Attached files
| file | filename |
|---|---|
| 8-K - 8-K - Intra-Cellular Therapies, Inc. | d147828d8k.htm |
| EX-99.1 - EX-99.1 - Intra-Cellular Therapies, Inc. | d147828dex991.htm |
| EX-99.2 - EX-99.2 - Intra-Cellular Therapies, Inc. | d147828dex992.htm |
| EX-99.4 - EX-99.4 - Intra-Cellular Therapies, Inc. | d147828dex994.htm |
Exhibit 99.3
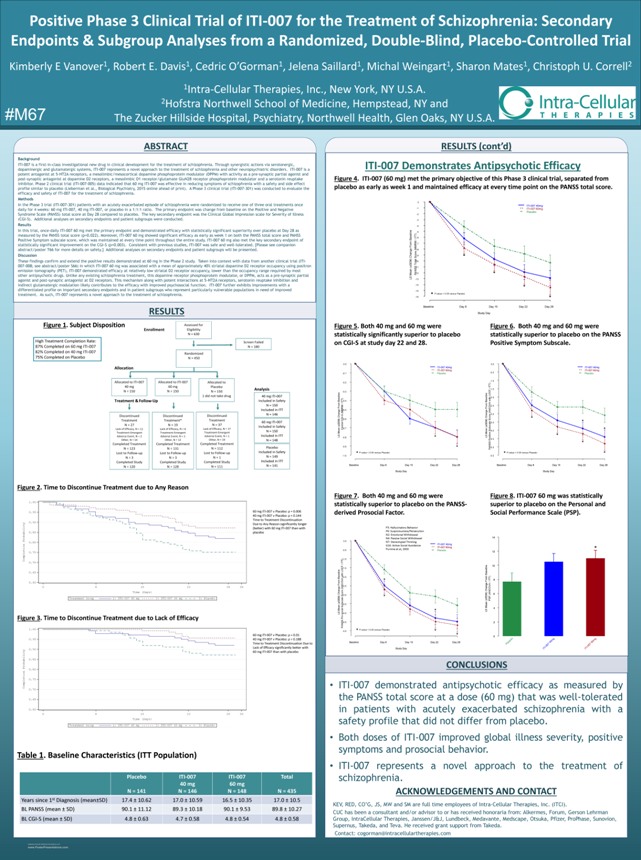
Positive Phase 3 Clinical Trial of ITI-007 for the Treatment of Schizophrenia: Secondary Endpoints & Subgroup Analyses from a Randomized, Double-Blind, Placebo-Controlled Trial Kimberly E Vanover1, Robert E. Davis1, Cedric O’Gorman1, Jelena Saillard1, Michal Weingart1, Sharon Mates1, Christoph U. Correll2 1Intra-Cellular Therapies, Inc., New York, NY U.S.A. 2Hofstra Northwell School of Medicine, Hempstead, NY and #M67 The Zucker Hillside Hospital, Psychiatry, Northwell Health, Glen Oaks, NY U.S.A. Intra-Cellular THERAPIES ADSTRACT Background ITI-007 is a first-in-class investigational new drug in clinical development for the treatment of schizophrenia. Through synergistic actions via serotonergic, dopaminergic and glutamatergic systems, ITI-007 represents a novel approach to the treatment of schizophrenia and other neuropsychiatric disorders. ITI-007 is a potent antagonist at 5-HT2A receptors, a mesolimbic/mesocortical dopamine phosphoprotein modulator (DPPM) with activity as a pre-synaptic partial agonist and post-synaptic antagonist at dopamine D2 receptors, a mesolimbic D1 receptor/glutamate GluN2B receptor phosphoprotein modulator and a serotonin reuptake inhibitor. Phase 2 clinical trial (ITI-007-005) data indicated that 60 mg ITI-007 was effective in reducing symptoms of schizophrenia with a safety and side effect profile similar to placebo (Lieberman et al., Biological Psychiatry, 2015 online ahead of print). A Phase 3 clinical trial (ITI-007-301) was conducted to evaluate the efficacy and safety of ITI-007 for the treatment of schizophrenia. Methods In the Phase 3 trial (ITI-007-301) patients with an acutely exacerbated episode of schizophrenia were randomized to receive one of three oral treatments once daily for 4 weeks: 60 mg ITI-007, 40 mg ITI-007, or placebo in a 1:1:1 ratio. The primary endpoint was change from baseline on the Positive and Negative Syndrome Scale (PANSS) total score at Day 28 compared to placebo. The key secondary endpoint was the Clinical Global Impression scale for Severity of Illness (CGI-S). Additional analyses on secondary endpoints and patient subgroups were conducted. Results In this trial, once-daily ITI-007 60 mg met the primary endpoint and demonstrated efficacy with statistically significant superiority over placebo at Day 28 as measured by the PANSS total score (p=0.022). Moreover, ITI-007 60 mg showed significant efficacy as early as week 1 on both the PANSS total score and PANSS Positive Symptom subscale score, which was maintained at every time point throughout the entire study. ITI-007 60 mg also met the key secondary endpoint of statistically significant improvement on the CGI-S (p=0.003). Consistent with previous studies, ITI-007 was safe and well-tolerated. [Please see companion abstract/poster T66 for more details on safety.] Additional analyses on secondary endpoints and patient subgroups will be presented. Discussion These findings confirm and extend the positive results demonstrated at 60 mg in the Phase 2 study. Taken into context with data from another clinical trial (ITI-007-008; see abstract/poster S66) in which ITI-007 60 mg was associated with a mean of approximately 40% striatal dopamine D2 receptor occupancy using positron emission tomography (PET), ITI-007 demonstrated efficacy at relatively low striatal D2 receptor occupancy, lower than the occupancy range required by most other antipsychotic drugs. Unlike any existing schizophrenia treatment, this dopamine receptor phosphoprotein modulator, or DPPM, acts as a pre-synaptic partial agonist and post-synaptic antagonist at D2 receptors. This mechanism along with potent interactions at 5-HT2A receptors, serotonin reuptake inhibition and indirect glutamatergic modulation likely contributes to the efficacy with improved psychosocial function. ITI-007 further exhibits improvements with a differentiated profile on important secondary endpoints and in patient subgroups who represent particularly vulnerable populations in need of improved treatment. As such, ITI-007 represents a novel approach to the treatment of schizophrenia. RESULTS Figure 1. Subject Disposition High Treatment Completion Rate: 87% Completed on 60 mg ITI-007 82% Completed on 40 mg ITI-007 75% Completed on Placebo Allocation Analysis 40 mg ITI-007 Treatment & Follow-Up Included in Safety N = 150 Included in ITT N = 146 60 mg ITI-007 Included in Safety N = 150 Included in ITT N = 148 Placebo Included in Safety N = 149 Included in ITT N = 141 Figure 2. Time to Discontinue Treatment due to Any Reason 60 mg ITI-007 v Placebo: p = 0.006 40 mg ITI-007 v Placebo: p = 0.144 Time to Treatment Discontinuation Due to Any Reason significantly longer (better) with 60 mg ITI-007 than with placebo Figure 3. Time to Discontinue Treatment due to Lack of Efficacy 60 mg ITI-007 v Placebo: p = 0.01 40 mg ITI-007 v Placebo: p = 0.188 Time to Treatment Discontinuation Due to Lack of Efficacy significantly better with 60 mg ITI-007 than with placebo Table 1. Baseline Characteristics (ITT Population) Placebo ITI-007 ITI-007 Total 40 mg 60 mg N = 141 N = 146 N = 148 N = 435 Years since 1st Diagnosis (mean±SD) 17.4 ± 10.62 17.0 ± 10.59 16.5 ± 10.35 17.0 ± 10.5 BL PANSS (mean ± SD) 90.1 ± 11.12 89.3 ± 10.18 90.1 ± 9.53 89.8 ± 10.27 BL CGI-S (mean ± SD) 4.8 ± 0.63 4.7 ± 0.58 4.8 ± 0.54 4.8 ± 0.58 RESULTS(cont’d) ITI-007 Demonstrates Antipsychotic Efficacy Figure 4. ITI-007 (60 mg) met the primary objective of this Phase 3 clinical trial, separated from placebo as early as week 1 and maintained efficacy at every time point on the PANSS total score. 0 ITI-007 40mg -1 ITI-007 60mg Placebo -2 -3 -4 -5 ITT)-6 Baseline/ From -7 (MMRM-8 Change Score-9 Total -10 (±SEM) -11 ANSS -12 Mean P LS -13 -14 -15 P-value < 0.05 versus Placebo -16 Baseline Day 8 Day 15 Day 22 Day 28 Study Day Figure 5. Both 40 mg and 60 mg were Figure 6. Both 40 mg and 60 mg were statistically significantly superior to placebo statistically superior to placebo on the PANSS on CGI-S at study day 22 and 28. Positive Symptom Subscale. 0.0 0.0 ITI-007 40mg ITI-007 40mg ITI-007 60mg ITI-007 60mg -0.1 Placebo -0.5 Placebo -1.0 -0.2 ITT) /-1.5 -0.3 LOCF with -2.0 Baseline -0.4 Baseline ITT) / From From -2.5 (MMRM-0.5 (ANCOVA S -3.0 Change—Change -0.6 Score CGI (±SEM) (±SEM) -3.5 Central-0.7 Subscale -4.0 Mean Mean LS LS -0.8 Positive-4.5 -0.9 PANSS-5.0 P-value < 0.05 versus Placebo P-value < 0.05 versus Placebo -1.0 -5.5 Baseline Day 8 Day 15 Day 22 Day 28 Baseline Day 8 Day 15 Day 22 Day 28 Study Day Study Day Figure 7. Both 40 mg and 60 mg were Figure 8. ITI-007 60 mg was statistically statistically superior to placebo on the PANSS- superior to placebo on the Personal and derived Prosocial Factor. Social Performance Scale (PSP). P3: Hallucinatory Behavior P6: Suspiciousness/Persecution N2: Emotional Withdrawal N4: Passive Social Withdrawal 14 0.0 N7: Stereotyped Thinking ITI-007 40mg G16: Active Social Avoidance ITI-007 60mg -0.5 Purnine et al, 2000 * Placebo 12 ITT)-1.0 / 10 LOCF-1.5 Baseline with Baseline -2.0 ITT) 8 From / From (ANCOVA-2.5 Change Change (ANCOVA 6 Score-3.0 (±SEM) PSP (±SEM) Subscale-3.5 ean M 4 Mean S L LS social-4.0 Pro—PANSS-4.5 2 P-value < 0.05 versus Placebo -5.0 0 o g g b e m m Baseline Day 8 Day 15 Day 22 Day 28 c 0 0 to l a 7 4 7 6 P 0 0—0—0 I I Study Day I T I T CONCLUSIONS • ITI-007 demonstrated antipsychotic efficacy as measured by the PANSS total score at a dose (60 mg) that was well-tolerated in patients with acutely exacerbated schizophrenia with a safety profile that did not differ from placebo. • Both doses of ITI-007 improved global illness severity, positive symptoms and prosocial behavior. • ITI-007 represents a novel approach to the treatment of schizophrenia. ACKNOWLEDGEMENTS AND CONTACT KEV, RED, CO’G, JS, MW and SM are full time employees of Intra-Cellular Therapies, Inc. (ITCI). CUC has been a consultant and/or advisor to or has received honoraria from: Alkermes, Forum, Gerson Lehrman Group, IntraCellular Therapies, Janssen/J&J, Lundbeck, Medavante, Medscape, Otsuka, Pfizer, ProPhase, Sunovion, Supernus, Takeda, and Teva. He received grant support from Takeda. Contact: cogorman@intracellulartherapies.com
