Attached files
| file | filename |
|---|---|
| 8-K - 8-K - Bellerophon Therapeutics, Inc. | a15-10084_18k.htm |
Exhibit 99.1
|
|
Company Presentation April 2015 Confidential |
|
|
Forward Looking Statements This presentation contains forward-looking statements that involve substantial risks and uncertainties. All statements, other than statements of historical facts, contained in this presentation, including statements regarding our strategy, future operations, future financial position, future revenues, projected costs, prospects, plans and objectives of management, are forward-looking statements. The words “anticipate,” “believe,” “estimate,” “expect,” “intend,” “may,” “plan,” “predict,” “project,” “target,” “potential,” “will,” “would,” “could,” “should,” “continue,” and similar expressions are intended to identify forward-looking statements, although not all forward-looking statements contain these identifying words. We may not actually achieve the plans, intentions or expectations disclosed in our forward-looking statements, and you should not place undue reliance on our forward-looking statements. Actual results or events could differ materially from the plans, intentions and expectations disclosed in the forward-looking statements we make due to a number of important factors, including risks and uncertainties relating to: the timing and outcomes of our ongoing and expected clinical trials for our product candidates; our ability to successfully develop, commercialize and market any of our product candidates; our ability to obtain, maintain and enforce intellectual property rights; competition; our reliance on third parties; our ability to obtain necessary financing; and those risk factors discussed in the “Risk Factors” section and elsewhere in our most recent Form 10-K and other periodic filings we make with the SEC. All forward-looking statements contained in this presentation reflect our current views with respect to future events. We assume no obligation, except as required by applicable law, to update any forward-looking statements publicly, or to update the reasons why actual results could differ materially from those anticipated in the forward-looking statements, even if new information becomes available in the future. |
|
|
Bellerophon Highlights Focused on developing novel therapies for severe cardiopulmonary and cardiac diseases Product candidates address opportunities at the intersection of drugs and devices with high unmet need BCM: Novel injectable treatment designed to prevent Congestive Heart Failure (CHF) Simple mechanism to prevent ventricular remodeling following a heart attack Pilot study results support safety and suggest morbidity/mortality benefit CE Mark registration trial enrollment complete with topline results in mid-2015 Approval will follow a device regulatory pathway, with potential for CE Mark approval in H1 2016 INOpulse: Extension of nitric oxide based therapy for Pulmonary Hypertension (PH) in chronic diseases Nitric oxide approved for use in hospital in neonates; over 450,000 patients treated since launch Novel delivery technology allows for use in serious chronic diseases Several potential applications include: PAH: Planning to initiate Phase 3 in 2015 PH-COPD: Planning Phase 2b Other opportunities may include PH-Idiopathic Pulmonary fibrosis, CTEPH and PH-Sarcoidosis Strong IP protection on core programs |
|
|
Expected Milestones INOpulse PAH Phase 2 trial Phase 3 trial* PH-COPD Phase 2b trial BCM CE Mark registration trial 1st Procedure safety trial Pivotal trial (for US) Q4 ’14 Q1 ’15 Q2 ’15 Q3 ’15 Q4 ’15 Q1 ’16 Q2 ’16 FDA EoPh2 Meeting Trial start Trial start Enrollment complete Topline results Trial start CE Mark approval Trial start * Includes ongoing long-term extension study for PAH EoPh2 = End of Phase 2 (Type B) meeting Topline results Mid ’18 Early ’17 Mid ’16 Mid ’18 Topline results expected |
|
|
Experienced Management Team Jon Peacock – Chairman & Chief Executive Officer Former CFO of Amgen; former CFO of Novartis Pharma Manesh Naidu – Chief Business Officer Former GM of INOpulse and Head of Marketing Strategy at Ikaria Reinilde Heyrman, M.D. – Chief Clinical Development Officer Former Chief Clinical Development Officer at Ikaria; former VP of Clinical Development at Daiichi Sankyo Martin Meglasson – Chief Scientific Officer Former Chief Scientific Officer for Ikaria; former VP and head of Research and Development at Ligand |
|
|
Experienced Management Team Martin Dekker – VP, Head of Device Engineering Former Director of Global Operations Engineering at Spacelabs Healthcare Deborah Quinn, M.D. – VP, Medical Lead, INOpulse Former Medical Director at Novartis, Lead for PAH Clinical Trials; Clinical Assistant Professor at Harvard Medical School; Physician at Massachusetts General Hospital |
|
|
BCM for Prevention of Remodeling after AMI |
|
|
Bioabsorbable Cardiac Matrix (BCM) Over 1.9 million patients have heart attacks (AMIs) annually in US & EU Emerging markets, including China and India, also have significant numbers AMI patients are at significant risk of developing Congestive Heart Failure (CHF) with an estimated 35 to 40% likelihood within 5 years CHF is an expensive disease with US treatment costs of $12 billion annually related to post-AMI patients Estimated lifetime medical costs following CHF >$100,000 per patient Average hospitalization costs estimated at ~$17,000 to $21,000 per admission BCM is being developed to prevent remodeling and progression to CHF after large AMIs Remodeling AMI CHF |
|
|
BCM is deployed as a liquid biomaterial by a single intracoronary injection Mode of Action* BCM is absorbed by the infarcted tissue Leaky capillaries allow BCM to be absorbed into the infarct zone The liquid changes into a semi-solid hydrogel within the infarct zone Ca2+ escapes from necrotic cardiomyocytes in the infarct zone BCM gels in the presence of the high extracellular Ca2+ level Visco-elastic properties of BCM hydrogel are similar to the normal extracellular matrix (ECM) Material turns back to liquid form after healing and is eliminated by 6 months after its deployment BCM is a Self Assembling Temporary Bio-mechanical Scaffold at the Infarct Site Infarct zone Coronary artery Catheter tip * Based on preclinical studies |
|
|
Comprehensive Preclinical Program Conducted Chronic toxicity study in pigs with AMI showed no abnormal changes in the structure or function of the internal organs Acute toxicity study in pigs with AMI demonstrated that BCM neither changed the cardiac rhythm nor caused coronary thrombi to form Pharmacokinetic studies demonstrated that alginate was rapidly and preferentially deposited in the infarct region Alginate was shown to be slowly excreted in the urine Alginate no longer detected by 6 months after BCM deployment FDA has agreed that the non-clinical safety package is complete and adequate for supporting clinical development and product registration |
|
|
BCM Reduced Remodeling and Improved Systolic Function in Pig Model of AMI Saline BCM BCM Saline Reduced Remodeling Improved Systolic Function (6 pigs/group) Similar findings observed in a dog model of AMI (Leor and Sabbah, European Society of Cardiology EuroPCR Meeting, 2012) *ESVI – Change in End Systolic Volume Index (mL/m2) AMI BCM (or saline) deployment AMI BCM (or saline) deployment 0 7 14 21 28 35 42 49 56 -20 -15 -10 -5 0 5 Study Day D E j e c t i o n F r a c t i o n P<0.05 0 7 14 21 28 35 42 49 56 0 5 10 15 20 Study Day D V e n t r i c u l a r V o l u m e * D = 9.5 mL/m 2 P<0.01 |
|
|
BCM Pilot Safety Trial Open label, single arm trial with sequential enrollment completed in 2009 27 patients with moderate to large AMI associated with ST-elevation (STEMI) recruited from multiple sites in Germany and Belgium BCM deployed within 7 days of successful primary percutaneous coronary intervention (PCI) Assessment at 30, 90, 180 days with annual follow-up for 5 years Acute Safety Findings: Primary safety endpoint results were consistent with expectations for the trial population BCM intracoronary artery deployment post-reperfusion was well tolerated No acute impact on thrombolysis in myocardial infarction (TIMI) flow or myocardial perfusion grade Frey N et al. Circulation: Cardiovascular Interventions, October 2014 |
|
|
Historical data* indicated that ventricular dilatation and reduced ejection fraction predicted heart failure and mortality at 6 months BCM pilot study** showed maintenance of ESVI and trend toward improving EF at 6 months Clinical endpoints at 4-year follow-up of 27 patients in BCM Study: 1 patient hospitalized for CHF and 1 patient had died from T-cell lymphoma, likely a preexisting condition¶ Published data suggests combined mortality + CHF hospitalization rates should be 35-40% at 5 years after a large AMI*** BCM Pilot Study in Patients with STEMI’s ¶ One patient who was alive at 36 months was lost to follow-up by the 48 months evaluation * Nicolosi G. et al. Eur. Heart J. (1996); ** Frey N. et al. Circ. Cardiovasc. Interv. (2014); *** Velagaleti R. et al. Circulation (2008) |
|
|
PRESERVATION I: International Study of BCM Population: Large STEMI, after successful PCI with stent Design: Randomized, double-blind, placebo-controlled trial 303 patients completed treatment procedure at approximately 90 sites in North America, Europe, Israel and Australia Device: placebo delivered in a 2:1 ratio Device delivered during secondary PCI procedure, 2 to 5 days post-AMI Endpoints: Primary: Change in left ventricular end-diastolic volume index after 6 months Secondary: Changes in 6-min walk distance and patient reported outcomes (Kansas City Cardiomyopathy Questionnaire) from baseline to 6 months Fully enrolled with procedure completed in 303 patients DSMB met several times and allowed study to continue to completion Topline data expected in mid-2015 |
|
|
Global Steering Committee Mitchell Krucoff, MD, FACC, FAHA, FSCAI: Chair of Steering Committee, Professor, Medicine/Cardiology, Duke University Medical Center, North Carolina, USA Sunil Rao, MD, FACC, FSCA: Principal Investigator, Associate Professor of Medicine, Duke University Medical Center, North Carolina, USA Uwe Zeymer, MD: Principal Investigator, Professor of Medicine, Klinikum Ludwigshafen, Germany Paul Vermeersch, MD, PhD: Antwerp Cardiovascular Institute, Belgium Jerome Roncalli, MD, PhD: Asst. Director Heart Failure Unit, Rangueil University Hospital; Professor of Cardiology of the Purpan School of Medicine, France Norbert Frey, MD: Professor, Head of Department of Cardiology, University of Kiel, Germany Jaroslaw Kasprzak, MD, FESC, FACC: Professor of Medicine, University of Lodz, Poland Jose Lopez-Sendon, MD: Chief of Cardiology, Hospital Universitario La Paz, Madrid, Spain Derek Chew, MBBS, MPH, FRACP, FACC: Director Cardiology, Flinders Cardiac Clinic, Australia Henry Krum, PhD, MBBS, FRACP, FCSANZ: Professor & Director Monash Centre, Australia Victor Guetta, MD: Deputy Director The Heart Institute Sheba Medical Center, Israel Jean-Francois Tanguay, MD, FACC, FAHA, FESC: Professor of Medicine, Montreal Heart Institute, Canada Timothy Henry, MD, FACC: Chief Cardiology, Cedars Sinai Heart Institute, Los Angeles, CA, USA Jay Traverse, MD, FACC, FAHA: Cardiologist at Minneapolis Heart Institute of Abbott Northwestern Hospital, Minneapolis, MN, USA |
|
|
BCM Regulatory Strategy & Milestones Agreement reached to follow device regulatory approval pathway with authorities in the US & 8 other countries European Notified Body: Preservation I is acceptable to support CE mark Key endpoints for US pivotal study expected to be composite of: Anatomical measures, such as left ventricular end diastolic index (LVEDI) or ejection fraction Functional assessment, such as six-minute walk distance (6MWD), and Patient reported outcomes, such as quality of life (QoL) e.g. Kansas City cardiomyopathy questionnaire (KCCQ) |
|
|
BCM Device Patents Patent Status Expiration Notes Composition of matter Issued-US Issued-RoW 3-2029 5-2024 Expected US patent-term extension to 2032-2034 Manufacturing process Pending WW 12-2032 Manufactured similar to a sterile parenteral drug Raw Materials: Medical grade Alginate supplied by FMC BioPolymer, a world leader in natural biopolymers Calcium Gluconate USP – same as the approved IV drug for hypocalcemia Product shelf life of 30 months BCM Manufacturing |
|
|
INOpulse Program |
|
|
Portable Delivery System Allows Outpatient Chronic Nitric Oxide Therapy Images are not to scale relative to each other Currently well established as a therapy for neonates in hospitals In-hospital device is bulky with large cylinders Continuous dosing is inefficient Pulsed iNO can deliver equivalent dose as continuous delivery with 5% of the volume; Allows for small portable ~2.5 lbs device Dynamic pulse is designed to deliver the prescribed dose accurately throughout the day Triple-lumen cannula designed to support accurate dosing and for use, when needed, alongside Long Term Oxygen Therapy (LTOT) Pulsing minimizes NO release which is important for chronic at-home use |
|
|
Clinical Application of Inhaled NO Nitric oxide is an endogenous molecule integral to normal vasodilation Well understood pathophysiology with FDA approved use in Persistent Pulmonary Hypertension in the Newborn for 10+ years Inhaled NO has ultra-local effect when targeted to the alveoli smooth muscle Metabolized rapidly as it contacts blood INOpulse is being developed as a safe and effective add-on to existing therapies cGMP Nitric Oxide cGMP Pathway sGC |
|
|
INOpulse Scientific Advisory Board Senior International Experts in PAH, PH-COPD and PH associated with other lung diseases Greg Elliot, MD, Utah: Professor of Medicine at the University of Utah and Chief of the Pulmonary and Critical Care Medicine Division at the LDS Nazzareno Galie, MD, Italy: Head of the Pulmonary Hypertension Center at the University of Bologna Ardi Ghofrani, MD, Germany: Associate Professor for Internal Medicine at University Hospital, Giessen Fernando Martinez, MD, NYC: Executive Vice Chair of Medicine, Weill Cornell Medical College and New York-Presbyterian Hospital/Weill Cornell Medical Center Robert Naeije, MD, PhD, Belgium: Professor and Chairman of the Department of Physiology and Pathophysiology at Erasme University Hospital, Brussels Steve Rennard, MD, Omaha: Larson Professor of Medicine in the Pulmonary and Critical Care Medicine, Department of Internal Medicine at the University of Nebraska Medical Center in Omaha Olivier Sitbon, MD, France: Professor of Respiratory Medicine at the South Paris University Lewis Rubin, MD, NYC: Emeritus Professor of Medicine at the University of California in San Diego; now consultant out of NY Vallerie McLaughlin, MD, Detroit: Director of the Pulmonary Hypertension Program at the University of Michigan and Attending Physician at the University of Michigan Health System in Ann Arbor, MI |
|
|
Potential Indications for Chronic Use of Pulsed iNO Pulmonary Arterial Hypertension (PAH) Several approved therapies but median survival still less than 5 years Orphan disease PH associated with Chronic Obstructive Pulmonary Disease (PH-COPD) No current drug therapies PH associated with Idiopathic Pulmonary Fibrosis (PH-IPF) No current drug therapies Orphan disease Chronic Thromboembolic Pulmonary Hypertension* (CTEPH) Riociguat recently approved for this condition Orphan disease PH associated with Sarcoidosis* No current drug therapies Orphan disease * Subject to finalizing discussions and entering into an agreement for additional licensing rights from Ikaria/Mallinckrodt |
|
|
INOpulse Device Patents Patent Status Expiration Notes Method of NO administration Issued-US Pending in other territories 1-2027 Covers consistent delivery of prescribed dose independent of respiratory rate Cannula Issued-US 12-2033 Covers accurate dose delivery and reduced NO2 formation Index valve Pending-US Pending-EU 5-2029 Ensures other cartridges cannot be used with INOpulse In addition to patent protection, we will have 7 years of market exclusivity in the US from Orphan Drug status* for PAH Orphan status filing for PAH planned for EU where orphan market exclusivity of 10 years may be available* * Contingent on INOpulse being the first inhaled nitric oxide therapy to receive FDA approval or EMA marketing authorization, respectively, in this indication |
|
|
INOpulse: Primary Indication in Pulmonary Arterial Hypertension (PAH) |
|
|
Pulmonary Arterial Hypertension (PAH) Disease of the Pulmonary Arteries Under 30 group at PHA Meeting They like going to karaoke at Disney World at PHA Meeting in Orlando Many are children and teenagers Diagnosed by right heart catheterization Despite the available therapies, PAH patients have a poor prognosis with high mortality rates resulting in a median survival of less than 5 years Only cure is lung transplantation More common in young women Approximately 20,000 patients in the US and EU have severe to very severe disease and are treated with multiple therapies, including many who are on Long Term Oxygen Therapy (LTOT) Pricing for existing treatments are in the range of ~$100K to $150K per patient per year in the US |
|
|
INOpulse Targets a New Pathway to Treat PAH Adapted from Humbert M et al. N Engl J Med. 2004;351:1425-1436. Endothelin receptor A Endothelin receptor B Endothelin-1 Endothelin Pathway Prostacyclin Pathway Prostacyclin (prostaglandin I2) IP receptor + sGC cGMP Sildenafil Nitric Oxide cGMP Pathway Riociguat + |
|
|
Pilot Study Indicated Efficacy of Pulsed iNO in PH Perez-Penate et al. J Heart Lung Transplant 2008;27:1326 7 patients with severe PAH who declined i.v. prostacyclin 4 patients with severe CTEPH Individualized pulsatile inhaled nitric oxide treatment administered for 8-12 months Change in Six Minute Walk Distance (6MWD) * Two patients did not complete 1 year evaluation; data are from 6 months test assessed as last measurement carried forward Change in WHO Severity Classification |
|
|
INOpulse for PAH: Phase 2 Trial Purpose of trial: Evaluate effect of iNO on hemodynamic measures and 6MWD in ambulatory patients with PAH on at least one approved therapy Design: Randomized, double-blind, placebo-controlled 16-weeks study with 80 patients in 52 sites Two active doses of 25 and 75 mcg/kg IBW/hr Endpoints: Primary: change in pulmonary vascular resistance (PVR) Target change of 190; powered for significance at 130 Secondary: change in 6MWD Clinically meaningful change is 30 to 35 meters Units for PVR: dynes sec.cm-5 Units for 6MWD: meters |
|
|
LTOT Users Were More Compliant to INOpulse Therapy Data shown as percentage of patients in group Higher adherence (>12 hrs of use per day) Lower adherence (<12 hrs of use per day) 71% 29% 56% 44% 32% 68% All On LTOT (at baseline) Not on LTOT (at baseline) |
|
|
Summary of Results: High Dose iNO Prevented Worsening of Hemodynamics and Showed Clinically Significant Improvement in Exercise Tolerance in LTOT Patients Units for PVR: dynes sec.cm-5; Units for 6MWD: meters N Placebo 25 iNO 75 iNO All patients 71 47.2 -54.1 -15.0 LTOT users 44 125.5 -47.1* -17.5 * p<0.05 vs. placebo Resting PVR: Change vs. Baseline (Mean) N Placebo 25 iNO 75 iNO All patients 71 7.5 4.7 22.8 LTOT users 43 -10.7 9.1 34.9* 6MWD: Change vs. Baseline (Mean) -100 -50 0 50 100 150 Placebo 25 INO 75 INO PVR (dynes.sec.cm - 5 ) All Patients LTOT -20 -10 0 10 20 30 40 Placebo 25 iNO 75 iNO Change 6MWD (meters) All Patients LTOT |
|
|
Inhaled Nitric Oxide Has Shown Significant Incremental Efficacy When Used With Oxygen Therapy ANOVA p Value is 0.0002 for mPAP and < 0.0001 for PVR mPAP and PVR for O2 + NO was different than for O2 and RA (p<0.05) PVR for O2 was different than for RA (p<0.05) Source: Atz et al, J Am Coll Cardiol 1999; 33:813-9 Academic study of 25 patients with PH, ranging in age from 5 months to 69 years, to evaluate acute vasoreactivity testing with oxygen alone and with nitric oxide versus room air = 5.7 = 12.8 = 5.8 = 9.6 |
|
|
Inhaled Nitric Oxide Has Improved Exercise Capacity in Heart Failure Patients With Pulmonary Hypertension In a prior academic study, patients with heart failure were evaluated for exercise capacity, measured as oxygen consumption (VO2) at peak exercise i.e. at the anaerobic threshold (AT) Exercise testing was performed with and without inhaled NO and patients were assessed by degree of PH measured as pulmonary arterial systolic pressure (PAS) Patients with high pulmonary artery pressures benefited more than patients with lower pressures and showed significant improvements in exercise capacity versus baseline These results show the importance of pulmonary circulation during exercise and the potential for iNO to impact exercise capacity Source: Koelling et al, Am. J of Card., June 15 1998 p < 0.05 0 5 10 15 20 25 30 <30 n = 6 >30 n = 7 VO 2 at AT , % change with NO PAS (mm Hg) |
|
|
Potential Mechanism of Action for Inhaled NO in PAH FDA analyzed 38 studies that they had reviewed and concluded only 5% of the change in 6MWD could be accounted for by change in PVR measured at rest Inhaled iloprost shows a significant decrease in PVR with inhalation, but after inhalation PVR at rest returned to baseline, but still causes a significant increase in 6MWD Improvements in 6MWD are related to both improvements in hemodynamics and the delivery of blood flow and oxygenation to exercising muscle During 6MWT, PAH patients may desaturate (SpO2 < 90%) by the end of the test, which could result in low delivery of oxygen to the periphery Lewis et al, Circulation. 2013;128:1470-1479.; Naeije et al, Am J Respir Crit Care Med Vol 187, Iss. 6, pp 576–583, Mar 15, 2013; Hasuda et al, Circulation. 2000;101:2066-2070; Lawrence et al., Contemporary Clinical Trials 33 (2012) 1217–1224; Olchewsky et al, N Engl J Med, Vol. 347, No. 5, August 1, 2002 INOpulse may improve 6MWD by blocking rise in PVR which occurs during exercise and by improving oxygen delivery to periphery |
|
|
Overall The Drug Was Well Tolerated Patients Placebo 25 iNO 75 iNO Number of patients 26 27 27 Total Adverse Events 23 22 26 Drug Related AEs 9 10 9 Total Serious Adverse Events 4 4 9 Drug Related SAEs 0 1 1 Deaths 1 0 0 Discontinuation due to AEs 1 1 2 The results were reviewed by the Data and Safety Monitoring Board and continuation of Part 2 of trial was approved |
|
|
Regulatory Pathway Following the recent End of Phase 2 meeting with FDA and preliminary input from EMA, we plan to conduct the Phase 3 program with 2 trials as follows: One trial with 1 active dose (75 mcg) vs placebo with ~90 patients per arm Another trial with 2 active doses (50 & 75 mcg) vs placebo with ~90 patients per arm Primary endpoint planned as change in 6MWD Secondary endpoint of Time to Clinical Worsening with analysis combining data across both trials Recruitment will focus on patients on LTOT and include a run-in period to enrich for adherence; Endpoints will be measured at 16 weeks after the run-in period Regulated as a drug-device combination Orphan Drug Designation granted in US Plan to apply for EU designation; Has been granted for other PAH drugs |
|
|
Phase 3 International Steering Committee Senior PAH Clinicians with Expertise in Clinical Trials Adaani Frost, MD, Co-Chair: Professor of Medicine at Baylor College of Medicine, Houston, Texas Ray Benza, MD: Professor of Medicine at Temple University School of Medicine, Philadelphia, PA Hap Farber, MD: Professor at Boston University and Boston Medical Center John Granton, BSc, MD, FRCPC: Director of the Pulmonary Hypertension program at the Toronto General Hospital Shelly Shapiro, MD, PhD: Clinical Professor of Medicine, UCLA and West Los Angeles Veterans Administration Healthcare System North America Europe Marius Hoeper, MD, Co-Chair: Professor, University of Hanover Medical School, Germany Marion Delcroix, MD: Professor of Medicine and of Respiratory Physiology at the Catholic Universities of Leuven, Belgium Andrew Peacock, MPhil, MD, FRCP: Professor in Medicine at the University of Glasgow and Director of the Scottish Pulmonary Vascular Unit, at the Golden Jubilee National Hospital |
|
|
INOpulse 2nd Indication: PH-COPD |
|
|
PH-COPD Patients Constitute a Large and Sick Patient Group US Patient Population All treated COPD patients ~12 mil. ~1.4 mil. PH-COPD patients COPD patients with Pulmonary Hypertension have poor prognosis and QoL Median life-expectancy is ~4 years High hospitalization rates Impaired exercise capacity No approved therapy for treating PH in these patients ~700K On LTOT |
|
|
INOpulse May Offer Unique Benefits in Treating COPD Patients with PH Existing PAH therapy lowers pulmonary pressures but negatively influences oxygenation in PH-COPD Pulsed iNO can be targeted to the alveoli Short pulse early in inspiration dilates vessels in best ventilated alveoli only, reduces pulmonary pressures, and prevents admixture of less oxygenated blood Local and fast metabolism prevents delivery to non-targeted alveoli Bianco 2010, Lederer 2012, Stolz 2008 |
|
|
High-Resolution Computed Tomography Imaging Study The objective of this exploratory study was to further validate the potential benefits for COPD patients by measuring changes in pulmonary vessels (i.e. vasodilation) as a function of short term iNO administration using INOpulse in subjects with PH associated with COPD on LTOT Acute Treatment with iNO 30 mcg/kg IBW/hr for at least 20 minutes not to exceed 90 minutes (n=6) No significant drop in blood oxygenation (SpO2) was observed during inhalation |
|
|
Comparison of Ventilation vs. Perfusion Lobe segmentation Blood vessels segmentation |
|
|
Vasodilation by pulsed iNO 30 in a patient with PH-COPD determined by HRCT and Computational Fluid Dynamics: Patient 2 30 mcg/kg IBW/hr for 20 minutes % Total |
|
|
30 mcg/kg IBW/hr for 20 minutes % Total Vasodilation by pulsed iNO 30 in a patient with PH-COPD determined by HRCT and Computational Fluid Dynamics: Patient 3 |
|
|
Good correlation between ventilation and vasodilation after iNO: better ventilated regions experience more vasodilation Each dot represents one lobe from one of 5 patients |
|
|
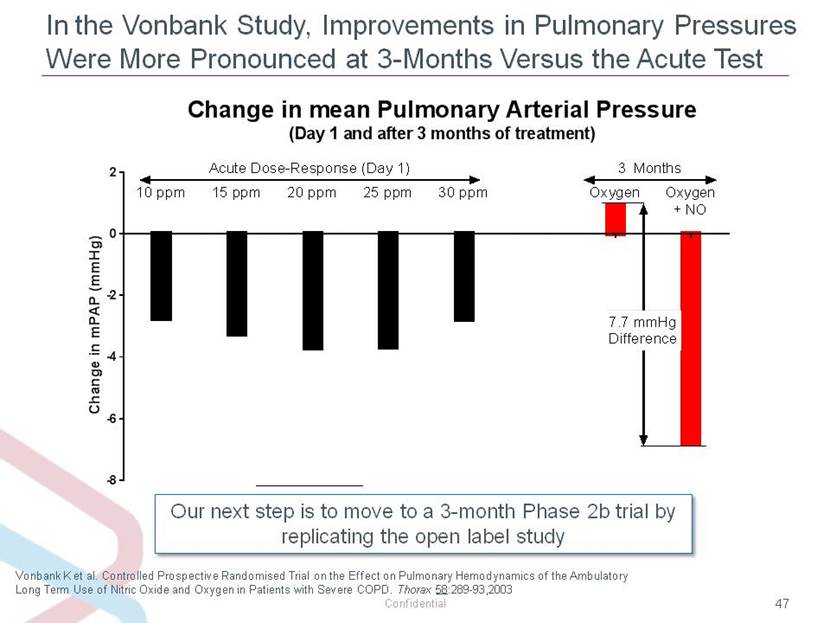
Pilot Studies Support Testing Long Term Benefit of iNO in PH-COPD Patients Vonbank K et al. Thorax 58:289-93,2003 PVRI = Pulmonary vascular resistance index PASP = Pulmonary artery systolic pressure iNO demonstrated sustained hemodynamic benefits in PH-COPD patients 3 month, open-label trial of pulsed iNO delivered using a prototype device Patients were randomized to LTOT alone (n=17) or LTOT + pulsed iNO (n=15) At 3 months, iNO reduced PVRI and PASP and increased cardiac output without negative impact on hypoxemia p < 0.001 = Improvement Oxygen alone Oxygen + iNO @ baseline @ 3 mo. p = 0.739 = No Deterioration Hemodynamics Hypoxemia 0 2 4 6 8 10 12 PaO2 (kPa) 0 100 200 300 400 500 600 PVRI (dyne/s/cm5/m2) |
|
|
INOpulse Testing Confirmed Impact on Pulmonary Hemodynamics Without Hypoxemia PASP = Pulmonary artery systolic pressure *PASP data consistently favor iNO at doses 10 – 75 mcg/kg IBW/hr, but statistical significance compared to placebo was not reached FDA asked us to establish a dose range with the INOpulse device and to confirm the efficacy and safety results seen in the open label study We have completed randomized placebo controlled acute test with 159 patients using the INOpulse device with doses ranging from 3 to 75 mcg/kg IBW/hr Oxygenation levels were similar to placebo across all doses tested PASP change vs. baseline was very similar to the open label study for doses >10 mcg/kg IBW/hr |
|
|
In the Vonbank Study, Improvements in Pulmonary Pressures Were More Pronounced at 3-Months Versus the Acute Test Vonbank K et al. Controlled Prospective Randomised Trial on the Effect on Pulmonary Hemodynamics of the Ambulatory Long Term Use of Nitric Oxide and Oxygen in Patients with Severe COPD. Thorax 58:289-93,2003 Our next step is to move to a 3-month Phase 2b trial by replicating the open label study |
|
|
Summary |
|
|
Major Institutional Stockholders |
|
|
Expected Milestones INOpulse PAH Phase 2 trial Phase 3 trial* PH-COPD Phase 2b trial BCM CE Mark registration trial 1st Procedure safety trial Pivotal trial (for US) Q4 ’14 Q1 ’15 Q2 ’15 Q3 ’15 Q4 ’15 Q1 ’16 Q2 ’16 FDA EoPh2 Meeting Trial start Enrollment complete Topline results CE Mark approval * Includes ongoing long-term extension study for PAH EoPh2 = End of Phase 2 (Type B) meeting Mid ’18 Early ’17 Mid ’16 Mid ’18 Topline results expected Topline results Trial start Trial start Trial start |
|
|
Bellerophon Highlights Focused on developing novel therapies for severe cardiopulmonary and cardiac diseases Product candidates address opportunities at the intersection of drugs and devices with high unmet need BCM: Novel injectable treatment designed to prevent Congestive Heart Failure (CHF) Simple mechanism to prevent ventricular remodeling following a heart attack Pilot study results support safety and suggest morbidity/mortality benefit CE Mark registration trial enrollment complete with topline results in mid-2015 Approval will follow a device regulatory pathway, with potential for CE Mark approval in H1 2016 INOpulse: Extension of nitric oxide based therapy for Pulmonary Hypertension (PH) in chronic diseases Nitric oxide approved for use in hospital in neonates; over 450,000 patients treated since launch Novel delivery technology allows for use in serious chronic diseases Several potential applications include: PAH: Planning to initiate Phase 3 in 2015 PH-COPD: Planning Phase 2b Other opportunities may include PH-Idiopathic Pulmonary fibrosis, CTEPH and PH-Sarcoidosis Strong IP protection on core programs |
|
|
Backup Slides 4/25/2015 |
|
|
We Expect That the Mark2 Device, Which is Substantially Lighter and More Intuitive, Will Improve Adherence ~8 lbs. weight LCD display with multiple menus/settings designed for use by RT’s in hospital Needs a backpack or wheeled bag to carry ~2.5 lbs. in weight Easy to use user interface with a three step start up Fits in small hip/shoulder bag; in usability testing, patients could carry in purse Images are not to scale Drug and battery indicator Alarm indicator and silence button Purge out (cannula) 3 Plug in (cannula) 2 Turn on 1 Physicians can set dose and download usage data INOpulse DS Mark2 |
|
|
Pulmonary Hypertension Independently Predicts Reduced Survival in Moderate-to-Severe COPD 1 Oswald-Mammosser, M et al. Prognostic Factors in COPD Patients Receiving Long-term Oxygen: Importance of Pulmonary Artery Pressure. Chest 1995; 107:1193-98 2 Andersen KH et al. Prevalence, Predictors and Survival in Pulmonary Hypertension Related to End-stage Chronic Obstructive Pulmonary Disease. Journal of Heart and Lung Transplantation 2012; 31: 373-380. mPAP < 25 mmHg mPAP > 25 mmHg Survival years Data published in 19951 Data published in 20122 mPAP < 25 mmHg mPAP > 25 mmHg 5 Year Survival mPAP < 25 mmHg: 62% mPAP > 25 mmHg: 36% 5 Year Survival mPAP < 25 mmHg: 63% mPAP > 25 mmHg: 37% |