Attached files
| file | filename |
|---|---|
| EX-99.2 - EX-99.2 - GLYCOMIMETICS INC | glyc-20160610ex9921be6c5.htm |
| 8-K - 8-K - GLYCOMIMETICS INC | glyc-20160610x8k.htm |
|
|
|
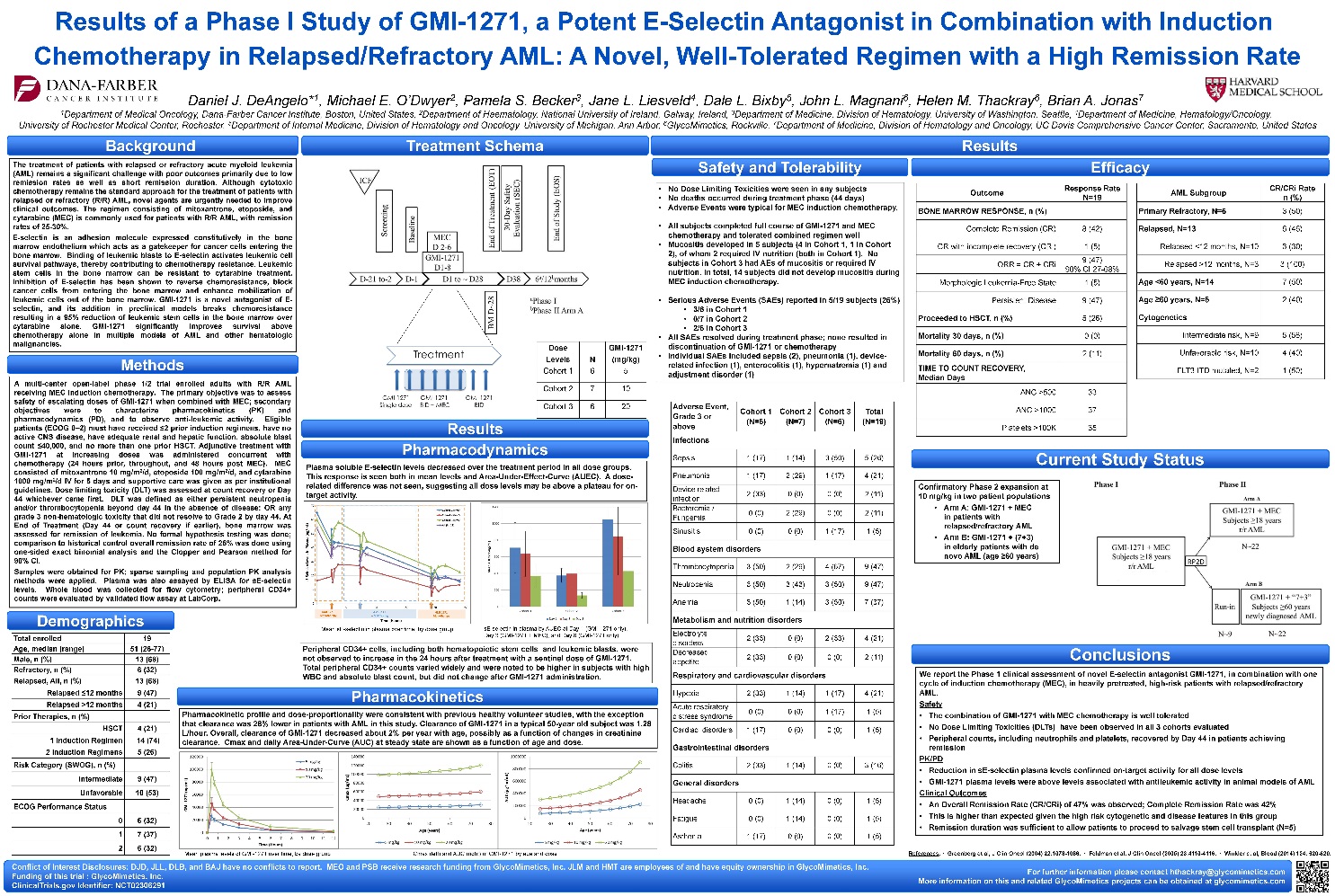
The treatment of patients with relapsed or refractory acute myeloid leukemia (AML) remains a significant challenge with poor outcomes primarily due to low remission rates as well as short remission duration. Although cytotoxic chemotherapy remains the standard approach for the treatment of patients with relapsed or refractory (R/R) AML, novel agents are urgently needed to improve clinical outcomes. The regimen consisting of mitoxantrone, etoposide, and cytarabine (MEC) is commonly used for patients with R/R AML, with remission rates of 25-30%. E-selectin is an adhesion molecule expressed constitutively in the bone marrow endothelium which acts as a gatekeeper for cancer cells entering the bone marrow. Binding of leukemic blasts to E-selectin activates leukemic cell survival pathways, thereby contributing to chemotherapy resistance. Leukemic stem cells in the bone marrow can be resistant to cytarabine treatment. Inhibition of E-selectin has been shown to reverse chemoresistance, block cancer cells from entering the bone marrow and enhance mobilization of leukemic cells out of the bone marrow. GMI-1271 is a novel antagonist of E-selectin, and its addition in preclinical models breaks chemoresistance resulting in a 95% reduction of leukemic stem cells in the bone marrow over cytarabine alone. GMI-1271 significantly improves survival above chemotherapy alone in multiple models of AML and other hematologic malignancies. A multi-center open-label phase 1/2 trial enrolled adults with R/R AML receiving MEC induction chemotherapy. The primary objective was to assess safety of escalating doses of GMI-1271 when combined with MEC; secondary objectives were to characterize pharmacokinetics (PK) and pharmacodynamics (PD), and to observe anti-leukemic activity. Eligible patients (ECOG 0–2) must have received ≤2 prior induction regimens, have no active CNS disease, have adequate renal and hepatic function, absolute blast count ≤40,000, and no more than one prior HSCT. Adjunctive treatment with GMI-1271 at increasing doses was administered concurrent with chemotherapy (24 hours prior, throughout, and 48 hours post MEC). MEC consisted of mitoxantrone 10 mg/m2/d, etoposide 100 mg/m2/d, and cytarabine 1000 mg/m2/d IV for 5 days and supportive care was given as per institutional guidelines. Dose limiting toxicity (DLT) was assessed at count recovery or Day 44 whichever came first. DLT was defined as either persistent neutropenia and/or thrombocytopenia beyond day 44 in the absence of disease; OR any grade 3 non-hematologic toxicity that did not resolve to Grade 2 by day 44. At End of Treatment (Day 44 or count recovery if earlier), bone marrow was assessed for remission of leukemia. No formal hypothesis testing was done; comparison to historical control overall remission rate of 25% was done using one-sided exact binomial analysis and the Clopper and Pearson method for 90% CI. Samples were obtained for PK; sparse sampling and population PK analysis methods were applied. Plasma was also assayed by ELISA for sE-selectin levels. Whole blood was collected for flow cytometry; peripheral CD34+ counts were evaluated by validated flow assay at LabCorp. No Dose Limiting Toxicities were seen in any subjects No deaths occurred during treatment phase (44 days) Adverse Events were typical for MEC induction chemotherapy. All subjects completed full course of GMI-1271 and MEC chemotherapy and tolerated combined regimen well Mucositis developed in 5 subjects (4 in Cohort 1, 1 in Cohort 2), of whom 2 required IV nutrition (both in Cohort 1). No subjects in Cohort 3 had AEs of mucositis or required IV nutrition. In total, 14 subjects did not develop mucositis during MEC induction chemotherapy. Serious Adverse Events (SAEs) reported in 5/19 subjects (26%) 3/6 in Cohort 1 0/7 in Cohort 2 2/6 in Cohort 3 All SAEs resolved during treatment phase; none resulted in discontinuation of GMI-1271 or chemotherapy Individual SAEs included sepsis (2), pneumonia (1), device-related infection (1), enterocolitis (1), hypernatremia (1) and adjustment disorder (1) Plasma soluble E-selectin levels decreased over the treatment period in all dose groups. This response is seen both in mean levels and Area-Under-Effect-Curve (AUEC). A dose-related difference was not seen, suggesting all dose levels may be above a plateau for on-target activity. Peripheral CD34+ cells, including both hematopoietic stem cells and leukemic blasts, were not observed to increase in the 24 hours after treatment with a sentinel dose of GMI-1271. Total peripheral CD34+ counts varied widely and were noted to be higher in subjects with high WBC and absolute blast count, but did not change after GMI-1271 administration. Pharmacokinetic profile and dose-proportionality were consistent with previous healthy volunteer studies, with the exception that clearance was 28% lower in patients with AML in this study. Clearance of GMI-1271 in a typical 50-year old subject was 1.28 L/hour. Overall, clearance of GMI-1271 decreased about 2% per year with age, possibly as a function of changes in creatinine clearance. Cmax and daily Area-Under-Curve (AUC) at steady state are shown as a function of age and dose. We report the Phase 1 clinical assessment of novel E-selectin antagonist GMI-1271, in combination with one cycle of induction chemotherapy (MEC), in heavily pretreated, high-risk patients with relapsed/refractory AML. Safety The combination of GMI-1271 with MEC chemotherapy is well tolerated No Dose Limiting Toxicities (DLTs) have been observed in all 3 cohorts evaluated Peripheral counts, including neutrophils and platelets, recovered by Day 44 in patients achieving remission PK/PD Reduction in sE-selectin plasma levels confirmed on-target activity for all dose levels GMI-1271 plasma levels were above levels associated with antileukemic activity in animal models of AML Clinical Outcomes An Overall Remission Rate (CR/CRi) of 47% was observed; Complete Remission Rate was 42% This is higher than expected given the high risk cytogenetic and disease features in this group Remission duration was sufficient to allow patients to proceed to salvage stem cell transplant (N=5) Confirmatory Phase 2 expansion at 10 mg/kg in two patient populations Arm A: GMI-1271 + MEC in patients with relapsed/refractory AML Arm B: GMI-1271 + (7+3) in elderly patients with de novo AML (age ≥60 years) sE-selectin in plasma by AUEC at Day 1 (GMI-1271 only), Day 3 (GMI-1271 + MEC), and Day 8 (GMI-1271 only) Mean sE-selectin in plasma over time, by dose group Mean plasma levels of GMI-1271 over time, by dose group References: · Greenberg et al, J Clin Oncol (2004) 22:1078-1086. · Feldman et al, J Clin Oncol (2005) 23:4110-4116. · Winkler et al, Blood (2014) 124: 620-620. Outcome Response Rate N=19 BONE MARROW RESPONSE, n (%) Complete Remission (CR) 8 (42) CR with incomplete recovery (CRi) 1 (5) ORR = CR + CRi 9 (47) 90% CI 27-68% Morphologic Leukemia-Free State 1 (5) Persistent Disease 9 (47) Proceeded to HSCT, n (%) 5 (26) Mortality 30 days, n (%) 0 (0) Mortality 60 days, n (%) 2 (11) TIME TO COUNT RECOVERY, Median Days ANC >500 33 ANC >1000 37 Platelets >100K 35 Adverse Event, Grade 3 or above Cohort 1 (N=6) Cohort 2 (N=7) Cohort 3 (N=6) Total (N=19) Infections Sepsis 1 (17) 1 (14) 3 (50) 5 (26) Pneumonia 1 (17) 2 (29) 1 (17) 4 (21) Device related infection 2 (33) 0 (0) 0 (0) 2 (11) Bacteremia / Fungemia 0 (0) 2 (29) 0 (0) 2 (11) Sinusitis 0 (0) 0 (0) 1 (17) 1 (5) Blood system disorders Thrombocytopenia 3 (50) 2 (29) 4 (67) 9 (47) Neutropenia 3 (50) 3 (43) 3 (50) 9 (47) Anemia 3 (50) 1 (14) 3 (50) 7 (37) Metabolism and nutrition disorders Electrolyte disorders 2 (33) 0 (0) 2 (33) 4 (21) Decreased appetite 2 (33) 0 (0) 0 (0) 2 (11) Respiratory and cardiovascular disorders Hypoxia 2 (33) 1 (14) 1 (17) 4 (21) Acute respiratory distress syndrome 0 (0) 0 (0) 1 (17) 1 (5) Cardiac disorders 1 (17) 0 (0) 0 (0) 1 (5) Gastrointestinal disorders Colitis 2 (33) 1 (14) 0 (0) 3 (16) General disorders Headache 0 (0) 1 (14) 0 (0) 1 (5) Fatigue 0 (0) 1 (14) 0 (0) 1 (5) Asthenia 1 (17) 0 (0) 0 (0) 1 (5) AML Subgroup CR/CRi Rate n (%) Primary Refractory, N=6 3 (50) Relapsed, N=13 6 (46) Relapsed <12 months, N=10 3 (30) Relapsed >12 months, N=3 3 (100) Age <60 years, N=14 7 (50) Age ≥60 years, N=5 2 (40) Cytogenetics Intermediate risk, N=9 5 (56) Unfavorable risk, N=10 4 (40) FLT3-ITD mutated, N=2 1 (50) Dose Levels N GMI-1271 (mg/kg) Cohort 1 6 5 Cohort 2 7 10 Cohort 3 6 20 Results of a Phase I Study of GMI-1271, a Potent E-Selectin Antagonist in Combination with Induction Chemotherapy in Relapsed/Refractory AML: A Novel, Well-Tolerated Regimen with a High Remission RateCmax (left) and AUC (right) of GMI-1271 by age and dose Total enrolled 19 Age, median (range) 51 (26-77) Male, n (%) 13 (68) Refractory, n (%) 6 (32) Relapsed, All, n (%) 13 (68) Relapsed ≤12 months 9 (47) Relapsed >12 months 4 (21) Prior Therapies, n (%) HSCT 4 (21) 1 Induction Regimen 14 (74) 2 Induction Regimens 5 (26) Risk Category (SWOG), n (%) Intermediate 9 (47) Unfavorable 10 (53) ECOG Performance Status 0 6 (32) 1 7 (37) 2 6 (32) Conflict of Interest Disclosures: DJD, JLL, DLB, and BAJ have no conflicts to report. MEO and PSB receive research funding from GlycoMimetics, Inc. JLM and HMT are employees of and have equity ownership in GlycoMimetics, Inc. Funding of this trial : GlycoMimetics, Inc. ClinicalTrials.gov Identifier: NCT02306291 For further information please contact hthackray@glycomimetics.com More information on this and related GlycoMimetics projects can be obtained at glycomimetics.com Background Treatment Schema Safety and Tolerability Results Efficacy Methods Results Pharmacodynamics Current Study Status Demographics Pharmacokinetics Conclusions |