Attached files
| file | filename |
|---|---|
| EX-23.3 - EX-23.3 - Signify Health, Inc. | d12124dex233.htm |
| EX-23.2 - EX-23.2 - Signify Health, Inc. | d12124dex232.htm |
| EX-23.1 - EX-23.1 - Signify Health, Inc. | d12124dex231.htm |
Table of Contents
As filed with the Securities and Exchange Commission on February 10, 2021
Registration No. 333-252231
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Amendment No. 3
to
FORM S-1
REGISTRATION STATEMENT
UNDER
THE SECURITIES ACT OF 1933
Signify Health, Inc.
(Exact Name of Registrant as Specified in Its Charter)
| Delaware | 8082 | 85-3481223 | ||
| (State or Other Jurisdiction of Incorporation or Organization) |
(Primary Standard Industrial Classification Code Number) |
(I.R.S. Employer Identification Number) |
800 Connecticut Avenue
Norwalk, CT 06854
(203) 541-4600
(Address, Including Zip Code, and Telephone Number, Including Area Code, of Registrant’s Principal Executive Offices)
Kyle Armbrester
Chief Executive Officer
Signify Health, Inc.
800 Connecticut Avenue
Norwalk, CT 06854
(203) 541-4600
(Name, Address, Including Zip Code, and Telephone Number, Including Area Code, of Agent For Service)
Copies to:
| Shane Tintle Deanna L. Kirkpatrick Davis
Polk & Wardwell LLP |
Joseph H. Kaufman Ryan R. Bekkerus Simpson Thacher & Bartlett LLP 425 Lexington Avenue New York, NY 10017 (212) 455-2000 |
Approximate date of commencement of proposed sale to the public: As soon as practicable after the effective date of this Registration Statement.
If any of the securities being registered on this form are to be offered on a delayed or continuous basis pursuant to Rule 415 under the Securities Act of 1933, check the following box. ☐
If this form is filed to register additional securities for an offering pursuant to Rule 462(b) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ☐
If this form is a post-effective amendment filed pursuant to Rule 462(c) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ☐
If this form is a post-effective amendment filed pursuant to Rule 462(d) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ☐
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
| Large accelerated filer | ☐ | Accelerated filer | ☐ | |||
| Non-accelerated filer | ☒ | Smaller reporting company | ☐ | |||
| Emerging growth company | ☒ | |||||
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 7(a)(2)(B) of the Securities Act. ☐
|
| ||||||||
| Title of Each Class of Securities to Be Registered |
Amount to be Registered(1)(2) |
Proposed Maximum Offering Price Per Share |
Proposed Maximum Aggregate |
Amount of Registration Fee(3) | ||||
| Class A common stock, par value $0.01 per share |
27,025,000 | $21.00 | $567,525,000 | $61,916.98 | ||||
|
| ||||||||
|
| ||||||||
| (1) | Includes additional shares of Class A common stock which the underwriters have the option to purchase to cover over-allotments. |
| (2) | Estimated solely for the purpose of computing the amount of the registration fee pursuant to Rule 457(a) under the Securities Act of 1933. |
| (3) | Of this amount, $56,020.12 was previously paid. |
The registrant hereby amends this registration statement on such date or dates as may be necessary to delay its effective date until the registrant shall file a further amendment which specifically states that this registration statement shall thereafter become effective in accordance with Section 8(a) of the Securities Act of 1933 or until the registration statement shall become effective on such date as the Commission, acting pursuant to said Section 8(a), may determine.
Table of Contents
The information in this prospectus is not complete and may be changed. We may not sell these securities until the registration statement filed with the Securities and Exchange Commission is effective. This prospectus is not an offer to sell these securities and we are not soliciting offers to buy these securities in any jurisdiction where the offer or sale is not permitted.
SUBJECT TO COMPLETION, DATED FEBRUARY 10, 2021
PRELIMINARY PROSPECTUS

23,500,000 Shares
Signify Health, Inc.
Class A common stock
Signify Health, Inc. is offering 23,500,000 shares of its Class A common stock. This is our initial public offering and no public market exists for our Class A common stock. We anticipate that the initial public offering price will be between $20.00 and $21.00 per share.
We will use all of the net proceeds we receive from this offering to purchase new membership interests of Cure TopCo, LLC, which we refer to as “LLC Units,” from Cure TopCo, LLC. No public market exists for the LLC Units. The purchase price for each LLC Unit will be equal to the initial public offering price of our Class A common stock net of underwriting discounts and commissions. We intend to cause Cure TopCo, LLC to use the net proceeds it receives from us in connection with this offering as described in “Use of proceeds.”
This offering is being conducted through what is commonly referred to as an “Up-C” structure, which is often used by partnerships and limited liability companies undertaking an initial public offering. The Up-C approach provides the existing owners with the tax treatment of continuing to own interests in a pass-through structure and provides potential future tax benefits for both the public company and the existing owners when they ultimately exchange their pass-through interests for shares of Class A common stock. Signify Health, Inc. is a holding company, and immediately after the consummation of the Reorganization Transactions and this offering its principal asset will be its ownership interests in Cure TopCo, LLC. We conduct our business through Cure TopCo, LLC and its subsidiaries. See “Organizational structure.” Upon the completion of this offering, Signify Health, Inc. and the Continuing Pre-IPO LLC Members (as defined herein) will hold 74.2% and 25.8% of Cure TopCo, LLC, respectively.
Upon completion of this offering, Signify Health, Inc. will have two classes of common stock. The Class A common stock offered hereby will have one vote per share and the Class B common stock will have one vote per share. Upon completion of this offering, the Pre-IPO LLC Members (as defined herein), including certain Pre-IPO LLC Members affiliated with New Mountain Capital, LLC (“New Mountain Capital”), will collectively hold shares of Class A common stock and Class B common stock that will entitle them to 89.4% (or 88.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full) of the combined voting power of our common stock. As a result, the Pre-IPO LLC Members will be able to control any action requiring the general approval of our stockholders, including the election of our board of directors, the adoption of amendments to our certificate of incorporation and bylaws and the approval of any merger or sale of the Company or substantially all of our assets. Accordingly, we will be a “controlled company” within the meaning of the corporate governance standards of the New York Stock Exchange (“NYSE”). See “Management.”
We will apply to list our Class A common stock on the NYSE under the symbol “SGFY.”
Investing in our Class A common stock involves risks. See “Risk factors” beginning on page 29.
We are an “emerging growth company” as defined under the federal securities laws and, as such, may elect, and have elected, to comply with certain reduced public company reporting requirements for future filings. See “Prospectus summary—Implications of being an emerging growth company.”
Neither the Securities and Exchange Commission nor any state securities commission has approved or disapproved of these securities or determined if this prospectus is truthful or complete. Any representation to the contrary is a criminal offense.
| Per Share | Total | |||||||
| Initial public offering price |
$ | $ | ||||||
| Underwriting discounts and commissions |
$ | $ | ||||||
| Proceeds to us before expenses(1) |
$ | $ | ||||||
| (1) | We have agreed to reimburse the underwriters for certain FINRA-related expenses. See “Underwriting.” |
At our request, the underwriters have reserved up to 1,175,000 shares of Class A common stock, or 5% of the shares of Class A common stock to be offered by this prospectus for sale, at the initial public offering price, through a directed share program for certain of our clinicians and employees and certain other individuals and entities. See “Underwriting—Directed share program.”
We have granted the underwriters the option to purchase an additional 3,525,000 shares of Class A common stock to cover over-allotments.
The underwriters expect to deliver the shares against payment on or about , 2021 through the book-entry facilities of The Depository Trust Company.
Joint Book-Running Managers
| Goldman Sachs & Co. LLC | J.P. Morgan | Barclays | Deutsche Bank Securities |
| BofA Securities | UBS Investment Bank | Baird | Piper Sandler |
William Blair | ||||
The date of this prospectus is , 2021.
Table of Contents
Table of Contents
We and the underwriters (and any of our or their affiliates) have not authorized anyone to provide any information or to make any representations other than those contained in this prospectus or in any free writing prospectuses we have prepared. We and the underwriters (and any of our or their affiliates) take no responsibility for, and can provide no assurance as to the reliability of, any other information that others may provide you. We are offering to sell, and seeking offers to buy, shares of Class A common stock only in jurisdictions where offers and sales are permitted. The information contained in this prospectus is accurate only as of the date of this prospectus, regardless of the time of delivery of this prospectus or of any sale of Class A common stock. Our business, financial condition, results of operations and prospects may have changed since the date on the front cover of this prospectus.
Basis of presentation
In this prospectus, unless the context otherwise requires, “Signify Health,” the “Company,” “we,” “us” and “our” refer (i) prior to the consummation of the reorganization transactions described under “Organizational structure—The Reorganization Transactions,” to Cure TopCo, LLC and its subsidiaries and (ii) after the reorganization transactions described under “Organizational structure—The Reorganization Transactions,” to Signify Health, Inc., Cure TopCo, LLC and their subsidiaries.
In 2019, through a series of transactions culminating on November 26, 2019, we acquired 100% of the outstanding equity of Remedy Partners, Inc. (“Remedy Partners”). A controlling interest was initially acquired by affiliates of New Mountain Capital on January 15, 2019, at which point we and Remedy Partners were considered to be under common control. Combined financial statements were presented from January 15, 2019 to November 26, 2019 and consolidated financial statements were presented through December 31, 2019. The audited consolidated financial statements of Remedy Partners as of and for the year ended December 31, 2018, together with the notes thereto, were prepared in accordance with generally accepted accounting principles (“GAAP”) and are included elsewhere in this prospectus. The audited consolidated financial statements of Remedy Partners as of and for the year ended December 31, 2018 reflect the application of Accounting Standards Codification 605. See Note 1 to the audited consolidated financial statements of Remedy Partners for further information.
i
Table of Contents
Market and industry data
This prospectus includes industry and market data that we obtained from periodic industry publications, third-party studies and surveys, as well as from filings of public companies in our industry and internal company surveys. These sources include government and industry sources. Industry publications and surveys generally state that the information contained therein has been obtained from sources believed to be reliable. Although we believe the industry and market data to be reliable as of the date of this prospectus, this information could prove to be inaccurate. Industry and market data could be wrong because of the method by which sources obtained their data and because information cannot always be verified with complete certainty due to the limits on the availability and reliability of raw data, the voluntary nature of the data gathering process and other limitations and uncertainties. In addition, we do not know all of the assumptions regarding general economic conditions or growth that were used in preparing the forecasts from the sources relied upon or cited herein.
Non-GAAP financial measures
We refer in this prospectus to the following non-GAAP financial measures:
| • | Adjusted EBITDA; and |
| • | Adjusted EBITDA Margin. |
These non-GAAP financial measures are not prepared in accordance with generally accepted accounting principles in the United States, or GAAP. They are supplemental financial measures of our performance only, and should not be considered a substitute for net loss or any other measure derived in accordance with GAAP.
As used in this prospectus, these non-GAAP financial measures have the following meanings:
| • | Adjusted EBITDA means net loss before interest expense, income tax expense, depreciation and amortization, and certain items of income and expense, including asset impairment, other (income) expense, net, transaction-related expenses, equity-based compensation, remeasurement of contingent consideration, management fees and non-recurring items; and |
| • | Adjusted EBITDA Margin means Adjusted EBITDA divided by total revenue. |
Adjusted EBITDA is a key metric used by management and our board of directors to assess the performance of our business. We believe that Adjusted EBITDA provides a useful measure to investors to assess our operating performance because it eliminates the impact of expenses that do not relate to ongoing business performance, and that the presentation of this measure enhances an investor’s understanding of the performance of our business. We believe that Adjusted EBITDA Margin is helpful to investors in measuring the profitability of our operations on a consolidated level. For a reconciliation of Adjusted EBITDA and Adjusted EBITDA Margin to net loss, see “Prospectus summary—Summary combined-consolidated financial and other data.”
Our use of the terms Adjusted EBITDA and Adjusted EBITDA Margin may vary from the use of similar terms by other companies in our industry and accordingly may not be comparable to similarly titled measures used by other companies. Adjusted EBITDA and Adjusted EBITDA Margin have important limitations as analytical tools. For example, Adjusted EBITDA and Adjusted EBITDA Margin:
| • | do not reflect any cash capital expenditure requirements for the assets being depreciated and amortized that may have to be replaced in the future; |
| • | do not reflect changes in, or cash requirements for, our working capital needs; |
| • | do not reflect the impact of certain cash charges resulting from matters we consider not to be indicative of our core operations; |
| • | do not reflect the interest expense or the cash requirements necessary to service interest or principal payments on our debt; |
| • | do not reflect equity-based compensation expense and other non-cash charges; and |
| • | exclude certain tax payments that may represent a reduction in cash available to us. |
ii
Table of Contents
This summary highlights selected information that is presented in greater detail elsewhere in this prospectus. This summary does not contain all of the information that you should consider before investing in our Class A common stock. You should read this entire prospectus carefully, including the “Risk factors” and “Management’s discussion and analysis of financial condition and results of operations” sections and the consolidated financial statements and the notes to those statements included elsewhere in this prospectus before deciding whether to purchase shares of our Class A common stock.
Overview
Our company
Signify Health is a leading healthcare platform that leverages advanced analytics, technology, and nationwide healthcare provider networks to create and power value-based payment programs. Our mission is to transform how care is paid for and delivered so that people can enjoy more healthy, happy days at home. Our customers include health plans, governments, employers, health systems and physician groups. We believe that we are a market leader in two fast-growing segments of the value-based healthcare payment industry: payment models based on individual episodes of care and in-home health evaluations (“IHEs”). Payment models based on individual episodes of care organize or bundle payments for all, or a substantial portion of, services received by a patient in connection with an episode of care, such as a surgical procedure, particular condition or other reason for a hospital stay. IHEs are health evaluations performed by a clinician in the home to support payors’ participation in Medicare Advantage and other government-run managed care plans. Our episode payment platform managed $6.1 billion of spend under the Medicare Bundled Payment for Care Improvement Advanced (“BPCI-A”) program in 2019, and the BPCI-A episodes we managed which were initiated in the last quarter of 2019 resulted in approximately 15% greater discharges home from acute-care facilities and approximately 10% lower readmissions when compared to the historical performance of our provider partners for similar episodes. Our mobile network of providers entered over 1 million unique homes to evaluate individuals in Medicare Advantage and other managed care plans in 2019. We believe that these core businesses have enabled us to become integral to how health plans and healthcare providers successfully participate in value-based payment programs, and that our platform lessens the dependence on facility-centric care for acute and post-acute services and shifts more services towards alternate sites and, most importantly, the home.
Value-based payment programs are rapidly transforming how governments, employers, and health plans pay for and manage healthcare services. The objective of these initiatives is to improve patient outcomes while lowering the overall cost of healthcare services. We believe that our differentiated data assets, proprietary analytics capabilities, comprehensive cloud-based software platforms, and healthcare provider networks enable success in the two dominant forms of value-based payments: population-based payment programs and episode-based payment programs. Medicare Advantage is one of the largest population-based payment initiatives and the Medicare Bundled Payment for Care Improvement (“BPCI”) initiative is one of the largest episode-based payment programs. We have leading positions serving both of these fast-growing sectors, as measured by our volume of IHEs and the program size of our episodes business, respectively.
Our solutions support value-based payment programs by aligning financial incentives around outcomes, providing tools to health plans and healthcare organizations designed to assess and manage risk and identify actionable opportunities for improved patient outcomes, coordination and cost-savings. Through our platform, we coordinate what we believe is a holistic suite of clinical, social, and behavioral services to address an individual’s healthcare needs and prevent adverse events that drive excess cost. Our business model is aligned with our customers as we generate revenue only when we successfully engage members for our health plan customers and generate savings for our provider customers.
1
Table of Contents
We serve 47 Medicare Advantage health plans ranging from the largest national organizations to smaller regional and provider-owned entities. We also serve thousands of healthcare provider organizations ranging from large integrated delivery systems to midsize and small urban and rural entities. We also serve large biopharmaceutical customers.
We believe we deliver a powerful value proposition to our health plan and provider customers and their members and patients by leveraging the following core assets:
| • | Insights to improve patient outcomes and lower costs. We build our software and services around the specific levers in each clinical episode that we believe have the most influence on patient outcomes and cost. This requires clinical expertise in disease progression and therapeutic interventions and the ability to identify factors that can be influenced during a patient’s episode of care. It also involves extensive data analytics to measure variations in treatment that can be influenced through more transparency and effective decision support. We believe this focus on critical levers has led to measurable outcomes, such as reductions in avoidable complications, reduced readmissions, reduced use of acute and post-acute facility services and increased delivery of services in the home, all of which benefit patients, while also lowering costs and generating savings for our health plan and healthcare provider customers. |
| • | Data analytics and reporting across the continuum. Our data analytics capabilities are focused on delivering decision support to all parties engaged in a value-based payment arrangement. Our platform analyzes data from a variety of sources that are designed to capture the patient’s condition not only from their visits to facility-based settings, but also from evaluations in the home and social services in their community. These sources include electronic health record (“EHR”) data in real time; claims and member data from private health plans, employers and the Centers for Medicare and Medicaid Services (“CMS”); care plan and case management data; data from comprehensive IHEs and device diagnostic data; laboratory and pharmacy data; and social determinants of health (“SDOH”) data. We use elements of this data to create longitudinal records of a patient’s health journey or to manage their care in an episode of care or other value-based payment arrangement, and to support our efforts to build decision support algorithms and predictive modeling tools. These data assets and decision support tools are designed to in turn help our providers efficiently and effectively deploy their resources and succeed in value-based payment programs. |
| • | National networks of healthcare providers. Our networks operate throughout the country, in both urban and rural locations, and encompass thousands of highly skilled medical professionals. We have three types of healthcare provider networks: |
| • | A flexible and mobile network of nearly 9,000 credentialed providers who are primarily deployed in an individual’s home and in post-acute facilities to collect critical patient data, assess an individual’s health status and coordinate care through our IHEs; |
| • | A nationwide network of hospitals and physicians that includes 3,500 value-based provider sites that are participating in payment programs run by the federal Medicare program, health plans, employers and other payors; and |
| • | A curated network of 200 community-based organizations (“CBOs”) and 200 clinical and social care coordinators that we connect to individuals and healthcare providers to meet individual member and patient needs. |
| • | Consumer engagement capabilities. Our proprietary, cloud-based technology platform, which was purpose-built for value-based payment programs, has a large array of engagement solutions intended to drive deeper and more meaningful engagement with the individuals we reach. We use advanced targeting and analytics, predictive models and our significant data assets to deploy a multi-modal approach to identifying and engaging individuals who may benefit from our services. We deploy email, |
2
Table of Contents
| SMS text messages, telephone outreach and digital-marketing campaigns to help us effectively engage individuals across the numerous value-based payment programs we support. |
| • | Innovative health benefit designs. We strive to drive transformation in how governments, health plans and employers pay for healthcare, and to facilitate healthcare organizations’ success under new programs that transfer risk and reward from health plans to providers. We work with governments, health plans and large employers to integrate episode-based program features into the health insurance plans they offer. We believe our ability to support numerous value-based payment arrangements and, importantly, to design and launch episode-based programs differentiates us in the market. For example, we recently successfully designed and launched new commercial episodes programs with a Northeastern state covering all state employees and retirees, as well as a large health insurer. We believe our ability to launch new, innovative programs will foster our long-term growth and impact on the healthcare system. |
| • | Workflow and logistics software. Our software tools are designed to improve the collection and accuracy of real-time patient information and to deliver effective decision support to health plans and healthcare providers. Our proprietary workflow software is used by our mobile network of providers to conduct comprehensive IHEs, as well as for the routing and logistics for such in-home visits; by hospitalists to guide discharge and referral decisions; by case managers to monitor patients and manage transitions of care; and by a wide variety of users to identify SDOH that may impact the achievement of optimal patient outcomes. |
We derive revenue from multiple sources. We receive administrative service fees and a share of savings generated in our episode-based payment programs, where we enter into at-risk contracts; health plans compensate us for conducting IHEs and virtual IHEs (“vIHEs”) and for helping launch and administer care coordination and episode-based payment programs; and health plans, health systems, government agencies and biopharmaceutical companies compensate us for delivering a variety of services, ranging from the management of post-acute care for accountable care organizations (“ACOs”), to managing SDOH, to complex care management and caregiver support services. Our relationships are grounded in long-term, multi-year contracts that we believe have the right incentives to align the performance of our services with the performance of our customers.
How we measure our progress
We operate our business in two segments: Home & Community Services, which focuses on reaching and engaging populations at home; and Episodes of Care Services, through which we manage episode-based payment programs. We provide our customers with measurable financial and patient outcome data to assess our performance. We believe that we are integral to how our health plan and provider customers manage value-based healthcare programs, making our success a material driver of the financial performance of our customers. We measure our success in the following ways:
| • | We measure our success in our Episodes of Care Services segment by how much medical spend we are responsible for managing; by the performance of the levers that drive clinical and financial success in episodes of care, including the amount of savings we help our providers generate; and by patient outcomes. |
| • | We measure success in our Home & Community Services segment by the number of health plans we serve and the number of health plan members we are able to reach, in their homes. We also measure our efficiency in reaching those health plan members in their homes. |
| • | We measure the success of our workflow software by its ability to identify when patients are likely to be attributed to an episode of care; by our ability to communicate decision support guidance to |
3
Table of Contents
| healthcare providers; by provider utilization of our decision support tools; and by how we ultimately perform on influencing a specific lever. We believe our focus on levers has led to measurable outcomes, such as reductions in avoidable complications, reduced readmissions, reduced use of acute and post-acute facility services and increased delivery of services in the home. |
Total U.S. healthcare spending exceeded $3.8 trillion in 2019 and we operate in the large market associated with payment for healthcare services. We serve needs of healthcare funding sources including Medicare, Medicaid, employers and private health plans. Signify Health operates in the value-based payment sector of the healthcare industry. We believe value-based payments have grown dramatically over the past ten years and are widely expected to eventually represent the majority of healthcare spending in the United States. According to recent studies, approximately 60% to 70% of total U.S. health spending is expected to be tied to quality and value by 2025 through the adoption of new payment models focused on value. We believe this will especially be the case as value-based payment models continue to penetrate the commercial insured and self-funded markets.
We believe we have demonstrated the ability to rapidly scale our customer base and operations and grow our business in our principal markets in large part due to the attractiveness of our services and our competitive scale in the market. We now serve 26 of the top 50 Medicare Advantage plans. We have increased the number of annual IHEs conducted from approximately 390,000 in 2015 to nearly 1.1 million in 2019, representing a compound annual growth rate of 28.9%. As the largest convener participant in BPCI-A by number of episodes managed and over 6 years of participating in BPCI-A and its predecessor BPCI, we also enjoy a leading position in the episodes of care industry and have continuously grown our networks of contracted at-risk provider organizations. We have increased the number of episodes of care we have managed from approximately 24,000 episodes under BPCI in 2014 to approximately 215,000 episodes under BPCI-A in 2019 based on our current estimates.
We believe our financial model is attractive with highly recurring revenues, strong EBITDA margins and high cash flow conversion. For the year ended December 31, 2019, our total revenue was $501.8 million, representing a 48.5% increase from $337.9 million in 2018, we incurred a net loss of $28.5 million, representing a 1.2% decrease from a net loss of $28.9 million in 2018, our Adjusted EBITDA was $93.3 million, representing an 18.0% increase from $79.1 million in 2018 and our Adjusted EBITDA Margin was 18.6%, a 4.8% decrease from 23.4% in 2018. For the nine months ended September 30, 2020, our total revenue was $417.1 million, representing a 13.2% increase from $368.5 million in the nine months ended September 30, 2019, we incurred a net loss of $15.2 million, representing a 25.8% decrease from a net loss of $20.5 million in the nine months ended September 30, 2019, our Adjusted EBITDA was $86.0 million, representing a 28.8% increase from $66.7 million in the nine months ended September 30, 2019 and our Adjusted EBITDA Margin was 20.6%, a 2.5% increase from 18.1% in the nine months ended September 30, 2019.
Our competitive strengths
| • | Scaled Episode-Based Payment Program. We are the largest convener participant in BPCI-A by number of episodes managed, with $6.1 billion of spend under management in 2019. We believe our leadership position in the BPCI-A program has allowed us to invest in and develop differentiated scale around networks, analytics, technology and relationships to grow rapidly as demand for services in the value-based payment industry increases over time. As a result of both the success and visibility of the BPCI-A program, commercial health plans, governments and employers are beginning to explore similar bundled arrangements. As a scaled leader in the industry, we believe we are a compelling partner to support these initiatives and believe we will benefit from a network effect as health plans and providers look to further capitalize on the benefits of value-based care. |
| • | Nationwide Home and Community-Based, Technology-Enabled Services Infrastructure. Signify Health is a leading provider of IHE services to third-party Medicare Advantage plans, as measured by our |
4
Table of Contents
| volume of IHEs. We have a network of nearly 9,000 credentialed providers that we deploy in the home, enabling patient evaluations, the delivery of a growing range of in-home services and care coordination. While in the home, our providers perform IHEs with the assistance of longitudinal patient records and our proprietary clinical workflow software with an integrated device hub. Our device hub captures important diagnostic patient data from interconnected devices that we use to conduct retinal exams to detect retinopathy, hemoglobin A1c tests for diabetes and microalbumin diptests to screen for chronic kidney disease, among other diagnostic services, all of which further extend our ability to deliver services in the home. The geographic density of our customers and the breadth of our mobile provider network allows us to cost-effectively reach patients in the home throughout the country, in both urban and rural locations. Combined with our community-based networks and platform applications, we work to bridge social needs identified in the home with solutions from the surrounding community. Our reach into the home, combined with our episode-specific focus, positions us to drive adoption of a wide range of emerging in-home monitoring and treatment modalities. |
| • | Access to the Home and Holistic Care Model. We believe patients achieve optimal health outcomes when all clinical and social factors influencing their health and recovery from specific events are addressed. We rely, therefore, on a holistic model of care in how we operate all our programs. We seek to assess every person in our programs on measures of physical health as well as SDOH. Our ability to capture clinical and social determinant data is complemented by our networks of providers and CBOs. We believe this enables our programs to have meaningful impact on the health and well-being of the individuals and families our programs touch. |
| • | Trusted Healthcare Brand. We believe we are a trusted healthcare platform in the health plan, provider and employer markets that adds value by leveraging advanced analytics, technology and national provider networks to create and power value-based payment programs in our two primary segments: Home & Community Services and Episodes of Care Services. In our Home & Community Services |
| segment, our IHEs have been shown to improve patient satisfaction among health plan members. In our Episodes of Care Services segment, our scale and success in the BPCI program encourages our provider customers to increase the volume and variety of bundles they participate in because of confidence in our ability to manage post-acute episodes. We have repeatedly leveraged our experience and leadership in these value-based payment programs to cross-sell and up-sell services across our two segments and deepen our relationships with customers. |
| • | Purpose-built Technology, Data and Analytics Platform. We provide our health plan and health system customers with a comprehensive suite of software, analytics, and services that fit with both population-based and episode-based models of value-based payments. As of September 30, 2020, our data chassis included data on approximately 35 million members. Both of our segments are supported by an advanced analytics team that is responsible for building decision support algorithms and predictive modeling, as well as for comprehensive monitoring and reporting, both internally and externally to our customers. |
| • | Established and Long-Standing Customer Relationships. We enjoy long-standing relationships and a history of collaborative innovation with many of our customers. Our top health plan customers that made up over 90% of our revenue in our Home & Community Services segment in 2019 have been with us for more than five years and we have had a strong presence in the BPCI program since its inception in 2013. We believe our wide footprint of customers, many of whom have long-term, multi-year contracts with us, allows us to better understand market needs and continue innovating in how we serve health plans, health systems and physician groups, as well as individuals in their homes. For example, in our Home & Community Services segment, we developed our IHE+ solution in collaboration with a large health insurer in Pennsylvania and have subsequently incorporated that into our broader offerings to all clients. We also worked with some of our large health plans to extend our IHE offering to serve their Medicaid populations. Similarly, in our Episodes of Care Services segment, |
5
Table of Contents
| we partnered with a large hospital system in Chicago to develop a transition of care program to support patients’ transition out of an acute setting and into a post-acute or home setting, which ultimately formed the basis of our Transition to Home (“TTH”) program. We believe our history of collaborative innovation uniquely positions us to capture additional opportunities as many organizations in the healthcare industry are vertically integrating, with health plans acquiring provider capabilities and vice versa. Signify Health partners with customers to provide more comprehensive services to help them succeed across the continuum of care. |
| • | Deeply Experienced Management Team and Mission-Driven Culture. Our management team has deep expertise in scaling technology-enabled services infrastructure, in servicing health plans, in provider contracting and in designing innovative products. We believe our deep base of knowledge in how healthcare is organized, financed and delivered enables us to tailor our software and service offerings to address highly specialized and complex challenges facing both the organizations that pay for healthcare and the organizations responsible for delivering that care. |
Our growth strategy
| • | Expand our in-home service offerings. We believe healthcare delivery will continue to move away from institutional settings and towards in-home services in the coming years. We believe we are positioned to capture a significant share of this fundamental trend towards home-based care delivery. We are able to deliver an expansive range of in-home services through our national scale, longitudinal patient records with an integrated device hub and access to patients. In response to the COVID-19 pandemic, we rapidly launched and scaled our vIHEs, a telehealth version of our in-home IHEs. Additionally, in 2020, we expanded our service offerings to include an “IHE+” in our Home & Community Services segment, through which our providers gather SDOH data while performing an IHE, our ACO service, which manages post-acute care for ACO patients, in our Episodes of Care Services segment and our TTH service, a support model for patients transitioning home from a hospital or a post-acute care facility that aims to reduce the likelihood of readmission, also in our Episodes of Care Services segment. Finally, we are rapidly expanding our remote patient monitoring and device connectivity capabilities via our device hub, which is integrated with several diagnostic devices we deploy in our service model. Our breadth of access and ability to rapidly deploy new technologies and services is helping to make the home an increasingly viable setting of care to manage a broadening population of patients. |
| • | Expand our episode of care programs. We intend to expand our Episodes of Care business by growing existing programs and launching new ones. Currently, we generate the majority of our revenue in our Episode of Care Services segment through the BPCI-A program. Participation in the BPCI-A program was locked in place at the end of 2020 through the end of the program in 2023, meaning that new healthcare providers will not be able to enter the program and participating providers will not be able to choose to participate in any additional episode types, which will impact our ability to increase the number of episodes managed or program size during this time. We intend, however, to continue growing our BPCI-A business by growing savings achieved under the program. We will also seek to capture new opportunities related to the June 2020 announcements from CMS of their intention to move to a more expansive and mandatory bundled payment program at the end of 2023. In addition, we are actively launching programs outside of the BPCI-A context with large employers and health plans to integrate new, innovative episode-based payment programs into their health plans and value-based payment programs. These new programs will aim to anchor our long-term growth, as we leverage our relationships with payors to build networks of providers under episode-based payment contracts. Our goal is to continuously increase the spend under management of these episode programs. |
| • | Expand our networks. We will continue to recruit more providers and CBOs into our Home & Community Services network. We will also continue to recruit health systems, physician groups and |
6
Table of Contents
| other provider organizations into our episode of care programs. By increasing the reach of our provider network, we have expanded the number of annual IHEs conducted from approximately 390,000 in 2015 to nearly 1.1 million in 2019. In addition, by expanding our network of hospital and physician organizations participating in our episodes business, we have increased the number of episodes of care we have managed from approximately 24,000 episodes under BPCI in 2014 to approximately 215,000 episodes under BPCI-A in 2019 based on our current estimates. |
| • | Grow our customer base and leverage our network effect. We have large addressable markets for our product and service offerings. Adding additional payor customers for our Episodes business within a given geography makes more providers eligible to participate in various episode types. Providers must exceed minimum episode volume requirements to be eligible for such episodes, and we are able to aggregate their episode volume across programs. We believe that greater episode participation drives increased commitment to care redesign among our provider partners and, in turn, increases our ability to manage post-acute care, as the increased patient volume increases program engagement among post-acute providers and results in the realization of additional savings. In addition, as our IHE customer base grows, the geographic density of our customers’ collective membership increases, which improves the efficiency and capacity of our mobile providers. This allows us to lower our cost of services to drive customer value, which we believe provides a key competitive advantage. As we continue to increase our scale, we believe this will both enhance our ability to attract new customers and incentivize existing customers to concentrate their business with us. |
| • | Improve our software and analytics capabilities. Our large existing base of customers provides feedback to our teams responsible for building software, analytics and decision support tools. We will seek to leverage this feedback and our customer relationships to continuously enhance the features and functionality of our software and service offerings; doing so is key to our ability to leverage our leadership position in the markets we serve. |
| • | Capitalize on our visible, recurring and capital efficient financial model. While the value-based initiatives that our customers undertake incorporate elements of upside and downside risk, our revenue model has historically been visible and recurring. Our insight into future demand for our services allows us to scale our operations in a manner we believe is in line with future demand, aiming to reduce waste and keep our investments efficient. |
| • | Selectively pursue acquisitions and partnerships. In recent years, we have expanded our product offerings in part through acquisitions, including Remedy Partners and TAV Health. We intend to complement our strong organic growth opportunities by evaluating the acquisition of complementary products and services. We will continue to selectively pursue strategic and complementary assets to support our clients’ needs. |
Impact of COVID-19 on our operations
Since mid-March 2020, our operations have been significantly affected by the COVID-19 pandemic. In our Home & Community Services segment, we temporarily halted IHEs as a precautionary measure in response to the pandemic beginning in March 2020. We resumed in-home visits beginning in July 2020. In response to the pandemic, we leveraged our technology capabilities to quickly pivot to offering vIHEs, a virtual version of our IHEs, beginning in April 2020. As a result, we were able to make up for the lost volume for IHEs through vIHEs and were able to perform approximately 380,000 vIHEs and over 560,000 in-person IHEs, or a total of approximately 940,000 IHEs, in the first nine months of 2020. By comparison, we performed approximately 835,000 IHEs in the first nine months of 2019.
As a result of the pandemic, many of our customers pushed in-person IHEs into the second half of 2020. Although we have seen some increase in IHE member cancellation rates in part as a result of the pandemic, overall we saw significant incremental IHE volumes in the second half of 2020 as certain customers increased
7
Table of Contents
the volumes they placed with us and in-home IHEs have represented the majority of those IHEs. In order to meet this volume growth, we have onboarded additional providers into our network, which has resulted in proportionally higher expenses.
In our Episodes of Care Services segment, various policies recommended and/or implemented by governmental authorities in response to the pandemic resulted in fewer elective procedures and a general reduction in individuals seeking medical care, which contributed to a substantially lower number of episodes managed in 2020. CMS also announced measures to address the impact COVID-19 would have otherwise had on the BPCI-A program, including allowing healthcare providers to exclude from reconciliation those episodes with a COVID-19 diagnosis or to exclude all episodes from reconciliation in 2020. These pandemic-related changes will reduce the number of episodes of care managed in 2020 and part of 2021. Subsequently, CMS announced that all episodes in 2021 with a COVID-19 diagnosis would be automatically excluded from reconciliation, and as a result, we expect a reduction in our overall program size in 2021 as well for as long as the COVID-19 pandemic is ongoing. Because our administrative fee is calculated as a percentage of program size and we receive a portion of the savings achieved in management of an episode, the decrease in episodes and related reduction in overall program size have had, and we expect will continue to have, a negative effect on our revenue. Some of these measures and challenges will likely continue for the duration of the COVID-19 pandemic, which is uncertain, and will harm the results of operations, liquidity and financial condition of our provider partners and our business. Lastly, our representatives may be prohibited from entering hospitals, skilled nursing facilities and other post-acute facilities as a result of the pandemic, which affects our ability to facilitate coordination among provider partners and could have a material impact on our savings rate.
The severity, magnitude and duration of the current COVID-19 pandemic is uncertain and rapidly changing. See “Risk Factors—Our operations have been, and may continue to be, significantly disrupted by the COVID-19 pandemic, and our business, financial condition and results of operations have been negatively impacted” and “Management’s discussion and analysis of financial condition and results of operations—Factors affecting our results of operations—COVID-19.”
Recent developments
Credit Agreement Amendments
On November 17, 2020 and December 7, 2020, we entered into amendments to the Credit Agreement (as defined herein) to incur additional indebtedness in the form of a new tranche of term loans in aggregate principal amounts of $125.0 million and $15.0 million, respectively. See “Management’s discussion and analysis of financial condition and results of operations—Liquidity and capital resources—Indebtedness.”
Preliminary Estimated Unaudited Financial Results for the Fiscal Year Ended December 31, 2020
The data presented below reflects our preliminary estimated unaudited financial results for the fiscal year ended December 31, 2020 (“Fiscal 2020”) based upon information available to us as of the date of this prospectus. This data is not a comprehensive statement of our financial results for Fiscal 2020, and our actual results may differ materially from this preliminary estimated data. The audit of our Fiscal 2020 financial statements has not been completed. During the course of the preparation of our financial statements and related notes and the completion of the audit for Fiscal 2020, additional adjustments to the preliminary estimated financial information presented below may be identified. Any such adjustments may be material. Our independent registered public accounting firm, Deloitte & Touche LLP, has not audited, reviewed, compiled or performed any procedures with respect to this preliminary financial data and, accordingly, Deloitte & Touche LLP does not express an opinion or any other form of assurance with respect thereto.
8
Table of Contents
Based upon such preliminary estimated financial results, we expect various key metrics for Fiscal 2020 to be between the ranges set out in the following table, as compared to Fiscal 2019:
| Year ended December 31, 2020 |
Year ended | |||||||||||
| Low | High | December 31, 2019 |
||||||||||
| (in millions, except percentages) | ||||||||||||
| Revenue |
$ | 600.0 | $ | 610.0 | $ | 501.8 | ||||||
| Home & Community Services |
444.0 | 450.0 | 377.0 | |||||||||
| Episodes of Care Services |
156.0 | 160.0 | 124.8 | |||||||||
| Net loss |
(17.0 | ) | (24.0 | ) | (28.5 | ) | ||||||
| Adjusted EBITDA(1) |
119.0 | 123.0 | 93.3 | |||||||||
| IHE Volume(2) |
1.4 | 1.4 | 1.1 | |||||||||
| Weighted Average Program Size(3) |
5,000.0 | 5,200.0 | 6,144.1 | |||||||||
| Weighted Average Savings Rate(4) |
7.0 | % | 7.3 | % | 5.3 | % | ||||||
| (1) | Adjusted EBITDA is a non-GAAP financial measure. We define Adjusted EBITDA as net income (loss) before interest expense, income tax expense, depreciation and amortization and certain items of income and expense, including asset impairment, other (income) expense, net, transaction-related expenses, equity-based compensation, remeasurement of contingent consideration, management fees and non-recurring expenses. We believe that Adjusted EBITDA provides a useful measure to investors to assess our operating performance because it eliminates the impact of expenses that do not relate to ongoing business performance, and that the presentation of this measure enhances an investor’s understanding of the performance of our business. |
The following table shows a reconciliation of net loss to Adjusted EBITDA for the periods presented:
| Year ended December 31, 2020 |
Year ended | |||||||||||
| Low | High | December 31, 2019 |
||||||||||
| (in millions) | ||||||||||||
| Net loss |
$ | (17.0 | ) | (24.0 | ) | $ | (28.5 | ) | ||||
| Interest expense |
22.0 | 23.0 | 21.2 | |||||||||
| Income tax expense |
0.5 | 1.0 | 0.1 | |||||||||
| Depreciation and amortization |
62.0 | 63.0 | 66.0 | |||||||||
| Asset impairment(a) |
0.5 | 1.0 | 6.4 | |||||||||
| Other (income) expense, net(b) |
8.0 | 10.0 | (1.6 | ) | ||||||||
| Transaction-related expenses(c) |
16.0 | 17.0 | 22.4 | |||||||||
| Equity-based compensation(d) |
12.0 | 13.0 | 4.5 | |||||||||
| Customer equity appreciation rights(e) |
12.0 | 13.0 | — | |||||||||
| Remeasurement of contingent consideration(f) |
— | 1.0 | 0.7 | |||||||||
| Management fees(g) |
— | — | 1.0 | |||||||||
| Non-recurring expenses(h) |
3.0 | 5.0 | 1.1 | |||||||||
|
|
|
|
|
|
|
|||||||
| Adjusted EBITDA |
$ | 119.0 | $ | 123.0 | $ | 93.3 | ||||||
| (a) | Asset impairment during the year ended December 31, 2019 was primarily related to the discontinued use of certain trade names following the Remedy Partners Acquisition (as defined below), which resulted in a $4.9 million asset impairment. Additionally, we discontinued the use of certain software resulting in an asset impairment of $1.5 million during the nine months ended September 30, 2019 and year ended December 31, 2019. Asset impairment in 2018 was primarily related to the discontinued use |
9
Table of Contents
| of certain trade names following the rebranding of the Company, which resulted in a $16.0 million asset impairment. Additionally, certain property and equipment was impaired for a total of $1.0 million in 2018. |
| (b) | Represents other non-operating (income) expense that consists primarily of the quarterly remeasurement of fair value of the outstanding customer equity appreciation rights (“EARs”), as well as interest and dividends earned on cash and cash equivalents. |
| (c) | Represents transaction-related expenses that consist primarily of expenses incurred in connection with acquisitions and other corporate development activities, such as mergers and acquisitions activity that did not proceed, strategic investments and similar activities. Expenses incurred in connection with this initial public offering, which cannot be netted against proceeds, are also included in transaction-related expenses. |
| (d) | Represents expense related to equity incentive awards, including profit interest units and stock options, granted to certain employees, officers and non-employee directors as long-term incentive compensation. We recognize the related expense for these awards ratably over the vesting period or as achievement of performance criteria become probable. |
| (e) | Represents the reduction of revenue related to the grant date fair value of the customer EARs granted pursuant to the customer EAR agreements we entered into in December 2019 (the “December 2019 EAR”) and September 2020 (the “September 2020 EAR”). See “Management’s discussion and analysis of financial condition and results of operations—Liquidity and capital resources—Customer Equity Appreciation Rights agreements.” |
| (f) | Represents the remeasurement of contingent consideration due to the selling shareholders of Censeo Health, a business acquired in 2017, pending the resolution of an Internal Revenue Service (“IRS”) tax matter. The matter was resolved in 2020. |
| (g) | Represents the annual advisory fee paid to New Mountain Capital under the Management Services Agreement. The Management Services Agreement was terminated in January 2019 in connection with the consummation of the Remedy Partners Acquisition. |
| (h) | Represents certain gains and expenses incurred that are not expected to recur, including those associated with the closure of certain facilities, the sale of certain assets and the early termination of certain contracts. |
| (2) | IHE Volume represents the total number of IHEs, including both in-home IHEs and vIHEs, completed and invoiced to customers during the period. We did not conduct any vIHEs in 2019. |
| (3) | Weighted Average Program Size represents the weighted average program size for performance obligation periods included in a calendar quarter or calendar year. We manage episodes in six-month blocks, which we refer to as performance measurement periods. Each performance measurement period, we reconcile those episodes of care that concluded during such performance measurement period. We recognize the revenue attributable to episodes reconciled during each six-month performance measurement period over a 13-month performance obligation period, which we refer to as performance obligation periods. Accordingly, our weighted average program size during a given calendar quarter or calendar year reflects the results of multiple overlapping performance obligation periods. We define program size for a performance obligation period as (x) the number of episodes we managed during the relevant performance measurement period multiplied by (y) the baseline price of each episode, which represents the benchmark price set by the relevant program prior to any discounts. We define weighted average program size as the sum of the following for each performance obligation period included in a calendar quarter or calendar year: (x) the program size for the relevant performance obligation period, (y) divided by 13, which represents the approximately 13-month performance obligation period required to complete performance obligations under our episodes programs, and (z) multiplied by the number of months of the relevant performance obligation period included in the calendar quarter or calendar year. For 2019, this does not include amounts related to the BPCI program, as these are not comparable to the current BPCI-A program and are not indicative of future performance. |
10
Table of Contents
| (4) | Weighted Average Savings Rate represents the weighted average savings rate generated during performance obligation periods included in a calendar quarter or calendar year. The gross savings for each performance obligation period (i.e., the 13-month period over which we recognize revenue attributable to episodes that concluded during a six-month performance measurement period) is equal to the gross amount of savings generated under the episode programs we manage during the performance measurement period to which such performance obligation period relates. The gross savings for a performance measurement period is defined as (x) the sum of the baseline episode prices of each such episode less (y) the total actual cost of each episode that concluded during such performance measurement period, which baseline prices represent the benchmark price set by the relevant program prior to any discounts. The weighted average savings rate is (i) the sum, for each performance obligation period included in a calendar quarter or calendar year, of (A) the gross savings for each such performance obligation period, divided by (B) 13, and multiplied by (C) the number of months of such performance obligation period included in such calendar quarter or calendar year, divided by (ii) the weighted average program size for such calendar quarter or calendar year. For the above purposes, the gross amount of savings is calculated prior to the deduction of our administrative fees and amounts shared with health plans and provider partners. For example, for BPCI-A, CMS receives a 3% discount, which is included in the gross amount of savings calculated for each performance measurement period. For 2019, the weighted average savings rate does not include amounts related to the predecessor BPCI program, as these are not comparable to the current BPCI-A program and are not indicative of future performance. |
Organizational structure
We currently conduct our business through Cure TopCo, LLC and its subsidiaries. Following this offering, Signify Health, Inc. will be a holding company and its sole material asset will be an ownership interest in Cure TopCo, LLC.
Prior to the consummation of the Reorganization Transactions (as defined below), the amended and restated limited liability company agreement of Cure TopCo, LLC will be amended and restated to, among other things, convert all outstanding equity interests into one class of non-voting common units (the “LLC Units”) and appoint Signify Health, Inc. as the sole managing member of Cure TopCo, LLC. We refer to the limited liability company agreement of Cure TopCo, LLC, as in effect at the time of this offering, as the “Amended LLC Agreement.” After these transactions and prior to the consummation of the Reorganization Transactions and the completion of this offering, all of Cure TopCo, LLC’s outstanding equity interests will be owned by the following persons (collectively, the “Pre-IPO LLC Members”):
| • | Affiliates of New Mountain Capital and certain other minority equityholders, indirectly through certain entities treated as corporations for U.S. tax purposes; |
| • | New Mountain Partners V (AIV-C), LP; |
| • | Cure Aggregator, LLC; and |
| • | Certain other equity holders in Cure TopCo, LLC (the “Other Legacy Signify Holders”). |
In connection with this offering, we intend to enter into the following series of transactions to implement an internal reorganization, which we collectively refer to as the “Reorganization Transactions.” We refer to the Pre-IPO LLC Members who will retain their equity ownership in Cure TopCo, LLC in the form of LLC Units immediately following the consummation of the Reorganization Transactions as “Continuing Pre-IPO LLC Members.”
| • | Our amended and restated certificate of incorporation that will be in effect upon the completion of this offering will authorize the issuance of two classes of common stock: Class A common stock and |
11
Table of Contents
| Class B common stock (collectively, our “common stock”). Each share of common stock will entitle its holder to one vote per share on all matters submitted to a vote of our stockholders. The Class B common stock is not entitled to economic interests in Signify Health, Inc. See “Description of capital stock.” |
| • | Prior to the completion of this offering, we will acquire, directly and indirectly, LLC Units through (i) the contribution of LLC Units in exchange for Class A common stock by New Mountain Partners V (AIV-C), LP (the “IPO Contribution”) and (ii) the “Mergers,” in which certain entities treated as corporations for U.S. tax purposes that hold LLC Units (individually, a “Blocker Company” and together, the “Blocker Companies”), will each simultaneously merge with a merger subsidiary created by us (and survive such merger as a wholly owned subsidiary of Signify Health, Inc.), after which each Blocker Company will immediately merge into Signify Health, Inc. (with each such merger into Signify Health, Inc. occurring simultaneously). The shareholders of the Blocker Companies (the “Reorganization Parties”), including affiliates of New Mountain Capital, will collectively hold 141,592,313 shares of Class A common stock of Signify Health, Inc. after the IPO Contribution and the Mergers. The Reorganization Parties will collectively receive a number of shares of our Class A common stock in the Mergers equal to the number of LLC Units held by the Blocker Companies prior to the Mergers, and will not directly hold interests in Cure TopCo, LLC. |
| • | Each Continuing Pre-IPO LLC Member will be issued a number of shares of our Class B common stock equal to the number of LLC Units held by such Continuing Pre-IPO LLC Member, except in the case of Cure Aggregator, LLC. Cure Aggregator, LLC is a special purpose investment vehicle through which certain members of Cure TopCo, LLC, primarily our employees and certain legacy investors, indirectly hold interests in Cure TopCo, LLC. Cure Aggregator, LLC holds LLC Units on behalf of such members on a one-for-one basis with each member’s interests in Cure Aggregator, LLC. Such common units in Cure Aggregator, LLC are subject to vesting as set forth under “Executive and Director Compensation—Other compensation plans—Incentive Units”. In connection with the Reorganization Transactions, shares of Class B common stock will be issued to the direct holders of common units in Cure Aggregator, LLC in proportion to their interests in Cure Aggregator, LLC, provided that such shares will not be entitled to any voting rights until such time as the common units of Cure Aggregator, LLC corresponding to such shares have vested. |
| • | Cure TopCo, LLC will enter into the Amended LLC Agreement. Under the Amended LLC Agreement, holders of LLC Units, including the Continuing Pre-IPO LLC Members, will have the right, from and after the completion of this offering (subject to the terms of the Amended LLC Agreement), to require Cure TopCo, LLC to redeem all or a portion of their LLC Units for, at our election, newly issued shares of Class A common stock on a one-for-one basis or a cash payment equal to the volume-weighted average market price of one share of our Class A common stock for each LLC Unit redeemed (subject to customary adjustments, including for stock splits, stock dividends and reclassifications) in accordance with the terms of the Amended LLC Agreement. Additionally, in the event of a redemption request from a holder of LLC Units, we may, at our option, effect a direct exchange of cash or Class A common stock for LLC Units in lieu of such a redemption. Shares of Class B common stock will be cancelled on a one-for-one basis if we, following a redemption request from a holder of LLC Units, redeem or exchange LLC Units of such holder pursuant to the terms of the Amended LLC Agreement. See “Certain relationships and related party transactions—Amended LLC Agreement.” Except for transfers to us or to certain permitted transferees pursuant to the Amended LLC Agreement, the LLC Units and corresponding shares of Class B common stock may not be sold, transferred or otherwise disposed of. |
| • | We will use all of the net proceeds from this offering (including net proceeds received if the underwriters exercise their option to purchase additional shares of Class A common stock in full) to acquire newly issued LLC Units from Cure TopCo, LLC at a purchase price per LLC Unit equal to the |
12
Table of Contents
| initial public offering price of Class A common stock, after deducting the underwriting discounts and commissions, collectively representing 10.6% of Cure TopCo, LLC’s outstanding LLC Units (or 12.0%, if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
| • | We will enter into a Tax Receivable Agreement that will obligate us to make payments to the Continuing Pre-IPO LLC Members, the Reorganization Parties, Optionholders (as defined in the Tax Receivable Agreement) of the Blocker Companies at the time of the Mergers, holders of synthetic equity units and any future party to the Tax Receivable Agreement (collectively, the “TRA Parties”) in the aggregate generally equal to 85% of the applicable cash savings that we actually realize as a result of (i) certain favorable tax attributes we will acquire from the Blocker Companies in the Mergers (including net operating losses, the Blocker Companies’ allocable share of existing tax basis and refunds of Blocker Company taxes attributable to pre-Merger tax periods), (ii) increases in our allocable share of existing tax basis and tax basis adjustments that may result from (x) future redemptions or exchanges of LLC Units by Continuing Pre-IPO LLC Members for cash or Class A common stock, (y) the IPO Contribution and (z) certain payments made under the Tax Receivable Agreement and (iii) deductions in respect of interest and certain compensatory payments made under the Tax Receivable Agreement. We will retain the benefit of the remaining 15% of these tax savings. |
| • | We will cause Cure TopCo, LLC to use the proceeds from the issuance of LLC Units to us (i) to pay fees and expenses of approximately $13.5 million in connection with this offering and the Reorganization Transactions and (ii) for general corporate purposes, including working capital and potential strategic acquisitions of, or investments in, other businesses or technologies that we believe will complement our current business and expansion strategies. See “Use of proceeds.” |
We will issue 23,500,000 shares of Class A common stock pursuant to this offering.
Because we will manage and operate the business and control the strategic decisions and day-to-day operations of Cure TopCo, LLC and because we will also have a substantial financial interest in Cure TopCo, LLC, we will consolidate the financial results of Cure TopCo, LLC, and a portion of our net income will be allocated to the noncontrolling interest to reflect the entitlement of the Continuing Pre-IPO LLC Members to a portion of Cure TopCo, LLC’s net income. In addition, because Cure TopCo, LLC will be under the common control of the Pre-IPO LLC Members before and after the Reorganization Transactions (both directly and indirectly through their ownership of us), we will account for the Reorganization Transactions as a reorganization of entities under common control and will initially measure the interests of the Continuing Pre-IPO LLC Members in the assets and liabilities of Cure TopCo, LLC at their carrying amounts as of the date of the completion of the consummation of the Reorganization Transactions.
The following diagram depicts our organizational structure immediately following the consummation of the Reorganization Transactions, the completion of this offering and the application of the net proceeds from this offering, based on an assumed initial public offering price of $20.50 per share of Class A common stock (the midpoint of the estimated price range set forth on the cover page of this prospectus) and assuming the
13
Table of Contents
underwriters do not exercise their option to purchase additional shares of Class A common stock. This chart is provided for illustrative purposes only and does not purport to represent all legal entities within our organizational structure.
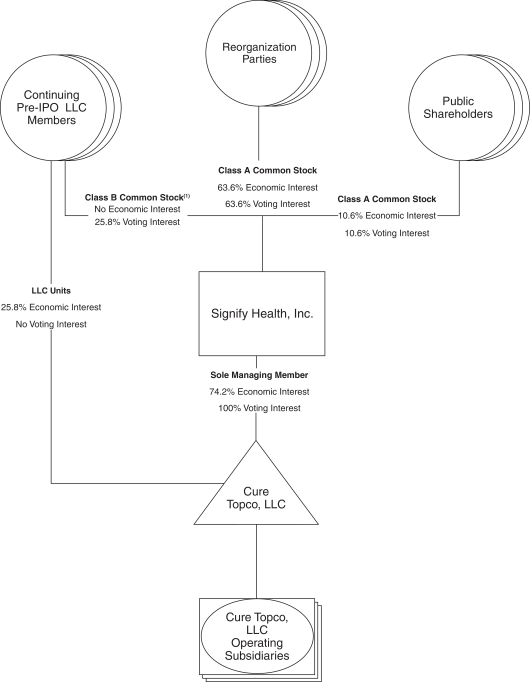
| (1) | Includes Class B common stock held directly by directors and officers who hold their interests in Cure TopCo, LLC indirectly through vested common units of Cure Aggregator, LLC. |
14
Table of Contents
Our corporate structure following the completion of this offering, as described above, is commonly referred to as an “Up-C” structure, which is commonly used by partnerships and limited liability companies when they undertake an initial public offering of their business. Our Up-C structure will allow the Continuing Pre-IPO LLC Members to continue to realize tax benefits associated with owning interests in an entity that is treated as a partnership, or “pass-through” entity, for income tax purposes following this offering. One of these benefits is that future taxable income of Cure TopCo, LLC that is allocated to such owners will be taxed on a flow-through basis and, therefore, will not be subject to corporate taxes at the entity level. Additionally, because the LLC Units that the Continuing Pre-IPO LLC Members will hold are redeemable for, at our election, either newly issued shares of Class A common stock on a one-for-one basis or a cash payment in accordance with the terms of the Amended LLC Agreement, our Up-C structure also provides the Continuing Pre-IPO LLC Members with potential liquidity that holders of nonpublicly traded limited liability companies are not typically afforded. See “Organizational structure” and “Description of capital stock.”
We will also hold LLC Units, and therefore receive the same benefits as the Continuing Pre-IPO LLC Members with respect to our ownership in an entity treated as a partnership, or “pass-through” entity, for income tax purposes. The acquisition of LLC Units from the Continuing Pre-IPO LLC Members in connection with this offering, future taxable redemptions or exchanges by the Continuing Pre-IPO LLC Members for shares of our Class A common stock or cash, the Mergers and other transactions described herein are expected to result in favorable tax attributes that will be allocated to us. These tax attributes would not be available to us in the absence of those transactions and are expected to reduce the amount of tax that we would otherwise be required to pay in the future. In connection with the Reorganization Transactions, we will enter into a Tax Receivable Agreement that will obligate us to make payments to the TRA Parties in the aggregate generally equal to 85% of the applicable cash savings that we actually realize as a result of these tax attributes and tax attributes resulting from certain payments made under the Tax Receivable Agreement. We will retain the benefit of the remaining 15% of these tax savings. See “Organizational structure—Holding company structure and the Tax Receivable Agreement.”
Under the Amended LLC Agreement, we will receive a pro rata share of any distributions, including tax distributions, made by Cure TopCo, LLC to its members. Such tax distributions will be calculated based upon an assumed tax rate, which, under certain circumstances, may cause Cure TopCo, LLC to make tax distributions that, in the aggregate, exceed the amount of taxes that Cure TopCo, LLC would have paid if it were a similarly situated corporate taxpayer. Funds used by Cure TopCo, LLC to satisfy its tax distribution obligations will not be available for reinvestment in our business. See “Risk factors—Risks related to our organizational structure.”
Upon completion of the transactions described above, this offering and the application of the Company’s net proceeds from this offering:
| • | Signify Health, Inc. will be appointed as the managing member of Cure TopCo, LLC and will hold 165,092,313 LLC Units, constituting 74.2% of the outstanding economic interests in Cure TopCo, LLC (or 168,617,313 LLC Units, constituting 74.6% of the outstanding economic interests in Cure TopCo, LLC if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
| • | The Pre-IPO LLC Members will collectively hold (i) (x) 141,592,313 shares of Class A common stock and (y) 57,264,580 LLC Units, which together directly and indirectly represent approximately 89.4% of the economic interest in Cure TopCo, LLC (or 88.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full) and (ii) through their collective ownership of 141,592,313 shares of Class A and 57,264,580 shares of Class B common stock, approximately 89.4% of the combined voting power of our common stock (or 88.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
15
Table of Contents
| • | Investors in this offering will collectively hold (i) 23,500,000 shares of our Class A common stock, representing approximately 10.6% of the combined voting power of our common stock (or 27,025,000 shares and 12.0%, respectively, if the underwriters exercise their option to purchase additional shares of Class A common stock in full) and (ii) through our direct and indirect ownership of LLC Units, indirectly will hold approximately 10.6% of the economic interest in Cure TopCo, LLC (or 12.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
Funds affiliated with New Mountain Capital, including the Reorganization Parties through their holdings of our Class A common stock and certain Continuing Pre-IPO LLC Members through their holdings of LLC Units and our Class B common stock, will collectively own 63.1% of the economic interest in Cure TopCo, LLC (or 62.1% if the underwriters exercise their option to purchase additional shares of Class A common stock in full), as well as an equal percentage of the voting power in Signify Health, Inc.
See “Organizational structure,” “Certain relationships and related party transactions” and “Description of capital stock” for more information on the rights associated with our common stock and the LLC Units.
Risk factors
An investment in shares of our Class A common stock involves substantial risks and uncertainties that may adversely affect our business, financial condition and results of operations and cash flows. Some of the more significant challenges and risks relating to an investment in our Class A common stock include those associated with the following:
| • | our operations have been, and may continue to be, significantly disrupted by the COVID-19 pandemic, and our business, financial condition and results of operations have been negatively impacted; |
| • | our revenues and operations are dependent upon a limited number of key customers; |
| • | a large portion of our revenues are substantially dependent on certain key government programs, primarily BPCI-A; |
| • | we have a history of net losses, we anticipate increasing expenses in the future, and we may not be able to achieve or maintain profitability; |
| • | our future revenues may not grow at the rates they historically have, or at all; |
| • | we may be unable to successfully execute on our growth initiatives, business strategies, or operating plans; |
| • | if we are unable to effectively adapt to changes in the healthcare industry, including changes to laws and regulations regarding or affecting the U.S. healthcare reform, our business may be harmed; |
| • | if our providers are characterized as employees, we would be subject to adverse effects on our business and employment and withholding liabilities; |
| • | changes in the rules governing Medicare or other federal healthcare programs could have a material adverse effect on our financial condition and results of operations; |
| • | our ability to effectively invest in, implement improvements to, and properly maintain the uninterrupted operation, security, and integrity of, our operating platform and other information technology and business systems; |
| • | security breaches or incidents, loss or misuse of data or other disruptions, arising either from internal or external sources, and whether or not intentional, could compromise sensitive information related to our business, customers or individuals, or prevent us from accessing critical information, and may expose us to operational disruptions, litigation, fines and penalties or other liability, any of which could materially adversely affect our business, results of operations and our reputation; |
16
Table of Contents
| • | disruptions of the information technology systems or infrastructure of certain of our third-party vendors and service providers could also disrupt our businesses, damage our reputation, increase our costs, and have a material adverse effect on our business, financial condition and results of operations; |
| • | we are a holding company and our principal asset after completion of this offering will be our 74.2% ownership interest in Cure TopCo, LLC, and we are accordingly dependent upon distributions from Cure TopCo, LLC to pay dividends, if any, and taxes, make payments under the Tax Receivable Agreement and pay other expenses; |
| • | in certain circumstances, Cure TopCo, LLC will be required to make distributions to us and the other holders of LLC Units, and the distributions that Cure TopCo, LLC will be required to make may be substantial; |
| • | we are controlled by the Pre-IPO LLC Members whose interests in our business may be different than yours, and certain statutory provisions afforded to stockholders are not applicable to us; |
| • | immediately following the consummation of this offering, the Continuing Pre-IPO LLC Members may require us to issue additional shares of our Class A common stock; and |
| • | some provisions of Delaware law and our certificate of incorporation and bylaws may deter third parties from acquiring us and diminish the value of our Class A common stock. |
Before you invest in our Class A common stock, you should carefully consider all the information in this prospectus, including matters set forth under the heading “Risk factors.”
Implications of being an emerging growth company
As a company with less than $1.07 billion (as adjusted for inflation pursuant to SEC rules from time to time) in revenue during our last fiscal year, we qualify as an “emerging growth company” under the Jumpstart Our Business Startups Act of 2012, or the JOBS Act. An emerging growth company may take advantage of reduced reporting requirements and is relieved of certain other significant requirements that are otherwise generally applicable to public companies. As an emerging growth company:
| • | we may present as few as two years of audited financial statements and two years of related management discussion and analysis of financial condition and results of operations; |
| • | we are exempt from the requirement to obtain an attestation report from our auditors on management’s assessment of our internal control over financial reporting under the Sarbanes-Oxley Act of 2002, or the Sarbanes-Oxley Act, for up to five years or until we no longer qualify as an emerging growth company; |
| • | we are permitted to provide reduced disclosure regarding our executive compensation arrangements pursuant to the rules applicable to smaller reporting companies, which means we do not have to include a compensation discussion and analysis and certain other disclosures regarding our executive compensation; and |
| • | we are not required to hold non-binding advisory votes on executive compensation or golden parachute arrangements. |
In addition to the relief described above, the JOBS Act permits us an extended transition period for complying with new or revised accounting standards affecting public companies. We have elected to use this extended transition period, which means that our financial statements may not be comparable to the financial statements of public companies that comply with such new or revised accounting standards on a non-delayed basis.
17
Table of Contents
In this prospectus we have elected to take advantage of the reduced disclosure requirements relating to executive compensation, and in the future we may take advantage of any or all of these exemptions for so long as we remain an emerging growth company. We will remain an emerging growth company until the earliest of (i) the end of the fiscal year during which we have total annual gross revenue of $1.07 billion (as adjusted for inflation pursuant to SEC rules from time to time) or more, (ii) the end of the fiscal year following the fifth anniversary of the completion of this offering, (iii) the date on which we have, during the previous three-year period, issued more than $1.0 billion in non-convertible debt or (iv) the date on which we are deemed to be a “large accelerated filer” under the Securities Exchange Act of 1934, as amended.
Our sponsor
New Mountain Capital is a New York-based investment firm that emphasizes business building and growth, rather than debt, as it pursues long-term capital appreciation. The firm currently manages private equity, public equity, and credit funds with over $30 billion in assets under management as of September 30, 2020. New Mountain Capital seeks out what it believes to be the highest quality growth leaders in carefully selected industry sectors and then works intensively with management to build the value of these companies.
Corporate information
Signify Health, Inc. was incorporated in the State of Delaware on October 1, 2020 to serve as the issuer of the Class A common stock in this offering. Our principal executive offices are located at 800 Connecticut Avenue, Norwalk, CT 06854 and our telephone number is (203) 541-4600. Our internet site is www.signifyhealth.com. Our website and the information contained therein or connected thereto is not incorporated into this prospectus or the registration statement of which it forms a part.
18
Table of Contents
THE OFFERING
| Class A common stock offered by us |
23,500,000 shares. |
| Option to purchase additional shares |
We have granted the underwriters an option for a period of 30 days to purchase up to 3,525,000 additional shares of Class A common stock from us. |
| Class A common stock to be outstanding after this offering |
165,092,313 shares (or 222,356,893 shares if all outstanding LLC Units held by the Continuing Pre-IPO LLC Members were redeemed or exchanged for a corresponding number of newly issued shares of Class A common stock). |
| If the underwriters exercise their option to purchase additional shares of Class A common stock in full, 168,617,313 shares (or 225,881,893 shares if all outstanding LLC Units held by the Continuing Pre-IPO LLC Members were redeemed or exchanged for a corresponding number of newly issued shares of Class A common stock) would be outstanding. |
| Class B common stock to be outstanding after this offering |
57,264,580 shares (or 0 shares if all outstanding LLC Units held by the Continuing Pre-IPO LLC Members were redeemed or exchanged for a corresponding number of newly issued shares of Class A common stock). |
| LLC Units to be held by us after this offering |
165,092,313 LLC Units, representing a 74.2% economic interest in Cure TopCo, LLC (or 168,617,313 LLC Units, representing a 74.6% economic interest in Cure TopCo, LLC, if the underwriters exercise their option to purchase additional shares of Class A common stock in full). The LLC Units are not entitled to voting interests in Cure TopCo, LLC. |
| Total LLC Units to be outstanding after this offering |
222,356,893 LLC Units (or 225,881,893 LLC Units if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
| Voting rights after giving effect to this offering |
Each share of Class A common stock will entitle its holder to one vote per share, representing an aggregate of 74.2% of the combined voting power of our issued and outstanding common stock upon completion of this offering (or 74.6% if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
| Each share of Class B common stock will entitle its holder to one vote per share, representing an aggregate of 25.8% of the combined voting power of our issued and outstanding common stock upon completion |
19
Table of Contents
| of this offering (or 25.4% if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
| Holders of all outstanding shares of our Class A common stock and Class B common stock will vote together as a single class on all matters submitted to a vote of our stockholders. See “Description of capital stock.” |
| Following the Reorganization Transactions and this offering, the Pre-IPO LLC Members will collectively hold through their ownership of 141,592,313 shares of Class A and 57,264,580 shares of Class B common stock, approximately 89.4% of the combined voting power of our common stock (or 88.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
| Redemption rights of the holders of LLC Units |
Under the Amended LLC Agreement, the holders of LLC Units will have the right, from and after the completion of this offering (subject to the terms of the Amended LLC Agreement), to require Cure TopCo, LLC to redeem all or a portion of their LLC Units for, at our election, newly issued shares of Class A common stock on a one-for-one basis or a cash payment equal to the volume weighted average market price of one share of our Class A common stock for each LLC Unit redeemed (subject to customary adjustments, including for stock splits, stock dividends and reclassifications) in accordance with the terms of the Amended LLC Agreement. Additionally, in the event of a redemption request by a holder of LLC Units, we may, at our option, effect a direct exchange of cash or Class A common stock for LLC Units in lieu of such a redemption. |
| Shares of Class B common stock will be cancelled on a one-for-one basis if we, following a redemption request of a holder of LLC Units, redeem or exchange LLC Units of such holder of LLC Units pursuant to the terms of the Amended LLC Agreement. See “Certain relationships and related party transactions—Amended LLC Agreement.” |
| Except for transfers to us pursuant to the Amended LLC Agreement or to certain permitted transferees, the LLC Units and corresponding shares of Class B common stock may not be sold, transferred or otherwise disposed of. |
| Use of proceeds |
We estimate that our net proceeds from this offering will be approximately $456.5 million (or approximately $524.9 million if the underwriters exercise their option to purchase additional shares of Class A common stock in full), after deducting underwriting discounts and commissions. |
20
Table of Contents
| We intend to use the net proceeds that we receive from this offering to purchase 23,500,000 newly issued LLC Units from Cure TopCo, LLC (or 27,025,000 LLC Units, if the underwriters exercise their option to purchase additional shares of Class A common stock in full) at a purchase price per LLC Unit equal to the initial public offering price per share of Class A common stock net of underwriting discounts and commissions. |
| Cure TopCo, LLC will use the proceeds from the issuance of LLC Units to Signify Health, Inc. (i) to pay fees and expenses of approximately $13.5 million in connection with this offering and the Reorganization Transactions and (ii) for general corporate purposes, including working capital and potential strategic acquisitions of, or investments in, other businesses or technologies that we believe will complement our current business and expansion strategies. See “Use of proceeds.” |
| Controlled company |
Upon the closing of this offering, a group of Pre-IPO LLC Members (as defined herein) comprised of entities affiliated with New Mountain Capital will beneficially own more than 50% of the voting power for the election of members of our board of directors. Consequently, we will be a “controlled company” under the NYSE rules. As a controlled company, we qualify for, and intend to rely on, exemptions from certain corporate governance requirements of the NYSE. See “Management—Controlled company exception.” |
| Directed share program |
At our request, the underwriters have reserved up to 1,175,000 shares of Class A common stock, or 5% of the shares of Class A common stock to be offered by this prospectus for sale, at the initial public offering price, through a directed share program for certain of our clinicians and employees and certain other individuals and entities. Shares purchased through the directed share program will not be subject to a lock-up restriction, except in the case of shares purchased by any of our directors or officers and certain of our employees and existing equityholders. The number of shares of Class A common stock available for sale to the general public will be reduced to the extent these individuals or entities purchase such reserved shares. Any reserved shares that are not so purchased will be offered by the underwriters to the general public on the same basis as the other shares offered by this prospectus. See “Certain relationships and related party transactions,” “Shares eligible for future sales” and “Underwriting—Directed share program.” |
| Tax Receivable Agreement |
Upon the completion of this offering, we will be a party to the Tax Receivable Agreement with the TRA Parties. Under the Tax Receivable Agreement, we generally will be required to pay to the TRA Parties 85% of the amount of cash savings, if any, in U.S. federal, state and local income tax that we actually realize as a result of (i) certain favorable tax attributes we will acquire from the Blocker Companies in the Mergers (including net operating losses, the |
21
Table of Contents
| Blocker Companies’ allocable share of existing tax basis and refunds of Blocker Company taxes attributable to pre-Merger tax periods), (ii) increases in our allocable share of existing tax basis and tax basis adjustments that may result from (x) future redemptions or exchanges of LLC Units by Continuing Pre-IPO LLC Members for cash or Class A common stock, (y) the IPO Contribution and (z) certain payments made under the Tax Receivable Agreement and (iii) deductions in respect of interest and certain compensatory payments made under the Tax Receivable Agreement. These payment obligations are our obligations and not the obligations of Cure TopCo, LLC. Our obligations under the Tax Receivable Agreement will also apply with respect to any person who is issued LLC Units in the future and who becomes a party to the Tax Receivable Agreement. See “Organizational structure—Holding company structure and the Tax Receivable Agreement.” |
| Dividend policy |
We do not currently expect to pay any cash dividends on our Class A common stock for the foreseeable future. Instead, we intend to retain future earnings, if any, for the future operation and expansion of our business. |
| The declaration and payment by us of any future dividends to holders of our Class A common stock will be at the sole discretion of our board of directors. See “Dividend policy.” |
| Following this offering and subject to funds being legally available, we intend to cause Cure TopCo, LLC to make pro rata distributions to the Continuing Pre-IPO LLC Members and us in an amount at least sufficient to allow us and the Continuing Pre-IPO LLC Members to pay all applicable taxes and allows us to make payments under the Tax Receivable Agreement and to pay our corporate and other overhead expenses. |
| Stock symbol |
SGFY |
Unless we indicate otherwise throughout this prospectus, the number of shares of our Class A common stock outstanding after this offering excludes:
| • | 3,525,000 shares of Class A common stock issuable upon the exercise of the underwriters’ option to purchase additional shares of Class A common stock from us; |
| • | 57,264,580 shares of Class A common stock reserved for issuance upon the redemption or exchange of LLC Units that will be held by the Continuing Pre-IPO LLC Members on a one-for-one basis; |
| • | 8,141,503 shares of Class A common stock reserved for issuance upon the redemption or exchange of LLC Units issued to Cure Aggregator, LLC in respect of common units of Cure Aggregator, LLC that are unvested; |
| • | 4,501,037 shares of Class A common stock that may be issued on a net basis upon the vesting and exercise of stock options outstanding based on an offer price of $20.50 per share (the midpoint of the range set forth on the cover page of this prospectus), which represents 6,281,119 of shares of Class A common stock that may be issued on a gross basis at an average weighted exercise price of $5.80; and |
22
Table of Contents
| • | 20,071,433 shares of Class A common stock reserved for future issuance under our Long-Term Incentive Plan, which is expected to become effective in connection with this offering (of which restricted stock units with respect to an estimated 74,144 shares and stock options exercisable for an estimated 872,500 shares (with an exercise price equal to the initial public offering price) are expected to be granted in connection with this offering), and our Employee Stock Purchase Plan, which is expected to become effective following this offering. |
Unless we indicate otherwise throughout this prospectus, all information in this prospectus:
| • | assumes an initial public offering price of $20.50 per share of Class A common stock, which is the midpoint of the price range set forth on the cover page of this prospectus; |
| • | assumes the underwriters’ option to purchase additional shares of Class A common stock has not been exercised; |
| • | assumes the completion of the reorganization transactions described under “Organizational structure—The reorganization transactions;” and |
| • | gives effect to our amended and restated certificate of incorporation and our amended and restated bylaws, which will become effective prior to or upon the closing of this offering. |
Unless otherwise indicated or the context otherwise requires, references in this prospectus to the exercise of the underwriters’ option to purchase additional shares of Class A common stock give effect to the use of the net proceeds therefrom.
23
Table of Contents
SUMMARY COMBINED-CONSOLIDATED FINANCIAL AND OTHER DATA
The following tables set forth summary historical financial and other data of Cure TopCo, LLC for the periods presented. Signify Health, Inc. was formed as a Delaware corporation on October 1, 2020 and has not, to date, conducted any activities other than those incident to its formation, those in preparation for the Reorganization Transactions (as defined herein) and the preparation of this prospectus and the registration statement of which this prospectus forms a part.
The statements of operations data for the years ended December 31, 2019 and 2018 and balance sheet data as of December 31, 2019 and 2018 have been derived from Cure TopCo, LLC’s audited combined-consolidated financial statements included elsewhere in this prospectus. The statements of operations data for the nine months ended September 30, 2020 and 2019 and balance sheet data as of September 30, 2020 have been derived from Cure TopCo, LLC’s unaudited combined-consolidated financial statements included elsewhere in this prospectus which, in the opinion of management, include all adjustments, consisting only of normal recurring adjustments, necessary for a fair statement of the results for the unaudited interim periods. In 2019, we acquired 100% of the outstanding equity of Remedy Partners. A controlling interest was initially acquired by New Mountain Capital on January 15, 2019 (the “Remedy Partners Acquisition”), at which point we and Remedy Partners were considered to be under common control and combined financial statements were presented from January 15, 2019 to November 26, 2019. On November 26, 2019, a series of transactions were effected which resulted in Remedy Partners becoming our wholly owned subsidiary and consolidated financial statements were presented from that date forward (the “Remedy Partners Combination” and together with the Remedy Partners Acquisition, the “Remedy Partners Transactions”). Because we were not under common control with and did not own Remedy Partners in 2018, our results of operations for the year ended December 31, 2019 are not directly comparable to our results of operations for the year ended December 31, 2018.
The pro forma statements of operations for the year ended December 31, 2019 and the nine months ended September 30, 2020 give effect to the Reorganization Transactions and Offering Adjustments (as defined below), in the manner described under “Unaudited pro forma consolidated financial information” and the notes thereto, as if they had occurred on January 1, 2019.
The pro forma balance sheet data as of September 30, 2020 gives effect, in the manner described under “Unaudited pro forma consolidated financial information” and the notes thereto, to the Reorganization Transactions and Offering Adjustments as if each had occurred on September 30, 2020. See “Unaudited pro forma consolidated financial information” and “Capitalization.”
24
Table of Contents
The summary historical and pro forma financial and other data presented below do not purport to be indicative of the results that can be expected for any future period and should be read together with “Capitalization,” “Unaudited pro forma consolidated financial information,” “Selected combined-consolidated financial data,” “Management’s discussion and analysis of financial condition and results of operations” and our consolidated financial statements and related notes thereto included elsewhere in this prospectus. The presentation of the unaudited pro forma consolidated financial information is prepared in conformity with Article 11 of Regulation S-X.
| Cure TopCo, LLC | Signify Health, Inc. Pro Forma (unaudited) |
|||||||||||||||||||||||
| Year Ended December 31, | Nine Months Ended September 30, (unaudited) |
Year Ended December 31, |
Nine Months Ended September 30, |
|||||||||||||||||||||
| 2019 | 2018 | 2020 | 2019 | 2019 | 2020 | |||||||||||||||||||
| (in millions) | ||||||||||||||||||||||||
| Statement of Operations Data: |
||||||||||||||||||||||||
| Revenue |
$ | 501.8 | $ | 337.9 | $ | 417.1 | $ | 368.5 | $ | 501.8 | $ | 417.1 | ||||||||||||
| Operating expenses |
||||||||||||||||||||||||
| Service expense (exclusive of depreciation and amortization shown below) |
247.2 | 196.3 | 203.4 | 188.2 | 247.2 | 203.4 | ||||||||||||||||||
| Selling, general and administrative expense (exclusive of depreciation and amortization shown below) |
168.6 | 67.9 | 148.5 | 119.1 | 173.9 | 151.3 | ||||||||||||||||||
| Transaction-related expenses |
22.4 | 21.0 | 10.8 | 15.9 | 30.9 | 9.9 | ||||||||||||||||||
| Asset impairment |
6.4 | 17.0 | — | 1.5 | 6.4 | — | ||||||||||||||||||
| Depreciation and amortization |
66.0 | 43.0 | 46.0 | 49.5 | 66.0 | 46.0 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total operating expenses |
510.6 | 345.2 | 408.7 | 374.2 | 524.4 | 410.6 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| (Loss) income from operations |
(8.8 | ) | (7.3 | ) | 8.4 | (5.7 | ) | (22.6 | ) | 6.5 | ||||||||||||||
| Interest expense |
21.2 | 21.4 | 16.2 | 16.1 | 26.6 | 20.5 | ||||||||||||||||||
| Other (income) expense, net |
(1.6 | ) | — | 6.9 | (1.4 | ) | (1.6 | ) | 6.9 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Other expense, net |
19.6 | 21.4 | 23.1 | 14.7 | 25.0 | 27.4 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Loss before income taxes |
(28.4 | ) | (28.7 | ) | (14.7 | ) | (20.4 | ) | (47.6 | ) | (20.9 | ) | ||||||||||||
| Income tax (benefit) expense |
0.1 | 0.2 | 0.5 | 0.1 | (5.6 | ) | — | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Net loss |
$ | (28.5 | ) | $ | (28.9 | ) | $ | (15.2 | ) | $ | (20.5 | ) | $ | (42.0 | ) | $ | (20.9 | ) | ||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Net loss attributed to contingently redeemable noncontrolling interest. |
— | — | — | — | (11.5 | ) | (5.4 | ) | ||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Net loss attributable to Signify Health, Inc. |
— | — | — | — | $ | (30.5 | ) | $ | (15.5 | ) | ||||||||||||||
| Cure TopCo, LLC | Signify Health, Inc. Pro Forma (unaudited) |
|||||||||||||||||||||||
| December 31, | September 30, (unaudited) |
September 30, | ||||||||||||||||||||||
| 2019 | 2018 | 2020 | 2020 | |||||||||||||||||||||
| (in millions) | ||||||||||||||||||||||||
| Balance Sheet Data: |
||||||||||||||||||||||||
| Cash and cash equivalents |
$ | 27.7 | $ | 20.4 | $ | 87.9 | $ | 602.3 | ||||||||||||||||
| Working capital |
140.9 | 33.9 | 153.6 | 656.6 | ||||||||||||||||||||
| Total assets |
1,392.4 | 601.7 | 1,468.7 | |
2,004.9 |
| ||||||||||||||||||
| Total liabilities |
434.8 | 317.7 | 577.3 | 694.4 | ||||||||||||||||||||
| Total members’ equity/stockholders’ equity |
957.6 | 284.0 | 891.4 | |
1,310.5 |
| ||||||||||||||||||
25
Table of Contents
| Cure TopCo, LLC | ||||||||||||||||
| Year Ended December 31, | Nine Months Ended September 30, (unaudited) |
|||||||||||||||
| 2019 | 2018 | 2020 | 2019 | |||||||||||||
| (in millions, except for percentages) |
||||||||||||||||
| Other Financial and Operating Data: |
||||||||||||||||
| Adjusted EBITDA(1) |
$ | 93.3 | $ | 79.1 | $ | 86.0 | $ | 66.7 | ||||||||
| Adjusted EBITDA Margin(1) |
18.6 | % | 23.4 | % | 20.6 | % | 18.1 | % | ||||||||
| IHE Volume(2) |
1.1 | 0.9 | 0.9 | 0.8 | ||||||||||||
| Weighted Average Program Size(3) |
$ | 6,144.1 | — | — | — | |||||||||||
| Weighted Average Savings Rate(4) |
5.3 | % | — | — | — | |||||||||||
| (1) | Adjusted EBITDA and Adjusted EBITDA Margin are non-GAAP financial measures. We define Adjusted EBITDA as net income (loss) before interest expense, income tax expense, depreciation and amortization and certain items of income and expense, including asset impairment, other (income) expense, net, transaction-related expenses, equity-based compensation, remeasurement of contingent consideration, management fees and non-recurring expenses. We believe that Adjusted EBITDA provides a useful measure to investors to assess our operating performance because it eliminates the impact of expenses that do not relate to ongoing business performance, and that the presentation of this measure enhances an investor’s understanding of the performance of our business. |
| We define Adjusted EBITDA Margin as Adjusted EBITDA divided by revenue. We believe that Adjusted EBITDA Margin is helpful to investors in measuring the profitability of our operations on a consolidated level. See “Non-GAAP financial measures.” |
The following table shows a reconciliation of net loss to Adjusted EBITDA and Adjusted EBITDA Margin:
| Cure TopCo, LLC | ||||||||||||||||
| Year Ended December 31, | Nine Months Ended September 30, (unaudited) |
|||||||||||||||
| 2019 | 2018 | 2020 | 2019 | |||||||||||||
| (in millions) | ||||||||||||||||
| Net loss |
(28.5 | ) | (28.9 | ) | (15.2 | ) | (20.5 | ) | ||||||||
| Interest expense |
21.2 | 21.4 | 16.2 | 16.1 | ||||||||||||
| Income tax expense |
0.1 | 0.2 | 0.5 | 0.1 | ||||||||||||
| Depreciation and amortization |
66.0 | 43.0 | 46.0 | 49.5 | ||||||||||||
| Asset impairment(a) |
6.4 | 17.0 | — | 1.5 | ||||||||||||
| Other (income) expense, net(b) |
(1.6 | ) | — | 6.9 | (1.4 | ) | ||||||||||
| Transaction-related expenses(c) |
22.4 | 21.0 | 10.8 | 15.9 | ||||||||||||
| Equity-based compensation(d) |
4.5 | 2.6 | 10.0 | 3.0 | ||||||||||||
| Customer equity appreciation rights (e) |
— | — | 7.5 | — | ||||||||||||
| Remeasurement of contingent consideration(f) |
0.7 | 0.9 | 0.2 | 0.7 | ||||||||||||
| Management fees(g) |
1.0 | 1.0 | — | 0.8 | ||||||||||||
| Non-recurring expenses(h) |
1.1 | 0.9 | 3.1 | 1.0 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Adjusted EBITDA |
93.3 | 79.1 | 86.0 | 66.7 | ||||||||||||
| Adjusted EBITDA Margin |
18.6 | % | 23.4 | % | 20.6 | % | 18.1 | % | ||||||||
| (a) | Asset impairment during the year ended December 31, 2019 was primarily related to the discontinued use of certain trade names following the Remedy Partners Acquisition, which resulted in a $4.9 million |
26
Table of Contents
| asset impairment. Additionally, we discontinued the use of certain software resulting in an asset impairment of $1.5 million during the nine months ended September 30, 2019 and year ended December 31, 2019. Asset impairment in 2018 was primarily related to the discontinued use of certain trade names following the rebranding of the Company, which resulted in a $16.0 million asset impairment. Additionally, certain property and equipment was impaired for a total of $1.0 million in 2018. |
| (b) | Represents other non-operating (income) expense that consists primarily of the quarterly remeasurement of fair value of the outstanding customer EARs, as well as interest and dividends earned on cash and cash equivalents. |
| (c) | Represents transaction-related expenses that consist primarily of expenses incurred in connection with acquisitions and other corporate development activities, such as mergers and acquisitions activity that did not proceed, strategic investments and similar activities. Expenses incurred in connection with this initial public offering, which cannot be netted against proceeds, are also included in transaction-related expenses. |
| (d) | Represents expense related to equity incentive awards, including profit interest units and stock options, granted to certain employees, officers and non-employee directors as long-term incentive compensation. We recognize the related expense for these awards ratably over the vesting period or as achievement of performance criteria become probable. |
| (e) | Represents the reduction of revenue related to the grant date fair value of the December 2019 EAR and September 2020 EAR. See “Management’s discussion and analysis of financial condition and results of operations—Liquidity and capital resources—Customer Equity Appreciation Rights agreements.” |
| (f) | Represents the remeasurement of contingent consideration due to the selling shareholders of Censeo Health, a business acquired in 2017, pending the resolution of an IRS tax matter. The matter was resolved in 2020. |
| (g) | Represents the annual advisory fee paid to New Mountain Capital under the Management Services Agreement. The Management Services Agreement was terminated in January 2019 in connection with the consummation of the Remedy Partners Acquisition. |
| (h) | Represents certain gains and expenses incurred that are not expected to recur, including those associated with the closure of certain facilities, the sale of certain assets and the early termination of certain contracts. |
| (2) | IHE Volume represents the total number of IHEs (as defined below), including both in-home IHEs and vIHEs (as defined below), completed and invoiced to customers during the period. We did not conduct any vIHEs in 2018 or 2019. |
| (3) | Weighted Average Program Size represents the weighted average program size for performance obligation periods (described below) included in a calendar quarter or calendar year. We manage episodes in six-month blocks, which we refer to as performance measurement periods. Each performance measurement period, we reconcile those episodes of care that concluded during such performance measurement period. We recognize the revenue attributable to episodes reconciled during each six-month performance measurement period over a 13-month performance obligation period, which we refer to as performance obligation periods. Accordingly, our weighted average program size during a given calendar quarter or calendar year reflects the results of multiple overlapping performance obligation periods. We define program size for a performance obligation period as (x) the number of episodes we managed during the relevant performance measurement period multiplied by (y) the baseline price of each episode, which represents the benchmark price set by the relevant program prior to any discounts. We define weighted average program size as the sum of the following for each performance obligation period included in a calendar quarter or calendar year: (x) the program size for the relevant performance obligation period, (y) divided by 13, which represents the approximately 13-month performance obligation period required to complete performance obligations under our episodes programs, and (z) multiplied by the number of months of the relevant performance obligation period included in the calendar quarter or calendar year. For 2019, this does not include amounts related to the BPCI program, as these are not comparable to the current BPCI-A program and are not indicative of future performance. The Remedy Partners Acquisition |
27
Table of Contents
| and the subsequent Remedy Partners Combination occurred in 2019, and as a result, we did not have any episodes of care programs in 2018. |
| (4) | Weighted Average Savings Rate represents the weighted average savings rate generated during performance obligation periods included in a calendar quarter or calendar year. The gross savings for each performance obligation period (i.e., the 13-month period over which we recognize revenue attributable to episodes that concluded during a six-month performance measurement period) is equal to the gross amount of savings generated under the episode programs we manage during the performance measurement period to which such performance obligation period relates. The gross savings for a performance measurement period is defined as (x) the sum of the baseline episode prices of each such episode less (y) the total actual cost of each episode that concluded during such performance measurement period, which baseline prices represent the benchmark price set by the relevant program prior to any discounts. The weighted average savings rate is (i) the sum, for each performance obligation period included in a calendar quarter or calendar year, of (A) the gross savings for each such performance obligation period, divided by (B) 13, and multiplied by (C) the number of months of such performance obligation period included in such calendar quarter or calendar year, divided by (ii) the weighted average program size for such calendar quarter or calendar year. For the above purposes, the gross amount of savings is calculated prior to the deduction of our administrative fees and amounts shared with health plans and provider partners. For example, for BPCI-A, CMS receives a 3% discount, which is included in the gross amount of savings calculated for each performance measurement period. For 2019, the weighted average savings rate does not include amounts related to the predecessor BPCI program, as these are not comparable to the current BPCI-A program and are not indicative of future performance. The Remedy Partners Acquisition and the subsequent Remedy Partners Combination occurred in 2019, and as a result, we did not have any episodes of care programs in 2018. |
28
Table of Contents
Investing in our Class A common stock involves a high degree of risk. These risks include, but are not limited to, those described below, each of which may be relevant to an investment decision. You should carefully consider the risks and uncertainties described below, together with all of the other information contained in this prospectus, including the section titled “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and our consolidated financial statements and the related notes, before deciding whether to invest in shares of our Class A common stock. If any of the following risks or other risks actually occur, our business, financial condition, results of operations, and future prospects could be materially harmed. In that event, the market price of our Class A common stock could decline, and you could lose part or all of your investment.
Risks related to our business and operations
Our operations have been, and may continue to be, significantly disrupted by the COVID-19 pandemic, and our business, financial condition and results of operations have been negatively impacted.
The global spread of the COVID-19 pandemic and measures introduced by local, state and federal governments to contain the virus and mitigate its public health effects have significantly impacted the U.S. economy. The duration and severity of the COVID-19 pandemic is unknown, and the extent of the business disruption and financial impact depend on factors beyond our knowledge and control. Given the uncertainty around the duration and extent of the COVID-19 pandemic, we expect that the evolving COVID-19 pandemic will continue to impact our business, results of operations, and financial condition and liquidity.
Our operations in our Home & Community Services segment have been significantly affected by the pandemic. Because the majority of the individuals we provide IHEs to participate in Medicare Advantage plans and are over 65, they are at higher risk for contracting COVID-19. Beginning in March 2020, we temporarily halted IHEs as a precautionary measure in response to the pandemic. We resumed in-home visits beginning in July 2020.
In response to the pandemic, we were able to quickly expand our business model to perform vIHEs beginning in April 2020 and have made up for the lost volume for IHEs through vIHEs. The fees we receive for vIHEs are slightly lower than the fees we receive for IHEs, although our overall margins associated with vIHEs are substantially similar to IHEs due to the lower costs associated with vIHEs. We were able to perform approximately 380,000 vIHEs and over 560,000 in-person IHEs, or a total of approximately 940,000 IHEs, in the first nine months of 2020. By comparison, we performed approximately 835,000 IHEs in the first nine months of 2019. As a result of the pandemic, many of our health plan customers pushed in-person IHEs into the second half of 2020. Although we have seen some increase in IHE member cancellation rates in part as a result of the pandemic, overall we saw significant incremental IHE volumes in the second half of 2020 as certain customers increased the volumes they have placed with us and in-home IHEs have represented the majority of those IHEs. In order to meet this volume growth, we have onboarded additional providers into our network. However, due to some provider unwillingness to perform in-person IHEs and increased competition from telehealth companies, which are generally experiencing upticks in business and hiring additional personnel due to the pandemic, we may have difficulty expanding our network of high-quality providers sufficiently to be able to complete all of the pending in-person visits. If we are unable to complete all of the in-person visits and do not receive the related fees for those visits, it would have a negative impact on our revenue for the year. Moreover, there has been a significant uptick in COVID-19 cases in the fourth quarter of 2020, and there can be no guarantee that we will be able to continue performing IHEs in person as the situation develops.
Our Episodes of Care Services segment has also been affected by the pandemic. In the United States, at certain times during the course of the pandemic, governmental authorities have recommended, and in certain cases required, that elective, specialty and other procedures and appointments, including certain acute and post-
29
Table of Contents
acute care services, be suspended or canceled to avoid non-essential patient exposure to medical environments and potential infection with the virus that causes COVID-19. In addition, the temporary suspension or cancellation of services was put in place to focus limited resources and personnel capacity toward the prevention of, and care for patients with, COVID-19. This has resulted in fewer elective procedures and a general reduction in individuals seeking medical care, which contributed to a substantially lower number of episodes being managed in 2020. In addition, CMS announced that healthcare providers could choose to eliminate upside and downside risk by excluding all episodes from reconciliation in 2020 or could choose to exclude from reconciliation those episodes with a COVID-19 diagnosis during the episode. Healthcare providers were required to make their election by September 25, 2020. The results of the elections made by healthcare providers will reduce the total number of episodes we manage during 2020 and 2021, and therefore reduce program size. This impact on program size was partially offset by a higher savings rate due to a combination of improved performance by some of our partners as well as partners that were underperforming choosing to exclude some or all of their episodes from reconciliation in 2020. Subsequently, CMS announced that all episodes in 2021 with a COVID-19 diagnosis would be automatically excluded from reconciliation, and as a result, we expect a reduction in our overall program size in 2021 as well for as long as the COVID-19 pandemic is ongoing. There can be no assurance that the positive impact on our savings rate in 2020 will continue in 2021.
Each of these pandemic-related changes has had a material impact on program size in 2020 and could have the effect of reducing program size for 2021 through 2023. Because our administrative fee is calculated as a percentage of program size and we receive a portion of the savings achieved in management of an episode, the decrease in episodes and related reduction in overall program size have had, and we expect will continue to have, a negative effect on our revenue. Some of these measures and challenges will likely continue for the duration of the COVID-19 pandemic, which is uncertain, and will harm the results of operations, liquidity and financial condition of our provider partners and our business. Lastly, our representatives may be prohibited from entering hospitals, skilled nursing facilities and other post-acute facilities as a result of the pandemic, which affects our ability to facilitate coordination among provider partners and could have a material impact on our savings rate.
There has been significant regional variability in the impact of the COVID-19 pandemic on our customers, and in certain regions, we faced significant pressure in the last several months from customers to renegotiate our contracts as they sought to minimize risk as much as possible in response to the pandemic. We entered into contractual amendments with certain of our provider partners to put in place alternative administrative fees and gain/loss sharing arrangements, which are also expected to lead to a decline in revenue in 2020.
We also launched several new solutions in 2019 and 2020, such as our ACO services and Commercial Episodes solutions. We may see lower market adoption of our new solutions as a result of the pandemic. For example, many provider partners that might otherwise be interested in participating in Commercial Episodes face financial uncertainty as a result of the COVID-19 pandemic and the decline in elective procedures, through which they make much of their revenue. While we have seen increased demand from healthcare providers for cost-effective, value-based solutions, in particular with respect to the non-elective or chronic conditions, we may see lower demand from healthcare providers for programs like our Commercial Episodes program.
The COVID-19 pandemic may also create risks to our overall business or corporate operations. Due to the shelter-in-place orders that are and/or were previously in effect across the country, we have implemented work-from-home policies for many employees which may impact productivity and disrupt our business operations. Our providers performing in-home visits also face an increased risk of infection with COVID-19, which may result in staffing shortages or claims, as well as increased expenses associated with personal protective equipment and compliance with applicable testing protocols.
During the fourth quarter of 2020, the average daily cases of COVID-19 have been increasing once again and parts of the United States are experiencing significant increases in the average daily cases of COVID-19. Given the inherent uncertainty surrounding COVID-19 due to changes in COVID-19 rates regionally and nationally, rapidly changing governmental directives, public health challenges and economic disruption and the
30
Table of Contents
duration of the foregoing, the potential impact that COVID-19 could have on the other Risk Factors described in this “Risk Factors” section remains unclear.
Our revenues and operations are dependent upon a limited number of key customers.
We are dependent on a concentrated number of health plans and provider partners with whom we contract to provide IHEs and other services. For example, when aggregating the revenue associated with each health plan (including its local affiliates), Humana and Aetna accounted for approximately 23% and 21%, respectively, of our total revenue for the year ended December 31, 2019 and for approximately 26% and 16%, respectively, of our total revenue for the nine months ended September 30, 2020; Optum accounted for approximately 12% of our total revenue for the nine months ended September 30, 2020. In addition, the revenue from our top 10 customers across our segments accounted for approximately 74% and 70% of our total revenue for the year ended December 31, 2019 and nine months ended September 30, 2020, respectively.
We believe that a majority of our revenues will continue to be derived from a limited number of key health plans and provider partners. Health plans and provider partners may seek to terminate and/or modify their contractual relationships with us for various reasons, such as changes in the regulatory landscape and poor performance by us, subject to certain conditions. Certain of our contracts can be terminated immediately upon the occurrence of certain events and others may be terminated immediately by the customer if we lose applicable licenses, go bankrupt, lose our liability insurance or receive an exclusion, suspension or debarment from state or federal government authorities. We may also terminate customer relationships from time to time. For example, if a health plan or provider partner were to lose applicable licenses, lose liability insurance, become insolvent, file for bankruptcy or receive an exclusion, suspension or debarment from state or federal government authorities, our contract with such customer could in effect be terminated. The sudden loss of any of our customers or the renegotiation of any of their contracts could materially and adversely affect our operating results. In addition, effective June 2020, we terminated a customer relationship with a significant customer in our Episodes of Care Services segment, representing approximately 5% of our total revenue for the year ended December 31, 2019 in connection with a contractual dispute.
In the ordinary course of business, we engage in active discussions and renegotiations with customers in respect of the services we provide and the terms of our agreements. As our customers respond to market dynamics and financial pressures, and as they make strategic business decisions in respect of the lines of business they pursue and programs in which they participate, our customers may seek to renegotiate or terminate their agreements with us or to utilize our services less under those agreements. For example, some of our larger customers are capable of performing certain of the services we provide, in particular our IHE services, and may decide to provide some or all of those services internally. Similarly, a customer could obtain services we provide, particularly our IHE services, from another third-party provider partner of such services. Such a decision could result in reductions to the fees and changes to the scope of services contemplated by our existing contractual relationships and consequently could negatively impact our revenues, business and prospects.
In our Home & Community Services segment, our business model and growth depends heavily on achieving various operational efficiencies with our provider network, which benefits from increased geographic density of our customers’ members. As the total number of our customers’ members increases, and as those members’ geographic density increases, we are increasingly able to efficiently send our providers to any neighborhood across the country, as needed. If a significant customer terminates its relationship with us, it could impact the geographic density of members we reach and make it less efficient for us to operate in certain jurisdictions, or we may need to increase our prices, which would negatively affect our business, results of operations and financial condition.
Because we rely on a limited number of health plans and provider partners for a significant portion of our revenues, we depend on the creditworthiness of these health plans and provider partners. Our customers are subject to a number of risks including the impact of COVID-19, reductions in payment rates from governmental programs, higher than expected healthcare costs and lack of predictability of financial results when entering new
31
Table of Contents
lines of business, particularly with high-risk populations. If the financial condition of our health plan and provider partners decline, or if there are delays in receiving payment due to internal payment policies or claims systems issues, our credit risk could increase. Should one or more of our significant customers declare bankruptcy, be declared insolvent or otherwise be restricted by state or federal laws or regulation from continuing in some or all of their operations, this could adversely affect our ongoing revenues, the collectability of our accounts receivable, our bad debt reserves and our net income.
A large portion of our revenues are substantially dependent on BPCI-A.
In our Episodes of Care Services segment, revenues from BPCI-A services and, previously BPCI services, provided to our customers represented approximately 20% of our total revenue and over 85% of our Episodes of Care Services segment revenue in 2019, and approximately 25% of our total revenue and over 90% of our Episodes of Care Services segment revenue in the nine months ended September 30, 2020. We contract directly with CMS and enter into back-to-back contracts with healthcare providers participating in the BPCI-A program. CMS has identified certain circumstances that could result in termination of our agreements under BPCI-A. CMS reserves the right to terminate a participant agreement as a result of any of the following factors, among others: (i) for issues warranting termination, if not addressed sufficiently, including, but not limited to, failure to comply with Medicare program requirements, rules or regulations; (ii) actions that threaten the health or safety of a beneficiary or other patient; or (iii) submission of false data or false representations, warranties, or certifications in connection with any aspect of BPCI-A. Termination could also result from changes to payment or program structures, such as: certain states entering an arrangement with CMS to implement a global or per-capita payment for services furnished to a population that includes BPCI-A beneficiaries; CMS determining that it no longer has the funds to support BPCI-A or that the BPCI-A voluntary episode payment model (the “Model”) should be terminated for other reasons; or CMS terminating or modifying the Model for any reason, including pursuant to Section 1115A(b)(3)(B) of the Social Security Act, which permits the Secretary of the U.S. Department of Health and Human Services (“HHS”) to terminate or modify the design and implementation of a model after testing has begun if the Secretary determines that model does not meet certain criteria. If we were to lose one or more of our contracts with CMS, our business, results of operations and financial condition would be materially and adversely affected.
Participation in the BPCI-A program was locked in place at the end of 2020 through the end of the program in 2023, meaning that new healthcare providers will not be able to enter the program, and participating healthcare providers will not be able to choose to participate in any additional episode types. Accordingly, our ability to grow our business under the BPCI-A program requires us to maximize savings rates and, in turn, our revenue. In addition, in September 2020, CMS announced changes to BPCI-A for 2021. These changes include an adjustment to the baseline period on which clinical episode prices are calculated, such that prices for 2021 will be calculated on the basis of historical experience that includes the first year of the BPCI-A program. As a result, benchmark episode prices could be lower than in prior years because BPCI-A care redesign and savings measures will be reflected in a portion of the benchmark period. In addition, CMS announced changes to the pricing methodology by which benchmark episode prices will be calculated, which could impact both (i) provider demand to take on certain episodes (and therefore affect program size), and (ii) savings rate opportunities. Further, when healthcare providers selected episodes for 2021 at the end of 2020, CMS required such selections to be made in groups of similar episodes, rather than individually. For example, a healthcare provider that previously only participated in hip replacement episodes may also be required to participate in knee and shoulder replacement episodes as well. This could impact provider demand for various episodes and correspondingly affect program size. Moreover, the clinical episodes selected by healthcare providers for 2021 will also apply to 2022 and 2023, meaning the selections will be binding through 2023. Any of these changes could lead to a decline in the program size and/or savings rates we are able to achieve for our BPCI-A services.
The BPCI-A Program in its current form expires at the end of 2023, and it is not currently clear whether the BPCI-A program will be renewed in 2023, or if renewed, what form it will take. If the BPCI-A program is not renewed at the end of 2023, and we have not diversified our revenue streams in our Episodes of Care Services
32
Table of Contents
segment by that time, our business, results of operations and financial condition will be negatively affected due to our substantial dependence on the BPCI-A program in this segment. Even if the BPCI-A program is renewed, if CMS materially changes the BPCI-A program as compared to its current form, our business, results of operations and financial condition could also be negatively affected. For example, the predecessor BPCI program (“BPCI Classic”) expired in the third quarter of 2018 and CMS launched the BPCI-A program in the fourth quarter of 2018. CMS made significant changes to BPCI-A as compared to BPCI Classic, including reducing the number of episodes that can be managed and modifying the definitions for many of the episodes, as well as opening the program up to new provider partners (most of whom did not have prior experience participating in episode of care programs). CMS also increased the discount used to generate the benchmark episode price from 2% to 3%. This had the effect of increasing the savings threshold that must be achieved before we are able to earn our administrative fee, or any incremental savings that are shared with our provider partners and ultimately reduced our savings rate in 2019 compared to the savings rate achieved under BPCI Classic in 2018. CMS could make similarly material changes to BPCI-A in 2023 or earlier. If the BPCI-A program is not renewed at the end of 2023, or is amended in any material way following the expiration of the current program in 2023, and we are not able to adapt our product offerings quickly in response to any changes to the program, our business, results of operations and financial condition will be negatively affected.
Our business depends on our ability to maintain and grow our network of high-quality providers. If we are unable to do so, our future growth would be limited and our business, financial condition and results of operations would be harmed.
Our success is dependent upon our continued ability to maintain and grow our credentialed network of high-quality providers. We compete with numerous healthcare providers, primarily hospitals, post-acute care facilities, telehealth operators and locum tenens staffing agencies in attracting and retaining physicians and nurse practitioners. As a result, providers could refuse to contract with us, limit or reduce the number of hours they allocate to work for us under their contracts, be unavailable or otherwise decline to work during key hours of the business day, demand higher payments or take other actions that could result in higher operating costs or less attractive service for our customers. In some markets, the lack of availability of providers has become a significant operating issue and could continue to be a significant operating issue in the future. This shortage may negatively impact our future growth and require us to continue to increase the fees we pay our providers in order to recruit and retain qualified providers.
Identifying high-quality providers, credentialing and negotiating contracts with them and evaluating, monitoring and maintaining our network requires significant time and resources. We employ the great majority of our providers on an independent contractor basis. If we are not successful in maintaining our relationships with providers, these providers may refuse to renew their contracts with us or may choose to spend fewer hours, or fewer key hours of the business day, working for us in lieu of our competitors. Our ability to develop and maintain satisfactory relationships with high-quality providers also may be negatively impacted by other factors not associated with us, such as regulatory changes impacting providers. In addition, the perceived value of our solutions and our reputation may be negatively impacted if the services provided by one or more of our providers are not satisfactory to customers and their members. Any such issue with one of our providers may expose us to public scrutiny, adversely affect our reputation, expose us to litigation or regulatory action, and otherwise make our operations vulnerable. Many of our providers have not provided services to us within the past 12 months and may not be available to us to meet future capacity needs. The failure to maintain or grow our selective network of providers or the failure of those providers to meet and exceed our customers’ expectations, may result in a loss of or inability to grow or maintain our customer base, which could adversely affect our business, financial condition and results of operations.
33
Table of Contents
If we do not continue to innovate and provide services that are useful to customers and achieve and maintain market acceptance, we may not remain competitive, and our revenue and results of operations could suffer.
Our success depends on our ability to keep pace with technological developments, satisfy increasingly sophisticated customer requirements, and achieve and maintain market acceptance on our existing and future services in the rapidly evolving market for the management and administration of healthcare services in the United States. In addition, market acceptance and adoption of our existing and future services depends on the acceptance by health plans and provider partners as to the distinct features, cost savings and other perceived benefits of our existing and future offerings as compared to competitive alternative services. Our competitors are constantly developing products and services that may become more efficient or appealing to our customers. As a result, we must continue to invest significant resources in research and development in order to enhance our existing services and introduce new services that our customers will want, while offering our existing and future services at competitive prices. If we are unable to predict customer preferences or industry changes, or if we are unable to modify our existing and future services on a timely or cost-effective basis, we may lose customers and our business financial condition and results of operations may be harmed.
Our latest developing services include, Biopharma solutions and IHE+ in the Home & Community Services segment and the Commercial Episodes of Care solutions, TTH and ACO services in our Episodes of Care Services segment. There is no guarantee that these solutions will prove effective, achieve market acceptance or generate revenue in the long term.
If we are not successful in demonstrating to existing and potential customers the benefits of our existing and future services, or if we are not able to achieve the support of health plans and provider partners for our existing and future services, our revenue may decline or we may fail to increase our revenue in line with our forecasts. Our results of operations would also suffer if our technology and other innovations are not responsive to the needs of our customers, are not timed to match the corresponding market opportunity, or are not effectively brought to market.
We have a limited operating history with certain of our solutions, which makes it difficult to predict our future results of operations.
We went live with certain solutions very recently. For example, in 2019 and 2020 we launched our ACO services, Biopharma, IHE+, Commercial Episodes of Care and TTH program. As a result of our limited operating history with these and other solutions, as well as limited amount of time serving certain customers, our ability to accurately forecast our future results of operations is limited and subject to a number of uncertainties, including our ability to plan for and model future growth. Our historical revenue and growth trends should not be considered indicative of our future performance. Our revenue growth could slow or decline for a number of reasons, including slowing demand for our more established solutions, but also because of a failure for customers to adopt our newer solutions, into which we have invested heavily and expect to continue to do so in the future. If our assumptions regarding the value proposition of and appropriate pricing for our newer solutions and solutions still under development prove incorrect or change based on any number of factors, our operating and financial results could differ materially from our expectations, and our business and prospects could suffer materially.
In particular, we intend to diversify our revenue streams in our Episodes of Care Services segment through our Commercial Episodes of Care program. While we have significant experience managing episodes through the BPCI-A program, our Commercial Episodes of Care program is substantially different from BPCI-A. For example, the suite of tools that we provide to customers is different, the various inputs that we use to estimate program size and savings are different and our entire administrative fee is at risk, meaning if a customer generates losses one year, we cannot recoup that through savings in a subsequent year. As a result, our experience managing episodes under BPCI-A may not translate into an ability to successfully manage episodes under our Commercial Episodes of Care program and we may not be successful at operating this program.
34
Table of Contents
We operate in a competitive industry, and if we are not able to compete effectively our business would be harmed.
The market for healthcare solutions and services is intensely competitive. We compete with large and small companies that are formulating innovative ways to transition the healthcare market to value-based care with an increasing focus on treating individuals within the home. The market for services supporting this transition is a highly fragmented market with direct and indirect competitors that offer varying levels of impact to key stakeholders, such as consumers, employers, health networks, healthcare providers and health plans. Our competitive success is contingent on our ability to simultaneously address the needs of key stakeholders efficiently and with superior outcomes at scale compared with competitors. Competition in our market involves rapidly changing technologies, evolving regulatory requirements and industry expectations, frequent new product and service introductions and changes in customer requirements. If we are unable to keep pace with the evolving needs of our customers and their members and patients or continue to develop and introduce new applications and services in a timely and efficient manner while being mindful of the pricing of our solutions and those of our competitors and addressing complex regulatory requirements, demand for our solutions and services may be reduced and our business and results of operations would be harmed. In addition, if we are unable to increase savings rates within managed episodes for our BPCI-A customers, demand for our BPCI-A solutions and services may also be reduced, which would also harm our business, financial condition results of operations and prospects.
Our business and future growth are highly dependent on gaining new customers and retaining existing customers in our Home & Community Services segment and increasing savings rates under our BPCI-A solution in our Episodes of Care Services segment. We currently face competition in the healthcare industry for our services and solutions from a range of companies and healthcare providers looking to innovate in the value-based care space. Many of our competitors offer similar and/or competing services, and are continuing to develop additional products and becoming more sophisticated and effective. Our principal competitors in both of our segments also vary considerably in type and identity by market. There have also been increasing indications of interest from non-traditional healthcare providers and others to enter the in-home diagnostic and evaluative services space and/or develop innovative technologies or business activities that could be disruptive to the healthcare risk management industry. For example, many large health plans use their considerable resources to invest in building similar provider networks or technology platforms. In addition, in recent years, health plans have and may continue to acquire in-home diagnostic and evaluative services capabilities, taking what we do in-house.
As a result, some of our competitors may have longer operating histories and significantly greater resources than we do. Further, our current or potential competitors may be acquired by third parties with greater available resources. As a result, our competitors may be able to respond more quickly and effectively than we can to new or changing opportunities, technologies, regulations or customer requirements and may have the ability to initiate or withstand substantial price competition. Accordingly, new competitors may emerge that have greater market share, a larger customer base, more sophisticated proprietary technologies, greater financial resources and larger sales forces than we have, which could put us at a competitive disadvantage. Our competitors could also be better positioned to serve certain segments of the healthcare market, which would limit our growth. In light of these factors, even if our solutions are more effective than those of our competitors, current customers may accept competitive solutions in lieu of purchasing our solutions. If we are unable to successfully compete in the value-based healthcare market, our business would be harmed.
Our sales cycle can be long and unpredictable and requires considerable time and expense. As a result, our sales, revenue, and cash flows are difficult to predict and may vary substantially from period to period, which may cause our results of operations to fluctuate significantly.
The timing of our sales, revenue, and cash flows is difficult to predict, in particular with respect to our new sales and cross-sell efforts, because of the length and unpredictability of our sales cycle. The sales cycle for our
35
Table of Contents
services from initial contact to implementation of services varies widely by potential customer. Some of our potential customers undertake a significant and prolonged evaluation process to determine whether our services meet the specific needs of their organization, as well as other goals, which frequently involves evaluation of not only our services but also an evaluation of other available services. Such evaluations have in the past resulted in extended sales cycles that, due to changes in corporate objectives or leadership involved in the selection process and other factors, may result in delayed or suspended decision-making in awarding the sale. In addition, when government programs we participate in change, it can take a significant period of time for existing customers to familiarize themselves with new programs and for us to engage new customers in these programs. For example, when the BPCI Classic program expired at the end of the third quarter of 2018 and the BPCI-A program launched in the fourth quarter of 2018, it took a significant amount of time for existing customers to become accustomed to the new program and it took several months to sign up new customers to the program. As we introduce new products, we also expect there to be a lengthy onboarding process with our customers as they learn more about our services and choose when and how to adopt them. For example, in 2020, we launched our Commercial Episodes of Care business. Once we have a payor customer that wants to sponsor an episode program, we do not begin generating any revenue until we have helped them design the program, signed up provider partners to participate in the program and initiated episodes, which further extends the length of time between initial contact to full implementation of services. Further, completed episodes are retrospectively reconciled following semiannual performance measurement periods, significantly delaying cash generation. In addition, our sales cycle may become more lengthy and difficult if prospective customers slow down their decision-making about purchasing new services due to the effects of COVID-19. During the sales cycle, we expend significant time and money on sales and marketing activities, which lowers our operating margins, particularly if no sale occurs. For example, there may be unexpected delays in a potential customer’s internal processes, which involve intensive technological, legal, financial, operational, and security reviews. In addition, our services represent a significant purchase and require customers to take on risk. In addition, the significance and timing of our offering enhancements, and the introduction of new products by our competitors, may also affect our potential customers’ purchases. For all of these reasons, it is difficult to predict whether a sale will be completed, the particular period in which a sale will be completed, or the period in which revenue from a sale will be recognized.
Our ability to complete IHEs can be negatively impacted by a variety of factors outside of our control.
Our ability to complete IHEs depends on the plan members provided by our customers for purposes of our TML agreeing to an IHE. Our outreach to members each year generally starts with a TML which is provided by our customers or created by us from information provided by our customers, which may be supplemented or amended during the year. Our ability to complete IHEs in a period or to do so in a cost-effective manner may be negatively affected if the initial TML includes a significant number of plan members in difficult-to-reach jurisdictions or if the members on the TML are less likely to accept an IHE for any number of reasons. Decisions by our customers with respect to the TML, including a reduction in the number of members included in the TML (or the member list from which it is derived), may impact the number of IHEs we are able to complete and, as a result, our revenue. In addition, our ability to schedule and complete IHEs may also be negatively affected if we receive incorrect or incomplete contact information for plan members on the TML. We are not able to call members to schedule an IHE if we have not received their contact information directly from the member or their health plan as a result of the Telephone Consumer Protection Act of 1991 (the “TCPA”), and as such if the contact information provided by health plans is incomplete or incorrect, we may have difficulty scheduling IHEs with members on our TML. In addition, from time to time, our telephone numbers may be mistakenly labeled as spam by cell phone carriers. If we do not timely catch any labeling of our telephone number as spam, the numbers of members answering our calls for scheduling IHEs would fall, any of which would also have a negative impact on our ability to complete IHEs, and as a result, our revenue.
36
Table of Contents
Seasonality may cause fluctuations in our sales and results of operations, and our quarterly results may fluctuate significantly, which could adversely impact the value of our Class A common stock.
Our quarterly results of operations, including our revenue, loss from operations, net loss and cash flows, have varied and may vary significantly in the future, and period-to-period comparisons of our results of operations may not be meaningful. Accordingly, our quarterly results should not be relied upon as an indication of future performance. Historically, quarterly financial results in our Home & Community Services segment have generally been lower in the fourth quarter as compared to other quarters as the volume of individuals on our TML who have yet to receive an IHE and whom we are still able to contact declines as the year progresses and we complete IHEs. In addition, revenue in our Episodes of Care Services segment generally is higher in the second and fourth quarters. Under the BPCI-A program, we recognize the revenue attributable to episodes reconciled during each six-month episode performance measurement period over a 13-month performance obligation period that commences in the second or fourth quarter of each year, depending on the relevant contract with our provider partners. See “Management’s discussion and analysis of financial condition and results of operations—Critical accounting policies.” As a result, during the first and third quarters of each year, we recognize three months of revenue for each of two overlapping performance obligation periods, and during the second and fourth quarter of each year, we recognize revenue relating to three overlapping performance obligation periods, representing three months of revenue from one performance obligation period, three months of revenue from a second, overlapping performance obligation period, and one month of revenue from a third, overlapping performance obligation period (representing the thirteenth month of the third performance obligation period). We also recognize episodes revenue based on our estimates of savings realized. The semiannual reconciliations for each performance measurement period under our episodes programs are received or generated in the second and fourth quarter of each year, and indicate the actual savings realized. As a result, we experience seasonality in our results of operations.
Our quarterly financial results may also fluctuate as a result of a variety of factors, many of which are outside of our control, including, without limitation, the following:
| • | the addition or loss of customers in either of our segments; |
| • | the amount and timing of operating expenses related to the maintenance and expansion of our business, operations and infrastructure, including upfront capital expenditures, costs related to provider recruitment (including incentive bonuses) and other costs related to developing new solutions and upgrading our technology; |
| • | our ability to effectively manage the size and composition of our proprietary network of providers relative to the level of demand for services from our customers; |
| • | the timing and success of introductions of new solutions by us; and |
| • | the timing of expenses related to the development or acquisition of technologies or businesses and potential future charges for impairment of goodwill from acquired companies. |
In addition, the seasonality of our businesses could create cash flow management risks if we do not adequately anticipate and plan for periods of comparatively decreased cash flow, which could negatively impact our ability to execute on our strategy, and in turn could harm our results of operations. Accordingly, our results for any particular quarter may vary for a number of reasons, and we caution investors to evaluate our quarterly results in light of these factors.
The information that we provide to our health plan and provider partners could be inaccurate or incomplete, which could harm our business, financial condition and results of operations.
We provide healthcare-related information for use by our health plan and provider partners. Because data in the healthcare industry is complex, fragmented in origin and inconsistent in format, the overall quality of data in the healthcare industry is poor, and we frequently encounter data issues and errors.
37
Table of Contents
With respect to our health plan customers in our Home & Community Services segment, IHEs that we submit to health plans may impact data that support the Medicare Risk Adjustment Factor (“RAF”) scores attributable to members. These RAF scores determine, in part, the revenue to which the health plans are entitled for specific members. Each health plan generally relies on us and our providers to appropriately document and support such RAF data. Each health plan also relies on us to appropriately code our IHEs. If the risk adjustment data we provide is the result of IHEs that have not been properly completed (e.g., if a provider failed to visit an individual at their home or incorrectly captured an individual’s data), unsubstantiated diagnoses or incorrect risk adjustment coding, our reputation may suffer and our ability to attract and retain future customers may be harmed. Although we have certain mechanisms in place to flag instances in which an IHE may not have taken place, given the breadth of our network, we are not able to monitor and detect all instances in which a provider fails to visit an individual. If we do not continue to improve our monitoring processes in place and a significant portion of the risk adjustment data we provide is the result of IHEs that did not actually take place, our reputation may also suffer. In addition, corrected or adjusted information may be reflected in financial statements for periods subsequent to the period in which the revenue was recorded. We might be required to refund a portion of the revenue that we received, which, depending on the magnitude of the refund, could damage our relationship with the applicable health plan and could have a material adverse effect on our business, results of operations, financial condition and cash flows.
Additionally, CMS audits Medicare Advantage plans for documentation to support RAF-related payments for members chosen at random. It is possible that claims associated with members with higher RAF scores could be subject to more scrutiny in a CMS or plan audit. There is a possibility that a health plan may seek repayment from us should CMS make any payment adjustments to the Medicare Advantage plan as a result of its audits and an assessment of the RAF scores our IHEs have supported. The plans also may seek to hold us liable for any penalties owed to CMS for inaccurate or unsupportable RAF scores provided by us. In addition, because the government or a whistleblower could argue that our errors caused the plan to submit false claims to CMS, we could potentially be liable for treble damages and per-violation penalties up to $22,363 to the government under the False Claims Act (“FCA”). If a plan is found similarly liable under the FCA for submitting false claims or making false statements to CMS, it may also seek indemnification or contribution from us to the extent it believes the liability was caused by errors in the information we provided. CMS has indicated that payment adjustments will not be limited to RAF scores for the specific Medicare Advantage enrollees for which errors are found but may also be extrapolated to the entire Medicare Advantage plan subject to a particular CMS contract. CMS has described its audit process as plan-year specific and stated that it will not extrapolate audit results for plan years prior to 2011. Because CMS has not stated otherwise, there is a risk that payment adjustments made as a result of one plan year’s audit would be extrapolated to prior plan years after 2011.
There can be no assurance that one of our health plan customers will not be selected or targeted for review by CMS or that the outcome of such a review will not result in a material adjustment in our revenue and profitability.
For our episodes and care redesign solutions, we assume the risk that the cost of services provided by our customers will be higher than benchmark prices for specific episodes.
In our Episodes of Care Services segment, we receive a percentage of all savings and are responsible for a percentage of any losses generated in connection with a specific episode of care as compared to the relevant benchmark price, in addition to receiving an administrative fee that is paid out of any savings generated. As a result, our ability to generate revenue under these contracts is dependent on our provider partners’ ability to achieve cost savings compared to the relevant benchmark price for any given episode, whether that price is set by CMS under the BPCI-A program or in collaboration with the relevant health plan customer in our Commercial Episodes of Care business. If any of our provider partners are unsuccessful at achieving such cost savings, it may negatively impact our business, results of operations and financial condition.
Generally, when provider partners first enter an episode of care program, the savings rates are low as they begin to implement care redesign and integrate with our systems, which can negatively impact our revenues for
38
Table of Contents
certain periods. We provide a variety of tools and services to our provider partners to help them achieve savings against established benchmark prices for specific episodes. For example, using our data analytics capabilities, we help them identify individuals that will be attributed to a BPCI-A bundle early in their care journey. If we are delayed in implementing our data feed, or if we misidentify individuals likely to be attributed to a BPCI-A bundle or experience delays in identifying such individuals, our customers may be less successful at achieving cost savings, which may also adversely affect our reputation and ability to attract future customers as well as our business, financial condition and results of operations. Historically, under the BPCI Classic program, savings rates increased over time as provider partners became more comfortable with the program, implemented care redesign and integrated with our systems, and by the end of the BPCI Classic program, our savings rate was approximately 10%. There can be no assurance that the same trend will continue under the BPCI-A program, which began in late 2018, or that we will see similar trends in our other episodes-based programs.
The tools and services we provide to participants in episode of care programs are in part covered by our administrative fees, which are paid out of any savings generated and are therefore at risk. Under many of our contracts, we are able to carry forward administrative fees not covered by savings in a given period. However, under certain contracts, in particular in our new Commercial Episodes of Care business, we do not in all instances have the ability to recoup administrative fees out of future program savings under our contracts with our customers. Any inability to recoup our administrative fees or obligation to pay for losses associated with the costs of episodes of care exceeding the relevant benchmark price may also have a negative impact on our business, results of operations and financial condition.
There are significant risks associated with estimating the program size and the amount of savings that we may be able to achieve under our agreements with health plans and provider partners under the BPCI-A program and other episode-based programs that we manage, and if our estimates of revenue are materially inaccurate, it could impact the timing and the amount of our revenue recognition or have a material adverse effect on our business, results of operations, financial condition and cash flows.
There are significant risks associated with estimating the amount of revenues that we recognize under our agreements with health plans and provider partners in a reporting period. Our revenue recognition for each semiannual reconciliation under the BPCI-A program is tied to a 13-month performance obligation for an episode of care beginning at the start of the episodes of care through receipt and validation of the semiannual reconciliation from CMS as well as the provision and explanation of statements of performance under the program to each of our customers. The transaction price is 100% variable and therefore we estimate an amount that we expect to be entitled to receive for each six-month set of episodes of care eligible for the program from our customers. We have similar variable transaction prices and periods over which we satisfy our performance obligation in the other episode-based contacts that we manage.
Under the BPCI-A program, for each partner agreement, we charge an administrative fee, which is based on a stated percentage of program size, and receive a defined share of program savings or losses, if any. Under certain contracts, our administrative fees and share of program savings or losses decrease as program size increases. In order to estimate this variable consideration, we estimate the expected program size as well as the expected savings rate for each six-month period of episodes of care. The estimate is performed both at the onset of each performance measurement period based on information available at the time and at the end of each reporting period. We adjust our estimates at the end of each performance measurement period, generally in the second and fourth quarter each year, and may further adjust at the end of each reporting period to the extent new information indicates a change is needed. Although our estimates are based on the information available to us at each reporting date, several factors may cause actual revenue earned to differ from the estimates recorded each period. These include, among others, limited historical experience as the current BPCI-A program only commenced in the fourth quarter of 2018 and the first reconciliation was not received until the fourth quarter of 2019, CMS-imposed restrictions on the definition of episodes and benchmark prices, healthcare provider participation and other limitations of the program beyond our control. In addition, in response to the COVID-19 pandemic, CMS has announced changes to the BPCI-A program that have allowed healthcare providers to
39
Table of Contents
exclude episodes under certain circumstances. This has introduced additional uncertainty into our ability to accurately estimate program size and savings. See “—Our operations have been, and may continue to be, significantly disrupted by the COVID-19 pandemic, and our business, financial condition and results of operations have been negatively impacted.”
We may not realize the benefits of our combination with Remedy Partners.
Our business is the product of various strategic combination transactions and there is no guarantee that the benefits of such combinations will be realized. In particular, our core businesses—payment models based on individual episodes of care and in-home patient health risk assessments—reflect the disparate businesses of legacy Remedy Partners and legacy Signify Health, respectively. We combined with Remedy Partners at the end of 2019 in an effort to become integral to how health plans and healthcare providers successfully implement value-based payments. Although we believe we have successfully integrated Remedy Partners into our operations, our revenue is generated from contracts with our customers within our two operating segments, Home & Community Services and Episodes of Care Services, that largely reflect the legacy businesses of Remedy Partners and Signify Health, respectively. These businesses have historically operated as two separate businesses and many of their operations are still being integrated. There remain significant questions as to whether the market will adopt our discrete solutions in a holistic and integrated fashion, if our customers only utilize a portion of our offerings in a selective manner it could materially impair our ability to drive value-based healthcare payment in a meaningfully way. Ultimately, this could impact our ability to convince customers of the benefits of our model and value proposition, which could materially adversely affect our business, results of operations and financial condition.
Changes in our health plan and provider partner mix could adversely affect our revenues and results of operation.
The amounts we receive for our services in our Home & Community Services segment are determined by a number of factors, including each health plan’s negotiated contract, the number of IHEs completed and the number and type of ancillary services selected by each health plan. Health plan mix can affect the average per-visit fee, the geographic mix of plan members we are visiting, the mix of members that are Medicare versus Medicaid recipients and the selection of IHE, vIHE or IHE+ solutions, which can also influence factors such as the conversion rate associated with the number of members who agree to receive IHEs, the total number of IHEs completed and number of ancillary services selected by the health plan for its members.
The amounts we receive for our services in our Episodes of Care Services segment are similarly determined by a number of factors, including the terms of each health plan or provider partner’s negotiated contract, the amount of our administrative fee, our share of episode savings and risk for episode losses and the health plans’ and provider partners’ share of savings, as well as the overall program size and the savings rate generated (and therefore are at risk) under each managed episode. We receive a percentage of the total program size as an administrative fee that is paid out of any savings generated and a portion of the net savings generated, if any, upon completion of an episode. Provider partner mix impacts the type of episodes managed, our administrative fee and our savings rate.
Risks related to our limited operating history, financial position and future growth
We have a history of net losses, we anticipate increasing expenses in the future, and we may not be able to achieve or maintain profitability.
We have incurred net losses on an annual basis since our inception in 2009. We incurred net losses of $28.5 million and $28.9 million for the years ended December 31, 2019 and 2018, respectively, and $15.2 million and $20.5 million for the nine months ended September 30, 2020 and 2019, respectively. Our accumulated deficit as of September 30, 2020 was $82.7 million. We have encountered and will continue to
40
Table of Contents
encounter risks and difficulties frequently experienced by growing companies in rapidly changing industries, including increasing expenses as we continue to grow our business. We anticipate our losses could continue as we expect to invest heavily in increasing our products and services, expanding our operations, hiring additional employees and operating as a public company. These efforts may prove more expensive than we currently anticipate, and we may not succeed in increasing our revenue sufficiently to offset these higher expenses. To date, we have financed our operations principally from revenue from our products, the sale of our equity and services and the incurrence of indebtedness. Although our cash flow from operations was positive for the years ended December 31, 2018 and 2019, and the nine months ended September 30, 2019 and 2020, we may not generate positive cash flow from operations or profitability in any given period, and our limited operating history may make it difficult for you to evaluate our current business and our future prospects. Moreover, under the Amended LLC Agreement that Cure TopCo, LLC will enter into in connection with the Reorganization Transactions, we may elect to satisfy the rights of the Continuing Pre-IPO LLC Members to redeem their LLC Units in cash instead of through the issuance of additional shares of Class A common stock. If the Continuing Pre-IPO LLC Members exercise their redemption rights over a significant portion of their LLC Units and we elect to satisfy those redemptions in cash, it may also negatively impact our cash position in future periods.
Investments in our business may be more costly than we expect, and if we do not achieve the benefits anticipated from these investments, or if the realization of these benefits is delayed, they may not result in increased revenue or growth in our business. If our growth rate were to decline significantly or become negative, it could adversely affect our financial condition and results of operations. If we are not able to achieve or maintain positive cash flow in the long term, we may require additional financing, which may not be available on favorable terms or at all and/or which would be dilutive to our stockholders. If we are unable to successfully address these risks and challenges as we encounter them, our business, results of operations and financial condition would be adversely affected. Our failure to achieve or maintain profitability could negatively impact the value of our Class A common stock.
Our future revenues may not grow at the rates they historically have, or at all.
We have experienced significant growth since our inception in 2009. Our relatively limited operating history makes it difficult to evaluate our current business and prospects and plan for our future growth. Revenue and our customer base may not grow at the same rates they historically have, or they may decline in the future. Our future growth will depend, in part, on our ability to:
| • | continue to attract new customers and maintain existing customers; |
| • | price our solutions effectively so that we are able to attract new customers, expand sales to our existing customers and maintain profitability; |
| • | demonstrate the value our solutions provide; |
| • | expand our solutions to meet changing customer demands; |
| • | achieve increasing savings for our customers; |
| • | retain and maintain relationships with high-quality and respected providers; and |
| • | attract and retain highly qualified personnel to support all customers. |
We may not successfully accomplish all or any of these objectives, which may affect our future revenue, and which makes it difficult for us to forecast our future results of operations. In addition, if the assumptions that we use to plan our business are incorrect or change in reaction to changes in our market, it may be difficult for us to achieve profitability. You should not rely on our revenue for any prior quarterly or annual periods as an indication of our future revenue or revenue growth.
41
Table of Contents
In addition, we expect to continue to expend substantial financial and other resources on:
| • | sales and marketing; |
| • | new solutions; |
| • | our technology infrastructure, including systems architecture, scalability, availability, performance and security; |
| • | acquisition of businesses to help achieve our growth strategy; and |
| • | general administration, including increased legal and accounting expenses associated with being a public company. |
These investments may not result in increased revenue growth in our business. If we are unable to increase our revenue at a rate sufficient to offset the expected increase in our costs, our business, financial position, and results of operations will be harmed, and we may not be able to maintain profitability over the long term. Additionally, we may encounter unforeseen operating expenses, difficulties, complications, delays and other unknown factors, such as burdens resulting from regulatory compliance and unexpected regulatory developments, that may result in losses in future periods. If our revenue growth does not meet our expectations in future periods, we may not maintain profitability in the future, our business, financial position and results of operations may be harmed.
We may be unable to successfully execute on our growth initiatives, business strategies, or operating plans.
We are continually executing on growth initiatives, strategies, and operating plans designed to enhance our business and extend our existing and future offerings to address evolving needs. For example, in 2019 and 2020, we developed our vIHE to address COVID-19 challenges, our TTH, ACO and Commercial Episodes services to expand our reach in the post-acute care management space, and our Biopharma and Signify Community services to expand our offerings in the in-home evaluation and care management space. The anticipated benefits from these efforts are based on several assumptions that may prove to be inaccurate. Moreover, we may not be able to successfully complete these growth initiatives, strategies, and operating plans and realize all of the benefits, including growth targets and cost savings, that we expect to achieve, or it may be more costly to do so than we anticipate. A variety of risks could cause us not to realize some or all of the expected benefits in the anticipated time period, or at all. These risks include, among others, delays in the anticipated timing of activities related to such growth initiatives, strategies, and operating plans, increased difficulty and cost in implementing these efforts, including difficulties in complying with regulatory requirements, the incurrence of other unexpected costs associated with operating our business, and lack of acceptance by our customers. Moreover, our continued implementation of these programs may disrupt our operations and performance. We also pride ourselves on our culture of compliance. As we continue to grow and add additional personnel to our teams, we may find it difficult to maintain this culture of compliance, which could negatively impact our future success. For example, as we grow our Commercial Episodes solution, we will need to increase the number of clinical episodes that we administer. If we are unable to hire additional personnel to process these claims in a timely and compliant manner, our ability to grow this solution may be negatively impacted. As a result, we cannot assure you that we will realize these benefits. If, for any reason, the growth we realize from any of our solutions is less than we estimate or the implementation of these growth initiatives, strategies, and operating plans adversely affect our operations or cost more or take longer to effectuate than we expect, or if our assumptions prove inaccurate, our business may be harmed.
Our level of indebtedness may increase and reduce our financial flexibility.
As of September 30, 2020, we had approximately $350.2 million of debt outstanding under our Credit Agreement, which includes $77.0 million drawn in the first nine months of 2020. Despite this level of indebtedness, we may incur substantial additional indebtedness under the Credit Agreement or otherwise in the
42
Table of Contents
future. Our borrowings, current and future, will require interest payments and need to be repaid or refinanced, which could require us to divert funds identified for other purposes to debt service and could create additional cash demands or impair our liquidity position and add financial risk for us. Diverting funds identified for other purposes for debt service may adversely affect our business and growth prospects. If we cannot generate sufficient cash flow from operations to service our debt, we may need to refinance our debt, dispose of assets, reduce or delay expenditures or issue equity to obtain necessary funds. We do not know whether we would be able to take any of these actions on a timely basis, on terms satisfactory to us or at all.
Our level of indebtedness could affect our operations in several ways, including the following:
| • | a significant portion of our cash flows could be used to service our indebtedness; |
| • | it may be difficult for us to satisfy our obligations with respect to our debt; |
| • | the covenants contained in the Credit Agreement or in future agreements governing our outstanding indebtedness may limit our ability to borrow additional funds, dispose of assets and make certain investments; |
| • | our debt covenants may also affect our flexibility in planning for, and reacting to, changes in the economy and in our industry; |
| • | a high level of debt would increase our vulnerability to general adverse economic and industry conditions; |
| • | a high level of debt may place us at a competitive disadvantage compared to our competitors that are less leveraged and therefore may be able to take advantage of opportunities that our indebtedness would prevent us from pursuing; and |
| • | a high level of debt may impair our ability to obtain additional financing in the future for working capital, capital expenditures, debt service requirements, acquisitions or other purposes. |
If we are unable to generate sufficient cash flows to pay the interest on our debt, future working capital, borrowings or equity financing may not be available to pay or refinance such debt. See “Management’s discussion and analysis of financial condition and results of operations—Liquidity and capital resources—Indebtedness.”
Risks related to governmental regulation
If we are unable to effectively adapt to changes in the healthcare industry, including changes to laws and regulations regarding or affecting the U.S. healthcare reform, our business may be harmed.
Due to the importance of the healthcare industry in the lives of all Americans, federal, state, and local legislative bodies frequently pass legislation and promulgate regulations relating to healthcare reform or that affect the healthcare industry. As has been the trend in recent years, it is reasonable to assume that there will continue to be increased government oversight and regulation of the healthcare industry in the future. This may be particularly true in coming years as a result of the COVID-19 pandemic. We cannot assure you as to the ultimate content, timing or effect of any new healthcare legislation or regulations, nor is it possible at this time to estimate the impact of potential new legislation or regulations on our business. It is possible that future legislation enacted by Congress or state legislatures, or regulations promulgated by regulatory authorities at the federal or state level, could adversely affect our business by making our solutions obsolete or making it difficult or impossible to create new service offerings. In particular, any changes to Medicare, Medicaid or other governmental healthcare programs, as well as newly promulgated constraints on data sharing, could negatively impact demand for our solutions, such as IHEs, or decrease participation, or result in the discontinuation of, government programs like BPCI-A, which could have a material adverse effect on our business, financial condition and results of operations.
43
Table of Contents
While we believe that we have structured our agreements and operations in material compliance with applicable healthcare laws and regulations, there can be no assurance that we will be able to successfully address changes in the current regulatory environment. We believe that our business operations materially comply with applicable healthcare laws and regulations. However, some of the healthcare laws and regulations applicable to us are subject to limited or evolving interpretations, and a review of our business or operations by a court, law enforcement or a regulatory authority might result in a determination that could have a material adverse effect on us. Furthermore, the healthcare laws and regulations applicable to us may be amended or interpreted in a manner that could have a material adverse effect on our business, prospects, results of operations and financial condition.
If our providers are characterized as employees, we would be subject to adverse effects on our business and employment and withholding liabilities.
We structure the majority of our relationships with our providers in a manner that we believe results in an independent contractor relationship, not an employee relationship. An independent contractor is generally distinguished from an employee by his or her degree of autonomy and independence in providing services. A high degree of autonomy and independence is generally indicative of a contractor relationship, while a high degree of control is generally indicative of an employment relationship. Although we believe that our providers are properly characterized as independent contractors, individuals, interest groups, tax or other regulatory authorities have in the past and may in the future challenge our characterization of these relationships. For example, we have been subject to allegations, lawsuits and inquiries challenging our characterization of these relationships in the past. While these past challenges have not had a material impact on us, there can be no assurance that similar challenges in the future will not have a material impact our business. If regulatory authorities or state or federal courts were to determine that our providers are employees, and not independent contractors, our mobile network of providers would be disrupted and we would be required to withhold income taxes, to withhold and pay social security, Medicare and similar taxes and to pay unemployment and other related payroll taxes. We would also be liable for unpaid past taxes, subject to penalties and increased operating costs moving forward. As a result, any determination that our providers are our employees could have a material adverse effect on our business, financial condition and results of operations.
Changes in the rules governing Medicare or other federal healthcare programs could have a material adverse effect on our financial condition and results of operations.
In our Home & Community Services segment, the majority of our revenues are derived from IHEs, which support our customers’ participation in Medicare Advantage. The Medicare program and related programs under Medicare are subject to frequent change. These include statutory and regulatory changes, rate adjustments (including retroactive adjustments), administrative or executive orders and government funding restrictions. Likewise, in our Episodes of Care Services segment, we generate the majority of our revenue through the BPCI-A program, which is also intended to benefit Medicare members. The BPCI-A program was established and is administered by the CMS Center for Medicare & Medicaid Innovation (“CMMI”). In turn, the Patient Protection and Affordable Care Act, as amended by the Health Care Education and Reconciliation Act (collectively, the “ACA”), established and continues to provide funding for CMMI and its initiatives, including the BPCI-A program. If the ACA were repealed or replaced, the BPCI-A program could be eliminated as a result, which would have an adverse effect on our business, results of operations and financial condition.
Since its enactment, there have been judicial and congressional challenges to certain aspects of the ACA, as well as recent efforts by the Trump administration to repeal or replace certain aspects of the ACA, and we expect such challenges and amendments to continue. For example, the Tax Cuts and Jobs Act of 2017 (“TCJA”) includes a provision reducing to $0, effective January 1, 2019, the tax-based shared responsibility payment imposed by the ACA on certain individuals who fail to maintain qualifying health coverage for all or part of a year that is commonly referred to as the “individual mandate.” On December 14, 2018, a U.S. District Court Judge in the Northern District of Texas, ruled that the individual mandate is a critical and inseverable feature of the ACA, and therefore, because it was modified under the TCJA, the remaining provisions of the ACA are
44
Table of Contents
invalid as well. On December 18, 2019, the U.S. Court of Appeals for the 5th Circuit upheld the District Court ruling that the individual mandate was unconstitutional and remanded the case back to the District Court to determine whether the remaining provisions of the ACA are invalid as well. On March 2, 2020, the United States Supreme Court granted the petitions for writs of certiorari to review this case, and oral argument is scheduled for November 10, 2020. It remains unclear when or how the Supreme Court will rule. It is also unclear how other efforts to challenge, repeal or replace the ACA will impact the ACA or our business. It is likely that there will be additional challenges and amendments to the ACA in the future.
The results of the 2020 U.S. presidential and congressional elections have created regulatory uncertainty, including with respect to the U.S. government’s role, in the U.S. healthcare industry. As a result of such elections, there are renewed and reinvigorated calls for health insurance reform, which could cause significant uncertainty in the U.S. healthcare market, could increase our costs or decrease our revenues or inhibit our ability to sell our services. We cannot predict with certainty what impact any federal and state health reforms will have on us, but such changes could impose new and/or more stringent regulatory requirements on our activities or adversely affect our business, results of operations and financial condition.
While specific changes and their timing are not yet apparent, enacted reforms and future legislative, regulatory, judicial, or executive changes, particularly any changes to Medicare or other federal health care programs, could have a material adverse effect on our business, results of operations, financial condition and cash flows. On September 10, 2020, the Office of the Inspector General (“OIG”) of HHS issued a report criticizing the use of in-home health risk assessments (which we refer to as IHEs) as a basis for determining risk-adjusted reimbursement rates under the Medicare Advantage program. The OIG report found that some Medicare Advantage plans may be using IHEs to collect diagnoses and maximize risk-adjusted payments without improving care coordination or follow-up care. The report also raised potential payment integrity concerns that inaccurate or unsupported diagnoses could result in inappropriate risk-adjustment payments. In the report, OIG recommended that CMS provide targeted oversight of (i) the parent organizations of the Medicare Advantage Organizations (“MAOs”) that drove most of the risk-adjusted payments resulting from IHEs and (ii) the MAOs that drove most of the risk-adjusted payments resulting from IHEs for beneficiaries who had no other service records in the encounter data. CMS responded to OIG and agreed with both recommendations.
OIG also recommended that CMS (i) require MAOs to implement best practices to ensure care coordination for diagnoses identified in IHEs, (ii) reassess the risks and benefits of allowing IHEs to be used as sources of diagnoses for risk adjustment, and reconsider excluding such diagnoses from risk-adjustment; and (iii) require MAOs to flag any MAO-initiated HRAs in their encounter data. CMS responded to the OIG and disagreed with each of these three recommendations. If, in the future, CMS were to adopt restrictions on the use of IHEs as a basis for determining risk-adjusted reimbursement rates, it could have a material adverse effect on demand for IHEs by Medicare Advantage plans.
There is also uncertainty regarding Medicare Advantage beneficiary enrollment, which, if reduced, would reduce our overall revenues and net income. Although Medicare Advantage and other health plan enrollment increased by approximately 9.7 million, or by 83%, between the enactment of the ACA in 2010 and 2018, there can be no assurance that this trend will continue. Because IHEs are primarily provided to Medicare Advantage members, uncertainty over Medicare Advantage enrollment presents a continuing risk to our business.
In our Home & Community Services segment, we are increasingly realizing opportunities through Medicaid managed care organizations. Medicaid is co-funded by federal and state governments; as a result, the regulations governing the program vary from state to state. With more Americans receiving health care coverage from Medicaid, it is reasonable to predict significant and varying efforts to contain Medicaid spending. These efforts, whether promulgated by CMS or approved via a program waiver, could disrupt existing or emerging business lines. Further, if the ACA were repealed or replaced, Medicaid enrollment could be significantly reduced as a result. The ACA gives states the option to expand the financial eligibility for Medicaid benefits from 100% of the federal poverty level to 133% of the federal poverty level. To date, 39 states and the District of Columbia have
45
Table of Contents
adopted the Medicaid expansion. If the ACA were repealed and any such states reduced the levels at which individuals qualified for Medicaid, it could reduce our Medicaid business and have an adverse effect on our business, results of operations and financial condition.
If we fail to adhere to all of the complex government laws and regulations that apply to our business, we could suffer severe consequences that could have a material adverse effect on our business, results of operations, financial condition, cash flows, reputation and stock price.
Our operations are subject to extensive federal, state and local government laws and regulations, such as:
| • | federal and state anti-kickback laws, which prohibit the knowing and willful offer, payment, solicitation or receipt of any bribe, kickback, rebate or other remuneration for referring an individual, in return for ordering, leasing, purchasing or recommending or arranging for or to induce the referral of an individual or the ordering, purchasing or leasing of items or services covered, in whole or in part, by any federal healthcare program, such as Medicare and Medicaid; |
| • | the FCA and associated laws that impose civil and criminal liability on individuals or entities that knowingly submit or cause to be submitted, false or fraudulent claims for payment to the government or knowingly make, or cause to be made, a false statement material to a false claim; |
| • | the Civil Monetary Penalty statute and associated regulations, which authorizes the government agent to impose civil money penalties, an assessment, and program exclusion for various forms of fraud and abuse involving the Medicare, Medicaid and other federal healthcare programs; |
| • | federal and state laws regarding the collection, use and disclosure of personally identifiable information (“PII”) or protected health information (“PHI”) (e.g., the Health Insurance Portability and Accountability Act of 1996, as amended by the Health Information Technology for Economic and Clinical Health Act of 2009, and their implementing regulations (collectively known as “HIPAA”)), 42 C.F.R. Part 2, state laws, etc., and related laws regarding communications with individuals and the more recent information blocking and interoperability regulations; |
| • | federal and state laws governing the manufacture, distribution, storage, handling, shipment, disposal and/or dispensing of pharmaceuticals and blood products and other biological materials; |
| • | state and federal statutes and regulations that govern workplace health and safety; |
| • | state laws governing the corporate practice of medicine and fee splitting; |
| • | federal and state laws and policies that require healthcare providers and/or sites of care to maintain licensure, certification or accreditation to provide professional healthcare services, to report certain changes in their operations to regulatory oversight agencies and, in some cases, seek new licensure when changes in direct or indirect ownership occur; and |
| • | federal and state laws pertaining to the provision of services by nurse practitioners and physician assistants in certain settings, physician supervision of those services, and reimbursement requirements that depend on the types of services provided and documented and relationships between physician supervisors and nurse practitioners and physician assistants. |
Moreover, the various laws and regulations that apply to our operations are often subject to varying interpretations and may be conflicting, and additional laws and regulations potentially affecting our customers continue to be promulgated that may impact us. As we expand our business lines, we may cross into differing regulations and regulatory structures with which we may have less experience or familiarity. A violation or departure from any of the legal requirements implicated by our business may result in, among other things, government audits, significant fines and penalties, the potential loss of certification, recoupment efforts or voluntary repayments termination of customer contracts. These legal requirements may be civil, criminal, contractual or administrative in nature depending on the law or requirement.
46
Table of Contents
We endeavor to comply with all legal requirements. We further endeavor to structure all of our relationships with providers in our mobile network and provider partners we work with in our episodes of care programs to comply with state and federal anti-kickback and Stark physician self-referral laws, as well as the various state prohibitions against the corporate practice of medicine, fee splitting and other applicable healthcare laws. We utilize considerable resources to monitor laws and regulations and implement necessary changes. However, the laws and regulations in these areas are complex, changing and often subject to varying interpretations. As a result, there is no guarantee that we will be able to adhere to all of the laws and regulations that apply to our business and there may be insufficient reporting for the detection and prevention of fraud, waste and abuse, and any failure to do so could have a material adverse impact on our business, results of operations, financial condition, cash flows and reputation.
Additionally, the federal government has used the FCA to prosecute a wide variety of alleged false claims and fraud allegedly perpetrated against Medicare, Medicaid and other federally funded health care programs. Such liability can attach to individuals or entities that do not directly submit claims if they knowingly or recklessly provide material false information to the entity submitting claims. For example, if an IHE with inaccurate diagnosis data is used by a plan customer to seek additional Medicare reimbursement, we could be held liable under these statutes if the requisite knowledge or reckless disregard of the inaccuracy exists. Moreover, amendments to the federal Anti-Kickback Statute (“AKS”) in the ACA make claims resulting from AKS violations potentially subject to liability under the FCA, including qui tam or whistleblower suits. The penalties for a violation of the FCA range from $5,500 to $11,000 (amounts not adjusted for inflation) for each false claim, plus three times the amount of damages caused by each such claim, which generally means the amount received directly or indirectly from the government. Most recently, on June 19, 2020, the Department of Justice (“DOJ”) issued a final rule announcing adjustments to FCA penalties, under which the per claim penalty range increases to a range from $11,665 to $23,331 for penalties assessed after June 19, 2020, so long as the underlying conduct occurred after November 2, 2015. Given the number of claims submitted by our provider partners based on information supplied by us, the potential is high for substantial penalties in connection with any alleged FCA violations.
In addition to the provisions of the FCA, which provide for civil enforcement, the federal government can use several criminal statutes to prosecute persons who are alleged to have submitted false or fraudulent claims for payment to the federal government or have caused such claims to have been submitted.
If any of our operations are found to violate these or other government laws or regulations, we could suffer severe consequences that would have a material adverse effect on our business, results of operations, financial condition, cash flows, reputation and stock price, including:
| • | suspension or termination of our participation in government payment programs or in the demand for our services by Medicare Advantage plans and/or Medicaid managed care organizations; |
| • | refunds of amounts received in violation of law or applicable payment program requirements dating back to the applicable statute of limitation periods; |
| • | criminal or civil liability, fines, damages or monetary penalties for violations of healthcare fraud and abuse laws, including the AKS, Civil Monetary Penalties Law, Stark Physician Self-Referral Law and FCA, or other failures to meet regulatory requirements; |
| • | enforcement actions and/or criminal prosecution by governmental agencies and/or state law claims for monetary damages by individuals who believe their PHI has been used, disclosed or not properly safeguarded in violation of federal or state patient privacy laws, including HIPAA and the Privacy Act of 1974; |
| • | imposition of, and compliance with, Corporate Integrity Agreements that could subject us to ongoing audits and reporting requirements as well as increased scrutiny of our business practices, which could lead to potential fines, among other things; and |
47
Table of Contents
| • | harm to our reputation which could negatively impact our business relationships, affect our ability to attract and retain customers, individuals and providers, affect our ability to obtain financing and decrease access to new business opportunities, among other things. |
Our use, disclosure, and other processing of PII, including PHI, is subject to HIPAA and other federal and state privacy and security regulations, and our failure to comply with those regulations or to adequately secure the information we hold could result in significant liability or reputational harm and, in turn, a material adverse effect on our customer base and revenue.
Numerous state and federal laws and regulations govern the collection, dissemination, use, privacy, confidentiality, security, availability, integrity, creation, receipt, transmission, storage and other processing of PHI and PII. These laws and regulations include HIPAA, 42 C.F.R. Part 2, and a range of other federal and state laws that protect data pertaining to specific conditions, such as HIV/AIDS, genetic disorders, mental and behavioral health, as well as more broadly to PII. HIPAA implemented the use of standard transaction code sets and standard identifiers that covered entities and their business associates must use when submitting or receiving certain electronic healthcare transactions, including activities associated with the billing and collection of healthcare claims. HIPAA establishes a set of national privacy and security standards for the protection of PHI by health plans, healthcare clearinghouses and certain healthcare providers, referred to as covered entities, and the business associates with whom such covered entities contract for services. We may be acting as a covered entity in certain instances and as a business associate in other instances. As a business associate to our customers, we are also obligated to additional contractual requirements. Other federal and state laws require additional levels of protection over discrete sets of data that we handle in our day-to-day business.
These laws require us and those with whom we do business to develop and maintain policies and procedures with respect to PHI that is used or disclosed, including the adoption of administrative, physical and technical safeguards to protect such information. As a result of the COVID-19 pandemic, HHS’s Office for Civil Rights (“OCR”), which enforces HIPAA, has issued a notice of enforcement discretion for telehealth remote communications, which states that OCR will exercise its enforcement discretion and will not impose penalties for noncompliance with regulatory requirements under HIPAA against HIPAA-covered healthcare providers in connection with the good-faith provision of telehealth during the COVID-19 nationwide public health emergency. During the COVID-19 pandemic, our vIHEs have at times been conducted using several applications that allow for audio-video communications, such as Apple Face Time, which OCR has stated that covered healthcare providers may use without risk that OCR might seek to impose a penalty for noncompliance with HIPAA. OCR has also stated that it will not impose penalties against covered healthcare providers for the lack of a HIPAA Business Associate Agreement with video communication vendors (such as Apple) or any other noncompliance with HIPAA that relates to the good-faith provision of telehealth services during the COVID-19 nationwide public health emergency.
HIPAA imposes mandatory penalties for certain violations. Penalties for violations of HIPAA and its implementing regulations have varied, with larger breaches for some organizations ranging from a couple million dollars to a $16 million penalty for one breach. HIPAA also authorizes state attorney generals to enforce the law on behalf of their residents. Courts may award damages, costs and attorneys’ fees related to violations of HIPAA in such cases. While HIPAA does not create a private right of action allowing individuals to sue us in civil court for violations of HIPAA, its standards have been used as the basis for duty of care in state civil suits such as those for negligence or recklessness in the misuse or breach of PHI or PII. Moreover, many state laws do create state-specific private rights of action for conduct that would otherwise violate HIPAA or state law obligations. Class-action lawsuits are becoming an expected and more common occurrence in cases of breaches.
In addition, HIPAA mandates that the HHS Secretary conduct periodic compliance audits of HIPAA covered entities and business associates for compliance with the HIPAA Privacy and Security Standards and an investigation especially in instances in which a breach affects over 500 individuals. It also tasks HHS with establishing a methodology whereby harmed individuals who were the victims of breaches of unsecured PHI may receive a percentage of the civil monetary penalty paid by the violator.
48
Table of Contents
HIPAA further requires that individuals be notified of any acquisition, access, use or disclosure of their unsecured PHI that compromises the privacy or security of such information, with certain limited exceptions. HIPAA specifies that such notifications must be made “without unreasonable delay and in no case later than 60 calendar days after discovery of the breach,” but many state laws require notification within a shorter time frame, such as within five calendar days of discovery, even if the full extent of the breach is not known. If a business associate is acting as an agent of a covered entity, then the covered entity must provide the required notifications to individuals based on the time when the business associate discovered the breach. If a breach affects 500 individuals or more, it must be reported to HHS without unreasonable delay, and HHS will post the name of the breaching entity on its public web site. Breaches affecting 500 individuals or more in the same state or jurisdiction must also be reported to the local media. If a breach involves fewer than 500 people, the covered entity must record it in a log and notify HHS at least annually.
In addition to HIPAA, numerous other federal and state laws and regulations designed to protect the collection, use, confidentiality, privacy, availability, creation, receipt, transmission, storage, integrity and security of PHI and other types of PII have been enacted, including the California Consumer Privacy Act (“CCPA”), which became effective on January 1, 2020. The effects of the CCPA are potentially far-reaching and may require us to modify certain of our policies and practices regarding the collection, use, processing, and sharing of certain personal information. Privacy and data security statutes and regulations vary from state to state, and these laws and regulations in many cases are more restrictive than, and may not be preempted by, HIPAA and its implementing rules. These laws and regulations are often uncertain, contradictory, and subject to changing or differing interpretations. We expect new laws, rules and regulations regarding privacy, data protection, and information security to be proposed and enacted in the future, and the interpretations of existing laws to change. In the event that new data security laws are implemented, we may not be able to timely comply with such requirements, compliance with such requirements could require expending significant resources, or such requirements may not be compatible with our current processes. Changing our processes could be time consuming and expensive, and failure to timely implement required changes could subject us to significant liability for noncompliance. In addition, our failure to adequately train or monitor our workforce with respect to the requirements of applicable privacy and data security laws and regulations, and our own policies and procedures, has exposed, and may in the future expose, us to risks, including risks resulting from inadvertent disclosures or unintentional acquisitions of, access to, or uses of PHI or PII. The complex, dynamic legal landscape regarding privacy, data protection and information security creates significant compliance challenges for us, potentially restricts our ability to collect, use and disclose data, and exposes us to additional expense, and, if we cannot comply with applicable laws in a timely manner or at all, adverse publicity, harm to our reputation, and liability. While we have implemented data privacy and security measures in an effort to comply with applicable laws and regulations relating to privacy, data protection, and information security, some PHI and other PII or confidential information is transmitted to us by third parties (including, but not limited to, vendors and other service providers), who may not implement adequate security and privacy measures, and it is possible that laws, rules and regulations relating to privacy, data protection, or information security may be interpreted and applied in a manner that is inconsistent with our practices or those of third parties who transmit PHI and other PII or confidential information to us. If we or these third parties are found to have violated such laws, rules or regulations, such violations could result in government-imposed fines, orders requiring that we or these third parties change our or their practices, or criminal charges, which could adversely affect our business and reputation. Complying with these various laws and regulations could cause us to incur substantial costs or require us to change our business practices, systems or compliance procedures in a manner that is adverse to our business.
We take steps to ensure that our policies and procedures describing how we handle and protect PHI and other PII are documented as appropriate and required by law. As appropriate, employees and third parties are trained and informed on such policies and procedures. If we or our employees do not comply with our own policies and procedures, including those regarding PHI and other PII, or if our security practices are found to be inadequate, we may be subject to claims of unfair or deceptive business practices, which could lead to significant liabilities and consequences, including, without limitation, costs of responding to investigations, defending
49
Table of Contents
against litigation, settling claims, and complying with regulatory or court orders. Any of the foregoing consequences could have a material adverse impact on our business and our financial results.
Evolving government regulations may result in increased costs or adversely affect our results of operations.
In a regulatory climate that is uncertain, our operations may be subject to direct and indirect adoption, expansion, or reinterpretation of various laws and regulations. There could also be laws and regulations applicable to our business that we have not identified or that, if changed, may be costly to us, and we cannot predict all the ways in which implementation of such laws and regulations may affect us. Furthermore, both state and federal regulation of managed care typically lag behind innovation. As a result, there is uncertainty as to how our offerings will be viewed by future lawmakers and/or regulators. Similarly, the predilections of the current regulators impact how laws and regulations are interpreted, applied and enforced. Compliance with future laws and regulations or the regulators’ interpretations of the laws and regulations may require us to change our practices at an undeterminable, and possibly significant, initial and annual expense. These additional monetary expenditures may increase future overhead, which could harm our business. Take, for example, the possibility that additional governmental action is taken to address the COVID-19 pandemic. In June 2020, CMS permitted participants in BPCI-A to opt out of both upside and downside risk entirely for 2020 or carve out the episodes in 2020 in which the patient was ultimately diagnosed with COVID-19, which negatively impacted our revenues during 2020. In addition, CMS subsequently announced that all episodes in 2021 with a COVID-19 diagnosis would automatically be excluded from reconciliation.
Currently, in the states in which we operate, we believe we comply with all applicable material regulations, but, due to the uncertain regulatory environment, there is always the concern that a state may determine that we are in violation of its laws and regulations. There is also the possibility that, due to an obscure interpretation or application, a state regulator could impose requirements that may be costly to us. We cannot predict all the ways in which implementation of such laws and regulations may affect us. To comply with the regulator’s interpretations, we could be required to modify our existing and future offerings in such states in a manner that undermines our existing and future services’ attractiveness to our customers. We could be subject to administrative action that results in fines, penalties and cease and desist orders. The regulatory environment may be so hostile to our business model that we elect to terminate our operations in such states. In each case, our revenue may decline and our business, financial condition, and results of operations could be adversely affected.
Additionally, the introduction of new offerings, including a Commercial Episodes of Care based on prospective payments rather than retrospective reconciliations, may require us to comply with additional, yet undetermined, laws and regulations. Compliance may require licensure or certification under state law, increased security measures and/or expenditure of additional resources to monitor state regulation. Failure to comply with regulations implicated by the prospective payment model could delay or possibly prevent our existing and future offerings from being extended to our customers, which could harm our business.
Our employment of and contractual relationships with our providers may subject us to licensing and other regulatory risks.
Our engagement with and use of physicians, nurse practitioners and other health care professionals may subject us to state and other licensing and regulatory risks. Although we license and credential our providers through an in-house National Committee for Quality Insurance certified program and monitor our providers to verify their licenses are current and have not expired, we cannot guarantee that any such expiration will be immediately detected. We do not monitor the expiration of each provider’s Medicare and Medicaid enrollment status, which can pose a financial risk if a health plan rejects a claim based on a provider not being a participating provider in a particular state’s Medicare or Medicaid program at the time. In addition, our providers’ use of telehealth services related to COVID-19 also may subject us to certain licensing and regulatory risks. For example, there may be restrictions on the ability of our employed and contracted providers to provide services to individuals residing in states outside of the state or states in which such providers are licensed or registered or meet applicable state telehealth delivery requirements. The services provided by our providers may be restricted by state regulatory requirements and subject to review by state or other regulatory bodies. In addition, any activities conducted by our providers that are in violation of practice rules could subject us to fines or other
50
Table of Contents
penalties. For example, as we expand our solutions to provide new services, our providers could be found to be practicing outside the scope of their respective licenses in violation of applicable laws. Further, if one of our providers is found to be acting outside the scope of their professional license in violation of the applicable state’s practice laws, such activity could result in disciplinary action against the provider by the applicable licensing agency. The definition of what constitutes the practice of medicine, nursing or other health professions varies by state.
In addition, although we have structured our operations to comply with all applicable state corporate practice of medicine and fee splitting rules, there remains some risk that we may be found in violation of those state laws, which may result in the imposition of civil or criminal penalties. Certain states prevent corporations from employing or being licensed as practitioners and prohibit certain providers such as physicians from practicing medicine or their respective health profession in partnership with non-professionals, such as business corporations. Certain activities other than those directly related to the delivery of healthcare may be considered an element of the practice of a health profession in certain states or be viewed as controlling the practice of a health profession. These laws, which vary by state, may also prevent the sharing of professional services income with non-professional or business entities. Any determination that we are acting in the capacity of a healthcare provider, exercising undue influence or control over a healthcare provider’s independent clinical judgment or impermissibly splitting fees with a healthcare provider, may damage our reputation, cause us to lose customers, result in significant sanctions against us and our providers, including civil and criminal penalties and fines, additional compliance requirements, expense, and liability to us, and require us to change or terminate some portions of our contractual arrangements or business.
Alleged violations of the Telephone Consumer Protection Act or the Controlling the Assault of Non-Solicited Pornography and Marketing (“CAN-SPAM”) Act may cause us to face litigation risk.
The TCPA places restrictions on making outbound calls, faxes, and SMS text messages to consumers using certain types of automated technology. Prior express consent, and in the case of marketing calls prior express written consent, of consumers may be required to override certain activities prohibited under the TCPA. The scope and interpretation of the TCPA, and other laws that are or may be applicable to making calls and delivering SMS text messages to consumers, are continuously evolving and developing. We schedule IHEs with individuals through a variety of methods, including telephone calls. As a result of the TCPA, we are not able call members to schedule an IHE if we did not receive their contact information directly from the member or their health plan. As a result of the TCPA restrictions, if the contact information provided by health plans is incomplete or incorrect, we may have difficulty scheduling IHEs with members on our TML. The CAN-SPAM Act regulates commercial email messages and specifies penalties for the transmission of commercial email messages that do not comply with certain requirements, such as providing an opt-out mechanism for stopping future emails from senders. To the extent these and similar laws, rules and regulations apply to our business, we are required to comply with them. We could face allegations that we have violated these laws, rules and regulations, and even if they are without merit, we could face liability and harm to our reputation. We could also become liable under these laws or regulations due to the failure of our customers or vendors to comply with these laws, and as a result we could face liability and harm to our reputation.
The effects of the interoperability and information blocking regulations on our business are unknown and may negatively impact our business and results of operations.
In 2020, HHS issued two final regulations designed to promote interoperability of information systems and prevent information blocking, one each from CMS and the Office of the National Coordinator (“ONC”). The rules regulate communications from provider partners and health plans. The implementation of the regulations is in process and the full implications continue to be evaluated. It is too early to accurately predict how these regulations may impact operations and contracts with customers and vendors and it is possible such regulations could adversely impact the manner in which we conduct our business.
51
Table of Contents
The expansion of our Commercial Episodes of Care business may subject us to additional licensing and other regulatory risks.
As we grow our Episodes of Care business, we will be required to comply with additional laws and regulations. This will occur if we expand our Commercial Episodes of Care services to additional states or if we offer Commercial Episodes of Care in different markets, such as the Medicaid managed care space.
Further, if we expand our Commercial Episodes of Care business to include a program based on prospective payments rather than retrospective reconciliations, we could be considered an insurer, third-party administrator or other regulated entity under some states’ laws. For example, depending on how it is structured, a prospective Commercial Episodes of Care offering may be considered an insurance product in some states, the offering of which would require us to obtain an insurance company license and meet statutory capital and surplus requirements. Even if insurance company license is not required, we may still be regulated as a managed care entity such as a third-party administrator, limited health service organization, preferred healthcare provider organization, network contracting entity or similar regulated entity. Failure to obtain a license or certification, register with the appropriate regulatory authority or comply with state-imposed requirements for regulated managed care entities, could result in fines, cease and desist orders or even, in some instances, criminal charges.
Our Commercial Episodes of Care offering may involve a number of arrangements that potentially implicate the AKS, because they may involve payments intended to influence behavior relative to Medicare, Medicaid or other federal healthcare program beneficiaries, including risk sharing and gainsharing arrangements. While there is no fixed definition of a “gainsharing” arrangement, the term typically refers to an arrangement in which a share of cost savings for patient care attributable in part to a healthcare provider’s efforts are shared with the healthcare provider. The OIG has recognized that there are legitimate interests in enlisting healthcare providers in efforts to reduce unnecessary costs from the health care system and, if appropriately structured, such gainsharing arrangements should not violate the AKS. With respect to BPCI-A and other CMS innovations models in which we may participate, the OIG and CMS jointly issued waivers of certain fraud and abuse laws, including the AKS. With respect to our Commercial Episodes of Care program, however, there are no such fraud and abuse waivers. While we endeavor to carefully structure these arrangements in accordance with applicable guidance to be in compliance with the fraud and abuse laws, such arrangements are subject to a case-by-case analysis based on the intent of the parties and the overall potential for abuse. If any of our business transactions or arrangements were found to violate the AKS or other fraud and abuse laws, we could face, among other things, criminal, civil or administrative sanctions, including possible exclusion from participation in Medicare, Medicaid and other state and federal healthcare programs. Any findings that we have violated these laws could have a material adverse impact on our business, results of operations, financial condition, cash flows, reputation and the price of our Class A common stock.
We face inspections, reviews, audits and investigations from health plans. These audits could have adverse findings that may negatively affect our business, including our results of operations, liquidity, financial condition and reputation.
Because we support our health plan customers’ participation in Medicare and other federal health care programs, we are subject to inspections, reviews, audits and investigations by them to verify our compliance with these programs and applicable laws and regulations. We also periodically conduct internal audits and reviews of our regulatory compliance. An adverse inspection, review, audit or investigation could result in:
| • | refunding amounts we have been paid by health plans; |
| • | state or federal agencies imposing fines, penalties and other sanctions on us; |
| • | decertification or exclusion from participation in one or more health plan networks; |
| • | self-disclosure of violations to applicable regulatory authorities; |
| • | damage to our reputation; and |
| • | loss of certain rights under, or termination of, our contracts with health plans. |
52
Table of Contents
We have in the past and will likely in the future be required to refund amounts we have been paid and/or pay fines and penalties as a result of these inspections, reviews, audits and investigations. If adverse inspections, reviews, audits or investigations occur and any of the results noted above occur, it could have a material adverse effect on our business and operating results. Furthermore, the legal, document production and other costs associated with complying with these inspections, reviews, audits or investigations could be significant.
The FDA could determine that certain of our software is a “device” under the FFDCA.
The U.S. Food and Drug Administration (“FDA”) has the statutory authority to regulate medical software if it falls within the definition of a “device” under the Federal Food, Drug, and Cosmetic Act (“FFDCA”). However, the FDA has exercised enforcement discretion for software said to be “low risk.” The December 2016 21st Century Cures Act clarified the FDA’s regulation of medical software by amending the definition of “device” in the FFDCA to exclude certain software functions, including EHR software functionality, administrative software functionality and certain qualified clinical decision support functionality. In December 2017, the FDA issued draft guidance documents to clarify how it intends to interpret and enforce these provisions of the Cures Act. In 2017, the FDA also issued a Digital Health Innovation Action Plan and launched a voluntary “Software Precertification (Pre-Cert) Pilot Program” for software developers. Then, in September 2019, the FDA issued several different digital health-focused final and draft guidance documents. Although we believe that our products are currently not subject to FDA regulation, we continue to follow the FDA’s guidance in this area, which is subject to change and, in some areas, only currently exists in draft form. As a result, certain of our software, such as our site-of-care decision support software, may potentially be subject to regulation by the FDA as a medical device or could become regulated as our product functionality evolves or the FDA’s guidance evolves. Such regulation could require, among other things, the registration of the applicable software design facility and listing of software products, application of burdensome record-keeping, complaint handling, reporting and software design control requirements, and requirements for FDA approval or clearance. The imposition of the FDA regulatory requirements could increase our costs and create delays, including potentially requiring us to discontinue the use of affected medical software, such as our site-of-care decision support software, pending FDA clearance or approval, which could adversely affect our business, financial condition and results of operations.
Government regulation, industry standards and other requirements create risks and challenges with respect to our compliance efforts and our business strategies.
The healthcare industry is highly regulated and subject to frequently changing laws, regulations, industry standards and other requirements. Many healthcare laws and regulations are complex, and their application to specific solutions, services and relationships may not be clear. Because our customers are subject to various requirements, we may be impacted as a result of our contractual obligations even when we are not directly subject to such requirements. In particular, many existing healthcare laws and regulations, when enacted, did not anticipate the solutions and services that we provide, and these laws and regulations may be applied to our solutions and services in ways that we do not anticipate. The ACA, efforts to repeal or materially change the ACA, and other federal and state efforts to reform or revise aspects of the healthcare industry or to revise or create additional legal and/or regulatory requirements could impact our operations, the use of our solutions and services, and our ability to market new solutions and services, or could create unexpected liabilities for us. We also may be impacted by laws, industry standards and other requirements that are not specific to the healthcare industry, such as consumer protection laws. These requirements may impact our operations and, if not followed, could result in fines, penalties and other liabilities and adverse publicity and injury to our reputation. Furthermore, the inability to follow such requirements could adversely affect our business if, for example, CMS canceled our contracts for our BPCI-A business, CMS ended the BPCI-A program or if health plans chose to discontinue using our IHE services as a result of such noncompliance.
53
Table of Contents
Risks related to intellectual property and information technology
Our business depends on our ability to effectively invest in, implement improvements to, and properly maintain the uninterrupted operation, security and integrity of, our operating platform and other information technology and business systems.
Our business is highly dependent on maintaining effective information technology systems as well as the integrity and timeliness of the data we use to serve our customers and their members and patients, support our partners and operate our business. It is possible that hardware failures or errors in our systems could result in data loss or corruption, or cause the information that we collect to be incomplete, or contain inaccuracies that our customers regard as significant. Because of the large amount of data that we collect and manage, if our data were found to be inaccurate or unreliable, or became inaccessible, whether due to failures, errors, or other reasons, or if we, or any of our third-party service providers, especially our third-party dialing and routing software systems, were to fail to effectively maintain such information systems and data integrity, we could experience operational disruptions that may impact our customers, individuals and partner teams, and hinder our ability to provide services, establish appropriate pricing for services, retain and attract customers, establish reserves, report financial results timely and accurately and maintain regulatory compliance, among other things.
Our information technology strategy and execution are critical to our continued success. We must continue to invest in long-term solutions that will enable us to anticipate customer needs and expectations, enhance our customer experience, act as a differentiator in the market, comply with applicable laws, and protect against cybersecurity risks and threats. Our success is dependent, in large part, on maintaining the effectiveness of existing technology systems and continuing to deliver and enhance technology systems that support our business processes in a cost-efficient and resource-efficient manner and enable us to analyze and manage data in a comprehensive manner. Increasing and shifting regulatory and legislative requirements are likely to place additional demands on our information technology infrastructure that could have a direct impact on resources available for other projects tied to our strategic initiatives.
Connectivity and interoperability among technologies is becoming increasingly important. As a result, we must also develop new systems to meet current market standards and keep pace with continuing changes in information processing technology, evolving industry and regulatory standards and customer needs. Failure to do so may present compliance challenges and impede our ability to deliver services in a competitive manner. Further, system development projects are long term in nature, may be more costly than expected to complete and may not deliver the expected benefits upon completion. In addition, we may not be able to adequately assess the functionality, and data integrity and security impacts, of new or significantly changed products, services, business processes or infrastructure that we use. Our failure to effectively invest in, implement improvements to and properly maintain the uninterrupted operation and integrity of our information technology and other business systems, as well as any write-downs in connection with the obsolescence of our technology, could materially and adversely affect our business, financial condition and results of operations.
Security breaches or incidents, loss or misuse of data or other disruptions, arising either from internal or external sources, and whether or not intentional, could compromise sensitive information related to our business, customers or individuals, or prevent us from accessing critical information, and may expose us to operational disruptions, litigation, fines and penalties or other liability, any of which could materially adversely affect our business, results of operations and our reputation.
In the ordinary course of our business, we collect, store, use, disclose and otherwise process sensitive data, including PHI, and other types of personal data or PII relating to our employees, customers, their members and patients, individuals and others. We also process and store, and use third-party service providers to process and store, sensitive information, including intellectual property, confidential information and other proprietary business information. We manage and maintain such sensitive data and information utilizing a combination of on-site systems, managed data center systems and cloud-based computing center systems.
54
Table of Contents
We are highly dependent on information technology networks and systems, including the internet, to securely process, transmit and store this sensitive data and information. We cannot guarantee that our controls for this secure processing, transmission and storage are sufficient. Security breaches of, or interruptions to, this infrastructure, including physical or electronic break-ins, computer viruses, attacks by hackers and similar breaches, or employee or contractor error, negligence or malfeasance, have in the past, and may in the future, create system disruptions or shutdowns, result in unauthorized access to, or disclosure, misuse, modification, or loss or destruction of, our or our customers’ (or their members’ and patients’) or employees’ data, or result in damage, disablement, or encryption of our data or our customers’ (or their members and patients’) or employees’ data. Such data may include sensitive data or information, including PHI or other PII.
We utilize third-party service providers for important aspects of the collection, storage, processing and transmission of employee and customer (and their members’ and patients’) information, and other confidential and sensitive information, and therefore rely on such third-party service providers to manage functions that have material cybersecurity risks. Because of the sensitivity of the PHI, other PII and other sensitive information we and our service providers collect, store, use, transmit, and otherwise process, the security of our technology and other aspects of our services, including those provided or facilitated by our third-party service providers, are important to our operations and business strategy. We take certain administrative, physical and technological safeguards to address these risks, such as by requiring contractors and other third-party service providers who handle this PHI, other PII and other sensitive information on our behalf to enter into agreements that contractually obligate them to use reasonable efforts to safeguard such PHI, other PII, and other sensitive information, and to comply with applicable laws regarding their collection, storage, processing, and transmission of such PHI and other PII. Measures taken to protect our systems, those of our contractors or third-party service providers, or the PHI, other PII, or other sensitive information we or our contractors or third-party service providers process or maintain, may not adequately protect us from the risks associated with the collection, storage, use, transmission and processing of such sensitive data and information. We have and may in the future be required to expend significant capital and other resources to protect against security breaches or to alleviate problems caused by security breaches, regardless of whether such breaches are of our systems or networks, or the systems or networks of our third-party service providers. Despite our implementation of data privacy and security measures in an effort to comply with applicable laws and regulations relating to privacy, data protection and information security, cyberattacks are becoming harder to detect and more sophisticated and frequent. As a result, we or our third-party service providers have and may in the future be unable to anticipate the techniques used to attack our or their systems or networks, or to implement adequate protective measures.
Information security risks for companies such as ours, and for our third-party service providers, have increased in recent years and can result in significant losses, in part because of the proliferation of new technologies, the use of the internet and telecommunications technologies to conduct financial transactions, and the increased sophistication and activities of organized crime, hackers, terrorists, activists, malicious state actors, and other internal and external parties.
Security breaches, privacy violations, interruptions of systems or other security incidents that we or our third party service providers experience, or the perception that such incidents have occurred, have and could in the future harm our reputation, compel us to comply with breach notification and other laws, expose us to legal liabilities, including litigation, regulatory enforcement, resolution agreements and orders, disputes, investigations, indemnity obligations, damages for contract breach or penalties for violation of applicable laws or regulations, cause us to incur significant costs for investigations and remediation, fines, penalties, notification to individuals and for measures intended to repair or replace systems or technology and to prevent future occurrences, and to potential increases in insurance premiums. Such an event may also require us to verify the accuracy of database contents, resulting in increased costs or loss of revenue. For example, in October 2020, we learned that one of our IT employees had posted his log-in credentials on an IT support website in violation of our policies. We hired a reputable third party IT forensics firm to conduct a full investigation and determined that PHI, including names, addresses and dates of birth of up to 1,700 patients treated by our provider partners could have potentially been exposed. In less than 300 cases, social security numbers may also have been exposed. The employee in
55
Table of Contents
question was terminated. We engaged outside legal counsel, are in the process of notifying our provider partners of this incident and will be notifying the potentially affected individuals, to whom we will be offering free credit monitoring for at least one year. We have also conducted a full review of our internal controls and added additional layers of security and training for all employees. There can be no guarantee that we will not experience similar data security incidents in the future. If we are unable to prevent or mitigate security breaches, privacy violations, interruptions of systems or other security incidents in the future, or to implement satisfactory remedial measures, or if it is perceived that we have been unable to do so, our operations could be disrupted, we may be unable to provide access to our systems, and we could suffer a loss of customers, and we may as a result suffer loss of reputation and individual and investor confidence. In addition, our customers may be adversely impacted, we may suffer financial losses, and could be subject to governmental investigations or other actions, regulatory or contractual penalties, or other claims and liability, including under laws and regulations that protect the privacy of individual health information or other information, such as HIPAA. We cannot ensure that any limitation of liability or indemnity provisions in our contracts, including with third-party vendors and service providers, for a security lapse or breach or other security incident would be enforceable or adequate or would otherwise protect us from any liabilities or damages with respect to any particular claim. These risks may increase as we continue to grow and collect, store, use, transmit and process increasingly large amounts of data. In addition, security breaches and other unauthorized access to, or acquisition or processing of, data can be difficult to detect, and any delay in identifying such incidents or in providing any notification of such incidents may lead to increased harm to our business and our customers and could subject us to governmental investigations or other actions, including penalties and resolution agreements.
Any such breach could also result in the compromise of our trade secrets and other proprietary information, which could adversely affect our business and competitive position. Our business relies on its digital technologies, computer and email systems, software, and networks to conduct its operations. Although we have information security procedures and controls in place, our and our third-party service providers’ technologies, systems and networks, as well as our customers’ devices, may become the target of cyberattacks or information security breaches. In addition, hardware, software or applications we develop internally or procure from third parties may contain defects in design or manufacture, or other problems that could unexpectedly compromise information security.
While we maintain insurance covering certain business interruptions, security and privacy damages and claim expenses, we may not carry insurance or maintain coverage sufficient to compensate for all liability, or all types of liability, or cover any indemnification claims against us relating to any security incident or breach, disruption in information technology services, and in any event, insurance coverage would not address the reputational damage that could result from a security incident. Moreover, we cannot be certain that insurance will continue to be available to us on commercially reasonable terms, or at all, or that any insurer will not deny coverage as to any future claim. The successful assertion of one or more large claims against us that exceed available insurance coverage, or the occurrence of changes in our insurance policies, including premium increases or the imposition of large deductible or co-insurance requirements, could adversely affect our business, financial condition and results of operations.
Disruptions of the information technology systems or infrastructure of certain of our third-party vendors and service providers could also disrupt our businesses, damage our reputation, increase our costs, and have a material adverse effect on our business, financial condition and results of operations.
We rely heavily on the communications and information systems of third parties to conduct our business. For instance, we rely on computing infrastructure operated by Amazon Web Services (“AWS”) and Microsoft Azure (“Azure”) to host or operate some or all of certain key products or functions of our business. Our customers need to be able to access our platform at any time, without interruption or degradation of performance. Our platform depends, in part, on the virtual cloud infrastructure hosted in AWS and Azure. Although we have disaster recovery plans that utilize multiple AWS and Azure locations, any incident affecting their infrastructure could adversely affect our cloud-native platform. A prolonged AWS or Azure service disruption affecting our cloud-native platform would adversely impact our ability to service our customers and could damage our
56
Table of Contents
reputation with current and potential customers, expose us to liability, result in substantial costs for remediation, could cause us to lose customers, or otherwise harm our business, financial condition and results of operations. We may also incur significant costs for using alternative hosting sources or taking other actions in preparation for, or in reaction to, events that damage the AWS or Azure services we use. Additionally, in the event that our AWS or Azure service agreements are terminated, or there is a lapse of service, elimination of AWS or Azure services or features that we utilize, or damage to such facilities, we could experience interruptions in access to our platform as well as significant delays and additional expenses in arranging for or creating new facilities or re-architecting our platform for deployment on a different cloud infrastructure service provider, which would adversely affect our business, financial condition, and results of operations.
As expectations regarding operational and information security practices have increased, our operating systems and infrastructure, and those of our third-party service providers, must continue to be safeguarded and monitored for potential failures, disruptions, breakdowns, and attacks. Our data processing systems, or other operating systems and facilities, and those of our third-party service providers, may stop operating properly or become disabled or damaged as a result of a number of factors, including events that are wholly or partially beyond our and our third-party service providers’ control. For example, there could be electrical or telecommunication outages, natural disasters such as earthquakes, tornadoes, or hurricanes; disease pandemics and related government orders; events arising from local or larger scale political or social matters, including terrorist acts; cyberattacks and other data security incidents, including ransomware, malware, phishing, social engineering, including some of the foregoing that target healthcare systems in particular. These incidents can range from individual attempts to gain unauthorized access to information technology systems to more sophisticated security threats involving cyber criminals, hacktivists, cyber terrorists, nation state actors, or the targeting of commercial financial accounts. These events can also result from internal compromises, such as human error or malicious internal actors, of our workforce or our vendors’ personnel.
While we have business continuity, disaster recovery and other policies and procedures designed to prevent or limit the effect of the failure, interruption or security breach of our information systems, there can be no assurance that any such failures, interruptions or security breaches will not occur or, if they do occur, that they will be adequately addressed. Furthermore, if such failures, interruptions or security breaches are not detected immediately, their effect could be compounded. Our risk and exposure to these matters remains heightened because of the evolving nature of these threats and our use of third-party service providers with access to our systems and data. As a result, cybersecurity and the continued development and enhancement of our controls, processes, and practices designed to protect our systems, computers, software, data, and networks from attack, damage or unauthorized access remain a focus for us. Disruptions or failures in the physical infrastructure or operating systems that support our businesses and customers, or cyberattacks or security breaches of our networks, systems or devices, or those that our customers or third-party service providers use to access our products and services, could result in customer attrition, financial loss, reputational damage, reimbursement or other compensation costs, and/or remediation costs, any of which could have a material effect on our results of operations or financial condition.
Changes in laws, regulations or standards relating to privacy or data protection (including the collection, storage, use, transfer, and processing of data), or any actual or perceived failure by us to comply with such laws, regulations or standards, or our own information security policies or contractual or other obligations relating to privacy, data use and protection, or the protection or transfer of personal data, could adversely affect our business.
We collect, receive, generate, use, process, and store significant and increasing volumes of sensitive information, such as employee, customer and individual PHI and other PII. We are subject to a variety of federal, state and local laws, directives and regulations, as well as contractual obligations, relating to the collection, use, storage, retention, security, disclosure, transfer, return, destruction and other processing of PHI, other PII, and other data. In many jurisdictions, enforcement actions and consequences for noncompliance with such laws, directives and regulations are rising, and the regulatory framework for privacy, data protection and data transfers
57
Table of Contents
is complex and rapidly evolving and is likely to remain uncertain for the foreseeable future. As required by certain laws, we publicly post documentation regarding our privacy practices concerning the collection, processing, use and disclosure of certain data. The publication of our privacy policy and other documentation that provide promises and assurances about privacy and security can subject us to potential state and federal action if they are found to be deceptive, unfair, or misrepresentative of our actual practices. In addition, although we endeavor to comply with our published policies and documentation, individuals could allege we have failed to do so, or we may at times actually fail to do so despite our efforts. Any failure by us, our third-party service providers or other parties with whom we do business to comply with this documentation or with laws or regulations applicable to our business could result in proceedings against us by governmental entities or others.
The U.S. federal and various state government bodies and agencies have adopted or are considering adopting laws and regulations limiting, or laws and regulations regarding the collection, distribution, use, disclosure, storage and security of personal information. For example, in June 2018, California enacted the CCPA, which became effective on January 1, 2020, and, among other things, requires covered companies to provide disclosures to California consumers, and afford such consumers data protection rights, including the ability to opt-out of certain sales of personal information. The CCPA provides for civil penalties for violations, as well as a private right of action for certain data breaches that result in the loss of PII that may increase data breach litigation. While CCPA may not apply to certain PHI, it still may require us to modify our data practices and policies and to incur substantial costs and expenses in an effort to comply.
In the United States, many state legislatures, government bodies and regulatory agencies have adopted legislation and regulations that regulate how businesses operate online, including measures relating to privacy, data security and data breaches. Additionally, some statutory and regulatory requirements in the United States, such as HIPAA, include obligations for companies to notify individuals of security breaches involving particular personal information, which could result from breaches experienced by us or our service providers. Laws in all 50 states and other United States territories require businesses to provide notice to individuals whose PII has been disclosed as a result of a data breach. Such laws are not always consistent, and compliance in the event of a widespread data breach is costly and may be challenging. States are also constantly amending existing laws, requiring attention to frequently changing requirements, and we expect these changes to continue.
In addition to government regulation, privacy advocates and industry groups may propose self-regulatory standards from time to time. These and other industry standards may legally or contractually apply to us, or we may elect to comply with such standards or to facilitate our customers’ compliance with such standards. We expect that there will continue to be new proposed laws and regulations concerning privacy, data protection, and information security, and we cannot yet determine the impact such future laws, regulations, and standards may have on our business. New laws, amendments to or re-interpretations of existing laws and regulations, industry standards, contractual and other obligations may require us to incur additional costs and restrict our business operations. Because the interpretation and application of laws, standards, contractual and other obligations relating to privacy and data protection are still uncertain and changing, it is possible that these laws, standards, contractual and other obligations may be interpreted and applied in a manner that is inconsistent with our data management practices, our privacy, data protection or data security policies or procedures or the features of our technology. If so, in addition to the possibility of fines, lawsuits, regulatory investigations, imprisonment of company officials and public censure, other claims and penalties, significant costs for remediation and damage to our reputation, we could be required to fundamentally change our business activities and practices or modify our technology, any of which could adversely affect our business. We may be unable to make such changes or modifications in a commercially reasonable manner, or at all, and our ability to develop new software or provide new services could be limited. Any inability to adequately address privacy, data protection or information security-related concerns, even if such concerns are unfounded, or to successfully negotiate privacy, data protection or information security-related contractual terms with customers, or to comply with applicable laws and regulations, or our policies relating to privacy, data protection, and information security, could result in additional cost and liability to us, harm our reputation and brand, and adversely affect our business, financial condition and results of operations.
58
Table of Contents
Disruptions in our disaster recovery systems or management continuity planning could limit our ability to operate our business effectively.
Our information technology systems facilitate our ability to conduct our business. While we have disaster recovery systems and business continuity plans in place, any disruptions in our disaster recovery systems or the failure of these systems to operate as expected could, depending on the magnitude of the problem, adversely affect our operating results by limiting our capacity to effectively conduct our operations. Despite our implementation of a variety of security measures, our information technology systems could be subject to physical or electronic compromises and similar disruptions from unauthorized tampering, or to weather-related disruptions where our systems are hosted. In addition, in the event that a significant number of our personnel were unavailable in the event of a disaster or we failed to recover office facilities or systems, our ability to effectively conduct business could be adversely affected. Any of the foregoing could have a material adverse effect on our business, financial condition and results of operations.
Any failure to obtain, maintain, protect and enforce our intellectual property and proprietary rights, or the failure of the scope of our intellectual property and proprietary rights to be sufficiently broad, could harm our business, financial condition, and results of operations.
Our success depends, in part, upon our ability to obtain, maintain, protect and enforce our intellectual property rights, including our proprietary technology and know-how. Our business depends on internally developed technology and content, including software, databases, confidential information and know-how, the protection of which is crucial to the success of our business. We rely on a combination of trademark, trade secret and copyright laws, as well as confidentiality procedures and contractual provisions in an effort to protect our intellectual property rights, including in our internally developed technology and content. Although currently we primarily rely on trade secret protection, we may, over time, increase our investment in protecting our intellectual property through additional trademark, patent and other intellectual property filings that could be expensive, time consuming and may not yield enforceable rights. Effective intellectual property protection is expensive to develop and maintain, both in terms of initial and ongoing registration requirements and the costs of defending our rights. The measures we take to obtain, maintain, protect and enforce our intellectual property rights, however, may not be sufficient to offer us meaningful protection. If we are unable to protect our intellectual property and proprietary rights, particularly with respect to our technology and proprietary software, our competitive position and our business could be harmed, as third parties may be able to commercialize and use technologies and software products or offer services that are substantially the same as, or functionally equivalent to, ours without incurring the development and licensing costs that we have incurred.
Any of our owned or licensed intellectual property rights, or rights we develop or license in the future, could be challenged, invalidated, circumvented, infringed or misappropriated, our trade secrets and other confidential information could be disclosed in an unauthorized manner to, or misappropriated by, third parties, or our owned or licensed intellectual property rights may not be sufficient to permit us to take advantage of current market trends or otherwise to provide us with competitive advantages, which could result in costly redesign efforts, discontinuance of certain offerings or other competitive harm.
There can be no guarantee that others will not infringe on our trademarks or other intellectual property rights, independently develop similar technology, duplicate any of our technology or services, or design around our intellectual property rights. Additionally, monitoring unauthorized use of our intellectual property rights is difficult and costly. From time to time, we seek to analyze our competitors’ services, and may in the future seek to enforce our rights against potential infringement. However, the steps we have taken to protect our intellectual property rights may not be adequate to prevent infringement, misappropriation or other violations of our intellectual property. We may not be able to detect unauthorized use of, or take appropriate steps to enforce, our intellectual property rights. Furthermore, intellectual property laws may change over time, and such changes may impair our ability to protect or enforce our intellectual property rights. Any inability to meaningfully protect and enforce our intellectual property rights could result in harm to our ability to compete and reduce demand for our
59
Table of Contents
technology and services. Moreover, our failure to develop and properly manage new intellectual property could adversely affect our market position and business opportunities, including in our Commercial Episodes of Care solution. Also, some of our services rely on technologies and software developed by or licensed from third parties, and we may not be able to maintain our relationships with such third parties or enter into similar relationships in the future on commercially reasonable terms, or at all.
Litigation may be necessary in the future to enforce our intellectual property rights, and such litigation could be costly, time consuming and distracting to management, regardless of whether we are successful or not, and could result in the impairment or loss of portions of our intellectual property. Our efforts to enforce our intellectual property rights may be met with defenses, counterclaims and countersuits attacking the validity and enforceability of our intellectual property rights, and, if such defenses, counterclaims or countersuits are successful, we could lose valuable intellectual property rights. In addition, we may be required to license additional technology from third parties to develop and market new technology features, which may not be available on commercially reasonable terms, or at all, and could adversely affect our ability to compete.
Uncertainty may result from changes to intellectual property legislation and from interpretations of intellectual property laws by applicable courts and agencies. Accordingly, despite our efforts, we may be unable to obtain and maintain the intellectual property rights necessary to provide us with a competitive advantage. Our failure to obtain, maintain and enforce our intellectual property rights could have a material adverse effect on our business, financial condition and results of operations.
Third parties may initiate legal proceedings alleging that we are infringing, misappropriating or otherwise violating their intellectual property rights, the outcome of which would be uncertain and could have a material adverse effect on our business, financial condition and results of operations.
Our commercial success depends, in part, on our ability to develop and commercialize our services and use our internally developed technology without infringing, misappropriating or otherwise violating the intellectual property or proprietary rights of third parties. We may become subject to intellectual property disputes, whether or not such allegations have merit. Intellectual property disputes can be costly to defend and may cause our business, operating results and financial condition to suffer. As the market for healthcare in the United States expands and more patents are issued, the risk increases that there may be patents or other intellectual property rights owned by third parties that relate to our technology, and of which we are not aware or that we must challenge to continue our operations as currently contemplated. Whether merited or not, we may face allegations that we, our partners or parties indemnified by us have infringed, misappropriated, or otherwise violated the patents, trademarks, copyrights or other intellectual property rights of third parties. Such claims may be made by competitors seeking to obtain a competitive advantage or by other parties. For example, in recent years, individuals and groups have begun purchasing intellectual property assets for the purpose of making claims of infringement and attempting to extract settlements from companies like ours. It may also be necessary for us to initiate litigation in order to determine the scope, enforceability or validity of third-party intellectual property or proprietary rights, or to establish our intellectual property rights. We may not be able to successfully settle or otherwise resolve such adversarial proceedings or litigation. If we are unable to successfully settle future claims on terms acceptable to us we may be required to engage in or to continue litigation. Regardless of whether third-party claims have merit, litigation can be time consuming, divert management’s attention and financial resources, and can be costly to evaluate and defend. Some third parties may be able to sustain the costs of complex litigation more effectively than we can because they have substantially greater resources. Results of any such litigation are difficult to predict and may require us to stop commercializing or using our technology, obtain licenses and pay royalties, modify our services and technology while we develop non-infringing substitutes, or incur substantial damages, settlement costs, or face a temporary or permanent injunction prohibiting us from marketing or providing the affected services.
With respect to any third-party claims regarding intellectual property rights, we may have to seek a license to continue operations found to be in violation of such rights. If we require a third-party license, it may not be
60
Table of Contents
available on commercially reasonable terms or at all, and we may have to pay substantial royalties, upfront fees or grant cross-licenses to our intellectual property rights. We may also have to redesign our technology or services so they do not infringe such third-party intellectual property rights, which may not be possible or may require substantial expenditures of money and time, during which our technology may not be available for commercialization or use. Even if we are party to an agreement pursuant to which a third party must indemnify us against such costs, the indemnifying party may be unable or otherwise unwilling to uphold its contractual obligations. If we cannot or do not obtain relevant third-party licenses, or cannot obtain such licenses on commercially reasonable terms, obtain similar technology from another source, or design new technology that is not infringing, our revenue and earnings could be adversely impacted.
We also license software from third-party vendors. Third parties may claim that our use of such licensed software infringes upon their intellectual property rights. Although we seek to secure indemnification protection from our software vendors to protect us against potential third-party infringement claims in connection with our use of such license software, not all of our vendors agree to provide us with sufficient indemnification protection, and in the instances where we do secure indemnification protection from our vendors, it is possible such vendors may not honor such indemnification obligations.
Even if resolved in our favor, litigation or other legal proceedings relating to intellectual property may cause us to incur significant expenses, and could distract our technical and management personnel from their normal responsibilities. In addition, there could be public announcements of the results of hearings, motions or other interim proceedings or developments, and if securities analysts or investors perceive these results to be negative, such announcements could have a material adverse effect on the price of our Class A common stock. Moreover, any uncertainties resulting from the initiation and continuation of any legal proceedings could have a material adverse effect on our ability to raise the funds necessary to continue our operations. Assertions by third parties that we violate their intellectual property rights could therefore have a material adverse effect on our business, financial condition and results of operations.
We may be subject to claims that we have wrongfully hired an employee from a competitor, or that our employees, consultants or independent contractors have wrongfully used or disclosed confidential information of third parties or that our employees have wrongfully used or disclosed alleged trade secrets of their former employers.
Many of our employees, consultants and advisors, or individuals that may in the future serve as our employees, consultants and advisors, are currently or were previously employed at companies including our competitors or potential competitors. Although we try to ensure that our employees, consultants, independent contractors and advisors do not use the confidential or proprietary information, trade secrets or know-how of others in their work for us, we may be subject to claims that we have, inadvertently or otherwise, used or disclosed confidential or proprietary information, trade secrets or know-how of these third parties, or that our employees, consultants or, independent contractors or advisors have, inadvertently or otherwise, used or disclosed confidential information, trade secrets or know-how of such individual’s current or former employer. If we fail in defending any such claims, in addition to paying monetary damages, we may lose valuable intellectual property rights or personnel. Litigation may be necessary to defend against these claims. Even if we are successful in defending against these claims, and whether or not such claims have merit, litigation could result in substantial cost and be a distraction to our management and employees. Claims that we, our employees, consultants or advisors have misappropriated the confidential or proprietary information, trade secrets or know-how of third parties could therefore have a material adverse effect on our business, financial condition and results of operations.
If we are unable to protect the confidentiality of our trade secrets, know-how and other proprietary and internally developed information, the value of our technology could be adversely affected.
We may not be able to protect our trade secrets, know-how and other internally developed information adequately. Although we use reasonable efforts to protect this internally developed information and technology,
61
Table of Contents
our employees, consultants and other parties (including independent contractors and companies with whom we conduct business) may unintentionally or willfully disclose our information or technology to competitors. Enforcing a claim that a third party illegally disclosed or obtained and is using any of our internally developed information or technology is difficult, expensive and time consuming, and the outcome is unpredictable. We rely, in part, on non-disclosure, confidentiality and assignment-of-invention agreements with our employees, independent contractors, consultants and companies with whom we conduct business to protect our trade secrets, know-how and other intellectual property rights and internally developed information. These agreements may not be self-executing, or they may be breached and we may not have adequate remedies for such breach. Moreover, third parties may independently develop similar or equivalent proprietary information or otherwise gain access to our trade secrets, know-how and other internally developed information. Additionally, as with other potential information security breaches, our trade secrets could also be compromised. Any of these events could materially and adversely affect our business, financial condition and results of operations.
Our use of “open source” software could adversely affect our ability to offer our services and subject us to possible litigation.
Our technology contains software modules licensed to us by third-party authors under so-called “open source” licenses, and we expect to continue to incorporate such open source software in our technology in the future. Use and distribution of open source software may entail greater risks than use of third-party commercial software, as open source licensors generally do not provide support, warranties, indemnification, or other contractual protections regarding infringement claims or the quality of the code. In addition, the public availability of such software may make it easier for others to compromise our technology.
Open source licenses contain various requirements, including, in some cases, requirements that we make available source code of any modifications or derivative works we create based on our use of such open source software, or grant third parties licenses to our intellectual property at no cost. If we were to combine our proprietary software with open source software in a certain manner, we could, under certain open source licenses, be required to release the source code of our proprietary software to the public or otherwise be in violation of the terms of the license. Release of our source code would allow our competitors to create similar offerings in less time and with lower development effort, and ultimately could result in a loss of our competitive advantages. Alternatively, to avoid the public release of the affected portions of our source code, we could be required to expend substantial time and resources to re-engineer some or all of our software, and could be subject to claims of infringement or breach of contract by the licensors of open source software modules. Additionally, some open source projects have known security vulnerabilities and architectural instabilities and are provided on an “as-is” basis, which, if not properly addressed, could negatively affect the performance of our technology. Any of these events could materially and adversely affect our business, financial condition and results of operations.
Any restrictions on our use of, or ability to license, data, or our failure to license data and integrate third-party technologies, could have a material adverse effect on our business, financial condition and results of operations.
We depend upon licenses from third parties for some of the technology and data used in our technology and services. We expect that we may need to obtain additional licenses from third parties in the future in connection with the development of our technology and services. In addition, we obtain a portion of the data that we use from government entities, public records and from our partners for specific partner engagements. We believe that we have all rights necessary to use the data that is incorporated into our services. We cannot, however, assure you that our licenses for information will allow us to use that information for all potential or contemplated applications. In addition, our ability to continue to support integrated healthcare for individuals depends on maintaining our database, which is partially populated with information disclosed to us by our partners with their consent. If these partners revoke their consent for us to maintain, use, de-identify and share this data, consistent with applicable law, our data assets could be degraded.
62
Table of Contents
In the future, data providers could withdraw their data from us or restrict our usage for any reason, including if there is a competitive reason to do so, if legislation is passed restricting the use of the data or if judicial interpretations are issued restricting use of the data that we currently use to support our services. In addition, data providers could fail to adhere to our quality control standards in the future, causing us to incur additional expense to appropriately use such data. If a substantial number of data providers were to withdraw or restrict our use of their data, or if they fail to adhere to our quality control standards, and if we are unable to identify and contract with suitable alternative data suppliers and integrate these data sources into our service offerings, our ability to provide services to our customers would be materially and adversely impacted, which could have a material adverse effect on our business, financial condition and results of operations. We also integrate third-party applications into our internally developed applications and use third-party software to support our technology infrastructure. Some of this software is proprietary and some is open source software. These technologies may not be available to us in the future on commercially reasonable terms or at all and could be difficult to replace once integrated into our own internally developed applications. Many of these licenses can be renewed only by mutual consent and most may be terminated if we breach the terms of the license and fail to cure the breach within a specified period of time. Our inability to obtain, maintain or comply with any of these licenses could delay development until equivalent technology can be identified, licensed and integrated, which would harm our business, financial condition and results of operations.
Most of our third-party licenses are nonexclusive and our competitors may obtain the right to use any of the technology covered by these licenses to compete directly with us. Our use of third-party technologies exposes us to increased risks, including, but not limited to, risks associated with the integration of new technology into our solutions, the diversion of our resources from development of our own internally developed technology and the potential inability to generate revenue from licensed technology sufficient to offset associated acquisition, use and maintenance costs. In addition, if our third-party licensors choose to discontinue support of their licensed technology in the future, we might not be able to modify or adapt our own solutions to compensate for that loss.
Risks related to our organizational structure
We are a holding company and our principal asset after completion of this offering will be our 74.2% ownership interest in Cure TopCo, LLC, and we are accordingly dependent upon distributions from Cure TopCo, LLC to pay dividends, if any, and taxes, make payments under the Tax Receivable Agreement and pay other expenses.
We are a holding company and, upon completion of the Reorganization Transactions and this offering, our principal asset will be our ownership of 74.2% of the outstanding LLC Units. See “Organizational structure.” We have no independent means of generating revenue. Cure TopCo, LLC is, and will continue to be, treated as a partnership for U.S. federal income tax purposes and, as such, will not be subject to U.S. federal income tax. Instead, the taxable income of Cure TopCo, LLC will be allocated to holders of LLC Units, including us. Accordingly, we will incur income taxes on our allocable share of any net taxable income of Cure TopCo, LLC. We will also incur expenses related to our operations, and will have obligations to make payments under the Tax Receivable Agreement. As the sole managing member of Cure TopCo, LLC, we intend to cause Cure TopCo, LLC to make distributions to the holders of LLC Units (including us) in amounts sufficient to (i) cover all applicable taxes payable by us and the other holders of LLC Units, (ii) allow us to make any payments required under the Tax Receivable Agreement we intend to enter into as part of the Reorganization Transactions, (iii) fund dividends to our stockholders in accordance with our dividend policy, to the extent that our board of directors declares such dividends and (iv) pay our expenses.
Deterioration in the financial conditions, earnings or cash flow of Cure TopCo, LLC and its subsidiaries for any reason could limit or impair their ability to pay such distributions. Additionally, to the extent that we need funds and Cure TopCo, LLC is restricted from making such distributions to us under applicable law or regulation, as a result of covenants in its debt agreements or otherwise, we may not be able to obtain such funds on terms acceptable to us, or at all, and, as a result, could suffer a material adverse effect on our liquidity and financial condition.
63
Table of Contents
In certain circumstances, Cure TopCo, LLC will be required to make distributions to us and the other holders of LLC Units, and the distributions that Cure TopCo, LLC will be required to make may be substantial.
Under the Amended LLC Agreement, Cure TopCo, LLC will generally be required from time to time to make pro rata distributions in cash to us and the other holders of LLC Units at certain assumed tax rates in amounts that are intended to be sufficient to cover the taxes on our and the other LLC Unit holders’ respective allocable shares of the taxable income of Cure TopCo, LLC. As a result of (i) potential differences in the amount of net taxable income allocable to us and the other LLC Unit holders, (ii) the lower tax rate applicable to corporations than individuals and (iii) the use of an assumed tax rate (based on the tax rate applicable to individuals) in calculating Cure TopCo, LLC’s distribution obligations, we may receive tax distributions significantly in excess of our tax liabilities and obligations to make payments under the Tax Receivable Agreement. Our board of directors will determine the appropriate uses for any excess cash so accumulated, which may include, among other uses, dividends, repurchases of our Class A common stock, the payment of obligations under the Tax Receivable Agreement and the payment of other expenses. We will have no obligation to distribute such cash (or other available cash other than any declared dividend) to our stockholders. No adjustments to the redemption or exchange ratio of LLC Units for shares of Class A common stock will be made as a result of either (i) any cash distribution by us or (ii) any cash that we retain and do not distribute to our stockholders. To the extent that we do not distribute such excess cash as dividends on our Class A common stock and instead, for example, hold such cash balances or lend them to Cure TopCo, LLC, holders of LLC Units would benefit from any value attributable to such cash balances as a result of their ownership of Class A common stock following a redemption or exchange of their LLC Units. See “Certain relationships and related party transactions—Amended LLC Agreement.”
We are controlled by the Pre-IPO LLC Members whose interests in our business may be different than yours, and certain statutory provisions afforded to stockholders are not applicable to us.
The Pre-IPO LLC Members will control approximately 89.4% of the combined voting power of our common stock (or 88.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full) after the completion of this offering and the application of the net proceeds from this offering.
This concentration of ownership and voting power may delay, defer or even prevent an acquisition by a third party or other change of control of our company, which could deprive you of an opportunity to receive a premium for your shares of Class A common stock and may make some transactions more difficult or impossible without the support of the Pre-IPO LLC Members, even if such events are in the best interests of minority stockholders. Furthermore, this concentration of voting power with the Pre-IPO LLC Members may have a negative impact on the price of our Class A common stock.
Further, pursuant to the stockholders agreement that we and certain of the Pre-IPO LLC Members will enter into, New Mountain Capital will have the right to nominate directors to our board of directors as follows: so long as affiliates of New Mountain Capital continue to own (A) at least 50% of the shares of common stock that New Mountain Capital owns immediately following this offering, New Mountain Capital shall be entitled to nominate directors representing a majority of the number of directors on our board of directors, (B) less than 50% but at least 25% of the shares of common stock that New Mountain Capital owns immediately following this offering, New Mountain Capital shall be entitled to nominate directors representing at least 25% of the number of directors on the board of directors and (C) less than 25% but at least 10% of the shares of common stock New Mountain Capital owns immediately following this offering, New Mountain Capital shall be entitled to nominate directors representing at least 10% of the number of directors on the board of directors. As a result, following this offering, New Mountain Capital will be able to designate at least half of the nominees for election to our board of directors. The stockholders agreement will also provide that for so long as New Mountain Capital has the right to designate at least one director, New Mountain Capital will have the right to nominate the pro rata share of the total number of members of each committee of our board of directors that is equal to the proportion that the number of directors designated by New Mountain Capital bears to the total number of directors then on our board
64
Table of Contents
of directors; provided that the right of any director designated by New Mountain Capital to serve on a committee will be subject to applicable laws and NYSE independence rules.
Moreover, for so long as New Mountain Capital continues to own at least 15% of the issued and outstanding common stock, written approval by New Mountain Capital will be required for certain significant corporate actions, including any consolidation, merger or other business combination of Signify or Cure TopCo, LLC into or with any other entity, entry into any new line of business or other significant change in the scope or nature of our or our subsidiaries’ business or operations, taken as a whole, our incurrence of any indebtedness in excess of $10 million, the sale, transfer or other disposition of in any transaction or series of related transactions of more than 25% of the fair market value of our and our subsidiaries’ consolidated assets, taken as a whole, and the entry into agreements by us in connection with acquisitions or dispositions in excess of $25 million and joint ventures or strategic partnerships. Other actions requiring New Mountain Capital’s written consent include the declaration or payment of dividends on our Class A common stock, the creation, issuance or sale of equity securities by us, including Class A common stock, any amendments to our certificate of incorporation or bylaws, or to the certificate of formation or operating agreement of Cure TopCo, LLC, any increase or decrease in the size of our board of directors, any change in our independent auditors, any hiring, termination, or replacement of our Chief Executive Officer or Chief Financial and Administrative Officer or any amendments to their employment agreements. See “Certain relationships and related party transactions—Stockholders agreement.”
We cannot predict whether our dual-class structure, combined with the concentrated control of the Pre-IPO LLC Members, will result in a lower or more volatile market price of our Class A common stock or in adverse publicity or other adverse consequences. For example, certain index providers have announced restrictions on including companies with multiple-class share structures in certain of their indexes. In July 2017, FTSE Russell announced that it plans to require new constituents of its indexes to have greater than 5% of the company’s voting rights in the hands of public stockholders, and S&P Dow Jones announced that it will no longer admit companies with multiple-class share structures to certain of its indexes. Because of our dual-class structure, we will likely be excluded from these indexes and we cannot assure you that other stock indexes will not take similar actions. Given the sustained flow of investment funds into passive strategies that seek to track certain indexes, exclusion from stock indexes would likely preclude investment by many of these funds and could make our Class A common stock less attractive to other investors. As a result, the market price of our Class A common stock could be adversely affected.
The Pre-IPO LLC Members’ interests may not be fully aligned with yours, which could lead to actions that are not in your best interests. Because the Pre-IPO LLC Members hold a majority of their economic interests in our business through Cure TopCo, LLC rather than through Signify Health, Inc., they may have conflicting interests with holders of shares of our Class A common stock. For example, the Continuing Pre-IPO LLC Members may have a different tax position from us, which could influence their decisions regarding whether and when we should dispose of assets or incur new or refinance existing indebtedness, especially in light of the existence of the Tax Receivable Agreement that we will enter into in connection with this offering, and whether and when we should undergo certain changes of control for purposes of the Tax Receivable Agreement or terminate the Tax Receivable Agreement. In addition, the structuring of future transactions may take into consideration these tax or other considerations even where no similar benefit would accrue to us. Pursuant to the Bipartisan Budget Act of 2015, for tax years beginning after December 31, 2017, if the IRS makes audit adjustments to Cure TopCo, LLC’s federal income tax returns, it may assess and collect any taxes (including any applicable penalties and interest) resulting from such audit adjustment directly from Cure TopCo, LLC. If, as a result of any such audit adjustment, Cure TopCo, LLC is required to make payments of taxes, penalties and interest, Cure TopCo, LLC’s cash available for distributions to us may be substantially reduced. These rules are not applicable to Cure TopCo, LLC for tax years beginning on or prior to December 31, 2017. See “Certain relationships and related party transactions—Tax Receivable Agreement.” In addition, the Pre-IPO LLC Members’ significant ownership in us and resulting ability to effectively control us may discourage someone from making a significant equity investment in us, or could discourage transactions involving a change in control, including transactions in which you as a holder of shares of our Class A common stock might otherwise receive a premium for your shares over the then-current market price.
65
Table of Contents
In addition, until such time as no Pre-IPO LLC Member party to the stockholders agreement owns 5% or more of our total voting power, we have opted out of Section 203 of the General Corporation Law of the State of Delaware, or DGCL, which prohibits a publicly held Delaware corporation from engaging in a business combination transaction with an interested stockholder for a period of three years after the interested stockholder became such unless the transaction fits within an applicable exemption, such as board approval of the business combination or the transaction which resulted in such stockholder becoming an interested stockholder. Therefore, after the 180-day lock-up period expires, the Pre-IPO LLC Members will be able to transfer control of us to a third party by transferring their shares of our common stock (subject to certain restrictions and limitations), which would not require the approval of our board of directors or our other stockholders.
Further, our certificate of incorporation will provide that, to the fullest extent permitted by law, none of New Mountain Capital or any of its affiliates or any director who is not employed by us (including any non-employee director who serves as one of our officers in both his or her director and officer capacities) or his or her affiliates will have any duty to refrain from (i) engaging in a corporate opportunity in the same or similar lines of business in which we or our affiliates now engage or propose to engage or (ii) otherwise competing with us or our affiliates. See “Description of capital stock.”
We are a “controlled company” within the meaning of the NYSE rules and, as a result, qualify for, and will rely on, exemptions from certain corporate governance requirements that provide protection to the stockholders of companies that are subject to such corporate governance requirements.
Upon completion of this offering, a group of Pre-IPO LLC Members composed of entities affiliated with New Mountain Capital will continue to beneficially own more than 50% of the voting power for the election of members of our board of directors. As a result, we will be a “controlled company” within the meaning of the corporate governance standards of the NYSE rules. Under these rules, a listed company of which more than 50% of the voting power is held by an individual, group or another company is a “controlled company” and may elect not to comply with certain NYSE corporate governance requirements.
As a controlled company, we will rely on certain exemptions from the NYSE standards that may enable us not to comply with certain NYSE corporate governance requirements. Therefore, immediately following the consummation of this offering, a majority of our directors will not be “independent.” In addition, although we have opted to have a compensation committee and a nominating and governance committee, such committees will not be fully independent. As a consequence of our reliance on certain exemptions from the NYSE standards provided to “controlled companies,” you will not have the same protections afforded to stockholders of companies that are subject to all of the corporate governance requirements of the NYSE. See “Management—Controlled company exception.”
We will be required to pay the Continuing Pre-IPO LLC Members, the Reorganization Parties, Optionholders of the Blocker Companies at the time of the Mergers, holders of synthetic equity units and any other persons that become parties to the Tax Receivable Agreement for certain tax benefits we may receive, and the amounts we may pay could be significant.
As described under “Organizational structure,” we will acquire certain favorable tax attributes from the Blocker Companies in the Mergers. In addition, future taxable redemptions or exchanges by the Continuing Pre-IPO LLC Members of LLC Units for shares of our Class A common stock or cash and the IPO Contribution, as well as other transactions described herein, are expected to result in favorable tax attributes for us. These tax attributes would not be available to us in the absence of those transactions and are expected to reduce the amount of tax that we would otherwise be required to pay in the future.
Upon the completion of this offering, we will be a party to the Tax Receivable Agreement with the TRA Parties. Under the Tax Receivable Agreement, we generally will be required to pay to the TRA Parties, in the aggregate, 85% of the amount of cash savings, if any, in U.S. federal, state and local income tax that we actually realize as a result of (i) certain favorable tax attributes we will acquire from the Blocker Companies in the Mergers (including net operating losses, the Blocker Companies’ allocable share of existing tax basis and refunds
66
Table of Contents
of Blocker Company taxes attributable to pre-Merger tax periods), (ii) increases in our allocable share of existing tax basis and tax basis adjustments that may result from (x) future redemptions or exchanges of LLC Units by Continuing Pre-IPO LLC Members for cash or Class A common stock, (y) the IPO Contribution and (z) certain payments made under the Tax Receivable Agreement and (iii) deductions in respect of interest and certain compensatory payments made under the Tax Receivable Agreement. The payment obligations under the Tax Receivable Agreement are our obligations and not the obligations of Cure TopCo, LLC.
We expect that the payments we will be required to make under the Tax Receivable Agreement will be substantial. The tax attributes available to us as a result of the Mergers and our allocable share of existing tax basis are expected to result in tax savings of approximately $56.3 million. We would be required to pay the TRA Parties approximately 85% of such amount, or $47.8 million, over the 15-year period from the date of the completion of this offering. Further, assuming no material changes in relevant tax law and that we earn sufficient taxable income to realize all tax benefits that are subject to the Tax Receivable Agreement, we expect that the tax savings associated with all tax attributes described above would aggregate to approximately $444.2 million over 15 years from the date of the completion of this offering, based on an assumed initial public offering price of $20.50 per share of Class A common stock, the midpoint of the estimated price range set forth on the cover page of this prospectus and assuming all future redemptions or exchanges would occur on the date of this offering. Under this scenario, we would be required to pay the TRA Parties approximately 85% of such amount, or $377.6 million, over the 15-year period from the date of the completion of this offering. The actual amounts we will be required to pay may materially differ from these hypothetical amounts, because potential future tax savings that we will be deemed to realize, and the Tax Receivable Agreement payments made by us, will be calculated based in part on the market value of our Class A common stock at the time of each redemption or exchange of an LLC Unit for cash or a share of Class A common stock and the prevailing applicable federal tax rate (plus the assumed combined state and local tax rate) applicable to us over the life of the Tax Receivable Agreement and will depend on our generating sufficient taxable income to realize the tax benefits that are subject to the Tax Receivable Agreement. See “Certain relationships and related party transactions—Tax Receivable Agreement.” Payments under the Tax Receivable Agreement are not conditioned on our existing owners’ continued ownership of us after this offering.
Payments under the Tax Receivable Agreement will be based on the tax reporting positions we determine, and the IRS or another tax authority may challenge all or a part of the deductions, existing tax basis, tax basis increases, NOLs or other tax attributes subject to the Tax Receivable Agreement, and a court could sustain such challenge. Payments we will be required to make under the Tax Receivable Agreement generally will not be reduced as a result of any taxes imposed on us, Cure TopCo, LLC or any direct or indirect subsidiary thereof that are attributable to a tax period (or portion thereof) ending on or before the Mergers, the IPO Contribution or the date of the completion of this offering, Further, the parties to the Tax Receivable Agreement will not reimburse us for any payments previously made if such tax attributes are subsequently disallowed, except that any excess payments made to a TRA Party will be netted against future payments otherwise to be made to such TRA Party under the Tax Receivable Agreement, if any, after our determination of such excess. In addition, the actual state or local tax savings we may realize may be different than the amount of such tax savings we are deemed to realize under the Tax Receivable Agreement, which will be based on an assumed combined state and local tax rate applied to our reduction in taxable income as determined for U.S. federal income tax purposes as a result of the tax attributes subject to the Tax Receivable Agreement. In both such circumstances, we could make payments to the TRA Parties that are greater than our actual cash tax savings and we may not be able to recoup those payments, which could negatively impact our liquidity. The Tax Receivable Agreement provides that (1) in the event that we breach any of our material obligations under the Tax Receivable Agreement, (2) at the election of the TRA Parties, upon certain changes of control or (3) if, at any time, we elect an early termination of the Tax Receivable Agreement, our obligations under the Tax Receivable Agreement (with respect to all LLC Units, whether or not LLC Units have been exchanged or acquired before or after such transaction) would accelerate and become payable in a lump sum amount equal to the present value of the anticipated future tax benefits calculated based on certain assumptions, including that we would have sufficient taxable income to fully utilize the deductions arising from the tax deductions, tax basis and other tax attributes subject to the Tax Receivable
67
Table of Contents
Agreement. The change of control provisions in the Tax Receivable Agreement may result in situations where the Pre-IPO LLC Members have interests that differ from or are in addition to those of our other stockholders.
Finally, because we are a holding company with no operations of our own, our ability to make payments under the Tax Receivable Agreement depends on the ability of Cure TopCo, LLC to make distributions to us. To the extent that we are unable to make payments under the Tax Receivable Agreement for any reason, such payments will be deferred and will accrue interest until paid; provided, however, that nonpayment for a specified period may constitute a breach of a material obligation under the Tax Receivable Agreement and therefore accelerate payments due under the Tax Receivable Agreement, which could negatively impact our results of operations and could also affect our liquidity in periods in which such payments are made.
Risks related to our Class A common stock and this offering
Immediately following the consummation of this offering, the Continuing Pre-IPO LLC Members may require us to issue additional shares of our Class A common stock.
After this offering, we will have an aggregate of more than 830,000,000 shares of Class A common stock authorized but unissued, including approximately 57,264,580 shares of Class A common stock issuable upon the redemption or exchange of LLC Units that will be held by the Continuing Pre-IPO LLC Members. We, the Continuing Pre-IPO LLC Members and Cure TopCo, LLC will enter into the Amended LLC Agreement, pursuant to which holders of LLC Units (other than us and our wholly owned subsidiaries), including the Continuing Pre-IPO LLC Members, will have the right, from and after the completion of this offering to require Cure TopCo, LLC to redeem all or a portion of their LLC Units for, at our election, newly issued shares of Class A common stock on a one-for-one basis or a cash payment equal to the volume-weighted average market price of one share of our Class A common stock for each LLC Unit redeemed or exchanged. Alternatively, we can elect to directly acquire LLC Units in exchange for newly issued shares of Class A common stock on a one-for-one basis or a cash payment equal to the volume-weighted average market price of one share of our Class A common stock for each LLC Unit redeemed or exchanged. If we elect to satisfy such redemption or exchange by issuing additional shares of Class A common stock instead of cash and such shares of Class A common stock are sold into the public market, it may cause the market price of our Class A common stock to decline.
Some provisions of Delaware law and our certificate of incorporation and bylaws may deter third parties from acquiring us and diminish the value of our Class A common stock.
Our certificate of incorporation and bylaws will provide for, among other things:
| • | a classified board of directors, as a result of which our board of directors will be divided into three classes, with each class serving for staggered three-year terms and with successors to the class of directors whose term expires at the first and second annual meetings of stockholders following the adoption of the certificate of incorporation, as applicable, elected for a term expiring at the third annual meeting following the annual meeting at which such directors were elected; |
| • | at any time after New Mountain Capital, together with its affiliates and permitted transferees, owns less than a majority of our outstanding common stock (the “Majority Ownership Requirement”), there will be: |
| • | restrictions on the ability of our stockholders to call a special meeting and the business that can be conducted at such meeting or to act by written consent; |
| • | supermajority approval requirements for amending or repealing provisions in the certificate of incorporation and bylaws; |
| • | the removal of directors for cause only upon the affirmative vote of the holders of at least 662⁄3% of the shares of common stock entitled to vote generally in the election of directors; |
| • | the authorization of undesignated preferred stock, the terms of which may be established and shares of which may be issued without stockholder approval; and |
| • | advance notice requirements for stockholder proposals. |
68
Table of Contents
These anti-takeover defenses could discourage, delay or prevent a transaction involving a change in control of our company. Even in the absence of a takeover attempt, the existence of these provisions may adversely affect the prevailing market price of our Class A common stock if they are viewed as discouraging future takeover attempts. These provisions could also make it more difficult for stockholders to nominate directors for election to our board of directors and take other corporate actions.
The provision of our amended and restated certificate of incorporation requiring exclusive forum in certain courts in the State of Delaware or the federal district courts of the United States for certain types of lawsuits may have the effect of discouraging lawsuits against our directors and officers.
Our amended and restated certificate of incorporation will require, to the fullest extent permitted by law, that (i) any derivative action or proceeding brought on our behalf, (ii) any action asserting a claim of breach of a fiduciary duty owed by any of our directors, officers or stockholders to us or our stockholders, (iii) any action asserting a claim against us arising pursuant to any provision of the DGCL or our amended and restated certificate of incorporation or our bylaws or (iv) any action asserting a claim against us governed by the internal affairs doctrine will have to be brought in a state court located within the state of Delaware (or if no state court of the State of Delaware has jurisdiction, the federal district court for the District of Delaware), in all cases subject to the court’s having personal jurisdiction over the indispensable parties named as defendants. The foregoing provision will not apply to claims arising under the Securities Act, the Exchange Act or other federal securities laws for which there is exclusive federal or concurrent federal and state jurisdiction.
Additionally, unless we consent in writing to the selection of an alternative forum, the federal district courts of the United States of America shall be the exclusive forum for the resolution of any complaint asserting a cause of action arising under the Securities Act.
Although we believe these exclusive forum provisions benefit us by providing increased consistency in the application of Delaware law and federal securities laws in the types of lawsuits to which each applies, the exclusive forum provisions may limit a stockholder’s ability to bring a claim in a judicial forum that it finds favorable for disputes with us or any of our directors, officers or stockholders, which may discourage lawsuits with respect to such claims. Further, in the event a court finds either exclusive forum provision contained in our amended and restated certificate of incorporation to be unenforceable or inapplicable in an action, we may incur additional costs associated with resolving such action in other jurisdictions, which could harm our business, operating results and financial condition.
We do not anticipate paying any cash dividends in the foreseeable future.
We currently intend to retain our future earnings, if any, for the foreseeable future, to fund the development and growth of our business. We do not intend to pay any dividends to holders of our Class A common stock. As a result, capital appreciation in the price of our Class A common stock, if any, will be your only source of gain on an investment in our Class A common stock. See “Dividend policy.”
However, under the Amended LLC Agreement, Cure TopCo, LLC will generally be required from time to time to make pro rata distributions in cash to us and the other holders of LLC Units at certain assumed tax rates in amounts that could be significant. See “—In certain circumstances, Cure TopCo, LLC will be required to make distributions to us and the other holders of LLC Units, and the distributions that Cure TopCo, LLC will be required to make may be substantial.”
We have identified a series of significant deficiencies in our internal controls over financial reporting and IT access controls that collectively amounted to a material weakness. If our remediation of these significant deficiencies that led to the material weakness is not effective, or if we experience additional material weaknesses in the future or otherwise fail to maintain an effective system of internal controls in the future, we may not be able to accurately or timely report our financial condition or results of operations, which may adversely affect investor confidence in us and, as a result, the value of our Class A common stock.
In connection with our audits of the consolidated financial statements in each of fiscal year 2018 and 2019, we identified a material weakness in our internal control over financial reporting. In 2018, the material weakness
69
Table of Contents
related to deficiencies in our controls, which ultimately led to a restatement of our 2018 financial statements. In 2019, we identified a number of significant deficiencies in the design and operation of our internal control over financial reporting that collectively amounted to a material weakness. The significant deficiencies primarily related to segregation of duty controls over the review and evaluation of the company’s combined-consolidated financial statements in order to prevent misstatements associated with various accounts, disclosures and statements in accordance with GAAP. Additionally, we did not have effective information technology controls related to governance over privileged access, security and change management. A number of these IT access control deficiencies had been identified in 2018 and had not been fully remediated ahead of the 2019 audit. No individual control deficiency identified in 2019 was considered to be of significance enough to individually escalate to the level of material weakness.
We are currently undertaking and otherwise evaluating a number of steps to enhance our internal control over financial reporting and address the material weaknesses, including: the hiring of additional accounting and financial reporting personnel with technical accounting and public company experience, enhancing and formalizing our internal review procedures during the financial statement close process, and designing and implementing IT general computer controls.
We cannot assure you that the measures we have taken to date, and actions we may take in the future, will be sufficient to remediate the control deficiencies that led to our material weaknesses in our internal control over financial reporting and IT access control or that they will prevent or avoid potential future material weaknesses. In addition, neither our management nor an independent registered public accounting firm has performed an evaluation of our internal control over financial reporting in accordance with the provisions of the Sarbanes-Oxley Act because no such evaluation has been required. Had we or our independent registered public accounting firm performed an evaluation of our internal control over financial reporting in accordance with the provisions of the Sarbanes-Oxley Act, additional material weaknesses may have been identified. As a public company, we will be required in future years to document and assess the effectiveness of our system of internal control over financial reporting to satisfy the requirements of the Sarbanes-Oxley Act.
If we fail to effectively remediate the material weaknesses in our internal control over financial reporting, if we identify future material weaknesses in our internal control over financial reporting or if we are unable to comply with the demands that will be placed upon us as a public company, including the requirements of Section 404 of the Sarbanes-Oxley Act, in a timely manner, we may be unable to accurately report our financial results, or report them within the time frames required by the SEC. In addition, if we are unable to assert that our internal control over financial reporting is effective, or if our independent registered public accounting firm is unable to express an opinion as to the effectiveness of our internal control over financial reporting, when required, investors may lose confidence in the accuracy and completeness of our financial reports, we may face restricted access to the capital markets and our stock price may be adversely affected.
Our internal controls over financial reporting may not be effective and our independent registered public accounting firm may not be able to certify as to their effectiveness, which could have a significant and adverse effect on our business and reputation.
We are not currently required to comply with SEC rules that implement Section 404 of the Sarbanes-Oxley Act and are therefore not required to make a formal assessment of the effectiveness of our internal controls over financial reporting for that purpose. We will not be required to formally assess our internal controls until we file our second annual report on Form 10-K and we will not be required to have our independent registered public accounting firm formally assess our internal controls for as long as we remain an “emerging growth company” as defined in the JOBS Act.
When evaluating our internal controls over financial reporting, we may identify material weaknesses that we may not be able to remediate in time to meet the applicable deadline imposed upon us for compliance with the requirements of Section 404 of the Sarbanes-Oxley Act. In addition, if we fail to achieve and maintain the
70
Table of Contents
adequacy of our internal controls, as such standards are modified, supplemented or amended from time to time, we may not be able to ensure that we can conclude on an ongoing basis that we have effective internal controls over financial reporting in accordance with Section 404 of the Sarbanes-Oxley Act. We cannot be certain as to the timing of completion of our evaluation, testing and any remediation actions or the impact of the same on our operations. If we are not able to implement the requirements of Section 404 of the Sarbanes-Oxley Act in a timely manner or with adequate compliance, our independent registered public accounting firm may issue an adverse opinion due to ineffective internal controls over financial reporting, and we may be subject to sanctions or investigation by regulatory authorities, such as the SEC. As a result, there could be a negative reaction in the financial markets due to a loss of confidence in the reliability of our financial statements. In addition, we may be required to incur costs in improving our internal control system and the hiring of additional personnel. Any such action could negatively affect our results of operations and cash flows.
General risks related to our business and this offering
If our existing customers do not continue or renew their contracts with us, renew at lower fee levels, decline to purchase additional services from us or reduce the services received from us pursuant to those contracts, it could have a material adverse effect on our business, financial condition and results of operations.
We expect to derive a significant portion of our revenue from renewal of existing customer contracts and sales of additional services to existing customers. As part of our growth strategy, for instance, we have recently focused on expanding our services among current customers, both in terms of the number of distinct services an existing customer uses and expanding the existing customer’s use of a particular service. As a result, selling additional services and expanding use of current services are critical to our future business, revenue growth and results of operations.
Factors that may affect our ability to sell additional services and expand use of current services include the following:
| • | the price, performance and functionality of our services; |
| • | the availability, price, performance and functionality of competing or replacement services; |
| • | our ability to develop and sell complementary services; |
| • | changes in healthcare laws, regulations or trends; |
| • | the business environment of our customers; and |
| • | the government programs in which our customers participate. |
Our contracts with our health plan customers for IHEs generally have stated initial terms of one to two years with automatic renewal at the end of each term unless terminated by the customer. We are paid a flat fee per IHE completed. Our ability to complete IHEs depends on the plan members provided by our customers for purposes of our target member list (“TML”) agreeing to an IHE. However, our customers typically have no obligation to accept such automatic renewal. In addition, our customers may negotiate terms less advantageous to us upon renewal, which may reduce our revenue from these customers. Our future results of operations also depend, in part, on our ability to expand across the continuum of care. If our customers fail to renew their contracts, renew their contracts upon less favorable terms or at lower fee levels or fail to purchase new services from us, our revenue may decline, or our future revenue growth may be constrained.
Our contracts with healthcare providers are also subject to renegotiation from time to time. Under our provider contracts, provider partners can typically terminate their contracts with or without cause upon advance notice to Signify. In addition, provider partners may seek to renegotiate the administrative fees and/or percentage of shared savings that we are entitled to under our contracts from time to time.
In addition, a significant number of our customer contracts (including contracts with many of our top 10 customers) allow health plan and provider partners to terminate such agreements for convenience, typically with
71
Table of Contents
one to three months advance notice. If a customer terminates its contract early and revenue and cash flows expected from a customer are not realized in the time period expected or not realized at all, our business, financial condition and results of operations could be adversely affected.
If we are unable to attract new customers, our business, financial condition and results of operations would be adversely affected.
To increase our revenue and achieve continued growth, we must continue to attract new customers. Our ability to do so depends in large part on the success of our sales and marketing efforts and the quality of our solutions, as potential customers may seek out other options. For example, in our Episodes of Care Services segment, potential customers might decline episode of care programs in favor of other value-based care models, such as ACOs, capitation models, or pay-for-performance programs. Therefore, we must demonstrate that our services and solutions are valuable and superior to alternatives. If we fail to provide high-quality solutions and convince customers of the benefits of our model and value proposition, we may not be able to attract new customers. If the markets for our solutions decline or grow more slowly than we expect, or if the number of customers that contract with us for our solutions declines or fails to increase as we expect, our financial results could be harmed. As markets in which we participate mature, services evolve and competitors begin to enter into the market and introduce differentiated solutions or services that are perceived to compete with ours, our ability to sell our solutions could be impaired. As a result of these and other factors, we may be unable to attract new customers, which would have an adverse effect on our business, financial condition and results of operations.
We may acquire other companies or technologies, which could divert our management’s attention, result in dilution to our stockholders, and otherwise disrupt our operations.
In the past, we have expanded our business in part through acquisitions, and we may seek to acquire or invest in additional businesses, applications, services, or technologies that we believe could complement or expand our existing and future offerings, enhance our technical capabilities, give us access to new markets or otherwise offer growth opportunities. However, we may not be successful in identifying acquisition targets or we may use estimates and judgments to evaluate the operations and future revenues of a target that turn out to be inaccurate. The pursuit of potential acquisitions may also divert the attention of management and cause us to incur various expenses in identifying, investigating, and pursuing suitable acquisitions, whether or not they are consummated. In addition, we have limited experience in acquiring other businesses and may have difficulty integrating acquired businesses. If we acquire additional businesses, we may not be able to integrate the acquired operations and technologies successfully, or effectively manage the combined business following the acquisition. Integration may prove to be difficult due to the necessity of integrating personnel that have disparate business backgrounds and are accustomed to different corporate cultures.
We also may not achieve the anticipated benefits from any acquired business due to a number of factors, including:
| • | inability to integrate or benefit from acquired technologies or services in a profitable manner; |
| • | unanticipated costs or liabilities, including legal liabilities, associated with the acquisition; |
| • | an incoherent customer experience as we integrate different technologies and systems; |
| • | difficulties and additional expenses associated with supporting legacy products and hosting infrastructure of the acquired business; |
| • | difficulty converting the customers of the acquired business into our current and future offerings and contract terms, including disparities in the revenue model of the acquired company; |
| • | diversion of management’s attention or resources from other business concerns; |
| • | adverse effects on our existing business relationships with customers, members, or strategic partners as a result of the acquisition; |
72
Table of Contents
| • | due diligence errors or poor execution; |
| • | a lack of understanding of the acquired business’ historical liabilities and existing insurance coverage; |
| • | the potential loss of key employees; and |
| • | use of substantial portions of our available cash to consummate the acquisition. |
We may issue equity securities or incur indebtedness to pay for any such acquisition or investment, which would cause dilution for our shareholders and could adversely affect our financial condition. Any such issuances of additional capital stock may cause stockholders to experience significant dilution of their ownership interests and the per share value of our Class A common stock to decline. In addition, a significant portion of the purchase price of any companies we acquire may be allocated to acquired goodwill and other intangible assets, which must be assessed for impairment at least annually. In the future, if our acquisitions do not yield expected returns, we may be required to take charges to our results of operations based on this impairment assessment process, which could adversely affect our results of operations.
The growth of our business and future success relies in part on our relationships with third parties and our business could be harmed if we fail to maintain or expand these relationships.
We selectively form relationships and engage with a range of third parties for our technology needs in implementation of our service. For example, we are particularly reliant on a vendor that provides us with software that allows us to engage in efficient, targeted outreach to members on our TML. We may fail to retain and expand these relationships for various reasons, and any such failure could harm our relationship with our customers, our prospects, and our business. In order to grow our business, we anticipate that we will continue to depend on relationships with third parties. As we seek to continue current relationships and form additional relationships, it is uncertain whether these efforts will be successful, or that these relationships will result in increased customer use of our solutions or increased revenue. In the event that we are unable to effectively utilize, maintain, and expand these relationships that we are dependent on, our results of operations and financial condition could be materially adversely affected.
If we fail to retain and motivate members of our management team or other key employees, or fail to attract additional qualified personnel to support our operations, our business and future growth prospects could be harmed.
Our success and future growth depend largely upon the continued services of our management team and our other key employees. From time to time, there may be changes in our executive management team or other key employees resulting from the hiring or departure of these personnel. Our executive officers and other key employees are employed on an at-will basis, which means that these personnel could terminate their employment with us at any time. The loss of one or more of our executive officers, or the failure by our executive team to effectively work with our employees and lead our company, could harm our business.
In addition, to execute our growth plan, we must attract and retain highly qualified personnel. Competition for these personnel is intense, especially for experienced sales, customer account management, digital product development and technology personnel. There is no guarantee we will be able to attract such personnel or that competition among potential employers will not result in increased salaries or other benefits. From time to time, we have experienced, and we expect to continue to experience, difficulty in hiring and retaining employees with appropriate qualifications. Many of the companies with which we compete for experienced personnel have greater resources than we have. If we hire employees from competitors or other companies, their former employers may attempt to assert that these employees or we have breached their legal obligations, resulting in a diversion of our time and resources. We expect prospective employees to evaluate us on a number of areas, such as diversity and inclusion and workplace conduct. If we are unable to foster a positive and inclusive working environment that is attractive to our existing and prospective employees, it could impact employee recruiting,
73
Table of Contents
engagement and retention and the willingness of customers and our partners to do business with us, which could have a material adverse effect on our business, results of operations and cash flows. In addition, prospective and existing employees often consider the value of the equity awards they receive in connection with their employment. If the perceived value of our equity awards declines, experiences significant volatility, or increases such that prospective employees believe there is limited upside to the value of our equity awards, it may adversely affect our ability to recruit and retain key employees. If we fail to attract new personnel or fail to retain and motivate our current personnel, our business and future growth prospects could be harmed.
We may be subject to legal proceedings and litigation, including intellectual property and privacy disputes, which are costly to defend and could materially harm our business and results of operations.
We may be party to lawsuits and legal proceedings in the ordinary course of business. These matters are often expensive and disruptive to normal business operations. We have in the past and may in the future face allegations, lawsuits, regulatory inquiries, audits or investigations regarding data privacy, data security, personal injury, malpractice or intellectual property infringement, including claims related to privacy, patents, publicity, trademarks, copyrights, trade secrets or other rights. We have in the past and may in the future be subject to allegations, lawsuits or inquiries relating to labor and employment, in the case of the past in particular, with respect to our characterization of independent contractor relationships. See “—Risks related to governmental regulation—If our providers are characterized as employees, we would be subject to adverse effects on our business and employment and withholding liabilities.” We may also face allegations or litigation related to our acquisitions, securities issuances or business practices, including public disclosures about our business. See “Business—Legal proceedings.” Litigation and regulatory proceedings may be protracted and expensive, and the results are difficult to predict. Certain of these matters may include speculative claims for substantial or indeterminate amounts of damages or for injunctive relief. Additionally, our litigation costs could be significant and are difficult to predict. Adverse outcomes with respect to allegations, lawsuits, regulatory inquiries, audits, or investigations may result in significant settlement costs or judgments, penalties and fines, or require us to modify our services or require us to stop serving certain customers or geographies, any of which could negatively impact our business. We have also in the past been subject to information requests and subpoenas in connection with investigations by government agencies into some of our customers. Complying with these requests can be costly and time consuming. Managing legal proceedings, litigation and audits, even if we achieve favorable outcomes, is time consuming and diverts management’s attention from our business. The results of regulatory proceedings, lawsuits, regulatory inquiries, audits and investigations cannot be predicted with certainty, and determining reserves for pending litigation and other legal, regulatory and audit matters requires significant judgment. There can be no assurance that our expectations will prove correct, and even if these matters are resolved in our favor or without significant cash settlements, these matters, and the time and resources necessary to litigate or resolve them, could harm our reputation, business, financial condition, results of operations and the market price of our Class A shares.
We also may be subject to lawsuits under the FCA and comparable state laws if the government or a whistleblower alleges that some misconduct or materially faulty services provided by us resulted in the health plan submitting allegedly false or fraudulent risk adjustment information to CMS under the Medicare Advantage program, among other potential legal theories under the FCA. These lawsuits, which may be initiated by government authorities as well as private party whistleblowers (also known as “relators”), can involve significant monetary damages, fines, attorney fees and the award of bounties to private plaintiffs who successfully bring these suits, as well as to the relevant government programs, or may lead to our exclusion from government programs we or our customers participate in. Such actions can also form the basis for exclusion from participation in those programs. In recent years, government oversight and law enforcement have become increasingly active and aggressive in investigating and taking legal action against potential fraud and abuse.
Furthermore, our business exposes us to professional negligence, personal injury and other related actions or claims that are inherent in the managing of healthcare services or a network of traveling personnel. These claims, with or without merit, could cause us to incur substantial costs, and could place a significant strain on our
74
Table of Contents
financial resources, divert the attention of management from our core business, harm our reputation and adversely affect our ability to attract and retain customers, any of which could have a material adverse effect on our business, financial condition and results of operations.
Although we maintain third-party liability insurance coverage, it is possible that claims against us may exceed the coverage limits of our insurance policies or may not be covered by our liability insurance coverage. Even if any professional liability loss is covered by an insurance policy, these policies typically have substantial deductibles for which we are responsible. Professional liability claims in excess of applicable insurance coverage could have a material adverse effect on our business, financial condition and results of operations. In addition, any professional liability claim brought against us, with or without merit, could result in an increase of our professional liability insurance premiums. Insurance coverage varies in cost and can be difficult to obtain, and we cannot guarantee that we will be able to obtain insurance coverage in the future on terms acceptable to us or at all. If our costs of insurance and claims increase, then our earnings could decline.
The emergence and effects related to a pandemic, epidemic, outbreak of an infectious disease or a natural or man-made disaster could negatively impact our operations and business.
If a pandemic, epidemic, outbreak of an infectious disease, other public health crisis or natural or man-made disaster were to occur in an area in which we or our provider partners operate, our operations could be negatively impacted. In particular, a public health crisis could reduce the demand for IHE visits from our providers, especially if such crisis is of an infectious nature. We have disaster plans in place and operate pursuant to infectious disease and other disaster protocols, but the potential emergence of a pandemic, epidemic, outbreak or natural or man-made disaster is difficult to predict and could harm our business and operations.
Further, a public health crisis or other public disaster may lead government agencies to provide forms of relief that could negatively impact our business. For example, in 2020 as a result of the COVID-19 pandemic, CMS announced that healthcare providers could choose to eliminate upside and downside risk by excluding all episodes from reconciliation in 2020 or could choose to exclude from reconciliation those episodes with a COVID-19 diagnosis during the episode. Subsequently, CMS announced that all episodes in 2021 with a COVID-19 diagnosis would be automatically excluded from reconciliation. See “—Our operations have been, and may continue to be, significantly disrupted by the COVID-19 pandemic, and our business, financial condition and results of operations have been negatively impacted.” As evidenced by the reduction in episodes due to COVID-19 diagnoses, if such measures were to be taken in connection with another pandemic, public health emergency or natural disaster, the program size we manage would decline, which would accordingly reduce our fees and ability to generate savings.
If the estimates and assumptions we use to determine the size of our total addressable market are inaccurate, our future growth rate may be impacted and our business would be harmed.
Market estimates and growth forecasts are subject to significant uncertainty and are based on assumptions and estimates that may prove to be inaccurate. Even if the market in which we compete meets our size estimates and forecasted growth, our business could fail to grow at rates similar to those at which it has historically grown, if at all. Our market opportunity is also based on the assumption that our existing and future solutions will be more attractive to our customers and potential customers than competing solutions. If these assumptions prove inaccurate, our business, financial condition, and results of operations could be adversely affected. For more information regarding our estimates of market opportunity and the forecasts of market growth included in this prospectus, see the section titled “Market and Industry Data.”
Our financial results may be adversely impacted by changes in accounting principles applicable to us.
Generally accepted accounting principles in the United States are set by and subject to interpretation by the Financial Accounting Standards Board, or FASB, and the SEC and new accounting principles are adopted from
75
Table of Contents
time to time. For example, in May 2014, the FASB issued accounting standards update No. 2014-09 (Topic 606), Revenue from Contracts with Customers, which superseded nearly all previously existing revenue recognition guidance under GAAP. The core principle of Topic 606 is that an entity should recognize revenue to depict the transfer of promised goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled in exchange for those goods or services.
We adopted this standard as of January 1, 2019 using the modified retrospective method. The adoption of this standard did not have a material impact on our consolidated financial statements. Remedy Partners also adopted this new accounting standard effective January 1, 2019, prior to our acquisition of Remedy Partners and its inclusion in our combined-consolidated financial statements. The adoption of this standard did have a material impact on Remedy Partners’ consolidated financial statements. We estimate net revenue for the year ended December 31, 2019 for Remedy Partners was approximately $25.0 million lower under Topic 606 than it would have been under previous revenue recognition guidance primarily due to changes in the timing of revenue recognition under Topic 606.
Under Topic 606, more estimates, judgments, and assumptions are required within the revenue recognition process than were previously required. Our reported financial position and financial results may be harmed if our estimates or judgments prove to be wrong, assumptions change, or actual circumstances differ from those in our assumptions. Any difficulties in implementing these pronouncements could cause us to fail to meet our financial reporting obligations, which could result in regulatory discipline and harm our business and the trading price of our Class A common stock.
If our estimates or judgments relating to our critical accounting policies prove to be incorrect or change, our results of operations could be harmed.
The preparation of financial statements in conformity with GAAP requires management to make judgments, estimates and assumptions that affect the reported amounts in the consolidated financial statements and accompanying notes. We base these estimates on historical experience and various other assumptions that we believe to be reasonable under the circumstances, as provided in “Management’s discussion and analysis of financial condition and results of operations—Critical accounting policies.” The results of these estimates form the basis for making judgments about the carrying values of assets, liabilities and equity and the amount of revenue and expenses that are not readily apparent from other sources. Significant assumptions and estimates used in preparing our consolidated financial statements include those related to revenue recognition, allowance for doubtful accounts, equity-based compensation, business combinations, impairment of long-lived assets, including intangible assets and goodwill and EARs. Our results of operations may be harmed if our assumptions change or if actual circumstances differ from those in our assumptions, which could cause our results of operations to fall below the expectations of securities analysts and investors, resulting in a decline in the trading price of our Class A common stock.
There may not be an active, liquid trading market for our Class A common stock.
Prior to this offering, there has been no public market for shares of our Class A common stock. We cannot predict the extent to which investor interest in our company will lead to the development of a trading market on the NYSE or how liquid that market may become. If an active trading market does not develop, you may have difficulty selling any of our Class A common stock that you purchase. The initial public offering price of shares of our Class A common stock is, or will be, determined by negotiation between us and the underwriters and may not be indicative of prices that will prevail following the completion of this offering. The market price of shares of our Class A common stock may decline below the initial public offering price, and you may not be able to resell your shares of our Class A common stock at or above the initial public offering price.
76
Table of Contents
We expect that our stock price will fluctuate significantly, and you may not be able to resell your shares at or above the initial public offering price.
The trading price of our Class A common stock is likely to be volatile and subject to wide price fluctuations in response to various factors, including:
| • | market conditions in the broader stock market in general, or in our industry in particular; |
| • | actual or anticipated fluctuations in our quarterly financial and operating results; |
| • | introduction of new products and services by us or our competitors; |
| • | issuance of new or changed securities analysts’ reports or recommendations; |
| • | sales of large blocks of our stock; |
| • | additions or departures of key personnel; |
| • | regulatory developments; |
| • | litigation and governmental investigations; and |
| • | economic and political conditions or events. |
These and other factors may cause the market price and demand for our Class A common stock to fluctuate substantially, which may limit or prevent investors from readily selling their shares of Class A common stock and may otherwise negatively affect the liquidity of our Class A common stock. In addition, in the past, when the market price of a stock has been volatile, holders of that stock have instituted securities class action litigation against the company that issued the stock. If any of our stockholders brought a lawsuit against us, we could incur substantial costs defending the lawsuit. Such a lawsuit could also divert the time and attention of our management from our business.
The trading market for our Class A common stock will also be influenced by the research and reports that industry or securities analysts publish about us or our business. If one or more of these analysts cease coverage of our company or fail to publish reports on us regularly, we could lose visibility in the financial markets, which in turn could cause our stock price or trading volume to decline. Moreover, if one or more of the analysts who cover us downgrade our stock, or if our results of operations do not meet their expectations, our stock price could decline.
If a substantial number of shares become available for sale and are sold in a short period of time, the market price of our Class A common stock could decline.
If our existing stockholders sell substantial amounts of our Class A common stock in the public market following this offering, the market price of our Class A common stock could decrease significantly. The perception in the public market that our existing stockholders might sell shares of Class A common stock could also depress our market price. Upon completion of this offering, we will have outstanding 165,092,313 shares of Class A common stock and options to purchase 7,153,619 shares of Class A common stock and restricted stock units with respect to an estimated 74,144 shares of Class A common stock. Our directors, executive officers and additional other holders of our Class A common stock will be subject to the lock-up agreements described in “Underwriting” and the Rule 144 holding period requirements described in “Shares eligible for future sale.” After all of these lock-up periods have expired and the holding periods have elapsed, 198,856,893 additional shares will be eligible for sale in the public market (assuming all LLC Units and corresponding shares of Class B common stock held by the Continuing Pre-IPO LLC Members are exchanged for shares of Class A common stock). The market price of shares of our Class A common stock may drop significantly when the restrictions on resale by our existing stockholders lapse. A decline in the price of shares of our Class A common stock might impede our ability to raise capital through the issuance of additional shares of our Class A common stock or other equity securities.
Our management may spend the proceeds of this offering in ways with which you may disagree or that may not be profitable.
Although we anticipate using the net proceeds from the offering as described under “Use of proceeds,” management will have broad discretion as to the application of the net proceeds and could use them for purposes other than those contemplated by this offering. You may not agree with the manner in which our management
77
Table of Contents
chooses to allocate and spend the net proceeds. Our management may use the proceeds for corporate purposes that may not increase our profitability or otherwise result in the creation of stockholder value. In addition, pending our use of the proceeds, we may invest the proceeds primarily in instruments that do not produce significant income or that may lose value.
New investors in our Class A common stock will experience immediate and substantial book value dilution after this offering.
The initial public offering price of our Class A common stock will be substantially higher than the pro forma net tangible book value per share of the outstanding common stock immediately after the offering. Based on an assumed initial public offering price of $20.50 per share (the midpoint of the price range set forth on the cover page of this prospectus) and our net tangible book value as of September 30, 2020, if you purchase our Class A common stock in this offering you will pay more for your shares than the amounts paid by our existing stockholders for their shares and you will suffer immediate dilution of approximately $21.53 per share in pro forma net tangible book value. As a result of this dilution, investors purchasing stock in this offering may receive significantly less than the full purchase price that they paid for the shares purchased in this offering in the event of a liquidation. See “Dilution.”
We also have outstanding stock options to purchase approximately 6,281,119 shares of Class A common stock on a gross basis with exercise prices that are below the assumed initial public offering price of the Class A common stock. To the extent that these options are exercised, there will be further dilution.
We will incur significantly increased costs and become subject to additional regulations and requirements as a result of becoming a public company, and our management will be required to devote substantial time to new compliance matters, which could lower our profits or make it more difficult to run our business.
As a public company, we will incur significant legal, regulatory, finance, accounting, investor relations and other expenses that we have not incurred as a private company, including costs associated with public company reporting requirements. As a result of having publicly traded common stock, we will also be required to comply with, and incur costs associated with such compliance with, the Sarbanes-Oxley Act and the Dodd-Frank Wall Street Reform and Consumer Protection Act, or the Dodd-Frank Act, as well as rules and regulations implemented by the SEC and the NYSE. The expenses incurred by public companies generally for reporting and corporate governance purposes have been increasing. We expect these rules and regulations to increase our legal and financial compliance costs and to make some activities more time consuming and costly. Our management will need to devote a substantial amount of time to ensure that we comply with all of these requirements, diverting the attention of management away from revenue-producing activities. These laws and regulations also could make it more difficult or costly for us to obtain certain types of insurance, including director and officer liability insurance, and we may be forced to accept reduced policy limits and coverage or incur substantially higher costs to obtain the same or similar coverage. These laws and regulations could also make it more difficult for us to attract and retain qualified persons to serve on our Board of Directors, our board committees or as our executive officers. Furthermore, if we are unable to satisfy our obligations as a public company, we could be subject to delisting of our Class A common stock, fines, sanctions and other regulatory action and potentially civil litigation.
We are an “emerging growth company” and we cannot be certain if the reduced disclosure requirements applicable to emerging growth companies will make our Class A common stock less attractive to investors.
We are an “emerging growth company,” as defined in the JOBS Act, and we intend to take advantage of certain exemptions from various reporting requirements that are applicable to other public companies that are not “emerging growth companies” including, but not limited to, not being required to comply with the auditor attestation requirements of Section 404 of the Sarbanes-Oxley Act, and reduced disclosure obligations regarding executive compensation in our periodic reports and proxy statements. We cannot predict if investors will find our Class A common stock less attractive if we rely on these exemptions. If some investors find our Class A common stock less attractive as a result, there may be a less active trading market for our Class A common stock and our stock price may be more volatile.
78
Table of Contents
SPECIAL NOTE REGARDING FORWARD-LOOKING STATEMENTS
We have made statements under the captions “Prospectus summary,” “Risk factors,” “Management’s discussion and analysis of financial condition and results of operations,” “Business” and in other sections of this prospectus that are forward-looking statements. In some cases, you can identify these statements by forward-looking words such as “may,” “might,” “will,” “should,” “expects,” “plans,” “anticipates,” “believes,” “estimates,” “predicts,” “potential” or “continue,” the negative of these terms and other comparable terminology. These forward-looking statements, which are subject to risks, uncertainties and assumptions about us, may include projections of our future financial performance, our anticipated growth strategies and anticipated trends in our business. These statements are only predictions based on our current expectations and projections about future events. There are important factors that could cause our actual results, level of activity, performance or achievements to differ materially from the results, level of activity, performance or achievements expressed or implied by the forward-looking statements, including those factors discussed under the caption entitled “Risk factors.” You should specifically consider the numerous risks outlined under “Risk factors.”
Although we believe the expectations reflected in the forward-looking statements are reasonable, we cannot guarantee future results, level of activity, performance or achievements. Moreover, neither we nor any other person assumes responsibility for the accuracy and completeness of any of these forward-looking statements. Some of the factors that could cause actual results to differ materially from those expressed or implied by the forward-looking statements include:
| • | the COVID-19 pandemic; |
| • | our dependence upon a limited number of key customers; |
| • | our dependence on certain key government programs; |
| • | our failure to maintain and grow our network of high-quality providers; |
| • | our failure to continue to innovate and provide services that are useful to customers and achieve and maintain market acceptance; |
| • | our limited operating history with certain of our solutions; |
| • | our failure to compete effectively; |
| • | the length and unpredictability of our sales cycle; |
| • | failure of our existing customers to continue or renew their contracts with us; |
| • | seasonality that may cause fluctuations in our sales and results of operations; |
| • | our failure to achieve or maintain profitability; |
| • | our revenue not growing at the rates they historically have, or at all; |
| • | our failure to successfully execute on our growth initiatives, business strategies, or operating plans; |
| • | inaccurate estimates and assumptions used to determine the size of our total addressable market; |
| • | changes in accounting principles applicable to us; |
| • | incorrect estimates or judgments relating to our critical accounting policies; |
| • | increase in our level of indebtedness; |
| • | our failure to effectively adapt to changes in the healthcare industry, including changes in the rules governing Medicare or other federal health care programs; |
| • | our failure to adhere to complex and evolving governmental laws and regulations; |
| • | our failure to comply with current and future federal and state privacy, security and data protection laws, regulations or standards; |
79
Table of Contents
| • | our employment of and contractual relationships with our providers subjecting us to licensing or other regulatory risks; |
| • | adverse findings from inspections, reviews, audits and investigations from health plans; |
| • | inadequate investment in or maintenance of our operating platform and other information technology and business systems; |
| • | security breaches or incidents, loss or misuse of data, a failure in or breach of our operational or security systems or other disruptions; |
| • | disruptions in our disaster recovery systems or management continuity planning; |
| • | our ability to comply with, and changes to, laws, regulations and standards relating to privacy or data protection; |
| • | our ability to obtain, maintain, protect and enforce our intellectual property; |
| • | our dependence on distributions from Cure TopCo, LLC to fund dividend payments, if any, and to pay our taxes and expenses, including payments under the Tax Receivable Agreement; |
| • | the Pre-IPO LLC Members’ control of us and our status as a controlled company; |
| • | our ability to realize any benefit from our organizational structure; and |
| • | the other risk factors described under “Risk factors.” |
Given these risks and uncertainties, you are cautioned not to place undue reliance on such forward-looking statements. The forward-looking statements contained in this prospectus are not guarantees of future performance and our actual results of operations, financial condition or liquidity, and the development of the industry and markets in which we operate, may differ materially from the forward-looking statements contained or incorporated by reference in this prospectus. In addition, even if our results of operations, financial condition or liquidity, and events in the industry and markets in which we operate, are consistent with the forward-looking statements contained or incorporated by reference in this prospectus, they may not be predictive of results or developments in future periods.
Any forward-looking statement speaks only as of the date of such statement. Except as required by law, we do not undertake any obligation to update or revise, or to publicly announce any update or revision to, any of the forward-looking statements, whether as a result of new information, future events or otherwise.
80
Table of Contents
Structure prior to the Reorganization Transactions
We currently conduct our business through Cure TopCo, LLC and its subsidiaries. Following this offering, we will be a holding company and our sole material asset will be an ownership interest in Cure TopCo, LLC. Signify Health, Inc. was incorporated as a Delaware corporation on October 1, 2020 to serve as the issuer of the Class A common stock offered hereby.
Prior to the consummation of the Reorganization Transactions, the amended and restated limited liability company agreement of Cure TopCo, LLC will be amended and restated to, among other things, convert all outstanding equity interests into one class of non-voting common units (the “LLC Units”) and appoint Signify Health, Inc. as the sole managing member of Cure TopCo, LLC. After these transactions and prior to the consummation of the Reorganization Transactions and the completion of this offering, all of Cure TopCo, LLC’s outstanding equity interests will be owned by the following persons (collectively, the “Pre-IPO LLC Members”):
| • | Affiliates of New Mountain Capital and certain other minority equityholders, indirectly through certain entities treated as corporations for U.S. tax purposes; |
| • | New Mountain Partners V (AIV-C), LP; |
| • | Cure Aggregator, LLC; and |
| • | Certain other equity holders in Cure TopCo, LLC (the “Other Legacy Signify Holders”). |
The Reorganization Transactions
In connection with this offering, we intend to enter into the Reorganization Transactions.
Because we will manage and operate the business and control the strategic decisions and day-to-day operations of Cure TopCo, LLC and because we will also have a substantial financial interest in Cure TopCo, LLC, we will consolidate the financial results of Cure TopCo, LLC, and a portion of our net income will be allocated to the noncontrolling interest to reflect the entitlement of the Continuing Pre-IPO LLC Members to a portion of Cure TopCo, LLC’s net income. In addition, because Cure TopCo, LLC will be under the common control of the Pre-IPO LLC Members before and after the Reorganization Transactions (both directly and indirectly through their ownership of us), we will account for the Reorganization Transactions as a reorganization of entities under common control and will initially measure the interests of the Continuing Pre-IPO LLC Members in the assets and liabilities of Cure TopCo, LLC at their carrying amounts as of the date of the completion of the consummation of the Reorganization Transactions.
Our amended and restated certificate of incorporation that will be in effect upon the completion of this offering will authorize the issuance of two classes of common stock: Class A common stock and Class B common stock. Each share of common stock will entitle its holder to one vote per share on all matters submitted to a vote of our stockholders. The Class B common stock is not entitled to economic interests in Signify Health, Inc. See “Description of capital stock.”
Prior to the completion of this offering, we will acquire, directly and indirectly, LLC Units through the IPO Contribution and the Mergers. The Reorganization Parties will collectively hold 141,592,313 shares of Class A common stock of Signify Health, Inc. after the IPO Contribution and the Mergers. The Reorganization Parties will collectively receive a number of shares of our Class A common stock in the Mergers equal to the number of LLC Units held by the Blocker Companies prior to the Mergers, and will not directly hold interests in Cure TopCo, LLC.
Each Continuing Pre-IPO LLC Member will be issued a number of shares of our Class B common stock in an amount equal to the number of LLC Units held by such Continuing Pre-IPO LLC Member, except in the case of Cure Aggregator, LLC. Cure Aggregator, LLC is a special purpose investment vehicle through which certain members of Cure TopCo, LLC, primarily our employees and certain legacy investors, indirectly hold interests in Cure TopCo, LLC. Cure Aggregator, LLC holds LLC Units on behalf of such members on a one-for-one basis
81
Table of Contents
with each member’s interests in Cure Aggregator, LLC. Such common units in Cure Aggregator, LLC are subject to vesting as set forth under “Executive and Director Compensation—Other compensation plans—Incentive Units”. In connection with the Reorganization Transactions, shares of Class B common stock will be issued to the direct holders of common units in Cure Aggregator, LLC in proportion to their interests in Cure Aggregator, LLC, provided that such shares will not be entitled to any voting rights until such time as the common units of Cure Aggregator, LLC corresponding to such shares have vested.
Cure TopCo, LLC will enter into the Amended LLC Agreement. Under the Amended LLC Agreement, holders of LLC Units (other than us and our wholly owned subsidiaries), including the Continuing Pre-IPO LLC Members, will have the right, from and after the completion of this offering (subject to the terms of the Amended LLC Agreement), to require Cure TopCo, LLC to redeem all or a portion of their LLC Units for, at our election, newly issued shares of Class A common stock on a one-for-one basis or a cash payment equal to the volume-weighted average market price of one share of our Class A common stock for each LLC Unit redeemed (subject to customary adjustments, including for stock splits, stock dividends and reclassifications) in accordance with the terms of the Amended LLC Agreement. Additionally, in the event of a redemption request from a holder of LLC Units, we may, at our option, effect a direct exchange of cash or Class A common stock for LLC Units in lieu of such a redemption. Shares of Class B common stock will be cancelled on a one-for-one basis if we, following a redemption request from a holder of LLC Units, redeem or exchange LLC Units of such holder pursuant to the terms of the Amended LLC Agreement. See “Certain relationships and related party transactions—Amended LLC Agreement.” Except for transfers to us or to certain permitted transferees pursuant to the Amended LLC Agreement, the LLC Units and shares of Class B common stock may not be sold, transferred or otherwise disposed of.
In connection with this offering, we will enter into the stockholders agreement with certain of the Pre-IPO LLC Members. Pursuant to the stockholders agreement, New Mountain Capital will have certain board nomination, committee nomination and consent and information rights. See “Certain relationships and related party transactions—Stockholders agreement.”
We will issue 23,500,000 shares of Class A common stock to the public pursuant to this offering.
We will use all of the net proceeds from this offering (including net proceeds received if the underwriters exercise their option to purchase additional shares of Class A common stock in full) to acquire newly issued LLC Units from Cure TopCo, LLC at a purchase price per LLC Unit equal to the initial public offering price of Class A common stock, after deducting the underwriting discounts and commissions, collectively representing 10.6% of Cure TopCo, LLC’s outstanding LLC Units (or 12.0%, if the underwriters exercise their option to purchase additional shares of Class A common stock in full).
We will enter into a Tax Receivable Agreement, that will obligate us to make payments to the TRA Parties in the aggregate generally equal to 85% of the applicable cash savings that we actually realize as a result of (i) certain favorable tax attributes we will acquire from the Blocker Companies in the Mergers (including net operating losses, the Blocker Companies’ allocable share of existing tax basis and refunds of Blocker Company taxes attributable to pre-Merger tax periods), (ii) increases in our allocable share of existing tax basis and tax basis adjustments that may result from (x) future redemptions or exchanges of LLC Units by Continuing Pre-IPO LLC Members for cash or Class A common stock, (y) the IPO Contribution and (z) certain payments made under the Tax Receivable Agreement and (iii) deductions in respect of interest and certain compensatory payments made under the Tax Receivable Agreement. We will retain the benefit of the remaining 15% of these tax savings.
We will cause Cure TopCo, LLC to use the proceeds from the issuance of LLC Units to us (i) to pay fees and expenses of approximately $13.5 million in connection with this offering and the Reorganization Transactions and (ii) for general corporate purposes, including working capital and potential strategic acquisitions of, or investments in, other businesses or technologies that we believe will complement our current business and expansion strategies. See “Use of proceeds.”
82
Table of Contents
Effect of the Reorganization Transactions and this offering
The Reorganization Transactions are intended to create a holding company that will facilitate public ownership of, and investment in, the Company and are structured in a tax-efficient manner for the Blocker Companies and Reorganization Parties. The Continuing Pre-IPO LLC Members will continue to hold their ownership interests in Cure TopCo, LLC until such time in the future as they may elect to cause us to redeem or exchange their LLC Units for a corresponding number of shares of our Class A common stock or cash.
We estimate that the offering expenses (other than the underwriting discounts and commissions) will be approximately $13.5 million. All of such offering expenses will be paid for by Cure TopCo, LLC. See “Use of proceeds.”
83
Table of Contents
The following diagram depicts our organizational structure immediately following the consummation of the Reorganization Transactions, the completion of this offering and the application of the net proceeds from this offering, based on an assumed initial public offering price of $20.50 per share of Class A common stock (the midpoint of the estimated price range set forth on the cover page of this prospectus) and assuming the underwriters do not exercise their option to purchase additional shares of Class A common stock. This chart is provided for illustrative purposes only and does not purport to represent all legal entities within our organizational structure.
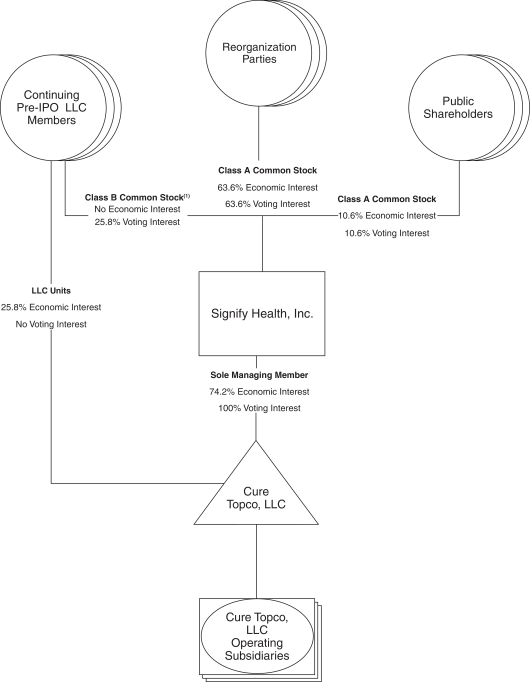
| (1) | Includes Class B common stock held directly by directors and officers who hold their interests in Cure TopCo, LLC indirectly through vested common units of Cure Aggregator, LLC. |
84
Table of Contents
Upon completion of the transactions described above, this offering and the application of the Company’s net proceeds from this offering:
| • | Signify Health, Inc. will be appointed as the managing member of Cure TopCo, LLC and will hold 165,092,313 LLC Units, constituting 74.2% of the outstanding economic interests in Cure TopCo, LLC (or 168,617,313 LLC Units, constituting 74.6% of the outstanding economic interests in Cure TopCo, LLC if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
| • | The Pre-IPO LLC Members will collectively hold (i) (x) 141,592,313 shares of Class A common stock and (y) 57,264,580 LLC Units, which together directly and indirectly represent approximately 89.4% of the economic interest in Cure TopCo, LLC (or 88.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full) and (ii) through their collective ownership of 141,592,313 shares of Class A and 57,264,580 shares of Class B common stock, approximately 89.4% of the combined voting power of our common stock (or 88.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
| • | Investors in this offering will collectively beneficially own (i) 23,500,000 shares of our Class A common stock, representing approximately 10.6% of the combined voting power of our common stock (or 27,025,000 shares and 12.0%, respectively, if the underwriters exercise their option to purchase additional shares of Class A common stock in full) and (ii) through our direct and indirect ownership of LLC Units, indirectly will hold approximately 10.6% of the economic interest in Cure TopCo, LLC (or 12.0% if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
Funds affiliated with New Mountain Capital, including the Reorganization Parties through their holdings of our Class A common stock and certain Continuing Pre-IPO LLC Members through their holdings of LLC Units and our Class B common stock, will collectively own 63.1% of the economic interest in Cure TopCo, LLC (or 62.1% if the underwriters exercise their option to purchase additional shares of Class A common stock in full), as well as an equal percentage of the voting power in Signify Health, Inc.
Holding company structure and the Tax Receivable Agreement
We are a holding company, and immediately after the consummation of the Reorganization Transactions and this offering, our sole material asset will be our ownership interests in Cure TopCo, LLC. The number of LLC Units that we will own directly and indirectly in the aggregate at any time will equal the aggregate number of outstanding shares of our Class A common stock. The economic interest represented by each LLC Unit that we own directly and indirectly will correspond to one share of our Class A common stock, and the total number of LLC Units owned directly and indirectly by us and the holders of our Class B common stock at any given time will equal the sum of the outstanding shares of all classes of our common stock.
We do not intend to list our Class B common stock on any stock exchange.
We will acquire certain favorable tax attributes from the Blocker Companies in the Mergers. In addition, acquisitions by us of LLC Units from Continuing Pre-IPO LLC Members in connection with the IPO Contribution and future redemptions or exchanges by the Continuing Pre-IPO LLC Members of LLC Units for shares of our Class A common stock or cash, and other transactions described herein are expected to result in favorable tax attributes that will be allocated to us. These tax attributes would not be available to us in the absence of those transactions and are expected to reduce the amount of tax that we would otherwise be required to pay in the future.
We intend to enter into a Tax Receivable Agreement with the TRA Parties. Under the Tax Receivable Agreement, we generally will be required to pay to the TRA Parties, in the aggregate, 85% of the amount of cash savings, if any, in U.S. federal, state and local income tax that we actually realize as a result of (i) certain favorable tax attributes we will acquire from the Blocker Companies in the Mergers (including net operating losses, the Blocker Companies’ allocable share of existing tax basis and refunds of Blocker company taxes
85
Table of Contents
attributable to pre-Merger tax periods), (ii) increases in our allocable share of existing tax basis and tax basis adjustments that may result from (x) future redemptions or exchanges of LLC Units by Continuing Pre-IPO LLC Members for cash or Class A common stock, (y) the IPO Contribution and (z) certain payments made under the Tax Receivable Agreement and (iii) deductions in respect of interest and certain compensatory payments made under the Tax Receivable Agreement.
The tax attributes available to us as a result of the Mergers and our allocable share of existing tax basis are expected to result in tax savings of approximately $56.3 million. We would be required to pay the TRA Parties approximately 85% of such amount, or $47.8 million, over the 15-year period from the date of the completion of this offering. Further, assuming no material changes in relevant tax law and that we earn sufficient taxable income to realize all tax benefits that are subject to the Tax Receivable Agreement, we expect that the tax savings associated with all tax attributes described above would aggregate to approximately $444.2 million over 15 years from the date of the completion of this offering, based on an assumed initial public offering price of $20.50 per share of Class A common stock, the midpoint of the estimated price range set forth on the cover page of this prospectus and assuming all future redemptions or exchanges would occur on the date of this offering. Under this scenario, we would be required to pay the TRA Parties approximately 85% of such amount, or $377.6 million, over the 15-year period from the date of the completion of this offering. The actual amounts we will be required to pay may materially differ from these hypothetical amounts, because potential future tax savings that we will be deemed to realize, and the Tax Receivable Agreement payments made by us, will be calculated based in part on the market value of our Class A common stock at the time of each redemption or exchange of an LLC Unit for cash or a share of Class A common stock and the prevailing applicable federal tax rate (plus the assumed combined state and local tax rate) applicable to us over the life of the Tax Receivable Agreement and will depend on our generating sufficient taxable income to realize the tax benefits that are subject to the Tax Receivable Agreement.
Payments under the Tax Receivable Agreement will be based on the tax reporting positions we determine, and the IRS or another tax authority may challenge all or part of the deductions, existing tax basis, tax basis increases, NOLs or other tax attributes subject to the Tax Receivable Agreement, and a court could sustain such challenge. Payments we will be required to make under the Tax Receivable Agreement generally will not be reduced as a result of any taxes imposed on us, Cure TopCo, LLC or any direct or indirect subsidiary thereof that are attributable to a tax period (or portion thereof) ending on or before the Mergers, the IPO Contribution or the date of the completion of this offering. Further, the TRA Parties will not reimburse us for any payments previously made if such tax attributes are subsequently challenged by a tax authority and are ultimately disallowed, except that any excess payments made to a TRA Party will be netted against future payments otherwise to be made to such TRA Party under the Tax Receivable Agreement, if any, after our determination of such excess. As a result, in such circumstances we could make future payments under the Tax Receivable Agreement that are greater than our actual cash tax savings and may not be able to recoup those payments, which could negatively impact our liquidity. See “Risk factors—Risks related to our organizational structure—We will be required to pay the Continuing Pre-IPO LLC Members, the Reorganization Parties and any other persons that become parties to the Tax Receivable Agreement for certain tax benefits we may receive, and the amounts we may pay could be significant.”
Our obligations under the Tax Receivable Agreement will also apply with respect to any person who is issued LLC Units in the future and who becomes a party to the Tax Receivable Agreement.
We are a holding company with no operations of our own and our ability to make payments under the Tax Receivable Agreement will depend on the ability of Cure TopCo, LLC to make distributions to us. Deterioration in the financial condition, earnings, or cash flow of Cure TopCo, LLC and its subsidiaries for any reason could limit or impair their ability to pay such distributions. To the extent that we are unable to make payments under the Tax Receivable Agreement for any reason, such payments generally will be deferred and will accrue interest until paid; provided, however, that nonpayment for a specified period may constitute a breach of a material obligation under the Tax Receivable Agreement and therefore accelerate payments due under the Tax Receivable Agreement, which could negatively impact our results of operations and could also affect our liquidity in periods in which such payments are made.
86
Table of Contents
We estimate that our net proceeds from this offering will be approximately $456.5 million, after deducting underwriting discounts and commissions, based on an assumed initial public offering price of $20.50 per share (the midpoint of the estimated initial public offering price range set forth on the cover page of this prospectus) and assuming the underwriters’ option to purchase additional shares of Class A common stock is not exercised. If the underwriters exercise their option to purchase additional shares of Class A common stock in full, we expect to receive approximately $524.9 million of net proceeds based on an assumed initial public offering price of $20.50 per share (the midpoint of the estimated initial public offering price range set forth on the cover page of this prospectus).
We estimate that the offering expenses (other than the underwriting discount and commissions) will be approximately $13.5 million. All of such offering expenses will be paid for or otherwise borne by Cure TopCo, LLC.
We will use all of the net proceeds from this offering (including net proceeds received if the underwriters exercise their option to purchase additional shares of Class A common stock) to acquire 23,500,000 newly issued LLC Units from Cure TopCo, LLC (or 27,025,000 LLC Units, if the underwriters exercise their option to purchase additional shares of Class A common stock in full) at a purchase price per LLC Unit equal to the initial public offering price of Class A common stock net of underwriting discounts and commissions, collectively representing 10.6% of Cure TopCo, LLC’s outstanding LLC Units (or 12.0%, if the underwriters exercise their option to purchase additional shares of Class A common stock in full).
Cure TopCo, LLC currently intends to use the net proceeds from this offering (i) to pay fees and expenses of approximately $13.5 million in connection with this offering and the Reorganization Transactions and (ii) for general corporate purposes, including working capital and potential strategic acquisitions of, or investments in, other businesses or technologies that we believe will complement our current business and expansion strategies. Although we routinely evaluate acquisition and investment opportunities that are aligned with our strategic goals, we do not have agreements or commitments to enter into any acquisitions at this time.
If the underwriters exercise their option to purchase additional shares of Class A common stock in full, we estimate that our additional net proceeds will be approximately $68.4 million. We will use the additional net proceeds we receive pursuant to any exercise of the underwriters’ option to purchase additional shares of Class A common stock to purchase additional LLC Units from Cure TopCo, LLC to maintain the one-to-one ratio between the number of shares of Class A common stock issued by us and the number of LLC Units owned by us. We intend to cause Cure TopCo, LLC to use such additional proceeds it receives for general corporate purposes.
A $1.00 increase (decrease) in the assumed initial public offering price of $20.50 per share would increase (decrease) the amount of proceeds to us from this offering available by approximately $22.3 million, assuming the number of shares offered by us, as set forth on the cover page of this prospectus, remains the same, and after deducting the estimated underwriting discounts and commissions. An increase (decrease) of 1,000,000 shares from the expected number of shares to be sold by us in this offering, assuming no change in the assumed initial public offering price per share, the midpoint of the estimated offering price range shown on the cover page of this prospectus, would increase (decrease) the amount of proceeds to us from this offering available by approximately $19.4 million.
87
Table of Contents
We do not currently expect to pay any cash dividends on our Class A common stock for the foreseeable future. Instead, we intend to retain future earnings, if any, for the future operation and expansion of our business, including for the development of new solutions and services and strategic acquisitions of, or investments in, business and technologies that we believe will complement our current business and expansion strategies. Any determination to pay dividends in the future will be at the discretion of our board of directors and will depend upon our results of operations, cash requirements, financial condition, contractual restrictions, restrictions imposed by applicable laws and other factors that our board of directors may deem relevant.
Signify Health, Inc. will be a holding company and will have no material assets other than its ownership of LLC Units in Cure TopCo, LLC, and as a consequence, our ability to declare and pay dividends to the holders of our Class A common stock, if our board of directors determines to do so, will be subject to the ability of Cure TopCo, LLC to provide distributions to us. If Cure TopCo, LLC makes such distributions, the holders of LLC Units will be entitled to receive equivalent distributions from Cure TopCo, LLC. However, because we must pay taxes, make payments under the Tax Receivable Agreement and pay our expenses, amounts ultimately distributed as dividends to holders of our Class A common stock are expected to be less than the amounts distributed by Cure TopCo, LLC to the other holders of LLC Units on a per share basis. See “Certain relationships and related party transactions—Tax Receivable Agreement.”
Assuming Cure TopCo, LLC makes distributions to its members in any given year, the determination to pay dividends, if any, to our Class A common stockholders out of the portion, if any, of such distributions remaining after our payment of taxes, Tax Receivable Agreement payments and expenses (any such portion, an “excess distribution”) will be made by our board of directors. Because our board of directors may determine to pay or not pay dividends to our Class A common stockholders, our Class A common stockholders may not necessarily receive dividend distributions relating to excess distributions, even if Cure TopCo, LLC makes such distributions to us.
In 2019 and 2018, Cure TopCo, LLC made cash distributions to its equity holders in aggregate amounts of $22.5 million and $18.3 million, respectively, in connection with equity holder tax obligations. In the nine months ended September 30, 2020, Cure TopCo, LLC made cash distributions to its equity holders in an aggregate amount of $8.1 million in connection with equity holder tax obligations.
88
Table of Contents
The following table sets forth our cash, cash equivalents and capitalization as of September 30, 2020:
| • | on an actual basis for Cure TopCo, LLC; |
| • | on an as adjusted basis to reflect the Reorganization Transactions and the Incremental Term Loans and the use of proceeds therefrom; and |
| • | on a pro forma basis giving effect to the Offering Adjustments described under “Unaudited pro forma consolidated financial information,” including the sale by us of 23,500,000 shares of Class A common stock in this offering and the application of the net proceeds from this offering as described in “Use of proceeds” and based on an assumed initial public offering price of $20.50 per share (the midpoint of the range set forth on the cover page of this prospectus). |
This table should be read in conjunction with “Organizational structure,” “Use of proceeds,” “Unaudited pro forma consolidated financial information,” “Selected combined-consolidated financial data,” “Management’s discussion and analysis of financial condition and results of operations” and the consolidated financial statements and notes thereto appearing elsewhere in this prospectus.
| September 30, 2020 | ||||||||||||
| Actual | As Adjusted |
Pro Forma(1) |
||||||||||
| (in millions) | ||||||||||||
| Cash and cash equivalents |
$ | 87.9 | $ | 145.8 | $ | 602.3 | ||||||
|
|
|
|
|
|
|
|||||||
| Long-term debt |
$ | 350.2 | $ | 413.2 | $ | 413.2 | ||||||
| Stockholders’ equity: |
||||||||||||
| Class A common stock; $0.01 par value per share; 141,592,313 shares outstanding on an as adjusted basis; 165,092,313 shares outstanding on a pro forma basis |
— | 1.4 | 1.7 | |||||||||
| Class B common stock; $0.01 par value per share; 57,264,580 shares outstanding on an as adjusted basis; 57,264,580 shares outstanding on a pro forma basis |
— | 0.6 | 0.6 | |||||||||
| Additional paid-in capital |
— | 607.8 | 972.8 | |||||||||
| Accumulated deficit |
— | — | (8.5 | ) | ||||||||
| Contingently redeemable noncontrolling interest |
— | 256.7 | 343.9 | |||||||||
| Total members’ equity/stockholders’ equity |
$ | 891.4 | $ | 866.5 | $ | 1,310.5 | ||||||
|
|
|
|
|
|
|
|||||||
| Total capitalization |
$ | 1,153.7 | $ | 1,133.9 | $ | 1,121.4 | ||||||
|
|
|
|
|
|
|
|||||||
| (1) | To the extent we change the number of shares of Class A common stock sold by us in this offering from the shares we expect to sell or we change the initial public offering price from the $20.50 per share assumed initial public offering price, representing the midpoint of the price range set forth on the cover page of this prospectus, or any combination of these events occurs, the net proceeds to us from this offering and each of pro forma total stockholders’ equity and total capitalization may increase or decrease. A $1.00 increase (decrease) in the assumed initial public offering price per share, assuming no change in the number of shares to be sold, would increase (decrease) the net proceeds that we receive in this offering and our pro forma total stockholders’ equity by approximately $22.3 million. An increase (decrease) of 1,000,000 shares in the expected number of shares to be sold in the offering, assuming no change in the assumed initial offering price per share, would increase (decrease) our net proceeds from this offering and our pro forma total stockholders’ equity by approximately $19.4 million. If the underwriters exercise in full their option to purchase additional shares of Class A common stock, the pro forma amount of each of cash, additional paid-in capital, total stockholders’ equity would increase by approximately $68.4 million, after deducting the underwriting discount, and we would have 168,617,313 shares of our Class A common stock issued and outstanding, pro forma. |
89
Table of Contents
If you invest in our Class A common stock, you will experience dilution to the extent of the difference between the initial public offering price per share of our Class A common stock and the pro forma net tangible book value per share of our Class A common stock. Dilution results from the fact that the per share offering price of the Class A common stock is substantially in excess of the pro forma net tangible book value per share attributable to the Continuing Pre-IPO LLC Members.
The Continuing Pre-IPO LLC Members will maintain their LLC Units in Cure TopCo, LLC after the Reorganization Transactions, but will be able to cause the redemption or exchange of their LLC Units for, at our election, shares of Class A common stock or cash. We have presented dilution in pro forma net tangible book value per share assuming that all of the holders of LLC Units (other than the Company) had their LLC Units redeemed or exchanged for newly issued shares of Class A common stock on a one-for-one basis (rather than for cash) and the cancellation for no consideration of all of their shares of Class B common stock (which are not entitled to receive distributions or dividends, whether cash or stock, from the Company) in order to more meaningfully present the dilutive impact on the investors in this offering.
Our pro forma net tangible book value as of September 30, 2020, would have been approximately $(215.9) million, or $(1.09) per share of our Class A common stock on a fully diluted basis. Pro forma net tangible book value represents the amount of total tangible assets less total liabilities, and pro forma net tangible book value per share represents pro forma net tangible book value divided by the number of shares of common stock outstanding, in each case after giving effect to the Reorganization Transactions (based on an assumed initial public offering price of $20.50 per share (the midpoint of the estimated initial public offering price range set forth on the cover page of this prospectus)), assuming that the Continuing Pre-IPO LLC Members redeem or exchange all of their LLC Units and shares of Class B common stock for newly issued shares of our Class A common stock on a one-for-one basis (assuming 23,500,000 shares of Class A common stock are sold in this offering).
After giving effect to the Reorganization Transactions, assuming that the Continuing Pre-IPO LLC Members redeem or exchange all of their LLC Units for newly issued shares of our Class A common stock on a one-for-one basis, and after giving further effect to the sale of 23,500,000 shares of Class A common stock in this offering at the assumed initial public offering price of $20.50 per share (the midpoint of the estimated price range on the cover page of this prospectus) and the use of the net proceeds from this offering, our pro forma as adjusted net tangible book value would have been approximately $228.0 million, or $1.03 per share, representing an immediate increase in net tangible book value of $2.11 per share to existing equity holders and an immediate dilution in net tangible book value of $21.53 per share to new investors.
The following table illustrates the per share dilution:
| Assumed initial public offering price per share |
$ | 20.50 | ||||||
| Pro forma net tangible book value per share as of September 30, 2020(1) |
$ | (1.09 | ) | |||||
| Increase in pro forma net tangible book value per share attributable to new investors |
2.11 | |||||||
| Pro forma adjusted net tangible book value per share after this offering(2) |
1.03 | |||||||
|
|
|
|||||||
| Dilution in pro forma net tangible book value per share to new investors |
$ | 21.53 | ||||||
|
|
|
| (1) | Reflects 198,856,893 outstanding shares of Class A common stock (assuming all LLC Units and corresponding shares of Class B common stock held by the Continuing Pre-IPO LLC Members are exchanged for shares of Class A common stock). |
| (2) | Reflects 222,356,893 outstanding shares, consisting of (i) 23,500,000 shares of Class A common stock to be issued in this offering and (ii) the 198,856,893 outstanding shares described in note (1) above. |
Dilution is determined by subtracting pro forma net tangible book value per share after this offering from the initial public offering price per share of Class A common stock.
90
Table of Contents
A $1.00 increase (decrease) in the assumed initial public offering price of $20.50 per share would increase (decrease) our pro forma net tangible book value after this offering by $22.3 million and the dilution per share to new investors by $0.10, in each case assuming the number of shares offered, as set forth on the cover page of this prospectus, remains the same. Each increase (decrease) of 1.0 million shares in the number of shares sold by us in this offering, as set forth on the cover page of this prospectus, would increase (decrease) the net proceeds to us from this offering by approximately $19.4 million, assuming the assumed initial public offering price of $20.50 per share (the midpoint of the estimated price range set forth on the cover page of this prospectus) remains the same.
To the extent the underwriters’ option to purchase additional shares of Class A common stock is exercised, there will be further dilution to new investors.
The following table illustrates, as of September 30, 2020, after giving effect to the Reorganization Transactions, assuming that the Continuing Pre-IPO LLC Members redeem or exchange all of their LLC Units for newly issued shares of our Class A common stock on a one-for-one basis, and after giving further effect to the sale by us of shares of our Class A common stock in this offering at the initial public offering price of $20.50 per share (the midpoint of the estimated initial public offering price range set forth on the cover page of this prospectus), the difference between the Pre-IPO LLC Members, and the investors purchasing shares of our Class A common stock in this offering with respect to the number of shares of our common stock purchased from us, the total consideration paid or to be paid to us, and the average price per share paid or to be paid to us, before deducting underwriting discounts and commissions and the estimated offering expenses payable by us:
| Shares of Class A Common Stock Purchased |
Total Consideration | Average Price Per Share of Class A Common Stock |
||||||||||||||||||
| Number | Percent | Amount | Percent | |||||||||||||||||
| (in millions) | ||||||||||||||||||||
| Pre-IPO LLC Members(1) |
198,856,893 | 89.4 | $ | 1,665,737,572 | 77.6 | $ | 8.38 | |||||||||||||
| Investors in this offering |
23,500,000 | 10.6 | 481,750,000 | 22.4 | 20.50 | |||||||||||||||
| Total |
222,356,893 | 100.0 | $ | 2,147,487,572 | 100.0 | $ | 9.66 | |||||||||||||
| (1) | Includes 57,264,580 shares of Class A common stock issuable to the Continuing Pre-IPO LLC Members upon redemption or exchange of all of their LLC Units and 141,592,313 shares of Class A common stock issued to the Reorganization Parties in connection with the IPO Contribution and the Mergers. |
We may choose to raise additional capital due to market conditions or strategic considerations even if we believe we have sufficient funds for our current or future operating plans. To the extent additional capital is raised through the sale of equity or convertible debt securities, the issuance of these securities could result in further dilution to holders of our Class A common stock.
91
Table of Contents
SELECTED COMBINED-CONSOLIDATED FINANCIAL DATA
The following tables set forth selected historical financial and other data of Cure TopCo, LLC for the periods presented. Signify Health, Inc. was formed as a Delaware corporation on October 1, 2020, and has not, to date, conducted any activities other than those incident to its formation, those in preparation for the Reorganization Transactions and the preparation of this prospectus and the registration statement of which this prospectus forms a part.
The statements of operations data for the years ended December 31, 2019 and 2018 and balance sheet data as of December 31, 2019 and 2018 have been derived from Cure TopCo, LLC’s audited combined-consolidated financial statements included elsewhere in this prospectus. The statements of operations data for the nine months ended September 30, 2020 and 2019 and balance sheet data as of September 30, 2020 have been derived from Cure TopCo, LLC’s unaudited combined-consolidated financial statements included elsewhere in this prospectus which, in the opinion of management, include all adjustments, consisting only of normal recurring adjustments, necessary for a fair statement of the results for the unaudited interim periods.
In 2019, we acquired 100% of the outstanding equity of Remedy Partners. A controlling interest was initially acquired by New Mountain Capital on January 15, 2019, at which point we and Remedy Partners were considered to be under common control and combined financial statements were presented from January 15, 2019 to November 26, 2019. On November 26, 2019, a series of transactions were effected which resulted in Remedy Partners becoming our wholly owned subsidiary and consolidated financial statements were presented from that date forward. Because we were not under common control with and did not own Remedy Partners in 2018, our results of operations for the year ended December 31, 2019 are not directly comparable to our results of operations for the year ended December 31, 2018.
The selected historical financial and other data presented below do not purport to be indicative of the results that can be expected for any future period and should be read together with “Capitalization,” “Summary combined-consolidated financial data,” “Management’s discussion and analysis of financial condition and results of operations” and our consolidated financial statements and related notes thereto included elsewhere in this prospectus.
| Cure TopCo, LLC | ||||||||||||||||
| Year Ended December 31, | Nine Months Ended September 30, (unaudited) |
|||||||||||||||
| 2019 | 2018 | 2020 | 2019 | |||||||||||||
| (in millions) | ||||||||||||||||
| Statement of Operations Data: |
||||||||||||||||
| Revenue |
$ | 501.8 | $ | 337.9 | $ | 417.1 | $ | 368.5 | ||||||||
| Operating expenses |
||||||||||||||||
| Service expense (exclusive of depreciation and amortization shown below) |
247.2 | 196.3 | 203.4 | 188.2 | ||||||||||||
| Selling, general and administrative expense (exclusive of depreciation and amortization shown below) |
168.6 | 67.9 | 148.5 | 119.1 | ||||||||||||
| Transaction-related expenses |
22.4 | 21.0 | 10.8 | 15.9 | ||||||||||||
| Asset impairment |
6.4 | 17.0 | — | 1.5 | ||||||||||||
| Depreciation and amortization |
66.0 | 43.0 | 46.0 | 49.5 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Total operating expenses |
510.6 | 345.2 | 408.7 | 374.2 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| (Loss) income from operations |
(8.8 | ) | (7.3 | ) | 8.4 | (5.7 | ) | |||||||||
| Interest expense |
21.2 | 21.4 | 16.2 | 16.1 | ||||||||||||
| Other (income) expense, net |
(1.6 | ) | — | 6.9 | (1.4 | ) | ||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Other expense, net |
19.6 | 21.4 | 23.1 | 14.7 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Loss before income taxes |
(28.4 | ) | (28.7 | ) | (14.7 | ) | (20.4 | ) | ||||||||
92
Table of Contents
| Cure TopCo, LLC | ||||||||||||||||
| Year Ended December 31, | Nine Months Ended September 30, (unaudited) |
|||||||||||||||
| 2019 | 2018 | 2020 | 2019 | |||||||||||||
| (in millions) | ||||||||||||||||
| Income tax expense |
0.1 | 0.2 | 0.5 | 0.1 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Net loss |
$ | (28.5 | ) | $ | (28.9 | ) | $ | (15.2 | ) | $ | (20.5 | ) | ||||
|
|
|
|
|
|
|
|
|
|||||||||
| Cure TopCo, LLC | ||||||||||||
| December 31, | September 30, (unaudited) |
|||||||||||
| 2019 | 2018 | 2020 | ||||||||||
| (in millions) | ||||||||||||
| Balance Sheet Data: |
||||||||||||
| Cash and cash equivalents |
$ | 27.7 | $ | 20.4 | $ | 87.9 | ||||||
| Working capital |
140.9 | 33.9 | 153.6 | |||||||||
| Total assets |
1,392.4 | 601.7 | 1,468.7 | |||||||||
| Total liabilities |
434.8 | 317.7 | 577.3 | |||||||||
| Total members’ equity |
957.6 | 284.0 | 891.4 | |||||||||
93
Table of Contents
UNAUDITED PRO FORMA CONSOLIDATED FINANCIAL INFORMATION
The unaudited pro forma statements of operations for the year ended December 31, 2019 and for the nine months ended September 30, 2020 and the unaudited pro forma balance sheet as of September 30, 2020 give effect to the pro forma adjustments related to (i) the Reorganization Transactions, which we refer to as the “Transaction Adjustments” and (ii) this offering, including the sale of 23,500,000 shares of Class A common stock and the application of the net proceeds from this offering, which we refer to as the “Offering Adjustments.” The unaudited pro forma statements of operations for the year ended December 31, 2019 and for the nine months ended September 30, 2020 give effect to the pro forma adjustments as if they had occurred on January 1, 2019 and the unaudited pro forma balance sheet as of September 30, 2020 gives effect to the pro forma adjustments as if they had occurred on September 30, 2020. See “Capitalization.” The unaudited pro forma financial information has been prepared by our management and is based on Cure TopCo, LLC’s historical financial statements and the assumptions and adjustments described in the notes to the unaudited pro forma financial information below. The presentation of the unaudited pro forma financial information is prepared in conformity with Article 11 of Regulation S-X rules effective January 1, 2021.
Our historical financial information for the year ended December 31, 2019 and as of and for the nine months ended September 30, 2020 have been derived from Cure TopCo, LLC’s combined-consolidated financial statements and accompanying notes included elsewhere in this prospectus.
We based the pro forma adjustments on available information and on assumptions that we believe are reasonable under the circumstances in order to reflect, on a pro forma basis, the impact of the relevant transactions on the historical financial information of Cure TopCo, LLC. See the notes to unaudited pro forma financial information below for a discussion of assumptions made. The unaudited pro forma financial information does not purport to be indicative of our results of operations or financial position had the relevant transactions occurred on the dates assumed and does not project our results of operations or financial position for any future period or date.
The unaudited pro forma financial information should be read together with “Capitalization,” “Selected combined-consolidated financial data,” “Management’s discussion and analysis of financial condition and results of operations” and our combined-consolidated financial statements and related notes thereto included elsewhere in this prospectus.
The pro forma adjustments related to the Reorganization Transactions, which we refer to as the “Transaction Adjustments,” are described in the notes to the unaudited pro forma consolidated financial information, and principally include the following:
| • | adjustments for the Reorganization Transactions, the entry into the Amended and Restated LLC Agreement and the entry into the Tax Receivable Agreement; |
| • | the recognition of a contingently redeemable noncontrolling interest in Cure TopCo, LLC held by the Continuing Pre-IPO LLC Members, which will be redeemable, at our election, for shares of Class A common stock on a one-for-one basis or a cash payment in accordance with the terms of the Amended LLC Agreement and which, if the redeeming member is an affiliate, the decision to redeem in cash or shares will be approved by the disinterested members of the Audit Committee; and |
| • | provision for federal and state income taxes of Signify Health, Inc. as a taxable corporation at an effective rate of 14.3% and 4.8% for the year ended December 31, 2019 and for the nine months ended September 30, 2020, respectively (calculated using a U.S. federal income tax rate of 21%). |
The Transaction Adjustments also include the incurrence of $125.0 million of additional indebtedness under the 2020 November Incremental Term Loans, some of which was used to repay the outstanding borrowings under our Revolving Credit Facility, and the incurrence of $15.0 million of additional indebtedness under the 2020 December Incremental Term Loans.
94
Table of Contents
The pro forma adjustments related to this offering, which we refer to as the “Offering Adjustments,” are described in the notes to the unaudited pro forma consolidated financial information, and principally include the following:
| • | the issuance of shares of our Class A common stock to the purchasers in this offering in exchange for net proceeds of approximately $456.5 million, assuming that the shares are offered at $20.50 per share (the midpoint of the price range listed on the cover page of this prospectus), after deducting underwriting discounts and commissions but before offering expenses; |
| • | the application by Signify Health, Inc. of the net proceeds from this offering to acquire newly issued LLC Units from Cure TopCo, LLC at a purchase price per LLC Unit equal to the initial public offering price of Class A common stock net of underwriting discounts and commissions; and |
| • | the application by Cure TopCo, LLC of a portion of the proceeds of the sale of LLC Units to Signify Health, Inc. to (i) pay fees and expenses of approximately $13.5 million in connection with this offering and (ii) for general corporate purposes, including working capital and potential strategic acquisitions of, or investments in, other businesses or technologies that we believe will complement our current business and expansion strategies. |
As a public company, we will be implementing additional procedures and processes for the purpose of addressing the standards and requirements applicable to public companies. We expect to incur additional annual expenses related to these steps and, among other things, additional directors’ and officers’ liability insurance, director fees, reporting requirements of the SEC, transfer agent fees, hiring additional accounting, legal and administrative personnel, increased auditing and legal fees and similar expenses. We have not included any pro forma adjustments relating to these costs.
95
Table of Contents
Unaudited pro forma combined-consolidated statement of operations (year ended December 31, 2019)
| Historical Cure TopCo, LLC |
Transaction adjustments |
Pro forma Signify Health, Inc. |
Offering adjustments |
Pro forma Signify Health, Inc. |
||||||||||||||||
| (in millions, except per unit/share data) | ||||||||||||||||||||
| Revenue |
$ | 501.8 | — | $ | 501.8 | — | $ | 501.8 | ||||||||||||
| Operating expenses |
||||||||||||||||||||
| Service expense (exclusive of depreciation and amortization shown below) |
247.2 | — | 247.2 | — | 247.2 | |||||||||||||||
| Selling, general and administrative expense (exclusive of depreciation and amortization shown below) |
168.6 | — | 168.6 | 5.3 | (6) | 173.9 | ||||||||||||||
| Transaction-related expenses |
22.4 | — | 22.4 | 8.5 | (5) | 30.9 | ||||||||||||||
| Asset impairment |
6.4 | — | 6.4 | — | 6.4 | |||||||||||||||
| Depreciation and amortization |
66.0 | — | 66.0 | — | 66.0 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total operating expenses |
510.6 | — | 510.6 | 13.8 | 524.4 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Loss from operations |
(8.8 | ) | — | (8.8 | ) | (13.8 | ) | (22.6 | ) | |||||||||||
| Interest expense |
21.2 | 5.4 | (4) | 26.6 | — | 26.6 | ||||||||||||||
| Other (income) expense, net |
(1.6 | ) | — | (1.6 | ) | — | (1.6 | ) | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Other expense, net |
19.6 | 5.4 | 25.0 | — | 25.0 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Loss before income taxes |
(28.4 | ) | (5.4 | ) | (33.8 | ) | (13.8 | ) | (47.6 | ) | ||||||||||
| Income tax (benefit) expense |
0.1 | (3.6 | )(1) | (3.5 | ) | (2.1 | ) | (5.6 | ) | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net loss |
$ | (28.5 | ) | (1.8 | ) | (30.3 | ) | (11.7 | ) | (42.0 | ) | |||||||||
| Net loss attributable to contingently redeemable noncontrolling interests |
— | 9.5 | (2) | (9.5 | ) | (2.0 | )(2) | (11.5 | ) | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net loss attributable to Signify Health, Inc. |
(28.5 | ) | (7.7 | ) | (20.8 | ) | (9.7 | ) | (30.5 | ) | ||||||||||
| Pro forma net loss per share data(3) |
||||||||||||||||||||
| Pro forma weighted average shares of Class A common stock outstanding |
||||||||||||||||||||
| Basic and diluted |
141.6 | 165.1 | ||||||||||||||||||
| Net loss per share of Class A common stock |
||||||||||||||||||||
| Basic and diluted |
(0.15 | ) | (0.18 | ) | ||||||||||||||||
See accompanying notes to unaudited pro forma financial information
96
Table of Contents
Notes to unaudited pro forma combined-consolidated statement of operations (year ended December 31, 2019)
| (1) | Following the Reorganization Transactions, Signify Health, Inc. will be subject to U.S. federal income taxes, in addition to state and local taxes. As a result, the pro forma statement of operations reflects an adjustment to income tax expense for corporate income taxes to reflect a statutory tax rate of 24.4%, which includes a provision for U.S. federal income taxes and assumes the highest statutory rates apportioned to each state and local jurisdiction. Cure TopCo, LLC is, and will continue to be, taxed as a partnership for federal income tax purposes and, as a result, its members, including Signify Health, Inc., will pay income taxes with respect to their allocable shares of its net taxable income. |
The pro forma adjustment for income tax expense represents tax expense on income that will be taxable in jurisdictions after our corporate reorganization that previously had not been taxable. The adjustment is calculated as pro forma income before income taxes multiplied by the ownership percentage of the controlling interest and multiplied by the effective tax rate of 14.3%.
| December 31, 2019 | ||||
| Pro forma income before income taxes |
(33.8 | ) | ||
| Ownership % of the controlling interest |
74.2 | % | ||
| Pro forma income attributable to the controlling interest |
(25.1 | ) | ||
| Pro forma effective tax rate |
14.3 | % | ||
| Reorganization Transaction adjustment |
$ | (3.60 | ) | |
| (2) | In connection with the Reorganization Transactions, we will be appointed as the sole managing member of Cure TopCo, LLC pursuant to the Amended LLC Agreement. As a result, while we will own less than 100% of the economic interest in Cure TopCo, LLC, we will have 100% of the voting power and control the management of Cure TopCo, LLC. Because we will manage and operate the business and control the strategic decisions and day-to-day operations of Cure TopCo, LLC and will also have a substantial financial interest in Cure TopCo, LLC, we will consolidate the financial results of Cure TopCo, LLC, and a portion of our net income (loss) will be allocated to the contingently redeemable noncontrolling interest to reflect the entitlement of the Continuing Pre-IPO LLC Members to a portion of Cure TopCo, LLC’s net income (loss). We will initially hold approximately 74.2% of Cure TopCo, LLC’s outstanding LLC Units (or approximately 74.6% if the underwriters exercise their option to purchase additional shares of Class A common stock in full), and the remaining LLC Units of Cure TopCo, LLC will be held by the Continuing Pre-IPO LLC Members. Immediately following the Reorganization Transactions, the ownership percentage held by the contingently redeemable noncontrolling interest will be approximately 25.8%. Net loss attributable to the contingently redeemable noncontrolling interest will represent approximately 27.4% of net loss. |
97
Table of Contents
| (3) | Pro forma basic net loss per share of Class A common stock is computed by dividing the pro forma net loss available to Class A common stockholders by the pro forma weighted-average shares of Class A common stock outstanding during the period. Pro forma diluted net loss per share of Class A common stock is computed by adjusting the pro forma net loss available to Class A common stockholders and the pro forma weighted-average shares of Class A common stock outstanding to give effect to potentially dilutive securities. |
| For the Year Ended December 31, 2019 |
||||
| |
(in millions, except share data) |
| ||
| Pro forma loss per share of Class A common stock |
||||
| Numerator: |
||||
| Pro forma net loss attributable to the Issuer’s Class A common stockholders (basic and diluted) |
$ | 30.5 | ||
| Denominator: |
||||
| Pro forma weighted average of shares of Class A common stock outstanding (basic and diluted) |
165,092,313 | |||
| Pro forma basic loss per share |
$ | (0.18 | ) | |
| Antidilutive shares excluded |
69,981,264 | |||
| (4) | The incurrence of $140.0 million of additional indebtedness under the 2020 Incremental Term Loans, some of which was used to repay the outstanding borrowings under our Revolving Credit Facility, results in an increase to interest expense of $5.4 million. |
| (5) | We incurred approximately $8.5 million in expenses in connection with this offering that were not reflected in our historical financial statements, which we do not expect to recur. |
| (6) | Compensation expense of $5.3 million associated with incentive grants at the IPO price, including stock options, restricted stock units and synthetic equity units. All of these awards are subject to time-based vesting conditions. |
98
Table of Contents
Unaudited pro forma combined-consolidated statement of operations (nine months ended September 30, 2020)
| Historical Cure TopCo, LLC |
Transaction adjustments |
Pro forma Signify Health, Inc. |
Offering adjustments |
Pro forma Signify Health, Inc. |
||||||||||||||||
| (in millions, except per unit/share data) | ||||||||||||||||||||
| Revenue |
$ | 417.1 | — | $ | 417.1 | — | $ | 417.1 | ||||||||||||
| Operating expenses |
||||||||||||||||||||
| Service expense (exclusive of depreciation and amortization shown below) |
203.4 | — | 203.4 | — | 203.4 | |||||||||||||||
| Selling, general and administrative expense (exclusive of depreciation and amortization shown below) |
148.5 | — | 148.5 | 2.8 | (6) | 151.3 | ||||||||||||||
| Transaction-related expenses |
10.8 | — | 10.8 | (0.9 | )(5) | 9.9 | ||||||||||||||
| Depreciation and amortization |
46.0 | — | 46.0 | — | 46.0 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total operating expenses |
408.7 | — | 408.7 | 1.9 | 410.6 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Income (loss) from operations |
8.4 | — | 8.4 | (1.9 | ) | 6.5 | ||||||||||||||
| Interest expense |
16.2 | 4.3 | (4) | 20.5 | — | 20.5 | ||||||||||||||
| Other (income) expense, net |
6.9 | — | 6.9 | — | 6.9 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Other expense, net |
23.1 | 4.3 | 27.4 | — | 27.4 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Loss before income taxes |
(14.7 | ) | (4.3 | ) | (19.0 | ) | (1.9 | ) | (20.9 | ) | ||||||||||
| Income tax (benefit) expense |
0.5 | (0.7 | )(1) | (0.2 | ) | 0.2 | — | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net loss |
$ | (15.2 | ) | (3.6 | ) | $ | (18.8 | ) | (2.1 | ) | (20.9 | ) | ||||||||
| Net loss attributable to contingently redeemable noncontrolling interests |
— | (5.4 | )(2) | (5.4 | ) | — | (2) | (5.4 | ) | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net loss attributable to Signify Health, Inc. |
(15.2 | ) | (1.8 | ) | (13.4 | ) | (2.1 | ) | (15.5 | ) | ||||||||||
| Pro forma net loss per share data(3) |
||||||||||||||||||||
| Pro forma weighted average shares of Class A common stock outstanding |
||||||||||||||||||||
| Basic and diluted |
141.6 | 165.1 | ||||||||||||||||||
| Net loss per share of Class A common stock |
||||||||||||||||||||
| Basic and diluted |
(0.09 | ) | (0.09 | ) | ||||||||||||||||
See accompanying notes to unaudited pro forma financial information
99
Table of Contents
Notes to unaudited pro forma combined-consolidated statement of operations (nine months ended September 30, 2020)
| (1) | Following the Reorganization Transactions, Signify Health, Inc. will be subject to U.S. federal income taxes, in addition to state and local taxes. As a result, the pro forma statement of operations reflects an adjustment to income tax expense for corporate income taxes to reflect a statutory tax rate of 24.4%, which includes a provision for U.S. federal income taxes and assumes the highest statutory rates apportioned to each state and local jurisdiction. Cure TopCo, LLC is, and will continue to be, taxed as a partnership for federal income tax purposes and, as a result, its members, including Signify Health, Inc., will pay income taxes with respect to their allocable shares of its net taxable income. |
The pro forma adjustment for income tax expense represents tax expense on income that will be taxable in jurisdictions after our corporate reorganization that previously had not been taxable. The adjustment is calculated as pro forma income before income taxes multiplied by the ownership percentage of the controlling interest and multiplied by the effective tax rate of 4.8%.
| September 30, 2020 | ||||
| Pro forma income before income taxes | (19.0 | ) | ||
| Ownership % of the controlling interest | 74.2 | % | ||
| Pro forma income attributable to the controlling interest | (14.1 | ) | ||
| Pro forma effective tax rate | 4.8 | % | ||
| Reorganization Transaction adjustment | (0.7 | ) | ||
| (2) | In connection with the Reorganization Transactions, we will be appointed as the sole managing member of Cure TopCo, LLC pursuant to the Amended LLC Agreement. As a result, while we will own less than 100% of the economic interest in Cure TopCo, LLC, we will have 100% of the voting power and control the management of Cure TopCo, LLC. Because we will manage and operate the business and control the strategic decisions and day-to-day operations of Cure TopCo, LLC and will also have a substantial financial interest in Cure TopCo, LLC, we will consolidate the financial results of Cure TopCo, LLC, and a portion of our net income (loss) will be allocated to the contingently redeemable noncontrolling interest to reflect the entitlement of the Continuing Pre-IPO LLC Members to a portion of Cure TopCo, LLC’s net income (loss). We will initially hold approximately 74.2% of Cure TopCo, LLC’s outstanding LLC Units (or approximately 74.6% if the underwriters exercise their option to purchase additional shares of Class A common stock in full), and the remaining LLC Units of Cure TopCo, LLC will be held by the Continuing Pre-IPO LLC Members. Immediately following the Reorganization Transactions, the ownership percentage held by the contingently redeemable noncontrolling interest will be approximately 25.8%. Net loss attributable to the contingently redeemable noncontrolling interest will represent approximately 25.7% of net loss. |
| (3) | Pro forma basic net loss per share of Class A common stock is computed by dividing the pro forma net loss available to Class A common stockholders by the pro forma weighted-average shares of Class A common stock outstanding during the period. Pro forma diluted net loss per share of Class A common stock is computed by adjusting the pro forma net loss available to Class A common stockholders and the pro forma weighted-average shares of Class A common stock outstanding to give effect to potentially dilutive securities. |
100
Table of Contents
| For the Nine Months Ended September 30, 2020 |
||||
| |
(in millions, except share data) |
| ||
| Pro forma loss per share of Class A common stock |
||||
| Numerator: |
||||
| Pro forma net loss attributable to the Issuer’s Class A common stockholders (basic and diluted) |
$ | (15.5 | ) | |
| Denominator: |
||||
| Pro forma weighted average of shares of Class A common stock outstanding (basic and diluted) |
165,092,313 | |||
| Pro forma basic loss per share |
$ | (0.09 | ) | |
| Antidilutive shares excluded |
69,981,264 | |||
| (4) | The incurrence of $140.0 million of additional indebtedness under the 2020 Incremental Term Loans, some of which was used to repay the outstanding borrowings under our Revolving Credit Facility, results in an increase to interest expense of $4.3 million. |
| (5) | Approximately $0.9 million of the transaction-related expenses are expenses incurred in connection with this offering that are presented in the transaction-related expenses for the year ended December 31, 2019 as if the transaction had occurred on January 1, 2019, which we do not expect to recur. This results in a decrease to transactions-related expenses of $0.9 million. |
| (6) | Compensation expense of $2.8 million associated with incentive grants at the IPO price, including stock options and synthetic equity units. All of these awards are subject to time-based vesting conditions. |
101
Table of Contents
Unaudited pro forma consolidated balance sheet (as of September 30, 2020)
| Historical Cure TopCo, LLC |
Transaction adjustments |
Pro forma Signify Health, Inc. |
Offering adjustments |
Pro forma Signify Health, Inc. |
||||||||||||||||
| (in millions, except per share data) | ||||||||||||||||||||
| ASSETS |
||||||||||||||||||||
| Current Assets: |
||||||||||||||||||||
| Cash and cash equivalents |
$ | 87.9 | 57.9 | (9) | $ | 145.8 | 456.5 | (1) | $ | 602.3 | ||||||||||
| Accounts receivable, net |
143.1 | — | 143.1 | — | 143.1 | |||||||||||||||
| Contract assets |
110.0 | — | 110.0 | — | 110.0 | |||||||||||||||
| Restricted cash |
4.4 | — | 4.4 | — | 4.4 | |||||||||||||||
| Prepaid expenses and other current assets |
11.7 | — | 11.7 | — | 11.7 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total current assets |
357.1 | 57.9 | 415.0 | 456.5 | 871.5 | |||||||||||||||
| Property and equipment, net |
26.7 | — | 26.7 | — | 26.7 | |||||||||||||||
| Goodwill |
578.8 | — | 578.8 | — | 578.8 | |||||||||||||||
| Intangible assets, net |
503.6 | — | 503.6 | — | 503.6 | |||||||||||||||
| Deferred tax assets |
— | 22.9 | (2) | 22.9 | — | 22.9 | ||||||||||||||
| Other assets |
2.5 | — | 2.5 | (1.1 | )(3) | 1.4 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total assets |
$ | 1,468.7 | $ | 80.8 | $ | 1,549.5 | $ | 455.4 | $ | 2,004.9 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| LIABILITIES AND MEMBERS’/STOCKHOLDERS’ EQUITY |
||||||||||||||||||||
| Current Liabilities: |
||||||||||||||||||||
| Accounts payable and accrued expenses |
$ | 95.6 | — | 95.6 | 11.4 | (1)(3) | 107.0 | |||||||||||||
| Contract liabilities |
35.0 | — | 35.0 | — | 35.0 | |||||||||||||||
| Current maturities of long-term debt |
2.8 | — | 2.8 | — | 2.8 | |||||||||||||||
| Due to shareholders |
54.0 | — | 54.0 | — | 54.0 | |||||||||||||||
| Other current liabilities |
16.1 | — | 16.1 | — | 16.1 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total current liabilities |
203.5 | — | 203.5 | 11.4 | 214.9 | |||||||||||||||
| Long-term debt |
263.8 | 134.9 | (9) | 398.7 | — | (1) | 398.7 | |||||||||||||
| Borrowings under Revolving Credit Facility |
77.0 | (77.0 | )(9) | — | — | — | ||||||||||||||
| Customer EAR liability |
14.4 | — | 14.4 | — | 14.4 | |||||||||||||||
| Tax Receivable Agreement liability |
— | 47.8 | (4) | 47.8 | — | 47.8 | ||||||||||||||
| Other noncurrent liabilities |
18.6 | — | 18.6 | — | 18.6 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total liabilities |
577.3 | 105.7 | 683.0 | 11.4 | 694.4 | |||||||||||||||
| Commitments and contingencies |
||||||||||||||||||||
| MEMBERS’/STOCKHOLDERS’ EQUITY |
||||||||||||||||||||
| Members’ equity—Series A Preferred (3,384,543 issued and outstanding at September 30, 2020) |
697.7 | (697.7 | )(7) | — | — | — | ||||||||||||||
| Members’ equity—Series B Preferred (3,402,608 issued and outstanding at September 30, 2020) |
264.3 | (264.3 | )(7) | — | — | — | ||||||||||||||
| Members’ equity—Class A common (0 issued and outstanding at September 30, 2020) |
— | — | — | — | — | |||||||||||||||
| Members’ equity—Class B common (108,977 issued and outstanding at September 30, 2020) |
4.9 | (4.9 | )(7) | — | — | — | ||||||||||||||
| Members’ equity—Class C common (83,244 issued and outstanding at September 30, 2020) |
7.2 | (7.2 | )(7) | — | — | — | ||||||||||||||
| Class A common stock (1,000,000,000 shares authorized, 165,092,313 shares issued and outstanding on a pro forma basis at September 30, 2020) |
1.4 | (5),(6) | 1.4 | 0.3 | (1),(5),(6) | 1.7 | ||||||||||||||
| Class B common stock (75,000,000 shares authorized, 57,264,580 shares issued and outstanding on a pro forma basis at September 30, 2020) |
0.6 | 0.6 | — | (6) | 0.6 | |||||||||||||||
| Additional paid-in capital |
|
607.8
|
(1),(2),(3),(4), (5),(7) |
607.8 | 365.0 | (5),(7) | 972.8 | |||||||||||||
| Accumulated deficit |
(82.7 | ) | 82.7 | — | (8.5 | )(10) | (8.5 | ) | ||||||||||||
| Contingently redeemable noncontrolling interest |
— | 256.7 | (5),(7) | 256.7 | 87.2 | (5),(6),(7),(8) | 343.9 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total members’/stockholders’ equity |
891.4 | (24.9 | ) | 866.5 | 444.0 | 1,310.5 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total liabilities and members’/stockholders’ equity |
$ | 1,468.7 | $ | 80.8 | $ | 1,549.5 | $ | 455.4 | $ | 2,004.9 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
See accompanying notes to unaudited pro forma financial information
102
Table of Contents
Notes to unaudited pro forma consolidated balance sheet (as of September 30, 2020)
| (1) | We estimate that our net proceeds from this offering will be approximately $456.5 million, after deducting underwriting discounts and commissions, based on an assumed initial public offering price of $20.50 per share (the midpoint of the estimated initial public offering price range set forth on the cover page of this prospectus) and assuming the underwriters’ option to purchase additional shares of Class A common stock is not exercised. If the underwriters exercise their option to purchase additional shares of Class A common stock in full, we expect to receive approximately $524.9 million of net proceeds based on an assumed initial public offering price of $20.50 per share (the midpoint of the estimated initial public offering price range set forth on the cover page of this prospectus). |
We estimate that the offering expenses inclusive of deferred costs (other than the underwriting discount and commissions) will be approximately $13.5 million. All of such offering expenses will be paid for or otherwise borne by Cure TopCo, LLC.
We intend to use all of the net proceeds from this offering (including net proceeds received if the underwriters exercise their option to purchase additional shares of Class A common stock) to acquire 23,500,000 newly issued LLC Units from Cure TopCo, LLC (or 27,025,000 if the underwriters exercise their option to purchase additional shares of Class A common stock in full) at a purchase price per LLC Unit equal to the initial public offering price of Class A common stock net of underwriting discounts and commissions, collectively representing 10.6% of Cure TopCo, LLC’s outstanding LLC Units (or 12.0%, if the underwriters exercise their option to purchase additional shares of Class A common stock in full).
Cure TopCo, LLC will use the proceeds from the issuance of LLC Units to Signify Health, Inc. (i) to pay fees and expenses of approximately $13.5 million in connection with this offering and the Reorganization Transactions and (ii) for general corporate purposes, including working capital and potential strategic acquisitions of, or investments in, other businesses or technologies that we believe will complement our current business and expansion strategies. See “Use of proceeds.”
| (2) | We are subject to U.S. federal, state and local income taxes and will file consolidated income tax returns for U.S. federal and certain state and local jurisdictions. This adjustment reflects the recognition of deferred taxes in connection with the Reorganization Transaction assuming the federal rates currently in effect and the highest statutory rates apportioned to each state and local jurisdiction. |
We have recorded a pro forma deferred tax asset adjustment of $22.9 million (or $26.3 million if the underwriters exercise in full their option to purchase additional shares of Class A common stock). The deferred tax asset includes (i) $18.9 million related to temporary differences in the book basis as compared to the tax basis of our investment in Cure TopCo, LLC (or $22.2 million if the underwriters exercise in full their option to purchase additional shares of Class A common stock) and (ii) $4.0 million related to tax benefits from future deductions. To the extent we determine it is more likely than not that we will not realize the full benefit represented by the deferred tax asset, we will record an appropriate valuation allowance based on an analysis of the objective or subjective negative evidence.
| (3) | We are deferring certain costs associated with this offering. These costs primarily represent legal, accounting and other direct costs and are recorded in other assets in our consolidated balance sheet. Upon completion of this offering, these deferred costs will be charged against the proceeds from this offering with a corresponding reduction to additional paid-in capital. |
| (4) | Reflects the recognition of a liability of $47.8 million, which represents 12.7% of the full obligation for applicable deferred tax assets under the terms of the Tax Receivable Agreement that we will enter into upon completion of this offering. Upon the completion of this offering, we will be a party to the Tax Receivable Agreement with the TRA Parties. Under the Tax Receivable Agreement, we generally will be required to pay to the TRA Parties 85% of the amount of cash savings, if any, in U.S. federal, state and local income tax that we actually realize as a result of (i) certain favorable tax attributes we will acquire from the Blocker Companies in the Mergers (including net operating losses, the Blocker Companies’ allocable share of existing tax basis and refunds of Blocker Company taxes attributable to pre-Merger tax periods), (ii) increases in our allocable share of existing tax basis and tax basis |
103
Table of Contents
| adjustments that may result from (x) future redemptions or exchanges of LLC Units by Continuing Pre-IPO LLC Members for cash or Class A common stock, (y) the IPO Contribution and (z) certain payments made under the Tax Receivable Agreement and (iii) deductions in respect of interest and certain compensatory payments made under the Tax Receivable Agreement. These payment obligations are our obligations and not obligations of Cure TopCo, LLC. Our obligations under the Tax Receivable Agreement will also apply with respect to any person who is issued LLC Units in the future and who becomes a party to the Tax Receivable Agreement. See “Organizational structure—Holding company structure and the Tax Receivable Agreement.” No adjustment has been made to reflect future redemptions or exchanges of LLC Units for cash or shares of our Class A common stock, as applicable. |
| (5) | As described in “Organizational structure—Effect of the Reorganization Transactions and this Offering,” upon completion of the Reorganization Transactions, this offering and the application of the net proceeds from this offering, we will be appointed as the managing member of Cure TopCo, LLC and will hold 165,092,313 LLC Units, constituting 74.2% of the outstanding economic interests in Cure TopCo, LLC (or 168,617,313 LLC Units, constituting 74.6% of the outstanding economic interests in Cure TopCo, LLC if the underwriters exercise their option to purchase additional shares of Class A common stock in full). |
Represents an adjustment to equity reflecting (i) par value of $1.4 million for Class A common stock and $0.6 million for Class B common stock to be outstanding following the Reorganization Transactions and (ii) a decrease in $256.7 million of additional paid-in capital to allocate a portion of Cure TopCo, LLC’s equity to the contingently redeemable noncontrolling interests.
| (6) | Represents an adjustment to stockholders’ equity reflecting (i) par value of $0.2 million for Class A common stock to be outstanding following the Offering Adjustments and (ii) a decrease of $87.2 million in members’ equity to allocate a portion of Signify Health, Inc.’s equity to the contingently redeemable noncontrolling interest. |
| (7) | The following table is a reconciliation of the adjustments impacting additional paid-in-capital: |
| Net adjustment from recognition of deferred tax asset and Tax Receivable Agreement |
$ | (24.9 | ) | |
| Net proceeds from offering of Class A common stock |
456.5 | |||
| Reclassification of offering expenses, other than discounts and commissions, inclusive of deferred costs, offset against additional paid-in capital |
(4.1 | ) | ||
| Adjustment for contingently redeemable noncontrolling interest |
(343.9 | ) | ||
| Reclassification of pre-IPO membership equity |
889.2 | |||
|
|
|
|||
| Total |
$ | 972.8 |
Other members’ equity was netted out as part of the $891.4 million adjustment for contingently redeemable noncontrolling interest.
| (8) | As described in “Organizational structure—Effect of the Reorganization Transactions and this offering,” under the Amended LLC Agreement, holders of LLC Units, including the Continuing Pre-IPO LLC Members, will have the right, from and after the completion of this offering (subject to the terms of the Amended LLC Agreement), to require Cure TopCo, LLC to redeem all or a portion of their LLC Units for, at our election, newly issued shares of Class A common stock on a one-for-one basis or a cash payment equal to the volume-weighted average market price of one share of our Class A common stock for each LLC Unit redeemed (subject to customary adjustments, including for stock splits, stock dividends and reclassifications) in accordance with the terms of the Amended LLC Agreement. Additionally, in the event of a redemption request from a holder of LLC Units, we may, at our option, effect a direct exchange of cash or Class A common stock for LLC Units in lieu of such a redemption. Shares of Class B common stock will be cancelled on a one-for-one basis if we, following a redemption request from a holder of LLC Units, redeem or exchange LLC Units of such holder pursuant to the terms of the Amended LLC Agreement. |
| (9) | We incurred $140.0 million of additional indebtedenss under the 2020 Incremental Term Loans, some of which was used to repay the $77.0 million in outstanding borrowings under our Revolving Credit Facility. We paid fees of approximately $5.1 million in connection with the 2020 Incremental Term Loans. |
| (10) | We expect to incur a total of approximately $9.8 million in expenses in connection with this offering, which we do not expect to recur. |
104
Table of Contents
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
The following discussion of our financial condition and results of operations should be read in conjunction with our audited consolidated financial statements as of and for the years ended December 31, 2019 and 2018, our unaudited combined-consolidated financial statements as of and for the nine months ended September 30, 2020 and 2019 and the notes thereto included elsewhere in this prospectus, as well as the information presented under “Presentation of Financial and Other Information” and “Selected Financial and Other Information.” The following discussion contains forward-looking statements that involve risks and uncertainties. Our actual results may differ materially from those discussed in the forward-looking statements as a result of various factors, including those set forth in “Forward-Looking Statements” and “Risk Factors.”
The following discussion contains references to calendar year 2019, calendar year 2018 and the nine months ended September 30, 2020 and 2019, which represents the consolidated and combined financial results of our predecessor Cure TopCo, LLC and its consolidated subsidiaries for the fiscal years ended December 31, 2019 and 2018 and the nine months ended September 30, 2020 and 2019, respectively.
Overview
Signify Health is a leading healthcare platform that leverages advanced analytics, technology, and nationwide healthcare provider networks to create and power value-based payment programs. Our mission is to transform how care is paid for and delivered so that people can enjoy more healthy, happy days at home. Our customers include health plans, governments, employers, health systems and physician groups. We believe that we are a market leader in two fast-growing segments of the value-based healthcare payment industry: payment models based on individual episodes of care and IHEs. Payment models based on individual episodes of care organize or bundle payments for all, or a substantial portion of, services received by a patient in connection with an episode of care, such as a surgical procedure, particular condition or other reason for a hospital stay. IHEs are health evaluations performed by a clinician in the home to support payors’ participation in Medicare Advantage and other government-run managed care plans. Our episode payment platform managed $6.1 billion of BPCI-A spend under the BPCI-A program in 2019, and the BPCI-A episodes we managed which were initiated in the last quarter of 2019 resulted in approximately 15% greater discharges home from acute-care facilities and approximately 10% lower readmissions when compared to the historical performance of our provider partners for similar episodes. Our mobile network of providers entered over 1 million unique homes to evaluate individuals in Medicare Advantage and other managed care plans in 2019. We believe that these core businesses have enabled us to become integral to how health plans and healthcare providers successfully participate in value-based payment programs, and that our platform lessens the dependence on facility-centric care for acute and post-acute services and shifts more services towards alternate sites and, most importantly, the home.
Our solutions support value-based payment programs by aligning financial incentives around outcomes, providing tools to health plans and healthcare organizations designed to assess and manage risk and identify actionable opportunities for improved patient outcomes, coordination and cost-savings. Through our platform, we coordinate what we believe is a holistic suite of clinical, social, and behavioral services to address an individual’s healthcare needs and prevent adverse events that drive excess cost. Our business model is aligned with our customers as we generate revenue only when we successfully engage members for our health plan customers and generate savings for our provider customers.
We serve 47 Medicare Advantage health plans ranging from the largest national organizations to smaller regional and provider-owned entities. We also serve thousands of healthcare provider organizations ranging from large integrated delivery systems to midsize and small urban and rural entities. We also serve large biopharmaceutical customers. For the year ended December 31, 2019, our total revenue was $501.8 million, representing a 48.5% increase from $337.9 million in 2018, we incurred a net loss of $28.5 million, representing a 1.2% decrease from a net loss of $28.9 million in 2018, our Adjusted EBITDA was $93.3 million, representing
105
Table of Contents
an 18.0% increase from $79.1 million in 2018 and our Adjusted EBITDA Margin was 18.6%, a 4.8% decrease from 23.4% in 2018. For the nine months ended September 30, 2020, our total revenue was $417.1 million, representing a 13.2% increase from $368.5 million in the nine months ended September 30, 2019, we incurred a net loss of $15.2 million, representing a 25.8% decrease from a net loss of $20.5 million in the nine months ended September 30, 2019, our Adjusted EBITDA was $86.0 million, representing a 28.8% increase from $66.7 million in the nine months ended September 30, 2019 and our Adjusted EBITDA Margin was 20.6%, a 2.5% increase from 18.1% in the nine months ended September 30, 2019.
Factors affecting our results of operations
As a result of a number of factors, our historical results of operations may not be comparable to our results of operations in future periods, and our results of operations may not be directly comparable from period to period. Set forth below is a brief discussion of the key factors impacting our results of operations.
Seasonality
Historically, there has been a seasonal pattern to our revenue in our Home & Community Services segment with the revenues in the fourth quarter of each calendar year generally lower than the other quarters. Each year, our IHE customers provide us with a TML, which may be supplemented or amended during the year. Our customers generally limit the number of times we may attempt to contact their members. Throughout the year, as we complete IHEs and attempt to contact members, the number of members who have not received an IHE and whom we are still able to contact declines, typically resulting in fewer IHEs scheduled during the fourth quarter. In 2020, the COVID-19 pandemic has led to a large number of in-person IHEs being scheduled in the second half of the year, and as a result, we may not see such historical seasonality with respect to in-person IHEs in 2020.
Revenue in our Episodes of Care Services segment generally is higher in the second and fourth quarters. We recognize the revenue attributable to episodes reconciled during each 6-month episode performance measurement period over a 13-month performance obligation period that commences in the second or fourth quarter of each year, depending on the relevant contract with our provider partners. The 13-month performance obligation period begins at the start of the relevant episodes of care and extends through the receipt or generation of the semiannual reconciliation for the relevant performance measurement period, as well as the provision and explanation of statements of performance to each of our customers. As a result, during the first and third quarters of each year, we recognize three months of revenue for each of two overlapping performance obligation periods (i.e., three months of revenue from one performance obligation period, and three months of revenue from a second, overlapping performance obligation period). In contrast, during the second and fourth quarter of each year, we recognize revenue relating to three overlapping performance obligation periods—three months of revenue from one performance obligation period, three months of revenue from a second, overlapping performance obligation period, and one month of revenue from a third, overlapping performance obligation period (representing the thirteenth month of the third performance obligation period). We also recognize Episodes revenue based on our estimates of savings realized. The semiannual reconciliations for each performance measurement period under our Episodes programs are received or generated in the second and fourth quarter of each year, and indicate the actual savings realized. See “—Critical accounting policies—Revenue recognition.” In addition, due to the semiannual reconciliations for our Episodes programs, and BPCI-A in particular, we typically receive cash during the first and third quarters of each year, which can cause our liquidity to fluctuate from quarter to quarter. See “—Liquidity and capital resources.”
Customer mix
Our customer mix can affect our revenue and profitability in both of our segments. For example, due to the different contractual arrangements we have with different health plans, health plan mix during the period can affect our average per-visit fee, the geographic mix of plan members we are visiting, the mix of members we see that are covered by Medicare versus Medicaid and the selection of IHE, vIHE or IHE+ solutions, each of which
106
Table of Contents
has a different price point and can affect the conversion rate associated with the number of members who agree to receive IHEs, the total number of IHEs completed and the number and type of ancillary services selected. The amounts we receive for our services in our Episodes of Care Services segment are similarly determined by customer mix, as the amount of our administrative fee, our share of episode savings and risk for episode losses and the health plans’ and providers’ share of savings, as well as the overall program size and the savings rate generated (and therefore are at risk) under each managed episode vary by customer.
Impact of IHE volume and margins
Our revenue and profitability in our Home & Community Services segment are affected by the number of IHEs we complete during a period and how cost effectively we are able to complete them. The number of IHEs we are able to complete during a period can be affected by a variety of factors. For example, decisions by our customers with respect to the TML, including any increase or reduction in the number of members included in the TML (or the member list from which it is derived), may impact our IHE completion rate and, as a result, our revenue. Similarly, our ability to complete IHEs is affected by the level of member engagement. In our experience, members of existing customers are more likely to have had an IHE from Signify Health in the past and are more likely to be responsive to our outreach. In contrast, for new customers, their members are often just getting to know Signify Health and may have never had an IHE before, which can make it harder to successfully contact them and obtain their consent to an IHE. Our ability to complete IHEs is also affected by the capacity of our mobile network of providers, which impacts our ability to efficiently reach all of the members on our TML. We believe we will benefit from demographic trends in the coming years. As the U.S. population ages, the number of Medicare eligible individuals is increasing. Moreover, Medicare Advantage is growing faster than the Medicare Classic or FFS program according to CMS. We believe we are well positioned to capture the growth in Medicare Advantage enrollment in the coming years and further increase the number of members we provide IHEs to.
Our long-term profitability in our Home & Community Services segment is also impacted by how cost-effectively we are able to complete IHEs. For example, it tends to be less costly for us to perform IHEs in densely populated urban areas and more costly for us to perform IHEs in difficult-to-reach jurisdictions. Our ability to cost-effectively perform IHEs is also affected by how efficiently we are able to schedule a provider’s day to maximize the number of IHEs he or she is able to complete in a day. The mix of providers we use may also impact our costs. We use a mix of physicians, nurse practitioners and physicians assistants, with physicians being the most costly to contract with for IHEs. If we increase or decrease our usage of a particular type of provider, it impacts the cost of performing IHEs and our margins.
Impact of program size and savings rate
Our revenue and profitability in our Episodes of Care Services segment are affected by the program size of our episodes programs and the savings rates we are able to achieve under these programs. Program size for a particular customer represents the number of episodes we managed for a customer during a period multiplied by the respective baseline price of each episode, which represents the benchmark price set by the relevant program prior to any discounts. Our program size is increased by increasing the number of episodes we manage. The weighted average program size for all of our programs in 2019 was $6.1 billion. In connection with our episodes offerings, we receive an administrative fee that is based on the program size we manage for a customer. The BPCI-A program in its current form expires at the end of 2023, and as of the end of 2020, participation in the BPCI-A program was locked in place, meaning that new healthcare providers cannot enter the program, and participating healthcare providers cannot choose to participate in any additional episode types. Accordingly, our ability to grow our revenue under the BPCI-A program going forward will require us to maximize savings rates.
Revenue in our Episodes of Care Services segment is also affected by the savings rate we are able to achieve. Under our contracts with provider partners in our episodes of care programs, we receive a share of any savings generated by the relevant provider for each episode managed. The savings rate during each period
107
Table of Contents
therefore affects our revenue period to period. The savings rate during each period is affected by a variety of factors, including how quickly new customers are able to integrate with our technology and data analytics tools, how long provider partners have been participating in an episode program and their resulting level of familiarity with the program and the degree of implementation of care redesign. The savings rate also varies by the type of solution we offer, and as a result the savings rate will fluctuate depending on the number of episodes we manage under one type of program, such as BPCI-A, versus another program, such as our Commercial Episodes of Care programs.
Our ability to increase program size and savings rate will depend on a number of factors, including the effectiveness of our advanced data analytics capabilities and operating platform, market adoption of our solutions and the adoption of care redesign and bundled payment models overall.
Investment in growth and technology
We continue to invest in sustaining significant growth, expanding our suite of solutions and being able to support a larger customer base over time. Achievement of our growth strategy will require additional investments and results in higher expenses incurred, particularly in developing new solutions, as well as in technology and human resources, as we aim to achieve this growth without diluting or decreasing the level and quality of services we provide. Developing new solutions can be time- and resource-intensive, and even once we launch a new solution, it can take a significant amount of time to contract with customers, provide them with our suite of technology and data analytics tools and have them actually begin generating revenue. This may increase our costs for one or more periods before we begin generating revenue from new solutions. In addition to developing new solutions, we are making significant investments in developing our existing solutions and increasing capacity. We will continue to invest in our technology platform and human resources to empower our providers and our customers to further improve results and optimize efficiencies. However, our investments may be more expensive or take longer to develop than we expect and may not result in operational efficiencies.
Changes to the BPCI program
Revenue generated by our BPCI solutions represented approximately 20% of our total revenue and 85% of our Episodes of Care Services segment revenue in 2019, and approximately 25% of our total revenue and over 90% of our Episodes of Care Services segment revenue in the nine months ended September 30, 2020. Our revenue and profitability are affected by changes to the BPCI program. Under our BPCI-A contracts, we earn an administrative fee, which is based on the size of the program, and also share in the savings or losses generated in conjunction with our provider partners as compared to BPCI-A’s benchmark episode price for a particular episode. Significant changes to the BPCI-A program can lead to a decline in the program size and/or savings rates we are able to achieve in conjunction with our provider partners under the program. For example, the predecessor BPCI Classic expired at the end of the third quarter of 2018 and CMS launched the BPCI-A program in the fourth quarter of 2018, which replaced BPCI Classic. CMS made significant changes to BPCI-A as compared to BPCI Classic, including reducing the number of episode types that can be managed, modifying the definitions for many of the episodes, as well as opening the program up to new healthcare providers (most of whom did not have prior experience participating in episode of care programs). CMS also increased the discount used to generate the benchmark episode price from 2% to 3%. This had the effect of increasing the savings threshold that must be achieved before we are able to earn our administrative fee, or any incremental savings that are shared with our provider partners. As a result of these changes, we saw a significant drop in the savings rate under BPCI-A during 2019 as compared to under the BPCI Classic program in 2018. This was partially offset by an increase in program size in 2019 under BPCI-A. Historically savings rates increased under the BPCI Classic program over time as healthcare providers integrated with our technology, implemented care redesign, developed a post-acute strategy, and adapted to the program. However, there can be no assurance that the same trend will continue under the BPCI-A program.
In September 2020, CMS announced changes to BPCI-A for 2021. These changes include an adjustment to the baseline period on which clinical episode prices are calculated, such that prices for 2021 will be calculated on
108
Table of Contents
the basis of historical experience that includes the first year of the BPCI-A program. As a result, benchmark episode prices could be lower than in prior years because BPCI-A care redesign and savings measures will be reflected in a portion of the benchmark period. In addition, CMS announced changes to the pricing methodology by which benchmark episode prices will be calculated, which could impact both (i) healthcare provider demand to take on certain episodes (and therefore affect program size), and (ii) savings rate opportunities. Further, when healthcare providers selected episodes for 2021 at the end of 2020, CMS required such selections to be made in groups of similar episodes, rather than individually. For example, a provider partner that previously only participated in hip replacement episodes may also be required to participate in knee and shoulder replacement episodes as well. This could impact provider partner demand for various episodes and correspondingly affect program size. Moreover, the clinical episodes selected by provider partners for 2021 will also apply to 2022 and 2023, meaning the selections will be binding through 2023. Lastly, in 2021, CMS will exclude from the BPCI-A program all episodes where the individual is ultimately diagnosed with COVID-19. In contrast, in 2020, such episodes could be included or excluded at the election of the provider partner. All of these changes could lead to a decline in the program size and/or savings rates we are able to achieve.
Finally, the BPCI-A program is scheduled to expire in 2023 and it is not clear in what form, if any, CMS will renew the program, although in September 2020 CMS announced that it anticipated launching a mandatory bundled payment model upon the expiration of the BPCI-A program. If CMS does not renew the program, or makes significant changes in any successor program, it may have an impact on the number of episodes we are able to manage, our savings rate and, consequently, revenue and profitability in future periods.
COVID-19
Our operations in our Home & Community Services segment have been significantly affected by the COVID-19 pandemic. As a precautionary measure in response to the pandemic, we temporarily halted IHEs in March 2020. Shortly following the suspension of in-home visits, we were able to expand the business model to perform vIHEs and have made up for some of the lost volume for IHEs through vIHEs. We resumed in-home visits beginning in July 2020. We established personal protective equipment protocols with our major customers in order to be able to return to IHEs.
As a result of the pandemic, many of our customers pushed in-person IHEs into the second half of 2020. Although we continue to see some increase in IHE member cancellation rates, overall we saw significant incremental IHE volumes in the second half of 2020 as certain customers increased the volumes they placed with us and in-home IHEs have represented the majority of those IHEs. In order to meet this volume growth, we have onboarded additional providers into our network, which has resulted in proportionally higher expenses. Additionally, in 2020, the COVID-19 pandemic and particularly the resulting shift to virtual evaluations which was most evident in the second quarter, has had an impact on the quarterly volume and results of operations for the Home & Community Services segment. The shift to virtual evaluations was due to a combination of the pause in in-person IHEs between March and July 2020, the decline in acceptance rates for in-person IHEs and an increase in IHE member cancellation rates as individuals have been less willing to receive IHEs in-person since the start of the pandemic. We have also seen some provider unwillingness to perform IHEs in the home during the pandemic. We will continue to monitor these trends in IHEs for as long as the pandemic is ongoing.
Our Episodes of Care Services segment has also been affected by the pandemic. In the United States, at certain times during the course of the pandemic, governmental authorities have recommended, and in certain cases required, that elective, specialty and other procedures and appointments, including certain acute and post-acute care services, be suspended or canceled to avoid non-essential patient exposure to medical environments and potential infection with the virus that causes COVID-19. In addition, the temporary suspension or cancellation of services was put in place to focus limited resources and personnel capacity toward the prevention of, and care for patients with, COVID-19. This has resulted in fewer elective procedures and a general reduction in individuals seeking medical care, which contributed to a substantially lower number of episodes being managed in 2020.
109
Table of Contents
In addition, CMS announced that healthcare providers could continue in the BPCI-A program with no change or they could choose one of the following two options:
| • | Healthcare providers can choose to eliminate upside and downside risk by excluding all episodes from reconciliation in 2020; or |
| • | Healthcare providers could choose to exclude from reconciliation those episodes with a COVID-19 diagnosis during the episode. |
Healthcare providers were required to make their election by September 25, 2020. The results of these elections made by the providers will reduce the total number of episodes we manage during 2020 and 2021, and therefore reduce our program size. This impact on program size was partially offset by a higher savings rate due to a combination of improved performance by some of our partners as well as partners that were underperforming choosing to exclude some or all of their episodes from reconciliation in 2020. Subsequently, CMS announced that all episodes in 2021 with a COVID-19 diagnosis would be automatically excluded from reconciliation, which will reduce program size for all of 2021. There can be no assurance that the positive impact on our savings rate in 2020 will continue in 2021.
Each of these pandemic-related changes has had a material impact on program size in 2020, is expected to have a material impact on program size during at least part of 2021 and could have the effect of reducing program size for 2021 through 2023. Because our administrative fee is calculated as a percentage of program size and we receive a portion of the savings achieved in management of an episode, the decrease in episodes and related reduction in overall program size have had, and we expect will continue to have, a negative effect on our revenue. Some of these measures and challenges will likely continue for the duration of the COVID-19 pandemic, which is uncertain, and will harm the results of operations, liquidity and financial condition of our provider partners and our business. Lastly, our representatives may be prohibited from entering hospitals, skilled nursing facilities and other post-acute facilities as a result of the pandemic, which affects our ability to manage post-acute care and could have a material impact on the savings rate being generated by the program.
During the fourth quarter of 2020, the average daily cases of COVID-19 have been increasing once again and parts of the United States are experiencing significant increases in the average daily cases of COVID-19. We continue to monitor trends related to COVID-19 and their impact on our business, results of operations and financial condition.
Remedy Partners Transactions
In 2019, we acquired 100% of the outstanding equity of Remedy Partners. A controlling interest was initially acquired by New Mountain Capital on January 15, 2019, which we refer to as the “Remedy Partners Acquisition.” At that point, we and Remedy Partners were considered to be under common control and combined financial statements were presented from January 15, 2019 to November 26, 2019. On November 26, 2019, a series of transactions were effected which resulted in Remedy Partners becoming our wholly owned subsidiary, which we refer to as the “Remedy Partners Combination,” and consolidated financial statements were presented from that date. In connection with the Remedy Partners Transactions, we incurred significant transaction costs, primarily diligence-related costs and professional fees, including those related to integration. We assigned values to the assets acquired and the liabilities assumed based upon their fair values at the acquisition date. We also acquired intangible assets, consisting primarily of customer relationships, with a value of $118.0 million, acquired software with a value of $43.0 million and a trade name with a value of $6.0 million, which we expect will increase our amortization expenses in future periods. As a result of the Remedy Partners Acquisition, we also recorded $408.4 million in goodwill, which represents the amount by which the purchase price exceeded the fair value of the net assets acquired.
Because we were not under common control with and did not own Remedy Partners in 2018 and due to the above factors, our results of operations for the year ended December 31, 2019 are not directly comparable to our results of operations for the year ended December 31, 2018.
110
Table of Contents
TAV Health acquisition
On March 31, 2019, we acquired TAV Health. TAV Health formed the basis for our Signify Community solution. As part of the TAV Health acquisition, we assigned values to the assets acquired and the liabilities assumed based upon their fair values at the acquisition date. We also acquired intangible assets, consisting primarily of acquired software with a value of $7.7 million and customer relationships with a value of $0.5 million, which we also expect will increase our amortization expenses in future periods. As a result of the TAV Health acquisition, we also recorded $47.9 million in goodwill, which represents the amount by which the purchase price exceeded the fair value of the net assets acquired. Because we did not own TAV Health in 2018 and due to the above factors, our results of operations for the year ended December 31, 2019 are not directly comparable to our results of operations for the year ended December 31, 2018.
Cost of being a public company
To operate as a public company, we will be required to continue to implement changes in certain aspects of our business and develop, manage and train management level and other employees to comply with ongoing public company requirements. We will also incur new expenses as a public company, including, among others, public reporting obligations, increased professional fees for accounting, proxy statements and stockholder meetings, equity plan administration, stock exchange fees, transfer agent fees, SEC and Financial Industry Regulatory Authority, Inc., or FINRA fees, filing fees, legal fees and offering expenses. In addition, upon the completion of this offering, we will be a party to the Tax Receivable Agreement with the TRA Parties and will be required to make certain distributions to them in accordance with the terms of the Tax Receivable Agreement. See “—Liquidity and capital resources—Tax Receivable Agreement.”
Effects of the reorganization on our corporate structure
Signify Health, Inc. was formed for the purpose of this offering and has engaged to date only in activities in contemplation of this offering. Signify Health, Inc. will be a holding company and its sole material asset will be its ownership interest in Cure TopCo, LLC. For more information regarding our reorganization and holding company structure, see “Organizational structure—The Reorganization Transactions.” Upon completion of this offering, all of our business will be conducted through Cure TopCo, LLC and its consolidated subsidiaries and affiliates, and the financial results of Cure TopCo, LLC and its consolidated subsidiaries will be included in the consolidated financial statements of Signify Health, Inc.
Cure TopCo, LLC is, and will continue to be, taxed as a partnership for federal income tax purposes and, as a result, its members, including Signify Health, Inc., will pay income taxes with respect to their allocable shares of its net taxable income.
Components of our results of operations
Revenue
Our revenue is generated from contracts with our customers within our two operating segments, Home & Community Services and Episodes of Care Services, under contracts that contain various fee structures. Through our Home & Community Services segment, we offer IHEs, performed either within the patient’s home, virtually or at a healthcare provider facility primarily to Medicare Advantage health plans (and to some extent Medicaid). Additionally, we offer certain diagnostic screening and other ancillary services and, through our Signify Community solution, services to address healthcare concerns related to SDOH. Through our Episodes of Care Services segment, we primarily provide services designed to improve the quality and efficiency of healthcare delivery by developing and managing episodic payment programs in partnership with healthcare providers primarily under the BPCI-A program with CMS.
In our Home & Community Services segment, we primarily generate revenue through IHEs. Revenue is recognized when the IHEs are submitted to our customers on a daily basis. Submission to the customer occurs
111
Table of Contents
after the IHEs are completed and coded, a process which may take one to several days after completion of the evaluation. We are paid a flat fee for each completed IHE regardless of the member’s location or the outcome of an IHE. We earn a separate fee for any additional diagnostic screenings the health plan elects to provide for the relevant member. Revenue is recognized when the additional screening occurs.
We have entered into EAR agreements with one of our customers. Beginning in 2020, revenue generated under the underlying customer contracts includes an estimated reduction in the transaction price for IHEs associated with the initial grant date fair value of the outstanding customer EARs. The total grant date fair value of the outstanding EAR agreements was $51.8 million and will be recorded against revenue through December 2022. See “—Liquidity and capital resources—Customer Equity Appreciation Rights agreements.”
In our Episodes of Care Services segment, we primarily generate revenue through episodes of care under the BPCI-A program. We participate as a “convener participant” under the BPCI-A program. As a convener participant, we hold a contract directly with CMS and are responsible for developing and monitoring a BPCI-A episode of care program in partnership with healthcare providers. We enter into back-to-back contracts with provider partners interested in participating in BPCI-A episode of care programs through which we assist with compliance with CMS rules and program requirements and provide a suite of analytic, technology and post-acute management services. Under the BPCI-A program, we recognize the revenue attributable to episodes reconciled during each six-month episode performance measurement period over a 13-month performance obligation period that commences in the second or fourth quarter of each year, depending on the relevant contract with our provider partners. The 13-month performance obligation period begins at the start of the relevant episodes of care and extends through the receipt or generation of the semiannual reconciliation for the relevant performance measurement period, as well as the provision and explanation of statements of performance to each of our customers. We are generally paid an administrative fee, which is paid out of savings, and also share in the savings or losses generated by our provider partners as compared to BPCI-A’s benchmark episode price for a particular episode. The transaction price is 100% variable, and therefore we estimate the amount which we expect to be entitled to receive for each episode performance measurement period over a 13-month performance obligation period. In making this estimate, we consider inputs such as the overall program size, which is defined by the historic cost and the frequency of occurrence of defined episodes of care. Additionally, we estimate rates for shared savings or losses by using data sources such as historical trend analysis together with indicative data of the current volume of episodes. Although our estimates are based on the information available to us at each reporting date, several factors may cause actual revenue earned to differ from the estimates recorded each period. These include, among others, limited historical experience, as the current BPCI-A program only commenced in the fourth quarter of 2018 and has been affected by the COVID-19 pandemic in 2020, and other limitations of the program beyond our control. See “Critical accounting policies—Revenue recognition.”
Operating expenses
Operating expenses are composed of:
| • | Service expense. Service expense represents direct costs associated with generating revenue. These costs include fees paid to providers for performing IHEs, provider travel expenses and the total cost of payroll, related benefits and other personnel expenses for employees in roles that serve to provide direct revenue generating services to customers. Additionally, service expense also includes costs related to the use of certain professional service firms, member engagement expenses, coding expenses and certain other direct costs. |
| • | Selling, general and administrative expense (“SG&A”). SG&A includes the total cost of payroll, related benefits and other personnel expense for employees who do not have a direct role associated with revenue generation, including those involved with developing new service offerings. SG&A includes all general operating costs including, but not limited to, rent and occupancy costs, telecommunications costs, information technology infrastructure and operations costs, software licensing costs, advertising and marketing expenses, recruiting expenses, costs associated with |
112
Table of Contents
| developing new service offerings and expenses related to the use of certain subcontractors and professional services firms. After the consummation of this offering, we expect to incur significant additional legal, accounting and other expenses associated with being a public company, including, among others, costs associated with our compliance with the Sarbanes-Oxley Act and other regulatory requirements. |
| • | Transaction-related expenses. Transaction-related expenses primarily consist of expenses incurred in connection with acquisitions and other corporate development such as mergers and acquisitions activity that did not proceed, strategic investments and similar activities, including consulting expenses, compensation expenses and other integration-type expenses. Additionally, expenses associated with our preparation for this offering are included in transaction-related expenses. |
| • | Asset impairment. Asset impairment includes charges resulting from the impairment of long-lived assets when it is determined that the carrying value exceeds the estimated fair value of the asset. |
| • | Depreciation and amortization. Depreciation expense includes depreciation of property and equipment, including leasehold improvements, computer equipment, furniture and fixtures and software. Amortization expense includes amortization of capitalized internal-use software and software development costs, customer relationships, acquired software and certain trade names. |
Other expense, net
Other expense, net is composed of:
| • | Interest expense. Interest expense consists of accrued interest and related payments on our outstanding long-term debt and Revolving Credit Facility, as well as the amortization of debt issuance costs. |
| • | Other (income) expense, net. Other (income) expense, net primarily consists of interest and dividends on cash and cash equivalents. Changes in fair value of the customer EARs as measured at the end of each period are also included in other (income) expense, net. |
Noncontrolling interest
In connection with the reorganization transactions, we will be appointed as the sole managing member of Cure TopCo, LLC pursuant to the Amended LLC Agreement. Because we will manage and operate the business and control the strategic decisions and day-to-day operations of Cure TopCo, LLC and will also have a substantial financial interest in Cure TopCo, LLC, we will consolidate the financial results of Cure TopCo, LLC, and a portion of our net income (loss) will be allocated to the noncontrolling interest to reflect the entitlement of the Continuing Pre-IPO LLC Members to a portion of Cure TopCo, LLC’s net income (loss). We will hold approximately 74.2% of Cure TopCo, LLC’s outstanding LLC Units (or approximately 74.6% if the underwriters exercise their option to purchase additional shares of Class A common stock in full), and the remaining LLC Units of Cure TopCo, LLC will be held by the Continuing Pre-IPO LLC Members.
Income tax expense
Our business was historically operated through Cure TopCo, LLC, a limited liability company treated as a partnership for U.S. federal income tax purposes, which is generally not subject to U.S. federal or certain state income taxes. In connection with the Reorganization Transactions and this offering, Signify Health, Inc. will acquire LLC Units in Cure TopCo, LLC. Accordingly, Signify Health, Inc. will be subject to U.S. federal and state income tax with respect to its allocable share of the income of Cure TopCo, LLC.
Results of operations
For the nine months ended September 30, 2020 and 2019
The following is a discussion of our combined-consolidated results of operations for each of the nine months ended September 30, 2020 and 2019. A discussion of the results by each of our two operating segments,
113
Table of Contents
Home & Community Services and Episodes of Care Services, follows the discussion of our combined-consolidated results.
The following table summarizes our combined-consolidated results of operations for the nine months ended September 30, 2020 and 2019:
| Nine Months Ended September 30, |
% Change | |||||||||||
| 2020 | 2019 | 2020 v. 2019 | ||||||||||
| (in millions) | ||||||||||||
| Revenue |
$ | 417.1 | $ | 368.5 | 13.2 | % | ||||||
| Operating expenses: |
||||||||||||
| Service expense |
203.4 | 188.2 | 8.1 | % | ||||||||
| Selling, general and administrative expense |
148.5 | 119.1 | 24.7 | % | ||||||||
| Transaction-related expenses |
10.8 | 15.9 | (32.1 | )% | ||||||||
| Asset impairment |
— | 1.5 | (96.9 | )% | ||||||||
| Depreciation and amortization |
46.0 | 49.5 | (7.2 | )% | ||||||||
|
|
|
|
|
|
|
|||||||
| Total operating expenses |
408.7 | 374.2 | 9.2 | % | ||||||||
| Income (loss) from operations |
8.4 | (5.7 | ) | (245.7 | )% | |||||||
| Interest expense |
16.2 | 16.1 | 1.1 | % | ||||||||
| Other expense (income), net |
6.9 | (1.4 | ) | (583.7 | )% | |||||||
|
|
|
|
|
|
|
|||||||
| Other expense, net |
23.1 | 14.7 | 57.8 | % | ||||||||
|
|
|
|
|
|
|
|||||||
| Loss before income taxes |
(14.7 | ) | (20.4 | ) | (27.8 | )% | ||||||
| Income tax expense |
0.5 | 0.1 | 333.0 | % | ||||||||
|
|
|
|
|
|
|
|||||||
| Net loss |
$ | (15.2 | ) | $ | (20.5 | ) | (25.8 | )% | ||||
Revenue
Our total revenue was $417.1 million for the nine months ended September 30, 2020, representing an increase of $48.6 million, or 13.2%, from $368.5 million for the nine months ended September 30, 2019. This increase was primarily driven by a $33.8 million increase in revenue from our Episodes of Care Services segment and a $14.8 million increase in revenue from our Home & Community Services segment. See “Segment results” below.
Operating expenses
Our total operating expenses were $408.7 million for the nine months ended September 30, 2020, representing an increase of $34.5 million, or 9.2%, from $374.2 million for the nine months ended September 30, 2019. This increase was driven by the following:
| • | Service expense—Our total service expense was $203.4 million for the nine months ended September 30, 2020, representing an increase of $15.2 million, or 8.1%, from $188.2 million for the nine months ended September 30, 2019. This increase was primarily driven by compensation-related expenses, which increased by $6.0 million to support the overall growth in our business. Additionally, expenses related to our network of providers increased by $3.3 million driven by the increase in IHE volume partially offset by an increase in vIHEs performed during the period, which have a lower price per evaluation than in-person IHEs; the costs of providing other ancillary services, including certain laboratory and testing fees, increased by $2.3 million; expenses related to member outreach increased by approximately $1.9 million; and other variable costs increased by $0.3 million. The impact of COVID-19 also resulted in approximately $1.5 million in incremental costs for personal protective equipment to be used by our providers while conducting IHEs during the pandemic and $1.0 million in one-time costs, including costs related to COVID-19 tests for our providers, which were partially offset |
114
Table of Contents
| by a decrease in travel and entertainment costs of $1.1 million due to the COVID-19 imposed travel restrictions. |
| • | Selling, general and administrative expense—Our total SG&A expense was $148.5 million for the nine months ended September 30, 2020, representing an increase of $29.4 million, or 24.7%, from $119.1 million for the nine months ended September 30, 2019. This increase was primarily driven by compensation-related expenses, which increased by $23.0 million to support the overall growth in our business, and includes a $7.2 million increase in stock-based compensation expense due to additional equity-based grants. Other costs also increased primarily to support the growth in our business, including: professional and consulting fees, which increased by $5.8 million; facilities-related expenses, including rent expense under our operating leases, which increased by $5.9 million; and other variable costs, which increased by $0.1 million. These increases were partially offset by a decrease in employee travel and entertainment of $2.4 million driven by COVID-19 related travel restrictions and a decrease in information technology expenses including infrastructure and software costs of $3.0 million. |
| • | Transaction-related expenses—Our total transaction-related expenses were $10.8 million for the nine months ended September 30, 2020, representing a decrease of $5.1 million, or 32.1%, from $15.9 million for the nine months ended September 30, 2019. In 2020, the transaction-related expenses related to the Remedy Partners Combination and integration of Remedy Partners, expenses incurred in connection with potential acquisitions and other corporate development activities that did not proceed, as well as costs incurred in connection with our initial public offering. These transaction-related expenses consisted primarily of consulting, compensation and integration-type expenses. In 2019, the transaction-related expenses related to the Remedy Partners Acquisition, the TAV Health acquisition, as well as certain integration-related expenses associated with acquisitions made in prior years. These transaction-related expenses consisted primarily of consulting, compensation and integration-type expenses. |
| • | Asset impairment—Our total asset impairment was $1.5 million for the nine months ended September 30, 2019. In 2019, we discontinued the use of certain software resulting in an asset impairment of $1.5 million. We did not have any significant asset impairments for the nine months ended September 30, 2020. |
| • | Depreciation and amortization—Our total depreciation and amortization expense was $46.0 million for the nine months ended September 30, 2020, representing a decrease of $3.5 million, or 7.2%, from $49.5 million for the nine months ended September 30, 2019. This decrease in depreciation and amortization was primarily driven by a decrease in amortization expense of $4.4 million primarily relating to assets becoming fully amortized in 2019 as well as the discontinued use of certain trade names following the Remedy Partners Acquisition, which resulted in an asset impairment in the fourth quarter of 2019. This decrease was partially offset by an increase in depreciation expense of $0.9 million related to additional capital expenditures over the past year. |
Other expense, net
Other expense, net was $23.1 million for the nine months ended September 30, 2020, representing an increase of $8.4 million, or 57.8%, from $14.7 million for the nine months ended September 30, 2019. This increase was primarily driven by an increase in other expense (income), net of $8.3 million and an increase in interest expense of $0.1 million. The increase in other expense (income), net was driven by an increase of $6.9 million related to the remeasurement of fair value of the customer EARs’ liability in 2020 and a decrease of $1.4 million in interest income related to lower interest rates and lower excess cash balances held throughout 2020 compared to 2019. Interest expense increased $0.1 million primarily driven by the borrowings under the Revolving Credit Facility in 2020, which was partially offset by lower interest rates and quarterly principal payments of long-term debt under our Credit Agreement.
115
Table of Contents
Income tax expense
Income tax expense was $0.5 million for the nine months ended September 30, 2020, representing an increase of $0.4 million, or 333.0%, from $0.1 million for the nine months ended September 30, 2019. This increase was primarily driven by additional taxes incurred in 2020 as a result of the increase in taxable income following the Remedy Partners Combination.
Segment results
We evaluate the performance of each of our two operating segments based on segment revenue and segment adjusted EBITDA. Service expense for each segment is based on direct expenses associated with revenue generating activities of each segment. We allocate SG&A expenses to each segment based on the relative proportion of direct employees.
The following table summarizes our segment revenue and the percentage of total combined-consolidated revenue for the nine months ended September 30, 2020 and 2019:
| Nine Months Ended September 30, |
% Change | |||||||||||||||||||
| 2020 | % of Total | 2019 | % of Total | 2020 v. 2019 | ||||||||||||||||
| (in millions) | ||||||||||||||||||||
| Revenue |
||||||||||||||||||||
| Home & Community Services: |
||||||||||||||||||||
| Evaluations |
$ | 294.9 | 70.7 | % | $ | 280.7 | 76.2 | % | 5.1 | % | ||||||||||
| Other |
6.9 | 1.7 | % | 6.3 | 1.7 | % | 9.7 | % | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total Home & Community Services revenue |
301.8 | 72.4 | % | 287.0 | 77.9 | % | 5.2 | % | ||||||||||||
| Episodes of Care Services: |
||||||||||||||||||||
| Episodes |
107.2 | 25.7 | % | 67.8 | 18.4 | % | 58.2 | % | ||||||||||||
| Other |
8.1 | 1.9 | % | 13.7 | 3.7 | % | (41.4 | )% | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total Episodes of Care Services revenue |
115.3 | 27.6 | % | 81.5 | 22.1 | % | 41.4 | % | ||||||||||||
| Segment Adjusted EBITDA |
||||||||||||||||||||
| Home & Community Services |
65.8 | N/ | A | 73.9 | N | /A | (10.9 | )% | ||||||||||||
| Episode of Care Services |
20.2 | N/ | A | (7.2 | ) | N/ | A | 380.5 | % | |||||||||||
Home & Community Services revenue was $301.8 million for the nine months ended September 30, 2020, representing an increase of $14.8 million, or 5.2%, from $287.0 million for the nine months ended September 30, 2019. This increase was primarily driven by increased IHE volume resulting in an increase in Evaluations revenue of $21.7 million. The increase in revenue resulting from the increased IHE volume was partially offset by an increase in vIHEs performed during the period, which have a lower price per evaluation than in-person IHEs. Additionally, Home & Community Services revenue for the nine months ended September 30, 2020 was reduced by $7.5 million as a result of the customer EAR agreements, which became effective in 2020. Additionally, other revenue increased by $0.6 million, primarily related to the TAV Health acquisition, which formed the basis for our Signify Community product and occurred in March 2019 and therefore revenue was not included for the full nine-month period during the nine months ended September 30, 2019.
Episodes of Care Services revenue was $115.3 million for the nine months ended September 30, 2020, representing an increase of $33.8 million, or 41.4%, from $81.5 million for the nine months ended September 30, 2019. This increase was primarily driven by an increase of $39.4 million in Episodes revenue, which was partially offset by a $5.6 million decrease in Other revenue. The increase in Episodes revenue was primarily driven by an improved savings rate, an increase in program size as a result of additional partners entering the program at the start of 2020 and the timing of the Remedy Partners Acquisition, which occurred on January 15, 2019 and therefore was not included for the full nine-month period ended September 30, 2019. During the nine
116
Table of Contents
months ended September 30, 2020, we recognized approximately $8.9 million of revenue representing changes in estimates of variable consideration upon receipt and analysis of reconciliations from CMS in the second quarter of 2020 as a result of the improved savings rate and changes in program size. During the nine months ended September 30, 2020, we also recorded approximately $9.2 million of revenue related to changes in estimates based on new information received primarily related to the impact of COVID-19 on program size and related CMS imposed changes offered to providers that had an overall beneficial impact on savings rates. During the nine months ended September 30, 2019, we recognized approximately $2.1 million of revenue representing changes in estimates of variable consideration upon receipt and analysis of reconciliations from CMS. Other revenue decreased by $5.6 million in the first nine months of 2020 driven by the termination and sale of two customer contracts in early 2019 that had been using our complex care management services and the shift in business strategy related to that product offering.
Home & Community Services Adjusted EBITDA was $65.8 million for the nine months ended September 30, 2020, representing a decrease of $8.1 million, or 10.9%, from $73.9 million for the nine months ended September 30, 2019. This decrease was primarily driven by the impact of COVID-19, including the shift to vIHEs, which have a lower price per evaluation than in-person IHEs, partially offset by the increase in revenue and higher operating expenses as a result of the investments to support our growth and technology.
Episodes of Care Services Adjusted EBITDA was $20.2 million for the nine months ended September 30, 2020, representing an increase of $27.4 million, or 380.5%, from $(7.2) million for the nine months ended September 30, 2019. This increase was primarily driven by the increase in revenue, including the impact of the improved savings rate, the increase in program size due to additional partners entering the program at the start of 2020 and changes in program size estimates, which resulted in changes in estimated revenue for the nine months ended September 30, 2020. Additionally, the Remedy Partners Acquisition occurred in January 2019. As a result, operating results for Remedy Partners were included for the full nine-month period ended September 30, 2020 but were not included for the full nine-month period ended September 30, 2019.
For the years ended December 31, 2019 and 2018
The following is a discussion of our combined-consolidated results of operations for each of the years ended December 31, 2019 and 2018. A discussion of the results by each of our two operating segments, Home & Community Services and Episodes of Care Services, follows the discussion of our combined-consolidated results.
117
Table of Contents
The following table summarizes our combined-consolidated results of operations for the years ended December 31, 2019 and 2018:
| Year Ended December 31, | % Change | |||||||||||
| 2019 | 2018 | 2019 v. 2018 | ||||||||||
| (in millions) | ||||||||||||
| Revenue |
$ | 501.8 | $ | 337.9 | 48.5 | % | ||||||
| Operating expenses: |
||||||||||||
| Service expense |
247.2 | 196.3 | 25.9 | % | ||||||||
| Selling, general and administrative expense |
168.6 | 67.9 | 148.5 | % | ||||||||
| Transaction-related expenses |
22.4 | 21.0 | 6.9 | % | ||||||||
| Asset impairment |
6.4 | 17.0 | (62.4 | )% | ||||||||
| Depreciation and amortization |
66.0 | 43.0 | 53.4 | % | ||||||||
|
|
|
|
|
|
|
|||||||
| Total operating expenses |
510.6 | 345.2 | 47.9 | % | ||||||||
| Loss from operations |
(8.8 | ) | (7.3 | ) | 21.3 | % | ||||||
| Interest expense |
21.2 | 21.4 | (1.0 | )% | ||||||||
| Other (income) expense, net |
(1.6 | ) | — | N.M. | ||||||||
|
|
|
|
|
|
|
|||||||
| Other expense, net |
19.6 | 21.4 | (8.2 | )% | ||||||||
|
|
|
|
|
|
|
|||||||
| Loss before income taxes |
(28.4 | ) | (28.7 | ) | (0.8 | )% | ||||||
| Income tax expense |
0.1 | 0.2 | (54.4 | )% | ||||||||
|
|
|
|
|
|
|
|||||||
| Net loss |
(28.5 | ) | (28.9 | ) | (1.2 | )% | ||||||
Revenue
Our total revenue was $501.8 million in 2019, representing an increase of $163.9 million, or 48.5%, from $337.9 million in 2018. This increase was primarily driven by a $96.9 million increase in revenue from our Episodes of Care Services segment as a result of the Remedy Partners Acquisition and a $67.0 million increase in revenue from our Home & Community Services segment. See “Segment results” below.
Operating expenses
Our total operating expenses were $510.6 million in 2019, representing an increase of $165.4 million, or 47.9%, from $345.2 million in 2018. This increase was driven by the following:
| • | Service expense—Our total service expense was $247.2 million in 2019, representing an increase of $50.9 million, or 25.9%, from $196.3 million in 2018. This increase was primarily driven by $30.7 million related to the Remedy Partners Acquisition. Additionally, expenses related to our network of providers increased by $8.9 million driven by the increase in IHE volume, the costs of providing other ancillary services, including certain laboratory and testing fees, increased by $5.2 million, compensation related expenses increased $5.2 million to support the overall growth in our business, including the impact of the TAV Health acquisition, and other variable costs increased by $0.9 million. |
| • | Selling, general and administrative expense—Our total SG&A expense was $168.6 million in 2019, representing an increase of $100.7 million, or 148.5%, from $67.9 million in 2018. $76.2 million of this increase was driven by the Remedy Partners Acquisition. In addition, compensation related expenses increased by $19.2 million to support the overall growth in our business, including the impact of the TAV Health acquisition. Other costs also increased primarily to support the growth in our business, including: employee travel and entertainment, which increased by $1.8 million, professional and consulting fees, which increased by $1.4 million, facilities-related expenses, including rent expense under our operating leases, which increased by $1.4 million and information technology expenses including infrastructure and software costs, which increased by $1.1 million. These increases were partially offset by a decrease of $0.4 million in other variable costs. |
118
Table of Contents
| • | Transaction-related expenses—Our total transaction-related expenses were $22.4 million in 2019, representing an increase of $1.4 million, or 6.9%, from $21.0 million in 2018. In 2019, the transaction-related expenses related to the acquisition and integration of Remedy Partners, including our initial combination with Remedy Partners in January 2019, the TAV Health acquisition, as well as certain integration-related expenses associated with acquisitions made in prior years. These transaction-related expenses related to consulting, compensation and integration-type expenses. In 2018, the transaction-related expenses primarily related to integration costs associated with acquisitions made in late 2017. These transaction-related expenses related to consulting, compensation and integration-type expenses. |
| • | Asset impairment—Our total asset impairment was $6.4 million in 2019, representing a decrease of $10.6 million, or 62.4%, from $17.0 million in 2018. The asset impairment in 2019 was primarily related to the discontinued use of certain trade names following the Remedy Partners Acquisition, which resulted in a $4.9 million asset impairment. Additionally, in 2019, we discontinued the use of certain software resulting in an asset impairment of $1.5 million. The asset impairment in 2018 was primarily related to the discontinued use of certain trade names following our rebranding, which resulted in a $16.0 million asset impairment. Additionally, certain property and equipment were impaired for a total of $1.0 million in 2018. |
| • | Depreciation and amortization—Our total depreciation and amortization expense was $66.0 million in 2019, representing an increase of $23.0 million, or 53.4%, from $43.0 million in 2018. This increase was primarily driven by $25.7 million related to the Remedy Partners Acquisition, which resulted in the acquisition of $167.0 million in intangible assets, comprised of customer relationships of $118.0 million, acquired software of $43.0 million and a trade name of $6.0 million, as well as $6.6 million in property and equipment. This increase in depreciation and amortization was partially offset by a decrease of $1.7 million in amortization expense primarily driven by impairment of certain software assets which were being amortized in 2018 and a decrease of $1.0 million in depreciation expense as a result of assets becoming fully depreciated during 2019. |
Other expense, net
Other expense, net was $19.6 million in 2019, representing a decrease of $1.8 million, or 8.2%, from $21.4 million in 2018. This decrease was primarily driven by an increase in other (income) expense, net of approximately $1.6 million and a decrease in interest expense of $0.2 million. The increase in other (income) expense, net was driven by an increase of $1.6 million in interest income on excess cash balances held throughout the year. The decrease in interest expense was primarily driven by lower interest rates partially offset by an increase in the outstanding principal of long-term debt under our Credit Agreement.
Income tax expense
Income tax expense was $0.1 million in 2019, representing a decrease of $0.1 million, or 54.4%, from $0.2 million in 2018. This decrease was primarily driven by additional taxes incurred in 2018 related to predecessor entities.
Segment results
We evaluate the performance of each of our two operating segments based on segment revenue and segment adjusted EBITDA. Service expense for each segment is based on direct expenses associated with revenue generating activities of each segment. We allocate SG&A expenses to each segment based on the relative proportion of direct employees.
119
Table of Contents
The following table summarizes our segment revenue and the percentage of total combined-consolidated revenue for the years ended December 31, 2019 and 2018:
| Year Ended December 31, |
% Change | |||||||||||||||||||
| 2019 | % of Total | 2018 | % of Total | 2019 v. 2018 | ||||||||||||||||
| (in millions) | ||||||||||||||||||||
| Revenue |
||||||||||||||||||||
| Home & Community Services: |
||||||||||||||||||||
| Evaluations |
$ | 369.6 | 73.6 | % | $ | 310.0 | 91.8 | % | 19.2 | % | ||||||||||
| Other |
7.4 | 1.5 | % | — | — | N.M. | ||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total Home & Community Services revenue |
377.0 | 75.1 | % | 310.0 | 91.8 | % | 21.6 | % | ||||||||||||
| Episodes of Care Services: |
||||||||||||||||||||
| Episodes |
107.8 | 21.4 | % | — | — | N.M. | ||||||||||||||
| Other |
17.0 | 3.5 | % | 27.9 | 8.2 | % | (39.0 | )% | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total Episodes of Care Services revenue |
124.8 | 24.9 | % | 27.9 | 8.2 | % | 347.9 | % | ||||||||||||
| Segment Adjusted EBITDA |
||||||||||||||||||||
| Home & Community Services |
90.5 | N/A | 76.1 | N/A | 19.0 | % | ||||||||||||||
| Episode of Care Services |
2.8 | N/A | 3.0 | N/A | (6.4 | )% | ||||||||||||||
Home & Community Services revenue was $377.0 million in 2019, representing an increase of $67.0 million, or 21.6%, from $310.0 million in 2018. This increase was primarily driven by increased IHE volume resulting in an increase in Evaluations revenue of $59.6 million, of which $57.9 million was driven by the expansion at existing customers and $1.7 million was driven by the addition of new customers. Additionally, other revenue was $7.4 million in 2019, primarily related to the TAV Health acquisition, which formed the basis for our Signify Community product and the introduction of other product offerings to our customers.
Episodes of Care Services revenue was $124.8 million in 2019, representing an increase of $96.9 million, or 347.9%, from $27.9 million in 2018. This increase was primarily driven by the Remedy Partners Acquisition which contributed $107.8 million in Episodes revenue for 2019. Other revenue decreased by $10.9 million driven by the termination and sale of two customer contracts using our complex care management services and the shift in business strategy related to that product offering.
Home & Community Services Adjusted EBITDA was $90.5 million in 2019, representing an increase of $14.4 million, or 19.0%, from $76.1 million in 2018. This increase was primarily driven by the increased revenue partially offset by higher operating expenses as a result of the investments to support our growth and technology.
Episodes of Care Services Adjusted EBITDA was $2.8 million in 2019, representing a decrease of $0.2 million, or 6.4%, from $3.0 million in 2018. This decrease was primarily driven by the termination and sale of two customer contracts using our complex care management services and the shift in business strategy related to that product offering which resulted in a decrease of approximately $3.8 million in segment Adjusted EBITDA. This decrease was partially offset by the Remedy Partners Acquisition, which since 2019 has comprised a majority of this segment, and contributed approximately $3.6 million in segment Adjusted EBITDA.
Quarterly Results of Operations
The following table sets forth unaudited statement of operations data for each of the quarters presented. We have prepared the quarterly statement of operations data on a basis consistent with the audited combined-consolidated financial statements included elsewhere in this prospectus. In the opinion of management, the financial information reflects all adjustments, consisting of normal recurring adjustments, which we consider necessary for a fair presentation of this data. This information should be read in conjunction with the combined-
120
Table of Contents
consolidated financial statements and related notes included elsewhere in this prospectus. The results of historical periods are not necessarily indicative of the results for any future period.
| Three months ended (unaudited) |
||||||||||||||||||||||||||||
| March 31, 2019 |
June 30, 2019 |
September 30, 2019 |
December 31, 2019 |
March 31, 2020 |
June 30, 2020 |
September 30, 2020 |
||||||||||||||||||||||
| (in millions) | ||||||||||||||||||||||||||||
| Revenue |
$ | 107.2 | $ | 133.0 | $ | 128.3 | $ | 133.3 | $ | 131.7 | $ | 130.7 | $ | 154.7 | ||||||||||||||
| Operating expenses: |
||||||||||||||||||||||||||||
| Service expense |
58.2 | 64.4 | 65.6 | 59.0 | 67.3 | 52.7 | 83.4 | |||||||||||||||||||||
| Selling, general and administrative expense |
31.3 | 42.2 | 45.6 | 49.5 | 51.1 | 47.0 | 50.4 | |||||||||||||||||||||
| Transaction-related expenses |
7.9 | 5.1 | 2.9 | 6.5 | 2.4 | 1.6 | 6.8 | |||||||||||||||||||||
| Asset impairment |
1.5 | — | — | 4.9 | — | — | — | |||||||||||||||||||||
| Depreciation and amortization |
15.8 | 17.4 | 16.3 | 16.5 | 14.5 | 15.7 | 15.8 | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Total operating expenses |
114.7 | 129.1 | 130.4 | 136.4 | 135.3 | 117.0 | 156.4 | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| (Loss) income from operations |
(7.5 | ) | 3.9 | (2.1 | ) | (3.1 | ) | (3.6 | ) | 13.7 | (1.7 | ) | ||||||||||||||||
| Interest expense |
5.1 | 5.6 | 5.4 | 5.1 | 5.2 | 5.9 | 5.1 | |||||||||||||||||||||
| Other (income) expense, net |
(0.7 | ) | (0.5 | ) | (0.2 | ) | (0.2 | ) | — | 0.6 | 6.3 | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Other expense, net |
4.4 | 5.1 | 5.2 | 4.9 | 5.2 | 6.5 | 11.4 | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| (Loss) income before income taxes |
(11.9 | ) | (1.2 | ) | (7.3 | ) | (8.0 | ) | (8.8 | ) | 7.2 | (13.1 | ) | |||||||||||||||
| Income tax expense |
0.1 | — | — | — | 0.1 | 0.2 | 0.2 | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Net (loss) income |
$ | (12.0 | ) | $ | (1.2 | ) | $ | (7.3 | ) | $ | (8.0 | ) | $ | (8.9 | ) | $ | 7.0 | $ | (13.3 | ) | ||||||||
Liquidity and capital resources
Liquidity describes our ability to generate sufficient cash flows to meet the cash requirements of our business operations, including working capital needs to meet operating expenses, debt service, acquisitions and other commitments and contractual obligations. We consider liquidity in terms of cash flows from operations and their sufficiency to fund our operating and investing activities.
Our primary sources of liquidity are our existing cash and cash equivalents, cash provided by operating activities and borrowings under our Credit Agreement. As of September 30, 2020, we had unrestricted cash and cash equivalents of $87.9 million. Our total indebtedness was $350.2 million as of September 30, 2020. See “—Indebtedness” below.
Our principal liquidity needs have been, and we expect them to continue to be, working capital and general corporate needs, debt service, capital expenditures and potential acquisitions. Our capital expenditures for property and equipment to support growth in the business were $12.6 million and $6.6 million for the years ended December 31, 2019 and 2018, respectively, and $13.0 million and $7.1 million for the nine months ended September 30, 2020 and 2019, respectively.
Our liquidity may fluctuate on a quarterly basis due to our agreement with CMS under the BPCI-A program. Cash receipts generated under this contract, which represents the majority of revenue in our Episodes of Care
121
Table of Contents
Services segment, are subject to a semiannual reconciliation cycle, which occurs in the second and fourth quarters of the year. As a result, we typically receive cash receipts under this contract during the first and third quarters of each year, which can cause our liquidity to fluctuate from quarter to quarter.
In October 2020, we paid $54.0 million to repurchase certain Series B preferred units that were originally issued to TAV Health in connection with the TAV Health acquisition. In November 2020, we entered into the 2020 November Incremental Term Loans under our existing Credit Agreement for a total of $125.0 million. The proceeds were used to repay the $77.0 million in borrowings outstanding under the Revolving Credit Facility, to fund a small acquisition and for general corporate purposes. In December 2020, we entered into the 2020 December Incremental Term Loans under our existing Credit Agreement for a total of $15.0 million. See “—Indebtedness.”
During 2020, the COVID-19 pandemic has had a negative impact on our liquidity, particularly in the Home & Community Services segment. IHEs were temporarily suspended and despite being able to pivot to vIHEs, the reduction in IHEs has impacted revenue growth and therefore, liquidity. Furthermore, as a result of the shift to vIHEs and other customer claims processing system delays, we have experienced certain temporary collection delays from a few large Home & Community Services customers, which temporarily resulted in a negative impact on operating cash flows during the nine months ended September 30, 2020. We collected a significant portion of these amounts in the fourth quarter of 2020 and continue to actively work with our customers to collect on these amounts. In our Episodes of Care Services segment, the lower number of episodes managed in 2020 has not yet had an impact on our liquidity because of the timing of the semiannual reconciliations and related cash receipts from CMS under the BPCI-A program. We expect to see the impact of the lower number of episodes managed on our liquidity reflected in the next cash payment we receive from CMS in the first quarter of 2021.
We believe that our cash flow from operations, availability under our Credit Agreement and available cash and cash equivalents will be sufficient to meet our liquidity needs for at least the foreseeable future. We anticipate that to the extent that we require additional liquidity, it will be funded through the proceeds from this offering, the incurrence of additional indebtedness, the issuance of additional equity, or a combination thereof. We cannot assure you that we will be able to obtain this additional liquidity on reasonable terms, or at all. Additionally, our liquidity and our ability to meet our obligations and fund our capital requirements are also dependent on our future financial performance, which is subject to general economic, financial and other factors that are beyond our control. See “Risk factors.” Accordingly, we cannot assure you that our business will generate sufficient cash flow from operations or that future borrowings will be available from additional indebtedness or otherwise to meet our liquidity needs. If we decide to pursue one or more significant acquisitions, we may incur additional debt or sell or issue additional equity to finance such acquisitions, which could possibly result in additional expenses or dilution.
Indebtedness
On December 21, 2017, our subsidiaries, Cure Intermediate 3, LLC (f/k/a Chloe Ox Intermediate 3, LLC and Ox Parent, LLC) as “Holdings” and Signify Health, LLC (f/k/a Cure Borrower, LLC and Chloe Ox Parent, LLC), as “Borrower,” entered into a credit agreement (as subsequently amended, restated, supplemented and/or otherwise modified from time to time, the “Credit Agreement”) with UBS AG, Stamford Branch as administrative agent and collateral agent (the “Administrative Agent”), the guarantors party thereto from time to time and the lenders party thereto from time to time, consisting of term loans in an aggregate principal amount of $260.0 million (the “Initial Term Loans”) and a revolving credit facility in an aggregate principal amount of $35.0 million (the “Revolving Credit Facility”). On June 22, 2018, Holdings, the Borrower, the Administrative Agent, the guarantors party thereto and the lenders party thereto entered into the first amendment to the Credit Agreement to amend and restate the Credit Agreement in order to, among other things, refinance the Initial Term Loans with a new tranche of term loans in an aggregate principal amount of $260.0 million (the “2018 Term Loans”). On April 23, 2019, Holdings, the Borrower, the Administrative Agent, the guarantors party thereto and the lenders party thereto executed the second amendment to the Credit Agreement to borrow an additional
122
Table of Contents
$20.0 million of term loans (the “2019 Term Loans”). On December 9, 2019, Holdings, the Borrower, the Administrative Agent, the guarantors party thereto and the lenders party thereto executed the third amendment to the Credit Agreement to increase the revolving credit commitments by an aggregate principal amount of $45.0 million, resulting in a total of $280.0 million of Term Loans outstanding and borrowing capacity of $80.0 million under the Revolving Credit Facility. On November 17, 2020, Holdings, the Borrower, the Administrative Agent, the guarantors party thereto and the lenders party thereto entered into the fourth amendment to the Credit Agreement to amend and restate the Credit Agreement in order to, among other things, incur additional indebtedness in the form of a new tranche of term loans in an aggregate principal amount of $125.0 million (the “2020 November Incremental Term Loans”). On December 7, 2020, Holdings, the Borrower, the Administrative Agent, the guarantors party thereto and the lenders party thereto entered into the fifth amendment to the Credit Agreement to borrow an additional $15.0 million of term loans (the “2020 December Incremental Loans” and together with the 2020 November Incremental Term Loans, the “Incremental Term Loans,” and, the Incremental Term Loans together with the 2018 Term Loans and the 2019 Term Loans, the “Term Loans”). The obligations under the Credit Agreement are secured by substantially all of the assets of Holdings, the Borrower and its wholly owned domestic subsidiaries (subject to customary exceptions and exclusions), including a pledge of the equity of each of its subsidiaries.
The Term Loans are payable in quarterly installments of 0.25% of the aggregate principal amount of Term Loans outstanding and mature on December 21, 2024. The Revolving Credit Facility matures on December 21, 2022.
Prior to June 22, 2018, the Initial Term Loans bore interest at a rate of the base rate plus 4.00% for base rate loans or the eurocurrency rate plus 5.00% for eurocurrency rate loans. Since June 22, 2018, the 2018 Term Loans and the 2019 Term Loans have had an interest rate of the base rate plus 3.50% for base rate loans or the eurocurrency rate plus 4.50% for eurocurrency rate loans. The Incremental Term Loans have an interest rate of the base rate plus 4.25% for base rate loans or the eurocurrency rate plus 5.25% for eurocurrency rate loans. Prior to June 22, 2018, borrowings under the Revolving Credit Facility bore interest at a rate of the base rate plus 4.00% for base rate loans or the eurocurrency rate plus 5.00% for eurocurrency rate loans and letter of credit fees and, undrawn commitment fees equal to 0.50%. From June 22, 2018 until delivery of financial statements for the first full quarter after June 22, 2018, borrowings under the Revolving Credit Facility bore interest at a rate of the base rate plus 3.50% for base rate loans or the eurocurrency rate plus 4.50% for eurocurrency rate loans and letter of credit fees and, in the case of undrawn commitment fees, 0.50%. Since delivery of financial statements for the first full quarter after June 22, 2018, the interest rate for borrowings under the Revolving Credit Facility has been based on the consolidated first lien net leverage ratio pricing grid below. In each case, eurocurrency rate loans are subject to a 1.00% floor for the 2018 Term Loans and the 2019 Term Loans and 0.00% for revolving loans. Term loans borrowed at the base rate are subject to a 2.00% floor.
| Pricing Level | Consolidated First Lien Net Leverage Ratio |
Eurocurrency Rate Loans and Letter of Credit Fees |
Base Rate Loans | Commitment Fee | ||||||||||
| 1 |
> 3.25:1.00 | 4.50 | % | 3.50 | % | 0.50 | % | |||||||
| 2 |
£ 3.25:1.00 and > 2.75:1.00 |
4.25 | % | 3.25 | % | 0.375 | % | |||||||
| 3 |
£ 2.75:1.00 | 4.00 | % | 3.00 | % | 0.250 | % | |||||||
In addition, the Credit Agreement contains covenants that, among other things, restrict the ability of the Borrower and its restricted subsidiaries to make certain restricted payments, incur additional debt, engage in certain asset sales, mergers, acquisitions or similar transactions, create liens on assets, engage in certain transactions with affiliates, change its business or make investments. Following our initial public offering, the Credit Agreement will continue to contain these covenants, including a covenant that restricts the Borrower’s ability to make dividends or other distributions to Signify Health, Inc. In addition, the Credit Agreement contains a springing financial covenant requiring the Borrower to maintain its Consolidated First Lien Net Leverage Ratio
123
Table of Contents
(as defined in the Credit Agreement) at or below 5.75:1.00 as of the last day of any fiscal quarter in which the principal amount of all revolving loans and letters of credit (other than undrawn letters of credit) exceed 35% of the revolving credit commitments at such time.
Comparative cash flows
The following table sets forth our cash flows for the periods indicated:
| Year Ended December 31, |
Nine Months Ended September 30, |
|||||||||||||||
| 2019 | 2018 | 2020 | 2019 | |||||||||||||
| (in millions) | ||||||||||||||||
| Net cash provided by operating activities |
$ | 41.7 | $ | 35.6 | $ | 40.7 | $ | 56.2 | ||||||||
| Net cash provided by (used in) investing activities |
82.9 | (13.1 | ) | (28.7 | ) | 91.6 | ||||||||||
| Net cash (used in) provided by financing activities |
(94.8 | ) | (21.9 | ) | 30.1 | (90.6 | ) | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Net increase in cash, cash equivalents and restricted cash |
29.8 | 0.6 | 42.1 | 57.2 | ||||||||||||
| Cash, cash equivalents and restricted cash—beginning of year |
20.4 | 19.8 | 50.2 | 20.4 | ||||||||||||
| Cash, cash equivalents and restricted cash—end of year |
$ | 50.2 | $ | 20.4 | $ | 92.3 | $ | 77.6 | ||||||||
Operating activities
Net cash provided by operating activities was $40.7 million for the nine months ended September 30, 2020, a decrease of $15.5 million, compared to $56.2 million for the nine months ended September 30, 2019. This decrease was primarily the result of a $35.6 million decrease related to the effect of changes in operating assets and a $1.8 million payment of contingent consideration partially offset by decrease in net loss of $5.3 million and a $15.5 million increase in non-cash items partially offset by a $1.1 million gain on sale of assets in 2019.
Net loss was $15.2 million for the nine months ended September 30, 2020, as compared to $20.5 million for the nine months ended September 30, 2019. The decrease was primarily due to the Remedy Partners Acquisition and growth in Home & Community Services revenue partially offset by an increase in operating expenses to support the growth in the business. Non-cash items were $79.9 million in 2019 as compared to $66.6 million in 2018. The increase in non-cash items was primarily driven by the Remedy Partners Acquisition and the associated increase in intangible assets subject to amortization.
The effect of changes in operating assets and liabilities was a cash decrease of $14.4 million for the nine months ended September 30, 2020, as compared to an increase of $21.2 million for the nine months ended September 30, 2019. The most significant drivers contributing to this net decrease of $35.9 million relate to the following:
| • | A decrease related to accounts receivable of $48.7 million; |
| • | A cash inflow of $25.0 million during the nine months ended September 30, 2020 primarily as a result of the collection of amounts outstanding at December 31, 2019 related to the Episodes of Care Services segment partially offset by an increase in amounts due from customers at September 30, 2020 related to the Home & Community Services segment driven by certain delays in collections from a few large clients; |
| • | A cash inflow of $73.7 million for the nine months ended September 30, 2019 primarily driven by the timing of collections related to the Remedy Partners Acquisition and an increase in revenue; |
| • | A net decrease related to contract assets and liabilities of $25.5 million driven by the timing of semiannual reconciliations and improvements in savings rate in the nine months ended September 30, 2020 resulting in an increase in estimated revenue under the BPCI-A program; |
124
Table of Contents
| • | A net increase related to accounts payable and accrued expenses of $25.9 million primarily due to timing of payments and the Remedy Partners Acquisition in 2019. Accounts payable and accrued expenses decreased $11.5 million for the nine months ended September 30, 2020 as compared to a decrease of $37.4 million for the nine months ended September 30, 2019; |
| • | A net increase related to other noncurrent liabilities of $7.5 million as a result of an increase in deferred rent due to additional facility space and the Remedy Partners Acquisition. Other noncurrent liabilities increased $10.6 million for the nine months ended September 30, 2020 as compared to a net increase of $3.1 million for the nine months ended September 30, 2019; and |
| • | A net increase related to other current liabilities of $6.8 million primarily driven by an increase in deferred revenue related to a payment in advance of services from a customer and an increase in the estimated sales tax reserve as described in the notes to our combined-consolidated financial statements included elsewhere in this prospectus. Other current liabilities increased $6.3 million for the nine months ended September 30, 2020 compared to a decrease of $0.5 million for the nine months ended September 30, 2019. |
Net cash provided by operating activities was $41.7 million in 2019, an increase of $6.1 million, compared to $35.6 million in 2018. This increase was primarily the result of a decrease in net loss of $0.4 million, a $13.3 million increase in non-cash items partially offset by a $1.1 million gain on sale of assets and a $6.5 million decrease related to the effect of changes in operating assets.
Net loss was $28.5 million in 2019, as compared to $28.9 million in 2018. The decrease was primarily due to the Remedy Partners Acquisition and growth in Home & Community Services revenue partially offset by an increase in operating expenses to support the growth in the business. Non-cash items were $79.9 million in 2019 as compared to $66.6 million in 2018. The increase in non-cash items was primarily driven by the Remedy Partners Acquisition and the associated increase in intangible assets subject to amortization.
The effect of changes in operating assets and liabilities was a cash decrease of $8.6 million in 2019, as compared to a decrease of $2.1 million in 2018. The most significant drivers contributing to this decrease relate to the following:
| • | An increase in accounts receivable of $37.8 million in 2019 primarily as a result of the Remedy Partners Acquisition which resulted in an increase of approximately $34.4 million and an increase of approximately $3.4 million driven by higher revenue and timing of collections compared to an increase of $8.0 million in 2018; |
| • | A net decrease in contract assets and liabilities for a net increase to cash impact of $17.4 million driven by the Remedy Partners Acquisition and timing of semiannual reconciliations and estimated revenue under the BPCI-A program; and |
| • | A net increase in other noncurrent liabilities of $5.8 million as a result of an increase in deferred rent due to additional facility space and the Remedy Partners Acquisition. Other noncurrent liabilities increased $6.8 million in 2019 as compared to a net increase of $1.0 million in 2018. |
Investing activities
Net cash used in investing activities was $28.7 million for the nine months ended September 30, 2020, a decrease of $120.3 million, compared to net cash provided by investing activities of $91.6 million for the nine months ended September 30, 2019. This decrease was primarily the result of cash acquired from the Remedy Partners Acquisition of $136.0 million in 2019, partially offset by the acquisition of TAV Health in 2019 for $28.8 million. Capital expenditures for property and equipment were $13.0 million for the nine months ended September 30, 2020 compared to $7.1 million for the nine months ended September 30, 2019. The $5.9 million increase in capital expenditures for property and equipment was primarily driven by investments in certain
125
Table of Contents
facilities and other requirements to support the growth in the business. Capital expenditures for internal-use software development were $15.7 million for the nine months ended September 30, 2020 compared to $9.7 million for the nine months ended September 30, 2019. The $6.0 million increase in capital expenditures for internal-use software development was primarily driven by additional investments in our technology platforms to support future growth.
Net cash provided by investing activities was $82.9 million in 2019, an increase of $96.0 million, compared to net cash used in investing activities of $13.1 million in 2018. This increase was primarily the result of cash acquired from the Remedy Partners Acquisition of $136.0 million in 2019, partially offset by the acquisition of TAV Health for $28.8 million. Capital expenditures for property and equipment were $12.6 million in 2019 compared to $6.6 million in 2018. The $6.0 million increase in capital expenditures for property and equipment was primarily driven by the Remedy Partners Acquisition. Capital expenditures for internal-use software development were $12.9 million in 2019 compared to $6.5 million in 2018. The $6.4 million increase in capital expenditures for internal-use software development was primarily driven by the Remedy Partners Acquisition and additional investments in our technology platforms to support future growth.
Financing activities
Net cash provided by financing activities was $30.1 million for the nine months ended September 30, 2020, an increase of $120.7 million, compared to net cash used in financing activities of $90.6 million for the nine months ended September 30, 2019. The source of cash for the nine months ended September 30, 2020 was primarily driven by a net $77.0 million in proceeds from borrowings under the Revolving Credit Facility and $1.0 million in net income tax refunds received on behalf of New Remedy Corp. (“New Remedy”) partially offset by payment of contingent consideration of $38.2 million, tax distributions to members of Cure Aggregator, LLC of $8.1 million and scheduled principal payments on long-term debt under our Credit Agreement of $2.1 million. The use of cash for the nine months ended September 30, 2019 was primarily driven by an $83.8 million payment to the sellers of Remedy Partners in connection with the Remedy Partners Acquisition, tax distributions to members of Cure Aggregator, LLC of $22.5 million, tax payments on behalf of New Remedy of $7.4 million and scheduled principal payments on long-term debt under our Credit Agreement of $2.1 million. These uses of cash were partially offset by $20.0 million in proceeds from issuance of long-term debt, $5.0 million in proceeds from borrowings under the Revolving Credit Facility and $3.0 million in proceeds from a third-party investor to which new member units in Cure Aggregator, LLC were issued.
Net cash used in financing activities in 2019 was $94.8 million, an increase of $72.9 million, compared to $21.9 million in 2018. The use of cash in 2019 was primarily driven by an $83.8 million payment to the sellers of Remedy Partners in connection with the Remedy Partners Acquisition. Additionally, in 2019, we made tax distributions to members of Cure Aggregator, LLC of $22.5 million, tax payments on behalf of New Remedy of $5.1 million, repurchased certain member units from certain former employee investors for $3.1 million and made scheduled principal payments on long-term debt under our Credit Agreement of $2.8 million. These financing outflows were partially offset by proceeds of $20.0 million in incremental long-term debt under our Credit Agreement to fund the TAV Health acquisition and $3.0 million in proceeds from a third-party investor to which new member units in Cure Aggregator, LLC were issued. The use of cash in financing activities for the year ended December 31, 2018 was primarily driven by tax distributions made to members of $18.3 million, the repurchase of certain member units from certain former employee investors for $4.1 million and scheduled principal payments on long-term debt under our Credit Agreement of $2.0 million. These financing outflows in 2018 were partially offset by $3.0 million in proceeds from a third-party investor to which new member units in Cure Aggregator, LLC were issued.
Future sources and uses of liquidity
Our initial sources of liquidity will be (1) cash on hand, (2) net working capital, (3) cash flows from operations and (4) our Credit Agreement. Based on our current expectations, we believe that these sources of
126
Table of Contents
liquidity will be sufficient to fund our working capital requirements and to meet our commitments into the foreseeable future.
We expect that our primary liquidity needs will be comprised of cash to (1) provide capital to facilitate the organic growth of our business, (2) pay operating expenses, including cash compensation to our employees, (3) make payments under our Tax Receivable Agreement, (4) pay interest and principal due on borrowings under our Credit Agreement, (5) pay income taxes and (6) acquire businesses to help achieve our growth strategy.
Dividend policy
Assuming Cure TopCo, LLC makes distributions to its members in any given year, the determination to pay dividends, if any, to our Class A common stockholders out of the portion, if any, of such distributions remaining after our payment of taxes, Tax Receivable Agreement payments and expenses (any such portion, an “excess distribution”) will be made at the sole discretion of our Board of Directors. Our Board of Directors may change our dividend policy at any time. See “Dividend policy.”
Tax Receivable Agreement
Upon the completion of this offering, we will be a party to the Tax Receivable Agreement with the TRA Parties. Under the Tax Receivable Agreement, we generally will be required to pay to the TRA Parties 85% of the amount of cash savings, if any, in U.S. federal, state and local income tax that we actually realize as a result of (i) certain favorable tax attributes we will acquire from the Blocker Companies in the Mergers (including net operating losses, the Blocker Companies’ allocable share of existing tax basis and refunds of taxes attributable to pre-Merger tax periods), (ii) increases in our allocable share of existing tax basis and tax basis adjustments that may result from (x) future redemptions or exchanges of LLC Units by Continuing Pre-IPO LLC Members for cash or Class A common stock, (y) the IPO Contribution and (z) certain payments made under the Tax Receivable Agreement and (iii) deductions in respect of interest and certain compensatory payments made under the Tax Receivable Agreement. These payment obligations are our obligations and not obligations of Cure TopCo, LLC. Our obligations under the Tax Receivable Agreement will also apply with respect to any person who is issued LLC Units in the future and who becomes a party to the Tax Receivable Agreement.
The tax attributes available to us as a result of the Mergers and our allocable share of existing basis are expected to result in tax savings of approximately $56.3 million. We would be required to pay the TRA Parties approximately 85% of such amount, or $47.8 million, over the 15-year period from the date of the completion of this offering. Further, assuming no material changes in relevant tax law and that we earn sufficient taxable income to realize all tax benefits that are subject to the Tax Receivable Agreement, we expect that the tax savings associated with all tax attributes described above would aggregate to approximately $444.2 million over 15 years from the date of the completion of this offering, based on an assumed initial public offering price of $20.50 per share of Class A common stock, the midpoint of the estimated price range set forth on the cover page of this prospectus and assuming all future redemptions or exchanges would occur on the date of this offering. Under this scenario, we would be required to pay the TRA Parties approximately 85% of such amount, or $377.6 million, over the 15-year period from the date of the completion of this offering. The actual amounts we will be required to pay may materially differ from these hypothetical amounts, because potential future tax savings that we will be deemed to realize, and the Tax Receivable Agreement payments made by us, will be calculated based in part on the market value of our Class A common stock at the time of each redemption or exchange of an LLC Unit for cash or a share of Class A common stock and the prevailing applicable federal tax rate (plus the assumed combined state and local tax rate) applicable to us over the life of the Tax Receivable Agreement and will depend on our generating sufficient taxable income to realize the tax benefits that are subject to the Tax Receivable Agreement.
Customer Equity Appreciation Rights agreements
In each of December 2019 and September 2020, we entered into EAR agreements with one of our customers. Pursuant to the agreement, certain revenue targets are established for the customer to meet in the next
127
Table of Contents
three years. If they meet those targets, they retain the EAR. If they do not meet such targets, they forfeit all or a portion of the EAR. Each EAR agreement allows the customer to participate in the future growth in the fair market value of our equity and can only be settled in cash (or, under certain circumstances, in whole or in part with a replacement agreement containing substantially similar economic terms as the original EAR agreement) upon a change-in-control of us, other liquidity event, or upon approval of our Board of Directors with consent by New Mountain Capital with certain terms and conditions. Each EAR will expire in 20 years from the date of grant, if not previously settled.
Pursuant to the terms of the EAR agreements, the value of the EARs will be calculated as an amount equal to the non-forfeited portion of a defined percentage (3.5% in the case of the December 2019 EAR and 4.5% in the case of the September 2020 EAR) of the excess of (i) the aggregate fair market value of the Reference Equity (as defined below) as of the applicable date of determination over (ii) a base threshold equity value defined in each agreement. Pursuant to the terms of each agreement, the “Reference Equity” following this offering will be the Class A common stock of the Company and the aggregate fair market value of the Reference Equity will be determined by reference to the volume-weighted average trading price of the Company’s Class A common stock (assuming all of the holders of LLC Units redeemed or exchanged their LLC Units for a corresponding number of newly issued shares of Class A common stock) over a period of 30 calendar days. In addition, following this offering, the base threshold equity value set forth in each agreement will be increased by the aggregate offering price of this offering.
If a change in control occurs on or prior to December 20, 2020, in the case of the December 2019 EAR, or July 1, 2021, in the case of the September 2020 EAR, the manner in which the value of each EAR is calculated is subject to adjustment. As defined in each EAR, a change in control prior to an initial public offering will be deemed to have occurred if New Mountain Capital ceases to beneficially own, directly or indirectly, at least a majority of the total voting power of Signify Health, LLC (f/k/a Cure Borrower, LLC) or ceases to have the right, directly or indirectly, to elect or designate for election at least a majority of the board of directors of Signify Health, LLC. Following an initial public offering, a change in control will be deemed to have occurred if any person or group of persons other than New Mountain Capital shall beneficially own 35% or more of the total voting power of Signify Health, LLC or New Mountain Capital ceases to have the right, directly or indirectly, to elect or designate for election at least a majority of the board of directors of Signify Health, LLC. New Mountain Capital will continue to hold a majority of our total voting power and continue to have the right, both by voting power and contractually, to designate for election at least a majority of the board of directors of Signify Health, LLC following the Reorganization Transactions and this offering, and as a result, the Reorganization Transactions and this offering are not expected to affect the EAR agreements or impact the manner in which the value of each EAR is calculated except as set forth above.
As of September 30, 2020, cash settlement was not considered probable, due to the change in control and liquidity provisions of each EAR. The grant date fair value of the December 2019 customer EAR was estimated to be $15.2 million and is being recorded as a reduction of revenue through December 31, 2022, coinciding with the three-year performance period. The grant date fair value of the September 2020 customer EAR was estimated to be $36.6 million and is being recorded as a reduction of revenue through December 31, 2022, coinciding with the 2.5-year performance period. As of September 30, 2020, the fair market value of the outstanding EAR agreements was approximately $79.7 million.
Non-GAAP financial measures
In this prospectus, we used Adjusted EBITDA and Adjusted EBITDA Margin. Adjusted EBITDA and Adjusted EBITDA Margin are not measures of financial performance under GAAP and should not be considered substitutes for GAAP measures, including net loss, which we consider to be the most directly comparable GAAP measure. Adjusted EBITDA and Adjusted EBITDA Margin have limitations as analytical tools, and when assessing our operating performance, you should not consider these non-GAAP financial measures in isolation or as substitutes for net loss or other consolidated income statement data prepared in accordance with GAAP. Other
128
Table of Contents
companies may calculate Adjusted EBITDA and Adjusted EBITDA Margin differently than we do, limiting its usefulness as a comparative measure. For more information on the use of non-GAAP financial information, including a reconciliation of Adjusted EBITDA and Adjusted EBITDA Margin to net income, as applicable, see “Prospectus summary—Summary combined-consolidated financial and other data.”
We define Adjusted EBITDA as net income (loss) before interest expense, income tax expense, depreciation and amortization and certain items of income and expense, including asset impairment, other (income) expense, net, transaction-related expenses, equity-based compensation, remeasurement of contingent consideration, management fees and non-recurring expenses. We believe that Adjusted EBITDA provides a useful measure to investors to assess our operating performance because it eliminates the impact of expenses that do not relate to ongoing business performance, and that the presentation of this measure enhances an investor’s understanding of the performance of our business.
Adjusted EBITDA increased by $14.2 million, or 18.0%, to $93.3 million for 2019 from $79.1 million for 2018. Adjusted EBITDA increased by $19.3 million, or 28.8%, to $86.0 million for the nine months ended September 30, 2020 from $66.7 million for the nine months ended September 30, 2019.
We define Adjusted EBITDA Margin as Adjusted EBITDA divided by revenue. We believe that Adjusted EBITDA Margin is helpful to investors in measuring the profitability of our operations on a consolidated level.
Adjusted EBITDA Margin decreased by 482 basis points to 18.6% for 2019 from 23.4% for 2018. Adjusted EBITDA Margin increased by 250 basis points to 20.6% for the nine months ended September 30, 2020 from 18.1% for the nine months ended September 30, 2019.
Contractual obligations and commitments
The following table presents information relating to our contractual obligations as of December 31, 2019. There were no material changes outside the ordinary course of business to our outstanding contractual obligations as of September 30, 2020, except as noted below.
| Contractual Obligations |
Total | Less than 1 year |
1-3 years | 3-5 years | More than 5 years |
|||||||||||||||
| (in millions) | ||||||||||||||||||||
| Operating lease obligations(1) |
49.8 | 7.0 | 15.0 | 9.9 | 17.9 | |||||||||||||||
| Credit agreement(2) |
357.4 | 20.4 | 40.3 | 296.7 | — | |||||||||||||||
| Contingent consideration(3) |
40.0 | — | 40.0 | — | — | |||||||||||||||
| Purchase obligations(4) |
15.7 | 10.6 | 4.5 | 0.6 | — | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total |
462.9 | 38.0 | 99.8 | 307.2 | 17.9 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| (1) | Represents amounts due under existing operating leases related to our offices and other facilities. |
| (2) | Includes $82.1 million of interest based on interest rates in place and the amounts outstanding as of December 31, 2019. Actual payments may differ as the interest rates under our Credit Agreement are variable. |
| (3) | Represents amount due to former sellers of Censeo Health, an entity we acquired in 2017. |
| (4) | Represents noncancelable commitments for the purchase of software, goods and services. |
During the second quarter of 2020, we ceased using certain office space in New York, New York and in the third quarter began subleasing the space. We have entered into non-cancelable lease agreements for new space in New York, New York that ultimately expire in 2029. Total lease commitments over the term of the lease agreements are approximately $25.7 million.
129
Table of Contents
On December 21, 2017, we acquired 100% of the outstanding equity of Censeo Health. The purchase price included contingent consideration with an initial fair value of $38.2 million, which required us to pay up to an additional $40.0 million to selling shareholders of Censeo Health, pending the resolution of an examination by the IRS regarding the classification of certain independent contractors. In May 2020, we received the final IRS determination letter closing the open matter related to the contingent consideration and as a result of the determination, the contingent consideration was payable in full. We made payment of the full $40.0 million on July 31, 2020 to the selling shareholders.
In November 2020, we entered into the 2020 November Incremental Term Loans under our Credit Agreement for a total of $125.0 million, due in December 2024.
In December 2020, we entered into the 2020 December Incremental Term Loans under our Credit Agreement for a total of $15.0 million, due in December 2024.
As of December 31, 2019 and September 30, 2020, cash settlement was not considered probable, due to the change in control and liquidity provisions of the EARs, and therefore an amount related to this commitment is not included in the above table.
Off-balance sheet arrangements
Except for operating leases and certain letters of credit entered into in the normal course of business, we do not have any off-balance sheet arrangements that have or are reasonably likely to have a current or future effect on our financial condition, changes in financial condition, revenue or expenses, results of operations, liquidity, capital expenditures or capital resources that is material to investors.
Quantitative and qualitative disclosures about market risks
In the ordinary course of our business activities, we are exposed to market risks that are beyond our control and which may have an adverse effect on the value of our financial assets and liabilities, future cash flows and earnings. The market risks that we are exposed to primarily relate to changes in interest rates associated with our long-term debt obligations and cash and cash equivalents.
At September 30, 2020, we had total variable rate debt outstanding under our Credit Agreement of $350.2 million. If the effective interest rate of our variable rate debt outstanding as of September 30, 2020 were to increase by 100 basis points (1%), our annual interest expense would increase by approximately $3.5 million.
At September 30, 2020, our total cash and cash equivalents were $87.9 million. Throughout the year, we invest any excess cash in short-term investments, primarily money market accounts, where returns effectively reflect current interest rates. As a result, market interest rate changes may impact our interest income. The impact will depend on variables such as the magnitude of rate changes and the level of excess cash balances. We do not consider this risk to be material. We manage such risk by continuing to evaluate the best investment rates available for short-term, high-quality investments.
Critical accounting policies
The discussion and analysis of our financial condition and results of operations is based upon our consolidated financial statements, which have been prepared in accordance with GAAP. The preparation of our financial statements requires us to make judgments, estimates and assumptions that affect the reported amounts of assets, liabilities, income and expenses and related disclosures of contingent assets and liabilities. We base these estimates on our historical experience and various other assumptions that we believe to be reasonable under the circumstances. Actual results experienced may vary materially and adversely from our estimates. Revisions to estimates are recognized prospectively. We believe the following critical accounting policies could potentially
130
Table of Contents
produce materially different results if we were to change underlying assumptions, estimates or judgments. See Note 3, “Significant Accounting Policies” to our combined-consolidated financial statements included elsewhere in this prospectus for a summary of our significant accounting policies.
Revenue recognition
We recognize revenue as the control of promised services is transferred to our customers and we generate all of our revenue from contracts with customers. The amount of revenue recognized reflects the consideration to which we expect to be entitled in exchange for these services. The measurement and recognition of revenue requires us to make certain judgments and estimates.
Effective January 1, 2019, we adopted the new accounting standard Accounting Standards Codification Topic 606, Revenue from Contracts with Customers (Topic 606), under the modified retrospective method. Under the modified retrospective method, we were not required to restate comparative financial information prior to the adoption of this standard and, therefore, such information presented prior to January 1, 2019 continues to be reported under our previous accounting policies.
We apply the five-step model to recognize revenue from customer contracts. The five-step model requires us to (i) identify the contract with the customer, (ii) identify the performance obligations in the contract, (iii) determine the transaction price, including variable consideration to the extent that it is probable that a significant future reversal will not occur, (iv) allocate the transaction price to the respective performance obligations in the contract, and (v) recognize revenue when, or as, we satisfy the performance obligation.
The unit of measure for revenue recognition is a performance obligation, which is a promise in a contract to transfer a distinct or series of distinct goods or services to the customer. A contract’s transaction price is allocated to each distinct performance obligation and recognized as revenue when, or as, the performance obligation is satisfied. We satisfy substantially all of our performance obligations, which generally are related to a series of distinct services as described below, and recognize revenue over time instead of at a point in time.
Our customer contracts have either (1) a single performance obligation as the promise to transfer services is not separately identifiable from other promises in the contracts and is, therefore, not distinct; (2) a series of distinct performance obligations; or (3) multiple performance obligations, most commonly due to the contract covering multiple service offerings. For contracts with multiple performance obligations, the contract’s transaction price is allocated to each performance obligation on the basis of the relative standalone selling price of each distinct service in the contract.
Home & Community Services
In our Home & Community Services segment, revenue is recognized when the IHEs are submitted to our customers on a daily basis. Submission to the customer occurs after the IHEs are completed and coded, a process which may take one to several days after completion of the evaluation. The pricing for the IHEs is generally based on a fixed transaction fee, which is directly linked to the usage of the service by the customer during a distinct service period. Customers are invoiced for evaluations performed each month and remit payment accordingly. The IHEs are recognized as a single performance obligation which qualify for point-in-time revenue recognition since the customer simultaneously receives and consumes the benefits provided daily as we perform.
The transaction price for certain of our IHEs is reduced by the grant date fair value of outstanding customer EARs. See “—Critical accounting policies—Customer Equity Appreciation Rights.”
The remaining sources of revenue in our Home & Community Services segment, which relate to ancillary diagnostic and evaluative services we provide, are recognized over time as the performance obligations are satisfied and are primarily based on a fixed fee. Therefore, they do not require estimates and assumptions by management. See Note 5, “Revenue Recognition” to our combined-consolidated financial statements included elsewhere in this prospectus for further details regarding revenue recognition policies.
131
Table of Contents
Episodes of Care Services
The episodes solutions we provide in our Episodes of Care Services segment are an integrated set of services which represent a single performance obligation in the form of a series of distinct services. This performance obligation is satisfied over time as the various services are delivered. We primarily offer these services to customers under the BPCI-A program.
Under the BPCI-A program, we recognize the revenue attributable to episodes reconciled during each six-month episode performance measurement period over a 13-month performance obligation period that commences in the second or fourth quarter of each year, depending on the relevant contract with our provider partners. The 13-month performance obligation period begins at the start of the relevant episodes of care and extends through the receipt or generation of the semiannual reconciliation for the relevant performance measurement period, as well as the provision and explanation of statements of performance to each of our customers. The transaction price is 100% variable and therefore we estimate an amount in which we expect to be entitled to receive for each six-month episode performance measurement period over a 13-month performance obligation period.
For each partner agreement, the fees are generally twofold, an administrative fee, which is based on a stated percentage of program size and is paid out of savings, and a defined share of program savings or losses, if any. In order to estimate this variable consideration, management estimates the expected program size as well as the expected savings rate for each six-month period of episodes of care. The estimate is performed both at the onset of each performance measurement period based on information available at the time and at the end of each reporting period. In making the estimate, we consider inputs such as the overall program size which is defined by the historic cost multiplied by the frequency of occurrence of defined episodes of care. Additionally, we estimate savings rates by using data sources such as historical trend analysis together with indicative data of the current volume of episodes.
We adjust our estimates at the end of each six-month performance measurement period, generally in the second and fourth quarter each year, and may further adjust at the end of each reporting period to the extent new information indicates a change is needed. We apply a constraint to the variable consideration estimate in circumstances where we believe the claims data received is incomplete or inconsistent, so as not to have the estimates result in a significant revenue reversal in future periods. Although our estimates are based on the information available to us at each reporting date, several factors may cause actual revenue earned to differ from the estimates recorded each period. These include, among others, limited historical experience as the current BPCI-A program only commenced in the fourth quarter of 2018, CMS-imposed restrictions on the definition of episodes and benchmark prices, healthcare provider participation, the impacts of the COVID-19 pandemic in 2020 and other limitations of the program beyond our control.
The remaining sources of revenue in our Episodes of Care Services segment are recognized over time when, or as, the performance obligations are satisfied and are primarily based on a fixed fee or per member per month fee. Therefore, they do not require significant estimates and assumptions by management. See Note 5, “Revenue Recognition” to our combined-consolidated financial statements included elsewhere in this prospectus for further details regarding revenue recognition policies.
Allowance for doubtful accounts
We continuously monitor collections and payments from our customers. We maintain an allowance for doubtful accounts based on the best facts available to management. We consider historical realization data, accounts receivable aging trends and other operational trends to estimate the collectability of receivables. After all reasonable attempts are made to collect a receivable, the receivable is written off against the allowance for doubtful accounts. As of September 30, 2020, we had an allowance for doubtful accounts of $5.1 million, which represented 3.5% of total accounts receivable, net. We continue to assess our receivable portfolio and collections in light of the current economic environment and its impact on our estimation of the adequacy of the allowance for doubtful accounts.
132
Table of Contents
Equity-based compensation
Equity-based compensation represents the cost related to equity-based awards granted to employees and non-employee directors. These awards are intended to be profits interest units for federal income tax purposes. The profits interest units have time-based and performance-based vesting criteria. We recognize equity-based compensation for all equity-based awards based on the grant date fair value of the award. Forfeitures are recorded as they occur.
Awards with time-based vesting generally vest over time, with a portion of the awards vesting on the grant date anniversary and other awards vesting on December 31 of each year. The resulting compensation expense related to time-based service awards is recognized on a straight-line basis over the requisite service period and is included within SG&A expense or service expense in the accompanying combined-consolidated statements of operations based on the role of the grantee. For those awards with performance-based vesting, the total cash on cash return of the private equity owners as defined in the award agreement must exceed certain multiples set forth in the award agreement in order to vest, and is also generally dependent upon the participant’s continued employment. The criteria associated with the performance-vesting criteria has not been probable to date. As such, we have not recorded any equity-based compensation expense related to the equity-based awards that are subject to performance-based vesting criteria.
Grant date fair value of the profits interest units is calculated based on a Monte Carlo option pricing simulation. Our total equity value represents a key input for determining the fair value of the underlying common units. A discount for lack of marketability is applied to the per unit fair value to reflect increased risk arising from the inability to readily sell our common units.
In order to estimate the fair value of our common units, we used a combination of the market approach and the income approach. We used a combination of these standard valuation techniques rather than picking just one overall approach, as we believe that the market approach on its own provides a less reliable evaluation of the fair value than an income approach because such an approach relies solely on data and trends of companies in similar market segments with similar characteristics. By contrast, the income approach incorporates management’s best estimates of future performance based on both company and industry-specific factors and incorporates management’s long-term strategy for positioning and operating the business.
For the market approach, we utilized the guideline company method by selecting certain companies that we considered to be the most comparable to us in terms of size, growth, profitability, risk and return on investment, among others. We then used these guideline companies to develop relevant market multiples and ratios. The market multiples and ratios were applied to our financial projections based on assumptions at the time of the valuation in order to estimate our total enterprise value. Since there is not an active market for our common units, a discount for lack of marketability was then applied to the resulting value.
For the income approach, we performed discounted cash flow analyses utilizing projected cash flows, which were discounted to the present value in order to arrive at an enterprise value. The key assumptions used in the income approach include management’s financial projections which are based on highly subjective assumptions as of the date of valuation, a discount rate, and a long-term growth rate.
The Monte Carlo simulation also requires additional inputs to estimate the grant date fair value of an award, including an assumption for expected volatility, expected dividend yield, risk-free rate and an expected life. Since we are privately held, we calculate expected volatility using comparable peer companies with publicly traded shares over a term similar to the expected term of the underlying award. At the time of grant, we had no intention to pay dividends on our common units, and therefore, the dividend yield percentage is zero. The risk-free interest rate is based on the U.S. Treasury constant maturity interest rate whose term is consistent with the expected life of the profits interests. Profits interest awards granted during the years ended December 31, 2019
133
Table of Contents
and 2018 and the nine months ended September 30, 2020 and 2019 included the following weighted average assumptions (annualized percentages):
| Year Ended December 31, | Nine Months Ended September 30, | |||||||||||||||
| 2019 | 2018 | 2020 | 2019 | |||||||||||||
| Expected volatility |
40.6% – 50.6 | % | 48.8% – 58.8 | % | 41.5% | 41.1% – 51.1 | % | |||||||||
| Expected dividend yield |
— | — | — | — | ||||||||||||
| Risk-free interest rate |
1.8 | % | 2.6 | % | 1.3 | % | 1.9 | % | ||||||||
| Expected life (years) |
3.5 | 4.6 | 2.9 | 3.6 | ||||||||||||
In addition, Remedy Partners historically maintained an equity incentive plan whereby certain employees and directors were granted stock options. In November 2019, at the conclusion of the Remedy Partners Acquisition, outstanding Remedy Partners stock options were converted to stock options in New Remedy. No additional stock option grants will be made following the Remedy Partners Acquisition. The grant date fair value of the outstanding stock options was estimated using a Black-Scholes option-pricing model, which requires the input of subjective assumptions, including estimated share price, volatility over the expected term of the awards, expected term, risk free interest rate and expected dividends, as described above. Expected volatility, expected dividend yield and risk-free interest rate were all calculated in similar ways for the Remedy Partners stock options as described above for the valuation of the profits interests. The expected term of the stock options represents the period the stock options are expected to be outstanding. We used the simplified method for estimating the expected term of the stock options. We continue to record equity-based compensation expense related to outstanding Remedy Partners stock options over the remaining vesting periods, to the extent the former Remedy Partners employees who received the stock option grants remain our employees.
Customer Equity Appreciation Rights
In December 2019 and September 2020, we entered into EAR agreements with one of our customers. See “—Liquidity and capital resources—Customer Equity Appreciation Rights agreements.” Although the initial EAR agreement was executed in December 2019, the service period did not begin until 2020 and, therefore, there was no impact on our results of operations until 2020.
The initial grant date fair value of the EARs are estimated in a similar manner, subject to the same management assumptions, as described for equity-based compensation as the EARs are a form of equity-based award. However, since the EARs are granted to a customer, they are also subject to accounting guidance for revenue recognition. Accordingly, their initial grant date fair values are recorded as a reduction to the transaction price over the service period for the associated customer’s IHE services. Forfeitures, if any, as a result of annual purchase commitments not being met, will be recognized as revenue in the period the forfeiture occurs.
As the awards will ultimately be settled in cash, they are classified as noncurrent liabilities with estimated changes in fair market value recorded each accounting period based on current management assumptions related to the valuation approaches described for equity-based compensation above. These changes in fair market value are recorded in other expense (income), net on the combined-consolidated statement of operations.
Business combinations
We account for business combinations under the acquisition method of accounting, which requires the acquiring entity in a business combination to recognize the fair value of all assets acquired, liabilities assumed and any noncontrolling interest in the acquiree, and establishes the acquisition date as the fair value measurement point. Accordingly, we recognize assets acquired and liabilities assumed in business combinations, including contingent assets and liabilities and noncontrolling interests in the acquiree, based on fair value estimates as of the date of acquisition.
134
Table of Contents
Discounted cash flow models are typically used in these valuations if quoted market prices are not available, and the models require the use of significant estimates and assumptions including, but not limited to (1) estimating future revenue, expenses and cash flows expected to be collected; and (2) developing appropriate discount rates, long-term growth rates and probability rates. Our estimates of fair value are based upon assumptions believed to be reasonable, but we recognize that the assumptions are inherently uncertain.
We recognize and measure goodwill, if any, as of the acquisition date, as the excess of the fair value of the consideration paid over the fair value of the identified net assets acquired. The primary drivers that generate goodwill are the value of synergies with our existing operations, ability to grow in the market, and estimates of market share at the date of purchase. Goodwill recorded in an acquisition is assigned to applicable reporting units based on expected revenues or expected cash flows. Identifiable intangible assets with finite lives are amortized over their useful lives.
Pushdown accounting establishes a new basis for the assets and liabilities of an acquired company based on a “pushdown” of the acquirer’s stepped-up basis to the acquired company in connection with a change-in-control event. We elected to apply pushdown accounting in the reporting period in which the change-in-control event occurred as it relates to the January 2019 acquisition of Remedy Partners. The decision to apply pushdown accounting is irrevocable. The election of pushdown accounting required the recognition of the new basis of accounting established for the individual assets and liabilities of Remedy Partners as of the date New Mountain Capital acquired Remedy Partners. Goodwill was calculated and recognized consistent with business combination accounting, resulting in the pushdown of $408.4 million in goodwill as of December 31, 2019.
Acquisition-related contingent consideration is initially measured and recorded at its estimated fair value as an element of consideration paid in connection with an acquisition. Subsequent adjustments are recognized in SG&A expense in the combined-consolidated Statements of Operations. We determine the fair value of acquisition-related contingent consideration, and any subsequent changes in fair value using a discounted probability-weighted approach. This approach takes into consideration certain Level 3 unobservable inputs. These unobservable inputs include probability assessments of expected future cash flows over the period in which the obligation is expected to be settled and applies a discount factor that captures the uncertainties associated with the obligation. Acquisition-related contingent consideration as of December 31, 2019 was $39.8 million, related to an acquisition made in 2017. This contingent consideration was paid in full for $40.0 million in July 2020.
Recoverability of goodwill, intangible assets, and other long-lived assets subject to amortization
Goodwill is an asset which represents the future economic benefits which arise from the excess of the purchase price over the fair value of acquired net assets in a business combination, including the amount assigned to identifiable intangible assets. Goodwill is not amortized, but rather is tested for impairment annually, or more frequently whenever there are triggering events or changes in circumstances which indicate that the carrying value of the asset may not be recoverable and an impairment loss may have been incurred. As of December 31, 2019, we had goodwill of approximately $578.8 million, which represented 42% of our consolidated total assets. As of September 30, 2020, we had goodwill of approximately $578.8 million, which represented 39% of our consolidated total assets.
We assess goodwill for impairment at least annually, during the fourth quarter, and more frequently if indicators of impairment exist. Impairment testing for goodwill is performed at the reporting unit level. A reporting unit is an operating segment or one level below an operating segment if the component constitutes a business for which discrete financial information is available, and management regularly reviews the operating results of that component. Our reporting units are the same as our reportable segments, Home & Community Services and Episodes of Care Services.
We perform an assessment of goodwill utilizing either a qualitative or quantitative impairment test. The qualitative impairment test assesses several factors to determine whether it is more likely than not that the fair
135
Table of Contents
value of a reporting unit is less than its carrying amount. If management concludes it is more likely than not that the fair value of the entity is less than its carrying amount, a quantitative fair value test is performed.
In a quantitative impairment test, management assesses goodwill by comparing the carrying amount of each reporting unit to its fair value. We estimate the fair value of each of our reporting units using either an income approach, a market valuation approach, a transaction valuation approach or a blended approach.
If the fair value exceeds the carrying value of a reporting unit, goodwill is not considered impaired. If the carrying value of a reporting unit exceeds its fair value, goodwill is considered impaired and we would recognize an impairment loss equal to the excess of a reporting unit’s carrying amount over its fair value, not to exceed the total amount of goodwill allocated to the reporting unit.
We perform discounted cash flow analyses which utilize projected cash flows as well as a residual value, which is discounted to the present value in order to arrive at a reporting unit fair value. The determination of whether or not goodwill has become impaired involves a significant level of judgment in the assumptions and estimates underlying the approach used to determine the value of our reporting units. Actual results could differ from management’s estimates, and such differences could be material to our combined-consolidated financial position and results of operations. See “Risk factors.”
We performed a qualitative assessment in 2019 for our Home & Community Services reporting unit and concluded it was not more likely than not that the reporting unit’s fair value was less than its carrying amount. We performed a quantitative assessment for our Episodes of Care Services reporting unit in 2019, the year we formed this segment through the Remedy Partners Acquisition. Given the significant excess of the estimated fair value over the carrying value for this reporting unit, we do not believe an inconsequential change in the underlying assumptions would have a significant impact on the results and result in a goodwill impairment. However, if there are any unfavorable changes in growth assumptions, particularly related to the impact of the COVID-19 pandemic, if growth related to new product lines does not materialize over time or if the long-term construct of the BPCI-A program or any successor program is materially changed, this could lead to a potential failure in the goodwill impairment testing process in future periods.
We review the carrying value of other long-lived assets or groups of assets, including property and equipment, internally developed software costs and other intangible assets, to be used in operations whenever events or changes in circumstances indicate that the carrying amount of the assets may not be recoverable.
Intangible assets with definite lives subject to amortization include customer relationships, acquired and capitalized software and trade names. Acquired intangible assets are initially recorded at fair value and are amortized on a basis consistent with the timing and pattern of expected cash flows used to value the intangible asset, generally on a straight-line basis over the estimated useful life. Capitalized software is recorded for certain costs incurred for the development of internal-use software. These costs are amortized on a straight-line basis over the expected economic life of the software.
We assess the recoverability of an asset or group of assets by determining whether the carrying value of the asset or group of assets exceeds the sum of the projected undiscounted cash flows expected to result from the use and eventual disposition of the assets over the remaining economic life of the asset or the primary asset in the group of assets. If such testing indicates the carrying value of the asset or group of assets is not recoverable, we estimate the fair value of the asset or group of assets using various valuation methodologies, including discounted cash flow models and quoted market values, as necessary. If the fair value of those assets or groups of assets is less than carrying value, we record an impairment loss equal to the excess of the carrying value over the estimated fair value.
There was no impairment of property and equipment during the year ended December 31, 2019. We incurred an asset impairment charge of $1.0 million on property and equipment that was no longer being used for
136
Table of Contents
the year ended December 31, 2018. This expense is included in asset impairment on the combined-consolidated Statements of Operations. We recorded an asset impairment charge of $4.9 million on a trade name during the year ended December 31, 2019 as a result of the discontinued use of certain trade names due to our rebranding which was announced in December 2019. We also recorded an asset impairment charge of $1.5 million related to certain acquired and capitalized software during the year ended December 31, 2019 as a result of the discontinued use of the software. We recorded an asset impairment charge of $16.0 million on trade names during the year ended December 31, 2018 as a result of the discontinued use of certain trade names due to our rebranding in 2018.
We did not incur any significant asset impairment charges during the nine months ended September 30, 2020.
Recent accounting pronouncements
Below, we include a description of certain recent accounting pronouncements that may have an impact on our financial statements. See Note 3 to our combined-consolidated financial statements included elsewhere in this prospectus for further information.
In May 2014, FASB issued Accounting Standards Update (“ASU”) 2014-09, Revenue from Contracts with Customers. The new revenue recognition standard provides a five-step model to determine when and how revenue is recognized. The core principle is that a company should recognize revenue to depict the transfer of promised goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled in exchange for those goods or services. This guidance was effective for nonpublic companies for annual periods beginning after December 15, 2018 and is applied either retrospectively to each period presented or as a cumulative-effect adjustment as of the date of adoption. We used the modified retrospective method to adopt the new revenue recognition guidance on January 1, 2019. Adoption of the new standard did not have a material impact to our revenue recognition, with approximately $0.2 million recognized as a cumulative impact increase in accumulated deficit upon adoption. Remedy Partners adopted this new accounting guidance effective January 1, 2019, prior to our acquisition of Remedy Partners and its inclusion in our combined-consolidated financial statements. This new guidance did have a material impact on the timing of revenue recognition for Remedy Partners.
In November 2019, the FASB issued ASU 2019-08, Compensation—Stock Compensation (Topic 718) and Revenue from Contracts with Customers (Topic 606): Codification Improvements—Share-Based Consideration Payable to a Customer (“ASU 2019-08”). ASU 2019-08 requires that an entity measure and classify share-based payment awards granted to a customer by applying the guidance in Topic 718. The amount recorded as a reduction of the transaction price is required to be measured on the basis of the grant-date fair value of the share-based payment award in accordance with Topic 718. The grant date is the date at which a grantor (supplier) and a grantee (customer) reach a mutual understanding of the key terms and conditions of a share-based payment award. ASU 2019-08 is effective for fiscal years beginning after December 15, 2019, and interim periods within fiscal years beginning after December 15, 2020. We elected to early adopt this new guidance for interim periods in 2020 as it relates to the customer EARs. The initial grant date fair value of the EAR agreements is being recorded as a reduction of the transaction price.
In February 2016, the FASB issued ASU 2016-02, Leases (Topic 842). The new lease standard requires lessees to recognize leases on the balance sheet by recording a right-of-use asset and lease liability. This guidance is effective for nonpublic entities for annual reporting periods beginning after December 15, 2021. Early adoption is permitted. We are evaluating the impact of this new guidance on our financial statements.
In June 2016, the FASB issued ASU 2016-13, Financial Instruments – Credit Losses (Topic 326) (“ASU 2016-13”). ASU 2016-13 introduces the current expected credit losses methodology for estimating allowances for credit losses. ASU 2016-13 applies to all financial instruments carried at amortized cost and off-balance-sheet
137
Table of Contents
credit exposures not accounted for as insurance, including loan commitments, standby letters of credit, and financial guarantees. The new accounting standard does not apply to trading assets, loans held for sale, financial assets for which the fair value option has been elected, or loans and receivables between entities under common control. ASU 2016-13 is effective for nonpublic entities for fiscal years beginning after December 15, 2022, including interim periods within those fiscal years. Early adoption is permitted. We are evaluating the impact of this new guidance on our financial statements.
Emerging growth company status
Pursuant to the JOBS Act, an emerging growth company is provided the option to adopt new or revised accounting standards that may be issued by FASB or the SEC either (i) within the same periods as those otherwise applicable to non-emerging growth companies or (ii) within the same time periods as private companies. We intend to take advantage of the exemption for complying with new or revised accounting standards within the same time periods as private companies. Accordingly, the information contained herein may be different than the information you receive from other public companies.
We also intend take advantage of some of the reduced regulatory and reporting requirements of emerging growth companies pursuant to the JOBS Act so long as we qualify as an emerging growth company, including, but not limited to, not being required to comply with the auditor attestation requirements of Section 404(b) of the Sarbanes-Oxley Act, reduced disclosure obligations regarding executive compensation and exemptions from the requirements of holding non-binding advisory votes on executive compensation and golden parachute payments.
138
Table of Contents
Our company
Signify Health is a leading healthcare platform that leverages advanced analytics, technology, and nationwide healthcare provider networks to create and power value-based payment programs. Our mission is to transform how care is paid for and delivered so that people can enjoy more healthy, happy days at home. Our customers include health plans, governments, employers, health systems and physician groups. We believe that we are a market leader in two fast-growing segments of the value-based healthcare payment industry: payment models based on individual episodes of care and in-home health evaluations (“IHEs”). Payment models based on individual episodes of care organize or bundle payments for all, or a substantial portion of, services received by a patient in connection with an episode of care, such as a surgical procedure, particular condition or other reason for a hospital stay. IHEs are health evaluations performed by a clinician in the home to support payors’ participation in Medicare Advantage and other government-run managed care plans. Our episode payment platform managed $6.1 billion of spend under the Medicare Bundled Payment for Care Improvement Advanced (“BPCI-A”) program in 2019, and the BPCI-A episodes we managed which were initiated in the last quarter of 2019 resulted in approximately 15% greater discharges home from acute-care facilities and approximately 10% lower readmissions when compared to the historical performance of our provider partners for similar episodes. Our mobile network of providers entered over 1 million unique homes to evaluate individuals in Medicare Advantage and other managed care plans in 2019. We believe that these core businesses have enabled us to become integral to how health plans and healthcare providers successfully participate in value-based payment programs, and that our platform lessens the dependence on facility-centric care for acute and post-acute services and shifts more services towards alternate sites and, most importantly, the home.
Value-based payment programs are rapidly transforming how governments, employers, and health plans pay for and manage healthcare services. The objective of these initiatives is to improve patient outcomes while lowering the overall cost of healthcare services. We believe that our differentiated data assets, proprietary analytics capabilities, comprehensive cloud-based software platforms, and healthcare provider networks enable success in the two dominant forms of value-based payments: population-based payment programs and episode-based payment programs. Medicare Advantage is one of the largest population-based payment initiatives and the Medicare Bundled Payment for Care Improvement (“BPCI”) initiative is one of the largest episode-based payment programs. We have leading positions serving both of these fast-growing sectors, as measured by our volume of IHEs and the program size of our episodes business, respectively.
Our solutions support value-based payment programs by aligning financial incentives around outcomes, providing tools to health plans and healthcare organizations designed to assess and manage risk and identify actionable opportunities for improved patient outcomes, coordination and cost-savings. Through our platform, we coordinate what we believe is a holistic suite of clinical, social, and behavioral services to address an individual’s healthcare needs and prevent adverse events that drive excess cost. Our business model is aligned with our customers as we generate revenue only when we successfully engage members for our health plan customers and generate savings for our provider customers.
We serve 47 Medicare Advantage health plans ranging from the largest national organizations to smaller regional and provider-owned entities. We also serve thousands of healthcare provider organizations ranging from large integrated delivery systems to midsize and small urban and rural entities. We also serve large biopharmaceutical customers.
We believe we deliver a powerful value proposition to our health plan and provider customers and their members and patients by leveraging the following core assets:
| • | Insights to improve patient outcomes and lower costs. We build our software and services around the specific levers in each clinical episode that we believe have the most influence on patient outcomes and cost. This requires clinical expertise in disease progression and therapeutic interventions and the ability |
139
Table of Contents
| to identify factors that can be influenced during a patient’s episode of care. It also involves extensive data analytics to measure variations in treatment that can be influenced through more transparency and effective decision support. We believe this focus on critical levers has led to measurable outcomes, such as reductions in avoidable complications, reduced readmissions, reduced use of acute and post-acute facility services and increased delivery of services in the home, all of which benefit patients, while also lowering costs and generating savings for our health plan and healthcare provider customers. |
| • | Data analytics and reporting across the continuum. Our data analytics capabilities are focused on delivering decision support to all parties engaged in a value-based payment arrangement. Our platform analyzes data from a variety of sources that are designed to capture the patient’s condition not only from their visits to facility-based settings, but also from evaluations in the home and social services in their community. These sources include electronic health record (“EHR”) data in real time; claims and member data from private health plans, employers and the Centers for Medicare and Medicaid Services (“CMS”); care plan and case management data; data from comprehensive IHEs and device diagnostic data; laboratory and pharmacy data; and social determinants of health (“SDOH”) data. We use elements of this data to create longitudinal records of a patient’s health journey or to manage their care in an episode of care or other value-based payment arrangement, and to support our efforts to build decision support algorithms and predictive modeling tools. These data assets and decision support tools are designed to in turn help our providers efficiently and effectively deploy their resources and succeed in value-based payment programs. |
| • | National networks of healthcare providers. Our networks operate throughout the country, in both urban and rural locations, and encompass thousands of highly skilled medical professionals. We have three types of healthcare provider networks: |
| • | A flexible and mobile network of nearly 9,000 credentialed providers who are primarily deployed in an individual’s home and in post-acute facilities to collect critical patient data, assess an individual’s health status and coordinate care through our IHEs; |
| • | A nationwide network of hospitals and physicians that includes 3,500 value-based provider sites that are participating in payment programs run by the federal Medicare program, health plans, employers and other payors; and |
| • | A curated network of 200 community-based organizations (“CBOs”) and 200 clinical and social care coordinators that we connect to individuals and healthcare providers to meet individual member and patient needs. |
| • | Consumer engagement capabilities. Our proprietary, cloud-based technology platform, which was purpose-built for value-based payment programs, has a large array of engagement solutions intended to drive deeper and more meaningful engagement with the individuals we reach. We use advanced targeting and analytics, predictive models and our significant data assets to deploy a multi-modal approach to identifying and engaging individuals who may benefit from our services. We deploy email, SMS text messages, telephone outreach and digital-marketing campaigns to help us effectively engage individuals across the numerous value-based payment programs we support. |
| • | Innovative health benefit designs. We strive to drive transformation in how governments, health plans and employers pay for healthcare, and to facilitate healthcare organizations’ success under new programs that transfer risk and reward from health plans to providers. We work with governments, health plans and large employers to integrate episode-based program features into the health insurance plans they offer. We believe our ability to support numerous value-based payment arrangements and, importantly, to design and launch episode-based programs differentiates us in the market. For example, we recently successfully designed and launched new commercial episodes programs with a Northeastern state covering all state employees and retirees, as well as a large health insurer. We believe our ability to launch new, innovative programs will foster our long-term growth and impact on the healthcare system. |
140
Table of Contents
| • | Workflow and logistics software. Our software tools are designed to improve the collection and accuracy of real-time patient information and to deliver effective decision support to health plans and healthcare providers. Our proprietary workflow software is used by our mobile network of providers to conduct comprehensive IHEs, as well as for the routing and logistics for such in-home visits; by hospitalists to guide discharge and referral decisions; by case managers to monitor patients and manage transitions of care; and by a wide variety of users to identify SDOH that may impact the achievement of optimal patient outcomes. |
We derive revenue from multiple sources. We receive administrative service fees and a share of savings generated in our episode-based payment programs, where we enter into at-risk contracts; health plans compensate us for conducting IHEs and virtual IHEs (“vIHEs”) and for helping launch and administer care coordination and episode-based payment programs; and health plans, health systems, government agencies and biopharmaceutical companies compensate us for delivering a variety of services, ranging from the management of post-acute care for accountable care organizations (“ACOs”), to managing SDOH, to complex care management and caregiver support services. Our relationships are grounded in long-term, multi-year contracts that we believe have the right incentives to align the performance of our services with the performance of our customers.
How we measure our progress
We operate our business in two segments: Home & Community Services, which focuses on reaching and engaging populations at home; and Episodes of Care Services, through which we manage episode-based payment programs. We provide our customers with measurable financial and patient outcome data to assess our performance. We believe that we are integral to how our health plan and provider customers manage value-based healthcare programs, making our success a material driver of the financial performance of our customers. We measure our success in the following ways:
| • | We measure our success in our Episodes of Care Services segment by how much medical spend we are responsible for managing; by the performance of the levers that drive clinical and financial success in episodes of care, including the amount of savings we help our providers generate; and by patient outcomes. |
| • | We measure success in our Home & Community Services segment by the number of health plans we serve and the number of health plan members we are able to reach, in their homes. We also measure our efficiency in reaching those health plan members in their homes. |
| • | We measure the success of our workflow software by its ability to identify when patients are likely to be attributed to an episode of care; by our ability to communicate decision support guidance to healthcare providers; by provider utilization of our decision support tools; and by how we ultimately perform on influencing a specific lever. We believe our focus on levers has led to measurable outcomes, such as reductions in avoidable complications, reduced readmissions, reduced use of acute and post-acute facility services and increased delivery of services in the home. |
Our platform and scalability
We believe we have demonstrated the ability to rapidly scale our customer base and operations and grow our business in our principal markets in large part due to the attractiveness of our services and our competitive scale in the market. We now serve 26 of the top 50 Medicare Advantage plans. We have increased the number of annual IHEs conducted from approximately 390,000 in 2015 to nearly 1.1 million in 2019, representing a compound annual growth rate of 28.9%. As the largest convener participant in BPCI-A by number of episodes managed and over 6 years of participating in BPCI-A and its predecessor BPCI, we also enjoy a leading position in the episodes of care industry and have continuously grown our networks of contracted at-risk provider organizations. We have increased the number of episodes of care we have managed from approximately 24,000 episodes under BPCI in 2014 to approximately 215,000 episodes under BPCI-A in 2019 based on our current estimates.
141
Table of Contents
We believe our financial model is attractive with highly recurring revenues, strong EBITDA margins and high cash flow conversion. For the year ended December 31, 2019, our total revenue was $501.8 million, representing a 48.5% increase from $337.9 million in 2018, we incurred a net loss of $28.5 million, representing a 1.2% decrease from a net loss of $28.9 million in 2018, our Adjusted EBITDA was $93.3 million, representing an 18.0% increase from $79.1 million in 2018 and our Adjusted EBITDA Margin was 18.6%, a 4.8% decrease from 23.4% in 2018. For the nine months ended September 30, 2020, our total revenue was $417.1 million, representing a 13.2% increase from $368.5 million in the nine months ended September 30, 2019, we incurred a net loss of $15.2 million, representing a 25.8% decrease from a net loss of $20.5 million in the nine months ended September 30, 2019, our Adjusted EBITDA was $86.0 million, representing a 28.8% increase from $66.7 million in the nine months ended September 30, 2019 and our Adjusted EBITDA Margin was 20.6%, a 2.5% increase from 18.1% in the nine months ended September 30, 2019.
Our platform has been designed to address the factors that we believe are critical to success in value-based payment programs. A recent Deloitte study cited four essential building blocks that rely on a holistic, longitudinal view of each patient in order to achieve success. We believe our advanced analytics and technology-enabled services address each of these building blocks.
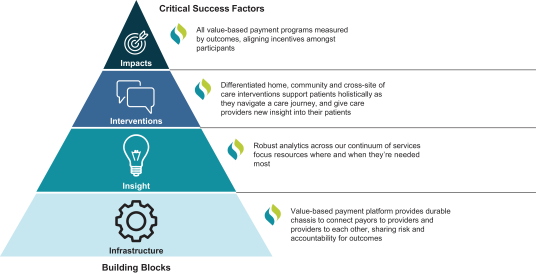
Industry trends and market opportunity
Total U.S. healthcare spending exceeded $3.8 trillion in 2019 and we operate in the large market associated with payment for healthcare services. We serve needs of healthcare funding sources including Medicare, Medicaid, employers and private health plans. Signify Health operates in the value-based payment sector of the healthcare industry. We believe value-based payments have grown dramatically over the past ten years and are expected to eventually represent the majority of healthcare spending in the United States according to studies by Health Care Payment Learning & Action Network and other research reports by industry analysts, which suggest that approximately 60% to 70% of total U.S. health spending is expected to be tied to quality and value by 2025 through the adoption of new payment models focused on value. We believe this will especially be the case as value-based payment models continue to penetrate the commercial insured and self-funded markets. Our leadership position in enabling some of the most significant risk programs has allowed us to invest in and develop differentiated scale and expertise around analytics, technology, networks, and relationships to grow rapidly as demand for services in the value-based payment industry increases over time.
142
Table of Contents
Industry reports estimate the current addressable market for value-based payor programs, such as Medicare Advantage and Medicaid, is at least $300 billion, with 79 million members enrolled in Medicare Advantage and Medicaid Managed Care. Under such payor value-based care programs, payor rates are set based upon overall population risk. Through these arrangements, payors take on risk and need to develop an accurate picture of the health of their patient population in order to receive appropriate funding. Adjusting funding based upon a member’s health helps stabilize payor value-based care programs and incentivizes payors to enroll both healthy and higher cost members. A critical element to developing and understanding the overall health of a patient population is an accurate health evaluation in the home and coding of each individual patient’s health conditions. While the overall cost to perform these activities is a small component of total spending, there is significant value from the resulting data that is captured.
According to the Health Care Payment Learning & Action Network (“HCP-LAN”), in 2018, approximately $400 billion of provider spending flowed through value-based payment models, which are alternatives, such as bundled payment models, to the traditional fee-for-service payment models. HCP-LAN reported that of this $400 billion, approximately $142 billion of spending was through value-based payment models where providers also assumed potential risk in the event of suboptimal outcomes, as opposed to models where providers only stood to benefit from shared savings without the possibility of bearing downside risk. Under provider value-based care programs, healthcare provider reimbursement is tied to the outcomes and the overall quality of care delivered to patients. Value-based care reimbursement is different from the standard fee-for-service model in that providers are reimbursed based on the financial value of the healthcare services they provide and are rewarded for both efficiency and effectiveness. In order for providers to be able to participate in value-based care models, they need to utilize solutions that can track and report on hospital readmissions, adverse events, population health, patient engagement, and more. They also need tools to help them analyze costs, redesign care and align incentives with other healthcare providers. These solutions are used to organize and finance healthcare delivery around a patient’s episode of care to ensure higher quality outcomes at improved costs.
Medicare
Medicare coverage is primarily available directly through traditional Medicare or through private health plans who participate in the Medicare Advantage program. There are approximately 63 million Americans covered by Medicare. We serve both the traditional Medicare program, with our BPCI-A program, and private health plans in the Medicare Advantage program, through our IHE and other service offerings. Medicare expenditures totaled $796 billion in 2019 and are expected to grow to $1.6 trillion by 2029.
Medicare Fee-for–Service (“FFS”)
The traditional Medicare program, often referred to as the Medicare FFS program generally includes Part A hospital services, Part B physician services and Part D drug coverage. Beneficiaries are automatically eligible for Part A and generally receive Part B coverage in exchange for a deduction from their social security payments. Expenditures in the Medicare Part A and Part B Fee for Service program were $414 billion in 2019 and are predicted to grow to $727 billion by 2029. Medicare has been aggressively promoting value-based payment models, which have bipartisan support in Congress. In just a few years, the Medicare FFS program has moved over $100 billion of spending into population-based payments and episode-based payment programs. We operate a large episode-based program serving the Medicare FFS program under the BPCI-A program. We believe the BPCI-A program contributes to the long-term sustainability of funding for the Medicare program and has been more effective than most other CMS value-based payment initiatives.
Medicare Advantage
Medicare Advantage is one of the largest population-based value-based payment programs. In Medicare Advantage, private health plans are offered to Medicare beneficiaries as an alternative to the default Medicare FFS program. Through CMS, Medicare pays private health plans monthly fees per beneficiary based on historical
143
Table of Contents
spending by the Medicare FFS Program, as adjusted by Medicare RAF scores attributable to beneficiaries. The IHEs that we provide to our health plan customers may be used, in part, to support RAF scores and, thus, payment adjustments made by CMS. Beneficiaries default into the Medicare FFS program and must make a choice to opt into Medicare Advantage. Once a beneficiary opts into Medicare Advantage, they may choose from which private health plan to receive coverage.
Medicare Advantage by many measures is a model of success. In particular, beneficiaries receive enhanced benefits that lower out of pocket expenses for covered and non-covered expenses. Medicare Advantage and other health plans have attracted approximately 40% of eligible beneficiaries as enrollment has nearly doubled over the past decade, reaching nearly 25 million enrollees as of September 2020. The Congressional Budget Office and the 2020 Medicare Trustees Report to Congress predict that by 2029 enrollment will grow by more than 15 million beneficiaries. The same report estimates payments to Medicare Advantage plans in 2019 reached approximately $271 billion and are expected to grow to $664 billion by 2029 according to the same Medicare Trustees report.
Employer-Based health insurance market
Employer-based, or commercial, health insurance is primarily administered by private health plans and third-party administrators. According to the Congressional Budget Office, approximately 159 million Americans receive employer-sponsored health insurance. The vast majority (70%) work in a business with over 200 employees. Health benefit spending in the private health insurance market has historically exceeded $1 trillion annually according to CMS.
The employer-based health insurance market faces a number of challenges that drive adoption of value-based payment initiatives in their benefit plans. Health benefit inflation continues unabated and outpaces most other expenses incurred by employers. Employer premiums grew by approximately 3.5% annually between 2016 and 2018. Additionally, the growth in each employee’s share of premiums and benefit costs has grown faster than income for over a decade. Since 2010, costs borne by employees, such as premium contributions and deductibles, have grown 55% and 111% percent, respectively, which far outstripped workers’ earnings growth of 27% over the same time period.
Employers are seeking to accomplish multiple goals as they manage health benefits. These goals include reducing overall costs to employers and to employees; encouraging employees and their dependents to take a more active role in selecting healthcare providers and choosing optimal courses of treatment; identifying and engaging high risk and high cost beneficiaries in programs that reduce their health risks and encourage appropriate health maintenance; and promoting competition among healthcare providers in the geographies where their employees seek health services.
Medicaid and other
Medicaid is a government insurance program for persons of all ages whose income and resources are insufficient to pay for healthcare. Medicaid provides free insurance for approximately 68 million low-income and disabled people in America. Medicaid is administered at the state level and the total annual cost of benefits is approximately $600 billion annually according to CMS.
Similar to value-based payment initiatives developed under the federal Medicare program, state Medicaid programs continue to implement a growing range of value-based payment arrangements. These payment arrangements vary considerably by state. Some states, including Indiana, Arkansas, Ohio and Tennessee, have rolled out episode-based payment programs similar to BPCI. This is a trend that is expected to continue as state budget shortfalls lead to the pursuit of new models for lowering the cost of covered healthcare benefits.
144
Table of Contents
Types of value-based payment models
Provider engagement with patients and utilization of services has historically centered around costly acute events rather than a comprehensive assessment of individuals’ clinical, social and behavioral factors in order to proactively avoid such events. For decades, policymakers and healthcare experts have acknowledged the fundamental challenges and opportunities for improvement in the delivery of healthcare in the United States. A rapidly growing share of healthcare payments in the U.S. are moving away from FFS reimbursement towards these value-based payment arrangements. The shift to value-based care is driven by the belief that the current FFS-based payment model offers incentives for providers to increase the volume of services provided and does not reward providers for improving health outcomes. Due to concerns about rising costs and poor performance on quality indicators, employers, health plans, and government purchasers of healthcare are pushing for a transition to value-based payment models. These models have been designed with financial incentives and penalties to encourage physicians, hospitals and other healthcare providers to focus on quality, outcome and cost measures. In addition, we believe the current COVID-19 pandemic has heightened the focus on adoption of value-based programs among providers because of the adverse impact on patient volumes that has occurred. Health plans and healthcare provider organizations are experimenting with variations and combinations of two main types of value-based payment models:
Population-based models
| • | Global capitation – An organization receives a per-person, per-month payment intended to pay for all of an individual’s care, regardless of what services that individual receives. The Medicare Advantage program is an example of the global capitation model, which often moves substantially all insurance risk from one party to another. |
| • | Shared savings and shared risk models – Shared savings models call for an organization to be paid using the traditional FFS model, but at the end of the year, total spending is compared with a target; if the organization’s spending is below the target, it can share some of the difference as a bonus. Most of the Medicare ACO program participants are participating in a shared savings model. In addition to shared savings, there are shared risk models in which participating organizations are “at-risk” for spending that exceeds targets. In these “downside risk” models, if spending exceeds targets, organizations may have to repay a portion of such excess as a penalty. |
Episode-based models
| • | Episode Payments (also called Bundled Payments) – Instead of paying separately for hospital, physician, and other services, a payor bundles payment for all, or a substantial portion, of services received by a patient in connection with an episode of care over a fixed period of time. An episode of care may be a surgical procedure, a particular condition, or the reason for a hospital stay. If the amount spent on care is lower than a pre-established benchmark price, an organization can keep the money it saves through the reduced spending. However, if the amount spent on such care is higher than a pre-established benchmark price, the organization may be responsible for all or a portion of the excess spending. The Model can be integrated into any population-based payment model as a mechanism for managing high-cost episodes of care or as a strategy to involve specialists in value-based programs. |
Our competitive strengths
| • | Scaled Episode-Based Payment Program. We are the largest convener participant in BPCI-A by number of episodes managed, with $6.1 billion of spend under management in 2019. We believe our leadership position in the BPCI-A program has allowed us to invest in and develop differentiated scale around networks, analytics, technology and relationships to grow rapidly as demand for services in the value-based payment industry increases over time. As a result of both the success and visibility of the BPCI-A program, commercial health plans, governments and employers are beginning to explore |
145
Table of Contents
| similar bundled arrangements. As a scaled leader in the industry, we believe we are a compelling partner to support these initiatives and believe we will benefit from a network effect as health plans and providers look to further capitalize on the benefits of value-based care. |
| • | Nationwide Home and Community-Based, Technology-Enabled Services Infrastructure. Signify Health is a leading provider of IHE services to third-party Medicare Advantage plans, as measured by our volume of IHEs. We have a network of nearly 9,000 credentialed providers that we deploy in the home, enabling patient evaluations, the delivery of a growing range of in-home services and care coordination. While in the home, our providers perform IHEs with the assistance of longitudinal patient records and our proprietary clinical workflow software with an integrated device hub. Our device hub captures important diagnostic patient data from interconnected devices that we use to conduct retinal exams to detect retinopathy, hemoglobin A1c tests for diabetes and microalbumin diptests to screen for chronic kidney disease, among other diagnostic services, all of which further extend our ability to deliver services in the home. The geographic density of our customers and the breadth of our mobile provider network allows us to cost effectively reach patients in the home throughout the country, in both urban and rural locations. Combined with our community-based networks and platform applications, we work to bridge social needs identified in the home with solutions from the surrounding community. Our reach into the home, combined with our episode-specific focus, positions us to drive adoption of a wide range of emerging in-home monitoring and treatment modalities. |
| • | Access to the Home and Holistic Care Model. We believe patients achieve optimal health outcomes when all clinical and social factors influencing their health and recovery from specific events are addressed. We rely, therefore, on a holistic model of care in how we operate all our programs. We seek to assess every person in our programs on measures of physical health as well as SDOH. Our ability to capture clinical and social determinant data is complemented by our networks of providers and CBOs. We believe this enables our programs to have meaningful impact on the health and well-being of the individuals and families our programs touch. |
| • | Trusted Healthcare Brand. We believe we are a trusted healthcare platform in the health plan, provider and employer markets that adds value by leveraging advanced analytics, technology and national provider networks to create and power value-based payment programs in our two primary segments: Home & Community Services and Episodes of Care Services. In our Home & Community Services segment, our IHEs have been shown to improve patient satisfaction among health plan members. In our Episodes of Care Services segment, our scale and success in the BPCI program encourages our provider customers to increase the volume and variety of bundles they participate in because of confidence in our ability to manage post-acute episodes. We have repeatedly leveraged our experience and leadership in these value-based payment programs to cross-sell and up-sell services across our two segments and deepen our relationships with customers. |
| • | Purpose-built Technology, Data and Analytics Platform. We provide our health plan and health system customers with a comprehensive suite of software, analytics, and services that fit with both population-based and episode-based models of value-based payments. As of September 30, 2020, our data chassis included data on approximately 35 million members. Both of our segments are supported by an advanced analytics team that is responsible for building decision support algorithms and predictive modeling, as well as for comprehensive monitoring and reporting, both internally and externally to our customers. |
| • | Established and Long-Standing Customer Relationships. We enjoy long-standing relationships and a history of collaborative innovation with many of our customers. Our top health plan customers that made up over 90% of our revenue in our Home & Community Services segment in 2019 have been with us for more than five years and we have had a strong presence in the BPCI program since its inception in 2013. We believe our wide footprint of customers, many of whom have long-term, multi-year contracts with us, allows us to better understand market needs and continue innovating in how we serve health plans, health systems and physician groups, as well as individuals in their homes. For example, |
146
Table of Contents
| in our Home & Community Services segment, we developed our IHE+ solution in collaboration with a large health insurer in Pennsylvania and have subsequently incorporated that into our broader offerings to all clients. We also worked with some of our large health plans to extend our IHE offering to serve their Medicaid populations. Similarly, in our Episodes of Care Services segment, we partnered with a large hospital system in Chicago to develop a transition of care program to support patients’ transition out of an acute setting and into a post-acute or home setting, which ultimately formed the basis of our TTH program. We believe our history of collaborative innovation uniquely positions us to capture additional opportunities as many organizations in the healthcare industry are vertically integrating, with health plans acquiring provider capabilities and vice versa. Signify Health partners with customers to provide more comprehensive services to help them succeed across the continuum of care. |
| • | Deeply Experienced Management Team and Mission-Driven Culture. Our management team has deep expertise in scaling technology-enabled services infrastructure, in servicing health plans, in provider contracting and in designing innovative products. We believe our deep base of knowledge in how healthcare is organized, financed and delivered enables us to tailor our software and service offerings to address highly specialized and complex challenges facing both the organizations that pay for healthcare and the organizations responsible for delivering that care. |
Our growth strategy
| • | Expand our in-home service offerings. We believe healthcare delivery will continue to move away from institutional settings and towards in-home services in the coming years. We believe we are positioned to capture a significant share of this fundamental trend towards home-based care delivery. We are able to deliver an expansive range of in-home services through our national scale, longitudinal patient records with an integrated device hub and access to patients. In response to the COVID-19 pandemic, we rapidly launched and scaled our vIHEs, a telehealth version of our in-home IHEs. Additionally, in 2020, we expanded our service offerings to include an “IHE+” in our Home & Community Services segment, our ACO service in our Episodes of Care Services segment, our TTH service, also in our Episodes of Care Services segment. Finally, we are rapidly expanding our remote patient monitoring and device connectivity capabilities via our device hub, which is integrated with several diagnostic devices we deploy in our service model. Our breadth of access and ability to rapidly deploy new technologies and services is helping to make the home an increasingly viable setting of care to manage a broadening population of patients. |
| • | Expand our episode of care programs. We intend to expand our Episodes of Care business by growing existing programs and launching new ones. Currently, we generate the majority of our revenue in our Episode of Care Services segment through the BPCI-A program. Participation in the BPCI-A program was locked in place at the end of 2020 through the end of the program in 2023, meaning that new healthcare providers will not be able to enter the program and participating providers will not be able to choose to participate in any additional episode types, which will impact our ability to increase the number of episodes managed or program size during this time. We intend, however, to continue growing our BPCI-A business by growing savings achieved under the program. We will also seek to capture new opportunities related to the June 2020 announcements from CMS of their intention to move to a more expansive and mandatory bundled payment program at the end of 2023. In addition, we are actively launching programs outside of the BPCI-A context with large employers and health plans to integrate new, innovative episode-based payment programs into their health plans and value-based payment programs. These new programs will aim to anchor our long-term growth, as we leverage our relationships with payors to build networks of providers under episode-based payment contracts. Our goal is to continuously increase the spend under management of these episode programs. |
| • | Expand our networks. We will continue to recruit more providers and CBOs into our Home & Community Services network. We will also continue to recruit health systems, physician groups and other provider organizations into our episode of care programs. By increasing the reach of our provider |
147
Table of Contents
| network, we have expanded the number of annual IHEs conducted from approximately 390,000 in 2015 to nearly 1.1 million in 2019. In addition, by expanding our network of hospital and physician organizations participating in our episodes business, we have increased the number of episodes of care we have managed from approximately 24,000 episodes under BPCI in 2014 to approximately 215,000 episodes under BPCI-A in 2019 based on our current estimates. |
| • | Grow our customer base and leverage our network effect. We have large addressable markets for our product and service offerings. Adding additional payor customers for our Episodes business within a given geography makes more providers eligible to participate in various episode types. Providers must exceed minimum episode volume requirements to be eligible for such episodes, and we are able to aggregate their episode volume across programs. We believe that greater episode participation drives increased commitment to care redesign among our provider partners and, in turn, increases our ability to manage post-acute care, as the increased patient volume increases program engagement among post-acute providers and results in the realization of additional savings. In addition, as our IHE customer base grows, the geographic density of our customers’ collective membership increases, which improves the efficiency and capacity of our mobile providers. This allows us to lower our cost of services to drive customer value, which we believe provides a key competitive advantage. As we continue to increase our scale, we believe this will both enhance our ability to attract new customers and incentivize existing customers to concentrate their business with us. |
| • | Improve our software and analytics capabilities. Our large existing base of customers provides feedback to our teams responsible for building software, analytics and decision support tools. We will seek to leverage this feedback and our customer relationships to continuously enhance the features and functionality of our software and service offerings; doing so is key to our ability to leverage our leadership position in the markets we serve. |
| • | Capitalize on our visible, recurring and capital efficient financial model. While the value-based initiatives that our customers undertake incorporate elements of upside and downside risk, our revenue model has historically been visible and recurring. Our insight into future demand for our services allows us to scale our operations in a manner we believe is in line with future demand, aiming to reduce waste and keep our investments efficient. |
| • | Selectively pursue acquisitions and partnerships. In recent years, we have expanded our product offerings in part through acquisitions, including Remedy Partners and TAV Health. We intend to complement our strong organic growth opportunities by evaluating the acquisition of complementary products and services. We will continue to selectively pursue strategic and complementary assets to support our clients’ needs. |
Our solutions
Home & Community Services
In our Home & Community Services segment, we offer a variety of solutions to help manage the health of our customers’ members in their homes.
In-home health evaluations and related services
We believe we have the largest mobile network of credentialed providers in the United States, which we deploy into the home primarily to conduct IHEs and to perform select diagnostic services. Through our IHEs, we create a comprehensive, documented record of the clinical, social, and behavioral needs of our health plan customers’ medically complex populations and seek to further engage them with the healthcare system. Working with data from our health plan customers, our operating platform and advanced data analytics seek to identify the highest priority individuals for an in-home evaluation. We then engage with those members to schedule visits to perform IHEs. While in the home, our providers perform IHEs with the assistance of our longitudinal patient
148
Table of Contents
records and our proprietary clinical workflow software with its integrated device hub. Our software guides clinical workflows as well as in-home diagnostic screenings, yielding a rich patient report of approximately 240 data points. The duration of our IHEs is up to 2.5 times longer than the average visit with a primary care physician (“PCP”). While performing these evaluations, we also seek to engage individuals more closely with the healthcare system. For example, the evaluation results of IHEs are provided to individuals’ PCPs. We believe sharing these results helps to fill gaps in care, while encouraging individuals who do not regularly visit their PCP to schedule a visit. In 2019, more than 90% of the members we evaluated followed up with a primary care visit.
In addition to providing health plans with insights into member health without taking members out of the home, the patient reports our IHEs produce form the basis of the RAF scores, which are required for health plans to effectively participate in value-based and risk-adjusted government programs like Medicare Advantage and affect the premiums health plans receive for Medicare Advantage beneficiaries. The data we gather is used by health plans to improve their Healthcare Effectiveness Data and Information Set (“HEDIS”) scores and Medicare Advantage Star Ratings (“Star Ratings”). Following our success in Medicare Advantage, we have entered new markets in recent years, such as Managed Medicaid in 17 states as well as supporting our customers’ Affordable Care Act Exchange lines of business, both of which are subject to quality-based payments and risk adjustment to varying degrees. We conducted nearly 1.1 million IHEs in 2019 and over 940,000 IHEs (including vIHEs) in the first nine months of 2020 alone.
Telehealth through virtual IHEs
In response to the COVID-19 pandemic and in close coordination with our customers, we accelerated our telehealth initiatives by quickly launching vIHEs in the second quarter of 2020. vIHEs primarily take place via videoconference. vIHEs have allowed us to engage with high-need, vulnerable individuals during a critical time, ensuring that our health plan customers maintain detailed insights into their members’ health and are able to coordinate services accordingly. Leveraging our technology and engagement tools, our staff and clinical network successfully completed more than 380,000 vIHEs using a combination of audio and video connectivity in the first nine months of 2020. We believe vIHEs will be a significant component of our business going forward, as customers have recognized the benefit of virtual engagement with members as a means to improve the IHE completion rate. We believe that our further development of this product over the course of 2020 has given us a strong, secure, and compliant foundation for ongoing and diversified telehealth services.
Social determinants of health
We bring CBOs together into outcomes-focused networks that are designed to address SDOH. In 2019, we started utilizing telephonic outreach and comprehensive, in-home evaluations to directly identify the social determinants of an individual’s health, such as food insecurity, slip and fall risk, access to transportation, social isolation, and the financial resources to afford medications. For certain customers, we combine this assessment with IHEs and refer to this combined product as an IHE+. Beginning in 2020, we began referring individuals directly to CBOs in our network through our Signify Community platform, leveraging the platform as a system of record for referral workflow and data capture. In one example of a new and promising program, in 2017 we deployed our SDOH model state-wide for the Iowa Department of Public Health in 2017 to manage Medicaid services for the state’s Title V maternal and childhood health program, in which 25 state agencies serve as the nodes on the network. Today, our CBO network extends across all 99 Iowa counties and includes local health departments, community action programs and organizations, Federally Qualified Health Centers, and home health providers. As a further example, in September 2020, we announced the launch of a network of CBOs in Philadelphia in partnership with a local health plan, connecting a local community center, wellness center, food security organizations and a legal clinic. Through our platform, these CBOs and the health plan are able to coordinate and manage individuals’ non-clinical needs. For our health plan customers, we believe this feature adds an advanced SDOH component to an already high-value IHE product and helps us to drive increased member engagement.
149
Table of Contents
Biopharmaceutical Services
In recent years, we have begun deploying our provider network in service of other sectors such as the biopharmaceutical sector. We approach this sector from two vantage points: approved therapies and decentralized trials. In the former, we are assisting patients in starting complex therapies more quickly, by providing them first-dose observations at home, in direct contract with major pharmaceutical manufacturers. In the latter, we leverage our deep domain expertise in addressing social determinants to provide caregiver support services designed to improve trial subject retention, lower trial costs and increase speed to trial completion.
Episodes of Care Services
We develop provider networks, build software and deliver services that support the organization and financing of healthcare around a patient’s episode of care. Our customers include the payors offering episode of care programs, as well as the providers who participate in such programs when delivering healthcare services.
We operate a large episode-based program, with $6.1 billion of BPCI-A spend under management in 2019. We have agreements with 85 healthcare provider organizations in 44 states and the District of Columbia, including hospital groups and physician groups. Our programs, platforms and networks drive care redesign to reduce costs and improve patient outcomes. We believe we accomplish these goals by reducing variations in care delivery, identifying cost saving opportunities and propelling recovery homeward. In so doing, we help to improve the coordination of care among clinicians, facilities and individuals along the care continuum. In 2019, we generated savings of $327 million through this program, while seeking also to improve key measures of patient outcomes. Furthermore, the BPCI-A episodes we managed which were initiated in the last quarter of 2019 resulted in approximately 15% greater discharges home from acute-care facilities and approximately 10% lower readmissions when compared to the historical performance of our provider partners for similar episodes.
The complexity and risk associated with episode of care programs leads payors and healthcare providers to seek expertise in the many disciplines required to achieve success in these programs. That is the role we play. Our episodes of care capabilities include the following:
| • | We own libraries of episode definitions and also work with open source versions of episode definitions to implement and develop clinical episodes. We are able to implement surgical or medical episodes, such as those for knee replacements, colonoscopies, pregnancy and newborn deliveries, as well as condition-centric episodes, including those addressing chronic conditions, such as diabetes and hypertension, and behavioral health conditions, such as depression, anxiety, or substance abuse disorders. |
| • | We have data analytics capabilities that enable us to analyze payment data from multiple sources in order to provide payors and providers with information about clinical episode initiation, real-time status and episode of care program performance for an individual patient, a participating provider’s practice and a payor’s overall program. |
| • | We use episode definitions to analyze data and help determine a fair benchmark price for a specific episode. We are able to utilize a payor or provider’s historical claims data and benchmark data, and trend that data forward to make predictions about future costs for individual episodes at the individual provider level. |
| • | We can help payors determine where and how episodes of care can improve care coordination, reduce expenditures and improve outcomes for their members, and we can help design an episode of care program, develop pricing, recruit and contract with participating providers, provide protocols for launching a program and engage directly with contracted providers on care optimization. |
| • | We have a field-based organization that recruits healthcare provider organizations into episode of care programs and then helps them implement care redesign and manage episode of care programs. |
| • | We have a proprietary suite of software tools, called Signify Connect, which includes our Episode Connect software and supports health systems and physician organizations in managing their episode |
150
Table of Contents
| of care programs. This platform includes workflow tools that identify patients using predictive analytics, assist with the creation and implementation of care coordination plans, facilitate communication between providers across a patient’s care team and enable providers to manage and track a patient’s care during an episode of care. |
| • | We have decision support tools to support providers when important decisions are being made upon discharge from an acute care facility on the next site of care. Our decision support tools are grounded in clinical information, at the individual episode level, to help healthcare providers transition patients to the optimal next care setting. For our Commercial Episodes of Care services, we also have decision support tools that support decision making around appropriate sites of care, such as whether a particular procedure should be performed at an acute-care hospital or an ambulatory surgery center. |
| • | We have an expansive analytics platform that includes a real-time dashboard that delivers information at the aggregate level as well as at the patient level, and a wide range of reports that enables users to configure how they want to see the data available from Episode Connect and the other data sources that populate our longitudinal view of individual patients. |
| • | We offer comprehensive administrative services that support the back-office activities required to launch and manage episode of care programs. |
In our Episodes of Care Services segment, we offer a variety of solutions to help our customers participate in episode-based programs.
Medicare Bundled Payment for Care Improvement (BPCI and BPCI-A)
We are the largest convener participant in the BPCI-A program by number of episodes managed. In this role, we hold contracts directly with CMS pursuant to which we are responsible for developing and monitoring a BPCI-A episode of care program in partnership with healthcare providers. We enter into back-to-back contracts with providers participating in the BPCI-A program, whereby we facilitate coordination among providers and share financial risk. To enable our provider partners to successfully participate in BPCI-A, we provide a suite of analytic, technology and post-acute management services in exchange for an administrative fee (which is paid out of savings) and a share of any incremental savings or losses related to episodes initiated by our provider partners.
BPCI-A employs (and BPCI employed) a retrospective payment system in which Medicare reimburses providers in accordance with their usual fee-for-service payment schedule, while also tracking the total fee-for-service costs for all billable services rendered during the episode period (generally 90 days from the date of discharge from the acute-care facility). Upon completion of each episode, CMS compares the total amount of all fee-for-service payments made during the episode against a predetermined benchmark price. If the total fee-for-service costs of the episode exceeds the benchmark price, the designated program participant owes the difference to CMS, and likewise, if total fee-for-service costs of the episode are lower than the benchmark price, then CMS pays the difference (representing the incremental savings achieved) to the designated program participant.
While increasing care coordination has been shown to improve health outcomes and reduce overall costs in the healthcare system, it can require significant time and specialized resources that many healthcare systems, hospitals and physician group practices lack. We address these needs and enable our provider partners to successfully participate in BPCI-A by providing data analytics, tools and support from the initial stages of care redesign, to identifying and tracking individuals, to managing patients’ post-acute care, through handling program reconciliation and the distribution of shared savings. Our services include the following:
| • | Data Integration & Patient Identification: We set up secure data feeds with our provider partners and are able to receive data from all leading EHR systems, which allows us access to real-time EHR data in order to quickly predict and identify individuals that are likely to be attributed to a BPCI-A bundle. When a clinical event or procedure occurs which initiates, or “triggers,” an episode, our proprietary software |
151
Table of Contents
| platform, Episode Connect, identifies the individual. This allows providers to begin tracking the individual’s care journey and enabling them to intervene at key moments in the journey. |
| • | Care Redesign Processes: Our approach is designed to create lasting change in the management of higher-risk patients in the acute and post-acute setting. We utilize locally based team members to engage with our provider partners in an effort to maximize patient recovery and stabilization. In the acute setting, we focus on key goals around effective transition to the appropriate post-acute facility for the patient by partnering directly within the acute-care hospital with all members of the typically interdisciplinary team treating a patient. In the post-acute setting, our team works directly with the facility and provider to align processes that support improved patient outcomes. |
| • | Decision Support Tools: Once an individual is ready to be discharged from the acute setting, our suite of tools provides recommendations on the most appropriate next site of care (e.g., home vs. post-acute facility), as well as information on the post-acute providers within our network that may best be able to support the patient’s needs. |
| • | Post-Acute Network Development & Management: To further facilitate coordination of care, we develop and manage local networks of high-quality, high-value healthcare providers, including skilled nursing facilities and home health agencies, which can serve individuals participating in bundles at each stage of care. Our team of post-acute specialists regularly meets with post-acute care providers to review care plans and promote adherence to evidence-based guidelines, providing guidance on early identification of clinical and social gaps that may impact readmissions risks. |
| • | Incentive Alignment, Gainsharing & Information Sharing: The BPCI-A program permits second-tier payment arrangements between the relevant program provider participant and a downstream healthcare provider who has participated in an individual’s care. Provider partners are permitted to share risk with downstream participating providers as a way to align financial incentives and improve cooperation among providers, generating more favorable patient outcomes and increased savings. We connect our provider partners with downstream providers, and we negotiate and administer these gainsharing agreements on behalf of our customers. We also act as the paying agent, distributing (or collecting) gainsharing payments in connection with each semiannual reconciliation. We also facilitate coordination among these providers. Episode Connect allows these providers to share data, further increasing coordination. For example, our provider partner can review patient-specific information throughout the post-acute care continuum, including patient progress to recovery goals as well as the transition from a post-acute facility to home health services. This type of coordination allows us and our provider partners to better track an individual’s progress and assess when they are ready to self-manage in the home. |
| • | Reconciliation Analysis, Benchmarking & Performance Review: At the end of each BPCI-A performance measurement period, we review reconciliation statements from CMS, identify errors and distribute shared savings. In addition, our platform generates reports on healthcare providers’ performance, showing their performance benchmarked both against their own historical performance, as well as against peers in their geography. In this way, we close the loop on an episode by providing actionable insights that a provider can use the next time an episode is initiated. |
Commercial Episodes of Care
In 2020, we began offering program sponsors, including health plans, employers and state government agencies, the analytics, software tools and services necessary to design, launch and administer episodes of care programs outside of the BPCI-A context. This opened new markets and, equally significant, new chronic care episodes to us. We believe expanding our business from Medicare’s bundles, which are triggered by a hospital stay, to episodes that are triggered with a diagnosis, significantly expands our total addressable market.
152
Table of Contents
As with our BPCI-A program, we deploy our care coordination resources directly in the field to create the relationship with the local providers that effectively drives process transformation. In addition to the services we provide in the BPCI-A program, we also offer the following services as part of our growing commercial business:
| • | Program Design: Using our advanced data analytics capabilities, we help program sponsors identify the potential benefits of an episode of care program, both from a financial and strategic perspective, and assist them with the initial program design, including episode of care selection and pricing. Importantly, our episode of care programs also include measures designed to improve patient outcomes by reducing the incidence of adverse events and potentially avoidable or wasteful services. |
| • | Provider Network Recruitment, Contracting & Support: Leveraging our expertise, credibility with providers established through the BPCI-A program and suite of provider tools, we recruit providers into the program sponsor’s episode of care program. By sharing risk with providers, we align incentives and build trust, which we believe puts us in a unique position to encourage program participation and takes the burden of network recruitment off program sponsors. We equip participating providers with tools designed to identify opportunities for improved patient care while achieving cost savings and educate them on the levers that support improved patient outcomes while generating savings within each clinical episode type (which differ considerably from those in the BPCI-A program). |
| • | Expanded Decision Support Tools: We expand our decision support tools to align to the specific decisions that a provider makes in the expanded episodes, such as the appropriate site of care for a surgery. These tools evaluate quality, cost and convenience. Our tools also update the provider on services that are being delivered during the patient’s care journey. |
| • | Additional Program Sponsor Support: We deliver to program sponsors a comprehensive analytics platform that includes episode pricing, monitoring and reporting of performance at the individual beneficiary, provider and program level. We perform program reconciliations, provide reconciliation statements to program sponsors and participating providers and collect and distribute program savings and losses among payors and providers. |
Transition to Home
In 2020, we introduced our TTH service, a support model for patients transitioning home from a hospital or a post-acute care facility that aims to reduce the likelihood of readmission. The readmission rate for BPCI-A patients can be greater than 30%, and we estimate that the average cost of a readmission of a BPCI-A patient, including related post-acute costs, is approximately $17,000. Leveraging our provider network and community-based services, we work to prevent readmissions by providing individuals with continued support from our social care coordinators and, when necessary, our nurses and nurse practitioners. We believe our TTH offering is able to provide the necessary support for both clinical and social needs, facilitate the appropriate care and fulfillment of social needs and promote patient engagement to reduce the likelihood of readmission, which could result in improved patient outcomes and a significant increase in cost savings.
Complex Care Management
We also offer health plans a solution to manage the clinical needs and well-being of their members with complex chronic conditions through a multi-disciplinary approach. Our providers engage with high-needs individuals in facilities. By looking at an individual’s medical needs and well-being holistically, the provider is able to address elements of the individual’s care plan such as medication adjustments, adherence to care plans and patient behavioral and nutritional needs.
ACO Services
In 2020, we began helping ACOs manage the post-acute care of their patient populations. This service offering grew out of demand from our BPCI-A provider partners, who we believe recognized our ability to
153
Table of Contents
manage costs, improve outcomes and generate savings in the BPCI-A program and wanted to apply the same services and tools to manage the post-acute care of their ACO populations. Our ACO solution expands on the BPCI-A definitions with a more comprehensive suite of episodic conditions that are managed through the post-acute setting. We use the same data analytics capabilities we use in our BPCI-A services to analyze historical data and identify opportunities for post-acute cost savings for ACOs. In addition, ACOs have access to our platform through which they can access data across care settings and follow the patient more closely throughout the post-acute episode. This information allows ACOs to make informed decisions with respect to, among other things, treatment, cost management, next site of care and length of post-acute care. Finally, we utilize our teams of acute and post-acute specialists to support the delivery of appropriate post-acute care to ACO patients.
Sales and marketing
In each of our segments, we focus our sales & marketing initiatives on three primary dimensions of growth: (1) sales to new customers, (2) cross-sales to existing customers and (3) product expansion with existing customers. In order to successfully obtain new customers and to cross-sell solutions to existing customers, we have a strong sales team that is organized by segment as well as by product/service offered. For example, we have sales representatives dedicated to selling our IHE solutions in our Home & Community Services segment. These representatives are responsible for selling our IHE solutions to new customers as well as cross-selling our IHE solutions to existing customers. For example, we expanded our IHE offerings in 2020 to include an IHE+ solution and these sales representatives are focused on expanding use of this solution among our existing customers.
Similarly, in our Episodes of Care Services segment, we have representatives dedicated to selling our solutions to new and existing customers. For example, since 2019, BPCI-A participants have not been able to change their convener and will not be able to do so until the program expires in 2023, assuming it is renewed. However, we are able to offer our full suite of solutions to self-conveners to support their participation in BPCI-A, even though they do not participate in BPCI-A through us. Our sales representatives that specialize in BPCI-A are currently focused on selling our services to self-convener participants that we do not currently work with. We also believe there are significant cross-selling opportunities in our Episodes of Care Services segment. For example, most of our BPCI-A customers also serve ACO populations and we have dedicated sales representatives focused on selling our ACO services to our BPCI-A customers. We believe organizing our sales teams by product/service offered ensures that our representatives have deep industry and product/service knowledge and are able to more effectively sell our products and services to new and existing customers.
In terms of product expansion with existing customers, we also have a certain number of sales representatives that are not organized by segment, but are instead responsible for managing significant existing customer relationships. These representatives focus on engaging with our customers and finding ways that we can expand and grow with our customers. For example, these representatives may focus on increasing the volume of IHEs we perform for existing customers in our Home & Community Services segment, or they may work with existing BPCI-A customers to see if there is different or better data available to guide a customer through the program. Currently, as BPCI-A participants make episode elections for 2021, these representatives are working with our existing customers to analyze which episodes make the most sense for them to take on given available data. We believe having representatives dedicated to particular customers allows our representatives to forge relationships with our existing customers and work closely with them to find additional ways we can support their operations.
Customers
Our customers consist primarily of health plans and providers and, to a lesser extent, state and government agencies, employers, biopharmaceutical companies and other risk-bearing entities. Revenue from our top ten customers across our segments accounted for approximately 74% of our total revenue for the year ended December 31, 2019 and 70% of our total revenue for the nine months ended September 30, 2020.
154
Table of Contents
In our Home & Community Services segment, our customers are primarily Medicare Advantage health plans and managed Medicaid organizations, as well as pharmaceutical manufacturers. We currently serve 51 health plans in the United States, including 26 of the 50 largest Medicare Advantage plans. In 2019, each of our two largest customers in this segment represented more than 10% of our total revenue.
In our Episodes of Care Services segment, we serve a variety of customers. All of our direct contracts to participate in the BPCI-A program are with CMS. Our customers for BPCI-A management services are primarily providers, including 85 healthcare provider organizations. Within our emerging businesses, our ACO management services are directed at ACOs participating in CMS’ Medicare Shared Savings Program; our Commercial Episodes of Care business is directed at health plans, employers, state and government agencies and providers looking to launch programs centered around care redesign; our TTH services will be offered to providers participating in the BPCI-A program, and our Complex Care Management business serves health plans.
Competition
The U.S. healthcare industry is highly competitive. We compete primarily in the market associated with payment for healthcare services, where large and small companies are formulating innovative ways to transition the healthcare market to value-based care with an increasing focus on treating individuals within the home. In our Home & Community Services segment, we compete with local and national providers of in-home diagnostic and evaluative services. Our competitors include pure-play competitors whose principal business is providing IHEs and similar services as well as large payors that have in-house capabilities for performing a portion of their IHEs in house. Among pure-play companies, our primary competitor is Matrix Medical Network, which we believe is the only other pure-play company providing IHEs with national scale. With respect to large payors, most large payors use a variety of different providers for their IHE volume and several large payors service a portion of their total volume with their own in-house capabilities. For example, Humana has a division called Your Home Advantage and UnitedHealth has a division called OptumCare, each of which performs IHEs for a portion of each payor’s plan members. As a result, we compete with these in-house capabilities for additional volume. Although large payors such as Humana and UnitedHealth have more resources than we do, because we focus principally on IHEs and have dedicated significant resources to building the breadth our national network, we believe we are able to more efficiently perform IHEs than these in-house divisions and we have consistently increased our volume with large payors such as Humana and UnitedHealth in recent years.
In our Home & Community Services segment, we also compete for, among other things, physicians, nurse practitioners, physician assistants and other medical and non-medical personnel. In particular, we face significant competition in attracting and retaining qualified providers for our mobile network, in particular from telehealth service providers.
In our Episodes of Care Services segment, we compete with healthcare risk management providers, primarily in the BPCI-A space. Our competitors include companies like us that convene (i.e., contract) with CMS on behalf of healthcare providers as well as physician group practices that “self-convene” under BPCI-A, meaning they contract directly with CMS to participate in BPCI-A rather than working through a company like Signify Health. In terms of traditional conveners, we compete with naviHealth (a subsidiary of UnitedHealth), OptumCare, Fusion5 and Archway. The largest self-conveners include Sound Physicians and other large physician group practices. To a lesser extent, we also compete with companies such as Change Healthcare that provide ancillary services to support the BPCI-A management process, such as software for patient tracking or analytics services. Because we provide a full suite of management solutions, we have not faced significant competition to date from these companies, although we may face more intense competition from them in the future.
In the commercial episodes of care space, we believe we are one of the only companies offering a comprehensive suite of services and technology solutions to help customers build episode programs and then recruit providers to participate. However, we do compete with companies offering episodes of care or bundled payment consulting services. In this space, we compete primarily with Aver, Cognizant and Cedar Gate.
155
Table of Contents
Our principal competitors in both of our segments vary considerably in type and identity by market. There have also been increasing indications of interest from non-traditional providers and others to enter the in-home diagnostic and evaluative services space and/or develop innovative technologies or business activities that could be disruptive to the healthcare risk management industry. Our growth strategy and our business could be adversely affected if we are not able to continue to penetrate existing markets, successfully expand into new markets, maintain or establish new relationships with health plans and providers, recruit qualified physicians, nurse practitioners and physician assistants, or if we experience significant customer attrition to our competitors. See “Risk factors—Risks related to our business and operations—We operate in a competitive industry, and if we are not able to compete effectively our business would be harmed.”
We believe the principal competitive factors for our industry include:
| • | ability to improve individuals’, health plans’ and providers’ health and/or financial outcomes; |
| • | level of individual, health plans and provider satisfaction; |
| • | ease of integration with employer and government programs; |
| • | price; |
| • | breadth and depth of platform functionality; |
| • | modern technology capabilities, including the ability to support virtual health evaluations; |
| • | ability to recruit and retain skilled physicians and nurse practitioners; |
| • | ability to accurately predict and reduce cost trends; |
| • | access to, ability to integrate with, and ability to derive insights, from large data sets; |
| • | regulatory compliance; |
| • | ability to rapidly innovate and respond to changing customer needs and legislative developments; |
| • | scalability of models; and |
| • | operational execution abilities. |
While certain of our competitors may have greater resources, recognition, larger customer bases, or longer-standing offerings, we believe that we compete favorably against our competitors based on these factors. We believe that our platform dramatically improves individuals’ experiences, encourages better health outcomes and reduces costs for health plans and providers.
Intellectual property
We believe that our intellectual property rights are important to our business. Our success depends in part upon our ability to obtain and maintain intellectual property protection for our brand, technology and inventions; to preserve the confidentiality of our trade secrets; to defend and enforce our intellectual property and proprietary rights; and to operate without infringing, misappropriating or otherwise violating the valid and enforceable patents and other intellectual property rights of third parties.
We rely on a combination of trademarks, service marks, copyrights and trade secrets to protect our proprietary technology and other intellectual property. As of September 30, 2020, we exclusively owned 20 trademark applications and registrations in the United States, including Signify Health. In addition, we have registered domain names for websites that we use or may use in our business. As of September 30, 2020, we had no issued patents and, other than one patent application which we intend to abandon, no pending patent applications anywhere in the world, and therefore, we do not have patent protection for any of our proprietary technology, including our proprietary software, mobile app or web portal.
156
Table of Contents
We rely upon trade secrets, confidential know-how and continuing technological innovation to develop and maintain our competitive position. However, trade secrets and confidential information are difficult to protect. We seek to control access to and distribution of our confidential and proprietary information, including our algorithms, source and object code, designs, and business processes, through physical, technical, and administrative security measures and contractual restrictions. We seek to limit access to our confidential and proprietary information on a “need to know” basis and enter into confidentiality and nondisclosure agreements with our employees, consultants, customers and vendors that may receive or otherwise have access to any confidential or proprietary information. We also obtain written invention assignment agreements from our employees, consultants, and vendors that assign to us all right, interest and title to inventions and work products developed during their employment or service engagement with us. However, these agreements may not provide meaningful protection. These agreements may also be breached, and we may not have an adequate remedy for any such breach.
Despite our efforts to protect our proprietary rights, unauthorized parties may attempt to copy aspects of our technology or obtain and use information that we regard as proprietary, or our technology and proprietary information could be unintentionally or intentionally misused by our employees. Third parties may independently develop the same or similar proprietary information or technology, or may otherwise gain access to our proprietary information or technology. As a result, we may be unable to meaningfully protect our trade secrets and proprietary information.
Intellectual property rights may not address all potential threats to our competitive advantage. See “Risk factors—Risks related to intellectual property and information technology” for a description of risks related to our intellectual property and information technology systems.
Government regulation
Our operations and those of the providers we employ and contract with are subject to extensive federal, state and local governmental laws and regulations. These laws and regulations require us to meet various standards relating to, among other things, billings and reports to government payment programs, equipment, dispensing of pharmaceuticals, personnel qualifications, maintenance of proper records, licensure, information privacy and security compliance, and quality assurance programs. If any of our operations or those of our providers are found to violate applicable laws or regulations, we could suffer severe consequences that would have a material adverse effect on our business, results of operations, financial condition, cash flows, reputation and stock price, including:
| • | suspension or termination of our participation in government payment programs or in the demand for our services by Medicare Advantage plans and/or Medicaid managed care organizations; |
| • | refunds of amounts received in violation of law or applicable payment program requirements dating back to the applicable statute of limitation periods; |
| • | criminal or civil liability, fines, damages or monetary penalties for violations of federal and state healthcare fraud and abuse laws, including the AKS, Civil Monetary Penalties Law, Stark Physician Self-Referral Law and FCA, or other regulatory requirements; |
| • | enforcement actions by governmental agencies and/or state law claims for monetary damages if PHI or PII has been used, disclosed or not properly safeguarded in violation of federal or state privacy and security laws, including HIPAA and the Privacy Act of 1974; and |
| • | harm to our reputation which could negatively impact our business relationships, affect our ability to attract and retain customers, individuals and providers, affect our ability to obtain financing and decrease access to new business opportunities, among other things. |
We expect that our industry will continue to be subject to substantial regulation, the scope and effect of which are difficult to predict. Our activities could be subject to investigations, audits and inquiries by various
157
Table of Contents
government and regulatory agencies and private members and payors with whom we contract at any time in the future. See “Risk factors—Risks related to governmental regulation.” Adverse findings from such investigations and audits could bring severe consequences that could have a material adverse effect on our business, results of operations, financial condition, cash flows, reputation and stock price.
Medicare, Medicare Advantage, Medicaid, Bundled Payment Initiatives and ACOs
Medicare
Medicare is a federal program administered by CMS through various contractors. Available to individuals age 65 or over, and certain other individuals, the Medicare program provides, among other things, healthcare benefits that cover, within prescribed limits, the major costs of most medically necessary care for such individuals, subject to certain deductibles and copayments.
CMS has established guidelines for the coverage and reimbursement of certain products and procedures by Medicare. In general, to be reimbursed by Medicare, a healthcare procedure furnished to a Medicare beneficiary must be reasonable and necessary for the diagnosis or treatment of an illness or injury, or to improve the functioning of a malformed body part. The methodology for determining coverage status and the amount of Medicare reimbursement varies based upon, among other factors, the setting in which a Medicare beneficiary received healthcare products and services. Medicare is subject to statutory and regulatory changes, retroactive and prospective rate adjustments, administrative rulings, interpretations of policy, intermediary determinations, and government funding restrictions, all of which may materially increase or decrease the rate of program payments to healthcare providers. Any such changes in federal legislation, regulations and policy affecting the entities with which we contact could have a material effect on our performance.
Medicare Advantage
Under the Medicare Advantage program, also known as Medicare Part C, the federal government contracts with private health insurers to provide members with Medicare Part A, Part B and Part D benefits. Medicare Advantage plans can be structured as Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs) or private fee-for-service plans. In addition to covering Part A and Part B benefits, the health insurers may choose to offer supplemental benefits and impose higher premiums and plan costs on beneficiaries. Medicare beneficiaries that choose to participate in Medicare Advantage choose which health plan through which to receive their Medicare coverage. To assist beneficiaries with plan selection, CMS established a five-star quality rating system. Using this system, CMS publishes Star Ratings based on a variety of quality, patient satisfaction and performance measures for health plans on an annual basis. These ratings are based on data gathered from a variety of sources, including HEDIS, the Consumer Assessment of Healthcare Providers and Systems program, the Medicare Health Outcome Survey, the Medicare Prescription Drug Program and CMS administrative data. According to CMS, over one-third of all Medicare enrollees participate in Medicare Advantage plans.
CMS generally pays health insurance plans that participate in the Medicare Advantage program on a per capita basis. CMS makes certain adjustments based on service benchmarks and quality ratings. The IHEs that we provide to our health plan customers may be used, in part, to support RAF scores attributable to the Medicare Advantage plan members and, thus, payment adjustments made by CMS. CMS audits Medicare Advantage plans for documentation to support RAF-related payments for members chosen at random. Such audits may result in payment adjustments to a Medicare Advantage plan, including extrapolation across the entire plan. Our health plan customers may seek to hold us liable for penalties owed to CMS for inaccurate or unsupportable RAF scores based on information provided by us. In addition, the government or a whistleblower could assert that our errors caused the plan to submit false claims to CMS, which could subject us to liability under the FCA.
158
Table of Contents
Medicaid
Medicaid programs provide medical assistance benefits to qualifying (typically low income or medically needy) persons. Medicaid programs are funded jointly by the federal government and the states and are administered by states under approved plans. Most state Medicaid program payments are made under a Prospective Payment System (PPS) or are based on negotiated payment levels. Medicaid reimbursement is often less than a healthcare provider’s cost of services. The ACA requires states to expand Medicaid coverage to all individuals under age 65 with incomes effectively at or below 138% of the federal poverty level. However, states may opt out of the expansion without losing existing federal Medicaid funding. Some states have opted out of the Medicaid expansion. Other states use, or have applied to use, waivers granted by CMS to implement expansion, impose different eligibility or enrollment restrictions, or otherwise implement programs that vary from federal standards. CMS has indicated its support of increased state flexibility in the administration of Medicaid programs, including allowing states to condition enrollment on work or other community engagement.
Because most state governments must operate with balanced budgets and because the Medicaid program is often the state’s largest program, states may adopt or consider adopting legislation designed to reduce their Medicaid expenditures. Budgetary pressures have, in recent years, resulted and likely will continue to result in decreased spending, or decreased spending growth, for Medicaid programs in many states. Many states have adopted, or are considering, legislation designed to reduce coverage, enroll Medicaid recipients in managed care programs and/or impose additional taxes on healthcare providers to help finance or expand the states’ Medicaid systems.
Federal funds under the Medicaid program may not be used to reimburse healthcare providers for medical assistance provided to treat certain provider-preventable conditions. Each state Medicaid program must deny payments to healthcare providers for the treatment of health care-acquired conditions designated by CMS as well as other provider-preventable conditions that may be designated by the state.
Congress has expanded the federal government’s involvement in fighting fraud, waste and abuse in the Medicaid program through the Medicaid Integrity Program. CMS employs Unified Program Integrity Contractors (“UPICs”) to perform post-payment audits of Medicaid claims, identify overpayments, and perform other program integrity activities, many of which were previously performed by Medicaid Integrity Contractors. The UPICs collaborate with states and coordinate healthcare provider investigations across the Medicare and Medicaid programs. In addition, state Medicaid agencies are required to establish Medicaid RAC programs. These programs vary by state in design and operation.
Bundled Payment Initiatives
CMMI is responsible for establishing demonstration projects and other initiatives in order to identify, develop, test and encourage the adoption of new methods of delivering and paying for healthcare that create savings under the Medicare and Medicaid programs, while improving quality of care. For example, healthcare providers participating in bundled payment initiatives agree to be responsible for the costs of services provided to Medicare patients experiencing certain medical conditions which trigger an episode of care, accepting accountability for costs and quality of care. By rewarding healthcare providers for increasing quality and reducing costs and penalizing healthcare providers if costs exceed a set amount, these models are intended to lead to higher quality, more coordinated care at a lower cost to the Medicare program. Healthcare providers may receive incentive payments or owe repayments to CMS depending on whether overall CMS spending per episode falls below or exceeds a target specified by CMS and whether quality standards are met. The CMMI has implemented bundled payment models, including the BPCI program and the BPCI-A program, the latter of which is voluntary and expected to run through December 2023. Participation in bundled payment programs is generally voluntary, but CMS has required healthcare providers in selected geographic areas to participate in a mandatory bundled program for specified orthopedic procedures, the Comprehensive Care for Joint Replacement (“CJR”) model, which is scheduled to run through December 2020. HHS has indicated that it plans to implement additional bundled payment programs, some of which will be mandatory.
159
Table of Contents
CMS continues to express support for shifting from traditional fee-for-service reimbursement models to alternative payment models that tie reimbursement to quality and/or value, including bundled payment and pay-for-performance programs. Several private third-party payers are increasingly employing such reimbursement models, which may increasingly shift financial risk to healthcare providers.
Accountable Care Organizations
An ACO is a network of healthcare providers and suppliers that work together to invest in infrastructure and redesign delivery processes to attempt to achieve high quality and efficient delivery of services. Promoting accountability and coordination of care, ACOs are intended to produce savings as a result of improved quality and operational efficiency. ACOs that achieve quality performance standards established by HHS are eligible to share in a portion of the amounts saved by the Medicare program. There are several types of ACO programs, including the Medicare Shared Savings Program, which was established pursuant to the ACA, and the Next Generation ACO Model.
Federal Anti-Kickback Statute
The AKS prohibits, among other things, knowingly and willfully offering, paying, soliciting or receiving remuneration, directly or indirectly, in cash or kind, to induce or reward either the referral of an individual for, or the purchase, order or recommendation of, any good or service, for which payment may be made in whole or in part under federal and state healthcare programs such as Medicare and Medicaid.
Federal criminal penalties for the violation of the AKS include imprisonment, fines and exclusion of the healthcare provider from future participation in the federal healthcare programs, including Medicare and Medicaid. Violations of the AKS are punishable by imprisonment for up to ten years, fines of up to $100,000 per kickback or both. Larger fines can be imposed upon corporations under the provisions of the U.S. Sentencing Guidelines and the Alternate Fines Statute. Individuals and entities convicted of violating the AKS are subject to mandatory exclusion from participation in Medicare, Medicaid and other federal healthcare programs for a minimum of five years. Civil penalties for violation of the AKS include up to $100,000 in monetary penalties per violation, repayments of up to three times the total payments between the parties to the arrangement and suspension from future participation in Medicare and Medicaid. Court decisions have held that the statute may be violated even if only one purpose of remuneration is to induce referrals. The ACA amended the AKS to clarify the intent that is required to prove a violation. Under the statute as amended, the defendant does not need to have actual knowledge of the AKS or have the specific intent to violate it. In addition, the ACA amended the AKS to provide that any claims for items or services resulting from a violation of the AKS are considered false or fraudulent for purposes of the FCA.
The AKS includes statutory exceptions and regulatory safe harbors that protect certain arrangements. These exceptions and safe harbors are voluntary. Business transactions and arrangements that are structured to comply fully with an applicable safe harbor do not violate the AKS. However, transactions and arrangements that do not satisfy all elements of a relevant safe harbor do not necessarily violate the law. When an arrangement does not satisfy a safe harbor, the arrangement must be evaluated on a case-by-case basis in light of the parties’ intent and the arrangement’s potential for abuse. Arrangements that do not satisfy a safe harbor may be subject to greater scrutiny by enforcement agencies.
Our episodes of care programs involve a number of arrangements that potentially implicate the AKS because they may involve payments intended to influence behavior relative to Medicare and other federal healthcare program beneficiaries, including risk sharing and “gainsharing” arrangements. While there is no fixed definition of a gainsharing arrangement, the term typically refers to an arrangement in which a share of cost savings for patient care attributable in part to a physician’s efforts are shared with the physician. The OIG has recognized that there are legitimate interests in enlisting physicians in efforts to reduce unnecessary costs from the healthcare system and, if appropriately structured, such gainsharing arrangements should not violate the
160
Table of Contents
AKS. With respect to BPCI-A and other CMS innovations models in which we may participate, the OIG and CMS jointly issued waivers of certain fraud and abuse laws, including the AKS. However, with respect to our Commercial Episodes of Care program and any other episode of care programs in which we may participate, there are no fraud and abuse waivers that are applicable. While we have carefully structured these arrangements in accordance with applicable guidance to be in compliance with the fraud and abuse laws, such arrangements are subject to a case-by-case analysis in light of the intent if the parties and the overall potential for abuse.
If any of our business transactions or arrangements were found to violate the AKS, we could face, among other things, criminal, civil or administrative sanctions, including possible exclusion from participation in Medicare, Medicaid and other state and federal healthcare programs. Any findings that we have violated these laws could have a material adverse impact on our business, results of operations, financial condition, cash flows, reputation and stock price.
Stark Law
The Physician Self-Referral Law (commonly referred to as the Stark Law) prohibits a physician who has a financial relationship, or who has an immediate family member who has a financial relationship, with entities providing Designated Health Services (“DHS”) from referring Medicare patients to such entities for the furnishing of DHS, unless an exception applies. Although uncertainty exists, federal agencies and at least one court have taken the position that the Stark Law also applies to Medicaid.
DHS is defined to include clinical laboratory services, physical therapy services, occupational therapy services, radiology services including magnetic resonance imaging, computerized axial tomography scans, and ultrasound services, radiation therapy services and supplies, durable medical equipment and supplies, parenteral and enteral nutrients, equipment and supplies, prosthetics, orthotics and prosthetic devices and supplies, home health services, outpatient prescription drugs, inpatient and outpatient hospital services and outpatient speech-language pathology services. The types of financial arrangements between a physician and an entity providing DHS that trigger the self-referral prohibitions of the Stark Law are broad and include direct and indirect ownership and investment interests and compensation arrangements. The Stark Law prohibits any entity providing DHS that has received a prohibited referral from presenting, or causing to be presented, a claim or billing for the services arising out of the prohibited referral. Similarly, the Stark Law prohibits an entity from “furnishing” a DHS to another entity in which it has a financial relationship when that entity bills for the service. The prohibition applies regardless of the reasons for the financial relationship and the referral. Unlike the AKS, the Stark Law is a strict liability statute where unlawful intent need not be demonstrated.
If the Stark Law is implicated, the financial relationship must fully satisfy a Stark Law exception. If an exception is not satisfied, then the parties to the arrangement could be subject to sanctions. Sanctions for violation of the Stark Law include denial of payment for claims for services provided in violation of the prohibition, refunds of amounts collected in violation of the prohibition, a civil penalty of up to $25,820 for each service arising out of the prohibited referral, a civil penalty of up to $172,137 against parties that enter into a scheme to circumvent the Stark Law prohibition, civil assessment of up to three times the amount claimed and potential exclusion from the federal healthcare programs, including Medicare and Medicaid. Amounts collected on claims related to prohibited referrals must be reported and refunded generally within 60 days after the date on which the overpayment was identified. Furthermore, Stark Law violations and failure to return overpayments in a timely manner can form the basis for FCA liability, as discussed below.
Our episode of care programs involve a number of arrangements that potentially implicate the Stark Law because they may involve payments between a physician and an entity providing DHS in connection with Medicare patients, including risk sharing and gainsharing arrangements. With respect to BPCI-A and other CMS innovations models in which we may participate, the OIG and CMS jointly issued waivers of certain fraud and abuse laws, including the Stark Law. With respect to our Commercial Episodes of Care program and any other episode of care programs in which we may participate, there are no fraud and abuse waivers that are applicable.
161
Table of Contents
While we have carefully structured these arrangements in accordance with applicable guidance to be in compliance with the fraud and abuse laws, such arrangements are subject to a case-by-case analysis to ensure compliance with the Stark Law.
If the CMS or other regulatory or enforcement authorities determine that claims have been submitted for referrals by us that violate the Stark Law, we would be subject to the penalties described above. In addition, it might be necessary to restructure existing compensation agreements with our doctors and nurse practitioners. Any such penalties and restructuring or other required actions could have a material adverse effect on our business, results of operations, financial condition and cash flows.
In June 2018, the CMS issued a request for information seeking input on how to address any undue regulatory impact and burden of the Stark Law. The CMS placed the request for information in the context of the Regulatory Sprint to Coordinated Care (“Regulatory Sprint”) discussed below and stated that it identified aspects of the Stark Law that pose potential barriers to coordinated care. The CMS thus sought comments on the impact and burden of the Stark Law, including whether it prevents or inhibits care coordination. The CMS has since issued a sweeping set of proposed regulations that introduce significant new value-based terminology, safe harbors and exceptions to the Stark Law. If implemented by the CMS, those or other changes may change the parameters of Stark Law exceptions that we rely on and thus impact our business, results of operations and financial condition.
The definition of DHS under the Stark Law does not include outpatient physician services. Since many services furnished to Medicare beneficiaries provided through our programs are outpatient physician services, our services do not always implicate the Stark Law referral prohibition. However, certain services we may provide, including certain diagnostic testing, may be considered DHS.
Fraud and abuse under state law
Some states have laws prohibiting physicians from having financial interests in or with healthcare facilities to which they refer patients. States also have laws similar to or stricter than the AKS that may affect our ability to enter into financial relationships with certain entities or individuals. Some state anti-kickback laws also include civil and criminal penalties. Some of these laws include exemptions that may be applicable to our physician relationships or for financial interests limited to shares of publicly traded stock. Some, however, may include no explicit exemption for certain types of agreements and/or relationships entered into with physicians. Such laws may be implicated if we expand our services to provide healthcare services directly, as opposed to the purely diagnostic and evaluative services we currently provide.
Similarly, states have beneficiary inducement prohibitions and consumer protection laws that may be triggered by the offering of inducements, incentives and other forms of remuneration to patients and prospective patients. Violations range from civil to criminal and could have a material adverse effect on our business, results of operations and financial condition.
The False Claims Act
The FCA is a means of policing false bills or false requests for payment in the healthcare delivery system. Among other things, the FCA authorizes the imposition of up to three times the government’s damages and significant per claim civil penalties on any “person” (including an individual, organization or company) who, among other acts:
| • | knowingly presents or causes to be presented to the federal government a false or fraudulent claim for payment or approval; |
| • | knowingly makes, uses or causes to be made or used a false record or statement material to a false or fraudulent claim; |
162
Table of Contents
| • | knowingly makes, uses or causes to be made or used a false record or statement material to an obligation to pay the government, or knowingly conceals or knowingly and improperly avoids or decreases an obligation to pay or transmit money or property to the federal government; or |
| • | conspires to commit the above acts. |
In addition, amendments to the FCA and Social Security Act impose severe penalties for the knowing and improper retention of overpayments collected from government payors. Under these provisions, within 60 days of identifying and quantifying an overpayment, a healthcare provider is required to notify the CMS or the Medicare Administrative Contractor of the overpayment and the reason for it and return the overpayment. An overpayment impermissibly retained could subject us to liability under the FCA, exclusion from government healthcare programs and penalties under the federal Civil Monetary Penalty statute. As a result of these provisions, our procedures for identifying and processing overpayments may be subject to greater scrutiny.
The penalties for a violation of the FCA range from $5,500 to $11,000 (amounts not adjusted for inflation) for each false claim, plus up to three times the amount of damages caused by each false claim, which can be as much as the amounts received directly or indirectly from the government for each such false claim. On June 19, 2020, the Department of Justice issued a final rule announcing adjustments to FCA penalties, under which the per claim penalty range increased to a range from $11,665 to $22,331 for penalties assessed after June 19, 2020, so long as the underlying conduct occurred after November 2, 2015.
The federal government has used the FCA to prosecute a wide variety of alleged false claims and fraud allegedly perpetrated against Medicare and state healthcare programs, including but not limited to coding errors, billing for services not rendered, the submission of false cost or other reports, billing for services at a higher payment rate than appropriate, billing under a comprehensive code as well as under one or more component codes included in the comprehensive code, billing for care that is not considered medically necessary and intentionally reporting of inaccurate risk-adjusted diagnostic codes to Medicare Advantage plans. The ACA provides that claims tainted by a violation of the AKS are false for purposes of the FCA. Some courts have held that filing claims or failing to refund amounts collected in violation of the Stark Law can form the basis for liability under the FCA. In addition to the provisions of the FCA, which provide for civil enforcement, the federal government can use several criminal statutes to prosecute persons who are alleged to have submitted false or fraudulent claims for payment to the federal government. Any allegations or findings that we have violated the FCA could have a material adverse impact on our business, results of operations and financial condition.
In addition to the FCA, the various states in which we operate have adopted their own analogs of the FCA. States are becoming increasingly active in using their false claims laws to police the same activities listed above, particularly with regard to Medicaid fee-for-service and Managed Medicaid programs.
Civil Monetary Penalties Statute
The Civil Monetary Penalties Statute, 42 U.S.C. § 1320a-7a, authorizes the imposition of civil monetary penalties, assessments and exclusion against an individual or entity based on a variety of prohibited conduct, including, but not limited to:
| • | presenting, or causing to be presented, claims for payment to Medicare or other federal healthcare programs that the individual or entity knows or should know are for an item or service that was not provided as claimed or is false or fraudulent; |
| • | offering remuneration to a Medicare or Medicaid program beneficiary that the individual or entity knows or should know is likely to influence the beneficiary to order or receive healthcare items or services from a particular healthcare provider; |
| • | arranging contracts with an entity or individual excluded from participation in the federal healthcare programs; |
163
Table of Contents
| • | violating the AKS; |
| • | being involved in a hospital or a critical access hospital knowingly making a payment, directly or indirectly, to a physician as an inducement to reduce or limit medically necessary services provided with respect to Medicare or Medicaid patients who are under the direct care of the physician; |
| • | making, using or causing to be made or used a false record or statement material to a false or fraudulent claim for payment for items and services furnished under a federal healthcare program; |
| • | making or causing to be made any false statement, omission or misrepresentation of a material fact in any application, bid or contract to participate or enroll as a provider of healthcare services or a supplier under a federal healthcare program, including MAOs and entities that apply to participate as healthcare providers of services or suppliers in such managed care organizations and such plans; and |
| • | failing to report and return an overpayment owed to the federal government. |
Our episodes of care programs involve a number of arrangements that potentially implicate aspects of the Civil Monetary Penalties Statute because they may involve payments intended to influence behavior of physicians relative to Medicare and other federal healthcare program beneficiaries, including risk sharing and gainsharing arrangements, that could be found to violate the AKS or the prohibition against hospitals making payments to physicians to reduce or limit medically necessary services. With respect to BPCI-A and other CMS innovations models in which we may participate, the OIG and CMS jointly issued waivers of certain fraud and abuse laws, including the Civil Monetary Penalties Statute. With respect to our Commercial Episodes of Care program and any other episode of care programs in which we may participate, there are no fraud and abuse waivers that are applicable. While we have carefully structured these arrangements in accordance with applicable guidance to be in compliance with the fraud and abuse laws, such arrangements are subject to a case-by-case analysis in light of the intent of the parties and the overall potential for abuse.
Substantial civil monetary penalties may be imposed under the federal Civil Monetary Penalty Statute and may vary depending on the underlying violation. In addition, an assessment of not more than three times the total amount claimed for each item or service may also apply and a violator may be subject to exclusion from federal and state healthcare programs.
We could be exposed to a wide range of allegations to which the federal Civil Monetary Penalty Statute would apply. We perform checks on our providers, our customers’ members, healthcare provider organizations, patients and certain affiliates and vendors using government databases to confirm that these individuals have not been excluded from federal programs. However, should an individual become excluded and we fail to detect it, a federal agency could require us to refund amounts attributable to all claims or services performed or sufficiently linked to an excluded individual. Thus, we cannot foreclose the possibility that we will face allegations subject to the Civil Monetary Penalty Statute with the potential for a material adverse impact on our business, results of operations and financial condition.
State corporate practice of medicine and fee splitting laws
We are subject to various state laws and regulations that regulate the corporate practice of medicine and fee splitting. The corporate practice of medicine doctrine generally prohibits corporate entities from practicing medicine or employing physicians (and, in some cases, other providers) to provide professional medical services. The doctrine reflects a variety of historical public policy concerns, including concerns that (a) allowing corporations to practice medicine or employ physicians will result in the commercialization of the practice of medicine, (b) a corporation’s obligation to its shareholders may not align with a physician’s obligation to his/her patients and (c) employment of a physician by a corporation may interfere with the physician’s independent medical judgment. While most (but not all) states have some form of the corporate practice of medicine doctrine, the scope and enforcement varies widely. In those states where the doctrine exists, it typically arises from the state’s medical practice act, but has been shaped over the years by state statutes, regulations, court decisions, attorney general opinions and actions by state medical licensing boards.
164
Table of Contents
Historically, the medical profession has recognized an ethical prohibition against physicians (and often other providers) paying professional peers and others for referrals. One form this has taken is the prohibition against fee splitting. Fee splitting occurs when a physician splits part of the professional fee earned from treating a referred patient in order to generate the referral. Among the public policy harms that have been cited in support of fee splitting prohibitions are (a) unnecessary operations and procedures, (b) incompetent specialists and (c) unnecessary medical services. Fee splitting prohibitions are aimed primarily at situations where a healthcare professional, in order to generate patient referrals from other licensed or unlicensed persons, splits part of the professional fee earned from treating the referred patient with the source of the referral. In response to legitimate concerns, states adopted prohibitions against fee splitting. Some of these prohibitions, however, reach far broader than necessary to deter this behavior and instead prohibit appropriate business relationships with entities that are not healthcare providers, such as billing agencies or management companies. States have taken a variety of legislative approaches to fee splitting, from near complete bans to bans with various exceptions to no prohibition at all. Depending on the approach that a particular state has taken, fee splitting laws may implicate a variety of otherwise legitimate activities such as management and billing companies.
Despite the existence of various state corporate practice of medicine and fee splitting laws, it is possible to develop legal structures that comply with these laws. The “captive” or “friendly” professional corporation model allows a legal entity (typically a professional corporation or professional limited liability company) whose shareholders are all physicians to employ the physicians (and other providers). The physician entity then contracts with a corporate entity referred to as a Management Services Organization, or “MSO,” to provide various management services. The physician entity is kept “friendly” through a stock transfer restriction agreement and/or other relationship between the MSO and the physician owners of the professional corporation. The fees under the management services arrangement must be carefully structured to comply with state fee splitting laws, which in some states may prohibit percentage-based fees.
Provider licensure and telehealth laws
We utilize the services of a variety of providers, including physicians, nurse practitioners, physician’s assistants, pharmacists and nurses, among others. States generally require providers providing professional healthcare services, whether in person or via telehealth, to a patient residing within the state to be licensed in that state. States have established a variety of licensing and other regulatory requirements around the provision of telehealth services. States also require notification of certain material events be provided to licensing agencies. These licensure requirements vary from state to state. We have established systems for ensuring that our providers are appropriately licensed under applicable state law and that their provision of telehealth to our members occurs in each instance in compliance with applicable laws and regulations governing telehealth. Failure to comply with these laws and regulations could result in licensure actions against the providers as well as civil, criminal or administrative penalties against the providers and/or those engaging the services of the provider.
Privacy and security
We are subject to federal and state laws and regulations that protect the use and disclosure of certain types of data. These include the federal regulations promulgated under the authority of HIPAA require us to provide certain protections to individuals and their health information. Further all 50 states and certain territories maintain additional laws regulating the privacy and security of PII. The HIPAA privacy and security regulations extensively regulate the use and disclosure of PHI and require covered entities, which include healthcare providers, and their business associates to implement and maintain administrative, physical and technical safeguards to protect the security of such information. Additional security requirements apply to electronic PHI. These regulations also provide individuals with substantive rights with respect to their health information.
The HIPAA privacy and security regulations also require us to enter into written agreements with our customers as the “covered entities” and our subcontractors, also known as business associates, to whom we
165
Table of Contents
disclose PHI. Covered entities and business associates may be subject to penalties for, among other activities and compliance issues, failing to enter into a business associate agreement where required by law or as a result of a business associates (including subcontractors) violating HIPAA. Business associates are also directly subject to liability under certain HIPAA privacy and security regulations.
Covered entities must notify affected individuals of breaches of unsecured PHI without unreasonable delay but no later than 60 days after discovery of the breach, and such timelines are generally shortened under state law obligations and standard practice when possible. If a business associate is acting as an agent of a covered entity, then the covered entity must provide the required notifications to individuals based on the time when the business associate discovered the breach. Reporting must also be made to the HHS OCR and, for breaches of unsecured PHI involving more than 500 residents of a state or jurisdiction, to the media. Generally impermissible uses or disclosures of unsecured PHI are presumed to be breaches unless the covered entity or business associate establishes that there is a low probability the PHI has been compromised. Various state laws and regulations may also require us to notify affected individuals in the event of a data breach involving personal information without regard to the probability of the information being compromised.
Violations of HIPAA by entities like us, including, but not limited to, failing to implement appropriate administrative, physical and technical safeguards, have resulted in enforcement actions and in some cases triggered settlement payments or civil monetary penalties. Penalties for violations of HIPAA and its implementing regulations have widely ranged, with larger breaches for some organizations ranging from a couple million dollars to a $16 million penalty for one breach. HIPAA also authorizes state attorneys general to enforce the law on behalf of their residents. In addition, HIPAA provides for criminal penalties of up to $250,000 and ten years in prison, with the severest penalties for obtaining and disclosing PHI with the intent to sell, transfer or use such information for commercial advantage, personal gain or malicious harm. Further, state attorneys general may bring civil actions seeking either injunction or damages in response to violations of the HIPAA privacy and security regulations that threaten the privacy of state residents. There can be no assurance that we will not be the subject of an investigation (arising out of a reportable breach incident, audit or otherwise) alleging noncompliance with HIPAA regulations in our maintenance of PHI. States attorneys general may also negotiate settlements for related cases and on behalf of their respective residents.
In addition to HIPAA, numerous state and federal laws and regulations govern the collection, dissemination, use, privacy, confidentiality, security, availability, integrity, creation, receipt, transmission, storage, and other processing of PHI and PII. Privacy and data security statutes and regulations vary from state to state, and these laws and regulations in many cases are more restrictive than, and may not be preempted by, HIPAA and its implementing rules. These laws and regulations include 42 C.F.R. Part 2, including the CCPA, and a range of other laws that protect data pertaining to specific conditions, such as HIV/AIDS, genetic disorders, and mental and behavioral health. The requirements of the CCPA are potentially far-reaching and may require us to modify certain policies and practices regarding the collection, use, processing and sharing of certain personal information. Privacy and data security laws and regulations are often uncertain, contradictory and subject to change or differing interpretations. The complex, dynamic legal landscape regarding privacy, data protection and information security creates significant compliance challenges for us, potentially restricts our ability to collect, use and disclose data, and exposes us to additional expense, and, if we cannot comply with applicable laws in a timely manner or at all, adverse publicity, harm to our reputation, and liability.
Telecommunications and telemarketing laws
We are subject to a variety of federal and state laws that regulate telecommunications and telemarketing activities, including the following.
The TCPA places restrictions on making certain telemarketing calls, non-telemarketing calls, faxes, and SMS text messages to consumers. Prior express consent of consumers may be required to override certain activities prohibited under the TCPA. The scope and interpretation of the TCPA, and other laws that are or may
166
Table of Contents
be applicable to making calls and delivering SMS text messages to consumers, are continuously evolving and developing. TCPA violations may be subject to penalties of $500 per violation and $1,500 for each willful or knowing violation. Recent expansion of the law through the Telephone Robocall Abuse Criminal Enforcement and Deterrence (“TRACED”) Act expanded the authority of the Federal Communications Commission (“FCC”) to impose civil penalties of up to $10,000 per call for intentional violations of federal robocall laws and increased the time period that the FCC can take action to against those who intentionally violate federal law to four years. This penalty is in addition to other penalties for TCPA violations.
The CAN-SPAM Act regulates commercial email messages. It prohibits the inclusion of deceptive or misleading information and subject headings and requires identifying information such as a return address in email messages. The CAN-SPAM Act also specifies penalties for the transmission of commercial email messages that do not comply with certain requirements, such as providing an opt-out mechanism for stopping future emails from senders.
Healthcare reform
In March 2010, broad healthcare reform legislation was enacted in the United States through the ACA. The ACA substantially changed the way healthcare is financed by both commercial and government payors and contains a number of provisions that impact our business and operations. Although many of the provisions of the ACA did not take effect immediately and continue to be implemented, and some have been and may be modified before or during their implementation, the reforms could continue to have an impact on our business in a number of ways. We cannot predict how employers, private payors or persons buying insurance might react to federal and state healthcare reform legislation, whether already enacted or enacted in the future.
Other aspects of the ACA may also affect our business, including provisions that impact the Medicare and Medicaid programs. These and other provisions of the ACA remain subject to ongoing uncertainty due to administrative actions and executive orders during the current Administration, as well as continuing political and legal challenges at both the federal and state levels. Since 2016, various administrative and legislative initiatives have been implemented that have had adverse impacts on the ACA and its programs. For example, in October 2017, the federal government announced that cost-sharing reduction payments to insurers would end, effective immediately, unless Congress appropriated the funds, and, in December 2017, Congress passed the Tax Cuts and Jobs Act, which includes a provision that reduces to $0 the penalty under the ACA’s individual mandate for individuals who fail to obtain a qualifying health insurance plan and could impact the future state of the exchanges. Moreover, in February 2018, Congress passed the Bipartisan Budget Act (the “BBA”) which, among other things, repealed the Independent Payment Advisory Board that was established by the ACA and intended to reduce the rate of growth in Medicare spending by extending sequestration cuts to Medicare payments through fiscal year 2027. The Coronavirus Aid, Relief, and Economic Security Act (the “CARES Act”), which was signed into law on March 27, 2020, included a temporary suspension of the 2% sequestration cuts from May 1, 2020 through December 31, 2020. The Consolidated Appropriations Act, 2021, extended the temporary suspension through March 31, 2021. The CARES Act also postponed the sunset of sequestration as it applies to Medicare to the end of 2030. The BBA also included provisions to expand the scope of benefits that Medicare Advantage plans may offer for certain chronically ill federal healthcare program beneficiaries beginning in 2020. Medicare Advantage plans now have the flexibility to target non-primarily health-related supplemental benefits to beneficiaries with chronic illnesses and to address social and environmental factors that may impact beneficiary health.
Since its enactment, there have been judicial and congressional challenges to certain aspects of the ACA, as well as efforts by the Trump Administration to repeal or replace certain aspects of the ACA, and we expect such challenges and amendments to continue. For example, the TCJA includes a provision reducing to $0, effective January 1, 2019, the tax-based shared responsibility payment imposed by the ACA on certain individuals who fail to maintain qualifying health coverage for all or part of a year that is commonly referred to as the “individual mandate.” On December 14, 2018, a U.S. District Court Judge in the Northern District of Texas, ruled that the
167
Table of Contents
individual mandate is a critical and inseverable feature of the ACA, and therefore, because it was modified under the TCJA, the remaining provisions of the ACA are invalid as well. On December 18, 2019, the U.S. Court of Appeals for the Fifth Circuit upheld the District Court ruling that the individual mandate was unconstitutional and remanded the case back to the District Court to determine whether the remaining provisions of the ACA are invalid as well. On March 2, 2020, the United States Supreme Court granted the petitions for writs of certiorari to review this case, and the Court held oral argument on November 10, 2020. The case is expected to be decided by mid-2021. It is unclear how this decision, and other efforts to challenge, repeal or replace the ACA will impact the ACA or our business. It is likely that there will be additional challenges and amendments to the ACA in the future.
While there may be significant changes to the healthcare environment in the future, the specific changes and their timing are not yet apparent. As a result, there is considerable uncertainty regarding the future with respect to the exchanges and other core aspects of the current health care marketplace. Future elections may create conditions for Congress to adopt new federal coverage programs that may disrupt our current revenue streams both from payors and other government programs. While specific changes and their timing are not yet apparent, such changes could lower our reimbursement rates or increase our expenses. Any failure to successfully implement strategic initiatives that respond to future legislative, regulatory, and executive changes could have a material adverse effect on our business, results of operations and financial condition.
The CMS and state Medicaid agencies also routinely adjust the RAF which is central to payment under Medicare Advantage programs in which our customers participate. The monetary “coefficient” values associated with diseases that our customers manage in their member populations are subject to change by the CMS and state agencies. Such changes could have a material adverse effect on our financial condition.
Regulatory Sprint to Coordinated Care
In an effort to help accelerate the transformation of the U.S. healthcare system from a fee-for-service to a value-based system, HHS launched its Regulatory Sprint initiative in 2018. The effort encompasses a number of federal statutes and regulations, including:
| • | Stark Law |
| • | AKS |
| • | Civil Monetary Penalties Statute |
| • | Privacy and Security of Health Information |
As part of HHS’s Regulatory Sprint, the OIG issued a request for information in August 2018 seeking input on regulatory provisions that may act as barriers to coordinated care or value-based care. Specifically, the OIG sought to identify ways in which it might modify or add new safe harbors to the AKS as well as exceptions to the definition of “remuneration” in the beneficiary inducements provision of the Civil Monetary Penalty statute in order to foster arrangements that promote care coordination and advance the delivery of value-based care, while also protecting against harms caused by fraud and abuse. Numerous federal agencies have requested comments and information from the public and have published proposed regulations as part of the Regulatory Sprint on areas that have historically been viewed as barriers to innovative care coordination arrangements. For example, the OIG and CMS each issued a sweeping set of proposed regulations that introduce significant new value-based terminology, safe harbors and exceptions to the AKS and the Stark Law. Additionally, the OIG has called for comments and issued proposed regulations related to modernizing the civil monetary penalty law governing inducements provided to Medicare and Medicaid beneficiaries. The OCR is also involved, and has called for information from the public regarding ways that the HIPAA regulations could be modernized to support coordinated, value-based care.
Additionally, the Substance Abuse and Mental Health Services Administration (“SAMHSA”) published proposed regulations related to the privacy of substance use disorder treatment records, and the CMS published
168
Table of Contents
proposals to revise its Stark advisory opinion process. On July 15, 2020, SAMHSA issued a final rule on the protection of substance use disorder (“SUD”) treatment records under 42 C.F.R. Part 2 (the “Part 2 Rule”). The Part 2 final rule aims to reduce delays and burdens in care coordination by more closely aligning Part 2 with the HIPAA Privacy Rule, while maintaining certain privacy protections specific to Part 2. This final rule became effective August 14, 2020. Also of note, under the CARES Act Congress itself made significant modifications to the authorizing statute for the Part 2 regulations, with the aim of aligning the Part 2 laws more strongly with the HIPAA privacy rule. The law directs the Secretary of HHS to revise the Part 2 regulations such that the amendments would apply to uses and disclosures of SUD records the date that is 12 months after the date of enactment of the CARES Act.
These changes in federal regulations are anticipated to have a significant impact on healthcare providers and other stakeholders. In addition, we anticipate that additional changes will continue to be proposed in the future. Many of the solutions we offer in our Episodes of Care Services segment focus on encouraging collaboration among provider partners and the sharing of accountability in order to improve medical outcomes. As a result, these changes could have a material effect on our business. Based on the proposed regulations, the effect appears to be largely positive but the full effect of these regulations will not be known until the final regulations are promulgated. When (and if) such regulations will be promulgated is unknown.
Other regulations
Our operations are subject to various state hazardous waste and non-hazardous medical waste disposal laws. These laws do not classify as hazardous most of the waste produced from medical services. Occupational Safety and Health Administration regulations require employers to provide workers who are occupationally subject to blood or other potentially infectious materials with prescribed protections. These regulatory requirements require employers to make a determination as to which employees may be exposed to blood or other potentially infectious materials and to have in effect a written exposure control plan. In addition, employers are required to provide or employ hepatitis B vaccinations, personal protective equipment and other safety devices, infection control training, post-exposure evaluation and follow-up, waste disposal techniques and procedures and work practice controls. Employers are also required to comply with various record-keeping requirements.
Federal and state law also governs the dispensing of controlled substances by physicians. For example, the Prescription Drug Marketing Act governs the distribution of drug samples. Any allegations or findings that we or our provider partners have violated any of these laws or regulations could have a material adverse impact on our business, results of operations and financial condition.
Employees and human capital resources
Our success depends on our ability to attract, retain and motivate highly qualified personnel. As of September 30, 2020, we had approximately 2,100 employees, of which approximately 1,900 employees were full time. Our employees are based primarily at our offices located in Norwalk, CT, Dallas, TX, New York, NY and Rapid City, SD. We also had nearly 9,000 credentialed physicians and nurse practitioners and other providers within our mobile network that we contract with on an independent contractor basis, either directly or through captive professional affiliates. These credentialed physicians and nurse practitioners form a mobile network of practitioners located all over the country. We consider our relationship with our independent contractors and employees to be good. None of our employees are represented by a labor union or party to a collective bargaining agreement.
We strive to foster an innovative culture as we further build our business and expand our products and services, and we view our human capital-related initiatives as an ongoing priority. Such initiatives include: (i) implementing a robust talent acquisition approach, including through competitive pay and benefits, (ii) implementing our Diversity, Equity and Inclusion initiative and Spirit of Signify programs to promote diversity and foster a sense of connection and community throughout our company, (iii) offering an array of learning and
169
Table of Contents
development opportunities, including live programs and online courses through our learning management system and (iv) conducting annual employee engagement surveys and developing action plans based on the survey outcomes.
Facilities
Our principal offices are located in Norwalk, Connecticut, New York, New York, Dallas, Texas and Rapid City, South Dakota, where we occupy facilities totaling 350,000 square feet. We use these facilities for administration, sales and marketing, technology and development and professional services.
We intend to procure additional space as we add team members and expand geographically. We believe that our facilities are adequate to meet our needs for the immediate future, and that, should it be needed, suitable additional space will be available to accommodate any such expansion of our operations.
Legal proceedings
From time to time, we may be involved in various legal proceedings and subject to claims that arise in the ordinary course of business. Although the results of litigation and claims are inherently unpredictable and uncertain, we are not currently a party to any legal proceedings the outcome of which, if determined adversely to us, are believed to, either individually or taken together, have a material adverse effect on our business, financial condition or results of operations. Regardless of the outcome, litigation has the potential to have an adverse impact on us because of defense and settlement costs, diversion of management resources, and other factors. See “Risk factors—Risks related to our business and operations—We may be subject to legal proceedings and litigation, including intellectual property and privacy disputes, which are costly to defend and could materially harm our business and results of operations.”
170
Table of Contents
Directors and executive officers
Set forth below is certain biographical and other information regarding our directors, after giving effect to the Reorganization Transactions, and our executive officers and key employees. We intend to appoint additional directors prior to the consummation of this offering.
| Name |
Age | Position | ||
| Matthew S. Holt |
44 | Chairman | ||
| Kyle Armbrester |
35 | Chief Executive Officer and Director | ||
| Steven Senneff |
51 | President, Chief Financial and Administrative Officer | ||
| Adam McAnaney |
43 | General Counsel and Secretary | ||
| Marc Rothman, MD |
50 | Chief Medical Officer | ||
| Peter Boumenot |
42 | Chief Product Officer | ||
| David Pierre |
41 | Chief Operating Officer | ||
| Josh Builder |
39 | Chief Technology Officer | ||
| Laurel Douty |
52 | Executive Vice President, Clinical Operations, Episodes of Care Services | ||
| Taj J. Clayton |
44 | Director | ||
| Brandon H. Hull |
60 | Director | ||
| Kevin M. McNamara |
64 | Director | ||
| Albert A. Notini |
63 | Director | ||
| Kyle B. Peterson |
35 | Director | ||
| Vivian E. Riefberg |
60 | Director | ||
| Stephen F. Wiggins |
64 | Director |
Matthew S. Holt has served as Chairman of our Board since December 2017. Mr. Holt serves as a Managing Director and President, Private Equity of New Mountain Capital LLC. Since August 2001, he has focused on growth buyouts across a range of industries including healthcare products, health technology, materials and infrastructure. Mr. Holt currently serves on the board of Avantor, Inc., where he also serves on the Compensation Committee. Mr. Holt serves as Lead Director or Chairman of CIOX Health, Cloudmed, Cytel, Emids, Ontario Systems, W20 and Zep, Inc. He also serves as a Director of Aceto, Topic Pharmaceuticals, and TRC Companies. He previously served as Lead Director of Bellerophon Therapeutics, Inc., Convey Health Solutions, Inc., Equian LLC, Gelest, Ikaria, Inc., Nusil Technology LLC and as a Director of MailSouth. Mr. Holt holds an AB in English and American Literature and Language from Harvard College. Mr. Holt was selected to serve on our board of directors because of his management and advisory experience with various companies in the healthcare industry and his extensive experience in the areas of finance, strategy, international business transactions and mergers and acquisitions.
Kyle Armbrester has served as Chief Executive Officer and a Director of the Company since April 2018. Prior to this, Mr. Armbrester was at athenahealth, where he served as Senior Vice President and Chief Product Officer from May 2015 to April 2018, leading the core product and operations division, and Vice President, Strategy & Corporate Development from May 2011 to May 2015, driving corporate development through strategic partnerships and investments. He has been a Director at The Mentor Network since September 2019 and Parexel International since November 2017. Mr. Armbrester holds an MBA from Harvard Business School and an AB in Government from Harvard University. Mr. Armbrester was selected to serve on our board of directors because of his management experience and expertise in the healthcare sector.
Steven Senneff has served as President and Chief Financial and Administrative Officer of the Company since November 2019. Prior to this, Mr. Senneff served as the Chief Financial Officer of Remedy Partners from March 2019 to November 2019 and as the Chief Financial Officer of DigitalOcean, Inc. from October 2017 to
171
Table of Contents
February 2019, where he was responsible for all of the accounting and finance activities at the respective companies. At Cotiviti, Inc., he served as Chief Financial Officer from October 2012 to April 2014 and from May 2015 to September 2017, where he was responsible for all of Cotiviti’s accounting and finance activities and part of the leadership team that took the company public, and Chief Operating Officer from May 2014 to April 2015, where he focused on growth opportunities during a post-acquisition integration period. Mr. Senneff holds an MBA from Purdue University, Krannert Graduate School of Management and a BBA in Accounting from the University of Iowa.
Adam McAnaney has served as General Counsel and Secretary of the Company since its acquisition of Remedy Partners in November 2019. He joined Remedy Partners as General Counsel and Secretary in June 2019. Prior to joining Remedy Partners, Mr. McAnaney was at Aetna where he served as Vice President, Head of Corporate Legal and Corporate Secretary from November 2017 to March 2019, overseeing legal support of SEC reporting and disclosure matters, corporate finance, mergers and acquisitions, subsidiary management, licensing, investments, executive compensation and human resources. Mr. McAnaney previously held the positions of Senior Corporate Counsel from May 2013 to October 2017 and Counsel from May 2011 to April 2012 at Aetna. From September 2004 to May 2011, he was an Associate in the New York, Frankfurt and London offices of Sullivan & Cromwell LLP focusing on capital markets and mergers and acquisitions. Mr. McAnaney holds a JD from Columbia Law School and a BA in Germanic Languages and Literatures from Yale University.
Marc Rothman has served as Chief Medical Officer of the Company since June 2020. Prior to this, Dr. Rothman served as Deputy Chief Medical Officer at Aspire Healthcare from May 2019 to June 2020, where he led a nationwide palliative care medical practice and implemented and grew new clinical models and business lines. Before that Dr. Rothman served as Enterprise Chief Medical Officer from January 2015 to December 2018 at Kindred Healthcare, Inc., where he oversaw medical affairs, clinical quality, patient experience and pharmacy services. He also served as the Chief Medical Officer of Kindred’s Nursing Center Division from November 2011 to December 2014, where he eventually led the medical and pharmacy leadership team. Dr. Rothman holds an MD from New York University School of Medicine and a BA in Philosophy from the University of Wisconsin, Madison. He completed his postgraduate clinical training at Yale New Haven Hospital and is triple boarded in Internal, Geriatric and Hospice & Palliative Medicine.
Peter Boumenot has served as Chief Product Officer of the Company since January 2020. Prior to this, Mr. Boumenot served as Senior Vice President, Product & Operations—Signify Community of the Company from August 2019 to January 2020. Prior to this, Mr. Boumenot was at athenahealth for nine years, serving as Vice President, Product Management from October 2017 to July 2019 leading patient engagement, population health and revenue cycle services and prior to that was Vice President, Client Solution Group from March 2014 to October 2017 and Director, Solution Design from March 2012 to March 2014, where he led a comprehensive pre-sale to post-go-live commercial organization of across all business segments. Mr. Boumenot holds a BS in Biology from Boston College.
David Pierre has served as Chief Operating Officer of the Company since December 2017. Prior to this, Mr. Pierre served as Chief Operating Officer of Advance Health from December 2016 to December 2017, where he drove operating scale until its successful sale and merger, which formed Signify Health. Mr. Pierre was at Cerner Corporation from August 2007 to December 2016 in various positions, including Vice President, General Manager and Managing Director, where he led several of Cerner Corporation’s business units, including Hospital Operations and Pediatrics. He is a Fellow of the American College of Healthcare Executives. Mr. Pierre holds an MBA from the University of Chicago Booth School of Business and a BA in Psychology from Southern Methodist University.
Josh Builder has served as Chief Technology Officer of the Company since June 2020. Prior to this, Mr. Builder served as Chief Technology & Product Officer of Rent the Runway from August 2016 to May 2020, where he was responsible for the customer experience, operational expansion, development of supply chain technology and data engineering. Before that, from June 2015 to July 2016, Mr. Builder was the Chief
172
Table of Contents
Technology Officer of Soulcycle where he was responsible for building its technology platform, product organization and customer data analytics. Prior to this, Mr. Builder was at The Orchard, serving as Chief Technology Officer from January 2010 to June 2015 and Vice President and Senior Director, Global Operations, Product Development & Engineering from November 2006 to January 2010, where he led its product management operations, mergers and acquisitions functions and go-private transaction. Mr. Builder holds a BA in Computer Information & Decision Systems & Financial Economics from Carnegie Mellon University.
Laurel Douty has served as Executive Vice President, Clinical Operations, Episodes of Care Services of the Company since February 2020. Prior to this, Ms. Douty was an independent consultant from January 2019 to February 2020 focused on designing and implementing a clinical managed care infrastructure for a large private equity-owned vision company. Prior to her independent consulting, Ms. Douty was at Magellan Health for almost 11 years with increasing responsibilities during her tenure. Ms. Douty started at Magellan Health in the specialty division from March 2008 to June 2015, progressing to Chief Operating Officer and Senior Vice President of Clinical and Service Operations. From July 2015 through December 2018, Ms. Douty’s role was expanded to Chief Operating Officer and Chief Experience Officer for the broader Magellan Health Care division, which included the following segments: Specialty Medical/Surgical, Behavioral Health, Employee Assistance Programs, ACO and provider care coordination, Medicaid/Medicare health plan and specialty pharmacy claims. Ms. Douty’s operational management during her tenure at Magellan included direct leadership of service and clinical operations, network contracting and network operations management, claims payment and payment integrity, innovation and implementation PMO, and divisional capital expenditure management. Ms. Douty holds a BA in Political Science from the University of Texas at Arlington.
Taj J. Clayton has served as a Director of the Company since July 2020. Mr. Clayton has served as a member of the Executive Advisory Council of New Mountain Capital since July 2020. Since September 2020, Mr. Clayton has served as a Partner at Kirkland & Ellis LLP. Prior to this, from March 2017 to August 2020, he was a Partner at Winston & Strawn, LLP. From September 2006 to December 2013, he was an Associate, and from January 2014 to March 2017, a Principal, at Fish & Richardson P.C. From September 2005 to September 2006, Mr. Clayton served as a Law Clerk to Chief Judge Mark L. Wolf in the United States Federal District Court of Massachusetts. Mr. Clayton is a member of the President’s Advisory Board for UT Southwestern Medical Center, a Member of the Board for the International Institute for Conflict Prevention and Resolution, a Member of the National Board of Directors for Girls Inc., a Member of the Board of the Hockaday School and a Member of the Advisory Board for the Coalition of Black Excellence. Mr. Clayton holds a JD from Harvard Law School and an AB in History from Harvard University. Mr. Clayton was selected to serve on our board of directors because of his extensive professional experience working with a variety of successful companies and previous board member experience.
Brandon H. Hull has served as a Director of the Company since April 2018. Since February 2018, Mr. Hull has served as an Industry Advisor for New Mountain Capital. Prior to this, from September 1996 to December 2017, he was the Managing General Partner and Co-Founder of Cardinal Partners. He has served on the Board of Asylon Aerospace since September 2015 and served on the Board of athenahealth as Lead Director from August 1999 to January 2019. He has also previously served as a Director of Equian, Sapphire Digital, Ivenix, QPID, Inc., Cureatr and CodeRyte, among many others. Mr. Hull holds an MBA from the Wharton School of the University of Pennsylvania and a BA in Literature & Philosophy from Wheaton College. Mr. Hull was selected to serve on our board of directors because of his extensive expertise in the healthcare sector and his management experience as a director of numerous companies.
Kevin M. McNamara has served as a Director of the Company since April 2013. He previously served as the Chief Executive Officer of CenseoHealth from February 2015 to June 2018. Mr. McNamara has served as the Founding Principal at McNamara Family Ventures since June 2012. From April 2013 to October 2014, he was an Operating Partner at Health Evolution Partners. He has been a Director of Tyson Foods, Inc. since August 2007 and currently serves as the Vice Chairman and Lead Independent Director. He has served as a Director of Luminex Corporation since May 2003. Mr. McNamara previously served on the Board of Leon Medical Centers,
173
Table of Contents
Agilum Healthcare Intelligence and Optimal Radiology Partners. Mr. McNamara holds a BS in Accounting from Virginia Commonwealth University and an MBA from the University of Richmond. Mr. McNamara was selected to serve on our board of directors because of his financial expertise and management experience as both a principal financial officer and director of public companies.
Albert A. Notini has served as a Director of the Company since December 2017. Since January 2012, he has served as a Managing Director at New Mountain Capital. Prior to this, he was the Chairman and Chief Executive Officer of Apptis Inc. from March 2007 to June 2011. From April 2004 to August 2007, he was the President and Chief Operating Officer of Sonus Networks, Inc. Mr. Notini currently serves as a Director of Western Dental, CIOX Health, Alteon Health, Sparta Systems, Emids and MAG Aerospace. Mr. Notini holds a JD from Boston College Law School, a MA from Boston University and a BA from Boston College. Mr. Notini was selected to serve on our board of directors because of his management experience as both an executive officer and director of various companies.
Kyle B. Peterson has served as Director of the Company since December 2017. He serves as a Managing Director of New Mountain Capital and has been with the firm since September 2011. Prior to this, he was an investment professional at Sageview Capital from August 2009 to September 2011. Prior to Sageview, Mr. Peterson worked in the Mergers and Acquisitions group at Merrill Lynch from June 2006 to July 2009. He currently serves as Chairman of the Board of Directors of Cytel since November 2017, as a Director on the board of Horizon Services since November 2019, and formerly served on the boards of Equian from November 2015 to July 2019 and Remedy Partners from January 2019 to November 2019. Mr. Peterson received his B.S. from Cornell University. Mr. Peterson was selected to serve on our board of directors because of his expertise in investment strategy and mergers and acquisitions and his management experience as both an executive officer and director of various companies.
Vivian E. Riefberg has served as a Director of the Company since February 2020. Since August 2020, she has served as the David C. Walentas Jefferson Scholars Foundation Professorship Chair and is a Professor of Practice at the University of Virginia Darden School of Business. Prior to this, from September 1987 to May 2020, Ms. Riefberg was at McKinsey & Company and held a variety of senior positions, including leading the Public Sector Practice for the Americas and co-leading the U.S. Health Care practice. She currently serves as an Emeritus Director and Senior Advisor with McKinsey & Company since June 2020. In 2018, Ms. Riefberg was elected as a Director to the board of the Public Broadcasting Service. She also serves on the board of Johns Hopkins Medicine since July 2020. She was previously on the Board of Governors for the NIH Clinical Center and was a Director on the boards for the Partnership for a Healthier America, Mentors, Inc. and McKinsey & Company. Ms. Riefberg holds an MBA from Harvard Business School and a BA in History from Harvard University. Ms. Riefberg was selected to serve on our board of directors because of her healthcare expertise across both public and private sectors and her management experience.
Stephen F. Wiggins has served as a Director of the Company since November 2019. Mr. Wiggins is an entrepreneur and private investor. Since May 2018, he has served as the Founder and Chairman of Wiggins Ventures. From September 2011 to January 2019, he was the Founder and Chairman of Remedy Partners. From March 2008 to August 2019, he was a Managing Director at EW Healthcare Partners. He was previously the Founder, Chairman and CEO of HealthMarket from September 1999 to April 2004 and Oxford Health Plans from September 1984 to December 2000. Mr. Wiggins holds an MBA from Harvard Business School and a BA in Urban Studies from Macalester College. Mr. Wiggins was selected to serve on our board of directors because of his management experience as a founder and chairman of numerous healthcare companies.
Board structure
Upon completion of the offering, our board of directors will consist of nine members. Our board has determined that each of Matthew S. Holt, Albert A Notini, Kyle B. Peterson, Brandon H. Hull, Vivian E. Riefberg and Taj J. Clayton is independent under applicable NYSE rules.
174
Table of Contents
In connection with this offering, we will amend and restate our certificate of incorporation to provide for a classified board of directors following this offering. Our board of directors will be divided into three classes with staggered three-year terms, with three directors in Class I (expected to be Matthew S. Holt, Kyle B. Peterson and Stephen F. Wiggins), three directors in Class II (expected to be Brandon H. Hull, Kevin M. McNamara and Albert A. Notini) and three directors in Class III (expected to be Kyle Armbrester, Taj J. Clayton and Vivian E. Riefberg). Successors to the class of directors whose term expires at the first and second annual meetings of stockholders following the adoption of the certificate of incorporation, as applicable, will be elected for a term expiring at the third annual meeting following the annual meeting at which such directors were elected.
Our board of directors will have discretion to determine the size of the board of directors. Subject to the terms of the stockholders agreement, we expect that any additional directorships resulting from an increase in the number of directors will be distributed among the three classes so that, as nearly as possible, each class will consist of one third of the directors. The division of our board of directors into three classes with staggered three-year terms may delay or prevent a change of our management or a change in control. See “Description of capital stock—Anti-takeover effects of our certificate of incorporation, stockholders agreement and bylaws—Classified board; election of directors.”
Controlled company exception
After the consummation of this offering, a group of Pre-IPO LLC Members comprised of entities affiliated with New Mountain Capital will, in the aggregate, beneficially own more than 50% of the voting power for the election of members of our board of directors. As a result, we will be a “controlled company” within the meaning of the NYSE rules and may elect not to comply with certain corporate governance standards, including that (i) a majority of our board of directors consists of “independent directors,” as defined under the NYSE rules; (ii) the nominating and corporate governance committee be composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; and (iii) the compensation committee be composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities. We intend to rely on certain of the foregoing exemptions provided to controlled companies under the NYSE rules. Therefore, immediately following the consummation of this offering, a majority of our directors will not be “independent.” In addition, although we have opted to have a compensation committee and a nominating and governance committee, such committees will not be fully independent. Accordingly, to the extent and for so long as we rely on these exemptions, you will not have the same protections afforded to stockholders of companies that are subject to all of these corporate governance requirements. In the event that we cease to be a “controlled company” and our Class A common stock continues to be listed on the NYSE, we will be required to comply with these provisions within the applicable transition periods.
Board committees
Upon the consummation of this offering, our board of directors will have four standing committees: an Audit Committee, a Nominating and Corporate Governance Committee, a Compensation Committee and a Corporate Development Committee. The following is a brief description of our committees.
Audit Committee
The members of our Audit Committee are Kevin M. McNamara, Taj J. Clayton and Kyle B. Peterson. Kevin M. McNamara is the chairman of our Audit Committee. Taj J. Clayton meets the requirements for independence under the current NYSE listing standards and SEC rules and regulations. We expect to appoint two new independent directors to the audit committee within the applicable timeframe required by the NYSE and the SEC and that the composition of our audit committee will satisfy the independence requirements of the NYSE and the SEC within the applicable timeframe. Each member of our Audit Committee is financially literate. In addition, our board of directors has determined that Kevin M. McNamara and Kyle B. Peterson each qualify as an “audit committee financial expert” as defined in Item 407(d)(5)(ii) of Regulation S-K promulgated under the Securities Act of 1933, as amended (the “Securities Act”). This designation does not impose on him any duties, obligations
175
Table of Contents
or liabilities that are greater than are generally imposed on members of our Audit Committee and our board of directors. Our Audit Committee is directly responsible for, among other things:
| • | selecting a firm to serve as the independent registered public accounting firm to audit our financial statements; |
| • | ensuring the independence of the independent registered public accounting firm; |
| • | discussing the scope and results of the audit with the independent registered public accounting firm and reviewing, with management and that firm, our interim and year-end operating results; |
| • | establishing procedures for employees to anonymously submit concerns about questionable accounting or audit matters; |
| • | considering the adequacy of our internal controls and internal audit function; |
| • | reviewing material related party transactions or those that require disclosure; and |
| • | approving or, as permitted, pre-approving all audit and non-audit services to be performed by the independent registered public accounting firm. |
Compensation Committee
The members of our Compensation Committee are Matthew S. Holt, Kevin M. McNamara and Albert A. Notini. Matthew S. Holt is the chairman of our Compensation Committee. Each of Matthew S. Holt and Albert A. Notini meets the requirements for independence under the current NYSE listing standards and SEC rules and regulations. Our Compensation Committee is responsible for, among other things:
| • | reviewing and approving, or recommending that our board of directors approve, the compensation of our executive officers; |
| • | reviewing and recommending to our board of directors the compensation of our directors; |
| • | administering our stock and equity incentive plans; |
| • | reviewing and approving, or making recommendations to our board of directors with respect to, incentive compensation and equity plans; and |
| • | reviewing our overall compensation philosophy. |
Nominating and Governance Committee
The members of our Nominating and Governance Committee are Matthew S. Holt, Kyle B. Peterson and Vivian E. Riefberg. Matthew S. Holt is the chairman of our Nominating and Governance Committee. Matthew S. Holt, Kyle B. Peterson and Vivian E. Riefberg all meet the requirements for independence under the current NYSE listing standards. Our Nominating and Governance Committee is responsible for, among other things:
| • | identifying and recommending candidates for membership on our board of directors; |
| • | reviewing and recommending our corporate governance guidelines and policies; |
| • | reviewing proposed waivers of the code of conduct for directors and executive officers; |
| • | overseeing the process of evaluating the performance of our board of directors; and |
| • | assisting our board of directors on corporate governance matters. |
Corporate Development Committee
The members of our Corporate Development Committee are Kyle B. Peterson, Brandon H. Hull and Stephen F. Wiggins. Kyle B. Peterson is the chairman of our Corporate Development Committee. Our Corporate Development Committee is responsible for, among other things, reviewing and approving the acquisitions, dispositions, joint ventures and strategic partnerships and investments of the Company.
176
Table of Contents
Code of ethics
In connection with this offering, our board of directors will adopt a code of ethics that applies to all of our employees, officers and directors, including our Chief Executive Officer, Chief Financial and Administrative Officer, Chief Operating Officer and other executive and senior financial officers. Upon completion of this offering, the full text of our codes of business conduct and ethics will be posted on the investor relations section of our website. We intend to disclose future amendments to our codes of business conduct and ethics, or any waivers of such code, on our website or in public filings.
Compensation committee interlocks and insider participation
None of our executive officers has served as a member of a compensation committee (or if no committee performs that function, the board of directors) of any other entity that has an executive officer serving as a member of our board of directors.
177
Table of Contents
EXECUTIVE AND DIRECTOR COMPENSATION
Executive compensation
The following tables set forth information concerning the compensation paid to or earned by our chief executive officer and our two other most highly compensated executive officers during our fiscal years ended December 31, 2020 and December 31, 2019 (collectively referred to as our “named executive officers” or “NEOs”).
Summary compensation table
| Name and Principal |
Year | Salary ($) |
Bonus ($)(3) | Stock Awards ($)(4) |
Non-Equity Incentive Plan Compensation ($)(5) |
All Other Compensation ($)(6) |
Total ($) | |||||||||||||||||||||
| Kyle Armbrester |
2020 | 604,615 | — | 13,128,663 | 1,200,000 | 17,026 | 14,950,304 | |||||||||||||||||||||
| Chief Executive Officer |
2019 | 600,000 | 4,120,036 | — | 726,000 | 15,641 | 5,461,677 | |||||||||||||||||||||
| Steven Senneff |
2020 | 500,000 | — | 2,010,212 | 800,000 | 8,650 | 3,318,862 | |||||||||||||||||||||
| Chief Financial & Administrative Officer |
2019 | (1) | 50,000 | 142,444 | — | 332,000 | 8,328 | 532,772 | ||||||||||||||||||||
| P. Tad Kendall(2) |
2020 | $ | 424,140 | — | 3,647,527 | 402,500 | 100 | 4,474,267 | ||||||||||||||||||||
| Chief Growth Officer |
||||||||||||||||||||||||||||
| (1) | Mr. Senneff commenced employment with us on November 26, 2019, in connection with the closing of the Remedy Partners Combination. These rows reflect compensation paid by us with respect to his 2019 service following such date. |
| (2) | Mr. Kendall was not a named executive officer in 2019 and his compensation information is therefore only being provided for 2020. Mr. Kendall’s employment with us terminated, effective February 1, 2021, and he will receive the severance payments described below under “—Executive severance arrangements”. |
| (3) | The amounts in this column represent, for 2019, (i) special discretionary bonuses paid to Messrs. Armbrester and Senneff in the first quarter of 2020 in recognition of our financial performance in 2019 and the successful navigation of the Remedy Partners Combination and (ii) a transaction bonus paid to Mr. Armbrester in recognition of the successful completion of the Remedy Partners Combination. |
| (4) | The amounts reported in this column represent the aggregate grant date fair value of the incentive unit awards granted to the named executive officers during 2020, as calculated in accordance with FASB Accounting Standards Codification Topic 718. The assumptions used in calculating the grant date fair value of the incentive unit awards in this column are described in Note 14 to our consolidated financial statements included elsewhere in this prospectus. |
| (5) | Represents (i) for 2020, (A) awards earned by Messrs. Armbrester and Senneff pursuant to our 2020 Cash Incentive Plan, as described below under “—2020 Cash Bonuses” and (B) a bonus of 115% of target payable to Mr. Kendall in connection with his termination of employment with us, as described below under “—Executive severance arrangements”, and (ii) for 2019, (A) awards earned by Messrs. Armbrester and Senneff pursuant to our 2019 Cash Incentive Plan and (B) a performance bonus earned by Mr. Armbrester based on the achievement of predetermined first quarter 2019 EBITDA performance goals. |
| (6) | The amounts in this column represent all other compensation paid to our NEOs in 2020, including (i) 401(k) matching contributions for Messrs. Armbrester and Senneff ($3,288 and $8,550 respectively); (ii) for Mr. Armbrester, $13,638 in Company-paid medical and dental premiums that are not made available to employees generally; and (iii) for Messrs. Armbrester, Senneff and Kendall, a COVID-19-related $100 incentive provided to all employees of the company. |
178
Table of Contents
Employment arrangements
Employment agreements
We have entered into employment agreements with each of our named executive officers (described in further detail below) which generally include the officer’s base compensation, annual bonus opportunity, entitlement to participate in our health and welfare benefit plans and certain restrictive covenants and severance entitlements on qualifying terminations of employment.
Kyle Armbrester
Mr. Armbrester’s employment agreement provides for Mr. Armbrester’s employment, commencing no later than June 18, 2018, as our Chief Executive Officer. Under the employment agreement, which does not have a set employment term, Mr. Armbrester’s initial base salary was set at $600,000 (which may be increased, but not decreased). Mr. Armbrester is eligible to receive an annual performance-based cash bonus having a target opportunity of 100% of base salary and a maximum opportunity of 200% of base salary, payable based on the attainment of one or more performance goals established by the board of directors for the applicable calendar year and at the time designated by the board of directors (or a committee thereof), subject to Mr. Armbrester’s employment through such payment date (except as described below). In addition, the employment agreement provides for a grant of profits interests of which approximately (i) 48% service-vests in quarterly installments over the four-year period following Mr. Armbrester’s start date and (ii) 52% performance-vests based on New Mountain Capital’s achievement of specified multiples of cash-on-cash returns, the terms of which are described under “—Other Compensation Plans; Incentive Units” below. The employment agreement also provides for paid time-off consistent with those provided to other senior executives (with a minimum of four weeks per calendar year), participation in employee benefit plans made available to other executives and a lump sum cash signing bonus equal to $2,000,000.
In the event of a termination of Mr. Armbrester’s employment without Cause or if he resigns for Good Reason (each as defined in the employment agreement), he will be entitled to receive the following severance payments and benefits: (i) a cash payment equal to the sum of then-current base salary and target annual bonus, payable 50% in a lump sum and 50% in equal installments over 12 months, (ii) a lump sum pro-rata bonus for the year of termination (based on actual results for such year), payable at such time bonuses for the year are paid to other executives, (iii) continued participation in group health plans for 18 months at the same expense as if Mr. Armbrester’s employment had continued and (iv) the prior year’s earned but unpaid annual bonus. In the event of a termination without Cause or Mr. Armbrester’s resignation for Good Reason that occurs within 90 days prior to or at any time following a Company Sale (as defined in the employment agreement), Mr. Armbrester will receive (i) a cash payment equal to 150% of the sum of his then-current base salary and target annual bonus, which is payable in a lump sum if the termination occurs within two years after the Company Sale or is otherwise paid 50% in a lump sum and 50% in equal installments over 12 months, and (ii) continued participation in group health plans for 18 months at the same expense as if Mr. Armbrester’s employment had continued. Receipt of severance is subject to Mr. Armbrester’s execution and non-revocation of a release of claims.
Pursuant to his employment agreement, Mr. Armbrester is subject to certain restrictive covenants, including confidentiality (perpetual), non-competition (during employment and for 18 months post-termination), employee non-solicitation and non-hire (during employment and for 18 months post-termination), non-disparagement (mutual and perpetual), investigation cooperation (during employment and for 12 months post-termination) and assignment of intellectual property rights.
Steven Senneff
Mr. Senneff commenced employment with us on November 26, 2019, in connection with the closing of the Remedy Partners Combination. Mr. Senneff’s employment agreement, which was entered into prior to the
179
Table of Contents
Remedy Partners Combination, provides for Mr. Senneff’s employment as Chief Financial Officer of our subsidiary. Under the employment agreement, Mr. Senneff’s initial base salary was set at $500,000. Mr. Senneff is eligible to receive an annual cash bonus having a target opportunity of 80% of base salary, payable based on the attainment of performance goals established by the board of directors, subject to Mr. Senneff’s employment on the payment date (except as described below). In addition, the employment agreement provides for a grant of stock options equal to 1% of the equity of Remedy Partners (which were granted on June 10, 2019 and were converted into stock options to purchase shares of New Remedy Class A common stock, par value $0.001 (“New Remedy Class A Shares”) in connection with the Remedy Partners Combination). The employment agreement also provides for paid time-off consistent with those provided to other executives and managerial employees and participation in employee benefit plans in effect for similarly situated executives.
In the event of a termination of Mr. Senneff’s employment without Cause (as defined in the employment agreement), Mr. Senneff is entitled to receive as severance continued base salary payments for a period of 18 months. Receipt of severance is subject to Mr. Senneff’s execution and the effectiveness of a release of claims.
Pursuant to his employment agreement, Mr. Senneff is subject to certain restrictive covenants, including confidentiality (perpetual), non-competition (during employment and for 18 months post-termination), customer non-solicit (during employment and for 18 months post-termination), employee non-solicitation and non-hire (during employment and for 18 months post-termination), and assignment of intellectual property rights.
P. Tad Kendall
In November 2019, we entered into an employment agreement with Mr. Kendall which provides for Mr. Kendall’s employment commencement on November 11, 2019. The employment agreement provides that Mr. Kendall will serve as our Chief Revenue Officer. Under the employment agreement, Mr. Kendall’s initial base salary was set at $400,000 (which may be increased but not decreased). Mr. Kendall is eligible to receive an annual cash bonus having a target value of $350,000. In addition, Mr. Kendall received a sign-on bonus equal to $250,000 pursuant to his employment agreement. The employment agreement also provides for Mr. Kendall’s participation in employee benefit plans and perquisite and fringe benefit programs made generally available to other executives.
In the event of a termination of Mr. Kendall’s employment without Cause or if he resigns for Good Reason (each as defined in the employment agreement), Mr. Kendall would be entitled to receive the following severance payments and benefits: (i) 12 months continued base salary payments, (ii) a lump sum pro-rata target bonus for the year of termination, payable at such time bonuses for the year are paid to other executives and (iii) the employer portion of the monthly premiums paid under our medical and dental benefit plans for up to 12 months. Receipt of severance is subject to Mr. Kendall’s execution and non-revocation of a release of claims.
Pursuant to his employment agreement, Mr. Kendall is subject to certain restrictive covenants, including confidentiality (perpetual), non-competition (during employment), customer non-solicit (during employment), employee non-solicit and non-hire (during employment and for 12 months post-termination), non-disparagement (perpetual) and assignment of intellectual property rights.
Mr. Kendall’s employment with us terminated effective February 1, 2021. Subject to his execution and non-revocation of a release of claims, Mr. Kendall will receive the severance payments and benefits described above under his employment agreement, and will also receive a bonus amount equal to 115% of target for calendar year 2020.
Restrictive covenant agreements
Each of our NEOs is subject to restrictive covenants as described above under “Employment agreements.” In addition, pursuant to the terms of the stock option agreement relating to the grant to Mr. Senneff of stock options to purchase New Remedy Class A Shares, Mr. Senneff is subject to restrictive covenants regarding
180
Table of Contents
confidentiality (perpetual), non-competition (during employment and for 12 months post-termination), employee non-solicit and non-hire (during employment and for 12 months post-termination), customer non-solicit (during employment and for 12 months post-termination), assignment of intellectual property rights and non-disparagement (perpetual).
In connection with the commencement of employment with us, Messrs. Armbrester and Senneff executed a confidentiality, invention assignment and non-disclosure agreement, which provides for restrictions on confidentiality (perpetual), employee and customer non-solicit and non-hire (during employment and for 12 months post-termination), non-disparagement (perpetual) and assignment of intellectual property rights.
2020 cash bonuses
2020 Cash Incentive Plan
Our named executive officers were eligible to participate in our annual Cash Incentive Plan (“CIP”) for the plan year beginning January 1, 2020 and ending December 31, 2020 (the “2020 CIP”). Under the 2020 CIP, each of our NEOs had a target bonus that was assigned by our compensation committee. Bonuses under the 2020 CIP were payable based on the achievement of the following corporate performance goals: evaluations revenue (25%), non-evaluations revenue (20%), EBITDA (45%) and employee turnover (10%). For 2020, the target bonuses for each of our NEOs were as follows: (i) Mr. Armbrester, $600,000; (ii) Mr. Senneff, $400,000; and (iii) Mr. Kendall, $350,000. For 2020, the 2020 CIP bonuses for Messrs. Armbrester and Senneff were paid out at 200% of target; accordingly, the amounts actually paid were as follows: (i) Mr. Armbrester, $1,200,000; and (ii) Mr. Senneff, $800,000. In connection with his termination of employment with us, Mr. Kendall will receive a bonus of $402,500 (equal to 115% of target) under the 2020 CIP, as described below under “Executive severance arrangements.”
Outstanding equity awards at December 31, 2020
The following table sets forth information concerning outstanding equity awards for our named executive officers as of the end of our fiscal year ended December 31, 2020.
| Option Awards | Stock Awards | |||||||||||||||||||||||||||||||||||||||
| Name |
Grant Date | Number of Securities Underlying Unexercised Options (#) Exercisable |
Number of Securities Underlying Unexercised Options (#) Unexercisable |
Equity Incentive Plan Awards: Number of Securities Underlying Unearned Unexercised Options (#) |
Option Exercise Price ($) |
Option Expiration Date |
Number of Shares or Units of Stock That Have Not Vested (#) |
Market Value of Shares or Units of Stock That Have Not Vested ($)(6) |
Equity Incentive Plan Awards: Number of Unearned Shares, Units or Other Rights That Have Not Vested (#) |
Equity Incentive Plan Awards: Market or Payout Value of Unearned Shares, Units or Other Rights That Have Not Vested ($)(6) |
||||||||||||||||||||||||||||||
| Kyle Armbrester |
7/12/2018 | (1) | — | — | — | — | — | 22,031 | $ | 8,440,957 | 63,750 | $ | 22,930,175 | |||||||||||||||||||||||||||
| 2/14/2020 | — | — | — | — | — | 94,315 | 19,759,936 | — | — | |||||||||||||||||||||||||||||||
| Steven Senneff |
6/10/2019 | (3) | — | 827,821 | 1,655,643 | $ | 3.01 | 6/10/2029 | — | — | — | — | ||||||||||||||||||||||||||||
| 2/14/2020 | (4) | — | — | — | — | — | 12,143 | 2,544,132 | 16,191 | 2,868,883 | ||||||||||||||||||||||||||||||
| P. Tad Kendall |
2/14/2020 | (5) | — | — | — | — | — | 23,696 | 4,964,444 | 31,594 | 5,025,658 | |||||||||||||||||||||||||||||
| (1) | Reflects a grant of 122,500 Class B Incentive Units (as defined under “Incentive Units” below), of which 58,750 are subject to time-vesting in equal quarterly installments over four years beginning on May 9, 2018, and 63,750 are subject to performance-vesting based upon the aggregate cash-on-cash returns achieved by New Mountain Capital and its affiliates (with 29,375 Class B Incentive Units vesting upon the achievement of 2.0 times the applicable cash-on-cash return and an additional 34,375 Class B Incentive Units vesting upon the achievement 3.0 times the applicable cash-on-cash return). Following this offering, the time-based Class B Incentive Units will accelerate in full upon the occurrence of an Acceleration Event (as defined below). The terms of the units are described in more detail under “—Other compensation plans; Incentive Units” below. |
| (2) | Reflects a grant of 181,085 Class C Incentive Units (as defined under “Incentive Units” below) subject to time-vesting over a four-year period beginning on January 1, 2019, with 25% vesting on January 1, 2020 and the remaining 75% in equal monthly installments over three years thereafter. Following this offering, the time-based Class C Incentive Units will accelerate in full upon the occurrence of an Acceleration Event (as defined below). The terms of the units are described in more detail under “—Other compensation plans; Incentive Units” below. |
| (3) | Reflects a grant of nonqualified stock options (“NQSOs”) to purchase New Remedy Class A Shares having an exercise price of $3.01 per share, of which 1,103,762 are subject to time-vesting in equal annual installments on each of the first four anniversaries of March 14, 2019, and 1,655,643 are subject to performance-vesting based upon the achievement by New Mountain Capital and its affiliates of specified multiple of invested capital return milestones (with 50% vesting at a return of 2.0 times or greater and 100% at a return of 2.5 times or greater). Following this offering, the NQSOs will accelerate in full upon the occurrence of a Change of Control (generally defined under the award agreements governing the NQSOs to include either a “Change of Control” of Signify Health or such time as New Mountain Capital and its affiliates cease to directly or indirectly control at least 25% of all classes of our common stock). The NQSOs are outstanding under the New Remedy Corp. Amended and Restated 2019 Equity Plan, which is described in more detail under “—Other compensation plans; New Remedy Corp. Amended and Restated 2019 Equity Plan” below. |
181
Table of Contents
| (4) | Reflects a grant of 32,381 Class C Incentive Units (as defined under “Incentive Units” below), of which 16,190.5 are subject to time-vesting in equal annual installments on each of the first four anniversaries of February 18, 2019, subject to his continued employment through the applicable vesting date, and 16,190.5 are subject to performance-vesting based upon the achievement of at least 1.75 times the applicable cash-on-cash returns by New Mountain Capital and its affiliates. Following this offering, the time-based Class C Incentive Units will accelerate in full upon the occurrence of an Acceleration Event. The terms of the units are described in more detail under “—Other compensation plans; Incentive Units” below. |
| (5) | Reflects a grant of 63,188 Class C Incentive Units (as defined under “Incentive Units” below) of which 31,594 are subject to time-vesting in equal annual installments on each of the first four anniversaries of November 26, 2019, subject to continued employment through the applicable vesting date, and 31,594 are subject to performance-vesting based upon the achievement of at least 2.0 times the applicable cash-on-cash returns by New Mountain Capital and its affiliates. Following this offering, the time-based Class C Incentive Units will accelerate in full upon the occurrence of an Acceleration Event. The terms of the units are described in more detail under “—Other compensation plans; Incentive Units” below. |
| (6) | Amounts reported are based on the appreciation in the value of Cure TopCo, LLC from and after the applicable grant date through the most recent valuation of Cure TopCo, LLC as of September 30, 2020. |
Cash IPO Bonuses
In recognition of their extraordinary efforts and contributions to the success of this offering, we intend to pay cash bonuses to certain of our executive officers in an aggregate amount of $500,000, including a $250,000 bonus payable to Mr. Senneff, which bonuses will be paid as soon as reasonably practical following the completion of this offering.
Other compensation plans
Incentive Units
Our NEOs have received awards in the form of Class B units and Class C units in Cure Aggregator, LLC (the “Class B Incentive Units” and “Class C Incentive Units,” respectively, and, collectively, the “Incentive Units”), which correspond to Class B units and Class C units issued by Cure TopCo, LLC to Cure Aggregator, LLC. These Incentive Units are intended to be treated as “profits interests” for U.S. federal income tax purposes and have economic characteristics similar to stock appreciation rights. Therefore, the Incentive Units only have value to the extent there is an appreciation in the value of Cure TopCo, LLC above the applicable floor amount from and after the applicable grant date. In connection with the Reorganization Transactions, the Incentive Units will be reclassified into common units of Cure Aggregator, LLC (with the corresponding Class B units and Class C units issued by Cure TopCo, LLC to Cure Aggregator, LLC reclassified into LLC Units of Cure TopCo, LLC (the “Reclassified Incentive Units”)) and will remain subject to the vesting terms described below. In connection with the Reorganization Transactions, shares of Class B common stock will be issued to each holder of Reclassified Incentive Units on a one-for-one basis to such holder’s Reclassified Incentive Units, provided that such shares of Class B common stock will not be entitled to any voting rights until such time as the Reclassified Incentive Units vest. Once vested, the holders of Reclassified Incentive Units will have the ability, pursuant to the terms of the amended and restated limited liability company agreement of Cure Aggregator, LLC, to exchange their Reclassified Incentive Units for LLC Units of Cure TopCo, LLC and immediately thereafter will have the right to require Cure TopCo, LLC to redeem their LLC Units for, at our election, either newly issued shares of Class A common stock on a one-for-one basis or a cash payment, pursuant to the terms of the Amended LLC Agreement. Should a holder of Reclassified Incentive Units choose to exchange their Reclassified Incentive Units for LLC Units and not immediately request a redemption of LLC Units, such holder will continue to hold the shares of Class B common stock received in connection with the Reorganization Transactions.
The Incentive Units granted to our NEOs include “time-vesting” awards subject to vesting terms based on the executive’s continued employment through the applicable vesting date (except as described below), as well as “performance-vesting” awards subject to the achievement of specified cash-on-cash returns received by New Mountain Capital and its affiliates based on its equity investment in Cure TopCo, LLC.
Mr. Armbrester received a grant of Class B Incentive Units, 48% of which are subject to time-vesting in equal quarterly installments over four years, subject to his continued employment through the applicable vesting date (except as described below), and 52% of which are subject to performance-vesting based on the achievement by New Mountain Capital and its affiliates of cash-on-cash returns (with 46% of the performance-vesting Incentive Units vesting at 2.0 times the applicable cash-on-cash return and the remaining 54% vesting at 3.0
182
Table of Contents
times the applicable cash-on-cash return, subject to Mr. Armbrester’s continued employment through the applicable vesting date (except as described below)). Mr. Armbrester also received a grant of Class C Incentive Units on February 14, 2020 that are subject only to time-vesting over a four-year period from January 1, 2019, with 25% vesting on January 1, 2020 and the remaining 75% vesting in equal monthly installments over three-years thereafter, subject to Mr. Armbrester’s continued employment through each vesting date (except as described below). In the event of Mr. Armbrester’s termination of employment without Cause or if he resigns for Good Reason (each as defined in his employment agreement), his time-vesting and performance-vesting Class B Incentive Units will remain outstanding and eligible to vest during the 12-month period following the termination date. At the end of such 12-month period, any remaining unvested Incentive Units will be canceled and forfeited.
Mr. Senneff received a grant of Class C Incentive Units on February 14, 2020, 50% of which are subject to time-vesting in equal annual installments on each of the first four anniversaries of February 18, 2019, subject to his continued employment through the applicable vesting date (except as described below), and 50% of which are subject to performance-vesting based on the achievement by New Mountain Capital and its affiliates of cash-on-cash returns of at least 1.75 times the applicable cash-on-cash return and are subject to his continued employment through the applicable vesting date.
Mr. Kendall received a grant of 63,188 Class C Incentive Units on February 14, 2020, 50% of which are subject to time-vesting in equal annual installments on each of the first four anniversaries of November 26, 2019, subject to his continued employment through the applicable vesting date (except as described below), and 50% of which are subject to performance-vesting based on the achievement by New Mountain Capital and its affiliates of cash-on-cash returns of at least 2.0 times the applicable cash-on-cash return subject to his continued employment through the applicable vesting date. In the event of Mr. Kendall’s termination of employment without Cause or if he resigns for Good Reason (each as defined in his employment agreement), his performance-vesting Incentive Units will remain outstanding and eligible to vest during the 6-month period following the termination date. At the end of such 6-month period, any remaining unvested Incentive Units will be canceled and forfeited.
Upon the occurrence of an “Acceleration Event” (which is generally defined under the award agreements governing the Reclassified Incentive Units to include either a “Change of Control” of Signify Health or such time as New Mountain Capital and its affiliates cease to beneficially own at least 25% of all classes of our common stock) that occurs after the completion of this offering, all outstanding time-based Reclassified Incentive Units will become fully vested, subject to the employee’s continued employment through such event. In addition, our compensation committee may, in its sole discretion, provide for the full acceleration of any portion of the Incentive Units (or, following the completion of this offering, the Reclassified Incentive Units) at any time and for any reason. On a termination of employment for any reason other than for Cause (as defined in the applicable award agreement), any unvested Incentive Units (or, following the completion of this offering, the Reclassified Incentive Units) will be forfeited, and on a termination of employment for Cause, all vested and unvested Incentive Units (or, following the completion of this offering, Reclassified Incentive Units) are forfeited. Vested Incentive Units (or, following the completion of this offering, Reclassified Incentive Units) are subject to a call right at a price equal to fair market value for 180 days following a termination of employment for any reason.
In connection with this offering, we intend to grant stock options to purchase shares of Class A common stock under our 2021 Long-Term Incentive Plan (described below) to certain holders of Reclassified Incentive Units in order to compensate such holders for the loss of leverage as a result of the reclassification of their Incentive Units into Reclassified Incentive Units and to retain these employees following the offering. These stock options will have an exercise price per share that is equal to the initial public offering price per share and will time-vest in equal annual installments over three years from the grant date. The aggregate number of shares of our Class A common stock covered by stock options that we grant to holders of Reclassified Incentive Units in connection with the offering is 872,500 shares, of which 600,000 shares would be granted to certain non-NEO executive officers. No stock options will be granted to our NEOs in connection with the offering.
183
Table of Contents
2021 Long-Term Incentive Plan
We expect that our 2021 Long-Term Incentive Plan (the “2021 Plan”) will become effective in connection with this offering. The 2021 Plan provides for the grant of equity-based awards to our employees, consultants, service providers and non-employee directors.
Administration. The 2021 Plan will be administered by the compensation committee (the “Committee”) of our board of directors, unless another committee is designated by our board of directors. The Committee will have the authority to, among other actions, determine eligible participants, the types of awards to be granted, the number of shares covered by any awards, the terms and conditions of any awards (and amend any terms and conditions) and the methods by which awards may be settled, exercised, cancelled, forfeited or suspended.
Shares Reserve; Adjustments. The maximum number of shares of our Class A common stock available for issuance under the 2021 Plan will not exceed a number of shares of our Class A common stock equal to 7% of the aggregate number of shares of Class A common stock and Class B common stock outstanding (on a fully diluted basis) on the effective date of this offering. The share pool will be increased on the first day of each year by the least of (i) a number of shares of Class A common stock equal to 6% of the aggregate number of shares of Class A common stock and Class B common stock outstanding (on a fully diluted basis) on the effective date of this offering, (ii) 3% of the aggregate number of shares of Class A common stock and shares of Class B common stock outstanding (on a fully diluted basis) on the last day of the immediately preceding fiscal year and (iii) an amount determined by the board of directors. Any shares underlying substitute awards, shares remaining available for grant under a plan of an acquired company and awards (including pre-IPO awards (as defined in the 2021 Plan)) that are forfeited, cancelled, expired, terminated or are otherwise lapsed, in whole or in part, or are settled in cash or withheld by us in respect of taxes, will become available for future grant under our 2021 Plan.
In the event of certain changes in our corporate structure, including any extraordinary dividend or other distribution, recapitalization, stock split, reorganization, merger, consolidation, spin-off, or other similar corporate transaction or event affecting our common stock, or changes in applicable laws, regulations or accounting principles, the Committee will make appropriate adjustments to prevent undue enrichment or harm to the number and type of common shares subject to awards, and to the grant, purchase, exercise or hurdle price for any award.
Non-Employee Director Limits. Under the 2021 Plan, the maximum number of shares of our Class A common stock subject to an award granted during a single fiscal year to any non-employee director, taken together with any cash fees paid during the fiscal year, in respect to the director’s service as a member of our board of directors during such year, shall not exceed $500,000 in total value. The independent directors may make exception to this limit for a non-executive chair of the board of directors, provided that the non-employee director receiving such additional compensation may not participate in the decision to award such compensation.
Stock Options. The 2021 Plan permits the grant of incentive stock options to employees and/or nonstatutory stock options to all eligible participants. The exercise price of stock options may not be less than the fair market value of our Class A common stock on the grant date, provided that if an incentive stock option is granted to a 10% stockholder, the exercise price may not be less than 110% of the fair market value of our Class A common stock. Each stock option agreement will set forth the vesting schedule of the options and the term of the options, which may not exceed 10 years (or five years in the case of an incentive stock option granted to a 10% stockholder). The Committee will determine the method of payment of the exercise price. The Committee may provide in an applicable award agreement that, to the extent a stock option is not previously exercised as to all of the shares of our Common Stock subject thereto, and, if the fair market value of one share of our Class A common stock is greater than the exercise price then in effect, then the stock option shall be deemed automatically exercised immediately before its expiration.
Stock Appreciation Rights. The 2021 Plan permits the grant of stock appreciation rights, which entitle the holder to receive shares of our Class A common stock or cash having an aggregate value equal to the
184
Table of Contents
appreciation in the fair market value of our Class A common stock between the grant date and the exercise date, times the number of shares of our Class A common stock subject to the award. The exercise price of stock appreciation rights may not be less than the fair market value of our common stock on the date of grant. Each stock appreciation rights agreement will set forth the vesting schedule of the stock appreciation rights. The Committee may provide in an applicable award agreement that, to the extent a stock appreciation right is not previously exercised as to all of the shares of our Common Stock subject thereto, and, if the fair market value of one common share is greater than the exercise price then in effect, then the stock appreciation right shall be deemed automatically exercised immediately before its expiration.
Restricted Stock and Restricted Stock Units. The 2021 Plan permits the grant of restricted stock and restricted stock units. Restricted stock awards are grants of shares of our Class A common stock, subject to certain condition and restrictions as specified in the applicable award agreement. Restricted stock units represent the right to receive shares of our Class A common stock (or a cash amount equal to the value of our Class A common stock) on future specified dates. The Committee will determine the form or forms in which payment of the amount owing upon settlement of a restricted stock unit may be made.
Performance Awards. The 2021 Plan permits the grant of performance awards which are payable upon the achievement of performance goals determined by the Committee. The Committee may, in its discretion, increase or reduce the amount of a settlement otherwise to be made in connection with a performance award.
Other Cash-Based Awards and Other Stock-Based Awards. The 2021 Plan permits the grant of other cash-based and other stock-based awards, the terms and conditions of which will be determined by the Committee and specified in the applicable award agreement.
Minimum Vesting Requirements. Awards granted under the 2021 Plan are required to vest over a period at not less than one year from the grant date, provided that (i) the Committee may accelerate the vesting of awards or otherwise lapse the minimum vesting requirement upon a participant’s death or disability or upon a change in control and (ii) up to 5% of shares available for issuance under the 2021 Plan may be granted not subject to this requirement.
Separation from Service. In the event of a participant’s separation from service, as defined in the 2021 Plan, the Committee may determine the extent to which an award may be exercised, settled, vested, paid or forfeited prior to the end of a performance period, or the vesting, exercise or settlement of such award.
Change in Control. In the event of a change in control, as defined in the 2021 Plan, the Committee may take certain actions with respect to outstanding awards, including the continuation or assumption of awards, substitution or replacement of awards by a successor entity, acceleration of vesting and lapse of restrictions, determination of the attainment of performance conditions for performance awards or cancellation of awards in consideration of a payment.
Dissolution or Liquidation. In the event of the dissolution or liquidation of our company, each award will be terminated immediately prior to the consummation of such action, unless otherwise determined by the Committee.
No Repricing. Except pursuant to an adjustment by the Committee permitted under the 2021 Plan, no action may directly or indirectly reduce the exercise or hurdle price of any award established at the time of grant without stockholder approval.
Plan Amendment or Suspension. The Committee has the authority to amend or suspend the 2021 Plan, provided that no such action may be taken without stockholder approval if the approval is necessary to comply with a tax or regulatory requirement or other applicable law for which the Committee deems it necessary or desirable to comply. No amendment may in general adversely and materially affect a participant’s rights under any award without such participant’s written consent.
185
Table of Contents
Term of the Plan. No awards may be granted under the 2021 Plan after our board of directors terminates the plan, the maximum number of shares available for issuance has been issued or 10 years from the effective date, whichever is earlier.
2021 Employee Stock Purchase Plan
We expect that our Employee Stock Purchase Plan (the “ESPP”) will become effective on a date to be specified by the Committee following the completion of this offering. The ESPP will provide our employees and employees of participating subsidiaries with an opportunity to acquire a proprietary interest in our company through the purchase of shares of our Class A common stock. Initially, the ESPP will not be intended to qualify as an “employee stock purchase plan” under Section 423 of the Internal Revenue Code of 1986, as amended (the “Code”). From and after such date as the Committee, in its discretion, determines that the ESPP is able to satisfying the requirements under Section 423 of the Code and that it will operate the ESPP in accordance with such requirements, the ESPP will be intended to qualify as an “employee stock purchase plan” under Section 423 of the Code and the ESPP will be interpreted in a manner that is consistent with that intent.
Administration. Our ESPP will be administered by the Committee, which will have the authority to take any actions necessary or desirable for the administration of the ESPP, including adopting sub-plans applicable to particular participating subsidiaries or locations, which sub-plans may be designed to be outside the scope of Section 423 of the Code, or special rules applicable to participants in particular participating subsidiaries or particular locations. The Committee may change the minimum amounts of compensation (as defined in the ESPP) for payroll deductions, the frequency with which a participant may elect to change his or her rate of payroll deductions, the dates by which a participant is required to submit an enrollment form and the effective date of a participant’s withdrawal from the ESPP due to a termination or transfer of employment or change in employment status.
Shares Reserved. The maximum number of shares of our Class A common stock available for issuance under the ESPP will initially not exceed in the aggregate a number of shares of our Class A common stock equal to 2% of the aggregate number of shares of Class A common stock and Class B common stock outstanding (on a fully diluted basis) on the effective date of this offering. The share pool will be increased on the first day of each fiscal year in an amount equal to the lesser of (i) a number of shares of our Class A common stock equal to 2% of the aggregate number of shares of Class A common stock and Class B common stock outstanding (on a fully diluted basis) on the effective date of this offering and (ii) 1% of the aggregate number of shares of our Class A common stock and Class B common stock outstanding (on a fully diluted basis) on the last day of the immediately preceding fiscal year.
Eligibility. Unless otherwise determined by the Committee in a manner that is consistent with Section 423 of the Code, any employee of ours or a participating subsidiary who is customarily employed for at least 20 hours per week and more than five months in any calendar year is eligible to participate in an offering period, subject to the requirements of Section 423 of the Code. An eligible employee will not be granted an option if such grant would result in the employee owning 5% or more of the total combined voting power or value of all classes of our and our subsidiaries’ stock or if such grant would permit the employee to purchase our and our subsidiaries’ stock at a rate that exceeds $25,000 of the fair market value of the stock for each calendar year in which such option is outstanding at any time.
Offering Periods. Unless otherwise determined by the Committee, each offering period under the ESPP will have a duration of six months commencing on January 1 or June 1. The initial offering period under the ESPP will commence on a date to be specified by the Committee following the completion of this offering.
Participation. Participation in the ESPP is voluntary. Eligible employees may elect to participate in the ESPP by completing an enrollment form and submitting it in accordance with the enrollment procedures established by the Committee, upon which the employee authorizes payroll deductions from his or her paycheck on each payroll date during the offering period in an amount equal to at least 1% of his or her compensation.
186
Table of Contents
Participants may decrease (but not increase) their rate of payroll deductions only once during an offering period (twice during the initial offering period) by submitting a new enrollment form which must be submitted at least fifteen (15) days before the purchase date (as defined in the ESPP). The deduction rate selected for an offering period will remain in effect for subsequent offering periods unless the participant (i) submits a new enrollment form authorizing a new rate of payroll deductions, (ii) withdraws from the ESPP or (iii) terminates employment or otherwise becomes ineligible to participate in the ESPP.
Grant and Exercise of Options. Each participant will be granted, on the first trading day of each offering period, an option to purchase, on the last trading day of the offering period, a number of shares of our Class A common stock determined by dividing the participant’s accumulated payroll deductions by the applicable purchase price. The purchase price for the option will equal to 85% of the fair market value of a share on the purchase date. A participant’s option will be exercised automatically on the purchase date to purchase the maximum number of whole shares of our Class A common stock that can be purchased with the amounts in the participant’s notional account. The maximum number of shares of our Class A common stock that may be purchased by all participants during a single offering period may not exceed the number of shares equal to 2% of the aggregate number of shares of Class A common stock and Class B common stock outstanding (on a fully diluted basis) on the effective date of this offering (the “Offering Period Limit”).
Withdrawal. Participants may withdraw from an offering at any time prior to the last day of the offering period by submitting a revised enrollment form indicating his or her election to withdraw at least fifteen (15) days before the purchase date. The accumulated payroll deductions held on behalf of the participant in his or her notional account will be paid to the participant promptly following receipt of the participant’s revised enrollment form indicating their election to withdraw, and the participant’s option will be automatically terminated.
Termination of Employment; Change in Employment Status; Transfer of Employment. On termination of a participant’s employment for any reason, or a change in the participant’s employment status following which the participant is no longer an eligible employee, the participant will be deemed to have withdrawn from the ESPP effective as of the date of such termination of employment or change in status, the accumulated payroll deductions remaining in the participant’s notional account will be returned to the participant, and the participant’s option will be automatically terminated.
Oversubscribed Offerings. If the Committee determines that, on a particular purchase date, the number of shares with respect to which options are to be exercised either exceeds the number of shares available under the ESPP or the Offering Period Limit, the shares will be allocated pro rata in a uniform manner as practicable and as the Committee deems equitable.
Adjustments Upon Changes in Capitalization; Corporate Transactions. In the event of any dividend or other distribution, recapitalization, stock split, reorganization, merger, consolidation, spin-off, combination, repurchase, or exchange of shares or other securities of our company or other change in our company’s structure affecting our Class A common stock, then in order to prevent dilution or enlargement of the benefits intended to be made available under the ESPP, the Committee will make equitable adjustments to the number and class of shares that may be issued under the ESPP, the purchase price per share, and the number of shares covered by each outstanding option.
In the event of a corporate transaction (as defined in the ESPP), each outstanding option will be assumed (or an equivalent option substituted) by the successor corporation or a parent or subsidiary of such successor corporation. If the successor corporation refuses to assume or substitute such option, the offering period will be shortened by setting a new purchase date on which the offering period will end. The new purchase date for the offering period will occur before the date of the corporate transaction.
Dissolution or Liquidation. Unless otherwise determined by the Committee, in the event of a proposed dissolution or liquidation of our company, any offering period in progress will be shortened by setting a new
187
Table of Contents
purchase date and the offering period will end immediately prior to the proposed dissolution or liquidation. Participants will be provided with written notice of the new purchase date and that the participant’s option will be exercised automatically on such date, unless before such time, the participant has withdrawn from the offering.
Amendment and Termination. The Committee may, in its sole discretion, amend, suspend or terminate the ESPP at any time and for any reason. The Committee may elect, upon termination of the ESPP, to terminate any outstanding offering period either immediately or once shares have been purchased on the next purchase date or permit the offering period to expire in accordance with its terms.
New Remedy Corp. Amended and Restated 2019 Equity Incentive Plan
In connection with the Remedy Partners Combination, the Remedy Partners 2019 Equity Incentive Plan was amended and restated as the New Remedy Corp. Amended and Restated 2019 Equity Incentive Plan (the “New Remedy 2019 Plan”). As of December 31, 2020, there were NQSOs outstanding under the New Remedy 2019 Plan with respect to 17,667,258 New Remedy Class A Shares having a weighted-average exercise price of $2.09 per New Remedy Class A Share. In connection with this offering, it is expected that the outstanding NQSOs will be converted into stock options with respect to shares of our Class A common stock, with the number of shares and the exercise price adjusted on a proportionate basis, and that the New Remedy 2019 Plan will be amended and restated (and renamed the Signify Health, Inc. Amended and Restated 2019 Equity Incentive Plan), to provide for the issuance of shares of our Class A common stock upon the exercise of stock options, and that no further grants will be made under the New Remedy 2019 Plan. The following description of the New Remedy 2019 Plan provides a summary of its key terms as currently in effect.
Purpose of the New Remedy 2019 Plan. The New Remedy 2019 Plan is intended promote the interests of New Remedy and its affiliates by (i) attracting and retaining exceptional employees and directors of, and consultants and advisors to, New Remedy or its affiliates and (ii) enabling such individuals to acquire an equity interest in, and participate in the long-term growth and financial success of, New Remedy by providing for the grant of awards thereunder.
Administration of the New Remedy 2019 Plan. The board of directors of New Remedy serves as the administrator of the New Remedy 2019 Plan. The administrator has discretionary authority to interpret the New Remedy 2019 Plan, determine eligibility for and grant awards thereunder, determine, modify or waive the terms and conditions of any award, determine the form of settlement of awards (whether in cash, shares of stock or other property), prescribe forms, rules and procedures relating to the plan and awards, and otherwise do all things necessary or desirable to carry out the purposes of the plan.
Shares subject to the New Remedy 2019 Plan. The aggregate number of New Remedy Class A Shares reserved for grant or issuance under the New Remedy 2019 Plan was 13,000,000, which does not include shares withheld in payment of the exercise price of an option or in satisfaction of tax withholding requirements with respect to an option and by excluding any shares underlying awards that may be settled in cash or that expire, become unexerciseable, terminate or are forfeited to or repurchased by New Remedy without the issuance of shares.
Types of awards; eligibility. The New Remedy 2019 Plan provides for the grant of stock options, which may be incentive stock options (“ISOs”) or NQSOs, stock appreciation rights (“SARs”), restricted stock, unrestricted stock, stock units (including RSUs), performance awards and other awards that are convertible into or otherwise base on stock to key employees, directors, consultants or advisors to New Remedy and its affiliates, subject to certain eligibility limitations under applicable tax rules.
Vesting. The administrator will determine the vesting terms of the applicable award. In addition, the administrator may accelerate the vesting or exercisability of an award, regardless of any adverse or potentially adverse tax or other consequences resulting from such acceleration.
188
Table of Contents
Awards requiring exercise. The exercise price (or base value from which appreciation is to be measured) of each award requiring exercise may be no less than 100% of the fair market value of the New Remedy Class A Shares on the date of grant (110% in the case of ISOs granted to a 10% stockholder within the meaning of Section 422(b)(6) of the Code). Awards, once granted, may only be repriced in accordance with the terms of the New Remedy 2019 Plan. The maximum term of awards requiring exercise may not exceed 10 years from the date of grant (or 5 years in the case of an ISO granted to a 10% stockholder within the meaning of Section 422(b)(6) of the Code).
Dividend equivalents. The administrator may provide for the payment of amounts in lieu of cash dividends or other cash distributions with respect to stock subject to an award, whether or not the holder of such award is otherwise entitled to share in the actual dividend or distribution in respect of such award.
Effect of termination of service. Unless the administrator expressly provides otherwise, awards under the New Remedy 2019 Plan will be subject to the following treatment upon a participant’s termination of service:
| • | Stock Options and SARs. In the event the participant’s service is terminated by New Remedy for Cause (as defined in the New Remedy 2019 Plan), all stock options and SARs (whether or not vested) will immediately terminate. In the event the participant’s service is terminated due to death or disability, all stock options and SARs, to the extent exercisable, will remain exercisable for the lesser of (i) a period of six months or (ii) the applicable expiration date. In the event the participant’s service is terminated by New Remedy without Cause or by the participant for Good Reason (as defined in the New Remedy 2019 Plan), all stock options and SARs, to the extent exercisable, will remain exercisable for the lesser of (i) a period of 60 days or (ii) the applicable expiration date. In the event the participant’s service is terminated for any other reason, all stock options and SARs will remain exercisable for the lesser of (i) a period of 30 days or (ii) the applicable expiration date. |
| • | Other Awards. Except as set forth above with respect to stock options and SARs, upon the cessation of a participant’s employment each award requiring exercise held by such participant, if any, will cease to be exercisable and will terminate, and all other awards held by such participant, if any, to the extent not already vested will be forfeited. |
Effect of a covered transaction. In the event of a Covered Transaction (as defined in the New Remedy 2019 Plan, and which would include the Up-C restructuring) the administrator may provide for (i) the assumption or continuation of outstanding awards; (ii) the substitution of awards; (iii) the cash-out of outstanding awards; or (iv) the acceleration of outstanding awards, in full or in part.
Effect of changes in and distributions with respect to stock. In the event of a stock dividend, stock split or combination of New Remedy Class A Shares (including a reverse stock split), recapitalization or other change in New Remedy’s capital structure that constitutes an equity restructuring within the meaning of the accounting rules, the administrator will make appropriate adjustments to the maximum number of New Remedy Class A Shares that may be issued under the New Remedy 2019 Plan and will make appropriate adjustments to outstanding awards. The administrator may also make adjustments to take into account distributions to stockholders other than those described above, or any other event, if the administrator determines that adjustments are appropriate to avoid distortion in the operation of the New Remedy 2019 Plan.
Clawback. The administrator may provide that outstanding awards (whether or not vested or exercisable) and the proceeds for the exercise or disposition of awards or stock acquired under awards will be subject to forfeiture and disgorgement to New Remedy if a participant violates (i) a non-competition, non-solicitation, confidentiality or other restrictive covenant, or (ii) any New Remedy policy applicable to the participant that provides for forfeiture or disgorgement with respect to incentive compensation that includes awards under the New Remedy 2019 Plan.
189
Table of Contents
Repurchase option. Upon a termination of employment of a participant for any reason, New Remedy will have the right to purchase all or any portion of the New Remedy Class A Shares received by the participant in respect of an award during the one year period following the later of (a) the date of the termination and (b) six months plus one day after the date of the acquisition of the applicable shares. In the event New Remedy becomes aware that the participant breached certain restrictive covenants within two years of the termination date, such period will be extended to two years following the date New Remedy becomes aware of such breach.
Amendment and termination. The New Remedy 2019 Plan will terminate on June 10, 2029, unless terminated at an earlier date by vote of New Remedy’s shareholders or the board of directors. The New Remedy 2019 Plan may be terminated and the New Remedy 2019 Plan or outstanding awards may be amended by the administrator, provided that no termination or amendment may, without the consent of a participant, adversely and materially affect the participant’s rights under such award, unless the administrator reserved the right to do so at the time the award was granted. Any amendments to the plan will be conditioned upon stockholder approval if required by law or applicable stock exchange requirements.
Governing law. The New Remedy 2019 Plan is construed and enforced in accordance with the law of the State of Delaware.
Cure TopCo, LLC Synthetic Equity Plan
Certain of our non-executive officer key employees hold synthetic equity units in Cure TopCo, LLC (the “SEUs”), which are cash-based awards that track the value of the Class C Incentive Units, and therefore only have value to the extent there is an appreciation in the value of Cure TopCo, LLC above the applicable floor amount from and after the applicable grant date. In connection with the Reorganization Transactions, the SEUs will be reclassified into synthetic common units of Cure TopCo, LLC (the “Reclassified SEUs”) in the same manner as described under “—Incentive Units” above, and will remain subject to the vesting terms described below. Upon vesting, the Reclassified SEUs will be settled by payment of a cash amount based on the 30-day volume weighted average price per share of our Class A common stock.
The SEUs are comprised of 50% “time-vesting” awards that vest in equal quarterly installments over four years, subject to the employee’s continued employment through the applicable vesting date (except as described below), and of 50% “performance-vesting awards” that vest based on the achievement by New Mountain Capital and its affiliates of at least 2.0 times the applicable cash-on-cash return. In the event of the employee’s termination of employment without Cause (as defined in the applicable award agreement) following this offering, any unvested Reclassified SEUs will be forfeited and any vested Reclassified SEUs to the extent not already settled, will be cashed out. In the event of the employee’s termination of employment for Cause, any vested Reclassified SEUs that have not yet been settled will be forfeited.
Upon the occurrence of an “Acceleration Event” (which is generally defined under the award agreements governing the Reclassified SEUs to include either a “Change of Control” of Signify Health or such time as New Mountain Capital and its affiliates cease to beneficially own at least 25% of all classes of our common stock) that occurs after the completion of this offering, all outstanding time-based Reclassified SEUs will become fully vested, subject to the employee’s continued employment through such event.
In connection with this offering, we intend to grant synthetic shares of our Class A common stock under our 2021 Plan (described above) to holders of Reclassified SEUs in order to compensate such holders for the loss of leverage as a result of the reclassification of their SEUs into Reclassified SEUs and to retain these employees following the offering. These synthetic shares will have a hurdle price that is equal to the initial public offering price per share, will time-vest in equal annual installments over three years from the grant date and will settle in cash upon vesting based on the 30-day volume weighted average price per share of our Class A common stock. The aggregate number of synthetic shares of our Class A common stock covered by these awards is 355,725 synthetic shares.
190
Table of Contents
Retirement benefits
We maintain a tax-qualified defined contribution plan (the “Signify 401(k) Plan”), under which employees of Signify Health and legacy Remedy Partners employees, including our named executive officers, are eligible to participate. Under the Signify 401(k) Plan, participants may defer a portion of their annual compensation on a pre-tax basis. In addition, we make a matching contribution of 50% of an employee’s contributions up to 6% of eligible compensation.
We do not provide a pension plan for employees and none of our named executive officers participates in a nonqualified deferred compensation plan.
Executive severance arrangements
Our NEOs are entitled to severance benefits under their respective employment agreements, as described under “—Employment arrangements—Employment agreements,” above. In connection with his termination of employment, Mr. Kendall will receive the following severance payments and benefits: (i) 12 months continued base salary payments, (ii) a bonus equal to 115% of target for 2020; (iii) a lump sum pro-rata target bonus for 2021; and (iv) the employer portion of the monthly premiums paid under our medical and dental benefit plans for up to 12 months. In addition, Mr. Kendall’s outstanding performance-vesting Incentive Units will remain outstanding and eligible to vest for six months post-termination (and will be canceled and forfeited if they remain unvested at the end of such 6-month period).
Director compensation
The following table sets forth information concerning the compensation earned by each of our non-employee directors during the fiscal year ended December 31, 2020.
|
Name(1) |
Fees Earned or Paid in Cash ($) |
Stock Awards ($)(2) |
Option Awards ($)(3) |
All Other Compensation ($)(4) |
Total ($) |
|||||||||||||||
| Matthew S. Holt |
— | — | — | — | — | |||||||||||||||
| Vigniesh M. Aier |
— | — | — | — | — | |||||||||||||||
| Mark Caputo |
— | — | — | — | — | |||||||||||||||
| Brett Carlson(4) |
— | — | — | 255,000 | 255,000 | |||||||||||||||
| Taj J. Clayton |
46,212 | 116,834 | — | — | 163,046 | |||||||||||||||
| Brandon H. Hull |
500,000 | — | — | — | 500,000 | |||||||||||||||
| Michael A. Krupka |
— | — | — | — | — | |||||||||||||||
| Kevin M. McNamara |
— | — | — | 247,026 | 247,026 | |||||||||||||||
| Albert A. Notini |
— | — | — | — | — | |||||||||||||||
| Kyle B. Peterson |
— | — | — | — | — | |||||||||||||||
| Vivian E. Riefberg |
94,643 | 89,127 | — | — | 183,770 | |||||||||||||||
| Stephen F. Wiggins |
— | — | — | — | — | |||||||||||||||
| (1) | No compensation was paid to Messrs. Holt, Aier, Caputo, Krupka, Notini, Peterson or Wiggins in 2020. Messrs. Caputo, Carlson and Krupka resigned from service on our board of directors, effective January 12, 2021. |
| (2) | The amounts reported in this column represent the aggregate grant date fair value of the incentive unit awards granted to the directors during 2020, as calculated in accordance with FASB Accounting Standards Codification Topic 718. The assumptions used in calculating the grant date fair value of the incentive unit awards in this column are described in Note 14 to our consolidated financial statements included elsewhere in this prospectus. The aggregate number of stock awards outstanding for each of our non-employee directors as of December 31, 2020 was: Mr. Clayton, 1,544 Class C Incentive Units; Mr. Hull, 40,000 Class B Incentive Units; Mr. McNamara, 40,000 Class B Incentive Units; and Ms. Riefberg, 1,544 Class C Incentive Units. No other non-employee director held any outstanding stock awards as of such date. |
| (3) | The aggregate number of option awards outstanding for each of our non-employee directors as of December 31, 2020 was: Mr. Carlson, 1,351,045 options; and Mr. Wiggins, 563,500 options. No other non-employee director held any outstanding options as of such date. |
191
Table of Contents
| (4) | The amounts in this column include (i) $255,000 in consulting fees paid to Mr. Carlson and (ii) $246,926 in consulting fees paid to Mr. McNamara and a COVID-19 related incentive payment. |
| (5) | All compensation payable to Mr. Carlson in his capacity as a director of the Company was paid to Eir Partners, LLC (“Eir”), a company founded by Mr. Carlson and for which he serves as Chief Executive Officer. |
We currently do not maintain a director compensation program or policy in which our non-employee directors participate. Rather, certain of our non-employee directors, Messrs. Carlson (who no longer serves on our board of directors, effective January 12, 2021), Hull and McNamara, have received compensation pursuant to individual arrangements with us. The agreement for Mr. Carlson was entered into between us and Eir, with Mr. Carlson serving as Eir’s representative on our board. The arrangements with our non-employee directors in 2020 generally provided for the following payments:
Cash. Messrs. Carlson, Hull and McNamara were entitled to annual cash payments in the following amounts: (i) Mr. Carlson, $180,000, (ii) Mr. Hull, $500,000 and (iii) Mr. McNamara, $225,000. Cash fees paid to Messrs. Carlson and McNamara were primarily for their services as our consultants, while fees paid to Mr. Hull are primarily for services as a member of our board.
Equity awards. In 2020, Mr. Clayton and Ms. Riefberg each received a one-time grant of 772 time-vesting and 772 performance-vesting Class C Incentive Units. In addition, in 2018, Messrs. Hull and McNamara each received a one-time grant of 16,000 time-vesting and 24,000 performance-vesting Class B Incentive Units. The terms of these Incentive Units are generally consistent with those described under “Incentive Units” above.
Benefits. Pursuant to his consulting arrangement, Mr. McNamara is entitled to reimbursement for annual premiums on life, accidental death and dismemberment, short-term disability and medical insurance.
Our board has approved the adoption of a non-employee director compensation policy pursuant to which each of our non-employee directors will be eligible to receive annual compensation for their services on our board. The directors will be eligible to receive an annual cash retainer of $60,000, plus additional annual cash compensation for service as non-executive chair or as a chair or member of a committee of our board, as follows: Board Chair: $100,000; Audit Committee Chair: $25,000; Audit Committee Member: $12,500; Compensation Committee Chair: $20,000; Compensation Committee Member: $10,000; Corporate Development Committee Chair: $20,000; Corporate Development Committee Member: $10,000; Nominating and Corporate Governance Committee Chair: $15,000; and Nominating and Corporate Governance Committee Member: $7,500. The annual cash compensation is payable in quarterly installments in arrears. Non-employee directors will have the opportunity to elect to receive restricted stock units under the 2021 Plan in lieu of the annual cash retainer.
The non-employee directors will also be eligible to receive the following equity-based compensation in the form of restricted stock units with respect to shares of our Class A common stock granted pursuant to the 2021 Plan:
| • | an initial grant in the amount of $190,000, vesting after one year, to be made to new directors who join our board after the effective date of this offering; and |
| • | an annual grant in the amount of $190,000, vesting after one year, to be made on or about the date of our annual stockholder meeting, beginning with the annual meeting that occurs during the 2022 fiscal year. |
In addition, in connection with this offering, each of our non-employee directors serving as a member of our board on the effective date of this offering will receive a grant of restricted stock units in the amount of $190,000, vesting one year after the grant date. Non-employee directors will have the opportunity to elect to defer settlement of their restricted stock units for a period of 5 or 10 years, or upon a separation from service.
All board compensation paid to any non-employee director who is an employee New Mountain Capital will be paid to New Mountain Capital, pursuant to an agreement entered into between the company and the director.
192
Table of Contents
CERTAIN RELATIONSHIPS AND RELATED PARTY TRANSACTIONS
We describe below transactions and series of similar transactions, during our last three fiscal years or currently proposed, to which we were a party or will be a party, in which:
| • | the amounts involved exceeded or will exceed $120,000; and |
| • | any of our directors, executive officers or beneficial holders of more than 5% of any class of our capital stock had or will have a direct or indirect material interest. |
Other than as described below, there have not been, nor are there any currently proposed, transactions or series of similar transactions meeting this criteria to which we have been or will be a party other than compensation arrangements, which are described where required under “Management—Board structure” and “Executive and director compensation.”
Reorganization agreement
In connection with the Reorganization Transactions, we will enter into a reorganization agreement and related agreements with Cure TopCo, LLC and each of the Pre-IPO LLC Members, which will effect the Reorganization Transactions.
The table below sets forth the consideration in LLC Units and Class B common stock to be received by our directors, officers and 5% equity holders in the Reorganization Transactions:
| Class B Common Stock and LLC Units to Be Issued in the Reorganization Transactions(1)(2) |
||||
| Name |
Number | |||
| Certain Pre-IPO LLC Members affiliated with New Mountain Capital |
43,070,294 | |||
| Kyle Armbrester |
2,402,349 | |||
| Steven Senneff |
110,140 | |||
| Adam McAnaney |
2,625 | |||
| Peter Boumenot |
33,033 | |||
| David Pierre |
245,372 | |||
| Laurel Douty |
15,755 | |||
| Brandon H. Hull |
301,996 | |||
| Kevin M. McNamara |
583,564 | |||
| Vivian E. Riefberg |
2,625 | |||
| (1) | Certain of our directors and officers indirectly hold their interests in Cure TopCo, LLC through common units of Cure Aggregator, LLC. The number of LLC Units includes the number of LLC Units held by Cure Aggregator, LLC on behalf of such directors and officers on a one-for-one basis with each director’s and officer’s interests in Cure Aggregator, LLC that have vested. |
| (2) | Includes Class B common stock in respect of common units of Cure Aggregator, LLC that will vest within 60 days of February 1, 2021. |
The consideration set forth above and otherwise to be received in the Reorganization Transactions is subject to adjustment based on the final public offering price of our Class A common stock in this offering.
Amended and restated Cure TopCo, LLC agreement
In connection with the Reorganization Transactions, Signify Health, Inc., Cure TopCo, LLC and each of the Continuing Pre-IPO LLC Members will enter into the Amended LLC Agreement. Following the Reorganization Transactions, and in accordance with the terms of the Amended LLC Agreement, we will operate our business through Cure TopCo, LLC. Pursuant to the terms of the Amended LLC Agreement, so long as the Continuing Pre-IPO LLC Members continue to own any LLC Units or securities redeemable or exchangeable into shares of our Class A common stock, we will not, without the prior written consent of such holders, engage in any business activity other than the
193
Table of Contents
management and ownership of Cure TopCo, LLC or own any assets other than securities of Cure TopCo, LLC and/or any cash or other property or assets distributed by or otherwise received from Cure TopCo, LLC, unless we determine in good faith that such actions or ownership are in the best interest of Cure TopCo, LLC.
As the sole managing member of Cure TopCo, LLC, we will have control over all of the affairs and decision making of Cure TopCo, LLC. As such, through our officers and directors, we will be responsible for all operational and administrative decisions of Cure TopCo, LLC and the day-to-day management of Cure TopCo, LLC’s business. We will fund any dividends to our stockholders by causing Cure TopCo, LLC to make distributions to the holders of LLC Units and us, subject to the limitations imposed by our debt agreements. See “Dividend policy.”
The holders of LLC Units will generally incur U.S. federal, state and local income taxes on their proportionate share of any net taxable income of Cure TopCo, LLC. Net profits and net losses of Cure TopCo, LLC will generally be allocated to its members pro rata in accordance with the percentages of their respective ownership of LLC Units. The Amended LLC Agreement will provide for pro rata cash distributions to the holders of LLC Units for purposes of funding their tax obligations in respect of the taxable income of Cure TopCo, LLC that is allocated to them. Generally, these tax distributions will be computed based on Cure TopCo, LLC’s estimate of the net taxable income of Cure TopCo, LLC allocable to each holder of LLC Units multiplied by an assumed tax rate equal to the highest effective marginal combined U.S. federal, state and local income tax rate prescribed for an individual or corporate resident of New York, New York (taking into account the non-deductibility of certain expenses and the character of our income). As a result of (i) potential differences in the amount of net taxable income allocable to us and the other LLC Unit holders, (ii) the lower tax rate applicable to corporations than individuals and (iii) the use of an assumed tax rate in calculating Cure TopCo, LLC’s distribution obligations, we may receive tax distributions significantly in excess of our tax liabilities and obligations to make payments under the Tax Receivable Agreement.
Except as otherwise determined by us, if at any time we issue a share of our Class A common stock, the net proceeds received by us with respect to such share, if any, shall be concurrently invested in Cure TopCo, LLC and Cure TopCo, LLC shall issue to us one LLC Unit, unless such share was issued by us solely to fund the purchase of an LLC Unit from a holder of LLC Units (upon an election by us to exchange such LLC Unit in lieu of redemption following a redemption request by such holder of LLC Units), in which case such net proceeds shall instead be transferred to the selling holder of LLC Units as consideration for such purchase, and Cure TopCo, LLC will not issue an additional LLC Unit to us. Similarly, except as otherwise determined by us, (i) Cure TopCo, LLC will not issue any additional LLC Units to us unless we issue or sell an equal number of shares of our Class A common stock and (ii) should Cure TopCo, LLC issue any additional LLC Units to the Continuing Pre-IPO LLC Members or any other person, we will issue an equal number of shares of our Class B common stock to such Continuing Pre-IPO LLC Members or any other person; provided, that, in the case of LLC Units issued to Cure Aggregator, LLC, Class B common stock will be issued directly to the holders of Reclassified Incentive Units. Conversely, if at any time any shares of our Class A common stock are redeemed, purchased or otherwise acquired by us, Cure TopCo, LLC will redeem, purchase or otherwise acquire an equal number of LLC Units held by us, upon the same terms and for the same price per security, as the shares of our Class A common stock are redeemed, purchased or otherwise acquired. In addition, Cure TopCo, LLC will not effect any subdivision (by any unit split, unit distribution, reclassification, reorganization, recapitalization or otherwise) or combination (by reverse unit split, reclassification, reorganization, recapitalization or otherwise) of the LLC Units unless it is accompanied by a substantively identical subdivision or combination, as applicable, of each class of our common stock, and we will not effect any subdivision or combination of any class of our common stock unless it is accompanied by a substantively identical subdivision or combination, as applicable, of the LLC Units.
Under the Amended LLC Agreement, the holders of LLC Units (other than us) will have the right, from and after the completion of this offering (subject to the terms of the Amended LLC Agreement), to require Cure TopCo, LLC to redeem all or a portion of their LLC Units for, at our election, newly-issued shares of Class A common stock on a one-for-one basis or a cash payment equal to the volume weighted average market price of one share of our Class A common stock for each LLC Unit redeemed (subject to customary adjustments, including for stock splits, stock dividends and reclassifications). If we decide to make a cash payment, the holder of an LLC Unit has the option to rescind its redemption request within a specified time period. Upon the exercise of the redemption right, the redeeming
194
Table of Contents
member will surrender its LLC Units to Cure TopCo, LLC for cancellation. The Amended LLC Agreement requires that we contribute cash or shares of our Class A common stock to Cure TopCo, LLC in exchange for an amount of newly-issued LLC Units in Cure TopCo, LLC equal to the number of LLC Units redeemed from the holders of LLC Units. Cure TopCo, LLC will then distribute the cash or shares of our Class A common stock to such holder of an LLC Unit to complete the redemption. In the event of a redemption request by a holder of an LLC Unit, we may, at our option, effect a direct exchange of cash or Class A common stock for LLC Units in lieu of such a redemption. Whether by redemption or exchange, we are obligated to ensure that at all times the number of LLC Units that we own equals the number of shares of Class A common stock issued by us (subject to certain exceptions for treasury shares and shares underlying certain convertible or exchangeable securities). Shares of Class B common stock will be canceled on a one-for-one basis if we, following a redemption request of a holder of an LLC Unit, redeem or exchange LLC Units of such holder of an LLC Unit pursuant to the terms of the Amended LLC Agreement.
The Amended LLC Agreement will provide that, in the event that a tender offer, share exchange offer, issuer bid, take-over bid, recapitalization or similar transaction with respect to our Class A common stock is proposed by us or our stockholders and approved by our board of directors or is otherwise consented to or approved by our board of directors, the holders of LLC Units (other than holders of unvested Reclassified Incentive Units indirectly holding LLC Units through Cure Aggregator, LLC) will be permitted to participate in such offer by delivery of a notice of redemption or exchange that is effective immediately prior to the consummation of such offer. In the case of any such offer proposed by us, we are obligated to use our reasonable best efforts to enable and permit the holders of LLC Units to participate in such offer to the same extent or on an economically equivalent basis as the holders of shares of our Class A common stock without discrimination. In addition, we are obligated to use our reasonable best efforts to ensure that the holders of LLC Units may participate in each such offer without being required to redeem or exchange LLC Units.
The Amended LLC Agreement will provide that, except for transfers to us as provided above or to certain permitted transferees, the LLC Units and shares of Class B common stock may not be sold, transferred or otherwise disposed of.
Subject to certain exceptions, Cure TopCo, LLC will indemnify all of its members and their officers and other related parties, against all losses or expenses arising from claims or other legal proceedings in which such person (in its capacity as such) may be involved or become subject to in connection with Cure TopCo, LLC’s business or affairs or the Amended LLC Agreement or any related document.
Cure TopCo, LLC may be dissolved upon (i) the determination by us to dissolve Cure TopCo, LLC or (ii) any other event which would cause the dissolution of Cure TopCo, LLC under the Delaware Limited Liability Company Act, unless Cure TopCo, LLC is continued in accordance with the Delaware Limited Liability Company Act. Upon dissolution, Cure TopCo, LLC will be liquidated and the proceeds from any liquidation will be applied and distributed in the following manner: (a) first, to creditors (including creditors who are members or affiliates of members) in satisfaction of all of Cure TopCo, LLC’s liabilities (whether by payment or by making reasonable provision for payment of such liabilities, including the setting up of any reasonably necessary reserves) and (b) second, to the members in proportion to their vested LLC Units.
Tax Receivable Agreement
As described under “Organizational structure,” we will acquire certain favorable tax attributes from the Blocker Companies in the Mergers. In addition, future redemptions or exchanges by Continuing Pre-IPO LLC Members of LLC Units for shares of our Class A common stock or cash, and other transactions described herein are expected to result in favorable tax attributes for us. These tax attributes would not be available to us in the absence of those transactions and are expected to reduce the amount of tax that we would otherwise be required to pay in the future.
Upon the completion of this offering, we will be a party to the Tax Receivable Agreement with the TRA Parties. Under the Tax Receivable Agreement, we generally will be required to pay to the TRA Parties, in the
195
Table of Contents
aggregate, 85% of the amount of cash savings, if any, in U.S. federal, state and local income tax that we actually realize as a result of (i) certain favorable tax attributes we will acquire from the Blocker Companies in the Mergers (including net operating losses, the Blocker Companies’ allocable share of existing tax basis and refunds of Blocker Company taxes attributable to pre-Merger tax periods), (ii) increases to our allocable share of existing tax basis and tax basis adjustments that may result from (x) future redemptions or exchanges of LLC Units by Continuing Pre-IPO LLC Members for cash or Class A common stock, (y) the IPO Contribution and (z) certain payments made under the Tax Receivable Agreement and (iii) deductions in respect of interest and certain compensatory payments made under the Tax Receivable Agreement. The payment obligations under the Tax Receivable Agreement are our obligations and not the obligations of Cure TopCo, LLC.
We expect that the payments we will be required to make under the Tax Receivable Agreement will be substantial. The tax attributes available to us as a result of the Mergers and our allocable share of existing tax basis are expected to result in tax savings of approximately $56.3 million. We would be required to pay the TRA Parties approximately 85% of such amount, or $47.8 million, over the 15-year period from the date of the completion of this offering. Further, assuming no material changes in relevant tax law and that we earn sufficient taxable income to realize all tax benefits that are subject to the Tax Receivable Agreement, we expect that the tax savings associated with all tax attributes described above would aggregate to approximately $444.2 million over 15 years from the date of the completion of this offering, based on an assumed initial public offering price of $20.50 per share of Class A common stock, the midpoint of the estimated price range set forth on the cover page of this prospectus and assuming all future redemptions or exchanges would occur on the date of this offering. Under this scenario, we would be required to pay the TRA Parties approximately 85% of such amount, or $377.6 million, over the 15-year period from the date of the completion of this offering. The actual amounts we will be required to pay may materially differ from these hypothetical amounts, because potential future tax savings that we will be deemed to realize, and the Tax Receivable Agreement payments made by us, will be calculated based in part on the market value of our Class A common stock at the time of each redemption or exchange of an LLC Unit for cash or a share of Class A common stock and the prevailing applicable federal tax rate (plus the assumed combined state and local tax rate) applicable to us over the life of the Tax Receivable Agreement and will depend on our generating sufficient taxable income to realize the tax benefits that are subject to the Tax Receivable Agreement. Payments under the Tax Receivable Agreement are not conditioned on our existing owners’ continued ownership of us after this offering.
Payments under the Tax Receivable Agreement will be based on the tax reporting positions we determine, and the IRS or another tax authority may challenge all or a part of the deductions, existing tax basis, tax basis increases, NOLs or other tax attributes subject to the Tax Receivable Agreement, and a court could sustain such challenge. Payments we will be required to make under the Tax Receivable Agreement generally will not be reduced as a result of any taxes imposed on us, Cure TopCo, LLC or any direct or indirect subsidiary thereof that are attributable to a tax period (or portion thereof) ending on or before the Mergers, the IPO Contribution or the date of the completion of this offering. Further, the parties to the Tax Receivable Agreement will not reimburse us for any payments previously made if such tax attributes are subsequently disallowed, except that any excess payments made to a TRA Party will be netted against future payments otherwise to be made to such TRA Party under the Tax Receivable Agreement, if any, after our determination of such excess. In addition, the actual state or local tax savings we may realize may be different than the amount of such tax savings we are deemed to realize under the Tax Receivable Agreement, which will be based on an assumed combined state and local tax rate applied to our reduction in taxable income as determined for U.S. federal income tax purposes as a result of the tax attributes subject to the Tax Receivable Agreement. In both such circumstances, we could make payments to the TRA Parties that are greater than our actual cash tax savings and we may not be able to recoup those payments, which could negatively impact our liquidity. The Tax Receivable Agreement provides that (1) in the event that we breach any of our material obligations under the Tax Receivable Agreement, (2) at the election of the TRA Parties, upon certain changes of control or (3) if, at any time, we elect an early termination of the Tax Receivable Agreement, our obligations under the Tax Receivable Agreement (with respect to all LLC Units, whether or not LLC Units have been exchanged or acquired before or after such transaction) would accelerate and become payable in a lump sum amount equal to the present value of the anticipated future tax benefits
196
Table of Contents
calculated based on certain assumptions, including that we would have sufficient taxable income to fully utilize the deductions arising from the tax deductions, tax basis and other tax attributes subject to the Tax Receivable Agreement. The change of control provisions in the Tax Receivable Agreement may result in situations where the Pre-IPO LLC Members have interests that differ from or are in addition to those of our other stockholders.
Finally, because we are a holding company with no operations of our own, our ability to make payments under the Tax Receivable Agreement depends on the ability of Cure TopCo, LLC to make distributions to us. To the extent that we are unable to make payments under the Tax Receivable Agreement for any reason, such payments will be deferred and will accrue interest until paid; provided, however, that nonpayment for a specified period may constitute a breach of a material obligation under the Tax Receivable Agreement and therefore accelerate payments due under the Tax Receivable Agreement, which could negatively impact our results of operations and could also affect our liquidity in periods in which such payments are made.
Registration rights agreement
Prior to the consummation of this offering, we will enter into a registration rights agreement with certain of the Pre-IPO LLC Members, including New Mountain and one of our directors, Stephen Wiggins. At any time beginning 180 days following the closing of this offering, subject to several exceptions, including underwriter cutbacks and our right to defer a demand registration under certain circumstances, the Pre-IPO LLC Members party to the registration rights agreement may require that we register for public resale under the Securities Act all shares of common stock constituting registrable securities that they request be registered at any time following this offering so long as the securities requested to be registered in each registration statement have an aggregate estimated market value of least $20 million. If we become eligible to register the sale of our securities on Form S-3 under the Securities Act, which will not be until at least twelve months after the date of this prospectus, the Pre-IPO LLC Members party to the registration rights agreement have the right to require us to register the sale of the registrable securities held by them on Form S-3, subject to offering size and other restrictions.
If we propose to register any of our securities under the Securities Act for our own account or the account of any other holder (excluding any registration related to an employee benefit plan or a corporate reorganization transaction), the Pre-IPO LLC Members party to the registration rights agreement are entitled to notice of such registration and to request that we include registrable securities for resale on such registration statement, and we are required, subject to certain exceptions, to include such registrable securities in such registration statement. We will undertake in the registration rights agreement to use our reasonable best efforts to file a shelf registration statement on Form S-3 to permit the resale of the shares of Class A common stock held by Pre-IPO LLC Members party to the registration rights agreement.
In connection with the transfer of their registrable securities, the parties to the registration rights agreement may assign certain of their respective rights under the registration rights agreement under certain circumstances.
Stockholders agreement
In connection with this offering, we will enter into the stockholders agreement with certain of the Pre-IPO LLC Members. Pursuant to the stockholders agreement, New Mountain Capital will have the right to nominate directors to our board of directors as follows: so long as affiliates of New Mountain Capital continue to own (A) at least 50% of the shares of common stock that New Mountain Capital owns immediately following this offering, New Mountain Capital shall be entitled to nominate directors representing a majority of the number of directors on our board of directors, (B) less than 50% but at least 25% of the shares of common stock that New Mountain Capital owns immediately following this offering, New Mountain Capital shall be entitled to nominate directors representing at least 25% of the number of directors on the board of directors and (C) less than 25% but at least 10% of the shares of common stock New Mountain Capital owns immediately following this offering, New Mountain Capital shall be entitled to nominate directors representing at least 10% of the number of directors on the board of directors. As a result, following this offering, New Mountain Capital will be able to designate at least half of the nominees for election to our board of directors.
197
Table of Contents
The stockholders agreement will also provide that for so long as New Mountain Capital has the right to designate at least one director, New Mountain Capital will have the right to nominate the pro rata share of the total number of members of each committee of our board of directors that is equal to the proportion that the number of directors designated by New Mountain Capital bears to the total number of directors then on our board of directors; provided that the right of any director designated by New Mountain Capital to serve on a committee will be subject to applicable laws and NYSE independence rules.
Pursuant to the stockholders agreement, for so long as New Mountain Capital continues to own at least 15% of the issued and outstanding Class A common stock and Class B common stock, written approval by New Mountain Capital will be required for certain corporate actions. These actions include: (a) the liquidation, dissolution or winding up of Signify or Cure TopCo, LLC; (b) (i) the consolidation or merger of Signify or Cure TopCo, LLC into or with any other entity, (ii) the sale, lease or other transfer of all or substantially all of the assets of Signify or Cure TopCo, LLC to another entity, or (iii) any other business combination transaction with another entity, in each case, where such transaction would result in any “person” or “group” (as such terms are used for purposes of Section 13(d) of the Exchange Act) becoming the beneficial owner, directly or indirectly, of more than 50% of the total voting power of our capital stock entitled to vote generally in the election of our directors or acquires the power to direct or cause the direction of the our management and policies, whether through the ownership of voting securities, by contract or otherwise; (c) entry into any new line of business or other significant change in the scope or nature of our or our subsidiaries’ business or operations, taken as a whole; (d) the incurrence by Signify or Cure TopCo, LLC of any indebtedness, including the entry into any guarantee in respect of indebtedness, in each case in excess of $10,000,000, other than working capital loans and other similar transactions in the ordinary course of business; (e) any amendments to credit agreements or other documents representing our material indebtedness; (f) the sale, transfer or other disposition of (which for purposes of clarification excludes inventory and other sales in the ordinary course of business) in any transaction or series of related transactions of more than 25% of the fair market value of our and our subsidiaries’ consolidated assets, taken as a whole; (g) the declaration or payment of dividends on Class A common stock, or distributions by Cure TopCo, LLC on LLC Units other than Tax Distributions as defined in the Third Amended and Restated Limited Liability Company Agreement of Cure TopCo, LLC; (h) the creation, issuance or sale (by reclassification, merger, consolidation, reorganization or otherwise) of equity securities by us, including Class A common stock and Class B common stock, or any securities convertible into our equity securities; provided, that the consent of New Mountain Capital shall not be required in connection with the grant or issuance of equity or equity-based awards to employees, officers, directors, consultants or other persons performing services for Signify or any of its subsidiaries, or in connection with the issuance of Class A common stock or Class B common stock upon the exercise, conversion or settlement of such awards, pursuant to any equity incentive plans as in existence on the date of the stockholders agreement or that are thereafter adopted by the board of directors; (i) any amendments to our certificate of incorporation or bylaws, or to the certificate of formation or operating agreement of Cure TopCo, LLC; (j) any increase or decrease in the size of our board of directors; (k) any change in our independent auditors; (l) any hiring, termination, or replacement of our Chief Executive Officer or Chief Financial and Administrative Officer; (m) any amendments to employment agreements with our Chief Executive Officer of Chief Financial and Administrative Officer; (n) entry into agreements by us in connection with (i) acquisitions or dispositions in excess of $25,000,000 and (ii) joint ventures or strategic partnerships outside the ordinary course of business; (o) any action or resolution inconsistent with Section 16 of our certificate of incorporation or (p) any agreement or commitment with respect to any of the foregoing.
In addition, until such time as New Mountain Capital owns less than 10% of our outstanding common stock, all parties to the stockholders agreement will have the right to receive certain information with respect to the Company. The stockholders agreement will also provide restrictions on the parties’ ability to sell, transfer or otherwise dispose of shares of Class B common stock, except (i) in the event of a merger, consolidation or other business combination of the Company as provided in the Amended LLC Agreement, (ii) with our written consent or (iii) to certain permitted transferees.
198
Table of Contents
Transactions with New Mountain and other related parties
Management services agreement
We entered into a management services agreement with New Mountain Capital L.L.C. in 2017, which indirectly owns a majority of our equity interests. Under the terms of this agreement, New Mountain Capital L.L.C. provided us with assistance in (i) establishing and maintaining banking, legal and other business relationships, (ii) developing and implementing corporate and business strategy, (iii) structuring and implementing equity participation plans, employee benefit plans and other incentive arrangements for key executives and (iv) providing professional employees, advisors and consultants to serve as directors and/or officers. Pursuant to the management services agreement, New Mountain Capital L.L.C. was entitled to (i) an annual fee of $1.0 million and (ii) at its request, reasonable fees in connection with the consummation of certain transactions. This agreement was terminated upon our combination with Remedy in November 2019. During each of the years ended December 31, 2018 and 2019, we incurred management services fees of $1.0 million per year relating to this agreement. These fees are included in selling, general and administrative expenses in our consolidated statements of income included elsewhere in this prospectus.
Consulting agreements
On March 7, 2019, we entered into a consulting agreement with Eir (as amended on June 18, 2020), pursuant to which Brett Carlson, a former director of Cure TopCo, LLC and the Chief Executive Officer of Eir, provides non-director related services to us. The agreement provides for a cash retainer equal to $15,000 per month, which is payable to Eir under the terms of the agreement. In addition, in the event that we complete a corporate transaction in which we acquire a company referred and introduced to us by Mr. Carlson, we will pay Eir a cash transaction fee of 3% of any deal consideration up to $10 million, plus an additional 1.5% on any incremental deal consideration above $10 million. See “Executive and director compensation—Director compensation.” Effective January 12, 2021, Mr. Carlson no longer serves on our board of directors.
On November 23, 2020, we entered into a letter agreement with Kevin McNamara, a director of Cure TopCo, LLC, which provides for payment to Mr. McNamara of an annual cash retainer of $225,000 for service as a member of our board of directors and for consulting services provided to us by Mr. McNamara. In addition, Mr. McNamara is entitled to reimbursement for annual premiums on life, accidental death and dismemberment, short-term disability and medical insurance.
Note receivable
On April 17, 2019, we issued a note receivable to our Chief Executive Officer for $2.0 million, which accrued interest at a rate of 2.52% per annum. In December 2019, our Chief Executive Officer repaid the note receivable and accrued interest thereon in full. The interest is included in other expense (income), net in our consolidated statement of income for the year ended December 31, 2019 included elsewhere in this prospectus.
Issuance of preferred units
In November 2019, Cure TopCo, LLC issued 3,050,000 Series B preferred units to New Mountain Partners V (AIV-C), LP in connection with the Remedy Combination.
In addition, as a holder of Series B preferred units, New Mountain Partners V (AIV-C), LP received tax distributions of $18.4 million and $16.6 million for the years ended December 31, 2019 and 2018, respectively, and $5.6 million and $16.6 million for the nine months ended September 30, 2020 and 2019, respectively.
Remedy Partners Combination agreement
On November 14, 2019, we entered into a combination agreement with Remedy Partners, Inc. pursuant to which Remedy Partners became our wholly owned subsidiary on November 26, 2019. As consideration for the
199
Table of Contents
combination, we issued 3,384,543 Series A preferred units to New Remedy, which is controlled indirectly by New Mountain Capital, in exchange for all of Remedy Partners’ outstanding equity interests. In addition, in connection with the recapitalization of Cure TopCo, LLC that occurred as part of the combination, all Class A common units of Cure TopCo, LLC, including those held by an entity affiliated with New Mountain Capital, that were outstanding as of immediately prior to the combination were converted on a one-for-one basis into Series B preferred units of Cure TopCo, LLC. See “—Transactions with New Mountain and other related parties—Issuance of preferred units.”
New Remedy Stockholders’ Agreement
In connection with our combination with Remedy Partners in November 2019, New Remedy entered into an amended and restated stockholders’ agreement with Remedy Acquisition, L.P., the controlling stockholder of New Remedy and an entity controlled by New Mountain Capital, and the other stockholders of Remedy Partners (the “New Remedy Stockholders’ Agreement”). The New Remedy Stockholders’ Agreement requires each stockholder of New Remedy to agree to cast all votes to elect to the board of New Remedy (i) a number of persons designated by Remedy Acquisition, L.P. that constitute a majority of directors on the board at such time and (ii) a number of persons designated by the minority stockholders in proportion to such stockholders’ ownership of New Remedy. A director may be removed only with the affirmative vote of the stockholders entitled to designate such director. In addition, pursuant to the New Remedy Stockholders’ Agreement, each stockholder of New Remedy agrees to vote their shares in the same proportion as Remedy Acquisition, L.P. votes its shares to approve certain significant transactions, including a sale, recapitalization, merger, consolidation, reorganization or other transaction for the transfer of shares that would constitute a change of control or that has been approved by Remedy Acquisition, L.P. The New Remedy Stockholders’ Agreement will be terminated in connection with this offering and the merger of New Remedy with and into Signify Health, Inc.
Related party transactions policies and procedures
Upon the completion of this offering, we will adopt a written Related Person Transaction Policy (the “policy”), which will set forth our policy with respect to the review, approval, ratification and disclosure of all related person transactions by our Audit Committee. In accordance with the policy, our Audit Committee will have overall responsibility for implementation of and compliance with the policy.
For purposes of the policy, a “related person transaction” is a transaction, arrangement or relationship (or any series of similar transactions, arrangements or relationships) in which we were, are or will be a participant and the amount involved exceeded, exceeds or will exceed $120,000 and in which any related person (as defined in the policy) had, has or will have a direct or indirect material interest. A “related person transaction” does not include any employment relationship or transaction involving an executive officer and any related compensation resulting solely from that employment relationship that has been reviewed and approved by our board of directors.
The policy will require that notice of a proposed related person transaction be provided to our legal department prior to entry into such transaction. If our legal department determines that such transaction is a related person transaction, the proposed transaction will be submitted to our Audit Committee for consideration at its next meeting. Under the policy, our Audit Committee may approve only those related person transactions that are in, or not inconsistent with, our best interests. In the event that we become aware of a related person transaction that has not been previously reviewed, approved or ratified under the policy and that is ongoing or is completed, the transaction will be submitted to the Audit Committee so that it may determine whether to ratify, rescind or terminate the related person transaction.
The policy will also provide that the Audit Committee review certain previously approved or ratified related person transactions that are ongoing to determine whether the related person transaction remains in our best interests and the best interests of our stockholders. Additionally, we will make periodic inquiries of directors and executive officers with respect to any potential related person transaction of which they may be a party or of which they may be aware.
200
Table of Contents
Directed share program
At our request, the underwriters have reserved up to 1,175,000 shares of Class A common stock, or 5% of the shares of Class A common stock to be offered by this prospectus for sale, at the initial public offering price, through a directed share program for certain of our clinicians and employees and certain other individuals and entities.
201
Table of Contents
The following table sets forth information regarding the beneficial ownership of our common stock as of February 1, 2021 (i) as adjusted to give effect to the Reorganization Transactions, but prior to this offering, and (ii) as adjusted to give effect to the Reorganization Transactions and this offering as described in “Use of proceeds” by:
| • | each person or group whom we know to own beneficially more than 5% of our common stock; |
| • | each of the directors and named executive officers individually; and |
| • | all directors and executive officers as a group. |
The numbers of shares of common stock beneficially owned, percentages of beneficial ownership and percentages of combined voting power before this offering that are set forth below are based on the number of shares of Class A common stock and Class B common stock to be issued and outstanding prior to this offering after giving effect to the Reorganization Transactions. See “Organizational structure.” The numbers of shares of common stock beneficially owned, percentages of beneficial ownership and percentages of combined voting power after this offering that are set forth below are based on the number of shares of Class A common stock and Class B common stock to be issued and outstanding immediately after this offering.
In connection with this offering, we will issue to each Continuing Pre-IPO LLC Member one share of Class B common stock for each LLC Unit such Continuing Pre-IPO LLC Member beneficially owns immediately prior to the consummation of this offering, except in the case of Cure Aggregator, LLC, in which case Class B common stock will be issued to the direct holders of common units in Cure Aggregator, LLC in proportion to their interests in Cure Aggregator, LLC. Shares of Class B common stock will be canceled on a one-for-one basis if we, following a redemption request of a Continuing Pre-IPO LLC Member, redeem or exchange LLC Units of such Continuing Pre-IPO LLC Member pursuant to the terms of the Amended LLC Agreement. See “Certain relationships and related party transactions—Amended LLC Agreement.” As a result, the number of shares of Class B common stock listed in the table below correlates to the number of LLC Units each Continuing Pre-IPO LLC Member will beneficially own immediately after this offering (or in the case of directors and officers that hold their interests in Cure TopCo, LLC indirectly through common units of Cure Aggregator LLC, to the number of LLC Units corresponding to common units of Cure Aggregator, LLC that have vested or will vest within 60 days of February 1, 2021). The number of shares of Class A common stock listed in the table below represents the Class A common stock that will be issued in connection with this offering and the shares of Class A common stock that were issued to the Reorganization Parties in connection with the IPO Contribution and the Mergers.
In accordance with the rules of the SEC, beneficial ownership includes voting or investment power with respect to securities and includes the shares issuable pursuant to stock options that are exercisable within 60 days of February 1, 2021. The number of shares of Class A common stock outstanding after this offering includes shares of common stock being offered for sale by us in this offering and the shares of Class A common stock that were issued to the Reorganization Parties in connection with the IPO Contribution and the Mergers. Unless otherwise indicated, the address for each listed stockholder is: c/o Signify Health, Inc., 800 Connecticut Avenue, Norwalk, CT 06854. To our knowledge, except as indicated in the footnotes to this table and pursuant to applicable community property laws, the persons named in the table have sole voting and investment power with respect to all shares of common stock.
202
Table of Contents
The following table assumes the underwriters’ option to purchase additional shares of Class A common stock is not exercised. In addition, the following table does not reflect any shares of Class A common stock that may be purchased in this offering or pursuant to our directed share program described under “Underwriting—Directed share program.”
| Shares owned before the offering | % of combined voting power before the offering(3) |
Shares owned after the offering | % of combined voting power after the offering(3) |
|||||||||||||||||||||||||||||||||||||
| Class A common stock(1) |
Class B common stock(2) |
Class A common stock(1) |
Class B common stock(2) |
|||||||||||||||||||||||||||||||||||||
| Name of beneficial owner |
Number | Percentage | Number | Percentage | Number | Percentage | Number | Percentage | ||||||||||||||||||||||||||||||||
| 5% stockholders |
||||||||||||||||||||||||||||||||||||||||
| Certain Pre-IPO LLC Members affiliated with New Mountain Capital(4) |
97,239,840 | 68.7 | % | 43,070,294 | 75.2 | % | 70.6 | % | 97,239,840 | 58.9 | % | 43,070,294 | 75.2 | % | 63.1 | % | ||||||||||||||||||||||||
| Directors and executive officers |
|
|||||||||||||||||||||||||||||||||||||||
| Kyle Armbrester |
— | — | 2,402,349 | 4.2 | % | 1.2 | % | — | — | 2,402,349 | 4.2 | % | 1.1 | % | ||||||||||||||||||||||||||
| Steven Senneff |
197,826 | * | 110,140 | * | * | 197,826 | * | 110,140 | * | * | ||||||||||||||||||||||||||||||
| Adam McAnaney |
23,897 | * | 2,625 | * | * | 23,897 | * | 2,625 | * | * | ||||||||||||||||||||||||||||||
| Marc Rothman, MD |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Peter Boumenot |
— | — | 33,033 | * | * | — | — | 33,033 | * | * | ||||||||||||||||||||||||||||||
| David Pierre |
— | — | 245,372 | * | * | — | — | 245,372 | * | * | ||||||||||||||||||||||||||||||
| Josh Builder |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Laurel Douty |
— | — | 15,755 | * | * | — | — | |
15,755 |
|
* | * | ||||||||||||||||||||||||||||
| Taj J. Clayton |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Matthew S. Holt |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Brandon H. Hull |
— | — | 301,996 | * | * | — | — | 301,996 | * | * | ||||||||||||||||||||||||||||||
| Kevin M. McNamara |
— | — | 583,564 | 1.0 | % | * | — | — | 583,564 | 1.0 | % | * | ||||||||||||||||||||||||||||
| Albert A. Notini |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Kyle B. Peterson |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Vivian E. Riefberg |
— | — | 2,625 | * | * | — | — | 2,625 | * | * | ||||||||||||||||||||||||||||||
| Stephen F. Wiggins(6) |
7,941,729 | 5.6 | % | — | — | 4.0 | % | 7,941,729 | 4.8 | % | — | — | 3.6 | % | ||||||||||||||||||||||||||
| All directors and executive officers as a group (16 persons) |
8,163,452 | 5.8 | % | 3,697,459 | 6.4 | % | 5.9 | % | 8,163,452 | 4.9 | % | |
3,697,459 |
|
6.4 | % | 5.3 | % | ||||||||||||||||||||||
| * | Less than 1% |
203
Table of Contents
The following table assumes the underwriters’ option to purchase additional shares of Class A common stock is exercised in full. In addition, the following table does not reflect any shares of Class A common stock that may be purchased in this offering or pursuant to our directed share program described under “Underwriting—Directed share program.”
| Shares owned before the offering | % of combined voting power before the offering(3) |
Shares owned after the offering | % of combined voting power after the offering(3) |
|||||||||||||||||||||||||||||||||||||
| Class A common stock(1) |
Class B common stock(2) |
Class A common stock(1) |
Class B common stock(2) |
|||||||||||||||||||||||||||||||||||||
| Name of beneficial owner |
Number | Percentage | Number | Percentage | Number | Percentage | Number | Percentage | ||||||||||||||||||||||||||||||||
| 5% stockholders |
||||||||||||||||||||||||||||||||||||||||
| Certain Pre-IPO LLC Members affiliated with New Mountain Capital(4) |
97,239,840 | 68.7 | % | 43,070,294 | 75.2 | % | 70.6 | % | 97,239,840 | 57.7 | % | 43,070,294 | 75.2 | % | 62.1 | % | ||||||||||||||||||||||||
| Directors and executive officers |
|
|||||||||||||||||||||||||||||||||||||||
| Kyle Armbrester |
— | — | 2,402,349 | 4.2 | % | 1.2 | % | — | — | 2,402,349 | 4.2 | % | 1.1 | % | ||||||||||||||||||||||||||
| Steven Senneff |
197,826 | * | 110,140 | * | * | 197,826 | * | 110,140 | * | * | ||||||||||||||||||||||||||||||
| Adam McAnaney |
23,897 | * | 2,625 | * | * | 23,897 | * | 2,625 | * | * | ||||||||||||||||||||||||||||||
| Marc Rothman, MD |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Peter Boumenot |
— | — | 33,033 | * | * | — | — | 33,033 | * | * | ||||||||||||||||||||||||||||||
| David Pierre |
— | — | 245,372 | * | * | — | — | 245,372 | * | * | ||||||||||||||||||||||||||||||
| Josh Builder |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Laurel Douty |
— | — | 15,755 | * | * | — | — | 15,755 | * | * | ||||||||||||||||||||||||||||||
| Taj J. Clayton |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Matthew S. Holt. |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Brandon H. Hull |
— | — | 301,996 | * | * | — | — | 301,996 | * | * | ||||||||||||||||||||||||||||||
| Kevin M. McNamara |
— | — | 583,564 | 1.0 | % | * | — | — | 583,564 | 1.0 | % | * | ||||||||||||||||||||||||||||
| Albert A. Notini |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Kyle B. Peterson |
— | — | — | — | — | — | — | — | — | — | ||||||||||||||||||||||||||||||
| Vivian E. Riefberg |
— | — | 2,625 | * | * | — | — | 2,625 | * | * | ||||||||||||||||||||||||||||||
| Stephen F. Wiggins(6) |
7,941,729 | 5.6 | % | — | — | 4.0 | % | 7,941,729 | 4.7 | % | — | — | 3.5 | % | ||||||||||||||||||||||||||
| All directors and executive officers as a group (16 persons) |
8,163,452 | 5.8 | % | 3,697,459 | 6.4 | % | 5.9 | % | 8,163,452 | 4.8 | % | |
3,697,459 |
|
6.4 | % | 5.2 | % | ||||||||||||||||||||||
* Less than 1%
| (1) | On a fully exchanged and converted basis. Subject to the terms of the Amended LLC Agreement, LLC Units are redeemable or exchangeable for shares of our Class A common stock on a one-for-one basis. Shares of Class B common stock will be canceled on a one-for-one basis if we redeem or exchange LLC Units pursuant to the terms of the Amended LLC Agreement. Beneficial ownership of shares of our Class A common stock reflected in this table does not include beneficial ownership of shares of our Class A common stock for which such LLC Units may be redeemed or exchanged. |
| (2) | On a fully exchanged and converted basis. All of the issued and outstanding shares of our Class B common stock is held by the Continuing Pre-IPO LLC Members, except in the case of Cure Aggregator, LLC, in which case shares of Class B common stock corresponding to the LLC Units held by Cure Aggregator, LLC are held by the holders of common units in Cure Aggregator, LLC in proportion to their interests in Cure Aggregator, LLC. Excludes shares of Class B common stock issued to holders of common units in Cure Aggregator, LLC that are unvested and do not have any voting rights. |
| (3) | Represents percentage of voting power of the Class A common stock and Class B common stock held by such person voting together as a single class. Each holder of Class A common stock and Class B common stock is entitled to one vote per share on all matters submitted to our stockholders for a vote. The Class B common stock is not entitled to economic interests in Signify Health, Inc. See “Description of capital stock—Common stock.” |
| (4) | The general partner of New Mountain Partners V (AIV-C), L.P. is New Mountain Investments V, L.L.C. and the manager of New Mountain Partners V (AIV-C), L.P. is New Mountain Capital, L.L.C. Steven B. Klinsky is the managing member of New Mountain Investments V, L.L.C. Matthew S. Holt, Albert A. Notini and Kyle B. Peterson, each members of our Board of Directors, are members of New Mountain Investments V, L.L.C. New Mountain Investments V, L.L.C. has decision-making power over the disposition and voting of shares of portfolio investments of New Mountain Partners V (AIV-C), L.P. New Mountain Capital, L.L.C. also has voting power over the shares of portfolio investments of New Mountain Partners V (AIV-C), L.P. Steven B. Klinsky, as the managing member of New Mountain Investments V, L.L.C., has voting and investment power over the shares held by New Mountain Investments V, L.L.C. |
The managing member of New Mountain Capital, L.L.C. is New Mountain Capital Group, L.P. The general partner of New Mountain Capital Group, L.P. is NM Holdings GP, L.L.C. Steven B. Klinsky is the managing member of NM Holdings GP, L.L.C. Since (a) New Mountain Investments V, L.L.C. has decision-making power over New Mountain Partners V (AIV-C), L.P. and (b) New Mountain Capital, L.L.C. has voting power over the shares of portfolio investments of New Mountain Partners V (AIV-C), L.P., Mr. Klinsky may be deemed to beneficially own the shares that New Mountain Partners V (AIV-C), L.P. holds of record or may be deemed to beneficially own.
Messrs. Klinsky, Holt, Notini and Peterson, New Mountain Investments V, L.L.C. and New Mountain Capital, L.L.C. expressly disclaim beneficial ownership over the shares held by New Mountain Partners V (AIV-C), L.P. The address of each of the foregoing is c/o New Mountain Capital, L.L.C., 1633 Broadway, 48th Floor, New York, New York 10019.
| (5) | Includes the equivalent Class A shares for 80,517.31 Class C LLC units in Cure Aggregator, LLC owned by Philippa Armbrester 2020 Irrevocable Trust and 6,252.18 Class C LLC units and 36,718.75 Class B LLC units in Cure Aggregator, LLC owned by the Kyle and Philippa Armbrester Family Trust. |
| (6) | Consists of 7,988,509 shares of Class A common stock beneficially owned directly by Mr. Wiggins and 4,103 shares of Class A common stock beneficially owned by RP Special Situations LLC, an entity controlled by Mr. Wiggins. |
204
Table of Contents
In connection with this offering, we will amend and restate our certificate of incorporation and our bylaws. The following is a description of the material terms of, and is qualified in its entirety by, our certificate of incorporation and bylaws, each of which will be in effect upon the consummation of this offering, the forms of which are filed as exhibits to the registration statement of which this prospectus forms a part. Under “Description of capital stock,” “we,” “us,” “our” and “our company” refer to Signify Health, Inc.
General
Upon the consummation of this offering, our authorized capital stock will consist of 1,000,000,000 shares of Class A common stock, par value $0.01 per share, 75,000,000 shares of Class B common stock, par value $0.01 per share, and 50,000,000 shares of preferred stock, par value $0.01 per share. Unless our board of directors determines otherwise, we will issue all shares of our capital stock in uncertificated form.
Common stock
Class A common stock
Holders of shares of our Class A common stock are entitled to one vote for each share held of record on all matters on which stockholders are entitled to vote generally, including the election or removal of directors. The holders of our Class A common stock do not have cumulative voting rights in the election of directors.
Holders of shares of our Class A common stock are entitled to receive dividends when and if declared by our board of directors out of funds legally available therefor, subject to any statutory or contractual restrictions on the payment of dividends and to any restrictions on the payment of dividends imposed by the terms of any outstanding preferred stock.
Upon our liquidation, dissolution or winding up and after payment in full of all amounts required to be paid to creditors and to the holders of preferred stock having liquidation preferences, if any, the holders of shares of our Class A common stock will be entitled to receive pro rata our remaining assets available for distribution.
All shares of our Class A common stock that will be outstanding at the time of the completion of the offering will be fully paid and non-assessable. The Class A common stock will not be subject to further calls or assessments by us. The rights, powers and privileges of our Class A common stock will be subject to those of the holders of any shares of our preferred stock or any other series or class of stock we may authorize and issue in the future.
Class B common stock
Each share of Class B common stock will entitle its holder to one vote per share on all matters submitted to a vote of our stockholders. If at any time the ratio at which LLC Units are redeemable or exchangeable for shares of our Class A common stock changes from one-for-one as described under “Certain relationships and related party transactions—Amended LLC Agreement,” the number of votes to which Class B common stockholders are entitled will be adjusted accordingly. The holders of our Class B common stock do not have cumulative voting rights in the election of directors.
Except for transfers to us pursuant to the Amended LLC Agreement or to certain permitted transferees, the LLC Units and corresponding shares of Class B common stock may not be sold, transferred or otherwise disposed of. Holders of shares of our Class B common stock will vote together with holders of our Class A common stock as a single class on all matters on which stockholders are entitled to vote, except as otherwise required by law.
205
Table of Contents
The Class B common stock is not entitled to economic interests in Signify Health, Inc. Holders of our Class B common stock do not have any right to receive dividends or to receive a distribution upon a liquidation or winding up of Signify Health, Inc. However, if Cure TopCo LLC makes distributions to Signify Health, Inc., the other holders of LLC Units, including the Continuing Pre-IPO LLC Members, will be entitled to receive distributions pro rata in accordance with the percentages of their respective LLC Units. The Class B common stock will not be subject to further calls or assessment by us.
Preferred stock
No shares of preferred stock will be issued or outstanding immediately after the offering contemplated by this prospectus. Our certificate of incorporation will authorize our board of directors to establish one or more series of preferred stock (including convertible preferred stock). Unless required by law or any stock exchange, the authorized shares of preferred stock will be available for issuance without further action by holders of our common stock. Our board of directors will be able to determine, with respect to any series of preferred stock, the powers (including voting powers), preferences and relative, participating, optional or other special rights, and the qualifications, limitations or restrictions thereof, including, without limitation:
| • | the designation of the series; |
| • | the number of shares of the series, which our board of directors may, except where otherwise provided in the preferred stock designation, increase (but not above the total number of authorized share of the class) or decrease (but not below the number of shares then outstanding); |
| • | whether dividends, if any, will be cumulative or non-cumulative and the dividend rate of the series; |
| • | the dates at which dividends, if any, will be payable; |
| • | the redemption rights and price or prices, if any, for shares of the series; |
| • | the terms and amounts of any sinking fund provided for the purchase or redemption of shares of the series; |
| • | the amounts payable on shares of the series in the event of any voluntary or involuntary liquidation, dissolution or winding up of the affairs of our company; |
| • | whether the shares of the series will be convertible into shares of any other class or series, or any other security, of our company or any other entity, and, if so, the specification of the other class or series or other security, the conversion price or prices or rate or rates, any rate adjustments, the date or dates as of which the shares will be convertible and all other terms and conditions upon which the conversion may be made; |
| • | restrictions on the issuance of shares of the same series or of any other class or series; and |
| • | the voting rights, if any, of the holders of the series. |
We could issue a series of preferred stock that could, depending on the terms of the series, impede or discourage an acquisition attempt or other transaction that some, or a majority, of the holders of our common stock might believe to be in their best interests or in which the holders of our common stock might receive a premium over the market price of the shares of common stock. Additionally, the issuance of preferred stock may adversely affect the holders of our common stock by restricting dividends on the common stock, diluting the voting power of the common stock or subordinating the liquidation rights of the common stock. As a result of these or other factors, the issuance of preferred stock could have an adverse impact on the market price of our common stock.
Authorized but unissued capital stock
Delaware law does not require stockholder approval for any issuance of authorized shares. However, the listing requirements of the NYSE, which would apply so long as the shares of Class A common stock remains
206
Table of Contents
listed on the NYSE, require stockholder approval of certain issuances equal to or exceeding 20% of the then outstanding voting power or the then outstanding number of shares of Class A common stock (we believe the position of the NYSE is that the calculation in this latter case treats as outstanding shares of Class A common stock issuable upon redemption or exchange of outstanding LLC Units not held by Signify Health, Inc.). These additional shares of Class A common stock may be used for a variety of corporate purposes, including future public offerings, to raise additional capital or to facilitate acquisitions.
One of the effects of the existence of unissued and unreserved common stock or preferred stock may be to enable our board of directors to issue shares to persons friendly to current management, which issuance could render more difficult or discourage an attempt to obtain control of our company by means of a merger, tender offer, proxy contest or otherwise, and thereby protect the continuity of our management and possibly deprive the stockholders of opportunities to sell their shares at prices higher than prevailing market prices.
Dividends
The DGCL permits a corporation to declare and pay dividends out of “surplus” or, if there is no “surplus,” out of its net profits for the fiscal year in which the dividend is declared and/or the preceding fiscal year. “Surplus” is defined as the excess of the net assets of the corporation over the amount determined to be the capital of the corporation by its board of directors. The capital of the corporation is typically calculated to be (and cannot be less than) the aggregate par value of all issued shares of capital stock. Net assets equal the fair value of the total assets minus total liabilities. The DGCL also provides that dividends may not be paid out of net profits if, after the payment of the dividend, remaining capital would be less than the capital represented by the outstanding stock of all classes having a preference upon the distribution of assets. Declaration and payment of any dividend will be subject to the discretion of our board of directors. See also “Dividend policy.”
Stockholder meetings
Our certificate of incorporation and our bylaws will provide that annual stockholder meetings will be held at a date, time and place, if any, as exclusively selected by our board of directors. Our certificate of incorporation will provide that, subject to any special rights of the holders as required by law, special meetings of the stockholders can only be called by the chairman of the board, the chief executive officer or the president of the Company, or, until the time that the Majority Ownership Requirement is no longer met, at the request of holders of a majority of the total voting power of our outstanding shares of common stock, voting together as a single class. Except as described above, stockholders are not permitted to call a special meeting or to require the board of directors to call a special meeting. To the extent permitted under applicable law, we may conduct meetings by remote communications, including by webcast.
Transferability, redemption and exchange
Under the Amended LLC Agreement, the holders of LLC Units will have the right, from and after the completion of this offering (subject to the terms of the Amended LLC Agreement), to require Cure TopCo, LLC to redeem all or a portion of their LLC Units for, at our election, newly issued shares of Class A common stock on a one-for-one basis or a cash payment equal to the volume weighted average market price of one share of our Class A common stock for each LLC Unit redeemed (subject to customary adjustments, including for stock splits, stock dividends and reclassifications) in accordance with the terms of the Amended LLC Agreement. Additionally, in the event of a redemption request by a holder of LLC Units, we may, at our election, effect a direct exchange of cash or Class A common stock for LLC Units in lieu of such a redemption. Shares of Class B common stock will be canceled on a one-for-one basis if we, following a redemption request of a holder of LLC Units, redeem or exchange LLC Units of such holder of LLC Units pursuant to the terms of the Amended LLC Agreement. See “Certain relationships and related party transactions—Amended LLC Agreement.”
Except for transfers to us pursuant to the Amended LLC Agreement or to certain permitted transferees, the LLC Units and corresponding shares of Class B common stock may not be sold, transferred or otherwise disposed of.
207
Table of Contents
Other provisions
Neither the Class A common stock nor the Class B common stock has any preemptive or other subscription rights.
There will be no redemption, conversion or sinking fund provisions applicable to the Class A common stock or Class B common stock.
At such time when no LLC Units remain redeemable or exchangeable for shares of our Class A common stock, our Class B common stock will be canceled.
Corporate opportunity
Our certificate of incorporation will renounce, to the maximum extent permitted from time to time by Delaware law, any interest or expectancy that we have in, or right to be offered an opportunity to participate in, specified business opportunities that are from time to time presented to our officers, directors or stockholders or their respective affiliates, other than those officers, directors, stockholders or affiliates who are our or our subsidiaries’ employees. Our certificate of incorporation will provide that, to the fullest extent permitted by law, none of New Mountain Capital or any of its affiliates or any director who is not employed by us (including any non-employee director who serves as one of our officers in both his director and officer capacities) or his or her affiliates will have any duty to refrain from (i) engaging in a corporate opportunity in the same or similar lines of business in which we or our affiliates now engage or propose to engage or (ii) otherwise competing with us or our affiliates.
In addition, to the fullest extent permitted by law, in the event that New Mountain Capital or any non-employee director acquires knowledge of a potential transaction or other business opportunity which may be a corporate opportunity for itself or himself or its or his affiliates or for us or our affiliates, such person will have no duty to communicate or offer such transaction or business opportunity to us or any of our affiliates and they may take any such opportunity for themselves or offer it to another person or entity.
Our certificate of incorporation will not renounce our interest in any business opportunity that is expressly offered to a non-employee director solely in his or her capacity as a director or officer of the Company. To the fullest extent permitted by law, no business opportunity will be deemed to be a potential corporate opportunity for us unless we would be permitted to undertake the opportunity under our amended and restated certificate of incorporation, we have sufficient financial resources to undertake the opportunity and the opportunity would be in line with our business.
Certain certificate of incorporation, bylaws and statutory provisions
The provisions of our certificate of incorporation and bylaws and of the DGCL summarized below may have an anti-takeover effect and may delay, defer or prevent a tender offer or takeover attempt that you might consider in your best interest, including an attempt that might result in your receipt of a premium over the market price for your shares of Class A common stock.
Anti-takeover effects of our certificate of incorporation and bylaws
Our certificate of incorporation and bylaws will contain certain provisions that are intended to enhance the likelihood of continuity and stability in the composition of our board of directors and that may have the effect of delaying, deferring or preventing a future takeover or change in control of our company unless such takeover or change in control is approved by our board of directors. These provisions include:
No cumulative voting. Under Delaware law, the right to vote cumulatively does not exist unless the certificate of incorporation specifically authorizes cumulative voting. Our certificate of incorporation will not authorize cumulative voting. Therefore, stockholders holding a majority in voting power of the shares of our common stock entitled to vote generally in the election of directors will be able to elect all our directors.
208
Table of Contents
Classified board; election of directors. Our certificate of incorporation provides that our board of directors will be divided into three classes of directors, with the classes to be as nearly equal in number as possible and serving staggered three-year terms. Successors to the class of directors whose term expires at the first and second annual meetings of stockholders following the adoption of the certificate of incorporation, as applicable, will be elected for a term expiring at the third annual meeting following the annual meeting at which such directors were elected.
Our certificate of incorporation and bylaws will provide that, subject to any rights of holders of preferred stock to elect additional directors under specified circumstances, the number of directors will be fixed from time to time exclusively pursuant to a resolution adopted by the board of directors. Our certificate of incorporation will also provide that, subject to the rights granted to one or more series of preferred stock then outstanding, any vacancies on our board will be filled only by the affirmative vote of a majority of the remaining directors, even if less than a quorum.
Removal of directors. Following the time when the Majority Ownership Requirement is no longer met, and subject to obtaining any required stockholder votes, directors may be removed, but for cause only, by the affirmative vote of holders of 662⁄3% of the total voting power of our outstanding shares of common stock, voting together as a single class. This requirement of a super-majority vote to remove directors could enable a minority of our stockholders to exercise veto power over any such removal. Prior to such time, directors may be removed, but for cause only, by the affirmative vote of the holders of a majority of the total voting power of our outstanding shares of common stock.
Action by written consent; special meetings of stockholders. Our certificate of incorporation will provide that, following the time that the Majority Ownership Requirement is no longer met, stockholder action can be taken only at an annual or special meeting of stockholders and cannot be taken by written consent in lieu of a meeting. Our certificate of incorporation will also provide that, subject to any special rights of the holders as required by law, special meetings of the stockholders can only be called by the chairman of the board of directors, the chief executive officer or the president of the company or, until the time that the Majority Ownership Requirement is no longer met, at the request of holders of a majority of the total voting power of our outstanding shares of common stock, voting together as a single class. Except as described above, stockholders are not permitted to call a special meeting or to require the board of directors to call a special meeting.
Advance notice procedures. Our bylaws will establish an advance notice procedure for stockholder proposals to be brought before an annual meeting of our stockholders, including proposed nominations of persons for election to the board of directors. Stockholders at an annual meeting will only be able to consider proposals or nominations specified in the notice of meeting or brought before the meeting by or at the direction of the board of directors or by a stockholder who was a stockholder of record on the record date for the meeting, who is entitled to vote at the meeting and who has given our Secretary timely written notice, in proper form, of the stockholder’s intention to bring that business before the meeting. Although the bylaws will not give our board of directors the power to approve or disapprove stockholder nominations of candidates or proposals regarding other business to be conducted at a special or annual meeting, the bylaws may have the effect of precluding the conduct of certain business at a meeting if the proper procedures are not followed or may discourage or deter a potential acquirer from conducting a solicitation of proxies to elect its own slate of directors or otherwise attempting to obtain control of our company.
Super-majority approval requirements. The DGCL generally provides that the affirmative vote of the holders of a majority of the total voting power of the shares entitled to vote on any matter is required to amend a corporation’s certificate of incorporation or bylaws, unless either a corporation’s certificate of incorporation or bylaws require a greater percentage. Our certificate of incorporation and bylaws will provide that, following the time that the Majority Ownership Requirement is no longer met, the affirmative vote of holders of 662⁄3% of the total voting power of our outstanding common stock eligible to vote in the election of directors, voting together as a single class, will be required to amend, alter, change or repeal specified provisions, including those relating to actions by written consent of stockholders, calling of special meetings of stockholders, election and removal of directors, business combinations and amendment of our certificate of incorporation and bylaws. This requirement of a super-majority vote to approve amendments to our certificate of incorporation and bylaws could enable a minority of our stockholders to exercise veto power over any such amendments.
209
Table of Contents
Authorized but unissued shares. The authorized but unissued shares of common stock and preferred stock are available for future issuance without stockholder approval, subject to any limitations imposed by the listing rules of the NYSE. The existence of authorized but unissued and unreserved common stock and preferred stock could make more difficult or discourage an attempt to obtain control of us by means of a proxy contest, tender offer, merger or otherwise. See “—Preferred stock” and “—Authorized but unissued capital stock” above.
Business combinations with interested stockholders. In general, Section 203 of the DGCL prohibits a publicly held Delaware corporation from engaging in a business combination, such as a merger, with a person or group owning 15% or more of the corporation’s voting stock for a period of three years following the date the person became an interested stockholder, unless (with certain exceptions) the business combination or the transaction in which the person became an interested stockholder is approved in a prescribed manner. We will expressly elect not to be governed by the “business combination” provisions of Section 203 of the DGCL until such time as no party to our stockholders agreement beneficially owns 5% or more of the then outstanding shares of our common stock, at which time we will automatically become subject to Section 203 of the DGCL.
Exclusive forum
Our certificate of incorporation will require, to the fullest extent permitted by law, that (i) any derivative action or proceeding brought on our behalf, (ii) any action asserting a claim of breach of a fiduciary duty owed by any of our directors, officers or stockholders to us or our stockholders, (iii) any action asserting a claim against us arising pursuant to any provision of the DGCL or our certificate of incorporation or our bylaws or (iv) any action asserting a claim against us governed by the internal affairs doctrine will have to be brought in a state court located within the state of Delaware (or if no state court of the State of Delaware has jurisdiction, the federal district court for the District of Delaware), in all cases subject to the court’s having personal jurisdiction over the indispensable parties named as defendants. Additionally, our certificate of incorporation will state that the foregoing provision will not apply to claims arising under the Securities Act, the Exchange Act or other federal securities laws for which there is exclusive federal or concurrent federal and state jurisdiction. Unless we consent in writing to the selection of an alternative forum, the federal district courts of the United States of America shall be the exclusive forum for the resolution of any complaint asserting a cause of action arising under the Securities Act. The exclusive forum provisions may limit a stockholder’s ability to bring a claim in a judicial forum that it finds favorable for disputes with us or any of our directors, officers or stockholders, which may discourage lawsuits with respect to such claims. See “Risk factors—Risks related to our Class A common stock and this offering—The provision of our amended and restated certificate of incorporation requiring exclusive forum in certain courts in the State of Delaware or the federal district courts of the United States for certain types of lawsuits may have the effect of discouraging lawsuits against our directors and officers.”
Directors’ liability; indemnification of directors and officers
Our certificate of incorporation will limit the liability of our directors to the fullest extent permitted by the DGCL and provides that we will provide them with customary indemnification. We expect to enter into customary indemnification agreements with each of our executive officers and directors that provide them, in general, with customary indemnification in connection with their service to us or on our behalf.
Listing
We will apply to have our Class A common stock approved for listing on the NYSE under the symbol “SGFY.”
Transfer agent and registrar
The transfer agent and registrar for the Class A common stock is American Stock Transfer & Trust Company, LLC.
210
Table of Contents
MATERIAL U.S. FEDERAL TAX CONSIDERATIONS FOR NON-U.S. HOLDERS OF COMMON STOCK
The following is a general discussion of the material U.S. federal income and estate tax consequences of the purchase, ownership and disposition of shares of our Class A common stock by a “non-U.S. holder.” A “non-U.S. holder” is a beneficial owner of a share of our Class A common stock that is, for U.S. federal income tax purposes:
| • | a non-resident alien individual, other than a former citizen or resident of the United States subject to U.S. tax as an expatriate, |
| • | a foreign corporation, or |
| • | a foreign estate or trust. |
If a partnership or other pass-through entity (including an entity or arrangement treated as a partnership or other type of pass-through entity for U.S. federal income tax purposes) owns our Class A common stock, the tax treatment of a partner or beneficial owner of the entity may depend upon the status of the partner or beneficial owner, the activities of the entity and certain determinations made at the partner or beneficial owner level. Partners and beneficial owners in partnerships or other pass-through entities that own our Class A common stock should consult their own tax advisors as to the particular U.S. federal income and estate tax consequences applicable to them.
This discussion is based on the “Code” and administrative pronouncements, judicial decisions and final, temporary and proposed Treasury regulations, changes to any of which subsequent to the date of this prospectus may affect the tax consequences described herein (possibly with retroactive effect). This discussion does not address all aspects of U.S. federal income and estate taxation that may be relevant to non-U.S. holders in light of their particular circumstances and does not address any U.S. federal gift, alternative minimum tax or Medicare contribution tax considerations or any tax consequences arising under the laws of any state, local or foreign jurisdiction. Prospective holders are urged to consult their tax advisors with respect to the particular tax consequences to them of owning and disposing of our Class A common stock, including the consequences under the laws of any state, local or non-U.S. jurisdiction.
Dividends
To the extent that we make a distribution of cash or other property in respect of our Class A common stock, other than certain pro rata distributions of our Class A common stock, the distribution generally will be treated as a dividend for U.S. federal income tax purposes to the extent it is paid out of our current or accumulated earnings and profits (as determined under U.S. federal income tax principles). Any portion of a distribution that exceeds our current and accumulated earnings and profits generally will be treated first as a tax-free return of capital that reduces the adjusted tax basis of a non-U.S. holder’s Class A common stock, and to the extent the amount of the distribution exceeds a non-U.S. holder’s adjusted tax basis in our Class A common stock, the excess will be treated as gain from the disposition of our Class A common stock (the tax treatment of which is discussed below under “—Gain on disposition of Class A common stock”).
Dividends paid to a non-U.S. holder generally will be subject to U.S. federal withholding tax at a 30% rate, or a reduced rate specified by an applicable income tax treaty, subject to the discussion of FATCA (as defined below) withholding taxes below. In order to obtain a reduced rate of withholding under an applicable income tax treaty, a non-U.S. holder generally will be required to provide a properly executed IRS Form W-8BEN or IRS Form W-8BEN-E, as applicable, certifying its entitlement to benefits under the treaty.
Dividends paid to a non-U.S. holder that are effectively connected with the non-U.S. holder’s conduct of a trade or business within the United States (and, if required by an applicable income tax treaty, are attributable to
211
Table of Contents
a permanent establishment or fixed base maintained by the non-U.S. holder in the United States) will not be subject to U.S. federal withholding tax if the non-U.S. holder provides a properly executed IRS Form W-8ECI. Instead, the effectively connected dividend income will generally be subject to regular U.S. income tax as if the non-U.S. holder were a U.S. person as defined under the Code. A non-U.S. holder that is treated as a corporation for U.S. federal income tax purposes receiving effectively connected dividend income may also be subject to an additional “branch profits tax” imposed at a rate of 30% (or a lower treaty rate) on its effectively connected earnings and profits (subject to certain adjustments).
A non-U.S. holder eligible for a reduced rate of U.S. federal withholding tax pursuant to an income tax treaty may obtain a refund of any excess amounts withheld by timely filing an appropriate claim for refund with the IRS.
Gain on disposition of Class A common stock
Subject to the discussions of backup withholding and FATCA withholding tax below, a non-U.S. holder generally will not be subject to U.S. federal income tax on gain realized on a sale or other disposition of Class A common stock unless:
| • | the gain is effectively connected with the conduct of a trade or business of the non-U.S. holder in the United States (and, if required by an applicable tax treaty, the gain is attributable to a permanent establishment or fixed base maintained by the non-U.S. holder in the United States), in which case the gain will be subject to U.S. federal income tax generally in the same manner as effectively connected dividend income as described above; |
| • | the non-U.S. holder is an individual present in the United States for 183 days or more in the taxable year of disposition and certain other conditions are met, in which case the gain (net of certain U.S.-source losses) generally will be subject to U.S. federal income tax at a rate of 30% (or a lower treaty rate); or |
| • | we are or have been a “United States real property holding corporation” (as described below) at any time within the five-year period preceding the disposition or the non-U.S. holder’s holding period, whichever period is shorter, and either (i) our Class A common stock is not regularly traded on an established securities market prior to the beginning of the calendar year in which the sale or disposition occurs or (ii) the non-U.S. holder has owned or is deemed to have owned, at any time within the five-year period preceding the disposition or the non-U.S. holder’s holding period, whichever period is shorter, more than 5% of our Class A common stock. |
We will be a United States real property holding corporation at any time that the fair market value of our “United States real property interests,” as defined in the Code and applicable Treasury regulations, equals or exceeds 50% of the aggregate fair market value of our worldwide real property interests and our other assets used or held for use in a trade or business (all as determined for the U.S. federal income tax purposes). We believe that we are not, and do not anticipate becoming in the foreseeable future, a United States real property holding corporation.
Information reporting and backup withholding
Distributions paid to a non-U.S. holder and the amount of any tax withheld with respect to such distributions generally will be reported to the IRS. Copies of the information returns reporting such distributions and any withholding may also be made available to the tax authorities in the country in which the non-U.S. holder resides under the provisions of an applicable income tax treaty.
A non-U.S. holder will not be subject to backup withholding on dividends received if such holder certifies under penalty of perjury that it is a non-U.S. holder (and the payor does not have actual knowledge or reason to know that such holder is a U.S. person as defined under the Code), or such holder otherwise establishes an exemption.
212
Table of Contents
Information reporting and, depending on the circumstances, backup withholding will apply to the proceeds of a sale or other disposition of our Class A common stock made within the United States or conducted through certain U.S.-related financial intermediaries, unless the non-U.S. holder complies with certification procedures to establish that it is not a U.S. person in order to avoid information reporting and backup withholding. The certification procedures required to claim a reduced rate of withholding under a treaty will generally satisfy the certification requirements necessary to avoid backup withholding as well.
Backup withholding is not an additional tax and the amount of any backup withholding from a payment to a non-U.S. holder will be allowed as a credit against the non-U.S. holder’s U.S. federal income tax liability and may entitle the non-U.S. holder to a refund, provided that the required information is furnished to the IRS in a timely manner.
FATCA withholding tax
Under Sections 1471 through 1474 of the Code (such Sections commonly referred to as “FATCA”), payments of dividends on and the gross proceeds of dispositions of our Class A common stock paid to (i) a “foreign financial institution” (as specifically defined in the Code) or (ii) a “non-financial foreign entity” (as specifically defined in the Code) will be subject to a withholding tax (separate and apart from, but without duplication of, the withholding tax described above) at a rate of 30%, unless various U.S. information reporting and due diligence requirements (generally relating to ownership by U.S. persons of interests in or accounts with those entities) have been satisfied or an exemption from these rules applies. Under proposed U.S. Treasury regulations promulgated by the Treasury Department on December 13, 2018, which state that taxpayers may rely on the proposed Treasury regulations until final Treasury regulations are issued, this withholding tax will not apply to the gross proceeds from the sale or disposition of our Class A common stock. An intergovernmental agreement between the United States and an applicable foreign country may modify these requirements. If a dividend payment is both subject to withholding under FATCA and subject to the withholding tax discussed above under “—Dividends,” the withholding under FATCA may be credited against, and therefore reduce, such other withholding tax. Non-U.S. holders should consult their tax advisors regarding the possible implications of this withholding tax on their investment in our Class A common stock.
Federal estate tax
Individual non-U.S. holders (as specifically defined for U.S. federal estate tax purposes) and entities the property of which is potentially includible in such an individual’s gross estate for U.S. federal estate tax purposes (for example, a trust funded by such an individual and with respect to which the individual has retained certain interests or powers) should note that our Class A common stock will be treated as U.S. situs property subject to U.S. federal estate tax, unless an applicable estate tax treaty provides otherwise.
213
Table of Contents
SHARES ELIGIBLE FOR FUTURE SALE
Prior to this offering, there has been no public market for our Class A common stock. We cannot make any prediction as to the effect, if any, that sales of Class A common stock or the availability of Class A common stock for future sales will have on the market price of our Class A common stock. The market price of our Class A common stock could decline because of the sale of a large number of shares of our Class A common stock or the perception that such sales could occur in the future. These factors could also make it more difficult to raise funds through future offerings of Class A common stock. See “Risk factors—Risks related to our Class A common stock and this offering—If a substantial number of shares become available for sale and are sold in a short period of time, the market price of our Class A common stock could decline.”
Sale of restricted shares
Upon the consummation of this offering, we will have 165,092,313 shares of Class A common stock (or 168,617,313 shares if the underwriters exercise their option to purchase additional shares of Class A common stock in full) outstanding. Of these shares, the 23,500,000 shares sold in this offering (or 27,025,000 shares if the underwriters exercise their option to purchase additional shares of Class A common stock in full) will be freely tradable, without further restriction or registration under the Securities Act, except any shares held by our “affiliates,” as that term is defined in Rule 144 under the Securities Act, or any shares purchased in our directed share program which are subject to the lock-up agreements described in “Underwriting.” In the absence of registration under the Securities Act, shares held by affiliates may only be sold in compliance with the limitations of Rule 144 described below or another exemption from the registration requirements of the Securities Act. As defined in Rule 144, an affiliate of an issuer is a person that directly, or indirectly through one or more intermediaries, controls, is controlled by or is under common control with the issuer. Upon the completion of this offering, approximately 141,592,313 of our outstanding shares of Class A common stock will be deemed “restricted securities,” as that term is defined under Rule 144, and would also be subject to the “lock-up” period noted below.
In addition, upon the consummation of the offering, the Continuing Pre-IPO LLC Members will own all of the 57,264,580 shares of our Class B common stock. The Continuing Pre-IPO LLC Members, from time to time following the offering may require Cure TopCo, LLC to redeem or exchange all or a portion of their LLC Units for newly-issued shares of Class A common stock on a one-for-one basis. Shares of our Class B common stock will be canceled on a one-for-one basis if we, following a redemption request of a Continuing Pre-IPO LLC Member, redeem or exchange LLC Units of such Continuing Pre-IPO LLC Member pursuant to the terms of the Amended LLC Agreement. Shares of our Class A common stock issuable to the Continuing Pre-IPO LLC Members upon a redemption or exchange of LLC Units would be considered “restricted securities,” as that term is defined under Rule 144 and would also be subject to the “lock-up” period noted below.
Restricted securities may be sold in the public market only if they qualify for an exemption from registration under Rule 144 under the Securities Act, which is summarized below, or any other applicable exemption under the Securities Act, or pursuant to a registration statement that is effective under the Securities Act. Immediately following the consummation of this offering, the holders of approximately 198,856,893 shares of our Class A common stock (on an assumed as-exchanged basis) will be entitled to dispose of their shares following the expiration of an initial 180-day underwriter “lock-up” period pursuant to the holding period, volume and other restrictions of Rule 144. Goldman Sachs & Co. LLC, J.P. Morgan Securities LLC and Barclays Capital Inc., as representatives of the underwriters, are entitled to waive these lock-up provisions at their discretion prior to the expiration dates of such lock-up agreements.
Rule 144
In general, a person who has beneficially owned restricted shares of our common stock for at least six months would be entitled to sell such securities, provided that (i) such person is not deemed to have been one of
214
Table of Contents
our affiliates at the time of, or at any time during the 90 days preceding, a sale and (ii) we are subject to the Exchange Act periodic reporting requirements for at least 90 days before the sale. Persons who have beneficially owned restricted shares of our common stock for at least six months but who are our affiliates at the time of, or any time during the 90 days preceding, a sale, would be subject to additional restrictions, by which such person would be entitled to sell within any three month period only a number of securities that does not exceed the greater of either of the following:
| • | 1% of the number of shares of our Class A common stock then outstanding, which will equal approximately 1,650,923 shares immediately after this offering, assuming no exercise of the underwriters’ option to purchase additional shares of Class A common stock; or |
| • | the average weekly trading volume of our Class A common stock on the NYSE during the four calendar weeks preceding the filing of a notice on Form 144 with respect to the sale; |
provided, in each case, that we are subject to the Exchange Act periodic reporting requirements for at least 90 days before the sale. Such sales both by affiliates and by non-affiliates must also comply with the manner of sale, current public information and notice provisions of Rule 144 to the extent applicable.
Rule 701
In general, under Rule 701, any of our employees, directors, officers, consultants or advisors who purchases shares from us in connection with a compensatory stock or option plan or other written agreement before the effective date of this offering is entitled to resell such shares 90 days after the effective date of this offering in reliance on Rule 144, without having to comply with the holding period requirements or other restrictions contained in Rule 701.
The SEC has indicated that Rule 701 will apply to typical stock options granted by an issuer before it becomes subject to the reporting requirements of the Exchange Act, along with the shares acquired upon exercise of such options, including exercises after the date of this prospectus. Securities issued in reliance on Rule 701 are restricted securities and, subject to the contractual restrictions described above, beginning 90 days after the date of this prospectus, may be sold by persons other than “affiliates,” as defined in Rule 144, subject only to the manner of sale provisions of Rule 144 and by “affiliates” under Rule 144 without compliance with its one-year minimum holding period requirement.
Stock issued under employee plans
We intend to file a registration statement on Form S-8 under the Securities Act to register stock issuable pursuant to awards granted under our 2021 Long-Term Incentive Plan and Employee Stock Purchase Plan and on the exercise of stock options outstanding under our Amended and Restated 2019 Equity Incentive Plan and Amended and Restated 2012 Equity Incentive Plan. This registration statement on Form S-8 is expected to be filed following the effective date of the registration statement of which this prospectus is a part and will be effective upon filing. Accordingly, shares of Class A common stock registered under such registration statement will be available for sale in the open market following the effective date, unless such shares are subject to vesting restrictions with us, Rule 144 restrictions applicable to our affiliates or the lock-up restrictions described above.
Registration rights
Our Registration Rights Agreement grants registration rights to the Continuing Pre-IPO LLC Members. See “Certain relationships and related party transactions—Registration rights agreement.”
Lock-up agreements
Our executive officers, directors and certain of our stockholders have agreed that, for a period of 180 days from the date of this prospectus, they will not, without the prior written consent of the representatives of the
215
Table of Contents
underwriters, dispose of or hedge any shares of our common stock or any securities convertible into or exchangeable for our common stock (including LLC Units) subject to certain exceptions (including dispositions in connection with the Reorganization Transactions).
Immediately following the consummation of this offering, stockholders subject to lock-up agreements will hold 198,856,893 shares of our Class A common stock (assuming the Continuing Pre-IPO LLC Members redeem or exchange all their Class B common stock and LLC Units for shares of our Class A common stock), representing approximately 89.4% of our then-outstanding shares of Class A common stock (or approximately 88.0% of our then-outstanding shares of Class A common stock if the underwriters exercise their option to purchase additional shares of Class A common stock in full and giving effect to the use of the net proceeds therefrom).
We have agreed, subject to certain exceptions, not to issue, sell or otherwise dispose of any shares of our Class A common stock or any securities convertible into or exchangeable for our Class A common stock (including LLC Units) during the 180-day period following the date of this prospectus.
216
Table of Contents
We have entered into an underwriting agreement with the underwriters named below with respect to the shares being offered. Subject to certain conditions, we have agreed to sell to the underwriters, and each underwriter has severally agreed to purchase the number of shares indicated in the following table. Goldman Sachs & Co. LLC, J.P. Morgan Securities LLC and Barclays Capital Inc. are the representatives of the underwriters.
| Underwriters |
Number of Shares |
|||
| Goldman Sachs & Co. LLC |
||||
| J.P. Morgan Securities LLC |
||||
| Barclays Capital Inc. |
||||
| Deutsche Bank Securities Inc. |
||||
| BofA Securities, Inc. |
||||
| UBS Securities LLC |
||||
| Robert W. Baird & Co. Incorporated |
||||
| Piper Sandler & Co. |
||||
| William Blair & Company, L.L.C. |
||||
|
|
|
|||
| Total |
23,500,000 | |||
|
|
|
|||
The underwriters are committed to take and pay for all of the shares being offered, if any are taken, other than the shares covered by the over-allotment option described below unless and until this over-allotment option is exercised.
The underwriters have an over-allotment option to buy up to an additional 3,525,000 shares to cover sales by the underwriters of a greater number of shares than the total number set forth in the table above. They may exercise that over-allotment option for 30 days. If any shares are purchased pursuant to this over-allotment option, the underwriters will severally purchase shares in approximately the same proportion as set forth in the table above.
The following table shows the per share and total underwriting discounts and commissions to be paid to the underwriters by us. Such amounts are shown assuming both no exercise and full exercise of the underwriters’ over-allotment option to purchase 3,525,000 additional shares.
| Paid |
No exercise |
Full exercise |
||||||
| Per share |
$ | $ | ||||||
| Total |
$ | $ | ||||||
Shares sold by the underwriters to the public will initially be offered at the initial public offering price shown on the cover page of this prospectus. Any shares sold by the underwriters to securities dealers may be sold at a discount of up to $ per share from the initial public offering price. After the initial offering of the shares, the representatives may change the offering price and the other selling terms. The offering of the shares by the underwriters is subject to receipt and acceptance and subject to the underwriters’ right to reject any order in whole or in part.
We, our executive officers, directors and certain of our stockholders have agreed that, for a period of 180 days from the date of this prospectus, they will not, without the prior written consent of the representatives of the underwriters, dispose of or hedge any shares of our common stock or any securities convertible into or exchangeable for our common stock (including LLC Units) subject to certain exceptions (including dispositions in connection with the Reorganization Transactions). See “Shares eligible for future sale.”
Prior to the offering, there has been no public market for the shares. The initial public offering price has been negotiated among us and the representatives. Among the factors to be considered in determining the initial
217
Table of Contents
public offering price of the shares, in addition to prevailing market conditions, will be our historical performance, estimates of our business potential and earnings prospects, an assessment of management and the consideration of the above factors in relation to market valuation of companies in related businesses.
We will apply to list our Class A common stock on the NYSE under the symbol “SGFY.”
In connection with the offering, the underwriters may purchase and sell shares of Class A common stock in the open market. These transactions may include short sales, stabilizing transactions and purchases to cover positions created by short sales. Short sales involve the sale by the underwriters of a greater number of shares than they are required to purchase in the offering, and a short position represents the amount of such sales that have not been covered by subsequent purchases. A “covered short position” is a short position that is not greater than the amount of additional shares for which the underwriters’ over-allotment option described above may be exercised. The underwriters may cover any covered short position by either exercising their over-allotment option to purchase additional shares or purchasing shares in the open market. In determining the source of shares to cover the covered short position, the underwriters will consider, among other things, the price of shares available for purchase in the open market as compared to the price at which they may purchase additional shares pursuant to the over-allotment option described above. “Naked” short sales are any short sales that create a short position greater than the amount of additional shares for which the over-allotment option described above may be exercised. The underwriters must cover any such naked short position by purchasing shares in the open market. A naked short position is more likely to be created if the underwriters are concerned that there may be downward pressure on the price of the Class A common stock in the open market after pricing that could adversely affect investors who purchase in the offering. Stabilizing transactions consist of various bids for or purchases of Class A common stock made by the underwriters in the open market prior to the completion of the offering.
The underwriters may also impose a penalty bid. This occurs when a particular underwriter repays to the underwriters a portion of the underwriting discount received by it because the representatives have repurchased shares sold by or for the account of such underwriter in stabilizing or short-covering transactions.
Purchases to cover a short position and stabilizing transactions, as well as other purchases by the underwriters for their own accounts, may have the effect of preventing or retarding a decline in the market price of our stock, and together with the imposition of the penalty bid, may stabilize, maintain or otherwise affect the market price of the Class A common stock. As a result, the price of the Class A common stock may be higher than the price that otherwise might exist in the open market. The underwriters are not required to engage in these activities and may end any of these activities at any time. These transactions may be effected on the NYSE, in the over-the-counter market or otherwise.
We estimate that our share of the total expenses of the offering, excluding underwriting discounts and commissions, will be approximately $13.5 million. We have also agreed to reimburse the underwriters for certain expenses in connection with this offering up to $40.0 thousand.
We have agreed to indemnify the several underwriters against certain liabilities, including liabilities under the Securities Act, and to contribute to payments that the underwriters may be required to make in respect of those liabilities.
The underwriters and their respective affiliates are full service financial institutions engaged in various activities, which may include sales and trading, commercial and investment banking, advisory, investment management, investment research, principal investment, hedging, market making, brokerage and other financial and non-financial activities and services. Certain of the underwriters and their respective affiliates have provided, and may in the future provide, a variety of these services to the issuer and to persons and entities with relationships with the issuer, for which they received or will receive customary fees and expenses. Deutsche Bank Securities Inc. acts as a joint lead arranger, joint bookrunner and documentation and syndication agent under our Credit Agreement.
218
Table of Contents
In the ordinary course of their various business activities, the underwriters and their respective affiliates, officers, directors and employees may purchase, sell or hold a broad array of investments and actively trade securities, derivatives, loans, commodities, currencies, credit default swaps and other financial instruments for their own account and for the accounts of their clients, and such investment and trading activities may involve or relate to assets, securities and/or instruments of the issuer (directly, as collateral securing other obligations or otherwise) and/or persons and entities with relationships with the issuer. The underwriters and their respective affiliates may also communicate independent investment recommendations, market color or trading ideas and/or publish or express independent research views in respect of such assets, securities or instruments and may at any time hold, or recommend to clients that they should acquire, long and/or short positions in such assets, securities and instruments.
Directed share program
At our request, the underwriters have reserved up to 1,175,000 shares of Class A common stock, or 5% of the shares of Class A common stock to be offered by this prospectus for sale, at the initial public offering price, through a directed share program for certain of our clinicians and employees and certain other individuals and entities. Shares purchased through the directed share program will not be subject to a lock-up restriction, except in the case of shares purchased by any of our directors or officers and certain of our employees and existing equityholders. The number of shares of Class A common stock available for sale to the general public will be reduced to the extent these individuals or entities purchase such reserved shares. Any reserved shares that are not so purchased will be offered by the underwriters to the general public on the same basis as the other shares offered by this prospectus. The underwriters will receive the same discount from such reserved shares as they will from other shares of our Class A common stock sold to the public in this offering. We have agreed to indemnify the underwriters against certain liabilities and expenses, including liabilities under the Securities Act, in connection with sales of the reserved shares.
Selling restrictions
Other than in the United States, no action has been taken by us or the underwriters that would permit a public offering of the securities offered by this prospectus in any jurisdiction where action for that purpose is required. The securities offered by this prospectus may not be offered or sold, directly or indirectly, nor may this prospectus or any other offering material or advertisements in connection with the offer and sale of any such securities be distributed or published in any jurisdiction, except under circumstances that will result in compliance with the applicable rules and regulations of that jurisdiction. Persons into whose possession this prospectus comes are advised to inform themselves about and to observe any restrictions relating to the offering and the distribution of this prospectus. This prospectus does not constitute an offer to sell or a solicitation of an offer to buy any securities offered by this prospectus in any jurisdiction in which such an offer or a solicitation is unlawful.
European Economic Area
In relation to each Member State of the European Economic Area (each, a “Relevant Member State”), an offer to the public of any shares may not be made in that Relevant Member State, except that an offer to the public in that Relevant Member State of any shares may be made at any time under the following exemptions under the Prospectus Regulation:
(a) to any legal entity which is a “qualified investor” as defined under the Prospectus Regulation;
(b) to fewer than 150 natural or legal persons (other than “qualified investors” as defined under the Prospectus Regulation), subject to obtaining the prior consent of the representatives for any such offer; or
(c) in any other circumstances falling within Article 1(4) of the Prospectus Regulation,
provided that no such offer of shares shall result in a requirement for the Issuer or any representative to publish a prospectus pursuant to Article 3 of the Prospectus Regulation or a supplemental prospectus pursuant to Article 23
219
Table of Contents
of the Prospectus Regulation. For the purposes of this provision, the expression an “offer to the public” in relation to any shares in any Relevant Member State means the communication in any form and by any means of sufficient information on the terms of the offer and any shares to be offered so as to enable an investor to decide to purchase or subscribe for any shares, and the expression “Prospectus Regulation” means Regulation (EU) 2017/1129.
United Kingdom
An offer to the public of any shares may not be made in the United Kingdom, except that an offer to the public in the United Kingdom of any shares may be made at any time under the following exemptions under the UK Prospectus Regulation:
(a) to any legal entity which is a “qualified investor” as defined under the UK Prospectus Regulation;
(b) to fewer than 150 natural or legal persons (other than “qualified investors” as defined under the UK Prospectus Regulation), subject to obtaining the prior consent of the representatives for any such offer; or
(c) in any other circumstances falling within section 86 of the Financial Services and Markets Act 2000 (as amended, “FSMA”),
provided that no such offer of shares shall result in a requirement for the Issuer or any representative to publish a prospectus pursuant to section 85 of the FSMA or a supplemental prospectus pursuant to Article 23 of the UK Prospectus Regulation. For the purposes of this provision, the expression an “offer to the public” in relation to any shares in the United Kingdom means the communication in any form and by any means of sufficient information on the terms of the offer and any shares to be offered so as to enable an investor to decide to purchase or subscribe for any shares, and the expression “UK Prospectus Regulation” means Regulation (EU) 2017/1129 as it forms part of domestic law by virtue of the European Union (Withdrawal) Act 2018.
In the United Kingdom, this prospectus is being distributed only to, and is directed only at, persons who are “qualified investors” (as defined in the UK Prospectus Regulation ) who are (i) persons having professional experience in matters relating to investments falling within Article 19(5) of the Financial Services and Markets Act 2000 (Financial Promotion) Order 2005 (as amended, the “Order”), or (ii) high net worth entities falling within Article 49(2)(a) to (d) of the Order, or (iii) persons to whom it would otherwise be lawful to distribute it, all such persons together being referred to as “Relevant Persons”. In the United Kingdom, the shares are only available to, and any invitation, offer or agreement to subscribe, purchase or otherwise acquire such shares will be engaged in only with, Relevant Persons. This prospectus and its contents are confidential and should not be distributed, published or reproduced (in whole or in part) or disclosed by any recipients to any other person in the United Kingdom. Any person in the United Kingdom that is not a Relevant Person should not act or rely on this prospectus or its contents. The shares are not being offered to the public in the United Kingdom.
Canada
The securities may be sold in Canada only to purchasers purchasing, or deemed to be purchasing, as principal that are accredited investors, as defined in National Instrument 45-106 Prospectus Exemptions or subsection 73.3(1) of the Securities Act (Ontario), and are permitted clients, as defined in National Instrument 31-103 Registration Requirements, Exemptions, and Ongoing Registrant Obligations. Any resale of the securities must be made in accordance with an exemption form, or in a transaction not subject to, the prospectus requirements of applicable securities laws.
Securities legislation in certain provinces or territories of Canada may provide a purchaser with remedies for rescission or damages if this prospectus (including any amendment thereto) contains a misrepresentation, provided that the remedies for rescission or damages are exercised by the purchaser within the time limit prescribed by the securities legislation of the purchaser’s province or territory. The purchaser should refer to any applicable provisions of the securities legislation of the purchaser’s province or territory of these rights or consult with a legal advisor.
220
Table of Contents
Pursuant to section 3A.3 of National Instrument 33-105 Underwriting Conflicts (NI 33-105), the underwriters are not required to comply with the disclosure requirements of NI 33-105 regarding underwriter conflicts of interest in connection with this offering.
Switzerland
This prospectus is not intended to constitute an offer or solicitation to purchase or invest in the shares. The shares may not be publicly offered, directly or indirectly, in Switzerland within the meaning of the Swiss Financial Services Act (“FinSA”) and no application has or will be made to admit the shares to trading on any trading venue (exchange or multilateral trading facility) in Switzerland. Neither this prospectus nor any other offering or marketing material relating to the shares constitutes a prospectus pursuant to the FinSA, and neither this prospectus nor any other offering or marketing material relating to the shares may be publicly distributed or otherwise made publicly available in Switzerland.
Dubai International Financial Centre (“DIFC”)
This document relates to an Exempt Offer in accordance with the Markets Rules 2012 of the Dubai Financial Services Authority (“DFSA”). This document is intended for distribution only to persons of a type specified in the Markets Rules 2012 of the DFSA. It must not be delivered to, or relied on by, any other person. The DFSA has no responsibility for reviewing or verifying any documents in connection with Exempt Offers. The DFSA has not approved this prospectus supplement nor taken steps to verify the information set forth herein and has no responsibility for this document. The securities to which this document relates may be illiquid and/or subject to restrictions on their resale. Prospective purchasers of the securities offered should conduct their own due diligence on the securities. If you do not understand the contents of this document you should consult an authorized financial advisor.
In relation to its use in the DIFC, this document is strictly private and confidential and is being distributed to a limited number of investors and must not be provided to any person other than the original recipient, and may not be reproduced or used for any other purpose. The interests in the securities may not be offered or sold directly or indirectly to the public in the DIFC.
United Arab Emirates
The shares have not been, and are not being, publicly offered, sold, promoted or advertised in the United Arab Emirates (including the Dubai International Financial Centre) other than in compliance with the laws of the United Arab Emirates (and the Dubai International Financial Centre) governing the issue, offering and sale of securities. Further, this prospectus does not constitute a public offer of securities in the United Arab Emirates (including the Dubai International Financial Centre) and is not intended to be a public offer. This prospectus has not been approved by or filed with the Central Bank of the United Arab Emirates, the Securities and Commodities Authority or the Dubai Financial Services Authority.
Australia
This prospectus:
| • | does not constitute a product disclosure document or a prospectus under Chapter 6D.2 of the Corporations Act 2001 (Cth) (the “Corporations Act”); |
| • | has not been, and will not be, lodged with the Australian Securities and Investments Commission (“ASIC”), as a disclosure document for the purposes of the Corporations Act and does not purport to include the information required of a disclosure document under Chapter 6D.2 of the Corporations Act; and |
221
Table of Contents
| • | may only be provided in Australia to select investors who are able to demonstrate that they fall within one or more of the categories of investors, or Exempt Investors, available under section 708 of the Corporations Act. |
The shares may not be directly or indirectly offered for subscription or purchased or sold, and no invitations to subscribe for or buy the shares may be issued, and no draft or definitive offering memorandum, advertisement or other offering material relating to any shares may be distributed in Australia, except where disclosure to investors is not required under Chapter 6D of the Corporations Act or is otherwise in compliance with all applicable Australian laws and regulations. By submitting an application for the shares, you represent and warrant to us that you are an Exempt Investor.
As any offer of shares under this document will be made without disclosure in Australia under Chapter 6D.2 of the Corporations Act, the offer of those securities for resale in Australia within 12 months may, under section 707 of the Corporations Act, require disclosure to investors under Chapter 6D.2 if none of the exemptions in section 708 applies to that resale. By applying for the shares you undertake to us that you will not, for a period of 12 months from the date of issue of the shares, offer, transfer, assign or otherwise alienate those securities to investors in Australia except in circumstances where disclosure to investors is not required under Chapter 6D.2 of the Corporations Act or where a compliant disclosure document is prepared and lodged with ASIC.
Hong Kong
The shares may not be offered or sold in Hong Kong by means of any document other than (i) in circumstances which do not constitute an offer to the public within the meaning of the Companies (Winding Up and Miscellaneous Provisions) Ordinance (Cap. 32 of the Laws of Hong Kong) (“Companies (Winding Up and Miscellaneous Provisions) Ordinance”) or which do not constitute an invitation to the public within the meaning of the Securities and Futures Ordinance (Cap. 571 of the Laws of Hong Kong) (“Securities and Futures Ordinance”), or (ii) to “professional investors” as defined in the Securities and Futures Ordinance and any rules made thereunder, or (iii) in other circumstances which do not result in the document being a “prospectus” as defined in the Companies (Winding Up and Miscellaneous Provisions) Ordinance, and no advertisement, invitation or document relating to the shares may be issued or may be in the possession of any person for the purpose of issue (in each case whether in Hong Kong or elsewhere), which is directed at, or the contents of which are likely to be accessed or read by, the public in Hong Kong (except if permitted to do so under the securities laws of Hong Kong) other than with respect to shares which are or are intended to be disposed of only to persons outside Hong Kong or only to “professional investors” in Hong Kong as defined in the Securities and Futures Ordinance and any rules made thereunder.
Singapore
This prospectus has not been registered as a prospectus with the Monetary Authority of Singapore. Accordingly, this prospectus and any other document or material in connection with the offer or sale, or invitation for subscription or purchase, of the shares may not be circulated or distributed, nor may the shares be offered or sold, or be made the subject of an invitation for subscription or purchase, whether directly or indirectly, to persons in Singapore other than (i) to an institutional investor (as defined under Section 4A of the Securities and Futures Act, Chapter 289 of Singapore (the “SFA”)) under Section 274 of the SFA, (ii) to a relevant person (as defined in Section 275(2) of the SFA) pursuant to Section 275(1) of the SFA, or any person pursuant to Section 275(1A) of the SFA, and in accordance with the conditions specified in Section 275 of the SFA or (iii) otherwise pursuant to, and in accordance with the conditions of, any other applicable provision of the SFA, in each case subject to conditions set forth in the SFA.
Where the shares are subscribed or purchased under Section 275 of the SFA by a relevant person which is a corporation (which is not an accredited investor (as defined in Section 4A of the SFA)) the sole business of which is to hold investments and the entire share capital of which is owned by one or more individuals, each of
222
Table of Contents
whom is an accredited investor, the securities (as defined in Section 239(1) of the SFA) of that corporation shall not be transferable for 6 months after that corporation has acquired the shares under Section 275 of the SFA except: (1) to an institutional investor under Section 274 of the SFA or to a relevant person (as defined in Section 275(2) of the SFA), (2) where such transfer arises from an offer in that corporation’s securities pursuant to Section 275(1A) of the SFA, (3) where no consideration is or will be given for the transfer, (4) where the transfer is by operation of law, (5) as specified in Section 276(7) of the SFA, or (6) as specified in Regulation 32 of the Securities and Futures (Offers of Investments) (Shares and Debentures) Regulations 2005 of Singapore (“Regulation 32”).
Where the shares are subscribed or purchased under Section 275 of the SFA by a relevant person which is a trust (where the trustee is not an accredited investor (as defined in Section 4A of the SFA)) whose sole purpose is to hold investments and each beneficiary of the trust is an accredited investor, the beneficiaries’ rights and interest (howsoever described) in that trust shall not be transferable for 6 months after that trust has acquired the shares under Section 275 of the SFA except: (1) to an institutional investor under Section 274 of the SFA or to a relevant person (as defined in Section 275(2) of the SFA), (2) where such transfer arises from an offer that is made on terms that such rights or interest are acquired at a consideration of not less than $200,000 (or its equivalent in a foreign currency) for each transaction (whether such amount is to be paid for in cash or by exchange of securities or other assets), (3) where no consideration is or will be given for the transfer, (4) where the transfer is by operation of law, (5) as specified in Section 276(7) of the SFA, or (6) as specified in Regulation 32.
Singapore Securities and Futures Act Product Classification—Solely for the purposes of its obligations pursuant to Sections 309B(1)(a) and 309B(1)(c) of the SFA, the issuer has determined, and hereby notifies all relevant persons (as defined in Section 309A of the SFA) that the shares are “prescribed capital markets products” (as defined in the Securities and Futures (Capital Markets Products) Regulations 2018) and “Excluded Investment Products” (as defined in MAS Notice SFA 04-N12: Notice on the Sale of Investment Products and MAS Notice FAA-N16: Notice on Recommendations on Investment Products).
Japan
The securities have not been and will not be registered under the Financial Instruments and Exchange Act of Japan (Act No. 25 of 1948, as amended), or the FIEA. The securities may not be offered or sold, directly or indirectly, in Japan or to or for the benefit of any resident of Japan (including any person resident in Japan or any corporation or other entity organized under the laws of Japan) or to others for reoffering or resale, directly or indirectly, in Japan or to or for the benefit of any resident of Japan, except pursuant to an exemption from the registration requirements of the FIEA and otherwise in compliance with any relevant laws and regulations of Japan.
Bermuda
Shares may be offered or sold in Bermuda only in compliance with the provisions of the Investment Business Act of 2003 of Bermuda which regulates the sale of securities in Bermuda. Additionally, non-Bermudian persons (including companies) may not carry on or engage in any trade or business in Bermuda unless such persons are permitted to do so under applicable Bermuda legislation.
Saudi Arabia
This document may not be distributed in the Kingdom of Saudi Arabia except to such persons as are permitted under the Offers of Securities Regulations as issued by the board of the Saudi Arabian Capital Market Authority (“CMA”) pursuant to resolution number 2-11-2004 dated 4 October 2004 as amended by resolution number 1-28-2008, as amended (the “CMA Regulations”). The CMA does not make any representation as to the accuracy or completeness of this document and expressly disclaims any liability whatsoever for any loss arising
223
Table of Contents
from, or incurred in reliance upon, any part of this document. Prospective purchasers of the securities offered hereby should conduct their own due diligence on the accuracy of the information relating to the securities. If you do not understand the contents of this document, you should consult an authorized financial adviser.
British Virgin Islands
The shares are not being, and may not be offered to the public or to any person in the British Virgin Islands for purchase or subscription by or on behalf of the Company. The shares may be offered to companies incorporated under the BVI Business Companies Act, 2004 (British Virgin Islands), but only where the offer will be made to, and received by, the relevant BVI Company entirely outside of the British Virgin Islands.
China
This prospectus will not be circulated or distributed in the People’s Republic of China (the “PRC”) and the shares will not be offered or sold, and will not be offered or sold to any person for re-offering or resale directly or indirectly to any residents of the PRC except pursuant to any applicable laws and regulations of the PRC. Neither this prospectus nor any advertisement or other offering material may be distributed or published in the PRC, except under circumstances that will result in compliance with applicable laws and regulations.
Korea
The shares have not been and will not be registered under the Financial Investments Services and Capital Markets Act of Korea and the decrees and regulations thereunder (the “FSCMA”), and the shares have been and will be offered in Korea as a private placement under the FSCMA. None of the shares may be offered, sold or delivered directly or indirectly, or offered or sold to any person for re-offering or resale, directly or indirectly, in Korea or to any resident of Korea except pursuant to the applicable laws and regulations of Korea, including the FSCMA and the Foreign Exchange Transaction Law of Korea and the decrees and regulations thereunder (the “FETL”). The shares have not been listed on any of securities exchanges in the world including, without limitation, the Korea Exchange in Korea. Furthermore, the purchaser of the shares shall comply with all applicable regulatory requirements (including but not limited to requirements under the FETL) in connection with the purchase of the shares. By the purchase of the shares, the relevant holder thereof will be deemed to represent and warrant that if it is in Korea or is a resident of Korea, it purchased the shares pursuant to the applicable laws and regulations of Korea.
Malaysia
No prospectus or other offering material or document in connection with the offer and sale of the shares has been or will be registered with the Securities Commission of Malaysia (“Commission”) for the Commission’s approval pursuant to the Capital Markets and Services Act 2007. Accordingly, this prospectus and any other document or material in connection with the offer or sale, or invitation for subscription or purchase, of the shares may not be circulated or distributed, nor may the shares be offered or sold, or be made the subject of an invitation for subscription or purchase, whether directly or indirectly, to persons in Malaysia other than (i) a closed end fund approved by the Commission; (ii) a holder of a Capital Markets Services License; (iii) a person who acquires the shares, as principal, if the offer is on terms that the shares may only be acquired at a consideration of not less than RM250,000 (or its equivalent in foreign currencies) for each transaction; (iv) an individual whose total net personal assets or total net joint assets with his or her spouse exceeds RM3 million (or its equivalent in foreign currencies), excluding the value of the primary residence of the individual; (v) an individual who has a gross annual income exceeding RM300,000 (or its equivalent in foreign currencies) per annum in the preceding 12 months; (vi) an individual who, jointly with his or her spouse, has a gross annual income of RM400,000 (or its equivalent in foreign currencies), per annum in the preceding 12 months; (vii) a corporation with total net assets exceeding RM10 million (or its equivalent in a foreign currencies) based on the last audited accounts; (viii) a partnership with total net assets exceeding RM10 million (or its equivalent in foreign currencies); (ix) a bank
224
Table of Contents
licensee or insurance licensee as defined in the Labuan Financial Services and Securities Act 2010; (x) an Islamic bank licensee or takaful licensee as defined in the Labuan Financial Services and Securities Act 2010; and (xi) any other person as may be specified by the Commission; provided that, in the each of the preceding categories (i) to (xi), the distribution of the shares is made by a holder of a Capital Markets Services License who carries on the business of dealing in securities. The distribution in Malaysia of this prospectus is subject to Malaysian laws. This prospectus does not constitute and may not be used for the purpose of public offering or an issue, offer for subscription or purchase, invitation to subscribe for or purchase any securities requiring the registration of a prospectus with the Commission under the Capital Markets and Services Act 2007.
Taiwan
The shares have not been and will not be registered with the Financial Supervisory Commission of Taiwan pursuant to relevant securities laws and regulations and may not be sold, issued or offered within Taiwan through a public offering or in circumstances which constitutes an offer within the meaning of the Securities and Exchange Act of Taiwan that requires a registration or approval of the Financial Supervisory Commission of Taiwan. No person or entity in Taiwan has been authorized to offer, sell, give advice regarding or otherwise intermediate the offering and sale of the shares in Taiwan.
South Africa
Due to restrictions under the securities laws of South Africa, no “offer to the public” (as such term is defined in the South African Companies Act, No. 71 of 2008 (as amended or re-enacted) (the “South African Companies Act”)) is being made in connection with the issue of the shares in South Africa. Accordingly, this document does not, nor is it intended to, constitute a “registered prospectus” (as that term is defined in the South African Companies Act) prepared and registered under the South African Companies Act and has not been approved by, and/or filed with, the South African Companies and Intellectual Property Commission or any other regulatory authority in South Africa. The shares are not offered, and the offer shall not be transferred, sold, renounced or delivered, in South Africa or to a person with an address in South Africa, unless one or other of the following exemptions stipulated in section 96 (1) applies:
Section 96 (1)(a)
The offer, transfer, sale, renunciation or delivery is to:
(i) persons whose ordinary business, or part of whose ordinary business, is to deal in securities, as principal or agent;
(ii) persons whose ordinary business, or part of whose ordinary business, is to deal in securities, as principal or agent;
(iii) persons or entities regulated by the Reserve Bank of South Africa;
(iv) authorised financial service providers under South African law;
(v) financial institutions recognised as such under South African law;
(vi) a wholly owned subsidiary of any person or entity contemplated in (c), (d) or (e), acting as agent in the capacity of an authorised portfolio manager for a pension fund, or as manager for a collective investment scheme (in each case duly registered as such under South African law); or
(vii) any combination of the person in (i) to (vi); or
225
Table of Contents
Section 96 (1)(b)
The total contemplated acquisition cost of the securities, for any single addressee acting as principal is equal to or greater than ZAR1,000,000 or such higher amount as may be promulgated by notice in the Government Gazette of South Africa pursuant to section 96(2)(a) of the South African Companies Act.
Information made available in this prospectus should not be considered as “advice” as defined in the South African Financial Advisory and Intermediary Services Act, 2002.
226
Table of Contents
The validity of the issuance of the shares of Class A common stock offered hereby will be passed upon for Signify Health, Inc. by Davis Polk & Wardwell LLP. Simpson Thacher & Bartlett LLP is representing the underwriters.
The financial statement of Signify Health, Inc., as of October 1, 2020, included in this prospectus, has been audited by Deloitte & Touche LLP, an independent registered public accounting firm, as stated in their report appearing herein. Such financial statement is included in reliance upon the report of such firm given upon their authority as experts in accounting and auditing.
The combined-consolidated financial statements of Cure TopCo, LLC, and its subsidiaries, and the related financial statement schedule, as of December 31, 2018 and 2019 and for the years then ended, included in this prospectus, have been audited by Deloitte & Touche LLP, an independent registered public accounting firm, as stated in their report appearing herein. Such financial statements and financial statement schedule are included in reliance upon the report of such firm given upon their authority as experts in accounting and auditing.
The financial statements of Remedy Partners, Inc. as of December 31, 2018 and for the year ended December 31, 2018 included in this prospectus have been so included in reliance on the report of RSM US LLP, an independent registered public accounting firm, given on the authority of said firm as experts in auditing and accounting.
WHERE YOU CAN FIND MORE INFORMATION
We have filed with the SEC a registration statement on Form S-1 under the Securities Act with respect to the Class A common stock offered hereby. This prospectus does not contain all of the information set forth in the registration statement and the exhibits and schedules thereto. For further information with respect to the company and its Class A common stock, reference is made to the registration statement and the exhibits and any schedules filed therewith. Statements contained in this prospectus as to the contents of any contract or other document referred to are not necessarily complete and in each instance, if such contract or document is filed as an exhibit, reference is made to the copy of such contract or other document filed as an exhibit to the registration statement, each statement being qualified in all respects by such reference. The SEC maintains an internet site at www.sec.gov that contains reports, proxy and information statements we have filed electronically with the SEC.
As a result of the offering, we will be required to file periodic reports and other information with the SEC. We also maintain an internet site at www.signifyhealth.com. Our website and the information contained therein or connected thereto shall not be deemed to be incorporated into this prospectus or the registration statement of which it forms a part.
227
Table of Contents
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
| Page | ||||
| Signify Health, Inc. |
||||
| Financial Statement |
||||
| F-2 | ||||
| F-3 | ||||
| F-4 | ||||
| Cure TopCo, LLC |
||||
| Condensed Combined-Consolidated Financial Statements (Unaudited) |
||||
| Condensed Consolidated Balance Sheets as of September 30, 2020 and December 31, 2019 |
F-5 | |||
| F-6 | ||||
| F-7 | ||||
| F-8 | ||||
| Notes to the Condensed Combined-Consolidated Financial Statements |
F-9 | |||
| Combined – Consolidated Financial Statements |
||||
| F-39 | ||||
| Consolidated Balance Sheets as of December 31, 2019 and 2018 |
F-40 | |||
| Combined-Consolidated Statements of Operations for the Years Ended December 31, 2019 and 2018 |
F-41 | |||
| F-42 | ||||
| Combined-Consolidated Statements of Cash Flows for the Years Ended December 31, 2019 and 2018 |
F-43 | |||
| F-44 | ||||
| Remedy Partners, Inc. |
||||
| Financial Statements |
||||
| F-79 | ||||
| F-80 | ||||
| Statement of Operations for the Year Ended December 31, 2018 |
F-81 | |||
| Statement of Changes in Members’ Equity for the Year Ended December 31, 2018 |
F-82 | |||
| Statement of Cash Flows for the Year Ended December 31, 2018 |
F-83 | |||
| F-84 | ||||
F-1
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Shareholder and Board of Directors of Signify Health, Inc.
Opinion on the Financial Statements
We have audited the accompanying balance sheet of Signify Health, Inc. (the “Company”) as of October 1, 2020, and the related notes (collectively referred to as the “financial statement”). In our opinion, the financial statement presents fairly, in all material respects, the financial position of the Company as of October 1, 2020, in conformity with accounting principles generally accepted in the United States of America.
Basis for Opinion
This financial statement is the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s financial statement based on our audit. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statement is free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audit, we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion.
Our audit included performing procedures to assess the risks of material misstatement of the financial statement, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statement. Our audit also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statement. We believe that our audit provides a reasonable basis for our opinion.
/s/ Deloitte & Touche LLP
Stamford, Connecticut
December 7, 2020 (January 19, 2021, as to the effects of the share issuance described in Note 5)
We have served as the Company’s auditor since 2020.
F-2
Table of Contents
Signify Health, Inc.
| October 1, 2020 | ||||
| ASSETS |
||||
| Current assets |
||||
| Cash and cash equivalents |
$ | — | ||
|
|
|
|||
| Total assets |
$ | — | ||
|
|
|
|||
| Commitments and contingencies (Note 4) |
||||
| STOCKHOLDERS’ EQUITY |
||||
| Common stock, par value $0.01 per share, 1,000 shares authorized, no shares issued or outstanding |
$ | — | ||
|
|
|
|||
| Total stockholders’ equity |
$ | — | ||
|
|
|
|||
F-3
Table of Contents
Signify Health, Inc.
Notes to the Financial Statements
| 1. | Nature of Operations and Basis of Presentation |
Signify Health, Inc. (“Signify Health”, the “Company”) was incorporated in the state of Delaware on October 1, 2020. Signify Health was formed for the purpose of completing an initial public offering (“IPO”) of its common stock and related transactions in which it will gain control of, and therefore consolidate the operations of Cure TopCo, LLC and its subsidiaries.
The accompanying balance sheet has been prepared in accordance with accounting principles generally accepted in the United States of America. Statements of income, stockholders’ equity and cash flows have not been presented because Signify Health has not engaged in any business or other activities except in connection with its formation.
| 2. | Significant Accounting Policies |
Underwriting Commissions and Offering Costs
Underwriting commissions and offering costs incurred in connection with the Company’s common share offering will be reflected as a reduction of additional paid-in capital upon completion of its IPO. Underwriting commissions and offering costs are not recorded in the Company’s balance sheet because such costs are not the Company’s liability until the Company completes its IPO.
| 3. | Stockholders’ Equity |
Signify Health is authorized to issue 1,000 shares of common stock, $0.01 par value per share. Holders of common stock are entitled to one vote for each share of common stock held on all matters submitted to shareholders for vote, consent or approval.
| 4. | Commitments and Contingencies |
Signify Health may be subject to legal proceedings that arise in the ordinary course of business. There are currently no material proceedings to which Signify Health is a party, nor does Signify Health have knowledge of any proceedings threatened against it.
| 5. | Subsequent Events |
Signify Health, Inc. performed an evaluation of subsequent events through December 7, 2020, the date the balance sheet was originally issued and through the re-issuance date of January 19, 2021, for events requiring recording or disclosure in the financial statements as of October 1, 2020. On January 5, 2021, Signify Health, Inc. issued 100 shares of common stock, par value $0.01 per share, to our Chief Executive Officer, which represents all outstanding common stock issued to date.
F-4
Table of Contents
Cure TopCo, LLC and Subsidiaries
Condensed Consolidated Balance Sheets (Unaudited, In millions, except units)
| September 30, | December 31, | |||||||
| 2020 | 2019 | |||||||
| ASSETS |
||||||||
| Current assets |
||||||||
| Cash and cash equivalents |
$ | 87.9 | $ | 27.7 | ||||
| Accounts receivable, net |
143.1 | 168.1 | ||||||
| Contract assets |
110.0 | 38.3 | ||||||
| Restricted cash |
4.4 | 22.5 | ||||||
| Prepaid expenses and other current assets |
11.7 | 6.9 | ||||||
|
|
|
|
|
|||||
| Total current assets |
357.1 | 263.5 | ||||||
| Property and equipment, net |
26.7 | 19.3 | ||||||
| Goodwill |
578.8 | 578.8 | ||||||
| Intangible assets, net |
503.6 | 528.5 | ||||||
| Other assets |
2.5 | 2.3 | ||||||
|
|
|
|
|
|||||
| Total assets |
$ | 1,468.7 | $ | 1,392.4 | ||||
|
|
|
|
|
|||||
| LIABILITIES AND MEMBERS’ EQUITY |
||||||||
| Current liabilities |
||||||||
| Accounts payable and accrued expenses |
$ | 95.6 | $ | 107.1 | ||||
| Contract liabilities |
35.0 | 3.1 | ||||||
| Current maturities of long-term debt |
2.8 | 2.8 | ||||||
| Due to shareholders |
54.0 | — | ||||||
| Other current liabilities |
16.1 | 9.6 | ||||||
|
|
|
|
|
|||||
| Total current liabilities |
203.5 | 122.6 | ||||||
| Long-term debt |
263.8 | 264.6 | ||||||
| Borrowings under revolving credit |
77.0 | — | ||||||
| Contingent consideration |
— | 39.8 | ||||||
| Customer EAR liability |
14.4 | — | ||||||
| Other noncurrent liabilities |
18.6 | 7.8 | ||||||
|
|
|
|
|
|||||
| Total liabilities |
577.3 | 434.8 | ||||||
| Commitments and Contingencies (Note 17) |
||||||||
| Members’ equity—Series A Preferred (3,384,543 issued and outstanding at September 30, 2020 and December 31, 2019) |
697.7 | 695.4 | ||||||
| Members’ equity—Series B Preferred (3,402,608 and 3,533,133 issued and outstanding at September 30, 2020 and December 31, 2019, respectively) |
264.3 | 325.5 | ||||||
| Members’ equity—Class A common (0 issued and outstanding at September 30, 2020 and December 31, 2019) |
— | — | ||||||
| Members’ equity—Class B common (108,977 and 93,311 issued and outstanding at September 30, 2020 and December 31, 2019, respectively) |
4.9 | 4.2 | ||||||
| Members’ equity—Class C common (83,244 and 0 issued and outstanding at September 30, 2020 and December 31, 2019, respectively) |
7.2 | — | ||||||
| Accumulated deficit |
(82.7 | ) | (67.5 | ) | ||||
|
|
|
|
|
|||||
| Total members’ equity |
891.4 | 957.6 | ||||||
|
|
|
|
|
|||||
| Total liabilities and members’ equity |
$ | 1,468.7 | $ | 1,392.4 | ||||
|
|
|
|
|
|||||
See accompanying notes to the condensed combined-consolidated financial statements.
F-5
Table of Contents
Cure TopCo, LLC and Subsidiaries
Condensed Combined-Consolidated Statement of Operations (Unaudited, in millions, except unit and per unit amounts)
| Nine months ended September 30, | ||||||||
| 2020 | 2019 | |||||||
| Revenue |
$ | 417.1 | $ | 368.5 | ||||
| Operating expenses: |
||||||||
| Service expense (exclusive of depreciation and amortization shown below) |
203.4 | 188.2 | ||||||
| Selling, general and administrative expense (exclusive of depreciation and amortization shown below) |
148.5 | 119.1 | ||||||
| Transaction-related expenses |
10.8 | 15.9 | ||||||
| Asset impairment |
— | 1.5 | ||||||
| Depreciation and amortization |
46.0 | 49.5 | ||||||
|
|
|
|
|
|||||
| Total operating expenses |
408.7 | 374.2 | ||||||
| Income (loss) from operations |
8.4 | (5.7 | ) | |||||
| Interest expense |
16.2 | 16.1 | ||||||
| Other (income) expense, net |
6.9 | (1.4 | ) | |||||
|
|
|
|
|
|||||
| Other expense, net |
23.1 | 14.7 | ||||||
|
|
|
|
|
|||||
| Loss before income taxes |
(14.7 | ) | (20.4 | ) | ||||
| Income tax expense |
0.5 | 0.1 | ||||||
|
|
|
|
|
|||||
| Net loss |
$ | (15.2 | ) | $ | (20.5 | ) | ||
|
|
|
|
|
|||||
| Loss per unit |
||||||||
| Former Class A and B Common Units |
$ | — | $ | (5.75 | ) | |||
| Class C Common Units |
$ | (2.15 | ) | — | ||||
| Weighted average units outstanding |
||||||||
| Former Class A and B Common Units |
— | 3,564,661 | ||||||
| Class C Common Units |
58,968 | — | ||||||
See accompanying notes to the condensed combined-consolidated financial statements.
F-6
Table of Contents
Cure TopCo, LLC and Subsidiaries
Condensed Combined-Consolidated Statements of Changes in Members’ Equity
(Unaudited, in millions, except units)
| Former Class A common units |
Former Class A members’ equity |
Class B common units |
Class B members’ equity |
Additional paid-in capital |
Accumulated deficit |
Total members’ equity |
||||||||||||||||||||||
| Balance at January 1, 2019 |
3,391,370 | $ | 320.2 | 52,240 | $ | 2.6 | $ | — | $ | (38.8 | ) | $ | 284.0 | |||||||||||||||
| ASC 606 adoption |
— | — | — | — | — | (0.2 | ) | (0.2 | ) | |||||||||||||||||||
| Contribution of Remedy |
— | — | — | — | 698.3 | — | 698.3 | |||||||||||||||||||||
| Acquisition of TAV Health |
130,525 | 26.1 | — | — | — | — | 26.1 | |||||||||||||||||||||
| Member contributions |
30,000 | 3.0 | — | — | — | — | 3.0 | |||||||||||||||||||||
| Member distributions (Note 14) |
— | (21.8 | ) | — | (0.7 | ) | — | — | (22.5 | ) | ||||||||||||||||||
| Repurchase of member units |
(18,762 | ) | (2.0 | ) | (6,300 | ) | (0.3 | ) | — | — | (2.3 | ) | ||||||||||||||||
| Tax payments on behalf of members |
— | — | — | — | (7.4 | ) | — | (7.4 | ) | |||||||||||||||||||
| Equity-based compensation |
— | — | 14,966 | 2.0 | 1.0 | — | 3.0 | |||||||||||||||||||||
| Proceeds from exercises of stock options |
— | — | — | — | 0.6 | — | 0.6 | |||||||||||||||||||||
| Net loss |
— | — | — | — | — | (20.5 | ) | (20.5 | ) | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Balance at September 30, 2019 |
3,533,133 | $ | 325.5 | 60,906 | $ | 3.6 | $ | 692.5 | $ | (59.5 | ) | $ | 962.1 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Series A preferred units |
Series A preferred members’ equity |
Series B preferred units |
Series B preferred members’ equity |
Class B common units |
Class B members’ equity |
Class C common units |
Class C members’ equity |
Accumulated deficit |
Total members’ equity |
|||||||||||||||||||||||||||||||
| Balance at January 1, 2020 |
3,384,543 | $ | 695.4 | 3,533,133 | $ | 325.5 | 93,311 | $ | 4.2 | — | $ | — | $ | (67.5 | ) | $ | 957.6 | |||||||||||||||||||||||
| Repurchase of member units |
— | — | (130,525 | ) | (54.0 | ) | (350 | ) | — | — | — | — | (54.0 | ) | ||||||||||||||||||||||||||
| Tax payments on behalf of members |
— | — | — | (7.2 | ) | — | (0.7 | ) | — | (0.2 | ) | (8.1 | ) | |||||||||||||||||||||||||||
| Equity-based compensation |
— | 1.2 | — | — | 16,016 | 1.4 | 83,244 | 7.4 | — | 10.0 | ||||||||||||||||||||||||||||||
| Proceeds from exercises of stock options |
— | 0.7 | — | — | — | — | — | — | 0.7 | |||||||||||||||||||||||||||||||
| Repurchase of stock on behalf of New Remedy Corp |
— | (0.6 | ) | — | — | — | — | — | — | — | (0.6 | ) | ||||||||||||||||||||||||||||
| Tax refunds received on behalf of New Remedy Corp |
— | 1.0 | — | — | — | — | — | — | — | 1.0 | ||||||||||||||||||||||||||||||
| Net loss |
— | — | — | — | — | — | — | — | (15.2 | ) | (15.2 | ) | ||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
| Balance at September 30, 2020 |
3,384,543 | $ | 697.7 | 3,402,608 | $ | 264.3 | 108,977 | $ | 4.9 | 83,244 | $ | 7.2 | $ | (82.7 | ) | $ | 891.4 | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
See accompanying notes to the condensed combined-consolidated financial statements.
F-7
Table of Contents
Cure TopCo, LLC and Subsidiaries
Condensed Combined-Consolidated Statements of Cash Flows (Unaudited, in millions)
| Nine months ended September 30, | ||||||||
| 2020 | 2019 | |||||||
| Operating activities |
||||||||
| Net loss |
$ | (15.2 | ) | $ | (20.5 | ) | ||
| Adjustments to reconcile net loss to net cash provided by operating activities: |
||||||||
| Depreciation and amortization |
46.0 | 49.5 | ||||||
| Loss on impairment |
— | 1.5 | ||||||
| Equity-based compensation |
10.0 | 3.0 | ||||||
| Customer equity appreciation right |
7.5 | — | ||||||
| Remeasurement of customer equity appreciation right |
6.9 | — | ||||||
| Amortization of deferred financing fees |
1.3 | 1.2 | ||||||
| Loss on extinguishment of debt |
— | 0.2 | ||||||
| Remeasurement of contingent consideration |
0.2 | 0.7 | ||||||
| Payment of contingent consideration |
(1.8 | ) | ||||||
| Gain on sale of assets |
— | (1.1 | ) | |||||
| Other |
0.2 | 0.5 | ||||||
| Changes in operating assets and liabilities: |
||||||||
| Accounts receivable |
25.0 | 73.7 | ||||||
| Prepaid expenses and other current assets |
(4.8 | ) | (3.5 | ) | ||||
| Contract assets |
(71.7 | ) | 23.4 | |||||
| Other assets |
(0.2 | ) | 0.1 | |||||
| Accounts payable and accrued expenses |
(11.5 | ) | (37.4 | ) | ||||
| Contract liabilities |
31.9 | (37.7 | ) | |||||
| Other current liabilities |
6.3 | (0.5 | ) | |||||
| Other noncurrent liabilities |
10.6 | 3.1 | ||||||
|
|
|
|
|
|||||
| Net cash provided by operating activities |
40.7 | 56.2 | ||||||
| Investing activities |
||||||||
| Capital expenditures—property and equipment |
(13.0 | ) | (7.1 | ) | ||||
| Capital expenditures—internal-use software development |
(15.7 | ) | (9.7 | ) | ||||
| Proceeds from sale of assets |
— | 1.2 | ||||||
| Business combinations, net of cash acquired |
— | (28.8 | ) | |||||
| Cash acquired from Remedy Partners Acquisition |
— | 136.0 | ||||||
|
|
|
|
|
|||||
| Net cash (used in) provided by investing activities |
(28.7 | ) | 91.6 | |||||
| Financing activities |
||||||||
| Repayment of long-term debt |
(2.1 | ) | (2.1 | ) | ||||
| Proceeds from issuance of long-term debt |
— | 20.0 | ||||||
| Repayment of borrowings under revolving credit facility |
(15.0 | ) | (20.0 | ) | ||||
| Proceeds from borrowings under revolving credit facility |
92.0 | 25.0 | ||||||
| Repayments of borrowings under financing agreement |
(0.2 | ) | — | |||||
| Proceeds from borrowings under financing agreement |
0.6 | — | ||||||
| Payment of contingent consideration |
(38.2 | ) | — | |||||
| Payment of debt issuance costs |
— | (0.7 | ) | |||||
| Payment to sellers of Remedy |
— | (83.8 | ) | |||||
| Member distributions |
(8.1 | ) | (22.5 | ) | ||||
| Payment of taxes on behalf of New Remedy Corp |
1.0 | (7.4 | ) | |||||
| Repurchase of member units |
— | (2.7 | ) | |||||
| Contributions from members |
— | 3.0 | ||||||
| Proceeds related to the issuance of New Remedy Corp common stock under stock plans |
0.1 | 0.6 | ||||||
|
|
|
|
|
|||||
| Net cash provided by (used in) financing activities |
30.1 | (90.6 | ) | |||||
| Increase in cash, cash equivalents and restricted cash |
42.1 | 57.2 | ||||||
| Cash, cash equivalents and restricted cash—beginning of year |
50.2 | 20.4 | ||||||
|
|
|
|
|
|||||
| Cash, cash equivalents and restricted cash—end of year |
$ | 92.3 | $ | 77.6 | ||||
|
|
|
|
|
|||||
| Supplemental disclosures of cash flow information |
||||||||
| Cash paid for interest |
$ | 14.9 | $ | 14.6 | ||||
| Cash paid for taxes (net of refunds) |
0.3 | 0.3 | ||||||
| Noncash transactions |
||||||||
| Issuance of membership units related to acquisition |
— | 26.1 | ||||||
| Capital expenditures not yet paid |
0.2 | — | ||||||
See accompanying notes to the condensed combined-consolidated financial statements.
F-8
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
| 1. | Nature of Operations |
Cure TopCo, LLC (formerly Chloe Ox Holdings, LLC, “we”, “our”, “us”) is a Delaware limited liability company formed on November 3, 2017. We have adopted a holding company structure and are the indirect parent company of Signify Health, LLC (“Signify”), a Delaware limited liability company formerly known as Cure Borrower, LLC.
Signify was formed on November 3, 2017. Operations are performed through our wholly-owned subsidiaries.
We are a healthcare platform that leverages advanced analytics, technology and nationwide healthcare provider networks. Our customers include health plans, governments, employers, health systems and physician groups. We operate in two segments of the value-based healthcare payment industry: payment models based on individual episodes of care, or Episodes of Care Services segment, and in-home health evaluations, or Home & Community Services segment. Our solutions support value-based payment programs by aligning financial incentives around, and providing tools to health plans and healthcare organizations designed to assess and manage, risk and identify actionable opportunities for improved patient outcomes, coordination and cost-savings.
In 2019, we acquired 100% of the outstanding equity of Remedy Partners, Inc. (“Remedy Partners”). A controlling interest in Remedy Partners was initially acquired by New Mountain Capital on January 15, 2019 (the “Remedy Partners Acquisition”), at which point we and Remedy Partners were considered to be under common control and combined financial statements were presented from January 15, 2019 to November 26, 2019. On November 26, 2019, a series of transactions were effected which resulted in Remedy Partners becoming our wholly-owned subsidiary and consolidated financial statements were presented from that date forward (the “Remedy Partners Combination” and together with the Remedy Partners Acquisition, the “Remedy Partners Transaction”).
On March 13, 2019, Signify acquired 100% of the outstanding equity of Triple Aim Ventures, LLC, a Delaware limited liability company (“TAV Health”).
| 2. | Significant Accounting Policies |
Basis of Presentation
Combination—Consolidation
The unaudited financial statements were consolidated as of September 30, 2020 and December 31, 2019 and for the nine months ended September 30, 2020. The financial statements were combined for the nine months ended September 30, 2019, see Note 1 Nature of Operations. These unaudited Condensed Combined-Consolidated Financial Statements should be read in conjunction with the 2019 audited Combined-Consolidated Financial Statements and the related notes thereto included elsewhere in this prospectus.
These Condensed Combined-Consolidated Financial Statements are unaudited and have been prepared by us in accordance with accounting principles generally accepted in the United States of America (“GAAP”) and following the rules and regulations of the SEC. In our opinion, they reflect all adjustments, including normal recurring items, that are necessary to present fairly the results of interim periods. Certain information and footnote disclosures normally included in annual financial statements prepared in accordance with GAAP have been condensed or omitted as permitted by such rules and regulations; however, we believe that the disclosures are adequate to make the information presented not misleading. Operating results for the periods presented herein are not necessarily indicative of the results that may be expected for future interim periods or the entire fiscal year. Our quarterly results of operations, including our revenue, income (loss) from operations, net loss and cash flows, have varied and may vary significantly in the future, and
F-9
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
period-to-period comparisons of our results of operations may not be meaningful. Accordingly, our interim results should not be relied upon as an indication of future performance.
The Condensed Combined-Consolidated Financial Statements include the accounts and financial statements of our wholly-owned subsidiaries and variable interest entities (VIEs) where we are the primary beneficiary. Results of operations of VIEs are included from the dates we became the primary beneficiary. All intercompany balances and transactions have been eliminated in consolidation.
We have two operating segments, Home & Community Services and Episodes of Care Services.
Use of Estimates
The accompanying unaudited Condensed Combined-Consolidated Financial Statements have been prepared in accordance with GAAP, which requires management to make estimates and assumptions affecting the reported amounts in the Condensed Combined-Consolidated Financial Statements and accompanying notes. These estimates are based on information available as of the date of the Condensed Combined-Consolidated Financial Statements; therefore, actual results could differ from those estimates. The significant estimates underlying our Condensed Combined-Consolidated Financial Statements include revenue recognition; allowance for doubtful accounts; recoverability of long-lived assets, intangible assets and goodwill; loss contingencies; accounting for business combinations, including amounts assigned to definite and indefinite lived intangible assets and contingent consideration; and equity-based compensation.
As of September 30, 2020, the impact of the outbreak of COVID-19 continues to unfold; See Note 3 COVID-19 Pandemic. As a result, many of our estimates and assumptions have required increased judgment and carry a higher degree of variability and volatility. As events continue to evolve and additional information becomes available, our estimates may change materially in the future.
Comprehensive Income (Loss)
We have not identified any incremental items that would be considered a component of comprehensive income (loss) and accordingly a statement of comprehensive loss is not reflected in the Condensed Combined-Consolidated Financial Statements because net loss and comprehensive loss are the same.
Restricted Cash
Under our Master Agreement with the Centers for Medicare and Medicaid Services (“CMS”), we are required to place certain funds in escrow for the benefit of CMS. This account, known as a Secondary Repayment Source (“SRS”), is based on the size of our participation in the legacy CMS Bundled Payments for Care Improvement (“BPCI”) program, the predecessor program of the Bundled Payments for Care Improvement—Advanced initiative (“BPCI-A”). These funds are available to CMS as a supplemental payment source if we fail to pay amounts owed to CMS. The funds will be returned to us 18 months after the conclusion of the effective period of the CMS Master Agreement, or when all financial obligations to CMS are fulfilled. As of September 30, 2020 and December 31, 2019, there was $0.5 and $16.3, respectively, in the SRS account included in restricted cash on the Condensed Consolidated Balance Sheets. In March 2020 and August 2020, $13.4 and $2.4, respectively, of these funds were released to us from escrow as the original BPCI program has ended, with the remaining balance of $0.5 as of September 30, 2020 related to BPCI-A.
We also withhold a portion of shared savings to customers in a “holding pool” to cover any potential subsequent negative adjustments through CMS’s subsequent reconciliation true-up process. These funds are
F-10
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
distributed to customers following the final true-up if there is no negative adjustment. These amounts represent consideration payable to the customer and therefore have reduced revenue in the period earned. The funds have been received by us from CMS and are held in a separate cash account, included as restricted cash on the Condensed Consolidated Balance Sheets. Since the funds are payable to the customer at the point the final CMS true-up is made or a negative adjustment is due to us, the amounts are also included in accounts payable and accrued expenses on the Condensed Consolidated Balance Sheets. As of September 30, 2020 and December 31, 2019, there was $3.9 and $6.2, respectively, of restricted cash in the holding pool.
The following table reconciles cash, cash equivalents, and restricted cash per the Condensed Combined-Consolidated Statements of Cash Flows to the Condensed Consolidated Balance Sheets:
| September 30, 2020 |
December 31, 2019 |
September 30, 2019 |
December 31, 2018 |
|||||||||||||
| Cash and cash equivalents |
$ | 87.9 | $ | 27.7 | $ | 46.2 | $ | 20.4 | ||||||||
| Restricted cash |
4.4 | 22.5 | 31.4 | — | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Total cash, cash equivalents, and restricted cash |
$ | 92.3 | $ | 50.2 | $ | 77.6 | $ | 20.4 | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
Accounts Receivable
Accounts receivable primarily consist of amounts due from customers and CMS and are stated at their net realizable value. Management evaluates all accounts periodically and an allowance is established based on the best facts available to management. Management considers historical realization data, accounts receivable aging trends and other operational trends to estimate the collectability of receivables. After all reasonable attempts to collect a receivable have been exhausted, the receivable is written off against the allowance for doubtful accounts. As of September 30, 2020 and December 31, 2019, we had an allowance for doubtful accounts of $5.1 and $4.8, respectively.
Recent Accounting Pronouncements
Recently adopted
In May 2014, FASB issued Accounting Standards Update (“ASU”) 2014-09, Revenue from Contracts with Customers (“ASC 606”). The new revenue recognition standard provides a five-step model to determine when and how revenue is recognized. The core principle is that a company should recognize revenue to depict the transfer of promised goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled in exchange for those goods or services. This guidance was effective for nonpublic companies for annual periods beginning after December 15, 2018 and is applied either retrospectively to each period presented or as a cumulative-effect adjustment as of the date of adoption. We used the modified retrospective method to adopt the new revenue recognition guidance on January 1, 2019. Adoption of the new standard did not have a material impact to our revenue recognition, with approximately $0.2 recognized as a cumulative impact increase in accumulated deficit upon adoption. Remedy Partners adopted this new accounting guidance effective January 1, 2019, prior to our acquisition of Remedy Partners and its inclusion in our Condensed Combined-Consolidated Financial Statements. This new guidance did have a material impact on the timing of revenue recognition for Remedy Partners.
In June 2018, the FASB issued Accounting Standards Update No. 2018-07, Compensation—Stock Compensation (Topic 718): Improvements to Nonemployee Share-Based Payment Accounting (“ASU 2018-07”). The amendments in ASU 2018-07 expand the scope of Topic 718 to include share-based
F-11
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
payment transactions for acquiring goods and services from nonemployees. ASU 2018-07 is effective for fiscal years beginning after December 15, 2019, and interim periods within fiscal years beginning after December 15, 2020. We elected to early adopt this new guidance for interim periods in 2020 with no significant impact to our financial statements.
In November 2019, the FASB issued ASU 2019-08, Compensation—Stock Compensation (Topic 718) and Revenue from Contracts with Customers (Topic 606): Codification Improvements—Share-Based Consideration Payable to a Customer (“ASU 2019-08”). ASU 2019-08 requires that an entity measure and classify share-based payment awards granted to a customer by applying the guidance in Topic 718. The amount recorded as a reduction of the transaction price is required to be measured on the basis of the grant-date fair value of the share-based payment award in accordance with Topic 718. The grant date is the date at which a grantor (supplier) and a grantee (customer) reach a mutual understanding of the key terms and conditions of a share-based payment award. ASU 2019-08 is effective for fiscal years beginning after December 15, 2019, and interim periods within fiscal years beginning after December 15, 2020. We elected to early adopt this new guidance for interim periods in 2020, which had an impact on the customer EAR agreements. The initial grant date fair value of the EAR agreements is being recorded as a reduction of the transaction price beginning in 2020. See Note 17 Commitments and Contingencies.
Pending Adoption
In February 2016, the FASB issued ASU 2016-02, Leases (Topic 842). The new lease standard requires lessees to recognize leases on the balance sheet by recording a right-of-use asset and lease liability. This guidance is effective for non-public entities for annual reporting periods beginning after December 15, 2021. Early adoption is permitted. We are currently assessing the impact of this guidance on the Condensed Combined-Consolidated Financial Statements.
In June 2016, the FASB issued ASU 2016-13, Financial Instruments—Credit Losses (Topic 326) (“ASU 2016-13”). ASU 2016-13 introduced the current expected credit losses methodology for estimating allowances for credit losses. ASU 2016-13 applies to all financial instruments carried at amortized cost and off-balance-sheet credit exposures not accounted for as insurance, including loan commitments, standby letters of credit, and financial guarantees. The new accounting standard does not apply to trading assets, loans held for sale, financial assets for which the fair value option has been elected, or loans and receivables between entities under common control. ASU 2016-13 is effective for non-public entities for fiscal years beginning after December 15, 2022, including interim periods within those fiscal years. Early adoption is permitted. We are evaluating the impact of this new guidance on our financial statements.
| 3. | The COVID-19 Pandemic |
During the first quarter of 2020, the COVID-19 outbreak rapidly evolved. In our Home & Community Services segment, in-home health evaluations (“IHEs”) were only moderately impacted during the first quarter of 2020. However, at the end of the first quarter of 2020, we temporarily suspended conducting IHEs. At the same time, we launched a new service, offering health plan customers a “virtual” health assessment (“vIHE”) to be supplemented, where possible, with a confirmatory IHE later in the year. Certain of our Home & Community Services health plan customers agreed to this new service, which we began providing on April 2, 2020. CMS provided temporary approval of this service in early April 2020. We also developed a number of new product offerings in support of the crisis, such as workplace screening and testing, which we quickly operationalized and began offering to employers as an additional service in early April 2020. As a result of these actions, more than 90% of health evaluations during the second quarter 2020 were vIHEs. In July 2020, we began to return to IHEs. For the third quarter of 2020, the number of health
F-12
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
risk assessments that were being performed on an in-home basis, had returned to historic levels. We established personal protective equipment protocols with our major customers in order to achieve this return to IHEs. We, together with our customers, continue to monitor the changing situation with COVID-19 cases on a state-by-state basis.
Within the Episodes of Care Services segment, we observed some evidence of reduced volumes of episodes of care as a result of the cancellation of elective surgeries in the final two weeks of the first quarter of 2020. Due to the nature of the BPCI-A program, however, there is a significant lag between us performing our services and CMS reporting the final outcomes of those services. We will continue to monitor any leading indicators and the potential impact on our operations and financial performance.
We also note that by virtue of the passage of time between when we perform our services and the confirmation of results and subsequent cash settlement by CMS, COVID-19 did not have an impact on the cash we received from CMS during 2020. We expect to receive our next cash payment from CMS in the first quarter of 2021 which will reflect the initial impact of COVID-19 on our business as described below.
In response to the COVID-19 pandemic, CMS announced healthcare providers may continue in the BPCI-A program with no change or they allowed healthcare providers an exception to previous rules of the program with two options as follows:
| • | Healthcare providers may choose to eliminate upside and downside risk by excluding all episodes from reconciliation in 2020; or |
| • | Healthcare providers may choose to exclude from reconciliation those episodes with a COVID-19 diagnosis during the episode. |
Healthcare providers were required to make their elections by September 25, 2020. The results of these elections made by the providers will reduce the total number of episodes we manage during 2020 and part of 2021, and therefore reduce program size. While these provider elections will temporarily reduce program size in the near term, this impact is partially offset by a higher savings rate achieved as a result of certain underperforming episodes being dropped. Subsequently, CMS announced that all episodes in 2021 with a COVID-19 diagnosis would be automatically excluded from reconciliation, which will further reduce program size for all of 2021.
During the fourth quarter of 2020, COVID-19 rates have been spiking once again and parts of the United States are experiencing peak levels of the virus. We continue to monitor trends related to COVID-19 and their impact on our business, results of operations and financial condition.
| 4. | Business Combinations |
Remedy Partners Acquisition
On January 15, 2019, affiliates of New Mountain Capital acquired a controlling interest in Remedy Partners for $405.0 in cash at which point we and Remedy Partners were considered to be under common control. The total enterprise value purchase consideration of the transaction was determined to be $664.0. We allocated the purchase price to the identifiable net assets acquired, based on the estimated fair values at the date of acquisition. The excess of the purchase price over the amount allocated to the identifiable assets and liabilities was recorded as goodwill. Goodwill represents the value of the acquired assembled workforce, specialized processes and procedures and operating synergies, none of which qualify as separate intangible assets.
We determined the estimated fair values of intangible assets acquired using estimates of future discounted cash flows to be generated by the business over the estimated duration of those cash flows. We base the
F-13
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
estimated cash flows on projections of future revenue, operating expenses, capital expenditures, working capital needs and tax rates. We estimated the duration of the cash flows based on the projected useful lives of the assets acquired. The discount rate was determined based on specific business risk, cost of capital and other factors.
The table below presents the fair value of net assets acquired and pushed down as of the acquisition date:
| Cash |
$ | 114.7 | ||
| Accounts receivable |
89.2 | |||
| Contract assets |
112.8 | |||
| Prepaid expenses and other current assets |
3.7 | |||
| Restricted cash |
21.3 | |||
| Property and equipment |
6.6 | |||
| Other assets |
0.8 | |||
| Intangible assets |
167.0 | |||
|
|
|
|||
| Total identifiable assets acquired |
516.1 | |||
| Accounts payable and accrued liabilities |
161.6 | |||
| Contract liabilities |
60.3 | |||
| Other current liabilities |
8.2 | |||
| Deferred tax liabilities |
30.4 | |||
|
|
|
|||
| Total liabilities assumed |
260.5 | |||
|
|
|
|||
| Net identifiable assets acquired |
255.6 | |||
| Goodwill |
408.4 | |||
|
|
|
|||
| Total of assets acquired and liabilities assumed |
$ | 664.0 | ||
|
|
|
The $167.0 of acquired intangible assets include customer relationships of $118.0 (weighted average useful life of 9 years), acquired software of $43.0 (5-year useful life) and a tradename of $6.0 (5-year useful life). The tradename was subsequently impaired following our rebranding upon the Remedy Partners Combination during the fourth quarter of 2019.
Accounts payable and accrued liabilities assumed includes $83.8 related to an excess cash distribution that was paid to the sellers of Remedy Partners in May 2019, in accordance with the terms of the purchase agreement.
None of the goodwill is deductible for tax purposes. At the time of the Remedy Partners Combination in November 2019, Remedy Partners was contributed as a limited liability company after a series of transactions in a tax-free transaction. As such, all tax attributes, including $3.9 of current tax liabilities included in other current liabilities above and $30.4 of deferred tax liabilities previously related to Remedy Partners are maintained at the New Remedy Corp. level (parent holding company). For presentation purposes, the tax treatment was as if New Remedy Corp. existed and held the tax attributes for the entire year ended December 31, 2019.
The acquisition resulted in common control by New Mountain Capital. As such, the financial results of Remedy Partners have been combined with our financial results and included in the Condensed Combined-Consolidated Financial Statements since the date of acquisition. At the time of the Remedy Partners Combination in November 2019, the financial results were consolidated with the financial results of the other entities of the Company. Total revenue and net loss of $67.8 and $30.3, respectively, related to Remedy Partners is included in the Condensed Combined-Consolidated Statements of Operations for the nine months ended September 30, 2019.
F-14
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
TAV Health Acquisition
On March 13, 2019, we acquired 100% of the outstanding equity of TAV Health. The purchase price was $55.0, comprised of $28.9 in cash and the issuance of 130,525 of our former Class A Common Units. We allocated the purchase price to the identifiable net assets acquired, based on the estimated fair values at the date of acquisition. The excess of the purchase price over the amount allocated to the identifiable assets and liabilities was recorded as goodwill. Goodwill represents the value of the acquired assembled workforce, specialized processes and procedures and operating synergies, none of which qualify as separate intangible assets.
We determined the estimated fair values of intangible assets acquired using estimates of future discounted cash flows to be generated by the business over the estimated duration of those cash flows. We base the estimated cash flows on projections of future revenue, operating expenses, capital expenditures, working capital needs and tax rates. We estimated the duration of the cash flows based on the projected useful lives of the assets acquired. The discount rate was determined based on specific business risk, cost of capital and other factors.
The table below presents the fair value of net assets acquired at the date of acquisition:
| Cash |
$ | 0.1 | ||
| Accounts receivable |
0.3 | |||
| Prepaid expenses and other current assets |
0.2 | |||
| Other assets |
0.1 | |||
| Property and equipment |
0.3 | |||
| Intangible assets |
8.2 | |||
|
|
|
|||
| Total identifiable assets acquired |
9.2 | |||
| Accounts payable and accrued liabilities |
0.1 | |||
| Other current liabilities |
2.0 | |||
|
|
|
|||
| Total liabilities assumed |
2.1 | |||
|
|
|
|||
| Net identifiable assets acquired |
7.1 | |||
| Goodwill |
47.9 | |||
|
|
|
|||
| Total of assets acquired and liabilities assumed |
$ | 55.0 | ||
|
|
|
The $8.2 of acquired intangible assets is comprised of acquired software of $7.7 (6-year useful life) and customer relationships of $0.5 (14-year useful life).
None of the goodwill is expected to be deductible for tax purposes.
The acquisition was not material to our Condensed Combined-Consolidated Statements of Operations. Therefore, pro forma results of operations related to this acquisition have not been presented. The financial results of TAV Health have been included in our Condensed Combined-Consolidated Financial Statements since the date of the acquisition.
| 5. | Variable Interest Entities |
We consolidate our affiliates when we are the primary beneficiary. The primary beneficiary of a Variable Interest Entity (“VIE”) is the party that has both the decision-making authority to direct the activities that most significantly impact the VIE’s economic performance and the right to absorb losses or receive benefits that could potentially be significant to the VIE. Consolidated VIEs at September 30, 2020 and December 31,
F-15
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
2019 include one and two, respectively, physician practices that require an individual physician to legally own the equity interests as certain state laws and regulations prohibit non-physician owned business entities from practicing medicine or employing licensed healthcare providers. We have determined we are the primary beneficiary of these VIEs as we have the obligation to absorb the losses from and direct activities of these operations. As a result, these VIEs are consolidated and any non-controlling interest is not presented. Recourse of creditors to these VIEs is limited to the assets of the VIE entities, which total $2.0 and $2.5 at September 30, 2020 and December 31, 2019, respectively.
In February 2019, we sold a VIE, Principium LLC and Medical Service Professionals of New Jersey PLC, to Clover Health LLC for $1.2 and recognized a gain on disposition of assets of $1.1, which is included in SG&A expenses on the Condensed Combined-Consolidated Statements of Operations.
The carrying amount and classification of the VIEs’ assets and liabilities included in the Condensed Consolidated Balance Sheets as of September 30, 2020 and December 31, 2019, net of intercompany amounts, are as follows:
| September 30, | December 31, | |||||||
| 2020 | 2019 | |||||||
| ASSETS |
||||||||
| Current assets |
||||||||
| Cash and cash equivalents |
$ | 0.1 | $ | 0.1 | ||||
| Accounts receivable, net |
1.9 | 2.4 | ||||||
|
|
|
|
|
|||||
| Total current assets |
2.0 | 2.5 | ||||||
|
|
|
|
|
|||||
| Total assets |
$ | 2.0 | $ | 2.5 | ||||
|
|
|
|
|
|||||
| LIABILITIES AND EQUITY |
||||||||
| Total liabilities |
— | — | ||||||
| Company capital |
(1.2 | ) | (0.1 | ) | ||||
| Retained earnings |
3.2 | 2.6 | ||||||
|
|
|
|
|
|||||
| Total equity |
2.0 | 2.5 | ||||||
|
|
|
|
|
|||||
| Total liabilities and equity |
$ | 2.0 | $ | 2.5 | ||||
|
|
|
|
|
|||||
| 6. | Revenue Recognition |
Under ASC 606, we recognize revenue as the control of promised services is transferred to our customers and we generate all of our revenue from contracts with customers. The amount of revenue recognized reflects the consideration to which we expect to be entitled in exchange for these services. The measurement and recognition of revenue requires us to make certain judgments and estimates.
We are dependent on a concentrated number of payors and provider partners with whom we contract to provide our services, see Note 20 Concentrations.
Disaggregation of Revenue
We earn revenue from our two operating segments, Home & Community Services and Episodes of Care Services, under contracts that contain various fee structures. Through our Home & Community Services segment, we offer health evaluations performed either within the patient’s home or at a healthcare provider facility primarily to Medicare Advantage health plans (and to some extent, Medicaid). Additionally, we
F-16
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
offer certain diagnostic screening and other ancillary services and through our Signify Community solution, we offer services to address healthcare concerns related to social determinants of health. Through our Episodes of Care Services segment, we primarily provide services designed to improve the quality and efficiency of healthcare delivery by developing and managing episodic payment programs in partnership with healthcare providers, primarily under the BPCI-A program with CMS. Additionally, we provide certain complex care management services. All of our revenue is generated in the United States.
The following table summarizes disaggregated revenue from contracts with customers for the nine months ended September 30, 2020 and 2019 by source of revenue, which we believe best depicts the nature, amount and timing of revenue.
| Nine months ended September 30, |
||||||||
| 2020 | 2019 | |||||||
| Evaluations |
$ | 294.9 | $ | 280.7 | ||||
| Other |
6.9 | 6.3 | ||||||
|
|
|
|
|
|||||
| Home & Community Services Total Revenue |
301.8 | 287.0 | ||||||
| Episodes |
107.2 | 67.8 | ||||||
| Other |
8.1 | 13.7 | ||||||
|
|
|
|
|
|||||
| Episodes of Care Services Total Revenue |
115.3 | 81.5 | ||||||
|
|
|
|
|
|||||
| Combined-Consolidated Revenue Total |
$ | 417.1 | $ | 368.5 | ||||
|
|
|
|
|
|||||
Performance Obligations
The unit of measure under ASC 606 is a performance obligation, which is a promise in a contract to transfer a distinct or series of distinct goods or services to the customer. A contract’s transaction price is allocated to each distinct performance obligation and recognized as revenue when, or as, the performance obligation is satisfied.
Our customer contracts have either (1) a single performance obligation as the promise to transfer services is not separately identifiable from other promises in the contracts and is, therefore, not distinct; (2) a series of distinct performance obligations; or (3) multiple performance obligations, most commonly due to the contract covering multiple service offerings. For contracts with multiple performance obligations, the contract’s transaction price is allocated to each performance obligation on the basis of the relative standalone selling price of each distinct service in the contract.
Home & Community Services
Home & Community Services revenue primarily consists of IHEs and related services, categorized as evaluations and other.
Revenue generated from IHEs relates to the assessments performed either within the patient’s home or at a healthcare provider facility as well as certain in-home clinical evaluations performed by our mobile network of providers.
Revenue is recognized when the IHEs are submitted to our customers on a daily basis. Submission to the customer occurs after the IHEs are completed and coded, a process which may take one to several days after completion of the evaluation. The pricing for the IHEs is generally based on a fixed transaction fee, which is directly linked to the usage of the service by the customer during a distinct service period. Customers are
F-17
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
invoiced for evaluations performed each month and remit payment accordingly. Each IHE represents a single performance obligation for which revenue is recognized at a point-in-time when control is transferred to the customer upon submission of the completed and coded evaluation.
See Note 17 Commitments and Contingencies for detail on the Customer Equity Appreciation Rights.
The remaining sources of revenue in our Home & Community Services segment, which relate to ancillary diagnostic and evaluative services we provide, are recognized over time as the performance obligations are satisfied and are primarily based on a fixed fee. Therefore, they do not require estimates and assumptions by management.
Episodes of Care Services
The episodes solutions we provide are an integrated set of services which represent a single performance obligation in the form of a series of distinct services. This performance obligation is satisfied over time as the various services are delivered. We primarily offer our services to customers under the BPCI-A program.
Under the BPCI-A program, we act in a convener capacity, as defined by CMS, for most of our customer contracts, with the exception of a few customer contracts whereby we act in a non-convener capacity. Under the BPCI-A program, we recognize the revenue attributable to episodes reconciled during each six-month episode performance measurement period over a 13-month performance obligation period that commences in the second or fourth quarter of each year, depending on the relevant contract with our provider partners. The 13-month performance obligation period begins at the start of the relevant episodes of care and extends through the receipt or generation of the semiannual reconciliation for the relevant performance measurement period, as well as the provision and explanation of statements of performance to each of our customers. The transaction price is 100% variable and therefore we estimate an amount in which we expect to be entitled to receive for each six-month episode performance measurement period over a 13-month performance obligation period.
For each partner agreement, the fees are generally two-fold, an administrative fee, which is based on a stated percentage of program size and is paid out of savings, and a defined share of program savings or losses, if any. In order to estimate this variable consideration, management estimates the expected program size as well as the expected savings rate for each six-month episode performance measurement period. The estimate is performed both at the onset of each performance measurement period based on information available at the time and at the end of each reporting period. In making the estimate we consider inputs such as the overall program size which is defined by the historic cost multiplied by the frequency of occurrence of defined episodes of care. Additionally, we estimate savings rates by using data sources such as historical trend analysis together with indicative data of the current volume of episodes.
We adjust our estimates at the end of each six-month performance measurement period, generally in the second and fourth quarter each year, and may further adjust at the end of each reporting period to the extent new information indicates a change is required. We apply a constraint to the variable consideration estimate in circumstances where we believe the claims data received is incomplete or inconsistent, so as not to have the estimates result in a significant revenue reversal in future periods. Although our estimates are based on the information available to us at each reporting date, several factors may cause actual revenue earned to differ from the estimates recorded in each period. These include, among others, limited historical experience as the current BPCI-A program only commenced in the fourth quarter of 2018, CMS-imposed restrictions on the definition of episodes and benchmark prices, provider partner participation, the impacts of the COVID-19 pandemic in 2020 and other limitations of the program beyond our control.
The overall goal of the BPCI-A program is to generate savings relative to CMS benchmark prices. In return for participating in the program, we and our customers can share in savings or losses generated compared to
F-18
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
the CMS benchmark prices, and those savings or losses are then shared with customers in accordance with the terms of our customer contracts. The customer’s share of the total savings represents consideration payable to customers and therefore is a reduction of the transaction price. We receive payment semi-annually from CMS for our customers in which we act as a convener or directly from our non-convener customers.
The remaining sources of revenue in our Episodes of Care Services segment are recognized over time when, or as, the performance obligations are satisfied and are primarily based on a fixed fee or per member per month fee. Therefore, they do not require significant estimates and assumptions by management.
During the nine months ended September 30, 2019, we recognized $2.1 of revenue representing changes in estimates related to variable consideration upon receipt and analysis of reconciliations from CMS in 2019 related to performance obligations satisfied in the year ended December 31, 2018.
During the nine months ended September 30, 2020, we recognized approximately $7.3 of revenue representing changes in estimates related to variable consideration upon receipt and analysis of reconciliations from CMS in the second quarter of 2020 related to performance obligations satisfied in the year ended December 31, 2019. In addition, during the nine months ended September 30, 2020, we recorded approximately $1.6 related to a cumulative catch up of a change in estimated transaction price upon the satisfaction of the performance obligations. During the nine months ended September 30, 2020, we also recorded approximately $9.2 of revenue related to changes in estimates for performance obligations in process based on new information received primarily related to the impact of COVID-19 on program size and related CMS imposed changes offered to providers.
During the nine months ended September 30, 2020, we recorded revenue of $3.3 related to a one-time termination fee associated with a customer in the Episodes of Care Services segment upon termination of the contract.
During the nine months ended September 30, 2020, we terminated a contract with a customer in our Episodes of Care Services segment, representing approximately 5% of our total revenue for the year ended December 31, 2019 in connection with a contractual dispute. Effective July 2020, we entered into an advisory services agreement with the customer to assist the customer with its ongoing participation in the BPCI-A program through December 31, 2023.
Related Balance Sheet Accounts
The following table provides information about accounts included on the Condensed Consolidated Balance Sheet as of September 30, 2020 and December 31, 2019.
| September 30, 2020 | December 31, 2019 | |||||||||||||||||||||||
| Episodes of Care Services |
Home & Community Services |
Total | Episodes of Care Services |
Home & Community Services |
Total | |||||||||||||||||||
| Assets |
||||||||||||||||||||||||
| Accounts receivable, net (1) |
$ | 25.1 | $ | 118.0 | $ | 143.1 | $ | 125.1 | $ | 43.0 | $ | 168.1 | ||||||||||||
| Contract assets (2) |
$ | 110.0 | $ | — | $ | 110.0 | $ | 38.3 | $ | — | $ | 38.3 | ||||||||||||
| Liabilities |
||||||||||||||||||||||||
| Shared savings payable (3) |
$ | 33.2 | $ | — | $ | 33.2 | $ | 58.2 | $ | — | $ | 58.2 | ||||||||||||
| Contract liabilities (4) |
$ | 35.0 | $ | — | $ | 35.0 | $ | 3.1 | $ | — | $ | 3.1 | ||||||||||||
| Deferred revenue (5) |
$ | 4.7 | $ | 1.4 | $ | 6.1 | $ | — | $ | 1.2 | $ | 1.2 | ||||||||||||
F-19
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
| (1) | Accounts receivable, net for Episodes of Care Services included $5.1 due from CMS as of September 30, 2020 primarily related to the second reconciliation period of the BPCI-A program. The remaining amount of accounts receivable for both Episodes of Care Services and Home & Community Services represent amounts to be received from customers. As a result of the shift to vIHEs and other customer claims processing system delays, we have experienced collection delays from certain Home & Community Services customers, which has temporarily resulted in a negative impact on operating cash flows during 2020. We continue to actively work with our customers to collect on these amounts. |
| (2) | Contract assets represents management’s estimate of amounts we expect to receive under the BPCI-A program related to the next two reconciliation periods. As of September 30, 2020, contract assets cover episodes of care for the period October 2019 through September 2020. Estimates for program size and savings rate are based on information available as of the date of the financial statements. We record an estimate of revenue related to these performance obligations over the 13-month period starting in the period the related episodes of care commence and through the estimated receipt of the semi-annual CMS reconciliation file. Any changes to these estimates based on new information will be recorded in the period such information is received. Total savings generated and revenue earned for the episodes of care in which the contract asset recorded as of September 30, 2020 relates to, will be included in the semi-annual reconciliations expected from CMS during the fourth quarter 2020 and second quarter of 2021. The increase in contract assets from December 31, 2019 to September 30, 2020 is primarily driven by the increase in estimated savings rate. |
| (3) | Total shared savings payable is included in accounts payable and accrued expenses on the Condensed Consolidated Balance Sheets. Shared savings payable for Episodes of Care Services included $13.3 due to CMS as of December 31, 2019, which represented management’s estimate of total fees that were constrained related to the first reconciliation period of the BPCI-A program. We settled this amount with CMS during the next semi-annual reconciliation period in the second quarter of 2020. Shared savings payable includes $29.3 as of September 30, 2020, which is expected to be paid to customers related to their portion of savings earned under the BPCI-A program. Additionally, there is $3.9 included in shared savings payable at September 30, 2020, which represents amounts withheld from customers under the BPCI-A program based on contractual withholding percentages. This amount has been received by us from CMS and is held as restricted cash. We expect to remit these amounts to customers at the conclusion of the program, at which time both restricted cash and the liability will be reduced. |
| (4) | Contract liabilities represent management’s estimate of savings amounts we expect to share with our customers based on contractual shared savings percentages related to the amounts we expect to be entitled to receive under the BPCI-A program related to the next two reconciliation periods. As of September 30, 2020, contract liabilities cover episodes of care for the period October 2019 through September 2020. These amounts offset the gross amount we expect to receive for the same period included in contract assets as of September 30, 2020. The increase in contract liabilities from December 31, 2019 to September 30, 2020 is primarily driven by the increase in estimated savings rate and therefore increase in amounts we expect to share with our customers. |
| (5) | Deferred revenue is included in other current liabilities on the Condensed Consolidated Balance Sheets and primarily relates to advance payments received from certain customers. |
F-20
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
The table below summarizes the activity recorded in the contract asset and liability accounts for the nine months ended September 30, 2020 and 2019.
| Contract Assets |
||||
| Balance at January 1, 2019 |
$ | — | ||
| Acquired in Remedy Partners Acquisition |
112.9 | |||
| Performance obligation completed, converted to accounts receivable |
(95.5 | ) | ||
| Estimated revenue recognized related to performance obligations satisfied over time |
72.1 | |||
|
|
|
|||
| Balance at September 30, 2019 |
$ | 89.5 | ||
|
|
|
|||
| Balance at January 1, 2020 |
$ | 38.3 | ||
| Performance obligation completed, converted to accounts receivable |
(43.9 | ) | ||
| Estimated revenue recognized related to performance obligations satisfied over time |
115.6 | |||
|
|
|
|||
| Balance at September 30, 2020 |
$ | 110.0 | ||
|
|
|
| Contract Liabilities |
||||
| Balance at January 1, 2019 |
$ | — | ||
| Assumed in Remedy Partners Acquisition |
60.3 | |||
| Performance obligation completed, converted to shared savings payable |
(55.9 | ) | ||
| Estimated amounts due to customer related to performance obligations satisfied over time |
18.2 | |||
|
|
|
|||
| Balance at September 30, 2019 |
$ | 22.6 | ||
|
|
|
|||
| Balance at January 1, 2020 |
$ | 3.1 | ||
| Performance obligation completed, converted to shared savings payable |
(4.6 | ) | ||
| Estimated amounts due to customer related to performance obligations satisfied over time |
36.5 | |||
|
|
|
|||
| Balance at September 30, 2020 |
$ | 35.0 | ||
|
|
|
F-21
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
| Deferred Revenue |
||||
| Balance at January 1, 2019 |
$ | 0.4 | ||
| Acquired in TAV Health acquisition |
1.0 | |||
| Payments received from customers |
2.6 | |||
| Revenue recognized upon completion of performance obligation |
(2.8 | ) | ||
|
|
|
|||
| Balance at September 30, 2019 |
$ | 1.2 | ||
|
|
|
|||
| Balance at January 1, 2020 |
$ | 1.2 | ||
| Payments received from customers |
10.1 | |||
| Revenue recognized upon completion of performance obligation |
(5.2 | ) | ||
|
|
|
|||
| Balance at September 30, 2020 |
$ | 6.1 | ||
|
|
|
| Shared Savings Payable |
||||
| Balance at January 1, 2019 |
$ | — | ||
| Assumed in Remedy Partners Acquisition |
65.5 | |||
| Amounts paid to customer and/or CMS |
(121.3 | ) | ||
| Amounts due to customer upon completion of performance obligation |
70.4 | |||
|
|
|
|||
| Balance at September 30, 2019 |
$ | 14.6 | ||
|
|
|
|||
| Balance at January 1, 2020 |
$ | 58.2 | ||
| Amounts paid to customer and/or CMS |
(94.6 | ) | ||
| Amounts due to customer upon completion of performance obligation |
69.6 | |||
|
|
|
|||
| Balance at September 30, 2020 |
$ | 33.2 | ||
|
|
|
Other Matters
We do not disclose, as amounts are not material or settled within a short period of time, the value of unsatisfied performance obligations for (a) contracts with an original expected length of one year or less; (b) contracts for which we recognize revenue at the amount to which we have the right to invoice for services performed; or (c) contracts for which the variable consideration is allocated entirely to a wholly unsatisfied performance obligation or to a wholly unsatisfied promise to transfer a distinct good or service that forms part of a single performance obligation, and the terms of the variable consideration relate specifically to our efforts to transfer the distinct service or to a specific outcome from transferring the distinct service.
As an accounting policy election, sales tax amounts collected from customers on behalf of government entities are not included in the transaction price with customers and any amounts collected are reported net in our financial statements.
F-22
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
| 7. | Property and Equipment |
As of September 30, 2020 and December 31, 2019, property and equipment, net were as follows:
| September 30, 2020 | December 31, 2019 | |||||||
| Leasehold Improvements |
$ | 17.6 | $ | 11.6 | ||||
| Computer equipment |
16.1 | 10.6 | ||||||
| Furniture and fixtures |
5.7 | 5.3 | ||||||
| Software |
2.5 | 3.4 | ||||||
| Projects in progress |
1.3 | 0.9 | ||||||
|
|
|
|
|
|||||
| Property and equipment, gross |
43.2 | 31.8 | ||||||
| Less: Accumulated depreciation and amortization |
(16.5 | ) | (12.5 | ) | ||||
|
|
|
|
|
|||||
| Property and equipment, net |
$ | 26.7 | $ | 19.3 | ||||
|
|
|
|
|
|||||
Depreciation and amortization expense for property and equipment, inclusive of amounts subsequently written off or disposed from accumulated depreciation, was $5.5 and $4.6 for the nine months ended September 30, 2020 and 2019, respectively. There was no impairment of property and equipment during the nine months ended September 30, 2020 or 2019. During the nine months ended September 30, 2019, we sold approximately $0.3 in property and equipment, included in the gain as discussed in Note 5 Variable Interest Entities.
| 8. | Goodwill |
There was no change in the carrying amount of goodwill for each reporting segment from December 31, 2019 to September 30, 2020. The carrying amount of goodwill for each reporting segment as of September 30, 2020 and December 31, 2019 is as follows:
| Home & Community Services |
Episodes of Care Services |
Total | ||||||||||
| Goodwill |
$ | 170.4 | $ | 408.4 | $ | 578.8 | ||||||
|
|
|
|
|
|
|
|||||||
There was no impairment related to goodwill during any period presented.
| 9. | Intangible Assets |
As of September 30, 2020 and December 31, 2019, intangible assets were as follows:
| September 30, 2020 | December 31, 2019 | |||||||||||||||||||||||||
| Estimated Useful Life (years) |
Gross Carrying Amount |
Accumulated amortization |
Net Carrying Value |
Gross Carrying Amount |
Accumulated amortization |
Net Carrying Value |
||||||||||||||||||||
| Customer relationships |
3 - 20 | $ | 530.5 | $ | (83.9 | ) | $ | 446.6 | $ | 530.5 | $ | (56.7 | ) | $ | 473.8 | |||||||||||
| Acquired and capitalized software |
3 - 6 | 107.1 | (50.1 | ) | 57.0 | 91.6 | (36.9 | ) | 54.7 | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Total |
$ | 637.6 | $ | (134.0 | ) | $ | 503.6 | $ | 622.1 | $ | (93.6 | ) | $ | 528.5 | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
F-23
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
We capitalized $15.7 and $9.7 of internally-developed software costs for the nine months ended September 30, 2020 and 2019, respectively.
Amortization expense for intangible assets, inclusive of amounts subsequently written off from accumulated amortization, was $40.5 and $44.9 for the nine months ended September 30, 2020 and 2019, respectively. Expected amortization expense as of September 30, 2020 related to intangible assets, including internal-use software development costs, was as follows:
| Remainder of 2020 |
$ | 14.1 | ||
| 2021 |
56.4 | |||
| 2022 |
48.6 | |||
| 2023 |
43.1 | |||
| 2024 |
32.5 | |||
| thereafter |
308.9 | |||
|
|
|
|||
| $ | 503.6 | |||
|
|
|
There was no significant impairment of intangible assets for the nine months ended September 30, 2020. We recorded an asset impairment charge of $1.5 related to certain acquired and capitalized software during the nine months ended September 30, 2019 as a result of the discontinued use of the software. This is included in asset impairment on the Condensed Combined-Consolidated Statements of Operations.
| 10. | Accounts Payable and Accrued Expenses |
Accounts payable and accrued expenses consist of the following:
| September 30, 2020 |
December 31, 2019 |
|||||||
| Shared savings payable |
$ | 33.2 | $ | 58.2 | ||||
| Accrued payroll and payroll-related expenses |
34.5 | 33.0 | ||||||
| Other accrued expenses |
23.0 | 12.4 | ||||||
| Accounts payable |
4.9 | 3.5 | ||||||
|
|
|
|
|
|||||
| Total accounts payable and accrued liabilities |
$ | 95.6 | $ | 107.1 | ||||
|
|
|
|
|
|||||
| 11. | Long-Term Debt |
Long-term debt was as follows at September 30, 2020 and December 31, 2019:
| September 30, 2020 |
December 31, 2019 |
|||||||
| Revolving Facility |
$ | 77.0 | $ | — | ||||
| Term Loan |
273.2 | 275.3 | ||||||
|
|
|
|
|
|||||
| Total debt |
350.2 | 275.3 | ||||||
| Unamortized debt issuance costs |
(4.9 | ) | (5.9 | ) | ||||
| Unamortized discount on debt |
(1.7 | ) | (2.0 | ) | ||||
|
|
|
|
|
|||||
| Total debt, net |
343.6 | 267.4 | ||||||
| Less current maturities |
(2.8 | ) | (2.8 | ) | ||||
|
|
|
|
|
|||||
| Total long-term debt |
$ | 340.8 | $ | 264.6 | ||||
|
|
|
|
|
|||||
F-24
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
On December 21, 2017, Signify entered into a Credit Agreement (the “Credit Agreement”) with an unaffiliated secured lender syndicate. Under the Credit Agreement, Signify incurred a term loan of $260.0 (the “Term Loan”) and a revolving credit facility (the “Revolving Facility”) with a $35.0 borrowing capacity, which could also be used to obtain letters of credit up to $5.0. The maturity date of the Term Loan is December 21, 2024 and the maturity date of the Revolving Facility is December 21, 2022. Signify is required to make amortization payments of 0.25% of the aggregate principal amount of the Term Loan, payable on a quarterly basis.
On December 9, 2019, Signify amended its Credit Agreement to increase the borrowing capacity under the Revolving Facility to $80.0.
The Credit Agreement is collateralized by substantially all of the assets of Signify and its subsidiaries. The Term Loan and Revolving Facility both have the option of being drawn at the Base Rate plus 3.50% or the Eurocurrency Rate plus 4.50%, subject to two 0.25% stepdowns in the case of the Revolving Facility based on the applicable Consolidated First Lien Net Leverage Ratio. At September 30, 2020 and December 31, 2019, the effective interest rate on Term Loan borrowings was 5.50% and 6.44%, respectively. At September 30, 2020, the effective interest rate on the Revolving Facility was 4.31%. There were no borrowings outstanding under the Revolving Facility at December 31, 2019.
The Credit Agreement is subject to certain financial and nonfinancial covenants, including a defined Consolidated First Lien Net Leverage Ratio applicable solely to the Revolving Facility. The term loan requires an excess cash flow (“ECF”) payment commencing with and including the period ended December 31, 2018. The prior year’s ECF payment is due within 10 business days after financial statements have been delivered. As our Consolidated First Lien Net Leverage Ratio was below the threshold requiring an ECF payment, there was no ECF payment due in 2019 or 2020. In addition, the Credit Agreement includes negative covenants which restrict Signify and its subsidiaries’ ability, among other things, to incur indebtedness, grant liens, make investments, sell or otherwise dispose of assets or enter into a merger, pay dividends or repurchase stock. As of September 30, 2020, the amount of Signify and its subsidiaries’ net assets restricted from transfer to the Company was zero as a result of the Remedy Partners Combination which allowed for the ability to make certain payments for up to one year following the Remedy Partners Combination in excess of the normal restrictions. This additional capacity on restricted payments will expire on the one-year anniversary of the Remedy Partners Combination, at which time, a significant portion of Signify and its subsidiaries’ net assets may be deemed restricted. Cure TopCo, LLC, the parent, has no stand-alone operations, including no cash or assets; its only activities relate to owning a controlling interest in its subsidiaries and the issuances of equity as described in Note 14 Members’ Equity. Signify did not make any distributions to the parent during the nine months ended September 30, 2020 or 2019. As of September 30, 2020 and December 31, 2019, we were in compliance with all covenants.
On March 12, 2019, we drew $20.0 from the Revolving Facility for the purpose of acquiring Triple Aim Ventures, LLC. On April 23, 2019, the $20.0 was converted to an Incremental Term Loan (as defined in the Credit Agreement) as allowed under the terms of the Credit Agreement. Such Incremental Term Loan is due December 21, 2024. As a result of the Incremental Term Loan, certain lenders were extinguished and replaced with additional term lenders, and we extinguished related deferred financing fees in the amount of $0.2, which is included in interest expense on the Condensed Combined-Consolidated Statements of Operations for the nine months ended September 30, 2019.
On March 18, 2020, we borrowed $77.0 under the Revolving Facility as a precautionary measure to ensure appropriate liquidity as a result of the potential risks associated with COVID-19.
On November 17, 2020, we entered into the fourth amendment to the existing Credit Agreement for $125.0 (the “2020 November Incremental Term Loans”). On December 7, 2020, we entered into the fifth amendment to the existing Credit Agreement for $15.0 (the “2020 December Incremental Term Loans” and together with the 2020 November Incremental Term Loans, the “Incremental Term Loans”). The maturity
F-25
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
date of the Incremental Term Loans is the same as that of the Term Loan, December 21, 2024. The Incremental Term Loans have an interest rate of the Base Rate plus 4.25% for base rate loans or the Eurocurrency Rate plus 5.25% for eurocurrency rate loans. The proceeds of the 2020 November Incremental Term Loans are intended for general corporate use and were used to repay the $77.0 in outstanding borrowings under the Revolving Facility in November 2020 and to fund the acquisition described in Note 22 Subsequent Events. Given that the outstanding borrowings under the Revolving Facility are expected to be refinanced on a long-term basis, the borrowings are classified as long-term as of September 30, 2020. We paid a total of approximately $5.0 in financing fees related to the Incremental Term Loans.
As of September 30, 2020, aggregate principal maturities of long-term debt for each of the next five years ending December 31 and thereafter are as follows:
| Remainder of 2020 |
$ | 0.7 | ||
| 2021 |
2.8 | |||
| 2022 |
2.8 | |||
| 2023 |
2.8 | |||
| 2024 |
341.1 | |||
|
|
|
|||
| $ | 350.2 | |||
|
|
|
| 12. | Fair Value Measurements |
Assets and liabilities measured at fair value on a recurring basis were as follows as of September 30, 2020 and December 31, 2019:
| September 30, 2020 | ||||||||||||||||||
| Balance Sheet Classification |
Type of Instrument | Level 1 | Level 2 | Level 3 | Total | |||||||||||||
| Customer EAR liability |
Customer equity appreciation rights | $ | — | $ | — | $ | 14.4 | $ | 14.4 | |||||||||
| December 31, 2019 | ||||||||||||||||||
| Balance Sheet Classification |
Type of Instrument | Level 1 | Level 2 | Level 3 | Total | |||||||||||||
| Cash equivalents |
Money market funds | $ | 11.1 | $ | — | $ | — | $ | 11.1 | |||||||||
| Contingent consideration |
Consideration due to sellers | $ | — | $ | — | $ | 39.8 | $ | 39.8 | |||||||||
There were no transfers between Level 1 and Level 2, or into or out of Level 3 during the nine months ended September 30, 2020 or 2019.
The changes in Level 3 liabilities measured at fair value on a recurring basis for the nine months ended September 30, 2020 and 2019 were as follows:
Contingent Consideration
| Balance at January 1, 2019 |
$ | 39.1 | ||
| Remeasurement of contingent consideration included in selling, general and administrative expense |
0.7 | |||
|
|
|
|||
| Balance at September 30, 2019 |
$ | 39.8 | ||
|
|
|
|||
| Balance at January 1, 2020 |
$ | 39.8 | ||
| Remeasurement of contingent consideration included in selling, general and administrative expense |
0.2 | |||
| Payment of contingent consideration |
(40.0 | ) | ||
|
|
|
|||
| Balance at September 30, 2020 |
$ | — |
F-26
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
Customer equity appreciation rights
| Balance at January 1, 2020 |
$ | — | ||
| Grant date fair value estimate recorded as reduction to revenue |
7.5 | |||
| Remeasurement of fair value included in other expense |
6.9 | |||
|
|
|
|||
| Balance at September 30, 2020 |
$ | 14.4 |
The valuation techniques and significant unobservable inputs used in recurring Level 3 fair value measurements were as follows as of September 30, 2020:
| Fair Value | Valuation Technique |
Significant Unobservable Inputs |
Assumption | |||||||
| Customer equity appreciation rights |
$ | 14.4 | Volatility | 40% -55% | ||||||
| Monte Carlo |
Dividend yield |
0% | ||||||||
| Risk-free rate |
0.13% - 1.67% | |||||||||
| Expected term (years) |
1.5 - 3.0 | |||||||||
| Fair Value | Valuation Technique |
Significant Unobservable |
Discount Rate | |||||||
| Consideration due to sellers |
$ | 39.8 | Discounted approach | Discount Rate | 2.3% | |||||
The fair value of the underlying equity related to the customer equity appreciation rights is estimated in a similar manner, subject to the same management assumptions, as described for equity-based compensation awards. See Note 14 Members’ Equity.
The fair value of our debt is measured at Level 3 and is determined based on fluctuations in current interest rates, the trends in market yields of debt instruments with similar credit ratings, general economic conditions and other quantitative and qualitative factors. The carrying value of our debt approximates its fair value.
The carrying amounts of accounts receivable and accounts payable approximate their fair value because of the relatively short-term maturity of these instruments.
| 13. | Employee Benefit Arrangements |
We provide two 401(k) retirement savings plans to eligible employees whereby each match 50% of every dollar contributed up to 6% of an employee’s eligible compensation and, under certain plans, may also make profit sharing contributions at our discretion. For the nine months ended September 30, 2020, we incurred total contribution expense of $2.7, of which $1.3 is included in service expense and $1.4 is included in SG&A expense on the Condensed Combined-Consolidated Statements of Operations. For the nine months ended September 30, 2019, we incurred total contribution expense of $2.6, of which $1.2 is included in service expense and $1.4 is included in SG&A expense on the Condensed Combined-Consolidated Statements of Operations.
F-27
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
| 14. | Member’s Equity |
Membership Units
In connection with the Remedy Partners Combination, our limited liability agreement (“LLC Agreement”) was amended and restated to authorize five classes of equity membership interests in us that are represented by Units: Series A Preferred Units, Series B Preferred Units, Class A Common Units, Class B Common Units, and Class C Common Units. In connection with the consummation of the Remedy Partners Combination, each outstanding Class A Common Unit that was outstanding prior to the Remedy Partners Combination was converted into a Series B Preferred Unit on a one-for-one basis and each Class B Common Unit remained outstanding. Also, in connection with the Remedy Partners Combination, 3,384,543 Series A Preferred Units were issued to New Remedy Corp in exchange for the contribution of $698.3 in net assets and tax attributes to us.
We had 3,384,543 units of Series A Preferred Units and 3,402,608 units of Series B Preferred Units outstanding as of September 30, 2020. We had zero Class A Common Units, 108,977 Class B Common Units and 83,244 Class C Common Units outstanding as of September 30, 2020.
The Series A Preferred Units have voting rights, being entitled to one vote per Series A Preferred Unit and have rights with respect to our profits and losses and distributions from us as set forth in our LLC Agreement. In the context of a liquidation or similar event, the Series A Preferred Units have a preference over other classes of Units, including, in certain circumstances, over the Series B Preferred Units. The preference with respect to the Series A Preferred Units is subject to forfeiture in certain scenarios based on the financial performance of Remedy Partners’ business and also in connection with an initial public offering of us or our successor entity. We did not make any tax or non-tax distributions on behalf of members holding Series A Preferred Units for the nine months ended September 30, 2020.
The Series B Preferred Units have voting rights, being entitled to one vote per Series B Preferred Unit, and have rights with respect to our profits and losses and distributions from us as set forth in our LLC Agreement. In the context of a liquidation or similar event, the Series B Preferred Units have a preference over other classes of Units, including, in certain circumstances, over the Series A Preferred Units. The preference with respect to the Series B Preferred Units is subject to forfeiture in certain scenarios based on the financial performance of Signify’s business and also in connection with an initial public offering of us or our successor entity. We made tax distributions of $7.2 and $21.8 on behalf of members holding Series B Preferred Units (formerly Class A Common Units) for the nine months ended September 30, 2020 and 2019, respectively. We did not make any non-tax distributions on behalf of members holding Series B Preferred Units for the nine months ended September 30, 2020 or 2019.
The Class A Common Units have voting rights, being entitled to one vote per Class A Common Unit, and have rights with respect to our profits and losses and distributions as set forth in our LLC Agreement. As of September 30, 2020 and December 31, 2019, there were no Class A Common Units issued or outstanding.
The Class B Common Units have no voting rights and are intended to be treated as profits interests for federal income tax purposes. Class B Common Units are issued from time to time to be held by Cure Aggregator, LLC, a member of our company (“Cure Aggregator”), on behalf of our employees and other service providers in connection with their respective performance of services for our benefit as designated by our Board of Directors or Compensation Committee. All Class B Common Units are issued pursuant to an award agreement that sets forth a distribution threshold in an amount intended for such Class B Common Units to qualify as profits interests for federal income tax purposes and vesting terms determined by our Board of Directors or Compensation Committee. The distribution thresholds and vesting terms of the Class B Common Units described above were not modified in connection with the Remedy Partners
F-28
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
Combination. We made tax distributions in the amount of $0.7 and $0.7 on behalf of members holding Class B Common Units during the nine months ended September 30, 2020 and 2019, respectively.
The Class C Common Units have no voting rights and are intended to be treated as profits interests for federal income tax purposes. Class C Common Units are issued from time to time to be held by Cure Aggregator, on behalf of our employees and other service providers in connection with their respective performance of services for our benefit as designated by our Board of Directors or Compensation Committee. All Class C Common Units are issued pursuant to an award agreement that sets forth a distribution threshold in an amount intended for such Class C Common Units to qualify as profits interests for federal income tax purposes and vesting terms determined by our Board of Directors or Compensation Committee. As of September 30, 2020, 83,244 Class C Common Units had been granted. As of December 31, 2019, no Class C Common Units had been granted by our Board of Directors or Compensation Committee. We made tax distributions of $0.2 on behalf of members holding Class C Common Units during the nine months ended September 30, 2020.
During the nine months ended September 30, 2019, we repurchased 18,762 Former Class A Common Units for $2.4, related to the termination of two former executives. These repurchases were made at amounts that exceeded the estimated fair market value as of the repurchase date by approximately $0.4. This excess over fair market value is included in transaction-related expenses in the Condensed Combined-Consolidated Statements of Operations during the nine months ended September 30, 2019.
As described in Note 4 Business Combinations, in March 2019, we issued 130,525 former Class A Common Units, which were subsequently converted to Series B preferred units as part of the purchase consideration to acquire TAV Health. In September 2020, we entered into an agreement to repurchase the 130,525 Series B preferred units for a total of $54.0, which is included in Due to Shareholders on the Condensed Consolidated Balance Sheet as of September 30, 2020. This repurchase was made on October 1, 2020 at amounts that approximated the estimated current fair market value as of the repurchase date.
Incentive Unit Awards and Equity-Based Compensation
In accordance with the LLC Agreement, our Board of Directors may grant awards of Class B Common Units and Class C Common Units for the benefit of key employees and service providers. The Board and/or Compensation Committee has approved equity-based awards with time-based and performance-based vesting criteria.
Awards of Class B Common Units and Class C Common Units are intended to be profits interest units for federal income tax purposes as described above. Awards with time-based vesting generally vest over time either on the grant date anniversary or on December 31 of each year. For those awards with performance-based vesting, the performance condition stipulates that in order for awards to vest, the total cash on cash return of the private equity owners as defined in the award agreement must exceed certain multiples set forth in the award agreement. The performance-based vesting condition is not probable as assessed at each reporting period; therefore, compensation expense related to these awards (or portions thereof) has not been recognized. Since December 31, 2019, no additional Class B Common Units have been granted and only Class C Common Units have been granted by our Board of Directors or Compensation Committee.
Grant date fair value of awards of Class B Common Units and Class C Common Units are estimated based on a Monte Carlo option pricing simulation. The equity value of the enterprise represents a key input for determining the fair value of the Class B Common Units and Class C Common Units. A discount for lack of marketability was applied to the per unit fair value to reflect increased risk arising from the inability to readily sell the Class B Common Units and Class C Common Units. The estimated fair values for awards
F-29
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
granted during the nine months ended September 30, 2020 and 2019 included the following weighted average assumptions (annualized percentages):
| September 30, 2020 | September 30, 2019 | |||
| Expected volatility |
41.50% | 41.1% - 51.1% | ||
| Expected dividend yield |
- | - | ||
| Risk-free interest rate |
1.3% | 1.9% | ||
| Expected life (years) |
2.9 | 3.6 |
Since we are privately held, we calculate expected volatility using comparable peer companies with publicly traded shares over a term similar to the expected term of the underlying award. At the time of grant, we had no intention to pay dividends on our common units, and therefore, the dividend yield percentage is zero. The risk-free interest rate is based on the U.S. Treasury constant maturity interest rate whose term is consistent with the expected life of the profits interests.
In order to estimate the equity value of the enterprise to determine the fair value of our common units, we used a combination of the market approach and the income approach. For the market approach, we utilized the guideline company method by selecting certain companies that we considered to be the most comparable to us in terms of size, growth, profitability, risk and return on investment, among others. We then used these guideline companies to develop relevant market multiples and ratios. The market multiples and ratios were applied to our financial projections based on assumptions at the time of the valuation in order to estimate our total enterprise value. Since there is not an active market for our common units, a discount for lack of marketability was then applied to the resulting value.
For the income approach, we performed discounted cash flow analyses utilizing projected cash flows, which were discounted to the present value in order to arrive at an enterprise value. The key assumptions used in the income approach include management’s financial projections which are based on highly subjective assumptions as of the date of valuation, a discount rate and a long-term growth rate.
The following table summarizes our Class B Common Unit activity for the nine months ended September 30, 2020 and 2019:
| 2020 | 2019 | |||||||||||||||
| Profits Interest Units |
Weighted Avg. Grant Date FMV |
Profits Interest Units |
Weighted Avg. Grant Date FMV |
|||||||||||||
| Outstanding at January 1 |
481,539 | $ | 52.28 | 453,250 | $ | 48.21 | ||||||||||
| Granted |
— | $ | — | 48,824 | $ | 68.15 | ||||||||||
| Forfeited |
(83,418 | ) | $ | 53.38 | (39,518 | ) | $ | 49.62 | ||||||||
| Cancelled |
— | $ | — | (50 | ) | $ | 49.66 | |||||||||
| Repurchased |
(350 | ) | $ | 73.08 | (6,300 | ) | $ | 43.15 | ||||||||
|
|
|
|
|
|||||||||||||
| Outstanding at September 30 |
397,771 | $ | 52.03 | 456,206 | $ | 50.29 | ||||||||||
During the nine months ended September 30, 2020 and 2019, we recognized $1.4 and $2.0, respectively, of equity-based compensation expense related to awards of Class B Common Units. Of this amount, $0.1 and $0.3 were included in service expense and $1.3 and $1.7 were included in SG&A expense on the Condensed Combined-Consolidated Statements of Operations for the nine months ended September 30, 2020 and 2019, respectively. As of September 30, 2020, there was $3.3 of total unrecognized compensation expense related to unvested equity-based compensation arrangements expected to be recognized over a weighted average period of 0.9 years. Additionally, there was approximately $11.5 of unrecognized compensation expense
F-30
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
related to equity-based awards with performance-based vesting, in which the vesting conditions are not probable of occurring as of September 30, 2020. The grant date fair value of units that vested during the nine months ended September 30, 2020 and 2019 were $0.8 and $0.7, respectively.
The following table summarizes our Class C Common Unit activity for the nine months ended September 30, 2020:
| Profits Interest Units |
Weighted Avg. Grant Date FMV |
|||||||
| Outstanding at January 1, 2020 |
— | $ | — | |||||
| Granted |
341,461 | $ | 73.56 | |||||
|
|
|
|||||||
| Outstanding at September 30, 2020 |
341,461 | $ | 73.56 | |||||
During the nine months ended September 30, 2020, we recognized $7.3 of equity-based compensation expense, included in SG&A expense on the Condensed Combined-Consolidated Statements of Operations, related to awards of Class C Common Units. As of September 30, 2020, there was $12.4 of total unrecognized compensation expense related to unvested equity-based compensation arrangements over a weighted average period of 1.36 years. Additionally, there was approximately $3.6 of unrecognized compensation expense related to equity-based awards with performance-based vesting, in which the vesting conditions are not probable of occurring as of September 30, 2020. The grant date fair value of units that vested during the nine months ended September 30, 2020 were $6.0.
Stock Options in New Remedy Corp
Remedy Partners maintained an equity incentive plan whereby certain employees and directors were granted stock options. In November 2019, at the time of the Remedy Partners Combination, outstanding Remedy Partners stock options were converted to stock options in New Remedy Corp. No additional stock option grants will be made following the Remedy Partners Combination. During the nine months ended September 30, 2020 and 2019, we recorded approximately $1.3 and $1.0, respectively, in share-based compensation expense included in SG&A expense on the Condensed Combined-Consolidated Statements of Operations related to outstanding stock options held by certain of our employees. As of September 30, 2020, there was approximately $4.3 of total unrecognized compensation expense related to unvested time-based stock options expected to be recognized over a weighted average period of 1.4 years. Additionally, there was approximately $2.6 of unrecognized compensation expense related to outstanding stock options with performance-based vesting, in which the vesting conditions are not probable of occurring as of September 30, 2020. As the underlying stock is in New Remedy Corp., the offset to the equity-based compensation expense is included in capital contributions on the Condensed Combined-Consolidated Statements of Changes in Members’ Equity.
| 15. | Loss Per Unit |
For the nine months ended September 30, 2019, basic loss per unit is computed by dividing the net loss by the weighted average number of Class A and Class B Common Units outstanding during the period. There were no potentially dilutive securities for the nine months ended September 30, 2019 and therefore, the basic and diluted loss per unit have been presented together. Common units consisted of former Class A Common Units and Class B Common Units.
For the nine months ended September 30, 2020, net loss per unit is computed using the “two-class” method. Five classes of member units became legally authorized as of the Remedy Partners Combination on
F-31
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
November 26, 2019. Therefore, net losses for the nine months ended September 30, 2020 are attributable to the Series A Preferred Units, the Series B Preferred Units and the Class B Common Units, and the Class C Common Units. There were no potentially dilutive securities for the nine months ended September 30, 2020 and therefore, the basic and diluted loss per unit have been presented together.
Loss per unit for the nine months ended September 30, 2019 is computed as follows:
| Net loss attributable to unitholders: |
||||
| Class A Common Units and Class B Common Units |
$ | (20.5 | ) | |
| Weighted average outstanding units: |
||||
| Class A Common Units and Class B Common Units |
3,564,661 | |||
| Basic and Diluted net loss per unit attributable to unitholders: |
||||
| Class A Common Units and Class B Common Units |
$ | (5.75 | ) |
Loss per unit for the nine months ended September 30, 2020 is computed as follows:
| Net loss attributable to unitholders: |
||||
| Series A Preferred Units |
$ | (7.3 | ) | |
| Series B Preferred Units and Class B Common Units |
(7.8 | ) | ||
| Class C Common Units |
(0.1 | ) | ||
| Weighted average outstanding units: |
||||
| Series A Preferred Units |
3,384,543 | |||
| Series B Preferred Units and Class B Common Units |
3,634,323 | |||
| Class C Common Units |
58,968 | |||
| Basic and Diluted net loss per unit attributable to unitholders: |
||||
| Series A Preferred Units |
$ | (2.15 | ) | |
| Series B Preferred Units and Class B Common Units |
(2.15 | ) | ||
| Class C Common Units |
(2.15 | ) |
| 16. | Transaction-related Expenses |
For the nine months ended September 30, 2020, we incurred $10.8 of transaction-related expenses related to the integration of Remedy Partners. These transaction-related expenses related to consulting, compensation and integration-type expenses. Additionally, approximately $0.9 of costs incurred in connection with our initial public offering are included in transaction-related expenses.
For the nine months ended September 30, 2019, we incurred $15.9 of transaction-related expenses related to the acquisition of Remedy Partners, the Remedy Partners Combination, the TAV Health acquisition as well as certain acquisitions made in prior years. These transaction-related expenses related to consulting, compensation and integration-type expenses.
F-32
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
Included within the compensation expense amounts described above for both nine months ended September 30, 2020 and 2019 is severance related to an approved plan by our Board of Directors. The following table summarizes the approved severance activity for the nine months ended September 30, 2020 and 2019.
| Balance at January 1, 2019 |
$ | 1.7 | ||
| Severance and related costs |
1.6 | |||
| Cash payments |
(1.8 | ) | ||
|
|
|
|||
| Balance at September 30, 2019 |
$ | 1.5 | ||
|
|
|
|||
| Balance at January 1, 2020 |
$ | 1.2 | ||
| Severance and related costs |
— | |||
| Cash payments |
(1.2 | ) | ||
|
|
|
|||
| Balance at September 30, 2020 |
$ | — | ||
|
|
|
As of September 30, 2020, there are no remaining amounts expected to be paid under approved severance plans.
| 17. | Commitments and Contingencies |
Lease Commitments
During the second quarter of 2020, we ceased using our former New York City office space and in the third quarter began subleasing the space. We have entered into non-cancelable lease agreements for new space in New York City that ultimately expire in 2029. Total lease commitments over the term of the lease are approximately $25.7.
We are obligated as lessee under certain non-cancellable operating leases. As of September 30, 2020, future minimum lease payments under non-cancellable operating leases were as follows:
| Remainder of 2020 |
$ | 1.9 | ||
| 2021 |
10.0 | |||
| 2022 |
9.2 | |||
| 2023 |
7.5 | |||
| 2024 |
5.5 | |||
| Thereafter |
36.8 | |||
|
|
|
|||
| $ | 70.9 | |||
|
|
|
Total rent expense associated with non-cancellable operating leases was $6.4 and $4.6 for the nine months ended September 30, 2020 and 2019, respectively, and was included within SG&A expenses on the Condensed Combined-Consolidated Statements of Operations.
Letters of Credit
As of September 30, 2020, we have outstanding letters of credit totaling $9.2 in favor of CMS which is required in the event of a negative outcome on certain episodes of care within the BPCI-A program and we do not settle the related amounts owed to CMS. However, the terms of BPCI-A also require that certain partners provide a related reciprocal letter of credit to us for the majority of this amount. As of September 30, 2020, we have three related letters of credit in our favor totaling $8.8.
F-33
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
Contingencies
Liabilities for loss contingencies arising from claims, assessments, litigation, fines, penalties and other sources are recorded when it is probable a liability has been incurred and the amount of the liability can be reasonably estimated. We are involved in various lawsuits, claims and administrative proceedings arising in the normal course of business. In management’s opinion, the ultimate resolution of these matters will not materially adversely affect our financial position, results of operations or cash flows.
On March 12, 2019, a Complaint was filed against us by Dr. Mohammad A. Gharavi, in the Superior Court, State of California, San Bernardino County. The claim was a wage and hour class action of all California contracted physicians from March 12, 2015 through the present and ongoing. The Complaint alleges that these physicians should have been classified as employees. The class action was settled for $1.2 at mediation in January 2020. This amount is included in other current liabilities on the Condensed Consolidated Balance Sheet at September 30, 2020. We expect to make payment during the fourth quarter of 2020 as the Court has recently approved the settlement.
Sales Tax Reserve
During the year ended December 31, 2019, it was determined that certain Episodes of Care Services may be subject to sales tax in certain jurisdictions. Historically, we have not collected sales tax from our Episodes of Care Services customers as we believed the services were not taxable. As of September 30, 2020 and December 31, 2019, we have a liability of $7.6 and $6.5, respectively, for potential sales tax exposure related to services performed in 2016 through the second quarter of 2020, included in other current liabilities on the Condensed Consolidated Balance Sheets. We expect to start collecting sales tax from customers in 2021 for 2020 services.
Equity Appreciation Rights
In December 2019, we entered into an equity appreciation fee right agreement (“EAR”) with a customer, which contains the following provisions: 1) commits the customer to purchase a minimum amount of services from one of our wholly-owned indirect operating subsidiaries for three years in accordance with specific terms and conditions and 2) granted the customer a contingent EAR. The EAR agreement allows for the customer to participate in the future growth in the fair market value of our equity and can only be settled in cash (or, under certain circumstances, in whole or in part with a replacement agreement that mimics the economics of the original EAR agreement) upon a change in control, other liquidity event, or upon approval of our Board of Directors with consent by New Mountain Capital with certain terms and conditions. The EAR will expire in 20 years from the date of grant, if not previously settled. As of December 31, 2019, the EAR was accounted for as a contingent contract liability instrument. We did not recognize an expense associated with the EAR for the year ended December 31, 2019 as cash settlement was not considered probable, due to the changes in control and liquidity provisions of the EAR. We adopted new accounting guidance in early 2020, which resulted in the initial fair value of the EAR being recorded as a reduction of revenue as this is consideration payable to a customer, and subsequent changes in fair value being recorded as other income (expense), net. Although the initial EAR agreement was executed in December 2019, the service period did not begin until 2020 and, therefore, there was no impact on our results of operations until 2020. The grant date fair value of this EAR was estimated to be $15.2 and is being recorded as a reduction of revenue through December 31, 2022, coinciding with the three year performance period.
Effective September 2020, we entered into a second EAR agreement with the same customer, containing similar provisions to the EAR agreement entered into in December 2019. We concurrently entered into an
F-34
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
amended customer contract which includes incremental evaluations volume from the customer beginning in 2020. The grant date fair value of this EAR was estimated to be $36.6 and is being recorded as a reduction of revenue through December 31, 2022, coinciding with the 2.5 year performance period.
As of September 30, 2020, there was approximately $44.3 of original grant date fair value unrecognized, which we expect to record as a reduction of revenue over the next 2.25 years. We remeasure the fair value of the outstanding EAR agreements at the end of each quarter and record any changes in fair value to other expense. See Note 12 Fair Value Measurements for changes in estimated fair value and valuation techniques used to estimate.
Synthetic Equity Plan
On February 14, 2020, the Board of Directors adopted a Synthetic Equity Plan (“SEP”) that provides for cash payments upon the satisfaction of certain criteria. The synthetic equity units granted under the SEP are subject to time and performance vesting and are paid out upon a change in control (as defined in the SEP) based upon the difference in the value of the Company at the time of the change in control event and a “floor amount”. During the nine months ended September 30, 2020, 14,536 synthetic equity units were granted. Since the vesting criteria are not probable of occurring as of September 30, 2020, we have not recognized any compensation expense related to these awards.
Contingent Consideration
On December 21, 2017, we acquired 100% of the outstanding equity of Censeo. The purchase price included contingent consideration with an initial fair value of $38.2, which required us to pay up to an additional $40.0 to selling shareholders of Censeo, pending the resolution of an examination by the IRS regarding the classification of certain independent contractors. If the IRS determined Censeo must employ any portion of its independent contractors prospectively, the incremental costs of such employment, multiplied by a factor of eight, would be deducted from the $40.0 to determine the remaining amount due to the selling shareholders under the acquisition agreement.
On February 11, 2019, we received a proposed assessment of employment taxes from the IRS in the amount of $5.5 related to tax year 2014. The assessment was based on the IRS’s position that all of Censeo’s service providers who performed health assessments during 2014 should have been classified as employees instead of independent contractors. We appealed this determination. There was no change to the fair value of the contingent liability due to this proposed assessment.
We had up to 12 months to make payment following a final determination, which had not yet been received as of December 31, 2019; therefore the estimated liability of $39.8 was included in non-current liabilities on the Condensed Consolidated Balance Sheet as of December 31, 2019. In May 2020, we received the final IRS determination letter closing the open matter related to the contingent consideration and as a result of the determination, the contingent consideration was payable in full. We made payment of the full $40.0 on July 31, 2020 to the selling shareholders, some of whom are also affiliated with us and/or are our equity holders.
| 18. | Income Taxes |
Income tax expense for the nine months ended September 30, 2020 and 2019, was $0.5 and $0.1, respectively, and consists of current state and local taxes. We have no deferred tax assets or liabilities as of September 30, 2020 or December 31, 2019.
F-35
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
Uncertain Tax Provisions
We recognize the impact of uncertain tax positions taken or expected to be taken on an income tax return in the financial statements at the amount that is more likely than not to be sustained upon audit by the relevant taxing authority. An uncertain tax position will not be recognized unless it is more likely than not to be sustained. We have evaluated our tax positions and have not identified any material uncertain tax positions that would not be sustained in federal or state income tax examination or that require disclosure. Accordingly, no provision for uncertainties in income taxes has been made in the accompanying Condensed Combined-Consolidated Financial Statements at September 30, 2020.
| 19. | Segment Reporting |
Operating segments are components of an enterprise for which separate financial information is available and evaluated regularly by our Chief Operating Decision Maker in deciding how to allocate resources and in assessing financial performance. Management views our operating performance in two reportable segments: Home & Community Services and Episodes of Care Services.
We evaluate the performance of each segment based on segment revenue and adjusted EBITDA. The operating results of the reportable segment are based on segment adjusted EBITDA, which includes revenue and expenses incurred by the segment, as well as an allocation of shared expenses. Shared expenses are generally allocated to each segment based on the segments’ proportionate employee headcount. Certain costs are not allocated to the segments, as described below, as these items are not considered in evaluating the segment’s overall performance.
See Note 6 Revenue Recognition for a summary of segment revenue by product type for the nine months ended September 30, 2020 and 2019. Our operating segment results for the periods presented were as follows:
| Nine months ended September 30, |
||||||||
| 2020 | 2019 | |||||||
| Revenue |
||||||||
| Home & Community Services |
$ | 301.8 | $ | 287.0 | ||||
| Episodes of Care Services |
115.3 | 81.5 | ||||||
| Segment Adjusted EBITDA |
||||||||
| Home & Community Services |
65.8 | 73.9 | ||||||
| Episodes of Care Services |
20.2 | (7.2 | ) | |||||
| Less: reconciling items to net loss: |
||||||||
| Unallocated costs (1) |
38.5 | 21.5 | ||||||
| Depreciation and amortization |
46.0 | 49.5 | ||||||
| Interest expense |
16.2 | 16.1 | ||||||
|
|
|
|
|
|||||
| Loss before income taxes |
$ | (14.7 | ) | $ | (20.4 | ) | ||
|
|
|
|
|
|||||
| (1) Unallocated costs as follows: |
||||||||
| Asset impairment |
— | 1.5 | ||||||
| Other income, net |
6.9 | (1.4 | ) | |||||
| Equity-based compensation |
10.0 | 3.0 | ||||||
| Customer equity appreciation rights |
7.5 | — | ||||||
| Transaction-related expenses |
10.8 | 15.9 | ||||||
| Non-allocated costs (2) |
3.3 | 2.5 | ||||||
|
|
|
|
|
|||||
| Total unallocated costs |
$ | 38.5 | $ | 21.5 | ||||
|
|
|
|
|
|||||
F-36
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
| (2) | Non-allocated costs included remeasurement of contingent consideration, management fees paid to our capital partner and certain non-recurring expenses, including those associated with the closure of certain facilities, the sale of certain assets, one-time expenses related to the COVID-19 pandemic and the early termination of certain contracts. These costs are not considered by our Chief Operating Decision Maker in making resource allocation decisions. |
Our Chief Operating Decision Maker does not receive or utilize asset information to evaluate performance of operating segments. Accordingly, asset-related information has not been presented.
| 20. | Concentrations |
During the normal course of operations, we maintain cash in bank accounts which exceed federally insured amounts. We have not experienced any losses in such accounts and do not believe we are exposed to any significant credit risk related to cash.
Accounts receivable potentially subject us to concentrations of credit risk. Management believes that its contract acceptance, billing and collection policies are adequate to minimize potential credit risk. We continuously evaluate the credit worthiness of our customers’ financial condition and generally do not require collateral.
We are dependent on a concentrated number of payors and provider partners with whom we contract to provide IHEs and other services. A significant portion of our revenues are generated from a small number of customers. For the nine months ended September 30, 2020, we had three customers which accounted for approximately 26%, 16% and 12%, respectively, of revenues. In addition, the revenue from our top ten customers accounted for approximately 72% of our total revenue for the nine months ended September 30, 2020. For the nine months ended September 30, 2019, we had two customers which accounted for approximately 24% and 23%, respectively, of revenues.
As of September 30, 2020, we had two customers which accounted for 31% and 14%, respectively, of accounts receivable. No customer accounted for greater than 10% of accounts receivable as of December 31, 2019.
While CMS is not our customer, a majority of the revenue generated by Episodes of Care Services is under the CMS administered BPCI-A program and payments are received under this program in certain cases from CMS rather than directly from the customer. During the nine months ended September 30, 2020, approximately 25% of total consolidated revenue was generated from the BPCI-A program.
| 21. | Related Party Transactions |
We were subject to a Management Services Agreement whereby we paid our capital partners an annual advisory fee of $1.0. As 100% of Signify’s income is derived from our operations, these amounts are expensed as incurred by us. During the nine months ended September 30, 2019, $0.8 of expense was recorded and included in SG&A expenses in the Condensed Combined-Consolidated Statements of Operations related to these services. The Management Services Agreement was terminated in connection with the consummation of the Remedy Partners Combination.
On April 17, 2019, we issued a note receivable to our Chief Executive Officer for $2.0 with simple interest accruing at a rate of 2.52% per annum and included in other expense (income), net on the Condensed Combined-Consolidated Statements of Operations. In December 2019, the outstanding principal and an insignificant amount of accrued interest under the note was repaid in full. There are no other outstanding amounts.
On March 7, 2019, we entered into a consulting agreement with Bret Carlson, a director, which currently provides for $0.2 annually (payable monthly) in compensation for consulting services provided to us. In the
F-37
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Condensed Combined-Consolidated Financial Statements
(Unaudited, in millions, except units and per unit amounts)
event that we complete a corporate transaction in which we acquire a company referred and introduced to us by Mr. Carlson, Mr. Carlson will be eligible to receive a cash transaction fee of 3% of any deal consideration up to $10 million, plus an additional 1.5% on any incremental deal consideration above $10 million.
On November 23, 2020, we entered into a letter agreement with Kevin McNamara, a director, which currently provides for payment of $0.2 annually (payable in accordance with the Company’s payroll practices) in compensation for service as a member of our board of directors and for consulting services provided to us. In addition, Mr. McNamara is entitled to reimbursement for annual premiums on life, accidental death and dismemberment, short-term disability and medical insurance.
| 22. | Subsequent Events |
For our Condensed Combined-Consolidated Financial Statements as of September 30, 2020, we performed an evaluation of subsequent events through December 7, 2020, the date the Condensed Combined-Consolidated Financial Statements were originally issued and through the re-issuance date of December 30, 2020, for events requiring recording or disclosure in the Condensed Combined-Consolidated Financial Statements for the interim period ended September 30, 2020.
On November 18, 2020, we completed an acquisition of PatientBlox, Inc., a technology company with expertise in applying distributed ledger technology in healthcare. The acquisition accelerates our prospective provider payment capabilities for episodes of care, supporting our commitment to advance value-based care through novel payment and risk arrangements. We paid cash consideration of $15.0, subject to certain adjustments, upon closing. Up to an additional $15.0 of cash consideration may be paid in the third quarter of 2021 and $5.0 of cash consideration may be paid in the third quarter of 2022, in each case contingent upon the completion of certain milestones. We are currently assessing the accounting impact of the transaction.
F-38
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Unitholders and the Board of Directors of Cure TopCo, LLC
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of Cure TopCo, LLC and its subsidiaries (the “Company”) as of December 31, 2019 and 2018, the related combined-consolidated statements of operations, changes in members’ equity, and cash flows, for each of the two years in the period ended December 31, 2019, and the related notes and Schedule II - Valuation and Qualifying Accounts (collectively referred to as the “financial statements”) (see Note 1). In our opinion, the financial statements present fairly, in all material respects, the financial position of the Company as of December 31, 2019 and 2018, and the results of its operations and its cash flows for each of the two years in the period ended December 31, 2019, in conformity with accounting principles generally accepted in the United States of America.
Basis for Opinion
These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB and in accordance with auditing standards generally accepted in the United States of America. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audits, we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion.
Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
/s/ Deloitte & Touche LLP
Stamford, Connecticut
October 19, 2020
We have served as the Company’s auditor since 2019.
F-39
Table of Contents
Cure TopCo, LLC and Subsidiaries
Consolidated Balance Sheets (In millions, except units)
| December 31, | ||||||||
| 2019 | 2018 | |||||||
| ASSETS |
||||||||
| Current assets |
||||||||
| Cash and cash equivalents |
$ | 27.7 | $ | 20.4 | ||||
| Accounts receivable, net |
168.1 | 40.9 | ||||||
| Contract assets |
38.3 | — | ||||||
| Restricted cash |
22.5 | — | ||||||
| Prepaid expenses and other current assets |
6.9 | 3.3 | ||||||
|
|
|
|
|
|||||
| Total current assets |
263.5 | 64.6 | ||||||
| Property and equipment, net |
19.3 | 7.0 | ||||||
| Goodwill |
578.8 | 122.5 | ||||||
| Intangible assets, net |
528.5 | 406.0 | ||||||
| Other assets |
2.3 | 1.6 | ||||||
|
|
|
|
|
|||||
| Total assets |
$ | 1,392.4 | $ | 601.7 | ||||
|
|
|
|
|
|||||
| LIABILITIES AND MEMBERS’ EQUITY |
||||||||
| Current liabilities |
||||||||
| Accounts payable and accrued expenses |
$ | 107.1 | $ | 26.7 | ||||
| Contract liabilities |
3.1 | — | ||||||
| Current maturities of long-term debt |
2.8 | 2.6 | ||||||
| Other current liabilities |
9.6 | 1.4 | ||||||
|
|
|
|
|
|||||
| Total current liabilities |
122.6 | 30.7 | ||||||
| Long-term debt |
264.6 | 246.9 | ||||||
| Contingent consideration |
39.8 | 39.1 | ||||||
| Other noncurrent liabilities |
7.8 | 1.0 | ||||||
|
|
|
|
|
|||||
| Total liabilities |
434.8 | 317.7 | ||||||
| Commitments and Contingencies (Note 17) |
||||||||
| Members’ equity—Series A Preferred (3,384,543 and 0 issued and outstanding at December 31, 2019 and 2018, respectively) |
695.4 | — | ||||||
| Members’ equity—Series B Preferred (3,533,133 and 0 issued and outstanding at December 31, 2019 and 2018, respectively) |
325.5 | |||||||
| Members’ equity—Class A common ( 0 and 3,391,370 issued and outstanding at December 31, 2019 and 2018, respectively) |
— | 320.2 | ||||||
| Members’ equity—Class B common (93,311 and 52,240 issued and outstanding at December 31, 2019 and 2018, respectively) |
4.2 | 2.6 | ||||||
| Members’ equity—Class C common (0 issued and outstanding at December 31, 2019 and 2018) |
— | — | ||||||
| Accumulated deficit |
(67.5 | ) | (38.8 | ) | ||||
|
|
|
|
|
|||||
| Total members’ equity |
957.6 | 284.0 | ||||||
|
|
|
|
|
|||||
| Total liabilities and members’ equity |
$ | 1,392.4 | $ | 601.7 | ||||
|
|
|
|
|
|||||
The accompanying notes are an integral part of these combined-consolidated financial statements.
F-40
Table of Contents
Cure TopCo, LLC and Subsidiaries
Combined-Consolidated Statement of Operations (In millions, except unit and per unit amounts)
| Year ended December 31, | ||||||||
| 2019 | 2018 | |||||||
| Revenue |
$ | 501.8 | $ | 337.9 | ||||
| Operating expenses: |
||||||||
| Service expense (exclusive of depreciation and amortization shown below) |
247.2 | 196.3 | ||||||
| Selling, general and administrative expense (exclusive of depreciation and amortization shown below) |
168.6 | 67.9 | ||||||
| Transaction-related expenses |
22.4 | 21.0 | ||||||
| Asset impairment |
6.4 | 17.0 | ||||||
| Depreciation and amortization |
66.0 | 43.0 | ||||||
|
|
|
|
|
|||||
| Total operating expenses |
510.6 | 345.2 | ||||||
| Loss from operations |
(8.8 | ) | (7.3 | ) | ||||
| Interest expense |
21.2 | 21.4 | ||||||
| Other (income) expense, net |
(1.6 | ) | — | |||||
|
|
|
|
|
|||||
| Other expense, net |
19.6 | 21.4 | ||||||
|
|
|
|
|
|||||
| Loss before income taxes |
(28.4 | ) | (28.7 | ) | ||||
| Income tax expense |
0.1 | 0.2 | ||||||
|
|
|
|
|
|||||
| Net loss |
$ | (28.5 | ) | $ | (28.9 | ) | ||
|
|
|
|
|
|||||
| Loss per unit |
||||||||
| Former Class A and B Common Units (pre-Remedy Partners Combination) |
$ | (5.10 | ) | $ | (8.44 | ) | ||
| Class B Common Units (post-Remedy Partners Combination) |
$ | (19.13 | ) | $ | (8.44 | ) | ||
| Weighted average units outstanding |
||||||||
| Former Class A and B Common Units (pre-Remedy Partners Combination) |
3,211,075 | 3,421,451 | ||||||
| Class B Common Units (post-Remedy Partners Combination) |
4,526 | — | ||||||
F-41
Table of Contents
Cure TopCo, LLC and Subsidiaries
Combined-Consolidated Statements of Changes in Members’ Equity
(In millions, except units)
| Series A preferred units |
Series A preferred members’ equity |
Series B preferred units |
Series B preferred members’ equity |
Former Class A common units |
Former Class A members’ equity |
Class B common units |
Class B members’ equity |
Additional paid-in capital |
Accumulated deficit |
Total members’ equity |
||||||||||||||||||||||||||||||||||
| Balance at January 1, 2018 |
— | $ | — | — | $ | — | 3,396,228 | $ | 339.6 | — | $ | — | $ | — | $ | (9.9 | ) | $ | 329.7 | |||||||||||||||||||||||||
| Member contributions |
— | — | — | — | 32,667 | 3.0 | — | — | — | — | 3.0 | |||||||||||||||||||||||||||||||||
| Member distributions (Note 14) |
— | — | — | — | — | (18.3 | ) | — | — | — | — | (18.3 | ) | |||||||||||||||||||||||||||||||
| Repurchase of member units |
— | — | — | — | (37,525 | ) | (4.1 | ) | — | — | — | — | (4.1 | ) | ||||||||||||||||||||||||||||||
| Equity-based compensation |
— | — | — | — | — | — | 52,240 | 2.6 | — | — | 2.6 | |||||||||||||||||||||||||||||||||
| Net loss |
— | — | — | — | — | — | — | — | — | (28.9 | ) | (28.9 | ) | |||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
| Balance at December 31, 2018 |
— | $ | — | — | $ | — | 3,391,370 | $ | 320.2 | 52,240 | $ | 2.6 | $ | — | $ | (38.8 | ) | $ | 284.0 | |||||||||||||||||||||||||
| ASC 606 adoption |
— | — | — | — | — | — | — | — | — | (0.2 | ) | (0.2 | ) | |||||||||||||||||||||||||||||||
| Contribution of Remedy |
— | — | — | — | — | — | — | — | 698.3 | — | 698.3 | |||||||||||||||||||||||||||||||||
| Acquisition of TAV Health |
— | — | — | — | 130,525 | 26.1 | — | — | — | — | 26.1 | |||||||||||||||||||||||||||||||||
| Member contributions |
— | — | — | — | 30,000 | 3.0 | — | — | — | — | 3.0 | |||||||||||||||||||||||||||||||||
| Member distributions (Note 14) |
— | — | — | — | — | (21.8 | ) | — | (0.7 | ) | — | — | (22.5 | ) | ||||||||||||||||||||||||||||||
| Repurchase of member units |
— | — | — | — | (18,762 | ) | (2.0 | ) | (10,300 | ) | (0.7 | ) | — | — | (2.7 | ) | ||||||||||||||||||||||||||||
| Remedy Partners Combination (Note 1) |
3,384,543 | 698.3 | — | — | — | — | — | — | (698.3 | ) | — | — | ||||||||||||||||||||||||||||||||
| Conversion of Class A common to Series B preferred |
— | — | 3,533,133 | 325.5 | (3,533,133 | ) | (325.5 | ) | — | — | — | — | — | |||||||||||||||||||||||||||||||
| Tax payments on behalf of members |
— | (5.1 | ) | — | — | — | — | — | — | — | — | (5.1 | ) | |||||||||||||||||||||||||||||||
| Equity-based compensation |
— | 0.2 | — | — | — | — | 51,371 | 3.0 | 1.3 | — | 4.5 | |||||||||||||||||||||||||||||||||
| Proceeds from exercises of stock options |
— | — | — | — | — | — | — | — | 0.7 | — | 0.7 | |||||||||||||||||||||||||||||||||
| Contribution to New Remedy Corp |
— | 2.0 | — | — | — | — | — | — | (2.0 | ) | — | — | ||||||||||||||||||||||||||||||||
| Net loss |
— | — | — | — | — | — | — | — | — | (28.5 | ) | (28.5 | ) | |||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
| Balance at December 31, 2019 |
3,384,543 | $ | 695.4 | 3,533,133 | $ | 325.5 | — | $ | — | 93,311 | $ | 4.2 | $ | — | $ | (67.5 | ) | $ | 957.6 | |||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
The accompanying notes are an integral part of these combined-consolidated financial statements.
F-42
Table of Contents
Cure TopCo, LLC and Subsidiaries
Combined-Consolidated Statements of Cash Flows (in millions)
| Year ended December 31, |
||||||||
| 2019 | 2018 | |||||||
| Operating activities |
||||||||
| Net loss |
$ | (28.5 | ) | $ | (28.9 | ) | ||
| Adjustments to reconcile net loss to net cash provided by operating activities: |
||||||||
| Depreciation and amortization |
66.0 | 43.0 | ||||||
| Loss on impairment |
6.4 | 17.0 | ||||||
| Equity-based compensation |
4.5 | 2.6 | ||||||
| Amortization of deferred financing fees |
1.5 | 1.7 | ||||||
| Loss on extinguishment of debt |
0.2 | 1.4 | ||||||
| Remeasurement of contingent consideration |
0.7 | 0.9 | ||||||
| Gain on sale of assets |
(1.1 | ) | — | |||||
| Other |
0.6 | — | ||||||
| Changes in operating assets and liabilities: |
||||||||
| Accounts receivable |
(37.8 | ) | (8.0 | ) | ||||
| Prepaid expenses and other current assets |
0.3 | (1.0 | ) | |||||
| Contract assets |
74.6 | — | ||||||
| Other assets |
0.3 | (0.7 | ) | |||||
| Accounts payable and accrued expenses |
2.8 | 5.2 | ||||||
| Contract liabilities |
(57.2 | ) | — | |||||
| Other current liabilities |
1.6 | 1.4 | ||||||
| Other noncurrent liabilities |
6.8 | 1.0 | ||||||
|
|
|
|
|
|||||
| Net cash provided by operating activities |
41.7 | 35.6 | ||||||
| Investing activities |
||||||||
| Capital expenditures—property and equipment |
(12.6 | ) | (6.6 | ) | ||||
| Capital expenditures—internal-use software development |
(12.9 | ) | (6.5 | ) | ||||
| Proceeds from sale of assets |
1.2 | — | ||||||
| Business combinations, net of cash acquired |
(28.8 | ) | — | |||||
| Cash acquired from Remedy Partners Acquisition |
136.0 | — | ||||||
|
|
|
|
|
|||||
| Net cash provided by (used in) investing activities |
82.9 | (13.1 | ) | |||||
| Financing activities |
||||||||
| Repayment of long-term debt |
(2.8 | ) | (2.0 | ) | ||||
| Proceeds from issuance of long-term debt |
20.0 | — | ||||||
| Repayment of borrowings under revolving credit facility |
(25.0 | ) | — | |||||
| Proceeds from borrowings under revolving credit facility |
25.0 | — | ||||||
| Payment of debt issuance costs |
(1.2 | ) | (0.5 | ) | ||||
| Payment to sellers of Remedy |
(83.8 | ) | — | |||||
| Member distributions |
(22.5 | ) | (18.3 | ) | ||||
| Payment of taxes on behalf of New Remedy Corp |
(5.1 | ) | — | |||||
| Repurchase of member units |
(3.1 | ) | (4.1 | ) | ||||
| Contributions from members |
3.0 | 3.0 | ||||||
| Proceeds related to the issuance of New Remedy Corp common stock under stock plans |
0.7 | — | ||||||
|
|
|
|
|
|||||
| Net cash used in financing activities |
(94.8 | ) | (21.9 | ) | ||||
| Increase in cash, cash equivalents and restricted cash |
29.8 | 0.6 | ||||||
| Cash, cash equivalents and restricted cash—beginning of year |
20.4 | 19.8 | ||||||
|
|
|
|
|
|||||
| Cash, cash equivalents and restricted cash—end of year |
$ | 50.2 | $ | 20.4 | ||||
|
|
|
|
|
|||||
| Supplemental disclosures of cash flow information |
||||||||
| Cash paid for interest |
$ | 19.3 | $ | 19.4 | ||||
| Cash paid for taxes (net of refunds) |
0.2 | 4.6 | ||||||
| Noncash transactions |
||||||||
| Contribution of assets to New Remedy Corp |
$ | 698.3 | $ | — | ||||
| Issuance of membership units related to acquisition |
26.1 | — | ||||||
| Capital expenditures not yet paid |
0.2 | 1.3 | ||||||
The accompanying notes are an integral part of these combined-consolidated financial statements.
F-43
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
| 1. | Nature of Operations |
Cure TopCo, LLC (formerly Chloe Ox Holdings, LLC, “we”, “our”, “us”) is a Delaware limited liability company formed on November 3, 2017. We have adopted a holding company structure and are the indirect parent entity of Cure Borrower, LLC, a Delaware limited liability company formerly known as Chloe Ox Parent, LLC (“Cure Borrower”).
Cure Borrower is a Delaware limited liability company formed on November 3, 2017. Operations are performed through our wholly-owned subsidiaries primarily under the name Signify Health, LLC, a Delaware limited liability company (“Signify Health”), and throughout 2019, also under the name Remedy Partners, LLC, a limited liability company formerly known as Remedy Partners, Inc. (“Remedy Partners”).
We are a healthcare platform that leverages advanced analytics, technology and nationwide healthcare provider networks. Our customers include health plans, governments, employers, health systems and physician groups. We operate in two segments of the value-based healthcare payment industry: payment models based on individual episodes of care and in-home health evaluations. Our solutions support value-based payment programs by aligning financial incentives around, and providing tools to health plans and healthcare organizations designed to assess and manage, risk and identify actionable opportunities for improved patient outcomes, coordination and cost-savings.
On December 21, 2017, certain investment funds affiliated with New Mountain Capital, LLC (“New Mountain Capital”) formed Cure Borrower and Cure Borrower acquired 100% of the equity of Censeo Health LLC, a Delaware limited liability company (“Censeo”), and 100% of the equity of Drynachan, LLC, a Delaware limited liability company (“Drynachan”). Drynachan operated as “Advance Health”. The acquisition and subsequent integration of these two legacy entities under the ownership and control of New Mountain Capital resulted in the rebranding to Signify Health in July 2018.
In 2019, we acquired 100% of the outstanding equity of Remedy Partners, Inc. (“Remedy Partners”). A controlling interest was initially acquired by New Mountain Capital on January 15, 2019 (the “Remedy Partners Acquisition”), at which point we and Remedy Partners were considered to be under common control and combined financial statements were presented from January 15, 2019 to November 26, 2019. On November 26, 2019, a series of transactions were effected which resulted in Remedy Partners becoming our wholly owned subsidiary and consolidated financial statements were presented from that date forward (the “Remedy Partners Combination” and together with the Remedy Partners Acquisition, the “Remedy Partners Transaction”). Because we were not under common control with and did not own Remedy Partners in 2018, our results of operations for the year ended December 31, 2019 are not directly comparable to our results of operations for the year ended December 31, 2018.
On March 13, 2019, Cure Borrower acquired 100% of the outstanding equity of Triple Aim Ventures, LLC, a Delaware limited liability company (“TAV Health”).
| 2. | Basis of Presentation |
Combination—Consolidation
The financial statements were consolidated for the year ended December 31, 2018 as Chloe Ox Holdings, LLC. See Note 1 Nature of Operations for a description of the combined-consolidated financial statements for the year ended December 31, 2019.
We have two operating segments, Home & Community Services, operated as part of Signify Health and Episodes of Care Services, primarily operated as part of Remedy Partners.
F-44
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
The Combined-Consolidated Financial Statements include the accounts and financial statements of our wholly-owned subsidiaries and variable interest entities (VIEs) where we are the primary beneficiary. Results of operations of VIEs are included from the dates we became the primary beneficiary. All intercompany balances and transactions have been eliminated in consolidation.
Certain prior year amounts have been reclassified (1) on the Combined-Consolidated Statements of Cash Flows to conform to the current year presentation, including capital expenditures presented in additional detail and other assets and other noncurrent liabilities have been split out to be separately presented and (2) in the revenue recognition footnote to conform to the segment presentation.
Use of Estimates
The preparation of combined-consolidated financial statements in conformity with accounting principles generally accepted in the United States of America (“GAAP”) requires management to make estimates and assumptions affecting the reported amounts in the combined-consolidated financial statements and accompanying notes. These estimates are based on information available as of the date of the Combined-Consolidated Financial Statements; therefore, actual results could differ from those estimates. The significant estimates underlying our Combined-Consolidated Financial Statements include revenue recognition; allowance for doubtful accounts; recoverability of long-lived assets, intangible assets and goodwill; loss contingencies; accounting for business combinations, including amounts assigned to definite and indefinite lived intangible assets and contingent consideration; and equity-based compensation.
Comprehensive Income (Loss)
We have not identified any incremental items that would be considered a component of comprehensive income (loss) and accordingly a statement of comprehensive loss is not reflected in the Combined-Consolidated Financial Statements because net loss and comprehensive loss are the same.
| 3. | Significant Accounting Policies |
Cash and Cash Equivalents
We consider all demand deposits with banks and all highly liquid short-term cash investments with an original or remaining maturity of three months or less to be cash equivalents.
Restricted Cash
Under our Master Agreement with the Centers for Medicare and Medicaid Services (“CMS”), we are required to place certain funds in escrow for the benefit of CMS. This account, known as a Secondary Repayment Source (SRS), is based on the size of our participation in the legacy CMS Bundled Payments for Care Improvement (“BPCI”) program, the predecessor program of the Bundled Payments for Care Improvement—Advanced initiative (“BPCI-A). These funds are available to CMS as a supplemental payment source if Remedy Partners fails to pay amounts owed to CMS. The funds will be returned to us 18 months after the conclusion of the effective period of the CMS Master Agreement, or when all financial obligations to CMS are fulfilled. As of December 31, 2019, there was $16.3 in the SRS account included in restricted cash on the Consolidated Balance Sheets. In March 2020 and August 2020, $13.4 and $2.4, respectively, of these funds were released from escrow as the original BPCI program has ended.
F-45
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
We also historically withhold a portion of shared savings to customers in a “holding pool” to cover any potential subsequent negative adjustments through CMS’s subsequent reconciliation true-up process. These funds are distributed to customers following the final true-up if there is no negative adjustment, generally three calendar quarters after the original reconciliation. These amounts represent consideration payable to the customer and therefore have reduced revenue in the period earned. The funds have been received by us from CMS and are held in a separate cash account, included as restricted cash on the Consolidated Balance Sheets. Since the funds are payable to the customer at the point the final CMS true-up is made or a negative adjustment is due to us, the amounts are also included in accounts payable and accrued expenses on the Consolidated Balance Sheets. As of December 31, 2019, there was $6.2 of restricted cash in the holding pool.
The following table reconciles cash, cash equivalents, and restricted cash per the Combined-Consolidated Statements of Cash Flows to the Consolidated Balance Sheets:
| December 31, | ||||||||
| 2019 | 2018 | |||||||
| Cash and cash equivalents |
$ | 27.7 | $ | 20.4 | ||||
| Restricted cash |
22.5 | — | ||||||
|
|
|
|
|
|||||
| Total cash, cash equivalents, and restricted cash |
$ | 50.2 | $ | 20.4 | ||||
|
|
|
|
|
|||||
Accounts Receivable
Accounts receivable primarily consist of amounts due from customers and CMS and are stated at their net realizable value. Management evaluates all accounts periodically and an allowance is established based on the best facts available to management. Management considers historical realization data, accounts receivable aging trends and other operational trends to estimate the collectability of receivables. After all reasonable attempts to collect a receivable have been exhausted, the receivable is written off against the allowance for doubtful accounts. As of December 31, 2019 and 2018, we had an allowance for doubtful accounts of $4.8 and $3.4, respectively.
Prepaid Expenses
Prepaid expenses consist primarily of prepaid insurance and other expenses paid in advance, but for which the services are incurred in the future. The portion of prepaid expenses related to services beyond 12 months from the date of the financial statements is included in other assets.
Property and Equipment
Property and equipment are stated at cost, net of salvage value, if applicable, less accumulated depreciation. Depreciation is computed using the straight-line method over the estimated useful life of the asset. When property and equipment are sold or otherwise disposed of, the costs and accumulated depreciation are removed from the accounts and any gain or loss is recognized in operating income. See Note 7 Property and Equipment.
F-46
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
The estimated useful lives used in computing depreciation and amortization are as follows:
| Estimated Useful Life | ||
| Leasehold improvements |
Shorter of lease term or asset life | |
| Computer equipment and software |
3 - 5 years | |
| Furniture and fixtures |
3 - 7 years |
Maintenance and repairs are expensed as incurred and improvements that increase the value of the property and extend the useful life are capitalized.
Internally-Developed Software
We capitalize certain costs for the development of internal-use software, including certain payroll, payroll-related costs for employees and consulting services that are directly associated with the software development. These capitalized costs are amortized on a straight-line basis over the expected economic life of the software, generally estimated to be three to six years. The costs related to internally-developed software, net of accumulated amortization, are included in intangible assets on the Consolidated Balance Sheets. Costs associated with preliminary stage activities, training, maintenance and all other post-implementation activities are expensed as incurred. We expense internal costs related to minor upgrades and enhancements, as it is impractical to separate these costs from normal maintenance activities.
Business Combinations
We account for business acquisitions under the acquisition method of accounting, which requires the acquiring entity in a business combination to recognize the fair value of all assets acquired, liabilities assumed and any noncontrolling interest in the acquiree, and establishes the acquisition date as the fair value measurement point. Accordingly, we recognize assets acquired and liabilities assumed in business combinations, including contingent assets and liabilities and noncontrolling interests in the acquiree, based on fair value estimates as of the date of acquisition. We recognize and measures goodwill, if any, as of the acquisition date, as the excess of the fair value of the consideration paid over the fair value of the identified net assets acquired.
Pushdown accounting establishes a new basis for the assets and liabilities of an acquired company based on a “pushdown” of the acquirer’s stepped-up basis to the acquired company in connection with a change-in-control event. We elected to apply pushdown accounting in the reporting period in which the change-in-control event occurred. The decision to apply pushdown accounting is irrevocable. The election of pushdown accounting required the recognition of the new basis of accounting established for the individual assets and liabilities of Remedy Partners as of the date New Mountain Capital acquired Remedy. Goodwill was calculated and recognized consistent with business combination accounting, resulting in the pushdown of $408.4 in goodwill as of December 31, 2019.
Recoverability of Goodwill
Goodwill is an asset representing the future economic benefits arising from other assets acquired in a business combination which are not individually identified and separately recognized. We do not amortize goodwill. We review goodwill for impairment annually or when a triggering event occurs that could indicate a potential impairment. We perform the annual goodwill impairment test for both of our reporting units during the fourth quarter.
F-47
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
We are permitted to first perform a qualitative assessment to determine whether it is more likely than not that the fair value of a reporting unit is less than its carrying amount. If the qualitative assessment can support the conclusion that it is more likely than not that the fair value of a reporting unit is greater than its carrying value amount, then we would not need to perform the quantitative impairment test. If the qualitative assessment cannot support such a conclusion, or we do not elect to perform the qualitative assessment, then we perform a quantitative assessment and compare the fair value of the reporting unit to its carrying value, including goodwill. We estimate the fair value of each of our reporting units using either an income approach, a market valuation approach, a transaction valuation approach or a blended approach. We recognize an impairment charge equal to the excess, if any, of a reporting unit’s carrying amount over its fair value, not to exceed the total amount of goodwill allocated to the reporting unit.
Recoverability of Intangible Assets and Other Long-Lived Assets Subject to Amortization
Intangible assets with definite lives subject to amortization include customer relationships, acquired and capitalized software and trade names. Acquired intangible assets are initially recorded at fair value and are amortized on a basis consistent with the timing and pattern of expected cash flows used to value the intangible asset, generally on a straight-line basis over the estimated useful life. Amortization expense is included in depreciation and amortization on the Combined-Consolidated Statements of Operations.
We review the carrying value of long-lived assets or groups of assets, including property and equipment, internally-developed software costs and acquired intangible assets, to be used in operations whenever events or changes in circumstances indicate that the carrying amount of the assets may not be recoverable. We assess the recoverability of an asset or group of assets by determining whether the carrying value of the asset or group of assets exceeds the sum of the projected undiscounted cash flows expected to result from the use and eventual disposition of the assets over the remaining economic life of the asset or the primary asset in the group of assets. If such testing indicates the carrying value of the asset or group of assets is not recoverable, we estimate the fair value of the asset or group of assets using various valuation methodologies, including discounted cash flow models and quoted market values, as necessary. If the fair value of those assets or groups of assets is less than carrying value, we record an impairment loss equal to the excess of the carrying value over the estimated fair value. See Note 9 Intangible Assets for details of impairment losses recognized during the years ended December 31, 2019 and 2018.
Revenue Recognition
In May 2014, the Financial Accounting Standards Board (“FASB”) issued a comprehensive new standard, ASC 606 Revenue from Contracts with Customers (“ASC 606”), which supersedes prior revenue recognition guidance. We adopted the new standard on January 1, 2019 by applying the modified retrospective method to all contracts open at that point in time. Results as reported in the Combined-Consolidated Statements of Operations of prior periods have not been adjusted and continue to be reported under the accounting standards in effect at that time. See Note 6 Revenue Recognition for further details.
Service Expense
Service expense represents direct costs associated with generating revenue. These costs include fees paid to providers for performing evaluations, provider travel expenses, the total cost of payroll, related benefits and other personnel expenses for employees in roles that serve to provide direct revenue generating services to customers. Additionally, service expense also includes costs related to the use of certain professional service firms, member engagement expenses, coding expenses and certain other direct costs. Service expense does
F-48
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
not include depreciation and amortization, which is stated separately in the Combined-Consolidated Statements of Operations.
Selling, General and Administrative (“SG&A”)
SG&A includes the total cost of payroll, related benefits and other personnel expense for employees who do not have a direct role associated with revenue generation including those involved with developing new service offerings. SG&A expenses include all general operating costs including, but not limited to, rent and occupancy costs, telecommunications costs, information technology infrastructure costs, technology development costs, software licensing costs, advertising and marketing expenses, recruiting expenses, costs associated with developing new service offerings and expenses related to the use of certain subcontractors and professional services firms. SG&A expenses do not include depreciation and amortization, which is stated separately in the Combined-Consolidated Statements of Operations.
Advertising and Marketing Costs
Advertising and marketing costs are included in SG&A expenses and are expensed as incurred. Advertising and marketing costs totaled $3.3 and $0.8 for the years ended December 31, 2019 and 2018, respectively.
Accounting for Leases
We lease various property and equipment. Amortization of assets accounted for as capital leases is computed utilizing the straight-line method over the shorter of the remaining lease term or the estimated useful life.
All other leases, primarily facility leases, are accounted for as operating leases. Rent expense for operating leases, which may have rent escalation provisions or rent holidays, is recorded on a straight-line basis over the noncancelable lease period. The difference between rent expensed and rent paid is recorded as deferred rent. Lease incentives received from landlords are recorded as a deferred rent credit and amortized to rent expense over the term of the lease. Deferred rent is included in other noncurrent liabilities and accounts payable and accrued expenses on the Consolidated Balance Sheet.
Income Taxes
We account for income taxes using the asset and liability method. The current and deferred tax consequences of a transaction are measured by applying the provisions of enacted tax laws to determine the amount of taxes payable or receivable currently or in future years. Deferred income taxes are provided for on temporary differences between the income tax basis of assets and liabilities and their carrying amounts for financial reporting purposes. The effect on deferred taxes of a change in tax rates is recognized in income in the period that includes the enactment date. Deferred tax assets are subject to a valuation allowance to reduce them to their net realizable value, on a more-likely-than-not basis.
We are organized as a Delaware limited liability company. Therefore, federal taxes are paid at the member level, rather than at the company level. LLCs may be subject to income tax in certain states and other jurisdictions. These taxes, if applicable, are paid by us and included in income tax expense.
We may recognize tax liabilities when, despite our belief that our tax return positions are supportable, we believe that certain positions may not be fully sustained upon review by the tax authorities. Benefits from tax positions are measured at the largest amount of benefit that is greater than fifty percent likely of being realized upon settlement. To the extent that the final tax outcome of these matters is different than the amounts recorded, such differences impact income tax expense in the period such determination is made.
F-49
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
At the time of the Remedy Partners Combination, Remedy Partners was converted from a Delaware corporation to a Delaware limited liability company after a series of transactions pursuant to which New Remedy Corp. was formed and became the sole equity holder of Remedy Partners. New Remedy Corp. then contributed 100% of the equity interests of Remedy Partners to us in exchange for our Series A Preferred Units. New Remedy Corp. is outside of our consolidated group. Certain federal and state tax attributes that previously related to Remedy Partners became attributes of New Remedy Corp. For presentation purposes, the tax treatment was as if New Remedy Corp. existed and held these tax attributes for the entire year ended December 31, 2019.
We recognize interest and penalties related to income taxes as a component of income tax expense.
Equity-Based Compensation
We recognize equity-based compensation for all equity-based awards granted to employees based on the grant date fair value of the award. The resulting compensation expense is generally recognized on a straight-line basis over the requisite service period. Forfeitures are recorded as they occur.
The determination of equity-based compensation expense related to profits interests is calculated based on an option pricing model as of the grant date. The determination of equity-based compensation expense related to stock options in New Remedy Corp is calculated using a Black-Scholes option pricing model and is affected by the estimated share price, volatility over the expected term of the awards, expected term, risk free interest rate and expected dividends.
Certain of the profits interests are subject to performance-vesting criteria, as set forth in the applicable award agreement. The vesting of the profits interests that are subject to performance-based vesting criteria is also generally dependent upon the participant’s continued employment. The criteria associated with the performance-vesting criteria, as defined in the applicable award agreements, is not probable as assessed at the end of each reporting period. As such, we have not recorded any equity-based compensation expense related to the portion of the equity awards that is subject to performance-based vesting criteria.
Loss Per Unit
Net loss per unit is computed using the “two-class” method. The two-class method requires net loss to be allocated between common member units and participating securities based on their respective right to receive distributions as if all income for the period had been distributed. All of our member units are participating securities as each class has the right to participate in distributions of the Company on a pro rata basis. Under the two-class method, basic net loss per unit is computed by dividing the net loss attributable to each respective class by the weighted average number of member units outstanding for the period. Net losses are allocated to both the preferred unitholders and the common unitholders in accordance with our LLC Agreement, which includes an obligation for all unitholders to share in our net losses in certain circumstances. In accordance with our LLC Agreement, under certain operating conditions, Class A preferred units could receive an additional distribution per member unit. Because this distribution is contingent on a liquidation event or operating metrics that have not yet occurred, it is not determined to be probable and has not been considered in the calculation of loss per unit. There were no dilutive securities in 2018 and 2019, and therefore, the basic and diluted loss per unit have been presented together.
F-50
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Debt Issuance Costs
Debt issuance costs incurred in connection with our borrowings are being presented as a reduction of debt and are amortized through interest expense using the effective interest rate method over the expected life of the related debt instruments.
Fair Value Measurement
We disclose the fair value of our financial instruments based on the following fair value hierarchy:
| • | Level 1—Quoted prices in active markets for identical assets or liabilities |
| • | Level 2—Inputs that are observable for the asset or liability, either directly or indirectly through market corroboration, for substantially the full term of the asset or liability |
| • | Level 3—Inputs that are unobservable for the asset or liability based on our evaluation of the assumptions market participants would use in pricing the asset or liability |
We may be required to pay additional consideration in relation to certain acquisitions based on certain future events. Acquisition-related contingent consideration is initially measured and recorded at fair value as an element of consideration paid in connection with an acquisition with subsequent adjustments recognized in SG&A expense in the Combined-Consolidated Statements of Operations. We determine the fair value of acquisition-related contingent consideration, and any subsequent changes in fair value using a discounted probability-weighted approach. This approach takes into consideration Level 3 unobservable inputs including probability assessments of expected future cash flows over the period in which the obligation is expected to be settled and applies a discount factor that captures the uncertainties associated with the obligation. Changes in these unobservable inputs could significantly impact the fair value of the obligation recorded in the accompanying Combined-Consolidated Financial Statements.
Recent Accounting Pronouncements
Recently adopted
In May 2014, FASB issued Accounting Standards Update (“ASU”) 2014-09, Revenue from Contracts with Customers (“ASC 606”). The new revenue recognition standard provides a five-step model to determine when and how revenue is recognized. The core principle is that a company should recognize revenue to depict the transfer of promised goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled in exchange for those goods or services. This guidance was effective for nonpublic companies for annual periods beginning after December 15, 2018 and is applied either retrospectively to each period presented or as a cumulative-effect adjustment as of the date of adoption. We used the modified retrospective method to adopt the new revenue recognition guidance on January 1, 2019. Adoption of the new standard did not have a material impact to our revenue recognition, with approximately $0.2 recognized as a cumulative impact increase in accumulated deficit upon adoption. Remedy Partners adopted this new accounting guidance effective January 1, 2019, prior to our acquisition of Remedy Partners and its inclusion in our combined-consolidated financial statements. This new guidance did have a material impact on the timing of revenue recognition for Remedy Partners.
In August 2016, the FASB issued ASU No. 2016-15, Classification of Certain Cash Receipts and Cash Payments (“ASU 2016-15”). ASU 2016-15 addresses eight specific cash flow issues to reduce the existing diversity in practice in how certain cash receipts and cash payments are presented and classified in the statement of cash flows. In November 2016, the FASB issued ASU No. 2016-18, Statement of Cash Flows:
F-51
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Restricted Cash (“ASU 2016-18”). ASU 2016-18 requires companies to include amounts generally described as restricted cash and restricted cash equivalents in cash and cash equivalents when reconciling beginning-of-period and end-of-period total amounts shown on the statement of cash flows. These ASUs are effective for fiscal years beginning after December 15, 2018, including interim reporting periods. Early adoption is permitted. We have implemented the impact of these updates in our Combined-Consolidated Financial Statements as of January 1, 2018 with no material impact.
In January 2017, the FASB issued ASU 2017-01, Business Combinations (Topic 805): Clarifying the Definition of a Business, which revises the definition of a business and provides guidance to assist entities with evaluating whether transactions should be accounted for as acquisitions (or disposals) of assets or businesses. The guidance is effective for the fiscal year, and interim periods within that fiscal year, beginning after December 15, 2018. Early adoption is permitted. We have adopted ASU 2017-01 as of January 1, 2018 with no material impact to our Combined-Consolidated Financial Statements.
In January 2017, the FASB issued ASU 2017-04, Goodwill and Other (Topic 350): Simplifying the Test for Goodwill Impairment (“ASU 2017-04”). This amendment simplified the manner in which an entity is required to test for goodwill impairment by eliminating Step 2 from the goodwill impairment test. Step 2 measured goodwill impairment loss by comparing the implied fair value of a reporting unit’s goodwill with the carrying amount of that goodwill. The amendment simplifies this approach by having the entity (1) perform its annual or interim goodwill impairment test by comparing the fair value of a reporting unit with its carrying amount, and (2) recognize an impairment charge for the amount by which the carrying amount exceeds the reporting unit’s fair value, with the understanding that the loss recognized should not exceed the total amount of goodwill allocated to that reporting unit. We elected to early adopt the new guidance in the fourth quarter of fiscal year 2018. The adoption of this guidance did not have a material effect on our Combined-Consolidated Financial Statements.
In June 2018, the FASB issued Accounting Standards Update No. 2018-07, Compensation—Stock Compensation (Topic 718): Improvements to Nonemployee Share-Based Payment Accounting (“ASU 2018-07”). The amendments in ASU 2018-07 expand the scope of Topic 718 to include share-based payment transactions for acquiring goods and services from nonemployees. ASU 2018-07 is effective for fiscal years beginning after December 15, 2019, and interim periods within fiscal years beginning after December 15, 2020. We elected to early adopt this new guidance for interim periods in 2020 with no significant impact to our financial statements.
In November 2019, the FASB issued ASU 2019-08, Compensation—Stock Compensation (Topic 718) and Revenue from Contracts with Customers (Topic 606): Codification Improvements—Share-Based Consideration Payable to a Customer (“ASU 2019-08”). ASU 2019-08 requires that an entity measure and classify share-based payment awards granted to a customer by applying the guidance in Topic 718. The amount recorded as a reduction of the transaction price is required to be measured on the basis of the grant-date fair value of the share-based payment award in accordance with Topic 718. The grant date is the date at which a grantor (supplier) and a grantee (customer) reach a mutual understanding of the key terms and conditions of a share-based payment award. ASU 2019-08 is effective for fiscal years beginning after December 15, 2019, and interim periods within fiscal years beginning after December 15, 2020. We elected to early adopt this new guidance for interim periods in 2020, which had an impact on the customer EAR. The initial grant date fair value of the EAR agreement is being recorded as a reduction of the transaction price beginning in 2020.
F-52
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Pending Adoption
In February 2016, the FASB issued ASU 2016-02, Leases (Topic 842). The new lease standard requires lessees to recognize leases on the balance sheet by recording a right-of-use asset and lease liability. This guidance is effective for non-public entities for annual reporting periods beginning after December 15, 2021. Early adoption is permitted. We are currently assessing the impact of this guidance on the Combined-Consolidated Financial Statements.
In June 2016, the FASB issued ASU 2016-13, Financial Instruments—Credit Losses (Topic 326) (“ASU 2016-13”). ASU 2016-13 introduces the current expected credit losses methodology for estimating allowances for credit losses. ASU 2016-13 applies to all financial instruments carried at amortized cost and off-balance-sheet credit exposures not accounted for as insurance, including loan commitments, standby letters of credit, and financial guarantees. The new accounting standard does not apply to trading assets, loans held for sale, financial assets for which the fair value option has been elected, or loans and receivables between entities under common control. ASU 2016-13 is effective for private entities for fiscal years beginning after December 15, 2022, including interim periods within those fiscal years. Early adoption is permitted. We are evaluating the impact of this new guidance on our financial statements.
| 4. | Business Combinations |
Remedy Partners Acquisition
On January 15, 2019, affiliates of New Mountain Capital acquired a controlling interest in Remedy Partners for $405.0 in cash at which point we and Remedy Partners were considered to be under common control. The total enterprise value purchase consideration of the transaction was determined to be $664.0. We allocated the purchase price to the identifiable net assets acquired, based on the estimated fair values at the date of acquisition. The excess of the purchase price over the amount allocated to the identifiable assets and liabilities was recorded as goodwill. Goodwill represents the value of the acquired assembled workforce, specialized processes and procedures and operating synergies, none of which qualify as separate intangible assets.
We determined the estimated fair values of intangible assets acquired using estimates of future discounted cash flows to be generated by the business over the estimated duration of those cash flows. We base the estimated cash flows on projections of future revenue, operating expenses, capital expenditures, working capital needs and tax rates. We estimated the duration of the cash flows based on the projected useful lives of the assets acquired. The discount rate was determined based on specific business risk, cost of capital and other factors.
F-53
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
The table below presents the fair value of net assets acquired and pushed down as of the acquisition date:
| Cash |
$ | 114.7 | ||
| Accounts receivable |
89.2 | |||
| Contract assets |
112.8 | |||
| Prepaid expenses and other current assets |
3.7 | |||
| Restricted cash |
21.3 | |||
| Property and equipment |
6.6 | |||
| Other assets |
0.8 | |||
| Intangible assets |
167.0 | |||
|
|
|
|||
| Total identifiable assets acquired |
516.1 | |||
| Accounts payable and accrued liabilities |
161.6 | |||
| Contract liabilities |
60.3 | |||
| Other current liabilities |
8.2 | |||
| Deferred tax liabilities |
30.4 | |||
|
|
|
|||
| Total liabilities assumed |
260.5 | |||
|
|
|
|||
| Net identifiable assets acquired |
255.6 | |||
| Goodwill |
408.4 | |||
|
|
|
|||
| Total of assets acquired and liabilities assumed |
$ | 664.0 | ||
|
|
|
The $167.0 of acquired intangible assets include customer relationships of $118.0 (weighted average useful life of 9 years), acquired software of $43.0 (5-year useful life) and a tradename of $6.0 (5-year useful life). The tradename was subsequently impaired following our rebranding upon the Remedy Partners Combination, see Note 9 Intangible Assets.
Accounts payable and accrued liabilities assumed includes $83.8 related to an excess cash distribution that was paid to the sellers of Remedy Partners in May 2019, in accordance with the terms of the purchase agreement.
None of the goodwill is expected to be deductible for tax purposes. At the time of the Remedy Partners Combination in November 2019, Remedy Partners was contributed as a limited liability company after a series of transactions in a tax-free transaction. As such, all tax attributes, including $3.9 of current tax liabilities included in other current liabilities above and $30.4 of deferred tax liabilities previously related to Remedy Partners are maintained at the New Remedy Corp. level (parent holding company). For presentation purposes, the tax treatment was as if New Remedy Corp. existed and held the tax attributes for the entire year ended December 31, 2019.
The acquisition resulted in common control by New Mountain Capital. As such, the financial results of Remedy Partners have been combined with our financial results and included in the Combined-Consolidated Financial Statements since the date of acquisition. At the time of the Remedy Partners Combination in November 2019, the financial results were consolidated with the financial results of the other entities of the company. Total revenue and net loss of $107.8 and $32.3, respectively, related to Remedy Partners is included in the Combined-Consolidated Statements of Operations for the year ended December 31, 2019.
TAV Health Acquisition
On March 13, 2019, we acquired 100% of the outstanding equity of Triple Aim Ventures, LLC (“TAV Health”). The purchase price was $55.0, comprised of $28.9 in cash and the issuance of 130,525 our former
F-54
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Class A Common Units. We allocated the purchase price to the identifiable net assets acquired, based on the estimated fair values at the date of acquisition. The excess of the purchase price over the amount allocated to the identifiable assets and liabilities was recorded as goodwill. Goodwill represents the value of the acquired assembled workforce, specialized processes and procedures and operating synergies, none of which qualify as separate intangible assets.
We determined the estimated fair values of intangible assets acquired using estimates of future discounted cash flows to be generated by the business over the estimated duration of those cash flows. We base the estimated cash flows on projections of future revenue, operating expenses, capital expenditures, working capital needs and tax rates. We estimated the duration of the cash flows based on the projected useful lives of the assets acquired. The discount rate was determined based on specific business risk, cost of capital and other factors.
The table below presents the fair value of net assets acquired at the date of acquisition:
| Cash |
$ | 0.1 | ||
| Accounts receivable |
0.3 | |||
| Prepaid expenses and other current assets |
0.2 | |||
| Other assets |
0.1 | |||
| Property and equipment |
0.3 | |||
| Intangible assets |
8.2 | |||
|
|
|
|||
| Total identifiable assets acquired |
9.2 | |||
| Accounts payable and accrued liabilities |
0.1 | |||
| Other current liabilities |
2.0 | |||
|
|
|
|||
| Total liabilities assumed |
2.1 | |||
|
|
|
|||
| Net identifiable assets acquired |
7.1 | |||
| Goodwill |
47.9 | |||
|
|
|
|||
| Total of assets acquired and liabilities assumed |
$ | 55.0 | ||
|
|
|
The $8.2 of acquired intangible assets is comprised of acquired software of $7.7 (6-year useful life) and customer relationships of $0.5 (14-year useful life).
None of the goodwill is expected to be deductible for tax purposes.
The acquisition was not material to our Combined-Consolidated Statements of Operations. Therefore, pro forma results of operations related to this acquisition have not been presented. The financial results of TAV Health have been included in our Combined-Consolidated Financial Statements since the date of the acquisition.
| 5. | Variable Interest Entities |
We consolidate our affiliates when we are the primary beneficiary. The primary beneficiary of a Variable Interest Entity (“VIE”) is the party that has both the decision-making authority to direct the activities that most significantly impact the VIE’s economic performance and the right to absorb losses or receive benefits that could potentially be significant to the VIE. Consolidated VIEs at December 31, 2019 and 2018 include two and three, respectively, physician practices that require an individual physician to legally own the equity interests as certain state laws and regulations prohibit non-physician owned business entities from practicing medicine or employing licensed healthcare providers. We have determined we are the primary
F-55
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
beneficiary of these VIEs as we have the obligation to absorb the losses from and direct activities of these operations. As a result, these VIEs are consolidated and any non-controlling interest is not presented. Recourse of creditors to these VIEs is limited to the assets of the VIE entities, which total $2.5 and $6.6 at December 31, 2019 and 2018, respectively.
In February 2019, we sold a VIE, Principium LLC and Medical Service Professionals of New Jersey PLC, to Clover Health LLC for $1.2 and recognized a gain on disposition of assets of $1.1, which is included in SG&A expenses on the Combined-Consolidated Statements of Operations.
The carrying amount and classification of the VIEs’ assets and liabilities included in the Consolidated Balance Sheets as of December 31, 2019 and 2018, net of intercompany amounts, are as follows:
| December 31, | ||||||||
| 2019 | 2018 | |||||||
| ASSETS |
||||||||
| Current assets |
||||||||
| Cash and cash equivalents |
$ | 0.1 | $ | 2.3 | ||||
| Accounts receivable, net |
2.4 | 4.0 | ||||||
|
|
|
|
|
|||||
| Total current assets |
2.5 | 6.3 | ||||||
| Property and equipment, net |
— | 0.3 | ||||||
|
|
|
|
|
|||||
| Total assets |
$ | 2.5 | $ | 6.6 | ||||
|
|
|
|
|
|||||
| LIABILITIES AND EQUITY |
||||||||
| Current liabilities |
||||||||
| Accounts payable and accrued expenses |
$ | — | $ | 0.5 | ||||
|
|
|
|
|
|||||
| Total current liabilities |
— | 0.5 | ||||||
|
|
|
|
|
|||||
| Total liabilities |
— | 0.5 | ||||||
| Company capital |
(0.1 | ) | 7.0 | |||||
| Retained earnings (accumulated deficit) |
2.6 | (0.9 | ) | |||||
|
|
|
|
|
|||||
| Total equity |
2.5 | 6.1 | ||||||
|
|
|
|
|
|||||
| Total liabilities and equity |
$ | 2.5 | $ | 6.6 | ||||
|
|
|
|
|
|||||
| 6. | Revenue Recognition |
Prior to the adoption of ASC 606, we recognized revenue when all of the following criteria were met: (i) persuasive evidence of an arrangement exists, (ii) delivery has occurred, (iii) the fee is fixed or determinable, and (iv) collectability is probable. Under ASC 606, we recognize revenue as the control of promised services is transferred to our customers and we generate all of our revenue from contracts with customers. The amount of revenue recognized reflects the consideration to which we expect to be entitled in exchange for these services. The measurement and recognition of revenue requires us to make certain judgments and estimates
We are dependent on a concentrated number of payors and provider partners with whom we contract to provide our services, See Note 20 Concentrations.
F-56
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Disaggregation of Revenue
We earn revenue from our two operating segments, Home & Community Services and Episodes of Care Services under contracts that contain various fee structures. Through our Home & Community Services segment, we offer health evaluations performed either within the patient’s home or at a healthcare provider facility primarily to Medicare Advantage health plans (and to some extent, Medicaid). Additionally, we offer certain diagnostic screening and other ancillary services and through our Signify Community solution, services to address healthcare concerns related to social determinants of health. Through our Episodes of Care Services segment, we primarily provide services designed to improve the quality and efficiency of healthcare delivery by developing and managing episodic payment programs in partnership with healthcare providers primarily under the BPCI-A program with CMS. Additionally, we provide certain complex care management services. All of our revenue is generated in the United States.
The following table summarizes disaggregated revenue from contracts with customers for the years ended December 31, 2019 and 2018 by source of revenue, which we believe best depicts the nature, amount and timing of revenue. Certain products have been reclassified from Home & Community Services to Episodes of Care Services to reflect changes made in 2020 associated with the integration related to the Remedy Partners Combination.
| Year ended December 31, | ||||||||
| 2019 | 2018 | |||||||
| Evaluations |
$ | 369.6 | $ | 310.0 | ||||
| Other |
7.4 | — | ||||||
|
|
|
|
|
|||||
| Home & Community Services Total Revenue |
377.0 | 310.0 | ||||||
| Episodes |
107.8 | — | ||||||
| Other |
17.0 | 27.9 | ||||||
|
|
|
|
|
|||||
| Episodes of Care Services Total Revenue |
124.8 | 27.9 | ||||||
|
|
|
|
|
|||||
| Combined-Consolidated Revenue Total |
$ | 501.8 | $ | 337.9 | ||||
|
|
|
|
|
|||||
Performance Obligations
The unit of measure under ASC 606 is a performance obligation, which is a promise in a contract to transfer a distinct or series of distinct goods or services to the customer. A contract’s transaction price is allocated to each distinct performance obligation and recognized as revenue when, or as, the performance obligation is satisfied.
Our customer contracts have either (1) a single performance obligation as the promise to transfer services is not separately identifiable from other promises in the contracts and is, therefore, not distinct; (2) a series of distinct performance obligations; or (3) multiple performance obligations, most commonly due to the contract covering multiple service offerings. For contracts with multiple performance obligations, the contract’s transaction price is allocated to each performance obligation on the basis of the relative standalone selling price of each distinct service in the contract.
Home & Community Services
Home & Community Services revenue primarily consists of in-home health evaluations and related services, categorized as evaluations and other.
F-57
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Revenue generated from in-home health evaluations (“IHEs”) relates to the assessments performed either within the patient’s home or at a healthcare provider facility as well as certain in-home clinical evaluations performed by our mobile network of providers.
Revenue is recognized when the IHEs are submitted to our customers on a daily basis. Submission to the customer occurs after the IHEs are completed and coded, a process which may take one to several days after completion of the evaluation. The pricing for the IHEs is generally based on a fixed transaction fee, which is directly linked to the usage of the service by the customer during a distinct service period. Customers are invoiced for evaluations performed each month and remit payment accordingly. Each IHE represents a single performance obligation for which revenue is recognized at a point-in-time when control is transferred to the customer upon submission of the completed and coded evaluation.
The remaining sources of revenue in our Home & Community Services segment, which relate to ancillary diagnostic and evaluative services we provide, are recognized over time as the performance obligations are satisfied and are primarily based on a fixed fee. Therefore, they do not require estimates and assumptions by management.
Episodes of Care Services
The episodes solutions we provide are an integrated set of services which represent a single performance obligation in the form of a series of distinct services. This performance obligation is satisfied over time as the various services are delivered. We primarily offer our services to customers under the BPCI-A program.
Under the BPCI-A program, we act in a convener capacity, as defined by CMS, for most of our customer contracts, with the exception of a few customer contracts whereby we act in a non-convener capacity. Under the BPCI-A program, we recognize the revenue attributable to episodes reconciled during each six-month episode performance measurement period over a 13-month performance obligation period that commences in the second or fourth quarter of each year, depending on the relevant contract with our provider partners. The 13-month performance obligation period begins at the start of the relevant episodes of care and extends through the receipt or generation of the semiannual reconciliation for the relevant performance measurement period, as well as the provision and explanation of statements of performance to each of our customers. The transaction price is 100% variable and therefore we estimate an amount in which we expect to be entitled to receive for each six-month episode performance measurement period over a 13-month performance obligation period.
For each partner agreement, the fees are generally two-fold, an administrative fee, which is based on a stated percentage of program size and is paid out of savings, and a defined share of program savings or losses, if any. In order to estimate this variable consideration, management estimates the expected program size as well as the expected savings rate for each six-month episode performance measurement period. The estimate is performed both at the onset of each performance measurement period based on information available at the time and at the end of each reporting period. In making the estimate we consider inputs such as the overall program size which is defined by the historic cost multiplied by the frequency of occurrence of defined episodes of care. Additionally, we estimate savings rates by using data sources such as historical trend analysis together with indicative data of the current volume of episodes.
We adjust our estimates at the end of each six-month performance measurement period, generally in the second and fourth quarter each year, and may further adjust at the end of each reporting period to the extent new information indicates a change is needed. We apply a constraint to the variable consideration estimate in circumstances where we believe the claims data received is incomplete or inconsistent, so as not to have the estimates result in a significant revenue reversal in future periods. Although our estimates are based on
F-58
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
the information available to us at each reporting date, several factors may cause actual revenue earned to differ from the estimates recorded each period. These include, among others, limited historical experience as the current BPCI-A program only commenced in the fourth quarter of 2018, CMS-imposed restrictions on the definition of episodes and benchmark prices, provider partner participation, the impacts of the COVID-19 pandemic in 2020 and other limitations of the program beyond our control.
The overall goal of the BPCI-A program is to generate savings relative to CMS benchmark prices. In return for participating in the program, we and our customers can share in savings or losses generated compared to the CMS benchmark prices, and those savings or losses are then shared with customers in accordance with the terms of our customer contracts. The customer’s share of the total savings, represents consideration payable to customers and therefore is a reduction of the transaction price. We receive payment semi-annually from CMS for our customers in which we act as a convener or directly from our non-convener customers.
During the year ended December 31, 2019, we recognized $2.1 of revenue representing changes in estimates related to variable consideration upon receipt and analysis of reconciliations from CMS in 2019 related to performance obligations satisfied in the year ended December 31, 2018. In addition, during the year ended December 31, 2019, we also recorded approximately $2.0 related to a cumulative catch up of a change in estimated transaction price upon the satisfaction of the performance obligations.
The remaining sources of revenue in our Episodes of Care Services segment are recognized over time when, or as, the performance obligations are satisfied and are primarily based on a fixed fee or per member per month fee. Therefore, they do not require significant estimates and assumptions by management.
The Episodes of Care Services segment was acquired as part of the Remedy Partners Acquisition on January 15, 2019. Remedy Partners had adopted ASC 606 effective January 1, 2019. Remedy Partners was not under common control for the year ended December 31, 2018 and therefore there is no impact on the comparative financial statements related to the change in revenue recognition.
Upon application of the modified retrospective method of adoption, we are required to disclose the impact on our statement of operations had we continued to follow the accounting policies under the previous revenue recognition guidance. We estimate net revenue for the year ended December 31, 2019 is approximately $25.0 lower as reported in the Combined-Consolidated Statements of Operations under ASC 606 than it would have been under previous revenue recognition guidance primarily due to changes in timing of revenue recognition. That difference results from the previous revenue recognition guidance, which required that the timing of revenue recognition occur when the amounts were fixed and determinable. In contrast, under ASC 606 revenue is estimated and recognized for variable consideration subject to a constraint.
F-59
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Related Balance Sheet Accounts
The following table provides information about accounts included on the Consolidated Balance Sheet as of December 31, 2019.
| Episodes of Care Services |
Home & Community Services |
Total | ||||||||||
| Assets |
||||||||||||
| Accounts receivable, net(1) |
$ | 125.1 | $ | 43.0 | $ | 168.1 | ||||||
| Contract assets(2) |
$ | 38.3 | $ | — | $ | 38.3 | ||||||
| Liabilities |
||||||||||||
| Shared savings payable(3) |
$ | 58.2 | $ | — | $ | 58.2 | ||||||
| Contract liabilities(4) |
$ | 3.1 | $ | — | $ | 3.1 | ||||||
| Deferred revenue(5) |
$ | — | $ | 1.2 | $ | 1.2 | ||||||
| (1) | Accounts receivable, net for Episodes of Care Services includes $99.5 due from CMS as of December 31, 2019 related to the first reconciliation period of the BPCI-A program. The remaining amount of accounts receivable for both Episodes of Care Services and Home & Community Services represent amounts to be received from customers. |
| (2) | Contract assets represents management’s estimate of amounts we expect to receive under the BPCI-A program related to the next two reconciliation periods covering episodes of care for the period April 2019 through March 2020. Estimates for program size and savings rate are based on information available as of the date of the financial statements. We record an estimate of revenue related to these performance obligations over the 13-month period starting in the period the related episodes of care commence and through the estimated receipt of the semi-annual CMS reconciliation file. Any changes to these estimates based on new information will be recorded in the period such information is received. Total savings generated and revenue earned for the episodes of care in which the contract asset recorded as of December 31, 2019 relates to will be included in the semi-annual reconciliations expected from CMS during 2020. |
| (3) | Total shared savings payable is included in accounts payable and accrued expenses on the Consolidated Balance Sheets. Shared savings payable for Episodes of Care Services included $13.3 due to CMS as of December 31, 2019, which represents management’s estimate of total fees that are constrained related to the first reconciliation period of the BPCI-A program. We settled this amount with CMS during the next semi-annual reconciliation period in the second quarter of 2020. Shared savings payable also includes $38.7 as of December 31, 2019, which we paid to customers during 2020 related to their portion of savings earned under the BPCI-A program. Additionally, there is $6.2 included in shared savings payable at December 31, 2019 which represents amounts previously withheld from customers under the original BPCI program based on contractual withholding percentages. This amount has been received by us from CMS and is held as restricted cash. We expect to remit these amounts to customers during 2020, at which time both restricted cash and the liability will be reduced. |
| (4) | Contract liabilities represent management’s estimate of savings amounts we expect to share with our customers based on contractual shared savings percentages related to the amounts we expect to be entitled to receive under the BPCI-A program for episodes of care for the period April 2019 through December 2019. These amounts offset the gross amount we expect to receive for the same period included in contract assets as of December 31, 2019. |
| (5) | Deferred revenue is included in other current liabilities on the Consolidated Balance Sheets and primarily relates to advance payments received from certain customers. |
F-60
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
The table below summarizes the activity recorded in the contract asset and liability accounts during the year ended December 31, 2019.
| Contract Assets |
||||
| Balance at January 1, 2019 |
$ | — | ||
| Acquired in Remedy Partners Acquisition |
112.9 | |||
| Performance obligation completed, converted to accounts receivable |
(112.9 | ) | ||
| Estimated revenue recognized related to performance obligations satisfied over time |
38.3 | |||
|
|
|
|||
| Balance at December 31, 2019 |
$ | 38.3 | ||
|
|
|
|||
| Contract Liabilities |
||||
| Balance at January 1, 2019 |
$ | — | ||
| Assumed in Remedy Partners Acquisition |
60.3 | |||
| Performance obligation completed, converted to shared savings payable |
(60.3 | ) | ||
| Estimated amounts due to customer related to performance obligations satisfied over time |
3.1 | |||
|
|
|
|||
| Balance at December 31, 2019 |
$ | 3.1 | ||
|
|
|
|||
| Deferred Revenue |
||||
| Balance at January 1, 2019 |
$ | 0.4 | ||
| Acquired in TAV Health acquisition |
1.0 | |||
| Payments received from customers |
2.8 | |||
| Revenue recognized upon completion of performance obligation |
(3.0 | ) | ||
|
|
|
|||
| Balance at December 31, 2019 |
$ | 1.2 | ||
|
|
|
|||
| Shared Savings Payable |
||||
| Balance at January 1, 2019 |
$ | — | ||
| Assumed in Remedy Partners Acquisition |
65.5 | |||
| Amounts paid to customer and/or CMS |
(129.9 | ) | ||
| Amounts due to customer upon completion of performance obligation |
122.6 | |||
|
|
|
|||
| Balance at December 31, 2019 |
$ | 58.2 | ||
|
|
|
|||
Other Matters
We do not disclose, as amounts are not material or settled within a short period of time, the value of unsatisfied performance obligations for (a) contracts with an original expected length of one year or less; (b) contracts for which we recognize revenue at the amount to which we have the right to invoice for services performed; or (c) contracts for which the variable consideration is allocated entirely to a wholly unsatisfied performance obligation or to a wholly unsatisfied promise to transfer a distinct good or service that forms part of a single performance obligation, and the terms of the variable consideration relate specifically to our efforts to transfer the distinct service or to a specific outcome from transferring the distinct service.
As an accounting policy election, sales tax amounts collected from customers on behalf of government entities are not included in the transaction price with customers and any amounts collected are reported net in our financial statements.
F-61
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
| 7. | Property and Equipment |
As of December 31, 2019 and 2018, property and equipment, net were as follows:
| December 31, 2019 | December 31, 2018 | |||||||
| Leasehold Improvements |
$ | 11.6 | $ | 0.8 | ||||
| Computer equipment |
10.6 | 6.1 | ||||||
| Furniture and fixtures |
5.3 | 3.2 | ||||||
| Software |
3.4 | 3.1 | ||||||
| Projects in progress |
0.9 | — | ||||||
|
|
|
|
|
|||||
| Property and equipment, gross |
31.8 | 13.2 | ||||||
| Less: Accumulated depreciation and amortization |
(12.5 | ) | (6.2 | ) | ||||
|
|
|
|
|
|||||
| Property and equipment, net |
$ | 19.3 | $ | 7.0 | ||||
|
|
|
|
|
|||||
Depreciation and amortization expense for property and equipment, inclusive of amounts subsequently written off or disposed from accumulated depreciation, was $6.8 and $6.3 for the years ended December 31, 2019 and 2018, respectively. There was no impairment of property and equipment during the year ended December 31, 2019. We incurred an asset impairment charge of $1.0 on property and equipment that was no longer being used for the year ended December 31, 2018. This expense is included in asset impairment on the Combined-Consolidated Statements of Operations. During the year ended December 31, 2019, we sold approximately $0.3 in property and equipment, included in the gain as discussed in Note 5 Variable Interest Entities.
| 8. | Goodwill |
The change in the carrying amount of goodwill for each reporting segment is as follows:
| Home & Community Services |
Episodes of Care Services |
Total | ||||||||||
| Balance at January 1, 2018 |
$ | 122.2 | $ | — | $ | 122.2 | ||||||
| Measurement period adjustments |
0.3 | — | 0.3 | |||||||||
|
|
|
|
|
|
|
|||||||
| Balance at December 31, 2018 |
$ | 122.5 | $ | — | $ | 122.5 | ||||||
| Business combinations |
47.9 | 408.4 | 456.3 | |||||||||
|
|
|
|
|
|
|
|||||||
| Balance at December 31, 2019 |
$ | 170.4 | $ | 408.4 | $ | 578.8 | ||||||
|
|
|
|
|
|
|
|||||||
The measurement period adjustment of $0.3 during the year ended December 31, 2018 relates to an adjustment of the assumed deferred tax liability and goodwill resulting from obtaining the final information regarding the tax obligation that existed at the time of the 2017 acquisition of Advance Health.
There was no impairment related to goodwill during the years ended December 31, 2019 or 2018.
F-62
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
| 9. | Intangible Assets |
As of December 31, 2019 and 2018, intangible assets were as follows:
| December 31, 2019 | December 31, 2018 | |||||||||||||||||||||||||||
| Estimated Useful Life (years) |
Gross Carrying Amount |
Accumulated amortization |
Net Carrying Value |
Gross Carrying Amount |
Accumulated amortization |
Net Carrying Value |
||||||||||||||||||||||
| Customer relationships |
3 - 20 | $ | 530.5 | $ | (56.7 | ) | $ | 473.8 | $ | 412.0 | $ | (21.2 | ) | $ | 390.8 | |||||||||||||
| Acquired and capitalized software |
3 - 6 | 91.6 | (36.9 | ) | 54.7 | 29.7 | (14.5 | ) | 15.2 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Total |
$ | 622.1 | $ | (93.6 | ) | $ | 528.5 | $ | 441.7 | $ | (35.7 | ) | $ | 406.0 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
We capitalized $12.9 and $6.5 of internally-developed software costs for the years ended December 31, 2019 and 2018, respectively.
Amortization expense for intangible assets, inclusive of amounts subsequently written off from accumulated amortization, was $59.2 and $36.7 for the years ended December 31, 2019 and 2018, respectively. Expected amortization expense related to intangible assets, including internal-use software development costs, for years subsequent to December 31, 2019 was as follows:
| 2020 |
$ | 51.7 | ||
| 2021 |
51.2 | |||
| 2022 |
43.3 | |||
| 2023 |
41.0 | |||
| 2024 |
32.4 | |||
| thereafter |
308.9 | |||
|
|
|
|||
| $ | 528.5 | |||
|
|
|
We recorded an asset impairment charge on a trade name during the year ended December 31, 2019 as a result of the discontinued use of certain trade names due to our rebranding which was announced in December 2019. We performed a quantitative test comparing the fair value of the trade name, as determined by projected cash flows, with the carrying amount. As future cash flows associated with the trade names were zero, we recorded an asset impairment charge of $4.9 for the year ended December 31, 2019, which is included in asset impairment on the Combined-Consolidated Statements of Operations.
We also recorded an asset impairment charge of $1.5 related to certain acquired and capitalized software during the year ended December 31, 2019 as a result of the discontinued use of the software. This is included in asset impairment on the Combined-Consolidated Statements of Operations.
We recorded an asset impairment charge on trade names during the year ended December 31, 2018 as a result of the discontinued use of certain trade names due to our rebranding in 2018. We performed a quantitative test comparing the fair value of the trade names, as determined by projected cash flows, with the carrying amount. As future cash flows associated with the trade names were zero, we recorded an asset impairment charge of $16.0 during the year ended December 31, 2018, which is included in asset impairment on the Combined-Consolidated Statements of Operations.
F-63
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
| 10. | Accounts Payable and Accrued Liabilities |
Accounts payable and accrued liabilities consist of the following:
| December 31, | ||||||||
| 2019 | 2018 | |||||||
| Shared savings payable |
$ | 58.2 | $ | — | ||||
| Accrued payroll and payroll-related expenses |
33.0 | 18.8 | ||||||
| Other accrued expenses |
12.4 | 6.3 | ||||||
| Accounts payable |
3.5 | 1.6 | ||||||
|
|
|
|
|
|||||
| Total accounts payable and accrued liabilities |
$ | 107.1 | $ | 26.7 | ||||
|
|
|
|
|
|||||
| 11. | Long-Term Debt |
Our long-term debt was as follows at December 31, 2019 and 2018:
| December 31, | ||||||||
| 2019 | 2018 | |||||||
| Revolving credit facility |
$ | — | $ | — | ||||
| Term loan |
275.3 | 258.1 | ||||||
|
|
|
|
|
|||||
| Total debt |
275.3 | 258.1 | ||||||
| Unamortized debt issuance costs |
(5.9 | ) | (6.4 | ) | ||||
| Unamortized discount on debt |
(2.0 | ) | (2.2 | ) | ||||
|
|
|
|
|
|||||
| Total debt, net |
267.4 | 249.5 | ||||||
| Less current maturities of long-term debt |
(2.8 | ) | (2.6 | ) | ||||
|
|
|
|
|
|||||
| Total long-term debt |
$ | 264.6 | $ | 246.9 | ||||
|
|
|
|
|
|||||
On December 21, 2017, in conjunction with the acquisition of Censeo and Advance, as described in Note 1 Nature of Operations, Cure Borrower entered into a Credit Agreement (the “Credit Agreement”) with an unaffiliated secured lender syndicate. Under the Credit Agreement, Cure Borrower incurred a term loan of $260.0 (the “Term Loan”) and a revolving credit facility (the “Revolving Facility”) with a $35.0 borrowing capacity, which could also be used to obtain letters of credit up to $5.0. The maturity date of the Term Loan is December 21, 2024 and the maturity date of the Revolving Facility is December 21, 2022. Cure Borrower is required to make amortization payments of 0.25% of the aggregate principal amount of the Term Loan, payable on a quarterly basis.
On December 9, 2019, Cure Borrower amended its Credit Agreement to increase the borrowing capacity under the Revolving Facility to $80.0.
The Credit Agreement is collateralized by substantially all of the assets of Cure Borrower and its subsidiaries. The Term Loan and Revolving Facility both have the option of being drawn at the Base Rate plus 3.50% or the Eurocurrency Rate plus 4.50%, subject to two 0.25% stepdowns in the case of the Revolving Facility based on the applicable Consolidated First Lien Net Leverage Ratio. At December 31, 2019 and 2018, the effective interest rate on borrowings was 6.44% and 6.89%, respectively.
The Credit Agreement is subject to certain financial and nonfinancial covenants, including a defined Consolidated First Lien Net Leverage Ratio applicable solely to the Revolving Facility. The term loan requires an excess cash flow (“ECF”) payment commencing with and including the period ended
F-64
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
December 31, 2018. The prior year’s ECF payment is due within 10 business days after financial statements have been delivered. As our Consolidated First Lien Net Leverage Ratio was below the threshold requiring an ECF payment, there was no ECF payment due in 2019 or 2020. In addition, the Credit Agreement includes negative covenants which restrict Cure Borrower and its subsidiaries’ ability, among other things, to incur indebtedness, grant liens, make investments, sell or otherwise dispose of assets or enter into a merger, pay dividends or repurchase stock. As of December 31, 2019, the amount of Cure Borrower and its subsidiaries’ net assets restricted from transfer to the Company was zero as a result of the Remedy Partners Combination which allowed for the ability to make certain payments for up to one year following the Remedy Partners Combination in excess of the normal restrictions. This additional capacity on restricted payments will expire on the one-year anniversary of the Remedy Partners Combination, at which time, a significant portion of Cure Borrower and its subsidiaries’ net assets may be deemed restricted. Cure TopCo, LLC, the parent, has no stand-alone operations, including no cash or assets; its only activities relate to owning a controlling interest in its subsidiaries and the issuances of equity as described in Note 14 Members’ Equity. Cure Borrower did not make any distributions to the parent during December 31, 2019 or 2018. As of December 31, 2019 and 2018, we were in compliance with all financial covenants.
On June 22, 2018, we amended the Credit Agreement to reduce the interest rates applicable to the term loan and revolving credit facility. Specifically, the amendment decreased the applicable Eurocurrency Rate Loan percentage and Base Rate percentage for the various pricing levels. As a result of the amendment, certain lenders were extinguished and replaced with additional term lenders, and we extinguished related deferred financing fees in the amount of $1.4 for the year ended December 31, 2018, which is included in interest expense on the Combined-Consolidated Statements of Operations for the year ended December 31, 2018.
On March 12, 2019, we drew $20.0 from the revolver for the purpose of acquiring Triple Aim Ventures, LLC. On April 23, 2019, the $20.0 was converted to an Incremental Term Loan (as defined under the Credit Agreement) as allowed under the terms of the Credit Agreement. Such Incremental Term Loan is due December 21, 2024. As a result of the Incremental Term Loan, certain lenders were extinguished and replaced with additional term lenders, and we extinguished related deferred financing fees in the amount of $0.2, which is included in interest expense on the Combined-Consolidated Statements of Operations for the year ended December 31, 2019.
As of December 31, 2019, aggregate principal maturities of long-term debt for each of the next five years ending December 31 and thereafter are as follows:
| 2020 |
$ | 2.8 | ||
| 2021 |
2.8 | |||
| 2022 |
2.8 | |||
| 2023 |
2.8 | |||
| 2024 |
264.1 | |||
|
|
|
|||
| $ | 275.3 | |||
|
|
|
F-65
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
| 12. | Fair Value Measurements |
Assets and liabilities measured at fair value on a recurring basis were as follows as of December 31, 2019 and 2018:
| December 31, 2019 | ||||||||||||||||||
| Balance Sheet Classification |
Type of Instrument |
Level 1 | Level 2 | Level 3 | Total | |||||||||||||
| Cash equivalents |
Money market funds |
$ | 11.1 | $ | — | $ | — | $ | 11.1 | |||||||||
| Contingent consideration |
Consideration due to sellers |
$ | — | $ | — | $ | 39.8 | $ | 39.8 | |||||||||
| December 31, 2018 | ||||||||||||||||||
| Balance Sheet Classification |
Type of Instrument |
Level 1 | Level 2 | Level 3 | Total | |||||||||||||
| Cash equivalents |
Money market funds |
$ | 3.0 | $ | — | $ | — | $ | 3.0 | |||||||||
| Contingent consideration |
Consideration due to sellers |
$ | — | $ | — | $ | 39.1 | $ | 39.1 | |||||||||
There were no transfers between Level 1 and Level 2, or into or out of Level 3 during the year ended December 31, 2018.
The changes in Level 3 liabilities measured at fair value on a recurring basis were as follows for the years ended December 31, 2019 and 2018:
| Balance at December 31, 2017 |
$ | 38.2 | ||
| Remeasurement of contingent consideration included in selling, general and administrative expense |
0.9 | |||
|
|
|
|||
| Balance at December 31, 2018 |
$ | 39.1 | ||
| Remeasurement of contingent consideration included in selling, general and administrative expense |
0.7 | |||
|
|
|
|||
| Balance at December 31, 2019 |
$ | 39.8 | ||
|
|
|
The valuation techniques and significant unobservable inputs used in recurring Level 3 fair value measurements were as follows for the years ended December 31, 2019 and 2018:
| Fair Value | Valuation Technique | Significant Unobservable Inputs |
Discount Rate |
|||||||||
| Consideration due to sellers |
$ | 39.8 | Discounted approach | Discount Rate |
2.3 | % | ||||||
The fair value of our debt is measured at Level 3 and is determined based on fluctuations in current interest rates, the trends in market yields of debt instruments with similar credit ratings, general economic conditions and other quantitative and qualitative factors. The carrying value of our debt approximates its fair value.
The carrying amounts of accounts receivable and accounts payable approximate their fair value because of the relatively short-term maturity of these instruments.
F-66
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
| 13. | Employee Benefit Arrangements |
We provide two 401(k) retirement savings plans to eligible employees whereby each match 50% of every dollar contributed up to 6% of an employee’s compensation and, under certain plans, may also make profit sharing contributions at our discretion. For the year ended December 31, 2019, we incurred total contribution expense of $3.4, of which $1.6 is included in service expense and $1.8 is included in SG&A expense on the Combined-Consolidated Statements of Operations.
In 2018, we provided various 401(k) savings plans to eligible employees whereby we matched either 100% of every dollar contributed up to 3% plus 50% of every dollar contributed up to an additional 2% of an employee’s compensation or we matched 50% of every dollar contributed up to 6% of an employee’s compensation and could also make profit sharing contributions at our discretion. For the year ended December 31, 2018, we incurred total contribution expense of $2.8, of which $1.1 is included in service expense and $1.7 is included in SG&A expense on the Combined-Consolidated Statements of Operations.
| 14. | Member’s Equity |
Membership Units
In connection with the Remedy Partners Combination, our limited liability agreement (“LLC Agreement”) was amended and restated to authorize five classes of equity membership interests in us that are represented by Units: Series A Preferred Units, Series B Preferred Units, Class A Common Units, Class B Common Units, and Class C Common Units. In connection with the consummation of the Remedy Partners Combination, each outstanding Class A Common Unit that was outstanding prior to the Remedy Partners Combination was converted into a Series B Preferred Unit on a one-for-one basis and each Class B Common Unit remained outstanding. Also, in connection with the Remedy Partners Combination, 3,384,543 Series A Preferred Units were issued to New Remedy Corp in exchange for the contribution of $698.3 in net assets and tax attributes to us.
We had 3,384,543 units of Series A preferred Units and 3,533,133 units of Series B preferred units outstanding as of December 31, 2019. We had zero Class A common units, 93,311 Class B common units and zero Class C common units outstanding as of December 31, 2019.
The Series A Preferred Units have voting rights, being entitled to one vote per Series A Preferred Unit and have rights with respect to our profits and losses and distributions from us as set forth in our LLC Agreement. In the context of a liquidation or similar event, the Series A Preferred Units have a preference over other classes of Units in certain circumstances, including, in certain circumstances, over the Series B Preferred Units. The preference with respect to the Series A Preferred Units is subject to forfeiture in certain scenarios based on the financial performance of Remedy Partners’ business and also in connection with an initial public offering of us or our successor entity. We did not make any tax or non-tax distributions on behalf of members holding Series A Preferred Units for the year ended December 31, 2019.
The Series B Preferred Units have voting rights, being entitled to one vote per Series B Preferred Unit, and have rights with respect to our profits and losses and distributions from us as set forth in our LLC Agreement. In the context of a liquidation or similar event, the Series B Preferred Units have a preference over other classes of Units, including, in certain circumstances, over the Series A Preferred Units. The preference with respect to the Series B Preferred Units is subject to forfeiture in certain scenarios based on the financial performance of Signify Health, LLC’s business and also in connection with an initial public offering us or our successor entity. We made tax distributions of $21.8 and $18.3 on behalf of members holding Series B Preferred Units (formerly Class A Common Units) for the years ended December 31, 2019
F-67
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
and 2018, respectively. We did not make any non-tax distributions on behalf of members holding Series B Preferred Units for the year ended December 31, 2019.
The Class A Common Units have voting rights, being entitled to one vote per Class A Common Unit, and have rights with respect to our profits and losses and distributions as set forth in our LLC Agreement. As of December 31, 2019, there were no Class A Common Units issued or outstanding.
The Class B Common Units have no voting rights and are intended to be treated as profits interests for federal income tax purposes. Class B Common Units are issued from time to time to be held by Cure Aggregator, LLC, a member of our company, on behalf of our employees and other service providers in connection with their respective performance of services for our benefit as designated by our Board of Directors or Compensation Committee. All Class B Common Units are issued pursuant to an award agreement that sets forth a distribution threshold in an amount intended for such Class B Common Units to qualify as profits interests for federal income tax purposes and vesting terms determined by our Board of Directors or Compensation Committee. The distribution thresholds and vesting terms of the Class B Common Units described above were not modified in connection with the Remedy Partners Combination. We made tax distributions in the amount of $0.7 on behalf of members holding Class B Common Units for the year ended December 31, 2019.
The Class C Common Units have no voting rights and are intended to be treated as profits interests for federal income tax purposes. Class C Common Units are issued from time to time to be held by Cure Aggregator, LLC, a holding member of our company, on behalf of our employees and other service providers in connection with their respective performance of services for our benefit as designated by our Board of Directors or Compensation Committee. All Class C Common Units are issued pursuant to an award agreement that sets forth a distribution threshold in an amount intended for such Class C Common Units to qualify as profits interests for federal income tax purposes and vesting terms determined by our Board of Directors or Compensation Committee. As of December 31, 2019, no Class C Common Units had been granted by our Board of Directors or Compensation Committee.
During the year ended December 31, 2019 and 2018, we repurchased 18,762 and 37,525 Former Class A Common Units for $2.4 and $5.0, respectively, related to the termination of two former executives. These repurchases were made at amounts that exceeded the estimated fair market value by approximately $0.4 and $0.9 during the years ended December 31, 2019 and 2018, respectively. This excess over fair market value is included in transaction-related expenses in the Combined-Consolidated Statements of Operations during the respective period.
Incentive Unit Awards and Equity-Based Compensation
In accordance with the LLC Agreement, our Board of Directors may grant awards of Class B Common Units and Class C Common Units for the benefit of key employees and service providers. The Board and/or Compensation Committee has approved equity-based awards with time-based and performance-based vesting criteria.
Awards of Class B Common Units and Class C Common Units are intended to be profits interest units for federal income tax purposes as described above. Awards with time-based vesting generally vest over time either on the grant date anniversary or on December 31 of each year. For those awards with performance-based vesting, the performance condition stipulates that in order for awards to vest, the total cash on cash return of the private equity owners as defined in the award agreement must exceed certain multiples set forth in the award agreement. The performance-based vesting condition is not probable as assessed at each reporting period; therefore, compensation expense related to these awards (or portions thereof) has not been
F-68
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
recognized. As of December 31, 2019, no Class C Common Units had been granted by our Board of Directors or Compensation Committee.
Grant date fair value of awards of Class B Common Units are estimated based on a Monte Carlo option pricing simulation. The equity value of the enterprise represents a key input for determining the fair value of the Class B Common Units. A discount for lack of marketability was applied to the per unit fair value to reflect increased risk arising from the inability to readily sell the Class B Common Units. The estimated fair values for awards granted during the years ended December 31, 2019 and 2018 included the following weighted average assumptions (annualized percentages):
| 2019 | 2018 | |||
| Expected volatility |
40.6% - 50.6% | 48.8% - 58.8% | ||
| Expected dividend yield |
— | — | ||
| Risk-free interest rate |
1.8% | 2.6% | ||
| Expected life (years) |
3.5 | 4.6 |
The following table summarizes our Class B Common Unit activity for the years ended December 31, 2019 and 2018:
| Profits Interest Units |
Weighted Avg. Grant Date FMV |
|||||||
| Outstanding at January 1, 2018 |
— | |||||||
| Granted |
530,750 | $ | 46.95 | |||||
| Forfeited |
(77,500 | ) | $ | 39.60 | ||||
|
|
|
|||||||
| Outstanding at December 31, 2018 |
453,250 | $ | 48.21 | |||||
| Granted |
80,824 | $ | 73.81 | |||||
| Forfeited |
(42,185 | ) | $ | 51.45 | ||||
| Cancelled |
(50 | ) | $ | 49.66 | ||||
| Repurchased |
(10,300 | ) | $ | 45.68 | ||||
|
|
|
|||||||
| Outstanding at December 31, 2019 |
481,539 | $ | 52.28 | |||||
During the years ended December 31, 2019 and 2018, we recognized $3.0 and $2.6, respectively, of equity-based compensation expense related to awards of Class B Common Units. Of this amount, $0.5 and $0.1 were included in service expense and $2.5 and $2.5 were included in SG&A expense on the Combined-Consolidated Statements of Operations for the years ended December 31, 2019 and 2018, respectively. As of December 31, 2019, there was $6.1 of total unrecognized compensation expense related to unvested equity-based compensation arrangements expected to be recognized over a weighted average period of 1.25 years. Additionally, there was approximately $14.0 of unrecognized compensation expense related to equity-based awards with performance-based vesting, in which the vesting conditions are not probable of occurring as of December 31, 2019. The grant date fair value of units that vested during the years ended December 31, 2019 and 2018 were $2.8 and $2.4, respectively.
Stock Options in New Remedy Corp
Remedy Partners maintained an equity incentive plan whereby certain employees and directors were granted stock options. In November 2019, at the time of the Remedy Partners Combination, outstanding Remedy Partners stock options were converted to stock options in New Remedy Corp. No additional stock option grants will be made following the Remedy Partners Combination. During the year ended December 31,
F-69
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
2019, we recorded approximately $1.5 in share-based compensation expense included in SG&A expense on the Combined-Consolidated Statements of Operations related to outstanding stock options held by certain of our employees. As of December 31, 2019, there was approximately $6.9 of total unrecognized compensation expense related to unvested time-based stock options expected to be recognized over a weighted average period of 1.7 years. Additionally, there was approximately $2.9 of unrecognized compensation expense related to outstanding stock options with performance-based vesting, in which the vesting conditions are not probable of occurring as of December 31, 2019. As the underlying stock is in New Remedy Corp, the offset to the equity-based compensation expense is included in capital contributions on the Combined-Consolidated Statements of Changes in Members’ Equity.
| 15. | Loss Per Unit |
For the year ended December 31, 2018, basic loss per unit is computed by dividing the net loss by the weighted average number of Class A and Class B common units outstanding during the period. There were no potentially dilutive securities in 2018 and therefore, the basic and diluted loss per unit have been presented together. Common units in 2018 consisted of former Class A common units and Class B common units.
For the year ended December 31, 2019, net loss per unit is computed using the “two-class” method prior and subsequent to the Remedy Partners Combination; however, subsequent to the Remedy Partners Combination, five classes of member units are issued or available to be issued compared to two classes of member units prior to the transaction. There were no Class A common units or Class C common units issued as of December 31, 2019. The five classes of member units became legally authorized as of the Remedy Partners Combination on November 26, 2019. Therefore, net losses in 2019 up until November 26, 2019 were attributed to the former Class A common units and Class B common units. The pre-Remedy Partners Combination net losses include the losses of Remedy Partners as our combined-consolidated statement of operations is presented under common control provisions. Therefore, the losses of Remedy Partners prior to the Remedy Partners Combination are being allocated to the former Class A common and Class B common units outstanding up until the Combination date, as those were the only legally outstanding member units of the Company. Subsequent to the Remedy Partners Combination date, net losses were attributable to the Series A preferred units, the Series B preferred units and the Class B common units. There were no potentially dilutive securities in 2018 and 2019 and therefore, the basic and diluted loss per unit have been presented together.
Loss per unit in 2018 is computed as follows:
| Net loss attributable to unitholders: |
||||
| Class A Common Units and Class B Common Units |
$ | (28.9 | ) | |
| Weighted average outstanding units: |
||||
| Class A Common Units and Class B Common Units |
3,421,451 | |||
| Basic and Diluted net loss per unit attributable to unitholders: |
||||
| Class A Common Units and Class B Common Units |
$ | (8.44 | ) |
F-70
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Loss per unit in 2019 is computed as follows:
| Net loss attributable to unitholders: |
||||
| Former Class A Common Units and Class B Common Units (pre-Remedy Partners Combination) |
$ | (16.4 | ) | |
| Series A Preferred Units |
(5.6 | ) | ||
| Series B Preferred Units and Class B Common Units (post-Remedy Partners Combination) |
(6.5 | ) | ||
| Weighted average outstanding units: |
||||
| Former Class A Common Units and Class B Common Units (pre-Remedy Partners Combination) |
3,211,075 | |||
| Series A Preferred Units |
324,545 | |||
| Series B Preferred Units and Class B Common Units (post-Remedy Partners Combination) |
343,320 | |||
| Basic and Diluted net loss per unit attributable to unitholders: |
||||
| Former Class A Common Units |
$ | (5.10 | ) | |
| Series A Preferred Units |
(17.18 | ) | ||
| Series B Preferred Units and Class B Common Units |
(19.13 | ) |
| 16. | Transaction-related Expenses |
In 2019, we incurred $22.4 of transaction-related expenses related to the acquisition and integration of Remedy Partners, the Remedy Partners Combination, the TAV Health acquisition as well as certain acquisitions made in prior years. These transaction-related expenses related to consulting, compensation and integration-type expenses.
In 2018, we incurred $21.0 of transaction-related expenses related to acquisitions made in 2017. These transaction-related expenses related to consulting, compensation and integration-type expenses.
Included within the compensation expense amounts above for both years ended December 31, 2019 and 2018 is severance related to an approved plan by our board of directors. The following table summarizes the approved severance activity for the years ended December 31, 2019 and 2018.
| Balance at January 1, 2018 |
$ | — | ||
| Severance and related costs |
2.4 | |||
| Cash payments |
(0.7 | ) | ||
|
|
|
|||
| Balance at December 31, 2018 |
$ | 1.7 | ||
| Severance and related costs |
1.6 | |||
| Cash payments |
(2.1 | ) | ||
|
|
|
|||
| Balance at December 31, 2019 |
$ | 1.2 | ||
|
|
|
As of December 31, 2019, amounts expected to be paid under approved severance plans of $1.2 was included in accounts payables and accrued expenses in the Consolidated Balance Sheet.
F-71
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
| 17. | Commitments and Contingencies |
Lease Commitments
We are obligated as lessee under certain non-cancellable operating leases. As of December 31, 2019, future minimum lease payments under non-cancellable operating leases were as follows:
| 2020 |
$ | 7.0 | ||
| 2021 |
8.0 | |||
| 2022 |
7.0 | |||
| 2023 |
5.3 | |||
| 2024 |
4.6 | |||
| Thereafter |
17.9 | |||
|
|
|
|||
| $ | 49.8 | |||
|
|
|
Total rent expense associated with non-cancellable operating leases was $6.3 and $3.6 for the years ended December 31, 2019 and 2018, respectively, and was included within SG&A expenses on the Combined-Consolidated Statements of Operations.
Letters of Credit
As of December 31, 2019, we have outstanding letters of credit totaling $9.2 in favor of CMS which is required in the event of a negative outcome on certain episodes of care within the BPCI-A program and we do not settle the related amounts owed to CMS. However, the terms of BPCI-A also require that certain partners provide a related reciprocal letter of credit to us for the majority of this amount. As of December 31, 2019, we have three related letters of credit in our favor totaling $8.8.
Contingencies
Liabilities for loss contingencies arising from claims, assessments, litigation, fines, penalties and other sources are recorded when it is probable a liability has been incurred and the amount of the liability can be reasonably estimated. We are involved in various lawsuits, claims and administrative proceedings arising in the normal course of business. In management’s opinion, the ultimate resolution of these matters will not materially adversely affect our financial position, results of operations or cash flows.
On March 12, 2019, a Complaint was filed against us by Dr. Mohammad A. Gharavi, in the Superior Court, State of California, San Bernardino County. The claim was a wage and hour class action of all California contracted physicians from March 12, 2015 through the present and ongoing. The Complaint alleges that these physicians should have been classified as employees. The class action was settled for $1.2 at mediation in January 2020. This amount is included in other current liabilities on the Consolidated Balance Sheet at December 31, 2019. Payment will not be made until the Court has approved the settlement, which is expected to occur in the fourth quarter of 2020.
Sales Tax Reserve
During the year ended December 31, 2019, it was determined that certain Episodes of Care Services may be subject to sales tax in certain jurisdictions. Historically, we have not collected sales tax from our Episodes of Care Services customers as we believed the services were not taxable. As of December 31, 2019, we have recorded a liability of $6.5 for potential sales tax exposure related to services performed in 2016 through 2019, included in other current liabilities on the Consolidated Balance Sheets.
F-72
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Equity Appreciation Rights
In December 2019, we entered into an equity appreciation fee right agreement (“EAR”) with a customer, which contains the following provisions: 1) commits the customer to purchase a minimum amount of services from one of our wholly-owned indirect operating subsidiaries for three years in accordance with specific terms and conditions and 2) granted the customer a contingent EAR. The EAR agreement allows for the customer to participate in the future growth in the fair market value of our equity and can only be settled in cash (or, under certain circumstances, in whole or in part with a replacement agreement that mimics the economics of the original EAR agreement) upon change in our control, other liquidity event, or upon approval of our Board of Directors with consent by New Mountain Capital with certain terms and conditions. The EAR will expire in 20 years from the date of grant, if not previously settled. As of December 31, 2019, the EAR is being accounted for as a contingent contract liability instrument. We did not recognize an expense associated with the EAR for the year ended December 31, 2019 as cash settlement is not considered probable, due to the changes in control and liquidity provisions of the EAR. We adopted new accounting guidance in early 2020, which results in the initial fair value of the EAR being recorded as a reduction of revenue and subsequent changes in fair value being recorded as other income (expense), net. Although the initial EAR agreement was executed in December 2019, the service period did not begin until 2020 and, therefore, there was no impact on our results of operations until 2020.
Contingent Consideration
On December 21, 2017, we acquired 100% of the outstanding equity of Censeo. The purchase price included contingent consideration with a fair value of $39.8 and $39.1 as of December 31, 2019 and 2018, respectively. The contingent consideration will require us to pay up to an additional $40.0 to selling shareholders of Censeo, pending the resolution of an examination by the IRS regarding the classification of certain independent contractors. If the IRS determines Censeo must employ any portion of its independent contractors prospectively, the incremental costs of such employment, multiplied by a factor of eight, will be deducted from the $40.0 to determine the remaining amount due to the selling shareholders under the acquisition agreement.
On February 11, 2019, we received a proposed assessment of employment taxes from the IRS in the amount of $5.5 related to tax year 2014. The assessment is based on the IRS’s position that all of Censeo’s service providers who performed health assessments during 2014 should have been classified as employees instead of independent contractors. We appealed this determination. There was no change to the fair value of the contingent liability due to this proposed assessment for the years ended December 31, 2018 or 2019.
In March 2020, we received verbal confirmation from the IRS that we will prevail in the case. The IRS is expected to formally close the matter once they resume normal operations following the COVID-19 crisis (See Note 22 Subsequent Events). We expect to make payment of the full $40.0 to the selling shareholders, some of whom are also affiliated with and/or equity holders, within 12 months following the formal IRS conclusion of the matter (See Note 22 Subsequent Events).
| 18. | Income Taxes |
Income tax expense for the years ended December 31, 2019 and 2018 was $0.1 and $0.2, respectively, and consists of current state and local taxes. We have no deferred tax assets or liabilities as of December 31, 2019 or 2018.
F-73
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
Uncertain Tax Provisions
We recognize the impact of uncertain tax positions taken or expected to be taken on an income tax return in the financial statements at the amount that is more likely than not to be sustained upon audit by the relevant taxing authority. An uncertain tax position will not be recognized unless it is more likely than not to be sustained. We have evaluated our tax positions and have not identified any material uncertain tax positions that would not be sustained in federal or state income tax examination or that require disclosure. Accordingly, no provision for uncertainties in income taxes has been made in the accompanying Combined-Consolidated Financial Statements at December 31, 2019.
| 19. | Segment Reporting |
Operating segments are components of an enterprise for which separate financial information is available and evaluated regularly by our Chief Operating Decision Maker in deciding how to allocate resources and in assessing financial performance. Management views our operating performance in two reportable segments: Home & Community Services and Episodes of Care Services.
We evaluate the performance of each segment based on segment revenue and segment adjusted EBITDA. The operating results of the reportable segment are based on segment adjusted EBITDA, which includes revenue and expenses incurred by the segment, as well as an allocation of shared expenses. Shared expenses are generally allocated to each segment based on the segments’ proportionate employee headcount. Certain costs are not allocated to the segments, as described below, as these items are not considered in evaluating the segment’s overall performance.
See Note 6 Revenue Recognition for a summary of segment revenue by product type for the years ended December 31, 2019 and 2018. Our operating segment results for the periods presented were as follows:
| Year ended December 31, | ||||||||
| 2019 | 2018 | |||||||
| Revenue |
||||||||
| Home & Community Services |
$ | 377.0 | $ | 310.0 | ||||
| Episodes of Care Services |
124.8 | 27.9 | ||||||
| Segment Adjusted EBITDA |
||||||||
| Home & Community Services |
90.5 | 76.1 | ||||||
| Episodes of Care Services |
2.8 | 3.0 | ||||||
| Less: reconciling items to net loss: |
||||||||
| Unallocated costs (1) |
34.5 | 43.4 | ||||||
| Depreciation and amortization |
66.0 | 43.0 | ||||||
| Interest expense |
21.2 | 21.4 | ||||||
|
|
|
|
|
|||||
| Loss before income taxes |
$ | (28.4 | ) | $ | (28.7 | ) | ||
|
|
|
|
|
|||||
| (1)Unallocated costs as follows: |
||||||||
| Asset impairment |
6.4 | 17.0 | ||||||
| Other income, net |
(1.6 | ) | — | |||||
| Equity-based compensation |
4.5 | 2.6 | ||||||
| Transaction-related expenses |
22.4 | 21.0 | ||||||
| Non-allocated costs (2) |
2.8 | 2.8 | ||||||
|
|
|
|
|
|||||
| Total unallocated costs |
$ | 34.5 | $ | 43.4 | ||||
|
|
|
|
|
|||||
F-74
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
| (2) | Non-allocated costs include remeasurement of contingent consideration, management fees paid to our capital partner and certain non-recurring expenses, including those associated with the closure of certain facilities, the sale of certain assets and the early termination of certain contracts. These costs are not considered by our Chief Operating Decision Maker in making resource allocation decisions. |
Our Chief Operating Decision Maker does not receive or utilize asset information to evaluate performance of operating segments. Accordingly, asset-related information has not been presented.
| 20. | Concentrations |
During the normal course of operations, we maintain cash in bank accounts which exceed federally insured amounts. We have not experienced any losses in such accounts and do not believe we are exposed to any significant credit risk related to cash.
Accounts receivable potentially subject us to concentrations of credit risk. Management believes that its contract acceptance, billing and collection policies are adequate to minimize potential credit risk. We continuously evaluate the credit worthiness of our customers’ financial condition and generally do not require collateral.
We are dependent on a concentrated number of payors and provider partners with whom we contract to provide IHEs and other services. A significant portion of our revenues are generated from a small number of customers. For the year ended December 31, 2019, we have two customers which accounted for approximately 23% and 21%, respectively, of revenues. In addition, the revenue from our top ten customers accounted for approximately 74% of our total revenue for the year ended December 31, 2019. No customer accounted for greater than 10% of accounts receivable as of December 31, 2019. For the year ended December 31, 2018, we had two customers which accounted for approximately 27% and 21% of revenues. As of December 31, 2018, three customers accounted for approximately 20%, 11% and 10%, respectively, of accounts receivable.
While CMS is not our customer, a majority of the revenue generated by Episodes of Care Services is under the CMS administered BPCI-A program and payments are received under this program in certain cases from CMS rather than directly from the customer. During the year ended December 31, 2019, approximately 20% of total combined-consolidated revenue was generated from the BPCI-A program. As of December 31, 2019, approximately 59% of the total accounts receivable was due from CMS related to payments expected to be received by us under the BPCI-A program.
| 21. | Related Party Transactions |
We are subject to a Management Services Agreement whereby we paid our capital partners an annual advisory fee of $1.0 beginning in 2018. As 100% of Cure Borrower’s income is derived from our operations, these amounts are expensed as incurred by us. During each of the years ended December 31, 2019 and 2018, $1.0 of expense was recorded and included in SG&A expenses in the Combined-Consolidated Statements of Operations related to these services. The Management Services Agreement was terminated in connection with the consummation of the Remedy Partners Combination.
On April 17, 2019, we issued a note receivable to our Chief Executive Officer for $2.0 with simple interest accruing at a rate of 2.52% per annum and included in other expense (income), net on the Combined-Consolidated Statements of Operations. In December 2019, the outstanding principal and an insignificant amount of accrued interest under the note was repaid in full. There are no other outstanding amounts.
F-75
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
On March 7, 2019, we entered into a consulting agreement with Brett Carlson, a director, which currently provides for $0.2 annually (payable monthly) in compensation for consulting services provided to us. In the event that we complete a corporate transaction in which we acquire all of the equity interests or all or substantially all of the assets of a company in our industry referred and introduced to us by Mr. Carlson, Mr. Carlson will be eligible to receive a cash transaction fee of 3% of any deal consideration up to $10 million, plus an additional 1.5% on any incremental deal consideration above $10 million.
We also have a consulting agreement with Kevin McNamara, a director, which currently provides for $0.2 annually (payable monthly) in compensation for consulting services provided to us. In addition, Mr. McNamara is entitled to reimbursement for annual premiums on life, accidental death and dismemberment, short-term disability and medical insurance.
| 22. | Subsequent Events |
We performed an evaluation of subsequent events through April 29, 2020, the date the financial statements were available to be issued. We updated such evaluation for disclosure purposes through October 19, 2020, the date on which the revised financial statements were reissued.
On February 14, 2020, the Board of Directors adopted a Synthetic Equity Plan (“SEP”) that provides for cash payments upon the satisfaction of certain criteria. The synthetic equity units granted under the SEP are subject to time and performance vesting and are paid out upon a change in control (as defined in the SEP) based upon the difference in the value of the Company at the time of the change in control event and a “floor amount”.
During the first quarter of 2020, the COVID-19 outbreak rapidly evolved. In the Home & Community Services segment, in-home health evaluations were only moderately impacted during the first quarter of 2020. However, at the end of the first quarter of 2020, we temporarily suspended conducting in-home health evaluations. At the same time, we launched a new service, offering health plan customers a “virtual” health assessment (“vIHE”) to be supplemented, where possible, with a confirmatory in-home health evaluation later in the year. Certain of our Home & Community Services health plan customers agreed to this new service, which we began providing on April 2, 2020. CMS provided temporary approval of this service in early April 2020. We also developed a number of new product offerings in support of the crisis, such as workplace screening and testing, which we quickly operationalized and began offering to employers as an additional service in early April 2020. As a result of these actions, more than 90% of health evaluations during the second quarter 2020 were vIHEs. In July 2020, we began to return to in-home health assessments. For the third quarter of 2020, the number of health risk assessments that were being performed on an in-home basis, had returned to historic levels. We established personal protective equipment protocols with our major customers in order to achieve this return to in-home assessments. We, together with our customers, continue to monitor the changing situation with COVID-19 cases on a state-by-state basis.
Within the Episodes of Care Services segment, we observed some evidence of reduced volumes of episodes of care as a result of the cancellation of elective surgeries in the final two weeks of the first quarter of 2020. Due to the nature of the BPCI-A program however, there is a significant lag between us performing our services and CMS reporting the final outcomes of those services. We will continue to monitor any leading indicators and the potential impact on operations and financial performance.
We also note that by virtue of the passage of time between when we perform our services and the confirmation of results and subsequent cash settlement by CMS, COVID-19 did not have an impact on the cash we received from CMS during 2020. We expect to receive our next cash payment from CMS in the first quarter of 2021 which will reflect the initial impact of COVID-19 on our business as described below.
F-76
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
In response to the COVID-19 pandemic, CMS announced healthcare providers may continue in the BPCI-A program with no change or they allowed healthcare providers an exception to previous rules of the program with two options as follows:
| • | Healthcare providers may choose to eliminate upside and downside risk by excluding all episodes from reconciliation in 2020; or |
| • | Healthcare providers may choose to exclude from reconciliation those episodes with a COVID-19 diagnosis during the episode. |
Healthcare providers were required to make their election by September 25, 2020. We have received preliminary information related to the elections made by healthcare providers, which we expect will reduce the total number of episodes we manage during 2020 and 2021, and therefore reduce program size. Subsequently, CMS announced that all episodes in 2021 with a COVID-19 diagnosis would be automatically excluded from reconciliation. We are evaluating the impact these healthcare provider elections will have on the savings rate and our overall revenue and results of operations for the year ended December 31, 2020.
As a precautionary measure related to COVID-19 concerns, in March 2020, we drew $77.0 in borrowings under the revolver.
As a result of the shift to vIHEs and other customer claims processing system delays, we have experienced collection delays from certain Home & Community Services customers, which has temporarily resulted in a negative impact on operating cash flows during 2020. We continue to actively work with our customers to collect on these amounts.
We continue to monitor trends related to COVID-19.
In addition to the impact that COVID-19 has had on our accounts receivable and operating cash flows, we agreed to perform a significant amount of incremental IHEs with one of our major customers in the second half of the year, which this has led to an increase in claims which we have not yet invoiced to the customer.
In May 2020, we received the final IRS determination letter closing the open matter related to the contingent consideration described in Note 17 Commitments and Contingencies. We made payment of the full $40.0 in July 2020 to the selling shareholders, some of whom are also affiliated with and/or our equity holders.
During the second quarter of 2020, we recognized approximately $7.3 of revenue representing changes in estimates related to variable consideration upon receipt and analysis of reconciliations from CMS in the second quarter of 2020 related to performance obligations satisfied in the year ended December 31, 2019. In addition, during the second quarter of 2020, we recorded approximately $1.6 related to a cumulative catch up of a change in estimated transaction price upon the satisfaction of the performance obligations.
During the second quarter of 2020, we recorded revenue of $3.3 related to a one-time termination fee associated with a customer in the Episodes of Care Services segment who terminated their contract.
Effective June 2020, we terminated a customer relationship with a customer in our Episodes of Care Services segment, representing approximately 5% of our total revenue for the year ended December 31, 2019 in connection with a contractual dispute. Effective July 2020, we entered into an advisory services agreement with the customer to assist the customer with its ongoing participation in the BPCI-A program through December 31, 2023.
During the second quarter of 2020, we ceased using our New York City office space and in the third quarter began subleasing the space. We have entered into a noncancelable lease agreement for new space in New
F-77
Table of Contents
Cure TopCo, LLC and Subsidiaries
Notes to the Combined-Consolidated Financial Statements
December 31, 2019 and 2018 (In millions, except units and per unit amounts)
York City that ultimately expires in 2029. Total lease commitments over the term of the lease are approximately $25.7.
As described in Note 4 Business Combinations, in March 2019, we issued 130,525 former Class A Common Units, which were subsequently converted to Series B preferred units as part of the purchase consideration to acquire TAV Health. In October 2020, we repurchased the 130,525 Series B preferred units for a total of $54.0.
Effective September 2020, we entered into a second EAR agreement with a customer (See Note 17 Commitments and Contingencies), containing similar provisions to the EAR agreement entered into in December 2019. We concurrently entered into an amended customer contract which includes incremental evaluations volume from the customer beginning in 2020.
F-78
Table of Contents
Board of Directors
Remedy Partners, Inc. and Subsidiaries
Report on the Financial Statements
We have audited the accompanying consolidated financial statements of Remedy Partners, Inc. and its subsidiaries (the Company), which comprise the consolidated balance sheet as of December 31, 2018, the related consolidated statements of income, changes in stockholders’ equity and temporary equity, and cash flows for the year then ended, and the related notes to the consolidated financial statements (collectively, the financial statements).
Management’s Responsibility for the Financial Statements
Management is responsible for the preparation and fair presentation of these financial statements in accordance with accounting principles generally accepted in the United States of America; this includes the design, implementation and maintenance of internal control relevant to the preparation and fair presentation of financial statements that are free from material misstatement, whether due to fraud or error.
Auditor’s Responsibility
Our responsibility is to express an opinion on these financial statements based on our audit. We conducted our audit in accordance with auditing standards generally accepted in the United States of America. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free from material misstatement.
An audit involves performing procedures to obtain audit evidence about the amounts and disclosures in the financial statements. The procedures selected depend on the auditor’s judgment, including the assessment of the risks of material misstatement of the financial statements, whether due to fraud or error. In making those risk assessments, the auditor considers internal control relevant to the entity’s preparation and fair presentation of the financial statements in order to design audit procedures that are appropriate in the circumstances, but not for the purpose of expressing an opinion on the effectiveness of the entity’s internal control. Accordingly, we express no such opinion. An audit also includes evaluating the appropriateness of accounting policies used and the reasonableness of significant accounting estimates made by management, as well as evaluating the overall presentation of the financial statements.
We believe that the audit evidence we have obtained is sufficient and appropriate to provide a basis for our audit opinion.
Opinion
In our opinion, the financial statements referred to above present fairly, in all material respects, the financial position of Remedy Partners, Inc. and its subsidiaries as of December 31, 2018, and the results of their operations and their cash flows for the year then ended in accordance with accounting principles generally accepted in the United States of America.
/s/ RSM US LLP
Stamford, Connecticut
April 30, 2019, except as to Note 2, which is as of October 14, 2020
F-79
Table of Contents
Remedy Partners, Inc. and Subsidiaries
Consolidated Balance Sheet
| December 31, | ||||
| 2018 | ||||
| ASSETS |
||||
| Current assets |
||||
| Cash and cash equivalents |
$ | 138,360,863 | ||
| Accounts receivable, net |
135,311,182 | |||
| Prepaid expenses and other current assets |
3,859,349 | |||
|
|
|
|||
| Total current assets |
277,531,394 | |||
| Property and equipment, net |
6,156,483 | |||
| Restricted cash |
21,307,192 | |||
| Goodwill |
13,901,155 | |||
| Intangible assets, net |
10,363,463 | |||
| Other assets |
768,870 | |||
|
|
|
|||
| Total assets |
$ | 330,028,557 | ||
|
|
|
|||
| LIABILITIES AND STOCKHOLDERS’ EQUITY |
||||
| Current liabilities |
||||
| Accounts payable and accrued expenses |
$ | 107,982,589 | ||
| Income taxes payable |
3,816,056 | |||
|
|
|
|||
| Total current liabilities |
111,798,645 | |||
| Indebtedness to related parties- noncurrent |
452,985 | |||
| Other liabilities |
22,684 | |||
| Net deferred tax liabilities, noncurrent |
2,654,795 | |||
|
|
|
|||
| Total liabilities |
114,929,109 | |||
| Commitments and Contingencies (Note 9) |
||||
| Series A preferred stock, $0.001 par value; 55,000 shares authorized; aggregate liquidation value
of $73,662,770 |
54,476,000 | |||
| Series B preferred stock, $0.001 par value; 41,413,600 shares authorized; aggregate liquidation
value of $78,205,683 |
60,002,898 | |||
| Stockholders’ equity |
||||
| Common stock, $0.001 par value; 350,000,000 shares authorized and 197,052,873 shares outstanding |
191,211 | |||
| Additional paid-in capital |
11,010,587 | |||
| Retained earnings |
89,418,752 | |||
|
|
|
|||
| Total stockholders’ equity |
100,620,550 | |||
|
|
|
|||
| Total liabilities, preferred stock and stockholders’ equity |
$ | 330,028,557 | ||
|
|
|
|||
See accompanying notes to the consolidated financial statements.
F-80
Table of Contents
Remedy Partners, Inc. and Subsidiaries
Consolidated Statement of Operations
| Year ended December 31, |
||||
| 2018 | ||||
| Revenue, net |
$ | 134,891,256 | ||
| Operating expenses: |
||||
| Service expense (exclusive of depreciation and amortization) |
27,457,306 | |||
| Selling, general and administrative expense (exclusive of depreciation and amortization) |
77,815,808 | |||
| Depreciation and amortization |
1,272,363 | |||
|
|
|
|||
| Total operating expenses |
106,545,477 | |||
| Income from operations |
28,345,779 | |||
| Interest income |
1,850,499 | |||
|
|
|
|||
| Income before income tax expense |
30,196,278 | |||
| Income tax expense |
10,277,285 | |||
|
|
|
|||
| Net income |
$ | 19,918,993 | ||
|
|
|
|||
See accompanying notes to the consolidated financial statements.
F-81
Table of Contents
Remedy Partners, Inc. and Subsidiaries
Consolidated Statement of Changes in Stockholders’ Equity and
Temporary Equity
| Common Stock | Additional Paid-in Capital |
Retained Earnings |
Total Stockholders’ Equity |
Preferred Stock | ||||||||||||||||||||||||||||||||
| Class A | Class B | |||||||||||||||||||||||||||||||||||
| Shares | Amount | Shares | Amount | Shares | Amount | |||||||||||||||||||||||||||||||
| Balance, December 31, 2017 |
195,481,167 | $ | 189,639 | $ | 9,662,842 | $ | 69,499,759 | $ | 79,352,240 | 54,476 | $ | 54,476,000 | 41,415,584 | $ | 60,002,898 | |||||||||||||||||||||
| Exercised shares for vested employees |
1,571,706 | 1,572 | 867,909 | — | 869,481 | — | — | — | — | |||||||||||||||||||||||||||
| Stock-based compensation |
— | — | 479,836 | — | 479,836 | — | — | — | — | |||||||||||||||||||||||||||
| Net income |
— | — | — | 19,918,993 | 19,918,993 | — | — | — | — | |||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
| Balance, December 31, 2018 |
197,052,873 | $ | 191,211 | $ | 11,010,587 | $ | 89,418,752 | $ | 100,620,550 | 54,476 | $ | 54,476,000 | 41,415,584 | $ | 60,002,898 | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
See accompanying notes to the consolidated financial statements.
F-82
Table of Contents
Remedy Partners, Inc. and Subsidiaries
Consolidated Statement of Cash Flows
| Year ended December 31, |
||||
| 2018 | ||||
| Cash flows from operating activities: |
||||
| Net income |
$ | 19,918,993 | ||
| Adjustments to reconcile net income to net cash provided by (used in) operating activities: |
||||
| Depreciation and amortization |
1,272,363 | |||
| Loss on disposal of assets |
237,644 | |||
| Stock-based compensation |
479,836 | |||
| Deferred income taxes |
187,323 | |||
| Changes in assets and liabilities |
||||
| Accounts receivable |
(22,718,613 | ) | ||
| Prepaid expenses and other current assets |
(2,130,907 | ) | ||
| Income taxes receivable |
1,760,890 | |||
| Restricted cash |
(72,296 | ) | ||
| Other assets |
6,270 | |||
| Accounts payable and accrued expenses |
56,552,325 | |||
| Income taxes payable |
3,816,056 | |||
| Other liabilities |
(5,316 | ) | ||
|
|
|
|||
| Net cash provided by operating activities |
59,304,568 | |||
|
|
|
|||
| Cash flows from investing activities: |
||||
| Purchase of property and equipment |
(9,948,288 | ) | ||
|
|
|
|||
| Net cash used in investing activities |
(9,948,288 | ) | ||
|
|
|
|||
| Cash flows provided by financing activities: |
||||
| Proceeds from options exercised |
869,481 | |||
|
|
|
|||
| Net cash provided by financing activities |
869,481 | |||
|
|
|
|||
| Net increase in cash and cash equivalents |
50,225,761 | |||
| Cash and cash equivalents: |
||||
| Beginning |
88,135,102 | |||
|
|
|
|||
| Ending |
$ | 138,360,863 | ||
|
|
|
|||
| Supplemental disclosure of cash flow information: |
||||
|
|
|
|||
| Cash payments for income taxes |
$ | 4,532,163 | ||
|
|
|
|||
See accompanying notes to consolidated financial statements.
F-83
Table of Contents
Remedy Partners, Inc. and Subsidiaries
Notes to Consolidated Financial Statements
Note 1. Organization, basis of presentation, and summary of accounting policies
Organization: Remedy Partners, Inc. and Subsidiaries (“Remedy” or “the Company”), a Delaware corporation, is an Awardee Convener contracted with the Centers for Medicare and Medicaid Services (“CMS”) under the Bundled Payments for Care Improvement (“BPCI”) program. The BPCI program was replaced by Bundled Payments for Care Improvement Advanced (“BPCI-A” and together, the “BPCI Programs”) on October 1, 2018, and Remedy became a Convener Participant on that date. Remedy’s role in BPCI-A is essentially the same as it was in BPCI. Remedy contracts with a variety of acute care hospitals, physician groups and post-acute care facilities and engages in care redesign efforts in order to reduce costs and improve the patient outcomes for certain Medicare beneficiaries undergoing an episode of care that begins with a hospitalization and continues for up to 90 days following discharge from the hospital. Specifically, Remedy and its client partners focus on improving the coordination of care as patients move from acute care settings to post-acute facilities or home recovery in order to increase efficiency, eliminate waste, and reduce unnecessary hospital readmissions of Medicare beneficiaries. Under the BPCI program, Remedy and its clients provide CMS between 2-3 percent savings (3 percent for BPCI-A) over prior period cost levels, and any additional savings accrue to the benefit of Remedy and its partners. After deducting an administrative fee of approximately 2 percent of program size to manage these programs, Remedy shares additional savings with its partners. In addition to its Convener Participant role in BPCI-A, Remedy also provides care coordination and analytics services for other Convener Participants in the BPCI-A program.
Basis of presentation: The accompanying consolidated financial statements include the accounts of Remedy Partners, Inc. and its wholly owned subsidiaries. All significant intercompany accounts and transactions have been eliminated in consolidation.
Use of estimates: The preparation of financial statements in conformity with accounting principles generally accepted in the United States of America, or GAAP, requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and the disclosure of contingent assets and liabilities at the date of the financial statements, as well as the reported amounts of revenues and expenses during the reporting period. Although actual results in subsequent periods will differ from these estimates, such estimates are developed based on the best information available to management and management’s best judgments at the time made. Significant estimates that are particularly susceptible to material change in the near term involve revenue recognition related to administrative fee revenue.
Comprehensive income (loss): The Company has not identified any incremental items that would be considered a component of comprehensive income (loss) and accordingly a statement of comprehensive loss is not reflected in the Consolidated Financial Statements because net income and net comprehensive income are the same.
Summary of Significant Accounting Policies
Cash and cash equivalents: The Company considers all highly liquid debt investments purchased with a maturity of three months or less to be cash equivalents.
Restricted cash: Under the Company’s Master Agreement with CMS, the Company is required to place certain funds in escrow for the benefit of CMS. This account, known as a Secondary Repayment Source (“SRS”), is based on the size of the Company’s BPCI Reprogram. These funds are available to CMS as a supplemental payment source if Remedy fails to pay amounts owed to CMS. The funds will be returned to the Company 18 months after the effective period of the CMS Master Agreement, or when all financial obligations to CMS are fulfilled. As of December 31, 2018, there was $15,689,729 in the SRS account.
F-84
Table of Contents
The Company also withholds a portion of shared savings payable to clients in a “holding pool” to cover any potential subsequent negative adjustments to NPRA through CMS’s true-up process (which corrects for errors and late-billed expenses that followed the original reconciliation process.) These funds are distributed clients following the final true-up, generally three quarters after the original reconciliation.
Since clients have earned these funds, the shared savings expense is accrued at the time of reconciliation and remains payable until the funds are either disbursed or used to pay a negative true-up. As of December 31, 2018, there was $5,617,463 of restricted cash in the holding pool.
Accounts receivable, net The Company carries its accounts receivable at net realizable value. Receivables are written down or written off when they are deemed to be uncollectable. Accounts receivable primarily consists of amounts due from customers and CMS and are stated at their net realizable value. Management evaluates all accounts periodically and an allowance is established based on the best facts available to management. Management considers historical realization data, accounts receivable aging trends, and other operational trends to estimate the collectability of receivables. The Company carries its accounts receivable at net realizable value. As of December 31, 2018, the Company does not have an allowance for doubtful accounts.
Property and equipment: Property and equipment is stated at cost less accumulated depreciation. The Company provides for depreciation using the straight-line method over the useful lives of the assets estimated as follows: computer equipment, five years; computer software, three years; and furniture and fixtures, five to seven years. Leasehold improvements are depreciated over the shorter of their useful life or the term of the lease. Expenditures for maintenance and repairs are charged to expense as incurred. Upon sale or retirement, the cost of the asset and the related accumulated depreciation are removed from the accounts, and the remaining gain or loss is included in the results of operations. Maintenance and repairs are expensed as incurred and improvements that increase the value of the property and extend the useful life are capitalized.
Internally-Developed Software: Certain software development costs are capitalized. Such costs include charges for employee costs and consulting services associated with programming, coding and testing such software. Costs incurred for software development prior to the application development stage are expensed in the period incurred. Once the application development stage is reached, development costs are capitalized until the product is ready for implementation or operational use. These capitalized costs are amortized on a straight-line basis over the expected economic life of the software, generally estimated to be three to six years. Amortization of capitalized software costs begins when the software is placed into service ready for intended use and is included in depreciation and amortization expense in the accompanying consolidated statements of income.
Goodwill: Goodwill represents the excess of acquisition consideration paid over the fair value of net tangible and identifiable intangible assets acquired. The Company evaluates goodwill and intangible assets in accordance with ASC 350, Goodwill and Other Intangible Assets (“ASC 350”). Goodwill is not amortized, but rather is reviewed for impairment on an annual basis (or more frequently if impairment indicators exist). The Company tests goodwill at the reporting unit level, which is the level for which there are distinct cash flows, products, capabilities and available financial information by first performing a qualitative assessment to determine if it is more likely than not that the carrying value of the entity exceeds its fair value. As of December 31, 2018, the Company had one reporting unit.
If there are indicators that goodwill may be impaired and a quantitative assessment is necessary, the Company must determine the fair value of each reporting unit and compare it to the reporting unit’s carrying value. Fair value of the reporting unit is determined based on the present value of estimated cash flows using available information regarding expected cash flows of each reporting unit, discount rates and the expected long-term cash
F-85
Table of Contents
flow growth rates. If the fair value of the reporting unit exceeds the carrying value, goodwill is not impaired, and no further testing is performed. The Company adopted ASU 2017-04 which requires the recording of impairment to the extent the fair value exceeds the carrying value and to the extent there is remaining goodwill in the reporting unit under a one-step model. There was no goodwill impairment recognized in any period presented in the consolidated financial statements.
Intangible assets: Intangible assets with finite lives include intellectual property and capitalized software. Intellectual property is amortized using the straight-line method over a period of five years and capitalized software, once placed into service and ready for intended use, is amortized using the straight-line method over a period of three to six years.
Impairment of long-lived assets: In accordance with Financial Accounting Standards Board’s (“FASB”) guidance, long-lived assets, such as property and equipment are reviewed for impairment whenever events or changes in circumstances indicate that the carrying amount of an asset may not be recoverable. If circumstances require a long-lived asset to be tested for possible impairment, the Company first compares undiscounted cash flows expected to be generated by an asset to the carrying value of the asset. If the carrying value of the long-lived asset is not recoverable on an undiscounted cash flow basis, impairment is recognized to the extent that the carrying value exceeds its fair value. Fair value is determined through various valuation techniques including discounted cash flow models, quoted market values and third-party independent appraisals, as considered necessary.
Stock-based compensation: Compensation cost relating to share-based payment transactions is recognized in financial statements based on the fair value of the equity or liability instruments issued. The Company measures the cost of employee services received in exchange for stock awards based on the grant date fair value of the awards, and recognizes the cost over the period the employee is required to provide services for the award, which is usually the vesting period. The Company uses the Black-Scholes valuation methodology in order to estimate the fair value of its share-based awards.
Revenue recognition: The Company primarily offers its services to customers under the CMS, BPCI, and BCPI-A program. The Company recognizes revenue when there is evidence of an arrangement, the service has been provided to the client, the collection of the fees is reasonably assured, and the amount of fees to be paid by the client is fixed or determinable.
The Company earns revenues from the BPCI program from two sources:
| a. | Administrative fees: based on a percentage of each client’s program size or number of BPCI-A episodes for certain BPCI-A partners. |
| b. | Shared savings revenues: in its role as a convener, funds available after administrative fees to the Company are paid from the net payment reconciliation amount, or (“NPRA”). NPRA is paid by CMS on a quarterly basis (semi-annually for BPCI-A) approximately 90 days following the receipt of a CMS Reconciliation which details savings amounts for a given performance period. |
Administrative fees: Administrative fees are recognized monthly, in the month that they are earned, using prior period volumes to estimate current period program size. For BPCI, administrative fee accruals are adjusted quarterly to actual values with the receipt of each quarterly CMS reconciliation. For BPCI Advanced, Administrative Fees will be adjusted semi-annually using both semi-annual CMS reconciliations and CMS claims file data.
F-86
Table of Contents
Shared savings revenues: Remedy accrues shared savings revenues on a quarterly basis (semi-annually for BPCI-A), after the receipt of the CMS reconciliation for a given performance period. At that point, NPRA, administrative fees and shared savings are all known for that performance quarter.
As of 2015, programs initiated by Remedy’s Episode Initiators that do not generate CMS’s minimum savings can have a negative NPRA for a performance quarter. Remedy must pay CMS for the negative NPRA, and is reimbursed for a portion of the negative NPRA by the Episode Initiator based on the terms of each Episode Initiator’s Participant Agreement. The unreimbursed portion of negative NPRA is deducted from shared savings revenue. For programs initiated by physician groups from April 1, 2015 to September 30, 2016, CMS did not collect negative NPRA. Beginning on October 1, 2016, all of Remedy’s programs operated under “full risk”, where CMS would collect from Remedy any negative NPRA generated from an Episode Initiator. The Company records shared savings expenses quarterly (semi-annually for BPCI-A), concurrent with the shared savings revenue. Shared savings payments made to partners are driven by individual contract terms. Shared savings expense includes shared savings payments to Episode Initiators and gainsharing payments (“NPRA Shared Payment in BPCI-A”) to providers who participate in care redesign, and are generally paid within 30 days of receipt of NPRA funds from CMS.
Outsourced field operations: The Company has contracts with certain clients that require the client to employ professionals to manage the program in lieu of Remedy personnel. The Company will reimburse these clients the cost of those personnel from NPRA payments, up to 1 percent of program size. For 2018, the Company incurred costs of approximately $17.2 million from its largest client for field staff. The Company pays these costs each quarter from positive NPRA payments. If there are insufficient NPRA funds to pay the full reimbursement to the client, Remedy pays out a portion that is pro rata with the percent of administrative fees that are received from the current NPRA payment. The balance of the outsourced field expenses is deferred and will be paid from future positive NPRA. Total outsourced field operations payable is included in accounts payable and accrued expenses on the Consolidated Balance Sheets.
Related Balance Sheet Accounts: The following table provides information about accounts included on the Consolidated Balance Sheet as of December 31, 2018:
| 2018 | ||||
| Assets |
||||
| Administrative fee receivable |
$ | 46,499,779 | ||
| Due from CMS |
87,460,723 | |||
| Shared savings receivable |
1,350,680 | |||
|
|
|
|||
| Total Accounts Receivable, net |
$ | 135,311,182 | ||
| Liabilities |
||||
| Outsourced field operations payable |
$ | 12,546,005 | ||
| Shared savings payable |
$ | 60,761,457 | ||
Service Expense: Service expense represents direct costs associated with generating revenue. These costs include payroll costs, travel expenses, related benefits, and other personnel expenses for employees in roles that serve to provide direct revenue generating services to customers. Additionally, service expense also includes costs related to the use of certain professional service firms, software expenses, licensing expenses and certain other direct costs. Service expense does not include depreciation and amortization, which is stated separately in the Consolidated Statements of Operations.
F-87
Table of Contents
Selling, General and Administrative (“SG&A”): SG&A includes the total cost of payroll, related benefits and other personnel expense for employees who do not have a direct role associated with revenue generation including those involved with developing new service offerings. SG&A expenses include all general operating costs including, but not limited to, rent and occupancy costs, telecommunications costs, information technology infrastructure costs, technology development costs, software licensing costs, advertising and marketing expenses, recruiting expenses, costs associated with developing new service offerings and expenses related to the use of certain subcontractors and professional services firms. SG&A expenses do not include depreciation and amortization, which is stated separately in the Consolidated Statements of Operations.
Advertising and Marketing Costs: Advertising and marketing costs are included in SG&A expenses and are expensed as incurred. Advertising and marketing costs totaled $1,449,031 for the year ended December 31, 2018.
Income taxes: The Company accounts for income taxes using the liability method. The current and deferred tax consequences of a transaction are measured by applying the provisions of enacted tax laws to determine the amount of taxes payable or receivable currently or in future years. Deferred income taxes are provided for on temporary differences between the income tax basis of assets and liabilities and their carrying amounts for financial reporting purposes. The effect on deferred taxes of a change in tax rates is recognized in income in the period that includes the enactment date. Deferred tax assets are subject to a valuation allowance to reduce them to their net realizable value, on a more-likely-than-not basis.
The Company may recognize tax liabilities when, despite the Company’s belief that its tax return positions are supportable, the company believes that certain positions may not be fully sustained upon review by the tax authorities. Benefits from tax positions are measured at the largest amount of benefit that is greater than 50 percent likely of being realized upon settlement. To the extent that the final tax outcome of these matters is different than the amounts recorded, such differences impact income tax expense in the period such determination is made. There was no liability for uncertain tax positions at December 31, 2018.
Recent accounting pronouncements: In November 2016, the FASB issued ASU 2016-18, Statement of Cash Flows (Topic 230): Restricted Cash (a consensus of the FASB Emerging Issues Task Force), which provides guidance on the presentation of restricted cash or restricted cash equivalents in the statement of cash flows. ASU 2016-18 will be effective for the Company beginning on January 1, 2019. ASU 2016-18 must be applied using a retrospective transition method with early adoption permitted. The adoption of ASU 2016-18 is not expected to have a material impact on the consolidated financial statements.
In February 2016, the FASB issued ASU 2016-02, Leases (Topic 842). The guidance in this ASU supersedes the leasing guidance in Topic 840, Leases. Under the new guidance, lessees are required to recognize lease assets and lease liabilities on the balance sheet for all leases with terms longer than 12 months. Leases will be classified as either finance or operating, with classification affecting the pattern of expense recognition in the income statement. The new standard is effective for fiscal years beginning after December 15, 2021 including interim periods within those fiscal years. A modified retrospective transition approach is required for lessees for capital and operating leases existing at, or entered into after, the beginning of the earliest comparative period presented in the financial statements, with certain practical expedients available. The Company is currently evaluating the impact of the pending adoption of the new standard on its consolidated financial statements.
In May 2014, the FASB issued ASU 2014-09, Revenue from Contracts with Customers (Topic 606), requiring an entity to recognize the amount of revenue to which it expects to be entitled for the transfer of promised goods or services to customers. The updated standard will replace most existing revenue recognition guidance in U.S. GAAP when it becomes effective and permits the use of either a full retrospective or retrospective with
F-88
Table of Contents
cumulative effect transition method. In August 2015, the FASB issued ASU 2015-14 which defers the effective date of ASU 2014-09 one year making it effective for annual reporting periods beginning after December 15, 2018. The Company has completed its initial assessment of the new standard and it does not expect that impact of adoption to be material to the Company’s financial statements. The Company continues to evaluate the disclosure requirements related to the new standard.
In March 2016, the FASB issued ASU No. 2016-09, Improvements to Employee Share-Based Payment Accounting, which intends to simplify several aspects of accounting for share-based payment transactions, including the income tax consequences, classification of awards as either equity or liabilities, a choice to recognize gross stock compensation expense with actual forfeitures recognized as they occur, as well as certain classifications on the statement of cash flows. The Company adopted this ASU in Fiscal 2018 and it did not have a material impact on the Company’s consolidated financial position, results of operations or cash flows.
In June 2018, the FASB issued an accounting pronouncement (FASB ASU 2018-07) to expand the scope of ASC Topic 718, Compensation—Stock Compensation, to include share-based payment transactions for acquiring goods and services from nonemployees. The pronouncement is effective for fiscal years, and for interim periods within those fiscal years, beginning after December 15, 2018, with early adoption permitted. We are currently in the process of evaluating the effects of this pronouncement on our consolidated financial statements.
Note 2. Accounting Policy Changes
The Company made the following changes to its consolidated financial statements which were dated April 30, 2019:
| (i) | Goodwill amortization—The Company previously amortized its goodwill over a 10 year period in accordance with an accounting alternative developed by the FASB’s Private Company Council. The resulting amortization has been reversed in these consolidated financial statements resulting in a decrease in amortization expense of approximately $1,390,000 for the year ended December 31, 2018 and an increase in goodwill of approximately $5,440,000 as of December 31, 2018. |
| (ii) | Preferred stock—The Company reclassified its preferred stock from stockholders’ equity to temporary equity to comply with requirements of Regulation S-X. See Note 6. |
The Company also reclassified various income statement items which had no impact on net income or stockholders’ equity.
Note 3. Property and Equipment
A summary of property and equipment, as of December 31, 2018 is as follows:
| 2018 | ||||
| Furniture and fixtures |
$ | 1,606,511 | ||
| Leasehold improvements |
5,050,798 | |||
| Computer equipment |
1,495,912 | |||
| Computer software |
1,297,798 | |||
|
|
|
|||
| 9,451,019 | ||||
| Less accumulated depreciation |
(3,294,536 | ) | ||
|
|
|
|||
| $ | 6,156,483 | |||
|
|
|
|||
Depreciation on property and equipment was $1,022,363 for the year ended December 31, 2018.
F-89
Table of Contents
Note 4. Intangible Assets
Intangible assets consisted of the following as of December 31, 2018:
| Gross carrying amount |
Accumulated amortization |
Net carrying value |
||||||||||
| Intellectual property |
$ | 1,250,000 | $ | (541,667 | ) | $ | 708,333 | |||||
| Capitalized software |
9,655,130 | — | 9,655,130 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total |
$ | 10,905,130 | $ | (541,667 | ) | $ | 10,363,463 | |||||
|
|
|
|
|
|
|
|||||||
The Company capitalized $4,580 of internally- developed software costs for the year ended December 31, 2018. Amortization of the software developed for internal-use had not begun as the software was not ready for its intended use as of December 31, 2018.
Amortization expense related to intellectual property for each of the years ended December 31, 2018 amounted to $250,000. Expected amortization expense of intangible assets for years subsequent to December 31, 2018 was as follows:
| 2019 |
$ | 250,000 | ||
| 2020 |
250,000 | |||
| 2021 |
208,333 | |||
| 2022 |
— | |||
| 2023 |
— | |||
| Thereafter |
— | |||
|
|
|
|||
| $ | 708,333 | |||
|
|
|
Note 5. Goodwill
The Company has $13.90 million of goodwill on its balance sheet that resulted from the business acquisition of Liberty Health Partners in 2015. Goodwill is not amortized and is tested for impairment in the fourth quarter of each year or when a change in circumstances indicate a possible impairment. The impairment testing can be performed on either a quantitative or qualitative basis. Upon evaluating the qualitative analysis, it was more likely than not that the fair value exceeded the carrying value of the reporting unit. As a result, there was no impairment related to goodwill during the year ended December 31, 2018.
Note 6. Preferred Stock and Stockholders’ Equity
The Company’s preferred stock features certain redemption rights that are considered to be outside of the Company’s control and subject to the occurrence of uncertain future events. Accordingly, preferred stock subject to possible redemption is presented as temporary equity on the Consolidated Balance Sheet as of December 31, 2018.
Series A Preferred stock: The holders of the preferred stock are entitled to a dividend of 8% per annum of the original cost. As of December 31, 2018, the value of the cumulative dividend was approximately $19.19 million. The Company has no obligation to pay the Series A cumulative dividends other than through a liquidation or by preference of distributions described below, unless the Company’s Board of Directors declares a dividend on the Series A preferred stock. The Company’s Board of Directors has not declared a dividend on the Series A
F-90
Table of Contents
preferred stock at December 31, 2018. Therefore, there was no liability at December 31, 2018. The preferred stockholders are entitled to one vote per share of preferred stock. Preferred Series A stockholders are allocated income and distributions after Series B preferred shares but in preference to common shares.
Series B Preferred stock: The holders of the preferred stock are entitled to a dividend of 8% per annum of the original cost. As of December 31, 2018, the value of the cumulative dividend was approximately $18.21 million. The Company has no obligation to pay the Series B cumulative dividends other than through a liquidation or by preference of distributions described below, unless the Company’s Board of Directors declares a dividend on the Series B preferred stock. The Company’s Board of Directors has not declared a dividend on the Series B preferred stock at December 31, 2018. Therefore, there was no liability at December 31, 2018. The preferred stockholders are entitled to one vote per share of preferred stock. Preferred Series B stockholders have preference to all other classes of shares.
Common stock: The Company has 350,000,000 shares authorized of common stock, which entitles holders to voting rights.
Note 7. Accounts Payable and Accrued Expenses
Accounts payable and accrued expenses consisted of the following as of December 31, 2018:
| 2018 | ||||
| Accounts payable |
$ | 2,223,522 | ||
| Accrued bonuses |
15,092,591 | |||
| Accrued transaction costs |
11,113,201 | |||
| Accrued-other |
3,532,786 | |||
| Deferred rent |
2,713,027 | |||
| Outsourced field operations payable |
12,546,005 | |||
| Shared savings payable |
60,761,457 | |||
|
|
|
|||
| Total accounts payable and accrued expenses |
$ | 107,982,589 | ||
|
|
|
|||
Note 8. Income Taxes
On December 22, 2017, the President of the United States signed into law the Tax Cuts and jobs Act tax reform legislation. This legislation made significant changes in U.S. tax law including a reduction in the corporate tax rates, changes to net operating loss carryforwards and carrybacks, and a repeal of the corporate alternative minimum tax. The legislation reduced the U.S. corporate tax rate from 35% to 21%. As a result of the enacted law, the Company was required to revalue deferred tax assets and liability at the enacted rate as of December 31, 2017. The other provisions of the Tax Cuts and Jobs Act did not have a material impact on the consolidated financial statements.
F-91
Table of Contents
The income tax expense differs from the amount of income tax expense determined by applying the United States federal income tax rate of 21 percent to pre-tax income for the years ended December 31, 2018 due to the following:
| 2018 | ||||
| Computed “expected” tax provision |
$ | 6,341,218 | ||
| Increase (decrease) in tax provision resulting from: |
||||
| Transaction costs |
2,445,601 | |||
| State taxes |
3,712,135 | |||
| R&D tax credit |
(1,101,596 | ) | ||
| Other |
(1,120,073 | ) | ||
|
|
|
|||
| $ | 10,277,285 | |||
|
|
|
|||
Deferred taxes are provided for the temporary differences between the financial and tax basis of assets and liabilities, applying presently enacted tax rates and laws. Significant components of the Company’s deferred tax liabilities and assets were as follows at December 31, 2018:
| 2018 | ||||
| Deferred tax assets (liabilities): |
||||
| Net operating loss carryforwards |
$ | 332,993 | ||
| Depreciation of property and equipment |
561,654 | |||
| Allowance for bad debt |
203,337 | |||
| Tenant allowance |
451,171 | |||
| Accrued expenses |
489,667 | |||
| Internally developed software |
(2,347,547 | ) | ||
| Amortization of intangible assets |
(151,307 | ) | ||
| Cash to accrual adjustment |
(2,194,763 | ) | ||
|
|
|
|||
| Net deferred tax liability |
$ | (2,654,795 | ) | |
|
|
|
|||
Note 9. Commitments and Contingencies
Lease commitments: The Company is obligated as lessee under certain non-cancellable operating leases. As of December 31, 2018, future minimum lease payments under non-cancellable operating leases were as follows:
| 2019 |
$ | 3,396,987 | ||
| 2020 |
3,278,310 | |||
| 2021 |
3,104,803 | |||
| 2022 |
2,072,254 | |||
| 2023 |
1,340,436 | |||
| thereafter |
2,165,704 | |||
|
|
|
|||
| $ | 15,358,494 | |||
|
|
|
Total rent expense associated with non-cancellable operating leases was $3,191,908 for the year ended December 31, 2018 and was included within SG&A expenses on the Consolidated Statement of Operations.
Contingent loss: As disclosed in Note 1, certain programs that do not generate savings can have a negative NPRA for a performance quarter. The Company must pay CMS the negative NPRA and recoup a portion of that
F-92
Table of Contents
payment from the Episode Initiator. The Company has recorded its share of negative NPRA as a reduction to shared savings revenue through the first two quarters of 2018. The Company has earned net positive NPRA for the third quarter of 2018, and those revenues will be reflected in the January 2019 financial statements. There is no liability recorded subsequent to September 30, 2018, as the Company does not have a reasonable basis to estimate if there is negative NPRA related to the last quarter of 2018. The Company has not had any quarter with program-wide negative NPRA (where total partner Negative NPRA is greater than Positive NPRA) since the inception of the BPCI program on October 1, 2013.
Legal Matters: From time to time, the Company may become involved in various legal matters. Management of the Company believes that there are no legal matters as of December 31, 2018 whose resolution could have a material adverse effect on the consolidated financial statements.
Note 10. Stock-Based Compensation
The Company’s Equity Incentive Plan authorizes granting key employees of the Company options to purchase 30,724,479 shares of common stock of the Company, at exercise prices as determined by the Board of Directors. The Board has the authority to grant “incentive unit-based options” within the meaning of Section 422(b) of the Internal Revenue Code, or “non-qualified unit options” as described in Treasury Regulation Section 1.83-7, or “restricted unit” awards.
Under this plan, unit-based options vest and become exercisable over three or four years, beginning one year after the grant date and expire ten years after the grant date. Compensation cost relating to unit- based payment transactions is recognized in the financial statements with measurement based upon the calculated value of the equity or liability instruments issued. For the years ended December 31, 2018, the Company recognized $479,836 in compensation expense for unit- based options.
We recognize the impact of forfeitures in stock-based compensation expense when they occur. Additionally, the Company issues options with the strike price equaling the fair value as of the grant date, resulting in zero intrinsic value at issuance.
A summary of the status of stock-based options at December 31, 2018 and changes during the year then ended is as follows:
| Options | Weighted- Average Exercise Price |
Weighted- (in Years) |
Aggregate Intrinsic Value |
|||||||||||||
| Outstanding, December 31, 2017 |
25,461,658 | 0.53 | 7.26 | — | ||||||||||||
| Granted |
6,965,419 | 0.82 | 9.12 | — | ||||||||||||
| Exercised |
(1,571,706 | ) | 0.55 | N/A | ||||||||||||
| Forfeited |
(2,747,535 | ) | 0.82 | N/A | — | |||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Outstanding, December 31, 2018 |
28,107,836 | $ | 0.57 | 6.58 | $ | — | ||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Exercisable, December 31, 2018 |
19,440,134 | $ | 0.43 | 5.70 | $ | — | ||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
The weighted-average grant date calculated fair value for options granted during 2018 was $0.15.
As of December 31, 2018, there was $1,003,575 of total unrecognized compensation cost related to non- vested unit options. That cost is expected to be recognized over a weighted-average period of 2.62 years.
F-93
Table of Contents
At December 31, 2018, there were 13,105,427 unit options available for future grants under the Company’s unit-based option plan.
Note 11. Related Party Transactions
In 2012, the Company issued a promissory note to fund the Company’s operations from one of the shareholders with the intention of repayment. The payable was noninterest bearing and had no specific repayment term. The
total outstanding balance due to the shareholder was $452,985 at December 31, 2018.
Note 12. Concentration of Credit Risk
The Company maintains its cash balances in accounts which, at times, may exceed federally insured limits. The Company has not experienced any losses in such accounts and believes there is little or no exposure to any significant credit risk.
Accounts receivable potentially subject the Company to concentrations of credit risk. Management believes that its contract acceptance, billing and collection policies are adequate to minimize potential credit risk. The Company continuously evaluates the credit worthiness of its customers’ financial condition and generally does not require collateral.
A significant portion of the Company’s revenues are generated from a few customers. For the year ended December 31, 2018, the Company had one customer which accounted for approximately 37.2% of revenues and 10.4% of accounts receivable as of December 31, 2018.
While CMS is not the Company’s customer, a majority of the revenue generated by Remedy is under the CMS administered BPCI-A program and payments are received under this program in certain cases from CMS rather than directly from the customer. As of December 31, 2018, approximately 64.6% of the total accounts receivable was due from CMS related to payments expected to be received by the Company under the BPCI-A program.
Note 13. Subsequent Events
The Company performed an evaluation of subsequent events through April 30, 2019, the date the financial statements were available to be issued.
On January 15, 2019, the Company’s shareholders sold 51% of the Preferred shares to Remedy Acquisition, L.P, an investment vehicle of New Mountain Capital Partners for approximately $405 million. All Remedy Partners Class A and Class B preferred shares were converted into shares of Remedy Partners, Inc. common as of that date with a one to one exchange ratio. Remedy Acquisition, L.P. received 135,993,425 shares of a newly created Senior Convertible Preferred Stock.
During the first quarter of 2020, the COVID-19 outbreak rapidly evolved. The former Remedy business saw some evidence of reduced volumes of episodes of care as a result of the cancellation of elective surgeries in the final two weeks of the first quarter of 2020 and through the second quarter. Due to the nature of the BPCI-A program however, there is a significant lag between the Company performing its services and CMS reporting the final performance outcomes of those services. The Company will continue to monitor any leading indicators and the potential impact on operations and financial performance.
F-94
Table of Contents
23,500,000 Shares
Class A common stock
Signify Health, Inc.

PRELIMINARY PROSPECTUS
| Goldman Sachs & Co. LLC | J.P. Morgan | Barclays | Deutsche Bank Securities |
| BofA Securities | UBS Investment Bank |
Baird | Piper Sandler | William Blair | ||||
Through and including , 2021 (the 25th day after the date of this prospectus), all dealers that buy, sell or trade our Class A common stock, whether or not participating in this offering, may be required to deliver a prospectus. This is in addition to the dealers’ obligation to deliver a prospectus when acting as underwriters and with respect to their unsold allotments or subscriptions.
, 2021
Table of Contents
PART II
INFORMATION NOT REQUIRED IN PROSPECTUS
Item 13. Other Expenses of Issuance and Distribution
| Amount to Be Paid |
||||
| SEC registration fee |
$ | 61,917 | ||
| FINRA filing fee |
85,629 | |||
| Listing fee |
158,100 | |||
| Transfer agent’s fees |
7,000 | |||
| Printing and engraving expenses |
800,000 | |||
| Legal fees and expenses |
4,800,000 | |||
| Accounting fees and expenses |
2,460,000 | |||
| Blue Sky fees and expenses |
— | |||
| Miscellaneous |
5,127,354 | |||
|
|
|
|||
| Total |
$ | 13,500,000 | ||
|
|
|
|||
Each of the amounts set forth above, other than the registration fee and the FINRA filing fee, is an estimate.
Item 14. Indemnification of Directors and Officers
Section 145 of the Delaware General Corporation Law provides that a corporation may indemnify directors and officers as well as other employees and individuals against expenses (including attorneys’ fees), judgments, fines and amounts paid in settlement actually and reasonably incurred by such person in connection with any threatened, pending or completed actions, suits or proceedings in which such person is made a party by reason of such person being or having been a director, officer, employee or agent to the registrant. The Delaware General Corporation Law provides that Section 145 is not exclusive of other rights to which those seeking indemnification may be entitled under any bylaw, agreement, vote of stockholders or disinterested directors or otherwise. The registrant’s Bylaws provide for indemnification by the registrant of its directors, officers and employees to the fullest extent permitted by the Delaware General Corporation Law. The registrant has entered into indemnification agreements with each of its current directors and executive officers to provide these directors and executive officers additional contractual assurances regarding the scope of the indemnification set forth in the registrant’s amended and restated certificate of incorporation and amended and restated bylaws and to provide additional procedural protections. There is no pending litigation or proceeding involving a director or executive officer of the registrant for which indemnification is sought.
Section 102(b)(7) of the Delaware General Corporation Law permits a corporation to provide in its certificate of incorporation that a director of the corporation shall not be personally liable to the corporation or its stockholders for monetary damages for breach of fiduciary duty as a director, except for liability (i) for any breach of the director’s duty of loyalty to the corporation or its stockholders, (ii) for acts or omissions not in good faith or which involve intentional misconduct or a knowing violation of law, (iii) for unlawful payments of dividends or unlawful stock repurchases, redemptions or other distributions, or (iv) for any transaction from which the director derived an improper personal benefit. The registrant’s Certificate of Incorporation provides for such limitation of liability.
The registrant maintains standard policies of insurance under which coverage is provided (a) to its directors and officers against loss rising from claims made by reason of breach of duty or other wrongful act, and (b) to the registrant with respect to payments which may be made by the registrant to such officers and directors pursuant to the above indemnification provision or otherwise as a matter of law.
The proposed form of underwriting agreement filed as Exhibit 1.1 to this registration statement provides for indemnification of directors and officers of the registrant by the underwriters against certain liabilities.
Table of Contents
Item 15. Recent Sales of Unregistered Securities
The following sets forth information regarding securities sold or issued by the predecessors to the registrant in the three years preceding the date of this registration statement. No underwriters were involved in these sales. There was no general solicitation of investors or advertising, and we did not pay or give, directly or indirectly, any commission or other remuneration, in connection with the offering of these shares. In each of the transactions described below, the recipients of the securities represented their intention to acquire the securities for investment only and not with a view to or for sale in connection with any distribution thereof, and appropriate legends were affixed to the securities issued in these transactions.
LLC Unit Issuances
(1) In November 2019, Cure TopCo, LLC issued 3,402,608 Series B preferred units to the existing owners of Cure TopCo, LLC, including 3,050,000 Series B preferred units to New Mountain Partners V (AIV-C), LP in connection with the Remedy Partners Combination.
(2) In November 2019, Cure TopCo, LLC issued 3,384,543 Series A preferred units to New Remedy in exchange for all of Remedy Partners’ outstanding equity interests in connection with the Remedy Partners Combination.
(3) In March 2019, Cure TopCo, LLC issued 130,525 Class A common units to the owners of TAV Health in connection with the TAV Health acquisition. These Class A common units were subsequently converted into Series B preferred units in connection with the Remedy Partners Combination. Cure TopCo, LLC entered into a securities purchase agreement to repurchase all of these Series B preferred units from TAV Health in September 2020.
(4) From December 2017 through October 2019, Cure TopCo, LLC issued 611,574 Class B common units to Cure Aggregator, LLC and the Other Legacy Signify Holders. As of December 31, 2020, 370,921 Class B common units remain outstanding.
(5) From February 14, 2020 to December 1, 2020, Cure TopCo, LLC issued 343,671 Class C units to Cure Aggregator, LLC. As of December 31, 2020, 328,231 Class C common units remain outstanding.
Profits Interest Grants
(6) From December 21, 2017 to October 28, 2019, Cure Aggregator, LLC granted 611,574 Class B common units to certain employees and directors, which correspond to 611,574 Class B common units issued by Cure TopCo, LLC to Cure Aggregator, LLC, which were intended to qualify as “profits interests” within the meaning of Revenue Procedures 93-27 (1993-2 C.B. 343) and 2001-43 (2001-2 C.B. 191) (“Profits Interests”).
(7) From February 14, 2020 to December 1, 2020, Cure Aggregator, LLC granted 343,671 Class C units to certain employees and directors, which correspond to 343,671 Class C units issued by Cure TopCo, LLC to Cure Aggregator, LLC, which were intended to qualify as Profits Interests.
The offers, sales and issuances of the securities described in (6) and (7) above were deemed to be exempt from registration in reliance upon Section 4(a)(2) or Rule 701 promulgated under Section 3(b) of the Securities Act as transactions between an issuer not involving any public offering within the meaning of Section 4(a)(2) or pursuant to benefit plans and contracts relating to compensation as provided under Rule 701 of the Securities Act. The recipients in each of these transactions acquired the securities for investment only and not with a view to or for sale in connection with any distribution thereof.
Table of Contents
Option Grants and Common Stock Issuances
(7) From March 1, 2012 through November 1, 2019, New Remedy (including its predecessor, Remedy Partners) has granted to its directors, officers, employees and consultants options to purchase an aggregate of 62,328,759 shares of its Class A common stock under its Amended and Restated 2019 Equity Incentive Plan (the “2019 Plan”), at exercise prices ranging from $0.05 to $3.01 per share.
(8) Since March 1, 2012, New Remedy (including its predecessor, Remedy Partners) has issued and sold to its directors, officers, employees and consultants an aggregate of 18,975,225 shares of its Class A common stock upon the exercise of options under the 2019 Plan at exercise prices ranging from $0.05 to $3.01 per share, for aggregate consideration of approximately $8.9 million. In addition, in January 2019, in connection with the Remedy Partners Acquisition by New Mountain Capital, 4,517,968 stock options were canceled and redeemed.
The offers, sales and issuances of the securities described in (7) and (8) above were deemed to be exempt from registration in reliance upon Section 4(a)(2) or Rule 701 promulgated under Section 3(b) as transactions between an issuer not involving any public offering within the meaning of Section 4(a)(2) of the Securities Act or pursuant to benefit plans and contracts relating to compensation as provided under Rule 701. The recipients in each of these transactions acquired the securities for investment only and not with a view to or for sale in connection with any distribution thereof.
Issuances in Connection with the Reorganization Transactions
(9) On January 5, 2021, in connection with its formation, the registrant issued 100 shares of common stock, par value $0.01 per share, to an officer of the registrant in exchange for $1.00. The issuance was exempt from registration under Section 4(a)(2) of the Securities Act as a transaction by an issuer not involving any public offering.
Item 16. Exhibits and Financial Statement Schedules
(a) The following documents are filed as part of this registration statement:
Table of Contents
Table of Contents
| ** | Previously filed. |
(b) Schedule II—Valuation and Qualifying Accounts of Cure TopCo, LLC
Table of Contents
Item 17. Undertakings
The undersigned registrant hereby undertakes:
(a) The undersigned registrant hereby undertakes to provide to the underwriter at the closing specified in the underwriting agreement certificates in such denominations and registered in such names as required by the underwriter to permit prompt delivery to each purchaser.
(b) Insofar as indemnification for liabilities arising under the Securities Act of 1933 may be permitted to directors, officers and controlling persons of the registrant pursuant to the provisions referenced in Item 14 of this registration statement, or otherwise, the registrant has been advised that in the opinion of the Securities and Exchange Commission such indemnification is against public policy as expressed in the Act and is, therefore, unenforceable. In the event that a claim for indemnification against such liabilities (other than the payment by the registrant of expenses incurred or paid by a director, officer, or controlling person of the registrant in the successful defense of any action, suit or proceeding) is asserted by such director, officer or controlling person in connection with the securities being registered hereunder, the registrant will, unless in the opinion of its counsel the matter has been settled by controlling precedent, submit to a court of appropriate jurisdiction the question of whether such indemnification by it is against public policy as expressed in the Act and will be governed by the final adjudication of such issue.
(c) The undersigned registrant hereby undertakes that:
(1) For purposes of determining any liability under the Securities Act of 1933, the information omitted from the form of prospectus filed as part of this registration statement in reliance upon Rule 430A and contained in a form of prospectus filed by the registrant pursuant to Rule 424(b)(1) or (4) or 497(h) under the Securities Act shall be deemed to be part of this registration statement as of the time it was declared effective.
(2) For the purpose of determining any liability under the Securities Act of 1933, each post-effective amendment that contains a form of prospectus shall be deemed to be a new registration statement relating to the securities offered therein, and the offering of such securities at that time shall be deemed to be the initial bona fide offering thereof.
Table of Contents
SIGNATURES
Pursuant to the requirements of the Securities Act of 1933, the registrant has duly caused this registration statement to be signed on its behalf by the undersigned, thereunto duly authorized, in the City of Norwalk, State of Connecticut, on the 10th day of February, 2021.
| Signify Health, Inc. | ||
| By: | /s/ Kyle Armbrester | |
| Name: Kyle Armbrester | ||
| Title: Chief Executive Officer | ||
Pursuant to the requirements of the Securities Act of 1933, this registration statement has been signed by the following persons in the capacities and on the dates indicated.
| Signature |
Title |
Date | ||
| * Matthew S. Holt |
Chairman |
February 10, 2021 | ||
|
/s/ Kyle Armbrester Kyle Armbrester |
Chief Executive Officer and Director |
February 10, 2021 | ||
|
* Steven Senneff |
President, Chief Financial and |
February 10, 2021 | ||
|
* Laurence Orton |
Chief Accounting Officer (principal accounting officer) |
February 10, 2021 | ||
| * Taj J. Clayton |
Director |
February 10, 2021 | ||
| * Brandon H. Hull |
Director |
February 10, 2021 | ||
| * Kevin M. McNamara |
Director |
February 10, 2021 | ||
| * Albert A. Notini |
Director |
February 10, 2021 | ||
| * Kyle B. Peterson |
Director |
February 10, 2021 | ||
| * Vivian E. Riefberg |
Director |
February 10, 2021 | ||
| * Stephen F. Wiggins |
Director |
February 10, 2021 | ||
| By: | /s/ Kyle Armbrester |
|||
| Attorney-in-Fact |
Table of Contents
Cure TopCo, LLC and Subsidiaries
Schedule II—Valuation and Qualifying Accounts
(in millions)
| Additions | Deductions | |||||||||||||||||||||||
| Description | Balance at Beginning of Period |
Charged to Operating Expenses |
Acquired from Acquisitions |
Write-offs | Recoveries | Balance at End of Period |
||||||||||||||||||
| Year Ended December 31, 2019 |
||||||||||||||||||||||||
| Allowance for doubtful accounts |
$ | 3.4 | 1.5 | 1.2 | (0.6 | ) | (0.7 | ) | $ | 4.8 | ||||||||||||||
| Year Ended December 31, 2018 |
||||||||||||||||||||||||
| Allowance for doubtful accounts |
$ | 0.7 | 2.7 | 0.1 | (0.1 | ) | — | $ | 3.4 | |||||||||||||||
