Attached files
| file | filename |
|---|---|
| 8-K - FORM 8-K - TEAM HEALTH HOLDINGS INC. | d41748d8k.htm |
Exhibit 99.1
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
| I. | EXECUTIVE SUMMARY |
A. Introduction
TeamHealth, Inc. (“TeamHealth”, “TMH” or the “Company”) is one of the largest suppliers of outsourced healthcare professional staffing and administrative services to hospitals and other healthcare providers in the United States, based upon revenues, patient visits, and number of clients. TeamHealth serves approximately 1,000 civilian and military hospitals in 47 states with a team of more than 14,000 affiliated healthcare professionals, including physicians, physician assistants, nurse practitioners and nurses. Since its inception in 1979, TeamHealth has focused primarily on providing outsourced services in emergency departments. The Company also provides comprehensive programs for anesthesiology, inpatient care (hospitalists comprising the specialties of internal medicine, orthopedic surgery, general surgery and OB/GYN), urgent care, pediatrics and other healthcare services, principally within hospitals and other healthcare facilities, enabling their management teams to outsource certain management, recruiting, hiring, payroll, billing and collection and benefits functions.
On August 4, 2015, TeamHealth entered into a definitive agreement to acquire IPC Healthcare, Inc., a leading national acute hospitalist and post-acute provider group practice in the United States, for total consideration of approximately $1.6 billion in cash (the “Acquisition”).
The Acquisition combines two physician-centric companies with leading market positions in their respective core service lines to create the nation’s leading physician services organization with a diversified, complementary business mix and significantly enhanced growth and cash flow profiles. The combined company will offer the leading emergency medicine and hospitalist services program and will possess an unmatched presence in the post-acute clinician services market, significantly enhancing each individual company’s positioning against an evolving healthcare landscape, including the migration to value based payment systems. The pro forma business will operate across 47 states in approximately 3,400 facilities. For the twelve months ended September 30, 2015, the combined company, after giving effect for full-year impact of previously closed acquisitions, had pro forma net revenue of approximately $4.5 billion and pro forma adjusted EBITDA (“EBITDA”) of $489 million.
1
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
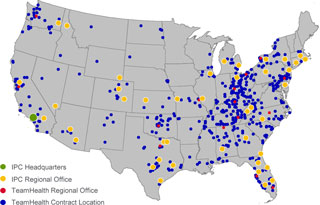
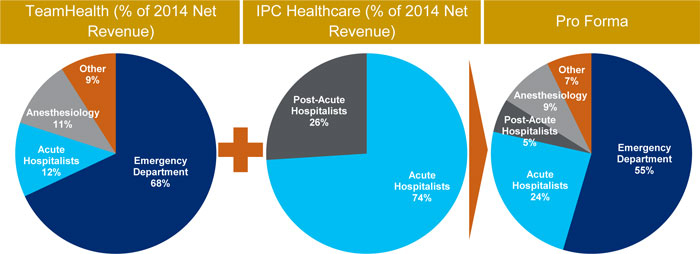
Figure 01 illustrates the percentage of net revenue for the year ended December 31, 2014 for each of TeamHealth, IPC Healthcare and the combined company by specialty / business line, demonstrating the enhanced diversification this combination creates.
Figure 01 – Combined Product Offering: ~3,400 Facilities and ~$4.5 billion in LTM Revenue
Source: Company filings, investor presentations and management analysis.
2
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
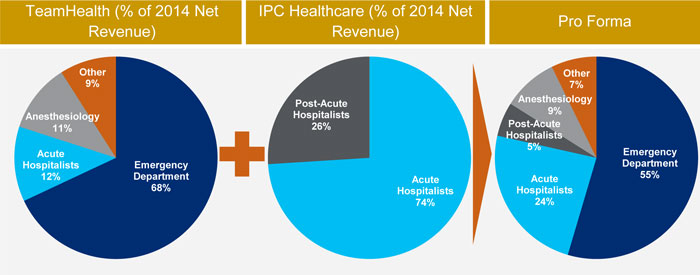
TeamHealth’s national footprint and high quality, long-standing relationships with its broad set of hospital and health system customers provides a significant opportunity to broaden IPC’s presence across the United States. TeamHealth’s current footprint in 47 states will extend IPC into 19 states in which it currently does not have operations today. Additionally, TeamHealth provides emergency medicine services in less than 20% of IPC’s roughly 375 acute-care sites of service, providing an attractive opportunity to grow TeamHealth’s core service lines by leveraging IPC’s high quality customer relationships. As illustrated in Figure 02, there is significant opportunity for TeamHealth to utilize its national presence to grow IPC’s current footprint in new markets and enhance bundled service options across the unique customer base of each company.
Figure 02 – Geographic Overlap
Source: TeamHealth management.
TeamHealth has identified a substantial synergy opportunity through its combination with IPC. TeamHealth’s management, which will be supplemented by key operational executives from IPC, believes it can achieve approximately $60 million of synergies within three years of closing the acquisition. This
3
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
estimated synergy opportunity is comprised of approximately $25 million in cost savings and identifiable revenue opportunities representing an approximately $35 million impact to EBITDA (primarily related to enhanced billing and collection processes and optimizing IPC’s managed care contracting efforts).
4
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
B. Sources and Uses
| Sources |
$ | % | Uses |
$ | % | |||||||||||||
| IPC Cash |
$ | 2 | 0.1 | % | Purchase IPCM Equity | $ | 1,485 | 88.4 | % | |||||||||
| Revolving Credit Facility Draw |
168 | 10.0 | Refinance IPCM Debt | 130 | 7.7 | |||||||||||||
| New Term Loan |
965 | 57.4 | Fees and Expenses | 65 | 3.9 | |||||||||||||
| New Unsecured Debt |
545 | 32.4 | ||||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Total Sources |
$ | 1,680 | 100.0 | % | Total Uses | $ | 1,680 | 100.0 | % | |||||||||
C. Pro Forma Capitalization
| ($ in millions) |
9/30/15 | Transaction Adjustment |
Pro Forma 9/30/15 |
|||||||||
| Cash |
$ | 18 | — | $ | 18 | |||||||
| Revolving Credit Facility |
$ | 170 | 168 | $ | 338 | |||||||
| Term Loan A |
585 | $ | 585 | |||||||||
| New Term Loan |
— | 965 | 965 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total Senior Secured Debt |
$ | 755 | $ | 1,133 | $ | 1,888 | ||||||
| New Unsecured Debt |
— | 545 | 545 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total Debt |
$ | 755 | $ | 1,678 | $ | 2,433 | ||||||
| Credit Statistics |
||||||||||||
| LTM PF Adj. EBITDA (09/30/15) |
$ | 380 | (1) | $ | 109 | (2) | $ | 489 | ||||
| Senior Secured Debt / LTM PF Adj. EBITDA |
2.0x | 3.9x | ||||||||||
| Total Debt / LTM PF Adj. EBITDA |
2.0 | 5.0 | ||||||||||
| Net Debt / LTM PF Adj. EBITDA |
1.9 | 4.9 | ||||||||||
|
|
|
|
|
|
|
|||||||
| TeamHealth Compliance Cert. PF Adj. EBITDA(3) |
$ | 414 | $ | 109 | $ | 523 | ||||||
| Senior Secured Debt / Compliance Cert. PF Adj. EBITDA |
1.8x | 3.6x | ||||||||||
| Total Debt / Compliance Cert. PF Adj. EBITDA |
1.8 | 4.7 | ||||||||||
| Net Debt / Compliance Cert. PF Adj. EBITDA |
1.8 | 4.6 | ||||||||||
|
|
|
|
|
|
|
|||||||
| (1) | Includes full-year impact of previously closed acquisitions. See next section for details. |
| (2) | Includes $25mm of expected cost synergies related to IPC transaction as well as other adjustments detailed in next section. |
| (3) | Based on TMH current credit agreement definition of EBITDA for the trailing twelve month period ending 9/30/15, which includes add back for non-cash component of professional liability insurance expense. |
5
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
D. Pro Forma Adjusted EBITDA
| Twelve Months Ended September 30, 2015 | ||||||||||||||||
| ($ in Millions) |
TeamHealth | IPC | Adj. | Pro Forma | ||||||||||||
| Historical Financials |
$ | 3,408.3 | $ | 728.8 | — | $ | 4,137.1 | |||||||||
| Acquisitions Pro Forma Adjustment |
253.1 | (1) | 79.1 | (1) | — | 332.3 | ||||||||||
| Net Revenues |
$ | 3,661.4 | $ | 807.9 | — | $ | 4,469.4 | |||||||||
| EBIT |
$ | 200.8 | $ | 47.3 | — | $ | 248.1 | |||||||||
| Depreciation & Amortization |
105.5 | 5.9 | — | 111.4 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| EBITDA |
$ | 306.4 | $ | 53.2 | $ | 359.6 | ||||||||||
| Equity Based Compensation |
16.7 | 8.4 | — | 25.1 | ||||||||||||
| Full Year Impact of Previous Acquisitions |
12.2 | (2) | 6.2 | (3) | — | 18.4 | ||||||||||
| Non-recurring Charges |
42.9 | (4) | 16.0 | (5) | — | 58.9 | ||||||||||
| Insurance Subsidiaries Interest Income |
2.1 | (4) | — | — | 2.1 | |||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| EBITDA Adjustments |
$ | 73.8 | $ | 30.6 | — | $ | 104.4 | |||||||||
| Expected Cost Synergies |
— | — | 25.0 | 25.0 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Pro Forma Adj. EBITDA |
$ | 380.2 | $ | 83.8 | $ | 25.0 | $ | 489.0 | ||||||||
| (1) | Includes full year impact of previously closed acquisitions. |
(2) (3) (4) (5) See tables below and sections VI A and B.
(2) Full-Year Impact of Previous Acquisitions – TeamHealth
| ($ in Millions) | ||||||
| Adjustment |
Amount | Detail | ||||
| Q4 2014 Acquisitions |
$ | 1.4 | Acquisition of 1 hospitalist, 1 emergency department, 1 scribe and 1 anesthesia practice with operations in California, Ohio, Texas and Washington D.C., respectively | |||
| Q1 2015 Acquisitions |
$ | 2.5 | Acquisition of 2 emergency department and 1 emergency department / hospitalist practice with operations in New York, Nevada and Texas, respectively | |||
| Q2 2015 Acquisitions |
$ | 5.6 | Acquisition of 1 anesthesia and 1 emergency department practice with operations in Ohio and New Jersey, respectively | |||
| Q3 2015 Acquisitions |
$ | 2.7 | Acquisition of 1 anesthesia practice in New York | |||
6
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
(3) Full-Year Impact of Previous Acquisitions – IPC
| ($ in Millions) | ||||||
| Adjustment |
Amount | Detail | ||||
| Q4 2014 Acquisitions |
$ | 0.3 | Acquisition of 7 hospitalist practices with operations in Ohio, Pennsylvania, Southeast Florida, West Michigan, Jacksonville, Southwest Florida, North Carolina, South Carolina and Virginia | |||
| Q1 2015 Acquisitions |
$ | 1.0 | Acquisition of 6 hospitalist practices with operations in Jacksonville, New York, Maryland, Tennessee and New Mexico | |||
| Q2 2015 Acquisitions |
$ | 2.3 | Acquisition of 7 hospitalist practices with operations in Georgia, Alabama, Houston, New York, North Carolina, South Carolina and Virginia | |||
| Q3 2015 Acquisitions |
$ | 2.6 | Acquisition of 7 hospitalist practices with operations in California, Tucson, Virginia, North Carolina, Tennessee, Ocala and Tampa | |||
7
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
(4) Other TeamHealth PF Adj. EBITDA Adjustments
| ($ in Millions) | ||||||
| Adjustment |
Amount | Description | ||||
| Other (Income) Expenses, Net |
($ | 1.3 | ) | Represents gains and losses related to the sale of certain assets and equity stakes as well as violation adjustments on SERP assets | ||
| Contingent Purchase & Other Acquisition Expense |
$ | 20.4 | Reflects expense recognized for historical and estimated future contingent payments and other compensation expense activity associated with acquisitions | |||
| Transaction Costs |
$ | 8.6 | Reflects expenses associated with accounting, legal, due diligence and other transaction fees related to acquisition activities | |||
| Severance & Other Charges |
$ | 11.6 | Severance costs related to acquisitions and management changes | |||
| Debt Refinancing Costs |
$ | 3.6 | Reflects the write-off of deferred financing costs from the previous term loan as well as certain fees and expenses associated with the debt amendment | |||
|
|
|
|||||
| Non-Recurring Charges Subtotal |
$ | 42.9 | ||||
| Insurance Subsidiaries Interest Income |
$ | 2.1 | Interest income from investments of captive insurance subsidiary | |||
(5) Other IPC PF Adj. EBITDA Adjustments
| ($ in Millions) | ||||||
| Adjustment |
Amount | Description | ||||
| Net Changes in Fair Value of Contingent Consideration |
$ | 6.5 | Adjustment to fair value of contingent consideration liability related to acquisitions updated quarterly for the actual performance of acquired practices | |||
| Costs Related to the False Claims Act Litigation |
$ | 1.7 | Legal expenses related False Claims Act litigation with the U.S. government | |||
| TeamHealth Transaction Expenses |
$ | 5.3 | Transaction costs incurred that related to the pending merger with TeamHealth | |||
| Transaction Expenses and CID Related Legal Expenses |
$ | 1.8 | Legal expenses related to transactions and defending against federal lawsuits | |||
| BPCI Overhead |
$ | 0.8 | One time expenses related to the preparation for BPCI program launch in mid 2015 | |||
8
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
E. Pro Forma Corporate Structure
Please refer to Debtdomain for detailed information about the pro forma corporate structure.
F. Description of the Term Loan
Please refer to Debtdomain for detailed information about the proposed facilities.
G. Business Description
TeamHealth Overview
TeamHealth is one of the largest suppliers of outsourced healthcare professional staffing and administrative services to hospitals and other healthcare providers in the United States, based upon revenues, patient visits, and number of clients. As of September 2015, the Company serves approximately 1,000 civilian and military hospitals, clinics and physician groups in 47 states with a team of more than 14,000 affiliated healthcare professionals, including physicians, physician assistants, nurse practitioners, and nurses. The Company recruits and contracts with healthcare professionals who then provide professional services within third-party healthcare facilities.
TeamHealth is a physician-founded organization with physician leadership throughout all levels of its organization. Since the Company’s inception in 1979, TeamHealth has provided outsourced services in emergency departments, or EDs. The Company also provides comprehensive programs for anesthesiology, inpatient services (hospitalists comprising the specialties of internal medicine, orthopedic surgery, general surgery and OB/GYN), urgent care, pediatrics and other healthcare services, by providing permanent staffing that enables the management teams of hospitals and other healthcare facilities to outsource certain management, recruiting, hiring, payroll, billing and collection and benefits functions. For the LTM period September 30, 2015, TeamHealth, after giving effect for full-year impact of previously closed acquisitions, generated net revenues of $3.7 billion and Adjusted EBITDA of $380 million (excluding the impact of the contemplated acquisition of IPC).
9
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
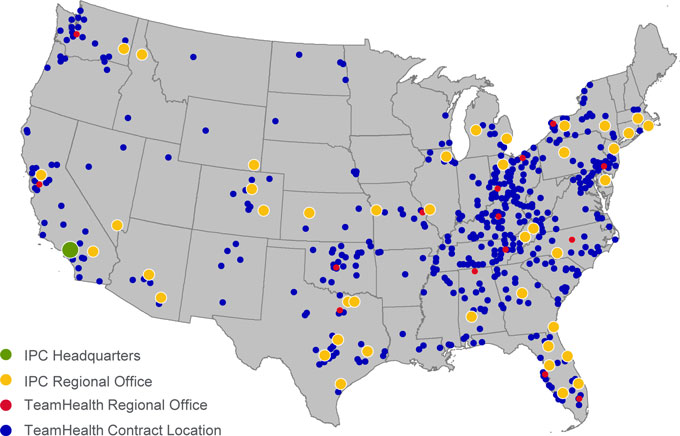
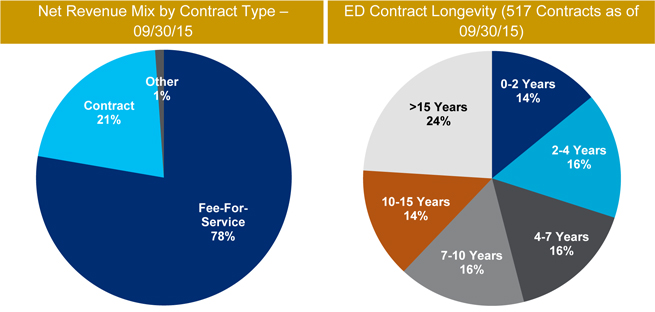
Figure 03 – TeamHealth Revenue Mix
Source: TeamHealth 2014 10-K and Q3 2015 earnings presentation.
IPC Healthcare Overview
IPC is a leading national acute hospitalist and post-acute provider group practice in the United States. Hospitalist medicine is organized around inpatient care, delivered primarily in acute care hospitals, and post-acute medicine is delivered primarily in skilled nursing facilities. IPC’s clinical services are focused on providing, managing and coordinating the entire episode of care of inpatients. IPC believes it is the largest dedicated hospitalist and post-acute provider in the United States based on revenues, patient encounters and number of affiliated clinicians. As of September 30, 2015, IPC’s approximately 2,100 affiliated clinicians, including physicians, nurse practitioners and physician assistants (collectively “affiliated clinicians”) practice in 375 hospitals and 2,025 other inpatient and post-acute care facilities primarily in 28 states. IPC has had approximately 24 million patient encounters since the beginning of 2012. Collectively, IPC’s affiliated clinicians work with more than 48,000 referring physicians and 3,500 health plans. IPC’s early entry into the emerging hospitalist industry has permitted it to establish a reputation and leadership position that IPC believes is closely identified with the success of hospitalist medicine.
10
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
IPC began operating its first hospitalist practice in 1998 and in recent years has also become a leading provider in the post-acute arena. Since that time, IPC has increased the number of practice groups to over 360 as of September 31, 2015. IPC’s affiliated clinicians are primarily full-time employees of wholly-owned subsidiaries or affiliated professional organizations.
IPC assists hospitals, post-acute care facilities and payors in improving quality of care, increasing operating efficiencies and reducing costs. Through IPC’s affiliated clinicians, IPC provides, manages and coordinates the care of hospitalized patients and serves as the inpatient partner of primary care physicians and specialists, allowing them to focus their time and resources on their office based practices or specialties. IPC provides its affiliated clinicians with the infrastructure, information management systems, specialized training programs and administrative support necessary to perform these services. These administrative services help reduce the burden associated with managing a physician practice, making IPC an attractive employer for hospitalists and post-acute clinicians whether practicing individually or in groups.
For the LTM period September 30, 2015, IPC, after giving effect for full-year impact of previously closed acquisitions, generated revenues of $808 million and Adjusted EBITDA of $84 million.
11
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 04 – IPC Healthcare Facility and Physician Overview
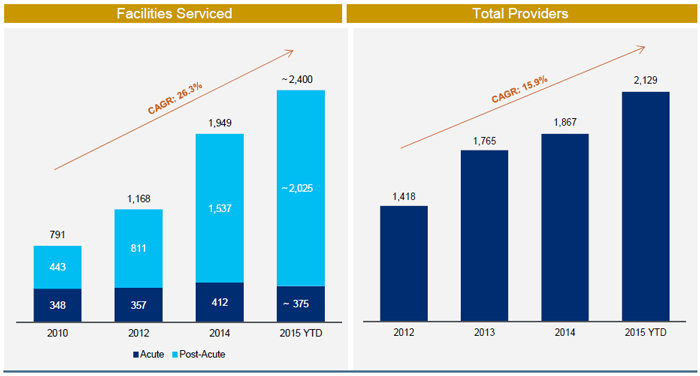
Source: Public filings.
H. Transaction Rationale
TeamHealth’s acquisition of IPC Healthcare creates a leading physician services organization spanning multiple specialties in the hospital based and post-acute settings. The combined company expects to realize several benefits from the Acquisition, including the following:
Diversifying and Highly Strategic Transaction Combines Two Physician-Centric Companies Creating the Nation’s Leading Physician Services Organization. TeamHealth is the market leader in emergency medicine (ED), servicing 17% of the 2,800 hospitals comprising TeamHealth’s target market and serving 12 million patients in 2014. The Company also enjoys a strong position in the hospital medicine and anesthesia markets, servicing 4% and 2%, respectively, of the hospitals comprising TeamHealth’s target market. IPC is a leading provider of physician outsourcing services and the largest pure-play hospitalist player. With approximately 2,100 affiliated providers serving approximately 2,400 facilities in 28 states, IPC is the largest dedicated hospitalist and post-acute provider in the United States based on revenues, patient encounters and number of affiliated clinicians. The addition of IPC’s service network will increase TeamHealth’s national presence in the acute
12
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
and post-acute markets, creating the leading physician outsourcing organization in multiple specialties. With >16,000 healthcare professionals nationwide, the combined company will have a powerful capability to manage patient care and influence outcomes while lowering costs across the continuum of care.
Combination Substantially Enhances Business Diversity, Scale and National Footprint. After consummation of the acquisition, TeamHealth expects to be one of the largest providers of multi-specialty outsourced healthcare services in the United States. The combined company’s >16,000 physicians and health-care professionals will operate in approximately 3,400 facilities across 47 states generating over $4.5bn in pro forma net revenue and approximately $490mm in pro forma adjusted EBITDA. TeamHealth believes its geographic diversification will provide it with a strong competitive position within the highly fragmented industries that the combined company will serve. The Company also believes its national scale and position as a large, public company operator has made and will continue to make it an attractive partner for physicians and service provider for clients. TeamHealth’s scalable national infrastructure drives value for customers and is a significant competitive advantage.
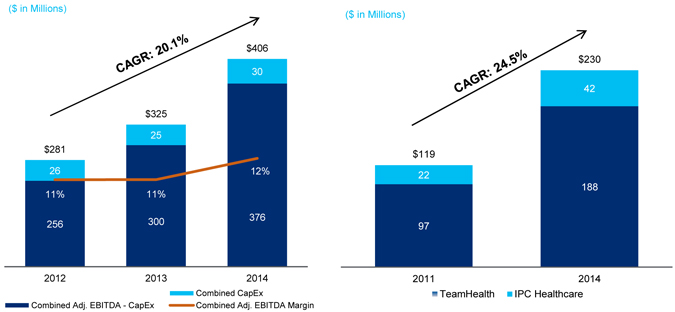
Figure 05 – Combination Enhances Scale
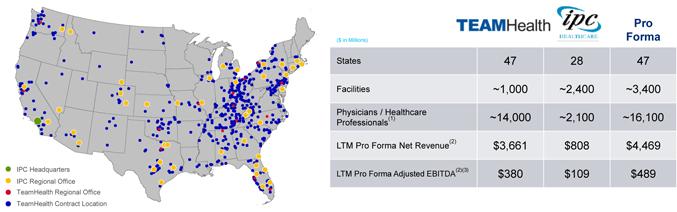
Source: TeamHealth management and public filings. See sections VI A and B for PF Adjusted EBITDA detail.
| (1) | TeamHealth physician / healthcare professionals count includes relationships with ~4,000 independent contractors. |
| (2) | Includes full year impact of previously closed acquisitions. |
| (3) | IPC Adjusted EBITDA includes $25mm of expected cost synergies. |
13
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Establishes a Leadership Position in the Large and Increasingly Strategic Post-Acute Setting. The post-acute setting represents one of the most impactable, yet expensive parts of healthcare delivery. Driven in part by trends towards value-based reimbursement models, TeamHealth’s health system customer base has increasingly expressed interest in post-acute coordination. IPC healthcare has the leading national post-acute platform, providing services in approximately 2,000 post-acute facilities across 28 states. IPC has demonstrated significant momentum in the buildout of its post-acute business, increasing the number of facilities it services from under 450 in 2010 to today’s level, representing a CAGR of 38% over the last ~5 years. TeamHealth believes there are no other competitors of scale in the post-acute space, a healthcare segment characterized as a highly fragmented and unpenetrated market comprised of approximately 15,000 facilities. Even as the clear leader in the market with significant growth in the platform over the last five years, IPC provides services in only roughly 13% of total post-acute facilities in the United States. The combined company’s expanded presence in the post-acute setting will provide TeamHealth with the powerful capability to manage patient care throughout the care continuum (from ED to post-acute) and to improve patient outcomes while lowering costs.
Enhances TeamHealth’s Positioning Relative to Key Trends Impacting the Healthcare Industry. The combined company, with its market leading service offerings in emergency medicine, hospitalist medicine, anesthesia and post-acute physician services, will be uniquely positioned to provide a differentiated suite of services to a variety of providers across the healthcare continuum. Additionally, the Acquisition enhances the positioning of the pro forma business relative to key trends impacting healthcare, including:
| • | Migration to value based reimbursement models (e.g., BPCI) |
| • | Growing importance of post-acute management |
| • | Continued outsourcing of critical hospital based physician services to large national and regional providers |
| • | Ongoing consolidation of commercial payors |
Annual Cost and Revenue Synergy Opportunity of Approximately $60 Million Within Three Years. Through its comprehensive diligence effort, TeamHealth identified a significant synergy opportunity related to the Acquisition and believes it can achieve identified annual synergies of approximately $60 million within three years of closing the transaction. The synergy opportunity is comprised of a combination of cost and revenue synergies, the realization of which will be based on an integration and synergy realization strategy that TeamHealth has successfully employed in dozens of previous acquisitions. Specifically, TeamHealth expects to achieve approximately $25 million of cost synergies as part of the IPC acquisition. This amount represents approximately 10% of the roughly $250 million of IPC corporate and combined hospital medicine regional overhead of the two companies. TeamHealth also expects to achieve EBITDA contribution of approximately $35 million related to revenue synergies as part of the IPC acquisition. The overwhelming majority of the revenue synergy opportunity is expected to be driven by leveraging TeamHealth’s robust managed care contracting and collections infrastructure (key components of the integration strategy TeamHealth has successfully employed in nearly all of its historical acquisitions).
14
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Enhances TeamHealth’s Already Attractive Financial Profile. The acquisition of IPC materially enhances TeamHealth’s already highly attractive financial profile and robust free cash flow generation, creating a pro forma company with the potential to delever quickly.
TeamHealth believes its experience and expertise in managing the complexities of high-volume EDs (a core component of its customer base) are competitive advantages and enable its hospital customers to provide higher quality and more efficient patient care. These competitive advantages, coupled with TeamHealth’s long history of demonstrated expertise, commitment to clinical excellence, superior customer service and focus on physician satisfaction, have enabled the Company to maintain long-standing relationships with many of its customers. IPC’s business model, which does not exclusively rely on contract-based revenues, will complement TeamHealth’s current business model. Additionally, TeamHealth expects the combined company to benefit from an accelerated, differentiated and diversified growth profile. While TeamHealth’s organic growth has been approximately 6% and 7% in 2013 and 2014, respectively, IPC has been able to deliver over 9% same-market revenue in each of the last three years. The Company expects IPC to continue its established track record of organic growth, which it believes to be immediately accretive to TeamHealth’s own organic growth profile.
Given the scale of each of TeamHealth’s and IPC’s businesses, and the ability to leverage administrative and support infrastructure, both companies have been able to demonstrate consistent and favorable Adjusted EBITDA margins of 10% to 12% over the last three years. Strong revenue growth coupled with stable margins and relatively low capital expenditures (roughly 1% of net revenue on a pro forma basis) and working capital requirements have resulted in strong and growing cash flows from operations. The combined company’s robust cash flow profile is expected to drive deleveraging, with a target of mid-to-low 4x leverage by the end of 2016, and to create significant capacity to continue to grow the business through a disciplined acquisition strategy.
Experienced TeamHealth Leadership Team Supplemented with Core IPC Executive Team. Upon completion of the merger, TeamHealth’s senior management team will be supplemented by members of the IPC executive team who have played a crucial role in growing IPC into the leading national acute hospitalist and post-acute provider. The new TeamHealth management team has extensive healthcare experience as well as a proven track record of successfully identifying, diligencing, executing and integrating acquisitions of physician practice groups. Jeff Taylor, IPC President and Chief Operating Officer, along with other key IPC executives, will join the combined company and will assist with the integration and the continuity of IPC’s operational plan. The combined executive team will have an average of twenty-nine years of relevant experience.
15
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
I. Industry Overview
TeamHealth estimates the size of the domestic outsourced healthcare professional staffing market for emergency medicine, hospital medicine and anesthesia to be approximately $50 billion. Over the last decade, healthcare facilities have experienced increased pressure from government and private payors both to improve the quality and to reduce the cost of care. With the increasing complexity of clinical, regulatory, managed care and reimbursement matters in today’s healthcare environment, healthcare facilities have increasingly outsourced the staffing and management of key clinical areas to companies such as TeamHealth and IPC that possess specialized skills, standardized models and information technology to improve service, increase the overall quality of care and reduce administrative costs.
TeamHealth and IPC target certain clinical areas within healthcare facilities, including emergency medicine (ED), hospital medicine, and anesthesiology. TeamHealth estimates the annual size of these markets in the United States to be approximately $12 billion, $12 billion and $21 billion, respectively.
16
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 06 – The Total Addressable Market Opportunity
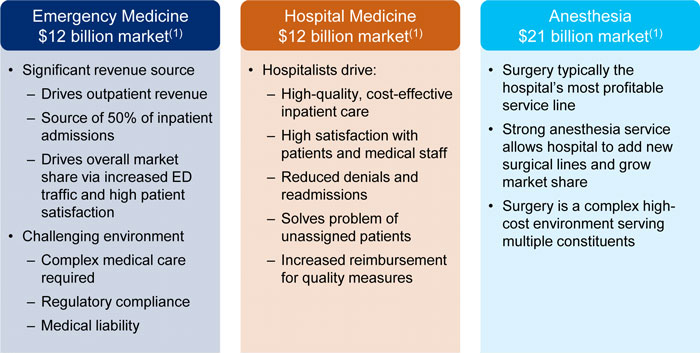
| (1) | Based on TeamHealth estimates. |
Each of these clinical areas currently faces severe physician shortages, and many healthcare facilities lack the resources necessary to identify and attract specialized, career-oriented physicians. Moreover, the market for outsourced services in each of these areas is highly fragmented and predominately served by small practice groups. TeamHealth believes these market conditions present attractive opportunities for future growth through continued consolidation and the ability to leverage its national platform and infrastructure to win new contracts.
17
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
J. Summary of Historical Financials
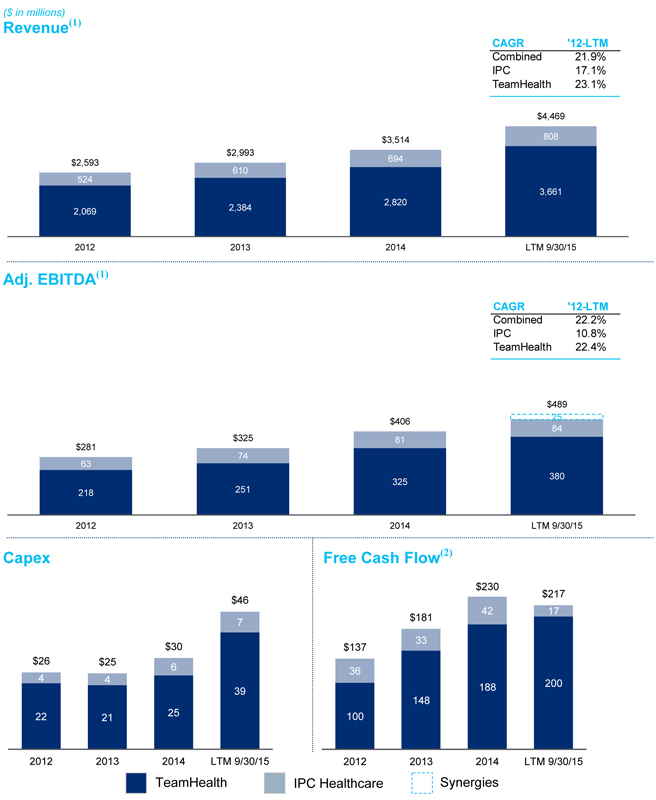
18
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Source: Public filings and TeamHealth Q3 2015 investor presentation. See sections VI A and B for PF Adj. EBITDA detail.
| (1) | LTM 9/30/15 includes full year impact of previously closed acquisitions. |
| (2) | Free cash flow represents operating cash flow plus contingent purchase payments, less capital expenditures, less net change in investments at insurance subsidiary. Figures represent actual historical financials for each company on a standalone basis and does not include pro forma adjustments for the contemplated acquisition. |
19
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
| II. | INVESTMENT HIGHLIGHTS |
A. Diversifying and Highly Strategic Transaction Combines Two Physician-Centric Companies to Create the Nation’s Leading Physician Services Organization
TeamHealth and IPC are physician-centric companies with leadership positions in their respective core service areas with vast networks of employed and affiliated physicians. The acquisition creates a leading, more diversified physician outsourcing company with complementary business mixes and cultures as well as significantly enhanced growth and free cash flow profiles. The combined company, with its service lines extending from urgent care to the post-acute setting will be even better positioned in an evolving healthcare landscape and to address the challenges facing physicians, health systems, payors and communities.
Figure 07 – Physician / Clinician Organization Spanning the Care Continuum
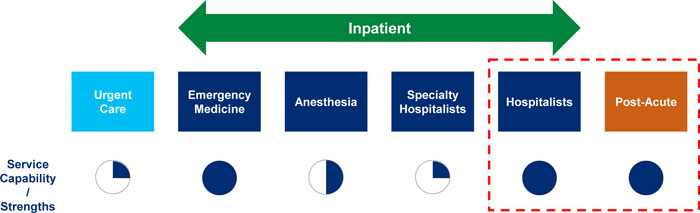
With presence in approximately 1,000 civilian and military hospitals in 47 states and affiliations with more than 14,000 healthcare professionals, TeamHealth is one of the largest suppliers of outsourced healthcare professional staffing and administrative services to hospitals and other healthcare providers in the United States. TeamHealth is a market leader in emergency medicine (ED), servicing 17% of the 2,800 hospitals comprising TeamHealth’s target market and serving 12 million patients in 2014. The Company also enjoys a strong position in the hospital medicine and anesthesia markets, servicing 4% and 2%, respectively, of the hospitals comprising TeamHealth’s target market. IPC is a leading provider of physician outsourcing services and the largest pure-play hospitalist player. With more than 2,100 affiliated providers serving approximately 2,400 facilities in 28 states, IPC is the largest dedicated hospitalist and post-acute provider in the United States based on revenues, patient encounters and number of affiliated clinicians.
The addition of IPC’s service network will increase TeamHealth’s national presence in the acute and post-acute markets, creating the leading physician outsourcing organization in multiple specialties. With >16,000 healthcare professionals nationwide, the combined company will have a powerful capability to manage patient care and influence outcomes while lowering costs across the continuum of care.
20
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
B. Combination Substantially Enhances Scale, Business Diversity, and National Footprint
The acquisition creates a combined company with significant business diversity and scale.
Figure 08 – Combination Enhances Scale
Source: TeamHealth management and public filings. See sections VI A and B for PF Adjusted EBITDA detail.
| (1) | TeamHealth physician / healthcare professionals count includes relationships with ~4,000 independent contractors. |
| (2) | Includes full year impact of previously closed acquisitions. |
| (3) | IPC Adjusted EBITDA includes $25mm of expected cost synergies. |
Market Leading, National Scale Provider of Critical Outsourced Physician Services. After consummation of the acquisition, TeamHealth expects to be one of the largest providers of multi-specialty outsourced healthcare services in the United States. The combined company’s >16,000 physicians and health-care professionals will operate in 3,400 facilities across 47 states generating over $4.5bn in pro forma net revenue and approximately $489mm in pro forma adjusted EBITDA. TeamHealth believes its
21
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
geographic diversification will provide it with a strong competitive position within the highly fragmented industries that the combined company will serve. The Company also believes its national scale and position as a large, public company operator has made and will continue to make it an attractive partner for physicians and service provider for clients. TeamHealth’s scalable national infrastructure drives value for customers and is a significant competitive advantage.
| • | 21 regional offices throughout the United States allow for local client facing support and market knowledge |
| • | Four billing centers offer national managed care contracting that works in tandem with regional operators and processes approximately fourteen million patient claims per year across a single IT platform |
| • | Centralized risk & claims management and professional liability insurance support an aggressive claims management process and captive professional liability insurance program |
| • | A centralized and well-funded administrative unit supports accounting, payroll, human resources, legal and compliance needs |
Diversifies Business and Establishes a Leadership Position in the Large and Increasingly Strategic Post-Acute Setting. After giving effect to the acquisition, TeamHealth will operate a diversified set of critical care physician services businesses with leading positions in service lines vital to the operations of acute care providers. Pro forma for the acquisition of IPC, TeamHealth’s concentration in emergency medicine will decline from 68% of 2014 net revenue to approximately 55% of pro forma 2014 net revenue. Despite acquiring the leading hospitalist medicine platform, hospitalist medicine will approximately comprise only 24% of pro forma 2014 net revenue.
Figure 09 – Combined PF Product Offering: ~3,400 facilities and LTM Revenue of ~$4.5bn
Source: TeamHealth 2014 10-K and Q3 2015 earnings presentation.
22
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
The post-acute setting represents one of the most impactable, yet expensive parts of healthcare delivery. Driven in part by trends towards value-based reimbursement models. TeamHealth’s health system customer base has increasingly expressed interest in post-acute coordination. IPC healthcare has the leading national post-acute platform, providing services in approximately 2,000 post-acute facilities across 28 states. IPC has demonstrated significant momentum in the buildout of its post-acute business, increasing the number of facilities it services from under 450 in 2010 to today’s level, representing a CAGR of 38% over the last ~5 years. TeamHealth believes IPC is the leader in the post-acute space, a healthcare segment characterized as a highly fragmented and unpenetrated market comprised of approximately 15,000 facilities. Even as the clear leader in the market, with significant growth in the platform over the last five years, IPC provides services in only roughly 13% of total post-acute facilities in the United States. The combined company’s expanded presence in the post-acute setting will provide TeamHealth with the powerful capability to manage patient care throughout the care continuum (from ED to post-acute) and to improve patient outcomes while lowering costs.
C. Enhances TeamHealth’s Positioning Relative to Key Trends Impacting the Healthcare Industry
The combined company, with its market leading service offerings in emergency medicine, hospitalist medicine, anesthesia and post-acute physician services, will be uniquely positioned to provide a differentiated suite of services to a variety of providers across the healthcare continuum. Additionally, the Acquisition enhances the positioning of the pro forma business relative to key trends impacting healthcare, including:
| • | Migration to value based reimbursement models (e.g., CMS value-based reimbursement initiatives such as Bundled Payments for Care Improvement (BPCI)) |
| • | Growing importance of post-acute management |
| • | Continued outsourcing of critical hospital based physician services to large national and regional providers |
| • | Ongoing consolidation of commercial payors |
Migration to Value Based Reimbursement Models and the BPCI Opportunity. Both commercial and government payors have articulated plans to increase the percentage of annual reimbursement paid through value-based programs in the coming years. In a January 26, 2015 press release, the Centers for Medicare and Medicaid Services (CMS) announced a goal of increasing the reimbursement of Medicare spending that flows through alternative payment models to 50% from today’s level of 20% by the end of 2018.
One such alternative payment program is the Bundled Payments for Care Improvement (“BPCI”) initiative, which illustrates the growing opportunity for providers who can efficiently and effectively coordinate patient care both within and beyond the hospital setting. Under this program, Medicare consolidates all payments for a hospitalization episode and pays a flat fee, including post-discharge care of up to 90 days, as opposed to the current system where Medicare pays on a procedure-by-procedure basis to every party involved. The BPCI program intends to consolidate payments to a single provider entity (such as a physician or hospital) with the goal of improving care coordination to ultimately drive better outcomes for patients and lower costs for
23
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Medicare. Savings are based on retrospective bundled payment arrangements, with actual expenditures reconciled against a target price for an episode of care. Providers will be incentivized under the program through a gain sharing construct whereby the provider will be entitled to a portion of total savings generated for specific patient encounters. Participating providers can select in which clinical conditions to participate and receive payment through an organization known as a “convener”. The convener enters into an agreement with CMS whereby it receives the difference between Medicare’s predetermined target price for a given clinical condition and the actual fee-for-service payment upon reconciliation of the patient episode. Successfully managing the episode of care for a lower cost than the Medicare assigned bundled payment rate results in program savings. The savings, after operating expenses and CMS’ retention of the first 2% of savings, is then distributed among the various entities involved. These entities can include physicians and other providers, hospitals, potential third-parties, the convener and TeamHealth or IPC.
Figure 10 depicts an illustrative distribution of the program gainshare to the combined company and its partners.
Figure 10 –Significant BPCI Opportunity
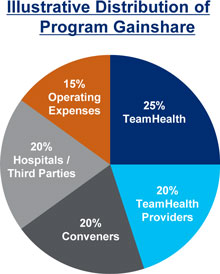
Source: TeamHealth management estimates.
This program represents a unique opportunity for the combined company given its strong pro forma presence across the continuum of care in the ED, hospital and post-acute settings. TeamHealth believes expertise across these key services will differentiate the Company’s ability to coordinate entire episodes of care for a large portion of eligible patient encounters. Select TeamHealth and IPC Healthcare provider groups began participation in phase II of the BPCI program effective July 1, 2015, leveraging state-of-the-art proprietary technology and infrastructure as well as post-acute expertise to manage a combined $2 billion of Medicare spend. While TeamHealth believes the BPCI program represents an attractive and potentially substantial opportunity, the Company has conservatively not included any revenue from BPCI in its identified synergy expectation.
24
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Growing Importance of Post-Acute Management. Estimated at a market size greater than $300 billion, the post-acute setting represents the most impactable and expensive part of healthcare delivery (CMS). With ~44% of Medicare patients discharged from acute care facilities to post-acute settings, a substantial portion of overall Medicare spend is generated in post-acute facilities today (MedPAC). That spend is expected to continue to grow as the number of Americans aged 65 and over (who represent the highest utilizers of acute care services) will increase approximately 36% to approximately 65 million by 2025 (U.S. Census Bureau). As Figure 11 demonstrates, TeamHealth anticipates the primary driver of savings for the BPCI program is post-acute management. These savings are expected to be achieved by a combination of care coordination initiatives, including procedural containment efforts, focus on clinically appropriate discharge timing and locations, reduction in average length of stay in post-acute facilities and a focus on reduction in readmit rates.
Figure 11 –Increasing Strategic Importance of Post-Acute Services
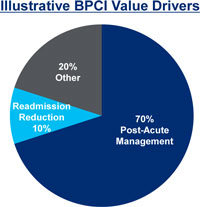
Source: TeamHealth management estimates.
Figure 12 illustrates post-acute Medicare spending has grown over 6% annually from 1999 to 2013.
25
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 12 – Growth in Medicare Spending from 1999 – 2013
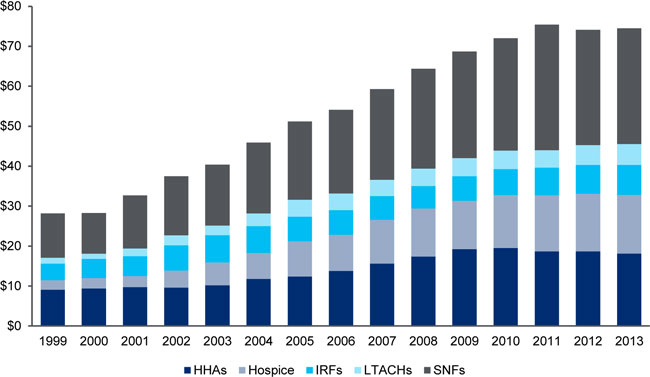
Source: CMS, MedPAC.
Shift towards national providers of physician outsourcing. Hospitals and other healthcare facilities are increasingly utilizing national providers of outsourced healthcare professionals for a variety of reasons. Third-party outsourcing services assist healthcare facilities in reducing operating expenses and in achieving targeted physician coverage levels, including addressing difficulties associated with hiring and retaining physicians. Additionally, companies such as TeamHealth and IPC are impactful to a variety of operational challenges faced by hospital administrators, including increasing operational efficiency, improving patient flow, reducing wait times, coordinating care, shortening lengths of stay and reducing readmission rates. Such improvements not only reduce the cost of care, but also improve patient outcomes, the overall quality of care and patient satisfaction. Hospitals and other healthcare providers continue to experience pressure from managed care companies and other payers to reduce costs while maintaining or improving their quality of service. Additionally, providers in general are increasingly faced with challenges related to the evolving healthcare environment, including increased administrative burdens driven by regulatory initiatives and the introduction of new reimbursement models (including bundled payments and at-risk models).
As these and other challenges continue to impact providers, TeamHealth believes hospitals and other contracting parties will increasingly turn to a single source with an established track record of success for outsourced physician staffing and administrative services. Further, partners such as TeamHealth and IPC are uniquely positioned to benefit customers through their operating models designed to provide localized presence with the benefits of scale in centralized administrative and other back office functions that accrue to larger, national companies. In 2012, approximately 65% of hospitals outsourced their emergency services and
26
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
approximately 50% of hospitals outsourced their anesthesiology services primarily to small local provider groups. However, hospitals and health systems are increasingly turning to national outsourced physician groups to meet their increasingly complex needs. The combined company is even better positioned to be a direct beneficiary of this continuing shift from smaller local groups to larger national provider organizations.
Payor Consolidation. With multiple large, pending mergers in the managed care sector, the potential exists for increased pressure on provider reimbursement from larger, more powerful commercial payors across numerous markets. Increasing scale and market relevance are amongst the key strategies for providers to employ to best counteract the potential impact of the wave of consolidation currently contemplated by the largest health insurers in the United States. The Merger not only enhances the scale and breadth of services of each of TeamHealth and IPC, but also positions the combined company to broaden its relevance in key markets through the expansion of service offerings, providing the Company with a stronger position from which to negotiate fair compensation for its high quality services. In addition, the complimentary nature of the leading emergency medicine and hospitalist medicine programs, particularly when coupled with post-acute expertise, has the potential to significantly impact cost of care while maintaining superior clinical outcomes. This dynamic should make TeamHealth a potentially powerful partner to payors seeking to steer patients towards providers with expertise across those critical clinical areas of service.
D. Strong, Stable Pro Forma Growth Profile Coupled with Robust Free Cash Flow Generation
TeamHealth and IPC represent two of the strongest and most stable high growth companies in the healthcare services sector. The acquisition of IPC enhances TeamHealth’s already attractive financial profile and robust free cash flow generation, creating a pro forma company with the potential to delever quickly.
Diversified and Recurring Revenue Stream. Both companies have a demonstrated track record of consistent growth driven by operational excellence, strong fundamentals and competitive differentiation. These characteristics are supported by market leading reputations in each of their respective core service lines as evidenced by long term customer relationships.
TeamHealth believes its experience and expertise in managing the complexities of high-volume EDs (a core component of its customer base) are competitive advantages and enable its hospital customers to provide higher quality and more efficient patient care. These competitive advantages, coupled with TeamHealth’s long history of demonstrated expertise, commitment to clinical excellence, superior customer service and focus on physician satisfaction, have enabled the Company to maintain long-standing relationships with many of its customers. The average ED contract length of TeamHealth’s top 50 customers by net revenue is approximately 13 years with many spanning over 25 years. TeamHealth’s contract stability is further demonstrated by the Company’s industry leading contract renewal rate (approximately 98% as of LTM September 30, 2015). TeamHealth has also built a diversified customer base, with no single individual staffing location accounting for more than 2% of total net revenue as of September 30, 2015.
27
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
IPC’s limited reliance on contract-based revenues will complement TeamHealth’s current business model. While hospitalist medicine contracts are in place for approximately 50% (based on revenue) of the acute care facilities in which IPC provides services, those contracts only provide IPC with access to patients admitted through the emergency department who do not have a primary care physician. IPC estimates inpatient admissions through the emergency department account for approximately only 30% of total inpatients at an average hospital, and are often patients with limited or no health insurance coverage. The remaining roughly 70% of inpatients are primarily admitted via referral by primary care or specialty physicians. These patients represent an important population of inpatients who could benefit from the oversight and care coordination IPC’s physicians provide through its market leading hospitalist medicine program. IPC is able to provide care to these patients by referral from the patient’s primary care or specialist physician. IPC relies on its well diversified referral network of over 48,000 primary and specialty care physicians as well as numerous payor relationships to provide service to this large population of patients. Importantly, IPC affiliated clinicians are able to provide hospitalist medicine services to any inpatient facility where they have credentials regardless of whether IPC has a contract with the facility. Thus, even if IPC loses a contract with a hospital, it can still provide service to patients admitted via its numerous referral sources. IPC’s patient volume at any given facility is often significantly weighted towards patients treated via referral rather than through patients seen due to contracts with the facility.
Enhancing to TeamHealth’s Already Attractive Total and Organic Growth Potential. TeamHealth expects the combined company to benefit from an accelerated, differentiated and diversified growth profile. While TeamHealth’s organic growth has been approximately 6% and 7% in 2013 and 2014, respectively, IPC has been able to deliver over 9% same-market growth in each of the last three years. The Company expects IPC to continue its established track record of organic growth, which it believes to be immediately accretive to TeamHealth’s own organic growth profile. To support its longer-term growth plan, IPC has made significant investment in growth driving functions and in re-engineering its physician retention efforts over the last year. Accordingly, IPC grew organic hires by 13% year-over-year in 2014, and year-to-date has increased new hires while lowering its physician turnover rates.
While IPC has been successful growing its business organically on a standalone basis, TeamHealth expects the combination has the potential to accelerate new contract growth. TeamHealth intends to utilize its broad geographic footprint in 47 states to expand IPC’s current presence into 20 new states and introduce IPC’s acute and post-acute services to a broad set of new potential clients leveraging TeamHealth’s long-standing customer relationships. IPC’s unique customer base also provides an attractive opportunity to expand TeamHealth’s portfolio of contracts across its suite of services. With TeamHealth providing emergency medicine services to only approximately 20% of the roughly 375 acute care facilities IPC services, a significant opportunity exists to enhance TeamHealth’s new organic contract pipeline. TeamHealth also expects industry fundamentals to drive continued tailwinds in the physician outsourcing space in both the acute and post-acute setting.
28
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 13 – Combines Two Stable and Fast Growing Providers
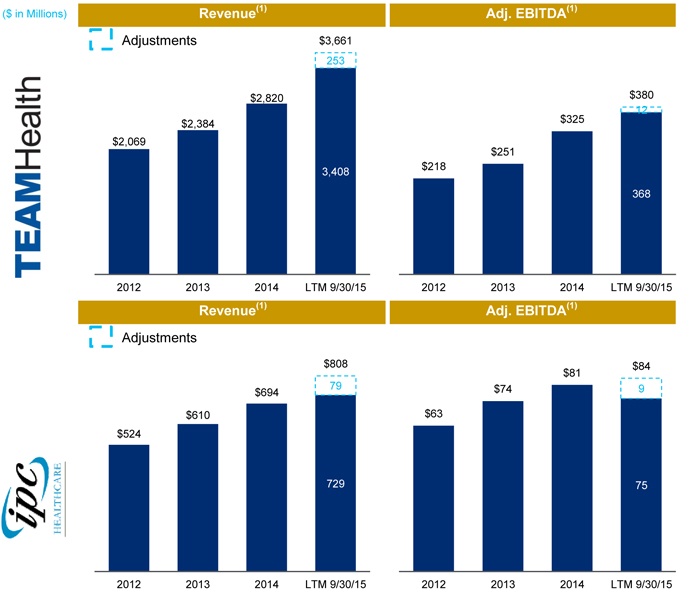
Source: Public filings and TeamHealth Q3 2015 investor presentation. See sections VI A and B for PF Adj. EBITDA detail.
| (1) | LTM 9/30/15 includes full year impact of previously closed acquisitions. |
Robust Cash Flow and Delevering Profile. Given the scale of each of TeamHealth’s and IPC’s businesses, and the ability to leverage administrative and support infrastructure, both companies have been able to demonstrate consistent and favorable Adjusted EBITDA margins of 10% to 12% over the last three years.
29
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Strong revenue growth coupled with stable margins and relatively low capital expenditures (roughly 1% of net revenue on a pro forma basis) and working capital requirements have resulted in strong and growing cash flows from operations. The combined company’s robust cash flow profile is expected to drive deleveraging, with a target of mid-to-low 4x leverage by the end of 2016, and to create significant capacity to continue to grow the business through a disciplined acquisition strategy.
Source: Public filings and TeamHealth investor presentations.
| (1) | Represent historical financials and does not include adjustments for combining companies. |
| (2) | Free cash flow represents operating cash flow plus contingent purchase payments, less capital expenditures, less net change in investments at insurance subsidiary. Figures represent actual historical financials for each company on a standalone basis and do not include pro forma adjustments for the contemplated acquisition. |
Continued Execution of Disciplined Capital Efficient M&A Opportunities. As illustrated in Figure 16, the Company’s total addressable market is characterized by significant fragmentation and comprised of a majority of local and regional competitors. Small practices and physician groups are increasingly under significant financial pressure driven in large part by growing administrative burdens due to a confluence of factors including costly and evolving regulation. As a result, these smaller physician practices are increasingly seeking to align with larger, financially stable organizations. The combined company’s broad national presence, robust infrastructure, financial resources and market leading positions in ED, hospital medicine and anesthesia, will make it an increasingly attractive partner for local and regional practice groups in those service lines.
30
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 16 – Significant M&A Opportunity in Highly Fragmented Markets
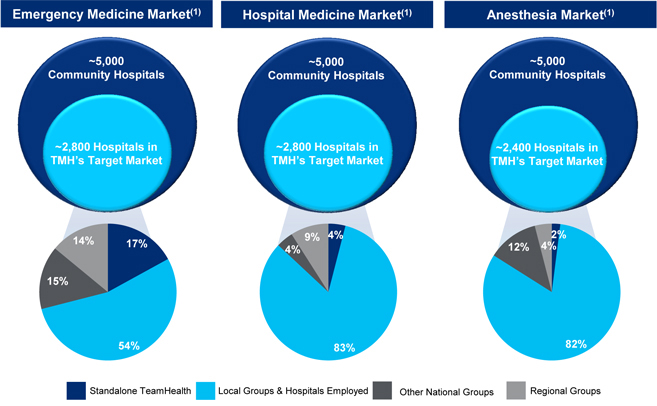
| (1) | Management Estimates |
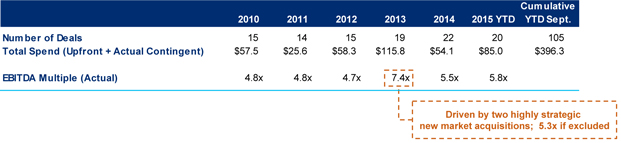
Both TeamHealth and IPC have a long track record of successfully acquiring and integrating practices of various sizes and achieving synergies. Since 2010, TeamHealth and IPC have successfully acquired 45 and 105 practices, respectively. Both companies have demonstrated an ability to source opportunities with attractive pro forma purchase multiple profiles achieved through execution on proven synergy realization strategies. Further, IPC’s leading position in the highly fragmented post-acute physician services segment provides TeamHealth with a substantial consolidation opportunity in a market largely comprised of smaller physician practices where acquisition opportunities are typically less competitive than TeamHealth’s core service lines.
31
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 17 – IPC’s Track Record of Accretive M&A
Source: IPC management.
E. Annual Cost and Revenue Synergy Opportunity of Approximately $60 Million Within Three Years
Through its comprehensive diligence effort, TeamHealth identified a significant synergy opportunity related to the Acquisition and believes it can achieve identified annual synergies of approximately $60 million within three years of closing the transaction. The synergy opportunity is comprised of a combination of cost and revenue synergies, the realization of which will be based on an integration and synergy realization strategy TeamHealth has successfully employed in dozens of previous acquisitions.
Cost Synergies. TeamHealth expects to achieve approximately $25 million of cost synergies as part of the IPC acquisition. This amount represents approximately 10% of the roughly $250 million of IPC corporate and combined hospital medicine regional overhead of the two companies. Specifically, synergies are expected to be realized through numerous initiatives including eliminating duplicative public company and corporate function costs, streamlining regional operating costs, moving to a centralized billing system and leveraging the purchasing power of the combined company to drive savings related to supply purchasing. Moreover, TeamHealth expects additional synergies will be realized through leveraging IPC-Link (IPC’s leading proprietary technology system that improves the operating efficiency of hospital medicine practice groups) in TeamHealth’s own hospitalist programs.
Revenue Synergies. TeamHealth expects to achieve EBITDA contribution of approximately $35 million related to revenue synergies as part of the IPC acquisition. The overwhelming majority of the revenue synergy opportunity is expected to be driven by leveraging TeamHealth’s robust managed care contracting and collections infrastructure (key components of the integration strategy TeamHealth has successfully employed in nearly all of its historical acquisitions). TeamHealth’s experience successfully executing on this component of the revenue synergy opportunity via its formulaic approach underpins management’s high degree of confidence around not only the total opportunity and ultimate achievability of this portion of the synergy target, but also in the ability to achieve a significant portion relatively quickly post-closing.
32
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Beyond the identified revenue synergy opportunities noted above, TeamHealth also believes additional revenue synergy opportunities exist in the form of an enhanced ED/Hospitalist medicine bundled physician services offering for acute care customers. The introduction of post-acute services to a broad array of TeamHealth’s current health system customers is also expected to contribute to the revenue synergy opportunity.
While TeamHealth only provides emergency medicine services in less than 20% of the roughly 375 acute care facilities IPC services, TeamHealth has not included any revenue from cross-selling TeamHealth and IPC core services into the unique customer bases of each individual company. Additionally, potential revenue generated from the BPCI initiative is not included in the identified revenue synergy range. Nevertheless, the BPCI opportunity potentially represents potential upside for the combined company.
F. Experienced TeamHealth Leadership Team Supplemented with Core IPC Executive Team
An integral component of TeamHealth’s integration plan for the acquisition of IPC is maintaining the continuity of IPC’s operational plan and key management. As part of the acquisition, Jeffrey Taylor, President and Chief Operating Officer of IPC, as well as other key operational leaders of IPC will join TeamHealth to supplement the executive team. These key IPC executives will continue to maintain responsibility for the execution of the IPC growth strategy and have been instrumental building, cultivating and maintaining IPCs broad physician and customer relationships over the course of IPC’s history.
TeamHealth’s senior management team, and the senior management team of IPC who will join TeamHealth upon completion of the acquisition, have extensive healthcare industry experience. The combined executive team will have an average of twenty-nine years of relevant experience.
Methodical and Well-Formulated Integration Strategy. With over 45 acquisitions successfully executed since 2010, physician group integration is a core competency of TeamHealth. While IPC represents the largest acquisition TeamHealth has made to date, many of the key integration initiatives mirror those of the numerous successful physician group practice acquisitions the Company has made throughout its history. TeamHealth and IPC executives are fully utilizing the time between signing and closing to progress integration while experienced team leaders have been identified and detailed execution plans have been developed for integration of key functional areas. To supplement management’s efforts, TeamHealth has engaged a premier management consulting group to help management coordinate key aspects of the integration.
33
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
| III. | OVERVIEW OF TEAMHEALTH |
A. Company Overview
TeamHealth is one of the largest suppliers of outsourced healthcare professional staffing and administrative services to hospitals and other healthcare providers in the United States, based upon revenues, patient visits, and number of clients. As of September 2015, the Company serves approximately 1,000 civilian and military hospitals, clinics and physician groups in 47 states with a team of more than 14,000 affiliated healthcare professionals, including physicians, physician assistants, nurse practitioners, and nurses. The Company recruits and contracts with healthcare professionals, who then provide professional services within third-party healthcare facilities.
TeamHealth is a physician-founded organization with physician leadership throughout all levels of its organization. Since the Company’s inception in 1979, TeamHealth has provided outsourced services in emergency departments, or EDs. The Company also provides comprehensive programs for anesthesiology, inpatient services (hospitalists comprising the specialties of internal medicine, orthopedic surgery, general surgery and OB/GYN), urgent care, pediatrics and other healthcare services, by providing permanent staffing that enables the management teams of hospitals and other healthcare facilities to outsource certain management, recruiting, hiring, payroll, billing and collection and benefits functions. For the LTM period September 30, 2015, TeamHealth, after giving effect for full-year impact of previously closed acquisitions, generated net revenues of $3.7 billion and Adjusted EBITDA of $380 million (excluding the impact of the contemplated acquisition of IPC).
Figure 18 – Diverse Service Offering with Particular Strength in the Emergency Department
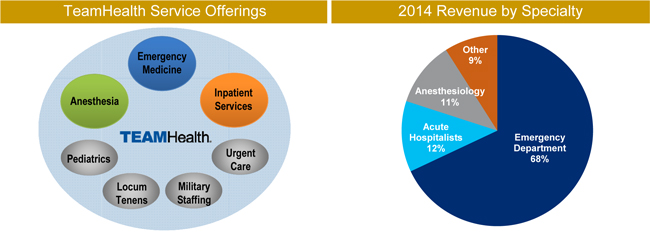
Source: TeamHealth 2014 10-K and TeamHealth investor presentations.
TeamHealth focuses on providing high-performance outsourced physician staffing solutions to hospitals. Under its business model, the Company signs exclusive contracts with hospitals that retain it to provide clinical staffing services. Once a relationship with a hospital has been formed, TeamHealth assigns affiliated physicians from its network of high-quality local physician groups to work with the hospital staff and to provide patient care. In addition,
34
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
TeamHealth works to recruit and maintain a network of top-notch local physician groups across the country. The range of physician and non-physician staffing and administrative services that TeamHealth provides to its clients include the following:
| • | Recruiting, schedule and credential coordination for clinical and non-clinical medical professionals |
| • | Coding, billing and collection of fees for services provided by medical professionals |
| • | Provision of experienced medical directors |
| • | Administrative support services, such as payroll, professional liability insurance coverage, continuing medical education services and management training |
| • | Claims and risk management services |
| • | Standardized procedures and operational consulting |
TeamHealth provides physicians and hospitals a compelling value proposition, demonstrated by a 93% physician retention rate and a 98% contract retention rate with affiliated hospitals (calculated on a preceding 12 month basis as of September 30, 2015 for ED operations). With respect to physicians, TeamHealth eases the administrative burdens associated with practice management while also providing physicians stable practice opportunities in well-regarded hospitals with competitive compensation. Furthermore, TeamHealth has demonstrated its commitment to building a strong physician-centric culture by employing physician leaders throughout all levels of its organization and by providing its physicians with continuing medical education and other opportunities for career advancement. For hospitals, TeamHealth delivers mission critical results via a robust operating platform. Supported by the resources of a national organization and 21 regional client service teams, the Company’s physicians offer hospitals customizable patient care and the option to “bundle” services.
TeamHealth is a national company delivering services through its regional operating units located in key geographic markets. This operating model enables the Company to provide a localized presence combined with the benefits of scale in centralized administrative and other back office functions that accrue to a larger, national company. The teams in TeamHealth’s regional offices are responsible for managing client relationships and for providing healthcare administrative services.
35
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
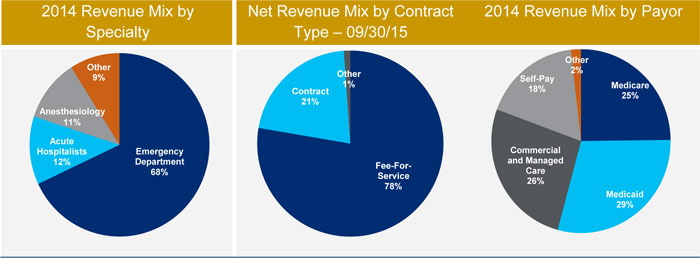
Figure 19 – TeamHealth’s National Presence
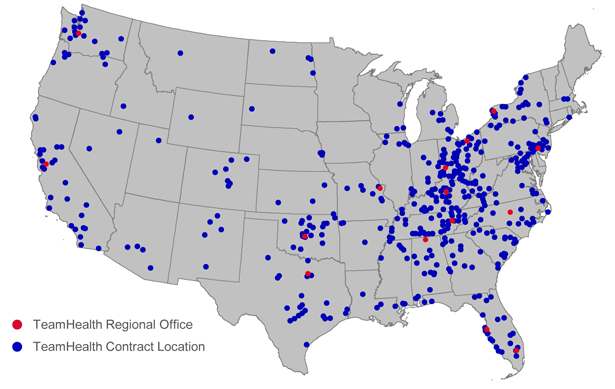
Source: TeamHealth management.
36
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 20 – Company History
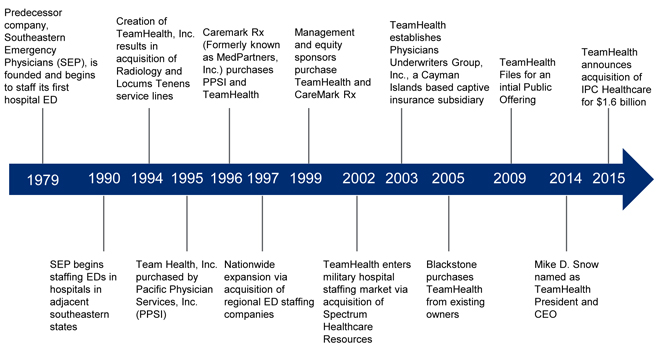
Service Lines
TeamHealth provides a full range of outsourced physician staffing and administrative services in emergency medicine, anesthesiology, inpatient services (hospitalists comprising the specialties of internal medicine, critical care, orthopedic surgery, general surgery, and OB/GYN), scribes, urgent care, pediatrics and other hospital-based functions. The Company also provides a full range of healthcare management services to military treatment and government facilities. In addition to physician-related services within a military treatment facility setting, TeamHealth also provides non-physician staffing services, including such services as para-professional providers, nursing, specialty technicians and administrative staffing to military and government facilities.
Emergency Department. TeamHealth is one of the largest providers of outsourced clinical staffing and administrative services for EDs in the United States, based upon revenues and patient visits. EDs are a significant source of hospital inpatient admissions with a majority of admissions for key medical service lines starting in EDs, making successful management of this department critical to a hospital’s patient satisfaction rates and overall success. This dynamic, combined with the challenges involved in billing and collections and physician recruiting and retention, is a primary driver for hospitals to outsource their clinical staffing and management services to companies such as TeamHealth. For the year ended December 31, 2014, the Company’s clinicians provided services to over 12 million patients within the Company’s EDs. Net revenues from ED contracts increased by approximately 72% from the beginning of 2010 through 2014, or at a compound annual growth rate of approximately 14.6%. As of December 31, 2014, TeamHealth independently contracted with or employed approximately 4,200 hospital-based emergency physicians. Net revenues derived from the ED service line were 69%, 67% and 68% of consolidated net revenues in 2012, 2013 and 2014, respectively.
37
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
TeamHealth contracts with hospitals to provide qualified emergency physicians, physician assistants and nurse practitioners for their EDs. In addition to the core services of contract management, recruiting, credentials coordination, staffing and scheduling, the Company provides client hospitals with enhanced services designed to improve the efficiency and effectiveness of their EDs. The Company has specific programs that apply proven process improvement methodologies to departmental operations. By providing these enhanced services, TeamHealth believes it increases the value of services provided to clients and improves client relations. Additionally, the Company differentiates itself from its competitors in sales situations and improves its chances of being selected in a competitive bidding process.
The EDs that TeamHealth staffs are generally located in mid-sized to larger hospitals. The Company believes that its experience and expertise in managing the complexities of these high-volume EDs enables its hospital clients to provide higher quality and more efficient physician and administrative services. In this type of setting, TeamHealth can establish stable long-term relationships, recruit and retain high quality physicians and other providers and staff, and obtain attractive payor mixes and reasonable margins. The Company has long-term relationships with customers under exclusive ED contracts with an approximate 98% renewal rate and a 93% physician retention rate as of September 30, 2015 (calculated on a preceding 12 months basis).
Anesthesiology. TeamHealth provides outsourced anesthesiology and pain management solutions to hospitals and ambulatory surgery centers on a ‘turn-key’ basis. The services provided by anesthesiologists, certified registered nurse anesthetists (CRNAs), and anesthesiologist assistants include anesthesia for the full range of surgical subspecialties, including cardiac, pediatric, trauma, ambulatory, orthopedic, obstetrical, general and ear, nose and throat, as well as interventional pain management. The Company also provides comprehensive administrative oversight and business management of these services, including processes designed to improve the efficiency and effectiveness of the anesthesiology department and the hospital’s surgical services. This, along with TeamHealth’s industry reputation and focus on high levels of customer service, provide the Company with key market differentiation. As of December 31, 2014, the Company independently contracted with or employed approximately 400 anesthesiologists. Net revenues derived from the anesthesiology service line were 8%, 10% and 11% of consolidated net revenues in 2012, 2013 and 2014, respectively.
Inpatient Services (Hospitalists Comprising the Specialties of Internal Medicine, Critical Care, Orthopedic Surgery, General Surgery and OB/GYN). TeamHealth provides physician staffing and administrative functions for inpatient services, which include hospital medicine, intensivist and house coverage services. Inpatient contracts with hospitals are generally on a cost-plus or flat rate basis. The Company also contracts directly with health plans. As of December 31, 2014, the Company independently contracted with or employed approximately 1,000 inpatient physicians. Net revenues derived from inpatient services operations were 11% of consolidated net revenues in 2012, 12% in 2013 and 12% in 2014.
38
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Other. In addition, TeamHealth operates the following business lines:
Military Staffing Services. TeamHealth provides physician and other non-physician staffing services, including such services as nursing, specialty technician and administrative staffing, primarily in military treatment and outpatient clinical facilities within the United States. These services are generally provided on an hourly contract basis. Net revenues derived from military staffing services line were 5%, of consolidated net revenues in 2012, and 2013 and 4% in 2014.
Temporary Staffing. TeamHealth provides temporary staffing (locum tenens) of physicians and advanced practice clinicians to hospitals and other healthcare organizations through a subsidiary, Daniel and Yeager, Inc., or D&Y. Temporary staffing specialties placed through D&Y include anesthesiology, hospitalists, primary care, radiology, psychiatry and emergency medicine, among others. Revenues from these services are generally derived from a standard contract rate based upon the type of service provided. Customers include hospitals, military treatment facilities and medical groups.
Pediatrics. TeamHealth provides outsourced pediatric physician staffing and administrative services for general and pediatric hospitals on a fee for service basis. These services include pediatric emergency medicine, neonatal intensive care, pediatric intensive care, urgent care centers, primary care centers, observation units and inpatient services. The Company also operates after-hours pediatric urgent care centers in Florida.
Scribes. Through its newly acquired medical scribes company, PhysAssist, TeamHealth provides documentation services to physicians and other medical personnel in a variety of healthcare environments.
Urgent Care and Occupational Medicine. TeamHealth provides cost-effective, high quality primary care physician staffing and administrative services in stand-alone urgent care clinics and in clinics located on the work-site of industrial clients. Urgent care is an emerging area that is an important part of the continuum of care and not only serves as a portal on the initial or front end of care but also as a site for the delivery of follow up post discharge care to patients.
Medical Call Center Services. Through a subsidiary, TeamHealth Medical Call Center, the Company provides medical call center services to hospitals, physician groups and managed care organizations. The 24-hour medical call center is staffed by registered nurses and specially trained telephone representatives with consultation available from practicing physicians. The services provided by TeamHealth Medical Call Center include: physician after-hours call coverage, community nurse lines, ED advice calls, physician referral, class scheduling, appointment scheduling, and web response
Contractual Arrangements
Revenues are earned from both fee for service arrangements and from flat-rate or hourly contracts. Neither form of contract requires any significant financial outlay, investment obligation or equipment purchase other than the professional expenses and administrative support costs associated with obtaining and staffing the contracts and the associated cost of working capital for such investments.
39
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
The Company’s contracts with hospitals generally have terms of three years. Present contracts with military treatment and government facilities are generally for one year. Both types of contracts often include automatic renewal options under similar terms and conditions unless either party gives notice to the other of an intent not to renew. Despite the fact that most contracts are terminable by either party upon notice of as little as 90 days, the average tenure of existing ED contracts is approximately eleven years. The termination of a contract is usually due to either an award of the contract to another staffing provider as a result of a competitive bidding process or the termination of the contract by the Company due to a lack of an acceptable profit margin on fee for service patient volumes coupled with inadequate contract subsidies. Contracts may also be terminated as a result of a hospital facility closing due to facility mergers or a hospital attempting to insource the services.
Figure 21 – Long-Term Relationships Generating Recurring Contractual Revenue
Source: TeamHealth Q3 2015 investor presentation.
Hospitals. TeamHealth provides outsourced physician staffing and administrative services to hospitals under fee for service contracts, flat-rate contracts and cost-plus contracts. Hospitals entering into fee for service contracts agree, in exchange for granting exclusivity to the Company for such services, to authorize the Company to bill and collect the professional component of the charges for such professional services. Under the fee for service arrangements, the Company bills patients and third-party payors for services rendered. Depending on the underlying economics of the services provided to the hospital, including its payor mix, TeamHealth may also receive supplemental revenue from the hospital. In a fee for service arrangement, TeamHealth accepts responsibility for billing and collections.
Under flat-rate contracts, the hospital usually performs the billing and collection services of the professional component and assumes the risk of collectibility. In return for providing the physician staffing and administrative services, the hospital pays the Company a contractually negotiated fee, often on an hourly basis. Under cost-plus contracts, the hospital typically reimburses the Company the amount of its total costs incurred in providing physicians and mid-level practitioners to perform the professional services, plus an agreed upon administrative management fee, less billings and collections of the professional component of the charges for such professional services.
40
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Physicians. TeamHealth contracts with physicians as independent contractors or employees to provide the professional services necessary to fulfill its contractual obligations to hospital clients. The Company typically pays physicians: (1) a base rate (generally for emergency physicians an hourly rate for each hour of coverage and a base salary for other physician specialties) provided at rates comparable to the market in which they work; (2) a productivity-based payment such as a relative value unit (RVU) based payment or (3) a combination of both a fixed rate and a productivity-based payment. The hourly rate varies depending on whether the physician is independently contracted or an employee. Independently contracted physicians are required to pay self-employment tax, social security, and workers’ compensation insurance premiums. By contrast, the Company pays these taxes and expenses for employed physicians.
Contracts with physicians generally have automatic renewal provisions and can be terminated at any time under certain circumstances by either party without cause, typically upon 90 to 180 days notice. Physician contracts may also be terminated immediately for cause under certain circumstances. In addition, TeamHealth has generally required physicians to sign non-competition and non-solicitation agreements. Although the terms of non-competition and non-solicitation agreements vary from physician to physician, they generally restrict the physician for two years after termination from divulging confidential information, soliciting or hiring employees and physicians, inducing termination of Company agreements, competing for and/or soliciting the Company’s clients and, in limited cases, providing services in a particular geographic region. As of September 30, 2015, TeamHealth had working relationships with approximately 6,900 physicians, of which approximately 3,900 were independently contracted.
Other Healthcare Professionals. The Company utilizes other advanced practice clinicians, such as physician assistants, nurse practitioners, certified registered nurse anesthetists and anesthesiologist assistants to assist physicians when staffing its hospital-based facilities. TeamHealth also provides other healthcare professionals such as nurses, specialty technicians and administrative support staff on a contractual basis to military treatment and government facilities. As of September 30, 2015, TeamHealth employed or contracted with approximately 7,600 other healthcare professionals.
Sales and Marketing. Contracts for outsourced physician staffing and administrative services are generally obtained either through direct selling efforts or requests for proposals. TeamHealth has a team of sales professionals located throughout the country. Each sales professional is responsible for developing sales opportunities for the operating unit in their territory. In addition to direct selling, the sales professionals are responsible for working in concert with the regional operating unit president and corporate development personnel to respond to requests for proposals or to take other steps to develop new business relationships. Although practices vary, healthcare facilities generally issue a request for proposal with demographic information of the facility department, a list of services to be performed, the length of the contract, the minimum qualifications of bidders, the selection criteria and the format to be followed in the bid. Supporting the sales professionals is a fully integrated marketing campaign comprised of an inside sales program, an internet website, journal advertising, direct mail, conventions/trade shows, online campaigns, social media, and a lead referral program.
41
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Payor Mix
The chart below summarizes TeamHealth’s approximate payor mix as a percentage of consolidated fee for service patient volume for the periods indicated:
Figure 22 – Continued Evolution Towards More Favorable Payor Mix
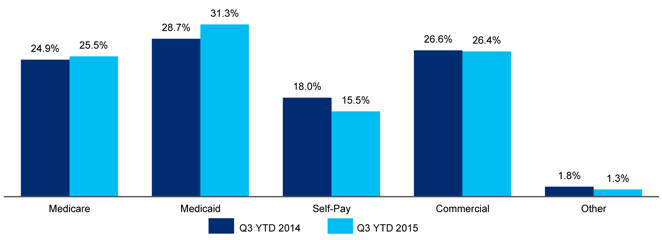
Source: TeamHealth Q3 2015 investor presentation.
Since implementation of the Patient Protection and Affordable Care Act (the PPACA), there has been a reduction in the number of uninsured patients. Accordingly, TeamHealth has begun to enjoy an improved payor mix as more patients —especially those visiting TeamHealth affiliated EDs— are insured. For the nine months ended September 30, 2015, self-pay has declined to 15.5% of total fee for service volume from 18.0% in the same period in 2014.
Service Offerings
The Company provides a full range of outsourced physician and non-physician healthcare professional staffing and administrative services, including the following:
Contract Management. The delivery of services for a clinical area of a healthcare facility is led by an experienced contract management team of clinical and other healthcare professionals. The team usually includes a regional medical director, an on-site medical director and a client services manager. The on-site medical director is a physician with the primary responsibility of coordinating the physician component of a clinical area of the facility. The medical director works with the team, in conjunction with the nursing staff and private medical staff, to improve clinical quality and operational effectiveness. Additionally, the medical director works closely with the regional operating unit’s operations staff to meet the client’s ongoing recruiting and staffing needs.
Operational Consulting. TeamHealth assists clients in achieving or exceeding their clinical, operational and financial goals through operational consulting. The Company focuses on improving patient satisfaction, reducing patient throughput times, managing resource utilization, ensuring integration among multiple service lines, improving clinical outcomes, and overall enhancing efficiency and quality of patient care. Physician and nurse coaches are utilized in providing this consulting service.
42
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Staffing. A full range of staffing services is provided to meet the unique needs of each healthcare facility. The dedicated clinical teams include qualified, career-oriented physicians and other healthcare professionals responsible for the delivery of high quality, cost-effective care. These teams also rely on managerial personnel, many of whom have clinical experience, who oversee the administration and operations of the clinical area. As a result of the Company’s staffing services, healthcare facilities can focus their efforts on improving their core business of providing healthcare services for their communities as opposed to recruiting and managing physician staffing. TeamHealth also provides temporary staffing services of physicians and other healthcare professionals to healthcare facilities on a national basis.
Recruiting. Many healthcare facilities lack the resources necessary to identify and attract specialized, career-oriented physicians. TeamHealth has a staff of more than 100 professionals dedicated to the recruitment of qualified physicians and other clinicians. These professionals are regionally located and focus on matching qualified, career-oriented physicians with healthcare facilities. Common recruiting methods include the use of robust residency relations program, proprietary national physician database, attendance at trade shows, the placement of website and professional journal advertisements, telemarketing efforts, and referrals from its existing providers.
The Company has committed significant infrastructure and personnel to the development of a proprietary national physician database to be shared among its regional operating units. This database is utilized at all of its operating units. Recruiters contact prospects through telemarketing, direct mail, conventions, journal advertising and over the Internet to confirm and update physicians’ information. Prospects expressing interest in one of the Company’s practice opportunities then provide more extensive background on their training, experience, and references, all of which are added to the database. TeamHealth’s goal is to ensure that the practitioner is a good match with both the facility and the community before proceeding with an interview.
Credentials Coordination. Primary source information is gathered regarding physicians to facilitate the review and evaluation of physicians’ credentials by the healthcare facility.
Scheduling. TeamHealth’s scheduling department assists the on-site medical directors in scheduling physicians and other healthcare professionals within the clinical area on a monthly basis.
Payroll Administration and Employee Benefits. The Company provides payroll administration services for the physicians and other healthcare professionals with whom there is contract. Clinical employees benefit significantly from the Company’s ability to aggregate eligible physicians and other healthcare professionals to negotiate more favorable employee benefit packages and to provide professional liability coverage at lower rates than many hospitals or physicians could negotiate individually. Additionally, healthcare facilities benefit from the elimination of the overhead costs associated with the administration of payroll and, where applicable, employee benefits.
Information Systems. TeamHealth has invested in advanced information systems and proprietary software packages designed to assist hospitals in lowering administrative costs while improving the efficiency and productivity of a clinical area. These systems include TeamWorks, a national physician database and software package that facilitates the recruitment and retention of physicians and supports contract requisition, credentials coordination, automated application generation, scheduling and payroll operations.
43
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
The strength of the Company’s electronic billing system and other information systems has enhanced its ability to properly collect patient payments and reimbursements in an orderly and timely fashion and has increased its billing and collections productivity. As a result of investments in information systems and the company-wide application of operational best practices policies, TeamHealth believes its average cost per patient billed and average recruiting cost per clinician are among the lowest in the industry.
Billing and Collections. The Company’s billing and collection services are a critical component of its business. The fee for service billing and collections operations are primarily conducted at one of four billing locations and operate on a uniform billing system using a state of the art billing and accounts receivable software package with comprehensive reporting capabilities. TeamHealth is able to maintain fee schedules that vary for the level of care rendered and to apply contractually agreed upon allowances (in the case of commercial and managed care insurance payors) and reimbursement policy parameters (in the case of governmental payors) to allow the Company to process payor reimbursements at levels that are less than the gross charges resulting from its fee schedules. TeamHealth’s billing system calculates the contractual allowances at the time of processing of third-party payor remittances. The contractual allowance calculation is used principally to determine the propriety of subsequent third-party payor payments. The nature of emergency care services and the requirement to treat all patients in need of such care and often times under circumstances where complete and accurate billing information is not readily available at the time of discharge, precludes the use of the Company’s billing system to accurately determine contractual allowances on an individual patient basis for financial reporting purposes. As a result, management estimates net revenues, which is the revenue estimated to be collected after considering contractual allowance obligations and estimates of doubtful accounts.
The Company has interfaced a number of other software systems with its billing system to further improve productivity and efficiency. Foremost among these is an electronic registration interface that has the capability to gather registration information directly from a hospital’s management information system. Additionally, TeamHealth has invested in electronic submission of claims and remittance posting, as well as electronic chart capture, workflow, and online coding. These programs have resulted in lower labor and postage expenses. During 2014, approximately 95% of the Company’s more than twelve million fee for service patient visits were processed by one of its four billing locations.
The Company also operates an internal collection agency. Substantially all collection placements generated from its billing locations are sent to the agency. Comparative analysis has shown that the internal collection agency is more cost effective than the use of outside agencies and has improved the collectability of existing placements. TeamHealth’s advanced comprehensive billing and collection systems allow the Company to have full control of accounts receivable at each step of the process.
Risk Management. Through the organization’s Patient Safety Organization (PSO), claims management staff, quality assurance staff, Chief Risk Officer, and medical directors, The Company manages an aggressive risk management program for loss prevention and early intervention. The Company is proactive in promoting early reporting, evaluation and resolution of serious incidents that may evolve into claims or suits. The risk management function is designed to prevent or minimize medical professional liability claims and includes:
| • | Incident reporting systems through which the Company monitors events that may potentially become claims |
44
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
| • | Tracking/trending the cause of events and claims looking for preventable sources of erroneous medical treatment or decision-making |
| • | Risk management quality improvement programs |
| • | Physician education and service programs, including peer review and monitoring and the provision of more than 300,000 hours of Category I continuing medical education credits in 2014 |
| • | Collection of loss prevention information available to affiliated providers, enabling them to review current topics in medical care |
| • | Early intervention in potential professional liability claims |
In addition, the Company has one of the most comprehensive risk management information systems on the market. TeamHealth uses this information system to enhance physician risk management assessments, malpractice claims/litigation management and the analysis of claims data to identify loss patterns/trends. The collection and analysis of claims data enables TeamHealth to evaluate losses and target risk management intervention to proactively address potential liability exposures.
Patient Safety Organization. TeamHealth has established a federally qualified PSO, whose mission is to improve patient care by conducting quality and safety analyses. Through the protection of the Patient Safety and Quality Improvement Act of 2005 and implementing regulations, confidentiality is afforded all patient safety work product analyzed within the PSO. The TeamHealth PSO creates a secure environment that enables professional analyses of clinical issues so that best practices can be developed and shared in a confidential environment that fosters a culture of continuous quality improvement in patient care and safety.
Continuing Medical Education Services. The TeamHealth Institute is fully accredited by the Accreditation Council for Continuing Medical Education and the American Nurses Credentialing Center. This allows the Company to grant its clinicians continuing medical education credits for both externally and internally developed educational programs at a lower cost than if such credits were earned through external programs. In addition to providing life support certification courses, TeamHealth has designed a series of client support educational seminars for physicians, nurses and other personnel to learn specific techniques for becoming more effective communicators and delivering top-quality customer service.
B. Business Strategy
TeamHealth intends to utilize its competitive strengths to capitalize on favorable industry trends and continue to drive growth by:
| • | Winning new contracts |
| • | Driving same contract revenue growth |
| • | Executing a disciplined M&A strategy |
| • | Enhancing profitability through operational focus |
| • | Increasing revenues from additional clinical areas |
45
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 23 – TeamHealth Has Seen Robust Revenue Growth in the Past Four Years
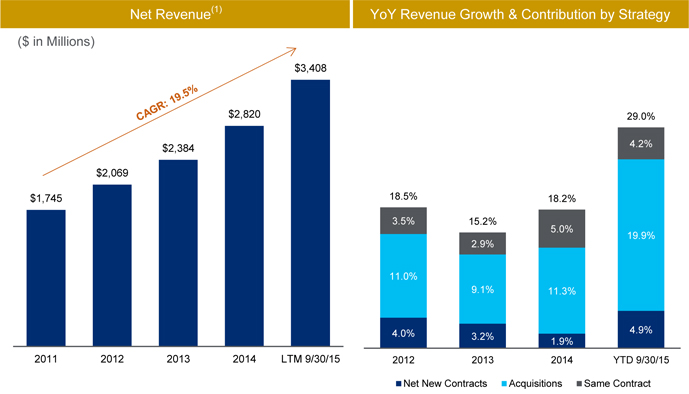
Source: Public filings and TeamHealth Q3 2015 investor presentation.
| (1) | LTM 9/30/15 excludes full year impact of previously closed acquisitions. |
Capitalizing on Outsourcing Opportunities to Win New Contracts
As hospitals and other healthcare providers continue to experience pressure from managed care companies and other payors to reduce costs while maintaining or improving their quality of service, TeamHealth believes hospitals and other contracting parties will increasingly turn to a single source with an established track record of success for outsourced physician staffing and administrative services. The Company believes it is well-positioned to capitalize on the growth in emergency medicine and other target outsourcing markets due to its:
| • | Demonstrated ability to improve productivity, patient satisfaction and quality of care while reducing overall cost to the healthcare facility |
| • | Successful record of recruiting and retaining high quality physicians and other healthcare professionals |
| • | National presence |
| • | Sophisticated information systems and standardized procedures that enable the Company to efficiently manage its core staffing and administrative services as well as the complexities of the billing and collections process |
| • | Financial strength and resources |
46
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Furthermore, the Company seeks to obtain new contracts that meet its financial targets by:
| • | Replacing competitors at hospitals that currently outsource their services |
| • | Obtaining new contracts from healthcare facilities that do not currently outsource |
| • | Expanding its present base of military treatment facility contracts by successfully competing for new staffing contracts |
Increasing Revenues from Existing Customers
As depicted above in Figure 23, TeamHealth’s net revenue growth increased at a 19.5% compound annual growth rate since 2011. Further illustrated in Figure 23 is TeamHealth’s strong record of achieving growth in revenues from its existing customer base. In 2013 and 2014, same contract revenue grew by approximately 2.9% and 5.0% on a year-over-year basis. As of September 30 2015, same contract revenue increased by 4.7% over the same period last year. The Company plans to continue to increase revenues from existing customers by:
| • | Capitalizing on increasing patient volumes |
| • | Implementing enhanced point of service capture of non-clinical patient data, resulting in improved billing and collection for services rendered |
| • | Continuing to improve documentation of clinical care delivered, thereby capturing appropriate reimbursement for services provided |
| • | Negotiating and implementing fee schedule increases, where appropriate |
| • | Cross-selling additional services within contracted healthcare facilities |
| • | Increasing staffing levels and expanding services at current military sites of service to retain patients who might otherwise receive services off-base |
| • | Participating in the BPCI program to more efficiently coordinate and manage episodes of care (as of July 2015) |
Pursuing Selective Acquisitions
The Company believes its fragmented industry provides a number of attractive opportunities for acquisitions, and estimates that approximately 68% of the ED outsourcing market is currently serviced by local and regional groups. Although TeamHealth is one of the largest providers of outsourced physician staffing and administrative services in the US, based on revenues and patient visits, its current ED and hospital medicine market shares are less than 20%.
TeamHealth has a long and successful record of executing efficiently executing on M&A opportunities. Since 2010, TeamHealth has successfully acquired 45 businesses for a combined price of $1.27 billion. The Company uses experienced teams of operations and financial personnel to conduct thorough diligence on potential targets and dedicated teams responsible for the integration of acquired centers and practices. The Company intends to continue using its robust internally generated cash flows selectively to acquire businesses at attractive multiples that would enhance both its strategic and competitive positions.
47
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Enhancing Profitability Through Operational Focus
Regional operating units supported by TeamHealth’s centralized national infrastructure are designed to continually drive operating leverage, improve efficiencies and align employee incentives to drive growth. Information systems and economy of scale allow the Company to enhance profitability with revenue growth without compromising the quality of operations or clinical care. Furthermore, TeamHealth believes its consolidated revenue platform and standardized processes related to managed care contracting, billing, coding, collection and compliance have driven a track record of strong revenue cycle management. The Company also believes its innovative patient safety and risk management initiatives and robust claims management processes have delivered favorable loss trends.
Increasing Revenues from Additional Clinical Areas
TeamHealth believes that it is well-positioned to increase market share in inpatient services (hospitalists comprising the specialties of internal medicine, orthopedic surgery, general surgery and OB/GYN), anesthesia, urgent care, locum tenens, pediatrics and medical call center areas due to its ability to leverage its infrastructure and existing client relationships as well as its recruiting and risk management expertise. The Company intends to grow its presence in these sectors by adding new clients with whom it does not currently have a relationship and cross-selling these services to existing clients.
C. Competition
The market for outsourced ED staffing and management services is highly fragmented. There are approximately 2,800 hospitals in the Company’s target market that operate full-time EDs, of which approximately 2,250 outsource to a national, regional or local emergency physician group. Of these hospitals that outsource, approximately 41% contract with a local provider, approximately 18% contract with a regional provider and approximately 41% contract with a national provider.
TeamHealth believes that EmCare Emergency Medicine, a subsidiary of Envision Healthcare (formerly Emergency Medical Services Corporation) has one of the largest shares of the ED services market based upon revenues. There are several smaller companies that provide outsourced ED services and that operate in multiple states.
Such competition could adversely affect the Company’s ability to obtain new contracts, retain existing contracts and increase profit margins. TeamHealth competes with national and regional healthcare services companies and physician groups. In addition, some of these entities may have greater access to physicians and potential clients than the Company. All of these competitors provide healthcare services that are similar in scope to some, if not all, of the services provided by the Company. TeamHealth therefore also competes against local physician groups and self-operated hospital EDs for satisfying staffing and scheduling needs.
The market for outsourced professional anesthesia services is large, diverse and highly fragmented, with approximately 2,400 hospitals in the Company’s target market, of which approximately 1,765 outsource to a national, regional or local anesthesia physician group. Of those that outsource, local groups hold the majority of the market, with approximately 75% of the hospitals outsourcing to local groups. The remaining 25% of the hospitals outsource to either regional or national groups.
48
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
TeamHealth believes that Mednax, Inc. and Sheridan Healthcare, a subsidiary of AmSurg Corp., are two of the largest providers in the anesthesia services market. There are several smaller companies, including several backed by private equity investors, that provide outsourced anesthesia services and that operate in multiple states.
The military has changed its approach toward providing most of its outsourced healthcare staffing needs through direct provider contracting on a competitive bid basis. As a result, competition for such outsourced military staffing contracts may be affected by such factors as:
| • | The lowest bid price |
| • | The ability to meet technical government bid specifications |
| • | The ability to recruit and retain qualified healthcare providers |
| • | Restrictions on the ability to competitively bid based on restrictive government bid lists or bid specifications designed to award government contracts to targeted business ownership forms, such as those determined to meet small business or minority ownership qualifications |
TeamHealth believes that it competes effectively in its industry for outsourced physician and other healthcare staffing and administrative services based, among other things, on:
| • | Ability to improve department productivity and patient satisfaction while reducing overall costs |
| • | Breadth of staffing and management services offered |
| • | Ability to recruit and retain qualified physicians, technicians and nurses |
| • | Billing and reimbursement expertise |
| • | Reputation for compliance with state and federal regulations |
| • | Financial stability |
D. Employees
As of September 30, 2015, TeamHealth had approximately 14,400 employees, of which approximately 4,100 worked in billing and collections, operations and administrative support functions, approximately 3,000 were physicians and approximately 7,600 were other healthcare providers. In addition, the Company had agreements with approximately 4,200 independent contractors, of whom approximately 3,900 were physicians.
E. Regulatory and Reimbursement Matters
On March 23, 2010, the Patient Protection and Affordable Care Act (the PPACA) was signed into law and is expected to significantly affect the U.S. healthcare system. While the ultimate impact of the PPACA and implementing regulations will not be known until all provisions are fully implemented, TeamHealth believes that the law will potentially benefit its operating performance by improving its payor mix and reducing its bad debt expense. These improvements are expected to occur because the PPACA is likely to create reductions in the number of uninsured patients, especially for EDs, which have more exposure to the uninsured than other medical specialties. Indeed, recent projections from the Congressional Budget Office reflect a 24 million reduction in the current estimate
49
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
of 52 million uninsured individuals over the three year period starting in 2015. Since implementation of the PPACA, TeamHealth has already begun to enjoy an improved payor mix. For the nine months ended September 30, 2015, self-pay has declined to 15.5% of total fee for service volume from 18.0% in the same period in 2014.
The Centers for Medicaid and Medicare Services (CMS) reimburses TeamHealth’s services to Medicare beneficiaries based upon the rates in the Medicare Physician Fee Schedule (MPFS), which are updated each year based on the Sustainable Growth Rate (SGR) formula enacted under the Balanced Budget Act of 1997. Medicare accounts for approximately 17% of the Company’s consolidated net revenue in 2014 and 19% YTD through September 2015. Additionally, many private payors use the MPFS to determine their own reimbursement rates. The application of the SGR formula to the MPFS yielded negative updates every year beginning in 2002, although CMS was able to take administrative steps to avoid a reduction in 2003 and Congress periodically acted each year to prevent reductions each year from 2004 through March 31, 2015. While the SGR has been an overhanging Medicare reimbursement risk to all physicians for many years, recent Congressional action has permanently addressed this issue. Legislation enacted on April 16, 2015 repeals the SGR and provides for an annual 0.5% increase to physician reimbursement rates for a five-year period (from July 1, 2015 through the end of 2019). In 2020 and subsequent years, physician payments will be tied to quality performance and participation in alternative payment models. For a comprehensive update on pending regulatory matters, please refer to the Company’s public filings available on EDGAR.
F. Proceedings and Insurance
TeamHealth is currently a party to various legal proceedings arising in the ordinary course of business, but does not believe the ultimate outcome of such proceedings, individually and in the aggregation, will have a material adverse effect on its financial position or operations. For a comprehensive update on pending legal matters, please refer to the Company’s public filings available on EDGAR.
TeamHealth requires the physicians with whom it contracts to obtain professional liability insurance coverage. For independently contracted physicians, TeamHealth typically arranges for, and for employed providers, typically provides for, claims-made coverage with per incident and annual aggregate per physician limits and per incident and annual aggregate limits for various corporate entities. These limits are deemed appropriate by management based upon historical claims, the nature and risks of the business and standard industry practice.
Additionally, the Company provides for a significant portion of its professional liability loss exposures through the use of a captive insurance company and through greater utilization of self-insurance reserves. The Company bases a substantial portion of its provision for professional liability losses on periodic actuarial estimates of such losses. The Company is usually obligated to arrange for the provision of tail coverage for claims against its clinicians for incidents that are incurred but not reported during periods for which the related risk was covered by claims-made insurance. With respect to those clinicians for whom the Company obligated to provide tail coverage, the Company accrues professional liability reserves based on the actuarial estimates of such incurred but not reported claims.
50
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
TeamHealth also maintains general liability, vicarious liability, automobile liability, property, directors and officers and other customary coverages in amounts deemed appropriate by management based upon historical claims and the nature and risks of the business.
51
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
G. Management
| Name | Title | Years Experience | ||
| Michael D. Snow | President, Chief Executive Officer and Director | 30 | ||
| David Jones | EVP, Chief Financial Officer | 23 | ||
| Oliver Rogers | EVP, Chief Operating Officer | 35 | ||
| Miles Snowden, M.D., MPH. | Chief Medical Officer | 28 | ||
| Joe Carman | Chief Administrative Officer | 26 | ||
| Steve Clifton | EVP, General Counsel, Corporate Secretary | 29 | ||
Michael D. Snow, President, Chief Executive Officer
Michael D. Snow joined TeamHealth as president in 2013, and in September 2014 assumed the additional role of chief executive officer and president of TeamHealth. He is also a member of the TeamHealth Board of Directors. As president and chief executive officer, Mr. Snow oversees the organization’s operations, revenue cycle, administrative services, sales and marketing. Throughout his career, Mr. Snow has held numerous executive-level positions in the healthcare arena, including president of HCA Gulf Coast Division, executive vice president and chief operating officer of HealthSouth Corporation, president and chief executive officer of Surgical Care Affiliates, president and chief executive officer of Wellmont Health System and chief operating officer of Amedisys, Inc. Mr. Snow earned his bachelor’s degree from the University of Alabama and a master’s degree in business administration from Troy State University.
David Jones, Executive Vice President, Chief Financial Officer
As chief financial officer, David Jones is responsible for all accounting and financial reporting matters of TeamHealth and works closely with executive management and the Board of Directors on the strategic direction and growth of TeamHealth. Mr. Jones first joined TeamHealth in 1994 as controller and was named chief financial officer in 1996, followed with his promotion to executive vice president and chief financial officer in 2010. Prior to joining TeamHealth, Mr. Jones worked for the accounting firm KPMG Peat Marwick in Nashville, Tennessee, and healthcare accounting and consulting firm Pershing Yoakley & Associates. Mr. Jones received his bachelor’s degree in business administration from The University of Tennessee, Knoxville.
52
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Oliver Rogers, Executive Vice President and Chief Operating Officer
As executive vice president and chief operating officer, Oliver Rogers oversees the national field operations of TeamHealth, including Emergency Medicine; Anesthesia; Hospital Medicine, including intensivists and post-acute providers; Specialty Hospitalists; Urgent Care; Spectrum (staffing for governmental healthcare facilities); Daniel and Yeager (locum tenens providers); and PhysAssist (medical scribes). Mr. Rogers has more than 35 years of management experience in a variety of healthcare organizations, including hospitals and large physician practice groups. He joined TeamHealth Southeast in 2003 as executive vice president and was promoted to CEO of that division in 2006. Under his leadership, TeamHealth Southeast experienced unprecedented growth and client retention. Mr. Rogers was promoted to president of TeamHealth Hospital Based Services in 2010 and was responsible for national contract management of TeamHealth’s emergency medicine, hospital medicine, anesthesia, urgent care and specialty hospitalist service lines. Mr. Rogers received his undergraduate degree in Business Administration from The University of North Carolina and a Master of Hospital Administration degree from Duke University.
Miles Snowden, M.D., MPH., Chief Medical Officer
As chief medical officer of TeamHealth, Dr. Miles Snowden is responsible for improving the overall quality of patient care provided by TeamHealth-affiliated physicians and advanced practice clinicians. Dr. Snowden also works to establish effective integration plans for hospital partners, provide educational support on important clinical topics and develop data-driven care plans and processes that measure improvement across the organization. He provides oversight for the TeamHealth Patient Safety Organization and supervises clinical data analysis and risk prevention education initiatives that help physician members enhance patient safety. With more than 30 years of clinical leadership experience, Dr. Snowden brings valuable knowledge of innovation, consultation and management to his role as chief medical officer of TeamHealth. Dr. Snowden’s professional background includes serving as the chief medical officer for Optum, UnitedHealth Group’s services division, and Delta Air Lines. Prior to these positions, Dr. Snowden held a private practice in Louisville, Kentucky, and founded an occupational health consulting business. Dr. Snowden received his medical degree from the University of Louisville School of Medicine. He completed an internal medicine residency at the University of Alabama – Birmingham and is board certified in internal medicine and preventive medicine. Dr. Snowden also holds a master’s of public health degree.
Steve Clifton, Executive Vice President, General Counsel and Corporate Secretary
As executive vice president, general counsel and corporate secretary for TeamHealth, Steve Clifton provides counsel to TeamHealth’s Board of Directors and clinical and administrative leadership. Mr. Clifton will also develop, direct and manage the legal functions of the organization, including corporate governance, mergers and acquisitions, regulatory and contractual compliance, partnerships and affiliations, and healthcare operations. Prior to joining TeamHealth, Mr. Clifton most recently served as senior vice president and general counsel at Health Management Associates (HMA), vice president of legal operations at Hospital Corporation of America (HCA), corporate counsel at Alliant Health System and associate attorney at Wyatt, Tarrant & Combs. He received his bachelor’s degree from Western Kentucky University and his law degree from the University of Kentucky.
53
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
| IV. | OVERVIEW OF IPC HEALTHCARE |
A. Company Overview
IPC is a leading national acute hospitalist and post-acute provider group practice in the United States. Hospitalist medicine is organized around inpatient care, delivered primarily in acute care hospitals, and post-acute medicine is delivered primarily in skilled nursing facilities. IPC’s clinical services are focused on providing, managing and coordinating the entire episode of care of inpatients. IPC believes it is the largest dedicated hospitalist and post-acute provider in the United States based on revenues, patient encounters and number of affiliated clinicians. As of September 30, 2015, IPC’s more than 2,100 affiliated clinicians, including physicians, nurse practitioners and physician assistants (collectively “affiliated clinicians”) practice in 375 hospitals and 2,025 other inpatient and post-acute care facilities primarily in 28 states. IPC has had approximately 24 million patient encounters since the beginning of 2012. Collectively, IPC’s affiliated clinicians work with more than 48,000 referring physicians and 3,500 health plans. IPC’s early entry into the emerging hospitalist industry has permitted it to establish a reputation and leadership position that IPC believes is closely identified with the success of hospitalist medicine. For the LTM period September 30, 2015, IPC, after giving effect for full-year impact of previously closed acquisitions, generated revenues of $808 million and Adjusted EBITDA of $84 million.
54
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 24 – IPC Facility Mix / IPC Revenue Mix / Provider Headcount Growth
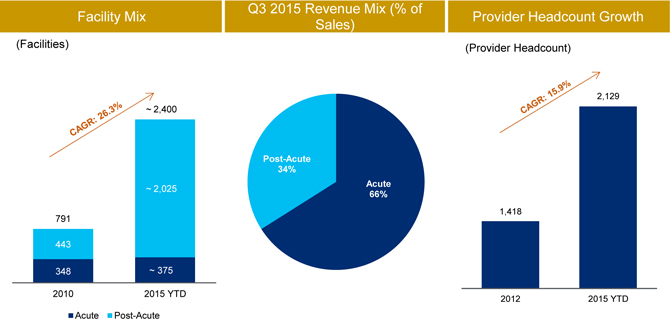
Source: Public filings and IPC Q3 2015 earnings call transcript.
IPC began operating its first hospitalist practice in 1998 and in recent years has also become a leading provider in the post-acute arena. Since that time, IPC has increased the number of practice groups to over 360 as of September 31, 2015. IPC’s affiliated clinicians are primarily full-time employees of wholly-owned subsidiaries or affiliated professional organizations.
IPC assists hospitals, post-acute care facilities and payors in improving quality of care, increasing operating efficiencies and reducing costs. Through IPC’s affiliated clinicians, IPC provides, manages and coordinates the care of hospitalized patients and serve as the inpatient partner of primary care physicians and specialists, allowing them to focus their time and resources on their office based practices or specialties. IPC provides its affiliated clinicians with the infrastructure, information management systems, specialized training programs and administrative support necessary to perform these services. These administrative services help reduce the burden associated with managing a physician practice, making IPC an attractive employer for hospitalists and post-acute clinicians whether practicing individually or in groups.
55
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Service Lines
IPC provides outsourced hospital medicine solutions to hospitals and post-acute facilities. IPC’s hospitalists assist hospitals, post-acute care facilities and payors in improving quality of care, increasing operating efficiencies and reducing costs. Specifically, hospitalists provide, manage and coordinate the care of hospitalized patients and serves as the inpatient partner of primary care physicians and specialists, allowing them to focus their time and resources on their office based practices or their specialties. IPC also provides its affiliated physicians with the infrastructure, information management systems, specialized training programs and administrative support necessary to perform these services. IPC generates the entirety of its revenue from its acute and post-acute hospital medicine services.
Business Model
Upon admission to a hospital or post-acute facility, a patient may be assigned to a hospitalist who provides, manages and coordinates the care of that patient. The hospitalist has an exclusive focus on facility-based care and possesses expertise in the diagnosis and treatment of conditions requiring facility admission. The hospitalist’s singular focus on the patient throughout the stay and discharge helps shorten a patient’s average length of stay, lowers readmission rates and generally improves patient outcomes. If a hospitalist is discharging a patient to a lower acuity setting, the hospitalist often has the ability to refer a patient to a post-acute service center staffed by IPC, generating an internal referral. Hospitalist care is reimbursed as a facility visit with one billable hospital visit per day, per patient. The coding is straightforward (only three coding options), which minimizes ambiguity and administrative issues for physicians. IPC often credentials and staffs their employees in facilities without negotiating a contract with the facility, instead relying on its vast referral network for patient volume.
Attractive Value Proposition to Physicians. The IPC business model allows for significant clinical autonomy within a large national practice group that relieves physicians of the administrative burden, strained resources and risk associated with smaller practices. Once a billable visit has been successfully entered into IPC-Link®, IPC’s administrative support takes care of the subsequent financial reporting, billing and collections, risk management and compliance related items. Additionally, being part of a larger physician practice allows for more negotiating powers with hospitals and
56
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
reduces much of the job security and mobility risk associated with smaller practices. Still, IPC strives to retain the entrepreneurial spirit of smaller private practices by offering competitive, performance-based compensation to motivate employees to outperform and stay with the company.
Attractive Value Proposition to Facilities. Facilities recognize that hospitalists are key influencers of lower readmission rates, appropriate lengths of stay and improved outcomes. With the continued move towards value-based care in the healthcare industry, the necessity of competent hospitalists is only becoming more apparent. IPC’s pure hospitalist focus has allowed them to be the lowest cost provider of hospitalist services in the healthcare industry. Additionally, IPC removes the administrative burden of billing, staffing, collecting and ongoing training for which a facility would otherwise bear responsibility. IPC’s significant scale and resources allows for assured, consistent solutions and bundled arrangements across multiple facilities.
Contractual Arrangements
Limited Reliance on Contract-Based Revenue. IPC’s affiliated clinicians, in general, provide services in any inpatient facility where they have credentials and call privileges, regardless of whether it has entered into a contract with the inpatient facility. Only 8% of IPC’s total revenue YTD through September 30, 2015 was paid by hospitals and post-acute facilities. When IPC contracts with hospitals and other inpatient or post-acute care facilities, it typically provides various professional services, including supporting the emergency department, assisting in bed allocation, planning patient discharge, coordinating with ancillary departments, cooperating with facility management, developing facility policies and procedures, training facility personnel and developing call schedules. IPC believes its facility contracts benefit the inpatient facility by establishing a stable and consistent provider of hospitalist and post-acute care services to that facility, while IPC benefits by having its affiliated clinicians obtain the opportunity to provide patient care services to patients admitted through the emergency department who do not have a primary care physician available to care for them, expanding the base of the referral relationships within the facility and strengthening IPC’s contractual revenue base. In these contracted facilities, billings to third-party payors for direct patient care constitute the most significant source of IPC’s revenue. The term of these contracts varies between facilities, but they typically can be terminated with cause for various reasons and usually contain provisions allowing for termination without cause by either party upon 90 days notice. Agreements with the inpatient facilities typically contain confidentiality provisions and requirements that the facilities maintain their own insurance. IPC has structured these contracts and agreements in accordance with the restrictions and requirements of applicable federal and state laws.
57
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Contracts with Health Plans. IPC’s regional management teams negotiate health plan contracts on behalf of its affiliated clinicians in their local markets. These agreements vary from plan to plan and payment is typically a negotiated fee per service. IPC’s regional management teams assist its affiliated clinicians with any required credentialing with these plans, provide ongoing contract management and maintain the relationships with the health plans. IPC believes that these health plan contracts can enhance its practices by capturing additional patient volumes as well as promoting prompt payment for services.
Affiliated Clinicians and Practice Groups. IPC’s practice groups and affiliated clinicians are responsible for the provision of medical care to patients. IPC’s affiliated clinicians are employees of either its wholly-owned subsidiaries or affiliated professional organizations. IPC’s affiliated professional organizations are separate legal entities, comprised of corporations, limited liability companies and limited partnerships. For financial reporting purposes, IPC consolidates the revenues and expenses of all its practice groups that IPC owns or manages because it has a controlling financial interest in these practices based on applicable accounting rules as described in IPC’s accompanying consolidated financial statements. IPC provides all of the non-medical, administrative and management services necessary for the operations of each of its affiliated professional organizations under comprehensive long-term management agreements. Under the terms of these agreements, IPC is paid for the provision of these non-medical management services based upon either the financial performance of the applicable practice group or a fixed fee. Each agreement is for a term of 20 years with 10 year automatic renewal periods, which IPC may terminate at any time, with or without cause, with 30 days prior written notice to the affiliated professional organization. Agreements with IPC’s affiliated professional organizations contain a confidentiality provision and a power of attorney appointing IPC as its attorney-in-fact.
Each affiliated professional organization is organized or qualified to do business in a state where only a physician-owned professional entity may provide medical services, and each affiliated professional organization is owned by a licensed physician. To ensure IPC’s continued affiliation with and management of the affiliated professional organizations, IPC has entered into a succession agreement with each affiliated professional organization and physician owner that prohibits the sale or transfer of the ownership interests of the affiliated professional organization to non-physicians and provides for the repurchase of such ownership interests by the affiliated professional organization for a nominal amount upon the occurrence of certain events. IPC has structured these arrangements in accordance with the restrictions and requirements of applicable state law, including state law that prohibits the corporate practice of medicine.
58
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
IPC’s affiliated clinicians are employed under contracts which typically have one or two year employment terms with automatic extensions. The contracts can be terminated with cause for various reasons, and generally contain provisions allowing for termination without cause by either party upon 30 to 60 days notice. Agreements with IPC’s affiliated clinicians generally contain a confidentiality provision and a non-compete and/or non-solicitation provision. The scope and enforceability of these provisions varies from state to state.
IPC’s affiliated clinicians generally are paid a competitive fixed base salary, and most are eligible to participate in IPC’s physician incentive compensation plan, which provides varying bonuses based upon productivity and practice group profitability. IPC typically provides professional liability and workers compensation coverage, along with vacation, sick leave, continuing medical education, health, disability and 401(k) benefits.
IPC also utilizes the services of independent contractors for certain of its health plan contracts. The independent contractors are paid on a per case basis.
Payor Mix
IPC generates approximately 92% of its net revenue from billings to third-party payors such as Medicare, Medicaid, managed care organizations and insurance companies. IPC generates the remaining 8% of its net revenue from hospitals and other inpatient and post-acute care facilities for organizing and managing clinical programs, providing medical directorships and providing coverage for patients admitted from the emergency department who otherwise have no assigned admitting physician.
59
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
With respect to revenue generated from billings to third-party payors, Figure 25 summarizes the approximate payor mix as a percentage of patient encounters for the periods indicated:
Figure 25 – IPC Payor Mix
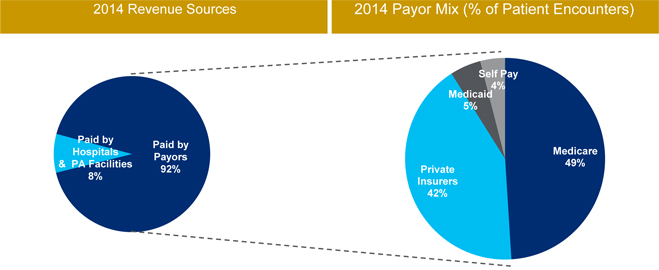
Source: IPC 2014 10-K.
Note: IPC payor mix reported as a percentage of patient encounters. IPC’s commercial payor mix includes commercial payor managed government programs (Managed Medicare and Managed Medicaid).
IPC derives a significant portion of its revenue from services rendered to beneficiaries of Medicare, Medicaid and other governmental healthcare programs. Participation in these programs requires compliance with stringent and often complex enrollment and reimbursement requirements. The applicable standards are subject to statutory and regulatory changes, administrative rulings, and new interpretations of policy that may be difficult to predict and that may require significant changes to IPC’ operations.
IPC relies upon its affiliated clinicians to appropriately and accurately complete necessary medical record documentation and assign appropriate reimbursement codes for their services. Reimbursement to IPC is conditioned on affiliated clinicians providing the correct procedure and diagnosis codes and properly documenting the services themselves, including the level of service provided, and the medical necessity for the services. If affiliated clinicians have provided incorrect or incomplete documentation or selected inaccurate reimbursement codes, this could result in nonpayment for services rendered or lead to allegations of billing fraud. This could subsequently lead to civil and criminal penalties, including exclusion from government healthcare programs, such as Medicare and Medicaid.
60
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Service Offerings
IPC provides its affiliated clinicians with administrative and professional services to support their practice of medicine, reduce their administrative burden and improve their operating efficiencies.
Regional Management. Each of IPC’s operating regions is led by an experienced executive director and team of marketing and administrative staff that is responsible for the overall non-clinical management of IPC’s affiliated practice groups within a region, as well as coordinating clinician recruitment, monitoring financial performance and contracting with facilities and payors. IPC’s regional executive directors and their staff provide its affiliated clinicians with direct, day-to-day access to an experienced management team that is familiar with the opportunities and challenges faced by IPC’s clinicians in a particular region.
Recruiting. As a national company, IPC has greater resources to commit to recruiting hospitalists and post-acute clinicians than most other practice groups do. IPC has a dedicated staff of recruiting professionals who are regionally assigned to source, screen and provide candidates to each of its local markets. IPC’s recruiting strategy includes advertising in national physician publications and websites, exhibiting at professional association meetings, establishing a regular presence at select residency programs and leveraging IPC’s existing clinician relationships.
Training. IPC has developed extensive training programs and tools for its newly hired clinicians and its existing affiliated clinicians. IPC’s newly hired clinicians are required to enroll in its comprehensive new hire training program prior to treating patients. The new hire training program emphasizes the role of the hospitalist or post-acute clinician in leading the clinical care team and provides training on billing and medical record documentation, compliance, risk management and other related topics regarding hospitalist and post-acute care practices. Newly hired clinicians are also paired with experienced local affiliated clinicians as part of the new-hire training program. IPC provides continuing medical education programs for its existing affiliated clinicians that are designed to enhance the skills of its affiliated clinicians in key areas, including clinical, risk management and compliance. IPC sponsors local and national retreats for its affiliated clinicians to foster better communication and learning and enhance their professional practices. Additionally, IPC uses the automated reporting capabilities of IPC-Link ® to allow its affiliated clinicians to compare and benchmark performance metrics. This information provides positive feedback to IPC’s affiliated clinicians when strong performance is achieved and helps to identify specific areas for improvement.
61
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Financial Reporting. Each month IPC provides its practice groups with a detailed financial statement that enables each of its affiliated clinicians to see the financial performance of their respective practices. IPC’s incentive compensation plan is based on these financial statements and provides transparency regarding bonus compensation to IPC’s affiliated clinicians.
Billing and Collections. IPC assumes responsibility for all billing, reimbursement and collection processes relating to clinical services provided by its affiliated clinicians and practice groups. To address the increasingly complex and time-consuming process for obtaining reimbursement for medical services, IPC has invested in both the technical and human resources necessary to create an efficient billing and reimbursement process. IPC provides extensive training to its affiliated clinicians, which emphasizes detailed documentation and proper coding protocol for services provided and procedures performed.
Risk Management. IPC provides risk management and quality management programs to its affiliated clinicians. IPC takes a proactive role in promoting early reporting, evaluation and resolution of incidents that may evolve into medical claims. IPC risk management program includes clinician education and a sophisticated claims management program. The collection and analysis of claims data enables IPC to identify loss patterns and trends to better target risk management intervention and proactively address potential liability. Risk management education is included in IPC’s core orientation program for newly hired clinicians, and advanced risk management topics are offered to its tenured affiliated clinicians.
Compliance. Compliance programs are an important part of IPC’s operations, which permit it and its affiliated clinicians to respond to new regulations and legislation as they arise. IPC has invested significant resources in developing and enhancing its compliance programs, including proprietary compliance issue tracking databases, routine checks of the U.S. Department of Health and Human Services Office of the Inspector General (OIG) list of Excluded Persons or Entities, automated monitoring of key claims management processes and facility contract analysis and monitoring. IPC also provides comprehensive monitoring and internal auditing processes by both internal staff and third-party coding specialists. Compliance education is an important component of IPC’s new hire training program for its entire staff.
62
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Information Management System. IPC provides its affiliated clinicians with access to IPC-Link® and other third party applications (collectively IPC-Link ® ) through IPC’s web-based “Virtual Office” portal to support their clinical, administrative and communications needs. IPC-Link ® is distinctive in its ability to capture the results of each doctor-patient encounter and organize these results into a searchable database. IPC-Link ® enables IPC’s affiliated clinicians to view and record important patient data, and allows clinicians in a practice group to share patient information as needed. Additionally, the technology enables IPC’s affiliated clinicians to communicate directly and securely to its clinical call center and risk management and compliance departments. IPC-Link ® includes a secure, HIPAA-compliant web interface, which allows IPC to assume responsibility for billing, collection and reimbursement for services rendered by its affiliated clinicians.
Transition Management. IPC uses IPC-Link® to create customized surveys for patients who are discharged to home from an inpatient facility. To assist in monitoring and documenting the patient’s discharge or transition to outpatient care, IPC-Link ® provides IPC’s call center with patient information and follow-up instructions. IPC’s system provides for its dedicated call center staff of patient representatives and nurses to contact the discharged patient, usually within 48 hours of discharge to home, to discuss the patient’s ability to understand post-discharge instructions, obtain prescribed medication, schedule an appointment with a primary care physician, and fulfill other health-related post-discharge needs. IPC’s system enables it to identify a patient’s post-discharge medical issues on a near real-time basis, coordinate care with the appropriate care provider, improve outcomes, lower the re-admission rate into inpatient facilities, and decrease IPC’s medical malpractice risk.
Geographic Coverage
IPC provides services primarily in the following 28 states: Alabama, Arizona, California, Colorado, Connecticut, Delaware, Florida, Georgia, Idaho, Illinois, Kansas, Kentucky, Maryland, Massachusetts, Michigan, Missouri, Nevada, New Jersey, New York, North Carolina, Ohio, Pennsylvania, Rhode Island, South Carolina, Tennessee, Texas, Virginia, and Washington.
63
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 26 – IPC’s Geographic Footprint

Source: TeamHealth management.
During 2014, 2013 and 2012 approximately 57%, 59% and 60%, respectively, of net revenue was generated by operations in five states. For 2014 the five states are Arizona, Florida, Massachusetts, Michigan, and Texas. For 2013 and 2012, the five states are Arizona, Florida, Michigan, Missouri and Texas. Over those same periods, operations in Florida and Texas accounted for approximately, 32%, 33% and 33% of net revenue, respectively. Although IPC continues to seek to diversify the geographic scope of its operations, primarily through acquisitions of physician group practices or by recruiting new clinicians or entering into new hospital or post-acute care facility contracts, IPC may not be able to successfully implement or realize the expected benefits of any of these initiatives. Adverse changes or conditions affecting states in which IPC’s operations are concentrated, such as healthcare reforms, changes in laws and regulations, reduced Medicaid reimbursements, loss of Medicaid Parity or government investigations, may have a material adverse effect on its business, financial condition and results of operations.
64
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
B. Competition
The healthcare industry is highly competitive, and the market for hospitalists and post-acute clinicians within this industry is highly fragmented. IPC believes it is the largest dedicated hospitalist and post-acute provider group practice in the United States based on revenues, patient encounters and number of affiliated clinicians. In each of IPC’s local markets and throughout the United States, there are acute and post-acute care practice groups of varying sizes, as well as privately-owned practices, with which IPC’s practice groups compete.
Companies in other segments of the healthcare industry, such as emergency department service companies, also provide hospitalist and post-acute care services. Competitors of this nature on a national basis include Envision.
In addition, because of the fragmented nature of this market and the ability of physicians to provide services in any hospital where they have certain credentials, competition for growth in existing and expanding markets is not limited to IPC’s large competitors with substantial financial resources available to them. IPC also competes against local physician groups for qualified physicians, and sometimes with hospitals themselves to provide hospitalist services.
IPC is also dependent on its affiliated clinicians to provide services and generate revenue. Competition for qualified physicians to act as hospitalists or post-acute clinicians is intense. IPC competes with many types of healthcare providers, including teaching, research and government institutions, hospitals and other practice groups, for the services of such physicians.
65
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
C. Employees
Figure 27 below illustrates an approximate break-down of the affiliated clinicians and non-clinical staff employed or contracted by IPC’s wholly-owned subsidiaries or its affiliated professional organizations by job classification as of September 30, 2015.
Figure 27 – 9/30/15 IPC Employee Break-Down
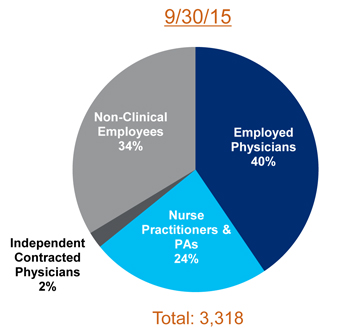
Source: IPC management.
In addition to the full-time and part-time employees and independent contractors included above, IPC has employment agreements with over 960 other physicians and non-physician providers, who provide episodic care as needed. All of IPC’s employees and independent contractors are located in the United States. None of IPC’s employees are covered by collective bargaining agreements. IPC has had no labor-related work stoppages, and IPC believes it have positive relations with its employees and independent contractors.
D. Regulatory and Reimbursement Matters
The Centers for Medicaid and Medicare Services (CMS) reimburses IPC’s services to Medicare beneficiaries based upon the rates in the Medicare Physician Fee Schedule (MPFS), which is updated each year based on the Sustainable Growth Rate (SGR) formula enacted under the Balanced Budget Act of 1997. Medicare accounts for approximately 49% of IPC’s revenue in 2014 and YTD through September 30, 2015 (measured as a percentage of patient encounters). Additionally, many private payors use the MPFS to determine their own reimbursement rates. The application of the SGR formula to the MPFS yielded negative updates every year beginning in 2002, although CMS was able to take administrative steps to avoid a reduction in 2003 and Congress periodically acted
66
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
each year to prevent reductions each year from 2004 through March 31, 2015. While the SGR has been an overhanging Medicare reimbursement risk to all physicians for many years, recent Congressional action has permanently addressed this issue. Legislation enacted on April 16, 2015 repeals the SGR and provides for an annual 0.5% increase to physician reimbursement rates for a five-year period (from July 1, 2015 through the end of 2019). In 2020 and subsequent years, physician payments will be tied to quality performance and participation in alternative payment models. For a comprehensive update on pending regulatory matters, please refer to IPC’s public filings available on EDGAR.
Florida Medicaid Reimbursement Suspension. IPC received notice on August 7, 2015 that the Florida Agency for Health Care Administration (“AHCA”) temporarily suspended Medicaid fee-for-service and Medicaid managed care payments to its Florida affiliate, InPatient Consultants of Florida, Inc. d/b/a IPC of Florida, because IPC of Florida is “under investigation by a state or federal agency.” Since receiving this notice, and based on its failure to contain the required specificity under the applicable federal regulations, IPC has sought additional information from AHCA regarding the basis of the payment suspension, including through repeated discussions with the responsible AHCA officials; by submitting a request for documents through the Florida Public Records Law (“PRL”) on August 27, 2015; and by filing a petition for formal administrative review on September 4, 2015.
Following these actions, IPC received a revised letter on September 9, 2015 in which AHCA clarified that the investigation causing the payment suspension concerns IPC of Florida’s alleged “up-coding” and “billing for the highest level of inpatient hospital care, which may not be medically necessary.” Since receipt of this revised notice, which still failed to contain the required specificity, IPC has continued to engage with AHCA to obtain information that would enable it to rebut the basis for the payment suspension. These efforts have included submitting a second PRL request on September 18, 2015; continuing to pursue formal administrative review of the payment suspension; and submitting a letter to AHCA providing information to support a determination by AHCA that it has “good cause” to discontinue the payment suspension, consistent with applicable federal regulations. On October 23, 2015, IPC received an order dismissing its petition for formal administrative review on the grounds that there is no final agency action and because the suspension is a contract action not appropriate for administrative hearing.
It is not possible to predict when any of the above matters may be resolved, the time or resources that IPC will need to devote to the matters, or what impact, if any, the outcome of any of the matters might have on its business, consolidated financial position, results of operations, or cash flows.
67
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
E. Legal Proceedings and Insurance
On June 7, 2010, IPC received a civil investigative demand (CID) issued by the Department of Justice (DOJ), U.S. Attorney’s Office for the Northern District of Illinois. The CID requested information concerning claims that IPC has submitted to Medicare and Medicaid. The CID covered the period from January 1, 2003, through June 4, 2010, and requested production of a range of documents relating to IPC’s Medicare and Medicaid participation, physician arrangements, operations, billings and compliance programs. IPC produced responsive documents and was in contact with representatives of the DOJ who informed IPC that the inquiry related to a qui tam whistleblower action filed under court seal in the U.S. District Court for the Northern District of Illinois (Chicago). IPC was also informed that several state attorneys general were examining its Medicaid claims in coordination with the DOJ.
Though IPC believes it has a strong compliance focus, that it operates with appropriate billing policies, procedures, provider training, and compliance programs and controls, and cooperated with the government’s investigation and would welcome a resolution to this matter, it is now in active litigation with the federal government regarding this matter and intend to contest the case vigorously. On December 6, 2013, the U.S. District Court partially lifted the seal on the civil False Claims Act case related to this investigation. The unsealed portions of the Court docket include the whistleblower’s Complaint, which contains allegations of improper billing to Medicare and Medicaid, a Notice of Election to Intervene filed by the federal government and a Notice of Election to Decline Intervention filed by the State of Illinois and 12 other states that participated in the investigation. On June 16, 2014, the federal government filed its Complaint in Intervention against IPC and several of its subsidiaries in the U.S. District Court. The Complaint in Intervention contains allegations of improper billing to Medicare, Medicaid and other federal programs from January 1, 2003 to the present, seeks to recover treble damages and civil penalties under the civil False Claims Act, and seeks to recover damages under the common law theories of payment by mistake and unjust enrichment. On August 13, 2014, IPC and the IPC subsidiary defendants filed a joint motion to dismiss the Complaint in Intervention or, in the alternative, to sever claims against the defendants. The federal government filed its response on September 18, 2014, to which the defendants replied on September 25, 2014. The court’s decision, which was filed on February 17, 2015, grants the motion to dismiss in part and denies it in part. The Court’s Opinion and Order dismisses the 29 IPC subsidiary and affiliate defendants without prejudice, but the Court denies the request to dismiss IPC, which remains the sole defendant in the lawsuit.
It is not possible to predict when this matter may be resolved, the time or resources that IPC will need to devote to this litigation, or what impact, if any, the outcome of this matter might have on IPC’s consolidated financial position, results of operations, or cash flows.
68
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Derivative Lawsuit. Although the underlying government lawsuit is still in an early stage and no liability has been found by a court, on October 20 and 24, 2014, shareholder derivative lawsuits were filed in the Court of Chancery of the State of Delaware against certain of IPC’s current and former directors and officers. On December 4, 2014, the derivative lawsuits were consolidated into one lawsuit. The litigation is in an early stage and it is not possible to predict when this matter may be resolved, the time or resources that IPC will need to devote to this litigation, or what impact, if any, the outcome of this matter might have on its consolidated financial position, results of operations, or cash flows.
For a comprehensive update on pending legal matters, please refer to IPC’s public filings available on EDGAR.
Professional Liability and Other Insurance Coverage. IPC contracts and pays premiums for third-party professional liability insurance that indemnifies IPC and its affiliated clinicians on a claims-made basis for losses incurred related to medical malpractice litigation. Professional liability coverage is required in order for IPC’s affiliated clinicians to maintain hospital privileges. IPC records in its consolidated financial statements estimates for its liabilities, on an undiscounted basis, for self-insured deductibles, claims incurred and reported and claims incurred but not reported during the policy period, based on actuarial loss projections using historical loss patterns. For claims incurred and reported, an insurance receivable from IPC’s carrier has been recorded pursuant to U.S. generally accepted accounting principles (GAAP).
IPC’s professional liability insurance policy, which ends December 31 of each year, is written on a claims-made basis providing first dollar coverage up to its policy limits on new claims reported in the policy period. In December 2014, IPC renewed its annual professional liability insurance policy for 2015, effective January 1, 2015, under the same terms as its 2014 policy.
IPC believes that its insurance coverage is appropriate based upon its claims experience and the nature and risks of its business. IPC also maintains general liability, casualty, worker’s compensation, director and officer, and other third-party insurance coverage subject to deductibles and other restrictions in accordance with industry standards.
69
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
F. Management
| Name | Title | Years Experience | ||
| Adam D. Singer, M.D. | Chairman and Chief Executive Officer | 28 | ||
| R. Jeffrey Taylor | President and Chief Operating Officer | 32 | ||
| Rick Kline | Chief Financial Officer | 5 | ||
| Kerry Weiner, M.D. | Chief Medical Officer | 34 | ||
| Richard Russell | EVP, Chief Development Officer | 26 | ||
Adam D. Singer M.D., Chairman and Chief Executive Officer
Dr. Adam D. Singer has been a director, Chairman, and Chief Executive Officer since he founded IPC in 1995, and in 2006, was designated as Chief Medical Officer. In 1991, Dr. Singer acquired a private practice in pulmonary medicine that shortly thereafter merged with two other pulmonary physicians to become part of Consultants For Lung Disease, Inc. (now the Institute for Better Breathing). Dr. Singer received his B.S. in Biology from the University of California, Los Angeles and his medical degree from the Chicago Medical School at Rosalind Franklin University. Dr. Singer performed a post-doctoral internship and residency in internal medicine and a fellowship in pulmonary medicine at University of Southern California.
R. Jeffrey Taylor, President and Chief Operating Officer
Jeffrey Taylor has been a director and President and Chief Operating Officer since he joined IPC in July 2000. Prior to joining IPC, Mr. Taylor was the executive vice president of Atlanta-based Mariner Post-Acute Network. Prior to that, Mr. Taylor was chief executive officer of American Outpatient Services, Inc. and held various positions including executive vice president, chief administrative officer and general counsel with American Medical International, Inc. (now Tenet Healthcare Corp.; NYSE-THC). Mr. Taylor also serves on the board of directors of Dormir, Inc. Mr. Taylor received a B.S. from the University of Utah and a J.D. from the University of Utah College of Law. Mr. Taylor has more than 25 years of experience in the areas of acute-care, sub-acute care and the outpatient dialysis segments of the healthcare industry.
70
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Rick Kline, Chief Financial Officer
Rick Kline joined IPC in November 2011 as Chief Financial Officer. From 2007 until March 2011, Mr. Kline served first as Vice President and Chief Financial Officer and later as President and Chief Operating Officer of Castle & Cooke, Inc., a consortium of businesses in real estate, hospitality, golf courses, restaurants, warehousing/logistics, building materials, aviation, life sciences, oil and gas, and transportation. From 1991 to 2007, Mr. Kline was with Ernst and Young, LLP, serving most recently as Partner of the Assurance and Advisory Business Services group in the Los Angeles office. He received his BS in Accounting from the University of Southern California
Kerry Weiner M.D., Chief Medical Officer
Dr. Kerry Weiner joined IPC in March 2011 in the newly created position of Chief Clinical Officer. Dr. Weiner leads the clinical functions of the Company and is charged with continuing the development of hospitalist leaders throughout IPC. Most recently, Dr. Weiner held the position of Chief Medical Officer for the Lakeside Medical Organization, a multispecialty group of 130 physicians and an IPA (Independent Practice Association) of approximately 2200 physicians. Dr. Weiner was one of the earliest proponents of hospitalists in Southern California, having utilized them at Lakeside since 1991. A co-founder of Lakeside Medical Group, Dr. Weiner served as president of the integrated medical group for 14 years. Dr. Weiner received his medical degree, masters in public health and bachelor’s degree from the University of California, Los Angeles.
Richard Russell, EVP, Chief Development Officer
Richard G. Russell. Mr. Russell has been Executive Vice President and Chief Development Officer since he joined IPC in March 2003. Prior to joining IPC, Mr. Russell was senior vice president of information technology and business planning for Cogent Healthcare, Inc., a national hospitalist organization, from 2002 to March 2003. Mr. Russell began his career as a senior consultant with McKinsey & Company and then held executive level positions in several entrepreneurial and healthcare operating companies. Mr. Russell received a B.S. in chemical engineering from the Case Western Reserve University and an M.B.A. from Harvard Business School and has 23 years of experience in health care services.
71
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
| V. | INDUSTRY OVERVIEW |
TeamHealth estimates the size of the domestic outsourced healthcare professional staffing market to be approximately $50 billion. Over the last decade, healthcare facilities have experienced increased pressure from the government and private payors both to improve the quality and to reduce the cost of care. With the increasing complexity of clinical, regulatory, managed care and reimbursement matters in today’s healthcare environment, healthcare facilities have increasingly outsourced the staffing and management of multiple clinical areas to companies —such as TeamHealth and IPC— that have specialized skills, standardized models and information technology to improve service, increase the overall quality of care and reduce administrative costs.
TeamHealth and IPC target certain clinical areas within healthcare facilities, including emergency medicine (ED), hospital medicine, and anesthesiology. TeamHealth estimates the annual size of these markets in the United States to be approximately $12 billion, $12 billion and $21 billion, respectively.
Figure 28 – TeamHealth Has Leading Positions in Several Highly Fragmented Markets
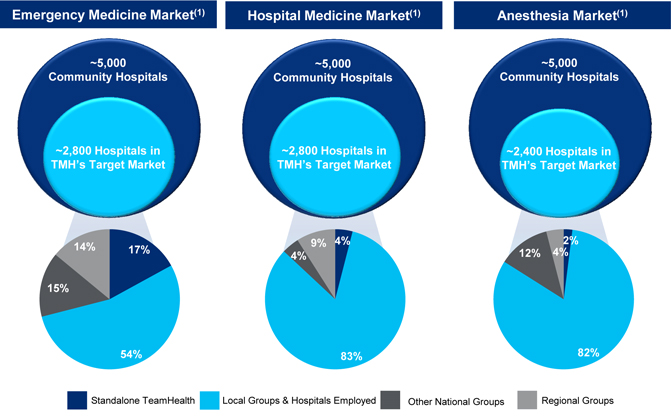
| (1) | Management Estimates |
Each of these clinical areas currently faces physician shortages, and many healthcare facilities lack the resources necessary to identify and attract specialized, career-oriented physicians. Moreover, the market for outsourced services in each of these areas is highly fragmented and predominately served by small practice groups.
72
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Thus, TeamHealth believes that these market conditions present enormous opportunities for future growth as the industry becomes more regulated and consolidated.
Figure 29 – The Total Addressable Market Opportunity
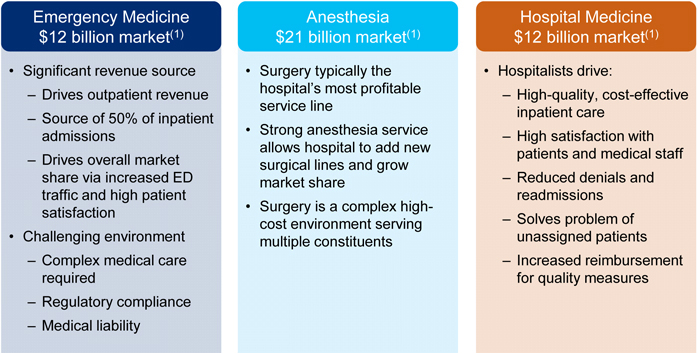
| (1) | Based on TeamHealth estimates. |
A. Emergency Medicine (ED)
TeamHealth estimates that the annual size of the ED market is approximately $12 billion. According to the American Hospital Association (AHA Hospital Statistics, 2011 edition), there were more than 5,000 community hospitals in the United States in 2009, and approximately 92% of those operated EDs. In 2011, hospitals treated more than 127.3 million patients in their EDs, representing a compound annual growth rate of approximately 2.5% from the 99.5 million ED patients treated in 1999. During the same time period, more than 140 EDs closed, which resulted in the average number of patient visits per ED to grow from approximately 21,800 to approximately 27,600 over the same period. Since EDs represent a majority of admissions for key medical service lines, the operation of an ED has significant implications for hospitals in terms of revenue, cost, quality, and the ability to grow market share.
With its origins dating back to the early 1970s, the ED is one of the most established service lines for clinical outsourcing. The market for outsourced ED staffing and management services is highly fragmented.
TeamHealth estimates that, of all hospitals that operate an ED, approximately 33% employ their emergency physicians and manage the function in-house, while the remaining 67% choose to outsource. The Company also
73
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
estimates that approximately 75% of the ED outsourcing market is currently serviced by local and regional groups. However, local providers often lack the operating capital, experience, breadth of services and sophisticated information systems necessary to meet the increasingly complex needs of hospitals. As a result, healthcare facilities seek third-party physician staffing and administrative service providers that can improve department quality, productivity and patient satisfaction while reducing overall costs. Moreover, healthcare facilities rely on third-party services to offer a breadth of staffing and management services, including billing and reimbursement expertise, compliance and financial oversight, and a demonstrated ability to recruit and retain qualified physicians, technicians and nurses. In particular, EDs face significant challenges with respect to capturing patient billing data and collecting relatively small dollar amounts billed to a high volume of patients. As a result, EDs seek third-party providers with the billing expertise, information technology infrastructure and systems necessary to reduce their administrative burden.
B. Hospital Medicine (Hospitalist)
TeamHealth estimates that the annual size of the hospitalist medicine market is approximately $12 billion. The field is expected to continue to grow as hospitals face additional cost pressures and added focus on improving patient outcomes. This market is currently serviced primarily by regional and local outsourced providers.
Founded approximately 20 years ago in the early 1990s, the field of hospitalist medicine continues to be an evolving and developing medical specialty. Hospitalists focus on a patient’s care from the time of admission to discharge, working in close consultation with primary care physicians, other referring physicians and medical providers to coordinate the acute and post-acute care delivery system and manage the entire inpatient episode of care. Hospitalists receive medical training generally in primary care, with the majority having experience in internal medicine, family practice or other medical specialties. Hospitalists and post-acute clinicians differ from primary care physicians and specialists by treating patients only in non-office based settings. By focusing exclusively on inpatient medicine, clinicians develop practice expertise in both the diagnosis and treatment of common conditions that require hospitalization and the optimization of patient care within a hospital or a post-acute care facility. Clinicians practice in inpatient facilities, including acute care hospitals, long-term acute care facilities, specialty hospitals, psychiatric facilities and post-acute care facilities. Acute care hospitals represent the largest component of inpatient facilities in which hospitalists practice. Clinicians serve a necessary and critical role in coordinating, managing and communicating with the different healthcare constituents within the inpatient care and post-hospital settings.
Hospitalists assume the inpatient care responsibilities that are otherwise provided by the primary care physician or attending physician and are reimbursed by third parties using the same visit-based or procedural billing codes as would be used by the primary care physician or attending physician. By practicing each day in the same facility, clinicians perform consistent functions, interact regularly with the same healthcare professionals and become highly accustomed to specific facility processes, which can result in greater efficiency, less process variability and better patient outcomes. TeamHealth believes hospitalists and post-acute clinicians are better able to achieve these results because of their exclusive focus on inpatient care without the inherent distraction of balancing both inpatient and outpatient care responsibilities. Likewise, hospitalists generate operating and cost efficiencies by managing the treatment of a large number of patients with similar clinical needs.
74
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
According to the Society of Hospitalist Medicine (SHM), the number of hospitalists has grown over the past decade from a few hundred to more than 44,000 at the end of 2014, making it one of the fastest-growing medical specialties in the United States. The SHM also reports that hospitalists now have a presence at a majority of hospitals nationwide.
The growing demand for hospitalists and post-acute clinicians is primarily driven by six significant changes in the healthcare delivery system:
| • | The primary care physician’s role in hospital care is decreasing due to the increasingly specialized nature of hospital care, the demands of treating higher acuity patients in an outpatient setting and the desire to reduce on-call obligations |
| • | Hospitals and post-acute care facilities have a greater need for consistent on-site physician availability, due to the need to admit patients from the emergency room, the increasing severity of illness required to justify hospital admissions, the need to reduce avoidable re-hospitalizations and external pressures to decrease the length of inpatient stays |
| • | Specialists have an increased desire to limit the scope of their practice to their own medical specialty |
| • | National residency accreditation organizations have established limitations on the number of hours that resident physicians in training may practice |
| • | Health plans are seeking alternative mechanisms to appropriately control the substantial increase in inpatient expenditures |
| • | There is a growing interest in providing a coordinated continuum of care for patients that move between different types of facilities to improve quality of patient care, improve patient satisfaction and to reduce costs over an entire episode of care |
C. Anesthesiology
TeamHealth estimates that the annual size of the anesthesiology market is $21 billion. The market is currently serviced primarily by hospitals, which self-operate their programs, and by small and local outsourced providers. These small groups of local providers are often very good clinicians, but often lack the resources to develop processes to optimize issues such as timely availability, operating room turnover, and proper preparation of patients to avoid surgical cancellations or delays. In hospitals, the perioperative environment is often the most profitable department, putting a heightened priority and value on the efficient functioning of this unit.
In current market conditions, where hospitals have a need for more sophisticated management of their anesthesiology departments, and where individual groups of anesthesiologists do not have the resources to either recruit enough providers to keep up with the increasing number of surgeries, or to address hospital priorities, demand has significantly increased for organized, national anesthesia management companies. There is significant opportunity for consolidation in this field as only 7% of the 43,000 anesthesiologists in the United States are part of a national or regional group (those consisting of more than 50 anesthesiologists). These favorable market characteristics offer the combined company tremendous opportunities for growth.
75
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
D. Post-Acute
Estimated at a market size of over $300 billion, the post-acute setting represents the most impactable and expensive part of healthcare delivery (CMS). Post-acute settings are comprised of home health and facilities (which include skilled nursing, inpatient rehabilitation (including psychiatric), assisted living and nursing homes). According to MedPac, in 2013, Medicare alone paid for 9.6 million encounters (including home health patients).
Also according to MedPAC, among Medicare beneficiaries enrolled in fee-for-service Medicare and discharged from an acute care hospital in 2013, roughly ~42% were discharged to a post-acute setting, with 20% being discharged to a skilled nursing facility, 17% discharged to home health agencies, 4% discharged to an inpatient rehabilitation facility and 1% discharged to a long-term acute care hospital. As the number of Americans aged 65 and over (who represent the highest utilizers of acute and post-acute care services) are expected to increase approximately 36% (to approximately 65 million) by 2025, post-acute expenditures are also expected to materially increase.
The market for the provision of post-acute clinician services is highly fragmented, with IPC representing the largest national provider. IPC provides services to approximately 2,000 of the roughly 15,000 post-acute facilities in the United States, or approximately 13%. Typical clinical specialties include post-acute hospitalist, psychology, psychiatry and geriatrics.
Figure 30 –Increasing Strategic Importance of Post-Acute Services
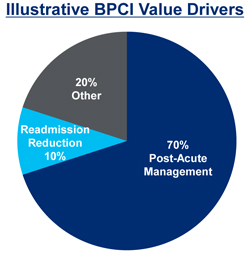
Source: TeamHealth management estimates.
Figure 31 illustrates post-acute Medicare spending has grown over 6% annually from 1999 to 2013 (CMS).
76
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Figure 31 – Growth in Medicare Spending from 1999 – 2013
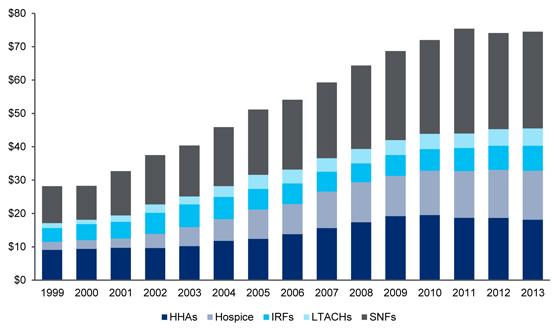
Source: CMS.
77
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
| VI. | HISTORICAL FINANCIAL INFORMATION |
Comprehensive historical financials and MD&A for TeamHealth and IPC can be found on EDGAR in public filings.
A. TeamHealth
| ($ in Millions) | Year Ended December 31, | Nine Months Ended September 30, (unaudited) |
LTM Ended September 30, |
|||||||||||||||||
| 2013 | 2014 | 2014 | 2015 | 2015 | ||||||||||||||||
| Net Revenues Before Provision for Uncollectibles |
$ | 4,313.8 | $ | 4,800.9 | $ | 3,493.9 | $ | 4,390.7 | $ | 5,697.7 | ||||||||||
| Provision for Uncollectibles |
1,930.3 | 1,981.2 | 1,464.9 | 1,773.1 | 2,289.4 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net Revenues |
$ | 2,383.6 | $ | 2,819.6 | $ | 2,029.0 | $ | 2,617.6 | $ | 3,408.3 | ||||||||||
| Operating Expenses Excluding Depreciation & Amortization |
2,170.9 | 2,558.5 | 1,827.0 | 2,359.5 | 3,090.9 | |||||||||||||||
| Depreciation & Amortization |
54.6 | 76.5 | 50.5 | 79.5 | 105.5 | |||||||||||||||
| Other (Income) Expenses, net |
(4.5 | ) | (4.6 | ) | (3.5 | ) | (0.2 | ) | (1.3 | ) | ||||||||||
| Loss on Refinancing of Debt |
— | 3.6 | — | — | 3.6 | |||||||||||||||
| Transaction Costs |
3.8 | 7.2 | 5.7 | 7.2 | 8.6 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Operating Income |
$ | 158.8 | $ | 178.4 | $ | 149.1 | $ | 171.7 | $ | 200.9 | ||||||||||
| Interest Expense, Net |
14.9 | 15.1 | 10.8 | 14.1 | 18.4 | |||||||||||||||
| EBITDA |
$ | 213.3 | $ | 254.6 | $ | 199.5 | $ | 251.2 | $ | 306.4 | ||||||||||
| Other (Income) expenses, net |
(4.5 | ) | (4.6 | ) | (3.5 | ) | (0.2 | ) | (1.3 | ) | ||||||||||
| Loss on Refinancing of Debt |
— | 3.6 | — | — | 3.6 | |||||||||||||||
| Contingent Purchase & Other Acq. Expense |
24.0 | 30.6 | 22.5 | 12.2 | 20.4 | |||||||||||||||
| Transaction Costs |
3.8 | 7.2 | 5.7 | 7.2 | 8.6 | |||||||||||||||
| Equity Based Compensation Expense |
9.9 | 16.2 | 12.7 | 13.2 | 16.7 | |||||||||||||||
| Insurance Subsidiaries Interest Income |
1.8 | 2.0 | 1.5 | 1.6 | 2.1 | |||||||||||||||
| Professional Liability Loss Adj. |
— | 7.1 | 7.1 | — | — | |||||||||||||||
| Severance & Other Charges |
3.1 | 8.6 | 1.6 | 4.6 | 11.6 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Adjusted EBITDA |
$ | 251.3 | $ | 325.2 | $ | 247.1 | $ | 289.8 | $ | 368.0 | ||||||||||
| Full Year Impact of Acquisitions Closed Before 9/30/15 |
12.2 | |||||||||||||||||||
|
|
|
|||||||||||||||||||
| PF Adjusted EBITDA |
$ | 380.2 | ||||||||||||||||||
Reported Net Earnings to Adjusted EBITDA Reconciliation
| YTD Sept | YTD Sept | LTM Sept | ||||||||||||||||||||||||||
| ($ in millions) | 2011 | 2012 | 2013 | 2014 | 2014 | 2015 | 2015 | |||||||||||||||||||||
| Net earnings, attributable to Team Health Holdings, Inc. |
$ | 65.5 | $ | 63.8 | $ | 87.4 | $ | 97.7 | $ | 81.6 | $ | 92.4 | $ | 108.5 | ||||||||||||||
| Interest expense, net |
12.8 | 16.3 | 14.9 | 15.1 | 10.8 | 14.1 | 18.4 | |||||||||||||||||||||
| Provision for income taxes |
43.3 | 40.6 | 56.3 | 65.2 | 56.5 | 65.2 | 73.9 | |||||||||||||||||||||
| Depreciation |
12.2 | 14.5 | 17.1 | 20.9 | 15.3 | 17.4 | 23.0 | |||||||||||||||||||||
| Amortization |
17.8 | 29.8 | 37.6 | 55.6 | 35.2 | 62.1 | 82.5 | |||||||||||||||||||||
| Other (income) expenses, net |
0.2 | (4.8 | ) | (4.5 | ) | (4.6 | ) | (3.5 | ) | (0.2 | ) | (1.3 | ) | |||||||||||||||
| Loss on extinguishment and refinancing of debt |
6.0 | 0.2 | — | 3.6 | — | — | 3.6 | |||||||||||||||||||||
| Contingent purchase and other acquisition compensation expense |
13.6 | 36.8 | 23.9 | 30.6 | 22.5 | 12.2 | 20.4 | |||||||||||||||||||||
| Transaction costs |
4.1 | 4.3 | 3.8 | 7.2 | 5.7 | 7.2 | 8.6 | |||||||||||||||||||||
| Equity based compensation expense |
4.1 | 6.8 | 9.9 | 16.2 | 12.7 | 13.2 | 16.7 | |||||||||||||||||||||
| Insurance subsidiary interest income |
2.2 | 1.9 | 1.8 | 2.0 | 1.5 | 1.6 | 2.1 | |||||||||||||||||||||
| Severance and other charges |
1.4 | 2.8 | 3.1 | 8.6 | 1.6 | 4.6 | 11.6 | |||||||||||||||||||||
| Actuarial adjustments associated with prior periods |
5.3 | 5.2 | — | 7.1 | 7.1 | — | — | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Adjusted EBITDA |
$ | 188.5 | $ | 218.2 | $ | 251.3 | $ | 325.2 | $ | 247.1 | $ | 289.8 | $ | 368.0 | ||||||||||||||
| Full year impact of previously closed acquisitions |
12.2 | |||||||||||||||||||||||||||
|
|
|
|||||||||||||||||||||||||||
| PF Adjusted EBITDA |
$ | 380.2 | ||||||||||||||||||||||||||
|
Free Cash Flow Calculation
|
||||||||||||||||||||||||||||
| Net cash provided by operating activities (as reported) |
$ | 96.8 | $ | 71.6 | $ | 154.4 | $ | 198.6 | $ | 106.7 | $ | 131.9 | $ | 223.9 | ||||||||||||||
| Contingent purchase payments |
15.5 | 31.3 | 29.1 | 24.5 | 21.9 | 12.2 | 14.8 | |||||||||||||||||||||
| Capital expenditures |
(12.0 | ) | (22.0 | ) | (21.4 | ) | (24.6 | ) | (16.8 | ) | (31.1 | ) | (38.9 | ) | ||||||||||||||
| Change in investments at insurance subsidiary, net(1) |
(3.7 | ) | 19.5 | (13.7 | ) | (10.5 | ) | (7.2 | ) | 3.7 | 0.4 | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Free Cash Flow |
$ | 96.6 | $ | 100.4 | $ | 148.4 | $ | 188.0 | $ | 104.6 | $ | 116.8 | $ | 200.2 | ||||||||||||||
| (1) | Excludes liquidation of investments from captive subsidiary acquired in 2014 transaction. |
Three Months Ended September 30, 2015 Compared to Three Months Ended September 30, 2014
Net revenue was $899.2 million for the quarter, an increase of 26.2% from $712.2 million for the third quarter of 2014. Acquisitions contributed 19.2%, net sales growth contributed 4.4%, and same contract revenue contributed 2.7% of the increase in quarter-over-quarter growth. Within the acquisitions category, new hospital contracting opportunities that were developed by TeamHealth’s sales and marketing process contributed 4.7% of overall net revenue growth between quarters. Same contract revenue increased $19.0 million, or 2.9%, to $672.9 million from $653.9 million in the third quarter of 2014. Acquisitions contributed $136.5 million of revenue growth and net new contract revenue increased by $31.4 million between quarters.
Adjusted EBITDA for the quarter increased 13.6% to $101.1 million from $89.0 million in the third quarter of 2014. Adjusted EBITDA margin was 11.2% in 2015 compared to 12.5% in 2014. Excluding the impact of Medicaid parity in both periods, Adjusted EBITDA margin would have been 11.2% in the third quarter of 2015 and 11.6% in 2014.
78
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Cash flow provided by operations for the nine months ended September 30, 2015 was $131.9 million compared to $106.7 million in 2014. There were $12.2 million contingent purchase payments in 2015 and $21.9 million contingent purchase payments in 2014. Excluding the impact of the 2015 and 2014 contingent purchase payments, operating cash flows increased $15.5 million to $144.2 million in 2015 compared to $128.7 million in 2014. The increase in operating cash flow between periods was due primarily to increased profitability compared to the prior period.
Year Ended December 31, 2014 Compared to Year Ended December 31, 2013
Net revenue was $2.82 billion for the year, an increase of 18.3% from $2.38 Billion in 2013. Acquisitions contributed 11.3%, net sales growth contributed 1.9%, and same contract revenue contributed 5.0% of the increase in year-over-year growth. Within the acquisitions category, new hospital contracting opportunities that were developed by TeamHealth’s sales and marketing process contributed 2.3% of overall net revenue growth between years. Same contract revenue increased $119.5 million, or 6.1%, to $2.09 billion from $1.97 billion in the 2013. Acquisitions contributed $270.1 million of revenue growth and net new contract revenue increased by $46.4 million between years.
Adjusted EBITDA for 2014 increased 29.4% to $325.2 million from $251.3 million in 2013. Adjusted EBITDA margin was 11.5% in 2014 compared to 10.5% in 2013. Excluding the impact of Medicaid parity in both periods, Adjusted EBITDA margin would have been 10.7% in the 2014 and 9.9% in 2013.
Cash flow provided by operations for the twelve months ended December 31, 2014 was $198.7 million compared to $154.4 million in 2013. There were $24.5 million contingent purchase payments in 2014 and $29.1 million contingent purchase payments in 2013. Excluding the impact of the 2014 and 2013 contingent purchase payments, operating cash flows increased $39.7 million or 21.6% between periods.
79
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
B. IPC Healthcare
| Nine Months Ended | LTM Ended | |||||||||||||||||||
| ($ in Millions) | Year Ended December 31, | September 30, (unaudited) | September 30, | |||||||||||||||||
| 2013 | 2014 | 2014 | 2015 | 2015 | ||||||||||||||||
| Net Revenues |
$ | 609.5 | $ | 694.0 | $ | 514.8 | $ | 549.6 | $ | 728.8 | ||||||||||
| Operating Expenses Excluding Depreciation & Amortization |
537.2 | 623.6 | 461.9 | 513.9 | 675.6 | |||||||||||||||
| Depreciation & Amortization |
4.7 | 5.4 | 4.0 | 4.5 | 5.9 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Operating Income |
$ | 67.6 | $ | 65.0 | $ | 48.8 | $ | 31.2 | $ | 47.3 | ||||||||||
| Interest Expense, Net |
0.5 | 1.3 | 1.1 | 0.9 | 1.2 | |||||||||||||||
| EBITDA |
$ | 72.3 | $ | 70.4 | $ | 52.9 | $ | 35.7 | $ | 53.2 | ||||||||||
| Net Change in Fair Value of Contingent Consideration |
(5.7 | ) | 2.3 | 1.3 | 5.5 | 6.5 | ||||||||||||||
| Incremental Costs Related to the False Claims Act Litigation |
— | — | — | 1.7 | 1.7 | |||||||||||||||
| TeamHealth Transaction Costs |
— | — | — | 5.3 | 5.3 | |||||||||||||||
| Equity Based Compensation Expense |
7.4 | 8.3 | 6.1 | 6.2 | 8.4 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Adjusted EBITDA |
$ | 73.9 | $ | 80.9 | $ | 60.3 | $ | 54.4 | $ | 75.1 | ||||||||||
| Full Year Impact of Acquisitions Closed Before 9/30/15 |
6.2 | |||||||||||||||||||
| Transaction Expenses and CID Related Legal Expenses |
1.8 | |||||||||||||||||||
| BPCI Overhead Adjustment |
0.8 | |||||||||||||||||||
|
|
|
|||||||||||||||||||
| PF Adjusted EBITDA |
$ | 83.8 | ||||||||||||||||||
Reported Net Earnings to Adjusted EBITDA Reconciliation
| YTD Sept | YTD Sept | LTM Sept | ||||||||||||||||||||||||||
| ($ in millions) | 2011 | 2012 | 2013 | 2014 | 2014 | 2015 | 2015 | |||||||||||||||||||||
| Net Earnings |
$ | 29.3 | $ | 32.6 | $ | 41.4 | $ | 39.0 | $ | 29.5 | $ | 18.8 | $ | 28.3 | ||||||||||||||
| Interest expense, net |
0.2 | 0.3 | 0.5 | 1.3 | 1.1 | 0.9 | 1.2 | |||||||||||||||||||||
| Provision for income taxes |
17.6 | 19.7 | 25.7 | 24.6 | 18.3 | 11.5 | 17.8 | |||||||||||||||||||||
| Depreciation & Amortization |
3.2 | 3.9 | 4.7 | 5.4 | 4.0 | 4.5 | 5.9 | |||||||||||||||||||||
| Net change in fair value of contingent consideration |
(1.0 | ) | 0.3 | (5.7 | ) | 2.3 | 1.3 | 5.5 | 6.5 | |||||||||||||||||||
| Equity based compensation expense |
4.8 | 6.3 | 7.4 | 8.3 | 6.1 | 6.2 | 8.4 | |||||||||||||||||||||
| Costs Related to the False Claims Act Litigation |
— | — | — | — | — | 1.7 | 1.7 | |||||||||||||||||||||
| TMH Transaction Expenses |
— | — | — | — | — | 5.3 | 5.3 | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Adjusted EBITDA |
$ | 54.0 | $ | 63.2 | $ | 73.9 | $ | 80.9 | $ | 60.3 | $ | 54.4 | $ | 75.1 | ||||||||||||||
| Full year impact of previously closed acquisitions |
6.2 | |||||||||||||||||||||||||||
| Transaction Expenses and CID Related Legal Expenses |
1.8 | |||||||||||||||||||||||||||
| BPCI Overhead Adjustment |
0.8 | |||||||||||||||||||||||||||
|
|
|
|||||||||||||||||||||||||||
| PF Adjusted EBITDA |
$ | 83.8 | ||||||||||||||||||||||||||
|
Free Cash Flow Calculation
|
||||||||||||||||||||||||||||
| Net cash provided by operating activities (as reported) |
$ | 25.8 | $ | 39.8 | $ | 36.8 | $ | 47.6 | $ | 53.8 | $ | 30.3 | $ | 24.1 | ||||||||||||||
| Capital expenditures |
(3.3 | ) | (3.6 | ) | (3.9 | ) | (5.8 | ) | (3.7 | ) | (4.8 | ) | (6.9 | ) | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Free Cash Flow |
$ | 22.5 | $ | 36.2 | $ | 32.9 | $ | 41.8 | $ | 50.1 | $ | 25.5 | $ | 17.1 | ||||||||||||||
Three Months Ended September 30, 2015 Compared to Three Months Ended September 30, 2014
Patient encounters for the three months ended September 30, 2015 increased by 249,000, or 14.2%, to 1,998,000, compared with 1,749,000 for the same period in the prior year. Net revenue for the three months ended September 30, 2015 was $184.8 million, an increase of $15.0 million, or 8.9%, from $169.8 million for the same period in the prior year. The difference between revenue growth and encounter growth is principally related to Medicaid Parity, which largely expired at the end of 2014, and the exiting of a few facility contracts during 2014. Of this $15.0 million increase, 32.5% was attributable to same-market area growth, including new hires and tuck-in acquisitions, and 67.5% was attributable to revenue generated from operations in new markets. Same-market encounters increased 7.3%, and same-market net revenue increased 2.9%. Adjusting for Medicaid Parity and the exiting of certain contracted facilities in 2014, same-market encounter growth and net revenue growth would have been approximately 11.7% and 12.2%, respectively.
Excluding stock-based compensation, adjusted G&A expenses were 16.0% of net revenue for the three months ended September 30, 2015, compared with 15.3% of net revenue for the same period in the prior year. This adjusted cost variance of 70 basis points as a percentage of revenue is largely related to the cessation of Medicaid Parity.
80
| CONFIDENTIAL INFORMATION MEMORANDUM | NOVEMBER 2015 |
Adjusted EBITDA for the three months ended September 30, 2015 decreased 20.6% to $14.3 million, or an adjusted EBITDA margin of 7.8%, compared with adjusted EBITDA of $18.1 million, or an adjusted EBITDA margin of 10.6% for the same period in the prior year.
Year Ended December 31, 2014 Compared to Year Ended December 31, 2013
Patient encounters for 2014 increased by 857,000, or 13.8%, to 7,068,000, compared with 6,211,000 for 2013. Net revenue for 2014 was $694.0 million, an increase of $84.5 million, or 13.9%, from $609.5 million for 2013. Of this $84.5 million increase, 64.7% was attributable to same-market area growth, including tuck-in acquisitions and new hires, and 35.3% was attributable to revenue generated from operations in new markets. Same-market revenue increased 9.1%, and same-market encounters increased 8.2%.
Adjusted EBITDA for 2014 increased 9.1% to $72.6 million, or an adjusted EBITDA margin of 10.5%, compared with adjusted EBITDA of $66.6 million, or an adjusted EBITDA margin of 10.9% for 2013. The adjusted EBITDA margin decrease of 40 basis points compared with the same period in the prior year is related to an increase in both physician practice expenses and general and administrative expenses as a percentage of revenue.
81