Attached files
| file | filename |
|---|---|
| 8-K - 8-K - Cardiff Oncology, Inc. | a13-22639_18k.htm |
Exhibit 99.1
|
|
A better clinical pathway for cancer monitoring Antonius Schuh, Ph.D. | Chief Executive Officer October 2013 |
|
|
Forward-Looking Statements Statements in this presentation about the Company's expectations, applications of its technology, markets, launch of tests and other statements that are not historical facts are "forward-looking statements" within the meaning of Section 27A of the Securities Act of 1933 and Section 21E of the Securities Exchange Act of 1934 and are based on management's current beliefs, assumptions, estimates and projections. Actual results may differ materially from those projected in the forward-looking statements for various reasons, including risks associated with product and test development, test transfer to contracting labs, government regulation, market acceptance, limited commercial experience, dependence on key personnel, obtaining financing and other factors discussed in the Company's periodic reports filed with the Securities and Exchange Commission. DISCLAIMER |
|
|
Our goal: Towards better treatment for cancer INTRODUCTION A better clinical pathway for cancer monitoring Novel clinical utility: non-invasive, near real-time detection of oncogene mutations for any tumor type |
|
|
Introduction Welcome to Trovagene, Inc. Addresses a high unmet need in cancer by enabling easier, more frequent monitoring of emergence of oncogene mutation status, disease progression and recurrence Unique IP around cell-free DNA in urine creates a powerful core diagnostic platform for the non-invasive detection of oncogene mutations, with urine providing the competitive advantages of ease of sampling and large volume Cancer monitoring based on urine testing is now ready for clinical use as improved PCR technologies and next generation sequencing platforms are available at much reduced cost CLIA certified, CAP accredited high complexity diagnostic laboratory to offer diagnostic services Technology development collaborations with leading corporate partners INTRODUCTION NASDAQ: TROV $180M market cap* Molecular Diagnostic Specialist founded in 1999 NASDAQ listing 2012 $55M invested in R&D and IP $27.M cash on hand as Sept. 30 Focused on oncology and infectious disease *as of 13 October 2013 |
|
|
Experienced Senior Management Team TROVAGENE CORE TEAM Thomas Adams, PhD (Chair) John P. Brancaccio, CPA Gary S. Jacob, PhD Antonius Schuh PhD CEO CEO Sorrento Therapeutics, AviaraDx, Arcturus Biosciences, Sequenom PhD Pharm. Chem Stephen Zaniboni CFO Mark Erlander PhD CSO Keith McCormick VP, Sales Michael Terry VP, Comm. Ops CFO, Awarepoint, XIFIN, Sorrento Therapeutics, AviaraDx, Arcturus, Sequenom CPA, BS Accounting, MBA Boston College CSO, bioTheranostics, AviaraDx, Arcturus Biosciences Research Fellow, J&J Assistant Professor, Scripps Research Institute BS, MS Biochem; Ph.D. Neuroscience Sr. Director, Sales Ops, bioTheranostics Director, Sales & Marketing, AviaraDx Management roles at Biogen Idec, Schering Plough, Dianon Systems BBA – Marketing MBA – Int’l Business President, Ligand DX, EVP Sequenom, EVP and MD of European Operations, Lumenis, Director-level position, GE Healthcare Medical BS Econ & Business, AD Int’l Business Paul Billings, MD, PhD Carlo M. Croce, MD Riccardo Dalla-Favera, MD Brunangelo Falini, MD Kunwar Shailubhai, PhD Antonius Schuh, PhD Stanley Tennant, MD Chris McGuigan, PhD Scientific Advisors Board of Directors |
|
|
Understanding “cell-free” DNA for cancer monitoring THE CLINICAL UTILITY OF CELL-FREE DNA FROM URINE Cell-free DNA is released by dying cells in the human body Cells in the body die continuously in a process known as “apoptosis” , releasing DNA/RNA into the bloodstream This “cell-free” DNA, detectable in the blood, has been the basis of minimal invasive diagnostic tests launched by Sequenom, Illumina/Verinata, Natera, Ariosa Dx, and facilitates real time cancer monitoring What is cell-free DNA? Dying cancer cells also release their mutated DNA into the bloodstream, enabling determination of mutation type and relative tumor volume |
|
|
Why not simply use a blood specimen? THE CLINICAL UTILITY OF CELL-FREE DNA FROM URINE Blood Draw Sample quantity is limited Sample frequency is limited Inconvenient for patient – requires an appointment Painful and perceived as threatening Requires a medical professional Specimen is a biohazard Requires urgent shipping/cold-chain support While routinely used and regarded by physicians as “non-invasive”, blood is far from an ideal choice of specimen Blood specimen |
|
|
Kidneys filter cell-free DNA from blood into the urine THE CLINICAL UTILITY OF CELL-FREE DNA FROM URINE By isolating cell-free DNA from urine, Trovagene eliminates the need for the cost, complexity and inconvenience of a blood sample Truly non-invasive Patient can self-sample at home or clinic No medical professional required for specimen collection Large volume can be collected High frequency of collection possible Non-biohazardous specimen No refrigeration required No infection risk Lower cost Urine contains cell-free “Transrenal” DNA or RNA Urine sample Blood after centrifugation Urine specimen |
|
|
Enabled by a confluence of emerging technologies THE CLINICAL UTILITY OF CELL-FREE DNA FROM URINE Ability to detect single DNA molecules in a urine sample Trovagene IP Next Gen sequencing Digital PCR RainDance Droplet Digital PCR up to 5,000,000 target sequences Oncogene mutations are rare events Tumors are small relative to the body and not genetically homogeneous Next Gen Sequencing Enables detection/monitoring panels |
|
|
Why Cell-free DNA? Cell-free DNA gives a global view of tumor heterogeneity for metastatic cancer patients THE CLINICAL UTILITY OF CELL-FREE DNA FROM URINE Detection of specific tumor mutations Monitoring of tumor load/response to therapy Detection of emerging tumor resistant mutations/new directed therapy Clinical Utility Tumors are heterogeneous in their tumor mutational make-up Would need multiple tissue/tumor biopsies to determine heterogeneity and optimal therapy Cell-free DNA from tumors is released into the blood plasma after cell-death Previously established that cell-free DNA increases with cancer stage in plasma Technology now available to detect mutations: Digital droplet PCR and Next Generation Sequencing Platforms |
|
|
Healthy Subject Oncogenic Mutation DRUG A CYCLE 1 CYCLE 2 CYCLE 3 CYCLE 4 SURVIVAL TUMOR MUTATION#1 Selective pressure of targeted drugs enrich tumor tissue with new mutant cells that are drug resistant Treatment SURVIVAL DRUG B DRUG C DRUG D SURVIVAL CELL DEATH CELL DEATH CELL DEATH MUTATION#2 MUTATION#3 Detecting & monitoring cancer mutations key to effective therapy COMMERCIAL FOCUS ON CANCER MONITORING Match up targeted drugs with mutation profile |
|
|
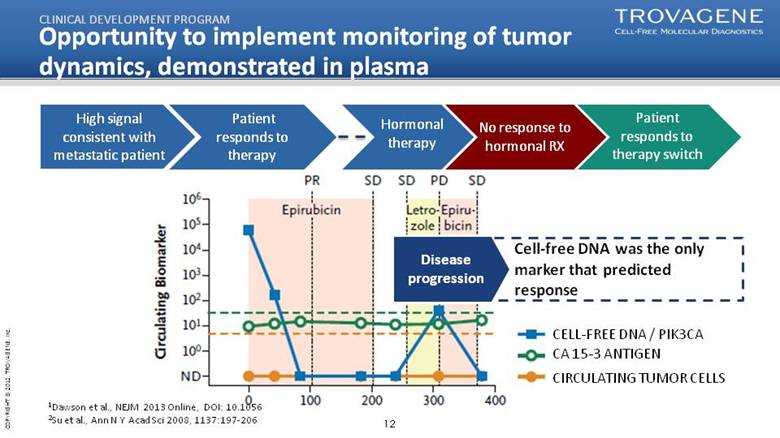
Opportunity to implement monitoring of tumor dynamics, demonstrated in plasma CLINICAL DEVELOPMENT PROGRAM Disease progression 1Dawson et al., NEJM 2013 Online, DOI: 10.1056 2Su et al., Ann N Y Acad Sci 2008, 1137:197-206 Cell-free DNA was the only marker that predicted response CELL-FREE DNA / PIK3CA CA 15-3 ANTIGEN CIRCULATING TUMOR CELLS Patient responds to therapy No response to hormonal RX High signal consistent with metastatic patient Patient responds to therapy switch Hormonal therapy |
|
|
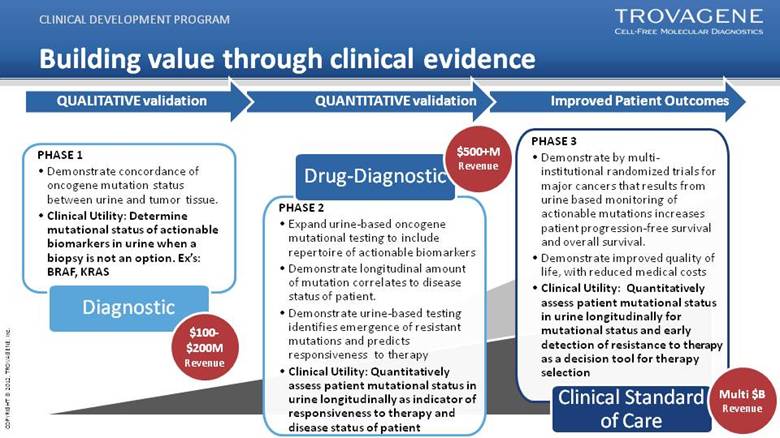
Improved Patient Outcomes Building value through clinical evidence CLINICAL DEVELOPMENT PROGRAM PHASE 1 Demonstrate concordance of oncogene mutation status between urine and tumor tissue. Clinical Utility: Determine mutational status of actionable biomarkers in urine when a biopsy is not an option. Ex’s: BRAF, KRAS Diagnostic $100-$200M Revenue PHASE 2 Expand urine-based oncogene mutational testing to include repertoire of actionable biomarkers Demonstrate longitudinal amount of mutation correlates to disease status of patient. Demonstrate urine-based testing identifies emergence of resistant mutations and predicts responsiveness to therapy Clinical Utility: Quantitatively assess patient mutational status in urine longitudinally as indicator of responsiveness to therapy and disease status of patient QUANTITATIVE validation QUALITATIVE validation Drug-Diagnostic PHASE 3 Demonstrate by multi-institutional randomized trials for major cancers that results from urine based monitoring of actionable mutations increases patient progression-free survival and overall survival. Demonstrate improved quality of life, with reduced medical costs Clinical Utility: Quantitatively assess patient mutational status in urine longitudinally for mutational status and early detection of resistance to therapy as a decision tool for therapy selection $500+M Revenue Clinical Standard of Care Multi $B Revenue |
|
|
Phase 1: Demonstrate concordance of urine-based DNA mutational testing with tumor tissue biopsy Principal Investigator: Filip Janku MD PhD; Investigational Cancer Therapeutics (Phase I Clinical Trials Program) MD Anderson Cancer Center Objective 1: Measure the degree of concordance between results of DNA mutation analysis from urine samples versus confirmed mutational status of tumor biopsy tissue. Objective 2: Longitudinal assessment over time of mutational status of urinary DNA in the treatment of metastatic cancer patients with correlation to therapeutic response and disease status of the patient. CLINICAL DEVELOPMENT PROGRAM Clinical Study: Detecting & Monitoring Tumor Mutations in Cell-free DNA from Urine in Metastatic Cancer Patients |
|
|
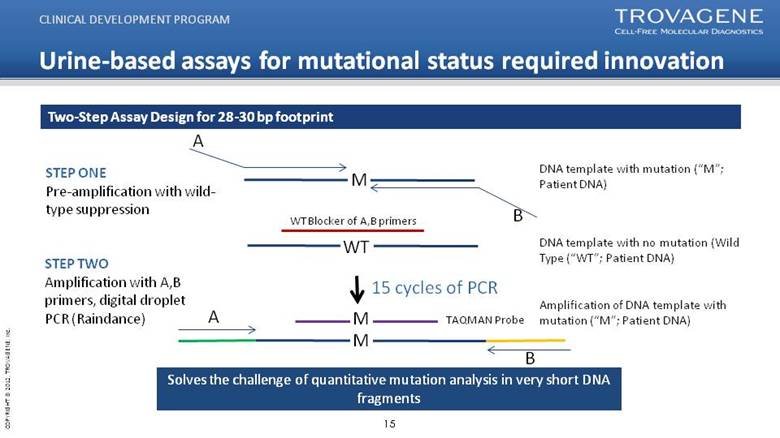
A STEP ONE Pre-amplification with wild-type suppression DNA template with mutation (“M”; Patient DNA) B STEP TWO Amplification with A,B primers, digital droplet PCR (Raindance) DNA template with no mutation (Wild Type (“WT”; Patient DNA) WT Blocker of A,B primers M WT A B M M TAQMAN Probe Amplification of DNA template with mutation (“M”; Patient DNA) 15 cycles of PCR Two-Step Assay Design for 28-30 bp footprint Urine-based assays for mutational status required innovation CLINICAL DEVELOPMENT PROGRAM Solves the challenge of quantitative mutation analysis in very short DNA fragments |
|
|
BRAF V600E mutation detection by droplet digital PCR CLINICAL DEVELOPMENT PROGRAM BRAF mutation Empty droplets No mutation (wild type) Healthy (negative) Control Positive Control Empty droplets No mutation (wild type) |
|
|
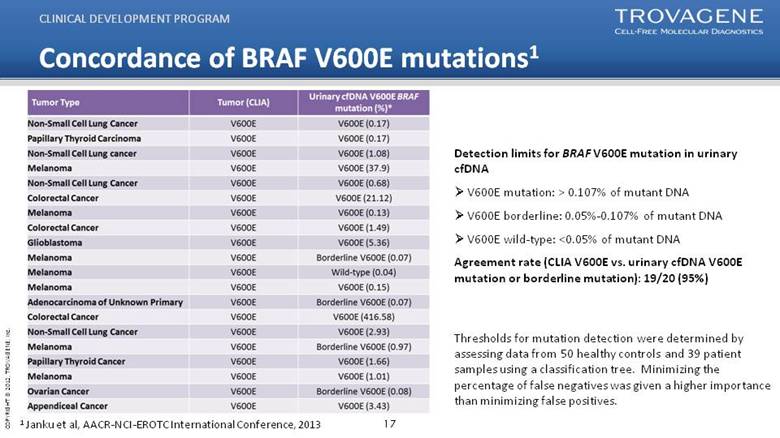
Concordance of BRAF V600E mutations1 CLINICAL DEVELOPMENT PROGRAM Thresholds for mutation detection were determined by assessing data from 50 healthy controls and 39 patient samples using a classification tree. Minimizing the percentage of false negatives was given a higher importance than minimizing false positives. 1 Janku et al, AACR-NCI-EROTC International Conference, 2013 Detection limits for BRAF V600E mutation in urinary cfDNA V600E mutation: > 0.107% of mutant DNA V600E borderline: 0.05%-0.107% of mutant DNA V600E wild-type: <0.05% of mutant DNA Agreement rate (CLIA V600E vs. urinary cfDNA V600E mutation or borderline mutation): 19/20 (95%) |
|
|
Longitudinal Urinary cf-DNA BRAF V600E Mutation Correlates with Therapy Response CLINICAL DEVELOPMENT PROGRAM Patient 5: Melanoma Progressive Disease Vemurafenib only |
|
|
Longitudinal Urinary cf-DNA BRAF V600E Mutation Correlates with Therapy Response CLINICAL DEVELOPMENT PROGRAM Progressing on Chemotherapy Patient 16 Colorectal Cancer Patient 44 Appendiceal Cancer Progressing on chemotherapy |
|
|
Summary A cell free DNA (cf-DNA) BRAF V600E mutation test from urine has high concordance with patient-matched known BRAF mutational status from tumor tissue biopsy BRAF mutations were detected in a range of tumor types including melanoma, colorectal, appendiceal, lung, glioblastoma, papillary thyroid and ovarian indicating that mutational detection in urine is not limited by tumor type. Patient longitudinal monitoring of urinary cf-DNA BRAF V600E spanning 2 to 10 months indicates concordance with therapeutic response and disease status of the patient. cf-DNA BRAF V600E testing in urine represents a truly non-invasive method for detecting clinically actionable mutations and monitoring responsiveness to therapy. CLINICAL DEVELOPMENT PROGRAM |
|
|
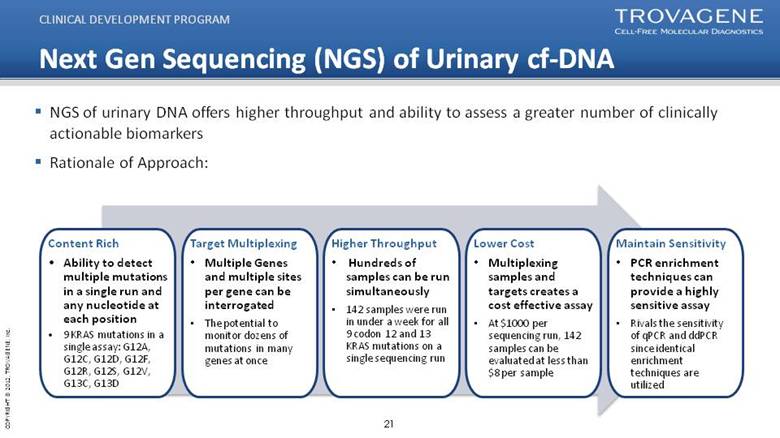
Content Rich Ability to detect multiple mutations in a single run and any nucleotide at each position 9 KRAS mutations in a single assay: G12A, G12C, G12D, G12F, G12R, G12S, G12V, G13C, G13D Target Multiplexing Multiple Genes and multiple sites per gene can be interrogated The potential to monitor dozens of mutations in many genes at once Higher Throughput Hundreds of samples can be run simultaneously 142 samples were run in under a week for all 9 codon 12 and 13 KRAS mutations on a single sequencing run Lower Cost Multiplexing samples and targets creates a cost effective assay At $1000 per sequencing run, 142 samples can be evaluated at less than $8 per sample Maintain Sensitivity PCR enrichment techniques can provide a highly sensitive assay Rivals the sensitivity of qPCR and ddPCR since identical enrichment techniques are utilized Next Gen Sequencing (NGS) of Urinary cf-DNA NGS of urinary DNA offers higher throughput and ability to assess a greater number of clinically actionable biomarkers Rationale of Approach: CLINICAL DEVELOPMENT PROGRAM |
|
|
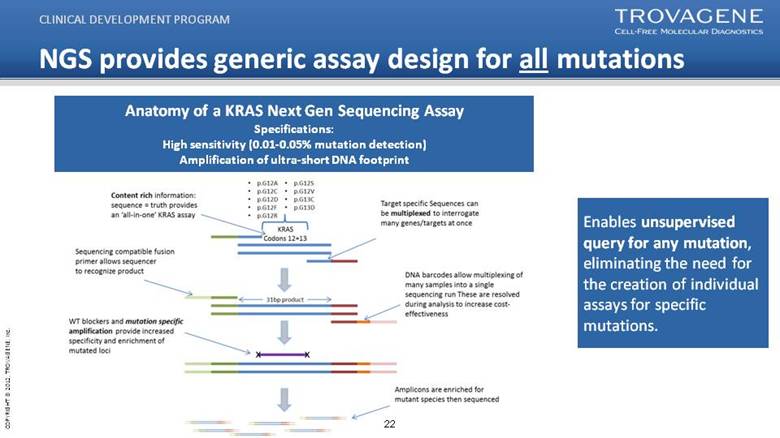
NGS provides generic assay design for all mutations CLINICAL DEVELOPMENT PROGRAM Enables unsupervised query for any mutation, eliminating the need for the creation of individual assays for specific mutations. Anatomy of a KRAS Next Gen Sequencing Assay Specifications: High sensitivity (0.01-0.05% mutation detection) Amplification of ultra-short DNA footprint |
|
|
cf-DNA NGS KRAS Assay Knowing KRAS mutational status in metastatic colorectal cancer patients is currently standard of care for anti-EGFR therapy To assess the performance of our assay we utilized mutant containing cell line DNA with known mutational status to optimize the performance with each mutation. A list of nucleotide substitutions for each of the KRAS mutations in codons 12/13 were tested in our assay. Seven mutations were validated using mutation containing cell line DNA. CLINICAL DEVELOPMENT PROGRAM KRAS |
|
|
NGS cf-DNA KRAS has high specificity CLINICAL DEVELOPMENT PROGRAM NGS assay of cell lines with 7 different known KRAS mutations indicates high specificity |
|
|
Fold Enrichment of KRAS G12D Mutation Actual Mutation Frequency Observed Frequency 50.00% 91.14% 12.50% 86.74% 3.13% 72.26% 0.78% 41.32% 0.20% 16.59% 0.05% 5.72% 0.01% 2.24% 0% 0.30% NGS assay has required detection sensitivity CLINICAL DEVELOPMENT PROGRAM |
|
|
NGS assay detects KRAS mutations in Urinary DNA from Metastatic Cancer Patients CLINICAL DEVELOPMENT PROGRAM Initial Study indicates high concordance 8 out of 9 KRAS mutations detected by NGS assay NGS assay enables quantitation of amount of mutation (versus normal) present in urine |
|
|
Summary NGS of cf-DNA from patient urine will enable a non-invasive method for mutation detection of the large number of clinically actionable biomarkers and longitudinally monitoring responsiveness to therapy. A NGS cf-DNA KRAS test is being developed to detect and quantitate mutational status for metastatic cancer patients with tumors harboring KRAS mutations. Initial studies indicate that the cf-DNA NGS KRAS assay has high specificity and sensitivity CLINICAL DEVELOPMENT PROGRAM |
|
|
Core IP extends into assay detection and development CORE INTELLECTUAL PROPERTY |
|
|
Reimbursement Strategy Our tests must be positioned as different from other mutation assays: New Technology Code “81479” being considered Allows for billing at list price Single Mutation - $400-500 Multiple Mutation Profile - $1500-2000 Appeal cases of low-pay or no-pay Medicare providership will be important Provides access to key networks, hospitals, physicians Up to one year window to bill for services Allows supporting data to be developed and published Short term revenue will be impacted Initial claims will be denied and appealed Developing data will support utility eventually Developing supporting materials for appeals Insure trials have viable clinical utility endpoints Utilize patent portfolio to emphasize unique technology Working with key consultants to optimize billing and appeals process Develop pricing strategies that ensures broadest insurance coverage New technology code allows most options for both ddPCR and NGS platform tests Evaluate new NGS codes when available (2014-2015) Evaluating Patient Registry Trials Provide means of evaluating utility of assay in a broad community setting Develops publishable data and can be used as part of appeals process What we are doing about it COMMERCIAL UPDATE |
|
|
2012 achievements Acquired CLIA laboratory CLIA-certified, cap-accredited high complexity molecular diagnostic lab Strengthened patent portfolio Issued U.S. Patent for NPM mutants to diagnose and monitor acute myeloid leukemia Issued European patent for detection of pathogenic infections Improved liquidity and access to capital Completed public offering of $10 million and began trading on NASDAQ Added to the Russell microcap and the MSCI microcap index Closed private placement of $4.4 million Initiated KRAS mutation detection development program Commenced validation program and commenced study at MD Anderson Cancer Center for transrenal KRAS mutation detection in pancreatic cancer Expanded of high risk HPV carrier screening development program Partnered with Strand Life Sciences to validate and offer urine-based HPV screening test in India Partnered with Barretos cancer hospital to evaluate urine-based HPV assay in Brazil COMMERCIAL DEVELOPMENT UPDATE |
|
|
2013 achievements Demonstrated proof of concept for tumor mutation detection from urine samples of metastatic cancer patients Validated the presence of BRAF, KRAS in multiple cancer types Initiated R&D partnership with PerkinElmer Collaborate to develop test to determine liver cancer risk Initiated R&D partnership with Illumina Collaborate to apply NGS for the analysis of transrenal sequence signals Extended oncogene mutation detection development program Began second study at MD Anderson cancer center focusing on BRAF and KRAS mutations in 2013 Initiated prospective colorectal cancer study with USC Norris Cancer Center Completed $15 million registered direct offering Released the first prospective data Indicating that oncogene mutation signal in urine correlates with response to therapy COMMERCIAL DEVELOPMENT UPDATE |
|
|
For further information Please contact: Antonius Schuh, CEO aschuh@trovagene.com Stephen Zaniboni, CFO szaniboni@trovagene.com |