Attached files
| file | filename |
|---|---|
| EX-99.2 - EX-99.2 - ACCELERON PHARMA INC | xlrn-20201113ex992.htm |
| EX-99.1 - EX-99.1 - ACCELERON PHARMA INC | xlrn-20201113ex991.htm |
| 8-K - 8-K - ACCELERON PHARMA INC | xlrn-20201113.htm |
Exhibit 99.3 AHA 2020 Virtual: Updates from the PULSAR and SPECTRA Trials of Sotatercept in PAH November 13, 2020 Sotatercept is an investigational therapy that is not approved for any use in any country.
Acceleron Forward-Looking Statements THIS PRESENTATION CONTAINS FORWARD-LOOKING STATEMENTS ABOUT THE COMPANY’S STRATEGY, FUTURE PLANS AND PROSPECTS, including statements regarding the development and commercialization of sotatercept in pulmonary arterial hypertension (“PAH”) and of the Company’s other compounds, the timeline for clinical development and regulatory approval of the Company’s compounds and the expected timing for reporting of data from ongoing clinical trials. The words “anticipate,” “believe,” “could,” “estimate,” “expect,” “goal,” “intend,” “may,” “plan,” “potential,” “project,” “should,” “target,” “will,” “would,” and similar expressions are intended to identify forward- looking statements, although not all forward-looking statements contain these identifying words. ACTUAL RESULTS COULD DIFFER MATERIALLY FROM THOSE INCLUDED IN THE FORWARD-LOOKING STATEMENTS DUE TO VARIOUS factors, risks and uncertainties, including, but not limited to, that preclinical testing of the Company's compounds and data from clinical trials may not be predictive of the results or success of ongoing or later clinical trials, that regulatory approval of the Company’s compounds in one indication or country may not be predictive of approval in another indication or country, that the development of the Company's compounds may take longer and/or cost more than planned, that the Company may be unable to successfully complete the clinical development of the Company’s compounds, that the Company may be delayed in initiating, enrolling or completing any clinical trials, that the Company's compounds may not receive regulatory approval or become commercially successful products, and that Breakthrough Therapy or Priority Medicines (PRIME) designation may not expedite the development or review of sotatercept. These and other risks and uncertainties are identified under the heading "Risk Factors" included in the Company's most recent Annual Report on Form 10-K, Quarterly Report on Form 10-Q, and other filings that the Company has made and may make with the SEC in the future. THE FORWARD-LOOKING STATEMENTS CONTAINED IN THIS PRESENTATION ARE BASED ON MANAGEMENT’S CURRENT VIEWS, PLANS, estimates, assumptions and projections with respect to future events, and the Company does not undertake and specifically disclaims any obligation to update any forward-looking statements. This presentation is for investor relations purposes only – Not for product promotional purposes. 2

Our Special Guest Presenters on Today’s Call Vallerie McLaughlin, MD Aaron Waxman, MD, PhD Professor of Cardiovascular Medicine; Director, Pulmonary Vascular Disease Program, Director of the Pulmonary Hypertension Program, Brigham and Women’s Hospital; University of Michigan Associate Professor of Medicine, Harvard Medical School Investigator in the PULSAR trial and a paid consultant to Acceleron Principal investigator in the SPECTRA trial and a paid consultant to Acceleron 3 This presentation is for investor relations purposes only – Not for product promotional purposes.
Habib Dable Chief Executive Officer This presentation is for investor relations purposes only – Not for product promotional purposes.

Sotatercept: Significant Progress in 2020 PRECLINICAL REGULATORY CLINICAL CLINICAL Upcoming Phase 3 Trial Starts Planned BREAKTHROUGH THERAPY DESIGNATION SCIENCE TRANSLATIONAL MEDICINE RESEARCH ARTICLE PRIME – PRIORITY MEDICINES This presentation is for investor relations purposes only – Not for product promotional purposes. 5
Presentations at AHA Scientific Sessions 2020 November 13-17, 2020 A virtual experience CLINICAL PRESENTATIONS • Sotatercept Improves Right Ventricular - Pulmonary Arterial Coupling and Right Ventricular Function in the PULSAR Study: A Phase 2, double-blind, placebo controlled, randomized study to compare the efficacy and safety of sotatercept versus placebo when added to standard of care for the treatment of pulmonary arterial hypertension (PAH) Cardiopulmonary Best Abstract Award • SPECTRA and Beyond: Signs of Disease Modification? PRECLINICAL PRESENTATIONS • Sotatercept Analog RAP-011 Inhibits Right Ventricular Remodeling and Restores Function in a Mouse Model of Pressure Overload This presentation is for investor relations purposes only – Not for product promotional purposes. 6

Vallerie McLaughlin, MD Professor of Cardiovascular Medicine; Director of the Pulmonary Hypertension Program, University of Michigan Investigator in the PULSAR trial and a paid consultant to Acceleron 7 This presentation is for investor relations purposes only – Not for product promotional purposes.
Sotatercept improves right ventricular – pulmonary arterial coupling and right ventricular function in the PULSAR study A Phase 2, double-blind, placebo controlled, randomized study to compare the efficacy and safety of sotatercept versus placebo when added to standard of care for the treatment of pulmonary arterial hypertension (PAH) 1Vallerie McLaughlin, 2Mardi Gomberg-Maitland, 3Solaiappan Manimaran, 3Jonathan Lu, 4Simon Gibbs. 1University of Michigan, AnnArbor, MI; 2GWMFA,George Washington University, Washington DC; 3Acceleron Pharma, Cambridge, MA; 4Imperial College London, London, UK. #AHA20
Disclosures Financial relationships with relevant commercial interests for three years preceding this presentation: Dr. McLaughlin reports grants and personal fees from Acceleron, Actelion, Bayer, Gossamer, and United Therapeutics; personal fees from Altavant, Caremark, CiVi Biopharma and Neuroderm and grants from Reata Pharm. and SonoVie, outside the presented work 9
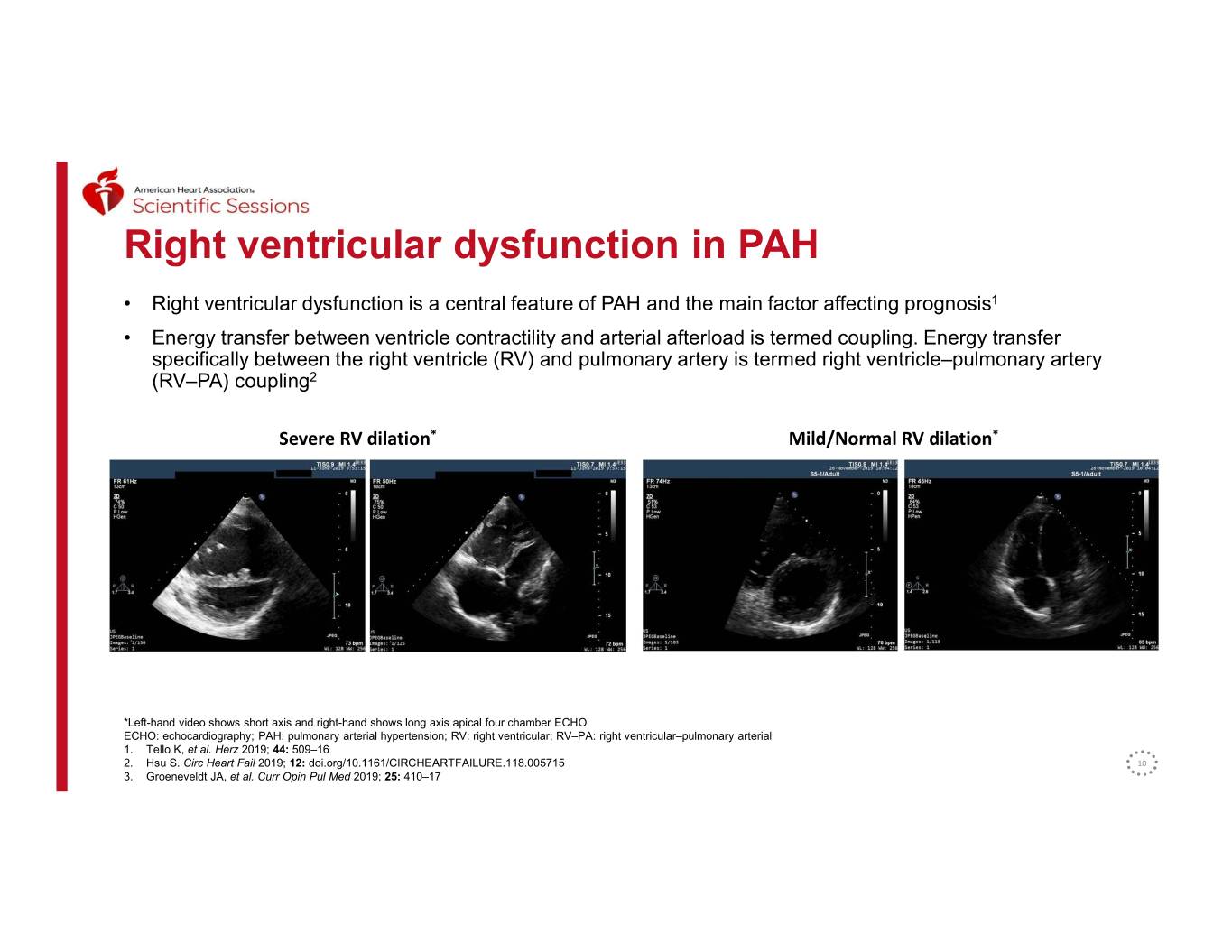
Right ventricular dysfunction in PAH • Right ventricular dysfunction is a central feature of PAH and the main factor affecting prognosis1 • Energy transfer between ventricle contractility and arterial afterload is termed coupling. Energy transfer specifically between the right ventricle (RV) and pulmonary artery is termed right ventricle–pulmonary artery (RV–PA) coupling2 Severe RV dilation* Mild/Normal RV dilation* *Left-hand video shows short axis and right-hand shows long axis apical four chamber ECHO ECHO: echocardiography; PAH: pulmonary arterial hypertension; RV: right ventricular; RV–PA: right ventricular–pulmonary arterial 1. Tello K, et al. Herz 2019; 44: 509–16 2. Hsu S. Circ Heart Fail 2019; 12: doi.org/10.1161/CIRCHEARTFAILURE.118.005715 10 3. Groeneveldt JA, et al. Curr Opin Pul Med 2019; 25: 410–17
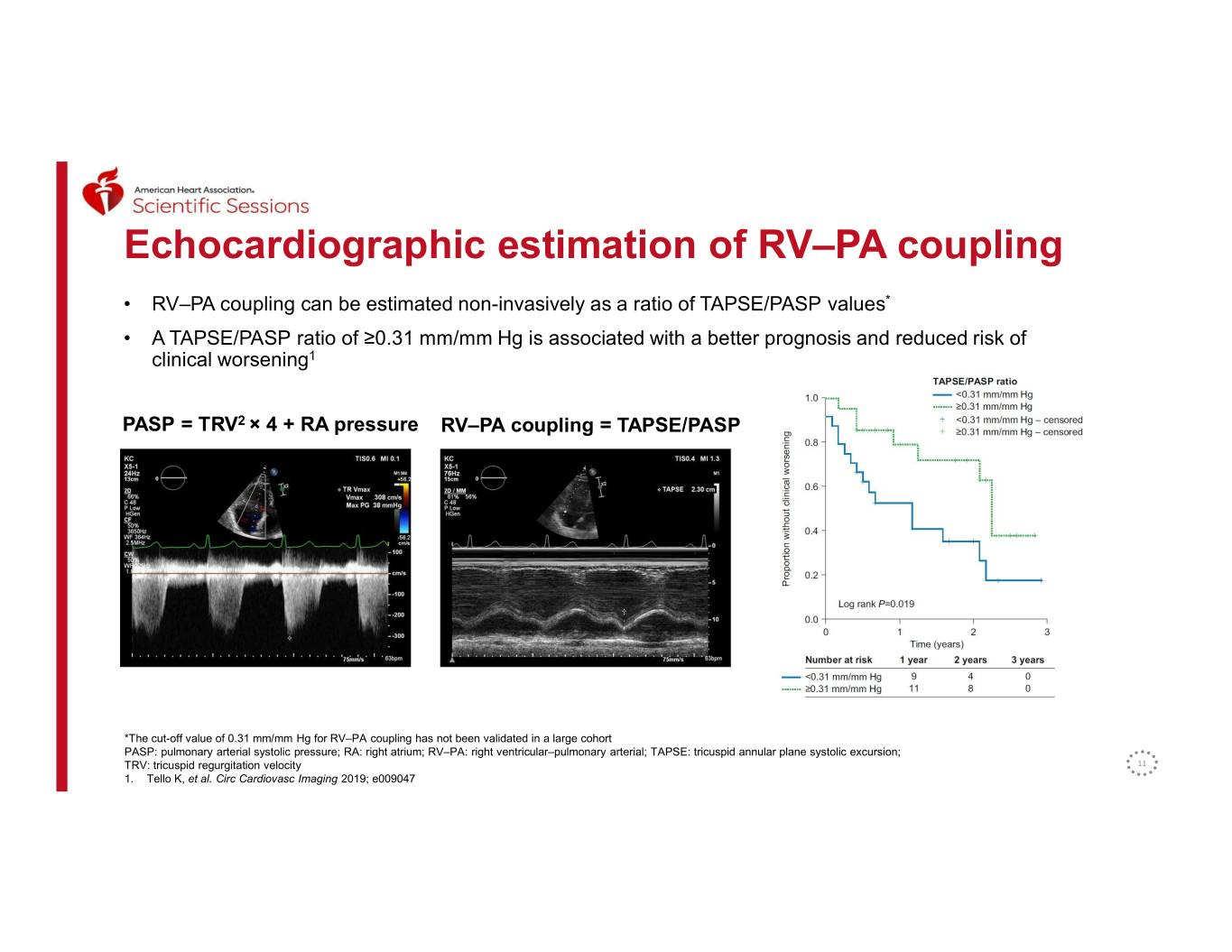
Echocardiographic estimation of RV–PA coupling • RV–PA coupling can be estimated non-invasively as a ratio of TAPSE/PASP values* • A TAPSE/PASP ratio of ≥0.31 mm/mm Hg is associated with a better prognosis and reduced risk of clinical worsening1 PASP = TRV2 × 4 + RA pressure RV–PA coupling = TAPSE/PASP *The cut-off value of 0.31 mm/mm Hg for RV–PA coupling has not been validated in a large cohort PASP: pulmonary arterial systolic pressure; RA: right atrium; RV–PA: right ventricular–pulmonary arterial; TAPSE: tricuspid annular plane systolic excursion; TRV: tricuspid regurgitation velocity 11 1. Tello K, et al. Circ Cardiovasc Imaging 2019; e009047
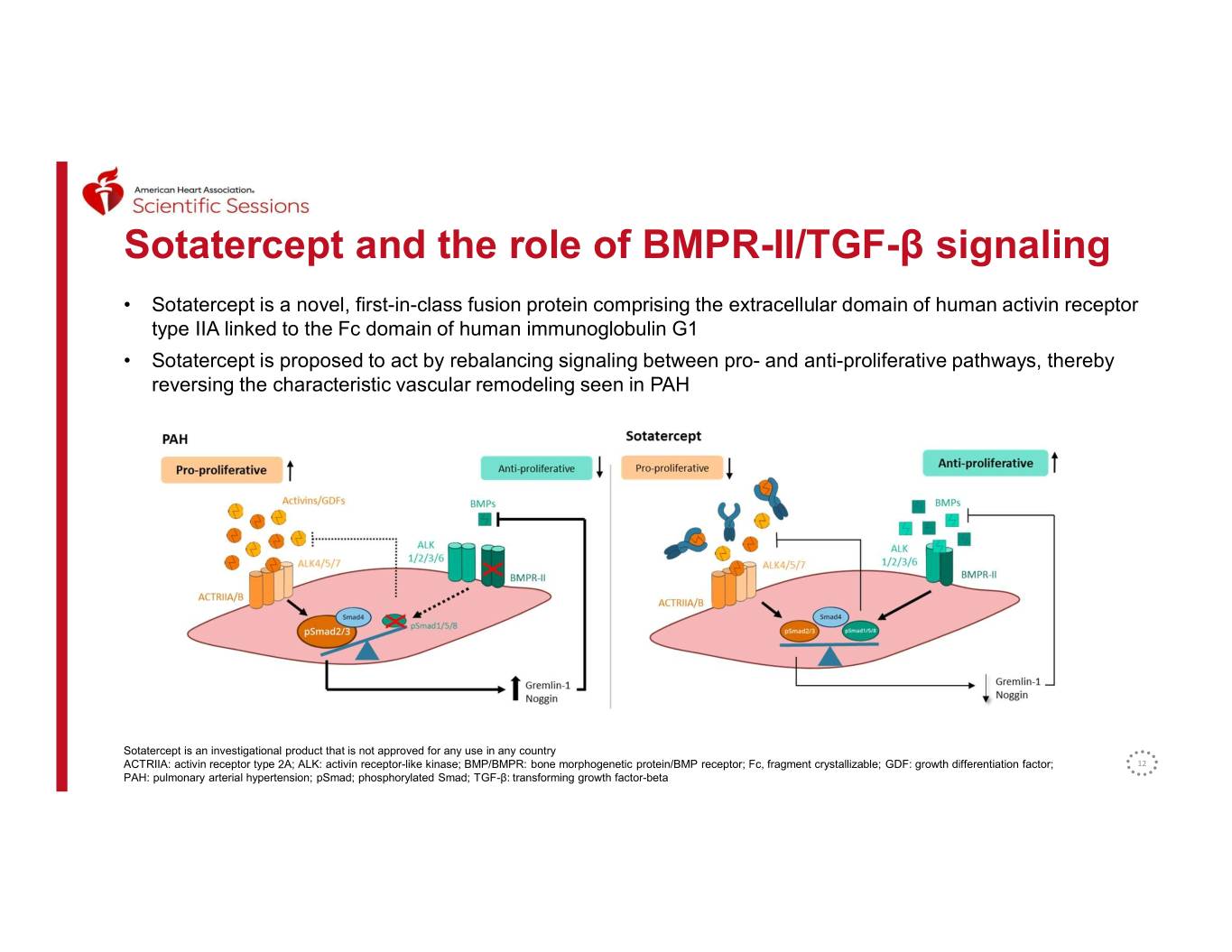
Sotatercept and the role of BMPR-II/TGF-β signaling • Sotatercept is a novel, first-in-class fusion protein comprising the extracellular domain of human activin receptor type IIA linked to the Fc domain of human immunoglobulin G1 • Sotatercept is proposed to act by rebalancing signaling between pro- and anti-proliferative pathways, thereby reversing the characteristic vascular remodeling seen in PAH Sotatercept is an investigational product that is not approved for any use in any country ACTRIIA: activin receptor type 2A; ALK: activin receptor-like kinase; BMP/BMPR: bone morphogenetic protein/BMP receptor; Fc, fragment crystallizable; GDF: growth differentiation factor; 12 PAH: pulmonary arterial hypertension; pSmad; phosphorylated Smad; TGF-β: transforming growth factor-beta
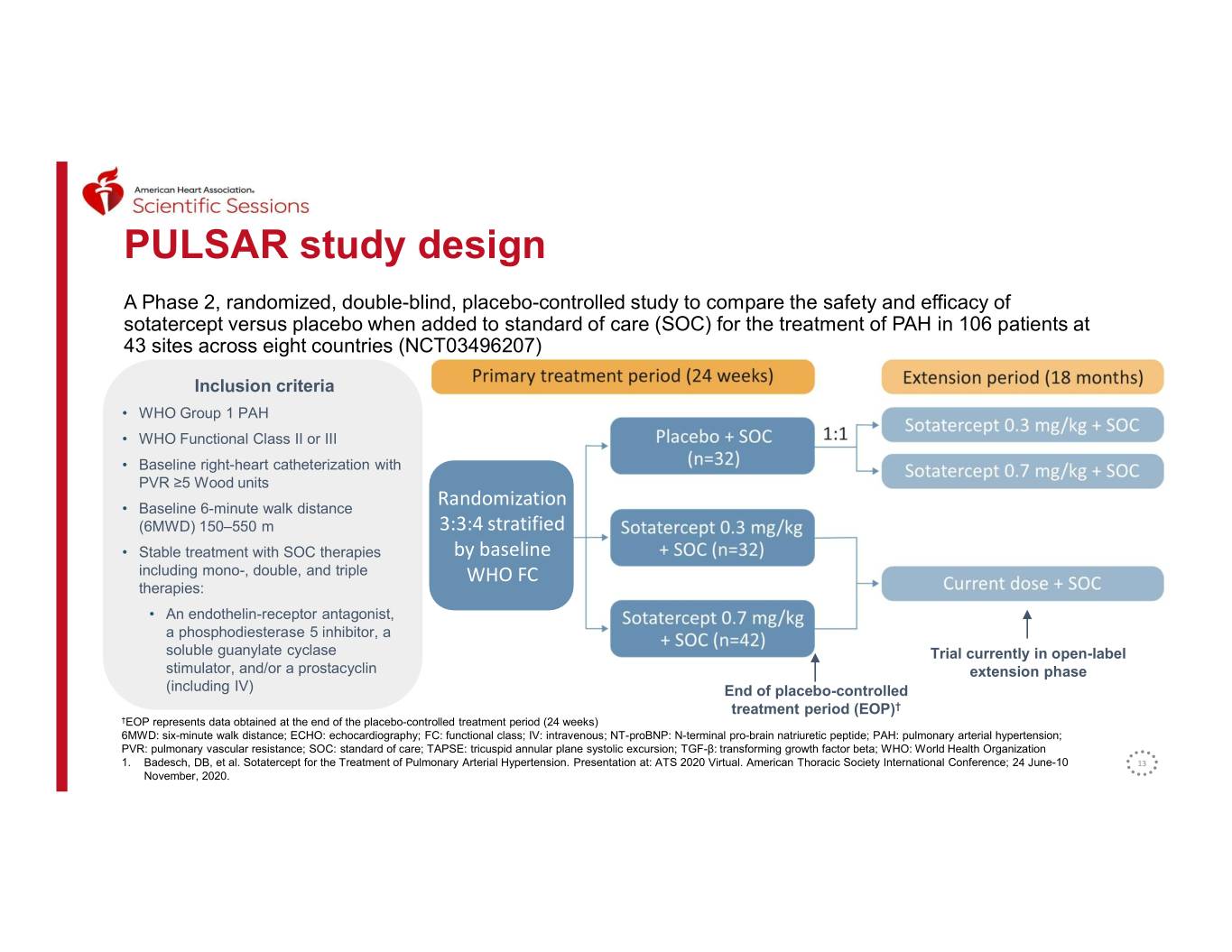
PULSAR study design A Phase 2, randomized, double-blind, placebo-controlled study to compare the safety and efficacy of sotatercept versus placebo when added to standard of care (SOC) for the treatment of PAH in 106 patients at 43 sites across eight countries (NCT03496207) Inclusion criteria • WHO Group 1 PAH • WHO Functional Class II or III • Baseline right-heart catheterization with PVR ≥5 Wood units • Baseline 6-minute walk distance Randomization (6MWD) 150–550 m 3:3:4 stratified • Stable treatment with SOC therapies by baseline including mono-, double, and triple WHO FC therapies: • An endothelin-receptor antagonist, a phosphodiesterase 5 inhibitor, a soluble guanylate cyclase Trial currently in open-label stimulator, and/or a prostacyclin extension phase (including IV) End of placebo-controlled treatment period (EOP)† †EOP represents data obtained at the end of the placebo-controlled treatment period (24 weeks) 6MWD: six-minute walk distance; ECHO: echocardiography; FC: functional class; IV: intravenous; NT-proBNP: N-terminal pro-brain natriuretic peptide; PAH: pulmonary arterial hypertension; PVR: pulmonary vascular resistance; SOC: standard of care; TAPSE: tricuspid annular plane systolic excursion; TGF-β: transforming growth factor beta; WHO: World Health Organization 1. Badesch, DB, et al. Sotatercept for the Treatment of Pulmonary Arterial Hypertension. Presentation at: ATS 2020 Virtual. American Thoracic Society International Conference; 24 June-10 13 November, 2020.
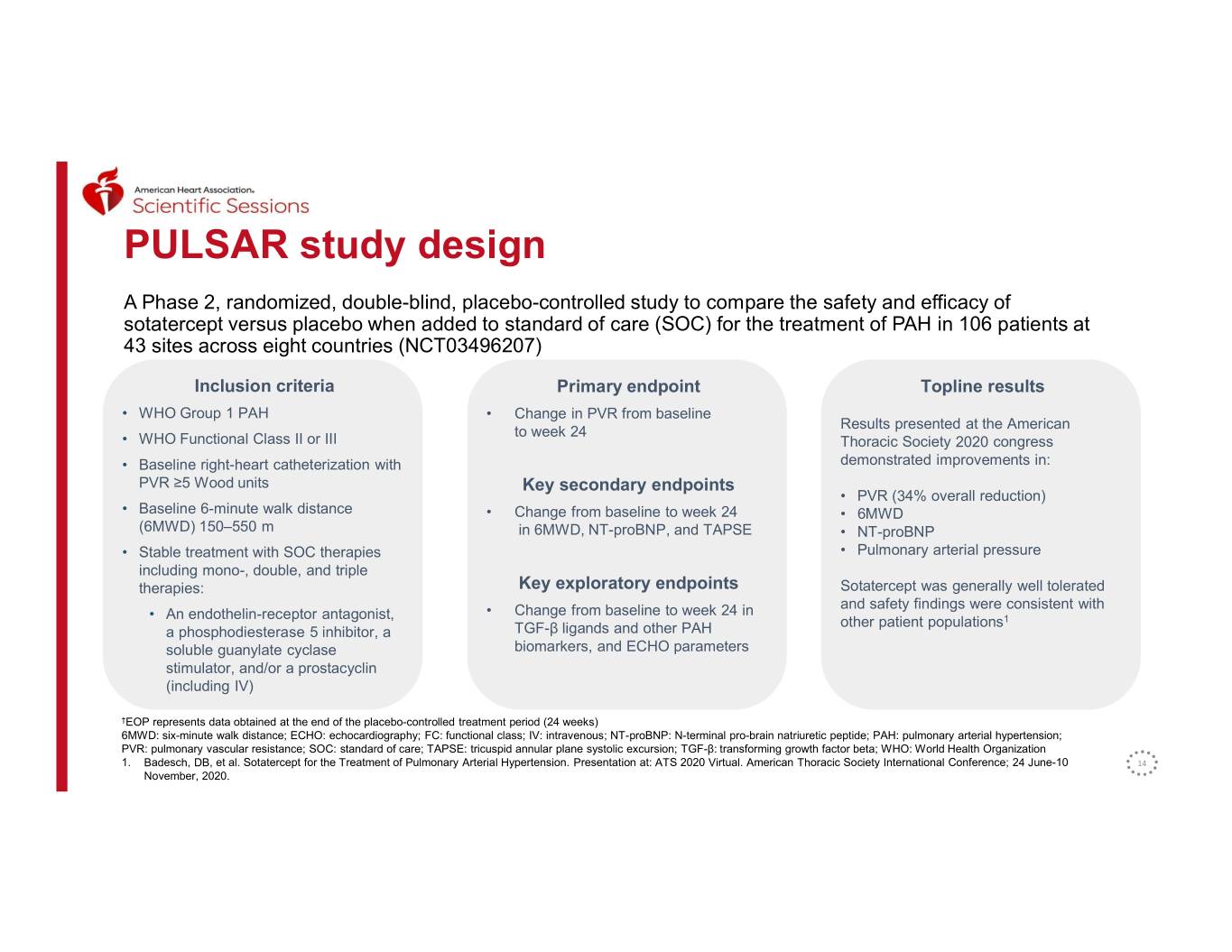
PULSAR study design A Phase 2, randomized, double-blind, placebo-controlled study to compare the safety and efficacy of sotatercept versus placebo when added to standard of care (SOC) for the treatment of PAH in 106 patients at 43 sites across eight countries (NCT03496207) Inclusion criteria Primary endpoint Topline results • WHO Group 1 PAH • Change in PVR from baseline Results presented at the American to week 24 • WHO Functional Class II or III Thoracic Society 2020 congress • Baseline right-heart catheterization with demonstrated improvements in: PVR ≥5 Wood units Key secondary endpoints • PVR (34% overall reduction) • Baseline 6-minute walk distance • Change from baseline to week 24 • 6MWD (6MWD) 150–550 m in 6MWD, NT-proBNP, and TAPSE • NT-proBNP • Stable treatment with SOC therapies • Pulmonary arterial pressure including mono-, double, and triple therapies: Key exploratory endpoints Sotatercept was generally well tolerated and safety findings were consistent with • An endothelin-receptor antagonist, • Change from baseline to week 24 in other patient populations1 a phosphodiesterase 5 inhibitor, a TGF-β ligands and other PAH soluble guanylate cyclase biomarkers, and ECHO parameters stimulator, and/or a prostacyclin (including IV) †EOP represents data obtained at the end of the placebo-controlled treatment period (24 weeks) 6MWD: six-minute walk distance; ECHO: echocardiography; FC: functional class; IV: intravenous; NT-proBNP: N-terminal pro-brain natriuretic peptide; PAH: pulmonary arterial hypertension; PVR: pulmonary vascular resistance; SOC: standard of care; TAPSE: tricuspid annular plane systolic excursion; TGF-β: transforming growth factor beta; WHO: World Health Organization 1. Badesch, DB, et al. Sotatercept for the Treatment of Pulmonary Arterial Hypertension. Presentation at: ATS 2020 Virtual. American Thoracic Society International Conference; 24 June-10 14 November, 2020.
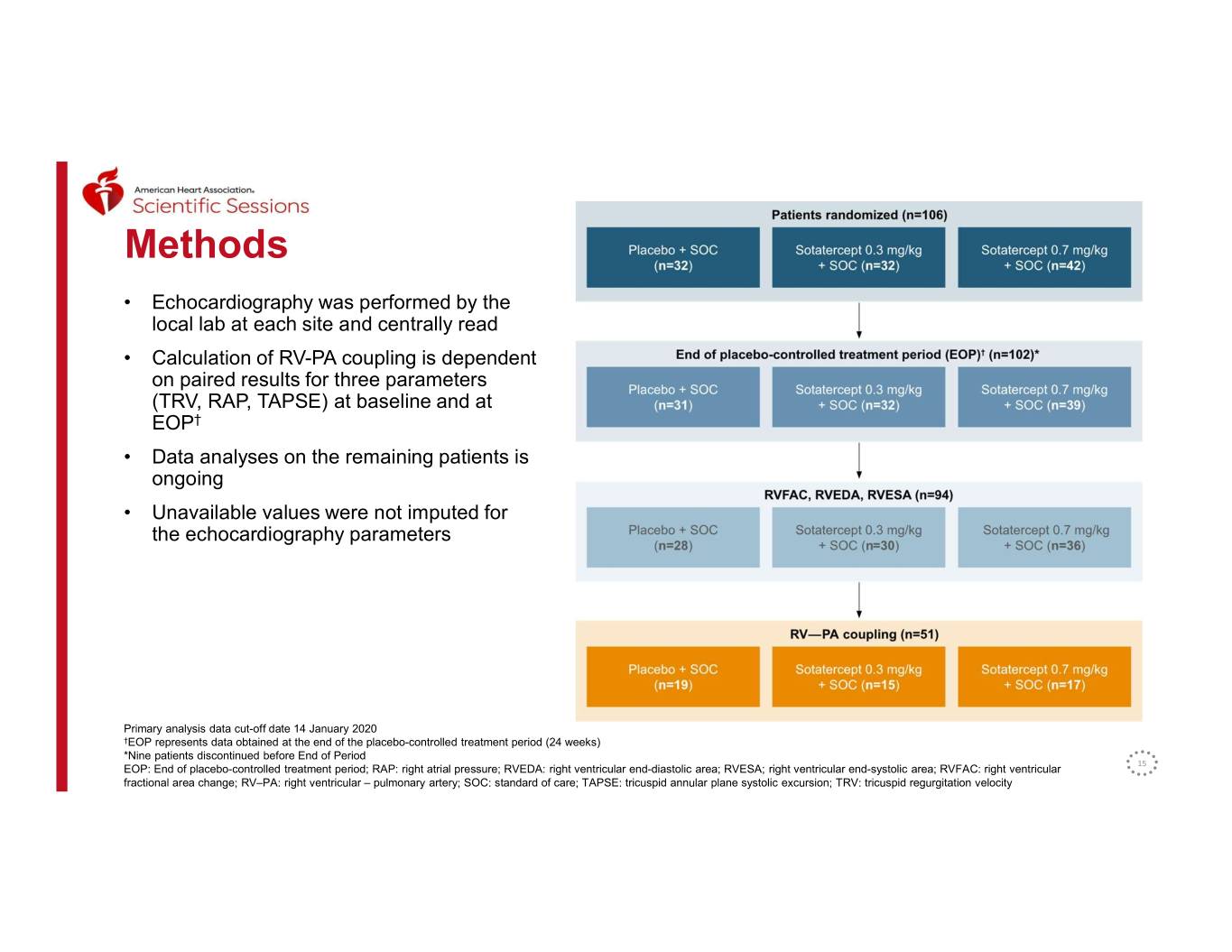
Methods • Echocardiography was performed by the local lab at each site and centrally read • Calculation of RV-PA coupling is dependent on paired results for three parameters (TRV, RAP, TAPSE) at baseline and at Placebo + SOC (n=30) EOP† • Data analyses on the remaining patients is ongoing • Unavailable values were not imputed for the echocardiography parameters Placebo + SOC (n=19) Primary analysis data cut-off date 14 January 2020 †EOP represents data obtained at the end of the placebo-controlled treatment period (24 weeks) *Nine patients discontinued before End of Period EOP: End of placebo-controlled treatment period; RAP: right atrial pressure; RVEDA: right ventricular end-diastolic area; RVESA; right ventricular end-systolic area; RVFAC: right ventricular 15 fractional area change; RV–PA: right ventricular – pulmonary artery; SOC: standard of care; TAPSE: tricuspid annular plane systolic excursion; TRV: tricuspid regurgitation velocity
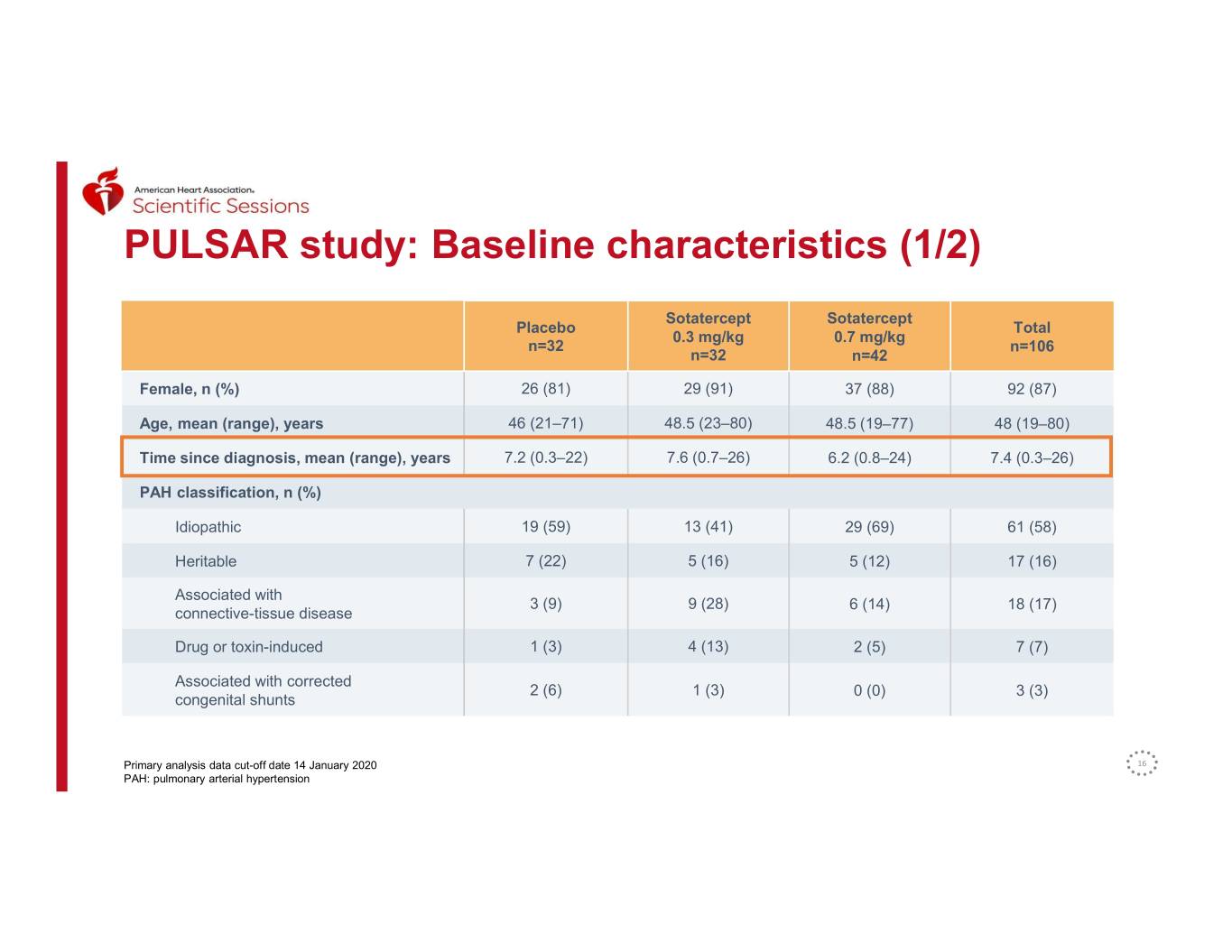
PULSAR study: Baseline characteristics (1/2) Sotatercept Sotatercept Placebo Total 0.3 mg/kg 0.7 mg/kg n=32 n=106 n=32 n=42 Female, n (%) 26 (81) 29 (91) 37 (88) 92 (87) Age, mean (range), years 46 (21–71) 48.5 (23–80) 48.5 (19–77) 48 (19–80) Time since diagnosis, mean (range), years 7.2 (0.3–22) 7.6 (0.7–26) 6.2 (0.8–24) 7.4 (0.3–26) PAH classification, n (%) Idiopathic 19 (59) 13 (41) 29 (69) 61 (58) Heritable 7 (22) 5 (16) 5 (12) 17 (16) Associated with 3 (9) 9 (28) 6 (14) 18 (17) connective-tissue disease Drug or toxin-induced 1 (3) 4 (13) 2 (5) 7 (7) Associated with corrected 2 (6) 1 (3) 0 (0) 3 (3) congenital shunts Primary analysis data cut-off date 14 January 2020 16 PAH: pulmonary arterial hypertension
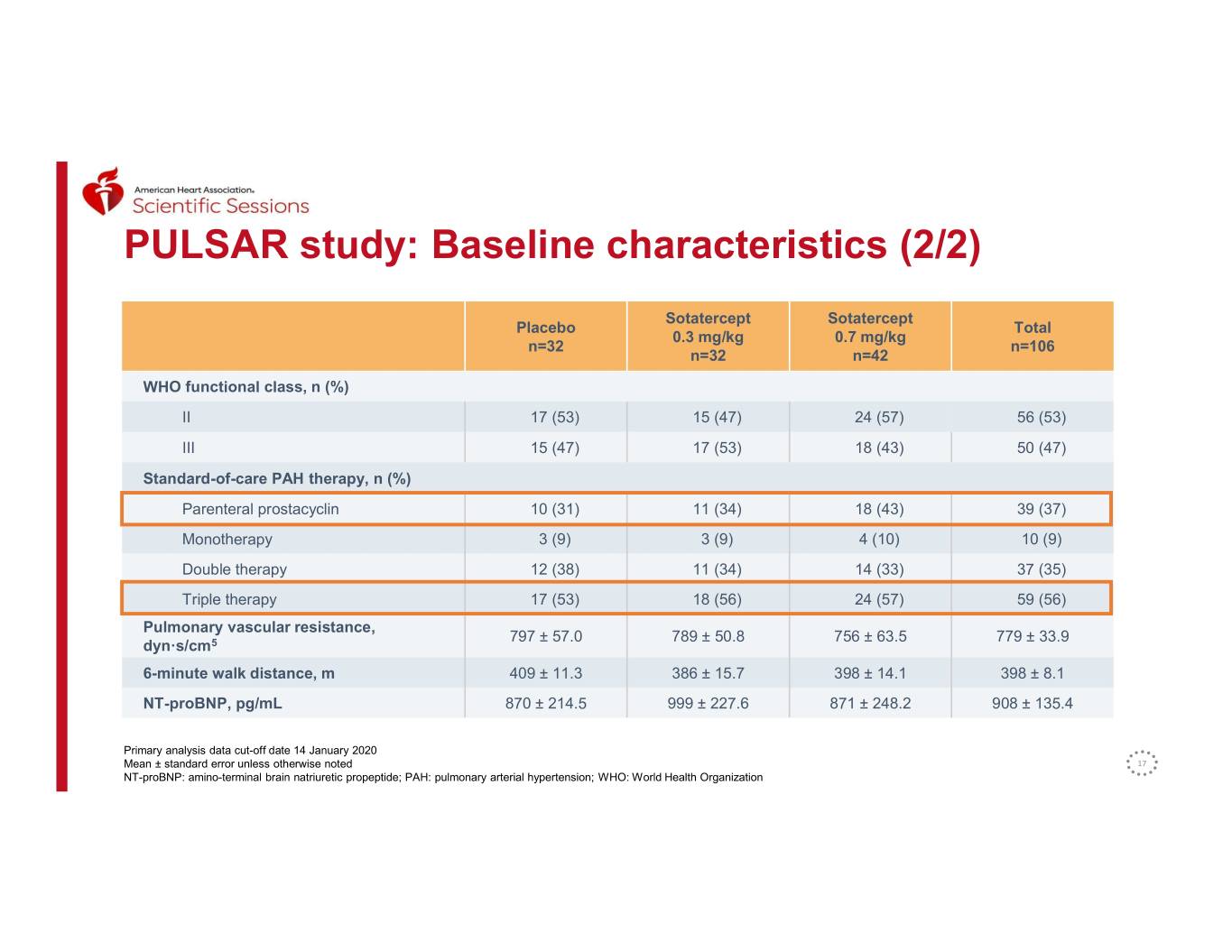
PULSAR study: Baseline characteristics (2/2) Sotatercept Sotatercept Placebo Total 0.3 mg/kg 0.7 mg/kg n=32 n=106 n=32 n=42 WHO functional class, n (%) II 17 (53) 15 (47) 24 (57) 56 (53) III 15 (47) 17 (53) 18 (43) 50 (47) Standard-of-care PAH therapy, n (%) Parenteral prostacyclin 10 (31) 11 (34) 18 (43) 39 (37) Monotherapy 3 (9) 3 (9) 4 (10) 10 (9) Double therapy 12 (38) 11 (34) 14 (33) 37 (35) Triple therapy 17 (53) 18 (56) 24 (57) 59 (56) Pulmonary vascular resistance, 797 ± 57.0 789 ± 50.8 756 ± 63.5 779 ± 33.9 dyn·s/cm5 6-minute walk distance, m 409 ± 11.3 386 ± 15.7 398 ± 14.1 398 ± 8.1 NT-proBNP, pg/mL 870 ± 214.5 999 ± 227.6 871 ± 248.2 908 ± 135.4 Primary analysis data cut-off date 14 January 2020 Mean ± standard error unless otherwise noted 17 NT-proBNP: amino-terminal brain natriuretic propeptide; PAH: pulmonary arterial hypertension; WHO: World Health Organization
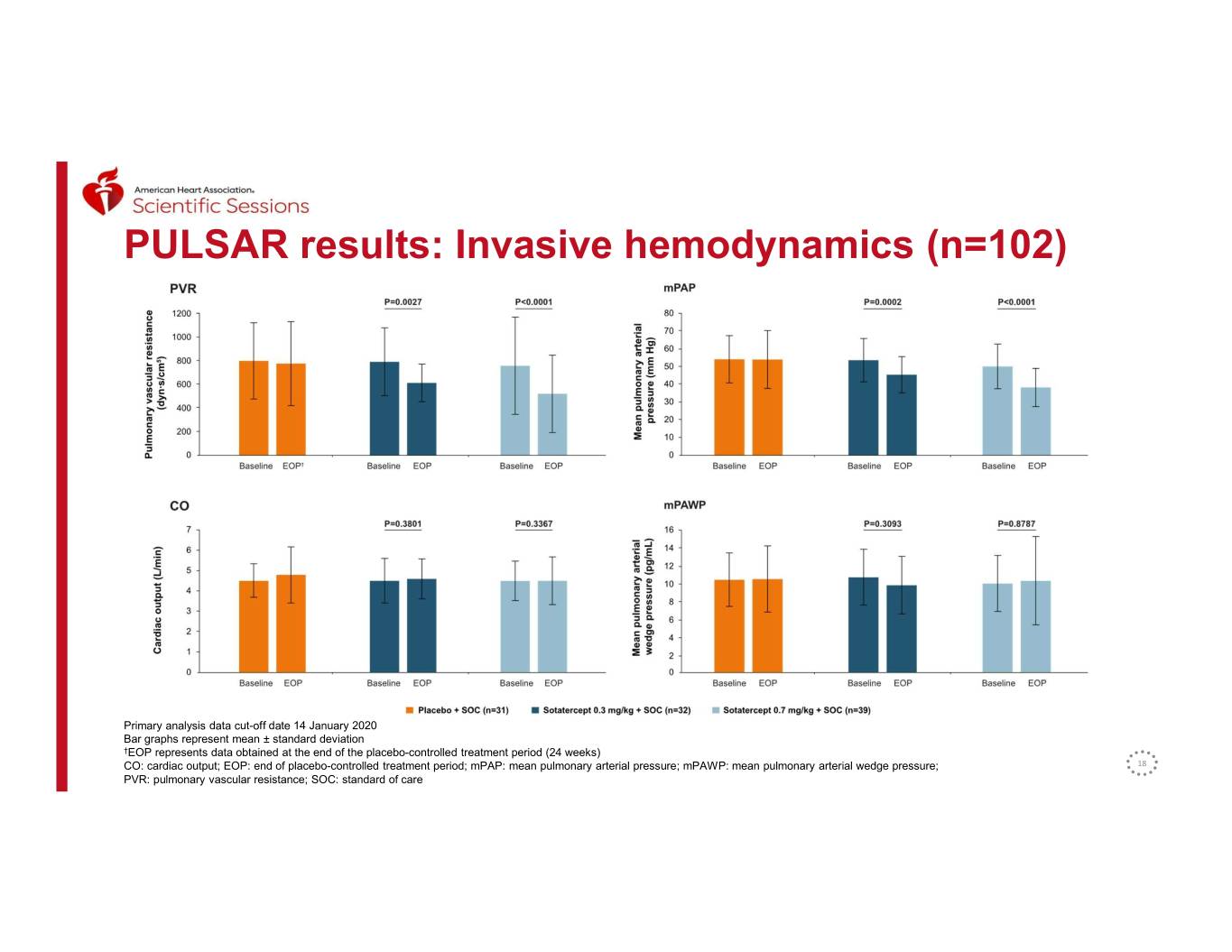
PULSAR results: Invasive hemodynamics (n=102) Primary analysis data cut-off date 14 January 2020 Bar graphs represent mean ± standard deviation †EOP represents data obtained at the end of the placebo-controlled treatment period (24 weeks) CO: cardiac output; EOP: end of placebo-controlled treatment period; mPAP: mean pulmonary arterial pressure; mPAWP: mean pulmonary arterial wedge pressure; 18 PVR: pulmonary vascular resistance; SOC: standard of care
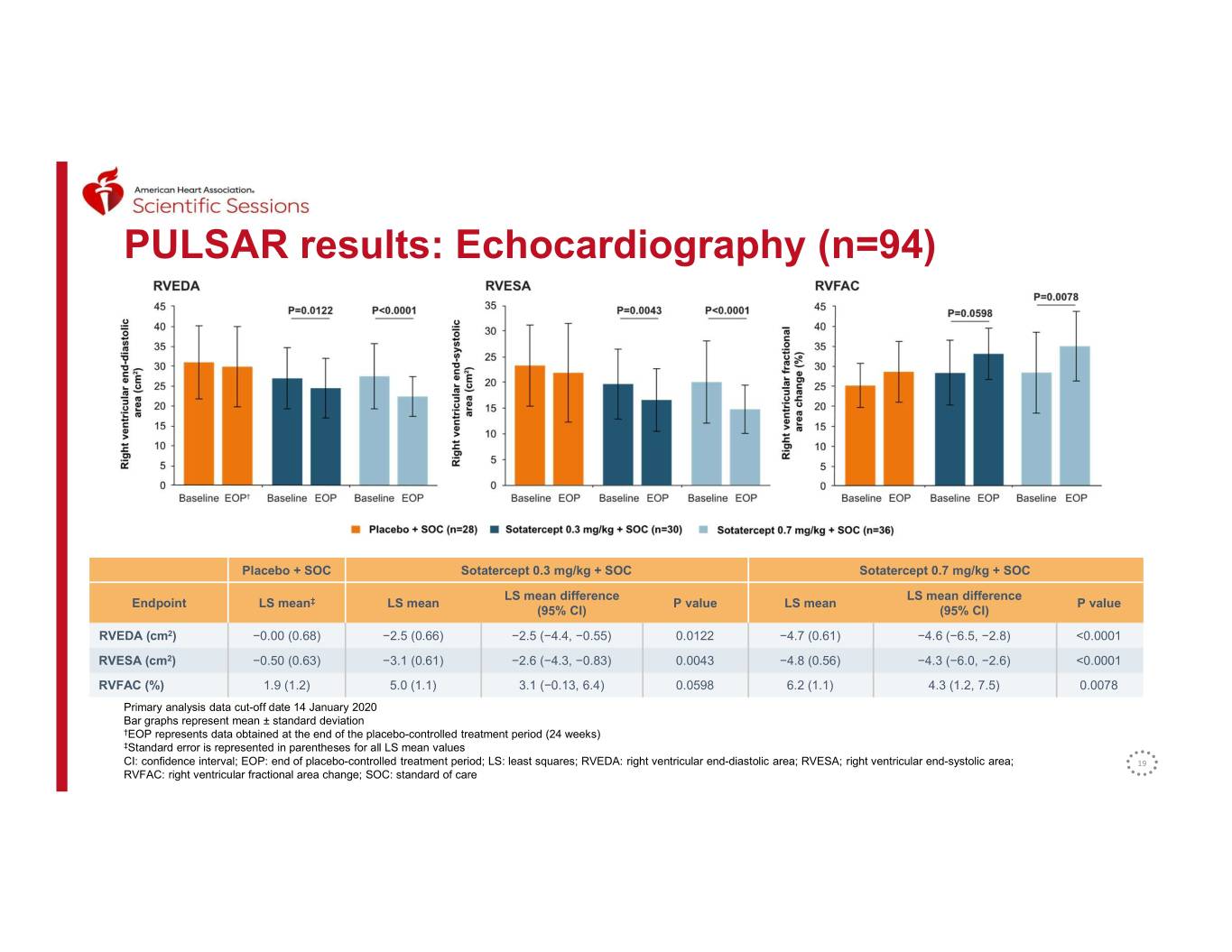
PULSAR results: Echocardiography (n=94) Placebo + SOC Sotatercept 0.3 mg/kg + SOC Sotatercept 0.7 mg/kg + SOC LS mean difference LS mean difference Endpoint LS mean‡ LS mean P value LS mean P value (95% CI) (95% CI) RVEDA (cm2) −0.00 (0.68) −2.5 (0.66) −2.5 (−4.4, −0.55) 0.0122 −4.7 (0.61) −4.6 (−6.5, −2.8) <0.0001 RVESA (cm2) −0.50 (0.63) −3.1 (0.61) −2.6 (−4.3, −0.83) 0.0043 −4.8 (0.56) −4.3 (−6.0, −2.6) <0.0001 RVFAC (%) 1.9 (1.2) 5.0 (1.1) 3.1 (−0.13, 6.4) 0.0598 6.2 (1.1) 4.3 (1.2, 7.5) 0.0078 Primary analysis data cut-off date 14 January 2020 Bar graphs represent mean ± standard deviation †EOP represents data obtained at the end of the placebo-controlled treatment period (24 weeks) ‡Standard error is represented in parentheses for all LS mean values CI: confidence interval; EOP: end of placebo-controlled treatment period; LS: least squares; RVEDA: right ventricular end-diastolic area; RVESA; right ventricular end-systolic area; 19 RVFAC: right ventricular fractional area change; SOC: standard of care
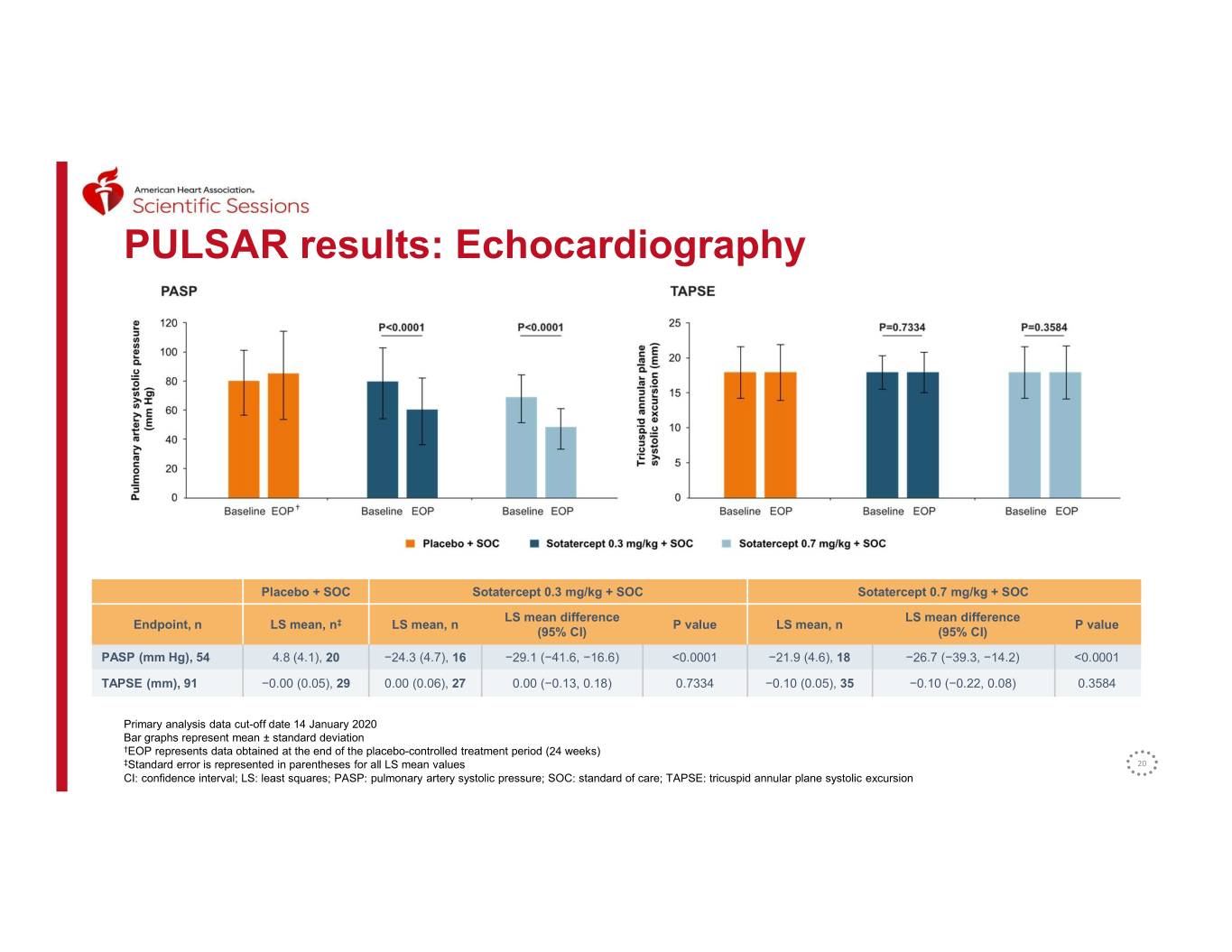
PULSAR results: Echocardiography † Placebo + SOC Sotatercept 0.3 mg/kg + SOC Sotatercept 0.7 mg/kg + SOC LS mean difference LS mean difference Endpoint, n LS mean, n‡ LS mean, n P value LS mean, n P value (95% CI) (95% CI) PASP (mm Hg), 54 4.8 (4.1), 20 −24.3 (4.7), 16 −29.1 (−41.6, −16.6) <0.0001 −21.9 (4.6), 18 −26.7 (−39.3, −14.2) <0.0001 TAPSE (mm), 91 −0.00 (0.05), 29 0.00 (0.06), 27 0.00 (−0.13, 0.18) 0.7334 −0.10 (0.05), 35 −0.10 (−0.22, 0.08) 0.3584 Primary analysis data cut-off date 14 January 2020 Bar graphs represent mean ± standard deviation †EOP represents data obtained at the end of the placebo-controlled treatment period (24 weeks) ‡Standard error is represented in parentheses for all LS mean values 20 CI: confidence interval; LS: least squares; PASP: pulmonary artery systolic pressure; SOC: standard of care; TAPSE: tricuspid annular plane systolic excursion
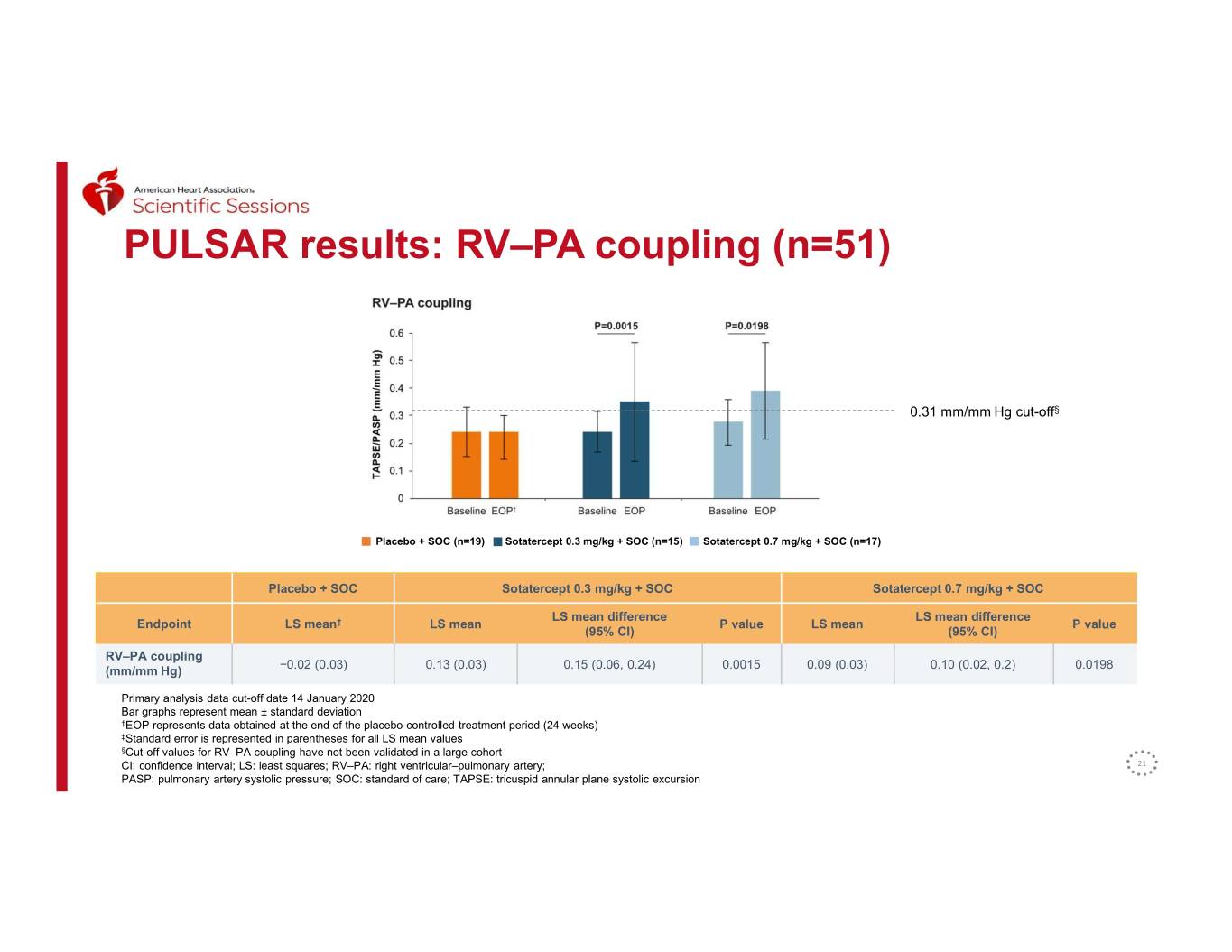
PULSAR results: RV–PA coupling (n=51) 0.31 mm/mm Hg cut-off§ Placebo + SOC (n=19) Sotatercept 0.3 mg/kg + SOC (n=15) Sotatercept 0.7 mg/kg + SOC (n=17) Placebo + SOC Sotatercept 0.3 mg/kg + SOC Sotatercept 0.7 mg/kg + SOC LS mean difference LS mean difference Endpoint LS mean‡ LS mean P value LS mean P value (95% CI) (95% CI) RV–PA coupling −0.02 (0.03) 0.13 (0.03) 0.15 (0.06, 0.24) 0.0015 0.09 (0.03) 0.10 (0.02, 0.2) 0.0198 (mm/mm Hg) Primary analysis data cut-off date 14 January 2020 Bar graphs represent mean ± standard deviation †EOP represents data obtained at the end of the placebo-controlled treatment period (24 weeks) ‡Standard error is represented in parentheses for all LS mean values §Cut-off values for RV–PA coupling have not been validated in a large cohort CI: confidence interval; LS: least squares; RV–PA: right ventricular–pulmonary artery; 21 PASP: pulmonary artery systolic pressure; SOC: standard of care; TAPSE: tricuspid annular plane systolic excursion
Conclusions • In this limited subgroup of the PULSAR study: o Treatment with sotatercept was associated with statistically significant improvements in RV–PA coupling and RV function when compared with placebo o Significant improvement from baseline to week 24 in both sotatercept dose groups versus placebo was observed in RV–PA coupling, RVEDA, RVESA, and PASP o For RVFAC, significance was seen at the sotatercept 0.7 mg/kg dose level and was trending at the sotatercept 0.3 mg/kg dose level but did not quite reach the 0.05 significance level o No changes were seen in TAPSE or in cardiac output • Sotatercept was generally well tolerated and safety findings were consistent with other patient populations • Sotatercept has the potential to be a new treatment option for PAH patients, with consistent and encouraging effects on RV–PA coupling and RV function in a post hoc analysis PAH: pulmonary arterial hypertension; PASP: pulmonary arterial systolic pressure; RV: right ventricular; RVEDA: right ventricular end-diastolic area; RVESA: right ventricular end-systolic area; 22 RVFAC: right ventricular fractional area change; RV–PA: right ventricular–pulmonary artery; TAPSE: tricuspid annular plane systolic excursion
PULSAR study: Acknowledgements • We thank all the patients, their families, and all the PULSAR study investigators who participated in the trial – PULSAR study investigators: Y. Adir, H. Alnuaimat, M. Andrade-Lima, J. Arakaki, R. Argula, A. Baloira, D. Baratz, J. Barberá, A. Bar-Shai, C. Berastagui, L. Bertoletti, M. Delcroix, D. Blanco, A. Bourdin, F. Campos, M. Chakinala, C. Church, J. Cifrian Martinez, J. Coghlan, T. Demarco, S. Eisenmann, P. Engel, P. Escribano-Subias, J. Feenstra, J. Feldman, M. Halank, L. Howard, O. Hussein, A. Keogh, M. Kramer, T. Lange, M. Lavender, M. Lazaro Salvador, G. Meyer, J. Michaelson, D. Montani, W. Nseir, K. Olsson, C. Opitz, C. Pison, D. Poch, F. Rahaghi, Y. Raviv, G. Reeves, F. Rischard, J. Robinson, Z. Safdar, R. Saggar, J. Schreiber, M. Segel, J. Segovia Cubero, D. Shitrit, N. Sood, L. Spikes, S. Steiglitz, JL. Vachiery, J. Wheatley, H. Wirtz • We also thank all members of the PULSAR trial steering committee including; D. Badesch, R. De Souza, M. Hoeper, M. Humbert, I. Preston and A. Waxman • The study was sponsored by Acceleron Pharma, Cambridge, MA, USA – Acceleron personnel: A. Atanasov, C. Barron, B. Budda, E. Davis, K. de Jong, R. Gerber, S. Harrison, J. Lu, J. Reynolds, J. Oram, C. Sanmarco, M. Troy, N. Yuen • The authors received editorial assistance from InterComm LTD, supported by Acceleron Pharma 23
Aaron Waxman, MD, PhD Director, Pulmonary Vascular Disease Program, Brigham and Women’s Hospital; Associate Professor of Medicine, Harvard Medical School Principal investigator in the SPECTRA trial and a paid consultant to Acceleron 24 This presentation is for investor relations purposes only – Not for product promotional purposes.
SPECTRA and Beyond: Signs of Disease Modification? Aaron B Waxman, MD, PhD Director, Pulmonary Vascular Disease Program Brigham and Women’s Hospital, Cardiovascular Medicine, Pulmonary and Critical Care #AHA20
Disclosures Financial relationships with relevant commercial interests for three years preceding this presentation: • Acceleron Pharma Sotatercept is an investigational product that is not approved for any use in any country 26
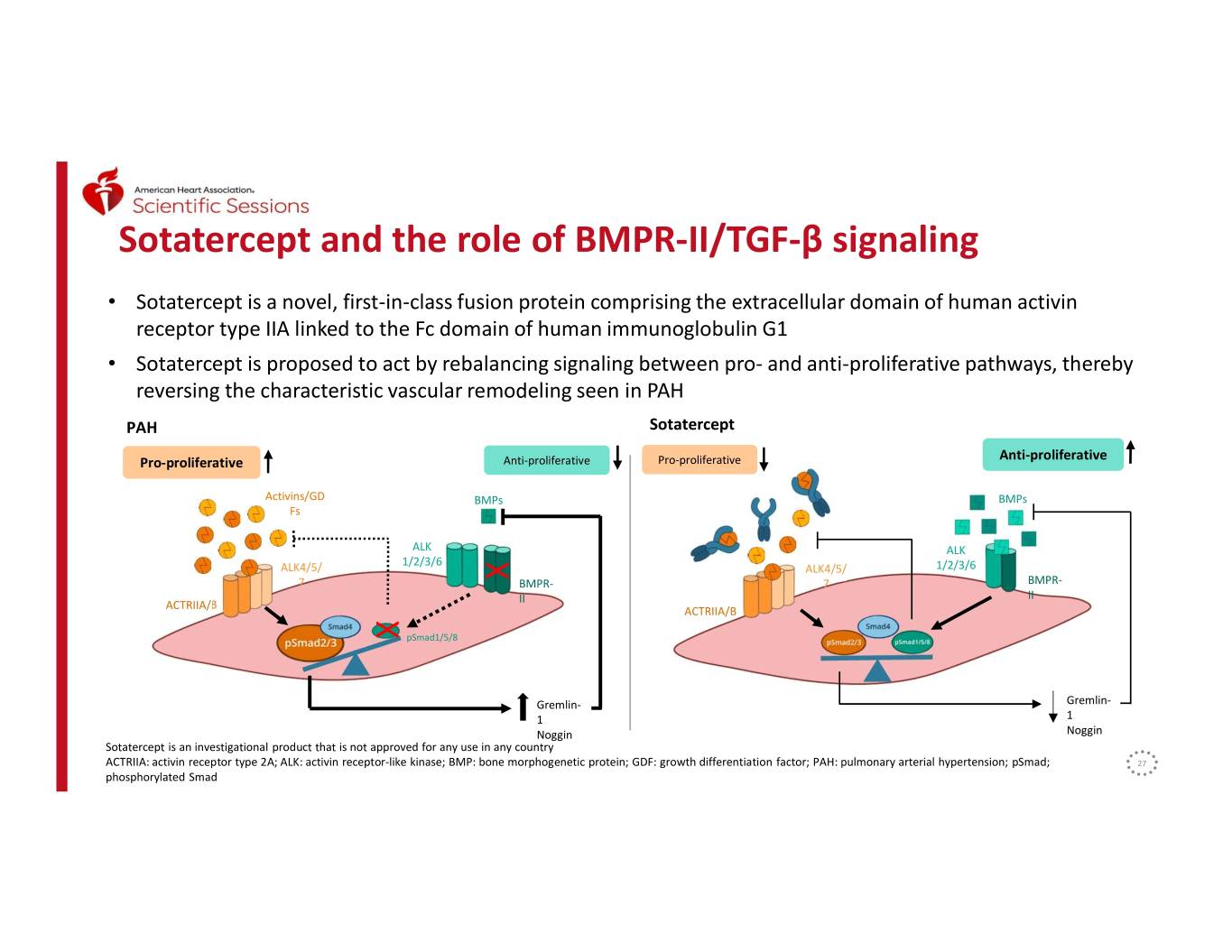
Sotatercept and the role of BMPR-II/TGF-β signaling • Sotatercept is a novel, first-in-class fusion protein comprising the extracellular domain of human activin receptor type IIA linked to the Fc domain of human immunoglobulin G1 • Sotatercept is proposed to act by rebalancing signaling between pro- and anti-proliferative pathways, thereby reversing the characteristic vascular remodeling seen in PAH PAH Sotatercept Anti-proliferative Pro-proliferative Anti-proliferative Pro-proliferative Activins/GD BMPs BMPs Fs ALK ALK 1/2/3/6 ALK4/5/ ALK4/5/ 1/2/3/6 7 X BMPR- 7 BMPR- II II ACTRIIA/B ACTRIIA/B X pSmad1/5/8 Gremlin- Gremlin- 1 1 Noggin Noggin Sotatercept is an investigational product that is not approved for any use in any country ACTRIIA: activin receptor type 2A; ALK: activin receptor-like kinase; BMP: bone morphogenetic protein; GDF: growth differentiation factor; PAH: pulmonary arterial hypertension; pSmad; 27 phosphorylated Smad
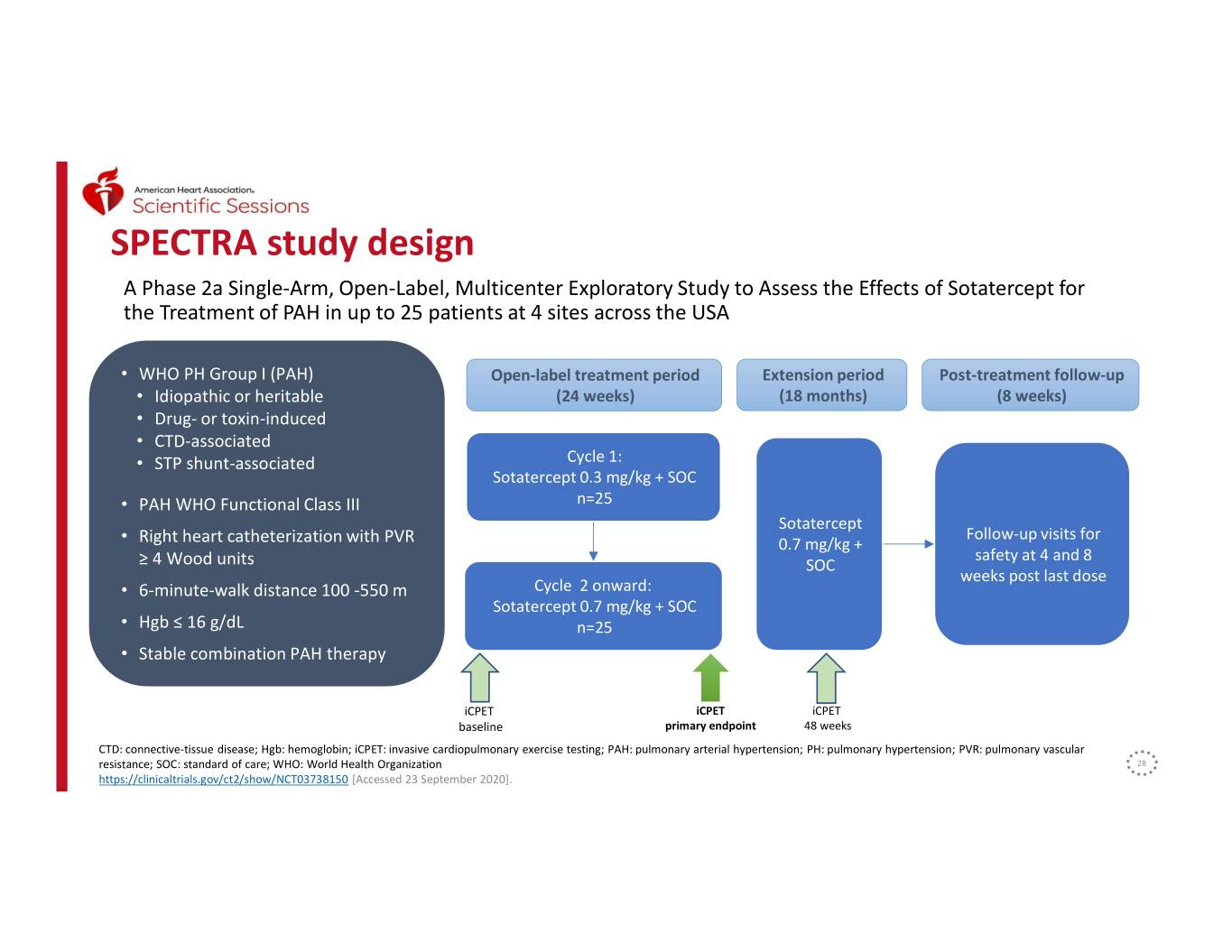
SPECTRA study design A Phase 2a Single-Arm, Open-Label, Multicenter Exploratory Study to Assess the Effects of Sotatercept for the Treatment of PAH in up to 25 patients at 4 sites across the USA • WHO PH Group I (PAH) Open-label treatment period Extension period Post-treatment follow-up • Idiopathic or heritable (24 weeks) (18 months) (8 weeks) • Drug- or toxin-induced • CTD-associated • STP shunt-associated Cycle 1: Sotatercept 0.3 mg/kg + SOC • PAH WHO Functional Class III n=25 Sotatercept Follow-up visits for • Right heart catheterization with PVR 0.7 mg/kg + safety at 4 and 8 ≥ 4 Wood units SOC weeks post last dose Cycle 2 onward: • 6-minute-walk distance 100 -550 m Stratified by Sotatercept 0.7 mg/kg + SOC baseline • Hgb ≤ 16 g/dL n=25 WHO FC • Stable combination PAH therapy iCPET iCPET iCPET baseline primary endpoint 48 weeks CTD: connective-tissue disease; Hgb: hemoglobin; iCPET: invasive cardiopulmonary exercise testing; PAH: pulmonary arterial hypertension; PH: pulmonary hypertension; PVR: pulmonary vascular resistance; SOC: standard of care; WHO: World Health Organization 28 https://clinicaltrials.gov/ct2/show/NCT03738150 [Accessed 23 September 2020].
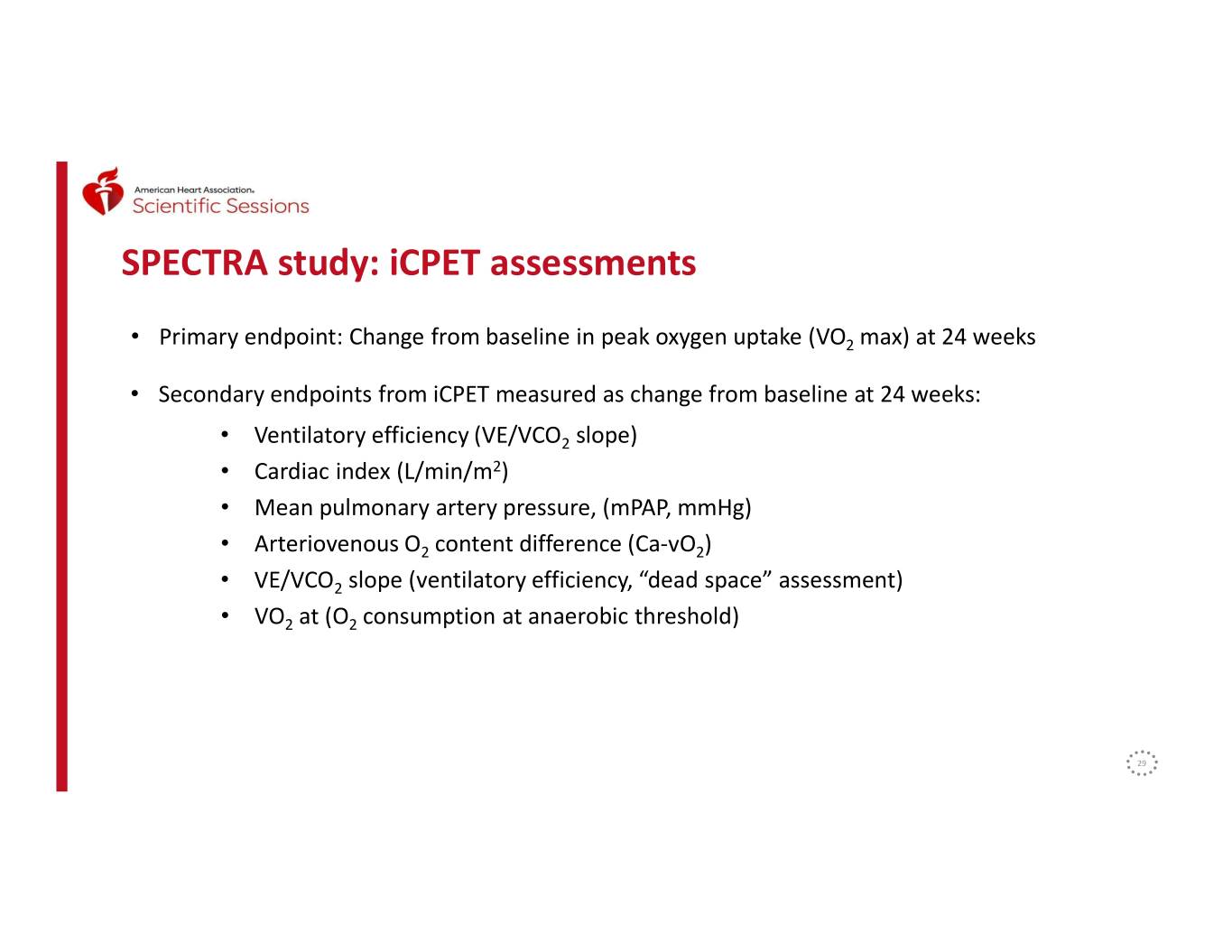
SPECTRA study: iCPET assessments • Primary endpoint: Change from baseline in peak oxygen uptake (VO2 max) at 24 weeks • Secondary endpoints from iCPET measured as change from baseline at 24 weeks: • Ventilatory efficiency (VE/VCO2 slope) • Cardiac index (L/min/m2) • Mean pulmonary artery pressure, (mPAP, mmHg) • Arteriovenous O2 content difference (Ca-vO2) • VE/VCO2 slope (ventilatory efficiency, “dead space” assessment) • VO2 at (O2 consumption at anaerobic threshold) 29
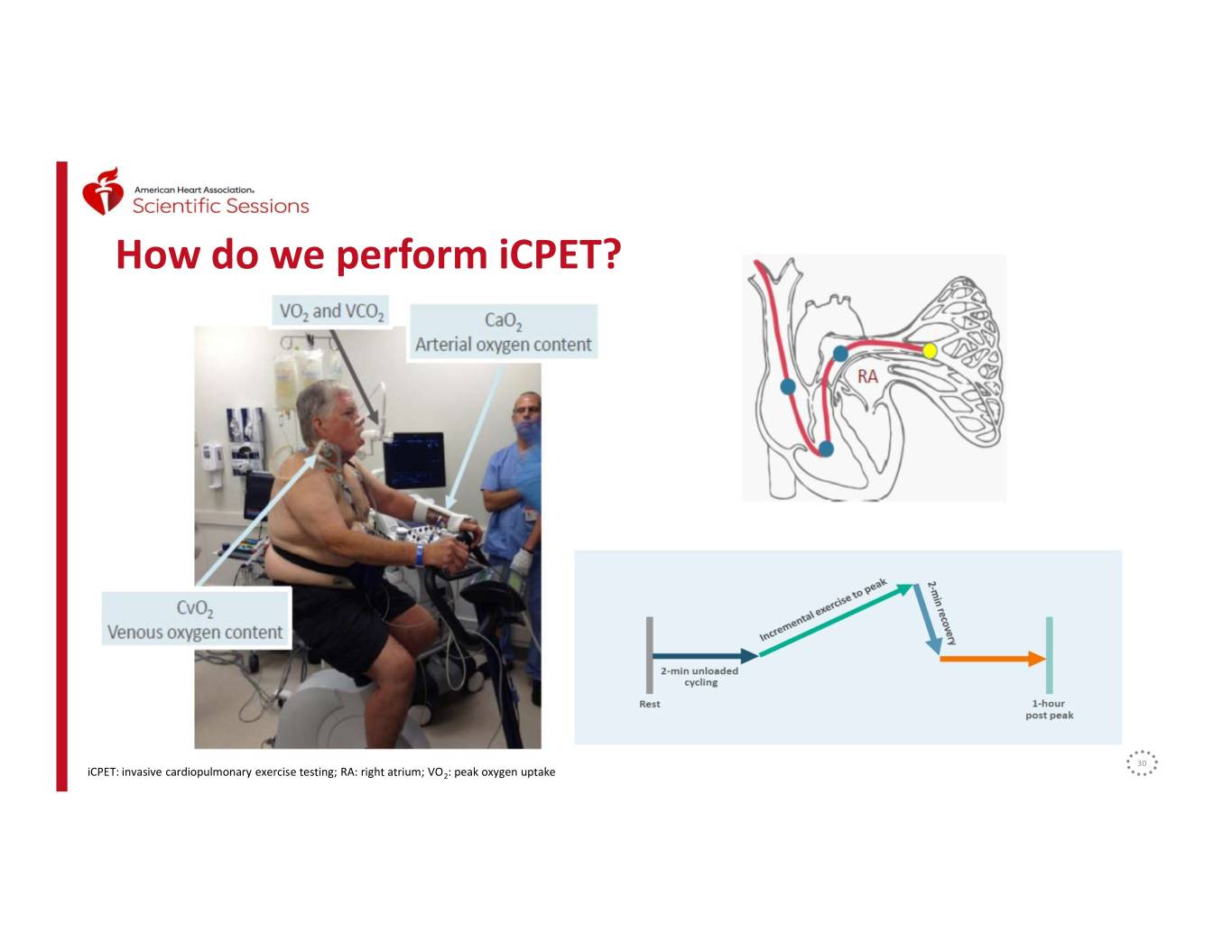
How do we perform iCPET? 30 iCPET: invasive cardiopulmonary exercise testing; RA: right atrium; VO2: peak oxygen uptake
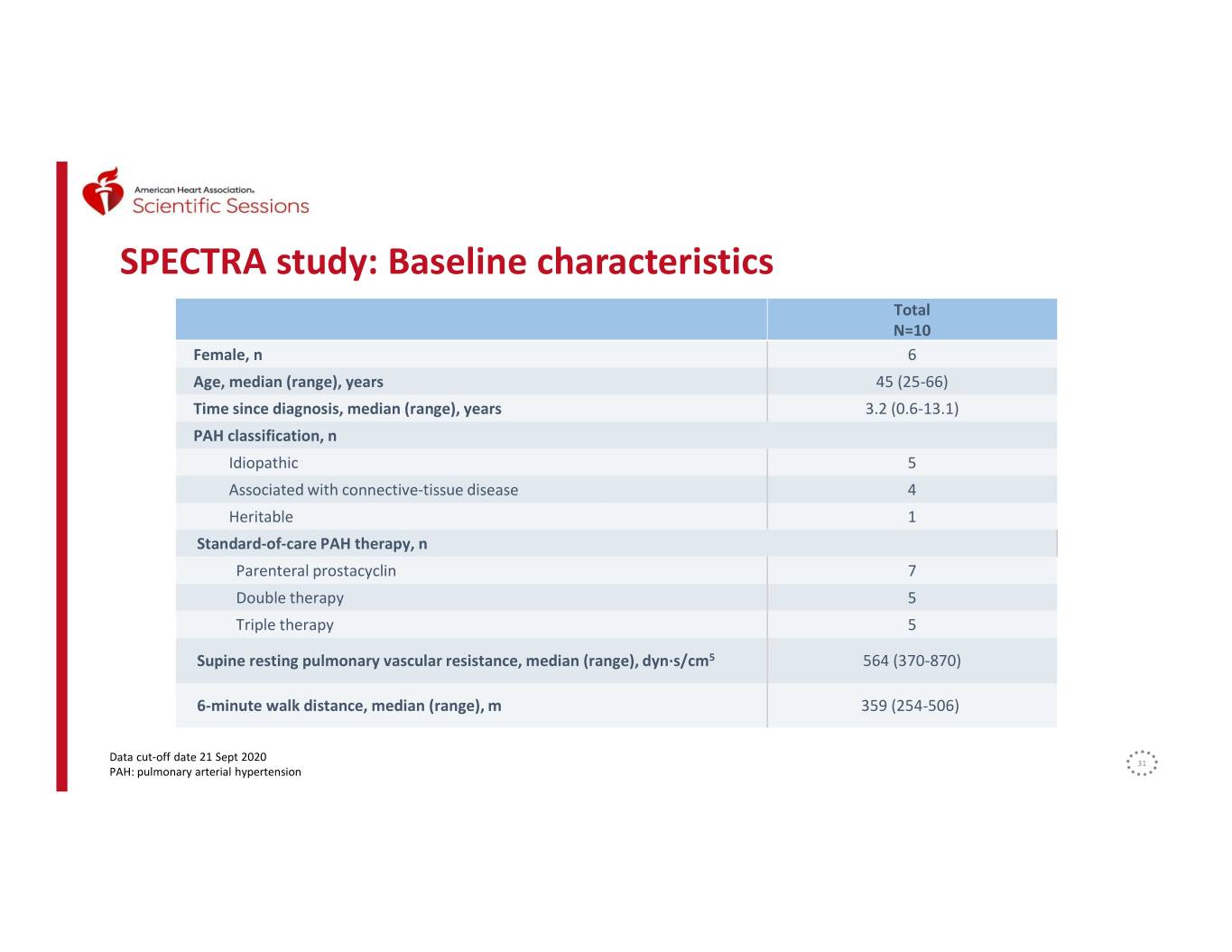
SPECTRA study: Baseline characteristics Total N=10 Female, n 6 Age, median (range), years 45 (25-66) Time since diagnosis, median (range), years 3.2 (0.6-13.1) PAH classification, n Idiopathic 5 Associated with connective-tissue disease 4 Heritable 1 Standard-of-care PAH therapy, n Parenteral prostacyclin 7 Double therapy 5 Triple therapy 5 Supine resting pulmonary vascular resistance, median (range), dyn·s/cm5 564 (370-870) 6-minute walk distance, median (range), m 359 (254-506) Data cut-off date 21 Sept 2020 31 PAH: pulmonary arterial hypertension
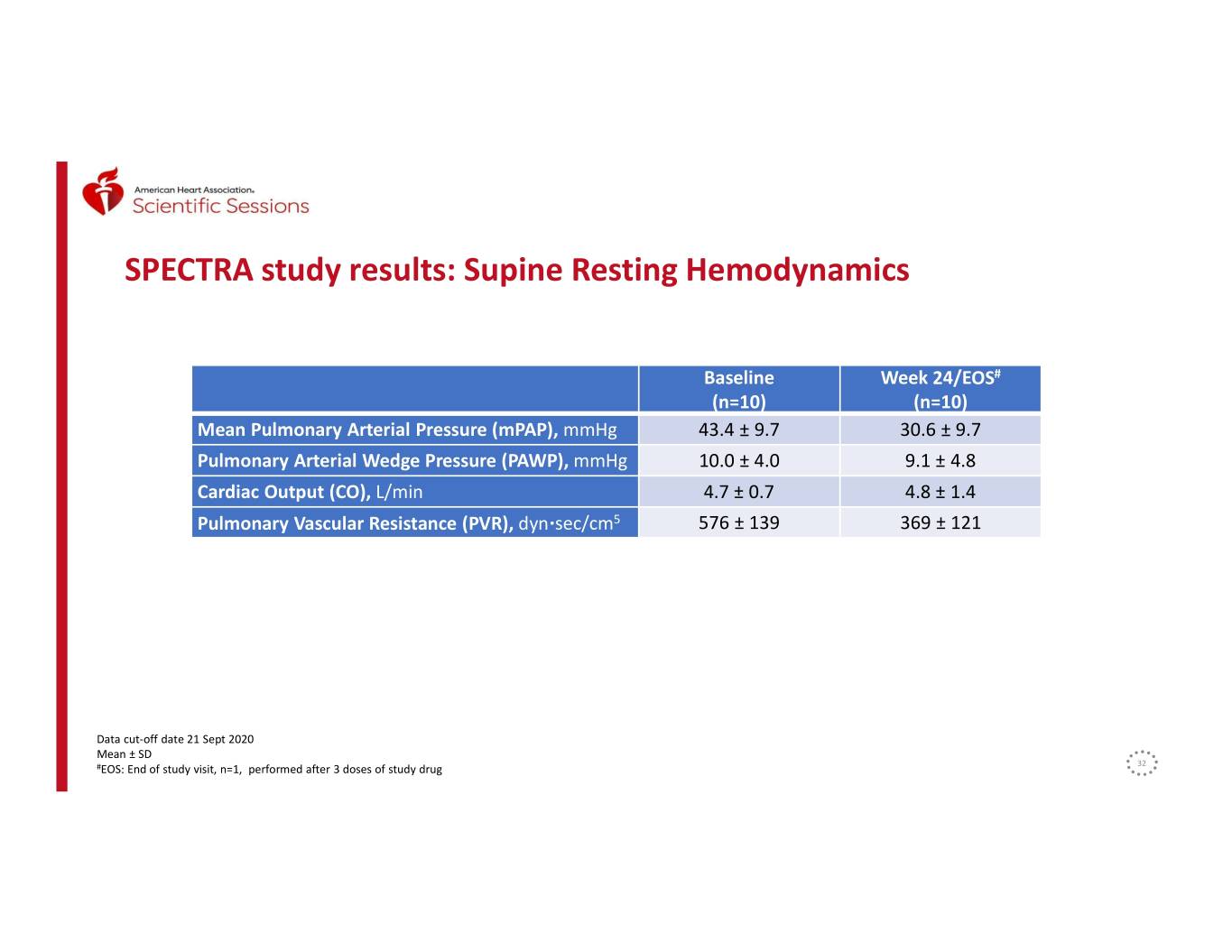
SPECTRA study results: Supine Resting Hemodynamics Baseline Week 24/EOS# (n=10) (n=10) Mean Pulmonary Arterial Pressure (mPAP), mmHg 43.4 ± 9.7 30.6 ± 9.7 Pulmonary Arterial Wedge Pressure (PAWP), mmHg 10.0 ± 4.0 9.1 ± 4.8 Cardiac Output (CO), L/min 4.7 ± 0.7 4.8 ± 1.4 Pulmonary Vascular Resistance (PVR), dyn·sec/cm5 576 ± 139 369 ± 121 Data cut-off date 21 Sept 2020 Mean ± SD #EOS: End of study visit, n=1, performed after 3 doses of study drug 32
SPECTRA Study: Safety Treatment Emergent Adverse Events (TEAE) reported: • 9/10 patients reported at least one TEAE • Arthralgia, dizziness, fluid overload, gingival bleeding, hematochezia, hemoglobin increased, infusion site pain, palpitations, pyrexia, upper respiratory tract infection, weight increased • Two SAEs reported (fluid overload, resolved; hematochezia, resolved), both considered not related to study drug and no dose interruption or reduction required. • One discontinuation due to AE (patient felt worsening pain at Remodulin® site injection) Data cut-off date 21 Sept 2020 AE: adverse event; SAE: serious adverse event: TEAE: treatment-emergent adverse event 33
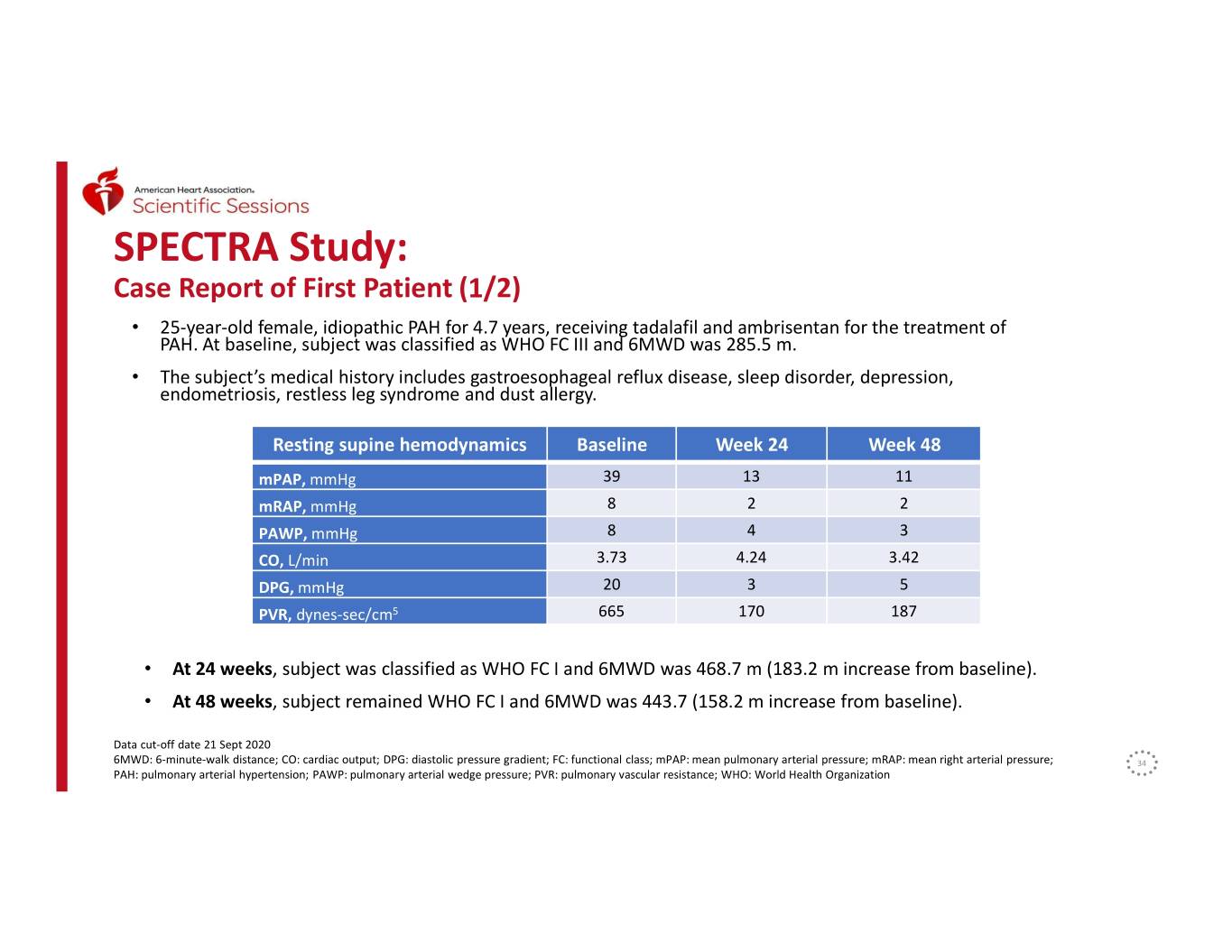
SPECTRA Study: Case Report of First Patient (1/2) • 25-year-old female, idiopathic PAH for 4.7 years, receiving tadalafil and ambrisentan for the treatment of PAH. At baseline, subject was classified as WHO FC III and 6MWD was 285.5 m. • The subject’s medical history includes gastroesophageal reflux disease, sleep disorder, depression, endometriosis, restless leg syndrome and dust allergy. Resting supine hemodynamics Baseline Week 24 Week 48 mPAP, mmHg 39 13 11 mRAP, mmHg 8 2 2 PAWP, mmHg 8 4 3 CO, L/min 3.73 4.24 3.42 DPG, mmHg 20 3 5 PVR, dynes-sec/cm5 665 170 187 • At 24 weeks, subject was classified as WHO FC I and 6MWD was 468.7 m (183.2 m increase from baseline). • At 48 weeks, subject remained WHO FC I and 6MWD was 443.7 (158.2 m increase from baseline). Data cut-off date 21 Sept 2020 6MWD: 6-minute-walk distance; CO: cardiac output; DPG: diastolic pressure gradient; FC: functional class; mPAP: mean pulmonary arterial pressure; mRAP: mean right arterial pressure; 34 PAH: pulmonary arterial hypertension; PAWP: pulmonary arterial wedge pressure; PVR: pulmonary vascular resistance; WHO: World Health Organization
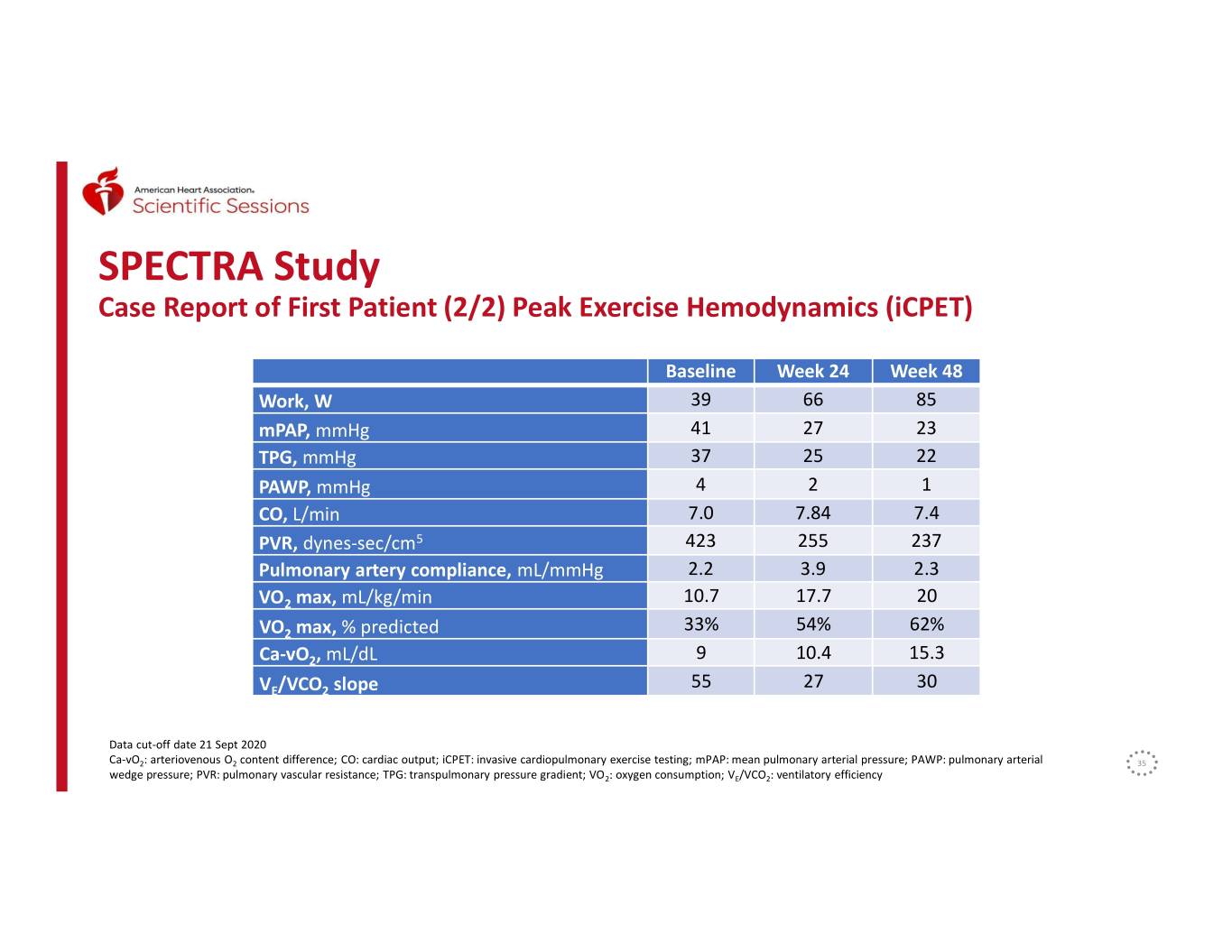
SPECTRA Study Case Report of First Patient (2/2) Peak Exercise Hemodynamics (iCPET) Baseline Week 24 Week 48 Work, W 39 66 85 mPAP, mmHg 41 27 23 TPG, mmHg 37 25 22 PAWP, mmHg 4 2 1 CO, L/min 7.0 7.84 7.4 PVR, dynes-sec/cm5 423 255 237 Pulmonary artery compliance, mL/mmHg 2.2 3.9 2.3 VO2 max, mL/kg/min 10.7 17.7 20 VO2 max, % predicted 33% 54% 62% Ca-vO2, mL/dL 9 10.4 15.3 VE/VCO2 slope 55 27 30 Data cut-off date 21 Sept 2020 Ca-vO2: arteriovenous O2 content difference; CO: cardiac output; iCPET: invasive cardiopulmonary exercise testing; mPAP: mean pulmonary arterial pressure; PAWP: pulmonary arterial 35 wedge pressure; PVR: pulmonary vascular resistance; TPG: transpulmonary pressure gradient; VO2: oxygen consumption; VE/VCO2: ventilatory efficiency
Conclusions • The ongoing SPECTRA study has shown substantial improvements in hemodynamics as well as exercise tolerance and capacity in the limited number of subjects studied to date. • Sotatercept was generally well tolerated, consistent with the previously reported safety profile in PAH1. • Additional data on sotatercept will be presented during AHA 2020: • McLaughlin V, et al. “Sotatercept improves right ventricular – pulmonary arterial coupling and right ventricular function in the PULSAR study”, Dickinson W. Richards Memorial Lecture, Cardiopulmonary Best Abstract Award, presentation number 287 • Joshi S, et al. “Sotatercept analog RAP-011 inhibits right ventricular remodeling and restores function in a mouse model of pressure overload”, poster number MP282 1 Badesch, DB, et al. Sotatercept for the Treatment of Pulmonary Arterial Hypertension. Presentation at: ATS 2020 Virtual. American Thoracic Society International Conference; 36 24 June-10 November, 2020.
SPECTRA study: Acknowledgements • We thank all the patients, their families, and all the SPECTRA study investigators who participated in the trial – SPECTRA study investigators: Aaron B. Waxman, MD, PhD, Franz Rischard, MD, Michael Risbano, MD, and Robert Frantz, MD. – The study was sponsored by Acceleron Pharma, Cambridge, MA, USA – Acceleron personnel: Jonathan Lu, Rebecca Young, Solaiappan Manimaran, Jennifer Barnes, Musa Mutyaba, Erica Davis, Atanas Atanasov, Saba Qamar, Carrie Barron, Jay Backstrom, Janethe Pena 37
Summary | Jay T. Backstrom, MD, MPH EVP, Head of Research & Development This presentation is for investor relations purposes only – Not for product promotional purposes.
AHA 2020: Key Highlights from the Sotatercept Presentations • Echo data received “Cardiopulmonary Best Abstract” • Sotatercept associated with measures of improved right ventricular function • Preliminary hemodynamic data consistent with PULSAR ― Reduction in PVR and mPAP ― Improvement in exercise tolerance and capacity Sotatercept is an investigational therapy that is not approved for any use in any country. This presentation is for investor relations purposes only – Not for product promotional purposes. 39
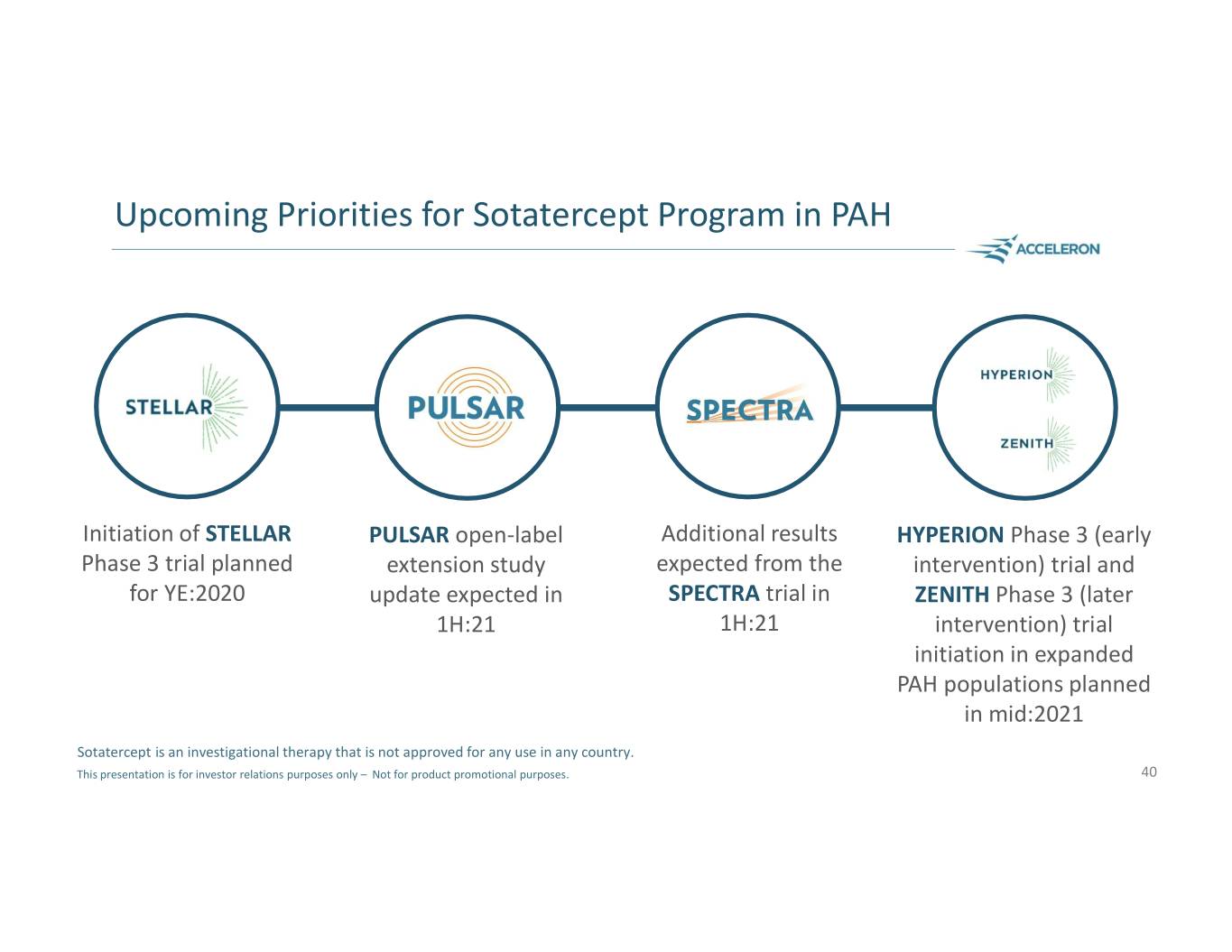
Upcoming Priorities for Sotatercept Program in PAH Initiation of STELLAR PULSAR open-label Additional results HYPERION Phase 3 (early Phase 3 trial planned extension study expected from the intervention) trial and for YE:2020 update expected in SPECTRA trial in ZENITH Phase 3 (later 1H:21 1H:21 intervention) trial initiation in expanded PAH populations planned in mid:2021 Sotatercept is an investigational therapy that is not approved for any use in any country. This presentation is for investor relations purposes only – Not for product promotional purposes. 40
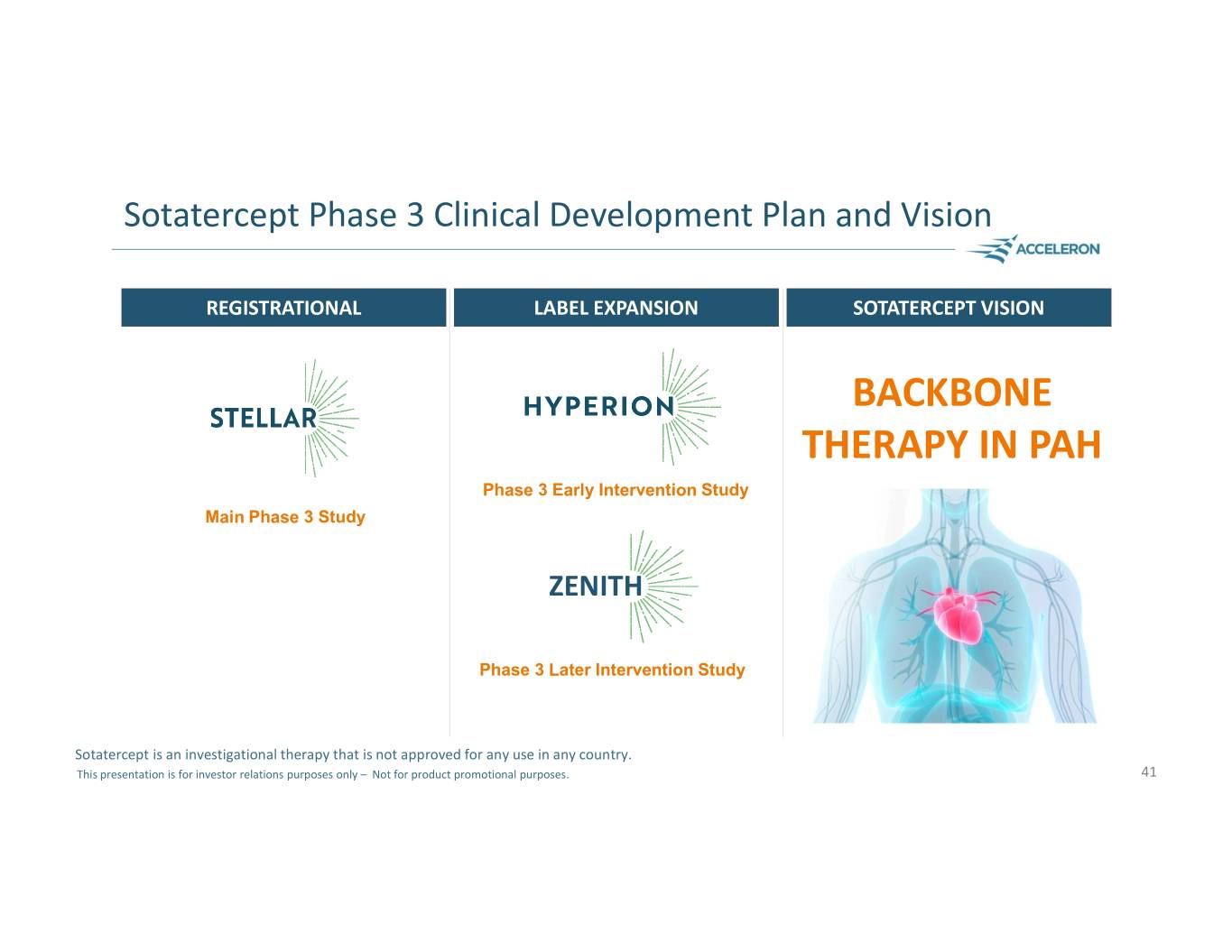
Sotatercept Phase 3 Clinical Development Plan and Vision REGISTRATIONAL LABEL EXPANSION SOTATERCEPT VISION BACKBONE THERAPY IN PAH Phase 3 Early Intervention Study Main Phase 3 Study ZENITH Phase 3 Later Intervention Study Sotatercept is an investigational therapy that is not approved for any use in any country. This presentation is for investor relations purposes only – Not for product promotional purposes. 41

Question & Answer Session Habib Dable Vallerie McLaughlin, MD* President & Chief Executive Officer Professor, Cardiovascular Medicine; Director, Pulmonary Hypertension Program, University of Michigan Jay T. Backstrom, MD, MPH EVP, Head of Research & Development Aaron Waxman, MD, PhD** Director, Pulmonary Vascular Disease Program, Brigham & Women’s Hospital; Sujay Kango Associated Professor of Medicine, EVP, Chief Commercial Officer Harvard Medical School Janethe Pena, MD, PhD Todd James VP, Medical Research, Pulmonary SVP, Corporate Affairs & Investor Relations *Investigator in the PULSAR trial and a paid consultant to Acceleron. **Principal investigator in the SPECTRA trial and a paid consultant to Acceleron. This presentation is for investor relations purposes only – Not for product promotional purposes. 42
