Attached files
| file | filename |
|---|---|
| EX-32.2 - EXHIBIT 32.2 - R1 RCM INC. | exhibit322-q22018.htm |
| EX-32.1 - EXHIBIT 32.1 - R1 RCM INC. | exhibit321-q22018.htm |
| EX-31.2 - EXHIBIT 31.2 - R1 RCM INC. | exhibit312-q22018.htm |
| EX-31.1 - EXHIBIT 31.1 - R1 RCM INC. | exhibit311-q22018.htm |
| EX-10.6 - EXHIBIT 10.6 - R1 RCM INC. | exhibit106ascensionmpsa-am.htm |
| EX-10.4 - EXHIBIT 10.4 - R1 RCM INC. | exhibit104-imhaddendum2.htm |
| 10-Q - 10-Q - R1 RCM INC. | q2201810q.htm |
EXHIBIT 10.5
EXECUTION VERSION
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SUPPLEMENT 26 TO
AMENDED AND RESTATED MASTER PROFESSIONAL SERVICES AGREEMENT
between
Ascension Health
and
R1 RCM Inc.
SUPPLEMENT 26 TO
AMENDED AND RESTATED MASTER PROFESSIONAL SERVICES AGREEMENT
This Supplement 26 (this “Supplement”) is made and entered into as of June 24, 2018 (the “Supplement Effective Date”) by and between Ascension Health (“Ascension Health”) and R1 RCM Inc., f/k/a Accretive Health, Inc. (“Supplier”) (together, the “Parties”). Capitalized terms used herein and not otherwise defined shall have the meanings ascribed to such terms in the MPSA (as defined below).
WHEREAS, the Parties are party to that certain Amended and Restated Master Professional Services Agreement, dated as of February 16, 2016 by and between Ascension Health and Supplier, as amended by that certain Amendment No. 1 to the Master Professional Services Agreement, dated as of the 28th of April, 2017 (as further amended, restated, supplemented, or otherwise modified, the “Master Professional Services Agreement” or “MPSA”), pursuant to which Supplier provides Dependent Services and Physician Advisory Services for Acute Care with respect to certain Eligible Recipients;
WHEREAS, Ascension Health has historically provided revenue cycle management services to certain Eligible Medical Groups (as defined in Section 1(c) below) through, among other resources, (a) Ascension Health’s National Revenue Service Center, and (b) the use of certain third party Platforms (as defined below);
WHEREAS, the Parties entered into that certain Term Sheet for Ascension Medical Group RCM Services, dated as of February 23, 2018 (“Term Sheet”), pursuant to which Supplier agreed to provide, and Ascension Health agreed to receive, the EMG Services (as defined in Section 4(a) below) in accordance with the terms set forth herein; and
WHEREAS, the Parties now desire for Supplier to provide the EMG Services, which will be deemed as New Services accepted and to be provided under the MPSA, to the Eligible Medical Groups pursuant to the terms and subject to the conditions set forth in this Supplement.
NOW THEREFORE, in consideration of the foregoing premises and mutual consents set forth below, the Parties hereby agree as follows:
1.Schedules and Attachments; Relationship with the MPSA; Scope and Authority.
(a) | Schedules, Exhibits, and Annexes. This Supplement includes each of the following attached Schedules, Exhibits, and Annexes, all of which are hereby incorporated into this Supplement by this reference: |
Schedule A | Current Non-Standard Third Party Eligible Medical Groups |
Schedule B | Supplier Technology Tools and Software |
Exhibit 1 Exhibit 2 Exhibit 3 Exhibit 4 | EMG Services EMG Base Fees EMG Incentive Fees Service Level Targets and Metrics |
Annex 1 | Form of EMG Services Addendum |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 1
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(b) | General Relationship with the MPSA. This Supplement is entered into pursuant and subject to, and, solely as provided herein, amends certain provisions of, the MPSA, the terms of which are incorporated herein by reference (as modified by this Supplement). In accordance with Section 1.1(c) of the MPSA, any amendment to the MPSA, including amendments made after the Supplement Effective Date, shall automatically, as of the amendment effective date, be incorporated into this Supplement, unless otherwise specifically set forth in such amendment. This Supplement shall be considered a “Supplement” for purposes of the MPSA, notwithstanding any deviations herein from the form set forth in Annex 1 of the MPSA. This Supplement sets forth a legal framework under which Supplier will provide EMG Services to Eligible Medical Groups that are the subject of this Supplement. Notwithstanding anything to the contrary in this Supplement or the MPSA: (i) the Parties agree that Exhibits 2-A, 2-B, 4-A, 4-B, 4-E, and 17 to the MPSA, and any provision of the MPSA that relates solely and exclusively to Acute Care, the Physician Advisory Services, or the transition or onboarding of Additional Book Eligible Recipients or New ABMs shall be disregarded and have no effect for purposes of this Supplement (except that references to Exhibit 4 to the MPSA in the body of the MPSA will be deemed to refer to Exhibit 2 and/or Exhibit 3 to this Supplement, as applicable); and (ii) solely with respect to the provision or receipt of the EMG Services, in the event of a conflict between the terms in this Supplement and the terms set forth in the MPSA, the terms of this Supplement shall prevail. Upon the execution and delivery of this Supplement by the Parties, the Term Sheet is hereby terminated, and this Supplement contains, and is intended as, a complete statement of all of the terms of the agreements between the Parties with respect to the matters provided for in the Term Sheet, and supersedes and terminates the Term Sheet. |
(c) | Eligible Medical Groups. Each physician group that is permitted to receive EMG Services from Supplier hereunder (each such physician group, an “Eligible Medical Group”, and collectively, the “Eligible Medical Groups”) will be either (x) an Entity that is a Controlled Affiliate of Ascension Health or an Ascension Health Affiliate, or a department operating under the control of Ascension Health or an Ascension Health Affiliate (each, an “Owned Eligible Medical Group”) or (y) subject to Section 1(e), a third party legal entity that is receiving revenue cycle services from Ascension Health or an Ascension Health Affiliate pursuant to contractual agreements between such third party legal entity and Ascension Health or an Ascension Health Affiliate (each such contract, a “PSA”, and each such entity, a “Third Party Eligible Medical Group”). To the extent a physician group is either an Owned Eligible Medical Group or, subject to Section 1(e), a Third Party Eligible Medical Group, the Parties agree that any such physician group included in one of the below groups, whether such physician group is currently existing or hereafter becomes acquired by, employed by, or party to a PSA with Ascension Health or an Ascension Health Affiliate, is an Eligible Medical Group and will receive EMG Services under this Supplement following the execution of an EMG Services Addendum (as defined in Section 1(g) below) covering the applicable physician group(s): |
(i) | all physician groups that receive revenue cycle management services through the Athena Platform (or any successor Platform that Ascension Health uses as its primary Platform with respect to revenue cycle management services), which physician groups are located in various U.S. states (“NRSC/Athena Group”); |
(ii) | all physician groups associated with Via Christi Health in Kansas that receive revenue cycle management services through the Cerner Platform (“Cerner Group”); and |
(iii) | all physician groups associated with Wheaton Franciscan Healthcare in Wisconsin that receive revenue cycle management services through the Epic Platform (“Epic Group”). |
(d) | Treatment of the Owned Eligible Medical Groups. Ascension Health shall be and remains responsible and liable to Supplier for all acts or omissions of an Owned Eligible Medical Group, including the physicians employed by the Owned Eligible Medical Group (each, an “Employed EMG Physician”), in connection with this Supplement and the EMG Services (including failure by an Owned Eligible Medical Group or Employed EMG Physician to perform in accordance with this Supplement or to |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 2
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
comply with any duties or obligations imposed on Ascension Health under this Supplement) to the same extent that such act or omission was committed by Ascension Health or Ascension Health employees hereunder. Any claims or rights that may accrue to any Owned Eligible Medical Group or Employed EMG Physician under this Supplement may be exercised only by Ascension Health against Supplier.
(e) | Treatment of Third Party Eligible Medical Groups. Following the Supplement Effective Date, Ascension Health and Supplier will work together in good faith to create a set of terms and conditions related to the receipt of EMG Services by Third Party Eligible Medical Groups from Supplier, to which Ascension Health may, in its sole discretion, bind any Third Party Eligible Medical Group in connection with such Third Party Eligible Medical Group’s receipt of EMG Services from Supplier (such terms and conditions, “Third Party Terms”). Ascension Health will take the lead in determining a strategy for approaching Third Party Eligible Medical Groups regarding their potential receipt of EMG Services from Supplier under this Supplement and Supplier shall comply with any such strategy determined by Ascension Health. The Parties anticipate that each Third Party Eligible Medical Group would receive all of the EMG Services described in Exhibit 1 of this Supplement, which receipt of EMG Services would be subject to and in accordance with this Supplement (including an applicable EMG Services Addendum) in the same manner as the Owned Eligible Medical Groups also receiving EMG Services under this Supplement (including such EMG Services Addendum); provided that [**]. Ascension Health shall be and remains responsible and liable to Supplier for all acts or omissions of a Third Party Eligible Medical Group, including the physicians employed by the Third Party Eligible Medical Group (each, an “Third Party EMG Physician”), receiving EMG Services under this Supplement (including any failure by a Third Party Eligible Medical Group or a Third Party EMG Physician to perform in accordance with this Supplement or to comply with any duties or obligations imposed on Ascension Health under this Supplement) to the same extent that such act or omission was committed by Ascension Health, an Ascension Health Affiliate, or its or their employees hereunder, notwithstanding any conflicting terms or conditions in the applicable PSA or any Third Party Terms. Any claims or rights that may accrue to any Third Party Eligible Medical Group or Third Party EMG Physician under this Supplement may be exercised only by Ascension Health against Supplier. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 3
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(f) | Onboarding of Eligible Medical Groups. In accordance with the terms of this Supplement, the provision of EMG Services to the Eligible Medical Groups will be transitioned to Supplier as soon as practicable, but in distinct phases and at different times during the Supplement Term, in accordance with the timelines set forth in this Section 1(f), Section 4.2(b) of the MPSA, and the initial transition plan provided to Ascension Health by Supplier. The Parties intend that both Owned Eligible Medical Groups and, subject to Section 1(e) above, Third Party Eligible Medical Groups included in the NRSC/Athena Group, Cerner Group or Epic Group will be transitioned to Supplier in accordance with the timeline below; provided that [**]. |
(g) | EMG Services Addenda. The Parties intend for Eligible Medical Groups included in the NRSC/Athena Group (excluding those located in Binghamton and Bridgeport, which will only receive Platform-Specific Services) to: (i) first receive Platform-Specific Services under an EMG Services Addendum covering the NRSC/Athena Group as a whole (i.e., “Enterprise 1” in the chart below) (“NRSC/Athena Addendum”); and (ii) thereafter, on an EMG Market-by-EMG Market basis, receive Medical Group Market Services (as defined in Section 4(a) below, which would be in addition to the Platform-Specific Services) under separate market-specific EMG Services Addenda for the Eligible Medical Groups included in the NRSC/Athena Group (each, a “Market Addendum”). Eligible Medical Groups in the Epic Group will receive all of the EMG Services under the Wisconsin Addendum (as defined below). Eligible Medical Groups in the Cerner Group will receive all of the EMG Services under an EMG Services Addendum covering only the Cerner Group (“Cerner Group Addendum”). The Parties intend for the aforementioned EMG Services Addenda to be executed in accordance with the timeline above. Supplier will have no obligation to provide EMG Services to any Eligible Medical Group, and Ascension Health will have no obligation to pay the EMG Base Fee (as defined in Section 5(a) below) in respect of any Eligible Medical Group, until Ascension Health and Supplier enter into an addendum to this Supplement in substantially the form set forth in Annex 1, which applies specifically to such Eligible Medical Group and sets forth: (i) an acknowledgment that the provision of revenue cycle management services for the applicable Eligible Medical Groups will be transitioned to Supplier; and (ii) any terms or conditions that deviate from, or are in addition to, the terms and conditions of this Supplement as specifically applied to such Eligible Medical Group (each such addendum, an “EMG Services Addendum”). Upon execution, each EMG Services Addendum will be automatically incorporated by reference into this Supplement. In the event of a conflict between the terms in this Supplement and the terms of an EMG Services Addendum, the terms of the EMG Services Addendum will control with respect to the applicable Eligible Medical Group. |
(h) | New Eligible Medical Groups. If: (i) (A) following the Supplement Effective Date, Ascension Health or an Ascension Health Affiliate acquires, employs, or enters into a PSA with, a physician group that is not automatically included in the NRSC/Athena Group, the Cerner Group or the Epic Group under the applicable EMG Services Addendum or (B) there is any physician group that, as of the Supplement |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 4
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Effective Date, is an Owned Eligible Medical Group or Third Party Eligible Medical Group but is not included in the NRSC/Athena Group, the Cerner Group, or the Epic Group (any such physician group described in this clause (i), a “New Eligible Medical Group”); and (ii) Ascension Health wishes to have Supplier perform the EMG Services for the applicable New Eligible Medical Group, then the Parties will enter into a separate EMG Services Addendum for such New Eligible Medical Group, which EMG Services Addendum shall describe the EMG Services to be provided to such New Eligible Medical Group, the EMG Service Commencement Date for such EMG Services, and the calculation of a separate or revised EMG Base Fee to include such New Eligible Medical Group, as determined in accordance with Exhibit 2. Supplier shall, subject to Section 1(e), offer to provide to each such New Eligible Medical Group the full scope of EMG Services set forth on Exhibit 1 of this Supplement. For the avoidance of doubt, this Section 1(h) does not apply with respect to physician groups that are automatically included in the NRSC/Athena Group, the Cerner Group or the Epic Group under the applicable EMG Services Addendum (as contemplated in Section 1(c) above), which physician groups will automatically receive EMG Services under the applicable EMG Services Addendum.
(i) | Divestitures of Eligible Medical Groups Receiving EMG Services. If, during the Supplement Term, Ascension Health or an Ascension Health Affiliate divests or sells an Eligible Medical Group then-currently receiving EMG Services under this Supplement to an unaffiliated third party (including if such divestiture is part of a divestiture to any unaffiliated third party of the Ascension Health Affiliate that Controls or owns such Owned Eligible Medical Group), then the Parties agree to undertake the obligations set forth in Section 4.6(b) of the MPSA, including, if all of the Owned Eligible Medical Groups within an EMG Market then-receiving EMG Services are divested (provided that for purposes of this sentence, the Oklahoma, Kansas, Alabama, Florida, Maryland and D.C. markets will each be considered separate EMG Markets), with respect to Acquirer Termination Charges and Divestiture Termination Charges (i.e., a one-time termination fee equal to 0.65% of the Cash Collections for the applicable sold or divested Owned Eligible Medical Groups for the applicable trailing twelve (12) month period, which percentage shall decrease to zero percent (0%) on a straight line basis over the five (5) year period beginning on the Supplement Effective Date), which shall be applied to this Supplement, mutatis mutandis. With respect to all divestitures or sales of an Owned Eligible Medical Group to an Affiliate of Ascension Health, the Parties agree to undertake the obligations set forth in Section 4.6(c) of the MPSA, which shall be applied to this Supplement, mutatis mutandis. For clarity, any Eligible Medical Group then-receiving EMG Services that is not divested or sold shall continue to receive EMG Services after such divestiture or sale in accordance with the terms of any applicable EMG Services Addendum. With respect to any divestiture covered under this Section, Supplier agrees to provide support relating to the winding down of legacy Ascension Health-owned accounts receivable for any divested Eligible Medical Group then-receiving EMG Services, the scope of which support shall be, on a case-by-case basis, separately negotiated and agreed by the Parties in good faith. |
(j) | Wisconsin. Effective as of October 1, 2018, the Parties intend to (i) terminate each of Supplement 23 (Wheaton), Supplement 24 (Ministry (MHS)) and Supplement 25 (Columbia St. Mary’s) (collectively, the “WI MG Supplements”) and (ii) replace the WI MG Supplements with an EMG Services Addendum applicable to the Wisconsin EMG Market (“Wisconsin Addendum”), which EMG Services Addendum will incorporate all of the schedules that had been attached to the WI MG Supplements. |
2. Definitions.
Exhibit 1 to the MPSA is hereby supplemented (solely for purposes of this Supplement) with the definitions set forth below and as otherwise defined herein.
(a) | “Athena Platform” means a Platform licensed, or otherwise provided, by athenahealth, Inc. (or any successor in interest) (“Athena”). |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 5
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(b) | “Cerner Platform” means the “OneChart” Platform (or any successor Platform) licensed, or otherwise provided, by Cerner Corporation (or any successor in interest). |
(c) | “EMG Market” means each of the following geographical physician group markets: 1) Wisconsin, 2) Indiana, 3) Tennessee, 4) Michigan, 5) Oklahoma/ Kansas, 6) Texas, 7) Alabama/ Florida, and 8) Maryland/D.C (as set forth in the table in Section 1(f) above). Where applicable, references in this Supplement to an EMG Market shall be deemed to also be a reference to all of the Eligible Medical Groups comprising such EMG Market. |
(d) | “EMG Service Commencement Date” means, for each EMG Service and the provision of such EMG Service to certain Eligible Medical Groups, the date set forth in the applicable EMG Services Addendum designated for the commencement of such EMG Service to such Eligible Medical Groups or, if no such date is set forth in the applicable EMG Services Addendum, the effective date of such EMG Services Addendum. |
(e) | “Epic Platform” means a Platform licensed, or otherwise provided, by Epic Systems Corporation (or any successor in interest). |
(f) | “Platform” means a practice management or patient accounting system. |
3. Supplement Term.
The Supplement Term shall commence as of 12:00:01 a.m., Central Time on the Supplement Effective Date and shall continue until the date that is ten (10) years from the Supplement Effective Date; provided that if the Parties elect not to extend the MPSA in accordance with Section 3.1 of the MPSA with respect to Acute Care, then, at any time following February 16, 2024, Ascension Health may elect to terminate this Supplement for convenience upon notice to Supplier at any time, effective no earlier than February 16, 2026. For the avoidance of doubt, the Parties acknowledge that (a) the expiration date of the MPSA is unchanged by virtue of this Supplement and (b) the termination rights in Section 20 of the MPSA apply to this Supplement.
4. Services.
(a) | EMG Services. Subject to and in accordance with Section 1(g), Supplier shall provide the Services set forth in Exhibit 1 to this Supplement (the “EMG Services”) in accordance with this Section 4 and Section 4.1 of the MPSA. |
(b) | Technology Tools and Software. In connection with the provision of the EMG Services, Supplier will make available to the Eligible Medical Groups, at Supplier’s cost, the technology tools and software set forth on Schedule B, which tools and software shall constitute Supplier Owned Materials and will be licensed to Ascension Health (solely for the benefit of the Eligible Medical Groups receiving the EMG Services) pursuant to Section 14.3 of the MPSA. |
(c) | Expansion of Services. The Parties agree to have good faith discussions regarding the possible expansion of the scope of EMG Services to cover the entire revenue cycle for all Eligible Medical Groups (e.g., to add front end services to the scope of EMG Services). The Parties will agree on appropriate pricing for any such adjustment to the scope of the EMG Services in connection with any such expansion. For clarity, such expansion of scope shall not include EMG Base Employees (as defined in Exhibit 2). |
(d) | Disclaimer Regarding Athena-Provided Services. The Parties understand and acknowledge that (i) Athena is a contractor of Ascension Health, (ii) as Supplier and Athena are not in privity of contract, Supplier does not have any contractual right to control or otherwise be responsible for Athena’s acts and omissions taken or made under its contract with Ascension Health or an Ascension Health Affiliate, and (iii) Supplier’s obligation to perform the EMG Services shall not include any tasks or |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 6
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
activities that Athena may undertake with respect to Ascension Health’s revenue cycle management operations. Without limiting the foregoing and notwithstanding anything in this Supplement to the contrary, Supplier expressly disclaims all claims, liability, and responsibility, and makes no representations or warranties (express or implied), with respect to any acts or omissions taken or made by Athena relating to its obligation to provide services or otherwise perform on behalf of Ascension Health or any Ascension Health Affiliate.
5. Pricing.
(a) | EMG Base Fees. Ascension Health shall pay to Supplier, in addition to the EMG Incentive Fees, base fees for the EMG Services (“EMG Base Fees”) in accordance with Exhibit 2 to this Supplement. With respect to the EMG Services and this Supplement, all references to “Base Fee” in the MPSA are hereby deemed to refer to the EMG Base Fee. |
(b) | EMG Incentive Fees. Ascension Health shall pay to Supplier, in addition to the EMG Base Fees, incentive fees for the EMG Services (“EMG Incentive Fees”) in accordance with Exhibit 3 to this Supplement. |
(c) | Cost Board. Any disagreement between the Parties regarding compensation for the EMG Services shall be finally resolved by the Cost Board (as defined in Section 1.5 of Exhibit 2 to this Supplement). |
6. Subcontractors.
Subcontractors that relate to the NRSC/Athena Group in a certain EMG Market (with respect to the Medical Group Market Services), the NRSC/Athena Group as a whole (with respect to the Platform-Specific Services), or the Cerner Group or Epic Group (with respect to the EMG Services) shall be set forth in the applicable EMG Services Addendum.
7. Initial Transition Plan.
The initial transition plan with respect to the transition to Supplier as the provider of the EMG Services will be provided by Supplier to Ascension Health prior to the EMG Service Commencement Date for each EMG Service to be provided under each EMG Services Addendum.
8. Service Level Agreements.
(a) | Service Levels. The Service Levels described in Exhibit 4 to this Supplement will apply to the EMG Services. |
(b) | Separate Treatment from Acute Care. Service Levels for the EMG Services shall be measured independently from the Service Levels applicable to the Dependent Services with respect to Acute Care. Any Service Level Credits resulting from a Service Level Default relating to EMG Services shall apply only to portions of the EMG Base Fee, as further described in Exhibit 4 and, conversely, any Service Level Credits resulting from a Service Level Default relating to Dependent Services for Acute Care shall not apply to any portion of the EMG Base Fee. Exhibit 4 sets forth the Service Level Defaults applicable to the EMG Services, which, for purposes of Section 20.1(b) of the MPSA, will be determined separately from any Service Level Default relating to the Dependent Services for Acute Care. For the avoidance of doubt, a trigger of Section 20.1(b)(i) or Section 20.1(b)(ii) of the MPSA resulting from Service Level Defaults in respect of EMG Services will result in Ascension Health’s right to terminate the EMG Services only (and not any Dependent Services for Acute Care). |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 7
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
9. | HIPAA. |
Supplier shall execute a Business Associate Addendum substantially similar to the form attached to Annex 3 to the MPSA if Ascension Health reasonably believes that any Eligible Medical Group receiving EMG Services is not covered by the BAA currently in effect between the Parties.
10. Addendum-Specific MPSA Modifications.
In connection with entering into each EMG Services Addendum, the Parties shall discuss in good faith whether any modifications are needed to the following Sections and Exhibits of the MPSA: Section 9.10 of the MPSA (Audit Rights), or Exhibits 7 (Facilities), 8 (Ascension Health Rules and Policies), 13 (Transitioned Employee Terms), or 14 (Reports and Data Sets) to the MPSA.
11. | Transitioned Employee Terms. |
With respect to this Supplement, the term “Affected Employees” means an In-Scope Employee (as defined in Section 5.1 of Exhibit 2) who does not have a clinical certification.
12. Governance.
(a) | Supplier Executive Sponsor |
In accordance with Section 8.3 of the MPSA, the Supplier Executive Sponsor is John Sparby.
(b) | Ascension Health Relationship Manager (for all Eligible Medical Groups) |
In accordance with Section 10.1(b) of the MPSA, the Ascension Health Relationship Manager (on behalf of all Eligible Medical Groups) is Stephanie Delks.
SIGNATURE PAGE FOLLOWS
[SPACE LEFT INTENTIONALLY BLANK]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 8
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
IN WITNESS WHEREOF, the Parties have caused this Supplement 26 to be executed by their respective duly authorized representatives as of the Supplement Effective Date.
R1 RCM INC. | ASCENSION HEALTH | |||
By: | /s/ John Sparby | By: | /s/ Rhonda Anderson | |
Name: | John Sparby | Name: | Rhonda Anderson | |
Title: | EVP Customer Operations, R1 RCM | Title: | Sr VP & CFO | |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Signature Page to Supplement 26
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE A
[**]
• | [**] |
• | [**] |
• | [**] |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 10
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE B
Supplier Technology Tools and Software
• | R1Access Suite |
• | R1Link |
• | R1Decision |
• | ePars |
• | R1Contact |
• | R1Insight |
• | R1Integrity |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Page 11
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Exhibit 1
EMG Services
The EMG Services described below are being undertaken for the purposes of optimizing the revenue cycle operations process to maximize compliant collections from the amounts billable as a result of operations of the Eligible Medical Group. None of the EMG Services described below are being undertaken to manage medical decisions or business operations of any Eligible Medical Group, nor are any of the Services intended to increase the volume of operations of the Eligible Medical Group.
With respect to each function in the revenue cycle operations of the Eligible Medical Groups, Schedule A to Exhibit 1 attached hereto sets forth ownership, applicable technology, and whether Supplier is responsible for implementing related processes and performance improvement.
1. | EMG Services. In accordance with Section 4 of this Supplement and Section 4.1 of the MPSA, Supplier shall provide the following EMG Services, subject to the allocation of tasks set forth in Schedule A of this Exhibit 1. |
a. | Medical Group Market Services. “Medical Group Market Services” shall include the following functional areas: |
i. | PRE-SERVICE – Supplier will provide leadership, management oversight, staffing and technical expertise of: |
•Authorization/Referral (Verification) – Supplier will (i) perform authorization clearance services for patients to verify that an authorization is in place, and (ii) document all required authorizations.
•Insurance Eligibility Verification (Financial Clearance) – Once the payer is identified, check benefit eligibility and obtain verification from insurance (governmental or commercial) that the patient reported insurance for the applicable service is still in force and will reimburse the provider for the service.
ii. | TIME OF SERVICE - Supplier will directly provide leadership, management oversight, staffing and technical expertise of, or indirectly support through implementation of “best practices” and process standardization, the following services: |
•Self-Pay Financial Advocacy and Eligibility of Services (e.g., self-pay conversions) (Financial Counseling) – For those patients that are unaware of what insurance they have, or declare they have no insurance, work diligently and use proprietary tools to gather information to understand what might be an acceptable source of reimbursement.
• Registration – Obtaining all required patient liability (i.e., outstanding balance), clinical, demographic, and financial information from patients that was not obtained during scheduling or pre-registration when the patient is present for service regardless of status (scheduled or walk-in). Obtaining information necessary to obtain financial clearance at time of service (to include collection of co-pay, deductible, or co-insurance).
•Collection of Residuals – Support and monitor the patient education and communication process, present the opportunity for patients to pay their patient balances as both a convenience and improvement to patient flow at the point of service.
iii. | POST-SERVICE - Supplier will directly provide leadership, management oversight, staffing and technical expertise of, or indirectly (depending on the applicable patient accounting system) support through implementation of “best practices” and process standardization, the following services: |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 1 Page 12
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
• Coding Supported Accounts Receivable Management – Once a medical record coding and/or charge entry is completed and submitted for billing, identify and remedy billing deficiencies in accordance with payer requirements and compliant billing practices. When required, utilize certified coding professional to review and correct billing editor rejections and payer denials to correct and resubmit claims.
• Charge Capture/ Pre-Bill, Post-Bill (Charge Optimization) - Use automated and manual methods, including retrospectively, to correctly bill gross revenue and to capture applicable and authorized charges on the bill that is sent to the payer/ patient, while remaining in compliance with all applicable laws and guidelines. For retrospective review, analyze claims after the bill has been sent to look for incorrect or missing charges or codes, and initiate confirmation and rebill processes to ensure all applicable and authorized charges have been captured by clinical departments and re-billed to the payer/ patient.
b. | Platform-Specific Services – “Platform-Specific Services” shall include the following functional areas: |
POST-SERVICE – Supplier will directly provide leadership, management oversight, staffing and technical expertise of, or indirectly (depending on the applicable patient accounting system) support through implementation of “best practices” and process standardization, the following services:
•Billing/Claims Processing, Claims Scrubbing/Preparation/Claims Submission - Send all required information to the billing editor application or system so that a claim proceeds to the applicable payer. Though the goal is to have no bill editor rejects, Supplier shall oversee processes to resolve all discrepancies in a timely manner for resubmission of the bill to the applicable payer. Once the insurance balance is resolved, confirm that the applicable patient billing system sends a bill for the residual patient responsibility. Recommend billing edits and bridge routines to improve the number of claims sent to the payer without intervention and/or to reduce denials.
• | Credits (Refund Processing) - Research credit balances and reasons for credit balances (e.g., over-contractualization, system processing issues, actual over-payments, etc.), and prepare appropriate payment alterations where no refund is due. Supplier shall process credit balances for refund payment for Ascension Health Affiliates’ review and consent. Implement processes necessary to comply with state escheatment laws for uncashed refund payments. |
•Unpostables – Research and gather all information necessary to support posting an “Unpostable” to the correct account. “Unpostables” are unidentified remittances, whether made by check, cash payment, remit or individual account balance, which do not contain sufficient information to accurately process and post such payments to a patient account.
•Credit Card Processing – Manage and/or support processes for patient and payer credit card processing.
•Cash Posting and Processing (Lockbox and Payment Posting) – Electronically and manually post cash from both payers’ and patients’ accounts and reconcile outstanding accounts receivable in a timely and accurate manner. Reconcile daily cash at patient account level to the extent reasonably feasible (except Ascension Health will be responsible for general ledger and patient accounting reconciliation). Post payments not processed electronically (e.g., over-the-counter deposits, payroll deductions, returned lockbox items, bank credit/debit adjustments, credit card chargebacks) on the day such items are received or in a longer timeframe determined by Ascension Health to be proper. Identify and reconcile unidentified cash receipts and daily lockbox deposits to payment posting in the patient accounting system on a daily basis.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 1 Page 13
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
•Third Party Collections and Self-Pay Follow-Up (internal and external collection activities) (AR Follow-up) - Manage the collection process in accordance with Ascension Health Standards, federal, state and local hospital policies and practices. Coordinate with third party collectors for debt in default. Attempt to resolve all issues (e.g. registration, coding, billing, clinical, etc.) which have caused a partial or full denial. Perform denial and appeal service on third party claims, including review Remittance Advice and/or Explanation of Benefits and determine payment discrepancies between actual payment and expected payment. Create and send appeal letters for accounts that have been denied by the insurance payer. As necessary, resubmit all applicable bills to the payer and make improvements to attempt reduction or elimination of re-occurrence of such events. This service includes all non-zero balances.
•Denial Management (Operational and Clinical) - Attempt to resolve all issues (e.g., registration, coding, billing, clinical, etc.) which have caused a partial or full denial. Resubmit the applicable bill to the payer as necessary and make systemic improvements to reduce or eliminate re-occurrence. Implement process improvements to reduce future denials based on root cause analysis of current denials.
•Customer Service (Patient Billing/Patient Financial Services) – Provide an inbound call center capability and mail response capabilities for patient inquires, complaints, and possible payment/resolutions via a phone number and address listed on the patient bill. Customer service agent shall handle and resolve a wide range of questions or issues to include disputes. Supplier shall record all relevant customer service calls and maintain recordings for a period of a least ninety (90) days after the date of call, making such recordings available to Ascension Health upon request. Manage all correspondence received by the call center or patient correspondence sent to an Eligible Medical Group’s lockbox. This function will also include processing post-service financial assistance applications, Medicaid applications, and other patient liability functions (e.g. bankruptcy, attorney requests, etc). This call center will receive calls for both acute care and professional fee patient balances at the mutual agreement of each Eligible Medical Group.
•Patient Statement/Pre-Collect – Manage processing of patient statements and perform patient/ authorized guarantor non-defaulted receivables collection services.
•Bad Debt Management (Self-Pay Collections) - Manage patient bad debt through internal means and/or third party vendors and maintain documentation to support bad debt logging.
•Underpayment Review/Recovery – Use a contract management system and other tools or vendors to identify claims (after all efforts related to AR follow-up have been exhausted) that were not technically paid correctly (commonly due to a payer mistake or a misinterpretation of or a vague contractual term). Once such claims have been identified, appeal such claims and follow-up until either the claim is paid correctly or the contract is clarified for re-modeling or changed.
• | Patient Billing / Secondary Billing – Identified as part of the registration process (preferred) or subsequently from the patient at time of patient billing. Send a secondary payer bill for the patient responsibility portion of such bill after the primary insurance is settled to gain reimbursement from a secondary insurance payer. |
•AR Oversight Support as Appropriate to Support General Operations – Provide oversight of open accounts receivable and escalate items as appropriate to assist the Eligible Medical Group to timely resolve items and maximize collections.
c. | OTHER SERVICES – The Platform-Specific Services and the Medical Group Market Services will include the additional services listed below, which Supplier will provide across all Pre-Service, Time of Service and Post-Service functional areas: |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 1 Page 14
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
•Revenue Cycle Analytics and Reporting - Provide detailed reports and analytical support to revenue cycle functions through data mining, analysis and report creation.
•Revenue Cycle Technology and Support - Revenue cycle support services including, but not limited to, technology support, training and special projects.
•Revenue Cycle Training - Conduct training and quality assurance across all revenue cycle processes.
•Vendor Management - Contracting for and management of vendor relationships specializing in revenue cycle sub-functions including areas such as authorization management, coding and debt collection.
1. | Out of Scope Services. |
Without limiting Section 4.1 of the MPSA, the Parties agree that any services that are not described in Section 1 of this Exhibit 1 shall be considered to be out-of-scope services unless agreed to in writing by Supplier and the applicable Eligible Medical Group. Notwithstanding the foregoing, the Parties acknowledge that (i) Supplier shall be responsible for overall performance improvement across the entire revenue cycle with respect to Eligible Medical Groups and will be accountable for revenue cycle performance of the Eligible Medical Groups through the Incentive Fee Payments (as defined in Exhibit 3) and Service Levels (as defined in Exhibit 4) and (ii) in the future, certain out-of-scope services may be provided by Supplier for any Eligible Medical Group in accordance with Section 4.3(a) of the MPSA.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 1 Page 15
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Schedule A to Exhibit 1
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 1 Page 16
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Exhibit 2
EMG Base Fees
For clarity, any reference in this Exhibit 2 to a particular Section shall be deemed a reference to a Section within this Exhibit 2 unless otherwise stated. Capitalized terms used in this Exhibit 2 and not otherwise defined will have the meanings ascribed to such terms elsewhere in the Supplement or, if such terms are not defined in the Supplement, the MPSA.
1. | Base Fees. |
For Supplier’s provision of EMG Services to the Eligible Medical Groups, Ascension Health will pay to Supplier a base fee (the “EMG Base Fee”), which EMG Base Fee shall be comprised of the following four components:
1.1. | with respect to all Eligible Medical Groups in the NRSC/Athena Group (“NRSC/Athena EMGs”) receiving Platform-Specific Services, a [**] fee (to be paid in accordance with Exhibit 4-D to the MPSA) equal to the product of: |
(i) | the [**] Rolling Average Cash Collections with respect to such [**] for all such Eligible Medical Groups (in the aggregate), |
multiplied by
(ii) | the result of: |
a. | the NRSC Cost to Collect Factor (as defined in Section 2.2) |
minus
b. | [**] |
(the portion of the EMG Base Fee described in this Section 1.1, the “NRSC Base Fee”)
and
1.2. | with respect to all NRSC/Athena EMGs that have commenced receiving Medical Group Market Services from Supplier, for each EMG Market, a [**] fee (to be paid in accordance with Exhibit 4-D to the MPSA) equal to the product of: |
(i) | the [**] Rolling Average Cash Collections with respect to such [**] for all such Eligible Medical Groups in such EMG Market (in the aggregate), |
multiplied by
(ii) | the EMG Market Cost to Collect Factor (as defined in Section 2.3) applicable to the NRSC/Athena EMGs in such EMG Market, |
(the portion of the EMG Base Fee described in this Section 1.2, together with the NRSC Base Fee, the “Combined Athena Base Fee”)
and
1.3. | with respect to all Eligible Medical Groups in the Epic Group receiving EMG Services, a [**] fee (to be paid in accordance with Exhibit 4-D to the MPSA) equal to the product of: |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 17
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(i) | the [**] Rolling Average Cash Collections with respect to such [**] for all such Eligible Medical Groups (in the aggregate), |
multiplied by
(ii) | the result of: |
a. | the Epic Cost to Collect Factor (as defined in Section 2.4) |
minus
b. | [**] |
(the portion of the EMG Base Fee described in this Section 1.3, the “Epic Base Fee”)
and
1.4. | with respect to all Eligible Medical Groups in the Cerner Group receiving EMG Services, a [**] fee (to be paid in accordance with Exhibit 4-D to the MPSA) equal to the product of: |
(i) | the [**] Rolling Average Cash Collections with respect to such [**] for all such Eligible Medical Groups (in the aggregate), |
multiplied by
(i) | the result of:. |
a. | the Cerner Cost to Collect Factor (as defined in Section 2.5) |
minus
b. | [**] |
(the portion of the EMG Base Fee described in this Section 1.4, the “Cerner Base Fee”).
It is the intent of the Parties for the EMG Service Commencement Date to occur on the first day of any month; however, in the event any EMG Service does not start on the first of a month, the Parties shall account for any proration in the EMG Base Fees in accordance with Section 11.1(c) of the MPSA.
1.5. | Certain Definitions |
(i) | “Cerner Assessment” means the inspections, examinations, or assessments performed by the Parties in connection with the onboarding of the Cerner Group (i.e., the transitioning to Supplier of the provision of all of the EMG Services to the Cerner Group), which will conclude prior to the execution of the Cerner Group Addendum in accordance with the Assessment Principles listed in Section 5, which will identify and analyze various costs and expenses relating to the Revenue Cycle Operations of such Eligible Medical Groups (including the allocation of costs relating to In-Scope Employees and non-payroll vendors). |
(ii) | “Cerner Baseline Year” means the most recent and concluded Ascension Health fiscal year or calendar year (as mutually agreed by the Parties) as of the time of the effective date of the Cerner Group Addendum. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 18
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(iii) | “Cost Board” shall mean a joint governance group that shall be tasked with decisions relating to cost allocation and EMG Base Fee calculation, as such decisions may be required under this Agreement, including relating to the determination of In-Scope Employees and In-Scope Vendors that will transition to the Supplier, and the resulting calculation of EMG Base Fees. The Cost Board shall have an equal number of members from each of Ascension Health and Supplier. The default members of the Cost Board shall at all times be comprised of two Ascension Health representatives (i.e., Executive Vice President and Chief Financial Officer, Ascension, and Senior Vice President and Chief Financial Officer, Ascension Health), and two Supplier representatives (i.e., Chief Executive Officer, R1 RCM Inc., and Managing Director, TowerBrook Capital Partners, L.P.). The Cost Board will meet on a periodic basis as mutually agreed to by the Parties. Decisions of the Cost Board shall require [**] representatives. In the event the Cost Board cannot resolve any disputes or other issues submitted to it, such disputes or issues shall be subject to formal mediation proceedings. If not resolved through such mediation proceedings, any such unresolved disputes or other issues shall be subject to final and binding arbitration proceedings. In the event a third party acquires, directly or indirectly, Control of Supplier, or a third party acquires all or substantially all of Supplier’s assets, the Cost Board shall be dissolved and all responsibilities and rights of the Cost Board shall be assumed by the JRB. |
(iv) | “EMG Assessment” means any of: (a) the NRSC Assessment, (b) the Epic Assessment, (c) the Cerner Assessment and (d) each Market Assessment. |
(v) | “EMG Numerator” means any of: (a) the NRSC Cost to Collect Numerator, (b) the Epic Cost to Collect Numerator, (c) the Cerner Cost to Collect Numerator Factor and (d) each Market Cost to Collect Numerator. |
(vi) | “Epic Assessment” means the inspections, examinations, or assessments performed by the Parties in connection with the onboarding of the Epic Group (i.e., the transitioning to Supplier of the provision of all of the EMG Services to the Epic Group), which will conclude prior to the execution of the Wisconsin Addendum in accordance with the Assessment Principles listed in Section 5, which will identify and analyze various costs and expenses relating to the Revenue Cycle Operations of such Eligible Medical Groups (including the allocation of costs relating to In-Scope Employees and non-payroll vendors). |
(vii) | “Epic Baseline Year” means the period actually used for purposes of calculating the Base Fee for the physician groups associated with the Wheaton ministry as set forth in the EMG Services Addendum for Wisconsin, which Base Fee shall be subject to any MG Realized Cost Savings (as defined in MPSA Amendment No. 1) for each ministry realized through [**], with [**] percent ([**]%) of the MG Realized Cost Savings applied to the EMG Base Fee. |
(viii) | “Initial EMG Cost to Collect Factor” means any of: (a) the Initial NRSC Cost to Collect Factor, (b) the Initial Epic Cost to Collect Factor, (c) the Initial Cerner Cost to Collect Factor and (d) each Initial Market Cost to Collect Factor. |
(ix) | “Market Assessment” means the inspection, examination, or assessment performed by the Parties in connection with the onboarding of each EMG Market (i.e., the transitioning to Supplier of the provision of Medical Group Market Services to the NRSC/Athena EMGs in such EMG Market) and in accordance with the Assessment Principles listed in Section 5 that will conclude prior to the execution of the applicable Market Addendum, which will identify and analyze various costs and expenses relating to the Revenue Cycle Operations of such EMG Market (including the allocation of costs relating to In-Scope Employees and non-payroll vendors). |
(x) | “Market Baseline Cash” means the aggregate amount of Cash Collections received by the NRSC/Athena EMGs in an EMG Market during the Market Baseline Year for such EMG Market. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 19
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(xi) | “Market Baseline Year” means (a) with respect to the NRSC/Athena EMGs in the Wisconsin EMG Market only, the period actually used for purposes of calculating the Base Fee for the physician groups associated with Ministry (MHS) and Columbia St. Mary’s ministries as set forth in the EMG Services Addendum for Wisconsin, which Base Fee shall be subject to any MG Realized Cost Savings (as defined in MPSA Amendment No. 1) for each ministry realized through [**], with [**] percent ([**]%) of the MG Realized Cost Savings applied to the EMG Base Fee, and (b) with respect to the NRSC/Athena EMGs in all other EMG Markets, the most recent and concluded Ascension Health fiscal year or calendar year (as mutually agreed by the Parties) as of the time of the effective date of the applicable EMG Services Addendum for that EMG Market. |
(xii) | “NRSC Assessment” means the inspections, examinations, or assessments performed by the Parties in connection with the onboarding of the NRSC (i.e., the transitioning to Supplier of the provision of Platform-Specific Services for the NRSC/Athena Group), which began before the Supplement Effective Date and will conclude prior to the execution of the NRSC/Athena Addendum in accordance with the Assessment Principles listed in Section 5, which will identify and analyze various costs and expenses relating to the Revenue Cycle Operations of such Eligible Medical Groups (including the allocation of costs relating to In-Scope Employees and non-payroll vendors). |
(xiii) | “NRSC Baseline Year” means [**]. |
(xiv) | “[**] Rolling Average Cash Collections” means, with respect to an Eligible Medical Group, the average for [**] Cash Collections received by such Eligible Medical Group based on the Cash Collections during the [**] period that ends [**] prior to the [**] of the [**] that includes the [**] for which the applicable portion of the EMG Base Fee is payable. |
For example, to calculate an Eligible Medical Group’s portion of the EMG Base Fee for [**], the [**] Rolling Average Cash Collections would equal the [**] Cash Collections received by such Eligible Medical Group in [**].
2. | Cost to Collect Factors. Each Initial EMG Cost to Collect Factor shall be determined by the Cost Board after completion of the corresponding EMG Assessment. |
2.1. | Calculation Principles. In addition to the principles listed in Section 5 below, the Cost Board shall follow the methodology below in order to establish an applicable Initial EMG Cost to Collect Factor: |
(i) | The “Initial NRSC Cost to Collect Factor” means the fraction (expressed as a percentage) representing the NRSC Cost to Collect Factor as of the completion of the NRSC Assessment, which will be calculated as follows: (i) the numerator is equal to the aggregate annual value of all costs and expenses associated with providing the Platform-Specific Services identified as part of the NRSC Assessment to the NRSC/Athena Group, as approved by the Cost Board, and otherwise normalized to account for any extraordinary costs that do not relate to the Platform-Specific Services provided to the NRSC/Athena Group during the NRSC Baseline Year or are not reasonably be expected to continue (collectively, the “NRSC Cost to Collect Numerator”); and (ii) the denominator is equal to the aggregate amount of Cash Collections received by the NRSC/Athena EMGs during the NRSC Baseline Year. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 20
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(ii) | The “Initial Market Cost to Collect Factor” means the fraction (expressed as a percentage) representing the EMG Market Cost to Collect Factor as of the completion of the Market Assessment for the NRSC/Athena EMGs in each EMG Market, which will be calculated as follows: (i) the numerator is equal to, for the EMG Market addressed in the applicable EMG Services Addendum, the aggregate annual value of all costs and expenses associated with providing the Medical Group Market Services that are identified as part of the Market Assessment, as approved by the Cost Board, and otherwise normalized to account for any extraordinary costs that do not relate to the applicable EMG Services provided during the applicable Market Baseline Year or are not reasonably be expected to continue (collectively, the “Market Cost to Collect Numerator”); and (ii) the denominator is equal to the Market Baseline Cash for the NRSC/Athena EMGs in such EMG Market. |
(iii) | The “Initial Epic Cost to Collect Factor” means the fraction (expressed as a percentage) representing the Epic Cost to Collect Factor as of the completion of the Epic Assessment, which will be calculated as follows: (i) the numerator is equal to the aggregate annual value of all costs and expenses associated with providing the EMG Services identified as part of the Epic Assessment to the Epic Group, as approved by the Cost Board, and otherwise normalized to account for any extraordinary costs that do not relate to the EMG Services provided to the Epic Group during the Epic Baseline Year or are not reasonably be expected to continue (collectively, the “Epic Cost to Collect Numerator”); and (ii) the denominator is equal to the aggregate amount of Cash Collections received by the Eligible Medical Groups in the Epic Group during the Epic Baseline Year. |
(iv) | The “Initial Cerner Cost to Collect Factor” means the fraction (expressed as a percentage) representing the Cerner Cost to Collect Factor as of the completion of the Cerner Assessment, which will be calculated as follows: (i) the numerator is equal to the aggregate annual value of all costs and expenses associated with providing the EMG Services identified as part of the Cerner Assessment to the Cerner Group, as approved by the Cost Board, and otherwise normalized to account for any extraordinary costs that do not relate to the EMG Services provided to the Cerner Group during the Cerner Baseline Year or are not reasonably be expected to continue (collectively, the “Cerner Cost to Collect Numerator”); and (ii) the denominator is equal to the aggregate amount of Cash Collections received by the Eligible Medical Groups in the Cerner Group during the Cerner Baseline Year. |
(v) | The Parties agree that one-time system implementation-related costs (i.e., costs for both (1) implementing systems and (2) stabilizing operations as a result of such implementation) will be excluded from the calculation of the EMG Base Fees. The Parties acknowledge that the EMG Base Fees are intended to compensate Supplier for steady-state revenue cycle management services and will exclude extraordinary costs for substantial or non-recurring projects (e.g., system implementation). If either Party believes that there were any anomalies, significant events or other cost-generating developments (including the recurrence of non-recurring costs) during the NRSC Baseline Year, Market Baseline Year, Epic Baseline Year and/or Cerner Baseline Year (as applicable), the Parties agree to reasonably address such concerns in good faith, with escalation to the Cost Board if necessary. |
2.2. | “NRSC Cost to Collect Factor” means the Initial NRSC Cost to Collect Factor determined by the Parties in accordance with this Exhibit 2, as such fraction may be adjusted if agreed by the Cost Board in accordance with Sections 2.6 and/or 2.7 below. |
For the avoidance of doubt, the NRSC Cost to Collect Factor that will be used in the EMG Base Fee calculation in Section 1.1 above shall equal the sum or difference of:
(i) | the Initial NRSC Cost to Collect Factor, |
plus (if the adjustment is upward) or minus (if the adjustment is downward)
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 21
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(ii) | the aggregated value of all adjustments (as may be agreed in accordance with Sections 2.6 and/or 2.7 below) associated with the provision of Platform-Specific Services to NRSC/Athena Group EMGs. |
For the further avoidance of doubt, the Initial NRSC Cost to Collect Factor shall not be changed except in accordance with Sections 2.6 and/or 2.7 below, and any such changes will be applied prospectively to EMG Base Fee calculations.
2.3. | “EMG Market Cost to Collect Factor” means, the Initial Market Cost to Collect Factor determined by the Parties in accordance with this Exhibit 2, as such fraction may be adjusted if agreed by the Cost Board in accordance with Sections 2.6 and/or Section 2.7 below. |
For the avoidance of doubt, the EMG Market Cost to Collect Factor that will be used in the EMG Base Fee calculation in Section 1.2 shall equal the sum or difference of:
(i) | the Initial Market Cost to Collect Factor for the NRSC/Athena EMGs in the applicable EMG Market, |
plus (if the adjustment is upward) or minus (if the adjustment is downward),
(ii) | the aggregated value of all adjustments (as may be agreed in accordance with Sections 2.6 and/or Section 2.7 below) associated with the provision of Medical Group Market Services to NRSC/Athena EMGs in the applicable EMG Market. |
For the further avoidance of doubt, the Initial Market Cost to Collect Factor shall not be changed except in accordance with Sections 2.6 and/or Section 2.7, and such changes will be applied prospectively to EMG Base Fee calculations.
2.4. | “Epic Cost to Collect Factor” means the Initial Epic Cost to Collect Factor determined by the Parties in accordance with this Exhibit 2, as such fraction may be adjusted if agreed by the Cost Board in accordance with Sections 2.6 and/or 2.7 below. |
For the avoidance of doubt, the Epic Cost to Collect Factor that will be used in the EMG Base Fee calculation in Section 1.3 above shall equal the sum or difference of:
(i) | the Initial Epic Cost to Collect Factor, |
plus (if the adjustment is upward) or minus (if the adjustment is downward)
(ii) | the aggregated value of all adjustments (as may be agreed in accordance with Sections 2.6 and/or 2.7 below) for Eligible Medical Groups in the Epic Group. |
For the further avoidance of doubt, the Initial Epic Cost to Collect Factor shall not be changed except in accordance with Sections 2.6 and/or 2.7 below, and any such changes will be applied prospectively to EMG Base Fee calculations.
2.5. | “Cerner Cost to Collect Factor” means the Initial Cerner Cost to Collect Factor determined by the Parties in accordance with this Exhibit 2, as such fraction may be adjusted if agreed by the Cost Board in accordance with Sections 2.6 and/or 2.7 below. |
For the avoidance of doubt, the Cerner Cost to Collect Factor that will be used in the EMG Base Fee calculation in Section 1.4 above shall equal the sum or difference of:
(i) | the Initial Cerner Cost to Collect Factor, |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 22
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
plus (if the adjustment is upward) or minus (if the adjustment is downward)
(ii) | the aggregated value of all adjustments (as may be agreed in accordance with Sections 2.6 and/or 2.7 below) for Eligible Medical Groups in the Cerner Group. |
For the further avoidance of doubt, the Initial Cerner Cost to Collect Factor shall not be changed except in accordance with Sections 2.6 and/or 2.7 below, and any such changes will be applied prospectively to EMG Base Fee calculations.
2.6. | Post-Assessment Adjustments to Initial NRSC Cost to Collect Factor, Initial Market Cost to Collect Factor, Initial Epic Cost to Collect Factor and Initial Cerner Cost to Collect Factor |
(i) | Prior to the EMG Service Commencement Date of each of the NRSC/Athena Addendum, any Market Addendum and the Cerner Group Addendum, Ascension Health shall keep Supplier reasonably apprised of any material developments, updates, and other process and organizational changes, including with respect to cost and scope of the services applicable to Eligible Medical Groups included in each of the NRSC/Athena Group, the Epic Group and/or the Cerner Group (as applicable) and the Parties will cooperate in good faith with respect to any implications on baselining and calculating the EMG Base Fee that may result from such changes. |
(ii) | Prior to the EMG Service Commencement Date of each of the NRSC/Athena Addendum, any Market Addendum and the Cerner Group Addendum, the Parties shall identify: (A) any areas of material change with respect to Eligible Medical Groups included in the NRSC/Athena Group, Epic Group or the Cerner Group (as applicable) that occurred between the Supplement Effective Date and the contemplated date of onboarding of such Eligible Medical Groups; (B) any areas that may result in material changes to the manner in which the EMG Services are provided to such Eligible Medical Groups (e.g., onboarding of material revenue amounts, materially substandard performance); and (C) any factors or conditions that may otherwise require investments in technology, employees and other infrastructure that may improve the operational performance of the EMG Services with respect to such Eligible Medical Groups. If any such changes, factors or conditions are identified, the Parties will, in good faith, make adjustments to the applicable Initial EMG Cost to Collect Factor to equitably reflect such changes, factors or conditions. |
(iii) | [**] |
2.7. | Other Post-EMG Assessment Adjustments to EMG Cost to Collect Factors |
If, after an EMG Assessment: (i) an Eligible Medical Group requests that Supplier provide an EMG Service that was not received by such Eligible Medical Group at the time of such EMG Assessment (such EMG Service, an “Unfurnished Service”); or (ii) the costs or expenses associated with such Unfurnished Service are not accounted for in the determination of the NRSC Cost to Collect Factor, the Epic Cost to Collect Factor, the Cerner Cost to Collect Factor or any EMG Market Cost to Collect Factor, as applicable, as of the date such Unfurnished Service would commence, then, subject to Cost Board approval, the NRSC Cost to Collect Factor, the Epic Cost to Collect Factor, the Cerner Cost to Collect Factor and/or the applicable EMG Market Cost to Collect Factor, as applicable, will be equitably increased by an amount to be determined by the Cost Board, and such adjustments shall be effective as of the date Supplier begins performing such Unfurnished Service. For the avoidance of doubt, the mere reconfiguration or natural evolution of an EMG Service (or multiple EMG Services) that had been provided by Supplier under this Supplement will not, by itself, trigger any Cost Board determination under this Section 2.7, and such reconfigured or naturally evolved EMG Service shall not constitute an Unfurnished Service.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 23
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
[**]
If, after an EMG Assessment, Ascension Health enters into an agreement (or a series of related agreements) to add (whether via acquisition, employment or PSAs) additional physician groups that will automatically receive EMG Services under an EMG Services Addendum pursuant to Section 1(c) of the main body of the Supplement, and either Party reasonably believes that such addition may result in an increase of [**]% or more of Net Patient Service Revenue (as measured over the then-current Ascension Health fiscal year to the subsequent Ascension Health fiscal year) across all of the Eligible Medical Groups in the aggregate, then such Party shall provide notice to the other Party of the same and the Parties will promptly perform and complete an assessment of such additional physician groups that is consistent with the assessments described in this Exhibit 2 and follows the principles set forth in Section 5 for purposes of determining whether an adjustment to the NRSC Cost to Collect Factor, the Epic Cost to Collect Factor, the Cerner Cost to Collect Factor or any EMG Market Cost to Collect Factor, as applicable, should be adjusted to account for such additional physician groups. Suppler acknowledges and agrees that the addition of such physician groups may cause the NRSC Cost to Collect Factor, the Epic Cost to Collect Factor, the Cerner Cost to Collect Factor and/or any EMG Market Cost to Collect Factor to decrease and the Parties agree that the results of any such assessment shall be submitted to the Cost Board and the Cost Board will determine the proper increase or decrease to the NRSC Cost to Collect Factor, the Epic Cost to Collect Factor, the Cerner Cost to Collect Factor and/or any EMG Market Cost to Collect Factor, as applicable, in accordance with the guidelines and principles of this Exhibit 2.
2.8. | New Services |
If any Eligible Medical Group requests that Supplier provide any services other than EMG Services, all such requested services shall be New Services under Section 4.3(a) of the MPSA.
3. | [**]. [**]. |
4. | Benefits Uplift. Ascension Health will have the option, in its sole discretion, to direct Supplier to provide a Benefits Uplift as described in and in accordance with Exhibit 13, Section 2.5(b) of the MPSA. |
5. | Guiding Principles for the EMG Assessments. The Parties agree that, in connection with each EMG Assessment undertaken by the Parties, the calculation of the corresponding EMG Numerator will be based on the following guidelines. |
5.1. | Payroll Expenses for Eligible Medical Groups: All payroll costs and expenses at each Eligible Medical Group for In-Scope Employees (defined below) that are [**] shall be [**]. |
“In-Scope Employees” means those employees which are responsible for performing functions that relate to “Job Titles,” which at the applicable physician group and at the applicable “Cost Center” (collectively, an “Area”) for EMG Services which are designated by the Parties, pursuant to the applicable EMG Assessment, as having an In-Scope Percentage (as defined below) that is: (A) greater than or equal to [**] percent ([**]%); and (B) higher than [**] percent ([**]%) but lower than [**] percent ([**]%), in each case of (A) and (B), subject to the right of the Cost Board to remove any such “Job Title”, job code, or some other categorical identifier, from the “In-Scope Employees.” Notwithstanding the foregoing, “In-Scope Employees” exclude (A) those employees working in departments which perform both EMG Services and services not qualifying as EMG Services, (B) all National Employees, and (C) all EMG Base Employees.
“In-Scope Percentage” shall mean, for any Area, the proportion of “In Scope FTEs” cost for such Area divided by the “Total FTEs” cost for such Area, in each case, as determined by the Parties in the applicable EMG Assessment.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 24
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
“EMG Base Employee” means those employees who are responsible for performing functions for EMG Services and such functions by their nature are performed at a physician’s office or clinic location.
“National Employee” shall mean any employee of Ascension Health engaged in Revenue Cycle Operations but without any operational responsibility for any Eligible Medical Group.
5.2. | IT Support Expenses for Eligible Medical Groups: The Parties will identify costs and expenses related to information technology support and real estate for Revenue Cycle Operations and agree on the proper allocation of such costs and expenses for inclusion in the applicable EMG Numerator. |
5.3. | Non-Payroll Expenses for Third-Party Vendors: Each EMG Numerator will include all costs and expenses related to In-Scope Vendors (defined below), all of which shall be [**], excluding any portion of the costs and expenses for Partially Related Vendors that are not related to the EMG Services. |
“In-Scope Vendors” means third party vendors that perform functions as part of or related to the EMG Services, including: (A) any vendor that, pursuant to the applicable EMG Assessment (as applicable), provides a product, solution or service (a “Vendor Service”) that is [**] percent ([**]%) related to the EMG Services; and (B) any vendor that is, pursuant to the applicable EMG Assessment, providing or offering a Vendor Service [**] related to the Services ([**]).
In-Scope Vendors shall not include: (i) the vendors of the Athena Platform, Cerner Platform or Epic Platform; and (ii) any vendor with respect to a Vendor Service that, pursuant to the applicable EMG Assessment, is not related to the EMG Services in any manner.
5.4. | [**]: For any [**], the portion of the cost of the [**] that relates to the EMG Services will be [**]. The Cost Board may review the list of vendors from time to time and, when appropriate, determine whether any such vendor is not an In-Scope Vendor (subject to Section 5.5). If a vendor is deemed not to be an In-Scope Vendor, an adjustment to the NRSC Cost to Collect Factor, the Epic Cost to Collect Factor, the Cerner Cost to Collect Factor or any EMG Market Cost to Collect Factor (as applicable) shall be made [**], and Supplier [**]. |
5.5. | Additional Considerations: |
(i) | If a termination fee or other termination-related costs or expenses must be paid to allow for the termination or any splitting of an existing In-Scope Vendor contract, such fee will be [**]. |
(ii) | The allocation of one-time, lump-sum implementation and/or license fees for a particular In-Scope Vendor which are greater than or equal to [**] dollars ($[**]) will be dependent on whether or not such fees will be determined to be in or out of the applicable EMG Numerator by the Cost Board. If the Cost Board does not make such a determination, allocation of such fee shall be submitted for resolution in accordance with the governance mechanism set forth in Exhibit 6 to the MPSA. Notwithstanding the foregoing, one-time, lump-sum implementation fees less than [**] dollars ($[**]) are included in each EMG Numerator and shall be [**]. |
(iii) | Supplier and Ascension Health shall each be responsible for its own incurred costs associated with information technology, such as interface development, file transfers, and custom programming related to the Supplier technology solutions and other third party vendors. |
(iv) | The allocation between the Parties of one-time costs related to information technology system conversion services, including consulting services, staff augmentation and training, shall be determined by mutual agreement of the Parties with any adjustment of the applicable EMG Numerator to be agreed by the Cost Board. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 25
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(v) | Recurring maintenance, support, service, license, or contingency fees for all In-Scope Vendor products, solutions, and services, shall be included in the applicable EMG Numerator and [**]. |
(vi) | Ascension Health reserves the right to separately contract with and utilize vendors for services not provided by Supplier, subject to such vendors being reviewed by the Cost Board to confirm that Supplier does not provide such service to any Eligible Medical Group. If the use of any such vendor results in additional [**] for Ascension Health, Supplier may: (A) [**] Ascension Health for the actual vendor cost; or (B) have such additional [**] solely purposes of calculating the EMG Base Fee (to the extent such additional [**]). |
6. | EMG Base Fee for New Eligible Medical Groups. With respect to any EMG Services that will be provided to New Eligible Medical Groups: (i) the Parties shall conduct an assessment of such New Eligible Medical Groups that is consistent in scope with the EMG Assessments; (ii) such assessment will identify any areas that may require investments in technology, employees, and other infrastructure that may improve the operational performance of the EMG Services with respect to such New Eligible Medical Groups; (iii) the results of any such assessment shall be submitted to the Cost Board; and (iv) the Parties will work together in good faith to determine the methodology for calculating the EMG Base Fee for such New Eligible Medical Group in accordance with guidelines and principles that are consistent with those set forth in this Exhibit 2. |
7. | Binghamton and Bridgeport Ministries. For Supplier’s provision of Platform-Specific Services to the physician groups associated with Binghamton and Bridgeport, Ascension Health will pay to Supplier the monthly NRSC Base Fee calculated in accordance with Section 1.1 of this Exhibit 2. The Parties acknowledge and agree that there shall be [**] with respect to the sale of either Binghamton or Bridgeport. |
8. | Windfall Situations and Changes in the Environment. |
8.1. | In the event that there is a Force Majeure Event, a material change in the environment in which the Eligible Medical Groups are operating their revenue cycles, or a material change in the laws and regulations that apply to Ascension Health, Supplier, or an individual Eligible Medical Group which significantly affects the economics of one or more of the Parties or frustrates the ability of a party to perform its obligations hereunder, through no fault of its own, the applicable Party shall have the right to request that the other Party or Parties consider a fair and appropriate adjustment to portions of the EMG Base Fee. Upon such request, the Parties will, in good faith, discuss the costs associated with the change in circumstance, with the outcome to equitably reflect the incremental change in costs to deliver EMG Services. |
8.2. | Examples of matters that could trigger a request to adjust the EMG Base Fee include the following: |
(i) | Material changes in the form of reimbursement by commercial or government payors, including changes to a payment model such as an at-risk or partial or fully capitated system; |
(ii) | Changes in the Laws governing portions of provider processes in the revenue cycle such as the way medical treatments are reported (an example would be mandated changes to the medical coding that will result due to CMS’s requirement to implement ICD 11 or any subsequent material changes to the ICD nomenclature); |
(iii) | Changes in payer or state regulation that may affect the performance of any functions comprising or included in the EMG Services (e.g., financial clearance, transcription, coding, billing, and payer follow-up); |
(iv) | An Eligible Medical Group’s investment in or adoption of new technologies that affect the level of, or type of, work conducted in the revenue cycle (e.g., advances in EMR or CPOE technology that reduce the need for transcription services); and |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 26
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(v) | Any large-scale system, which shall include any patient accounting system (e.g., EPIC, Cerner/Siemens, Meditech, McKesson), is replaced or undergoes a vendor change or other fundamental or significant conversion or modification. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 2 Page 27
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Exhibit 3
EMG Incentive Fees
1. | Incentive Payments |
1.1. | General. Supplier will deliver a set of core strategies and management services designed to improve and optimize the revenue cycle operations for Eligible Medical Groups receiving EMG Services. Ascension Health shall pay to Supplier EMG Incentive Fees in the form of Incentive Fee Payments subject to, and in accordance with, the terms of this Exhibit 3. Whether Supplier qualifies for an Incentive Fee Payment will be determined separately with respect to each Applicable Phase by measuring Supplier’s Actual Performance against a pre-determined and mutually agreed set of Operating Metrics for all of the Eligible Medical Groups receiving the EMG Services in such Applicable Phase. The EMG Incentive Fees will be determined separately for each Applicable Phase for each Measurement Period; provided, however, that after the completion of the fourth (4th) Contract Year with respect to the Kansas EMG Market, the Parties shall meet to discuss combining the calculation of the EMG Incentive Fees for the Kansas EMG Market together with the calculation for the Phase 1 Group. |
The Incentive Fee Payments will relate to Supplier’s ability to deliver the EMG Services efficiently and in compliance with all applicable rules and regulations.
For the avoidance of doubt, Exhibit 4-B of the MPSA shall not apply to EMG Incentive Fees.
1.2. | Definitions. |
For purposes of this Exhibit 3, the following terms will have the meanings set forth below:
a) | “Actual Performance” means the actual result achieved for an Operating Metric with respect to an Applicable Phase during the Measurement Period. |
b) | “Applicable Phase” means, as applicable, (i) the Phase 1 Group or (ii) the Kansas EMG Market. |
c) | “Applicable Platform” means (i) with respect to the Eligible Medical Groups in the NRSC/Athena Group, the Athena Platform, (ii) with respect to the Eligible Medical Groups in the Cerner Group, the Cerner Platform, and (iii) with respect to the Eligible Medical Groups in the Epic Group, the Epic Platform. |
d) | “Contract Year” means, for each Applicable Phase, a period commencing on the Commencement Date for EMG Services (and, for each subsequent Contract Year, each anniversary thereof) for such Applicable Phase and ending twelve (12) months thereafter. For the avoidance of doubt, the Phase 1 Group will be in a different Contract Year than the Kansas EMG Market at any given time during the Term. For the Phase 1 Group, the Commencement Date will be deemed to be [**]. |
e) | “Fiscal Year” means Ascension Health’s fiscal year, which shall begin on July 1 (or, in the initial Contract Year for any Applicable Phase, its Commencement Date for EMG Services) and end on June 30. |
f) | “Lower Bound Score” means with respect to an Applicable Phase: (i) for any Measurement Period in which the YTD Lift Percentage for such Applicable Phase is less than [**] percent ([**]%), [**] percent ([**]%); and (ii) for any Measurement Period in which the YTD Lift Percentage for such Applicable Phase is greater than or equal to [**] percent ([**]%), [**] percent ([**]%). |
g) | “Measurement Period” means any Ascension Health fiscal quarter. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 28
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
h) | “Metric Lift” means, with respect to an Applicable Phase for any Measurement Period, the dollar value assigned to the Operating Metric representing increased Cash Collections for the Applicable Phase during such Measurement Period for such Operating Metric as compared to the Performance Baseline value for such Operating Metric. |
i) | “Performance Baseline” means, with respect to any Operating Metric, the Actual Performance for such Operating Metric with respect to the Applicable Phase during the applicable baseline period described in Section 3 below. |
j) | [**] |
k) | “Performance Score” means with respect to an Applicable Phase: |
(i) | if for any Measurement Period the YTD Lift Percentage for such Applicable Phase is greater than or equal to [**] percent ([**]%), then the result of the following (expressed as a percentage): the sum of (A) the result of (x) the difference of the YTD Lift Percentage and the Lower Bound, divided by (y) the difference of the applicable Upper Bound Score and the applicable Lower Bound Score, multiplied by (z) [**], and (B) [**]. An illustrated example of this [**] Performance Score is set forth in Appendix D. |
[**] = Performance Score
For example, a YTD Lift Percentage of [**]% would result in a Performance Score of [**]% since
[**]
or
ii) | if for any Measurement Period the YTD Lift Percentage for such Applicable Phase is less than [**] percent ([**]%), then the result of the following (expressed as a percentage): (A) the difference of the YTD Lift Percentage and the applicable Lower Bound, divided by (B) the difference of the applicable Upper Bound Score and the applicable Lower Bound Score, multiplied by (C) [**]. An illustrated example of this [**] Performance Score is set forth in Appendix E. |
[**] = Performance Score
For example, a YTD Lift Percentage of [**]% would result in a Performance Score of [**]% since
[**]
Notwithstanding the foregoing, in each case, the maximum Performance Score is [**] percent ([**]%) and the minimum Performance Score is [**] percent ([**]%).
l) | “Phase 1 Group” means all of the EMG Markets other than the Kansas EMG Market. |
m) | “Quarterly Aggregate Lift” means, with respect to an Applicable Phase for any Measurement Period, the sum of the Metric Lifts for each Operating Metric for such Applicable Phase during such Measurement Period. |
n) | “Upper Bound Score” means with respect to an Applicable Phase: (i) for any Measurement Period in which the YTD Lift Percentage for such Applicable Phase is less than [**] percent ([**]%), [**] |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 29
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
percent ([**]%); and (ii) for any Measurement Period in which the YTD Lift Percentage for such Applicable Phase is greater than or equal to [**] percent ([**]%), [**] percent ([**]%).
o) | “YTD Aggregate Lift” means, with respect to an Applicable Phase, the sum of the Quarterly Aggregate Lifts for each Measurement Period to date in the applicable Fiscal Year. For example, when calculated at the end of the third fiscal quarter in a Fiscal Year, the YTD Aggregate Lift equals the sum of the applicable Quarterly Aggregate Lifts in each of the first, second, and third fiscal quarters in such Fiscal Year. |
p) | “YTD Cash” means, with respect to an Applicable Phase, the aggregate Cash Collections to date of such Applicable Phase for the applicable Fiscal Year. |
q) | “YTD Lift Percentage” means, with respect to an Applicable Phase, the YTD Aggregate Lift divided by the YTD Cash. |
2. | Operating Metrics Scorecard |
2.1. | General. Separate Operating Metrics Scorecards will be utilized for each Applicable Phase to determine the Performance Score for the Applicable Phase for each Measurement Period in order to determine the amount of any Incentive Fee Payment earned by Supplier for such Measurement Period. For Metric 1, Metric 2 and Metric 3, the Operating Metrics Scorecards will be populated with the requisite financial performance data from (i) the Applicable Platforms used by the Applicable Phase for each Measurement Period until the Parties mutually agree that the Crowe RCA System is ready for use in connection with such Metrics, and (ii) thereafter, the Crowe RCA System. For Metric 4, and Metric 5, the Operating Metrics Scorecards will be populated with the requisite financial performance data from Supplier’s system of record; provided that Ascension Health will have the right to approve and audit Supplier’s calculations. The Applicable Platform for each Eligible Medical Group will be the sole source of data for the applicable Operating Metrics Scorecard. Each Operating Metrics Scorecard will also include the supporting information that is used to determine the Actual Performance for each Operating Metric and the overall Performance Scores. |
2.2. | Metrics. For purposes of this Supplement 26, the “Operating Metrics” are comprised of the following five (5) revenue cycle operating metrics, as each is further described and defined in Appendix A to this Exhibit 3. The Operating Metrics will be calculated separately for each Applicable Phase: |
a. | Metric 1: [**] |
b. | Metric 2: [**] |
c. | Metric 3: [**] |
d. | Metric 4: [**] |
e. | Metric 5: [**] |
3. | Operating Metric Performance Baselines |
Ascension Health and Supplier will calculate the Performance Baselines in accordance with this Section 3 for each Operating Metric in the Operating Metrics Scorecard. The Performance Baseline for each Operating Metric for: (i) the Phase 1 Group will be calculated using the twelve (12) month period beginning [**]; and (ii) the Kansas EMG Market using the most recent completed Ascension Health fiscal year or calendar year (as mutually agreed by the Parties) prior to the Commencement Date for the Kansas EMG Market.
4. | Operating Metric Scorecard Performance |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 30
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
An Operating Metric report card (the “Operating Metric Scorecard”) will be generated at the end of each Measurement Period for each Applicable Phase summarizing Supplier’s overall Operating Metrics Scorecard performance for the Measurement Period, including the Performance Score, Quarterly Aggregate Lift, YTD Aggregate Lift, YTD Lift Percentage, and YTD Cash. For clarity, no Operating Metric Scorecard will be generated for the Kansas EMG Market until the first Measurement Period following the Commencement Date for the Kansas EMG Market.
5. | Timing of Calculation |
The Operating Metrics Scorecard for each Applicable Phase will be calculated at the end of each Measurement Period. The calculation will be based on the [**] of the applicable Measurement Period for each Applicable Phase, and will [**] on the first day of each subsequent Fiscal Year [**]. The Operating Metrics will be measured quarterly, on a cumulative basis within any single Fiscal Year.
6. | Calculation of Incentive Fee Payments |
Supplier shall be eligible for Incentive Fee Payments as calculated pursuant to this Section 6, in accordance with the Operating Metric Scorecard performance, and subject to the Performance Caps.
“Incentive Fee Earned Year-to-Date” means, with respect to an Applicable Phase for any Measurement Period, an amount equal to the product of:
(i) | YTD Cash for such Applicable Phase, |
multiplied by
(ii) | [**], |
multiplied by
(iii) the applicable Performance Score for such Applicable Phase in such Measurement Period.
“Incentive Fee Earned In Period” means, with respect to an Applicable Phase for any Measurement Period, an amount equal to the result of:
(i) | The Incentive Fee Earned Year-to-Date for such Applicable Phase, |
less
(ii) | The Incentive Fee Earned Year-to-Date for such Applicable Phase as of the end of the prior Measurement Period within the same Fiscal Year. |
“Incentive Fee Payment” means, with respect to an Applicable Phase for any Measurement Period, an amount equal to the result of:
(i) | The lesser of: |
(a) | The sum of all Incentive Fees Earned In Period for the applicable Measurement Period for such Applicable Phase and all previous Measurement Periods within the applicable Fiscal Year |
and
(b) | [**] for such Applicable Phase for such Measurement Period |
less
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 31
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
(ii) | The sum of all Incentive Fee Payments for such Applicable Phase for all previous Measurement Periods within the applicable Fiscal Year. |
For the avoidance of doubt a schedule detailing a sample of this calculation has been included in Appendix C and a range of scenarios for the calculation of Performance Scores has been included in Appendix F.
7. | Review and Invoicing Process |
Step 1: | Operating Metric Scorecards will be provided and distributed by Supplier to Ascension Health for each Applicable Phase in accordance with Section 2.1 above by the [**] day of the month following the end of each Measurement Period. |
Step 2: | Ascension Health and Supplier will have [**] days from the delivery of the Operating Metric Scorecards to review such Operating Metric Scorecards for the Applicable Phases, perform audits of Applicable Platform data as appropriate, and work to reach agreement on the Operating Metrics Scorecards for the Measurement Period. In the event that a potential error is identified in an Operating Metrics Scorecard which error may, as determined by either Party, have a material impact on the measurement of the Operating Metrics Scorecard performance for the Measurement Period, the Parties will work to identify the range of impact of the potential error and shall establish a mutually agreed upon plan to review and resolve such potential error, which error will be resolved effective retroactively as the date that the error impacted the applicable measurement. Absent exceptional circumstances, the Parties will work to resolve all such issues within [**] days of discovery of such issue. |
Step 3: | Supplier will invoice Ascension Health for each Incentive Fee Payment for each Applicable Phase no later than [**] days following the end of the Measurement Period for which the EMG Incentive Fees accrued. The invoice shall not include amounts associated with unresolved potential errors identified in Step 2 above. If any Incentive Fee Payment amount is negative for any particular Measurement Period, then such amount shall be held as a credit against EMG Incentive Fees owed in future Measurement Periods. |
Step 4: | Incentive Fee Payments shall be jointly reviewed quarterly by Ascension Health and Supplier promptly following the delivery of Operating Metric Scorecard results by Supplier to Ascension Health. To the extent that neither Party delivers written notice of objection to such results within [**] days following such delivery to Ascension Health, the performance results and the resulting Incentive Fee Payments shall be final and binding on the Parties. |
8. | Adjustments to Measurement Metrics |
When appropriate, Ascension Health and Supplier can mutually agree to adjust the calculation of one or more metrics (the “Prospective Adjustment”) when market events or actions outside of either Party’s control compromise the ability to accurately compare Actual Performance to Performance Baselines. Any such adjustments shall only take effect on a prospective basis from and after the Measurement Period during which the Parties agree to such adjustments. The Parties agree that a Prospective Adjustments may take into account any prior Measurement Periods affected by such Prospective Adjustment beginning as of the date either Party provides a formal written request for adjustment to the other Party (the “Adjustment Request”) and any Measurement Periods thereafter. For the avoidance of doubt, a Prospective Adjustment may affect any Measurement Period during and after the Adjustment Request is made but not any Measurement Periods prior to the Adjustment Request.
9. | Governance Principles |
9.1. | Code Mapping. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 32
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
a. | Ascension Health will be responsible for mapping the transaction codes and planning codes within the Applicable Platforms to the applicable figures in the Operating Metrics, and shall provide Supplier with sufficient time to review, discuss and concur with such mapping of transaction codes and planning codes before they are implemented. |
b. | If Supplier does not agree to any mapping of any transaction code or planning code proposed by Ascension Health, then the Parties shall seek to resolve the dispute in good faith. However, if the Parties are unable to resolve the dispute, then the issue will be escalated to the Cost Board for resolution. |
9.2. | Notification. Supplier agrees to promptly notify Ascension Health of any proposed changes in the processes or technology under their management that are reasonably likely to impact any of the revenue cycle operating metrics including but not limited to the use of transaction codes or management of accounts receivables. Ascension Health will have sufficient time to review and discuss the proposed changes before they are implemented and, if requested by Ascension Health, Supplier will provide an account sampling to ensure that any such proposed changes will be accurate. |
9.3. | Records. Supplier and Ascension Health will maintain a reconciled record of the key assumptions used to derive targets and/or make decisions to support development and management of the Operating Metrics Scorecard. |
9.4. | Supplier Access. Ascension Health shall provide to Supplier access to the Applicable Platform databases to review, reconcile and validate the data used to populate the Operating Metrics Scorecard. Supplier will have the right to audit the Applicable Platform database. In the event the Supplier’s auditor requires information regarding or from the database or access to the database in connection with its audit related to Supplier’s financial or operating controls, Ascension Health shall reasonably cooperate with Supplier to secure that information for Supplier’s auditors. Any data or database deficiencies will be addressed by Ascension Health (on behalf of the applicable Eligible Medical Group) in a timely manner. |
9.5. | Windfall Situations and Changes in the Environment. In the event that there is a Force Majeure Event, a material change in the environment in which the Eligible Medical Groups are operating their revenue cycles, or a material change in the laws and regulations that apply to Ascension Health, Supplier, or an individual Eligible Medical Group which significantly impacts the economics of one or more of the Parties or frustrates the ability of a Party to perform its obligations hereunder, through no fault of its own, the applicable Party shall have the right to request that the other Party consider a fair and appropriate adjustment to the Operating Metrics Scorecard. Upon such request, Supplier and Ascension Health will discuss the impact associated with the change in circumstance, with the outcome to equitably reflect the impact on the Operating Metrics Scorecard. Examples of material matters that could affect one or more metrics on the Operating Metrics Scorecard performance include, but are not limited to, the following: |
• | Payor bankruptcies. |
• | A pattern of services to patients for whom an Eligible Medical Group is not certified by a payor to bill for such services and thus not entitled to reimbursement. |
• | Changes in Self-Pay Discounts and/or changes in Charity Policy. |
• | Material growth or decline in self pay population or patient residual balance after insurance. |
• | Changes in accounts receivable write-off policies or Medicaid Pending aging policies |
• | Implementation of new systems outside the control of Supplier (e.g., new patient accounting system). |
• | Regulatory changes, including changes to the ICD nomenclature (e.g., ICD-11) or changes to the status of Medicaid Expansion in a given state. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 33
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
APPENDIX A – Operating Metrics Calculation Methods
Set forth below are the details of each of the Operating Metrics.
1. | Metric: [**] |
Calculation:
[**]
Metric Lift = [**]
Measurement Period: | Measured Fiscal Year to Date on a quarterly basis |
Performance Baseline: [**] calculated during the baseline period
Applicable Definitions/Other Notes:
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
2. | Metric: [**] |
Calculation:
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 34
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
[**]
Metric Lift = [**]
Measurement Period: | Measured Fiscal Year to Date on a quarterly basis |
Performance Baseline: [**] calculated during the baseline period
Applicable Definitions/Other Notes:
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 35
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
3. | Metric: [**] |
Calculation:
[**]
Metric Lift = [**]
Measurement Period: | Measured Fiscal Year to Date on a quarterly basis |
Performance Baseline: [**] calculated during the baseline period
Applicable Definitions/Other Notes: | For the Performance Baseline, the component (b) [**] will be the defined term [**]; while during the Measurement Periods it will be the defined term [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**] |
• | [**]. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 36
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
4. | Metric: [**] |
Calculation:
Metric Lift = [**]
Measurement Period: | Measured quarterly |
Performance Baseline: Baseline value = $0
Applicable Definitions/Other Notes:
• | [**] |
• | [**] |
• | [**] |
5. | Metric: [**] |
Calculation:
Metric Lift = [**]
Measurement Period: | Measured quarterly. |
Performance Baseline: Baseline value = $0
Applicable Definitions/Other Notes:
• | [**] |
• | [**] |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 37
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
APPENDIX B – [**]
Phase 1 Group
Measurement Period End Date | Applicable Measurement Period (Fiscal Quarter) | Contract Year Quarter | [**] | [**] |
9/30/2018 | FY19-Q1 | N/A | [**] | [**] |
12/31/2018 | FY19-Q2 | CY1-Q1 | [**] | [**] |
3/31/2019 | FY19-Q3 | CY1-Q2 | [**] | [**] |
6/30/2019 | FY19-Q4 | CY1-Q3 | [**] | [**] |
[**] | [**] | |||
9/30/2019 | FY20-Q1 | CY1-Q4 | [**] | [**] |
12/31/2019 | FY20-Q2 | CY2-Q1 | [**] | [**] |
3/31/2020 | FY20-Q3 | CY2-Q2 | [**] | [**] |
6/30/2020 | FY20-Q4 | CY2-Q3 | [**] | [**] |
[**] | [**] | |||
9/30/2020 | FY21-Q1 | CY2-Q4 | [**] | [**] |
12/31/2020 | FY21-Q2 | CY3-Q1 | [**] | [**] |
3/31/2021 | FY21-Q3 | CY3-Q2 | [**] | [**] |
6/30/2021 | FY21-Q4 | CY3-Q3 | [**] | [**] |
[**] | [**] | |||
9/30/2021 | FY22-Q1 | CY3-Q4 | [**] | [**] |
12/31/2021 | FY22-Q2 | CY4-Q1 | [**] | [**] |
3/31/2022 | FY22-Q3 | CY4-Q2 | [**] | [**] |
6/30/2022 | FY22-Q4 | CY4-Q3 | [**] | [**] |
[**] | [**] | |||
9/30/2022 | FY23-Q1 | CY4-Q4 | [**] | [**] |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 38
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Kansas EMG Market
Measurement Period End Date | Applicable Measurement Period (Fiscal Quarter) | Contract Year Quarter | [**] | [**] |
9/30/2019 | FY19-Q1 | N/A | [**] | [**] |
12/31/2019 | FY19-Q2 | CY1-Q1 | [**] | [**] |
3/31/2020 | FY19-Q3 | CY1-Q2 | [**] | [**] |
6/30/2020 | FY19-Q4 | CY1-Q3 | [**] | [**] |
[**] | [**] | |||
9/30/2020 | FY20-Q1 | CY1-Q4 | [**] | [**] |
12/31/2020 | FY20-Q2 | CY2-Q1 | [**] | [**] |
3/31/2021 | FY20-Q3 | CY2-Q2 | [**] | [**] |
6/30/2021 | FY20-Q4 | CY2-Q3 | [**] | [**] |
[**] | [**] | |||
9/30/2021 | FY21-Q1 | CY2-Q4 | [**] | [**] |
12/31/2021 | FY21-Q2 | CY3-Q1 | [**] | [**] |
3/31/2022 | FY21-Q3 | CY3-Q2 | [**] | [**] |
6/30/2022 | FY21-Q4 | CY3-Q3 | [**] | [**] |
[**] | [**] | |||
9/30/2022 | FY22-Q1 | CY3-Q4 | [**] | [**] |
12/31/2022 | FY22-Q2 | CY4-Q1 | [**] | [**] |
3/31/2023 | FY22-Q3 | CY4-Q2 | [**] | [**] |
6/30/2023 | FY22-Q4 | CY4-Q3 | [**] | [**] |
[**] | [**] | |||
9/30/2023 | FY23-Q1 | CY4-Q4 | [**] | [**] |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 39
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
APPENDIX C – Quarterly Invoice Sample
[**]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 40
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
APPENDIX D – [**] Performance Score Example
[**]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 41
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
APPENDIX E – [**] Performance Score Example
[**]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 42
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
APPENDIX F –Performance Score Scenarios
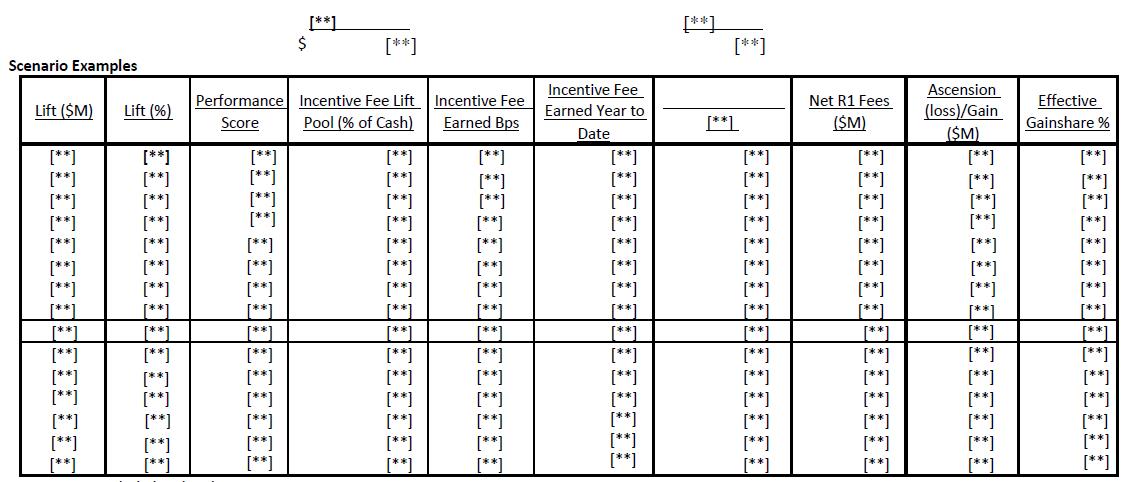
Assumptions included in the above:
1) [**]
2) This example is shown for the NRSC cash only but would hold methodically for other Applicable Phases
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 3 Page 43
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Exhibit 4
Service Level Targets and Metrics
For clarity, any reference in this Exhibit 4 to a particular Section shall be deemed a reference to a Section within this Exhibit 4 unless otherwise stated. Capitalized terms used in this Exhibit 4 and not otherwise defined will have the meanings ascribed to such terms elsewhere in the Supplement or, if such terms are not defined in the Supplement, the MPSA.
1. | Definitions. |
• | “AMG-Wide Service Levels” means each of Service Level 1, Service Level, 3, Service Level 4, Service Level 5, and Service Level 11. |
• | “Current Service Levels” means the AMG-Wide Service Levels and the Group-Specific Service Levels listed in this Exhibit 4 as of the Supplement Effective Date. |
• | “Future Service Levels” means Service Level 2 and any additional Service Levels agreed by the Parties after the date hereof. |
• | “Group-Specific Service Levels” means Service Level 6 and Service Level 8. |
• | “Measurement Window” means the time during, or frequency by, which a Service Level shall be measured. The Measurement Window shall be quarterly, unless otherwise specified. |
• | “Root Cause Analysis” is the formal process, specified in the Policy and Procedures Manual, to be used by Supplier to diagnose problems at the lowest reasonable level so that corrective action can be taken that will eliminate, to the extent reasonably possible, repeat failures. |
• | “Service Level” means, with respect to this Supplement, any service level described in one of the following Sections (and any additional service levels agreed to by the Parties): Section 3.1 (“Service Level 1”), Section 3.2 (“Service Level 2”), Section 3.3 (“Service Level 3”), Section 3.4 (“Service Level 4”), Section 3.5 (“Service Level 5”), Section 3.6 (“Service Level 6”), Section 3.8 (“Service Level 8”), Section 3.11 (“Service Level 11”). |
• | “Service Level Default” means Supplier’s level of performance for a particular Service Level fails to meet the applicable Target Level for such Service Level during the applicable Measurement Window. |
• | “Service Level Effective Date” means, with respect to each Service Level as applied to a particular Eligible Medical Group, the date that such Service Level will be effective and enforced, which shall be the date that is [**] months after the EMG Service Commencement Date for the EMG Service against which the applicable Service Level is applied. For clarity, the Service Level Effective Date for any particular Service Level can vary among different groupings of Eligible Medical Groups (i.e., the Service Level Effective Date for Service Level 1 for the Cerner Group can be different from the Service Level Effective Date for Service Level 1 for the Epic Group). |
• | “SLA Measurement Commencement Date” means, with respect to each Service Level as applied to a particular Eligible Medical Group, the date that such Service Level will start to be measured, tracked, and recorded, which shall be the EMG Service Commencement Date for the EMG Service against which the applicable Service Level is applied. |
2. | General. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 4 Page 44
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
2.1 | As of the SLA Measurement Commencement Date for each of the NRSC/Athena Group, the Epic Group, or the Cerner Group (as applicable), Supplier shall perform the EMG Services with the intention to meet or exceed the Target Levels (as defined below) for each of the Service Levels by its applicable Service Level Effective Date. For the avoidance of doubt, in no event shall Supplier be liable for any Service Level Default (including any Service Level Credits) with respect to any Service Level prior to its applicable Service Level Effective Date. |
2.2 | The Current Service Levels apply solely to Supplier’s performance of the Platform-Specific Services. In connection with any Future Service Levels, the Parties shall agree upon (i) whether the Future Service Level will be applied against a Platform-Specific Service or a Medical Group Market Service, (ii) whether, for purposes of the Service Level Credits, the Future Service Level will be an AMG-Wide Service Level or a Group-Specific Service Level (or if the applicable Service Level Credit should apply in another mutually agreed manner), (iii) the applicable SLA Measurement Commencement Date and Service Level Effective Date (which may vary among different groupings of Eligible Medical Groups) and (iv) any other relevant adjustments to this Exhibit 4 for purposes of measuring and enforcing such Future Service Levels. |
2.3 | Supplier shall report to Ascension Health regarding Supplier’s performance against each of the Service Levels for each Measurement Window. With respect to all of the Service Levels other than Service Level 4, such reports shall provide information and data at a state-by-state level. |
2.4 | Ascension Health will have the right to receive Service Level Credits to be applied against the [**], in accordance with Section 7 below (subject to the last sentence of Section 2.1 above). |
2.5 | Supplier shall provide Ascension Health with the performance reporting for the EMG Services as specified in Section 6 below and as set forth in Section 9.2 of the MPSA. |
2.6 | As of the SLA Measurement Commencement Date for each Service Level and continuing throughout the duration of the Supplement Term, Supplier shall, in accordance with this Section 2.6, monitor, measure, collect, and record Supplier’s performance with respect to the metric applicable to each such Service Level. Commencing on the applicable Service Level Effective Date for each Service Level, the Target Levels with respect to such Service Level shall equal the applicable Target Level agreed pursuant to this Exhibit 4. |
2.7 | The Parties shall agree upon the Target Levels for each of the Current Service Levels by no later than September 14, 2018. The Parties acknowledge and agree that, for purposes of this Supplement, the Target Levels and Service Level metrics are intended to reflect rational and reasonable standards of performance in line with industry standards, but are not intended to be in the top quartile of performance standards; provided that the Parties may, in accordance with Section 5, mutually agree to increase any Target Levels or Service Level metrics during the Supplement Term to be in such top quartile. |
2.8 | For the avoidance of doubt, all of the Current Service Levels, metrics, and measurement standards will be the same for each of the NRSC/Athena Group, the Epic Group and the Cerner Group. The Parties may mutually agree that Future Service Levels, and its associated metrics, and measurement standards will vary based on the identity of the applicable Eligible Medical Group. |
3. | Service Level Criteria – Supplier will measure Supplier’s performance against the following Service Levels. |
3.1 | Service Level 1 - Customer Service Mean Speed to Answer (mean wait time, in seconds, to answer calls at Supplier’s customer service centers). This Service Level shall mean, for a given Measurement Window, for the Eligible Medical Groups then-receiving Platform-Specific Services (as a whole), (a) the Aggregate Hold Time divided by (b) the number of calls to Supplier’s customer service center for which the caller requested to speak with a Supplier representative during the Measurement Window. For purposes of calculating this Service Level, “Aggregate Hold Time” means the aggregated total amount of time during the Measurement Window that all callers to Supplier’s customer service center for all of the Eligible Medical Groups then-receiving Platform-Specific Services collectively (including “hang-ups”) remained on hold or in the interactive |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 4 Page 45
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
voice response unit after such callers requested to speak with a Supplier representative with respect to Supplier’s customer service center for the Eligible Medical Groups then-receiving Platform-Specific Services (as a whole).
3.2 | Service Level 2 - Financial Clearance. By September 14, 2018, the Parties shall agree upon a Service Level which measures Supplier’s ability to contact and interact with a patient, identify a patient’s eligibility and verify the requisite insurance authorization. |
3.3 | Service Level 3 – Percentage of financial assistance applications completed in less than [**] days in compliance with Ascension Health policies and CMS Refund Rules and Regulations. This Service Level shall mean, for a given Measurement Window, for the Eligible Medical Groups then-receiving Platform-Specific Services (as a whole), (a) the number of patients who have completed applications for financial assistance that were received by Supplier during such Measurement Window, for which, in accordance with [**] Practices, (i) the application has been evaluated, (ii) a determination has been made as to the application and (iii) the patient has been notified of the determination within [**] days or less from Supplier’s receipt of the completed application divided by (b) the number of patients who have completed applications for financial assistance that were received by Supplier during such Measurement Window. |
3.4 | Service Level 4 - Associate Engagement. The Parties will apply the protocol agreed to by the Parties for measuring associate engagement related to Dependent Services. This metric will be, for a given Measurement Window, measured for the Eligible Medical Groups then-receiving Platform-Specific Services (as a whole). |
3.5 | Service Level 5 - Patient Satisfaction survey. The Parties will utilize the patient satisfaction survey methodology agreed to by the Parties for Dependent Services to measure patient satisfaction with Supplier’s Financial Clearance Center, Medical Financial Solutions (pre-collect services) team, and customer service centers. This metric will be, for a given Measurement Window, measured for the Eligible Medical Groups then-receiving Platform-Specific Services (as a whole). |
3.6 | Service Level 6 – Credit AR Days. This Service Level shall mean, for a given Measurement Window, for each of the NRSC/Athena Group, the Epic Group and the Cerner Group respectively, (a) the negative balance accounts receivable as of the last day of the Measurement Window, divided by (b) the average daily GPSR for such Measurement Window. Average daily GPSR is calculated by dividing the total GPSR for the applicable Measurement Window by the number of calendar days during such Measurement Window. With respect to the NRSC/Athena Group, the source data for measurement will be the Athena Platform. With respect to the Cerner Group or the Epic Group, the source data for measurement will be the Cerner Platform or the Epic Platform, respectively. |
3.7 | Intentionally Deleted. |
3.8 | Service Level 8 – Remittance Resolution: Accountable Unpostables and Unposted Cash. |
a. | For the NRSC/Athena Group: this Service Level shall mean, for the NRSC/Athena Group as a whole, during any Measurement Window, (a) the Trailing Period Monthly Average Unpostables (as defined below) for the NRSC/Athena Group, divided by (b) the average daily NPSR for such Measurement Window. |
“Trailing Period Monthly Average Unpostables” shall mean, the result of (i) the sum of the aggregate amount of the Accountable Unpostables as of the last day of each of the most recent three months ended on or prior to the date of measurement, divided by (ii) three.
“Accountable Unpostables” shall mean, for the NRSC/Athena Group as a whole, the sum of the aggregate balances of the NRSC Unpostables that are aged greater than [**] days from the date that such item first appeared in the Supplier’s work queue as reflected by the Athena Platform.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 4 Page 46
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
“NRSC Unpostables” shall mean those NRSC appropriate groups from the Unpostables dashboard in the Athena Platform designated by the Parties to measure unidentified remittances that do not contain sufficient information for payments to be processed and posted. The Parties will designate the groups for the NRSC Unpostables by no later than September 14, 2018.
b. | For Eligible Medical Groups in the Epic Group and the Cerner Group respectively: this Service Level shall mean, for the Epic Group or the Cerner Group (as applicable), during any Measurement Window, the absolute value of the quotient of (i) the Trailing Period Monthly Average Unposted Cash (as defined below) as of the last day of such Measurement Window, divided by (ii) the Trailing Period Daily Average NPSR as of the last day of such Measurement Window. For purposes of the foregoing: |
“Trailing Period Monthly Average Unposted Cash” shall mean, the result of (i) the sum of the aggregate amount of Unposted Cash as of the last day of each of the most recent three month ended on or prior to the date of measurement, divided by (ii) three.
“Unposted Cash” shall mean, for the Epic Group or the Cerner Group (as applicable), the sum of the aggregate balances in each of the accounts used to hold unposted or unidentified cash; provided, however, that any portion of such balances for which Supplier has provided instruction or recommendation for the proper posting of such amounts shall be deducted from the calculation of Unposted Cash.
c. | Section 2.5 above, Section 6 below and the data and reporting requirements of Section 2.6 above shall not apply with respect to Service Level 8 for the Epic Group or the Cerner Group. Ascension Health shall provide Supplier, within 5 business days following the end of each month, with reports setting forth for each of the Epic Group and the Cerner Group, respectively: (i) the Trailing Period Monthly Average Unposted Cash (including a detailed itemization of the applicable balances of each account holding Unposted Cash) and (ii) the Trailing Period Daily Average NPSR together with all supporting data reasonably necessary for Supplier to verify such amounts and calculations. Additionally, Ascension Health shall provide (or cause the applicable Eligible Medical Groups to provide) Supplier with continuous, direct access to review the balances of each account holding Unposted Cash through PeopleSoft or similar reporting applications. |
In the event that Ascension Health or any Eligible Medical Group changes the manner (including accounting methods, principles or procedures) in which unposted cash is accounted for, or changes any accounting methodology, principles or procedures related to the accounts holding Unposted Cash, then Service Level 8 shall be deemed to be of no effect whatsoever with respect to any such Eligible Medical Group for which such changes have been employed until such time as Supplier and Ascension Health agree on reasonable modifications to the metrics for Service Level 8 and the Target Level applicable thereto.
3.9 | Intentionally Deleted. |
3.10 | Intentionally Deleted. |
3.11 | Service Level 11 – Customer Service Abandonment Rate. This Service Level shall mean, for a given Measurement Window, for the Eligible Medical Groups then-receiving Platform-Specific Services (as a whole), (A) the number of calls to Supplier’s Customer Service Center entering the queue that are abandoned after at least 20 seconds in the queue, divided by (B) the total number of inbound calls. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 4 Page 47
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
4. | Target Levels. |
The target level for each of the Service Levels (“Target Level”) will be mutually agreed by the Parties in accordance with the terms of this Exhibit 4.
5. | Changes to Existing Service Levels. |
The number of Service Levels will not exceed eleven (11). An opportunity to reset the target for each of the Service Levels will occur every [**] during the Term. In the [**] months prior to the applicable anniversary of the Supplement Effective Date, Supplier and Ascension Health will meet to discuss whether to reset any targets. The baseline reset methodology to be discussed will allow the target for each Service Level to increase or decrease, and may reflect or be derived from the following as mutually agreed upon information and factors:
- External benchmarks; and/or
- Then-current performance.
Any adjustment to any Service Level resulting from this Section 5 must be mutually agreed, shall apply prospectively only and shall not be applied to any period of time preceding the written agreement of the Parties with respect to such adjustment.
6. | Measurement and Reporting. |
6.1 | Supplier’s performance against the Service Levels will be measured for each Measurement Window as of the Service Level Effective Date for such Service Level. |
6.2 | Supplier will implement automated or other measurement and monitoring tools and procedures reasonably acceptable to Ascension Health to measure Supplier’s performance against the Service Levels in a manner and at a level of detail approved by Ascension Health. Supplier will provide Ascension Health and the Eligible Medical Groups then-receiving EMG Services with access to up-to-date problem management data and other data reasonably requested by Ascension Health regarding the status of failures and/or user inquiries. |
6.3 | If Supplier fails to measure its performance with respect to a Service Level so that it is not possible to confirm whether the level of performance specified for the Service Level has been achieved for a given Measurement Window (including if and to the extent the Parties are unable to timely agree upon the Target Levels), then, unless such failure to measure was previously excused in writing by Ascension Health, such failure will be deemed a Service Level Default for the applicable Measurement Window. |
6.4 | Supplier shall provide to the Eligible Medical Groups then-receiving EMG Services, as part of Supplier’s monthly performance reports, a set of hard- and soft-copy reports to verify Supplier’s performance and compliance with the Service Levels where data is available monthly. |
6.5 | Supplier shall provide detailed supporting information for each report to the Eligible Medical Groups then-receiving EMG Services in machine-readable form suitable for use on a personal computer. The data and detailed supporting information shall be Ascension Health Confidential Information, and the applicable Eligible Medical Groups may access such information online, where technically feasible and permissible under Supplier’s applicable third party agreements, at any time. |
7. | Service Level Credits. |
7.1 | If Supplier fails to meet any Service Level, then Supplier will pay or credit Ascension Health for the amounts described below (each, a “Service Level Credit”). Service Level Credits are not exclusive remedies and will in no way limit the rights of an Eligible Medical Group or Ascension Health at law or in equity. Service Level |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 4 Page 48
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Credits will be deemed to be reductions in the charges reflecting the impact on the Services as a result of the failure, and not as a penalty.
7.2 | If Supplier’s performance relative to any one of the Service Levels does not achieve the Target Level during a particular Measurement Window, such failure shall be deemed a Service Level Default, and Supplier will perform the problem analysis described in Section 8. Supplier will also propose a corrective action plan to improve Supplier’s performance in the upcoming Measurement Window, subject to the approval of the affected Eligible Medical Groups. Unless mutually agreed upon by Supplier and the affected Eligible Medical Groups, the measurement of Supplier’s performance for a Measurement Window will be completed no later than [**] days after the completion of such Measurement Window. |
7.3 | Calculation of AMG-Wide Service Level Credits. With respect to each of the AMG-Wide Service Levels, if Supplier’s performance within a Measurement Window for such Service Level does not achieve the applicable Target Level, resulting in a Service Level Default for such Service Level, then Supplier shall apply a Service Level Credit equal to the product of (i) [**] percent ([**]%) divided by the number of Service Levels then in effect, multiplied by (ii) [**] for such Measurement Window, which Service Level Credit shall be applied on the first day of the second month following the applicable Measurement Window (e.g., May 1 for a Service Level Default for the first quarter Measurement Window) for such Service Level Default. If more than one AMG-Wide Service Level has experienced a Service Level Default for any Measurement Window, Supplier will apply the sum of the Service Level Credit amounts for each of the AMG-Wide Service Levels that had Service Level Defaults during such Measurement Window as described in this Section 7.3. There shall be up to [**] percent ([**]%) of the [**] at risk with respect to such Measurement Window (excluding any portion of such [**] that, [**], and Supplier shall in no event be liable for Service Level Credits in excess of such at-risk amount with respect to AMG-Wide Service Levels. |
7.4 | Calculation of Group-Specific Service Level Credits. With respect to each of the Group-Specific Service Levels, if Supplier’s performance within a Measurement Window for such Service Level for the NRSC/Athena Group, the Epic Group, or the Cerner Group does not achieve the applicable Target Level, resulting in a Service Level Default for such Service Level with respect to the NRSC/Athena Group, the Epic Group, or the Cerner Group (as applicable), then Supplier shall apply a Service Level Credit equal to the product of (i) [**] percent ([**]%) divided by the number of Service Levels then in effect with respect to the NRSC/Athena Group, the Epic Group, or the Cerner Group (as applicable), multiplied by (ii) [**], for such Measurement Window, which Service Level Credit shall be applied on the first day of the second month following the applicable Measurement Window (e.g., May 1 for a Service Level Default for the first quarter Measurement Window) for such Service Level Default. If more than one Group-Specific Service Level within the NRSC/Athena Group, the Epic Group, or the Cerner Group (as applicable) has experienced a Service Level Default for any Measurement Window, Supplier will apply the sum of the Service Level Credit amounts for each such Group-Specific Service Level that had Service Level Defaults during such Measurement Window as described in this Section 7.4. There shall be up to [**] percent ([**]%) of the [**], at risk with respect to such Measurement Window (excluding, with respect to [**]), and Supplier shall in no event be liable for Service Level Credits in excess of such at-risk amount with respect to Group-Specific Service Levels. |
7.5 | Except as otherwise expressly set forth in Section 20.1(b)(ii) of the MPSA, if Supplier’s performance on the Service Level that experienced a Service Level Default achieves the Target Level in the subsequent Measurement Window, Ascension Health will remit the previously paid applicable Service Level Credit on the first day of the second month following the next Measurement Window (“Earnback”). However, if Supplier’s performance on such Service Level fails to achieve the Target Level during the next Measurement Window, Supplier will no longer have an opportunity to earn back the applicable Service Level Credit. |
7.6 | The mechanism for applying Service Level Credits and Earnback credits to the EMG Base Fee invoice and payment schedule is set forth in Exhibit 4-D to the MPSA. |
8. | Problem Analysis and Correction. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 4 Page 49
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
Supplier shall promptly investigate and correct each failure to meet a Service Level, by (i) promptly investigating and reporting on the causes of the problem; (ii) providing a Root Cause Analysis of such failure as soon as practicable after such failure or at the request of the affected Eligible Medical Groups; (iii) correcting the problem as soon as practicable or coordinate the correction of the problem if Supplier does not have responsibility for the cause of the problem; (iv) advising the affected Eligible Medical Groups of the status of remedial efforts being undertaken with respect to such problem; (v) demonstrating that the causes of such problem have been or will be corrected on a prospective basis; and (vi) taking corrective actions to prevent any recurrence of such problem. Supplier shall complete the Root Cause Analysis as quickly as possible, but in all events within [**] days, and shall notify such affected Eligible Medical Groups prior to the end of the initial [**] day period as to the status of the Root Cause Analysis and the estimated completion date. The Parties shall report on Service Level Defaults at each meeting of the JRB, including any disputes regarding problem analysis and correction steps, and without limiting any obligations of the Parties to implement any other decision of the JRB, each Party shall promptly implement or facilitate implementation of any resolutions determined by the JRB (e.g., Supplier cooperating with any exercise of step-in rights by Ascension Health as required by Section 4.4 of the MPSA).
9. | Windfall Situations; Environmental Changes and Other Issues. |
If any of the events described in Section 8.1 or Section 8.2 of Exhibit 2 to the Supplement occur, and such event significantly affects the Service Level measurement, Supplier’s performance under any Service Level (including the amount of resources required to maintain such performance) or Supplier’s ability to measure its performance with respect to any of the Service Levels, then either Party shall have the right to request that the other Party consider a fair and appropriate adjustment to the affected Service Levels and/or Target Levels. Upon such a request, the Parties will, in good faith, discuss the impact of such event on (i) Supplier’s performance under each such Service Level; (ii) the amount of resources required to maintain performance at or above the applicable Target Levels and (iii) Supplier’s ability to measure such Service Levels, with the outcome to equitably reflect the impact of such event(s).
With respect to the NRSC/Athena Group, in the event that the Athena Platform experiences any outage, bugs or other support issue not attributable to Supplier that materially affects Supplier's ability to meet any Service Levels, as applicable ("Athena Support Issue"), Ascension Health shall promptly work to resolve the Athena Support Issue. Until such time that the Athena Support Issue is resolved or a reasonable work around is implemented that eliminates the adverse effect of the Athena Support Issue on the NRSC/Athena Group and Supplier, the impacted Service Levels, as applicable, will be calculated as if failure to meet such Service did not occur due to the Athena Support Issue.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Exhibit 4 Page 50
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
ANNEX 1
Form of EMG Services Addendum
EMG SERVICES ADDENDUM [X] TO SUPPLEMENT 26 TO
AMENDED AND RESTATED MASTER PROFESSIONAL SERVICES AGREEMENT
FOR [NRSC/ATHENA GROUP / MEDICAL GROUP MARKET/ ELIGIBLE MEDICAL GROUP]
[Instructions for use of this document: This document is intended only as a template. The Sections and Schedules referred to below can be included or omitted as applicable for the particular Eligible Medical Group(s) being onboarded.]
This EMG Services Addendum No. [x] (this “Addendum”) to the AMG Supplement (as defined below) is made and entered into as of the ___ day of ______, 20___ (the “Addendum Effective Date”) by and between Ascension Health (“Ascension”) and R1 RCM Inc., f/k/a Accretive Health, Inc. (“Supplier”) (together, the “Parties”). Capitalized terms used herein and not otherwise defined shall have the meanings ascribed to such terms in the AMG Supplement, and if not defined therein, then in the MPSA (as defined below).
This Addendum is entered into pursuant to and subject to (a) that certain Supplement 26 of the MPSA (as defined below), dated as of June 20, 2018 (the “AMG Supplement”) and (b) that certain Amended and Restated Master Professional Services Agreement (“Master Professional Services Agreement” or “MPSA”) dated as of February 16, 2016, in each case, by and between Ascension Health and Supplier, the terms of which, except as expressly modified or excluded herein, are incorporated herein by reference. In accordance with Section 1.1(c) of the MPSA, any amendment to the MPSA (or the AMG Supplement), including amendments made after the Addendum Effective Date, shall automatically, as of the amendment effective date, be incorporated into this Addendum, unless otherwise specifically set forth in such amendment.
NOW THEREFORE, in consideration of the premises and mutual consents set forth below, the Parties hereby agree as follows:
1. | Schedules and Attachments. |
This Addendum includes each of the following attached Schedules, all of which are incorporated into this Addendum by this reference:
Schedule A | Transitioned Employees |
Schedule B | Contract Employee Roster |
Schedule C | Subcontractors |
Schedule D | Ascension Health Facilities |
Schedule E | Supplier Facilities |
Schedule F | Managed Third Party Agreements |
Schedule G | Assigned Third Party Contracts |
Schedule H | Ascension Health Provided Equipment |
Schedule I | Local EMGs |
Schedule J | Administered Expenses |
2. Definitions.
Section 2 of the AMG Supplement is hereby supplemented with the definitions set forth below:
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Form of EMG Services Addendum Page 51
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
[List any additional definitions specific to this Addendum.]
The definitions added to Section 2 of the AMG Supplement by this Addendum shall apply only with respect to the EMG Services provided under this Addendum.
3. Addendum Term.
The term of this Addendum shall commence as of 12:00:01 a.m., ____ Time on the Addendum Effective Date and shall continue for the Supplement Term, unless this Addendum is terminated as provided in the MPSA, in which case the term of this Addendum shall end at 11:59:59 p.m., Central Time, on the effective date of such termination.
4. Applicable Eligible Medical Group(s) and EMG Services.
This Addendum shall cover the provision of EMG Services by Supplier to the Owned Eligible Medical Groups and Third Party Eligible Medical Groups set forth in Schedule I (the “Local EMGs”) in accordance with the AMG Supplement. For the avoidance of doubt, if a physician group is an Owned Eligible Medical Group or, subject to Section 1(e) of the AMG Supplement, a Third Party Eligible Medical Group that is (i) included in the [NRSC/Athena Group / Epic Group / Cerner Group], (ii) is not listed on Schedule I and (iii) hereafter becomes acquired by, employed by, or party to a PSA with Ascension Health, then such physician group will automatically be deemed included in Schedule I.
[Schedule I will differentiate between Owned Eligible Medical Groups and Third Party Eligible Medical Groups. If there are any special terms or conditions related to Local EMGs, they can be listed here.]
5. EMG Services.
Supplier shall provide to the Local EMGs the [Platform-Specific Services/Medical Group Market Services/other EMG Services] set forth in Exhibit 1 of the AMG Supplement.
[If there are any changes to the scope of EMG Services (including any provision of out-of-scope services), they can be listed here.]
6. Pricing.
The EMG Base Fee shall be determined in accordance with Exhibit 2 to the AMG Supplement. The EMG Incentive Fees shall be determined in accordance with Exhibit 3 to the AMG Supplement.
[Parties may add an updated Cost to Collect Factor.]
7. List of Transitioned Employees and Key Supplier Personnel.
7.1 | List of Transitioned Employees. Schedule A to this Addendum lists the Ascension Health Personnel to whom offers of employment shall be made by Supplier, its Affiliates or Subcontractors pursuant to the terms of Exhibit 13 to the MPSA. |
7.2 | Key Supplier Personnel. In accordance with Sections 8.2(a)(i) and 8.2(b) of the MPSA, the Key Supplier Personnel positions under this Addendum are listed below: |
[Please identify the Site Lead.]
8. Contract Employee Rosters.
In accordance with Exhibit 5 of the MPSA, the Contract Employee Roster applicable to the provision of EMG Services to the Local EMGs is set forth in Schedule B.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Form of EMG Services Addendum Page 52
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
[This may be deleted if not applicable.]
9. Subcontractors.
The Subcontractors identified on Schedule C are approved by the Local EMGs for the purposes of the EMG Services.
10. Facilities.
10.1 | Ascension Health Facilities. In accordance with Section 6.1(a) and 6.2 of the MPSA, Supplier may provide any of the EMG Services at or from those Ascension Health Facilities set forth in Schedule D or any other office-based/practice-based facility from which the Local EMGs provides services, and Local EMGs shall provide Supplier with access to and the use of the foregoing locations (or equivalent space). |
10.2 | Supplier Facilities. In accordance with Section 6.1(a) and 6.2 of the MPSA, Supplier may provide any of the EMG Services at or from the [the locations identified in Schedule E.] |
11. Managed Third Party Agreements; Assigned Contracts.
The Managed Third Party Agreements listed on Schedule F shall not be assigned to Supplier. The Third Party Contracts to be assigned to Supplier shall be set forth in Schedule G.
12. Ascension Health Provided Equipment.
In accordance with Section 6.5(e) of the MPSA, the applicable Eligible Medical Group shall provide Supplier with the Ascension Health Provided Equipment listed on Schedule H, for the purpose of performing the EMG Services for Local EMGs during the term of this Addendum.
13. Administered Expenses.
In accordance with Section 11.2(a) of the MPSA, the Administered Expenses are set forth in Schedule J.
14. Initial Transition Plan.
Supplier shall deliver to Ascension Health an initial transition plan for the Local EMGs by [_____].
15. Other Terms.
[●]
SIGNATURE PAGE FOLLOWS
[SPACE LEFT INTENTIONALLY BLANK]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Form of EMG Services Addendum Page 53
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
IN WITNESS WHEREOF, the Parties have caused this Addendum to be executed by their respective duly authorized representatives as of the Addendum Effective Date.
R1 RCM INC. | ASCENSION HEALTH | |||
By: | By: | |||
Name: | Name: | |||
Title: | Title: | |||
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Signature Page to Form Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
NRSC/ATHENA ADDENDUM TO SUPPLEMENT 26 TO
AMENDED AND RESTATED MASTER PROFESSIONAL SERVICES AGREEMENT
This NRSC/Athena Addendum (this “Addendum”) to the AMG Supplement (as defined below) for the provision of Platform-Specific Services to the NRSC/Athena Group is made and entered into as of June 24, 2018 (the “Addendum Effective Date”) by and between Ascension Health (“Ascension”) and R1 RCM Inc., f/k/a Accretive Health, Inc. (“Supplier”) (together, the “Parties”). Capitalized terms used herein and not otherwise defined shall have the meanings ascribed to such terms in the AMG Supplement, and if not defined therein, then in the MPSA (as defined below).
This Addendum is entered into pursuant to and subject to (a) that certain Supplement 26 of the MPSA (as defined below), dated as of June 20, 2018 (the “AMG Supplement”) and (b) that certain Amended and Restated Master Professional Services Agreement (“Master Professional Services Agreement” or “MPSA”) dated as of February 16, 2016, in each case, by and between Ascension Health and Supplier, the terms of which, except as expressly modified or excluded herein, are incorporated herein by reference. The Parties have entered into this Addendum to set forth additional terms and conditions pursuant to which Supplier shall provide the Platform-Specific Services to the NRSC/Athena Group. In accordance with Section 1.1(c) of the MPSA, any amendment to the MPSA (or the AMG Supplement), including amendments made after the Addendum Effective Date, shall automatically, as of the amendment effective date, be incorporated into this Addendum, unless otherwise specifically set forth in such amendment.
NOW THEREFORE, in consideration of the premises and mutual consents set forth below, the Parties hereby agree as follows:
1. | Schedules and Attachments. |
This Addendum includes each of the following attached Schedules, all of which are incorporated into this Addendum by this reference:
Schedule A | Transitioned Employees |
Schedule B | Contract Employee Roster |
Schedule C | Subcontractors |
Schedule D | Ascension Health Facilities |
Schedule E | Supplier Facilities |
Schedule F | Managed Third Party Agreements |
Schedule G | Assigned Third Party Contracts |
Schedule H | Ascension Health Provided Equipment |
Schedule I | Local EMGs |
Schedule J | Administered Expenses |
2. Definitions.
Reserved.
3. Addendum Term.
The term of this Addendum shall commence as of 12:00:01 a.m., Central Time on the Addendum Effective Date and shall continue for the Supplement Term, unless this Addendum is terminated as provided in the MPSA, in which case the term of this Addendum shall end at 11:59:59 p.m., Central Time, on the effective date of such termination. The EMG Service Commencement Date for all of the Platform-Specific Services provided under this Addendum is October 1, 2018.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL NRSC/Athena Addendum Page 2
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
4. Applicable Eligible Medical Group(s) and Scope of EMG Services.
This Addendum shall cover the provision of Platform-Specific Services by Supplier to the Owned Eligible Medical Groups and Third Party Eligible Medical Groups, in each case, included in the NRSC/Athena Group (“Local EMGs”) in accordance with the AMG Supplement. The Parties shall, on or prior to October 1, 2018, amend this Addendum to include Schedule I listing all of the Local EMGs. For the avoidance of doubt, if a physician group is an Owned Eligible Medical Group or, subject to Section 1(e) of the AMG Supplement, a Third Party Eligible Medical Group that is (i) included in the NRSC/Athena Group, (ii) is not listed on Schedule I and (iii) hereafter becomes acquired by, employed by, or party to a PSA with Ascension Health, then such physician group will automatically be to deemed included in Schedule I.
5. EMG Services.
Supplier shall provide to the Local EMGs the Platform-Specific Services set forth in Exhibit 1 of the AMG Supplement.
6. Pricing.
(a) | The NRSC Base Fee shall be determined in accordance with Exhibit 2 to the AMG Supplement. The EMG Incentive Fees shall be determined in accordance with Exhibit 3 to the AMG Supplement. |
(b) | As a result of the NRSC Assessment conducted in accordance with Section 5 of Exhibit 2 to the AMG Supplement, for purposes of calculating the portion of the NRSC Base Fee, the Initial NRSC Cost to Collect Factor shall equal the result of [**] divided by [**] (i.e., [**]%). |
7. List of Transitioned Employees and Key Supplier Personnel.
7.1 | List of Transitioned Employees. The Parties shall, on or prior to October 1, 2018, amend this Addendum to include Schedule A listing the Ascension Health Personnel to whom offers of employment shall be made by Supplier, its Affiliates or Subcontractors pursuant to the terms of Exhibit 13 to the MPSA. |
7.2 | Key Supplier Personnel. In accordance with Sections 8.2(a)(i) and 8.2(b) of the MPSA, the Key Supplier Personnel is Roger Carroll. |
8. Contract Employee Rosters.
The Parties shall, on or prior to October 1, 2018, amend this Addendum to include Schedule B, the Contract Employee Roster applicable to the provision of Platform-Specific Services to the Local EMGs, in accordance with Exhibit 5 to the MPSA.
9. Subcontractors.
The Subcontractors identified on Schedule C are approved by the Local EMGs for the provision of the Platform-Specific Services.
10. Facilities.
10.1 | Ascension Health Facilities. In accordance with Section 6.1(a) and 6.2 of the MPSA, Supplier may provide any of the EMG Services at or from those Ascension Health Facilities set forth in Schedule D or any other office-based/practice-based facility from which Local EMGs provide services, and Local EMGs shall provide Supplier with access to and the use of the foregoing locations (or equivalent space). |
10.2 | Supplier Facilities. In accordance with Section 6.1(a) and 6.2 of the MPSA, Supplier may provide any of the EMG Services at or from any of the locations (or equivalent space) identified in Schedule E. |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL NRSC/Athena Addendum Page 3
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
11. Managed Third Party Agreements; Assigned Contracts.
The Managed Third Party Agreements listed on Schedule F shall not be assigned to Supplier. The Third Party Contracts to be assigned to Supplier shall be set forth in Schedule G.
12. Ascension Health Provided Equipment.
The Parties shall, on or prior to October 1, 2018, amend this Addendum to include Schedule H, the list of Ascension Health Provided Equipment to be provided by the NRSC in accordance with Section 6.5(e) of the MPSA, for the purpose of performing the Platform-Specific Services for the Local EMGs during the term of this Addendum.
13. Administered Expenses.
In accordance with Section 11.2(a) of the MPSA, the Administered Expenses are set forth in Schedule J.
14. Initial Transition Plan.
Supplier shall deliver to Ascension Health an initial transition plan for the Local EMGs by August 1, 2018.
SIGNATURE PAGE FOLLOWS
[SPACE LEFT INTENTIONALLY BLANK]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL NRSC/Athena Addendum Page 4
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
IN WITNESS WHEREOF, the Parties have caused this Addendum to be executed by their respective duly authorized representatives as of the Addendum Effective Date.
R1 RCM, INC. | ASCENSION HEALTH | |||
By: | By: | |||
Name: | Name: | |||
Title: | Title: | |||
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL NRSC/Athena Addendum Signature Page
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE A
TRANSITIONED EMPLOYEES
[Schedule to be inserted following October 1, 2018]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule A to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE B
CONTRACT EMPLOYEE ROSTER
[Schedule to be inserted following October 1, 2018]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule B to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE C
SUBCONTRACTORS
To the extent that any of the following vendors constitute Data Subcontractors, such vendors are hereby approved for the provision of the services applicable to such vendor:
Vendor Name |
[**] |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule C to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE D
ASCENSION HEALTH FACILITIES
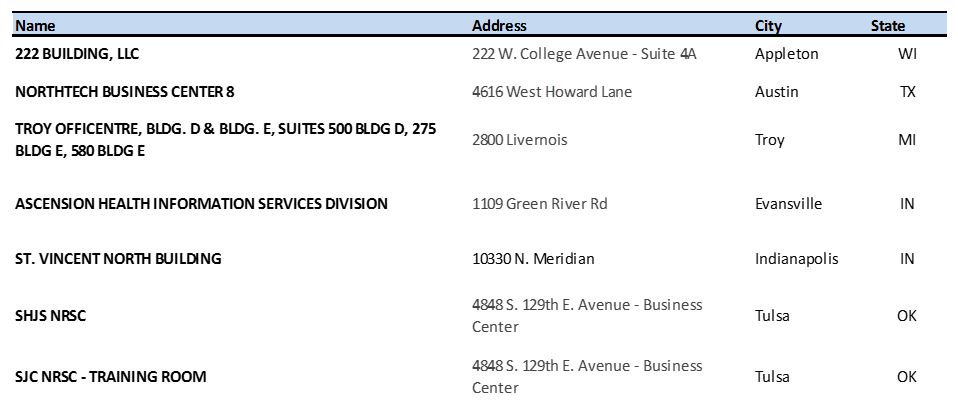
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule D to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE E
SUPPLIER FACILITIES
1. | Supplier Facilities. |
In accordance with Section 6.1 of the MPSA, the Supplier Facilities owned or operated by Supplier are set forth below:
SUPPLIER FACILITY | LOCATIONS | APPROVED SERVICE TYPES | |
1. | Chicago | 401 N. Michigan Avenue, Chicago, Illinois 60611 | • Revenue Cycle Training• Vendor Management • Revenue Cycle Technology and Support • Revenue Cycle Analytics and Reporting • Charge Optimization |
2. | Michigan Customer Contact Center | 225-229 & 234 N. Rose Street, Kalamazoo, Michigan 49007 | • Authorization / Referral Verification • Insurance Eligibility Verification • Collection of Residuals • Pre-Service Collections • Patient Billing Customer Service/Patient Financial Services • Prior Balance Found Insurance • Patient Liability Collections |
3. | Southeast Customer Contact Center | 950 22nd Street North, Birmingham, Alabama 35203 | • Authorization / Referral Verification • Insurance Eligibility Verification • Pre-Service Collections |
4. | Underpayment Center | 725 N. Highway A1A, Jupiter, Florida 33477 | • Underpayment Review/Recovery |
5. | Contract Modeling/Analytics | 2811 Wintergreen Drive, Cape Girardeau, Missouri 63701 | • Revenue Cycle Technology and Support (R1 Contract) • Underpayment Review / Recovery • Revenue Cycle Analytics and Reporting (for Contract Modeling (R1 Contract)) |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule E to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SUPPLIER FACILITY | LOCATIONS | APPROVED SERVICE TYPES | |
6. | Michigan Shared Services Center | Travelers Tower II, 26533 Evergreen Road, Southfield, Michigan | • Billing (patient and payer) • Secondary Billing • Self-Pay Financial Advocacy and Eligibility of Services • Prior Balance Found Insurance • Cash Applications • Patient Billing Customer Service/Patient Financial Services • Denial Management (e.g., Medicaid and other Third Party Payer Follow Up, and Rejections follow up) • Collection of Residuals • Prior Balance Found Insurance • Charge Optimization • Bad Debt Management • Revenue Cycle Analytics and Reporting |
7. | Noida Shared Services Center | Building 3 and Building 9 Situated at IT/ITeS Sez, Sector 135 Noida, India | • Billing (patient and payer) • Secondary Billing • Denial Management (e.g., Medicaid and other Third Party Payer Follow Up , and Rejections Follow Up) • Cash Applications • Credits • Revenue Cycle Technology and Support No patient facing-activities associated with the above functions will be performed at this location. |
8. | Gurgaon Shared Services Center | Building 2, Tower A Situated at IT/ITeS Sez, Sector 21, Dundahera, Gurgaon, Haryana, India | • Authorization/Referral Verification • Insurance Eligibility Verification • Billing (patient and payer) • Secondary Billing • Prior Balance Found Insurance • Denial Management (e.g., Medicaid and other Third-Party Payer Follow Up, and Rejections Follow Up) • Cash Applications • Revenue Cycle Analytics and Reporting • Credits No patient facing-activities associated with the above functions will be performed at this location. |
9. | Various U. S. Employee Residences | Various addresses | • Denial Management (ie - Coding Follow Up) |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule E to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SUPPLIER FACILITY | LOCATIONS | APPROVED SERVICE TYPES | |
10. | Hyderabad Shared Services Center | NSL SEZ Arena, Survey No- 1, Plot No. 6, Ramanthapur Road, Uppal, Gaddi, annaram, Hyderbad, Telangana 500039, India | • Authorization/Referral Verification • Insurance Eligibility Verification • Billing (patient and payer) • Secondary Billing • Prior Balance Found Insurance • Denial Management (e.g., Medicaid and other Third-Party Payer Follow Up, and Rejections Follow Up) • Cash Applications • Revenue Cycle Analytics and Reporting • Credits • Revenue Cycle Technology and Support No patient facing-activities associated with the above functions will be performed at this location. |
11. | Tikri Shared Services Center | Candor Gurgaon One Reality Projects, Private Limited IT/ITES, SEZ, 2nd, 3rd and 4th floor, Building No. 1, Village Tikri, Sector 48, Gurugram 122001, Haryana, India | • Authorization/Referral Verification • Insurance Eligibility Verification • Billing (patient and payer) • Secondary Billing • Prior Balance Found Insurance • Denial Management (e.g., Medicaid and other Third-Party Payer Follow Up, and Rejections Follow Up) • Cash Applications • Revenue Cycle Analytics and Reporting • Credits No patient facing-activities associated with the above functions will be performed at this location. |
12. | Indianapolis Shared Services Center | 10330 N. Meridian Street, 2nd Floor, Indianapolis, 46290 | • Billing (patient and payer) • Secondary Billing • Self-Pay Financial Advocacy and Eligibility of Services • Prior Balance Found Insurance • Cash Applications • Patient Billing Customer Service/Patient Financial Services • Denial Management (e.g., Medicaid and other Third-Party Payer Follow Up, and Rejections follow up) • Collection of Residuals • Prior Balance Found Insurance • Charge Optimization • Bad Debt Management • Revenue Cycle Analytics and Reporting |
13. | RCS (formerly NRIT) | 3030 Salt Creek Lane, Suite 301, Arlington Heights, IL 60005 | • Underpayment Review / Recovery • Charge Optimization |
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule E to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule E to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE F
MANAGED THIRD PARTY AGREEMENTS
Each agreement described in Schedule C hereto shall be deemed to be a Managed Third Party Agreement until such time as such agreement is either assigned to Supplier or terminated (either at Supplier’s direction or otherwise).
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule F to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE G
ASSIGNED THIRD PARTY CONTRACTS
None.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule G to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE H
ASCENSION HEALTH PROVIDED EQUIPMENT
[Schedule to be inserted following October 1, 2018]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule H to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE I
LOCAL EMGS
[Schedule to be inserted following October 1, 2018]
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule I to NRSC Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
SCHEDULE J
ADMINISTERED EXPENSES
None.
R1 RCM AND ASCENSION HEALTH
CONFIDENTIAL Schedule J to NRSC/Athena Addendum
[**] Indicates that text has been omitted which is the subject of a confidential treatment request. The text has been separately filed with the Securities and Exchange Commission.
