Attached files
| file | filename |
|---|---|
| 8-K - 8-K - Vanda Pharmaceuticals Inc. | d892669d8k.htm |
Exhibit 99.1

Vanda Reports results from the EPIONE study of Tradipitant in the treatment of Pruritus in Atopic Dermatitis
| • | Tradipitant antipruritic effects not seen in moderate or severe Atopic Dermatitis and the study did not meet its primary endpoint |
| • | Tradipitant significantly improved severe itch and nighttime sleep in patients with mild Atopic Dermatitis |
| • | Pruritus improved in over 70% of patients with mild Atopic Dermatitis and seen after the first day of treatment |
WASHINGTON, Feb. 25, 2020 /PRNewswire/ — Vanda Pharmaceuticals Inc. (Vanda) (Nasdaq:VNDA) today announced results from a Phase III clinical trial (EPIONE) of tradipitant for the treatment of pruritus in atopic dermatitis (AD) in adults. The EPIONE study did not meet its primary endpoint in reduction of pruritus across the overall study population. However, the antipruritic effect of tradipitant was robust in the mild AD study population. Mild AD represents over 60% of the total AD population in the U.S.1, 2 The EPIONE study continued to demonstrate that tradipitant is safe and well-tolerated.
“Although we are disappointed that EPIONE did not meet its primary endpoint, the profile of efficacy demonstrated in this study potentially addresses a highly unmet need of treating intractable pruritus for a large portion of AD patients,” said Mihael H. Polymeropoulos, M.D., Chief Executive Officer of Vanda. “Due to their potent immuno-suppressive effects, current systemic therapies for AD are typically only used in moderate to severe AD. The safe profile of tradipitant, coupled with a significant and immediate onset of itch reduction by the first full day of treatment, may provide a much-needed therapy for the majority of AD patients that experience mild AD lesion severity but still suffer from significant pruritus.”
EPIONE was a randomized, placebo-controlled Phase III study (n=341) in AD patients with severe pruritus with a range of disease severity presentation from mild (23%) to moderate (64%) and severe (13%) as determined by the Investigator’s Global Assessment scale (IGA). Patients were randomized 1:1 to receive either tradipitant or placebo for a treatment period of 8 weeks. Patients were assessed at baseline and post-randomization with a number of symptomatic and disease severity scales at regular intervals.
The EPIONE study examined the hypothesis that tradipitant dosed at 85 mg twice a day offers improvement of the disease symptoms and signs of AD over the evaluation period. At week 8, tradipitant and placebo patients demonstrated significant and meaningful improvement in
pruritus as measured by the Worst Itch Numeric Rating Scale (WI-NRS), but while the tradipitant magnitude of improvement was greater than that of placebo, the difference between treatment groups was not statistically significant. A significant interaction was observed between baseline disease severity (IGA 1-4) and treatment (p=0.0004). This suggests that study participants with different baseline disease severity experienced different treatment outcomes. When accounting for baseline disease severity and treatment interaction, a significantly larger improvement in WI-NRS was seen with tradipitant at the pre-specified endpoint of Week 8 in the full trial population (p=0.0217). Similar effects were seen throughout the treatment periods at all post-randomization visits comprising weeks 2, 4, 6 and 8 (Table 1).
Given the observed significant interaction between baseline disease severity and treatment, a subgroup analysis showed that patients with mild disease severity (23% of study patients, IGA 1, 2) experienced the largest improvement over placebo. Specifically, in the mild AD group, tradipitant significantly improved WI-NRS over placebo at every visit (Table 1, Figure 1). The categorical WI-NRS responder analysis (>4 point improvement) showed that 72.5% of tradipitant patients had a clinically meaningful response as compared to 33.3% of placebo patients.
These results suggest a large and significant antipruritic effect of tradipitant in mild AD, and were confirmed with patient daily diary entries. For mild AD patients, a time course of response also showed that the antipruritic effect was seen immediately after the first full day of tradipitant dosing, suggesting a large and immediate therapeutic effect. Similar improvement was observed for nighttime sleep, often disrupted in patients with severe pruritus.
Results from the EPIONE study (Figure 2) and scientific literature suggest that mild and severe AD appear to be distinct endotypes with different sets of causative factors and course.3, 4 The American Academy of Dermatology (AAD) atopic dermatitis guidelines lists pruritus as an essential feature of atopic dermatitis.5 The significant pruritus associated with mild AD and the worsening of lesions through scratching, along with the sleep disruption, continue to represent a significant unmet medical need.
“The majority of AD patients across all age groups from children to seniors suffer from a form of atopic dermatitis characterized by mild lesions. Yet these patients might still have severe pruritus and suffer from impacts to quality of life, as well as sleep. With a beneficial safety profile and assuming this significant improvement in itch in the mild-type atopic dermatitis is confirmed in a future study, this therapy would be of interest to all these mild-type AD patients,” said Dr. Sonja Stander, professor of Dermatology and Neurodermatology at the Department of Dermatology, and head of the Interdisciplinary Center for Chronic Pruritus (KCP) of the University Hospital Münster, Germany.
Dr. Stander added, “we also see patients with moderate-to-severe disease where immunomodulatory therapies may have a profound effect on healing lesions in the short term but they still suffer from significant itch. The NK-1 antagonist mechanism may work well for this population where only the severe itch is left and their disease is mild or almost clear after steroids, an interleukin inhibitor, or another immunomodulatory therapy has been used.”
The results of the EPIONE study suggest that tradipitant can produce a large and rapid antipruritic effect in mild AD. Currently, American Academy of Dermatology (AAD) treatment guidelines indicate and recommend immunomodulatory medications only after topical regimens and phototherapy are found to not adequately control the disease.6 A well-tolerated, systemic antipruritic agent with rapid onset of action, like tradipitant, could add significant value to patients and take a primary place in the treatment algorithm of atopic dermatitis.
The results of the EPIONE study will need to be confirmed in a follow up study. Vanda plans to reassess the ongoing EPIONE2 study of pruritus in AD as it continues to analyze the results and determines next steps.
About Vanda Pharmaceuticals Inc.
Vanda is a global biopharmaceutical company focused on the development and commercialization of innovative therapies to address high unmet medical needs and improve the lives of patients. For more on Vanda Pharmaceuticals Inc., please visit www.vandapharma.com.
Corporate Contact:
AJ Jones II
Chief Corporate Affairs and Communications Officer
Vanda Pharmaceuticals Inc.
202-734-3400
pr@vandapharma.com
CAUTIONARY NOTE REGARDING FORWARD LOOKING STATEMENTS
Various statements in this release, including, without limitation, statements regarding the efficacy of traidipitant in the treatment of pruritus in patients with mild atopic dermatitis and the potential commercial opportunity for tradipitant, are “forward-looking statements” under the securities laws. Forward-looking statements are based upon current expectations that involve risks, changes in circumstances, assumptions and uncertainties. Important factors that could cause actual results to differ materially from those reflected in Vanda’s forward-looking statements include, among others: the ability of tradipitant to provide significant benefit in the treatment of pruritus in patients with mild atopic dermatitis; the results of Vanda’s clinical development activities for tradipitant; delays in the completion of Vanda’s clinical development of tradipitant; a failure of tradipitant to be demonstrably safe and effective; tradipitant’s potential to become a first line pharmacological option in the treatment of pruritis in patients with mild atopic dermatitis; and other factors that are set forth in the “Risk Factors” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations”
sections of Vanda’s annual report on Form 10-K for the fiscal year ended December 31, 2018 and quarterly report on Form 10-Q for the fiscal quarter ended September 30, 2019, which are on file with the SEC and available on the SEC’s website at www.sec.gov. Additional factors may be set forth in those sections of Vanda’s annual report on Form 10-K for the fiscal year ended December 31, 2019, to be filed with the SEC in the first quarter of 2020. In addition to the risks described above and in Vanda’s annual report on Form 10-K and quarterly reports on Form 10-Q, other unknown or unpredictable factors also could affect Vanda’s results. There can be no assurance that the actual results or developments anticipated by Vanda will be realized or, even if substantially realized, that they will have the expected consequences to, or effects on, Vanda. Therefore, no assurance can be given that the outcomes stated in such forward-looking statements and estimates will be achieved. All written and verbal forward-looking statements attributable to Vanda or any person acting on its behalf are expressly qualified in their entirety by the cautionary statements contained or referred to herein. Vanda cautions investors not to rely too heavily on the forward-looking statements Vanda makes or that are made on its behalf. The information in this release is provided only as of the date of this release, and Vanda undertakes no obligation, and specifically declines any obligation, to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise.
Table 1. EPIONE Summary Results
|
Endpoints1 |
Visit | Tradipitant | Placebo | Diff | P-value | |||||||||||||||
| WI-NRS |
Week 2 | -1.68 | -1.44 | 0.23 | 0.3092 | |||||||||||||||
| ITT (n=341) |
Week 4 | -2.58 | -2.20 | 0.39 | 0.1664 | |||||||||||||||
| Tradipitant (n=171) |
Week 6 | -3.00 | -2.89 | 0.11 | 0.7105 | |||||||||||||||
| Placebo (n=170) |
Week 8 | -3.61 | -3.43 | 0.18 | 0.5667 | |||||||||||||||
| WI-NRS Adjusting for IGA Severity |
Week 2 | -2.43 | -1.29 | 1.14 | 0.0069 | |||||||||||||||
| ITT (n=341) |
Week 4 | -3.34 | -2.05 | 1.29 | 0.0042 | |||||||||||||||
| Week 6 | -3.75 | -2.74 | 1.01 | 0.0284 | ||||||||||||||||
| Week 8 | -4.36 | -3.28 | 1.08 | 0.0217 | ||||||||||||||||
| WI-NRS |
Week 2 | -2.59 | -0.98 | 1.61 | 0.0003 | |||||||||||||||
| IGA 1, 2 (n=79) |
Week 4 | -3.39 | -1.48 | 1.92 | 0.0005 | |||||||||||||||
| Tradipitant (n=40) |
Week 6 | -4.18 | -2.32 | 1.86 | 0.0024 | |||||||||||||||
| Placebo (n=39) |
Week 8 | -4.74 | -3.14 | 1.60 | 0.0152 | |||||||||||||||
| Diary WI-NRS |
Week 2 | -1.54 | -0.36 | 1.18 | 0.0002 | |||||||||||||||
| IGA 1, 2 (n=79) |
Week 4 | -2.78 | -1.07 | 1.71 | 0.0002 | |||||||||||||||
| Week 6 | -3.48 | -1.72 | 1.76 | 0.0011 | ||||||||||||||||
| Week 8 | -4.23 | -2.14 | 2.09 | 0.0010 | ||||||||||||||||
| Responder Analysis (%)2 (n=79) |
||||||||||||||||||||
| WI-NRS ³4 Improvement |
Week 8 | 72.5 | 33.3 | 39.2 | 0.0007 | |||||||||||||||
| SCORAD 50% Improvement |
Week 8 | 55.0 | 30.8 | 24.2 | 0.0411 | |||||||||||||||
| IGA 0 or 1 |
Week 8 | 60.0 | 38.5 | 21.5 | 0.0729 | |||||||||||||||
| 1. | P-values are from MMRM analysis. |
| 2. | P-values are from Fisher’s exact test. |
Figure 1. WI-NRS Change by Week
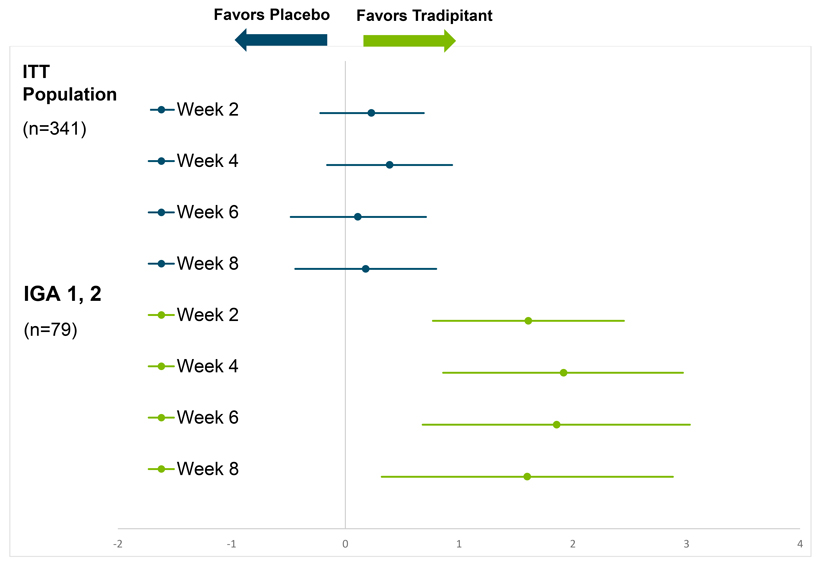
Figure 2. EPIONE Baseline Study Population by IGA Disease Severity
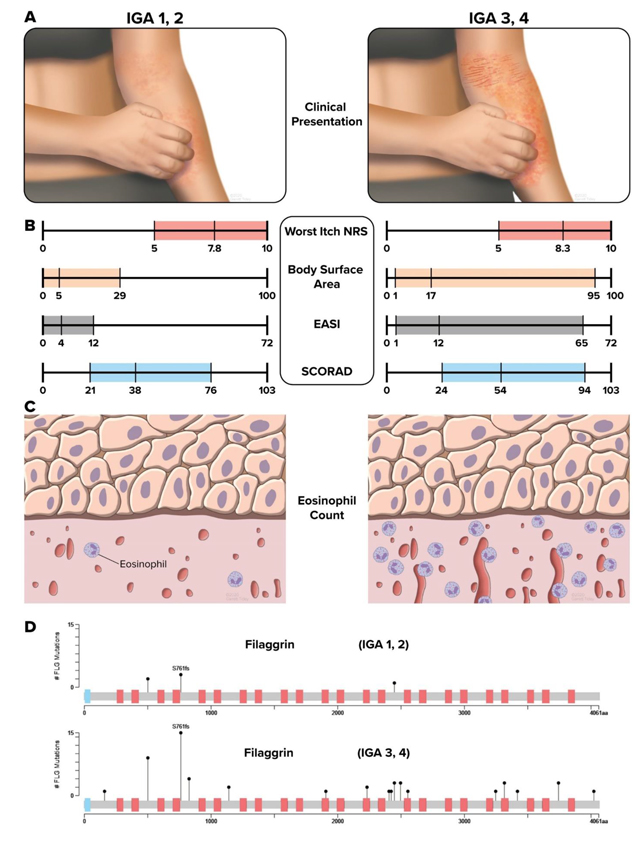
| A. | Distinct endotypes and clinical presentation of AD as defined by IGA 1 and 2 (mild) and IGA 3 and 4 (moderate and severe) |
| B. | Distribution of clinical variables across endotypes as defined by IGA 1 and 2 (mild) and IGA 3 and 4 (moderate and severe) |
| C. | Significant differences in Eosinophil counts across endotypes as defined by IGA 1 and 2 (mild) and IGA 3 and 4 (moderate and severe) |
| D. | Lollipop plots display the location and frequency of the identified variants in Filaggrin. We observe a significant enrichment of rare LOF variants in FLG detected in IGA 3 and 4 AD patients (moderate and severe) as compared to IGA 1 and 2 AD patients (mild). |
Figure 3. Substance P in Atopic Dermatitis
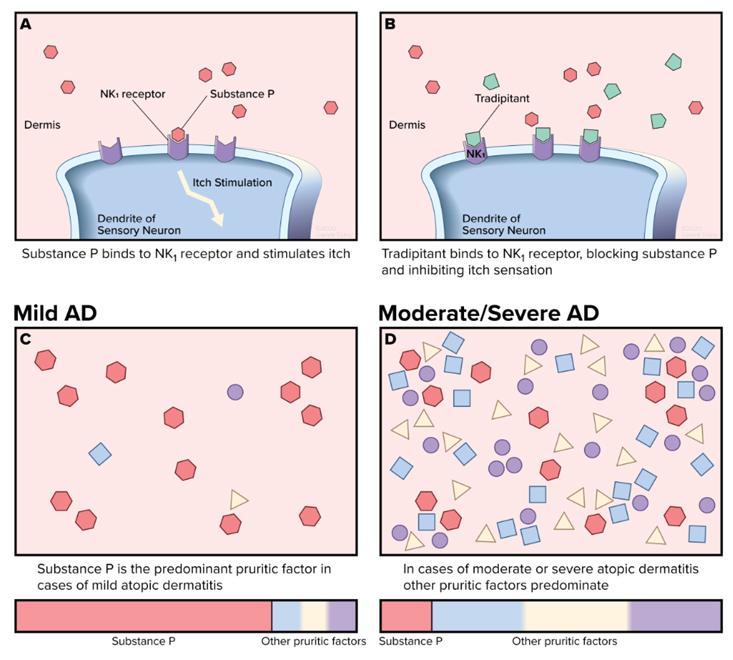
Pruritus-related mechanisms comprise interleukins as well as neuropeptides that are relevant to neurogenic inflammation such as substance P and the pruritogen-keratinocyte communication (Yosipovitch 2020).7 In the mild AD population (C), relatively fewer itch mediation factors including cytokines, serotonin, histamine, and eosinophils are present, leaving substance P as the predominant factor in itch. In contrast, in the more severe AD population (D), there are increasingly multiple factors other than Substance P involved in the cause of itch.
References:
| 1. | Chiesa Fuxench ZC, Block J, Boguniewicz M, et al. Atopic Dermatitis in America Study: a cross-sectional study examining the prevalence and disease burden of atopic dermatitis in the US adult population. J Invest Dermatol. 2019 Mar; 139(3): 583-590. |
| 2. | Silverberg JI, Simpson EL. Associations of childhood eczema severity: a US population-based study. Dermatitis. 2014; 25(3): 107–114. |
| 3. | Czarnowicki T, He H, Krueger, JG, Guttman-Yassky E. Atopic Dermatitis endotypes and implications for targeted therapeutics. J Allergy Clin Immunol. 2019 Jan; 143(1): 1-11. |
| 4. | Brown SJ, McLean WHI, Eczema Genetics: Current State of Knowledge and Future Goals. J Invest Dermatol. 2009; 129: 543–552. |
| 5. | Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: Section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014; 70: 338–51. |
| 6. | Sidbury R, Davis DM, Cohen DE, et al. Guidelines of care for the management of atopic dermatitis: Section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014; 71: 327–49. |
| 7. | Yosipovitch G, Berger T, Fassett MS. Neuroimmune interactions in chronic itch of atopic dermatitis. J Eur Acad Dermatol Venereol. 2020 Feb; 34(2): 239-250. |
