Attached files
| file | filename |
|---|---|
| EX-23.1 - EX-23.1 - GLAUKOS Corp | gkos-20171231ex231e8ae79.htm |
| EX-32.2 - EX-32.2 - GLAUKOS Corp | gkos-20171231ex322a144ef.htm |
| EX-32.1 - EX-32.1 - GLAUKOS Corp | gkos-20171231ex321f758d0.htm |
| EX-31.2 - EX-31.2 - GLAUKOS Corp | gkos-20171231ex312ce74da.htm |
| EX-31.1 - EX-31.1 - GLAUKOS Corp | gkos-20171231ex311654ade.htm |
| EX-21 - EX-21 - GLAUKOS Corp | gkos-20171231ex214c20005.htm |
| EX-10.22 - EX-10.22 - GLAUKOS Corp | gkos-20171231ex10227d811.htm |
| EX-10.21 - EX-10.21 - GLAUKOS Corp | gkos-20171231ex102175848.htm |
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
(Mark one)
☒ ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
For the fiscal year ended December 31, 2017
OR
☐ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
For the transition period from: to
Commission File No. 001-37463
GLAUKOS CORPORATION
(Exact name of registrant as specified in its charter)
|
Delaware |
|
33-0945406 |
|
(State or other jurisdiction of incorporation or organization) |
|
(I.R.S. Employer Identification No.) |
|
|
|
|
|
229 Avenida Fabricante |
|
92672 |
|
(Address of principal executive office) |
|
(Zip Code) |
(949) 367-9600
(Registrant’s telephone number, including area code)
Securities registered pursuant to Section 12(b) of the Act:
|
Common Stock, $0.001 par value per share |
|
New York Stock Exchange |
|
(Title of each class) |
|
(Name of each exchange on which registered) |
Securities registered pursuant to Section 12(g) of the Act: None.
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☒ No ☐
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or 15(d) of the Act. Yes ☐ No ☒
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports) and (2) has been subject to such filing requirements for the past 90 days. Yes ☐ No ☒
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ☒ No ☐
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of the registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. ☒
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, or a smaller reporting company. (See definitions of “large accelerated filer”, “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Exchange Act).
|
|
|
|
|
|
|
|
|
|
|
Large accelerated filer ☒ |
|
Accelerated filer ☐ |
|
Non-accelerated filer ☐ |
|
Smaller reporting company ☐ |
|
Emerging growth company ☐ |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ◻
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes ☐ No ☒
As of June 30, 2017, the last business day of the registrant’s most recently completed second quarter, the aggregate market value of common stock held by non-affiliates of the registrant, based on the closing sales price for the registrant’s common stock as reported on The New York Stock Exchange, was $1,268 million.
The number of shares of the Registrant’s common stock outstanding as of February 26, 2018 (latest practicable date) was 34,740,886 shares.
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the Registrant's Proxy Statement for the 2018 Annual Meeting of Stockholders are incorporated herein by reference in Part III of this Annual Report on Form 10-K to the extent stated herein. Such Proxy Statement will be filed with the Securities and Exchange Commission within 120 days after the close of the registrant's fiscal year ended December 31, 2017.
We use Glaukos, our logo, iStent, iStent Inject, iStent Infinite, iStent SA, iStent Supra, iPrism, iDose, MIGS and other marks as trademarks. This report contains references to our trademarks and service marks and to those belonging to other entities. Solely for convenience, trademarks and trade names referred to in this report, including logos, artwork and other visual displays, may appear without the ® or ™ symbols, but such references are not intended to indicate in any way that we will not assert, to the fullest extent under applicable law, our rights or the rights of the applicable licensor to these trademarks and trade names. We do not intend our use or display of other entities’ trade names, trademarks or service marks to imply a relationship with, or endorsement or sponsorship of us by, any other entity.
References throughout this document to “we,” “us,” “our,” or “Glaukos” refer to Glaukos Corporation and its consolidated subsidiaries.
i
SPECIAL NOTE REGARDING FORWARD-LOOKING STATEMENTS AND INDUSTRY DATA
This Annual Report on Form 10-K contains forward‑looking statements within the meaning of Section 27A of the Securities Act of 1933, as amended, and Section 21E of the Securities Exchange Act of 1934, as amended (Exchange Act). These statements are based on management’s beliefs and assumptions and on information currently available to management. Some of the statements under Item 1 - “Business,” Item 1A - “Risk Factors,” Item 7 - “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and elsewhere in this Annual Report on Form 10-K contain forward‑looking statements. In some cases, you can identify forward‑looking statements by the following words: “may,” “will,” “could,” “would,” “should,” “expect,” “intend,” “plan,” “anticipate,” “believe,” “estimate,” “predict,” “project,” “potential,” “continue,” “ongoing” or the negative of these terms or other comparable terminology, although not all forward‑looking statements contain these words.
These statements involve risks, uncertainties and other factors that may cause actual results, levels of activity, performance or achievements to be materially different from the information expressed or implied by these forward‑looking statements. Although we believe that we have a reasonable basis for each forward‑looking statement contained in this report, we caution you that these statements are based on a combination of facts and factors currently known by us and our projections of the future, about which we cannot be certain.
In addition, you should refer to the “Risk Factors” section of this report for a discussion of other important factors that may cause actual results to differ materially from those expressed or implied by the forward‑looking statements. As a result of these factors, we cannot assure you that the forward‑looking statements in this report will prove to be accurate. Furthermore, if the forward‑looking statements prove to be inaccurate, the inaccuracy may be material. In light of the significant uncertainties in these forward‑looking statements, you should not regard these statements as a representation or warranty by us or any other person that we will achieve our objectives and plans in any specified time frame, or at all. We undertake no obligation to publicly update any forward‑looking statements, whether as a result of new information, future events or otherwise, except as required by law.
This Annual Report on Form 10-K contains market data and industry forecasts that were obtained from industry publications. These data involve a number of assumptions and limitations, and you are cautioned not to give undue weight to such information. Although we believe that the industry publications on which the market and industry statements are based are reliable and we are not aware of any misstatements regarding any market data or industry forecasts presented herein, we have not independently verified any of the third party information. Statements in this Annual Report on Form 10-K regarding our market position, market opportunity, market size and our general expectations involve risks and uncertainties and are subject to change based on various factors, including those discussed under Item 1A - “Risk Factors” and Item 7 - “Management’s Discussion and Analysis of Financial Condition and Results of Operations” included elsewhere in this Annual Report on Form 10-K.
ii
Overview
We are an ophthalmic medical technology and pharmaceutical company focused on the development and commercialization of surgical devices and sustained pharmaceutical therapies designed to treat glaucoma, one of the world’s leading causes of blindness. We developed Micro‑Invasive Glaucoma Surgery (MIGS) to serve as an alternative to the traditional glaucoma treatment and management paradigm. We launched the iStent, our first MIGS device, in the United States in July 2012 and we are developing additional products designed to treat a full range of glaucoma progression.
Glaucoma is a group of eye diseases characterized by progressive, irreversible and largely asymptomatic vision loss caused by optic nerve damage which is most commonly associated with elevated levels of pressure within the eye, or intraocular pressure. Elevated intraocular pressure often occurs when aqueous humor, the thin watery fluid that fills the front part of the eye, is not circulating normally and draining properly. Glaucoma is a chronic condition that progresses slowly over long periods of time and can have a devastating impact on a patient’s vision and quality of life.
Reducing intraocular pressure is the only proven treatment for glaucoma. Glaucoma has traditionally been treated through a range of approaches that often require patients to use multiple types of prescription eye drops for the rest of their lives, and sometimes undergo complex and invasive eye surgery. Unfortunately, these medications can be ineffective over time due to patient noncompliance and other factors. Complex and invasive glaucoma surgical options are typically reserved for more advanced glaucoma and have remained largely unchanged since the 1970’s.
We developed MIGS to address the shortcomings of traditional glaucoma treatment options. MIGS procedures involve the insertion of a micro‑scale device or drug delivery system from within the eye’s anterior chamber through a small corneal incision. Our MIGS devices are designed to reduce intraocular pressure by restoring the natural outflow pathways for aqueous humor. Our MIGS drug delivery systems are designed to reduce intraocular pressure by continuously eluting a glaucoma drug from within the eye, potentially providing sustained pharmaceutical therapy for extended periods of time.
Our iStent, a micro‑bypass stent that is designed to reduce intraocular pressure by restoring the natural physiologic pathways for aqueous humor, was the first commercially available MIGS treatment solution. Approved by the United States (U.S.) Food and Drug Administration (FDA) for insertion in combination with cataract surgery, the iStent procedure is currently reimbursed by Medicare and all major national private payors. Our next product, the iStent Inject, includes two stents pre‑loaded in an auto‑injection inserter that are also designed to lower intraocular pressure. The iStent Inject was commercially available in 2017 in certain European Union countries, Canada, Australia, Brazil and South Africa. In these markets, it is approved for use in conjunction with cataract surgery or as a standalone procedure, even though reimbursement may not be available for all such procedures. We are currently seeking FDA approval to market the iStent Inject in the U.S.
We are developing four additional iStent pipeline products: the iStent Inject (in the U.S.), the iStent SA, the iStent Infinite and the iStent Supra. In an effort to obtain approval to market the iStent Inject in the U.S. in conjunction with cataract surgery, we completed a U.S. investigational device exemption (IDE) pivotal trial and submitted a premarket approval application (PMA) for the iStent Inject in 2017. The iStent SA is designed for use as a standalone glaucoma procedure. Similar to the iStent Inject, the iStent SA is a two-stent product that is slightly wider than the iStent Inject and uses a different auto‑injection inserter designed for use in a standalone procedure. The iStent SA is currently being studied in a U.S. pivotal IDE study as a standalone treatment for lowering intraocular pressure in pseudophakic glaucoma patients. We recently submitted an IDE application for the iStent Infinite, which includes three stents pre-loaded in an auto-injection inserter and is intended to lower intraocular pressure in refractory glaucoma patients. The iStent Supra is designed to access an alternative drainage space within the eye and is being evaluated in a U.S. pivotal IDE trial. We completed enrollment for the U.S. pivotal IDE trial for the iStent Supra in 2017.
We are also pursuing regulatory approval of our first sustained pharmaceutical therapy using our iDose drug delivery system. A U.S. investigational new drug (IND) Phase II study of our initial iDose platform product, iDose
1
Travoprost, was completed in 2017 and we intend to commence U.S. Phase III clinical trials for this product in the first half of 2018. We are also conducting research and development (R&D) activities to explore other potential drugs that may benefit from the use of the iDose drug delivery system. In addition, other proprietary R&D efforts are underway on early-stage technologies, including, without limitation, an intraocular pressure sensor (IOP) system that is designed to capture and store a glaucoma patient’s short-interval IOP measurements over extended periods of time, and transmit data to the patient’s physician in order to enhance treatment decisions.
We have a commercial organization which includes a direct sales force in the United States and 16 other countries, as well as distribution partners in regions of Europe, Asia Pacific, Latin America and other targeted international geographies. Information about geographic revenue is set forth in Note 12 of our notes to consolidated financial statements included in Part II, Item 8 of this Annual Report on Form 10-K.
Our net sales increased to $159.3 million in 2017 from $114.4 million in 2016 and $71.7 million in 2015, and we incurred a net loss of $0.1 million for the year ended December 31, 2017, compared with net income of $4.5 million for the year ended December 31, 2016, and a net loss of $38.3 million for the year ended December 31, 2015.
Glaucoma Treatment Overview and Limitations
Glaucoma and the eye’s drainage system
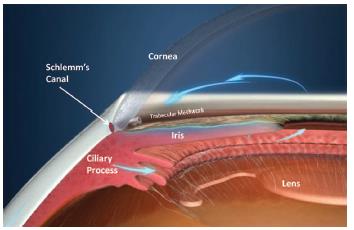
Glaucoma is a group of eye diseases characterized by progressive, irreversible and largely asymptomatic vision loss in which elevated levels of intraocular pressure are often associated with optic nerve damage. While some glaucoma patients do not experience an increase in intraocular pressure, it is widely considered a major risk factor in glaucoma’s progression and reduction in intraocular pressure is the only clinically proven treatment. Elevated intraocular pressure occurs when aqueous humor is not circulating normally or properly draining from the front part of the eye. Normally, this fluid flows through the trabecular meshwork, an area of spongy mesh‑like tissue in the eye located around the base of the cornea, and into Schlemm’s canal, a circular channel in the eye that collects the aqueous humor and delivers it back into the bloodstream. This trabecular meshwork pathway is also known as the conventional outflow pathway.
A second outflow pathway is located in the suprachoroidal space, which lies between the sclera and the choroid, where we estimate 20% of the eye’s total aqueous humor outflow occurs. This pathway is also known as the unconventional or uveoscleral pathway. The suprachoroidal space is characterized as an area of less venous resistance to aqueous humor outflow than Schlemm’s canal.
2
The following image depicts the blockage of aqueous humor outflow in an eye with open‑angle glaucoma.
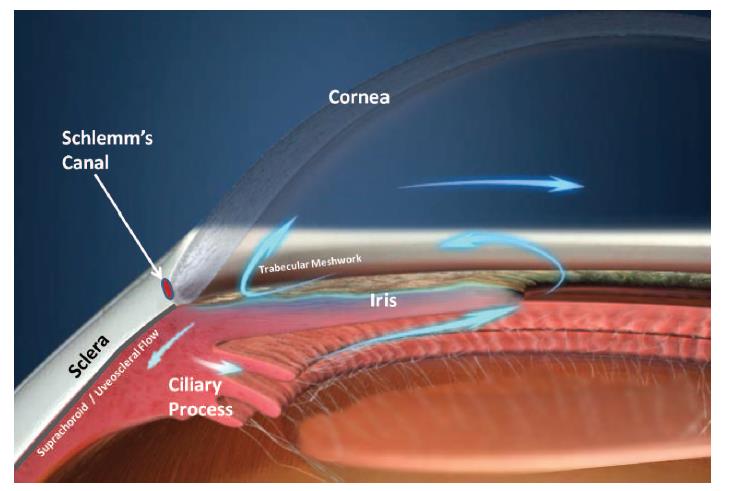
Open‑angle glaucoma is the most common type of glaucoma. In open‑angle glaucoma, structures of the eye may appear normal, but aqueous humor outflow through the trabecular meshwork and into Schlemm’s canal is reduced due to gradual degeneration and obstruction causing a permanent and progressive loss of retinal cells and associated vision loss. Direct causes of this blockage are unknown, but the disease is linked to age, ethnicity and hereditary factors. Loss of aqueous humor drainage leads to increased resistance and thus a chronic, painless buildup of pressure in the eye.
Glaucoma is a progressive disease that can be categorized based by severity levels ranging from ocular hypertension (or pre‑glaucoma) to severe glaucoma. An eye doctor usually diagnoses glaucoma as part of a comprehensive exam that includes measuring intraocular pressure and corneal thickness, evaluating optic nerve damage and testing visual fields. Intraocular pressure is measured in millimeters of mercury (mm Hg), with normal eye pressures ranging from 10 to 21 mm Hg. Glaucoma is typically characterized by an intraocular pressure greater than 21 mm Hg.
Glaucoma treatment overview
The traditional treatment of glaucoma encompasses a variety of medication regimens, laser treatments and surgical procedures to lower intraocular pressure.
Multiple clinical trials have shown that medications can reduce intraocular pressures to baseline targets that can minimize vision loss. However, poor adherence to and lack of persistence with glaucoma medication regimens have been documented in numerous independent studies, which often place the incidence of patient noncompliance up to or above 50%, particularly in patients on two or more prescription eye drops. Even daily glaucoma single medication use has been associated with noncompliance rates as high as 75%.
Because glaucoma progresses slowly and with few symptoms, patients often do not adhere to their medication regimens as prescribed until the disease has progressed to the point of significant vision loss. As a result, despite the availability of medication therapies to combat glaucoma, progressive visual loss and blindness still occur.
Laser treatments have been developed to provide an alternative to lifelong medication treatments. Typically performed at an outpatient surgical center, these treatments involve the use of lasers to create changes in eye tissue and improve aqueous humor outflow. Ophthalmic surgeons may perform laser procedures as an initial treatment or for patients who are noncompliant with prescription eye drops or whose intraocular pressure is not well controlled by
3
medications. According to Market Scope, selective laser trabeculoplasty (SLT) is the most frequently performed glaucoma laser procedure in the United States. Although SLT can help to lower intraocular pressure, the procedure’s effectiveness often wears off within one to five years according to the Glaucoma Research Foundation. While a second procedure can be performed, the results of repeated laser surgeries are less predictable and less effective than those of the first surgery. Additionally, medication therapy may still be required post‑treatment.
Where medication therapy and laser treatment are unsuccessful in managing glaucoma, invasive surgical procedures such as trabeculectomies or implantation of tube shunts are performed, usually as outpatient procedures. In a trabeculectomy, the surgeon cuts open the conjunctiva and sclera to create flaps, removes a plug of scleral tissue and sometimes a portion of the trabecular meshwork to create an opening into the anterior chamber. The conjunctiva and scleral flaps are sutured back down and a small blister, or bleb, is created between the conjunctiva and sclera. The surgery results in a new drainage channel that allows increased outflow of aqueous humor into the bleb. While some patients experience significant reductions in intraocular pressure, trabeculectomy failure rates can approach 50% according to published research. A common complication is scarring, which can prevent fluid drainage from the eye and interfere with the proper function of the bleb. If the bleb doesn’t work properly, more surgery may be needed. Among the other complications associated with trabeculectomies are blurred vision, bleeding in the eye, bleb leaks, low intraocular pressure or hypotony, infection, persistent corneal edema, choroidal detachment and cataract development. Implantations of tube shunts, devices that divert the aqueous humor from the anterior chamber, are generally reserved for eyes in which a trabeculectomy has failed or has a poor likelihood of success. A tube shunt surgery is similar to a trabeculectomy, except that the device’s tube is inserted through the scleral channel to maintain the channel and the device’s reservoir end is placed deep under the conjunctiva to maintain the drainage space. While invasive glaucoma surgery often leads to significant reductions in intraocular pressure, it is associated with high long‑term failure rates, long recovery times and significant complication risks. Additionally, as with laser treatment, the effects may dissipate over time, requiring additional procedures, and medication therapy may still be required post‑treatment.
We believe that because of the limitations of medications and laser treatments, and the morbidity associated with invasive surgical therapies, a clear unmet medical need exists in the management of open‑angle glaucoma patients.
Our Products
We pioneered the development of MIGS in order to address the shortcomings of traditional pharmaceutical and surgical options.
In contrast to invasive surgical approaches, MIGS procedures access the anterior chamber of the eye through small corneal incisions or penetrations. MIGS devices are designed to reduce intraocular pressure by restoring the natural physiologic pathways for aqueous humor outflow in a procedure that preserves more eye tissue and allows for faster recovery times and fewer complications than invasive glaucoma surgical options.
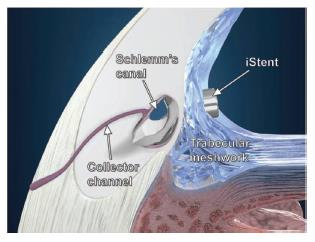
iStent trabecular micro-bypass stent. We launched our first micro‑scale MIGS treatment solution, the iStent, in the United States following FDA approval in June 2012. The iStent was the first FDA‑approved surgical device available for insertion in conjunction with cataract surgery for the reduction of intraocular pressure in adult patients with mild‑to‑moderate open‑angle glaucoma. The iStent is a micro‑bypass stent made of surgical‑grade non‑ferromagnetic titanium that is coated with heparin and is 1.0 mm long and 0.33 mm wide. Packaged in a sterile, pre‑loaded configuration, the iStent is inserted through the small corneal incision made during cataract surgery and placed into Schlemm’s canal. Once inserted, the iStent is designed to improve aqueous humor outflow while fitting naturally within Schlemm’s canal. The ergonomic rail design protects and accesses underlying collector channels while the iStent’s three retention arches help ensure secure placement. The iStent is currently approved in the U.S. only for insertion in conjunction with cataract surgery because this was the product usage in the U.S. IDE clinical trial information that was included in the PMA. The iStent is commercially available in the U.S., certain European Union countries, Brazil, Canada, Australia, Japan and other countries.
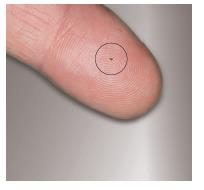
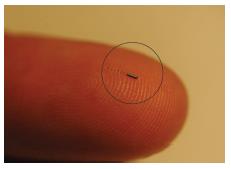
The image below left shows a gloved hand holding the pre‑loaded iStent inserter; the image below center is a magnified view of the insertion tip and iStent device; the image below right shows an iStent on the tip of a finger (inside circle).
4
|
|
|
|
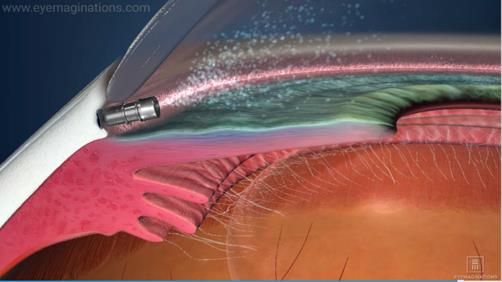
The following series of graphics illustrates the effect of iStent in the eye: (left) after placement of the iStent, aqueous humor outflow is restored; (right) close‑up illustration of iStent placement in Schlemm’s canal.
|
|
|
iStent Inject trabecular micro‑bypass stent (Outside of the U.S). The iStent Inject, which includes two stents pre‑loaded in an auto‑injection inserter, is also designed to lower intraocular pressure. Each iStent Inject stent is approximately one‑third the size of the iStent and relies on a similar fluidic method of action to improve aqueous humor outflow into Schlemm’s canal. Packaged in a two‑stent, pre-loaded, auto‑inject mechanism, the iStent Inject is designed to allow the surgeon to inject these stents into multiple trabecular meshwork locations through a single corneal entry. The iStent Inject has been approved for marketing in the European Union, Canada, Brazil, Australia and certain other countries, primarily in the Middle East. In these markets, it is approved for use in conjunction with cataract surgery or as a standalone procedure. In 2017, the iStent Inject was commercially available in certain European Union countries, Canada, Australia, Brazil and South Africa, even though reimbursement may not be available for all such procedures.
The image below left is the iStent Inject injection system, pre‑loaded with two iStent Inject devices; the image below center is a magnified view of two iStent Inject devices; the image below right shows two iStent Inject devices on a penny (inside circle).
5
|
|
|
|
Our Pipeline
We are developing five additional pipeline products: the iStent Inject (U.S.), the iStent SA, the iStent Infinite, the iStent Supra and iDose Travoprost.
iStent Inject trabecular micro bypass stent (in the U.S.). We are seeking FDA approval to market the iStent Inject in the U.S. We submitted a PMA application to the FDA at the end of 2017 after completing the U.S. pivotal IDE clinical trial to evaluate the iStent Inject for the reduction of intraocular pressure in mild‑to‑moderate open‑angle glaucoma in combination with cataract surgery.
iStent SA trabecular micro-bypass system. The iStent SA is designed for use as a standalone glaucoma procedure. Similar to the iStent Inject, the iStent SA is a two-stent product that is slightly wider than the iStent Inject and uses a different auto‑injection inserter designed for use in a standalone procedure. The system allows the surgeon to inject stents into multiple trabecular meshwork locations through a single corneal entry point and is designed to make its own self‑sealing corneal needle penetration in order to achieve insertion without an incision. A U.S. pivotal IDE trial evaluating the iStent SA for the reduction of intraocular pressure in pseudophakic mild-to-moderate open-angle glaucoma patients is currently underway. Pseudophakic refers to patients who have previously undergone cataract surgery and no longer have a natural crystalline lens. We have not commercialized the iStent SA.
iStent Infinite trabecular micro-bypass system. The iStent Infinite is designed for use as a standalone procedure in patients with refractory glaucoma (or on maximally tolerated topical glaucoma medications). The iStent Infinite consists of three stents that are pre-loaded in an auto-injection system that allows the surgeon to inject stents across a span of five to six clock hours of Schlemm’s canal. In early 2018, we submitted an IDE application seeking authorization to study the iStent Infinite in order to seek regulatory clearance through a 510(k) pre-market submission. We have not commercialized the iStent Infinite.
The image below left is a magnified view of two iStent SA devices; the image below center is a magnified view of three iStent Infinite devices; the image below right is a magnified view of the iStent Infinite inserter.
|
|
|
|
iStent Supra suprachoroidal micro‑bypass stent. The iStent Supra is designed to reduce intraocular pressure by accessing the suprachoroidal space in the eye, an area that we estimate is responsible for 20% of its total aqueous outflow. Enrollment for the U.S. pivotal IDE trial for the iStent Supra used in conjunction with cataract surgery was completed in 2017 and the two-year follow-up will conclude in 2019. The iStent Supra device has been approved for
6
marketing in the European Union and certain other countries, primarily in the Middle East. We have not commercialized the iStent Supra.
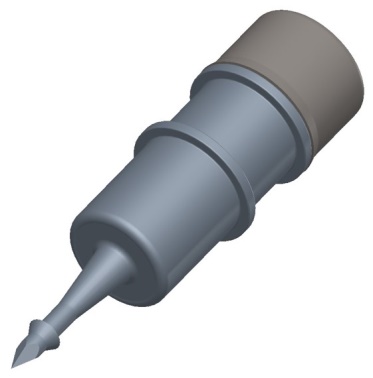
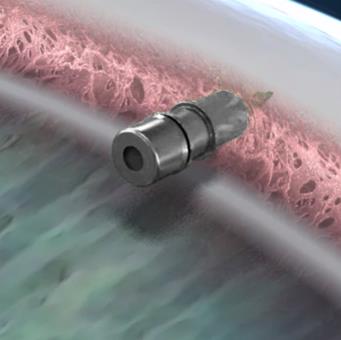
The image below left is a magnified view of the iStent Supra; the image below center illustrates the iStent Supra device implanted into the suprachoroidal space of the eye; the image below right shows the iStent Supra device on the tip of a finger (inside circle).
|
|
|
|
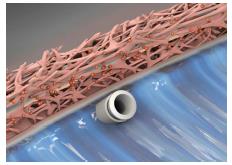
iDose. The iDose drug delivery system is a targeted injectable implant that is based on our micro‑scale device-platform designed to be pre‑loaded into a small gauge needle and injected into the eye via a self‑sealing corneal needle penetration, where it is secured within the eye. Once secured in the eye, the iDose implant is designed to continuously deliver therapeutic levels of medication from within the eye for extended periods of time. The titanium implant is similar in size to the Company’s other proprietary MIGS devices. The implant is capped with a membrane that is designed for continuous controlled drug elution into the anterior chamber. When depleted, the implant can be removed and replaced in a similar, subsequent procedure. Glaukos has designed the product to be an alternative to chronic, daily prescription eye drop treatments, which may have high rates of patient noncompliance and cause long‑term ocular surface damage to glaucomatous eyes.
In November 2015, the Company submitted an IND application to the FDA seeking authorization to study our initial iDose platform product, iDose Travoprost, for investigational use in the reduction of elevated intraocular pressure in patients with glaucoma. In December 2015, the FDA notified the Company that it was allowing the Phase II IND clinical trial to proceed. In this Phase II clinical trial, the iDose Travoprost implant was filled with a special formulation of travoprost, a prostaglandin analog used to reduce elevated intraocular pressure. In 2017, the Company completed the 154-patient, randomized, 12-week masked Phase II clinical trial, which was designed to assess the safety and preliminary efficacy of two models of iDose Travoprost with different travoprost elution rates compared to topical timolol maleate ophthalmic solution, 0.5% and conducted an End-of-Phase II meeting with the FDA. The Company is currently making preparations to initiate Phase III IND clinical trials for iDose Travoprost in the first half of 2018. We have not commercialized the iDose Travoprost.
The image below left is a magnified view of the iDose implant; the image below center is a close-up illustration of the iDose implant placement in the eye; the image below right is a graphic illustrating the effect of iDose after implantation.
7
|
|
|
|
Research & Development
Our research and development efforts are focused primarily on continuous improvement of our iStent devices, iDose drug delivery systems, related injector systems and development of new innovations that are based on our proprietary MIGS surgical and sustained pharmaceutical therapy platforms. Our research and development objectives are:
|
· |
To advance glaucoma patient care through continuous improvement of our MIGS platforms by providing viable MIGS alternatives to lifelong medication regimens and invasive surgical procedures for intraocular pressure management; |
|
· |
To introduce micro‑scale injectable therapies—including our iStent Inject, iStent SA, iStent Supra, iStent Infinite and iDose Travoprost pipeline products—that can be performed in minor surgical suites or in‑office settings with topical anesthetic; and |
|
· |
To leverage our expertise in micro-scale design and continue to expand our core research and development capabilities in order to identify and develop additional micro-invasive ophthalmic innovations that complement our existing product offerings and address important unmet clinical needs. |
As of December 31, 2017, our research and development team consisted of 132 employees. Our research and development process is supported by multiple clinical trials and regulatory affairs activities. Our research and development expenses were approximately $38.9 million, $29.2 million, and $25.0 million in the years ended December 31, 2017, 2016 and 2015, respectively. We expect our research and development expenditures to increase as we continue to devote significant resources to clinical trials and regulatory approvals of our new products.
Sales and Marketing
In the United States, we sell our products through a direct sales organization that, as of December 31, 2017, consisted of 119 sales professionals, including regional business managers, sales directors, clinical relations personnel and reimbursement specialists. Our sales organization is primarily responsible for training ophthalmic surgeons on the iStent procedure, helping these physicians integrate the technology into their practices and providing resources to support reimbursement, while also identifying and supporting investigational sites for clinical trials of our pipeline technologies. We continue to recruit experienced sales professionals with extensive sales and/or clinical experience in ophthalmic medical technologies.
We invest significant time and expense to provide comprehensive training to our sales professionals so that they are proficient in all aspects of our iStent technologies, including features and benefits, procedure techniques and reimbursement. In addition, we provide technical education regarding the eye’s anatomy, glaucoma diagnosis, disease states and treatment, and cataract surgery.
Outside the United States, we sell our products through direct sales organizations in 16 countries and a network of distribution partners in other markets. As of December 31, 2017, our direct sales organization outside the United States consisted of 87 sales professionals. We continually monitor our international sales progress and consider conversion to a direct sales approach on a country‑by‑country basis, depending on our assessment of market conditions,
8
net sales and profitability trends, reimbursement coding and coverage potential, and other factors. As of December 31, 2017, we had agreements with approximately 18 distributor organizations. No single distributor accounted for more than 10% of our total net sales for the years ended December 31, 2017, 2016 or 2015.
Our global sales efforts and promotional activities are currently aimed at ophthalmic surgeons and other eye care professionals. Our primary customers include hospitals and ambulatory surgery centers (ASCs).
Reimbursement
United States reimbursement
Reimbursement for iStent procedures
There are three key aspects of reimbursement in the United States:
|
· |
Coding refers to distinct numeric and alphanumeric billing codes that are used by healthcare providers to report the provision of medical procedures and the use of supplies for specific patients to payors. There are different categories of Current Procedural Terminology (CPT) codes (Category I, II and III) based on the procedure or supply. |
|
· |
Coverage refers to decisions made by individual payors as to whether or not to pay for a specific procedure and related supplies and if so, under what conditions (i.e., for which specific diagnoses and clinical indications). Payors typically base coverage decisions on reviews of the published medical literature. |
|
· |
Payment refers to the amount paid to providers for specific procedures and supplies. Payment is generally determined for the specific billing code and, in addition, there may be separate numeric codes, under which the billing code is classified, to establish a payment amount. |
In 2008, in consultation with and with the approval of the American Academy of Ophthalmology, we applied for and received a temporary Category III CPT code to describe insertion of devices such as the iStent using MIGS procedures.
Category III codes expire five years after the date they become effective. Prior to expiration, there are two options: submit an application to convert to a Category I code; or submit an application for a five-year extension of Category III status. CPT code 0191T, which describes the insertion of the iStent, as well as the iStent Inject, iStent SA, and iStent Infinite devices, was first effective in 2008 and our most recent application for an additional extension was approved in early 2017 and expires on December 31, 2023.
The iStent is approved by the FDA for reduction of intraocular pressure in adult patients with mild‑to‑moderate open‑angle glaucoma undergoing cataract surgery who are currently treated with prescription eye drops. Based on data released by Centers for Medicare & Medicaid Services (CMS) regarding total cataract surgery volume in the Medicare Fee for Service program and data published by Market Scope, we estimate that Medicare pays for approximately 80% of all cataract surgeries performed in the United States.
We estimate that 20% of patients who meet the FDA indication for iStent insertion are covered by private health insurance companies and we have secured coverage policies for iStent insertion with all major national private payors.
iStent insertion in the United States is almost always performed in an outpatient setting and virtually all U.S. iStent sales are to ASCs and hospital outpatient departments (HOPDs). National payment rates by Medicare to ASCs and HOPDs are determined each year through a complex formula, which takes into account reported costs for each claim submitted. When two procedures are performed in an ASC on the same patient on the same day (e.g., iStent insertion and cataract surgery), Medicare reduces the payment of the lower‑paying procedure by 50%. The ASC facility payment for cataract surgery is generally lower than the payment for iStent insertion. Therefore, when these two procedures are performed together in an ASC, the payment for cataract surgery is reduced by 50%.
For iStent insertion and cataract procedures performed in HOPDs, the Medicare fee-for-service facility reimbursement is a single, all‑inclusive payment. We estimate that approximately 25% of U.S. iStent procedures are
9
currently performed in HOPDs and that a majority of these procedures are reimbursed through traditional Medicare fee‑for‑service.
Physicians are paid separately from the facility for surgical procedures. Unlike the CPT code used to pay facilities for iStent insertion, there is no published Medicare payment schedule at the national level for the physician payment, leaving the amount of such payment to the discretion of the individual Medicare contractor. Recently, several Medicare contractors have reduced the amount of the physician payment. One of the factors a surgeon evaluates when deciding whether to adopt or to continue to perform procedures is whether or not payment for the procedure adequately covers the surgeon’s time. As with the facility payment, the incremental payment the physician receives for inserting the iStent device in conjunction with cataract surgery over and above what he or she would receive for performing cataract surgery alone plays a role in a surgeon’s decision to adopt or to continue to use the technology.
Unlike Medicare, commercial payors do not publish fee schedules. In general, based on selected feedback from facilities and surgeons, payments for iStent insertion from the commercial payors who cover the procedure are generally comparable to local Medicare payments.
Reimbursement for future products
We have also filed and received approval of applications for CPT codes that describe our pipeline iStent devices. Our application for a CPT code to describe insertion of the iStent Supra was approved by the American Medical Association (AMA), in 2011 resulting in the creation of a Category III CPT code 0253T. Our application for another extension of the Category III status of code 0253T was approved in early 2017 and expires on December 31, 2023. Our application for a CPT code to describe the insertion of additional trabecular meshwork stents (as with the iStent Inject, iStent SA, and iStent Infinite procedures) was approved by the AMA in early 2014 resulting in the creation of Category III CPT code 0376T. While this code was available beginning on January 1, 2015 for the reporting of procedures in which more than one iStent is inserted in the same eye, it currently does not result in any incremental facility or professional fee payment from Medicare. In addition, it is unclear whether any other third‑party payor will provide reimbursement for the insertion of a second stent or that a professional fee payment for a second stent will be adequate. Our application for an extension of the Category III status of code 0376T was approved in early 2017 and expires on December 31, 2023. We have not yet filed any applications for CPT codes that describe our iDose drug delivery system.
Reimbursement outside the United States
Outside the United States, reimbursement levels vary significantly by country and by region within some countries. Reimbursement is obtained from a variety of sources, including government-sponsored and private health insurance plans, and combinations of both. Some countries require additional clinical data before granting or expanding coverage and reimbursement for our products. In general, obtaining broad‑based reimbursement and adequate payment for new technologies is more difficult in these markets than in the United States. Many countries require new medical technologies to not only be safe and effective, but also to be able to demonstrate clinical benefits that outweigh the costs when compared to the standard of care.
In some countries, applications for reimbursement can be approved, but additional approvals or negotiations for payment have to be obtained. For example, in France, our customers can obtain reimbursement from the government by obtaining a code that describes iStent insertion. Certain customers, including hospitals, can obtain an incremental facility fee if the iStent were to be included on the list of devices approved for pass-through payment. In 2013, our application for a code to describe iStent insertion and our application to add the iStent to the list of devices approved for pass-through payment were denied. Following publication of data on iStent Inject, we submitted new applications for both devices in 2014. In November 2015, the French government approved the iStent application for reimbursement, but since the iStent has not been added to the list of devices approved for pass-through payment, the incremental facility payment has never been paid. Thus, as in this situation, obtaining full or even partial reimbursement can be difficult and time consuming and there can be no assurance that full or partial reimbursement will be made even though our products have been approved for reimbursement at some level.
10
In other countries, there are no codes that specifically describe the insertion of a trabecular stent or there is no mechanism to provide incremental payment for the iStent when insertion is in conjunction with cataract surgery.
As in the United States, reimbursement decisions can change, resulting in the elimination or reduction of reimbursement payments. For example, in Australia, the iStent and iStent Inject were initially included on the Department of Health’s (ADOH) prosthesis listing, which provided for a separate reimbursement payment for these devices. Last year, the Australian government began a comprehensive review of the approximately 5,600 items on the Medicare Benefits Schedule (MBS), including the prosthesis listing, in an effort to ensure all MBS items were aligned with contemporary clinical evidence and practice and improved health outcomes for patients. In connection with this review, the Company we were advised that effective May 1, 2017, the iStent and iStent Inject would no longer be reimbursed under the current code. Following petitions by the Company, on May 4, 2017, the ADOH created a temporary MBS code for the implantation of iStent and iStent Inject. This temporary code is set to expire on December 31, 2018. Concurrently, we submitted a request to the ADOH for the creation of permanent MBS code for the implantation of iStent and iStent Inject. The ADOH is considering the request for a new permanent MBS procedure code for the implantation of iStent and iStent Inject. Recently, we received correspondence advising us that ADOH’s medical services advisory committee has expressed written support for the inclusion of a permanent MBS code for implantation of iStent and iStent Inject in conjunction with cataract surgery. The advisory committee did not, however, support at this time the inclusion of a permanent code for a standalone procedure. Even though the ADOH has received the recommendations of the advisory committee, it has yet to make a final decision on the Company’s application for the creation of a permanent code.
Competition
Until recently, our iStent was the only MIGS device approved for sale in the United States by the FDA. Thus, we had for several years commercialized the iStent in the United States without any direct MIGS competitors. Alcon, Inc. (which acquired Transcend Medical, Inc., a MIGS competitor) obtained FDA approval and commenced a commercial launch of its CyPass® suprachoroidal implant, a competitive MIGS device, in 2016. The CyPass device is indicated for use in conjunction with cataract surgery for the reduction of IOP in adult patients with mild to moderate primary open-angle glaucoma. Also in 2016, Allergan plc (which acquired AqueSys, Inc., a MIGS competitor) obtained FDA approval and commenced a commercial launch of its Xen® Glaucoma Treatment System for use in the U.S. The Xen device is indicated for the management of refractory glaucoma where previous surgical treatment has failed or in patients with primary open angle glaucoma and pseudoexfoliative or pigmentary glaucoma with open angles that are unresponsive to maximum tolerated medical therapy. We are aware of several other companies, such as Santen Pharmaceutical Co., Ltd. (which recently acquired InnFocus, Inc., a MIGS competitor) and Ivantis Inc., that are conducting FDA‑approved IDE clinical trials or have filed for regulatory approval of MIGS devices. If these MIGS products or other products that may be developed receive regulatory approval, we will have additional direct MIGS competitors. These new MIGS products could achieve greater commercial acceptance, demonstrate better safety or effectiveness, clinical results, ease of use or lower costs than our iStent or our other products under development, which may reduce demand for our primary product, the iStent, as well as for our products in development.
We also compete with the use of medication therapy for treating glaucoma and with manufacturers of medical devices used in surgical therapy procedures for treating glaucoma, including Alcon, Inc., Johnson & Johnson (through its acquisition of Abbott Medical Optics Inc.), Allergan plc, STAAR Surgical Company, Lumenis Ltd., NeoMedix, Inc., New World Medical, Inc., Iridex Corporation and Ellex Medical Lasers Limited. Alcon, Inc. and Johnson & Johnson (through its acquisition of Abbott Medical Optics Inc.) are the leading manufacturers of aqueous shunts, and Alcon, Inc. also markets the EX‑PRESS Glaucoma Filtration Device. Lumenis Ltd. is a leading manufacturer of selective laser trabeculoplasty equipment. Neomedix, Inc. markets an electrosurgical device. New World Medical, Inc. offers a surgical device. Iridex Corporation offers laser systems. And, Ellex Medical Lasers Limited markets a canaloplasty device that some physicians employ to lower intraocular pressure in glaucoma.
Many of our current and potential competitors (including MIGS competitors) are large publicly traded companies or divisions of publicly‑traded companies and have several competitive advantages, including:
|
· |
greater financial and human resources for product development, sales and marketing and patent litigation; |
|
· |
significantly greater name recognition; |
11
|
· |
longer operating histories; |
|
· |
established relationships with healthcare professionals, customers and third‑party payors; |
|
· |
additional lines of products and the ability to offer rebates or bundle products to offer higher discounts or incentives; |
|
· |
more established sales and marketing programs and distribution networks; and |
|
· |
greater experience in conducting research and development, manufacturing, clinical trials, preparing regulatory submissions and obtaining regulatory clearance or approval for drug and device products and marketing approved products. |
In addition to competing for market share for our products, we also compete against these companies for personnel, including qualified sales representatives that are necessary to grow our business, as well as scientific and clinical personnel from universities and research institutions that are important to our research and development efforts.
We believe the principal competitive factors in our market include:
|
· |
improved outcomes for glaucoma; |
|
· |
acceptance by ophthalmic surgeons; |
|
· |
ease of use and reliability; |
|
· |
product price and availability of reimbursement; |
|
· |
technical leadership; |
|
· |
effective marketing and distribution; and |
|
· |
speed to market. |
Facilities, Manufacturing and Distribution
Our corporate headquarters and our manufacturing operations are located in an approximately 86,000 square foot campus in San Clemente, California which is comprised of two main buildings. This location serves as our sole manufacturing location where we manufacture, inspect, package, release and ship nearly all of our final products. All of our headquarters‑based employees, including our manufacturing and distribution employees, work at this campus. While these facilities are sufficient for our current needs, we will require additional space as our business expands. Our international subsidiaries also lease facilities in Australia, Brazil, Canada, Germany, Japan and the United Kingdom.
We manufacture, inspect, package and ship finished products from our San Clemente facility. We source components used in our proprietary manufacturing process from outside vendors and we assemble them to produce iStent devices and disposable insertion instruments. These components include both off‑the‑shelf materials and custom made parts. The iStent device and some insertion instrument components are supplied by single vendors. While we believe that there are at least several other vendors that could make any one of these items, we strive to maintain a minimum inventory of three to six months’ supply to help mitigate any supply interruptions. We source the heparin used in our iStent heparin coating from one supplier. We maintain a stock of several years’ worth of heparin material and have FDA approval to retest and extend the shelf life of the material indefinitely for U.S. product.
We have received International Standards Organization (ISO) 13485 certification which includes design control requirements. Our manufacturing processes have been validated as required by the FDA and other regulatory bodies. As a medical device manufacturer, our manufacturing facility and the facilities of our critical suppliers are subject to periodic inspection by the FDA and other regulatory agencies.
12
Intellectual Property
The strength of our competitive position depends substantially upon our ability to obtain and enforce intellectual property rights protecting our technology both domestically and internationally. We rely on a combination of intellectual property rights, including patents, trademarks, service marks, copyrights, trade secrets and other similar intellectual property, as well as customary contractual protections and security measures used to protect our proprietary, trade secret information.
In the aggregate, our intellectual property assets are of material importance to our business. We are significantly dependent on our patent and other intellectual property rights and the failure to protect such rights or succeed in litigation could negatively impact our ability to sell current or future products, or prohibit us from enforcing our patents or other intellectual property rights against others. For additional information see “Risks Related to Our Intellectual Property.”
As of December 31, 2017, we owned or exclusively licensed in certain fields of use 158 issued patents and 87 pending patent applications, including 64 U.S. patents and 32 U.S. patent applications. We may, from time to time, choose to acquire or license additional patents and patent applications, or we may choose to abandon, sell, or license certain Company patents and patent applications, depending on the needs of the Company. Our issued patents that protect our commercial products and current product pipeline will expire between 2020 and 2034. While we have pursued and continue to pursue patent protection for our existing and pipeline technologies in the U.S. and certain jurisdictions abroad, we do not know how many of our pending patent applications will result in the issuance of patents or the extent to which the examination process could require us to narrow our claims. In addition, any of our issued patents may be successfully challenged and invalidated or found to lack the scope necessary to prevent a competitor from entering the marketplace.
The ophthalmology industry in which we operate has been subject to a large number of patent filings and patent infringement litigation. Whether we infringe any patent claim owned by a third party will not be known with certainty unless and until a court interprets the patent claim in the context of litigation. If an infringement allegation is made against us, we may seek to invalidate the asserted patent claim and may allege non‑infringement of the asserted patent claim. Also, for business reasons, we may take similar actions before any such infringement allegation is made. In order for us to invalidate a U.S. patent claim, we would need to rebut the presumption of validity afforded to issued patents in the United States with clear and convincing evidence of invalidity, which is a high burden of proof. Similar or greater effort and proof may be required to invalidate foreign patents owned by third parties, including those owned by our competitors.
In some circumstances, we may rely on trade secrets to protect our technology. However, trade secrets can be difficult to protect. We seek to protect our proprietary technology and manufacturing processes, in part, by confidentiality and invention assignment agreements with employees and certain third-party service providers.
We also seek to preserve the integrity and confidentiality of our data and trade secrets by maintaining physical security of our premises and physical and electronic security of our information technology systems. While we have confidence in these individuals, organizations and systems, agreements or security measures may be breached and we may not have adequate remedies for any breach. In addition, our trade secrets may otherwise become known or be independently discovered by competitors. To the extent that our consultants, contractors or collaborators use intellectual property owned by others in their work for us, disputes may arise as to the rights in related or resulting know‑how and inventions.
Government Regulation
Our products and operations are subject to extensive and rigorous regulation by the FDA and other federal, state and local authorities, as well as foreign regulatory authorities. The FDA regulates, among other things, the research, development, testing, manufacturing, approval, labeling, storage, recordkeeping, advertising, promotion and marketing, distribution, post approval monitoring and reporting and import and export of medical devices (such as our iStent products), as well as combination drug/device products (such as iDose) in the United States to assure the safety and effectiveness of medical products for their intended use. The Federal Trade Commission also regulates the advertising of
13
our products. Further, we are subject to laws directed at preventing fraud and abuse, which subject our sales and marketing, training and other practices to government scrutiny.
U.S. government regulation—medical devices
Unless an exemption applies, each new or significantly modified medical device we seek to commercially distribute in the United States will require either a premarket notification to the FDA requesting permission for commercial distribution under Section 510(k) of the Federal Food, Drug and Cosmetic Act (FDCA), also referred to as a 510(k) clearance, or approval from the FDA of a PMA. Both the 510(k) clearance and PMA processes can be expensive, and lengthy, and require payment of significant user fees, unless an exemption is available.
Device classification
Under the FDCA, medical devices are classified into one of three classes—Class I, Class II or Class III—depending on the degree of risk associated with each medical device and the extent of control needed to provide reasonable assurances with respect to safety and effectiveness.
Class I devices are those for which safety and effectiveness can be reasonably assured by adherence to a set of regulations, referred to as General Controls, which require compliance with the applicable portions of the FDA’s Quality System Regulation (QSR), facility registration and product listing, reporting of adverse events and malfunctions, and appropriate, truthful and non‑misleading labeling and promotional materials. Some Class I devices, also called Class I reserved devices, also require premarket clearance by the FDA through the 510(k) premarket notification process described below. Most Class I products are exempt from the premarket notification requirements.
Class II devices are those that are subject to the General Controls, as well as Special Controls, which can include performance standards, guidelines and postmarket surveillance. Most Class II devices are subject to premarket review and clearance by the FDA. Premarket review and clearance by the FDA for Class II devices is accomplished through the 510(k) premarket notification process. Under the 510(k) process, the manufacturer must submit to the FDA a premarket notification, demonstrating that the device is “substantially equivalent,” as defined in the statute, to either:
|
· |
a device that was legally marketed prior to May 28, 1976, the date upon which the Medical Device Amendments of 1976 were enacted, or |
|
· |
another commercially available, similar device that was cleared through the 510(k) process. |
To be “substantially equivalent,” the proposed device must have the same intended use as the predicate device, and either have the same technological characteristics as the predicate device or have different technological characteristics and not raise different questions of safety or effectiveness than the predicate device. Clinical data is sometimes required to support substantial equivalence.
After a device receives 510(k) clearance, any modification that could significantly affect its safety or effectiveness, or that would constitute a new or major change in its intended use, will require a new 510(k) clearance or, depending on the modification, could require a PMA application. If the FDA disagrees with a manufacturer’s determination regarding whether a new premarket submission is required for the modification of an existing device, the FDA can require the manufacturer to cease marketing and/or recall the modified device until 510(k) clearance or approval of a PMA application is obtained.
If the FDA determines that the device is not “substantially equivalent” to a predicate device, or if the device is automatically classified into Class III, the device sponsor must then fulfill the much more rigorous premarketing requirements of the PMA approval process, or seek reclassification of the device through the de novo process. Pursuant to amendments to the statute in 2012, a manufacturer can also submit a petition for direct de novo review if the manufacturer is unable to identify an appropriate predicate device and the new device or new use of the device presents a moderate or low risk.
Class III devices include devices deemed by the FDA to pose the greatest risk such as life‑supporting or life‑sustaining devices, or implantable devices, in addition to those deemed not substantially equivalent following the
14
510(k) process. These devices are subject to the PMA application process, which is generally more costly and time consuming than the 510(k) process. Through the PMA application process, the applicant must submit data and information demonstrating reasonable assurance of the safety and effectiveness of the device for its intended use to the FDA’s satisfaction. Accordingly, a PMA application typically includes, but is not limited to, extensive technical information regarding device design and development, pre‑clinical and clinical trial data, manufacturing information, labeling and financial disclosure information for the clinical investigators in device studies. The PMA application must provide valid scientific evidence that demonstrates to the FDA’s satisfaction reasonable assurance of the safety and effectiveness of the device for its intended use.
The investigational device process
In the United States, absent certain limited exceptions, human clinical trials intended to support medical device clearance or approval require an IDE application. Some types of studies deemed to present “non‑significant risk” are deemed to have an approved IDE once certain requirements are addressed and Institutional Review Board (IRB) approval is obtained. If the device presents a “significant risk” to human health, as defined by the FDA, the sponsor must submit an IDE application to the FDA and obtain IDE approval prior to commencing the human clinical trials. The IDE application must be supported by appropriate data, such as animal and laboratory testing results, showing that it is safe to test the device in humans and that the testing protocol is scientifically sound. The IDE application must be approved in advance by the FDA for a specified number of subjects. Generally, clinical trials for a significant risk device may begin once the IDE application is approved by the FDA and the study protocol and informed consent are approved by appropriate institutional review boards at the clinical trial sites. There can be no assurance that submission of an IDE will result in the ability to commence clinical trials, and although the FDA’s approval of an IDE allows clinical testing to go forward for a specified number of subjects, it does not bind the FDA to accept the results of the trial as sufficient to prove the product’s safety and efficacy, even if the trial meets its intended success criteria.
All clinical trials must be conducted in accordance with the FDA’s IDE regulations that govern investigational device labeling, prohibit promotion and specify an array of recordkeeping, reporting and monitoring responsibilities of study sponsors and study investigators. Clinical trials must further comply with the FDA’s regulations for institutional review board approval and for informed consent and other human subject protections. Required records and reports are subject to inspection by the FDA. The results of clinical testing may be unfavorable, or, even if the intended safety and efficacy success criteria are achieved, may not be considered sufficient for the FDA to grant marketing approval or clearance of a product. The commencement or completion of any clinical trial may be delayed or halted or be inadequate to support approval of a PMA application for numerous reasons, including, but not limited to, the following:
|
· |
the FDA or other regulatory authorities do not approve a clinical trial protocol or a clinical trial, or place a clinical trial on hold; |
|
· |
patients do not enroll in clinical trials at the rate expected; |
|
· |
patients do not comply with trial protocols; |
|
· |
patient follow‑up is not at the rate expected; |
|
· |
patients experience adverse events; |
|
· |
patients die during a clinical trial, even though their death may not be related to the products that are part of our trial; |
|
· |
device malfunctions occur with unexpected frequency or potential adverse consequences; |
|
· |
institutional review boards and third‑party clinical investigators may delay or reject the trial protocol; |
|
· |
third‑party clinical investigators decline to participate in a trial or do not perform a trial on the anticipated schedule or consistent with the clinical trial protocol, good clinical practices or other FDA requirements; |
|
· |
we or third‑party organizations do not perform data collection, monitoring and analysis in a timely or accurate manner or consistent with the clinical trial protocol or investigational or statistical plans; |
15
|
· |
third‑party clinical investigators have significant financial interests related to us or our study such that the FDA deems the study results unreliable, or we or investigators fail to disclose such interests; |
|
· |
regulatory inspections of our clinical trials or manufacturing facilities, which may, among other things, require us to undertake corrective action or suspend or terminate our clinical trials; |
|
· |
changes in government regulations or administrative actions; |
|
· |
the interim or final results of the clinical trial are inconclusive or unfavorable as to safety or efficacy; or |
|
· |
the FDA concludes that our trial design is inadequate to demonstrate safety and efficacy. |
The PMA approval process
Following receipt of a PMA application, the FDA conducts an administrative review to determine whether the application is sufficiently complete to permit a substantive review. If it is not, the agency will refuse to file the PMA. If it is, the FDA will accept the application for filing and begin the review. The FDA, by statute and by regulation, has 180 days to review a filed PMA application, although the review of an application more often occurs over a significantly longer period of time. During this review period, the FDA may request additional information or clarification of information already provided, and the FDA may issue a major deficiency letter to the applicant, requesting the applicant’s response to deficiencies communicated by the FDA. The FDA considers a PMA or PMA supplement to have been voluntarily withdrawn if an applicant fails to respond to an FDA request for information (e.g., major deficiency letter) within a total of 360 days. Before approving or denying a PMA, an FDA advisory committee may review the PMA at a public meeting and provide the FDA with the committee’s recommendation on whether the FDA should approve the submission, approve it with specific conditions, or not approve it. Prior to approval of a PMA, the FDA may conduct a bioresearch monitoring inspection of the clinical trial data and clinical trial sites and a QSR inspection of the manufacturing facility and processes. Overall, the FDA review of a PMA application generally takes between one and three years, but may take significantly longer. The FDA can delay, limit or deny approval of a PMA application for many reasons, including:
|
· |
the device may not be shown safe or effective to the FDA’s satisfaction; |
|
· |
the data from pre‑clinical studies and clinical trials may be insufficient to support approval; |
|
· |
the manufacturing process or facilities may not meet applicable requirements; and |
|
· |
changes in FDA approval policies or adoption of new regulations may require additional data. |
If the FDA evaluation of a PMA is favorable, the FDA will issue either an approval letter, or an approvable letter, which usually contains a number of conditions that must be met in order to secure final approval of the PMA. When and if those conditions have been fulfilled to the satisfaction of the FDA, the agency will issue a PMA approval letter authorizing commercial marketing of the device, subject to the conditions of approval and the limitations established in the approval letter. If the FDA’s evaluation of a PMA application or manufacturing facilities is not favorable, the FDA will deny approval of the PMA or issue a not approvable letter. The FDA also may determine that additional tests or clinical trials are necessary, in which case the PMA approval may be delayed for several months or years while the trials are conducted and data is submitted in an amendment to the PMA, or the PMA is withdrawn and resubmitted when the data are available. The PMA process can be expensive, uncertain and lengthy and a number of devices for which FDA approval has been sought by other companies have never been approved by the FDA for marketing.
New PMA applications or PMA supplements may be required for modification to the manufacturing process, labeling, device specifications, materials or design of a device that has been approved through the PMA process. PMA supplements often require submission of the same type of information as an initial PMA application, except that the supplement is limited to information needed to support any changes from the device covered by the approved PMA application and may or may not require as extensive technical or clinical data or the convening of an advisory panel, depending on the nature of the proposed change.
16
In approving a PMA application, the FDA may also require some form of postmarket studies or postmarket surveillance, whereby the applicant follows certain patient groups for a number of years and makes periodic reports to the FDA on the clinical status of those patients when necessary to protect the public health or to provide additional safety and effectiveness data for the device. FDA may also require postmarket surveillance for certain devices cleared under a 510(k) notification, such as implants or life‑supporting or life‑sustaining devices used outside a device user facility. The FDA may also approve a PMA application with other post‑approval conditions intended to ensure the safety and effectiveness of the device, such as, among other things, restrictions on labeling, promotion, sale, distribution and use.
The FDA approved the iStent PMA on June 25, 2012, for the indication for use in combination with cataract surgery for the reduction of intraocular pressure in adult patients with mild‑to‑moderate open‑ angle glaucoma currently treated with prescription eye drops. The FDA imposed conditions of approval, including three postmarket studies (two of which are now completed), and a requirement that we implement a three‑part training program for physicians who will use the iStent device.
We are required to file new PMA applications or PMA supplement applications for significant modifications to the manufacturing process, labeling and design of a device for which we have received approval through the PMA approval process.
Post‑approval requirements
After the FDA permits a device to enter commercial distribution, numerous regulatory requirements apply. These include, but are not limited to:
|
· |
the registration and listing regulation, which requires manufacturers to register all manufacturing facilities and list all medical devices placed into commercial distribution; |
|
· |
the QSR, which requires manufacturers, including third‑party manufacturers, to follow elaborate design, testing, production, control, supplier/contractor selection, complaint handling, documentation and other quality assurance procedures during the manufacturing process; |
|
· |
labeling regulations and unique device identification requirements; |
|
· |
advertising and promotion requirements; |
|
· |
restrictions on sale, distribution or use of a device; |
|
· |
PMA annual reporting requirements; |
|
· |
the FDA’s general prohibition against promoting products for unapproved or “off‑label” uses; |
|
· |
the Medical Device Reporting (MDR) regulation, which requires that manufacturers report to the FDA if their device may have caused or contributed to a death or serious injury or malfunctioned in a way that would likely cause or contribute to a death or serious injury if it were to reoccur; |
|
· |
medical device correction and removal reporting regulations, which require that manufacturers report to the FDA field corrections and product recalls or removals if undertaken to reduce a risk to health posed by the device or to remedy a violation of the FDCA that may present a risk to health; |
|
· |
recall requirements, including a mandatory recall if there is a reasonable probability that the device would cause serious adverse health consequences or death; |
|
· |
an order of repair, replacement or refund; |
|
· |
device tracking requirements; and |
|
· |
postapproval study and postmarket surveillance requirements. |
17
Our facilities, records and manufacturing processes are subject to periodic unscheduled inspections by the FDA. Failure to comply with the applicable United States medical device regulatory requirements could result in, among other things, warning letters, untitled letters, fines, injunctions, consent decrees, civil penalties, unanticipated expenditures, repairs, replacements, refunds, recalls or seizures of products, operating restrictions, total or partial suspension of production, the FDA’s refusal to issue certificates to foreign governments needed to export products for sale in other countries, the FDA’s refusal to grant future premarket clearances or approvals, withdrawals or suspensions of current product clearances or approvals and criminal prosecution.
U.S. government regulation—drug delivery implant
In the United States, the FDA regulates drugs and combination drug/device products under the FDCA and related regulations. Drugs are also subject to other federal, state and local statutes and regulations, which along with the FDCA govern, among other things, the research, development, testing, manufacture, storage, recordkeeping, approval, labeling, advertising, promotion and marketing, distribution, post‑approval monitoring and reporting, and import and export of pharmaceutical products. Failure to comply with the applicable U.S. regulatory requirements at any time during the drug product development process, approval process or post‑approval, may subject an applicant to administrative or judicial sanctions, including refusal by the FDA to approve pending applications, withdrawal of an approval, imposition of a clinical hold, issuance of warning letters and other types of letters, product recalls, product seizures, total or partial suspension of production or distribution, injunctions, fines, refusals of government contracts, restitution, disgorgement of profits, or civil or criminal investigations and penalties brought by FDA and the Department of Justice, or other governmental entities. Any agency or judicial enforcement action could have a material adverse effect on us.
The steps required before a drug may be approved for marketing in the United States generally include:
|
· |
completion of preclinical laboratory tests and animal tests conducted in compliance with the FDA’s Good Laboratory Practices; |
|
· |
the submission to the FDA of an IND which must become effective before human clinical trials commence in the United States; |
|
· |
approval by an IRB at each clinical trial site before each trial may be initiated; |
|
· |
obtaining informed consent from the participants in a clinical trial; |
|
· |
performance of adequate and well‑controlled human clinical trials to establish the safety and efficacy of the product for each intended use and conducted in accordance with Good Clinical Practices (GCP); |
|
· |
the submission to the FDA of an NDA seeking marketing authorization for the drug product; |
|
· |
satisfactory completion of an FDA pre‑approval inspection of the facility or facilities at which the product is manufactured to assess compliance with FDA’s current Good Manufacturing Practices (cGMPs) to assure that the facilities, methods and controls are adequate to preserve the drug’s identity, strength, quality and purity; |
|
· |
satisfactory completion of a potential review by an FDA advisory committee, if applicable; and |
|
· |
FDA acceptance, review and approval of the NDA. |
The investigational new drug process
An IND is a request for authorization from the FDA to administer an investigational drug to humans. Such authorization must be obtained prior to administration to humans of any new drug or dosage form, including a new use of a previously approved drug, that is not the subject of an approved NDA, except under limited circumstances.
To conduct a clinical study of an investigational new drug product, we are required to file an IND with the FDA. The IND submission must include the general investigational plan and the protocol(s) for human studies, as well as results of animal studies or other human studies, as appropriate, analytical data and any available data or literature to
18
support the use of the investigational new drug. An IND must become effective before human clinical trials may begin. An IND will automatically become effective 30 days after receipt by the FDA, unless before that time the FDA raises concerns or questions related to the proposed clinical trials as outlined in the IND. If the FDA raises questions, the IND may be placed on clinical hold and the IND sponsor and the FDA must resolve any outstanding concerns or questions before clinical trials can begin. Accordingly, submission of an IND may or may not result in the FDA allowing clinical trials to begin. A separate submission to an existing IND must also be made for each successive clinical trial conducted during product development.
Clinical trials involve the administration of the investigational drug to patients under the supervision of qualified investigators in accordance with GCPs. Clinical trials are conducted under protocols detailing, among other things, the objectives of the study, how the study will be carried out, the parameters to be used in monitoring safety, and the efficacy criteria to be evaluated. A protocol for each clinical trial and any subsequent protocol amendments must be submitted to the FDA as part of the IND. Additionally, approval must also be obtained from the IRB at each clinical site before the trials may be initiated. The IRB will consider, among other things, ethical factors, the safety of human subjects and the possible liability of the institution. The IRB must also monitor the trial until completed. Either FDA or an IRB may suspend or terminate an ongoing clinical trial at any time for a variety of reasons, including safety concerns or lack of protection of patient rights. All participants in our clinical trials must provide their informed consent in writing. In addition, there are requirements and industry guidelines that require the posting of ongoing clinical trials on public registries and the disclosure of designated clinical trial results. The IRB must also review and approve all clinical trial recruitment plans and materials.
The clinical investigation of an investigational drug product is generally divided into three phases. Although the phases are usually conducted sequentially, they may overlap or be combined. The three phases of investigational new drug investigation are as follows:
|
· |
Phase I. Phase I includes the initial introduction of an investigational new drug into humans. Phase I clinical trials are typically closely monitored and may be conducted in patients with the target disease or condition or healthy volunteers. These studies are designed to evaluate the safety, dosage tolerance, metabolism and pharmacologic actions of the investigational drug product in humans, the side effects associated with increasing doses, and if possible, to gain early evidence on effectiveness. During Phase I clinical trials, sufficient information about the investigational drug’s pharmacokinetics and pharmacological effects may be obtained to permit the design of well‑controlled and scientifically valid Phase II clinical trials. The total number of participants included in Phase I clinical trials varies, but is generally in the range of 20 to 80. |
|
· |
Phase II. Phase II includes the controlled clinical trials conducted to preliminarily evaluate the effectiveness of the investigational drug for a particular indication in patients with the disease or condition under study, to determine dosage tolerance and optimal dosage, and to identify possible adverse side effects and safety risks associated with the drug product. Phase II clinical trials are typically well‑controlled, closely monitored, and conducted in a limited patient population, usually involving no more than several hundred participants. |
|
· |
Phase III. Phase III clinical trials are generally controlled clinical trials conducted in an expanded patient population generally at multiple clinical trial sites. They are performed after preliminary evidence suggesting effectiveness of the drug product has been obtained and are intended to further evaluate dosage, clinical effectiveness and safety, to establish the overall benefit‑risk profile of the investigational drug product, and to provide an adequate basis for product approval and adequate information for product labeling. Phase III clinical trials usually involve several hundred to several thousand participants. In most cases, the FDA requires two adequate and well‑controlled Phase III clinical trials to demonstrate the efficacy of the drug. The FDA has the legal discretion to approve a drug on the basis of a single well‑controlled clinical trial although this is less common and typically is subject to significant restrictions. |
The FDA’s primary objectives in reviewing an IND are to assure the safety and rights of patients and to help assure that the quality of the investigation will be adequate to permit an evaluation of the drug’s effectiveness and safety. The decision to terminate development of an investigational drug product may be made by either the FDA, an IRB or ethics committee, or by the study sponsor for various reasons. Clinical trials may be overseen by an independent group
19
of qualified experts organized by the trial sponsor, known as a data safety monitoring board or committee. Data safety monitoring boards provide review blinded study data at designated check points for safety risks. Suspension or termination of development during any phase of clinical trials can occur if it is determined that the participants or patients are being exposed to an unacceptable risk to health. Other reasons for suspension or termination may include changes in business objectives or the economic environment.
The NDA approval process
In order to obtain approval to market a drug product in the United States, a marketing application must be submitted to the FDA that includes data to establish the safety and effectiveness of the new drug product for the proposed indication. The NDA includes all relevant data available from pertinent preclinical and clinical trials, including negative or ambiguous results as well as positive findings, together with detailed information relating to the product’s chemistry, manufacturing, controls and proposed labeling, among other things. The NDA filing must also be accompanied by a substantial user fee, although there may be some instances in which the user fee is waived.
The FDA has 60 days from its receipt of an NDA to determine whether the application will be accepted for filing based on the agency’s threshold determination that it is sufficiently complete to permit substantive review. The FDA has substantial discretion in the approval process and may refuse to accept any incomplete application. Incomplete applications must be resubmitted with any deficiencies corrected and may be subject to an additional user fee.
Once the NDA has been accepted for filing, the FDA begins an in‑depth substantive review and sets a Prescription Drug User Fee Act date that informs the applicant of the specific date by which the FDA intends to complete its review. The FDA has agreed to certain performance goals in the review of NDAs through a two‑tiered classification system, Standard Review and Priority Review. Priority Review designation is given to drugs that treat serious diseases or conditions that offer significant improvements over existing therapies. The FDA endeavors to review applications subject to Standard Review within 10 to 12 months, whereas the FDA’s goal is to review Priority Review applications within six to eight months, depending on whether the drug is a new molecular entity. The review process is often extended by FDA requests for additional information or clarification. The FDA reviews NDAs to determine, among other things, whether the proposed product is safe and effective for its intended use, and whether the product is being manufactured in accordance with cGMP to assure and preserve the product’s identity, strength, quality and purity. Before approving an NDA, the FDA will review the proposed product labeling and may request changes. FDA will also inspect the facilities at which the product is manufactured. The FDA will not approve the product unless it determines that the manufacturing processes and facilities are in compliance with cGMP requirements and adequate to assure consistent production of the product within required specifications. In addition, before approving an NDA, the FDA will typically inspect one or more clinical sites to assure compliance with GCP. If the FDA determines the application, manufacturing process or manufacturing facilities are not acceptable, it will communicate the deficiencies to the applicant and often will request additional testing or information, including new clinical trials. Even with the submission of additional information, the FDA ultimately may decide that the application does not satisfy the regulatory standards for approval.
After the FDA evaluates the NDA and the manufacturing facilities, it issues either an approval letter or a complete response letter which indicates that the review cycle for an application is complete but that the application is not ready for approval. A complete response letter generally outlines the deficiencies in the submission and may require substantial additional testing (including clinical testing), or information, in order for the FDA to reconsider the application. Even with submission of this additional information, the FDA may ultimately decide that an application does not satisfy the regulatory criteria for approval. If, or when, the deficiencies have been addressed to the FDA’s satisfaction in a resubmission of the NDA, the FDA will issue an approval letter. An approval letter authorizes commercial marketing of the drug with specific prescribing information for specific indications.
The clinical testing and drug approval process requires substantial time, effort and financial resources, and each may take several years to complete. Data obtained from clinical activities are not always conclusive and may be susceptible to varying interpretations, which could delay, limit or prevent regulatory approval. The FDA may not grant approval on a timely basis, or at all. Even if the FDA approves a product, the agency may limit the approved indications for use, impose prominent warnings, or place other conditions on approval that could restrict the commercial application of the products, such as special risk management measures through a Risk Evaluation and Mitigation Strategy. After
20
approval, some types of changes to the approved product, such as adding new indications, manufacturing changes and additional labeling claims, are subject to further testing requirements and FDA review and pre-approval.
Section 505 of the FDCA describes three types of NDAs: (1) an application that contains full reports of investigations of safety and effectiveness (section 505(b)(1)); (2) an application that contains full reports of investigations of safety and effectiveness but where at least some of the information required for approval comes from studies not conducted by or for the applicant and for which the applicant has not obtained a right of reference (section 505(b)(2)); and (3) an application that contains information to show that the proposed product has the same active ingredient, dosage form, strength, route of administration, labeling, quality, performance characteristics, and intended use, among other things, to a previously approved product (section 505(j)).
Our iDose implant may be eligible for the Section 505(b)(2) application pathway if and when we are prepared to submit an application for marketing to the FDA. Section 505(b)(2) expressly permits the FDA to rely, in approving an NDA, on data not developed by the applicant. Thus, if a 505(b)(2) applicant can establish that reliance on the FDA’s previous findings of safety and effectiveness is scientifically appropriate, it may eliminate the need to conduct certain preclinical or clinical studies of the new product. We are pursuing a Section 505(b)(2) NDA regulatory strategy for our iDose implant which we expect will allow us to rely in our NDA filing on certain nonclinical and clinical safety findings made by the FDA in previous approvals. For changes to a previously approved drug product, an application may rely on the FDA’s finding of safety and effectiveness of the previously approved drug, coupled with the information needed to support the change from the approved drug product. The additional information could be new studies conducted by the applicant or published data. The FDA may approve the new product candidate for all, or some, of the label indications for which the reference drug has been approved, as well as for any new indication sought by the 505(b)(2) applicant.
The filing or approval of a Section 505(b)(2) application may be delayed due to patent or exclusivity protections covering an approved product. Section 505(b)(2) applications must include patent certifications and must provide notice of certain patent certifications to the NDA holder and patent owner. A Section 505(b)(2) application may be granted three years of Hatch-Waxman data exclusivity if one or more of the clinical investigations, other than bioavailability/bioequivalence studies, was essential to approval of the application and was conducted or sponsored by the applicant. Such exclusivity would cover only the new condition of use that was supported by the clinical trials that were essential to approval.
Circumstances could change that may cause a Section 505(b)(2) application for our product to no longer be an appropriate pathway. For example, if an equivalent drug product were approved before our application is submitted, the applicable pathway for our drug product might be an Abbreviated New Drug Application (ANDA). An ANDA seeks approval of a drug product that has the same active ingredient(s), dosage form, strength, route of administration, and conditions of use (labeling) as a so‑called “reference listed drug” approved under an NDA with full supporting data to establish safety and effectiveness. Limited exceptions exist to this ANDA sameness requirement, including certain limited variations approved by the FDA through a special petition process. An ANDA must contain certifications relating to patents for the reference listed drug. An ANDA also generally contains limited clinical data to demonstrate that the product covered by the ANDA is absorbed in the body at the same rate and to the same extent as the reference listed drug, which is known as bioequivalence. In addition, the ANDA must contain information regarding the manufacturing processes and facilities that will be used to ensure product quality, and must contain certifications to patents listed with the FDA for the reference listed drug.
Post‑approval regulation
After regulatory approval of a drug or combination drug/device product is obtained under an NDA, we are required to comply with pervasive and continuing regulation by the FDA, including, among other things, requirements relating to drug listing and registration, recordkeeping, periodic reporting, product sampling and distribution, advertising, marketing and promotion and reporting of adverse experiences with the product. For example, as a condition of approval of an NDA, the FDA may require post‑marketing testing, including Phase IV clinical trials, and surveillance to further assess and monitor the product’s safety and effectiveness after commercialization. In addition, the holder of an approved NDA would be required to report, among other things, certain adverse events and production problems to the FDA, and to provide updated safety and efficacy information to the FDA. Drugs may be marketed only for the approved indications and in accordance with the provisions of the approved label, and even if the FDA approves a product, it may
21
limit the approved indications for use for the product or impose other conditions, including labeling or distribution restrictions or other risk‑management mechanisms. For a combination drug/device product, such as our iDose implant, certain device reporting requirements might also apply, such as MDR requirements and reports of corrections and removal.
Quality control and manufacturing procedures must continue to conform to cGMP after approval. In addition, medical device quality system regulations would apply to the device component of a combination drug/device product, either all the QSR regulations or particular QSR regulations supplementing the drug cGMP in accordance with FDA regulations in 21 C.F.R. Part 4. The FDA periodically inspects manufacturing facilities to assess compliance with cGMP and QSR. In addition, changes to the manufacturing process are strictly regulated, and, depending on the significance of the change, may require prior FDA approval before being implemented. FDA regulations also require investigation and correction of any deviations from cGMP or QSR and impose reporting and documentation requirements upon us and any third‑party manufacturers that we may decide to use. Accordingly, manufacturers must continue to expend time, money and effort in the area of production and quality control to maintain compliance with cGMP, QSR, and other aspects of regulatory compliance.
After approval, most changes to the approved product, such as adding new indications or other labeling claims, as well as some manufacturing and supplier changes, are subject to prior FDA review and approval of a new NDA or an NDA supplement. An NDA supplement for a new indication typically requires clinical data and the FDA uses similar procedures in reviewing NDA supplements as it does in reviewing NDAs. The manufacturer and/or sponsor under an approved NDA are also subject to annual product and establishment user fees, as well as new application fees for certain supplemental applications.
Discovery of previously unknown problems with a product or the failure to comply with applicable requirements may result in restrictions on a product, manufacturer or holder of an approved NDA, including withdrawal or recall of the product from the market or other voluntary, FDA‑initiated or judicial action that could delay or prohibit further marketing. Other potential consequences include, among other things:
|
· |
fines, warning letters or holds on post‑approval clinical trials; |
|
· |
refusal of the FDA to approve pending applications or supplements to approved applications, or suspension or revocation of product license approvals; |
|
· |
product seizure or detention, or refusal to permit the import or export of products; or |
|
· |
injunctions or the imposition of civil or criminal penalties. |
Newly discovered or developed safety or effectiveness data may require changes to a product’s approved labeling, including the addition of new warnings and contraindications, and also may require the implementation of other risk management measures and/or additional clinical studies. In addition, the FDA strictly regulates marketing, labeling, advertising and promotion of products that are placed on the market. Drugs may be promoted only for the approved indications and in accordance with the provisions of the approved label. The FDA and other agencies actively enforce the laws and regulations prohibiting the promotion of off‑label uses, and a company that is found to have improperly promoted off‑label uses may be subject to significant liability.
New government requirements, including those resulting from new legislation, may be established, or the FDA’s policies may change, which could delay or prevent regulatory approval of our products under development and/or could significantly impact the requirements imposed on us after approval.
Available special regulatory procedures
Formal meetings
In the United States, there are different types of official meetings that may occur between us and the FDA. Each meeting type is subject to different procedures. Conclusions and agreements from each of these meetings are captured in the official final meeting minutes issued by the FDA.
22
Advice from the FDA is typically provided based on questions concerning quality (chemistry, manufacturing and controls testing), pre‑clinical testing and clinical studies, and pharmacovigilance plans and risk‑management programs. Advice is not legally binding with regard to any future marketing application for the drug product.
To obtain binding commitments from the FDA on the design and size of clinical trials intended to form the primary basis of an effectiveness claim for a new drug product, Special Protocol Assessment (SPA) procedures are available. Where the FDA agrees to an SPA, the agreement may not be changed by either the sponsor or the FDA except if the sponsor and the FDA agree to a change, or a senior FDA official determines that a substantial scientific issue essential to determining the safety or effectiveness of the product was identified after the testing began. An SPA is not binding if new circumstances arise, and there is no guarantee that a study will ultimately be adequate to support an approval even if the study is conducted according to the terms of an SPA.
Other healthcare laws
We are also subject to healthcare regulation and enforcement by the federal government and the states and foreign governments in which we conduct our business. These laws include, without limitation, state and federal anti‑kickback, fraud and abuse, false claims, and physician sunshine laws and regulations.
The federal Anti‑Kickback Statute prohibits, among other things, the offer, receipt, or payment of remuneration in exchange for or to induce the use of products or services that are paid for in whole or part by Medicare, Medicaid or other federal healthcare programs. Remuneration has been broadly defined to include anything of value, including cash, improper discounts, and free or reduced price items and services. The government has enforced the Anti‑Kickback Statute to reach large settlements with healthcare companies based on sham research or consulting and other financial arrangements with physicians. Further, a person or entity does not need to have actual knowledge of the statute or specific intent to violate it. In addition, the government may assert that a claim including items or services resulting from a violation of the federal Anti‑Kickback Statute constitutes a false or fraudulent claim for purposes of the federal False Claims Act (FCA). Many states have similar laws that apply to their state healthcare programs as well as private payors. Violations of the Anti‑Kickback Statute can result in exclusion from federal healthcare programs and substantial civil and criminal penalties.
The FCA imposes civil liability on persons who, among other things, present or cause to be presented false or fraudulent claims for payment by a federal healthcare program. The FCA has been used to prosecute persons submitting claims for payment that are inaccurate or fraudulent, that are for services not provided as claimed, or for services that are not medically necessary. Manufacturers can be held liable under these laws if they are deemed to “cause” the submission of false or fraudulent claims by, for example, providing inaccurate billing or coding information to customers or promoting a product off‑label. Actions under the FCA may be brought by the Attorney General or as a qui tam action by a private individual in the name of the government. Violations of the FCA can result in significant monetary penalties and treble damages. The federal government is using the FCA, and the accompanying threat of significant liability, in its investigation and prosecution of device companies throughout the country, for example, in connection with the promotion of products for unapproved uses and other improper sales and marketing practices. The government has obtained multi‑million and multi‑billion dollar settlements under the FCA. In addition, companies have been forced to implement extensive corrective action plans, and have often become subject to consent decrees or corporate integrity agreements, severely restricting the manner in which they conduct their business.
In addition, there has been a trend of increased federal and state regulation of payments made to physicians and other healthcare providers. The Affordable Care Act (ACA), among other things, imposed new annual reporting requirements on certain device manufacturers for payments made by them to physicians and teaching hospitals, as well as certain ownership and investment interests held by physicians and their immediate family members. Failure to submit required information may result in civil monetary penalties of up to $1 million. Certain states also mandate implementation of commercial compliance programs and/or require the tracking and reporting of gifts, compensation and other remuneration to physicians.
The shifting commercial compliance environment and the need to build and maintain robust systems to comply with different compliance and/or reporting requirements in multiple jurisdictions increase the possibility that a healthcare company may violate one or more of the requirements. If our operations are found to be in violation of any of such laws or any other governmental regulations that apply to us, we may be subject to penalties, including, without limitation,
23
civil and criminal penalties, damages, fines, the curtailment or restructuring of our operations, exclusion from participation in federal and state healthcare programs and imprisonment, any of which could adversely affect our ability to operate our business and our financial results.
Regulation outside the United States
In addition to regulations in the United States, we are subject to a variety of regulations in other jurisdictions governing clinical trials and commercial sales and distribution of our products. Whether or not we obtain FDA approval for a product, we must obtain authorization before commencing clinical trials or obtain marketing authorization or approval of a product under the comparable regulatory authorities of countries outside the United States before we can commence clinical trials or marketing of the product in those countries. The approval process varies from country to country and the time may be longer or shorter than that required for FDA approval. The requirements governing the conduct of clinical trials, product licensing, pricing and reimbursement vary greatly from country to country.
Other
Our operations and many of the products we manufacture or sell are subject to extensive regulation by numerous other governmental agencies, both within and outside the United States. In the United States, apart from the agencies discussed above, our facilities, operations, employees, products (their manufacture, sale, import and export) and services are regulated by Environmental Protection Agency, the Occupational Health & Safety Administration, the Department of Labor, Customs and Border Protection, the Department of Commerce, the Department of Treasury, the Department of Justice and others. Furthermore, because we supply products and services to healthcare providers that are reimbursed by federally funded programs such as Medicare, our activities are also subject to regulation by the Centers for Medicare and Medicaid Services and enforcement by the Office of the Inspector General within the Department of Health and Human Services. We are also required to report payments and other transfers of value to physicians and teaching hospitals, among others. State agencies also regulate our facilities, operations, employees, products and services within their respective states. Government agencies outside the United States also regulate public health, product registration, manufacturing, environmental conditions, labor, exports, imports and other aspects of our global operations.
Employees
As of December 31, 2017, we had 387 employees, with 183 in sales and marketing, 132 in research and development, clinical, regulatory and quality assurance, 44 in general and administrative, and 28 in manufacturing and distribution. We often supplement our research and development and clinical, regulatory and quality assurance departments with independent consultants on a project basis. We believe that our future success will depend in part on our continued ability to attract, hire and retain qualified personnel. None of our employees is represented by a labor union. We consider our relationship with our employees to be good.
Available Information
Our Annual Report on Form 10-K, Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and amendments to reports filed or furnished pursuant to Sections 13(a) and 15(d) of the Exchange Act, are available on our web site at www.glaukos.com, free of charge, as soon as reasonably practicable after the electronic filing of these reports with, or furnishing of these reports to, the Security and Exchange Commission (SEC). Any materials we file with the SEC are available at the SEC’s Public Reference Room at 100 F Street, NE, Washington, DC 20549. Additional information about the operation of the Public Reference Room can also be obtained by calling the SEC at 1-800-SEC-0330. In addition, the SEC maintains a web site at www.sec.gov that contains reports, proxy and information statements, and other information regarding issuers that file electronically with the SEC, including us.
The risks discussed below are not the only ones facing our business but do represent those risks that we believe are material to us. Additional risks and uncertainties not presently known to us or that we currently deem immaterial
24
may also harm our business. Please read the cautionary notice regarding forward-looking statements under the heading “Management’s Discussion and Analysis of Financial Condition and Results of Operations.”
Risks Related to Our Business
We have incurred significant losses since inception and there can be no guarantee that we reach or sustain profitability.
Since the Company’s inception in July 1998, we have incurred significant operating losses. For the fiscal year ended December 31, 2017, we incurred a net loss of approximately $0.1 million and for the fiscal year ended December 31, 2016 we had net income of $4.5 million. As of December 31, 2017, we had an accumulated deficit of approximately $192.2 million. Losses have resulted principally from costs incurred in our clinical trial, research and development programs and from our general and administrative expenses. Losses in the fiscal year ended December 31, 2017 were primarily attributable to our purchase of certain IOP sensor system assets from DOSE Medical Corporation (DOSE), which resulted in a $5.3 million charge to in-process research and development expense in April 2017. To date, we have financed our operations primarily through the sale of equity securities, debt financing, and cash generated from net sales. We have devoted substantially all of our resources to the research and development of our products, the commercial launch of the iStent, the development of our proprietary sales network, and the assembly of a management team to build our business.
To implement our global business strategies we need to, among other things, further grow our global sales and marketing infrastructure to increase global market acceptance of our products and any other products that receive FDA or equivalent foreign approval, fund ongoing research and development activities, expand our manufacturing capabilities, and obtain regulatory clearance or approval to commercialize our existing products in international markets or to commercialize those currently under development in the United States and internationally. As a result, we expect our expenses to increase significantly as we pursue these objectives. Our ability to sustain profitability is highly uncertain, especially given our limited commercial history selling our products globally and an increasingly competitive landscape, which makes forecasting our sales more difficult. We will need to generate significant additional net sales to maintain profitability. We cannot be sure that we will remain profitable for any substantial period of time. Our failure to sustain profitability could have an adverse effect on the value of our common stock.
Substantially all of our net sales are generated from sales of the iStent, which has an increasingly competitive landscape, and we are completely dependent on its success. If competition or other factors slow the market acceptance or usage of the iStent or our other products under development, our business will suffer.
Our primary sales‑generating commercial product is the iStent, which we began selling in the United States in the third quarter of 2012. We rely heavily upon sales in the United States, which comprised 88% and 92% of our net sales for the years ended December 31, 2017 and 2016, respectively. We expect to continue to derive a significant portion of our net sales from sales of the iStent in the United States, even if we are successful in continuing to commercialize our iStent products outside the United States, or receive necessary approvals to commercialize the iStent Inject, iStent SA, iStent Infinite, iStent Supra, iDose Travoprost and the IOP Sensor System in the United States and other countries. Accordingly, our ability to generate net sales is highly dependent on our ability to market and sell the iStent.
We developed MIGS to provide an alternative to the traditional glaucoma treatment and management paradigm. The iStent is our first MIGS device and we are developing other products to treat glaucoma. MIGS and our MIGS devices may experience a slowdown of market acceptance among eye care professionals, patients, healthcare payors and the medical community. There are a number of other available therapies marketed for the treatment of glaucoma, including medication therapies that are well established and are widely accepted by the medical community. There are also other MIGS devices that are currently available in the United States and globally or are in development by third parties that have entered or could enter the market and which may affect adoption of or demand for our products. For example, Alcon, Inc. (which acquired Transcend Medical, Inc., a MIGS competitor) obtained FDA approval and commenced a commercial launch of its CyPass® suprachoroidal implant, a competitive MIGS device, in 2016. The CyPass device is indicated for use in conjunction with cataract surgery for the reduction of IOP in adult patients with mild to moderate primary open-angle glaucoma. Also in 2016, Allergan plc (which acquired AqueSys, Inc., a MIGS competitor) obtained FDA approval and commenced a commercial launch of its Xen® Glaucoma Treatment System, a
25
competitive MIGS device, for use in the U.S. This Xen device is indicated for the management of refractory glaucoma, where previous surgical treatment has failed or in patients with primary open angle glaucoma, and pseudoexfoliative or pigmentary glaucoma with open angles that are unresponsive to maximum tolerated medical therapy. We are aware of several other companies, including Santen Pharmaceutical Co., Ltd. (which recently acquired InnFocus, Inc., a MIGS competitor), Istar Medical SA and Ivantis Inc. that are conducting FDA‑approved IDE clinical trials or have filed for regulatory approval of MIGS devices. If these MIGS products, or other products that may be developed, receive regulatory approval, we will have additional direct MIGS competitors. These new MIGS products could achieve greater commercial acceptance or demonstrate better safety or effectiveness, clinical results, ease of use or lower costs than our iStent or other products under development, which may reduce demand for our primary product, the iStent, as well as for our products in development.
Eye care professionals, patients, healthcare payors and the medical community globally may be slow or fail to adopt our products for a variety of reasons, including, among others:
|
· |
lack of experience with our products; |
|
· |
lack of availability of adequate coverage and reimbursement for hospitals, ambulatory surgery centers and physicians; |
|
· |
our inability to convince key opinion leaders to provide recommendations regarding our products, or to convince eye care professionals, patients and healthcare payors that our products are attractive alternatives to other products and treatment solutions; |
|
· |
lack of evidence supporting cost benefits or cost‑effectiveness of our products over existing alternatives; |
|
· |
perception that our products are unproven, investigational or experimental; |
|
· |
the price of our products relative to competing treatment alternatives; |
|
· |
physician preference for competitive MIGS devices in the market; |
|
· |
liability risks generally associated with the use of new products and procedures; and |
|
· |
training required to use new products. |
Our growth depends on our ability to develop and commercialize additional products, including, our pipeline products consisting of the iStent Inject, the iStent SA, the iStent Infinite, the iStent Supra and the iDose Travoprost. If we are not able to commercialize additional products, including any or each of such pipeline products, in a timely manner, our products may become obsolete over time, customers may not buy our products, our net sales and profitability may decline, and we may not experience growth in our business.
Demand for our products may change in ways we may not anticipate due to:
|
· |
changing coverage and reimbursement, coding and payments; |
|
· |
changing customer needs; |
|
· |
the introduction of new products and technologies; |
|
· |
evolving surgical practices; |
|
· |
evolving industry standards; and |
|
· |
other unforeseen reasons. |
As a result, it is important that we continue to build a more complete product offering. Developing additional products is expensive and time‑consuming, and could divert management’s attention away from expanding acceptance of the iStent and harm our business. Even if we are successful in developing our additional pipeline products, including those currently in development, the success of our new product offerings, if any, will depend on a variety of factors, including our ability to:
|
· |
properly identify and anticipate customer needs; |
26
|
· |
commercialize new products in a cost‑effective and timely manner; |
|
· |
manufacture and deliver products in sufficient volumes on time; |
|
· |
obtain regulatory approval for new products; |
|
· |
receive adequate coverage and reimbursement for procedures performed with our products; |
|
· |
differentiate our offerings from competitors’ offerings; |
|
· |
achieve positive clinical outcomes; |
|
· |
satisfy the increased demands from healthcare payors, providers and patients for lower‑cost procedures; |
|
· |
innovate and develop new materials, product designs and surgical techniques; and |
|
· |
provide adequate medical and consumer education relating to new products and attract key ophthalmologists and other eye care professionals to advocate these new products. |
Moreover, we will need to make a substantial investment in research and development before we can determine the commercial viability of any innovations, and we may not have the financial resources required to fund such research and development. In addition, even if we are able to successfully develop product enhancements or new products, these enhancements or new products may not produce net sales in excess of the costs of development, or they may be quickly rendered obsolete by changing customer preferences or the introduction by our competitors of products embodying superior technologies or features.
Research programs to identify new products will require substantial technical, financial and human resources, whether or not any such products are ultimately identified. We may determine that one or more of our pre‑clinical programs does not have sufficient potential to warrant the allocation of such resources. Our research programs may initially show promise in identifying potential products, yet fail to yield product candidates for clinical development for many reasons, including the following:
|
· |
the research methodology used may not be successful in identifying potential products; |
|
· |
competitors may develop alternatives that render our future products, if any, obsolete; |
|
· |
our products may not be deployed safely or effectively; |
|
· |
our future products, if any, may, on further study, be shown to have harmful side effects or other characteristics that indicate they are unlikely to be effective; |
|
· |
our clinical trials may not be successful; and |
|
· |
we may not receive regulatory approval. |
If we are not successful in obtaining market acceptance of our products globally, overall utilization of our products may fall below targeted levels. If we are unable to establish a global sales and marketing organization, we may not be able to effectively commercialize our products, which would adversely affect our business prospects, results of operations and financial condition.
Because of the numerous risks and uncertainties associated with our global commercialization efforts, our products may not obtain market acceptance outside of the United States, which would adversely impact the overall utilization of our products. International markets differ significantly from the U.S. market, including as a result of differences in payor systems, reimbursement, competitive dynamics, market size, regulations and patient treatment regimens. As a result of the differences in these markets, you should not compare our financial results in the U.S. market to any potential results in the international markets nor should you rely on our past results as an indication of our future performance.
In order to generate increased sales, we will need to establish a global sales organization. Our future success will depend largely on our ability to train, retain and motivate skilled regional sales managers and direct sales representatives and distributors around the world with significant technical knowledge of MIGS and the iStent and our other products. Because of the competition for their services, we cannot assure you we will be able to retain such
27
representatives on favorable or commercially reasonable terms, if at all. If we are unable to establish a global sales and marketing organization, we may not be able to effectively commercialize our products globally, which would adversely affect our business prospects, results of operations and financial condition.
Our global growth strategy requires us to enter new foreign markets to increase international sales. If we fail to obtain and maintain the regulatory approvals or the favorable reimbursement coverage or payment levels necessary to market our products in foreign jurisdictions, our market penetration opportunities will be limited. Foreign governments tend to impose strict price controls, which could negatively impact our profitability. Additionally, our existing and new potential international operations subject us to certain operating risks, which could adversely impact our results of operations and financial condition.
To implement our global growth strategy, we must continue to market our iStent and other medical device products in the international jurisdictions in which we are currently authorized, as well as expand such operations into additional foreign countries. In order to market our products in the European Union, Asia or other foreign jurisdictions, we must obtain and maintain separate regulatory approvals and comply with numerous and varying regulatory requirements. The approval procedure varies from country to country and can involve additional testing. The time required to obtain approval abroad may be longer than the time required to obtain FDA clearance or approval. Foreign regulatory approval processes include many of the risks associated with obtaining FDA clearance or approval and we may not obtain foreign regulatory approvals on a timely basis, if at all. FDA clearance or approval does not ensure approval by regulatory authorities in other countries, and approval by one foreign regulatory authority does not ensure approval by regulatory authorities in other foreign countries. However, the failure to obtain clearance or approval in one jurisdiction may have a negative impact on our ability to obtain clearance or approval elsewhere. If we do not obtain or maintain necessary approvals to commercialize our products in markets outside the United States, it would negatively affect our overall market penetration.
Even when we receive the necessary approvals to market our products in a foreign jurisdiction, we face challenges to reaching or maintaining profitability. In some foreign countries, particularly in the European Union, the pricing of medical devices is subject to governmental control. In these countries, pricing negotiations with governmental authorities can take considerable time after the receipt of marketing approval for a product. To obtain reimbursement or pricing approval in some countries, we may be required to supply data that compares the cost‑effectiveness of our products to other available therapies. If reimbursement of our products is unavailable or limited in scope or amount, or if pricing is set at unsatisfactory levels, it may not be profitable to sell our products in certain foreign countries, which could negatively affect the long‑term growth of our business.
Our existing foreign operations, as well as our planned international growth, expose us to additional uncertainty and risks beyond regulatory authorization and reimbursement levels. Outside the United States, we sell our products through direct sales organizations in 16 countries and a network of third-party distribution partners in other markets. These international operations expose us and our subsidiaries and third-party distributors to a variety of risks including, without limitation, the following:
|
· |
compliance with foreign regulations and laws, as well as U.S. laws that apply to activities in foreign jurisdictions, the adherence to which can be costly. Such regulations and laws expose us to penalties for non-compliance. These laws and regulations include various anti-bribery laws, including the U.S. Foreign Corrupt Practices Act, the United Kingdom Bribery Act, the French Sunshine Act, as well as export control regulations. Any failure to comply with applicable legal and regulatory obligations could impact us in a variety of ways that include, but are not limited to, significant criminal, civil and administrative penalties, including imprisonment of individuals, fines and penalties, denial of export privileges, seizure of shipments, restrictions on certain business activities and exclusion or debarment from government contracting; |
|
· |
difficulties enforcing our intellectual property rights and defending against third-party threats and intellectual property enforcement actions against us, our distributors, or any of our third-party suppliers; |
|
· |
reduced or varied protection for intellectual property rights in some countries; |
|
· |
pricing pressure that we may experience internationally; |
|
· |
foreign currency exchange rate fluctuations; |
28
|
· |
a shortage of high-quality sales people and distributors, and the difficulties of managing foreign operations; |
|
· |
the availability and level of third-party coverage and reimbursement within prevailing foreign healthcare systems that may require some of the patients who would be good candidates for the iStent or our other products to directly absorb medical costs, the ability of those patients to elect to privately pay for the iStent or our other products, or the potential necessity to reduce the selling prices of our products; |
|
· |
relative disadvantages compared to competitors with more recognizable names, longer operating histories and better established distribution networks and customer relationships; |
|
· |
the imposition of additional U.S. and foreign governmental controls or regulations; |
|
· |
political and economic instability; |
|
· |
changes in duties and tariffs, license obligations and other non-tariff barriers to trade; |
|
· |
the imposition of restrictions on the activities of foreign agents, representatives and distributors; |
|
· |
scrutiny of foreign tax authorities that could result in significant fines, penalties and additional taxes being imposed on us; |
|
· |
laws and business practices favoring local companies; |
|
· |
longer sales and payment cycles; |
|
· |
difficulties in maintaining consistency with our internal guidelines; |
|
· |
difficulties in enforcing agreements and collecting receivables through certain foreign legal systems; |
|
· |
the imposition of costly and lengthy new export licensing requirements and restrictions, particularly relating to technology; |
|
· |
International terrorism and anti-U.S. sentiment; |
|
· |
the imposition of U.S. or international sanctions against a country, company, person or entity with whom we do business that would restrict or prohibit continued business with the sanctioned country, company, person or entity; and |
|
· |
the imposition of new trade restrictions. |
If we experience any of these risks, our sales in non-U.S. jurisdictions may be harmed, our results of operations would suffer and our business prospects would be negatively impacted.
We face manufacturing risks that may adversely affect our ability to manufacture products and could reduce our gross margins and negatively affect our operating results.
Our business strategy depends on our ability to manufacture our current and proposed products in sufficient quantities and on a timely basis so as to meet customer demand, while adhering to product quality standards, complying with regulatory requirements and managing manufacturing costs.
Our corporate headquarters and our manufacturing operations are located in an approximately 86,000 square foot campus located in San Clemente, California, comprised of two main buildings. This location serves as our sole manufacturing location where we manufacture, inspect, package, release and ship nearly all of our final products pursuant to numerous U.S. and foreign regulatory approvals. If this facility suffers a crippling event, or a force majeure event, this could materially impact our ability to operate. If we are unable to continue to expand our manufacturing facility in compliance with regulatory requirements or to hire additional necessary manufacturing personnel, we may encounter operational interruptions, delays or additional costs in achieving our research, development and commercialization objectives, including in obtaining regulatory approvals of our product candidates and meeting customer demand, which could materially damage our business and financial position. As our business expands, we will require additional space, which could also result in a higher cost structure that could reduce our gross margin and negatively affect our operating results.
29
We are also subject to numerous other risks relating to our manufacturing capabilities, including:
|
· |
quality and reliability of product components that we source from third‑party suppliers, including the risk of receiving contaminated heparin or sourcing quality heparin in quantities sufficient to coat our products; |
|
· |
our inability to secure product components in a timely manner, in sufficient quantities or on commercially reasonable terms; |
|
· |
our inability to maintain compliance with quality system requirements; |
|
· |
our failure to increase production capacity or volumes to meet demand; |
|
· |
our inability to design or modify production processes to enable us to produce efficiently future products or implement changes in current products in response to design or regulatory requirements; and |
|
· |
difficulty identifying and qualifying alternative suppliers for components in a timely manner. |
As demand for our products increases, we will have to invest additional resources to purchase components, hire and train employees and enhance our manufacturing processes. If we fail to increase our production capacity efficiently, our sales may not increase in line with our expectations and our operating margins could fluctuate or decline. In addition, although we expect some of our products in development to share product features and components with the iStent, the manufacture of these products may require the modification of our current production processes or unique production processes, the hiring of specialized employees, the identification of new suppliers for specific components or the development of new manufacturing technologies. It may not be possible for us to manufacture these products at a cost or in quantities sufficient to make these products commercially viable or to maintain current operating margins.
We depend on a limited number of third‑party suppliers for certain components and pharmaceuticals, and the loss of any of these suppliers, or their inability to provide us with an adequate supply of materials, could harm our business.
We rely on a limited number of third‑party suppliers to supply components for the iStent, the iStent Inject and its unique injector system and our other pipeline products, as well as drugs for our iDose drug delivery system in development. Other than agreements with key suppliers, we generally do not enter into long‑term supply agreements with our suppliers, and we order most components and other products on a purchase order basis. In some cases, we have a sole supplier or a limited number of suppliers. For example, we rely on one machining company to manufacture the titanium iStent implant and one pharmaceutical supplier for the heparin used in the iStent’s heparin coating. While we believe that there are at least several other vendors that could supply the titanium implant, and other pharmaceutical vendors that could supply heparin, we have not yet qualified any of these vendors, which could cause delay, thereby impairing our ability to meet the demand of our customers. Although we maintain inventory to mitigate supply interruptions, we are nevertheless exposed to risks, including limited control over costs, availability, quality and delivery schedules.
We have been and may continue to be required to make significant “last time” purchases of components that are being discontinued by the supplier to ensure supply continuity. In addition, given our limited experience with certain suppliers, it may be difficult for us to assess their ability to timely meet our demand in the future based on past performance. If any one or more of our suppliers cease to provide us with sufficient quantities of components or drugs in a timely manner or on terms acceptable to us, we would have to seek alternative sources of supply. Because of factors such as the proprietary nature of our products, our quality control standards and regulatory requirements, we cannot quickly engage additional or replacement suppliers for some of our critical components. Even if we are able to identify and qualify a suitable second source to replace one of our key suppliers, if necessary, that replacement supplier would not have access to our previous supplier’s proprietary processes and would therefore be required to develop its own, which could result in further delay.
Failure of any of our suppliers to deliver products at the level our business requires would limit our ability to meet our sales commitments, which could harm our reputation and could have a material adverse effect on our business. We may also have difficulty obtaining similar components or drugs from other suppliers that are acceptable to the FDA or other regulatory agencies, and the failure of our suppliers to comply with strictly enforced regulatory requirements could expose us to regulatory action including warning letters, product recalls, termination of distribution, product seizures or civil penalties. It could also require us to cease using the components or drugs, seek alternative components, drugs or technologies and modify our products to incorporate alternative components, drugs or technologies, which
30
could result in a requirement to seek additional regulatory approvals. Our suppliers may also encounter financial or other hardships unrelated to our demand for their products, which could inhibit their ability to fulfill our orders and meet our requirements. Any disruption of this nature or increased expense could harm our commercialization efforts and adversely affect our operating results.
In addition, we rely on our suppliers to supply us with components and pharmaceuticals that comply with regulatory requirements, Current Good Manufacturing Practices and quality control standards, and meet agreed upon specifications at acceptable costs and on a timely basis. Although we expect our third‑party suppliers to act consistent with such standards, we do not control our suppliers, as they operate and oversee their own businesses. There is a risk that our suppliers will not always act consistent with our best interests, and may not always supply components that meet our needs. Unexpected safety or efficacy concerns can arise with respect to marketed products, whether or not scientifically justified, leading to product recalls, withdrawals, or declining sales, as well as product liability, consumer fraud and/or other claims, including potential civil or criminal governmental actions. Accordingly, if we fail to obtain sufficient quantities of high‑quality components and pharmaceuticals to meet demand for our products on a timely basis, we could lose customer orders, our reputation may be harmed and our business could suffer.
We currently operate primarily at a facility in a single location and any crippling accident, natural disaster or other force majeure event or disruption at this facility could materially affect our ability to operate and produce saleable products and could shut down our manufacturing capacity for an extended period.
Our principal office and manufacturing facility is located in San Clemente, California, adjacent to U.S. Marine Corps Base Camp Pendleton and wilderness area susceptible to brushfires, earthquakes and other natural disasters. Thus, substantially all of our operations are conducted primarily at a single location, including our manufacturing processes, research and development activities, customer and technical support, and management and administrative functions. In addition, substantially all of our inventory of component supplies and finished goods are held at a single location. Despite our efforts to safeguard this facility, including acquiring insurance on commercially reasonable terms, adopting environmental health and safety protocols and utilizing off‑site storage of computer data, vandalism, terrorism or a natural or other disaster, such as an earthquake, fire or flood, could damage or destroy our manufacturing equipment or our inventory of component supplies or finished goods, cause substantial delays in our operations, result in the loss of key information, and cause us to incur additional expenses, including relocation expenses. Our insurance may not cover our losses in any particular case, or insurance may not be available on commercially reasonable terms to cover certain of these catastrophic events. In addition, regardless of the level of insurance coverage, damage to our facilities may have a material adverse effect on our business, financial condition and operating results.
Failure to secure and maintain adequate coverage or reimbursement by third‑party payors for procedures using the iStent or our other products in development, or changes in current coverage or reimbursement, could materially impact our net sales and future growth.
We currently derive nearly all our net sales from sales of the iStent in the United States and expect this to continue for the next several years. Hospitals and ambulatory surgery centers that purchase the iStent typically bill various third‑party payors, including Medicare, Medicaid, private commercial insurance companies, health maintenance organizations and other healthcare‑related organizations, to cover all or a portion of the costs and fees associated with the MIGS procedures in which the iStent is used and bill patients for any applicable deductibles or co‑payments. Access to adequate coverage and reimbursement for the procedures using the iStent (and our other products in development) by third‑party payors is essential to the acceptance of our products by our customers.
Because there is generally no separate reimbursement for medical devices and other supplies used in such procedures, including the iStent, the additional cost associated with the use of our iStent device could impact the profit margin of the hospital or surgery center where the cataract surgery is performed if the incremental facility fee payment is not sufficient. Some of our target customers may be unwilling to adopt our iStent in light of the additional associated cost. Further, any decline in the amount payors are willing to reimburse our customers for MIGS procedures could make it difficult for existing customers to continue using, or new customers to adopt, our iStent devices and could create additional pricing pressure for us. If we are forced to lower the price we charge for our products, our gross margins would decrease, which would adversely affect our ability to invest in and grow our business.
In addition, a key component of our global expansion strategy is obtaining reimbursement for the iStent device and procedure by governmental or private payors within the foreign countries in which we are seeking to commercialize
31
our products. The requirements and processes for obtaining approval for such reimbursement may vary significantly from country to country, entail prolonged delay, or be more difficult for foreign manufacturers with new, unfamiliar products and treatments. If we face one or more of these challenges as we pursue commercializing our products internationally, our business prospects will suffer.
Third‑party payors, whether foreign or domestic, or governmental or commercial, are developing increasingly sophisticated methods of controlling healthcare costs. In addition, in the United States, no uniform policy of coverage and reimbursement for medical device products and services exists among third‑party payors. Therefore, coverage and reimbursement for medical device products and services can differ significantly from payor to payor. In addition, payors continually review new technologies for possible coverage and can, without notice, deny coverage for these new products and procedures. As a result, the coverage determination process is often a time‑consuming and costly process that will require us to provide scientific and clinical support for the use of our products to each payor separately, with no assurance that coverage and adequate reimbursement will be obtained, or maintained if obtained.
Many third‑party payors in the United States model their coverage policies and payment amounts after those determined by CMS, the federal agency responsible for administering the Medicare program. CMS relies on an extensive network of Medicare Administrative Contractors (MACs) to develop coverage policies when no national coverage determination exists for a procedure. Because there currently is no Medicare national coverage determination for procedures using our iStent devices, we are required to provide scientific and clinical support for the use of the iStent (including the iStent Inject device and iStent Supra device, if approved) to each MAC separately, with no assurance that coverage and adequate reimbursement will be obtained. Although all MACs currently provide coverage and reimbursement for the MIGS procedure using the iStent, difficulties in processing reimbursement or regional differences or reductions in the reimbursement amount for the physician professional services could negatively impact iStent penetration or usage by customers. These differences in MAC reimbursement could also negatively impact the amount paid by private commercial insurance companies, further negatively affecting customer penetration or usage.
Third‑party payors, including CMS, regularly assess and propose changes to their coverage and reimbursement policies. Changes in these current policies impact the profit margin of the hospital or surgery center where the surgery is performed and increase costs to customers. For example, beginning in 2016, Medicare started to make a single, comprehensive payment for combination iStent insertion and cataract procedures performed in hospital outpatient departments (HOPDs), eliminating the separate payments that were available for the procedures in prior years and reducing the total reimbursement amount for the combination procedure in the HOPD. Further, any decline in the amount payors are willing to reimburse our customers for MIGS procedures could make it difficult for existing customers to continue using, or new customers to adopt, our iStent devices and could create additional pricing pressure for us. If we were forced to lower the price we charge for our products, our gross margins would decrease, which would adversely affect our ability to invest in and grow our business. Conversely, although the reimbursement payments from Medicare to surgery centers for the iStent procedure was increased effective January 1, 2017, there can be no assurance that this increase will remain in effect in future years or that the amount of reimbursement will not be decreased in future years. Any reduction in the amount of Medicare reimbursement payments will have a negative effect on our net sales.
Some third‑party payors in the United States, including Medicaid and certain commercial payors, have developed policies that deny coverage for the MIGS procedure using the iStent. To support changes in these policies, we may need to conduct prospective, randomized controlled clinical trials and present data from such trials to these payors to demonstrate the medical necessity or cost‑effectiveness of the iStent. There can be no assurance that coverage for our products will be expanded. In addition, those private payors that do not follow the Medicare guidelines may adopt different coverage and reimbursement policies for MIGS procedures performed with the iStent, though we cannot predict whether coverage will be sufficient or if there will be coverage at all. Failure to obtain favorable payor policies could have a material adverse effect on our business and operations.
We believe that Medicare coverage and existing coverage by third‑party payors represents more than 90% of our target patient population. U.S. third‑party payors representing more than 90% of individuals covered by commercial insurance currently reimburse the iStent procedure. While we anticipate gaining coverage and reimbursement from additional third‑party payors, we cannot guarantee that we will be successful or that coverage and reimbursement will be at levels that support continued penetration and usage by our customers. Moreover, compliance with the administrative procedures and requirements of third‑party payors may result in delays in processing approvals by those third‑party payors for customers to obtain coverage and reimbursement for procedures using the iStent. Failure to secure or maintain adequate coverage or reimbursement for procedures using the iStent by third‑party payors, or delays in processing
32
approvals by those payors, could result in the cancellations of procedures to insert the iStent in combination with cataract surgery, resulting in the loss of net sales from these procedures. If these issues remain unresolved, they could have a material adverse effect on our business, financial condition and operating results.
In addition, although we have obtained temporary Category III Current Procedural Terminology (CPT) codes for the MIGS procedures associated with the insertion of our iStent products, there is no guarantee that these billing codes or the payment amounts associated with such codes will not change in the future. Category III codes expire five years after the date they become effective. Prior to expiration, there are two options: submit an application to convert to a permanent Category I code; or submit an application for a five-year extension of Category III status. If we are unable to maintain our existing codes or obtain new permanent Category I codes for procedures using our iStent products, or obtain new reimbursement codes for our other products in development, we will be subject to significant pricing pressure, which could harm our business, results of operations, financial condition and prospects. Additionally, if we do obtain a permanent Category I Code for procedures using our iStent products, national reimbursement levels for such procedures may be adjusted at that time. Reimbursement levels may be decreased or significantly decreased, which would have a material adverse effect on our business, financial condition and operating results.
Physicians are typically paid separately from the facility for surgical procedures involving the iStent. Unlike the facility payment associated with the CPT code that describes iStent insertion, there is no published Medicare payment schedule at the national level, and the physician payment rate is left to the discretion of the individual MAC. In order to adopt a new procedure, one of the factors that the surgeon evaluates is whether or not payment for the procedure adequately covers the surgeon’s time. As with the facility payment, the incremental payment the physician receives for inserting the iStent device plays a role in a surgeon’s decision to adopt the technology. Accordingly, changes in the payment the physician receives could affect the extent to which physicians recommend the iStent procedure to patients, which could have a material adverse effect on our business, financial condition and operating results.
Further, we believe that future coverage and reimbursement will likely be subject to increased restrictions both in the United States and in international markets. Coverage decisions may depend upon clinical and economic standards that disfavor new products when more established or lower cost therapeutic alternatives are already available or subsequently become available. Adequate coverage and reimbursement from governmental and commercial payors are critical to new product acceptance. Third‑party coverage and reimbursement for our products or any of our product candidates for which we may receive regulatory approval may not be available or adequate in either the United States or international markets.
If our competitors are better able to develop and market products that are safer, more effective, less costly or otherwise more attractive than the iStent or any new products that we may develop, our commercial opportunity may be reduced or eliminated.
The medical device industry is highly competitive and subject to rapid and profound technological, market and product-related changes. Our success depends, in part, upon our ability to maintain a competitive position in the development of MIGS products. Our competitors, medical companies, academic and research institutions or others could develop new drugs, therapies, medical devices or surgical procedures to treat glaucoma that could render our products obsolete.
Until recently, our iStent was the only MIGS device approved for sale in the United States by the FDA. Thus, we had for several years commercialized the iStent in the United States without any direct MIGS competitors. Alcon, Inc. (which acquired Transcend Medical, Inc., a MIGS competitor) obtained FDA approval and commenced a commercial launch of its CyPass® suprachoroidal implant, a competitive MIGS device, in 2016. The CyPass device is indicated for use in conjunction with cataract surgery for the reduction of IOP in adult patients with mild to moderate primary open-angle glaucoma. Also in 2016, Allergan plc (which acquired AqueSys, Inc., a MIGS competitor) obtained FDA approval and commenced a commercial launch of its Xen® Glaucoma Treatment System, a competitive MIGS device, for use in the U.S. The Xen device is indicated for the management of refractory glaucoma, where previous surgical treatment has failed or in patients with primary open angle glaucoma, and pseudoexfoliative or pigmentary glaucoma with open angles that are unresponsive to maximum tolerated medical therapy. We are aware of several other companies, including Santen Pharmaceutical Co., Ltd. (which recently acquired InnFocus, Inc., a MIGS competitor), Istar Medical SA and Ivantis Inc. that are conducting FDA‑approved investigational device exemption (IDE) clinical trials or have filed for regulatory approval of MIGS devices. If these MIGS products, or other products that may be developed, receive regulatory approval, we will have additional direct MIGS competitors. These new MIGS products
33
could achieve greater commercial acceptance or demonstrate better safety or effectiveness, clinical results, ease of use or lower costs than our iStent or other products under development, which may reduce demand for our primary product, the iStent, as well as for our products in development. Demand for the iStent or our future products may decline when such products and technologies are introduced, and our business may be harmed.
We also compete with the use of medication therapy for treating glaucoma and with manufacturers of medical devices used in surgical therapy procedures for treating glaucoma, including Alcon, Inc., Johnson & Johnson (through its acquisition of Abbott Medical Optics Inc.), Allergan plc, STAAR Surgical Company, Lumenis Ltd., NeoMedix, Inc., New World Medical, Inc., Iridex Corporation and Ellex Medical Lasers Limited. Alcon, Inc. and Johnson & Johnson (through its acquisition of Abbott Medical Optics Inc.) are the leading manufacturers of aqueous shunts, and Alcon, Inc. also markets the EX‑PRESS Glaucoma Filtration Device. Lumenis Ltd. is a leading manufacturer of selective laser trabeculoplasty equipment. Neomedix, Inc. markets an electrosurgical device. New World Medical, Inc. offers a surgical device. Iridex Corporation offers laser systems. And, Ellex Medical Lasers Limited markets a canaloplasty device that some physicians employ to lower intraocular pressure in glaucoma.
Many of our current and potential competitors (including MIGS competitors) are large publicly traded companies or divisions of publicly traded companies and have several competitive advantages, including:
|
· |
greater financial and human resources for product development, sales and marketing and patent litigation; |
|
· |
significantly greater name recognition; |
|
· |
longer operating histories; |
|
· |
established relationships with healthcare professionals, customers and third‑party payors; |
|
· |
additional lines of products, and the ability to offer rebates or bundle products to offer higher discounts or incentives; |
|
· |
more established sales and marketing programs and distribution networks; and |
|
· |
greater experience in conducting research and development, manufacturing, clinical trials, preparing regulatory submissions and obtaining regulatory clearance or approval for drug and device products and marketing approved products. |
As discussed above, the Xen device is being marketed by Allergan plc, a publicly traded company, and the CyPass is being marketed by Alcon, Inc., which is a division of Novartis International AG, a publicly traded multinational pharmaceutical company. InnFocus, Inc. was acquired by Santen Pharmaceutical Co., Ltd., a publicly traded multinational pharmaceutical company dedicated to the ophthalmic field. As a result of these transactions, we are competing directly against other MIGS providers that have the efficiencies and advantages identified above.
The training required for surgeons to use our products could reduce the market acceptance of our products.
As with any new method or technique, ophthalmic surgeons must undergo a thorough training program before they are qualified to perform procedures using our products. Surgeons could experience difficulty with the technique necessary to successfully insert our products, including intraoperative gonioscopy, and not achieve the technical competency necessary to be qualified to insert our devices. Also, even after successfully completing the training program, the physicians could experience difficulty inserting our products and cease utilizing them or limit their use significantly in practice. Surgeons may also experience greater success or competency with a competitive MIGS product.
We could also experience difficulty meeting expected levels of ophthalmic surgeons who complete our training program. This could happen due to less demand than expected, preference for competitive MIGS products, the length of time necessary to train each surgeon being longer than expected, the capacity of our sales representatives to train surgeons being less than anticipated, or if we are unable to sufficiently increase our sales organization. All of these events would lead to fewer trained ophthalmic surgeons qualified to insert our products, which could negatively impact our operating and financial results.
34
Ophthalmic surgeons may not use our products if they do not believe they are safe, efficient, effective and preferable alternatives to other treatment solutions in the market. If subsequent or continuing patient studies on the iStent, or patient outcomes, demonstrate results that are inferior to or inconsistent with our existing data, our sales could be adversely impacted. Additionally, ophthalmic surgeons not completing the iStent training program may nevertheless elect to perform iStent procedures and experience inferior clinical outcomes.
We believe that ophthalmic surgeons will not use our products unless they conclude that our products provide a safe, efficient, effective and preferable alternative to currently available treatment options. If longer‑term patient studies or clinical experience indicate that treatment with our products is less effective, less efficient or less safe than our current data suggest, our sales would be harmed, and we could be subject to significant liability. Further, unsatisfactory patient outcomes or patient injury could cause negative publicity for our products, particularly in the early phases of product introduction for our products currently under development. In addition, physicians may be slow to adopt our products if they perceive liability risks arising from their use. It is also possible that as our products become more widely used, latent defects could be identified, creating negative publicity and liability problems for us and adversely affecting demand for our products. Physicians may also conclude that the products offered by our MIGS competitors have greater efficacy than our products, which could result in a decline in our sales.
Ophthalmic surgeons may also determine not to use our products due to other potential risks to patients. For example, the iStent is rated “MRI Conditional” by the American Society for Testing and Materials. This means that a patient implanted with the iStent can be scanned via magnetic resonance imaging (MRI) only under the following conditions specified on the product label: static magnetic field of 3‑Tesla or less, and maximum spatial magnetic field gradient of 4,000‑Gauss/cm or less. Therefore, it may not be safe for iStent recipients to undergo MRIs in environments that do not match these specified conditions. Physicians may choose not to implant iStents because of this limitation, which could have an adverse impact on our net sales growth and financial results.
Additionally, inferior patient outcomes, or patient injury, may result if untrained or unqualified ophthalmic surgeons elect to perform iStent procedures. Although our sales representatives manage the training program for ophthalmic surgeons to become qualified to insert the iStent in combination with cataract surgery, once training is completed the surgeon and/or surgical facility that the surgeon utilizes are cleared to purchase and maintain an iStent supply. There is a risk that untrained or unqualified ophthalmic surgeons could gain access to iStent devices from a facility’s inventory and conduct iStent procedures without having received qualified status from us. If performing iStent procedures by unqualified ophthalmic surgeons were to become pervasive, this could raise the risk of complications and inferior clinical outcomes, which could result in negative patient experiences or experiences being published and damaging our reputation and that of the iStent. This could result in lower penetration and utilization by ophthalmic surgeons and could have a material adverse effect on our net sales growth, expected operating results and financial condition.
If an increasing number of ophthalmic surgeons do not continue to adopt the use of our products, our operating and financial results will be negatively impacted.
Product liability suits brought against us could cause us to incur substantial liabilities, limit sales of our existing products and limit commercialization of any products that we may develop.
If our product offerings, including the iStent, are defectively designed or manufactured, contain defective components, or are used or deployed improperly, or if someone claims any of the foregoing, whether or not such claims are meritorious, we may become subject to substantial and costly litigation. Any product liability claims brought against us, with or without merit, could divert management’s attention from our business, be expensive to defend, result in sizable damage awards against us, damage our reputation, increase our product liability insurance rates, prevent us from securing continuing coverage, or prevent or interfere with commercialization of our products. In addition, we may not have sufficient insurance coverage for all future claims. Product liability claims brought against us in excess of our insurance coverage would likely be paid out of cash reserves, harming our financial condition and results of operations.
35
Operating results could be unpredictable and may fluctuate significantly from quarter to quarter, which could adversely affect our business, financial condition, results of operations and the trading price of our common stock.
Our net sales from the sale of the iStent may experience volatility due to a number of factors, many of which are beyond our control, including:
|
· |
our ability to drive increased sales of our products; |
|
· |
our ability to establish and maintain an effective and dedicated sales organization; |
|
· |
fluctuations in the demand for our products; |
|
· |
pricing pressure applicable to our products, including adverse third‑party coverage and reimbursement outcomes and competitor pricing; |
|
· |
results of clinical research and trials on our products; |
|
· |
fluctuations in the number of cataract procedures performed by our customers, which could decrease significantly during holiday seasons and summer months, when significant numbers of physicians and patients may schedule vacations; |
|
· |
timing of new product offerings, acquisitions, licenses or other significant events by us or our competitors; |
|
· |
deferrals of customer orders in anticipation of the introduction of new products or product enhancements by us; |
|
· |
regulatory approvals and legislative changes affecting the products we may offer or those of our competitors; |
|
· |
interruption in the manufacturing or distribution of our products; |
|
· |
the ability of our suppliers to timely provide us with an adequate supply of product components; |
|
· |
the effect of competing technological, industry and market developments; |
|
· |
changes in our ability to obtain regulatory clearance or approval for our products or to obtain or maintain our CE Certificates of Conformity for our products; |
|
· |
variances in the sales terms, timing or volume of customer orders from period to period; |
|
· |
the length of our sales cycle, which varies and may be unpredictable; and |
|
· |
our ability to expand the geographic reach of our sales and marketing efforts. |
As a result, you should not rely on our results in any past period as an indication of future results and you should anticipate that fluctuations in our quarterly and annual operating results may continue and could generate volatility in the price of our common stock. We believe that quarterly comparisons of our financial results should not be relied upon as an indication of our future performance.
If we fail to manage our anticipated growth effectively, our business could suffer.
Since the commercial launch of the iStent in July 2012, we have seen significant period‑to‑period growth in our business. We anticipate that this growth will continue in the near term as the iStent continues to gain market acceptance and we develop and introduce new products. Not only do we expect this growth to continue, but we must continue to grow in order to meet our business and financial objectives. However, continued growth may create numerous challenges, including:
|
· |
new and increased responsibilities for our management team; |
|
· |
increased pressure on our operating, financial and reporting systems; |
|
· |
increased pressure from our competitors; |
|
· |
increased pressure to anticipate and satisfy market demand; |
36
|
· |
additional manufacturing capacity requirements; |
|
· |
strain on our ability to source a larger supply of components that meet our required specifications on a timely basis; |
|
· |
management of an increasing number of relationships with our customers, suppliers and other third parties; |
|
· |
entry into new international territories with unfamiliar regulations and business approaches, and |
|
· |
the need to hire, train and manage additional qualified personnel. |
If we fail to manage any of the above challenges effectively, our business may be harmed.
Our future growth depends on our ability to retain members of our senior management and other key employees. If we are unable to retain or recruit qualified personnel for growth, our business results could suffer.
We have benefited substantially from the leadership and performance of our senior management as well as certain key employees. For example, our chief executive officer, as well as other key members of our senior management, has experience successfully developing novel technologies and scaling early‑stage medical device companies to achieve profitability. Our success will depend on our ability to retain our current management and key employees, and to attract and retain qualified personnel in the future. Competition for senior management and key employees in our industry is intense and we cannot guarantee that we will be able to retain our personnel or attract new, qualified personnel. The loss of services of certain members of our senior management or key employees could prevent or delay the implementation and completion of our strategic objectives, or divert management’s attention to seeking qualified replacements. Each member of senior management as well as our key employees may terminate employment without notice and without cause or good reason. The members of our senior management are not subject to non‑competition agreements. Accordingly, the adverse effect resulting from the loss of certain members of senior management could be compounded by our inability to prevent them from competing with us.
In addition to competing for market share for our products, we also compete against our competitors for personnel, including qualified sales representatives that are necessary to grow our business. Also, we compete with universities and research institutions for scientific and clinical personnel that are important to our research and development efforts.
We also rely on consultants and advisors in our research, operations, clinical and commercial efforts to implement our business strategies. Our consultants and advisors may be employed by employers other than us and may have commitments under consulting or advisory contracts with other entities that may limit their availability to us.
Our strategic plan requires us to continue growing our sales, marketing, clinical and operational infrastructure in order to generate, and meet, the demand for our products. If we fail to retain or attract these key personnel, we could fail to take advantage of the market for our iStent technologies and our business, financial condition and operating results could be adversely affected.
Our iDose implant will be regulated as a drug and be subject to a different regulatory approval process than our other products in development. iDose is in early stages of development and may never be commercialized.
As a drug delivery implant, iDose will be subject to a regulatory approval process similar to that for pharmaceuticals. This process is often a more lengthy, costly and complex process than obtaining regulatory approval for a medical device. The future success of our iDose product depends on our ability to complete clinical trials, and will require significant development activities, clinical trials, regulatory approvals, and substantial additional investment.
This development program may not lead to a commercially viable product for several reasons. For example, we may fail to demonstrate safety and efficacy in pre‑clinical tests or clinical trials, or we may have inadequate financial or other resources to pursue drug development efforts. From time to time, we may establish and announce certain development goals for our iDose product candidate; however, it is difficult to predict accurately if and when we will achieve these goals. We may be unsuccessful in advancing this drug delivery implant into clinical testing or in obtaining FDA approval, and our long‑term business prospects could be harmed.
37
Our business requires substantial capital and operating expenditures to operate and grow.
Although we raised net proceeds of approximately $113.6 million from our IPO and generate net sales from our approved products, we may nevertheless need to raise substantial additional capital in the future to:
|
· |
expand our sales and marketing organization in the United States and internationally; |
|
· |
fund our operations, clinical trials and commercialization efforts for new products, if any such products receive regulatory approval for commercial sale; |
|
· |
scale‑up our manufacturing operations; |
|
· |
pursue additional research and development; |
|
· |
enforce or defend, in litigation or otherwise, our patent or other intellectual property rights against infringement, misappropriation or other violation by third parties or any claims that we infringe or have otherwise violated third‑party patent or other intellectual property rights; and |
|
· |
acquire companies or in‑license products or intellectual property. |
We believe that our available cash, cash equivalents, investment balances and interest we earn on these balances and cash generated from sales of our iStent products will be sufficient to fund our operations and satisfy our liquidity requirements for at least the next 12 months from the date our consolidated financial statements for the year ended December 31, 2017 are made publicly available. However, our future funding requirements will depend on many factors, including:
|
· |
the scope, rate of progress and cost of our clinical trials and other research and development activities; |
|
· |
the cost of filing and prosecuting patent applications and defending and enforcing our patent and other intellectual property rights; |
|
· |
the cost of asserting or defending, in litigation or otherwise, our patent or other intellectual property rights against infringement, misappropriation or other violation by third parties or any claims that we infringe or have otherwise violated third‑party patent or other intellectual property rights; |
|
· |
the terms and timing of any collaborative, licensing and other arrangements that we may establish; |
|
· |
the cost and timing of regulatory approvals; |
|
· |
the cost and timing of establishing sales, marketing and distribution capabilities; |
|
· |
the cost of establishing clinical and commercial supplies of our products and any products that we may develop; |
|
· |
the effect of competing technological and market developments; |
|
· |
licensing technologies for future development; and |
|
· |
the extent to which we acquire or invest in businesses, products and technologies, although we currently have no commitments or agreements relating to any of these types of transactions. |
If we raise additional funds through further issuances of equity or issuances of convertible debt securities, our existing stockholders could suffer significant dilution, and any new equity securities we issue could have rights, preferences and privileges superior to those of holders of our common stock. Any debt financing obtained by us in the future would likely be senior to our common stock, would likely cause us to incur interest expense, and could involve restrictive covenants relating to our capital raising activities and other financial and operational matters, which may increase our expenses and make it more difficult for us to obtain additional capital and to pursue business opportunities, including potential acquisitions. We may also be required to secure any such debt obligations with some or all of our assets.
We cannot assure you that we will be able to obtain additional financing on terms favorable to us, if at all. If we are unable to obtain adequate financing or financing on terms satisfactory to us when we require it, or if we expend
38
capital on projects that are not successful, our ability to continue to support our business growth and to respond to business challenges could be significantly limited, or we may even have to scale back our operations.
We may enter into acquisitions, collaborations, in‑licensing agreements, joint ventures, alliances or partnerships with third parties that fail to result in a commercial product or net sales.
We may enter into acquisitions, collaborations, in‑licensing agreements, joint ventures, alliances, partnerships or undertake one or more of these transactions in order to retain our competitive position within the marketplace or to expand into new markets. However, we cannot assure you that we would be able to successfully complete any acquisition we choose to pursue, or that we would be able to successfully integrate any acquired business, product or technology in a cost‑effective and non‑disruptive manner. If we were unable to integrate any acquired businesses, products or technologies effectively, our business would likely suffer.
Failure to protect our information technology infrastructure against cyber-based attacks, network security breaches, service interruptions or data corruption could materially disrupt our operations and adversely affect our business and operating results.
The efficient operation of our business depends on our information technology systems. We rely on our information technology systems to effectively manage sales and marketing data, accounting and financial functions, inventory management, product development tasks, clinical data, customer service and technical support functions. Our information technology systems are vulnerable to damage or interruption from earthquakes, fires, floods and other natural disasters, terrorist attacks, cyber-based attacks, attacks by computer viruses or hackers, power losses, computer system or data network failures, security breaches and data corruption. In addition, a variety of our software systems are cloud‑based data management applications, hosted by third‑party service providers whose security and information technology systems are subject to similar risks.
The failure of either our or our service providers’ information technology could disrupt our entire operation or result in decreased sales, increased overhead costs and product shortages, all of which could have a material adverse effect on our reputation, business, financial condition and operating results.
We cannot be certain that our net operating loss tax carryforwards will be available to offset future taxable income.
As of December 31, 2017, we had net operating loss carryforwards of approximately $125.7 million for U.S. federal income tax purposes, approximately $94.2 million of net operating loss carryforwards for state income tax purposes and approximately $18.0 million of net operating loss carryforwards for foreign purposes. The federal net operating loss carryforwards begin to expire in 2018 and $2.5 million of the state net operating loss carryforwards expired in 2017 and the remainder will begin to expire in 2028. The foreign net operating loss carryforwards will begin to expire no earlier than 2023, if not utilized sooner. At December 31, 2017, we had federal and state research and development carryforwards of approximately $7.5 million and $7.0 million, respectively, which begin to expire in 2021 for federal purposes and carry over indefinitely for state purposes. We have recorded a full valuation allowance against these tax attributes because we believe that uncertainty exists with respect to the future realization of the tax attributes as well as with respect to the amount of the tax attributes that will be available in future periods. To the extent available, we intend to use these net operating loss carryforwards to offset future taxable income associated with our operations. There can be no assurance that we will generate sufficient taxable income in the carryforward period to utilize any remaining net operating loss carryforwards before they expire.
In addition, Section 382 of the Internal Revenue Code of 1986, as amended (the Code) contains rules that limit for U.S. federal income tax purposes the ability of a corporation that undergoes an “ownership change” to utilize its net operating losses (and certain other tax attributes) existing as of the date of such ownership change. Under these rules, a corporation is treated as having had an “ownership change” if there is more than a 50% increase in stock ownership by one or more “five percent shareholders,” within the meaning of Section 382 of the Code, during a rolling three‑year period. We believe a portion of our existing net operating losses are subject to limitations arising from previous ownership changes, and if we undergo an ownership change, our ability to utilize our net operating losses to offset future taxable income could be further limited, which could have a negative effect on our liquidity. For these reasons, we may not be able to utilize a material portion of our net operating losses, even if we continue to achieve profitability.
39
Risks Related to the Regulatory Environment
Our failure to obtain and maintain regulatory clearances or approvals on a timely basis, or at all, could prevent us from commercializing our current or pipeline products in the U.S., which could severely impede our ability to grow our business and/or harm our business, financial condition and operating results.
The iStent is classified as a medical device. As a result, we are subject to extensive government regulation in the United States by the FDA and state regulatory authorities and by foreign regulatory authorities in the countries in which we conduct business. These regulations relate to, among other things, research and development, design, testing, clinical trials, manufacturing, clearance or approval, environmental controls, safety and efficacy, labeling, advertising, promotion, pricing, recordkeeping, reporting, import and export, post‑approval studies and the sale and distribution of the iStent and our other products in development.
In the United States, before we can market a new medical device, or a new use of, new claim for, or significant modification to, an existing product, we must first receive either clearance under Section 510(k) of the Federal Food, Drug and Cosmetic Act (FDCA) or approval of a premarket approval application (PMA) from the FDA, unless an exemption applies. The process of obtaining PMA approval, which was required for the iStent, is much more costly and uncertain than the 510(k) clearance process. In the 510(k) clearance process, the FDA must determine that a proposed device is “substantially equivalent” to a device legally on the market, known as a “predicate” device, in order to clear the proposed device for marketing. To be “substantially equivalent,” the proposed device must have the same intended use as the predicate device, and either have the same technological characteristics as the predicate device or have different technological characteristics and not raise different questions of safety or effectiveness than the predicate device. Clinical data is sometimes required to support substantial equivalence. In the PMA approval process, the FDA must determine that a proposed device is safe and effective for its intended use based, in part, on extensive data, including, but not limited to, technical, pre‑clinical, clinical trial, manufacturing and labeling data. The PMA process is typically required for devices for which the 510(k) process cannot be used and that are deemed to pose the greatest risk.
To the extent clinical data is required to support a 510(k) clearance or PMA approval process, clinical testing must be conducted in compliance with FDA requirements pertaining to human research. Depending on the risk posed by a device, we may be required to obtain an IDE from the FDA prior to beginning any clinical trial; similar notifications are required in other countries. Among other requirements, we must obtain approval from an independent Institutional Review Board (IRB) before such studies may begin. We may not be able to obtain FDA and/or IRB approval to undertake clinical trials in the United States for any new devices we intend to market in the United States. If the IDE application is approved, there can be no assurance the FDA will determine that the data derived from the trials support the safety and effectiveness of the device or warrant the continuation of clinical trials. We must also comply with other FDA requirements such as obtaining informed consent, monitoring, record-keeping, reporting and the submission of information regarding certain clinical trials to a public database maintained by the National Institutes of Health. Compliance with these requirements can require significant time and resources and if the FDA determines that we have not complied with such requirements, it may refuse to consider the data to support our applications or initiate enforcement actions.
Modifications to products that are approved through a PMA application generally need FDA approval. Similarly, some modifications made to products cleared through a 510(k) may require a new 510(k). The FDA’s 510(k) clearance process usually takes from three to 12 months, but may last longer. The process of obtaining a PMA generally takes from one to three years, or even longer, from the time the PMA is submitted to the FDA until an approval is obtained. Any delay or failure to obtain necessary regulatory approvals would have a material adverse effect on our business, financial condition and prospects.
The FDA can delay, limit or deny clearance or approval of a device for many reasons, including:
|
· |
our inability to demonstrate to the satisfaction of the FDA or the applicable regulatory entity or notified body that our products are safe or effective for their intended uses; |
|
· |
the disagreement of the FDA or the applicable foreign regulatory body with the design or implementation of our clinical trials or the interpretation of data from pre‑clinical studies or clinical trials; |
40
|
· |
failure of clinical sites to conduct the clinical trial in accordance with applicable regulatory requirements or our clinical protocols; |
|
· |
serious and unexpected adverse effects experienced by participants in our clinical trials; |
|
· |
the data from our pre‑clinical studies and clinical trials may be insufficient to support clearance or approval, where required; |
|
· |
our inability to demonstrate that the clinical and other benefits of the device outweigh the risks; |
|
· |
the manufacturing process or facilities we use may not meet applicable requirements; and |
|
· |
the potential for approval policies or regulations of the FDA or applicable foreign regulatory bodies to change significantly in a manner rendering our clinical data or regulatory filings insufficient for clearance or approval. |
The research, testing, manufacturing, labeling, approval, selling, import, export, marketing and distribution of drug products is also subject to extensive regulation by the FDA and other regulatory authorities in the United States and other countries, which regulations differ from country to country. We are not permitted to market any drug product candidate in the United States until we receive FDA approval of a NDA or other appropriate drug product application. Prior to submitting a marketing application, human clinical studies are required. In order for clinical studies of a new drug to commence in the United States, an Investigational New Drug (IND) application must be filed with the FDA; similar notifications are required in other countries. Informed consent also must be obtained from study participants. In general, studies may begin in the United States without specific approval by the FDA after a 30‑day review period has passed. However, the FDA may prevent studies from moving forward, and may suspend or terminate studies once initiated. Studies are also subject to review by an independent Institutional Review Board (IRB) responsible for overseeing studies at particular sites and protecting human research study subjects. An IRB may prevent a study from beginning or suspend or terminate a study once initiated. Furthermore, the FDA may suggest amendments to any study protocol that may be necessary for the results to support approval. These amendments and the associated discussions with the FDA may further delay study initiation and, as a result, approval of our drug product. Generally, studies also may not commence until after receiving approval by an independent IRB. The IRB is responsible for overseeing studies at particular sites and protecting human research study subjects. An IRB may disapprove a study or suspend or terminate an approved study once initiated.
The FDA or other applicable foreign regulatory bodies can delay, limit or deny approval of a drug candidate for many reasons, including, but not limited to, the following:
|
· |
our inability to demonstrate to the satisfaction of the FDA or the applicable foreign regulatory body that the drug candidate is safe and effective for the requested indication; |
|
· |
the FDA’s or the applicable foreign regulatory body’s disagreement with design or implementation of our clinical trials or the interpretation of data from preclinical studies or clinical trials; |
|
· |
serious and unexpected drug‑related side effects experienced by participants in our clinical trials or by individuals using drugs similar to our product candidates; |
|
· |
our inability to demonstrate that the clinical and other benefits of the drug candidate outweigh any safety or other perceived risks; |
|
· |
the FDA’s or the applicable foreign regulatory body’s requirement for additional preclinical or clinical studies; |
|
· |
the FDA’s or the applicable foreign regulatory body’s non‑approval of the drug candidate’s chemistry, manufacturing or controls or labeling; |
|
· |
the FDA’s or the applicable foreign regulatory body’s failure to approve the manufacturing processes or facilities of third‑party manufacturers; or |
|
· |
the potential for approval policies or regulations of the FDA or applicable foreign regulatory bodies to change significantly in a manner rendering our clinical data or regulatory filings insufficient for approval. |
41
Further, we are subject to laws directed at preventing fraud and abuse, which subject our marketing, training and other practices to government scrutiny. To ensure compliance with Medicare, Medicaid and other regulations, government agencies or their contractors often conduct routine audits and request customer records and other documents to support claims submitted for payment of services rendered. Government agencies or their contractors also periodically open investigations and obtain information from healthcare providers. Violations of federal and state regulations can result in severe criminal, civil and administrative penalties and sanctions, including debarment, suspension or exclusion from Medicare, Medicaid and other government reimbursement programs, any of which would have a material adverse effect on our business.
Legislative or regulatory reform of the healthcare system may affect our ability to sell our products profitably.
In the United States and in certain foreign jurisdictions, there have been a number of legislative and regulatory proposals to change the regulatory and healthcare systems in ways that could impact our ability to sell our products profitably, if at all. In the United States in recent years, new legislation has been proposed and adopted at the federal and state levels that is effecting major changes in the healthcare system. In addition, new regulations and interpretations of existing healthcare statutes and regulations are frequently adopted.
For example, in 2011, the FDA announced a Plan of Action to modernize and improve the FDA’s premarket review of medical devices, and has implemented, and continues to implement, reforms intended to improve the timeliness and predictability of the premarket review process. In addition, as part of the Food and Drug Administration Safety and Innovation Act of 2012, Congress enacted several reforms entitled the Medical Device Regulatory Improvements and additional miscellaneous provisions that will further affect medical device regulation both pre‑and post‑approval.
Further, in December 2016, Congress enacted the 21st Century Cures Act (Cures Act), which contained several provisions related to the review and approval of new medical technologies. Along with other changes, the Cures Act established a statutory program for “breakthrough” devices. The FDA will apply additional resources to help speed the approval or clearance of devices that are designated as breakthrough devices. The Cures Act also included provisions related to the “least burdensome” principle with respect to demonstrating substantial equivalence or reasonable assurance of safety and effectiveness and expanded the number of patients that could be treated by a device approved under a Humanitarian Device Exemption, among other provisions.
Similarly, in August 2017, Congress enacted the FDA Reauthorization Act of 2017 (FDARA). FDARA reauthorized the FDA to collect device user fees, including a new user fee for de novo classification requests, and contained substantive amendments to the device provisions of the FDCA. Among other changes, FDARA required that the FDA update and revise its processes for scheduling inspections of device establishments, communicating about those inspections with manufacturers and providing feedback on the manufacturer’s responses to Form 483s. The statute also required that the FDA study the impact of device servicing, including third party servicers, and creates a new process for device sponsors to request classification of accessory devices as part of the PMA application for the parent device or to request a separate classification of accessory devices.
If, as a result of legislative or regulatory healthcare reform, we cannot sell the iStent (or our other products in development, if approved) profitably, our business would be harmed. In addition, any change in the laws or regulations that govern the clearance and approval processes relating to our current and future products could make it more difficult and costly to obtain clearance or approval for new products, or to produce, market and distribute existing products.
In March 2010, the Affordable Care Act, as amended by the Health Care and Education Reconciliation Act (ACA) was signed into law. While the goal of health care reform is to expand coverage to more individuals, it also involves increased government price controls, additional regulatory mandates and other measures designed to constrain medical costs. The ACA substantially changes the way healthcare is financed by both governmental and private insurers, encourages improvements in the quality of healthcare items and services and significantly impacts the medical device industry. Among other things, the ACA:
|
· |
imposes an annual excise tax of 2.3% on any entity that manufactures or imports medical devices offered for sale in the United States, with limited exceptions (described in more detail below), which, under the PATH Act, was suspended from January 1, 2016 to December 31, 2017, and, pursuant to HR 195 passed on January 22, 2018, was further suspended through December 31, 2019; |
42
|
· |
establishes a new Patient‑Centered Outcomes Research Institute to oversee and identify priorities in comparative clinical effectiveness research in an effort to coordinate and develop such research; |
|
· |
implements payment system reforms including a national pilot program on payment bundling to encourage hospitals, physicians and other providers to improve the coordination, quality and efficiency of certain healthcare services through bundled payment models; and |
|
· |
creates an independent payment advisory board that will submit recommendations to Congress to reduce Medicare spending if projected Medicare spending exceeds a specified growth rate. |
In addition, other legislative changes have been proposed and adopted since the ACA was enacted. On August 2, 2011, the Budget Control Act of 2011 was signed into law, which, among other things, created the Joint Select Committee on Deficit Reduction to recommend to Congress proposals in spending reductions. The Joint Select Committee did not achieve a targeted deficit reduction of at least $1.2 trillion for the years 2013 through 2021, triggering the legislation’s automatic reduction to several government programs. This includes reductions to Medicare payments to providers of up to 2% per fiscal year, which went into effect on April 1, 2013 and, due to subsequent legislation, will remain in effect through 2025 unless additional Congressional action is taken. On January 2, 2013, the American Taxpayer Relief Act of 2012 was signed into law, which, among other things, further reduced Medicare payments to several providers, including hospitals, and increased the statute of limitations period for the government to recover overpayments to providers from three to five years. On April 16, 2015, President Obama signed into law the Medicare Access and CHIP Reauthorization Act of 2015, which, among other things, repealed the formula by which Medicare made annual payment adjustments to physicians and replaced the former formula with fixed annual updates and a new system of incentive payments scheduled to begin in 2019 that are based on various performance measures and physicians’ participation in alternative payment models such as accountable care organizations.
The medical device excise tax moratorium imposed by the PATH Act for 2016 and 2017 favorably impacted our gross profit margin in 2017, and will continue to do so through 2019, based upon its recent extension. However, this impact will not continue in 2020 when the tax is automatically reinstated, absent further legislation, as the iStent was subject to this excise tax prior to the moratorium and the other products in our pipeline potentially will be subject to this tax. There are no assurances that our business will not be materially adversely affected by the current, or possible future additional tax, provisions implemented under healthcare reform or appropriate legislation. It is also possible that legislation may be introduced and passed by Congress repealing the ACA in whole or in part and signed into law by President Trump. Because of the continued uncertainty about the likelihood or extent of a potential repeal of that legislation, we cannot quantify or predict with any certainty the likely impact of a repeal of ACA on our business model, prospects, financial condition or results of operations.
Additional state and federal healthcare reform measures may be adopted in the future, any of which could limit the amounts that federal and state governments will pay for healthcare products and services, which could result in reduced demand for our products or product candidates or additional pricing pressures.
In May 2017, the EU adopted a new Medical Devices Regulation (EU) 2017/745 (MDR), which will repeal and replace the Medical Device Directive (MDD). The MDR will take effect beginning May 25, 2020. The MDR does not set out a substantially different regulatory system, but provides for stricter controls of medical devices, including, among other things, strengthening of conformity assessment procedures, increased requirements as regards clinical data for devices and pre-market regulatory review of high-risk devices. The MDR also provides for greater control over conformity assessment notified bodies and their standards, increased transparency, more robust device vigilance requirements and clarification of the rules for clinical investigations. Under provisions that govern the transition period until the MDR takes effect, medical devices with notified body certificates issued under the MDD prior to May 26, 2020 may continue to be marketed and sold as long as those certificates are valid, until May 27, 2024 at the latest. After the expiration of any applicable transitional period, only devices that have been CE marked under the MDR may be placed on the market in the EU. If, as a result of these regulatory changes, we cannot obtain or maintain the approvals necessary to sell the iStent or our other products (including pipeline products, if approved) in the EU, our business would be harmed.
43
The clinical trial process required to obtain regulatory approvals is lengthy and expensive with uncertain outcomes, and could result in delays in new product introductions.
Because of the indication we chose to pursue for the iStent, the FDA required that we seek PMA approval rather than clearance under the 510(k) process. In order to obtain PMA and FDA approval for a product, the sponsor must conduct well‑controlled clinical trials designed to assess the safety and efficacy of the product candidate. We also will be required to conduct clinical trials to obtain approval of products using the iDose drug delivery system, new indications for the iStent or new product candidates. Conducting clinical trials is a complex and expensive process, can take many years, and outcomes are inherently uncertain. We incur substantial expense for, and devote significant time to, clinical trials but cannot be certain that the trials will ever result in commercial sales. We may suffer significant setbacks in clinical trials, even after earlier clinical trials showed promising results, and failure can occur at any time during the clinical trial process. Any of our products may malfunction or may produce undesirable adverse effects that could cause us or regulatory authorities to interrupt, delay or halt clinical trials. We, the clinical trial investigators, the reviewing IRB, the FDA, or another regulatory authority may suspend or terminate clinical trials at any time to avoid exposing trial participants to unacceptable health risks.
Successful results of pre‑clinical studies are not necessarily indicative of future clinical trial results, and predecessor clinical trial results may not be replicated in subsequent clinical trials. Additionally, the FDA may disagree with our interpretation of the data from our pre‑clinical studies and clinical trials, or may find the clinical trial design, conduct or results inadequate to prove safety or efficacy, and may require us to pursue additional pre‑clinical studies or clinical trials, which could further delay the clearance or approval of our products. The data we collect from our pre‑ clinical studies and clinical trials may not be sufficient to support FDA clearance or approval, and if we are unable to demonstrate the safety and efficacy of our future products in our clinical trials, we will be unable to obtain regulatory clearance or approval to market our products.
In addition, we may estimate and publicly announce the anticipated timing of the accomplishment of various clinical, regulatory and other product development goals, which are often referred to as milestones. These milestones could include the right to affix the CE Mark in the European Union; the submission to the FDA of an IDE application, or an IND application, to commence a clinical trial for a new product candidate; the enrollment of patients in clinical trials; the release of data from clinical trials; and other clinical and regulatory events. The actual timing of these milestones could vary dramatically compared to our estimates, in some cases for reasons beyond our control. We cannot assure you that we will meet our projected milestones and if we do not meet these milestones as publicly announced, the commercialization of our products may be delayed and, as a result, our stock price may decline.
Clinical trials are necessary to support PMA applications for our device product candidates and may be necessary to support PMA supplements for modified versions of our marketed device products. This would require the enrollment of large numbers of suitable subjects, which may be difficult to identify, recruit and maintain as participants in the clinical trial. The clinical trials supporting the PMA application for the iStent involved 289 randomized patients. We conducted an extended follow-up post-approval study with 108 patients from the pivotal study, and are currently conducting a post-approval study of 180 patients who will be implanted with the iStent in combination with cataract surgery and then monitored for three years thereafter. If the FDA were to require us to submit data on a greater number of patients or a longer follow‑up period, we would incur additional expenses that could be significant. Adverse outcomes in the post‑approval studies could also result in restrictions or withdrawal of approval of the PMA.
Before we can obtain regulatory approval for any drug product candidate, such as our iDose drug delivery implant, we must undertake extensive clinical testing in humans to demonstrate safety and efficacy to the satisfaction of the FDA and other regulatory agencies. Clinical trials of drug product candidates are expensive and take years to complete, and the outcome of such trials is uncertain. We completed a U.S. IND Phase II clinical trial of iDose Travoprost in 2017 and we intend to commence U.S. Phase III clinical trials in the first half of 2018. Our ability to conduct additional iDose clinical trials depends on many factors, including the data obtained in the Phase III clinical trials.
Delays in the commencement or completion of clinical trials or testing could significantly affect our product development costs. We do not know whether planned clinical trials will begin on time, need to be redesigned, enroll an
44
adequate number of patients in a timely manner or be completed on schedule, if at all. The commencement and completion of clinical trials can be delayed or terminated for a number of reasons, including delays or failures related to:
|
· |
the FDA or comparable foreign regulatory authorities disagreeing as to the design or implementation of our clinical studies; |
|
· |
obtaining regulatory approval to commence a clinical trial; |
|
· |
reaching agreement on acceptable terms with prospective clinical research organizations, or CROs, and trial sites, the terms of which can be subject to extensive negotiation and may vary significantly among different CROs and trial sites; |
|
· |
manufacturing sufficient quantities of a product candidate for use in clinical trials; |
|
· |
obtaining IRB or ethics committees approval to conduct a clinical trial at each prospective site; |
|
· |
recruiting and enrolling patients and maintaining their participation in clinical trials; |
|
· |
having clinical sites observe trial protocol or continue to participate in a trial; |
|
· |
addressing any patient safety concerns that arise during the course of a clinical trial; |
|
· |
addressing any conflicts with new or existing laws or regulations; and |
|
· |
adding a sufficient number of clinical trial sites. |
Patient enrollment in clinical trials and completion of patient follow‑up depend on many factors, including the size of the patient population, the nature of the trial protocol, the proximity of patients to clinical sites, the eligibility criteria for the clinical trial, patient compliance, competing clinical trials and clinicians’ and patients’ perceptions as to the potential advantages of the product being studied in relation to other available therapies, including any new treatments that may be approved for the indications we are investigating. For example, patients may be discouraged from enrolling in our clinical trials if the trial protocol requires them to undergo extensive post‑treatment procedures or follow‑up to assess the safety and efficacy of a product candidate, or they may be persuaded to participate in contemporaneous clinical trials of a competitor’s product candidate. In addition, patients participating in our clinical trials may drop out before completion of the trial or suffer adverse medical events unrelated to our products. Delays in patient enrollment or failure of patients to continue to participate in a clinical trial may delay commencement or completion of the clinical trial, cause an increase in the costs of the clinical trial and delays, or result in the failure of the clinical trial.
We could also encounter delays if the FDA concluded that our financial relationships with our principal investigators resulted in a perceived or actual conflict of interest that may have affected the interpretation of a study, the integrity of the data generated at the applicable clinical trial site or the utility of the clinical trial itself. Principal investigators for our clinical trials may serve as scientific advisors or consultants to us from time to time and receive cash compensation and/or stock options in connection with such services. If these relationships and any related compensation to or ownership interest by the clinical investigator carrying out the study result in perceived or actual conflicts of interest, or the FDA concludes that the financial relationship may have affected interpretation of the study, the integrity of the data generated at the applicable clinical trial site may be questioned and the utility of the clinical trial itself may be jeopardized, which could result in the delay or rejection of our marketing application by the FDA. Any such delay or rejection could prevent us from commercializing any of our products currently in development.
Further, clinical trials may also be delayed as a result of ambiguous or negative interim results. In addition, a clinical trial may be suspended or terminated by us, the FDA, the IRB overseeing the clinical trial at issue, the Data Safety Monitoring Board for such trial, any of our clinical trial sites with respect to that site, or other regulatory authorities due to a number of factors, including:
|
· |
failure to conduct the clinical trial in accordance with applicable regulatory requirements or our clinical protocols; |
|
· |
inspection of the clinical trial operations or trial sites by the FDA or other regulatory authorities resulting in the imposition of a clinical hold; |
45
|
· |
inability of a clinical investigator or clinical trial site to continue to participate in the clinical trial; |
|
· |
unforeseen safety issues or adverse side effects; |
|
· |
failure to demonstrate a benefit from using the product candidate; and |
|
· |
lack of adequate funding to continue the clinical trial. |
Additionally, changes in regulatory requirements and guidance may occur and we may need to amend clinical trial protocols to reflect these changes. Amendments may require us to resubmit our clinical trial protocols to IRBs for reexamination, which may impact the costs, timing or successful completion of a clinical trial. If we experience delays in completion of, or if we terminate, any of our clinical trials, the commercial prospects for our product candidates may be harmed and our ability to generate product revenues from these product candidates will be delayed or not realized at all. In addition, any delays in completing our clinical trials will increase our costs, slow down our product candidate development and approval process and jeopardize our ability to commence product sales and generate revenues. Any of these occurrences may significantly harm our business, financial condition and prospects significantly. In addition, many of the factors that cause, or lead to, a delay in the commencement or completion of a clinical trial may also ultimately lead to the denial of regulatory approval of the subject product candidate.
If the FDA does not conclude that the iDose drug delivery implant satisfies the requirements for the Section 505(b)(2) regulatory approval pathway, or if the requirements for approval of the iDose drug delivery implant under Section 505(b)(2) are not as we expect, the approval pathway will likely take significantly longer, cost significantly more and encounter significantly more complications and risks than anticipated, and in any case may not be successful.
We intend to seek FDA approval of an NDA under Section 505(b)(2) of the FDCA for our drug delivery implant, iDose. The Drug Price Competition and Patent Term Restoration Act of 1984, also known as the Hatch‑Waxman Act, added Section 505(b)(2) to the FDCA. Section 505(b)(2) permits the filing of an NDA where at least some of the information required for approval comes from studies that were not conducted by or for the applicant.
If the FDA does not allow us to pursue the 505(b)(2) regulatory pathway for iDose as anticipated, we may need to conduct additional clinical trials, provide additional data and information and meet additional standards for regulatory approval. If this were to occur, the time and financial resources required to obtain FDA approval would likely substantially increase. Moreover, the inability to pursue the 505(b)(2) regulatory pathway could result in new competitive products reaching the market faster than our product candidate, which could materially adversely impact our competitive position and prospects. In addition, circumstances could change that would render a 505(b)(2) application for the product no longer appropriate. Even if we are allowed to pursue the 505(b)(2) regulatory pathway for iDose, we cannot assure you that we will receive the requisite or timely approvals for commercialization of this product candidate.
We and our suppliers are subject to extensive post‑marketing regulatory requirements and failure to comply with applicable requirements could subject us to enforcement actions, including substantial penalties, and might require us to recall or withdraw a product from the market.
Once a medical device is approved, a manufacturer must notify the FDA of any modifications to the device. Any modification to a device that has received FDA clearance or approval that could significantly affect its safety or effectiveness, or that would constitute a major change in its intended use, design or manufacture, requires premarket clearance or approval from the FDA pursuant to a new 510(k) clearance or approval of a PMA supplement. The FDA requires every manufacturer to make the determination in the first instance regarding whether a modification to a cleared or approved device necessitates the filing of a new 510(k) notification or PMA supplement. The FDA may review any manufacturer’s decision and can disagree. If the FDA disagrees with any future determination by us that a new clearance or approval is not required, we may need to cease marketing or to recall the modified product until and unless we obtain clearance or approval. In addition, we could also be subject to significant regulatory fines or penalties. Any of these outcomes could harm our business.
A manufacturer must also submit periodic reports to the FDA as a condition of PMA approval. These reports include safety and effectiveness information about the device after its approval. Failure to submit such reports, or failure to submit the reports in a timely manner, could result in enforcement action by the FDA. Following its review of the periodic reports, the FDA might ask for additional information or initiate further investigation.
46
The PMA approval for the iStent is subject to several conditions of approval, including postmarket study and registry study requirements. Failure to comply with the conditions of approval could result in the withdrawal of PMA approval, and the inability to continue to market the device. Failure to conduct the required studies in accordance with IRB and informed consent requirements could also be grounds for withdrawal of approval of the PMA.
Medical devices are also subject to other postmarket requirements including establishment registration and device listing, quality system requirements, reporting of adverse events and device malfunctions, reporting of corrections and removals, labeling requirements, and promotional restrictions. The regulations to which we are subject are complex and have become more stringent over time. Regulatory changes could result in restrictions on our ability to continue or expand our operations, higher than anticipated costs, or lower than anticipated sales. Even after we have obtained the proper regulatory clearance or approval to market a product, we have ongoing responsibilities under FDA regulations and applicable foreign laws and regulations. The FDA, state and foreign regulatory authorities have broad enforcement powers. Our failure to comply with applicable regulatory requirements could result in enforcement action by the FDA, state or foreign regulatory authorities, which may include any of the following sanctions:
|
· |
untitled letters or warning letters; |
|
· |
fines, injunctions, consent decrees and civil penalties; |
|
· |
recalls, termination of distribution, administrative detention, or seizure of our products; |
|
· |
customer notifications or repair, replacement or refunds; |
|
· |
operating restrictions or partial suspension or total shutdown of production; |
|
· |
delays in or refusal to grant our requests for future 510(k) clearances, PMA approvals or foreign regulatory approvals of new products, new intended uses, or modifications to existing products; |
|
· |
withdrawals or suspensions of current 510(k) clearances or PMAs or foreign regulatory approvals, resulting in prohibitions on sales of our products; |
|
· |
FDA refusal to issue certificates to foreign governments needed to export products for sale in other countries; and |
|
· |
criminal prosecution. |
Any of these sanctions could result in higher than anticipated costs or lower than anticipated sales and have a material adverse effect on our reputation, business, results of operations and financial condition.
We must continually monitor the performance of our products once approved and marketed for signs that their use may elicit serious and unexpected adverse effects. Any recall of our products, either voluntarily or at the direction of the FDA or another governmental authority, or the discovery of serious safety issues with our products that leads to corrective actions, could have a significant adverse impact on us.
Our ability to achieve our strategic objectives will depend, among other things, on the long‑term clinical performance of the iStent for lowering intraocular pressure in mild‑to‑moderate open‑angle glaucoma patients undergoing cataract surgery. Our original PMA approval for the iStent included several post‑marketing study requirements and future approvals may be subject to similar requirements. Failure to conduct required post‑marketing studies in a timely manner could result in the revocation of the clearance or approval for the product that is subject to such a requirement and could also result in the recall or withdrawal of the product, which would prevent us from generating sales from that product in the United States.
Although we believe follow‑up at three years continues to support efficacy and safety of the iStent for lowering intraocular pressure in mild‑to‑moderate open‑angle glaucoma patients undergoing cataract surgery, in the future, longer term study outcomes could demonstrate conflicting clinical effectiveness, a reduction of effectiveness, no clinical effectiveness or longer term safety issues with the iStent. This type of differing data could have a detrimental effect on the market penetration and usage of the iStent by customers treating mild‑to‑moderate open‑angle glaucoma and/or the risk/benefit profile of using the iStent to treat mild‑to‑moderate open‑angle glaucoma in combination with cataract surgery. As a result, our sales may decline or expected growth would be negatively impacted. This could put pressure on
47
our ability to execute key components of our business strategy and/or negatively impact our operating condition and financial results.
More generally, all medical devices, such as the iStent, can experience performance problems that require review and possible corrective action by us or a component supplier. We cannot provide assurance that component failures, manufacturing errors, noncompliance with quality system requirements or good manufacturing practices, design defects and/or labeling inadequacies in any device or drug products that could result in an unsafe condition or injury to the patient will not occur. The FDA and similar foreign governmental authorities have the authority to require the recall of commercialized products in the event of material deficiencies or defects in design or manufacture of a product or in the event that a product poses an unacceptable risk to health. Manufacturers may also, under their own initiative, stop shipment or recall a product if any material deficiency is found, take corrective action with respect to product in the field, or withdraw a product to improve device performance or for other reasons. A government‑mandated or voluntary recall by us or one of our distributors could occur as a result of an unacceptable risk to health, component failures, manufacturing errors, noncompliance with good manufacturing practices or quality system requirements, design or labeling defects or other deficiencies and issues. Similar regulatory agencies in other countries have similar authority to recall products because of material deficiencies or defects in design or manufacture that could endanger health. Any recall would divert management attention and financial resources, could cause the price of our stock to decline and expose us to product liability or other claims and harm our reputation with customers. A recall involving our products could be particularly harmful to our business, financial and operating results.
The FDA requires that certain corrections or removals be reported to the FDA within 10 working days after the recall is initiated. Notice to the FDA of a correction or removal is required when undertaken to reduce a risk to health, including when there is a reasonable probability that the product will cause serious adverse health consequences or death, or when use of the device may cause temporary or medically reversible adverse health consequences or an outcome where the probability of serious adverse health consequences is remote. In addition, companies are required to maintain certain records of corrections and removal, even if they are not reportable to the FDA or similar foreign governmental authorities. We may initiate voluntary recalls involving our products in the future that we determine do not require notification of the FDA or foreign governmental authorities. If the FDA or foreign governmental authorities disagree with our determinations, they could require us to report those actions as recalls. A future recall announcement could harm our reputation with customers and negatively affect our sales. In addition, the FDA or a foreign governmental authority could take enforcement action for failing to report the recalls when they were conducted.
Depending on the corrective action we take to redress a product’s deficiencies or defects, the FDA or applicable foreign regulatory authority may require, or we may decide, that we will need to obtain new approvals or clearances for the device before we may market or distribute the corrected device. Seeking such approvals or clearances may delay our ability to replace the recalled devices in a timely manner. Moreover, we may face additional regulatory enforcement action, including FDA warning letters, product seizure, injunctions, administrative penalties, civil penalties or criminal fines. We may also be required to bear other costs or take other actions that may have a negative impact on our sales as well as face significant adverse publicity or regulatory consequences, which could harm our business, including our ability to market our products in the future.
In addition, under the FDA’s medical device reporting regulations, we are required to report to the FDA any incident in which our product may have caused or contributed to a death or serious injury or in which our product malfunctioned and, if the malfunction were to recur, would likely cause or contribute to death or serious injury. Repeated product malfunctions may result in a voluntary or involuntary product recall. We are subject to similar obligations in the EEA and other countries in which we market our products.
Depending on the corrective action we take to redress a product’s deficiencies or defects, the FDA or applicable foreign regulatory authority may require, or we may decide, that we will need to obtain new approvals or clearances for the device before we may market or distribute the corrected device. Seeking such approvals or clearances may delay our ability to replace the recalled devices in a timely manner. Moreover, we may face additional regulatory enforcement action, including FDA warning letters, product seizure, injunctions, administrative penalties, civil penalties or criminal fines. We may also be required to bear other costs or take other actions that may have a negative impact on our sales as well as face significant adverse publicity or regulatory consequences, which could harm our business, including our ability to market our products in the future.
48
Any adverse event involving our products, whether in the United States or abroad, could result in future voluntary corrective actions, such as recalls or customer notifications, or agency action, such as inspection, mandatory recall, orders of repair, replacement or refund or other enforcement action. Any corrective action, whether voluntary or involuntary, as well as defending ourselves in a lawsuit, will require the dedication of our time and capital, distract management from operating our business and may harm our reputation and financial results.
If we or our component manufacturers fail to comply with the FDA’s Quality System Regulation or Good Manufacturing Practice regulations, our manufacturing operations could be interrupted, and our product sales and operating results could suffer.
We and some of our component manufacturers are required to comply with regulatory requirements known as the FDA’s Quality System Regulation (QSR), which covers the procedures and documentation of the design, testing, production, control, quality assurance, inspection, complaint handling, recordkeeping, management review, labeling, packaging, sterilization, storage and shipping of our device products. The FDA’s Current Good Manufacturing Practices (cGMPs) also apply to the manufacture of our products. The FDA audits compliance with these regulatory requirements through periodic announced and unannounced inspections of manufacturing and other facilities. The FDA may conduct inspections or audits at any time, and we and some of our component suppliers are subject to such inspections. Although we believe our manufacturing facilities and those of our critical component suppliers are in material compliance with the QSR requirements and with applicable cGMPs, we cannot provide assurance that any future inspection will not result in adverse findings. If our manufacturing facilities or those of any of our component suppliers are found to be in violation of applicable laws and regulations, or we or our suppliers have significant noncompliance issues or fail to timely and adequately respond to any adverse inspectional observations or product safety issues, or if any corrective action plan that we or our suppliers propose in response to observed deficiencies is not sufficient, the FDA could take enforcement action, including any of the following sanctions:
|
· |
untitled letters or warning letters; |
|
· |
fines, injunctions, consent decrees and civil penalties; |
|
· |
customer notifications or repair, replacement, refunds, recall, detention or seizure of our products; |
|
· |
operating restrictions or partial suspension or total shutdown of production; |
|
· |
refusing or delaying our requests for clearance or approval of new products or modified products; |
|
· |
withdrawing clearances or approvals that have already been granted; |
|
· |
refusal to grant export approval for our products; or |
|
· |
criminal prosecution. |
Any of these sanctions could adversely affect our business, financial conditions and operating results.
Outside the United States, our products and operations are also often required to comply with standards set by industrial standards bodies, such as the ISO. Foreign regulatory bodies may evaluate our products or the testing that our products undergo against these standards. The specific standards, types of evaluation and scope of review differ among foreign regulatory bodies. If we fail to adequately comply with any of these standards, a foreign regulatory body may take adverse actions similar to those within the power of the FDA. Any such action may harm our reputation and could have an adverse effect on our business, results of operations and financial condition.
We may be subject to fines, penalties, injunctions or other enforcement actions if we are determined to be promoting the use of our products for unapproved or “off‑label” uses, resulting in damage to our reputation and business.
Our promotional materials and training methods must comply with FDA and other applicable laws and regulations, including the prohibition of the promotion of a drug or medical device for a use that has not been cleared or approved by the FDA. Use of a drug or device outside of its cleared or approved indications is known as “off‑label” use. Physicians may use our products off‑label, as the FDA does not restrict or regulate a physician’s choice of treatment within the practice of medicine. However, if the FDA determines that our promotional materials or training constitutes promotion of an off‑label use, it could request that we modify our training or promotional materials or subject us to
49
regulatory or enforcement actions, including the issuance of warning letters, untitled letters, fines, penalties, consent decrees, injunctions, or seizures, which could have an adverse impact on our reputation and financial results. We could also be subject to enforcement action under other federal or state laws, including the federal False Claims Act (FCA). While we may request additional indications for our products, the FDA may deny those requests, require additional expensive clinical data to support any additional indications or impose limitations on the intended use of any cleared or approved product as a condition of clearance or approval.
In addition to promoting our products in a manner consistent with our clearances, we must have adequate substantiation for the claims we make for our products. If any of our claims are determined to be false, misleading or deceptive, our products could be considered to be misbranded under the FDCA or to violate the Federal Trade Commission Act. We could also face lawsuits from our competitors under the Lanham Act alleging that our marketing materials are false or misleading.
Failure to comply with the Federal Health Insurance Portability and Accountability Act of 1996, the Health Information Technology for Economic and Clinical Health Act, and implementing regulations affecting the transmission, security and privacy of health information could result in significant penalties.
Numerous federal and state laws and regulations, including the Federal Health Insurance Portability and Accountability Act of 1996 (HIPAA), and the Health Information Technology for Economic and Clinical Health Act (HITECH Act) govern the collection, dissemination, security, use, disclosure and confidentiality of patient‑identifiable health information. HIPAA and the HITECH Act may require us to comply with standards for the use and disclosure of patient-identifiable health information. The Privacy Standards and Security Standards under HIPAA establish a set of basic national privacy and security standards for the protection of patient-identifiable health information by health plans, healthcare clearinghouses and certain healthcare providers, referred to as covered entities, and the business associates with whom such covered entities contract for services. Notably, whereas HIPAA previously directly regulated only these covered entities, the HITECH Act makes certain of HIPAA’s privacy and security standards also directly applicable to covered entities’ business associates. As a result, both covered entities and business associates are now subject to significant civil and criminal penalties for failure to comply with the Privacy Standards and Security Standards.
HIPAA and the HITECH Act also include standards for common healthcare electronic transactions and code sets, such as claims information, plan eligibility and payment information. Covered entities, such as healthcare providers, are required to conform to such transaction set standards pursuant to HIPAA.
HIPAA requires covered entities to develop and maintain policies and procedures with respect to the use and disclosure of patient-identifiable health information and the adoption of administrative, physical and technical safeguards to protect such information. The HITECH Act expands the notification requirement for breaches of patient‑identifiable health information, restricts certain disclosures and sales of patient‑identifiable health information and provides a tiered system for civil monetary penalties for HIPAA violations. The HITECH Act also increased the civil and criminal penalties that may be imposed against covered entities, business associates and possibly other persons and gave state attorneys general new authority to file civil actions for damages or injunctions in federal courts to enforce the federal HIPAA laws and seek attorney fees and costs associated with pursuing federal civil actions. Additionally, certain states have adopted comparable privacy and security laws and regulations, some of which may be more stringent than HIPAA.
If we do not comply with applicable existing or new laws and regulations related to patient health information, we could be subject to criminal or civil sanctions. New health information standards, whether implemented pursuant to HIPAA, the HITECH Act, congressional action or otherwise, could have a significant effect on the manner in which we handle healthcare‑related data and the cost of complying with these standards could be significant.
The 2013 final HITECH Act omnibus rule modified the breach reporting standard in a manner that will likely make more data security incidents qualify as reportable breaches. Any liability from a failure to comply with the applicable requirements of HIPAA or the HITECH Act could adversely affect our financial condition. The costs of complying with privacy and security‑related legal and regulatory requirements are burdensome and could have a material adverse effect on our results of operations. These provisions, as modified, will be subject to interpretation by various courts and other governmental authorities, thus creating potentially complex compliance issues for us, as well as our clients and strategic partners. In addition, we are unable to predict what changes to the HIPAA Privacy Standards and Security Standards might be made in the future or how those changes could affect our business. Any new legislation or regulation in the area of privacy and security of personal information, including personal health information, could also
50
adversely affect our business operations.
If we fail to comply with state and federal healthcare regulatory laws, we could face substantial penalties, damages, fines, disgorgement, exclusion from participation in governmental healthcare programs, and the curtailment of our operations, any of which could adversely affect our business, operations, and financial condition.
Although we do not provide healthcare services, submit claims for third‑party reimbursement, or receive payments directly from Medicare, Medicaid or other third‑party payors for our products, we are subject to healthcare fraud, abuse and transparency regulation and enforcement by federal and state governments, which could significantly impact our business. To ensure compliance with Medicare, Medicaid and other regulations, government agencies or their contractors often conduct routine audits and request customer records and other documents to support claims submitted for payment of services rendered. Government agencies or their contractors also periodically open investigations and obtain information from healthcare providers. Violations of federal and state regulations can result in severe criminal, civil and administrative penalties and sanctions, including debarment, suspension or exclusion from Medicare, Medicaid and other government reimbursement programs, any of which would have a material adverse effect on our business.
The laws that may affect our ability to operate include, but are not limited to:
|
· |
the federal Anti‑Kickback Statute, which prohibits, among other things, persons and entities from knowingly and willfully soliciting, receiving, offering, or paying remuneration, directly or indirectly, in cash or in kind, in exchange for or to induce either the referral of an individual for, or the purchase, lease, order or recommendation of, any good, facility, item or service for which payment may be made, in whole or in part, under federal healthcare programs such as Medicare and Medicaid. A person or entity does not need to have actual knowledge of this statute or specific intent to violate it; |
|
· |
the civil False Claims Act (FCA), which prohibits, among other things, individuals or entities from knowingly presenting, or causing to be presented, claims for payment from Medicare, Medicaid or other Federal payors that are false or fraudulent; knowingly making using, or causing to be made or used, a false record or statement to get a false or fraudulent claim paid or approved by the government; or knowingly making, using, or causing to be made or used, a false record or statement to avoid, decrease or conceal an obligation to pay money to the federal government; |
|
· |
the criminal FCA, which imposes criminal fines or imprisonment against individuals or entities who make or present a claim to the government knowing such claim to be false, fictitious or fraudulent; |
|
· |
HIPAA, which created federal criminal laws that prohibit executing a scheme to defraud any healthcare benefit program or making false statements relating to healthcare matters; |
|
· |
the federal civil monetary penalties statute, which prohibits, among other things, the offering or giving of remuneration to a Medicare or Medicaid beneficiary that the person knows or should know is likely to influence the beneficiary’s selection of a particular supplier of items or services reimbursable by a Federal or state governmental program; |
|
· |
the federal Physician Payments Sunshine Act under ACA, which require certain manufacturers of drugs, devices, biologics, and medical supplies to report annually to the U.S. Department of Health and Human Services information related to payments and other transfers of value to physicians, other healthcare providers, and teaching hospitals, and ownership and investment interests held by physicians and other healthcare providers and their immediate family members. Manufacturers must submit such reports by the 90th day of each subsequent calendar year; and |
|
· |
state law equivalents of each of the above federal laws, such as anti‑kickback and false claims laws that may apply to items or services reimbursed by any third‑party payor, including commercial insurers; state laws that require pharmaceutical companies to comply with the device industry’s voluntary compliance guidelines and the relevant compliance guidance promulgated by the federal government, or otherwise restrict payments that may be made to healthcare providers and other potential referral sources; and state laws that require device manufacturers to report information related to payments and other transfers of value to physicians and other healthcare providers or marketing expenditures. |
51
Further, the ACA, among other things, amended the intent requirements of the federal Anti‑Kickback Statute and certain criminal statutes governing healthcare fraud. A person or entity can now be found guilty of violating the statute without actual knowledge of the statute or specific intent to violate it. In addition, ACA provided that the government may assert that a claim including items or services resulting from a violation of the federal Anti‑Kickback Statute constitutes a false or fraudulent claim for purposes of the FCA.
While we do not submit claims and our customers make the ultimate decision on how to submit claims, from time to time, we may provide reimbursement guidance to our customers. If a government authority were to conclude that we provided improper advice to our customers or encouraged the submission of false claims for reimbursement, we could face action against us by government authorities. Any violations of these laws, or any action against us for violation of these laws, even if we successfully defend against it, could result in a material adverse effect on our reputation, business, results of operations and financial condition.
We have entered into consulting and scientific advisory board arrangements with physicians and other healthcare providers, including some who influence the ordering of and use of our products in procedures they perform. Compensation for some of these arrangements includes the provision of stock options. In addition, in connection with our clinical trial recruitment activities, we have entered into compensation arrangements with some of the physicians who recruit subjects to our clinical trials. While we believe we are in material compliance with applicable laws, because of the complex and far‑reaching nature of these laws, regulatory agencies may view these transactions as prohibited arrangements that must be restructured, or discontinued, or that affect our ability to use all of the data from the clinical trial to support our marketing applications, or for which we could be subject to other significant penalties. We could be adversely affected if regulatory agencies interpret our financial relationships with providers who influence the ordering of and use our products to be in violation of applicable laws.
The scope and enforcement of each of these laws is uncertain and subject to rapid change in the current environment of healthcare reform, especially in light of the lack of applicable precedent and regulations. Federal and state enforcement bodies scrutinize of interactions between healthcare companies and healthcare providers, which has led to a number of investigations, prosecutions, convictions and settlements in the healthcare industry. Responding to investigations can be time‑ and resource‑consuming and can divert management’s attention from the business. Additionally, as a result of these investigations, healthcare providers and entities may have to agree to additional onerous compliance and reporting requirements as part of a consent decree or corporate integrity agreement. Any such investigation or settlement could increase our costs or otherwise have an adverse effect on our business.
If our operations are found to be in violation of any of the laws described above or any other government regulations that apply to us, we may be subject to penalties, including civil and criminal penalties, damages, fines, disgorgement, imprisonment, exclusion from participation in federal and state healthcare programs and the curtailment or restricting of our operations, any of which could harm our ability to operate our business and our financial results.
Our operations involve hazardous materials, and we must comply with environmental laws and regulations, which can be expensive.
We are subject to a variety of federal, state and local regulations relating to the use, handling, storage and disposal of, and human exposure to, hazardous and toxic materials. We could incur costs, fines, and civil and criminal sanctions, third‑party property damage or personal injury claims, or could be required to incur substantial investigation or remediation costs, if we were to violate or become liable under environmental laws. Compliance with current or future environmental and safety laws and regulations could restrict our ability to expand our facilities, impair our research, development or production efforts, or require us to incur other significant expenses. There can be no assurance that violations of environmental laws or regulations will not occur in the future as a result of the inability to obtain permits, human error, accident, equipment failure or other causes.
Risks Related to Our Intellectual Property
If we are unable to adequately protect our intellectual property, our competitors and other third parties could develop and commercialize products similar or identical to ours, which would substantially impair our ability to compete.
Our success and ability to compete depends significantly upon our ability to maintain and protect our proprietary rights to the technologies and inventions used in or embodied by our products. We rely on a combination of patents and trademark rights, and to a lesser extent on trade secrets and copyrights, together with licenses and
52
nondisclosure agreements to protect our intellectual property. These legal means, however, afford only limited protection and may not adequately protect our intellectual property rights. We also have not pursued or maintained, and may not pursue or maintain in the future, patent protection for our products in every country or territory in which we sell or will in the future sell our products. In addition, we cannot be sure that any of our pending patent applications or pending trademark applications will issue or that, if issued, they will issue in a form that will be advantageous to us. The United States Patent and Trademark Office (USPTO) or other foreign patent offices may deny or significantly narrow claims made under our patent applications and our issued patents may be successfully challenged, may be designed around, or may otherwise be of insufficient scope to provide us with any meaningful protection for our present or future commercial products. Further, the USPTO or other foreign trademark offices may deny our trademark applications and, even if published or registered, these trademarks may be ineffective in protecting our brand and goodwill and may be successfully opposed or challenged.
The patent prosecution process itself is expensive and time consuming, and we may not be able to file and prosecute all necessary or desirable patent applications at a reasonable cost or in a timely manner. The patent prosecution process requires compliance with complex laws, rules and regulations imposed by patent authorities. Failure to comply with these laws, rules and regulations may derive, among other bases, from various defects of form in the preparation or filing of our patents or patent applications, which may include defects that relate to our making proper priority claims and inventorship determinations. If any such defects are identified, we may need to take corrective action. For example, we have filed petitions with the USPTO to request in part that Dr. Richard Hill, one of our consultants, be added as an inventor on patents related to our iStent, iStent Inject, iStent SA, iStent Infinite and iStent Supra product candidate that were developed during Dr. Hill’s consultancy. Dr. Hill has assigned his rights in these patents and certain other patent applications to us pursuant to the terms of his consulting agreement. Because Dr. Hill was employed as an Associate Professor at the University of California, Irvine, or the University, during the period when these patents and patent applications were developed in December 2014, we entered into an agreement with the University pursuant to which the University agreed not to challenge our ownership of these patents and patent applications. In addition, if any material defects are found in the form or preparation of any of our patents or patent applications, such patents or applications may be invalid and unenforceable. Any of these outcomes could impair our ability to prevent competition from third parties, which could harm our business. Moreover, the USPTO and various foreign governmental patent agencies require compliance with a number of procedural, documentary, fee payment and other similar provisions during the patent application process. In addition, periodic maintenance fees on issued patents often must be paid to the USPTO and foreign patent agencies over the lifetime of the patent. Noncompliance with these requirements can result in abandonment or lapse of the patent or patent application, resulting in partial or complete loss of patent rights in the relevant jurisdiction. If we fail to maintain the patents and patent applications covering our products or procedures, we may not be able to stop a competitor from marketing products that are the same as or similar to our products, which would have a material adverse effect on our business. In addition, patents are limited in term. Once all of the patents covering a particular product of ours in a particular jurisdiction have expired, we will no longer be able to stop competitors from marketing a product that is the same as or similar to our product in that jurisdiction, which could have a material adverse effect on our business.
The patent position of medical device companies is generally highly uncertain, involves complex legal and factual questions and has in recent years been the subject of much litigation and administrative proceedings, such as post-grant or inter partes review proceedings at the USPTO. In the United States and in many foreign jurisdictions, policies regarding the breadth of claims allowed in patents can be inconsistent. The U.S. Supreme Court and the Court of Appeals for the Federal Circuit have made, and will likely continue to make, changes in how the patent laws of the United States are interpreted. Similarly, foreign courts have made, and will likely continue to make, changes in how the patent laws in their respective jurisdictions are interpreted. We cannot predict future changes in the interpretation of patent laws or changes to patent laws that might be enacted into law by U.S. and foreign legislative bodies. Those changes may materially affect our patents or patent applications and our ability to obtain patents. Future protection for our proprietary rights is uncertain because legal means afford only limited protection and may not adequately protect our rights or permit us to gain or keep our competitive advantage, which could adversely affect our business, financial condition and results of operations.
Patent reform legislation could increase the uncertainties and costs surrounding the prosecution of our patent applications and the enforcement or defense of our issued patents. On September 16, 2011, the Leahy‑Smith America Invents Act, or the Leahy‑Smith Act, was signed into law. The Leahy‑Smith Act includes a number of significant changes to U.S. patent law. These include provisions that affect the way patent applications are prosecuted, redefine
53
prior art, affect patent litigation or administrative proceedings at the USPTO, and switch the U.S. patent system from a “first‑to‑invent” system to a “first‑to‑file” system. Under a “first‑to‑file” system, assuming the other requirements for patentability are met, the first inventor to file a patent application generally will be entitled to the patent on an invention regardless of whether another inventor had made the invention earlier. The USPTO developed new regulations and procedures to govern administration of the Leahy‑Smith Act, and many of the substantive changes to patent law associated with the Leahy‑Smith Act, and in particular, the first‑to‑file provisions, only became effective on March 16, 2013. Accordingly, it is not clear what, if any, impact the Leahy‑Smith Act will have on the operation of our business. However, the Leahy‑Smith Act and its implementation could increase the uncertainties and costs surrounding the prosecution of our patent applications and the enforcement or defense of our issued patents, all of which could have a material adverse effect on our business and financial condition. In addition, patent reform legislation may pass in the future, in the U.S. or elsewhere, that could lead to additional uncertainties and increased costs surrounding the prosecution, enforcement, and defense of our patents and applications.
We may be subject to a third‑party pre-issuance submission of prior art to the USPTO or to another foreign patent office, or become involved in opposition, interference, derivation, reexamination, inter partes review, post‑grant review, or other patent office proceedings or litigation, in the United States or elsewhere, challenging our patent rights or the patent rights of others. An adverse determination in any such submission, proceeding or litigation could reduce the scope of, or invalidate, our patent rights, allow third parties to commercialize our technology or products and compete directly with us, without payment to us, or result in our inability to manufacture or commercialize products without infringing third‑party patent rights.
We have a number of foreign patents and patent applications, and expect to pursue patent protection in the most significant markets in which we do business. The laws of other countries in which our product offerings are or may be sold may not protect our product offerings and intellectual property to the same extent as U.S. laws, if at all. Many companies have encountered significant difficulties in obtaining, protecting and defending such rights in such markets. In addition, many countries limit the enforceability of patents against other parties, including government agencies or government contractors. In these countries, the patent owner may have limited remedies, and certain countries have compulsory licensing laws under which a patent owner may be compelled to grant licenses to other parties. We also may be unable to protect our rights in trade secrets and unpatented proprietary technology in these countries. If we encounter such difficulties or we are otherwise precluded from effectively protecting our intellectual property rights in these jurisdictions, our business, financial condition and results of operations could be substantially harmed.
Despite our efforts to safeguard our intellectual property rights, we may not be successful in doing so, or the steps taken by us in this regard may not be adequate to detect or deter misappropriation of our technology or to prevent an unauthorized third party from copying or otherwise obtaining and using our products, technology or other information that we regard as proprietary. Moreover, our competitors may independently develop equivalent knowledge, methods and know‑how. Competitors could purchase our products and attempt to replicate some or all of the competitive advantages we derive from our development efforts, infringe our intellectual property rights, design around our protected technology or develop their own competitive technologies that fall outside of our intellectual property rights. Our inability to adequately protect our intellectual property could allow our competitors and other third parties to produce products based on our patented or proprietary technology and other intellectual property rights, which could substantially impair our ability to compete.
We may not be able to accurately estimate or control our future operating expenses in relation to obtaining, enforcing and/or defending intellectual property, which could lead to cash shortfalls. Our operating expenses may fluctuate significantly in the future as a result of the costs of preparing, filing, prosecuting, defending and enforcing patent claims and other patent related costs, including litigation costs and the results of such litigation or costs associated with administrative proceedings and the results of such proceedings.
We have been and may in the future become involved in patent and other intellectual property litigation or administrative proceedings to enforce or defend our intellectual property rights, which could be costly, time consuming and unsuccessful and could interfere with our ability to successfully commercialize our products.
We have asserted and may in the future need to assert claims of infringement against third parties to protect our intellectual property.
54
Regardless of the final outcome, any litigation to enforce our intellectual property rights in patents, copyrights, trade secrets or trademarks is highly unpredictable and could result in substantial costs and diversion of resources, which could have a material adverse effect on our business, financial condition and results of operations. Any claims we assert against alleged infringers could provoke these third parties to assert counterclaims against us alleging that we infringe their own intellectual property rights, or that our rights are invalid or unenforceable. A court could hold that some or all of our asserted intellectual property rights are not infringed, or could invalidate our rights, hold our rights unenforceable, or substantially narrow the scope of protection. Any such adverse result would undermine our competitive position. In addition, there could be public announcements of the results of hearings, motions or other interim proceedings or developments. If securities analysts or investors perceive these results to be negative, it could hurt the price of our common stock. Such litigation proceedings could substantially increase our operating losses and reduce the resources available for development activities or any future sales, marketing or distribution activities.
We may become subject to claims of infringement or misappropriation of the intellectual property rights of others, which could prohibit us from selling our products, require us to obtain licenses from third parties, require us to develop non‑infringing alternatives and/or subject us to substantial monetary damages and injunctive relief.
The medical device industry is characterized by the existence of a large number of patents and frequent litigation based on allegations of patent infringement. Third parties could assert infringement or misappropriation claims against us with respect to our current or future commercial products. Moreover, because patent applications can take many years to issue, there may be currently pending applications, unknown to us, which may later result in issued patents that materially and adversely affect our business. Our competitors or other interested parties could also pursue additional patent protection related to their earlier patent disclosures with the intent to cover our products. Whether or not any such claims are valid, we cannot be certain that we have not infringed and will not in the future infringe the intellectual property rights of such third parties or others. Additionally, for business reasons, we have challenged and may in the future seek to invalidate or challenge the intellectual property rights of a third party, including those rights owned by our competitors, before any infringement assertion is made. This action could include seeking a declaration or decision from a court or patent office that one or more of our products do not infringe one or more patents or other intellectual property rights owned by third parties and/or that one or more patents owned by one or more third parties are invalid.
Any infringement or misappropriation claim or validity or infringement challenge could result in significant costs, substantial damages and our inability to manufacture, market or sell our existing or future products that are found to infringe. Even if we were to prevail in any such action, the litigation or administrative proceeding could result in substantial cost and diversion of resources that could materially and adversely affect our business. If a court determined, or if we independently discovered, that our product offerings violated third‑party proprietary rights, there can be no assurance that we would be able to re‑engineer our products to avoid those rights or to obtain a license under those rights on commercially reasonable terms, if at all. As a result, we could be prohibited from selling products that are found to infringe, or we could elect not to sell or to stop selling products that we believe have a substantial probability of infringing a third‑party’s intellectual property rights. Even if obtaining a license were feasible, it may be costly and time‑consuming. A court could also enter orders that temporarily, preliminarily or permanently enjoin us or our customers from making, using, selling, offering to sell, distributing, exporting or importing the iStent or future products, such as the iStent Inject, iStent SA, iStent Infinite, iStent Supra or iDose Travoprost, or could enter orders mandating that we undertake certain remedial activities. A court could also order us to pay compensatory damages for such infringement, plus prejudgment interest, and if we are found to have willfully infringed third‑party rights, could in addition treble the compensatory damages and award attorneys’ fees. These damages could be substantial and could harm our reputation, business, financial condition and results of operations.
Even if resolved in our favor, litigation or other legal or administrative proceedings relating to intellectual property claims may cause us to incur significant expenses, and could distract our technical and management personnel from their normal responsibilities. In addition, there could be public announcements of the results of hearings, motions or other interim proceedings or developments. If securities analysts or investors perceive these results to be negative, it could hurt the price of our common stock. Such litigation or administrative proceedings could substantially increase our operating losses and reduce the resources available for development activities or any future sales, marketing or distribution activities. We may not have sufficient financial or other resources to conduct such litigation or administrative proceedings adequately. Some of our competitors may be able to sustain the costs of such litigation or administrative proceedings more effectively than we can because of their greater financial resources. Uncertainties
55
resulting from the initiation and continuation of patent litigation or other proceedings could compromise our ability to compete in the marketplace.
If any of our employees, consultants or others breach their proprietary information agreements, our competitive position could be harmed.
We protect our proprietary technology, in part, through proprietary information and inventions agreements with employees, consultants and other parties. These agreements with employees and consultants generally contain standard provisions requiring those individuals to assign to us, without additional consideration, inventions conceived or reduced to practice by them while employed or retained by us, subject to customary exceptions. Although it is our policy to require each of our employees, consultants and any other parties who may be involved in the development of intellectual property on our behalf to execute such agreements, we may be unsuccessful in doing so with each party who in fact develops intellectual property that we regard as our own. The relevant assignment provisions may not be self‑executing or may be breached. As a result, our competitors may learn our trade secrets or we may be required to pursue litigation in order to determine the ownership of the intellectual property rights at issue.
Even if we file suit to prevent or stop such disclosure, there is a risk that a court could find we have not adequately protected the information as a trade secret and allow use of the disclosed information by our competitors. Additionally, we may need to file suit to force the employee, consultant or other party in breach to assign his, her or its rights to us, or we may need to pay additional compensation to such employee, consultant or other party in order to quiet or obtain legal title to the intellectual property rights at issue.
We may be subject to claims that we or our employees have misappropriated the intellectual property of a third party, including trade secrets or know‑how, or are in breach of non‑competition or non‑solicitation agreements with our competitors and third parties may claim an ownership interest in intellectual property we regard as our own.
Many of our employees and consultants were previously employed at or engaged by other medical device, biotechnology or pharmaceutical companies, including our competitors or potential competitors. Some of these employees, consultants and contractors, may have executed proprietary rights, non‑disclosure and non‑competition agreements in connection with such previous employment. Although we try to ensure that our employees and consultants do not use the intellectual property, proprietary information, know‑how or trade secrets of others in their work for us, we may be subject to claims that we or these individuals have, inadvertently or otherwise, misappropriated the intellectual property or disclosed the alleged trade secrets or other proprietary information, of these former employers or competitors. Additionally, we may be subject to claims from third parties challenging our ownership interest in intellectual property we regard as our own, based on claims that our employees or consultants have breached an obligation to assign inventions to another employer, to a former employer, or to another person or entity. Litigation may be necessary to defend against claims, and it may be necessary or we may desire to enter into a license to settle any such claim; however, there can be no assurance that we would be able to obtain a license on commercially reasonable terms, if at all. If our defense to those claims fails, in addition to paying monetary damages, a court could prohibit us from using technologies or features that are essential to our products, if such technologies or features are found to incorporate or be derived from the trade secrets or other proprietary information of the former employers. An inability to incorporate technologies or features that are important or essential to our products could have a material adverse effect on our business, and may prevent us from selling our products. In addition, we may lose valuable intellectual property rights or personnel. Even if we are successful in defending against these claims, litigation could result in substantial costs and could be a distraction to management. Any litigation or the threat thereof may adversely affect our ability to hire employees or contract with independent sales representatives. A loss of key personnel or their work product could hamper or prevent our ability to commercialize our products, which could have an adverse effect on our business, results of operations and financial condition.
Risks Related to Being a Public Company
If we experience material weaknesses in, or otherwise fail to maintain an effective system of, internal controls in the future, we may not be able to accurately report our financial condition or results of operations, which may adversely affect investor confidence in us and, as a result, the value of our common stock.
The Sarbanes‑Oxley Act requires, among other things, that we assess the effectiveness of our internal control over financial reporting annually and the effectiveness of our disclosure controls and procedures quarterly. In particular,
56
Section 404(a) of the Sarbanes‑Oxley Act requires us to perform system and process evaluation and testing of our internal control over financial reporting to allow management to report on the effectiveness of our internal control over financial reporting. We are no longer an “emerging growth company” as of December 31, 2017, and consequently, Section 404(b) of the Sarbanes‑Oxley Act requires our independent registered public accounting firm to annually attest to the effectiveness of our internal control over financial reporting commencing with the year ending December 31, 2017.
Investor perceptions of our company may suffer if deficiencies are found, and this could cause a decline in the market price of our stock. Regardless of compliance with Section 404, any failure of our internal control over financial reporting could have a material adverse effect on our stated operating results and harm our reputation. If we are unable to implement these requirements effectively or efficiently, it could harm our operations, financial reporting, or financial results and could result in an adverse opinion on our internal controls from our independent registered public accounting firm.
Risks Related to our Common Stock and Ownership of Our Common Stock
We expect that the price of our common stock may fluctuate substantially.
The market price for our common stock may fluctuate depending upon many factors, including, but not limited to:
|
· |
the depth and liquidity of the market for our common stock; |
|
· |
volume, timing and nature of orders for our products; |
|
· |
developments generally affecting medical device companies; |
|
· |
actual or anticipated quarterly variation in our results of operations or the results of our competitors; |
|
· |
the announcements by us or our competitors of new products or product enhancements, significant contracts, commercial relationships or capital commitments; |
|
· |
developments or disputes concerning our intellectual property or other proprietary rights; |
|
· |
issuance of new or changes in earnings estimates or recommendations or reports by securities analysts; |
|
· |
investor perceptions of us and our business, including changes in market valuations of medical device companies; |
|
· |
actions by institutional or other large stockholders; |
|
· |
commencement of, or our involvement in, litigation; |
|
· |
failure to achieve significant sales; |
|
· |
manufacturing disruptions that could occur if we were unable to successfully expand our production in our current or an alternative facility; |
|
· |
any future sales of our common stock or other securities; |
|
· |
any major change to the composition of our board of directors or management; |
|
· |
our results of operations and financial performance; and |
|
· |
general economic, industry and market conditions. |
In addition, the market price of the stocks of medical device, medical technology, pharmaceutical, biotechnology and other life science companies have experienced significant volatility that often does not relate to the operating performance of the companies represented by the stock. Further, there has been particular volatility in the market price of securities of early‑stage and development‑stage life science and medical device companies. These broad market and industry factors may seriously harm the market price of our common stock, regardless of our operating performance.
57
If securities or industry analysts publish unfavorable research about our business, our stock price and trading volume could decline.
The trading market for our common stock will rely in part on the research and reports that equity research analysts publish about us and our business. We will not have any control over the analysts or the content and opinions included in their reports. The price of our stock could decline if one or more equity research analysts downgrade our stock or issue other unfavorable commentary or research. If one or more equity research analysts ceases coverage of our company or fails to publish reports on us regularly, demand for our stock could decrease, which in turn could cause our stock price or trading volume to decline..
Our officers, directors and principal stockholders have significant voting power and may take actions that may not be in the best interests of our other stockholders.
Our executive officers, directors and stockholders holding more than 5% of our outstanding common stock currently collectively own or control a significant amount of our outstanding common stock. As a result, our executive officers, directors and stockholders holding more than 5% of our outstanding common stock, acting as a group, have substantial influence over the outcome of corporate actions requiring stockholder approval, including the election of directors, any merger, consolidation or sale of all or substantially all of our assets or any other significant corporate transactions. These stockholders may also have the effect of delaying or preventing a change in control of us, even if such a change of control would benefit our other stockholders. This significant concentration of stock ownership may adversely affect the trading price of our common stock due to investors’ perception that conflicts of interest may exist or arise.
Two members of our board of directors are directors of DOSE. In addition, there is significant overlap between our current stockholders and the stockholders of DOSE. Their interests may conflict with those of our other stockholders.
Two of our current directors, Thomas W. Burns and William J. Link, Ph.D., serve as the only two members of the board of directors of DOSE. This could result in conflicts of interest between their obligations to our company and DOSE. In addition, there is significant overlap between our stockholders and the stockholders of DOSE. DOSE’s interests and the interests of its stockholders may be different from ours or those of our other stockholders and this could result in conflicts. The resolution of any of these conflicts may not always be in our or your best interest.
Anti‑takeover provisions in our charter documents and under Delaware law could make an acquisition of us, which may be beneficial to our stockholders, more difficult and may prevent attempts by our stockholders to replace or remove our current management and limit the market price of our common stock.
Provisions in our restated certificate of incorporation and amended and restated bylaws may have the effect of delaying or preventing a change of control or changes in our management. Our restated certificate of incorporation and amended and restated bylaws include provisions that:
|
· |
authorize our board of directors to issue, without further action by the stockholders, up to 5,000,000 shares of undesignated preferred stock; |
|
· |
require that any action to be taken by our stockholders be effected at a duly called annual or special meeting and not by written consent; |
|
· |
specify that special meetings of our stockholders may be called only by our board of directors, the chairman of the board of directors, the chief executive officer or the president; |
|
· |
establish an advance notice procedure for stockholder approvals to be brought before an annual meeting of our stockholders, including proposed nominations of persons for election to our board of directors; |
|
· |
establish that our board of directors is divided into three classes, Class I, Class II and Class III, with each class serving staggered three year terms; |
|
· |
provide that our directors may be removed only for cause by a supermajority vote of our stockholders; |
|
· |
provide that vacancies on our board of directors may be filled only by a majority of directors then in office, even though less than a quorum; |
58
|
· |
specify that no stockholder is permitted to cumulate votes at any election of directors; and |
|
· |
require a supermajority vote of the stockholders and a majority vote of the board to amend certain of the above‑mentioned provisions and our bylaws. |
These provisions may frustrate or prevent any attempts by our stockholders to replace or remove our current management by making it more difficult for stockholders to replace members of our board of directors, which is responsible for appointing the members of our management. In addition, because we are incorporated in Delaware, we are governed by the provisions of Section 203 of the Delaware General Corporation Law, which limits the ability of stockholders owning in excess of 15% of our outstanding voting stock to merge or combine with us.
We have never paid dividends on our capital stock and do not anticipate paying cash dividends in the foreseeable future.
We have never declared or paid cash dividends on our capital stock. We currently intend to retain all available funds and any future earnings for use in the operation and expansion of our business and do not anticipate paying any cash dividends in the foreseeable future. Accordingly, you may have to sell some or all of your shares of our common stock in order to generate cash flow from your investment. You may not receive a gain on your investment when you sell shares and you may lose the entire amount of the investment.
ITEM 1B.UNRESOLVED STAFF COMMENTS
None.
As of December 31, 2017, we leased or owned approximately 94,000 square feet of office and operations space. This space includes our corporate headquarters and production facilities in San Clemente, California as well as smaller administrative offices and sales offices in the United States, Germany, Australia, Canada, Brazil, Japan and the United Kingdom.
Neither we nor any of our subsidiaries is a party to, and none of their respective property is the subject of, any material legal proceeding, although we are from time to time party to legal proceedings that arise in the ordinary course of our business.
ITEM 4.MINE SAFETY DISCLOSURES
Not applicable.
59
ITEM 5. MARKET FOR REGISTRANT’S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
Market Information for Common Stock
Our common stock trades on the NYSE under the symbol “GKOS”. The table below sets forth, for the periods indicated, the high and low intra‑day sales prices per share of our common stock as reported on the NYSE.
|
|
|
High |
|
Low |
|
||
|
2017 |
|
|
|
|
|
|
|
|
First Quarter |
|
$ |
52.49 |
|
$ |
33.18 |
|
|
Second Quarter |
|
$ |
52.48 |
|
$ |
36.51 |
|
|
Third Quarter |
|
$ |
43.49 |
|
$ |
30.22 |
|
|
Fourth Quarter |
|
$ |
36.20 |
|
$ |
23.08 |
|
|
|
|
|
High |
|
|
Low |
|
|
2016 |
|
|
|
|
|
|
|
|
First Quarter |
|
$ |
25.97 |
|
$ |
14.25 |
|
|
Second Quarter |
|
$ |
30.01 |
|
$ |
16.26 |
|
|
Third Quarter |
|
$ |
39.82 |
|
$ |
28.26 |
|
|
Fourth Quarter |
|
$ |
39.02 |
|
$ |
28.72 |
|
As of February 26, 2018, we had 22 holders of record of our common stock. The actual number of stockholders is greater than this number of record holders, and includes stockholders who are beneficial owners but whose shares are held in street name by brokers and other nominees. The number of record holders also does not include stockholders whose shares may be held in trust by other entities.
Stock Performance Graph
The following performance graph shows the cumulative total stockholder return of an investment of $100 at the close of market on June 25, 2015 (the first day of trading of our common stock on the NYSE) in (i) our common stock, (ii) the S&P Small Cap 600 index and (iii) the S&P Small Cap 600 Healthcare index. The graph assumes that all
60
dividends were reinvested. Stockholder returns over the indicated period should not be considered indicative of future stockholder returns.
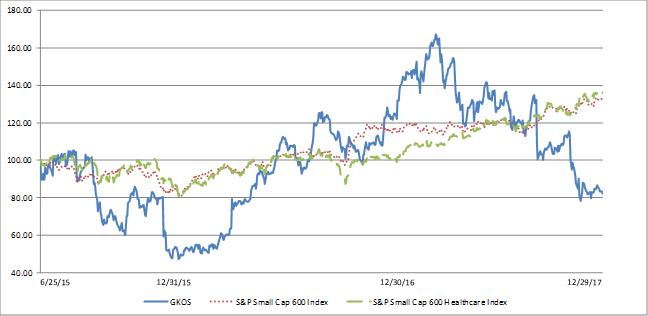
|
|
|
6/25/2015 |
|
12/31/2015 |
|
12/30/2016 |
|
12/29/2017 |
|
||||
|
GKOS |
|
$ |
100.00 |
|
$ |
79.08 |
|
$ |
109.87 |
|
$ |
82.16 |
|
|
S&P Small Cap 600 index |
|
$ |
100.00 |
|
$ |
92.03 |
|
$ |
116.47 |
|
$ |
131.89 |
|
|
S&P Small Cap 600 Healthcare index |
|
$ |
100.00 |
|
$ |
98.73 |
|
$ |
100.89 |
|
$ |
135.91 |
|
This performance graph shall not be deemed “filed” for purposes of Section 18 of the Exchange Act, or otherwise subject to the liabilities under that section and shall not be deemed to be incorporated by reference into any of our filings under the Securities Act of 1933, as amended, or the Exchange Act.
Dividend Policy
We have never declared or paid any cash dividends on our common stock or any other securities. We anticipate that we will retain all available funds and any future earnings, if any, for use in the operation of our business and do not anticipate paying cash dividends in the foreseeable future. In addition, our ability to pay dividends may be restricted by the terms of any future credit agreement or any future debt or preferred equity securities of us or of our subsidiaries Payment of future cash dividends, if any, will be at the discretion of our board of directors after taking into account various factors, including our financial condition, operating results, current and anticipated cash needs, the requirements of then existing debt instruments and other factors our board of directors may deem relevant.
61
ITEM 6.SELECTED FINANCIAL DATA
The selected consolidated financial information set forth below for each of the years ended December 31, 2017, 2016, 2015, 2014 and 2013 has been derived from our audited consolidated financial statements. The information below should be read in conjunction with “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the audited consolidated financial statements and notes thereto included in Items 7 and 8, respectively, of this Annual Report on Form 10-K.
|
|
|
Year ended December 31, |
|
|
|
|
||||||||||
|
(in thousands, except per share amounts) |
|
2017 |
|
2016 |
|
|
2015 |
|
2014 |
|
2013 |
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Statements of Operations Data: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Net sales |
|
$ |
159,254 |
|
$ |
114,397 |
|
$ |
71,700 |
|
$ |
45,587 |
|
$ |
20,946 |
|
|
Cost of sales |
|
|
21,050 |
|
|
16,177 |
|
|
12,988 |
|
|
11,418 |
|
|
2,535 |
|
|
Gross profit |
|
|
138,204 |
|
|
98,220 |
|
|
58,712 |
|
|
34,169 |
|
|
18,411 |
|
|
Operating expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Selling, general and administrative |
|
|
96,260 |
|
|
64,756 |
|
|
43,961 |
|
|
28,135 |
|
|
17,098 |
|
|
In-process research and development |
|
|
5,320 |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
Research and development |
|
|
38,905 |
|
|
29,223 |
|
|
25,047 |
|
|
19,205 |
|
|
15,511 |
|
|
Total operating expenses |
|
|
140,485 |
|
|
93,979 |
|
|
69,008 |
|
|
47,340 |
|
|
32,609 |
|
|
(Loss) income from operations |
|
|
(2,281) |
|
|
4,241 |
|
|
(10,296) |
|
|
(13,171) |
|
|
(14,198) |
|
|
Loss on deconsolidation of DOSE |
|
|
— |
|
|
— |
|
|
(25,685) |
|
|
— |
|
|
— |
|
|
Total other income (expense), net |
|
|
2,282 |
|
|
324 |
|
|
(2,307) |
|
|
(868) |
|
|
(23) |
|
|
Provision for income taxes |
|
|
93 |
|
|
43 |
|
|
33 |
|
|
18 |
|
|
6 |
|
|
Net (loss) income |
|
$ |
(92) |
|
$ |
4,522 |
|
$ |
(38,321) |
|
$ |
(14,057) |
|
$ |
(14,227) |
|
|
Net loss attributable to noncontrolling interest |
|
|
— |
|
|
— |
|
|
(1,080) |
|
|
(1,931) |
|
|
(1,588) |
|
|
Net (loss) income attributable to Glaukos Corporation |
|
$ |
(92) |
|
$ |
4,522 |
|
$ |
(37,241) |
|
$ |
(12,126) |
|
$ |
(12,639) |
|
|
Basic net (loss) income per share attributable to Glaukos Corporation stockholders |
|
$ |
(0.00) |
|
$ |
0.14 |
|
$ |
(2.13) |
|
$ |
(5.29) |
|
$ |
(6.21) |
|
|
Diluted net (loss) income per share attributable to Glaukos Corporation stockholders |
|
$ |
(0.00) |
|
$ |
0.12 |
|
$ |
(2.13) |
|
$ |
(5.29) |
|
$ |
(6.21) |
|
|
Weighted average shares used to compute basic net (loss) income per share attributable to Glaukos Corporation stockholders |
|
|
34,381 |
|
|
32,928 |
|
|
17,474 |
|
|
2,294 |
|
|
2,036 |
|
|
Weighted average shares used to compute diluted net (loss) income per share attributable to Glaukos Corporation stockholders |
|
|
34,381 |
|
|
36,459 |
|
|
17,474 |
|
|
2,294 |
|
|
2,036 |
|
62
|
|
|
As of December 31, |
|
|
|
|
||||||||||
|
(in thousands) |
|
2017 |
|
2016 |
|
|
2015 |
|
2014 |
|
2013 |
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Balance Sheet Data: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cash and cash equivalents |
|
$ |
24,508 |
|
$ |
6,494 |
|
|
21,572 |
|
$ |
2,304 |
|
$ |
6,728 |
|
|
Short-term investments |
|
|
94,506 |
|
|
89,268 |
|
|
69,552 |
|
|
— |
|
|
— |
|
|
Net working capital (deficit) |
|
|
122,672 |
|
|
103,085 |
|
|
83,778 |
|
|
(9,633) |
|
|
6,487 |
|
|
Total assets |
|
|
165,836 |
|
|
134,371 |
|
|
116,661 |
|
|
26,021 |
|
|
30,877 |
|
|
Total liabilities |
|
|
27,634 |
|
|
17,097 |
|
|
21,470 |
|
|
29,546 |
|
|
23,709 |
|
|
Convertible preferred stock |
|
|
— |
|
|
— |
|
|
— |
|
|
157,379 |
|
|
156,210 |
|
|
Additional paid in capital |
|
|
331,073 |
|
|
308,815 |
|
|
291,853 |
|
|
8,155 |
|
|
6,073 |
|
|
Total stockholders’ equity (deficit) |
|
|
138,202 |
|
|
117,274 |
|
|
95,191 |
|
|
(151,299) |
|
|
(141,298) |
|
|
Noncontrolling interest |
|
|
— |
|
|
— |
|
|
— |
|
|
(9,605) |
|
|
(7,744) |
|
|
Total equity (deficit) |
|
|
138,202 |
|
|
117,274 |
|
|
95,191 |
|
|
(160,904) |
|
|
(149,042) |
|
ITEM 7.MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
You should read the following discussion and analysis of our financial condition and results of operations together with “Selected financial data” and our audited consolidated financial statements and related notes included in Items 6 and 8, respectively, of this Annual Report on Form 10-K. This discussion and analysis and other parts of this Annual Report on Form 10-K contain forward-looking statements that reflect our current plans, expectations, estimates and beliefs that involve risks, uncertainties and assumptions, such as statements regarding our plans, objectives, expectations, intentions and projections. Our actual results and the timing of selected events may differ materially from those discussed in these forward-looking statements. You should carefully read Item 1A - “Risk Factors” included in this Annual Report on Form 10-K to gain an understanding of the important factors that could cause actual results to differ materially from our forward-looking statements. Please also see the section entitled “Special Note Regarding Forward-Looking Statements and Industry Data.”
Overview
We are an ophthalmic medical technology and pharmaceutical company focused on the development and commercialization of novel surgical devices and sustained pharmaceutical therapies designed to treat glaucoma, one of the world’s leading causes of blindness. We developed Micro‑Invasive Glaucoma Surgery (MIGS) to address the shortcomings of traditional glaucoma treatment options. MIGS procedures involve the insertion of a micro‑scale device or drug delivery system from within the eye’s anterior chamber through a small corneal incision. Our MIGS devices are designed to reduce intraocular pressure by restoring the natural outflow pathways for aqueous humor. Our MIGS drug delivery systems are designed to reduce intraocular pressure by continuously eluting a glaucoma drug from within the eye, potentially providing sustained pharmaceutical therapy for extended periods of time.
Our iStent, a micro‑bypass stent that is designed to reduce intraocular pressure by restoring the natural physiologic pathways for aqueous humor, was the first commercially available MIGS treatment solution. Approved by the United States (U.S.) Food and Drug Administration (FDA) for insertion in combination with cataract surgery, the iStent procedure is currently reimbursed by Medicare and all major national private payors. Our next product, the iStent Inject, includes two stents pre‑loaded in an auto‑injection inserter that are also designed to lower intraocular pressure. The iStent Inject was commercially available in 2017 in certain European Union countries, Canada, Australia, Brazil and South Africa. In these markets, it is approved for use in conjunction with cataract surgery or as a standalone procedure, even though reimbursement may not be available for all such procedures. We are currently seeking FDA approval to market the iStent Inject in the U.S.
We are developing four additional iStent pipeline products: the iStent Inject (in the U.S.), the iStent SA, the iStent Infinite and the iStent Supra. In an effort to obtain approval to market the iStent Inject in the U.S. in conjunction with cataract surgery, we completed a U.S. investigational device exemption (IDE) pivotal trial and submitted a premarket approval application (PMA) for the iStent Inject in 2017. The iStent SA is designed for use as a standalone
63
glaucoma procedure. Similar to the iStent Inject, the iStent SA is a two-stent product that is slightly wider than the iStent Inject and uses a different auto‑injection inserter designed for use in a standalone procedure. The iStent SA is currently being studied in a U.S. pivotal IDE study as a standalone treatment for lowering intraocular pressure in pseudophakic glaucoma patients. We recently submitted an IDE application for the iStent Infinite, which includes three stents pre-loaded in an auto-injection inserter and is intended to lower intraocular pressure in refractory glaucoma patients. The iStent Supra is designed to access an alternative drainage space within the eye and is being evaluated in a U.S. pivotal IDE trial. We completed enrollment for the U.S. pivotal IDE trial for the iStent Supra in 2017.
We are also pursuing regulatory approval of our first sustained pharmaceutical therapy using our iDose drug delivery system. A U.S. investigational new drug (IND) Phase II study of our initial iDose platform product, iDose Travoprost, was completed in 2017 and we intend to commence U.S. Phase III clinical trials for this product in the first half of 2018. We are also conducting research and development activities to explore other potential drugs that may benefit from the use of the iDose drug delivery system. In addition, other proprietary R&D efforts are underway on early-stage technologies, including, without limitation, an intraocular pressure sensor (IOP) system that is designed to capture and store a glaucoma patient’s short-interval IOP measurements over extended periods of time, and transmit data to the patient’s physician in order to enhance treatment decisions.
Prior to 2016, we had never been profitable and had incurred operating losses in each year since our inception. Our net sales increased to $159.3 million for the year ended December 31, 2017 from $114.4 million and $71.7 million for the years ended December 31, 2016 and 2015, respectively. We incurred a net loss of $0.1 million for the year ended December 31, 2017. We achieved net income of $4.5 million for the year ended December 31, 2016 and we incurred a net loss of $38.3 million for the year ended December 31, 2015.
As of December 31, 2017, we had an accumulated deficit of $192.2 million.
We have made and expect to continue to make significant investments in our global sales force, marketing programs, research and development activities and clinical studies. FDA‑approved IDE studies and new product development programs in our industry are expensive, and we have incurred a significant increase in administrative costs since we began operating as a public company. Accordingly, although we achieved profitability in 2016, we incurred a loss in 2017 and there can be no assurance that we will be profitable in future.
Components of results of operations
Net sales
We currently operate in one reportable segment, ophthalmic medical devices, and substantially all of our net sales are derived from sales of our iStent products, net of customer returns and allowances. We recognize net sales when goods are shipped, title and risk of loss transfer to our customers, persuasive evidence of an arrangement exists and collectability is reasonably assured.
We sell our products through a direct sales organization in the United States, and outside the United States we sell our products primarily through direct sales subsidiaries in sixteen countries and through independent distributors in certain countries in which we do not have a direct presence. The primary end‑user customers for our products are hospitals and surgery centers.
We anticipate our net sales will increase as we expand our global sales and marketing infrastructure and continue to increase awareness of our products by expanding our sales base and increasing our marketing efforts. We also expect that our net sales within a fiscal year may be impacted seasonally and reflect seasonality patterns generally consistent with U.S. cataract procedure volumes, which are typically softer in the first quarter and stronger in the fourth quarter of a given year. However, until recently, our iStent was the only MIGS device approved for sale in the United States by the FDA. Thus, we had for several years commercialized the iStent in the United States without any direct MIGS competitors. Other MIGS devices have now become available in the United States and globally, or are in development by third parties that have entered or could enter the market and which may affect adoption of or demand for our products. These new MIGS products could achieve greater commercial acceptance than our iStent or our pipeline products under development, which may reduce demand for our products and reduce our net sales.
64
In 2017, the Australian Department of Health (ADOH) initiated a comprehensive review of its Medicare Benefits Schedule (MBS), a list of approximately 5,600 codes used to determine reimbursement. As part of this review, reimbursement of the surgeon fee code for implantation of iStent devices was suspended effective May 1, 2017. Prior to suspension of the code, the Company filed an application with the ADOH to obtain a new code for reimbursement of the surgeon fee. On May 4, 2017 the ADOH created a temporary MBS code for the implantation of iStent and iStent Inject, which is set to expire on December 31, 2018. The Company has submitted a request to the ADOH for the creation of a permanent MBS code for the implantation of iStent and iStent Inject. See Item 1, Business above for additional information.
Cost of sales
Cost of sales reflects the aggregate costs to manufacture our products and includes raw material costs, labor costs, manufacturing overhead expenses and the effect of changes in the balance of reserves for excess and obsolete inventory. We manufacture our iStent products at our headquarters in San Clemente, California using components manufactured by third parties. Due to the relatively low production volumes of our iStent products compared to our potential capacity for those products, a significant portion of our per unit costs is comprised of manufacturing overhead expenses. These expenses include quality assurance, material procurement, inventory control, facilities, equipment and operations supervision and management.
Beginning in late 2013, cost of sales has included amortization of the $17.5 million intangible asset we recognized in connection with our royalty buyout agreement with GMP Vision Solutions, Inc. (GMP) in November 2013. See “Indebtedness-Notes payable to GMP Vision Solutions” for additional information. The amortization expense was $3.5 million in each of the years ended December 31, 2017, 2016 and 2015 and is estimated to be $3.0 million in 2018, after which it will be fully amortized.
Beginning in 2015, cost of sales includes a charge equal to a low single‑digit percentage of worldwide net sales of certain current and future products, including our iStent products, with a required minimum annual payment of $500,000, which amount became payable to the Regents of the University of California (University) in connection with our December 2014 agreement with the University (UC Agreement) related to a group of the Company’s U.S. patents (Patent Rights). This ongoing product payment obligation will terminate on the date the last of the Patent Rights expires, which is currently expected to be in 2022.
Under the Protecting Americans from Tax Hikes Act of 2015 (PATH Act), the 2.3% federal medical device excise tax on U.S. sales of medical devices manufactured by us was suspended from January 1, 2016 to December 31, 2017, and, pursuant to HR 195 passed on January 22, 2018, was further suspended through December 31, 2019.
Our future gross profit as a percentage of net sales, or gross margin, will be impacted by numerous factors including commencement of sales of products in our pipeline, or any other future products, which may have higher product costs. Our gross margin will also be affected by manufacturing inefficiencies that we may experience as we attempt to manufacture our products on a larger scale, manufacture new products and change our manufacturing capacity or output. Additionally, our gross margin will continue to be affected by the aforementioned intangible asset amortization and expense related to the UC Agreement.
Selling, general and administrative
Our selling, general and administrative (SG&A) expenses primarily consist of personnel‑related expenses, including salaries, sales commissions, bonuses, fringe benefits and stock‑based compensation for our executive, financial, marketing, sales, and administrative functions. Other significant SG&A expenses include marketing programs, advertising, conferences and congresses, and travel expenses, as well as the costs associated with obtaining and maintaining our patent portfolio, professional fees for accounting, auditing, consulting and legal services, travel and allocated overhead expenses.
We expect SG&A expenses to continue to grow as we increase our sales and marketing infrastructure globally and our clinical education and general administration infrastructure in the United States. We also expect other nonemployee‑related costs, including sales and marketing program activities for new products, outside services and accounting and general legal costs to increase as our overall operations grow. The timing of these increased expenditures
65
and their magnitude are primarily dependent on the commercial success and sales growth of our products, as well as on the timing of any new product launches and other potential business and operational activities. In addition, we have incurred increased SG&A expenses resulting from becoming a public company, which we expect will increase in 2018 now that, as of the end of fiscal year 2017, we are no longer able to rely on certain “emerging growth company” exemptions that we are afforded under the Jumpstart Our Business Startups Act.
In-process research and development
Our in-process research and development (IPR&D) expense consists of the cost associated with purchasing the IOP Sensor System from DOSE on April 12, 2017. The IOP Sensor System was in the development-stage at the time of purchase.
Research and development
Our research and development (R&D) activities primarily consist of new product development projects, pre‑clinical studies, IDE studies, and other clinical trials. Our R&D expenses primarily consist of personnel‑related expenses, including salaries, fringe benefits and stock‑based compensation for our R&D employees; research materials; supplies and services; and the costs of conducting clinical studies, which include payments to investigational sites and investigators, clinical research organizations, consultants, and other outside technical services and the costs of materials, supplies and travel. We expense R&D costs as incurred. We expect our R&D expenses to increase as we initiate and advance our development programs and clinical trials, the most costly of which are expected to be our iStent Inject, iStent Supra, iDose Travoprost, iStent SA and iStent Infinite product candidates. Additionally, we expect our R&D expenses to increase as we incur developmental spend on the IOP Sensor System product line we purchased from DOSE in April 2017.
Completion dates and costs for our clinical development programs include seeking regulatory approvals and our research programs can vary significantly for each current and future product candidate and are difficult to predict. As a result, while we expect our R&D costs to continue to increase for the foreseeable future, we cannot estimate with any degree of certainty the costs we will incur in connection with the development of our product candidates. We anticipate we will make determinations as to which programs and product candidates to pursue and how much funding to direct to each program and product candidate on an ongoing basis in response to the scientific success of early research programs, results of ongoing and future clinical trials, as well as ongoing assessments as to each current or future product candidate’s commercial potential and our likelihood of obtaining necessary regulatory approvals.
Other income (expense), net
Other income (expense), net primarily consists of interest income derived from our short-term investments, interest expense during the time our secured notes payable were outstanding during 2016, and until the common stock warrants were exercised during the first three months of 2016, changes in the fair value of our stock warrant liability. Also included are unrealized gains and losses arising from exchange rate fluctuations on transactions denominated in a currency other than the U.S. dollar, primarily related to intercompany loans.
Income taxes
The provision for income taxes is determined using an estimated annual effective tax rate which is generally lower than the U.S. federal statutory rate primarily due to the utilization of net operating loss carryforwards, the benefit of which had not previously been recognized due to a full valuation allowance. The annual effective tax rate may be subject to fluctuations during the year as new information is obtained which may affect the assumptions used to estimate the annual effective tax rate, including factors such as expected utilization of net operating loss carryforwards, changes in or the interpretation of tax laws in jurisdictions where the we conduct business, our expansion into new states or foreign countries, and the amount of valuation allowances against deferred tax assets.
The Tax Cuts and Jobs Act (the "Act") was enacted on December 22, 2017. Among other changes, the Act reduces the US federal corporate tax rate from 34 percent to 21 percent for federal tax purposes. In accordance with Staff
66
Accounting Bulletin 118, as of December 31, 2017, we have not completed the accounting for the tax effects of enactment of the Act; however, in certain cases, as described below, we have made a reasonable estimate of the effects on the existing deferred tax balances. In all cases, we will continue to make and refine calculations as additional analysis is completed. In addition, estimates may also be affected as we gain a more thorough understanding of the Act.
We remeasured certain deferred tax assets and liabilities based on the rates at which they are expected to reverse in the future, which is generally 21%. However, we are still analyzing certain aspects of the Act and refining calculations, which could potentially affect the measurement of these balances or give rise to new deferred tax amounts. The provisional amount recorded related to the remeasurement of the deferred tax balance was $25.2 million, which was fully offset by a decrease in the valuation allowance.
Due to uncertainties which currently exist in the interpretation of the provisions of the Act regarding Internal Revenue Code (IRC) Section 162(m), we are still evaluating the potential impacts of IRC Section 162(m) as amended by the Act.
Results of operations
Comparison of years ended December 31, 2017 and 2016
|
|
|
Year ended |
|
|
|
||||
|
|
|
December 31, |
|
% Increase |
|
||||
|
(in thousands) |
|
2017 |
|
2016 |
|
(decrease) |
|
||
|
Statements of operations data: |
|
|
|
|
|
|
|
|
|
|
Net sales |
|
$ |
159,254 |
|
$ |
114,397 |
|
39 |
% |
|
Cost of sales |
|
|
21,050 |
|
|
16,177 |
|
30 |
% |
|
Gross profit |
|
|
138,204 |
|
|
98,220 |
|
41 |
% |
|
Operating expenses: |
|
|
|
|
|
|
|
|
|
|
Selling, general and administrative |
|
|
96,260 |
|
|
64,756 |
|
49 |
% |
|
In-process research and development |
|
|
5,320 |
|
|
— |
|
NM |
|
|
Research and development |
|
|
38,905 |
|
|
29,223 |
|
33 |
% |
|
Total operating expenses |
|
|
140,485 |
|
|
93,979 |
|
49 |
% |
|
(Loss) income from operations |
|
|
(2,281) |
|
|
4,241 |
|
NM |
|
|
Total other income, net |
|
|
2,282 |
|
|
324 |
|
604 |
% |
|
Provision for income taxes |
|
|
93 |
|
|
43 |
|
116 |
% |
|
Net (loss) income |
|
$ |
(92) |
|
$ |
4,522 |
|
NM |
|
Net sales
Net sales for the years ended December 31, 2017 and 2016 were $159.3 million and $114.4 million, respectively, reflecting an increase of $44.9 million or 39%. The increase in net sales resulted from unit volume increases worldwide, an increase in the average selling price of iStents sold to U.S. ASCs related to an increase in Medicare reimbursement payments, and expansion of the Company’s direct sales operations into new international markets. Net sales in the United States represented $140.9 million and $105.0 million of net sales for the years ended December 31, 2017 and 2016, respectively, increasing by 34%. International sales for the years ended December 31, 2017 and 2016 were $18.4 million and $9.4 million, respectively, increasing by 95%. Net sales at our subsidiaries in Australia, Germany, Japan and the United Kingdom accounted for the majority of the increase internationally.
Cost of sales
Cost of sales for the years ended December 31, 2017 and 2016 were $21.1 million and $16.2 million, respectively, reflecting an increase of $4.9 million or 30%. Our gross margin for the year ended December 31, 2017 was approximately 87% compared to approximately 86% in 2016.
67
Selling, general and administrative expenses
SG&A expenses for the years ended December 31, 2017 and 2016 were $96.3 million and $64.8 million, respectively, reflecting an increase of $31.5 million or 49%. The increase in SG&A expenses was primarily the result of an increase of approximately $11.7 million in salary and related expenses and stock-based compensation associated with our increased number of domestic employees, an increase in SG&A expenses incurred by our foreign subsidiaries of approximately $8.9 million and an increase of approximately $4.4 million in consulting and professional services fees.
Research and development expenses
R&D expenses for the years ended December 31, 2017 and 2016 were $38.9 million and $29.2 million, respectively, reflecting an increase of $9.7 million or 33%. The increase in R&D expenses primarily resulted due to approximately $6.2 million in salary and related expenses, stock-based compensation, travel and other costs associated with our increased number of personnel, primarily in our clinical and regulatory affairs functions, required to manage the increased number of global clinical studies with associated investigational sites and study investigators, an increase of approximately $2.0 million in product costs for supplies and inventory requisitions for iStent Inject and an increase of approximately $1.8 million in consulting and professional services fees. Partially offsetting these increases was a reduction in U.S. clinical trial expenses of approximately $1.8 million given we achieved full enrollment in a U.S.-based clinical study during the fiscal year ended 2017.
Other income, net
We had other income, net for the years ended December 31, 2017 and December 31, 2016 of $2.3 million and $0.3 million, respectively. The increase in interest and other income reflects higher interest rates on a comparatively higher balance of short-term investments and the recognition of greater unrealized foreign currency gains due to higher intercompany loan balances.
Provision for income taxes
Our effective tax rate for the year ended 2017 was not meaningful. For the years ended December 31, 2017 and 2016, we recorded a provision for income taxes of $93,000 and $43,000, respectively, which were primarily comprised of federal alternative minimum tax and state income taxes.
Comparison of years ended December 31, 2016 and 2015
|
|
|
Year ended |
|
|
|
||||
|
|
|
December 31, |
|
% Increase |
|
||||
|
(in thousands) |
|
2016 |
|
2015 |
|
(decrease) |
|
||
|
Statements of operations data: |
|
|
|
|
|
|
|
|
|
|
Net sales |
|
$ |
114,397 |
|
$ |
71,700 |
|
60 |
% |
|
Cost of sales |
|
|
16,177 |
|
|
12,988 |
|
25 |
% |
|
Gross profit |
|
|
98,220 |
|
|
58,712 |
|
67 |
% |
|
Operating expenses: |
|
|
|
|
|
|
|
|
|
|
Selling, general and administrative |
|
|
64,756 |
|
|
43,961 |
|
47 |
% |
|
Research and development |
|
|
29,223 |
|
|
25,047 |
|
17 |
% |
|
Total operating expenses |
|
|
93,979 |
|
|
69,008 |
|
36 |
% |
|
Income (loss) from operations |
|
|
4,241 |
|
|
(10,296) |
|
NM |
|
|
Loss on deconsolidation of DOSE |
|
|
— |
|
|
(25,685) |
|
NM |
|
|
Total other income (expense), net |
|
|
324 |
|
|
(2,307) |
|
NM |
|
|
Provision for income taxes |
|
|
43 |
|
|
33 |
|
30 |
% |
|
Net income (loss) |
|
$ |
4,522 |
|
$ |
(38,321) |
|
NM |
|
68
Net sales
Net sales for the years ended December 31, 2016 and 2015 were $114.4 million and $71.7 million, respectively, reflecting an increase of $42.7 million or 60%. Net sales in the United States represented $105.0 million and $67.7 million of net sales for the years ended December 31, 2016 and 2015, respectively, increasing by 55% and accounting for 87% of the overall increase in net sales. Increases in both the number of customer facilities purchasing our iStent products and the average utilization of iStent in our customers’ available MIGS-appropriate procedures accounted for the growth in unit sales in the United States. International sales for the year ended December 31, 2016 and 2015 were $9.4 million and $4.0 million, respectively, increasing by $5.4 million or 135%, and accounting for 13% of the Company’s worldwide net sales increase. Net sales at our Australian and Canadian subsidiaries accounted for the majority of the increase internationally. Worldwide, increased unit volume due to increased iStent utilization across our expanding customer base was responsible for the majority of the increase in net sales.
Cost of sales
Cost of sales for the years ended December 31, 2016 and 2015 were $16.2 million and $13.0 million, respectively, reflecting an increase of $3.2 million or 25%. Our gross margin for the year ended December 31, 2016 was approximately 86% compared to approximately 82% in 2015. The increased gross margin percentage reflects that our fixed costs within cost of sales, such as certain manufacturing overhead costs and the intangible asset amortization in both the 2016 and 2015 periods, represent a smaller percentage of the larger 2016 revenue amount. Also, there was no medical device excise tax in cost of sales for the year ended 2016 due to the suspension of the excise tax pursuant to the PATH Act.
Selling, general and administrative expenses
SG&A expenses for the years ended December 31, 2016 and 2015 were $64.8 million and $44.0 million, respectively, reflecting an increase of $20.8 million or 47%. The increase in SG&A expenses was primarily the result of an increase of approximately $6.5 million in salary, commissions, bonuses, stock-based compensation, travel and other costs associated with our domestic sales force; an increase in SG&A expenses incurred by our foreign subsidiaries of approximately $6.4 million; and an increase of approximately $5.3 million for additional administrative and marketing personnel.
Research and development expenses
R&D expenses for the years ended December 31, 2016 and 2015 were $29.2 million and $25.0 million, respectively, reflecting an increase of $4.2 million or 17%. Most of the increase in R&D expenses resulted from the cost of additional personnel, primarily in our clinical affairs function, required to manage the increased number of clinical studies and associated investigational sites and study investigators. Also contributing to the increase in R&D expenses were higher clinical study costs, which included payments to investigational sites and study investigators and consultants.
Other income (expense), net
We recorded other income, net for the year ended December 31, 2016 of $0.3 million and other expense, net for the year ended December 31, 2015 of approximately $28.0 million. The 2016 period primarily reflected interest income from our short-term investments of approximately $0.9 million, offset by interest expense on our secured notes payable and changes in the fair value of our stock warrant liability. The 2015 period includes a charge of $25.7 million incurred with the deconsolidation of the non‑glaucoma related assets of DOSE and elimination of the noncontrolling interest.
Liquidity and capital resources
From our inception through 2015, we incurred losses and negative cash flow from our operations. For the 12 months ended December 31, 2016, we generated net income of $4.5 million and for the 12 months ended December 31, 2017, we incurred a $0.1 million net loss but generated $25.5 million of cash from operations. As of December 31, 2017, we had an accumulated deficit of approximately $192.2 million. We have funded our operations to date from the sale of
69
equity securities, including our June 2015 initial public offering (IPO), the issuance of notes payable, cash exercises of stock options and warrants to purchase equity securities and cash generated from operations. We have made and expect to continue to make significant investments in our global sales force, marketing programs, research and development activities and clinical studies. FDA‑approved IDE studies and new product development programs in our industry are expensive, and we have also incurred a significant increase in administrative costs since we began operating as a public company in 2015. Accordingly, although we were profitable in 2016, and have generated cash from operations, there can be no assurance that we will continue to be profitable or continue to generate cash from operations.
At December 31, 2017, we had $119.0 million in cash, cash equivalents and short-term investments. We plan to fund our operations and capital funding needs using existing cash and investments and cash generated from commercial operations, and we may seek to obtain additional financing in the future through debt or equity financings. There can be no assurance that we will be able to obtain additional financing on terms acceptable to us, or at all. We believe that our available cash, cash equivalents, investment balances and interest we earn on these balances and cash generated from sales of our iStent products will be sufficient to fund our operations and satisfy our liquidity requirements for at least the next 12 months from the date our financial statements for the year ended December 31, 2017 are made publicly available.
Cash flows
Our historical cash outflows have primarily been associated with cash used for operating activities such as the purchase and growth of inventory, expansion of our sales, marketing and R&D activities and other working capital needs; the acquisition of intellectual property; and expenditures related to equipment and improvements used to increase our manufacturing capacity, to improve our manufacturing efficiency and for overall facility expansion. For the year ended December 31, 2017 we generated cash from operations.
The following table is a summary of our cash flows for the periods indicated:
|
|
|
Year ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
(in millions) |
|
2017 |
|
2016 |
|
2015 |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Net cash provided by (used in): |
|
|
|
|
|
|
|
|
|
|
|
Operating activities |
|
$ |
25.5 |
|
$ |
12.3 |
|
$ |
(2.2) |
|
|
Investing activities |
|
|
(11.7) |
|
|
(26.1) |
|
|
(85.6) |
|
|
Financing activities |
|
|
4.7 |
|
|
(1.7) |
|
|
107.1 |
|
|
Exchange rate changes |
|
|
(0.5) |
|
|
0.4 |
|
|
— |
|
|
Net increase (decrease) in cash and cash equivalents |
|
$ |
18.0 |
|
$ |
(15.1) |
|
$ |
19.3 |
|
At December 31, 2017, our cash, cash equivalents and short-term investments were held for working capital purposes. We do not enter into investments for trading or speculative purposes. Our policy is to invest any cash in excess of our immediate requirements in investments designed to preserve the principal balance and provide liquidity.
Operating activities
In the years ended December 31, 2017 and December 31, 2016, our operating activities generated net cash of $25.5 million and $12.3 million, respectively, and in the year ended December 31, 2015, our operating activities used $2.2 million of net cash.
The improvement in net cash generation from operating activities primarily reflects an increase in cash generated from significantly higher net sales of our iStent partially offset by increases in our total operating expenses. For the year ended December 31, 2017, the total net change in operating assets and liabilities provided cash of $2.7 million due to an increase in accounts payable and accrued liabilities of $9.7 million partially offset by increases in accounts receivable and inventory of $6.3 million. The remaining adjustments to reconcile net loss to net cash provided
70
by operating activities provided cash of $22.9 million, primarily consisting of stock‑based compensation expense of $17.6 million and depreciation and amortization of $5.5 million.
For the year ended December 31, 2016, the total net change in operating assets and liabilities reflected cash usage of $6.3 million due to increases in accounts receivable and inventory of $9.7 million, partially offset by an increase in accounts payable of $5.1 million. The remaining adjustments to reconcile net income to net cash used in operating activities provided cash of $14.1 million, primarily consisting of stock‑based compensation expense of $8.8 million and depreciation and amortization of $4.7 million.
For the year ended December 31, 2015, the total net change in operating assets and liabilities reflected cash usage of $3.4 million due to increases in accounts receivable and inventory of approximately $4.0 million, partially offset by an increase in accounts payable of $1.5 million. All other adjustments to reconcile net loss to net cash used in operating activities totaled $39.5 million, primarily consisting of the $25.7 million loss on the deconsolidation of DOSE. The remaining adjustments primarily consisted of stock‑based compensation expense of $7.9 million and depreciation and amortization of $4.3 million.
Investing activities
In the years ended December 31, 2017, 2016 and 2015, we used approximately $11.7 million, $26.1 million and $85.6 million, respectively, of net cash in investing activities.
In the year ended December 31, 2017, we used approximately $94.3 million for purchases of short-term investments, and received proceeds from sales and maturities of short-term investments of $88.9 million.
In the year ended December 31, 2016, we used approximately $75.2 million for purchases of short-term investments, and received proceeds from sales and maturities of short-term investments of $55.4 million.
In the year ended December 31, 2015, we used approximately $69.8 million for purchases of short-term investments, and we used $15.0 million for the purchase of the iDose product line from DOSE.
Cash used for purchases of property and equipment was approximately $6.3 million, $6.3 million and $0.9 million for the years ended December 31, 2017, 2016 and 2015, respectively.
We expect to increase our investment in property and equipment in the future as we expand our manufacturing capacity for current and new products, improve our manufacturing efficiency and for overall facility expansion.
Financing activities
In the years ended December 31, 2017, 2016 and 2015, our financing activities provided (used) net cash of $4.7 million, ($1.7) million and $107.1 million of cash, respectively.
In the year ended December 31, 2017, we received net cash proceeds of approximately $4.7 million from the exercises of stock options and purchases of our common stock by employees pursuant to our Employee Stock Purchase Plan.
In the year ended December 31, 2016, we received net cash proceeds of approximately $8.0 million from the exercises of stock options and warrants and purchases of our common stock by employees pursuant to our Employee Stock Purchase Plan, and we used net cash of approximately $9.7 million for note payments.
In the year ended December 31, 2015, we received net cash proceeds of approximately $113.6 million from our IPO, approximately $6.9 million in net proceeds from senior secured term and draw-to term loans, and approximately $3.3 million from the exercises of stock options, warrants and purchases of our common stock by employees pursuant to our Employee Stock Purchase Plan. Additionally, we used approximately $7.8 million for note payments, approximately
71
$7.0 million to pay off and fully retire the senior secured term and draw-to term loans, and used approximately $1.9 million for net payments on the line of credit.
Indebtedness
Notes payable to GMP Vision Solutions
In November 2013, we entered into an agreement with GMP pursuant to which we bought out all remaining royalties payable to GMP in connection with the prior January 2017 agreement with GMP in exchange for the issuance of $17.5 million in secured promissory notes to GMP and a party related to GMP. These notes were secured by all of our assets, excluding intellectual property, and were previously subordinate to the rights of our bank lender in connection with our Amended Credit Agreement (as defined below) prior to the repayment in full of that facility in July 2015. The notes carried an interest rate of 5% per annum and required monthly interest‑only payments from November 30, 2013 through December 31, 2014 of $72,900, followed by 24 equal monthly principal and interest payments of $0.8 million, which we began paying on January 31, 2015 and were fully paid as of December 31, 2016. The buyout agreement also calls for payment of up to $2.0 million in the event of a sale of the Company that meets certain criteria. In connection with this buyout agreement, we recognized an intangible asset valued at $17.5 million. After determining that the pattern of future cash flows associated with this intangible asset could not be reliably estimated with a high level of precision, we concluded that the intangible asset would be amortized to cost of sales in our statements of operations on a straight line basis over the estimated useful life of five years.
In each of the years ended December 31, 2017, 2016 and 2015, we recorded related amortization expense of $3.5 million in cost of sales. Estimated amortization expense will be $3.0 million in 2018, after which it will be fully amortized.
Purchase commitments
The Company had $0.9 million in commitments for capital expenditures as of December 31, 2017.
Contractual obligations
The following table summarizes our significant contractual obligations as of December 31, 2017 and the effect those obligations are expected to have on our liquidity and cash flows in future periods.
|
|
|
Payments due by period |
|
|||||||||||||
|
Contractual obligations |
|
|
|
|
Less than |
|
|
|
|
|
|
|
More than |
|
||
|
(in millions) |
|
Total |
|
1 year |
|
1 - 3 years |
|
3 - 5 years |
|
5 years |
|
|||||
|
Operating lease obligations |
|
$ |
5,382 |
|
$ |
1,513 |
|
$ |
2,618 |
|
$ |
1,251 |
|
$ |
— |
|
|
Firm purchase commitments |
|
|
11,365 |
|
|
9,897 |
|
|
1,468 |
|
|
— |
|
|
— |
|
|
Total contractual obligations |
|
$ |
16,747 |
|
$ |
11,410 |
|
$ |
4,086 |
|
$ |
1,251 |
|
$ |
— |
|
Off‑balance sheet arrangements
We do not have any off‑balance sheet arrangements as defined in the rules and regulations of the SEC. We do not have any relationships with unconsolidated entities or financial partnerships, such as entities often referred to as structured finance or special purpose entities, which would have been established for the purpose of facilitating off‑balance sheet arrangements or for any other contractually narrow or limited purpose. However, from time to time we enter into certain types of contracts that contingently require us to indemnify parties against third‑party claims including in connection with certain real estate leases, and supply purchase agreements, and with directors and officers. The terms of such obligations vary by contract and in most instances a maximum dollar amount is not explicitly stated therein. Generally, amounts under these contracts cannot by reasonably estimated until a specific claim is asserted, thus no liabilities have been recorded for these obligations on our balance sheets for any of the periods presented.
72
Inflation
We may experience pressure on our iStent selling prices resulting from potential future reductions in reimbursement payments to our customers, particularly from governmental payors such as Medicare or Medicaid but also from private payors. We could also be impacted by rising costs for certain inflation‑sensitive operating expenses such as labor and employee benefits. However, we do not believe that inflation has had a material effect on our business, financial condition or results of operations presented herein. If our costs were to become subject to significant inflationary pressures, we may not be able to fully offset such higher costs through selling price increases. Our inability or failure to do so could adversely affect our business, financial condition and results of operations.
Critical accounting policies and significant estimates
Management’s discussion and analysis of our financial condition and results of operations are based on our financial statements, which have been prepared in accordance with U.S. generally accepted accounting principles (GAAP). The preparation of these financial statements requires us to make estimates and judgments that affect the reported amounts of assets and liabilities and related disclosure of contingent assets and liabilities, revenue and expenses at the date of the financial statements. Generally, we base our estimates on historical experience and on various other assumptions in accordance with GAAP that we believe to be reasonable under the circumstances. Actual results may differ materially from these estimates under different assumptions or conditions and such differences could be material to our financial position and results of operations.
While our significant accounting policies are more fully described in the Notes to our consolidated financial statements appearing elsewhere in this Annual Report on Form 10-K, we believe the following accounting policies to be most critical for fully understanding and evaluating our financial condition and results of operations.
Revenue recognition
Our revenue is generated primarily from sales of our iStent products to customers in the United States and internationally. Our customers are comprised of ASCs, hospitals and distributors in certain international locations where we currently do not have a direct commercial presence. We recognize revenue from product sales when the following criteria are met: goods are shipped, title and risk of loss has transferred to our customers, persuasive evidence of an arrangement exists and collectability is reasonably assured. Persuasive evidence of an arrangement exists when we have a contractual arrangement in place with the customer. Delivery has occurred when a product is shipped. If persuasive evidence of an arrangement exists and delivery has occurred, we determine whether the invoiced amount is fixed or determinable and collectability of the invoiced amount is reasonably assured. We assess whether the invoiced amount is fixed or determinable based on the existing arrangement with the customer, including whether we have sufficient history with a customer to reliably estimate the customer’s payment patterns. We assess collectability by evaluating historical cash receipts and individual customer outstanding balances. To the extent all criteria set forth above are not satisfied at the time of shipment, revenue is recognized when cash is received from the customer.
We permit returns of product if such product is returned in good condition and from normal distribution channels, and we provide a warranty on our products for one year from the date of shipment. Estimated allowances for sales returns and warranty replacements are based upon the historical patterns of our product returns and warranty replacements matched against sales, and our evaluation of specific factors that may increase the risk of product returns and warranty replacements. Product returns and warranty replacements to date have been immaterial.
Clinical trial expense accruals
As part of our R&D expenses, we accrue at each balance sheet date the estimated costs of clinical study activities performed by third‑party clinical sites with whom we have agreements providing for fees based upon the quantities of subjects enrolled and clinical evaluation visits that occur over the life of the study. The estimates are determined based upon a review of the agreements and data collected by internal and external clinical personnel as to the status of enrollment and subject visits, and are based upon the facts and circumstances known to us at each financial reporting date. If the actual timing of performance of activities varies from the assumptions used in the estimates, we
73
adjust the accruals accordingly. There have been no material adjustments to our prior period accrued estimates for clinical trial activities through December 31, 2017. If we underestimate or overestimate the activity or fees associated with a study or service at a given point in time, adjustments to R&D expenses may be necessary in future periods. Subsequent changes in estimates may result in a material change in our accruals. Nonrefundable advance payments for goods and services, including fees for process development or manufacturing and distribution of clinical supplies that will be used in future research and development activities, are deferred and recognized as expense in the period that the related goods are consumed or services are performed.
Inventory valuation
We value inventory at the lower of cost or market (net realizable value). Cost is determined by the first‑in, first‑out method. This policy requires us to make estimates regarding the market value of our inventory, including an assessment of excess or obsolete inventory. We evaluate inventory for excess quantities and obsolescence based on an estimate of the future demand for our product within a specified time horizon, and record an allowance to reduce the carrying value of inventory as determined necessary. The estimates we use for demand are also used for near‑term capacity planning and inventory purchasing and are consistent with our revenue forecasts. If our actual demand is less than our forecast demand, we may be required to take additional excess inventory charges, which would decrease gross margin and adversely impact net operating results in the future.
Stock‑based compensation expense
Stock‑based compensation expense for stock options is measured at the date of grant, based on the estimated fair value of the award using the Black‑Scholes option pricing model.
Stock-based compensation expense for restricted stock units is also measured at the date of grant, based on the closing price of our common stock.
For awards subject to time‑based vesting conditions, we recognize stock‑based compensation expense over the employee’s requisite service period on a straight‑line basis, net of estimated forfeitures. We account for stock‑based compensation arrangements with non‑employees using a fair value approach. Stock options granted to non‑employees are subject to periodic revaluation over their vesting terms.
The estimation of the fair value of each stock‑based option grant or issuance on the date of grant involves numerous assumptions by management. Although we calculate the fair value under the Black‑Scholes option pricing model, which is a standard option pricing model, this model still requires the use of numerous assumptions, including, among others, the expected life (turnover), volatility of the underlying equity security, a risk free interest rate and expected dividends. Because we have a limited operating history as a public company, there is a lack of company‑specific historical and implied volatility data, and therefore we have estimated stock price volatility based upon an index of the historical volatilities of a group of comparable publicly‑traded medical device peer companies. We will continue to apply this process until a sufficient amount of historical information regarding the volatility of our own stock price becomes available. We have estimated the expected term of our employee stock options using the “simplified” method, whereby the expected life equals the average of the vesting term and the original contractual term of the option. The model and assumptions also attempt to account for changing employee behavior as the stock price changes and capture the observed pattern of increasing rates of exercise as the stock price increases. The use of different values by management in connection with these assumptions in the Black‑Scholes option pricing model could produce substantially different results.
In July 2014, we granted stock options to purchase an aggregate of 1.2 million shares of common stock, which options contained a performance condition such that they only become exercisable in the event that our common stock is listed on a national securities exchange within one year from the date of grant. In accordance with authoritative guidance, we did not record any compensation expense associated with the grants until the performance condition was satisfied in the three month period ended June 30, 2015. Upon the completion of the IPO on June 30, 2015, we immediately recognized cumulative compensation cost of $3.8 million for the grants as if the method had been applied since the date of grant using the required graded accelerated attribution method, and we will record compensation expense over the
74
remainder of the four‑year vesting period using this method. Stock options granted subsequent to July 2014 do not contain a performance condition.
Recent Accounting Pronouncements
For a description of recent accounting pronouncements, see Note 2 of the notes to our consolidated financial statements included in Part II, Item 8 of this Annual Report on Form 10-K.
ITEM 7A.Quantitative and qualitative disclosures about market risk
Interest Rate Risk
We are exposed to market risks in the ordinary course of our business. Our cash and cash equivalents include cash in readily available checking and money market accounts, as well as a certificate of deposit. These securities are not dependent on interest rate fluctuations that could cause the principal amount of these assets to fluctuate and thus do not pose any interest rate risk to the Company. While we believe our cash and cash equivalents do not contain excessive risk, we cannot provide absolute assurance that in the future our investments will not be subject to adverse changes in market value.
In addition, we maintain significant amounts of cash and cash equivalents at one or more financial institutions that are in excess of federally insured limits.
Foreign currency exchange risk
The financial statements of our foreign subsidiaries and their sales to customers are denominated in the foreign subsidiaries’ respective functional currencies, and therefore we have exposure to foreign currency exchange rates. The remainder of our business is primarily denominated in U.S. dollars. The effect of a 10% adverse change in exchange rates on foreign denominated cash, receivables and payables would not have been material for the periods presented. As our operations in countries outside of the United States grow, our results of operations and cash flows will be subject to fluctuations due to changes in foreign currency exchange rates, which could harm our business in the future. To date, we have not entered into any material foreign currency hedging contracts although we may do so in the future.
75
ITEM 8.FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
Index to consolidated financial statements
| 77 | |
| 78 | |
| 79 | |
| 80 | |
|
Consolidated statements of convertible preferred stock and stockholders’ equity (deficit) |
81 |
| 82 | |
| 83 |
76
Report of Independent Registered Public Accounting Firm
To the Shareholders and the Board of Directors of Glaukos Corporation
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of Glaukos Corporation (the Company) as of December 31, 2017 and 2016, the related consolidated statements of operations, comprehensive (loss) income, convertible preferred stock and stockholders' equity (deficit), and cash flows for each of the three years in the period ended December 31, 2017, and the related notes (collectively referred to as the “consolidated financial statements”). In our opinion, the consolidated financial statements present fairly, in all material respects, the financial position of the Company at December 31, 2017 and 2016, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2017, in conformity with U.S. generally accepted accounting principles.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the Company's internal control over financial reporting as of December 31, 2017, based on criteria established in Internal Control–Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) and our report dated February 28, 2018 expressed an unqualified opinion thereon.
Basis for Opinion
These financial statements are the responsibility of the Company's management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
/s/ Ernst & Young LLP
We have served as the Company’s auditor since 2006.
Irvine, California
February 28, 2018
77
Glaukos Corporation
(in thousands, except par values)
|
|
|
December 31, |
|
||||
|
|
|
2017 |
|
2016 |
|
||
|
|
|
|
|
|
|
|
|
|
Assets |
|
|
|
|
|
|
|
|
Current assets: |
|
|
|
|
|
|
|
|
Cash and cash equivalents |
|
$ |
24,508 |
|
$ |
6,494 |
|
|
Short-term investments |
|
|
94,506 |
|
|
89,268 |
|
|
Accounts receivable, net |
|
|
16,656 |
|
|
14,305 |
|
|
Inventory, net |
|
|
11,222 |
|
|
6,844 |
|
|
Prepaid expenses and other current assets |
|
|
2,568 |
|
|
3,032 |
|
|
Restricted cash |
|
|
— |
|
|
80 |
|
|
Total current assets |
|
|
149,460 |
|
|
120,023 |
|
|
Property and equipment, net |
|
|
11,794 |
|
|
7,593 |
|
|
Intangible assets, net |
|
|
3,147 |
|
|
6,567 |
|
|
Deferred tax asset, net |
|
|
235 |
|
|
— |
|
|
Deposits and other assets |
|
|
1,200 |
|
|
188 |
|
|
Total assets |
|
$ |
165,836 |
|
$ |
134,371 |
|
|
Liabilities and stockholders' equity |
|
|
|
|
|
|
|
|
Current liabilities: |
|
|
|
|
|
|
|
|
Accounts payable |
|
$ |
6,244 |
|
$ |
2,967 |
|
|
Accrued liabilities |
|
|
20,449 |
|
|
13,911 |
|
|
Deferred rent |
|
|
95 |
|
|
60 |
|
|
Total current liabilities |
|
|
26,788 |
|
|
16,938 |
|
|
Other liabilities |
|
|
846 |
|
|
159 |
|
|
Total liabilities |
|
|
27,634 |
|
|
17,097 |
|
|
Commitments and contingencies (Note 10) |
|
|
|
|
|
|
|
|
Stockholders’ equity: |
|
|
|
|
|
|
|
|
Preferred stock, $0.001 par value; 5,000 shares authorized; no shares issued and outstanding |
|
|
— |
|
|
— |
|
|
Common stock, $0.001 par value; 150,000 shares authorized; 34,647 and 33,971 shares issued and 34,619 and 33,943 shares outstanding at December 31, 2017 and 2016, respectively |
|
|
35 |
|
|
34 |
|
|
Additional paid-in capital |
|
|
331,073 |
|
|
308,815 |
|
|
Accumulated other comprehensive (loss) income |
|
|
(591) |
|
|
648 |
|
|
Accumulated deficit |
|
|
(192,183) |
|
|
(192,091) |
|
|
Less treasury stock (28 shares as of December 31, 2017 and 2016) |
|
|
(132) |
|
|
(132) |
|
|
Total stockholders’ equity |
|
|
138,202 |
|
|
117,274 |
|
|
Total liabilities and stockholders' equity |
|
$ |
165,836 |
|
$ |
134,371 |
|
See accompanying notes to consolidated financial statements.
78
Glaukos Corporation
Consolidated statements of operations
(in thousands, except per share amounts)
|
|
|
Year ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Net sales |
|
$ |
159,254 |
|
$ |
114,397 |
|
$ |
71,700 |
|
|
Cost of sales |
|
|
21,050 |
|
|
16,177 |
|
|
12,988 |
|
|
Gross profit |
|
|
138,204 |
|
|
98,220 |
|
|
58,712 |
|
|
Operating expenses: |
|
|
|
|
|
|
|
|
|
|
|
Selling, general and administrative |
|
|
96,260 |
|
|
64,756 |
|
|
43,961 |
|
|
In-process research and development |
|
|
5,320 |
|
|
— |
|
|
— |
|
|
Research and development |
|
|
38,905 |
|
|
29,223 |
|
|
25,047 |
|
|
Total operating expenses |
|
|
140,485 |
|
|
93,979 |
|
|
69,008 |
|
|
(Loss) income from operations |
|
|
(2,281) |
|
|
4,241 |
|
|
(10,296) |
|
|
Other income (expense), net |
|
|
|
|
|
|
|
|
|
|
|
Interest and other income |
|
|
2,326 |
|
|
889 |
|
|
82 |
|
|
Loss on deconsolidation of DOSE |
|
|
— |
|
|
— |
|
|
(25,685) |
|
|
Loss on extinguishment of debt |
|
|
— |
|
|
— |
|
|
(195) |
|
|
Interest and other expense, net |
|
|
(44) |
|
|
(608) |
|
|
(1,062) |
|
|
Change in fair value of stock warrant liability |
|
|
— |
|
|
43 |
|
|
(1,132) |
|
|
Total other income (expense), net |
|
|
2,282 |
|
|
324 |
|
|
(27,992) |
|
|
Income (loss) before taxes |
|
|
1 |
|
|
4,565 |
|
|
(38,288) |
|
|
Provision for income taxes |
|
|
93 |
|
|
43 |
|
|
33 |
|
|
Net (loss) income |
|
|
(92) |
|
|
4,522 |
|
|
(38,321) |
|
|
Net loss attributable to noncontrolling interest |
|
|
|
|
|
— |
|
|
(1,080) |
|
|
Net (loss) income attributable to Glaukos Corporation |
|
$ |
(92) |
|
$ |
4,522 |
|
$ |
(37,241) |
|
|
Basic net (loss) income per share, attributable to Glaukos Corporation stockholders |
|
$ |
(0.00) |
|
$ |
0.14 |
|
$ |
(2.13) |
|
|
Diluted net (loss) income per share, attributable to Glaukos Corporation stockholders |
|
$ |
(0.00) |
|
$ |
0.12 |
|
$ |
(2.13) |
|
|
Weighted-average shares used to compute basic net (loss) income per share attributable to Glaukos Corporation stockholders |
|
|
34,381 |
|
|
32,928 |
|
|
17,474 |
|
|
Weighted-average shares used to compute diluted net (loss) income per share attributable to Glaukos Corporation stockholders |
|
|
34,381 |
|
|
36,459 |
|
|
17,474 |
|
See accompanying notes to consolidated financial statements.
79
Glaukos Corporation
Consolidated statements of comprehensive (loss) income
(in thousands)
|
|
|
Year ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Net (loss) income |
|
$ |
(92) |
|
$ |
4,522 |
|
$ |
(38,321) |
|
|
Other comprehensive (loss) income: |
|
|
|
|
|
|
|
|
|
|
|
Foreign currency translation (loss) gain |
|
|
(1,115) |
|
|
542 |
|
|
155 |
|
|
Unrealized (loss) gain on short-term investments, net of tax |
|
|
(124) |
|
|
55 |
|
|
(148) |
|
|
Other comprehensive (loss) income |
|
|
(1,239) |
|
|
597 |
|
|
7 |
|
|
Total comprehensive (loss) income |
|
|
(1,331) |
|
|
5,119 |
|
|
(38,314) |
|
|
Comprehensive loss attributable to noncontrolling interest |
|
|
— |
|
|
— |
|
|
(1,080) |
|
|
Comprehensive (loss) income attributable to Glaukos Corporation |
|
$ |
(1,331) |
|
$ |
5,119 |
|
$ |
(37,234) |
|
See accompanying notes to consolidated financial statements.
80
Glaukos Corporation
Consolidated statements of convertible preferred stock and stockholders’ equity (deficit)
(in thousands, except per share amounts)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Accumulated |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Convertible |
|
|
|
|
|
|
Additional |
|
other |
|
|
|
|
|
|
|
|
|
Non- |
|
Total |
|
|||||||
|
|
|
preferred stock |
|
Common stock |
|
paid-in |
|
comprehensive |
|
Accumulated |
|
Treasury stock |
|
controlling |
|
equity |
|
||||||||||||||
|
|
|
Shares |
|
Amount |
|
Shares |
|
Amount |
|
capital |
|
income |
|
deficit |
|
Shares |
|
Amount |
|
interest |
|
(deficit) |
|
||||||||
|
Balance at December 31, 2014 |
|
21,642 |
|
$ |
157,379 |
|
2,470 |
|
$ |
6 |
|
$ |
8,155 |
|
$ |
44 |
|
$ |
(159,372) |
|
(28) |
|
$ |
(132) |
|
$ |
(9,605) |
|
$ |
(160,904) |
|
|
Issuance of Series D convertible preferred stock at $18.00 per share in connection with exercises of preferred stock warrants |
|
94 |
|
|
1,698 |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
Conversion of preferred stock into common stock |
|
(21,736) |
|
|
(159,077) |
|
21,736 |
|
|
17 |
|
|
159,060 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
159,077 |
|
|
Issuance of common stock in initial public offering |
|
— |
|
|
— |
|
6,900 |
|
|
7 |
|
|
113,582 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
113,589 |
|
|
Common stock issued under stock plans |
|
— |
|
|
— |
|
1,097 |
|
|
2 |
|
|
2,979 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
2,981 |
|
|
Exercise of common stock warrant |
|
— |
|
|
— |
|
6 |
|
|
— |
|
|
188 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
188 |
|
|
Share-based compensation |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
7,889 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
7,889 |
|
|
Other comprehensive income |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
7 |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
7 |
|
|
Deconsolidation of DOSE |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
10,685 |
|
|
10,685 |
|
|
Net loss |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
(37,241) |
|
— |
|
|
— |
|
|
(1,080) |
|
|
(38,321) |
|
|
Balance at December 31, 2015 |
|
— |
|
$ |
— |
|
32,209 |
|
$ |
32 |
|
$ |
291,853 |
|
$ |
51 |
|
$ |
(196,613) |
|
(28) |
|
$ |
(132) |
|
$ |
— |
|
$ |
95,191 |
|
|
Common stock issued under stock plans |
|
— |
|
|
— |
|
1,756 |
|
|
2 |
|
|
8,064 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
8,066 |
|
|
Exercise of common stock warrant |
|
— |
|
|
— |
|
6 |
|
|
— |
|
|
112 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
112 |
|
|
Share-based compensation |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
8,786 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
8,786 |
|
|
Other comprehensive income |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
597 |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
597 |
|
|
Net income |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
4,522 |
|
— |
|
|
— |
|
|
— |
|
|
4,522 |
|
|
Balance at December 31, 2016 |
|
— |
|
$ |
— |
|
33,971 |
|
$ |
34 |
|
$ |
308,815 |
|
$ |
648 |
|
$ |
(192,091) |
|
(28) |
|
$ |
(132) |
|
$ |
— |
|
$ |
117,274 |
|
|
Common stock issued under stock plans |
|
— |
|
|
— |
|
676 |
|
|
1 |
|
|
4,666 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
4,667 |
|
|
Share-based compensation |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
17,592 |
|
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
17,592 |
|
|
Other comprehensive loss |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
(1,239) |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
(1,239) |
|
|
Net loss |
|
— |
|
|
— |
|
— |
|
|
— |
|
|
— |
|
|
— |
|
|
(92) |
|
— |
|
|
— |
|
|
— |
|
|
(92) |
|
|
Balance at December 31, 2017 |
|
— |
|
$ |
— |
|
34,647 |
|
$ |
35 |
|
$ |
331,073 |
|
$ |
(591) |
|
$ |
(192,183) |
|
(28) |
|
$ |
(132) |
|
$ |
— |
|
$ |
138,202 |
|
See accompanying notes to consolidated financial statements.
81
Glaukos Corporation
Consolidated statements of cash flows
(in thousands)
|
|
|
Year ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Operating Activities |
|
|
|
|
|
|
|
|
|
|
|
Net (loss) income |
|
$ |
(92) |
|
$ |
4,522 |
|
$ |
(38,321) |
|
|
Adjustments to reconcile net (loss) income to net cash provided by (used) in operating activities: |
|
|
|
|
|
|
|
|
|
|
|
Depreciation and amortization |
|
|
5,482 |
|
|
4,722 |
|
|
4,267 |
|
|
Loss on disposal of fixed assets |
|
|
6 |
|
|
40 |
|
|
— |
|
|
Stock-based compensation |
|
|
17,592 |
|
|
8,786 |
|
|
7,889 |
|
|
Loss on deconsolidation of DOSE |
|
|
— |
|
|
— |
|
|
25,685 |
|
|
Loss on extinguishment of debt |
|
|
— |
|
|
— |
|
|
186 |
|
|
Change in fair value of stock warrant liability |
|
|
— |
|
|
(43) |
|
|
1,132 |
|
|
Unrealized foreign currency (gains) losses |
|
|
(951) |
|
|
368 |
|
|
192 |
|
|
Amortization of premium on short-term investments |
|
|
20 |
|
|
210 |
|
|
51 |
|
|
Amortization of debt discount and deferred financing costs |
|
|
— |
|
|
— |
|
|
15 |
|
|
Deferred rent |
|
|
722 |
|
|
(31) |
|
|
91 |
|
|
Changes in operating assets and liabilities: |
|
|
|
|
|
|
|
|
|
|
|
Accounts receivable, net |
|
|
(2,181) |
|
|
(6,791) |
|
|
(2,163) |
|
|
Inventory, net |
|
|
(4,162) |
|
|
(2,935) |
|
|
(1,848) |
|
|
Prepaid expenses and other current assets |
|
|
494 |
|
|
(1,762) |
|
|
(755) |
|
|
Restricted cash |
|
|
80 |
|
|
— |
|
|
— |
|
|
Accounts payable and accrued liabilities |
|
|
9,741 |
|
|
5,096 |
|
|
1,518 |
|
|
Deferred tax asset, net |
|
|
(235) |
|
|
— |
|
|
— |
|
|
Other assets |
|
|
(1,008) |
|
|
127 |
|
|
(127) |
|
|
Net cash provided by (used in) operating activities |
|
|
25,508 |
|
|
12,309 |
|
|
(2,188) |
|
|
Investing activities |
|
|
|
|
|
|
|
|
|
|
|
Purchases of property and equipment |
|
|
(6,311) |
|
|
(6,278) |
|
|
(877) |
|
|
Purchase of iDOSE product line and related assets from DOSE Medical |
|
|
— |
|
|
— |
|
|
(15,000) |
|
|
Purchases of short-term investments |
|
|
(94,307) |
|
|
(75,192) |
|
|
(69,751) |
|
|
Proceeds from sales and maturities of short-term investments |
|
|
88,891 |
|
|
55,354 |
|
|
— |
|
|
Net cash used in investing activities |
|
|
(11,727) |
|
|
(26,116) |
|
|
(85,628) |
|
|
Financing activities |
|
|
|
|
|
|
|
|
|
|
|
Proceeds from public offering, net of issuance costs |
|
|
— |
|
|
— |
|
|
113,589 |
|
|
Proceeds from senior secured term and draw-to term loans |
|
|
— |
|
|
— |
|
|
6,852 |
|
|
Payments of senior secured term and draw-to term loans |
|
|
— |
|
|
— |
|
|
(7,000) |
|
|
Proceeds from line of credit |
|
|
— |
|
|
— |
|
|
1,750 |
|
|
Payments of line of credit |
|
|
— |
|
|
— |
|
|
(3,600) |
|
|
Payments of subordinated notes |
|
|
— |
|
|
(9,696) |
|
|
(7,804) |
|
|
Proceeds from exercise of stock options |
|
|
3,699 |
|
|
6,059 |
|
|
1,734 |
|
|
Share purchases under Employee Stock Purchase Plan |
|
|
968 |
|
|
1,945 |
|
|
1,161 |
|
|
Proceeds from exercise of stock warrants |
|
|
— |
|
|
50 |
|
|
428 |
|
|
Net cash provided by (used in) financing activities |
|
|
4,667 |
|
|
(1,642) |
|
|
107,110 |
|
|
Effect of exchange rate changes on cash and cash equivalents |
|
|
(434) |
|
|
371 |
|
|
(26) |
|
|
Net increase (decrease) in cash and cash equivalents |
|
|
18,014 |
|
|
(15,078) |
|
|
19,268 |
|
|
Cash and cash equivalents at beginning of period |
|
|
6,494 |
|
|
21,572 |
|
|
2,304 |
|
|
Cash and cash equivalents at end of period |
|
$ |
24,508 |
|
$ |
6,494 |
|
$ |
21,572 |
|
|
Supplemental disclosures of cash flow information |
|
|
|
|
|
|
|
|
|
|
|
Interest paid |
|
$ |
— |
|
$ |
285 |
|
$ |
834 |
|
|
Taxes paid, net of refunds |
|
$ |
12 |
|
$ |
513 |
|
$ |
25 |
|
|
Supplemental schedule of noncash investing and financing activities |
|
|
|
|
|
|
|
|
|
|
|
Purchase of intangible assets in exchange for future payments |
|
$ |
— |
|
$ |
— |
|
$ |
243 |
|
|
Conversion of preferred stock into common stock |
|
$ |
— |
|
$ |
— |
|
$ |
159,077 |
|
|
Reduction of liability upon vesting of stock options previously exercised for unvested stock |
|
$ |
4 |
|
$ |
62 |
|
$ |
86 |
|
See accompanying notes to consolidated financial statements.
82
Glaukos Corporation
Notes to consolidated financial statements
1.Organization and basis of presentation
Organization and business
Glaukos Corporation (Glaukos or the Company), incorporated in Delaware on July 14, 1998, is an ophthalmic medical technology and pharmaceutical company focused on the development and commercialization of novel surgical devices and sustained pharmaceutical therapies designed to treat glaucoma, one of the world’s leading causes of blindness. The accompanying consolidated financial statements include the accounts of Glaukos, its wholly owned subsidiaries and, through June 30, 2015, affiliated entity DOSE Medical Corporation (DOSE) (see Note 11). All significant intercompany balances and transactions among the consolidated entities have been eliminated in consolidation.
Liquidity
From inception through 2015, the Company was not profitable and incurred operating losses in each year. For the year ended December 31, 2017, the Company incurred a net loss of $0.1 million, generated $25.5 million of cash from operations and as of December 31, 2017 had an accumulated deficit of $192.2 million. For the year ended December 31, 2016, the Company generated net income of approximately $4.5 million. The Company has financed operations to date primarily through private placements of equity securities, the issuance of common stock in the initial public offering (IPO) completed in June 2015, debt financings and cash generated by its commercial operations. While the Company became profitable in 2016, it may not be able to sustain profitability on a recurring basis in the future, as evidenced by losses incurred in 2017. The Company plans to fund its operations and capital funding needs using existing cash and investments, cash generated from commercial operations, and through future debt and equity financings. There can be no assurance that the Company will be able to obtain additional financing on terms acceptable to it, or at all. Any equity financing may result in dilution to existing stockholders and any additional debt financing may include restrictive covenants. As of December 31, 2017, the Company had cash, cash equivalents and short-term investments totaling $119.0 million and net working capital of $123.0 million. The Company has performed an analysis and concluded substantial doubt does not exist with respect to the Company being able to continue as a going concern through one year from the date of issuance of the consolidated financial statements for the year ended December 31, 2017.
Initial public offering
On June 30, 2015, the Company completed its IPO, selling 6.9 million newly issued shares of common stock at a price of $18.00 per share. The IPO generated net cash proceeds of approximately $113.6 million, after deducting underwriting discounts and commissions of approximately $8.7 million and other related expenses of approximately $1.9 million. The underwriting discounts and commissions and offering costs were recorded as a reduction to the IPO proceeds included in additional paid‑in capital.
Immediately prior to the closing of the IPO, all unexercised warrants to purchase shares of Series D convertible preferred stock were net exercised at the IPO price per share, and then all outstanding shares of convertible preferred stock automatically converted into approximately 21.7 million shares of common stock. Following the completion of the IPO, there were no shares of preferred stock and no warrants to purchase shares of Series D convertible preferred stock outstanding. An additional 4.5 million shares of common stock were reserved for issuance under the Company’s 2015 Omnibus Incentive Compensation Plan and 450,000 shares of common stock were reserved for the Company’s 2015 Employee Stock Purchase Plan.
83
Acquisition of the IOP Sensor System and certain assets from DOSE Medical
On April 12, 2017, the Company entered into an IOP Sensor System Purchase Agreement (the Purchase Agreement), between the Company and DOSE, to purchase from DOSE its intraocular pressure (IOP) sensor system, including all patents, license rights and tangible assets, and to assume certain liabilities related thereto (collectively, the IOP Sensor System), for consideration consisting of an initial cash payment of $5.5 million, plus performance-based consideration of up to $9.5 million upon achievement of certain development, clinical and regulatory milestones. The Company completed the purchase of the IOP Sensor System concurrent with the execution of the Purchase Agreement.
The transaction was accounted for as an asset acquisition. Of the $5.5 million initial cash payment, $5.3 million was immediately charged to in-process research and development expense as management determined there was no alternative future use related to the assets purchased. Of the remaining $0.2 million, the majority was capitalized to fixed assets and will be depreciated over the corresponding asset’s useful life, and a small portion was recorded as a prepaid asset and will be amortized to general and administrative expense as the underlying amounts are utilized.
DOSE was previously a wholly-owned subsidiary of the Company. In 2010, it was spun-out as a standalone entity and was accounted for as a consolidated variable interest entity. In 2015, the Company acquired the iDose product line and related assets from DOSE for a cash payment of $15.0 million and upon the acquisition, the Company derecognized DOSE as a consolidated entity in the financial statements. In addition to an asset purchase, the parties agreed to an amended and restated patent license agreement and an amended and restated transition services agreement that provides for limited support from the Company to DOSE for a period of up to three years, which period was extended through June 30, 2021 in connection with the Purchase Agreement (see Note 11).
Thomas W. Burns, the Company’s President, Chief Executive and a member of its board of directors, and William J. Link, Ph.D., Chairman of the Company’s board of directors, currently serve on the board of directors of DOSE and certain members of the Company’s management and board of directors hold an equity interest in DOSE.
2.Summary of significant accounting policies
Basis of presentation
The accompanying consolidated financial statements have been prepared in accordance with accounting principles generally accepted in the United States of America (GAAP).
Use of estimates
The preparation of the financial statements in conformity with GAAP requires management to make informed estimates and assumptions that affect the reported amounts in the financial statements and accompanying notes. Actual results could differ materially from those estimates and assumptions. Management considers many factors in selecting appropriate financial accounting policies and controls and in developing the estimates and assumptions that are used in the preparation of these financial statements. Management must apply significant judgment in this process. In addition, other factors may affect estimates, including expected business and operational changes, sensitivity and volatility associated with the assumptions used in developing estimates, and whether historical trends are expected to be representative of future trends. The estimation process often may yield a range of potentially reasonable estimates of the ultimate future outcomes, and management must select an amount that falls within that range of reasonable estimates. The most significant estimates in the accompanying consolidated financial statements relate to revenue recognition and stock‑based compensation expense. Although these estimates are based on the Company’s knowledge of current events and actions it may undertake in the future, this process may result in actual results differing materially from those estimated amounts used in the preparation of the financial statements.
84
Foreign currency translation
The accompanying consolidated financial statements are presented in United States (U.S.) dollars. The Company considers the local currency to be the functional currency for its international subsidiaries. Accordingly, their assets and liabilities are translated into U.S. dollars using the exchange rate in effect on the balance sheet date. Revenues and expenses are translated at average exchange rates prevailing throughout the periods presented. Currency translation adjustments arising from period to period are charged or credited to accumulated other comprehensive (loss) income in stockholders’ equity. For the year ended December 31, 2017, the Company reported a loss from foreign currency translation adjustments of approximately $1.1 million, and for the years ended December 31, 2016 and 2015, the Company reported income from foreign currency translation adjustments of approximately $0.5 million and $0.2 million, respectively.
Realized gains and losses resulting from foreign currency transactions are included in selling, general and administrative expense in the consolidated statements of operations. For the year ended December 31, 2017, the Company reported a foreign currency transaction gain of approximately $0.1 million, and for the years ended December 31, 2016 and 2015, the Company reported foreign currency transaction losses of approximately $0.2 million and $0.1 million, respectively.
Unrealized gains and losses that arise from exchange rate fluctuations on transactions denominated in a currency other than the functional currency, primarily gains and losses on intercompany loans, are included in the consolidated statements of operations as a component of other income, net. For the year ended December 31, 2017, the Company reported a net foreign currency transaction gain of $1.0 million and for the years ended December 31, 2016 and 2015, the Company reported net foreign currency transaction losses of $0.4 million and $0.2 million, respectively.
Cash, cash equivalents and short-term investments
The Company invests its excess cash in marketable securities, including money market funds, money market securities, bank certificates of deposit, corporate bonds, corporate commercial paper, U.S. government bonds and U.S. government agency bonds. For financial reporting purposes, liquid investment instruments purchased with an original maturity of three months or less are considered to be cash equivalents. Cash and cash equivalents are recorded at face value or cost, which approximates fair market value. From time to time, the Company maintains cash balances in excess of amounts insured by the Federal Deposit Insurance Commission (FDIC). Investments are stated at fair value as determined by quoted market prices. Investments are considered available‑for‑sale and, accordingly, unrealized gains and losses are included in accumulated other comprehensive (loss) income within stockholders’ equity.
The Company’s entire investment portfolio, except for restricted cash, is considered to be available for use in current operations and, accordingly, all such investments are stated at fair value using quoted market prices and classified as current assets, although the stated maturity of individual investments may be one year or more beyond the balance sheet date. The Company did not have any trading securities or restricted investments at December 31, 2017, 2016 and 2015.
Realized gains and losses and declines in value, if any, judged to be other‑than‑temporary on available‑for‑sale securities, are reported in other income, net. When securities are sold, any associated unrealized gain or loss previously reported as a separate component of stockholders’ equity is reclassified out of stockholders’ equity and recorded in the statements of operations in the period sold using the specific identification method. Accrued interest and dividends are included in other income, net. The Company periodically reviews its available‑for‑sale securities for other‑than‑temporary declines in fair value below the cost basis, and whenever events or changes in circumstances indicate that the carrying amount of an asset may not be recoverable.
Concentration of credit risk and significant customers
Financial instruments, which potentially subject the Company to significant concentration of credit risk, consist primarily of cash, cash equivalents, short-term investments and accounts receivable. The Company maintains deposits in federally insured financial institutions in excess of federally insured limits and management believes that the Company is not exposed to significant credit risk due to the financial position of the depository institutions in which those deposits are held. Additionally, the Company has established guidelines regarding investment instruments and their maturities
85
which are designed to maintain preservation of principal and liquidity. The Company believes that the concentration of credit risk in its accounts receivable is mitigated by its credit evaluation process, relatively short collection terms and the level of credit worthiness of its customers. During 2017, 2016 and 2015, none of the Company’s customers accounted for more than 10% of revenues.
Accounts receivable
The Company sells its products directly to hospitals, surgery centers and distributors in the U.S. and internationally. The Company periodically assesses the payment performance of these customers and establishes reserves for anticipated losses when necessary, which losses historically have not been significant and have not exceeded management’s estimates. Accounts receivable are recorded at the invoiced amount and do not bear interest. The Company maintains an allowance for doubtful accounts based on historical collection experience and expectations of future collection based on current market conditions. The allowance for doubtful accounts is management’s best estimate of the amount of probable credit losses. Account balances are charged against the allowance when it is probable the receivable will not be recovered. The Company’s allowance for doubtful accounts was approximately $0.6 million, $0.5 million and $0.1 million as of December 31, 2017, 2016 and 2015, respectively. Additionally, no customers accounted for more than 10% of net accounts receivable as of either date.
The Company generally permits returns of product from customers if such product is returned in a timely manner and in good condition. Estimated allowances for sales returns are based upon the Company’s historical patterns of product returns matched against sales, and management’s evaluation of specific factors that may increase or decrease the risk of product returns. The Company’s sales return reserve was approximately $0.3 million, $0.2 million and $0.1 million as of December 31, 2017, 2016 and 2015, respectively.
Inventory
Inventory is valued at the lower of cost or market (net realizable value). Cost is determined by the first‑in, first‑out method. Management evaluates inventory for excess quantities and obsolescence and records an allowance to reduce the carrying value of inventory as determined necessary.
Long lived assets
Property and equipment is recorded at cost. Depreciation of property and equipment is generally provided using the straight‑line method over the estimated useful lives of the assets, which range from three to five years. Leasehold improvements are amortized over their estimated useful life or the related lease term, whichever is shorter. Maintenance and repairs are expensed as incurred.
All long lived assets are reviewed for impairment in value when changes in circumstances dictate, based upon undiscounted future operating cash flows, and appropriate losses are recognized and reflected in current earnings to the extent the carrying amount of an asset exceeds its estimated fair value, determined by the use of appraisals, discounted cash flow analyses or comparable fair values of similar assets. The Company recorded no impairment charges during 2017 and 2015 and $14,000 in 2016.
Intangible assets
Intangible assets are recorded at cost and are amortized over the estimated useful life. Intangible assets in the accompanying balance sheets are currently comprised of the cost of the Company’s buyout of a royalty payment obligation and the value of non-compete agreements entered with three former international distributors. (See Note 5).
Fair value of financial instruments
The carrying amounts of cash equivalents, accounts receivable, accounts payable, and accrued liabilities are considered to be representative of their respective fair values because of the short‑term nature of those instruments.
86
The valuation of assets and liabilities is subject to fair value measurements using a three‑tiered approach and fair value measurements are classified and disclosed by the Company in one of the following three categories:
Level 1: Unadjusted quoted prices in active markets that are accessible at the measurement date for identical, unrestricted assets or liabilities;
Level 2: Quoted prices for similar assets and liabilities in active markets, quoted prices in markets that are not active, or inputs which are observable, either directly or indirectly, for substantially the full term of the asset or liability; and
Level 3: Prices or valuation techniques that require inputs that are both significant to the fair value measurement and unobservable (i.e., supported by little or no market activity).
Revenue recognition
The Company recognizes revenue from product sales when the following criteria are met: goods are shipped, title and risk of loss has transferred to its customers, persuasive evidence of an arrangement exists and collectability is reasonably assured. Persuasive evidence of an arrangement exists when there is a contractual arrangement in place with the customer. Delivery has occurred when a product is shipped. If persuasive evidence of an arrangement exists and delivery has occurred, the Company determines whether the invoiced amount is fixed or determinable and collectability of the invoiced amount is reasonably assured. The Company assesses whether the invoiced amount is fixed or determinable based on the existing arrangement with the customer, including whether the Company has sufficient history with a customer to reliably estimate the customer’s payment patterns. The Company assesses collectability by evaluating historical cash receipts and individual customer outstanding balances. To the extent all criteria set forth above are not satisfied at the time of shipment, revenue is recognized when cash is received from the customer.
Customers are not granted specific rights of return; however, the Company may permit returns of product from customers if such product is returned in a timely manner and in good condition. The Company provides a warranty on its products for one year from the date of shipment, and any product found to be defective or out of specification will be replaced at no charge during the warranty period. Estimated allowances for sales returns and warranty replacements are recorded at the time of sale of the product and are estimated based upon the historical patterns of product returns matched against sales, and an evaluation of specific factors that may increase the risk of product returns. Product returns and warranty replacements to date have been consistent with amounts reserved or accrued and have not been significant.
Shipping and handling costs
All shipping and handling costs are expensed as incurred and are charged to general and administrative expense. Charges to customers for shipping and handling are credited to general and administrative expense.
Advertising costs
All advertising costs are expensed as incurred. Advertising costs incurred during the years ended December 31, 2017, 2016 and 2015 were approximately $2.1 million, $1.6 million and $0.8 million, respectively.
Income taxes
Income taxes are accounted for using an asset and liability approach that requires the recognition of deferred tax assets and liabilities for the expected future tax consequences of temporary differences between the financial reporting basis and the tax basis of the Company’s assets and liabilities at the applicable tax rates, along with net operating loss and tax credit carryovers. The Company records a valuation allowance against its deferred tax assets to reduce the net carrying value to an amount that it believes is more likely than not to be realized. Management has considered estimated taxable income and ongoing prudent and feasible tax planning strategies in assessing the amount of the valuation allowance. Based upon the weight of available evidence, which includes the Company’s historical operating performance and limited potential to utilize tax credit carryforwards, the Company has determined that total deferred tax assets should
87
be fully offset by a valuation allowance. When the Company establishes or reduces the valuation allowance against its deferred tax assets, its provision for income taxes will increase or decrease, respectively, in the period such determination is made.
The Company is required to file federal and state income tax returns in the United States and various other state jurisdictions. The preparation of these state income tax returns requires the company to interpret the applicable tax laws and regulations in effect in such jurisdictions, which could affect the amount of tax paid by us.
Additionally, the Company follows an accounting standard addressing the accounting for uncertainty in income taxes that prescribes rules for recognition, measurement, and classification in the financial statements of tax positions taken or expected to be taken in a tax return.
The Tax Cuts and Jobs Act (the "Act") was enacted on December 22, 2017. Among other changes, the Act reduces the US federal corporate tax rate from 34 percent to 21 percent. In accordance with Staff Accounting Bulletin 118, as of December 31, 2017, the Company has not completed the accounting for the tax effects of enactment of the Act; however, in certain cases, as described below, the Company has made a reasonable estimate of the effects on the existing deferred tax balances. In all cases, the Company will continue to make and refine calculations as additional analysis is completed. In addition, estimates may also be affected as the Company gains a more thorough understanding of the Act.
The Company remeasured certain deferred tax assets and liabilities based on the rates at which they are expected to reverse in the future, which is generally 21% for federal tax purposes. However, the Company is still analyzing certain aspects of the Act and refining calculations, which could potentially affect the measurement of these balances or give rise to new deferred tax amounts. The provisional amount recorded related to the remeasurement of the deferred tax balance was $25.2 million, which was fully offset by a decrease in the valuation allowance.
Due to uncertainties which currently exist in the interpretation of the provisions of the Act regarding Internal Revenue Code (IRC) Section 162(m), the Company is still evaluating the potential impacts of IRC Section 162(m) as amended by the Act.
Research and development expenses
Major components of research and development expense include personnel costs, preclinical studies, clinical trials and related clinical product manufacturing, materials and supplies, and fees paid to consultants. Research and development costs are expensed as goods are received or services are rendered. Costs to acquire technologies to be used in research and development that have not reached technological feasibility and have no alternative future use are also expensed as incurred.
At each financial reporting date, the Company accrues the estimated costs of clinical study activities performed by third party clinical sites with whom the Company has agreements that provide for fees based upon the quantities of subjects enrolled and clinical evaluation visits that occur over the life of the study. The cost estimates are determined based upon a review of the agreements and data collected by internal and external clinical personnel as to the status of enrollment and subject visits, and are based upon the facts and circumstances known to the Company at each financial reporting date. If the actual performance of activities varies from the assumptions used in the cost estimates, the accruals are adjusted accordingly. There have been no material adjustments to the Company’s prior period accrued estimates for clinical trial activities through December 31, 2017.
Stock‑based compensation
The Company recognizes compensation expense for all stock-based awards granted to employees and nonemployees, including members of its board of directors.
The fair value of stock option awards is estimated at the grant date using the Black-Scholes option pricing model, and the portion that is ultimately expected to vest is recognized as compensation cost over the requisite service
88
period using the straight-line method. The determination of the fair value-based measurement of stock options on the date of grant using an option pricing model is affected by the determination of the fair value of the underlying stock as well as assumptions regarding a number of highly complex and subjective variables. These variables include, but are not limited to, the Company’s stock price volatility over the expected term of the grants, and actual and projected employee stock option exercise behaviors. In the future, as additional empirical evidence regarding these estimates becomes available, the Company may change or refine its approach of deriving them, and these changes could impact the fair value-based measurement of stock options granted in the future. Changes in the fair value-based measurement of stock awards could materially impact the Company’s operating results.
The fair values of stock option awards made to nonemployees are remeasured at each reporting period using the Black-Scholes option pricing model. Compensation expense for these stock option awards is determined by applying the remeasured fair values to the shares that have vested during a period.
The fair value of restricted stock unit (RSU) awards made to employees and nonemployees is equal to the closing market price of the Company’s common stock on the grant date.
Comprehensive (loss) income
All components of comprehensive (loss) income, including net (loss) income, are reported in the financial statements in the period in which they are recognized. Comprehensive (loss) income is defined as the change in equity during a period from transactions and other events and circumstances from non‑owner sources, including unrealized gains and losses on marketable securities and foreign currency translation adjustments.
Net (loss) income per share
Basic net (loss) income per share is calculated by dividing the net (loss) income by the weighted average number of common shares that were outstanding for the period, without consideration for common stock equivalents.
For periods when the Company realizes a net loss, no common stock equivalents are included in the calculation of weighted average number of dilutive common stock equivalents as the effect of applying the treasury stock method is considered anti-dilutive.
For periods when the Company realizes net income, diluted net income per share is calculated by dividing the net income by the weighted average number of common shares plus the sum of the weighted average number of dilutive common stock equivalents outstanding for the period determined using the treasury stock method. Common stock equivalents are comprised of stock options outstanding under the Company’s stock option plans, shares issuable under the Company’s Employee Stock Purchase Plan (ESPP), and stock warrants.
89
The Company’s computation of net (loss) income per share is as follows (in thousands, except per share amounts):
|
|
|
|
|
|
As of |
|
||||
|
|
|
|
|
|
December 31, |
|
||||
|
|
|
|
2017 |
|
|
2016 |
|
|
2015 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Numerator: |
|
|
|
|
|
|
|
|
|
|
|
Net (loss) income - basic |
|
$ |
(92) |
|
$ |
4,522 |
|
$ |
(37,241) |
|
|
Denominator: |
|
|
|
|
|
|
|
|
|
|
|
Weighted average number of common shares outstanding - basic |
|
|
34,381 |
|
|
32,928 |
|
|
17,474 |
|
|
Common stock equivalents from outstanding common stock options |
|
|
- |
|
|
3,514 |
|
|
- |
|
|
Common stock equivalents for ESPP |
|
|
- |
|
|
16 |
|
|
- |
|
|
Common stock equivalents from outstanding common stock warrants |
|
|
- |
|
|
1 |
|
|
- |
|
|
Weighted average number of common shares outstanding - diluted |
|
|
34,381 |
|
|
36,459 |
|
|
17,474 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Basic net (loss) income per share |
|
$ |
(0.00) |
|
$ |
0.14 |
|
$ |
(2.13) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diluted net (loss) income per share |
|
$ |
(0.00) |
|
$ |
0.12 |
|
$ |
(2.13) |
|
Potentially dilutive securities not included in the calculation of diluted net (loss) income per share because to do so would be anti‑dilutive were as follows (in common stock equivalent shares, in thousands):
|
|
|
|
As of |
|
||||||
|
|
|
|
December 31, |
|
||||||
|
|
|
|
2017 |
|
|
2016 |
|
|
2015 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Stock options outstanding |
|
|
5,689 |
|
|
1,099 |
|
|
5,701 |
|
|
Employee stock purchase plan |
|
|
28 |
|
|
— |
|
|
89 |
|
|
Common stock warrants outstanding |
|
|
— |
|
|
— |
|
|
6 |
|
|
|
|
|
5,717 |
|
|
1,099 |
|
|
5,796 |
|
Recently adopted accounting pronouncements
In March 2016, the Financial Accounting Standards Board (FASB) issued Accounting Standards Update (ASU) No. 2016-09, Compensation – Stock Compensation (Topic 718): Improvements to Employee Share-Based Payment Accounting (ASU 2016-09), which modifies certain aspects of the accounting for share-based payment transactions, including income taxes, classification of awards, and classification in the statement of cash flows. The amendments are intended to improve the accounting for employee share-based payments and affect all organizations that issue share-based payment awards to their employees. Several aspects of the accounting for share-based payment award transactions are simplified, including: (a) income tax consequences; (b) classification of awards as either equity or liabilities; and (c) classification on the statement of cash flows. The amendments were effective for annual periods beginning after December 15, 2016, and interim periods within those annual periods and the Company adopted ASU 2016-09 in its first quarter 2017. As a result of the prospective adoption of ASU 2016-09 on January 1, 2017, excess tax benefits of $13.1 million were recorded to the Company’s net operating loss carryover resulting in an increase in the Company’s deferred tax assets with an identical increase in the associated valuation allowance, and no prior periods have been adjusted.
Recently issued accounting pronouncements not yet adopted
In May 2014, the FASB issued guidance in ASU 2014-09 which was codified in Accounting Standards Codification (ASC) 606, Revenue Recognition – Revenue from Contracts with Customers (ASC 606). ASC 606 provides a single comprehensive model for entities to use in accounting for revenue arising from contracts with customers, and is
90
principles-based, such that revenue is recognized to depict the transfer of goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled in exchange for those goods or services.
ASU 2015-14 deferred the effective date of ASC 606 to annual reporting periods beginning after December 15, 2017 (including interim periods within those periods) and while early adoption is permitted, the Company adopted ASC 606 on January 1, 2018. Companies are required to apply ASC 606 retrospectively; however, companies may use either a full retrospective or a modified retrospective approach when adopting the standard. The Company will be using the modified retrospective approach, and adoption of ASC 606 will not result in a cumulative catch-up adjustment to the opening balance sheet of retained earnings at the effective date.
The Company has performed an analysis and does not believe adoption of the standard will have a material impact on its consolidated financial statements with the exception of enhanced disclosure requirements required by ASC 606. In the analysis, the Company has concluded it generally has one performance obligation, the transaction price is not impacted by any variable consideration or other factors noted in ASC 606, except for offering a right of return, and the Company’s performance obligations are generally satisfied when products are shipped.
In February 2016, the FASB issued ASU No. 2016-02, Leases (Topic 842). The ASU requires management to recognize almost all leases with a term greater than one year as a right-of-use asset and corresponding liability, measured at the present value of the lease payments. The new standard must be adopted using the modified retrospective approach and will be effective for the Company starting in the first quarter of 2019. Early adoption is permitted. The Company is currently evaluating the impact this guidance will have on its consolidated financial statements; however, the Company anticipates recognition of additional assets and corresponding liabilities on its consolidated financial statements.
In November 2016, the FASB issued ASU No. 2016-18, Statement of Cash Flows (Topic 230): Restricted Cash (ASC 2016-18), which enhances and clarifies the guidance on the classification and presentation of restricted cash in the statement of cash flows. ASU 2016-18 was effective for the Company starting January 1, 2018. Currently, the Company's restricted cash balance is not significant and the Company does not expect the adoption of the guidance will have a material impact on its consolidated financial statements.
In January 2017, the FASB issued ASU No. 2017-01, Business Combinations (Topic 805): Clarifying the Definition of a Business (ASU 2017-01), clarifying the definition of a business. The amendments are intended to help companies evaluate whether transactions should be accounted for as acquisitions (or disposals) of assets or businesses. When substantially all of the fair value of gross assets acquired is concentrated in a single asset (or a group of similar assets), the assets acquired would not represent a business. This introduces an initial required screening that, if met, eliminates the need for further assessment. To be considered a business, an acquisition would have to include an input and a substantive process that together significantly contribute to the ability to create outputs. To be a business without outputs, there will need to be an organized workforce. The ASU also narrows the definition of the term “outputs” to be consistent with how it is described in ASC 606, Revenue Recognition - Revenue from Contracts with Customers. The amendments are effective for annual periods beginning after December 15, 2017, including interim periods within those periods with early adoption permitted. The Company does not expect the adoption of the guidance will have a material impact on its consolidated financial statements.
91
3.Balance sheet details
Short-term investments
Short-term investments consisted of the following (in thousands):
|
|
|
|
|
|
At December 31, 2017 |
|
||||||||||
|
|
|
|
Maturity |
|
Amortized cost |
|
Unrealized |
|
Unrealized |
|
Estimated |
|
||||
|
|
|
|
(in years) |
|
or cost |
|
gains |
|
losses |
|
fair value |
|
||||
|
U.S. government bonds |
|
|
less than 2 |
|
$ |
1,799 |
|
$ |
— |
|
$ |
(17) |
|
$ |
1,782 |
|
|
U.S. government agency bonds |
|
|
less than 2 |
|
|
2,698 |
|
|
— |
|
|
(17) |
|
|
2,681 |
|
|
Bank certificates of deposit |
|
|
less than 1 |
|
|
10,300 |
|
|
1 |
|
|
(3) |
|
|
10,298 |
|
|
Commercial paper |
|
|
less than 1 |
|
|
11,598 |
|
|
— |
|
|
(5) |
|
|
11,593 |
|
|
Corporate notes |
|
|
less than 3 |
|
|
51,532 |
|
|
6 |
|
|
(121) |
|
|
51,417 |
|
|
Asset-backed securities |
|
|
less than 3 |
|
|
16,796 |
|
|
— |
|
|
(61) |
|
|
16,735 |
|
|
Total |
|
|
|
|
$ |
94,723 |
|
$ |
7 |
|
$ |
(224) |
|
$ |
94,506 |
|
|
|
|
|
|
|
At December 31, 2016 |
|
||||||||||
|
|
|
|
Maturity |
|
Amortized cost |
|
Unrealized |
|
Unrealized |
|
Estimated |
|
||||
|
|
|
|
(in years) |
|
or cost |
|
gains |
|
losses |
|
fair value |
|
||||
|
U.S. government agency bonds |
|
|
1-3 |
|
$ |
9,535 |
|
$ |
2 |
|
$ |
(22) |
|
$ |
9,515 |
|
|
Bank certificates of deposit |
|
|
less than 2 |
|
|
11,101 |
|
|
13 |
|
|
(1) |
|
|
11,113 |
|
|
Commercial paper |
|
|
less than 1 |
|
|
17,011 |
|
|
1 |
|
|
(2) |
|
|
17,010 |
|
|
Corporate notes |
|
|
less than 3 |
|
|
45,178 |
|
|
7 |
|
|
(61) |
|
|
45,124 |
|
|
Asset-backed securities |
|
|
less than 2 |
|
|
6,503 |
|
|
3 |
|
|
— |
|
|
6,506 |
|
|
Total |
|
|
|
|
$ |
89,328 |
|
$ |
26 |
|
$ |
(86) |
|
$ |
89,268 |
|
Accounts receivable, net
Accounts receivable consisted of the following (in thousands):
|
|
|
December 31, |
|
||||
|
|
|
2017 |
|
2016 |
|
||
|
|
|
|
|
|
|
|
|
|
Accounts receivable |
|
$ |
17,248 |
|
$ |
14,800 |
|
|
Less allowance for doubtful accounts |
|
|
(592) |
|
|
(495) |
|
|
|
|
$ |
16,656 |
|
$ |
14,305 |
|
Inventory, net
Inventory consisted of the following (in thousands):
|
|
|
December 31, |
|
||||
|
|
|
2017 |
|
2016 |
|
||
|
|
|
|
|
|
|
|
|
|
Finished goods |
|
$ |
4,225 |
|
$ |
2,014 |
|
|
Work in process |
|
|
2,368 |
|
|
2,105 |
|
|
Raw material |
|
|
4,629 |
|
|
2,725 |
|
|
|
|
$ |
11,222 |
|
$ |
6,844 |
|
92
Property and equipment, net
Property and equipment consisted of the following (in thousands):
|
|
|
December 31, |
|
||||
|
|
|
2017 |
|
2016 |
|
||
|
|
|
|
|
|
|
|
|
|
Buildings |
|
$ |
874 |
|
$ |
874 |
|
|
Equipment |
|
|
8,311 |
|
|
5,342 |
|
|
Furniture and fixtures |
|
|
1,382 |
|
|
639 |
|
|
Leasehold improvements |
|
|
4,568 |
|
|
3,474 |
|
|
Computer equipment and software |
|
|
1,980 |
|
|
1,239 |
|
|
Construction in progress |
|
|
1,134 |
|
|
1,320 |
|
|
|
|
|
18,249 |
|
|
12,888 |
|
|
Less accumulated depreciation and amortization |
|
|
(6,455) |
|
|
(5,295) |
|
|
|
|
$ |
11,794 |
|
$ |
7,593 |
|
Depreciation and amortization expense related to property and equipment was $2.1 million, $1.1 million and $0.8 million for the years ended December 31, 2017, 2016 and 2015, respectively.
Accrued liabilities
Accrued liabilities consisted of the following (in thousands):
|
|
|
December 31, |
|
||||
|
|
|
2017 |
|
2016 |
|
||
|
|
|
|
|
|
|
|
|
|
Accrued contract payments (see Note 10) |
|
$ |
1,033 |
|
$ |
823 |
|
|
Accrued sales commissions |
|
|
506 |
|
|
1,641 |
|
|
Accrued clinical study payments |
|
|
609 |
|
|
1,167 |
|
|
Accrued bonuses |
|
|
9,106 |
|
|
6,122 |
|
|
Accrued vacation benefits |
|
|
2,121 |
|
|
1,382 |
|
|
Accrued Employee Stock Purchase Plan liability |
|
|
1,517 |
|
|
4 |
|
|
Other accrued liabilities |
|
|
5,557 |
|
|
2,772 |
|
|
|
|
$ |
20,449 |
|
$ |
13,911 |
|
4.Fair value measurements
Fair value is an exit price, representing the amount that would be received to sell an asset or paid to transfer a liability in an orderly transaction between market participants. As such, fair value is a market‑based measurement that should be determined based on assumptions that market participants would use in pricing an asset or liability.
The following tables present information about the Company’s financial assets measured at fair value on a recurring basis as of December 31, 2017 and 2016, and indicates the fair value hierarchy of the valuation techniques
93
utilized by the Company to determine such fair value (in thousands). The Company did not have any financial liabilities measured at fair value on a recurring basis as of December 31, 2017 and December 31, 2016.
|
|
|
At December 31, 2017 |
|
||||||||||
|
|
|
|
|
|
|
|
|
Significant |
|
|
|
|
|
|
|
|
|
|
|
Quoted prices in |
|
other |
|
Significant |
|
|||
|
|
|
|
|
|
active markets for |
|
observable |
|
unobservable |
|
|||
|
|
|
December 31, |
|
identical assets |
|
inputs |
|
inputs |
|
||||
|
|
|
2017 |
|
(Level 1) |
|
(Level 2) |
|
(Level 3) |
|
||||
|
Assets |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Money market funds (i) |
|
$ |
2,370 |
|
$ |
2,370 |
|
$ |
— |
|
$ |
— |
|
|
U.S. government agency bonds (ii) |
|
|
2,681 |
|
|
— |
|
|
2,681 |
|
|
— |
|
|
U.S. Government bonds (ii) |
|
|
1,782 |
|
|
— |
|
|
1,782 |
|
|
— |
|
|
Bank certificates of deposit (ii) |
|
|
10,298 |
|
|
— |
|
|
10,298 |
|
|
— |
|
|
Commercial paper (ii)(iii) |
|
|
14,593 |
|
|
— |
|
|
14,593 |
|
|
— |
|
|
Corporate notes (ii) |
|
|
51,417 |
|
|
— |
|
|
51,417 |
|
|
— |
|
|
Asset-backed securities (ii) |
|
|
16,735 |
|
|
— |
|
|
16,735 |
|
|
— |
|
|
Total assets |
|
$ |
99,876 |
|
$ |
2,370 |
|
$ |
97,506 |
|
$ |
— |
|
|
(i) |
Included in cash and cash equivalents with a maturity of three months or less from date of purchase on the consolidated balance sheets. |
|
(ii) |
Included in short-term investments on the consolidated balance sheets. |
|
(iii) |
One commercial paper investment totaling $3,000 (in thousands) is included in cash and cash equivalents on the condensed consolidated balance sheets, as the investment has a maturity of three months or less from the date of purchase on the condensed consolidated balance sheets. |
|
|
|
|
At December 31, 2016 |
|
|||||||||
|
|
|
|
|
|
|
|
|
Significant |
|
|
|
|
|
|
|
|
|
|
|
Quoted prices in |
|
other |
|
Significant |
|
|||
|
|
|
|
|
|
active markets for |
|
observable |
|
unobservable |
|
|||
|
|
|
December 31, |
|
identical assets |
|
inputs |
|
inputs |
|
||||
|
|
|
2016 |
|
(Level 1) |
|
(Level 2) |
|
(Level 3) |
|
||||
|
Assets |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Money market funds (i) |
|
$ |
80 |
|
$ |
80 |
|
$ |
— |
|
$ |
— |
|
|
U.S. government agency bonds (ii) |
|
|
9,515 |
|
|
— |
|
|
9,515 |
|
|
— |
|
|
Bank certificates of deposit (ii) |
|
|
11,113 |
|
|
— |
|
|
11,113 |
|
|
— |
|
|
Commercial paper (ii) |
|
|
17,010 |
|
|
— |
|
|
17,010 |
|
|
— |
|
|
Corporate notes (ii) |
|
|
45,124 |
|
|
— |
|
|
45,124 |
|
|
— |
|
|
Asset-backed securities (ii) |
|
|
6,506 |
|
|
— |
|
|
6,506 |
|
|
— |
|
|
Total assets |
|
$ |
89,348 |
|
$ |
80 |
|
$ |
89,268 |
|
$ |
— |
|
|
(i) |
Included in cash and cash equivalents with a maturity of three months or less from date of purchase on the consolidated balance sheets. |
|
(ii) |
Included in short-term investments on the consolidated balance sheets. |
Money market funds and currency are highly liquid investments and are actively traded. The pricing information on these investment instruments is readily available and can be independently validated as of the measurement date. This approach results in the classification of these securities as Level 1 of the fair value hierarchy.
U.S. government bonds, U.S. government agency bonds, bank certificates of deposit, commercial paper, corporate notes and asset-backed securities are measured at fair value using Level 2 inputs. The Company reviews trading activity and pricing for these investments as of each measurement date. When sufficient quoted pricing for identical securities is not available, the Company uses market pricing and other observable market inputs for similar securities obtained from third party data providers. These inputs represent quoted prices for similar assets in active
94
markets or these inputs have been derived from observable market data. This approach results in the classification of these securities as Level 2 of the fair value hierarchy.
There were no transfers between levels within the fair value hierarchy during the periods presented.
5.Long‑term debt and intangible assets
Notes payable in connection with GMP Vision Solutions
In January 2007, the Company entered into an agreement (the Original GMP Agreement) with GMP Vision Solutions, Inc. (GMP) to acquire certain in‑process research and development in exchange for periodic royalty payments equal to a single‑digit percentage of revenues received for royalty‑bearing products and periodic royalty payments at a higher royalty rate applied to all amounts received in connection with the grant of licenses or sub-licenses of the related intellectual property.
In November 2013, the Company entered into an amended agreement with GMP in which remaining royalties payable to GMP (the Buyout Agreement) were canceled in exchange for the issuance of $17.5 million in promissory notes payable to GMP and a party related to GMP.
The Company concluded that the $17.5 million transaction represented the purchase of an intangible asset. The Company estimated a useful life of five years over which the intangible asset is being amortized to cost of sales in the accompanying statements of operations, which amortization period was determined after consideration of the projected outgoing royalty payment stream had the Buyout Agreement not occurred, and the remaining life of the patents obtained in the Original GMP Agreement. After determining that the pattern of future cash flows associated with this intangible asset could not be reliably estimated with a high level of precision, the Company concluded that the intangible asset will be amortized on a straight‑line basis over the estimated useful life. For each of the years ended December 31, 2017, 2016 and 2015, the Company recorded amortization expense of $3.5 million related to this intangible asset in cost of sales.
Bank loan facility
In February 2015, the Company and its primary bank executed an Amended and Restated Revolving Credit and Term Loan Agreement (the Amended Credit Agreement) which provided for a $5.0 million senior secured term loan, a $5.0 million senior secured draw‑to term loan and an $8.0 million senior secured revolving credit facility. Amounts owed under the Amended Credit Agreement were secured by a first priority security interest in all of the Company’s assets, excluding intellectual property. The Amended Credit Agreement included certain reporting and financial covenants which, if not met, could have constituted an event of default under the Amended Credit Agreement.
On the closing date, the Company received $5.0 million cash under the senior secured term loan. The Company incurred loan origination fees of $41,000 which was recorded as a loan discount, and debt issuance costs of $0.1 million which was recorded as a deferred asset. As of July 31, 2015, the Company had drawn $2.0 million under the draw‑to term loan. The senior secured term loan and draw‑to term loan would have matured and would have been required to be fully paid by February 23, 2019. The entire unpaid principal amount plus any accrued but unpaid interest under the revolving line of credit were due to become payable in full on February 23, 2017.
On July 31, 2015, the Company paid off in full all amounts outstanding under the Amended Credit Agreement with the payment of $7.0 million in principal plus all interest and fees payable through the payoff date, and recorded a loss on extinguishment of debt in the amount of $0.2 million. Accordingly, this facility was terminated and is no longer outstanding and available to the Company.
Intangible assets
In 2015, the Company entered into agreements with two international distributors pursuant to which their distribution rights with the Company were terminated effective as of December 31, 2015. In 2016 and 2017, the Company entered into agreements with two additional international distributors pursuant to which their distribution
95
rights with the Company were terminated effective as of January 1, 2017 and March 31, 2017, respectively. As part of the agreements the distributors agreed to provide certain services to, and not compete with, the Company for one-to-two years in exchange for payments calculated based on single-digit percentages of the Company’s future revenues in those years in the respective countries that had comprised their distributors’ territories. Management recorded the estimated fair value of the non-compete provisions as intangible assets. As of December 31, 2017, the net non-compete intangible assets totaled approximately $0.2 million, and are being amortized on a straight-line basis to selling, general and administrative expense over the one-to-two year period. For the years ended December 31, 2017 and 2016, the Company recorded amortization expense related to the non-compete provisions of approximately $0.3 million and $0.2 million, respectively.
The following reflects the composition of intangible assets, net (in thousands):
|
|
|
December 31, |
|
December 31, |
|
||
|
|
|
2017 |
|
2016 |
|
||
|
|
|
|
|
|
|
|
|
|
GMP royalty buyout |
|
$ |
17,500 |
|
$ |
17,500 |
|
|
Non-compete agreements |
|
|
524 |
|
|
243 |
|
|
|
|
|
18,024 |
|
|
17,743 |
|
|
Accumulated amortization |
|
|
(14,877) |
|
|
(11,176) |
|
|
Total |
|
$ |
3,147 |
|
$ |
6,567 |
|
|
Weighted average amortization period (in months) |
|
|
60 |
|
|
60 |
|
Estimated amortization expense will be $3.1 million in 2018 after which the above mentioned intangible assets will be fully amortized.
6.Convertible preferred stock and stockholders’ equity
Convertible preferred stock
Immediately prior to the completion of the IPO, and after all unexercised warrants to purchase shares of Series D convertible preferred stock were net exercised at the IPO price per share, the Company had outstanding 21,736,367 shares of convertible preferred stock which automatically converted into 21,736,367 shares of the Company’s common stock. The related carrying value of $159.1 million was reclassified to additional paid-in capital in the period ending June 30, 2015, and no shares of convertible preferred stock were outstanding thereafter.
Preferred stock
The Company is authorized to issue 5.0 million shares of its preferred stock. No shares of preferred stock have been issued.
Common stock
Prior to the completion of the Company’s IPO in June 2015, all common stock issued resulted from the founding of the Company and the exercises of stock options. On June 30, 2015, the Company completed its IPO, selling 6.9 million newly issued shares of common stock at a price of $18.00 per share. Immediately prior to the closing of the IPO, all unexercised warrants to purchase shares of Series D convertible preferred stock were net exercised at the IPO price per share, and then all outstanding shares of convertible preferred stock automatically converted into approximately 21.7 million shares of common stock.
In 2013, the Company repurchased at fair market value and placed into treasury 28,000 shares of its common stock that had been acquired in connection with the exercise of a stock option.
96
7.Stock-based compensation
The Company has four stock‑based compensation plans (collectively, the Stock Plans)—the 2001 Stock Option Plan (the 2001 Stock Plan), the 2011 Stock Plan (the 2011 Stock Plan), the 2015 Omnibus Incentive Compensation Plan (the 2015 Stock Plan) and the 2015 Employee Stock Purchase Plan (the ESPP). The 2015 Stock Plan permits grants of restricted stock units (RSUs).
The Company has historically granted stock options, but the Company began to award RSU grants to certain employees during the fiscal year ended 2017. RSU awards vest 25% on each of the first, second, third and fourth anniversaries of the grant date.
The purpose of these plans is to provide incentives to employees, directors and nonemployee consultants. The Company no longer grants any awards under the 2001 Stock Plan and the 2011 Stock Plan. The maximum term of any stock options granted under the Stock Plans is 10 years. Stock options generally vest 25% on the first anniversary of the original vesting date, with the balance vesting monthly or annually over the remaining three years. Stock options are granted at exercise prices at least equal to the fair value of the underlying stock at the date of the grant.
The ESPP permits eligible employees to purchase shares of the Company’s common stock, using contributions via payroll deduction of up to 15% of their earnings, at a price per share equal to 85% of the lower of the stock’s fair market value on the offering date or purchase date. The ESPP is intended to qualify as an “employee stock purchase plan” under Section 423 of the Internal Revenue Code.
As of January 1, 2018, the Company has reserved an aggregate of 9.5 million shares of common stock for issuance under the 2015 Stock Plan, and 1.5 million shares of common stock for issuance under the ESPP.
Stock options granted pursuant to the 2001 Stock Plan and 2011 Stock Plan permitted optionees to elect to exercise unvested options in exchange for restricted common stock. All unvested shares issued upon the early exercise of stock options, so long as they remain unvested, are subject to the Company’s right of repurchase at the optionee’s original exercise price for a 90‑day period beginning on the date that an optionee’s service with the Company voluntarily or involuntarily terminates. Consistent with authoritative guidance, early exercises are not considered exercises for accounting purposes. Cash received for the exercise of unvested options is recorded as a liability, which liability is released to equity at each reporting date as the shares vest. During the years ended December 31, 2017, 2016 and 2015, there were option exercises for 0, 0 and 337 unvested shares, respectively. As of December 31, 2017 and 2016, 27 and 977 shares, respectively, remained subject to a repurchase right by the Company. As of December 31, 2017 and 2016, the related liability, which is included in other accrued liabilities in the accompanying consolidated balance sheets, was approximately $0 and $4,000, respectively.
In July 2014, the Company granted stock options to purchase an aggregate of 1.2 million shares of common stock, which options contain a performance condition such that they would only become exercisable in the event that the Company’s common stock was listed on a national securities exchange within one year from the date of grant. In accordance with authoritative guidance, the Company did not record any compensation expense associated with the grants until the performance condition was satisfied on June 30, 2015. Upon the completion of the IPO on June 30, 2015, the Company immediately recognized cumulative compensation cost of $3.8 million for the grants as if the method had been applied since the date of grant using the required graded accelerated attribution method, and the Company will record compensation expense over the remainder of the four‑year vesting period using this method. Stock options granted subsequent to July 2014 do not contain a performance condition.
97
Stock options
The following table summarizes stock option activity under the 2001 Stock Plan, 2011 Stock Plan and 2015 Stock Plan (in thousands):
|
|
|
Number of |
|
|
|
|
Weighted- |
|
|
|
|
|
|
|
shares |
|
Weighted- |
|
average |
|
Aggregate |
|
||
|
|
|
underlying |
|
average |
|
remaining |
|
intrinsic |
|
||
|
|
|
options |
|
exercise price |
|
contractual |
|
value (in |
|
||
|
|
|
(in thousands) |
|
per share |
|
life (in years) |
|
thousands) |
|
||
|
Outstanding at December 31, 2014 |
|
5,657 |
|
$ |
3.93 |
|
6.3 |
|
$ |
16,131 |
|
|
Granted |
|
1,139 |
|
|
18.07 |
|
|
|
|
|
|
|
Exercised |
|
(1,022) |
|
|
1.70 |
|
|
|
|
9,174 |
|
|
Canceled/forfeited/expired |
|
(73) |
|
|
6.56 |
|
|
|
|
|
|
|
Outstanding at December 31, 2015 |
|
5,701 |
|
$ |
7.10 |
|
6.7 |
|
$ |
102,390 |
|
|
Granted |
|
1,979 |
|
|
21.24 |
|
|
|
|
|
|
|
Exercised |
|
(1,660) |
|
|
3.65 |
|
|
|
|
42,458 |
|
|
Canceled/forfeited/expired |
|
(109) |
|
|
20.00 |
|
|
|
|
|
|
|
Outstanding at December 31, 2016 |
|
5,911 |
|
$ |
12.59 |
|
7.3 |
|
$ |
129,591 |
|
|
Granted |
|
1,877 |
|
|
43.85 |
|
|
|
|
|
|
|
Exercised |
|
(639) |
|
|
5.76 |
|
|
|
|
22,105 |
|
|
Canceled/forfeited/expired |
|
(123) |
|
|
23.79 |
|
|
|
|
|
|
|
Outstanding at December 31, 2017 |
|
7,026 |
|
$ |
21.36 |
|
7.3 |
|
$ |
69,555 |
|
|
Vested and expected to vest at December 31, 2017 |
|
6,893 |
|
$ |
21.13 |
|
7.2 |
|
$ |
69,080 |
|
|
Exercisable at December 31, 2017 |
|
3,687 |
|
$ |
10.58 |
|
5.9 |
|
$ |
57,987 |
|
Intrinsic value is calculated as the difference between the exercise price of the underlying options and the fair value of the common stock for the options that had exercise prices that were lower than the fair value per share of the common stock on the date of exercise.
The weighted average estimated grant date fair value per share of stock options granted during the years ended December 31, 2017, 2016 and 2015 was $20.62, $10.81 and $9.77, respectively.
The total fair value of stock options that vested during the years ended December 31, 2017 and 2016 was $12.9 million and $5.7 million, respectively.
Restricted Stock Units
The following table summarizes the activity of unvested restricted stock units under the Stock Plans during the year ended December 31, 2017 (in thousands):
|
|
|
|
|
|
Weighted- |
|
|
|
|
|
|
Number of |
|
average |
|
|
|
|
|
|
shares |
|
grant date |
|
|
|
|
|
|
(in thousands) |
|
fair value |
|
|
|
Unvested at December 31, 2016 |
|
|
— |
|
$ |
— |
|
|
Granted |
|
|
173 |
|
|
39.10 |
|
|
Vested |
|
|
— |
|
|
— |
|
|
Canceled/forfeited |
|
|
— |
|
|
— |
|
|
Unvested at December 31, 2017 |
|
|
173 |
|
|
39.10 |
|
No restricted stock units vested during the year ended December 31, 2017.
98
Valuation and expense recognition of stock-based awards
The Company accounts for the measurement and recognition of compensation expense for all share‑based awards made to the Company’s employees and nonemployees based on the estimated fair value of the awards.
The fair value of RSU awards made to employees and nonemployees is equal to the closing marking proce of the Company’s common stock price on the grant date.
The Company uses the Black‑Scholes option‑pricing model to estimate the fair value of stock options and shares purchased under the ESPP. The determination of fair value using the Black‑Scholes option‑pricing model is affected by the estimated fair market value per share of the Company’s common stock as well as assumptions regarding a number of highly complex and subjective variables, including expected stock price volatility, risk‑free interest rate, expected dividends and expected option life and generally requires significant management judgment to determine.
Risk‑free interest rate. The risk‑free interest rate is equal to the U.S. Treasury Note interest rate for the comparable term for the expected option life as of the valuation date. If the expected option life is between the U.S. Treasury Note rates of two published terms, then the risk‑free interest rate is based on the straight‑line interpolation between the U.S. Treasury Note rates of the two published terms as of the valuation date.
Expected dividend yield. The expected dividend yield is based on the Company’s history and expectation of dividend payouts. The Company has never declared or paid any cash dividends and does not presently plan to pay cash dividends in the foreseeable future.
Expected volatility. The Company only recently began to have publicly traded equity and has a limited operating history and a lack of Company‑specific historical and implied volatility data, and therefore has estimated its stock price volatility based upon an index of the historical volatilities of a group of comparable publicly‑traded medical device peer companies. The historical volatility data was computed using the historical daily closing prices for the selected peer companies’ shares during the equivalent period of the calculated expected term of the Company’s stock options. The Company will continue to apply this process until a sufficient amount of historical information regarding the volatility of its own stock price becomes available.
Expected term. The Company has concluded that its stock option exercise history does not provide a reasonable basis upon which to estimate expected term, and therefore it uses the simplified method for estimating the expected term of stock option grants. Under this approach, the weighted‑average expected term is presumed to be the average of the vesting term and the contractual term of the option.
Fair value of common stock. Historically, and until the June 30, 2015 completion of the Company’s IPO, the fair value of the shares of common stock underlying the stock options has been the responsibility of and determined by the Company’s Board of Directors. Because there had been no public market for the Company’s common stock, the Board of Directors determined the fair value of common stock at the time of grant of the option by considering a number of objective and subjective factors including independent third‑party valuations of the Company’s common stock, sales prices of convertible preferred stock to unrelated third parties, operating and financial performance, the lack of liquidity of capital stock and general and industry specific economic outlook, among other factors. Subsequent to the date of the Company’s IPO in June 2015, the Company has used the daily market prices in the determination of the fair value of its common stock.
99
Stock‑based awards to employees
The weighted‑average assumptions used to estimate the fair value of stock options granted to employees were as follows:
|
|
|
|
Year ended |
|
||||||
|
|
|
|
December 31, |
|
||||||
|
|
|
|
2017 |
|
|
2016 |
|
|
2015 |
|
|
Risk-free interest rate |
|
|
2.13 |
% |
|
1.59 |
% |
|
1.77 |
% |
|
Expected dividend yield |
|
|
0.0 |
% |
|
0.0 |
% |
|
0.0 |
% |
|
Expected volatility |
|
|
46.5 |
% |
|
52.9 |
% |
|
56.0 |
% |
|
Expected term (in years) |
|
|
6.04 |
|
|
6.04 |
|
|
6.07 |
|
Forfeiture rate. The Company reduces employee share‑based compensation expense for estimated forfeitures. Forfeitures are estimated at the time of grant based on historical experience, and revised, if necessary, in subsequent periods if actual forfeitures differ from those estimates.
The weighted‑average per share exercise price of options granted to employees during the years ended December 31, 2017, 2016 and 2015 was $43.85, $21.24 and $17.79, respectively.
Stock‑based awards to nonemployees
The fair values of stock‑based awards made to nonemployees are remeasured at the end of the reporting period using the Black‑Scholes option pricing model. The expected life for each option is determined based on the time remaining until the expiration of the option as of the date of remeasurement. Compensation expense for these share‑based awards is determined by applying the recalculated fair values to the shares that have vested during a period.
Through December 31, 2016, in conjunction with various consulting agreements, the Company issued options to nonemployees to purchase 891,400 shares of common stock at exercise prices ranging from $0.25 to $25.91 per share. For the years ended December 31, 2017, 2016 and 2015, the Company recorded nonemployee stock‑based compensation expense of $0.5 million, $0.8 million and $1.1 million, respectively. No stock options were issued to nonemployees in 2017.
The following table summarizes the allocation of stock‑based compensation related to stock options and restricted stock units in the accompanying consolidated statements of operations (in thousands):
|
|
|
Year ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Cost of sales |
|
$ |
597 |
|
$ |
233 |
|
$ |
251 |
|
|
Selling, general & administrative |
|
|
13,006 |
|
|
6,475 |
|
|
5,773 |
|
|
Research and development |
|
|
3,989 |
|
|
2,078 |
|
|
1,865 |
|
|
Total |
|
$ |
17,592 |
|
$ |
8,786 |
|
$ |
7,889 |
|
In the years ended December 31, 2017, 2016, and 2015, the related tax benefits were $5.4 million, $9.9 million and $0.5 million, respectively, relating to stock-based compensation.
At December 31, 2017, the total unamortized stock‑based compensation expense is approximately $49.5 million. Of the approximately $49.5 million in unamortized stock-based compensation expense, $43.9 million is attributable to stock options and is to be recognized over the stock options’ remaining vesting terms of approximately 4.0 years (2.7 years on a weighted average basis). The remaining $5.6 million is attributable to restricted stock units and is to be recognized over the restricted stock units’ vesting terms of approximately 4.0 years (3.5 years on a weighted-average basis).
100
The total stock-based compensation cost capitalized in inventory was $0.1 million, $0.1 million and $43,000 for the years ended December 31, 2017, 2016 and 2015, respectively.
Common stock reserved for future issuance
Common stock reserved for issuance is as follows (in thousands):
|
|
|
As of |
|
|
|
|
December 31, |
|
|
|
|
2017 |
|
|
|
|
|
|
|
Stock options issued and outstanding—2001 Plan |
|
811 |
|
|
Stock options issued and outstanding—2011 Plan |
|
2,001 |
|
|
Stock options issued and outstanding—2015 Plan |
|
4,388 |
|
|
Employee stock purchase plan |
|
838 |
|
|
Authorized for future stock awards or option grants |
|
3,443 |
|
|
|
|
11,481 |
|
8.Income taxes
United States and foreign income (loss) before income taxes was as follows (in thousands):
|
|
|
Year ended December 31, |
|
|||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
United States |
|
$ |
12,543 |
|
$ |
12,214 |
|
$ |
(36,750) |
|
|
Foreign |
|
|
(12,542) |
|
|
(7,649) |
|
|
(1,538) |
|
|
Total |
|
$ |
1 |
|
$ |
4,565 |
|
$ |
(38,288) |
|
The provision for income taxes was as follows (in thousands):
|
|
|
December 31, |
|
|||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
Current: |
|
|
|
|
|
|
|
|
|
|
|
Federal |
|
$ |
235 |
|
$ |
(28) |
|
$ |
— |
|
|
State |
|
|
93 |
|
|
71 |
|
|
33 |
|
|
Foreign |
|
|
— |
|
|
— |
|
|
— |
|
|
|
|
|
328 |
|
|
43 |
|
|
33 |
|
|
Deferred: |
|
|
|
|
|
|
|
|
|
|
|
Federal |
|
|
(235) |
|
|
— |
|
|
— |
|
|
State |
|
|
— |
|
|
— |
|
|
— |
|
|
Foreign |
|
|
— |
|
|
— |
|
|
— |
|
|
|
|
|
(235) |
|
|
— |
|
|
— |
|
|
Provision for income taxes |
|
$ |
93 |
|
$ |
43 |
|
$ |
33 |
|
The tax provision for the noncontrolling interest was $0 in 2015; therefore, no tax benefit or expense was allocated to the net loss attributable to noncontrolling interest.
101
The reconciliations of the U.S. federal statutory tax expense to the combined effective tax provision are as follows:
|
|
|
Year ended |
|
||||
|
|
|
December 31, |
|
||||
|
(amounts in thousands) |
|
2017 |
|
2016 |
|
2015 |
|
|
Statutory rate of tax expense |
$ |
- |
$ |
1,552 |
$ |
(13,018) |
|
|
State income taxes, net of federal benefit |
|
(17) |
|
530 |
|
(1,347) |
|
|
Permanent and other items |
|
(5,199) |
|
789 |
|
1,307 |
|
|
Deconsolidation of DOSE |
|
- |
|
- |
|
4,558 |
|
|
Nondeductible offering costs |
|
- |
|
7 |
|
- |
|
|
Research credits |
|
(2,215) |
|
(1,945) |
|
(1,745) |
|
|
Uncertain tax positions |
|
1,108 |
|
940 |
|
865 |
|
|
Change in tax rate |
|
1,013 |
|
1,337 |
|
68 |
|
|
Tax Cuts and Jobs Act |
|
25,216 |
|
- |
|
- |
|
|
Valuation allowance |
|
(19,813) |
|
(3,167) |
|
9,345 |
|
|
Provision for income taxes |
$ |
93 |
$ |
43 |
$ |
33 |
|
Significant components of the Company’s net deferred tax assets at December 31, 2017 and 2016 are as follows (in thousands):
|
|
|
December 31, |
|
||||
|
|
|
2017 |
|
2016 |
|
||
|
Deferred tax assets: |
|
|
|
|
|
|
|
|
Net operating loss carryforwards |
|
$ |
37,571 |
|
$ |
41,144 |
|
|
Tax credits |
|
|
6,713 |
|
|
4,913 |
|
|
Depreciation and amortization |
|
|
10,765 |
|
|
16,748 |
|
|
Stock-based compensation |
|
|
7,184 |
|
|
5,310 |
|
|
Reserves and accruals |
|
|
3,739 |
|
|
3,920 |
|
|
Other, net |
|
|
— |
|
|
233 |
|
|
Total deferred tax assets |
|
|
65,972 |
|
|
72,268 |
|
|
|
|
|
|
|
|
|
|
|
Deferred tax liabilities: |
|
|
|
|
|
|
|
|
Other, net |
|
$ |
(42) |
|
$ |
— |
|
|
|
|
|
|
|
|
|
|
|
Valuation allowance |
|
|
(65,695) |
|
|
(72,268) |
|
|
Net deferred tax assets |
|
$ |
235 |
|
$ |
— |
|
Based on the weight of available evidence, management has established a valuation allowance for all of the deferred tax assets, with the exception of known refundable federal credits, as it is more likely than not that the deferred tax assets will not be realized. The net change in the valuation allowance was $(6.6) million in 2017.
At December 31, 2017, the Company had approximately $125.7 million, $94.2 million and $18.0 million of net operating loss carryforwards for federal, state and foreign purposes, respectively, available to offset future taxable income. The federal and state net operating loss carryforwards begin to expire in 2018 and 2028, respectively. The tax losses in foreign jurisdictions, if not utilized sooner, will begin to expire no earlier than 2023.
At December 31, 2017, the Company had federal and state research and development credit carryforwards of $7.5 million and $7.0 million, respectively, which begin to expire in 2021 for federal purposes and carry over indefinitely for state purposes.
Utilization of the net operating loss and tax credit carryforwards will be subject to annual limitations under Sections 382 and 383 of the Internal Revenue Code of 1986 and similar state provisions due to several ownership changes that have occurred previously or that could occur in the future. These ownership changes will limit the amount
102
of net operating loss and tax credit carryforwards and other deferred tax assets that can be utilized to offset future taxable income and tax. In general, all ownership changes as defined by IRC Section 382 result from transactions increasing ownership of certain stockholders in the stock of the Company by more than 50 percentage points over a three‑year period. An analysis was performed by the Company which indicated that several ownership changes have occurred in previous years which created annual limitations on the Company’s ability to utilize net operating loss and tax credit carryforwards. Such limitations will result in approximately $0.1 million of tax benefits related to net operating loss and tax credit carryforwards that will expire unused. Accordingly, the related net operating loss and tax credit carryforwards have been removed from deferred tax assets accompanied by a corresponding reduction in the valuation allowance. The Company has not, however, conducted a IRC Section 382 study for any periods subsequent to December 31, 2009 and as such, the Company cannot provide any assurance that a change in ownership within the meaning of IRC has not occurred since that date. Due to the existence of the valuation allowance, limitations created by future ownership changes, if any, will not impact the Company’s effective tax rate.
The Company considers all earnings and profits of its foreign subsidiaries to be indefinitely reinvested. Due to losses incurred, there are no unrecorded income taxes associated with unrepatriated foreign earnings as of December 31, 2017.
A reconciliation of the beginning and ending amount of gross unrecognized tax benefits for 2017, 2016 and 2015, excluding interest and penalties, is as follows (in thousands):
|
|
|
December 31, |
|||||||
|
|
|
2017 |
|
2016 |
|
2015 | |||
|
Balance at beginning of the year |
|
$ |
5,947 |
|
$ |
4,848 |
|
$ |
4,066 |
|
Reductions for tax positions—prior years |
|
|
— |
|
|
(49) |
|
|
(284) |
|
Additions for tax positions—current year |
|
|
1,280 |
|
|
1,148 |
|
|
1,066 |
|
Balance at end of the year |
|
$ |
7,227 |
|
$ |
5,947 |
|
$ |
4,848 |
As of December 31, 2017, there would be no impact on the effective tax rate if the uncertain tax benefits were recognized.
The Company’s policy is to recognize interest expense and penalties related to income tax matters as a component of income tax expense. There was no accrued interest and penalties associated with uncertain tax positions as of December 31, 2017, 2016 and 2015. It is not anticipated that there will be a significant change in the unrecognized tax benefits over the next 12 months.
Due to the Company’s net operating loss carryforwards, its federal, state and foreign income tax returns are open to examination by the Internal Revenue Service and state jurisdictions for all years since inception.
The Tax Cuts and Jobs Act
The Tax Cuts and Jobs Act (the "Act") was enacted on December 22, 2017. Among other changes, the Act reduces the US federal corporate tax rate from 34 percent to 21 percent. In accordance with Staff Accounting Bulletin 118, as of December 31, 2017, the Company has not completed the accounting for the tax effects of enactment of the Act; however, in certain cases, as described below, the Company has made a reasonable estimate of the effects on the existing deferred tax balances. In all cases, the Company will continue to make and refine calculations as additional analysis is completed. In addition, estimates may also be affected as the Company gains a more thorough understanding of the Act.
The Company remeasured certain deferred tax assets and liabilities based on the rates at which they are expected to reverse in the future, which is generally 21%. However, the Company is still analyzing certain aspects of the Act and refining calculations, which could potentially affect the measurement of these balances or give rise to new deferred tax amounts. The provisional amount recorded related to the remeasurement of the deferred tax balance was $25.2 million, which was fully offset by a decrease in the valuation allowance.
Due to uncertainties which currently exist in the interpretation of the provisions of the Act regarding Internal
103
Revenue Code Section 162(m), the Company has not evaluated the potential impacts of IRC Section 162(m) as amended by the Act in its consolidated financial statements.
9.Employee benefits
Defined contribution plan
The Company sponsors a defined contribution plan pursuant to section 401(k) of the United States Internal Revenue Code that allows participating employees to contribute up to 100% of their salary, to an annual maximum of $18,000 in 2017 and 2016 ($24,000 in 2017 and 2016 for employees over the age of 50). Through December 31, 2017, the Company has only made “qualified nonelective contributions” to maintain compliance with IRS regulations. No plan contributions were made by the Company in 2016 and 2015. Beginning in 2017, the Company will contribute a $0.50 match for every $1.00 contributed by a participating employee up to 6% of plan-eligible earnings, with such Company contributions becoming vested when participating employees reach the 3-year anniversary from their date of hire, giving credit for past service. For the fiscal year ended December 31, 2017, Company contributions totaled approximately $1.0 million.
Deferred compensation plan
Effective April 1, 2017, the Company established a deferred compensation plan (the Deferred Compensation Plan) for eligible senior level employees. The plan is designed to permit eligible employees to make elective deferrals of compensation to which he or she will become entitled in the future. The Company also established a rabbi trust that serves as an investment to shadow the Deferred Compensation Plan liability. The investments of the rabbi trust consist of company-owned life insurance policies (COLIs). The fair value of the Deferred Compensation Plan liability, included in other liabilities on the consolidated balance sheets, was approximately $0.6 million as of December 31, 2017 and the cash surrender value of the COLIs, included in deposits and other assets on the consolidated balance sheets, which reflects the underlying assets at fair value, was approximately $0.7 million as of December 31, 2017.
10.Commitments and contingencies
The Company, from time to time, is involved in legal proceedings or regulatory encounters or other matters in the ordinary course of business that could result in unasserted or asserted claims or litigation. Management is not aware of any legal proceedings where the likelihood of a loss contingency is reasonably possible and the amount or range of reasonably possible losses is material to the Company’s results of operations, financial condition or cash flows.
Operating leases
The Company leases its main headquarters and manufacturing facility and facilities for some of its foreign subsidiaries. Certain of the Company’s leases contain renewal options, rent escalation clauses, and/or landlord incentives. Rent expense for noncancelable operating leases with scheduled rent increases and/or landlord incentives is recognized on a straight-line basis over the lease term beginning with the lease commencement date, or the date the Company takes control of the leased space, whichever is sooner. The excess of straight-line rent expense over scheduled payment amounts and landlord incentives is recorded as a deferred rent liability.
The Company leases two adjacent facilities located in San Clemente, California, both of which are subject to leases that expire on December 31, 2021. The agreements each contain an option to extend the leases for up to two additional three-year periods at market rates. The total square footage of both facilities equals approximately 77,000. The lease landlord agreed to provide the Company with a tenant improvement allowance after January 1, 2017 in the amount of the cost of any leasehold improvements, not to exceed approximately $264,000 upon the Company providing the necessary documentation evidencing the costs of the allowable leasehold improvements.
The Company’s remaining U.S.-based and foreign subsidiaries’ leased office space totals less than 14,000 square feet.
104
The Company recorded deferred rent of $0.3 million and $0.2 million as of December 31, 2017 and 2016, respectively, in conjunction with its facilities lease agreements. Rent expense was $1.5 million, $1.1 million and $0.6 million for the years ended December 31, 2017, 2016 and 2015, respectively.
Future minimum payments under the aforementioned noncancelable operating leases for each of the five succeeding years are as follows (in thousands):
|
2018 |
|
$ |
1,513 |
|
|
2019 |
|
|
1,340 |
|
|
2020 |
|
|
1,278 |
|
|
2021 |
|
|
1,251 |
|
|
2022 |
|
|
— |
|
|
Thereafter |
|
|
— |
|
|
|
|
$ |
5,382 |
|
Purchase commitment
As of December 31, 2017, the Company did not have any noncancelable, firm purchase commitments due beyond one year.
Regents of the University of California
On December 30, 2014, the Company executed an agreement (the UC Agreement) with the Regents of the University of California (the University) to correct inventorship in connection with a group of the Company’s U.S. patents (the Patent Rights) and to obtain from the University a covenant that it did not and would not claim any right or title to the Patent Rights and will not challenge or assist any others in challenging the Patent Rights. In connection with the UC Agreement, Glaukos paid the University a low single‑digit percentage of worldwide net sales of certain current and future products, including the Company’s iStent products, with a required minimum annual payment of $0.5 million. This ongoing product payment terminates on the date that the last of the Patent Rights expires, which is currently expected to be in 2022. For the years ended December 31, 2017, 2016 and 2015, the Company recorded approximately $3.9 million, $2.8 million and $1.8 million in cost of sales, respectively, in connection with the product payment obligation.
11.Variable interest entity
In October 2009, the Company formed a wholly‑owned subsidiary, DOSE Medical Corporation and in April 2010, the Company distributed all of its shares of common stock of DOSE via a stock dividend to the Company’s stockholders of record as of the close of business on March 31, 2010. Since its formation, the Company had provided DOSE with a small number of leased employees, management services and space, all of which had been charged to DOSE and pursuant to written agreements between the parties. Additionally, the Company had provided DOSE the cash required to fund its operations that, together with accrued interest and charges for the aforementioned services, the Company had recorded in an intercompany receivable account. Up until the transaction on June 30, 2015 described below, the Company had accounted for DOSE as a variable interest entity in which it had a variable interest in all reporting periods since the formation of DOSE. Accordingly, the Company’s consolidated financial statements include the accounts of DOSE, with all intercompany balances eliminated and with the deficit balance of DOSE’s net assets reflected as noncontrolling interest, up to but excluding June 30, 2015.
On June 30, 2015, the Company completed a transaction initially executed in July 2014, the closing of which was contingent upon the successful completion of an IPO. Pursuant to the terms of the asset purchase agreement, the Company acquired from DOSE certain assets, including the iDose product line, in exchange for payment of $15.0 million in cash and the elimination of the $10.9 million intercompany receivable owed by DOSE to the Company as of the closing date. The Company reconsidered its relationship with DOSE as a result of the transaction and determined it was no longer considered to be the primary beneficiary with the power to direct operations and the right to receive benefits/absorb losses of DOSE; therefore, upon the close of the transaction, the Company derecognized DOSE
105
and no longer considered it a consolidated entity in its financial statements. Accordingly, in the three months ended June 30, 2015, the Company recorded a charge to other expense in the amount of $25.7 million to reflect the deconsolidation of DOSE’ non‑glaucoma related assets and noncontrolling interest.
In addition to the asset purchase agreement, the parties agreed to an amended and restated patent license agreement and an amended and restated transition services agreement that provides for limited support from the Company to DOSE for a period of up to three years, which period was extended through June 30, 2021 in connection with the Purchase Agreement. Either party can terminate the transition services agreement upon adequate written notice.
Consolidation of DOSE’s results of operations included the following (in thousands):
|
|
|
Year ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Selling, general & administrative |
|
$ |
— |
|
$ |
— |
|
$ |
105 |
|
|
Research and development |
|
|
— |
|
|
— |
|
|
890 |
|
|
Interest expense |
|
|
— |
|
|
— |
|
|
85 |
|
|
Net loss of DOSE |
|
$ |
— |
|
$ |
— |
|
$ |
1,080 |
|
Consolidation of DOSE’s cash flows included the following (in thousands):
|
|
|
Year ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Cash used in operating activities |
|
$ |
— |
|
$ |
— |
|
$ |
(1,134) |
|
|
Cash used in investing activities |
|
|
— |
|
|
— |
|
|
(33) |
|
|
Cash provided by financing activities |
|
|
— |
|
|
— |
|
|
1,158 |
|
|
(Decrease) increase in cash and cash equivalents of DOSE |
|
$ |
— |
|
$ |
— |
|
$ |
(9) |
|
12.Business segment information
Operating segments are identified as components of an enterprise about which segment discrete financial information is available for evaluation by the chief operating decision maker in making decisions regarding resource allocation and assessing performance. The Company operates its business on the basis of one reportable segment—ophthalmic medical devices.
|
|
|
Year ended |
|
|||||||
|
|
|
December 31, |
|
|||||||
|
Geographic net sales information (in thousands) |
|
2017 |
|
2016 |
|
2015 |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
United States |
|
$ |
140,902 |
|
$ |
104,995 |
|
$ |
67,698 |
|
|
International |
|
|
18,352 |
|
|
9,402 |
|
|
4,002 |
|
|
Total net sales |
|
$ |
159,254 |
|
$ |
114,397 |
|
$ |
71,700 |
|
|
|
|
Property and equipment, net |
|
Depreciation and amortization |
|
Capital expenditures |
|
|||||||||||||||||||||
|
|
|
As of December 31, |
|
Year ended December 31, |
|
Year ended December 31, |
|
|||||||||||||||||||||
|
|
|
2017 |
|
2016 |
|
2015 |
|
2017 |
|
2016 |
|
2015 |
|
2017 |
|
2016 |
|
2015 |
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
United States |
|
$ |
11,677 |
|
$ |
7,463 |
|
$ |
2,012 |
|
$ |
5,406 |
|
$ |
4,654 |
|
$ |
4,180 |
|
$ |
6,051 |
|
$ |
6,493 |
|
$ |
972 |
|
|
International |
|
|
117 |
|
|
130 |
|
|
142 |
|
|
76 |
|
|
68 |
|
|
87 |
|
|
221 |
|
|
56 |
|
|
62 |
|
|
Total |
|
$ |
11,794 |
|
$ |
7,593 |
|
$ |
2,154 |
|
$ |
5,482 |
|
$ |
4,722 |
|
$ |
4,267 |
|
$ |
6,272 |
|
$ |
6,549 |
|
$ |
1,034 |
|
106
13.Selected Quarterly Financial Information (Unaudited)
|
|
|
Three months ended |
|
||||||||||
|
|
|
March 31, |
|
June 30, |
|
September 30, |
|
December 31, |
|
||||
|
(in thousands, except per share amounts) |
|
2017 |
|
2017 |
|
2017 |
|
2017 |
|
||||
|
Net sales |
|
$ |
35,907 |
|
$ |
41,285 |
|
$ |
40,412 |
|
$ |
41,650 |
|
|
Cost of sales |
|
|
5,180 |
|
|
5,522 |
|
|
5,718 |
|
|
4,630 |
|
|
Gross profit |
|
|
30,727 |
|
|
35,763 |
|
|
34,694 |
|
|
37,020 |
|
|
Operating expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Selling, general and administrative |
|
|
21,481 |
|
|
24,675 |
|
|
24,141 |
|
|
25,963 |
|
|
In-process research and development |
|
|
— |
|
|
5,320 |
|
|
— |
|
|
— |
|
|
Research and development |
|
|
8,942 |
|
|
9,633 |
|
|
9,805 |
|
|
10,525 |
|
|
Total operating expenses |
|
|
30,423 |
|
|
39,628 |
|
|
33,946 |
|
|
36,488 |
|
|
Income (loss) from operations |
|
|
304 |
|
|
(3,865) |
|
|
748 |
|
|
532 |
|
|
Total other income (expense), net |
|
|
629 |
|
|
586 |
|
|
630 |
|
|
437 |
|
|
Provision for income taxes |
|
|
55 |
|
|
22 |
|
|
53 |
|
|
(37) |
|
|
Net income (loss) |
|
$ |
878 |
|
$ |
(3,301) |
|
$ |
1,325 |
|
$ |
1,006 |
|
|
Net income (loss) per share (1): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Basic |
|
$ |
0.03 |
|
$ |
(0.10) |
|
$ |
0.04 |
|
$ |
0.03 |
|
|
Diluted |
|
$ |
0.02 |
|
$ |
(0.10) |
|
$ |
0.04 |
|
$ |
0.03 |
|
|
|
|
Three months ended |
|
||||||||||
|
|
|
March 31, |
|
June 30, |
|
September 30, |
|
December 31, |
|
||||
|
(in thousands, except per share amounts) |
|
2016 |
|
2016 |
|
2016 |
|
2016 |
|
||||
|
Net sales |
|
$ |
23,092 |
|
$ |
28,556 |
|
$ |
29,577 |
|
$ |
33,172 |
|
|
Cost of sales |
|
|
3,121 |
|
|
4,359 |
|
|
3,886 |
|
|
4,811 |
|
|
Gross profit |
|
|
19,971 |
|
|
24,197 |
|
|
25,691 |
|
|
28,361 |
|
|
Operating expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Selling, general and administrative |
|
|
12,288 |
|
|
15,120 |
|
|
16,854 |
|
|
20,494 |
|
|
Research and development |
|
|
7,062 |
|
|
6,955 |
|
|
7,807 |
|
|
7,399 |
|
|
Total operating expenses |
|
|
19,350 |
|
|
22,075 |
|
|
24,661 |
|
|
27,893 |
|
|
Income from operations |
|
|
621 |
|
|
2,122 |
|
|
1,030 |
|
|
468 |
|
|
Total other income (expense), net |
|
|
276 |
|
|
210 |
|
|
269 |
|
|
(431) |
|
|
Provision for income taxes |
|
|
— |
|
|
— |
|
|
140 |
|
|
(97) |
|
|
Net income |
|
$ |
897 |
|
$ |
2,332 |
|
$ |
1,159 |
|
$ |
134 |
|
|
Net income per share (1): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Basic |
|
$ |
0.03 |
|
$ |
0.07 |
|
$ |
0.03 |
|
$ |
0.00 |
|
|
Diluted |
|
$ |
0.03 |
|
$ |
0.06 |
|
$ |
0.03 |
|
$ |
0.00 |
|
|
(1) |
Net income or loss per share is computed independently for each of the quarters presented. Therefore, the sum of the quarterly per-share amounts will not necessarily equal the annual per share amount. |
14. Subsequent events
None.
107
ITEM 9.CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE
None.
ITEM 9A.CONTROLS AND PROCEDURES
Evaluation of Disclosure Controls and Procedures
The term “disclosure controls and procedures,” as defined in Rules 13a-15(e) and 15d-15(e) under the Exchange Act, refers to controls and procedures that are designed to ensure that information required to be disclosed by a company in the reports that it files or submits under the Exchange Act is recorded, processed, summarized and reported within the time periods specified in the SEC’s rules and forms. Disclosure controls and procedures include, without limitation, controls and procedures designed to ensure that information required to be disclosed by a company in the reports that it files or submits under the Exchange Act is accumulated and communicated to the company’s management, including its principal executive and principal financial officers, or persons performing similar functions, as appropriate to allow timely decisions regarding required disclosure. Our management recognizes that any controls and procedures, no matter how well designed and operated, can provide only reasonable assurance of achieving their objectives and our management necessarily applies its judgment in evaluating the cost-benefit relationship of possible controls and procedures. Our management, with the participation of our chief executive officer and our chief financial officer, evaluated the effectiveness of our disclosure controls and procedures as of the end of the period covered by this Annual Report on Form 10-K. Based on that evaluation, our chief executive officer and our chief financial officer concluded that our disclosure controls and procedures were effective, at the reasonable assurance level, as of December 31, 2017.
Management’s Annual Report on Internal Control Over Financial Reporting and Attestation Report of the Registered Public Accounting Firm
Our management is responsible for establishing and maintaining adequate internal control over financial reporting as defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act to provide reasonable assurance regarding the reliability of our financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. Internal control over financial reporting includes those policies and procedures that (i) pertain to the maintenance of records that in reasonable detail accurately and fairly reflect the transactions and dispositions of our assets; (ii) provide reasonable assurance that the transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that our receipts and expenditures are being made only in accordance with authorizations of our management and our directors; and (iii) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use or disposition of our assets that could have a material effect on the financial statements.
Our management conducted an evaluation of the effectiveness of our internal control over financial reporting as of the end of the period covered by this Annual Report on Form 10-K based on the framework in Internal Control – Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission. Based on this evaluation, management concluded that the Company’s internal control over financial reporting was effective as of December 31, 2017.
Ernst & Young LLP, our independent registered public accounting firm, which audited the consolidated financial statements included in this Annual Report on Form 10‑K, has issued an audit report on our internal control over financial reporting. See Report of Independent Registered Public Accounting Firm herein.
Changes in Internal Control over Financial Reporting
There have been no changes in our internal control over financial reporting, as such term is defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act, during our fourth fiscal quarter of 2017 that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
108
Report of Independent Registered Public Accounting Firm
To the Shareholders and the Board of Directors of Glaukos Corporation
Opinion on Internal Control over Financial Reporting
We have audited Glaukos Corporation’s internal control over financial reporting as of December 31, 2017, based on criteria established in Internal Control–Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) (the COSO criteria). In our opinion, Glaukos Corporation (the Company) maintained, in all material respects, effective internal control over financial reporting as of December 31, 2017, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the consolidated balance sheets of the Company as of December 31, 2017 and 2016, the related consolidated statements of operations, comprehensive (loss) income, convertible preferred stock and stockholders’ equity (deficit), and cash flows for each of the three years in the period ended December 31, 2017, and the related notes and our report dated February 28, 2018 expressed an unqualified opinion thereon.
Basis for Opinion
The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Annual Report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects.
Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
Definition and Limitations of Internal Control Over Financial Reporting
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/s/ Ernst & Young LLP
Irvine, California
February 28, 2018
109
110
ITEM 10.DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE
We have adopted a written code of business conduct and ethics that applies to our directors, executive officers and employees, including our principal executive officer, principal financial officer, principal accounting officer or controller, or persons performing similar functions. A current copy of the code is posted on the investor section of our web site, www.glaukos.com. To the extent required by rules adopted by the SEC and NYSE, we intend to promptly disclose future amendments to certain provisions of the code, or waivers of such provisions granted to executive officers and directors, in the Corporate Governance section of our Investor Relations web site at investors.glaukos.com.
The remaining information required by this Item 10 will be included in our Proxy Statement for the 2018 Annual Meeting of Stockholders, which will be filed with the SEC no later than 120 days after the close of the fiscal year ended December 31, 2017, and is incorporated herein by reference.
ITEM 11.EXECUTIVE COMPENSATION
The information required by this Item 11 will be included in our Proxy Statement for the 2018 Annual Meeting of Stockholders, which will be filed with the SEC no later than 120 days after the close of the fiscal year ended December 31, 2017, and is incorporated herein by reference.
ITEM 12.SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS
The information required by this Item 12 will be included in our Proxy Statement for the 2018 Annual Meeting of Stockholders, which will be filed with the SEC no later than 120 days after the close of the fiscal year ended December 31, 2017, and is incorporated herein by reference.
ITEM 13.CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE
The information required by this Item 13 will be included in our Proxy Statement for the 2018 Annual Meeting of Stockholders, which will be filed with the SEC no later than 120 days after the close of the fiscal year ended December 31, 2017, and is incorporated herein by reference.
ITEM 14.PRINCIPAL ACCOUNTING FEES AND SERVICES
The information required by this Item 14 will be included in our Proxy Statement for the 2018 Annual Meeting of Stockholders, which will be filed with the SEC no later than 120 days after the close of the fiscal year ended December 31, 2017, and is incorporated herein by reference.
111
ITEM 15.EXHIBITS, FINANCIAL STATEMENT SCHEDULES
|
(a) |
List of documents filed as part of this Annual Report on Form 10-K: |
|
(1) |
Financial Statements |
The financial statements included in Part II, Item 8 of this document are filed as part of this Annual Report on Form 10-K.
|
(2) |
Financial Statement Schedules |
Schedules have been omitted because they are not applicable or the amounts are immaterial or the required information is presented in the financial statements or notes thereto.
|
(b) |
Exhibits |
The exhibits listed in the Exhibit Index (following the signatures page of this report) below are filed, furnished or incorporated by reference as part of this Annual Report on Form 10-K.
None.
112
INDEX TO EXHIBITS
|
Exhibit |
|
Description |
|
2.1† |
|
|
| 3.1 |
|
|
| 3.2 |
|
|
| 10.1 |
|
|
| 10.2 |
|
|
| 10.3 |
|
|
|
10.4+ |
|
|
|
10.5+ |
|
|
|
10.6+ |
|
|
|
10.7+ |
|
|
|
10.8+ |
|
|
|
10.9+ |
|
|
|
10.10+ |
|
|
|
10.11+ |
|
|
|
10.12+ |
|
|
|
10.13+ |
|
113
|
Exhibit |
|
Description |
|
10.14+ |
|
|
|
10.15+ |
|
|
|
10.16+ |
|
|
|
10.17+ |
|
|
|
10.18+ |
|
|
|
10.19+ |
|
|
|
10.20+ |
|
|
|
10.21*+ |
|
|
|
10.22*+ |
|
|
| 10.23 |
|
|
| 10.24 |
|
|
| 10.25 |
|
|
|
10.26† |
|
|
| 10.27 |
|
|
|
21* |
|
|
|
23.1* |
|
|
|
31.1* |
|
|
|
31.2* |
|
|
|
32.1** |
|
114
|
Exhibit |
|
Description |
|
32.2** |
|
|
|
101.INS* |
|
XBRL Instance Document |
|
101.SCH* |
|
XBRL Taxonomy Schema Linkbase Document |
|
101.CAL* |
|
XBRL Taxonomy Calculation Linkbase Document |
|
101.DEF* |
|
XBRL Taxonomy Definition Linkbase Document |
|
101.LAB* |
|
XBRL Taxonomy Labels Linkbase Document |
|
101.PRE* |
|
XBRL Taxonomy Presentation Linkbase Document |
+ Indicates a management contract or compensatory plan or arrangement.
† Schedules and exhibits are omitted pursuant to Item 601(b)(2) of Regulation S-K. The Company agrees to furnish supplementally a copy of any omitted schedule or exhibit to the U.S. Securities and Exchange Commission upon request.
* Filed Herewith.
** Furnished Herewith.
115
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized, in the City of San Clemente, State of California, on February 28, 2018.
|
|
GLAUKOS CORPORATION |
|
|
|
|
|
|
|
By: |
/s/ Thomas W. Burns |
|
|
|
Thomas W. Burns |
|
|
|
Chief Executive Officer and President |
|
|
|
|
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed by the following persons in the capacities and on the dates indicated.
|
Signature |
|
Title |
|
Date |
|
|
|
|
|
|
|
/s/ Thomas W. Burns |
|
Chief Executive Officer, President and |
|
February 28, 2018 |
|
Thomas W. Burns |
|
Director (Principal Executive Officer) |
|
|
|
|
|
|
|
|
|
/s/ Joseph E. Gilliam |
|
Chief Financial Officer & SVP, Corporate Development |
|
February 28, 2018 |
|
Joseph E. Gilliam |
|
(Principal Accounting and Financial Officer) |
|
|
|
|
|
|
|
|
|
/s/ William J. Link |
|
Chairman of the Board |
|
February 28, 2018 |
|
William J. Link, Ph.D. |
|
|
|
|
|
/s/ Mark J. Foley |
|
Director |
|
February 28, 2018 |
|
Mark J. Foley |
|
|
|
|
|
|
|
|
|
|
|
/s/ David F. Hoffmeister |
|
Director |
|
February 28, 2018 |
|
David F. Hoffmeister |
|
|
|
|
|
|
|
|
|
|
|
/s/ Gilbert H. Kliman |
|
Director |
|
February 28, 2018 |
|
Gilbert H. Kliman, M.D. |
|
|
|
|
|
|
|
|
|
|
|
/s/ Jonathan T. Silverstein |
|
Director |
|
February 28, 2018 |
|
Jonathan T. Silverstein |
|
|
|
|
|
|
|
|
|
|
|
/s/ Marc A. Stapley |
|
Director |
|
February 28, 2018 |
|
Marc A. Stapley |
|
|
|
|
|
|
|
|
|
|
|
/s/ Aimee S. Weisner |
|
Director |
|
February 28, 2018 |
|
Aimee S. Weisner |
|
|
|
|
116