2016, the Company executed a Third Amendment ("Third Revolver Amendment") to amend the Amended Revolver. The Third Amendment modified the terms of the Amended Mortgage Loan Agreement by increasing the Company’s letter of credit sublimit from $10,000 to $15,000.
Effective June 30, 2017, the Company entered into a Second Amendment (the "Second Term Amendment") to amend the Amended Mortgage Loan. The Second Term Amendment amended the terms of the Amended Mortgage Loan Agreement by increasing the Company's term loan facility by $7,500.
Effective February 27, 2018, the Company executed a Fifth Amendment to the Amended Revolver and a Third Amendment to the Amended Mortgage Loan. Under the terms of the Amendments, the minimum fixed charge coverage ratio shall not be less than 1.01 to 1.00 as of March 31, 2018 and for each quarter thereafter.
As of March 31, 2018, the Company had $16,000 borrowings outstanding under the Amended Revolver compared to $16,000 outstanding as of December 31, 2017. The outstanding borrowings on the revolver were used primarily to compensate for accumulated Medicaid and Medicare receivables at recently acquired facilities as these facilities proceed through the change in ownership process with Centers for Medicare & Medicaid Services (“CMS”). Annual fees for letters of credit issued under the Amended Revolver are 3.0% of the amount outstanding. The Company has eleven letters of credit with a total value of $13,620 outstanding as of March 31, 2018. Considering the balance of eligible accounts receivable, the letters of credit, the amounts outstanding under the revolving credit facility and the maximum loan amount of $39,468 the balance available for borrowing under the Amended Revolver was $9,848 at March 31, 2018.
The Company’s debt agreements contain various financial covenants, the most restrictive of which relates to debt service coverage ratios. The Company is in compliance with all such covenants at March 31, 2018.
Interest Rate Swap Transaction
As part of the debt agreements entered into in April 2013, the Company entered into an interest rate swap agreement with a member of the bank syndicate as the counterparty. The Company designated its interest rate swap as a cash flow hedge and the earnings component of the hedge, net of taxes, is reflected as a component of other comprehensive income (loss). In conjunction with the February 26, 2016 amendment to the Credit Agreement, the Company amended the terms of its interest rate swap. The interest rate swap agreement has the same effective date and maturity date as the Amended Mortgage Loan, and has an amortizing notional amount that was $28,355 as of March 31, 2018. The interest rate swap agreement requires the Company to make fixed rate payments to the bank calculated on the applicable notional amount at an annual fixed rate of 5.79% while the bank is obligated to make payments to the Company based on LIBOR on the same notional amount.
The Company assesses the effectiveness of its interest rate swap on a quarterly basis, and at March 31, 2018, the Company determined that the interest rate swap was highly effective. The interest rate swap valuation model indicated a net asset of $492
12
at March 31, 2018. The fair value of the interest rate swap is included in “other noncurrent assets” on the Company’s interim consolidated balance sheet. The asset related to the change in the interest rate swap included in accumulated other comprehensive income at March 31, 2018 is $335 net of the income tax provision of $157. As the Company’s interest rate swap is not traded on a market exchange, the fair value is determined using a valuation based on a discounted cash flow analysis. This analysis reflects the contractual terms of the interest rate swap agreement and uses observable market-based inputs, including estimated future LIBOR interest rates. The interest rate swap valuation is classified in Level 2 of the fair value hierarchy, in accordance with the FASB guidance set forth in ASC 820, Fair Value Measurement.
13
6. COMMITMENTS AND CONTINGENCIES
Professional Liability and Other Liability Insurance
The Company has professional liability insurance coverage for its nursing centers that, based on historical claims experience, is likely to be substantially less than the claims that are expected to be incurred. Effective July 1, 2013, the Company established a wholly-owned, offshore limited purpose insurance subsidiary, SHC Risk Carriers, Inc. (“SHC”), to replace some of the expiring commercial policies. SHC covers losses up to specified limits per occurrence. All of the Company's nursing centers in Florida, and Tennessee are now covered under the captive insurance policies along with most of the nursing centers in Alabama, Kentucky, and Texas. The insurance coverage provided for these centers under the SHC policy provides coverage limits of at least $500 per medical incident with a sublimit per center of $1,000 and total annual aggregate policy limits of $5,000. All other centers within the Company's portfolio are covered through various commercial insurance policies which provide similar coverage limits per medical incident, per location, and on an aggregate basis for covered centers. The deductibles for these policies are covered through the insurance subsidiary.
Reserve for Estimated Self-Insured Professional Liability Claims
Because the Company’s actual liability for existing and anticipated professional liability and general liability claims will likely exceed the Company’s limited insurance coverage, the Company has recorded total liabilities for reported and estimated future claims of $20,536 as of March 31, 2018. This accrual includes estimates of liability for incurred but not reported claims, estimates of liability for reported but unresolved claims, actual liabilities related to settlements, including settlements to be paid over time, and estimates of legal costs related to these claims. All losses are projected on an undiscounted basis and are presented without regard to any potential insurance recoveries. Amounts are added to the accrual for estimates of anticipated liability for claims incurred during each period, and amounts are deducted from the accrual for settlements paid on existing claims during each period.
The Company evaluates the adequacy of this liability on a quarterly basis. Semi-annually, the Company retains a third-party actuarial firm to assist in the evaluation of this reserve. Since May 2012, Merlinos & Associates, Inc. (“Merlinos”) has assisted management in the preparation of the appropriate accrual for incurred but not reported general and professional liability claims based on data furnished as of May 31 and November 30 of each year. Merlinos primarily utilizes historical data regarding the frequency and cost of the Company's past claims over a multi-year period, industry data and information regarding the number of occupied beds to develop its estimates of the Company's ultimate professional liability cost for current periods.
On a quarterly basis, the Company obtains reports of asserted claims and lawsuits incurred. These reports, which are provided by the Company’s insurers and a third-party claims administrator, contain information relevant to the actual expense already incurred with each claim as well as the third-party administrator’s estimate of the anticipated total cost of the claim. This information is reviewed by the Company quarterly and provided to the actuary semi-annually. Based on the Company’s evaluation of the actual claim information obtained, the semi-annual estimates received from the third-party actuary, the amounts paid and committed for settlements of claims and on estimates regarding the number and cost of additional claims anticipated in the future, the reserve estimate for a particular period may be revised upward or downward on a quarterly basis. Any increase in the accrual decreases results of operations in the period and any reduction in the accrual increases results of operations during the period.
As of March 31, 2018, the Company is engaged in 73 professional liability lawsuits. Ten lawsuits are currently scheduled for trial or arbitration during the next twelve months, and it is expected that additional cases will be set for trial or hearing. The Company’s cash expenditures for self-insured professional liability costs from continuing operations were $1,093 and $2,071 for the three months ended March 31, 2018 and 2017, respectively.
The Company follows the FASB ASU, "Presentation of Insurance Claims and Related Insurance Recoveries," that clarifies that a health care entity should not net insurance recoveries against a related professional liability claim and that the amount of the claim liability should be determined without consideration of insurance recoveries. Accordingly, the estimated insurance recovery receivables are included within "Other Current Assets" on the Consolidated Balance Sheet. As of March 31, 2018 there are no estimated insurance recovery receivables.
Although the Company adjusts its accrual for professional and general liability claims on a quarterly basis and retains a third-party actuarial firm semi-annually to assist management in estimating the appropriate accrual, professional and general liability claims are inherently uncertain, and the liability associated with anticipated claims is very difficult to estimate. Professional liability cases have a long cycle from the date of an incident to the date a case is resolved, and final determination of the Company’s actual liability for claims incurred in any given period is a process that takes years. As a result, the Company’s actual liabilities may vary significantly from the accrual, and the amount of the accrual has and may continue to fluctuate by a material amount in any given period. Each change in the amount of this accrual will directly affect the Company’s reported earnings and financial position for the period in which the change in accrual is made.
14
Civil Investigative Demand ("CID")
In July 2013, the Company learned that the United States Attorney for the Middle District of Tennessee ("DOJ") had commenced a civil investigation of potential violations of the False Claims Act ("FCA").
In October 2014, the Company learned that the investigation was started by the filing under seal of a false claims action against the two centers that were subject of the original civil investigative demand ("CID"). In connection with this matter, between July 2013 and early February 2016, the Company received three civil investigative demands (a form of subpoena) for documents. The Company has responded to those demands and also provided voluntarily additional information requested by the DOJ. The DOJ has also taken testimony from current and former employees of the Company. The investigation relates to the Company’s practices and policies for rehabilitation, and other services, for preadmission evaluation forms ("PAEs") required by TennCare and for Pre-Admission Screening and Resident Reviews ("PASRRs") required by the Medicare program.
In June 2016, the Company received an authorized investigative demand (a form of subpoena) for documents in connection with a criminal investigation by the DOJ related to our practices with respect to PAEs and PASRRs, and the Company has provided documents responsive to this subpoena and continues to provide additional information as requested. The Company cannot predict the outcome of these investigations or the related lawsuits, and the outcome could have a materially adverse effect on the Company, including the imposition of treble damages, criminal charges, fines, penalties and/or a corporate integrity agreement. Additionally, the uncertainty regarding the outcome of this investigation makes it more difficult for the Company to pursue strategic possibilities, longer term initiatives or to make significant financial commitments outside of the normal course of its business. The Company is committed to provide caring and professional services to its patients and residents in compliance with applicable laws and regulations.
Other Insurance
With respect to workers’ compensation insurance, substantially all of the Company’s employees became covered under either a prefunded deductible policy or state-sponsored programs. The Company has been and remains a non-subscriber to the Texas workers’ compensation system and is, therefore, completely self-insured for employee injuries with respect to its Texas operations. From June 30, 2003 until June 30, 2007, the Company’s workers’ compensation insurance programs provided coverage for claims incurred with premium adjustments depending on incurred losses. For the period from July 1, 2007 until June 30, 2008, the Company is completely insured for workers' compensation exposure. From the period from July 1, 2008 through March 31, 2018, the Company is covered by a prefunded deductible policy. Under this policy, the Company is self-insured for the first $500 per claim, subject to an aggregate maximum of $3,000. The Company funds a loss fund account with the insurer to pay for claims below the deductible. The Company accounts for premium expense under this policy based on its estimate of the level of claims subject to the policy deductibles expected to be incurred. The liability for workers’ compensation claims is $802 at March 31, 2018. The Company has a non-current receivable for workers’ compensation policies covering previous years of $1,061 as of March 31, 2018. The non-current receivable is a function of payments paid to the Company’s insurance carrier in excess of the estimated level of claims expected to be incurred.
As of March 31, 2018, the Company is self-insured for health insurance benefits for certain employees and dependents for amounts up to $200 per individual annually. The Company provides reserves for the settlement of outstanding self-insured health claims at amounts believed to be adequate. The liability for reported claims and estimates for incurred but unreported claims is $1,687 at March 31, 2018. The differences between actual settlements and reserves are included in expense in the period finalized.
7. | STOCK-BASED COMPENSATION |
Overview of Plans
In June 2008, the Company adopted the Advocat Inc. 2008 Stock Purchase Plan for Key Personnel (“Stock Purchase Plan”). The Stock Purchase Plan provides for the granting of rights to purchase shares of the Company's common stock to directors and officers. The Stock Purchase Plan allows participants to elect to utilize a specified portion of base salary, annual cash bonus, or director compensation to purchase restricted shares or restricted share units (“RSU's”) at 85% of the quoted market price of a share of the Company's common stock on the date of purchase. The restriction period under the Stock Purchase Plan is generally two years from the date of purchase and during which the shares will have the rights to receive dividends, however, the restricted share certificates will not be delivered to the shareholder and the shares cannot be sold, assigned or disposed of during the restriction period. In June 2016, our shareholders approved an amendment to the Stock Purchase Plan to increase the number of shares of our common stock authorized under the Plan from 150 shares to 350 shares. No grants can be made under the Stock Purchase Plan after April 25, 2028.
In April 2010, the Compensation Committee of the Board of Directors adopted the 2010 Long-Term Incentive Plan (“2010 Plan”), followed by approval by the Company's shareholders in June 2010. The 2010 Plan allows the Company to issue stock appreciation
rights, stock options and other share and cash based awards. In June 2017, our shareholders approved an amendment to the Long-Term Incentive Plan to increase the number of shares of our common stock authorized under the Plan from 380 shares to 680 shares. No grants can be made under the 2010 Plan after May 31, 2027.
Equity Grants and Valuations
During the three months ended March 31, 2018 and 2017, the Compensation Committee of the Board of Directors approved grants totaling approximately 90 and 88 shares of restricted common stock to certain employees and members of the Board of Directors, respectively. The fair value of restricted shares is determined as the quoted market price of the underlying common shares at the date of the grant. The restricted shares typically vest 33% on the first, second and third anniversaries of the grant date. Unvested shares may not be sold or transferred. During the vesting period, dividends accrue on the restricted shares, but are paid in additional shares of common stock upon vesting, subject to the vesting provisions of the underlying restricted shares. The restricted shares are entitled to the same voting rights as other common shares. Upon vesting, all restrictions are removed.
Prior to 2017, the Compensation Committee of the Board of Directors also approved grants of Stock Only Stock Appreciation Rights (“SOSARs”) and Stock Options at the market price of the Company's common stock on the grant date. The SOSARs and Options vest 33% on the first, second and third anniversaries of the grant date, and expire 10 years from the grant date.
In computing the fair value estimates using the Black-Scholes-Merton valuation method, the Company took into consideration the exercise price of the equity grants and the market price of the Company's stock on the date of grant. The Company used an expected volatility that equals the historical volatility over the most recent period equal to the expected life of the equity grants. The risk free interest rate is based on the U.S. treasury yield curve in effect at the time of grant. The Company used the expected dividend yield at the date of grant, reflecting the level of annual cash dividends currently being paid on its common stock.
Summarized activity of the equity compensation plans is presented below:
Weighted | ||||||
Options/ | Average | |||||
SOSARs | Exercise Price | |||||
Outstanding, December 31, 2017 | 212 | $ | 6.64 | |||
Granted | 30 | 8.14 | ||||
Exercised | — | — | ||||
Expired or cancelled | (15 | ) | 10.88 | |||
Outstanding, March 31, 2018 | 227 | $ | 6.56 | |||
Exercisable, March 31, 2018 | 207 | $ | 6.40 | |||
Weighted | ||||||
Average | ||||||
Restricted | Grant Date | |||||
Shares | Fair Value | |||||
Outstanding, December 31, 2017 | 164 | $ | 9.95 | |||
Granted | 90 | 8.14 | ||||
Dividend Equivalents | 1 | 7.52 | ||||
Vested | (79 | ) | 10.27 | |||
Cancelled | (1 | ) | 10.17 | |||
Outstanding, March 31, 2018 | 175 | $ | 8.85 | |||
15
Summarized activity of the Restricted Share Units for the Stock Purchase Plan is as follows:
Weighted | ||||||
Average | ||||||
Restricted | Grant Date | |||||
Share Units | Fair Value | |||||
Outstanding, December 31, 2017 | 44 | $ | 9.59 | |||
Granted | 16 | 8.14 | ||||
Dividend Equivalents | 1 | 7.52 | ||||
Vested | (17 | ) | 8.91 | |||
Outstanding, March 31, 2018 | 44 | $ | 9.30 | |||
The SOSARs and Options were valued and recorded in the same manner, and will be settled with issuance of new stock for the difference between the market price on the date of exercise and the exercise price. The Company estimated the total recognized and unrecognized compensation related to SOSARs and stock options using the Black-Scholes-Merton equity grant valuation model.
In computing the fair value estimates using the Black-Scholes-Merton valuation model, the Company took into consideration the exercise price of the equity grants and the market price of the Company's stock on the date of grant. The Company used an expected volatility that equals the historical volatility over the most recent period equal to the expected life of the equity grants. The risk free interest rate is based on the U.S. treasury yield curve in effect at the time of grant. The Company used the expected dividend yield at the date of grant, reflecting the level of annual cash dividends currently being paid on its common stock.
The following table summarizes information regarding stock options and SOSAR grants outstanding as of March 31, 2018:
Weighted | ||||||||||||||||||
Average | Intrinsic | Intrinsic | ||||||||||||||||
Range of | Exercise | Grants | Value-Grants | Grants | Value-Grants | |||||||||||||
Exercise Prices | Prices | Outstanding | Outstanding | Exercisable | Exercisable | |||||||||||||
$8.14 to $10.88 | $ | 9.32 | 60 | $ | 56 | 40 | $ | 19 | ||||||||||
$2.37 to $6.21 | $ | 5.56 | 167 | $ | 741 | 167 | $ | 741 | ||||||||||
227 | 207 | |||||||||||||||||
Stock-based compensation expense is non-cash and is included as a component of general and administrative expense or operating expense based upon the classification of cash compensation paid to the related employees. The Company recorded total stock-based compensation expense of $284 and $241 in the three month periods ended March 31, 2018 and 2017, respectively.
8. | EARNINGS (LOSS) PER COMMON SHARE |
Information with respect to basic and diluted net income (loss) per common share is presented below in thousands, except per share:
Three Months Ended March 31, | |||||||
2018 | 2017 | ||||||
Net income (loss) | |||||||
Income (loss) from continuing operations | $ | (81 | ) | $ | 1,348 | ||
Loss from discontinued operations, net of income taxes | (22 | ) | (15 | ) | |||
Net income (loss) | $ | (103 | ) | $ | 1,333 | ||
16
Three Months Ended March 31, | |||||||
2018 | 2017 | ||||||
Net income (loss) per common share: | |||||||
Per common share – basic | |||||||
Income (loss) from continuing operations | $ | (0.01 | ) | $ | 0.22 | ||
Loss from discontinued operations | — | — | |||||
Net income (loss) per common share – basic | $ | (0.01 | ) | $ | 0.22 | ||
Per common share – diluted | |||||||
Income (loss) from continuing operations | $ | (0.01 | ) | $ | 0.21 | ||
Loss from discontinued operations | — | — | |||||
Net income (loss) per common share – diluted | $ | (0.01 | ) | $ | 0.21 | ||
Weighted Average Common Shares Outstanding: | |||||||
Basic | 6,314 | 6,233 | |||||
Diluted | 6,314 | 6,440 | |||||
The effects of 30 and 46 SOSARs and options outstanding were excluded from the computation of diluted earnings per common share in the three months ended March 31, 2018 and 2017, respectively, because these securities would have been anti-dilutive.
9. | BUSINESS DEVELOPMENTS AND OTHER SIGNIFICANT TRANSACTIONS |
2017 Acquisition
During the year ended December 31, 2017, the Company expanded its operations to acquire a center that complements its current portfolio. On June 8, 2017, the Company entered into an Asset Purchase Agreement (the "Purchase Agreement") with Park Place Nursing and Rehabilitation Center, LLC, Dunn Nursing Home, Inc., Wood Properties of Selma LLC, and Homewood of Selma, LLC to acquire a 103-bed skilled nursing center in Selma, Alabama, for an aggregate purchase price of $8,750. In connection with the funding of the acquisition, on June 30, 2017, the Company amended the terms of its Second Amended and Restated Term Loan Agreement to increase the facility by $7,500, which is described in Note 5 to the interim consolidated financial statements herein. The acquisition transaction closed on July 1, 2017. In accordance with ASC 805, this transaction was accounted for as a business combination, which resulted in the expensing of $140 of acquisition costs and a $925 recorded gain on bargain purchase for the Company for the year ended December 31, 2017. The operating results of the acquired center have been included in the Company's consolidated statement of operations since the acquisition date. Supplemental pro forma information regarding the acquisition is not material to the consolidated financial statements. The allocation of the purchase price to the net assets acquired is as follows:
Park Place | ||||
Purchase Price | $ | 8,750 | ||
Gain on bargain purchase | 925 | |||
$ | 9,675 | |||
Allocation: | ||||
Building | $ | 8,435 | ||
Land | 760 | |||
Land Improvements | 145 | |||
Furniture, Fixtures and Equipment | 335 | |||
$ | 9,675 | |||
17
2018 Assets Held for Sale
During the first quarter of 2018, three of the Company's skilled nursing facilities met the accounting criteria to be classified as held for sale, but did not meet the accounting criteria to be reported as discontinued operations. The Company is selling the property and equipment affiliated with these centers. The recorded values of these centers' assets are $13,228. The centers' assets are classified as held for sale in the accompanying interim consolidated balance sheets.
2017 Lease Termination
On September 30, 2017, the Company entered into an Agreement with Trend Health and Rehab of Carthage, LLC ("Trend Health") to terminate the lease and the Company's right of possession of the center in Carthage, Mississippi. In consideration of the early termination of the lease, Trend Health provided the Company with a $250 cash termination payment which is included in lease termination receipts in the accompanying interim consolidated statements of operations for the year ended December 31, 2017. For accounting purposes, this transaction was not reported as a discontinued operation as this disposal did not represent a strategic shift that has (or will have) a major effect on the Company's operations and financial results.
2016 Sale of Investment in Unconsolidated Affiliate
On October 28, 2016, the Company and its partners entered into an asset purchase agreement to sell the pharmacy joint venture. The sale resulted in a $1,366 gain in the fourth quarter of 2016. Subsequently, we recognized an additional gain of $733 in the first quarter of 2017, related to the final liquidation of remaining net assets affiliated with the partnership.
18
ITEM 2 – MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
Overview
Diversicare Healthcare Services, Inc. (together with its subsidiaries, “Diversicare” or the “Company”) provides long-term care services to nursing center patients in ten states, primarily in the Southeast, Midwest, and Southwest. The Company’s centers provide a range of health care services to their patients and residents that include nursing, personal care, and social services. Additionally, the Company’s nursing centers also offer a variety of comprehensive rehabilitation services, as well as nutritional support services. The Company's continuing operations include centers in Alabama, Florida, Indiana, Kansas, Kentucky, Mississippi, Missouri, Ohio, Tennessee, and Texas.
As of March 31, 2018, the Company’s continuing operations consist of 76 nursing centers with 8,456 licensed nursing beds. The Company owns 18 and leases 58 of its nursing centers. Our nursing centers range in size from 48 to 320 licensed nursing beds. The licensed nursing bed count does not include 497 licensed assisted living and residential beds.
Key Performance Metrics
Skilled Mix. Skilled mix represents the number of days our Medicare or Managed Care patients are receiving services at the skilled nursing facilities divided by the total number of days (less days from assisted living services) from all payor sources are receiving services as the skilled nursing facilities for any given period.
Average rate per day. Average rate per day is the revenue by primary payor source for a period at the skilled nursing facility divided by actual patient days for the revenue source for a given period.
Average daily skilled nursing census. Average daily skilled nursing census is the average number of patients who are receiving skilled nursing care as a percentage of total number of patient days.
Strategic Operating Initiatives
We identified several key strategic objectives to increase shareholder value through improved operations and business development. These strategic operating initiatives include: improving our facilities' quality metrics, improving skilled mix in our nursing centers, improving our average Medicare rate, implementing and maintaining Electronic Medical Records (“EMR”) to improve Medicaid capture, and completing strategic acquisitions and divestitures. We have experienced success in these initiatives and expect to continue to build on these improvements. In light of challenges facing the industry and the Company specifically, including the unresolved governmental investigation, we believe that now is not the time to attempt to engage in a company-wide strategic transaction.
Improving skilled mix and average Medicare rate:
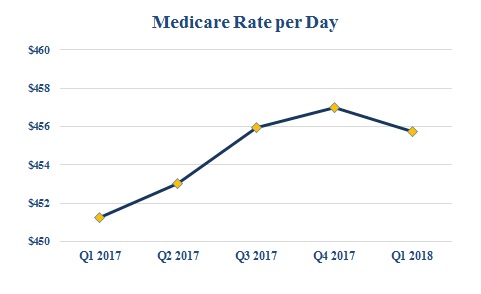
Our strategic operating initiatives of improving our skilled mix and our average Medicare rate required investing in nursing and clinical care to treat more acute patients along with nursing center-based marketing representatives to attract these patients. These initiatives developed referral and Managed Care relationships that have attracted and are expected to continue to attract payor sources for patients covered by Medicare and Managed Care. The Company's skilled mix for the three months ended March 31, 2018 and 2017 was 16.1% and 15.7%, respectively. The graph below illustrates our success with increasing our average Medicare rate per day:
19
Utilizing Electronic Medical Records to improve Medicaid acuity capture:
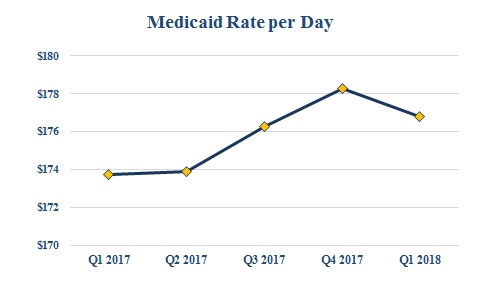
As another part of our strategic operating initiatives, we successfully completed a full implementation of EMR to improve Medicaid acuity capture, primarily in our states where the Medicaid payments are acuity based. We completed the implementation on time and under budget, and since implementation, have increased our average Medicaid rate despite rate cuts in certain acuity based states by accurate and timely capture of care delivery. The graph below illustrates our success with increasing our average Medicaid rate per day since implementation:
Completing strategic acquisitions and dispositions:
Our strategic operating initiatives include a renewed focus on completing strategic acquisitions and dispositions. We continue to pursue and investigate opportunities to acquire, lease or develop new centers, focusing primarily on opportunities within our existing geographic areas of operation. We expect to announce additional development projects in the near future.
Effective July 1, 2017, we acquired a 103-bed skilled nursing center in Selma, Alabama, for an aggregate purchase price of $8,750,000, pursuant to an Asset Purchase Agreement with Park Place Nursing and Rehabilitation Center, LLC, Dunn Nursing Home, Inc., Wood Properties of Selma LLC, and Homewood of Selma, LLC. This transaction is further discussed in Note 9 "Business Development and Other Significant Transactions" to the interim consolidated financial statements.
During the first quarter of 2018, three of the Company's skilled nursing facilities met the accounting criteria to be classified as held for sale, but did not meet the accounting criteria to be reported as discontinued operations. The Company is selling the property and equipment affiliated with these centers. The recorded values of these centers' assets are $13,228. The centers' assets are classified as held for sale in the accompanying interim consolidated balance sheets.
As part of our strategic efforts, we have also performed thorough analysis on our existing centers in order to determine whether continuing operations within certain markets or regions was in line with the short-term and long-term strategy of the business. As a result, we ceased operations at our Carthage, Mississippi, facility in September 2017 thus terminating our lease agreements with the lessor. This transaction was not reported as discontinued operations as described in Note 9 to the interim consolidated financial statements.
Basis of Financial Statements
Our patient revenues consist of the fees charged for the care of patients in the nursing centers we own and lease. Our operating expenses include the costs, other than lease, professional liability, depreciation and amortization expenses, incurred in the operation of the nursing centers we own and lease. Our general and administrative expenses consist of the costs of the corporate office and regional support functions. Our interest, depreciation and amortization expenses include all such expenses across the range of our operations.
Critical Accounting Policies and Judgments
A “critical accounting policy” is one which is both important to the understanding of our financial condition and results of operations and requires management’s most difficult, subjective or complex judgments often involving estimates of the effect of matters that are inherently uncertain. Actual results could differ from those estimates and cause our reported net income or loss to vary significantly from period to period. Our critical accounting policies are more fully described in our 2017 Annual Report on Form 10-K.
20
21
Revenue Sources
We classify our revenues from patients and residents into four major categories: Medicaid, Medicare, Managed Care, and Private Pay and other. Medicaid revenues are composed of the traditional Medicaid program established to provide benefits to those in need of financial assistance in the securing of medical services. Medicare revenues include revenues received under both Part A and Part B of the Medicare program. Managed Care revenues include payments for patients who are insured by a third-party entity, typically called a Health Maintenance Organization, often referred to as an HMO plan, or are Medicare beneficiaries who assign their Medicare benefits to a Managed Care replacement plan often referred to as Medicare replacement products. The Private Pay and other revenues are composed primarily of individuals or parties who directly pay for their services. Included in the Private Pay and other payors are patients who are hospice beneficiaries as well as the recipients of Veterans Administration benefits. Veterans Administration payments are made pursuant to renewable contracts negotiated with these payors.
The following table sets forth net patient and resident revenues related to our continuing operations by primary payor source for the periods presented (dollar amounts in thousands). The difference between 2018 revenue reported below and in the accompanying statements of operations is due to the implementation of ASC 606. Refer to Note 4 "Revenue Recognition" to the interim consolidated financial statements.
Three Months Ended March 31, | |||||||||||||||||
2018 | 2018 | 2017 | |||||||||||||||
As reported | As Adjusted to Legacy GAAP | As reported | |||||||||||||||
Medicaid | $ | 63,886 | 45.2 | % | $ | 73,214 | 50.7 | % | $ | 72,873 | 51.5 | % | |||||
Medicare | 29,751 | 21.1 | % | 38,139 | 26.4 | % | 38,011 | 26.9 | % | ||||||||
Managed Care | 14,212 | 10.1 | % | 12,092 | 8.4 | % | 10,806 | 7.6 | % | ||||||||
Private Pay and other | 33,436 | 23.6 | % | 21,047 | 14.5 | % | 19,810 | 14.0 | % | ||||||||
Total | $ | 141,285 | 100.0 | % | $ | 144,492 | 100.0 | % | $ | 141,500 | 100.0 | % | |||||
The following table sets forth average daily skilled nursing census by primary payor source for our continuing operations for the periods presented:
Three Months Ended March 31, | |||||||||||
2018 | 2017 | ||||||||||
Medicaid | 4,589 | 67.9 | % | 4,649 | 68.7 | % | |||||
Medicare | 783 | 11.6 | 792 | 11.7 | |||||||
Managed Care | 303 | 4.5 | 273 | 4.0 | |||||||
Private Pay and other | 1,081 | 16.0 | 1,056 | 15.6 | |||||||
Total | 6,756 | 100.0 | % | 6,770 | 100.0 | % | |||||
Consistent with the nursing home industry in general, changes in the mix of a facility’s patient population among Medicaid, Medicare, Managed Care, and Private Pay and other can significantly affect the profitability of the facility’s operations.
Health Care Industry
The health care industry is subject to regulation by numerous federal, state, and local governments. These laws and regulations include, but are not limited to, matters such as licensure, accreditation, government health care program participation requirements, reimbursement for patient services, quality of patient care and Medicare and Medicaid fraud and abuse. Over the last several years, government activity has increased with respect to investigations and allegations concerning possible violations by health care providers of a number of statutes and regulations, including those regulating fraud and abuse, false claims, patient privacy and quality of care issues. Violations of these laws and regulations could result in exclusion from government health care programs together with the imposition of significant fines and penalties, as well as significant repayments for patient services previously billed. Compliance with such laws and regulations is subject to ongoing government review and interpretation, as well as regulatory actions in which government agencies seek to impose fines and penalties. The Company is involved in regulatory actions of this type from time to time.
In recent years, the U.S. Congress and some state legislatures have considered and enacted significant legislation concerning health care and health insurance. The most prominent of these efforts, The Affordable Care Act affects how health care services are covered, delivered and reimbursed. As currently structured, the Affordable Care Act expands coverage through a combination of public program expansion and private sector reforms, provides for reduced growth in Medicare program spending, and promotes initiatives that tie reimbursement to quality and care coordination. Some of the provisions, such as the requirement that large
22
employers provide health insurance benefits to full-time employees, have increased our operating expenses. The Affordable Care Act expands the role of home-based and community services, which may place downward pressure on our sustaining population of Medicaid patients. Reforms that we believe may have a material impact on the long-term care industry and on our business include, among others, possible modifications to the conditions of qualification for payment, bundling of payments to cover both acute and post-acute care and the imposition of enrollment limitations on new providers. However, there is considerable uncertainty regarding the future of the Affordable Care Act. The Presidential administration and certain members of Congress have expressed their intent to repeal or make significant changes to the law, its implementation or its interpretation. For example, in 2017, Congress eliminated the financial penalty associated with the individual mandate, effective January 1, 2019.
Skilled nursing centers are required to bill Medicare on a consolidated basis for certain items and services that they furnish to patients, regardless of the cost to deliver these services. This consolidated billing requirement essentially makes the skilled nursing center responsible for billing Medicare for all care services delivered to the patient during the length of stay. CMS has instituted a number of test programs designed to extend the reimbursement and financial responsibilities under consolidating billing beyond the traditional discharge date to include a broader set of bundled services. Such examples may include, but are not exclusive to, home health, durable medical equipment, home and community based services, and the cost of re-hospitalizations during a specified bundled period. Currently, these test programs for bundled reimbursement are confined to a small set of clinical conditions, but CMS has indicated that it is developing additional bundled payment models. This bundled form of reimbursement could be extended to a broader range of diagnosis related conditions in the future. The potential impact on skilled nursing center utilization and reimbursement is currently unknown. The process for defining bundled services has not been fully determined by CMS and therefore is subject to change during the rule making process.
On April 27, 2018, CMS published a proposed rule outlining Medicare payment rates for skilled nursing facilities that, if approved as proposed, would be effective October 1, 2018. CMS proposes that the SNF market basket be updated by 2.4% as required by the Bipartisan Budget Act of 2018. Additionally, the proposed rule includes proposals relating to the SNF Quality Reporting Program and the Skilled Nursing Facility Value-Based Purchasing ("VBP") Program, that, as proposed, would affect Medicare payment beginning on October 1, 2018. CMS is also proposing a new Patient-Driven Payment Model ("PDPM") to replace the existing case-mix methodology, the Resource Utilization Group ("RUG-IV") model. CMS indicates that the proposed PDPM is expected to better account for patient characteristics by relating payment to patients' conditions and clinical needs rather than on volume-based services and reduce the administrative burden on providers. If finalized as proposed, the PDPM would be effective October 1, 2019 and implemented in lieu of the previously proposed Resident Classification System, Version I ("RCS-I").. CMS proposes to use a budget neutrality factor to satisfy the requirement that PDPM be budget neutral relative to RUG-IV, given that CMS states that it intends for the new model to not to change the aggregate amount of Medicare payments to SNFs, but to more accurately reflect resource utilization without incentivizing inappropriate care delivery. The proposed rule is currently open for public comment, after which the details of the final rule may vary from those summarized above.
Contractual Obligations and Commercial Commitments
We have certain contractual obligations of continuing operations as of March 31, 2018, summarized by the period in which payment is due, as follows (dollar amounts in thousands):
Contractual Obligations | Total | Less than 1 year | 1 to 3 Years | 3 to 5 Years | After 5 Years | ||||||||||||||
Long-term debt obligations (1) | $ | 103,665 | $ | 17,895 | $ | 85,735 | $ | 35 | $ | — | |||||||||
Settlement obligations (2) | 949 | 949 | — | — | — | ||||||||||||||
Elimination of Preferred Stock Conversion feature (3) | 343 | 343 | — | — | — | ||||||||||||||
Operating leases (4) | 1,059,914 | 58,342 | 120,238 | 123,714 | 757,620 | ||||||||||||||
Required capital expenditures under operating leases (5) | 11,347 | 1,205 | 2,410 | 2,410 | 5,322 | ||||||||||||||
Total | $ | 1,176,218 | $ | 78,734 | $ | 208,383 | $ | 126,159 | $ | 762,942 | |||||||||
(1) | Long-term debt obligations include scheduled future payments of principal and interest of long-term debt and amounts outstanding on our capital lease obligations. Our long-term debt obligations increased $0.2 million between December 31, 2017 and March 31, 2018, which is related to assumption of operation for the Golden Living centers and purchase of the center in Selma, Alabama. See Note 5, "Long-Term Debt and Interest Rate Swap," to the interim consolidated financial statements included in this report for additional information. |
(2) | Settlement obligations relate to professional liability cases that are expected to be paid within the next twelve months. The professional liabilities are included in our current portion of self-insurance reserves. |
(3) | Payments to Omega Health Investors ("Omega"), from which we lease 35 nursing centers, for the elimination of the preferred stock conversion feature in connection with restructuring the preferred stock and master lease agreements. Monthly payments of approximately $57,000 will be made through the end of the initial lease period that ends in September 2018. |
23
(4) | Represents lease payments under our operating lease agreements. Assumes all renewal periods are enacted. Our operating lease obligations decreased $5.7 million between December 31, 2017 and March 31, 2018. |
(5) | Includes annual expenditure requirements under operating leases. Our required capital expenditures decreased $0.6 million between December 31, 2017 and March 31, 2018. |
We have employment agreements with certain members of management that provide for the payment to these members of amounts up to two times their annual salary in the event of a termination without cause, a constructive discharge (as defined therein), or upon a change of control of the Company (as defined therein). The maximum contingent liability under these agreements is approximately $1.9 million as of March 31, 2018. The terms of such agreements are for one year and automatically renew for one year if not terminated by us or the employee. In addition, upon the occurrence of any triggering event, those certain members of management may elect to require that we purchase equity awards granted to them for a purchase price equal to the difference in the fair market value of our common stock at the date of termination versus the stated equity award exercise price. Based on the closing price of our common stock on March 31, 2018, the potential contingent liability for the repurchase of the equity grants is $0.2 million.
Results of Operations
The following tables present the unaudited interim consolidated statements of operations and related data for the three month periods ended March 31, 2018 and 2017:
(in thousands) | Three Months Ended March 31, | |||||||||||||
2018 | 2017 | Change | % | |||||||||||
PATIENT REVENUES, net | $ | 141,285 | $ | 141,500 | $ | (215 | ) | (0.2 | )% | |||||
EXPENSES: | ||||||||||||||
Operating | 112,278 | 110,667 | 1,611 | 1.5 | % | |||||||||
Lease and rent expense | 13,713 | 13,743 | (30 | ) | (0.2 | )% | ||||||||
Professional liability | 2,775 | 2,670 | 105 | 3.9 | % | |||||||||
General and administrative | 8,139 | 8,973 | (834 | ) | (9.3 | )% | ||||||||
Depreciation and amortization | 2,881 | 2,487 | 394 | 15.8 | % | |||||||||
Total expenses | 139,786 | 138,540 | 1,246 | 0.9 | % | |||||||||
OPERATING INCOME | 1,499 | 2,960 | (1,461 | ) | (49.4 | )% | ||||||||
OTHER INCOME (EXPENSE): | ||||||||||||||
Gain on sale of investment in unconsolidated affiliate | — | 733 | (733 | ) | (100.0 | )% | ||||||||
Other income | 51 | — | 51 | 100.0 | % | |||||||||
Interest expense, net | (1,669 | ) | (1,483 | ) | (186 | ) | (12.5 | )% | ||||||
(1,618 | ) | (750 | ) | (868 | ) | (115.7 | )% | |||||||
INCOME (LOSS) FROM CONTINUING OPERATIONS BEFORE INCOME TAXES | (119 | ) | 2,210 | (2,329 | ) | (105.4 | )% | |||||||
BENEFIT (PROVISION) FOR INCOME TAXES | 38 | (862 | ) | 900 | 104.4 | % | ||||||||
INCOME FROM CONTINUING OPERATIONS | $ | (81 | ) | $ | 1,348 | $ | (1,429 | ) | (106.0 | )% | ||||
24
Percentage of Net Revenues | Three Months Ended March 31, | ||||
2018 | 2017 | ||||
PATIENT REVENUES, net | 100.0 | % | 100.0 | % | |
EXPENSES: | |||||
Operating | 79.5 | 78.2 | |||
Lease and rent expense | 9.7 | 9.7 | |||
Professional liability | 2.0 | 1.9 | |||
General and administrative | 5.8 | 6.3 | |||
Depreciation and amortization | 2.0 | 1.8 | |||
Total expenses | 99.0 | 97.9 | |||
OPERATING INCOME | 1.0 | 2.1 | |||
OTHER INCOME (EXPENSE): | |||||
Gain on sale of investment in unconsolidated affiliate | — | 0.5 | |||
Other income | — | — | |||
Interest expense, net | (1.2 | ) | (1.0 | ) | |
(1.2 | ) | (0.5 | ) | ||
INCOME (LOSS) FROM CONTINUING OPERATIONS BEFORE INCOME TAXES | (0.2 | ) | 1.6 | ||
BENEFIT (PROVISION) FOR INCOME TAXES | — | (0.6 | ) | ||
INCOME (LOSS) FROM CONTINUING OPERATIONS | (0.2 | )% | 1.0 | % | |
25
Three Months Ended March 31, 2018 Compared With Three Months Ended March 31, 2017
Patient Revenues
Patient revenues were $141.3 million and $141.5 million for the three months ended March 31, 2018 and 2017, respectively, a decrease of $(0.2) million. The following summarizes the revenue fluctuations attributable to our portfolio growth (in thousands):
Three Months Ended March 31, | |||||||||||||||
2018 | 2017 | ||||||||||||||
As reported | As adjusted to Legacy GAAP | As reported | Change | ||||||||||||
Same-store revenue | $ | 138,938 | $ | 142,145 | $ | 141,500 | $ | 645 | |||||||
2017 acquisition revenue | 2,347 | 2,347 | — | 2,347 | |||||||||||
Total revenue | $ | 141,285 | $ | 144,492 | $ | 141,500 | $ | 2,992 | |||||||
The difference between patient revenues for the first quarter of 2018 is due to the implementation of ASC 606. Refer to Note 4 "Revenue Recognition" to the interim consolidated financial statements.
The overall increase in revenues as adjusted to legacy GAAP of $3.0 million is primarily attributable to revenue contributions from the acquisition of the Park Place operations during the first quarter of 2018 of $2.3 million.
On a same-store center basis, the average Medicare and Medicaid rate per patient day for the first quarter of 2018 increased compared to the first quarter of 2017, resulting in increases in revenue of $0.3 million and $1.1 million, respectively, or 0.9% and 1.5%, respectively. Our same-store Medicare, Medicaid and Private average daily census for the first quarter of 2018 decreased $0.5 million, $0.8 million and $0.4 million, or 1.7%, 1.1% and 3.4%, respectively. Conversely our Managed Care average daily census for the first quarter of 2018 increased $0.9 million or 9.9%.
The following table summarizes key revenue and census statistics for continuing operations for each period:
Three Months Ended March 31, | |||||||||||
2018 | 2017 | ||||||||||
Skilled nursing occupancy | 79.9 | % | 80.1 | % | |||||||
As a percent of total census: | |||||||||||
Medicare census | 11.6 | % | 11.7 | % | |||||||
Medicaid census | 67.9 | % | 68.7 | % | |||||||
Managed Care census | 4.5 | % | 4.0 | % | |||||||
As a percent of total revenues: | |||||||||||
Medicare revenues | 26.4 | % | 26.9 | % | |||||||
Medicaid revenues | 50.7 | % | 51.5 | % | |||||||
Managed Care revenues | 8.4 | % | 7.6 | % | |||||||
Average rate per day: | |||||||||||
Medicare | $ | 455.72 | $ | 451.26 | |||||||
Medicaid | $ | 176.78 | $ | 173.75 | |||||||
Managed Care | $ | 391.96 | $ | 381.54 | |||||||
26
Operating Expense
Operating expense increased in the first quarter of 2018 to $112.3 million as compared to $110.7 million in the first quarter of 2017. Operating expense increased as a percentage of revenue at 79.5% for the first quarter of 2018 as compared to 78.2% for the first quarter of 2017. The following table summarizes the expense increases attributable to our portfolio growth (in thousands):
Three Months Ended March 31, | |||||||||||||||
2018 | 2017 | ||||||||||||||
As reported | As adjusted to Legacy GAAP | As reported | Change | ||||||||||||
Same-store operating expense | $ | 110,709 | $ | 114,172 | $ | 110,667 | $ | 3,505 | |||||||
2017 acquisition expense | 1,569 | 1,569 | — | 1,569 | |||||||||||
Total expense | $ | 112,278 | $ | 115,741 | $ | 110,667 | $ | 5,074 | |||||||
The overall increase in operating expense of $5.1 million is partially attributable to the acquisition of the Park Place operations during the first quarter of 2018 of $1.6 million.
On a same-store center basis, operating expenses slightly increased by $3.5 million, which is attributable to unfavorable variances in provider taxes and salaries and related taxes of $2.3 million and $2.1 million, respectively, in first quarter of 2018 compared to the first quarter of 2017. The change in provider taxes is due to the $2.2 million refund from the state of Kentucky during the first quarter of 2017. Conversely our same-store health insurance costs decreased by $0.9 million in first quarter of 2018 compared to the first quarter of 2017.
One of the largest components of operating expenses is wages, which increased to $67.1 million during the first quarter of 2018 as compared to $65.0 million in the first quarter of 2017, which, consistent with above, is due primarily to acquisition activity.
Lease Expense
Lease expense in the first quarter of 2018 remained consisted with the first quarter of 2017 at $13.7 million.
Professional Liability
Professional liability expense was $2.8 million and $2.7 million in the first quarters of 2018 and 2017, respectively. Our cash expenditures for professional liability costs of continuing operations were $1.1 million and $2.1 million for the first quarters of 2018 and 2017, respectively. Professional liability expense and cash expenditures fluctuate from year to year based respectively on the results of our third-party professional liability actuarial studies and on the costs incurred in defending and settling existing claims. See “Liquidity and Capital Resources” for further discussion of the accrual for professional liability.
General and Administrative Expense
General and administrative expense was $8.1 million in the first quarter of 2018 as compared to $9.0 million in the first quarter of 2017. General and administrative expense decreased as a percentage of revenue from 6.3% in 2017 to 5.8% in 2018. The decrease in general and administrative expense is attributable to a decrease in corporate wages and payroll taxes by $0.9 million. The acquisition of 22 centers in the fourth quarter of 2016 resulted in an increase in salary expenses during the first quarter of 2017.
Depreciation and Amortization
Depreciation and amortization expense was approximately $2.9 million in the first quarter of 2018 as compared to $2.5 million in 2017. The increase in depreciation expense relates to the fixed asset acquisition of a center located in Selma, Alabama during the third quarter of 2017.
Interest Expense, Net
Interest expense was $1.7 million in the first quarter of 2018 and $1.5 million in the first quarter of 2017, an increase of $0.2 million. The increase was primarily attributable to the amendment of the term loan facility that occurred in June 2017.
Loss from Continuing Operations before Income Taxes; Loss from Continuing Operations per Common Share
As a result of the above, continuing operations reported a loss of $0.1 million before income taxes for the first quarter of 2018 as compared to income of $2.2 million for the first quarter of 2017. The benefit for income taxes was $0.1 million for the first quarter of 2018, and the provision for income taxes was $0.9 million for the first quarter of 2017. Both basic and diluted loss per common share from continuing operations were $0.01 for the first quarter of 2018 as compared to basic and diluted income per common share from continuing operations of $0.22 and $0.21, respectively, in the first quarter of 2017.
27
Liquidity and Capital Resources
Liquidity
Our primary source of liquidity is the net cash flow provided by the operating activities of our centers. We believe that these internally generated cash flows will be adequate to service existing debt obligations, fund required capital expenditures as well as provide cash flows for investing opportunities. In determining priorities for our cash flow, we evaluate alternatives available to us and select the ones that we believe will most benefit us over the long-term. Options for our use of cash include, but are not limited to, capital improvements, dividends, purchase of additional shares of our common stock, acquisitions, payment of existing debt obligations as well as initiatives to improve nursing center performance. We review these potential uses and align them to our cash flows with a goal of achieving long-term success.
Net cash provided by operating activities of continuing operations totaled $5.2 million for the three months ended March 31, 2018, compared to net cash used in operating activities of continuing operations of $0.8 million in the same period of 2017. The primary driver of the increase in cash provided by operating activities from continuing operations is due to the timing of accounts receivable collections.
Our cash expenditures related to professional liability claims of continuing operations were $1.1 million and $2.1 million for three months ended March 31, 2018 and 2017, respectively. Although we work diligently to limit the cash required to settle and defend professional liability claims, a significant judgment entered against us in one or more legal actions could have a material adverse impact on our cash flows and could result in our being unable to meet all of our cash needs as they become due.
Investing activities of continuing operations used cash of $2.0 million and $2.2 million for the three months ended in 2018 and 2017, respectively. The cash used for investing activities relates to the purchase of property and equipment at the centers we operate.
Financing activities of continuing operations provided cash of $0.2 million for the three months ended March 31, 2018 compared to cash provided of $2.8 million for the three months ended March 31, 2017. The decrease is primarily due to draws on the Company's revolving credit facility in 2017.
Dividends
On April 26, 2018, the Board of Directors declared a quarterly dividend of $0.055 per common share payable to shareholders of record as of June 30, 2018, to be paid on July 16, 2018. While the Board of Directors intends to pay quarterly dividends, the Board will make the determination of the amount of future cash dividends, if any, to be declared and paid based on, among other things, the Company’s financial condition, funds from operations, the level of its capital expenditures and its future business prospects and opportunities.
Professional Liability
The Company has professional liability insurance coverage for its nursing centers that, based on historical claims experience, is likely to be substantially less than the claims that are expected to be incurred. Effective July 1, 2013, the Company established a wholly-owned, offshore limited purpose insurance subsidiary, SHC Risk Carriers, Inc. (“SHC”), to replace some of the expiring commercial policies. SHC covers losses up to specified limits per occurrence. On a per claim basis, coverage for losses in excess of those covered by SHC is maintained through unaffiliated commercial reinsurance carriers. All of the Company's nursing centers in Florida and Tennessee are now covered under the captive insurance policies along with most of the nursing centers in Alabama, Kentucky, and Texas. The insurance coverage provided for these centers under the SHC policy include coverage limits of $0.5 million per medical incident with a sublimit per center of $1.0 million and total annual aggregate policy limits of $5.0 million. All other centers within the Company’s portfolio are covered through various commercial insurance policies which provide similar coverage limits per medical incident, per location, and on an aggregate basis for covered centers. The deductibles for these policies are covered through the insurance subsidiary.
As of March 31, 2018, we have recorded total liabilities for reported and settled professional liability claims and estimates for incurred, but unreported claims of $20.5 million. Our calculation of this estimated liability is based on an assumption that the Company will not incur a severely adverse judgment with respect to any asserted claim; however, a significant judgment could be entered against us in one or more of these legal actions, and such a judgment could have a material adverse impact on our financial position and cash flows.
28
Capital Resources
As of March 31, 2018, we had $90.3 million of outstanding long-term debt and capital lease obligations. The $90.3 million total includes $1.1 million in capital lease obligations and $16.0 million currently outstanding on the revolving credit facility. The balance of the long-term debt is comprised of $73.2 million owed on our mortgage loan, which includes $64.0 million on the term loan facility, $9.0 million on the acquisition loan facility and $0.2 million notes payable to finance equipment.
On February 26, 2016, the Company executed an Amended and Restated Credit Agreement (the "Credit Agreement") which modified the terms of the Original Mortgage Loan and the Original Revolver Agreements dated April 30, 2013. The Credit Agreement increases the Company's borrowing capacity to $100.0 million allocated between a $72.5 million Mortgage Loan ("Amended Mortgage Loan") and a $27.5 million Revolver ("Amended Revolver"). The Amended Mortgage Loan consists of a $60 million term loan facility and a $12.5 million acquisition loan facility. Loan acquisition costs associated with the Amended Mortgage Loan and the Amended Revolver were capitalized in the amount of $2.2 million and are being amortized over the five-year term of the agreements.
Under the terms of the amended agreements, the syndicate of banks provided the Amended Mortgage Loan with an original balance of $72.5 million with a five-year maturity through February 26, 2021, and a $27.5 million Amended Revolver through February 26, 2021. The Amended Mortgage Loan has a term of five years, with principal and interest payable monthly based on a 25-year amortization. Interest on the term and acquisition loan facilities is based on LIBOR plus 4.0% and 4.75%, respectively. A portion of the Amended Mortgage Loan is effectively fixed at 5.79% pursuant to an interest rate swap with an initial notional amount of $30.0 million. As of March 31, 2018, the interest rate related to the Amended Mortgage Loan was 5.75%. The Amended Mortgage Loan is secured by eighteen owned nursing centers, related equipment and a lien on the accounts receivable of these centers. The Amended Mortgage Loan and the Amended Revolver are cross-collateralized and cross-defaulted. The Company’s Amended Revolver has an interest rate of LIBOR plus 4.0% and is secured by accounts receivable and is subject to limits on the maximum amount of loans that can be outstanding under the revolver based on borrowing base restrictions.
Effective October 3, 2016, the Company entered into the Second Amendment ("Second Revolver Amendment") to amend the Amended Revolver. The Second Revolver Amendment increased the Amended Revolver capacity from the $27.5 million in the Amended Revolver to $52.3 million; provided that the maximum revolving facility be reduced to $42.3 million on August 1, 2017. Subsequently, on June 30, 2017, the Company executed a Fourth Amendment (the "Fourth Revolver Amendment") to amend the Amended Revolver, which modifies the capacity of the revolver to remain at $52.3 million.
On December 29, 2016, the Company executed a Third Amendment ("Third Revolver Amendment") to amend the Amended Revolver. The Third Amendment modifies the terms of the Amended Mortgage Loan Agreement by increasing the Company’s letter of credit sublimit from $10.0 million to $15.0 million.
Effective June 30, 2017, the Company entered into a Second Amendment (the "Second Term Amendment") to amend the Amended Mortgage Loan. The Second Term Amendment amends the terms of the Amended Mortgage Loan Agreement by increasing the Company's term loan facility by $7.5 million.
Effective February 27, 2018, the Company executed a Fifth Amendment to the Amended Revolver and a Third Amendment to the Amended Mortgage Loan. Under the terms of the Amendments, the minimum fixed charge coverage ratio shall not be less than 1.01 to 1.00 as of March 31, 2018 and for each quarter thereafter.
As of March 31, 2018, the Company had $16.0 million borrowings outstanding under the Amended Revolver compared to $16.0 outstanding as of December 31, 2017. The outstanding borrowings on the revolver primarily compensate for accumulated Medicaid and Medicare receivables at recently acquired facilities as these facilities proceed through the change in ownership process with CMS. Annual fees for letters of credit issued under the Amended Revolver are 3.00% of the amount outstanding. The Company has eleven letters of credit with a total value of $13.6 million outstanding as of March 31, 2018. Considering the balance of eligible accounts receivable, the letters of credit, the amounts outstanding under the revolving credit facility and the maximum loan amount of $39.5 million, the balance available for borrowing under the Amended Revolver was $9.8 million at March 31, 2018.
Our lending agreements contain various financial covenants, the most restrictive of which relates to debt service coverage ratios. We are in compliance with all such covenants at March 31, 2018.
29
Our calculated compliance with financial covenants is presented below:
Requirement | Level at March 31, 2018 | ||
Minimum fixed charge coverage ratio | 1.01:1.00 | 1.03:1.00 | |
Minimum adjusted EBITDA | $13.0 million | $17.9 million | |
EBITDAR (mortgaged centers) | $10.0 million | $16.5 million | |
Current ratio (as defined in agreement) | 1.00:1.00 | 1.30:1.00 | |
As part of the debt agreements entered into in February 2016, we amended our interest rate swap agreement with a member of the bank syndicate as the counterparty. The interest rate swap agreement has the same effective date and maturity date as the Amended Mortgage Loan, and carries an initial notional amount of $30.0 million. The interest rate swap agreement requires us to make fixed rate payments to the bank calculated on the applicable notional amount at an annual fixed rate of 5.79% while the bank is obligated to make payments to us based on LIBOR on the same notional amounts. We entered into the interest rate swap agreement to mitigate the variable interest rate risk on our outstanding mortgage borrowings.
Receivables
Our operations could be adversely affected if we experience significant delays in reimbursement from Medicare, Medicaid or other third-party revenue sources. Our future liquidity will continue to be dependent upon the relative amounts of current assets (principally cash, accounts receivable and inventories) and current liabilities (principally accounts payable and accrued expenses). In that regard, accounts receivable can have a significant impact on our liquidity. Continued efforts by governmental and third-party payors to contain or reduce the acceleration of costs by monitoring reimbursement rates, by increasing medical review of bills for services, or by negotiating reduced contract rates, as well as any delay by us in the processing of our invoices, could adversely affect our liquidity and financial position.
Accounts receivable attributable to patient services of continuing operations totaled $75.1 million at March 31, 2018 compared to $79.2 million at December 31, 2017, representing approximately 47 days and 49 days revenue in accounts receivable, respectively. The decrease in accounts receivable is due to the timing of accounts receivable payments.
The allowance for doubtful accounts and other contractual allowances was $15.1 million at March 31, 2018 as compared to $14.2 million at December 31, 2017. We continually evaluate the adequacy of our bad debt reserves based on patient mix trends, aging of older balances, payment terms and delays with regard to third-party payors, collateral and deposit resources, as well as other factors. We continue to evaluate and implement additional procedures to strengthen our collection efforts and reduce the incidence of uncollectible accounts.
Off-Balance Sheet Arrangements
We have eleven letters of credit outstanding with an aggregate value of approximately $13.6 million as of March 31, 2018. Ten of these letters of credit serve as a security deposits for certain center leases, while one was issued in conjunction with the initial funding of our wholly-owned captive insurance company. These letters of credit were issued under our revolving credit facility. Our accounts receivable serve as the collateral for this revolving credit facility.
Forward-Looking Statements
The foregoing discussion and analysis provides information deemed by management to be relevant to an assessment and understanding of our consolidated results of operations and financial condition. This discussion and analysis should be read in conjunction with our interim consolidated financial statements included herein. Certain statements made by or on behalf of us, including those contained in this “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and elsewhere, are forward-looking statements as defined in the Private Securities Litigation Reform Act of 1995. Actual results could differ materially from those contemplated by the forward-looking statements made herein. Forward-looking statements are predictive in nature and are frequently identified by the use of terms such as "may," "will," "should," "expect," "believe," "estimate," "intend," and similar words indicating possible future expectations, events or actions. In addition to any assumptions and other factors referred to specifically in connection with such statements, other factors, many of which are beyond our ability to control or predict, could cause our actual results to differ materially from the results expressed or implied in any forward-looking statements including, but not limited to:
• | our ability to successfully integrate the operations of our new nursing centers in Alabama, as well as successfully operate all of our centers, |
30
• | our ability to increase census at our centers and occupancy rates at our centers, |
• | changes in governmental reimbursement, |
• | government regulation, |
• | the impact of the Affordable Care Act, efforts to repeal or significantly modify the Affordable Care Act, and other health care reform initiatives, |
• | any increases in the cost of borrowing under our credit agreements, |
• | our ability to comply with covenants contained in those credit agreements, |
• | our ability to comply with the terms of our master lease agreements, |
• | our ability to renew or extend our leases at or prior to the end of the existing lease terms, |
• | the outcome of professional liability lawsuits and claims, |
• | our ability to control ultimate professional liability costs, |
• | the accuracy of our estimate of our anticipated professional liability expense, |
• | the impact of future licensing surveys, |
• | the outcome of proceedings alleging violations of state or Federal False Claims Acts, |
• | laws and regulations governing quality of care or other laws and regulations applicable to our business including HIPAA and laws governing reimbursement from government payors, |
• | the costs of investing in our business initiatives and development, |
• | our ability to control costs, |
• | our ability to attract and retain qualified healthcare professionals, |
• | changes to our valuation of deferred tax assets, |
• | changing economic and competitive conditions, |
• | changes in anticipated revenue and cost growth, |
• | changes in the anticipated results of operations, |
• | the effect of changes in accounting policies as well as others. |
Investors also should refer to the risks identified in this “Management's Discussion and Analysis of Financial Condition and Results of Operations” as well as risks identified in “Part I. Item 1A. Risk Factors” in our annual report on Form 10-K for the year ended December 31, 2017, for a discussion of various risk factors of the Company and that are inherent in the health care industry. Given these risks and uncertainties, we can give no assurances that these forward-looking statements will, in fact, transpire and, therefore, caution investors not to place undue reliance on them. These assumptions may not materialize to the extent assumed, and risks and uncertainties may cause actual results to be different from anticipated results. These risks and uncertainties also may result in changes to the Company’s business plans and prospects. Such cautionary statements identify important factors that could cause our actual results to materially differ from those projected in forward-looking statements. In addition, we disclaim any intent or obligation to update these forward-looking statements.
ITEM 3. QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK
The chief market risk factor affecting our financial condition and operating results is interest rate risk. As of March 31, 2018, we had outstanding borrowings of approximately $89.2 million, $60.8 million of which was subject to variable interest rates. In connection with our February 2016 financing agreement, we entered into an interest rate swap with an initial notional amount of $30.0 million to mitigate the floating interest rate risk of a portion of such borrowing. In the event that interest rates were to change 1%, the impact on future pre-tax cash flows would be approximately $0.6 million annually, representing the impact of increased or decreased interest expense on variable rate debt.
ITEM 4. CONTROLS AND PROCEDURES
Evaluation of Disclosure Controls and Procedures
As required by Rule 13a-15(b) of the Securities Exchange Act of 1934, as amended (the Exchange Act), our management, including our chief executive officer and chief financial officer, conducted an evaluation of the effectiveness of the design and operation of our disclosure controls and procedures (as defined in Exchange Act Rule 13a-15(e)) as of March 31, 2018. Disclosure controls and procedures include controls and procedures designed to ensure that information required to be disclosed in our reports filed or submitted under the Exchange Act, such as this Quarterly Report on Form 10-Q, is properly recorded, processed, summarized and reported within the time periods required by the Securities and Exchange Commission’s rules and forms. Management necessarily applied its judgment in assessing the costs and benefits of such controls and procedures that, by their nature, can
31
provide only reasonable assurance regarding management’s control objectives. Management does not expect that its disclosure controls and procedures will prevent all errors and fraud. A control system, irrespective of how well it is designed and operated, can only provide reasonable assurance, and cannot guarantee that it will succeed in its stated objectives.
Based on an evaluation of the effectiveness of the design and operation of disclosure controls and procedures, our chief executive officer and chief financial officer concluded that, as of March 31, 2018, our disclosure controls and procedures were effective in reaching a reasonable level of assurance that information required to be disclosed by us in the reports that we file or submit under the Exchange Act is recorded, processed, summarized and reported within the time period specified in the Securities and Exchange Commission’s rules and forms.
Changes in Internal Control Over Financial Reporting
We completed certain changes to our accounting processes related to our implementation of ASC 606, which was adopted on January 1, 2018. We updated our control activities for the adoption of the new accounting standard and the new accounting processes and methodologies established to evaluate contracts with our customers and determine the transaction price to allocate to our performance obligations with those customers as required in the five-step revenue recognition model in ASC 606.
Other than the items described above, there have been no changes in our internal control over financial reporting during the quarter ended March 31, 2018 that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
PART II — OTHER INFORMATION
ITEM 1. LEGAL PROCEEDINGS.
The provision of health care services entails an inherent risk of liability. Participants in the health care industry are subject to lawsuits alleging malpractice, negligence, violations of false claims acts, product liability, or related legal theories, many of which involve large claims and significant defense costs. Like many other companies engaged in the long-term care profession in the United States, we have numerous pending liability claims, disputes and legal actions for professional liability and other related issues. It is expected that we will continue to be subject to such suits as a result of the nature of our business. Further, as with all health care providers, we are periodically subject to regulatory actions seeking fines and penalties for alleged violations of health care laws and are potentially subject to the increased scrutiny of regulators for issues related to compliance with health care fraud and abuse laws and with respect to the quality of care provided to residents of our facilities. Like other health care providers, in the ordinary course of our business, we are also subject to claims made by employees and other disputes and litigation arising from the conduct of our business.
As of March 31, 2018, we are engaged in 73 professional liability lawsuits. Ten lawsuits are currently scheduled for trial or arbitration during the next twelve months, and it is expected that additional cases will be set for trial or hearing. The ultimate results of any of our professional liability claims and disputes cannot be predicted. We have limited, and sometimes no, professional liability insurance with regard to most of these claims. A significant judgment entered against us in one or more of these legal actions could have a material adverse impact on our financial position and cash flows.
In July 2013, the Company learned that the United States Attorney for the Middle District of Tennessee ("DOJ") had commenced a civil investigation of potential violations of the False Claims Act ("FCA"). In October 2014, the Company learned that the investigation was started by the filing under seal of a false claims action against the two centers that were the subject of the original civil investigative demand ("CID"). In connection with this matter, between July 2013 and early February 2016, the Company received three civil investigative demands (a form of subpoena) for documents and information. The Company has responded to those demands and also provided voluntarily additional information requested by the DOJ. The DOJ has also taken testimony from current and former employees of the Company. The investigation relates to the Company’s practices and policies for rehabilitation, and other services, for preadmission evaluation forms ("PAEs") required by TennCare and for Pre-Admission Screening and Resident Reviews ("PASRRs") required by the Medicare program.
In June 2016, the Company received an authorized investigative demand (a form of subpoena) for documents in connection with a criminal investigation by the DOJ related to our practices with respect to PAEs and PASRRs, and the Company has provided documents responsive to this subpoena and continues to provide additional information as requested. The Company cannot predict the outcome of these investigations or the related lawsuits, and the outcome could have a materially adverse effect on the Company, including the imposition of treble damages, criminal charges, fines, penalties and/or a corporate integrity agreement. Additionally, the uncertainty regarding the outcome of these investigations makes it more difficult for the Company to pursue strategic possibilities, longer term initiatives or to make significant financial commitments outside of the normal course of its business. The Company is committed to provide caring and professional services to its patients and residents in compliance with applicable laws and regulations.
32
In January 2009, a purported class action complaint was filed in the Circuit Court of Garland County, Arkansas against the Company and certain of its subsidiaries and Garland Nursing & Rehabilitation Center (the “Center”). The Company answered the original complaint in 2009, and there was no other activity in the case until May 2017. At that time, plaintiff filed an amended complaint asserting new causes of action. The amended complaint alleges that the defendants breached their statutory and contractual obligations to the patients of the Center over a multi-year period by failing to meet minimum staffing requirements, failing to otherwise adequately staff the Center and failing to provide a clean and safe living environment in the Center. The Company has filed an answer to the amended complaint denying plaintiffs’ allegations and has asked the Court to dismiss the new causes of action asserted in the amended complaint because the Company was prejudiced by plaintiff’s long delay in filing the amended complaint. The Court has not yet ruled on the motion to dismiss, so the lawsuit remains in its early stages and has not yet be certified by the court as a class action. The Company intends to defend the lawsuit vigorously.
We cannot currently predict with certainty the ultimate impact of any of the above cases on our financial condition, cash flows or results of operations. Our reserve for professional liability expenses do not include any amounts for the pending DOJ investigation or the purported class action against the Arkansas center. An unfavorable outcome in any of these lawsuits, any of our professional liability actions, any regulatory action, or any investigation or lawsuit alleging violations of fraud and abuse laws or of elderly abuse laws or any state or Federal False Claims Act law could subject us to fines, penalties and damages, including exclusion from the Medicare or Medicaid programs, and could have a material adverse impact on our financial condition, cash flows or results of operations.
ITEM 1A. RISK FACTORS.
In addition to the other information contained in this Quarterly Report, the risks and uncertainties that we believe could materially affect our business, financial condition or future results and are most important for you to consider are discussed in Part I, “Item 1A. Risk Factors” in our Annual Report on Form 10-K filed with the SEC on March 1, 2018. Additional risks and uncertainties which are not presently known to us, which we currently deem immaterial or which are similar to those faced by other companies in our industry or business in general, may also materially and adversely affect any of our business, financial position or future results.
ITEM 2. UNREGISTERED SALES OF EQUITY SECURITIES AND USE OF PROCEEDS.
None.
ITEM 3. DEFAULTS UPON SENIOR SECURITIES.
None.
ITEM 4. MINE SAFETY DISCLOSURE.
Not applicable.
ITEM 5. OTHER INFORMATION.
None.
ITEM 6. EXHIBITS
The following exhibits are filed as part of this report on Form 10-Q.
33
Exhibit Number | Description of Exhibits | ||
3.1 | Certificate of Incorporation of the Registrant (incorporated by reference to Exhibit 3.1 to the Company’s Registration Statement No. 33-76150 on Form S-1 filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Certificate of Designation of Registrant (incorporated by reference to Exhibit 3.5 to the Company’s quarterly report on Form 10-Q for the quarter ended September 30, 2006). | |||
3.3 | Bylaws of the Company (incorporated by reference to Exhibit 3.2 to the Company’s Registration Statement No. 33-76150 on Form S-1 filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Bylaw Amendment adopted November 5, 2007 (incorporated by reference to Exhibit 3.4 to the Company’s annual report on Form 10-K for the year ended December 31, 2007). | |||
3.5 | Amendment to Certificate of Incorporation dated March 23, 1995 (incorporated by reference to Exhibit A of Exhibit 1 to the Company’s Form 8-A filed March 30, 1995 filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Certificate of Designation of Registrant (incorporated by reference to Exhibit 3.4 to the Company’s quarterly report on Form 10-Q for the quarter ended March 31, 2001). | |||
Certificate of Ownership and Merger of Diversicare Healthcare Services, Inc. with and into Advocat Inc. (incorporated by reference to Exhibit 3.1 to the Company's current report on Form 8-K filed March 14, 2013). | |||
Amendment to Certificate of Incorporation dated June 9, 2016 (incorporated by reference to Exhibit 3.8 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2016). | |||
Bylaw Second Amendment adopted April 14, 2016. | |||
4.1 | Form of Common Stock Certificate (incorporated by reference to Exhibit 4 to the Company's Registration Statement No. 33-76150 on Form S-1 filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Certification of Chief Executive Officer pursuant to Rule 13a-14(a) or Rule 15d-14(a). | |||
Certification of Chief Financial Officer pursuant to Rule 13a-14(a) or Rule 15d-14(a). | |||
Certification of Chief Executive Officer and Chief Financial Officer pursuant to Rule 13a-14(b) or Rule 15d-14(b). | |||
101.INS | XBRL Instance Document | ||
101.SCH | XBRL Taxonomy Extension Schema Document | ||
101.CAL | XBRL Taxonomy Extension Calculation Linkbase Document | ||
101.LAB | XBRL Taxonomy Extension Labels Linkbase Document | ||
101.PRE | XBRL Taxonomy Extension Presentation Linkbase Document | ||
34
SIGNATURES
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned thereunto duly authorized.
Diversicare Healthcare Services, Inc. | |||
May 3, 2018 | |||
By: | /s/ Kelly J. Gill | ||
Kelly J. Gill | |||
President and Chief Executive Officer, Principal Executive Officer and | |||
An Officer Duly Authorized to Sign on Behalf of the Registrant | |||
By: | /s/ James R. McKnight, Jr. | ||
James R. McKnight, Jr. | |||
Executive Vice President and Chief Financial Officer and | |||
An Officer Duly Authorized to Sign on Behalf of the Registrant | |||
35
