Attached files
| file | filename |
|---|---|
| EX-32.2 - EX-32.2 - Nabriva Therapeutics plc | a2234062zex-32_2.htm |
| EX-32.1 - EX-32.1 - Nabriva Therapeutics plc | a2234062zex-32_1.htm |
| EX-31.2 - EX-31.2 - Nabriva Therapeutics plc | a2234062zex-31_2.htm |
| EX-31.1 - EX-31.1 - Nabriva Therapeutics plc | a2234062zex-31_1.htm |
| EX-23.2 - EX-23.2 - Nabriva Therapeutics plc | a2234062zex-23_2.htm |
| EX-23.1 - EX-23.1 - Nabriva Therapeutics plc | a2234062zex-23_1.htm |
| EX-21.1 - EX-21.1 - Nabriva Therapeutics plc | a2234062zex-21_1.htm |
| EX-10.18 - EX-10.18 - Nabriva Therapeutics plc | a2234062zex-10_18.htm |
| EX-10.17 - EX-10.17 - Nabriva Therapeutics plc | a2234062zex-10_17.htm |
| EX-10.16 - EX-10.16 - Nabriva Therapeutics plc | a2234062zex-10_16.htm |
Use these links to rapidly review the document
TABLE OF CONTENTS
INDEX TO FINANCIAL STATEMENTS
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Form 10-K
| (Mark one) | ||
| ý | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 | |
For the fiscal year ended December 31, 2017 |
||
Or |
||
o |
TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
|
For the transition period from to |
||
Commission file number 001-37558
Nabriva Therapeutics plc
(Exact name of registrant as specified in its charter)
| Ireland (State or jurisdiction of organization) |
Not applicable (I.R.S. Employer Identification No.) |
|
25-28 North Wall Quay IFSC, Dublin 1, Ireland (Address of principal executive offices) |
Not applicable (Zip Code) |
+353 1 649 2000
(Registrant's telephone number, including area code)
Securities registered pursuant to Section 12(b) of the Act:
| Title of each class | Name of each exchange on which registered | |
|---|---|---|
| Ordinary Shares, nominal value $0.01 per share | The Nasdaq Stock Market LLC |
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes o No ý
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes o No ý
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ý No o
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ý No o
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant's knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. o
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company or an emerging growth company. See the definitions of "large accelerated filer," "accelerated filer," "smaller reporting company" and "emerging growth company" in Rule 12b-2 of the Exchange Act.
| Large accelerated filer o | Accelerated filer ý | Non-accelerated filer o (Do not check if a smaller reporting company) |
Smaller reporting company o Emerging growth company ý |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to section 13(a) of the Exchange Act. ý
Indicate by check mark whether the registrant is a shell company (as defined in Rule12b-2 of the Act). Yes o No ý
As of June 30, 2017 (the last business day of the registrant's most recently completed second fiscal quarter), the aggregate market value of the registrant's voting securities held by non-affiliates was approximately $166.7 million based on the last reported sale price of the registrant's ordinary shares on June 30, 2017. As of February 28, 2018, the registrant had 36,716,356 ordinary shares outstanding.
NABRIVA THERAPEUTICS AG
INDEX TO REPORT ON FORM 10-K
This Annual Report contains forward-looking statements that involve substantial risks and uncertainties. All statements contained in this Annual Report, other than statements of historical fact, including statements regarding our strategy, future operations, future financial position, future revenues, projected costs, prospects, plans and objectives of management, are forward-looking statements. The words "anticipate, "around" "believe," "estimate," "expect," "intend," "may," "plan," "predict," "project," "target," "potential," "will," "would," "could," "should," "continue," and similar expressions are intended to identify forward-looking statements, although not all forward-looking statements contain these identifying words. The forward-looking statements in this report include, among other things, statements about:
- •
- the timing and conduct of our clinical trials of our lead product candidate, lefamulin, including statements regarding the timing and
completion of the trials, and the period during which the results of the trials will become available;
- •
- our expectations regarding how far into the future our cash on hand will fund our ongoing operations;
- •
- the timing of and our ability to submit applications for, obtain and maintain marketing approval of lefamulin;
- •
- the potential receipt of revenues from future sales of lefamulin;
- •
- our plans to pursue development of lefamulin for additional indications other than community-acquired bacterial pneumonia, or CABP;
- •
- our plans to pursue research and development of other product candidates;
- •
- our ability to establish and maintain arrangements for manufacture of our product candidates;
- •
- our sales, marketing and distribution capabilities and strategy;
- •
- our ability to successfully commercialize lefamulin and our other product candidates;
- •
- the potential advantages of lefamulin and our other product candidates;
- •
- our estimates regarding the market opportunities for lefamulin and our other product candidates;
- •
- the rate and degree of market acceptance and clinical benefit of lefamulin and our other product candidates;
- •
- our ability to establish and maintain collaborations;
- •
- our ability to acquire or in-license additional products, product candidates and technologies;
- •
- our future intellectual property position;
- •
- our estimates regarding future expense, capital requirements and needs for additional financing;
- •
- our ability to effectively manage our anticipated growth;
- •
- our ability to maintain the level of our expenses consistent with our internal budgets and forecasts;
- •
- the demand for securities of pharmaceutical and biotechnology companies in general and our ordinary shares in particular;
- •
- competitive factors;
- •
- compliance with current or prospective governmental regulation;
- •
- general economic and market conditions;
- •
- our ability to attract and retain qualified employees and key personnel; and,
- •
- other risks and uncertainties, including those described in the "Risk Factors" section of this Form 10-K.
We may not actually achieve the plans, intentions or expectations disclosed in our forward-looking statements, and you should not place undue reliance on our forward-looking statements. Actual results or events could differ materially from the plans, intentions and expectations disclosed in the forward-looking statements we make. We have included important factors in the cautionary statements included in this Annual Report, particularly in the "Risk Factors" section of this Annual Report, that we believe could cause actual results or events to differ materially from the forward-looking statements that we make. Our forward-looking statements do not reflect the potential impact of any future acquisitions, mergers, dispositions, joint ventures or investments we may make.
You should read this Annual Report and the documents that we have filed as exhibits to this Annual Report completely and with the understanding that our actual future results may be materially different from what we expect. We do not assume any obligation to update any forward-looking statements, except as required by applicable law.
This Annual Report includes statistical and other industry and market data that we obtained from industry publications and research, surveys and studies conducted by third parties. Industry publications and third-party research, surveys and studies generally indicate that their information has been obtained from sources believed to be reliable, although they do not guarantee the accuracy or completeness of such information.
SPECIAL NOTE REGARDING THE REDOMICILIATION
On June 23, 2017, Nabriva Therapeutics plc, a public limited company organized under the laws of Ireland, or Nabriva Ireland, became the successor issuer to Nabriva Therapeutics AG, a stock corporation (Aktiengesellschaft) organized under the laws of Austria, or Nabriva Austria, for certain purposes under both the Securities Act of 1933, as amended, and the Securities Exchange Act of 1934, as amended, or the Exchange Act. Such succession occurred following the conclusion of a tender offer related to the exchange of American Depositary Shares and common shares of Nabriva Austria for ordinary shares of Nabriva Ireland, which resulted in Nabriva Ireland, a new Irish holding company, becoming the ultimate holding company of Nabriva Austria (the predecessor registrant and former ultimate holding company) and its subsidiaries, which we refer to as the Redomiciliation Transaction. On October 19, 2017, Nabriva Austria was converted into a limited liability company under Austrian law and renamed Nabriva Therapeutics GmbH.
Unless the context requires otherwise, all references in this Annual Report to "Nabriva," "the Nabriva Group," "the Company," "we," "ours," "us," or similar terms on or prior to June 23, 2017 (the effective date of the Redomiciliation Transaction), refer to our predecessor, Nabriva Therapeutics AG, together with its subsidiaries.
Overview
We are a clinical stage biopharmaceutical company engaged in the research and development of novel anti-infective agents to treat serious infections, with a focus on the pleuromutilin class of antibiotics. We are developing our lead product candidate, lefamulin, to be the first pleuromutilin antibiotic available for systemic administration in humans. We are developing both intravenous, or IV, and oral formulations of lefamulin for the treatment of community-acquired bacterial pneumonia, or CABP and may potentially develop lefamulin for additional indications other than CABP.
We initiated the first of two pivotal, international Phase 3 clinical trials of lefamulin, which we refer to as Lefamulin Evaluation Against Pneumonia 1, or LEAP 1, in September 2015 and initiated the second trial, which we refer to as LEAP 2, in April 2016. On September 18, 2017, we announced positive top-line results for LEAP 1. In LEAP 1, which enrolled 551 patients, lefamulin met all of the primary endpoints of non-inferiority compared to moxifloxacin with or without linezolid as required by the U.S. Food and Drug Administration, or FDA, and European Medicines Agency, or EMA. Lefamulin also showed a favorable tolerability profile in the LEAP 1 trial, with no unexpected safety signals or evidence of off-target activity. We completed patient enrollment of 738 adult patients in LEAP 2 in December 2017 and expect to have top-line data available from LEAP 2 in the spring of 2018. If the results of LEAP 2 are also favorable, including achievement of the primary efficacy endpoints of the trial, we expect to submit a new drug application, or NDA, for marketing approval of lefamulin for the treatment of CABP in adults in the United States in the second half of 2018. We also expect to submit a marketing authorization application, or MAA, for lefamulin for the treatment of CABP in adults in Europe a few months after our NDA filing.
We believe that pleuromutilin antibiotics can help address the major public health threat posed by bacterial resistance, which the World Health Organization, or WHO, characterized in 2017 as one of the biggest threats to human health. Increasing resistance to antibiotics used to treat CABP is a growing concern and has become an issue in selecting the appropriate initial antibiotic treatment prior to determining the specific microbiological cause of the infection, referred to as empiric treatment. For example, the U.S. Centers for Disease Control and Prevention, or CDC, has classified Streptococcus pneumoniae, the most common respiratory pathogen, as a serious threat to human health as a result of increasing resistance to currently available antibiotics. In addition, the CDC recently reported on the growing evidence of widespread resistance to macrolides, widely used antibiotics that disrupt bacterial protein synthesis, in Mycoplasma pneumoniae, a common cause of CABP that is associated with significant morbidity and mortality. Furthermore, Staphylococcus aureus, including methicillin-resistant S. aureus, or MRSA, which has also been designated as a serious threat to human health by the CDC, has emerged as a more common cause of CABP in some regions of the world, and a possible pathogen to be covered with empiric therapy.
As a result of increasing resistance to antibiotics and the wide array of potential pathogens that cause CABP, the current standard of care for hospitalized patients with CABP whose treatment is initiated in the hospital usually involves first-line empiric treatment with a combination of antibiotics (beta-lactams and macrolides) to address all likely bacterial pathogens or monotherapy with a fluoroquinolone. Combination therapy presents the logistical challenge of administering multiple drugs with different dosing regimens, with some drugs available only as IV, and increases the risk of drug-drug interactions and the potential for serious side effects. Fluoroquinolones are associated with safety and tolerability concerns, including a relatively high risk for developing Clostridium difficile infection and increasing rates of resistance for uropathogens. We believe these concerns have resulted in a decreasing use of flouroquinolones and restriction of their use within a growing number of hospitals. In addition, in May 2016, the FDA announced that an FDA safety review has shown that
1
fluoroquinolones, when used systemically, in the form of tablets, capsules and injectable, are associated with disabling and potentially permanent serious side effects that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system. Fluoroquinolones are typically administered in combination with other antibiotics, if community-acquired MRSA is suspected. In addition, many currently available antibiotic therapies are only available for IV administration and are prescribed for seven to fourteen days, meaning continued treatment requires prolonged hospitalization or a switch to a different antibiotic administered orally, with the attendant risk that the patient might respond differently.
Effective January 1, 2017, the Joint Commission & Center for Medicare and Medicaid Services, or CMS, began requiring all U.S. hospitals to have Antibiotic Management guidelines, also known as "Stewardship" Committees, in place to identify antibiotics most appropriate and targeted to each individual patient's infection. Past efforts to "cast the widest net possible" with broad-spectrum antibiotics that affect many types of bacteria have caused problems, such as C. difficile infections, by killing good bacteria or increased antibiotic resistance in other bacteria in different areas of the body. Additionally, in 2016, the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America, or IDSA/SHEA, updated their Antibiotic Stewardship guidelines for antibiotic use. We believe that three key goals from these guidelines are applicable to the treatment of CABP:
- •
- Reduce the risk of antibiotics associated with a high risk of C. difficile infections;
- •
- Increase use of oral antibiotics as a strategy to improve outcomes or decrease costs; and
- •
- Reduce antibiotic therapy to the shortest effective duration.
Consistent with the Antimicrobial Stewardship principles, we believe that lefamulin could be well suited as either a first-line or second-line empiric monotherapy for the treatment of CABP patients in the hospital setting, outpatient-transition of care or in the community setting, because of its novel mechanism of action, complete spectrum of activity for CABP pathogens, including against multidrug resistant strains, achievement of substantial drug concentrations in lung fluids and lung immune cells, and flexibility as step down oral agent with both the IV and oral formulations and favorable safety and tolerability profile.
In recognition of the growing need for the development of new antibiotics, recent regulatory changes, including priority review and regulatory guidance enabling smaller clinical trials, have led to renewed interest from the pharmaceutical industry in anti-infective development. For example, the Food and Drug Administration Safety and Innovation Act became law in 2012 and included the Generating Antibiotic Incentives Now Act, or the GAIN Act, which provides incentives, including access to expedited FDA review for approval, fast track designation and five years of potential data exclusivity extension for the development of new QIDPs.
Our Strategy
Our goal is to become a fully integrated biopharmaceutical company focused on the research, development and commercialization of novel anti-infective products. The key elements of our strategy to achieve this goal are:
- •
- Complete Phase 3 clinical development of lefamulin for CABP. We are devoting a significant portion of our financial resources and business efforts to completing the clinical development of lefamulin for the treatment of CABP. We initiated two international Phase 3 clinical trials of lefamulin for the treatment of moderate to severe CABP. We initiated the first of these trials, LEAP 1, in September 2015 and the second trial, LEAP 2, in April 2016. In September 2017, we reported positive top-line results from our LEAP 1 trial. With respect to LEAP 2, we completed patient enrollment in December 2017, and we anticipate receiving top-line data for LEAP 2 in
2
- •
- Maximize the commercial potential of lefamulin for CABP. We own exclusive, worldwide rights to lefamulin. We expect that our initial target patient population for lefamulin will consist of patients with moderate to severe CABP. If lefamulin receives marketing approval from the FDA for the treatment of CABP, we plan to commercialize it in the United States with our own targeted sales and marketing organization that we plan to establish. We believe lefamulin has an innovative profile which, if approved, would support its adoption in the United States for adult CABP patients, treated both as in-patients in a hospital setting as well as outpatient transition of care from the hospital, which we believe represents a significant commercial opportunity. We believe that we will be able to effectively communicate lefamulin's differentiating characteristics and key attributes to clinicians, hospital pharmacies and payors with the goal of establishing favorable reimbursement as well as a favorable formulary status in the targeted hospitals.
the spring of 2018. If the results of the LEAP 2 trials are favorable, including achievement of the primary efficacy endpoints, we expect to submit applications for marketing approval for lefamulin for the treatment of CABP in the United States in the second half of 2018 and in Europe a few months later.
- •
- Pursue the continued development of lefamulin in additional
indications. We are evaluating the continued development of lefamulin for indications in addition to CABP. Pediatric oral formulation development
is ongoing, and we anticipate intiating a Phase 1 clinical trial in pediatric patients in mid-2018. We believe lefamulin has potential to treat acute bacterial skin and skin structure infection
(ABSSSI), ventilator-associated bacterial pneumonia (VABP) or hospital-acquired bacterial pneumonia (HABP) and sexually transmitted infections (STIs). In addition, we may explore longer duration of
treatment with lefamulin to support development of a treatment for osteomyelitis and prosthetic joint infections. We believe that lefamulin would be differentiated from other treatment options for
these potential indications because of its novel mechanism of action, spectrum of activity, including activity against multi-drug resistant pathogens, achievement of substantial concentrations in
relevant tissues, availability as both an IV and oral formulation and favorable safety and tolerability profile.
- •
- Advance the development of other pleuromutilin product candidates and possibly compounds in other
classes. We are currently evaluating additional pleuromutilin product candidates by using our deep understanding of this class of antibiotics. Our product candidate BC-7013 has
completed a Phase 1 clinical trial. We believe that this pleuromutilin compound is well suited for the topical treatment of a variety of Gram-positive infections, including uncomplicated skin
and skin structure infections, or uSSSIs. Furthermore, we own diverse libraries of compounds in other antibacterial classes, such as ß-lactams and acremonic acids, which are a potential
basis for the discovery and development of novel antibacterial agents.
- •
- Evaluate business development opportunities and potential collaborations. We plan to evaluate the merits of entering into collaboration agreements with other pharmaceutical or biotechnology companies that may contribute to our ability to efficiently advance our product candidates, build our product pipeline, concurrently advance a range of research and development programs and leverage our commercial infrastructure. Potential collaborations may provide us with funding and access to the scientific, development, regulatory and commercial capabilities of the collaborators. We also plan to encourage local and international government entities and non-government organizations to provide additional funding and support for our development programs. We may expand our product pipeline through opportunistically in-licensing or acquiring the rights to
If lefamulin receives marketing approval outside the United States for the treatment of CABP, we expect to utilize a variety of types of collaboration, distribution and other marketing arrangements with one or more third parties to commercialize lefamulin in such markets.
3
complementary products, product candidates and technologies for the treatment of a range of infectious diseases.
Background
Anti-Bacterial Market and Scientific Overview
Bacteria are broadly classified as Gram-positive or Gram-negative. Gram-positive bacteria possess a single membrane and a thick cell wall and turn dark-blue or violet when subjected to a laboratory staining method known as Gram's method. Gram-negative bacteria have a thin cell wall layered between an inner cytoplasmic cell membrane and a bacterial outer membrane and, as a result, do not retain the violet stain used in Gram's method. Antibiotics that are active against both Gram-positive and Gram-negative bacteria are referred to as broad spectrum, while those that are active only against a select subset of Gram-positive or Gram-negative bacteria are referred to as narrow spectrum. Bacteria that cause infections are often referred to as bacterial pathogens. Because it often takes from 24 to 48 hours to definitively diagnose the particular bacterial pathogen causing an infection, the causative pathogen often remains unidentified and narrow spectrum antibiotics are not generally used as empiric monotherapy for first-line treatment of hospitalized patients with serious infections.
Since the introduction of antibiotics in the 1940s, numerous new antibiotic classes have been discovered and developed for therapeutic use. The development of new antibiotic classes and new antibiotics within a class is important because of the ability of bacteria to develop resistance to existing mechanisms of action of currently approved antibiotics. However, the pace of discovery and development of new antibiotic classes slowed considerably in the past few decades. The CDC estimates that the pathogens responsible for more than 70% of U.S. hospital infections are resistant to at least one of the antibiotics most commonly used to treat them. The CDC also estimated in 2013, based on data collected from evaluations performed between 2006 and 2011, that annually in the United States at least two million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die as a direct result of these infections.
Antibiotic resistance is primarily caused by genetic mutations in bacteria selected by exposure to antibiotics that do not kill all of the bacteria. In addition to mutated bacteria being resistant to the drug used for treatment, many bacterial strains can also become cross-resistant, meaning that they become resistant to multiple classes of antibiotics. As a result, the effectiveness of many antibiotics has declined, limiting physicians' options to treat serious infections and exacerbating a global health issue. For example, the WHO estimated in 2014 that people with infections caused by MRSA, a highly resistant form of bacteria, are 64% more likely to die than people with a non-resistant form of the infection. Resistance can increase the cost of healthcare because of the potential for lengthier hospital stays and more intensive care. Growing antibiotic resistance globally, together with the low level of investment in research and development, is considered one of the biggest global health threats. In 2010, the WHO stated that antibiotic resistance is one of the three greatest threats to human health. Partially in response to this threat, the U.S. Congress passed the GAIN Act in 2012, which provides incentives, including access to expedited FDA review for approval, fast track designation and five years of potential data exclusivity extension for the development of new QIDPs. Additional legislation is also being considered in the United States, including the Antibiotic Development to Advance Patient Treatment Act of 2013, which is intended to accelerate the development of anti-infective products, and the Developing an Innovative Strategy for Antimicrobial Resistant Microorganisms Act of 2014, which is intended to establish a new reimbursement framework to enable premium pricing of anti-infective products.
In 2016, sales of antibiotics totaled approximately $39 billion globally. Although judicious use of antibiotics is important to reduce the rate of antibiotic resistance, this approach alone cannot fully
4
address the threat from increasing antibiotic resistance. New antibiotics, and particularly new antibiotic classes, are needed to ensure the availability of effective antibiotic therapy in the future.
Community-Acquired Bacterial Pneumonia (CABP)
Market Overview
The WHO estimated in 2002 that there were approximately 450 million pneumonia cases reported per year worldwide, causing approximately 4.0 million deaths in 2002. According to an article published in 2011 in the peer-reviewed medical journal Therapeutic Advances in Respiratory Disease, the annual incidence of community-acquired pneumonia is between five and 11 cases per 1,000 people, with the incidence rate rising in elderly patients. In a study published in 2004 in the peer-reviewed medical journal Clinical Infectious Diseases in which more than 46,000 people in the state of Washington were monitored over three years, the incidence of CABP among those 65 to 69 years of age was 18.2 cases per 1,000 people per year and increased to 52.3 cases per 1,000 people per year in those over 85 years of age.
The U.S. National Center for Health Statistics estimated that between 1988 and 1994 there were approximately 5.6 million cases of pneumonia per year in the United States. More recently, based on our combined analysis of the CDC's 2007 National Ambulatory Medical Care Survey, the National Hospital Ambulatory Medical Care Survey and 2013 data from the Healthcare Cost and Utilization Project we estimate that over 5.0 million adults are treated annually for CABP in the United States and that the majority of these adult CABP patients have their treatment initiated in a hospital, including emergency departments. According to the Healthcare Cost and Utilization Project, or HCUP, in 2013, approximately 3.1 million adults sought treatment in a U.S. hospital for CABP. In addition, in 2013, approximately 2.4 million adults were admitted to U.S. hospitals for in-patient care with a diagnosis of CABP and approximately 700,000 adults were seen in an emergency department at U.S. hospitals for treatment of CABP and then released.
Additionally, in 2014, based on CDC data approximately 50,000 patients died from CABP in the United States. Based on data collected from July 1, 2012 through June 30, 2015, on the Medicare.gov Hospital Compare website, the current national rate of readmissions for Medicare pneumonia patients is 17.1%, which is the percentage of patients who have had a recent hospital stay that must return to a hospital for unplanned care within 30 days of being discharged. The national average death rate for Medicare pneumonia patients, excluding Medicare Advantage plan data, is 16.3%, which is the percentage of patients who die, for any reason, within 30 days of admission to a hospital.
Based on data from Arlington Medical Resources, or AMR, a leading provider of medical data from hospitals and other healthcare facilities, who reported that the number of antibiotic treatment courses for CABP adult patients in hospitals in the United States exceeded 6.8 million for full-year 2015, we estimate approximately 5.3 million of these CABP courses were for IV/injectable antibiotics for adult CABP patients, while approximately 1.5 million CABP oral antibiotic courses were prescribed for adult CABP patients in the hospital setting. Additionally, for the twelve months ending September 30, 2016, Source Health Solutions estimates that once adult CABP patients are discharged home from U.S. hospitals, approximately 4.2 million antibiotic oral prescriptions are written annually for their outpatient antibiotic treatment. Relative to the approximately 6.6 million adult CABP outpatient oral antibiotic prescriptions that Health Source Solutions estimates are written over the same time-period, approximately 6 out of every 10 oral antibiotic prescriptions for adult CABP results as a transition of care from hospital-initiated treatment to outpatient therapy. The remaining CABP prescriptions originate from prescribers in community clinics, primary care offices and at other non-hospital based sites of urgent care.
5
Causes of CABP
Pneumonia can be caused by a variety of micro-organisms, with bacteria being the most common identifiable cause. CABP refers to bacterial pneumonia that is acquired outside of a hospital setting. Signs and symptoms of CABP include cough, fever, sputum production and chest pain. A number of different types of bacteria can cause CABP, including both Gram-positive and Gram-negative bacteria. Pneumonia that is caused by atypical bacterial pathogens often has different symptoms and responds to different antibiotics than pneumonia caused by pathogens referred to as typical bacteria. However, atypical bacteria are not uncommon. The most common bacterial pathogens noted in current treatment guidelines from the Infectious Diseases Society of America, or IDSA, for hospitalized CABP patients who are not in the intensive care unit are Streptococcus pneumoniae, Mycoplasma pneumoniae, Haemophilus influenzae, Chlamydophila pneumoniae, and Legionella species. In addition, IDSA notes the emergence of resistance to commonly utilized antibiotics for CABP, specifically drug-resistant S. pneumoniae and community-acquired MRSA, or CA-MRSA, as a major consideration in choosing empiric therapy. However, a majority of patients do not have a pathogen identified using routine diagnostic tests available to physicians.
Currently Available Treatment Options
In 2007, based on the most likely bacteria to cause CABP, IDSA and the American Thoracic Society, or ATS, recommend empiric treatment of hospitalized patients with CABP who do not require treatment in an intensive care unit with either:
- •
- a combination of a cephalosporin, an antibiotic that disrupts the cell wall of bacteria, plus a macrolide, an antibiotic that disrupts
bacterial protein synthesis; or
- •
- monotherapy with a respiratory fluoroquinolone, an antibiotic that disrupts bacterial protein synthesis.
In the event CA-MRSA is suspected, these guidelines recommend that vancomycin, an antibiotic that disrupts the cell wall of bacteria, or linezolid, an antibiotic that disrupts bacterial protein synthesis, be used or added to the current regimen.
In addition, physicians need to be aware of the local susceptibility profiles of the common bacterial pathogens associated with CABP because of increasing resistance to first-line antibiotics. For example, rates of pneumococcal resistance to recommended first-line macrolides exceed 40% in some areas, while resistance in M. pneumoniae associated with severe disease has been recently reported by the CDC in the United States.
Limitations of Currently Available Treatment Options
When confronted with a new patient suffering from a serious infection caused by an unknown pathogen, a physician may be required to quickly initiate first-line empiric antibiotic treatment, often with a combination of antibiotics, to stabilize the patient prior to definitively diagnosing the particular bacterial infection. However, currently available antibiotic therapies for first-line empiric treatment of CABP suffer from significant limitations.
Bacterial Resistance and Spectrum of Activity
As a result of bacterial resistance, the effectiveness of many antibiotics has declined. For example, the CDC estimates that in 30% of severe S. pneumoniae cases, the bacterial pathogen is fully resistant to one or more clinically relevant antibiotics, with 44% of strains resistant to a macrolide in the United States. In addition, fluoroquinolone resistance in S. pneumoniae has increased from less than 0.5% to more than 3% of cases in some regions of North America, which parallels increased total fluoroquinolone prescriptions. Antibiotic resistance has a significant impact on mortality and
6
contributes heavily to healthcare system costs worldwide. According to the CDC, cases of resistant pneumococcal pneumonia result in 32,000 additional doctor visits, approximately 19,000 additional hospitalizations and 7,000 deaths each year. None of the currently available treatment options provides a spectrum of antibacterial coverage as a monotherapy that sufficiently covers all of the most common bacterial causes of CABP, including multi-drug resistant strains.
Difficult, Inconvenient and Costly Regimens
Currently available antibiotics used to treat CABP and other serious infections can be difficult, inconvenient and costly to administer. Physicians typically prefer IV administration for patients hospitalized with more serious illness to ensure adequate delivery of the drug rapidly. Many IV antibiotics are prescribed for seven to 14 days or more and patients can be hospitalized for much or all of this period or require in-home IV therapy. The diagnosis related group, or DRG, reimbursement system often used in the U.S. hospital setting pays a fixed fee for an episode of CABP that may not fully compensate hospitals for the duration of hospitalized care. Prolonged IV treatment that extends the period of hospitalization may cause hospital costs to increase in excess of the fixed reimbursement fee, resulting in significant negative impact on healthcare institutions. In addition, to address all likely bacterial pathogens in a patient with a more serious illness, IDSA guidelines recommend using a combination of antibiotics. Combination therapy presents the logistical challenge of administering multiple drugs with different dosing regimens and increases the risk of drug-drug interactions. While IV treatment delivers the drug more rapidly than is possible orally, once a patient is stabilized, oral treatment with the same drug would allow for more convenient and cost-effective out-patient treatment. Because many commonly used antibiotics are only available in IV form, a switch to an oral therapy requires changing to a different antibiotic, which may be less effective for the patient.
Adverse Effects
Currently available antibiotic therapies can have serious side effects. These side effects may include severe allergic reaction, decreased blood pressure, nausea and vomiting, suppression of platelets, pain and inflammation at the site of injection, muscle, renal and oto-toxicities, optic and peripheral neuropathies and headaches. At times, these side effects may be significant and require discontinuation of therapy. As a result, some treatments require clinicians to closely monitor patients' blood levels and other parameters, increasing the expense and inconvenience of treatment. This risk may be increased with combination therapy, which exposes patients to potential adverse effects from each of the antibiotics used in treatment. For example, fluoroquinolones are associated with tendon rupture and peripheral neuropathy. In addition, fluoroquinolones have been associated with an increased frequency of C. difficile colitis, an overgrowth of a bacteria in the colon that produces a toxin that results in inflammation of the colon and repeated bouts of watery diarrhea. This has resulted in limitations on the use of fluoroquinolones in several countries. In November 2015, the FDA convened an Advisory Committee meeting to review the benefits and risks of fluoroquinolones in less severe indications, such as uncomplicated UTI, acute bacterial sinusitis and acute bacterial exacerbations of chronic bronchitis. Based on the committee's recommendation, in July 2016, the FDA approved changes to the labels of fluoroquinolones to indicate that fluoroquinolones should be reserved for use in patients who have no other treatment options for the indications mentioned above, because the risk of these serious side effects generally outweighs the benefits in these patients. These changes included a requirement that a separate patient Medication Guide be given with each prescription that describes the safety issues associated with this class of drugs.
7
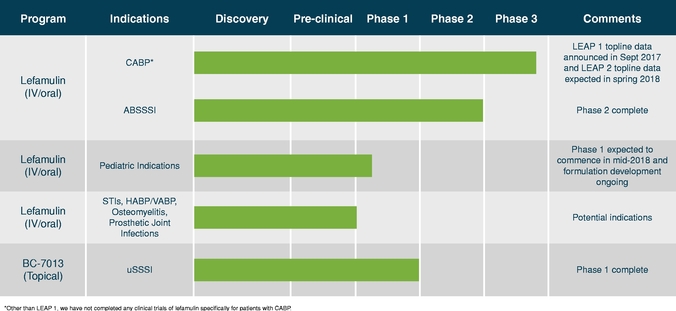
Our Product Development Pipeline
The following table summarizes the indications for which we are developing our product candidates and the status of development.
Lefamulin
Overview
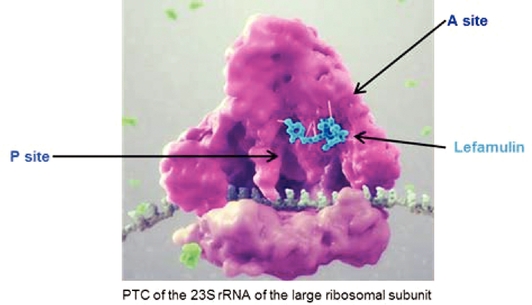
We are developing lefamulin to be the first pleuromutilin antibiotic available for systemic administration in humans. Lefamulin is a semi-synthetic derivative of the naturally occurring antibiotic, pleuromutilin, which was originally identified from a fungus called Pleurotus mutilius. Lefamulin inhibits the synthesis of bacterial protein, which is required for bacteria to grow. Lefamulin acts by binding to the peptidyl transferase center, or PTC, on the bacterial ribosome in such a way that it interferes with the interaction of protein production at two key sites known as the "A" site and the "P" site, resulting in the inhibition of bacterial proteins and the cessation of bacterial growth. Lefamulin's binding occurs with high affinity, high specificity and at molecular sites that are different than other antibiotic classes. We believe that lefamulin's novel mechanism of action is responsible for the lack of cross-resistance with other antibiotic classes that we have observed in our preclinical studies and clinical trials and a
8
low propensity for development of bacterial resistance to lefamulin. The binding of lefamulin to the PTC on the bacterial ribosome is depicted in the graphic below.
We are developing both IV and oral formulations of lefamulin. We believe that lefamulin is well suited to be used empirically as monotherapy for the treatment of respiratory tract infections, such as CABP, because of its spectrum of antibacterial activity against both the typical and atypical pathogens causing CABP, including multi-drug resistant pathogens such as MRSA. In addition, in preclinical studies, lefamulin showed potent antibacterial activity against a variety of Gram-positive bacteria, Gram-negative bacteria and atypical bacteria, including multi-drug resistant strains. In preclinical studies and in Phase 1 clinical trials, lefamulin achieved substantial concentrations in the epithelial lining fluid, or ELF, of the lung, the site infected during pneumonia. Lefamulin also provides the ability to switch from IV to oral therapy and maintain therapy with the same antibacterial treatment.
The FDA has designated each of the IV and oral formulations of lefamulin as a qualified infectious disease product, or QIDP, which provides for the extension of statutory exclusivity periods in the United States for an additional five years upon FDA approval of the product for the treatment of CABP and granted fast track designation to these formulations of lefamulin. Fast track designation is granted by the FDA to facilitate the development and expedite the review of drugs that treat serious conditions and fill an unmet medical need. The fast track designation for the IV and oral formulations of lefamulin will allow for more frequent interactions with the FDA, the opportunity for a rolling review of any new drug application, or NDA, we submit and eligibility for priority review and a shortening of the FDA's goal for taking action on a marketing application from ten months to six months.
We own exclusive, worldwide rights to lefamulin. Lefamulin is protected by issued patents in the United States, Europe and Japan covering composition of matter, which are scheduled to expire no earlier than 2028. We also have been granted patents for lefamulin relating to process and pharmaceutical crystalline salt forms in the United States, which are scheduled to expire no earlier than 2031. In addition, we own a family of pending patent applications directed to pharmaceutical compositions of lefamulin, which if issued would be scheduled to expire no earlier than 2036.
9
Key Attributes of Lefamulin
We believe that the combination of the following key attributes of lefamulin, observed in clinical trials and preclinical studies, differentiates lefamulin from currently available antibiotics and make lefamulin well suited for use as a first-line or second-line empiric monotherapy for the treatment of CABP.
The preclinical studies and clinical trials we have conducted to date suggest that lefamulin's novel mechanism of action is responsible for the lack of cross resistance observed with other antibiotic classes and a low propensity for development of bacterial resistance to lefamulin. As a result of the favorable safety and tolerability profile we have observed in our clinical trials to date, we believe lefamulin has the potential to present fewer complications relative to the use of current therapies. Based on our research, we also believe that the availability of both IV and oral formulations of lefamulin, and an option to switch to oral treatment, could reduce the length of a patient's hospital stay and the overall cost of care.
Targeted Spectrum of Activity for CABP pathogens and Low Propensity for the Development of Bacterial Resistance
We expect lefamulin's spectrum of antibacterial activity against typical and atypical pathogens could eliminate the need to use a combination of antibiotics for the treatment of CABP. In our completed Phase 2 clinical trial, IV lefamulin achieved a high cure rate against multi-drug resistant Gram-positive bacteria, including MRSA. In addition, in preclinical studies, lefamulin showed activity against a variety of Gram-positive bacteria, including S. pneumoniae and S. aureus, that are resistant to other classes of antibiotics, Gram-negative bacteria, including H. influenzae and M. catarrhalis, and atypical bacteria, including C. pneumoniae, M. pneumoniae and L. pneumophila. Included in lefamulin's spectrum of activity are all bacterial pathogens identified by IDSA as the most common causes of CABP for hospitalized patients who are not in the intensive care unit, as well as strains of the above listed bacteria that are resistant to other classes of antibiotics, including penicillins, cephalosporins, fluoroquinolones and macrolides.
Based on observations from our preclinical studies and clinical trials of lefamulin, as well as industry experience with pleuromutilins used in vetinary medicine over the last 30 years, we believe that lefamulin's novel mechanism of action is responsible for the lack of cross-resistance observed with other antibiotic classes and a low propensity for development of bacterial resistance to lefamulin.
Convenient Dosing Regimen; Potential for Switching from IV to Oral Treatment
We have developed both an IV and oral formulation of lefamulin, which we are utilizing in our clinical trials of lefamulin for the treatment of CABP. The administration of lefamulin as a monotherapy avoids the need for the complicated dosing regimens typical of multi-drug cocktails. We believe the availability of both IV and oral administration, and an option to switch to oral treatment, would be more convenient for patients and could reduce the length of a patient's hospital stay and the overall cost of care. The potential reduction in the overall cost of care could be particularly meaningful to healthcare institutions, as the DRG reimbursement system pays a fixed fee for the treatment of CABP regardless of the length of hospital stay. We believe that our Phase 3 trial design will permit us to submit for approval of both IV and oral formulations of lefamulin, subject to obtaining favorable results in LEAP 2, including achievement of the primary efficacy endpoints of the trials.
We designed our Phase 3 clinical trials to follow the draft guidance published by the FDA for the development of drugs for CABP and guidance from the European Medicines Agency, or EMA, for the development of antibacterial agents with the goal of positioning lefamulin as a first-line empiric monotherapy for the treatment of CABP. We reached agreement with the FDA in September 2015 on a SPA regarding the study design for our first Phase 3 clinical trial and obtained input from select
10
European authorities in anticipation of submitting a new drug application with the FDA and a marketing authorization application, or MAA, with the EMA, in each case, for the treatment of CABP. In April 2016, we reached agreement with the FDA regarding an amendment to the SPA. We also plan to conduct a number of studies to support FDA approval of lefamulin, including studies in patients with hepatic insufficiency and renal impairment. On September 18, 2017, we announced positive top-line results for LEAP 1. In LEAP 1, which enrolled 551 patients, lefamulin met all of the primary endpoints of non-inferiority compared to moxifloxacin with or without linezolid as required by the FDA, and EMA. Lefamulin also showed a favorable tolerability profile in the LEAP 1 trial, with no unexpected safety signals or evidence of off-target activity.
LEAP 1—IV/Oral Phase 3 Clinical Trial
LEAP 1 was a multi-center, randomized, controlled, double-blind, global study comparing lefamulin to moxifloxacin, with or without linezolid, in adults with CABP who have a Pneumonia Outcomes Research Team, or PORT Class, of 3, 4 or 5. After providing informed consent and completing screening procedures, patients were randomized in a 1:1 ratio to receive lefamulin or moxifloxacin. At the time of randomization, if the investigator suspected methicillin-resistant S aureus, also called MRSA, patients randomized to receive moxifloxacin could also receive linezolid, while patients receiving lefamulin would have had placebo added. All patients initially received 3 days of IV study medication, after which the option to switch to oral therapy was permitted in each treatment arm based on whether a patient met predefined signs of improvement and the investigator discretion. Patients completed a total of 7 days of study drug unless they were suspected to have MRSA infection, in which case then they received 10 days of treatment. The lefamulin dosing was 150 mg IV or 600 mg orally every 12 hours; moxifloxacin was dosed at 400 mg for both IV and oral once-daily, and linezolid was dosed at 600 mg for both IV and orally every 12 hours.
During the study, there were several pre-defined time points at which efficacy was assessed. The first time point, called the early clinical response assessment, or ECR, occurred at 96 +/– 24 hours after the first dose of study drug. The ECR is an on-therapy assessment and is the primary efficacy assessment required by the FDA. This endpoint assessed the four cardinal patient reported signs and symptoms of CABP. For a patient to be deemed to have a successful ECR, they must have had improvement in at least two of the four CABP symptoms, with none of the symptoms worsening, they also must have been alive and, must not have received a non-study antibacterial agent for the treatment of their CABP. The non-inferiority margin for the FDA primary endpoint is 12.5%, with a power >90%.
The EMA primary efficacy endpoint is the Investigator Assessment of Clinical Response, or the IACR, in both the modified ITT and Clinically Evaluable populations at the test of cure, or TOC. In order for a patient to be deemed to have had a successful IACR, they must have had their signs and symptoms of CABP improved or resolved in the investigator's judgement such that no additional antibacterial therapy was administered for their CABP. The non-inferiority margin for the EMA primary endpoints was 10%, with an 80% power.
Of the 551 patients enrolled in LEAP 1, there were 276 in the lefamulin arm versus 275 in the moxifloxacin with or without linezolid arm. Patients who were 65 or older were 47.8% in the lefamulin arm versus 39.3% in the moxifloxacin with or without linezolid arm. The lefamulin arm enrolled 196 (71.0%), 76 (27.5%) and 4 (1.4%) patients with a PORT score of III, IV and V, respectively. The moxifloxacin with or without linezolid arm enrolled 1 (0.4%), 201 (73.1%), 70 (25.5%) and 3 (1.1%) patients with a PORT score of II, III, IV and V, respectively.
11
Topline Results
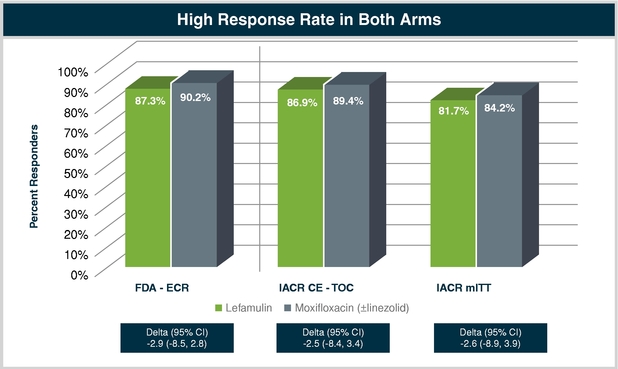
In LEAP 1, lefamulin met the FDA's primary efficacy endpoint of early clinical response measured at 96 +/– 24 hours after the first dose of study medication in the ITT population. The early clinical response rate observed in the lefamulin treatment arm was 87.3% compared to a 90.2% response rate in the moxifloxacin with or without linezolid treatment arm. The difference in the point estimate for the ECR was –2.9 with a 95% confidence internal between –8.5 and +2.8. Lefamulin also met the EMA's primary endpoint of Investigator assessment of clinical response, or IACR, measured 5 to 10 days after the last dose of study drug, or the TOC, in both the modified ITT and clinically evaluable populations. In the CE-population the IACR was 86.9% compared to 89.4% in the lefamulin and moxifloxacin arms, respectively. The difference in the point estimate was –2.5, with a 95% confidence interval between –8.4 and +3.4. In the mITT population the IACR was 81.7% compared to 84.2% in the lefamulin and moxifloxacin arms, respectively. The difference in the point estimate was –2.6, with a 95% confidence interval between –8.9 and +3.9.
12
ECR by Baseline Pathogen—micro ITT
ECR by Baseline Pathogen—Typical Pathogens [micro ITT]
| |
Lefamulin | Moxifloxacin (±Linezolid) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Microbiological ITT (microITT)
|
N = 159 (57.6%) |
N = 159 (57.8%) |
|||||||||
| |
|
ECR (%) |
|
ECR (%) |
|||||||
Baseline Pathogen |
|||||||||||
Gram Positive |
|||||||||||
S. pneumoniae |
82/93 | 88.2 | % | 91/97 | 93.8 | % | |||||
Penicillin Susceptible |
17/21 | 81.0 | % | 16/18 | 88.9 | % | |||||
Penicillin Intermediate |
5/5 | 100 | % | 2/2 | 100 | % | |||||
Penicillin Resistant |
2/2 | 100 | % | 2/3 | 66.7 | % | |||||
Multi-Drug Resistant |
6/6 | 100 | % | 5/6 | 83.3 | % | |||||
Macrolide-Resistant |
6/6 | 100 | % | 5/6 | 83.3 | % | |||||
S. aureus |
10/10 | 100 | % | 4/4 | 100 | % | |||||
Gram Negative |
|||||||||||
H. influenzae |
47/51 | 92.2 | % | 54/57 | 94.7 | % | |||||
M. catarrhalis |
23/25 | 92.0 | % | 11/11 | 100 | % | |||||
Atypicals |
|||||||||||
M. pneumoniae |
16/19 | 84.2 | % | 18/20 | 90.0 | % | |||||
L. pneumophila |
16/18 | 88.9 | % | 12/14 | 85.7 | % | |||||
C. pneumoniae |
10/11 | 90.9 | % | 18/19 | 94.7 | % | |||||
Lefamulin achieved a high clinical response against all of the most common bacterial causes of CABP. As expected, S. pneumoniae was the most common baseline pathogen identified and both lefamulin and moxifloxacin had high clinical success rates. Although a small number of S. pneumoniae resistant to at least one antibiotic was identified, the clinical success rate for lefamulin was 100% compared to with moxifloxacin's response rate of 67 to 83%.
The second most common isolate identified at baseline was H. influenza, with 51 and 57 isolates recovered in the lefamulin and moxifloxacin treatment arms, respectively. The clinical response rate was excellent in both treatment groups, with 92.2% and 94.7% achieving ECR in the lefamulin and moxifloxacin arms, respectively.
S. aureus was identified in 10 subjects receiving lefamulin and 4 subjects in the moxifloxacin +/– linezolid treatment arm, with 100% achieving ECR. All strains of S. aureus were methicillin susceptible. Lastly, against the atypical pathogens, M. pneumoniae, L. pneumophila and C. pneumoniae, both lefamulin and moxifloxacin performed very well with response rates between 84.2 and 94.7%.
LEAP 1 Adverse Events
In the LEAP 1 trial, a similar rate of treatment-emergent adverse events, or TEAEs, was observed in the lefamulin arm (38.1%) and the moxifloxacin with or without linezolid arm (37.7%). In addition, the rates of TEAEs leading to study drug discontinuation were 2.9% for lefamulin versus 4.4% for moxifloxacin with or without linezolid, and the rates of withdrawal from the trial were 1.8% for lefamulin versus 4.0% for moxifloxacin with or without linezolid. Death occurred with similar frequency in both arms, with 6 patients dying in the lefamulin arm (2.2%) and 5 patients dying in the moxifloxacin with or without linezolid arm (1.8%).
Gastrointestinal TEAEs were reported in 13% of patients on moxifloxacin as compared to 6.6% in the lefamulin arm. Of note, although no documented cases of Clostridium difficile infection were
13
reported, diarrhea was observed in 7.7% of those receiving moxifloxacin as compared to 0.7% of those receiving lefamulin.
The chart below provides all of the TEAEs that occurred in >2% of patients in either treatment group. Overall, both treatments were well tolerated, with only hypokalemia, nausea, insomnia, infusion site pain, infusion site phlebitis reported in >2% of lefamulin treated patients, and hypokalemia, nausea, Alanine transaminase increase, hypertension and diarrhea reported in >2% of moxifloxacin treated patients. In addition, no meaningful differences between the lefamulin and moxifloxacin with or without linezolid arms were observed in cardiac (2.9% versus 4.0%) or hepatobiliary (0.7% versus 1.5%) TEAEs.
Preferred Term
|
Lefamulin (n=273) |
Moxifloxacin (±Linezolid) (n=273) |
||
|---|---|---|---|---|
Hypokalemia |
8 (2.9)% | 6 (2.2)% | ||
Nausea |
8 (2.9)% | 6 (2.2)% | ||
Insomnia |
8 (2.9)% | 5 (1.8)% | ||
Infusion Site Pain |
8 (2.9)% | 0 (0.0)% | ||
Infusion Site Phlebitis |
6 (2.2)% | 3 (1.1)% | ||
ALT Increase |
5 (1.8)% | 6 (2.2)% | ||
Hypertension |
2 (0.7)% | 6 (2.2)% | ||
Diarrhea |
2 (0.7)% | 21 (7.7)% |
A summary of the maximum post baseline liver function enzyme elevations is shown below. Approximately 2% of patients in each treatment group had a >5x upper limit of normal ALT, 0.7% having a >5x ULN AST and 1.1% having a total bilirubin >1.5x ULN. In the lefamulin treatment group, one patient had a >10x ULN ALT and one patient had a >10x ULN AST. Neither patient had a baseline value reported and both patients' values reduced to near normal by the TOC visit. Additionally, no patients in either group met criteria for Hy's law.
Lab Parameter
|
Lefamulin | Moxifloxacin (±Linezolid) |
||
|---|---|---|---|---|
Any Post Baseline ALT |
||||
>3xULN |
19/268 (7.1)% | 17/267 (6.4)% | ||
>5xULN |
6/268 (2.2)% | 5/267 (1.9)% | ||
>10xULN |
1/268 (0.4)% | 0/267 (0.0)% | ||
Any Post Baseline AST |
||||
>3xULN |
11/268 (4.1)% | 7/267 (2.6)% | ||
>5xULN |
2/268 (0.7)% | 2/267 (0.7)% | ||
>10xULN |
1/268 (0.4)% | 0/267 (0.0)% | ||
Any Post Baseline Total Bilirubin |
||||
>1.5xULN |
3/268 (1.1)% | 3/267 (1.1)% | ||
>2xULN |
0/268 (0.0)% | 2/267 (0.7)% | ||
Any Post Baseline Alkaline Phosphatase |
||||
>2xULN |
5/268 (1.9)% | 5/267 (1.9)% |
A summary of the post dose QTc changes is shown below. The change in QTcF was measured post dose at the time expected to result in peak concentration of study drug on day 3 which was when both drugs were expected to be at steady state concentrations. Overall, low rates of post dose increases in QTcF were reported in both treatment arms, with no patient in the lefamulin treatment arm
14
experiencing the clinically relevant combination of a post dose change in QTcF >60 msec and an absolute total QtcF >480 msec.
Parameter
|
Lefamulin | Moxifloxacin (±Linezolid) |
||
|---|---|---|---|---|
Post Dose Increase 30 - 60 msec |
12 (4.6)% | 14 (5.4)% | ||
Post Dose Increase > 60 msec |
0 (0.0)% | 1 (0.4)% | ||
Post Dose Value > 500 msec |
1 (0.4)% | 1 (0.4)% |
LEAP 2—Phase 3 Clinical Trial of Oral Lefamulin
Our second Phase 3 clinical trial of lefamulin for the treatment of CABP is a multi-center, randomized, controlled, double-blind study comparing oral lefamulin to moxifloxacin, a fluoroquinolone antibiotic. This trial is designed to assess the non-inferiority of oral lefamulin compared to moxifloxacin. The study population included male and female patients of at least 18 years of age. Enrollment of 738 patients was completed in December 2017. We anticipate that topline clinical results will be available in the spring of 2018. If the results of LEAP 2 are also favorable, including achievement of the primary efficacy endpoints of the trial, we expect to submit an NDA for marketing approval of lefamulin for the treatment of CABP in adults in the United States in the second half of 2018. We also expect to submit an MAA for lefamulin for the treatment of CABP in adults in Europe a few months after our NDA filing.
In LEAP 2, lefamulin was dosed orally at 600mg every 12 hours. The comparator drug moxifloxacin was dosed according to approved labeling at 400 mg daily. All medications were administered according to a double-blind and double-dummy design.
All patients enrolled in this trial were classified as PORT severity of at least 2 and no greater than 4 on a scale of 1 to 5 which corresponds to moderate disease. Patients who had previously taken no more than one dose of a short acting, potentially effective antibiotic for the treatment of the current CABP episode within 24 hours of receiving the first dose of study medication were allowed to participate in the trial but were limited to only up to 25% of the total intent to treat, or ITT, population. Investigators obtained baseline Gram's stain and culture of suitable specimens from the site of infection. Patients were treated for five days with lefamulin or for seven days with moxifloxacin. We assessed patients between 72 and 120 hours from the start of treatment, at the end of treatment, or EOT, within 48 hours of administration of the final dose of study medication, at a TOC visit between five and ten days after administration of the final dose of study medication and at a telephone follow-up 30 days after administration of the first dose of study medication.
We will evaluate the following patient subsets:
- •
- an ITT population consisting of all randomized patients regardless of whether they have received study medication;
- •
- a MITT population consisting of all randomized subjects who receive any amount of study drug;
- •
- a microITT, population consisting of all subjects in the ITT population who have at least one baseline bacterial pathogen known to cause CABP, Legionella
pneumophila from an appropriate microbiological specimen, or CABP caused by Mycoplasma
pneumoniae or Chlamydophila pneumoniae;
- •
- a clinically evaluable, or CE, population which is a subset of the ITT population that will include subjects who meet the criteria for CABP and who have received at least the pre-specified minimal amount of the intended dose of study drug and duration of treatment, do not have an indeterminate response based on the investigator's assessment of clinical response at EOT for the CE-EOT population and at TOC for the CE-TOC population, did not receive concomitant
15
- •
- a microbiologically evaluable, or ME, population consisting of all subjects who meet the criteria for inclusion in both the microITT, CE-EOT and ME-EOT populations or the CE-TOC and ME-TOC populations.
antibacterial therapy that is potentially effective against CABP pathogens (except in the case of clinical failure) from the first dose of study drug through the EOT visit for the CE-EOT population and through the TOC visit for the CE-TOC population, and for whom there are no other confounding factors that interfere with the assessment of the outcome; and
The primary efficacy endpoint for the trial for the FDA is the proportion of patients in the ITT population for the lefamulin treatment group and for the moxifloxacin treatment group who are alive, have improvement in at least two of the four cardinal symptoms of CABP as outlined in the current FDA guidance, have no worsening in any of the four cardinal symptoms of CABP and have not received a concomitant antibiotic for the treatment of CABP up through 120 hours after the first dose of study medication. This endpoint is also referred to as early clinical response. The non-inferiority margin for the FDA primary endpoint is 10.0%, with a power of 90%.
The primary efficacy endpoint for the EMA is the clinical success rate at the TOC visit for lefamulin in both the CE and MITT populations compared to moxifloxacin. Clinical success is based on the investigator's assessment that a patient has clinically responded to treatment, which means that the patient has complete resolution or significant improvement of all local and systemic signs and symptoms of infection such that no additional antibiotic treatment is administered for the treatment of the current episode of CABP. The non-inferiority margin for the EMA primary endpoints is 10%, with a greater than 90% power.
Key secondary efficacy and exploratory endpoints for our second Phase 3 clinical trial include the following:
- •
- assessment of response for the primary efficacy outcome of early clinical response (the FDA primary endpoint) in the microITT population;
- •
- assessment of response in each treatment group with an investigator assessment of clinical response at TOC (the EMA primary endpoint) in the
microITT and ME-TOC populations;
- •
- assessment of the microbiological response by pathogen for the microITT and ME-TOC populations at TOC; and
- •
- assessment of all-cause mortality through day 28 in the ITT population.
Completed Phase 2 Clinical Trial in ABSSSI
ABSSSI
Acute bacterial skin and skin structure infections are common and are characterized by a wide range of disease presentations. Gram-positive bacteria, in particular S. aureus, S. pyogenes and S. agalactiae, are the most common pathogens in ABSSSI. The rising frequency of ABSSSI caused by MRSA and the significant increase in the occurrence of CA-MRSA infections over the past 15 years is an increasing concern. According to IDSA Skin and Skin Structure Infection guidelines 2014, in most U.S. cities, CA-MRSA is now the most common pathogen cultured from patients with ABSSSI in emergency departments. While the current standard of care for MRSA infections is vancomycin, the efficacy of this treatment is being compromised because of decreased susceptibility, or even resistance, of S. aureus to vancomycin. In addition, although linezolid is approved for ABSSSI due to MRSA, its use has been limited because of potential adverse events and drug-drug interactions with commonly prescribed concomitant medications such as antidepressants.
16
The emerging incidence of resistance to multiple antibiotics in pathogens makes ABSSSI increasingly difficult to treat and results in a need for alternate therapies. Based on our preclinical studies and clinical trials, we believe that lefamulin has potential to treat ABSSSI. In preclinical studies, lefamulin has shown in vitro antibacterial activity against the most relevant pathogens responsible for ABSSSI including S. aureus (MSSA, MRSA, and CA-MRSA), S. pyogenes, and S. agalactiae.
In 2011, we completed a multi-center, randomized, double-blind Phase 2 clinical trial in the United States evaluating the efficacy, safety and pharmacokinetics of two different doses of the IV formulation of lefamulin administered over five to 14 days compared to vancomycin in patients with ABSSSI, and the clinical success rate at test of cure for lefamulin was similar to that of vancomycin. We selected ABSSSI as the indication for the trial to ensure that there would be a significant population of patients with multi-drug resistant Gram-positive bacteria. Gram-positive bacteria are the prevalent pathogens in ABSSSI. We selected vancomycin as the comparison therapy because vancomcyin is one of the antibiotics recommended by IDSA guidelines for the treatment of ABSSSI.
We have discussed the design of a proposed Phase 3 clinical trial to evaluate the efficacy and safety of lefamulin for the treatment of ABSSSI with the FDA and several E.U. regulatory authorities.
Efficacy
In the trial, the patients in the lefamulin treatment groups experienced a similar clinical success rate at the TOC visit as patients in the vancomycin treatment group, in each of the ITT, MITT, CE and ME patient subsets. These results are summarized in the table below. In addition, the clinical success rate in the trial was high for important subgroups of patients based on factors such as primary infection type and diabetes mellitus status. The table below also shows the 95% confidence interval, a statistical determination that demonstrates the range of possible differences in the point estimate of success that will arise 95% of the time that the endpoint is measured. However, this trial was not statistically powered to determine differences between treatment groups. The sample size chosen was to provide clinically meaningful information on efficacy, safety and tolerability. In this table and other tables appearing below, the abbreviation "N" refers to the number of patients or subjects in each group or subgroup.
Clinical Success Rate at the TOC Visit (ITT, MITT, CE and ME Populations)
Population
|
Clinical Response | Lefamulin 100 mg |
Lefamulin 150 mg |
Vancomycin 1,000 mg |
||||
|---|---|---|---|---|---|---|---|---|
ITT |
N=70 | N=71 | N=66 | |||||
|
Success N (%) | 60 (85.7) | 59 (83.1) | 54 (81.8) | ||||
|
Failure N (%) | 9 (12.9) | 8 (11.3) | 9 (13.6) | ||||
|
Not determined N (%) | 1 (1.4) | 4 (5.6) | 3 (4.5) | ||||
|
95% CI | (75.3, 92.9) | (72.3, 91.0) | (70.4, 90.2) | ||||
MITT |
N=50 |
N=51 |
N=51 |
|||||
|
Success N (%) | 41 (82.0) | 42 (82.4) | 42 (82.4) | ||||
|
Failure N (%) | 8 (16.0) | 6 (11.8) | 6 (11.8) | ||||
|
Not determined N (%) | 1 (2.0) | 3 (5.9) | 3 (5.9) | ||||
|
95% CI | (68.6, 91.4) | (69.1, 91.6) | (69.1, 91.6) | ||||
CE |
N=60 |
N=54 |
N=51 |
|||||
|
Success N (%) | 54 (90.0) | 48 (88.9) | 47 (92.2) | ||||
|
Failure N (%) | 6 (10.0) | 6 (11.1) | 4 (7.8) | ||||
|
95% CI | (79.5, 96.2) | (77.4, 95.8) | (81.1, 97.8) | ||||
ME |
N=46 |
N=43 |
N=40 |
|||||
|
Success N (%) | 40 (87.0) | 38 (88.4) | 38 (95.0) | ||||
|
Failure N (%) | 6 (13.0) | 5 (11.6) | 2 (5.0) | ||||
|
95% CI | (73.7, 95.1) | (74.9, 96.1) | (83.1, 99.4) |
17
In the trial, the patients in the lefamulin treatment groups also experienced a similar clinical response at the day 3 visit as patients in the vancomycin treatment group in each of the ITT, MITT, CE and ME patient subsets. The clinical response results for the ITT patient subset are presented in the table below. Importantly, the assessment at day 3 included evaluation of a new primary endpoint recommended by the FDA of at least a 20% reduction in area of erythema, or redness.
Clinical Response at Day 3 (ITT Population)
Definition of Responder Used
|
Lefamulin 100 mg (N=70) N (%) |
Lefamulin 150 mg (N=71) N (%) |
Vancomycin 1,000 mg (N=66) N (%) |
|||
|---|---|---|---|---|---|---|
Overall clinical response |
53 (88.3) | 48 (88.9) | 44 (86.3) | |||
Absence of fever at Day 3 |
67 (95.7) | 67 (94.4) | 61 (92.4) | |||
No increase in area of erythema plus absence of fever |
60 (85.7) | 59 (83.1) | 53 (80.3) | |||
No increase in area of erythema and swelling and absence of fever |
53 (75.7) | 53 (74.6) | 49 (74.2) | |||
>20% reduction in area of erythema |
52 (74.3) | 50 (70.4) | 47 (71.2) |
A list of all pathogens identified at baseline along with the corresponding eradication rate by treatment group in the MITT patient subset is presented in the table below. Microbiological eradication rate was defined as the proportion of patients with a microbiological outcome of eradication or presumed eradication based on cultures from both the primary infection site and blood cultures. Patients with indeterminate or missing clinical responses were considered non-eradication. Overall, in the MITT population, microbiological success was achieved in 40 of 50 patients (80.0%) in the lefamulin 100 mg group, 43 of 51 patients (84.3%) in the lefamulin 150 mg group, and 42 of 51 patients (82.4%) in the vancomycin group. We did not observe development of decreased susceptibility to lefamulin or vancomycin during the trial. In this table, the abbreviation "n" refers to the number of patients who had a microbiological outcome of eradication or presumed eradication for each specified pathogen.
Sponsor-Assessed Microbiological Eradication Rate at the TOC Visit by Baseline Target Pathogen (MITT Population)
Baseline Pathogen
|
Lefamulin 100mg (N=50) n/N (%) |
Lefamulin 150mg (N=51) n/N (%) |
Vancomycin 1,000mg (N=51) n/N (%) |
|||
|---|---|---|---|---|---|---|
Staphylococcus aureus |
35/44 (79.5) | 41/47 (87.2) | 40/47 (85.1) | |||
MRSA |
28/34 (82.4) | 28/32 (87.5) | 32/39 (82.1) | |||
MSSA |
8/11 (72.7) | 13/15 (86.7) | 8/8 (100.0) | |||
Streptococcus species |
6/7 (85.7) | 3/5 (60.0) | 4/7 (57.1) | |||
Streptococcus pyogenes |
2/3 (66.7) | 1/2 (50.0) | 1/4 (25.0) | |||
Streptococcus agalactiae |
2/2 (100.0) | 2/3 (66.7) | 0/0 (0.0) | |||
Streptococcus Group C |
0/0 (0.0) | 0/0 (0.0) | 1/1 (100.0) | |||
Streptococcus Group F |
1/1 (100.0) | 0/0 (0.0) | 0/0 (0.0) | |||
Streptococcus Group G |
0/0 (0.0) | 0/1 (0.0) | 1/1 (100.0) | |||
Streptococcus constellatus |
1/1 (100.0) | 0/0 (0.0) | 0/0 (0.0) | |||
Streptococcus intermedius |
1/1 (100.0) | 0/0 (0.0) | 2/2 (100.0) |
We evaluated the clinical success of lefamulin against S. aureus, which is the most commonly identified cause of ABSSSI. The clinical success rate against a variety of subsets of S. aureus based on in vitro antibiotic susceptibility (methicillin-resistance), as well as the presence or absence of the virulence factors PVL-positivity or USA300, are clinically important, as limited therapeutic options exist to treat such infection. A summary of the clinical success rate against S. aureus is presented in the table
18
below. The clinical success rates for lefamulin against PVL-positive MRSA and USA300 MRSA strains were similar to, or numerically higher than, the corresponding clinical success rates for vancomycin. In this table, the abbreviation "n" refers to the number of patients with clinical success for each specified pathogen.
Clinical Success Rate at the TOC Visit by Baseline Target Pathogens (S. aureus) (MITT Population)
Baseline Pathogen PVL/PFGE Type |
Lefamulin 100 mg (N=50) n/N (%) |
Lefamulin 150 mg (N=51) n/N (%) |
Vancomycin 1,000 mg (N=51) n/N (%) |
|||
|---|---|---|---|---|---|---|
Staphylococcus aureus |
36/44 (81.8) | 41/47 (87.2) | 40/47 (85.1) | |||
MRSA |
29/34 (85.3) | 28/32 (87.5) | 32/39 (82.1) | |||
PVL positive |
27/32 (84.4) | 27/31 (87.1) | 30/37 (81.1) | |||
PFGE USA300 |
21/25 (84.0) | 18/19 (94.7) | 21/27 (77.8) | |||
MSSA |
8/11 (72.7) | 13/15 (86.7) | 8/8 (100.0) | |||
PVL positive |
4/6 (66.7) | 7/8 (87.5) | 4/4 (100.0) |
The mean duration of exposure to study medication treatment was approximately seven days for all groups, and almost 70% of patients completed therapy within that time.
Safety and tolerability
Lefamulin was well tolerated in this trial. No patient in the trial suffered any serious adverse events that were found to be related to lefamulin, and no patient in the trial died. The percentage of patients in the trial arms that experienced any treatment emergent adverse event were similar across treatment groups: 71.4% in the lefamulin 100 mg group, 69.0% in the lefamulin 150 mg group and 74.2% in the vancomycin group. Most of the treatment emergent adverse events were mild to moderate in severity. The table below shows the adverse events experienced by patients in the trial that were assessed by the investigator as possibly or probably related to study medication.
19
Drug-Related Treatment-Emergent Adverse Events by Preferred Term Reported by More Than 2% of Patients in the ITT Population
Adverse Event
|
Lefamulin 100 mg (N=70) N (%) |
Lefamulin 150 mg (N=71) N (%) |
Vancomycin 1,000 mg (N=66) N (%) |
|||
|---|---|---|---|---|---|---|
Headache |
5 (7.1) | 9 (12.7) | 10 (15.2) | |||
Nausea |
5 (7.1) | 6 (8.5) | 10 (15.2) | |||
Infusion site phlebitis |
4 (5.7) | 2 (2.8) | 0 (0.0) | |||
Diarrhea |
3 (4.3) | 4 (5.6) | 4 (6.1) | |||
Vomiting |
3 (4.3) | 2 (2.8) | 3 (4.5) | |||
Alanine aminotransferase increased |
2 (2.9) | 2 (2.8) | 3 (4.5) | |||
Pruritus generalized |
2 (2.9) | 1 (1.4) | 4 (6.1) | |||
Creatine phosphokinase increased |
2 (2.9) | 1 (1.4) | 0 (0.0) | |||
Phlebitis |
2 (2.9) | 0 (0.0) | 0 (0.0) | |||
Vulvovaginal mycotic infection |
2 (2.9) | 0 (0.0) | 0 (0.0) | |||
Abdominal pain |
1 (1.4) | 2 (2.8) | 0 (0.0) | |||
Aspartate aminotransferase increased |
1 (1.4) | 1 (1.4) | 2 (3.0) | |||
Pruritus |
0 (0.0) | 2 (2.8) | 8 (12.1) | |||
Infusion site pain |
0 (0.0) | 2 (2.8) | 0 (0.0) | |||
Tinnitus |
0 (0.0) | 2 (2.8) | 0 (0.0) | |||
Infusion site reaction |
0 (0.0) | 2 (2.8) | 0 (0.0) | |||
Constipation |
0 (0.0) | 1 (1.4) | 3 (4.5) | |||
Insomnia |
0 (0.0) | 0 (0.0) | 2 (3.0) |
The incidences of pain, tenderness, itching, erythema, swelling and thrombosis at the infusion site were higher for the lefamulin 100 mg group and the lefamulin 150 mg group than for the vancomycin group. The majority of these local tolerability symptoms were mild in severity. No patient had a severe local tolerability issue of erythema or swelling. No patient had a local tolerability issue of necrosis. When summarized on an infusion basis, the proportions of infusions with local tolerability events were similar for the treatment groups.
Four patients discontinued study medication following a drug-related adverse event: one patient (1.4%) in the lefamulin 100 mg group (events of hyperhidrosis, vomiting and headache), two patients (2.8%) in the lefamulin 150 mg group (infusion site pain in one patient and dyspnea in the other), and one patient (1.5%) in the vancomycin group (drug eruption).
Because the potential for mild effect on ECG measurements was observed in preclinical studies, we have continued to assess this potential in all human clinical trials we have conducted. In the Phase 2 clinical trial, no change in ECG measurements was considered to be of clinical significance, and no drug-related cardiovascular adverse event was reported. Both lefamulin and vancomycin treatment were associated with a small increase in the QT interval. The QT interval is a measure of the heart's electrical cycle, with a lengthened QT interval representing a marker for potential ventricular arrhythmia. We plan to continue to evaluate the effect of lefamulin on the QT interval in our Phase 3 clinical trials of lefamulin for CABP.
Pharmacokinetics
The table below summarizes selected pharmacokinetic parameters we obtained from pharmacokinetic sampling in the trial. Cmax refers to the maximum observed peak blood plasma concentration of study medication. AUC refers to the area under the curve in a plot of concentration of study medication in blood plasma over time, representing total drug exposure over time. In this table, the abbreviation "SD" refers to the standard deviation of the results. Standard deviation is a
20
statistical measure used to quantify the amount of variation within a set of data values. A standard deviation close to zero indicates that the data points do not vary greatly from the mean, while a high standard deviation indicates that the data points are spread over a wider range of values.
Summary Statistics for PK Exposure and Secondary PK Parameters
| |
Dose (mg) | Mean (SD) | |||
|---|---|---|---|---|---|
Cmax (Day 1) |
100 | 1.57 (0.974) | |||
(µg/mL) |
150 | 1.90 (0.705) | |||
Cmax (Day 5) |
100 | 1.67 (0.974) | |||
(µg/mL) |
150 | 2.06 (0.737) | |||
AUC0[ib]-12hr (Day 1) |
100 | 5.14 (2.95) | |||
(µg·hr/mL) |
150 | 6.59 (2.69) | |||
AUC0[ib]-12hr (Day 5) |
100 | 6.23 (3.02) | |||
(µg·hr/mL) |
150 | 8.27 (3.11) | |||
Half-life |
100 | 11.0 (5.18) | |||
(hour) |
150 | 13.2 (5.79) | |||
Efficacy for the pleuromutilin class of antibiotics is related to the ratio of total drug exposure over time, measured by the AUC, to minimum inhibitory concentration, or MIC. MIC is the minimum concentration of an antibiotic needed to inhibit growth of an organism. The plasma concentration data obtained from the Phase 2 clinical trial are the first data that describe how lefamulin is absorbed, distributed around the body, metabolized and eliminated in patients suffering from an infection.
Phase 1 Clinical Development
The objectives of our Phase 1 clinical trial program have been to understand the absorption and distribution of lefamulin in the blood and target tissues, evaluate the metabolism and elimination route of lefamulin and obtain safety and tolerability data to help predict safe and effective doses of lefamulin for the treatment of patients. In our Phase 1 clinical trials, subjects were exposed to single or multiple doses of IV or oral lefamulin.
Our ongoing Phase 1 trials include two special populations studies (renal and hepatic impairment), one drug-drug interaction study, and a hADME study. All studies have completed enrollment but have not yet been reported.
In the clinical Phase1 trials completed to date 382 male and female subjects, including elderly healthy subjects, were exposed to lefamulin in 12 studies where lefamulin was administered orally and in 10 studies with lefamulin administered intravenously. In these trials, there were no observed systemic adverse events of clinical concern and no serious adverse events in any of the Phase1 clinical trials with oral or IV administration of lefamulin.
Pharmacokinetic Overview
Our key observations from our Phase 1 clinical trials include the following:
- •
- lefamulin is rapidly absorbed and distributed throughout the body after either IV or oral administration;
- •
- lefamulin achieves therapeutic concentrations in a variety of target tissues, including the lung, skin and soft tissue;
- •
- lefamulin has a half-life between 8.6 and 11.8 hours, which enables a twice daily regimen, and is eliminated primarily through non-renal pathways;
21
- •
- lefamulin is a weak inhibitor of some liver enzymes, and we expect it to have limited adverse drug-drug interaction potential;
- •
- no statistically significant effects of age, gender, body weight or height, body mass index or other demographics on the pharmacokinetic
parameters of lefamulin;
- •
- the absolute oral bioavailability of a 600 mg immediate release, or IR, tablet formulation of lefamulin were 25.8% in the fasted and 21% in the
fed condition in healthy subjects; and
- •
- in the assessment of relative bioavailability, bioequivalence was demonstrated for the fasted IR tablet and the IV dose, exposure was slightly lower for the fed IR tablet than the IV dose.
Absorption
Lefamulin is absorbed rapidly after oral dosing with or without food. In our Phase 1 clinical trials, steady state blood levels were achieved after two days of dosing every 12 hours, irrespective of the route of administration, and the variability after oral dosing was similar to the variability after IV infusion. Because the ability of pleuromutilin antibiotics to kill bacteria is dependent on the AUC, or total lefamulin exposure over time, to MIC ratio, and IV doses of 150 mg every 12 hours and oral doses of 600 mg every 12 hours achieve similar AUCs, we believe that both regimens are capable of providing a similar therapeutic benefit.
Distribution
Following IV infusion, lefamulin is rapidly distributed throughout the body over approximately 30 minutes. We have observed rapid distribution of lefamulin into tissues, including the skin and ELF of the lung. In CABP, the lung is the target organ where pathogens replicate and cause inflammation that results in mucous production, cough and shortness of breath. Therefore, in 2010, we conducted a Phase 1 clinical trial to assess the pharmacokinetics of lefamulin in 12 healthy subjects. After a single IV administration of 150 mg of lefamulin over 60 minutes, we performed a bronchoalveolar lavage, or BAL, a medical procedure to collect fluid from the lung. We performed BAL analyses in groups of three subjects at 1, 2, 4 and 8 hours after the start of the lefamulin infusion and measured lefamulin concentrations in the ELF, the muscle tissue, soft tissue and blood plasma. In this trial, the exposure of free lefamulin, or the amount of lefamulin not bound to proteins and therefore available to inhibit bacterial growth, achieved in the ELF was approximately six times greater than free lefamulin exposure observed in blood plasma.
Metabolism
The average half-life, or the time it takes the body to eliminate one-half of the concentration of lefamulin present, is 9 to 12 hours. The major route lefamulin is eliminated from the body is the gastrointestinal tract, with limited metabolism of lefamulin occurring mainly through a liver and gut wall enzyme called CYP3A4, which is responsible for the metabolism of a wide variety of medication. We have identified only one metabolite, called BC-8041, as exceeding 10% of lefamulin concentrations in the plasma and only when lefamulin was given orally. None of the metabolites of lefamulin have any antibacterial properties.
Drug Interaction Potential
We continue to perform studies recommended by regulatory authorities to assess the drug-drug interaction potential of new drug products, including the assessment of the impact of potent P-glycoprotein and CYP3A4 inducers on the PK of lefamulin, and the impact of lefamulin on drugs metabolized via CYP3A4. Six drug-drug interaction studies have been completed to date.
22
Safety and Tolerability
Lefamulin has been well tolerated in all Phase 1 trials completed to date. We did not observe any systemic adverse events of clinical concern or any drug-related serious adverse events in these trials. In addition, we did not observe any changes of clinical concern in laboratory safety parameters or vital signs in any subject in any of the trials. The most commonly observed adverse effects with oral administration of lefamulin were related to the gastrointestinal tract, including nausea and abdominal discomfort, while the most commonly observed adverse effects related to IV administration were related to irritation at the infusion site. In addition, lefamulin produced a transient, predictable and reproducible prolongation of the QT interval based on the maximum concentration of the drug in the blood plasma. At therapeutic doses, we expect that the drug will not produce large effects on the QT interval that would be of clinical relevance. We did not observe any drug-related cardiac adverse events, such as increase in ectopic ventricular activity or other cardiac arrhythmia, or clinically relevant ECG findings during the conduct of any of our Phase 1 clinical trials.
Intravenous Formulation
We have administered IV lefamulin as single and repeat doses every 12 hours for up to 14 days. The most frequently reported adverse events in our Phase 1 clinical trials were pain or erythema at the site of the IV infusion. To further assess local tolerability, we conducted a Phase 1 clinical trial in 2013 to evaluate the local tolerability of two different IV formulations of lefamulin dosed every twelve hours for 7.5 days. In this trial, we compared lefamulin infusions given in normal saline solution, a sterile sodium chloride solution commonly used to administer IV medications, with lefamulin infusions given in a sterile saline solution buffered by a citrate salt that adjusted the pH, or level of acidity, of the solution. We enrolled 60 healthy subjects in the trial, of which 25 received the normal saline solution, 25 received the citrate buffered solution and ten received a matching placebo solution. Although we did not observe any difference between treatment arms over the first three days of study infusions, over the entire treatment period, the incidence of local pain or redness of at least moderate severity was statistically higher with lefamulin in the saline solution (84%), as compared to the citrate buffered infusions (36%) or placebo (10%). There was no statistical difference between citrate buffered infusions and placebo at any time period during the trial. As a result, we will administer lefamulin IV infusions in a citrate buffered saline solution in our Phase 3 clinical trials for CABP.
Oral Formulation
Initially, we administered lefamulin orally in capsules as single and repeat doses for up to five days. Oral administration of lefamulin was generally well tolerated with infrequent reports of mild gastrointestinal findings, such as nausea, abdominal pain and diarrhea. We subsequently developed 600 mg IR tablets that we have investigated in single and repeat dose studies. These tablets have been well tolerated and shown favorable pharmacokinetics. We will utilize the 600 mg tablets in our Phase 3 clinical trials.
Electrocardiogram Measurements
In our Phase 1 clinical trials, lefamulin was associated with a Cmax-dependent, transient, predictable, reversible and reproducible prolongation of the QT interval. We have closely monitored ECG measurements in all our trials. We did not observe any drug-related cardiac adverse events, such as increase in ectopic ventricular activity or other cardiac arrhythmia, or clinically relevant ECG findings during the conduct of any of our Phase 1 clinical trials. None of the ECG stopping criteria defined in the trial protocols was reached in any clinical trial. We plan to continue to assess the effects of lefamulin on the QT interval in our planned clinical trials.
23
Preclinical Development
In our preclinical studies, administration of lefamulin was well tolerated in a variety of animal models. Lefamulin was active against a broad range of bacteria, suggesting possible use as monotherapy for CABP with a low propensity for development of bacterial resistance.
Nonclinical Safety
In several nonclinical safety studies, including repeat dose toxicity, local tolerance, genotoxicity, development and reproductive toxicity, and safety pharmacology testing in both rodent and non-rodent species, lefamulin was well tolerated. When we treated rats or monkeys for up to three months with either oral or IV lefamulin, we did not identify any systemic target organ toxicity. Lefamulin was not associated with genetic damage, effects on fertility or teratogenicity. We are also conducting toxicity studies in juvenile animals. A potential for QT/QTc interval prolongation was noted in nonclinical studies. The nonclinical safety package to support an NDA for lefamulin in the treatment of CABP in adults has been completed.
Antimicrobial Spectrum of Lefamulin
We have extensively studied the in vitro antimicrobial activity of lefamulin against a variety of respiratory, or aerobic, and non-respiratory, or anaerobic, bacterial pathogens representing more than 22,500 clinical isolates collected from patients worldwide. A summary of our observations is presented in the table below. MIC90 indicates the concentration of drug that inhibits 90% of the pathogens in vitro, while MIC50 indicates the concentration of drug that inhibits 50% of the pathogens in vitro.
Antimicrobial Activity of Lefamulin Against Gram-Positive, Gram-Negative and Atypical Bacteria
| |
|
|
MIC [µg/mL] | |||||
|---|---|---|---|---|---|---|---|---|
Organism
|
n | 50% | 90% | Range | ||||
Aerobic and facultative anaerobic Gram-positive microorganisms |
||||||||
S. aureus |
9630 | 0.06 | 0.12 | £0.008 - ³32 | ||||
S. aureus, MSSA |
5475 | 0.06 | 0.12 | £0.008 - ³32 | ||||
S. aureus, MRSA |
4155 | 0.12 | 0.25(a) | £0.008 - ³32 | ||||
CA-MRSA (USA 300/400) |
50 | 0.12 | 0.12 | 0.06 - 0.12 | ||||
S. aureus, Vancomycin non-susceptible (VRSA, VISA, hVISA) |
30 | 0.06 | 0.25 | 0.03 - 0.5 | ||||
Coagulase negative Staphylococcus spp. |
1133 | 0.06 | 0.12 | £0.008 - ³32 | ||||
S. epidermidis |
474 | 0.06 | 0.25 | £0.008 - ³32 | ||||
S. pneumoniae |
5658 | 0.12 | 0.25 | £0.008 - 1 | ||||
S. pneumoniae, penicillin non-susceptible(b) |
358 | 0.12 | 0.25 | 0.015 - 0.5 | ||||
S. pneumoniae, macrolide-resistant(c) |
1867 | 0.12 | 0.25 | £0.008 - 1 | ||||
S. pneumoniae, levofloxacin-resistant(d) |
57 | 0.06 | 0.25 | 0.015 - 1 | ||||
S. pyogenes (Group A Streptococcus spp.) |
472 | 0.03 | 0.03 | £0.008 - 0.12 | ||||
S. agalactiae (Group B Streptococcus spp.) |
503 | 0.03 | 0.06 | £0.008 - 16 | ||||
Group C Streptococcus spp. |
116 | 0.03 | 0.06 | 0.015 - 0.5 | ||||
Group G Streptococcus spp. |
160 | 0.03 | 0.06 | 0.015 - 0.25 | ||||
Viridans Group Streptococcus spp. |
445 | 0.12 | 0.5 | £0.008 - 4 | ||||
E. faecalis |
50 | ³32 | ³32 | 4 - ³32 | ||||
E. faecium |
850 | 0.12 | 8(e) | 0.015 - ³32 | ||||
E. faecium, VSE |
361 | 0.12 | ³32 | 0.03 - ³32 | ||||
E. faecium, VRE |
389 | 0.06 | 0.5 | 0.015 - ³32 | ||||
24
| |
|
|
MIC [µg/mL] | |||||
|---|---|---|---|---|---|---|---|---|
Organism
|
n | 50% | 90% | Range | ||||
B. pertussis |
6 | 0.03 | 0.03 - 0.03 | |||||
H. influenzae |
1628 | 0.05 | 1 | 0.015 - ³8 | ||||
H. influenzae, ß-lactamase positive |
336 | 0.5 | 1 | 0.06 - 8 | ||||
H. ducreyi |
6 | — | — | £0.015 - 0.25 | ||||
L. pneumophila(f) |
30 | 0.12 (0.06) | 0.5 (0.5) | 0.12 - 1 (0.06 - 1) | ||||
M. catarrhalis |
1076 | 0.06 | 0.12 | £0.008 - 1 | ||||
N. gonorrhoeae |
344 | 0.25 | 1 | £0.008 - 2 | ||||
N. gonorrhoeae, azithromycin-resistant |
123 | 0.5 | 1 | 0.016 - 2 | ||||
E. coli |
26 | 16 | 32 | 4 - 64 | ||||
Anaerobic microorganisms |
||||||||
C. difficile |
43 | 4 | 8 | 0.25 - ³64 | ||||
Clostridium spp.(g) |
10 | 1 | >16 | 0.06 - ³32 | ||||
Peptostreptococcus spp.(h) |
10 | 0.06 | 1 | 0.03 - 2 | ||||
Porphyromonas spp.(i) |
10 | 0.03 | 0.03 | 0.03 | ||||
B. fragilis |
11 | 16 | ³32 | 2 - ³32 | ||||
B. fragilis group |
11 | ³32 | ³32 | 1 - ³32 | ||||
Prevotella spp.(j) |
10 | 0.5 | 4 | 0.015 - ³32 | ||||
Propionibacterium spp.(k) |
17 | 0.008 | 0.12 | 0.008 - 0.25 | ||||
Other microorganisms |
||||||||
C. pneumoniae |
50 | 0.02 | 0.04 | 0.02 - 0.08 | ||||
C. trachomatis |
15 | 0.02 | 0.04 | 0.01 - 0.04 | ||||
M. genitalium(l) |
5 | — | — | 0.016 - 0.06 | ||||
M. genitalium |
41 | £0.08 | 0.06 | 0.005 - 0.06 | ||||
M. pneumoniae |
50 | 0.006 | 0.006 | £0.003 - 0.024 | ||||
M. pneumoniae(m) |
50 | 0.001 | 0.002 | £0.00025 - 0.004 | ||||
M. pneumoniae, macrolide-resistant |
7 | £0.001 | 0.002 | £0.001 - 0.008 | ||||
- (a)
- 89.8%
of MRSA isolates inhibited at 0.12 µg/mL
- (b)
- Using
parenteral non-meningitis breakpoints of CLSI, 2017
- (c)
- Using
the erythromycin breakpoint of CLSI, 2017
- (d)
- Using
the 2017 CLSI breakpoints
- (e)
- 82.6%
of E. faecium isolates inhibited at 0.5 µg/mL
- (f)
- MIC
values determined by microbroth dilution using charcoal supplemented BCYEa medium; MIC values in brackets show MIC values
determined in BYEa medium without charcoal supplementation
- (g)
- C. butyricum (n=1), C. cadaveris (n=1), C.
clostridioforme (n=2), C. innocuum (n=1), C. perfringens (n=5)
- (h)
- Finegoldia magna (n=3), P. anaerobius (n=1), P. asaccharolyticus (n=2), P. micros (n=2), P. tetradius
(n=2)
- (i)
- P. gingivalis (n=9), non-specified Porphyromonas (n=1)
- (j)
- P. bivia (n=4), P. intermedia (n=2), P.
melaninogenica (n=2), and P. oralis (n=2)
- (k)
- P. acnes (n = 5). P. avidum (n = 5), P. granulosum (n = 7)
25
- (l)
- MDR
clinical isolates from patients failing treatment with high doses of azithromycin, moxifloxacin, and doxycycline
- (m)
- 72% of M. pneumoniae isolates were resistant to macrolides
The tables below compare the in vitro activity of lefamulin and various antibiotics for CABP and ABSSSI pathogens against various strains of bacteria, including those resistant to current antibiotics. Unlike other CABP antibiotics, such as ß-lactam/ß-lactamase inhibitor combinations, glycopeptides and oxazolidinones, lefamulin was active against the vast majority of potential respiratory pathogens collected in 2010, 2015 and 2016. When an alternative antibiotic from the same drug class was utilized, it is footnoted within the table and below.
Lefamulin in vitro Activity Against CABP Bacteria
Organism (Number of Strains Tested) |
Lefamulin MIC90 [µg/mL] |
Levofloxacin MIC90 [µg/mL] |
Azithromycin MIC90 [µg/mL] |
Doxcycline MIC90 [µg/mL] |
Ceftriaxone MIC90 [µg/mL] |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
Streptococcus pneumoniae (5,396) |
0.25 | 1 | >4 | 8 | 1 | |||||
Haemophilus influenzae (1,446) |
1 | <0.5 | 2 | 0.5 | <0.06 | |||||
Moraxella catarrhalis (920) |
0.12 | <0.5 | <0.25 | 0.25 | 0.5 | |||||
Staphylococcus aureus incl. MRSA (8,446) |
0.12 | >4 | >4 | 0.25 | * | |||||
Legionella pneumophila (30) |
0.5 | 0.015 | 0.015 | * | * | |||||
Mycoplasma pneumoniae (60) |
0.002 | 0.25(a) | >32 | 0.25 | * | |||||
Chlamydophila pneumoniae (50)(b) |
0.04 | 0.32 - 1.28 | 0.08 - 0.16 | 0.04 | * |
- (a)
- Moxifloxacin
used instead of levofloxacin against M. pneumoniae.
- (b)
- Only
two strains tested for comparators.
- *
- Not determined.
Lefamulin displayed potent antibacterial activity against bacterial pathogens predominantly causing skin and blood stream infections, such as S. aureus, coagulase-negative staphylococci, ß-hemolytic and viridans group streptococci, as well as E. faecium, including vancomycin-resistant strains, or VRE. Isolates were collected in the SENTRY surveillance study in 2010.
Lefamulin in vitro Activity Against ABSSSI Bacteria and Pathogens Causing Bacteremia
Organism (Number of Strains Tested) |
Lefamulin MIC90 [µg/mL] |
Erythromycin MIC90 [µg/mL] |
Doxycycline MIC90 [µg/mL] |
Vancomycin MIC90 [µg/mL] |
||||
|---|---|---|---|---|---|---|---|---|
S. aureus (5,527) |
0.12 | >4 | 0.25 | 1 | ||||
MSSA (3,157) |
0.12 | >4 | 0.25 | 1 | ||||
MRSA (2,370) |
0.25 | >4 | 1 | 1 | ||||
CoNS (878) |
0.12 | >4 | 2 | 2 | ||||
E. faecium (536) |
4 | >4 | >8 | >16 | ||||
Vancomycin non-susceptible (304) |
0.25 | >4 | >8 | >16 | ||||
ß-hemolytic Streptococcus species (763) |
0.03 | >4 | 8 | 0.5 | ||||
S. pyogenes (267) |
0.03 | £0.25 | 8 | 0.5 | ||||
S. agalactiae (334) |
0.03 | >4 | 8 | 0.5 | ||||
Viridans group Streptococcus species (245) |
0.5 | >4 | >8 | 0.5 |
26
Activity Against Resistant Strains and Low Propensity for Development of Bacterial Resistance
When tested against bacterial organisms resistant to macrolides, tetracyclines, quinolones, trimethoprim/sulfamethoxazole, vancomycin, mupirocin or ß-lactams, we did not observe any cross-resistance with lefamulin. Lefamulin displayed activity in vitro against drug-resistant N. gonorrhoeae, VRE, MRSA, multi-drug resistant S. pneumoniae, VISA/hVISA, erythromycin-resistant group A Streptococcus species and clindamycin-resistant group B Streptococcus species, all of which are listed as urgent, serious or concerning threats by the CDC. We utilized the interpretative criteria of the Clinical and Laboratory Standards Institute, or CLSI, to categorize the in vitro activity of each comparator against the organisms listed in the table below as sensitive (%S), intermediate (%I) or resistant (%R).
27
Lefamulin in vitro Activity Against Resistant Bacterial Pathogens Listed as Urgent, Serious or Concerning Threats According to CDC
| |
|
MIC [µg/mL] | CLSI | |||||
|---|---|---|---|---|---|---|---|---|
Organism
|
N | 50% | 90% | %S /%I /%/R | ||||
Urgent Threats |
||||||||
Drug-resistant Neisseria gonorrhoeae |
||||||||
Lefamulin |
93 | 0.12 | 0.5 | — /—/— | ||||
Azithromycin |
58 | 0.12 | 1 | 81.0 /6.9 / 12.1(b) | ||||
Tetracycline |
58 | 0.5 | 2 | 19.0 / 56.9 / 24.1(c) | ||||
Ciprofloxacin |
58 | 0.25 | 16 | 37.9 / 20.7 /41.4(c) | ||||
Ceftriaxone |
54 | 0.015 | 0.06 | 100.0 / 0.0 /0.0(c) | ||||
Serious Threats |
||||||||
Methicillin-resistant Staphylococcus aureus (MRSA) |
||||||||
Lefamulin |
3,308 | 0.12 | 0.12 | — /—/ — | ||||
Azithromycin |
3,308 | >4 | >4 | 23.8 / 0.7 / 75.5 | ||||
Ceftaroline |
3,308 | 1 | 2 | 84.5 / 15.0 / 0.4 | ||||
Clindamycin |
3,308 | £0.25 | >2 | 63.1 / 0.1 / 36.8 | ||||
Doxycycline |
3,308 | 0.12 | 0.12 | 95.7 / 3.6 / 0.7 | ||||
Erythromycin |
3,308 | >4 | >4 | 17.4 / 2.0 / 80.7 | ||||
Levofloxacin |
3,308 | >4 | >4 | 26.6 / 1.9 / 71.5 | ||||
Linezolid |
3,308 | 1 | 1 | 100.0 /—/ 0.0 | ||||
Moxifloxacin |
3,308 | 2 | >4 | 29.7 / 18.5 / 51.9 | ||||
Oxacillin |
3,308 | >2 | >2 | 0.0 /—/ 100.0 | ||||
Trimethoprim-sulfamethoxazole |
3,308 | £0.5 | £0.5 | 95.6 /—/ 4.4 | ||||
Vancomycin |
3,308 | 1 | 1 | 100.0 /—/ 0.0 | ||||
Drug-resistant Streptococcus pneumoniae |
||||||||
Lefamulin |
1,867 | 0.12 | 0.25 | — /—/ — | ||||
Azithromycin |
1,867 | >4 | >4 | 0.5 / 1.1 / 98.4 | ||||
Ceftriaxone (non-meningitis) |
1,867 | 0.5 | 2 | 85.4 / 11.7 / 2.9 | ||||
Erythromycin |
1,867 | >2 | >2 | 0.0 /—/ 100.0 | ||||
Levofloxacin |
1,867 | 1 | 1 | 98.0 / 0.1 / 2.0 | ||||
Penicillin (oral penicillin V) |
1,867 | 0.5 | 4 | 26.6 / 37.5 / 35.9 | ||||
Tetracycline |
1,867 | >4 | >4 | 39.4 / 0.8 / 59.7 | ||||
Trimethoprim/sulfamethoxazole |
1,867 | 1 | >4 | 45.8 / 16.0 / 38.2 | ||||
Vancomycin |
1,867 | 0.25 | 0.5 | 100.0 /—/ 0.0 | ||||
Vancomycin-resistant Enterococcus faecium |
|
|
|
|
||||
Lefamulin |
304 | 0.06 | 0.25 | — /—/— | ||||
Ampicillin |
304 | ³8 | ³8 | 0.3 /—/ 99.7 | ||||
Daptomycin |
304 | 2 | 2 | 100.0 /—/— | ||||
Linezolid |
304 | 1 | 1 | 98.7 /—/ 0.7 | ||||
Vancomycin |
304 | ³16 | ³16 | 0.0 / 99.3 | ||||
28
| |
|
MIC [µg/mL] | CLSI | |||||
|---|---|---|---|---|---|---|---|---|
Organism
|
N | 50% | 90% | %S /%I /%/R | ||||
Concerning Threats |
||||||||
Vancomycin-resistant Staphylococcus aureus |
||||||||
Lefamulin |
10 | 0.06 | 0.12 | —/—/— | ||||
Ceftaroline |
10 | 1 | 1 | 100.0 /—/— | ||||
Daptomycin |
10 | 0.5 | 0.5 | 100.0 /—/— | ||||
Linezolid |
10 | 1 | 1 | 100.0 /—/— | ||||
Oxacillin |
10 | >4 | >4 | —/—/ 100.0 | ||||
Quinupristin/dalfopristin |
10 | 0.25 | 0.5 | 100.0 /—/— | ||||
Tigecycline |
10 | 0.06 | 0.12 | 100.0 /—/— | ||||
Vancomycin |
10 | >32 | >32 | —/—/100.0 | ||||
Erythromycin-resistant Group A Streptococcus species |
|
|
|
|
||||
Lefamulin |
43 | 0.015 | 0.03 | —/—/— | ||||
Clindamycin |
43 | £0.25 | ³2 | 60.5 / 0.0 / 39.5 | ||||
Doxycycline |
25 | 8 | 8 | 32.0 / 4.0 / 64.0(d) | ||||
Erythromycin |
43 | >4 | >4 | 0.0 / 0.0 / 100.0 | ||||
Levofloxacin |
43 | £0.5 | 1 | 97.7 / 0.0 / 2.3 | ||||
Penicillin |
43 | £0.03 | £0.03 | 100.0 /—/— | ||||
Vancomycin |
43 | 0.25 | 0.5 | 100.0 /—/— | ||||
Clindamycin-resistant Group B Streptococcus species |
|
|
|
|
||||
Lefamulin |
108 | 0.03 | 0.06 | —/—/— | ||||
Clindamycin |
108 | ³2 | ³2 | —/—/100.0 | ||||
Doxycycline |
71 | 8 | >8 | 7.0 / 1.4 / 91.5(d) | ||||
Erythromycin |
108 | >4 | >4 | 3.7 / 0.0 / 96.3 | ||||
Levofloxacin |
108 | 1 | 1 | 95.4 /0.0 / 4.6 | ||||
Penicillin |
108 | £0.03 | 0.06 | 100.0 /—/— | ||||
Vancomycin |
108 | 0.5 | 0.5 | 100.0 /—/— | ||||
- (a)
- Criteria
as published by CLSI (2011).
- (b)
- No
breakpoints by CLSI available; criteria as published by the European Committee on Antimicrobial Susceptibility Testing (2017).
- (c)
- Criteria
as published by CLSI (2017).
- (d)
- No breakpoints by CLSI available; criteria as published by the European Committee on Antimicrobial Susceptibility Testing (2017).
Lefamulin has shown low potential for resistance development in vitro, which we believe is the result of the specific interaction with a binding site on the ribosome. Repeated exposure to low levels of lefamulin in laboratory tests resulted in a slow and step-wise development of resistance in S. aureus, Streptococcus species, and E. faecium. We believe that lefamulin's low potential for resistance is further supported by the fact that we observed isolates with consistently low MICs during our Phase 2 clinical trial in ABSSSI and that, despite the use of pleuromutilins in veterinary medicine for decades, the incidence of pleuromutilin-resistant isolates remains relatively low. Cross-resistance between lefamulin and other classes of antibiotics has also been rarely observed in our completed studies to date. Based on global surveillance studies in more than 16,743 staphylococcal and streptococcal clinical isolates, fewer than 0.44% of isolates contain mutations responsible for modifying the interaction between lefamulin and the binding site of the bacterial ribosome. One example of these resistance determinants is the cfrgene, which when present has resulted in observed elevations in the MIC90 to lefamulin as well as other antibiotics, such as chloramphenicol and linezolid. In 2010 one of 5,527 isolates, in 2015 and in
29
2016 no cfr positive isolates have been collected among 1273 and 1646 S. aureus isolates in the course of surveillance studies. Among coagulase-negative staphylococci 2 cfr, positive isolates have been collected in each of 2010 and 2016.
Earlier Stage Product Pipeline
Additional Indications for Lefamulin
Pediatric Indications
Not unlike treatment of infectious diseases in adults, the management of pediatric infections has become more difficult due to the continuing rise in resistance in bacteria. Further complicating antimicrobial selection in the pediatric population is the need for agents to be very well tolerated and available in a final dosage form that can be easily administered to children. Based upon the in vitro antimicrobial spectrum of activity, along with the safety profile observed to date, we believe lefamulin is appropriate for evaluation for the treatment of a variety of pediatric infections, including those affecting the respiratory tract and skin and skin structure. We have agreed PiP, or Pediatric Investigation Plan, and PSP, or Pediatric Study Plan, with EMA and FDA, respectively. Pediatric oral formulation development is ongoing and we anticipate intiating a Phase 1 clinical trial in pediatric patients in mid-2018.
HABP/VABP
One of the major causative organisms of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia is S. aureus, including MRSA. We are evaluating whether to investigate the utility of lefamulin in the treatment of HABP and VABP.
STIs
Urethritis and cervicitis caused by N. gonorrhoeae, C. trachomatis or M. genitalium are frequently occurring sexually transmitted infections in the United States and Europe. Left untreated, these infections can cause serious health problems, particularly in women, including chronic pelvic pain, life-threatening ectopic pregnancy and infertility. Resistance in these organisms to the most commonly prescribed antibacterial treatments poses a serious public health threat. For example, the CDC estimates that 30% of the clinical isolates of N. gonorrhoeae are resistant to at least one currently available antibiotic.
In preclinical studies, lefamulin has shown high potency against N. gonorrhoeae, C. trachomatis and M. genitalium, including strains resistant to currently available antibacterial agents. As a result, we are actively assessing a non-clinical and clinical development plan to support the development of lefamulin as a first-line treatment for urethritis, cervicitis and pelvic inflammatory disease.
Osteomyelitis
The incidence of osteomyelitis, which is an infection of the bone, is increasing. The most common causative organism is S. aureus. In the United States, the prevalence of MRSA in these cases ranges from 33% to 55%. Up to 90% of cases of hematogenous osteomyelitis, most frequently in children, are caused by S. aureus. We believe that lefamulin has the potential to be an effective treatment option for osteomyelitis. Lefamulin has shown substantial tissue penetration and activity against the most common causative organism in all forms of osteomyelitis. We believe that based on the safety profile observed to date, lefamulin will be well tolerated for the long term use necessary for the treatment of both adult and pediatric patients with osteomyelitis. The current standard of care for these infections is treatment with vancomycin. We believe the ability to administer lefamulin by either the IV or oral route would provide a significant advantage over agents, such as vancomycin, that can only be administered by IV.
30
Prosthetic Joint Infections
Infection occurs in approximately 1% of joint replacement surgeries. Although the incidence of infection has been decreasing, the total number of replacement operations has been rising, such that, overall, there is increasing morbidity. The majority of these infections are caused by three organisms: coagulase negative staphylococci, S. aureus (including MRSA) and streptococci, all organisms that are sensitive to lefamulin. The preferred treatment for joint infections with MRSA is vancomycin, with daptomycin and linezolid as alternatives. Vancomycin and daptomycin are administered only by IV for this indication, and linezolid has side effects that affect long term use. We believe that lefamulin could provide an alternative for both IV and oral therapy for these infections cases.
BC-7013 (Topical)
BC-7013 is a semi-synthetic compound derived from pleuromutilin with the potential to be developed for the topical treatment of Gram-positive infections, including uSSSIs.
BC-7013 is highly active against key bacterial pathogens causing skin and ocular infections. The MIC90 values for BC-7013 against MRSA are up to 20-fold lower than for mupirocin and 8-fold lower than for retapamulin, an FDA-approved topical pleuromutilin. Furthermore, BC-7013 has demonstrated potent activity against Chlamydia trachomatis, the leading cause of blindness in the world, and Propionibacterium acnes, the causative agent of acne.
We observed activity in a superficial skin infection model in mice infected with MRSA. BC-7013 was well tolerated following intranasal administration of an ointment formulation in a Phase 1 clinical trial.
Pleuromutilin Molecule Platform
Our pleuromutilin research program is based on our large and diverse proprietary compound library. We believe that our expertise in the areas of medicinal chemistry, pharmacology and toxicology have enabled targeted discovery of novel pleuromutilins through modification of side chains and core positions in the mutilin moiety. These modifications have resulted in alterations in microbial activity, ADME and toxicity of the semi-synthetic molecules.
Compounds in Other Antibiotic Classes
In addition to the pleuromutilin research program, we own a ß-lactam library encompassing approximately 2,000 novel broad spectrum cephalosporins and approximately 150 novel ß-lactamase inhibitor molecules. We own all rights and hold one active patent application on file covering ß-lactamase inhibitors.
We also own a library of approximately 200 acremonic acid derivatives which inhibit bacterial protein translation and have an antibacterial profile that covers primarily Gram-positive bacteria, such as S. aureus, MRSA and mupirocin-resistant strains, as well as ß-hemolytic streptococci (Streptococci that are not S. pneumoniae or members of the Viridans family). The first molecules in this series also displayed improved activity against isolates showing resistance against fusidic acid and showed no cross-resistance with other classes of antibiotics tested.
The existing compound libraries of ß-lactam/ß-lactamase inhibitors and acremonic acid derivatives represent an unrecognized portion of our pipeline. The current allocation of our funds and staff are dedicated to advancing the pleuromutilin compounds. Assessment of the ß-lactam/ß-lactamase inhibitors and acremonic acid derivatives compound libraries will be dependent upon additional funding.
31
Commercialization Strategy
We own exclusive, worldwide rights to lefamulin. We expect that our initial target population for lefamulin will consist of patients with moderate to severe CABP whose antibiotic treatment is hospital-initiated. If lefamulin receives marketing approval from the FDA for the treatment of CABP, we plan to pursue commercialization strategies that maximize the value of lefamulin in the United States with our own targeted hospital sales and marketing organization that we plan to establish. Based on our market research and experts' insight, we believe lefamulin has an innovative profile supporting adoption in the United States for adult hospital- initiated CABP patients, treated both as in-patients as well as outpatient-transition of care from the hospital to the community, which we believe represents a significant commercial opportunity. We believe that we will be able to effectively communicate lefamulin's differentiating characteristics and key attributes to clinicians, hospital pharmacies and payors with the goal of establishing favorable reimbursement for outpatients as well as a favorable formulary status in targeted hospitals. Additionally, we believe that our plans for an initial targeted hospital-focused sales force should allow us to address—on our own—the hospital-initiated treatment market for CABP in the United States in an efficient and effective way. There is also a significant opportunity for lefamulin to be used in the community for CABP patients, given the versatile profile, and this may represent a future expanded use. We plan to continue our pre-commercialization activities to prepare for a potential commercial launch of lefamulin, subject to receiving marketing approval in the United States. If lefamulin receives marketing approval outside of the United States for the treatment of CABP, we expect to utilize a variety of types of collaboration, distribution and other marketing arrangements with one or more third parties to commercialize lefamulin in such markets.
Along with additional market research, we believe that medical education will be a key component of our commercialization efforts and, following potential commercial launch, plan to invest in these activities to maximize the commercial potential of lefamulin. With a targeted initial prescribing base predominantly in the hospital setting, we expect that a targeted hospital sales and marketing organization would be relatively smaller than competitors who are focused on both the hospital and community prescribing base. We believe that lefamulin's novel mechanism of action, status as the only member of a new class of systemically administered pleuromutilins and anticipated clinical profile will support its potential favorable reimbursement, its potential inclusion on formularies and in local and national treatment guidelines, subject to and following marketing approval.
We plan to evaluate the merits of entering into collaboration agreements with other pharmaceutical or biotechnology companies that may contribute to our ability to efficiently advance our product candidates, build our product pipeline and concurrently advance a range of research and development programs for a variety of indications outside the United States.
Manufacturing
We do not own or operate, and currently have no plans to establish, manufacturing facilities for the production of clinical or commercial quantities of lefamulin, or any of the other compounds that we are evaluating in our discovery program. We currently rely, and expect to continue to rely, on third parties for the manufacture of lefamulin and any further products that we may develop. We have significant in-house knowledge and experience in the relevant chemistry associated with our product candidate and use these internal resources, alongside third-party consultants, to manage our manufacturing contractors.
We have engaged a limited number of third-party manufacturers to provide all of our raw materials, drug substance and finished product for use in clinical trials. The active pharmaceutical ingredients, or API, and drug products have been produced under master service contracts and specific work orders from these manufacturers pursuant to agreements that include specific supply timelines and volume and quality expectations. We choose the third-party manufacturers of the drug substance
32
based on the volume required and the regulatory requirements at the relevant stage of development. All lots of drug substance and drug products used in clinical trials are manufactured under current good manufacturing practices. Separate third-party manufacturers have been responsible for fill and finish services, and for labeling and shipment of the final drug product to the clinical trial sites.
We have entered into a long-term commercial supply agreement with SEL Biochem Xinjiang Co., Ltd, or Sel, and Fountain International Development Holding Limited for the supply of pleuromutilin, which is the key intermediate for lefamulin API production. Under this agreement, Sel is required to manufacture and supply and we are required to purchase from Sel a specified percentage of our commercial requirements of pleuromutilin. The agreement expires on August 28, 2022, subject to automatic renewal for successive three-year periods. Either party may elect not to renew the agreement by providing two-year prior written notice before the end of the initial term or the then-current renewal term. Either party may terminate the agreement for the other party's uncured material breach or upon the occurrence of specified bankruptcy events.
The agreement includes customary supply terms, including product specifications, price, payment terms, requirements forecasting, delivery mechanics and quality assurance. [Under the agreement, we have also negotiated a quality technical agreement pursuant to which Sel will conduct all quality control and release testing for the pleuromutilin produced under the agreement.
We have also entered into a long-term commercial supply agreement with Patheon UK Limited, or Patheon, for the supply of IV vials of lefamulin. Under this agreement, Patheon is required to supply and we are required to purchase a specified percentage of our commercial requirements of IV vials of lefamulin. The agreement expires on December 31, 2023, subject to automatic renewal for successive two-year periods. Either party may elect not to renew the agreement by providing two-year prior written notice before the end of the initial term, and after the initial term, either party may terminate the agreement with 24-months prior written notice at any time. Either party may also terminate the agreement for the other party's uncured material breach or upon the occurrence of specified bankruptcy events. We may also terminate the agreement if a governmental authority takes action that prevents us from importing, exporting, purchasing or selling the IV vials of lefamulin. Finally, Patheon may terminate the agreement if we assign any of our rights under the agreement to an assignee that it does not consider to be a creditworthy substitute or is a competitor of Patheon.
The agreement includes customary supply terms, including product specifications, batch size requirements, price, payment terms, requirements forecasting, delivery mechanics and quality assurance. [Under the agreement, we have also negotiated a quality agreement pursuant to which Patheon will conduct all quality control testing for the IV vials of lefamulin.
In addition, we have entered into a long-term commercial supply agreement with Almac Pharma Services Limited, or Almac, for the commercial supply of lefamulin tablets. Under this agreement, Almac is required to supply and we are required to purchase services relating to the manufactured tablets equaling a specified minimum annual spend. The initial term of the agreement expires on August 7, 2022, but it will remain in force until it is terminated by either party with 24-months prior written notice, expiring on or at any time after the expiry of the initial term. Either party may also terminate the agreement for the other party's uncured material breach or upon the occurrence of specified bankruptcy events. The agreement includes customary supply terms, including payment terms, requirements forecasting, delivery mechanics and quality assurance. Under the agreement, we have also negotiated a quality technical agreement pursuant to which Almac will conduct all quality control testing for the tablets.
These three commercial supply agreements are filed as exhibits to this Form 10-K. Other than these three agreements, we do not have long-term agreements with any other third parties for the manufacture of commercial supplies of lefamulin, but we intend to enter into additional agreements
33
with third-party contract manufacturers for additional commercial supplies of lefamulin pending potential regulatory approval.
Our product candidate is a semi-synthetic organic compound of low molecular weight. The pleuromutilin core of the molecule is produced by fermentation and is manufactured on a significant scale by various manufacturers. We have selected the compound based on its efficacy and safety profile, although it is also associated with reasonable cost of goods, ready availability of starting materials and ease of synthesis. The development stage production of lefamulin was carried out at a significant scale and we believe the synthetic route to lefamulin is amenable to further scale-up. The synthetic route does not require unusual, or specialized, equipment in the manufacturing process. Therefore, if any of our current or future drug substance manufacturers were to become unavailable for any reason, we believe there are a number of potential replacements, although delays may be incurred in identifying and qualifying such replacements.
Competition
The biotechnology and pharmaceutical industries are characterized by rapidly advancing technologies, intense competition and a strong emphasis on proprietary products. While we believe that our technologies, knowledge, experience and scientific resources provide us with competitive advantages, we face potential competition from many different sources, including major pharmaceutical, specialty pharmaceutical and biotechnology companies, academic institutions, government agencies and private and public research institutions. Any product candidates that we successfully develop and commercialize will compete with existing therapies and new therapies that may become available in the future.
Many of our competitors may have significantly greater financial resources and expertise in research and development, manufacturing, preclinical testing, conducting clinical trials, obtaining regulatory approvals and marketing approved products than we do. These competitors also compete with us in recruiting and retaining qualified scientific and management personnel and establishing clinical trial sites and patient registration for clinical trials, as well as in acquiring technologies complementary to, or necessary for, our programs. Smaller or early stage companies may also prove to be significant competitors, particularly through collaborative arrangements with large and established companies.
Our commercial opportunity could be reduced or eliminated if our competitors develop and commercialize products that are safer, more effective, have fewer or less severe side effects, are more convenient or are less expensive than any products that we may develop. Our competitors also may obtain marketing approvals for their products more rapidly than we obtain approval for ours, which could result in our competitors establishing a strong market position before we are able to enter the market. In addition, our ability to compete may be affected because in some cases insurers or other third-party payors seek to encourage the use of generic products. This may have the effect of making branded products less attractive, from a cost perspective, to buyers. We expect that if lefamulin is approved for CABP, it will be priced at a significant premium over competitive generic products. This may make it difficult for us to replace existing therapies with lefamulin.
The key competitive factors affecting the success of our product candidates are likely to be their efficacy, safety, convenience, price and the availability of coverage and reimbursement from government and other third-party payors.
There are a variety of available therapies marketed for the treatment of CABP. Currently, the treatment of CABP is dominated by generic products. For hospitalized patients, combination therapy is frequently used. Many currently approved drugs are well-established therapies and are widely accepted by physicians, patients and third-party payors. We also are aware of various drugs under development for the treatment of CABP, including solithromycin, for which an NDA was filed by Cempra Inc. (now
34
Melinta Therapeutics Inc.) and a complete response letter issued by the FDA in December 2016, omadacycline (under Phase 3 clinical development by Paratek Pharmaceuticals Inc.), delafloxacin which was approved by the FDA in June 2017 for ABSSSI, and is marketed by Melinta Therapeutics Inc. who also have an ongoing phase 3 clinical trial of delafloxacin for CABP and oral nafithromycin (under Phase 2 clinical development by Wockhardt Ltd.).
Intellectual Property
Our success depends in large part on our ability to obtain and maintain proprietary protection for our product candidates, technology and know-how, to operate without infringing the proprietary rights of others and to prevent others from infringing our proprietary rights. We strive to protect the proprietary technology that we believe is important to our business by, among other methods, seeking and maintaining patents, where available, that are intended to cover our product candidates, compositions and formulations, their methods of use and processes for their manufacture and any other inventions that are commercially important to the development of our business. We also rely on trade secrets, know-how, continuing technological innovation and in-licensing opportunities to develop and maintain our proprietary and competitive position.
As of January 31, 2018, we owned 22 different families of patents and patent applications, including 21 families directed to the various pleuromutilin derivatives as compositions of matter, processes for their manufacture, and their use in pharmaceutical compositions and methods of treating disease. The remaining family is directed to ß-lactamase inhibitors. Our patent portfolio includes 23 issued U.S. patents, 22 granted European patents and 18 granted Japanese patents, as well as patents in other jurisdictions. We also have pending patent applications in the United States, Europe, Japan and other countries and regions, including Asia, Australia, Eastern Europe, and South America, including notably Canada, Brazil, China, Israel, India and Taiwan among others.
All of these patents and patent applications are assigned solely to us and were either originally filed by us or originally filed by Sandoz and subsequently assigned to us.
As of January 31, 2018, our lead product candidate, lefamulin, was protected by the following six patent families:
- •
- The first patent family includes patents and applications with claims directed to generic classes of compounds that include lefamulin and/or
their use in the treatment of microbial infections. This family includes issued patents in the United States, Europe and Japan, as well as issued patents in 11 other jurisdictions. The standard term
for patents in this family expires in 2021.
- •
- The second patent family includes patents and applications with claims that specifically recite lefamulin and/or its use in the treatment of
microbial infections. This family includes two issued patents in each of the United States, Europe and Japan, as well as issued patents in 21 other jurisdictions and 5 pending patent applications in
other jurisdictions, including one divisional application in the United States. The standard term for patents in this family expires in 2028. A patent term adjustment of 303 days has already
been obtained in the United States for one patent.
- •
- The third patent family includes patents and applications with claims directed to the processes for the manufacture of lefamulin, crystalline
intermediates useful in the processes, and the resulting crystalline salts. This family includes 14 granted patents including issued patents in the United States, Europe and Japan and 15 pending
patent applications one each in Europe and Japan and 13 in other jurisdictions. The standard term for patents in this family expires in 2031.
- •
- The fourth patent family includes patents and applications with claims directed to processes for the synthetic manufacture of crystalline intermediates useful in the manufacture of lefamulin. This family includes granted patents in Europe, the United States and Japan and granted
35
- •
- The fifth patent family includes patents and applications with claims directed to pharmaceuticals and treatments for Helicobacter infection,
including pleuromutilins, such as lefamulin. This family includes issued patents in the United States, Europe and one other
jurisdiction. The standard term for patents in this family expires in 2023. A patent term adjustment of 921 days has already been obtained for the U.S. patent.
- •
- A further patent family is directed to pharmaceutical compositions of lefamulin and the PCT-application was recently published. The family
covers 17 pending patent applications in various jurisdictions.
- •
- During 2017 a priority application relating to a method for purification of pleuromutilins was filed. The application is not yet published.
patents in other jurisdictions and further pending applications. The standard term for patents in this family expires in 2031.
Our second most advanced product candidate, BC-7013, is covered specifically in one patent family with patents granted in the United States, Europe and Japan, as well as eight other jurisdictions, and pending patent applications in other jurisdictions. The standard term for patents in this family expires in 2027.
The remaining 13 pleuromutilin patent families are directed to either molecules in the intellectual property landscape surrounding our product candidates in development or molecules which can be potentially further developed by us but have not yet been pursued. All patent applications in these families have been filed at least in the United States and Europe, and most have been filed in other countries. The majority of these patent applications have already resulted in granted patents.
Finally, we own one patent family directed to ß-lactamase inhibitor compounds. Patent applications in this family have been filed and granted in the United States and Europe. The standard term for patents in this family expires in 2030.
The term of individual patents depends upon the legal term for patents in the countries in which they are obtained. In most countries, including the United States, the patent term is 20 years from the filing date of a non-provisional patent application. In the United States, a patent's term may, in certain cases, be lengthened by patent term adjustment, which compensates a patentee for administrative delays by the U.S. Patent and Trademark Office, or the USPTO, in examining and granting a patent, or may be shortened if a patent is terminally disclaimed over an earlier filed patent. The term of a U.S. patent that covers a drug, biological product or medical device approved pursuant to a pre-market approval, or PMA, may also be eligible for patent term extension when FDA approval is granted, provided that certain statutory and regulatory requirements are met. The length of the patent term extension is related to the length of time the drug is under regulatory review while the patent is in force. The Drug Price Competition and Patent Term Restoration Act of 1984, or the Hatch-Waxman Act, permits a patent term extension of up to five years beyond the expiration date set for the patent. Patent extension cannot extend the remaining term of a patent beyond a total of 14 years from the date of product approval, only one patent applicable to each regulatory review period may be granted an extension and only those claims reading on the approved drug may be extended. Similar provisions are available in Europe and certain other foreign jurisdictions to extend the term of a patent that covers an approved drug, provided that statutory and regulatory requirements are met. Thus, in the future, if and when our product candidates receive approval by the FDA or foreign regulatory authorities, we expect to apply for patent term extensions on issued patents covering those products, depending upon the length of the clinical trials for each drug and other factors. The expiration dates of our patents and patent applications referred to above are without regard to potential patent term extension or other market exclusivity that may be available to us.
36
In addition to patents, we may rely, in some circumstances, on trade secrets to protect our technology and maintain our competitive position. However, trade secrets can be difficult to protect. We seek to protect our proprietary technology and processes, in part, by confidentiality agreements with our employees, corporate and scientific collaborators, consultants, scientific advisors, contractors and other third parties. We also seek to preserve the integrity and confidentiality of our data and trade secrets by maintaining physical security of our premises and physical and electronic security of our information technology systems.
Government Regulation
Government authorities in the United States, at the federal, state and local level, and in other countries and jurisdictions, including the European Union, extensively regulate, among other things, the research, development, testing, manufacture, quality control, approval, pricing, packaging, storage, recordkeeping, labeling, advertising, promotion, distribution, marketing, post-approval monitoring and reporting, and import and export of pharmaceutical products. The processes for obtaining regulatory approvals in the United States and in foreign countries and jurisdictions, along with subsequent compliance with applicable statutes and regulations and other regulatory authorities, require the expenditure of substantial time and financial resources.
Review and Approval of Drugs in the United States
In the United States, the FDA reviews, approves and regulates drugs under the federal Food, Drug, and Cosmetic Act, or FDCA, and associated implementing regulations. The failure to comply with the applicable U.S. requirements at any time during the product development process, approval process or post-approval may result in delays to the conduct of study, regulatory review and subject an applicant and/or sponsor to a variety of administrative or judicial sanctions, including refusal by the FDA to approve pending applications, withdrawal of an approval, imposition of a clinical hold, issuance of warning letters and other types of letters, product recalls, product seizures, total or partial suspension of production or distribution, adverse publicity, injunctions, fines, refusals of government contracts, restitution, disgorgement of profits, and civil or criminal investigations and penalties brought by the FDA and the U.S. Department of Justice, or DOJ, or other governmental entities, including state agencies.
An applicant seeking approval to market and distribute a new drug product in the United States must typically undertake the following before a product candidate will be appoved by the FDA:
- •
- completion of preclinical laboratory tests, animal studies and formulation studies in compliance with the FDA's good laboratory practice, or
GLP, regulations;
- •
- submission to the FDA of an investigational new drug application, or IND, which must take effect before human clinical trials may begin;
- •
- approval by an independent institutional review board, or IRB, representing each clinical site before each clinical trial may be initiated;
- •
- performance of adequate and well-controlled human clinical trials in accordance with good clinical practices, or GCP, to establish the safety
and efficacy of the proposed drug product for each indication;
- •
- preparation and submission to the FDA of a new drug application, or NDA, summarizing available data to support the proposed approval of the new
drug product for the proposed use;
- •
- review of the product application by an FDA advisory committee, where appropriate or if applicable and as may be requested by the FDA;
37
- •
- satisfactory completion of one or more FDA inspections of the manufacturing facility or facilities at which the product, or components thereof,
are produced to assess compliance with current Good Manufacturing Practices, or cGMP, requirements and to assure that the facilities, methods and controls are adequate to preserve the product's
identity, strength, quality and purity;
- •
- satisfactory completion of FDA audits of clinical trial sites to assure compliance with GCPs and the integrity of the clinical data;
- •
- payment of PDUFA fees and securing FDA approval of the NDA; and
- •
- compliance with any post-approval requirements, including the potential requirement to implement a Risk Evaluation and Mitigation Strategy, or REMS, where applicable, and the potential to conduct post-approval studies required by the FDA.
Preclinical Studies
Before an applicant begins testing a compound with potential therapeutic value in humans, the drug candidate enters the preclinical testing stage. Preclinical studies include laboratory evaluation of the purity and stability of the manufactured drug substance or active pharmaceutical ingredient and the formulated drug or drug product, as well as in vitro and animal studies to assess the safety and activity of the drug for initial testing in humans and to establish a rationale for therapeutic use. The conduct of preclinical studies is subject to federal regulations and requirements, including GLP regulations. The results of the preclinical tests, together with manufacturing information, analytical data, any available clinical data or literature and plans for clinical studies, among other things, are submitted to the FDA as part of an IND. Additional long-term preclinical testing, such as animal tests of reproductive adverse events and carcinogenicity, may continue after the IND is submitted.
Companies usually must complete some long-term preclinical testing, such as animal tests of long term exposure and reproductive adverse events, and must also develop additional information about the chemistry and physical characteristics of the investigational product and finalize a process for manufacturing the product in commercial quantities in accordance with cGMP requirements. The manufacturing process must be capable of consistently producing quality batches of the candidate product and, among other things, the manufacturer must develop methods for testing the identity, strength, quality and purity of the final product. Additionally, appropriate packaging must be selected and tested and stability studies must be conducted to demonstrate that the candidate product does not undergo unacceptable deterioration over its shelf life.
The IND and IRB Processes
An IND is an exemption from the FDCA that allows an unapproved drug to be shipped in interstate commerce for use in an investigational clinical trial and a request for FDA authorization to administer an investigational drug to humans. Such authorization must be secured prior to interstate shipment and administration of any new drug that is not the subject of an approved NDA. In support of a request for an IND, applicants must submit a protocol for each clinical trial and any subsequent protocol amendments must be submitted to the FDA as part of the IND. In addition, the results of the preclinical tests, together with manufacturing information, analytical data, any available clinical data or literature and plans for clinical trials, among other things, are submitted to the FDA as part of an IND. The FDA requires a 30-day waiting period after the filing of each IND before clinical trials may begin. This waiting period is designed to allow the FDA to review the IND to determine whether human research subjects will be exposed to unreasonable health risks. At any time during this 30-day period, the FDA may raise concerns or questions about the conduct of the trials as outlined in the IND and impose a clinical hold or partial clinical hold. In this case, the IND sponsor and the FDA must resolve any outstanding concerns before clinical trials can begin.
38
Following commencement of a clinical trial under an IND, the FDA may also place a clinical hold or partial clinical hold on that trial. A clinical hold is an order issued by the FDA to the sponsor to delay a proposed clinical investigation or to suspend an ongoing investigation. A partial clinical hold is a delay or suspension of only part of the clinical work requested under the IND. For example, a specific protocol or part of a protocol is not allowed to proceed, while other protocols may do so. No more than 30 days after imposition of a clinical hold or partial clinical hold, the FDA will provide the sponsor a written explanation of the basis for the hold. Following issuance of a clinical hold or partial clinical hold, an investigation may only resume after the FDA has notified the sponsor that the investigation may proceed. The FDA will base that determination on information provided by the sponsor correcting the deficiencies previously cited or otherwise satisfying the FDA that the investigation can proceed.
A sponsor may choose, but is not required, to conduct a foreign clinical study under an IND. When a foreign clinical study is conducted under an IND, all FDA IND requirements must be met unless waived. When the foreign clinical study is not conducted under an IND, the sponsor must ensure that the study complies with FDA certain regulatory requirements in order to use the study as support for an IND or application for marketing approval. Specifically, on April 28, 2008, the FDA amended its regulations governing the acceptance of foreign clinical studies not conducted under an investigational new drug application as support for an IND or a new drug application. The final rule provides that such studies must be conducted in accordance with good clinical practice, or GCP, including review and approval by an independent ethics committee, or IEC, and informed consent from subjects. The GCP requirements in the final rule encompass both ethical and data integrity standards for clinical studies. The FDA's regulations are intended to help ensure the protection of human subjects enrolled in non-IND foreign clinical studies, as well as the quality and integrity of the resulting data. They further help ensure that non-IND foreign studies are conducted in a manner comparable to that required for IND studies.
In addition to the foregoing IND requirements, an IRB representing each institution participating in the clinical trial must review and approve the plan for any clinical trial before it commences at that institution, and the IRB must conduct continuing review and reapprove the study at least annually. The IRB must review and approve, among other things, the study protocol and informed consent information to be provided to study subjects. An IRB must operate in compliance with FDA regulations. An IRB can suspend or terminate approval of a clinical trial at its institution, or an institution it represents, if the clinical trial is not being conducted in accordance with the IRB's requirements or if the product candidate has been associated with unexpected serious harm to patients.
Additionally, some trials are overseen by an independent group of qualified experts organized by the trial sponsor, known as a data safety monitoring board or committee, or DSMB. This group provides authorization as to whether or not a trial may move forward at designated check points based on unblinded safety data from the study to which only the DSMB has access. Suspension or termination of development during any phase of clinical trials may occur if it is determined that the participants or patients are being exposed to an unacceptable health risk. Other reasons for suspension or termination may be made by us based on evolving business objectives and/or competitive climate.
Information about certain clinical trials must be submitted within specific timeframes to the National Institutes of Health, or NIH, for public dissemination on its ClinicalTrials.gov website.
Human Clinical Studies in Support of an NDA
Clinical trials involve the administration of the investigational product to human subjects under the supervision of qualified investigators in accordance with GCP requirements, which include, among other things, the requirement that all research subjects provide their informed consent in writing before their participation in any clinical trial. Clinical trials are conducted under written study protocols
39
detailing, among other things, the inclusion and exclusion criteria, the objectives of the study, the parameters to be used in monitoring safety and the effectiveness criteria to be evaluated.
Human clinical trials are typically conducted in the following four sequential phases, which may overlap or be combined:
- •
- Phase 1: The drug is initially introduced into healthy human subjects or, in certain indications such as cancer, patients with the
target disease or condition and tested for safety, dosage tolerance, absorption, metabolism, distribution, excretion and, if possible, to gain an early indication of its effectiveness and to determine
optimal dosage.
- •
- Phase 2: The drug is administered to a limited patient population to identify possible adverse effects and safety risks, to
preliminarily evaluate the efficacy of the product for specific targeted diseases and to determine dosage tolerance and optimal dosage.
- •
- Phase 3: The drug is administered to an expanded patient population, generally at geographically dispersed clinical trial sites, in
well-controlled clinical trials to generate enough data to statistically evaluate the efficacy and safety of the product for approval, to establish the overall risk-benefit profile of the product, and
to provide adequate information for the labeling of the product.
- •
- Phase 4: Post-approval studies, which are conducted following initial approval, are typically conducted to gain additional experience and data from treatment of patients in the intended therapeutic indication.
Progress reports detailing the results of the clinical trials must be submitted at least annually to the FDA and more frequently if serious adverse events occur. In addition, IND safety reports must be submitted to the FDA for any of the following: serious and unexpected suspected adverse reactions; findings from other studies or animal or in vitro testing that suggest a significant risk in humans exposed to the drug; and any clinically important increase in the case of a serious suspected adverse reaction over that listed in the protocol or investigator brochure. Phase 1, Phase 2 and Phase 3 clinical trials may not be completed successfully within any specified period, or at all. Furthermore, the FDA or the sponsor may suspend or terminate a clinical trial at any time on various grounds, including a finding that the research subjects are being exposed to an unacceptable health risk. Similarly, an IRB can suspend or terminate approval of a clinical trial at its institution, or an institution it represents, if the clinical trial is not being conducted in accordance with the IRB's requirements or if the drug has been associated with unexpected serious harm to patients. The FDA will typically inspect one or more clinical sites to assure compliance with GCP and the integrity of the clinical data submitted.
Concurrent with clinical trials, companies often complete additional animal studies and must also develop additional information about the chemistry and physical characteristics of the drug as well as finalize a process for manufacturing the product in commercial quantities in accordance with cGMP requirements. The manufacturing process must be capable of consistently producing quality batches of the drug candidate and, among other things, must develop methods for testing the identity, strength, quality, purity, and potency of the final drug. Additionally, appropriate packaging must be selected and tested and stability studies must be conducted to demonstrate that the drug candidate does not undergo unacceptable deterioration over its shelf life.
Special Protocol Assessment Agreements
A Special Protocol Assessment, or SPA, agreement is an agreement between a drug manufacturer and the FDA on the design and size of studies and clinical trials that can be used for approval of a drug or biological product. The FDA's guidance on such agreements states that an agreement may not be changed by the manufacturer or the agency unless through a written agreement of the two entities or if FDA determines a substantial scientific issue essential to determining the safety or effectiveness of
40
the drug. The protocols that are eligible for SPA agreements are: animal carcinogenicity protocols, final product stability protocols and clinical protocols for Phase 3 trials whose data will form the primary basis for an efficacy claim.
Specifically, under the FDCA, the FDA may meet with sponsors, provided certain conditions are met, for the purpose of reaching a SPA agreement on the design and size of clinical trials intended to form the primary basis of an efficacy claim in a marketing application. If a sponsor makes a reasonable written request to meet with the FDA for the purpose of reaching agreement on the design and size of a clinical trial, then the FDA will meet with the sponsor. If an agreement is reached, the FDA will reduce the agreement to writing and make it part of the administrative record. An agreement may not be changed by the sponsor or FDA after the trial begins, except with the written agreement of the sponsor and FDA, or if the director of the FDA reviewing division determines that "a substantial scientific issue essential to determining the safety or effectiveness of the drug" was identified after the testing began. If a sponsor and the FDA meet regarding the design and size of a clinical trial and the parties cannot agree that the trial design is adequate to meet the goals of the sponsor, the FDA will clearly state the reasons for the disagreement in a letter to the sponsor. We reached agreement with the FDA in September 2015 on a SPA regarding the study design of our first Phase 3 clinical trial of lefamulin for the treatment of CABP.
Submission of an NDA to the FDA
Assuming successful completion of required clinical testing and other requirements, the results of the preclinical and clinical studies, together with detailed information relating to the product's chemistry, manufacture, controls and proposed labeling, among other things, are submitted to the FDA as part of an NDA requesting approval to market the drug product for one or more indications. Under federal law, the submission of most NDAs is subject to an application user fee, which for federal fiscal year 2018 is $2,421,495 for an application requiring clinical data. The sponsor of an approved NDA is also subject to an annual program fee, which for fiscal year 2018 is $304,162. Exceptions or waivers for these fees exist for a small company (fewer than 500 employees, including employees and affiliates) satisfying certain requirements and products with orphan drug designation for a particular indication are not subject to a fee provided there are no other intended uses in the NDA.
Following submission of an NDA, the FDA conducts a preliminary review of an NDA generally within 60 calendar days of its receipt and strives to inform the sponsor by the 74th day after the FDA's receipt of the submission whether the application is sufficiently complete to permit substantive review. The FDA may request additional information rather than accept an NDA for filing. In this event, the application must be resubmitted with the additional information. The resubmitted application is also subject to review before the FDA accepts it for filing. Once the submission is accepted for filing, the FDA begins an in-depth substantive review. The FDA has agreed to certain performance goals in the review process of NDAs. Standard review, representing most such applications are meant to be reviewed within ten months from the date of filing. Priority review applications are meant to be reviewed within six months of filing. The review process and the Prescription Drug User Fee Act goal date may be extended by the FDA for three additional months to consider new information or clarification provided by the applicant to address an outstanding deficiency identified by the FDA following the original submission. Under the FDA Reauthorization Act of 2017, the FDA must implement a protocol to expedite review of responses to inspection reports pertaining to certain applications, including applications for products in shortage or those for which approval is dependent on remediation of conditions identified in the inspection report.
Before approving an NDA, the FDA typically will inspect the facility or facilities where the product is or will be manufactured. These pre-approval inspections may cover all facilities associated with an NDA submission, including drug component manufacturing (such as active pharmaceutical ingredients), finished drug product manufacturing, and control testing laboratories. The FDA will not approve an
41
application unless it determines that the manufacturing processes and facilities are in compliance with cGMP requirements and adequate to assure consistent production of the product within required specifications. Additionally, before approving an NDA, the FDA will typically inspect one or more clinical sites to assure compliance with GCP.
In addition, as a condition of approval, the FDA may require an applicant to develop a REMS. REMS use risk minimization strategies beyond the professional labeling to ensure that the benefits of the product outweigh the potential risks. To determine whether a REMS is needed, the FDA will consider the size of the population likely to use the product, seriousness of the disease, expected benefit of the product, expected duration of treatment, seriousness of known or potential adverse events, and whether the product is a new molecular entity. REMS can include medication guides, physician communication plans for healthcare professionals, and elements to assure safe use, or ETASU. ETASU may include, but are not limited to, special training or certification for prescribing or dispensing, dispensing only under certain circumstances, special monitoring, and the use of patient registries. The FDA may require a REMS before approval or post-approval if it becomes aware of a serious risk associated with use of the product. The requirement for a REMS can materially affect the potential market and profitability of a product.
The FDA may refer an application for a novel drug to an advisory committee or explain why such referral was not made. Typically, an advisory committee is a panel of independent experts, including clinicians and other scientific experts, that reviews, evaluates and provides a recommendation as to whether the application should be approved and under what conditions. The FDA is not bound by the recommendations of an advisory committee, but it considers such recommendations carefully when making decisions relating to approval of a new drug product.
Fast Track, Breakthrough Therapy, Priority Review and Regenerative Advanced Therapy Designations
The FDA is authorized to designate certain products for expedited review if they are intended to address an unmet medical need in the treatment of a serious or life-threatening disease or condition. These programs are referred to as fast track designation, breakthrough therapy designation, priority review designation and regenerative advanced therapy designation.
Specifically, the FDA may designate a product for Fast Track review if it is intended, whether alone or in combination with one or more other products, for the treatment of a serious or life-threatening disease or condition, and it demonstrates the potential to address unmet medical needs for such a disease or condition. For Fast Track products, sponsors may have greater interactions with the FDA and the FDA may initiate review of sections of a Fast Track product's application before the application is complete. This rolling review may be available if the FDA determines, after preliminary evaluation of clinical data submitted by the sponsor, that a Fast Track product may be effective. The sponsor must also provide, and the FDA must approve, a schedule for the submission of the remaining information and the sponsor must pay applicable user fees. However, the FDA's time period goal for reviewing a Fast Track application does not begin until the last section of the application is submitted. In addition, the Fast Track designation may be withdrawn by the FDA if the FDA believes that the designation is no longer supported by data emerging in the clinical trial process.
Second, a product may be designated as a Breakthrough Therapy if it is intended, either alone or in combination with one or more other products, to treat a serious or life-threatening disease or condition and preliminary clinical evidence indicates that the product may demonstrate substantial improvement over existing therapies on one or more clinically significant endpoints, such as substantial treatment effects observed early in clinical development. The FDA may take certain actions with respect to Breakthrough Therapies, including holding meetings with the sponsor throughout the development process; providing timely advice to the product sponsor regarding development and
42
approval; involving more senior staff in the review process; assigning a cross-disciplinary project lead for the review team; and taking other steps to design the clinical trials in an efficient manner.
Third, the FDA may designate a product for priority review if it is a product that treats a serious condition and, if approved, would provide a significant improvement in safety or effectiveness. The FDA determines, on a case- by-case basis, whether the proposed product represents a significant improvement when compared with other available therapies. Significant improvement may be illustrated by evidence of increased effectiveness in the treatment of a condition, elimination or substantial reduction of a treatment-limiting product reaction, documented enhancement of patient compliance that may lead to improvement in serious outcomes, and evidence of safety and effectiveness in a new subpopulation. A priority designation is intended to direct overall attention and resources to the evaluation of such applications, and to shorten the FDA's goal for taking action on a marketing application from ten months to six months.
With passage of the 21st Century Cures Act, or the Cures Act, in December 2016, Congress authorized the FDA to accelerate review and approval of products designated as regenerative advanced therapies. A product is eligible for this designation if it is a regenerative medicine therapy that is intended to treat, modify, reverse or cure a serious or life-threatening disease or condition and preliminary clinical evidence indicates that the product has the potential to address unmet medical needs for such disease or condition. The benefits of a regenerative advanced therapy designation include early interactions with FDA to expedite development and review, benefits available to breakthrough therapies, potential eligibility for priority review and accelerated approval based on surrogate or intermediate endpoints.
Accelerated Approval Pathway
The FDA may grant accelerated approval to a drug for a serious or life-threatening condition that provides meaningful therapeutic advantage to patients over existing treatments based upon a determination that the drug has an effect on a surrogate endpoint that is reasonably likely to predict clinical benefit. The FDA may also grant accelerated approval for such a drug when the product has an effect on an intermediate clinical endpoint that can be measured earlier than an effect on irreversible morbidity or mortality, or IMM, and that is reasonably likely to predict an effect on irreversible morbidity or mortality or other clinical benefit, taking into account the severity, rarity, or prevalence of the condition and the availability or lack of alternative treatments. Drugs granted accelerated approval must meet the same statutory standards for safety and effectiveness as those granted traditional approval.
For the purposes of accelerated approval, a surrogate endpoint is a marker, such as a laboratory measurement, radiographic image, physical sign, or other measure that is thought to predict clinical benefit, but is not itself a measure of clinical benefit. Surrogate endpoints can often be measured more easily or more rapidly than clinical endpoints. An intermediate clinical endpoint is a measurement of a therapeutic effect that is considered reasonably likely to predict the clinical benefit of a drug, such as an effect on IMM. The FDA has limited experience with accelerated approvals based on intermediate clinical endpoints, but has indicated that such endpoints generally may support accelerated approval where the therapeutic effect measured by the endpoint is not itself a clinical benefit and basis for traditional approval, if there is a basis for concluding that the therapeutic effect is reasonably likely to predict the ultimate clinical benefit of a drug.
The accelerated approval pathway is most often used in settings in which the course of a disease is long and an extended period of time is required to measure the intended clinical benefit of a drug, even if the effect on the surrogate or intermediate clinical endpoint occurs rapidly. Thus, accelerated approval has been used extensively in the development and approval of drugs for treatment of a variety of cancers in which the goal of therapy is generally to improve survival or decrease morbidity and the
43
duration of the typical disease course requires lengthy and sometimes large trials to demonstrate a clinical or survival benefit. The accelerated approval pathway is usually contingent on a sponsor's agreement to conduct, in a diligent manner, additional post-approval confirmatory studies to verify and describe the drug's clinical benefit. As a result, a drug candidate approved on this basis is subject to rigorous post-marketing compliance requirements, including the completion of Phase 4 or post-approval clinical trials to confirm the effect on the clinical endpoint. Failure to conduct required post-approval studies, or confirm a clinical benefit during post-marketing studies, would allow the FDA to withdraw the drug from the market on an expedited basis. All promotional materials for drug candidates approved under accelerated regulations are subject to prior review by the FDA.
Limited Population Antibacterial Drug Pathway
With passage of the CURES Act, Congress authorized FDA to approve an antibacterial or antifungal drug, alone or in combination with one or more other drugs, as a "limited population drug." To qualify for this approval pathway, the drug must be intended to treat a serious or life-threatening infection in a limited population of patients with unmet needs; the standards for approval of drugs and biologics under the FDCA and PHSA must be satisfied; and FDA must receive a written request from the sponsor to approve the drug as a limited population drug pursuant to this provision. The FDA's determination of safety and effectiveness for such a product must reflect the benefit-risk profile of such drug in the intended limited population, taking into account the severity, rarity, or prevalence of the infection the drug is intended to treat and the availability or lack of alternative treatment in such a limited population.
Any drug or biologic approved under this pathway must be labeled with the statement "Limited Population" in a prominent manner and adjacent to the proprietary name of the drug or biological product. The prescribing information must also state that the drug is indicated for use in a limited and specific population of patients and copies of all promotional materials relating to the drug must be submitted to FDA at least 30 days prior to dissemination of the materials. If FDA subsequently approves the drug for a broader indication, the agency may remove any post-marketing conditions, including requirements with respect to labeling and review of promotional materials applicable to the product. Nothing in this pathway to approval of a limited population drug prevents sponsors of such products from seeking designation or approval under other provisions of the FDCA, such as accelerated approval.
The FDA's Decision on an NDA
On the basis of the FDA's evaluation of the NDA and accompanying information, including the results of the inspection of the manufacturing facilities, the FDA may issue an approval letter or a complete response letter. An approval letter authorizes commercial marketing of the product with specific prescribing information for specific indications. A complete response letter generally outlines the deficiencies in the submission and may require additional, sometimes substantial, testing or information in order for the FDA to reconsider the application. If and when those deficiencies have been addressed to the FDA's satisfaction in a resubmission of the NDA, the FDA will issue an approval letter. The FDA has committed to reviewing such resubmissions in two or six months depending on the type of information included. Even with submission of this additional information, the FDA ultimately may decide that the application does not satisfy the regulatory criteria for approval.
If the FDA approves a new product, it may limit the approved indications for use for the product, require that contraindications, warnings or precautions be included in the product labeling, require that post-approval studies, including Phase 4 clinical trials, be conducted to further assess the drug's safety after approval, require testing and surveillance programs to monitor the product after commercialization, or impose other conditions, including distribution restrictions or other risk management mechanisms, including REMS, which can materially affect the potential market and
44
profitability of the product. The FDA may prevent or limit further marketing of a product based on the results of post-market studies or surveillance programs. After approval, many types of changes to the approved product, such as adding new indications, manufacturing changes and additional labeling claims, are subject to further testing requirements and FDA review and approval.
Post-Approval Regulation
Drugs manufactured or distributed pursuant to FDA approvals are subject to pervasive and continuing regulation by the FDA, including, among other things, requirements relating to recordkeeping, periodic reporting, product sampling and distribution, advertising and promotion and reporting of adverse experiences with the product. After approval, most changes to the approved product, such as adding new indications or other labeling claims, are subject to prior FDA review and approval. There also are continuing, annual user fee requirements for any marketed products and the establishments at which such products are manufactured, as well as new application fees for supplemental applications with or without clinical data.
In addition, drug manufacturers and other entities involved in the manufacture and distribution of approved drugs are required to register their establishments with the FDA and state agencies, and are subject to periodic unannounced inspections by the FDA and these state agencies for compliance with cGMP requirements. Changes to the manufacturing process are strictly regulated and often require prior FDA approval before being implemented. FDA regulations also require investigation and correction of any deviations from cGMP and impose reporting and documentation requirements upon the sponsor and any third-party manufacturers that the sponsor may decide to use. Accordingly, manufacturers must continue to expend time, money and effort in the area of production and quality control to maintain cGMP compliance.
Once an approval is granted, the FDA may withdraw the approval if compliance with regulatory requirements and standards is not maintained or if problems occur after the product reaches the market. Later discovery of previously unknown problems with a product, including adverse events of unanticipated severity or frequency, or with manufacturing processes, or failure to comply with regulatory requirements, may result in revisions to the approved labeling to add new safety information; imposition of post-market studies or clinical trials to assess new safety risks; or imposition of distribution or other restrictions under a REMS program. Other potential consequences include, among other things:
- •
- restrictions on the marketing or manufacturing of the product, suspension of the approval, or complete withdrawal of the product from the
market or product recalls;
- •
- fines, warning letters or holds on post-approval clinical trials;
- •
- refusal of the FDA to approve pending NDAs or supplements to approved NDAs, or suspension or revocation of product license approvals;
- •
- product seizure or detention, or refusal to permit the import or export of products; or
- •
- injunctions or the imposition of civil or criminal penalties.
The FDA strictly regulates the marketing, labeling, advertising and promotion of prescription drug products placed on the market. This regulation includes, among other things, standards and regulations for direct-to-consumer advertising, communications regarding unapproved uses, industry-sponsored scientific and educational activities, and promotional activities involving the Internet and social media. Promotional claims about a drug's safety or effectiveness are prohibited before the drug is approved. After approval, a drug product generally may not be promoted for uses that are not approved by the FDA, as reflected in the product's prescribing information. In the United States, health care professionals are generally permitted to prescribe drugs for such uses not described in the drug's
45
labeling, known as off-label uses, because the FDA does not regulate the practice of medicine. However, FDA regulations impose rigorous restrictions on manufacturers' communications and prohibit the promotion of off-label uses. It may be permissible, under very specific, narrow conditions, for a manufacturer to engage in nonpromotional, non-misleading communication regarding off-label information, such as distributing scientific or medical journal information.
If a company is found to have promoted off-label uses, it may become subject to adverse public relations and administrative and judicial enforcement by the FDA, the Department of Justice, or the Office of the Inspector General of the Department of Health and Human Services, as well as state authorities. This could subject a company to a range of penalties that could have a significant commercial impact, including civil and criminal fines and agreements that materially restrict the manner in which a company promotes or distributes drug products. The federal government has levied large civil and criminal fines against companies for alleged improper promotion, and has also requested that companies enter into consent decrees or permanent injunctions under which specified promotional conduct is changed or curtailed.
In addition, the distribution of prescription pharmaceutical products is subject to the Prescription Drug Marketing Act, or PDMA, and its implementing regulations, as well as the Drug Supply Chain Security Act, or DSCA, which regulate the distribution and tracing of prescription drug samples at the federal level, and set minimum standards for the regulation of drug distributors by the states. The PDMA, its implementing regulations and state laws limit the distribution of prescription pharmaceutical product samples and the DSCA imposes requirements to ensure accountability in distribution and to identify and remove counterfeit and other illegitimate products from the market.
Section 505(b)(2) NDAs
NDAs for most new drug products are based on two full clinical studies which must contain substantial evidence of the safety and efficacy of the proposed new product for the proposed use. These applications are submitted under Section 505(b)(1) of the FDCA. The FDA is, however, authorized to approve an alternative type of NDA under Section 505(b)(2) of the FDCA. This type of application allows the applicant to rely, in part, on the FDA's previous findings of safety and efficacy for a similar product, or published literature. Specifically, Section 505(b)(2) applies to NDAs for a drug for which the investigations made to show whether or not the drug is safe for use and effective in use and relied upon by the applicant for approval of the application "were not conducted by or for the applicant and for which the applicant has not obtained a right of reference or use from the person by or for whom the investigations were conducted."
Thus, Section 505(b)(2) authorizes the FDA to approve an NDA based on safety and effectiveness data that were not developed by the applicant. NDAs filed under Section 505(b)(2) may provide an alternate and potentially more expeditious pathway to FDA approval for new or improved formulations or new uses of previously approved products. If the Section 505(b)(2) applicant can establish that reliance on the FDA's previous approval is scientifically appropriate, the applicant may eliminate the need to conduct certain preclinical or clinical studies of the new product. The FDA may also require companies to perform additional studies or measurements to support the change from the approved product. The FDA may then approve the new drug candidate for all or some of the label indications for which the referenced product has been approved, as well as for any new indication sought by the Section 505(b)(2) applicant.
Abbreviated New Drug Applications for Generic Drugs
In 1984, with passage of the Hatch-Waxman Amendments to the FDCA, Congress authorized the FDA to approve generic drugs that are the same as drugs previously approved by the FDA under the NDA provisions of the statute. To obtain approval of a generic drug, an applicant must submit an
46
abbreviated new drug application, or ANDA, to the agency. In support of such applications, a generic manufacturer may rely on the preclinical and clinical testing previously conducted for a drug product previously approved under an NDA, known as the reference listed drug, or RLD.
Specifically, in order for an ANDA to be approved, the FDA must find that the generic version is identical to the RLD with respect to the active ingredients, the route of administration, the dosage form, and the strength of the drug. At the same time, the FDA must also determine that the generic drug is "bioequivalent" to the innovator drug. Under the statute, a generic drug is bioequivalent to a RLD if "the rate and extent of absorption of the drug do not show a significant difference from the rate and extent of absorption of the listed drug."
Upon approval of an ANDA, the FDA indicates whether the generic product is "therapeutically equivalent" to the RLD in its publication "Approved Drug Products with Therapeutic Equivalence Evaluations," also referred to as the "Orange Book." Physicians and pharmacists consider a therapeutic equivalent generic drug to be fully substitutable for the RLD. In addition, by operation of certain state laws and numerous health insurance programs, the FDA's designation of therapeutic equivalence often results in substitution of the generic drug without the knowledge or consent of either the prescribing physician or patient.
Under the Hatch-Waxman Amendments, the FDA may not approve an ANDA until any applicable period of non-patent exclusivity for the RLD has expired. The FDCA provides a period of five years of non-patent data exclusivity for a new drug containing a new chemical entity. For the purposes of this provision, a new chemical entity, or NCE, is a drug that contains no active moiety that has previously been approved by the FDA in any other NDA. An active moiety is the molecule or ion responsible for the physiological or pharmacological action of the drug substance. In cases where such exclusivity has been granted, an ANDA may not be filed with the FDA until the expiration of five years unless the submission is accompanied by a Paragraph IV certification, in which case the applicant may submit its application four years following the original product approval. The FDCA also provides for a period of three years of exclusivity if the NDA includes reports of one or more new clinical investigations, other than bioavailability or bioequivalence studies, that were conducted by or for the applicant and are essential to the approval of the application. This three-year exclusivity period often protects changes to a previously approved drug product, such as a new dosage form, route of administration, combination or indication.
The FDCA also provides for a period of three years of exclusivity if the NDA includes reports of one or more new clinical investigations, other than bioavailability or bioequivalence studies, that were conducted by or for the applicant and are essential to the approval of the application. This three-year exclusivity period often protects changes to a previously approved drug product, such as a new dosage form, route of administration, combination or indication. Three-year exclusivity would be available for a drug product that contains a previously approved active moiety, provided the statutory requirement for a new clinical investigation is satisfied. Unlike five-year NCE exclusivity, an award of three-year exclusivity does not block the FDA from accepting ANDAs seeking approval for generic versions of the drug as of the date of approval of the original drug product. The FDA typically makes decisions about awards of data exclusivity shortly before a product is approved.
The FDA must establish a priority review track for certain generic drugs, requiring the FDA to review a drug application within eight (8) months for a drug that has three (3) or fewer approved drugs listed in the Orange Book and is no longer protected by any patent or regulatory exclusivities, or is on the FDA's drug shortage list. The new legislation also authorizes FDA to expedite review of "competitor generic therapies" or drugs with inadequate generic competition, including holding meetings with or providing advice to the drug sponsor prior to submission of the application.
47
Hatch-Waxman Patent Certification and the 30-Month Stay
Upon approval of an NDA or a supplement thereto, NDA sponsors are required to list with the FDA each patent with claims that cover the applicant's product or an approved method of using the product. Each of the patents listed by the NDA sponsor is published in the Orange Book. When an ANDA applicant files its application with the FDA, the applicant is required to certify to the FDA concerning any patents listed for the reference product in the Orange Book, except for patents covering methods of use for which the ANDA applicant is not seeking approval. To the extent that the Section 505(b)(2) applicant is relying on studies conducted for an already approved product, the applicant is required to certify to the FDA concerning any patents listed for the approved product in the Orange Book to the same extent that an ANDA applicant would.
Specifically, the applicant must certify with respect to each patent that:
- •
- the required patent information has not been filed;
- •
- the listed patent has expired;
- •
- the listed patent has not expired, but will expire on a particular date and approval is sought after patent expiration; or
- •
- the listed patent is invalid, unenforceable or will not be infringed by the new product.
A certification that the new product will not infringe the already approved product's listed patents or that such patents are invalid or unenforceable is called a Paragraph IV certification. If the applicant does not challenge the listed patents or indicates that it is not seeking approval of a patented method of use, the ANDA application will not be approved until all the listed patents claiming the referenced product have expired (other than method of use patents involving indications for which the ANDA applicant is not seeking approval).
If the ANDA applicant has provided a Paragraph IV certification to the FDA, the applicant must also send notice of the Paragraph IV certification to the NDA and patent holders once the ANDA has been accepted for filing by the FDA. The NDA and patent holders may then initiate a patent infringement lawsuit in response to the notice of the Paragraph IV certification. The filing of a patent infringement lawsuit within 45 days after the receipt of a Paragraph IV certification automatically prevents the FDA from approving the ANDA until the earlier of 30 months after the receipt of the Paragraph IV notice, expiration of the patent, or a decision in the infringement case that is favorable to the ANDA applicant.
To the extent that the Section 505(b)(2) applicant is relying on studies conducted for an already approved product, the applicant is required to certify to the FDA concerning any patents listed for the approved product in the Orange Book to the same extent that an ANDA applicant would. As a result, approval of a Section 505(b)(2) NDA can be stalled until all the listed patents claiming the referenced product have expired, until any non-patent exclusivity, such as exclusivity for obtaining approval of a new chemical entity, listed in the Orange Book for the referenced product has expired, and, in the case of a Paragraph IV certification and subsequent patent infringement suit, until the earlier of 30 months, settlement of the lawsuit or a decision in the infringement case that is favorable to the Section 505(b)(2) applicant.
Pediatric Studies and Exclusivity
Under the Pediatric Research Equity Act of 2003, an NDA or supplement thereto must contain data that are adequate to assess the safety and effectiveness of the drug product for the claimed indications in all relevant pediatric subpopulations, and to support dosing and administration for each pediatric subpopulation for which the product is safe and effective. With enactment of the FDASIA in 2012, sponsors must also submit pediatric study plans prior to the assessment data. Those plans must
48
contain an outline of the proposed pediatric study or studies the applicant plans to conduct, including study objectives and design, any deferral or waiver requests, and other information required by regulation. The applicant, the FDA, and the FDA's internal review committee must then review the information submitted, consult with each other, and agree upon a final plan. The FDA or the applicant may request an amendment to the plan at any time.
For drugs intended to treat a serious or life-threatening disease or condition, the FDA must, upon the request of an applicant, meet to discuss preparation of the initial pediatric study plan or to discuss deferral or waiver of pediatric assessments. In addition, FDA will meet early in the development process to discuss pediatric study plans with sponsors and FDA must meet with sponsors by no later than the end-of-phase 1 meeting for serious or life-threatening diseases and by no later than ninety (90) days after FDA's receipt of the study plan.
The FDA may, on its own initiative or at the request of the applicant, grant deferrals for submission of some or all pediatric data until after approval of the product for use in adults, or full or partial waivers from the pediatric data requirements. Additional requirements and procedures relating to deferral requests and requests for extension of deferrals are contained in the FDASIA. Unless otherwise required by regulation, the pediatric data requirements do not apply to products with orphan designation.
Pediatric exclusivity is another type of non-patent marketing exclusivity in the United States and, if granted, provides for the attachment of an additional six months of marketing protection to the term of any existing regulatory exclusivity, including the non-patent and orphan exclusivity. This six-month exclusivity may be granted if an NDA sponsor submits pediatric data that fairly respond to a written request from the FDA for such data. The data do not need to show the product to be effective in the pediatric population studied; rather, if the clinical trial is deemed to fairly respond to the FDA's request, the additional protection is granted. If reports of requested pediatric studies are submitted to and accepted by the FDA within the statutory time limits, whatever statutory or regulatory periods of exclusivity or patent protection cover the product are extended by six months. This is not a patent term extension, but it effectively extends the regulatory period during which the FDA cannot approve another application.
Orphan Drug Designation and Exclusivity
Under the Orphan Drug Act, the FDA may designate a drug product as an "orphan drug" if it is intended to treat a rare disease or condition (generally meaning that it affects fewer than 200,000 individuals in the United States, or more in cases in which there is no reasonable expectation that the cost of developing and making a drug product available in the United States for treatment of the disease or condition will be recovered from sales of the product). A company must request orphan product designation before submitting an NDA. If the request is granted, the FDA will disclose the identity of the therapeutic agent and its potential use. Orphan product designation does not convey any advantage in or shorten the duration of the regulatory review and approval process, although it does convey certain advantages such as taxbenefits and exemption from PDUFA fees.
If a product with orphan status receives the first FDA approval for the disease or condition for which it has such designation or for a select indication or use within the rare disease or condition for which it was designated, the product generally will receive orphan product exclusivity. Orphan product exclusivity means that the FDA may not approve any other applications for the same product for the same indication for seven years, except in certain limited circumstances. Competitors may receive approval of different products for the indication for which the orphan product has exclusivity and may obtain approval for the same product but for a different indication. If a drug or drug product designated as an orphan product ultimately receives marketing approval for an indication broader than what was designated in its orphan product application, it may not be entitled to exclusivity.
49
Orphan drug exclusivity will not bar approval of another product under certain circumstances, including if a subsequent product with the same drug for the same condition is shown to be clinically superior to the approved product on the basis of greater efficacy or safety, or provid ing a major contribution to patient care, or if the company with orphan drug exclusivity is not able to meet market demand. This is the case despite an earlier court opinion holding that the Orphan Drug Act unambiguously required the FDA to recognize orphan exclusivity regardless of a showing of clinical superiority.
GAIN Exclusivity for Antibiotics
In 2012, Congress passed legislation known as the Generating Antibiotic Incentives Now Act, or GAIN Act. This legislation is designed to encourage the development of antibacterial and antifungal drug products that treat pathogens that cause serious and life-threatening infections. To that end, the law grants an additional five years of exclusivity upon the approval of an NDA for a drug product designated by FDA as a QIDP. Thus, for a QIDP, the periods of five-year new chemical entity exclusivity, three-year new clinical investigation exclusivity, and seven-year orphan drug exclusivity, would become ten years, eight years, and twelve years, respectively.
A QIDP is defined in the GAIN Act to mean "an antibacterial or antifungal drug for human use intended to treat serious or life-threatening infections, including those caused by (1) an antibacterial or antifungal resistant pathogen, including novel or emerging infectious pathogens" or (2) certain "qualifying pathogens." A "qualifying pathogen" is a pathogen that has the potential to pose a serious threat to public health (such as resistant Gram-positive pathogens, multi-drug resistant Gram-negative bacteria, multi-drug resistant tuberculosis, and C. difficile) and that is included in a list established and maintained by FDA. A drug sponsor may request the FDA to designate its product as a QIDP any time before the submission of an NDA. The FDA must make a QIDP determination within 60 days of the designation request. A product designated as a QIDP will be granted priority review by the FDA and can qualify for "fast track" status.
The additional five years of exclusivity under the GAIN Act for drug products designated by the FDA as QIDPs applies only to a drug that is first approved on or after July 9, 2012. Additionally, the five year exclusivity extension does not apply to: a supplement to an application under FDCA Section 505(b) for any QIDP for which an extension is in effect or has expired; a subsequent application filed with respect to a product approved by the FDA for a change that results in a new indication, route of administration, dosing schedule, dosage form, delivery system, delivery device or strength; or a product that does not meet the definition of a QIDP under Section 505(g) based upon its approved uses. The FDA has designated each of the IV and oral formulations of lefamulin as a QIDP and also granted fast track designations to each of these formulations of lefamulin.
Patent Term Restoration and Extension
A patent claiming a new drug product may be eligible for a limited patent term extension under the Hatch-Waxman Act, which permits a patent restoration of up to five years for patent term lost during product development and the FDA regulatory review. The restoration period granted on a patent covering a product is typically one-half the time between the effective date of a clinical investigation involving human beings is begun and the submission date of an application, plus the time between the submission date of an application and the ultimate approval date. Patent term restoration cannot be used to extend the remaining term of a patent past a total of 14 years from the product's approval date. Only one patent applicable to an approved drug product is eligible for the extension, and the application for the extension must be submitted prior to the expiration of the patent in question. A patent that covers multiple products for which approval is sought can only be extended in connection with one of the approvals. The United States Patent and Trademark Offices reviews and approves the application for any patent term extension or restoration in consultation with the FDA.
50
The 21st Century Cures Act
On December 13, 2016, President Obama signed the 21st Century Cures Act, or Cures Act, into law. The Cures Act is designed to modernize and personalize healthcare, spur innovation and research, and streamline the discovery and development of new therapies through increased federal funding of particular programs. It authorizes increased funding for the FDA to spend on innovation projects. The new law also amends the Public Health Service Act to reauthorize and expand funding for the National Institutes of Health. The Act establishes the NIH Innovation Fund to pay for the cost of development and implementation of a strategic plan, early stage investigators and research. It also charges NIH with leading and coordinating expanded pediatric research. Further, the Cures Act directs the Centers for Disease Control and Prevention to expand surveillance of neurological diseases.
With amendments to the FDCA and the Public Health Service Act, or PHSA, Title III of the Cures Act seeks to accelerate the discovery, development, and delivery of new medicines and medical technologies. To that end, and among other provisions, the Cures Act reauthorizes the existing priority review voucher program for certain drugs intended to treat rare pediatric diseases until 2020; creates a new priority review voucher program for drug applications determined to be material national security threat medical countermeasure applications; revises the FDCA to streamline review of combination product applications; requires FDA to evaluate the potential use of "real world evidence" to help support approval of new indications for approved drugs; provides a new "limited population" approval pathway for antibiotic and antifungal drugs intended to treat serious or life-threatening infections; and authorizes FDA to designate a drug as a "regenerative advanced therapy," thereby making it eligible for certain expedited review and approval designations.
Regulation Outside the United States
In order to market any product outside of the United States, a company must also comply with numerous and varying regulatory requirements of other countries and jurisdictions regarding quality, safety and efficacy and governing, among other things, clinical trials, marketing authorization, commercial sales and distribution of drug products. Whether or not it obtains FDA approval for a product, the company would need to obtain the necessary approvals by the comparable foreign regulatory authorities before it can commence clinical trials or marketing of the product in those countries or jurisdictions. The approval process ultimately varies between countries and jurisdictions and can involve additional product testing and additional administrative review periods. The time required to obtain approval in other countries and jurisdictions might differ from and be longer than that required to obtain FDA approval. Regulatory approval in one country or jurisdiction does not ensure regulatory approval in another, but a failure or delay in obtaining regulatory approval in one country or jurisdiction may negatively impact the regulatory process in others.
Regulation and Marketing Authorization in the European Union
The process governing approval of medicinal products in the European Union follows essentially the same lines as in the United States and, likewise, generally involves satisfactorily completing each of the following:
- •
- preclinical laboratory tests, animal studies and formulation studies all performed in accordance with the applicable E.U. Good Laboratory
Practice regulations;
- •
- submission to the relevant national authorities of a clinical trial application, or CTA, which must be approved before human clinical trials
may begin;
- •
- performance of adequate and well-controlled clinical trials to establish the safety and efficacy of the product for each proposed indication;
51
- •
- submission to the relevant competent authorities of a marketing authorization application, or MAA, which includes the data supporting safety
and efficacy as well as detailed information on the manufacture and composition of the product in clinical development and proposed labelling;
- •
- satisfactory completion of an inspection by the relevant national authorities of the manufacturing facility or facilities, including those of
third parties, at which the product is produced to assess compliance with strictly enforced cGMP;
- •
- potential audits of the non-clinical and clinical trial sites that generated the data in support of the MAA; and
- •
- review and approval by the relevant competent authority of the MAA before any commercial marketing, sale or shipment of the product.
Preclinical Studies
Preclinical tests include laboratory evaluations of product chemistry, formulation and stability, as well as studies to evaluate toxicity in animal studies, in order to assess the potential safety and efficacy of the product. The conduct of the preclinical tests and formulation of the compounds for testing must comply with the relevant E.U. regulations and requirements. The results of the preclinical tests, together with relevant manufacturing information and analytical data, are submitted as part of the CTA.
Clinical Trial Approval
Requirements for the conduct of clinical trials in the European Union including Good Clinical Practice, or GCP, are set forth in the Clinical Trials Directive 2001/20/EC and the GCP Directive 2005/28/EC. Pursuant to Directive 2001/20/EC and Directive 2005/28/EC, as amended, a system for the approval of clinical trials in the European Union has been implemented through national legislation of the E.U. member states. Under this system, approval must be obtained from the competent national authority of each E.U. member state in which a study is planned to be conducted. To this end, a CTA is submitted, which must be supported by an investigational medicinal product dossier, or IMPD, and further supporting information prescribed by Directive 2001/20/EC and Directive 2005/28/EC and other applicable guidance documents. Furthermore, a clinical trial may only be started after a competent ethics committee has issued a favorable opinion on the clinical trial application in that country.
In April 2014, the E.U. passed the new Clinical Trials Regulation, (EU) No 536/2014, which will replace the current Clinical Trials Directive 2001/20/EC. The Regulation was published on June 16, 2014 but is not expected to apply until 2019. To ensure that the rules for clinical trials are identical throughout the European Union, the new E.U. clinical trials legislation was passed as a regulation that is directly applicable in all E.U. member states. All clinical trials performed in the European Union are required to be conducted in accordance with the Clinical Trials Directive 2001/20/EC until the new Clinical Trials Regulation (EU) No 536/2014 becomes applicable. The Clinical Trials Directive 2001/20/EC will, however, still apply three years from the date of entry into application of the Clinical Trials Regulation to (i) clinical trials applications submitted before the entry into application and (ii) clinical trials applications submitted within one year after the entry into application if the sponsor opts for the old system.
The new Clinical Trials Regulation aims to simplify and streamline the approval of clinical trial in the European Union. The main characteristics of the regulation include:
- •
- a streamlined application procedure via a single entry point, the E.U. portal;
52
- •
- a single set of documents to be prepared and submitted for the application as well as simplified reporting procedures that will spare sponsors
from submitting broadly identical information separately to various bodies and different member states;
- •
- a harmonized procedure for the assessment of applications for clinical trials, which is divided in two parts. Part I is assessed jointly
by all member states concerned. Part II is assessed separately by each member state concerned;
- •
- strictly defined deadlines for the assessment of clinical trial applications; and
- •
- the involvement of the ethics committees in the assessment procedure in accordance with the national law of the member state concerned but within the overall timelines defined by the Clinical Trials Regulation.
Marketing Authorization
Authorization to market a product in the member states of the European Union proceeds under one of four procedures: a centralized authorization procedure, a mutual recognition procedure, a decentralized procedure or a national procedure.
Centralized Authorization Procedure
The centralized procedure enables applicants to obtain a marketing authorization that is valid in all E.U. member states based on a single application. Certain medicinal products, including products developed by means of biotechnological processes must undergo the centralized authorization procedure for marketing authorization, which, if granted by the European Commission, is automatically valid in all 28 E.U. member states. The EMA and the European Commission administer this centralized authorization procedure pursuant to Regulation (EC) No 726/2004.
Pursuant to Regulation (EC) No 726/2004, this procedure is mandatory for:
- •
- medicinal products developed by means of one of the following biotechnological processes:
- •
- recombinant DNA technology;
- •
- controlled expression of genes coding for biologically active proteins in prokaryotes and eukaryotes including transformed
mammalian cells; and
- •
- hybridoma and monoclonal antibody methods;
- •
- advanced therapy medicinal products as defined in Article 2 of Regulation (EC) No 1394/2007 on advanced therapy medicinal products;
- •
- medicinal products for human use containing a new active substance that, on the date of effectiveness of this regulation, was not authorized in
the European Union, and for which the therapeutic indication is the treatment of any of the following diseases:
- •
- acquired immune deficiency syndrome;
- •
- cancer;
- •
- neurodegenerative disorder;
- •
- diabetes;
- •
- auto-immune diseases and other immune dysfunctions; and
- •
- viral diseases; and
- •
- medicinal products that are designated as orphan medicinal products pursuant to Regulation (EC) No 141/2000.
53
The centralized authorization procedure is optional for other medicinal products if they contain a new active substance or if the applicant shows that the medicinal product concerned constitutes a significant therapeutic, scientific or technical innovation or that the granting of authorization is in the interest of patients in the European Union.
Administrative Procedure
Under the centralized authorization procedure, the EMA's Committee for Medicinal Products for Human Use, or CHMP serves as the scientific committee that renders opinions about the safety, efficacy and quality of medicinal products for human use on behalf of the EMA. The CHMP is composed of experts nominated by each member state's national authority for medicinal products, with one of them appointed to act as Rapporteur for the co-ordination of the evaluation with the possible assistance of a further member of the Committee acting as a Co-Rapporteur. After approval, the Rapporteur(s) continue to monitor the product throughout its life cycle. The CHMP has 210 days, to adopt an opinion as to whether a marketing authorization should be granted. The process usually takes longer in case additional information is requested, which triggers clock-stops in the procedural timelines. The process is complex and involves extensive consultation with the regulatory authorities of member states and a number of experts. When an application is submitted for a marketing authorization in respect of a drug that is of major interest from the point of view of public health and in particular from the viewpoint of therapeutic innovation, the applicant may pursuant to Article 14(9) Regulation (EC) No 726/2004 request an accelerated assessment procedure. If the CHMP accepts such request, the time-limit of 210 days will be reduced to 150 days but it is possible that the CHMP can revert to the standard time-limit for the centralized procedure if it considers that it is no longer appropriate to conduct an accelerated assessment. Once the procedure is completed, a European Public Assessment Report, or EPAR, is produced. If the opinion is negative, information is given as to the grounds on which this conclusion was reached. After the adoption of the CHMP opinion, a decision on the MAA must be adopted by the European Commission, after consulting the E.U. member states, which in total can take more than 60 days.
Conditional Approval
In specific circumstances, E.U. legislation (Regulation (EC) No 726/2004 and Regulation (EC) No 507/2006 on Conditional Marketing Authorisations for Medicinal Products for Human Use) enables applicants to obtain a conditional marketing authorization prior to obtaining the comprehensive clinical data required for an application for a full marketing authorization. Such conditional approvals may be granted for product candidates (including medicines designated as orphan medicinal products), if (1) the risk-benefit balance of the product candidate is positive, (2) it is likely that the applicant will be in a position to provide the required comprehensive clinical trial data, (3) the product fulfills unmet medical needs and (4) the benefit to public health of the immediate availability on the market of the medicinal product concerned outweighs the risk inherent in the fact that additional data are still required. A conditional marketing authorization may contain specific obligations to be fulfilled by the marketing authorization holder, including obligations with respect to the completion of ongoing or new studies, and with respect to the collection of pharmacovigilance data. Conditional marketing authorizations are valid for one year, and may be renewed annually, if the risk-benefit balance remains positive, and after an assessment of the need for additional or modified conditions and/or specific obligations. The timelines for the centralized procedure described above also apply with respect to the review by the CHMP of applications for a conditional marketing authorization.
Marketing Authorization Under Exceptional Circumstances
Under Regulation (EC) No 726/2004, products for which the applicant can demonstrate that comprehensive data (in line with the requirements laid down in Annex I of Directive 2001/83/EC, as
54
amended) cannot be provided (due to specific reasons foreseen in the legislation) might be eligible for marketing authorization under exceptional circumstances. This type of authorization is reviewed annually to reassess the risk-benefit balance. The fulfillment of any specific procedures/obligations imposed as part of the marketing authorization under exceptional circumstances is aimed at the provision of information on the safe and effective use of the product and will normally not lead to the completion of a full dossier/approval.
Market Authorizations Granted by Authorities of E.U. Member States
In general, if the centralized procedure is not followed, there are three alternative procedures to obtain a marketing authorization in (one or several) E.U. member states as prescribed in Directive 2001/83/EC:
- •
- The decentralized procedure allows applicants to file identical applications to several E.U. member states and receive simultaneous national
approvals based on the recognition by E.U. member states of an assessment by a reference member state.
- •
- The national procedure is only available for products intended to be authorized in a single E.U. member state.
- •
- A mutual recognition procedure similar to the decentralized procedure is available when a marketing authorization has already been obtained in at least one E.U. member state.
A marketing authorization may be granted only to an applicant established in the European Union.
Pediatric Studies
Prior to obtaining a marketing authorization in the E.U., applicants have to demonstrate compliance with all measures included in an EMA-approved Pediatric Investigation Plan, or PIP, covering all subsets of the pediatric population, unless the EMA has granted a product-specific waiver, a class waiver, or a deferral for one or more of the measures included in the PIP. The respective requirements for all marketing authorization procedures are set forth in Regulation (EC) No 1901/2006, which is referred to as the Pediatric Regulation. This requirement also applies when a company wants to add a new indication, pharmaceutical form or route of administration for a medicine that is already authorized. The Pediatric Committee of the EMA, or PDCO, may grant deferrals for some medicines, allowing a company to delay development of the medicine in children until there is enough information to demonstrate its effectiveness and safety in adults. The PDCO may also grant waivers when development of a medicine in children is not needed or is not appropriate, such as for diseases that only affect the elderly population.
Before a marketing authorization application can be filed, or an existing marketing authorization can be amended, the EMA determines that companies actually comply with the agreed studies and measures listed in each relevant PIP.
Period of Authorization and Renewals
A marketing authorization, other than a conditional marketing authorization, is initially valid for five years and the marketing authorization may be renewed after five years on the basis of a re-evaluation of the risk-benefit balance by the EMA or by the competent authority of the authorizing member state. To this end, the marketing authorization holder must provide the EMA or the competent authority with a consolidated version of the file in respect of quality, safety and efficacy, including all variations introduced since the marketing authorization was granted, at least six months before the marketing authorization ceases to be valid. Once renewed, the marketing authorization is valid for an unlimited period, unless the European Commission or the competent authority decides, on justified grounds relating to pharmacovigilance, to proceed with one additional five-year renewal. Any authorization which is not followed by the actual placing of the drug on the E.U. market (in case of centralized procedure) or on the market of the authorizing member state within three years after authorization ceases to be valid (the so-called sunset clause).
55
Regulatory Data Protection
European Union legislation also provides for a system of regulatory data and market exclusivity. According to Article 14(11) of Regulation (EC) No 726/2004, as amended, and Article 10(1) of Directive 2001/83/EC, as amended, upon receiving marketing authorization, new chemical entities approved on the basis of complete independent data package benefit from eight years of data exclusivity and an additional two years of market exclusivity. Data exclusivity prevents regulatory authorities in the European Union from referencing the innovator's data to assess a generic (abbreviated) application. During the additional two-year period of market exclusivity, a generic marketing authorization application can be submitted, and the innovator's data may be referenced, but no generic medicinal product can be marketed until the expiration of the market exclusivity. The overall ten-year period will be extended to a maximum of eleven years if, during the first eight years of those ten years, the marketing authorization holder, or MAH, obtains an authorization for one or more new therapeutic indications which, during the scientific evaluation prior to their authorization, are held to bring a significant clinical benefit in comparison with existing therapies. Even if a compound is considered to be a new chemical entity and the innovator is able to gain the period of data exclusivity, another company nevertheless could also market another version of the drug if such company obtained marketing authorization based on an MAA with a complete independent data package of pharmaceutical test, preclinical tests and clinical trials.
Orphan Drug Designation and Exclusivity
Regulation (EC) No. 141/2000, as implemented by Regulation (EC) No. 847/2000 provides that a drug can be designated as an orphan drug by the European Commission if its sponsor can establish: that the product is intended for the diagnosis, prevention or treatment of (1) a life-threatening or chronically debilitating condition affecting not more than five in ten thousand persons in the E.U. when the application is made, or (2) a life-threatening, seriously debilitating or serious and chronic condition in the E.U. and that without incentives it is unlikely that the marketing of the drug in the E.U. would generate sufficient return to justify the necessary investment. For either of these conditions, the applicant must demonstrate that there exists no satisfactory method of diagnosis, prevention or treatment of the condition in question that has been authorized in the E.U. or, if such method exists, the drug will be of significant benefit to those affected by that condition.
Once authorized, orphan medicinal products are entitled to 10 years of market exclusivity in all E.U. Member States and in addition a range of other benefits during the development and regulatory review process including scientific assistance for study protocols, authorization through the centralized marketing authorization procedure covering all member countries and a reduction or elimination of registration and marketing authorization fees. However, marketing authorization may be granted to a similar medicinal product with the same orphan indication during the 10-year period with the consent of the marketing authorization holder for the original orphan medicinal product or if the manufacturer of the original orphan medicinal product is unable to supply sufficient quantities. Marketing authorization may also be granted to a similar medicinal product with the same orphan indication if this product is safer, more effective or otherwise clinically superior to the original orphan medicinal product. The period of market exclusivity may, in addition, be reduced to six years if it can be demonstrated on the basis of available evidence that the original orphan medicinal product is sufficiently profitable not to justify maintenance of market exclusivity.
Transparency
There is an increasing trend in the E.U. towards greater transparency and, while the manufacturing or quality information in marketing authorization dossiers is currently generally protected as confidential information, the EMA and national regulatory authorities are now liable to disclose much of the non-clinical and clinical information, including the full clinical study reports, in
56
response to freedom of information requests after the marketing authorization has been granted. In October 2014, the EMA adopted a policy under which clinical study reports would be posted on the agency's website following the grant, denial or withdrawal of a marketing authorization application, subject to procedures for limited redactions and protection against unfair commercial use. Additional transparency provisions are contained in the new Clinical Trials Regulation (EU) No 536/2014 that will take effect in May 2016 at the earliest.
Regulatory Requirements After a Marketing Authorization has been Obtained
If we obtain authorization for a medicinal product in the European Union, we will be required to comply with a range of requirements applicable to the manufacturing, marketing, promotion and sale of medicinal products:
Pharmacovigilance and Other Requirements
We will, for example, have to comply with the E.U.'s stringent pharmacovigilance or safety reporting rules, pursuant to which post-authorization studies and additional monitoring obligations can be imposed. E.U. regulators may conduct inspections to verify our compliance with applicable requirements, and we will have to continue to expend time, money and effort to remain compliant. Non-compliance with E.U. requirements regarding safety monitoring or pharmacovigilance, and with requirements related to the development of products for the pediatric population, can also result in significant financial penalties in the European Union. Similarly, failure to comply with the European Union's requirements regarding the protection of individual personal data can also lead to significant penalties and sanctions. Individual E.U. member states may also impose various sanctions and penalties in case we do not comply with locally applicable requirements.
Manufacturing
The manufacturing of authorized drugs, for which a separate manufacturer's license is mandatory, must be conducted in strict compliance with the EMA's GMP requirements and comparable requirements of other regulatory bodies in the European Union, which mandate the methods, facilities and controls used in manufacturing, processing and packing of drugs to assure their safety and identity. The EMA enforces its GMP requirements through mandatory registration of facilities and inspections of those facilities. The EMA may have a coordinating role for these inspections while the responsibility for carrying them out rests with the member states competent authority under whose responsibility the manufacturer falls. Failure to comply with these requirements could interrupt supply and result in delays, unanticipated costs and lost revenues, and could subject the applicant to potential legal or regulatory action, including but not limited to warning letters, suspension of manufacturing, seizure of product, injunctive action or possible civil and criminal penalties.
Marketing and Promotion
The marketing and promotion of authorized drugs, including industry-sponsored continuing medical education and advertising directed toward the prescribers of drugs and/or the general public, are strictly regulated in the European Union under Directive 2001/83EC, as amended. The applicable regulations aim to ensure that information provided by holders of marketing authorizations regarding their products is truthful, balanced and accurately reflects the safety and efficacy claims authorized by the EMA or by the competent authority of the authorizing member state. Failure to comply with these requirements can result in adverse publicity, warning letters, corrective advertising and potential civil and criminal penalties.
57
Patent Term Extension
To compensate the patentee for delays in obtaining a marketing authorization for a patented product, a supplementary certificate, or SPC, may be granted extending the exclusivity period for that specific product by up to five years. Applications for SPCs must be made to the relevant patent office in each E.U. member state and the granted certificates are valid only in the member state of grant. An application has to be made by the patent owner within six months of the first marketing authorization being granted in the European Union (assuming the patent in question has not expired, lapsed or been revoked) or within six months of the grant of the patent (if the marketing authorization is granted first). In the context of SPCs, the term "product" means the active ingredient or combination of active ingredients for a medicinal product and the term "patent" means a patent protecting such a product or a new manufacturing process or application for it. The duration of an SPC is calculated as the difference between the patent's filing date and the date of the first marketing authorization, minus five years, subject to a maximum term of five years.
A six-month pediatric extension of an SPC may be obtained where the patentee has carried out an agreed pediatric investigation plan, the authorized product information includes information on the results of the studies and the product is authorized in all member states of the European Union.
Brexit and the Regulatory Framework in the United Kingdom
On June 23, 2016, the electorate in the United Kingdom voted in favor of leaving the E.U. (commonly referred to as "Brexit"). Thereafter, on March 29, 2017, the country formally notified the E.U. of its intention to withdraw pursuant to Article 50 of the Lisbon Treaty. The withdrawal of the U.K. from the European Union will take effect either on the effective date of the withdrawal agreement or, in the absence of agreement, two years after the U.K. provides a notice of withdrawal pursuant to the E.U. Treaty. Since the regulatory framework for pharmaceutical products in the U.K. covering quality, safety and efficacy of pharmaceutical products, clinical trials, marketing authorization, commercial sales and distribution of pharmaceutical products is derived from E.U. directives and regulations, Brexit could materially impact the future regulatory regime which applies to products and the approval of product candidates in the U.K. It remains to be seen how, if at all, Brexit will impact regulatory requirements for product candidates and products in the U.K.
Pharmaceutical Coverage, Pricing and Reimbursement
In the United States and markets in other countries, patients who are prescribed treatments for their conditions and providers performing the prescribed services generally rely on third-party payors to reimburse all or part of the associated healthcare costs. Significant uncertainty exists as to the coverage and reimbursement status of products approved by the FDA and other government authorities. Thus, even if a product candidate is approved, sales of the product will depend, in part, on the extent to which third-party payors, including government health programs in the United States such as Medicare and Medicaid, commercial health insurers and managed care organizations, provide coverage, and establish adequate reimbursement levels for, the product. The process for determining whether a payor will provide coverage for a product may be separate from the process for setting the price or reimbursement rate that the payor will pay for the product once coverage is approved. Third-party payors are increasingly challenging the prices charged, examining the medical necessity, and reviewing the cost-effectiveness of medical products and services and imposing controls to manage costs. Third-party payors may limit coverage to specific products on an approved list, also known as a formulary, which might not include all of the approved products for a particular indication.
To secure coverage and reimbursement for any product that might be approved for sale, a company may need to conduct expensive pharmacoeconomic studies in order to demonstrate the medical necessity and cost-effectiveness of the product, in addition to the costs required to obtain FDA
58
or other comparable marketing approvals. Nonetheless, product candidates may not be considered medically necessary or cost effective. A decision by a third-party payor not to cover a product candidate could reduce physician utilization once the product is approved and have a material adverse effect on sales, results of operations and financial condition. Additionally, a payor's decision to provide coverage for a product does not imply that an adequate reimbursement rate will be approved. Further, one payor's determination to provide coverage for a drug product does not assure that other payors will also provide coverage and reimbursement for the product, and the level of coverage and reimbursement can differ significantly from payor to payor.
The containment of healthcare costs also has become a priority of federal, state and foreign governments and the prices of drugs have been a focus in this effort. Governments have shown significant interest in implementing cost-containment programs, including price controls, restrictions on reimbursement and requirements for substitution of generic products. Adoption of price controls and cost-containment measures, and adoption of more restrictive policies in jurisdictions with existing controls and measures, could further limit a company's revenue generated from the sale of any approved products. Coverage policies and third-party reimbursement rates may change at any time. Even if favorable coverage and reimbursement status is attained for one or more products for which a company or its collaborators receive marketing approval, less favorable coverage policies and reimbursement rates may be implemented in the future.
Outside the United States, ensuring adequate coverage and payment for a product also involves challenges. Pricing of prescription pharmaceuticals is subject to governmental control in many countries. Pricing negotiations with governmental authorities can extend well beyond the receipt of regulatory marketing approval for a product and may require a clinical trial that compares the cost effectiveness of a product to other available therapies. The conduct of such a clinical trial could be expensive and result in delays in commercialization.
In the European Union, pricing and reimbursement schemes vary widely from country to country. Some countries provide that products may be marketed only after a reimbursement price has been agreed. Some countries may require the completion of additional studies that compare the cost-effectiveness of a particular drug candidate to currently available therapies or so called health technology assessments, in order to obtain reimbursement or pricing approval. For example, the European Union provides options for its member states to restrict the range of products for which their national health insurance systems provide reimbursement and to control the prices of medicinal products for human use. E.U. European Union member states may approve a specific price for a product or it may instead adopt a system of direct or indirect controls on the profitability of the company placing the product on the market. Other member states allow companies to fix their own prices for products, but monitor and control prescription volumes and issue guidance to physicians to limit prescriptions. Recently, many countries in the European Union have increased the amount of discounts required on pharmaceuticals and these efforts could continue as countries attempt to manage healthcare expenditures, especially in light of the severe fiscal and debt crises experienced by many countries in the European Union. The downward pressure on health care costs in general, particularly prescription drugs, has become intense. As a result, increasingly high barriers are being erected to the entry of new products. Political, economic and regulatory developments may further complicate pricing negotiations, and pricing negotiations may continue after reimbursement has been obtained. Reference pricing used by various European Union member states, and parallel trade, i.e., arbitrage between low-priced and high-priced member states, can further reduce prices. There can be no assurance that any country that has price controls or reimbursement limitations for pharmaceutical products will allow favorable reimbursement and pricing arrangements for any products, if approved in those countries.
59
Healthcare Law and Regulation
Healthcare providers and third-party payors play a primary role in the recommendation and prescription of drug products that are granted marketing approval. Arrangements with providers, consultants, third party payors and customers are subject to broadly applicable fraud and abuse, anti-kickback, false claims laws, reporting of payments to physicians and teaching physicians and patient privacy laws and regulations and other healthcare laws and regulations that may constrain business and/or financial arrangements. Restrictions under applicable federal and state healthcare laws and regulations, include the following:
- •
- the federal Anti-Kickback Statute prohibits, among other things, persons and entities from knowingly and willfully soliciting, offering,
paying, receiving or providing remuneration, directly or indirectly, in cash or in kind, to induce or reward either the referral of an individual for, or the purchase, order or recommendation of, any
good or service, for which payment may be made, in whole or in part, under a federal healthcare program such as Medicare and Medicaid;
- •
- the federal civil and criminal false claims laws, including the civil False Claims Act and civil monetary penalty laws, which prohibit
individuals or entities from, among other things, knowingly presenting, or causing to be presented, to the federal government, claims for payment that are false, fictitious or fraudulent or knowingly
making, using or causing to be made or used a false record or statement to avoid, decrease or conceal an obligation to pay money to the federal government;
- •
- the federal Health Insurance Portability and Accountability Act of 1996, or HIPAA, which created additional federal criminal laws that
prohibit, among other things, knowingly and willfully executing, or attempting to execute, a scheme to defraud any healthcare benefit program or making false statements relating to healthcare matters;
- •
- HIPAA, as amended by the Health Information Technology for Economic and Clinical Health Act and their regulations, including the Final Omnibus
Rule published in January 2013, which impose obligations, including mandatory contractual terms, with respect to safeguarding the privacy, security and transmission of individually identifiable health
information;
- •
- the federal false statements statute, which prohibits knowingly and willfully falsifying, concealing or covering up a material fact or making
any materially false statement in connection with the delivery of or payment for healthcare benefits, items or services;
- •
- the federal transparency requirements known as the federal Physician Payments Sunshine Act, under the Patient Protection and Affordable Care
Act, as amended by the Health Care Education Reconciliation Act, or the Affordable Care Act, which requires certain manufacturers of drugs, devices, biologics and medical supplies to report annually
to the Centers for Medicare & Medicaid Services, or CMS, within the United States Department of Health and Human Services, information related to payments and other transfers of value made by
that entity to physicians and teaching hospitals, as well as ownership and investment interests held by physicians and their immediate family members; and
- •
- analogous state and foreign laws and regulations, such as state anti-kickback and false claims laws, which may apply to healthcare items or services that are reimbursed by non-governmental third-party payors, including private insurers.
Some state laws require pharmaceutical companies to comply with the pharmaceutical industry's voluntary compliance guidelines and the relevant compliance guidance promulgated by the federal government in addition to requiring drug manufacturers to report information related to payments to physicians and other health care providers or marketing expenditures. State and foreign laws also govern the privacy and security of health information in some circumstances, many of which differ from
60
each other in significant ways and often are not preempted by HIPAA, thus complicating compliance efforts.
Healthcare Reform
A primary trend in the United States healthcare industry and elsewhere is cost containment. There have been a number of federal and state proposals during the last few years regarding the pricing of pharmaceutical and biopharmaceutical products, limiting coverage and reimbursement for drugs and other medical products, government control and other changes to the healthcare system in the United States.
In March 2010, the United States Congress enacted the Affordable Care Act, or the ACA, which, among other things, includes changes to the coverage and payment for products under government health care programs. Among the provisions of the Affordable Care Act of importance to potential drug candidates are:
- •
- an annual, nondeductible fee on any entity that manufactures or imports specified branded prescription drugs and biologic agents, apportioned
among these entities according to their market share in certain government healthcare programs, although this fee would not apply to sales of certain products approved exclusively for orphan
indications;
- •
- expansion of eligibility criteria for Medicaid programs by, among other things, allowing states to offer Medicaid coverage to certain
individuals with income at or below 133% of the federal poverty level, thereby potentially increasing a manufacturer's Medicaid rebate liability;
- •
- expanded manufacturers' rebate liability under the Medicaid Drug Rebate Program by increasing the minimum rebate for both branded and generic
drugs and revising the definition of "average manufacturer price," or AMP, for calculating and reporting Medicaid drug rebates on outpatient prescription drug prices and extending rebate liability to
prescriptions for individuals enrolled in Medicare Advantage plans;
- •
- addressed a new methodology by which rebates owed by manufacturers under the Medicaid Drug Rebate Program are calculated for drugs that are
inhaled, infused, instilled, implanted or injected;
- •
- expanded the types of entities eligible for the 340B drug discount program;
- •
- established the Medicare Part D coverage gap discount program by requiring manufacturers to provide a 50% point-of-sale-discount off the
negotiated price of applicable brand drugs to eligible beneficiaries during their coverage gap period as a condition for the manufacturers' outpatient drugs to be covered under Medicare Part D;
- •
- a new Patient-Centered Outcomes Research Institute to oversee, identify priorities in, and conduct comparative clinical effectiveness research,
along with funding for such research;
- •
- the Independent Payment Advisory Board, or IPAB, which has authority to recommend certain changes to the Medicare program to reduce
expenditures by the program that could result in reduced payments for prescription drugs. However, the IPAB implementation has been not been clearly defined. PPACA provided that under certain
circumstances, IPAB recommendations will become law unless Congress enacts legislation that will achieve the same or greater Medicare cost savings; and
- •
- established the Center for Medicare and Medicaid Innovation within CMS to test innovative payment and service delivery models to lower Medicare and Medicaid spending, potentially including prescription drug spending. Funding has been allocated to support the mission of the Center for Medicare and Medicaid Innovation from 2011 to 2019.
61
Other legislative changes have been proposed and adopted since the ACA was enacted. These changes include the Budget Control Act of 2011, which, among other things, led to aggregate reductions to Medicare payments to providers of up to 2% per fiscal year that started in 2013 and will stay in effect through 2024 unless additional Congressional action is taken, and the American Taxpayer Relief Act of 2012, which, among other things, reduced Medicare payments to several types of providers and increased the statute of limitations period for the government to recover overpayments to providers from three to five years. These new laws may result in additional reductions in Medicare and other healthcare funding and otherwise affect the prices we may obtain for any of our product candidates for which we may obtain regulatory approval or the frequency with which any such product candidate is prescribed or used. Further, there have been several recent U.S. congressional inquiries and proposed state and federal legislation designed to, among other things, bring more transparency to drug pricing, review the relationship between pricing and manufacturer patient programs, reduce the costs of drugs under Medicare and reform government program reimbursement methodologies for drug products.
These healthcare reforms, as well as other healthcare reform measures that may be adopted in the future, may result in additional reductions in Medicare and other healthcare funding, more rigorous coverage criteria, new payment methodologies and additional downward pressure on the price for any approved product and/or the level of reimbursement physicians receive for administering any approved product. Reductions in reimbursement levels may negatively impact the prices or the frequency with which products are prescribed or administered. Any reduction in reimbursement from Medicare or other government programs may result in a similar reduction in payments from private payors. Since enactment of the ACA, there have been numerous legal challenges and Congressional actions to repeal and replace provisions of the law. In May 2017, the U.S. House of Representatives passed legislation known as the American Health Care Act of 2017. Thereafter, the Senate Republicans introduced and then updated a bill to replace the ACA known as the Better Care Reconciliation Act of 2017. The Senate Republicans also introduced legislation to repeal the ACA without companion legislation to replace it, and a "skinny" version of the Better Care Reconciliation Act of 2017. In addition, the Senate considered proposed healthcare reform legislation known as the Graham-Cassidy bill. None of these measures was passed by the U.S. Senate.
The Trump Administration has also taken executive actions to undermine or delay implementation of the ACA. In January 2017, President Trump signed an Executive Order directing federal agencies with authorities and responsibilities under the ACA to waive, defer, grant exemptions from, or delay the implementation of any provision of the ACA that would impose a fiscal or regulatory burden on states, individuals, healthcare providers, health insurers, or manufacturers of pharmaceuticals or medical devices. In October 2017, the President signed a second Executive Order allowing for the use of association health plans and short-term health insurance, which may provide fewer health benefits than the plans sold through the ACA exchanges. At the same time, the Administration announced that it will discontinue the payment of cost-sharing reduction (CSR) payments to insurance companies until Congress approves the appropriation of funds for such CSR payments. The loss of the CSR payments is expected to increase premiums on certain policies issued by qualified health plans under the ACA. A bipartisan bill to appropriate funds for CSR payments was introduced in the Senate, but the future of that bill is uncertain.
More recently, with enactment of the Tax Cuts and Jobs Act of 2017, which was signed by the President on December 22, 2017, Congress repealed the "individual mandate." The repeal of this provision, which requires most Americans to carry a minimal level of health insurance, will become effective in 2019. According to the Congressional Budget Office, the repeal of the individual mandate will cause 13 million fewer Americans to be insured in 2027 and premiums in insurance markets may rise. Additionally, on January 22, 2018, President Trump signed a continuing resolution on appropriations for fiscal year 2018 that delayed the implementation of certain ACA-mandated fees,
62
including the so-called "Cadillac" tax on certain high cost employer-sponsored insurance plans, the annual fee imposed on certain health insurance providers based on market share, and the medical device excise tax on non-exempt medical devices. The Congress will likely consider other legislation to replace elements of the ACA, during the next Congressional session.
Further, there have been several recent U.S. congressional inquiries and proposed federal and proposed and enacted state legislation designed to, among other things, bring more transparency to drug pricing, review the relationship between pricing and manufacturer patient programs, reduce the costs of drugs under Medicare and reform government program reimbursement methodologies for drug products. At the federal level, Congress and the Trump administration have each indicated that it will continue to seek new legislative and/or administrative measures to control drug costs. At the state level, individual states are increasingly aggressive in passing legislation and implementing regulations designed to control pharmaceutical and biological product pricing, including price or patient reimbursement constraints, discounts, restrictions on certain product access and marketing cost disclosure and transparency measures, and, in some cases, designed to encourage importation from other countries and bulk purchasing. In addition, regional health care authorities and individual hospitals are increasingly using bidding procedures to determine what pharmaceutical products and which suppliers will be included in their prescription drug and other health care programs. These measures could reduce the ultimate demand for our products, once approved, or put pressure on our product pricing.
Employees
As of January 31, 2018, we had 88 employees, 39 of our employees are located in Vienna, Austria and 49 of our employees located in the U.S., with 31 located in King of Prussia, Pennsylvania and the remaining 18 employees in the field.
Our employees in Austria are subject to the collective bargaining agreement of the chemical industry. This is an annual agreement between the employer representatives and the trade union of an industry. It defines conditions of employment, such as minimum wages, working hours and conditions, overtime payments, vacations and other matters.
We consider our relations with our employees to be good.
Our Corporate Information
On March 1, 2017, Nabriva Ireland was incorporated in Ireland under the name Hyacintho 2 plc, and was renamed to Nabriva Therapeutics plc on April 10, 2017, in order to effectuate the change of the jurisdiction of incorporation of the ultimate parent company of the Nabriva Group from Austria to Ireland. Nabriva Ireland replaced Nabriva Austria as the ultimate parent company on June 23, 2017, following the conclusion of a tender offer in which holders of the outstanding share capital of Nabriva Austria exchanged their holdings for ordinary shares, $0.01 nominal value per share, of Nabriva Ireland. The ordinary shares of Nabriva Ireland were issued on a one-for-ten basis to the holders of the Nabriva Austria common shares and on a one-for-one basis to the holders of the Nabriva Austria American Depositary Shares, or Nabriva Austria ADSs. On June 26, 2017, the ordinary shares of Nabriva Ireland began trading on the NasdaqGlobal Market under the symbol "NBRV," the same symbol under which the Nabriva Austria ADSs were previously traded. This transaction was accounted for as a merger between entities under common control; accordingly, the historical financial statements of Nabriva Austria for periods prior to this transaction are considered to be the historical financial statements of Nabriva Ireland. Our executive offices are located at 25-28 North Wall Quay IFSC, Dublin 1, Ireland, and our telephone number is +353 1 649 2000.
The predecessor of Nabriva Ireland, Nabriva Austria, was incorporated in Austria as a spin-off from Sandoz GmbH in October 2005 under the name Nabriva Therapeutics Forschungs GmbH, a limited liability company organized under Austrian law and commenced operations in February 2006. In
63
2007, Nabriva Austria transformed into a stock corporation (Aktiengesellschaft) under the name Nabriva Therapeutics AG. On October 19, 2017, Nabriva Austria was converted into a private limited liability company under Austrian law and renamed Nabriva Therapeutics GmbH.
Our U.S. operations are conducted by our wholly-owned subsidiary Nabriva Therapeutics US, Inc., a Delaware corporation established in August 2014 and located at 1000 Continental Drive, Suite 600, King of Prussia, PA 19406.
Our website address is www.nabriva.com. The information contained on, or that can be accessed from, our website does not form part of this Annual Report. Our agent for service of process in the United States is CT Corporation System, 111 Eighth Avenue, New York, New York 10011.
Available Information
We make available free of charge through our website our annual report on Form 10-K, quarterly reports on Form 10-Q, current reports on Form 8-K and amendments to those reports filed or furnished pursuant to Sections 13(a) and 15(d) of the Securities Exchange Act of 1934, as amended, or the Exchange Act. We make these reports available through our website as soon as reasonably practicable after we electronically file such reports with, or furnish such reports to, the SEC. Previously, as a foreign private issuer, we filed our Annual Report on Form 20-F and furnished information on Form 6-K. You can find, copy and inspect information we file at the SEC's public reference room, which is located at 100 F Street, N.E., Room 1580, Washington, DC 20549. Please call the SEC at 1-800-SEC-0330 for more information about the operation of the SEC's public reference room. You can review our electronically filed reports and other information that we file with the SEC on the SEC's web site at http://www.sec.gov. We also make available, free of charge on our website, the reports filed with the SEC by our executive officers, directors and 10% shareholders pursuant to Section 16 under the Exchange Act as soon as reasonably practicable after copies of those filings are provided to us by those persons. The information contained on, or that can be accessed through, our website is not a part of or incorporated by reference in this Annual Report on Form 10-K.
64
You should consider carefully the risks and uncertainties described below, together with all of the other information in this Annual Report on Form 10-K. If any of the following risks are realized, our business, financial condition, results of operations and prospects could be materially and adversely affected. The risks described below are not the only risks facing us. Risks and uncertainties not currently known to us or that we currently deem to be immaterial also may materially adversely affect our business, financial condition, results of operations and/or prospects.
Risks Related to Our Financial Position and Need for Additional Capital
We have incurred significant losses since our inception. We expect to incur losses for at least the next several years and may never generate profits from operations or maintain profitability.
Since inception, we have incurred significant operating losses. Our net losses were $74.4 million for the year ended December 31, 2017, $54.9 million for the year ended December 31, 2016 and $47.0 million for the year ended December 31, 2015. As of December 31, 2017, we had an accumulated deficit of $279.2 million. To date, we have financed our operations primarily through the sale of our equity securities, convertible loans and research and development support from governmental grants and loans. We have devoted substantially all of our efforts to research and development, including clinical trials. We have not completed development of any drugs. We expect to continue to incur significant expenses and increasing operating losses for at least the next several years. The net losses we incur may fluctuate significantly from quarter-to-quarter and year-to-year.
We anticipate that our expenses will increase substantially as we progress our second of two international Phase 3 clinical trials of our lead product candidate, lefamulin, for the treatment of community-acquired bacterial pneumonia, or CABP and prepare to commercialize lefamulin, if it receives marketing approval. We initiated the first of our Phase 3 clinical trials, which we refer to as LEAP 1, in September 2015 and initiated the second trial, which we refer to as LEAP 2, in April 2016. In September 2017, we announced positive top-line results for LEAP 1. In December 2017, we announced completion of enrollment for LEAP 2. If the results of LEAP 2 are also favorable, including achievement of the primary efficacy endpoints of the trials, we expect to submit a new drug application, or NDA, for marketing approval of lefamulin for the treatment of CABP in adults in the United States in the second half of 2018. We also expect to submit a marketing authorization application, or MAA, for lefamulin for the treatment of CABP in adults in Europe a few months after our NDA filing. We also continue to characterize the clinical pharmacology of lefamulin. If we obtain marketing approval of lefamulin for CABP or another indication, we also expect to incur significant additional sales, marketing, distribution and manufacturing expenses.
In addition, our expenses will increase if and as we:
- •
- initiate or continue the research and development of lefamulin for additional indications and of our other product candidates;
- •
- seek to discover and develop additional product candidates;
- •
- seek marketing approval for any product candidates that successfully complete clinical development;
- •
- continue to establish a medical affairs, sales, marketing and distribution infrastructure and scale up manufacturing capabilities to
commercialize any product candidates for which we receive marketing approval;
- •
- in-license or acquire other products, product candidates or technologies;
- •
- maintain, expand and protect our intellectual property portfolio;
65
- •
- expand our physical presence in the United States and Ireland;
- •
- establish and expand manufacturing arrangements with third parties; and
- •
- add operational, financial and management information systems and personnel, including personnel to support our product development, our operations as a public company and our planned future commercialization efforts.
Our ability to generate profits from operations and remain profitable depends on our ability to successfully develop and commercialize drugs that generate significant revenue. Based on our current plans, we do not expect to generate significant revenue unless and until we obtain marketing approval for, and commercialize, lefamulin. We do not expect to obtain marketing approval before 2019, if at all. This will require us to be successful in a range of challenging activities, including:
- •
- obtaining favorable results from our LEAP 2 clinical trial of lefamulin for the treatment of CABP;
- •
- subject to obtaining favorable results from our LEAP 2 clinical trial, applying for and obtaining marketing approval for lefamulin;
- •
- expanding medical affairs, sales, marketing and distribution capabilities to effectively market and sell lefamulin in the United States;
- •
- establishing collaboration, distribution or other marketing arrangements with third parties to commercialize lefamulin in markets outside the
United States;
- •
- protecting our rights to our intellectual property portfolio related to lefamulin;
- •
- contracting for the manufacture of and obtaining commercial quantities of lefamulin; and
- •
- negotiating and securing adequate reimbursement from third-party payors for lefamulin.
We may never succeed in these activities and, even if we do, may never generate revenues that are significant enough to generate profits from operations. Even if we do generate profits from operations, we may not be able to sustain or increase profitability on a quarterly or annual basis. Our failure to generate profits from operations and remain profitable would decrease the value of our company and could impair our ability to raise capital, expand our business, maintain our research and development efforts, diversify our product offerings or continue our operations. A decline in the value of our company could also cause our shareholders to lose all or part of their investment.
We will need substantial additional funding. If we are unable to raise capital when needed or on acceptable terms, we could be forced to delay, reduce or eliminate our product development programs or future commercialization efforts.
We expect our research and development, commercialization and other expenses to increase substantially in connection with our ongoing activities, particularly as we continue development of and seek marketing approval for lefamulin and, possibly, other product candidates and continue our research activities. Our expenses will increase if we suffer any delays in our Phase 3 clinical program for lefamulin for CABP, including regulatory delays. If we obtain marketing approval for lefamulin or any other product candidate that we develop, we expect to incur significant commercialization expenses related to product sales, marketing, distribution and manufacturing.
Furthermore, we expect to continue to incur additional costs associated with operating as a public company. Accordingly, we will need to obtain substantial additional funding in connection with our continuing operations. If we are unable to raise capital when needed or on attractive terms, we could be forced to delay, reduce or eliminate our research and development programs or any future commercialization efforts.
66
We expect that our existing cash, cash equivalents and short-term investments, will be sufficient to enable us to fund our operating expenses and capital expenditure requirements into the fourth quarter of 2018 and to obtain top-line data for LEAP 2. We have based these estimates on assumptions that may prove to be wrong, and we could use our capital resources sooner than we currently expect. Furthermore, while these estimates are based on our current assumptions regarding our operating expenses and capital expenditure requirements, we also believe that by reducing certain planned pre-commercialization activities our existing cash, cash equivalents and short-term investments could fund our primary business focus of seeking regulatory approval for lefamulin, our lead product candidate, subject to positive LEAP 2 topline data, into the first quarter of 2019. These estimates assume, among other things, that we do not obtain any additional funding through grants and clinical trial support, collaboration agreements, equity or debt financings.
Our future capital requirements will depend on many factors, including:
- •
- the progress, costs and results of our clinical trials for lefamulin, including our LEAP 2 trial;
- •
- the costs and timing of process development and manufacturing scale-up activities associated with lefamulin;
- •
- the costs, timing and outcome of regulatory review of lefamulin;
- •
- the costs of commercialization activities for lefamulin if we receive, or expect to receive, marketing approval, including the costs and timing
of establishing product sales, marketing, distribution and outsourced manufacturing capabilities, including the costs of building finished product inventory and its components in preparation of
initial marketing of lefamulin;
- •
- subject to receipt of marketing approval, revenue received from commercial sales of lefamulin;
- •
- the costs of developing lefamulin for the treatment of additional indications;
- •
- our ability to establish collaborations on favorable terms, if at all;
- •
- the scope, progress, results and costs of product development of any other product candidates that we may develop;
- •
- the extent to which we in-license or acquire rights to other products, product candidates or technologies;
- •
- the costs of preparing, filing and prosecuting patent applications, maintaining and protecting our intellectual property rights and defending
against intellectual property-related claims;
- •
- the continued availability of Austrian governmental grants;
- •
- the rate of the expansion of our physical presence in the United States and Ireland; and
- •
- the costs of operating as a public company in the United States.
Conducting clinical trials is a time consuming, expensive and uncertain process that takes years to complete, and we may never generate the necessary data or results required to obtain marketing approval and achieve product sales. Our commercial revenues, if any, will be derived from sales of lefamulin or any other products that we successfully develop, in-license or acquire, none of which we expect to be commercially available for more than a year, if at all. In addition, if approved, lefamulin or any other product candidate that we develop, in-license or acquire may not achieve commercial success. Accordingly, we will need to obtain substantial additional financing to achieve our business objectives.
Adequate additional financing may not be available to us on acceptable terms, or at all. In addition, we may seek additional capital due to favorable market conditions or strategic considerations, even if we believe that we have sufficient funds for our current or future operating plans.
67
Raising additional capital may cause dilution to our security holders, restrict our operations or require us to relinquish rights to our technologies or product candidates.
Until such time, if ever, as we can generate substantial product revenues, we expect to finance our cash needs through a combination of equity offerings, debt financings, collaborations, and funding from local and international government entities and non-government organizations in the disease areas addressed by our product candidates and marketing, distribution or licensing arrangements. To the extent that we raise additional capital through the sale of equity or convertible debt securities, your ownership interest will be diluted, and the terms of these securities may include liquidation or other preferences that adversely affect your rights as a security holder. Debt financing, if available, may involve agreements that include covenants limiting or restricting our ability to take specific actions, such as incurring additional debt, making capital expenditures or declaring dividends. In addition, debt service obligations under any debt financings may limit the availability of our cash for other purposes, and we may be unable to make interest payments or repay the principal of such debt financings when due.
If we raise additional funds through collaborations, strategic alliances or marketing, distribution or licensing arrangements with third parties, we may have to relinquish valuable rights to our technologies, future revenue streams, research programs or product candidates or to grant licenses on terms that may not be favorable to us. If we are unable to raise additional funds through equity or debt financings when needed, we may be required to delay, limit, reduce or terminate our product development or future commercialization efforts or grant rights to develop and market product candidates that we would otherwise prefer to develop and market ourselves.
Our limited operating history may make it difficult for you to evaluate the success of our business to date and to assess our future viability.
Our operations to date have been limited to organizing and staffing our company, developing and securing our technology, raising capital and undertaking preclinical studies and clinical trials of our product candidates. We have not yet demonstrated our ability to successfully complete development of any product candidates, obtain marketing approvals, manufacture a commercial scale product, or arrange for a third party to do so on our behalf, or conduct sales and marketing activities necessary for successful product commercialization. Consequently, any predictions you make about our future success or viability may not be as accurate as they could be if we had a longer operating history.
In addition, as a new business, we may encounter unforeseen expenses, difficulties, complications, delays and other known and unknown factors. We will need to transition from a company with a research and development focus to a company capable of supporting commercial activities. We may not be successful in such a transition.
We have relied on, and expect to continue to rely on, certain government grants and funding from the Austrian government. Should these funds cease to be available, or our eligibility be reduced, or if we are required to repay any of these funds, this could impact our ongoing need for funding and the timeframes within which we currently expect additional funding will be required.
As a company that carries out extensive research and development activities, we benefit from the Austrian research and development support regime, under which we are eligible to receive a research premium from the Austrian government equal to 12% (10%, in the case of fiscal years prior to 2016) of a specified research and development cost base. Qualifying expenditures largely comprise research and development activities conducted in Austria, however, the research premium is also available for certain related third-party expenses with additional limitations. We received research premiums of $5.9 million for the year ended December 31, 2016 and $4.3 million for the year ended December 31, 2015. We have not received any research premium for our qualified 2017 expenditures as of
68
December 31, 2017. As we increase our personnel and expand our business outside of Austria, we may not be able to continue to claim research premiums to the same extent as we have in previous years, as some research and development activities may no longer be considered to occur in Austria. As research premiums that have been paid out already may be audited by the tax authorities, there is a risk that parts of the submitted cost base may not be considered as eligible and therefore repayments may have to be made.
The intended efficiency of our corporate structure depends on the application of the tax laws and regulations in the countries where we operate, and we may have exposure to additional tax liabilities or our effective tax rate could change, which could have a material impact on our results of operations and financial position.
As a company with international operations, we are subject to income taxes, as well as non-income based taxes, in both the United States and various foreign jurisdictions. We have designed our corporate structure, the manner in which we develop and use our intellectual property, and our intercompany transactions between our subsidiaries in a way that is intended to enhance our operational and financial efficiency. The application of the tax laws and regulations of various countries in which we operate and to our global operations is subject to interpretation. We also must operate our business in a manner consistent with our corporate structure to realize such efficiencies. The tax authorities of the countries in which we operate may challenge our methodologies for valuing developed technology or for transfer pricing. If, for one or more of these reasons, tax authorities determine that the manner in which we operate results in our business not achieving the intended tax consequences, our effective tax rate could increase and harm our financial position and results of operations.
A change in the tax law in the jurisdictions in which we do business, including an increase in tax rates, an adverse change in the treatment of an item of income or expense, a decrease in tax rates in a jurisdiction in which we have significant deferred tax assets, or a new or different interpretation of applicable tax law, could result in a material increase in tax expense.
Risks Related to Product Development and Commercialization
We depend heavily on the success of our lead product candidate, lefamulin, which we are developing for CABP and other indications. If we are unable to complete our Phase 3 clinical program for lefamulin for CABP as and when expected and obtain marketing approvals for lefamulin, or if thereafter we fail to commercialize lefamulin or experience significant delays in doing so, our business will be materially harmed.
We have invested a significant portion of our efforts and financial resources in the development of lefamulin. There remains a significant risk that we will fail to successfully develop lefamulin for CABP or any other indication. In September 2017, we announced positive top-line results for LEAP 1, the first of our two pivotal, international Phase 3 clinical trials of lefamulin for the treatment of CABP. Patient enrollment for our second Phase 3 clinical trial of lefamulin for the treatment of CABP was completed in December 2017. We currently expect availability of top-line data for LEAP 2 in the spring of 2018. Our ability to meet our target timing will depend on data analysis for LEAP 2. A significant delay in data analysis would result in delays to our development timelines and additional development costs beyond what we have budgeted. If we ultimately obtain favorable results from LEAP 2, we expect to submit an NDA for marketing approval for lefamulin for the treatment of CABP in adults in the United States in the second half of 2018. We also expect to submit an MAA for lefamulin for the treatment of CABP in adults in Europe a few months after our NDA filing.
69
Our ability to generate product revenues, which may not occur for several years, if ever, will depend heavily on our obtaining marketing approval for and commercializing lefamulin. The success of lefamulin will depend on a number of factors, including the following:
- •
- obtaining favorable safety and efficacy results from clinical trials, particularly LEAP 2;
- •
- making arrangements with third-party manufacturers for commercial supply and receiving regulatory approval of our manufacturing processes and
our third-party manufacturers' facilities from applicable regulatory authorities;
- •
- receipt of marketing approvals from applicable regulatory authorities for lefamulin for the treatment of CABP;
- •
- launching commercial sales of lefamulin, if and when approved, whether alone or in collaboration with third parties;
- •
- acceptance of lefamulin, if and when approved, by patients, the medical community and third- party payors;
- •
- effectively competing with other therapies;
- •
- maintaining a continued acceptable safety profile of lefamulin following approval;
- •
- obtaining and maintaining patent and trade secret protection and regulatory exclusivity; and
- •
- protecting our rights in our intellectual property portfolio.
Successful development of lefamulin for the treatment of additional indications, if any, or for use in other patient populations and our ability, if it is approved, to broaden the label for lefamulin will depend on similar factors.
If we do not achieve one or more of these factors in a timely manner or at all, we could experience significant delays or an inability to successfully commercialize lefamulin for CABP or for any additional indications, which would materially harm our business.
If clinical trials of lefamulin or any of our other product candidates fail to demonstrate safety and efficacy to the satisfaction of the U.S. Food and Drug Administration, or FDA, regulatory authorities in the European Union, or other regulatory authorities or do not otherwise produce favorable results, we may incur additional costs or experience delays in completing, or ultimately be unable to complete, the development and commercialization of lefamulin or any other product candidate.
Before obtaining marketing approval from regulatory authorities for the sale of any product candidate, we must complete preclinical development and early clinical trials, including Phase 1 clinical trials, in addition to extensive later-stage Phase 3 clinical trials, to demonstrate the safety and efficacy of our product candidates in humans. Clinical testing is expensive, difficult to design and implement, can take many years to complete and is uncertain as to outcome. A failure of one or more clinical trials can occur at any stage of testing. The outcome of preclinical testing and early clinical trials may not be predictive of the success of later clinical trials, and interim results of a clinical trial do not necessarily predict final results. The design of a clinical trial can determine whether its results will support approval of a product, and flaws in the design of a clinical trial may not become apparent until the clinical trial is well advanced or completed. Moreover, preclinical and clinical data are often susceptible to varying interpretations and analyses, and many companies that have believed their product candidates performed satisfactorily in preclinical studies and clinical trials have nonetheless failed to obtain marketing approval of their products.
LEAP 2 and other clinical trials we conduct may not be successful, and the results of our completed clinical trials may not predict success in LEAP 2 or any other clinical trials. Notably, the
70
LEAP 1 and LEAP 2 trial designs are not the same, as the LEAP 2 trial is evaluating a patient population with CABP that is less severe than those patients evaluated in LEAP 1, and LEAP 2 is only investigating oral lefamulin, among other differences. Positive results from LEAP 1 do not guarantee favorable results from LEAP 2. Although we believe that the collective data from prior trials and our preclinical studies provide support for concluding that lefamulin is well suited for treatment of CABP, we may fail to obtain favorable results in our LEAP 2 clinical trial of lefamulin for CABP or regulatory authorities could disagree with our interpretations or analyses of our clinical data. If the results of our LEAP 2 clinical trial are not favorable, including failure to achieve the primary efficacy endpoints of the trial, or regulatory authorities disagree with our interpretations or analyses of our clinical data, we may need to conduct additional clinical trials at significant cost or altogether abandon development of lefamulin for CABP.
If we are required to conduct additional clinical trials or other testing of lefamulin or any other product candidate that we develop beyond those that we contemplate, if we are unable to successfully complete our clinical trials or other testing, if the results of these trials or tests are not positive or are only modestly positive or if there are safety concerns, we may:
- •
- be delayed in obtaining marketing approval for our product candidates;
- •
- not obtain marketing approval at all;
- •
- obtain approval for indications or patient populations that are not as broad as intended or desired;
- •
- obtain approval with labeling that includes significant use or distribution restrictions or safety warnings, including boxed warnings;
- •
- be subject to additional post-marketing testing requirements or restrictions; or
- •
- have the product removed from the market after obtaining marketing approval.
The occurrence of any of the developments listed above could materially harm our business, financial condition, results of operations and prospects.
If we experience any of a number of possible unforeseen events in connection with our LEAP 2 clinical trial of lefamulin for CABP or other clinical trials, the potential marketing approval or commercialization of lefamulin or other product candidates could be delayed or prevented.
We may experience numerous unforeseen events during, or as a result of, our LEAP 2 clinical trial of lefamulin for CABP or other clinical trials we conduct that could delay or prevent our ability to receive marketing approval or commercialize lefamulin or our other product candidates, including:
- •
- clinical trials of lefamulin or our other product candidates may produce negative or inconclusive results, and we may decide, or regulators may
require us, to conduct additional clinical trials or abandon product development programs;
- •
- the number of patients required for LEAP 2, lefamulin for other indications or our other product candidates may be larger than we anticipate,
enrollment in these clinical trials may be slower than we anticipate or participants may drop out of these clinical trials at a higher rate than we anticipate;
- •
- our third-party contractors may fail to comply with regulatory requirements or meet their contractual obligations to us in a timely manner, or
at all;
- •
- regulators, institutional review boards or independent ethics committees may not authorize us or our investigators to commence a clinical trial or conduct a clinical trial at a prospective trial site or may require that we or our investigators suspend or terminate clinical research for various
71
- •
- we may experience delays in reaching or fail to reach agreement on acceptable clinical trial contracts or clinical trial protocols with
prospective trial sites;
- •
- we may have to suspend or terminate clinical trials of our product candidates for various reasons, including a finding that the participants
are being exposed to unacceptable health or safety risks;
- •
- the cost of clinical trials of our product candidates may be greater than we anticipate;
- •
- the supply or quality of our product candidates or other materials necessary to conduct clinical trials of our product candidates may be
insufficient or inadequate; and
- •
- our product candidates may have undesirable side effects or other unexpected characteristics, causing us or our investigators, regulators, institutional review boards or independent ethics committees to suspend or terminate the trials.
reasons, including noncompliance with regulatory requirements or a finding that the participants are being exposed to unacceptable health risks;
Our product development costs will increase if we experience delays in enrollment in our clinical development program or our non-clinical development program or in obtaining marketing approvals. We do not know whether any additional non-clinical tests or clinical trials will be required, or if they will begin as planned, or if they will need to be restructured or will be completed on schedule, or at all. Significant non-clinical development program delays, including chemistry, manufacturing and control activities, or clinical trial delays also could shorten any periods during which we may have the exclusive right to commercialize our product candidates or allow our competitors to bring products to market before we do and impair our ability to successfully commercialize our product candidates and may harm our business and results of operations.
If we experience delays or difficulties in the enrollment of patients in our clinical trials, our receipt of necessary marketing approvals could be delayed or prevented.
We may not be able to initiate or continue clinical trials of lefamulin or any other product candidate that we develop if we are unable to locate and enroll a sufficient number of eligible patients to participate in these clinical trials. Some of our competitors have ongoing clinical trials for product candidates that could be competitive with lefamulin, and patients who would otherwise be eligible for our clinical trials may instead enroll in clinical trials of our competitors' product candidates.
Patient enrollment is affected by other factors including:
- •
- severity of the disease under investigation;
- •
- eligibility criteria for the clinical trial in question;
- •
- perceived risks and benefits of the product candidate under study;
- •
- approval of other therapies to treat the disease under investigation;
- •
- efforts to facilitate timely enrollment in clinical trials;
- •
- patient referral practices of physicians;
- •
- the time of year in which the trial is initiated or conducted;
- •
- the geographic distribution of global trial sites, given the timing of pneumonia season globally, and the seasonal variation in the number of
patients suffering from pneumonia, including a decline in the number of patients with CABP during the summer months;
- •
- the ability to monitor patients adequately during and after treatment;
72
- •
- proximity and availability of clinical trial sites for prospective patients;
- •
- delays in the receipt of required regulatory approvals, or the failure to receive required regulatory approvals, in the jurisdictions in which
clinical trials are expected to be conducted; and
- •
- delays in the receipt of approvals, or the failure to receive approvals, from the relevant institutional review board or ethics committee at clinical trial sites.
Enrollment delays in our clinical trials may result in increased development costs for our product candidates, which would cause the value of the company to decline and limit our ability to obtain additional financing. Our inability to enroll a sufficient number of patients in any of our clinical trials would result in significant delays or may require us to abandon one or more clinical trials altogether.
If serious adverse or undesirable side effects are identified during the development of lefamulin or any other product candidate that we develop, we may need to abandon or limit our development of that product candidate.
All of our product candidates are in clinical or preclinical development and their risk of failure is high. It is impossible to predict when or if any of our product candidates will prove effective or safe in humans or will receive marketing approval. If our product candidates are associated with undesirable side effects or have characteristics that are unexpected, we may need to abandon their development or limit development to certain uses or subpopulations in which the undesirable side effects or other characteristics are less prevalent, less severe or more acceptable from a risk-benefit perspective. Many compounds that initially showed promise in clinical or earlier stage testing have later been found to cause side effects or other safety issues that prevented further development of the compound.
In LEAP 1, lefamulin was generally well tolerated and exhibited a similar rate of treatment-emergent adverse events to the comparator drug. However, 104 patients in the lefamulin arm of the trial reported at least one treatment-emergent adverse event and eight patients withdrew from the trial following an adverse event. Furthermore, at least 2.0% of patients in LEAP 1 who were dosed with lefamulin reported the following adverse events: hypokalemia, nausea, insomnia, infusion site pain and infusion site phlebitis. Fewer than 2.0% of trial patients dosed with lefamulin also experienced hypertension and an increase in alanine aminotransaminase, although no patients met Hy's Law criteria, which is an indicator for severe liver damage.
In addition, lefamulin was well tolerated in our Phase 2 clinical trial for ABSSSI. No patient in the trial suffered any serious adverse events that were found to be related to lefamulin, and no patient in the trial died. Some patients experienced adverse events that were assessed by the investigator as possibly or probably related to study medication. The majority of their symptoms were mild in severity. Four patients discontinued study medication following a drug-related event, three of whom were in a lefamulin treatment group: one patient experienced events of hyperhidrosis, vomiting and headache; one patient experienced infusion site pain; and one patient experienced dyspnea.
Because the potential for mild effect on electrocardiogram, or ECG, measurements was observed in preclinical studies, we have continued to assess this potential in all human clinical trials we have conducted. In the Phase 2 clinical trial, no change in ECG measurements was considered to be of clinical significance, and no drug-related cardiovascular adverse event was reported. Both lefamulin and vancomycin treatment were associated with a small increase in the QT interval. The QT interval is a measure of the heart's electrical cycle, and a prolonged QT interval is a risk factor for a potential ventricular arrhythmia. In LEAP 1, while changes in QT that were of potential clinical concern were uncommon, one patient treated with lefamulin had an increase in absolute QT interval to greater than 500 msec. We are continuing to evaluate the effect of lefamulin on the QT interval in LEAP 2.
73
There were no systemic adverse events of clinical concern and no drug-related serious adverse events observed in any of our completed Phase 1 clinical trials of lefamulin. In these trials, the most commonly observed adverse effects with oral administration of lefamulin were related to the gastrointestinal tract, including nausea and abdominal discomfort, while the most commonly observed adverse effects related to IV administration were related to irritation at the infusion site. In addition, lefamulin produced a transient, predictable and reproducible prolongation of the QT interval based on the maximum concentration of the drug in the blood plasma. At the doses administered in the Phase 3 clinical trials for lefamulin for CABP, we expect that the drug will not produce large effects on the QT interval that would be of clinical relevance. We did not observe any drug-related cardiac adverse events, such as increase in ectopic ventricular activity or other cardiac arrhythmia, or clinically relevant ECG findings during the conduct of any of our completed Phase 1 clinical trials. If we observe clinically relevant effects on the QT interval in our Phase 3 clinical trials of lefamulin for CABP or in any other clinical trial of lefamulin, our ability to successfully develop lefamulin for CABP or any other indication may be significantly delayed or prevented.
If we elect or are forced to suspend or terminate any clinical trial of lefamulin or any other product candidates that we are developing, the commercial prospects of lefamulin or such other product candidates will be harmed and our ability to generate product revenues, if at all, from lefamulin or any of these other product candidates will be delayed or eliminated. Any of these occurrences could materially harm our business, financial condition, results of operations and prospects.
Even if lefamulin or any other product candidate receives marketing approval, it may fail to achieve the degree of market acceptance by physicians, patients, third-party payors and others in the medical community necessary for commercial success and the market opportunity for lefamulin may be smaller than we estimate.
If lefamulin or any of our other product candidates receive marketing approval, it or they may nonetheless fail to gain sufficient market acceptance by physicians, patients, third-party payors and others in the medical community. For example, current treatments for pneumonia, including generic options, are well established in the medical community, and doctors may continue to rely on these treatments without lefamulin. In addition, our efforts to effectively communicate lefamulin's differentiating characteristics and key attributes to clinicians and hospital pharmacies with the goal of establishing favorable formulary status for lefamulin may fail or may be less successful than we expect. If lefamulin does not achieve an adequate level of acceptance, we may not generate significant product revenues or any profits from operations. The degree of market acceptance of our product candidates, if approved for commercial sale, will depend on a number of factors, including:
- •
- the efficacy and potential advantages compared to alternative treatments;
- •
- lefamulin's ability to limit the development of bacterial resistance in the pathogens it targets;
- •
- the prevalence and severity of any side effects;
- •
- the ability to offer our product candidates for sale at competitive prices, including in comparison to generic competition;
- •
- convenience and ease of administration compared to alternative treatments;
- •
- the willingness of the target patient population to try new therapies, physicians to prescribe these therapies and hospitals to approve the
cost and use by their physicians of these therapies;
- •
- the strength of marketing and distribution support;
- •
- the availability of third-party coverage and adequate reimbursement; and
- •
- the timing of any marketing approval in relation to other product approvals.
74
Although we believe that the mechanism of action for pleuromutilin antibiotics may result in a low propensity for development of bacterial resistance to lefamulin or our other pleuromutilin product candidates, bacteria might nevertheless develop resistance to lefamulin or our other pleuromutilin product candidates more rapidly or to a greater degree than we anticipate. If bacteria develop such resistance or if lefamulin is not effective against drug-resistant bacteria, the efficacy of these product candidates would decline, which would negatively affect our potential to generate revenues from these product candidates.
Our ability to negotiate, secure and maintain third-party coverage and reimbursement may be affected by political, economic and regulatory developments in the United States, the European Union and other jurisdictions. Governments continue to impose cost containment measures, and third-party payors are increasingly challenging prices charged for medicines and examining their cost effectiveness, in addition to their safety and efficacy. If the level of reimbursement is below our expectations, our revenue and gross margins would be adversely affected. Obtaining formulary approval from third-party payors can be an expensive and time-consuming process. We cannot be certain if and when we will obtain formulary approval to allow us to sell lefamulin or any future product candidates into our target markets. Even if we do obtain formulary approval, third-party payors, such as government or private health care insurers, carefully review and increasingly question the coverage of, and challenge the prices charged for, drugs. These and other similar developments could significantly limit the degree of market acceptance of lefamulin or any of our other product candidates that receive marketing approval.
If we are unable to establish sales, marketing and distribution capabilities or enter into sales, marketing and distribution agreements with third parties, we may not be successful in commercializing lefamulin or any other product candidate if and when they are approved.
We do not have a sales, marketing or distribution infrastructure, and as a company we have no experience in the sale, marketing or distribution of pharmaceutical products. To achieve commercial success for any approved product, we must either develop a sales, marketing and distribution organization or outsource these functions to third parties. If lefamulin receives marketing approval, we plan to commercialize it in the United States with our own targeted hospital sales and marketing organization that we plan to establish. In addition, we expect to utilize a variety of types of collaboration, distribution and other marketing arrangements with one or more third parties to commercialize lefamulin in markets outside the United States.
There are risks involved with establishing our own sales, marketing and distribution capabilities and entering into arrangements with third parties to perform these services. For example, recruiting and training a sales force is expensive and time consuming and could delay any product launch. If the commercial launch of a product candidate for which we recruit a sales force and establish marketing and distribution capabilities is delayed or does not occur for any reason, we would have prematurely or unnecessarily incurred these commercialization expenses. This may be costly, and our investment would be lost if we cannot retain or reposition our sales and marketing personnel.
Factors that may inhibit our efforts to commercialize our products on our own include:
- •
- our inability to recruit, train and retain adequate numbers of effective sales and marketing personnel;
- •
- the inability of sales personnel to obtain access to or persuade adequate numbers of physicians to prescribe any future products;
- •
- the lack of complementary products to be offered by sales personnel, which may put our sales representatives at a competitive disadvantage relative to sales representatives from companies with more extensive product lines; and
75
- •
- unforeseen costs and expenses associated with creating an independent sales, marketing and distribution organization.
If we enter into arrangements with third parties to perform sales, marketing and distribution services, our product revenues or the profitability of these product revenues to us are likely to be lower than if we were to market, sell and distribute ourselves any products that we develop. In addition, we may not be successful in entering into arrangements with third parties to sell, market and distribute our product candidates or may be unable to do so on terms that are favorable to us. We likely will have little control over such third parties, and any of them may fail to devote the necessary resources and attention to sell and market our products effectively. If we do not establish sales, marketing and distribution capabilities successfully, either on our own or in collaboration with third parties, we will not be successful in commercializing our product candidates.
We face substantial competition, which may result in others discovering, developing or commercializing products before or more successfully than we do.
The development and commercialization of new drug products is highly competitive. We face competition with respect to lefamulin and any other products we may seek to develop or commercialize in the future from major pharmaceutical companies, specialty pharmaceutical companies and biotechnology companies worldwide. Potential competitors also include academic institutions, government agencies and other public and private research organizations that conduct research, seek patent protection and establish collaborative arrangements for research, development, manufacturing and commercialization.
There are a variety of available therapies marketed for the treatment of CABP. Currently the treatment of CABP is dominated by generic products. For hospitalized patients, combination therapy is frequently used. Many currently approved drugs are well-established therapies and are widely accepted by physicians, patients and third-party payors. We also are aware of various drugs under development for the treatment of CABP, including omadacycline (under Phase 3 clinical development by Paratek Pharmaceuticals Inc.), delafloxacin (under Phase 3 clinical development by Melinta Therapeutics Inc.) and oral nafithromycin (under Phase 2 clinical development by Wockhardt Ltd.).
Our commercial opportunity could be reduced or eliminated if our competitors develop and commercialize products that are safer, more effective, have fewer or less severe side effects, are approved for broader indications or patient populations, are more convenient or are less expensive than any products that we may develop. Our competitors may also obtain marketing approvals for their products more rapidly than we may obtain approval for ours, which could result in our competitors establishing a strong market position before we are able to enter the market. In addition, our ability to compete may be affected because in some cases insurers or other third-party payors seek to encourage the use of generic products. This may have the effect of making branded products less attractive, from a cost perspective, to buyers. We expect that if lefamulin is approved for CABP, it will be priced at a significant premium over competitive generic products. This may make it difficult for us to replace existing therapies with lefamulin. The key competitive factors affecting the success of our product candidates are likely to be their efficacy, safety, convenience, price and the availability of coverage and reimbursement from government and other third-party payors.
Many of our competitors may have significantly greater financial resources and expertise in research and development, manufacturing, preclinical testing, conducting clinical trials, obtaining approvals from regulatory authorities and marketing approved products than we do. Mergers and acquisitions in the pharmaceutical and biotechnology industries may result in even more resources being concentrated among a smaller number of our competitors. Smaller and other early stage companies may also prove to be significant competitors, particularly through collaborative arrangements with large and established companies. These third parties compete with us in recruiting and retaining
76
qualified scientific and management personnel, establishing clinical trial sites and patient registration for clinical trials, as well as in acquiring technologies complementary to or necessary for our programs.
Even if we are able to commercialize lefamulin or any other product candidate that we develop, the product may become subject to unfavorable pricing regulations, third-party reimbursement practices or healthcare reform initiatives, which would harm our business.
The regulations that govern marketing approvals, pricing, coverage and reimbursement for new drug products vary widely from country to country. Current and future legislation may significantly change the approval requirements in ways that could involve additional costs and cause delays in obtaining approvals. Some countries require approval of the sale price of a drug before it can be marketed. In many countries, the pricing review period begins after marketing or product licensing approval is granted. In some foreign markets, prescription pharmaceutical pricing remains subject to continuing governmental control even after initial approval is granted. As a result, we might obtain marketing approval for a product in a particular country, but then be subject to price regulations that delay our commercial launch of the product, possibly for lengthy time periods, and negatively impact the revenues we are able to generate from the sale of the product in that country. Adverse pricing limitations may hinder our ability to recoup our investment in one or more product candidates, even if our product candidates obtain marketing approval.
Our ability to commercialize lefamulin or any other product candidate successfully also will depend in part on the extent to which coverage and adequate reimbursement for these products and related treatments will be available from government health administration authorities, private health insurers and other organizations. Government authorities and other third-party payors, such as private health insurers and health maintenance organizations, decide which medications they will pay for and establish reimbursement levels. A major trend in the healthcare industries in the European Union and the United States and elsewhere is cost containment. Government authorities and other third-party payors have attempted to control costs by limiting coverage and the amount of reimbursement for particular medications. Increasingly, third-party payors are requiring that drug companies provide them with predetermined discounts from list prices and are challenging the prices charged for medical products. We cannot be sure that coverage and reimbursement will be available for lefamulin or any other product that we commercialize and, if coverage and reimbursement are available, the level of reimbursement. Reimbursement may impact the demand for, or the price of, any product candidate for which we obtain marketing approval. Obtaining and maintaining adequate reimbursement for lefamulin may be particularly difficult because of the number of generic drugs, which are typically available at lower prices, that are available to treat CABP. In addition, third-party payors are likely to impose strict requirements for reimbursement of a higher priced drug, such as lefamulin. If reimbursement is not available or is available only to limited levels, we may not be able to successfully commercialize lefamulin or other product candidates for which we obtain marketing approval.
There may be significant delays in obtaining coverage and reimbursement for newly approved drugs, and coverage may be more limited than the purposes for which the drug is approved by the applicable regulatory authority. Moreover, eligibility for coverage and reimbursement does not imply that any drug will be paid for in all cases or at a rate that covers our costs, including research, development, manufacture, sale and distribution. Interim reimbursement levels for new drugs, if applicable, may also not be sufficient to cover our costs and may not be made permanent. Reimbursement rates may vary according to the use of the drug and the clinical setting in which it is used, may be based on reimbursement levels already set for lower cost drugs, and may be incorporated into existing payments for other services. Net prices for drugs may be reduced by mandatory discounts or rebates required by government healthcare programs or private payors and by any future relaxation of laws that presently restrict imports of drugs from countries where they may be sold at lower prices than in the United States. In the United States, third-party payors often rely upon Medicare coverage
77
policy and payment limitations in setting their own reimbursement policies. In the European Union, reference pricing systems and other measures may lead to cost containment and reduced prices. Our inability to promptly obtain coverage and adequate reimbursement rates from both government-funded and private payors for any approved products that we develop could have a material adverse effect on our operating results, our ability to raise capital needed to commercialize products and our overall financial condition.
Product liability lawsuits against us could divert our resources, cause us to incur substantial liabilities and to limit commercialization of any products that we may develop or in-license.
We face an inherent risk of product liability exposure related to the testing of lefamulin and any other product candidate that we develop in human clinical trials and will face an even greater risk if we commercially sell any products that we may develop or in-license. If we cannot successfully defend ourselves against claims that our product candidates or products caused injuries, we will incur substantial liabilities. Regardless of merit or eventual outcome, liability claims may result in:
- •
- reduced resources of our management to pursue our business strategy;
- •
- decreased demand for any product candidates or products that we may develop;
- •
- injury to our reputation and significant negative media attention;
- •
- withdrawal of clinical trial participants;
- •
- significant costs to defend the related litigation;
- •
- substantial monetary awards to trial participants or patients;
- •
- loss of revenue; and
- •
- the inability to commercialize any products that we may develop.
We maintain clinical trial liability insurance that covers bodily injury to patients participating in our clinical trials up to a $10.0 million annual aggregate limit and subject to a per event deductible. This amount of insurance may not be adequate to cover all liabilities that we may incur. We will need to increase our insurance coverage when and if we begin commercializing lefamulin or any other product candidate that receives marketing approval. Insurance coverage is increasingly expensive. We may not be able to maintain insurance coverage at a reasonable cost or in an amount adequate to satisfy any liability that may arise.
Risks Related to Our Dependence on Third Parties
Use of third parties to manufacture our product candidates may increase the risk that we will not have sufficient quantities of our product candidates or products or such quantities at an acceptable cost, which could delay, prevent or impair our development or commercialization efforts.
We do not own or operate manufacturing facilities for the production of lefamulin that could be used in product candidate development, including clinical trial supply, or for commercial supply, or for the supply of any other compound that we are developing or evaluating in our research program. We have limited personnel with experience in drug manufacturing and lack the resources and the capabilities to manufacture any of our product candidates on a clinical or commercial scale. We currently rely on third parties for supply of lefamulin, and our strategy is to outsource all manufacturing, packaging, testing, serialization and distribution of our product candidates and products to third parties.
We have entered into agreements, and expect to enter into additional agreements, with third-party manufacturers for the long-term commercial supply of lefamulin. We obtained the pleuromutilin
78
starting material for the clinical trial supply of lefamulin from a single third-party manufacturer, Sandoz GmbH, or Sandoz, a division of Novartis AG, or Novartis. Novartis stopped manufacturing pleuromutilin for us in June 2015 and will not be a commercial supplier of pleuromutilin for us. We have identified an alternative supplier that we believe will be able to provide pleuromutilin starting material for the commercial supply of lefamulin. Another third-party manufacturer synthesizes lefamulin from the pleuromutilin starting material and provides our supply of the active pharmaceutical ingredient. We engage separate manufacturers to provide tablets, sterile vials, and sterile diluent that we are using in our clinical trials of lefamulin. We may be unable to conclude agreements for commercial supply with additional third-party manufacturers, or may be unable to do so on acceptable terms.
Even if we are able to establish and maintain arrangements with third-party manufacturers, reliance on third-party manufacturers entails risks, including:
- •
- reliance on the third party for regulatory compliance and quality assurance;
- •
- an event at one of our manufacturers or suppliers causing an unforeseen disruption of the manufacture or supply of our product candidates;
- •
- the possible breach of the manufacturing agreement by the third party;
- •
- the possible misappropriation of our proprietary information, including our trade secrets and know-how; and
- •
- the possible termination or nonrenewal of the agreement by the third party at a time that is costly or inconvenient for us.
Third-party manufacturers may not be able to comply with current good manufacturing practice, or cGMP, regulations or similar regulatory requirements outside the United States. Our failure, or the failure of our third-party manufacturers, to comply with applicable regulations could result in sanctions being imposed on us, including fines, injunctions, civil penalties, delays, suspension or withdrawal of approvals, license revocation, seizures or recalls of product candidates or products, operating restrictions and criminal prosecutions, any of which could significantly and adversely affect supplies of our product candidates and products.
Our product candidates and any products that we may develop may compete with other product candidates and products for access to manufacturing facilities. There are a limited number of manufacturers that operate under cGMP regulations and that might be capable of manufacturing for us.
If the third parties that we engage to supply any materials or manufacture product for our non-clinical testing and clinical trials should cease to continue to do so for any reason, we likely would experience delays in advancing these trials while we identify and qualify replacement suppliers and we may be unable to obtain replacement supplies on terms that are favorable to us. For example, there are only a limited number of known manufacturers that produce the pleuromutilin starting material used in the synthesis of lefamulin. In early 2015, Novartis completed the sale of its animal health division, including its veterinary products, to a third party. As a result, we have identified an alternative supplier that currently manufactures pleuromutilin starting material for veterinary products, that we believe will be able to provide pleuromutilin starting material for the commercial scale manufacture of lefamulin. In addition, if we are not able to obtain adequate supplies of our product candidates or the drug substances used to manufacture them, it will be more difficult for us to develop our product candidates and compete effectively.
Our current and anticipated future dependence upon others for the manufacture of our product candidates may adversely affect our future profit margins and our ability to develop product candidates and commercialize any products that receive marketing approval on a timely and competitive basis.
79
We rely on third parties to conduct our clinical trials and those third parties may not perform satisfactorily, including failing to meet deadlines for the completion of such trials.
We do not independently conduct clinical trials for our product candidates. We rely on third parties, such as contract research organizations, clinical data management organizations, medical institutions and clinical investigators, to perform this function. We expect to continue to rely on such third parties in conducting our clinical trials of lefamulin, and expect to rely on these third parties to conduct clinical trials of any other product candidate that we develop. Any of these third parties may terminate their engagements with us at any time. If we need to enter into alternative arrangements, it would delay our product development activities.
Our reliance on these third parties for clinical development activities reduces our control over these activities but does not relieve us of our responsibilities. For example, we remain responsible for ensuring that each of our clinical trials is conducted in accordance with the general investigational plan and protocols for the trial. Moreover, the FDA requires us to comply with standards, commonly referred to as Good Clinical Practices, or GCP, for conducting, recording and reporting the results of clinical trials to assure that data and reported results are credible and accurate and that the rights, integrity and confidentiality of trial participants are protected. We also are required to register ongoing clinical trials and post the results of completed clinical trials on a U.S. government-sponsored database, ClinicalTrials.gov, within certain timeframes. Failure to do so can result in fines, adverse publicity and civil and criminal sanctions. Similar GCP and transparency requirements apply in the European Union. Failure to comply with such requirements, including with respect to clinical trials conducted outside the European Union, can also lead regulatory authorities to refuse to take into account clinical trial data submitted as part of an MAA.
Furthermore, third parties that we rely on for our clinical development activities may also have relationships with other entities, some of which may be our competitors. If these third parties do not successfully carry out their contractual duties, meet expected deadlines or conduct our clinical trials in accordance with regulatory requirements or our stated protocols, we will not be able to obtain, or may be delayed in obtaining, marketing approvals for our product candidates and will not be able to, or may be delayed in our efforts to, successfully commercialize our product candidates. Our product development costs will increase if we experience delays in testing or obtaining marketing approvals.
We also rely on other third parties to store and distribute drug supplies for our clinical trials. Any performance failure on the part of our distributors could delay clinical development or marketing approval of our product candidates or commercialization of our products, producing additional losses and depriving us of potential product revenue.
We may enter into collaborations with third parties for the development or commercialization of lefamulin and our other product candidates. If those collaborations are not successful, we may not be able to capitalize on the market potential of these product candidates.
If lefamulin receives marketing approval, we plan to commercialize it in the United States with our own targeted hospital sales and marketing organization. Outside the United States, we expect to utilize a variety of types of collaboration, distribution and other marketing arrangements with one or more third parties to commercialize lefamulin. We also may seek third-party collaborators for development and commercialization of other product candidates or for lefamulin for indications other than CABP. Our likely collaborators for any sales, marketing, distribution, development, licensing or broader collaboration arrangements include large and mid-size pharmaceutical companies, regional and national pharmaceutical companies and biotechnology companies. We are not currently party to any such arrangement. However, if we do enter into any such arrangements with any third parties in the future, we will likely have limited control over the amount and timing of resources that our collaborators dedicate to the development or commercialization of our product candidates. Our ability to generate
80
revenues from these arrangements will depend on our collaborators' abilities and efforts to successfully perform the functions assigned to them in these arrangements.
Collaborations involving our product candidates would pose numerous risks to us, including the following:
- •
- collaborators have significant discretion in determining the efforts and resources that they will apply to these collaborations and may not
perform their obligations as expected;
- •
- collaborators may deemphasize or not pursue development and commercialization of our product candidates or may elect not to continue or renew
development or commercialization programs based on clinical trial results, changes in the collaborators' strategic focus, product and product candidate priorities, available funding, or external
factors such as an acquisition that diverts resources or creates competing priorities;
- •
- collaborators may delay clinical trials, provide insufficient funding for a clinical trial program, stop a clinical trial or abandon a product
candidate, repeat or conduct new clinical trials or require a new formulation of a product candidate for clinical testing;
- •
- collaborators could independently develop, or develop with third parties, products that compete directly or indirectly with our products or
product candidates if the collaborators believe that competitive products are more likely to be successfully developed or can be commercialized under terms that are more economically attractive than
ours;
- •
- a collaborator with marketing and distribution rights to one or more products may not commit sufficient resources to the marketing and
distribution of such product or products;
- •
- collaborators may not properly maintain or defend our intellectual property rights or may use our proprietary information in such a way as to
invite litigation that could jeopardize or invalidate our intellectual property or proprietary information or expose us to potential litigation;
- •
- collaborators may infringe the intellectual property rights of third parties, which may expose us to litigation and potential liability;
- •
- disputes may arise between the collaborator and us as to the ownership of intellectual property arising during the collaboration;
- •
- we may grant exclusive rights to our collaborators, which would prevent us from collaborating with others;
- •
- disputes may arise between the collaborators and us that result in the delay or termination of the research, development or commercialization
of our products or product candidates or that result in costly litigation or arbitration that diverts management attention and resources; and
- •
- collaborations may be terminated and, if terminated, may result in a need for additional capital to pursue further development or commercialization of the applicable product candidates.
Collaboration agreements may not lead to development or commercialization of product candidates in the most efficient manner or at all. If a collaborator of ours were to be involved in a business combination, the continued pursuit and emphasis on our product development or commercialization program could be delayed, diminished or terminated.
If we are not able to establish collaborations, we may have to alter our development and commercialization plans.
The potential commercialization of lefamulin and the development and potential commercialization of other product candidates will require substantial additional cash to fund expenses.
81
For some of our product candidates, we may decide to collaborate with pharmaceutical and biotechnology companies for the development and potential commercialization of those product candidates. For example, we intend to seek to commercialize lefamulin through a variety of types of collaboration arrangements outside the United States.
We face significant competition in seeking appropriate collaborators. Whether we reach a definitive agreement for a collaboration will depend, among other things, upon our assessment of the collaborator's resources and expertise, the terms and conditions of the proposed collaboration and the proposed collaborator's evaluation of a number of factors. Those factors may include the design or results of clinical trials, the likelihood of approval by the FDA or similar regulatory authorities outside the United States, the potential market for the subject product candidate, the costs and complexities of manufacturing and delivering such product candidate to patients, the potential of competing products, the existence of uncertainty with respect to our ownership of technology, which can exist if there is a challenge to such ownership without regard to the merits of the challenge, and industry and market conditions generally. The collaborator may also consider alternative product candidates or technologies for similar indications that may be available to collaborate on and whether such a collaboration could be more attractive than the one with us for our product candidate. We may also be restricted under future license agreements from entering into agreements on certain terms with potential collaborators. Collaborations are complex and time-consuming to negotiate and document. In addition, there have been a significant number of recent business combinations among large pharmaceutical companies that have resulted in a reduced number of potential future collaborators.
If we are unable to reach agreements with suitable collaborators on a timely basis, on acceptable terms, or at all, we may have to curtail the development of a product candidate, reduce or delay its development program or one or more of our other development programs, delay its potential commercialization or reduce the scope of any sales or marketing activities, or increase our expenditures and undertake development or commercialization activities at our own expense. If we elect to fund and undertake development or commercialization activities on our own, we may need to obtain additional expertise and additional capital, which may not be available to us on acceptable terms or at all. If we fail to enter into collaborations and do not have sufficient funds or expertise to undertake the necessary development and commercialization activities, we may not be able to further develop our product candidates or bring them to market and generate product revenue.
Risks Related to Our Intellectual Property
If we are unable to obtain and maintain patent protection for our technology and products, or if the scope of the patent protection is not sufficiently broad, our competitors could develop and commercialize technology and products similar or identical to ours, and our ability to successfully commercialize our technology and products may be adversely affected.
Our success depends in large part on our ability to obtain and maintain patent protection in the United States and other countries with respect to our proprietary technology and products. We seek to protect our proprietary position by filing patent applications in the United States, Europe and in certain additional foreign jurisdictions related to our novel technologies and product candidates that are important to our business. This process is expensive and time-consuming, and we may not be able to file and prosecute all necessary or desirable patent applications at a reasonable cost or in a timely manner. It is also possible that we will fail to identify patentable aspects of our research and development output before it is too late to obtain patent protection. Moreover, if we license technology or product candidates from third parties in the future, these license agreements may not permit us to control the preparation, filing and prosecution of patent applications, or to maintain or enforce the patents, covering this intellectual property. These agreements could also give our licensors the right to enforce the licensed patents without our involvement, or to decide not to enforce the patents at all. Therefore, in these circumstances, these patents and applications may not be prosecuted and enforced in a manner consistent with the best interests of our business.
82
The patent position of biotechnology and pharmaceutical companies generally is highly uncertain, involves complex legal and factual questions and has in recent years been the subject of much litigation. As a result, the issuance, scope, validity, enforceability and commercial value of our patent rights are highly uncertain. Our pending and future patent applications may not result in patents being issued which protect our technology or products, in whole or in part, or which effectively prevent others from commercializing competitive technologies and products. Changes in either the patent laws or interpretation of the patent laws in the United States and other countries may diminish the value of our patents or narrow the scope of our patent protection.
The laws of foreign countries may not protect our rights to the same extent as the laws of the United States. For example, European patent law restricts the patentability of methods of treatment of the human body more than U.S. law does. We also may not pursue or obtain patent protection in all major markets or may not obtain protection that enables us to prevent the entry of third parties onto the market. Assuming the other requirements for patentability are met, currently, the first to file a patent application is generally entitled to the patent. However, prior to March 16, 2013, in the United States, the first to invent was entitled to the patent. Publications of discoveries in the scientific literature often lag behind the actual discoveries, and patent applications in the United States and other jurisdictions are typically not published until 18 months after filing, or in some cases not at all. Therefore, we cannot know with certainty whether we were the first to make the inventions claimed in our U.S. patents or pending U.S. patent applications, or that we were the first to file for patent protection of such inventions.
Moreover, we may be subject to a third-party pre-issuance submission of prior art to the U.S. Patent and Trademark Office, or USPTO, or become involved in opposition, derivation, reexamination, inter partes review, post grant review, interference proceedings or other patent office proceedings or litigation, in the United States or elsewhere, challenging our patent rights or the patent rights of others. An adverse determination in any such submission, proceeding or litigation could reduce the scope of, or invalidate, our patent rights, allow third parties to commercialize our technology or products and compete directly with us, without payment to us, or result in our inability to manufacture or commercialize products without infringing third-party patent rights. In addition, if the breadth or strength of protection provided by our patents and patent applications is threatened, it could dissuade companies from collaborating with us to license, develop or commercialize current or future product candidates.
Even if our patent applications issue as patents, they may not issue in a form that will provide us with any meaningful protection, prevent competitors from competing with us or otherwise provide us with any competitive advantage. Our competitors may be able to circumvent our owned or any future licensed patents by developing similar or alternative technologies or products in a non-infringing manner. In addition, other companies may attempt to circumvent any regulatory data protection or market exclusivity that we obtain under applicable legislation, which may require us to allocate significant resources to preventing such circumvention. Legal and regulatory developments in the European Union and elsewhere may also result in clinical trial data submitted as part of an MAA becoming publicly available. Such developments could enable other companies to circumvent our intellectual property rights and use our clinical trial data to obtain marketing authorizations in the European Union and in other jurisdictions. Such developments may also require us to allocate significant resources to prevent other companies from circumventing or violating our intellectual property rights. Our attempts to prevent third parties from circumventing our intellectual property and other rights may ultimately be unsuccessful. We may also fail to take the required actions or pay the necessary fees to maintain our patents.
The issuance of a patent is not conclusive as to its inventorship, scope, validity or enforceability, and our owned and licensed patents may be challenged in the courts or patent offices in the United States and abroad. Such challenges may result in loss of exclusivity or freedom to operate or in patent
83
claims being narrowed, invalidated or held unenforceable, in whole or in part, which could limit our ability to stop others from using or commercializing similar or identical technology and products, or limit the duration of the patent protection of our technology and products. Given the amount of time required for the development, testing and regulatory review of new product candidates, patents protecting such candidates might expire before or shortly after such candidates are commercialized. As a result, our patent portfolio may not provide us with sufficient rights to exclude others from commercializing products similar or identical to ours.
We may become involved in lawsuits to protect or enforce our patents or other intellectual property, which could be expensive, time consuming and unsuccessful.
Competitors may infringe our patents, trademarks, copyrights or other intellectual property. To counter such infringement or unauthorized use, we may be required to file claims, which can be expensive and time consuming. Any claims we assert against perceived infringers could provoke these parties to assert counterclaims against us alleging that we infringe their intellectual property. In addition, in a patent infringement proceeding, a court may decide that a patent of ours is invalid or unenforceable, in whole or in part, construe the patent's claims narrowly or may refuse to stop the other party from using the technology at issue on the grounds that our patents do not cover the technology in question.
Third parties may initiate legal proceedings alleging that we are infringing their intellectual property rights, the outcome of which would be uncertain and could have a material adverse effect on the success of our business.
Our commercial success depends upon our ability and the ability of our collaborators to develop, manufacture, market and sell our product candidates and use our proprietary technologies without infringing the intellectual property and other proprietary rights of third parties. There is considerable intellectual property litigation in the biotechnology and pharmaceutical industries, and we may become party to, or threatened with, future adversarial proceedings or litigation regarding intellectual property rights with respect to our products and technology, including interference, derivation, inter partes review or post-grant review proceedings before the USPTO. The risks of being involved in such litigation and proceedings may increase as our product candidates approach commercialization, and as we gain greater visibility as a public company. Third parties may assert infringement claims against us based on existing or future intellectual property rights. We may not be aware of all such intellectual property rights potentially relating to our product candidates. Any freedom-to-operate search or analysis previously conducted may not have uncovered all relevant patents and patent applications, and there may be pending or future patent applications that, if issued, would block us from commercializing lefamulin. Thus, we do not know with certainty whether lefamulin, any other product candidate, or our commercialization thereof, does not and will not infringe any third party's intellectual property.
If we are found to infringe a third party's intellectual property rights, or to avoid or settle litigation, we could be required to obtain a license to continue developing and marketing our products and technology. However, we may not be able to obtain any required license on commercially reasonable terms or at all. Even if we were able to obtain a license, it could be non-exclusive, thereby giving our competitors access to the same technologies licensed to us, and could require us to make substantial payments. We could be forced, including by court order, to cease commercializing the infringing technology or product. In addition, we could be found liable for monetary damages, including treble damages and attorneys' fees if we are found to have willfully infringed a patent or other intellectual property right. A finding of infringement could prevent us from commercializing our product candidates or force us to cease some of our business operations, which could materially harm our business. Claims that we have misappropriated the confidential information or trade secrets of third parties could have a similar negative impact on our business.
84
We may be subject to claims by third parties asserting that we or our employees have misappropriated their intellectual property, or claiming ownership of what we regard as our own intellectual property.
Many of our employees were previously employed at universities or other biotechnology or pharmaceutical companies, including our competitors or potential competitors. Although we try to ensure that our employees do not use the proprietary information or know-how of others in their work for us, we may be subject to claims that we or these employees have used or disclosed intellectual property, including trade secrets or other proprietary information, of any such employee's former employer. Litigation may be necessary to defend against these claims.
In addition, while we typically require our employees and contractors who may be involved in the development of intellectual property to execute agreements assigning such intellectual property to us, we may be unsuccessful in executing such an agreement with each party who in fact develops intellectual property that we regard as our own. Our business was founded as a spin-off from Sandoz. Although all patent applications are fully owned by us and were either filed by Sandoz with all rights fully transferred to us, or filed in our sole name, because we acquired certain of our patents from Sandoz, we must rely on their prior practices, with regard to the assignment of such intellectual property. Our and their assignment agreements may not be self-executing or may be breached, and we may be forced to bring claims against third parties, or defend claims they may bring against us, to determine the ownership of what we regard as our intellectual property.
If we fail in prosecuting or defending any such claims, in addition to paying monetary damages, we may lose valuable intellectual property rights or personnel. Even if we are successful in prosecuting or defending against such claims, litigation could result in substantial costs and be a distraction to management.
Intellectual property litigation could cause us to spend substantial resources and could distract our personnel from their normal responsibilities.
Even if resolved in our favor, litigation or other legal proceedings relating to intellectual property claims may cause us to incur significant expenses, and could distract our technical and management personnel from their normal responsibilities. In addition, there could be public announcements of the results of hearings, motions or other interim proceedings or developments. If securities analysts or investors perceive these results to be negative, it could have a substantial adverse effect on the price of our ordinary shares. Such litigation or proceedings could substantially increase our operating losses and reduce the resources available for development, sales, marketing or distribution activities. We may not have sufficient financial or other resources to adequately conduct such litigation or proceedings. Some of our competitors may be able to sustain the costs of such litigation or proceedings more effectively than we can because of their greater financial resources. Uncertainties resulting from the initiation and continuation of patent litigation or other proceedings could have a material adverse effect on our ability to compete in the marketplace.
If we are unable to protect the confidentiality of our trade secrets, our business and competitive position would be harmed.
In addition to seeking patents for some of our technology and products, we also rely on trade secrets, including unpatented know-how, technology and other proprietary information, to maintain our competitive position. We seek to protect these trade secrets, in part, by entering into non-disclosure and confidentiality agreements with parties who have access to them, such as our employees, corporate collaborators, outside scientific collaborators, contract manufacturers, consultants, advisors and other third parties. We also enter into confidentiality and invention or patent assignment agreements with our employees and consultants. However, we cannot guarantee that we have executed these agreements with each party that may have or have had access to our trade secrets or that the agreements we have
85
executed will provide adequate protection. Any party with whom we have executed such an agreement may breach that agreement and disclose our proprietary information, including our trade secrets, and we may not be able to obtain adequate remedies for such breaches. Enforcing a claim that a party illegally disclosed or misappropriated a trade secret is difficult, expensive and time-consuming, and the outcome is unpredictable. In addition, some courts inside and outside the United States are less willing or unwilling to protect trade secrets. If any of our trade secrets were to be lawfully obtained or independently developed by a competitor, we would have no right to prevent them, or those to whom they communicate it, from using that technology or information to compete with us. If any of our trade secrets were to be obtained or independently developed by a competitor, our competitive position would be harmed.
We have not yet registered our trademarks in all of our potential markets, and failure to secure those registrations could adversely affect our business.
Our trademark applications may not be allowed for registration, and our registered trademarks may not be maintained or enforced. During trademark registration proceedings, we may receive rejections. Although we are given an opportunity to respond to those rejections, we may be unable to overcome such rejections. In addition, in the USPTO and in comparable agencies in many foreign jurisdictions, third parties are given an opportunity to oppose pending trademark applications and to seek to cancel registered trademarks. Opposition or cancellation proceedings may be filed against our trademarks, and our trademarks may not survive such proceedings. If we do not secure registrations for our trademarks, we may encounter more difficulty in enforcing them against third parties than we otherwise would.
Risks Related to Regulatory Approval and Marketing of Our Product Candidates and Other Legal Compliance Matters
Even if we complete the necessary non-clinical studies and clinical trials, the marketing approval process is expensive, time-consuming and uncertain and may prevent us from obtaining approvals for the commercialization of some or all of our product candidates. If we are not able to obtain, or if there are delays in obtaining, required regulatory approvals, in particular in the United States or the European Union, we will not be able to commercialize our product candidates in those markets, and our ability to generate revenue will be materially impaired.
Our product candidates, including lefamulin, and the activities associated with their development and commercialization, including their design, testing, manufacture, safety, efficacy, recordkeeping, labeling, storage, approval, advertising, promotion, sale and distribution, are subject to comprehensive regulation by the FDA and by comparable authorities in other countries. Failure to obtain marketing approval for a product candidate will prevent us from commercializing the product candidate. We have not received approval to market lefamulin or any of our other product candidates from regulatory authorities in any jurisdiction.
We have no experience in filing and supporting the applications necessary to obtain marketing approvals for product candidates and expect to rely on third-parties to assist us in this process. Securing marketing approval requires the submission of extensive non-clinical and clinical data and supporting information to various regulatory authorities for each therapeutic indication to establish the product candidate's safety and efficacy. Securing marketing approval also requires the submission of information about the product manufacturing process to, and inspection of manufacturing facilities by, the regulatory authorities. Regulatory authorities may determine that lefamulin or any of our other product candidates are not effective or only moderately effective, or have undesirable or unintended side effects, toxicities, safety profiles or other characteristics that preclude us from obtaining marketing approval or that prevent or limit commercial use.
86
The process of obtaining marketing approvals is expensive, may take many years, if approval is obtained at all, and can vary substantially based upon a variety of factors, including the type, complexity and novelty of the product candidates involved. Changes in marketing approval policies during the development period, changes in or the enactment of additional statutes or regulations, or changes in regulatory review for each submitted product application, may cause delays in the approval or rejection of an application. For example, on June 23, 2016, eligible members of the electorate in the United Kingdom decided by referendum to leave the European Union, commonly referred to as "Brexit". On March 29, 2017, the United Kingdom formally notified the European Union of its intention to withdraw pursuant to Article 50 of the Lisbon Treaty. Because a significant proportion of the regulatory framework in the United Kingdom is derived from European Union directives and regulations, the referendum could materially change the regulatory regime applicable to the approval of any of our product candidates in the United Kingdom. In addition, because the European Medicines Agency, or EMA, is currently located in the United Kingdom but expected to move to the Netherlands as a result of the Brexit, the implications for the regulatory review process in the European Union has not been fully clarified and could result in disruption to the EMA review process.
The FDA and comparable regulatory authorities in other countries have substantial discretion in the approval process and may refuse to accept any application or may decide that our data are insufficient for approval and require additional preclinical, clinical or other studies. In addition, varying interpretations of the data obtained from non-clinical and clinical testing could delay, limit or prevent marketing approval of a product candidate. Any marketing approval we ultimately obtain may be limited or subject to restrictions or post-approval commitments that render the approved product not commercially viable.
Accordingly, if we or our collaborators experience delays in obtaining approval or if we or they fail to obtain approval of our product candidates, the commercial prospects for our product candidates may be harmed and our ability to generate revenues will be materially impaired.
Our failure to obtain marketing approval in jurisdictions other than the United States and Europe would prevent our product candidates from being marketed in these other jurisdictions, and any approval we are granted for our product candidates in the United States and Europe would not assure approval of product candidates in other jurisdictions.
In order to market and sell lefamulin and our other product candidates in jurisdictions other than the United States and Europe, we must obtain separate marketing approvals and comply with numerous and varying regulatory requirements. The approval process varies among countries and can involve additional testing. The time required to obtain approval may differ from that required to obtain FDA approval or approvals from regulatory authorities in the European Union. The regulatory approval process outside the United States and Europe generally includes all of the risks associated with obtaining FDA approval or approvals from regulatory authorities in the European Union. In addition, some countries outside the United States and Europe require approval of the sales price of a drug before it can be marketed. In many countries, separate procedures must be followed to obtain reimbursement and a product may not be approved for sale in the country until it is also approved for reimbursement. We may not obtain marketing, pricing or reimbursement approvals outside the United States and Europe on a timely basis, if at all. Approval by the FDA or regulatory authorities in the European Union does not ensure approval by regulatory authorities in other countries or jurisdictions, and approval by one regulatory authority outside the United States and Europe does not ensure approval by regulatory authorities in other countries or jurisdictions or by the FDA or regulatory authorities in the European Union. We may not be able to file for marketing approvals and may not receive necessary approvals to commercialize our products in any market. Marketing approvals in countries outside the United States and Europe do not ensure pricing approvals in those countries or
87
in any other countries, and marketing approvals and pricing approvals do not ensure that reimbursement will be obtained.
Even if we obtain marketing approvals for our product candidates, the terms of approvals and ongoing regulation of our products may limit how we manufacture and market our products and compliance with such requirements may involve substantial resources, which could materially impair our ability to generate revenue.
Even if marketing approval of a product candidate is granted, an approved product and its manufacturer and marketer are subject to ongoing review and extensive regulation, including the potential requirements to implement a risk evaluation and mitigation strategy or to conduct costly post-marketing studies or clinical trials and surveillance to monitor the safety or efficacy of the product. We must also comply with requirements concerning advertising and promotion for any of our product candidates for which we obtain marketing approval. Promotional communications with respect to prescription drugs are subject to a variety of legal and regulatory restrictions and must be consistent with the information in the product's approved labeling. Thus, we will not be able to promote any products we develop for indications or uses for which they are not approved. In addition, manufacturers of approved products and those manufacturers' facilities are required to comply with extensive FDA requirements including ensuring that quality control and manufacturing procedures conform to cGMP, which include requirements relating to quality control and quality assurance as well as the corresponding maintenance of records and documentation and reporting requirements. We and our contract manufacturers could be subject to periodic unannounced inspections by the FDA to monitor and ensure compliance with cGMP.
Accordingly, assuming we receive marketing approval for one or more of our product candidates, we and our contract manufacturers will continue to expend time, money and effort in all areas of regulatory compliance, including manufacturing, production, product surveillance and quality control. If we are not able to comply with post-approval regulatory requirements, we could have the marketing approvals for our products withdrawn by regulatory authorities and our ability to market any future products could be limited, which could adversely affect our ability to achieve or sustain profitability. Thus, the cost of compliance with post-approval regulations may have a negative effect on our operating results and financial condition.
Any product candidate for which we obtain marketing approval will be subject to strict enforcement of post-marketing requirements and we could be subject to substantial penalties, including withdrawal of our product from the market, if we fail to comply with all regulatory requirements or if we experience unanticipated problems with our product candidates, when and if any of them are approved.
Any product candidate for which we obtain marketing approval, along with the manufacturing processes, post-approval clinical data, labeling, advertising and promotional activities for such product, will be subject to continual requirements of and review by the FDA and other regulatory authorities. These requirements include, but are not limited to, restrictions governing promotion of an approved product, submissions of safety and other post-marketing information and reports, registration and listing requirements, cGMP requirements relating to manufacturing, quality control, quality assurance and corresponding maintenance of records and documents, and requirements regarding the distribution of samples to physicians and recordkeeping. In addition, even if marketing approval of a product candidate is granted, the approval may be subject to limitations on the indicated uses for which the product may be marketed or to the conditions of approval.
The FDA and other federal and state agencies, including the U.S. Department of Justice, or DOJ, closely regulate compliance with all requirements governing prescription drug products, including requirements pertaining to marketing and promotion of drugs in accordance with the provisions of the approved labeling and manufacturing of products in accordance with cGMP requirements.
88
The FDA and DOJ impose stringent restrictions on manufacturers' communications regarding off-label use and if we do not market our products for their approved indications, we may be subject to enforcement action for off-label marketing. Violations of such requirements may lead to investigations alleging violations of the Food, Drug and Cosmetic Act and other statutes, including the False Claims Act and other federal and state health care fraud and abuse laws as well as state consumer protection laws.
Our failure to comply with all regulatory requirements, and later discovery of previously unknown adverse events or other problems with our products, manufacturers or manufacturing processes, may yield various results, including:
- •
- litigation involving patients taking our products;
- •
- restrictions on such products, manufacturers or manufacturing processes;
- •
- restrictions on the labeling or marketing of a product;
- •
- restrictions on product distribution or use;
- •
- requirements to conduct post-marketing studies or clinical trials;
- •
- warning or untitled letters;
- •
- withdrawal of the products from the market;
- •
- refusal to approve pending applications or supplements to approved applications that we submit;
- •
- recall of products;
- •
- fines, restitution or disgorgement of profits or revenues;
- •
- suspension or withdrawal of marketing approvals;
- •
- damage to relationships with any potential collaborators;
- •
- unfavorable press coverage and damage to our reputation;
- •
- refusal to permit the import or export of our products;
- •
- product seizure; or
- •
- injunctions or the imposition of civil or criminal penalties.
Non-compliance by us or any future collaborator with regulatory requirements regarding safety monitoring or pharmacovigilance, and with requirements related to the development of products for the pediatric population, can also result in significant financial penalties. Similarly, failure to comply with regulatory requirements regarding the protection of personal information can also lead to significant penalties and sanctions.
Non-compliance with European Union requirements regarding safety monitoring or pharmacovigilance, and with requirements related to the development of products for the pediatric population, also can result in significant financial penalties. Similarly, failure to comply with the European Union's requirements regarding the protection of personal information can also lead to significant penalties and sanctions.
Governments outside the United States tend to impose strict price controls, which may adversely affect our revenues, if any.
In some countries, particularly the member states of the European Union, the pricing of prescription pharmaceuticals is subject to governmental control. In these countries, pricing negotiations with governmental authorities can take considerable time after the receipt of marketing approval for a
89
product. Also, there can be considerable pressure by governments and other stakeholders on prices and reimbursement levels, including as part of cost containment measures. Political, economic and regulatory developments may further complicate pricing negotiations, and pricing negotiations may continue after reimbursement has been obtained. Reference pricing used by various European Union member states and parallel distribution, or arbitrage between low-priced and high-priced member states, can further reduce prices. In some countries, we may be required to conduct a clinical trial or other studies that compare the cost-effectiveness of our product candidate to other available therapies to obtain or maintain reimbursement or pricing approval. Publication of discounts by third-party payors or authorities may lead to further pressure on prices or reimbursement levels within the country of publication and other countries. If reimbursement of our products is unavailable or limited in scope or amount, or if pricing is set at unsatisfactory levels, our business could be adversely affected.
The FDA's agreement to a Special Protocol Assessment, or SPA, with respect to the study design of our first Phase 3 clinical trial of lefamulin for CABP does not guarantee any particular outcome from regulatory review, including ultimate approval, and may not lead to a faster development or regulatory review or approval process.
We reached agreement with the FDA in September 2015 on a SPA, which was later amended in April 2016, regarding the study design of our first Phase 3 clinical trial of lefamulin for the treatment of CABP. The SPA process is designed to facilitate the FDA's review and approval of drugs by allowing the FDA to evaluate the proposed design and size of Phase 3 clinical trials that are intended to form the primary basis for determining a product candidate's efficacy and safety. Upon specific request by a clinical trial sponsor, the FDA will evaluate the protocol and respond to a sponsor's questions regarding, among other things, primary efficacy endpoints, trial conduct and data analysis, within 45 days of receipt of the request. The FDA ultimately assesses whether the protocol design and planned analysis of the trial are acceptable to support regulatory approval of the product candidate with respect to the effectiveness in the indication studied.
Our agreement with the FDA regarding the SPA may not lead to faster development, regulatory review or approval for lefamulin. Once the FDA and an applicant reach an agreement under the special protocol assessment process regarding the design and size of a clinical trial, the agreement generally cannot be changed after the clinical trial begins. Nevertheless, the FDA may revoke or alter a SPA under defined circumstances, such as changes in the relevant data or assumptions provided by the sponsor or the emergence of new public health concerns. A revocation or alteration in our SPA could significantly delay or prevent approval of any marketing applications we submit for lefamulin.
Fast track designation by the FDA may not actually lead to a faster development or regulatory review or approval process and does not assure FDA approval of our product candidate.
If a drug is intended for the treatment of a serious or life threatening condition and the drug demonstrates the potential to address unmet medical need for this condition, the drug sponsor may apply for FDA fast track designation. The FDA has designated each of the IV and oral formulations of lefamulin as a qualified infectious disease product, or QIDP, and granted fast track designations to each of these formulations of lefamulin. However, neither the QIDP nor the fast track designation ensures that lefamulin will receive marketing approval or that approval will be granted within any particular timeframe. We may also seek fast track designation for our other product candidates. We may not experience a faster development process, review or approval compared to conventional FDA procedures. In addition, the FDA may withdraw fast track designation if it believes that the designation is no longer supported by data from our clinical development program. Fast track designation alone does not guarantee qualification for the FDA's priority review procedures.
90
Priority review designation by the FDA may not lead to a faster regulatory review or approval process and, in any event, does not assure FDA approval of our product candidate.
If the FDA determines that a product candidate offers major advances in treatment or provides a treatment where no adequate therapy exists, the FDA may designate the product candidate for priority review. A priority review designation means that the FDA's goal to review an application is six months, rather than the standard review period of ten months. Because the FDA designated each of the IV and oral formulations of lefamulin as a QIDP, lefamulin also will receive priority review. We may also request priority review for other product candidates. The FDA has broad discretion with respect to whether or not to grant priority review status to a product candidate, so even if we believe a particular product candidate is eligible for such designation or status, the FDA may decide not to grant it. Moreover, a priority review designation does not necessarily mean a faster regulatory review process or necessarily confer any advantage with respect to approval compared to conventional FDA procedures. Receiving priority review from the FDA does not guarantee approval within the six-month review cycle or thereafter.
Designation of our product candidate, lefamulin, as a Qualified Infectious Disease Product does not assure FDA approval of this product candidate.
A QIDP is an antibacterial or antifungal drug intended to treat serious or life-threatening infections, including those caused by an antibacterial or antifungal resistant pathogen, including novel or emerging infectious pathogens or certain "qualifying pathogens." Upon the approval of an NDA for a drug product designated by the FDA as a QIDP, the product is granted an additional period of five years of regulatory exclusivity. Even though we have received QIDP designation for the IV and oral formulations of lefamulin, there is no assurance that this product candidate will be approved by the FDA.
Under the CURES Act and the Trump Administration's regulatory reform initiatives, the FDA's policies, regulations and guidance may be revised or revoked and that could prevent, limit or delay regulatory approval of our product candidates, which would impact our ability to generate revenue.
In December 2016, the 21st Century Cures Act, or Cures Act, was signed into law. The Cures Act, among other things, is intended to modernize the regulation of drugs and spur innovation, but its ultimate implementation is unclear. If we are slow or unable to adapt to changes in existing requirements or the adoption of new requirements or policies, or if we are not able to maintain regulatory compliance, we may lose any marketing approval that we may have obtained and we may not achieve or sustain profitability, which would adversely affect our business, prospects, financial condition and results of operations.
We also cannot predict the likelihood, nature or extent of government regulation that may arise from future legislation or administrative or executive action, either in the United States or abroad. For example, certain policies of the Trump administration may impact our business and industry. Namely, the Trump administration has taken several executive actions, including the issuance of a number of Executive Orders, that could impose significant burdens on, or otherwise materially delay, the FDA's ability to engage in routine regulatory and oversight activities such as implementing statutes through rulemaking, issuance of guidance, and review and approval of marketing applications. An under-staffed FDA could result in delays in the FDA's responsiveness or in its ability to review submissions or applications, issue regulations or guidance, or implement or enforce regulatory requirements in a timely fashion or at all. Moreover, on January 30, 2017, President Trump issued an Executive Order, applicable to all executive agencies, including the FDA, which requires that for each notice of proposed rulemaking or final regulation to be issued in fiscal year 2017, the agency shall identify at least two existing regulations to be repealed, unless prohibited by law. These requirements are referred to as the "two-for-one" provisions. This Executive Order includes a budget neutrality provision that requires the
91
total incremental cost of all new regulations in the 2017 fiscal year, including repealed regulations, to be no greater than zero, except in limited circumstances. For fiscal years 2018 and beyond, the Executive Order requires agencies to identify regulations to offset any incremental cost of a new regulation and approximate the total costs or savings associated with each new regulation or repealed regulation. In interim guidance issued by the Office of Information and Regulatory Affairs within the Office of Management and Budget on February 2, 2017, the administration indicates that the "two-for-one" provisions may apply not only to agency regulations, but also to significant agency guidance documents. In addition, on February 24, 2017, President Trump issued an executive order directing each affected agency to designate an agency official as a "Regulatory Reform Officer" and establish a "Regulatory Reform Task Force" to implement the two-for-one provisions and other previously issued executive orders relating to the review of federal regulations, however it is difficult to predict how these requirements will be implemented, and the extent to which they will impact the FDA's ability to exercise its regulatory authority. If these executive actions impose constraints on the FDA's ability to engage in oversight and implementation activities in the normal course, our business may be negatively impacted.
Our relationships with healthcare providers, physicians and third-party payors will be subject to applicable anti-kickback, fraud and abuse and other healthcare laws and regulations, which in the event of a violation could expose us to criminal sanctions, civil penalties, contractual damages, reputational harm and diminished profits and future earnings.
Healthcare providers, physicians and third-party payors will play a primary role in the recommendation and prescription of any product candidates, including lefamulin, for which we obtain marketing approval. Our future arrangements with healthcare providers, physicians and third-party payors may expose us to broadly applicable fraud and abuse and other healthcare laws and regulations that may constrain the business or financial arrangements and relationships through which we market, sell and distribute any products for which we obtain marketing approval. Restrictions under applicable federal and state healthcare laws and regulations, include the following:
- •
- the federal Anti-Kickback Statute prohibits, among other things, persons from knowingly and willfully soliciting, offering, receiving or
providing remuneration, directly or indirectly, in cash or in kind, to induce or reward, or in return for, either the referral of an individual for, or the purchase, order or recommendation or
arranging of, any good or service, for which payment may be made under a federal healthcare program such as Medicare and Medicaid;
- •
- the federal False Claims Act imposes criminal and civil penalties, including through civil whistleblower or qui tam actions, against
individuals or entities for, among other things, knowingly presenting, or causing to be presented, false or fraudulent claims for payment by a federal healthcare program or making a false statement or
record material to payment of a false claim or avoiding, decreasing or concealing an obligation to pay money to the federal government, with potential liability including mandatory treble damages and
significant per-claim penalties, currently set at $5,500 to $11,000 per false claim;
- •
- the federal Health Insurance Portability and Accountability Act of 1996, or HIPAA, imposes criminal and civil liability for executing a scheme
to defraud any healthcare benefit program or making false statements relating to healthcare matters;
- •
- HIPAA, as amended by the Health Information Technology for Economic and Clinical Health Act and its implementing regulations, also imposes obligations, including mandatory contractual terms, with respect to safeguarding the privacy, security and transmission of individually identifiable health information;
92
- •
- the federal Physician Payments Sunshine Act requires applicable manufacturers of covered products to report payments and other transfers of
value to physicians and teaching hospitals, with data collection beginning in August 2013; and
- •
- analogous state and foreign laws and regulations, such as state anti-kickback and false claims laws and transparency statutes, may apply to sales or marketing arrangements and claims involving healthcare items or services reimbursed by non-governmental third party payors, including private insurers.
Some state laws require pharmaceutical companies to comply with the pharmaceutical industry's voluntary compliance guidelines and the relevant compliance guidance promulgated by the federal government and may require product manufacturers to report information related to payments and other transfers of value to physicians and other healthcare providers or marketing expenditures. State and foreign laws also govern the privacy and security of health information in some circumstances, many of which differ from each other in significant ways and often are not pre-empted by HIPAA, thus complicating compliance efforts.
If our operations are found to be in violation of any of the laws described above or any governmental regulations that apply to us, we may be subject to penalties, including civil and criminal penalties, damages, fines and the curtailment or restructuring of our operations. Any penalties, damages, fines, curtailment or restructuring of our operations could adversely affect our financial results. We are developing and implementing a corporate compliance program designed to ensure that we will market and sell any future products that we successfully develop from our product candidates in compliance with all applicable laws and regulations, but we cannot guarantee that this program will protect us from governmental investigations or other actions or lawsuits stemming from a failure to be in compliance with such laws or regulations. If any such actions are instituted against us and we are not successful in defending ourselves or asserting our rights, those actions could have a significant impact on our business, including the imposition of significant fines or other sanctions.
Efforts to ensure that our business arrangements with third parties will comply with applicable healthcare laws and regulations will involve substantial costs. It is possible that governmental authorities will conclude that our business practices may not comply with current or future statutes, regulations or case law involving applicable fraud and abuse or other healthcare laws and regulations. If our operations are found to be in violation of any of these laws or any other governmental regulations that may apply to us, we may be subject to significant civil, criminal and administrative penalties, damages, fines, imprisonment, exclusion of products from government funded healthcare programs, such as Medicare and Medicaid, and the curtailment or restructuring of our operations. If any of the physicians or other healthcare providers or entities with whom we expect to do business is found to be not in compliance with applicable laws, they may be subject to criminal, civil or administrative sanctions, including exclusions from government funded healthcare programs.
Current and future legislation may increase the difficulty and cost for us and any future collaborators to obtain marketing approval of and commercialize our product candidates and affect the prices we, or they, may obtain.
In the United States and some foreign jurisdictions, there have been a number of legislative and regulatory changes and proposed changes regarding the healthcare system that could, among other things, prevent or delay marketing approval of lefamulin or any of our other product candidates, restrict or regulate post-approval activities and affect our ability, or the ability of any collaborators, to profitably sell any product candidates, including lefamulin, for which we, or they, obtain marketing approval. We expect that current laws, as well as other healthcare reform measures that may be adopted in the future, may result in more rigorous coverage criteria and in additional downward pressure on the price that we, or any future collaborators, may receive for any approved products.
93
In March 2010, President Obama signed into law the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act, or collectively the ACA. Among the provisions of the ACA of potential importance to our business and our product candidates are the following:
- •
- an annual, non-deductible fee on any entity that manufactures or imports specified branded prescription products and biologic agents;
- •
- an increase in the statutory minimum rebates a manufacturer must pay under the Medicaid Drug Rebate Program;
- •
- expansion of healthcare fraud and abuse laws, including the civil False Claims Act and the federal Anti-Kickback Statute, new government
investigative powers and enhanced penalties for noncompliance;
- •
- a new Medicare Part D coverage gap discount program, in which manufacturers must agree to offer 50% point-of-sale discounts off
negotiated prices;
- •
- extension of manufacturers' Medicaid rebate liability;
- •
- expansion of eligibility criteria for Medicaid programs;
- •
- expansion of the entities eligible for discounts under the Public Health Service pharmaceutical pricing program;
- •
- new requirements to report certain financial arrangements with physicians and teaching hospitals;
- •
- a new requirement to annually report product samples that manufacturers and distributors provide to physicians; and
- •
- a new Patient-Centered Outcomes Research Institute to oversee, identify priorities in, and conduct comparative clinical effectiveness research, along with funding for such research.
In addition, other legislative changes have been proposed and adopted since the ACA was enacted. These changes include the Budget Control Act of 2011, which among other things, led to aggregate reductions to Medicare payments to providers of up to 2% per fiscal year that started in 2013 and, due to subsequent legislative amendments to the statutes, will stay in effect through 2025 unless additional Congressional action is taken, and the American Taxpayer Relief Act of 2012, which, among other things, reduced Medicare payments to several types of providers and increased the statute of limitations period for the government to recover overpayments to providers from three to five years. These new laws may result in additional reductions in Medicare and other healthcare funding and otherwise affect the prices we may obtain for any of our product candidates for which we may obtain regulatory approval or the frequency with which any such product candidate is prescribed or used. Further, there have been several recent U.S. congressional inquiries and proposed state and federal legislation designed to, among other things, bring more transparency to drug pricing, review the relationship between pricing and manufacturer patient programs, reduce the costs of drugs under Medicare and reform government program reimbursement methodologies for drug products.
We expect that these healthcare reforms, as well as other healthcare reform measures that may be adopted in the future, may result in additional reductions in Medicare and other healthcare funding, more rigorous coverage criteria, new payment methodologies and additional downward pressure on the price that we receive for any approved product and/or the level of reimbursement physicians receive for administering any approved product we might bring to market. Reductions in reimbursement levels may negatively impact the prices we receive or the frequency with which our products are prescribed or administered. Any reduction in reimbursement from Medicare or other government programs may result in a similar reduction in payments from private payors. Since enactment of the ACA, there have
94
been numerous legal challenges and Congressional actions to repeal and replace provisions of the law. In May 2017, the U.S. House of Representatives passed legislation known as the American Health Care Act of 2017. Thereafter, the Senate Republicans introduced and then updated a bill to replace the ACA known as the Better Care Reconciliation Act of 2017. The Senate Republicans also introduced legislation to repeal the ACA without companion legislation to replace it, and a "skinny" version of the Better Care Reconciliation Act of 2017. In addition, the Senate considered proposed healthcare reform legislation known as the Graham-Cassidy bill. None of these measures was passed by the United States Senate.
The Trump Administration has also taken executive actions to undermine or delay implementation of the ACA. In January 2017, President Trump signed an Executive Order directing federal agencies with authorities and responsibilities under the ACA to waive, defer, grant exemptions from, or delay the implementation of any provision of the ACA that would impose a fiscal or regulatory burden on states, individuals, healthcare providers, health insurers, or manufacturers of pharmaceuticals or medical devices. In October 2017, the President signed a second Executive Order allowing for the use of association health plans and short-term health insurance, which may provide fewer health benefits than the plans sold through the ACA exchanges. At the same time, the Administration announced that it will discontinue the payment of cost-sharing reduction (CSR) payments to insurance companies until Congress approves the appropriation of funds for such CSR payments. The loss of the CSR payments is expected to increase premiums on certain policies issued by qualified health plans under the ACA. A bipartisan bill to appropriate funds for CSR payments was introduced in the Senate, but the future of that bill is uncertain.
More recently, with enactment of the Tax Cuts and Jobs Act of 2017, which was signed by the President on December 22, 2017, Congress repealed the "individual mandate." The repeal of this provision, which requires most Americans to carry a minimal level of health insurance, will become effective in 2019. According to the Congressional Budget Office, the repeal of the individual mandate will cause 13 million fewer Americans to be insured in 2027 and premiums in insurance markets may rise. Further, each chamber of the Congress has put forth multiple bills designed to repeal or repeal and replace portions of the ACA. Although none of these measures has been enacted by Congress to date, Congress may consider other legislation to repeal and replace elements of the ACA. The Congress will likely consider other legislation to replace elements of the ACA, during the next Congressional session.
We will continue to evaluate the effect that the ACA and its possible repeal and replacement could have on our business. It is possible that repeal and replacement initiatives, if enacted into law, could ultimately result in fewer individuals having health insurance coverage or in individuals having insurance coverage with less generous benefits. While the timing and scope of any potential future legislation to repeal and replace ACA provisions is highly uncertain in many respects, it is also possible that some of the ACA provisions that generally are not favorable for the research-based pharmaceutical industry could also be repealed along with ACA coverage expansion provisions. Accordingly, such reforms, if enacted, could have an adverse effect on anticipated revenue from product candidates that we may successfully develop and for which we may obtain marketing approval and may affect our overall financial condition and ability to develop commercialize product candidates.
The costs of prescription pharmaceuticals in the United States has also been the subject of considerable discussion in the United States, and members of Congress and the Administration have stated that they will address such costs through new legislative and administrative measures. The pricing of prescription pharmaceuticals is also subject to governmental control outside the United States. In these countries, pricing negotiations with governmental authorities can take considerable time after the receipt of marketing approval for a product. To obtain reimbursement or pricing approval in some countries, we may be required to conduct a clinical trial that compares the cost-effectiveness of our product candidates to other available therapies. If reimbursement of our products is unavailable or
95
limited in scope or amount, or if pricing is set at unsatisfactory levels, our ability to generate revenues and become profitable could be impaired. In the European Union, similar political, economic and regulatory developments may affect our ability to profitably commercialize our products. In addition to continuing pressure on prices and cost containment measures, legislative developments at the European Union or member state level may result in significant additional requirements or obstacles that may increase our operating costs.
Moreover, legislative and regulatory proposals have also been made to expand post-approval requirements and restrict sales and promotional activities for pharmaceutical drugs. We cannot be sure whether additional legislative changes will be enacted, or whether the FDA regulations, guidance or interpretations will be changed, or what the impact of such changes on the marketing approvals of our drug candidates, if any, may be. In addition, increased scrutiny by the United States Congress of the FDA's approval process may significantly delay or prevent marketing approval, as well as subject us and any future collaborators to more stringent drug labeling and post-marketing testing and other requirements.
We are subject to anti-corruption laws, as well as export control laws, customs laws, sanctions laws and other laws governing our operations. If we fail to comply with these laws, we could be subject to civil or criminal penalties, other remedial measures and legal expenses, which could adversely affect our business, results of operations and financial condition.
Our operations are subject to anti-corruption laws, including the U.S. Foreign Corrupt Practices Act, or FCPA, and other anti-corruption laws that apply in countries where we do business and may do business in the future. The FCPA and these other laws generally prohibit us, our officers, and our employees and intermediaries from bribing, being bribed or making other prohibited payments to government officials or other persons to obtain or retain business or gain some other business advantage. We may in the future operate in jurisdictions that pose a high risk of potential FCPA violations, and we may participate in collaborations and relationships with third parties whose actions could potentially subject us to liability under the FCPA or local anti-corruption laws. In addition, we cannot predict the nature, scope or effect of future regulatory requirements to which our international operations might be subject or the manner in that existing laws might be administered or interpreted.
Compliance with the FCPA is expensive and difficult, particularly in countries in which corruption is a recognized problem. In addition, the FCPA presents particular challenges in the pharmaceutical industry, because, in many countries, hospitals are operated by the government, and doctors and other hospital employees are considered foreign officials. Certain payments to hospitals in connection with clinical trials and other work have been deemed to be improper payments to government officials and have led to FCPA enforcement actions.
We are also subject to other laws and regulations governing our international operations, including regulations administered by the governments of the United States, and authorities in the European Union, including applicable export control regulations, economic sanctions on countries and persons, customs requirements and currency exchange regulations, collectively referred to as the trade control laws.
There is no assurance that we will be effective in ensuring our compliance with all applicable anti-corruption laws, including the FCPA or other legal requirements, including trade control laws. If we are not in compliance with the FCPA and other anti-corruption laws or trade control laws, we may be subject to criminal and civil penalties, disgorgement and other sanctions and remedial measures, and legal expenses, which could have an adverse impact on our business, financial condition, results of operations and liquidity. Likewise, any investigation of any potential violations of the FCPA, other anti-corruption laws or trade control laws by U.S. or other authorities could also have an adverse impact on our reputation, our business, results of operations and financial condition.
96
If we fail to comply with environmental, health and safety laws and regulations, we could become subject to fines or penalties or incur costs that could have a material adverse effect on the success of our business.
We are subject to numerous environmental, health and safety laws and regulations, including those governing laboratory procedures and the handling, use, storage, treatment and disposal of hazardous materials and wastes. Our operations currently, and may in the future, involve the use of hazardous and flammable materials, including chemicals and medical and biological materials, and produce hazardous waste products. Even if we contract with third parties for the disposal of these materials and wastes, we cannot eliminate the risk of contamination or injury from these materials. In the event of contamination or injury resulting from our use of hazardous materials or disposal of hazardous wastes, we could be held liable for any resulting damages, and any liability could exceed our resources.
Although we maintain workers' compensation insurance to cover us for costs and expenses we may incur due to injuries to our employees resulting from the use of hazardous materials, this insurance may not provide adequate coverage against potential liabilities. We also maintain a general liability program for some of the risks, but our insurance program includes limited environmental damage coverage, which has an annual aggregate coverage limit of $2.0 million. Although we maintain an umbrella policy with an annual aggregate coverage limit of $10.0 million, which may provide some environmental coverage, we do not maintain a separate policy covering environmental damages.
In addition, we may incur substantial costs to comply with current or future environmental, health and safety laws and regulations. These current or future laws and regulations may impair our research, development or production efforts. Failure to comply with these laws and regulations also may result in substantial fines, penalties or other sanctions.
Our employees may engage in misconduct or other improper activities, including non-compliance with regulatory standards and requirements, which could cause significant liability for us and harm our reputation.
We are exposed to the risk of employee fraud or other misconduct, including intentional failures to comply with FDA regulations or similar regulations of comparable non-U.S. regulatory authorities, provide accurate information to the FDA or comparable non-U.S. regulatory authorities, comply with manufacturing standards we have established, comply with federal and state healthcare fraud and abuse laws and regulations and similar laws and regulations established and enforced by comparable non-U.S. regulatory authorities, report financial information or data accurately or disclose unauthorized activities to us. In particular, sales, marketing and business arrangements in the healthcare industry are subject to extensive laws and regulations intended to prevent fraud, kickbacks, self-dealing and other abusive practices. These laws and regulations may restrict or prohibit a wide range of pricing, discounting, marketing and promotion, sales commission, customer incentive programs and other business arrangements.
Employee misconduct could also involve the improper use of information obtained during clinical trials, which could result in regulatory sanctions and serious harm to our reputation. It is not always possible to identify and deter employee misconduct, and the precautions we take to detect and prevent this activity may not be effective in controlling unknown or unmanaged risks or losses or in protecting us from governmental investigations or other actions or lawsuits stemming from a failure to be in compliance with such laws, standards or regulations. If any such actions are instituted against us, and we are not successful in defending ourselves or asserting our rights, those actions could have a significant impact on our business and results of operations, including the imposition of significant fines or other sanctions.
97
We rely significantly on information technology and any failure, inadequacy, interruption or security lapse of that technology, including any cyber security incidents, could harm our ability to operate our business effectively.
Despite the implementation of security measures, our internal computer systems and those of third parties with which we contract are vulnerable to damage from cyber-attacks, computer viruses, unauthorized access, natural disasters, terrorism, war and telecommunication and electrical failures. System failures, accidents or security breaches could cause interruptions in our operations, and could result in a material disruption of our drug development programs and commercialization activities and business operations, in addition to possibly requiring substantial expenditures of resources to remedy. The loss of clinical trial data could result in delays in our regulatory approval efforts and significantly increase our costs to recover or reproduce the data. To the extent that any disruption or security breach were to result in a loss of, or damage to, our data or applications, or inappropriate disclosure of confidential or proprietary information, we could incur liability and our product research, development and commercialization efforts could be delayed.
We are subject to various laws protecting the confidentiality of certain patient health information, and our failure to comply could result in penalties and reputational damage.
Certain countries in which we operate have, or are developing, laws protecting the confidentiality of certain patient health information. European Union, or EU, member states and other jurisdictions have adopted data protection laws and regulations, which impose significant compliance obligations.
For example, the EU Data Protection Directive, as implemented into national laws by the EU member states, imposes strict obligations and restrictions on the ability to collect, analyze and transfer personal data, including health data from clinical trials and adverse event reporting. Data protection authorities from different EU member states may interpret the EU Data Protection Directive and national laws differently, which adds to the complexity of processing personal data in the EU, and guidance on implementation and compliance practices are often updated or otherwise revised. The EU Data Protection Directive prohibits the transfer of personal data to countries outside of the EU member states that are not considered by the European Commission to provide an adequate level of data protection, and transfers of personal data to such countries can only be made in certain circumstances—for example, where the transfer is required by law or the data subject (i.e. the individual to whom the personal data relates) has given his or her consent to the transfer. Nevertheless, any failure to comply with the rules arising from the EU Data Protection Directive and related national laws of EU member states, as well as privacy laws in other countries in which we operate, could lead to government enforcement actions and significant sanctions or penalties against us, adversely impact our results of operations and subject us to negative publicity.
The EU Data Protection Regulation, which will replace the current EU Data Protection Directive, was adopted in 2016 and will become enforceable on May 25, 2018. The EU Data Protection Regulation will introduce new data protection requirements in the EU and substantial fines for breaches of the data protection rules, may increase our responsibility and liability in relation to personal data that we process and may require us to put in place additional mechanisms to ensure compliance with the new EU data protection rules.
Risks Related to Employee Matters and Managing Growth
Our future success depends on our ability to retain our chief executive officer and other key executives and to attract, retain and motivate qualified personnel.
We are highly dependent on Dr. Colin Broom, our Chief Executive Officer, and the other principal members of our management and scientific teams. Although we have formal employment agreements with each of our executive officers, these agreements do not prevent our executives from terminating
98
their employment with us at any time. We do not maintain "key person" insurance on any of our executive officers. The unplanned loss of the services of any of these persons might impede the achievement of our research, development and commercialization objectives.
Recruiting and retaining qualified scientific, clinical, manufacturing and sales and marketing personnel, including in the United States and Ireland where we plan to expand our physical presence, will also be critical to our success. We may not be able to attract and retain these personnel on acceptable terms given the competition among numerous pharmaceutical and biotechnology companies for similar personnel. We also experience competition for the hiring of scientific and clinical personnel from universities and research institutions. In addition, we rely on consultants and advisors, including scientific and clinical advisors, to assist us in formulating our research and development and commercialization strategy. Our consultants and advisors may be employed by employers other than us and may have commitments under consulting or advisory contracts with other entities that may limit their availability to us.
We expect to expand our development, regulatory and sales and marketing capabilities, and as a result, we may encounter difficulties in managing our growth, which could disrupt our operations.
We expect to experience significant growth in the number of our employees and the scope of our operations, particularly in the areas of drug development, regulatory affairs and sales and marketing. To manage our anticipated future growth, we must continue to implement and improve our managerial, operational and financial systems, expand our facilities and continue to recruit and train additional qualified personnel. Due to our limited financial resources and the limited experience of our management team in managing a company with such anticipated growth, we may not be able to effectively manage the expansion of our operations or recruit and train additional qualified personnel. The physical expansion of our operations may lead to significant costs and may divert our management and business development resources. Any inability to manage growth could delay the execution of our business plans or disrupt our operations.
Risks Related to Ownership of Our Ordinary Shares
An active trading market for our ordinary shares may not be sustained.
Following the Redomiciliation Transaction, our ordinary shares began trading on the Nasdaq Global Market on June 26, 2017. Given the limited trading history of our ordinary shares, there is a risk that an active trading market for our ordinary shares will not be sustained, which could put downward pressure on the market price of our ordinary shares and thereby affect the ability of our security holders to sell their shares.
The price of our ordinary shares may be volatile and fluctuate substantially.
The trading price of our ordinary shares has been and is likely to continue to be volatile. The stock market in general and the market for smaller biopharmaceutical companies in particular have experienced significant volatility that has often been unrelated to the operating performance of particular companies. The market price for our ordinary shares may be influenced by many factors, including:
- •
- the success of competitive products or technologies;
- •
- results of clinical trials of our product candidates or those of our competitors;
- •
- regulatory delays and greater government regulation of potential products due to adverse events;
- •
- regulatory or legal developments in the United States, the European Union and other countries;
99
- •
- developments or disputes concerning patent applications, issued patents or other proprietary rights;
- •
- the recruitment or departure of key scientific or management personnel;
- •
- the level of expenses related to any of our product candidates or clinical development programs;
- •
- the results of our efforts to discover, develop, acquire or in-license additional product candidates or products;
- •
- one of our manufacturers or suppliers could have an event which causes an unforeseen disruption of the manufacture or supply of our product
candidates;
- •
- actual or anticipated changes in estimates as to financial results, development timelines or recommendations by securities analysts;
- •
- variations in our financial results or those of companies that are perceived to be similar to us;
- •
- changes in the structure of healthcare payment systems;
- •
- market conditions in the pharmaceutical and biotechnology sectors;
- •
- general economic, industry and market conditions; and
- •
- the other factors described in this "Risk Factors" section.
In the past, following periods of volatility in the market price of a company's securities, securities class-action litigation has often been instituted against that company. We also may face securities class-action litigation if we cannot obtain regulatory approvals for or if we otherwise fail to commercialize lefamulin or any of our other product candidates or if our securities experience volatility for any reason. Such litigation, if instituted against us, could cause us to incur substantial costs to defend such claims and divert management's attention and resources.
Our executive officers, directors and principal shareholders, if they choose to act together, have the ability to significantly influence most matters submitted to shareholders for approval.
Our executive officers and directors, combined with our shareholders, and their respective affiliates who owned more than 5% of our outstanding ordinary shares as of December 31, 2017 in the aggregate, beneficially owned approximately 43.7% of our share capital. As a result, if these shareholders were to choose to act together, they would have significant influence over most matters submitted to our shareholders for approval, as well as our management and affairs. For example, these persons, if they choose to act together, would have significant influence over the election of directors and approval of any merger, consolidation or sale of all or substantially all of our assets.
Our ordinary shares do not trade on any exchange outside of the United States.
Our ordinary shares are listed only in the United States on The Nasdaq Global Market, and we have no plans to list our ordinary shares in any other jurisdiction. As a result, a holder of ordinary shares outside of the United States may not be able to effect transactions in our ordinary shares as readily as the holder may if our ordinary shares were listed on an exchange in that holder's home jurisdiction.
The sale of a substantial number of ordinary shares may cause the market price of our ordinary shares to decline.
Sales of a substantial number of our ordinary shares, or the perception in the market that these sales could occur, could reduce the market price of our ordinary shares. We had 36,707,685 ordinary
100
shares outstanding as of December 31, 2017. To the extent any of these shares are sold into the market, particularly in substantial quantities, the market price of our ordinary shares could decline.
Future issuances of ordinary shares pursuant to our equity incentive plans could also result in additional dilution of the percentage ownership of our shareholders. We have filed registration statements on Form S-8 registering all of the ordinary shares that we may issue under our equity compensation plans. These shares can be freely sold in the public market upon issuance and once vested, subject to volume, notice and manner of sale limitations applicable to affiliates. The majority of ordinary shares that may be issued under our equity compensation plans remain subject to vesting in tranches over a four-year period. As of December 31, 2017, an aggregate of 989,656 options to purchase our ordinary shares had vested and become exercisable.
In addition, in March 2018, we entered into a sales agreement with Cantor Fitzgerald & Co., or Cantor, pursuant to which, from time to time, we may offer and sell our ordinary shares having an aggregate offering price of up to $50,000,000 through Cantor pursuant to an effective universal shelf registration statement. Sales of our ordinary shares, if any, under the agreement with Cantor may be made in sales deemed to be an "at-the-market offering" as defined in Rule 415(a)(4) under the Securities Act of 1933, as amended.
If a large number of our ordinary shares are sold in the public market after they become eligible for sale, the sales could reduce the trading price of our ordinary shares and impede our ability to raise future capital.
We are an "emerging growth company", and the reduced disclosure requirements applicable to emerging growth companies may make our ordinary shares less attractive to investors.
We are an "emerging growth company," as that term is used in the Jumpstart Our Business Startups Act of 2012, or the JOBS Act, and may remain an emerging growth company until December 31, 2020 or such earlier time that we are no longer an emerging growth company. For so long as we remain an emerging growth company, we are permitted and may take advantage of specified reduced reporting and other burdens that are otherwise applicable generally to public companies. These provisions include:
- •
- an exemption from compliance with the auditor attestation requirement of Section 404 of the Sarbanes-Oxley Act of 2002, or the
Sarbanes-Oxley Act, on the design and effectiveness of our internal controls over financial reporting;
- •
- an exemption from compliance with any requirement that the Public Company Accounting Oversight Board may adopt regarding mandatory audit firm
rotation or a supplement to the auditor's report providing additional information about the audit and the financial statements;
- •
- reduced disclosure about the company's executive compensation arrangements; and
- •
- exemptions from the requirements to obtain a non-binding advisory vote on executive compensation or a shareholder approval of any golden parachute arrangements.
We may choose to take advantage of some, but not all, of the available exemptions. We may take advantage of these provisions until December 31, 2020 or such earlier time that we are no longer an emerging growth company. We would cease to be an emerging growth company upon the earlier to occur of: the last day of the fiscal year in which we have more than $1 billion (as may be inflation-adjusted by the SEC from time-to-time) in annual revenues; the date we qualify as a "large accelerated filer," with more than $700 million in market value of our share capital held by non-affiliates; or the issuance by us of more than $1 billion of non-convertible debt over a three-year period.
We may choose to take advantage of some, but not all, of the available benefits under the JOBS Act. We cannot predict whether investors will find our ordinary shares less attractive if we rely on such
101
exemptions. If some investors find our ordinary shares less attractive as a result, there may be a less active trading market for our ordinary shares and the market price of our ordinary shares may be more volatile.
In addition, the JOBS Act also provides that an emerging growth company can take advantage of an extended transition period for complying with new or revised accounting standards. This allows an emerging growth company to delay the adoption of certain accounting standards until those standards would otherwise apply to private companies. We have irrevocably elected not to avail ourselves of this exemption and, therefore, we will adopt new or revised accounting standards on the relevant dates on which adoption of such standards is required for other public companies that are not emerging growth companies.
We have broad discretion in the use of our funds and may not use them effectively.
Our management has broad discretion in the application of our available funds and could spend the funds in ways that do not improve our results of operations or enhance the value of our ordinary shares. The failure by our management to apply these funds effectively could result in financial losses that could have a material adverse effect on our business, cause the price of our ordinary shares to decline and delay the development of our product candidates. Pending their use, we may invest funds in a manner that does not produce income or that loses value.
We incur increased costs as a result of operating as a public company, and our management is required to devote substantial time to new compliance initiatives and corporate governance practices.
As a public company we incur, and particularly after we are no longer an emerging growth company, we will incur significant legal, accounting and other expenses that we did not incur as a private company. In addition, the Sarbanes-Oxley Act, the Dodd-Frank Wall Street Reform and Consumer Protection Act, the listing requirements of The Nasdaq Global Market and other applicable securities rules and regulations impose various requirements on public companies, including establishment and maintenance of effective disclosure and financial controls and corporate governance practices. Our management and other personnel need to devote a substantial amount of time to these compliance initiatives. Moreover, these rules and regulations have increased our legal and financial compliance costs and make some activities more time-consuming and costly. For example, these rules and regulations have made it more expensive for us to obtain director and officer liability insurance, which in turn could make it more difficult for us to attract and retain qualified members of our board.
For as long as we remain an emerging growth company, we may take advantage of certain exemptions from various reporting requirements that are applicable to other public companies that are not emerging growth companies as described elsewhere in this "Risk Factors" section. We may remain an emerging growth company until December 31, 2020, although if the market value of our share capital that is held by non-affiliates exceeds $700 million as of any June 30 before that time or if we have annual gross revenues of $1 billion or more in any fiscal year (as may be inflation adjusted by the SEC from time-to-time), we would cease to be an emerging growth company as of December 31 of the applicable year. We also would cease to be an emerging growth company if we issue more than $1 billion of non-convertible debt over a three-year period.
If we fail to maintain an effective system of internal control over financial reporting, we may not be able to accurately report our financial results or prevent fraud. As a result, security holders could lose confidence in our financial and other public reporting, which would harm our business and the trading price of our ordinary shares.
Effective internal control over financial reporting is necessary for us to provide reliable financial reports and, together with adequate disclosure controls and procedures, is designed to prevent fraud.
102
Any failure to implement required new or improved controls, or difficulties encountered in their implementation could cause us to fail to meet our reporting obligations. In addition, any testing by us, as and when required, conducted in connection with Section 404 of the Sarbanes-Oxley Act, or Section 404, or any subsequent testing by our independent registered public accounting firm, as and when required, may reveal deficiencies in our internal control over financial reporting that are deemed to be material weaknesses or that may require prospective or retroactive changes to our financial statements or identify other areas for further attention or improvement. Inferior internal controls could also cause investors to lose confidence in our reported financial information, which could have a negative effect on the trading price of our ordinary shares.
Pursuant to Section 404, we will be required to furnish a report by our management on our internal control over financial reporting. However, as an emerging growth company, we will not be required to include an attestation report on internal control over financial reporting issued by our independent registered public accounting firm until we are no longer an emerging growth company. To achieve compliance with Section 404 within the prescribed period, we are engaged in a process to document and evaluate our internal control over financial reporting, which is both costly and challenging. In this regard, we will need to continue to dedicate internal resources, potentially engage outside consultants and adopt a detailed work plan to assess and document the adequacy of internal control over financial reporting, continue steps to improve control processes as appropriate, validate through testing that controls are functioning as documented and implement a continuous reporting and improvement process for internal control over financial reporting. Despite our efforts, there is a risk that we will not be able to conclude within the prescribed timeframe that our internal control over financial reporting is effective as required by Section 404. This could result in an adverse reaction in the financial markets due to a loss of confidence in the reliability of our financial statements.
United States investors may have difficulty enforcing judgments against us, our directors and executive officers.
We are incorporated under the laws of Ireland, and our registered offices and a substantial portion of our assets are located outside of the United States. In addition, one of our directors is a resident of a jurisdiction other than the United States. As a result, it may not be possible to effect service of process on such person or us in the United States or to enforce judgments obtained in courts in the United States against such person or us based on civil liability provisions of the securities laws of the United States.
There is no treaty between Ireland and the United States providing for the reciprocal enforcement of foreign judgments. The following requirements must be met before the foreign judgment will be deemed to be enforceable in Ireland:
- •
- the judgment must be for a definite sum;
- •
- the judgment must be final and conclusive; and
- •
- the judgment must be provided by a court of competent jurisdiction.
An Irish court will also exercise its right to refuse judgment if the foreign judgment (1) was obtained by fraud; (2) violates Irish public policy; (3) is in breach of natural justice; or (4) is irreconcilable with an earlier judgment. Further, an Irish court may stay proceedings if concurrent proceedings are being brought elsewhere. Judgments of U.S. courts of liabilities predicated upon U.S. federal securities laws may not be enforced by Irish courts if deemed to be contrary to public policy in Ireland.
103
We do not expect to pay dividends in the foreseeable future.
We have not paid any dividends on our ordinary shares since our incorporation. Even if future operations lead to significant levels of distributable profits, we currently intend that earnings, if any, will be reinvested in our business and that dividends will not be paid until we have an established revenue stream to support continuing dividends. If we propose to pay dividends in the future, we must do so in accordance with Irish law, which provides that distributions including dividend payments, share repurchases and redemptions be funded from "distributable reserves." Payment of future dividends to security holders will be at the discretion of our board, after taking into account various factors including our business prospects, cash requirements, financial performance, debt covenant limitations and new product development.
We are exposed to risks related to currency exchange rates.
A significant portion of our expenses are denominated in currencies other than the U.S. dollar. Because our financial statements are presented in U.S. dollars, changes in currency exchange rates have had and could have a significant effect on our operating results. Exchange rate fluctuations between foreign currencies and the U.S. dollar create risk in several ways, including the following:
- •
- weakening of the U.S. dollar may increase the U.S. dollar cost of overseas research and development expenses;
- •
- strengthening of the U.S. dollar may decrease the value of our revenues denominated in other currencies;
- •
- the exchange rates on non-U.S. dollar transactions and cash deposits can distort our financial results; and
- •
- commercial pricing and profit margins are affected by currency fluctuations.
As a holding company, our operating results, financial condition and ability to pay dividends or other distributions are entirely dependent on funding, dividends and other distributions received from our subsidiaries, which may be subject to restrictions.
Our ability to pay dividends or other distributions and to pay our obligations in the future will depend on the level of funding, dividends and other distributions, if any, received from our subsidiaries and any new subsidiaries we establish in the future. The ability of our companies to make loans or distributions (directly or indirectly) to us may be restricted as a result of several factors, including restrictions in financing agreements and the requirements of applicable law and regulatory and fiscal or other restrictions. In particular, our subsidiaries and any new subsidiaries may be subject to laws that restrict dividend payments, authorize regulatory bodies to block or reduce the flow of funds from those subsidiaries to us, or limit or prohibit transactions with affiliates. Restrictions and regulatory action of this kind could impede access to funds that we may need to make dividend payments.
Furthermore, we may guarantee some of the payment obligations of certain of our subsidiaries from time to time. These guarantees may require us to provide substantial funds or assets to our subsidiaries or their creditors or counterparties at a time when we are in need of liquidity to fund our own obligations.
The ownership percentage of our shareholders may be diluted in the future.
As with any publicly traded company, the ownership percentage of our shareholders may be diluted in the future because of equity issuances for acquisitions, capital market transactions or otherwise, including equity awards that we intend to continue to grant to our directors, officers and
104
employees. From time to time, we may issue additional options or other share awards to our directors, officers and employees under our benefits plans.
In addition, our articles of association authorize us to issue, without the approval of our shareholders, one or more classes or series of preferred shares having such designation, powers, preferences and relative, participating, optional and other special rights, including preferences over our ordinary shares respecting dividends and distributions, as our board of directors generally may determine. The terms of one or more classes or series of preferred shares could dilute the voting power or reduce the value of our ordinary shares. Similarly, the repurchase or redemption rights or liquidation preferences we could assign to holders of preferred shares could affect the residual value of the ordinary shares.
The rights of our shareholders may differ from the rights typically offered to shareholders of a U.S. corporation. We are incorporated as a public limited company under Irish law.
The rights of our shareholders are governed by our memorandum and articles of association and Irish law. The rights associated with our ordinary shares are different to the rights generally associated with shares held in a U.S. corporation. Material differences between the rights of shareholders of a U.S. corporation and the rights of our shareholders include differences with respect to, among other things, distributions, dividends, repurchases and redemptions, dividends in shares / bonus issues, the election of directors, the removal of directors, the fiduciary and statutory duties of directors, conflicts of interests of directors, the indemnification of directors and officers, limitations on director liability, the convening of annual meetings of shareholders and special shareholder meetings, notice provisions for meetings, the quorum for shareholder meetings, the adjournment of shareholder meetings, the exercise of voting rights, shareholder suits, rights of dissenting shareholders, anti-takeover measures and provisions relating to the ability to amend the articles of association.
As an Irish public limited company, certain capital structure decisions require shareholder approval, which may limit our flexibility to manage our capital structure.
Under Irish law, our board of directors may increase our authorized share capital and issue new ordinary or preferred shares up to a maximum amount equal to the authorized but unissued share capital, without shareholder approval, once authorized to do so by our articles of association or by an ordinary resolution of our shareholders. Additionally, subject to specified exceptions, Irish law grants statutory preemption rights to existing shareholders where shares are being issued for cash consideration but allows shareholders to disapply such statutory preemption rights either in our articles of association or by way of special resolution. Such disapplication can either be generally applicable or be in respect of a particular allotment of shares. Accordingly, our articles of association contain, as permitted by Irish company law, provisions authorizing our board of directors to issue new shares, and to disapply statutory preemption rights. The authorization of our board of directors to issue shares and the disapplication of statutory preemption rights must both be renewed by the shareholders at least every five years, and we cannot provide any assurance that these authorizations will always be approved, which could limit our ability to issue equity and thereby adversely affect the holders of our ordinary shares.
Irish law differs from the laws in effect in the U.S. with respect to defending unwanted takeover proposals and may give our board less ability to control negotiations with hostile offerors.
We are subject to the Irish Takeover Panel Act, 1997, Takeover Rules, 2013. Under those Irish Takeover Rules, the board is not permitted to take any action that might frustrate an offer for our ordinary shares once the board has received an approach that may lead to an offer or has reason to believe that such an offer is or may be imminent, subject to certain exceptions. Potentially frustrating actions such as (i) the issue of ordinary shares, options or convertible securities, (ii) material
105
acquisitions or disposals, (iii) entering into contracts other than in the ordinary course of business or (iv) any action, other than seeking alternative offers, which may result in frustration of an offer, are prohibited during the course of an offer or at any earlier time during which the board has reason to believe an offer is or may be imminent. These provisions may give the board less ability to control negotiations with hostile offerors and protect the interests of holders of ordinary shares than would be the case for a corporation incorporated in a jurisdiction of the United States.
We will be exposed to the risk of future changes in law, which could materially adversely affect us.
We are subject to Irish law. As a result, we are subject to the risk of future adverse changes in Irish law (including Irish corporate and tax law). In addition, we and our subsidiaries are also subject to the risk of future adverse changes in Austrian and U.S. law, as well as changes of law in other countries in which we and our subsidiaries operate.
Future adverse changes in law could result in our not being able to maintain a worldwide effective corporate tax rate that is competitive in our industry.
While we believe that being incorporated in Ireland should not affect our ability to maintain a worldwide effective corporate tax rate that is competitive in our industry, we cannot give any assurance as to what our effective tax rate will be because of, among other things, uncertainty regarding the tax policies of the jurisdictions where we will operate. The tax laws of Ireland, Austria, the United States, and other jurisdictions could change in the future, and such changes could cause a material change in our worldwide effective corporate tax rate. In particular, legislative action could be taken by Ireland, Austria, the United States or other jurisdictions which could override tax treaties upon which we expect to rely and adversely affect our effective tax rate. As a result, our actual effective tax rate may be materially different from our expectation.
A transfer of our ordinary shares, other than a transfer effected by means of the transfer of book-entry interests in the Depository Trust Company, may be subject to Irish stamp duty.
Transfers of our ordinary shares effected by means of the transfer of book entry interests in the Depository Trust Company, or "DTC", will not be subject to Irish stamp duty. However, if you hold our ordinary shares directly rather than beneficially through DTC, any transfer of your shares could be subject to Irish stamp duty (currently at the rate of 1% of the higher of the price paid or the market value of the shares acquired). Payment of Irish stamp duty is generally a legal obligation of the transferee. The potential for stamp duty could adversely affect the price of our ordinary shares.
Our ordinary shares received by means of a gift or inheritance could be subject to Irish capital acquisitions tax.
Irish capital acquisitions tax, or "CAT" could apply to a gift or inheritance of our ordinary shares irrespective of the place of residence, ordinary residence or domicile of the parties. This is because our ordinary shares will be regarded as property situated in Ireland. The person who receives the gift or inheritance has primary liability for CAT. Gifts and inheritances passing between spouses are exempt from CAT. Children have a tax-free threshold of €310,000 in respect of taxable gifts or inheritances received from their parents.
We may be classified as a passive foreign investment company for our tax year ending December 31, 2018, which may result in adverse U.S. federal income tax consequence to U.S. holders.
Based on our estimated gross income and average value of our gross assets and the nature of our business, we do not believe that we were a "passive foreign investment company," or PFIC, for U.S. federal income tax purposes for our tax years ended December 31, 2015, 2016 or 2017. A corporation
106
organized outside the United States generally will be classified as a PFIC for U.S. federal income tax purposes (1) in any taxable year in which at least 75% of its gross income is passive income or on average at least 50% of the gross value of its assets is attributable to assets that produce passive income or are held for the production of passive income and (2) as to a given holder who was a holder in such year and regardless of such corporation's income or asset composition, in any subsequent taxable year, unless certain elections are made by that holder that can discontinue that classification as to that holder, at the risk of imposing substantial tax costs to that holder. Passive income for this purpose generally includes dividends, interest, royalties, rents and gains from commodities and securities transactions. Our status in any taxable year will depend on our assets and activities in each year, and because this is a factual determination made annually after the end of each taxable year, there can be no assurance that we will not be considered a PFIC for the current taxable year or any future taxable year. The market value of our assets may be determined in large part by reference to the market price of our ordinary shares, which may fluctuate considerably given that market prices of biotechnology companies have been especially volatile. If we were to be treated as a PFIC for the tax year ending December 31, 2017, or any other future taxable year during which a U.S. holder held our ordinary shares, however, certain adverse U.S. federal income tax consequences could apply to the U.S. holder. We currently intend to make available the information necessary to permit a U.S. holder to make a valid QEF election, which may mitigate some of the adverse U.S. federal income tax consequences that could apply to a U.S. holder of ordinary shares. However, we may choose not to provide such information at a future date.
ITEM 1B. UNRESOLVED STAFF COMMENTS
None.
Facilities
Our facilities consist of approximately 3,100 square meters of leased laboratory and office space in Vienna, Austria. We lease approximately 15,000 square feet of office space in King of Prussia, Pennsylvania. We also lease office space in Dublin, Ireland. We believe that our existing facilities are adequate to meet our current needs. However, we may seek to negotiate new leases or evaluate additional or alternate space as we plan for the growth of our commercial operations in the United States. We believe that suitable additional or alternative space will be available in the future on commercially reasonable terms.
None
ITEM 4. MINE SAFETY DISCLOSURES
Not applicable.
107
ITEM 5. MARKET FOR REGISTRANT'S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
Market Information
Our ordinary shares have been listed on the Nasdaq Global Market since June 26, 2017 following the Redomiciliation and trade on the Nasdaq Global Market under the symbol "NBRV". Prior to the Redomiciliation, the ADSs, representing the common shares of our predecessor, Nabriva Austria, had traded on the NASDAQ Global Market under the same symbol since September 18, 2015. Each ADS represented one tenth (1/10) of a common share of Nabriva Austria.
The following table sets forth, for the periods indicated, the reported high and low intraday sale prices of Nabriva Austria's ADSs from January 1, 2016 through June 25, 2017 and the high and low intraday sales prices of our ordinary shares since June 26, 2017, in each case, as reported by the Nasdaq Global Market.
Nabriva Austria's American Depositary Shares
| |
High | Low | |||||
|---|---|---|---|---|---|---|---|
Year ended December 31, 2016 |
|||||||
First quarter |
$ | 9.80 | $ | 6.61 | |||
Second quarter |
$ | 9.70 | $ | 6.85 | |||
Third quarter |
$ | 8.85 | $ | 7.01 | |||
Fourth quarter |
$ | 7.50 | $ | 3.52 | |||
Year ending December 31, 2017 |
|||||||
First quarter |
$ | 12.00 | $ | 5.97 | |||
Second quarter (through June 25, 2017) |
$ | 12.54 | $ | 8.58 | |||
Our Ordinary Shares
| |
High | Low | |||||
|---|---|---|---|---|---|---|---|
Year ended December 31, 2017 |
|||||||
Second quarter (from June 26, 2017) |
$ | 11.79 | $ | 10.35 | |||
Third quarter |
$ | 14.10 | $ | 6.52 | |||
Fourth Quarter |
$ | 8.54 | $ | 4.75 | |||
Stockholders
As of January 31, 2018, there were thirteen holders of record of ordinary shares. The number of record holders may not be representative of the number of beneficial owners because many of our ordinary shares are held by depositories, brokers or other nominees.
Securities Authorized for Issuance Under Equity Compensation Plans
Information regarding securities authorized for issuance under our equity compensation plans is contained in Part III, Item 12 of this Annual Report.
Dividend Policy
We have never declared or paid any cash dividends on our capital stock. We currently intend to retain all available funds and any future earnings to support our operations and finance the growth and
108
development of our business. We do not intend to pay cash dividends on our ordinary shares for the foreseeable future.
Performance Graph
The performance graph below compares the cumulative total holder return on our equity securities beginning on September 18, 2015, the date Nabriva Austria's ADSs began trading on the Nasdaq Global Market through and including December 31, 2017 with the cumulative return of the Nasdaq Composite Index and Nasdaq Biotechnology Index for the periods presented.
The performance graph comparison assumes $100 was invested in our equity securities and in each of the other indices described above on September 18, 2015. The performance shown on the graph below is not necessarily indicative of future price performance.
Cumulative Total Return
Assumes $100 Initial Investment
December 31, 2017
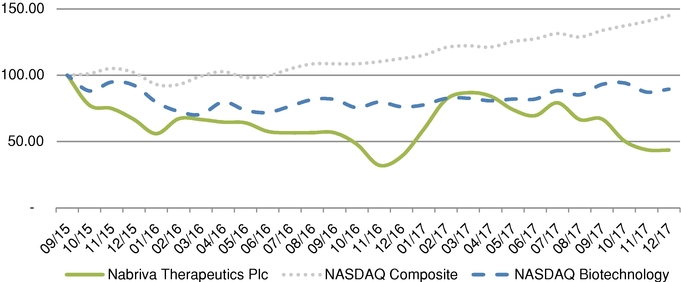
The performance graph above is being furnished solely to accompany this Annual Report on Form 10-K pursuant to Item 201(e) of Regulation S-K, is not being filed for purposes of Section 18 of the Exchange Act, shall not be deemed to be "soliciting material" or subject to Rule 14A of the Exchange Act and is not to be incorporated by reference into any of our filings with the SEC, whether made before or after the date hereof, except to the extent that we specifically incorporate this information by reference into such filing.
Recent Sales of Unregistered Securities
We did not sell any of our equity securities or any options, warrants, or rights to purchase our equity securities during the year ended December 31, 2017 that were not registered under the Securities Act of 1933, as amended, or the Securities Act.
Purchase of Equity Securities
We did not purchase any of our registered equity securities during the period covered by this Annual Report on Form 10-K.
109
Use of Proceeds from Registered Securities
We effected the initial public offering of our ADSs, each representing one tenth (1/10) of a common share, through a Registration Statement on Form F-1 (File No. 333-205073) that was declared effective by the Securities and Exchange Commission on September 17, 2015. On September 23, 2015, we completed the sale of 9,000,000 ADSs, representing 900,000 of our common shares, at a public offering price of $10.25 per ADS, before underwriting discounts. In addition, we granted the underwriters a 30-day option to purchase up to 1,350,000 additional ADSs to cover over allotments, if any. On September 30, 2015, we completed the additional sale of 1,350,000 ADSs under this option at a price to the public of $10.25 per ADS, resulting in aggregate net proceeds to us of approximately $92.4 million after deducting underwriting discounts and commissions of $7.4 million and offering expenses of $6.3 million. None of the underwriting discounts and commissions or other offering expenses were paid to directors or officers of ours or their associates or to persons owning 10% or more of any class of our equity securities or to any affiliates of ours. Leerink Partner LLC, RBC Capital Markets, LLC, Needham & Company, LLC and Wedbush PacGrow Inc. were the underwriters for our initial public offering.
There has been no material change in our planned use of the net proceeds from our initial public offering as described in our final prospectus filed with the SEC pursuant to Rule 424(b)(4) on September 21, 2015.
Our management retains broad discretion in the allocation and use of the net proceeds of our initial public offering.
ITEM 6. SELECTED FINANCIAL DATA
The selected financial data set forth below for the years ended December 31, 2017, 2016 and 2015 and as of December 31, 2017 and 2016 has been derived from our audited consolidated financial statements which have been prepared in accordance with generally accepted accounting practices in the United States and included elsewhere in this Annual Report. Financial data set forth below for the years ended December 31, 2013 and 2014 and as of December 31, 2015, 2014 and 2013 has been derived from the audited consolidated financial statements and not included in this Annual Report. The following selected consolidated financial data should be read in conjunction with Item 7, "Management's Discussion and Analysis of Financial Condition and Results of Operations" and the consolidated financial statements and the notes thereto included elsewhere in this Annual Report. The selected financial data in this section are not intended to replace our consolidated financial statements
110
and the related notes. Our historical results are not necessarily indicative of the results that may be expected in the future.
| |
Year ended December 31, | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2013 | 2014 | 2015 | 2016 | 2017 | |||||||||||
Consolidated Operations Data: |
||||||||||||||||
Revenues |
$ | 3,194 | $ | 2,398 | $ | 3,767 | $ | 6,482 | $ | 5,319 | ||||||
Costs and Expenses: |
||||||||||||||||
Research and development |
(10,471 | ) | (9,355 | ) | (23,604 | ) | (47,994 | ) | (49,615 | ) | ||||||
General and administrative |
(3,582 | ) | (3,739 | ) | (7,921 | ) | (13,535 | ) | (29,472 | ) | ||||||
| | | | | | | | | | | | | | | | | |
Total operating expenses |
(14,053 | ) | (13,094 | ) | (31,525 | ) | (61,529 | ) | (79,087 | ) | ||||||
| | | | | | | | | | | | | | | | | |
Loss from operations |
(10,859 | ) | (10,696 | ) | (27,758 | ) | (55,047 | ) | (73,768 | ) | ||||||
Other income (expense): |
||||||||||||||||
Other income (expense), net |
31,805 | (524 | ) | 2,427 | (783 | ) | 492 | |||||||||
Interest income |
5 | 2 | 14 | 343 | 318 | |||||||||||
Interest expense |
(2,856 | ) | (2,910 | ) | (22,092 | ) | (75 | ) | (43 | ) | ||||||
| | | | | | | | | | | | | | | | | |
Income (loss) before income taxes |
18,095 | (14,128 | ) | (47,409 | ) | (55,562 | ) | (73,001 | ) | |||||||
| | | | | | | | | | | | | | | | | |
Income tax (expense) benefit |
(1,030 | ) | (94 | ) | 445 | 672 | (1,355 | ) | ||||||||
| | | | | | | | | | | | | | | | | |
Net income (loss) |
$ | 17,065 | $ | (14,222 | ) | $ | (46,964 | ) | $ | (54,890 | ) | $ | (74,356 | ) | ||
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
Loss per share
|
2013 | 2014 | 2015 | 2016 | 2017 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Basic |
$ | 5.26 | $ | (4.44 | ) | $ | (4.80 | ) | $ | (2.56 | ) | $ | (2.49 | ) | ||
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
Diluted |
$ | 4.61 | $ | (4.44 | ) | $ | (4.80 | ) | $ | (2.56 | ) | $ | (2.49 | ) | ||
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
Weighted average number of shares: |
||||||||||||||||
Basic |
3,247,030 | 3,247,030 | 10,583,950 | 21,478,320 | 29,830,669 | |||||||||||
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
Diluted |
3,699,930 | 3,247,030 | 10,583,950 | 21,478,320 | 29,830,669 | |||||||||||
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
| |
As of December 31, | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2013 | 2014 | 2015 | 2016 | 2017 | |||||||||||
Consolidated Balance Sheet Data: |
||||||||||||||||
Cash and cash equivalents and short-term investments |
$ | 4,539 | $ | 2,150 | $ | 111,440 | $ | 83,884 | $ | 86,879 | ||||||
Total assets |
7,343 | 4,812 | 117,711 | 93,240 | 95,763 | |||||||||||
Long term liabilities |
2,856 | 5,741 | 84 | 107 | 435 | |||||||||||
Total liabilities |
25,969 | 33,192 | 9,005 | 15,984 | 13,695 | |||||||||||
Mezzanine equity |
— | 634 | — | — | — | |||||||||||
Accumulated deficit |
(106,173 | ) | (120,587 | ) | (171,426 | ) | (204,842 | ) | (279,198 | ) | ||||||
Total stockholder's equity (deficit) |
(18,626 | ) | (29,014 | ) | 108,706 | 77,256 | 82,068 | |||||||||
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
111
ITEM 7. MANAGEMENT'S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
You should read the following discussion and analysis of our financial condition and results of operations together with our historical consolidated financial statements and the related notes thereto appearing elsewhere in this Annual Report. Some of the information contained in this discussion and analysis or set forth elsewhere in this Annual Report, including information with respect to our plans and strategy for our business and related financing, includes forward-looking statements that involve risks and uncertainties. As a result of many factors, including those factors set forth in the "Risk Factors" section of this Annual Report, our actual results could differ materially from the results described in or implied by the forward-looking statements contained in the following discussion and analysis.
Overview
We are a clinical stage biopharmaceutical company engaged in the research and development of novel anti-infective agents to treat serious infections, with a focus on the pleuromutilin class of antibiotics. We are developing our lead product candidate, lefamulin, to be the first pleuromutilin antibiotic available for systemic administration in humans. We are developing both intravenous, or IV, and oral formulations of lefamulin for the treatment of community-acquired bacterial pneumonia, or CABP and may potentially develop lefamulin for additional indications other than CABP.
We initiated the first of two pivotal, international Phase 3 clinical trials of lefamulin, which we refer to as Lefamulin Evaluation Against Pneumonia 1, or LEAP 1, in September 2015 and initiated the second trial, which we refer to as LEAP 2, in April 2016. On September 18, 2017, we announced positive top-line results for LEAP 1. In LEAP 1, which enrolled 551 patients, lefamulin met all of the primary endpoints of non-inferiority compared to moxifloxacin with or without linezolid as required by the U.S. Food and Drug Administration, or FDA, and European Medicines Agency, or EMA. Lefamulin also showed a favorable tolerability profile in the LEAP 1 trial, with no unexpected safety signals or evidence of off-target activity. We completed patient enrollment of 738 adult patients in LEAP 2 in December 2017 and expect to have top-line data available from LEAP 2 in the spring of 2018. If the results of LEAP 2 are also favorable, including achievement of the primary efficacy endpoints of the trial, we expect to submit a new drug application, or NDA, for marketing approval of lefamulin for the treatment of CABP in adults in the United States in the second half of 2018. We also expect to submit a marketing authorization application, or MAA, for lefamulin for the treatment of CABP in adults in Europe a few months after our NDA filing.
We believe that pleuromutilin antibiotics can help address the major public health threat posed by bacterial resistance, which the World Health Organization, or WHO, characterized in 2017 as one of the biggest threats to human health. Increasing resistance to antibiotics used to treat CABP is a growing concern and has become an issue in selecting the appropriate initial antibiotic treatment prior to determining the specific microbiological cause of the infection, referred to as empiric treatment. For example, the U.S. Centers for Disease Control and Prevention, or CDC, has classified Streptococcus pneumoniae, the most common respiratory pathogen, as a serious threat to human health as a result of increasing resistance to currently available antibiotics. In addition, the CDC recently reported on the growing evidence of widespread resistance to macrolides, widely used antibiotics that disrupt bacterial protein synthesis, in Mycoplasma pneumoniae, a common cause of CABP that is associated with significant morbidity and mortality. Furthermore, Staphylococcus aureus, including methicillin-resistant S. aureus, or MRSA, which has also been designated as a serious threat to human health by the CDC, has emerged as a more common cause of CABP in some regions of the world, and a possible pathogen to be covered with empiric therapy.
As a result of increasing resistance to antibiotics and the wide array of potential pathogens that cause CABP, the current standard of care for hospitalized patients with CABP whose treatment is
112
initiated in the hospital usually involves first-line empiric treatment with a combination of antibiotics (beta-lactams and macrolides) to address all likely bacterial pathogens or monotherapy with a fluoroquinolone. Combination therapy presents the logistical challenge of administering multiple drugs with different dosing regimens, with some drugs available only as IV, and increases the risk of drug-drug interactions and the potential for serious side effects. Fluoroquinolones are associated with safety and tolerability concerns, including a relatively high risk for developing Clostridium difficile infection and increasing rates of resistance for uropathogens. These concerns have resulted in a decreasing use of flouroquinolones and restriction of their use within a growing number of hospitals. In addition, in May 2016, the FDA announced that an FDA safety review has shown that fluoroquinolones, when used systemically, in the form of tablets, capsules and injectable, are associated with disabling and potentially permanent serious side effects that can occur together. These side effects can involve the tendons, muscles, joints, nerves, and central nervous system. Fluoroquinolones are typically administered in combination with other antibiotics, if community-acquired MRSA is suspected. In addition, many currently available antibiotic therapies are only available for IV administration and are prescribed for seven to fourteen days, meaning continued treatment requires prolonged hospitalization or a switch to a different antibiotic administered orally, with the attendant risk that the patient might respond differently.
Effective January 1, 2017, the Joint Commission & Center for Medicare and Medicaid Services, or CMS, began requiring all U.S. hospitals to have Antibiotic Management guidelines, also known as "Stewardship" Committees, in place to identify antibiotics most appropriate and targeted to each individual patient's infection. Past efforts to "cast the widest net possible" with broad-spectrum antibiotics that affect many types of bacteria have caused problems, such as C. difficile infections, by killing good bacteria or increased antibiotic resistance in other bacteria in different areas of the body. Additionally, in 2016, the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America, or IDSA/SHEA, updated their Antibiotic Stewardship guidelines for antibiotic use. We believe that three key goals from these guidelines are applicable to the treatment of CABP:
- •
- Reduce the risk of antibiotics associated with a high risk of C. difficile infections;
- •
- Increase use of oral antibiotics as a strategy to improve outcomes or decrease costs; and
- •
- Reduce antibiotic therapy to the shortest effective duration.
Consistent with the Antimicrobial Stewardship principles, we believe that lefamulin is well suited as either a first- or second-line empiric monotherapy for the treatment of CABP patients as in-hospital, outpatient-transition of care as well as in the community, because of its novel mechanism of action, complete spectrum of activity for CABP pathogens, including against multidrug resistant strains, achievement of substantial drug concentrations in lung fluids and lung immune cells, and flexibility as step down oral agent with both the IV and oral formulations and favorable safety and tolerability profile.
In recognition of the growing need for the development of new antibiotics, recent regulatory changes, including priority review and regulatory guidance enabling smaller clinical trials, have led to renewed interest from the pharmaceutical industry in anti-infective development. For example, the Food and Drug Administration Safety and Innovation Act became law in 2012 and included the Generating Antibiotic Incentives Now Act, or the GAIN Act, which provides incentives, including access to expedited FDA review for approval, fast track designation and five years of potential data exclusivity extension for the development of new QIDPs.
On March 1, 2017, Nabriva Therapeutics plc, or Nabriva Ireland, was incorporated in Ireland under the name Hyacintho 2 plc, and was renamed to Nabriva Therapeutics plc on April 10, 2017, in order to effectuate the change of the jurisdiction of incorporation of the ultimate company of the
113
group from Austria to Ireland. Nabriva Ireland replaced Nabriva Therapeutics AG, or Nabriva Austria, as the ultimate parent company on June 23, 2017, following the conclusion of a tender offer, or the Exchange Offer, in which holders of 98.6% of the outstanding share capital of Nabriva Austria exchanged their holdings for ordinary shares, $0.01 nominal value per share, of Nabriva Ireland, which we refer to as the Redomiciliation Transaction. The ordinary shares of Nabriva Ireland were issued on a one-for-ten basis to the holders of the Nabriva Austria common shares and on a one-for-one basis to the holders of the Nabriva Austria American Depositary Shares, or Nabriva Austria ADSs, participating in the Exchange Offer. On June 26, 2017, the ordinary shares of Nabriva Ireland began trading on the Nasdaq Global Market under the symbol "NBRV," the same symbol under which the Nabriva Austria ADSs were previously traded. This transaction was accounted for as a merger between entities under common control; accordingly, the historical financial statements of Nabriva Austria for periods prior to this transaction are considered to be the historical financial statements of Nabriva Ireland. As of August 18, 2017, 100% of Nabriva Austria share capital had been exchanged for ordinary shares of Nabriva Ireland.
Nabriva Austria was incorporated in October 2005 in Austria under the name Nabriva Therapeutics Forschungs GmbH, a limited liability company organized under Austrian law, as a spin-off from Sandoz GmbH and commenced operations in February 2006. In 2007, Nabriva Austria transformed into a stock corporation (Aktiengesellschaft) under the name Nabriva Therapeutics AG. On October 19, 2017, Nabriva Austria was converted into a limited liability company under Austrian law and renamed Nabriva Therapeutics GmbH. In 2014, we established our wholly owned U.S. subsidiary, which began operations in August 2014.
Since inception, we have incurred significant operating losses. As of December 31, 2017, we had an accumulated deficit of $279.2 million. To date, we have financed our operations primarily through our 2017 equity offering, our 2016 rights offering, our 2015 initial public offering, private placements of our equity securities, convertible loans and research and development support from governmental grants and loans. We have devoted substantially all of our efforts to research and development, including clinical trials. Our ability to generate profits from operations and remain profitable depends on our ability to successfully develop and commercialize drugs that generate significant revenue.
We expect to continue to incur significant expenses and increasing operating losses for at least the next several years. We expect our expenses to increase substantially in connection with our ongoing activities, particularly as we continue the development of and seek marketing approval for lefamulin and, possibly, other product candidates and continue our research activities. Our expenses will increase if we suffer any delays in our Phase 3 clinical program for lefamulin for CABP, including regulatory delays. If we obtain marketing approval for lefamulin or any other product candidate that we develop, we expect to incur significant commercialization expenses related to product sales, marketing, distribution and manufacturing.
Based on our current plans, we do not expect to generate significant revenue unless and until we obtain marketing approval for, and commercialize, lefamulin. We do not expect to obtain marketing approval before 2019, if at all. Accordingly, we will need to obtain substantial additional funding in connection with our continuing operations. Adequate additional financing may not be available to us on acceptable terms, or at all. If we are unable to raise capital when needed or on attractive terms, we could be forced to delay, reduce or eliminate our research and development programs or any future commercialization effort.
114
Financial Operations Overview
Revenue
To date we have not generated any revenues from product sales. and we do not expect to generate any revenue from the sale of products in the near future. We do not expect to generate significant revenue unless and until we obtain marketing approval for, and commercialize, lefamulin. We do not expect to obtain marketing approval before 2019, if at all. If our development efforts result in clinical success and regulatory approval we may also enter into collaboration agreements with third parties and we may generate revenue from those agreements.
Our revenue consists principally of governmental research premiums, non-refundable government grants and the benefit of government loans at below-market interest rates, which are more fully described below under "Critical Accounting Policies."
Research and Development Expenses
Research and development expenses represented 74.9%, 78.0% and 62.7% of our total operating expenses for the years ended December 31, 2015, 2016 and 2017, respectively.
For each of our research and development programs, we incur both direct and indirect expenses. Direct expenses include third party expenses related to these programs such as expenses for manufacturing services, non-clinical and clinical studies and other third party development services. Indirect expenses include salaries and related costs, including stock-based compensation, for personnel in research and development functions, infrastructure costs allocated to research and development operations, costs associated with obtaining and maintaining intellectual property associated with our research and development operations, laboratory consumables, consulting fees related to research and development activities and other overhead costs. We utilize our research and development staff and infrastructure resources across multiple programs, and many of our indirect costs historically have not been specifically attributable to a single program. Accordingly, we cannot state precisely our total indirect costs incurred on a program-by-program basis.
The following table summarizes our direct research and development expenses by program and our indirect costs.
| |
Year Ended December 31, | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | 2017 | |||||||
Direct costs |
||||||||||
Lefamulin |
$ | 14,487 | $ | 36,003 | $ | 34,538 | ||||
Other programs and initiatives |
7 | 71 | 223 | |||||||
Indirect Costs |
9,110 | 11,920 | 14,854 | |||||||
| | | | | | | | | | | |
Total |
$ | 23,604 | $ | 47,994 | $ | 49,615 | ||||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
We expect to continue to incur research and development expenses in connection with our activities related to our ongoing LEAP 2 clinical trial of lefamulin for the treatment of CABP, our subsequent NDA and MAA filings and the pursuit of the clinical development of lefamulin for additional indications and engage in earlier stage research and development activities. It is difficult to estimate the duration and completion costs of our research and development programs.
115
The successful development and commercialization of our product candidates is highly uncertain. This is due to the numerous risks and uncertainties associated with product development and commercialization, including the uncertainty of:
- •
- the scope, progress, costs and results of clinical trials and other research and development activities;
- •
- the costs, timing and outcome of regulatory review of our product candidates;
- •
- the efficacy and potential advantages of our product candidates compared to alternative treatments, including any standard of care, and our
ability to achieve market acceptance for any of our product candidates that receive marketing approval;
- •
- the costs and timing of commercialization activities, including product sales, marketing, distribution and manufacturing, for any of our
product candidates that receive marketing approval; and
- •
- the costs and timing of preparing, filing and prosecuting patent applications, maintaining, enforcing and protecting our intellectual property rights and defending against any intellectual property-related claims.
A change in the outcome of any of these variables with respect to the development of our product candidates could result in a significant change in the costs and timing associated with the development of that product candidate. For example, if the FDA or another regulatory authority were to require us to conduct clinical trials or other testing beyond those that we have completed or currently contemplate will be required for the completion of clinical development of any product candidate, or if we experience significant delays in enrollment in any of our clinical trials, we could be required to expend significant additional resources and time on the completion of clinical development of that product candidate.
General and Administrative Expenses
General and administrative expenses represented 25.1%, 22.0% and 37.3% of our total operating expenses for the years ended December 31, 2015, 2016 and 2017, respectively.
General and administrative expenses consist primarily of salaries and related costs, including share-based compensation not related to research and development activities for personnel in our finance, information technology, commercial, medical affairs and administrative functions. General and administrative expenses also include costs related to professional fees for auditors, lawyers and tax advisors and consulting fees not related to research and development operations, as well as functions that are partly or fully outsourced by us, such as accounting, payroll processing and information technology.
We expect general and administrative expenses to increase with the expansion of our staff and management team in anticipation of the commercialization of lefamulin particularly commercial, medical affairs, technical operations and business development functions.
Additionally, we expect to incur significant marketing, commercial and manufacturing supply chain costs if LEAP 2 data is positive.
Critical Accounting Policies
Our management's discussion and analysis of our financial condition and results of operations is based on our consolidated financial statements, which we have prepared in accordance with generally accepted accounting principles in the United States, or U.S. GAAP. The preparation of our consolidated financial statements requires us to make estimates and assumptions that affect the
116
reported amounts of assets and liabilities and the disclosure of contingent assets and liabilities at the end of the reporting period, as well as the reported revenues and expenses during the reporting periods. We base our estimates on our limited historical experience, known trends and events and various other factors that we believe are reasonable under the circumstances, the results of which form the basis for making judgments about the carrying values of assets and liabilities that are not readily apparent from other sources. Actual results may differ from these estimates under different assumptions or conditions.
Our significant accounting policies are described in more detail in the notes to our consolidated financial statements appearing at the end of this filing. However, we believe that the following accounting policies are the most critical to aid you in fully understanding and evaluating our financial condition and results of operations.
Research Premium and Grant Revenue
As a company that carries out extensive research and development activities, we benefit from the Austrian research and development support regime, under which we are eligible to receive a research premium from the Austrian government equal to 12% (10%, in the case of fiscal years prior to 2016) of a specified research and development cost base. Qualifying expenditures largely comprise research and development activities conducted in Austria, however, the research premium is also available for certain related third-party expenses with additional limitations. We received research premiums of $5.9 million for the year ended December 31, 2016 and $4.3 million for the year ended December 31, 2015. We have not received any research premium for our qualified 2017 expenditures as of December 31, 2017. We recognize the research premium, as long as we have incurred research and development expenses. Significant judgment is required in determining which expenditures are eligible to be included in the research and development costs base and such costs are subject to review by the Austrian government.
Research and Development Expenses
Research expenses are defined as costs incurred for current or planned investigations undertaken with the prospect of gaining new scientific or technical knowledge and understanding. Development expenses are defined as costs incurred for the application of research findings or specialist knowledge to production, production methods, services or goods prior to the commencement of commercial production or use. We expense all research and development costs as incurred.
As part of the process of preparing our consolidated financial statements, we are required to estimate our accrued research and development expenses. This process involves reviewing open contracts and purchase orders, communicating with our applicable personnel to identify services that have been performed on our behalf and estimating the level of service performed and the associated cost incurred for the service when we have not yet been invoiced or otherwise notified of actual costs. We make estimates of our accrued expenses as of each balance sheet date in the consolidated financial statements based on facts and circumstances known to us at that time. Examples of estimated accrued research and development expenses include fees paid to:
- •
- vendors in connection with preclinical development activities;
- •
- the production of preclinical and clinical trial materials;
- •
- CROs in connection with clinical trials; and,
- •
- investigative sites in connection with clinical trials.
117
Implications of Being an Emerging Growth Company
We qualify as an "emerging growth company" as defined in the Jumpstart Our Business Startups Act of 2012, or the JOBS Act. An emerging growth company may take advantage of specified reduced reporting and other burdens that are otherwise applicable generally to public companies. These provisions include:
- •
- an exemption from compliance with the auditor attestation requirement of Section 404 of the Sarbanes-Oxley Act of 2002 on the design and
effectiveness of our internal controls over financial reporting;
- •
- an exemption from compliance with any requirement that the Public Company Accounting Oversight Board may adopt regarding mandatory audit firm
rotation or a supplement to the auditor's report providing additional information about the audit and the financial statements;
- •
- reduced disclosure about the company's executive compensation arrangements; and
- •
- exemptions from the requirements to obtain a non-binding advisory vote on executive compensation or a shareholder approval of any golden parachute arrangements.
We may take advantage of these provisions until December 31, 2020 or such earlier time that we are no longer an emerging growth company. We would cease to be an emerging growth company upon the earlier to occur of: the last day of the fiscal year in which we have more than $1 billion in annual revenues (as may be inflation adjusted by the SEC from time-to-time); the date we qualify as a "large accelerated filer," with at least more than $700 million in market value of our share capital held by nonaffiliates; or the issuance by us of more than $1 billion of non-convertible debt over a three-year period. We may choose to take advantage of some, but not all, of the available benefits under the JOBS Act. We have taken advantage of some reduced reporting burdens in this Annual Report. Accordingly, the information contained herein may be different than the information you receive from other public companies in which you hold stock.
In addition, the JOBS Act provides that an emerging growth company can take advantage of an extended transition period for complying with new or revised accounting standards. This provision allows an emerging growth company to delay the adoption of some accounting standards until those standards would otherwise apply to private companies. We have irrevocably elected not to avail ourselves of delayed adoption of new or revised accounting standards and, therefore, we will adopt new or revised accounting standards on the relevant dates on which adoption of such standards is required by for non-emerging growth companies.
118
Results of Operations
Comparison of Years Ended December 31, 2016 and 2017
| |
Year ended December 31, |
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2016 | 2017 | Change | |||||||
Consolidated Operations Data: |
||||||||||
Revenues |
$ | 6,482 | $ | 5,319 | $ | (1,163 | ) | |||
Costs and Expenses: |
||||||||||
Research and development |
(47,994 | ) | (49,615 | ) | (1,621 | ) | ||||
General and administrative |
(13,535 | ) | (29,472 | ) | (15,937 | ) | ||||
| | | | | | | | | | | |
Total operating expenses |
(61,529 | ) | (79,087 | ) | (17,558 | ) | ||||
| | | | | | | | | | | |
Loss from operations |
(55,047 | ) | (73,768 | ) | (18,721 | ) | ||||
Other income (expense): |
||||||||||
Other income (expense), net |
(783 | ) | 492 | 1,275 | ||||||
Interest income (expense), net |
268 | 275 | 7 | |||||||
| | | | | | | | | | | |
Loss before income taxes |
(55,562 | ) | (73,001 | ) | (17,439 | ) | ||||
Income tax (expense) benefit |
672 | (1,355 | ) | (2,027 | ) | |||||
Net loss |
$ | (54,890 | ) | $ | (74,356 | ) | $ | (19,466 | ) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
Revenues
Revenues, consisting primarily of research premium and grant revenue, decreased by $1.2 million from $6.5 million for the year ended December 31, 2016 to $5.3 million for the year ended December 31, 2017. The change was primarily due to a $1.4 million decrease in grant revenue from research premiums provided to us by the Austrian government as a result of lower applicable research and development expenses, which was offset by a $0.2 million increase in grant income.
Research and Development Expenses
Research and development expenses increased by $1.6 million from $48.0 million for the year ended December 31, 2016 to $49.6 million for the year ended December 31, 2017. The increase was primarily due to a $2.1 million increase in staff costs due to the addition of employees and a $1.2 million increase in share-based compensation expense also due to the inclusion of additional employees in our share-based compensation plan, partially offset by a $1.5 million decrease in direct costs for purchased services related to the development of lefamulin and a $0.2 million decrease of advisory and external consultancy, travel and other expenses .
General and Administrative Expenses
General and administrative expense increased by $16.0 million from $13.5 million for the year ended December 31, 2016 to $29.5 million for the year ended December 31, 2017. The increase was primarily due to a $4.1 million increase in legal fees mainly related to the redomiciliation of our parent company from Austria to Ireland, a $6.1 million increase of advisory and external consultancy expenses primarily related to pre-commercialization activities and professional service fees, a $2.0 million increase in share-based compensation expense due to the inclusion of additional employees in our share-based compensation plan, a $2.8 million increase in staff costs due to the addition of employees, a $0.7 million increase in VAT tax expenses, and a $0.3 million increase in support, infrastructure and other corporate costs.
119
Other income (expense), net
Other income (expense), net decreased by $1.3 million from a net expense of $0.8 million for the year ended December 31, 2016 to net income of $0.5 million for the year ended December 31, 2017. The increase was primarily due to re-measurements of our foreign currency account balances.
Interest expense, net
During the year ended December 31, 2017, net interest income was relatively flat compared to the same period in 2016.
Income tax (Expense) Benefit
Our income tax expense was $1.4 million for the year ended December 31, 2017 compared to an income tax benefit of $0.7 million for the year ended December 31, 2016. The year over year change was primarily due to the recognition of a valuation allowance against deferred tax assets in our foreign subsidiaries. Our income tax (expense) benefit includes Irish, Austrian and U.S. income taxes at statutory rates and the effects of various permanent differences.
Comparison of Years Ended December 31, 2015 and 2016
| |
Year ended December 31, |
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | Change | |||||||
Consolidated Operations Data: |
||||||||||
Revenues |
$ | 3,767 | $ | 6,482 | $ | 2,715 | ||||
Costs and Expenses: |
||||||||||
Research and development |
(23,604 | ) | (47,994 | ) | (24,390 | ) | ||||
General and administrative |
(7,921 | ) | (13,535 | ) | (5,614 | ) | ||||
| | | | | | | | | | | |
Total operating expenses |
(31,525 | ) | (61,529 | ) | (30,004 | ) | ||||
| | | | | | | | | | | |
Loss from operations |
(27,758 | ) | (55,047 | ) | (27,289 | ) | ||||
Other income (expense): |
||||||||||
Other income (expense), net |
2,427 | (783 | ) | (3,210 | ) | |||||
Interest income (expense), net |
(22,078 | ) | 268 | (22,346 | ) | |||||
Loss before income taxes |
(47,409 | ) | (55,562 | ) | (8,153 | ) | ||||
| | | | | | | | | | | |
Income tax (expense) benefit |
445 | 672 | 227 | |||||||
Net loss |
$ | (46,964 | ) | $ | (54,890 | ) | $ | (7,926 | ) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
Revenues
Revenues, consisting primarily of research premium and grant revenue, increased by $2.7 million from $3.8 million from the year ended December 31, 2015 to $6.5 million for the year ended December 31, 2016. The change was primarily due to a $2.6 million increase in grant revenue from research premiums provided to us by the Austrian government as a result of increases in our applicable research and development expenses.
Research and Development Expenses
Research and development expenses increased by $24.4 million from $23.6 million for the year ended December 31, 2015 to $48.0 million for the year ended December 31, 2016. The increase was primarily due to higher costs related to our Phase 3 clinical trials of lefamulin. Research materials and purchased services for our other programs and initiatives were relatively limited during both periods.
120
Staff costs related to research and development increased for the year ended December 31, 2016 compared to the year ended December 31, 2015, primarily due to the addition of employees and increased clinical development costs.
General and Administrative Expenses
General and administrative expense increased by $5.6 million from $7.9 million for the year ended December 31, 2015 to $13.5 million for the year ended December 31, 2016. The increase was primarily due to increased staff costs related to the hiring of additional employees and increased professional service fees related to operating as a public company.
Other income (expense), net
Other income (expense), net decreased by $3.2 million to a $0.8 million loss during the year ended December 31, 2016 compared to the same period in 2015. The change was primarily due to an increase in losses from the re-measurement of foreign currency balances as a result of the change in our functional currency.
Interest expense, net
During the year ended December 31, 2016, net interest expenses decreased by $22.3 million compared to the same period in 2015 primarily due to the decrease in the effective interest accrued under the convertible loan agreements, which were converted into equity securities in connection with our April 2015 financing, and the decrease in interest expense on the Kreos loan, which was fully repaid in November 2015.
Liquidity and Capital Resources
Since our inception, we have incurred net losses and generated negative cash flows from our operations. To date, we have financed our operations through the sale of equity securities, including our initial public offering, public follow-on offerings and private placements of our equity securities, convertible debt financings and research and development support from governmental grants and loans.
As of December 31, 2017, we had cash, cash equivalents and short term investments of $86.9 million.
In March 2018, we entered into a sales agreement with Cantor Fitzgerald & Co., or Cantor, pursuant to which, from time to time, we may offer and sell our ordinary shares having an aggregate offering price of up to $50.0 million through Cantor pursuant to an effective universal shelf registration statement. Sales of our ordinary shares, if any, under the agreement with Cantor may be made in sales deemed to be an "at-the-market offering" as defined in Rule 415(a)(4) under the Securities Act of 1933, as amended.
On September 22, 2017 we completed an underwritten public offering of 9,411,765 ordinary shares at a public offering price of $8.50 per share, resulting in gross proceeds of $80.0 million and net proceeds to us of $73.3 million, after deducting underwriting discounts and commissions and offering expenses.
On December 19, 2016, we completed a rights offering and a related underwritten offering for the sale of an aggregate of 588,127 common shares resulting in aggregate gross proceeds of approximately $24.8 million and net proceeds to us of $20.6 million, after deducting underwriting fees and offering expenses.
In the rights offering, holders of American Depositary Shares, or ADSs, received 0.276 ADS rights for each ADS owned of record on November 29, 2016. One ADS right entitled an ADS holder to
121
subscribe for and purchase one new ADS at the subscription price of $4.32 per ADS, the U.S. dollar equivalent of €4.014 per ADS. An aggregate of 1,592,750 ADSs, representing 159,275 common shares, were subscribed for by holders of ADSs. Each ADS represents one tenth of a common share.
In the rights offering, holders of common shares received the common share right to subscribe for and purchase 0.276 new common shares, at a subscription price of €40.14 per new common share for each common share owned of record on November 29, 2016. An aggregate of 102,077 new common shares were subscribed for by holders of common shares.
Pursuant to an underwriting agreement that we entered into with Cantor Fitzgerald & Co., dated December 14, 2016, Cantor Fitzgerald & Co. agreed to purchase 326,775 common shares, representing all of the unsubscribed common shares in the rights offering, at a purchase price of €40.14 per common share for purposes of resale of ADSs representing such unsubscribed common shares.
On September 23, 2015 we completed our initial public offering on the Nasdaq Global Market issuing 9,000,000 ADSs at a price to the public of $10.25 per ADS, representing 900,000 of our common shares. On September 30, 2015 the underwriters of our initial public offering exercised in full their over-allotment option to purchase an additional 1,350,000 ADSs, representing 135,000 common shares, at the initial public offering price of $10.25 per ADS, less underwriting discounts. Including the over-allotment ADSs, we sold an aggregate of 10,350,000 ADSs representing 1,035,000 common shares, in our initial public offering, which resulted in gross proceeds of $106.1 million and net proceeds to us of $92.4 million, after deducting underwriting discounts and offering expenses.
In March 2015, we entered into an agreement with certain existing and new investors to issue and sell common shares with contractual preference rights under a shareholders agreement. We refer to this transaction as our April 2015 financing. In connection with our April 2015 financing, we agreed to sell common shares with contractual preference rights under the shareholders agreement in two tranches. In April 2015, we closed the sale of the first tranche of 730,162 common shares, including the sale of 511,188 common shares at a price per share of €82.35 ($87.71) for €42.1 million ($44.8 million) in cash consideration and the sale of 218,974 common shares in exchange for certain contributions in-kind consisting of the conversion of outstanding convertible loans and silent partnership interests. We also agreed to sell a second tranche of common shares with contractual preference rights under the shareholders agreement to these investors at their option for an aggregate purchase price of $70.0 million if we did not complete a public offering in the United States within specified parameters or by a specified date. Upon the closing of our initial public offering and the issuance of the shares for nominal value in satisfaction of the preferred dividends rights, all contractual preference rights under the shareholders agreement terminated.
Cash Flows
Comparison of Years Ended December 31, 2016 and 2017
The following table summarizes our cash flows for the years ended December 31, 2016 and 2017:
| |
Year ended December 31, |
||||||
|---|---|---|---|---|---|---|---|
(in thousands)
|
2016 | 2017 | |||||
Net cash (used in) provided by: |
|||||||
Operating activities |
$ | (48,325 | ) | $ | (69,348 | ) | |
Investing activities |
23,352 | 49,749 | |||||
Financing activities |
22,301 | 72,219 | |||||
Effect of foreign currency translation on cash |
(996 | ) | 1,371 | ||||
| | | | | | | | |
Net increase (decrease) in cash and cash equivalents |
$ | (3,668 | ) | $ | 53,991 | ||
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
122
Operating Activities
Cash flow utilized by operating activities increased by $21.0 million from $48.3 million for the year ended December 31, 2016 to $69.3 million for the year ended December 31, 2017 primarily due to a $16.1 million increase in net loss, after adjustments for non-cash amounts included in net loss and higher working capital of $4.9 million primarily due to changes in accrued expenses and other current liabilities.
Investing Activities
Cash flow provided by investing activities increased by $26.4 million from $23.4 million cash inflow in the year ended December 31, 2016 to $49.7 million cash inflow in the year ended December 31, 2017 primarily due to an increase of $15.0 million in proceeds from sale of available-for-sale securities to fund operational cash out flows and a decrease of $57.0 million in purchases of available-for sale-securities in 2017. The year over year increase in investing activities was partially offset by a $45.0 million decrease in proceeds from maturities of term deposits.
Financing Activities
Cash flow provided by financing activities increased by $49.9 million from $22.3 million for the year ended December 31, 2016 to $72.2 million for the year ended December 31, 2017 primarily due to the gross proceeds of $80.0 million from our 2017 equity financing, compared to the proceeds of $24.8 million from our rights offering and related underwritten offering in December 2016. The year-over-year increase in financing cash inflows was partially offset by a $5.3 million increase in equity transaction costs.
Comparison of Years Ended December 31, 2015 and 2016
The following table summarizes our cash flows for the years ended December 31, 2015 and 2016:
| |
Year ended December 31, |
||||||
|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | |||||
Net cash (used in) provided by: |
|||||||
Operating activities |
$ | (21,858 | ) | $ | (48,325 | ) | |
Investing activities |
(76,704 | ) | 23,352 | ||||
Financing activities |
133,018 | 22,301 | |||||
Effect of foreign currency translation on cash |
(160 | ) | (996 | ) | |||
| | | | | | | | |
Net increase (decrease) in cash and cash equivalents |
$ | 34,296 | $ | (3,668 | ) | ||
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
Operating Activities
Cash flow utilized by operating activities increased by $26.4 million from $21.9 million for the year ended December 31, 2015 to $48.3 million for the year ended December 31, 2016 primarily due to a $27.4 million increase in net loss, after adjustments for non-cash amounts included in net loss partially offset by improved working capital of $1.0 million primarily from higher trade payables and other liabilities.
Investing Activities
Cash flow from investing activities changed by $100.1 million from $76.7 million cash outflow for the year ended December 31, 2015 to a $23.4 million cash inflow in the year ended December 31, 2016 primarily due to the redemption of term deposits. Other investing activities were relatively insignificant in both periods and related primarily to the acquisition of equipment in support of our research and development activities.
123
Financing Activities
Cash flow generated from financing activities decreased by $110.7 million from $133.0 million for the year ended December 31, 2015 to $22.3 million for the year ended December 31, 2016 primarily due to proceeds of $44.8 million from our April 2015 financing and proceeds of $106.1 million from our initial public offering in September 2015, $3.4 million from the issuance of an additional convertible loan in January 2015 and proceeds of $0.9 million from a silent partnership agreement entered into in January 2015. The year-over-year decrease in financing cash inflows was partially offset by proceeds of $24.8 million from our December 2016 rights offering, a $7.4 million decrease of cash outflows for repayments of long-term borrowings and a $12.1 million decrease in equity transaction costs.
Operating and Capital Expenditure Requirements
We anticipate that our expenses will increase substantially as we continue the development of and seek marketing approval for lefamulin and, possibly, other product candidates and continue our research activities. Our expenses will increase if we suffer any delays in our Phase 3 clinical program for lefamulin for the treatment of CABP, including regulatory delays. If we obtain marketing approval for lefamulin or any other product candidate that we develop, we expect to incur significant commercialization expenses related to product sales, marketing, distribution and manufacturing.
In addition, our expenses will increase if and as we:
- •
- initiate or continue the research and development of lefamulin for additional indications and of our other product candidates;
- •
- seek to discover and develop additional product candidates;
- •
- seek marketing approval for any product candidates that successfully complete clinical development;
- •
- continue to establish a medical affairs, sales, marketing and distribution infrastructure and build up inventory of finished product and its
components to commercialize any product candidates for which we receive marketing approval;
- •
- in-license or acquire other products, product candidates or technologies;
- •
- maintain, expand and protect our intellectual property portfolio;
- •
- establish and expand manufacturing arrangements with third parties;
- •
- expand our physical presence in the United States and Ireland; and,
- •
- add operational, financial and management information systems and personnel, including personnel to support our product development, our operations as a public company and our planned future commercialization efforts.
We expect that our existing cash, cash equivalents and short-term investments will be sufficient to enable us to fund our operating expenses and capital expenditure requirements into the fourth quarter of 2018. We have based these estimates on assumptions that may prove to be wrong, and we could use our capital resources sooner than we currently expect. Furthermore, while these estimates are based on our current assumptions regarding our operating expenses and capital expenditure requirements, we also believe that by reducing certain planned pre-commercialization activities our existing cash, cash equivalents and short-term investments could fund our primary business focus of seeking regulatory approval for lefamulin, our lead product candidate, subject to positive LEAP 2 topline data, into the first quarter of 2019. These estimates assume, among other things, that we do not obtain any additional funding through grants and clinical trial support, collaboration agreements or equity or debt financings.
124
Our future capital requirements will depend on many factors, including:
- •
- the progress, costs and results of our clinical trials for lefamulin, including our LEAP 2 trial;
- •
- the costs and timing of process development and manufacturing scale-up activities associated with lefamulin;
- •
- the costs, timing and outcome of regulatory review of lefamulin;
- •
- the costs of commercialization activities for lefamulin if we receive, or expect to receive, marketing approval, including the costs and timing
of establishing product sales, marketing, distribution and outsourced manufacturing capabilities, including the costs of building finished product inventory and its components in preparation of
initial marketing of lefamulin;
- •
- subject to receipt of marketing approval, revenue received from commercial sales of lefamulin;
- •
- the costs of developing lefamulin for the treatment of additional indications;
- •
- our ability to establish collaborations on favorable terms, if at all;
- •
- the scope, progress, results and costs of product development of any other product candidates that we may develop;
- •
- the extent to which we in-license or acquire rights to other products, product candidates or technologies;
- •
- the costs of preparing, filing and prosecuting patent applications, maintaining and protecting our intellectual property rights and defending
against intellectual property-related claims;
- •
- the continued availability of Austrian governmental grants;
- •
- the rate of the expansion of our physical presence in the United States and Ireland; and
- •
- the costs of operating as a public company in the United States.
Conducting clinical trials is a time-consuming, expensive and uncertain process that takes years to complete, and we may never generate the necessary data or results required to obtain marketing approval and achieve product sales. Our commercial revenues, if any, will be derived from sales of lefamulin or any other products that we successfully develop, in-license or acquire, none of which we expect to be commercially available for more than a year, if at all. In addition, if approved, lefamulin or any other product candidate that we develop, in-license or acquire may not achieve commercial success. Accordingly, we will need to obtain substantial additional financing to achieve our business objectives. Adequate additional financing may not be available to us on acceptable terms, or at all. In addition, we may seek additional capital due to favorable market conditions or strategic considerations, even if we believe that we have sufficient funds for our current or future operating plans.
Until such time, if ever, as we can generate substantial product revenues, we expect to finance our cash needs through a combination of equity offerings, debt financings, collaborations, and funding from local and international government entities and non-government organizations in the disease areas addressed by our product candidates and marketing, distribution or licensing arrangements. For example, in March 2018, we entered into an agreement with Cantor pursuant to which, from time to time, we may offer and sell up to $50.0 million of our ordinary shares "at the market" through Cantor pursuant to an effective universal shelf registration statement. To the extent that we raise additional capital through the sale of equity or convertible debt securities, the ownership interest of our shareholders will be diluted, and the terms of these securities may include liquidation or other preferences that adversely affect the rights of our shareholders. Debt financing, if available, may involve agreements that include covenants limiting or restricting our ability to take specific actions, such as incurring additional debt, making capital expenditures or declaring dividends.
125
If we raise additional funds through collaborations, strategic alliances or marketing, distribution or licensing arrangements with third parties, we may have to relinquish valuable rights to our technologies, future revenue streams, research programs or product candidates or to grant licenses on terms that may not be favorable to us. If we are unable to raise additional funds through equity or debt financings when needed, we may be required to delay, limit, reduce or terminate our product development or future commercialization efforts or grant rights to develop and market product candidates that we would otherwise prefer to develop and market ourselves.
Capital Expenditures
Capital expenditures were $603,000 and $1.2 million for the years ended December 31, 2016 and 2017, respectively. We made no significant investments in intangible assets during the years ended December 31, 2016 and 2017. Currently, there are no material capital projects planned in 2018.
Contractual Obligations and Commitments
The table below sets forth our contractual obligations and commercial commitments as of December 31, 2017 that are expected to have an impact on liquidity and cash flow in future periods. The amounts disclosed are the contractual undiscounted cash flow values.
| |
Payments Due by Period | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
Less than 1 year |
Between 1 and 3 years |
Between 3 and 5 years |
More than 5 years |
Total | |||||||||||
Operating lease obligations |
$ | 776 | 1,522 | 1,029 | — | 3,327 | ||||||||||
Other contractual commitments |
10,550 | — | — | — | 10,550 | |||||||||||
| | | | | | | | | | | | | | | | | |
Total |
$ | 11,326 | 1,522 | 1,029 | — | 13,877 | ||||||||||
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | |
Operating lease obligations include rental agreements for our facilities in Ireland, Austria and the United States.
Other contractual commitments relate to contracts entered into with contract research organizations and contract manufacturing organizations in connection with the conduct of clinical trials and other research and development activities. The estimated payments to the services providers included in the table above are based solely on the estimated work to be performed by them to complete the trials and other activities along with anticipated achievement of the milestones included within the agreements. Also, some of these contracts include early termination clauses exercisable at our discretion. Minimum required payments, if any, under these agreements are deemed to be immaterial.
Off-Balance Sheet Arrangements
We did not have during the periods presented, and we do not currently have, any off-balance sheet arrangements, as defined under SEC rules, other than our operating lease obligations for our facilities in Austria and the United States.
ITEM 7A. QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK
We are exposed to a variety of financial risks in the ordinary course of our business: market risk, credit risk and liquidity risk. Our overall risk management program focuses on preservation of capital given the unpredictability of financial markets. These market risks are principally limited to interest rate and foreign currency fluctuations.
126
Market Risk
We do not have any significant credit risk exposure to any single counterparty or any group of counterparties having similar characteristics. The credit risk on liquid funds (bank accounts, cash balances, marketable securities and term deposits) is limited because the counterparties are banks with high credit ratings from international credit rating agencies. The primary objective of our investment activities is to preserve principal and liquidity while maximizing income without significantly increasing risk. We do not enter into investments for trading or speculative purposes.
We are exposed to foreign exchange risk arising from various currency exposures, primarily with respect to the euro and the British pound. Our functional currency is the U.S. dollar, but we receive payments and acquire materials, in each of these other currencies. We have not established any formal practice to manage the foreign exchange risk against our functional currency. However, we attempt to minimize our net exposure by buying or selling foreign currencies at spot rates upon receipt of new funds to facilitate committed or anticipated foreign currency transactions.
Interest rate risk may arise from short-term or long-term debt. As of December 31, 2017, we had no debt that exposed us to interest rate risk. As of December 31, 2017, we had neither significant long-term interest-bearing assets nor significant long-term interest-bearing liabilities, other than a de minimis government loan we have received at a below-market rate of interest from the Austrian Research Promotion Agency (Österreichische Forschungsförderungsgesellschaft, or FFG). Due to the short-term nature of our investment portfolio, we do not believe an immediate 10% increase in interest rates would have a material effect on the fair market value of our portfolio, and accordingly we do not expect our operating results or cash flows to be materially affected by a sudden change in market interest rates.
Liquidity Risk
Since our inception, we have incurred net losses and generated negative cash flows from our operations. Based on our current operating plans, we believe that our existing cash, cash equivalents and short-term investments will be sufficient to enable us to fund our operating expenses and capital expenditure requirements into the fourth quarter of 2018. We have based these estimates on assumptions that may prove to be wrong, and we could use our capital resources sooner than we currently expect. Furthermore, while these estimates are based on our current assumptions regarding our operating expenses and capital expenditure requirements, we also believe that by reducing certain planned pre-commercialization activities our existing cash, cash equivalents and short-term investments could fund our primary business focus of seeking regulatory approval for lefamulin, our lead product candidate, subject to positive LEAP 2 topline data, into the first quarter of 2019.
We anticipate that our expenses will increase substantially as we continue the development of and seek marketing approval for lefamulin and, possibly, other product candidates and continue our research activities. If we obtain marketing approval for lefamulin or any other product candidate that we develop, in-license or acquire, we expect to incur significant commercialization expenses related to product sales, marketing, distribution and manufacturing. We have developed plans to mitigate this risk, which primarily consist of raising additional capital through a combination of equity or debt financings, new collaborations, and reducing cash expenditures.
However, there can be no assurance that we will be successful in acquiring additional capital at level sufficient to fund our operations or on terms favorable to us. These conditions raise substantial doubt about our ability to continue as a going concern for a period of one year from the date of the issuance of our consolidated financial statements for the year ended December 31, 2017.
If we are unable to raise capital when needed or on attractive terms, we could be forced to delay, reduce to eliminate our research and development programs or any future commercialization effort.
127
ITEM 8. FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
Our financial statements, together with the report of our independent registered public accounting firm, appear on pages F-1 through F-30 of this Annual Report on Form 10-K.
ITEM 9. CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE
On May 24, 2017, the audit committee of the supervisory board of Nabriva Austria dismissed PwC Wirtschaftsprüfung GmbH, or PwC, as its independent registered public accounting firm and approved the engagement of KPMG LLP as its independent registered public accounting firm for the fiscal year ended December 31, 2017. During the fiscal years ended December 31, 2016 and 2015 and the subsequent interim period through May 24, 2017, there were no disagreements with PwC on any matter of accounting principles or practices, financial statement disclosure, or auditing scope and procedure, which disagreements, if not resolved to PwC's satisfaction, would have caused PwC to make reference to the subject matter of the disagreement in connection with reports for such periods or (2) reportable events (as described in Item 304(a)(i)(v) of Regulation S-K).
ITEM 9A. CONTROLS AND PROCEDURES
Conclusions Regarding the Effectiveness of Disclosure Controls and Procedures
We have carried out an evaluation of the effectiveness of the design and operation of our disclosure controls and procedures (as such term is defined in Rules 13a-15(e) and 15d-15(e) under the Exchange Act) under the supervision and the participation of the company's management, which is responsible for the management of the internal controls, and which includes our Chief Executive Officer and Chief Financial Officer (our principal executive officer and principal financial officer, respectively). The term "disclosure controls and procedures," as defined in Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934, means controls and other procedures of a company that are designed to ensure that information required to be disclosed by a company in the reports that it files or submits under the Securities Exchange Act of 1934 is recorded, processed, summarized and reported within the time periods specified in the Securities and Exchange Commission's rules and forms.
Disclosure controls and procedures include, without limitation, controls and procedures designed to ensure that information required to be disclosed by a company in the reports that it files or submits under the Securities Exchange Act of 1934 is accumulated and communicated to the company's management, including its principal executive and principal financial officers, as appropriate to allow timely decisions regarding required disclosure. There are inherent limitations to the effectiveness of any system of disclosure controls and procedures, including the possibility of human error and the circumvention or overriding of the controls and procedures. Accordingly, even effective disclosure controls and procedures can only provide reasonable assurance of achieving their control objectives. Based upon our evaluation of our disclosure controls and procedures as of December 31, 2017, our Chief Executive Officer and Chief Financial Officer concluded that, as of such date, our disclosure controls and procedures were effective at a reasonable level of assurance.
Management's Annual Report on Internal Control Over Financial Reporting
Internal control over financial reporting refers to the process designed by, or under the supervision of, our Chief Executive Officer and Chief Financial Officer, and effected by our board of directors, management and other personnel, to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles, and includes those policies and procedures that: (1) pertain to the maintenance of records that in reasonable detail accurately and fairly reflect the transactions and
128
dispositions of our assets; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that our receipts and expenditures are being made only in accordance with authorizations of our management and board of directors; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use or disposition of the company's assets that could have a material effect on the financial statements.
Internal control over financial reporting cannot provide absolute assurance of achieving financial reporting objectives because of its inherent limitations. Internal control over financial reporting is a process that involves human diligence and compliance and is subject to lapses in judgment and breakdowns resulting from human failures. Internal control over financial reporting also can be circumvented by collusion or improper management override. Because of such limitations, there is a risk that material misstatements may not be prevented or detected on a timely basis by internal control over financial reporting. However, these inherent limitations are known features of the financial reporting process. Therefore, it is possible to design into the process safeguards to reduce, though not eliminate, this risk.
Management is responsible for establishing and maintaining adequate internal control over our financial reporting, as such term is defined in Rules 13a-15(f) and 15d-15(e) under the Exchange Act. Under the supervision and with the participation of our management, including our Chief Executive Officer and Chief Financial Officer, we conducted an evaluation of the effectiveness of our internal control over financial reporting. Management has used the framework set forth in the report entitled "Internal Control—Integrated Framework (2013)" published by the Committee of Sponsoring Organizations of the Treadway Commission to evaluate the effectiveness of our internal control over financial reporting. Based on its evaluation, management has concluded that our internal control over financial reporting was effective as of December 31, 2017, the end of our most recent fiscal year.
Our independent registered public accounting firm has not performed an evaluation of our internal control over financial reporting during any period in accordance with the provisions of the Sarbanes-Oxley Act. For as long as we remain an "emerging growth company" as defined in the JOBS Act, we intend to take advantage of the exemption permitting us not to comply with the requirement that our independent registered public accounting firm provide an attestation on the effectiveness of our internal control over financial reporting.
Changes in Internal Control over Financial Reporting
There were no changes in our internal control over financial reporting (as defined in Exchange Act Rule 13a-15(f)) that occurred during the three months ended December 31, 2017 that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
None.
129
ITEM 10. DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE
Board of Directors
Set forth below are the names and certain biographical information about each member of our board of directors as of March 1, 2018. The information presented includes each director's principal occupation and business experience for at least the past five years and the names of other public companies of which he or she has served as a director during the past five years.
Name
|
Age | Position | |||
|---|---|---|---|---|---|
Daniel Burgess(1)(3) |
56 | Director, Chairman of the Board | |||
Colin Broom, MD |
62 | Director, Chief Executive Officer | |||
Axel Bolte(2) |
46 | Director | |||
Carrie Bourdow(2) |
55 | Director | |||
Mark Corrigan, MD(3) |
61 | Director | |||
Charles A. Rowland, Jr.(1)(2) |
60 | Director | |||
George H. Talbot, MD |
69 | Director | |||
Stephen Webster(1)(3) |
57 | Director | |||
- (1)
- Member
of the audit committee.
- (2)
- Member
of the compensation committee.
- (3)
- Member of the nominating and corporate governance committee.
Daniel Burgess has served on our board of directors since June 23, 2017. Mr. Burgess was a member of the supervisory board of Nabriva Austria and served as its chairman from October 2016 until the Redomiciliation. Mr. Burgess has been a venture partner at SV Life Sciences since 2014. He was previously president and chief executive officer of Rempex Pharmaceuticals, an antibiotics company he co-founded in 2011 and that was subsequently sold to The Medicines Company in 2013. Prior to this, Mr. Burgess was president and chief executive officer of Mpex Pharmaceuticals from 2007 until its acquisition by Aptalis Inc. in 2011. He also served as chief operating officer and chief financial officer of Hollis-Eden Pharmaceuticals from 1999 to 2007 and chief financial officer at Nanogen Inc. from 1998 to 1999. Prior to this, Mr. Burgess spent 10 years at Gensia Sicor, Inc. (acquired by Teva Pharmaceutical Industries Ltd), where he held a variety of executive-level positions with responsibility for overall finance for the company. He began his career at Castle & Cooke, and Smith Barney, Harris Upham and Company. Mr. Burgess also is chairman of the board of directors of Atox Bio, a private biotechnology company, and of Pulmocide Ltd., a private drug discovery company; and a member of the boards of directors of Cidara Therapeutics, Inc., a public biotechnology company; Arbutus Biopharma Corp., a public biotechnology company; and Leiter's Inc., a private compounding pharmacy. Mr. Burgess was a member of the board of directors of Santarus, Inc., from 2004 until its acquisition in 2014 by Salix Pharmeceuticals Inc. (now Valeant Pharmaceuticals International, Inc.). He received his B.A. in economics from Stanford University and an M.B.A. from Harvard University. We believe Mr. Burgess is qualified to serve as a director because of his expertise and experience as an executive in the pharmaceutical industry and his educational background.
Colin Broom has served on our board of directors since June 23, 2017 and as our chief executive officer since April 12, 2017. Dr. Broom was previously chief executive officer of Nabriva Austria from August 2014 until the Redomiciliation. Prior to joining Nabriva Austria, he served as chief scientific officer at ViroPharma Incorporated from 2004 until it was acquired by Shire plc in 2014. Dr. Broom served as vice president of clinical development and medical affairs in Europe for Amgen Inc. from 2000 to 2003 and previously held several leadership positions with Hoechst Marion Roussel (now
130
Sanofi), SmithKline Beecham and Glaxo (now GlaxoSmithKline). Dr. Broom served as a member of the board of directors of NPS Pharmaceuticals, Inc. from 2009 until its acquisition by Shire in 2015. He is a member of the U.K. Royal College of Physicians and a fellow of the Faculty of Pharmaceutical Medicine. Dr. Broom received his B.Sc. from University College London and M.B.B.S. from St. George's Hospital Medical School. We believe that Dr. Broom is qualified to serve as a director due to his extensive experience in all stages of drug development and commercialization.
Axel Bolte has served on our board of directors since June 23, 2017. He previously served on the supervisory board of Nabriva Austria from 2007 until the Redomiciliation. In February 2017, Mr. Bolte began serving as president and chief executive officer of Inozyme Pharma Inc., and he has served as managing member of Healthcare Advisors GmbH since March 2017. Previously, Mr. Bolte was a venture partner at HBM Partners AG, a provider of investment advisory services in the life sciences industry, and he served as an investment advisor to HBM Partners AG from 2003 to February 2017. Previously, he was an investment manager at NMT New Medical Technologies AG from 2001 to 2003, and prior to that, Mr. Bolte served as a scientist at Serono SA. He currently serves on the board of directors of Inozyme Pharma Inc., Ophthotech Corporation, Allena Pharmaceuticals and Tripex Pharmaceuticals, and previously served on the board of directors of PTC Therapeutics, Inc., Kolltan Pharmaceuticals, Inc. and Lux Biosciences. Mr. Bolte received a degree from the Swiss Federal Institute of Technology and an M.B.A. from the University of St. Gallen. We believe that Mr. Bolte is qualified to serve as a director because of his many years of service on our board, his extensive experience as a venture capital investor in the life sciences industry and his service on the boards of directors of other life sciences companies.
Carrie Bourdow has served on our board of directors since June 23, 2017. Since February 2018, Ms. Bourdow has served as executive vice president and chief operating officer of Trevena, Inc., and she was chief commercial officer of Trevena from May 2015 to February 2017. Previously, she was vice president of marketing, reimbursement and operations at Cubist Pharmaceuticals, Inc. from May 2013 until it was acquired by Merck & Co., Inc. in 2015. Prior to joining Cubist, she spent more than 20 years at Merck, where she held various leadership positions including marketing lead for the U.S. hospital and anti-infectives franchise. Ms. Bourdow holds a B.A. degree from Hendrix College and an M.B.A. from Southern Illinois University. We believe Ms. Bourdow is qualified to serve as a director due to her extensive experience in the biopharmaceutical industry, including her experience with anti-infectives and with the commercialization of new drugs.
Mark Corrigan has served on our board of directors since June 23, 2017. Dr. Corrigan previously served on the supervisory board of Nabriva Austria from October 2016 until the Redomiciliation. Since January 2015, Dr. Corrigan has been executive chairman of BlackThorn Therapeutics. Dr. Corrigan served as president and chief executive officer of Zalicus, Inc. from January 2010 until July 2014. Previously, Dr. Corrigan was executive vice president of research and development at the specialty pharmaceutical company Sepracor Inc., and prior to this, he spent 10 years with Pharmacia & Upjohn, most recently as Group Vice President of Global Clinical Research and Experimental Medicine. Before entering the healthcare industry, Dr. Corrigan was in academic research at the University of North Carolina at Chapel Hill School of Medicine, where he maintains a faculty appointment as Adjunct Professor in the Psychiatry Department. Dr. Corrigan currently serves on the boards of directors of BlackThorn Therapeutics, Inc., a private clinical-stage biopharmaceutical company, Novelin Therapeutics, Inc., a public biopharmaceutical company, Cardiome Pharma Corporation, a public biopharmaceutical company, Quartet Medicine, a private biotechnology company, and Accele BioPharma Inc., a private biopharmaceutical company, and previously served on the boards of directors of CoLucid Pharmaceuticals, Inc., Cubist Pharmaceuticals, Inc., Avanair Pharmaceuticals, Inc., and EPIRUS Biopharmaceuticals, Inc., where he served as chairman of the board of directors. Dr. Corrigan holds an M.D. from the University of Virginia and received specialty training in psychiatry at Maine Medical Center and Cornell University. We believe Dr. Corrigan is qualified to serve as a director due
131
to his extensive experience in the biopharmaceutical industry as both an executive and a board member and because of his education and training.
George H. Talbot has served on our board of directors since June 23, 2017. Dr. Talbot previously served on the supervisory board of Nabriva Austria from 2009 until the Redomiciliation. Dr. Talbot has been the principal at Talbot Advisors LLC, a biopharmaceutical company consultancy, since 2007 and prior to that, from 2000 to 2006. From 2006 to 2007, he served as chief medical officer and executive vice president of Cerexa, Inc. prior to its acquisition by Forest Laboratories, Inc. Dr. Talbot also worked closely with Calixa Therapeutics, Inc. and Durata Therapeutics, Inc., prior to their acquisitions by Cubist Pharmaceuticals, Inc. and Actavis plc, respectively. He was an initial member of the Infectious Diseases Society of America's Antimicrobial Availability Task Force ("Bad Bugs, No Drugs") and recently completed a seven-year tenure as co-chair of the Foundation for the National Institutes of Health (FNIH) Biomarkers Consortium Projects for Endpoint Development in Acute Bacterial Skin and Skin Structure Infections, Community-acquired Bacterial Pneumonia, and Hospital-acquired Bacterial Pneumonia/Ventilator-associated Bacterial Pneumonia, which made evidence-based recommendations to the Food and Drug Administration for its Guidance development in these indications. Dr. Talbot received his B.A. from Wesleyan University, his M.D. from the Yale University School of Medicine, and his Infectious Diseases fellowship training at the University of Pennsylvania. After serving as a faculty member of the Infectious Diseases Section at the University of Pennsylvania, he joined the anti-infectives group at Rhone-Poulenc-Rorer in 1990. We believe that Dr. Talbot is qualified to serve as a director due to his education, training and extensive experience in the biopharmaceutical industry.
Charles A. Rowland, Jr. has served on our board of directors since June 23, 2017. Mr. Rowland previously served on the supervisory board of Nabriva Austria from January 2015 until the Redomiciliation. Mr. Rowland served as chief executive officer of Aurinia Pharmaceuticals Inc. from April 2016 to January 2017. Mr. Rowland previously served as vice president and chief financial officer of ViroPharma Incorporated from 2008 until it was acquired by Shire plc in 2014. Prior to joining ViroPharma, Mr. Rowland served as executive vice president and chief financial officer, as well as interim co-chief executive officer, for Endo Pharmaceuticals Inc. from 2006 to 2008 and chief financial officer at Biovail Corporation from 2004 to 2006. He previously held finance and operational positions of increasing responsibility at Breakaway Technologies, Inc., Pharmacia, Novartis International AG and Bristol-Myers Squibb Company. Mr. Rowland currently serves as a member of the board of directors for Blueprint Medicines Corporation, a public biopharmaceutical company, and Viking Therapeutics, a public, clinical-stage biopharmaceutical company, and PsiOxus Therapeutics Ltd., a privately held biopharmaceutical company. Previously, he served on the board of directors at Idenix Pharmaceuticals, Inc., Vitae Pharmaceuticals, Inc., Bind Therapeutics Inc. and Aurinia Pharmaceuticals Inc. Mr. Rowland received his B.S. from Saint Joseph's University and M.B.A. from Rutgers University. We believe that Mr. Rowland is qualified to serve as a director due to his extensive experience in pharmaceutical operations and all areas of finance and accounting.
Stephen Webster has served on our board of directors since June 23, 2017. Mr. Webster previously served on the supervisory board of Nabriva Austria from October 2016 until the Redomiciliation. Mr. Webster has been chief financial officer of Spark Therapeutics since July 2014. He was previously senior vice president and chief financial officer of Optimer Pharmaceuticals, Inc. from June 2012 until its acquisition by Cubist Pharmaceuticals in November 2013. Prior to this, Mr. Webster served as senior vice president and chief financial officer of Adolor Corporation, also acquired by Cubist, from 2008 to 2011. Previously, Mr. Webster served as managing director, Investment Banking Division, Health Care Group for Broadpoint Capital Inc. (formerly First Albany Capital). He also was a co-founder and served as president and chief executive officer of Neuronyx, Inc. Prior to this, Mr. Webster held positions of increasing responsibility, including as director, Investment Banking Division, Health Care Group, for PaineWebber Incorporated. Mr. Webster is currently a member of the board of directors of
132
Viking Therapeutics, Inc. He holds an A.B. in economics from Dartmouth College and an M.B.A. from the University of Pennsylvania. We believe that Mr. Webster is qualified to serve as a director due to his extensive experience in the biopharmaceutical industry, particularly his service as a chief financial officer and in other executive management roles.
Board Committees
Our board of directors has established an audit committee, a compensation committee and a nominating and corporate governance committee, each of which operates under a charter that has been approved by our board. Copies of the committee charters are posted under the heading "Corporate Governance" on the Investor section of our website, which is located at http://investors.nabriva.com. For the discussion below, references to our board committees include the committees of the supervisory board of our predecessor, Nabriva Austria, prior to the Redomicilaion.
Audit Committee
Our audit committee consists of Charles A. Rowland, Jr., Daniel Burgess and Stephen Webster, and Charles A. Rowland, Jr. is the chair of the audit committee. The audit committee oversees our accounting and financial reporting processes and the audits of our consolidated financial statements. The audit committee is responsible for, among other things:
- •
- making recommendations to our board regarding the ratification by the annual general meeting of shareholders of our independent auditors;
- •
- overseeing the work of the independent auditors, including resolving disagreements between management and the independent auditors relating to
financial reporting;
- •
- pre-approving all audit and non-audit services permitted to be performed by the independent auditors;
- •
- reviewing the independence and quality control procedures of the independent auditors;
- •
- reviewing and approving all proposed related-party transactions;
- •
- discussing the annual audited consolidated and statutory financial statements with management;
- •
- annually reviewing and reassessing the adequacy of our audit committee charter;
- •
- meeting separately with the independent auditors to discuss critical accounting policies, recommendations on internal controls, the auditor's
engagement letter and independence letter and other material written communications between the independent auditors and the management; and
- •
- attending to such other matters as are specifically delegated to our audit committee by our board from time to time.
Our Board has determined that Charles A. Rowland, Jr. is an "audit committee financial expert" as defined in the applicable SEC rules.
Compensation Committee
Our compensation committee consists of Axel Bolte, Carrie Bourdow and Charles A. Rowland, Jr.Axel Bolte was the chair of the compensation committee until December 5, 2017, and Charles A. Rowland, Jr. has been chair since December 5, 2017. The compensation committee assists the board in reviewing and approving or recommending our compensation structure, including all forms of
133
compensation relating to our directors and management. The compensation committee is responsible for, among other things:
- •
- reviewing and making recommendations to the board with respect to compensation of our board of directors and management;
- •
- reviewing and approving the compensation, including equity compensation, change-of-control benefits and severance arrangements, of our chief
executive officer, chief financial officer and such other members of our management as it deems appropriate;
- •
- overseeing the evaluation of our management;
- •
- reviewing periodically and making recommendations to our board with respect to any incentive compensation and equity plans, programs or similar
arrangements;
- •
- exercising the rights of our board under any equity plans, except for the right to amend any such plans unless otherwise expressly authorized
to do so; and
- •
- attending to such other matters as are specifically delegated to our compensation committee by our board from time to time.
Nominating and Corporate Governance Committee
Our nominating and corporate governance committee consists of Daniel Burgess, Mark Corrigan and Stephen Webster, and Daniel Burgess is the chair of the nominating and corporate governance committee. The nominating and corporate governance committee assists the board in selecting individuals qualified to become our directors and in determining the composition of the board and its committees. The nominating and corporate governance committee is responsible for, among other things:
- •
- recommending to the board persons to be nominated for election or re-election to the board at any meeting of shareholders;
- •
- overseeing the board's annual review of its own performance and the performance of its committees; and
- •
- considering, preparing and recommending to the board a set of corporate governance guidelines.
Compensation Committee Interlocks and Insider Participation
For the fiscal year ended December 31, 2017, the members of our compensation committee (including the compensation committee of our predecessor, Nabriva Austria) were Axel Bolte, Carrie Bourdow, Chau Khuong and Charles Rowland, Jr.. No member of our compensation committee (including the compensation committee of Nabriva Austria) is, or has been, an officer or employee of ours or any subsidiary of ours. None of our executive officers served as a director or a member of a compensation committee (or other committee serving an equivalent function) of any other entity that had one or more executive officers serving as a director or member of our compensation committee during the year ended December 31, 2017.
134
Executive Officers
The following table sets forth information regarding our executive officers as of March 1, 2018:
Name
|
Age | Position | |||
|---|---|---|---|---|---|
Colin Broom |
62 | Chief Executive Officer | |||
Robert Crotty |
44 | General Counsel and Secretary | |||
Steven Gelone |
50 | Chief Scientific Officer | |||
Francesco Maria Lavino |
44 | Chief Commercial Officer | |||
Gary Sender |
55 | Chief Financial Officer | |||
In addition to the biographical information for Dr. Broom, which is set forth above under "Board of Directors," set forth below is certain biographical information about Dr. Gelone and Messrs. Crotty, Lavino and Sender:
Robert Crotty has served as our general counsel and secretary since June 23, 2017. Mr. Crotty joined Nabriva Austria as general counsel and secretary prior to the Redomiciliation on June 14, 2017. Previously, Mr. Crotty served as vice president, general counsel, chief compliance officer and secretary of Vernalis Therapeutics, Inc. from January 2016 to June 2017. Prior to joining Vernalis, Mr. Crotty held several positions at Dendreon Corporation from April 2012 to July 2015, including president, general counsel and secretary from February 2015 to July 2015, executive vice president, general counsel and secretary from March 2014 to February 2015, and vice president, assistant general counsel and assistant secretary from April 2012 to February 2014. Before Dendreon, Mr. Crotty was senior counsel at NPS Pharmaceuticals from 2009 until 2012 and at ImClone Systems, Inc. from 2006 to 2009. Prior to going in-house, Mr. Crotty was an associate at Morgan, Lewis & Bockius and Norton Rose Fulbright. Mr. Crotty received his B.A. from Princeton University and J.D. from University of Pennsylvania.
Steven Gelone has served as our chief scientific officer since June 30, 2017. Dr. Gelone previously served as Nabriva Austria's chief development officer and head of business development from 2014 until the Redomiciliation and our chief development officer from the Redomiciliation until June 30, 2017. Prior to joining Nabriva Austria, he served as head of clinical research and development at Spark Therapeutics, Inc. in 2014 and vice president of clinical and preclinical development at ViroPharma Incorporated from 2005 to 2014. Dr. Gelone also served as director of medical affairs at Vicuron Pharmaceuticals from 2002 to 2003 and director of clinical pharmacology and experimental medicine at GlaxoSmithKline Pharmaceuticals from 2000 to 2002. Dr. Gelone received his B.S. Pharm. and Pharm.D. from Temple University.
Francesco Maria Lavino has served as our chief commercial officer since July 10, 2017. Previously, Mr. Lavino served as associate vice president and global brand leader for the anti-infective portfolio at Merck & Co. from September 2015 to July 2017. Prior to Merck, Mr. Lavino was vice president of international marketing for Cubist Pharmaceuticals from December 2013 until September 2015. Before joining Cubist, Mr. Lavino spent 10 years with Merck & Co. in various roles, including serving as executive director and global brand leader for Merck's anti-fungal portfolio from January 2011 to November 2013. Mr. Lavino began his career in pharmaceutical sales at UCB S.A. and 3M Company in Italy. He has a B.A. in Pharmacy from the Federico II University of Napoli, Italy and an M.B.A. from SDA Bocconi School of Management in Milan, Italy.
Gary Sender has served as our chief financial officer since April 12, 2017. Mr. Sender previously served as our chief financial officer from May 2016 until the Redomiciliation. Prior to joining Nabriva Austria, he served as chief financial officer and executive vice president at Synergy Pharmaceuticals from 2015 to 2016. From 2009 until 2015, Mr. Sender served as senior vice president, Finance at Shire plc., supporting its Specialty Pharmaceuticals business and subsequently its Global Commercial businesses. He was responsible for financial management and support of all commercial areas of Shire's
135
Specialty Pharmaceutical and Rare Disease businesses, with an emphasis on resource allocation, financial forecasting, business cases and mergers and acquisitions. Prior to joining Shire, Mr. Sender was the founding CFO of Tengion, Inc. Mr. Sender also spent 15 years in a number of leadership roles within Merck. Mr. Sender received his B.S. from Boston University and an M.B.A from Carnegie-Mellon University.
Code of Business Conduct and Ethics
Our Code of Business Conduct and Ethics is applicable to all of our directors, officers and employees and is available on our website at http://investors.nabriva.com. Our Code of Business Conduct and Ethics provides that our directors, officers and employees are expected to avoid any action, position or interest that conflicts with the interests of our company or gives the appearance of a conflict. We expect that any amendment to this code, or any waivers of its requirements, will be disclosed on our website. Information contained on, or that can be accessed through, our website is not incorporated by reference into this document, and you should not consider information on our website to be part of this document.
Section 16(a) Beneficial Ownership Reporting Compliance
Section 16(a) of the Exchange Act requires our directors, executive officers and holders of more than 10% of our ordinary shares to file with the SEC initial reports of ownership of our ordinary shares and other equity securities on a Form 3 and reports of changes in such ownership on a Form 4 or Form 5. Our directors, executive officers and holders of more than 10% of our ordinary shares are required by SEC regulations to furnish us with copies of all Section 16(a) forms they file. Based solely on a review of our records and representations made by the persons required to file these reports, we believe that, during the year ended December 31, 2017, our directors, executive officers and holders of more than 10% of any class of equity securities complied with all Section 16(a) filing requirements applicable to them, except a late Form 4 was filed on May 17, 2017 on behalf of George Talbot reporting certain option exercises.
Deadline for Submission of Shareholder Proposals for 2018 Annual General Meeting of Shareholders
We currently intend to hold our Annual General Meeting of Shareholders, or the 2018 Annual Meeting, on Wednesday, August 1, 2018. The exact time and location of the 2018 Annual Meeting will be specified in our proxy statement for the 2018 Annual Meeting.
Proposals of shareholders intended to be presented at our 2018 Annual Meeting pursuant to Rule 14a-8 promulgated under the Exchange Act must be received by us at our offices at 25-28 North Wall Quay, Dublin 1, Ireland, Attention: Secretary, no later than May 15, 2018, in order to be included in the proxy statement and proxy card relating to that meeting. Such deadline has been extended from the deadline disclosed in our proxy statement filed with the SEC on August 18, 2017 in connection with our Extraordinary General Meeting of Shareholders, in order to reflect a reasonable time before we expect to begin to print and send our proxy materials to our shareholders for the 2018 Annual Meeting.
In addition, our memorandum and articles of association also provide that we be given advance notice of shareholder nominations for election to our board of directors and of other matters which shareholders wish to present for action at an annual general meeting of shareholders, other than matters included in our proxy statement in accordance with Rule 14a-8 of the Exchange Act. The required proper written notice must be received by the Secretary at our registered office at the address noted above, no later than 10th day following the day on which we first publicly announce the date of the 2018 Annual Meeting.
136
ITEM 11. EXECUTIVE COMPENSATION
The following discussion provides the amount of compensation paid, and benefits in-kind granted, by us and our subsidiaries to the members of our board of directors and certain executives for services provided in all capacities to us and our subsidiaries for the year ended December 31, 2017.
Executive and Director Compensation Processes
Our executive compensation program is administered by the compensation committee of our board of directors, subject to the oversight and approval of our full board of directors. Our compensation committee reviews our executive compensation practices on an annual basis and based on this review approves, or, as appropriate, makes recommendations to our board of directors for approval of our executive compensation program.
In designing our executive compensation program, our compensation committee considers publicly available compensation data for national and regional companies in the biotechnology/pharmaceutical industry to help guide its executive compensation decisions at the time of hiring and for subsequent adjustments in compensation. Since 2016, our compensation committee has retained Radford, a part of Aon Hewitt, a business unit of Aon plc, as its independent compensation consultant, to provide comparative data on executive compensation practices in our industry and to advise on our executive compensation program generally. The committee also has retained Radford for guidelines and review of non-employee director compensation. Although our compensation committee considers the advice and guidelines of Radford as to our executive compensation program, our compensation committee ultimately makes its own decisions about these matters. In the future, we expect that our compensation committee will continue to engage independent compensation consultants to provide additional guidance on our executive compensation programs and to conduct further competitive benchmarking against a peer group of publicly traded companies.
Our director compensation program is administered by our board of directors with the assistance of the compensation committee. The compensation committee conducts an annual review of director compensation and makes recommendations to the board of directors with respect thereto.
Summary Compensation Table
Our "named executive officers" for the year ended December 31, 2017 were as follows: Dr. Broom, our chief executive officer; Dr. Seltzer, our former chief medical officer Mr. Sender, our Chief Financial Officer and Dr. Gelone, our Chief Scientific Officer. The following table sets forth
137
information regarding compensation awarded to, earned by or paid to our named executive officers for the periods presented.
Name and principal position
|
Year | Salary($) | Option Awards ($)(1) |
Non-Equity Incentive Plan Compensation ($)(2) |
All Other Compensation ($)(3) |
Total ($) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Colin Broom |
2017 | 457,387 | 1,235,835 | 183,501 | 40,158 | 1,916,881 | |||||||||||||
Chief Executive Officer |
2016 | 410,354 | 769,798 | 175,776 | 43,043 | 1,398,971 | |||||||||||||
Elyse Seltzer |
2017 |
303,005 |
535,055 |
108,635 |
253,134 |
1,199,829 |
|||||||||||||
Chief Medical Officer(4) |
2016 | 365,022 | 284,978 | 106,505 | 23,735 | 780,241 | |||||||||||||
Gary Sender |
2017 |
360,303 |
535,055 |
104,125 |
32,997 |
1,032,480 |
|||||||||||||
Chief Financial Officer |
2016 | — | — | — | — | — | |||||||||||||
Steve Gelone |
2017 |
370,278 |
535,055 |
93,766 |
15,942 |
1,015,041 |
|||||||||||||
Chief Scientific Officer |
2016 | — | — | — | — | — | |||||||||||||
- (1)
- The
amounts reported in the "Option Awards" column reflect the aggregate fair value of share-based compensation awarded during the year computed in accordance with
the provisions of ASC Topic 718. See Note 10 to the consolidated audited financial statements regarding assumptions underlying the valuation of equity awards.
- (2)
- The
amounts reported in the "Non-Equity Incentive Plan Compensation" column represent awards to our named executive officers under our annual cash bonus program.
- (3)
- The
compensation included in the "All Other Compensation" column consists of amounts we contributed to our 401(k) plan and medical insurance premiums paid by us on
behalf of such individual. This column also includes severance benefits for Dr. Seltzer.
- (4)
- Dr. Seltzer resigned from her position as chief medical officer effective as of September 30, 2017.
Narrative Disclosure to Summary Compensation Table
Base Salary
In 2017, we paid annualized base salaries of $457,800 to Dr. Broom; $394,472 to Dr. Seltzer; $360,500 to Mr. Sender; and $390,000 to Dr. Gelone.. In 2016, we paid annualized base salaries of $436,000 to Dr. Broom; $368,740 to Dr. Seltzer; $350,000 to Mr. Sender; and $318,270 to Dr. Gelone.
In January 2018, our board of directors, following approval and recommendation from the compensation committee and consistent with the recommendations of the compensation committee's independent compensation consultant, approved an increase to the base salaries of our named executive officers for 2018 as follows: $471,534 for Dr. Broom, $$371,315 for Mr. Sender and $409,500 for Dr. Gelone. The board also approved 2018 base salaries for Mr. Crotty, our general counsel and secretary, of $341,250 and Mr. Lavino, our chief commercial officer, of $360,500, which also were consistent with the recommendation of the compensation committee's independent consultant.
None of our named executive officers is currently party to an employment agreement or other agreement or arrangement that provides for automatic or scheduled increases in base salary.
138
Annual Performance-Based Compensation
Our executive officers, which include the named executive officers, participate in our performance-based bonus program. All annual cash bonuses for our executives under the performance-based bonus program are tied to the achievement of strategic and operational corporate goals for the company, which are set by the compensation committee and approved by the board. There are no discretionary individual goals under the bonus program. The 2017 strategic and operational goals for Nabriva related to the following objectives:
- •
- corporate structure, including completing restructuring following the Redomiciliation;
- •
- finance, specifically fundraising;
- •
- commercial strategy, including hiring a chief commercial officer;
- •
- clinical development, including executing on both our Phase 3 clinical trials and critical path regulatory activities;
- •
- chemistry, manufacturing, and control (CMC), including manufacturing drug product registration batches and finalizing commercial supply
agreements with a risk mitigation plan for commercial supply;
- •
- discovery programs, specifically selecting a lead compound for development.
Under their respective employment agreements, the annual target bonus for Dr. Broom is 50% of his current base salary and the annual target bonus for each of Mr. Sender, Dr. Gelone, Mr. Crotty and Mr. Lavino is 35% of their respective current base salaries. The annual target bonus for Dr. Seltzer was 35% of her then-current base salary.
At a meeting held in December 2017, our compensation committee reviewed the accomplishments of the named executive officers as measured against the aforementioned 2017 goals. The compensation committee reviewed whether each goal had been obtained and the weight such goals should be given in determining the bonus payout for 2017 performance. Based on its review, the compensation committee recommended an 97.5% payout of the target bonuses for 2017, which were paid in January 2018. Accordingly, the 2017 bonus payouts were $223,177 for Dr. Broom, $123,021 for Mr. Sender and $126,822 for Dr. Gelone. Dr. Seltzer received a lump sum cash payment of $138,065 in full satisfaction of any bonus as part of her separation agreement.
Equity Incentive Awards
We believe that equity grants provide our executive officers with a strong link to our long-term performance, create an ownership culture and help to align the interests of our executive officers and our shareholders. In addition, we believe that equity grants with a time-based vesting feature promote executive retention because this feature incents our executive officers to remain in our employment during the vesting period. Accordingly, our board of directors periodically reviews the equity incentive compensation of our executive officers, which includes the named executive officers, and from time to time may grant equity incentive awards to them in the form of stock options. We also generally make stock option grants to new executive officers in connection with the commencement of their employment.
We have historically granted stock options with exercise prices that are set at no less than the fair market value of the underlying award on the date of grant, as determined by contemporaneous valuations and reviewed, and approved by our compensation committee or our board.
On January 31, 2018, our board of directors granted stock options under the 2017 Share Incentive Plan to Dr. Broom, Mr. Sender and Dr. Gelone. The options will vest over a four-year period beginning on January 31, 2018. Twenty-five percent (25%) of the option will vest on January 31, 2019,
139
and the remaining seventy-five percent (75%) will vest on a monthly pro-rata basis over the remaining vesting period. Each of the option awards had an exercise price $6.47 per share, which was the equivalent of the closing sale price of our ordinary shares on the Nasdaq Global Market on the grant date. Dr. Broom, Mr. Sender and Dr. Gelone were also granted Restricted Stock Units, or RSUs. Vesting of the RSUs is subject to U.S. Food and Drug Administration, or the FDA, approval of a new drug application, or NDA, for lefamulin. Fifty percent (50%) of each RSU award will vest upon FDA approval of an NDA for lefamulin, and the remaining fifty percent (50%) will vest on the one year anniversary of such approval. If the FDA does not approve an NDA for lefamulin within two years of the grant date, the RSU award will terminate in full. The award of RSUs to Dr. Broom is contingent upon shareholder approval of an amendment to our 2017 Share Incentive Plan.
The following table sets forth the number of our ordinary shares issuable upon exercise of the share awards granted to our named executive officers in 2018:
Name
|
Option Award (#) |
RSU Award (#) |
|||||
|---|---|---|---|---|---|---|---|
Colin Broom |
200,000 | 67,500 | |||||
Gary Sender |
100,000 | 22,500 | |||||
Steve Gelone |
100,000 | 22,500 | |||||
On February 7, 2017, our board of directors granted stock options under the Stock Option Plan 2015 to Drs. Broom, Seltzer and Gelone and Mr. Sender. Vesting of the options began on February 28, 2017 and will end on February 28, 2021. Twenty-five percent (25%) of the option vested on February 28, 2018, and the remaining seventy-five percent (75%) will vest on a monthly pro-rata basis over the remaining vesting period. Prior to the Redomiciliation, each of the option awards had an exercise price of €79.63 ($85.00) per share, which was the equivalent of the closing sale price of Nabriva Austria's common shares underlying its American Depositary Shares on the Nasdaq Global Market on the grant date. Following the Redomiciliation and effective June 23, 2017, each of Nabriva Austria's Stock Option Plan 2007 and Stock Option Plan 2015 was amended to take account of certain requirements under Irish law, and we assumed the existing awards thereunder. In connection with such amendment and assumption, each outstanding stock option granted under the Stock Option Plan 2015 was substituted for an economically identical option, denominated in our ordinary shares, with each option to acquire one Nabriva Austria common share becoming an option to acquire ten of our ordinary shares on the same terms and conditions. Prior to the Redomiciliation, the options also had a grant date fair value of €44.36 ($47.35) per share, as determined in accordance with ASC Topic 718.
The following table sets forth the number of our ordinary shares issuable upon exercise of the stock options granted in 2017:
Name
|
Option Award (#) |
|||
|---|---|---|---|---|
Colin Broom |
261,000 | |||
Gary Sender |
113,000 | |||
Steve Gelone |
113,000 | |||
Elyse Seltzer |
113,000 | |||
140
Outstanding Equity Awards as of December 31, 2017
The following table sets forth information regarding outstanding stock options held by our named executive officers as of December 31, 2017:
| |
Option Awards | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Name
|
Number of securities underlying unexercised options (#) exercisable |
Number of securities underlying unexercised options (#) unexercisable |
Option exercise price ($) |
Option expiration date |
|||||||
Colin Broom |
131,892 | 26,378 | (1) | 7.21 | 7/5/2025 | ||||||
|
118,960 | 77,940 | (2) | 7.21 | 7/5/2025 | ||||||
|
69,208 | 81,792 | (3) | 8.34 | 2/4/2026 | ||||||
|
— | 261,000 | (4) | 8.50 | 2/7/2027 | ||||||
Elyse Seltzer(5) |
57,344 |
22,197 |
(5) |
7.21 |
7/5/2025 |
||||||
|
25,621 | 13,975 | (6) | 8.34 | 2/4/2026 | ||||||
|
— | 51,792 | (7) | 8.50 | 2/28/2027 | ||||||
Gary Sender |
35,150 |
53,650 |
(9) |
7.08 |
5/31/2026 |
||||||
|
— | 113,000 | (8) | 8.50 | 2/7/2027 | ||||||
Steve Gelone |
59,800 |
28,990 |
(11) |
7.21 |
7/5/2025 |
||||||
|
25,621 | 30,279 | (11) | 8.34 | 2/4/2026 | ||||||
|
— | 113,000 | (8) | 8.50 | 2/7/2027 | ||||||
- (1)
- Dr. Broom's
option to purchase 158,270 of our ordinary shares vests over four years, with 25% of the options vesting on August 31, 2015, and the
remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period.
- (2)
- Dr. Broom's
option to purchase 196,900 of our ordinary shares vests over four years, with 25% of the options vesting on July 31, 2016, and the
remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period.
- (3)
- Dr. Broom's
option to purchase 151,000 of our ordinary shares vests over four years, with 25% of the options vesting on February 28, 2017, and the
remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period.
- (4)
- Dr. Broom's
option to purchase 261,000 of our ordinary shares vests over four years, with 25% of the options vesting on February 28 2018, and the
remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period.
- (5)
- Dr. Seltzers's
option to purchase 88,790 of our ordinary shares vests over four years, with 25% of the options vesting on May 31, 2016, and the
remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period. Dr. Seltzer will forfeit 9,249 options upon the expiration of her
consulting agreement.
- (6)
- Dr. Seltzer's
option to purchase 55,900 of our ordinary shares vests over four years, with 25% of the options vesting on February 28, 2017, and the
remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period. Dr. Seltzer will forfeit 16,304 options upon the expiration of her
consulting agreement.
- (7)
- Dr. Seltzer's option to purchase 113,000 of our ordinary shares vests over four years, with 25% of the options vesting on February 28, 2018, and the remaining 75% of the option vesting on a
141
monthly pro-rata basis over the remaining three years of the vesting period. Dr. Seltzer will forfeit 61,208 options upon the expiration of her consulting agreement.
- (8)
- Mr. Sender's
and Dr. Gelone's option to purchase 113,000 of our ordinary shares vests over four years, with 25% of the options vesting on
February 28, 2018, and the remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period.
- (9)
- Mr. Sender's
option to purchase 88,800 of our ordinary shares vests over four years, with 25% of the options vesting on May 31, 2017, and the remaining
75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period.
- (10)
- Dr. Gelone's
option to purchase 88,790 of our ordinary shares vests over four years, with 25% of the options vesting on May 31, 2016, and the
remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period.
- (11)
- Dr. Gelone's option to purchase 55,900 of our ordinary shares vests over four years, with 25% of the options vesting on February 28, 2017, and the remaining 75% of the option vesting on a monthly pro-rata basis over the remaining three years of the vesting period.
Employment Agreements with Executive Officers
Agreement with Colin Broom, Chief Executive Officer and Director
Dr. Broom was appointed chief executive officer of Nabriva Austria and entered into an employment agreement dated and effective as of August 28, 2014, which was amended and restated as of June 17, 2016. He was appointed our chief executive officer on April 12, 2017 and also serves on our board. His employment agreement automatically renews each August 28 for an additional one-year term, unless either we or Dr. Broom timely provide a notice of non-renewal, as described below.
The employment agreement, and Dr. Broom's employment, may be terminated as follows: (1) either party may notify the other, in writing and not less than 90 days prior to the applicable term's expiration date, of its intention not to renew the term of employment; (2) upon Dr. Broom's death or "disability" (as disability is defined in his employment agreement); (3) at our election, with or without "cause" (as cause is defined in his employment agreement); and (4) at Dr. Broom's election, with or without "good reason" (as good reason is defined in his employment agreement).
In the event of the termination of Dr. Broom's employment by us without cause, including as a result of a termination of his employment following our delivery to Dr. Broom of a notice of non-renewal, or by him for good reason prior to, or more than twelve months following, a "change in control" (as change in control is defined in his employment agreement), Dr. Broom will be entitled to his base salary that has accrued and to which he is entitled as of the termination date. In addition, subject to his execution and nonrevocation of a release of claims in our favor and his continued compliance with his proprietary rights, non-disclosure and developments agreement with us, he is entitled to (1) continued payment of his base salary, in accordance with our regular payroll procedures, for a period of 18 months (2) provided he is eligible for and timely elects to continue receiving group medical insurance under COBRA and the payments would not result in the violation of nondiscrimination requirements of applicable law, payment by us of the portion of health coverage premiums we pay for similarly-situated, active employees who receive the same type of coverage, for a period of up to 18 months following his date of termination, (3) a lump sum payment equal to any earned but unpaid annual bonus for a previously completed calendar year and (4) a lump sum payment equal to a prorated annual bonus for the year in which Dr. Broom's employment is terminated based on the number of days he provided services to us during the year in which his employment is terminated.
142
In the event of the termination of Dr. Broom's employment by us without cause, including as a result of a termination of his employment following our delivery to Dr. Broom of a notice of non-renewal, or by him for good reason prior to, or by him for good reason within twelve months following a change in control, subject (as described above with respect to certain payments), to his execution and nonrevocation of a release of claims in our favor and his continued compliance with his proprietary rights, non-disclosure and developments agreement with us, Dr. Broom would be entitled to the same payments and benefits as described in the preceding paragraph, except that, in lieu of a pro-rated annual bonus payment, he would be entitled to receive a lump sum payment equal to 100% of his target bonus for the year in which his employment is terminated and he shall also be entitled to full vesting acceleration of his then-unvested equity awards, whether granted under the 2017 Share Incentive Plan or any successor equity incentive plan, such that his equity awards become fully exercisable and non-forfeitable as of the termination date.
If Dr. Broom's employment is terminated for any other reason, including as a result of his death or disability, for cause, or voluntarily by Dr. Broom without good reason, our obligations under the employment agreement cease immediately, and Dr. Broom is only entitled to his base salary that has accrued and to which he is entitled as of the termination date and solely if his employment is terminated as a result of his death or disability, subject to his execution and nonrevocation of a release of claims in our favor and his continued compliance with his proprietary rights, non-disclosure and developments agreement with us, he or his estate, as applicable, is entitled to any earned but unpaid annual bonus from a previously completed calendar year.
Pursuant to his amended and restated employment agreement, Dr. Broom is entitled to receive an annual base salary of $471,534. His base salary is reviewed by our compensation committee and the board of directors in the first quarter of each fiscal year and any adjustment to his base salary is retroactively effective to the first day of such fiscal year. In addition, Dr. Broom is eligible for an annual discretionary bonus of 50% of his current base salary. He is also eligible to receive equity awards at such times and on such terms and conditions as the Board may determine and is also entitled to participate in any and all benefit programs that we make available to our named executive officers, for which he may be eligible, under the plan documents governing such programs.
As a condition of his employment, Dr. Broom signed a proprietary rights, non-disclosure and developments agreement.
Agreements with other Executive Officers
Mr. Sender was appointed chief financial officer of Nabriva Austria and entered into an employment agreement dated and effective as of May 2, 2016. He was appointed our chief financial officer on April 12, 2017. Dr. Gelone was appointed chief development officer and entered into an employment agreement dated and effective as of December 1, 2014, which was amended and restated as of May 26, 2016. Mr. Crotty was appointed general counsel and secretary of Nabriva Austria and entered into an employment agreement dated and effective as of June 14, 2017. Dr. Gelone was appointed as our chief development officer and Mr. Crotty was appointed our general counsel and secretary effective as of June 23, 2017. Dr. Gelone was subsequently appointed our chief scientific officer on June 30, 2017. Mr. Lavino was appointed our chief commercial officer and entered into an employment agreement dated and effective as of July 10, 2017. Each of these employment agreements provides that such executive officer is an at-will employee, and his or her employment with us can be terminated by the respective executive officer or us at any time and for any reason.
The employment agreements and the employment of each of Mr. Sender, Dr. Gelone, Mr. Crotty and Mr. Lavino may be terminated in one of three ways: (1) upon the death or "disability" (as disability is defined in the applicable employment agreement) of such executive officer; (2) at our election, with or without "cause" (as cause is defined in the applicable employment agreement); and
143
(3) at such executive officer's election, with or without "good reason" (as good reason is defined in the applicable employment agreement).
In the event of the termination of such executive officer's employment by us without cause or by him or her for good reason prior to, or more than twelve months following, a "change in control" (as change in control is defined in the applicable employment agreement), such executive officer will be entitled to his or her base salary that has accrued and to which he or she is entitled as of the termination date. In addition, subject to such executive officer's execution and nonrevocation of a release of claims in our favor and his or her continued compliance with his or her proprietary rights, non-disclosure and developments agreement with us, such executive officer is entitled to (1) continued payment of such executive officer's base salary, in accordance with our regular payroll procedures, for a period of 12 months, (2) provided he or she is eligible for and timely elects to continue receiving group medical insurance under COBRA and the payments would not result in the violation of nondiscrimination requirements of applicable law, payment by us of the portion of health coverage premiums we pay for similarly-situated, active employees, who receive the same type of coverage, for a period of up to 12 months following the date of termination, (3) a lump sum payment equal to any earned but unpaid annual bonus for a previously completed calendar year and (4) a lump sum payment equal to a prorated annual bonus for the year in which such executive officer's employment is terminated based on the number of days such executive officer provided services to us during the year in which such executive officer's employment is terminated.
In the event of the termination of the executive officer's employment by us without cause or by him or her for good reason within twelve months following a change in control, subject (as describe above with respect to certain payments) to such executive officer's execution and nonrevocation of a release of claims in our favor and his or her continued compliance with his or her proprietary rights, non-disclosure and developments agreement with us, such executive officer will be entitled to the same payments and benefits as described in the preceding paragraph, except that, in lieu of a pro-rated annual bonus payment, such executive officer will be entitled to receive a lump sum payment equal to 100% of such executive officer's target bonus for the year in which his or her employment is terminated, and such executive officer shall also be entitled to full vesting acceleration of his or her then-unvested equity awards, whether granted under the 2017 Share Incentive Plan or any successor equity incentive plan, such that his or her equity awards become fully exercisable and non-forfeitable as of the termination date.
If such executive officer's employment is terminated for any other reason, including as a result of his or her death or disability, for cause, or voluntarily by such executive officer without good reason, our obligations under the applicable employment agreement cease immediately, and such executive officer is only entitled to his or her base salary that has accrued and to which he or she is entitled as of the termination date and, solely if such executive officer's employment is terminated as a result of his or her death or disability and subject to his or her execution and nonrevocation of a release of claims in our favor and his or her continued compliance with his or her proprietary rights, non-disclosure and developments agreement with us, such executive officer or the estate of such executive officer, as applicable, is entitled to any earned but unpaid annual bonus from a previously completed calendar year.
Pursuant to their respective employment agreements, each of these executive officers is entitled to an annual base salary, as follows: Mr. Sender: $371,315; Dr. Gelone: $409,500; Mr. Crotty: $341,250 and Mr. Lavino: $360,500. Such base salary is reviewed by our compensation committee and the board of directors in the first quarter of each fiscal year and any adjustment to such base salary is retroactively effective to the first day of such fiscal year. In addition, such executive officers are eligible for an annual discretionary bonus of 35% of their current base salary. Each executive officer is also eligible to receive equity awards at such times and on such terms and conditions as the Board may determine and is also entitled to participate in any and all benefit programs that we make available to
144
our executive officers, for which he or she may be eligible, under the plan documents governing such programs.
As a condition to their employment, each of Mr. Sender, Dr. Gelone, Mr. Crotty and Mr. Lavino signed a proprietary rights, non-disclosure and developments agreement.
Agreements with Elyse Seltzer, former Chief Medical Officer
Dr. Seltzer was appointed chief medical officer of Nabriva Austria and entered into an employment agreement dated and effective as of April 14, 2015, which was amended and restated as of May 26, 2016. Dr. Seltzer resigned as chief medical officer, effective September 30, 2017. Under her amended and restated employment agreement, she was entitled to an annual base salary of $394,552. We entered into a Separation and Release of Claims Agreement, or the Separation Agreement, with Dr. Seltzer prior to her resignation. We also agreed to enter into a Consulting Agreement with Dr. Seltzer, effective as of the date of her resignation, pursuant to which Dr. Seltzer agreed to provide to us, upon the request of our chief executive officer, consulting and advisory services in the areas of clinical development, regulatory affairs and drug safety from October 1, 2017 through December 31, 2018.
Under the Separation Agreement, Dr. Seltzer is entitled to the following severance benefits: (1) cash payment of $394,472, which represents her current annual base salary, paid in two lump sum payments at the beginning and end of the six-month period following the date of her resignation, less all applicable taxes and withholdings, a portion of which may be allocated to professional fees at Dr. Seltzer's direction and (2) a lump sum cash payment of $138,065 in full satisfaction of any bonus to which Dr. Seltzer may have been entitled for 2017, paid no later than March 15, 2018. Furthermore, under her Separation Agreement, Dr. Seltzer has until September 30, 2019 to exercise all of her vested outstanding options to purchase our ordinary shares. In addition, we agreed to pay for the our share of the cost of Dr. Seltzer's group health coverage under any our benefit plans for up to twelve months in accordance with the Consolidated Omnibus Budget Reconciliation Act of 1985. Pursuant to the Separation Agreement, Dr. Seltzer also executed a release of all claims and reaffirmed her confidentiality, non-solicitation and non-compete obligations under her existing agreement with the Company.
Under the Consulting Agreement, Dr. Seltzer (1) is paid a retainer of $32,879.33 per month for her performance of services from October 1, 2017 through March 31, 2018, (2) receives consulting fees at a rate of $500.00 per hour for her performance of services from April 1, 2018 until December 31, 2018 and (3) is entitled to the continued vesting of her unvested options to purchase our ordinary shares through December 31, 2018. The Consulting Agreement may be terminated (1) by us if Dr. Seltzer materially breaches the Consulting Agreement or the Separation Agreement; (2) by Dr. Seltzer if we materially breach the Consulting Agreement or the Separation Agreement; (3) at any time upon the mutual written consent of the parties; or (4) automatically upon the death, physical incapacitation or mental incompetence of Dr. Seltzer. In the event Dr. Seltzer dies during the term of the Consulting Agreement, the compensation and continued vesting will inure to the benefit of her estate.
Equity Incentive Plans
In this section, we describe our 2017 Share Incentive Plan, Stock Option Plan 2015 and Stock Option Plan 2007. Prior to the Redomiciliation, Nabriva Austria granted awards to eligible recipients under both the Stock Option Plan 2007 and the Stock Option Plan 2015. In connection with the Redomiciliation, both plans were amended to take account of certain requirements under Irish law and assumed by us, with each option to acquire one Nabriva Austria common share becoming an option to acquire ten of our ordinary shares on the same terms and conditions. We currently make share awards
145
to eligible recipients solely under our 2017 Share Incentive Plan. On September 27, 2017, our Stock Option Plan 2007 terminated according to its terms.
2017 Share Incentive Plan
The 2017 Share Incentive Plan permits the award of share options, share appreciation rights, or SARs, restricted shares, restricted share units or RSUs, and other share-based awards to our employees, officers, directors, consultants and advisers. Our board of directors will administer the 2017 Share Incentive Plan. As of January 31, 2018, under our 2017 Share Incentive Plan, there were 3,423,141 ordinary shares available for issuance under the plan. Shares covered by awards under the 2017 Share Incentive Plan that expire or are terminated, surrendered, or cancelled without having been fully exercised or are forfeited in whole or in part or that result in any shares not being issued will again be available for the grant of awards under the 2017 Share Incentive Plan (subject, in the case of incentive share options, to any limitations under the Internal Revenue Code, or the Code).
Options and SARs granted under the 2017 Share Incentive Plan may not have an exercise price or measurement price, respectively, that is less than 100% of the fair market value of our ordinary shares on the date of grant; provided, however, that if our board of directors approves the grant of an option or SAR with an exercise price or measurent price to be determined on a future date, such price may not be less than 100% of the fair market value of our ordinary shares on such future date. Such options and SARs will be exercisable at such times and subject to such terms and conditions as the board may specify in the applicable option or SAR agreement. No option or SAR will be granted with a term in excess of ten years.
Restricted shares and RSUs granted under the 2017 Share Incentive Plan will determine the terms and conditions of restricted shares and RSUs, including the conditions for vesting and repurchase (or forfeiture) and the issue price, if any.
If, during the term of the 2017 Share Incentive Plan, there is a change in our capital or a restructuring measure which has an effect on our capital, such as a share split or reverse share split, which change or measure results in a change in the value of the share-based awards outstanding under the 2017 Share Incentive Plan, the board will make appropriate adjustments to the price or the amount of such outstanding awards.
The 2017 Share Incentive Plan also contains provisions addressing the consequences of any reorganization event. A reorganization event is defined as (a) any merger or consolidation of us with or into another entity as a result of which all of our ordinary shares are converted into or exchanged for the right to receive cash, securities or other property, or are cancelled, (b) any transfer or disposition of all of our ordinary shares for cash, securities or other property pursuant to a share exchange or other transaction or (c) our liquidation or dissolution; any one of which, (a), (b) or (c), may be effected pursuant to the laws of the Republic of Ireland.
The 2017 Share Incentive Plan provides that, if a reorganization event occurs, the board of directors may take one or more of the following actions to all or any outstanding awards other than restricted shares on such terms as the board of directors determines: (1) provide that such awards will be assumed, or substantially equivalent awards will be substituted, by the acquiring or succeeding corporation (or an affiliate thereof), (2) upon written notice to a participant, provide that all of the participant's unvested awards will be forfeited immediately prior to the consummation of such reorganization event and/or that all of the participant's unexercised awards will terminate immediately prior to the consummation of such reorganization event unless exercised by the participant (to the extent then exercisable) within a specified period following the date of such notice, (3) provide that outstanding awards will become exercisable, realizable, or deliverable, or restrictions applicable to an award will lapse, in whole or in part prior to or upon such reorganization event, (4) in the event of a reorganization event under the terms of which holders of our ordinary shares will receive, upon
146
consummation thereof, a cash payment for each share surrendered in the reorganization event, which we refer to as the Acquisition Price, make or provide for a cash payment to participants with respect to each award held by a participant equal to (A) the number of ordinary shares subject to the vested portion of the award (after giving effect to any acceleration of vesting that occurs upon or immediately prior to such reorganization event) multiplied by (B) the excess, if any, of (I) the Acquisition Price over (II) the exercise, measurement or purchase price of such award and any applicable tax withholdings, in exchange for the termination of such award, (5) provide that, in connection with our liquidation or dissolution, awards will convert into the right to receive liquidation proceeds (if applicable, net of the exercise, measurement or purchase price thereof and any applicable tax withholdings) and (6) any combination of the foregoing. Our board is not obligated to treat all awards, all awards held by a participant, or all awards of the same type, identically.
No award may be grnted under the 2017 Share Incentive Plan after September 14, 2027. The board of directors may, at any time, amend, suspend or terminate the 2017 Share Incentive Plan or any portion thereof. However, if shareholder approval is required, including by application of Irish law, the board may not effect such modification or amendment without such approval.
Stock Option Plan 2015
The Stock Option Plan 2015 provided for the grant of options to purchase our ordinary shares to our employees, including executive officers, and to directors. As of January 31, 2018, under our Stock Option Plan 2015, there were options to purchase an aggregate of 3,015,849 of our ordinary shares at a weighted average exercise price of $8.35 per share and no ordinary shares were available for issuance under the plan. Following the approval of the 2017 Share Incentive Plan by our shareholders on September 15, 2017, we ceased granting awards under the Stock Option Plan 2015, Unless the context specifically indicates otherwise, references to our Stock Option Plan 2015 in this Annual Report on Form 10-K refer to the Stock Option Plan 2015, as amended and adopted by us.
Options granted under the Stock Option Plan 2015 entitle beneficiaries thereof to purchase our ordinary shares at an exercise price equal to 100% of the fair market value per share on the beneficiary's date of participation, which following the Redomiciliation was derived from the closing sale price of our ordinary shares on the Nasdaq Global Market. Options granted under the Stock Option Plan 2015 generally vest over four years from the beneficiary's date of participation. Typically, 25% of the options subject to a particular grant vest on the last day of the last calendar month of the first year of the vesting period, and the remaining 75% vests on a monthly pro-rata basis over the second, third and fourth years of the vesting period (i.e., 2.083% per month). Any alternative vesting period determined by us is subject to approval by our executive officers, board of directors or shareholders, in accordance with any applicable voting requirements.
The Stock Option Plan 2015 provides that, if a liquidity event (as defined below) occurs, all options outstanding under the Stock Option Plan 2015 will be assumed (or substantially equivalent awards will be substituted by an acquiring or succeeding corporation (or an affiliate of the acquiring or succeeding corporation)), and any then-unvested options shall continue to vest in accordance with the beneficiary's original vesting schedule. If a beneficiary is terminated due to a good leaver event (within the meaning of the Stock Option Plan 2015), on or prior to the first anniversary of the date of the liquidity event, the beneficiary's options will be immediately exercisable in full as of the date of such termination. If the acquiring or succeeding corporation (or an affiliate of the acquiring or succeeding corporation) refuses to assume the options outstanding under the Stock Option Plan 2015 or to substitute substantially equivalent options therefor, all then-unvested options under the Stock Option Plan 2015 will automatically vest in full upon the liquidity event. For purposes of the Stock Option Plan 2015, a liquidity event generally refers to an exclusive license of or the sale, lease or other disposal of all or substantially all of our assets, a sale or other disposal (but not a pledge) of 50% or more of our shares, a merger or consolidation of us with or into any third party, or our liquidation, winding up or other form of dissolution of us.
147
Unless otherwise specifically permitted in an option agreement or resolved upon by the board of directors, the exercise of vested options is permitted under the Stock Option Plan 2015 only during specified periods and on specified terms in the case of a liquidity event or following an initial public offering occurring during the term of the option. A beneficiary is entitled to exercise vested options at any time during the remaining term of the option while the beneficiary is providing services to us, and within the three-month period following a termination of the beneficiary's services due to a good leaver event. Options granted under the Stock Option Plan 2015 will have a term of no more than ten years from the beneficiary's date of participation.
If, during the term of the Stock Option Plan 2015, there is a change in our capital or a restructuring measure which has an effect on our capital, such as a stock split or reverse stock split, which change or measure results in a change in the value of the options outstanding under the Stock Option Plan 2015, the board may make appropriate adjustments to the price or the amount of such outstanding options.
The board of directors may, at any time, amend, suspend or terminate the Stock Option Plan 2015 in whole or in part. However, if shareholder approval is required, including by application of Irish law, the board may not effect such modification or amendment without such approval.
Stock Option Plan 2007
Prior to the Redomiciliation, the Stock Option Plan 2007 provided for the grant of options to purchase common shares of Nabriva Austria to certain of our employees, including our executive officers, directors, and other beneficiaries. After September 27, 2017, no options were permitted to be exercised under the Stock Option Plan 2007. Any options not exercised by September 27, 2017 were automatically terminated and forfeited.
401(k) Plan
We maintain a defined contribution employee retirement plan for our U.S.-based employees. Our 401(k) plan is intended to qualify as a tax-qualified plan under Section 401 of the Internal Revenue Code, so that contributions to our 401(k) plan, and income earned on such contributions, are not taxable to participants until withdrawn or distributed from the 401(k) plan. Our 401(k) plan provides that each participant may contribute up to 90% of his or her pre-tax compensation, up to a statutory limit, which is $18,000 for 2017. Participants who are at least 50 years old can also make "catch-up" contributions, which in 2017 may be up to an additional $6,000 above the statutory limit. Under our 401(k) plan, each employee is fully vested in his or her deferred salary contributions. Employee contributions are held and invested by the plan's trustee, subject to participants' ability to give investment directions by following certain procedures. We match 100.0% of the first 3.0% of the employee's voluntary contribution to the 401(k) plan and 50.0% of the next 2.0% contributed by the employee.
Risk Considerations in Our Compensation Program
Our compensation committee has reviewed and evaluated the philosophy and standards on which our compensation plans have been developed and implemented across our company. It is our belief that our compensation programs do not encourage inappropriate actions or risk taking by our executive officers. We do not believe that any risks arising from our employee compensation policies and practices are reasonably likely to have a material adverse effect on our company. In addition, we do not believe that the mix and design of the components of our executive compensation program encourage management to assume excessive risks.
148
Summary Compensation Table
The following table sets forth a summary of the compensation earned by the members of the board of directors for the year ended December 31, 2017. These amounts include compensastion earned for service on the supervisory board of our predecessor, Nabriva Austria, during the year ended December 31, 2017.
Name
|
Fees Earned or Paid in Cash ($)(1) |
Option Awards ($)(2) |
Total ($) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
Daniel Burgess(3) |
78,781 | 37,552 | (6) | 116,333 | ||||||
Axel Bolte(4) |
— | — | — | |||||||
Chau Khuong(8) |
19,836 | — | 19,836 | |||||||
George Talbot(3) |
36,764 | 37,552 | (6) | 74,316 | ||||||
Charles Rowland, Jr.(3) |
58,178 | 37,552 | (6) | 95,730 | ||||||
Stephen Webster(3) |
48,319 | 37,552 | (6) | 85,871 | ||||||
Mark Corrigan(3) |
40,429 | 37,552 | (6) | 77,981 | ||||||
Carrie Bourdow(7) |
22,181 | 159,944 | (5) | 182,125 | ||||||
- (1)
- Fees
paid in cash consist of director retainer fees.
- (2)
- The
amounts reported in the "Option Awards" column reflect the aggregate fair value of share-based compensation awarded during 2017 computed in accordance with the
provisions of ASC Topic 718.
- (3)
- Represents
the pro-rata amount of the annual cash retainer fees approved by the shareholders of Nabriva Austria at its annual general meeting of shareholders in
August 2017 and the pro-rata amount of the annual cash retainer fees approved by our shareholders at our extraordinary general meeting of shareholders in September 2017.
- (4)
- Mr. Bolte
has declined to accept either cash or equity compensation for his services on the Nabriva Austria supervisory board and our board of directors.
- (5)
- Represents
the grant of (i) an option to purchase 10,100 of our ordinary shares vesting with respect to all of the shares on the last date of the month of the
first anniversary of the grant date, and (ii) an option to purchase 20,200 of our ordinary shares vesting over a three-year period on a monthly pro-rata basis at the end of each successive
month following the date of the initial grant.
- (6)
- Represents
the grant of an option to purchase 10,100 of our ordinary shares vesting with respect to all of the shares on the last date of the month of the first
anniversary of the grant date.
- (7)
- Represents
the pro-rata amount of the annual cash retainer fees approved by our shareholders at the extraordinary general meeting of shareholders in September 2017.
- (8)
- Represents the pro-rata amount of the annual cash retainer fees approved by the shareholders of Nabriva Austria at its annual general meeting of shareholders in August 2017.
Director Compensation Arrangements
At the Nabriva Austria annual general meeting of shareholders in August 2016, the shareholders of Nabriva Austria approved a compensation plan for its non-employee supervisory board members,
149
effective as of the date of such meeting. The Nabriva Austria non-employee supervisory board member compensation policy provided for the following:
- •
- each new non-employee supervisory board member received an initial grant of an option under the Stock Option Plan 2015 to purchase 2,020 of
Nabriva Austria's common shares upon his or her initial election to the supervisory board;
- •
- each non-employee supervisory board member received an annual grant of an option under Stock Option Plan 2015 to purchase 1,010 of Nabriva
Austria's common shares on the date of Nabriva Austria's annual general meeting of shareholders;
- •
- each non-employee supervisory board member received an annual cash fee of $35,000;
- •
- the chairman of Nabriva Austria's supervisory board received an additional annual cash fee of $25,000;
- •
- each non-employee supervisory board member who was a member of the audit committee received an additional annual cash fee of $7,500 ($15,000
for the audit committee chair);
- •
- each non-employee supervisory board member who was a member of the compensation committee received an additional annual cash fee of $5,000
($10,000 for the compensation committee chair); and
- •
- each non-employee supervisory board member who was a member of the nominating and corporate governance committee received an additional annual cash fee of $3,500 ($7,500 for the nominating and corporate governance committee chair).
The stock options granted to Nabriva Austria's non-employee supervisory board members under its non-employee supervisory board member compensation policy had an exercise price equal to the fair market value of the Nabriva Austria common shares on the date of grant and will expire ten years after the date of grant. The initial stock options granted to newly elected Nabriva Austria non-employee supervisory board members vest, subject to such member's continued service on the board, over a three-year period on a monthly pro-rata basis at the end of each successive month following the date of the initial grant. The annual stock options granted to the Nabriva Austria non-employee supervisory board members vest, subject to such member's continued service on the board, fully on the last date of the month of the first anniversary of the grant date.
Prior to the Redomiciliation, the annual cash fee was payable to supervisory board members in arrears in four equal quarterly installments payable the week following the end of each quarter. The amount of each payment was prorated for any portion of a quarter that a member was not serving on the supervisory board. Each non-employee supervisory board member was also entitled to reimbursement for reasonable travel and other expenses incurred in connection with attending meetings of the supervisory board and any committee on which he or she served or otherwise in direct service of the company. Those amounts are excluded from the table above.
Following the Redomiciliation, the Nabriva Austria non-employee supervisory board member compensation policy was terminated and in July 2017, we adopted a non-employee director compensation policy for our directors, which provides for the following:
- •
- each new non-employee director receives an initial grant of an option to purchase 20,200 of our ordinary shares upon his or her initial
election to the board of directors;
- •
- each non-employee director receives an annual grant of an option to purchase 10,100 of our ordinary shares on the date of our annual general
meeting of shareholders;
- •
- each non-employee director receives an annual cash fee of $38,500;
- •
- the chairman of our board of directors receives an additional annual cash fee of $27,500;
150
- •
- each non-employee director who is a member of the audit committee receives an additional annual cash fee of $8,250 ($16,500 for the audit
committee chair);
- •
- each non-employee director who is a member of the compensation committee receives an additional annual cash fee of $5,500 ($11,000 for the
compensation committee chair); and
- •
- each non-employee director who is a member of the nominating and corporate governance committee receives an additional annual cash fee of $3,850 ($8,250 for the nominating and corporate governance committee chair).
The stock options to be granted to our non-employee directors under our non-employee director compensation policy have an exercise price equal to the fair market value of our ordinary shares on the date of grant and will expire ten years after the date of grant. The initial stock options granted to newly elected director vest, subject to such director's continued service on the board, over a three-year period on a monthly pro-rata basis at the end of each successive month following the date of the initial grant. The annual stock options granted to directors will vest, subject to such director's continued service on the board, fully on the last date of the month of the first anniversary of the grant date.
Under our non-employee director compensation policy, the annual cash fees are payable in arrears in four equal quarterly installments payable the week following the end of each quarter. Each non-employee director is also entitled to reimbursement for reasonable travel and other expenses incurred in connection with attending meetings of the board of directors and any committee on which he or she serves or otherwise in direct service of the company.
ITEM 12. SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS
The following table sets forth information with respect to the beneficial ownership of our ordinary shares as of January 31, 2018 by:
- •
- each of our directors and director nominees;
- •
- each of our "named executive officers";
- •
- all of our directors and executive officers as a group; and
- •
- each person, or group of affiliated persons, who is known by us to beneficially own more than 5% of our ordinary shares.
The percentages in the columns entitled "Percentage of Shares Beneficially Owned" are based on a total of 36,715,652 ordinary shares outstanding as of January 31, 2018.
Beneficial ownership is determined in accordance with the rules and regulations of the SEC and includes voting or investment power with respect to our ordinary shares. Our ordinary shares subject to options that are currently exercisable or exercisable within 60 days of January 31, 2018 are considered outstanding and beneficially owned by the person holding the options for the purpose of calculating the percentage ownership of that person but not for the purpose of calculating the percentage ownership of any other person. Except as otherwise noted, the persons and entities in this table have sole voting and investing power with respect to all of the ordinary shares beneficially owned by them, subject to
151
community property laws, where applicable. Except as otherwise set forth below, the address of the beneficial owner is c/o Nabriva Therapeutics plc, 25-28 North Wall Quay, Dublin 1, Ireland.
Name and Address of Beneficial Owner
|
Number of Shares Beneficially Owned |
Percentage of Shares Beneficially Owned |
|||||
|---|---|---|---|---|---|---|---|
Directors, Director Nominees and Named Executive Officers: |
|||||||
Daniel Burgess(1) |
20,761 | * | % | ||||
Axel Bolte(2) |
— | * | % | ||||
George H. Talbot(3) |
69,907 | * | % | ||||
Mark Corrigan(1) |
20,761 | * | % | ||||
Stephen Webster(1) |
20,761 | * | % | ||||
Charles A. Rowland, Jr.(4) |
20,767 | * | % | ||||
Carrie Bourdow |
4,489 | * | % | ||||
Colin Broom (5) |
582,385 | 1.57 | % | ||||
Steve Gelone(6) |
137,808 | * | % | ||||
Gary Sender(7) |
75,504 | * | % | ||||
Elyse Seltzer(8) |
125,012 | * | % | ||||
All current directors and executive officers as a group (12 individuals)(9) |
1,079,724 | 2.87 | % | ||||
5% Shareholders: |
|||||||
Entities affiliated with Vivo Capital(10) |
4,074,190 | 11.10 | % | ||||
OrbiMed Private Investments V, L.P.(11) |
3,919,600 | 10.68 | % | ||||
Novo A/S(12) |
2,924,822 | 7.97 | % | ||||
HBM Healthcare Investments (Cayman) Ltd. and an affiliated entity(13) |
2,334,008 | 6.36 | % | ||||
venBio Global Strategic Fund II, L.P.(14) |
2,222,962 | 6.05 | % | ||||
- *
- Less
than one percent.
- (1)
- Consists
of 20,761 ordinary shares issuable upon exercise of stock options within 60 days of January 31, 2018.
- (2)
- Mr. Bolte,
one of our directors, is an advisor to HBM Partners AG. HBM Partners AG provides investment management services to HBM Healthcare Investments
(Cayman) Ltd. and HBM BioCapital Invest Ltd. Mr. Bolte has no voting or investment power over the shares held by HBM Healthcare Investments (Cayman) Ltd. or HBM BioCapital
Invest Ltd. and disclaims beneficial ownership of such shares.
- (3)
- Consists
of (i) 33,140, ordinary shares and (ii) 36,767 ordinary shares issuable upon exercise of stock options within 60 days of
January 31, 2018.
- (4)
- Consists
of 20,767 ordinary shares issuable upon exercise of stock options within 60 days of January 31, 2018.
- (5)
- Consists
of (i) 87,151 ordinary shares directly owned by Dr. Broom, (ii) 72,849 ordinary shares held by the Colin Broom Grantor Trusts I and II,
and (iii) 422,385 ordinary shares issuable upon exercise of share options within 60 days of January 31, 2018.
- (6)
- Consists
of (i) 12,740 ordinary shares and (ii) 125,068 ordinary shares issuable upon exercise of stock options within 60 days of
January 31, 2018.
- (7)
- Consists of (i) 4,200 ordinary shares and (ii) 71,304 ordinary shares issuable upon exercise of stock options within 60 days of January 31, 2018.
152
- (8)
- Consists
of (i) 2,400 ordinary shares and (ii) 122,612 ordinary shares issuable upon exercise of stock options within 60 days of
January 31, 2018.
- (9)
- Consists
of (i) 214,049 ordinary shares and (ii) 865,675 ordinary shares issuable upon exercise of stock options within 60 days of
January 31, 2018. Such amounts include 1,569 ordinary shares held by executive officers not listed in the table above.
- (10)
- Based
solely upon Schedule 13G filed on February 12, 2018, which sets forth beneficial ownership as of December 31, 2017. Consists of
(i) 3,579,861 ordinary shares and held by Vivo Hong Kong VIII Co, Limited, wholly owned subsidiary of Vivo Capital Fund VIII, L.P. and (ii) 494,329 ordinary shares held by
Vivo Hong Kong VIII Surplus Co., Limited, wholly owned subsidiary of Vivo Capital Surplus Fund VIII, L.P. Vivo Capital VIII, LLC is the general partner of both Vivo Capital Fund
VIII, L.P. and Vivo Capital Surplus Fund VIII, L.P. The voting members of Vivo Capital VIII, LLC are Frank Kung, Albert Cha, Edgar Engleman, Chen Yu and Shan Fu, none of whom has
individual voting or investment power with respect to these shares and each of whom disclaims beneficial ownership of such shares. The address for Vivo Capital VIII, LLC is 505 Hamilton
Avenue, Suite 207, Palo Alto, California 94301.
- (11)
- Based
solely upon the Schedule 13D filed on January 26, 2018, which sets forth beneficial ownership as of January 24, 2018 for OrbiMed Private
Investments V-NB B.V., or OPI V-NB and OrbiMed Private Investments V, L.P., or OPI V. OrbiMed Private Investments V Cooperatief U.A., or Cooperatief, is the sole stockholder of OPI V-NB.
OPI V, is the majority member of Cooperatief, and OrbiMed Capital GP V LLC, or GP V, is the sole general partner of OPI V. OrbiMed Advisors LLC, or OrbiMed Advisors, is the
managing member of GP V. GP V and OrbiMed Advisors may be deemed to have beneficial ownership of the shares held by OPI V and OPI V-NB. OrbiMed Advisors exercises its investment and
voting power with respect to the shares held by OPI V-NB and OPI V through a management committee comprised of Carl L. Gordon, Sven H. Borho and Jonathan T. Silverstein, each of whom disclaims
beneficial ownership of such shares. Each of GP V and OrbiMed Advisors disclaims beneficial ownership of the shares held by OPI V and OPI V-NB except to the extent of its or his pecuniary
interest therein, if any. The address for these entities is 601 Lexington Avenue, 54th floor, New York, New York 10022.
- (12)
- Based
solely upon Schedule 13G filed on February 2, 2018, which sets forth beneficial ownership as of December 31, 2017. Novo Holdings
A/S, a Danish limited liability company, is wholly owned by Novo Nordisk Fonden (the "Foundation"), a Danish commercial foundation. Novo A/S changed its name to Novo Holdings A/S on June 23,
2017. Novo Holdings A/S is the holding company in the group of Novo companies (currently comprised of Novo Nordisk A/S, Novozymes A/S and NNIT A/S) and is responsible for managing the
Foundation's assets, including its financial assets. Based on the governance structure of Novo Holdings A/S and the Foundation, the Foundation disclaims any beneficial ownership of the shares held by
Novo Holdings A/S. Novo Holdings A/S, through its board of directors (the "Novo Board"), has the sole power to vote and dispose of the shares. Sten Scheibye, Francis Michael Cyprian Cuss, Goran Ando,
Jean-Luc Butel, Jeppe Christiansen, Steen Riisgaard, Per Wold-Olsen and Lars Rebien Sorensen serve on the Novo Board and may exercise voting and dispositive control over the shares only with the
support of a majority of the Novo Board. As such, no individual member of the Novo Board is deemed to hold any beneficial ownership or reportable pecuniary interest in the shares. The business address
of Novo Holdings A/S is Tuborg Havnevej 19, 2900 Hellerup, Denmark.
- (13)
- Based solely upon the Schedule 13G filed on October 10, 2017 by HBM Healthcare Investments (Cayman) Ltd. and HBM BioCapital Invest Ltd., which sets forth beneficial ownership as of September 22, 2017. Consists of 2,334,008 ordinary shares held by HBM Healthcare Investments (Cayman) Ltd. The board of directors of HBM Healthcare Investments (Cayman) Ltd. has sole voting and investment power with respect to the shares held by such entity. The board of directors
153
of HBM Healthcare Investments (Cayman) Ltd. is comprised of Jean-Marc LeSieur, Richard Coles, Sophia Harris, Dr. Andreas Wicki, Paul Woodhouse and John Urquhart, none of whom has individual voting or investment power with respect to these shares and each of whom disclaims beneficial ownership of the shares held by HBM Healthcare Investments (Cayman) Ltd., except to the extent of any pecuniary interest therein. The address for HBM Healthcare Investments (Cayman) Ltd. is Governor's Square, Suite # 4-212-2, 23 Lime Tree Bay Avenue, West Bay, Grand Cayman, Cayman Islands.
- (14)
- Based solely upon Schedule 13G filed on February 9, 2018, which sets forth beneficial ownership as of December 31, 2017. Consists of 2,122,960 ordinary shares held by venBio Global Strategic Fund II, L.P. (the "Fund"). venBio Global Strategic GP II, L.P. (the "General Partner") is the sole general partner of the Fund, and venBio Global Strategic GP II, Ltd. (the "GP Ltd.") is the sole general partner of the General Partner. The General Partner and GP Ltd., as well as Robert Adelman and Corey Goodman, as directors of GP Ltd. may be deemed beneficially own the shares. The business address of venBio Global Strategic Fund II, L.P.is c/o venBio Partners, LLC, 1700 Owens Street, Suite 595, San Francisco, California 94158.
Securities Authorized for Issuance under Equity Compensation Plans
The following table contains information about our equity compensation plans as of December 31, 2017, as adjusted to reflect our assumption of the option granted under the Stock Option Plan 2015 in connection with the Redomiciliation. As of December 31, 2017, Nabriva had two equity compensation plans, the 2017 Share Incentive Plan and the Stock Option Plan 2015, each of which were approved by our shareholders.
Plan category
|
Number of securities to be issued upon exercise of outstanding options, warrants and rights |
Weighted-average exercise price of outstanding options, warrants and rights |
Number of securities remaining available for future issuance under equity compensation plans (excluding securities reflected in column(a)) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| |
(a) |
(b) |
(c) |
|||||||
Equity compensation plans approved by security holders |
3,338,999 | $ | 8.22 | 3,099,991 | ||||||
Equity compensation plans not approved by security holders |
— | — | — | |||||||
Total |
3,338,999 | $ | 8.22 | 3,099,991 | ||||||
ITEM 13. CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE
Board Determination of Independence
Applicable Nasdaq rules require a majority of a listed company's board of directors to be comprised of independent directors within one year of listing. In addition, the Nasdaq rules require that, subject to specified exceptions, each member of a listed company's audit, compensation and nominating and corporate governance committees be independent under the Securities Exchange Act of 1934, as amended, or the Exchange Act. Audit committee members must also satisfy the independence criteria set forth in Rule 10A-3 under the Exchange Act, and compensation committee members must also satisfy the independence criteria set forth in Rule 10C-1 under the Exchange Act. Under applicable Nasdaq rules, a director will only qualify as an "independent director" if, in the opinion of the listed company's board of directors, that person does not have a relationship that would interfere with the exercise of independent judgment in carrying out the responsibilities of a director. To be
154
considered independent for purposes of Rule 10A-3, a member of an audit committee of a listed company may not, other than in his or her capacity as a member of the audit committee, the board of directors, or any other board committee, accept, directly or indirectly, any consulting, advisory, or other compensatory fee from the listed company or any of its subsidiaries or otherwise be an affiliated person of the listed company or any of its subsidiaries. In order to be considered independent for purposes of Rule 10C-1, the board must consider, for each member of a compensation committee of a listed company, all factors specifically relevant to determining whether a director has a relationship to such company which is material to that director's ability to be independent from management in connection with the duties of a compensation committee member, including, but not limited to: (1) the source of compensation of the director, including any consulting, advisory or other compensatory fee paid by such company to the director; and (2) whether the director is affiliated with the company or any of its subsidiaries or affiliates.
In March 2018, our board of directors undertook a review of the independence of each director. Based upon information requested from and provided by each director concerning his or her background, employment and affiliations, including family relationships, our board has determined that each of our directors, with the exception of George H. Talbot and Colin Broom, is an "independent director" as defined under applicable Nasdaq rules, including, in the case of all the members of our audit committee, the independence criteria set forth in Rule 10A-3 under the Exchange Act, and in the case of all the members of our compensation committee, the independence criteria set forth in Rule 10C-1 under the Exchange Act. In making such determination, our board considered the relationships that each such director has with us, including each of the transactions described below in "—Board Policies—Related Person Transactions—Certain Relationships and Related Transactions," and all other facts and circumstances that our board deemed relevant in make such independence determination.
Board Policies
Related Person Transactions
Our board of directors has adopted written policies and procedures for the review of any transaction, arrangement or relationship in which the company is a participant, the amount involved exceeds $120,000 and one of our executive officers, directors, director nominees or 5% shareholders, or their immediate family members, each of whom we refer to as a "related person," has a direct or indirect material interest.
If a related person proposes to enter into such a transaction, arrangement or relationship, which we refer to as a "related person transaction," the related person must report the proposed related person transaction to our chief financial officer or general counsel. The policy calls for the proposed related person transaction to be reviewed and, if deemed appropriate, approved by our audit committee. Whenever practicable, the reporting, review and approval will occur prior to entry into the transaction. If advance review and approval is not practicable, the committee will review, and, in its discretion, may ratify the related person transaction. The policy also permits the chair of the audit committee to review and, if deemed appropriate, approve proposed related person transactions that arise between committee meetings, subject to ratification by the committee at its next meeting. Any related person transactions that are ongoing in nature will be reviewed annually.
A related person transaction reviewed under the policy will be considered approved or ratified if it is authorized by the audit committee after full disclosure of the related person's interest in the transaction. As appropriate for the circumstances, the audit committee will review and consider:
- •
- the related person's interest in the related person transaction;
- •
- the approximate dollar value of the amount involved in the related person transaction;
155
- •
- the approximate dollar value of the amount of the related person's interest in the transaction without regard to the amount of any profit or
loss;
- •
- whether the transaction was undertaken in the ordinary course of our business;
- •
- whether the terms of the transaction are no less favorable to us than terms that could have been reached with an unrelated third party;
- •
- the purpose of, and the potential benefits to us of, the transaction; and
- •
- any other information regarding the related person transaction or the related person in the context of the proposed transaction that would be material to investors in light of the circumstances of such transaction.
Our audit committee may approve or ratify the transaction only if it determines that, under all of the circumstances, the transaction is in our best interests. Our audit committee may impose any conditions on the related person transaction that it deems appropriate.
In addition to the transactions that are excluded by the instructions to the SEC's related person transaction disclosure rule, our board of directors has determined that the following transactions do not create a material direct or indirect interest on behalf of related persons and, therefore, are not related person transactions for purposes of this policy:
- •
- interests arising solely from the related person's position as an executive officer of another entity, whether or not the person is also a
director of the entity, that is a participant in the transaction where the related person and all other related persons own in the aggregate less than a 10% equity interest in such entity, the related
person and his or her immediate family members are not involved in the negotiation of the terms of the transaction and do not receive any special benefits as a result of the transaction and the amount
involved in the transaction is less than the greater of $200,000 or 5% of the annual gross revenues of the company receiving payment under the transaction; and
- •
- a transaction that is specifically contemplated by provisions of our memorandum and articles of association.
The policy provides that transactions involving compensation of our executive officers shall be reviewed and approved by our compensation committee in the manner specified in the compensation committee's charter.
In addition, under our Code of Business Conduct and Ethics, our directors, executive officers and employees have an affirmative responsibility to disclose any transaction or relationship that reasonably could be expected to give rise to a conflict of interest.
Certain Relationships and Related Transactions
Since January 1, 2017, we have engaged in the following transactions with our executive officers, directors and holders of more than 5% of our voting securities, and affiliates of our executive officers, directors and 5% shareholders. We believe that all of the transactions described below were made on terms no less favorable to us than could have been obtained from unaffiliated third parties:
September 2017 Financing
In September 2017, we completed an underwritten offering for the sale of an aggregate of 9,411,765 ordinary shares. In connection with such offerings, Novo A/S, a 5% shareholder, purchased an aggregate of 1,000,000 ordinary shares at a purchase price of $8.50 per ordinary share.
156
ITEM 14. PRINCIPAL ACCOUNTING FEES AND SERVICES
The following table sets forth, for each of the years indicated, the aggregate fees billed or expected to be billed to us for services rendered by KPMG LLP, or KPMG, and PwC Wirtschaftsprüfung GmbH, or PwC, our independent registered public accounting firms during the periods indicated. Effective June 2017, we engaged KPMG as our independent registered public accounting firm replacing PwC, as further described in Part II, Item 9 "Changes in and Disagreements with Accountants on Accounting and Financial Disclosure".
| |
Year Ended December 31, |
||||||
|---|---|---|---|---|---|---|---|
(in thousands)
|
2017 | 2016 | |||||
Audit Fees |
$ | 467 | $ | 417 | |||
Audit-Related Fees(1) |
— | 253 | |||||
Tax Fees(2) |
24 | 30 | |||||
All Other Fees(3) |
1,210 | 989 | |||||
| | | | | | | | |
Total |
$ | 1,701 | $ | 1,689 | |||
| | | | | | | | |
- (1)
- Fees
for the performance of assurance reporting on historical information
- (2)
- Fees
related to services rendered on tax compliance, tax advice and tax planning.
- (3)
- Fees related to consulting services and services associated with Nabriva Austria's rights offering and our 2017 Public Offering.
Pre-Approval Policies and Procedures
Our audit committee has adopted policies and procedures relating to the approval of all audit and non-audit services that are to be performed by our independent registered public accounting firm. This policy generally provides that we will not engage our independent registered public accounting firm to render audit or non-audit services unless the service is specifically approved in advance by our audit committee or the engagement is entered into pursuant to a de minimis exception in accordance with applicable SEC rules.
All of the services provided to us by KPMG LLP and PwC Wirtschaftsprüfung GmbH during the last fiscal year were approved by the audit committee.
157
ITEM 15. EXHIBITS AND FINANCIAL STATEMENT SCHEDULES
| (a) | (1) | Financial Statements: See Index to Consolidated Financial Statements on page F-1. | ||
| (2) | No financial statement schedules have been filed as part of this Annual Report on Form 10-K because they are not applicable, not required or because the information is otherwise included in our financial statements or notes thereto. | |||
| (3) | The exhibits listed on the Exhibit Index set forth immediately following Item 16 are filed or furnished as part of this Annual Report. The Exhibit Index is incorporated herein by reference. |
Not Applicable.
| |
|
Incorporated by Reference | |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exhibit Number |
Description of Exhibit | Form | File Number | Date of Filing |
Exhibit Number |
Filed Herewith |
||||||||
| 3.1 | Memorandum and Articles of Association of Nabriva Therapeutics plc. | 8-K | 001-38132 | 06/26/2017 | 3.1 | |||||||||
10.1 |
Form of Indemnification Agreement. |
8-K |
001-38132 |
06/26/2017 |
10.1 |
|||||||||
10.2 |
# |
2017 Share Incentive Plan. |
10-Q |
001-37558 |
11/09/2017 |
10.2 |
||||||||
10.3 |
# |
Stock Option Plan 2007, as Amended. |
8-K |
001-38132 |
06/26/2017 |
10.2 |
||||||||
10.4 |
# |
Stock Option Plan 2015, as Amended. |
8-K |
001-38132 |
06/26/2017 |
10.3 |
||||||||
10.5 |
Lease Agreement, dated March 16, 2007, by and between Nabriva Therapeutics AG and CONTRA Liegenschaftsverwaltung GmbH |
F-1 |
333-205073 |
06/18/15 |
10.4 |
|||||||||
10.6 |
Sublease Agreement, dated July 7, 2015, by and between Nabriva Therapeutics AG and Card Connect, LLC |
F-1 |
333-205073 |
8/24/15 |
10.11 |
|||||||||
10.7 |
# |
Amended and Restated Employment Agreement dated June 17, 2016 by and between Nabriva Therapeutics US, Inc. and Colin Broom |
6-K |
001-37558 |
08/09/16 |
10.1 |
||||||||
10.8 |
# |
Employment Agreement dated May 2, 2016 by and between Nabriva Therapeutics US, Inc. and Gary Sender |
6-K |
001-37558 |
08/09/16 |
10.2 |
||||||||
158
159
- #
- Management
contract or compensatory plan or arrangement filed in response to Item 15(a)(3) of the Instructions to the Annual Report on Form 10-K.
- *
- Confidential treatment has been requested as to certain portions, which portions have been omitted and separately filed with the Securities and Exchange Commission.
160
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| Date: March 16, 2018 | NABRIVA THERAPEUTICS PLC | |||
By: |
/s/ COLIN BROOM Colin Broom Chief Executive Officer |
|||
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated:
Signature
|
Title
|
Date
|
||
|---|---|---|---|---|
| /s/ COLIN BROOM Colin Broom |
Director, Chief Executive Officer (Principal Executive Officer) |
March 16, 2018 | ||
/s/ GARY SENDER Gary Sender |
Chief Financial Officer (Principal Financial and Accounting Officer) |
March 16, 2018 |
||
/s/ DANIEL BURGESS Daniel Burgess |
Chairman of the Board |
March 16, 2018 |
||
/s/ AXEL BOLTE Axel Bolte |
Director |
March 16, 2018 |
||
/s/ CARRIE BOURDOW Carrie Bourdow |
Director |
March 16, 2018 |
||
/s/ GEORGE TALBOT George Talbot |
Director |
March 16, 2018 |
||
/s/ CHARLES A. ROWLAND JR. Charles A. Rowland Jr. |
Director |
March 16, 2018 |
161
Signature
|
Title
|
Date
|
||
|---|---|---|---|---|
| /s/ STEPHEN WEBSTER Stephen Webster |
Director | March 16, 2018 | ||
/s/ MARK CORRIGAN Mark Corrigan |
Director |
March 16, 2018 |
162
F-1
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To
the Stockholders and Board of Directors
Nabriva Therapeutics plc.:
Opinion on the Consolidated Financial Statements
We have audited the accompanying consolidated balance sheets of Nabriva Therapeutics plc and subsidiaries (the Company) as of December 31, 2016 and 2017, the related consolidated statements of operations and comprehensive income (loss), changes in stockholders' equity (deficit), and cash flows for the years then ended, and the related notes (collectively, the consolidated financial statements). In our opinion, the consolidated financial statements present fairly, in all material respects, the financial position of the Company as of December 31, 2016 and 2017, and the results of its operations and its cash flows for the years ended, in conformity with U.S. generally accepted accounting principles.
Going Concern
The accompanying consolidated financial statements have been prepared assuming that the Company will continue as a going concern. As discussed in Note 1 to the consolidated financial statements, the Company has incurred recurring losses and negative cash flows from operations that raise substantial doubt about its ability to continue as a going concern. Management's plans in regard to these matters are also described in Note 1. The consolidated financial statements do not include any adjustments that might result from the outcome of this uncertainty.
Basis for Opinion
These consolidated financial statements are the responsibility of the Company's management. Our responsibility is to express an opinion on these consolidated financial statements based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the consolidated financial statements are free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audits, we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company's internal control over financial reporting. Accordingly, we express no such opinion.
Our audits included performing procedures to assess the risks of material misstatement of the consolidated financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the consolidated financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the consolidated financial statements. We believe that our audits provide a reasonable basis for our opinion.
/s/
KPMG LLP
We have served as the Company's auditor since 2017.
Philadelphia, Pennsylvania
March 16, 2018
F-2
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Board of Directors and Stockholders of Nabriva Therapeutics plc
In our opinion, the consolidated statements of operations and comprehensive income (loss), of changes in stockholders' equity (deficit) and of cash flows for the year ended December 31, 2015 present fairly, in all material respects, the results of operations and cash flows of Nabriva Therapeutics plc (formerly known as Nabriva Therapeutics AG) and its subsidiary for the year ended December 31, 2015, in conformity with accounting principles generally accepted in the United States of America. These financial statements are the responsibility of the Company's management. Our responsibility is to express an opinion on these financial statements based on our audit. We conducted our audit of these financial statements in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, and evaluating the overall financial statement presentation. We believe that our audit provides a reasonable basis for our opinion.
/s/
PwC Wirtschaftsprüfung GmbH
Vienna, Austria
March 24, 2017, except for the effects of the merger between entities under common control discussed in Note 1 to the consolidated financial statements, as to which the date is
March 16, 2018
/s/ Alexandra Rester |
F-3
NABRIVA THERAPEUTICS plc
Consolidated Balance Sheets
(in thousands, except share data)
|
As of December 31, 2016 |
As of December 31, 2017 |
|||||
|---|---|---|---|---|---|---|---|
Assets |
|||||||
Current assets: |
|||||||
Cash and cash equivalents |
$ | 32,778 | $ | 86,769 | |||
Short-term investments |
51,106 | 110 | |||||
Other receivables |
5,561 | 5,402 | |||||
Prepaid expenses |
1,176 | 1,558 | |||||
| | | | | | | | |
Total current assets |
90,621 | 93,839 | |||||
Property, plant and equipment, net |
519 | 1,327 | |||||
Intangible assets, net |
270 | 172 | |||||
Long-term receivables |
420 | 425 | |||||
Deferred tax assets |
1,410 | — | |||||
| | | | | | | | |
Total assets |
$ | 93,240 | $ | 95,763 | |||
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
Liabilities and equity |
|||||||
Current liabilities: |
|||||||
Accounts payable |
$ | 2,551 | $ | 5,136 | |||
Accrued expense and other current liabilities |
13,326 | 8,124 | |||||
| | | | | | | | |
Total current liabilities |
15,877 | 13,260 | |||||
Non-current liabilities |
|||||||
Long-term debt |
— | 232 | |||||
Other non-current liabilities |
107 | 203 | |||||
| | | | | | | | |
Total non-current liabilities |
107 | 435 | |||||
| | | | | | | | |
Total liabilities |
15,984 | 13,695 | |||||
| | | | | | | | |
Commitments and contingencies (Note 14) |
|||||||
Stockholders' Equity: |
|||||||
Common shares, no par value, 2,719,695 common shares issued and outstanding at December 31, 2016; None issued and outstanding at December 31, 2017 |
2,939 | — | |||||
Ordinary shares, nominal value $0.01, 1,000,000,000 ordinary shares authorized at December 31, 2017; 36,707,685 issued and outstanding at December 31, 2017 |
— | 367 | |||||
Preferred shares, par value $0.01, 100,000,000 shares authorized at December 31, 2017; None issued and outstanding at December 31, 2017 |
— | — | |||||
Additional paid in capital |
279,149 | 360,872 | |||||
Accumulated other comprehensive income |
10 | 27 | |||||
Accumulated deficit |
(204,842 | ) | (279,198 | ) | |||
| | | | | | | | |
Total stockholders' equity |
77,256 | 82,068 | |||||
| | | | | | | | |
Total liabilities and stockholders' equity |
$ | 93,240 | $ | 95,763 | |||
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
The accompanying notes form an integral part of these consolidated financial statements.
F-4
NABRIVA THERAPEUTICS plc
Consolidated Statements of Operations and Comprehensive Income (Loss)
| |
Year ended December 31, | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands, except per share data)
|
2015 | 2016 | 2017 | |||||||
Revenues: |
||||||||||
Research premium and grant revenue |
$ | 3,767 | $ | 6,482 | $ | 5,319 | ||||
Operating expenses: |
||||||||||
Research and development |
(23,604 | ) | (47,994 | ) | (49,615 | ) | ||||
General and administrative |
(7,921 | ) | (13,535 | ) | (29,472 | ) | ||||
| | | | | | | | | | | |
Total operating expenses |
(31,525 | ) | (61,529 | ) | (79,087 | ) | ||||
| | | | | | | | | | | |
Loss from operations |
(27,758 | ) | (55,047 | ) | (73,768 | ) | ||||
Other income (expense): |
||||||||||
Other income (expense), net |
2,427 | (783 | ) | 492 | ||||||
Interest income |
14 | 343 | 318 | |||||||
Interest expense |
(22,092 | ) | (75 | ) | (43 | ) | ||||
| | | | | | | | | | | |
Loss before income taxes |
(47,409 | ) | (55,562 | ) | (73,001 | ) | ||||
Income tax (expense) benefit |
445 | 672 | (1,355 | ) | ||||||
| | | | | | | | | | | |
Net loss |
(46,964 | ) | (54,890 | ) | (74,356 | ) | ||||
Other comprehensive income (loss), net of tax |
||||||||||
Exchange differences on translating foreign operations |
2,026 | — | — | |||||||
Unrealized losses on available-for-sale securities |
(68 | ) | (18 | ) | (26 | ) | ||||
Reclassification to net income |
— | 68 | 43 | |||||||
| | | | | | | | | | | |
Other comprehensive income, net of tax |
1,958 | 50 | 17 | |||||||
| | | | | | | | | | | |
Comprehensive loss |
$ | (45,006 | ) | $ | (54,840 | ) | $ | (74,339 | ) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
Loss per share
|
|
|
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
Basic and diluted |
$ | (4.80 | ) | $ | (2.56 | ) | $ | (2.49 | ) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
Weighted average number of shares: |
||||||||||
Basic and diluted |
10,583,950 | 21,478,320 | 29,830,669 | |||||||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
The accompanying notes form an integral part of these consolidated financial statements.
F-5
NABRIVA THERAPEUTICS plc
Consolidated Statements of Changes in Stockholders' Equity (Deficit)
| |
Common Stock/Ordinary Shares |
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
Treasury Shares | |
Accumulated other comprehensive income (loss) |
|
|
|
|
||||||||||||||||||||||||
| |
|
|
Total Stockholders' Equity (Deficit) |
|
|
||||||||||||||||||||||||||
(in thousands)
|
Number of shares |
Amount | Number of shares |
Amount | Additional paid in capital |
Accumulated deficit |
Mezzanine Equity |
Total Equity (Deficit) |
|||||||||||||||||||||||
January 1, 2015 |
328 | $ | 432 | 3 | $ | (25 | ) | $ | 89,295 | $ | 1,871 | $ | (120,587 | ) | $ | (29,014 | ) | $ | 634 | $ | (28,380 | ) | |||||||||
Issuance of Silent Partnership Agreement, net of transaction fees |
— | — | — | — | — | — | — | — | 962 | 962 | |||||||||||||||||||||
Issuance of common stock |
1,563 | 1,725 | — | — | 149,218 | — | — | 150,943 | — | 150,943 | |||||||||||||||||||||
Conversion of convertible loans |
204 | 222 | — | — | 22,519 | — | — | 22,741 | — | 22,741 | |||||||||||||||||||||
Conversion of silent partnerships |
15 | 17 | — | — | 2,733 | — | — | 2,750 | (2,750 | ) | — | ||||||||||||||||||||
Exercise of Kreos options |
9 | 10 | — | — | 1,420 | — | — | 1,430 | — | 1,430 | |||||||||||||||||||||
Exercise of stock options |
1 | 1 | — | — | 124 | — | — | 125 | — | 125 | |||||||||||||||||||||
Equity transaction costs related to Initial Public Offering |
— | — | — | — | (13,616 | ) | — | — | (13,616 | ) | — | (13,616 | ) | ||||||||||||||||||
Equity transaction costs related to April 2015 financing |
— | — | — | — | (1,313 | ) | — | — | (1,313 | ) | — | (1,313 | ) | ||||||||||||||||||
Stock based compensation expense |
— | — | — | — | 1,249 | — | — | 1,249 | — | 1,249 | |||||||||||||||||||||
Beneficial conversion feature of silent partnership |
— | — | — | — | 2,561 | — | — | 2,561 | (2,561 | ) | — | ||||||||||||||||||||
Adjustment to redemption value of silent partnership |
— | — | — | — | — | — | (3,875 | ) | (3,875 | ) | 3,875 | — | |||||||||||||||||||
Beneficial conversion feature of convertible loans |
— | — | — | — | 18,993 | — | — | 18,993 | — | 18,993 | |||||||||||||||||||||
Extension of CLA repayment date—Modification |
— | — | — | — | 738 | — | — | 738 | — | 738 | |||||||||||||||||||||
Unrealized loss on available-for-sale securities |
— | — | — | — | — | (68 | ) | — | (68 | ) | — | (68 | ) | ||||||||||||||||||
Cumulative translation adjustment, net of tax |
— | — | — | — | — | 2,026 | — | 2,026 | (160 | ) | 1,866 | ||||||||||||||||||||
Net loss |
— | — | — | — | — | — | (46,964 | ) | (46,964 | ) | — | (46,964 | ) | ||||||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
December 31, 2015 |
2,120 | 2,407 | 3 | (25 | ) | 273,921 | 3,829 | (171,426 | ) | 108,706 | — | 108,706 | |||||||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Change in functional currency |
(99 | ) | — | 3 | (17,509 | ) | (3,869 | ) | 21,474 | — | — | — | |||||||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
January 1, 2016 |
2,120 | 2,308 | 3 | (22 | ) | 256,412 | (40 | ) | (149,952 | ) | 108,706 | — | 108,706 | ||||||||||||||||||
Issuance of common stock |
588 | 618 | — | — | 24,204 | — | — | 24,822 | — | 24,822 | |||||||||||||||||||||
Exercise of stock options |
12 | 13 | (3 | ) | 22 | 235 | — | — | 270 | — | 270 | ||||||||||||||||||||
Equity transaction costs |
— | — | — | — | (4,247 | ) | — | — | (4,247 | ) | — | (4,247 | ) | ||||||||||||||||||
Stock based compensation expense |
— | — | — | — | 2,545 | — | — | 2,545 | — | 2,545 | |||||||||||||||||||||
Other comprehensive income, net of tax |
— | — | — | — | — | 50 | — | 50 | — | 50 | |||||||||||||||||||||
Net loss |
— | — | — | — | — | — | (54,890 | ) | (54,890 | ) | — | (54,890 | ) | ||||||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
December 31, 2016 |
2,720 | 2,939 | — | — | 279,149 | 10 | (204,842 | ) | 77,256 | — | 77,256 | ||||||||||||||||||||
Issuance of common stock |
9,412 | 94 | — | — | 79,906 | — | — | 80,000 | — | 80,000 | |||||||||||||||||||||
Exercise of stock options |
54 | 3 | — | — | 51 | — | — | 54 | — | 54 | |||||||||||||||||||||
Equity transaction costs |
— | — | — | — | (6,635 | ) | — | — | (6,635 | ) | — | (6,635 | ) | ||||||||||||||||||
Redomiciliation share exchange |
24,522 | (2,669 | ) | — | — | 2,669 | — | — | — | — | — | ||||||||||||||||||||
Stock based compensation expense |
— | — | — | — | 5,732 | — | — | 5,732 | — | 5,732 | |||||||||||||||||||||
Other comprehensive income, net of tax |
— | — | — | — | — | 17 | — | 17 | — | 17 | |||||||||||||||||||||
Net loss |
— | — | — | — | — | — | (74,356 | ) | (74,356 | ) | — | (74,356 | ) | ||||||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
December 31, 2017 |
36,708 | $ | 367 | — | $ | — | $ | 360,872 | $ | 27 | $ | (279,198 | ) | $ | 82,068 | $ | — | $ | 82,068 | ||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
The accompanying notes form an integral part of these consolidated financial statements.
F-6
NABRIVA THERAPEUTICS plc
Consolidated Statements of Cash Flows
| |
Year ended December 31 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | 2017 | |||||||
Cash flows from operating activities |
||||||||||
Net loss |
$ | (46,964 | ) | $ | (54,890 | ) | $ | (74,356 | ) | |
Adjustments to reconcile net loss to net cash used in operating activities: |
||||||||||
Non-cash other income, net |
144 | 996 | (1,371 | ) | ||||||
Non-cash interest income |
(1 | ) | (52 | ) | — | |||||
Non-cash interest expense |
21,465 | 35 | — | |||||||
Depreciation and amortisation expense |
153 | 233 | 432 | |||||||
Stock-based compensation |
1,351 | 2,545 | 5,732 | |||||||
Deferred income taxes |
(627 | ) | (794 | ) | 1,410 | |||||
Other, net |
(5 | ) | 1 | 131 | ||||||
Changes in operating assets and liabilities: |
||||||||||
Changes in long-term receivables |
(71 | ) | 10 | (5 | ) | |||||
Changes in other receivables |
(3,181 | ) | (1,932 | ) | (223 | ) | ||||
Changes in accounts payable |
2,651 | (383 | ) | 2,585 | ||||||
Changes in accrued expenses and other liabilities |
3,971 | 6,034 | (3,778 | ) | ||||||
Changes in other non-current liabilities |
9 | 24 | 96 | |||||||
Changes in income tax liabilities |
(753 | ) | (152 | ) | (1 | ) | ||||
| | | | | | | | | | | |
Net cash used in operating activities |
(21,858 | ) | (48,325 | ) | (69,348 | ) | ||||
| | | | | | | | | | | |
Cash flows from investing activities |
||||||||||
Purchases of plant and equipment and intangible assets |
(216 | ) | (603 | ) | (1,173 | ) | ||||
Purchases of available-for-sale securities |
(30,603 | ) | (57,035 | ) | — | |||||
Purchases of term deposits |
(45,885 | ) | (10 | ) | (30 | ) | ||||
Proceeds from sale of property, plant and equipment |
— | — | 2 | |||||||
Proceeds from maturities of term deposits |
— | 45,000 | — | |||||||
Proceeds from sales of available-for-sale securities |
— | 36,000 | 50,950 | |||||||
| | | | | | | | | | | |
Net cash (used in) provided by investing activities |
(76,704 | ) | 23,352 | 49,749 | ||||||
| | | | | | | | | | | |
Cash flows from financing activities |
||||||||||
Proceeds from initial public offering |
106,088 | — | — | |||||||
Proceeds from April 2015 financing |
44,836 | — | — | |||||||
Proceeds from December 2016 financing |
— | 24,822 | — | |||||||
Proceeds from September 2017 public offering |
— | — | 80,000 | |||||||
Other proceeds from shareholders |
29 | — | ||||||||
Proceeds from silent partnership |
943 | — | — | |||||||
Proceeds from long-term borrowings |
— | — | 228 | |||||||
Proceeds from exercise of stock options |
5 | 269 | 83 | |||||||
Proceeds from convertible loans |
3,436 | — | — | |||||||
Repayments of participation rights |
(6 | ) | — | — | ||||||
Repayments of long-term borrowings |
(7,383 | ) | — | — | ||||||
Equity transaction costs |
(14,930 | ) | (2,790 | ) | (8,092 | ) | ||||
| | | | | | | | | | | |
Net cash provided by financing activities |
133,018 | 22,301 | 72,219 | |||||||
| | | | | | | | | | | |
Effects of foreign currency translation on cash and cash equivalents |
(160 | ) | (996 | ) | 1,371 | |||||
| | | | | | | | | | | |
Net increase (decrease) in cash and cash equivalents |
34,296 | (3,668 | ) | 53,991 | ||||||
Cash and cash equivalents at beginning of year |
2,150 | 36,446 | 32,778 | |||||||
| | | | | | | | | | | |
Cash and cash equivalents at end of year |
$ | 36,446 | $ | 32,778 | $ | 86,769 | ||||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
Supplemental disclosures of cash flow information: |
||||||||||
Interest paid |
$ | (1,057 | ) | $ | (41 | ) | $ | (1 | ) | |
Taxes paid |
$ | (939 | ) | $ | (867 | ) | $ | (5 | ) | |
Equity transaction costs included in accrued expenses |
$ | — | $ | 1,451 | $ | 28 | ||||
The accompanying notes form an integral part of these consolidated financial statements.
F-7
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements
(in thousands, except per share data)
1. Organization and Business Activities
Nabriva Therapeutics plc ("Nabriva Ireland"), together with its wholly owned and consolidated subsidiaries, Nabriva Therapeutics GmbH ("Nabriva Austria"), Nabriva Therapeutics US, Inc., Nabriva Therapeutics Ireland DAC, and Nabriva Therapeutics One DAC (In Voluntary Liquidation) (collectively, "Nabriva", the "Nabriva Group" or the "Company") is a clinical stage biopharmaceutical company engaged in the research and development of novel anti-infective agents to treat serious infections, with a focus on the pleuromutilin class of antibiotics. The Company's headquarters are located at 25-28 North Wall Quay, Dublin, Ireland.
On March 1, 2017, Nabriva Ireland was incorporated in Ireland under the name Hyacintho 2 plc, and was renamed to Nabriva Therapeutics plc on April 10, 2017, in order to effectuate the change of the jurisdiction of incorporation of the ultimate parent company of the Nabriva Group from Austria to Ireland. Nabriva Ireland replaced Nabriva Austria as the ultimate parent company on June 23, 2017, following the conclusion of a tender offer (the "Exchange Offer") in which holders of 98.5% of the outstanding share capital of Nabriva Austria exchanged their holdings for ordinary shares, $0.01 nominal value per share, of Nabriva Ireland (the "Redomiciliation Transaction"). The ordinary shares of Nabriva Ireland were issued on a one-for-ten basis to the holders of the Nabriva Austria common shares ("Nabriva Austria common shares") and on a one-for-one basis to the holders of the Nabriva Austria American Depositary Shares ("Nabriva Austria ADSs") participating in the Exchange Offer. On June 26, 2017, the ordinary shares of Nabriva Ireland began trading on the Nasdaq Global Market under the symbol "NBRV," the same symbol under which the American Depositary Shares of Nabriva Austria were previously traded. This transaction was accounted for as a merger between entities under common control; accordingly, the historical financial statements of Nabriva Austria for periods prior to this transaction are considered to be the historical financial statements of Nabriva Ireland. As of August 18, 2017, 100% of Nabriva Austria share capital had been exchanged for ordinary shares of Nabriva Ireland.
Nabriva Austria was incorporated in Austria as a spin-off from Sandoz GmbH in October 2005 and commenced operations in February 2006 as Nabriva Therapeutics AG. On October 19, 2017, Nabriva Austria was converted into a private limited liability company under Austrian law and renamed Nabriva Therapeutics GmbH. Nabriva Therapeutics US, Inc. was founded and began operations in the United States in August 2014. In February 2017, Nabriva Austria purchased all shares issued in the capital of Hyacintho DAC, a designated activity company incorporated by a nominee company in December 2016; it renamed the company to Nabriva Therapeutics Ireland DAC on April 10, 2017 and renamed the company again to Nabriva Therapeutics One DAC on October 13, 2017 ("One DAC"). From April 2017, One DAC held a license of all of the intellectual property rights of the Nabriva Group from Nabriva Austria. In October 2017, the Company purchased all shares issued in the capital of a new Irish designated activity company, Nabriva Therapeutics Ireland DAC ("Nabriva DAC") from a nominee company. On October 19, 2017, Nabriva Austria terminated the intellectual property rights license in place with One DAC and put in place a new intellectual property rights license with Nabriva DAC in respect of all of the intellectual property rights of the Nabriva Group. On February 8, 2018, Nabriva Austria passed a shareholder resolution to approve the voluntary and solvent liquidation of One DAC.
Throughout these Notes to the Consolidated Financial Statements, unless the context requires otherwise, all references to "Nabriva," "the Nabriva Group," "the Company," or similar terms on or
F-8
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
1. Organization and Business Activities (Continued)
prior to June 23, 2017 (the effective date of the Redomiciliation Transaction), refer to our predecessor, Nabriva Austria, together with its subsidiaries.
Certain share and per share amounts have been retrospectively adjusted to reflect the Exchange Offer and the Redomiciliation Transaction.
Liquidity
As of December 31, 2016, the Company adopted the provisions of Financial Accounting Standards Board ("FASB") Accounting Standards Codification ("ASC") Topic 205-40, Presentation of Financial Statements—Going Concern ("ASC 205-40"), which requires management to assess the Company's ability to continue as a going concern for one year after the date the financial statements are issued. This standard requires management to 1) identify and disclose if there are initial conditions indicating substantial doubt about the Company's ability to continue as a going concern within one year of the issuance date of the financial statements, 2) disclose the principal conditions that gave rise to substantial doubt, 3) disclose management's evaluation of the significance of those conditions in relation to the Company's ability to meet its obligations and 4) disclose management's plans that are intended to mitigate the adverse conditions. In accordance with the accounting standard, when considering management's plans to mitigate the conditions giving rise to substantial doubt, management can only consider those plans which are probable to be successfully implemented.
Since its inception, the Company has incurred net losses and generated negative cash flows from its operations. To date, it has financed its operations through the sale of equity securities, including its initial public offering of Nabriva Austria ADSs, public follow-on offerings and private placements of its Nabriva Austria common shares, convertible debt financings and research and development support from governmental grants and loans.
As of December 31, 2017, the Company had cash, cash equivalents and short-term investments of $86.9 million. The Company anticipates that its expenses will increase substantially as it continues the development of and seeks marketing approval for lefamulin and, possibly, other product candidates and continues its research activities. The Company's expenses will increase if it suffers any delays in its Phase 3 clinical program for lefamulin for the treatment of community-acquired bacterial pneumonia ("CABP"). If the Company obtains marketing approval for lefamulin or any other product candidate that it develops, it expects to incur significant commercialization expenses related to product sales, marketing, distribution and manufacturing.
The Company expects to seek additional funding in future periods. While the Company has raised capital in the past, the ability to raise capital in future periods is not considered probable, as defined under the accounting standards. As such, under the requirements of ASC 205-40, management may not consider the potential for future capital raises in their assessment of the Company's ability to meet its obligations for the next twelve months.
If the Company is not able to secure adequate additional funding in future periods, the Company may make reductions in certain expenditures. This may include extending payment terms with suppliers, liquidating assets, and suspending or curtailing planned programs. The Company may also have to delay, reduce the scope of, suspend or eliminate one or more research and development programs or its commercialization efforts.
F-9
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
1. Organization and Business Activities (Continued)
As a result, in accordance with the requirements of ASC 205-40, management has concluded that substantial doubt exists about the Company's ability to continue as a going concern for one year from the date these financial statements are issued. A failure to raise the additional funding or to effectively implement cost reductions could harm the Company's business, results of operations and future prospects.
The Company expects that its existing cash, cash equivalents and short-term investments will be sufficient to enable the Company to fund its operating expenses and capital expenditure requirements into the fourth quarter of 2018. Furthermore, while these estimates are based on the Company's current assumptions regarding its operating expenses and capital expenditure requirements, the Company also believes that by reducing certain planned pre-commercialization activities its existing cash, cash equivalents and short-term investments could fund its primary business focus of seeking regulatory approval for lefamulin, the Company's lead product candidate, subject to positive LEAP 2 topline data, into the first quarter of 2019. The consolidated financial statements have been prepared assuming that the Company will continue as a going concern, which contemplates continuity of operations, the realization of assets and the satisfaction of liabilities and commitments in the normal course of business.
2. Summary of Significant Accounting Policies
Basis of Preparation
The consolidated financial statements have been prepared in accordance with generally accepted accounting principles in the United States of America ("US GAAP") and US Securities and Exchange Commission ("SEC") regulations for annual reporting.The consolidated financial statements include the accounts of Nabriva Therapeutics plc and its wholly-owned subsidiaries. All intercompany accounts and transactions have been eliminated in consolidation.
Functional and presentation currency
Effective January 1, 2016, the Company's functional and reporting currency changed to the U.S. dollar ("USD"). Prior to January 1, 2016, the consolidated financial statements were presented in euro ("€"), which was the Company's functional and presentation currency. With the expansion of Nabriva's operations to the United States, the Company's assets, liabilities, revenues and expenses are expected to be predominantly denominated in USD, and accordingly, the use of USD to measure and report the Company's financial performance and financial position was considered to be more appropriate. The impact of the currency translation up to January 1, 2016 is recorded in accumulated other comprehensive income (loss). Upon the change in functional currency on January 1, 2016, all assets and liabilities of the Company's operations were translated from their euro functional currency into USD using the exchange rates in effect on the balance sheet date, equity was translated at the historical rates and revenues, expenses, and cash flows were translated at the average rates during the reporting period presented. The resulting translation adjustments are reported under comprehensive income (loss) as a separate component of stockholders'equity.
F-10
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
2. Summary of Significant Accounting Policies (Continued)
Transactions and balances
In preparing the consolidated financial statements, transactions in currencies other than the entity's functional currency (foreign currencies) are recognized at the exchange rates prevailing at the dates of the transactions. Foreign currency exchange gains and losses resulting from the settlement of such transactions and from the translation at year-end exchange rates of monetary assets and liabilities denominated in foreign currencies are recognized in the consolidated statement of comprehensive income (loss).
Use of Estimates
The preparation of financial statements in conformity with US GAAP requires management to make estimates and assumptions that affect the amount of assets and liabilities and disclosure of contingent assets and liabilities at the date of the consolidated financial statements and the reported amounts of revenues and espenses during the reporting period. Actual results could differ from those estimates.
Cash and Cash Equivalents
The company considers highly liquid investments with original maturities of three months or less to be cash equivalents.
Short-term Investments
The Company has designated its investments in securities as available-for-sale securities and measures these securities at their respective fair values. Investments that mature in one year or less are classified as short-term available-for-sale securities. Investments that are not considered available for use in current operations are classified as long-term available-for-sale securities. Changes in the fair value of available-for-sale investments are recognized in other comprehensive income (loss).
Property, Plant and Equipment
Property, plant and equipment are stated at cost less accumulated depreciation. Depreciation is calculated using the straight-line method over the estimated useful lives of the assets. The estimated useful lives of property, plant and equipment are as follows: 3-5 years for IT equipment, 5-10 years for laboratory equipment and 3-10 years for other plant and office equipment. The assets' residual values and useful lives are reviewed, and adjusted if appropriate, at each reporting date. When assets are sold or otherwise disposed of, the difference between the net proceeds, if any, and the net carrying amount of the asset is recognized as a gain or a loss in other operating income or expenses.
Intangible Assets and Other Long-lived Assets
Intangible assets, such as acquired computer software licenses, are capitalized on the basis of the costs incurred to acquire the software and bring it into use. These costs are amortized on a straight-line basis over their estimated useful lives (3-10 years).
Long-lived assets are assessed for potential impairment when there is evidence that events or changes in circumstances indicate that the carrying amount of an asset may not be recovered. An
F-11
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
2. Summary of Significant Accounting Policies (Continued)
impairment loss would be recognized when undiscounted cash flows expected to be generated by an asset, is less than its carrying amount. The impairment loss would be measured as the amount by which the asset's carrying value exceeds its fair value and recognized in these financial statements.
Research Premium and Grant Revenue
Grant revenue comprises (a) the research premium from the Austrian government, (b) grants received from the Vienna Center for Innovation and Technology (Zentrum für Innovation, or ZIT) and the Vienna Business Promotion Fund (Wiener Wirtschaftsförderungsfonds, or WWFF), (c) grants received from the Austrian Research Promotion Agency (Österreichische Forschungsförderungsgesellschaft, or FFG), and (d) the benefit of government loans at below-market interest rates. Please refer to Note 3 for further details on all forms of grant revenue.
The research premium the Company receives from the Austrian government is calculated at a specified percent of specified research and development cost base. The Company recognizes the research premium as long as it has incurred research and development expenses. The ZIT grants are provided to support specific research projects and are recognized according to the progress of the respective project. The WWFF grant is paid out through the landlord in the form of a monthly reduction in lease payments and is recognized over the period from grant date in March 2010 until end of the lease termination waiver term in December 2017. All grants are non-refundable as long as the conditions of the grant are met. Nabriva is and has been in full compliance with the conditions of the grants and all related regulations.
The benefit of a government loan at a below-market rate of interest is treated as a government grant. The benefit due to the difference between the market rate of interest and the rate of interest charged by the governmental organization is measured as the difference between the initial carrying value of the loan determined and the proceeds received. This benefit is deferred, and recognized through profit and loss over the term of the corresponding liabilities.
Research and Development Expenses
All research and development costs are expensed as incurred. Research and development costs included direct personnel and material costs, related overheads, depreciation of equipment used for research or development purposes; costs for clinical research; costs for the utilization of third parties' patents for research and development purposes and other taxes related to research facilities.
Share-Based Payments
The Company measures the cost of employee services received in exchange for an award of equity instruments based on the grant-date fair value of the award in accordance with ASC 718, Compensation—Stock Compensation," using the Black-Scholes model. All grants under share-based payment programs are accounted for at fair value and that cost is recognized over the period during which an employee is required to provide service in exchange for the award—the requisite service period (vesting period). The Company accounts for forfeitures as incurred. Compensation expense for options granted to non-employees is determined as the fair value of the consideration received or the fair value of the equity instruments issued, whichever is more reliably measured. The fair value of awards granted to non-employees is re-measured each period until the related service is complete.
F-12
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
2. Summary of Significant Accounting Policies (Continued)
Income Taxes
The Company accounts for income taxes under the asset and liability method, which requires the recognition of deferred tax assets and liabilities for the expected future tax consequences of events that have been included in the financial statements. Under this method, the Company determines deferred tax assets and liabilities on the basis of the differences between the financial statement and tax bases of assets and liabilities by using enacted tax rates in effect for the year in which the differences are expected to reverse. The effect of a change in tax rates on deferred tax assets and liabilities is recognized in income in the period that includes the enactment date.
The Company recognizes deferred tax assets to the extent that it believes that these assets are more likely than not to be realized. In making such a determination, the Company considers all available positive and negative evidence, including future reversals of existing taxable temporary differences, projected future taxable income, tax-planning strategies, and results of recent operations. If the Company determines that it would be able to realize its deferred tax assets in the future in excess of their net recorded amount, we would make an adjustment to the deferred tax asset valuation allowance, which would reduce the provision for income taxes.
In recognizing the benefit of tax positions, the Company has taken or expects to take, the Company determines whether it is more likely than not that the tax positions will be sustained on the basis of the technical merits of the position and for those tax positions that meet the more-likely-than-not recognition threshold, the Company recognizes the largest amount of tax benefit that is more than 50 percent likely to be realized upon ultimate settlement with the related tax authority.
The Company's policy is to record interest and penalties related to tax matters in income tax expense.
On December 22, 2017, the U.S. government enacted comprehensive tax legislation commonly referred to as the Tax Cuts and Jobs Act (the "Tax Act"). The Tax Act makes broad and complex changes to the U.S. tax code, including, but not limited to, reducing the top U.S. federal corporate tax rate from 35 percent to 21 percent; eliminating the corporate alternative minimum tax (AMT) and changing how existing AMT credits can be realized; creating the base erosion anti-abuse tax (BEAT), a new minimum tax; creating a new limitation on deductible interest expense; and, changing rules related to uses and limitations of net operating loss carryforwards created in tax years beginning after December 31, 2017.
The Tax Act reduces the U.S. corporate income tax rate from 35% to 21%, effective January 1, 2018. Deferred tax assets and liabilities are measured using enacted tax rates expected to apply to taxable income in the years in which those temporary differences are expected to reverse. As a result of the reduction in the U.S. corporate income tax rate from 35% to 21% under the Tax Act, the Company revalued the ending net deferred tax assets and liabilities of our U.S. subsidiary at December 31, 2017.
Mezzanine Equity
Silent partnership agreements entered into in 2014 and 2015, which entitled the silent partners to a proportionate share in the fair value of the Company, similar to a shareholder, including a share in profit or loss, according to an agreed participation rate, were classified as mezzanine equity pursuant to
F-13
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
2. Summary of Significant Accounting Policies (Continued)
ASC 480, Distinguishing Liabilities from Equity ("ASC 480"), and ASC 815, Derivatives and Hedging ("ASC 815"). The silent partnership interests were evaluated for equity or mezzanine classification based upon the nature of the partnerships settlement provisions which unilaterally provided the Company the option to settle the obligation in cash or a variable number of shares. However, when a settlement in shares cannot always be presumed, irrespective of probability of the event occurring, a classification outside of stockholders' equity is required. Mezzanine equity was initially measured at fair value and subsequently at the redemption value at each reporting period, representing the proceeds resulting from an exit event (trade sale or initial public offering), and such amount recognized in retained earnings.
Subsequent Events
Material subsequent events are evaluated and disclosed through the report issuance date.
Recent Accounting Pronouncements
From time to time, new accounting pronouncements are issued by the FASB or other standard setting bodies that the Company adopts as of the specified effective date.
Adopted as of the current period:
- •
- In November 2015, the FASB issued Accounting Standards Update ("ASU") 2015-17, Income Taxes: Balance Sheet
Classification of Deferred Taxes. ASU 2015-17 simplifies the balance sheet classification of deferred taxes and requires that all deferred taxes be presented as noncurrent. ASU
2015-17 was effective for fiscal years beginning after December 15, 2016. The impact of adopting this standard did not have a material effect on the Company's financial position, results of
operation or cash flow and related disclosures.
- •
- In March 2016, the FASB issued ASU 2016-09, Improvements to Employee Share-Based Payment Accounting. ASU 2016-09 provides for simplification of certain aspects of employee share-based payment accounting including income taxes, classification of awards as either equity or liabilities, accounting for forfeitures and classification on the statement of cash flows. ASU 2016-09 was effective for the fiscal years beginning after December 15, 2016, and interim periods within those fiscal years. The impact of adopting this standard did not have a material effect on the Company's financial position, results of operation or cash flow and related disclosures.
To be adopted in future periods:
- •
- In May 2014, the FASB issued ASU 2014-09, Revenue from Contracts with Customers, an updated standard on revenue recognition. ASU 2014-09 provides enhancements to the quality and consistency of how revenue is reported by companies while also improving comparability in the financial statements of companies reporting using International Financial Reporting Standards or US GAAP. The main purpose of the new standard is for companies to recognize revenue to depict the transfer of goods or services to customers in amounts that reflect the consideration to which a company expects to be entitled in exchange for those goods or services. The new standard also will result in enhanced revenue disclosures, provide guidance for transactions that were not previously addressed comprehensively and improve guidance for multiple-element
F-14
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
2. Summary of Significant Accounting Policies (Continued)
- •
- In February 2016, the FASB issued ASU 2016-02, Leases (Topic 842). ASU 2016-02 establishes a
right-of-use ("ROU") model that requires a lessee to record a ROU asset and a lease liability on the balance sheet for all leases with terms longer than 12 months. Leases will be classified as
either finance or operating, with classification affecting the pattern of expense recognition in the income statement. ASU 2016-02 is effective for annual periods beginning after December 15,
2018, and interim periods within those fiscal years, with early adoption permitted. A modified retrospective transition approach is required for lessees of capital and operating leases existing at, or
entered into after, the beginning of the earliest comparative period presented in the financial statements, with certain practical expedients available. The Company is currently evaluating the impact
that the standard will have on its financial position, results of operation or cash flow and related disclosures.
- •
- In May 2017, the FASB issued ASU 2017-09, Compensation—Stock Compensation: Scope of Modification Accounting. ASU 2017-09 clarifies which changes to the terms or conditions of a share-based payment award require an entity to apply modification accounting in Topic 718, Compensation—Stock Compensation. ASU 2017-09 is effective for annual periods beginning after December 15, 2017. An entity should apply the amendments prospectively to a modification that occurs on or after the adoption date. The Company does not anticipate the initial adoption of the provisions of this guidance in the first quarter of fiscal year 2018 to have a material impact on its financial position, results of operation or cash flow and related disclosures.
arrangements. The effective date of ASU 2014-09 for the Company is the first quarter of fiscal year 2018 and may be applied on a full retrospective or modified retrospective approach. The adoption of ASU 2014-09 will have no impact on the Company until it begins to generate product revenue.
3. Short-term investments
The Company's short-term investments were as follows:
| |
As of December 31, 2017 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
Amortized Cost |
Unrealized Gains |
Unrealized Losses |
Fair Value |
|||||||||
Short-term investments: |
|||||||||||||
Available-for-sale securities |
$ | 76 | $ | — | $ | (26 | ) | $ | 50 | ||||
Term deposits |
60 | — | — | 60 | |||||||||
| | | | | | | | | | | | | | |
Total |
$ | 136 | $ | — | $ | (26 | ) | $ | 110 | ||||
| | | | | | | | | | | | | | |
| | | | | | | | | | | | | | |
| | | | | | | | | | | | | | |
F-15
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
3. Short-term investments (Continued)
| |
As of December 31, 2016 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
Amortized Cost |
Unrealized Gains |
Unrealized Losses |
Fair Value |
|||||||||
Short-term investments: |
|||||||||||||
Available-for-sale securities |
$ | 51,094 | $ | — | $ | (18 | ) | $ | 51,076 | ||||
Term deposits |
30 | — | — | 30 | |||||||||
| | | | | | | | | | | | | | |
Total |
$ | 51,124 | $ | — | $ | (18 | ) | $ | 51,106 | ||||
| | | | | | | | | | | | | | |
| | | | | | | | | | | | | | |
| | | | | | | | | | | | | | |
As of December 31, 2017 and 2016 the Company's short-term investments were classified as available-for-sale and comprised a (i) money market fund that invests all of its assets, excluding cash and deposits, in short term USD-denominated debt securities, and (ii) a U.S. treasury note.
4. Fair Value Measurement
US GAAP establishes a valuation hierarchy for disclosure of the inputs to valuation used to measure fair value. This hierarchy prioritizes the inputs into three broad levels as follows:
- •
- Level 1: Quoted prices (unadjusted) in active markets for identical assets or liabilities.
- •
- Level 2: Inputs other than quoted prices included within Level 1 that are observable for the asset or liability, either directly
(as prices) or indirectly (as exchange rates).
- •
- Level 3: Valuation techniques that include inputs for the asset or liability that are not based on observable market data (those are unobservable inputs) and significant to the overall fair value measurement.
The following table presents the financial instruments measured at fair value and classified by level according to the fair value measurement hierarchy:
(in thousands)
|
Level 1 | Level 2 | Level 3 | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
December 31, 2017 |
|||||||||||||
Assets: |
|||||||||||||
Short-term investments: |
|||||||||||||
Available-for-sale securities |
$ | — | $ | 50 | $ | — | $ | 50 | |||||
Term deposits |
60 | — | — | 60 | |||||||||
| | | | | | | | | | | | | | |
Total Assets |
$ | 60 | $ | 50 | $ | — | $ | 110 | |||||
| | | | | | | | | | | | | | |
| | | | | | | | | | | | | | |
| | | | | | | | | | | | | | |
(in thousands)
|
Level 1 | Level 2 | Level 3 | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
December 31, 2016 |
|||||||||||||
Assets: |
|||||||||||||
Short-term investments: |
|||||||||||||
Available-for-sale securities |
$ | 15,017 | $ | 36,059 | $ | — | $ | 51,076 | |||||
Term deposits |
30 | — | — | 30 | |||||||||
Total Assets |
$ | 15,047 | $ | 36,059 | $ | — | $ | 51,106 | |||||
| | | | | | | | | | | | | | |
| | | | | | | | | | | | | | |
| | | | | | | | | | | | | | |
F-16
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
4. Fair Value Measurement (Continued)
As of December 31, 2017 and December 31, 2016, the Company held short-term investments classified as both Level 1 and Level 2, and the Company did not hold any Level 3 financial instruments measured at fair value. There were no transfers between Level 1 and 2 in the years ended December 31, 2017 and December 31, 2016. There were no changes in valuation techniques during the year ended December 31, 2017.
As of December 31, 2017 and December 31, 2016, the Company did not hold any financial instruments as liabilities that were held at fair value.
Other receivables and accounts payable are carried at their historical cost which approximates fair value due to their short-term nature.
5. Other receivables
| |
As of December 31 | ||||||
|---|---|---|---|---|---|---|---|
(in thousands)
|
2016 | 2017 | |||||
Research premium |
$ | 5,346 | $ | 5,124 | |||
VAT and other taxes |
46 | 28 | |||||
Receivables from grant revenue |
144 | 231 | |||||
Other receivables |
25 | 19 | |||||
| | | | | | | | |
Total current receivables |
$ | 5,561 | $ | 5,402 | |||
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
6. Property, Plant and Equipment
| |
As of December 31 | ||||||
|---|---|---|---|---|---|---|---|
(in thousands)
|
2016 | 2017 | |||||
IT equipment |
$ | 642 | $ | 1,060 | |||
Laboratory equipment |
2,613 | 3,299 | |||||
Other equipment |
15 | 15 | |||||
| | | | | | | | |
|
3,270 | 4,374 | |||||
Less: Accumulated depreciation |
(2,751 | ) | (3,047 | ) | |||
| | | | | | | | |
Property, plant and equipment, net |
$ | 519 | $ | 1,327 | |||
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
F-17
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
7. Accrued Expenses and Other Current Liabilities
Accrued expenses and other current liabilities include the following:
| |
As of December 31 | ||||||
|---|---|---|---|---|---|---|---|
(in thousands)
|
2016 | 2017 | |||||
Research and development related costs |
$ | 8,716 | $ | 2,308 | |||
Payroll and related costs |
2,345 | 4,426 | |||||
Accounting, tax and audit services |
484 | 231 | |||||
Other |
1,781 | 1,159 | |||||
| | | | | | | | |
Total other current liabilities |
$ | 13,326 | $ | 8,124 | |||
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
Other non-current liabilities include an obligation to pay jubilee benefits to it Austrian employees of $ 137 and $107 at December 31, 2017 and 2016, respectively, arising under the collective bargaining agreement for the chemical industry in Austria, by which employees are entitled to receive jubilee payments after being employed for a certain number of years.
The Company's net obligation in respect of the jubilee payments is calculated annually by an independent actuary in accordance with ASC 710-10-25 using the projected unit credit method. The principle actuarial assumptions used were as follows:
Discount rates of 1.7% and 1.3% used for the 2017 and 2016 calculations, respectively, retirement at the age of 61.5-65 for men and 56.5-65 for women and future annual salary increases of 3%.
8. Stockholders' Equity
On September 22, 2017 the Company completed an underwritten public offering of 9,411,765 ordinary shares at a public offering price of $8.50 per share, resulting in gross proceeds of $80.0 million and net proceeds to the Company of $73.3 million, after deducting underwriting discounts and commissions and offering expenses.
On December 19, 2016, the Company completed a rights offering and a related underwritten offering for the sale of an aggregate of 588,127 common shares resulting in aggregate gross proceeds of $24.8 million and net proceeds of $20.6 million, after deducting underwriting fees and offering expenses.
On September 23, 2015 the Company completed its initial public offering on the Nasdaq Global Market issuing 9,000,000 ADSs at a price to the public of $10.25 per ADS, representing 900,000 of its common shares. Each ADS represents one tenth of a common share. On September 30, 2015 the underwriters of its initial public offering exercised in full their over-allotment option to purchase an additional 1,350,000 ADSs, representing 135,000 common shares, at the initial public offering price of $10.25 per ADS, less underwriting discounts. Including the over-allotment ADSs, the Company sold an aggregate of 10,350,000 ADSs representing 1,035,000 common shares, in its initial public offering, which resulted in gross proceeds of $106.1 million and net proceeds to the Company of $92.4 million, after deducting underwriting discounts and offering expenses.
In connection with the Company's April 2015 financing, it sold 730,162 common shares with contractual preference rights under a shareholders agreement, including the sale of 511,188 common
F-18
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
8. Stockholders' Equity (Continued)
shares at a price per share of €82.35 ($87.71) for €42.1 million ($44.8 million) in cash consideration and the sale of 218,974 common shares in exchange for certain contributions in-kind consisting of the conversion of outstanding convertible loans and silent partnership interests. The Company also agreed to sell a second tranche of common shares with contractual preference rights under the shareholders agreement to the investors in its April 2015 financing at their option for an aggregate purchase price of $70.0 million if the Company did not complete a public offering in the United States within specified parameters or by a specified date. As a result of the preferred dividend rights, which were not legally separable, the Company was deemed to have issued common shares accompanied by preferred dividends that may be settled for cash or shares. Accordingly, the proceeds from the April 2015 financing, including the consideration from conversion of the convertible loan agreements and silent partnership interests, were recorded as mezzanine equity. A mezzanine equity classification arises as a result of the dividend provision in the Shareholders Agreement 2015, which the Company's shareholders have covenanted to vote in favor of the requisite shareholder resolutions to allow it to satisfy the preferred dividend rights. As a result, (i) the Company could not avoid fulfilling the preferred dividend rights if a triggering event occurred that was outside its control, and (ii) could not always presume a settlement in shares. Therefore, when a settlement in shares cannot always be presumed for an event not solely within the control of the issuer, irrespective of probability of the event occurring, a classification outside of stockholders' equity is required. Mezzanine equity was initially measured at fair value and subsequently at the redemption value at each reporting period, representing the proceeds resulting from an exit event (trade sale or initial public offering), and such amount recognized in retained earnings.
Upon the closing of its initial public offering and the issuance of the shares for nominal value in satisfaction of the preferred dividend rights, all contractual preference rights under the shareholders agreement terminated.
In connection with this April 2015 financing, all existing convertible loan agreements and silent partnership interests were converted to common shares with contractual preference rights under the Shareholders Agreement 2015.
On March 31, 2015, the Company, its existing investors and new investors in the April 2015 financing signed the Investment and Subscription Agreement 2015, or ISA 2015.
The signing of the ISA 2015 resulted in the following effects with respect to the Company's existing financial instruments:
- a)
- the
lenders under all existing convertible loan agreements, or CLAs, irrevocably waived their claims for payment of interest accrued on the loan amounts,
- b)
- all
CLA lenders irrevocably waived and acknowledged the termination of their call option rights granted under the CLAs, and
- c)
- all silent partners irrevocably agreed to the forfeiture of their claims for payment of interest accrued on their silent partnership investments.
The April 2015 financing and the related conversion of the Company's outstanding convertible loan agreements and silent partnership interests resulted in total consideration of $77.3 million which was recorded in mezzanine equity. Upon the closing of the Company's initial public offering in
F-19
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
8. Stockholders' Equity (Continued)
September 2015, a triggering event occurred as described above, and the holders of the preferred dividend right received 17,149 additional shares against payment of the nominal amount of €1.00 per share, effectively removing the mezzanine equity classification.
9. Research Premium and Grant Revenue
Research premium and grant revenue consists of the following items:
| |
Year ended December 31, | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | 2017 | |||||||
Research premium |
$ | 3,594 | $ | 6,232 | $ | 4,842 | ||||
Government grants |
67 | — | 369 | |||||||
Grants from WWFF and ZIT |
106 | 250 | 108 | |||||||
| | | | | | | | | | | |
Total |
$ | 3,767 | $ | 6,482 | $ | 5,319 | ||||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
10. Share-Based Payments
Stock Option Plan 2007
On September 12, 2007 the Company's management and supervisory boards resolved to implement a stock option plan ("SOP 2007") for all employees (including members of the management board) with open-ended contracts of employment with the Company and for selected members of the supervisory board of the Company and further participants. The stock option plan became effective on September 28, 2007. In connection with the Redomiciliation Transaction, the SOP 2007 was amended to take account of certain requirements under Irish law and assumed by Nabriva Ireland, with each option to acquire one Nabriva Austria common share becoming an option to acquire ten ordinary shares of Nabriva Ireland on the same terms and conditions. As of September 27, 2017, all outstanding options under the SOP 2007 automatically terminated and were forfeited.
Movements in the number of share options outstanding and their related weighted average exercise prices concerning the SOP 2007 are as follows:
| |
2015 | 2016 | 2017 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Stock Option Plan 2007
|
Weighted average exercise price in $ per share |
Options | Weighted average exercise price in $ per share |
Options | Weighted average exercise price in $ per share |
Options | Aggregate intrinsic value |
|||||||||||||||
Outstanding as of January 1 |
0.73 | 241,330 | 0.73 | 234,760 | 0.73 | 109,960 | ||||||||||||||||
Granted |
— | — | — | — | — | — | ||||||||||||||||
Exercised |
0.73 | (6,570 | ) | 0.73 | (124,540 | ) | 0.73 | (108,440 | ) | |||||||||||||
Forfeited |
— | — | 0.73 | (260 | ) | 0.73 | (1,520 | ) | ||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | |
Outstanding as of December 31 |
0.73 | 234,760 | 0.73 | 109,960 | — | — | $ | — | ||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
Vested and exercisable as of December 31 |
0.73 | 229,270 | 0.73 | 107,900 | — | — | $ | — | ||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
F-20
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
10. Share-Based Payments (Continued)
As a result of the Redomiciliation Transaction, the 2015 and 2016 movements in the number of share options outstanding and their related weighted average exercise prices have been adjusted on a one-for-ten basis from the Nabriva Austria common shares, to the Nabriva Ireland ordinary shares.
The total intrinsic value of options exercised during the years ended December 31, 2015, 2016 and 2017 was $119, $860 and $899, respectively.
Stock-based compensation expense under the SOP 2007 for the years ended December 31, 2015, 2016 and 2017 was $78, $95 and $40, respectively.
Stock Option Plan 2015
On April 2, 2015, the Company's shareholders, management board and supervisory board adopted the Stock Option Plan 2015 (the "SOP 2015") and the shareholders approved an amended and restated version of the SOP 2015 on June 30, 2015. An amendment to the amended and restated SOP 2015 was approved by the shareholders on July 22, 2015. SOP 2015 became effective on July 3, 2015 upon the registration with the commercial register in Austria of the conditional capital increase approved by the shareholders on June 30, 2015. The SOP 2015 initially provided for the grant of options for up to 95,000 Nabriva Austria common shares to the Company's employees, including members of the management board, and to members of the supervisory board. Following the closing of the initial public offering of the Company, the overall number of options increased to 177,499 Nabriva Austria common shares. Following approval by the Company's shareholders at its 2016 annual general meeting, the number of shares available for issuance under the SOP 2015 was increased to 346,235 Nabriva Austria common shares. In connection with the Redomiciliation Transaction, the SOP 2015 was amended to take account of certain requirements under Irish law and assumed by Nabriva Ireland, with each option to acquire one Nabriva Austria common share becoming an option to acquire ten ordinary shares of Nabriva Ireland on the same terms and conditions.
Each vested option grants the beneficiary the right to acquire one share in the Company. The vesting period for the options is four years following the grant date. On the last day of the last calendar month of the first year of the vesting period, 25% of the options attributable to each beneficiary are automatically vested. During the second, third and fourth years of the vesting period, the remaining 75% of the options vest on a monthly pro rata basis (i.e. 2.083% per month). Options granted under the SOP 2015 have a term of no more than ten years from the beneficiary's date of participation. Since the closing of the initial public offering of the Company on September 23, 2015 the beneficiaries are entitled to exercise their vested options until the 10th anniversary of the date of their participation. The beneficiaries are not entitled to transfer vested options except to individuals by way of inheritance or bequest. Options do not entitle beneficiaries to exercise any shareholder rights. Beneficiaries may only exercise shareholder rights if and to the extent he holds shares.
F-21
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
10. Share-Based Payments (Continued)
Movements in the number of share options outstanding and their related weighted average exercise prices concerning the SOP 2015 are as follows:
| |
2015 | 2016 | 2017 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Stock Option Plan 2015
|
Weighted average exercise price in $ per share |
Options | Weighted average exercise price in $ per share |
Options | Weighted average exercise price in $ per share |
Options | Aggregate intrinsic value |
|||||||||||||||
Outstanding as of January 1 |
— | — | 7.61 | 1,092,300 | 7.83 | 1,794,360 | ||||||||||||||||
Granted |
7.61 | 1,093,550 | 8.02 | 922,130 | 9.02 | 1,458,300 | ||||||||||||||||
Exercised |
— | — | 7.21 | (23,360 | ) | — | — | |||||||||||||||
Forfeited |
7.21 | (1,250 | ) | 7.64 | (196,710 | ) | 8.60 | (207,761 | ) | |||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | |
Outstanding as of December 31 |
7.61 | 1,092,300 | 7.83 | 1,794,360 | 8.35 | 3,044,899 | $ | 9 | ||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
Vested and exercisable as of December 31 |
7.21 | 86,620 | 7.52 | 425,210 | 7.68 | 989,656 | $ | 3 | ||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
The total intrinsic value of options exercised during the years ended December 31, 2015, 2016 and 2017 was $0, $181 and $0, respectively.
The Company has 3,044,899 option grants outstanding at December 31, 2017 with exercise prices ranging from $4.06 per share to $11.00 per share and a weighted average remaining contractual life of 8.4 years.
Stock-based compensation expense under the SOP 2015 was $1,274, $2,450 and $5,610 for the years ended December 31, 2015, 2016 and 2017, respectively. The weighted average fair value of the options granted during the years ended December 31, 2015, 2016 and 2017 was $7.07 per share, $4.76 per share and $5.05 per share, respectively.
The grant date fair value of each option grant was estimated throughout the year using the Black-Scholes option-pricing model using the following assumptions:
Input parameters
|
2015 | 2016 | 2017 | |||
|---|---|---|---|---|---|---|
Expected volatility |
55.0% - 70.0% | 59.8% - 67.2% | 55.6% - 62.0% | |||
Expected term of options |
2.0 years | 6.0 years | 6.1 years | |||
Risk-free interest rate |
(0.40)% - (0.21)% | 1.15% - 2.09% | 1.89% - 2.10% | |||
Expected dividend yield |
— | — | — |
The expected price volatility is based on historical trading volatility for the publicly traded peer companies under consideration of the remaining life of the options. The risk free interest rate for the year 2015, is based on the 6 year euro area market yield for AAA-rated European central government bonds and for the years 2016 and 2017, is based on the average of 5 and 7 year market yield on U.S. treasury securities in effect at the time of grant.
As of December 31, 2017, there was $10.1 million of unrecognized compensation expense, related to unvested options granted under the SOP 2015 Plan, which will be recognized over the weighted average remaining vesting period of 1.3 years.
F-22
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
10. Share-Based Payments (Continued)
2017 Share Incentive Plan
On July 26, 2017, the Company's board of directors adopted the 2017 Share Incentive Plan (the "2017 Plan") and the shareholders approved the 2017 Plan at the Company's Extraordinary General Meeting of Shareholders on September 15, 2017. Following shareholder approval of the 2017 Plan, the Company ceased making awards under the SOP 2015, and future awards will be made under the 2017 Plan. However, all outstanding awards under SOP 2015 will remain in effect and continue to be governed by the terms of the SOP 2015. The 2017 Plan permits the award of share options (both incentive and nonstatutory options), share appreciation rights ("SARs"), restricted shares, restricted share units ("RSUs"), and other share-based awards to the Company's employees, officers, directors, consultants and advisers. The 2017 Plan is administered by the Company's board of directors.
Under the 2017 Plan, the number of ordinary shares that will be reserved for issuance will be the sum of (1) 3,000,000 ordinary shares; plus (2) a number of ordinary shares (up to 3,438,990 ordinary shares) which is equal to the sum of the number of the Company's ordinary shares then available for issuance under the SOP 2015 and the number of ordinary shares subject to outstanding awards under the SOP 2015 that expire, terminate or are otherwise surrendered, cancelled, forfeited or repurchased by the Company at their original issuance price pursuant to a contractual repurchase right; plus (3) an annual increase, to be added on the first day of each fiscal year beginning in the fiscal year ending December 31, 2018 and continuing until, and including, the fiscal year ending December 31, 2027, equal to the least of (i) 2,000,000 ordinary shares, (ii) 4% of the number of outstanding ordinary shares on such date and (iii) an amount determined by the board of directors.
At December 31, 2017, 3,394,091 ordinary shares were available for issuance under the 2017 Plan.
Options and SARs granted will be exercisable at such times and subject to such terms and conditions as the board may specify in the applicable option agreement; provided, however, that no option or SAR will be granted with a term in excess of ten years. The board will also determine the terms and conditions of restricted shares and RSUs, including the conditions for vesting and repurchase (or forfeiture) and the issue price, if any.
The following table summarizes information regarding our stock option awards under the 2017 Plan at December 31, 2017:
| |
2017 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
2017 Plan
|
Weighted average exercise price in $ per share |
Options | Aggregate intrinsic value |
|||||||
Outstanding as of January 1, 2017 |
— | — | ||||||||
Granted |
6.92 | 294,100 | ||||||||
Exercised |
— | — | ||||||||
Forfeited |
— | — | ||||||||
| | | | | | | | | | | |
Outstanding as of December 31, 2017 |
6.92 | 294,100 | $ | — | ||||||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
Vested and exercisable as of December 31, 2017 |
— | — | $ | — | ||||||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
F-23
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
10. Share-Based Payments (Continued)
There were no options exercised during the year ended December 31, 2017.
The Company has 294,100 option grants outstanding at December 31, 2017 with exercise prices ranging from $5.98 per share to $8.35 per share and a weighted average remaining contractual life of 9.8 years.
Stock-based compensation expense under the 2017 Plan was $82 for the year ended December 31, 2017. The weighted average fair value of the options granted during year ended December 31, 2017 was $3.98 per share based on a Black Scholes option pricing model using
The significant inputs into the model were as follows:
Input parameters
|
|
|
|---|---|---|
Range of expected volatility |
59.5% - 63.0% | |
Expected term of options (in years) |
6.0 | |
Range of risk-free interest rate |
1.93% - 2.27% | |
Dividend yield |
— |
The expected price volatility is based on historical trading volatility for the publicly traded peer companies under consideration of the remaining life of the options. The risk free interest rate is based on the average of 5 and 7 year market yield on U.S. treasury securities in effect at the time of grant.
As of December, 2017, there was $1.1 million of total unrecognized compensation expense, related to unvested options granted under the 2017 Plan, which will be recognized over the weighted-average remaining vesting period of 1.7 years
Our share-based compensation expense has been allocated to research and development and general and administrative expenses in the Consolidated Statement of Operations and Comprehensive Loss as follows:
| |
December 31, | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | 2017 | |||||||
Research and development |
$ | 418 | $ | 894 | $ | 2,128 | ||||
General and administrative |
933 | 1,651 | 3,604 | |||||||
| | | | | | | | | | | |
Total |
$ | 1,351 | $ | 2,545 | $ | 5,732 | ||||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
11. Post-employment benefit obligations
As required under Austrian labor law, the Company makes contributions to a state plan classified as defined contribution plan (Mitarbeitervorsorgekasse) for its employees in Austria. Monthly contributions to the plan are 1.53% of salary with respect to each employee and are recognized as expense in the period incurred. In the years ended December 31, 2017, 2016 and 2015, contribution costs amounted to $58, $59 and $58, respectively.
For employees of Nabriva Therapeutics US, Inc., the Company makes contributions to a defined contribution plan as defined in subsection 401(k) of the Internal Revenue Code. The Company matches 100% of the first 3% of the employee's voluntary contribution to the plan and 50% of the next 2%
F-24
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
11. Post-employment benefit obligations (Continued)
contributed by the employee. Contributions are recognized as expense in the period incurred. In the years ended December 31, 2017, 2016 and 2015 contribution expenses were $213, $152 and $57, respectively.
12. Income tax (expense) benefit
Loss before income taxes attributable to domestic and international operations, consists of the following:
| |
Year ended December 31 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | 2017 | |||||||
Domestic |
$ | (46,300 | ) | $ | (54,509 | ) | $ | (66,109 | ) | |
Foreign |
(1,109 | ) | (1,053 | ) | (6,892 | ) | ||||
| | | | | | | | | | | |
Loss before income taxes |
$ | (47,409 | ) | $ | (55,562 | ) | $ | (73,001 | ) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
Income tax (expense) benefit consists of the following:
| |
Year ended December 31 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | 2017 | |||||||
Current tax |
||||||||||
Domestic |
$ | (3 | ) | $ | (4 | ) | $ | — | ||
Foreign |
(172 | ) | (118 | ) | 55 | |||||
Deferred tax |
||||||||||
Domestic |
— | — | — | |||||||
Foreign |
620 | 794 | (1,410 | ) | ||||||
| | | | | | | | | | | |
Total income tax (expense) benefit |
$ | 445 | $ | 672 | $ | (1,355 | ) | |||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
The reconciliation to our effective tax rate from the Austrian statutory income tax rate of 25% for the years ended December 31, 2015 and 2016 and from the Irish statutory income tax rate of 12.5% for the year ended December 31, 2017 is as follows:
| |
Year ended December 31 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(% of pre-tax income)
|
2015 | 2016 | 2017 | |||||||
Statutory income tax rate |
25.0 | % | 25.0 | % | 12.5 | % | ||||
Non-deductible expenses |
(0.1 | ) | (0.2 | ) | (0.8 | ) | ||||
Income not subject to tax |
1.9 | 2.8 | 0.9 | |||||||
Impairment |
— | — | 1.4 | |||||||
Tax credits |
— | 0.4 | 0.2 | |||||||
Foreign rate differential |
(5.0 | ) | (2.5 | ) | 21.0 | |||||
Other |
0.2 | 0.2 | (1.4 | ) | ||||||
Valuation allowance |
(21.1 | ) | (24.5 | ) | (35.6 | ) | ||||
| | | | | | | | | | | |
Effective income tax rate |
0.9 | % | 1.2 | % | (1.8 | )% | ||||
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
F-25
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
12. Income tax (expense) benefit (Continued)
The following table summarizes the components of deferred income tax balances:
(in thousands)
|
2016 | 2017 | |||||
|---|---|---|---|---|---|---|---|
Deferred tax assets: |
|||||||
Net operating loss carryforwards |
$ | 54,220 | $ | 70,871 | |||
Tax loss on liquidation of subsidiary |
— | 7,846 | |||||
Equity compensation |
1,025 | 1,450 | |||||
Non-deductible reserves |
409 | 57 | |||||
| | | | | | | | |
Total deferred tax assets |
55,654 | 80,224 | |||||
| | | | | | | | |
Valuation allowance |
(54,114 | ) | (80,087 | ) | |||
| | | | | | | | |
Net deferred tax assets |
1,540 | 137 | |||||
| | | | | | | | |
Deferred tax liabilities: |
|||||||
Financial liabilities |
95 | 80 | |||||
Property, plant and equipment |
35 | 57 | |||||
| | | | | | | | |
Total deferred tax liability |
130 | 137 | |||||
| | | | | | | | |
Deferred tax, net |
$ | 1,410 | $ | — | |||
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
The table below summarizes changes in the deferred tax valuation allowance:
| |
Year ended December 31, | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
2015 | 2016 | 2017 | |||||||
Balance at beginning of year |
$ | (30,507 | ) | $ | (40,487 | ) | $ | (54,114 | ) | |
Tax benefit |
(9,980 | ) | (13,627 | ) | (25,973 | ) | ||||
Balance at end of year |
$ | (40,487 | ) | $ | (54,114 | ) | $ | (80,087 | ) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
The following table summarizes carryforwards of net operating losses as of December 31, 2017.
(in thousands)
|
Amount | Expiration | |||
|---|---|---|---|---|---|
Ireland |
$ | 27,490 | Indefinite | ||
Austria |
$ | 268,285 | Indefinite | ||
United States |
$ | 200 | 2037 | ||
Due to uncertainty regarding the ability to realize the benefit of deferred tax assets primarily relating to net operating loss carryforwards, valuation allowances have been established to reduce deferred tax assets to an amount that is more likely than not to be realized.
On the basis of this evaluation, as of December 31, 2017, 2016 and 2015, the Company has recorded a valuation allowance of $80,087, $54,114 and $40,487, respectively, to recognize only the portion of the deferred tax asset that is more likely than not to be realized. The amount of the deferred tax asset considered realizable, however, could be adjusted if estimates of future taxable income during the carryforward period are reduced or increased or if objective negative evidence in the
F-26
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
12. Income tax (expense) benefit (Continued)
form of cumulative losses is no longer present and additional weight is given to subjective evidence such as our projections for growth.
The Tax Cuts and Jobs Act (the "TCJA") was enacted on December 22, 2017 and became effective January 1, 2018. The Tax Act had significant changes to U.S. tax law, lowering U.S. corporate income tax rates, implementing a territorial tax system, and modified the taxation of other income and expense items.
The TCJA reduces the U.S. corporate income tax rate from 35% to 21%, effective January 1, 2018. Deferred tax assets and liabilities are measured using enacted tax rates expected to apply to taxable income in the years in which those temporary differences are expected to reverse. As a result of the reduction in the U.S. corporate income tax rate from 35% to 21% under the TCJA, the Company revalued the ending net deferred tax assets and liabilities of its U.S. subsidiary as of December 31, 2017. The tax impact of the revaluation of these deferred tax assets, net was $0.8 million, which was wholly offset by a corresponding reduction in the valuation allowance for these net deferred tax assets resulting in a no net impact to income tax expense.
At December 31, 2017 and 2016, the Company had no uncertain tax positions and does not expect any material increase or decrease in income tax expense related to examinations or changes in uncertain tax positions.
The Company files income tax returns in Ireland. In addition, the Company's foreign subsidiaries file separate income tax returns in Austria and the United States and state jurisdictions in which they are located. Tax years 2012 and forward remain open for examination for Austrian tax purposes and years 2014 and forward remain open for examination for United States tax purposes.
The Company's policy is to record interest and penalties related to tax matters in income tax expense.
13. Earnings (Loss) per Share
Basic and diluted loss per share
Basic and diluted loss per share is calculated by dividing the net loss attributable to shareholders by the weighted average number of shares outstanding during the year. Diluted net loss per share is the
F-27
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
13. Earnings (Loss) per Share (Continued)
same as basic net loss per share during the periods presented as the effects of the Company's common stock equivalents are antidilutive and thus not included in the calculation.
| |
Year ended December 31, | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
(in thousands, except per share data)
|
2015 | 2016 | 2017 | |||||||
Net loss for the period |
$ | (46,964 | ) | $ | (54,890 | ) | $ | (74,356 | ) | |
Adjustment to redemption value of silent partnerships |
(3,875 | ) | — | — | ||||||
| | | | | | | | | | | |
Net loss attributable to shareholders |
(50,839 | ) | (54,890 | ) | (74,356 | ) | ||||
Weighted average number of shares outstanding |
10,583,950 | 21,478,320 | 29,830,669 | |||||||
Excluded treasury shares on December 31 |
2,819 | — | — | |||||||
| | | | | | | | | | | |
Basic and diluted loss per share |
$ | (4.80 | ) | $ | (2.56 | ) | $ | (2.49 | ) | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
The following common stock equivalents were excluded from the calculations of diluted loss per share as their effect would be anti-dilutive:
| |
Year ended December 31, | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| |
2015 | 2016 | 2017 | |||||||
Stock options |
1,327,060 | 1,904,320 | 3,338,999 | |||||||
14. Commitments and Contingencies
In March 2007, a lease agreement for an unlimited period starting in December 2007 was entered into for the use of business and research premises in Vienna. Within the first 10 years the contract can only be terminated under certain conditions.
In July 2015, a lease agreement was entered into for the use of approximately 15,000 square feet of office space in King of Prussia, PA, with the lease term continuing until December 2023 with no renewal options.
We also enter into lease agreements for equipment such as copiers and printers.
Lease expense was $1,264, $1,263 and $861 for the years ended December 31, 2017, 2016 and 2015, respectively.
Future minimum contractual obligations and commitments at December 31, 2017 are as follows:
| |
Year ending December 31, | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
(in thousands)
|
Total | 2018 | 2019 | 2020 | 2021 | 2022 | Therafter | |||||||||||||||
Operating lease obligations |
$ | 3,327 | $ | 776 | $ | 500 | $ | 507 | $ | 515 | $ | 522 | $ | 507 | ||||||||
Other contractual commitments |
10,550 | 10,550 | — | — | — | — | — | |||||||||||||||
| | | | | | | | | | | | | | | | | | | | | | | |
Total |
$ | 13,877 | $ | 11,326 | $ | 500 | $ | 507 | $ | 515 | $ | 522 | $ | 507 | ||||||||
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | |
F-28
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
14. Commitments and Contingencies (Continued)
In addition to the agreements described above, the Company has other contractual commitments related primarily to contracts entered into with contract research organizations and contract manufacturing organizations in connection with the conduct of clinical trials and other research and development activities. The estimated payments to the services providers included in the table above are based solely on the estimated work to be performed by them to complete the trials and other activities along with the anticipated achievement of milestones included within the agreements. Also, some of these contracts are subject to early termination clauses exercisable at the discretion of the Company. The Company is not obligated to make minimum required payments under these service agreements.
The Company has no contingent liabilities in respect of legal claims arising in the ordinary course of business.
15. Selected Quarterly Financial Information (Unaudited)
The table summarizes the unaudited consolidated financial results of operations for the quarters ended:
(amounts in thousands, except per share data)
|
March 31 | June 30 | September 30 | December 31 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
2017 Quarter Ended |
|||||||||||||
Revenues |
$ | 1,678 | $ | 1,051 | $ | 1,468 | $ | 1,122 | |||||
Operating expenses |
(16,878 | ) | (16,613 | ) | (22,193 | ) | (23,403 | ) | |||||
Loss from operations |
(15,200 | ) | (15,562 | ) | (20,725 | ) | (22,281 | ) | |||||
Other income (expense) |
326 | (7 | ) | 328 | 120 | ||||||||
Income tax (expense) benefit |
(349 | ) | 967 | (1,872 | ) | (101 | ) | ||||||
Net loss |
(15,223 | ) | (14,602 | ) | (22,269 | ) | (22,262 | ) | |||||
Basic and diluted loss per share(1) |
$ | (0.56 | ) | $ | (0.54 | ) | $ | (0.79 | ) | $ | (0.61 | ) | |
2016 Quarter Ended |
|||||||||||||
Revenues |
$ | 1,419 | $ | 1,785 | $ | 971 | $ | 2,307 | |||||
Operating expenses |
(16,121 | ) | (13,311 | ) | (15,050 | ) | (17,047 | ) | |||||
Loss from operations |
(14,702 | ) | (11,526 | ) | (14,079 | ) | (14,740 | ) | |||||
Other income (expense) |
1,086 | (590 | ) | 107 | (1,118 | ) | |||||||
Income tax (expense) benefit |
17 | 12 | (28 | ) | 671 | ||||||||
Net loss |
(13,599 | ) | (12,104 | ) | (14,000 | ) | (15,187 | ) | |||||
Basic and diluted loss per share(1) |
$ | (0.64 | ) | $ | (0.57 | ) | $ | (0.66 | ) | $ | (0.68 | ) | |
- (1)
- Net loss per share amounts may not agree to the per share amounts for the full year due to the use of weighted average shares for each period. Additionally, loss per share for the quarter ended March 31, 2017 and all the quarters in 2016 are recast to reflect the Redomicilation Transaction, accordingly the loss per share presented is based on the equivalent number of Nabriva Ireland ordinary shares outstanding in all periods.
F-29
NABRIVA THERAPEUTICS plc
Notes to the Consolidated Financial Statements (Continued)
(in thousands, except per share data)
16. Subsequent Events
The Company evaluated all events or transactions that occurred subsequent to December 31, 2017 through the date the consolidated financial statements were issued, and have not identified any such events.
F-30
