Attached files
| file | filename |
|---|---|
| EX-99.1 - EX-99.1 - Change Healthcare Inc. | d904010dex991.htm |
| EX-32.2 - EX-32.2 - Change Healthcare Inc. | d904010dex322.htm |
| EX-32.1 - EX-32.1 - Change Healthcare Inc. | d904010dex321.htm |
| EX-31.2 - EX-31.2 - Change Healthcare Inc. | d904010dex312.htm |
| EX-31.1 - EX-31.1 - Change Healthcare Inc. | d904010dex311.htm |
| EX-23.1 - EX-23.1 - Change Healthcare Inc. | d904010dex231.htm |
| EX-21.1 - EX-21.1 - Change Healthcare Inc. | d904010dex211.htm |
| EX-10.57 - EX-10.57 - Change Healthcare Inc. | d904010dex1057.htm |
| EX-10.56 - EX-10.56 - Change Healthcare Inc. | d904010dex1056.htm |
| EX-10.55 - EX-10.55 - Change Healthcare Inc. | d904010dex1055.htm |
| EX-10.54 - EX-10.54 - Change Healthcare Inc. | d904010dex1054.htm |
| EX-10.53 - EX-10.53 - Change Healthcare Inc. | d904010dex1053.htm |
| EX-10.52 - EX-10.52 - Change Healthcare Inc. | d904010dex1052.htm |
| EX-4.11 - EX-4.11 - Change Healthcare Inc. | d904010dex411.htm |
Table of Contents
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, D.C. 20549
FORM 10-K
| ☒ | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended March 31, 2020
or
| ☐ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
Commission file number 001-38961

Change Healthcare Inc.
(Exact Name of Registrant as Specified in its Charter)
| Delaware | 82-2152098 | |
| (State or Other Jurisdiction of Incorporation or Organization) |
(I.R.S. Employer Identification No.) | |
| 3055 Lebanon Pike, Suite 1000 Nashville, TN |
37214 | |
| (Address of Principal Executive Offices) | (Zip Code) | |
(615) 932-3000
(Registrant’s Telephone Number, Including Area Code)
Securities registered pursuant to Section 12(b) of the Act:
| Title of each class |
Trading Symbol(s) |
Name of each exchange on which registered | ||
| Common Stock, par value $.001 per share | CHNG | The Nasdaq Stock Market LLC | ||
| 6.00% Tangible Equity Units | CHNGU | The Nasdaq Stock Market LLC |
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☐ No ☒
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ☐ No ☒
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ☒ No ☐
Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T (§ 232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit such files). Yes ☒ No ☐
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer”, “smaller reporting company” and “emerging growth company” in Rule 12b-2 of the Exchange Act. (Check one):
| Large accelerated filer | ☐ | Accelerated filer | ☐ | |||
| Non-accelerated filer | ☒ | Smaller reporting company | ☐ | |||
| Emerging growth company | ☒ | |||||
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). Yes ☐ No ☒
As of September 30, 2019, the aggregate market value of the registrant’s voting and non-voting common equity held by non-affiliates was $597,490,716.
Number of shares of common stock outstanding on June 1, 2020: 303,526,591
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the registrant’s definitive proxy statement for the 2020 Annual Meeting of Stockholders are incorporated by reference into Part III of this Annual Report on Form 10-K.
Table of Contents
| PART I |
||||||
| Item 1. |
5 | |||||
| Item 1A. |
29 | |||||
| Item 1B. |
71 | |||||
| Item 2. |
71 | |||||
| Item 3. |
71 | |||||
| Item 4. |
71 | |||||
| PART II |
||||||
| Item 5. |
72 | |||||
| Item 6. |
73 | |||||
| Item 7. |
Management’s Discussion and Analysis of Financial Condition and Results of Operations |
74 | ||||
| Item 7A. |
97 | |||||
| Item 8. |
98 | |||||
| Item 9. |
Changes in and Disagreements with Accountants on Accounting and Financial Disclosures |
154 | ||||
| Item 9A. |
154 | |||||
| Item 9B. |
155 | |||||
| PART III |
||||||
| Item 10. |
155 | |||||
| Item 11. |
155 | |||||
| Item 12. |
Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
155 | ||||
| Item 13. |
Certain Relationships and Related Transactions, and Director Independence |
155 | ||||
| Item 14. |
155 | |||||
| PART IV |
||||||
| Item 15. |
155 | |||||
| Item 16. |
162 |
2
Table of Contents
Cautionary Notice Regarding Forward-Looking Statements
This Annual Report on Form 10-K contains “forward-looking statements” within the meaning of federal securities laws. Any statements made in this Annual Report that are not statements of historical fact, including statements about our beliefs and expectations, are forward-looking statements. Forward-looking statements include information concerning possible or assumed future results of operations, including descriptions of our business plans and strategies. These statements often include words such as “anticipate,” “expect,” “suggest,” “plan,” “believe,” “intend,” “estimate,” “target,” “project,” “should,” “could,” “would,” “may,” “will,” “forecast,” “outlook,” “potential,” “continues,” “seeks,” “predicts,” and the negatives of these words and other similar expressions.
Although we believe that these forward-looking statements are based on reasonable assumptions, you should be aware that factors affecting our actual financial results could cause actual results to differ materially from those expressed in the forward-looking statements. Factors that could materially affect our financial results or such forward-looking statements include, among others, the following factors:
| • | our ability to retain or renew existing customers and attract new customers; |
| • | macroeconomic and industry trends and adverse developments in the debt, consumer credit and financial services markets; |
| • | uncertainty and risks related to the impact of the COVID-19 pandemic on the national and global economy, our business, suppliers, customers, and employees; |
| • | our ability to connect a large number of payers and providers; |
| • | our ability to provide competitive services and prices while maintaining our margins; |
| • | further consolidation in our end-customer markets; |
| • | our ability to effectively manage our costs; |
| • | our ability to effectively develop and maintain relationships with our channel partners; |
| • | a decline in transaction volume in the United States (U.S.) healthcare industry; |
| • | our ability to timely develop new services and the market’s willingness to adopt our new services; |
| • | our ability to maintain our access to data sources; |
| • | our ability to maintain the security and integrity of our data; |
| • | our ability to deliver services timely without interruption; |
| • | our ability to make acquisitions and integrate the operations of acquired businesses; |
| • | government regulation and changes in the regulatory environment; |
| • | economic and political instability in the U.S. and international markets where we operate; |
| • | risks related to our international operations; |
| • | the ability of our outside service providers and key vendors to fulfill their obligations to us; |
| • | litigation or regulatory proceedings; |
| • | our ability to protect and enforce our intellectual property, trade secrets and other forms of unpatented intellectual property; |
| • | our ability to defend our intellectual property from infringement claims by third parties; |
| • | changes in local, state, federal and international laws and regulations, including related to taxation; |
| • | our reliance on key management personnel; |
3
Table of Contents
| • | our ability to manage and expand our operations and keep up with rapidly changing technologies; |
| • | our adoption of new, or amendments to existing, accounting standards; |
| • | losses against which we do not insure; |
| • | our ability to make timely payments of principal and interest on our indebtedness; |
| • | our ability to satisfy covenants in the agreements governing our indebtedness; |
| • | our ability to maintain our liquidity; |
| • | the potential dilutive effect of future issuances of our common stock; and |
| • | the impact of anti-takeover provisions in our organizational documents and under Delaware law, which may discourage or delay acquisition attempts. |
You should carefully consider the statements under Item 1A. Risk Factors and other sections of this report, which describe factors that could cause our actual results to differ from those set forth in the forward-looking statements.
Our forward-looking statements made herein speak only as of the date on which made. We expressly disclaim any intent, obligation or undertaking to update or revise any forward-looking statements made herein to reflect any change in our expectations with regard thereto or any change in events, conditions or circumstances on which any such statements are based. All subsequent written and oral forward-looking statements attributable to us or persons acting on our behalf are expressly qualified in their entirety by the cautionary statements contained in this report.
4
Table of Contents
PART I
| ITEM 1. | BUSINESS |
We are a leading independent healthcare technology platform that provides data and analytics-driven solutions to improve clinical, financial, administrative, and patient engagement outcomes in the U.S. healthcare system. We offer a comprehensive suite of software, analytics, technology-enabled services and network solutions that drive improved results in the complex workflows of healthcare system payers and providers. Our solutions are designed to improve clinical decision making, simplify billing, collection and payment processes, and enable a better patient experience.
We began our operations on March 1, 2017 upon completion of certain joint venture transactions whereby McKesson Corporation (“McKesson”) contributed the majority of its technology solutions segment and Change Healthcare Inc. (formerly HCIT Holdings, Inc.) contributed substantially all of Change Healthcare Performance, Inc.’s (formerly Change Healthcare, Inc.) legacy business to Change Healthcare LLC (the “Joint Venture”). From the time of its formation on June 17, 2016 until March 1, 2017, the Joint Venture had no substantive assets or operations. On July 1, 2019, Change Healthcare Inc., the owner of approximately 30% of the Joint Venture, completed its initial public offering. The proceeds of the offering were subsequently contributed to the Joint Venture in exchange for additional units of the Joint Venture, which together with the Company’s existing holding represented an approximate 41% interest in the Joint Venture immediately following the initial public offering. On March 10, 2020, Change Healthcare Inc. combined with a subsidiary of McKesson and the owner of the remaining 58% of the Joint Venture (“SpinCo”) in a two-step all-stock “Reverse Morris Trust” transaction that involved (1) a separation of SpinCo from McKesson followed by (2) the merger of SpinCo with and into Change Healthcare Inc., with Change Healthcare Inc. as the surviving company. In connection with the transaction, electing McKesson stockholders received shares of Change Healthcare Inc. common stock in exchange for McKesson common stock. As a result, the Joint Venture became a wholly owned subsidiary of Change Healthcare Inc. and McKesson no longer has any ownership interest in the Joint Venture.
We offer comprehensive, end-to-end solutions with modular capabilities to address our customers’ needs. Working with our customers to analyze workflows used before, during, and after care has been delivered to patients, we design and commercialize innovative solutions for various points in the healthcare delivery continuum. Our offerings range from discrete data and analytics solutions to broad enterprise-wide solutions, which include workflow software and technology-enabled services that help our customers achieve operational objectives. As payers and providers become larger and more sophisticated, and manage increasingly complex workflows, we believe they will increasingly seek strategic partners with scale and comprehensive, high-value solutions designed to scale.
Our Intelligent Healthcare Network was created to facilitate the transfer of data among participants and is one of the largest clinical and financial healthcare networks in the U.S. In the fiscal year ended March 31, 2020, we facilitated over 15 billion healthcare transactions and approximately $1.5 trillion in adjudicated claims or more than one-third of all U.S. healthcare expenditures. We serve the vast majority of U.S. payers and providers. Our customer base includes approximately 2,400 government and commercial payer connections, 1,000,000 physicians, 125,000 dentists, 39,000 pharmacies, 6,000 hospitals and 700 laboratories. This network transacts clinical records for over 85 million unique patients, approximately one-quarter of the estimated total U.S. population. With insights gained from our pervasive network, extensive applications and analytics portfolio, and our services operations, we have designed analytics solutions that include trusted, industry-leading franchises supported by extensive intellectual property and regularly updated content.
In addition to the advantages of scale, we believe we offer the collaborative benefits of a mission-critical partner. We seek to establish and develop enduring relationships with each customer through solutions that deliver measurable results, embedded in their complex daily workflows that deliver measurable results. Our customer retention rate for our top 50 provider and top 50 payer customers was 99% for the fiscal year ended
5
Table of Contents
March 31, 2020. We believe our size, scale, expertise, and prevalence throughout the healthcare ecosystem help make us a preferred partner for technology companies and industry associations focused on driving innovation, standardization and efficiencies in the healthcare industry.
We believe that our solutions play a mission-critical role in the following important areas of the healthcare system:
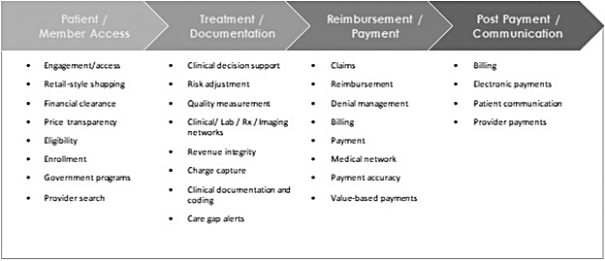
We seek to help healthcare system constituents address fundamental operating needs.
6
Table of Contents
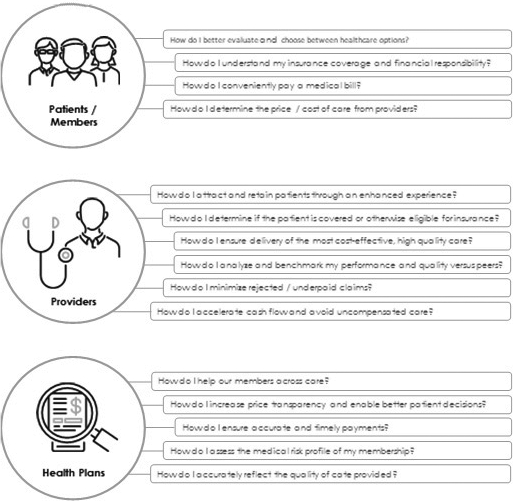
Our analytics-driven solutions are designed to improve delivery of care through better clinical decision-making and simplify billing and payment functions by reducing administrative errors and improving documentation. In addition, we seek to improve payers’ and providers’ relationships with consumers by offering solutions that enable transparency, empower their decision making and support. We believe that our solutions enable our customers to operate more efficiently and thereby improve their competitive positioning. Our solutions have generated measurable financial and operational return on investment and improved quality of care and patient experience. Some examples include:
| • | Provider organizations were able to resolve $527 million in patient accounts using Coverage Insight, netting $144 million. |
| • | Health systems and hospitals using Change Healthcare Financial Clearance Services received $869 million in reimbursement via the identification and enrollment of self-pay patients in government benefits. |
| • | A provider using the Change Healthcare Workflow Intelligence™ medical imaging workflow rules engine shortened emergency department (ED) wait times by 40 minutes per patient. |
| • | Over 60 payer customers achieved approximately $3.3 billion in incremental Medicaid add-on net revenue (from 2002 to 2018) through analytics-driven services that identify dual eligible members who are eligible for both Medicare Advantage (MA) and Medicaid benefits. |
| • | A large, national payer achieved $12 million in annual financial benefits through electronic provider payment penetration rates in excess of 90%. |
7
Table of Contents
| • | Payers using our pre-submission editing solution decreased evaluation and management (E/M) overbillings by an average of 34.7%.; decreased the cost of E/M claims by an average of 3.9%; and improved billing behavior among 80% of affiliated providers. |
| • | Payers using our comprehensive out of network management services saved an average of 36% on out-of-network claims. |
| • | Payers using our Audit and Recovery Services saved an average of $5,750 per claim. |
| • | Medicare Advantage health plans using our Natural Language Processing (NLP)-enabled coding realized a 20-30% increase in risk capture. Coding, combined with our risk adjustment analytics engine, has helped these plans realize an average ROI of 13:1 with an earned average increase of $10 million in revenue. |
| • | Payers using our primary claims editor realize a collective $12 billion in savings per year. |
Innovation
We have a consistent track record of innovation. Our pervasive network connectivity combined with our use of Artificial Intelligence (AI) and Machine Learning (ML) enable us to regularly improve our solutions and uncover new insights as our customers’ needs evolve. During fiscal 2020, we added a number of new solutions to our business platform through new product development, including:
| • | We launched Market Insights, a comprehensive analytic dataset that provides unparalleled views into utilization, population health, and financial trends that drive the U.S. healthcare system. Drawn from the Change Healthcare Intelligent Healthcare Platform™ (IHP), Market Insights gives payers, providers, and those serving the healthcare industry views spanning all major types of care and delivery models. In addition, it enables deep comparative analysis to “best in class” in local markets over time. |
| • | We introduced the API & Services Connection™ marketplace for open, standards-based application programming interface (API) products and comprehensive enablement tools for any healthcare organization––payers, providers, vendors––to leverage the same capabilities that power our healthcare financial, clinical, and engagement solutions. |
| • | We enhanced our claims attachment solution creating the industry’s first nationwide offering that enables providers to submit documents and data, such as claims attachments, electronically to all payers. Built on the Change Healthcare IHP, the claim attachments solution goes beyond fragmented workflows and paper-based processes that providers currently use to exchange clinical and other supporting documentation with payers in a single workflow. |
| • | Our Eligibility product, available through an API, can verify new applicants across multiple payers and deliver rapid implementations. The API, which makes the solution easily accessible to the market, extends the value of our solutions and enhances flexibility for our customers. |
| • | Our Coordination of Benefits solution helps payers determine the existence of any alternate coverage sources for their members. The solution helps payers avoid paying inappropriate claims and expenses associated with retroactive recovery attempts. |
| • | We debuted Shop Book and Pay™, offering consumers personalized pricing and a quality digital shopping experience, deployable by providers to drive patient acquisition, increase collections, and differentiate their business in a competitive market. |
| • | We unveiled Virtual Front Desk, a digital patient access solution for enabling a touchless registration, check-in, and waiting experience for patients. |
Our ability to innovate is supported by approximately 1,500 technology professionals including PhDs, masters-level health policy experts, design professionals, data scientists, programmers and statisticians in our research and development centers located in key markets such as Silicon Valley, Seattle, Boston, Philadelphia,
8
Table of Contents
Nashville, Minneapolis, and Tel Aviv. We believe that our deep reach across the healthcare ecosystem and our history of commercializing innovations position us to be a preferred partner for customers and leading healthcare and technology companies.
We believe we are well positioned for growth across the markets we serve. Our growth strategy is to increase the breadth and depth of our capabilities organically and through acquisitions. We continue to increase our business with a strong base of long-standing customers by expanding our enterprise relationships and positioning them for success in their markets. Our comprehensive end-to-end solutions can reduce the complexity of our customer’s environments, yet are modular to meet their specific needs. We seek to use our data products and analytics, pervasive connectivity and our position as a trusted partner to develop innovative ways to create high-value clinical and administrative solutions. We believe we are in the early stages of growth related to these opportunities.
Market Opportunity
We compete in the market for data and analytics-driven solutions that help ensure clinically appropriate care, increase efficiency and reduce waste in the healthcare industry. We believe the following trends impacting payers, providers and consumers represent a significant opportunity for us.
Wasteful spending amidst rising costs in the U.S. healthcare system.
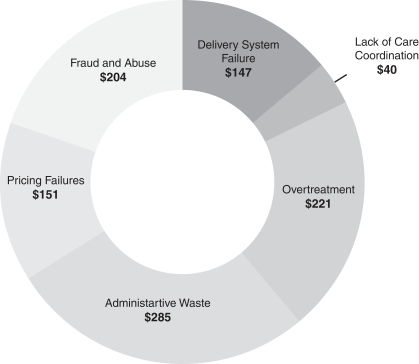
Note: Dollars in billions
Sources: Wasteful spending categories based upon Journal of American Medical Association (“JAMA”) “Waste in the US Health Care System”; and Dollar amounts of wasteful spending calculated based on JAMA categories and percentages applied to the implied 2019 wasteful spending amount.
Research cited by the Journal of the American Medical Association estimates that nearly 30% of U.S. healthcare spending is wasteful, implying approximately $1 trillion of wasteful healthcare spending in 2019.
9
Table of Contents
Examples of waste include failure to adhere to best care practices and lack of care coordination, which leads to unnecessary readmissions and inappropriate levels of care delivery. Wasteful spending includes significant variation among providers in the cost and quality of similar care from provider to provider, and market to market (not explained by geography alone); and also includes overtreatment, which is testing and care that is not medically beneficial.
Additionally, the U.S. healthcare system relies on many inefficient processes that are manual, complex, frequently changing, time consuming, prone to error, costly and requiring undue amounts of clinicians’ and other professionals’ time. In addition, improper payments, according to the Office of Management and Budget, have represented approximately 10% of all Medicare and Medicaid payments since 2015. Such improper payments and fraudulent billing create costly and labor-intensive follow-up. According to CMS, U.S. healthcare spending is expected to grow from $3.6 trillion in 2018, or 18% of U.S. gross domestic product, to $6.2 trillion, or approximately 20% of U.S. gross domestic product, by 2028. This implies that healthcare spending is increasing at a 5.4% annual growth rate, or 3.4% higher than expected inflation over the same period. Given the significant and lasting financial burden of ongoing rising costs and wasteful spending, both government and commercial payers and providers are increasingly focused on reducing costs attributable to administrative complexity and errors, excessive manual labor, and uncoordinated, unproductive, or ineffective processes. As a result, we expect continued strong demand for solutions that can aid in reducing waste, improving efficiency and help ensure delivery of clinically appropriate, value-based care.
Healthcare system exposure to growing chronically ill and higher risk populations. While the overall U.S. population is expected to increase 6.9% from 2019 to 2029, the population of adults age 65 and older is expected to increase 32.3% over the same period, according to the U.S. Census Bureau. This segment of the population has the highest prevalence of chronic conditions, with average annual healthcare spending approximately three times higher than working adults and approximately five times higher than the under-18 demographic, according to CMS. As those older than 65 years of age access complex care at growing rates, they are also increasingly enrolling in managed care plans that bear the risk of healthcare utilization. For example, enrollment in MA, which according to CMS, has increased from 24% to 36% of eligible lives between 2010 and 2020, is expected to increase to 51% of eligible lives by 2030, according to the Congressional Budget Office. Additionally, according to CMS, while health plans administering Medicaid covered 82% of eligible lives as of 2017, only roughly half of total Medicaid spending was managed, primarily because most dual eligibles, who are typically among the most chronically ill and disproportionately expensive beneficiaries for both programs, are not benefiting from any form of integrated care. Federal and state governmental agencies, Congress, and CMS are seeking ways to better service this group and promote efficient and effective avenues to access care. As the country’s elderly population continues to grow, and the healthcare system serves more chronically ill and higher risk populations, providers and payers will need tools to onboard and manage these populations. These include the ability to deliver appropriate care for medically complex patients, and the ability to document risk and outcomes to attain the appropriate reimbursement rates associated with these populations.
Increasing prevalence of value-based care and reimbursement models. The traditional fee-for-service reimbursement model is viewed as having facilitated growth in healthcare spending beyond the value provided from additional services. In response, both public and private sectors are shifting towards alternative payment models that are designed to incentivize value and quality throughout an “episode of care,” which encompasses most or all of the services provided to a patient to diagnose, treat, and manage a clinical condition before, during, and after care is delivered. In recent years, HHS has set quality and value targets for certain Medicare alternative payment models and private payers are accelerating their focus in a similar fashion. These payment models require a high level of documentation, robust data, sophisticated payment attribution capabilities, and advanced analytics that can adapt to new rules and goals to ensure compliance. Further, solutions seek to optimize the design, implementation, and monitoring of care delivery throughout an episode of care. Many payers and providers are still building the capabilities, expertise, and administrative processes to manage these changes adequately. They are increasingly partnering with third parties to demonstrate the achievement of the outcomes
10
Table of Contents
required under these value-based payment models, which requires a fundamentally different skillset than what they have deployed historically.
Increasing patient financial responsibility and consumerism in healthcare. As healthcare expenditures have continued to rise, employers and health plans have shifted costs to patients through increased adoption of high-deductible health plans. Enrollment in high deductible health plans with a savings option (HDHP/SO) has increased over the past five years, from 20% of covered workers in 2014 to 30% in 2019, according to the Kaiser Family Foundation. This trend is expected to continue. Increases in patient financial responsibility require providers to obtain payment from the patient before and after the point of care, which in turn requires more advanced billing and collection workflows. As providers become more consumer-oriented, they require increasingly sophisticated, dynamic, and personalized solutions, which generally necessitate scale for efficient implementation and cost-effectiveness. Likewise, as patient out-of-pocket costs continue to increase, they are becoming more quality- and cost-conscious consumers, likely to make more calculated decisions regarding their healthcare consumption. These empowered “healthcare consumers” are demanding price transparency and decision support from their health plans to help select caregivers who deliver the highest value of care at the lowest price. Health plans are consequently partnering with third parties to provide their members with tools which enable them to assess quality and cost based on individual plan benefits. At the same time, providers seek to effectively communicate the quality and value of their services, determine patients’ upfront insurance eligibility, coverage, and ability to pay their portion of healthcare bills, and simplify the payment process to improve patient experience and satisfaction.
Proliferation of healthcare data. The U.S. government funded almost $40 billion of incentive payments to healthcare providers between 2011 and July 2018 to adopt electronic health record (EHR) technology. This has resulted in 80% of physicians and 96% of hospitals in the U.S. having certified EHR systems as of 2017, according to the Office of the National Coordinator for Health Information Technology. These EHRs, other digitized healthcare data, and the increasing amount of personal health data from smartphones, wearables, and other devices have generated unprecedented amounts of healthcare data in the U.S., and that volume is expected to grow to more than 2,300 exabytes by the end of 2020, according to the 2018 Global Big Data in Healthcare Market report by BIS Research. However, healthcare data is often siloed and unstructured, and has historically been difficult for all constituents to understand and use in a timely manner. Both healthcare professionals and consumers increasingly demand tools and solutions that standardize the transfer and collection of data, as well as the ability to mine and analyze it for actionable insights. Advancements in ML and AI are making it easier to cost-effectively utilize data at scale in real time to identify actionable insights that help improve outcomes and decrease cost. As healthcare data can be used more effectively, we expect that leading technology companies will increasingly seek partners who can effectively develop new software and analytics solutions to help payers and providers improve workflows and deliver higher quality care at lower cost to consumers.
Our Strengths
Embedded in our customers’ end-to-end, mission-critical, daily workflows. Our solutions are embedded in our customers’ core business functions, including member enrollment, patient access, treatment, documentation, reimbursement and payment, claims and financial management, and post-payment and communication. We believe our collaborative and comprehensive approach, combined with modular capabilities, is important to our customers’ ability to operate efficiently and cost-effectively. We earn the loyalty of our customers with solutions designed to help them meet financial and operational objectives and improve their recurring and evolving processes.
Leading healthcare-specific technology infrastructure. We have developed industry-leading data and analytics solutions and services that deliver direct value to our customers. Our Intelligent Healthcare Platform™ (IHP) provides a cloud-based, robust, and agile platform for our solutions. Our IHP enables us to innovate with our customers and partners and to anticipate and meet customer needs. We continue to employ advanced technology to support our expansive network. Our commitment to maintaining industry-leading infrastructure creates
11
Table of Contents
significant leverage and speed for each of our businesses, and helps our customers deliver services faster and more effectively.
Financial Platform Supported by Clinical Insight. The Change Healthcare IHP sits at the center of everything we do as we continue to drive our transformation to a platform company. Over the last year, we have increased the maturity of our platform, facilitated adoption of platform services, enabled new revenue opportunities, and driven time-to-market benefits for products across the Change Healthcare portfolio. All of this is designed to help our customers innovate faster and more effectively. Examples include:
| • | We collaborated with AWS for our cloud-based network, in order to increase our efficiency, transparency, and security. |
| • | We continue to drive consistency, continuity, and scalability across our solutions via platform services. As an example, we have developed 45 API products representing over 120 standards-based APIs available to our internal developers and to the healthcare industry. |
| • | We added over two billion data records to our single, holistic data store, enhanced with comprehensive access and rights management capabilities, and made this available to existing applications and to internal users. This robust process has enabled the growth of our Data Solutions business, providing access to rights-managed data that is converted into insights, ultimately generating products sold in the AWS Data Exchange. |
| • | We are embedding AI into our platform, eliminating inefficiencies from our customers’ workflows. |
| • | We are becoming an interoperable platform, eliminating cost barriers and addressing federally mandated requirements. |
Scale and reach define us as a preferred technology partner. The pervasive nature of our solutions and network in the workflows of our more than 30,000 customers, and our breadth of industry relationships position us to introduce best-in-class technologies to the healthcare industry at scale. We provide solutions supporting approximately 2,400 government and commercial payer connections, 1,000,000 physicians, 125,000 dentists, 39,000 pharmacies, 6,000 hospitals and 700 laboratories. This network transacts clinical records for over 85 million unique patients, approximately one-quarter of the estimated total U.S. population. Our customers increasingly leverage our industry-leading data and analytics-driven solutions while taking advantage of our innovations in AI, ML and robotic process automation (RPA) to improve clinical, financial, and patient engagement outcomes. Our collaboration with technology leaders helps further broaden our scale and reach with new, innovative solutions.
| • | AWS: We are establishing a new cloud-based network infrastructure to promote more efficient, transparent, and secure administrative and financial transactions by shifting our solutions to AWS. |
| • | Google: We are building a pervasive, scalable, and cost-effective infrastructure, collaboration and AI platform for medical imaging specialists with Google Cloud. |
| • | Adobe and Microsoft: We leverage the Change Healthcare Intelligent Healthcare Network, Adobe Experience Cloud, and Microsoft Azure to collect, aggregate, and utilize consumer data from disparate healthcare IT sources, then employ behavioral science, personalization and engagement tools, to enable a more secure method for providing customers with improved healthcare experiences designed to protect their privacy. We are leveraging these partnerships to go to market with our Patient Experience solutions. |
| • | TIBCO: We currently incorporate TIBCO Spotfire for health data visualization to enable users to visually explore data for both enterprise and department-level needs. This technology also provides value for our Enterprise Imaging and Dental Network organizations. |
Modular and flexible solutions designed to serve a diverse, extensive customer base. We deploy our solutions through complementary software and analytics, technology-enabled services, and a network delivery model with
12
Table of Contents
the power to help customers improve revenue opportunities and reduce operational costs. At the same time, our solutions are modular and flexible, providing us with the ability to address a customer’s trajectory of needs with either point solutions or an end-to-end suite of services. In addition, we have the ability to deliver integrated solutions throughout our business.
For example, a medical network customer that utilizes our EDI can also use our Coding Advisor solution that leverages medical network transactions to improve coding accuracy, or an electronic payment solution that leverages the customer’s medical network to deliver electronic remittance advice. For their MA members, a customer can use Dx Gap Advisor to improve the comprehensiveness of claims submissions and help ensure appropriate reimbursement. As the needs of our customers evolve, our proprietary flexible architecture will enable us to offer scaled, comprehensive solutions and remain a partner of choice.
Proven ability to serve the evolving needs of our customers with industry-leading solution franchises. During FY2020, we added a number of new solutions to our business platform through new product development. As of March 31, 2020, our payment accuracy solutions were embedded in the workflow of 19 of the 20 largest U.S. commercial payers based on covered lives, while our InterQual solutions were used by roughly 4,200 hospitals and facilities, and by health plans covering over 125 million members. As a long-time leader in healthcare data interoperability, we provide open APIs based on Fast Healthcare Interoperability Resources (FHIR) and other industry standards, which help us integrate and innovate with customers and partners across the industry. The ability to quickly and accurately sort through massive amounts of data from multiple sources and determine relevant patient information is crucial to outcomes. Enterprise Imaging houses more than 41 petabytes of imaging data and one billion exams through our systems.
Examples of our innovative and growing solutions include:
| • | Clearance Estimator Patient Direct: A patient-facing web-based tool that allows patients to easily obtain cost estimates for common procedures and services––helping health systems meet CMS requirements with personalized out-of-pocket estimates |
| • | Enterprise Viewer: A new clinical image viewer provides unique interactive views of a patient’s complete clinical history, alongside images, for all users and clinical specialties. Now, for the first time, on a single platform, the entire care team can readily access aligned clinical information and diagnostic-quality images in a navigable timeline to facilitate quick treatment decisions, diagnoses, and disease tracking |
| • | CommonWell Health Alliance Services: CommonWell, the nationwide health information exchange network, awarded Change Healthcare a six-year contract to be its exclusive interoperability service provider. |
| • | ClaimsXten Cloud Services: Change Healthcare Cloud Services leverages AWS to deliver greater accuracy across the complex payment continuum, as well as savings through real-time integration and expanded editing capabilities. Its rules-based engine and technical enhancements are heightened by our investments in AI, data mining, and analytics to identify missed opportunities, and locate objects that can be moved from post pay audit and recovery into an earlier position on the extensive payment continuum. By driving efficiencies and improving accuracy earlier in the process, claims are more likely to be paid correctly the first time around, resulting in a reduced burden on providers and improved member satisfaction. Importantly the solution is scalable––servicing both large national as well as regionally focused payers. |
| • | Member Payments: A consumer payment solution enabling health plans to display consolidated patient financial information in a single destination and empowers consumers to better understand and manage their healthcare finances |
| • | Claims Attachments: Enhanced to create the industry’s first nationwide solution to enable providers to submit documents and data, such as claims attachments, electronically to all payers in both the Medical and Workers’ Compensation market segments. |
Data Stewardship and security. As the amount of data in healthcare grows and the ability to use that data becomes more essential to effective delivery, management, and administration, we expect data security to
13
Table of Contents
become increasingly important for our customers. Our history of delivering solutions while prioritizing data security and fidelity enables us to be the platform of choice for large customers and partners. We have multiple certifications on multiple offerings, including HITRUST, HIPAA, PCI, FISMA, ISO 27001, SOC2, and EHNAC, and we implement security procedures and policies informed by applicable law and recommended practices. We also aim to drive industry maturity through appointed leadership roles with HITRUST Alliance and H-ISAC (Healthcare Information Security and Analysis Center). We believe our customers will increasingly consolidate solutions providers to a handful of entrusted parties that can address large-scale healthcare cost and quality issues securely. We believe strong relationships with existing customers position us to benefit from this expected trend.
Predictable revenue profile and attractive, scalable model. Change Healthcare has an attractive operating profile given the predictable, recurring nature of a significant portion of our revenue combined with a scalable financial model. Our revenue is largely derived from recurring transactional, monthly-subscription and per-click formats, as well as contingency-based or long-term contracts. During the fiscal year ended March 31, 2020, 87% of solutions revenue was Recurring Revenue. Our customer base is highly diversified, as no customer represented more than 4% of solutions revenue in the fiscal year ended March 31, 2020. Additionally, we benefit from high customer retention across a diversified customer base composed of approximately 58% providers and 42% payers based on solutions revenue for the fiscal year ended March 31, 2020. Our business model requires moderate capital spending to grow, with capital expenditures of 8.4% of solutions revenue for the fiscal year ended March 31, 2020. We continue to streamline costs and have instituted cost improvement initiatives throughout the organization. We believe our Recurring Revenue, combined with the opportunities for continued operating improvement following the Transactions, will provide us with increasing flexibility to allocate and deploy our capital.
Growth Strategy
Develop, augment and commercialize capabilities at scale. We work closely with our customers to integrate our offerings into their workflows and business processes. Change Healthcare develops new products and services, partners with industry-leading companies and selectively acquires complementary technologies and businesses to enhance our offerings. We introduce solutions through one of three methods: internal development, commercial partnerships and acquisitions.
| • | Internal development—We cultivate and leverage feedback from our customers, our partners and the analytical capabilities of our platform and suite of solutions to drive commercial innovations. We utilize our decades of industry experience, technology and services capabilities to identify new insights along the administrative and clinical care continuum. Through dialogue with our customers and our position as a scaled partner to payers, providers and others, we target commercial opportunities where these insights can be applied. Working with Google Cloud, we are building a cloud-native solution to reduce cost and complexity in Enterprise Imaging. |
| • | Commercial partnerships—We had over 700 channel partners as of March 31, 2020, including the major EHR providers supporting workflow integration, as well as go-to-market channel partners who expand the sales and distribution reach of our software, data, network and payment solutions. We believe that our industry-leading customer base and platform allow us to collaborate with other software and technology leaders to develop and rapidly deploy complementary software and services. These partnerships are expansive and flexible ranging from limited scope sales relationships to arrangements in which we are a significant customer. |
| • | Acquisitions—We have acquired and expect to continue to acquire assets and businesses that strengthen the value we deliver to our customers. Since the Transactions (defined herein), we have completed and successfully integrated three acquisitions. We have a successful track record of identifying, integrating and scaling new and complementary capabilities. |
14
Table of Contents
Maximize wallet share with customers through cross selling. Change Healthcare has significant opportunities to expand the suite of services that our long tenured and highly loyal customer base purchases from us through focused cross selling. While we seek to continually improve our product and service offerings, our sales force is focused on expanding the scope and depth of our customer relationships. Our omni-channel sales force covers medium and larger customers with direct field sales teams and uses inside sales for direct coverage of smaller customers. In addition, our sales teams are focused on embedding our technology in our partners’ applications and solutions. We leverage our communication with and feedback from our customers to identify and execute on opportunities which expand and deepen relationships while increasing the benefits they receive through our connectivity, software, analytics and services.
Deliver comprehensive, end-to-end and modular solutions to customers. Our solutions are comprehensive in that they meet a significant portion of our customers’ clinical and administrative needs and are integrated to improve functionality and usability, yet modular to meet the specific needs of our customers. We believe the ability to be comprehensive and integrated, yet flexible, will be increasingly attractive as customers seek to consolidate outside vendor relationships and improve their return on investment. Our ability to deliver technology-enabled services as part of our comprehensive offerings significantly increases growth opportunities with our software, analytics and network solutions customers. Our goal is to deliver offerings flexible enough to work with the legacy technologies still used by many of our customers, while also delivering more sophisticated and advanced solutions to customers as they upgrade their technology platforms.
Use our large and growing data assets to deliver tangible value to customers. We continue to develop data-driven solutions to drive tangible returns for our customers. We leverage our pervasive network connectivity and position as a trusted partner to create clinical and administrative solutions that incorporate a multi-party, independent, longitudinal perspective, integrated technology and service assets. Our position as a trusted partner before, during, and after care enables us to view the healthcare system from a holistic standpoint and deliver solutions that we believe are difficult to replicate. We routinely take insights from our connectivity, software, and services and integrate them into complementary products and workflows. Through our large and growing data assets and associated analytics, we have created personalized, episodic, and population-based solutions for our customers to deliver high quality, low-cost solutions at scale. As payment and care models evolve, we believe scaled data assets and pervasive network connectivity across constituents will be essential to delivering meaningful and sustainable cost and care improvements.
Our Solutions
We offer clinical, financial, and patient engagement solutions in three business segments—Software and Analytics, Network Solutions, and Technology-Enabled Services—that help create a stronger, more collaborative healthcare system. Through our interconnected position at the center of healthcare, we utilize our broad portfolio of solutions to serve stakeholders throughout the healthcare system, including commercial and government payers, employers, hospitals and health systems, physicians and other providers, pharmacies, labs, and consumers. A summary of our various products and solutions is included below.
Software and Analytics
Our industry-leading software solutions seek to enable our customers to achieve financial performance, operational excellence, and payment and network optimization, ultimately helping them navigate the shift to value-based care. In the software and analytics segment, we provide solutions for revenue cycle management, provider network management, payment accuracy, value-based payments, clinical decision support, consumer engagement, risk adjustment and quality performance, and imaging and clinical workflow.
Network Solutions
We leverage our Intelligent Healthcare Network—with an industry-leading 15+ billion transactions and approximately $1.5 trillion in adjudicated claims during fiscal year 2020—to enable and optimize connectivity
15
Table of Contents
and transactions among healthcare system participants and to generate insight using healthcare data to help meet their analytical needs. Through our network solutions segment, we provide solutions for financial, administrative and clinical transactions, electronic payments, and aggregation and analytics of clinical and financial data.
Technology-Enabled Services
We provide expertise, resources, and scalability to allow our customers to streamline operations, optimize clinical and financial performance, and focus on patient care. Through our Technology-Enabled Services segment, we provide solutions for revenue cycle and practice management, value-based care enablement, communications and payments, pharmacy benefits administration, and consulting.
| Software & Analytics | Network Solutions | Technology Enabled Services | ||||
| Key Solution Areas | • Network & Financial Management • Value-Based Payment Analytics • Payment Accuracy Analytics & Services • Provider Network Management Analytics • Risk Adjustment & Quality Performance • Decision Analytics • Clinical Review Services • Consumer Engagement • Member Enrollment & Outreach • Transparency & Provider Search • Clinical Decision Support • Revenue Cycle Management • Imaging and Clinical Workflow Solutions • Imaging and Workflow Solutions • Capacity Planning |
• Connected Consumer Health • Intelligent Healthcare Network™ • Medical Network • Dental Network • Clinical Exchange Network • MedRx Network • Common Well Health Alliance • Electronic Payments • B2B Payment Solutions • C2B Payment Solutions • Data Solutions • Market Insights • Data Platform • Data Commercialization |
• Revenue Cycle Management • Patient Access Center Services • Financial Clearance Services • Revenue Integrity Services • Hospital Reimbursement Management Services • Physician Group Management Services • Physician Revenue Cycle Management Services • Value-Based Care Enablement Services • Network Development and Physician Recruiting • Risk Management and Population Health Services • Third-Party Admission • Business Process as a Service • Communication & Payment Services • Communication and Payments • Payment and Claims Automation • Conversion of Print to Electronic • Pharmacy Benefits Administration • Consulting | |||
| Customers | • Commercial & Government Payers • Hospitals / Health Systems • Physicians and Other Providers • Imaging Centers • Health IT Vendors |
• Commercial & Government Payers • Hospitals / Health Systems • Physicians and Other Providers • Reference Labs • Imaging Centers • Retail Pharmacies • Health IT Vendors |
• Commercial & Government Payers • Hospitals / Health Systems • Physicians and Other Providers | |||
16
Table of Contents
Software and Analytics
| • | Network & Financial Management: We help commercial and government payers improve claims operations performance, payment model innovation, and provider network management through a comprehensive solution supporting payers across the entire payment continuum in the transition to value-based care and alternative payment models. |
| • | Value-Based Payment Analytics: We combine an advanced, cloud-based analytics platform and over 90 clinically validated episodes of care definitions with visibility into over 97 million individuals and our customers represent more than one-third of the commercially insured lives in the U.S. |
| • | Payment Accuracy Analytics & Services: Our comprehensive suite of solutions is designed to help payers combat risk of fraud, waste, and abuse at every stage of the claim, from pre-submission to post-payment. Health plans covering over 200 million members, including all of the top 10 U.S. health plans based on covered lives, used these products in 2020. As of December 31, 2020, our payment accuracy solutions were embedded in the workflow of 19 of the 20 largest U.S. commercial payers based on covered lives. |
| • | Risk Adjustment & Quality Performance: We help payers and risk-bearing providers improve financial performance by supporting reimbursement for government-sponsored health plans—including risk adjustment and quality measures, such as the National Committee for Quality Assurance’s Healthcare Effectiveness Data and Information Set (“HEDIS”)—for the Medicare, Medicaid, and the Commercial Affordable Care Act markets. |
| • | Decision Analytics: We provide a comprehensive set of analytics-driven solutions for risk adjustment and quality performance that aligns with how government-sponsored plans are reimbursed. |
| • | Clinical Review Services: We provide solutions for medical records retrieval, coding, and abstraction for payers who want to increase incremental revenue and quality ratings for HEDIS and STARS (a CMS system to help beneficiaries compare performance and quality). With over 20 years of experience, our team retrieves 2.5 million charts and codes 2.7 million charts annually to support our payer customers with risk adjustment and quality programs compliance. |
| • | Consumer Engagement: We help commercial and government payers adapt to the evolving needs of a more value-based, consumer-driven environment with consumer-facing tools used to support enrollment and ongoing health management processes. Our consumer engagement solutions help payers respond to many of the industry’s most pressing consumer engagement challenges, from addressing social determinants of health to engaging high-need populations, such as dual eligibles. |
| • | Member Enrollment & Outreach: We provide member-centric solutions for payers—focusing on Medicare and Medicaid programs—to improve revenue, increase member satisfaction, and improve engagement in maintaining or improving their health. We have helped Medicaid managed care payers add $3.6 billion in net revenue through dual enrollment. Additionally, our enrollment AI services pinpoint those individuals with the highest likelihood to qualify for full or partial Medicare and Medicaid dual eligibility with up to 94% accuracy. |
| • | Clinical Decision Support: Our industry-leading clinical criteria, InterQual, assists payers, providers and government organizations in making clinically appropriate medical utilization decisions to help determine the right care, at the right time, and at the right cost. Our InterQual solutions were used by over 4,200 hospitals and facilities, and health plans covering over 125 million lives as of March 2020. |
| • | Revenue Cycle Management: We provide end-to-end revenue cycle management workflow and analytics to streamline reimbursement and time-to-revenue for hospitals, physician offices, laboratories, and other ancillary care providers by providing timely insights that reduce denials. |
| • | Imaging and Clinical Workflow Solutions: We help providers improve clinical, operational and financial performance through enterprise imaging, care delivery and capacity planning solutions for acute and post-acute care settings. We are building from the ground-up cloud-native solutions to showcase the flexible |
17
Table of Contents
| nature of cloud services and delivery. The network will enhance and optimize medical imaging data––enabling providers to improve clinical, financial, and operational outcomes. |
Network Solutions
| • | Digital Patient Experience: We help providers transform their patient engagement and access activities to meet consumer demand for digital interactions. Our solutions help providers acquire new patients and deliver a patient experience to assist with building loyalty. |
| • | Healthcare eCommerce: Our solutions help providers offer transparent pricing and deliver a retail-style shopping experience. Providers can enable public-facing pricing transparency in competitive markets or keep patients within their organization by offering an exclusive, in-network shopping experience. |
| • | Touchless Patient Access: Our solution assists providers with creating a touchless patient registration, check-in and form completion experience to help maintain social distancing requirements and reduce potential exposure to others that might be infected. |
| • | Intelligent Healthcare Network: Over the past three decades, we have built one of the largest financial and administrative healthcare networks in the U.S. Our Intelligent Healthcare Network provides pervasive connectivity that benefits all major healthcare stakeholders, including commercial and governmental payers, employers, hospitals, physicians, laboratories, pharmacies, and consumers. |
| • | Medical Network: Our network provides support for healthcare financial and administrative transactions, including eligibility, claims, durable medical equipment, electronic remittance advice, claim status, pre-authorization, and medical attachments. Our medical network is integrated with our payments network, which allows payers and providers to reconcile consumer out-of-pocket cash and credit card payments with payer electronic funds transfer and check payments to settle bills and claims. |
| • | Dental Network: We provide eligibility, claims, electronic remittance advice, and payment solutions to dental practices primarily through software channel partners. Our solutions further simplify claims through our attachment technology, which tightly integrates claims processing workflows to ensure only essential attachments required by a payer are connected to a claim and delivered according to payer preferences. |
| • | Clinical Exchange Network: Our Clinical Exchange Network provides an efficient mechanism for EHRs and laboratories to connect with each other and maintain regulatory certifications without the cost of expensive and redundant direct connections. |
| • | MedRx Network: Our medical pharmacy network provides pharmacies with connectivity to commercial and government payers, supporting billing medical claims, such as durable medical equipment and immunizations, directly from the pharmacy management system. |
| • | CommonWell Health Alliance: As the national service provider for CommonWell Health Alliance, we support an industry-wide interoperability effort to make available silos of data that reside within care settings and disparate health IT systems. Our services for CommonWell members include: (i) registration and unique identification of each individual enrolled; (ii) record locator services; (iii) linking of each individual’s clinical records across the care continuum; and (iv) data query and retrieval to enable caregivers to search, select and receive data. |
| • | Electronic Payments: Our electronic payment solutions support both business-to-business (“B2B”) and consumer-to-business (“C2B”) payments. We believe we are well positioned to further drive the healthcare industry’s adoption of convenient and cost-saving payment processes through our comprehensive network of payers and providers. |
| • | B2B Payment Solutions: We offer payers and providers the ability to distribute and receive payments in the most efficient manner—via electronic funds transfer, direct payment, card-based or check. We also assist our customers in automating these processes. |
18
Table of Contents
| • | C2B Payment Solutions: We help providers efficiently bill consumers and offer consumer-friendly options to help reduce bad debt while enhancing the consumer billing and payment experience. |
| • | Data Solutions: We help payers, providers, life sciences companies, and commercial data providers address increasing demands for data to support analytical needs related to performance improvement, consumer engagement, and value-based care. |
| • | Data Platform: We enable our customers to acquire and aggregate clinical, financial, and operational data from across the care continuum, analyze the data and make it available through applications or via direct feeds to a customer’s existing enterprise data warehouse and other analytics systems. |
| • | Data Commercialization: We provide de-identified data feeds informed by regulatory compliant formats and create applications and tools directly for customers or via third party channel partners. We believe that the scale, diversity, and timeliness of our data provide differentiated value. |
Technology-Enabled Services
| • | Revenue Cycle Management: We are a leader in revenue cycle management with demonstrated ability to help improve collections, optimize operational efficiency, and enhance patient experience. We are well positioned to grow as industry-wide margin pressure, coupled with increasing complexity of compliance and reimbursement, drive a robust demand for outsourcing. |
| • | Patient Access Services: We enable health systems and physician practices to provide a broad range of patient access services to their patients. We leverage call center technology with the flexibility to utilize EHR and practice management capabilities, providing a single source of accountability with reporting and continuous quality monitoring. |
| • | Revenue Integrity Services and Consulting: Our Revenue Integrity services help providers mitigate risk, and include charge audit services, coding augmentation, coding quality audit, clinical documentation improvement staffing, and compliance review. |
| • | Hospital Reimbursement Management Services and Physician Revenue Cycle Management Services: We deliver billing and accounts receivable management to address government, commercial, and self-pay payments for hospitals, health systems, independent and hospital-employed physician practices, fire and emergency medical service agencies, and other healthcare organizations, such as independent and hospital-employed laboratories. |
| • | Practice Management: We provide turnkey oversight and operations services for hospital-employed physicians and independent group practices handling a broad scope of administrative tasks including accounting, billing, collections, human resources, scheduling, finance, and managed care contracting. |
| • | Value-Based Care Enablement Services: We provide a broad scope of technologies, tools and services ranging from consulting and project support to full turn-key operations that enable providers, payers, accountable care organizations, and government agencies to succeed in the transition from fee-for-service reimbursement to payment models that reward high-quality and cost-effective care. |
| • | Network Development and Physician Recruiting: We help commercial payers and managed care organizations successfully develop, manage, and scale clinically integrated networks. |
| • | Risk Management and Population Health Services: We enable providers to drive growth and improve margin performance under all value-based payment models, ranging from capitation to shared savings programs. |
| • | Third-Party Administration: We provide fully delegated, licensed third-party administration services that enable risk-bearing providers and payers to reduce the burden of foundational health plan administration, allowing for greater focus on strategic activities such as new product development and member engagement. |
19
Table of Contents
| • | Business Process as a Service (BPaaS): At the core of our BPaaS solution is our next-generation CMS compliant, real-time benefits administration and claims processing platform for all lines of business built entirely on contemporary technology. Our platform offers unlimited flexibility in defining benefit plans, provider contracts, and core business processes using “healthcare business rules” language that can be read and written by non-technical people. |
| • | Communications and Payment Services: We provide communication and payment solutions for payers, providers, channel partners and other stakeholders in the healthcare system. |
| • | Communications and Payments: We help payers produce and distribute explanation of benefits, explanation of payments, checks, claims and correspondence. |
| • | Patient Payment Solutions: We offer providers patient-facing, digital payment solutions to collect patient self-pay obligations. |
| • | Patient Billing and Statements: For providers and channel partners, we manage patient statements and related correspondence, integrated with our digital payment solution. |
| • | Payment and Claims Automation: We provide payment and claims automation solutions that facilitate, expedite, and automate payment processing and posting activities. |
| • | Pharmacy Benefits Administration (PBA): Our PBA solutions provide healthcare management and other administrative services for pharmacy payers and state Medicaid programs, as well as claims processing and other administrative solutions, in real-time, according to customer benefit plan designs, and present a cost-effective alternative to an in-house pharmacy claims adjudication system. |
| • | Consulting: Our healthcare consulting solutions help healthcare customers analyze, develop and implement business and technology strategies that are designed to align with healthcare trends and overall business goals |
Our Customers
We generally provide solutions to payer and provider customers on a per transaction, per document, per communication, per member per month, per provider per month, monthly flat-fee, contingent fee, or hourly fee, and software license, with recurring maintenance fee, basis. Our customer contracts are generally one to three years in term and automatically renew for successive annual terms unless terminated.
| • | Payers: The payer market primarily consists of national commercial insurers, regional private insurers, BlueCross Blue Shield plans, Medicare/Medicaid plans, provider-sponsored payers, third party administrators, emerging technology and data-driven health plans and other specialty health benefits insurers. We are directly connected to their workflows and administrative and clinical systems and provide products and services to nearly all payers. The average tenure for our top ten payer customers is 25 years as of May 2019. We also have low payer customer concentration, with the top ten payers representing approximately 16% of total revenue for the fiscal year ended March 31, 2020. |
| • | Providers: The provider market is comprised of hospitals and health systems, physician practices, dentists, pharmacies, skilled nursing facilities, home health agencies, telehealth providers, senior care facilities, laboratories, and other healthcare providers. We currently have contractual or submitter relationships, directly or through channel partners, with approximately 1,000,000 physicians, 125,000 dentists, 39,000 pharmacies, 6,000 hospitals, approximately 700 channel partners and 700 laboratories. The average tenure for our top 10 provider customers is 23 years as of March 31, 2020. We have low provider customer concentration, with the top 10 providers representing approximately 8% of total solutions revenue for the fiscal year ended March 31, 2020. |
20
Table of Contents
Our Competition
The Company competes on the basis of the breadth and functionality of the solutions it offers on an integrated as well as modular basis, the return on investment realized by its customers from its solutions, the alignment it has with its customers due to not being owned by a payer or provider organization, the size and reach of its network, its value proposition and its pricing models. The Company’s solutions compete with:
| • | healthcare transaction processing companies, including those providing electronic data interchange services and/or internet-based services and those providing services through other means, such as paper and fax; |
| • | healthcare information system vendors that support providers or payers with their revenue and payment cycle management, imaging usage, retrieval and management, capacity and resource management, and clinical information exchange processes, including physician and dental practice management, hospital information, imaging and workflow solutions and EHR vendors; |
| • | IT and healthcare consulting service providers; |
| • | healthcare insurance companies, pharmacy benefit management and pharmacy benefit administrator companies, hospital management companies and pharmacies that provide or are developing electronic transaction and payment distribution services for use by providers and/or by their members and customers; |
| • | healthcare payments and communication solutions providers, including financial institutions and payment processors that have invested in healthcare data management assets, and print and mail vendors; |
| • | healthcare eligibility and enrollment services companies; |
| • | healthcare payment accuracy companies; |
| • | healthcare engagement and transparency companies; |
| • | healthcare billing and coding services companies; |
| • | providers of other data products and data analytics solutions, including healthcare risk adjustment, quality, economic statistics and other data; and other data and analytics solutions; and |
| • | licensors of de-identified healthcare information. |
The Company also competes in some cases with certain of its customers who themselves provide some of the same solutions that the Company offers, as well as with alliances formed by its competitors. In addition, certain major software, hardware, information systems and business process outsourcing companies, both with and without healthcare companies as their partners, offer or have announced their intention to offer competitive products or services.
Regulatory Matters
Substantially all of our business is directly or indirectly related to the healthcare industry and is affected by changes in the healthcare industry, including regulatory changes and fluctuations in healthcare spending. In the U.S. and other countries, the healthcare industry is highly regulated and subject to frequently changing political, legislative, regulatory and other influences. Although some regulatory requirements do not directly apply to our operations, these requirements affect the business of our payer and provider customers and the demand for our solutions. We also may be impacted by non-healthcare laws, requirements and industry standards. For example, banking and financial services industry regulations and privacy and data security regulations may impact our operations as a result of the electronic payment and remittance services we offer directly or through third-party vendors.
We are subject to a number of U.S. federal, state, local and foreign laws and regulations that involve matters central to our business. Failure to satisfy those legal and regulatory requirements, or the adoption of new laws or regulations, could have a significant negative impact on our results of operations, financial condition or liquidity.
21
Table of Contents
U.S. federal, state, local and foreign laws and regulations are evolving and can be subject to significant change. In addition, the application and interpretation of these laws and regulations are often uncertain. These laws are enforced by federal, state and local regulatory agencies in the jurisdictions where we operate, and in some instances also through private civil litigation. For a discussion of the risks and uncertainties affecting our business related to compliance with federal, state and other laws and regulations and other requirements, please see “Risk Factors—Risks Related to Our Business and Industry—Recent and future developments in the healthcare industry could have a material adverse impact on our business, results of operation or financial condition,” “Risk Factors—Risks Related to our Business and Industry—Government regulation, industry standards and other requirements create risks and challenges with respect to our compliance efforts and our business strategies,” and “Risk Factors—Risks Related to our Business and Industry—We are unable to predict what changes to laws, regulations and other requirements, including related contractual obligations, might be made in the future or how those changes could affect our business or the costs of compliance.”
Examples of the most significant of these laws include, but are not limited to, the following:
HIPAA Privacy and Security Requirements
There are numerous federal and state laws and regulations related to the privacy and security of health information. In particular, regulations promulgated pursuant to HIPAA establish privacy and security standards that limit the use and disclosure of certain individually identifiable health information (known as “protected health information”) and require the implementation of administrative, physical and technological safeguards to protect the privacy of protected health information and ensure the confidentiality, integrity and availability of electronic protected health information. The privacy regulations established under HIPAA also provide patients with rights related to understanding and controlling how their protected health information is used and disclosed. As a provider of services to entities subject to HIPAA, we are directly subject to certain provisions of the regulations as a “Business Associate.” We are also directly subject to the HIPAA privacy and security regulations as a “Covered Entity” with respect to our operations as a healthcare clearinghouse and with respect to our clinical care visit services.
When acting as a Business Associate under HIPAA, to the extent permitted by applicable privacy regulations and contracts and associated Business Associate Agreements with our customers, we are permitted to use and disclose protected health information to perform our solutions and for other limited purposes, but other uses and disclosures, such as marketing communications, require written authorization from the patient or must meet an exception specified under the privacy regulations. To the extent we are permitted to de-identify protected health information and use de-identified information for our purposes, determining whether such protected health information has been sufficiently de-identified to comply with the HIPAA privacy standards and our contractual obligations may require complex factual and statistical analyses and may be subject to interpretation.
Other Privacy and Security Requirements. In addition to HIPAA, numerous other U.S. federal and state laws govern the collection, dissemination, use, access to and confidentiality of personal information. Certain federal and state laws protect types of personal information that may be viewed as particularly sensitive. For example, the Confidentiality of Substance Use Disorder Patient Records (42 C.F.R. Part 2) is a federal law that protects information that would reveal if an individual has or had a substance abuse disorder. Similarly, New York’s Public Health Law, Article 27-F protects information that could reveal confidential HIV-related information about an individual. Some states have enacted or are considering new laws and regulations that would further protect this information, such as the California Consumer Privacy Act of 2018, which builds upon and is more stringent in many respects than other state laws currently in effect in the U.S. In many cases, state laws are more restrictive than, and not preempted by, HIPAA, and may allow personal rights of action with respect to privacy or security breaches, as well as fines. State laws are contributing to increased enforcement activity and may also be subject to interpretation by various courts and other governmental authorities. Further, Congress and a number of states have considered prohibitions or limitations on the disclosure of personal and other information to individuals or entities located outside of the U.S. The U.S. Congress is also currently considering a generally applicable national privacy law that may supplant California’s and other states’ privacy laws.
22
Table of Contents
There also are numerous international privacy and security laws that govern the collection, dissemination, use, access, retention, protection, transfer and confidentiality of personal information. For example, the GDPR, which became effective on May 25, 2018 is more stringent than laws and regulations governing personal information in the U.S. Certain of our solutions involve the transmission and storage of customer data in various jurisdictions, which subjects the operation of that service to privacy or data protection laws and regulations in those jurisdictions.
Data Protection and Breaches
Most states require holders of personal information to maintain safeguards and take certain actions in response to a data breach, such as providing prompt notification of the breach to affected individuals or the state’s attorney general. In some states, these laws are limited to electronic data, but states increasingly are enacting or considering stricter and broader requirements. Additionally, HIPAA imposes certain notification requirements on both Covered Entities and Business Associates. In certain circumstances involving large breaches, requirements may even involve notification to the media. A non-permitted use or disclosure of protected health information is presumed to be a breach under HIPAA unless the Covered Entity or Business Associate establishes that there is a low probability the information has been compromised consistent with requirements enumerated in HIPAA.
Further, the FTC has prosecuted certain data breach cases as unfair and deceptive acts or practices under the Federal Trade Commission Act. In addition, by regulation, the FTC requires creditors, which may include some of our customers, to implement identity theft prevention programs to detect, prevent and mitigate identity theft in connection with customer accounts. Although Congress passed legislation that restricts the definition of “creditor” and exempts many healthcare providers from complying with this identity theft prevention rule, we may be required to apply additional resources to our existing processes to assist our affected customers in complying with this rule.
HIPAA Transaction and Identifier Standards
HIPAA and our implementing regulations mandate format and data content standards and provider identifier standards (known as the National Provider Identifier) that must be used in certain electronic transactions, such as claims, payment advice and eligibility inquiries. HHS has established standards that health plans must use for electronic fund transfers with providers, has established operating rules for certain transactions, and is in the process of establishing operating rules to promote uniformity in the implementation of the remaining types of covered transactions. The ACA also requires HHS to establish standards for health claims attachment transactions. HHS has modified the standards for electronic healthcare transactions (e.g., eligibility, claims submission and payment and electronic remittance) from Version 4010/4010A to Version 5010. Further, as of 2015, HHS requires the use of updated standard code sets for diagnoses and procedures known as the ICD-10 code sets. Enforcement of compliance with these standards falls under HHS and is carried out by CMS.
Anti-Kickback Laws and Anti-Referral Laws
A number of federal and state laws govern patient referrals, financial relationships with physicians and other referral sources and inducements to providers and patients, including restrictions contained in amendments to the Social Security Act, commonly known as the “federal Anti-Kickback Statute (“AKS”).” The AKS prohibits any person or entity from offering, paying, soliciting or receiving, directly or indirectly, anything of value with the intent of generating referrals of patients covered by Medicare, Medicaid or other federal healthcare programs. Courts have interpreted the law to provide that a financial arrangement may violate this law if any one of the purposes of an arrangement is to encourage patient referrals or other federal healthcare program business, regardless of whether there are other legitimate purposes for the arrangement. Violation of the AKS is a felony, and penalties for AKS violations can be severe, and include imprisonment, criminal fines, civil penalties with treble damages (when the federal False Claims Act (“FCA”) is implicated) and exclusion from participation in
23
Table of Contents
federal healthcare programs. The ACA broadened the reach of the AKS by amending the intent requirement, such that a person or entity no longer needs to have actual knowledge of the AKS or specific intent to violate it in order to have committed a violation. In addition, as further discussed below, the ACA provided that the government may assert that a claim which includes items or services resulting from a violation of the AKS constitutes a false or fraudulent claim for purposes of the FCA, as well as restrictions contained in amendments to the Social Security Act, commonly known as the federal Civil Monetary Penalties Law (“CMP”). The AKS contains a limited number of exceptions, and the Office of the Inspector General (“OIG”) of HHS has created regulatory safe harbors to the AKS. Activities that comply with a safe harbor are deemed protected from prosecution under the AKS. Failure to meet a safe harbor does not automatically render an arrangement illegal under the AKS. The arrangement, however, does risk increased scrutiny by government enforcement authorities, based on our particular facts and circumstances. Our contracts and other arrangements may not meet an exception or a safe harbor. Additionally, many states have similar anti-kickback laws that are not necessarily limited to items or services for which payment is made by a federal healthcare program. In addition, federal laws restricting certain physician self-referrals (also known as the “Stark Law”), as well as state counterparts, may prohibit payment for patient referrals, patient brokering, remuneration of patients, or billing based on referrals between individuals or entities that have various financial, ownership, or other business relationships with physicians or other healthcare providers. The Stark Law is very complex, and state anti-referral laws vary widely. As noted below, to the extent we undertake billing and coding for designated health services, such activities may be subject to the Stark Law.
False or Fraudulent Claim Laws; Medical Billing and Coding
Medical billing, coding and collection activities are governed by numerous federal and state civil and criminal laws, regulations, and sub-regulatory guidance. We provide billing and coding services, claims processing and other solutions to providers that relate to, or directly involve, the reimbursement of health services covered by Medicare, Medicaid, other federal and state healthcare programs and private payers. In addition, as part of our data transmission and claims submission services, we may employ certain edits, using logic, mapping and defaults, when submitting claims to third-party payers. Such edits are utilized when the information received from providers is insufficient to complete individual data elements requested by payers. We also provide solutions including risk analytics, chart reviews, clinical care visits, payment accuracy, audit functions and enrollment and eligibility, to Medicaid and Medicare managed care plans, commercial plans and other entities. These solutions, which include identifying diagnosis codes with respect to hierarchical condition categories, impact the amounts paid by Medicare and Medicaid to managed care plans. In addition, solutions we offer to customers that enable customers to certify to compliance with certain requirements and standards, such as EHR Meaningful Use requirements. We rely on our customers to provide us with accurate and complete information and to appropriately use analytics, codes, reports and other information in connection with the solutions we provide to them, but they may not always do so. As a result of these aspects of our business, we may be subject to, or contractually required to comply with, numerous federal and state laws that prohibit false or fraudulent claims including but not limited to the FCA, the CMP, and state equivalents.
In addition, the FCA prohibits the knowing submission of false claims or statements to the federal government, including to the Medicare and Medicaid programs. The FCA also contains qui tam, or whistleblower provisions, which allow private individuals to sue on behalf of the federal government alleging that the defendant has defrauded the federal government.
Exclusion from participation in government healthcare programs. We are also subject to the exclusion rules of the OIG of HHS whereby OIG may or must exclude individuals and entities convicted of program-related crimes from participation in the Medicare and Medicaid programs. A company that employs or contracts with an OIG-excluded individual and submits a claim for reimbursement to a federal healthcare program, or causes such a claim to be submitted, may itself be excluded or may be subject to significant penalties under the CMP, plus treble damages, for each item or service furnished during the period in which the individual or entity was excluded. A company contracting with providers has an affirmative duty to check the exclusion status of individuals and entities prior to entering into employment or contractual relationships and periodically re-check thereafter, or run the risk of liability under the CMP.
24
Table of Contents
FDA and International Regulation of Medical Software
Certain of our products are classified as medical devices and are subject to regulation by the Food and Drug Administration (the “FDA”) and numerous other federal, state and foreign governmental authorities. In the U.S., the FDA permits commercial distribution of a new medical device after the device has received clearance under Section 510(k) of the Federal Food, Drug and Cosmetic Act (the “FDCA”), or is the subject of an approved premarket approval application, unless the device is specifically exempt from those requirements. Moreover, the FDA has increasingly focused on the regulation of medical software and health information technology products as medical devices under the FDCA. For example, in February 2015, the FDA issued guidance to inform manufacturers and distributors of medical device data systems that it did not intend to enforce compliance with regulatory controls that apply to medical device data systems, medical image storage devices, and medical image communication devices. The Cures Act, enacted in December 2016, builds on the FDA’s efforts to limit the regulation of low-risk medical devices by exempting certain categories of software functions from the definition of “medical device” under the FDCA, including software functions intended for administrative support of a healthcare facility and certain functions related to the exchange and use of electronic medical records. However, a software function may not be excluded from the device definition if the FDA determines that use of the software function would be reasonably likely to have serious adverse health consequences.
Foreign governmental authorities that regulate the manufacture and sale of medical devices have become increasingly stringent and, where we sell our medical device solutions internationally, we are subject to international regulation regarding these medical device solutions. For example, in May 2017, the EU Medical Devices Regulation (“MDR”) (Regulation 2017/745) was adopted and in May 2020 the MDR came into effect. The MDR repeals and replaces the EU Medical Devices Directive. Unlike directives, which must be implemented into the national laws of the EU Member States, the MDR is directly applicable in the EU Member States and on the basis of the European Economic Area (“EEA”) agreement in Iceland, Lichtenstein and Norway. The MDR, among other things, is intended to establish a uniform, transparent, predictable and sustainable regulatory framework across the EEA for medical devices and ensure a high level of safety and health while supporting innovation. The MDR, among other things:
| • | Strengthens the clinical data requirements related to medical devices; |
| • | Imposes additional scrutiny during the conformity assessment procedure for high risk medical devices; |
| • | Imposes on manufacturers and authorized representative the obligation to have a person responsible for regulatory compliance continuously at their disposal; |
| • | Requires that authorized representatives be held legally responsible and liable for defective products placed on the EEA market jointly with the device manufacturers; |
| • | Reinforces post market surveillance requirements applicable to CE marked medical devices; |
| • | Improves the traceability of medical devices throughout the supply chain to the end-user or patient through a Unique Device Identification System; and |
| • | Increases transparency. Information from several databases concerning economic operators, CE Certificates of Conformity, conformity assessment, clinical investigations, the Unique Device Identification system, adverse event reporting and market surveillance will be available to the public. |
25
Table of Contents
Interoperability Requirements
There is increasing demand among customers, industry groups and government authorities that healthcare IT products provided by various vendors be compatible with each other and allow for the efficient exchange of EHR information. In 2013, in order to address this demand for interoperability, a number of other healthcare IT companies co-founded the CommonWell Health Alliance with the aim of developing a standard for data sharing among physicians, hospitals, clinics and pharmacies. Certain federal and state agencies also are developing standards that could eventually become mandatory for software and systems purchased by these agencies, or used by our customers. For example, under the Cures Act, the Office of the National Coordinator for Health Information Technology (“ONC”) within HHS is required to develop a “trusted exchange framework” and common agreement for the secure exchange of health information between networks. Although the Cures Act does not make implementation of the trusted exchange framework mandatory, the Cures Act encourages its adoption through the establishment of a publicly available directory of networks that are capable of trusted exchange and by permitting federal agencies to require implementation of the trusted exchange framework by network contractors as the contractors update their health IT or operational practices.
The Cures Act also encourages interoperability through changes to EHR certification standards implemented as part of HHS’s programs to promote interoperability. In particular, the amended EHR certification standards will require developers (i) to publish application programming interfaces that permit exchange of EHR and other health information among different health IT systems, (ii) to successfully test the “real world use” of interoperability technology, and (iii) to attest that they will not engage in “information blocking” or otherwise inhibit the appropriate exchange, access, and use of electronic health information.
Restrictions on Communications
Communications with our customers and our customers’ patients are subject to laws and regulations governing communications, including the Telephone Consumer Protection Act of 1991 (the “TCPA”), the CAN-SPAM Act, and additional fax regulations under the Junk Fax Act and data privacy rules under the California Consumer Privacy Act of 2018, as well as potentially under non-U.S. laws that regulate communications and messaging and that affect our operations, such as Canada’s Anti-Spam Law (“CASL”), GDPR, and the European Union’s e-Privacy Directive and implementing member state laws (and any subsequent changes to such laws). We also use email and social medial platforms as marketing tools. For example, we maintain social media accounts and may occasionally email customers offers and promotions. As laws and regulations, including FTC enforcement, rapidly evolve to govern the use of these platforms and devices, we will become subject to such laws and regulations.
Financial Services Related Laws, Regulations and Industry Standards
Financial services and electronic payment processing services are subject to numerous laws, regulations and industry standards. These laws may subject us, our vendors and our customers to liability as a result of our communication and payment solutions. Although we do not act as a bank, we offer solutions that involve banks, or vendors who contract with banks and other regulated providers of financial services. We rely on relationships with such banks, vendors and providers. If we fail to maintain these relationships or if we maintain them under new terms that are less favorable to us, our business, results of operations or financial condition could suffer. The various payment modalities that we offer our customers directly and through banks, vendors, or other regulated providers may be deemed regulated activity at the federal or state level, and, as a result, we may be affected by banking and financial services industry laws, regulations and standards, such as licensing requirements, solvency standards, reporting and disclosure obligations and requirements to maintain the privacy and security of nonpublic personal financial information. In addition, our communication and payment solutions may be affected by payment card industry operating rules and security standards, certification requirements, state prompt payment laws and other rules governing electronic funds transfers. Moreover, in addition to regulatory requirements related to electronic funds transfers, payment transactions processed using the Automated Clearing
26
Table of Contents
House Network are subject to network operating rules promulgated by the National Automated Clearing House Association, and these rules may affect our payment practices. Certain payment transactions may be subject to card association and network rules and standards. Finally, as we expand our financial services offerings we may be subject to additional laws and regulations, including certain consumer protection laws such as the Fair Debt Collections Practices Act (the “FDCPA”), the Fair Credit Reporting Act (the “FCRA”) and various other state laws implicated by such financial services.
Foreign Corrupt Practices Act and Bribery Laws
The U.S. Foreign Corrupt Practices Act (“FCPA”) and similar international bribery laws make it unlawful for entities to make payments to foreign government officials to assist in obtaining and maintaining business. Specifically, the anti-bribery provisions of the FCPA prohibit any offer, payment, promise to pay, or authorizing the payment of money or anything of value to any person, while knowing that all or a portion of such money or thing of value will be offered, given or promised, directly or indirectly, to a foreign official to do or omit to do an act in violation of his or her duty, or to secure any improper advantage in order to assist in obtaining or retaining business for or with, or directing business, to any person. In addition to the anti-bribery provisions of the FCPA, the statute also contains accounting requirements designed to operate in tandem with the anti-bribery provisions. Covered companies are required to make and keep books and records that accurately and fairly reflect the transactions of the company and devise and maintain an adequate system of internal accounting controls.
Physician Payments Sunshine Act
The Physician Payments Sunshine Act of 2010 (the “Sunshine Act”) requires manufacturers of medical devices covered by Medicare, Medicaid, and the Children’s Health Insurance Program to collect and track all financial relationships with physicians and teaching hospitals and to report annually such data to CMS. Medical device manufacturers must report to CMS payments or “transfers of value” made to physicians, including meals, travel reimbursement, consulting fees and research payments. In addition, several states and the District of Columbia have passed laws requiring that medical device manufacturers report various details of their financial relationships with physicians. The Sunshine Act authorizes significant civil monetary penalties for each payment or transfer of value not accurately or completely reported.
Payment Card Industry Standards
We accept credit card, eCheck, ACH Payments, and payments via online portal, phone/Interactive Voice Response system or by mail. We also enable payers to collect member premium payments. These transactions are regulated at the federal, state and international levels as well as by certain industry groups, such as the Payment Card Industry Security Standards Council, the National Automated Clearing House Association and individual credit card issuers. Federal, state, international and industry groups also may consider and implement from time to time new privacy and security requirements that apply to our business. Compliance with contractual obligations and evolving privacy and security laws, requirements and regulations may result in cost increases due to necessary systems changes, new limitations or constraints on our business and the development of new administrative processes. If we fail to adequately control fraudulent ACH, credit card and debit card transactions, we may face civil liability, diminished public perception of our security measures and significantly higher ACH, credit card and debit card related costs, each of which could adversely affect our business, financial condition and results of operations. The termination of our ability to process payments through ACH transactions or on any major credit or debit card would adversely affect our ability to operate our business.
Other State Healthcare Laws
Many states in which we provide clinical care in-home assessment services prohibit corporations and other non-licensed entities from practicing medicine, nursing and other licensed professions by employing physicians and certain non-physician practitioners. These prohibitions on the corporate practice of medicine, nursing and
27
Table of Contents
other licensed professions impact how we structure our relationships with physicians and other affected non-physician practitioners. In addition, some states have restrictions on physicians and other healthcare practitioners splitting fees with non-practitioners or restrict the ability of practitioners to assign claims for reimbursement from government healthcare programs. Some states have interpreted these laws to prevent business service providers from charging their physician clients on the basis of a percentage of collections or charges. Furthermore, we hold certain state licenses and enrollments in government healthcare programs which subject us to additional requirements and scrutiny by government regulators.
Intellectual Property
The Company relies upon a combination of trade secrets, copyrights, trademarks, patents, license agreements, confidentiality policies and procedures, nondisclosure agreements and technical measures designed to protect the intellectual property and commercially valuable confidential information and data used in its business. The Company generally enters into nondisclosure agreements with our employees, consultants, vendors and customers. It also seeks to control access to and distribution of its technology, documentation and other proprietary information.
The Company uses numerous trademarks, trade names and service marks for its solutions and has a number of patents and patent applications covering solutions it provides, including software applications. However, the Company does not believe its solutions are dependent upon any one patent or patent application, or family or families of the same. It also licenses from third parties a variety of content, data and other intellectual property. Although we believes that alternative technologies and work-arounds are likely to be available should these agreements terminate or expire, there is no guarantee that third-party technologies will continue to be available to the Company on commercially reasonable terms or that work-arounds would be readily available for deployment on a commercially reasonable time-frame.
The steps the Company has taken to protect its trade secrets, copyrights, trademarks, service marks, patents and other intellectual property may not be adequate, and third parties could infringe, misappropriate or misuse its intellectual property. If this were to occur, it could harm the Company’s reputation and adversely affect its competitive position or results of operations.
Employees
As of March 31, 2020, we had approximately 15,000 employees. None of these employees are represented by a labor union. We consider our relationships with our employees to be good.
Seasonality
The nature of the Company’s customers’ end-market results in moderate seasonality reflected in revenue differences during the year with a slightly greater positive variance in our fiscal fourth quarter related to the regulatory impact of data submission deadlines due to HEDIS, which may drive timing of analytics activity. Following the adoption of new revenue recognition guidance on April 1, 2019, the Company believes that the moderate seasonality will continue to be reflected in its financial results but with potentially differing patterns than under the prior recognition method. Finally, quarter to quarter financial performance may vary from historical seasonal trends as the Company further expands and diversifies its business and increases the portion of its revenue generated from new offerings.
Available Information
Our website is www.changehealthcare.com. Available on this website, free of charge, are our annual reports on Form 10-K, quarterly reports on Form 10-Q, current reports on Form 8-K and all amendments to those reports as soon as reasonably practical after such material is electronically filed or furnished to the SEC. Alternatively, you may access these reports at the SEC’s website at www.sec.gov.
28
Table of Contents
The risks described below could have a material adverse impact on our business, financial condition or operating results. Although it is not possible to predict or identify all such risks and uncertainties, they may include, but are not limited to, the factors discussed below. The risks described herein are not the only risks we may face. Additional risks and uncertainties not currently known to us or that we currently deem to be immaterial may also materially adversely affect our business, financial condition or operating results.
Risks Related to Our Business and Industry
If we are unable to retain our existing customers or attract new customers, our business, financial condition or results of operations could suffer.
Our success depends substantially upon the retention of existing customers and the attraction of new customers. We may not be able to retain our existing customers or attract new customers if we are unable to provide solutions or services that existing or prospective payer customers believe enable them to achieve improved efficiencies and cost-effectiveness or allow them to more effectively manage their revenue cycle, increase reimbursement rates and improve cash flows.
Success in retaining and attracting customers will also depend, in part, on our ability to innovate successfully and be responsive to technological developments, pricing pressures and changing business models.
To remain competitive in the evolving healthcare information technology (“IT”) markets, we must continuously upgrade our existing solutions and develop and introduce new solutions on a timely basis. Future advances in healthcare IT could lead to new technologies, products or services that are competitive with existing solutions, resulting in pricing pressure or rendering such solutions obsolete or not competitive. In addition, because we deliver enterprise-wide and single entity clinical, patient care, financial, imaging, supply chain and strategic management software solutions to payers, hospitals, physicians and other providers, our ability to integrate these software solutions could be challenged, which may impair our ability to retain customers and harm our reputation with existing and prospective customers. We also may not be able to retain or attract customers if our solutions contain errors or otherwise fail to perform properly, if our pricing structure is not competitive or if we are unable to renegotiate customer contracts upon expiration.
Our revenue depends in part upon maintaining high customer retention rates and our future growth depends on attracting new customers. If we are unable to maintain customer retention rates, or to attract new customers, our business, results of operations or financial condition could be adversely impacted.
An economic downturn or volatility like we are currently experiencing due to COVID-19 could have a material adverse impact on our business, results of operations or financial condition.
The U.S. and world economies have experienced significant economic uncertainty and volatility during recent years and that uncertainty has become more acute in the last several months as a result of the COVID-19 pandemic. A weakening of economic conditions has led to reductions in demand for our solutions. As a result of volatile or uncertain economic conditions, we may experience the negative effects of increased financial pressures on payer and provider customers. For instance, our business has been and is likely to continue to be negatively impacted by increased competitive pricing pressure and a decline in our customers’ creditworthiness, which could result in us incurring increased bad debt expense. Additionally, volatile or uncertain economic conditions in the U.S. and other parts of the world could lead government customers to terminate, or elect not to renew, existing contracts with us, or not enter into new contracts with us. If we are not able to timely and appropriately adapt to changes resulting from the current weak economic environment, it could have a material adverse impact on our business, results of operations or financial condition.
29
Table of Contents
Our business has been and continues to be negatively affected by the ongoing COVID-19 pandemic and may face similar impacts from any future outbreaks of disease.
Our operations have and continue to be affected by the ongoing global COVID-19 pandemic and the resulting volatility and uncertainty it has caused in the U.S. and international markets. In March 2020, the World Health Organization (the “WHO”) declared the COVID-19 outbreak a pandemic and recommended containment and mitigation measures worldwide. On March 13, 2020, President Trump declared a National Emergency relating to the disease. The widespread infection in the U.S. and abroad has caused significant volatility and uncertainty in U.S. and international markets, which could result in a prolonged economic downturn that has disrupted and is expected to continue to disrupt our business.
While national, state and local quarantine, shelter-in-place, curfew and similar isolation measures have begun to ease, such government orders and other restrictions may continue in effect or may be reinstituted if outbreaks increase or fail to decrease. Such measures have had adverse impacts on the U.S. and foreign economies of uncertain severity and duration and have and may continue to negatively impact our ongoing operations, including our revenue and supply chain. For example, a portion of our business is tied to overall volumes of activity in the healthcare system, and as a result of the significant reduction, or in some cases elimination, of elective medical procedures and healthcare visits, without a corresponding increase in COVID-19 related transactions, we have seen a significant temporary decline in transactions across our medical and dental networks. In addition, for a portion of our technology-enabled services business we get paid on a contingency basis based on collections, which has also been impacted by a delay in elective procedures.
As a result of the ongoing COVID-19 outbreak, we and several of our business partners have transitioned the majority of our workforce to a temporary remote working model, which may result in us experiencing lower work efficiency and productivity, which in turn may adversely affect our business. As our employees and business partners’ employees work from home and access our system remotely, we may be subject to heightened security and privacy risks, including the risks of cyber attacks and privacy incidents. Additionally, we have a limited number of employees who continue to work in our facilities or perform services at our customers’ facilities who may be subject to heightened risks for COVID-19 exposure thus potentially impacting their health and future worker compensation claims against us. We may also be subject to lawsuits from employees and others exposed to COVID-19 at our facilities, which could involve large demands and substantial defense costs. Our professional and general liability insurance may not cover all claims against us. Furthermore, if any of our employees are unable to perform his or her duties for a period of time, including as the result of illness, our results of operations or financial condition could be adversely affected. Finally, the widespread pandemic has caused and is expected to continue to cause significant disruption of global financial markets, which may reduce or impair our ability to access capital (or access capital on reasonable terms) temporarily during this period.
While the COVID-19 outbreak may provide us with new business opportunities, including supporting customers offering novel telemedicine, telehealth, and data and analytics products and solutions, we may experience compliance and related business development risks associated with these new business opportunities if customers request, and we attempt to offer, these products and solutions on an expedited basis in support of COVID-19 efforts.
We cannot reasonably estimate the length or severity of the COVID-19 pandemic or the related response, including the length of time it may take for normal economic and operating conditions to resume or the extent to which the disruption may materially impact our business, consolidated financial position, consolidated results of operations or consolidated cash flows. To the extent the COVID-19 pandemic adversely affects our business, operations, financial position or consolidated cash flows, it may also have the effect of heightening many of the other risks described herein.
If we are unable to connect to a large number of payers and providers, our solutions would be limited and less desirable to customers.
Our business largely depends upon our ability to connect electronically to a substantial number of payers, such as insurance companies, Medicare and Medicaid agencies and pharmacy benefit managers and
30
Table of Contents
administrators, and providers, such as hospitals, physicians, clinics, dentists, laboratories and pharmacies. The attractiveness of some of the solutions we offer to providers, such as claims management and submission services, depends in part on our ability to connect to a large number of payers, which allows it to streamline and simplify workflows for providers. These connections may be made either directly or through a clearinghouse. We may not be able to maintain our connections with a large number of payers on satisfactory terms and may not be able to develop new connections, either directly or through other clearinghouses, on satisfactory terms. The failure to maintain these connections could cause our solutions to be less attractive to provider customers. In addition, payer customers view our relationships with providers as desirable in allowing them to receive a high volume of transactions electronically and realize the resulting cost efficiencies through the use of our solutions. Competing EDI service providers can easily establish connections with payers and providers and thereby may replicate these solutions. Any failure to maintain existing connections with payers, providers and other clearinghouses or to develop new connections as circumstances warrant, or an increase in the utilization of direct links between payers and providers, could cause our electronic transaction processing systems to be less desirable to healthcare constituents, which would reduce the number of transactions that we process, which would reduce our revenue and could have a material adverse impact on our business, results of operations or financial condition.
We face significant competition, which may harm our business, results of operations or financial condition.
We face substantial competition from many healthcare information systems companies and other IT companies, including the growing presence of large technology companies entering the healthcare market. This vigorous competition requires us to provide high quality, innovative products at a competitive price. These competitive threats will likely remain or expand in the future. Our key competitors include:
| • | healthcare transaction processing companies, including those providing electronic data interchange (“EDI”) services and/or internet-based services and those providing services through other means, such as paper and fax; |
| • | healthcare information system vendors that support providers or payers with their revenue and payment cycle management, imaging usage, retrieval and management, capacity and resource management, and clinical information exchange processes, including physician and dental practice management, hospital information, imaging and workflow solutions and Electronic Health Records (“EHR”) vendors; |
| • | IT and healthcare consulting service providers; |
| • | healthcare insurance companies, pharmacy benefit management and pharmacy benefit administrator companies, hospital management companies and pharmacies that provide or are developing electronic transaction and payment distribution services for use by providers and/or by their members and customers; |
| • | healthcare payments and communication solutions providers, including financial institutions and payment processors that have invested in healthcare data management assets, and print and mail vendors; |
| • | healthcare eligibility and enrollment services companies; |
| • | healthcare payment accuracy companies; |
| • | healthcare engagement and transparency companies; |
| • | healthcare billing and coding services companies; |
| • | providers of other data products and data analytics solutions, including healthcare risk adjustment, quality, economic statistics and other data; and |
| • | licensors of de-identified healthcare information. |
In addition, the increasing standardization of certain healthcare IT products and services has made it easier for companies to enter these markets with competitive products and services. Many software, hardware,
31
Table of Contents
information systems and business process outsourcing companies, both with and without healthcare companies as their partners, offer or have announced their intention to offer products or services that are competitive with solutions that we offer. There have been a number of recent entrants that have successfully marketed competitive solutions and they may expand these offerings in the future. We cannot fully anticipate whether or when companies in adjacent or other product, service or technology areas may launch competitive products, and any such entry may lead to product obsolescence, loss of market share or erosion of prices. The extent of this competition varies by the size of companies, geographical coverage and scope and breadth of products and services offered. Within certain of the markets in which we operate, our competitors are significantly larger and have greater financial or other resources and have established reputations for success. In addition, many of the world’s largest and most well-funded technology companies are aggressively pursuing opportunities to enter the healthcare market, and we expect such initiatives to accelerate in light of the COVID-19 pandemic.
Additionally, the pace of change in the healthcare information systems market is rapid, and there are frequent new solution introductions, solution enhancements and evolving industry standards and requirements. We cannot guarantee that we will be able to upgrade our existing solutions or services, or introduce new solutions or services at the same rate as our competitors, or at all, nor can it guarantee that such upgrades or new solutions or services will achieve market acceptance over or among competitive offerings, or at all. Competitors may also commercialize products, services or technologies that render our solutions obsolete or less marketable.
These competitive pressures could have a material adverse impact on our business, results of operations or financial condition.
Competition with some customers, or decisions by customers to perform internally some of the same solutions or services that we offer, could harm our business, results of operations or financial condition.
Some of our existing customers compete with us, or may do so in the future, and some customers belong to alliances that compete with us, or may do so in the future, either with respect to the solutions or services we provide to them now, or with respect to other lines of business. For example, some payer customers currently offer, through affiliated clearinghouses, web portals and other means, electronic data transmission services to providers that allow the provider to bypass third-party EDI service providers such as us, and additional payers may do so in the future. The ability of payers to replicate these solutions and the ability of providers to connect directly with payers may adversely affect the terms and conditions we are able to negotiate in our agreements with payers and our transaction volume with them, which directly relates to our revenue. In addition, to the extent that customers elect to perform internally any of the business processes our solutions address, either because they believe they can provide such processes more efficiently internally or otherwise, we may lose such customers, or the volume of our business with such customers may be reduced, which could harm our business, results of operations or financial condition.
In recent years, the healthcare industry has been subject to increasing consolidation. Many healthcare organizations, including a number of our customers, have consolidated to create larger enterprises with greater market power. This consolidation trend could give the resulting enterprises greater bargaining power, which may lead to downward price pressure on our solutions or services, or less demand for them, or both. In addition, when our customers combine, they often consolidate infrastructure including IT systems, which in turn may erode the diversity of our customer and revenue base. Any of these effects could harm our business, results of operations or financial condition.
If our solutions do not interoperate with our customers’ or their vendors’ networks and infrastructures, or if customers or their vendors implement new system updates that are incompatible with our solutions, sales of those solutions could be adversely affected.
Our solutions must interoperate with our customers’ and their vendors’ existing infrastructures, which often have different specifications, rapidly evolve, utilize multiple protocol standards, deploy products and applications
32
Table of Contents
from multiple vendors, and contain multiple generations of products that have been added to that infrastructure over time. Some of the technologies supporting our customers and their vendors are changing rapidly and we must continue to adapt to these changes in a timely and effective manner at an acceptable cost. In addition, our customers and their vendors may implement new technologies into their existing networks and systems infrastructures that may not immediately interoperate with our solutions. our continued success will depend on our ability to adapt to changing technologies, manage and process ever-increasing amounts of data and information and improve the performance, features and reliability of our services in response to changing customer and industry demands. If we encounter complications related to network configurations or settings, we may have to modify our solutions to enable them to interoperate with customers’ and their vendors’ networks and manage customers’ transactions in the manner intended. For example, if customers or their vendors implement new encryption protocols, it may be necessary for us to obtain a license to implement or interoperate with such protocols, and there can be no assurance that we will be able to obtain such a license on acceptable terms, if at all. These difficulties, and other difficulties we may experience, could delay or prevent the successful design, development, testing, introduction or marketing of our solutions. As a consequence of any of the foregoing, our ability to sell our solutions may be impaired, which could have a material adverse impact on our business, results of operations or financial condition.
Failure to maintain relationships with channel partners or significant changes in the terms of agreements with channel partners may have an adverse effect on our ability to successfully market our solutions.
We have entered into contracts with channel partners to market and sell some of our solutions. Most of these contracts are on a non-exclusive basis. However, under contracts with some channel partners, we may be bound by provisions that restrict our ability to market and sell solutions to potential customers. Our arrangements with some of these channel partners involve negotiated payments to them based on percentages of revenue they generate. If the payments prove to be too high, we may be unable to realize acceptable margins, but if the payments prove to be too low, channel partners may not be motivated to produce a sufficient volume of revenue. The success of these partnerships will depend in part upon the channel partners’ own competitive, marketing and strategic considerations, including the relative advantages of using alternative solutions being developed and marketed by them or by competitors. If any of these channel partners is unsuccessful in marketing our solutions or seeks to amend the financial or other terms of the contracts they have with us may need to broaden our marketing efforts to increase focus on the solutions they sell and alter our distribution strategy, which may divert planned efforts and resources from other projects and increase our costs generally. In addition, as part of the packages these channel partners sell, they may offer a choice to their customers between solutions what we supply and similar solutions offered by competitors or by the channel partners directly. If our solutions are not chosen for inclusion in these packages, the revenue we earn from our channel partner relationships will decrease. Lastly, we could be subject to claims and liability as a result of the activities, products or services of these channel partners or other resellers of our solutions. Even if these claims do not result in liability, investigating and defending these claims could be expensive, time-consuming and result in adverse publicity that could have a material adverse impact on our business, results of operations or financial condition.
We have faced and will continue to face pressure to reduce prices, which may reduce our margins, profitability and competitive position.
As electronic transaction processing has further penetrated the healthcare market and has become highly standardized, competition among revenue cycle management software and EDI providers is increasingly focused on providing value added services and capabilities to customers. This competition has placed pressure, and could place further pressure, on us to add functionality and keep prices competitive in order to retain market share. Likewise, as a result of Medicare or Medicaid payment reductions and other reimbursement changes, our provider customers have sought, and may attempt in the future to seek, price concessions. If we are unable to reduce costs sufficiently to offset declines in prices, or if we are unable to introduce new, innovative offerings with higher margins, our business, results of operations or financial condition may be materially adversely impacted.
33
Table of Contents
In addition, many healthcare industry constituents are consolidating to create integrated healthcare delivery systems with greater market power. As provider networks, such as hospitals, and payer organizations, such as private insurance companies, consolidate, competition to provide the types of solutions we provide may become more intense and the importance of establishing and maintaining relationships with key healthcare industry constituents could increase. These healthcare industry constituents have used in the past, and likely will try to use in the future, their market power—particularly where it has been increased following mergers and consolidations—to negotiate price reductions for our solutions. If we are forced to further reduce prices, margins will decrease and results of operations could deteriorate, unless we are able to achieve corresponding reductions in expenses.
We are highly dependent on transaction volumes in the U.S. healthcare industry, particularly payment and reimbursement transaction volumes, and any temporary or sustained decrease in healthcare transaction, payment or reimbursement volumes in the U.S. could have a material adverse impact on our business, results of operations or financial condition.
A significant portion of our revenue attributable to the ongoing use of or subscription to a service or solution after an initial sale or renewal without additional selling efforts is earned on a per transaction basis (or is derived from transaction-related services). As a result, much of our revenue is tied to customer transaction, payment and reimbursement volumes and generally is not contractually required to be paid in the absence of the occurrence of healthcare transactions, which themselves are not subject to any minimum or other similar volume requirements under customer contracts. In addition, some contracts with customers generally can be terminated or not renewed without penalty and on little or no advance notice. As a result, this “recurring” revenue is highly dependent on us maintaining our customer base as well as on the transaction volume generally in the U.S. healthcare industry since such revenue directly correlates with healthcare transaction, payment and reimbursement volumes in the U.S. For example, in the U.S. our revenue can be adversely affected by the impact of lower healthcare utilization trends currently being driven by COVID-19 and likely to continue to be driven by higher unemployment and other negative economic factors. Further, weakened economic conditions or a recession could reduce the amounts patients are willing or able to spend on healthcare services. As a result, patients may elect to delay or forgo seeking healthcare services and recent increases in unemployment rates are likely to cause commercial payer membership to decline, which could further reduce healthcare utilization and transaction volumes. In addition, such events could decrease payer or provider demand for our solutions, which could further adversely impact revenue, including “recurring” revenue.
Various factors may cause continued temporary or sustained disruption to U.S. healthcare transaction volumes. The impact such disruptions would have on our business will depend upon the magnitude and duration of any such disruption. These factors include, among others:
| • | the financial stability of customers and the U.S. healthcare industry generally, and the impact of any fundamental corporate changes to healthcare providers and payers, such as hospital and insurance consolidations, on the cost and availability of, and the rate of reimbursement for, healthcare services, including due to the aftermath of COVID-19; |
| • | political, legislative, regulatory and other changes in how healthcare services are covered, delivered and reimbursed, including any future changes to the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (collectively, the “ACA”), Medicare, Medicaid and other federal, state and local healthcare regulations, as well as any future changes due to the COVID-19 pandemic; |
| • | factors that may affect demand for healthcare services, such as high unemployment, rising healthcare costs and increased copayment requirements; and |
| • | general economic conditions. |
34
Table of Contents
Any temporary or sustained decrease in healthcare transaction, payment or reimbursement volumes in the U.S. could have a material adverse impact on our business, results of operations or financial condition.
Our ability to generate revenue could suffer if we do not continue to update and improve existing solutions and develop new ones.
We must continually improve the functionality of our existing solutions in a timely manner and introduce new and valuable healthcare IT and service solutions in order to respond to technological and regulatory developments and customer demands and, thereby, retain existing customers and attract new ones. For example, from time to time, government agencies may alter format and data code requirements applicable to electronic transactions. In addition, customers may request that solutions be customized to satisfy particular security protocols, modifications and other contractual terms in excess of industry norms and standard configurations. We may not be successful in responding to technological and regulatory developments or changing customer needs. In addition, these regulatory or customer-imposed requirements may impact the profitability of particular solutions and customer engagements. The pace of change in the markets served by us is rapid, and there are frequent new product and service introductions by competitors and channel partners who use our solutions in their offerings. If we do not respond successfully to technological and regulatory changes, as well as evolving industry standards and customer demands, our solutions may become obsolete. Technological changes also may result in the offering of competitive solutions at lower prices than we are charging for our solutions, which could result in us losing sales unless we lower the prices we charge or provide additional efficiencies or capabilities to the customer. If we lower our prices on some of our solutions, we will need to increase margins on other solutions in order to maintain overall profitability.
Achieving market acceptance of new or updated solutions is necessary in order for them to become profitable and will likely require significant efforts and expenditures.
Our future financial results will depend in part on whether new or updated solutions receive sufficient customer acceptance. Achieving market acceptance for new or updated solutions is likely to require substantial marketing efforts and expenditure of significant funds to create awareness and demand by existing or prospective customers. In addition, deployment of new or updated solutions may require the use of additional resources for training existing sales force and customer service personnel and for hiring and training additional salespersons and customer service personnel. Failure to achieve broad penetration in target markets with respect to new or updated solutions could have a material adverse impact on our business, results of operations or financial condition.
Our business would be adversely affected if we cannot obtain, process or distribute the highly regulated data we require to provide our solutions.
Our business relies on our ability to obtain, process, monetize and distribute highly regulated data in the healthcare industry and in other industries, in a manner that complies with applicable laws, regulations and contractual and technological restrictions. The failure of either us or our data suppliers and processors to obtain such data in a compliant manner could have a harmful effect on our ability to use and disclose such data which in turn could impair our functions and operations, including our ability to share such data with third parties or incorporate it into our services and offerings. In addition to complying with requirements in obtaining the data, the use, processing and distribution of such data may require us or our data suppliers and processors to obtain consent from third parties or follow additional laws, regulations or contractual and technological restrictions that apply to the healthcare industry and other industries. These requirements could interfere with or prevent creation or use of rules and analyses or limit other data-driven activities that benefit us. Moreover, we may be subject to claims or liability for use or disclosure of information by reason of lack of valid notice, permission or waiver. We have policies and procedures in place addressing the proper handling and use of data, but could face claims that our data practices may occur in a manner not permitted under applicable laws or our agreements with or obligations to data providers, individuals or other third parties, as more specifically described below. These
35
Table of Contents
claims or liabilities and other failures to comply with applicable requirements could subject us to unexpected costs and adversely affect our operating results.
There are increased risks of performance problems and breaches during times when we are making significant changes to our solutions or systems we use to provide our solutions. In addition, changes to our solutions or systems, including cost savings initiatives, may cost more than anticipated, may not provide the benefits expected, may take longer than anticipated to develop and implement or may increase the risk of performance problems.
In order to respond to technological changes, such as continuing development in the areas of data analytics, ML, AI and blockchain, among others, as well as regulatory changes and evolving security risks and industry standards, our solutions and the software and systems we use to provide our solutions must be continually updated and enhanced. Because some of the software and systems that we use to provide solutions to customers are inherently complex, changing, updating, enhancing or creating new versions of our solutions or the software or systems we use to provide our solutions introduces a risk of errors or performance problems, despite testing and quality control. We cannot be certain that errors will not arise in connection with any such changes, updates, enhancements or new versions, especially when first introduced. Even if our new, updated or enhanced solutions do not have performance problems, technical and customer service personnel may have difficulties installing them or providing any necessary training and support to customers, and customers may not follow our guidance on appropriate training, support and implementation for such new, updated or enhanced solutions. In addition, changes in technology and systems may not provide the additional functionality or other benefits that were expected.
Implementation of changes in our technology and systems may cost more or take longer than originally expected and may require more testing than initially anticipated. While new, updated or enhanced solutions will be tested before they are used in production, we cannot be sure that the testing will uncover all problems that may occur in actual use.
We also periodically implement efficiency measures and other cost-saving initiatives to improve our operating performance. These efficiency measures and other cost-saving initiatives may not provide the benefits anticipated or do so in the expected time frame. Implementation of these measures may also increase the risk of performance issues due to unforeseen impacts on our organization, systems and processes.
If significant problems occur as a result of these changes, we may fail to meet our contractual obligations to customers, which could result in claims being made against us or in the loss of customer relationships.
Breaches and failures of our IT systems and the security measures protecting them, and the sensitive information we transmit, use and store, expose us to potential liability and reputational harm.
Our business relies on sophisticated information systems to obtain, rapidly process, analyze, and manage data, affecting our ability to manufacture, purchase, distribute, and process products and services. To the extent our IT systems are not successfully implemented or fail, our business and results of operations may be adversely affected. Our business and results of operations may also be adversely affected if a vendor servicing our IT systems does not perform satisfactorily, or if the IT systems are interrupted or damaged by unforeseen events, including the actions of third parties. Further, our business relies to a significant degree upon the secure transmission, use and storage of sensitive information, including protected health information and other personally identifiable information, financial information and other confidential information and data within these systems.
To protect this information, we seek to implement commercially reasonable security measures and maintain information security policies and procedures informed by requirements under applicable law and recommended practices, in each case, as applicable to the data collected, hosted and processed. Despite our security
36
Table of Contents
management efforts with respect to physical and technological infrastructure, employee training, vendor (and sub-vendor) controls and contractual relationships, our infrastructure, data or other operation centers and systems used in connection with our business operations, including the internet and related systems of our vendors (including vendors to which we outsource data hosting, storage and processing functions) are vulnerable to, and from time to time experience, unauthorized access to data and/or breaches of confidential information due to criminal conduct, physical break-ins, hackers, employee or insider malfeasance and/or improper employee or contractor access, computer viruses, programming errors, denial-of-service attacks, ransomware events, phishing schemes, fraud, terrorist attacks, human error or other breaches by insiders or third parties or similar disruptive problems. It is not possible to prevent all security threats to our systems and data. Techniques used to obtain unauthorized access, disable or degrade service or sabotage systems change frequently and may be difficult to detect for long periods of time. Further, defects in the design or manufacture of the hardware, software or applications we develop or procure from third parties could compromise our IT systems. These events, including unauthorized access, misappropriation, disclosure or loss of sensitive information (including financial or personal health information) or a significant disruption of our network, expose us to risks including risks to our ability to provide our solutions and fulfill contractual demands, management distraction and the obligation to devote significant financial and other resources to mitigate such problems and increases to our future information security costs, including through organizational changes, deploying additional personnel and protection technologies, further training of employees, changing vendor (and sub-vendor) control practices, and engaging third-party experts and consultants. Moreover, unauthorized access, use or disclosure of certain sensitive information in our possession or our failure to satisfy legal requirements, including requirements relating to safeguarding protected health information under the Health Insurance Portability and Accountability Act (“HIPAA”) and personal information under the European Union (“EU”)’s General Data Protection Regulations (“GDPR”) or state data privacy laws, as discussed further below, could result in civil and criminal liability and regulatory action, which could result in potential fines and penalties, as well as costs relating to investigation of an incident or breach, corrective actions, required notifications to regulatory agencies and customers, credit monitoring services and other necessary expenses. In addition, actual or perceived breaches of our security management efforts can cause existing customers to terminate their relationship with us and deter existing or prospective customers from using or purchasing our solutions in the future. These events can have a material adverse impact on our business, results of operations, financial condition and reputation.
Because our products and services involve the storage, use and transmission of personal information of consumers, we and other industry participants have been and expect to routinely be the target of attempted cyber and other security threats by outside third parties, including technically sophisticated and well-resourced bad actors attempting to access or steal the data we store. Vendor, insider or employee cyber and security threats also occur and are a significant concern for all companies, including us. Recently, there have been a number of high profile security breaches involving the improper dissemination of personal information of individuals both within and outside of the healthcare industry. These breaches have resulted in lawsuits and governmental enforcement actions that have sought or obtained significant fines and penalties, and have required companies to enter into agreements with government regulators that impose ongoing obligations and requirements, including internal and external (third party) monitorships for five years or more. While we maintain liability insurance coverage including coverage for errors and omissions and cyber-liability, claims may not be covered or could exceed the amount of our applicable insurance coverage, if any, or such coverage may not continue to be available on acceptable terms or in sufficient amounts.
If we are unable to successfully expand our sales force productivity, and execute on cross-selling opportunities, sales of our solutions and the growth of our business and financial performance could be harmed.
We continue to invest significantly in our sales force to obtain new customers and increase sales to existing customers. Our ability to achieve revenue growth will depend, in large part, on our success in recruiting, training and retaining sufficient numbers of qualified sales personnel to support our sales efforts. A portion of current sales personnel are new to us, and new hires require significant training and may require a lengthy onboarding
37
Table of Contents
process before they achieve full productivity. Recent hires and planned hires may not become productive as quickly as expected. If we are unable to recruit, train and retain a sufficient number of productive sales personnel, sales of our solutions and the growth of our business could be harmed. Additionally, if efforts to improve sales force productivity do not result in increased revenue, operating results could be negatively impacted due to increased operating expenses associated with these efforts.
In addition, our ability to generate growth partly depends on our ability to cross-sell solutions to existing customers and new customers. We have identified our ability to successfully cross-sell our solutions as a key part of our business strategy and therefore one of the most significant factors influencing growth. We may not be successful in cross-selling our solutions because customers may find additional solutions unnecessary, unattractive or cost-ineffective. Failure to sell additional solutions to existing and new customers could negatively affect our ability to grow our business.
Poor service, system errors or failures of our solutions to conform to specifications could cause unforeseen liabilities or injury, harm our reputation and have a material adverse impact on our business, results of operations or financial condition.
We must meet our customers’ service level expectations and our contractual obligations with respect to our solutions. Failure to do so could subject us to liability or cause us to lose customers. In some cases, we rely upon third-party contractors (which, along with suppliers and other third-party vendors, are referred to as “vendors”) to assist us in providing our solutions. Our ability to meet our contractual obligations and customer expectations thus may be impacted by the performance of our vendors and their ability to comply with applicable laws and regulations. For example, our electronic payment and remittance solutions depend in part on the ability of our vendors to comply with applicable banking, financial service and payment card industry requirements and their failure to do so could cause an interruption in the solutions we provide or require us to seek alternative solutions or relationships. We likely will incur increased development costs to upgrade our software to be in compliance with changing and evolving standards, and delays may result in connection therewith. If our solutions are not in compliance with these evolving standards, our market position and sales could be adversely affected and we may have to invest significantly in changes and updates to our solutions, which could materially and adversely impact our financial condition and operating results.
Some of our solutions are intended to provide information to healthcare professionals in the course of delivering patient care. Although our contracts disclaim liability for medical decisions and responsibility for patient care, if use of or inability to use our solutions leads to faulty clinical decisions or injury to patients, such disclaimers may be unenforceable and we could be subject to claims or litigation, including product liability and warranty claims, by healthcare professionals, their patients or customers. Product liability and warranty claims often involve very large or indeterminate amounts, including punitive damages. The magnitude of potential losses from product liability lawsuits may remain unknown for substantial periods of time, and the related legal defense costs may be significant. We could experience material warranty or product liability losses in the future and incur significant costs to defend these claims. In addition, if any of our products or services are, or are alleged to be, defective, we may voluntarily participate, or be required by regulatory authorities to participate, in a recall of that product or service. In the event of a recall, we may lose sales and be exposed to individual or class-action litigation claims. Further, negative publicity regarding a quality or safety issue, whether accurate or inaccurate, could harm our reputation, decrease demand for our solutions, lead to withdrawals of our solutions or impair our ability to successfully launch and market our solutions in the future. Product liability, warranty and recall costs may have a material adverse effect on our business, financial condition, results of operations and cash flows.
Some of the software and systems that we use to provide our solutions are inherently complex. Errors or downtime in the software and systems we use to provide our solutions could negatively impact our customers. For example, because of the large amount of data we collect and manage, it is possible that hardware failures and errors in our systems could result in data loss or corruption or cause the information that we collect to be
38
Table of Contents
incomplete or contain inaccuracies that our customers could regard as significant. In addition, errors in our transaction processing systems could result in payers paying the wrong amount, payers making payments to the wrong payee or delayed payments. Although we seek to address any errors or downtime with updates to the software and systems, if we are unable to promptly remedy any errors or our customers do not implement system updates, the software and systems could be compromised or our customers could experience prolonged downtimes relating to the software and systems. If problems occur or persist, our customers may seek compensation from us, seek to terminate their contracts, withhold payments, seek refunds from us of part or all of the fees charged under our contracts, ask us to reconstruct lost or corrupted data at our expense, request a loan or advancement of funds or initiate litigation or other dispute resolution procedures. We also may be subject to claims by others affected by any such problems. Further, some of our existing and prospective customers may be reluctant or unwilling to use cloud-based services, because they have concerns regarding the risks associated with the security and reliability of the technology delivery model associated with these services. If our existing or prospective customers do not perceive the benefits of our services, then the market for these solutions may not expand as much or develop as quickly as we expect, either of which would adversely affect our business, financial condition, or operating results.
We attempt to limit, by contract, our liability for damages arising from our negligence, errors, mistakes or security breaches. However, contractual limitations on liability may not be accepted by our customers, may not be enforceable or may otherwise not provide sufficient protection to us from liability for damages. We maintain liability insurance coverage, including coverage for errors and omissions and cyber-liability. It is possible, however, that claims could be denied or exceed the amount of our applicable insurance coverage, if any, or that this coverage may not continue to be available on acceptable terms or in sufficient amounts. Even if these claims do not result in liability to us, investigating and defending against them could be expensive and time consuming and could divert management’s attention away from our operations. In addition, negative publicity caused by these events may negatively impact our customer relationships, market acceptance of our solutions, including unrelated solutions, or may harm our reputation and business.
Disruptions in service or damages to our data or other operation centers, or other software or systems failures, could have a material adverse impact on our business, results of operations or financial condition.
Our data and network operations centers are essential to our business. our business operations depend on our ability to maintain and protect our network and computer systems, many of which are located in our primary data and operations centers that we own and operate and some of which are outsourced to certain third-party hosting providers. We have consolidated several satellite data centers and plans to continue such consolidation. We also provide remote and cloud hosting services that involve operating both our software and the software of vendors for our customers. The ability to access the systems, applications, and data that we host and support on demand is important to our customers.
Our operations and facilities are vulnerable to interruption and/or damage from a number of sources, many of which are beyond our control, including, without limitation: (1) power loss and telecommunications failures; (2) fire, flood, hurricane, tornado and other natural disasters; (3) software and hardware errors, failures or crashes; and (4) cyber and ransomware attacks, computer viruses, hacking, break-ins, sabotage, intentional acts of vandalism and other similar disruptive problems. The occurrence of any of these events could result in interruptions, delays or cessations in service to users of our solutions, which could impair or prohibit our ability to provide our solutions, reduce the attractiveness of our solutions to our customers and could have a material adverse impact on our business, results of operations or financial condition. If customers’ access to our solutions is interrupted because of problems in our operations or our facilities, we could be in breach of our agreements with customers and/or exposed to significant claims, particularly if the access interruption is associated with problems in the timely delivery of medical care.
We attempt to mitigate these risks through various means including disaster recovery and business continuity plans, penetration testing, vulnerability scans, patching and other information security procedures and
39
Table of Contents
cybersecurity and ransomware measures, insurance against fires, floods, other natural disasters, cyber-liability and general business interruptions, and customer and employee training and awareness, but our precautions cannot protect against all risks. Any significant instances of system downtime could negatively affect our reputation and ability to provide our solutions or remote hosting services, which could have a material adverse impact on our business, results of operations or financial condition.
We also rely on a number of vendors, such as cloud service providers, to provide us with a variety of solutions and services, including cloud-based data hosting, telecommunications and data processing services necessary for our transaction services and processing functions and software developers for the development and maintenance of certain software products we use to provide our solutions. As a result, our disaster recovery and business continuity plans may rely, in part, upon vendors of related services. If these vendors do not fulfill their contractual obligations, have system failures or choose to discontinue their products or services, our business and operations could be disrupted, our brand and reputation could be harmed and our financial condition or operating results could be adversely affected.
We rely on internet infrastructure, bandwidth providers, data center providers, other third parties and our own systems in providing certain of our solutions to our customers, and any failure or interruption in the services provided by these third parties or our own systems could expose us to litigation and negatively impact our relationships with customers, adversely affecting our brand and our business.
Our ability to deliver our solutions is dependent on the development and maintenance of the infrastructure of the Internet and other telecommunications services by third parties. This includes maintenance of a reliable network connection with the necessary speed, data capacity and security for providing reliable Internet access and services and reliable telephone and facsimile services. As a result, our information systems require an ongoing commitment of significant resources to maintain and enhance existing systems and develop new systems in order to keep pace with continuing changes in information technology, emerging cybersecurity risks and threats, evolving industry and regulatory standards and changing preferences of our customers.
Our solutions are designed to operate without interruption in accordance with our service level commitments. However, we have experienced limited interruptions in these systems in the past, including server failures that temporarily slow down the performance of our solutions, and we may experience more significant interruptions in the future. We rely on internal systems as well as vendors, including bandwidth and telecommunications equipment providers, to provide our solutions. We do not maintain redundant systems or facilities for some of these services. Interruptions in these systems, whether due to system failures, computer viruses, physical or electronic break-ins or other catastrophic events, could affect the security or availability of our solutions and prevent or inhibit the ability of our customers to access our solutions.
If a catastrophic event were to occur with respect to one or more of these systems or facilities, we may experience an extended period of system unavailability, which could result in substantial costs to remedy those problems or negatively impact our relationship with our partners, our business, results of operations and financial condition. To operate without interruption, both us and our vendors must guard against:
| • | damage from fire, power loss, tornado and other natural disasters; |
| • | telecommunications failures; |
| • | software and hardware errors, failures and crashes; |
| • | security breaches, computer viruses and similar disruptive problems; and |
| • | other potential interruptions. |
Any disruption in the network access, telecommunications or co-location services provided by vendors, or any failure of or by vendors’ systems or our own systems to handle current or higher volume of use could
40
Table of Contents
significantly harm our business. We exercise limited control over these vendors, which increases our vulnerability to problems with services they provide. Any errors, failures, interruptions or delays experienced in connection with these vendor technologies and information services or our own systems could negatively impact our relationships with partners and adversely affect our business and could expose us to liabilities. Although we maintain insurance for our business, the coverage under our policies may not be adequate to compensate us for all losses that may occur. In addition, we cannot provide assurance that we will continue to be able to obtain adequate insurance coverage at an acceptable cost.
The reliability and performance of our internet connection may be harmed by increased usage or by denial-of-service attacks. The internet has experienced a variety of outages and other delays as a result of damage to portions of our infrastructure, and it could face outages and delays in the future. These outages and delays could reduce the level of Internet usage as well as the availability of the internet to us for delivery of our internet-based solutions.
As a result of the complexity of the issues facing healthcare providers and payers and the inherent complexity of our solutions to such issues, our customers depend on our support organization to resolve any technical issues relating to our offerings. In addition, our sales process is highly dependent on the quality of our offerings, on our business reputation and on strong recommendations from our existing customers. Any failure to maintain high-quality and highly responsive technical support, or a market perception that we do not maintain high-quality and highly responsive support, could harm our reputation, adversely affect our ability to sell our offering to existing and prospective customers, and harm our business, operating results and financial condition.
We offer technical support services with our offerings, and we may be unable to respond quickly enough to accommodate short-term increases in customer demand for support services, particularly as we increase the size of our customer base. We also may be unable to modify the format of our support services to compete with changes in support services provided by our competitors. It is difficult to predict customer demand for technical support services and, if customer demand increases significantly, we may be unable to provide satisfactory support services to our customers and their constituents. Additionally, increased customer demand for these services, without corresponding revenue, could increase costs and adversely affect our operating results.
The market price of shares of our Common Stock has been and is likely to continue to be volatile, which could cause the value of your investment to decline.
The market price of our Common Stock has been and is likely to continue to be highly volatile and subject to wide fluctuations. Securities markets worldwide experience significant price and volume fluctuations and have become especially volatile due to the COVID-19 pandemic. This market volatility, as well as general economic, market or political conditions, could reduce the market price of shares of our Common Stock regardless of our operating performance. We expect a high level of volatility to continue as the effects of COVID-19 continue to impact the economy, healthcare industry and our business. In addition, our operating results could be below the expectations of public market analysts and investors due to a number of potential factors, including variations in our quarterly operating results or dividends, if any, to stockholders, the impact of COVID-19 on our business, additions or departures of key management personnel, failure to meet analysts’ earnings estimates, publication of research reports about our industry, litigation and government investigations, changes or proposed changes in laws or regulations or differing interpretations or enforcement thereof affecting our business, adverse market reaction to any indebtedness we may incur or securities we may issue in the future, changes in market valuations of similar companies or speculation in the press or investment community, announcements by competitors of significant contracts, acquisitions, dispositions, strategic partnerships, joint ventures or capital commitments, adverse publicity about the industries we participate in or individual scandals, and in response the market price of shares of our Common Stock could decrease significantly. Stock markets and the price of shares of our Common Stock may experience extreme price and volume fluctuations. In the past, following periods of volatility in the overall market and the market price of a company’s securities, securities class action litigation has often been instituted against these companies. This litigation, if instituted against us, could result in substantial costs and a diversion of our management’s attention and resources.
41
Table of Contents
Our business will suffer if we fail to successfully integrate acquired businesses and technologies or to appropriately assess the risks in particular transactions.
We have historically acquired, and in the future may acquire, businesses, technologies, services, product lines and other assets. For example, on May 1, 2020, we closed on the acquisition of eRx Network and are currently in the process of integrating its business, assets and personnel. The successful integration of any businesses and assets we have acquired or may acquire can be critical to our future performance. The amount and timing of the expected benefits of any acquisition, including potential synergies, are subject to risks and uncertainties. These risks and uncertainties include, but are not limited to, those relating to:
| • | our ability to maintain relationships with the customers and suppliers of the acquired business; |
| • | our ability to cross-sell solutions to customers with which we have established relationships and those with which the acquired businesses have established relationships; |
| • | our ability to retain or replace key personnel of the acquired business; |
| • | potential conflicts in payer, provider, vendor or marketing relationships; |
| • | our ability to coordinate organizations that are geographically diverse and may have different business cultures; |
| • | the diversion of management’s attention to the integration of the operations of businesses or other assets we have acquired; |
| • | the continued coordination and cooperation with sellers pursuant to transition services agreements; |
| • | difficulties in the integration or migration of IT systems, including secure data sharing across networks securely and maintaining the security of the IT systems; and |
| • | compliance with regulatory, contracting and other requirements, including internal control over contracting and financial reporting. |
We cannot guarantee that any acquired businesses, technologies, services, product lines or other assets will be successfully integrated with our operations in a timely or cost-effective manner, or at all. Failure to successfully integrate acquired businesses or to achieve anticipated operating synergies, revenue enhancements or cost savings could have a material adverse impact on our business, results of operations or financial condition.
Although our management attempts to evaluate the risks inherent in each transaction and to evaluate acquisition candidates appropriately, we may not properly ascertain all such risks and the acquired businesses or other assets may not perform as we expect or enhance our value as a whole. Acquired companies or businesses also may have larger than expected liabilities that are not covered by the indemnification, if any, that we are able to obtain from the sellers. Furthermore, the historical financial statements of the companies we have acquired or may acquire in the future are prepared by management of such companies and are not independently verified by our management. In addition, any pro forma financial statements prepared by us to give effect to such acquisitions may not accurately reflect the results of operations of such companies that would have been achieved had the acquisition of such entities been completed at the beginning of the applicable periods. There are also no assurances that we will continue to acquire businesses at valuations consistent with our prior acquisitions or that we will complete acquisitions at all. If we are unable to successfully complete and integrate strategic acquisitions in a timely manner, our business and growth strategies could be negatively affected.
We may not realize the anticipated benefits of divestitures.
From time to time we may divest assets or businesses. We may encounter difficulty in finding or completing divestiture opportunities or alternative exit strategies on acceptable terms or in a timely manner. These circumstances could delay the achievement of our strategic objectives or cause us to incur additional expenses with respect to assets or a business that we want to dispose of, or we may dispose of assets or a business at a
42
Table of Contents
price or on terms that are less favorable than we anticipated. Additionally, such dispositions could result in disruption to other parts of our business, potential loss of employees or customers, exposure to unanticipated liabilities or result in ongoing obligations and liabilities to us following any such divestiture. For example, in connection with a disposition, we may be contractually obligated with respect to certain continuing obligations to customers, vendors, or other third parties, and we may also have continuing indemnities and obligations for pre-existing liabilities related to the assets or businesses. Such obligations could have a material adverse impact on our business, results of operations or financial condition.
Recent and future developments in the healthcare industry could have a material adverse impact on our business, results of operations or financial condition.
Almost all of our revenue is derived from the healthcare industry, which is highly regulated and subject to changing political, legislative, regulatory and other influences. For example, the ACA changes how healthcare services are covered, delivered and reimbursed. The ACA mandates that substantially all U.S. citizens maintain health insurance coverage, expands health insurance coverage through a combination of public program expansion and private sector reforms, reduces Medicare program spending and promotes value-based purchasing. However, efforts by the current presidential administration and certain members of Congress to repeal or make significant changes to the ACA, our implementation and/or our interpretation have cast uncertainty onto the future of the law. For example, in December 2017, tax reform legislation was enacted that, effective January 2019, eliminates the financial penalty for individuals who fail to maintain health insurance coverage, a change that may result in fewer individuals electing to purchase health insurance. Further, the Centers for Medicare & Medicaid Services (“CMS”) has indicated that it intends to increase flexibility in state Medicaid programs, including by expanding the scope of waivers under which states may implement Medicaid expansion provisions, imposing different eligibility or enrollment restrictions, or otherwise implementing programs that vary from federal standards. At the same time, members of Congress have proposed measures that would expand the role of government-sponsored coverage, including single payer or so-called “Medicare-for-All” proposals, which could have far-reaching implications for the healthcare industry if enacted. Furthermore, in light of the COVID-19 pandemic, additional changes to the ACA may be proposed and calls for an expanded government healthcare coverage could accelerate.
We are unable to predict the full impact of the ACA and other health reform initiatives on our operations in light of the uncertainty regarding whether, when and how the ACA will be further changed, what alternative reforms (including single payer proposals), if any, may be enacted, the timing of enactment and implementation of alternative provisions and the impact of alternative provisions on various healthcare industry participants. In particular, because many of our solutions designed to assist customers in effectively navigating the shift to value-based healthcare, the elimination of, or significant revisions to, various value-based healthcare initiatives may adversely impact our business.
While many of the provisions of the ACA and other health reform initiatives may not be directly applicable to us, such initiatives affect the businesses of our customers and the Medicaid programs of the states with which we have contracts. For example, as a result of Medicare payment reductions and other reimbursement changes mandated under the ACA, our customers may attempt to seek price concessions from us or reduce their use of our solutions, especially if provisions expanding coverage are repealed without eliminating the payment reductions or other reimbursement changes. Thus, the ACA may result in a reduction of expenditures by customers or potential customers in the healthcare industry, which could have a material adverse impact on our business, results of operations or financial condition. In addition, certain government programs, such as the Bundled Payments for Care Improvement initiative and the Accountable Care Organization Shared Savings Program, may impact reimbursement to our customers, which could have a material adverse impact on our business, results of operations or financial condition. Further, the general uncertainty of healthcare reform efforts, particularly if Congress repeals provisions of the ACA but delays the implementation date of repeal or fails to enact replacement provisions at the time of repeal, may negatively impact purchase decisions or demand for our solutions.
43
Table of Contents
Moreover, there are currently numerous federal, state and private initiatives seeking to increase the use of IT in healthcare as a means of improving care and reducing costs. For example, the Health Information Technology for Economic and Clinical Health (“HITECH”) Act, which was enacted in 2009, and the 21st Century Cures Act (the “Cures Act”), which was enacted in 2016, contain incentives and penalties to promote the use of Electronic Health Records (“EHR”) technology and the efficient exchange of health information electronically. Further, the Cures Act provides for penalties to be imposed on IT developers, health information exchanges or networks and health providers that are found to improperly block the exchange of health information. These and other initiatives may result in additional or costly legal or regulatory requirements that are applicable to us and our customers, may encourage more companies to enter our markets, may provide advantages to our competitors and may result in the development of technology solutions that compete with us. Any such initiatives also may result in a reduction of expenditures by existing or potential customers, which could have a material adverse impact on our business, results of operations or financial condition.
In addition, other general reductions in expenditures by healthcare industry constituents could result from, among other things, government regulation or private initiatives that affect the manner in which providers interact with patients, payers or other healthcare industry constituents, including changes in pricing or means of delivery of healthcare solutions. In addition, cost containment efforts at the federal and state levels may affect industry expenditures. For example, the Budget Control Act of 2011 requires automatic spending reductions to reduce the federal deficit. CMS began imposing a 2% reduction on payments of Medicare claims in 2013. These reductions have been extended through 2029.
Even if general expenditures by healthcare industry constituents remain the same or increase, other developments in the healthcare industry may result in reduced spending on healthcare IT and services or in some or all of the specific markets we serve or are planning to serve. In addition, our customers’ expectations regarding pending or potential healthcare industry developments also may affect their budgeting processes and spending plans with respect to the types of solutions we provide. For example, use of our solutions could be affected by:
| • | changes in the billing patterns of providers; |
| • | changes in the design of health insurance plans; |
| • | changes in the contracting methods payers use in their relationships with providers; |
| • | decreases in marketing expenditures by pharmaceutical companies or medical device manufacturers, as a result of governmental regulation or private initiatives that discourage or prohibit promotional activities by pharmaceutical or medical device companies or other factors; and |
| • | implementation of government programs that streamline and standardize eligibility enrollment processes, which could result in decreased pricing or demand for our eligibility and enrollment solutions. |
The healthcare industry has changed significantly in recent years, and we expect that significant changes will continue to occur. The timing and impact of developments in the healthcare industry are difficult to predict. We cannot be sure that the markets for our solutions will continue to exist at their current levels, will not change in ways that adversely affect us or that we will have adequate technical, financial and marketing resources to react to changes in those markets.
Government regulation, industry standards and other requirements create risks and challenges with respect to our compliance efforts and our business strategies.
The healthcare industry is highly regulated and subject to frequently changing laws, regulations, industry standards and other requirements. Many healthcare laws and regulations are complex, and their application to specific solutions, services and relationships may not be clear. Because our customers are subject to various requirements, we may be impacted as a result of our contractual obligations even when we are not directly
44
Table of Contents
subject to such requirements. In particular, many existing healthcare laws and regulations, when enacted, did not anticipate the healthcare IT solutions and services that we provide, and these laws and regulations may be applied to our solutions in ways that we do not anticipate. The ACA, efforts to repeal or materially change the ACA, and other federal and state efforts to reform or revise aspects of the healthcare industry or to revise or create additional legal or regulatory requirements could impact our operations, the use of our solutions and our ability to market new solutions, or could create unexpected liabilities for us.
We also may be impacted by non-healthcare laws, industry standards and other requirements. For example, laws, regulations and industry standards regulating the banking and financial services industry may impact our operations as a result of the payment and remittance services we offer directly or through vendors. Additionally, laws and regulations governing how we communicate with our customers and our customers’ patients may impact our operations and, if not followed, would result in fines, penalties and other liabilities and adverse publicity and injury to our reputation.
We are unable to predict what changes to laws, regulations and other requirements, including related contractual obligations, might be made in the future or how those changes could affect our business or the costs of compliance.
We have attempted to structure our operations to comply with laws, regulations and other requirements applicable to us directly and to our customers and contractors, but there can be no assurance that our operations will not be challenged or impacted by enforcement initiatives. We have been, and in the future may become, involved in governmental investigations, audits, reviews and assessments. Certain of our businesses have been reviewed or are currently under review, including for compliance with various legal, regulatory or other requirements. Any determination by a court or agency that our solutions violate, or cause our customers to violate, applicable laws, regulations or other requirements could subject us or our customers to civil or criminal penalties. Such a determination also could require us to modify or terminate portions of our business, disqualify us from serving customers that do business with government entities or cause us to refund some or all of our service fees or otherwise compensate our customers. In addition, failure to satisfy laws, regulations or other requirements could adversely affect demand for our solutions and could force us to expend significant capital, research and development and other resources to address the failure. Even an unsuccessful challenge by regulatory and other authorities or private whistleblowers could be expensive and time-consuming, could result in loss of business, exposure to adverse publicity and injury to our reputation and could adversely affect our ability to retain and attract customers. Laws, regulations and other requirements impacting our operations include the following:
HIPAA. If we are unable to properly protect the privacy and security of protected health information entrusted to it, we could be found to have breached our contracts with our customers and be subject to investigation by the U.S. Department of Health and Human Services (“HHS”) Office for Civil Rights (“OCR”). In the event OCR finds that we have failed to comply with applicable HIPAA privacy and security standards, we could face civil and criminal penalties. In addition, OCR performs compliance audits of Covered Entities and Business Associates in order to proactively enforce the HIPAA privacy and security standards. OCR has become an increasingly active regulator and has signaled its intention to continue this trend. OCR has the discretion to impose penalties without being required to attempt to resolve violations through informal means; further OCR may require companies to enter into resolution agreements and corrective action plans which impose ongoing compliance requirements. OCR enforcement activity can result in financial liability and reputational harm, and responses to such enforcement activity can consume significant internal resources. In addition to enforcement by OCR, state attorneys general are authorized to bring civil actions under either HIPAA or relevant state laws seeking either injunctions or damages in response to violations that threaten the privacy of state residents. Although we have implemented and maintained policies, processes and a compliance program infrastructure (e.g., a Privacy Office) to assist us in complying with these laws and regulations and our contractual obligations, we cannot provide assurance regarding how these laws and regulations will be interpreted, enforced or applied to our operations. In addition to the risks associated with enforcement activities and potential contractual liabilities,
45
Table of Contents
our ongoing efforts to comply with evolving laws and regulations at the federal and state levels also might require us to make costly system purchases and/or modifications or otherwise divert significant resources to HIPAA compliance initiatives from time to time.
HIPAA and our implementing regulations mandate format and data content standards and provider identifier standards (known as the National Provider Identifier) that must be used in certain electronic transactions, such as claims, payment advice and eligibility inquiries. HHS has established standards that health plans must use for electronic fund transfers with providers, has established operating rules for certain transactions, and is in the process of establishing operating rules to promote uniformity in the implementation of the remaining types of covered transactions. The ACA also requires HHS to establish standards for health claims attachment transactions. HHS has modified the standards for electronic healthcare transactions (e.g., eligibility, claims submission and payment and electronic remittance) from Version 4010/4010A to Version 5010. Further, as of 2015, HHS requires the use of updated standard code sets for diagnoses and procedures known as the ICD-10 code sets. Enforcement of compliance with these standards falls under HHS and is carried out by CMS.
In the event new requirements are imposed, we will be required to modify our systems and processes to accommodate these changes. We will seek to modify our systems and processes as needed to prepare for and implement changes to the transaction standards, code sets operating rules and identifier requirements; however, we may not be successful in responding to these changes, and any responsive changes we make to our systems and processes may result in errors or otherwise negatively impact our service levels. In addition, the compliance dates for new or modified transaction standards, operating rules and identifiers may overlap, which may further burden our resources.
We also may experience complications related to supporting customers that are not fully compliant with the revised requirements as of the applicable compliance or enforcement date. Some payers and healthcare clearinghouses with which we conduct business interpret HIPAA transaction requirements differently than we do or may require us to use legacy formats or include legacy identifiers as they transition to full compliance with the revised requirements. For example, we continue to process transactions using legacy identifiers for non-Medicare claims that are sent to us to the extent that the intended recipients have not instructed us to suppress those legacy identifiers. Where payers or healthcare clearinghouses require conformity with their interpretations or require us to accommodate legacy transactions or identifiers as a condition of successful transactions, we seek to comply with their requirements. We continue to work with payers, providers, practice management system vendors and other healthcare industry constituents to implement the transaction standards and identifier standards. However, we cannot provide assurances regarding how CMS will enforce the transaction and identifier standards or how CMS will view our practice of accommodating requests to process transactions that include legacy formats or identifiers for non-Medicare claims. It is possible that us, or our customers, could be subject to enforcement actions as a result of these accommodations. Any regulatory change, clarification or enforcement action by CMS that prohibited the processing by healthcare clearinghouses or private payers of transactions containing legacy formats or identifiers could have a material adverse impact on our business, results of operations or financial condition.
Other Privacy and Security Requirements. There also are numerous U.S. federal, state and international privacy and security laws that govern the collection, dissemination, use, access, retention, protection, transfer and confidentiality of personal information. For example, GDPR, which became effective on May 25, 2018, is more stringent than laws and regulations governing personal information in the U.S. Certain of our solutions involve the transmission and storage of customer data in various jurisdictions, which subjects the operation of that service to privacy or data protection laws and regulations in those jurisdictions. While we believe these solutions comply with current regulatory and security requirements in the jurisdictions in which we provide these solutions, there can be no assurance that such requirements will not change or that we will not otherwise be subject to legal or regulatory actions. These laws and regulations are rapidly evolving and changing, and could have an adverse impact on our operations. These laws and regulations are subject to uncertainty in how they may be interpreted and enforced by government authorities and regulators. The costs of compliance with, and the
46
Table of Contents
other burdens imposed by, these and other laws or regulatory actions may increase our operational costs, prevent us from providing our solutions, and/or impact our ability to invest in or jointly develop our solutions. We also may face audits or investigations by one or more domestic or foreign government agencies relating to our compliance with these laws and regulations. An adverse outcome under any such investigation or audit could result in fines, penalties, other liability, or could result in adverse publicity or a loss of reputation, and adversely affect our business. Any failure or perceived failure by us or by our solutions to comply with these laws and regulations may subject us to legal or regulatory actions, damage our reputation or adversely affect our ability to provide our solutions in the jurisdiction that has enacted the applicable law or regulation. Moreover, if these laws and regulations change, or are interpreted and applied in a manner that is inconsistent with our policies and processes or the operation of our solutions, we may need to expend resources in order to change our business operations, policies and processes or the manner in which we provide our solutions. This could adversely affect our business, financial condition and results of operations.
Anti-Kickback and Anti-Referral Laws. A number of federal and state laws govern patient referrals, financial relationships with physicians and other referral sources and inducements to providers and patients, including restrictions contained in amendments to the Social Security Act, commonly known as the “federal Anti-Kickback Statute (“AKS”).” The AKS contains a limited number of exceptions, and the Office of the Inspector General (“OIG”) of HHS has created regulatory safe harbors to the AKS. Activities that comply with a safe harbor are deemed protected from prosecution under the AKS. Our contracts and other arrangements may not meet an exception or a safe harbor. Additionally, many states have similar anti-kickback laws that are not necessarily limited to items or services for which payment is made by a federal healthcare program. In addition, federal laws restricting certain physician self-referrals (also known as the “Stark Law”), as well as state counterparts, may prohibit payment for patient referrals, patient brokering, remuneration of patients, or billing based on referrals between individuals or entities that have various financial, ownership, or other business relationships with physicians or other healthcare providers. To the extent we undertake billing and coding for designated health services, such activities may result in allegations that claims that we have processed or forwarded are improper.
The laws and regulations in this area are both broad and vague and judicial interpretation can also be inconsistent. We review our practices with regulatory experts in an effort to comply with all applicable laws and regulatory requirements. However, we are unable to predict how these laws and regulations will be interpreted or the full extent of their application, particularly to services that are not directly reimbursed by federal healthcare programs, such as transaction processing services. Any determination by a federal or state regulatory authority that any of our activities or those of our customers or vendors violate any of these laws or regulations could: (i) subject us to civil or criminal penalties, (ii) require us to enter into corporate integrity agreements or similar agreements with government regulators to meet ongoing compliance obligations, (iii) require us to change or terminate some portions of our business, (iv) require us to refund a portion of our service fees, (v) disqualify us from providing services to customers that are, or do business with, government programs and/or (vi) have a material adverse impact on our business, results of operations or financial condition. Even an unsuccessful challenge by a regulatory authority of our activities could result in adverse publicity and could require a costly response from us.
False or Fraudulent Claim Laws; Medical Billing and Coding. Medical billing, coding and collection activities are governed by numerous federal and state civil and criminal laws, regulations, and sub-regulatory guidance. We may be subject to, or contractually required to comply with, numerous federal and state laws that prohibit false or fraudulent claims including but not limited to the FCA, the CMP, and state equivalents. For example, errors or the unintended consequences of data manipulations by us or our systems with respect to the entry, formatting, preparation or transmission of claims, coding, audit, eligibility and other information, may result in allegations of false or fraudulent claims. False or fraudulent claims under the FCA and other laws include, but are not limited to, billing for services not rendered, making or causing to be made or used a false record or statement that is material to a false claim, failing to refund known overpayments, misrepresenting actual services rendered, improper coding and billing for medically unnecessary items or services. Some of these laws, including CMP, require a lower burden of proof than other fraud, waste and abuse laws. Federal and state
47
Table of Contents
authorities increasingly assert liability under CMP, especially where they believe they cannot meet the higher burden of proof requirements under the various criminal healthcare fraud provisions. Current penalties under CMP are significant, up to $100,000 per prohibited kickback and assessments of up to three times the amount claimed or received. Further, violations of the FCA are punishable by treble damages and penalties of up to $22,363 per false claim, and whistleblowers may receive a share of amounts recovered. Civil monetary penalties, including those imposed under the AKS and the FCA, are updated annually based on changes to the consumer price index.
In addition, the FCA prohibits the knowing submission of false claims or statements to the federal government, including to the Medicare and Medicaid programs. The FCA also contains qui tam, or whistleblower provisions, which allow private individuals to sue on behalf of the federal government alleging that the defendant has defrauded the federal government. Although simple negligence will not give rise to liability under the FCA, “knowingly” is defined broadly by the FCA and submitting a claim with reckless disregard to its truth or falsity can constitute “knowingly” submitting a false claim and may result in liability. Several states, including states in which we operate, have adopted their own false claims provisions and their own whistleblower provisions whereby a private individual may file a civil lawsuit in state court. Civil penalties also may be imposed for the failure to report and return an overpayment made by the federal government within 60 days of identifying the overpayment and also may result in liability under the FCA. The FCA provides that submission of a claim for an item or service generated in violation of the AKS constitutes a false or fraudulent claim under the FCA. Whistleblowers and federal authorities have taken the position, and some courts have held, that providers who allegedly violated other statutes, such as Stark Law, have thereby submitted false claims under the FCA. Although we believe our processes are consistent with applicable reimbursement rules and industry practice, a court, government authority or whistleblower could challenge these processes. In addition, we cannot guarantee that federal and state authorities will regard any billing and coding errors we process or make as inadvertent or will not hold us responsible for any compliance issues related to claims, reports and other information we handle on behalf of providers and payers. We cannot predict the impact of any enforcement actions under the various false claims and fraud, waste and abuse laws applicable to our operations. Even an unsuccessful challenge of our practices could cause us to incur adverse publicity and significant legal and related costs.
Exclusion from participation in government healthcare programs. We are also subject to the exclusion rules of the OIG of HHS whereby OIG may or must exclude individuals and entities convicted of program-related crimes from participation in the Medicare and Medicaid programs. While we regularly screen for excluded individuals as part of our initial hiring and continued employment as well as excluded individuals and entities as part of our contractor practices, but we may not always identify all excluded individuals and entities.
FDA and International Regulation of Medical Software. Certain of our products are classified as medical devices and are subject to regulation by the Food and Drug Administration (the “FDA”) and numerous other federal, state and foreign governmental authorities. If the FDA chooses to regulate more of our solutions as medical devices, or subsequently changes or reverses its guidance regarding not enforcing certain regulatory controls, we may be obligated to comply with extensive requirements. Any additional FDA regulations governing healthcare software products may increase the cost and time-to-market of new or existing solutions or may prevent us from marketing our solutions. If we fail to maintain regulatory approvals and clearances, or are unable to obtain, or experience significant delays in obtaining, FDA clearances or approvals for our future products or product enhancements, our ability to commercially distribute and market these products could suffer. Modifications to our medical device products may require new regulatory approvals or clearances, including 510(k) or de novo clearances or premarket approvals, or require us to recall or cease marketing the modified devices until these clearances or approvals are obtained. Once a device is on the market, we must comply with numerous additional regulations which may require us to file adverse event reports and recalls as well as manufacture the software in accordance with a quality management system. Compliance with applicable regulatory requirements is subject to continual review and is monitored through periodic inspections by the FDA. In addition, we must comply with requirements and restrictions related to advertising, marketing and promotion
48
Table of Contents
of FDA-approved medical devices, as well as more stringent requirements applicable to medical devices that are pending FDA approval. If we fail to comply with regulatory requirements in the U.S. or experience delays in obtaining necessary regulatory approvals or clearances, this could delay production of our medical device products and lead to fines, difficulties in obtaining regulatory approvals or clearances, recalls, enforcement actions, including injunctive relief or consent decrees, or other consequences, which could, in turn, have an adverse effect on our financial condition or results of operations.
Foreign governmental authorities that regulate the manufacture and sale of medical devices have become increasingly stringent and, where we sell our medical device solutions internationally, we are subject to international regulation regarding these medical device solutions. These international regulations could cause us to incur increased costs as they impose increased compliance obligations.
Interoperability Requirements. There is increasing demand among customers, industry groups and government authorities that healthcare IT products provided by various vendors be compatible with each other and allow for the efficient exchange of EHR information. Although several of our healthcare IT solutions have received certification, rules regarding interoperability and certification standards are subject to regular revision and updates. In March 2020, the ONC and CMS released final regulations concerning interoperability and information blocking. The final ONC rule address, among other things, the kinds of industry behaviors that do and do not constitute information blocking under the Cures Act and includes new criteria involving exporting electronic health information and standardized APIs for patient services. Health IT developers, exchanges, or networks that do engage in such information blocking by knowingly adopting practices that are likely to interfere with, prevent, or materially discourage the access, exchange, or use of electronic health information, may be subject to civil monetary penalties of up to $1 million per violation. The final CMS rule, among other things, effectively mandates interoperability as a condition for participating in Medicare. While we believe we are well positioned to address these new rules, it is too early to tell the impact these rules will have on our business and the industry we serve. In October 2016, HHS published rules establishing processes to facilitate ONC’s direct review and evaluation of the performance of certified health IT in certain circumstances, including in response to problems or issues that could pose serious risks to public health or safety. As a result of changing requirements, we may incur increased development costs and delays in receiving certification for our solutions, and changing or supplementing rules also may lengthen our sales and implementation cycle. We also may incur costs in periods prior to the corresponding recognition of revenue. To the extent these requirements subsequently are changed or supplemented, or our prior certifications are no longer valid, or we are delayed in receiving new certifications for our solutions, customers may postpone or cancel their decisions to purchase or implement these solutions.
Restrictions on Communications. Communications with our customers and our customers’ patients increasingly are scrutinized under laws and regulations governing communications. For example, the TCPA subjects us and our vendors to various rules regarding contacting our customers and our customers’ patients via telephone, fax or text message and may impact our operations. In the last few years, there has been a significant increase in class action lawsuits brought under the TCPA. This increase has been driven, in part, by more expansive interpretations of the activity subject to regulation under the TCPA by some courts and by the FCC, as well as by the significant statutory damages that are potentially available to successful plaintiffs. Because our solutions need and rely upon various messaging components to achieve successful outcomes for us and our customers, our ability to communicate with our customers and their patients may be affected by the TCPA, its implementing regulations and litigation pursuant to the TCPA. In addition, because of the scope and interpretation of the TCPA is continuing to evolve and develop, we inadvertently could fail to comply or be alleged to have failed to comply with the TCPA, and consequently be subject to significant statutory damages and negative publicity associated with class action litigation and/or costs associated with modifying our solutions and business strategies. Furthering the compliance challenges posed by the TCPA is the fact that the FCC continues to review dozens of petitions from parties in various industries that seek interpretation of the TCPA’s various regulations. To the extent the FCC issues an order that alters current understanding and accepted interpretation of the TCPA’s regulations, we may be required to modify our solutions in ways that may make
49
Table of Contents
them less attractive to our customers and/or require us to alter our business strategies and incur increased costs. In addition, we also may be subject to claims alleging failure to comply with email and marketing regulations under the CAN-SPAM Act, and additional fax regulations under the Junk Fax Act and data privacy rules under the California Consumer Privacy Act of 2018, as well as potentially under non-U.S. laws that regulate communications and messaging and that affect our operations, such as CASL, GDPR, and the European Union’s e-Privacy Directive and implementing member state laws (and any subsequent changes to such laws). As laws and regulations, including FTC enforcement, rapidly evolve to govern the use of these platforms and devices, the failure by us, our employees or third parties acting at our direction to abide by applicable laws and regulations in the use of these platforms and devices could adversely impact our business, financial condition and results of operations or subject us to fines or other penalties.
Financial Services Related Laws, Regulations and Industry Standards. Financial services and electronic payment processing services are subject to numerous laws, regulations and industry standards. These laws may subject us, our vendors and our customers to liability as a result of our communication and payment solutions. If we fail to comply with any applicable communication and payment rules or requirements, we may be subject to fines and changes in transaction fees and may lose our ability to process payment transactions or facilitate other types of billing and payment solutions. Moreover, in addition to regulatory requirements related to electronic funds transfers, payment transactions processed using the Automated Clearing House Network are subject to network operating rules promulgated by the National Automated Clearing House Association, and these rules may affect our payment practices. Certain payment transactions may be subject to card association and network rules and standards. Failure to comply with such rules or standards could subject us to fines or penalties imposed by such card associations and networks. If any changes in such rules or standards increase the cost of doing business or limit our ability to provide our solutions, our business, results of operations or financial condition could suffer. Further, our communication and payment solutions may impact the ability of our payer customers to comply with state prompt payment laws. These laws require payers to pay healthcare claims meeting the statutory or regulatory definition of a “clean claim” within a specified time frame. Finally, as we expand our financial services offerings we may be subject to additional laws and regulations, including certain consumer protection laws such as the Fair Debt Collections Practices Act (the “FDCPA”), the Fair Credit Reporting Act (the “FCRA”) and various other state laws implicated by such financial services.
Foreign Corrupt Practices Act and Bribery Laws. With our international businesses, we could incur significant fines and penalties, as well as criminal liability, if we fail to comply with either the anti-bribery or accounting requirements of the FCPA, or similar international bribery laws. Even an unsuccessful challenge of our compliance with these laws could cause us to incur adverse publicity and significant legal and related costs.
Physician Payments Sunshine Act. As a medical device manufacturer, we must report to CMS payments or “transfers of value” made to physicians, including meals, travel reimbursement, consulting fees and research payments. The Sunshine Act authorizes significant civil monetary penalties for each payment or transfer of value not accurately or completely reported. Although we have processes in place to track and timely report such financial relationships, we inadvertently may fail to track and report all such financial relationships and thus may be subject to penalties for such non-compliance.
U.S. Postal Service Laws and Regulations. Our communication and payment solutions provide mailing services primarily delivered by the U.S. Postal Service (“USPS” or the “Postal Service”). Postage is the most significant cost incurred in the delivery of our communication and payment solutions. Although we generally pass increases in postage costs through to our customers, in some circumstances we may be unable to do so, or the resulting increases in our charges could cause our customers to reduce the volume of our services they purchase. While we cannot predict the magnitude of these effects, they could have a material effect on our business, operating results or financial condition if large enough.
First, the Postal Service could increase the rates of postage that we must pay. Most of the mail that we send uses market-dominant mail products, whose postal rates are subject to maximum rate regulation. Current
50
Table of Contents
regulatory rules generally limit the average rate increase for each class of market-dominant mail to the rate of increase of the Consumer Price Index (“CPI”). The Postal Service, however, has argued for eliminating or loosening this restriction, and the Postal Regulatory Commission is now considering proposed rule changes that would have this effect. It is also possible that Congress could eliminate or loosen the restriction on postal rate increases through legislation, particularly if the Postal Service continues to report financial losses.
Second, even under current regulatory standards, the Postal Service has broad flexibility to raise rates on individual rate categories within a class of mail faster than the CPI, as long as the average rates for the affected mail class as a whole do not increase than the CPI-based rate cap.
Third, most of the postal rates that we pay reflect significant discounts from the basic USPS postage rate structure. These discounts could be changed or discontinued at any time on short notice. The Postal Service also could require more costly or difficult mail preparation (e.g., presorting, barcoding, bundling or destination entry) requirements as a condition for continuing to use the discounted rates. More onerous preparation requirements could force us to incur substantial additional mail preparation costs or pay higher rates of postage.
Fourth, it is possible that the Postal Service, the Postal Inspection Service, or other law enforcement officials could allege that we did not prepare past mailings as required to qualify for the discounted rates at which the mailings were mailed, and that we now owe additional postage. Further, if the government concludes that the noncompliance was intentional or reckless, the government could seek to recover treble damages and civil penalties of up to $22,363 per false claim (adjusted annually to reflect changes in the Consumer Price Index). If the volume of mail subject to these allegations is large enough, the recovery sought could have a material effect on our business, operating results, or financial condition.
Payment Card Industry Standards. We accept credit card, eCheck, ACH Payments, and payments via online portal, phone/Interactive Voice Response system or by mail. Compliance with contractual obligations and evolving privacy and security laws, requirements and regulations may result in cost increases due to necessary systems changes, new limitations or constraints on our business and the development of new administrative processes. If we fail to adequately control fraudulent ACH, credit card and debit card transactions, we may face civil liability, diminished public perception of our security measures and significantly higher ACH, credit card and debit card related costs, each of which could adversely affect our business, financial condition and results of operations. The termination of our ability to process payments through ACH transactions or on any major credit or debit card would adversely affect our ability to operate our business.
Other State Healthcare Laws. Most states have a variety of laws that potentially impact our operations and business practices. If our arrangements with physicians or other practitioners were found to violate a corporate practice of medicine, nursing and other licensed professions prohibition or fee-splitting prohibition, we may be subject to civil or criminal penalties, be required to terminate or make changes to our contractual arrangements with practitioners in such states or to our business generally, or be required to remit portions of our services fees to practitioners, which, in turn, may adversely affect both our operations and profitability. Further, we could face sanctions for aiding and abetting the violation of the state’s professional licensure statutes. In addition, we hold certain state licenses and enrollments in government healthcare programs which subject us to additional requirements and scrutiny by government regulators. Failure to comply with requirements and obligations imposed by such licensure and enrollments may result in civil and criminal penalties and may otherwise adversely affect our business. We continually monitors legislative, regulatory and judicial developments related to licensure and engagement arrangements with professionals; however, new agency interpretations, federal or state legislation or regulations, or judicial decisions could require us to change how we operate, may increase our costs of services and could have a material adverse impact on our business, results of operations or financial condition.
51
Table of Contents
Our infrastructure, data or other operation centers and systems used in our business operations, including the internet and related systems of our vendors are vulnerable to, and from time to time experience, unauthorized access to data and/or breaches of confidential information.
In recent years, there have been a number of well-publicized data breaches involving the improper dissemination of personal information of individuals both within and outside of the healthcare industry. Most states require holders of personal information to maintain safeguards and take certain actions in response to a data breach, such as providing prompt notification of the breach to affected individuals or the state’s attorney general. In some states, these laws are limited to electronic data, but states increasingly are enacting or considering stricter and broader requirements. Additionally, HIPAA imposes certain notification requirements on both Covered Entities and Business Associates. In certain circumstances involving large breaches, requirements may even involve notification to the media. A non-permitted use or disclosure of protected health information is presumed to be a breach under HIPAA unless the Covered Entity or Business Associate establishes that there is a low probability the information has been compromised consistent with requirements enumerated in HIPAA.
Further, the FTC has prosecuted certain data breach cases as unfair and deceptive acts or practices under the Federal Trade Commission Act. In addition, by regulation, the FTC requires creditors, which may include some of our customers, to implement identity theft prevention programs to detect, prevent and mitigate identity theft in connection with customer accounts. Although Congress passed legislation that restricts the definition of “creditor” and exempts many healthcare providers from complying with this identity theft prevention rule, we may be required to apply additional resources to our existing processes to assist our affected customers in complying with this rule.
Despite our security management efforts with respect to physical and technological infrastructure, employee training, vendor (and sub-vendor) controls and contractual relationships, our infrastructure, data or other operation centers and systems used in our business operations, including the internet and related systems of our vendors (including vendors to whom we outsource data hosting, storage and processing functions) are vulnerable to, and from time to time experience, unauthorized access to data and/or breaches of confidential information due to criminal conduct, physical break-ins, hackers, employee or insider malfeasance and/or improper employee or contractor access, computer viruses, programming errors, denial-of-service attacks, ransomware events, phishing schemes, fraud, terrorist attacks, human error or other breaches by insiders or third parties or similar disruptive problems. It is not possible to prevent all security threats to our systems and data. See “—Breaches and failures of our IT systems and the security measures protecting them, and the sensitive information we transmit, use and store, expose us to potential liability and reputational harm.”
Legislative changes and contractual limitations may impede our ability to utilize our offshore service capabilities.
In our operations, we have contractors and employees located outside of the U.S. who may have access to personal information, including protected health information in order to assist us in performing services for our customers. From time to time, Congress considers legislation that would restrict the transmission of personal information regarding a U.S. resident to any foreign affiliate, subcontractor or unaffiliated third party without adequate privacy protections or without providing notice to the identifiable individual of the transmission and an opportunity to opt out. Some of the proposals considered would have required patient consent and imposed liability on healthcare businesses arising from the improper sharing or other misuse of personal information. Congress also has considered creating a private civil cause of action that would allow an injured party to recover damages sustained as a result of a violation of these proposed restrictions. Furthermore, a number of states have considered prohibitions or limitations on the disclosure of personal information to individuals or entities located outside of the U.S. If legislation of this type is enacted, our ability to utilize offshore resources may be impeded, and we may be subject to sanctions for failure to comply with the new mandates of the legislation. In addition, the enactment of such legislation could result in such work being performed at a lower margin of profitability, or even at a loss. In addition, CMS requires that some of our customers, including Medicare Advantage
52
Table of Contents
organizations and Medicare Part D prescription drug plans and their subcontractors, submit certain information regarding their offshore subcontractors and attest that measures have been taken to mitigate risk associated with sharing personal information with such offshore subcontractors. As a result, we may be required to submit information or an attestation and may be impacted by our customer’s failure to submit accurate and complete information or attestations. Further, as a result of concerns regarding the possible misuse of personal information, some of our customers have contractually limited or may seek to limit our ability to use our offshore resources which may increase our costs. Use of offshore resources may increase our risk of violating our contractual obligations to our customers to protect the privacy and security of personal information provided to us, which could adversely impact our reputation and our business. In addition, depending on the location of contractors and employees accessing personal information outside of the U.S., we may have additional compliance obligations under non-U.S. laws applicable to accessing, using, or otherwise processing personal information and transmitting that information back to the U.S.
We are subject to risks associated with our international operations.
We market, sell and support our solutions internationally. We plan to continue to expand our non-U.S. operations and continue to focus on developing successful direct and indirect non-U.S. sales and support channels. Non-U.S. operations are subject to inherent risks, and our business, results of operations and financial condition, including our revenue growth and profitability, could be adversely affected by a variety of uncontrollable and changing factors. These include, but are not limited to:
| • | greater difficulty in collecting accounts receivable and longer collection periods; |
| • | difficulties and costs of staffing and managing non-U.S. operations; |
| • | the impact of global economic and political market conditions; |
| • | effects of sovereign debt conditions, including budgetary constraints; |
| • | unfavorable or volatile foreign currency exchange rates; |
| • | legal compliance costs or business risks associated with our global operations where: (i) local laws and customs differ from, or are more stringent than those in the U.S., such as those relating to data privacy and data security, or (ii) risk is heightened with the FCPA, the U.K. Anti-Bribery Act and similar laws and regulations in foreign jurisdictions; |
| • | certification, licensing, or regulatory requirements, including obligations imposed on manufacturers and distributors of medical devices by non-U.S. regulatory agencies, and unexpected changes to those requirements; |
| • | changes to or reduced protection of intellectual property rights in certain countries; |
| • | greater difficulty in protecting, maintaining and obtaining registered intellectual property, such as patents and trademarks; |
| • | potentially adverse tax consequences as a result of changes in tax laws or otherwise, and difficulties associated with repatriating cash generated or held abroad in a tax-efficient manner; |
| • | different or additional functionality requirements or preferences; |
| • | trade protection measures; |
| • | economic sanctions; |
| • | export control regulations; |
| • | disruption of, or loss of access to, regional information technology or telecommunication networks; |
| • | health service provider or government spending patterns or government-imposed austerity measures; |
| • | natural disasters, war or terrorist acts; and |
| • | labor disruptions that may occur in a country. |
53
Table of Contents
We rely on vendors and other third parties including vendors outside the U.S., for some of our IT infrastructure, development and maintenance, quality assurance, operations, and customer support.
We currently depend on various vendors and other third parties for substantial business functions, including with respect to our IT systems (including infrastructure, application development, purchase and distribution, payment processing, manufacturing, and maintenance), business process outsourcing, call center services, customer support and similar services. Specifically, we outsource some of our software development and design, quality assurance, and operations activities to third-party vendors that have employees and consultants located outside the U.S. In February 2018, the Joint Venture entered into a ten-year contract with Wipro in which it initially committed to purchase from Wipro at least $1.0 billion in outsourced professional services over the ten-year term of the contract, and in March 2020, that commitment amount was adjusted to $975.0 million. If the Joint Venture fails to meet this minimum commitment, it may be forced to pay to Wipro 25% of the shortfall relative to the minimum commitment at the end of the term, thus increasing our costs without a commensurate increase in services provided to our business. If we had terminated the Wipro contract on March 31, 2020, we estimate that the termination fee would have been approximately $220.8 million, which represents the greater of (i) a termination fee equal to 25% of the remaining unspent minimum commitment and (ii) the remaining unrecovered costs incurred by Wipro in connection with its performance under the agreement. In addition, the Joint Venture’s dependence on Wipro and our dependence on other third-party vendors creates a number of business risks—in particular, the risk that we may not maintain service quality, control or effective management with respect to these outsourcing arrangements of our business operations and that we cannot control the information systems, facilities or networks of such vendors.
Our results of operations could be adversely affected if the information systems, facilities or networks of a third party vendor are disrupted (including disruption of access), are damaged or fail, whether due to physical disruptions, such as fire, natural disaster, pandemic or power outage, or due to cyber-security incidents, ransomware or other actions of vendors, including labor strikes, political unrest and terrorist attacks. Moreover, because certain of our third-party vendors conduct operations for us outside the U.S., the political and military events in foreign jurisdictions could have an adverse impact on our outsourced operations. If we experiences problems with our third-party vendors, if the costs charged by our third-party vendors increase or if our agreements with our third-party vendors are terminated, we may not be able to develop new solutions, enhance or operate existing solutions, or provide customer support in an alternate manner that is equally or more efficient and cost-effective.
Failure by our customers to obtain proper permissions or provide us with accurate and appropriate information may result in claims against us or may limit or prevent our use of information, which could harm our business. Additionally, privacy concerns relating to our business could damage our reputation and deter current and potential customers from using our solutions.
To the extent we are not otherwise permitted to use and/or disclose customer information, we require our customers to provide necessary notices and obtain necessary permissions for the use and disclosure of the information that we receive from our member engagement, member eligibility, billing and coding and other solutions. If they do not provide necessary notices or obtain necessary permissions, then our use and disclosure of information that we receive from them or on their behalf may be limited or prohibited by federal or state privacy or other laws. Such failures by our customers could impair our functions, processes and databases that reflect, contain or are based upon such information. For example, as part of our claims submission services, we rely on our customers to provide us with accurate and appropriate information and directives for our actions. While we have implemented features and safeguards relating to the accuracy and completeness of claims content, these features and safeguards may not be sufficient to prevent inaccurate claims data from being submitted to payers. In addition, such failures by our customers could interfere with or prevent creation or use of rules, analyses or other data-driven activities that benefit us or make our solutions less useful. Accordingly, we may be subject to claims or liability for inaccurate claims data submitted to payers or for use or disclosure of information by reason of lack of valid notice or permission. As another example, we rely on our customers to provide us with accurate and appropriate billing and coding information, including provider enrollment information and medical
54
Table of Contents
necessity information. While we have implemented features and safeguards relating to provider enrollment and medical necessity requirements, these features and safeguards may not be sufficient to prevent inaccurate or incomplete billing and coding claims from being submitted to payers. Accordingly, we may be subject to claims or liability for inaccurate or incomplete billing and coding claims. These claims or liabilities could damage our reputation, subject us to unexpected costs and could have a material adverse impact on our business, results of operations or financial condition.
Additionally, in recent years, consumer advocates, media and elected officials increasingly and publicly have criticized companies in data focused industries regarding the collection, storage and use of personal data, including the licensing of de-identified data, by such companies. Concerns about our practices with regard to the collection, use, disclosure or security of personal information, the licensing of de-identified data, or other privacy related matters, even if unfounded, could damage our reputation and adversely affect our business, results of operations or financial condition.
Certain of our solutions present the potential for embezzlement, identity theft or other similar illegal behavior by our employees or vendors and a failure of our employees or vendors to observe quality standards or adhere to environmental, social and governance standards could damage our reputation.
Among other things, our solutions include printing and mailing checks and/or facilitating electronic funds transfers for our payer customers and handling mail and payments from payers and from patients for many of our provider customers. These services frequently include handling original checks, payment card information, banking account information and may include currency. Even in those cases in which we do not facilitate payments or handle original documents or mail, our services also involve the use and disclosure of personal and business information that could be used to impersonate third parties or otherwise gain access to their data or funds. If any of our employees or vendors or other bad actors takes, converts or misuses such funds, documents or information, or we experience a data breach creating a risk of identity theft, we could be liable for damages, and our reputation could be damaged or destroyed. In addition, we could be perceived to have facilitated or participated in illegal misappropriation of funds, documents or data and, therefore, be subject to civil or criminal liability. Federal and state regulators may take the position that a data breach or misdirection of data constitutes an unfair or deceptive act or trade practice. We also may be required to notify individuals affected by any data breaches. Further, a data breach or similar incident could impact the ability of our customers that are creditors to comply with the federal “red flags” rules, which require the implementation of identity theft prevention programs to detect, prevent and mitigate identity theft in connection with customer accounts.
Many of our licensees, as well as vendors are subject to specified product quality standards and other requirements pursuant to the related licensing or supply agreements. The non-compliance by these entities with the terms and conditions of their respective contracts that pertain to health and safety standards, quality control, product consistency, compliance with law, or proper marketing or other business practices, may adversely impact the goodwill of our business. We may not be able to adequately prevent such practices, which could harm the value of our business, result in the abandonment, dilution or invalidity of trademarks associated with our business and adversely affect our results of operations or financial condition. In addition, such licensees and suppliers could violate environmental, social and governance standards or engage in unethical conduct. Further, despite our policies to the contrary, we may not be able to control the conduct of every individual actor, and our employees and personnel may violate environmental, social or governance standards or engage in other unethical conduct. These acts could adversely impact the reputation of our business.
Contractual relationships with customers that are governmental agencies or are funded by government programs may impose special burdens on us and provide special benefits to those customers.
A portion of our revenue comes from customers that are governmental agencies or are funded by government programs. our contracts and subcontracts may be subject to some or all of the following:
| • | termination when appropriated funding for the current fiscal year is exhausted; |
55
Table of Contents
| • | termination for the governmental customer’s convenience, subject to a negotiated settlement for costs incurred and profit on work completed, along with the right to place contracts out for bid before completion of the full contract term, as well as the right to make unilateral changes in contract requirements, subject to negotiated price adjustments; |
| • | compliance and reporting requirements related to, among other things, agency-specific policies and regulations, information security, subcontracting requirements, equal employment opportunity, affirmative action for veterans and workers with disabilities and accessibility for the disabled; |
| • | broad audit rights; |
| • | ownership of inventions made with federal funding under the Bayh-Dole Act; and |
| • | specialized remedies for breach and default, including setoff rights, risk allocation, retroactive price adjustments and civil or criminal fraud penalties, re-procurement expenses, as well as mandatory administrative dispute resolution procedures instead of state contract law remedies. |
In addition, certain violations of federal and state law may result in termination of our contracts and subcontracts, and under certain circumstances, suspension and/or debarment from future government contracts. We are also subject to conflict-of-interest rules that may affect our eligibility for some federal, state and local government contracts and subcontracts, including rules applicable to all U.S. government contracts and subcontracts, as well as rules applicable to the specific agencies with which we have contracts or with which we may seek to enter into contracts.
The protection of our intellectual property requires substantial resources and protections of our proprietary rights may not be adequate.
We rely upon a combination of trade secret, copyright and trademark laws, patents, license agreements, confidentiality procedures, nondisclosure agreements and technical measures designed to protect the intellectual property used in our business. The steps we have taken to protect and enforce our proprietary rights and intellectual property may not be adequate. For instance, we may not be able to secure trademark or service mark registrations for marks in the U.S. or in foreign countries or take similar steps to secure patents for our proprietary processes, methods and technologies. Even if we are successful in obtaining patent and/or trademark registrations, these registrations may be opposed or invalidated by a third party. In addition, our agreements with employees, consultants and others who develop intellectual property for or on behalf of us could be breached and could result in our trade secrets and confidential information being publicly disclosed. We may not have adequate remedies for any such breach. Third parties also may infringe upon or misappropriate our copyrights, trademarks, service marks, patents and other intellectual property rights. If we believe a third party has misappropriated our intellectual property, litigation may be necessary to enforce and protect those rights, which would divert management resources, would be expensive and may not effectively protect our intellectual property. Even if we establish infringement, a court may decide not to grant an injunction against further infringing activity and instead award only monetary damages, which may or may not be an adequate remedy. Furthermore, because of the substantial amount of discovery required in connection with intellectual property litigation, there is a risk that some of our confidential information could be compromised by disclosure during litigation. There could also be public announcements of the results of hearings, motions or other interim proceedings or developments. If securities analysts or investors perceive these results to be negative, it could have a material adverse effect on the price of shares of our Common Stock. Moreover, there can be no assurance that we will have sufficient financial or other resources to file and pursue such infringement claims, which typically last for years before they are concluded. Even if we ultimately prevail in such claims, the monetary cost of such litigation and the diversion of the attention of our management and scientific personnel could outweigh any benefit we receive as a result of the proceedings. As a result, if we fail to maintain adequate intellectual property protection or if a third party infringes or misappropriates our intellectual property, it may have a material adverse impact on our business, results of operations or financial condition. Our currently pending or future patent applications may not result in issued patents, or be approved on a timely basis, if at all. Similarly,
56
Table of Contents
any term extensions that we seek may not be approved on a timely basis, if at all. In addition, our issued patents, or any patents that may issue in the future, may not contain claims sufficiently broad to protect us against third parties with similar technologies or products or provide us with any competitive advantage, including exclusivity in a particular product area. The validity and scope of our patent claims also may vary between countries, as individual countries have their own patent laws. The validity, enforceability, scope and effective term of patents can be highly uncertain and often involve complex legal and factual questions and proceedings that vary based on the local law of the relevant jurisdiction. Our ability to enforce our patents also depends on the laws of individual countries and each country’s practice with respect to enforcement of intellectual property rights. Patent protection must be obtained on a jurisdiction-by-jurisdiction basis, and we only pursue patent protection in countries where we think it makes commercial sense for the given product. In addition, if we are unable to maintain our existing license agreements or other agreements pursuant to which third parties grant us rights to intellectual property, including because such agreements terminate, our financial condition and results of operations could be materially adversely affected.
Patent law reform in the U.S. and other countries may also weaken our ability to enforce our patent rights, or make such enforcement financially unattractive. For instance, in September 2011, the U.S. enacted the America Invents Act, which permits enhanced third-party actions for challenging patents and implements a first-to-invent system. These reforms could result in increased costs to protect our intellectual property or limit our ability to obtain and maintain patent protection for our products in these jurisdictions. Additionally, certain foreign governments have indicated that compulsory licenses to patents may be granted in the case of national emergencies, which could diminish or eliminate sales and profits from those regions and materially adversely affect our financial condition and results of operations.
Our trademarks, logos, and brands may provide us with a competitive advantage in the market as they may be known or trusted by consumers. In order to maintain the value of such brands, we must be able to enforce and defend our trademarks. We have pursued and will pursue the registration of trademarks, logos and service marks in the U.S. and internationally; however, enforcing rights against those who knowingly or unknowingly dilute or infringe our brands can be difficult. Effective trademark, service mark, trade dress or related protections may not be available in every country in which our solutions are available. Enforcement is especially difficult in first-to-file countries where ‘‘trademark squatters’’ can prevent us from obtaining adequate protections for our brands. There can be no assurance that the steps we have taken and will take to protect our proprietary rights in our brands and trademarks will be adequate or that third parties will not infringe, dilute or misappropriate our brands, trademarks, trade dress or other similar proprietary rights.
Many of our products are based on or incorporate proprietary information. We actively seek to protect our proprietary information, including our trade secrets and proprietary know-how, by generally requiring our employees, consultants, other advisors and other third parties to execute proprietary information and confidentiality agreements upon the commencement of their employment, engagement or other relationship. Despite these efforts and precautions, we may be unable to prevent a third party from copying or otherwise obtaining and using our trade secrets or our other intellectual property without authorization and legal remedies may not adequately compensate us for the damages caused by such unauthorized use.
In addition, there can be no assurance that our competitors will not independently develop products or services that are equivalent or superior to our solutions.
We may not be able to protect our intellectual property rights throughout the world.
Third parties may attempt to commercialize competitive products or services in foreign countries where we do not have any patents or patent applications and where legal recourse may be limited. This may have a significant commercial impact on our foreign business operations.
57
Table of Contents
Filing, prosecuting and defending patents on our solutions in all countries throughout the world would be prohibitively expensive, and our intellectual property rights in some countries outside the U.S. may be less extensive than those in the U.S. The requirements for patentability may differ in certain countries, particularly developing countries. For example, Europe has a heightened requirement for patentability of software inventions. Thus, even in countries where we do pursue patent protection, there can be no assurance that any patents will issue with claims that cover our solutions. In addition, the laws of some foreign countries do not protect intellectual property rights to the same extent as laws in the U.S. Consequently, we may not be able to prevent third parties from practicing our inventions in all countries outside the U.S. Competitors may use our technologies in jurisdictions where we have not obtained patent protection to develop their own products and services and further, may export otherwise infringing products and services to territories where we have patent protection, but enforcement on infringing activities is inadequate. These products or services may compete with our products or services, and our patents or other intellectual property rights may not be effective or sufficient to prevent them from competing.
Many companies have encountered significant problems in protecting and defending intellectual property rights in foreign jurisdictions. The legal systems of certain countries, particularly certain developing countries, do not favor the enforcement of patents and other intellectual property protection, which could make it difficult for us to stop the infringement of our patents or marketing of competing products in violation of our proprietary rights generally. Proceedings to enforce our patent rights in foreign jurisdictions could result in substantial costs and divert our efforts and attention from other aspects of our business, could put our patents at risk of being invalidated or interpreted narrowly and our patent applications at risk of not issuing, and could provoke third parties to assert claims against us. We may not prevail in any lawsuits that we initiate, and the damages or other remedies awarded, if any, may not be commercially meaningful. In addition, certain countries in Europe and certain developing countries, including India and China, have compulsory licensing laws under which a patent owner may be compelled to grant licenses to third parties. In those countries, we may have limited remedies if our patents are infringed or if we are compelled to grant a license to our patents to a third party, which could materially diminish the value of those patents. This could limit our potential revenue opportunities. Accordingly, our efforts to enforce our intellectual property rights around the world may be inadequate to obtain a significant commercial advantage from the intellectual property that we own or license. Finally, our ability to protect and enforce our intellectual property rights may be adversely affected by unforeseen changes in foreign intellectual property laws.
Third parties may claim that we or our distributors or licensors are infringing their intellectual property, and we could suffer significant litigation or licensing expenses or be prevented from selling certain solutions.
We or our distributors and licensors could be subject to claims that we are misappropriating or infringing intellectual property (including patents, trademarks, trade dress, copyrights, trade secrets, domain names) or other proprietary rights of others. We may become subject to preliminary or provisional rulings in the course of any such litigation, including potential preliminary injunctions requiring us to cease some or all of our operations. Similarly, if any litigation to which we are a party is resolved adversely, we may be subject to an unfavorable judgment that may not be reversed upon appeal. These claims, even if not meritorious, could be expensive to defend and divert management’s attention from our operations and even if we believe it does not infringe a validly existing third-party right we may choose to license such rights. If we or our distributors or licensors become liable to third parties for infringing these rights, we could be required to pay a substantial damage award, including treble damages in some cases, and to develop non-infringing technology, obtain a license, which may not be available on commercially reasonable terms, or stop activities or services that use or contain the infringing intellectual property, which could include a recall or cessation of sales in the future. We may also decide to settle such matters on terms that are unfavorable to us. We may be unable to develop non-infringing solutions or obtain a license on commercially reasonable terms, or at all. We also may be required to indemnify our customers if they become subject to third party claims relating to intellectual property that we license or otherwise provide to them, which could be costly.
58
Table of Contents
The intellectual property positions of pharmaceutical and health IT services frequently involve complex legal and factual questions. For example, while we generally enter into proprietary information agreements with our employees and third parties which assign intellectual property rights to us, these agreements may not be honored or may not effectively assign intellectual property rights to us under the local laws of some countries or jurisdictions. We cannot be certain that a competitor or other third party does not have or will not obtain rights to intellectual property that may prevent us from manufacturing, developing or marketing certain of our products, regardless of whether we believe such intellectual property rights are valid and enforceable or we believe we would otherwise be able to develop a more commercially successful product, which may materially adversely affect our business, financial condition and results of operations.
We may be subject to claims that our employees, consultants or independent contractors have wrongfully used or disclosed confidential information of third parties.
We have received confidential and proprietary information from third parties. In addition, we may employ individuals who were previously employed at other healthcare companies. We may be subject to claims that us or our employees, consultants or independent contractors have inadvertently or otherwise improperly used or disclosed confidential information of these third parties or our employees’ former employers. Further, we may be subject to ownership disputes in the future arising, for example, from conflicting obligations of consultants or others who are involved in developing our solutions. We may also be subject to claims that former employees, consultants, independent contractors or other third parties have an ownership interest in our patents or other intellectual property. Litigation may be necessary to defend against these and other claims challenging our right to and use of confidential and proprietary information. In addition to paying monetary damages, if we fail in defending against any such claims we may lose our rights therein, which could have a material adverse effect on our business. Even if we are successful in defending against these claims, litigation could result in substantial cost and be a distraction to our management and employees.
Our solutions depend, in part, on intellectual property and technology licensed from third parties.
Much of our business and many of our solutions rely on key technologies or content developed or licensed by third parties. For example, many of our software offerings are developed using software components or other intellectual property licensed from third parties, including both proprietary and open source licenses. These third-party software components may become obsolete, defective or incompatible with future versions of our solutions, or our relationship with the third party licensor may deteriorate, or our contracts with the third party licensor may expire or be terminated. In addition, like most other service providers in the healthcare industry, many of our products rely on proprietary healthcare codes, descriptive terms and other content, such as Current Procedural Terminology codes (“CPT” codes), that third parties, such as the American Medical Association (“AMA”) develop and license for the purpose of maintaining standard language and coding throughout the healthcare industry. Because CPT codes are licensed by the AMA on reasonable and non-discriminatory terms, we anticipate the continued availability of such content; however, if we are unable to maintain an ongoing license for such content, certain of our products may become partially or entirely incompatible with the healthcare industry. We may also face legal or business disputes with licensors that may threaten or lead to the disruption of inbound licensing relationships. In order to remain in compliance with the terms of our licenses, we must carefully monitor and manage our use of third-party software components, including both proprietary and open source license terms that may require the licensing or public disclosure of our intellectual property without compensation or on undesirable terms. Because the availability and cost of licenses from third parties depends upon the willingness of third parties to deal with us on the terms we request, there is a risk that third parties who license to our competitors either will refuse to license to us at all, or refuse to license to us on terms equally favorable to those granted to our competitors. Consequently, we may lose a competitive advantage with respect to these intellectual property rights or we may be required to enter into costly arrangements in order to terminate or limit these rights. Additionally, some of these licenses may not be available to us in the future on terms that are acceptable or that allow our solutions to remain competitive. our inability to obtain licenses or rights on favorable terms could have a material effect on our business, including our financial condition and results of
59
Table of Contents
operations. In addition, it is possible that as a consequence of a merger or acquisition, third parties may obtain licenses to some of our intellectual property rights or our business may be subject to certain restrictions that were not in place prior to such transaction. Because the availability and cost of licenses from third parties depends upon the willingness of third parties to deal with us on the terms we request, there is a risk that third parties who license to our competitors either will refuse to license to us at all, or refuse to license to us on terms equally favorable to those granted to our competitors. Consequently, we may lose a competitive advantage with respect to these intellectual property rights or we may be required to enter into costly arrangements in order to terminate or limit these rights.
Our use of open source technology could impose limitations on our ability to commercialize our solutions.
Our solutions incorporate open source software components that are licensed to us under various public domain licenses. Some open source software licenses require users who distribute open source software as part of their software to publicly disclose all or part of the source code to such software or make available any derivative works of the open source code on unfavorable terms or at no cost. There is little or no legal precedent governing the interpretation of many of these licenses and therefore the potential impact of such licenses on our business is not fully known or predictable. There is a risk that such licenses could be construed in a manner that imposes unanticipated conditions or restrictions on our ability to market our solutions.
While we monitor our use of open source software and try to ensure that none is used in a manner that would require us to disclose our source code or that would otherwise breach the terms of an open source license, such use could inadvertently occur and we may be required to release our proprietary source code, pay damages for breach of contract, re-code or engineer one or more of our offerings, discontinue sales of one or more of our solutions in the event re-engineering cannot be accomplished on a timely basis or take other remedial action that may divert resources away from our development efforts, any of which could cause us to breach obligations to our customers, harm our reputation, result in customer losses or claims, increase our costs or otherwise adversely affect our business and operating results.
U.S. federal tax reform could adversely affect our results of operations.
On December 22, 2017, the Tax Cuts and Jobs Act of 2017 was signed into law, which made significant changes to the Code. Among other changes, Section 163(j) of the Code was amended to limit the deductibility of net interest expense paid or accrued on debt properly allocable to a trade or business to 30% of “adjusted taxable income,” subject to certain exceptions. Any deduction in excess of the limitation is carried forward and may be used in a subsequent year, subject to the 30% limitation. Adjusted taxable income is determined without regard to certain deductions, including those for net interest expense, net operating loss carryforwards and, for taxable years beginning before January 1, 2022, depreciation, amortization and depletion. While the impact of this rule is not completely clear and could change due to the issuance of additional interpretive guidance or changes in our level of indebtedness, we expect these rules will limit the amount of net interest expense that we and our subsidiaries can use as a deduction against taxable income and, as a result, may negatively impact our financial condition and results of operations.
A write-off or acceleration of amortization of all or a part of our long-lived assets (including identifiable intangible assets and goodwill) would adversely affect our operating results and reduce our net worth.
We have significant long-lived assets which include property and equipment, identifiable intangible assets, other noncurrent assets and goodwill. As of March 31, 2020, we had $206.2 million of property and equipment, $4,365.8 million of identifiable intangible assets, $338.9 million of other noncurrent assets and $3,795.3 million of goodwill on our balance sheet, which collectively represented in excess of 86% of our total assets. We amortize property and equipment, identifiable intangible assets and relevant other noncurrent assets over their estimated useful lives. Though we are not permitted to amortize goodwill under GAAP, we evaluate our goodwill for impairment at least annually. In the event of anticipated obsolescence or impairment of our long-lived assets,
60
Table of Contents
we may write-off all or part of the affected assets or accelerate the related amortization of these assets. We performed a goodwill impairment test as of March 31, 2020, and as a result of the expected impacts to our financial results arising out of the COVID-19 pandemic, we recorded a non-cash goodwill impairment charge of $561.2 million. Other risks and future developments that we ae unable to anticipate as of the testing date may require us to further revise future projected cash flows, which could adversely affect the fair value of reporting units in future periods. A write-off or acceleration of amortization in the future would result in an immediate one-time charge to earnings in the event of an impairment of assets and, in the event of anticipated obsolescence of assets that do not reach the level of an impairment, regular reductions to earnings over the remaining lives of the affected assets. Although it would not affect our cash flow, a write-off or acceleration of amortization in future periods of all or a part of these long-lived assets would adversely affect our financial condition and operating results.
Our success depends in part on our ability to identify, recruit and retain skilled management and technical personnel. If we fail to recruit and retain suitable candidates or if our relationship with our employees changes or deteriorates, there could be a material adverse impact on our business, results of operations or financial condition.
Our future success depends upon our continuing ability to identify, attract, hire and retain highly qualified personnel, including skilled management, product, technology, sales and marketing personnel, all of whom are in high demand and are often subject to competing offers. Competition for qualified personnel in the healthcare IT industry is intense, and we may not be able to hire or retain a sufficient number of qualified personnel to meet our requirements, or be able to do so at salary, benefit and other compensation costs that are acceptable to us. A loss of a substantial number of qualified employees, or an inability to attract, retain and motivate additional highly skilled employees required for expansion of our business, could have a material adverse impact on our business, results of operations or financial condition. In addition, while none of our employees currently are unionized, unionization of our employees is possible in the future. Such unionizing activities could be costly to address and, if successful, likely would adversely impact our operations.
Lengthy sales, installation and implementation cycles for some of our solutions may result in delays or an inability to generate revenue from these solutions.
Some of our solutions have long sales, installation and implementation cycles, which could range from a few months to years or more from initial contact with the customer to completion of implementation and generation of revenue. How and when to implement, replace, or expand an information system, or modify or add business processes, are important decisions for healthcare organizations, and some customers may be reluctant to change or modify existing systems or processes. Some of the solutions we provide require significant capital expenditures and time commitments by our customers. Sales may be subject to delays due to customers’ internal procedures for deploying new systems and processes, and implementation may be subject to delays based on the availability of the internal customer resources needed. We may be unable to control many of the factors that will influence the timing of the buying decisions of existing or prospective customers or the pace at which installation and training may occur, including decisions by our customers to delay or cancel implementations. If we experience longer sales, installation and implementation cycles for our solutions, we may experience delays in generating, or a decreased ability to generate, revenue from these solutions, which could have a material adverse impact on our business, results of operations or financial condition. Furthermore, significant delays or failures to meet milestones established in our customer contracts may result in breach of contract, termination of the contract, damages and/or penalties as well as a reduction in our margins or a delay in our ability to recognize revenue.
61
Table of Contents
We may be a party to legal, regulatory and other proceedings that could result in unexpected adverse outcomes.
From time to time, we have been, are and may in the future be, a party to legal and regulatory proceedings and investigations, including matters involving governmental agencies and entities with which we do business and other proceedings and investigations arising in the ordinary course of business, as described in more detail above. In addition, there are an increasing number of, and we may be subject to, investigations and proceedings in the healthcare industry generally that seek recovery under HIPAA, AKS, the FCA, the CMP, the Stark Law, the Sunshine Act, state laws and other statutes and regulations applicable to our business as described in more detail above. For example, we are currently subject to two overlapping putative class action complaints in Wisconsin federal court, alleging that we charged a fee to obtain certified healthcare bills for patients provided in the ordinary course of business in excess of Wisconsin state statutory limits. These and other similar statutory requirements impose statutory penalties for proven violations, which could become significant. While we intend to vigorously defend itself, the ultimate outcome and potential financial impact to us is not determinable at this time given the preliminary stage of these proceedings. We also may be subject to legal proceedings under non-healthcare federal, state and international laws affecting our business, such as the TCPA, FDCPA, FCRA, CAN-SPAM Act, Junk Fax Act, FCPA, the California Consumer Privacy Act of 2018, GDPR, employment, banking and financial services and USPS laws and regulations, as further detailed above. Such proceedings are inherently unpredictable, and the outcome can result in verdicts and/or injunctive relief that may affect how we operate our business or we may enter into settlements of claims for monetary payments. In some cases, substantial non-economic remedies or punitive damages may be sought. Governmental investigations, audits and other reviews could also result in criminal penalties or other sanctions, including restrictions, changes in the way we conduct business or exclusion from participation in government programs. We evaluate our exposure to these legal and regulatory proceedings and establish reserves for the estimated liabilities in accordance with GAAP. Assessing and predicting the outcome of these matters involves substantial uncertainties. Unexpected outcomes in these legal proceedings, or changes in management’s evaluations or predictions and accompanying changes in established reserves, could have a material adverse impact on our business, results of operations or financial condition.
Litigation is costly, time-consuming and disruptive to normal business operations. The defense of these matters could also result in continued diversion of our management’s time and attention away from business operations, which could also harm our business. Even if these matters are resolved in our favor, the uncertainty and expense associated with unresolved legal proceedings could harm our business and reputation.
The failure to successfully implement a new enterprise resource planning system could adversely impact our business and results of operations.
We are in a multi-year process of implementing a new Enterprise Resource Planning (“ERP”) business solution to create a system of integrated applications to manage our businesses and automate many functions related to financial reporting, human resources and other services. It is our intent through this ERP to integrate the major facets of our organization in order to improve planning, development, processes, sales, human resources management and other applications as they affect our evolving business model. ERP implementations are complex and time-consuming projects that require transformations of business and financial processes in order to reap the benefits of the ERP system; any such transformation involves risk inherent in the conversion to a new computer system, including loss of information and potential disruption to normal operations. Additionally, if the ERP system is not effectively implemented as planned, or the system does not operate as intended, the effectiveness of our internal controls over financial reporting could be adversely affected or our ability to assess those controls adequately could be delayed. Any failure(s) during this continued implementation process to develop, implement or maintain effective internal controls or to improve our internal controls could harm our operating results or cause us to fail to meet our reporting obligations. In addition, if we experience interruptions in service or operational difficulties and are unable to effectively manage our business during or following the implementation of the ERP, our business and results of operations could be harmed.
62
Table of Contents
Changes in accounting standards issued by the Financial Accounting Standards Board (“FASB”) or other standard-setting bodies may adversely affect our financial statements.
Our financial statements are subject to the application of GAAP, which is periodically revised and/or expanded. From time to time, we are required to adopt new or revised accounting standards issued by recognized authoritative bodies. For example, in April 2019 we adopted ASC 606, which replaced most prior general and industry specific revenue recognition guidance with a principles-based comprehensive revenue recognition framework. The adoption of ASC 606 resulted in significant changes to, among other things, how we report revenue resulting in increased expense to us and decreased comparability of our financial statements to prior historic periods. It is possible that future accounting standards we are required to adopt may require changes to the current accounting treatment that we apply to our consolidated financial statements and may require us to make significant changes to our systems and incur additional costs. Such changes could result in a material adverse impact on our financial position and results of operations.
Substantial indebtedness of our subsidiaries could adversely affect our financial condition, adversely affect our ability to operate our business, adversely affect our ability to react to changes in the economy or our industry, adversely affect our subsidiaries’ ability to meet obligations under our outstanding indebtedness and divert our cash flow from operations for debt payments.
Our subsidiaries have a substantial amount of debt, which requires significant interest and principal payments. As of March 31, 2020, our total was approximately $4,989.1 million. In addition, as of March 31, 2020, we had $529.9 million of availability to incur additional indebtedness under the senior secured revolving credit facility (the “Revolving Facility”). On July 3, 2019 the commitment amount of the Revolving Facility was increased from $500.0 million to $785.0 million. Subject to the limits contained in the credit agreement (the “Credit Agreement”) that governs the Revolving Facility and the senior secured term loan facility the (“Term Loan Facility” and, together with the Revolving Facility, the “Senior Credit Facilities”) and the indenture that governs the senior notes (the “Senior Notes”), we may be able to incur substantial additional debt from time to time to finance working capital, capital expenditures, investments or acquisitions, or for other purposes. If we do so, the risks related to the high level of debt could increase. Specifically, the high level of debt could have important consequences, including the following:
| • | it may be difficult for our subsidiaries to satisfy their obligations, including debt service requirements under outstanding debt; |
| • | our ability to obtain additional financing for working capital, capital expenditures, debt service requirements, acquisitions or other general corporate purposes may be impaired; |
| • | a substantial portion of cash flow from operations are required to be dedicated to the payment of principal and interest on indebtedness, therefore reducing our ability to use our cash flow to fund our operations, capital expenditures, future business opportunities and other purposes; |
| • | we could be more vulnerable to economic downturns and adverse industry conditions and our flexibility to plan for, or react to, changes in our business or industry is more limited; |
| • | our ability to capitalize on business opportunities and to react to competitive pressures, as compared to our competitors, may be compromised due to our high level of debt and the restrictive covenants in the Credit Agreement that governs the Senior Credit Facilities and the indenture that governs the Senior Notes; |
| • | our ability to borrow additional funds or to refinance debt may be limited; and |
| • | such indebtedness may cause potential or existing customers to not contract with it due to concerns over our ability to meet our financial obligations under such contracts. |
63
Table of Contents
Our subsidiaries’ ability to make scheduled payments on and to refinance our indebtedness depends on and is subject to our financial and operating performance, which in turn is affected by general and regional economic, financial, competitive, business and other factors and reimbursement actions of governmental and commercial payers, all of which are beyond our control, including the availability of financing in the international banking and capital markets. We cannot assure you that our business will generate sufficient cash flow from operations or that future borrowings will be available to it in an amount sufficient to enable it to service our debt, to refinance our debt or to fund our other liquidity needs. Any refinancing or restructuring of the such indebtedness could be at higher interest rates and may require it to comply with more onerous covenants that could further restrict our business operations. Moreover, in the event of a default, the holders of such indebtedness could elect to declare such indebtedness be due and payable and/or elect to exercise other rights, such as the lenders under the Revolving Facility terminating their commitments thereunder and ceasing to make further loans or the lenders under the Senior Credit Facilities instituting foreclosure proceedings against their collateral, any of which could materially adversely affect our results of operations and financial condition.
Furthermore, all of the debt under the Senior Credit Facilities bears interest at variable rates. If interest rates increase, our debt service obligations on our Senior Credit Facilities would increase even though the amount borrowed remained the same, and our net income and cash flows, including cash available for servicing our indebtedness, would correspondingly decrease.
Our subsidiaries’ debt agreements impose significant operating and financial restrictions, which may prevent us from capitalizing on business opportunities.
The Credit Agreement that governs the Senior Credit Facilities and the indenture that governs the Senior Notes each impose significant operating and financial restrictions on us. These restrictions will limit our ability to, among other things:
| • | incur or guarantee additional debt or issue disqualified stock or preferred stock; |
| • | pay dividends and make other distributions on, or redeem or repurchase, capital stock; |
| • | make certain investments; |
| • | incur certain liens; |
| • | enter into transactions with affiliates; |
| • | merge or consolidate; |
| • | enter into agreements that restrict the ability of restricted subsidiaries to make dividends or other payments; |
| • | designate restricted subsidiaries as unrestricted subsidiaries; and |
| • | transfer or sell assets. |
As a result of these restrictions, we may be limited as to how we conduct our business, and we may be unable to raise additional debt or equity financing to compete effectively or to take advantage of new business opportunities. The terms of any future indebtedness we may incur could include more restrictive covenants. We cannot assure you that our subsidiaries will be able to maintain compliance with these covenants in the future and, if they fail to do so, that they will be able to obtain waivers from the lenders and/or amend the covenants. Failure to comply with the restrictive covenants described above as well as the terms of any future indebtedness could result in an event of default, which, if not cured or waived, could result in it being required to repay these borrowings before their due date. If our subsidiaries were forced to refinance these borrowings on less favorable terms or cannot refinance these borrowings, our results of operations and financial condition could be adversely affected.
64
Table of Contents
Changes in the method for determining LIBOR or the elimination of LIBOR could affect our results of operations or financial condition.
In July 2017, the Financial Conduct Authority (the authority that regulates LIBOR) announced it intends to stop compelling banks to submit rates for the calculation of LIBOR after 2021. The Alternative Reference Rates Committee (“ARRC”) has proposed that the Secured Overnight Financing Rate (“SOFR”) is the rate that represents best practice as the alternative to USD-LIBOR for use in derivatives and other financial contracts that are currently indexed to USD-LIBOR. The ARRC has proposed a paced market transition plan to SOFR from USD-LIBOR and organizations are currently working on industry wide and company specific transition plans as it relates to derivatives and cash markets exposed to USD-LIBOR. We are not able to predict when LIBOR will cease to be available or when there will be sufficient liquidity in the SOFR markets. Any changes adopted by the Financial Conduct Authority or other governing bodies in the method used for determining LIBOR may result in a sudden or prolonged increase or decrease in reported LIBOR. We have material contracts that are indexed to USD-LIBOR and is monitoring this activity and evaluating the related risks.
We are dependent upon distributions from our subsidiaries to pay taxes, pay any dividends, make any share repurchases and meet any debt obligations.
We have no material assets other than our ownership of our subsidiaries and therefore, no independent means of generating revenue. Our subsidiaries make distributions in amounts sufficient to cover all applicable taxes and dividends, if any, declared by us. Payments of dividends or repurchases of shares in the future, if any, will be at the discretion of our board of directors after taking into account various factors, including our business, operating results and financial condition, current and anticipated cash needs, plans for expansion and any legal or contractual limitations on our ability to pay dividends or repurchase shares. The existing Senior Secured Credit Facilities and Senior Notes include, and any financing arrangement that we enter into in the future may include, restrictive covenants that limit our ability to pay dividends and repurchase shares.
The amounts we or our subsidiaries will be required to pay under their tax receivable agreements could be significant and, in certain circumstances, could differ significantly (in both timing and amount) from the underlying tax benefits they actually realize.
Change, the Joint Venture and Change Healthcare Performance, Inc. (collectively, the “TRA Affiliates”), are a party to certain tax receivable agreements (collectively, the “tax receivable agreements”) and other similar agreements with current and former owners. One of the existing tax receivable agreements (the “McKesson Tax Receivable Agreement”) generally provides for the payment by the Joint Venture to affiliates of McKesson (the “McKesson TRA Parties”) of 85% of certain cash tax savings realized (or, in certain circumstances, deemed to be realized) by us and our subsidiaries in certain periods ending on or after the date on which McKesson ceases to own at least 20% of the Joint Venture (i.e. for periods commencing March 31, 2020 and onwards) as a result of (i) certain amortizable tax basis in assets transferred to the Joint Venture at the consummation of the Joint Venture Transactions and (ii) imputed interest deductions and certain other tax attributes arising from payments under the McKesson Tax Receivable Agreement. Change, the Joint Venture, McKesson and certain of McKesson’s affiliates have also entered into an amended and restated letter agreement (the “Letter Agreement”) pursuant to which McKesson may choose to allocate an amount of deductions related to certain amortizable tax basis in assets transferred to the Joint Venture at the consummation of the Joint Venture Transactions to us in excess of a specified minimum threshold, in which case we may be required to make cash payments to McKesson equal to 100% of our tax savings attributable to such excess deductions for any tax period ending prior to the date on which McKesson ceases to own at least 20% of the Joint Venture. Because McKesson ceased to own at least 20% of the Joint Venture during the year ended March 31, 2020, the Letter Agreement applies only to tax benefits obtained in the periods ended March 31, 2019 and earlier, of which we estimate there are none.
65
Table of Contents
Another existing tax receivable agreement (the “2017 Tax Receivable Agreement”) generally provides for the payment by Change Healthcare Performance, Inc. to affiliates of the Sponsors and certain other former stockholders of Change Healthcare Performance, Inc. (the “2017 TRA Parties”) of 85% of the net cash tax savings realized (or, in certain circumstances, deemed to be realized) by Change Healthcare Performance, Inc. and our subsidiaries in respect of periods ending on or after the Joint Venture Transactions as a result of certain net operating losses and certain other tax attributes of Change Healthcare Performance, Inc. as of the date of the Joint Venture Transactions.
A predecessor to Change Healthcare Performance, Inc. is party to certain tax receivable agreements (the “2009—2011 Tax Receivable Agreements,” and together with the 2017 Tax Receivable Agreement, the “Legacy CHC Tax Receivable Agreements”) which were assumed by the Joint Venture in connection with the Joint Venture Transactions and obligate the Joint Venture to make payments to certain of the former Legacy CHC Stockholders (the “2009—2011 CHC TRA Parties,” and collectively, with the McKesson TRA Parties and the 2017 TRA Parties, the “TRA Parties”), equal to 85% of the applicable cash savings that the Joint Venture realizes (or is deemed to realize) as a result of tax attributes arising from certain previous transactions. Because covered changes of control with respect to the 2009—2011 Tax Receivable Agreements previously occurred as a result of the Joint Venture Transactions and other previous reorganizations, payments the Joint Venture makes under the 2009—2011 Tax Receivable Agreements are calculated using certain valuation assumptions, including that the Joint Venture will have sufficient taxable income to use the applicable tax attributes and that certain of such tax attributes will be used by the Joint Venture on a pro rata basis from the date of the Joint Venture Transactions (or in certain cases from the date of certain previous transactions) through the expiration of the applicable tax attribute.
The payments the TRA Affiliates may be required to make under these tax receivable agreements could be substantial. The amount and timing of any payments under the tax receivable agreements will vary depending upon a number of factors, including the amount and timing of the taxable income we generate in the future and the tax rate then applicable. We expect that, assuming no material changes in tax law and that the Joint Venture earns sufficient taxable income to realize the full potential tax benefit of the tax attributes in respect of which it is required to make payments under the Legacy CHC Tax Receivable Agreements and McKesson Tax Receivable Agreements, future payments under the Tax Receivable Agreements will range from $17.6 million to $85.8 million per year over the next 11 years and from $0.0 to $13.7 million per year over the following 10 years. As of March 31, 2020, we expect total remaining payments under the Tax Receivable Agreements of approximately $479.4 million. See Note 17, Tax Receivable Agreement Obligations within Item 8 of this Form 10-K. Because payments under the McKesson Tax Receivable Agreement are contingent upon McKesson’s determination to allocate certain excess deductions to us, which may be subject to change until the filing of a tax return for a relevant period, the amount of any payments under such agreement may change if McKesson alters the allocations estimated as of March 31, 2020 prior to filing the tax return for the period.
There may be circumstances in which the payments under the tax receivable agreements differ significantly (in both timing and amount) from the underlying tax benefits the TRA Affiliates actually realize. Pursuant to the tax receivable agreements, upon a covered change of control, the TRA Affiliates could be required to make payments that significantly exceed the actual cash tax savings from the tax benefits giving rise to such payments. As noted above, with respect to the 2009—2011 Tax Receivable Agreements, covered changes of control previously occurred as a result of the Joint Venture Transactions and other previous reorganizations. Moreover, in certain circumstances, the TRA Affiliates will have the option to terminate the tax receivable agreements in exchange for a lump-sum payment (based on an assumption that all expected potential tax benefits actually will be realized). In addition, under the tax receivable agreements, none of the TRA Parties will reimburse the TRA Affiliates for any payments previously made if such tax benefits are subsequently disallowed, except that excess payments made to a TRA Party will be netted against payments otherwise to be made, if any, after the determination of such excess. As a result, in such circumstances, the TRA Affiliates could make payments under the tax receivable agreements that are greater than the actual cash tax savings and may not be able to recoup those payments. Any difference between the payments the TRA Affiliates are required to make under the tax
66
Table of Contents
receivable agreements and the underlying tax benefits actually realized could adversely affect our business or financial condition. Furthermore, because certain of the TRA Affiliates are holding companies with no operations of their own, their ability to make payments under each relevant tax receivable agreement is substantially dependent on the ability of their subsidiaries to make distributions to them. To the extent that the TRA Affiliates are unable to make payments under the tax receivable agreements for any reason, such payments will be deferred and will accrue interest until paid.
We continue to rely on McKesson and our affiliates for certain transition services. The inability or unwillingness of McKesson or our affiliates to provide such services in a timely or effective manner could materially adversely affect our business, results of operations or financial condition.
We continue to rely on McKesson to provide us with certain services for our business and customers pursuant to the terms of a transition services agreement (the “McKesson Transition Services Agreement”). Certain of these services are essential to our efficient operation. After the transition period, we may be unable to provide these services internally because of financial or other constraints, and we may be unable to implement substitute arrangements on a timely and cost-effective basis on terms that are favorable to us, or at all. In addition, McKesson may fail to perform such transition services in a timely or effective manner, or at all, during the term of the McKesson Transition Services Agreement, either due to our inability or unwillingness to continue such services or for other reasons. If there is an interruption in such services prior to expiration of the McKesson Transition Services Agreement, or if such services are inadequate, we will be required to provide these services itself or to obtain substitute arrangements with third parties on a faster timeline than anticipated, which may be challenging without significant effort or expense. Any failure by McKesson to perform such transition services, or any failure by us to replace such transition services with acceptable arrangements when necessary, could have a material adverse impact on our business, results of operations or financial condition. See “Other Agreements and Other Related Party Transactions—Transition Services Agreements.”
Our internal controls over financial reporting currently do not meet all of the standards contemplated by Section 404 of the Sarbanes-Oxley Act, and failure to achieve and maintain effective internal controls over financial reporting in accordance with Section 404 of the Sarbanes-Oxley Act could have a material adverse effect on our business and common stock price.
Our internal controls over financial reporting currently do not meet all of the standards contemplated by Section 404 of the Sarbanes-Oxley Act that eventually we will be required to meet. Because currently we do not have comprehensive documentation of our internal controls and have not yet tested our internal controls in accordance with Section 404, we cannot conclude in accordance with Section 404 that it does not have a material weakness in our internal controls or a combination of significant deficiencies that could result in the conclusion that we have a material weakness in our internal controls. Once we are no longer an emerging growth company, which we expect to occur with respect to fiscal year 2021, our independent registered public accounting firm will be required to attest to the effectiveness of our internal control over financial reporting on an annual basis. If we are not able to complete our initial assessment of our internal controls and otherwise implement the requirements of Section 404 in a timely manner or with adequate compliance, our independent registered public accounting firm may not be able to certify as to the adequacy of our internal controls over financial reporting.
Matters impacting our internal controls may cause us to be unable to report our financial information on a timely basis and thereby subject us to adverse regulatory consequences, including sanctions by the SEC or violations of applicable stock exchange listing rules, which may result in a breach of the covenants under existing or future financing arrangements. There also could be a negative reaction in the financial markets due to a loss of investor confidence in us and the reliability of our financial statements. Confidence in the reliability of our financial statements also could suffer if we or our independent registered public accounting firm were to report a material weakness in our internal controls over financial reporting. This could materially adversely affect us and lead to a decline in the price of our Common Stock.
67
Table of Contents
If securities or industry analysts do not publish research or reports about our business, or if they downgrade their recommendations regarding our Common Stock, the price and trading volume of our Common Stock could decline.
The trading market for our Common Stock is influenced by the research and reports that industry or securities analysts publish about us or our business. If any of the analysts who cover us downgrade our Common Stock or publish inaccurate or unfavorable research about our business, the trading price of our Common Stock may decline. If analysts cease coverage of us or fail to regularly publish reports on us, we could lose visibility in the financial markets, which in turn could cause the trading price or trading volume of our Common Stock to decline and our Common Stock to be less liquid.
You may be diluted by the future issuance of additional shares of our Common Stock in connection with our incentive plans, acquisitions or otherwise.
As of March 31, 2020, we had approximately 8,696,600,000 shares of our Common Stock authorized but unissued. Our Amended and Restated Certificate of Incorporation authorizes us to issue authorized but unissued shares of our Common Stock and options, rights, warrants and appreciation rights relating to our Common Stock for the consideration and on the terms and conditions established by our board of directors in our sole discretion, whether in connection with acquisitions or otherwise. Additionally, there are an aggregate of 25,000,000 shares of our Common Stock reserved for issuance under our 2019 Omnibus Incentive Plan, 19,114,543 shares of our Common Stock reserved for issuance under or that may otherwise vest pursuant to outstanding equity awards issued pursuant to our legacy 2009 equity incentive plan and an aggregate of 15,000,000 shares of our Common Stock reserved for issuance under our Employee Stock Purchase Plan (“ESPP”). Any Common Stock that we issue, including under our Omnibus Incentive Plan, our legacy 2009 equity incentive plan, our ESPP or other equity incentive plans that we may adopt in the future, would dilute the percentage ownership held by our stockholders.
As of March 31, 2020, we also have 5,137,345 TEUs outstanding. Unless settled earlier as described below, each purchase contract that is a component of a TEU will settle automatically on the mandatory settlement date into between 3.2051 and 3.8461 shares of our Common Stock, subject to certain anti-dilution adjustments. The number of shares of Common Stock issuable upon settlement will be determined based on the average volume weighted average price per share of Common Stock over the 20 consecutive trading day period beginning on and including the 21st scheduled trading day immediately preceding the mandatory settlement date in accordance with the purchase contract agreement. Assuming automatic settlement at the rate of 3.8461 shares of Common Stock per purchase contract assuming the maximum number of shares issuable upon automatic settlement of such purchase contracts, up to 2,181,086 shares of Common Stock are issuable upon settlement of the purchase contracts that are a component of the TEUs, subject to certain anti-dilution adjustments.
At any time prior to the second scheduled trading day immediately preceding June 30, 2022, holders of the purchase contracts may elect to settle purchase contracts early and we will deliver shares of our Common Stock at the minimum settlement rate of shares of our Common Stock per purchase contract, subject to certain anti-dilution adjustments. If holders elect to settle any purchase contracts early in connection with a fundamental change, such purchase contracts will be settled at the fundamental change early settlement rate, which may be greater than the minimum settlement rate. See “Description of Change Healthcare Inc. Tangible Equity Units.”
Any of these issuances may dilute your ownership interest and any of these events or the perception that these events and/or issuances could occur may have an adverse impact on the price of our Common Stock.
68
Table of Contents
Our TEUs may adversely affect the market price of our Common Stock.
The market price of our Common Stock is likely to be influenced by the TEUs. For example, the market price of our Common Stock could become more volatile and could be depressed by:
| • | investors’ anticipation of the potential resale in the market of a substantial number of additional shares of our Common Stock received upon settlement of the purchase contracts that are a component of the TEUs; |
| • | possible sales of our Common Stock by investors who view the TEUs as a more attractive means of equity participation in us than owning shares of our Common Stock; and |
| • | hedging or arbitrage trading activity that may develop involving the TEUs and our Common Stock. |
We may issue preferred stock whose terms could adversely affect the voting power or value of our Common Stock.
Our Amended and Restated Certificate of Incorporation authorizes us to issue, without the approval of our stockholders, one or more classes or series of preferred stock having such designations, preferences, limitations and relative rights, including preferences over our Common Stock respecting dividends and distributions, as our board of directors may determine. The terms of one or more classes or series of preferred stock could adversely impact the voting power or value of our Common Stock. For example, we might grant holders of preferred stock the right to elect some number of directors in all events or on the happening of specified events or the right to veto specified transactions. Similarly, the repurchase or redemption rights or liquidation preferences that might be assigned to holders of preferred stock could affect the residual value of our Common Stock.
Sales or issuances of a substantial amount of shares of our Common Stock in the public market, particularly sales by directors, executive officers and significant stockholders, or the perception that these sales or issuances may occur, or the settlement of the purchase contracts, could cause the market price of our Common Stock to decline and may make it more difficult for investors to sell their common stock at a time and price that they deem appropriate.
The sale or issuance of substantial amounts of shares of our Common Stock or other securities convertible or exchangeable into shares of Common Stock in the public market, or the settlement of the purchase contracts that are a component of the TEUs, or the perception that such sales or issuances could occur, could harm the prevailing market price of shares of our Common Stock. This could also impair our ability to raise additional capital through the sale of equity securities. Future sales or issuances of our Common Stock or other equity-related securities could be dilutive to our stockholders and could adversely affect their voting and other rights and economic interests, including holders of any shares of our Common Stock issued upon settlement of the purchase contracts. Our stockholders, including holders of any shares of our Common Stock issued upon settlement of the purchase contracts, may also experience additional dilution upon future vesting events, equity issuances, exercise of options to purchase our Common Stock or the settlement of restricted stock units granted to employees, executive officers and directors.
Beginning on June 8, 2020, certain of our legacy stockholders that continue to own a substantial amount of our Common Stock will have the right, subject to certain exceptions and conditions, to require us to register our shares of Common Stock owned by them under the Securities Act of 1933, as amended (the “Securities Act”) and they will have the right to participate in future registrations of securities by us. Registration of any of these outstanding shares of our Common Stock would result in such shares becoming freely tradable without compliance with Rule 144 upon effectiveness of the registration statement.
The market price of shares of our Common Stock could drop significantly if these stockholders are perceived by the market as intending to sell them. These factors could also make it more difficult for us to raise additional funds through future offerings of our Common Stock or other securities.
69
Table of Contents
Anti-takeover provisions in our organizational documents and Delaware law might discourage or delay acquisition attempts that you might consider favorable.
Our Amended and Restated Certificate of Incorporation and our Amended and Restated Bylaws contain provisions that may make the merger or acquisition of us more difficult without the approval of our board of directors. Among other things, these provisions:
| • | would allow us to authorize the issuance of shares of one or more series of preferred stock, including in connection with a stockholder rights plan, financing transactions or otherwise, the terms of which series may be established and the shares of which may be issued without stockholder approval, and which may include super voting, special approval, dividend, or other rights or preferences superior to the rights of our stockholders; |
| • | prohibit stockholder action by written consent from and after the date on which the parties to our stockholders agreement and their affiliates cease to beneficially own at least 30% of the total voting power of all then outstanding shares of our capital stock entitled to vote generally in the election of directors unless such action is recommended by all directors then in office; |
| • | provide for certain limitations on convening special stockholder meetings; |
| • | provide (i) that the board of directors is expressly authorized to make, alter, or repeal our Amended and Restated Bylaws and (ii) that, at any time the Sponsors beneficially own, in the aggregate, less than 30% in voting power of the stock entitled to vote generally in the election of directors, our stockholders may only amend our Amended and Restated Bylaws with the approval of 80% or more of all of the outstanding shares of our capital stock entitled to vote; and |
| • | establish advance notice requirements for nominations for elections to our board or for proposing matters that can be acted upon by stockholders at stockholder meetings. |
Further, as a Delaware corporation, we are also subject to provisions of Delaware law, which may impede or discourage a takeover attempt that our stockholders may find beneficial. These anti-takeover provisions and other provisions under Delaware law could discourage, delay or prevent a transaction involving a change in control of us, including actions that our stockholders may deem advantageous, or could negatively affect the trading price of our Common Stock. These provisions could also discourage proxy contests and make it more difficult for you and other stockholders to elect directors of your choosing and to cause us to take other corporate actions you desire. For a further discussion of these and other such anti-takeover provisions, see “Description of Change Healthcare Inc. Capital Stock—Anti-Takeover Effects of our Amended and Restated Certificate of Incorporation and Amended and Restated Bylaws and Certain Provisions of Delaware Law.”
Our Amended and Restated Certificate of Incorporation designates the Court of Chancery of the State of Delaware as the sole and exclusive forum for certain types of actions and proceedings that may be initiated by our stockholders, which could limit our stockholders’ ability to obtain a favorable judicial forum for disputes with us or our directors, officers or other employees.
Our Amended and Restated Certificate of Incorporation provides that, unless we consent in writing to the selection of an alternative forum, any (i) derivative action or proceeding brought on behalf of us, (ii) action asserting a claim of breach of a fiduciary duty owed by any of our directors, officers, stockholder or employees, (iii) action asserting a claim arising pursuant to any provision of the DGCL or our Amended and Restated Certificate of Incorporation or our Amended and Restated Bylaws or (iv) action asserting a claim governed by the internal affairs doctrine, shall, to the fullest extent permitted by law, be exclusively brought in the Court of Chancery of the State of Delaware or, if such court does not have subject matter jurisdiction thereof, the federal district court of the State of Delaware. The Court of Chancery of the State of Delaware is not the sole and exclusive forum for actions brought under the federal securities laws. Section 27 of the Exchange Act creates exclusive federal jurisdiction over all suits brought to enforce any duty or liability created by the Exchange Act
70
Table of Contents
or the rules and regulations thereunder, and Section 22 of the Securities Act creates concurrent jurisdiction for federal and state courts over all suits brought to enforce any duty or liability created by the Securities Act or the rules and regulations thereunder. Our Amended and Restated Certificate of Incorporation provides that notwithstanding anything otherwise to the contrary therein, the forum selection provisions will not apply to suits brought to enforce a duty or liability created by the federal securities laws or any other claim for which the federal courts have exclusive jurisdiction. Any person or entity purchasing or otherwise acquiring any interest in any shares of our capital stock shall be deemed to have notice of and to have consented to the forum provisions in our Amended and Restated Certificate of Incorporation. These choice-of-forum provisions may limit a stockholder’s ability to bring a claim in a different judicial forum, including one that it may find favorable or convenient for specified class of disputes with us or our directors, officers, other stockholders or employees, which may discourage such lawsuits. Alternatively, if a court were to find these provisions of our Amended and Restated Certificate of Incorporation inapplicable or unenforceable with respect to one or more of the specified types of actions or proceedings, we may incur additional costs associated with resolving such matters in other jurisdictions, which could materially and adversely affect our business, financial condition and results of operations and result in a diversion of the time and resources of our management and board of directors.
ITEM 1B. UNRESOLVED STAFF COMMENTS
None.
Our corporate headquarters is located in leased office space in Nashville, Tennessee, and consists of approximately 178,000 square feet. The lease expires on October 31, 2022.
We also lease a number of operations, business and sales offices and other facilities in several states and in international locations. We believe that our facilities are generally adequate for our current anticipated and future use, although we may from time to time lease additional facilities or vacate existing facilities as our operations require.
The Company is involved in various legal proceeds in the ordinary course of business. We believe that the ultimate disposition of such proceedings will not have a material adverse effect on the Company’s consolidated financial position, results of operations or liquidity. See Note 20, Legal Proceedings, to our consolidated financial statements.
ITEM 4. MINE SAFETY DISCLOSURES
Not applicable.
71
Table of Contents
PART II
ITEM 5. MARKET FOR THE REGISTRANT’S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
Common Stock
The Company’s common stock is listed on The Nasdaq Stock Market under the ticker symbol “CHNG”.
Holders
As of June 1, 2020, we had approximately 108 holders of record of the Company’s common stock. The actual number of stockholders is greater than this number of record holders and includes stockholders who are beneficial owners but whose shares are held in street name by brokers and other nominees.
Dividends
The Company has not declared or paid any dividends on shares of common stock and does not intend to pay dividends in the foreseeable future. The declaration, amount, and payment of any future dividend will be at the sole discretion of the Company’s board of directors, and the Company may reduce or discontinue entirely the payment of such dividends at any time. The board of directors may take into account general and economic conditions, its financial condition and operating results, its available cash and current and anticipated cash needs, capital requirements, contractual, legal, tax and regulatory restrictions and implications on the payment of dividends by the Company to its stockholders or by its subsidiaries (including the Joint Venture) to it, and such other factors as its board of directors may deem relevant.
Issuer Purchases of Equity Securities
We did not purchase any shares of our common stock during the three months ended March 31, 2020.
Unregistered Sales of Equity Securities and Use of Proceeds
None.
Performance Graph
The following graph compares the cumulative stockholder return on our common stock between June 27, 2019 (the date of our initial public offering) and March 31, 2020, to the cumulative total returns of the S&P 500 Health Care Index and the NASDAQ Composite Index over the same period.
All values assume a $100 initial investment at market close on June 27, 2019. The initial public offering price of our common stock, which had a closing stock price of $15.00 on June 27, 2019, was $13.00 per share. The comparisons are based on historical data and are not indicative of, nor intended to forecast, the future performance of our common stock.
72
Table of Contents
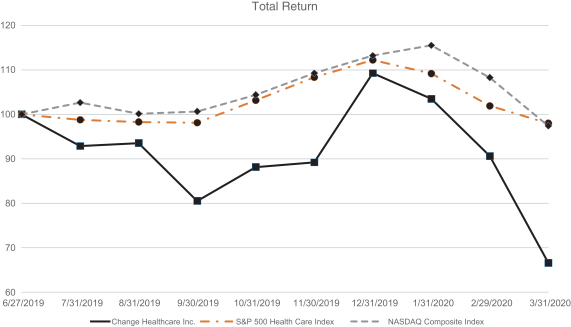
| Pricing Date |
CHNG ($) | S&P 500 Health Care Index ($) |
NASDAQ Composite Index ($) |
|||||||||
| 6/27/2019 | 100.00 | 100.00 | 100.00 | |||||||||
| 7/31/2019 | 92.87 | 98.77 | 102.65 | |||||||||
| 8/31/2019 | 93.53 | 98.28 | 100.13 | |||||||||
| 9/30/2019 | 80.53 | 98.12 | 100.66 | |||||||||
| 10/31/2019 | 88.13 | 103.14 | 104.40 | |||||||||
| 11/30/2019 | 89.20 | 108.33 | 109.25 | |||||||||
| 12/31/2019 | 109.27 | 112.22 | 113.21 | |||||||||
| 1/31/2020 | 103.47 | 109.17 | 115.51 | |||||||||
| 2/29/2020 | 90.60 | 101.89 | 108.27 | |||||||||
| 3/31/2020 | 66.60 | 98.00 | 97.41 | |||||||||
ITEM 6. SELECTED FINANCIAL DATA
Change Healthcare Inc.
| (in thousands, except per share amount) Statement of Operations Data: |
Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
Period of June 22, 2016 (inception) to March 31, 2017 |
||||||||||||
| Net revenue |
$ | 196,792 | $ | — | $ | — | $ | — | ||||||||
| Loss from Equity Method Investment in the Joint Venture |
$ | 380,713 | $ | 70,487 | $ | 58,680 | $ | 43,103 | ||||||||
| Net income (loss) |
$ | (947,597 | ) | $ | (52,012 | ) | $ | 60,955 | $ | (26,294 | ) | |||||
| Net income (loss) per share - basic |
$ | (6.92 | ) | $ | (0.69 | ) | $ | 0.81 | $ | (3.18 | ) | |||||
| Net income (loss) per share - diluted |
$ | (6.92 | ) | $ | (0.69 | ) | $ | 0.78 | $ | (3.18 | ) | |||||
73
Table of Contents
| Balance Sheet Data (at period end): |
March 31, 2020 |
March 31, 2019 |
March 31, 2018 |
|||||||||
| Current assets |
$ | 1,401,181 | $ | 5,563 | $ | 16,129 | ||||||
| Long-term assets |
$ | 8,706,199 | $ | 1,293,260 | $ | 1,357,875 | ||||||
| Current liabilities |
$ | 1,059,789 | $ | 6,343 | $ | 16,129 | ||||||
| Long-term liabilities |
$ | 5,762,144 | $ | 159,993 | $ | 18,303 | ||||||
Change Healthcare LLC
| (in thousands, except per share amount) Statement of Operations Data: |
Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
Period of June 22, 2016 (inception) to March 31, 2017 |
||||||||||||
| Net revenue |
$ | 3,302,973 | $ | 3,281,729 | $ | 3,298,843 | $ | 309,587 | ||||||||
| Cost of operations (exclusive of depreciation and amortization) |
$ | 1,345,920 | $ | 1,354,655 | $ | 1,407,893 | $ | 133,688 | ||||||||
| Customer postage |
$ | 228,079 | $ | 238,618 | $ | 274,397 | $ | 26,132 | ||||||||
| Net income (loss) |
$ | (5,617 | ) | $ | 176,670 | $ | 192,442 | $ | (83,592 | ) | ||||||
| Net income (loss) per share - basic |
$ | (0.02 | ) | $ | 0.70 | $ | 0.76 | $ | (3.03 | ) | ||||||
| Net income (loss) per share - diluted |
$ | (0.02 | ) | $ | 0.70 | $ | 0.76 | $ | (3.03 | ) | ||||||
| Balance Sheet Data (at period end): |
March 31, 2020 |
March 31, 2019 |
March 31, 2018 |
|||||||||
| Current assets |
$ | 1,424,547 | $ | 980,463 | $ | 901,712 | ||||||
| Long-term assets |
$ | 5,205,619 | $ | 5,223,675 | $ | 5,299,215 | ||||||
| Current liabilities |
$ | 1,186,791 | $ | 889,783 | $ | 969,495 | ||||||
| Long-term liabilities |
$ | 5,346,955 | $ | 6,219,141 | $ | 6,297,612 | ||||||
ITEM 7. MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
The following Management’s Discussion and Analysis of Financial Condition and Results of Operations (“MD&A”) is intended to help the reader understand our results of operations and financial condition. The MD&A is provided as a supplement to, and should be read in conjunction with, Change Healthcare Inc.’s and Change Healthcare LLC’s audited financial statements and the accompanying notes.
In addition to historical data, the discussion contains forward-looking statements about the business, operations and financial performance of Change Healthcare Inc. and Change Healthcare LLC based on current expectations that involve risks, uncertainties and assumptions. Actual results may differ materially from those discussed in the forward-looking statements as a result of various factors, including but not limited to those discussed in “Cautionary Notice Regarding Forward-Looking Statements” and “Risk Factors” above.
For a discussion of the comparison of the fiscal years ended March 31, 2019 and 2018, see the Results of Operations section disclosed in “Management’s Discussion and Analysis of Financial Condition and Results of Operations” of our registration statement on Form S-4, as amended (Registration No. 333-236234), which was declared effective by the Securities and Exchange Commission on February 28, 2020.
74
Table of Contents
Change Healthcare Inc.
Overview
Change Healthcare Inc. (formerly HCIT Holdings, Inc.), a Delaware corporation, was formed on June 22, 2016 to hold an equity investment in Change Healthcare LLC, a joint venture between Change Healthcare Inc. and McKesson Corporation (“McKesson”), which we refer to as the Joint Venture. Prior to the Merger described below, Change Healthcare Inc. accounted for this investment using the equity method of accounting. Subsequent to the Merger, Change Healthcare Inc. owns 100% of Change Healthcare LLC, and as a result, consolidates the financial statements of Change Healthcare LLC.
Due to the timing of the Merger, Change Healthcare Inc. had no substantive assets apart from its investment in the Joint Venture for the majority of its fiscal year. As a result, Change Healthcare Inc. believes the financial statements of the Joint Venture are more relevant to an investor than Change Healthcare Inc.’s financial statements as they include greater detail regarding the financial condition and results of operations of the business.
Recent Developments
Effective June 26, 2019, Change Healthcare Inc.’s Registration Statement on Form S-1 for the initial public offering of 49.3 million shares of common stock and the concurrent offering of 5.75 million tangible equity units (“TEUs”) was declared effective by the Securities and Exchange Commission (“SEC”) and Change Healthcare Inc. subsequently amended its charter to authorize 9.0 billion shares of common stock and effected a 126.4 for 1 split of its common stock. Change Healthcare Inc.’s common stock and TEUs began trading the next day on the NASDAQ under the “CHNG” and “CHNGU” ticker symbols, respectively.
On July 1, 2019, the offerings of common stock and TEUs were consummated and resulted in Change Healthcare Inc. receiving net proceeds of $608.7 million and $278.9 million respectively, before consideration of offering costs paid subsequent to the offering from available cash. The proceeds of the offering of common stock were subsequently contributed to the Joint Venture in exchange for 49.3 million additional units of the Joint Venture, thereby resulting in an additional ownership in the Joint Venture of approximately 11%. The proceeds of the offering of TEUs were used to acquire TEUs of the Joint Venture that substantially mirror the terms of the TEUs issued by Change Healthcare Inc. in the offering. The Joint Venture, in turn, used the proceeds received from Change Healthcare Inc. to repay $805.0 million of its indebtedness under the Term Loan Facility (as defined herein) without penalty in July 2019.
In March 2020, McKesson completed a split-off of its interest in the Joint Venture (“Qualified McKesson Exit”) through an exchange offer of its common stock for shares of PF2 SpinCo, Inc, a Delaware corporation and wholly owned subsidiary of McKesson (“SpinCo”). On March 10, 2020 (the “Merger Effective Date”), pursuant to the Agreement and Plan of Merger, dated December 20, 2016 (the “Merger Agreement”), by and among Change Healthcare Inc., McKesson and SpinCo, Change Healthcare Inc. combined with SpinCo in a two-step all-stock “Reverse Morris Trust” transaction that involved (i) a separation of SpinCo from McKesson pursuant to the Separation and Distribution Agreement, dated February 10, 2020 (the “Separation Agreement”), followed by (ii) the merger of SpinCo with and into Change Healthcare Inc., with Change Healthcare Inc. as the surviving company (such merger, together with the other transactions contemplated by the Merger Agreement, the “Merger”).
The Merger was consummated pursuant to the Merger Agreement and the Separation Agreement. As a result, the Joint Venture became a wholly owned subsidiary of Change Healthcare Inc. Pursuant to the Merger Agreement, McKesson accepted 15,426,537 shares of its own common stock, par value $0.01 in exchange for all 175,995,192 issued and outstanding shares of SpinCo common stock, par value $0.001 per share (the “SpinCo Common Stock”). All shares of SpinCo Common Stock were then converted into an equal number of shares of common stock of Change Healthcare Inc., par value $0.001, which Change Healthcare Inc. issued to the former holders of SpinCo Common Stock, together with cash in lieu of any fractional shares.
75
Table of Contents
Subsequent to the Merger, McKesson no longer holds any equity or voting interest in the Joint Venture.
Factors Affecting Results of Operations
Qualified McKesson Exit
Through the Merger, Change Healthcare Inc. acquired the interest in the Joint Venture that it did not own prior to the transaction. As a result, for the period from March 10, 2020 to March 31, 2020, Change Healthcare LLC was a wholly-owned subsidiary of Change Healthcare Inc. and consolidated the financial position and results of Change Healthcare LLC in its financial statements as of and for the year ended March 31, 2020.
Change Healthcare Inc. accounted for the Qualified McKesson Exit and related transactions as a business combination achieved in stages in accordance with Financial Accounting Standards Board (“FASB”) Accounting Standards Codification (“ASC”) 805, Business Combinations, resulting in a new basis of accounting. As a result, Change Healthcare Inc. remeasured its investment in the Joint Venture to fair value as of the date control was obtained and recognized a loss in its statement of operations for the difference in the carrying value and fair value of this investment of approximately $230.2 million. Further, Change Healthcare Inc. recognized the consideration transferred, as well as the acquired business’s identifiable assets, liabilities and noncontrolling interests at their acquisition date fair value. The excess of the consideration transferred over the fair value of the identifiable assets, liabilities and noncontrolling interest, was recorded as goodwill.
As a result of the accounting for these transactions and the change in basis of accounting, the consolidated results of Change Healthcare Inc. in periods following the Merger will not be comparable to the consolidated results of the Joint Venture in periods prior to the Merger. The following are certain of the more significant changes resulting from the Qualified McKesson Exit that will affect the comparability of financial results and operations:
| • | Increased tangible and intangible assets resulting from adjusting the basis of the assets to their fair value, which will also result in increased depreciation and amortization expense. |
| • | Decrease in long-term debt as a result of adjustments to state the long-term debt at its fair value. |
| • | Decreased deferred revenue as a result of recognizing deferred revenue only to the extent that contractual obligations remain to be fulfilled. These decreases will result in decreased solutions revenue in the near term. |
| • | Income currently attributable to the Joint Venture and not subject to U.S. federal income taxes and most state and local income taxes will become subject to such taxes, resulting in an increase in Change Healthcare Inc.’s effective tax rate compared with the historical effective tax rate of the Joint Venture. |
See Note 2, Business Combinations for additional information.
Macroeconomic and Industry Trends
The spread of COVID-19 both globally and in the U.S. has driven lower healthcare utilization as a result of the significant reduction in, or in some cases elimination of, elective medical procedures and healthcare visits, without a corresponding increase in COVID-19 related transactions. A portion of Change Healthcare Inc.’s business is tied to overall volumes of activity in the healthcare system, and therefore has been adversely impacted by this industry trend. Further, weakened economic conditions or a recession could reduce the amounts patients are willing or able to spend on healthcare services. As a result, patients may elect to delay or forgo seeking healthcare services and recent increases in unemployment rates is likely to cause commercial payer membership to decline, which could further reduce healthcare utilization and transaction volumes. While we began to see the impact of COVID-19 on our business and financial results late in fiscal year 2020, we expect to see a much more significant impact starting in the first quarter of fiscal year 2021.
76
Table of Contents
In response to COVID-19, we initiated a number of actions with our employees’ health being our first priority. We also focused on serving our customers and introducing new products and services to address their previously unexpected but now urgent needs related to COVID-19. To ensure our business continuity and the safety and welfare of our team members, we moved the majority of our employees to work from home, shifted to a virtual meeting environment, suspended all non-critical business travel, and expanded telehealth and COVID-19 related PTO coverage to all employees. We also did a comprehensive review of our cost structure to balance costs with interim variability in our revenue and have actively aligned our staffing level, primarily in our Technology-Enabled Services segment to address lower interim volume. Starting in March 2020, we initiated hiring freezes, began contractor reductions and made other staffing reductions, primarily in the form of furloughs to provide us with greater flexibility to scale back up as volumes recover. We expect to start to see the impact of these actions late in the first quarter and into the second quarter of fiscal year 2021.
While lower healthcare utilization will impact our results negatively this year, we cannot predict the length of time it may take for normal healthcare volumes to return and the extent to which our business, results of operations, financial condition or liquidity will ultimately be impacted by COVID-19. However, we continue to assess its impact on our business and are actively managing our response as the pandemic evolves. We believe the solutions we provide our customers will be as important, if not more, post-COVID-19. For further details on the potential impact of COVID-19 on our business, refer to Risk Factors in Item 1A of this Form 10-K.
Post-Merger Consolidation
As referenced above, Change Healthcare Inc. consolidated the results of the Joint Venture for the period subsequent to the Merger. While this 21-day period is included in Change Healthcare Inc.’s results, Change Healthcare Inc. believes the results of operations of the Joint Venture are more meaningful to an investor. Therefore, below are the key factors affecting the results of operations that are not related to the consolidated results of the Joint Venture.
Loss from Equity Method Investment in the Joint Venture
Loss from equity method investment in the Joint Venture generally represents Change Healthcare Inc.’s proportionate share of the income or loss from this investment, including basis adjustments related to amortization expense associated with equity method intangible assets, property and equipment, deferred revenue and other items. Loss from equity method investment in the Joint Venture was $380.7 million, $70.5 million, and $58.7 million for the years ended March 31, 2020, 2019 and 2018, respectively.
For the year ended March 31, 2020, the loss from equity method investment was impacted by the remeasurement of Change Healthcare Inc.’s investment in the Joint Venture, resulting in a loss of approximately $230.2 million. For the year ended March 31, 2019, the Joint Venture recognized a gain of $111.4 million during the year ended March 31, 2019 related to the sale of its extended care business in July 2018; however, its effect on Change Healthcare Inc.’s loss from equity method investment was almost completely offset by the required write-off of the equity method intangible asset basis differences attributable to this business.
General and Administrative Expense and Management Fees
In addition to its loss from its equity method investment in the Joint Venture, prior to the Merger, Change Healthcare Inc. also periodically incurred certain other operating expenses, including professional service fees, general liability insurance, and other fees associated with being an SEC registrant.
To the extent any such fees Change Healthcare Inc. incurs were required to facilitate or maintain its status as a public company, however, the limited liability company agreement of the Joint Venture (the “LLC Agreement”) contemplated that Change Healthcare Inc. be reimbursed for such costs by the Joint Venture.
77
Table of Contents
Goodwill Impairment
Goodwill was established through the application of the guidance for a business combination achieved in stages in accordance with ASC 805 as of the date of the Merger. Subsequent to the Merger, Change Healthcare Inc. concluded a triggering event had occurred due to the expected impacts to its financial results arising out of the COVID-19 pandemic beginning in the first quarter of fiscal year 2021. Change Healthcare Inc. performed a goodwill impairment test as of March 31, 2020, and as a result, recorded a non-cash goodwill impairment charge of $561.2 million. Other risks and future developments that Change Healthcare Inc. was unable to anticipate as of the testing date may require it to further revise future projected cash flows, which could adversely affect the fair value of reporting units in future periods. As a result, Change Healthcare Inc. may be required to record additional impairment charges. Refer to Note 9, Goodwill and Intangible Assets, for further information.
Loss (Gain) on Sale of Interests in the Joint Venture
Under the terms of the LLC Agreement, Change Healthcare Inc. and the Joint Venture agreed to cooperate to ensure a 1:1 ratio of outstanding shares of common stock of Change Healthcare Inc. to the units of the Joint Venture (“LLC Units”) held by Change Healthcare Inc. as long as the subsidiaries of McKesson that serve as members of the Joint Venture (the “McK Members”) hold LLC Units. This provision required that Change Healthcare Inc. be issued an additional LLC Unit for each share of common stock that Change Healthcare Inc. issued. Similarly, for any share that Change Healthcare Inc. repurchases, the Joint Venture is required to repurchase a respective LLC Unit from Change Healthcare Inc. The Joint Venture’s repurchase of LLC Unit(s) results in Change Healthcare Inc. recognizing a gain or loss equal to the difference in the fair value of such LLC Units and the proportionate carrying value of Change Healthcare Inc.’s investment in the Joint Venture associated with such repurchased LLC Units.
Gain on Forward Purchase Contract
Gain on forward purchase contract was $14.8 million, $0 and $0 for the years ended March 31, 2020, 2019 and 2018. The gain on forward purchase contract reflects the change in the fair value of the forward contract that is a component of the TEUs.
Income Taxes
As the Joint Venture is treated as a partnership for income tax purposes, Change Healthcare Inc. was subject to income taxes for its allocable portion of the Joint Venture’s taxable income until the Merger. In conjunction with the consolidation of the Joint Venture by Change Healthcare Inc. as a result of the Merger, the tax provision for the year ended March 31, 2020 reflects the consolidated results for the period from March 10, 2020 to March 31, 2020. In addition, Change Healthcare Inc. elected to begin recording its deferred tax assets and liabilities with respect to its investment in the Joint Venture under the look through approach. The result of the above was an income tax benefit of $143.3 million (which resulted in an effective income tax rate of 13.1%) for the year ended March, 31, 2020, compared with an income tax benefit of $18.6 million (which resulted in an effective income tax rate of 26.3%) for the year ended March 31, 2019. See Note 18, Income Taxes, for further discussion.
Acquisitions and Divestitures
Change Healthcare Inc. actively evaluates opportunities to improve and expand its business through targeted acquisitions that are consistent with its strategy. On occasion, Change Healthcare Inc. also may dispose of certain components of its business that no longer fit within its overall strategy. Because of Change Healthcare Inc.’s acquisition and divestiture activity, as well as the shifting revenue mix of its business due to this activity, the results of operations may not be directly comparable among periods.
78
Table of Contents
On May 1, 2020, Change Healthcare Inc. completed the sale of its Connected Analytics business for total consideration of $55.0 million (subject to a customary working capital adjustment), including a $25.0 million note receivable from the buyer. In addition, also on May 1, 2020, Change Healthcare Inc. completed the acquisition of eRx Network Holdings, Inc. (“eRx”) at a purchase price of $212.9 million plus cash on the balance sheet. On June 1, 2020, Change Healthcare Inc. completed the purchase of PDX, Inc. for a purchase price of $208.0 million.
Liquidity and Capital Resources
Overview
Change Healthcare Inc.’s principal sources of liquidity are cash flows provided by operating activities, cash and cash equivalents on hand, and potential funds available under its Revolving Facility (defined herein). Principal uses of liquidity are working capital, capital expenditures, debt service, business acquisitions and other general corporate purposes. Change Healthcare Inc. anticipates cash on hand, cash generated from operations, and funds available under the Revolving Facility will be sufficient to fund planned capital expenditures, debt service obligations, business acquisitions and operating needs for the next twelve months. Change Healthcare Inc. may, however, elect to raise funds through debt or equity financing in the future to fund significant investments or acquisitions that are consistent with its growth strategy.
Cash and cash equivalents totaled $410.4 million and $3.4 million at March 31, 2020 and 2019, respectively, of which $22.2 million and $0 was held outside the U.S., respectively. As of March 31, 2020, $250.0 million had been drawn and $5.1 million had been issued in letters of credit against the Revolving Facility, leaving $529.9 million available for borrowing. Change Healthcare Inc. also has the ability to borrow up to an additional $1,354.8 million, or such amount that the senior secured net leverage ratio does not exceed 4.9 to 1.0, whichever is greater, under the Senior Credit Facilities (defined herein), subject to certain additional conditions and commitments by existing or new lenders to fund any additional borrowings.
The balance retained in cash and cash equivalents is consistent with Change Healthcare Inc.’s short-term cash needs and investment objectives. Change Healthcare Inc. may be required to make additional principal payments on the Term Loan Facility (defined herein) based on excess cash flows of the prior year, as defined in the agreement governing the Term Loan Facility.
Refer to Change Healthcare LLC—Liquidity and Capital Resources—Overview for discussion on cash flows.
Debt
Senior Credit Facilities and Senior Notes
In March 2017, the Joint Venture entered into a $5,100.0 million term loan facility (the “Term Loan Facility”), and a $500.0 million revolving credit facility (the “Revolving Facility”, together with the Term Loan Facility, the “Senior Credit Facilities”). Additionally, the Joint Venture issued $1,000.0 million of 5.75% senior notes due 2025 (the “Senior Notes”).
The Joint Venture used the initial public offering proceeds received from Change Healthcare Inc. to repay $805 million of its indebtedness under the Term Loan Facility without penalty in July 2019. The Joint Venture repaid an additional $270 million of its indebtedness under the Term Loan Facility without penalty for a total paydown of $1,075 million subsequent to the initial public offering.
In July 2019, the Joint Venture amended the Revolving Facility, the primary effects of which were to increase the maximum amount that can be borrowed from $500.0 million to $785.0 million and to extend the maturity date until July 2024. In the event the outstanding balance under the Term Loan Facility exceeds $1,100.0 million on December 1, 2023, amounts due, if any, under the Revolving Facility become due and
79
Table of Contents
payable on December 1, 2023. As of March 31, 2020, $250.0 million had been drawn and $5.1 million had been issued in letters of credit against the Revolving Facility, leaving $529.9 million available for borrowing.
Tangible Equity Units
In July 2019, the Joint Venture issued a debt arrangement to Change Healthcare Inc. on terms that substantially mirror the economics of the amortizing note component of the Change Healthcare Inc. TEUs. The Joint Venture agreed to pay Change Healthcare Inc. an aggregate principal amount of $47.4 million in quarterly installments of principal and interest (5.5% per year) on March 30, June 30, September 30, and December 30 of each year through June 30, 2022.
Hedges
From time to time, Change Healthcare Inc. executes interest rate cap agreements with various counterparties that effectively cap its LIBOR exposure on a portion of its existing Term Loan Facility or similar replacement debt. The following table summarizes the terms of Change Healthcare Inc.’s interest rate cap agreements at March 31, 2020.
| Effective Date |
Expiration Date | Notional Amount | Receive LIBOR Exceeding(1) |
Pay Fixed Rate |
||||||||||
| August 31, 2018 | December 31, 2021 | $ | 600,000,000 | 1.00 | % | 1.82 | % | |||||||
| August 31, 2018 | December 31, 2021 | $ | 900,000,000 | 1.00 | % | 1.82 | % | |||||||
| March 31, 2020 | March 31, 2024 | $ | 250,000,000 | 1.00 | % | 0.18 | % | |||||||
| March 31, 2020 | March 31, 2024 | $ | 250,000,000 | 1.00 | % | 0.18 | % | |||||||
| March 31, 2020 | March 31, 2024 | $ | 250,000,000 | 1.00 | % | 0.18 | % | |||||||
| March 31, 2020 | March 31, 2024 | $ | 250,000,000 | 1.00 | % | 0.19 | % | |||||||
| (1) | All based on 1-month LIBOR. |
LIBOR Transition
The London Inter-bank Offered Rate (“LIBOR”) is a commonly used indicative measure of the average interest rate at which major global banks could borrow from one another. In July 2017, the Financial Conduct Authority (the authority that governs LIBOR) announced it intends to stop compelling banks to submit rates for the calculation of LIBOR after 2021. The Alternative Reference Rates Committee (“ARRC”) has proposed that the Secured Overnight Financing Rate (“SOFR”) is the rate that represents best practice as the alternative to USD-LIBOR for use in derivatives and other financial contracts that are currently indexed to USD-LIBOR. The ARRC has proposed a paced market transition plan to SOFR from USD-LIBOR and organizations are currently working on industry-wide and company-specific transition plans as it relates to derivatives and cash markets exposed to USD-LIBOR. Change Healthcare Inc. has material contracts that are indexed to USD-LIBOR and is monitoring this activity and evaluating the related risks.
Effect of Certain Debt Covenants
A breach of any of the covenants under the agreements governing Change Healthcare Inc.’s debt could limit its ability to borrow funds and could result in a default under the Term Loan Facility. Upon the occurrence of an event of default under the Term Loan Facility, the lenders could elect to declare all amounts then outstanding to be immediately due and payable and terminate all commitments to extend further credit. If Change Healthcare Inc. were unable to repay the amounts declared due, the lenders could proceed against any collateral granted to secure that indebtedness.
80
Table of Contents
With certain exceptions, the Term Loan Facility obligations are secured by a first-priority security interest in substantially all of the assets of the Joint Venture, including its investment in subsidiaries. The Term Loan Facility contains various restrictions and nonfinancial covenants, along with a senior secured net leverage ratio test. The nonfinancial covenants include restrictions on dividends, investments, dispositions, future borrowings and other specified payments, as well as additional reporting and disclosure requirements. The senior secured net leverage test must be met as a condition to incur additional indebtedness, but otherwise is applicable only to the extent that amounts drawn exceed 35% of the Revolving Facility at the end of any fiscal quarter. As of March 31, 2020, Change Healthcare Inc. was in compliance with all debt covenants.
Change Healthcare Inc.’s ability to meet its liquidity needs depends on its subsidiaries’ earnings and cash flows, the terms of Change Healthcare Inc. and its subsidiaries’ indebtedness, and other contractual restrictions.
Off-Balance Sheet Arrangements
As of March 31, 2020, Change Healthcare Inc. had no off-balance sheet arrangements.
Contractual Obligations
The following table presents a summary of contractual obligations for future fiscal years as of March 31, 2020:
| Payments by Period | ||||||||||||||||||||
| (amounts in millions) | Total | 2021 | 2022 - 2023 | 2024 - 2025 | Thereafter | |||||||||||||||
| Senior Credit Facilities and other long-term obligations(1) |
$ | 4,117.6 | $ | 278.8 | $ | 30.1 | $ | 3,808.7 | $ | — | ||||||||||
| Senior Notes(2) |
1,000.4 | — | — | 1,000.4 | — | |||||||||||||||
| Expected interest(3) |
979.9 | 250.5 | 454.7 | 274.7 | — | |||||||||||||||
| 2009-2011 Tax Receivable Agreements(4) |
199.1 | 18.7 | 40.2 | 37.3 | 102.9 | |||||||||||||||
| 2017 Tax Receivable Agreement(5) |
115.7 | 1.5 | 49.7 | 35.0 | 29.5 | |||||||||||||||
| McKesson Tax Receivable Agreement(6) |
164.6 | — | 18.4 | 43.1 | 103.1 | |||||||||||||||
| Operating lease obligations(7) |
141.0 | 40.5 | 58.5 | 26.2 | 15.9 | |||||||||||||||
| Contingent consideration obligation(8) |
3.0 | 3.0 | — | — | — | |||||||||||||||
| Purchase obligations and other(9) |
1,162.5 | 126.9 | 349.0 | 347.6 | 339.0 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total contractual obligations(10) |
$ | 7,883.8 | $ | 719.9 | $ | 1,000.6 | $ | 5,573.0 | $ | 590.3 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
As a result of displaying amounts in millions, rounding differences may exist in the table above.
| (1) | Represents the principal amount of indebtedness under the Senior Credit Facilities and the Joint Venture’s deferred financing obligations. See Note 11, Long-Term Debt. |
| (2) | Represents the principal amount of indebtedness under the Senior Notes without reduction for any original issue discount. See Note 11, Long-Term Debt. |
| (3) | Consists of interest payable under the Senior Credit Facilities and Senior Notes. Interest related to the Senior Credit Facilities is based on Change Healthcare Inc.’s interest rates in effect as of March 31, 2020 and assumes that payments are made in quarterly installments of 1% of the original principal amount until their maturity. Because the interest rates under the Senior Credit Facilities are variable, actual payments may differ. |
| (4) | Represents expected amounts due without reduction for any fair value adjustments recognized in prior acquisition method accounting. See Note 17, Tax Receivable Agreements. |
| (5) | Represents expected amounts due; however, the timing and/or amount of aggregate payments may vary based on a number of factors, including differences in the expected and actual utilization of prior net operating losses and changes in the tax rate then applicable, whether due to statutory changes or changes in apportionment. See Note 17, Tax Receivable Agreements. |
81
Table of Contents
| (6) | Represents expected amounts due; however, the timing and/or amount of aggregate payments may vary based on a number of factors. See Note 17, Tax Receivable Agreements. |
| (7) | Represents amounts due under existing operating leases related to Change Healthcare Inc.’s offices and other facilities. See Note 19, Commitments. |
| (8) | Contingent consideration transferred in connection with acquisitions includes a contingent obligation to make additional payments based on the achievement of certain future performance objectives. Because the ultimate timing and amount of payments are dependent on the outcome of future events, the timing and/or amount of these additional payments may vary from this estimate. See Note 19, Commitments. |
| (9) | Represents contractual obligations, including the Wipro Agreement. See Note 19, Commitments. |
Critical Accounting Estimates
The preparation of financial statements in accordance with GAAP requires Change Healthcare Inc. to make estimates and assumptions that affect reported amounts and related disclosures. Change Healthcare Inc. considers an accounting estimate to be critical if:
| • | it requires assumptions to be made that were uncertain at the time the estimate was made; and |
| • | changes in the estimate or different estimates that could have been made could have a material impact on Change Healthcare Inc.’s results of operations and financial condition. |
See Note 3, Significant Accounting Policies, as well as the Critical Accounting Estimates section for Change Healthcare LLC, for information about other critical accounting policies.
Equity Method Investment in the Joint Venture
As disclosed in Note 3, Significant Accounting Policies, Change Healthcare Inc. evaluated its equity method investment for impairment review whenever an event or change in circumstances occurs that may have a significant adverse impact on the carrying value of the investment. If a loss in value occurs that is deemed to be an other-than-temporary impairment (“OTTI”), an impairment loss would be recognized.
Subsequent to its initial public offering, Change Healthcare Inc. had a publicly available indication of the value of its investment in the Joint Venture. Change Healthcare Inc. considered various factors in determining whether an OTTI had occurred, including Change Healthcare Inc.’s ability and intent to hold the investment, the trading history available, the implied EBITDA valuation multiples compared to public guideline companies, the Joint Venture’s ability to achieve milestones and any operational and strategic changes by the Joint Venture that might have negatively impacted the fair value. In the periods prior to the Merger, Change Healthcare Inc. determined that an OTTI had not occurred.
Goodwill
Goodwill from Change Healthcare Inc.’s acquisitions is accounted for using the acquisition method of accounting. Change Healthcare Inc. assesses its goodwill for impairment annually (as of January 1 of each year) or whenever significant indicators of impairment are present. Change Healthcare Inc. first assesses whether it can reach a more likely than not conclusion that goodwill is not impaired via qualitative analysis alone. To the extent such a conclusion cannot be reached based solely on a qualitative assessment, Change Healthcare Inc., using the assistance of a valuation specialist as appropriate, compares the fair value of each reporting unit to its associated carrying value. Change Healthcare Inc. will generally recognize an impairment charge for the amount, if any, by which the carrying amount of the reporting unit exceeds its fair value.
When necessary, Change Healthcare Inc. estimates the fair value of its reporting units using a methodology that considers both income and market approaches. Each approach requires the use of certain assumptions. The income approach requires management to exercise judgment in making assumptions regarding the reporting
82
Table of Contents
unit’s future income stream, a discount rate and a constant rate of growth after the initial forecast period utilized. These assumptions are subject to change based on business and economic conditions and could materially affect the indicated values of the Joint Venture’s reporting units.
The market approach requires management to exercise judgment in its selection of guideline companies, as well in its selection of the most relevant transaction multiple. Guideline companies selected are comparable to Change Healthcare Inc. in terms of product or service offerings, markets and/or customers, among other characteristics. See Note 9, Goodwill and Intangible Assets, for further discussion.
Change Healthcare Inc. believes the current assumptions and other considerations used to estimate amounts reflected in its financial statements are appropriate. However, if actual experience differs from the assumptions and other considerations used in estimating amounts reflected in Change’s financial statements, the resulting changes could have a material adverse effect on Change Healthcare Inc.’s results of operations and financial condition.
Related Party Balances and Transactions
See Note 22, Related Party Transactions for information regarding our related party balances and transactions.
Recent Accounting Pronouncements
See Note 3, Significant Accounting Policies for information about recent accounting pronouncements and the potential impact on the Change Healthcare Inc.’s consolidated financial statements.
Change Healthcare LLC
Overview
The Joint Venture is a leading independent healthcare technology company, formed through the combination of substantially all of the businesses of Change Healthcare Performance, Inc. (formerly Change Healthcare, Inc.) (“Legacy CHC”) and a majority of the McKesson Technology Solutions business (“Core MTS”), which was completed on March 1, 2017. The Joint Venture offers a comprehensive suite of software, analytics, technology-enabled services and network solutions that drive improved results in the complex workflows of healthcare system payers and providers. The Joint Venture’s solutions are designed to improve clinical decision making, simplify billing, collection and payment processes and enable a better patient experience. On March 10, 2020, the Joint Venture became a wholly-owned subsidiary of Change Healthcare Inc.
The Joint Venture offers comprehensive end-to-end solutions with modular capabilities to address its customers’ needs. Working with its customers to analyze workflows before, during and after care has been delivered to patients, the Joint Venture designs and commercializes innovative solutions for various points in the healthcare delivery timeline. The Joint Venture’s offerings range from discrete data and analytics solutions to broad enterprise-wide solutions, which include workflow software and technology-enabled services that help its customers achieve their operational objectives.
The Joint Venture’s Intelligent Healthcare Network was created to facilitate the transfer of data among participants and is one of the largest clinical and financial healthcare networks in the U.S. With insights gained from its pervasive network, extensive applications and analytics portfolio and its services operations, the Joint Venture has designed analytics solutions that include industry-leading and trusted franchises supported by extensive intellectual property and regularly updated content.
83
Table of Contents
Segments
The Joint Venture reports its financial results in the following three reportable segments: Software and Analytics, Network Solutions and Technology-Enabled Services.
| • | Software and Analytics provides software and analytics solutions for financial performance, payment accuracy, clinical decision management, value-based payment, provider and consumer engagement and imaging and clinical workflow. |
| • | Network Solutions enables financial, administrative and clinical transactions, electronic business-to-business and consumer-to-business payments and aggregation and analytics of clinical and financial data. |
| • | Technology-Enabled Services provides solutions for financial and administrative management, value-based care, communication and payment, pharmacy benefits administration and healthcare consulting. |
In April 2019, the Joint Venture made certain changes in the way that it manages its business and allocates costs. Specifically, the Joint Venture made the following changes:
| • | Moved its consumer payments solution from the Network Solutions segment to the Technology-Enabled Services segment. |
| • | Moved its consumer engagement solutions from the Software and Analytics segment to the Network Solutions segment. |
| • | Made certain changes in the way that costs are assigned to segments. |
In November 2019, the Joint Venture moved certain of its revenue optimization services solutions from the Software and Analytics segment to the Technology-Enabled Services segment.
The presentation of revenue and Adjusted EBITDA included within MD&A has been retrospectively adjusted for all periods presented to reflect the above described changes.
Factors Affecting Change Healthcare LLC’s Results of Operations
The following are certain key factors that affect, will affect, or have recently affected, the Joint Venture’s results of operations:
Post-Contribution Cost Synergies
In connection with the Transactions, the Joint Venture identified opportunities to implement certain cost synergies based on its analyses of existing operating structures, estimated spend by category, resource requirements and industry benchmarks for similar activities. The Joint Venture expects such cost synergies to include, among others, (i) product integration, network efficiencies and combining common products; (ii) procurement savings from the elimination of duplicate orders, leveraging scale and optimization of providers; (iii) utilization of global talent; and (iv) reduction of management redundancies and duplicative roles.
By the end of fiscal year 2021, the Joint Venture expects to have implemented operational initiatives to fully realize these synergies, which are expected to result in significant annual run-rate cost savings and efficiencies. The Joint Venture has incurred significant non-recurring expenses and expects to continue to incur such expenses in order to achieve these cost synergies.
84
Table of Contents
Macroeconomic and Industry Trends
The spread of COVID-19 both globally and in the U.S. has driven lower healthcare utilization as a result of the significant reduction in, or in some cases elimination of, elective medical procedures and healthcare visits, without a corresponding increase in COVID-19 related transactions. A portion of the Joint Venture’s business is tied to overall volumes of activity in the healthcare system, and therefore has been adversely impacted by this industry trend. Further, weakened economic conditions or a recession could reduce the amounts patients are willing or able to spend on healthcare services. As a result, patients may elect to delay or forgo seeking healthcare services and recent increases in unemployment rates is likely to cause commercial payer membership to decline, which could further reduce healthcare utilization and transaction volumes. While we began to see the impact of COVID-19 on our business and financial results late in fiscal year 2020, we expect to see a much more significant impact starting in the first quarter of fiscal year 2021.
In response to COVID-19, we initiated a number of actions with our employees’ health being our first priority. We also focused on serving our customers and introducing new products and services to address their previously unexpected but now urgent needs related to COVID-19. To ensure our business continuity and the safety and welfare of our team members, we moved the majority of our employees to work from home, shifted to a virtual meeting environment, suspended all non-critical business travel, and expanded telehealth and COVID-19 related PTO coverage to all employees. We also did a comprehensive review of our cost structure to balance costs with interim variability in our revenue and have actively aligned our staffing level, primarily in our Technology-Enabled Services segment to address lower interim volume. Starting in March 2020, we initiated hiring freezes, began contractor reductions and made other staffing reductions, primarily in the form of furloughs to provide us with greater flexibility to scale back up as volumes recover. We expect to start to see the impact of these actions late in the first quarter and into the second quarter of fiscal year 2021.
While lower healthcare utilization will impact our results negatively this year, we cannot predict the length of time it may take for normal healthcare volumes to return and the extent to which our business, results of operations, financial condition or liquidity will ultimately be impacted by COVID-19. However, we continue to assess its impact on our business and are actively managing our response as the pandemic evolves. We believe the solutions we provide our customers will be as important, if not more, post-COVID-19. For further details on the potential impact of COVID-19 on our business, refer to Risk Factors in Item 1A of this Form 10-K.
Revenue Convergence
In April 2019, the Joint Venture adopted ASC 606, which replaces most prior general and industry specific revenue recognition guidance with a principles-based comprehensive revenue recognition framework.
ASC 606 was adopted using the modified retrospective transition method applied only to contracts that were not completed as of the date of initial application. The adoption of ASC 606 resulted in a cumulative effect adjustment to reduce members’ equity (deficit) as of April 1, 2019 by $159.9 million. After assessing all potential impacts of adopting the new standard on its consolidated financial statements, related disclosures, and necessary control and process changes, the Joint Venture noted the following to be the most notable impacts of adopting the new standard:
| • | Revenue for certain contingent fee service arrangements is accelerated as revenue for these arrangements is recognized as the services are performed. |
| • | Revenue related to certain time-based software and content license agreements is accelerated. The license component for certain time-based software is recognized upon delivery to the customer (“point in time”), or in the case of software that requires significant production, modification or customization, recognized as the implementation work is performed. A non-license component (i.e., technical support) is recognized over the respective contract terms (“over time”). |
85
Table of Contents
| • | Incremental costs to obtain contracts and qualifying costs to fulfill is capitalized and amortized over the period of benefit. The net result of this change was an increase to capitalized contract costs on the balance sheet; these capitalized costs are amortized and recognized as expense over an incrementally longer period of time. |
Refer to Note 2, Summary of Significant Accounting Policies, in the audited financial statements of the Joint Venture included as Exhibit 99.1 for a full description of the impact of the adoption of ASC 606 on the Joint Venture’s financial statements.
Equity-based Compensation
Change Healthcare Inc. grants equity-based awards of Change Healthcare Inc. common stock to certain employees, officers and directors of Change Healthcare Inc. and the Joint Venture. For grants to employees, equity-based awards are generally measured at the date of grant and recognized as expense over each employee’s service period. Because the Joint Venture’s employees were not considered employees of Change Healthcare Inc. before the Merger, prior to the adoption of ASU 2018-07 on April 1, 2019, the Joint Venture was generally required to re-measure these equity-based awards at fair value each quarter until the earlier of the completion of required service or the performance commitment date. As a result, the Joint Venture’s results of operations for the year ended March 31, 2019 and 2018 have historically reflected volatility from the periodic re-measurement of its equity-based awards.
After the adoption of ASU 2018-07, the Joint Venture is required to treat equity awards granted to non-employees similarly to awards to employees. As a result, the Joint Venture expects to significantly lessen the volatility on equity-based compensation that has historically resulted from changes in the fair value of the underlying stock of Change Healthcare Inc., stock price volatility among its peer companies, changes in interest rates and the passage of time.
In connection with the initial public offering, the board of directors adopted, and the stockholders approved, the Change Healthcare Inc. 2019 Omnibus Incentive Plan (the “Omnibus Incentive Plan”), which became effective as of the date of the initial public offering. The purpose of the Omnibus Incentive Plan is to provide a means to attract and retain key personnel and to provide a means whereby the Joint Venture’s directors, officers, employees, consultants and advisors (and those Change Healthcare Inc. and the Joint Venture’s subsidiaries) can acquire and maintain an equity interest in Change Healthcare Inc. or be paid incentive compensation. The Omnibus Incentive Plan allows for implementation of a new market-based long-term incentive program to align the executive compensation package with similarly situated public companies.
As part of the 2019 Omnibus Incentive Plan, the board of directors may, from time to time, grant awards to one or more eligible persons. All awards granted under the Omnibus Incentive Plan shall vest and become exercisable in such manner and on such dates or upon such events as determined by the Board of Directors, including attainment of performance conditions.
Refer to Note 17, Incentive Compensation Plans, in the audited financial statements of the Joint Venture included as Exhibit 99.1 for a full description of the new awards included in the long-term incentive program.
Acquisitions and Divestitures
The Joint Venture actively evaluates opportunities to improve and expand its business through targeted acquisitions that are consistent with its strategy. On occasion, the Joint Venture also may dispose of certain components of its business that no longer fit within its overall strategy. Because of the Joint Venture’s acquisition and divestiture activity, as well as the shifting revenue mix of its business due to this activity, the Joint Venture’s results of operations may not be directly comparable among periods.
86
Table of Contents
Income Taxes
The Joint Venture’s effective income tax rate is affected by several factors. The following table and subsequent commentary reconciles the Joint Venture’s federal statutory rate to its effective income tax rate and the subsequent commentary describes the more significant of the reconciling factors:
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Statutory U.S. federal tax rate (1) |
21.00 | % | 21.00 | % | 31.50 | % | ||||||
| State income taxes (net of federal benefit) |
(184.40 | ) | 2.80 | (1.32 | ) | |||||||
| Income passed through to Members |
102.80 | (20.62 | ) | (8.78 | ) | |||||||
| Remeasurement of deferred tax assets and liabilities arising from the Tax Legislation |
— | — | (42.95 | ) | ||||||||
| Transition tax arising from the Tax Legislation |
— | (0.89 | ) | 1.68 | ||||||||
| Change in valuation allowance |
23.70 | (0.88 | ) | (11.97 | ) | |||||||
| Accretion and changes in estimate, net |
(7.90 | ) | (0.06 | ) | (5.47 | ) | ||||||
| Equity compensation |
(49.10 | ) | (0.08 | ) | 1.03 | |||||||
| Research and development credits (net of uncertain tax position liability) |
132.10 | (4.39 | ) | (1.44 | ) | |||||||
| Other |
(81.70 | ) | 0.52 | 0.80 | ||||||||
|
|
|
|
|
|
|
|||||||
| Effective income tax rate |
(43.50 | )% | (2.60 | )% | (36.92 | )% | ||||||
|
|
|
|
|
|
|
|||||||
| (1) | The statutory U.S. federal tax rate for the year ended March 31, 2018 was calculated using the U.S. corporate federal income tax rate of 35.0% in the period from April 1, 2017 to December 31, 2017 and 21.0% in the period from January 1, 2018 to March 31, 2018. |
State Income Taxes – The Joint Venture’s effective tax rate for state income taxes is generally impacted by changes in its apportionment.
Income Passed through to Members – Certain of the Joint Venture’s subsidiaries are organized as limited liability corporations and report income that is distributed to the Members where it is subject to income taxes.
Change in Valuation Allowance – The Joint Venture records valuation allowances or reverses existing valuation allowances related to assumed future income tax benefits depending on circumstances and factors related to its business. During the year ended March 31, 2020, the Joint Venture released a valuation allowance related to prior deferred tax assets as a result of its change in judgment resulting from forecasted earnings and tax planning strategies that provide for future taxable income in the relevant jurisdictions.
Research and development credits (net of uncertain tax position liability) – The Joint Venture records credits against income taxes for certain research and development expenditures in the U.S. and Canada net of the portion that is estimated to be included in Change Healthcare Inc.’s unrecognized tax benefits.
Results of Operations
Year Ended March 31, 2020 (ASC 605 Basis) compared to Year Ended March 31, 2019
The Joint Venture adopted the new revenue recognition accounting standard, ASC 606, effective April 1, 2019 on a modified retrospective basis. Its results of operations as presented within the following discussion and analysis includes financial results for reporting periods during fiscal 2020, which are disclosed in compliance with ASC 606. Historical financial results have not been retroactively restated and are presented in conformity
87
Table of Contents
with amounts previously disclosed under the prior revenue recognition standard, ASC 605. The Joint Venture included additional information regarding the impacts from the adoption of ASC 606 for the year ended March 31, 2020 and included financial results during fiscal 2020 under ASC 605 for comparison to the prior year.
The following table summarizes our consolidated results of operations for the years ended March 31, 2020 and 2019:
| Year Ended March 31, 2020 | ||||||||||||||||||||||||
| (amounts in millions, except percentages) (1) |
As Reported | Impacts from Adoption |
Without Adoption (ASC 605) |
Year Ended March 31, 2019 |
$ Change |
% Change |
||||||||||||||||||
| Revenue |
||||||||||||||||||||||||
| Solutions revenue |
$ | 3,074.9 | $ | 3.0 | $ | 3,077.9 | $ | 3,043.1 | $ | 34.8 | 1.1 | % | ||||||||||||
| Postage revenue |
228.1 | — | 228.1 | 238.6 | (10.5 | ) | (4.4 | ) | ||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Total revenue |
3,303.0 | 3.0 | 3,306.0 | 3,281.7 | 24.3 | 0.7 | ||||||||||||||||||
| Operating expenses |
||||||||||||||||||||||||
| Costs of operations (exclusive of depreciation and amortization below) |
$ | 1,345.9 | 3.3 | 1,349.2 | 1,354.7 | (5.5 | ) | (0.4 | ) | |||||||||||||||
| Research and development |
205.0 | — | 205.0 | 202.2 | 2.8 | 1.4 | ||||||||||||||||||
| Sales, marketing, general and administrative |
742.8 | 20.4 | 763.2 | 821.1 | (57.9 | ) | (7.1 | ) | ||||||||||||||||
| Customer postage |
228.1 | — | 228.1 | 238.6 | (10.5 | ) | (4.4 | ) | ||||||||||||||||
| Depreciation and amortization |
315.9 | — | 315.9 | 278.0 | 37.9 | 13.6 | ||||||||||||||||||
| Accretion and changes in estimate with related parties, net |
15.0 | — | 15.0 | 19.3 | (4.3 | ) | (22.3 | ) | ||||||||||||||||
| Tax receivable agreement charge |
164.6 | — | 164.6 | — | 164.6 | |||||||||||||||||||
| Gain on sale of the Extended Care Business |
— | — | — | (111.4 | ) | 111.4 | (100.0 | ) | ||||||||||||||||
| Impairment of long-lived assets and related costs |
0.5 | — | 0.5 | 0.7 | (0.2 | ) | (28.6 | ) | ||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Total operating expenses |
$ | 3,017.8 | $ | 23.7 | $ | 3,041.5 | $ | 2,803.2 | $ | 238.3 | 8.5 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Operating income |
$ | 285.2 | $ | (20.7 | ) | $ | 264.5 | $ | 478.5 | $ | (214.0 | ) | (44.7 | ) | ||||||||||
| Non-operating (income) and expense |
||||||||||||||||||||||||
| Interest expense |
283.7 | — | 283.7 | 325.4 | (41.7 | ) | (12.8 | ) | ||||||||||||||||
| Loss on extinguishment of debt |
20.0 | — | 20.0 | — | 20.0 | |||||||||||||||||||
| Contingent consideration |
(0.1 | ) | — | (0.1 | ) | (0.8 | ) | 0.7 | (87.5 | ) | ||||||||||||||
| Other, net |
(14.6 | ) | — | (14.6 | ) | (18.3 | ) | 3.7 | (20.2 | ) | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Non-operating (income) and expense |
$ | 289.0 | — | 289.0 | 306.3 | (17.3 | ) | (5.6 | ) | |||||||||||||||
| Income (loss) before income tax provision (benefit) |
(3.8 | ) | (20.7 | ) | (24.5 | ) | 172.2 | (196.7 | ) | (114.2 | ) | |||||||||||||
| Income tax provision (benefit) |
1.7 | 2.0 | 3.7 | (4.5 | ) | 8.2 | (182.2 | ) | ||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Net income (loss) |
$ | (5.5 | ) | $ | (22.7 | ) | $ | (28.2 | ) | $ | 176.7 | $ | (204.9 | ) | (116.0 | )% | ||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| (1) | As a result of displaying amounts in millions, rounding differences may exist in the table above. |
88
Table of Contents
Revenues
Solutions Revenue
Solutions revenue increased $34.8 million for the year ended March 31, 2020, compared with the prior year. Factors affecting the Joint Venture’s solutions revenue are described in the various segment discussions below.
Postage Revenue
Postage revenue decreased $10.5 million for the year ended March 31, 2020 as compared with the prior year. See “Customer Postage” below for an explanation of the decline.
Expenses
Costs of Operations (Exclusive of Depreciation and Amortization)
Costs of operations decreased $5.5 million for the year ended March 31, 2020 as compared with the prior year. The decrease in the Joint Venture’s costs of operations is primarily attributable to cost synergies associated with network efficiencies and reduction or elimination of duplicative roles, among other factors.
Research and Development
Research and development expenses increased $2.8 million for the year ended March 31, 2020 as compared with the prior year. The increase is primarily attributable to increases in investments, offset by synergies associated with reduction or elimination of duplicative roles.
Sales, Marketing, General and Administrative
Sales, marketing, general and administrative expenses decreased $57.9 million for the year ended March 31, 2020 as compared with the prior year. Sales, marketing, general and administrative expense for each year reflects significant integration related costs, including professional and consulting fees related to rationalizations of information technology, business process re-engineering, implementation of human resource and finance information technology systems, severance and other costs. The amount of such costs decreased by $32.4 million in the year ended March 31, 2020 as compared to the prior year due to the completion of certain integration projects during the year ended March 31, 2020.
Customer Postage
Customer postage decreased $10.5 million for the year ended March 31, 2020 as compared with the prior year. Customer postage is affected by the declines in print volumes within communication and payment solutions, which were partially offset by the effect of a USPS postage rate increase in January 2019 (i.e., an increase in first-class postage of 10%). Because customer postage is a pass-through cost to the Joint Venture’s customers, changes in volume of customer postage generally have no net effect on operating income.
Depreciation and Amortization
Depreciation and amortization increased $37.9 million for the year ended March 31, 2020 as compared with the prior year. Depreciation and amortization were generally affected by routine amortization of tangible and intangible assets existing at March 31, 2019 as well as the routine amortization and depreciation of additions to property, equipment, and software.
89
Table of Contents
Accretion and changes in estimate with related parties, net
Accretion and changes in estimate with related parties, net decreased $4.3 million for the year ended March 31, 2020 as compared with the prior year. Accretion is routinely affected by changes in the expected timing or amount of cash flows related to tax receivable agreements which may result from various factors, including changes in tax rates.
Tax receivable agreement charge
The tax receivable charge of $164.6 million for the year ended March 31, 2020 represents the establishment of the liability for the McKesson tax receivable agreement that went into effect subsequent to the Merger.
Non-Operating Income and Expense
Interest expense
Interest expense decreased $41.7 million for the year ended March 31, 2020 as compared with prior year. This decrease is primarily attributable to the repayment of approximately $805.0 million of variable interest rate debt in July 2019 from the proceeds of the initial public offering as well as additional repayments totaling $270.0 million subsequent to the initial public offering.
Loss on Extinguishment of Debt
Loss on extinguishment of debt for the year ended March 31, 2020 of $20.0 million is related to the write-off of unamortized discounts and debt issuance costs associated with debt repayments.
Other, net
Other, net primarily represents income the Joint Venture receives from McKesson and eRx Network related to transitional and other services that the Joint Venture provides them following the closing of the Transactions in March 2017.
Income Tax Provision (Benefit)
The income tax benefit was $1.7 million (effective tax rate of (43.5)%) for the year ended March 31, 2020 as compared to an income tax benefit of $4.5 million (effective tax rate of (2.6)%) for the year ended March 31, 2019. The Joint Venture’s income taxes and related effective tax rate are routinely affected by it and its subsidiaries’ legal organization. Certain of the Joint Venture’s subsidiaries are organized as limited liability corporations and report income that is distributed to the Members where it is subject to income taxes. Other subsidiaries are organized as corporations, for which the tax effects are directly reflected in the Joint Venture’s financial statements.
90
Table of Contents
Solutions Revenue and Adjusted EBITDA
| Year Ended March 31, 2020 | ||||||||||||||||||||||||
| (amounts in millions, except percentages) (1) | As Reported | Impacts from Adoption |
Without Adoption (ASC 605) |
Year Ended March 31, 2019 |
$ Change |
% Change |
||||||||||||||||||
| Solutions revenue (2) |
||||||||||||||||||||||||
| Software and Analytics |
$ | 1,612.8 | $ | 2.4 | $ | 1,615.2 | $ | 1,579.0 | $ | 36.2 | 2.3 | % | ||||||||||||
| Network Solutions |
$ | 588.7 | $ | — | $ | 588.7 | $ | 556.5 | $ | 32.2 | 5.8 | % | ||||||||||||
| Technology-Enabled Services |
$ | 978.7 | $ | 0.7 | $ | 979.3 | $ | 1,005.3 | $ | (26.0 | ) | (2.6 | )% | |||||||||||
| Adjusted EBITDA |
||||||||||||||||||||||||
| Software and Analytics |
$ | 663.0 | $ | (14.3 | ) | $ | 648.7 | $ | 610.4 | $ | 38.3 | 6.3 | % | |||||||||||
| Network Solutions |
$ | 353.5 | $ | (1.9 | ) | $ | 351.6 | $ | 337.4 | $ | 14.2 | 4.2 | % | |||||||||||
| Technology-Enabled Services |
$ | 175.1 | $ | (3.0 | ) | $ | 172.1 | $ | 175.4 | $ | (3.3 | ) | (1.9 | )% | ||||||||||
| (1) | As a result of displaying amounts in millions, rounding differences may exist in the table above. |
| (2) | Includes intersegment revenues. |
Software and Analytics
Software and Analytics revenue increased $36.2 million for the year ended March 31, 2020 as compared with the prior year. Software and Analytics revenue reflects core revenue growth which was partially offset by ongoing efforts to rationalize the connected analytics solution, the effect on revenue of the sale of the extended care business in July 2018, and a COVID-19 impact of $3.1 million mainly due to deal timing. Related to the extended care business, we recognized revenue of $0 and $9.2 million for years ended March 31, 2020 and 2019, respectively.
Software and Analytics Adjusted EBITDA increased $38.3 million for the year ended March 31, 2020 as compared with the prior year, primarily attributable to revenue growth and operational synergies. This increase was partially offset by a $1.1 million decrease in Adjusted EBITDA that resulted from the divestiture of the extended care business, ongoing efforts to rationalize the connected analytics solution, and a COVID-19 impact of $3.1 million mainly due to deal timing.
Network Solutions
Network Solutions revenue increased $32.2 million for the year ended March 31, 2020 as compared with the prior year. Network Solutions revenue reflects growth from the implementation of new customers in the business to business payments solution, new contracts in data solutions, payments, and dental, stronger medical network volumes and a one-time customer true-up for prior periods of $7.3 million, partially offset by lower dental and medical network volumes of $1.5 million resulting from COVID-19.
Network Solutions Adjusted EBITDA increased $14.2 million for the year ended March 31, 2020 as compared with the prior year. The increase in Adjusted EBITDA was attributable to revenue growth, partially offset by investments to support new product launches and market expansion opportunities in the core network, data solutions, and B2B payments and the integration of network capabilities as well as lower volumes of $1.1 million due to COVID-19.
Technology-Enabled Services
Technology-Enabled Services revenue decreased $26.0 million for the year ended March 31, 2020 as compared with the prior year. Technology-Enabled Services revenue decreased $123.7 million due to customer attrition (including the Joint Venture’s decision to exit certain contracts). The decrease was partially offset by
91
Table of Contents
new sales and same store organic growth of $97.8 million, which includes a negative impact of $1.6 million due to COVID-19. Customer attrition reflects the full year impact of attrition that occurred throughout fiscal year 2019 in the physician and health system revenue cycle management and communication and payment services solutions, driven by industry consolidation.
Technology-Enabled Services Adjusted EBITDA decreased $3.3 million for the year ended March 31, 2020 as compared with the prior year. Technology-Enabled Services Adjusted EBITDA reflects the decrease in revenue and increased costs associated with repositioning certain of our physician and health system revenue cycle management and communication and payment solutions as well as a $2.6 million COVID-19 impact which was partially offset by productivity initiatives and cost synergies.
Significant Changes in Assets and Liabilities
The Joint Venture repaid approximately $1,075.0 million of variable rate debt subsequent to the initial public offering and also made a draw on its revolving debt instrument of $250.0 million in March 2020. Additionally, the Joint Venture recorded a liability of approximately $164.6 million related to the establishment of the reserve for the McKesson tax receivable agreement that was recorded subsequent to the Merger.
Within the Joint Venture’s network solutions business, the Joint Venture regularly receives funds from certain pharmaceutical industry participants in advance of its obligation to remit these funds to participating retail pharmacies. Such funds are not restricted; however, these funds are generally paid out in satisfaction of the processing obligations within three business days of their receipt. At the time of receipt, the Joint Venture records a corresponding liability within accrued expenses on its consolidated balance sheets. At March 31, 2020, the Joint Venture reported $29.1 million of such pass-through payment obligations which were subsequently paid in the first week of April 2020. At March 31, 2019, the Joint Venture reported $7.4 million of such pass-through payment obligations.
Liquidity and Capital Resources
Overview
The Joint Venture’s principal sources of liquidity are cash flows provided by operating activities, cash and cash equivalents on hand, and potential funds available under the Revolving Facility. The Joint Venture’s principal uses of liquidity are working capital, capital expenditures, debt service, business acquisitions and other general corporate purposes. We anticipate cash on hand, cash generated from operations, and funds available under the Revolving Facility will be sufficient to fund planned capital expenditures, debt service obligations, business acquisitions and operating needs for the next twelve months. The Joint Venture may, however, elect to raise funds through debt or equity financing in the future to fund significant investments or acquisitions that are consistent with its growth strategy.
Cash, cash equivalents and restricted cash totaled $407.7 million and $48.9 million at March 31, 2020 and 2019, respectively, of which $22.2 million and $28.1 million was held outside the U.S. As of March 31, 2020, $250.0 million had been drawn and $5.1 million had been issued in letters of credit against the Revolving Facility leaving $529.9 million available for borrowing. The Joint Venture also has the ability to borrow up to an additional $1,354.8 million, or such amount that the senior secured net leverage ratio does not exceed 4.9 to 1.0, whichever is greater, under the Senior Credit Facilities, subject to certain additional conditions and commitments by existing or new lenders to fund any additional borrowings.
The balance retained in cash and cash equivalents is consistent with the Joint Venture’s short-term cash needs and investment objectives. The Joint Venture may be required to make additional principal payments on the Term Loan Facility based on excess cash flows of the prior year, as defined in the agreement governing the Term Loan Facility.
92
Table of Contents
The following table summarizes the Joint Venture’s net cash flow from operating, investing and financing activities:
| (amounts in millions) (1) | Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
|||||||||
| Cash provided by (used in) operating activities |
$ | 593.3 | $ | 287.7 | $ | 324.8 | ||||||
| Cash provided by (used in) investing activities |
(247.7 | ) | (105.7 | ) | (260.7 | ) | ||||||
| Cash provided by (used in) financing activities |
14.2 | (182.1 | ) | (197.5 | ) | |||||||
| Effects of exchange rate changes on cash, cash equivalents and restricted cash |
(1.0 | ) | (1.0 | ) | (4.7 | ) | ||||||
|
|
|
|
|
|
|
|||||||
| Net change in cash, cash equivalents and restricted cash |
$ | 358.8 | $ | (1.1 | ) | $ | (138.1 | ) | ||||
|
|
|
|
|
|
|
|||||||
| (1) | As a result of displaying amounts in millions, rounding differences may exist in the tables above. |
Operating Activities
Cash provided by operating activities is primarily affected by operating income, including the impact of debt service payments, integration related costs and the timing of collections and related disbursements. Cash provided by operating activities includes $21.7 million and $3.0 million as a source of cash related to pass-through funds for the years ended March 31, 2020 and 2019, respectively, and $1.1 million as a use of cash for the year ended March 31, 2018.
Investing Activities
Cash used in investing activities primarily reflects routine capital expenditures related to purchase of property and equipment and the development of software, as well as expenditures related to significant software development efforts necessary to integrate the contributed businesses in both periods. Cash provided by investing activities in the year ended March 31, 2019 was primarily impacted by the proceeds from the sale of the extended care business.
Financing Activities
Cash used in financing activities reflects cash payments under the Term Loan Facility, receipts under interest rate cap agreements, and payments for deferred financing obligations. Cash used in financing activities was primarily impacted by the proceeds from the initial public offering and resulting increased payments under the Term Loan Facility in the year ended March 31, 2020.
Capital Expenditures
The Joint Venture incurs capital expenditures to grow its business by developing new and enhanced capabilities to increase the effectiveness and efficiency of the organization and to reduce risk. Additionally, the Joint Venture incurs capital expenditures for product development, disaster recovery, security enhancements, regulatory compliance and the replacement and upgrade of existing equipment at the end of its useful life.
93
Table of Contents
Debt
Refer to Change Healthcare Inc.—Liquidity and Capital Resources—Debt for information on debt obligations.
Off-Balance Sheet Arrangements
As of March 31, 2020, the Joint Venture had no off-balance sheet arrangements.
Contractual Obligations
Refer to Change Healthcare Inc.—Liquidity and Capital Resources—Contractual Obligations for information on the contractual obligations.
Critical Accounting Policies and Estimates
The preparation of financial statements in accordance with GAAP requires the Joint Venture to make estimates and assumptions that affect reported amounts and related disclosures. The Joint Venture considers an accounting estimate to be critical if:
| • | it requires assumptions to be made that were uncertain at the time the estimate was made; and |
| • | changes in the estimate or different estimates that could have been made could have a material impact on the Joint Venture’s consolidated results of operations and financial condition. |
The following discussion of critical accounting estimates is not intended to be a comprehensive list of all of the Joint Venture’s accounting policies that require estimates and highlights only those policies that involve estimates that it believes entail a higher degree of judgment and complexity. The Joint Venture believes the current assumptions and other considerations used to estimate amounts reflected in the Joint Venture’s consolidated financial statements are appropriate. However, if actual experience differs from the assumptions and other considerations used in estimating amounts reflected in the Joint Venture’s consolidated financial statements, the resulting changes could have a material adverse effect on the Joint Venture’s consolidated results of operations and financial condition.
Refer to Note 2, Summary of Significant Accounting Policies in the audited financial statements of the Joint Venture included as Exhibit 99.1 for additional information about other critical accounting policies.
Revenue Recognition
In April 2019, the Joint Venture adopted ASC 606 which replaced most prior general and industry specific revenue recognition guidance with a principles-based comprehensive revenue recognition framework. Under this revised framework, a company recognizes revenue to depict the transfer of promised goods and services to customers in an amount that reflects the consideration to which the company expects to be entitled in exchange for those goods and services.
The Joint Venture generates most of its solutions revenue by using technology solutions (generally Software as a Service (“SaaS”)) to provide services to its customers that automate and simplify business and administrative functions for payers, providers, pharmacies, and channel partners and through the licensing of software, software systems (consisting of software, hardware and maintenance support) and content.
The Joint Venture recognizes revenue when the customer obtains control of the good or service through the Joint Venture satisfying a performance obligation by transferring the promised good or service to the customer.
94
Table of Contents
Refer to Note 3, Revenue Recognition in the audited financial statements of the Joint Venture included as Exhibit 99.1 for additional information.
Business Combinations
The Joint Venture recognizes the consideration transferred (i.e., purchase price) in a business combination as well as the acquired business’ identifiable assets, liabilities and noncontrolling interests at their acquisition date fair value. The excess of the consideration transferred over the fair value of the identifiable assets, liabilities and noncontrolling interest, if any, is recorded as goodwill. Any excess of the fair value of the identifiable assets acquired and liabilities assumed over the consideration transferred, if any, is generally recognized within earnings as of the acquisition date.
The fair value of the consideration transferred, assets, liabilities and noncontrolling interests is estimated based on one or a combination of income, cost or market approaches as determined based on the nature of the asset or liability and the level of inputs available to the Joint Venture (i.e., quoted prices in an active market, other observable inputs or unobservable inputs).
With respect to assets, liabilities and noncontrolling interest, the determination of fair value requires management to make subjective judgments as to projections of future operating performance, the appropriate discount rate to apply, long-term growth rates, etc. The effect of these judgments then impacts the amount of the goodwill that is recorded and the amount of depreciation and amortization expense to be recognized in future periods related to tangible and intangible assets acquired.
With respect to the consideration transferred, certain of the Joint Venture’s acquisitions may include contingent consideration, the fair value of which is generally required to be measured each quarter until resolution of the contingency. In addition to the judgments applicable to valuing tangible and intangible assets, the determination of the fair value of the attainment of certain specified financial performance measures requires management to make subjective judgments as to the probability and timing of the attainment of certain specified financial performance measures. The determination of the fair value of the contingent consideration is particularly sensitive to judgments relative to the probability of achieving the specified financial performance measures.
Goodwill and Intangible Assets
Goodwill and intangible assets from the Joint Venture’s acquisitions are accounted for using the acquisition method of accounting. Intangible assets with definite lives are amortized on a straight-line basis over the estimated useful lives of the related assets.
With respect to intangible assets (excluding goodwill), the Joint Venture reviews for impairment whenever events or changes in circumstances indicate that carrying amounts may not be recoverable. For those assets that are held and used, the Joint Venture recognizes an impairment loss only if its carrying amount is not recoverable through its undiscounted cash flows and measure the impairment loss based on the difference between the carrying amount and fair value. Assets held for sale are reported at the lower of cost or fair value less costs to sell.
The Joint Venture assesses its goodwill for impairment annually (as of January 1 of each year) or whenever significant indicators of impairment are present. The Joint Venture first assesses whether it can reach a more likely than not conclusion that goodwill is not impaired via qualitative analysis alone. To the extent such a conclusion cannot be reached based solely on a qualitative assessment, the Joint Venture, using the assistance of a valuation specialist as appropriate, compares the fair value of each reporting unit to its associated carrying value. The Joint Venture will generally recognize an impairment charge for the amount, if any, by which the carrying amount of the reporting unit exceeds its fair value.
95
Table of Contents
When necessary, the Joint Venture estimates the fair value of its reporting units using a methodology that considers both income and market approaches. Each approach requires the use of certain assumptions. The income approach requires management to exercise judgment in making assumptions regarding the reporting unit’s future income stream, a discount rate and a constant rate of growth after the initial forecast period utilized. These assumptions are subject to change based on business and economic conditions and could materially affect the indicated values of the Joint Venture’s reporting units.
The market approach requires management to exercise judgment in its selection of guideline companies, as well in its selection of the most relevant transaction multiple. Guideline companies selected are comparable to the Joint Venture in terms of product or service offerings, markets and/or customers, among other characteristics.
Income Taxes
The Joint Venture records deferred income taxes for the tax effect of differences between book and tax bases of its assets and liabilities, as well as differences related to the timing of recognition of income and expenses.
Deferred income taxes reflect the available net operating losses and the net tax effect of temporary differences between the carrying amounts of assets and liabilities for financial reporting purposes and the amounts used for income tax purposes. Realization of the future tax benefits related to deferred tax assets is dependent on many factors, including the Joint Venture’s past earnings history, expected future earnings, the character and jurisdiction of such earnings, reversing taxable temporary differences, unsettled circumstances that, if unfavorably resolved would adversely affect utilization of the Joint Venture’s deferred tax assets, carryback and carryforward periods and tax strategies that could potentially enhance the likelihood of realization of a deferred tax asset.
The Joint Venture recognizes tax benefits for uncertain tax positions at the time that it concludes the tax position, based solely on its technical merits, is more likely than not to be sustained upon examination. The benefit, if any, is measured as the largest amount of benefit, determined on a cumulative probability basis that is more likely than not to be realized upon ultimate settlement. Tax positions failing to qualify for initial recognition are recognized in the first subsequent interim period that they meet the more likely than not standard, are resolved through negotiation or litigation with the taxing authority or on expiration of the statute of limitations.
Tax Receivable Agreement Obligations
Upon the consummation of the Transactions, the Joint Venture assumed obligations related to certain tax receivable agreements (collectively, the “tax receivable agreements”) with our current and former owners. Because the assets and obligations of the predecessor businesses were contributed to the Joint Venture at their historical carrying values, these tax receivable agreements are subject to differing accounting models. The Joint Venture established a liability related to the McKesson Tax Receivable Agreement upon the reduction of McKesson’s ownership in the Joint Venture below 20%, which occurred on the date of the Merger. Refer to Note 20, Tax Receivable Agreement Obligations in the audited financial statements of the Joint Venture included as Exhibit 99.1 for additional information.
Related Party Balances and Transactions
Refer to Note 21, Other Related Party Transactions in the audited financial statements of the Joint Venture included as Exhibit 99.1.
96
Table of Contents
Recent Accounting Pronouncements
Refer to Note 2, Summary of Significant Accounting Policies in the audited financial statements of the Joint Venture included as Exhibit 99.1.
ITEM 7A. QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK
Change Healthcare Inc. is exposed to market risk in the normal course of business.
Interest Rate Risk
Change Healthcare Inc. has interest rate risk primarily related to borrowings under the Joint Venture’s Senior Credit Facilities. Borrowings under the Senior Credit Facilities bear interest at a rate equal to either (i) LIBOR for the relevant interest period, adjusted for statutory reserve requirements (the Term Loan Facility, is subject to a floor of 1.00% per annum and the Revolving Facility is subject to a floor of 0.00% per annum), plus an applicable margin or (ii) a base rate equal to the highest of (a) the rate of interest in effect as publicly announced by the administrative agent as its prime rate, (b) the federal funds effective rate plus 0.50% and (c) adjusted LIBOR for an interest period of one month plus 1.00% (the Term Loan Facility may be subject to a floor of 2.00% per annum), in each case, plus an applicable margin.
As of March 31, 2020, Change Healthcare Inc. had Term Loan borrowings of $3,808.3 million (before unamortized debt discount) and Revolving Facility borrowings of $250.0 million under the Senior Credit Facilities. As of March 31, 2020, the LIBOR-based interest rate on the Term Loan Facility was LIBOR plus 2.5% and on the Revolving Facility LIBOR plus 2.25%.
Change Healthcare Inc. manages economic risks, including interest rate, liquidity and credit risk, primarily by managing the amount, sources and duration of its debt funding and the use of derivative financial instruments. Specifically, Change Healthcare Inc. enters into interest rate cap agreements to manage exposures that arise from business activities that result in the receipt or payment of future known and uncertain cash amounts, the value of which are determined by interest rates. Change Healthcare Inc.’s interest rate cap agreements are used to manage differences in the amount, timing and duration of its known or expected cash receipts and its known or expected cash payments principally related to its borrowings. As of March 31, 2020, Change Healthcare Inc.’s outstanding interest rate cap agreements were designated as cash flow hedges of interest rate risk and were determined to be highly effective.
A change in interest rates on variable rate debt may impact Change Healthcare Inc.’s pretax earnings and cash flows. Based on the outstanding debt as of March 31, 2020, and assuming that its mix of debt instruments, derivative financial instruments and other variables remain the same, the annualized effect of a one percentage point change in variable interest rates would have an annualized pretax impact on the earnings and cash flows of approximately $15.6 million.
In the future, in order to manage Change Healthcare Inc.’s interest rate risk, it may refinance its existing debt, enter into additional interest rate cap agreements, modify its existing interest rate cap agreements or make changes that may impact its ability to treat its interest rate cap agreements as a cash flow hedge. However, Change Healthcare Inc. does not intend or expect to enter into derivative or interest rate cap agreement transactions for speculative purposes.
97
Table of Contents
ITEM 8. FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
Page
98
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the stockholders and Board of Directors of Change Healthcare Inc.
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of Change Healthcare Inc. and subsidiaries (the “Company”) as of March 31, 2020 and March 31, 2019, the related consolidated statements of operations, comprehensive income (loss), stockholders’ equity, and cash flows, for each of the three years in the period ended March 31, 2020, and the related notes (collectively referred to as the “financial statements”). In our opinion, the financial statements present fairly, in all material respects, the financial position of the Company as of March 31, 2020 and March 31, 2019, and the results of its operations and its cash flows for each of the three years in the period ended March 31, 2020, in conformity with accounting principles generally accepted in the United States of America.
Change in Accounting Principle
As discussed in Note 3 to the financial statements, effective April 1, 2019, Change Healthcare LLC, an equity method investee of the Company until March 10, 2020, adopted Accounting Standards Codification (“ASC”) Topic 606, Revenue From Contracts With Customers, using the modified retrospective approach. The adoption had a material effect on the financial statements through a proportionate amount of the cumulative effect adjustment to Change Healthcare LLC’s Members’ Deficit that was recorded in the Company’s stockholders’ equity.
Basis for Opinion
These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audits, we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion.
Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
| /s/ Deloitte & Touche LLP |
| Atlanta, Georgia |
| June 4, 2020 |
We have served as the Company’s auditor since 2017.
99
Table of Contents
Consolidated Statements of Operations
(amounts in thousands, except share and per share amounts)
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Revenue |
||||||||||||
| Solutions revenue |
$ | 184,161 | $ | — | $ | — | ||||||
| Postage revenue |
12,631 | — | — | |||||||||
|
|
|
|
|
|
|
|||||||
| Total revenue |
196,792 | — | — | |||||||||
| Operating expenses |
||||||||||||
| Sales, marketing, general and administrative |
39,893 | 1,159 | 180 | |||||||||
| Cost of operations (exclusive of depreciation and amortization below) |
71,435 | — | — | |||||||||
| Research and development |
11,559 | — | — | |||||||||
| Customer postage |
12,631 | — | — | |||||||||
| Depreciation and amortization |
30,838 | — | — | |||||||||
| Accretion and changes in estimate with related parties, net |
15,823 | — | — | |||||||||
| Tax Receivable Agreement charges |
164,633 | — | — | |||||||||
| Goodwill impairment charge |
561,164 | — | — | |||||||||
|
|
|
|
|
|
|
|||||||
| Total operating expenses |
907,976 | 1,159 | 180 | |||||||||
|
|
|
|
|
|
|
|||||||
| Operating income (loss) |
(711,184 | ) | (1,159 | ) | (180 | ) | ||||||
| Non-operating (income) expense |
||||||||||||
| Loss from Equity Method Investment in the Joint Venture |
380,713 | 70,487 | 58,680 | |||||||||
| (Gain) Loss on sale of interests in the Joint Venture |
— | (661 | ) | (14 | ) | |||||||
| Management fee income |
(1,108 | ) | (378 | ) | (180 | ) | ||||||
| Interest expense, net |
16,652 | — | — | |||||||||
| (Gain) loss on other investments |
(15,881 | ) | — | — | ||||||||
| Other, net |
(709 | ) | — | — | ||||||||
|
|
|
|
|
|
|
|||||||
| Total non-operating (income) expense |
379,667 | 69,448 | 58,486 | |||||||||
|
|
|
|
|
|
|
|||||||
| Income (loss) before income tax provision (benefit) |
(1,090,851 | ) | (70,607 | ) | (58,666 | ) | ||||||
| Income tax provision (benefit) |
(143,254 | ) | (18,595 | ) | (119,621 | ) | ||||||
|
|
|
|
|
|
|
|||||||
| Net income (loss) |
$ | (947,597 | ) | $ | (52,012 | ) | $ | 60,955 | ||||
|
|
|
|
|
|
|
|||||||
| Net income (loss) per share: |
||||||||||||
| Basic |
$ | (6.92 | ) | $ | (0.69 | ) | $ | 0.81 | ||||
| Diluted |
$ | (6.92 | ) | $ | (0.69 | ) | $ | 0.78 | ||||
| Weighted average common shares outstanding: |
||||||||||||
| Basic |
136,996,624 | 75,513,130 | 75,590,613 | |||||||||
| Diluted |
136,996,624 | 75,513,130 | 77,801,096 | |||||||||
See accompanying notes to consolidated financial statements.
100
Table of Contents
Consolidated Statements of Comprehensive Income (Loss)
(amounts in thousands)
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Net income (loss) |
$ | (947,597 | ) | $ | (52,012 | ) | $ | 60,955 | ||||
| Other comprehensive income (loss): |
||||||||||||
| Foreign currency translation adjustment |
(5,519 | ) | (2,833 | ) | 1,242 | |||||||
| Changes in fair value of interest rate cap, net of taxes |
981 | (3,449 | ) | 1,606 | ||||||||
| Unrealized gain (loss) on available for sale debt securities of the Joint Venture, net of taxes |
1,045 | — | — | |||||||||
| Realized gain (loss) on available for sale debt securities of the Joint Venture |
(1,045 | ) | — | — | ||||||||
|
|
|
|
|
|
|
|||||||
| Other comprehensive income (loss) |
(4,538 | ) | (6,282 | ) | 2,848 | |||||||
|
|
|
|
|
|
|
|||||||
| Total comprehensive income (loss) |
$ | (952,135 | ) | $ | (58,294 | ) | $ | 63,803 | ||||
|
|
|
|
|
|
|
|||||||
See accompanying notes to consolidated financial statements.
101
Table of Contents
Consolidated Balance Sheets
(amounts in thousands, except share and per share amounts)
| March 31, 2020 |
March 31, 2019 |
|||||||
| Assets |
||||||||
| Current assets: |
||||||||
| Cash & cash equivalents |
$ | 410,405 | $ | 3,409 | ||||
| Accounts receivable, net of allowance for doubtful accounts |
740,105 | — | ||||||
| Contract assets |
132,704 | — | ||||||
| Due from Joint Venture |
— | 373 | ||||||
| Prepaid expenses and other current assets |
117,495 | — | ||||||
| Income taxes receivable |
472 | 1,781 | ||||||
|
|
|
|
|
|||||
| Total current assets |
1,401,181 | 5,563 | ||||||
| Property and equipment, net |
206,196 | — | ||||||
| Goodwill |
3,795,325 | — | ||||||
| Intangible assets, net |
4,365,806 | — | ||||||
| Dividend receivable |
— | 81,264 | ||||||
| Investment in the Joint Venture |
— | 1,211,996 | ||||||
| Investment in business purchase option |
146,500 | — | ||||||
| Other noncurrent assets, net |
192,372 | — | ||||||
|
|
|
|
|
|||||
| Total assets |
$ | 10,107,380 | $ | 1,298,823 | ||||
|
|
|
|
|
|||||
| Liabilities |
||||||||
| Current liabilities: |
||||||||
| Accounts payable |
$ | 68,169 | $ | — | ||||
| Accrued expenses |
390,294 | 176 | ||||||
| Deferred revenues |
302,313 | — | ||||||
| Due to related parties, net |
20,234 | — | ||||||
| Current portion of long-term debt |
278,779 | — | ||||||
| Due to the Joint Venture |
— | 6,167 | ||||||
|
|
|
|
|
|||||
| Total current liabilities |
1,059,789 | 6,343 | ||||||
| Long-term debt, excluding current portion |
4,710,294 | — | ||||||
| Deferred income tax liabilities |
615,904 | 159,993 | ||||||
| Tax receivable agreement obligations to related parties |
177,826 | — | ||||||
| Tax receivable agreement obligation |
164,633 | — | ||||||
| Other long-term liabilities |
93,487 | — | ||||||
|
|
|
|
|
|||||
| Total liabilities |
6,821,933 | 166,336 | ||||||
|
|
|
|
|
|||||
| Commitments and contingencies |
||||||||
| Stockholders’ Equity |
||||||||
| Common Stock (par value, $.001), 9,000,000,000 and 252,800,000 shares authorized and 303,428,142 and 75,474,654 shares issued and outstanding at March 31, 2020 and 2019, respectively |
303 | 75 | ||||||
| Class X common stock (par value, $.001), 0 and 1 share authorized and no shares issued and outstanding at March 2020 and 2019, respectively |
— | — | ||||||
| Preferred stock (par value, $.001), 900,000,000 and 0 shares authorized and no shares issued and outstanding at March 31, 2020 and 2019, respectively |
— | — | ||||||
| Additional paid-in capital |
4,222,580 | 1,153,509 | ||||||
| Accumulated other comprehensive income (loss) |
(7,372 | ) | (3,256 | ) | ||||
| Accumulated deficit |
(930,064 | ) | (17,841 | ) | ||||
|
|
|
|
|
|||||
| Total stockholders’ equity |
3,285,447 | 1,132,487 | ||||||
|
|
|
|
|
|||||
| Total liabilities and stockholders’ equity |
$ | 10,107,380 | $ | 1,298,823 | ||||
|
|
|
|
|
|||||
See accompanying notes to consolidated financial statements.
102
Table of Contents
Consolidated Statements of Stockholders’ Equity
(amounts in thousands, except share and per share amounts)
| Common Stock Shares |
Common Stock |
Additional Paid-in Capital |
Accumulated Deficit |
Accumulated Other Comprehensive Income (Loss) |
Total Stockholders’ Equity |
|||||||||||||||||||
| Balance at March 31, 2017 |
75,478,369 | $ | 75 | $ | 1,114,771 | $ | (26,294 | ) | $ | (312 | ) | $ | 1,088,240 | |||||||||||
| Equity compensation expense |
— | — | 24,700 | — | — | 24,700 | ||||||||||||||||||
| Repurchase of the Company’s common stock, net of taxes |
(8,974 | ) | — | (171 | ) | — | — | (171 | ) | |||||||||||||||
| Issuance of the Company’s common stock upon exercise of equity awards |
279,723 | — | — | — | — | — | ||||||||||||||||||
| Net income (loss) |
— | — | — | 60,955 | — | 60,955 | ||||||||||||||||||
| Foreign currency translation adjustment of the Joint Venture |
— | — | — | — | 1,242 | 1,242 | ||||||||||||||||||
| Change in fair value of interest rate swap, net of taxes of the Joint Venture |
— | — | — | — | 1,606 | 1,606 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Balance at March 31, 2018 |
75,749,118 | $ | 75 | $ | 1,139,300 | $ | 34,661 | $ | 2,536 | $ | 1,176,572 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Cumulative effect of accounting change by the Joint Venture-ASU 2017-12 |
— | — | — | (490 | ) | 490 | — | |||||||||||||||||
| Equity compensation expense |
— | 20,135 | — | — | 20,135 | |||||||||||||||||||
| Repurchase of the Company’s common stock, net of taxes |
(342,418 | ) | — | (5,926 | ) | — | — | (5,926 | ) | |||||||||||||||
| Issuance of the Company’s common stock upon exercise of equity awards |
67,953 | — | — | — | — | — | ||||||||||||||||||
| Net income (loss) |
— | — | — | (52,012 | ) | — | (52,012 | ) | ||||||||||||||||
| Foreign currency translation adjustment of the Joint Venture |
— | — | — | — | (2,833 | ) | (2,833 | ) | ||||||||||||||||
| Change in fair value of interest rate swap of the Joint Venture, net of taxes |
— | — | — | — | (3,449 | ) | (3,449 | ) | ||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Balance at March 31, 2019 |
75,474,654 | $ | 75 | $ | 1,153,509 | $ | (17,841 | ) | $ | (3,256 | ) | $ | 1,132,487 | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Cumulative effect of accounting change by the Joint Venture-ASC 606 |
— | — | — | 35,796 | — | 35,796 | ||||||||||||||||||
| Cumulative effect of accounting change by the Joint Venture-ASU 2018-02 |
— | — | — | (422 | ) | 422 | — | |||||||||||||||||
| Equity compensation expense |
— | — | 30,372 | — | — | 30,372 | ||||||||||||||||||
| Issuance of the Company’s common stock upon initial public offering |
49,285,713 | 49 | 608,630 | — | — | 608,679 | ||||||||||||||||||
103
Table of Contents
| Common Stock Shares |
Common Stock |
Additional Paid-in Capital |
Accumulated Deficit |
Accumulated Other Comprehensive Income (Loss) |
Total Stockholders’ Equity |
|||||||||||||||||||
| Effect of initial public offering issuance costs on Joint Venture equity |
— | — | (4,160 | ) | — | — | (4,160 | ) | ||||||||||||||||
| Issuance of tangible equity units |
— | — | 232,929 | — | — | 232,929 | ||||||||||||||||||
| Unrealized gain (loss) on available for sale debt securities of the Joint Venture |
— | — | — | — | 1,045 | 1,045 | ||||||||||||||||||
| Realized gain (loss) on available for sale debt securities of the Joint Venture |
— | — | — | — | (1,045 | ) | (1,045 | ) | ||||||||||||||||
| Issuance of the Company’s common stock upon exercise of equity awards |
708,962 | 1 | 6,023 | — | — | 6,024 | ||||||||||||||||||
| Net income (loss) |
— | — | — | (947,597 | ) | — | (947,597 | ) | ||||||||||||||||
| Foreign currency translation adjustment |
— | — | — | — | (5,519 | ) | (5,519 | ) | ||||||||||||||||
| Change in fair value of interest rate swap, net of taxes |
— | — | — | — | 981 | 981 | ||||||||||||||||||
| Issuance of the Company’s common stock upon Merger |
175,995,192 | 176 | 2,194,484 | — | — | 2,194,660 | ||||||||||||||||||
| Conversion of tangible equity units |
1,963,621 | 2 | (2 | ) | — | — | — | |||||||||||||||||
| Other |
— | — | 795 | — | — | 795 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Balance at March 31, 2020 |
303,428,142 | $ | 303 | $ | 4,222,580 | $ | (930,064 | ) | $ | (7,372 | ) | $ | 3,285,447 | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
See accompanying notes to consolidated financial statements.
104
Table of Contents
Consolidated Statements of Cash Flows
(amounts in thousands)
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Cash flows from operating activities: |
||||||||||||
| Net income (loss) |
$ | (947,597 | ) | $ | (52,012 | ) | $ | 60,955 | ||||
| Adjustments to reconcile net income (loss) to net cash provided by (used in) operating activities: |
||||||||||||
| Loss from Equity Method Investment in the Joint Venture |
380,713 | 70,487 | 58,680 | |||||||||
| Depreciation and amortization |
30,838 | — | — | |||||||||
| Accretion and changes in estimate, net |
15,823 | — | — | |||||||||
| Tax receivable agreement charges |
164,633 | — | — | |||||||||
| Equity compensation |
1,701 | — | — | |||||||||
| Deferred income tax expense (benefit) |
(143,822 | ) | (18,595 | ) | (119,621 | ) | ||||||
| (Gain) Loss on Sale of Interests in the Joint Venture |
— | (661 | ) | (14 | ) | |||||||
| (Gain) loss on other investments |
(15,881 | ) | — | — | ||||||||
| Goodwill impairment charge |
561,164 | — | — | |||||||||
| Amortization of debt discount and issuance costs |
2,235 | — | — | |||||||||
| Other |
(1,110 | ) | — | — | ||||||||
| Changes in operating assets and liabilities: |
||||||||||||
| Accounts receivable |
(21,211 | ) | — | — | ||||||||
| Prepaid expenses and other |
(7,528 | ) | — | — | ||||||||
| Due from the Joint Venture |
(2,516 | ) | (72 | ) | 524 | |||||||
| Income taxes receivable |
1,309 | 14,047 | (15,828 | ) | ||||||||
| Accounts payable |
7,532 | — | — | |||||||||
| Accrued expenses and other liabilities |
(195,207 | ) | (125 | ) | (524 | ) | ||||||
| Deferred Revenue |
11,304 | — | — | |||||||||
| Due to the Joint Venture |
3,692 | (9,661 | ) | 15,828 | ||||||||
|
|
|
|
|
|
|
|||||||
| Net cash provided by (used in) operating activities |
(153,928 | ) | 3,408 | — | ||||||||
|
|
|
|
|
|
|
|||||||
| Cash flows from investing activities: |
||||||||||||
| Proceeds from sale of interests in the Joint Venture |
— | 6,503 | 171 | |||||||||
| Capitalized expenditures |
(13,002 | ) | — | — | ||||||||
| Acquisitions, net of cash acquired |
330,667 | — | — | |||||||||
| Investment in debt and equity securities of the Joint Venture |
(278,875 | ) | — | — | ||||||||
| Proceeds from investments in debt securities of the Joint Venture |
7,332 | — | — | |||||||||
| Investment in the Joint Venture |
(610,784 | ) | — | — | ||||||||
|
|
|
|
|
|
|
|||||||
| Net cash provided by (used in) investing activities |
(564,662 | ) | 6,503 | 171 | ||||||||
|
|
|
|
|
|
|
|||||||
| Cash flows from financing activities: |
||||||||||||
| Proceeds from initial public offering, net of issuance costs |
608,679 | — | — | |||||||||
| Proceeds from issuance of equity component of tangible equity units, net of issuance costs |
232,929 | — | — | |||||||||
| Proceeds from issuance of debt component of tangible equity units |
47,367 | — | — | |||||||||
| Payment of loan costs |
(1,421 | ) | — | — | ||||||||
| Repayment of senior amortizing notes |
(11,094 | ) | — | — | ||||||||
| Proceeds from draw on revolver |
250,000 | — | — | |||||||||
| Payments to acquire common stock |
— | (6,502 | ) | (171 | ) | |||||||
| Receipts (payments) on derivative instruments |
(890 | ) | — | — | ||||||||
|
|
|
|
|
|
|
|||||||
| Net cash provided by (used in) financing activities |
1,125,570 | (6,502 | ) | (171 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Effect of exchange rate changes on cash and cash equivalents |
16 | — | — | |||||||||
105
Table of Contents
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Net increase (decrease) in cash, cash equivalents and restricted cash |
406,996 | 3,409 | — | |||||||||
| Cash, cash equivalents and restricted cash at beginning of period |
3,409 | — | — | |||||||||
|
|
|
|
|
|
|
|||||||
| Cash, cash equivalents and restricted cash at end of period |
$ | 410,405 | $ | 3,409 | $ | — | ||||||
|
|
|
|
|
|
|
|||||||
| Supplemental disclosures of cash flow information |
||||||||||||
| Cash paid for interest |
$ | 265,633 | $ | — | $ | — | ||||||
|
|
|
|
|
|
|
|||||||
| Cash paid for income taxes |
$ | (714 | ) | $ | — | $ | 15,828 | |||||
|
|
|
|
|
|
|
|||||||
| Supplemental disclosures of noncash transactions |
||||||||||||
| Issuance of common stock upon exercise of equity awards: |
||||||||||||
| Investment in the Joint Venture |
$ | 5,077 | $ | 1,297 | $ | 5,306 | ||||||
|
|
|
|
|
|
|
|||||||
| Dividend receivable |
$ | (5,077 | ) | $ | (1,297 | ) | $ | (5,306 | ) | |||
|
|
|
|
|
|
|
|||||||
| Change Healthcare Inc. portion of the Joint Venture equity transactions: |
||||||||||||
| Investment in the Joint Venture |
$ | 13,902 | $ | (2,377 | ) | $ | 10,898 | |||||
|
|
|
|
|
|
|
|||||||
| Additional paid in capital |
$ | (11,133 | ) | $ | (6,043 | ) | $ | (7,427 | ) | |||
|
|
|
|
|
|
|
|||||||
| Accumulated other comprehensive income |
$ | (2,769 | ) | $ | 8,420 | $ | (3,471 | ) | ||||
|
|
|
|
|
|
|
|||||||
| Capitalized Expenditures: |
||||||||||||
| Property and equipment, net |
$ | 5,295 | $ | — | $ | — | ||||||
|
|
|
|
|
|
|
|||||||
| Other noncurrent assets, net |
$ | 14,169 | $ | — | $ | — | ||||||
|
|
|
|
|
|
|
|||||||
| Intangibles, net |
$ | 2,855 | $ | — | $ | — | ||||||
|
|
|
|
|
|
|
|||||||
| Drafts and accounts payable |
$ | (9,843 | ) | $ | — | $ | — | |||||
|
|
|
|
|
|
|
|||||||
| Accrued expenses |
$ | (12,476 | ) | $ | — | $ | — | |||||
|
|
|
|
|
|
|
|||||||
Additionally, the exchange of shares and inclusion of the previously held equity interests and dividend receivable in the purchase price of the Merger are considered noncash transactions. See Note 2, Business Combinations.
See accompanying notes to consolidated financial statements.
106
Table of Contents
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
1. Nature of Business and Organization
Business Overview
Change Healthcare Inc. (the “Company”) is an independent healthcare technology platform that provides data and analytics-driven solutions to improve clinical, financial and patient engagement outcomes in the U.S. healthcare system. It offers a suite of software, analytics, technology-enabled services and network solutions that drive improved results in the complex workflows of healthcare system payers and providers. The Company’s solutions are designed to improve clinical decision-making, simplify billing, collection and payment processes and enable a better patient experience.
Organization
The Company, a Delaware corporation, was formed on June 22, 2016 to hold an equity investment in Change Healthcare LLC (the “Joint Venture”) a joint venture between the Company and McKesson Corporation (“McKesson”).
The Transactions
In June 2016, the Company, the Joint Venture, Change Healthcare Holdings, LLC, Change Healthcare Intermediate Holdings, LLC, Change Healthcare Performance, Inc. (formerly Change Healthcare, Inc.) (“Legacy CHC”) and its stockholders—including affiliates of The Blackstone Group, L.P. (“Blackstone”) and Hellman & Friedman LLC (“Hellman & Friedman”)—entered into an Agreement of Contribution and Sale (the “Contribution Agreement”) with McKesson Corporation (together with the Company, the “Members”). Under the terms of the Contribution Agreement, the parties agreed to form the Joint Venture, a joint venture that combined the majority of the McKesson Technology Solutions businesses excluding McKesson’s Enterprise Information Solutions business and RelayHealth Pharmacy Network (such contributed businesses, “Core MTS”), with substantially all of the assets and operations of Legacy CHC, but excluding Legacy CHC’s pharmacy claims switching and prescription routing businesses (such excluded business, the “eRx Network” and the businesses contributed by Legacy CHC, together with Core MTS, the “Contributed Businesses”). The creation of the Joint Venture, including the contribution of the Contributed Businesses and related transactions, is collectively referred to as the “Transactions”. The Transactions closed on March 1, 2017. Upon completion of the Transactions, the Company owned approximately 30% of the Joint Venture.
Pursuant to the terms of the Contribution Agreement, the Legacy CHC stockholders, directly and indirectly, transferred ownership of substantially all of Legacy CHC to the Joint Venture in consideration of (a) the payment at the closing of the Transactions by the Joint Venture to Legacy CHC’s stockholders and certain participants in the Legacy CHC Amended and Restated 2009 Equity Incentive Plan (the “Legacy CHC Equity Plan”) of approximately $1,800,000, stock in eRx Network Holdings, Inc., and the 2017 Tax Receivable Agreement (as described in Note 18. Tax Receivable Agreements) and (b) the issuance to the Company of membership interests in the Joint Venture. In addition, McKesson caused Core MTS to be transferred to the Joint Venture in consideration of (a) the assumption and subsequent payment at the closing of the Transactions by the Joint Venture to McKesson of a promissory note in the amount of approximately $1,300,000, (b) the issuance of membership interests in the Joint Venture and (c) an interest in a tax receivable agreement from the Joint Venture.
In connection with the Transactions, the Joint Venture, through its subsidiaries, entered into new senior secured credit facilities, consisting of a Term Loan Facility in the amount of $5,100,000 and a Revolving Credit
107
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Facility in an aggregate principal amount of $500,000, and issued $1,000,000 of 5.75% senior notes due 2025. The proceeds were used to make all payments to the Legacy CHC stockholders, certain participants in the Legacy CHC Equity Plan and McKesson described above, to refinance certain of Legacy CHC’s existing indebtedness and to pay fees and expenses incurred in connection with the Transactions.
Amendment of Certificate of Incorporation
Effective June 26, 2019 and in contemplation of its initial public offering of common stock, the Company amended its certificate of incorporation to effect a 126.4 for 1 stock split for all previously issued shares of common stock, to increase the authorized number of common stock, and to authorize shares of preferred stock. Following this amendment, the authorized shares include 9,000,000,000 shares of common stock (par value $.001 per share), one share of Class X stock (par value $.001 per share), and 900,000,000 shares of preferred stock (par value $.001 per share). Effective upon the consummation of the Merger (see Note 2, Business Combinations), the Class X stock is no longer available. All issued or outstanding shares or related share-based payment arrangement disclosures included herein have been retrospectively adjusted for the stock split.
Initial Public Offering
Effective July 1, 2019, the Company completed its initial public offering of 49,285,713 shares of common stock and a concurrent offering of 5,750,000 of tangible equity units (“TEUs”) for net proceeds of $608,679 and $278,875, respectively. The proceeds of the offering of common stock were subsequently contributed to the Joint Venture in exchange for 49,285,713 additional units of the Joint Venture, which together with the Company’s existing holdings represented an approximate 41% interest in the Joint Venture immediately following the initial public offering. The proceeds of the offering of TEUs were used to acquire TEUs of the Joint Venture that substantially mirror the terms of the TEUs included in the offering. The Joint Venture, in turn, used the proceeds received from the Company to repay $805,000 of its indebtedness under the Term Loan Facility without penalty in July 2019.
McKesson Exit
On March 10, 2020, McKesson completed a split-off of its interest in the Joint Venture through an exchange offer of its common stock for shares of PF2 SpinCo, Inc, a Delaware corporation and wholly owned subsidiary of McKesson (“SpinCo”). Immediately following consummation of the exchange offer, SpinCo was merged with and into the Company. As a result, McKesson no longer owns any voting or economic interest in the Joint Venture. See Note 2, Business Combinations, for more information.
COVID-19 Considerations
On March 11, 2020, the World Health Organization declared the current coronavirus (“COVID-19”) outbreak to be a global pandemic. In response to this declaration and the rapid spread of COVID-19 within the U.S., federal, state and local governments throughout the country have imposed varying degrees of restrictions on social and commercial activity to promote social distancing in an effort to slow the spread of the illness. These measures have led to weakened conditions in many sectors of the economy, including a decline in healthcare transaction volumes that are integral to the Company’s business.
While COVID-19 had a limited impact on the Company’s results of operations for the year ended March 31, 2020, the Company expects the COVID-19 outbreak to have an adverse impact on its financial results in future
108
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
periods. As a result of this change in financial outlook, the Company recognized a non-cash impairment charge during the fourth quarter of the year-ended March 31, 2020, as detailed in Note 9, Goodwill and Intangible Assets. The Company is not presently aware of events or circumstances arising from COVID-19 that would require it to revise the carrying value of any other of its assets or liabilities, nor does the Company expect the impacts of COVID-19 to cause it to be unable to comply with its debt covenants or meet its other contractual obligations.
2. Business Combinations
The Merger
On March 10, 2020 (the “Merger Effective Date”), pursuant to the Agreement and Plan of Merger, dated December 20, 2016 (the “Merger Agreement”), by and among the Company, McKesson and SpinCo, the Company combined with SpinCo in a two-step all-stock “Reverse Morris Trust” transaction that involved (i) a separation of SpinCo from McKesson pursuant to the Separation and Distribution Agreement, dated February 10, 2020 (the “Separation Agreement” and, the transactions contemplated by the Separation Agreement, the “Separation”), followed by (ii) the merger of SpinCo with and into the Company, with the Company as the surviving company (such merger, together with the other transactions contemplated by the Merger Agreement, the “Merger”).
The Merger was consummated pursuant to the Merger Agreement and the Separation Agreement. On the Merger Effective Date, SpinCo merged with and into the Company, with the Company as the surviving company. As a result, the Joint Venture became a wholly owned subsidiary of the Company. Pursuant to the Merger Agreement, McKesson accepted 15,426,537 shares of its own common stock, par value $0.01 (the “McKesson Common Stock”) in exchange for all 175,995,192 issued and outstanding shares of SpinCo common stock, par value $0.001 per share (the “SpinCo Common Stock”). All shares of SpinCo Common Stock were then converted into an equal number of shares of common stock of the Company, par value $0.001 (the “Change Common Stock”), which the Company issued to the former holders of SpinCo Common Stock, together with cash in lieu of any fractional shares.
Immediately after consummation of the Merger, approximately 58% of the outstanding Change Common Stock was held by pre-Merger holders of McKesson Common Stock and approximately 42% of the outstanding Change Common Stock was held by pre-Merger holders of Change Common Stock.
Prior to the Merger, the Company accounted for its investment in the Joint Venture under the equity method of accounting. Therefore, the Company’s acquisition of control of the Joint Venture was accounted for as a business combination achieved in stages under the acquisition method, in accordance with Accounting Standards Codification (“ASC”) 805, Business Combinations. Accordingly, the Company remeasured its previously held equity interest in the Joint Venture to fair value by reference to the publicly traded price of the common shares issued to SpinCo shareholders in exchange for the remaining 58% equity interest in the Joint Venture. Upon remeasurement of its investment, the Company recognized a loss of $230,229 which is included in Loss from Equity Method Investment in the Joint Venture in the consolidated statement of operations. The loss represents the amount by which the carrying value of the Company’s investment in the Joint Venture exceeded the fair value of its 42% interest immediately prior to the Merger.
The fair values of the assets acquired and the liabilities assumed were determined based on information that is currently available to the Company. Additional information is being gathered to finalize the provisional measurements with respect to deferred taxes. Accordingly, the measurement of the deferred tax assets acquired
109
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
and deferred tax liabilities assumed may change upon finalization of the Company’s valuations and completion of the purchase price allocation, both of which are expected to occur no later than one year from the acquisition date. The Company considers its accounting for the other assets acquired and liabilities assumed in the Merger to be complete. The following table summarizes the fair values of the identifiable assets and liabilities at the date of the acquisition.
| Net Assets acquired |
||||
| Cash |
$ | 330,665 | ||
| Accounts receivable, net of allowance for doubtful accounts of $22,059 |
718,895 | |||
| Contract assets |
132,704 | |||
| Prepaid and other current assets |
115,265 | |||
| Investment in business purchase option |
146,500 | |||
| Property and equipment, net |
206,751 | |||
| Goodwill |
4,360,648 | |||
| Other noncurrent assets |
169,539 | |||
| Identified intangible assets: |
||||
| Customer relationships (life 12-16 years) |
3,056,000 | |||
| Tradenames (life 18 years) |
146,000 | |||
| Technology-based intangible assets (life 6-12 years) |
1,188,000 | |||
| Drafts and accounts payable |
(60,637 | ) | ||
| Accrued expenses |
(559,456 | ) | ||
| Deferred revenues, current |
(292,528 | ) | ||
| Current portion of long-term debt |
(28,969 | ) | ||
| Other current liabilities |
(22,732 | ) | ||
| Long-term debt, excluding current portion |
(4,713,565 | ) | ||
| Deferred income tax liabilities |
(578,076 | ) | ||
| Tax receivable agreement obligations with related parties |
(176,586 | ) | ||
| Other long-term liabilities |
(102,675 | ) | ||
|
|
|
|||
| Net Assets acquired |
$ | 4,035,743 | ||
|
|
|
|||
| Summary of purchase consideration: |
||||
| Fair value of shares issued to SpinCo shareholders |
||||
| (175,995,192 shares at $12.47 per share): |
||||
| Common Stock, $0.001 par value |
$ | 176 | ||
| Additional paid-in capital |
2,194,484 | |||
| Fair value of Joint Venture equity interest previously held |
1,589,040 | |||
| Fair value of Joint Venture equity interest previously held through TEUs |
216,764 | |||
| Settlement of dividend receivable |
42,778 | |||
| Repayment of advances to member |
(7,499 | ) | ||
|
|
|
|||
| Purchase consideration |
$ | 4,035,743 | ||
|
|
|
|||
The goodwill recognized in the Merger is primarily attributable to expected synergies of the combined businesses and the acquisition of an assembled workforce knowledgeable of the healthcare and information
110
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
technology industries in which the Company operates. The goodwill is not expected to be deductible for tax purposes.
Acquisition costs related to the Merger were not material for the year ended March 31, 2020.
Supplemental Information
The supplemental pro forma results below were calculated after applying the Company’s accounting policies and adjusting the results of the acquired Joint Venture businesses to reflect (i) the additional depreciation and amortization that would have been charged resulting from the fair value adjustments to property and equipment and intangible assets, (ii) the additional interest expense associated with the consolidation of the Joint Venture’s long-term borrowings, and (iii) the decrease to revenue resulting from the fair value adjustment of assumed deferred revenue obligations, assuming the acquisition occurred on April 1, 2018.
| (Unaudited) Year ended March 31, |
||||||||
| 2020 | 2019 | |||||||
| Results of acquired business since acquisition date of March 10, 2020: |
||||||||
| Revenue |
$ | 196,792 | n/a | |||||
| Net income (loss) |
$ | 297 | n/a | |||||
| Supplemental pro forma data for combined entity: |
||||||||
| Revenue |
$ | 3,290,734 | $ | 3,133,907 | ||||
| Net income (loss) |
$ | (228,234 | ) | $ | (128,889 | ) | ||
| Net income (loss) per share, basic and diluted |
$ | (0.75 | ) | $ | (0.43 | ) | ||
3. Significant Accounting Policies
Basis of Presentation
The accompanying consolidated financial statements have been prepared in accordance with U.S. generally accepted accounting principles (“GAAP”) and include all subsidiaries and entities that are controlled by the Company. The results of operations for companies acquired are included in the consolidated financial statements from the effective date of acquisition. All intercompany accounts and transactions have been eliminated in the financial statements. Because of the significance of the Joint Venture to the Company’s financial position and results of operations, the Company is required to provide consolidated financial statements of the Joint Venture pursuant to Rule 3-09 of Regulation S-X.
Accounting Estimates
The preparation of financial statements in conformity with GAAP requires management to make estimates and assumptions that affect the amounts reported in the financial statements and accompanying notes. The Company bases its estimates on historical experience, current business factors and various other assumptions that the Company believes are necessary to consider in order to form a basis for making judgments about the carrying values of assets and liabilities, the recorded amounts of expenses and disclosure of contingent assets and liabilities. The Company is subject to uncertainties such as the impact of future events, economic, environmental and political factors and changes in the Company’s business environment; therefore, actual results could differ from these estimates. Accordingly, the accounting estimates used in the preparation of the Company’s financial statements will change as new events occur, as more experience is acquired, as additional information is obtained
111
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
and as the Company’s operating environment changes. Changes in estimates are made when circumstances warrant. Such changes in estimates and refinements in estimation methodologies are reflected in the reported results of operations; and if material, the effects of changes in estimates are disclosed in the notes to the financial statements. Estimates and assumptions by management affect: the allowance for doubtful accounts; the fair value assigned to assets acquired and liabilities assumed in business combinations; tax receivable agreement obligations; the fair value of interest rate cap agreement obligations; measurement of the components of tangible equity units; contingent consideration; loss accruals; the carrying value of the Company’s investments; the carrying value of long-lived assets (including goodwill and intangible assets); the amortization period of long-lived assets (excluding goodwill); the carrying value, capitalization and amortization of software development costs; the provision and benefit for income taxes and related deferred tax accounts; certain accrued expenses; revenue recognition; contingencies; and the value attributed to equity awards; the provision and benefit for income taxes and related deferred tax accounts; certain accrued expenses.
Business Combinations
The Company recognizes the consideration transferred (i.e., purchase price) in a business combination, as well as the acquired business’ identifiable assets, liabilities and noncontrolling interests at their acquisition date fair value. The excess of the consideration transferred over the fair value of the identifiable assets, liabilities and noncontrolling interest, if any, is recorded as goodwill. Any excess of the fair value of the identifiable assets acquired and liabilities assumed over the consideration transferred, if any, is generally recognized within earnings as of the acquisition date.
The fair value of the consideration transferred, assets, liabilities and noncontrolling interests is estimated based on one or a combination of income, costs or market approaches as determined based on the nature of the asset or liability and the level of inputs available to the Company (i.e., quoted prices in an active market, other observable inputs or unobservable inputs). To the extent that the Company’s initial accounting for a business combination is incomplete at the end of a reporting period, provisional amounts are reported for those items which are incomplete.
Equity Method Investment in the Joint Venture
Prior to the Merger, the Company accounted for its investment in the Joint Venture using the equity method. During that period, the Company evaluated its equity method investment for impairment whenever an event or change in circumstances occurred that had a potentially significant adverse impact on the carrying value of the investment. During the period from the inception of the Joint Venture through the date of the Merger, the Company did not identify any loss in the value of its investment that it deemed other than temporary, and therefore did not recognize any loss from impairment.
Cash and Cash Equivalents
The Company considers all highly liquid investments with an original maturity from the date of purchase of three months or less to be cash equivalents.
The Company’s cash and cash equivalents are deposited with several financial institutions. Deposits may exceed the amounts insured by the Federal Deposit Insurance Corporation in the U.S. and similar deposit insurance programs in other jurisdictions. The Company mitigates the risk of our short-term investment portfolio by depositing funds with reputable financial institutions and monitoring risk profiles.
112
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
The Company’s cash balances from time to time include funds it manages for customers, the most significant of which relates to funds remitted to retail pharmacies. Such funds are not restricted; however, these funds are generally paid out in satisfaction of the processing obligations pursuant to the management contracts. At the time of receipt, the Company records a corresponding liability within accrued expenses on the accompanying consolidated balance sheets. Such liabilities are summarized as “Pass-through payments” within Note 11, Accrued Expenses.
Allowance for Doubtful Accounts
The allowance for doubtful accounts was $22,360 at March 31, 2020 and $0 at March 31, 2019 and all prior balance sheet dates. The allowance for doubtful accounts reflects the Company’s best estimate of losses inherent in the Company’s receivables portfolio determined on the basis of historical experience, specific allowances for known troubled accounts and other currently available evidence. The following table summarizes activity related to the allowance for doubtful accounts:
| Year Ended March 31, 2020 |
Year Ended March 31, 2020 |
|||||||
| Balance at beginning of period |
$ | — | $ | — | ||||
| Acquisition in Merger |
22,059 | — | ||||||
| Provisions |
905 | — | ||||||
| Write-offs |
(604 | ) | — | |||||
|
|
|
|
|
|||||
| Balance at end of period |
$ | 22,360 | $ | — | ||||
|
|
|
|
|
|||||
Capitalized Software Developed for Internal Use
The Company provides services to many of its customers using software developed for internal use. The costs that are incurred to develop such software are expensed as incurred during the preliminary project stage and classified within research and development in the consolidated statements of operations. Once certain criteria have been met, direct costs incurred in developing or obtaining computer software are capitalized. Training and maintenance costs are expensed as incurred. Capitalized software costs are included in other noncurrent assets, net on the consolidated balance sheets and are generally amortized over the estimated useful life of three years.
Capitalized Software Developed for Sale
Development costs for software developed for sale to external customers are capitalized once a project has reached the point of technological feasibility. Completed projects are amortized after reaching the point of general availability using the straight-line method based on an estimated useful life of approximately three years. At each balance sheet date, or earlier if an indicator of an impairment exists, the Company evaluates the recoverability of unamortized capitalized software costs based on estimated future undiscounted revenues net of estimated related costs over the remaining amortization period.
Property and Equipment
Property and equipment are stated at cost, net of accumulated depreciation. Depreciation, including that related to assets under capital lease, is computed using the straight-line method over the estimated useful lives of the related assets. Expenditures for maintenance, repair and renewals of minor items are expensed as incurred. Expenditures for repair and renewals that extend the useful life of an asset are capitalized.
113
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Goodwill and Intangible Assets
Goodwill and intangible assets resulting from the Company’s acquisitions are accounted for using the acquisition method of accounting. Intangible assets with definite lives are amortized over their useful lives either on a straight-line basis or using an accelerated method, depending on the pattern that the Company expects the economic benefits of the assets to be consumed. Useful lives of the related assets generally are as follows:
| Customer relationships | 12-16 years | |||
| Tradenames | 18 years | |||
| Technology-based intangible assets | 6-12 years |
The Company assesses its goodwill for impairment annually (as of January 1 of each year) or whenever significant indicators of impairment are present. The Company first assesses whether it can reach a more likely than not conclusion that goodwill is not impaired via qualitative analysis alone. To the extent such a conclusion cannot be reached based on a qualitative assessment alone, the Company, using the assistance of a valuation specialist as appropriate, compares the fair value of each reporting unit to its associated carrying value. The Company will generally recognize an impairment charge for the amount, if any, by which the carrying amount of the reporting unit exceeds its fair value.
Long-Lived Assets
Long-lived assets used in operations are reviewed for impairment whenever events or changes in circumstances indicate that carrying amounts may not be recoverable. For long-lived assets to be held and used, the Company recognizes an impairment loss only if its carrying amount is not recoverable through its undiscounted cash flows and measures the impairment loss based on the difference between the carrying amount and fair value. Long-lived assets held for sale are reported at the lower of cost or fair value less costs to sell.
Derivatives
Derivative financial instruments are used to manage the Company’s interest rate exposure. The Company does not enter into financial instruments for speculative purposes. Derivative financial instruments are accounted for and measured at fair value. For derivative instruments that are designated and qualify as a cash flow hedge, the gain or loss on the derivative instrument is reported as a component of other comprehensive income and reclassified into earnings in the same line item associated with the forecasted transaction in the same period or periods during which the hedged transaction affects earnings (for example, in “interest expense” when the hedged transactions are interest cash flows associated with floating-rate debt). Receipts and payments under the derivative instruments are classified within cash flows from financing activities on the accompanying statements of cash flows.
Tangible Equity Units
In connection with the initial public offering, the Company completed an offering of TEUs. Each TEU comprises an amortizing note and purchase contract, both of which are freestanding instruments and separate units of account. The amortizing notes were issued at par and are classified as debt on the accompanying condensed consolidated balance sheet, with scheduled principal payments over the next twelve months reflected in current maturities of long-term debt. The purchase contracts are accounted for as prepaid forward contracts and classified as equity. The TEU proceeds and issuance costs were allocated to the amortizing notes and purchase contracts on a relative fair value basis. See Note 13, Tangible Equity Units for further discussion.
114
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Other Investments
The proceeds of the offering of TEUs were used to acquire TEUs of the Joint Venture that substantially mirror the terms of the TEUs included in the offering. Under these mirrored arrangements, the Joint Venture is required to make cash payments or to transfer LLC Units to the Company concurrent with any cash payments or issuance of shares by the Company pursuant to the terms of its TEUs.
Prior to the Merger, the Company accounted for these mirror arrangements as investments in debt and equity securities. The Company’s investment in debt securities were classified as “available-for-sale” and its investment in forward purchase contracts were considered equity securities measured at fair value. Changes in unrealized gains and losses for the Company’s debt securities were recognized as adjustments to other comprehensive income (loss) while changes in unrealized gains and losses for the Company’s investment in forward purchase contracts are recognized as adjustments to pretax income (loss). After the Merger, the Company’s investment in the TEUs of the Joint Venture is eliminated in the consolidated financial statements.
See Note 22, Related Party Transactions, for a discussion regarding the Investment in business purchase option.
Equity Compensation
The Company measures stock-based compensation cost at the grant date based on the estimated fair value of the award and recognizes the expense over the requisite service period, typically on a straight-line basis. The Company recognizes stock-based compensation cost for awards with performance conditions if and when it concludes that it is probable that the performance conditions will be achieved. The fair value of equity awards is recognized as an asset or expense in the same period and in the same manner as if the Company had paid cash for the goods or services. The Company recognizes forfeitures as they occur.
Prior to the Merger, these equity awards, as well as awards granted under the Company’s previous equity incentive plan, were granted to employees of the Company’s equity method investee, and therefore were subject to the accounting framework for awards granted to non-employees. Under this framework, the Company measured the compensation expense for equity awards based on the estimated fair value of such awards at the grant date, in a manner consistent with the recognition of expense for awards to employees. The recognized pre-Merger equity-based compensation is classified within loss from equity method investment in the Joint Venture on the consolidated statement of operations. However, as a result of a requirement that the Joint Venture issue an additional LLC Unit to the Company upon the exercise of each Company equity award (as described in Note 22, Related Party Transactions), the Company recognized an offsetting amount (i.e., a deemed dividend) within the same caption on the consolidated statements of operations.
Prior to the Merger, the Company recognized this deemed dividend as a receivable equal to the cumulative amount of stock compensation expense recognized by the Joint Venture for any outstanding equity awards. The dividend receivable was relieved upon exercise of the respective underlying equity awards. The Company’s dividend receivable from the Joint Venture was settled upon completion of the Merger.
Revenue
The Company recognizes revenue at an amount that reflects the consideration it expects to be entitled to in exchange for transferring goods or services to a customer, in accordance with ASC 606, Revenue from Contracts with Customers (“ASC 606”). See Note 4, Revenue Recognition, for additional information.
115
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Income Taxes
The Company records deferred income taxes for the tax effect of differences between book and tax bases of its assets and liabilities, as well as differences relating to the timing of recognition of income and expenses. Deferred income taxes reflect the available net operating losses and the net tax effect of temporary differences between the carrying amounts of assets and liabilities for financial reporting purposes and the amounts used for income tax purposes. Realization of the future tax benefits related to deferred tax assets is dependent on many factors, including the Company’s past earnings history, expected future earnings, the character and jurisdiction of such earnings, reversing taxable temporary differences, unsettled circumstances that, if unfavorably resolved, would adversely affect utilization of its deferred tax assets, carryback and carryforward periods and tax strategies that could potentially enhance the likelihood of realization of a deferred tax asset.
The Company recognizes tax benefits for uncertain tax positions at the time the Company concludes that the tax position, based solely on its technical merits, is more likely than not to be sustained upon examination. The benefit, if any, is measured as the largest amount of benefit, determined on a cumulative probability basis that is more likely than not to be realized upon ultimate settlement. Tax positions failing to qualify for initial recognition are recognized in the first subsequent interim period that they meet the more likely than not standard, upon resolution through negotiation or litigation with the taxing authority or on expiration of the statute of limitations.
Warranties
In the normal course of business, the Company provides warranties regarding the performance of software and products it sells. The Company’s liability under these warranties is to bring the product into compliance with previously agreed upon specifications. For software products, this may result in additional project costs, which are reflected in our estimates used for the percentage of completion method of accounting for software installations services within these contracts. In addition, most of the Company’s customers who purchase software and automation products also purchase annual maintenance agreements. Revenues from these maintenance agreements are recognized on a straight-line basis over the contract period and the cost of servicing product warranties is charged to expense when claims become estimable. As of March 31, 2020 and 2019, accrued warranty costs were immaterial.
Classification of Distributions Received from the Joint Venture
Prior to the Merger, the Company classifies distributions received from the Joint Venture in its consolidated statement of cash flows according to the nature of the distribution.
Accounting Pronouncements Not Yet Adopted
In June 2016, the Financial Accounting Standards Board (“FASB”) issued Accounting Standards Update (“ASU”) No. 2016-13, as amended by ASU No. 2018-19, which requires that a financial asset (or group of financial assets) measured at amortized cost be presented at the net amount expected to be collected based on relevant information about past events, including historical experience, current conditions and reasonable and supportable forecasts that affect the collectability of the reported amount. This update is scheduled to be effective for the Company beginning April 1, 2020. The Company is currently assessing the potential effects this update may have on its consolidated financial statements.
In August 2018, the FASB issued ASU 2018-13, which modifies the disclosure requirements for fair value measurements. ASU 2018-13 is effective for the Company beginning April 1, 2020. Early adoption is permitted
116
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
for either the entire standard or only the provisions that eliminate or modify requirements. The Company is currently assessing the potential effects this update may have on its financial statement disclosures.
In February 2016, the FASB issued ASU No. 2016-02, which generally requires that all lease obligations be recognized on the balance sheet at the present value of the remaining lease payments with a corresponding right of use asset (“ROU asset)”. As originally issued, the standard required that companies adopt the standard using the modified retrospective transition method and report a cumulative effect adjustment to the opening balance of retained earnings in the earliest comparative period presented. In July 2018, the FASB issued ASU No. 2018-11 which provides companies with the option to apply this cumulative effect adjustment to the opening balance of retained earnings in the period of adoption instead of the earliest comparative period presented. This update is effective for the Company beginning April 1, 2020, with early adoption permitted. The Company will utilize the modified retrospective approach upon adoption. While the Company is finalizing the assessment on the effect of adoption, the most significant impact is expected to relate to the recognition of new ROU assets and lease liabilities on the Company’s consolidated balance sheet for operating leases, as well as additional disclosures. Consequently, with adoption, the Company expects to recognize additional ROU assets and corresponding operating lease liabilities of between $110,000 and $125,000.
In August 2018, the FASB issued ASU No. 2018-15, which aligns the requirements for capitalizing implementation costs incurred in a hosting arrangement that is a service contract with the requirements for capitalizing implementation costs incurred to develop or obtain internal-use software. This update also requires that the effects of such capitalized costs be classified in the same respective caption of the statement of operations, balance sheet and cash flows as the underlying hosting arrangement. Upon adoption, a company may elect to either retrospectively restate each prior reporting period or apply the update prospectively to all implementation costs incurred after the effective date. This update is scheduled to be effective for the Company beginning April 1, 2020. The Company will adopt the new guidance prospectively and is assessing the potential effects this update may have on its consolidated financial statements.
The Company does not believe that any other recently issued, but not yet effective accounting standards, if adopted, would have a material impact on the consolidated financial statements.
Recently Adopted Accounting Pronouncements
In April 2019, the Company adopted ASU No. 2018-16, which adds the Overnight Index Swap rate based on the Secured Overnight Financing Rate as a benchmark interest rate for hedging purposes. As the adoption of this update applies only to qualifying new or redesignated hedging relationships entered into following the date of adoption, its adoption had no immediate effect on the consolidated financial statements.
In April 2019, the Company adopted ASU No. 2018-02, which allows a reclassification from accumulated other comprehensive income to retained earnings for stranded tax effects resulting from the Tax Cuts and Jobs Act of 2017 (“Tax Legislation”). The adoption of this update was not material and is limited to the separate disclosure in Note 26, Accumulated Other Comprehensive Income related to the reclassification of such stranded costs from accumulated comprehensive income (loss) to accumulated deficit.
In April 2019, the Company adopted ASU No. 2018-07, which expands the scope of Topic 718 to include share-based payment transactions for acquiring goods and services from nonemployees. Among other provisions, the measurement date for awards to nonemployees changed from the earlier of the date at which a commitment for performance by the counterparty is reached or the date at which performance is complete under the previous guidance to the grant date under this update. Because the Company’s equity-based compensation was previously
117
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
subject to remeasurement at fair value each quarter under the previous authoritative literature, the effect of the adoption of this update had no material effect on the consolidated financial statements.
In April 2019, the Company and the Joint Venture adopted ASC 606 on a modified retrospective basis. ASC 606 replaced most prior general and industry specific revenue recognition guidance with a principles-based comprehensive revenue recognition framework. Under this revised framework, a company recognizes revenue to depict the transfer of promised goods and services to customers in an amount that reflects the consideration to which the company expects to be entitled in exchange for those goods and services. Prior to the Merger, the Company’s operations consisted principally of an investment in the Joint Venture, its financial statements reflected no revenue and, accordingly, the Company recognized no direct impact on its financial statements from the adoption of this update. However, upon adoption, the Joint Venture recognized a cumulative effect adjustment to its Members’ deficit. As a result of the impact of the adoption of ASC 606 to the Joint Venture’s Members’ deficit, the Company was required to recognize a proportionate amount of this cumulative effect adjustment to its April 1, 2019 retained earnings as well. The effect is disclosed within a separate caption of the accompanying consolidated statement of stockholders’ equity.
The adoption of the new standard had an immaterial impact on the Company’s consolidated statement of cash flows for the fiscal year ended March 31, 2020. See Note 4, Revenue Recognition for more information.
4. Revenue Recognition
The Company generates most of its solutions revenue by using technology solutions (generally Software as a Service (“SaaS”)) to provide services to its customers that automate and simplify business and administrative functions for payers, providers, pharmacies, and channel partners and through the licensing of software, software systems (consisting of software, hardware and maintenance support) and content.
The Company recognizes revenue when the customer obtains control of the good or service through the Company satisfying a performance obligation by transferring the promised good or service to the customer.
Prior to the Merger, the Company’s principal operations were limited to its investment in the Joint Venture, and the Company therefore did not recognize revenue in its statement of operations.
Principal Revenue Generating Products and Services
Hosted solutions and SaaS - The Company enters into arrangements whereby the Company provides the customer access to a Company-owned software solution, which are generally marketed under annual and multi-year arrangements. The customer is only provided “access” (not a license) to the software application. In these arrangements, the customer does not purchase equipment nor does the customer take physical possession of the software. The related revenue is recognized ratably over the contracted term. For fixed fee arrangements, revenue recognition begins after set-up and implementation are complete. For per-transaction fee arrangements, revenue is recognized as transactions are processed beginning on the service start date. Revenue for hosted solutions and SaaS, which is included in solutions revenue, is generated by the Software and Analytics, Network Solutions, and Technology-Enabled Services segments.
Transaction processing services - The Company provides transaction processing (such as claims processing) services to hospitals, pharmacies and health systems via a cloud-based (SaaS) platform. The promised service is to stand ready to process transactions for our customers over the contractual period on an as needed basis. The revenue related to these services is recognized over time as the transactions are processed, and the revenue is
118
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
recognized over the individual days in which the services are performed. Revenue for these services is recognized as solutions revenue in the Software and Analytics, Network Solutions, and Technology-Enabled Services segments, with the exception of revenue related to postage that is generated through the delivery of certain of these services. Postage revenue is further discussed below and is separately presented on the consolidated statement of operations. Any fixed annual fees and implementation fees are recognized ratably over the contract period.
Contingent fee services - The Company provides services to customers in which the transaction price is contingent on future occurrences, such as savings generated or amounts collected on behalf of its customers through the delivery of its services. In some cases, the Company performs services in advance of invoicing the customer, thereby creating a contract asset. Revenue in these arrangements is estimated and constrained until the Company determines that it is probable a significant revenue reversal will not occur, and variable consideration is allocated to the performance obligation for which the Company earns a contingent fee. The Company uses the expected value method when estimating variable consideration, as the Company has a large number of contracts with similar characteristics and considers a portfolio of data from other similar contracts to form its estimate of expected value. Revenue for contingent fee services, which is included in solutions revenue, is generated by the Software and Analytics and Technology-Enabled Services segments.
Content license subscriptions and time-based software - The Company’s content license subscriptions and time-based software arrangements provide a license to use a software for a specified period of time. At the end of the contractual period, the customer either renews the license for an additional term or ceases to use the software. Software licenses are typically delivered to the customer with functionality that the customer can benefit from the software on its own or together with readily available resources. As contracts for these solutions generally do not price individual components separately, the Company allocates the transaction price to the license and ongoing support performance obligations based on standalone selling price, primarily determined by historical value relationships between licenses and ongoing support and updates. Revenue allocated to content license subscriptions and time-based software license agreements is generally recognized at the point-in-time of delivery of the license or the content update upon transfer of control of the underlying license to the customer. Generally, software implementation fees are recognized over the implementation period through an input measure of progress method. Revenue allocated to maintenance and support is recognized ratably over the period covered by the agreements, as passage of time represents a faithful depiction of the transfer of these services. In some cases, software arrangements provide licenses to several software applications that are highly integrated with the implementation services and software updates and cannot function separately. The bundle is a single performance obligation since the individually promised goods and services are not distinct in the context of the contract because the related implementation services significantly modify and customize the software and the updates provided to the integrated software solution are critical to the software’s utility. The related revenue is recognized on a straight-line basis, ratably over the contractual term due to the frequency and criticality of the updates throughout the license period. Revenue for content license subscriptions and time-based software, which is included in solutions revenue, is generated by the Software and Analytics segment.
Perpetual software licenses and software systems - The Company’s perpetual software arrangements provide a license for a customer to use software in perpetuity. Software licenses are typically delivered to the customer with functionality from which the customer can benefit from the license on its own or together with readily available resources. Perpetual software arrangements are recognized at the time of delivery or through an input measure of progress method over the installation period if the arrangements require significant production or modification or customization of the software. Contracts accounted for through an input measure of progress method are generally measured based on the ratio of labor hours incurred to date to total estimated labor hours to be incurred. Software implementation fees are recognized as the work is performed or under the input method for perpetual
119
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
software. Hardware revenues are generally recognized upon delivery. Maintenance is recognized ratably over the term of the agreement as passage of time represents a faithful depiction of the transfer of these services. License, implementation, hardware and maintenance revenue for these arrangements, which is included in solutions revenue, is generated by the Software and Analytics segment.
Professional services - The Company provides training and consulting services to its customers, and the services may be fixed fee or time and materials based. Consulting services that fall outside of the standard implementation services vary depending on the scope and complexity of the service requested by the customer. Consulting services are deemed to be capable of being distinct from other products and services, and the services are satisfied either at a point of time or over time based on delivery and are recognized as solutions revenue in the Software and Analytics and Technology-Enabled Services segments. Training services are usually provided as an optional service to enhance the customer’s experience with a software product or provides additional education surrounding the general topic of the solution. Training services are capable of being distinct from other products and services. The Company treats training services as a distinct performance obligation, and they are satisfied at a point of time and recognized as solutions revenue in the Software and Analytics and Technology-Enabled Services segments.
Contract Balances
The Company’s payment terms vary by customer and product type. For certain products or services, the Company requires upfront payments before control of the product or service has transferred to the customer. For other products and services, the Company invoices the customer in arrears after providing the products or services. In addition, for certain contingent fee services, customers are billed in arrears, typically based upon a percentage of collections the Company makes on the customer’s behalf.
Under the new revenue standard, the Company generally recognizes a contract asset when revenue is recognized in advance of invoicing on a customer contract, unless the right to payment for that revenue is unconditional (i.e. requiring no further performance and only the passage of time). If a right to payment is determined to meet the criteria to be considered ‘unconditional’, then the Company will recognize a receivable.
Neither the Company nor the Joint Venture recognized any impairment losses on accounts receivable or contract assets during the year ended March 31, 2020.
The Company records deferred revenues when billings or payments are received from customers in advance of its performance. Deferred revenue is generally recognized when transfer of control to customers occurs. The deferred revenue balance is driven by multiple factors, including the frequency of renewals, invoice timing, and invoice duration. As of March 31, 2020, the Company expects 94% of the deferred revenue balance to be recognized in one year or less. Prior to the Merger, the Company did not recognize revenue from contracts with customers, and therefore did not have deferred revenue on its balance sheet at March 31, 2019. Upon completion of the Merger and consolidation of the Joint Venture, the Company assumed deferred revenue of $311,200 as part of purchase accounting. The Company recognized $25,601 of that deferred revenue balance during the year ended March 31, 2020.
Costs to Obtain or Fulfill a Contract
Sales commissions and certain other incentive payments (e.g., bonuses that are contingent solely on obtaining a contract or a pool of contracts) are capitalized as incremental costs to obtain a contract. The Company typically does not offer commissions on contract renewals. Decremented commissions upon renewal
120
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
(i.e., non-commensurate with initial commissions) are offered to the Company’s sales associates for certain customers and are immaterial. All commissions and other qualifying incentive payments capitalized are amortized over an expected period of benefit defined as the initial contract term plus anticipated renewals. In determining the appropriate period of benefit, the Company evaluates both qualitative and quantitative factors such as the expected customer relationship period and technology obsolescence. In addition, prior to solution go-live, the Company incurs certain contract fulfillment costs primarily related to SaaS setup for our clients. These costs are capitalized to the extent they are directly related to a contract, are recoverable, and create a resource used to deliver the Company’s SaaS services. Capitalized costs to fulfill a contract are amortized over the expected period of benefit.
In accounting for the Merger, the Company did not recognize an asset for costs to obtain or fulfill a contract that had been previously capitalized by the Joint Venture, but the Company began capitalizing only qualifying costs to obtain and fulfill a contract that were incurred after the date of the Merger. Consequently, the Company did not have a material balance of capitalized costs to obtain or fulfill a contract at March 31, 2020, nor did it recognize a material amount of amortization of such costs during the year ended March 31, 2020.
Postage Revenues
Postage revenues are the result of providing delivery services to customers in the Company’s payment and communication solutions. Postage revenues are generally billed as a pass-through cost to the Company’s customers. The service is part of a combined performance obligation with the printing and handling services provided to the customer because the postage services are not distinct within the context of the contract. The Company presents Postage Revenue separately from Solutions Revenue on the consolidated statements of operations as doing so makes the financial statements more informative for the users. The revenue related to the combined performance obligation of the postage, printing, and handling service is recognized as the transactions are processed, and the revenue is recognized over the individual days in which the services are performed.
Arrangements with Multiple Performance Obligations
The Company engages in customer arrangements which may include multiple performance obligations, such as any combination of software, hardware, implementation, SaaS-based offerings, consulting services, or maintenance services. For such arrangements, the Company allocates revenues to each performance obligation on a relative standalone selling price basis. For substantially all such arrangements, a performance obligation’s standalone selling price is determined based on the directly observable prices charged to customers. When directly observable prices charged to customers are not available, other methods are used such as the adjusted market assessment approach, the expected cost plus a margin approach, or other approaches in cases where distinct performance obligations are not sold separately but instead sold at a bundled price. For performance obligations with historical pricing that is highly variable, the residual approach is used. Such instances primarily relate to the Company’s perpetual software arrangements in which the Company sells the same products to different customers for a broad range of amounts.
Remaining Performance Obligations
The aggregate amount of transaction price allocated to performance obligations that are unsatisfied (or partially unsatisfied) for executed contracts includes deferred revenue and other revenue yet to be recognized from non-cancellable contracts. As of March 31, 2020, the Company’s total remaining performance obligations approximated $1,141,000, of which approximately 55% is expected to be recognized over the next twelve months, and the remaining 45% thereafter.
121
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
In this balance, the Company does not include the value of unsatisfied performance obligations related to those contracts for which it recognizes revenue at the amount for which it has the right to invoice for services performed. Additionally, this balance does not include revenue related to performance obligations that are part of a contract with an original expected duration of one year or less. Lastly, this balance does not include variable consideration allocated to the individual goods or services in a series of distinct goods or services that are substantially the same and that have the same pattern of transfer to the customer. Examples includes variable fees associated with transaction processing and contingent fee services.
Disaggregated Revenue
Beginning in fiscal year 2021, the Company plans to report segment information consistent with the presentation of operating segments at the Joint Venture as it believes doing so best depicts how the nature, amount, timing and uncertainty of the Company’s revenue are affected by economic factors. Additionally, the Company plans to disaggregate revenue between revenue that is recognized over time and revenue that is recognized at a point in time. Given the short portion of the year during which the Company consolidated the results of the Joint Venture and recognized revenue in its financial statements, the Company does not consider disaggregation of the amount of revenue recognized in its consolidated statement of operations for the year ended March 31, 2020 to be meaningful. A full year disaggregation of revenues from contracts with customers is included in the accompanying financial statements of the Joint Venture.
Customer Incentives
Certain customers, which include the Company’s channel partners, may receive cash-based incentives or rebates based on actual sales and achievement of a cumulative level of sales, which are accounted for as variable consideration. The Company considers these amounts to be consideration payable to the customer, and therefore, the Company estimates these amounts based on the expected amount to be provided to customers and reduces the transaction price accordingly.
Practical Expedients and Exemptions
The Company has elected to utilize either the right to invoice practical expedient or the series-based variable consideration allocation framework for most transaction processing services not subject to contingencies. The Company also has elected to exclude sales taxes and other similar taxes from the measurement of the transaction price in contracts with customers. Therefore, revenue is recognized net of such taxes.
In certain customer arrangements with customers, the Company determined there are certain promised goods or services which are immaterial in the context of the contract from both a quantitative and qualitative perspective, and therefore, the goods and services are disregarded when assessing the performance obligations in the customer arrangement.
The Company has elected to apply the significant financing practical expedient, and as a result, the Company will not adjust the promised amount of consideration in a customer contract for the effects of a significant financing component when the period of time between when the Company transfers a promised good or service to a customer and when the customer pays for the good or service will be one year or less.
5. Concentration of Credit Risk
The Company maintains its cash and cash equivalent balances in either insured depository accounts or money market mutual funds. The money market mutual funds are limited to investments in low-risk securities such as U.S. or government agency obligations, or repurchase agreements secured by such securities.
122
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
6. Equity Method Investment in Change Healthcare LLC
Exchange of Equity Method Investments
In connection with the Transactions, the Company exchanged its 45.615% investment in Legacy CHC for 30% of the membership units of the Joint Venture. The Joint Venture used proceeds from the issuance of debt referred to previously to acquire the remaining 54.385% of Legacy CHC. The Company has accounted for this exchange of investments as a non-monetary transaction at their respective carrying values. Prior to the Transactions, the investors of Legacy CHC accounted for their investments at fair value. As a result, the book basis and fair value of the Company’s investment in Legacy CHC were generally the same such that no gain was recognized as a result of the Transactions.
The fair value of the Joint Venture was determined at March 1, 2017 using a combination of the income and the market valuation approaches. Under the income approach, a discounted cash flow model was used in which cash flows anticipated over several periods, plus a terminal value at the end of that time horizon, are discounted to their present value using an appropriate expected rate of return. The discount rate used for cash flows reflects capital market conditions and the specific risks associated with the business. Under the market approach, valuation multiples of reasonably similar publicly traded companies or guideline companies are applied to the operating data of the subject business to derive the estimated fair value. These valuation approaches are considered a Level 3 fair value measurement. Fair value determination requires complex assumptions and judgment by management in projecting future operating results, selecting guideline companies for comparisons, determining appropriate market value multiples, selecting the discount rate to measure the risks inherent in the future cash flows and assessing the business’s life cycle and the competitive trends impacting the business, including considering technical, legal, regulatory, or economic barriers to entry. Any material changes in key assumptions, including failure to meet business plans, deterioration in the financial market, an increase in interest rate or an increase in the cost of equity financing by market participants within the industry or other unanticipated events and circumstances, may affect such estimates.
Additional Ownership Interest
Following the initial public offering, the Company contributed the proceeds of the offering of common stock to the Joint Venture in exchange for 49,285,713 additional units of the Joint Venture, which represented approximately 11% of additional ownership interest. As a result of the additional ownership interest acquired, the Company measured additional basis differences at July 1, 2019 based on the fair value of the Joint Venture’s assets and liabilities as of the date of the initial public offering, and using valuation approaches substantially similar to those used as of the date of the Transactions.
Equity Method Investment in the Joint Venture
Prior to the Merger, the Company accounted for its investment in the Joint Venture using the equity method of accounting. During the period from April 1, 2019 to March 10, 2020, and the years ended March 31, 2019 and 2018, the Company recorded a proportionate share of the loss from this investment of $380,713, $70,487, and $58,680, respectively, which included transaction and integration expenses incurred by the Joint Venture and basis adjustments, including amortization expenses, associated with equity method intangible assets. The amount is in Loss from Equity Method Investment in the Joint Venture in the consolidated statements of operations.
Following completion of the Merger, the Company consolidates the Joint Venture and no longer accounts for its ownership interest as an equity method investment.
123
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Summarized financial information of the Joint Venture is as follows:
| Statement of Operations Data: | Period of April 1, 2019 to March 10, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
|||||||||
| Net revenue |
$ | 3,092,875 | $ | 3,281,729 | $ | 3,298,843 | ||||||
| Cost of operations (exclusive of depreciation and amortization) |
$ | 1,263,244 | $ | 1,354,655 | $ | 1,407,893 | ||||||
| Customer postage |
$ | 215,448 | $ | 238,618 | $ | 274,397 | ||||||
| Net income (loss) |
$ | 123,771 | $ | 176,670 | $ | 192,442 | ||||||
| Balance Sheet Data (at period end): | March 10, 2020 |
March 31, 2019 |
||||||
| Current assets |
$ | 1,339,908 | $ | 980,463 | ||||
| Long-term assets |
$ | 5,187,220 | $ | 5,223,675 | ||||
| Current liabilities |
$ | 1,112,875 | $ | 889,783 | ||||
| Long-term liabilities |
$ | 5,185,304 | $ | 6,219,141 | ||||
Other Investments
The Company invested in a unit purchase contract and a debt instrument of the Joint Venture on terms that substantially mirror the economics of the TEUs (see Note 13, Tangible Equity Units). Prior to the Merger, the Company accounted for these mirror arrangements as investments in debt and equity securities. After the Merger, the Company’s investments in the TEUs of the Joint Venture are eliminated in consolidation.
The following table presents a reconciliation of the activity related to the other investments:
| Year Ended March 31, 2020 |
||||
| Balance at beginning of period |
$ | — | ||
| Acquisition of forward purchase contracts |
232,928 | |||
| Acquisition of available-for-sale debt securities |
45,946 | |||
| Receipt of payments on debt securities |
(7,332 | ) | ||
| Change in fair value of forward purchase contracts |
14,836 | |||
| Change in fair value of debt securities |
1,489 | |||
| TEU conversions of forward purchase contracts |
(31,000 | ) | ||
| Settlement of investment in forward purchase contracts (1) |
(216,764 | ) | ||
| Elimination of investment in debt securities (2) |
(40,103 | ) | ||
|
|
|
|||
| Balance at end of period |
$ | — | ||
|
|
|
|||
| (1) | Amount is included as part of the Merger purchase price. See Note 2, Business Combinations for additional information. |
| (2) | Amount is eliminated as part of consolidation. |
7. Prepaid Expenses and Other Current Assets
Prepaid expenses and other current assets generally include items for which the Company has paid the related vendor or supplier in advance of receiving the related service. Prepaid expenses and other current assets consisted of the following:
124
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
| March 31, 2020 |
March 31, 2019 |
|||||||
| Prepaid expenses |
$ | 73,354 | $ | — | ||||
| Other current assets |
44,141 | — | ||||||
|
|
|
|
|
|||||
| Total prepaid expenses and other current assets |
$ | 117,495 | $ | — | ||||
|
|
|
|
|
|||||
8. Property and Equipment
Property and equipment consisted of the following:
| March 31, 2020 |
March 31, 2019 |
|||||||
| Land |
$ | 406 | $ | — | ||||
| Buildings and leasehold improvements |
51,460 | — | ||||||
| Computer equipment |
95,079 | — | ||||||
| Production equipment |
17,591 | — | ||||||
| Office equipment, furniture and fixtures |
31,302 | — | ||||||
| Construction in process |
13,318 | — | ||||||
|
|
|
|
|
|||||
| Property and equipment, gross |
209,156 | — | ||||||
| Less accumulated depreciation |
(2,960 | ) | — | |||||
|
|
|
|
|
|||||
| Property and equipment, net |
$ | 206,196 | $ | — | ||||
|
|
|
|
|
|||||
Depreciation expense was $2,960, $0, and $0 for the years ended March 31, 2020, 2019 and 2018, respectively.
9. Goodwill and Intangible Assets
Goodwill
The Company evaluates goodwill for impairment on an annual basis as of January 1 each year and at an interim date, if indicators of potential impairment exist. Goodwill impairment testing is conducted at the reporting unit level, which is generally defined as an operating segment or one level below an operating segment (also known as a component), for which discrete financial information is available and segment management regularly reviews the operating results of that reporting unit. As described in Note 24, Segment Reporting, management expects to view the Company’s operating results based on the same three reportable segments that currently comprise the Joint Venture: (a) Software & Analytics, (b) Network Solutions and (c) Technology-Enabled Services.
Goodwill was recognized on March 10, 2020 as a result of the Merger in accordance with ASC 805 and allocated to the Company’s reporting units on a relative fair value basis. Subsequent to the Merger, the Company concluded a triggering event had occurred due to the expected impacts to its financial results arising out of the COVID-19 pandemic beginning in the first quarter of fiscal year 2021. Therefore, the Company performed a goodwill impairment test as of March 31, 2020 to compare the carrying value and fair value of the Company’s reporting units. The fair value of each reporting unit was determined using a combination of an income approach based on a discounted cash flow model and a market approach based on appropriate valuation multiples observed for the reporting unit’s guideline public companies. Fair value estimates result from a complex series of judgments about future events and uncertainties and rely heavily on estimates and assumptions that have been
125
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
deemed reasonable by management as of the measurement date. The estimates considered most impactful to the goodwill impairment test are the Company’s expectation of timing of a return to a normal level of healthcare activity, the discount rate used in the income approach, and the market multiples used in the market approach. If the timing of the return to a normal level of healthcare activity is later than expected, or if macroeconomic conditions worsen, additional impairment charges may be required. Fair value assessments of the reporting units are considered a Level 3 measurement due to the significance of unobservable inputs developed using company specific information.
Based on the results of the interim impairment test, the Company recorded a non-cash pre-tax goodwill impairment charge of $561,164 as the Company determined that the carrying value of each of the three reporting units exceeded their estimated fair value. This charge is recorded under the caption Goodwill impairment charge in the consolidated statement of operations. The goodwill impairment was not deductible for income tax purposes. The following table presents the changes in the carrying amount of goodwill for the year ended March 31, 2020:
| Software and Analytics |
Network Solutions |
Technology- Enabled Services |
Total | |||||||||||||
| Balance at March 31, 2019 |
$ | — | $ | — | $ | — | $ | — | ||||||||
| Acquisitions |
1,901,116 | 1,944,701 | 514,831 | 4,360,648 | ||||||||||||
| Goodwill impairment |
(126,839 | ) | (298,870 | ) | (135,455 | ) | (561,164 | ) | ||||||||
| Effects of foreign currency |
(4,159 | ) | — | — | (4,159 | ) | ||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Balance at March 31, 2020 |
$ | 1,770,118 | $ | 1,645,831 | $ | 379,376 | $ | 3,795,325 | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
Intangible Assets
Intangible assets subject to amortization at March 31, 2020 consisted of the following:
| Weighted Average Remaining Life |
Gross Carrying Amount |
Accumulated Amortization |
Net | |||||||||||||
| Customer relationships |
15.2 | $ | 3,056,000 | $ | (13,064 | ) | $ | 3,042,936 | ||||||||
| Technology-based intangible assets |
9.2 | 1,188,000 | (10,290 | ) | 1,177,710 | |||||||||||
| Tradenames |
18.0 | 146,000 | (840 | ) | 145,160 | |||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total |
$ | 4,390,000 | $ | (24,194 | ) | $ | 4,365,806 | |||||||||
|
|
|
|
|
|
|
|||||||||||
The Company did not have any intangible assets subject to amortization as of March 31, 2019. Amortization expense was $24,194, $0 and $0 for the years ended March 31, 2020, 2019 and 2018, respectively.
Aggregate amortization expense for intangible assets future fiscal years is estimated to be:
| 2021 |
$ | 441,268 | ||
| 2022 |
469,741 | |||
| 2023 |
421,556 | |||
| 2024 |
381,546 | |||
| 2025 |
349,177 | |||
| Thereafter |
2,302,518 | |||
|
|
|
|||
| Total |
$ | 4,365,806 | ||
|
|
|
126
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
10. Accrued Expenses
Accrued expenses generally represent items for which the Company has received a service from a vendor in advance of being invoiced for that service. Accrued expenses consisted of the following:
| March 31, 2020 |
March 31, 2019 |
|||||||
| Customer deposits |
$ | 37,357 | $ | — | ||||
| Accrued compensation |
113,959 | — | ||||||
| Accrued outside services |
28,822 | — | ||||||
| Accrued insurance |
14,293 | — | ||||||
| Accrued income, sales and other taxes |
10,129 | 176 | ||||||
| Accrued interest |
5,892 | — | ||||||
| Interest rate cap agreements |
28,131 | — | ||||||
| Pass-through payments |
29,518 | — | ||||||
| Other accrued liabilities |
122,193 | — | ||||||
|
|
|
|
|
|||||
| Total accrued expenses |
$ | 390,294 | $ | 176 | ||||
|
|
|
|
|
|||||
11. Long-Term Debt
The Company’s long-term indebtedness is comprised of a senior secured term loan facility (the “Term Loan Facility”), a revolving credit facility (the “Revolving Facility”; together with the Term Loan Facility, the “Senior Credit Facilities”), and 5.75% senior notes due 2025 (the “Senior Notes”).
Long-term debt as of March 31, 2020 and 2019, consisted of the following:
| March 31 2020 |
March 31, 2019 |
|||||||
| Senior Credit Facilities |
||||||||
| $5,100,000 Term Loan Facility, due March 1, 2024, net of unamortized discount of $125,793 and $0 at March 31, 2020 and 2019, respectively (effective interest rate of 4.42%) |
$ | 3,682,457 | $ | — | ||||
| $785,000 Revolving Facility, expiring July 3, 2024, and bearing interest at a variable interest rate (1) |
250,000 | — | ||||||
| Senior Notes |
||||||||
| $1,000,000 5.75% Senior Notes due March 1, 2025, net of unamortized discount of $2,228 and $0 at March 31, 2020 and 2019, respectively (effective interest rate of 5.80%) |
997,772 | — | ||||||
| Tangible Equity Unit Senior Amortizing Note |
||||||||
| $47,367 Senior Amortizing Notes due June 30, 2022, net of unamortized discount of $842 and $0 at March 31, 2020 and 2019, respectively (effective interest rate of 7.44%) |
35,431 | — | ||||||
| Other |
23,413 | — | ||||||
| Less current portion |
(278,779 | ) | — | |||||
|
|
|
|
|
|||||
| Long-term debt |
$ | 4,710,294 | $ | — | ||||
|
|
|
|
|
|||||
| (1) | The weighted average interest rate at March 31, 2020 was 3.25%. |
127
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Senior Credit Facilities
The Senior Credit Facilities provide the Company with the right at any time to request additional term loan tranches and/or term loan increases, increases in the revolving commitments and/or additional revolving credit facilities up to the sum of (i) (a) the greater of $1,080,000 or an amount equal to 100% of EBITDA for the most recently ended four consecutive fiscal quarters, plus (b) certain voluntary prepayments, repurchases, redemptions and other retirements of indebtedness and commitments under our Senior Credit Facilities, incremental equivalent debt, and refinancings thereof, plus (ii) an additional aggregate amount such that, after giving pro forma effect to such incurrence, (x) if such additional amounts are secured on a pari passu basis with the first lien obligations under our Senior Credit Facilities, our consolidated first lien net leverage ratio does not exceed 4.90 to 1.00, (y) if such additional amounts are secured on a junior lien basis to the first lien obligations under our Senior Credit Facilities, our consolidated secured net leverage ratio does not exceed 5.75 to 1.00 and (z) if such additional amounts are unsecured, either our consolidated total net leverage ratio does not exceed 6.00 to 1.00 or the Company could incur at least $1.00 of additional indebtedness under a consolidated interest coverage ratio test under our Senior Credit Facilities of 2.00 to 1.00. The lenders under the Senior Credit Facilities will not be under any obligation to provide any such incremental commitments or loans, which are uncommitted, and any such addition of or increase in commitments or loans will be subject to obtaining commitments and certain customary conditions precedent in the Company’s Senior Credit Facilities. The applicable margin for loans under the Term Loan Facility is subject to reduction from and after a Qualified IPO (as defined in the Senior Credit Facilities).
Borrowings under the Senior Credit Facilities bear interest at a rate equal to either (i) LIBOR for the relevant interest period, adjusted for statutory reserve requirements (the Term Loan Facility is subject to a floor of 1.0% per annum and the Revolving Facility is subject to a floor of 0.0% per annum), plus an applicable margin or (ii) a base rate equal to the highest of (a) the rate of interest in effect as publicly announced by the administrative agent as its prime rate, (b) the federal funds effective rate plus 0.5% and (c) adjusted LIBOR for an interest period of one month plus 1.0% (the Term Loan Facility may be subject to a floor of 2.0% per annum), in each case, plus an applicable margin. The applicable margin under the Revolving Facility is subject to reduction after the completion of the Company’s first full fiscal quarter after the closing of its Senior Credit Facilities based upon its consolidated first lien net leverage ratio, as well as following a Qualified IPO.
In July 2019, the Company amended its Revolving Facility, primarily to increase the capacity from $500,000 to $785,000 and to extend the maturity date to July 2, 2024. However, in the event the Term Loan Facility exceeds $1,100,000 on December 1, 2023, amounts due, if any, under the Revolving Facility become due and payable on December 1, 2023.
In March 2020, the Company borrowed $250,000 under the Revolving Facility. The borrowings are classified as short-term based on the anticipated repayment date. The Revolving Facility has a total borrowing capacity of $785,000 less outstanding letters of credit which totaled $5,118 and $4,880 at March 31, 2020 and 2019, respectively. This leaves $529,882 and $495,120 available for borrowing as of March 31, 2020 and 2019, respectively.
In addition to paying interest on outstanding principal under the Senior Credit Facilities, the Company is required to pay a commitment fee of 0.375% per annum to the lenders under the Revolving Facility in respect of the unutilized commitments thereunder. The Company must also pay customary letter of credit fees and an annual administrative agency fee.
The Senior Credit Facilities requires the Company to prepay outstanding term loans, subject to certain exceptions, with:
128
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
| • | 50% of the Parent Borrower’s (as defined in the Senior Credit Facilities) annual Excess Cash Flow (as defined in the Senior Credit Facilities) commencing with the first full fiscal year completed after the closing of the Senior Credit Facilities (percentage will be reduced to 25% and 0% if the Company achieves and maintains specified consolidated first lien net leverage ratios), subject to certain credits and exceptions; |
| • | 100% of the net cash proceeds of non-ordinary course asset sales or other dispositions of property, including insurance condemnation proceeds (percentage will be reduced to 50%, 25% and 0% if the Company achieves and maintains specified consolidated first lien net leverage ratios), subject to certain exceptions, in excess of a minimum amount threshold set forth in the Senior Credit Facilities and subject to our right to reinvest the proceeds; and |
| • | 100% of the net cash proceeds of any incurrence of debt by the borrowers or their restricted subsidiaries, other than proceeds from debt permitted to be incurred by the terms of the Senior Credit Facilities. |
The foregoing mandatory prepayments will be applied, subject to certain exceptions, to the term loans outstanding under the Senior Credit Facilities then outstanding as directed by the Parent Borrower.
The Company may voluntarily repay outstanding loans or reduce outstanding commitments under the Senior Credit Facilities at any time without premium or penalty, subject to reimbursements of the lenders’ redeployment costs actually incurred in the case of a prepayment of LIBOR borrowings prior to the last day of the relevant interest period. The foregoing voluntary prepayments may be applied to the scheduled installments of principal of the Term Loan Facility in such order as directed by the Parent Borrower and applied to any class of loans under the Senior Credit Facilities as directed by the Parent Borrower.
The Term Loan Facility amortizes in equal quarterly installments in aggregate annual amounts equal to 1.0% of the principal amount of the Term Loan Facility outstanding as of the date of the closing of the Senior Credit Facilities, with the balance being payable at maturity. Principal amounts outstanding under the Revolving Facility are due and payable in full at maturity. The Company does not have any remaining quarterly amortization payments.
All obligations of the borrowers under the Senior Credit Facilities and under any swap agreements and cash management arrangements that are entered into are unconditionally guaranteed by all material wholly owned direct and indirect domestic restricted subsidiaries of the borrowers and by the direct parent of the Parent Borrower, with customary exceptions including, among other things, where providing such guarantees is not permitted by law, regulation or contract or would result in adverse tax consequences.
All obligations of the borrowers under the Senior Credit Facilities and under any swap agreements and cash management arrangements are secured, subject to permitted liens and other exceptions, by substantially all of the assets of the borrowers and each guarantor, including but not limited to: (i) a perfected pledge of all of the capital stock issued by the parent borrower and each direct wholly owned domestic restricted subsidiary of the borrowers or any subsidiary guarantor (subject to certain exceptions) and up to 65% of the capital stock issued and outstanding by each direct wholly owned foreign restricted subsidiary of the borrowers or any subsidiary guarantor (subject to certain exceptions) and (ii) perfected security interests in and mortgages on substantially all tangible and intangible personal property and material owned real property of the borrowers and the subsidiary guarantors (subject to certain exceptions and exclusions).
As of March 31, 2020, the Company was in compliance with all of the applicable covenants under the Senior Credit Facilities.
129
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Senior Notes
The Senior Notes bear interest at an annual rate of 5.75% with interest payable semi-annually on March 1 and September 1 of each year and mature on March 1, 2025.
The Company may redeem the Senior Notes, in whole or in part, at any time on or after March 1, 2020 at the applicable redemption price, plus accrued and unpaid interest.
If the Company experiences specific kinds of changes in control, it must offer to purchase the Senior Notes at a price equal to 101% of the principal amount, plus accrued and unpaid interest.
The Senior Notes are senior unsecured obligations and rank equally in right of payment with all of the Company’s existing and future indebtedness and senior in right of payment to all of its existing and future subordinated indebtedness. The Company’s obligations under the Senior Notes are guaranteed on a senior basis by all of its existing and subsequently acquired or organized wholly owned U.S. restricted subsidiaries that guarantee the Senior Credit Facilities. The Senior Notes and the related guarantees are effectively subordinated to the Company’s existing and future secured obligations and that of its affiliate guarantors to the extent of the value of the collateral securing such obligations and are structurally subordinated to all existing and future indebtedness and other liabilities of any of the Company’s subsidiaries that do not guarantee the Senior Notes.
As of March 31, 2020, the Company was in compliance with all of the applicable covenants under the Senior Notes.
Tangible Equity Unit Senior Amortizing Note
Refer to Note 13, Tangible Equity Units for information.
Other
From time to time, the Company enters into deferred financing arrangements with certain vendors. The obligations under such arrangements are recorded at the present value of the scheduled payments. Such future payments totaled approximately $21,454 at March 31, 2020.
Aggregate Future Maturities
The aggregate amounts of future maturities by fiscal year under long-term debt arrangements are as follows:
| 2021 |
$ | 278,778 | ||
| 2022 |
25,432 | |||
| 2023 |
4,658 | |||
| 2024 |
3,808,682 | |||
| 2025 |
1,000,382 | |||
| Thereafter |
— | |||
|
|
|
|||
| Total |
$ | 5,117,932 | ||
|
|
|
12. Interest Rate Cap Agreements
Risk Management Objective of Using Derivatives
The Company is exposed to certain risks arising from both its business operations and economic conditions. The Company principally manages its exposures to a wide variety of business and operational risks through
130
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
management of its core business activities. The Company manages economic risks, including interest rate, liquidity and credit risk, primarily by managing the amount, sources and duration of its debt funding and the use of derivative financial instruments. Specifically, the Company enters into derivative financial instruments to manage differences in the amount, timing and duration of the Company’s known or expected cash receipts and its known or expected cash payments principally related to the Company’s borrowings.
Cash Flow Hedges of Interest Rate Risk
The Company’s objectives in using interest rate derivatives are to add stability to interest expense and to manage its exposure to interest rate movements. To accomplish these objectives, the Company primarily uses interest rate cap agreements as part of its interest rate risk management strategy. Payments and receipts related to interest rate cap agreements are included in cash flows from financing activities in the Company’s consolidated statements of cash flows.
In March 2016 and 2017, Legacy CHC and the Joint Venture, respectively, executed annuitized interest rate cap agreements with a combined notional amount of $650,000 and $750,000, respectively, to limit the exposure of the variable component of interest rates under the then existing term loan facility or future variable rate indebtedness, each beginning March 31, 2017 and expired March 31, 2020. Due to the proximity of this maturity to the date of the Merger, these interest rate cap agreements were not redesignated as cash flow hedges by the Company. Instead, the Company recognized an immaterial amount of interest expense related to the change in fair value of these instruments in its consolidated statement of operations for the year ended March 31, 2020.
In August 2018, the Joint Venture executed additional annuitized interest rate cap agreements with notional amounts of $500,000, accreting to $1,500,000 to limit the exposure of the variable component of interest rates under the Term Loan Facility or future variable rate indebtedness to a maximum of 1.0%. The interest rate cap agreements became effective August 31, 2018, accreted to $1,500,000 and expire December 31, 2021. Upon completion of the Merger, these agreements were redesignated as cash flow hedges of the Company.
In March 2020, the Company executed additional annuitized interest rate cap agreements with notional amounts totaling $1,000,000 to limit the exposure of the variable component of the interest rates under the Term Loan Facility or future variable rate indebtedness to a maximum of 1.0%. Each interest rate cap agreement became effective March 31, 2020 and expires March 31, 2024.
At March 31, 2020, each of the Company’s outstanding interest rate cap agreements were designated as cash flow hedges of interest rate risk and was determined to be highly effective.
Amounts reported in accumulated other comprehensive income related to derivatives will be reclassified to interest expense as interest payments are made on the Company’s variable-rate debt. The Company estimates that $1,203 will be reclassified as an increase to interest expense within one year.
131
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
The fair value of the Company’s derivative instruments at March 31, 2020 and 2019 is as follows:
| Fair Values of Derivative Financial Instruments Asset (Liability) |
||||||||||
| Derivative financial instruments designated as hedging instruments: |
Balance Sheet Location |
March 31, 2020 | March 31, 2019 | |||||||
| Interest rate cap agreements |
Prepaid and other current assets | $ | — | $ | — | |||||
| Interest rate cap agreements |
Accrued expenses | (28,131 | ) | — | ||||||
| Interest rate cap agreements |
Other long-term liabilities | (19,277 | ) | — | ||||||
|
|
|
|
|
|||||||
| $ | (47,408 | ) | $ | — | ||||||
|
|
|
|
|
|||||||
Effect of Derivative Instruments on the Statement of Operations
The effect of the derivative instruments on the accompanying consolidated statements of operations for the years ended March 31, 2020, 2019 and 2018 is as follows:
| Derivative financial instruments in cash flow hedging relationships: |
Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
|||||||||
| Gain/(loss) related to derivative financial instruments recognized in other comprehensive income (loss) |
$ | (1,361 | ) | $ | — | $ | — | |||||
|
|
|
|
|
|
|
|||||||
| Gain/ (loss) related to portion of derivative financial instruments reclassified from accumulated other comprehensive income (loss) to interest expense |
$ | (22 | ) | $ | — | $ | — | |||||
|
|
|
|
|
|
|
|||||||
Credit Risk-Related Contingent Features
The Company has agreements with each of its derivative counterparties providing that if the Company defaults on any of its indebtedness, including a default where repayment of the indebtedness has not been accelerated by the lender, then the Company also could be declared in default on its derivative obligations.
As of March 31, 2020, the termination value of derivative financial instruments in a net liability position, which includes accrued interest but excludes any adjustment for nonperformance risk, was $51,020. If the Company had breached any of these provisions at March 31, 2020, the Company could have been required to settle its obligations under the agreements at this termination value. The Company does not offset any derivative financial instruments and the derivative financial instruments are not subject to collateral posting requirements.
132
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
13. Tangible Equity Units
In July 2019, the Company completed its offering of 5,750,000 TEUs. Total proceeds, net of underwriting discounts, were $278,875. Each TEU, which has a stated amount of $50, is comprised of a stock purchase contract and a senior amortizing note due June 30, 2022. The Company allocated the proceeds from the issuance of the TEUs to equity and debt based on the relative fair values of the respective components of each TEU. The value allocated to the stock purchase contracts is reflected net of issuance costs in additional paid in capital. The value allocated to the senior amortizing notes is reflected in debt on the consolidated balance sheets, with payments expected in the next twelve months reflected in current maturities of long-term debt. Issuance costs, reflected as a reduction of the face amount of the amortizing notes, are being accreted to the face amount of the debt under the effective interest method.
The aggregate values assigned upon issuance of the TEUs, based on the relative fair value of the respective components of each TEU, were as follows:
| Equity Component | Debt Component | Total | ||||||||||
| Price per TEU |
$ | 41.7622 | $ | 8.2378 | $ | 50.00 | ||||||
| Gross proceeds |
240,133 | 47,367 | 287,500 | |||||||||
| Issuance costs |
(7,204 | ) | (1,421 | ) | (8,625 | ) | ||||||
|
|
|
|
|
|
|
|||||||
| Net proceeds |
$ | 232,929 | $ | 45,946 | $ | 278,875 | ||||||
|
|
|
|
|
|
|
|||||||
Each senior amortizing note has an initial principal amount of $8.2378 and bears interest at 5.5% per year. On each March 30, June 30, September 30 and December 30, the Company pays equal quarterly cash installments of $0.7500 per amortizing note (except for the September 30, 2019 installment payment, which was $0.7417 per amortizing note). Each installment constitutes a payment of interest and partial payment of principal. Unless settled earlier, each purchase contract will automatically settle on June 30, 2022. The Company will deliver between a minimum of 18,429,325 shares and a maximum of 22,115,075 shares of the Company’s common stock, subject to adjustment, based on the Applicable Market Value (as defined below) of the Company’s common stock as described below:
| • | If the Applicable Market Value is greater than $15.60 per share, holders will receive 3.2051 shares of common stock per purchase contract. |
| • | If the Applicable Market Value is less than or equal to $15.60 per share but greater than or equal to $13.00 per share, the holder will receive a number of shares of the Company’s common stock per purchase contract equal to $50, divided by the Applicable Market Value; and |
| • | If the Applicable Market Value is less than $13.00 per share, the holder will receive 3.8461 shares of common stock per purchase contract. |
The Applicable Market Value is defined as the arithmetic average of the volume weighted average price per share of the Company’s common stock over the twenty consecutive trading day period immediately preceding the balance sheet date, or June 30, 2022, for settlement of the stock purchase contracts.
The TEUs have a dilutive effect on the Company’s net income (loss) per share. The 18,429,325 minimum shares to be issued are included in the calculation of basic net income (loss) per share. The difference between the minimum shares and the maximum shares are potentially dilutive securities, and accordingly, are included in the Company’s diluted net income (loss) per share on a pro rata basis to the extent the Applicable Market Value is higher than $13.00 but is less than $15.60 at period end.
After the initial issuance date, the Company may elect to have the purchase contracts settled prior to the mandatory settlement date, June 30, 2022. Upon settlement, each purchase contract will be settled for Joint Venture units equal to 3.2051 units per purchase contract.
133
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
The following table summarizes TEU activity for the year ended March 31, 2020:
| Tangible Equity Units |
||||
| Outstanding at beginning of year |
— | |||
| Issued |
5,750,000 | |||
| Conversions |
(612,655 | ) | ||
|
|
|
|||
| Outstanding at end of year |
5,137,345 | |||
|
|
|
|||
14. Net Income (Loss) Per Share
The following table sets forth the computation of basic net income (loss) per share of common stock:
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Basic net income (loss) per share: |
||||||||||||
| Numerator: |
||||||||||||
| Net income (loss) |
$ | (947,597 | ) | $ | (52,012 | ) | $ | 60,955 | ||||
| Denominator: |
||||||||||||
| Weighted average common shares outstanding |
123,387,547 | 75,513,130 | 75,590,613 | |||||||||
| Minimum shares issuable under purchase contracts |
13,609,077 | — | — | |||||||||
|
|
|
|
|
|
|
|||||||
| 136,996,624 | 75,513,130 | 75,590,613 | ||||||||||
|
|
|
|
|
|
|
|||||||
| Basic net income (loss) per share |
$ | (6.92 | ) | $ | (0.69 | ) | $ | 0.81 | ||||
|
|
|
|
|
|
|
|||||||
| Diluted net income per share: |
||||||||||||
| Numerator: |
||||||||||||
| Net income (loss) |
$ | (947,597 | ) | $ | (52,012 | ) | $ | 60,955 | ||||
| Denominator: |
||||||||||||
| Number of shares used in basic computation |
136,996,624 | 75,513,130 | 75,590,613 | |||||||||
| Weighted average effect of dilutive securities |
||||||||||||
| Time-Vesting Options |
— | — | 2,051,346 | |||||||||
| Restricted Share Units |
— | — | 159,137 | |||||||||
|
|
|
|
|
|
|
|||||||
| 136,996,624 | 75,513,130 | 77,801,096 | ||||||||||
|
|
|
|
|
|
|
|||||||
| Diluted net income (loss) per share |
$ | (6.92) | $ | (0.69) | $ | 0.78 | ||||||
|
|
|
|
|
|
|
|||||||
Due to their antidilutive effect, the following securities have been excluded from diluted net income (loss) per share:
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Dilutive shares issuable under purchase contracts |
1,829,437 | — | — | |||||||||
| Time-Vesting Options |
1,259,594 | 1,869,456 | 4,570,624 | |||||||||
| Restricted Share Units |
1,345,211 | — | — | |||||||||
| Deferred Stock Units |
20,371 | — | — | |||||||||
134
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
15. Incentive Compensation Plans
Prior to the Merger, the Company provided equity awards to employees of the Joint Venture which were subject to the accounting framework for awards granted to non-employees. Under this framework, the Company recognized stock compensation expense within the Loss from Equity Method Investment in the Joint Venture caption on the consolidated statements of operations for its proportionate amount of stock compensation expense included in the operating results of the Joint Venture as well as the amount funded for the benefit of the McKesson member. However, due to requirements of the LLC Agreement, as described in Note 22, Related Party Transactions, the Company recognized a dividend receivable equal to the cumulative amount of stock compensation expense recognized by the Joint Venture for any outstanding equity awards with an offset to the Loss from Equity Method Investment in Joint Venture. As a result, no net equity compensation expense of the Joint Venture was recognized in the financial statements of the Company.
Legacy CHC Equity Plan
In connection with the Transactions, the Company assumed and amended the Legacy CHC Equity Plan. Pursuant to the amended Legacy CHC Equity Plan, 37.9 million shares of the Company’s common stock have been reserved for the issuance of equity awards to employees, directors and consultants of the Joint Venture and its affiliates.
The Company granted equity-based awards of its common stock to certain employees, officers and directors of the Joint Venture under terms of awards that are described below. Grants under the Legacy CHC Equity Plan consist of one or a combination of time-vested and/or performance-based awards. In most circumstances, the shares issued upon exercise of the equity awards are subject to certain call rights by the Company in the event of termination of service of an award holder and put rights by the award holder or his/her beneficiary in the event of death or disability.
The Company expects to repurchase shares of common stock held by former Joint Venture employees no earlier than six months following the issuance of such shares.
Replacement Awards
In connection with the Transactions, the Company was obligated to either assume obligations under Legacy CHC’s prior equity award plans or to issue substantially equivalent equity awards. The Company elected to issue replacement awards with vesting and exercisability terms generally identical to the awards which were replaced. Because the stock of eRx Network and the 2017 Tax Receivable Agreement were distributed to Legacy CHC stockholders immediately prior to the Transactions, certain participants in the Legacy CHC Equity Plan also received equity awards in eRx Network and the right to receive a cash payment related to a proportionate value of the 2017 Tax Receivable Agreement in connection with the Transactions.
These replacement awards granted under the Legacy CHC Equity Plan consisted of one, or a combination of, time-vested awards and/or performance-based awards.
Vested Awards: Vested awards consist of the following:
| (i) | Tier I Time-Vesting Awards became immediately vested in connection with the Transactions, 54.4% of which were liquidated for cash upon the closing of the Transactions. The remaining 45.6% of such options were exchanged for vested options of the Company with exercise prices and expiration terms that correspond with those of the original grant to Legacy CHC Equity Plan participants (“Replacement Time-Vesting Options”). These Legacy CHC Equity Plan participants also received vested options in eRx Network with exercise prices equal to 25% of the fair value of the eRx Network stock and a cash payment related to the proportionate value of the 2017 Tax Receivable Agreement at the time of the Transactions. |
135
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
| (ii) | Tier II Time-Vesting Awards became immediately vested in connection with the Transactions but because the original exercise price of these awards was greater than the fair value of the stock at the time of the Transactions, none of the awards were liquidated and they were replaced with vested Replacement Time-Vesting Options with an exercise price equal to the original exercise price as reduced by the fair value of one share of eRx Network stock. |
| (iii) | 2.0x Exit-Vesting Awards became immediately vested in connection with the Transactions as a result of meeting the specified performance and market conditions outlined in the original award terms. As with the Tier I Time-Vesting Awards, 54.4% were liquidated for cash upon the closing of the Transactions. The remaining 45.6% of such options were exchanged for vested Replacement Time-Vesting Options with exercise prices and expiration terms that correspond with those of the original grant to the Legacy CHC Equity Plan participants. The Legacy CHC Equity Plan participants also received vested options in eRx Network with exercise prices equal to 25% of the fair value of the eRx Network stock and a cash payment related to the proportionate value of the 2017 Tax Receivable Agreement at the time of the Transactions. |
Unvested Awards: Certain awards granted by Legacy CHC contained conditions that were not satisfied at the time of the Transactions. These awards generally consisted of awards that vest subject to the employee’s continued employment through the date when Blackstone has sold at least 25% of the maximum number of Legacy CHC’s shares held by it (i.e. a liquidity event) and achieved specified rates of return that vary by award. In connection with the Transactions, these unvested equity awards were replaced with unvested restricted stock of the Company (“Replacement Exit-Vesting Restricted Stock”) with an aggregate intrinsic value and vesting conditions which were identical to the original Legacy CHC awards. Legacy CHC Equity Plan participants also received unvested restricted stock of eRx Network and a right, contingent upon vesting of the awards, to receive a future cash payment related to the proportionate value of the 2017 Tax Receivable Agreement at the time of the Transactions.
Restricted Stock Units: Vesting of Legacy CHC restricted share units was not affected by the Transactions. 54.4% of the vested portion of such restricted share units were liquidated in connection with the Transactions and the remainder of the vested and unvested restricted share units were replaced with vested and unvested Company restricted share units (“Replacement Restricted Share Units”) with terms identical to the original awards. Legacy CHC Equity Plan participants also received vested and unvested restricted share units of eRx Network and a right to receive a future cash payment upon vesting related to the proportionate value of the 2017 Tax Receivable Agreement at the time of the Transactions.
The total fair value of shares vested during the years ended March 31, 2020, 2019 and 2018 was $0, $0 and $1,440, respectively.
The following table summarizes Replacement Time-Vesting Option activity for the year ended March 31, 2020:
| Replacement Time- Vesting Options |
Weighted Average Exercise Price |
Weighted Average Remaining Contractual Term |
Aggregate Intrinsic Value |
|||||||||||||
| Outstanding at April 1, 2019 |
4,529,291 | $ | 11.76 | 4.4 | $ | 39,896 | ||||||||||
| Exercised |
(708,969 | ) | 15.66 | — | 5,077 | |||||||||||
| Forfeited |
(361,578 | ) | — | — | 74 | |||||||||||
|
|
|
|||||||||||||||
| Outstanding at March 31, 2020 |
3,458,744 | $ | 11.95 | 3.3 | $ | 4,083 | ||||||||||
|
|
|
|||||||||||||||
| Exercisable at March 31, 2020 |
3,458,744 | $ | 11.95 | 3.3 | $ | 4,083 | ||||||||||
|
|
|
|||||||||||||||
136
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
The following table summarizes Replacement Exit-Vesting Restricted Stock activity for the year ended March 31, 2020:
| Replacement Exit-Vesting Restricted Stock |
||||
| Unvested at April 1, 2019 |
1,261,599 | |||
| Canceled |
(255,881 | ) | ||
|
|
|
|||
| Unvested at March 31, 2020 |
1,005,718 | |||
|
|
|
|||
Time-Vesting Options
Time-vesting options were granted with an exercise price equal to the fair value of the Company’s common stock on the date of grant and generally vest in equal 25% installments on the first through fourth anniversary of the designated vesting start date, subject to the award holders continued employment through such vesting date. The Company estimates the fair value of the time-vesting options using the Black-Scholes option pricing model. As of March 31, 2020, unrecognized expense related to the time-vesting options was $3,611. This expense is expected to be recognized over a weighted average period of 1.3 years.
Exit-Vesting Options
Exit-vesting options were granted with an exercise price equal to the fair value of the Company’s common stock on the date of grant and vest, subject to the award holder’s continued employment through the vesting date, on the earlier to occur of (i) the date that affiliates of Blackstone sell 25% of the equity interests of the Joint Venture held by it on March 1, 2017 (the “Transaction Date”) at a specified weighted average price per share and McKesson distributes more than 50% of the equity interests of the Joint Venture held by it on the Transaction Date or (2) McKesson and affiliates of Blackstone collectively sell more than 25% of the aggregate equity interests held by McKesson and Blackstone on the Transaction Date at a specified weighted average price per share.
In May 2018, the terms of the Exit-Vesting Options and Replacement Exit-Vesting Restricted Stock were modified to permit, in addition to existing vesting provisions, vesting to occur in three equal installments commencing on the earlier to occur of the date that (i) affiliates of Blackstone sell more than 25% of the equity interests of the Joint Venture held by it on March 1, 2017 (the “Transaction Date”) and McKesson distributes more than 50% of the equity interests of the Joint Venture held by it on the Transaction Date or (ii) McKesson and affiliates of Blackstone collectively sell more than 25% of the aggregate equity interests held by McKesson and Blackstone on the Transaction Date. No effect on compensation expense was recognized in connection with this modification as the vesting of the affected awards remained not probable following the modification.
The following table summarized time-vesting and exit-vesting option activity for the year ended March 31, 2020:
| Awards | Weighted Average Exercise Price |
Weighted Average Remaining Contractual Term |
Aggregate Intrinsic Value |
|||||||||||||||||||||||||||||
| Time- Vesting Options |
Exit- Vesting Options |
Time- Vesting Options |
Exit- Vesting Options |
Time- Vesting Options |
Exit- Vesting Options |
Time- Vesting Options |
Exit- Vesting Options |
|||||||||||||||||||||||||
| Outstanding at April 1, 2019 |
6,988,403 | 6,504,544 | $ | 18.99 | $ | 18.99 | 8.0 | 8.0 | $ | 11,058 | $ | 10,292 | ||||||||||||||||||||
| Forfeited |
(1,256,156 | ) | (1,250,440 | ) | 18.99 | 18.99 | — | — | — | — | ||||||||||||||||||||||
|
|
|
|
|
|||||||||||||||||||||||||||||
| Outstanding at March 31, 2020 |
5,732,247 | 5,254,104 | 18.99 | 18.99 | 7.6 | 7.6 | — | — | ||||||||||||||||||||||||
|
|
|
|
|
|||||||||||||||||||||||||||||
| Exercisable at March 31, 2020 |
3,743,688 | — | $ | 18.99 | $ | — | 7.5 | — | $ | $ | ||||||||||||||||||||||
|
|
|
|
|
|||||||||||||||||||||||||||||
137
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Valuation Assumptions
The following table summarizes the weighted average fair value of awards using the Black-Scholes and Monte Carlo Simulation option pricing models, as appropriate, and the weighted average assumptions used to develop the fair value estimates under each of the valuation models for the years ended March 31, 2020 and 2019.
| Time-Vesting Options |
Exit-Vesting Options |
Replacement Exit-Vesting Restricted Stock |
||||||||||
| Year Ended March 31, 2020: |
||||||||||||
| Weighted average fair value |
$ | 2.10 | $ | 0.08 | $ | 2.15 | ||||||
| Expected dividend yield |
— | % | — | % | — | % | ||||||
| Expected volatility |
52.0 | % | 50.9 | % | 76.9 | % | ||||||
| Risk-free interest rate |
0.3 | % | 0.3 | % | 0.9 | % | ||||||
| Expected term (years) |
3.8 | 4.1 | 0.9 | |||||||||
| Year Ended March 31, 2019: |
||||||||||||
| Weighted average fair value |
$ | 9.78 | $ | 5.90 | $ | 12.80 | ||||||
| Expected dividend yield |
— | % | — | % | — | % | ||||||
| Expected volatility |
52.5 | % | 52.9 | % | 62.2 | % | ||||||
| Risk-free interest rate |
2.2 | % | 2.2 | % | 2.3 | % | ||||||
| Expected term (years) |
4.5 | 5.1 | 1.9 | |||||||||
| • | Expected dividend yield – Prior to the Merger, the Company was subject to limitations on the payment of dividends under the LLC Agreement. An increase in the dividend yield will decrease compensation expense. |
| • | Expected volatility – Expected volatility is a measure of the amount by which the price of the equity instrument has fluctuated or is expected to fluctuate. The expected volatility was based on the levered median historical volatility of a group of guideline companies. An increase in the expected volatility will increase compensation expense. |
| • | Risk-free interest rate – This is the U.S. Treasury rate as of the measurement date having a term approximating the expected life of the award. An increase in the risk-free interest rate will increase compensation expense. |
| • | Expected term – This is the period of time over which the awards are expected to remain outstanding. The Company estimates the expected term as the mid-point between the actual or expected vesting date and the contractual term. An increase in the expected term will increase compensation expense. |
Omnibus Incentive Plan
Effective as of the Company’s initial public offering, the Company adopted the Change Healthcare Inc. 2019 Omnibus Incentive Plan (the “Omnibus Incentive Plan”) pursuant to which 25.0 million shares of the Company’s common stock have been reserved for issuance to employees, directors and consultants of the Company, the Joint Venture and its affiliates.
In connection with the Omnibus Incentive Plan, Change Healthcare Inc., during the year ended March 31, 2020, granted to the Company’s and the Joint Venture’s employees and directors one or a combination of time-vesting restricted stock units (RSUs), time-vesting deferred stock units, performance stock units, and cash settled restricted stock units under vesting terms that generally vary from one to four years from the date of grant. Each of these instruments are described below.
138
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Restricted Stock Units (“RSUs”) –The RSUs are subject to either a graded vesting schedule over four years, or a one or four year cliff vesting schedule, depending on the terms of the specific award. Upon vesting, the RSUs are exchanged for shares of the Company’s common stock.
Performance Stock Units (“PSUs”) – The PSUs consist of two tranches, one for which the quantity of awards expected to vest varies based on the Joint Venture’s compound annual revenue growth rate over a three year period in comparison to a target percentage and one for which the quantity of awards expected to vest varies based on the Joint Venture’s compound annual Adjusted EBITDA growth rate over a three year period in comparison to a target percentage. The awards earned upon satisfaction of the performance conditions become vested on the fourth anniversary of the vesting commencement date of the award (i.e., continued service is required beyond the satisfaction of the performance condition prior to vesting). The Company recognizes compensation expense for the PSUs based on the number of awards that are considered probable to vest. Recognition of expense is based on the probability of achievement of performance targets and is periodically reevaluated.
Cash Settled Restricted Stock Units (“CSRSUs”) – The CSRSUs are expected to vest ratably over three years. Upon vesting, however, the Company is required to pay cash in settlement of such CSRSUs based on their fair value at the date such CSRSUs vest. Prior to the Merger, the Company was reimbursed by the Joint Venture for any cash settlements.
Deferred Stock Units (“DSUs”) – The DSUs vest 100% upon the one-year anniversary of the date of grant. Unlike the RSUs, the DSUs are exchanged for shares of the Company’s common stock only following the participant’s separation from service.
The following table summarizes Omnibus Incentive Plan activity for the year ended March 31, 2020:
| Restricted Stock Units |
Deferred Stock Units |
Cash Settled Restricted Stock Units |
Performance Stock Units |
|||||||||||||
| Outstanding at April 1, 2019 |
— | — | — | — | ||||||||||||
| Granted |
4,846,058 | 45,704 | 597,006 | 1,079,621 | ||||||||||||
| Cancelled |
(377,969 | ) | — | (119,445 | ) | (113,932 | ) | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Outstanding at March 31, 2020 |
4,468,089 | 45,704 | 477,561 | 965,689 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
During the year ended March 31, 2020, the Company recognized compensation expense of $1,701. At March 31, 2020, aggregate unrecognized compensation expense related to awards granted under the Omnibus Incentive Plan was $89,182.
16. Retirement Plans and Other Postretirement Benefits
Defined Contribution Plans
Employees may participate in one of the Company’s 401k plans, which provide for matching contributions. Expenses related to these 401k plans were immaterial for the years ended March 31, 2020, 2019 and 2018.
Deferred Compensation Plans
Certain of the Company’s employees are eligible to participate in deferred compensation plans. Pursuant to these deferred compensation plans, certain executives and other highly compensated employees may defer a portion of their salaries and incentive compensation at their discretion.
139
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
The following table summarizes the liabilities related to this plan at March 31, 2020 and 2019:
| Balance Sheet Location | March 31, 2020 |
March 31, 2019 |
||||||
| Accrued expenses |
$ | 1,772 | $ | — | ||||
| Other long-term liabilities |
15,880 | — | ||||||
|
|
|
|
|
|||||
| Total deferred compensation |
$ | 17,652 | $ | — | ||||
|
|
|
|
|
|||||
Post-employment Benefits
The Company generally offers post-employment benefits to its employees in the case of certain employee termination events consisting of severance and outplacement services. The extent of such benefits varies based on employee title and accumulates based on the respective employee’s years of service. Due to the episodic nature of severance benefit history at the Joint Venture and the inability to reasonably predict future termination events, no accrual for accumulating severance benefits is accrued until the point that the payment of a severance benefit is probable and can be reasonably estimated. As of March 31, 2020 and 2019, the Company recognized liabilities related to these benefits of $5,927 and $0, respectively.
17. Tax Receivable Agreements
Upon the consummation of the Merger, the Company assumed obligations related to certain tax receivable agreements (collectively, the “tax receivable agreements”) entered into by the Joint Venture with its current and former owners. Depending on whether the respective tax receivable agreements were assumed as part of the Merger or became effective after the Merger, the liabilities related to the tax receivable agreements are subject to differing accounting models as explained below.
2009 - 2011 Tax Receivable Agreements
Under the 2009 - 2011 Tax Receivable Agreements assumed by the Company in connection with the Merger, the Company is obligated to make payments to certain of the former Legacy CHC stockholders, equal to 85% of the applicable cash savings that the Joint Venture expects to realize as a result of tax attributes arising from certain previous transactions. As a result of the covered change of control with respect to the tax receivable agreements that occurred in connection with the Transactions, payments the Joint Venture makes under the 2009 - 2011 Tax Receivable Agreements are required to be calculated using certain valuation assumptions, including that the Joint Venture will have sufficient taxable income to use the applicable tax attributes and that certain of such tax attributes will be used by the Joint Venture on a pro rata basis from the date of the Transactions (or in certain cases from the date of certain previous transactions) through the expiration of the applicable tax attribute. The 2009 - 2011 Tax Receivable Agreements was measured at its fair value as part of the Merger and is recognized at its initial fair value plus recognized accretion to date on the Company’s consolidated balance sheet.
2017 Tax Receivable Agreement
The 2017 Tax Receivable Agreement generally provides for the payment by Change Healthcare Performance, Inc. (a subsidiary of the Company) to affiliates of Blackstone and Hellman & Friedman of 85% of the net cash tax savings realized (or, in certain circumstances, deemed to be realized) in periods ending on or after the Transactions as a result of certain net operating losses and certain other tax attributes of Change
140
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Healthcare Performance, Inc. as of the date of the Transactions. The 2017 Tax Receivable Agreement was measured at its fair value as part of the Merger and is recognized at its initial fair value plus recognized accretion to date on the Company’s consolidated balance sheet.
Based on facts and circumstances at March 31, 2020, the Company estimates the aggregate payments due under these tax receivable agreements in future fiscal years to be as follows:
| 2009 - 2011 Tax Receivable Agreements |
2017 Tax Receivable Agreement |
Total | ||||||||||
| 2021 |
$ | 18,714 | $ | 1,520 | 20,234 | |||||||
| 2022 |
20,113 | 2,281 | 22,394 | |||||||||
| 2023 |
20,084 | 47,384 | 67,468 | |||||||||
| 2024 |
19,358 | 26,551 | 45,909 | |||||||||
| 2025 |
17,917 | 8,441 | 26,358 | |||||||||
| Thereafter |
102,942 | 29,479 | 132,421 | |||||||||
|
|
|
|
|
|
|
|||||||
| Gross expected payments |
199,128 | 115,656 | 314,784 | |||||||||
| Less: Amounts representing discount |
(55,945 | ) | (60,779 | ) | (116,724 | ) | ||||||
|
|
|
|
|
|
|
|||||||
| Total tax receivable agreement obligations due to related parties |
143,183 | 54,877 | 198,060 | |||||||||
| Less: Current portion due (included in due to related parties, net) |
(18,714 | ) | (1,520 | ) | (20,234 | ) | ||||||
|
|
|
|
|
|
|
|||||||
| Tax receivable agreement long-term obligations due to related parties |
$ | 124,469 | $ | 53,357 | $ | 177,826 | ||||||
|
|
|
|
|
|
|
|||||||
McKesson Tax Receivable Agreement
In connection with the closing of the Transactions, the Joint Venture, the McK Members, McKesson and the Company entered into a tax receivable agreement (the “McKesson Tax Receivable Agreement”). The McKesson Tax Receivable Agreement generally requires payment to affiliates of McKesson (the “McKesson TRA Parties”) of 85% of certain cash tax savings realized (or, in certain circumstances, deemed to be realized) by the Company in periods ending on or after the date on which McKesson ceases to own at least 20% of the Joint Venture as a result of (i) certain amortizable tax basis in assets transferred to the Joint Venture at the Contribution Agreement Closing and (ii) imputed interest deductions and certain other tax attributes arising from payments under the McKesson Tax Receivable Agreement. Following the McKesson exit and based on anticipated amortization allocations McKesson advised, the Company recorded an obligation of $164,633 as of March 31, 2020 for the McKesson Tax Receivable estimated payments, which represents a loss contingency under ASC 450 and is included in the other long-term liabilities caption within the accompanying consolidated balance sheet. Future changes in this value will be reflected within pretax income or loss.
Based on facts and circumstances at March 31, 2020, the Joint Venture estimates the aggregate payments due under the McKesson Tax Receivable Agreement in future fiscal years to be as follows:
| McKesson Tax Receivable Agreement |
||||
| 2021 |
$ | — | ||
| 2022 |
128 | |||
| 2023 |
18,306 | |||
141
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
| 2024 |
19,905 | |||
| 2025 |
23,150 | |||
| Thereafter |
103,144 | |||
|
|
|
|||
| Gross expected payments |
164,633 | |||
| Less: Amounts representing discount |
— | |||
|
|
|
|||
| Total tax receivable agreement obligation |
164,633 | |||
| Less: Current portion due (included in accrued expenses) |
— | |||
|
|
|
|||
| Tax receivable agreement long-term obligation (included in other long-term liabilities) |
$ | 164,633 | ||
|
|
|
The timing and/or amount of aggregate payments due may vary based on a number of factors, including the amount of net operating losses and income tax rates.
18. Income Taxes
The income tax provision (benefit) for the years ended March 31, 2020, 2019, and 2018 was as follows:
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Current: |
||||||||||||
| Federal |
$ | — | $ | — | $ | — | ||||||
| State |
568 | — | — | |||||||||
|
|
|
|
|
|
|
|||||||
| Current income tax provision (benefit) |
568 | — | — | |||||||||
|
|
|
|
|
|
|
|||||||
| Deferred: |
||||||||||||
| Federal |
(113,523 | ) | (15,468 | ) | (116,563 | ) | ||||||
| State |
(30,299 | ) | (3,127 | ) | (3,058 | ) | ||||||
|
|
|
|
|
|
|
|||||||
| Deferred income tax provision (benefit) |
(143,822 | ) | (18,595 | ) | (119,621 | ) | ||||||
|
|
|
|
|
|
|
|||||||
| Total income tax provision (benefit) |
$ | (143,254 | ) | $ | (18,595 | ) | $ | (119,621 | ) | |||
|
|
|
|
|
|
|
|||||||
Effective Tax Rate
The reconciliation between the federal statutory rate and the effective income tax rate is as follows:
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
Year Ended March 31, 2018 |
||||||||||
| Statutory U.S. federal tax rate |
21.0 | % | 21.0 | % | 31.5 | % | ||||||
| State income taxes (net of federal benefit) |
2.1 | 3.5 | 3.6 | |||||||||
| Remeasurement of deferred tax assets and liabilities arising from the Tax Legislation |
— | — | 166.9 | |||||||||
| Change in fair value of equity based awards |
(1.2 | ) | 1.0 | — | ||||||||
| Look through accounting policy election |
2.1 | |||||||||||
| Research and development credit |
0.2 | 1.6 | 2.4 | |||||||||
| Goodwill impairment charge |
(10.8 | ) | ||||||||||
| Other |
(0.3 | ) | (0.8 | ) | (0.5 | ) | ||||||
|
|
|
|
|
|
|
|||||||
| Effective income tax rate |
13.1 | % | 26.3 | % | 203.9 | % | ||||||
|
|
|
|
|
|
|
|||||||
142
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Deferred Tax Assets and Liabilities
For the years ended March 31, 2019 and earlier, the Company recorded its deferred tax assets and liabilities with respect to its investment in the Joint Venture under the outside basis approach. As a result of the Merger, the Company elected to begin recording those deferred tax assets and liabilities under the look through approach. As a result, the change in the deferred tax assets and liabilities in the year ended March 31, 2020 reflects the impact of both the Company’s change in accounting for its investment in the Joint Venture to the look through approach as well as the application of the guidance in ASC 805 for a business combination achieved in stages as described in Note 2, Business Combinations. The change from the outside basis approach to the look through approach resulted in the reduction of the Company’s deferred tax liability associated with its investment in the Joint Venture by $28,576.
Significant components of the Company’s deferred tax assets (liabilities) were as follows:
| March 31, 2020 |
March 31, 2019 |
|||||||
| Investment in the Joint Venture |
$ | — | $ | (190,448 | ) | |||
| Depreciation and amortization |
(1,034,407 | ) | — | |||||
| Accounts receivable |
5,793 | — | ||||||
| Fair value of interest rate cap agreements |
14,011 | — | ||||||
| Accruals and reserves |
15,680 | — | ||||||
| Net operating losses |
348,329 | 19,958 | ||||||
| Debt discount and interest |
(9,661 | ) | — | |||||
| Equity compensation |
18,560 | — | ||||||
| Valuation allowance |
(29,350 | ) | — | |||||
| Tax receivable agreements obligations to related parties |
68,900 | — | ||||||
| 163(j) Business interest expense limitation |
23,842 | 7,711 | ||||||
| Tax credits |
16,629 | 2,786 | ||||||
| Accounting method change (ASC 606 adoption) |
(31,886 | ) | — | |||||
| Residual deferred tax asset |
12,072 | — | ||||||
| Other |
(3,696 | ) | — | |||||
|
|
|
|
|
|||||
| Net deferred tax assets (liabilities) |
$ | (585,184 | ) | $ | (159,993 | ) | ||
|
|
|
|
|
|||||
| Reported as: |
||||||||
| Non-current deferred tax assets |
30,720 | — | ||||||
| Non-current deferred tax liabilities |
(615,904 | ) | (159,993 | ) | ||||
|
|
|
|
|
|||||
| Net deferred tax assets (liabilities) |
$ | (585,184 | ) | $ | (159,993 | ) | ||
|
|
|
|
|
|||||
At March 31, 2020, the Company and its subsidiaries had net operating loss carryforwards for federal, state and foreign income tax purposes of $1,174,862, $1,833,161, and $15,260, respectively, which expire from 2026 through 2040, 2020 through 2040 and 2028 through 2037, respectively. A portion of net operating loss carryforwards may be subject to an annual limitation regarding their utilization against taxable income in future periods due to “change of ownership” provisions of the Internal Revenue Code and similar state provisions. However, we do not believe that the limitation will impact the Company’s ability to utilize the net operating loss carryforwards.
At March 31, 2020, the Company and its subsidiaries had research and development (R&D) tax credit carryforwards for federal and state income tax purposes of $16,302 and $413, respectively. The federal credits
143
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
expire from 2038 through 2040, while $116 of the state credits have an indefinite carryforward period and $197 of the state credits expire from 2033 through 2035.
The Company believes that it is more likely than not that the benefit from certain state and foreign net operating loss carryforwards and a residual deferred tax asset recorded in the look through approach will not be realized. In recognition of this risk, the Company has provided a valuation allowance of $17,279 on the deferred tax assets related to these state and foreign net operating loss carryforwards and a valuation allowance of $12,701 on the residual deferred tax asset. If recognized, the tax benefits related to any reversal of the valuation allowance on deferred tax assets as of March 31, 2020, will be accounted for as a reduction of income tax expense of $26,403.
Unrecognized Tax Benefits
The federal, state, and foreign net operating loss carryforwards and R&D and tax credits within the income tax returns filed included unrecognized tax benefits. The deferred tax assets recognized for those net operating losses and R&D credits are presented net of these unrecognized tax benefits.
A reconciliation of unrecognized tax benefits is as follows:
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
|||||||
| Beginning unrecognized benefit |
$ | 863 | $ | — | ||||
| Decreases from prior period tax positions |
(2 | ) | — | |||||
| Increases from prior period tax positions |
— | 432 | ||||||
| Increases from current period tax positions |
769 | 431 | ||||||
| Increases from acquisition |
54,547 | — | ||||||
|
|
|
|
|
|||||
| Ending unrecognized benefit |
$ | 56,177 | $ | 863 | ||||
|
|
|
|
|
|||||
If the above unrecognized tax benefits were recognized, $46,672 would affect the effective income tax rate.
The Company recognizes interest income and expense (if any) related to income taxes as a component of income tax expense. The Company recognized interest and penalties of $138, $0, and $0 for the years ended March 31, 2020, 2019 and 2018, respectively.
The Company and its subsidiaries file income tax returns in the U.S. federal jurisdiction and various states and foreign jurisdictions. The U.S. federal and state income tax returns for certain subsidiaries of the Company remain subject to examination by the Internal Revenue Service for the tax years 2012 and beyond (i.e., periods prior to the Transactions). With respect to state and local jurisdictions and international countries, the Company and its subsidiaries are typically subject to examination for a number of years after the income tax returns have been filed. Although the outcome of tax audits is always uncertain, the Company believes that adequate amounts of tax, interest and penalties have been provided for in the consolidated financial statements for any adjustments that may be incurred due to state, local or foreign audits.
Tax Legislation Updates
On March 27, 2020, the Coronavirus Aid, Relief, and Economic Security Act (“CARES Act”) was enacted. Included in the CARES Act are numerous income tax provisions including changes to the net operating loss rules and the business interest expense deduction rules under Code Section 163(j). The Company anticipates benefiting
144
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
from the changes to the business interest expense deduction rules which temporarily increase the amount of interest expense that businesses are allowed to deduct on their tax returns by increasing the 30% Adjusted Taxable Income limitation to 50% for corporations for tax years 2019 and 2020. Such benefit resulted in an increase in the amount of deductible interest available to the Company. However, this did not result in any immediate change to the Company’s tax position given the amount of net operating losses currently available.
In addition, the CARES Act accelerates the remaining alternative minimum tax (“AMT”) credit refund allowances resulting in taxpayers being able to immediately claim a refund in full for any AMT credit carryforwards, which should provide the Company with the accelerated receipt of its AMT credit refund of $869.
19. Commitments
Lease Commitments
The Company leases its offices and other facilities under operating lease agreements that expire at various dates through 2029. The Company recognizes lease expense on a straight-line basis, including predetermined fixed escalations, over the initial lease term including reasonably assured renewal periods from the time that the Company controls the leased property. Total rent expense for all operating leases was $3,048, $0 and $0 for the years ended March 31, 2020, 2019, and 2018, respectively.
Other Commitments
In February 2018, the Joint Venture, through one its wholly-owned subsidiaries, entered into a Master Services Agreement (the “Agreement”) with Wipro, LLC and Wipro Limited (jointly, “Wipro”). The term of the Agreement is ten years, with the Company having three one-year renewal options. The Company initially committed to purchase services from Wipro through the initial ten-year term of the Agreement (the “Minimum Commitment”) in an aggregate amount of $1 billion; the Minimum Commitment was subsequently adjusted in March 2020 to $975 million. Under the Agreement, Wipro will globally provide the Company with professional services for information technology (including infrastructure, application development and maintenance), business process outsourcing, call center services and similar services. As the Company orders specific services under the Agreement, the parties will execute Statements of Work describing the specific scope of the services to be performed by Wipro. The amount of the Minimum Commitment may be reduced on the occurrence of certain events, some of which also provide the Company the right to terminate the Agreement. If the Company has not fully satisfied the Minimum Commitment (as reduced) by the end of the initial ten-year term, it is required to pay Wipro 25% of the shortfall.
In connection with the Agreement, the Company expects to incur significant severance costs related to the transition of services currently performed by the Company to Wipro. However, pending execution of future Statements of Work, the Company cannot reliably estimate the timing or amount of such future severance costs. Accordingly, the consolidated balance sheet reflects no accrual for such costs associated with the Agreement.
Minimum Commitments
Future minimum commitments by fiscal year as of March 31, 2020 consisted of the following:
| Payments by Period | ||||||||||||||||||||||||||||
| Total | 2021 | 2022 | 2023 | 2024 | 2025 | Thereafter | ||||||||||||||||||||||
| Operating lease obligations |
$ | 141,010 | $ | 40,476 | $ | 34,750 | $ | 23,761 | $ | 15,393 | $ | 10,780 | $ | 15,850 | ||||||||||||||
| Contingent consideration obligation |
3,000 | 3,000 | — | — | — | — | — | |||||||||||||||||||||
| Purchase obligations and other |
1,162,529 | 126,900 | 174,516 | 174,516 | 173,805 | 173,805 | 338,987 | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Total contractual obligations |
$ | 1,306,539 | $ | 170,376 | $ | 209,266 | $ | 198,277 | $ | 189,198 | $ | 184,585 | $ | 354,837 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
145
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
| (1) | The Company expects to receive $1,562 of minimum rentals in the future under noncancelable subleases. |
20. Legal Proceedings
The Company is subject to various claims with customers and vendors, pending and potential legal actions for damages, investigations relating to governmental laws and regulators and other matters arising out of the normal conduct of its business.
Government Subpoenas and Investigations
From time to time, the Company receives subpoenas or requests for information from various government agencies. The Company generally responds to such subpoenas and requests in a cooperative, thorough and timely manner. These responses sometimes require time and effort and can result in considerable costs being incurred by the Company. Such subpoenas and requests also can lead to the assertion of claims or the commencement of civil or criminal proceedings against the Company and other members of the health care industry, as well as to settlements.
Other Matters
In the ordinary course of business, the Company is involved in various claims and legal proceedings. While the ultimate resolution of these matters has yet to be determined, the Company does not believe that it is reasonably possible that their outcomes will have a material adverse effect on the Company’s consolidated financial position, results of operations, or liquidity.
21. Stockholders’ Equity
Under the amended certificate of incorporation and until the Merger, the Company was authorized to issue 9,000,000,001 shares of stock consisting of 9,000,000,000 shares of common stock (“Common Stock”) and one share of Class X stock (“Class X Stock”), each with a par value of $0.001 per share. Each holder of Common Stock is entitled to one vote for each share of Common Stock held with respect to matters on which stockholders are generally entitled to vote. The share of Class X Stock was issuable to McKesson only in the event that the Company breached the terms of the Agreement and Plan of Merger between the Company and McKesson dated December 20, 2016 and only during the period following a qualified initial public offering and prior to a McKesson exit. In the event of issuance of Class X Stock, the holder would have received the right to appoint an additional director to the Company’s board of directors.
As of March 31, 2020 and 2019, the Company has a total of 303,428,142 and 75,474,654 shares of Common Stock outstanding, respectively, and no Class X Stock outstanding. Furthermore, as a result of the Merger, the Class X Stock is no longer available for issuance as McKesson no longer has an ownership interest in the Joint Venture.
22. Related Party Transactions
Registration Rights Agreement
The Joint Venture, certain subsidiaries of the Joint Venture, McKesson and the Company are party to a registration rights agreement providing each of McKesson and the Legacy CHC Stockholders party thereto with
146
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
customary demand and piggyback registration rights with respect to the Company’s common stock. These registration rights include the rights to register shares of the Company in an initial public offering, the rights to register shares of the Company during certain specified time windows and the rights to freely register shares of the Company after such specified time windows.
Advances Received from the Joint Venture
Under the terms of the LLC Agreement, the Joint Venture was required to periodically advance to its members amounts necessary to fund their respective tax obligations on an interim basis, subject to recoupment in the event that such advances exceed the final tax obligations of the respective Members for such year. Once the final tax obligations of each of the Members was determined for such year, the Joint Venture was obligated to formally distribute such amounts to the respective Members. To the extent that the amounts to be distributed were subject to interim advances, additional cash was distributed only to the extent that the interim advances were insufficient to fund the respective Member’s final tax obligation. Distributions up to the amount of interim advances resulted in full settlement of any advances to the respective Member.
The Company received advances of $625 during the year ended March 31, 2020, repaid $9,869 of previous advances during the year ended March 31, 2019 and received advances of $15,828 during the year ended March 31, 2018. Prior to the Merger, such amounts were classified within Due to the Joint Venture on the consolidated balance sheets.
Dilution
Under the terms of the LLC Agreement, the Company and the Joint Venture agreed to cooperate to ensure a 1:1 ratio of Company shares outstanding to units of the Joint Venture held by the Company for as long as the McKesson members hold units of the Joint Venture. Specifically, the parties agreed that:
| • | In the event that the Company issues additional shares, the Joint Venture is required to issue a corresponding number of units to the Company. |
| • | Any net proceeds received by the Company with respect to a Company share must be concurrently contributed to the Joint Venture. |
| • | Any stock split or combination of other equity restructuring involving Company shares must be concurrent with an equivalent unit split or other equity restructuring of the Joint Venture. |
| • | The Company may not redeem, repurchase or otherwise acquire any Company shares unless substantially simultaneously the Joint Venture redeems, repurchases, or otherwise acquires from the Company an equal number of units for the same price per security. |
| • | The Joint Venture may not redeem, repurchase or otherwise acquire any units held by the Company unless substantially simultaneously the Company redeems, repurchases, or otherwise acquires an equal number of Company shares for the same price per security. |
Services Provided to the Company by the Joint Venture
Prior to the Merger, the Company generally had no substantive independent assets or operations apart from its investment in the Joint Venture. As a result, the Company received certain services from the Joint Venture and its employees for which the Joint Venture was not reimbursed. These services include the utilization of office space and a portion of the salaries of the Company’s officers who are considered employees of the Joint Venture. In addition, the Joint Venture was responsible for funding certain costs incurred in connection with the
147
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Company’s contemplated initial public offering and the Merger. Accordingly, the consolidated statements of operations reflect no expense related to these services through the date of the Merger for the year ended March 31, 2020 and for the full years ended March 31, 2019 and 2018.
Management Fees
Under the terms of the LLC Agreement, the Joint Venture was required to fund the cost of preparing for and executing an initial registration statement. Such costs may include legal, accounting and other professional service fees. To the extent that these fees are incurred for the benefit of the Joint Venture and funded by the Joint Venture, they are excluded from the Company’s financial statements. For other costs that are incurred by the Company for its benefit but funded by the Joint Venture, the reimbursement of such costs has been presented in the consolidated statements of operations as Management fees.
Letter Agreement
The Company, the Joint Venture, McKesson and certain of McKesson’s affiliates entered into a letter agreement relating to the Contribution Agreement (the “Letter Agreement”). The Letter Agreement addressed miscellaneous tax-related matters, including (i) technical clarifications and modifications to the manner in which the Joint Venture allocates certain items of taxable income, loss and deduction among, and calculates and makes required tax distributions to, its members, (ii) the sharing of certain contingent tax benefits and expenses not addressed by the McKesson Tax Receivable Agreement or the tax matters agreement that the Company entered into with McKesson in connection with a spin-off or split-off transaction (or a combination of the foregoing) that McKesson could, at its election, initiate and complete that would result, among other things, in the acquisition by the Company of all of McKesson’s LLC Units and the issuance by the Company to McKesson and/or McKesson’s securityholders of an equal number of shares of its common stock and (iii) procedures applicable in the case of certain tax proceedings.
In particular, pursuant to the terms of the Letter Agreement, McKesson was permitted to adjust the manner in which depreciation or amortization deductions in respect of assets transferred to the Joint Venture at the closing of the Transactions are allocated among the Company, McKesson and certain of McKesson’s affiliates. If McKesson chose to allocate an amount of deductions to the Company in excess of a specified minimum threshold, the Company was required to make cash payments to McKesson equal to 100% of the tax savings of the Company attributable to such excess deductions for any tax period ending prior to the date on which McKesson ceased to own at least 20% of the outstanding LLC Units of the Joint Venture, after which the terms of the McKesson Tax Receivable Agreement would control. Effective with the consummation of the Merger, McKesson no longer holds an ownership interest in the Joint Venture and the matters addressed by the Letter Agreement are governed by the terms of McKesson Tax Receivable Agreement.
eRx Network Option Agreement
Prior to the Transactions, the equity interests for entities representing the eRx Network were distributed to the former Legacy CHC stockholders, and in connection therewith a Legacy CHC subsidiary and the Legacy CHC Stockholders entered into an option agreement for a subsidiary of the Joint Venture to acquire the eRx Network (the “Option Agreement”). Under the terms of the Option Agreement, the option to acquire the eRx Network will only become exercisable at any such time that McKesson owns (directly or indirectly), in the aggregate, less than 5% of the outstanding Units of the Joint Venture. Such option will expire, unexercised or unexercisable, on the fifth anniversary of the Transactions. Under the Option Agreement, upon exercise of the option, a Legacy CHC subsidiary will be required to pay an exercise price of $1.00 plus a fixed multiple of the incremental increase (if any) in the EBITDA (as defined in the Option Agreement) of the eRx Network for the
148
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
trailing 12 months preceding the exercise of the option over a baseline level of such EBITDA. Upon completion of the Merger, the Option became exercisable. As a result, the Option Agreement was recognized as an Investment in business purchase option acquired as part of the purchase price allocation described in Note 2, Business Combinations. The value of the option was determined using a Monte Carlo simulation that utilizes assumptions with regard to future cash flows, which were then discounted to present value using an appropriate discount rate, and no adjustment to the carrying value of the option occurred between the Merger Effective Date and March 31, 2020. As of March 31, 2020, the option had not been exercised, but the Company subsequently exercised the option and completed its acquisition of eRx Network in May 2020. See Note 26, Subsequent Events, for additional information.
23. Fair Value Measurements
Assets and Liabilities Measured at Fair Value on a Recurring Basis
The Company’s assets and liabilities that are measured at fair value on a recurring basis consist of derivative financial instruments and contingent consideration obligations and prior to the Merger, a freestanding derivative. The following table below summarize these items, aggregated by the level in the fair value hierarchy within which those measurements fall, as of March 31, 2020 and 2019:
| Description |
Balance at March 31, 2020 |
Quoted in Markets Identical (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) |
||||||||||||
| Interest rate cap agreements |
$ | (47,408 | ) | $ | — | $ | (47,408 | ) | $ | — | ||||||
| Contingent consideration obligation |
(3,000 | ) | — | — | (3,000 | ) | ||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Total |
$ | (50,408 | ) | $ | — | $ | (47,408 | ) | $ | (3,000 | ) | |||||
|
|
|
|
|
|
|
|
|
|||||||||
| Description |
Balance at March 31, 2019 |
Quoted in Markets Identical (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) |
||||||||||||
| Freestanding derivative |
$ | 81,264 | $ | — | $ | — | $ | 81,264 | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Total |
$ | 81,264 | $ | — | $ | — | $ | 81,264 | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
Derivative Financial Instruments
The valuation of the Company’s derivative financial instruments is determined using widely accepted valuation techniques, including a discounted cash flow analysis on the expected cash flows of each derivative. This analysis reflects the contractual terms of the derivative, including the period to maturity, and uses observable market-based inputs, including interest rate curves. The fair value of the interest rate cap agreements are determined using the market standard methodology of netting the discounted future fixed cash payments (or receipts) and the discounted expected variable cash receipts (or payments) using the overnight index swap rate as the discount rate.
The Company incorporates credit valuation adjustments to appropriately reflect both its own nonperformance risk and the respective counterparty’s nonperformance risk in the fair value measurements. In adjusting the fair value of its derivative contracts for the effect of nonperformance risk, the Company considered the impact of netting and any applicable credit enhancements and measures the credit risk of its derivative financial instruments that are subject to master netting agreements on a net basis by counterparty portfolio.
149
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Although the Company has determined that the majority of the inputs used to value its derivatives fall within Level 2 of the fair value hierarchy, the credit valuation adjustments utilize Level 3 inputs to evaluate the likelihood of default by itself and its counterparties. As of March 31, 2020, the Company determined that the credit valuation adjustments are not significant to the overall valuation of its derivatives. As a result, the derivative valuations are classified in Level 2 of the fair value hierarchy.
Contingent Consideration
The valuation of the Company’s contingent consideration obligations was determined using a discounted cash flow method that involved a Monte Carlo simulation. This analysis reflects the contractual terms of the purchase agreements (i.e., minimum and maximum payments, length of earn-out periods, manner of calculating amounts due, etc.) and utilizes assumptions with regard to future cash flows that were determined using a Monte Carlo simulation which were then discounted to present value using an appropriate discount rate. Significant increases with respect to assumptions as to future revenue would have resulted in a higher fair value measurement while an increase in the discount rate would have resulted in a lower fair value measurement.
Freestanding Derivative
Prior to the Merger, the Company was entitled to receive an additional LLC Unit for each share of stock issued by the Company. In the case of equity-based awards, the requirement to receive an additional LLC Unit upon exercise of such awards represented a freestanding derivative. Because the fair value measurement of this derivative involved significant unobservable inputs, the most significant of which in the value of the Company’s stock, the Company determined that it represented a Level 3 fair value measurement.
Because the freestanding derivative was directly related to the Company’s equity-based compensation awards, the valuation of the derivative was determined with the valuation of the underlying equity-based awards. Changes in the value of the derivative are generally expected to fluctuate with changes in the value of the Company’s stock.
As the dividend receivable was initially received in connection with the contribution of assets to the Joint Venture, the initial fair value was treated as a component of the Company’s contribution of assets and receipt of its Investment in the Joint Venture. During the years ended March 31, 2020 and 2019, the Company recognized changes in the Dividend Receivable as a component of Loss from Equity Method Investment in the Joint Venture. The result is that no net equity-based compensation related to employees of the Joint Venture was recognized in the financial statements of the Company prior to the Merger.
Following the adoption of FASB ASU No. 2018-07, however, the measurement of equity-based compensation generally becomes fixed at the date of grant such that the fair value of the dividend receivable was no longer correlated with the amount of equity compensation recognized. As a result, following the adoption of FASB ASU No. 2018-07, the Loss from Equity Method Investment in the Joint Venture was subject to variability associated with changes in the fair value of the equity-based awards.
This freestanding derivative was settled as a result of the Merger and the fair value was included as part of the total purchase price of the transaction. The fair value of the freestanding derivative at March 31, 2020 and 2019 was $0 and $81,264, respectively. This was presented within Dividend receivable on the consolidated balance sheets.
The following table presents a reconciliation of the fair value of the freestanding derivative for which the Company uses significant unobservable inputs:
150
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
| Year Ended March 31, 2020 |
Year Ended March 31, 2019 |
|||||||
| Balance at beginning of period |
$ | 81,264 | $ | 59,116 | ||||
| Increase in fair value based on ASC 505 equity-based compensation |
— | 20,135 | ||||||
| Settlements due to exercise of awards |
(5,077 | ) | (1,297 | ) | ||||
| Change in fair value of equity-based awards |
(33,409 | ) | 3,310 | |||||
| Settlement as component of Merger purchase price |
(42,778 | ) | — | |||||
|
|
|
|
|
|||||
| Balance at end of period |
$ | — | $ | 81,264 | ||||
|
|
|
|
|
|||||
Assets and Liabilities Measured at Fair Value upon Initial Recognition
The carrying amount and the estimated fair value of financial instruments held by the Company as of March 31, 2020 and 2019 were as follows:
| March 31, 2020 | March 31, 2019 | |||||||||||||||
| Carrying Amount |
Fair Value | Carrying Amount |
Fair Value | |||||||||||||
| Cash and cash equivalents |
$ | 410,405 | $ | 410,405 | $ | 3,409 | $ | 3,409 | ||||||||
| Accounts receivable |
$ | 740,105 | $ | 740,105 | $ | — | $ | — | ||||||||
| Investment in business purchase option |
$ | 146,500 | $ | 146,500 | $ | — | $ | — | ||||||||
| Senior Credit Facilities (Level 2) |
$ | 3,682,457 | $ | 3,452,687 | $ | — | $ | — | ||||||||
| Senior Notes (Level 2) |
$ | 997,772 | $ | 950,000 | $ | — | $ | — | ||||||||
| Debt component of tangible equity units (Level 2) |
$ | 35,431 | $ | 34,806 | $ | — | $ | — | ||||||||
Additionally, the assets acquired and liabilities assumed as part of the Merger were recorded at fair value upon initial recognition. See Note 2, Business Combinations, for additional information.
As described in Note 9, Goodwill and Intangible Assets, fair value assessments of the reporting units used in the Company’s impairment analysis are considered a Level 3 measurement due to the significance of unobservable inputs developed using company specific information.
Investments in Businesses
In December 2018, the Joint Venture purchased $15,000 of preferred shares of a health care company and $500 of shares in a related company holding certain intellectual property, each of which is classified within Other noncurrent assets, net on the accompanying consolidated balance sheets. Because this investment has no readily determinable fair value, the Joint Venture measures this investment at cost minus impairment, if any, plus or minus changes resulting from observable price changes in orderly transactions for the identical or a similar investment of the same issuer.
24. Segment Reporting
Beginning in fiscal year 2021, management expects to view the Company’s operating results based on the same three reportable segments that currently comprise the Joint Venture: (a) Software & Analytics, (b) Network Solutions and (c) Technology-Enabled Services.
151
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Prior to the Merger, the Company had minimal operations outside of its investment in the Joint Venture, and its standalone operating results were not utilized by management to make operating decisions, assess performance, or allocate resources. The Company’s chief operating decision maker (“CODM”) and management team, which is the same CODM and management team as of the Joint Venture, did not request or review financial results of the consolidated Company for the period from the date of the Merger through March 31, 2020. Management instead considers the results of its reportable segments for the year ended March 31, 2020 to be best summarized in Note 26, Segment Reporting of the Joint Venture’s consolidated financial statements, which are included as Exhibit 99.1 to the Company’s Form 10-K.
25. Accumulated Other Comprehensive Income (Loss)
The following is a summary of the accumulated other comprehensive income (loss) activity for the years ended March 31, 2020, 2019 and 2018. Prior to the Merger, the activity in accumulated other comprehensive income (loss) reflects the Company’s proportionate share of the Joint Venture’s accumulated other comprehensive income (loss), net of taxes.
| Available For Sale Debt Security |
Foreign Currency Translation Adjustment |
Cash Flow Hedge |
Accumulated Other Comprehensive Income (Loss) |
|||||||||||||
| Balance at March 31, 2017 |
$ | — | $ | 26 | $ | (338 | ) | $ | (312 | ) | ||||||
| Change associated with foreign currency translation |
— | 1,242 | — | 1,242 | ||||||||||||
| Change associated with current period hedging (net of taxes of $623) |
— | — | 1,267 | 1,267 | ||||||||||||
| Reclassification into earnings |
— | — | 339 | 339 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Balance at March 31, 2018 |
$ | — | $ | 1,268 | $ | 1,268 | $ | 2,536 | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Cumulative effect of accounting change by the Joint Venture-ASU 2017-12 |
— | — | 490 | 490 | ||||||||||||
| Change associated with foreign currency translation |
— | (2,833 | ) | — | (2,833 | ) | ||||||||||
| Change associated with current period hedging (net of taxes of $2,139) |
— | — | (1,671 | ) | (1,671 | ) | ||||||||||
| Reclassification into earnings |
— | — | (1,778 | ) | (1,778 | ) | ||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Balance at March 31, 2019 |
$ | — | $ | (1,565 | ) | $ | (1,691 | ) | $ | (3,256 | ) | |||||
|
|
|
|
|
|
|
|
|
|||||||||
| Cumulative effect of accounting change of the Joint Venture-ASU 2018-02 |
— | — | 422 | 422 | ||||||||||||
| Unrealized gain (loss) on available for sale debt securities of the Joint Venture |
1,045 | — | — | 1,045 | ||||||||||||
| Realized gain (loss) on available for sale debt securities of the Joint Venture |
(1,045 | ) | — | — | (1,045 | ) | ||||||||||
| Change associated with foreign currency translation |
— | (5,519 | ) | — | (5,519 | ) | ||||||||||
| Change associated with current period hedging (net of taxes of $607) |
— | — | 981 | 981 | ||||||||||||
| Reclassification into earnings |
— | — | — | — | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Balance at March 31, 2020 |
$ | — | $ | (7,084 | ) | $ | (288 | ) | $ | (7,372 | ) | |||||
|
|
|
|
|
|
|
|
|
|||||||||
152
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
Effective April 1, 2018, the Joint Venture adopted ASU No. 2017-12, which significantly changed the framework by which hedge accounting is recognized, presented and disclosed in the Joint Venture’s financial statements. The adoption of this update by the Joint Venture resulted in a reclassification between accumulated other comprehensive income (loss) and accumulated earnings (deficit).
Effective April 1, 2019, the Joint Venture adopted ASU No. 2018-02, which allows a reclassification from accumulated other comprehensive income to retained earnings for stranded tax effects resulting from the Tax Cuts and Jobs Act of 2017. The adoption of this update resulted in a reclassification between accumulative other comprehensive income (loss) and accumulated earnings (deficit).
26. Subsequent Events
Senior Note Issuance
On April 21, 2020, the Company issued $325,000 of 5.75% unsecured senior notes due 2025 (“Senior Notes”) at 100% of their principal amount. The Senior Notes were issued as part of the same series as the $1,000,000 of 5.75% senior notes due 2025 issued in February 2017.
Connected Analytics Divestiture
On May 1, 2020, the Company completed the sale of its Connected Analytics business for total consideration of $55,000, subject to a customary working capital adjustment, including a $25,000 note receivable from the buyer.
eRx Network Option
On May 1, 2020, the Company exercised its option to purchase and completed the acquisition of eRx Network, a leading provider in comprehensive, innovative and secure data-driven solutions for pharmacies. The Company acquired 100% of the ownership interest for a purchase price of $212,900 plus cash on the balance sheet. The Company expects to account for this transaction as a business combination. The initial accounting, including the identification and allocation of consideration to assets acquired and liabilities assumed, is not complete given the proximity of the acquisition to the financial statement filing date.
PDX Acquisition
On June 1, 2020, the Company completed the purchase of PDX, Inc. (“PDX”), a company focused on delivering patient centric and innovative technologies for pharmacies and health systems. The Company acquired 100% of the ownership interest for a purchase price of $208,000, and the Company expects to account for this transaction as a business combination. The initial accounting, including the identification and allocation of consideration to assets acquired and liabilities assumed, is not complete given the proximity of the acquisition to the financial statement filing date.
27. Quarterly Financial Information (unaudited)
Selected quarterly financial information is as follows:
153
Table of Contents
Change Healthcare Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share and per share amounts)
| Total Revenue | Income (Loss) Before Income Tax |
Net Income (Loss) |
Basic Net Income (Loss) Per Unit |
Diluted Net Income (Loss) Per Unit |
||||||||||||||||
| Quarter Ended: |
||||||||||||||||||||
| June 30, 2019 |
$ | — | $ | (39,701 | ) | $ | (37,517 | ) | $ | (0.50 | ) | $ | (0.50 | ) | ||||||
| September 30, 2019 |
— | (107,555 | ) | (93,935 | ) | (0.66 | ) | (0.66 | ) | |||||||||||
| December 31, 2019 |
— | 65,975 | 50,735 | 0.35 | 0.35 | |||||||||||||||
| March 31, 2020 (1) |
196,792 | (1,009,571 | ) | (866,881 | ) | (4.65 | ) | (4.65 | ) | |||||||||||
| Total Revenue | Income (Loss) Before Income Tax |
Net Income (Loss) |
Basic Net Income (Loss) Per Unit |
Diluted Net Income (Loss) Per Unit |
||||||||||||||||
| Quarter Ended: |
||||||||||||||||||||
| June 30, 2018 |
$ | — | $ | (22,302 | ) | (17,501 | ) | $ | (0.23 | ) | $ | (0.23 | ) | |||||||
| September 30, 2018 |
— | (25,374 | ) | (18,591 | ) | (0.25 | ) | (0.25 | ) | |||||||||||
| December 31, 2018 |
— | (17,468 | ) | (12,388 | ) | (0.16 | ) | (0.16 | ) | |||||||||||
| March 31, 2019 |
— | (5,463 | ) | (3,532 | ) | (0.05 | ) | (0.05 | ) | |||||||||||
| (1) | Results for the quarter ended March 31, 2020 were impacted by the Merger and recognition of a goodwill impairment charge. See Note 2, Business Combinations and Note 9, Goodwill and Intangible Assets, for additional information. |
ITEM 9. CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURES
None.
ITEM 9A. CONTROLS AND PROCEDURES
Evaluation of Disclosure Control and Procedures
Our management, with the participation of our Chief Executive Officer and Chief Financial Officer, evaluated the effectiveness of our disclosure controls and procedures as of March 31, 2020. The term “disclosure controls and procedures” as defined in Rules 13a-15(e) and 15d-15(e) under the Exchange Act means controls and other procedures of a company that are designed to ensure that information required to be disclosed by a company in the reports that it files or submits under the Exchange Act is recorded, processed, summarized and reported, within the time periods specified in the SEC’s rules and forms and that such information is accumulated and communicated to management including the Chief Executive Officer and Chief Financial Officer, as appropriate, to allow timely discussions regarding required disclosures.
Management recognizes that any controls and procedures, no matter how well designed and operated, can provide only reasonable, not absolute, assurance of achieving their desired control objectives. Based on the evaluation of disclosure controls and procedures as of March 31, 2020, our Chief Executive Officer and Chief Financial Officer concluded that, as of such date, our disclosure controls and procedures were effective at a reasonable assurance level.
Management’s Annual Report on Internal Control over Financial Reporting
This Annual Report on Form 10-K does not include a report of management’s assessment regarding internal control over financial reporting or an attestation report of our registered public accounting firm due to a transition period established by rules of the SEC for newly public companies.
154
Table of Contents
Changes in Internal Control over Financial Reporting
During the quarter covered by this report, there have been no changes in the Company’s internal controls over financial reporting that have materially affected or are reasonably likely to materially affect, the Company’s internal controls over financial reporting.
None.
PART III
ITEM 10. DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE
The information required by this item is incorporated by reference to our definitive proxy statement for our 2020 Annual Meeting of Stockholders, which will be filed with the SEC not later than 120 days subsequent to March 31, 2020.
ITEM 11. EXECUTIVE COMPENSATION
The information required by this item is incorporated by reference to our definitive proxy statement for our 2020 Annual Meeting of Stockholders, which will be filed with the SEC not later than 120 days subsequent to March 31, 2020.
ITEM 12. SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AN MANAGEMENT AND RELATED STOCKHOLDER MATTERS
The information required by this item is incorporated by reference to our definitive proxy statement for our 2020 Annual Meeting of Stockholders, which will be filed with the SEC not later than 120 days subsequent to March 31, 2020.
ITEM 13. CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE
The information required by this item is incorporated by reference to our definitive proxy statement for our 2020 Annual Meeting of Stockholders, which will be filed with the SEC not later than 120 days subsequent to March 31, 2020.
ITEM 14. PRINCIPAL ACCOUNTANT FEES AND SERVICES
The information required by this item is incorporated by reference to our definitive proxy statement for our 2020 Annual Meeting of Stockholders, which will be filed with the SEC not later than 120 days subsequent to March 31, 2020.
ITEM 15. EXHIBITS AND FINANCIAL STATEMENT SCHEDULES
The following documents are filed as part of this report:
| a) | Financial Statements – The consolidated financial statements and related notes, together with the report of Deloitte & Touche LLP, Independent Registered Public Accounting Firm, appear in Part II, Item 8 Financial Statements and Supplementary Data, on this Form 10-K. |
| b) | Financial Statement Schedules – All schedules have been omitted as they are not required, or the required information is shown in the financial statements or notes thereto. |
| c) | Exhibits – The exhibits listed on the accompanying Exhibit Index are filed, furnished or incorporated by reference (as stated therein) as part of this Annual Report. |
155
Table of Contents
Exhibit Index
156
Table of Contents
157
Table of Contents
158
Table of Contents
159
Table of Contents
| 10.33† | Form of Replacement 2.5x Restricted Stock Grant Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (incorporated by reference to Exhibit 10.33 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.34† | Form of Replacement Tranche I Nonqualified Stock Option Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (incorporated by reference to Exhibit 10.34 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.35† | Form of Replacement Tranche II Nonqualified Stock Option Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (incorporated by reference to Exhibit 10.35 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.36† | Form of Replacement Tranche III Nonqualified Stock Option Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (incorporated by reference to Exhibit 10.36 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.37† | Form of Nonqualified Exit Vesting Stock Option Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (Neil de Crescenzo) (incorporated by reference to Exhibit 10.37 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.38† | Form of Nonqualified Time Vesting Stock Option Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (Neil de Crescenzo) (incorporated by reference to Exhibit 10.38 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.39† | Form of Nonqualified Stock Option Agreement Under the HCIT Holdings, Inc. Amended and Restated 2009 Equity Incentive Plan (Exit Vesting—Frederik Eliasson) (incorporated by reference to Exhibit 10.39 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.40† | Replacement Unvested Stock Appreciation Rights Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (Howard Lance) (incorporated by reference to Exhibit 10.40 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.41† | Replacement Vested Stock Appreciation Rights Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (Howard Lance) (incorporated by reference to Exhibit 10.41 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.42† | McKesson Technologies LLC Supplemental 401(k) Plan (incorporated by reference to Exhibit 10.42 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.43† | First Amendment to the McKesson Technologies Inc. Supplemental 401(k) Plan (incorporated by reference to Exhibit 10.43 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.44† | McKesson Technologies Inc. Deferred Compensation Administration Plan (incorporated by reference to Exhibit 10.44 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.45† | First Amendment to the McKesson Technologies Inc. Deferred Compensation Administration Program (incorporated by reference to Exhibit 10.45 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.46† | Change Healthcare LLC U.S. Executive Severance Benefit Guidelines (incorporated by reference to Exhibit 10.46 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.47† | Form of Nonqualified Stock Option Agreement Under the HCIT Holdings, Inc. 2009 Equity Incentive Plan (Directors) (incorporated by reference to Exhibit 10.47 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
| 10.48† | Employment Agreement, dated as of February 25, 2017, between Rod O’Reilly and Change Healthcare LLC (incorporated by reference to Exhibit 10.48 to the Company’s Registration Statement on Form S-4 filed on February 4, 2020) | |
160
Table of Contents
161
Table of Contents
| 101.LAB* | XBRL Taxonomy Extension Label Linkbase Document | |
| 101.PRE* | XBRL Taxonomy Extension Presentation Linkbase Document | |
| * | Filed herewith. |
| † | Indicates management contract or compensatory plan. |
Certain agreements and other documents filed as exhibits to this Form 10-K contain representations and warranties that the parties thereto made to each other. These representations and warranties have been made solely for the benefit of the other parties to such agreements and may have been qualified by certain information that has been disclosed to the other parties to such agreements and other documents and that may not be reflected in such agreements and other documents. In addition, these representations and warranties may be intended as a way of allocating risks among parties if the statements contained therein prove to be incorrect, rather than as actual statements of fact. Accordingly, there can be no reliance on any such representations and warranties as characterizations of the actual state of facts. Moreover, information concerning the subject matter of any such representations and warranties may have changed since the date of such agreements and other documents.
None.
162
Table of Contents
SIGNATURES
Pursuant to the requirements of Section 13 or 15 (d) of the Securities Exchange Act of 1934, as amended, the Registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| CHANGE HEALTHCARE INC. | ||||||
| Date: June 4, 2020 | By: | /s/ Neil E. de Crescenzo | ||||
| Neil E. de Crescenzo | ||||||
| Chief Executive Officer and Director | ||||||
| (Principal Executive Officer) | ||||||
| Date: June 4, 2020 | By: | /s/ Fredrik Eliasson | ||||
| Fredrik Eliasson | ||||||
| Executive Vice President, Chief Financial Officer | ||||||
| (Principal Financial Officer) |
| Date: June 4, 2020 | By: | /s/ Paul Rareshide | ||||
| Paul Rareshide | ||||||
| Senior Vice President, Corporate Controller | ||||||
| (Principal Accounting Officer) |
Pursuant to the requirements of the Securities Exchange Act of 1934, as amended, the report has been signed below by the following persons on behalf of the Registrant and in the capacities and on the dates indicated.
| Signature |
Title |
Date | ||
| /s/ Neil E. de Crescenzo |
Chief Executive Officer and Director | June 4, 2020 | ||
| Neil E. de Crescenzo | (Principal Executive Officer) | |||
| /s/ Nella Domenici |
Director | June 4, 2020 | ||
| Nella Domenici | ||||
| /s/ Nicholas L. Kuhar |
Director | June 4, 2020 | ||
| Nicholas L. Kuhar | ||||
| /s/ Howard L. Lance |
Director | June 4, 2020 | ||
| Howard L. Lance | ||||
| /s/ Diana L. McKenzie |
Director | June 4, 2020 | ||
| Diana L. McKenzie | ||||
| /s/ Phillip M. Pead |
Director | June 4, 2020 | ||
| Philip M. Pead | ||||
| /s/ Phillip W. Roe |
Director | June 4, 2020 | ||
| Phillip W. Roe | ||||
| /s/ Neil P. Simpkins |
Director | June 4, 2020 | ||
| Neil P. Simpkins | ||||
163
Table of Contents
| /s/ Robert J. Zollars |
Director | June 4, 2020 | ||
| Robert J. Zollars | ||||
| /s/ Fredrik Eliasson |
Chief Financial Officer | June 4, 2020 | ||
| Fredrik Eliasson | (Principal Financial Officer) | |||
| /s/ Paul Rareshide |
SVP, Corporate Controller | June 4, 2020 | ||
| Paul Rareshide | (Principal Accounting Officer) | |||
164
