Attached files
| file | filename |
|---|---|
| EX-21 - SUBSIDIARIES - Benefytt Technologies, Inc. | d489881dex21.htm |
| EX-31.1 - CERT - Benefytt Technologies, Inc. | d489881dex311.htm |
| EX-32 - CERT - Benefytt Technologies, Inc. | d489881dex32.htm |
| EX-31.2 - CERT - Benefytt Technologies, Inc. | d489881dex312.htm |
| EX-23.1 - CONSENT - Benefytt Technologies, Inc. | d489881dex231.htm |
Table of Contents
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, DC 20549
FORM 10-K
| x | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2012
| ¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
COMMISSION FILE NUMBER 001-35811
Health Insurance Innovations, Inc.
(Exact name of registrant as specified in its charter)
| Delaware | 46-1282634 | |
| (State or other jurisdiction of incorporation or organization) |
(IRS Employer Identification No.) |
15438 North Florida Avenue, Suite 201
Tampa, Florida 33613
(Address of principal executive offices) (zip code)
Registrant’s telephone number, including area code:
(877) 376-5831
SECURITIES REGISTERED PURSUANT TO SECTION 12(b) OF THE ACT:
| Title of each class |
Name of each exchange on which registered | |
| Class A common stock, par value $0.001 per share | NASDAQ Global Market |
SECURITIES REGISTERED PURSUANT TO SECTION 12(g) OF THE ACT: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ¨ No x
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Exchange Act. Yes ¨ No x
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the Registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ¨ No x
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§ 232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ¨ No ¨
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. ¨
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer or a smaller reporting company. See the definitions of “large accelerated filer”, “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Exchange Act. (Check one):
| Large accelerated filer | ¨ | Accelerated filer | ¨ | |||
| Non-accelerated filer | ¨ (Do not check if a smaller reporting company) | Smaller reporting company | x | |||
Indicate by check mark whether the registrant is a shell company (as defined in Exchange Act Rule 12b-2). Yes ¨ No x
The aggregate market value of the common stock held by non-affiliates of the registrant, as of March 27, 2013, was approximately $73,313,260 million. Such aggregate market value was computed by reference to the closing price of the common stock as reported on the NASDAQ Global Market on March 27, 2013. For purposes of making this calculation only, the registrant has defined affiliates as including only directors and executive officers and shareholders holding greater than 10% of the common stock of the registrant as of March 27, 2013. The registrant used March 27, 2013 as the measurement date because its common stock was not publicly traded as of the last business day of its most recently completed second fiscal quarter.
As of March 27, 2013, there were 5,295,167 shares of the registrant’s Class A common stock, $0.001 par value per share, outstanding and 8,566,667 shares of the registrant’s Class B common stock, $0.001 par value per share, outstanding.
Table of Contents
| 1 | ||||||
| 1 | ||||||
| 2 | ||||||
| ITEM 1. |
2 | |||||
| ITEM 1A. |
18 | |||||
| ITEM 1B. |
35 | |||||
| ITEM 2. |
35 | |||||
| ITEM 3. |
35 | |||||
| ITEM 4. |
35 | |||||
| 36 | ||||||
| ITEM 5. |
36 | |||||
| ITEM 6. |
37 | |||||
| ITEM 7. |
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS |
38 | ||||
| ITEM 7A. |
53 | |||||
| ITEM 8. |
53 | |||||
| ITEM 9. |
CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE |
53 | ||||
| ITEM 9A. |
54 | |||||
| ITEM 9B. |
55 | |||||
| 56 | ||||||
| ITEM 10. |
56 | |||||
| ITEM 11. |
59 | |||||
| ITEM 12. |
SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS |
61 | ||||
| ITEM 13. |
CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE |
62 | ||||
| ITEM 14. |
64 | |||||
| F-1 | ||||||
| ITEM 15. |
F-1 | |||||
| F-19 | ||||||
Table of Contents
In this report, unless the context otherwise requires, “HII,” the “Company,” “we,” “us” and “our” refer to (1) prior to the consummation of the reorganization described under “Item 1. Business—Our History and the Reorganization of Our Corporate Structure,” Health Plan Intermediaries, LLC, and (2) after giving pro forma effect to the reorganization, Health Insurance Innovations, Inc., a Delaware corporation, and its consolidated subsidiaries, including Health Plan Intermediaries Holdings, LLC. References to “Series B Membership Interests” in this report are to Health Plan Intermediaries Holdings, LLC Series B Membership Interests. The term “Predecessor” refers to our Company prior to the acquisition described under “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Basis of Presentation,” and the term “Successor” refers to our Company following such acquisition. Unless otherwise indicated, all references to the year ended December 31, 2012 relate to the year ended December 31, 2012 of the Successor. All references to the nine months ended September 30, 2011 relate to the nine-month period ended September 30, 2011 of the Predecessor. All references to the year ended December 31, 2011 relate to the combined three-month period ended December 31, 2011 of the Successor and the nine-month period ended September 30, 2011 of the Predecessor. The presentation of combined Predecessor and Successor operating results (which is the arithmetic sum of the Predecessor and Successor amounts) is a presentation not incompliance with United States Generally Accepted Accounting Principles (“GAAP”), which is provided as a convenience solely for the purpose of facilitating comparisons of current results with combined results over the same period in the prior year. For more information about the reorganization and our recent initial public offering, including a diagram of our organizational structure, see “Item 1. Business—Our History and the Reorganization of Our Corporate Structure.”
SPECIAL NOTE REGARDING FORWARD-LOOKING STATEMENTS
We have made statements in “Item 1A. Risk Factors,” “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations,” “Item 1. Business” and in other sections of this report that are forward-looking statements. All statements other than statements of historical fact included in this report are forward-looking statements. You can identify forward-looking statements by the fact that they do not relate strictly to historical or current facts. These statements may include words such as “may,” “might,” “will,” “should,” “expects,” “plans,” “anticipates,” “believes,” “estimates,” “predicts,” “potential” or “continue,” the negative of these terms and other comparable terminology. These forward-looking statements, which are subject to risks, uncertainties and assumptions about us, may include projections of our future financial performance, our anticipated growth strategies, anticipated trends in our business and other future events or circumstances. These statements are only predictions based on our current expectations and projections about future events. There are important factors that could cause our actual results, level of activity, performance or achievements and other future events or circumstances to differ materially from the results, level of activity, performance or achievements, events or circumstances expressed or implied by the forward-looking statements, including those factors discussed “Item 1A. Risk Factors.” You should specifically consider the numerous risks outlined under “Item 1A. Risk Factors.”
Although we believe the expectations reflected in the forward-looking statements are reasonable, we cannot guarantee future results, level of activity, performance, achievements, events or circumstances. We are under no duty to update any of these forward-looking statements after the date of this report to conform our prior statements to actual results or revised expectations.
1
Table of Contents
| ITEM 1. | BUSINESS |
Overview
Our Company
We are a leading developer and administrator of affordable, web-based individual health insurance plans and ancillary products. Our highly scalable, proprietary, web-based technology platform allows for mass distribution of, and online enrollment in, our large and diverse portfolio of affordable health insurance offerings.
Our technology platform provides customers, who we refer to as members, immediate access to our products through our distribution partners anytime, anyplace. The health insurance products we develop are underwritten by insurance carrier companies, and we assume no underwriting, insurance or reimbursement risk. Members can price and tailor product selections to meet their needs, buy policies and print policy documents and identification cards in real-time. Our sales are executed online and offer instant electronic fulfillment. Our technology platform uses abbreviated online applications, some with health questionnaires, to provide an immediate accept or reject decision on applications for all products that we offer. Once an application is accepted, individuals can use our automated payment system to complete the enrollment process and obtain instant electronic access to their policy fulfillment documents, including the insurance policy, benefits schedule and identification cards. We receive credit card and Automated Clearing House (“ACH”) payments directly from members at the time of sale. Our technology platform provides significant operating leverage as we add members and reduces the costs associated with marketing, selling, underwriting and administering policies.
We are an industry leader in the sale of 12-month short-term medical (“STM”) insurance plans, an alternative to traditional Individual Major Medical (“IMM”) plans, which provide lifetime renewable coverage. STM plans generally offer qualifying individuals comparable benefits for fixed short-term durations of six or 12 months at approximately half the cost of IMM plans. While applications for IMM insurance may take up to 60 days to process, STM plans feature a streamlined underwriting process offering immediate coverage options. We also offer guaranteed-issue hospital indemnity plans for individuals under the age of 65, which pay fixed cash benefits for covered procedures and services, and a variety of ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans that are frequently purchased as supplements to STM and hospital indemnity plans. We design and structure insurance products on behalf of insurance carrier companies, market them to individuals through our large network of distributors and manage member relations via our online member portal, which is available 24 hours a day, seven days a week. Our online enrollment process allows us to aggregate and analyze consumer data and purchasing habits to track market trends and drive product innovation. We have established relationships with several highly rated insurance carriers, including Starr Indemnity & Liability Company, Companion Life, United States Fire, ING, Markel and CIGNA, among others. In addition, as of December 31, 2012, the large independent distribution network we access consists of 46 licensed agent call centers and 262 wholesalers, including Marsh, eHealthInsurance and MasterCard, among others, that work with over 8,275 licensed brokers. Our data-driven product design, technology platform and extensive distribution network have enabled us to grow our revenues from $29,878,000 in 2011 to $41,940,000 in 2012.
We focus on the large and under-penetrated segment of the U.S. population who are uninsured or underinsured, which includes individuals who are unable to afford traditional IMM premiums, individuals not covered by employer-sponsored insurance plans, such as those who are self-employed as well as small business owners and their employees, and underserved “gap populations” that require insurance due to changes caused by life events, such as new graduates, divorcees, early retirees, military discharges, the unemployed, part-time and seasonal employees and temporary workers. Our target market consists of approximately 64 million Americans, including approximately 50 million Americans who were uninsured in 2010, according to the U.S. Census Bureau, and approximately 14 million non-elderly Americans who purchased individual health insurance plans in 2010, according to a 2010 Kaiser Family Foundation survey. As of December 31, 2012, we had 23,747 STM members. We expect the number of uninsured and underinsured to significantly increase due to the rising costs and burdensome underwriting requirements of traditional IMM plans and a decline in employer-sponsored health insurance programs.
As of December 31, 2012, we had 23,747 STM plans in force, compared with 18,059 on December 31, 2011, with an average monthly retention rate of 79% from December 31, 2011 to December 31, 2012. We earn our revenues from commissions and fees related to the sale of products to our members. Our ancillary products have created several additional revenue streams and resulted in a significant portion of our business being generated by monthly member renewals. For the year ended December 31, 2012, our premium equivalents, revenues and EBITDA were $75,872,000, $41,940,000 and $4,543,000, respectively, representing a 42.6%, 40.4% and 65.7% increase compared to premium equivalents, revenues and EBITDA of $53,206,000, $29,878,000 and $2,742,000, respectively, for the year ended December 31, 2011. For more detail about the use of premium equivalents as a business metric and a reconciliation of premium equivalents to revenues, see “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Key Business Metrics—Premium Equivalents.”
2
Table of Contents
Health Insurance Industry and Market Opportunity
We believe ongoing changes in the health insurance industry will expand and reshape our target market. For example, the Patient Protection and Affordable Care Act, or PPACA, and the Health Care and Education Reconciliation Act of 2010, or HCERA, which we refer to, collectively, as “Healthcare Reform”, were signed into law on March 23, 2010. After facing a number of legal challenges, Healthcare Reform was upheld by the U.S. Supreme Court on June 28, 2012. Healthcare Reform includes a mandate requiring individuals to carry health insurance or face tax penalties; a mandate that certain employers with over 50 employees offer their employees group health insurance coverage or face tax penalties; prohibitions against insurance companies that offer traditional IMM insurance plans using pre-existing health conditions as a reason to deny an application for health insurance; and medical loss ratio (“MLR”) requirements that require each health insurance carrier to spend a certain percentage of its IMM premium revenue on reimbursement for clinical services and activities that improve healthcare quality.
According to a 2011 McKinsey survey, the implementation of Healthcare Reform will likely increase the number of Americans in the individual health insurance market from 14 million to more than 100 million starting in 2014. We believe this increase will be primarily driven by two key factors: employers dropping group coverage and an additional 45 million uninsured Americans entering the individual insurance market. The McKinsey survey estimates that approximately 30% of employers would “definitely” or “probably” drop employer-sponsored insurance starting in 2014. The estimated penalty employers will face for not providing their employees coverage is $2,000 per employee for employers with over 50 employees (there is no penalty for employers with less than 50 employees), which is significantly less than the estimated price currently paid for employee coverage ($9,000 to $14,000 per employee). Assuming a 30% drop in employer-sponsored insurance, approximately 50 million Americans would join the individual health insurance market starting in 2014. In addition, because Americans will face penalties if they are uninsured, we expect that a large number of the current uninsured population of 50 million will enter the individual health insurance market. Accordingly, after 2014, we expect that the individual health insurance market will grow more than 600% to over 100 million policyholders, representing annual individual aggregate health insurance premiums in the United States of approximately $361 billion, compared with approximately $50 billion in 2010.
We believe certain dynamics in the health insurance industry present an opportunity to increase our market share in the individual health insurance market. For example, the minimum MLR thresholds require that IMM carriers use 80% of all premiums collected to pay claims. This has significantly reduced distributor commission rates on traditional IMM policies, forcing many distributors to abandon the traditional face-to-face IMM sales model. Starting in 2014, IMM carriers will also be subject to a pre-existing condition mandate, requiring them to accept all customers regardless of their pre-existing conditions. This “must-carry” pre-existing conditions requirement will further increase the costs of IMM coverage. Unlike traditional IMM plans, our STM products are exempt from the minimum MLR thresholds and “must-carry” pre-existing conditions requirements under Healthcare Reform, allowing us to offer attractive distributor commission rates while providing affordable products for individuals. In addition, Healthcare Reform also requires that states establish health insurance exchanges where uninsured individuals can select and purchase health insurance plans. We believe that these exchanges will further the transition from group-based insurance coverage to individual health insurance coverage and that our STM products will be an attractive option in the non-subsidized exchange environment. Moreover, consumers are increasingly accessing the Internet to find affordable health insurance solutions. The current number of Internet users in the United States continues to grow and, according to a report published by Pew Research Center, represented 74% of the population in 2010. In addition, according to the same report, 33% of Internet users in 2010 looked online for information related to health insurance. This represents approximately 75 million Americans who used the Internet to access information related to health insurance in 2010.
We intend to aggressively pursue opportunities to help consumers identify our STM products as the right choice for healthcare coverage, and we believe our technology platform, product focus and industry expertise will allow us to gain an increasing share of this growing market.
Our Solutions
We believe that our products address a significant portion of the issues facing the healthcare system in the United States and improve access to coverage for certain underserved segments of the population.
| • | Lack of Access to Health Insurance. Due to the streamlined underwriting process for our STM plans, we are able to provide an instant decision regarding acceptance. Individuals applying for STM coverage only have to answer an abbreviated, online questionnaire regarding the status of their health to screen for risks that cannot be supported by the rate structure and design of the plan before a decision is generated. We also offer hospital indemnity plans under which members are paid fixed dollar amounts by procedure or service according to a defined schedule which includes doctor visits, lab tests, surgeries and hospitalizations. As these plans are not based on an individual’s health status, they guarantee issuance to individuals under the age of 65 and provide a viable coverage alternative for otherwise uninsurable individuals. |
| • | Growing Number of Uninsured and Underinsured Americans. We focus on the large and under-penetrated segment of the U.S. population that is uninsured or underinsured. According to the U.S. Census Bureau, 16% of Americans were uninsured in 2011, representing approximately 50 million individuals. In addition, the percentage of non-elderly Americans with employer-sponsored insurance decreased from 68% in 2000 to 59% in 2009, driving more Americans into the individual health insurance market. The number of uninsured and underinsured Americans continues to grow in part due to reductions in employer-provided health benefits. |
| • | High Cost of Health Insurance. We offer affordable alternatives to IMM. According to the U.S. Census Bureau, approximately 34 million of the 50 million uninsured Americans in 2011 were members of families with annual incomes of less than $50,000. Based on these figures, we estimate that a sizable portion of the uninsured population chooses not to purchase insurance primarily due to its high cost. According to a 2010 Kaiser Family Foundation survey, traditional IMM premiums increased an average of approximately 20% over a 12-month period, while the cost of our STM plans remained stable. In addition, as a result of Healthcare Reform, IMM premiums are expected to increase significantly in price as a result of guaranteed issue requirements for individuals with pre-existing health conditions. For individuals with pre-existing conditions, we currently offer guaranteed-issue hospital indemnity plans and, only where required by state mandate, STM plans. The implementation of Healthcare Reform will not expand our coverage of such individuals, allowing us to continue to offer attractive distributor commission rates while providing affordable products for members. |
3
Table of Contents
Our Competitive Strengths
We have the following key competitive strengths that we believe collectively provide significant barriers to entry:
| • | Value Generated for All Key Constituents. By combining extensive management experience with our technology platform, we have developed a business model that we believe enables us to create a “win-win” proposition for our key constituents. |
| • | Our Carriers. We offer carriers access to a large member base with no covered pre-existing conditions. Our technology platform connects our carriers directly to a large independent distribution network. Our platform also provides our carriers access to real-time sales and membership data. We use this information to assist our carriers in designing products that cater to their target populations. We currently utilize several carrier companies, including Starr Indemnity & Liability Company, Companion Life, United States Fire, ING, Markel and CIGNA, among others. Our management team has long-standing relationships with most of the major carrier companies we utilize and has not lost a carrier relationship in over 10 years. |
| • | Our Distributors. At a time when commission rates on many health insurance products, including traditional IMM plans, are declining, we provide our distributors with specialized, highly sought-after product offerings and a compensation structure characterized by attractive commission rates and advanced payments. We believe our long-standing relationships with most of the major carriers we utilize, as well as our technology platform, which enables real-time underwriting decisions, immediate sales conversions and access to commission data and selling tools, drive demand for distributors to partner with us. We also offer a turnkey solution that allows us to design products that best meet our distributors’ needs. This solution enables us to assist our distributors in choosing between insurance carriers on a single website and allows them to create customized products for their customers by bundling our STM and hospital indemnity products with our various ancillary products into one package. As of December 31, 2012, we utilized a network of 46 licensed agent call centers and 262 wholesalers that work with over 8,275 licensed brokers nationally. |
| • | Our Members. We provide our members with easy access to health insurance coverage at an affordable price. For qualifying individuals, our STM plans offer benefits comparable to traditional IMM plans at approximately half the cost. For example, according to a 2010 Kaiser Family Foundation survey, the average cost for an IMM plan is $3,606 for an individual and $7,102 for a family. However, the average cost for one of our 12-month STM plans is $1,800 for an individual and $3,600 for a family. Our technology platform allows our members to compare and quote prices for a broad spectrum of STM and hospital indemnity products and, after they have made informed purchase decisions, to buy and print policies online. In addition to STM and hospital indemnity plans, we allow our members the opportunity to purchase high quality ancillary products with automatic, monthly renewals at rates that fit our members’ budgets, all at the click of a button. For example, during the year ended December 31, 2012, in addition to the 59,877 STM plans that we sold, we successfully cross-sold 44,064 new ancillary products. |
| • | Proprietary, Web-Based Technology Platform. We believe our technology platform represents a distinct competitive advantage as it reduces the need for customer care agents and provides significant operating leverage as we add members and product offerings. Our primary technology platform is named A.R.I.E.S. (“Automated Real-Time Integrated E System”). We believe our business benefits from the increasing trend of Internet use by individuals to research and purchase health insurance. The Internet offers a means of providing individuals access to health insurance products 24 hours a day, seven days a week and, for the carriers and distributors, reduces the cost and time associated with marketing, selling, underwriting and administering these products. We believe our target market is increasingly researching and applying for health insurance products online and shifting away from more traditional buying patterns. We believe our technology platform positions us for strong continued growth due to the following factors: |
| • | Plan and Product Design. Our technology platform provides real-time data that enables us, our carriers and our distributors to receive immediate information on our members, and allows us to design products that meet the changing demands of the market. Our platform also allows individuals to supplement our STM and hospital indemnity offerings with ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans and makes it possible for us to instantly offer these products, which can be bundled to fit member needs. |
4
Table of Contents
| • | Sales. Our technology platform combined with our customer service model drives faster sale conversions. The entire underwriting procedure is processed through our technology platform, which uses abbreviated, online health questionnaires and provides an immediate accept or reject decision, allowing for instant electronic fulfillment. Individuals can obtain full access to our technology platform through our distribution partners and can price products, buy policies and print their policy documents and identification cards anytime, anyplace. Our call centers use our technology platform to, among other functions, perform online, real-time electronic quoting, to process electronic applications and to provide instant electronic approval and fulfillment, back-office administrative support and commission reporting. |
| • | Distribution. Our technology platform allows for low cost mass distribution of our products and provides significant operating leverage. Our automated payment system allows us to collect credit card and ACH payments electronically and directly from members and to disburse commission payments to our distributors in advance, weekly or monthly. In addition, the system provides distributors with direct access to commission statements, selling tools, reporting tools (for example, information as to cancelations, failed credit card and ACH payments and persistency, renewal and cross-sell rates) and custom links to support their business. |
| • | Compliance. In addition to our A.R.I.E.S. platform, we have obtained a license to use a technology platform called HiiVe, which we use to implement a highly automated compliance program that has enhanced quality while minimizing overhead and allowed us to offer higher commissions to our distributors. The compliance program enables us to record each enrollment phone call, retrieve archived calls within seconds and score calls based on script adherence. |
| • | Established Long-Standing Insurance Carrier Relationships. Our access to carriers is essential to our business. Our management team has developed close relationships with the senior management teams of many of our insurance carriers, some lasting over 15 years. Our management team has not lost a carrier relationship in over 10 years. We believe that the nature of our relationships with our insurance carriers, combined with our product knowledge and technology platform, allow us to provide value-added products to our members. |
| • | Extensive Long-Term Relationships with Licensed Insurance Distributors. We believe our product expertise, our relationships with multiple insurance carriers, our focus on compliance and our technology platform make us a partner of choice for our distributors. We offer an appealing, incentive-based compensation structure that we believe drives demand for distributors to partner with us. We have extensive knowledge of the individual health insurance products that we design and administer, which allows us to assist our distribution partners in placing business. Our management team has built a broad distribution network and continuously adds new distributors. As of December 31, 2012, we utilized a network of 46 licensed agent call centers and 262 wholesalers that work with over 8,275 licensed brokers. Over the last 12 months, we added over 4,675 licensed brokers, 24 independent licensed broker call centers and 73 wholesalers to our national distributor network. |
| • | Seasoned Management Team. Our management team has substantial experience and long-standing relationships developed over an average of 25 years in the insurance industry. Our management team draws on its industry experience to identify opportunities to expand our business and collaborate with insurance carriers and distributors to help develop products and respond to market trends. In addition, the majority of our management team has worked together under the leadership of Michael W. Kosloske, our Chairman, President, and Chief Executive Officer, for more than a decade. |
Our Strategy
Our objective is to continue to expand our business and increase our presence in the affordable, web-based health insurance solutions market. Our principal strategies to meet this objective are:
| • | Expand and Enhance Distributor Relationships, Distribution Channels and Lead Generation Methods. We believe we will continue to attract new distributors as the insurance marketplace continues to evolve, and we intend to continue to identify large distributor and lead relationships through the following strategies: |
| • | Advanced Commission Structure. We will continue to focus on attracting additional distributors through expansion of our advanced commission structure. We believe distributors increasingly demand alternative methods to fund the large and growing costs of lead generation. We estimate that these costs usually range from $2 to $20 per lead and represent a significant startup cost for our distributors. We are in the process of growing our advanced commission structure, whereby we pay distributors commissions on policies sold in advance of when they would ordinarily be due to the distributor. Commissions are advanced for up to six months and are made to distributors with an established track record of selling our products. In return, we reduce subsequent commission fees payable to the distributor by up to 2% of premiums for each month that we advance commissions. We believe this structure will assist our distributors in funding their lead generation costs and will provide us with a competitive advantage in attracting and retaining distributors and will increase sales. |
5
Table of Contents
| • | Call Centers. We believe we can grow our distribution network organically by developing call center managers and incentivizing them via attractive commissions. As part of this strategy, we assist in enhancing the sales model of many of our current call centers in order to increase efficiencies and maximize returns, and we established our Insurance Center for Excellence, LLC (“ICE” or “Insurance Academy”) in June 2012 to expand the number of call centers selling our products. We anticipate that our Insurance Academy operations will closely resemble a “franchise model,” in that we will provide the tools (sales scripts, key metrics, lead programs, compensation programs, technology systems, etc.) for building a profitable and successful call center that focuses on selling our products and leverages our technology. Our goal is to assist in the training of owners and managers, who in return agree to enter into long-term agreements with us, under which they are required to market our products. We anticipate establishing relationships with 10 to 20 new call centers per year through our Insurance Academy initiative. We believe that this will enhance our ability to convert leads from our current distribution channels into sales. |
| • | Lead Generation and Innovative Distributor Relationships. We will continue to identify large and innovative distributor and lead relationships that we believe will increase revenue and diversify distribution. For example, in September 2012, we entered into an agreement whereby MasterCard, through its approved pre-paid card member networks, will assist us in targeting and acquiring new relationships or “leads” for marketing our products. Upon notification from MasterCard of a prospective lead, we will negotiate a separate referral fee arrangement with MasterCard at which point such prospective lead will be identified to us. We will then attempt to enter into an agreement with the prospective lead under which it will provide us with a list of its customers who hold MasterCard prepaid cards or it will directly market our products to those customers on our behalf. For example, we have entered into such an agreement with KEEPS America LLC, (“KEEPS”) for our prescription benefits cards. When sending their own pre-paid cards to customers, KEEPS includes our prescription benefits cards in the mailing. If the KEEPS customer uses our card, we pay KEEPS and MasterCard referral fees in connection with the distribution. To further expand our lead generation efforts, we will also continue to explore methods of screening member data for key demographic factors to identify populations for whom our products are well suited. |
| • | Increase Sales of Hospital Indemnity and Ancillary Products. We believe we have a significant opportunity to expand our market share in the hospital indemnity market. Our hospital indemnity plans in force have grown with 5,243 plans in force at December 31, 2011 and 8,141 plans in force at December 31, 2012. After the implementation of Healthcare Reform in 2014, we expect hospital indemnity plans to be used increasingly to supplement high deductible plans. In addition, our technology platform enables us to sell ancillary products that carry higher profit margins than our core STM products and that can be issued to a broader population than STM plans. Our members demand a wide range of ancillary products, including pharmacy benefit cards and dental, cancer and critical illness plans. Ancillary product policies in force grew from 6,649 at December 31, 2011 to 26,230 at December 31, 2012. We believe we are well-positioned to take advantage of these additional opportunities at the time of sale. |
| • | Enhance Product and Name Recognition. We are focused on increasing our marketing efforts to consumers. We intend to aggressively pursue opportunities to help consumers identify our products as the right choice for health insurance coverage. We are pursuing multiple avenues to increase our brand awareness among distributors, carriers and our target market, such as through our arrangement with MasterCard that introduces our products and name to MasterCard’s large pre-paid card member networks. |
| • | Develop and Establish New and Specialized Products to Meet Consumer Needs. We plan to continue to develop and add new products to our existing portfolio of offerings. By leveraging our technology platform member data, feedback gathered by customer service agents and distributors and expertise in plan design, we believe we are well-positioned to design and bundle products that meet customer needs and add a viable source of revenue for us, our distributors and our carriers. For example, in June 2012, we introduced our cancer plan. We sold 1,491 of these policies during the year ended December 31, 2012, and we are currently developing new products, including fully-insured prescription cards. |
| • | Supplement Our Growth through Strategic Acquisitions. Part of our continuing business strategy is to acquire or invest in, companies, products or technologies that complement our current products, enhance our market coverage, technical capabilities or production capacity, or offer growth opportunities. |
Our Products
Our differentiated product offering allows us to build leading positions in our target markets for insurance products and related services. The key products we provide include:
| • | Short-Term Medical Plans. Our STM plans cover individuals for up to six- and 12-month periods with a wide range of co-pay and deductible options at approximately half the cost of traditional IMM plans. For example, according to a 2010 Kaiser Family Foundation survey, the average cost for an IMM plan is $3,606 for an individual and $7,102 for a family. However, the average cost for one of our 12-month STM plans is $1,800 for an individual and $3,600 for a family. STM plans offer similar benefits for qualifying individuals as IMM plans. For example, both STM plans and IMM plans offer a choice of deductibles, a choice of coinsurance, coverage for emergency room care, surgeries, x-rays, lab work, diagnostics, doctor office co-payments, and preferred provider organization network discounts. However, while IMM plans cover prescription drugs, pre-existing conditions and |
6
Table of Contents
| preventive care, STM plans provide optional coverage for prescription drugs and do not cover pre-existing conditions or preventive care unless such coverage is mandated by the state. STM plans do not cover certain medical events such as pregnancy. Additionally, while IMM plans have guaranteed renewability and can be of a permanent duration, STM plan renewal is not guaranteed and STM plans have a limited duration of up to 12 months. Our STM plans provide up to $2 million of lifetime coverage for each insured individual, allow members to choose any doctor or hospital, offer $50 physician office and urgent care co-pays, cover foreign travel and offer phone access to physician services. As of December 31, 2012, we had 23,747 STM plans in force. For the year ended December 31, 2012, revenues associated with the sale of our STM plans accounted for approximately 63% of our revenues for the period. |
| • | Hospital Indemnity Plans. Our hospital indemnity plans provide a daily cash benefit for hospital treatment and doctor office visits as well as accidental injury and death or dismemberment benefits. The claims process for hospital indemnity plans is streamlined: the member simply provides proof of hospitalization and the carrier pays the benefits. These policies are primarily used by customers who do not have adequate health insurance and do not qualify for our STM plans or who wish to supplement existing coverage, typically in conjunction with high deductible plans. As of December 31, 2012, we had 8,141 hospital indemnity plans in force. For the year ended December 31, 2012, revenues associated with the sale of our hospital indemnity plans accounted for approximately 27% of our revenues for the period. |
| • | Ancillary Products. We provide numerous low-cost ancillary insurance products, including pharmacy benefit cards, dental plans and cancer/critical illness plans. These are typically monthly policies with automatic renewal. As of December 31, 2012, we had 26,230 ancillary product plans in force. For the year ended December 31, 2012, revenues associated with the sale of our ancillary products accounted for approximately 10% of our revenues for the period. |
Healthcare Laws and Regulations
Our business is subject to extensive, complex and rapidly changing federal and state laws and regulations. Various federal and state agencies have discretion to issue regulations and interpret and enforce healthcare laws. While we believe we comply in all material respects with applicable healthcare laws and regulations, these regulations can vary significantly from jurisdiction to jurisdiction, and interpretation of existing laws and regulations may change. Federal and state legislatures also may enact various legislative proposals that could materially impact certain aspects of our business. The following are summaries of key federal and state laws and regulations that impact our operations:
Healthcare Reform
In March 2010, Healthcare Reform was signed into law. Healthcare Reform contains provisions that have changed and will continue to change the health insurance industry in substantial ways. For example, Healthcare Reform includes a mandate requiring individuals to be insured or face tax penalties; a mandate that employers with over 50 employees offer their employees group health insurance coverage or face tax penalties; prohibitions against insurance companies that offer traditional IMM plans using pre-existing health conditions as a reason to deny an application for health insurance; MLR requirements that require each health insurance carrier to spend a certain percentage of their premium revenue on reimbursement for clinical services and activities that improve healthcare quality; establishment of state and/or federal health insurance exchanges to facilitate access to, and the purchase of, health insurance; subsidies and cost-sharing credits to make health insurance more affordable for those below certain income levels; and expanded eligibility for Medicaid for individuals and families with incomes of up to 133% of the poverty level.
Healthcare Reform amended various provisions in many federal laws, including the Internal Revenue Code, the Employee Retirement Income Security Act of 1974 and the Public Health Services Act. Healthcare Reform is being implemented by the Department of Health and Human Services, the Department of Labor and the Department of Treasury. These agencies have already issued a number of proposed, interim final and final regulations, as well as general guidance, on key aspects of Healthcare Reform. While many aspects of Healthcare Reform do not become effective until 2014, health insurance carriers have been required to maintain MLRs of 80% in their individual and family health insurance business since the beginning of 2011.
These laws have been the subject of multiple constitutional challenges and the U.S. Supreme Court held hearings in March 2012 in National Federation of Independent Business v. Sebelius to review the constitutionality of Healthcare Reform. On June 28, 2012, the United States Supreme Court released its decision, upholding Healthcare Reform’s mandate requiring individuals to purchase health insurance. Also, under the U.S. Supreme Court’s ruling, states are able to opt out of expanding Medicaid eligibility to families and individuals with incomes up to 133% of the poverty level. Despite the decision, some uncertainty about whether parts of Healthcare Reform or Healthcare Reform in its entirety will remain in effect is expected to continue with the possibility of future litigation with respect to certain provisions as well as legislative efforts to repeal and defund portions of Healthcare Reform or Healthcare Reform in its entirety. We cannot predict the outcome of any future legislation or litigation related to Healthcare Reform. As described under “Item 1. Business—Health Insurance Industry and Market Opportunity,” we expect Healthcare Reform to result in profound changes to the individual health insurance market and our business.
7
Table of Contents
Anti-Kickback Laws
In the United States, there are federal and state anti-kickback laws that generally prohibit the payment or receipt of kickbacks, bribes or other remuneration in exchange for the referral of patients or other health-related business. The United States federal healthcare programs’ Anti-Kickback Statute makes it unlawful for individuals or entities knowingly and willfully to solicit, offer, receive or pay any kickback, bribe or other remuneration, directly or indirectly, in exchange for or to induce the referral of an individual to a person for the furnishing or arranging for the furnishing of any item or service for which payment may be made in whole or in part under a federal healthcare program or the purchase, lease or order, or arranging for or recommending purchasing, leasing, or ordering, any good, facility, service, or item for which payment may be made in whole or in part under a federal healthcare program. Penalties for violations include criminal penalties and civil sanctions such as fines, imprisonment, and possible exclusion from federal healthcare programs.
Federal Civil False Claims Act and State False Claims Laws
The federal civil False Claims Act imposes liability on any person or entity who, among other things, knowingly presents, or causes to be presented, a false or fraudulent claim for payment by a federal healthcare program. The “qui tam” or “whistleblower” provisions of the False Claims Act allow a private individual to bring actions on behalf of the federal government alleging that the defendant has submitted a false claim to the federal government, and to share in any monetary recovery. Our future activities relating to the manner in which we sell and market our services may be subject to scrutiny under these laws.
HIPAA, Privacy and Data Security Regulations
By processing data on behalf of our clients and customers, we are subject to specific compliance obligations under privacy and data security-related laws, including the Health Insurance Portability and Accountability Act (“HIPAA”), the Health Information Technology for Economic and Clinical Health Act (the “HITECH Act”), and related state laws. We are also subject to federal and state security breach notification laws, as well as state laws regulating the processing of protected personal information, including laws governing the collection, use and disclosure of social security numbers and related identifiers.
The regulations that implement HIPAA and the HITECH Act establish uniform standards governing the conduct of certain electronic healthcare transactions and protecting the security and privacy of individually identifiable health information maintained or transmitted by healthcare providers, health plans, and healthcare clearinghouses, all of which are referred to as “covered entities,” and their “business associates” (which is anyone who performs a service on behalf of a covered entity involving the use or disclosure of protected health information and is not a member of the covered entity’s workforce). Our carrier companies’ and our clients’ health plans generally will be covered entities, and as their business associate they may ask us to contractually comply with certain aspects of these standards by entering into requisite business associate agreements.
As part of the payment-related aspects of our business, we may also undertake security-related obligations arising out of the Gramm-Leach-Bliley Act and the Payment Card Industry guidelines applicable to card systems. These requirements generally require safeguards for the protection of personal and other payment related information.
HIPAA Healthcare Fraud Standards
The HIPAA healthcare fraud statute created a class of federal crimes known as the “federal healthcare offenses,” including healthcare fraud and false statements relating to healthcare matters. The HIPAA healthcare fraud statute prohibits, among other things, executing a scheme to defraud any healthcare benefit program while the HIPAA false statements statute prohibits, among other things, concealing a material fact or making a materially false statement in connection with the payment for healthcare benefits, items or services. Entities that are found to have aided or abetted in a violation of the HIPAA federal healthcare offenses are deemed by statute to have committed the offense and are punishable as a principal.
State Privacy Laws
In addition to federal regulations issued under HIPAA, some states have enacted privacy and security statutes or regulations, or State Privacy Laws, that govern the use and disclosure of a person’s medical information or records and, in some cases, are more stringent than those issued under HIPAA. These State Privacy Laws include regulation of health insurance providers and agents, regulation of organizations that perform certain administrative functions such as utilization review or third-party administration, issuance of notices of privacy practices, and reporting and providing access to law enforcement authorities. In those cases, it may be necessary to modify our operations and procedures to comply with these more stringent State Privacy Laws. If we fail to comply with applicable State Privacy Laws, we could be subject to additional sanctions.
Consumer Protection Laws
Federal and state consumer protection laws are being applied increasingly by the United States Federal Trade Commission, or FTC, and states’ attorneys general to regulate the collection, use, storage and disclosure of personal or patient information, through websites or otherwise, and to regulate the presentation of web site content. Courts may also adopt the standards for fair information practices promulgated by the FTC, which concern consumer notice, choice, security and access.
8
Table of Contents
State Insurance Laws
Some of the states in which we operate have laws prohibiting unlicensed persons or business entities, including corporations, from making certain direct and indirect payments or fee-splitting arrangements with licensed insurance agents and brokers. Possible sanctions for violation of these restrictions include loss of license and civil penalties. These statutes vary from state to state, are often vague and have seldom been interpreted by the courts or regulatory agencies.
State insurance laws also require us to maintain an insurance agency or broker license in each state in which we transact health insurance business and adhere to sales, documentation and administration practices specific to that state. In addition, each of our employees who solicits, negotiates, sells or transacts health insurance business for us must maintain an individual insurance agent or broker license in one or more states. Because we transact business in the majority of states, compliance with health insurance-related laws, rules and regulations is difficult and imposes significant costs on our business.
State regulations may also require that individuals enroll in group programs or associations in order to access certain insurance products, benefits and services. We have entered into relationships with such associations in order to provide individuals access to our products. For example, we have an agreement with Med-Sense Guaranteed Association (“Med-Sense”), a non-profit association that provides membership benefits to individuals and gives members access to certain of our products. Under the agreement, we primarily market membership in the association and collect certain fees and dues on its behalf. In return, we have sole access to its membership list, and Med-Sense exclusively endorses the insurance products that we offer. Under the agreement, we receive a monthly fee per member. Our agreement with Med-Sense is automatically renewable for one-year terms, unless terminated on 120 days written notice by either party. The agreement is also terminable on 15 days written notice by either party under certain circumstances, such as in the case of a breach of the agreement.
Sales and Marketing
Our sales and marketing initiatives primarily consist of hiring seasoned sales professionals who have worked with or been referred to us by our distributors in order to strengthen our relationships with such distributors, marketing campaigns and attendance at meetings and conferences associated with acquiring new distributors. As we do not distribute insurance products to individuals, we utilize third-party distributors to market our products directly to potential members, and are engaged in their own sales and marketing efforts that include investments in lead acquisition, online marketing and customer referrals. We focus on building brand awareness among our distributors and members, increasing the number of distributors and converting sales leads into buyers. Our marketing initiatives include:
Third-Party Distributors. Our third-party distributor acquisition channel consists of independent licensed agent call centers and individual insurance brokers who market directly to individuals. We have established several initiatives to assist these call centers and distributors in helping individuals select our products, including the provision of sales scripting and monitoring services through the HiiVe technology platform discussed below. We generally compensate our distributors for their individual health insurance sales based on the consumer submitting a health insurance application to us. If a marketing partner is licensed to sell health insurance, we may share a percentage of the commission revenue we earn from the health insurance carrier for each member referred by that distributor.
Marketing Partners. Our marketing partner member acquisition channel consists of a network of affiliate partners, including credit card companies, national banks and database marketing services who make our products available to individuals. We have established a pay-for-performance network that drives individuals to our products. These partners generally fall into one of the following categories:
| • | Financial and online services partners in industries such as credit card services, banking, insurance and mortgage and association partners; and |
| • | Employers who do not offer health insurance benefits to their employees or to one or more classes of their employees. |
Carrier Relationships
One of our core strengths is our deep integration with some of the leading insurance carriers in the United States, which enables us to offer our STM, hospital indemnity and ancillary products on our technology platform. We currently have relationships with several insurance carriers, including Starr Indemnity & Liability Company, Companion Life, United States Fire, ING, Markel and CIGNA, among others. We have entered into written contracts with each of these carriers pursuant to which we are authorized to sell the carriers’ health plans and products in exchange for the payment of commissions that vary by carrier and by plan. These contracts are typically non-exclusive and terminable on short notice by either party for any reason. In some cases, the amendment or termination of an agreement we have with a health insurance carrier may impact the commissions we are paid on health insurance plans and products that we have already sold through the carrier.
9
Table of Contents
For the year ended December 31, 2012, Starr Indemnity & Liability Company accounted for approximately 46% of our premium equivalents. The commission percentage used to calculate our commissions under our agreement with Starr Indemnity & Liability Company is based on net written premium and varies by the state of a member’s domicile. The agreement is terminable on 180 days written notice by either party for any reason and may be terminated on shorter notice under certain circumstances, such as in the case of a breach of the agreement.
For the year ended December 31, 2012, United States Fire accounted for approximately 25% of our premium equivalents. The commission percentage used to calculate our commissions under our agreement with United States Fire is based on gross collected premium. Our agreement with United States Fire is for automatically renewable one-year terms, unless otherwise terminated. The agreement is terminable on 120 days written notice by either party for any reason and may be terminated on shorter notice under certain circumstances, such as in the case of a breach of the agreement.
For the year ended December 31, 2012, Companion Life accounted for approximately 22% of our premium equivalents. The commission percentage used to calculate our commissions under our agreement with Companion Life is based on gross written premium. The agreement is terminable on 180 days written notice by either party for any reason and may be terminated on shorter notice under certain circumstances, such as in the case of a breach of the agreement.
To create an improved experience for our members, we regularly evaluate insurance carriers by comparing their market presence and brand, cost competitiveness, breadth of plans, emphasis on improving the customer experience, and ability to integrate with our data systems. We plan to continue to expand and adjust the number of insurance carriers with which we partner.
Technology
Since we began operations in 2008, we have invested significant financial and human resources in building a unique and scalable proprietary, web-based technology platform. Our technology represents a distinct competitive advantage as it reduces the need for customer care agents, the time associated with billing, underwriting, fulfillment, sale and marketing and provides significant operating leverage as we add members and product offerings. We purchased the intellectual property rights to certain of the software in August 2012.
The key components of our technology platform include:
| • | Automated Real-Time Integrated E System. A.R.I.E.S. is the core of our technology platform. This proprietary technology reduces the need for the continual involvement of customer care representatives after a member has enrolled by allowing him or her to change payment information and print identification cards anytime, anyplace. A.R.I.E.S. also offers distributors an unprecedented ability to manage their business by providing direct access to real-time commission statements, commission payment and real-time sales and membership data (including cancelations, failed credit card and ACH payments, persistency, renewal and cross-sell rates). Key elements of A.R.I.E.S. include: |
| • | Quote-Buy-Print. Individuals access our technology platform through our distribution partners and can quote products and buy and print their policy documents and identification cards anytime, anyplace. |
| • | Automated Underwriting. The entire underwriting process is handled by A.R.I.E.S. through the use of health questionnaires. Because our STM products are largely targeted to healthy individuals who do not have pre-existing conditions, we do not have a traditional underwriting department. Underwriting is an immediate accept or reject decision based on a prospective member’s answers to an abbreviated online health-related questionnaire. |
| • | Multiple Value-Added Products. Consumers can purchase multiple plans and specialty products with the click of a button. Consumers are able to supplement our core STM and hospital indemnity offerings with ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans. Our technology platform makes it possible for us to instantly offer these bundled products to fit member needs. |
| • | Turn-Key Solution. Our technology platform is a turnkey solution, allowing distributors to tailor their offering to meet member needs and can be customized to enhance the experience of an affinity group or employer. |
| • | Payment. Our sales are executed online and offer instant electronic fulfillment through our platform, through which we receive credit card ACH payments directly from members at the time of sale. |
| • | Member Services. Members have the ability to log-in and change payment information and print new identification cards, all without the need of a customer service representative. |
| • | HiiVe. The HiiVe technology system streamlines compliance by providing real-time sales scripting and monitoring for distributors to ensure customers are making informed purchase decisions. The compliance system enables us to record each enrollment phone call, retrieve archived calls within seconds and score calls based on script adherence. In addition, this technology has also allowed us to automate our compliance program, enhancing quality while minimizing overhead and thereby allowing us to offer higher commissions to our distributors. |
10
Table of Contents
We rely on BimSym eBusiness Solutions, Inc. (“BimSym”) and other vendors to provide various services relating to our A.R.I.E.S. technology platform, including hosting, support, maintenance and development services, for which we pay both recurring and one-off fees. A.R.I.E.S. was placed in service in March 2011 through an informal relationship with BimSym. On August 1, 2012, we entered into a software assignment agreement with BimSym pursuant to which we acquired certain proprietary rights to the A.R.I.E.S. software for a one-time payment of $45,000. On August 1, 2012, we also entered into a master services agreement with BimSym with respect to the hosting, support, maintenance and development of our A.R.I.E.S. technology platform. This agreement obligates us to make minimum future payments of $312,000 per year for the next five years. Thereafter, this agreement provides for automatic one-year renewals, unless we notify BimSym of our intent not to renew. Additionally, on August 1, 2012, we entered into an exclusivity agreement with BimSym whereby neither BimSym nor any of its affiliates will create, market or sell a software, system or service with the same or similar functionality as that of A.R.I.E.S., under which we are required to make monthly payments of $16,000 for five years. Prior to March 2011, the Company contracted with a third party vendor, Carpe Datum L.L.C., to provide some of the services now provided through A.R.I.E.S. The HiiVe technology system is based on software we license from a third-party. For more information see “Item 1A. Risk Factors—We rely on third-party vendors to develop, host, maintain, service and enhance our technology platform” and “Item 1A. Risk Factors—Our failure to obtain, maintain and enforce the intellectual property rights on which our business depends could have a material adverse effect on our business, financial condition and results of operations.”
Seasonality
Our business of marketing individual STM insurance plans is subject to seasonal fluctuations. A large number of undergraduate and post-graduate students complete their studies during the second fiscal quarter of each year and are no longer eligible for health insurance coverage through the insurance plans of their parents or educational institutions. As a result, we experience a higher volume of new member enrollment from these demographics during the third fiscal quarter when such students purchase our products, producing a seasonal increase in revenue. During the fourth quarter of each fiscal year, many of our call centers and licensed agents are closed or maintain shorter business hours for varying periods of time due to the holiday season. We experience a lower volume of new member enrollment during the fourth quarter compared with other quarters, resulting in a seasonal decrease commission revenue. As our business matures, other seasonality trends may develop and the existing seasonality and consumer behavior that we experience may change.
Competition
The market for selling insurance products is highly competitive and the sale of health insurance over the Internet is rapidly evolving. We compete with individuals and entities that offer and sell health insurance products utilizing traditional distribution channels, as well as the Internet. Our current or potential competitors include:
Traditional local insurance agents. There are tens of thousands of local insurance agents across the United States who sell health insurance products in their communities. We believe that the vast majority of these local agents offer health insurance without significantly utilizing the Internet or technology other than simple desktop applications such as word processing and spreadsheet programs. Some traditional insurance agents, however, utilize general agents that offer online quoting services and other tools to obtain quotes from multiple carriers and prepare electronic benefit proposals to share with their potential customers. These general agents typically offer their services only for the small and mid-sized group markets (not the individual and family markets) and operate in only a limited geographic region. Additionally, some local agents use the Internet to acquire new consumer referrals from companies that have expertise in Internet marketing. These “lead aggregator” companies utilize keyword search, primarily paid keyword search listings on Google, Bing and Yahoo! and other forms of Internet advertising, to drive Internet traffic to the lead aggregator’s website. The lead aggregator then collects and sells consumer information to agents and, to a lesser extent, to carriers, both of whom endeavor to close the referrals through traditional offline sales methods.
Health insurance carriers’ “direct-to-member” sales. Some carriers directly market and sell their plans and products to consumers through call centers and their own websites. Although we offer health insurance plans and products for many of these carriers, they also can compete with us by offering their products directly to consumers. Most of these carriers have superior brand recognition, extensive marketing budgets and significant financial resources to influence consumer preferences for searching and buying health insurance online. The carriers we choose to represent, however, do not have a competitive price advantage over us. Because individual and family plan health insurance prices are regulated in all U.S. jurisdictions, a consumer is entitled to pay the same price for a particular plan, whether the consumer purchased the plan directly from one of our carrier companies or from us.
Online agents. There are a number of agents that operate websites and provide a limited online shopping experience for consumers interested in purchasing health insurance (e.g., online quoting of health insurance product prices). Most of these online agents operate in only one or very few states, and some represent only one or a limited number of health insurance carriers. Some online agents also sell non-health insurance products such as auto insurance, life insurance and home insurance. We are one of the leading sources of STM insurance products.
11
Table of Contents
National insurance brokers. Although insurance brokers have traditionally not focused on the affordable STM market, they may enter our markets and could compete with us. These large agencies have existing relationships with many of our carrier companies, are licensed nationwide and have large customer bases and significant financial, technical and marketing resources to compete in our markets. Some of these large agencies and financial services companies, such as eHealthInsurance have partnered with us in order to offer our services to their customer and member bases.
We believe the principal factors that determine our competitive advantage in the online distribution of health insurance include the following:
| • | value added healthcare products; |
| • | strength of carrier relationships and depth of technology integration with carriers; |
| • | proprietary, web-based technology platform; |
| • | data-driven product design; |
| • | highly automated compliance program; |
| • | strength of distribution relationships; and |
| • | proven capabilities measured in years of delivering sales and creating and using reliable technology. |
Employees
As of December 31, 2012, we had 79 employees, of which 73 were full-time employees. We have not experienced any work stoppages and consider our employee relations to be good. None of our employees is represented by a labor union.
Intellectual Property
Our success depends, in part, on our ability to protect our intellectual property and proprietary technology, and to operate our business without infringing or violating the intellectual property or proprietary rights of others. We rely on a combination of copyrights, trademarks, domain names, and trade secrets, intellectual property licenses and other contractual rights (including confidentiality and non-disclosure agreements) to establish and protect our intellectual property and proprietary technology. However, these intellectual property rights may not prevent others from creating a competitive online platform or otherwise competing with us.
We may be unable to obtain, maintain and enforce the intellectual property rights on which our business depends, and assertions by third-parties that we violate their intellectual property rights could have a material adverse effect on our business, financial condition and results of operations. For more information see “Item 1A. Risk Factors—Our failure to obtain, maintain and enforce the intellectual property rights on which our business depends could have a material adverse effect on our business, financial condition and results of operations” and “Item 1A. Risk Factors—Assertions by third-parties that we violate their intellectual property rights could have a material adverse effect on our business, financial condition and results of operations.”
Our History and the Reorganization of Our Corporate Structure
Overview
Our business began operations in 2008, and historically, we operated through Health Plan Intermediaries, LLC. In anticipation of our recent initial public offering (the “IPO”), on November 7, 2012, Health Plan Intermediaries, LLC assigned the operating assets of our business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC.
Health Insurance Innovations, Inc. was incorporated as a Delaware corporation on October 26, 2012. Immediately prior to the completion of the IPO, we amended and restated our certificate of incorporation to, among other things, authorize two classes of common stock, Class A common stock and Class B common stock. We also granted the underwriters, which consisted of Credit Suisse, Citigroup, BofA Merrill Lynch and Raymond James, the right to purchase additional shares of Class A common stock to cover over-allotments. Our Class A common stock was issued to investors in the IPO and is held by certain of our employees. As of March 27, 2013, all of our Class B common stock is held by Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (a subsidiary of Health Plan Intermediaries, LLC that was formed on October 31, 2012 in connection with the IPO), which are beneficially owned by our Chairman, President, and Chief Executive Officer, Michael Kosloske. Shares of our Class B common stock vote together with shares of our Class A common stock as a single class, except as otherwise required by law. As of March 27, 2013, Mr. Kosloske beneficially owns 62.4% of our outstanding Class A and Class B common stock on a combined basis, which equals his combined economic interest in our Company, and will have effective control over the outcome of votes on all matters requiring approval by our stockholders. As described in more detail below, each Series B Membership Interest of Health Plan Intermediaries Holdings, LLC can be exchanged (together with one share of Class B common stock) for one share of Class A common stock. Health Insurance Innovations, Inc. was formed for purposes of the IPO and prior to the IPO engaged only in activities in contemplation of the IPO. Following the IPO, Health Insurance Innovations, Inc. remains a holding company owning as its principal asset Series A Membership Interests in Health Plan Intermediaries Holdings, LLC.
12
Table of Contents
The diagram below shows our organizational structure immediately after completion of the IPO and the reorganization.
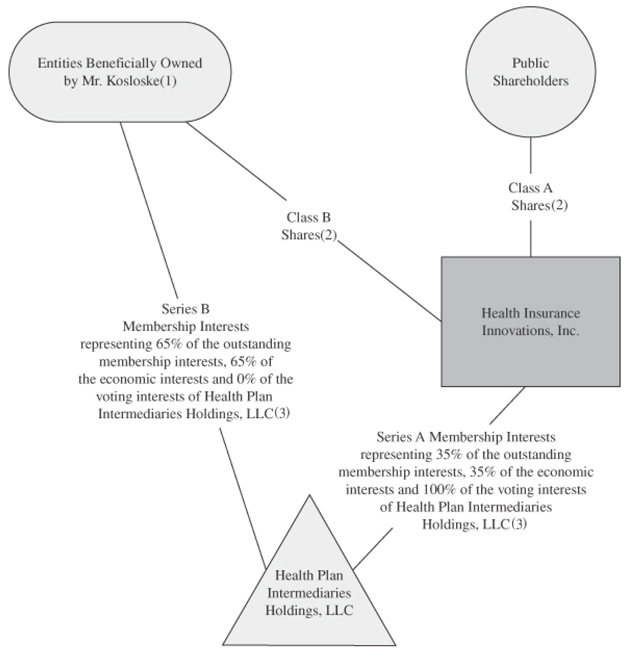
| (1) | The members of Health Plan Intermediaries Holdings, LLC, other than us, include Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. |
| (2) | Class A shares represent 100% of the economic rights of the holders of all classes of our common stock to share in our distributions. Class B shares do not entitle their holders to any dividends paid by, or rights upon liquidation of, Health Insurance Innovations, Inc. Each share of our Class A common stock and our Class B common stock entitle its holder to one vote. |
| (3) | As of March 27, 2013, (i) the Series A Membership Interests held by Health Insurance Innovations, Inc. represent 37.6% of the outstanding membership interests, 37.6% of the economic interests and 100% of the voting interests in Health Plan Intermediaries Holdings, LLC and (ii) the Series B Membership Interests held by the entities beneficially owned by Mr. Kosloske represent 62.4% of the outstanding membership interests, 62.4% of the economic interests and 0% of the voting interests in Health Plan Intermediaries Holdings, LLC. |
13
Table of Contents
Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC
Following our reorganization and the IPO, we have operated our business through Health Plan Intermediaries Holdings, LLC. The operations of Health Plan Intermediaries Holdings, LLC, and the rights and obligations of its members, are governed by the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC. The following is a description of the material terms of that amended and restated limited liability company agreement.
Governance
We serve as sole managing member of Health Plan Intermediaries Holdings, LLC. As such, we control its business and affairs and will be responsible for the management of its business. No other members of Health Plan Intermediaries Holdings, LLC, in their capacity as such, we have any authority or right to control the management of Health Plan Intermediaries Holdings, LLC or to bind it in connection with any matter.
Voting and Economic Rights of Members
Health Plan Intermediaries Holdings, LLC has two series of outstanding equity: Series A Membership Interests, which may only be issued to Health Insurance Innovations, Inc., as sole managing member, and Series B Membership Interests. The Series B Membership Interests are held by Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (a subsidiary of Health Plan Intermediaries, LLC that was formed on October 31, 2012 in connection with the IPO), entities beneficially owned by Mr. Kosloske. The Series A Membership Interests and Series B Membership Interests entitle their holders to equivalent economic rights meaning an equal share in the profits and losses of, and distributions from, Health Plan Intermediaries Holdings, LLC. Holders of Series B Membership Interests have no voting rights, except for the right to approve certain amendments to the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC. As of March 27, 2013, (i) the Series A Membership Interests held by Health Insurance Innovations, Inc. represent 37.6% of the outstanding membership interests, 37.6% of the economic interests and 100% of the voting interests in Health Plan Intermediaries Holdings, LLC and (ii) the Series B Membership Interests held by the entities beneficially owned by Mr. Kosloske represent 62.4% of the outstanding membership interests, 62.4% of the economic interests and 0% of the voting interests in Health Plan Intermediaries Holdings, LLC.
Net profits and losses of Health Plan Intermediaries Holdings, LLC generally will be allocated, and distributions made, to its members pro rata in accordance with the number of Membership Interests (Series A or Series B, as the case may be) they hold. Accordingly, as of March 27, 2013, net profits and net losses of Health Plan Intermediaries Holdings, LLC would be allocated, and distributions would be made, 37.6% to us and 62.4% to the holders of Series B Membership Interests.
Subject to the availability of net cash flow at the Health Plan Intermediaries Holdings, LLC level and to applicable legal and contractual restrictions, we intend to cause Health Plan Intermediaries Holdings, LLC to distribute to us, and to the other holders of Membership Interests, cash payments for the purposes of funding tax obligations in respect of any net taxable income that is allocated to us and the other holders of Membership Interests as members of Health Plan Intermediaries Holdings, LLC, to fund dividends, if any, declared by us and to make any payments due under the tax receivable agreement, as described below. See “Tax Consequences” below. If Health Plan Intermediaries Holdings, LLC makes distributions to its members in any given year, the determination to pay dividends, if any, to our Class A common stockholders will be made by our board of directors. We do not, however, expect to declare or pay any cash or other dividends in the foreseeable future on our Class A common stock, as we intend to reinvest any cash flow generated by operations in our business. Class B common stock will not be entitled to any dividend payments. We may enter into credit agreements or other borrowing arrangements in the future that prohibit or restrict our ability to declare or pay dividends on our Class A common stock.
Coordination of Health Insurance Innovations, Inc. and Health Plan Intermediaries Holdings, LLC
Except with respect to shares of Class A common stock issued pursuant to the exercise of the underwriters’ over-allotment option, whenever we issue one share of Class A common stock for cash, the net proceeds will be transferred promptly to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC will issue to us one Series A Membership Interest. If we issue other classes or series of equity securities, we will contribute to Health Plan Intermediaries Holdings, LLC the net proceeds we receive in connection with such issuance, and Health Plan Intermediaries Holdings, LLC will issue to us an equal number of equity securities with designations, preferences and other rights and terms that are substantially the same as our newly issued equity securities. Conversely, if we repurchase any shares of Class A common stock (or equity securities of other classes or series) for cash, Health Plan Intermediaries Holdings, LLC will, immediately prior to our repurchase, redeem an equal number of Series A Membership Interests (or its equity securities of the corresponding classes or series), upon the same terms and for the same price, as the shares of our Class A common stock (or our equity securities of such other classes or series) are repurchased. Membership Interests and shares of our common stock will be subject to equivalent stock splits, dividends and reclassifications.
We will not conduct any business other than the management and ownership of Health Plan Intermediaries Holdings, LLC and its subsidiaries, or own any other assets (other than on a temporary basis), although we may take such actions and own such assets as are necessary to comply with applicable law, including compliance with our responsibilities as a public company under the U.S. federal securities laws, and may incur indebtedness and may take other actions if we determine that doing so is in the best interest of Health Plan Intermediaries Holdings, LLC.
14
Table of Contents
Issuances of Membership Interests
Series A Membership Interests may be issued only to us as the sole managing member of Health Plan Intermediaries Holdings, LLC. Series B Membership Interests may be issued only to persons or entities we permit, which initially will be Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. Such issuances shall be in exchange for cash or other consideration. Series B Membership Interests may not be transferred as Series B Membership Interests except to certain permitted transferees and in accordance with the restrictions on transfer set forth in the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC, and any such transfer must be accompanied by the transfer of an equal number of shares of our Class B common stock.
Exchange Agreement
On February 13, 2013, we entered into an exchange agreement with the holders of Series B Membership Interests. Pursuant to and subject to the terms of the exchange agreement and the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC, holders of Series B Membership Interests, at any time and from time to time, may exchange one or more Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock on a one-for-one basis, subject to equitable adjustments for stock splits, stock dividends and reclassifications.
Holders will not have the right to exchange Series B Membership Interests if we determine that such exchange would be prohibited by law or regulation or would violate other agreements to which we may be subject. We may impose additional restrictions on exchange that we determine necessary or advisable so that Health Plan Intermediaries Holdings, LLC is not treated as a “publicly traded partnership” for U.S. federal income tax purposes. If the Internal Revenue Service were to contend successfully that Health Plan Intermediaries Holdings, LLC should be treated as a “publicly traded partnership” for U.S. federal income tax purposes, Health Plan Intermediaries Holdings, LLC would be treated as a corporation for U.S. federal income tax purposes and thus would be subject to entity-level tax on its taxable income.
A holder that exchanges Series B Membership Interests will also be required to deliver an equal number of shares of our Class B common stock. In connection with each exchange, Health Plan Intermediaries Holdings, LLC will cancel the delivered Series B Membership Interests and issue to us Series A Membership Interests on a one-for-one basis. Thus, as holders exchange their Series B Membership Interests for Class A common stock, our interest in Health Plan Intermediaries Holdings, LLC will increase.
We and the exchanging holder will each generally bear our own expenses in connection with an exchange, except that, subject to a limited exception, we are required to pay any transfer taxes, stamp taxes or duties or other similar taxes in connection with such an exchange.
Exculpation and Indemnification
The amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC contains provisions limiting the liability of its managing member, members, officers and their respective affiliates to Health Plan Intermediaries Holdings, LLC or any of its members. Moreover, the amended and restated limited liability company agreement contains broad indemnification provisions for Health Plan Intermediaries Holdings, LLC’s managing member, members, officers and their respective affiliates. Because Health Plan Intermediaries Holdings, LLC is a limited liability company, these provisions are not subject to the limitations on exculpation and indemnification contained in the Delaware General Corporation Law with respect to the indemnification that may be provided by a Delaware corporation to its directors and officers.
Voting Rights of Class A Stockholders and Class B Stockholders
Each share of our Class A common stock and our Class B common stock entitles its holder to one vote.
Tax Consequences
Holders of Membership Interests, including Health Insurance Innovations, Inc., generally will incur U.S. federal, state and local income taxes on their proportionate shares of any net taxable income of Health Plan Intermediaries Holdings, LLC. Net profits and net losses of Health Plan Intermediaries Holdings, LLC generally will be allocated to its members pro rata in proportion to the number of Membership Interests they hold. The amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC provides for cash distributions to its members in an amount at least equal to the members’ assumed tax liability attributable to Health Plan Intermediaries Holdings, LLC. Generally, distributions in respect of the members’ assumed tax liability
15
Table of Contents
will be computed based on our estimate of the net taxable income of Health Plan Intermediaries Holdings, LLC allocable per Membership Interest multiplied by an assumed tax rate. In accordance with this agreement, Health Plan Intermediaries Holdings, LLC intends to make distributions to its members in respect of such assumed tax liability and to fund dividends, if any, declared by us, as well as any payments we are obligated to make under the tax receivable agreement, described below.
Health Plan Intermediaries Holdings, LLC intends to make an election under Section 754 of the Internal Revenue Code of 1986, as amended, which is effective for 2013 and for each taxable year in which occurs an exchange of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock. We expect that, as a result of this election, the acquisition of Series B Membership Interests from Health Plan Intermediaries, LLC with the net proceeds of the sale of over-allotment shares, as well as any future exchanges of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock, will result in increases in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC at the time of such acquisition or exchange, which will increase the tax depreciation and amortization deductions available to us and which could create other tax benefits. Any such increases in tax basis and tax depreciation and amortization deductions or other tax benefits could reduce the amount of tax that we would otherwise be required to pay in the future. We will be required to pay a portion of the cash savings we actually realize from such increase (or are deemed to realize in the case of an early termination payment by us, a change in control or a material breach by us of our obligations under the tax receivable agreement, as described below) to certain holders of Series B Membership Interests pursuant to the tax receivable agreement. Furthermore, payments under the tax receivable agreement, as described below, will give rise to additional tax benefits and therefore to additional payments under the tax receivable agreement itself. To the extent that we are unable to make payments under the income tax receivable agreement for any reason, such payments will be deferred and will accrue interest until paid. See “Tax Receivable Agreement” below.
Tax Receivable Agreement
The IPO is not anticipated to result in an increase in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. However, the purchase of Series B Membership Interests (together with an equal number of shares of our Class B common stock) with the net proceeds of the sale of over-allotment shares, as well as subsequent exchanges of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock, are expected to increase our tax basis in our share of Health Plan Intermediaries Holdings, LLC’s tangible and intangible assets. These increases in tax basis are expected to increase our depreciation and amortization deductions and create other tax benefits and therefore may reduce the amount of tax that we would otherwise be required to pay in the future.
On February 13, 2013, we entered into a tax receivable agreement with the holders of Series B Membership Interests (currently Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske). The agreement requires us to pay to such holders 85% of the cash savings, if any, in U.S. federal, state and local income tax we realize (or are deemed to realize in the case of an early termination payment, a change in control or a material breach by us of our obligations under the tax receivable agreement, as discussed below) as a result of any possible future increases in tax basis described above and of certain other tax benefits related to entering into the tax receivable agreement, including tax benefits attributable to payments under the tax receivable agreement itself. This is our obligation and not an obligation of Health Plan Intermediaries Holdings, LLC. We will benefit from the remaining 15% of any realized cash savings. For purposes of the tax receivable agreement, cash savings in income tax is computed by comparing our actual income tax liability with our hypothetical liability had we not been able to utilize the tax benefits subject to the tax receivable agreement itself. The tax receivable agreement became effective upon completion of the IPO and will remain in effect until all such tax benefits have been used or expired, unless the agreement is terminated early, as described below. Estimating the amount of payments to be made under the tax receivable agreement cannot be done reliably at this time because any increase in tax basis, as well as the amount and timing of any payments under the tax receivable agreement, will vary depending on a number of factors, including:
| • | the timing of exchanges of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for shares of our Class A common stock—for instance, the increase in any tax deductions will vary depending on the fair market value of the depreciable and amortizable assets of Health Plan Intermediaries Holdings, LLC at the time of the exchanges, and this value may fluctuate over time; |
| • | the price of our Class A common stock at the time of exchanges of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for shares of our Class A common stock—the increase in our share of the basis in the assets of Health Plan Intermediaries Holdings, LLC, as well as the increase in any tax deductions, will be related to the price of our Class A common stock at the time of these exchanges; |
16
Table of Contents
| • | the tax rates in effect at the time we use the increased amortization and depreciation deductions or realize other tax benefits; and |
| • | the amount, character and timing of our taxable income. We will be required to pay 85% of the tax savings, as and if realized. Except in certain circumstances, if we do not have taxable income in a given taxable year, we will not be required to make payments under the tax receivable agreement for that taxable year because no tax savings will have been realized. |
The payments that we make under the tax receivable agreement could be substantial. Assuming no material changes in relevant tax law and based on our current operating plan and other assumptions, including our estimate of the tax basis of our assets as of December 31, 2012, if all of the Series B Membership Interests were acquired by us in taxable transactions for a price of $14.00 per Series B Membership Interest, we estimate that the maximum amount that we would be required to pay under the tax receivable agreement could be approximately $53,001,000. The actual amount may differ materially from this hypothetical amount as potential future payments will vary depending on a number of factors, including those listed above.
We have the right to terminate the tax receivable agreement at any time. In addition, the tax receivable agreement will terminate early if we (or our successors) breach our obligations under the tax receivable agreement or upon certain mergers, asset sales, other forms of business combinations or other changes of control. If we exercise our right to terminate the tax receivable agreement, or if the tax receivable agreement is terminated early in accordance with its terms, our (or our successors’) payment obligations under the tax receivable agreement with respect to certain exchanged or acquired Membership Interests would be accelerated and would become due and payable based on certain assumptions, including that we would have sufficient taxable income to use in full the deductions arising from the increased tax basis and certain other benefits. As a result, we could make payments under the tax receivable agreement that are substantial and in excess of our actual cash savings in income tax.
Decisions made in the course of running our business, such as with respect to mergers, asset sales, other forms of business combinations or other changes in control, may influence the timing and amount of payments we make under the tax receivable agreement. For example, the earlier disposition of assets following an exchange or acquisition transaction will generally accelerate payments under the tax receivable agreement and increase the present value of such payments. In these situations, our obligations under the tax receivable agreement could have a substantial negative impact on our liquidity and could have the effect of delaying, deferring or preventing certain mergers, asset sales, other forms of business combinations or other changes of control.
Payments are generally due under the tax receivable agreement within a specified period of time following the filing of our tax return for the taxable year with respect to which the payment obligation arises, although interest on such payments will begin to accrue at a rate of LIBOR from the due date (without extensions) of such tax return. Late payments generally accrue interest at a rate of LIBOR plus 300 basis points. However, to the extent, based on certain specified reasons, that we do not have available cash to satisfy our payment obligations under the tax receivable agreement, such deferred payments would accrue interest at a rate of LIBOR.
Were the Internal Revenue Service to challenge successfully the tax basis increases described above, we would not be reimbursed for any payments previously made under the tax receivable agreement although future payments under the tax receivable agreement, if any, would be adjusted to reflect the result of any such successful challenge by the Internal Revenue Service. As a result, we could make payments under the tax receivable agreement in excess of our actual cash savings in income tax.
17
Table of Contents
| ITEM 1A. | RISK FACTORS |
Risks Relating to Our Business and Industry
The market for health insurance in the United States is rapidly evolving, which makes it difficult to forecast demand for our products.
The market for health insurance in the United States is rapidly evolving. Accordingly, our future financial performance will depend in part on growth in this market and on our ability to adapt to emerging demands in this market. We believe demand for our products has been driven in large part by recent regulatory changes, broader use of the Internet and advances in technology. It is difficult to predict with any precision the future growth rate and size of our target market. The rapidly evolving nature of the market in which we operate, as well as other factors that are beyond our control, reduce our ability to evaluate accurately our long-term outlook and forecast annual performance. A reduction in demand for our products caused by lack of acceptance, technological challenges, competing offerings or other factors would result in a lower revenue growth rate or decreased revenue, either of which could negatively impact our business and results of operations. In addition, our business, financial condition and results of operations may be adversely affected if Healthcare Reform is not implemented in accordance with our expectations and we cannot successfully execute our growth strategies. For example, our STM plans are currently classified as “short-term limited duration” plans under Healthcare Reform. Accordingly, “short-term limited duration” plans are exempt under Healthcare Reform from the minimum MLR thresholds and “must-carry” pre-existing conditions requirements, the requirements for the extension of dependent coverage, certain documentation, reporting and appeals process requirements and the prohibitions against excessive waiting periods, lifetime or annual limits, rescissions and more generally, discrimination against individuals and discrimination on the provision of health care. If our STM plans were no longer classified as short-term limited duration plans, or we were not able to take advantage of certain current exemptions for any other reason, our business could be negatively affected.
If we are unable to retain our members, our business and results of operations would be harmed.
Our revenue is primarily derived from commissions that insurance carriers pay to us for the health insurance plans and products that we market and that remain in effect. When one of these plans or products is cancelled, or if we otherwise do not remain the administrator of record on the policy, we no longer receive the related commission revenue. Members may choose to discontinue their insurance policies for a number of reasons. For example, members may determine that they cannot afford our products or may decide not to renew their policies due to future increases in premiums. In addition, our members may choose to purchase new plans or products using a different administrator if, for example, they are not satisfied with our customer service or the plans or products that we offer. Further, members may discontinue their policies because they no longer need STM insurance because, for example, they have received coverage through an employer or spouse. Insurance carriers may also terminate health insurance plans or products
18
Table of Contents
purchased by our members for a variety of reasons. Our cost in acquiring a new member is substantially greater than the cost involved in maintaining our relationship with an existing member. If we are not able to successfully retain existing members and limit member turnover, our revenue and operating margins could be adversely affected.
Our business would be harmed if we lose our relationships with insurance carriers, fail to maintain good relationships with insurance carriers, become dependent upon a limited number of insurance carriers or fail to develop new relationships with insurance carriers.
We typically enter into contractual agency relationships with insurance carriers that are non-exclusive and terminable on short notice by either party for any reason. In many cases, insurance carriers also have the ability to amend the terms of our agreements unilaterally on short notice. Insurance carriers may be unwilling to underwrite our health insurance plans or products or may amend our agreements with them for a variety of reasons, including for competitive or regulatory reasons. Insurance carriers may decide to rely on their own internal distribution channels, including traditional in-house agents, carrier websites or other sales channels, or to market their own plans or products, and, in turn, could limit or prohibit us from marketing their plans or products. Insurance carriers may decide not to underwrite insurance plans or products in the individual health insurance market in certain geographies or altogether. The termination or amendment of our relationship with an insurance carrier could reduce the variety of health insurance plans or products we offer. We also could lose a source of, or be paid reduced commissions for, future sales and could lose renewal commissions for past sales. Our business could also be harmed if we fail to develop new carrier relationships or are unable to offer members a wide variety of health insurance plans and products.
The private health insurance industry in the United States has experienced substantial consolidation over the past several years, resulting in a decrease in the number of insurance carriers. For example, for the year ended December 31, 2012, Starr Indemnity & Liability Company accounted for 46% of our premium equivalents, United States Fire accounted for 25% of our premium equivalents, and Companion Life accounted for 22% of our premium equivalents. In the future, it may become necessary for us to offer insurance plans and products from a reduced number of insurance carriers or to derive a greater portion of our revenue from a more concentrated number of carriers as our business and the health insurance industry evolve. Each of these insurance carriers may terminate our agreements with them, and, in some cases, as a result of the termination we may lose our right to receive future commissions for policies we have sold. In addition, one or more of our carrier companies could experience a failure of its business due to a decline in sales volumes, unavailability of reinsurance, failure of business strategy or otherwise. Should our dependence on a smaller number of insurance carriers increase, whether as a result of the termination of carrier relationships, further insurance carrier consolidation, business failure, bankruptcy or any other reason, we may become more vulnerable to adverse changes in our relationships with our carriers, particularly in states where we offer health insurance plans and products from a relatively small number of carriers or where a small number of insurance carriers dominate the market. The termination, amendment or consolidation of our relationships with our insurance carriers could harm our business, results of operations and financial condition.
Our business would be harmed if we lose our relationships with distributors, fail to maintain good relationships with distributors, become dependent upon a limited number of distributors or fail to develop new relationships with distributors.
We depend on distributors to sell our products. We typically enter into contractual agency relationships with distributors that are non-exclusive and terminable on short notice by either party for any reason. In many cases, distributors also have the ability to amend the terms of our agreements unilaterally on short notice. Distributors may be unwilling to sell our health insurance plans or products or may amend our agreements with them for a variety of reasons, including for competitive or regulatory reasons. For example, distributors may decide to sell plans and products that bring them a higher commission than our plans and products or may decide not to sell STM plans at all. Because we rely on a diverse distributor network to sell our products, any loss of relationships with distributors or failure to maintain good relationships with distributors could harm our business, results of operations and financial condition. Further, we believe that we must grow our distributor network in order to achieve our growth plans. If we are unable to grow our distributor network and develop new relationships with distributors, our revenue could be adversely impacted.
We depend on relationships with third-parties for certain services that are important to our business. An interruption or cessation of such services by any third party could have a material adverse effect on our business.
We depend on a number of third-party relationships to enhance our business. For instance, state regulations may require that individuals enroll in group programs or associations in order to access certain insurance products, benefits and services. We have entered into relationships with such associations in order to provide individuals access to our products. For example, we have an agreement with Med-Sense Guaranteed Association, or Med-Sense, a non-profit association that provides membership benefits to individuals and gives members access to certain of our products. Under the agreement, we primarily market membership in the association and collect certain fees and dues on its behalf. In return, we have sole access to its membership list, and Med-Sense exclusively endorses the insurance products that we offer. Members of the association are given access to a wide variety of our products that are otherwise unavailable to non-members. For the year ended December 31, 2012, approximately 80.9% of our business was derived from individuals who became members of Med-Sense. We intend to establish an affiliation with Savers Choice of America, an association offering similar benefits, as an alternative to Med-Sense. We intend to have several of our carriers issue policies to Savers Choice of America members beginning in the first half of 2013. While we believe we could replace Med-Sense with other group programs or associations, there can be no assurance we could find such a replacement on a timely basis or at all. If we were to lose our relationship with Med-Sense and were unable to find another group program or association on a timely basis or at all, this would have a material adverse effect on our business.
19
Table of Contents
In addition, we develop and maintain strategic relationships with our partners in order for them to market our products to their end users. While we have entered into agreements with certain partners pursuant to which our products may be made available to their end-users, such agreements are not exclusive and generally do not obligate the partner to market or distribute our service. For example, we have entered into an agreement with MasterCard whereby MasterCard, through its approved pre-paid card member networks, will assist us in targeting and acquiring new leads for marketing our products. Under such agreement, MasterCard will use good-faith efforts to identify prospective leads.
Our ability to offer our services and operate our business is therefore dependent on maintaining our relationships with third-party partners, particularly Med-Sense, and entering into new relationships to meet the changing needs of our business. Any deterioration in our relationships with such partners, or our failure to enter into agreements with partners in the future would harm our business, results of operations and financial condition. If our partners are unable or unwilling to provide the services necessary to support our business, or if our agreements with such partners are terminated, our operations could be significantly disrupted. We may also incur substantial costs, delays and disruptions to our business in transitioning such services to ourselves or other third-party partners. In addition, third-party partners may not be able to provide the services required in order to meet the changing needs of our business.
Insurance carriers could reduce the commissions paid to us or change their plan pricing practices in ways that reduce the commissions paid to us, which could harm our revenue and results of operations.
Our commission rates are negotiated between us and each carrier. Insurance carriers have altered, and may in the future alter, the contractual relationships we have with them, either by renegotiation or unilateral action. Also, insurance carriers may adjust their commission rates to comply with regulatory guidelines. If these contractual changes result in reduced commissions, our revenue may decline. For example, on June 1, 2011, we entered into a new contract with Starr Indemnity & Liability Company which replaced a previous contract with Starr Global Accident and Health Insurance Agency, LLC to provide similar services for slightly lower commission rates. The reduced commissions had no material impact on our revenue or results of operations, however, as the contract also provided for additional administrative fees paid to us to offset the lower commission rates.
In addition, insurance carriers periodically adjust the premiums they charge to individuals for their insurance policies. These premium changes may cause members to cancel their existing policies and purchase a replacement policy from a different insurance carrier, either through our platform or through another administrator. We may receive a reduced commission or no commission at all when a member purchases a replacement policy. Also, because insurance rates may vary between insurance carriers, plans and enrollment dates, changes in our enrollment mix may impact our commission revenue. Future changes in carrier pricing practices could harm our business, results of operations and financial condition.
We face intense competition and compete with a broad range of market participants within the health insurance industry. If competition increases, our growth and profits may decline.
The market for selling individual health insurance and ancillary products is highly competitive and, except for regulatory considerations, there are limited barriers to entry. Currently, we believe the cost-effective, high-quality STM solutions that we distribute to the individual health insurance market are somewhat rare among our competitors. However, if we achieve our goal of becoming a leader in the distribution of individual health insurance products, we believe that competition for our business model will substantially increase. Because the barriers to entry in our markets are not substantial and members have the flexibility to select new health insurance providers, we believe that the addition of new competitors, or the adoption of our business model by existing competitors, may occur relatively quickly.
We compete with entities and individuals that offer and sell products similar to ours utilizing traditional distribution channels, including insurance agents and brokers across the United States who sell health insurance products in their communities. Some local agents use “lead aggregator” services that use the Internet to find individuals interested in purchasing health insurance and are compensated for referring those individuals to a traditional insurance agent. In addition to health insurance brokers and agents, many insurance carriers directly market and sell their plans and products to individuals through call centers and their own websites. Although we offer health insurance plans and products for many of these insurance carriers, they also compete with us by offering their plans and products directly to individuals or may elect to compete with us by offering their plans and products directly to individuals in the future. We may not be able to compete successfully against our current or future competitors. Some of our current and potential competitors have longer operating histories in the health insurance industry, access to larger customer bases, greater name recognition and significantly greater financial, technical, marketing and other resources than we do. As compared to us, our current and future competitors may be able to:
| • | undertake more extensive marketing campaigns for their brands and services; |
| • | devote more resources to website and systems development; |
| • | negotiate more favorable commission rates; and |
| • | attract potential employees, marketing partners and third-party service providers. |
20
Table of Contents
Further, there are many alternatives to the individual health insurance products that we currently provide. We can make no assurances that we will be able to compete effectively with the various individual health insurance products that are currently available or may become available in the future. Competitive pressures may result in our experiencing increased marketing costs and loss of market share, or may otherwise harm our business, results of operations and financial condition.
Changes and developments in the health insurance system in the United States, in particular the implementation of Healthcare Reform, could harm our business.
Our business depends upon the private sector of the U.S. insurance system, its role in financing healthcare delivery, and insurance carriers’ use of, and payment of commissions to, agents, brokers and other organizations to market and sell health insurance plans and products.
Healthcare Reform contains provisions that have changed and will continue to change the industry in which we operate in substantial ways. Many aspects of Healthcare Reform do not take effect until 2014, although certain provisions currently are effective, such as medical loss ratio requirements for individual, family and small business health insurance and a prohibition against using pre-existing health conditions as a reason to deny health coverage for children. In addition, state governments have adopted, and will continue to adopt, changes to their existing laws and regulations in light of Healthcare Reform and related regulations. Future changes may not be beneficial to us.
Notwithstanding the recent U.S. Supreme Court decision largely upholding the constitutionality of Healthcare Reform, certain key members of Congress have expressed a desire to withhold the funding necessary to implement Healthcare Reform as well as the desire to repeal or amend all or a portion of Healthcare Reform. Any partial or complete repeal or amendment or implementation difficulties, or uncertainty regarding such events, could increase our costs of compliance and adversely affect our results of operations and financial condition. The implementation of Healthcare Reform could have negative effects on us, including:
| • | increasing our competition; |
| • | reducing or eliminating the need for health insurance agents and brokers and/or demand for the health insurance that we sell through the manner in which the federal government and the states implement health insurance exchanges and the process for receiving subsidies and cost-sharing credits; |
| • | decreasing the number of types of health insurance plans and products that we sell, as well as the number of insurance carriers offering such plans and products; |
| • | causing insurance carriers to change the benefits and/or premiums for the plans and products they sell; |
| • | causing insurance carriers to reduce the amount they pay for our services or change their relationships with us in other ways; |
| • | causing STM to not qualify as adequate healthcare coverage, resulting in STM policyholders having to pay the government a penalty or tax; |
| • | causing STM policies to be subject to MLR threshold requirements; or |
| • | causing STM policies to be subject to “must carry” pre-existing condition requirements. |
Any of these effects could materially harm our business, results of operations and financial condition. For example, the manner in which the federal government and the states implement Healthcare Reform could substantially increase our competition and member turnover and substantially reduce the number of individuals who purchase insurance through us. Various aspects of Healthcare Reform could cause insurance carriers to limit the type of health insurance plans and products we are able to sell and the geographies in which we are able to sell them. Changes in the law could also cause insurance carriers to exit the business of selling insurance plans and products in a particular jurisdiction, to eliminate certain categories of products or to attempt to move members into new plans and products for which we receive lower commissions. If insurance carriers decide to limit our ability to sell their plans and products or determine not to sell individual health insurance plans and products altogether, our business, results of operations and financial condition would be materially harmed.
21
Table of Contents
Compliance with the strict regulatory environment applicable to the health insurance industry and the specific products we sell is difficult and costly. If we fail to comply with the numerous laws and regulations that are applicable to our business, our business and results of operations would be harmed.
The health insurance industry is heavily regulated by each state in the United States. For instance, state regulators require us to maintain a valid license in each state in which we transact health insurance business and further require that we adhere to sales, documentation and administration practices specific to each state. In addition, each distributor who transacts health insurance business on our behalf must maintain a valid license in one or more states. Because we do business in the majority of states and the District of Columbia, compliance with health insurance-related laws, rules and regulations is difficult and imposes significant costs on our business. Each jurisdiction’s insurance department typically has the power, among other things, to:
| • | grant and revoke licenses to transact insurance business; |
| • | conduct inquiries into the insurance-related activities and conduct of agents and agencies; |
| • | require and regulate disclosure in connection with the sale and solicitation of health insurance; |
| • | authorize how, by which personnel and under what circumstances insurance premiums can be quoted and published and an insurance policy sold; |
| • | determine which entities can be paid commissions from carriers; |
| • | regulate the content of insurance-related advertisements, including web pages; |
| • | approve policy forms, require specific benefits and benefit levels and regulate premium rates; |
| • | impose fines and other penalties; and |
| • | impose continuing education requirements on agents and employees. |
Although we believe we are currently in compliance with applicable insurance laws and regulations, due to the complexity, periodic modification and differing interpretations of insurance laws and regulations, we may not have always been, and we may not always be, in compliance with such laws and regulations. Failure to comply could result in significant liability, additional department of insurance licensing requirements or the revocation of licenses in a particular jurisdiction, which could significantly reduce our revenue, increase our operating expenses, prevent us from transacting health insurance business in a particular jurisdiction and otherwise harm our business, results of operations and financial condition. Moreover, an adverse regulatory action in one jurisdiction could result in penalties and adversely affect our license status or reputation in other jurisdictions due to the requirement that adverse regulatory actions in one jurisdiction be reported to other jurisdictions. Even if the allegations in any regulatory or other action against us are proven false, any surrounding negative publicity could harm member, distributor or health insurance carrier confidence in us, which could significantly damage our reputation. Because some members, distributors and health insurance carriers may not be comfortable with the concept of purchasing health insurance using the Internet, any negative publicity may affect us more than it would others in the health insurance industry and would harm our business, results of operations and financial condition.
In addition, we may in the future receive inquiries from state insurance regulators regarding our marketing and business practices. We may modify our practices in connection with any such inquiry. Any modification of our marketing or business practices in response to future regulatory inquiries could harm our business, results of operations or financial condition.
Regulation of the sale of health insurance is subject to change, and future regulations could harm our business and results of operations.
The laws and regulations governing the offer, sale and purchase of health insurance are subject to change, and future changes may be adverse to our business. For example, once health insurance pricing is set by the carrier and approved by state regulators, it is fixed and not generally subject to negotiation or discounting by insurance companies or agents. Additionally, state regulations generally prohibit carriers, agents and brokers from providing financial incentives, such as rebates, to their members in connection with the sale of health insurance. As a result, we do not currently compete with carriers or other agents and brokers on the price of the health insurance products offered on our website. We are also currently allowed to base our revenue structure on various commissions and fees, including commissions from insurance premiums and enrollment, monthly administrative fees and discount benefit fees. However, future laws and regulations could negatively adjust the commissions and fees we receive. If current laws or regulations change, we could be forced to reduce prices, commissions and fees or provide rebates or other incentives for the health insurance products sold through our online platform, which would harm our business, results of operations and financial condition.
Because we use the Internet as our distribution platform, we are subject to additional insurance regulatory risks. In many cases, it is not clear how existing insurance laws and regulations apply to Internet-related health insurance advertisements and transactions. To the extent that new laws or regulations are adopted that conflict with the way we conduct our business, or to the extent that existing laws and regulations are interpreted adversely to us, our business, results of operations and financial condition would be harmed.
22
Table of Contents
Our business may not grow if individuals are not informed about the availability and accessibility of affordable health insurance.
Numerous health insurance plans and products are available to individuals in any given market. Most of these plans and products vary by price, benefits and other policy features. Health insurance terminology and provisions are often confusing and difficult to understand. As a result, researching, selecting and purchasing health insurance can be a complex process. We believe that this complexity has contributed to a perception held by many individuals that individual health insurance is prohibitively expensive and difficult to obtain. If individuals are not informed about the availability and accessibility of affordable health insurance, our business may not grow and our results of operations and financial condition would be harmed.
Changes in the quality and affordability of the health insurance plans and products that carriers offer to us for sale through our technology platform could harm our business and results of operations.
The demand for health insurance marketed through our technology platform is affected by, among other things, the variety, quality and price of the health insurance plans and products we offer. If health insurance carriers do not continue to allow us to sell a variety of high-quality, affordable health insurance plans and products in our markets, or if their offerings are limited or terminated as a result of consolidation in the health insurance industry, the implementation of Healthcare Reform or otherwise, our sales may decrease and our business, results of operations and financial condition would be harmed.
If we are not able to maintain and enhance our name recognition, our business and results of operations will be harmed.
We believe that maintaining and enhancing our name recognition is critical to our relationships with existing members, distributors and carriers and to our ability to attract new members, distributors and carriers. The promotion of our name may require us to make substantial investments and we anticipate that, as our market becomes increasingly competitive, these marketing initiatives may become increasingly difficult and expensive. Our marketing activities may not be successful or yield increased revenue, and to the extent that these activities yield increased revenue, the increased revenue may not offset the expenses we incur and our results of operations could be harmed. If we do not successfully maintain and enhance our name recognition, our business may not grow and we could lose our relationships with carriers, distributors and/or members, which would harm our business, results of operations and financial condition.
In addition, we cannot be certain of the impact of media coverage on our business. If it were to be reduced, the number of distributors selling our products could decrease, and our cost of acquiring members could increase, both of which could harm our business, results of operations and financial condition.
If individuals or carriers opt for more traditional or alternative channels for the purchase and sale of health insurance, our business will be harmed.
Our success depends in part upon widespread individual and carrier acceptance of the Internet as a marketplace for the purchase and sale of health insurance. Individuals and carriers may choose to depend more on traditional sources, such as individual agents, or alternative sources may develop, including as a result of Healthcare Reform. Our future growth, if any, will depend in part upon:
| • | the growth of the Internet as a commerce medium generally, and as a market for individual health insurance plans and services specifically; |
| • | individuals’ willingness to conduct their own health insurance research; |
| • | our ability to make the process of purchasing health insurance online an attractive alternative to traditional and new means of purchasing health insurance; |
| • | our ability to successfully and cost-effectively market our services as superior to traditional or alternative sources for health insurance to a sufficiently large number of individuals; and |
| • | carriers’ willingness to use us and the Internet as a distribution channel for health insurance plans and products. |
If individuals and carriers determine that other sources of health insurance and health insurance applications are superior, our business will not grow and our results of operations and financial condition would be harmed.
Any legal liability, regulatory penalties, or negative publicity for the information on our platform or that we otherwise distribute or provide will likely harm our business and results of operations.
We provide information on our platform, through our call center partners and in other ways regarding health insurance in general and the health insurance plans and products we market and sell, including information relating to insurance premiums, coverage, benefits, provider networks, exclusions, limitations, availability, plan comparisons and insurance company ratings. A significant amount of both automated and manual effort is required to maintain the considerable amount of insurance plan information on our platform. We also regularly provide health insurance plan information in the scripts used by our customer call center partners. If the information we provide on our platform, through our customer call center partners or otherwise is not accurate or is construed as
23
Table of Contents
misleading, or if we do not properly assist individuals and businesses in purchasing health insurance, members, carriers and others could attempt to hold us liable for damages, our relationships with carriers could be terminated and regulators could attempt to subject us to penalties, revoke our licenses to transact health insurance business in a particular jurisdiction, and/or compromise the status of our licenses to transact health insurance business in other jurisdictions, which could result in our loss of our commission revenue. In the ordinary course of operating our business, we have received complaints that the information we provided was not accurate or was misleading. Although in the past we have resolved these complaints without significant financial cost, we cannot guarantee that we will be able to do so in the future. In addition, these types of claims could be time-consuming and expensive to defend, could divert our management’s attention and other resources and could cause a loss of confidence in our services. As a result, these claims could harm our business, results of operations and financial condition.
In the ordinary course of our business, we may receive inquiries from state regulators relating to various matters. We may in the future become involved in litigation in the ordinary course of our business. If we are found to have violated laws or regulations, we could lose our relationship with carriers and be subject to various fines and penalties, including revocation of our licenses to sell insurance, and our business, results of operations and financial condition would be materially harmed. We would also be harmed to the extent that related publicity damages our reputation as a trusted source of information relating to health insurance and its affordability. It could also be costly to defend ourselves regardless of the outcome. As a result, inquiries from regulators or our becoming involved in litigation could adversely affect our business, results of operations and financial condition.
If we do not continue to attract new individual customers, we may not achieve our revenue projections, and our results of operations would be harmed.
In order to grow our business, we must continually attract new distributors and individual customers. Our ability to do so depends in large part on the success of our sales and marketing efforts. Potential individual customers may seek out other options for purchasing insurance. Therefore, we must demonstrate that our products provide a viable solution for individual customers to obtain high quality coverage at an attractive price and provide a valuable business opportunity to our distributors. If we fail to provide high quality solutions and convince individual customers and distributors of our value proposition, we may not be able to retain existing customers or attract new individual customers. Additionally, there is no guarantee that the market for our services will grow as we expect. If the market for our services declines or develops more slowly than we expect, or if the number of individual customers or distributors that use our solutions declines or fails to increase as we expect, our revenue, results of operations, financial condition, business and prospects could be harmed.
Advanced commission arrangements between us and some of our distributors expose us to the credit risks of such distributors and may increase our costs and expenses, which could in turn have an adverse effect on our business, financial condition, and results of operations.
We make advanced commission payments to some of our licensed distributors in order to assist them with the cost of lead acquisition. As of December 31, 2012, we had a prepayment balance for advanced commissions of approximately $297,000 under such contracts. Part of our strategy is to expand the practice of paying advanced commissions, so we expect such balance to increase significantly in the future. In all such cases where we make advanced commission payments, we receive collateral and personal guarantees. At a minimum, our collateral includes a claim against all future compensation owed to the distributor for all products sold. As a result, our claims for such payments would rank as secured claims. Depending on the amount of future compensation owed to the distributor, we could be exposed to the credit risks of our distributors in the event of their insolvency or bankruptcy. Where the amount owed to us exceeds the value of the collateral, our claims against the defaulting distributors would rank below those of other secured creditors, which would undermine our chances of obtaining the return of our advance commission payments. We may not be able to recover such advanced payments and we may suffer losses should the distributors fail to fulfill their sales obligations under the contracts. Accordingly, any of the above scenarios could harm our business, results of operations and financial condition.
Seasonality may cause fluctuations in our financial results.
The number of member enrollments through our technology platform has generally increased in our third fiscal quarter. Conversely, we have generally experienced a decline in member enrollments in our fourth fiscal quarter. Although we believe that these trends may be influenced by an increase in new enrollments of college graduates in the third quarter and a decrease in new enrollments due to call center closures and reduced operating hours in the fourth quarter, we believe that the sale of health insurance plans and products through the Internet is still in its early stages, and, therefore, the reasons for these seasonal patterns are not entirely apparent. As the use of the Internet for the purchase and sale of health insurance becomes more widely accepted, other seasonality trends may develop and the existing seasonality and member behavior that we experience may change. Any seasonality that we experience may cause fluctuations in our financial results.
24
Table of Contents
If we are unable to successfully introduce new technology solutions or services or fail to keep pace with advances in technology, our business, financial condition and results of operations will be adversely affected.
Our business depends on our ability to adapt to evolving technologies and industry standards and introduce new technology solutions and services accordingly. If we cannot adapt to changing technologies, our technology solutions and services may become obsolete, and our business would suffer. Because the healthcare insurance market is constantly evolving, our existing technology may become obsolete and fail to meet the requirements of current and potential members. Our success will depend, in part, on our ability to continue to enhance our existing technology solutions and services, develop new technology that addresses the increasingly sophisticated and varied needs of our members and respond to technological advances and emerging industry standards and practices on a timely and cost-effective basis. The development of our online platform entails significant technical and business risks. We may not be successful in developing, using, marketing, or maintaining new technologies effectively or adapting our technology to evolving customer requirements or emerging industry standards, and, as a result, our business and reputation could suffer. We may not be able to introduce new technology solutions on schedule, or at all, or such solutions may not achieve market acceptance. We also engage third-party vendors to develop, maintain and enhance our technology solutions, and our ability to develop and implement new technologies is therefore dependent on our ability to engage suitable vendors. We may also need to license software or technology from third parties in order to maintain, expand or modify our technology platform. However, there is no guarantee we will be able to enter into such agreements on acceptable terms or at all. Moreover, competitors may develop competitive products that could adversely affect our results of operations. A failure by us to introduce new solutions or to introduce these solutions on schedule could have an adverse effect on our business, financial condition and results of operations.
Our failure to obtain, maintain and enforce the intellectual property rights on which our business depends could have a material adverse effect on our business, financial condition and results of operations.
We rely upon intellectual property laws in the United States, and non-disclosure, confidentiality and other types of agreements with our employees, members and other parties, to establish, maintain and enforce our intellectual property and proprietary rights. However, any of our owned or licensed intellectual property rights could be challenged, invalidated, circumvented, infringed or misappropriated, our trade secrets and other confidential information could be disclosed in an unauthorized manner to third-parties, or our intellectual property rights may not be sufficient to permit us to take advantage of current market trends or otherwise to provide us with competitive advantages, which could result in costly redesign efforts, discontinuance of certain offerings or other competitive harm. Efforts to enforce our intellectual property rights may be time consuming and costly, distract management’s attention and resources and ultimately be unsuccessful. In addition, such efforts may result in our intellectual property rights being challenged, limited in scope, or declared invalid or unenforceable. Moreover, our failure to develop and properly manage new intellectual property could adversely affect our market positions and business opportunities.
We may not be able to obtain, maintain and enforce the intellectual property rights that may be necessary to protect and grow our business and to provide us with a meaningful competitive advantage. Also, some of our business and services may rely on technologies and software developed by or licensed from third-parties, and we may not be able to maintain our relationships with such third-parties or enter into similar relationships in the future on reasonable terms or at all. Our failure to obtain, maintain and enforce our intellectual property rights could therefore have a material adverse effect on our business, financial condition and results of operations.
Assertions by third-parties that we violate their intellectual property rights could have a material adverse effect on our business, financial condition and results of operations.
Third-parties may claim that we, our members, our licensees or parties indemnified by us are infringing upon or otherwise violating their intellectual property rights. Such claims may be made by competitors seeking to obtain a competitive advantage or by other parties. Additionally, in recent years, individuals and groups have begun purchasing intellectual property assets for the purpose of making claims of infringement and attempting to extract settlements from companies like ours. Any claims that we violate a third-party’s intellectual property rights can be time consuming and costly to defend and distract management’s attention and resources, even if the claims are without merit. Such claims may also require us to redesign affected products and services, enter into costly settlement or license agreements or pay costly damage awards, or face a temporary or permanent injunction prohibiting us from marketing or providing the affected products and services. Even if we have an agreement to indemnify us against such costs, the indemnifying party may be unable to uphold its contractual obligations. If we cannot or do not license the infringed technology at all, license the technology on reasonable terms or substitute similar technology from another source, our revenue and earnings could be adversely impacted.
In addition, we may use open source software in connection with our products and services. Companies that incorporate open source software into their products have, from time to time, faced claims challenging the ownership of open source software and/or compliance with open source license terms. As a result, we could be subject to suits by parties claiming ownership of what we believe to be open source software or noncompliance with open source licensing terms. Some open source software licenses require users who distribute open source software as part of their software to publicly disclose all or part of the source code to such software and/or make available any derivative works of the open source code on unfavorable terms or at no cost. Any requirement to disclose our proprietary source code or pay damages for breach of contract could have a material adverse effect on our business, financial condition and results of operations.
25
Table of Contents
Assertions by third-parties that we violate their intellectual property rights could therefore have a material adverse effect on our business, financial condition and results of operations.
If we fail to effectively manage our growth, our business and results of operations could be harmed.
We have expanded our operations significantly since 2008. This has increased the significant demands on our management, our operational and financial systems and infrastructure and other resources. If we do not effectively manage our growth, the quality of our services could suffer. In order to successfully expand our business, we must effectively integrate, develop and motivate new employees, and we must maintain the beneficial aspects of our corporate culture. We may not be able to hire new employees quickly enough to meet our needs. If we fail to effectively manage our hiring needs and successfully integrate our new hires, our efficiency and ability to meet our forecasts and our employee morale, productivity and retention could suffer, and our business and results of operations could be harmed. We also need to continue to improve our existing systems for operational and financial management, including our reporting systems, procedures and controls. These improvements could require significant capital expenditures and place increasing demands on our management. We may not be successful in managing or expanding our operations or in maintaining adequate financial and operating systems and controls. If we do not successfully manage these processes, our business and results of operations will be harmed.
If we are unable to maintain a high level of service, our business and prospects may be harmed.
One of the key attributes of our business is providing high quality service to our carriers, distributors and members. We may be unable to sustain these levels of service, which would harm our reputation and our business. Alternatively, we may only be able to sustain high levels of service by significantly increasing our operating costs, which would materially adversely affect our results of operations. The level of service we are able to provide depends on our personnel to a significant extent. Our personnel must be well-trained in our processes and able to handle customer calls effectively and efficiently. Any inability of our personnel to meet our demand, whether due to absenteeism, training, turnover, disruptions at our facilities, bad weather, power outages or other reasons, could adversely impact our business. If we are unable to maintain high levels of service performance, our reputation could suffer and our results of operations and prospects would be harmed.
We are subject to privacy and data protection laws governing the transmission, security and privacy of health information, which may impose restrictions on the manner in which we access personal data and subject us to penalties if we are unable to fully comply with such laws.
Numerous federal, state and international laws and regulations govern the collection, use, disclosure, storage and transmission of individually identifiable health information. These laws and regulations, including their interpretation by governmental agencies, are subject to frequent change. These regulations could have a negative impact on our business, for example:
| • | HIPAA and its implementing regulations were enacted to ensure that employees can retain and at times transfer their health insurance when they change jobs, and to simplify healthcare administrative processes. The enactment of HIPAA also expanded protection of the privacy and security of personal health information and required the adoption of standards for the exchange of electronic health information. Among the standards that the Department of Health and Human Services has adopted pursuant to HIPAA are standards for electronic transactions and code sets, unique identifiers for providers, employers, health plans and individuals, security, electronic signatures, privacy and enforcement. Failure to comply with HIPAA could result in fines and penalties that could have a material adverse effect on us. |
| • | The HITECH Act, enacted as part of the American Recovery and Reinvestment Act of 2009, also known as the “Stimulus Bill,” effective February 22, 2010, sets forth health information security breach notification requirements and increased penalties for violation of HIPAA. The HITECH Act requires individual notification for all breaches, media notification of breaches of over 500 individuals and at least annual reporting of all breaches to the Department of Health and Human Services. The HITECH Act also replaced the prior penalty system of one tier of penalties of $100 per violation and an annual maximum of $25,000 with a four-tier system of sanctions for breaches. Penalties now range from the original $100 per violation and an annual maximum of $25,000 for the first tier to a fourth-tier minimum of $50,000 per violation and an annual maximum of $1.5 million. Failure to comply with the HITECH Act could result in fines and penalties that could have a material adverse effect on us. |
| • | Other federal and state laws restricting the use and protecting the privacy and security of individually identifiable information may apply, many of which are not preempted by HIPAA. |
| • | Federal and state consumer protection laws are increasingly being applied by the United States Federal Trade Commission, or FTC, and states’ attorneys general to regulate the collection, use, storage and disclosure of personal or individually identifiable information, through websites or otherwise, and to regulate the presentation of website content. |
26
Table of Contents
We are required to comply with federal and state laws governing the transmission, security and privacy of individually identifiable health information that we may obtain or have access to in connection with the provision of our services. Despite the security measures that we have in place to ensure compliance with privacy and data protection laws, our facilities and systems, and those of our third-party vendors and subcontractors, are vulnerable to security breaches, acts of vandalism or theft, computer viruses, misplaced or lost data, programming and human errors or other similar events. Due to the recent enactment of the HITECH Act, we are not able to predict the extent of the impact such incidents may have on our business. Our failure to comply may result in criminal and civil liability because the potential for enforcement action against business associates is now greater. Enforcement actions against us could be costly and could interrupt regular operations, which may adversely affect our business. While we have not received any notices of violation of the applicable privacy and data protection laws and believe we are in compliance with such laws, there can be no assurance that we will not receive such notices in the future.
Under the HITECH Act, as a business associate we may also be liable for privacy and security breaches and failures of our subcontractors. Even though we provide for appropriate protections through our agreements with our subcontractors, we still have limited control over their actions and practices. A breach of privacy or security of individually identifiable health information by a subcontractor may result in an enforcement action, including criminal and civil liability, against us. In addition, numerous other federal and state laws protect the confidentiality of individually identifiable information as well as employee personal information, including state medical privacy laws, state social security number protection laws, and federal and state consumer protection laws. These various laws in many cases are not preempted by HIPAA and may be subject to varying interpretations by the courts and government agencies, creating complex compliance issues for us and our members and potentially exposing us to additional expense, adverse publicity and liability, any of which could adversely affect our business.
Our business is subject to online security risks, and if we are unable to safeguard the security and privacy of confidential data, our reputation and business will be harmed.
Our services involve the collection and storage of confidential information of members and the transmission of this information to carriers. For example, we collect names, addresses, social security, bank account and credit card numbers, and information regarding the medical history of members in connection with their applications for insurance. In certain cases such information is provided to third-parties, for example to the service providers who provide hosting services for our technology platform, and we may therefore be unable to control the use of such information or the security protections employed by such third-parties. We may be required to expend significant capital and other resources to protect against security breaches or to alleviate problems caused by security breaches. Despite our implementation of security measures, techniques used to obtain unauthorized access or to sabotage systems change frequently. As a result, we may be unable to anticipate these techniques or to implement adequate preventative measures. Any compromise or perceived compromise of our security (or the security of our third-party service providers who have access to our members’ confidential information) could damage our reputation and our relationship with our members, distributors and carriers, could reduce demand for our services and could subject us to significant liability as well as regulatory action. In addition, in the event that new data security laws are implemented, or our carrier or other partners determine to impose new requirements on us relating to data security, we may not be able to timely comply with such requirements, or such requirements may not be compatible with our current processes. Changing our processes could be time consuming and expensive, and failure to timely implement required changes could result in our inability to sell health insurance plans and products in a particular jurisdiction or for a particular carrier, or subject us to liability for non-compliance.
Our services present the potential for embezzlement, identity theft or other similar illegal behavior by our employees or subcontractors with respect to third-parties.
Among other things, our services involve handling information from members, including credit card information and bank account information. Our services also involve the use and disclosure of personal information that could be used to impersonate third-parties or otherwise gain access to their data or funds. If any of our employees or subcontractors takes, converts or misuses such funds, documents or data, we could be liable for damages, and our business reputation could be damaged. In addition, we could be perceived to have facilitated or participated in illegal misappropriation of funds, documents or data and therefore be subject to civil or criminal liability. Any such illegal activity by our employees or subcontractors could have an adverse effect on our business, financial condition and results of operations.
System failures or capacity constraints could harm our business and results of operations.
The performance, reliability and availability of our technology platform, customer service call center and underlying network infrastructures are critical to our financial results and our relationship with members, distributors and insurance carriers. Although we regularly attempt to enhance and maintain our technology platform, customer service call center and system infrastructure, system failures and interruptions may occur if we are unsuccessful in these efforts or experience difficulties with transitioning existing systems to upgraded systems, if we are unable to accurately project the rate or timing of increases in our platform traffic or customer service call center call volume or for other reasons, some of which are completely outside our control. Significant failures and interruptions, particularly during peak enrollment periods, could harm our business, results of operations and financial condition.
27
Table of Contents
We rely in part upon third-party vendors, including data center and bandwidth providers, to operate and maintain our technology platform. We cannot predict whether additional network capacity will be available from these vendors as we need it, and our network or our suppliers’ networks might be unable to achieve or maintain a sufficiently high capacity of data transmission to allow us to process health insurance applications in a timely manner or effectively download data, especially if our platform traffic increases. Any system failure that causes an interruption in, or decreases the responsiveness of, our services could impair our revenue-generating capabilities, harm our image and subject us to potential liability. Our database and systems are vulnerable to damage or interruption from human error, earthquakes, fire, floods, power loss, telecommunications failures, physical or electronic break-ins, computer viruses, acts of terrorism, other attempts to harm our systems and similar events.
We depend upon third-parties, including telephone service providers and third-party software providers, to operate our customer service call center. Any failure of the systems upon which we rely in the operation of our customer service call center could negatively impact sales as well as our relationship with members, which could harm our business, results of operations and financial condition.
We rely on third-party vendors to develop, host, maintain, service and enhance our technology platform.
We rely on third-party vendors to develop, host, maintain, support and enhance our technology platform. In particular, we are party to an agreement with BimSym pursuant to which BimSym provides various professional services relating to our A.R.I.E.S. technology platform, including hosting, support, maintenance and development services. Our ability to offer our services and operate our business is therefore dependent on maintaining our relationships with third-party vendors, particularly BimSym, and entering into new relationships to meet the changing needs of our business. Any deterioration in our relationships with such vendors, or our failure to enter into agreements with vendors in the future would harm our business, results of operations and financial condition. If our vendors are unable or unwilling to provide the services necessary to support our business, or if our agreements with such vendors are terminated, our operations could be significantly disrupted. We may also incur substantial costs, delays and disruptions to our business in transitioning such services to ourselves or other third-party vendors. In addition, third-party vendors may not be able to provide the services required in order to meet the changing needs of our business.
Carriers and distributors depend upon third-party service providers to access our online platform, and our business and results of operations could be harmed as a result of technical difficulties experienced by these service providers.
Carriers and distributors using our online platform depend upon Internet and other service providers for access to our platform. Many of these service providers have experienced significant outages, delays and other difficulties in the past and could experience them in the future. Any significant interruption in access to our technology platform or increase in our platform’s response time as a result of these difficulties could damage our relationship with carriers, distributors and existing and potential members and could harm our business, results of operations and financial condition.
Economic conditions and other factors beyond our control may negatively impact our business, results of operations and financial condition.
Our revenue depends upon demand for our insurance products, which can be influenced by a variety of factors beyond our control. We have no control over the economic and other factors that influence such demand. We cannot be certain of the future impact that the recent recession will have on our business. A further softening of demand for our products and the services offered by us, whether caused by changes in individual preferences or the regulated environment in which we operate, or by a weak economy, including as a result of recent disruptions in the global financial markets or a decrease in general consumer confidence, will result in decreased revenue and growth. Members may attempt to reduce expenses by canceling existing plans and products purchased through us, not purchasing new plans and products through us or purchasing plans with lower premiums for which we receive lower commissions. A continuing negative economic environment could also adversely impact the carriers whose plans and products are offered on our platform, and they may, among other things, determine to reduce their commission rates, increase premiums or reduce benefits, any of which could negatively impact our business, results of operations and financial condition.
To the extent the economy or other factors adversely impact our member retention, the number or type of insurance applications submitted through us and that are approved by carriers, or the commissions that we receive from carriers, our rate of growth will decline and our business and results of operations will be harmed.
The loss of any member of our management team and our inability to make up for such loss with a qualified replacement could harm our business.
Competition for qualified management in our industry is intense. Many of the companies with which we compete for management personnel have greater financial and other resources than we do or are located in geographic areas which may be considered by some to be more desirable places to live. If we are not able to retain any of our key management personnel, our business could be harmed.
28
Table of Contents
Our acquisitions and other strategic transactions may be difficult to integrate, divert management resources, result in unanticipated costs or dilute our stockholders.
Part of our continuing business strategy is to acquire or invest in, companies, products or technologies that complement our current products, enhance our market coverage, technical capabilities or production capacity, or offer growth opportunities or make other strategic transactions. For example, in March 2013, we completed a transaction with TSG Agency, LLC (“TSG”) and its principal, Ivan Spinner (“Spinner”), which is further described in “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—General.” Such acquisitions could pose numerous risks to our operations, including:
| • | difficulty integrating the purchased operations, technologies or products; |
| • | incurring substantial unanticipated integration costs; |
| • | assimilating the acquired businesses may divert significant management attention and financial resources from our other operations and could disrupt our ongoing business; |
| • | acquisitions could result in the loss of key employees, particularly those of the acquired operations; |
| • | difficulty retaining or developing the acquired businesses’ customers; |
| • | acquisitions could adversely affect our existing business relationships with suppliers and members; |
| • | failing to realize the potential cost savings or other financial benefits and/or the strategic benefits of the acquisitions; and |
| • | incurring liabilities from the acquired businesses for infringement of intellectual property rights or other claims, and we may not be successful in seeking indemnification for such liabilities or claims. |
The TSG transaction poses some of these risks, including the potential that TSG and Spinner might not generate the revenues that we anticipate and that we might not retain Spinner for a sufficient time period to realize anticipated benefits.
In connection with these acquisitions or investments, we could incur debt, amortization expenses related to intangible assets, large and immediate write-offs, assume liabilities or issue stock that would dilute our current stockholders’ percentage of ownership. We may not be able to complete acquisitions or integrate the operations, products or personnel gained through any such acquisition without a material adverse effect on our business, financial condition and results of operations.
The requirements of being a public company may strain our resources and distract our management, which could make it difficult to manage our business, particularly after we are no longer an “emerging growth company.”
We are required to comply with various regulatory and reporting requirements, including those required by the Securities and Exchange Commission (the “SEC”). Complying with these reporting and other regulatory requirements will be time-consuming and will result in increased costs to us and could have a negative effect on our business, financial condition and results of operations.
As a public company, we are subject to the reporting requirements of the Securities Exchange Act of 1934 (as amended, the “Exchange Act”) and the requirements of the Sarbanes-Oxley Act of 2002 (as amended, the “Sarbanes-Oxley Act”). These requirements may place a strain on our systems and resources. The Exchange Act requires that we file annual, quarterly and current reports with respect to our business and financial condition. The Sarbanes-Oxley Act requires that we maintain effective disclosure controls and procedures and internal controls over financial reporting. To maintain and improve the effectiveness of our disclosure controls and procedures, we will need to commit significant resources, hire additional staff and provide additional management oversight. We will be implementing additional procedures and processes for the purpose of addressing the standards and requirements applicable to public companies. Sustaining our growth also will require us to commit additional management, operational and financial resources to identify new professionals to join our company and to maintain appropriate operational and financial systems to adequately support expansion. These activities may divert management’s attention from other business concerns, which could have a material adverse effect on our business, financial condition and results of operations.
As an “emerging growth company” as defined in the Jumpstart Our Business Startups Act of 2012 (the “JOBS Act”), we intend to take advantage of certain temporary exemptions from various reporting requirements, including, but not limited to, not being required to comply with the auditor attestation requirements of Section 404 of the Sarbanes-Oxley Act and reduced disclosure obligations regarding executive compensation in our periodic reports and proxy statements. In addition, we have elected under the JOBS Act to delay adoption of new or revised accounting pronouncements applicable to public companies until such pronouncements are made applicable to private companies.
When these exemptions cease to apply, we expect to incur additional expenses and devote increased management effort toward ensuring compliance with them. We cannot predict or estimate the amount of additional costs we may incur as a result of becoming a public company or the timing of such costs.
Risks Related to Our Structure
We are a holding company and our only material asset is our interest in Health Plan Intermediaries Holdings, LLC and, accordingly, we are dependent upon distributions from Health Plan Intermediaries Holdings, LLC to pay taxes and other expenses.
We are a holding company and have no material assets other than our ownership of Series A Membership Interests of Health Plan Intermediaries Holdings, LLC. We have no independent means of generating revenue. Health Plan Intermediaries Holdings, LLC is treated as a partnership for U.S. federal income tax purposes and, as such, is not itself be subject to U.S. federal income tax. Instead,
29
Table of Contents
its net taxable income is generally allocated to its members, including us, pro rata according to the number of membership interests each member owns. Accordingly, we incur income taxes on our proportionate share of any net taxable income of Health Plan Intermediaries Holdings, LLC and also incur expenses related to our operations. We intend to cause Health Plan Intermediaries Holdings, LLC to distribute cash to its members, including us, in an amount at least equal to the amount necessary to cover their respective tax liabilities, if any, with respect to their allocable share of the net income of Health Plan Intermediaries Holdings, LLC and to cover dividends, if any, declared by us, as well as any payments due under the tax receivable agreement, as described below. To the extent that we need funds to pay our tax or other liabilities or to fund our operations, and Health Plan Intermediaries Holdings, LLC is restricted from making distributions to us under applicable agreements, laws or regulations or does not have sufficient cash to make these distributions, we may have to borrow funds to meet these obligations and operate our business, and our liquidity and financial condition could be materially adversely affected. To the extent that we are unable to make payments under the income tax receivable agreement for any reason, such payments will be deferred and will accrue interest until paid.
We will be required to pay the existing and certain future holders of Series B Membership Interests most of the tax benefits that we may receive as a result of the purchase of Series B Membership Interests with the net proceeds of the sale of over-allotment shares, future exchanges of Series B Membership Interests for our Class A common stock and payments made under the tax receivable agreement itself, and the amounts we pay could be substantial.
We expect that the purchase of Series B Membership Interests (together with an equal number of shares of our Class B common stock) with the net proceeds of the sale of over-allotment shares, as well as any future exchanges of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for shares of our Class A common stock, will result in increases in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. Any such increases in tax basis could reduce the amount of tax that we would otherwise be required to pay in the future.
We entered into a tax receivable agreement with the members of Health Plan Intermediaries Holdings, LLC (Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske) and certain future members of Health Plan Intermediaries Holdings, LLC, pursuant to which we will pay them 85% of the amount of the cash savings, if any, in U.S. federal, state and local income tax that we realize (or are deemed to realize in the case of an early termination payment by us, a change in control or a material breach by us of our obligations under the tax receivable agreement, as discussed below) as a result of these possible increases in tax basis resulting from our purchases or exchanges of Series B Membership Interests as well as certain other benefits attributable to payments under the tax receivable agreement itself. Any actual increases in tax basis, as well as the amount and timing of any payments under the tax receivable agreement, cannot be predicted reliably at this time. The amount of any such increases and payments will vary depending upon a number of factors, including the timing of exchanges, the price of our Class A common stock at the time of the exchanges, the amount, character and timing of our income and the tax rates then applicable. The payments that we may be required to make pursuant to the tax receivable agreement could be substantial for periods in which we generate taxable income. Assuming no material changes in the relevant tax law and based on our current operating plan and other assumptions, including our estimate of the tax basis of our assets as of December 31, 2012, if we acquired all of the Series B Membership Interests in taxable transactions for a price of $14.00 per Series B Membership Interest, we estimate that the maximum amount that we would be required to pay under the tax receivable agreement could be approximately $53,001,000. The actual amount may materially differ from this hypothetical amount, as potential future payments will be calculated using the market value of our Class A common stock at the time of relevant exchange and prevailing tax rates in future years and will be dependent on us generating sufficient future taxable income to realize the benefit. See “Item 1. Business—Our History and the Reorganization of Our Corporate Structure—Tax Receivable Agreement.”
In addition, the tax receivable agreement provides that in the case that we exercise our right to early termination of the tax receivable agreement or in the case of a change in control or a material breach by us of our obligations under the tax receivable agreement, the tax receivable agreement will terminate, and we will be required to make a payment equal to the present value of future payments under the tax receivable agreement, which payment would be based on certain assumptions, including those relating to our future taxable income. In these situations, our obligations under the tax receivable agreement could have a substantial negative impact on our liquidity and could have the effect of delaying, deferring or preventing certain mergers, asset sales, other forms of business combinations or other changes of control. These provisions of the tax receivable agreement may result in situations where Mr. Kosloske may have interests that differ from or are in addition to those of other shareholders. Because we are controlled by Mr. Kosloske, Mr. Kosloske will have effective control over the outcome of votes on all matters requiring approval by our stockholders and accordingly actions that affect such obligations under the tax receivable agreement may be taken even if other stockholders oppose them.
If the Internal Revenue Service successfully challenges the tax basis increases, we will not be reimbursed for any payments made under the tax receivable agreement (although future payments under the tax receivable agreement, if any, would be adjusted to reflect the result of any such successful challenge by the Internal Revenue Service). As a result, in certain circumstances, we could be required to make payments under the tax receivable agreement in excess of our cash tax savings.
30
Table of Contents
We may not be able to realize all or a portion of the tax benefits that are expected to result from the purchase of Series B Membership Interests with the net proceeds of the sale of over-allotment shares, future exchanges of Series B Membership Interests for our Class A common stock and payments made under the tax receivable agreement itself.
Our ability to benefit from any depreciation or amortization deductions or to realize other tax benefits that we currently expect to be available as a result of the increases in tax basis created by the purchase of Series B Membership Interests (together with an equal number of shares of our Class B common stock) with the net proceeds of the sale of any over-allotment shares, as well as any future exchanges of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for our Class A common stock, and our ability to realize certain other tax benefits attributable to payments under the tax receivable agreement itself depend on a number of assumptions, including that we earn sufficient taxable income each year during the period over which such deductions are available and that there are no adverse changes in applicable law or regulations. If our actual taxable income were insufficient and/or there were adverse changes in applicable law or regulations, we may be unable to realize all or a portion of these expected benefits and our cash flows and stockholders’ equity could be negatively affected.
Risks Related to Ownership of Our Class A Common Stock
There may not be an active, liquid trading market for our Class A common stock.
Prior to February 2013, there was no public market for shares of our Class A common stock. We cannot predict the extent to which investor interest in our Company will lead to the development of an active trading market on the NASDAQ Global Market or how liquid that market may become. If an active trading market does not develop, you may have difficulty selling any shares of our Class A common stock that you purchase.
We expect that our stock price will fluctuate significantly, and you may not be able to resell your shares at or above the purchase price.
The trading price of our Class A common stock is likely to be volatile and subject to wide price fluctuations in response to various factors, including:
| • | market conditions in the broader stock market in general, or in our industry in particular; |
| • | actual or anticipated fluctuations in our quarterly financial and results of operations; |
| • | our ability to satisfy our ongoing capital needs and unanticipated cash requirements, particularly with respect to our advanced commissions structure; |
| • | additional indebtedness incurred in the future; |
| • | introduction of new products and services by us or our competitors; |
| • | issuance of new or changed securities analysts’ reports or recommendations; |
| • | sales of large blocks of our stock; |
| • | additions or departures of key personnel; |
| • | regulatory developments; |
| • | litigation and governmental investigations; and |
| • | economic and political conditions or events. |
These and other factors may cause the market price and demand for our Class A common stock to fluctuate substantially, which may limit or prevent investors from readily selling their shares of Class A common stock and may otherwise negatively affect the liquidity of our Class A common stock. In addition, in the past, when the market price of a stock has been volatile, holders of that stock have instituted securities class action litigation against the company that issued the stock. If any of our stockholders brought a lawsuit against us, we could incur substantial costs defending the lawsuit. Such a lawsuit could also divert the time and attention of our management from our business.
The trading market for our Class A common stock may also be influenced by the research and reports that industry or securities analysts publish about us or our business. If one or more of these analysts cease coverage of our company or fail to publish reports on us regularly, we could lose visibility in the financial markets, which in turn could cause our stock price or trading volume to decline. Moreover, if one or more of the analysts who cover us downgrades our stock, or if our results of operations do not meet their expectations, our stock price could decline.
If a substantial number of shares become available for sale and are sold in a short period of time, the market price of our Class A common stock could decline.
If our existing stockholders sell substantial amounts of our Class A common stock in the public market, the market price of our Class A common stock could decrease significantly. The perception in the public market that our existing stockholders might sell
31
Table of Contents
shares of Class A common stock could also depress our market price. As of March 27, 2013, we have 5,295,167 shares of Class A common stock outstanding. In addition, some of our employees and directors hold stock options that are subject to lock-up agreements and Rule 144 holding period requirements. The market price of shares of our Class A common stock may drop significantly when the restrictions on resale by our existing stockholders lapse. A decline in the price of shares of our Class A common stock might impede our ability to raise capital through the issuance of additional shares of our Class A common stock or other equity securities.
We are a “controlled company” within the meaning of the rules of the NASDAQ Global Market and, as a result, qualify for, and intend to rely on, exemptions from certain corporate governance requirements. You will not have the same protections afforded to stockholders of companies that are subject to such requirements.
Entities controlled by Michael W. Kosloske, our Chairman, President and Chief Executive Officer, control a majority of the combined voting power of all classes of our voting stock. As a result, we are a “controlled company” within the meaning of the corporate governance standards of the NASDAQ Global Market. Under NASDAQ Global Market rules, a company of which more than 50% of the voting power is held by an individual, group or another company is a “controlled company” and may elect not to comply with certain corporate governance requirements, including:
| • | the requirement that a majority of the board of directors consist of independent directors; |
| • | the requirement that we have a nominating and corporate governance committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; |
| • | the requirement that we have a compensation committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; and |
| • | the requirement for an annual performance evaluation of the nominating and corporate governance and compensation committees. |
We intend to utilize these exemptions if we continue to qualify as a “controlled company.” If we utilize these exemptions we will not have a majority of independent directors and our nominating and corporate governance and compensation committees will not consist entirely of independent directors and such committees will not be subject to annual performance evaluations. Accordingly, you will not have the same protections afforded to stockholders of companies that are subject to all of the corporate governance requirements of the NASDAQ Global Market.
We are controlled by entities associated with Mr. Kosloske, whose interests may differ from those of our public stockholders.
We are controlled by entities associated with Mr. Kosloske. Mr. Kosloske beneficially owns in the aggregate approximately 62.4% of the combined voting power of our common stock. As a result of this ownership, Mr. Kosloske has effective control over the outcome of votes on all matters requiring approval by our stockholders, including the election of directors, the adoption of amendments to our certificate of incorporation and bylaws and approval of a sale of the company and other significant corporate transactions, including such corporate transactions that may affect our obligations under the tax receivable agreement. See “We will be required to pay the existing and certain future holders of Series B Membership Interests most of the tax benefits that we may receive as a result of the purchase of Series B Membership Interests with the net proceeds of the sale of over-allotment shares, future exchanges of Series B Membership Interests for our Class A common stock and payments made under the tax receivable agreement itself, and the amounts we pay could be substantial.” Mr. Kosloske can also take actions that have the effect of delaying or preventing a change in control of us or discouraging others from making tender offers for our shares, which could prevent stockholders from receiving a premium for their shares. These actions may be taken even if other stockholders oppose them.
The market price of our Class A common stock could decline due to the large number of shares of Class A common stock eligible for future sale upon the exchange of Series B Membership Interests.
The market price of our Class A common stock could decline as a result of sales of a large number of shares of our Class A common stock eligible for future sale upon the exchange of Series B Membership Interests (together with an equal number of shares of our Class B common stock), or the perception that such sales could occur. These sales, or the possibility that these sales may occur, may also make it more difficult for us to raise additional capital by selling equity securities in the future, at a time and price that we deem appropriate.
As of March 27, 2013, 5,295,167 Series A Membership Interests and 8,566,667 Series B Membership Interests of Health Plan Intermediaries Holdings, LLC are outstanding. Each Series B Membership Interest, together with one share of our Class B common stock, is exchangeable for one share of Class A common stock. We have entered into a registration rights agreement with Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC pursuant to which we granted them registration rights with respect to their shares of Class A common stock delivered in exchange for their Series B Membership Interests. See “Item 13. Certain Relationships and Related Transactions and Director Independence—Exchange Agreement.”
32
Table of Contents
Some provisions of Delaware law, our amended and restated certificate of incorporation and amended and restated bylaws and the beneficial ownership of a majority of our shares by one person may deter third-parties from acquiring us.
Our amended and restated certificate of incorporation and amended and restated bylaws provide for, among other things:
| • | restrictions on the ability of our stockholders to fill a vacancy on the board of directors; |
| • | prohibit stockholder action by written consent after the date on which Mr. Kosloske ceases to beneficially own at least a majority of all of the outstanding shares of our capital stock entitled to vote; |
| • | prohibit cumulative voting in the election of directors, which would otherwise allow holders of less than a majority of stock to elect some directors; |
| • | provide that special meetings of stockholders may be called only by the board of directors, the chairman of the board of directors or the chief executive officer; provided, however, if Mr. Kosloske beneficially owns at least a majority of all of the outstanding shares of our capital stock entitled to vote, special meetings of stockholders may be called by the holders of a majority of the total voting power of our then outstanding capital stock; |
| • | establish advance notice procedures for the nomination of candidates for election as directors or for proposing matters that can be acted upon at stockholder meetings; |
| • | provide that on and after the date Mr. Kosloske collectively ceases to beneficially own a majority of all of the outstanding shares of our capital stock entitled to vote, (a) directors may be removed only for cause and only upon the affirmative vote of holders of at least 75% of all of the outstanding shares of our capital stock entitled to vote, and (b) certain provisions of our amended and restated certificate of incorporation may only be amended upon the affirmative vote of holders of at least 75% of all of the outstanding shares of our capital stock entitled to vote; and |
| • | the authorization of undesignated preferred stock, the terms of which may be established and shares of which may be issued without stockholder approval. As of March 27, 2013, Mr. Kosloske beneficially owned 62.4% of the combined voting power of our common stock. |
These anti-takeover defenses, the beneficial ownership of a majority of our shares by one person and other factors could discourage, delay or prevent a transaction involving a change in control of our company. These provisions could also discourage proxy contests and make it more difficult for you and other stockholders to elect directors of your choosing and cause us to take other corporate actions that you desire.
We do not anticipate paying any cash dividends in the foreseeable future.
We currently intend to retain our future earnings, if any, for the foreseeable future, to repay indebtedness and to fund the development and growth of our business. We do not intend to pay any dividends to holders of our Class A common stock. As a result, capital appreciation in the price of our Class A common stock, if any, will be your only source of gain on an investment in our Class A common stock.
We have identified a material weakness in our internal control over financial reporting that, if not corrected, could result in material misstatements in our financial statements.
In connection with the preparation of our financial statements for the years ended December 31, 2012 and 2011 and for the nine months ended September 30, 2012, we identified a certain matter involving our internal control over financial reporting that constitutes a material weakness under standards established by the Public Company Accounting Oversight Board (“PCAOB”). The PCAOB defines a material weakness as a deficiency, or combination of deficiencies, in internal control over financial reporting, such that there is a reasonable possibility that a material misstatement of a company’s annual or interim financial statements will not be prevented or detected on a timely basis.
We identified a material weakness where we did not have effective controls over the design and operation of the financial statement close process, which process impacts most of our significant accounts included in the financial statements. The deficiencies in the design and operation of the financial statement close process that resulted in the material weakness included the following:
| • | lack of a formal process for reviewing period-end cutoff of revenues and expenses to ensure amounts are captured in the period earned or incurred under the accrual basis of accounting; |
| • | no process in place to ensure all expenses incurred during the period are accrued as of the month-end date, including expenses for which estimates are required; |
| • | absence of a mechanism through which the accounting implications of significant or unusual events and transactions are formally evaluated; and |
| • | no process to ensure formally executed agreements regarding all significant arrangements with third parties and others are obtained. |
33
Table of Contents
We are taking steps to address this material weakness by hiring additional personnel with technical accounting expertise and by implementing enhanced training for our finance and accounting personnel to familiarize them with our accounting policies. However, the material weakness will be ongoing until these controls are fully implemented and we will not be able to confirm that we have remediated this material weakness until our newly implemented procedures have been working for a sufficient period of time. As a result of this and similar activities, management’s attention may be diverted from other business concerns, which could have a material adverse effect on our business, financial condition and results of operations.
If the remedial policies and procedures we implement and resources we hire are insufficient to address the identified material weakness, or if additional material weaknesses or significant deficiencies in our internal controls are discovered in the future, we may fail to meet our future reporting obligations, our financial statements may contain material misstatements and our operating results may be adversely affected.
Our internal controls over financial reporting may not be effective and our independent registered public accounting firm may not be able to certify as to their effectiveness, which could have a significant and adverse effect on our business and reputation.
We are not currently required to comply with SEC rules that implement Section 404 of the Sarbanes-Oxley Act and are therefore not required to make a formal assessment of the effectiveness of our internal controls over financial reporting for that purpose. We will be required, pursuant to the Exchange Act, to furnish a report by management on, among other things, the effectiveness of our internal control over financial reporting for the first fiscal year beginning after February 13, 2013, the effective date of our initial public offering.
When evaluating our internal controls over financial reporting, we may identify material weaknesses that we may not be able to remediate in time to meet the applicable deadline imposed upon us for compliance with the requirements of Section 404 of the Sarbanes-Oxley Act. In addition, if we fail to achieve and maintain the adequacy of our internal controls, as such standards are modified, supplemented or amended from time to time, we may not be able to ensure that we can conclude, on an ongoing basis, that we have effective internal controls over financial reporting in accordance with Section 404 of the Sarbanes-Oxley Act. We cannot be certain as to the timing of completion of our evaluation, testing and any remediation actions or the impact of the same on our operations. If we are not able to implement the requirements of Section 404 of the Sarbanes-Oxley Act in a timely manner or with adequate compliance, we may be subject to sanctions or investigation by regulatory authorities, such as the SEC. As a result, there could be a negative reaction in the financial markets due to a loss of confidence in the reliability of our financial statements. In addition, we may be required to incur costs in improving our internal control system and the hiring of additional personnel. Any such action could negatively affect our results of operations and cash flows.
We are an “emerging growth company” and we cannot be certain if the reduced disclosure requirements applicable to emerging growth companies will make our Class A common stock less attractive to investors.
We are an “emerging growth company,” as defined in the JOBS Act, and we intend to take advantage of certain exemptions from various reporting requirements that are applicable to other public companies that are not “emerging growth companies” including, but not limited to, not being required to comply with the auditor attestation requirements of Section 404 of the Sarbanes-Oxley Act, which may increase the risk that weaknesses or deficiencies in our internal control over financial reporting go undetected, and reduced disclosure obligations regarding executive compensation in our periodic reports and proxy statements, which may make it more difficult for investors and securities analysts to evaluate our Company. In addition, we have elected under the JOBS Act to delay adoption of new or revised accounting pronouncements applicable to public companies until such pronouncements are made applicable to private companies. As a result of this election, our financial statements may not be comparable to companies that comply with public company effective dates. We cannot predict if investors will find our Class A common stock less attractive if we rely on these exemptions. If some investors find our Class A common stock less attractive as a result, there may be a less active trading market for our Class A common stock and our stock price may be more volatile. We may take advantage of these reporting exemptions until we are no longer an emerging growth company, which in certain circumstances could be up to five years.
We have broad discretion in using the net proceeds of our recent initial public offering, and we may not effectively expend the proceeds.
We used the net proceeds of our recent initial public offering to repay all of the outstanding debt, and intend to use the remaining net proceeds to provide the funds necessary to expand our advanced commission structure and for general corporate purposes, including acquisitions. We have significant flexibility and broad discretion in applying the net proceeds, and we may not apply them effectively. Our management might not be able to yield a significant return, if any, on any investment of the net proceeds. You do not have the opportunity to influence our decisions on how to use the net proceeds.
Our business and stock price may suffer as a result of our lack of public company operating experience.
We were a privately-held company from the beginning of our operations in 2008 until February 2013. Our lack of public company operating experience may make it difficult to forecast and evaluate our future prospects. If we are unable to execute our business strategy, either as a result of our inability to effectively manage our business in a public company environment or for any other reason, our prospects, financial condition and results of operations may be harmed.
34
Table of Contents
| ITEM 1B. | UNRESOLVED STAFF COMMENTS |
None.
| ITEM 2. | PROPERTIES |
We lease 7,858 square feet of space for our headquarters in Tampa, Florida under a lease that expires in 2015. In addition, we sublease approximately 4,000 square feet of space for our Insurance Academy in Boca Raton, Florida under a lease that expires in 2015. We believe that suitable additional or alternative space will be available in the future on commercially reasonable terms to accommodate our foreseeable future expansion.
| ITEM 3. | LEGAL PROCEEDINGS |
We are not currently a party to any material litigation proceedings. From time to time, however, we may be a party to litigation and subject to claims incident to the ordinary course of business. Regardless of the outcome, litigation can have an adverse impact on us because of defense and settlement costs, diversion of management resources and other factors.
| ITEM 4. | MINE SAFETY DISCLOSURES |
Not applicable.
35
Table of Contents
| ITEM 5. | MARKET FOR REGISTRANT’S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES |
Our Class A common stock is listed on the NASDAQ Global Market under the symbol “HIIQ.” On March 27, 2013, the last reported sale price of our Class A common stock on the NASDAQ Global Market was $15.16 per share. Our shares of Class A common stock have been publicly traded since February 8, 2013. Prior to that time there was no public market for our Class A common stock. As a result, we have not set forth quarterly information with respect to the high and low prices of our Class A common stock for the two most recent fiscal years. Between February 8, 2013 and March 27, 2013, the closing price of our Class A common stock as reported on the NASDAQ Global Market ranged from a high of $15.55 per share to a low of $12.32 per share.
There is no public market for our Class B common stock.
HOLDERS
As of March 27, 2013, 5,295,167 shares of our Class A common stock and 8,566,667 shares of our Class B common stock were issued and outstanding, and there were two Class A common stockholders of record and two Class B stockholders of record.
DIVIDEND POLICY
We currently anticipate that we will retain all available funds for use in the operation and expansion of our business, and do not anticipate paying any cash dividends in the foreseeable future. Class B common stock will not be entitled to any dividend payments.
EQUITY COMPENSATION PLAN INFORMATION
Prior to our corporate reorganization in anticipation of our initial public offering on February 7, 2013, we did not have any equity securities authorized for issuance under equity compensation plans. The following table contains information about our equity compensation plans as of March 27, 2013:
| Equity Compensation Plan Information | ||||||||||||
| (a) | (b) | (c) | ||||||||||
| Plan Category |
Number of securities to be issued upon exercise of outstanding options, warrants and rights |
Weighted-average exercise price of outstanding options, warrants and rights |
Number of securities remaining available for future issuance under equity compensation plans (excluding securities reflected in column (a)) |
|||||||||
| Equity compensation plans approved by security holders(1) |
678,500 | $ | 13.97 | 571,500 | ||||||||
| Equity compensation plans not approved by security holders |
— | — | — | |||||||||
|
|
|
|
|
|
|
|||||||
| Total |
678,500 | $ | 13.97 | 571,500 | ||||||||
|
|
|
|
|
|
|
|||||||
| (1) | Refers to the Health Insurance Innovations, Inc. Long Term Incentive Plan. |
UNREGISTERED SALES OF EQUITY SECURITIES
None.
USE OF PROCEEDS
On February 7, 2013, a registration statement (Registration No. 333-185596) relating to our initial public offering of our Class A common stock was declared effective by the Securities and Exchange Commission. Under this registration statement, we registered 4,666,667 shares of our Class A common stock, and another 700,000 shares subject to the over-allotment option of the underwriters of the initial public offering. The offering closed on February 13, 2013. All 4,666,667 shares of Class A common stock registered under the registration statement and 100,000 shares covered by the over-allotment option were sold at a price to the public of $14.00 per share.
36
Table of Contents
The offering did not terminate until after the sale of all of the shares registered on the registration statement. The aggregate gross proceeds from the shares of Class A common stock sold by us were $65,333,000. The aggregate net proceeds to us from the offering were approximately $60,760,000, after deducting an aggregate of $4,573,000 in underwriting discounts and commissions paid to the underwriters and other expenses incurred in connection with the offering.
As of March 27, 2013, we had used $3,230,000 of the net proceeds to pay all of our outstanding debt under our loans from a third-party bank. We used $1,302,000 of the proceeds from the sale of shares through the over-allotment option to acquire Series B Membership Interests, together with an equal number of shares of our Class B common stock, from Health Plan Intermediaries, LLC, which is controlled by Mr. Kosloske, our Chairman, President, and Chief Executive Officer, which Series B Membership Interests were immediately recapitalized into Series A Membership Interests. We also used $5,500,000 of the net proceeds to complete the transaction with TSG and Spinner, which is described in further detail in “Item 1A. Risk Factors” and “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—General.” We expect to use the remaining proceeds of the offering to expand our advanced commission structure and for general corporate purposes, including potential acquisitions that are complementary to our business or enable us to enter new markets or provide new products or services. The remaining proceeds are currently held in short-term, highly liquid investment accounts.
| ITEM 6. | SELECTED FINANCIAL DATA AND OPERATIONAL DATA |
This item is not applicable for smaller reporting companies.
37
Table of Contents
ITEM 7. MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
Management’s Discussion and Analysis of Financial Condition and Results of Operations below presents the Company’s operating results for each of the two years in the period ended December 31, 2012, and its financial condition as of December 31, 2012. Except for the historical information contained herein, this report and other written and oral statements that the Company makes from time to time contain forward-looking statements, which involve substantial known and unknown risks, uncertainties and other important factors that could cause the actual results, performance or achievements of results to differ materially from any future results, performance or achievements expressed or implied by such forward-looking statements. See the section of this report entitled “Special Note Regarding Forward-Looking Statements.” Among the factors that could cause actual results to differ materially are those discussed in “Risks Factors” in Item 1A of this report. In addition, the following Management’s Discussion and Analysis of Financial Condition and Results of Operations should be read in connection with the information presented in the Company’s consolidated financial statements and the related notes to its consolidated financial statements included in Part IV of this report.
Overview
We are a leading developer and administrator of affordable, web-based individual health insurance plans and ancillary products. Our highly scalable, proprietary, web-based technology platform allows for mass distribution of and online enrollment in our large and diverse portfolio of affordable health insurance offerings.
Our technology platform provides customers, who we refer to as members, immediate access to our products through our distribution partners anytime, anyplace. The health insurance products we develop are underwritten by insurance carrier companies, and we assume no underwriting, insurance or reimbursement risk. Members can price and tailor product selections to meet their needs, buy policies and print policy documents and identification cards in real-time. Our sales are executed online and offer instant electronic fulfillment. Our technology platform uses abbreviated online applications, some with health questionnaires, to provide an immediate accept or reject decision on applications for all products that we offer. Once an application is accepted, individuals can use our automated payment system to complete the enrollment process and obtain instant electronic access to their policy fulfillment documents, including the insurance policy, benefits schedule and identification cards. We receive credit card and Automated Clearing House (“ACH”) payments directly from members at the time of sale. Our technology platform provides significant operating leverage as we add members and reduces the costs associated with marketing, selling, underwriting and administering policies.
We are an industry leader in the sale of 12-month STM insurance plans, an alternative to traditional IMM plans which provide lifetime renewable coverage. STM plans generally offer qualifying individuals comparable benefits for fixed short-term durations of six or 12 months at approximately half the cost of IMM plans. While applications for IMM insurance may take up to 60 days to process, STM plans feature a streamlined underwriting process offering immediate coverage options. We also offer guaranteed-issue hospital indemnity plans for individuals under the age of 65, which pay fixed cash benefits for covered procedures and services, and a variety of ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans that are frequently purchased as supplements to STM and hospital indemnity plans. We design and structure insurance products on behalf of insurance carrier companies, market them to individuals through our large network of distributors and manage member relations via our online member portal, which is available 24 hours a day, seven days a week. Our online enrollment process allows us to aggregate and analyze consumer data and purchasing habits to track market trends and drive product innovation. We have established relationships with several highly rated insurance carriers, including Starr Indemnity & Liability Company, Companion Life, United States Fire, ING, Markel and CIGNA, among others. In addition, as of December 31, 2012, the large independent distribution network we access consists of 46 licensed agent call centers and 264 wholesalers, including Marsh, eHealthInsurance and MasterCard, among others, that work with over 8,275 licensed brokers. Our data-driven product design, technology platform and extensive distribution network have enabled us to grow our revenues from $29,878,000 in 2011 to $41,940,000 in 2012.
We focus on the large and under-penetrated segment of the U.S. population who are uninsured or underinsured, which includes individuals who are unable to afford traditional IMM premiums, individuals not covered by employer-sponsored insurance plans, such as those who are self-employed as well as small business owners and their employees, and underserved “gap populations” that require insurance due to changes caused by life events, such as new graduates, divorcees, early retirees, military discharges, the unemployed, part-time and seasonal employees and temporary workers. Our target market consists of approximately 64 million Americans, including approximately 50 million Americans who were uninsured in 2010, according to the U.S. Census Bureau, and approximately 14 million non-elderly Americans who purchased individual health insurance plans in 2010, according to a 2010 Kaiser Family Foundation survey. As of December 31, 2012, we had 23,747 STM members. We expect the number of uninsured and underinsured to significantly increase due to the rising costs and burdensome underwriting requirements of traditional IMM plans and a decline in employer-sponsored health insurance programs.
38
Table of Contents
As of December 31, 2012, we had 23,747 STM plans in force, compared with 18,059 on December 31, 2011, with an average monthly retention rate of 79% from December 31, 2011 to December 31, 2012. We earn our revenues from commissions and fees related to the sale of products to our members. Our ancillary products have created several additional revenue streams and resulted in a significant portion of our business being generated by monthly member renewals. For the year ended December 31, 2012, our premium equivalents, revenue and EBITDA were $75,872,000, $41,940,000 and $4,543,000, respectively, representing a 42.6%, 40.4% and 65.7% increase compared to premium equivalents, revenues and EBITDA of $53,206,000, $29,878,000 and $2,742,000, respectively, for the year ended December 31, 2011. For more detail about the use of premium equivalents and EBITDA as business metrics and a reconciliation of premium equivalents and EBITDA to revenues, see “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Key Business Metrics—Premium Equivalents” and “EBITDA.”
Basis of Presentation
On September 28, 2011, we entered into an agreement to purchase of the units of Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC. Prior to the purchase (the “Acquisition”), Health Plan Intermediaries, LLC was 50% owned by Naylor Group Partners, LLC and 50% owned by Mr. Kosloske. Following the Acquisition, Mr. Kosloske became the sole member of Health Plan Intermediaries, LLC. The Acquisition was accounted for as a purchase and the purchase price was reflected on our financial statements using push-down accounting. Accordingly, purchase accounting adjustments have been reflected in our financial statements for the period commencing on October 1, 2011. The new basis of accounting reflects the estimated fair value of the our assets and liabilities as of the date of the Acquisition. We used October 1, 2011, as the effective date of the transaction, since the operating activity between that date and the September 28, 2011 transaction date was not material.
The following discussion and analysis of our financial condition and results of operations covers periods before and after the Acquisition. The discussion and analysis of periods prior to September 30, 2011 do not reflect the purchase accounting adjustments discussed above and in the financial statements and notes thereto included elsewhere in this report. However, the general nature of our operations was not impacted by the Acquisition. As such, for comparative purposes we will discuss changes between the periods without reference to the effects of the Predecessor and Successor periods, which is consistent with the manner in which we evaluate the results of operations. All references to the year ended December 31, 2012 relate to the annual period ended December 31, 2012 of the Successor. All references to the year ended December 31, 2011 relate to the combined three-month period ended December 31, 2011 of the Successor and the nine-month period ended September 30, 2011 of the Predecessor. The presentation of combined Predecessor and Successor operating results (which is the arithmetic sum of the Predecessor and Successor amounts) is a non-GAAP presentation, which is provided as a convenience solely for the purpose of facilitating comparisons of current results with combined results over the same period in the prior year. Effects of the Acquisition will be discussed where applicable.
Effects of the Reorganization of our Corporate Structure
Historically, our business was operated through Health Plan Intermediaries, LLC. In anticipation of the IPO, on November 7, 2012, Health Plan Intermediaries, LLC assigned the operating assets of our business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC.
Health Insurance Innovations, Inc. was formed for the purpose of our recently completed IPO. Since November 2012, all of our business is conducted through Health Plan Intermediaries Holdings, LLC. The financial results of Health Plan Intermediaries Holdings, LLC will be consolidated in our financial statements.
Health Insurance Innovations, Inc. is a holding company whose principal asset is its interest in Health Plan Intermediaries Holdings, LLC. All of the equity of Health Plan Intermediaries Holdings, LLC outstanding prior to the reorganization has been exchanged for Series B Membership Interests of Health Plan Intermediaries Holdings, LLC and an equal number of shares of our Class B common stock.
We expect that future exchanges of Series B Membership Interests (together with an equal number of our Class B common shares) for shares of our Class A common stock, as well as the Acquisition with net proceeds of the sale of over-allotment shares, of Series B Membership Interests (together with an equal number of shares of our Class B common stock) from Health Plan Intermediaries, LLC (which Series B Membership Interests will immediately be recapitalized into Series A Membership Interests) will result in increases in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. We expect that these increases in tax basis, which would not have been available but for our new holding company structure, will reduce the amount of tax that we would otherwise be required to pay in the future. We will be required to pay a portion of the cash savings we actually realize from such increase (or are deemed to realize in the case of an early termination payment by us, a change in control or a material breach by us of our obligations under the tax receivable agreement, as discussed above) to the existing and certain future holders of Series B Membership Interests (currently Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske), pursuant to a tax receivable agreement. Furthermore, payments under the tax receivable agreement will give rise to additional tax benefits and therefore additional payments under the tax receivable agreement itself. Our
39
Table of Contents
former operating entity, Health Plan Intermediaries, LLC, is taxed as an S corporation for income tax purposes. Therefore, we have not been subject to entity-level federal or state income taxation. Health Plan Intermediaries Holdings, LLC is currently taxed as a partnership for federal income tax purposes; and as a result, the members of Health Plan Intermediaries Holdings, LLC pay taxes with respect to their allocable shares of its net taxable income. The earnings of Health Insurance Innovations, Inc. are subject to federal income taxation.
Factors Affecting Our Results of Operations
As the managing general underwriter of our individual health insurance plans and ancillary products, we receive all amounts due in connection with our plans on behalf of the providers of the services. We refer to these total collections as premium equivalents, which typically represent a combination of premiums, fees for discount benefit plans (a non-insurance benefit product that supplements or enhances an insurance product), fees for distributors and our enrollment fees. From premium equivalents, we remit risk premium to carriers and amounts earned by discount benefit plan providers, who we refer to as third-party obligors, such carriers and third-party obligors being the ultimate parties responsible for providing the insurance coverage or discount benefits to the member. Our revenues consist of the balance of the premium equivalents.
We collect premium equivalents upon the initial sale of the plan and then monthly upon each subsequent periodic payment under such plan. We receive most premium equivalents through online credit card or ACH processing. As a result, we have limited accounts receivable. We remit the risk premium to the applicable carriers and the amounts earned by third-party obligors on a monthly basis based on the respective compensation arrangements.
Commission revenue and fees attributable to revenues from STM plans and hospital indemnity policies represented substantially all of our revenues for the periods presented. Our commissions represent premiums and fees for discount benefit plans, net of risk premium and amounts earned by third-party obligors, respectively. We recognize commissions as we collect the premiums and fees for discount benefit plans.
Commission rates for all insurance plans are approved in advance by the relevant carrier. Our commission rates and the length of the commission period typically vary by carrier and plan type. Under our carrier compensation arrangements, the commission rate schedule that is in effect on the policy effective date will govern the commissions over the life of the plan.
We continue to receive a commission payment until the plan expires or is terminated. Accordingly, a portion of our monthly revenues is predictable on a month-to-month basis and revenues increase in direct proportion to the growth we experience in the number of plans in force.
We pay fees to distributors for their services in selling our plans, which are included in our operating costs and expenses.
Key Business Metrics
In addition to traditional financial metrics, we rely upon the following key business metrics to evaluate our business performance and facilitate long-term strategic planning:
Premium equivalents. We define this metric as the combination of premiums, fees for discount benefit plans, fees for distributors and our enrollment fees. All amounts not paid out as risk premium to carriers or paid out to other third-party obligors are considered to be revenues for financial reporting purposes. We have included premium equivalents in this report because it is a key measure used by our management to understand and evaluate our core operating performance and trends, to prepare and approve our annual budget and to develop short- and long-term operational plans. In particular, the inclusion of premium equivalents can provide a useful measure for period-to-period comparisons of our business.
The following table presents a reconciliation of premium equivalents to revenues for the years ended December 31, 2012 and 2011:
| December 31, | ||||||||
| 2012 | 2011 | |||||||
| (in thousands) | ||||||||
| Premium equivalents |
$ | 75,872 | $ | 53,206 | ||||
| Less risk premium |
(32,346 | ) | (22,108 | ) | ||||
| Less amounts earned by third party obligors |
(1,586 | ) | (1,220 | ) | ||||
|
|
|
|
|
|||||
| Revenues |
$ | 41,940 | $ | 29,878 | ||||
|
|
|
|
|
|||||
Plans in force. We consider a plan to be in force when we have issued a member his or her insurance policy or discount benefit plan and have collected the applicable premium payments and/or discount benefit fees. Our plans in force are an important indicator of our expected revenues, as we receive a monthly commission for up to six months for our six-month STM plan, up to 12 months for
40
Table of Contents
our 12-month STM plan and often more than 12 months for our hospital indemnity and discount benefit plans, provided that the policy or discount benefit plan is not cancelled. A member may be enrolled in more than one policy or discount benefit plan simultaneously. A plan becomes inactive upon notification to us of termination of its policy or discount benefit plan, when the member’s policy or discount benefit plan expires or following non-payment of premiums or discount benefit fees when due.
EBITDA. We define this metric as net income before interest expense, income taxes and depreciation and amortization. We have included EBITDA in this report because it is a key measure used by our management and board of directors to understand and evaluate our core operating performance and trends, to prepare and approve our annual budget and to develop short- and long-term operational plans. In particular, the exclusion of certain expenses in calculating EBITDA can provide a useful measure for period-to-period comparisons of our business.
The following table presents a reconciliation of net income to EBITDA for the years ended December 31, 2012 and 2011:
| Year
Ended December 31, 2012 |
Year Ended December 31, 2011 |
|||||||
| (in thousands) | ||||||||
| Net income |
$ | 3,260 | $ | 2,373 | ||||
| Interest expense |
271 | 71 | ||||||
| Depreciation and amortization |
1,012 | 298 | ||||||
|
|
|
|
|
|||||
| EBITDA |
$ | 4,543 | $ | 2,742 | ||||
|
|
|
|
|
|||||
Key Components of Our Statements of Operations
Revenues
Our revenues consist primarily of commissions earned for our insurance policies and discount benefit plans issued to members, enrollment fees paid by members and administration fees paid by members as a direct result of our enrollment services. We recognize revenues upon the member’s acceptance of a policy. We expect our revenues to increase as we add new members.
Operating Costs and Expenses
Operating costs and expenses consist of fees and commissions paid to distributors for selling our products to members, credit card or ACH processing fees and general and administrative expenses. We expect our operating costs and expenses to represent a decreasing percentage of our revenues due to the scalable nature of our technology platform that allows for mass distribution and online enrollment of our products, requiring minimal maintenance and incremental costs.
Third-party Commissions
Our third-party commissions consist of fees and commissions paid to distributors for selling our products to members, which we pay monthly for existing members and on a weekly basis for new members. We expect third-party commissions as a percentage of revenue to remain generally consistent with prior periods.
Credit Card and ACH Fees
Our credit card and ACH fees are fees paid to our banks and processors for the collection of credit card and ACH payments. We expect credit card and ACH fees as a percentage of revenue to remain generally consistent with prior periods.
General and Administrative Expenses
Our general and administrative expenses primarily consist of personnel costs, which represent salaries, bonuses, commissions, payroll taxes and benefits. General and administrative expenses also include marketing campaign expenditures and travel costs associated with obtaining new distributor relationships. In addition, these expenses also include technology expenses and personnel costs and expenses for outside professional services, including legal, audit and financial services. We expect general and administrative expenses to increase due to the anticipated growth of our business and infrastructure and the costs associated with becoming a public company, such as costs associated with SEC reporting and compliance, developing and maintaining internal controls over financial reporting, insurance, investor relations and other related costs. We also expect general and administrative expenses to increase as a result of equity-based compensation under our long-term incentive plan.
Depreciation and Amortization
Depreciation and amortization expense is primarily a function of amortization of the intangible assets acquired as a result of the Acquisition described above as well as depreciation of property and equipment used in our business.
41
Table of Contents
Interest Expense
Interest expense primarily consists of interest incurred on our outstanding bank note. On February 13, 2013, we repaid our term loan with a portion of the net proceeds raised from the IPO.
Other Income
Other income includes fees charged to distributors for advanced commissions, whereby we pay distributors commissions on policies sold in advance of when they would ordinarily be due to the distributor. These advanced commissions are made to distributors with an established track record of selling our products. Advanced commission fees range from 0% up to 2% of the premiums for each month that we advance commissions. Advanced commissions to a distributor are based upon the number of future months of expected premium equivalent multiplied by a distributor’s commission rate. We expect other income to increase as we expand our advanced commission structure with the application of the net proceeds of the IPO.
Income Tax Expense
Our former operating entity, Health Plan Intermediaries, LLC, is taxed as an S corporation for income tax purposes. Therefore, we have not been subject to entity-level federal or state income taxation. Health Plan Intermediaries Holdings, LLC is currently taxed as a partnership for federal income tax purposes; and as a result, the members of Health Plan Intermediaries Holdings, LLC pay taxes with respect to their allocable shares of its net taxable income. The earnings of Health Insurance Innovations, Inc. are subject to federal income taxation. Health Insurance Innovations, Inc. accounts for income taxes in accordance under the provisions GAAP. Based on this guidance, our historical statements of operations would have reflected total income tax expense in the amount of approximately $1,250,000 and $896,000 for the years ended December 31, 2012 and 2011, respectively.
Noncontrolling Interest
On June 1, 2012, we and TSG acquired ICE. ICE is a call center training facility for our distributors. Pursuant to the terms of the transaction, we contributed $80,000 in cash, and TSG contributed $20,000 in cash to the newly created limited liability company. In connection with the transaction, we received an 80% controlling interest in ICE and TSG received a 20% noncontrolling interest in ICE. The intent of this transaction was to attract potential call centers and educate them on our model and best practices with the ultimate goal of these call centers joining our distribution network. Subsequent to the initial contributions, we contributed an additional $240,000, and TSG contributed an additional $60,000, respectively, to ICE during the year ended December 31, 2012. As of December 31, 2012, our total investment in ICE is $320,000, representing an 80% controlling interest.
Results of Operations
The following table is a summary of our statements of operations as a percentage of our total revenues.
| Year Ended December 31, | ||||||||
| 2012 | 2011 | |||||||
| Revenues |
100.0 | % | 100.0 | % | ||||
| Third-party commissions |
66.4 | % | 72.6 | % | ||||
| Credit cards and ACH fees |
2.3 | % | 2.2 | % | ||||
| General and administrative expenses |
20.5 | % | 15.9 | % | ||||
| Depreciation and amortization |
2.4 | % | 1.0 | % | ||||
|
|
|
|
|
|||||
| Total operating costs and expenses |
91.6 | % | 91.7 | % | ||||
| Other expenses (income): |
||||||||
| Interest expense |
0.7 | % | 0.2 | % | ||||
| Other income |
(0.1 | )% | 0.0 | % | ||||
|
|
|
|
|
|||||
| Net income |
7.8 | % | 8.1 | % | ||||
|
|
|
|
|
|||||
| Net loss attributable to noncontrolling interests in subsidiary |
(0.2 | )% | 0.0 | % | ||||
| Net income attributable to Health Plan Intermediaries, LLC |
8.0 | % | 8.1 | % | ||||
|
|
|
|
|
|||||
42
Table of Contents
Comparison of 2012 and 2011
The following table presents our historical results of operations and the changes in these results in dollars and as a percentage for the years presented:
| Year Ended December 31, | ||||||||||||||||
| 2012 | 2011 | Change ($) | Change (%) | |||||||||||||
| (in thousands, except percentages) | ||||||||||||||||
| Revenues |
$ | 41,940 | $ | 29,878 | $ | 12,062 | 40.4 | % | ||||||||
| Third-party commissions |
27,858 | 21,704 | 6,154 | 28.4 | % | |||||||||||
| Credit cards and ACH fees |
963 | 670 | 293 | 43.7 | % | |||||||||||
| General and administrative expenses |
8,611 | 4,762 | 3,849 | 80.8 | % | |||||||||||
| Depreciation and amortization |
1,012 | 298 | 714 | >100.0 | % | |||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total operating costs and expenses |
38,444 | 27,434 | 11,010 | 40.1 | % | |||||||||||
| Other expenses (income): |
||||||||||||||||
| Interest expense |
271 | 71 | 200 | >100 | % | |||||||||||
| Other income |
(35 | ) | — | (35 | ) | >100 | % | |||||||||
|
|
|
|
|
|
|
|||||||||||
| Net income |
3,260 | 2,373 | 887 | 37.4 | % | |||||||||||
| Net loss attributable to noncontrolling interests in subsidiary |
(89 | ) | — | (89 | ) | >100 | % | |||||||||
|
|
|
|
|
|
|
|||||||||||
| Net income attributable to Health Plan Intermediaries, LLC |
3,349 | 2,373 | 976 | 41.1 | % | |||||||||||
|
|
|
|
|
|
|
|||||||||||
Revenues
Revenues for 2012 were $41,940,000, an increase of $12,062,000, or 40.4%, compared to 2011. The increase was primarily due to a 94.0% increase in the number of policies in force. The number of hospital indemnity and ancillary policies in force as of December 31, 2012 and 2011 increased as we increased our focus on the sales of our other products to complement our STM sales. The following table presents the number of our policies in force by product type as of December 31, 2012 and 2011:
| December 31, | ||||||||||||
| 2012 | 2011 | Change (%) | ||||||||||
| STM |
23,747 | 18,059 | 31.5 | % | ||||||||
| Hospital indemnity |
8,141 | 5,243 | 55.3 | % | ||||||||
| Ancillary products |
26,230 | 6,649 | >100 | % | ||||||||
|
|
|
|
|
|||||||||
| Total |
58,118 | 29,951 | 94.0 | % | ||||||||
|
|
|
|
|
|||||||||
Third-party Commissions
Third-party commissions for 2012 were $27,858,000, an increase of $6,154,000, or 28.4%, compared to 2011. The increase in third-party commissions was primarily due to an increase in the number of plans in force. Third-party commissions represented 66.4% of revenues for 2012 as compared to 72.6% of revenues for 2011. This decrease is primarily due to a shift in our core business from hospital indemnity policies to STM policies. Generally, STM policies incur lower commissions than hospital indemnity policies.
Credit Card and ACH Fees
Credit card and ACH fees for 2012 were $963,000, an increase of $293,000, or 43.7%, compared to 2011. The increase in credit card and ACH fees was primarily due to the increase in the number of plans in force. Credit card and ACH fees represented 2.3% and 2.2% of revenues for 2012 and 2011, respectively.
General and Administrative Expenses
General and administrative expenses for 2012 were $8,611,000, an increase of $3,849,000, or 80.8%, compared to 2011. The increase in general and administrative expenses was driven by an increase in personnel costs of approximately $1,761,000, professional fees of approximately $1,273,000 and selling, marketing expenses and other expenses of approximately $848,000. Personnel costs increased primarily due to additional sales and financial reporting personnel added to accommodate our growth. Professional fees increased as a result of legal fees, accounting and financial consulting costs and for the maintenance of our administrative technology platform. The increase in selling and marketing expenses was primarily due to our adoption of a revised sales strategy and the hiring of additional sales employees to implement the strategy.
Depreciation and Amortization
Depreciation and amortization expenses for 2012 were $1,012,000, an increase of $714,000, compared to 2011. The increase in depreciation and amortization from was primarily driven by the amortization of intangible assets that were recognized from the Acquisition and the acquisition of intellectual property rights during 2012. For further information related to the Acquisition, see Note 2 in the accompanying audited financial statements.
43
Table of Contents
Other Expenses (Income)
Interest expense for 2012 was $271,000, an increase of $200,000, compared to 2011. Interest expense increased due to the bank loan agreement that commenced during the third quarter of 2011 to finance the Acquisition.
Other income for 2012 was $35,000, as compared to no other income during 2011. Other income primarily included fees charged to distributors for advanced commissions. We began to distribute advanced commissions during the fourth quarter of 2011.
Liquidity and Capital Resources
General
As of December 31, 2012, we had $750,000 of cash. Since the fourth quarter of fiscal 2009, we have funded our operations primarily with cash flows from operations and, to a lesser extent, working capital and borrowings, as described below.
During the year ended December 31, 2012, Health Plan Intermediaries, LLC declared cash distributions of $4,010,000 to Mr. Kosloske in accordance with the terms of its Operating Agreement. Of this 2012 declared distribution, $773,000 is payable as of December 31, 2012. Such payments made to members in 2011 totaled $1,301,000 ($681,000 was paid to Naylor Group Partners, LLC and $620,000 was paid to Mr. Kosloske). Mr. Kosloske contributed capital in the amount of $1,135,000 during the year ended December 31, 2011 to partially fund the Acquisition.
We experienced positive cash flows from operations during 2012. We expect that we will continue to generate positive cash flows from operations on an annual basis, although this may fluctuate significantly on a quarterly basis. We believe that our available cash, cash flows expected to be generated from operations and net proceeds from the IPO will be adequate to satisfy our current and planned operations for at least the next 12 months. We believe that the net proceeds from the IPO will be sufficient to implement our advanced commission strategy.
On February 13, 2013, Health Insurance Innovations, Inc. completed an initial public offering by issuing 4,666,667 shares of its Class A common stock, par value $0.001 to the public at a price of $14.00 per share common stock. In conjunction with the offering, Health Plan Innovations, Inc. obtained a 35% membership interest, a 35% economic interest and 100% of the voting interest in Health Plan Intermediaries Holdings, LLC.
On March 14, 2013, we entered into an agreement to terminate certain contract rights with TSG, a managing general agent of the Company, for an aggregate cash price of $5,500,000. Pursuant to Financial Accounting Standards Board (“FASB”) guidance, the full amount plus transaction costs is expected to be expensed during the first quarter of 2013. We do not expect to incur any material future expenses associated with the transaction.
Our Indebtedness
Term Loan Agreement. In September 2011, we entered into a bank loan agreement with a third-party bank with a principal amount of $4,250,000. The purpose of this bank loan was to finance the Acquisition of the remaining 50% interest in Health Plan Intermediaries, LLC. Borrowings under the loan were secured by all of our assets and by a personal unlimited guarantee by Mr. Kosloske and Lori Kosloske, our Chief Broker Compliance Officer and Mr. Kosloske’s wife, and certain real properties owned by Mr. Kosloske and Mrs. Kosloske.
As of December 31, 2012, the outstanding balance of the term loan was $3,294,000, including a current portion of $813,000. On February 13, 2013, we paid $3,232,000 to repay all of the outstanding debt under our term loan, using a portion of the net proceeds from the IPO.
Cash Flows
The following summary of cash flows for the periods indicated has been derived from our financial statements included elsewhere in this report (in thousands):
| Year Ended December 31, | ||||||||
| 2012 | 2011 | |||||||
| Statements of Cash Flows Data: |
||||||||
| Net cash provided by operating activities |
$ | 5,342 | $ | 2,247 | ||||
| Net cash used in investing activities |
$ | (251 | ) | $ | (5,392 | ) | ||
| Net cash (used in) provided by financing activities |
$ | (4,959 | ) | $ | 3,756 | |||
44
Table of Contents
Cash Flows from Operating Activities
We experienced positive cash flows from operating activities during 2012 and 2011 primarily as a result of our increased revenues and the resulting net income during these periods. Our primary source of cash from operating activities is retention of commissions from premium equivalents. Our primary uses of cash for operating activities are for compensation-related expenditures, settlement of accounts payable to vendors and to fund our advanced commission structure.
During the year ended December 31, 2012, cash provided by operating activities was $5,342,000 as compared to net cash provided in operations of $2,247,000 for the year ended December 31, 2011. This increase of $3,095,000 was primarily due to revenue growth and our scalable technology platform.
Cash Flows from Investing Activities
Our primary investing activities have consisted of the Acquisition, purchases of equipment and loans to our distributors. Our capital expenditures primarily consist of purchases of computer equipment, furniture and fixtures and computer software. In the future, we expect that we will continue to incur capital expenditures to support our expanding operations.
During the year ended December 31, 2012, cash used in investing activities was $251,000 as compared to $5,392,000 for the year ended December 30, 2011. The decrease of $5,141,000 was primarily due to payments made in 2011 for the Acquisition.
Cash Flows from Financing Activities
Our financing activities have consisted primarily of issuance of long-term debt, periodic repayments of debt, payment of fees for equity issuance, capital contributions from members and distributions of earnings to our members.
During the year ended December 31, 2012, cash used by financing activities was $4,959,000 as compared to cash provided of $3,756,000 for the year ended December 31, 2011. Cash used by financing activities during the year ended December 31, 2012 consisted of payments made on debt and other obligations of $905,000, payments made with respect to equity issuance costs of $1,009,000, and, distributions to members of $3,237,000 less proceeds received from issuance of note payable of $100,000 and proceeds of $92,000 from the issuance of noncontrolling interest in Insurance Center for Excellence, LLC. Cash provided by financing activities for the year ended December 31, 2011 consisted of bank loan proceeds of $4,250,000 and member contributed capital in the amount of $1,135,000 less payments on debt and other obligations in the amount of $328,000 and distributions made to members in the amount of $1,301,000.
Contractual Obligations
The following summarizes our contractual obligations as of December 31, 2012:
| Payments Due by Period | ||||||||||||||||||||
| Total | Less Than 1 Year | 1 to 3 Years | 3 to 5 Years | More Than 5 Years | ||||||||||||||||
| (in thousands) | ||||||||||||||||||||
| Contractual Obligations: |
||||||||||||||||||||
| Operating leases |
$ | 556 | $ | 222 | $ | 333 | $ | 1 | $ | — | ||||||||||
| Software maintenance |
1,430 | 312 | 624 | 494 | — | |||||||||||||||
| Exclusivity agreement |
880 | 192 | 384 | 304 | — | |||||||||||||||
| Payments on debt obligations, including interest(1) |
3,642 | 968 | 1,937 | 737 | — | |||||||||||||||
| Capital lease obligations |
7 | 3 | 4 | — | — | |||||||||||||||
| Other |
54 | 54 | — | — | — | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total contractual obligations(2) |
$ | 6,569 | $ | 1,751 | $ | 3,282 | $ | 1,536 | $ | — | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| (1) | On February 13, 2013, we repaid our term loan with a portion of the net proceeds raised from the IPO. |
| (2) | Payments to holders of Series B Membership Interests pursuant to our tax receivable agreement are excluded from our contractual obligations. For additional information, see “Item 1. Business—Our History and the Reorganization of Our Corporate Structure—Tax Receivable Agreement”. |
Unaudited Pro Forma Financial Information
The following unaudited pro forma consolidated statements of operations for the years ended December 31, 2012 and 2011 and the unaudited pro forma consolidated balance sheet as of December 31, 2012 present our consolidated results of operations and financial position to give pro forma effect to the purchase of the units of Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC described under “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations”, the reorganization transactions described in “Item 1. Business—Our History and the Reorganization of Our Corporate Structure” and the sale of shares in the IPO (excluding shares issuable upon any exercise of the underwriters’ over-allotment option) and the application of the net proceeds
45
Table of Contents
from the IPO as if all such transactions had been completed as of January 1, 2011 with respect to the unaudited consolidated pro forma statements of operations data and as of December 31, 2012 with respect to the unaudited pro forma consolidated balance sheet data. The unaudited pro forma consolidated financial statements reflect pro forma adjustments that are described in the accompanying notes and are based on available information and certain assumptions we believe are reasonable, but are subject to change. We have made, in our opinion, all adjustments that are necessary to present fairly the pro forma financial data.
The unaudited pro forma financial information should be read together with “Item 1. Business—Our History and the Reorganization of Our Corporate Structure,” “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the historical financial statements and related notes included elsewhere in this report.
The pro forma adjustments principally give effect to:
| • | the reorganization transactions described in “Item 1. Business—Our History and the Reorganization of Our Corporate Structure,” including (i) the issuance by Health Plan Intermediaries Holdings, LLC of Series A membership interests to Health Insurance Innovations, Inc. pursuant to the Third Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC, (ii) the consolidation of Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries into Health Insurance Innovations, Inc.’s financial statements pursuant to FASB guidance and the resulting increase of additional paid-in-capital to allocate a portion of Health Plan Intermediaries Holdings, LLC’s equity to the noncontrolling interest, (iii) the conversion of each share of Health Insurance Innovations, Inc.’s outstanding common stock into 86,667.67 shares of Class B common stock pursuant to Health Insurance Innovations, Inc.’s Amended and Restated Certificate of Incorporation and (iv) the issuance of shares of Class A common stock of Health Insurance Innovations, Inc. in connection with the IPO; |
| • | with regard to the unaudited pro forma consolidated statements of operations, a provision for corporate income taxes on the income attributable to Health Insurance Innovations, Inc. at an effective rate of 37.8%, which includes a provision for U.S. Federal income taxes and assumes the highest statutory rates apportioned to each state, local and /or foreign jurisdiction; |
| • | the purchase of the units of Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC; |
| • | the grant to Michael D. Hershberger, our Chief Financial Officer, of restricted stock in connection with the IPO; and |
| • | the application of a portion of the proceeds from the IPO to repay outstanding indebtedness, as described in “Item 5. Market for Registrant’s Common Equity, Related Shareholder Matters and Issuer Purchases of Equity Securities—Use of Proceeds.” |
The IPO and the reorganization transactions did not result in an immediate step-up in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. However, future purchases or exchanges of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock are expected to increase the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. The step-up in tax basis would be initially depreciable and amortizable for tax purposes over a period of approximately 15 years. We entered into a tax receivable agreement with the holders of Series B Membership Interests after giving effect to the reorganization and certain future holders of Series B Membership Interests that will require us to pay such holders 85% of the amount of cash savings, if any, in U.S. federal, state and local income tax that we actually realize (or are deemed to realize in the case of an early termination payment, a change in control or a material breach by us of our obligations under the tax receivable agreement) as a result of the increases in tax basis and of certain other tax benefits related to entering into the tax receivable agreement, including tax benefits attributable to payments under the tax receivable agreement. Assuming all Series B Membership Interests of Health Plan Intermediaries Holdings, LLC beneficially owned by Mr. Kosloske were acquired by us in a taxable transaction as of the date of the IPO, the step-up in the tax basis in our share of the tangible and intangible assets and the resulting estimated maximum payment due under the tax receivable agreement would be $162,348,000 and $53,001,000, respectively, based on our estimate of the tax basis in Health Plan Intermediaries Holdings, LLC’s assets as of December 31, 2012. We are not currently a party to any other agreements or commitments for any such acquisitions, and we have no current understandings with respect to any other such transactions. The actual amount of the tax receivable payment may materially differ from this hypothetical amount, as potential future payments will be calculated using the market value of our Class A common stock at the time of relevant exchange and prevailing tax rates in future years and will be dependent on us generating sufficient future taxable income to realize the benefit. Payments are generally due under the tax receivable agreement within a specified period of time following the filing of our tax return for the taxable year with respect to which the payment obligation arises, although interest on such payments will begin to accrue at a rate of LIBOR from the due date (without extensions) of such tax return. Late payments generally accrue interest at a rate of LIBOR plus 300 basis points. However, to the extent, based on certain specified reasons, that we do not have available cash to satisfy our payment obligations under the tax receivable agreement, such deferred payments would accrue interest at a rate of LIBOR.
The pro forma adjustments above give effect to activities directly related to completion of the IPO on February 13, 2013. Certain events subsequent to that date were not considered events directly related to the IPO, but rather subsequent events that occurred in the first quarter of 2013 and part of normal, recurring operations and standard, ordinary compensation of members of our board of directors or other unanticipated subsequent events. Those events include the following:
| • | On March 8, 2013, our compensation committee approved equity awards for our executive officers and certain other senior management under our Long Term Incentive Plan. The equity awards consist of an aggregate of 78,500 shares of our Class A common stock. |
| • | On March 8, 2013, 100,000 shares of Class A common stock were issued through the over-allotment option. |
| • | On March 14, 2013, we entered into an agreement to terminate certain contract rights with TSG, a managing general agent of the Company, for an aggregate cash price of $5,500,000. |
The unaudited pro forma financial data are presented for informational purposes only and should not be considered indicative of actual results of operations that would have been achieved had the reorganization transactions and the IPO been consummated on the dates indicated, and do not purport to be indicative of statements of financial condition or results of operations as of any future date or any future period.
46
Table of Contents
HEALTH INSURANCE INNOVATIONS, INC.
Unaudited Pro Forma Consolidated Balance Sheet
As of December 31, 2012
(in thousands)
| Health Plan Intermediaries, LLC Historical(1) |
Reorganization Adjustments |
Health Insurance Innovations, Inc. (2) Pro Forma |
Offering Adjustments |
Health Insurance Innovations, Inc. (2) Pro Forma as Adjusted |
||||||||||||||||
| Assets |
||||||||||||||||||||
| Current assets: |
||||||||||||||||||||
| Cash |
$ | 750 | — | $ | 750 | $ | 56,779 | (4) | $ | 57,529 | ||||||||||
| Cash held on behalf of others |
3,839 | — | 3,839 | — | 3,839 | |||||||||||||||
| Credit card transactions receivable |
588 | — | 588 | — | 588 | |||||||||||||||
| Accounts receivable |
273 | — | 273 | — | 273 | |||||||||||||||
| Advanced commissions |
297 | — | 297 | — | 297 | |||||||||||||||
| Prepaid expenses and other current assets |
217 | — | 217 | — | 217 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total current assets |
5,964 | — | 5,964 | 56,779 | 62,743 | |||||||||||||||
| Property and equipment, net of accumulated depreciation |
213 | — | 213 | — | 213 | |||||||||||||||
| Capitalized offering costs |
1,819 | — | 1,819 | (1,819 | )(4) | — | ||||||||||||||
| Goodwill |
5,906 | — | 5,906 | — | 5,906 | |||||||||||||||
| Intangible assets, net of accumulated amortization |
3,959 | — | 3,959 | — | 3,959 | |||||||||||||||
| Other assets |
100 | — | 100 | (78 | ) | 22 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total assets |
$ | 17,961 | $ | — | $ | 17,961 | $ | 54,882 | $ | 72,843 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Liabilities and member’s equity |
||||||||||||||||||||
| Current liabilities: |
||||||||||||||||||||
| Accounts payable and accrued expenses |
$ | 2,062 | — | $ | 2,062 | $ | — | $ | 2,062 | |||||||||||
| Carriers and vendors payable |
2,790 | — | 2,790 | — | 2,790 | |||||||||||||||
| Commissions payable |
1,533 | — | 1,533 | — | 1,533 | |||||||||||||||
| Current portion of long-term debt |
813 | — | 813 | (813 | )(4) | — | ||||||||||||||
| Current portion of noncompete obligation |
155 | — | 155 | — | 155 | |||||||||||||||
| Due to members |
773 | — | 773 | — | 773 | |||||||||||||||
| Other current liabilities |
345 | — | 345 | — | 345 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total current liabilities |
8,471 | — | 8,471 | (813 | ) | 7,658 | ||||||||||||||
| Long-term debt, less current portion |
2,481 | — | 2,481 | (2,481 | )(4) | — | ||||||||||||||
| Noncompete obligation |
626 | — | 626 | — | 626 | |||||||||||||||
| Other liabilities |
45 | — | 45 | — | 45 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total liabilities |
11,623 | — | 11,623 | (3,294 | ) | 8,329 | ||||||||||||||
| Member’s equity |
6,335 | (6,335 | ) | — | — | — | ||||||||||||||
| Class A par value |
— | — | — | 5 | (5) | 5 | ||||||||||||||
| Class B par value |
— | 9 | (3) | 9 | — | 9 | ||||||||||||||
| Additional paid in capital |
— | 851 | (3) | 851 | 20,435 | (5) | 21,286 | |||||||||||||
| Accumulated earnings |
— | 1,358 | (3) | 1,358 | (78 | )(5) | 1,280 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total equity attributable to Health Insurance Innovations, Inc. |
6,335 | (4,117 | ) | 2,218 | 20,362 | 22,580 | ||||||||||||||
| Noncontrolling interest |
3 | 4,117 | 4,120 | 37,814 | (5) | 41,934 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total liabilities and equity |
$ | 17,961 | $ | — | $ | 17,961 | $ | 54,882 | $ | 72,843 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
47
Table of Contents
| (1) | We have historically operated our business through Health Plan Intermediaries, LLC. On November 7, 2012, Health Plan Intermediaries, LLC assigned all of the operating assets of its business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC and began conducting operations. As a result, Health Plan Intermediaries Holdings, LLC currently operates all of our business. Pursuant to FASB guidance, we assessed whether any pro forma adjustments in connection with the assignment were necessary. First, we concluded that Health Plan Intermediaries, LLC and Health Plan Intermediaries Holdings, LLC were under common control at the time of the assignment. In addition, after eliminating the effects of intra-entity transactions, the results of operations of the entities before and after the assignment were substantially the same. Accordingly, we determined that the transactions did not result in any pro forma effect. Accordingly, the unaudited pro forma consolidated statements of operations for the years ended December 31, 2012 and 2011 and the unaudited pro forma consolidated balance sheet as of December 31, 2012 present the historical results of Health Plan Intermediaries, LLC as a starting point for the pro forma amounts. |
| (2) | As a newly formed entity, Health Insurance Innovations, Inc. did not have assets or results of operations until the recent completion of the IPO. |
| (3) | Represents adjustments to reflect (i) the portion of Health Plan Intermediaries Holdings, LLC’s accumulated earnings that Health Insurance Innovations, Inc. received in connection with the conversion of the existing shares of common stock of Health Insurance Innovations, Inc. into shares of Class B common stock and (ii) the related additional amount paid in capital resulting from the transaction. |
As described in “Item 1. Business—Our History and the Reorganization of Our Corporate Structure,” after the IPO and the reorganization transactions that transpired, our only material asset was the ownership of approximately 35% of the Membership Interests in Health Plan Intermediaries Holdings, LLC and our only business will be to act as the sole managing member of Health Plan Intermediaries Holdings, LLC. Accordingly, pursuant to FASB guidance, we will consolidate the financial results of Health Plan Intermediaries Holdings, LLC into our financial statements.
Under FASB guidance, Health Plan Intermediaries Holdings, LLC meets the definition of a variable interest entity. Further, Health Insurance Innovations, Inc. is the primary beneficiary of Health Plan Intermediaries Holdings, LLC as a result of its 100% voting power and control over Health Plan Intermediaries Holdings, LLC and as a result of its obligation to absorb losses and its right to receive benefits of Health Plan Intermediaries Holdings, LLC that could potentially be significant to Health Plan Intermediaries Holdings, LLC. As a result, Health Insurance Innovations, Inc. will consolidate the financial results of Health Plan Intermediaries Holdings, LLC and record a noncontrolling interest for the economic interest in Health Plan Intermediaries Holdings, LLC held by the existing members to the extent that the book value of their interest in Health Plan Intermediaries Holdings, LLC is greater than zero. Health Insurance Innovations, Inc.’s and the noncontrolling membership pro forma economic interest in Health Plan Intermediaries Holdings, LLC are 35% and 65%, respectively, as of December 31, 2012. Pro forma net income attributable to the noncontrolling interest on the statements of operations represents the portion of earnings or loss attributable to the economic interest in Health Plan Intermediaries Holdings, LLC held by the noncontrolling members. Noncontrolling interest on the balance sheet represents the portion of net assets of Health Plan Intermediaries Holdings, LLC attributable to the noncontrolling members based on total membership interest of Health Plan Intermediaries Holdings, LLC owned by such member.
| (4) | We received net proceeds from the IPO of $56,779,000 based on an aggregate underwriting discount of $4,573,000 and estimated offering expenses of $2,506,000. We used $3,294,000 of the net proceeds of the IPO to repay all of the outstanding debt under our term loan. The following table reconciles the gross proceeds from the IPO to the net cash provided to Health Insurance Innovations, Inc. ($ in thousands): |
| Assumed share price |
$ | 14.00 | ||
| Class A shares offered hereby |
4,666,667 | |||
|
|
|
|||
| Gross proceeds from offering |
65,333,000 | |||
| Offering costs |
(7,079,000 | ) | ||
| Offering costs already incurred |
1,819,000 | |||
| Debt repayment |
(3,294,000 | ) | ||
|
|
|
|||
| Net cash provided |
$ | 56,779,000 | ||
|
|
|
| (5) | Represents adjustments to reflect the allocation of offering proceeds between controlling and noncontrolling membership interests. |
48
Table of Contents
HEALTH INSURANCE INNOVATIONS, INC.
Unaudited Pro Forma Statements of Operations
Year Ended December 31, 2011
(in thousands)
| Historical(1) | ||||||||||||||||||||||||||||||||
| Three Months Ended December 31, 2011 (Successor) |
Nine Months Ended September 30, 2011 (Predecessor) |
Naylor Acquisition Adjustments |
Health Plan Intermediaries, LLC(1) Pro Forma |
Reorganization Adjustments |
Health Insurance Innovations, Inc. Pro Forma as Adjusted(2) |
Offering Adjustments |
Health Insurance Innovations, Inc.(2) Pro Forma as Further Adjusted |
|||||||||||||||||||||||||
| Revenue |
$ | 8,090 | $ | 21,788 | — | $ | 29,878 | — | $ | 29,878 | — | $ | 29,878 | |||||||||||||||||||
| Third-party commissions |
5,601 | 16,103 | — | 21,704 | — | 21,704 | — | 21,704 | ||||||||||||||||||||||||
| Credit cards and ACH fees |
197 | 473 | — | 670 | — | 670 | — | 670 | ||||||||||||||||||||||||
| General and administrative expenses |
1,421 | 3,341 | — | 4,762 | — | 4,762 | 3,487 | (3) | 8,249 | |||||||||||||||||||||||
| Depreciation and amortization |
269 | 29 | 705 | (4) | 1,003 | — | 1,003 | — | 1,003 | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Total operating costs and expenses |
7,488 | 19,946 | 705 | 28,139 | — | 28,139 | 3,487 | 31,626 | ||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Income (loss) from operations |
602 | 1,842 | (705 | ) | 1,739 | — | 1,739 | (3,487 | ) | (1,748 | ) | |||||||||||||||||||||
| Other expenses (income): |
||||||||||||||||||||||||||||||||
| Interest expense |
71 | — | 185 | (4) | 256 | — | 256 | (256 | )(5) | — | ||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Pre tax income (loss) |
531 | 1,842 | (890 | ) | 1,483 | — | 1,483 | (3,231 | ) | (1,748 | ) | |||||||||||||||||||||
| Income tax |
— | — | — | — | 574 | (6) | 574 | (1,173 | )(7) | (599 | ) | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Net income (loss) |
531 | 1,842 | (890 | ) | 1,483 | (574 | ) | 909 | (2,058 | ) | (1,149 | ) | ||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Net income (loss) attributable to non-controlling interest |
— | — | — | — | 591 | 591 | (1,338 | )(8) | (747 | ) | ||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Net income (loss) attributable to Health Insurance Innovations, Inc. |
$ | 531 | $ | 1,842 | $ | (890 | ) | $ | 1,483 | $ | (1,165 | ) | $ | 318 | $ | (720 | ) | $ | (402 | ) | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Weighted average shares Class A common stock outstanding |
||||||||||||||||||||||||||||||||
| Basic |
— | — | — | — | — | — | — | 4,826,667 | ||||||||||||||||||||||||
| Diluted |
— | — | — | — | — | — | — | 4,826,667 | ||||||||||||||||||||||||
| Net income available to Class A common stock per share(9) |
||||||||||||||||||||||||||||||||
| Basic |
— | — | — | — | — | — | — | $ | (0.08 | ) | ||||||||||||||||||||||
| Diluted |
— | — | — | — | — | — | — | $ | (0.08 | ) | ||||||||||||||||||||||
49
Table of Contents
HEALTH INSURANCE INNOVATIONS, INC.
Unaudited Pro Forma Consolidated Statement of Operations
Year Ended December 31, 2012
(in thousands, except share and per share amounts)
| Health Plan Intermediaries, LLC Historical(1) |
Reorganization Adjustments |
Health Insurance Innovations, Inc.(2) Pro Forma |
Offering Adjustments |
Health Insurance Innovations, Inc.(2) Pro Forma as Adjusted |
||||||||||||||||
| Revenue |
$ | 41,940 | — | $ | 41,940 | — | $ | 41,940 | ||||||||||||
| Third-party commissions |
27,858 | — | 27,858 | — | 27,858 | |||||||||||||||
| Credit cards and ACH fees |
963 | — | 963 | — | 963 | |||||||||||||||
| General and administrative expenses |
8,611 | — | 8,611 | 1,253 | (3) | 9,864 | ||||||||||||||
| Depreciation and amortization |
1,012 | — | 1,012 | — | 1,012 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total operating costs and expenses |
38,444 | — | 38,444 | 1,253 | 39,697 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Income from operations |
3,496 | — | 3,496 | (1,253 | ) | 2,243 | ||||||||||||||
| Other expenses (income): |
||||||||||||||||||||
| Interest expense |
271 | — | 271 | (271 | )(5) | — | ||||||||||||||
| Other income |
(35 | ) | — | (35 | ) | — | (35 | ) | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Pre tax income |
3,260 | — | 3,260 | (982 | ) | 2,278 | ||||||||||||||
| Income tax |
— | 1,250 | (6) | 1,250 | (390 | )(7) | 860 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income |
3,260 | (1,250 | ) | 2,010 | (592 | ) | 1,418 | |||||||||||||
| Net income attributable to noncontrolling interest in subsidiary |
(89 | ) | 1,365 | 1,276 | (296 | )(8) | 980 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income attributable to Health Insurance Innovations, Inc. |
$ | 3,349 | $ | (2,615 | ) | $ | 734 | $ | (296 | ) | $ | 438 | ||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Weighted average shares Class A common stock outstanding |
||||||||||||||||||||
| Basic |
— | — | — | — | 4,906,667 | |||||||||||||||
| Diluted |
— | — | — | — | 5,005,189 | |||||||||||||||
| Net income available to Class A common stock per share(9) |
||||||||||||||||||||
| Basic |
— | — | — | — | $ | 0.09 | ||||||||||||||
| Diluted |
— | — | — | — | $ | 0.09 | ||||||||||||||
| (1) | We have historically operated our business through Health Plan Intermediaries, LLC. On November 7, 2012, Health Plan Intermediaries, LLC assigned all of the operating assets of its business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC and began conducting operations. As a result, Health Plan Intermediaries Holdings, LLC currently operates all of our business. Pursuant to FASB guidance, we assessed whether any pro forma adjustments in connection with the assignment were necessary. First, we concluded that Health Plan Intermediaries, LLC and Health Plan Intermediaries Holdings, LLC were under common control at the time of the assignment. In addition, after eliminating the effects of intra-entity transactions, the results of operations of the entities before and after the assignment were substantially the same. Accordingly, we determined that the transactions did not result in any pro forma effect. Accordingly, the unaudited pro forma consolidated statements of operations for the years ended December 31, 2012 and 2011 and the unaudited pro forma consolidated balance sheet as of December 31, 2012 present the historical results of Health Plan Intermediaries, LLC as a starting point for the pro forma amounts. |
| (2) | As a newly formed entity, Health Insurance Innovations, Inc. had no assets or results of operations until the completion of the IPO. |
50
Table of Contents
| (3) | Represents expected total stock compensation expense related to Mr. Hershberger’s restricted stock grant calculated in accordance with FASB guidance. Upon the consummation of the IPO, Mr. Hershberger was granted to an amount equal to 3% of Health Insurance Innovations, Inc.’s enterprise value. We calculated total stock compensation expense over the term of the grant by accounting for an estimated 400,000 shares granted and a grant date price of $14.00, which represents the IPO price, to arrive at a total stock compensation amount of $5,600,000. Taking into consideration the accelerated graded vesting schedule of the grant whereby 40% of the total shares granted vest in 2013 and then the remaining shares vest 20% every October 1 from 2014 through 2016, we calculated $3,487,000 and $1,253,000 of estimated stock compensation expense for the pro forma twelve months ended December 31, 2011 and December 31, 2012, respectively. |
| (4) | On September 28, 2011, we entered into an agreement to purchase the units of Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC for $5,330,000 plus closing costs of $135,000. Prior to this purchase, Health Plan Intermediaries, LLC was 50% owned by Naylor Group Partners, LLC and 50% owned by our Chairman, President and Chief Executive Officer, Mr. Kosloske. Following the purchase, Mr. Kosloske became the sole member of Health Plan Intermediaries, LLC. Adjustments represent the amortization of the intangible assets that resulted from the acquisition and the interest expense related to the bank loan agreement with SunTrust Bank for the purpose of financing the acquisition. |
| (5) | Represents amounts to be eliminated in connection with the IPO following application of a portion of the net proceeds of the IPO to pay off all of our outstanding debt, which represent a five-year term loan bearing fixed interest at 5.25%. |
| (6) | Health Plan Intermediaries Holdings, LLC is not currently subject to entity-level federal income taxation and taxes with respect to income of Health Plan Intermediaries Holdings, LLC are payable by Health Plan Intermediaries Holdings, LLC’s equity holders at rates applicable to them. Following the IPO, and the reorganization that we are undertaking in connection therewith, earnings recorded by us will be subject to federal income taxation. |
| (7) | Following the IPO, Health Insurance Innovations, Inc. will be subject to U.S. federal income taxes, in addition to state and local taxes, with respect to its allocable share of any taxable income of Health Plan Intermediaries Holdings, LLC. As a result, the pro forma consolidated statement of operations reflects an adjustment to our provision for corporate income taxes to reflect an effective rate of 38%, which includes provision for U.S. federal income taxes. |
| (8) | As described in “Item 1. Business—Our History and the Reorganization of Our Corporate Structure,” immediately after the IPO and the reorganization transactions that transpired, our only material asset was the ownership of approximately 35% of the Membership Interests in Health Plan Intermediaries Holdings, LLC and our only business will be to act as the sole managing member of Health Plan Intermediaries Holdings, LLC. Accordingly, pursuant to FASB guidance, we will consolidate the financial results of Health Plan Intermediaries Holdings, LLC into our financial statements. The ownership interests of the other members of Health Plan Intermediaries Holdings, LLC (Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC) will be accounted for as a noncontrolling interest in our consolidated financial statements after the IPO. Represents adjustments to reflect noncontrolling interest resulting from the existing members’ ownership interest of 100% of the Series B Membership Interests of Health Plan Intermediaries Holdings, LLC. Immediately following the IPO, the noncontrolling interest is approximately 65%. Net income (loss) attributable to the noncontrolling interest represents 65%, or $980,000 of net income of $1,418,000 for the year ended December 31, 2012 and 65%, or $747,000 of net loss of $1,149,000 for the year ended December 31, 2011. These amounts have been determined based on the initial public offering price of $14.00 and the assumption that the underwriter’s option to purchase additional shares is not exercised. |
| (9) | Pro forma basic and diluted net income per share was computed by dividing the pro forma net income attributable to our Class A stockholders by the 4,666,667 shares of Class A common stock that we issued and sold in the IPO and the vested shares of Mr. Hershberger’s Class A restricted stock grant. The shares of Class B common stock do not share in our earnings and are therefore not included in the weighted average shares outstanding or net income available per share. |
Off-Balance Sheet Arrangements
Through December 31, 2012, we had not entered into any off-balance sheet arrangements, other than the operating leases noted above, and do not have any holdings in variable interest entities.
Critical Accounting Policies
Our financial statements are prepared in accordance with GAAP. The preparation of these financial statements requires our management to make estimates, assumptions and judgments that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements, and the reported amounts of revenues and expenses during the applicable periods. We base our estimates, assumptions and judgments on historical experience and on various other factors that we believe to be reasonable under the circumstances. Different assumptions and judgments could change the estimates used in the preparation of our financial statements, which, in turn, could change the results from those reported. We evaluate our estimates, assumptions and judgments on an ongoing basis. The critical accounting estimates, assumptions and judgments that we believe have the most significant impact on our financial statements are described below. We have elected under the JOBS Act to delay adoption of new or revised accounting pronouncements applicable to public companies until such pronouncements are made applicable to private companies. As a result of this election, our financial statements may not be comparable to companies that comply with public company effective dates.
51
Table of Contents
Revenue Recognition
Our revenues consist primarily of commissions earned for our insurance policies and discount benefit plans issued to members, enrollment fees paid by members and administration fees paid by members as a direct result of our enrollment services. The member’s payment includes a combination of premiums, fees for discount benefit plans, fees for distributors and enrollment fees, which are collectively referred to as “premium equivalents.” Reported revenues are net of risk premium remitted to insurance carriers and amounts earned by third-party obligors. Commissions and fees attributable to the sale of STM plans and hospital indemnity policies represent substantially all our revenues for the periods presented. Revenues are net of an allowance for policies expected to be cancelled by members during a limited cancellation period. We establish the allowance for estimated policy cancellations through a charge to revenue. The allowance is estimated using historical data to project future experience. Such estimates and assumptions could change in the future as more information becomes known, which could impact the amounts reported. We periodically review the adequacy of the allowance and record adjustments as necessary. The net allowance for estimated policy cancellations was $77,000 as of December 31, 2012.
Revenue is earned at the time of sale. Commission rates for all of our products are agreed to in advance with the relevant insurance carrier and vary by carrier and policy type. Under our carrier compensation arrangements, the commission rate schedule that is in effect on the policy effective date governs the commissions over the life of the policy. In addition, we earn enrollment and administration fees on policies issued.
We report our revenues net of amounts paid to our contracted insurance carrier companies and third-party obligors as we are not the ultimate party responsible for providing the insurance coverage or discount benefits to the member. As a result, we recognize the net amount of revenues earned as the agent in these transactions.
Goodwill and Other Intangible Assets
Goodwill
Under the FASB guidance, the process of evaluating the potential impairment of goodwill involves a two-step process and requires significant judgment at many points during the analysis. In the first step, we determine whether there is an indication of impairment by comparing the fair value of the reporting unit to its carrying amount, including goodwill. Our annual impairment test is performed with a measurement date of October 1. If, based on the first step, we determine that there is an indication of goodwill impairment, we assess the impairment in step two in accordance with the FASB guidance.
In the first step, we determine the fair value using a combination of three valuation approaches: the cost approach, the market approach and the income approach. The cost approach uses multiples from publicly available transactional data of acquired comparable target companies. Transactions are identified that have occurred over the past three years in the subject Company’s industry. The market approach uses a guideline company methodology which is based upon a comparison of the reporting unit to similar publicly-traded companies within our industry. We derive a market value of invested capital or business enterprise value for each comparable company by multiplying the price per share of common stock of the publicly traded companies by their total common shares outstanding and adding each company’s current level of debt. We calculate a business enterprise multiple based on revenue and earnings from each company, then apply those multiples to our revenue and earnings to calculate a business enterprise value. Assumptions regarding the selection of comparable companies are made based on, among other factors, capital structure, operating environment and industry. As the comparable companies were typically larger and more diversified than our business, multiples were adjusted prior to application to our revenues and earnings to reflect differences in margins, long-term growth prospects and market capitalization.
The income approach uses a discounted debt-free cash flow analysis to measure fair value by estimating the present value of future economic benefits. To perform the discounted debt-free cash flow analysis, we develop a pro forma analysis of the reporting unit to estimate future available debt-free cash flow and discounting estimated debt-free cash flow by an estimated industry weighted average cost of capital based on the same comparable companies used in the market approach. Per the FASB guidance, the weighted average cost of capital is based on inputs (e.g., capital structure, risk, etc.) from a market participant’s perspective and not necessarily from the reporting unit’s perspective. Future cash flow is projected based on assumptions for our economic growth, industry expansion, future operations and the discount rate, all of which require significant judgments by management.
After computing a separate business enterprise value under the above approaches, we apply a weighting to them to derive the business enterprise value of the reporting unit. The weightings are evaluated each time a goodwill impairment assessment is performed and give consideration to the relative reliability of each approach at that time. Based on these weightings, we calculated a business enterprise value for the reporting unit. We then add debt-free liabilities of the reporting unit to the calculated business enterprise value to derive an implied fair value of the reporting unit. The implied fair value is then compared to the reporting unit’s carrying value. Upon completion of the analysis in step one, we determined that the fair value of the business exceeded its respective carrying value. As such, a step two analysis was not required.
52
Table of Contents
Other intangible assets
Our intangible assets consist of in-force members, our brand, the carrier network, distributor relationships, capitalized software and a non-compete agreement. Finite-lived intangible assets are amortized over their useful lives from two to seven years.
Advanced Commissions
Advanced commissions consist of amounts advanced to certain third-party distributors. We began advancing commissions in November 2011. We perform ongoing credit evaluations of our distributors, all of which are located in the United States. We recover the advanced commissions from future commissions earned on premiums collected. We have not experienced any credit losses from commission advances and accordingly, have not recognized any provision for bad debt expense at December 31, 2012. A fee for the advanced commission of up to 2% of the insurance premiums advanced is charged to the distributors and recognized as other income as earned. Advanced commissions outstanding at December 31, 2012 and December 31, 2011 totaled approximately $297,000 and $24,000, respectively.
Property and Equipment
Property and equipment is carried at cost, less accumulated depreciation. As a result of the Acquisition and the related application of purchase accounting to the acquired assets and liabilities, there is a new basis of property and equipment subsequent to the acquisition date. Depreciation expense for property and equipment is computed using the straight-line method over the estimated useful lives of the respective assets, with two to three years for computer equipment and seven years for furniture and fixtures. Leasehold improvements are depreciated over the shorter of the lease term or estimated useful life. We periodically review long-lived assets for impairment whenever events or changes in business circumstances indicate that the carrying value of the assets may not be recoverable. No impairment losses were recognized for the periods presented.
Recent Accounting Pronouncements
In December 2011, the FASB issued guidance which requires disclosures of both gross and net information about instrument and transactions eligible for offset as well as transactions subject to an agreement similar to a master netting agreement. This guidance is effective for annual periods beginning on or after January 1, 2013 and interim periods within those annual periods and must be applied retrospectively. As this guidance is limited to presentation only, adoption of this guidance is not expected to have a material impact on our financial position or results of operations.
In July 2012, the FASB issued amended guidance relating to goodwill and other intangible assets which permits an entity to first assess qualitative factors to determine whether it is more likely than not that an indefinite-lived intangible asset is impaired as a basis for determining whether it is necessary to perform the quantitative impairment test in accordance with GAAP. The more-likely-than-not threshold is defined as having a likelihood of more than 50%. If, after assessing the totality of events and circumstances, an entity concludes that it is not more likely than not that the indefinite-lived intangible asset is impaired, then no further action is required. This guidance is effective as of January 1, 2013 with early adoption permitted. Since this guidance only changes the manner in which we assess indefinite-lived intangible assets for impairment, adoption is not expected to have a material effect on our financial position or results of operations.
Legal and Other Contingencies
None.
| ITEM 7A. | QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK |
As a smaller reporting company we are not required to provide the information required by this Item.
| ITEM 8. | FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA |
Financial statements and exhibits filed under this item are listed in the index appearing in Item 15 of this report.
| ITEM 9. | CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE |
None.
53
Table of Contents
| ITEM 9A. | CONTROLS AND PROCEDURES |
Evaluation of Disclosure Controls and Procedures
Disclosure Controls and Procedures
The Company has evaluated, under the supervision of the Company’s principal executive officer and the principal financial officer, the effectiveness of its disclosure controls and procedures as of December 31, 2012. The term “disclosure controls and procedures” (as defined in Exchange Act Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934) means controls and other procedures of a company that are designed to ensure that information a company is required to disclose in reports that are filed or submitted under the Securities Exchange Act of 1934 is (i) recorded, processed, summarized and reported within the time periods specified in SEC rules and forms, and (ii) accumulated and communicated to a company’s management, including its principal executed officer and principal financial officer, as appropriate to allow timely decisions regarding required disclosure. In designing and evaluating the disclosure controls and procedures, management recognizes that any controls and procedures, no matter how well designed and operated, can provide only reasonable assurance of achieving the desired control objectives.
Based on this evaluation for 2012, the principal executive officer and principal financial officer concluded that the Company’s disclosure controls and procedures were not effective as of December 31, 2012, due to a material weakness (as defined under standards established by the Public Company Accounting Oversight Board) in the controls over the design and operation of the financial statement close process, which process impacts most of the Company’s significant accounts included in the financial statements. The deficiencies in the design and operation of the financial statement close process that resulted in the material weakness included the following:
| • | lack of a formal process for reviewing period-end cutoff of revenues and expenses to ensure amounts are captured in the period earned or incurred under the accrual basis of accounting; |
| • | no process in place to ensure all expenses incurred during the period are accrued as of the month-end date, including expenses for which estimates are required; |
| • | absence of a mechanism through which the accounting implications of significant or unusual events and transactions are formally evaluated; and |
| • | no process to ensure formally executed agreements regarding all significant arrangements with third parties and others are obtained. |
As discussed below, we are taking steps to remedy this material weakness.
Management’s Report on Internal Control Over Financial Reporting
This annual report on Form 10-K does not include a report of management’s assessment regarding internal control over financial reporting or an attestation report of the Company’s registered public accounting firm due to the transition period established by the rules of the SEC for newly public companies.
Changes in Internal Control Over Financial Reporting
We are taking steps to address the material weakness described above by hiring additional personnel with technical accounting expertise and by implementing enhanced training for our finance and accounting personnel to familiarize them with our accounting policies. The material weakness will be ongoing until these controls are fully implemented, and we will not be able to confirm that we have remediated this material weakness until our newly implemented procedures have been working for a sufficient period of time.
If the remedial policies and procedures we implement and resources we hire are insufficient to address the identified material weakness, or if additional material weaknesses or significant deficiencies in our internal controls are discovered in the future, we may fail to meet our future reporting obligations, our financial statements may contain material misstatements and our operating results may be adversely affected.
54
Table of Contents
Except for these changes in response to the material weakness identified above, there were no changes in the Company’s internal control over financial reporting during the last fiscal quarter that have materially affected, or are reasonably likely to materially affect, the Company’s internal control over financial reporting.
| ITEM 9B. | OTHER INFORMATION |
None.
55
Table of Contents
| ITEM 10. | DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE |
The following table sets forth information regarding our executive officers and directors as of March 27, 2013:
| Name |
Age | Position | ||||
| Michael W. Kosloske | 49 | Chairman, President and Chief Executive Officer | ||||
| Michael D. Hershberger | 50 | Chief Financial Officer, Treasurer and Secretary | ||||
| Gary Raeckers | 70 | Director, Chief Operating Officer | ||||
| Scott Lingle | 44 | Chief Sales Officer | ||||
| Lori Kosloske | 37 | Chief Broker Compliance Officer | ||||
| Bryan Krul | 37 | Senior Vice President of Sales and Operations | ||||
| Joan Rodgers | 50 | Chief Accounting Officer | ||||
| Paul E. Avery | 53 | Lead Director | ||||
| Anthony J. Barkett | 66 | Director | ||||
| Liana O’Drobinak | 49 | Director | ||||
| Adelaide A. Sink | 64 | Director | ||||
| A. Gordon Tunstall | 68 | Director | ||||
Michael W. Kosloske, our founder, has served as our President and Chief Executive Officer since we began operations in 2008. Mr. Kosloske has served as our Chairman since 2012. Prior to founding our Company, from 1987 to 2007, Mr. Kosloske was president of Health Plan Administrators, Inc., or HPA, a fully-insured niche and individual health insurance company that focused on online sales. In 2005, Mr. Kosloske sold HPA to Independence Holding Company, a New York Stock Exchange-listed holding company engaged in the life and health insurance business, and he remained president of HPA until 2007. Previously, from 1986 to 1987, Mr. Kosloske was marketing manager for Dun & Bradstreet Plan Services, Inc., a third-party administrator in Tampa, Florida. Mr. Kosloske holds a bachelor of science degree in risk management and insurance from Florida State University. Mr. Kosloske is married to our Chief Broker Compliance Officer, Lori Kosloske.
Michael D. Hershberger has served as our Chief Financial Officer since 2011. Mr. Hershberger served as senior manager at Baker Tilly, a full service accounting and advisory firm, from 2005 to 2011, where he was responsible for managing housing research. From 2009 until joining us in 2011, Mr. Hershberger also served as president of Med-Sense Guaranteed Association, a non-profit association that provides membership benefits to individuals and gives members access to certain of our products. Previously, from 1996 until 2012, Mr. Hershberger served as president of Urban Solutions, Inc. (formerly Hersh Group, Ltd), a real-estate advisory consulting firm. Prior to 2005, Mr. Hershberger served as chief financial officer of HPA from 1992 to 2002, where he was responsible for oversight of financial reporting and financial operations of certain third-party insurance administrators. From 1988 to 1992, Mr. Hershberger served as commercial loan officer at Draper & Kramer. He served as senior accountant at Coopers & Lybrand from 1985 to 1987. Mr. Hershberger holds a bachelor of science degree in accounting from Augustana College and earned his masters of science degree in urban land economics/finance from the University of Wisconsin Graduate School of Business. He is a Certified Public Accountant in the State of Illinois.
Gary Raeckers has been our Chief Operating Officer since 2010 and has served as a director since February 2013. From 2002 to 2004, Mr. Raeckers served as chief operating officer of HPA under the leadership of Mr. Kosloske. From 2009 to 2010, Mr. Raeckers served as the director of operations of Premier Administrative Solutions, where he was responsible for administration, customer service and claims processing. Prior to that, from 2005 to 2009, he served as chief operating officer and chief financial officer of Special Markets Insurance Consultants, Inc. From 2004 to 2005, Mr. Raeckers served as senior vice president of Advantec Solutions, Inc. where he was responsible for benefit administration. Prior to his service with HPA, from 1974 to 2002, Mr. Raeckers served in varying capacities, including chief executive officer and chief operating officer, at Health Plan Services, Inc. and its predecessor company, Plan Services Inc. From 1978 to 1994, Plan Services, Inc. was a wholly owned subsidiary of Dun & Bradstreet Plan Services, Inc.
Scott Lingle has served as our Chief Sales Officer since October 2011. Prior to joining us in 2011, Mr. Lingle served in various roles, including vice president of sales, at Golden Rule/United Healthcare beginning in 1992. Mr. Lingle holds a bachelor of business management degree from Olivet Nazarene University as well as a registered health underwriter designation from American College.
Lori Kosloske has served as our Chief Broker Compliance Officer since 2008. Mrs. Kosloske has served in various capacities with us since we began operations in 2008. Previously, Mrs. Kosloske served as our Vice President from 2011 to 2012 and our Vice President of Special Markets from 2008 to 2011. Prior to joining us, Mrs. Kosloske worked as a reinsurance broker at MarketRe (now ParkRe), a reinsurance brokerage company. From 1998 to 2003, Mrs. Kosloske held various positions at Innovative Insurance Group (InnRe), a reinsurance managing general underwriter, where she served as senior underwriter beginning in 2002. Mrs. Kosloske holds a bachelor of business administration degree from Temple University. Mrs. Kosloske is married to our Chairman, President and Chief Executive Officer, Michael W. Kosloske.
56
Table of Contents
Bryan Krul has served as our Senior Vice President of Sales and Operations since 2010. Prior to joining us, Mr. Krul spent 2005 to 2010 at Independence Holding Company, a New York Stock Exchange-listed holding company engaged in the life and health insurance business, where he most recently served as vice president of eBusiness solutions. From 1998 to 2005, Mr. Krul also served in varying capacities, including director of eCommerce, at HPA under the leadership of Mr. Kosloske. Mr. Krul holds a bachelor of arts degree in communications from the University of South Florida.
Joan Rodgers has served as our Chief Accounting Officer since November 2012. Prior to joining us, Ms. Rodgers held various titles from 2007 to 2012 at Quality Distribution, Inc. (“Quality”), which operates the largest chemical bulk tank truck network and is the largest provider of intermodal tank container and depot services in North America. While at Quality, Ms. Rodgers served as director of financial reporting, director of investor relations and director of internal audit. From 2005 to 2007, Ms. Rodgers served as manager of corporate accounting and SEC compliance for Syniverse Technologies, Inc., a global leader in mobile interoperability and communications. Prior to that, Ms. Rodgers served as vice president at Communications Equity Associates, LLC, an advisory and banking services firm, from 1998 to 2005 where she was responsible for capital funding activities for construction projects and financial reporting for subsidiaries. She served as an audit associate at PricewaterhouseCoopers, LLP from 1996 to 1998. In addition, Ms. Rodgers was an adjunct instructor at the University of South Florida’s School of Accountancy from 1998 to 2005 where she taught financial accounting, management accounting and federal income tax. Ms. Rodgers holds a bachelor of science degree and master of accountancy degree from the University of South Florida. She is a Certified Public Accountant in the State of Florida.
Paul E. Avery has served as director since February 2013 and as the Lead Director of our board of directors since March 2013. Mr. Avery currently serves as chief executive officer of World of Beer Franchising, Inc. and as chief executive officer and principal of Avery Management Group, a developer of a franchisee network of Carsmetics Expert Accident Repair Centers throughout the Northeast and Texas, a position he has held since February 2010. From 2005 to 2009, Mr. Avery served as chief operating officer of OSI Restaurant Partners, Inc. In 1998, Mr. Avery was elected to the board of directors of OSI Restaurant Partners, Inc. and served as director until 2004. From 1997 to 2004, Mr. Avery served as president of Outback Steakhouse Inc. Mr. Avery holds an associate degree in hotel and restaurant management from Middlesex County College and a bachelor of science degree from Kean University.
Anthony J. Barkett has served as a director since March 2013. Anthony J. Barkett currently serves as vice-president at Amalie Oil Co., an oil company that develops high-quality, well-engineered petroleum products, a position he has held since 1977. At Amalie Oil Co., Mr. Barkett is responsible for overseeing and coordinating activities in accounting, marketing, sales, operations, information technology and administration. He is also responsible for developing and approving internal controls. From 2007 to 2012, Mr. Barkett was a board member of the Florida Hospital Foundation and he is currently a committee member at FARA ACE for CURE.
Liana O’Drobinak has served as a director since February 2013. Ms. O’Drobinak currently serves as chief executive officer of Bay Consulting Partners, an organization focused on strategic and risk advisory consulting services, a position she has held since 2010. From 2005 to 2010, Ms. O’Drobinak served as the managing director for Florida and the vice president for the South Region of Jefferson Wells International, Inc., a subsidiary of Manpower Inc. Prior to joining Jefferson Wells, Inc., Ms. O’Drobinak founded Acclaris, Inc., a global business process outsourcing company, where she was president and chief executive officer from 2001 to 2005. From 1985 to 2001, Ms. O’Drobinak held several positions at Arthur Andersen LLP, including partner in charge, business process outsourcing for the Southeast Region of the United States. While at Arthur Andersen LLP, Ms. O’Drobinak led SEC reporting for several initial public offerings and was involved in merger and acquisition activity across a variety of industries, qualifying her as a financial expert. In 2011, Ms. O’Drobinak was appointed to a second term as a board member of the Florida Prepaid College Board, where she currently serves as chair of a new audit committee and as a member of the investment committee. Ms. O’Drobinak also served on the board and as finance committee chair for St. Joseph’s—Baptist Hospital, served as an audit committee member of Baycare Inc. and on the board and audit committees of Acclaris, Inc. Ms. O’Drobinak holds a master of business administration and bachelor of science degree in accounting from the University of South Florida. She is a Certified Public Accountant and Certified Internal Auditor in the State of Florida.
Adelaide A. Sink has served as a director since March 2013. Ms. Sink presently serves as a Senior Advisor with Tampa, Florida-based Hyde Park Capital, an investment banking firm specializing in mergers, acquisitions, and capital raising. Ms. Sink is also currently serving as Founder and Chair of Florida Next Foundation, a non-profit, non-partisan organization focused on diversifying Florida’s economy through the growth of small businesses and entrepreneurship. Previously, Ms. Sink served as the State of Florida’s Chief Financial Officer from 2007 to 2011 as one of four statewide elected officials. She managed over $15 billion in state treasury funds, was responsible for state accounting and implemented reforms in contracting and transparency for citizens. She also directed the state’s insurance consumer advocacy work, focusing on strengthening laws to protect seniors against insurance fraud. In 2010, she was the state’s Democratic nominee for governor. Prior to elected office, Ms. Sink had a 26-year career with Bank of America. She retired as president of Florida operations in 2000, managing the state’s largest bank with $40 billion in deposits, leading 9,000 employees in over 800 branches.
A. Gordon Tunstall has served as a director since February 2013. Mr. Tunstall is the founder, and for more than 25 years has served as president, of Tunstall Consulting, Inc., a provider of strategic consulting and financial planning services. Mr. Tunstall currently serves as a director on the boards of Kforce Inc. and CareKinesis, and he previously served as a director for JLM Industries, Inc., Orthodontics Center of America, Inc., Discount Auto Parts, Inc., Advanced Lighting Technologies Inc., Horizon Medical Products Inc., excelleRX and L.A.T. Sportswear. Mr. Tunstall holds a bachelor of science degree in accounting from Widener College. We engaged Tunstall Consulting, Inc. for its consulting services in connection with our recent initial public offering.
Expertise, Qualifications, Attributes and Skills of Our Board Members
Set forth below are the specific expertise, qualifications, attributes and skills that each member of our board brings to our board which have led the board to conclude that such member should serve on our board.
Michael W. Kosloske brings direct knowledge and experience with the Company, based on his service as founder and principal executed officer of the Company, as well as extensive experience in the insurance industry.
57
Table of Contents
Gary Raeckers brings direct knowledge and experience with the Company, based on his service as COO of the Company. He also has extensive experience in and knowledge of the insurance industry, based on service as executive officer with many companies involved in the insurance industry, including Health Plan Services, Inc.
Paul E. Avery brings business knowledge and experience based on his service as principal executive officer of Outback Steakhouse, Inc. and his involvement in various other business enterprises.
Anthony J. Barkett brings business knowledge and experience based on his service as principal executive officer of Amalie Oil Co.
Liana O’Drobinak brings financial expertise and status as a financial expert, based on her service as a partner with Arthur Andersen LLP and her work with Jefferson Wells, Inc. She has business knowledge and experience, based on her service as a founder and CEO of Acclaris, Inc.
Adelaide A. Sink brings business knowledge and experience and financial expertise based on her long experience as a bank executive and insurance industry knowledge and experience based on her service as Chief Financial Officer of the State of Florida.
A. Gordon Tunstall brings business knowledge and experience and financial expertise based on his long experience as a consultant to a number of companies, as well as knowledge of public company governance and executive compensation, based on his service as a director of a number of public companies.
Controlled Company
For purposes of the rules of the NASDAQ Global Market, we are considered a “controlled company”. Controlled companies under those rules are companies of which more than 50% of the voting power for the election of directors is held by an individual, a group or another company. Mr. Kosloske beneficially owns more than 50% of the combined voting power of our common stock and has the right to designate a majority of the members of our board of directors for nomination for election and the voting power to elect such directors. Accordingly, we are eligible to, and we intend to, take advantage of certain exemptions from corporate governance requirements provided in rules of the NASDAQ Global Market. Specifically, as a controlled company, we are not required to have (1) a majority of independent directors, (2) a nominating and corporate governance committee composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities, (3) a compensation committee composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities, or (4) an annual performance evaluation of the nominating and corporate governance and compensation committees. Accordingly, our stockholders will not have the same protections afforded to stockholders of companies that are subject to all of the applicable rules of the NASDAQ Global Market.
Board Structure
Our board of directors consists of seven members. Our board has determined that each of Mr. Avery, Ms. O’Drobinak, Ms. Sink and Mr. Barkett are independent under applicable NASDAQ rules. Mr. Avery serves as our Lead Director. In accordance with our amended and restated certificate of incorporation and our amended and restated bylaws, each of our directors will serve for a one-year term or until his or her successor is elected and qualified. At each annual meeting of our stockholders, our stockholders will elect the members of our board of directors. There will be no limit on the number of terms a director may serve on our board of directors.
Board Committees
Audit Committee
The audit committee, which consists of Ms. O’Drobinak (Chair), Mr. Avery and Ms. Sink, assists the board in overseeing our accounting and financial reporting processes and the audits of our financial statements. In addition, the audit committee is directly responsible for the appointment, compensation, retention and oversight of the work of our independent registered public accounting firm. The board of directors has determined that Ms. O’Drobinak qualifies as an “audit committee financial expert,” as such term is defined in the rules of the SEC and that Ms. O’Drobinak, Mr. Avery and Ms. Sink qualify as independent, as such term is defined in the rules of the SEC. Mr. Tunstall served on our audit committee from February 7, 2103 to March 8, 2013. We relied on the phase-in rules of the SEC and the NASDAQ Global Market with respect to the independence of our audit committee. These rules permit us to have an audit committee that has one member that is independent upon the effectiveness of our registration statement for our IPO, a majority of members that are independent within 90 days thereafter and all members that are independent within one year thereafter.
Compensation Committee
Our compensation committee consists of Mr. Tunstall (Chairman), Mr. Avery, Ms. O’Drobinak and Mr. Barkett. Our compensation committee is responsible for assisting our board of directors in discharging its responsibilities relating to (1) setting our compensation program and compensation of our executive officers and directors; (2) monitoring our incentive and equity-based compensation plans; and (3) preparing our compensation committee report required to be included in our proxy statement under the rules and regulations of the SEC.
58
Table of Contents
Nominating and Corporate Governance Committee
Our nominating and corporate governance committee consists of Mr. Avery (Chairman), Ms. O’Drobinak, Mr. Barkett and Mr. Tunstall. Our nominating and corporate governance committee assists our board of directors in identifying individuals qualified to become members of our board of directors consistent with criteria established by our board and in developing our corporate governance principles. This committee’s responsibilities include: (1) evaluating the composition, size and governance of our board of directors and its committees and making recommendations regarding the appointment of directors to our committees; (2) considering stockholder nominees for election to our board of directors; (3) evaluating and recommending candidates for election to our board of directors; (4) leading the self-evaluation process of our board of directors; (5) developing and reviewing our corporate governance guidelines and providing recommendations to the board regarding possible changes; (6) evaluating and recommending management candidates; and (7) performing any other activities the committee deems appropriate, are set forth in the corporate governance guidelines or are requested by the board.
Section 16(a) Beneficial Ownership Reporting Compliance
Our directors, executive officers and beneficial owners of more than 10% of our common stock are required under Section 16(a) of the Securities Exchange Act of 1934, as amended, to file reports of ownership and changes in ownership of our securities with the SEC. We completed the IPO on February 13, 2013, and accordingly, we did not have a class of securities registered pursuant to Section 12 of the Exchange Act in 2012.
Code of Ethics
Our board of directors has adopted a code of business conduct and ethics that applies to all of our directors, officers and other employees, including our principal executive officer, principal financial officer and principal accounting officer. Any waiver of the code for directors or executive officers may be made only by our board of directors and will be promptly disclosed to our stockholders through publication on our website, www.hiiquote.com. Amendments to the code must be approved by our board of directors and will be promptly disclosed (other than technical, administrative or non-substantive changes). A copy of our code of business conduct and ethics is posted on our website.
Compensation Committee Interlocks and Insider Participation
None of our executive officers has served as a member of a compensation committee (or if no committee performs that function, the board of directors) of any other entity that has an executive officer serving as a member of our board of directors.
| ITEM 11. | EXECUTIVE COMPENSATION |
The following table sets forth information concerning the compensation earned by our chief executive officer and our two other most highly compensated executive officers during our fiscal years ended December 31, 2012 and December 31, 2011.
Summary Compensation Table
| Name and Principal Position |
Year | Salary ($) |
Bonus ($) |
All Other Compensation ($) |
Total ($) |
|||||||||||||||
| Michael W. Kosloske |
2012 | 400,000 | 39,559 | (1) | 439,559 | |||||||||||||||
| (Chairman, President and Chief Executive Officer) |
2011 | 100,000 | 615,378 | (2) | 22,962 | (3) | 738,340 | |||||||||||||
| Gary Raeckers |
2012 | 217,708 | 217,708 | |||||||||||||||||
| (Chief Operating Officer) |
2011 | 145,000 | 145,000 | |||||||||||||||||
| Scott Lingle |
2012 | 219,510 | 99,996 | 319,506 | ||||||||||||||||
| (Chief Sales Officer) |
2011 | 50,000 | 56,666 | 106,666 | ||||||||||||||||
| (1) | Reflects an automobile allowance of $32,857 and club dues of $6,702. |
| (2) | Reflects amounts earned in respect of the 2011 fiscal year. |
| (3) | Reflects an automobile allowance of $16,260 and club dues of $6,702. |
Outstanding Equity Awards at Fiscal Year End
We had no outstanding equity awards as of the end of our fiscal year ended December 31, 2012.
Employment, Severance, Retirement and Change in Control Arrangements
We have entered into an employment agreement with Mr. Kosloske with a term beginning on February 13, 2013 and ending on December 31, 2013. Under his agreement, Mr. Kosloske is entitled to an annual salary of $595,000 and is eligible to participate in our long term incentive plan (described below) in accordance with its terms. Unless prior written notice of termination is given by either party prior to its expiration date, the term of the agreement will be automatically extended for successive one-year periods. In the
59
Table of Contents
event that we determine not to extend Mr. Kosloske’s agreement, terminate Mr. Kosloske’s employment without cause (as defined in the agreement) or Mr. Kosloske terminates his employment for good reason (as defined in the agreement), Mr. Kosloske will be entitled to an amount equal to two times the sum of his annual base salary and the greater of (i) his most recently earned annual bonus and (ii) his average annual bonus earned in the three most recently completed calendar years, payable in 24 equal monthly installments beginning on the termination date, provided that Mr. Kosloske executes a general release in our favor. Mr. Kosloske is subject to non-competition, non-disparagement and non-solicitation covenants that expire 24 months following termination of his employment. Mr. Kosloske is not entitled to any change in control benefits.
We are party to “at will” employment agreements with Mr. Raeckers and Mr. Lingle pursuant to which each is entitled to a current annual base salary of $250,000 and $200,000, respectively. Mr. Raeckers and Mr. Lingle are each subject to non-solicitation and non-competition covenants that expire 12 months after termination of employment. Neither Mr. Raeckers nor Mr. Lingle is entitled to any change in control benefits.
We do not maintain any tax-qualified or supplemental retirement or pension plans. We anticipate that we will adopt a tax-qualified 401(k) defined contribution plan.
Restricted Stock Agreements
On February 13, 2013, we granted to Mr. Hershberger an award of 400,000 restricted shares of our Class A common stock in accordance with his employment agreement, 20% of which will vest on the six-month anniversary of our initial public offering and 20% of which will vest on October 1 of each of 2013, 2014, 2015 and 2016, subject to Mr. Hershberger’s continued employment through the relevant vesting date. Any unvested shares will vest upon Mr. Hershberger’s death or disability, or termination of employment without cause or for good reason. In addition, any unvested shares will vest if Mr. Kosloske ceases to be either our Chief Executive Officer or Chairman of our board.
Director Compensation
Each outside director will receive a board meeting fee of $2,000 per meeting. Additionally, the Company will compensate each outside director for his or her attendance at board committee meetings in the amount of $1,500 per meeting. The Company will pay a reduced rate of $1,000 per board or committee meeting if the meeting is held by teleconference. Certain board members will also receive retainers for their role as board committee chairs. The Company will pay annual retainers of $20,000 to the audit committee chair, $10,000 to the compensation committee chair, and $5,000 to the nominating and corporate governance committee chair. Our directors did not earn nor receive any compensation for their service in 2012.
On March 8, 2013, the compensation committee awarded each outside director stock settled appreciation rights (“SSARs”) under the 2013 Outside Director Compensation Program. The Company awarded each outside director 30,000 SSARs, of which 33% of the SSARs vest on August 6, 2013, 33% vest on May 1, 2014, and the remaining unvested SSARs vest on May 1, 2015. Each SSAR has a grant price of $13.97 and expires seven years after the grant date.
Long Term Incentive Plan and Awards
On February 7, 2013, we adopted our Health Insurance Innovations, Inc. Long Term Incentive Plan (“LTIP”), which permits us to grant an array of equity-based and cash incentive awards to our named executive officers and other employees and service providers. The purpose of the LTIP is to motivate and reward those employees and other individuals who are expected to contribute significantly to our success to perform at the highest level and to further our best interests and those of our shareholders. Our compensation committee administers the plan and has discretion of the types of awards issued under the plan. The LTIP expires after ten years, unless prior to that date the maximum number of shares available for issuance under the plan has been issued or our board of directors terminates the plan.
60
Table of Contents
| ITEM 12. | SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS |
Health Insurance Innovations, Inc. has two classes of outstanding capital stock: Class A common stock and Class B common stock. Class A shares represent 100% of the economic rights of the holders of all classes of our common stock to share in our distributions. Class B shares do not entitle their holders to any dividends paid by, or rights upon liquidation of, Health Insurance Innovations, Inc. Shares of our Class A common stock vote together with shares of our Class B common stock as a single class, except as otherwise required by law. Each share of our Class A common stock and our Class B common stock entitles its holder to one vote.
Health Insurance Innovations, Inc. is a holding company owning as its principal asset Series A Membership Interests in Health Plan Intermediaries Holdings, LLC. Since the IPO, we have operated our business through Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries. Health Plan Intermediaries Holdings, LLC has two series of outstanding equity: Series A Membership Interests, which may only be issued to Health Insurance Innovations, Inc., as sole managing member, and Series B Membership Interests. The Series B Membership Interests are held by Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (a subsidiary of Health Plan Intermediaries, LLC that was formed on October 31, 2012 in connection with the IPO), entities beneficially owned by our Chairman, President and Chief Executive Officer, Michael Kosloske. As of March 27, 2013, (i) the Series A Membership Interests held by Health Insurance Innovations, Inc. represent 37.6% of the outstanding membership interests, 37.6% of the economic interests and 100% of the voting interests in Health Plan Intermediaries Holdings, LLC and (ii) the Series B Membership Interests held by the entities beneficially owned by Mr. Kosloske represent 62.4% of the outstanding membership interests, 62.4% of the economic interests and 0% of the voting interests in Health Plan Intermediaries Holdings, LLC. Pursuant to and subject to the terms of an exchange agreement and the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC, holders of Series B Membership Interests, at any time and from time to time, may exchange one or more Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock on a one-for-one basis, subject to equitable adjustments for stock splits, stock dividends and reclassifications.
For greater detail regarding our organizational structure, our capitalization, the exchange agreement referenced above and related matters, see “Item 1. Business—Our History and the Reorganization of Our Corporate Structure.”
The following table sets forth information regarding beneficial ownership of our Class A common stock and Class B common as of March 27, 2013 by:
| • | each person whom we know to own beneficially more than 5% of our Class A common stock or Class B common stock; |
| • | each of the directors and named executive officers individually; and |
| • | all directors and executive officers as a group. |
Except as set forth below, the following information is given as of March 27, 2013. In the case of percentage ownership, the information is based on 5,295,167 shares of the Company’s Class A common stock and 8,566,667 shares of the Company’s Class B common stock being outstanding as of March 27, 2013.
| Name of Beneficial Owner |
Shares of Class A Common Stock Beneficially Owned |
Percentage of Shares of Class A Common Stock Beneficially Owned |
Shares of Class B Common Stock Beneficially Owned |
Percentage of Shares of Class B Common Stock Beneficially Owned |
||||||||||||
| Named executive officers and directors: |
||||||||||||||||
| Michael W. Kosloske(1) |
8,900 | (2) | * | 8,566,667 | (1) | 100.0 | % | |||||||||
| Gary Raeckers(3) |
12,500 | * | — | — | ||||||||||||
| Scott Lingle(4) |
9,200 | * | — | — | ||||||||||||
| Paul E. Avery |
4,000 | * | — | — | ||||||||||||
| Anthony Barkett |
— | * | — | — | ||||||||||||
| Liana O’Drobinak |
5,000 | * | — | — | ||||||||||||
| Adelaide A. Sink |
— | * | — | — | ||||||||||||
| A. Gordon Tunstall |
— | * | — | — | ||||||||||||
| All directors and executive officers as a group (12 persons) |
459,200 | 8.67 | % | 8,566,667 | (1) | 100.0 | % | |||||||||
| Greater than 5% Stockholders: |
||||||||||||||||
| Health Plan Intermediaries, LLC(1) |
— | — | 8,566,667 | (1) | 100.0 | % | ||||||||||
| Michael D. Hershberger(5) |
400,000 | 7.55 | % | — | — | |||||||||||
| * | Less than 1.0% |
| (1) | Consists of 8,480,000 shares of Class B common stock held of record by Health Plan Intermediaries, LLC and 86,667 shares of Class B common stock held by Health Plan Intermediaries Sub, LLC. As managing member of Health Plan Intermediaries Sub, LLC, Health Plan Intermediaries, LLC has sole voting and dispositive power over the shares held by Health Plan Intermediaries Sub, LLC. Michael W. Kosloske, our Chairman, President and Chief Executive Officer, is the sole member and primary manager of Health Plan Intermediaries, LLC and has sole voting and dispositive power over the shares held by Health Plan Intermediaries, LLC. We refer to Health Plan Intermediaries, LLC, Health Plan Intermediaries Sub, LLC and Mr. Kosloske as the Existing Stockholders. The Existing Stockholders may be deemed to have formed a “group” within the meaning of Section 13(d) under the Exchange Act, and the group may be deemed, collectively, to beneficially own all the shares of Class B common stock held of record by each of Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC. As of March 27, 2013, the shares of Class B common stock, together with the Series B Membership Interests of Health Plan Intermediaries Holdings, LLC owned of record by the Existing Stockholders, are exchangeable at the Existing Stockholders’ option into an equal number of shares of Class A common stock, representing 62.4% of the shares of Class A common outstanding stock. Under SEC rules, the Existing Stockholders are deemed the beneficial owner of such number of shares of Class A common stock. The shares of Class A common stock and Class B common stock vote together as a single class on matters submitted to a vote of our stockholders. The address of each Existing Stockholder is 15438 N. Florida Avenue, Suite 201, Tampa, Florida 33613. |
| (2) | Consists of 8,900 shares of unvested restricted stock owned by Lori Kosloske, Michael Kosloske’s wife. Mrs. Kosloske has the right to vote, but not dispose of, the shares of unvested restricted stock. |
| (3) | Consists of 12,500 shares of unvested restricted stock. Mr. Raeckers has the right to vote, but not to dispose of, the shares of unvested restricted stock. |
| (4) | Consists of 12,500 shares of unvested restricted stock. Mr. Lingle has the right to vote, but not to dispose of, the shares of unvested restricted stock. |
| (5) | Consists of 400,000 shares of unvested restricted stock owned by Mr. Hershberger. Mr. Hershberger has the right to vote, but not to dispose of, the shares of his unvested restricted stock. |
| (6) | See footnotes (1) through (5). Shares for all current executive officers and directors as a group also include 8,900 unvested restricted shares owned by Mr. Krul, plus 300 shares owned outright by Mr. Krul and 7,100 unvested restricted shares owned by Ms. Rodgers. Mr. Krul and Ms. Rodgers have the right to vote, but not dispose of, the shares of unvested restricted stock. |
61
Table of Contents
| ITEM 13. | CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE |
In addition to the compensation arrangements with directors and executive officers described under “Executive Compensation,” the following is a description of each transaction since January 1, 2011, and each currently proposed transaction in which:
| • | we have been or are to be a participant; |
| • | the amount involved exceeded or will exceed $120,000; and |
| • | any of our directors, executive officers, beneficial holders of more than 5% of our capital stock, or any member of their immediate family or person sharing their household had or will have a direct or indirect material interest. |
Transactions with Health Insurance Innovations, Inc.
In connection with the reorganization, we engaged in certain transactions with entities controlled by Mr. Kosloske, our Chairman, President and Chief Executive Officer, that became beneficial owner of 5% or more of our voting securities through ownership of shares of our Class B common stock. These transactions are described in detail under “Item 1. Business—Our History and the Reorganization of Our Corporate Structure.”
Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC
We operate our business through Health Plan Intermediaries Holdings, LLC. The operations of Health Plan Intermediaries Holdings, LLC, and the rights and obligations of its members are governed by the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC. We serve as sole managing member of Health Plan Intermediaries Holdings, LLC. As such, we control its business and affairs and will be responsible for the management of its business.
The amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC establishes two classes of equity: Series A Membership Interests and Series B Membership Interests. Series A Membership Interests may be issued only to us as the sole managing member of Health Plan Intermediaries Holdings, LLC. Series B Membership Interests may be issued only to persons or entities we permit, which initially will be Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. See “Item 1. Business—Our History and the Reorganization of Our Corporate Structure—Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC.”
Exchange Agreement
On February 13, 2013, we entered into an exchange agreement with holders of Series B Membership Interests of Health Plan Intermediaries Holdings, LLC, including Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. Pursuant to and subject to the terms of the exchange agreement and the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC, holders of Series B Membership Interests, at any time and from time to time, may exchange one or more Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock on a one-for-one basis, subject to equitable adjustments for stock splits, stock dividends and reclassifications. See “Item 1. Business—Our History and the Reorganization of Our Corporate Structure—Exchange Agreement.”
Tax Receivable Agreement
On February 13, 2013, we entered into a tax receivable agreement with the existing and certain future holders of Series B Membership Interests (initially Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske). The agreement requires us to pay to such holders 85% of the cash savings, if any, in U.S. federal, state and local income tax we realize (or are deemed to realize in the case of an early termination payment, a change in control or a material breach by us of our obligations under the tax receivable agreement) as a result of any possible future increases in tax basis described above and of certain other tax benefits related to entering into the tax receivable agreement, including tax benefits attributable to payments under the tax receivable agreement itself. This will be our obligation and not an obligation of Health Plan Intermediaries Holdings, LLC. We will benefit from the remaining 15% of any realized cash savings. See “Item 1. Business—Our History and the Reorganization of Our Corporate Structure—Tax Receivable Agreement.”
Purchase of Membership Interest in Health Plan Intermediaries, LLC
On September 28, 2011, we entered into an agreement to purchase the units of Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC for $5,330,000 plus closing costs of $135,000. This purchase was financed with a loan from a bank for $4,250,000 and by a cash payment of $1,135,000 made by Mr. Kosloske to the Naylor Group Partners, LLC. Borrowings under the loan were secured by all of our assets, including, but not limited to, cash accounts, accounts receivable and property and equipment. The loan was further secured with a personal unlimited guarantee by Mr. Kosloske and Mrs. Kosloske and certain real properties owned by Mr. Kosloske and Mrs. Kosloske. On February 13, 2013, we repaid the loan with a portion of the net proceeds of the IPO.
62
Table of Contents
Prior to the purchase, Health Plan Intermediaries, LLC was 50% owned by Naylor Group Partners, LLC and 50% owned by Mr. Kosloske. Following the purchase, Mr. Kosloske became the sole member of Health Plan Intermediaries, LLC.
Employment Contracts
In August 2008, we entered into an employment arrangement with Mr. Kosloske under which he receives on an annual basis all net revenues from the sale of certain prescription contracts, in an amount not to exceed $214,000, plus commissions based on yearly revenues. This compensation is treated as guaranteed payments and totaled $615,000 for 2011 and $485,000 for 2010. Such compensation does not relate to any investment in us made by Mr. Kosloske. The employment agreement terminated on September 28, 2011. Mr. Kosloske has not received revenues from the sale of prescription contracts or commissions based on yearly revenues since October 2011, and he will not receive such revenues under any current or proposed employment contract. We have entered into a new employment contract with Mr. Kosloske in connection with this offering. See “Item 11. Executive Compensation.”
Other Relationships
During the year ended December 31, 2012, we paid Mr. Kosloske approximately $126,000 for unreimbursed expenses paid by Mr. Kosloske on behalf of the Company. This amount represented commissions payable to Lori Kosloske of approximately $93,000 and general business expenses of approximately $33,000.
In February 2012, we entered into a relationship with Tunstall Consulting Inc. for consulting services in connection with the IPO. A. Gordon Tunstall, one of our directors, is the founder and president of Tunstall Consulting Inc. During the year ended December 31, 2012, we paid $407,000 to Tunstall Consulting Inc.
In March 2008, we entered into a relationship with Med-Sense, a non-profit association that provides membership benefits to individuals and gives members access to certain of our products. Michael D. Hershberger, our Chief Financial Officer, was president of Med-Sense until October 2011, when he resigned as president and joined us as one of our officers. We paid $434,000 to Med-Sense in 2011.
Executive Management Fees
The Naylor Group Partners, LLC, the former owners of 50% of the units of the Health Plan Intermediaries, LLC, performed certain executive management services for us in 2011 and 2010. These executive management services generally consisted of advice in connection with participation in board of managers meetings. The amount paid totaled $231,000 for 2011 and $25,000 for 2010. We terminated the services arrangement with the Naylor Group Partners, LLC in connection with the transaction described above under the heading “Purchase of Membership Interest in Health Plan Intermediaries, LLC.”
Distribution to Members
In accordance with terms of its Operating Agreement, Health Plan Intermediaries, LLC declared cash distributions during the years ended December 31, 2012 and 2011 of $4,010,000, all of which was distributed to Mr. Kosloske, and $1,301,000, respectively. Of the $1,301,000 paid during the year ended December 31, 2011, $681,000 was paid to Naylor Group Partners, LLC and $620,000 was paid to Mr. Kosloske, respectively.
Exercise of Over-allotment Option
We used $1,302,000 of the proceeds from the sale of shares through the over-allotment option to acquire Series B Membership Interests, together with an equal number of shares of our Class B common stock, from Health Plan Intermediaries, LLC, which is controlled by Mr. Kosloske, which Series B Membership Interests were immediately recapitalized into Series A Membership Interests.
Employment Arrangements with Immediate Family Members of Our Executive Officers
Lori Kosloske is married to Mr. Kosloske. Mrs. Kosloske is employed by us. During 2012 and 2011, Mrs. Kosloske had total cash compensation of $199,402 and $290,101, respectively. For more information on Mrs. Kosloske’s employment arrangement, see “Item 11. Executive Compensation—Employment, Severance, Retirement and Change in Control Arrangements.”
Registration Rights Agreement
On February 13, 2013, we entered into a registration rights agreement with Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske, to register for sale under the Securities Act shares of our Class A common stock delivered in exchange for Series B Membership Interests in the circumstances described below. This agreement provides these two entities (and their affiliates) with the right to require us, at our expense, to register shares of our Class A common stock that are issuable upon exchange of Series B Membership Interests (and an equal number of shares of our Class B common stock) for shares of our Class A common stock. The agreement also provides that we pay certain expenses of Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (and their affiliates) relating to such registrations and indemnify them against certain liabilities, which may arise under the Securities Act.
Demand Rights
Subject to certain limitations, at any time after completion of the IPO, Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (and their affiliates) have the right, by delivering written notice to us, to require us to register the number of our shares of Class A common stock requested to be so registered in accordance with the registration rights agreement. Within 10 days of receipt of notice of a demand registration, we are required to give written notice to all other holders of registrable shares of Class A common stock. Subject to certain limitations as described below, we will include in the registration all securities with respect to which we receive a written request for inclusion in the registration within 10 days after we give our notice.
Piggyback Rights
Any holder of registrable shares of Class A common stock will be entitled to request to participate in, or “piggyback” on, registrations of any of our securities for sale by us at any time after the IPO. This piggyback right will apply to any registration following the IPO other than a demand registration described above, a registration on Form S-4 or S-8 or a registration solely in connection with an exchange offer or any employee benefit or dividend reinvestment plan.
Conditions and Limitations
The registration rights outlined above are subject to conditions and limitations, including the right of the underwriters to limit the number of shares to be included in a registration statement and our right to delay, suspend or withdraw a registration statement under specified circumstances. For example, our board may, in its good faith judgment, defer any filing for up to 75 days (which deferral may not be used more than once in any 12-month period). Furthermore, our board may, in its good faith judgment, suspend a registration on Form S-3 (which suspension may not be more than an aggregate of 90 days in any 12-month period), for such period of time as is reasonably necessary not in excess of 75 days. Additionally, in certain circumstances we may withdraw a registration upon request by the holder of registrable securities.
If requested by the managing underwriter or underwriters, holders of securities with registration rights will not be able to make any sale of our equity securities (including sales under Rule 144) or give any demand notice during a period commencing on the date of the request and continuing for a period not to exceed 90 days (with respect to any underwritten public offering, other than the IPO, made prior to the second anniversary of the IPO, and thereafter 60 days rather than 90 days) or such shorter period as may be requested by the underwriters. The managing underwriters for the relevant offering may agree to shorten this period.
63
Table of Contents
Policies and Procedures for Related Party Transactions
Our board of directors adopted a written related person transaction policy setting forth the policies and procedures for the review and approval or ratification of related person transactions. This policy covers any transaction, arrangement or relationship, or any series of similar transactions, arrangements or relationships, in which we were or are to be a participant and a related person had or will have a direct or indirect material interest, as determined by the audit committee of our board of directors, including, purchases of goods or services by or from the related person or entities in which the related person has a material interest, and indebtedness, guarantees of indebtedness or employment by us of a related person. In reviewing any such proposal, our audit committee is tasked to consider all relevant facts and circumstances, including the commercial reasonableness of the terms, the benefit or perceived benefit, or lack thereof, to us, opportunity costs of alternate transactions, the materiality and character of the related person’s direct or indirect interest and the actual or apparent conflict of interest of the related person.
All related party transactions that occurred prior to the adoption of this policy were not subject to the approval and review procedures set forth in the policy.
| ITEM 14. | PRINCIPAL ACCOUNTANT FEES AND SERVICES |
Aggregate fees for professional services rendered by Ernst & Young, LLP to us for work performed during and related to the fiscal years ended December 31, 2012 and 2011 are summarized in the table below.
| 2012 | 2011 | |||||||
| Type of Fees |
||||||||
| Audit fees |
$ | 1,577,000 | $ | 185,000 | ||||
| Audit-related fees |
— | — | ||||||
| Tax fees |
11,000 | — | ||||||
| All other fees |
— | — | ||||||
|
|
|
|
|
|||||
| Total |
$ | 1,588,000 | $ | 185,000 | ||||
|
|
|
|
|
|||||
Audit Fees
Audit fees are composed of fees for professional services related to the audits of our annual financial statements and the review of financial statements included in our SEC filings.
Tax Fees
Tax fees are composed of fees for professional services rendered in relation to our reorganization.
Since the IPO, our audit committee has adopted a policy that we will not engage our registered public accounting firm to render audit or non-audit services unless the service is specifically approved in advance by our audit committee.
64
Table of Contents
| ITEM 15. | EXHIBITS AND FINANCIAL STATEMENT SCHEDULES |
FINANCIAL STATEMENTS
Health Plan Intermediaries, LLC and Subsidiaries
| Page | ||||
| Audited Consolidated Financial Statements |
||||
| F-2 | ||||
| F-3 | ||||
| F-4 | ||||
| F-5 | ||||
| F-6 | ||||
| F-7 | ||||
F-1
Table of Contents
Report of Independent Registered Public Accounting Firm
Member of Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
We have audited the accompanying consolidated balance sheet of Health Plan Intermediaries, LLC d/b/a Health Insurance Innovations (the Company) as of December 31, 2012, and the related consolidated statements of operations, member’s equity, and cash flows for the year ended December 31, 2012 (Successor), the period from October 1, 2011 to December 31, 2011 (Successor) and the period from January 1, 2011 to September 30, 2011 (Predecessor). These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. We were not engaged to perform an audit of the Company’s internal control over financial reporting. Our audits included consideration of internal control over financial reporting as a basis for designing audit procedures that are appropriate in the circumstances, but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion. An audit also includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, and evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated financial position of Health Plan Intermediaries, LLC d/b/a Health Insurance Innovations at December 31, 2012 (Successor), and the consolidated results of its operations and its cash flows for the year ended December 31, 2012 (Successor), the period from October 1, 2011 to December 31, 2011 (Successor), and the period from January 1, 2011 to September 30, 2011 (Predecessor) in conformity with U.S. generally accepted accounting principles.
| /s/ Ernst & Young LLP |
| Certified Public Accountants |
Tampa, Florida
April 1, 2013
F-2
Table of Contents
Health Plan Intermediaries, LLC and Subsidiaries
d/b/a Health Insurance Innovations
Consolidated Balance Sheet (Successor)
(in thousands)
| December 31, 2012 |
||||
| Assets |
||||
| Current assets: |
||||
| Cash |
$ | 750 | ||
| Cash held on behalf of others |
3,839 | |||
| Credit card transactions receivable |
588 | |||
| Accounts receivable |
273 | |||
| Advanced commissions |
297 | |||
| Prepaid expenses and other current assets |
217 | |||
|
|
|
|||
| Total current assets |
5,964 | |||
| Property and equipment, net of accumulated depreciation |
213 | |||
| Capitalized offering costs |
1,819 | |||
| Goodwill |
5,906 | |||
| Intangible assets, net of accumulated amortization |
3,959 | |||
| Other assets |
100 | |||
|
|
|
|||
| Total assets |
$ | 17,961 | ||
|
|
|
|||
| Liabilities and member’s equity |
||||
| Current liabilities: |
||||
| Accounts payable and accrued expenses |
$ | 2,062 | ||
| Carriers and vendors payable |
2,790 | |||
| Commissions payable |
1,533 | |||
| Current portion of long-term debt |
813 | |||
| Current portion of noncompete obligation |
155 | |||
| Due to member |
773 | |||
| Other current liabilities |
345 | |||
|
|
|
|||
| Total current liabilities |
8,471 | |||
| Long-term debt, less current portion |
2,481 | |||
| Noncompete obligation |
626 | |||
| Other liabilities |
45 | |||
|
|
|
|||
| Total liabilities |
11,623 | |||
| Member’s equity |
6,335 | |||
| Noncontrolling interest in subsidiaries |
3 | |||
|
|
|
|||
| Total member’s equity |
6,338 | |||
|
|
|
|||
| Total liabilities and member’s equity |
$ | 17,961 | ||
|
|
|
|||
See accompanying notes.
F-3
Table of Contents
Health Plan Intermediaries, LLC and Subsidiaries
d/b/a Health Insurance Innovations
Consolidated Statements of Operations
(in thousands)
| Successor | Predecessor | |||||||||||||
| Year Ended December 31, 2012 |
Three-Month Period Ended December 31, 2011 |
Nine-Month Period Ended September 30, 2011 |
||||||||||||
| Revenues (premium equivalents of $75,872, $14,949, and $38,257 for the Successor year ended December 31, 2012, Successor period ended December 31, 2011, and the Predecessor period ended September 30, 2011, respectively) |
$ | 41,940 | $ | 8,090 | $ | 21,788 | ||||||||
| Third-party commissions |
27,858 | 5,601 | 16,103 | |||||||||||
| Credit cards and ACH fees |
963 | 197 | 473 | |||||||||||
| General and administrative expenses |
8,611 | 1,421 | 3,341 | |||||||||||
| Depreciation and amortization |
1,012 | 269 | 29 | |||||||||||
|
|
|
|
|
|
|
|||||||||
| Total operating costs and expenses |
38,444 | 7,488 | 19,946 | |||||||||||
|
|
|
|
|
|
|
|||||||||
| Income from operations |
3,496 | 602 | 1,842 | |||||||||||
| Other expenses (income): |
||||||||||||||
| Interest expense |
271 | 71 | — | |||||||||||
| Other income |
(35 | ) | — | — | ||||||||||
|
|
|
|
|
|
|
|||||||||
| Net income |
3,260 | 531 | 1,842 | |||||||||||
|
|
|
|
|
|
|
|||||||||
| Net loss attributable to noncontrolling interest in subsidiaries |
(89 | ) | — | — | ||||||||||
|
|
|
|
|
|
|
|||||||||
| Net income attributable to Health Plan Intermediaries, LLC |
$ | 3,349 | $ | 531 | $ | 1,842 | ||||||||
|
|
|
|
|
|
|
|||||||||
See accompanying notes.
F-4
Table of Contents
Health Plan Intermediaries, LLC and Subsidiaries
d/b/a Health Insurance Innovations
Consolidated Statements of Member’s Equity
| Member’s equity |
Noncontrolling interest in subsidiaries |
Total | ||||||||||
| Balance as of January 1, 2011 (Predecessor) |
$ | (77 | ) | — | $ | (77 | ) | |||||
| Net income |
1,842 | — | 1,842 | |||||||||
| Distributions to members |
(1,301 | ) | — | (1,301 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Balance as of September 30, 2011 (Predecessor)
|
|
464
|
|
|
—
|
|
|
464
|
| |||
| Balance as of October 1, 2011 (Successor) |
464 | — | 464 | |||||||||
| Net income |
531 | — | 531 | |||||||||
| Contributions from member |
1,135 | — | 1,135 | |||||||||
| Purchase of member’s interest in Company and adjustment to member’s equity to reflect fair value |
4,866 | — | 4,866 | |||||||||
|
|
|
|
|
|
|
|||||||
| Balance as of December 31, 2011 (Successor) |
6,996 | — | 6,996 | |||||||||
| Net income (loss) |
3,349 | (89 | ) | 3,260 | ||||||||
| Contributions from minority partner |
— | 92 | 92 | |||||||||
| Distributions to member |
(4,010 | ) | — | (4,010 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Balance as of December 31, 2012 (Successor) |
$ | 6,335 | $ | 3 | $ | 6,338 | ||||||
|
|
|
|
|
|
|
|||||||
See accompanying notes.
F-5
Table of Contents
Health Plan Intermediaries, LLC and Subsidiaries
d/b/a Health Insurance Innovations
Consolidated Statements of Cash Flows
(in thousands)
| Successor | Predecessor | |||||||||||||
| Year Ended December 31, 2012 |
Three-Month Period Ended December 31, 2011 |
Nine-Month Period Ended September 30, 2011 |
||||||||||||
| Operating activities |
||||||||||||||
| Net income |
$ | 3,260 | $ | 531 | $ | 1,842 | ||||||||
| Adjustments to reconcile net income to net cash provided by operating activities: |
||||||||||||||
| Depreciation and amortization |
1,012 | 269 | 29 | |||||||||||
| Amortization of deferred financing costs |
44 | 13 | — | |||||||||||
| Change in operating assets and liabilities: |
||||||||||||||
| Increase in cash held on behalf of others |
(809 | ) | (204 | ) | (414 | ) | ||||||||
| (Increase) decrease in credit card transactions receivable |
(62 | ) | 17 | (461 | ) | |||||||||
| (Increase) decrease in accounts receivable |
(19 | ) | 94 | (179 | ) | |||||||||
| Increase in advanced commissions |
(273 | ) | (24 | ) | — | |||||||||
| Decrease (increase) in gateway processor deposit |
400 | — | (400 | ) | ||||||||||
| (Increase) decrease in prepaid expenses and other current assets |
(76 | ) | (119 | ) | 83 | |||||||||
| Increase (decrease) in carriers and vendors payable |
536 | (156 | ) | 1,267 | ||||||||||
| Increase (decrease) in accounts payable, accrued and deferred expenses |
919 | 18 | (182 | ) | ||||||||||
| Increase in commissions payable |
277 | 45 | 412 | |||||||||||
| Increase in other liabilities |
259 | — | — | |||||||||||
| (Decrease) increase in amounts due to member |
(126 | ) | 126 | (360 | ) | |||||||||
|
|
|
|
|
|
|
|||||||||
| Net cash provided by operating activities |
5,342 | 610 | 1,637 | |||||||||||
| Investing activities |
||||||||||||||
| Purchases of property and equipment |
(141 | ) | (24 | ) | (38 | ) | ||||||||
| Loan to distributor |
(245 | ) | — | — | ||||||||||
| Proceeds from repayment of loan to distributor |
135 | — | — | |||||||||||
| Payments made on business acquisition |
— | (5,330 | ) | — | ||||||||||
|
|
|
|
|
|
|
|||||||||
| Net cash used in investing activities |
(251 | ) | (5,354 | ) | (38 | ) | ||||||||
| Financing activities |
||||||||||||||
| Proceeds from issuance of long-term debt |
— | 4,250 | — | |||||||||||
| Principal payments on notes payable |
(67 | ) | — | — | ||||||||||
| Proceeds from issuance of notes payable |
100 | — | — | |||||||||||
| Principal payments on long-term debt |
(768 | ) | (188 | ) | — | |||||||||
| Payment of financing costs |
— | (135 | ) | — | ||||||||||
| Payment of fees for equity issuance |
(1,009 | ) | — | — | ||||||||||
| Payment of noncompete obligation |
(62 | ) | ||||||||||||
| Payments on capital leases |
(8 | ) | (1 | ) | (4 | ) | ||||||||
| Capital contribution |
— | 1,135 | — | |||||||||||
| Proceeds from issuance of noncontrolling interest in subsidiaries |
92 | — | — | |||||||||||
| Distributions to member |
(3,237 | ) | — | (1,301 | ) | |||||||||
|
|
|
|
|
|
|
|||||||||
| Net cash (used in) provided by financing activities |
(4,959 | ) | 5,061 | (1,305 | ) | |||||||||
|
|
|
|
|
|
|
|||||||||
| Net increase in cash |
132 | 317 | 294 | |||||||||||
| Cash at beginning of period |
618 | 301 | 7 | |||||||||||
|
|
|
|
|
|
|
|||||||||
| Cash at end of period |
$ | 750 | $ | 618 | $ | 301 | ||||||||
|
|
|
|
|
|
|
|||||||||
| Supplemental disclosures of cash flow information |
||||||||||||||
| Cash paid for interest |
$ | 198 | $ | 56 | $ | — | ||||||||
|
|
|
|
|
|
|
|||||||||
| Supplemental disclosure of non-cash investing and financing activities |
||||||||||||||
| Software acquired through accounts payable |
$ | 45 | $ | — | $ | — | ||||||||
|
|
|
|
|
|
|
|||||||||
| Purchase of insurance through premium financing agreement |
$ | 21 | $ | — | $ | — | ||||||||
|
|
|
|
|
|
|
|||||||||
| Noncompete agreement acquired through issuance of long-term payable |
$ | 843 | $ | — | $ | — | ||||||||
|
|
|
|
|
|
|
|||||||||
| Capitalized offering costs in accounts payable and accrued expenses |
$ | 810 | $ | — | $ | — | ||||||||
|
|
|
|
|
|
|
|||||||||
| Declared but unpaid member distribution |
$ | 773 | $ | — | $ | — | ||||||||
|
|
|
|
|
|
|
|||||||||
See accompanying notes.
F-6
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements
December 31, 2012
| 1. | Organization, Basis of Presentation, and Summary of Significant Accounting Policies |
Description of the Company
Health Plan Intermediaries, LLC, which operates under the name Health Insurance Innovations (“the Company”), is a developer and administrator of affordable individual health insurance and discount benefit plans that are sold throughout the United States. The Company’s main product, short-term medical (“STM”) insurance, is an alternative to traditional individual major medical plans and generally offers comparable benefits for qualifying individuals. The Company also offers guaranteed-issue hospital indemnity plans for individuals under the age of 65 and a variety of ancillary products that are frequently purchased together with the STM and hospital indemnity plans as supplements. The Company designs and structures insurance products on behalf of the Company’s contracted insurance carrier companies; markets them to individuals through a network of distributors; and manages the member relationship through customer service agents. The Company’s sales are primarily executed online and offer real-time fulfillment through a proprietary web-based technology platform, through which the Company receives credit card and automated clearing house payments directly from the purchasing customers, whom are referred to as “members,” at the time of sale. In certain cases, premiums are collected from the distributor. The plans are underwritten by contracted insurance carrier companies, and the Company assumes no underwriting or insurance risk.
Noncontrolling interests are included in the consolidated balance sheet within equity separate from the Company’s equity. The Company reports consolidated net income inclusive of both the Company’s and the noncontrolling interests’ shares and, separately, the amounts of consolidated net income attributable to the Company and noncontrolling interests.
The Company was formed as a Florida limited liability company in April 2003. On August 21, 2008, the Naylor Group Partners, LLC (“Naylor”) made a capital contribution to the Company in exchange for a 50% ownership interest in the Company. On September 28, 2011, the Company purchased all of the units owned by Naylor for $5,330,000, plus deferred financing costs of $135,000. The Company financed a portion of the purchase by entering into a loan agreement with a bank for $4,250,000. The remaining purchase price was funded with the Company’s cash and a capital contribution from Michael Kosloske (“Kosloske”), the current sole member of the Company.
In June 2012, the Company and a minority partner acquired the Insurance Center for Excellence (“ICE” or “Insurance Academy”), a marketing call center. The Company owns an 80% interest in ICE, which has been consolidated in the accompanying consolidated financial statements.
On October 26, 2012, Health Insurance Innovations, Inc. was incorporated in the State of Delaware to facilitate the Company’s recently completed initial public offering (“IPO”).
On November 7, 2012, interests in the assets and liabilities of the Company were transferred to two subsidiaries, Health Plan Intermediaries Holdings, LLC (99.0099%) and Health Plan Intermediaries Subsidiary, LLC (0.9901% each of which was created in October 2012).
On November 8, 2012, a capital contribution of $12,010 was made to Health Plan Intermediaries Subsidiary, LLC from Health Plan Intermediaries II, LLC, a related party, and that cash along with the 0.9901% interest was contributed by Health Plan Intermediaries Subsidiary, LLC to Health Plan Intermediaries Holdings, LLC in exchange for a 1.0% interest in Health Plan Intermediaries Holdings, LLC.
Health Insurance Innovations, Inc. sold 4,666,667 shares of common stock for $14.00 per share in an IPO on February 13, 2013. Simultaneous with the offering, Health Insurance Innovations, Inc. obtained a 35% membership interest, 35% economic interest and 100% of the voting interest in Health Plan Intermediaries Holdings, LLC.
Upon completion of the offering, Health Insurance Innovations, Inc. became a holding company the principal asset of which is its interest in Health Plan Intermediaries Holdings, LLC. All of Health Insurance Innovations, Inc. business will be conducted through Health Plan Intermediaries Holdings, LLC. Health Insurance Innovations, Inc. will be the sole managing member of Health Plan Intermediaries Holdings, LLC and will therefore have 100% of the voting rights and control.
Basis of Presentation
The consolidated financial statements include the accounts of the Company and its wholly owned and majority controlled subsidiaries. Intercompany accounts and transactions have been eliminated in consolidation.
F-7
Table of Contents
The September 2011 business acquisition was accounted for as a purchase and the purchase price was “pushed down” to the Company’s financial statements. When using the push-down basis of accounting, the acquired company’s financial statements reflect the new accounting basis recorded by the acquirer. Accordingly, purchase accounting adjustments have been reflected in the Company’s financial statements for the period commencing on October 1, 2011. The new basis of accounting reflects the estimated fair value of the Company’s assets and liabilities as of the date of the transaction. The Company used October 1, 2011, as the effective date of the transaction, since the operating activity between that date and the September 28, 2011 transaction date was not material.
The Company, as it existed prior to the October 1, 2011 acquisition, is referred to as “Predecessor.” The Company, as it existed on and after October 1, 2011, is referred to as the “Successor.”
The accompanying Predecessor historical financial statements for the periods ended September 30, 2011 and prior represent the financial position and corporate structure as of the dates indicated. The Predecessor’s financial statements are presented at historical cost values and do not reflect the effects of the Company’s new capital structure (debt and ownership) and accounting for the acquired intangible assets and goodwill. Therefore, the result of operations, changes in member’s equity, and cash flows for the predecessor and successor periods are not comparable.
The accompanying financial statements have been prepared in accordance with U.S. generally accepted accounting principles (“GAAP”).
All dollar amounts in the footnotes are rounded to the nearest thousand.
Use of Estimates
The preparation of the financial statements in conformity with GAAP requires management to make estimates, judgments, and assumptions that affect the reported amounts of assets and liabilities at the date of the financial statements. These estimates also affect the reported amounts of revenue and expenses during the reporting periods. Actual results could differ from those estimates.
Revenue Recognition
The Company’s revenues consist of commissions earned for health insurance policies and discount benefit plans issued to members, enrollment fees paid by members, and administration fees paid by members as a direct result of the Company’s enrollment services. The member’s payment includes a combination of risk premium, fees for discount benefit plans, fees for distributors and an enrollment fee, which are collectively referred to as “Premium equivalents.” Revenues reported by the Company are net of premiums remitted to insurance carriers and fees paid for discount benefit plans. Commissions and fees attributable to the sale of six- or 12-month STM plans and hospital indemnity policies represent substantially all of the Company’s revenue for the periods presented. Revenues are net of an allowance for policies expected to be cancelled by members during a limited cancellation period. The Company establishes the allowance for estimated policy cancellations through a charge to revenues. The allowance is estimated using historical data to project future experience. Such estimates and assumptions could change in the future as more information becomes known, which could impact the amounts reported. The Company periodically reviews the adequacy of the allowance and records adjustments as necessary. The net allowance for estimated policy cancellations as of December 31, 2012 (Successor) was $77,000.
Revenue is earned at the time of sale. Commission rates for all of the Company’s products are agreed to in advance with the relevant insurance carrier and vary by carrier and policy type. Under the Company’s carrier compensation arrangements, the commission rate schedule that is in effect on the policy effective date governs the commissions over the life of the policy. In addition, the Company earns enrollment and administration fees on policies issued. All amounts due to insurance carriers and discount benefit vendors are reported and paid to them according to the procedures provided for in the contractual agreements between the Company and the individual carrier or vendor. Risk premiums are typically reported and remitted to insurance carriers on the 15th of the month following the end of the month in which they are collected.
In concluding that revenues should be reported on a net basis, the Company considered Financial Accounting Standards Board (“FASB”) requirements and whether it has the responsibility to provide the goods or services to the customer or if it relies on a supplier to provide the goods or services to the customer. The Company is not the ultimate party responsible for providing the insurance coverage or discount benefits to the member and, therefore, the Company is not the primary obligor in the arrangement. The supplier, or insurance carrier, bears the risk for that insurance coverage. The Company therefore reports its revenues net of amounts paid to its contracted insurance carrier companies and discount benefit vendors.
Third-Party Commissions
The Company utilizes a broad network of licensed third-party distributors to sell the plans developed by the Company. The Company pays commissions to these distributors based on a percentage of the policy premium that varies by type of policy. The Company pays fees to the distributors for discount benefit plans issued.
F-8
Table of Contents
Cash Held on Behalf of Others
In the Company’s capacity as the policy administrator, the Company collects premiums from members and distributors and, after deducting the Company’s earned commissions, remits these premiums to the Company’s contracted insurance carriers, discount benefit vendors and distributors. The Company holds the unremitted funds in a fiduciary capacity until they are disbursed and the use of such funds is restricted. The Company holds these funds in bank accounts. These unremitted amounts are reported as cash held on behalf of others in the accompanying consolidated balance sheet with the related liabilities reported as carriers and vendors payable and commissions payable. Cash held on behalf of others at December 31, 2012 (Successor) was approximately $3,839,000.
Accounts Receivable
Accounts receivable represent amounts due to the Company for premiums collected by a third party and are generally considered delinquent 15 days after the due date. The underlying insurance contracts are cancelled retroactively if the payment remains delinquent. The Company has not experienced any credit losses from accounts receivable and has not recognized a provision for uncollectible accounts receivable.
Credit Card Transactions Receivable
Members may pay their policy premiums to the Company by credit card or through automatic check withdrawal (“ACH”) transfers. The credit card vendor remits cash for these transactions to the Company periodically. Credit card transactions processed by the credit card vendor, but not yet remitted to the Company are recorded as credit card transactions receivable. A portion of the amount receivable from these transactions is related to carrier premiums, discount benefit plan fees, and commissions. The balance related to carrier premiums, discount benefit plan fees, and commissions was $484,000 as of December 31, 2012 and is included in credit card transactions receivable on the accompanying balance sheet.
The Company incurs fees for these transactions that are expensed as incurred.
Advanced Commissions
Advanced commissions consist of amounts advanced to certain third-party distributors. The Company began advancing commissions in November 2011. The Company performs ongoing credit evaluations of their distributors, all of which are located in the United States. The Company recovers the advanced commissions from future commissions earned on premiums collected. The Company has not experienced any credit losses from commission advances and accordingly, has not recognized any provision for bad debt expense for the periods presented. A fee for the advanced commission of up to 2% of the insurance premium sold is charged to the distributors and recognized as interest income as earned. The interest income earned from advanced commissions for the year ended December 31, 2012 (Successor) and period ended December 31, 2011 (Successor) was approximately $35,000 and $2,000, respectively. There was no interest income earned from advanced commissions for the period ending September 30, 2011 (Predecessor). Advanced commissions outstanding as of December 31, 2012 (Successor) totaled approximately $297,000.
Capitalization of Offering Costs
Capitalized offering costs are costs directly attributable to the Company’s offering of its equity securities. The Company’s capitalized offering costs as of December 31, 2012 (Successor) were approximately $1,819,000.
Property and Equipment
Property and equipment is recorded at cost, less accumulated depreciation, in the accompanying consolidated balance sheet. As a result of the acquisition and the related application of purchase accounting to the acquired assets and liabilities, there is a new basis of property and equipment subsequent to the acquisition date. See Note 2 for a discussion of the new basis of accounting for property and equipment. Depreciation expense for property and equipment is computed using the straight-line method over the following estimated useful lives:
| Computer equipment | 5 years | |
| Furniture and fixtures | 7 years | |
| Leasehold improvements | Shorter of the lease term or estimated useful life |
The Company periodically reviews long-lived assets for impairment whenever events or changes in business circumstances indicate that the carrying value of the assets may not be recoverable. No impairment losses were recognized for the periods presented.
F-9
Table of Contents
Goodwill and Other Intangible Assets
Goodwill
Under the FASB guidance, the process of evaluating the potential impairment of goodwill involves a two-step process and requires significant judgment at many points during the analysis. In the first step, the Company determines whether there is an indication of impairment by comparing the fair value of the reporting unit to its carrying amount, including goodwill. The Company’s annual impairment test is performed with a measurement date of October 1. If, based on the first step, the Company determines that there is an indication of goodwill impairment, the Company assesses the impairment in step two in accordance with the FASB guidance.
In the first step, the Company determines the fair value using a combination of three valuation approaches: the cost approach, the market approach and the income approach. The cost approach uses multiples from publicly available transactional data of acquired comparable target companies. Transactions are identified that have occurred over the past three years in the subject company’s industry.
The market approach uses a guideline company methodology which is based upon a comparison of the reporting unit to similar publicly-traded companies within the Company’s industry. The Company derives a market value of invested capital or business enterprise value for each comparable company by multiplying the price per share of common stock of the publicly traded companies by their total common shares outstanding and adding each company’s current level of debt. The Company calculates a business enterprise multiple based on revenue and earnings from each company, then apply those multiples to the Company’s revenue and earnings to calculate a business enterprise value. Assumptions regarding the selection of comparable companies are made based on, among other factors, capital structure, operating environment and industry. As the comparable companies were typically larger and more diversified than our business, multiples were adjusted prior to application to the Company’s revenues and earnings to reflect differences in margins, long-term growth prospects and market capitalization.
The income approach uses a discounted debt-free cash flow analysis to measure fair value by estimating the present value of future economic benefits. To perform the discounted debt-free cash flow analysis, the Company develops a pro forma analysis of the reporting unit to estimate future available debt-free cash flow and discounting estimated debt-free cash flow by an estimated industry weighted average cost of capital based on the same comparable companies used in the market approach. Per the FASB guidance, the weighted average cost of capital is based on inputs (e.g., capital structure, risk, etc.) from a market participant’s perspective and not necessarily from the reporting unit’s perspective. Future cash flow is projected based on assumptions for the Company’s economic growth, industry expansion, future operations and the discount rate, all of which require significant judgments by management.
After computing a separate business enterprise value under the above approaches, the Company applies a weighting to them to derive the business enterprise value of the reporting unit. The weightings are evaluated each time a goodwill impairment assessment is performed and give consideration to the relative reliability of each approach at that time. Based on these weightings, the Company calculated a business enterprise value for the reporting unit. The Company then added debt-free liabilities of the reporting unit to the calculated business enterprise value to derive an implied fair value of the reporting unit. The implied fair value is then compared to the reporting unit’s carrying value. Upon completion of the analysis in step one, the Company determined that the fair value of business exceeded its respective carrying value. As such, a step two analysis was not required.
Other intangible assets
Other intangible assets consist of in-force members, our brand, the carrier network, distributor relationships, capitalized software and a noncompete agreement. Finite-lived intangible assets are amortized over their useful lives from two to seven years.
Fair Value of Financial Instruments
The Company measures and reports financial assets and liabilities at fair value on a recurring basis. Fair value is defined as the exchange price that would be received for an asset or paid to transfer a liability (referred to as an exit price) in the principal or most advantageous market for the asset or liability in an orderly transaction between market participants on the measurement date. Valuation techniques used to measure fair value must maximize the use of observable inputs and minimize the use of unobservable inputs. The fair value of the Company’s financial assets and liabilities is determined by using three levels of input, which are defined as follows:
| Level 1: | Quoted prices in active markets for identical assets or liabilities | |
| Level 2: | Quoted prices in active markets for similar assets or liabilities, quoted prices for identical or similar assets or liabilities in markets that are not active, or inputs other than quoted prices that are observable for the asset or liability | |
| Level 3: | Unobservable inputs for the asset or liability | |
The categorization of a financial instrument within the valuation hierarchy is based upon the lowest level of input that is significant to the fair value measurement.
F-10
Table of Contents
The Company utilizes the market approach to measure the fair value of their financial assets. The Company’s long-term debt and non-compete obligation are valued based on Level 2 inputs, and primarily valued using quoted market prices for similar instruments and nonbinding market prices that are corroborated by observable market data. The inputs and fair value are reviewed for reasonableness and may be further validated by comparison to publicly available information or compared to multiple independent valuation sources.
The carrying amounts of financial assets and liabilities reported in the accompanying consolidated balance sheet for cash, cash held on behalf of others, credit card transactions receivable, accounts receivable, advanced commissions, carriers and vendors payable, commissions payable, and accounts payable and accrued expenses at December 31, 2012 (Successor) approximate fair value because of the short-term duration of these instruments. See Note 5 to the consolidated financial statements for further discussion of the Company’s borrowings outstanding under debt agreements.
The Company’s long-term debt and noncompete obligation measured at fair value were as follows:
| Fair Value Measurements at December 31, 2012 (Successor) |
||||||||||||||||
| Carrying Value at December 31, 2012 (Successor) |
Level 1 | Level 2 | Level 3 | |||||||||||||
| Long-term debt, including current portion |
$ | 3,294,000 | $ | — | $ | 3,314,000 | $ | — | ||||||||
| Noncompete obligation, including current portion |
781,000 | — | 779,000 | — | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| $ | 4,075,000 | $ | — | $ | 4,093,000 | $ | — | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||
Recent Accounting Pronouncements
In December 2011, the FASB issued guidance which requires disclosures of both gross and net information about instrument and transactions eligible for offset as well as transactions subject to an agreement similar to a master netting agreement. This guidance is effective for annual periods beginning on or after January 1, 2013 and interim periods within those annual periods and must be applied retrospectively. As this guidance is limited to presentation only, adoption of this guidance is not expected to have a material impact on the Company’s financial position or results of operations.
In July 2012, the FASB issued amended guidance relating to goodwill and other intangible assets which permits an entity to first assess qualitative factors to determine whether it is more likely than not that an indefinite-lived intangible asset is impaired as a basis for determining whether it is necessary to perform the quantitative impairment test in accordance with GAAP. The more-likely-than-not threshold is defined as having a likelihood of more than 50%. If, after assessing the totality of events and circumstances, an entity concludes that it is not more likely than not that the indefinite-lived intangible asset is impaired, then no further action is required. This guidance is effective as of January 1, 2013 with early adoption permitted. Since this guidance only changes the manner in which the Company assess indefinite-lived intangible assets for impairment, adoption is not expected to have a material effect on the Company’s financial position or results of operations.
| 2. | Business Acquisitions |
Acquisition of Naylor ownership
On September 28, 2011, the Company purchased the member units owned by Naylor, which represented a 50% ownership interest in the Company, for $5,330,000 plus financing costs of $135,000. The Company financed a portion of the purchase price by entering into a loan agreement with a bank for $4,250,000. The remaining purchase price was funded with the Company’s cash and a contribution from Michael Kosloske, the current sole member of the Company.
The amount of the purchase price that exceeded the fair value of the net identified tangible and intangible assets acquired is recorded as goodwill. The purchase price was allocated to the assets acquired and liabilities assumed based on their respective fair values.
F-11
Table of Contents
The following table summarizes the allocation of the purchase price for the Company’s business acquisition as of September 28, 2011:
| Cash |
$ | 3,127,000 | ||
| Receivables |
891,000 | |||
| Deposits |
406,000 | |||
| Property and equipment, net |
112,000 | |||
| Carriers payable |
(2,410,000 | ) | ||
| Commissions payable |
(1,210,000 | ) | ||
| Accrued expenses and other liabilities |
(452,000 | ) | ||
| Intangible asset—in-force insureds |
240,000 | |||
| Intangible asset—brand |
400,000 | |||
| Intangible asset—carrier network |
40,000 | |||
| Intangible asset—distributor relationships |
3,610,000 | |||
| Goodwill |
5,906,000 | |||
|
|
|
|||
| Total fair value |
$ | 10,660,000 | ||
|
|
|
Acquisition of Insurance Center for Excellence, LLC
On June 1, 2012, the Company and TSG Agency, LLC (“TSG”) acquired ICE. ICE is a call center training facility for the Company’s distributors. In connection with the transaction, the Company received an 80% controlling interest in ICE and was required to contribute $80,000 in capital contributions, and TSG received a 20% noncontrolling interest in the business and was required to contribute $20,000 in capital contributions. Subsequent to the initial contributions, the Company contributed an additional $240,000, and TSG contributed an additional $60,000, respectively, to ICE during the year ended December 31, 2012. As of December 31, 2012, the Company’s total investment in ICE is $320,000, representing and 80% controlling interest. As of December 31, 2012 (Successor), the required contributions by the controlling and noncontrolling interests were met.
Insurance Academy entered into employment agreements with employees of The Amacore Group, Inc. (“Amacore”) contemporaneously with the June 1, 2012 formation of ICE, and at the date of formation, former Amacore employees comprise the full staff of Insurance Academy. Insurance Academy additionally assumed a month-to-month lease for space that was occupied by Amacore immediately prior to the formation of Insurance Academy.
Concurrent with the formation of ICE, ICE additionally entered into a sublease agreement (“Lease Agreement”) with Amacore for additional space effective June 1, 2012. Under the Lease Agreement, ICE assumed all rights, responsibilities, obligations, terms and conditions of the original lease, which expires on April 30, 2015. Amacore agreed to transfer to ICE a security deposit previously paid by Amacore of approximately $13,000; Amacore contributed $15,000 to ICE for the purchase of property and equipment; and Amacore contributed certain office and computer equipment, and rights to certain 800 numbers, to Insurance Academy that have minimal value. The Company is recognizing the consideration provided by Amacore as a lease incentive that is being amortized over the term of the lease on a straight-line basis.
Additionally, concurrent with the June 1, 2012 formation of Insurance Academy, ICE entered into an Agent Producer Agreement and an Assignment of Commissions Agreement with Amacore (“collectively referred to as Agent Agreement”). Under the Agent Agreement, ICE assigned its commissions with respect to Assurant dental sales to Amacore in return for production incentives, training, marketing materials, commission payments and reporting, advances on commissions and ongoing sales support.
The transaction with Amacore as described above is a business combination, and no assets or liabilities, including intangible assets or goodwill, were recognized other than those described above.
On March 14, 2013, we entered into an agreement to terminate certain contract rights with TSG. As a result of this transaction, Ivan Spinner, who controls TSG, became an employee of the Company. This transaction had no effect on our ownership percentage of control of ICE. See Note 16 for additional information on this transaction.
| 3. | Property and Equipment |
Property and equipment, net, are comprised of the following:
| December 31, 2012 (Successor) |
||||
| Computer equipment |
$ | 85,000 | ||
| Furniture and fixtures |
102,000 | |||
| Leasehold improvements |
84,000 | |||
|
|
|
|||
| Total property and equipment |
271,000 | |||
| Less accumulated depreciation |
(58,000 | ) | ||
|
|
|
|||
| Total property and equipment, net |
$ | 213,000 | ||
|
|
|
|||
F-12
Table of Contents
Depreciation expense, including depreciation related to assets acquired through capital leases, was approximately $52,000, $11,000 and $29,000, respectively, for the year ended December 31, 2012 (Successor), the three months ended December 31, 2011 (Successor) and the nine months ended September 30, 2011 (Predecessor).
| 4. | Goodwill and Intangible Assets |
The changes in the carrying amount of goodwill are as follows:
| Balance as of January 1, 2012 (Successor) |
5,906,000 | |||
| Goodwill acquired during the period |
— | |||
| Impairment of goodwill |
— | |||
|
|
|
|||
| Balance as of December 31, 2012 (Successor) |
$ | 5,906,000 | ||
|
|
|
Major classes of amortizable intangible assets at December 31, 2012 (Successor) consist of the following:
| Weighted- Average Amortization Period (In Years) |
Gross Carrying Amount |
Accumulated Amortization |
Intangible Asset, net |
|||||||||||||
| Distributor relationships |
7 | $ | 3,610,000 | $ | 645,000 | $ | 2,965,000 | |||||||||
| Carrier network |
5 | 40,000 | 10,000 | 30,000 | ||||||||||||
| Brand |
2 | 400,000 | 250,000 | 150,000 | ||||||||||||
| Capitalized software |
5 | 45,000 | 4,000 | 41,000 | ||||||||||||
| Noncompete agreement |
5 | 843,000 | 70,000 | 773,000 | ||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total intangible assets |
6.2 | $ | 4,938,000 | $ | 979,000 | $ | 3,959,000 | |||||||||
|
|
|
|
|
|
|
|||||||||||
Amortization expense for the year ended December 31, 2012 (Successor) and three months ended December 31, 2011 (Successor) was approximately $960,000 and $258,000, respectively. There was no amortization expense for the nine months ended September 30, 2011 (Predecessor).
Amortization expense expected to be recognized subsequent to December 31, 2012 (Successor) is as follows:
| 2013 |
$ | 851,000 | ||
| 2014 |
701,000 | |||
| 2015 |
701,000 | |||
| 2016 |
699,000 | |||
| 2017 |
619,000 | |||
| Thereafter |
388,000 | |||
|
|
|
|||
| Total |
$ | 3,959,000 | ||
|
|
|
| 5. | Debt |
During September 2011, the Company entered into a bank loan agreement with a principal balance of $4,250,000. The purpose of this credit loan was to finance a portion of the acquisition of the remaining 50% interest in the Company as discussed in Note 2. Borrowings under the facility are secured by all of the Company’s assets, including, but not limited to, cash accounts, accounts receivable, and property and equipment. The loan is further secured with a personal unlimited guarantee by Mr. Kosloske and certain real properties owned by Mr. Kosloske. The loan is a self-amortizing five-year loan bearing fixed interest at 5.25% with equal monthly payments of approximately $81,000, which consists of principal and interest. As of December 31, 2012 (Successor) a balance of $3,294,000 was outstanding, including current portions of $813,000.
The loan is subject to customary covenants and restrictions which, among other things, limit the Company’s ability to incur additional indebtedness. In addition, the loan agreement also includes certain nonfinancial covenants that would require immediate payment if the Company, among other things, reorganizes, merges, consolidates, or otherwise changes ownership or business structure without the bank’s prior written consent.
The loan agreement also contains customary representations and warranties and events of default. The payment of outstanding principal under the loan and accrued interest thereon may be accelerated and become immediately due and payable upon default of payment or failure to meet certain other performance obligations or failure to comply with other covenants in the loan agreement, subject to applicable notice requirements and cure periods as provided in the loan agreement.
F-13
Table of Contents
On August 11, 2012, the Company and Health Plan Intermediaries Holdings, LLC (“HPIH”) entered into an Assumption and Reaffirmation of Loan Documents and Consent to Assignment (“Assignment”) with the lender to conditionally transfer the loan from the Company to HPIH. The Assignment required two post-closing conditions to be met. The first condition was met on September 18, 2012. The second condition was met on November 7, 2012.
As of December 31, 2012 (Successor), the Company was in compliance with all applicable covenants.
Future principal payments on the loan subsequent to December 31, 2012 (Successor) are as follows:
| 2013 |
$ | 813,000 | ||
| 2014 |
857,000 | |||
| 2015 |
904,000 | |||
| 2016 |
720,000 | |||
|
|
|
|||
| Total minimum payments |
$ | 3,294,000 | ||
|
|
|
On February 13, 2013 the outstanding balance of the loan in the amount of $3,232,000 was repaid using a portion of the proceeds of the initial public offering of the common stock of Health Insurance Innovations, Inc. See Note 16 for further information on the initial public offering.
| 6. | Deferred Financing Costs |
Deferred financing costs which is included in other assets in the consolidated balance sheet consist primarily of consulting and legal fees directly related to the bank loan. These amounts are amortized over the life of the related debt using the effective interest rate method. Deferred financing costs reported on the consolidated balance sheet was approximately $78,000 as of December 31, 2012 (Successor). Amortization of the loan costs was approximately $44,000 for the year ended December 31, 2012 (Successor) and $13,000 for the nine months ended December 31, 2011 (Successor). There was no amortization for the nine months ended September 30, 2011 (Predecessor). The deferred financing costs were written off on February 13, 2013, when the Company repaid the term loan.
| 7. | Accounts Payable and Accrued Expenses |
Accounts payable and accrued expenses consisted of the following at:
| December 31, 2012 (Successor) |
||||
| Accounts payable |
$ | 735,000 | ||
| Accrued Interest |
12,000 | |||
| Accrued professional fees |
683,000 | |||
| Accrued refunds |
467,000 | |||
| Deferred salaries |
19,000 | |||
| Accrued wages |
90,000 | |||
| Accrued credit card/ACH fees |
56,000 | |||
|
|
|
|||
| Total accounts payable and accrued expenses |
$ | 2,062,000 | ||
|
|
|
|||
| 8. | Segments |
Operating segments are defined as components of an enterprise about which separate financial information is available that is evaluated regularly by the chief operating decision-maker, or decision-making group, in deciding how to allocate resources and in assessing performance of the Company. The Company’s chief operating decision-maker is considered to be the chief executive officer (“CEO”). The CEO reviews the Company’s financial information in a manner substantially similar to the accompanying consolidated financial statements. In addition, the Company’s operations, revenues, and decision-making functions are based solely in the United States. Therefore, management has concluded that the Company operates in one operating and geographic segment.
| 9. | Related-Party Transactions |
On August 22, 2012, the Company entered into a promissory note with Ivan Spinner who controls TSG, the 20% owner of ICE, in the amount of $100,000 for the purpose of funding advanced commissions. The note is non-interest bearing and requires equal monthly payments of $25,000 beginning September 20, 2012 and ending December 20, 2012. This loan was modified on October 18, 2012 whereby the November and December payments were deferred to January 2, 2013 and February 1, 2013, respectively.
F-14
Table of Contents
Under an employment agreement, Kosloske received compensation from prescription contracts plus commissions based on annual revenues. This compensation was treated as guaranteed payments during the Predecessor periods. The agreement was terminated in conjunction with the acquisition discussed in Note 2. The guaranteed payment expense totaled approximately $615,000 for the Predecessor period ended September 30, 2011 and was recorded as general and administrative expenses in the consolidated statements of operations.
As of December 31, 2012 (Successor), $773,000 was due to the member.
The Company incurred management fees for accounting and administrative services performed by Naylor, in the amount of $93,000, which are included in general and administrative expenses on the consolidated statements of operations for the nine months ended September 30, 2011 (Predecessor).
| 10. | Commitments and Contingencies |
Call and Put Option for ICE
In accordance with the ICE operating agreement, the Company has the right of first refusal to purchase any membership units that another member may desire to transfer. Written notice shall be provided to the Company and contain a full description of the proposed transfer including the type of transfer, the units of the proposed transfer, purchase price and payment method of proposed transfer, and the true identity of the parties involved in the proposed transfer. If the Company desires to purchase all or a portion of the units proposed to be transferred, it must give a binding written notice of the exercise of its option along with the specific number of units it intends to purchase. The Company shall have 60 days after it provides notice to close the purchase.
In the event of Ivan Spinner’s death or disability or a change of control of TSG (“Termination Event”), the Company additionally has the option to repurchase all the membership units of TSG or its affiliates. At any time a TSG Affiliate (i.e., TSG, Ivan Spinner and any permitted transferee of TSG or Ivan Spinner, collectively referred to as “TSG Affiliates”) may elect to sell to the Company all of the units owned by the TSG Affiliates by delivering a single written notice to the Company. The Company then has a period of 10 days following receipt of such notice by delivering a written notice to TSG to either (1) elect to purchase all of the TSG Affiliate units or (2) elect to sell to TSG all of the units owned by the Company and its permitted transferees. In the event the Company does not deliver the aforementioned notice, then the Company shall be deemed to have agreed to purchase all of the TSG Affiliate units. Transfers with respect to a Termination Event or TSG Affiliate are based upon fair market value as determined by a nationally recognized independent appraiser.
BimSym Agreements
On August 1, 2012, the Company entered into a software assignment agreement (“Agreement”) with BimSym eBusiness Solutions, Inc. (“BimSym”) for the Company’s exclusive ownership of all rights, title and interest in the technology platform (“A.R.I.E.S. System”) developed by BimSym and utilized by the Company. As a result of the executed Agreement, the Company purchased the A.R.I.E.S. System for $45,000 of which $30,000 remains to be paid and is recorded as an accounts payable and accrued expense on the accompanying consolidated balance sheet as of December 31, 2012 (Successor). The consideration of $45,000 was capitalized and recorded as an intangible asset. In connection with this agreement, the Company simultaneously entered into a master services agreement for the technology, under which the Company is required to make monthly payments of $26,000 for 5 years. After the five-year term, this agreement automatically renews for one-year terms unless 60 days’ notice is given by the Company.
Additionally, the Company also entered into an exclusivity agreement with BimSym whereby neither BimSym nor any of its affiliates will create, market or sell a software, system or service with the same or similar functionality as that of A.R.I.E.S. System under which the Company is required to make monthly payments of $16,000 for 5 years. The present value of these payments has been capitalized and recorded as an intangible asset with a corresponding liability, on the accompanying consolidated balance sheet as of December 31, 2012 (Successor).
Legal Proceedings
As of December 31, 2012 (Successor), the Company had no significant outstanding legal proceedings. The Company is subject to certain legal proceedings and claims that may arise in the ordinary course of business. In the opinion of management, the Company does not have a potential liability related to any current legal proceedings and claims that would individually, or in the aggregate, have a material adverse effect on the Company’s financial condition, liquidity, results of operations, or cash flows.
| 11. | Concentrations of Credit Risk and Significant Customers |
Financial instruments that are potentially subject to concentrations of credit risk consist primarily of cash, credit card transactions receivable, accounts receivable, and advanced commissions.
F-15
Table of Contents
Cash is maintained in noninterest-bearing accounts at depository institutions and amounts held at these institutions were fully insured by the Federal Deposit Insurance Corporation as of December 31, 2012 (Successor).
The Company generally does not require collateral for credit card transactions receivable or accounts receivable. However, advanced commissions are collateralized by renewal commissions. The Company has not experienced any credit losses related to these receivables and advances.
Advanced commissions were approximately $297,000 as of December 31, 2012 (Successor). As of December 31, 2012 (Successor) a single agency comprised 37% of the advanced commissions balance.
Accounts receivable were approximately $273,000 as of December 31, 2012 (Successor). As of December 31, 2012 (Successor), a single distributor made up 83% of the accounts receivable balance.
Revenues consist of commissions earned for health insurance policies and discount benefit plans issued to members, enrollment fees paid by members, and monthly administration fees paid by members as a direct result of enrollment services provided by the Company. None of the Company’s members individually accounted for 10% or more of the Company’s revenue for the year ended December 31, 2012 (Successor), three-month period ended December 31, 2011 (Successor), or nine-month period ended September 30, 2011 (Predecessor).
During the year ended December 31, 2012 (Successor), three carriers represented 46%, 25% and 22% of premium equivalents, respectively.
| 12. | Capital Lease Obligations |
The Company has entered into capital lease obligations to finance certain equipment. The leases have terms expiring beginning in 2015. As of December 31, 2012 (Successor), future cash payment commitments related to these leases are as follows:
| 2013 |
$ | 3,000 | ||
| 2014 |
3,000 | |||
| 2015 |
1,000 | |||
|
|
|
|||
| Total minimum lease payments |
7,000 | |||
| Less amounts representing interest |
— | |||
|
|
|
|||
| Total capital lease obligations |
$ | 7,000 | ||
|
|
|
| 13. | Operating Leases |
The Company leases office facilities under an operating lease, which expires in 2015. The operating lease agreement contains rent holidays and rent escalation provisions. Rent holidays and rent escalation provisions are considered in determining straight-line rent expense to be recorded over the lease term. The difference between cash rent payments and straight-line rent expense was approximately $63,000 as of December 31, 2012 (Successor).
Total rent expense under all operating leases, which includes equipment for the was approximately $193,000, $28,000 and $78,000, for the year ended December 31, 2012 (Successor) and the three months ended December 31, 2011 (Successor) and the nine months ended September 30, 2011 (Predecessor), respectively, and is included in general and administrative expenses in the accompanying consolidated statements of operations.
As of December 31, 2012 (Successor), the future minimum lease payments under noncancellable operating leases were as follows:
| 2013 |
$ | 222,000 | ||
| 2014 |
226,000 | |||
| 2015 |
107,000 | |||
| 2016 |
1,000 | |||
|
|
|
|||
| Total minimum lease payments |
$ | 556,000 | ||
|
|
|
| 14. | Income Tax |
The Company was treated as a partnership for tax purposes prior to the change in ownership on September 28, 2011. Subsequently, the Company became a single-member LLC treated as a disregarded entity not separate from its owner for income tax purposes. Income tax for the Company for both its time as a partnership and then as a single-member LLC, is the responsibility of its member. As a result, no provision for income taxes is reflected in the accompanying consolidated financial statements. On January 1, 2012, the Company elected to be taxed as an S Corporation under the provisions of the Internal Revenue Code. Furthermore, on November 7, 2012, the Company transferred all of its assets and liabilities to Health Plan Intermediaries Holdings, LLC, in exchange
F-16
Table of Contents
for a member interest therein. Health Plan Intermediaries Holdings, LLC is treated as a partnership for tax purposes. Income tax for Health Plan Intermediaries Holdings, LLC is the responsibility of its members (the Company and Health Plan Intermediaries Sub, LLC). Income tax for the Company during the period of the S Corporation election is the responsibility of its shareholder. As a result, no provision for income taxes is reflected in the accompanying consolidated financial statements either for the Company or for Health Plan Intermediaries Holdings, LLC. Net income for financial statement purposes may differ significantly from taxable income attributable to members as a result of differences between the tax basis and the financial reporting basis of assets and liabilities.
| 15. | Pro Forma Disclosure (Unaudited) |
Health Insurance Innovations, Inc. will operate and control all of the businesses and affairs of Health Plan Intermediaries Holdings, LLC. Under GAAP requirements related to consolidation, Health Plan Intermediaries Holdings, LLC meets the definition of a variable interest entity. Further, Health Insurance Innovations, Inc. will be the primary beneficiary of Health Plan Intermediaries Holdings, LLC as a result of its 100% voting power and control over Health Plan Intermediaries Holdings, LLC and as a result of its obligation to absorb losses and its right to receive benefits of Health Plan Intermediaries Holdings, LLC that could potentially be significant to Health Plan Intermediaries Holdings, LLC. As a result, Health Insurance Innovations, Inc. is expected to consolidate the financial results of Health Plan Intermediaries Holdings, LLC and record a noncontrolling interest for the economic interest in Health Plan Intermediaries Holdings, LLC held by the existing members to the extent that the book value of their interest in Health Plan Intermediaries Holdings, LLC is greater than zero. Health Insurance Innovations, Inc.’s and the noncontrolling membership pro forma economic interest in Health Plan Intermediaries Holdings, LLC is estimated to be 35% and 65%, respectively, as of December 31, 2012. Pro forma net income attributable to the noncontrolling interest on the statements of operations represents the portion of earnings or loss attributable to the economic interest in Health Plan Intermediaries Holdings, LLC held by the noncontrolling members. Noncontrolling interest on the balance sheet represents the portion of net assets of Health Plan Intermediaries Holdings, LLC attributable to the noncontrolling members based on total membership interest of Health Plan Intermediaries Holdings, LLC owned by such members.
The Company has elected to be taxed as an S-Corporation under the provisions of the Internal Revenue Code. The Company directly sustained business operations until November 7, 2012, and indirectly receives, together with Health Plan Intermediaries Sub, LLC, the entire share of business operations subsequent to that date. Accordingly, the Company, together with Health Plan Intermediaries Sub, LLC, continues to incur the entire share of business operations for the year ended December 31, 2012. The following unaudited pro forma information reflects the reconciliation between the estimated total statutory provision for income taxes and the total actual provision relating to the income tax expense that would have been incurred if the S-Corporation were subject to U.S. federal and state income taxes. The Company would account for income taxes under the provisions of FASB guidance, which requires recognition of deferred tax assets and liabilities for the expected future consequences of events that have been included in the financial statements or tax returns. Under this method, deferred income tax assets and liabilities are determined based on the difference between the financial statement and tax bases of assets and liabilities using enacted tax rates for the year in which the differences are expected to reverse. Further, the effect of a change in tax rates on deferred tax assets and liabilities under this method is recognized in income in the period that includes the enactment date.
Uncertain tax positions are recorded under this method on the basis of a two-step process whereby (1) the Company determines whether it is more likely than not that the tax positions will be sustained based on the technical merits of the position, and (2) for those tax positions that meet the more-likely-than-not recognition threshold, the Company recognizes the largest amount of tax benefit that is greater than 50 percent likely to be realized upon ultimate settlement with the related tax authority. Based on its analysis, the Company determined that the Company does not have any uncertain positions requiring recognition under this method. The Company accounts for interest and penalties under this method as a component of tax expense, and none were included in the Company’s financial statements as there are not uncertain tax positions outstanding as of December 31, 2012. The Company’s 2012 tax year remains subject to examination by tax authorities.
| Year
Ended December 31, 2012 (Successor) |
Three
Months Ended December 31, 2011 (Successor) |
Nine
Months Ended September 30, 2011 (Predecessor) |
||||||||||||
| Pro forma statutory tax provision |
$ | 1,139,000 | $ | 180,000 | $ | 626,000 | ||||||||
| State income taxes, net |
79,000 | 12,000 | 43,000 | |||||||||||
| Nondeductible expenses |
32,000 | 9,000 | 26,000 | |||||||||||
|
|
|
|
|
|
|
|||||||||
| Pro forma total provision for income taxes |
$ | 1,250,000 | $ | 201,000 | $ | 695,000 | ||||||||
|
|
|
|
|
|
|
|||||||||
The carrying value of the Company’s assets and liabilities recorded in the financial statements differs from the tax basis of its assets and liabilities primarily with respect to a $1,278,000 excess of financial statement basis over tax basis in intangible and fixed assets, and a $3,007,000 excess of financial statement basis over tax basis in goodwill.
Pro forma net income per common share outstanding: Pro forma basic and diluted net income per share was computed by dividing the pro forma net income attributable to our Class A stockholders by the 4,666,667 shares of Class A common stock and the vested shares of Mr. Hershberger’s Class A restricted stock grant. For
F-17
Table of Contents
the year ended December 31, 2011, there was no effect of dilutive restricted shares due to the pro forma net loss position. For the year ended December 31, 2012, the dilutive effect of the restricted shares was 61,478 shares. The shares of Class B common stock do not share in our earnings and are therefore not included in the weighted average shares outstanding or net income available per share.
| Year
Ended December 31, 2012 |
Year
Ended December 31, 2011 |
|||||||
| (Successor) | (Successor) | |||||||
| (in thousands, except shares and per share amounts) |
||||||||
| Pro forma net income (loss) |
$ | 1,418 | $ | (1,149 | ) | |||
| Net income (loss) attributable to noncontrolling interest |
980 | (747 | ) | |||||
|
|
|
|
|
|||||
| Net income (loss) attributable to Health Insurance Innovations, Inc. |
$ | 438 | $ | (402 | ) | |||
|
|
|
|
|
|||||
| Weighted average shares Class A common stock outstanding |
||||||||
| Basic |
4,906,667 | 4,826,667 | ||||||
| Diluted |
5,005,189 | 4,826,667 | ||||||
| Net income available to Class A common stock per share |
||||||||
| Basic |
$ | 0.09 | $ | (0.08 | ) | |||
| Diluted |
$ | 0.09 | $ | (0.08 | ) | |||
The pro forma adjustments above give effect to activities directly related to completion of the IPO on February 13, 2013. Certain events subsequent to that date were not considered events directly related to the IPO, but rather subsequent events that occurred in the first quarter of 2013 and part of normal, recurring operations and standard, ordinary compensation of members of our board of directors or other unanticipated subsequent events. Those events include the following:
| • | On March 8, 2013, the Compensation Committee approved equity awards for its executive officers and certain other senior management under the Company’s Long Term Incentive Plan. The equity awards consist of an aggregate of 78,500 shares of the Company’s Class A Common Stock. |
| • | On March 8, 2013, 100,000 shares of Class A common stock were issued through the over-allotment option. |
| • | On March 14, 2013, the Company entered into an agreement to terminate certain contract rights with TSG, a managing general agent of the Company, for an aggregate cash price of $5,500,000. |
| 16. | Subsequent Events |
Initial Public Offering of Health Insurance Innovations, Inc. Common Stock
On February 13, 2013, Health Insurance Innovations, Inc. completed an initial public offering by issuing 4,666,667 shares of its Class A common stock, par value $0.001 per share, at a price to the public of $14.00 per share common stock. In conjunction with the offering, Health Plan Innovations, Inc. obtained a 35% membership interest, a 35% economic interest and 100% of the voting interest in Health Plan Intermediaries Holdings, LLC.
The Company used $1,302,000 of the proceeds from the sale of shares through the over-allotment option to acquire Series B Membership Interests, together with an equal number of shares of our Class B common stock, from Health Plan Intermediaries, LLC, which is controlled by Mr. Kosloske, the Company’s Chairman, President and Chief Executive Officer, which Series B Membership Interests were immediately recapitalized into Series A Membership Interests.
Upon completion of the offering, Health Insurance Innovations, Inc. became a holding company, the principal asset of which is its interest in Health Plan Intermediaries Holdings, LLC. All of Health Insurance Innovations, Inc. business will be conducted through Health Plan Intermediaries Holdings, LLC. Health Insurance Innovations, Inc. will be the sole managing member of Health Plan Intermediaries Holdings, LLC and will have 100% of the voting rights and control.
Issuance of Equity Compensation Awards
On March 8, 2013, the Compensation Committee approved equity awards for its executive officers and certain other senior management under the Company’s Long Term Incentive Plan. The equity awards consist of an aggregate of 78,500 shares of the Company’s Class A Common Stock, of which 20% vest on each of the first through third anniversary dates of the grant date, and the balance vest on the fourth anniversary date of the grant date. The terms of the Company’s Long Term Incentive Plan and related equity awards were disclosed by the Company pursuant to the Company’s Current Reports on Form 8-K filed with the U.S. Securities and Exchange Commission on February 13, 2013 and March 14, 2013.
Termination of Certain Contract Rights
On March 14, 2013, the Company entered into an agreement to terminate certain contract rights with TSG, a managing general agent of the Company, for an aggregate cash price of $5,500,000. Pursuant to FASB guidance, the full amount plus transaction costs is expected to be expensed during the first quarter of 2013. We do not expect to incur any material future expenses associated with the transaction. In conjunction with this transaction, Ivan Spinner, who controls TSG, became an employee of the Company, and the Company maintained a majority interest in ICE.
F-18
Table of Contents
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| HEALTH INSURANCE INNOVATIONS, INC. | ||
| By: | /s/ Michael W. Kosloske | |
| Michael W. Kosloske | ||
| President and Chief Executive Officer | ||
| (Principal Executive Officer) | ||
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the Registrant and in the capacities and on the dates indicated.
| DATE |
SIGNATURE |
TITLE | ||
| April 1, 2013 |
/s/ Michael W. Kosloske |
Chairman of the Board of Directors, President and Chief Executive Officer (Principal Executive Officer) | ||
| Michael W. Kosloske | ||||
| April 1, 2013 |
/s/ Michael D. Hershberger |
Chief Financial Officer, Treasurer and Secretary (Principal Financial Officer) | ||
| Michael D. Hershberger | ||||
| April 1, 2013 |
/s/ Joan Rodgers |
Chief Accounting Officer (Principal Accounting Officer) | ||
| Joan Rodgers | ||||
| April 1, 2013 |
/s/ Paul E. Avery |
Lead Director | ||
| Paul E. Avery | ||||
| April 1, 2013 |
/s/ Anthony J. Barkett |
Director | ||
| Anthony J. Barkett | ||||
| April 1, 2013 |
/s/ Liana O’Drobinak |
Director | ||
| Liana O’Drobinak | ||||
| April 1, 2013 |
/s/ Gary Raeckers |
Director | ||
| Gary Raeckers | ||||
| April 1, 2013 |
/s/ Adelaide A. Sink |
Director | ||
| Adelaide A. Sink | ||||
| April 1, 2013 |
/s/ A. Gordon Tunstall |
Director | ||
| A. Gordon Tunstall | ||||
F-19
Table of Contents
HEALTH INSURANCE INNOVATIONS, INC. AND SUBSIDIARIES
EXHIBIT INDEX
| Page(s) | ||||
| Exhibit No. |
Description | |||
| 3.1 | Amended and Restated Certificate of Incorporation of Health Insurance Innovations, Inc. Incorporated by reference to Exhibit 3.1 of Form 8-K filed February 13, 2013. | |||
| 3.2 | Certificate of Correction to the Amended and Restated Certificate of Incorporation of Health Insurance Innovations, Inc. Incorporated by reference to Exhibit 3.2 of Form 8-K filed February 13, 2013. | |||
| 3.3 | Amended and Restated Bylaws of Health Insurance Innovations, Inc. Incorporated by reference to Exhibit 3.3 of Form 8-K filed February 13, 2013. | |||
| 4 | Registration Rights Agreement among Health Insurance Innovations, Inc. and the stockholders named therein. Incorporated by reference to Exhibit 4.1 of Form 8-K filed February 13, 2013. | |||
| 10.1 | Third Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC. Incorporated by reference to Exhibit 10.1 of Form 8-K filed February 13, 2013. | |||
| 10.2 | Contribution Agreement between Health Plan Intermediaries Holdings, LLC and Health Plan Intermediaries, LLC. Incorporated by reference to Exhibit 10.2 of the Draft Registration Statement on Form S-1 (File No. 333-00034 / Film No. 121193612) filed November 9, 2012. | |||
| 10.3 | Tax Receivable Agreement among Health Insurance Innovations, Inc., Health Plan Intermediaries Holdings, LLC and Series B Members of Health Plan Intermediaries Holdings, LLC. Incorporated by reference to Exhibit 10.2 of Form 8-K filed February 13, 2013. | |||
| 10.4 | Exchange Agreement among Health Insurance Innovations, Inc., Health Plan Intermediaries Holdings, LLC and Series B Members of Health Plan Intermediaries Holdings, LLC. Incorporated by reference to Exhibit 10.3 of Form 8-K filed February 13, 2013. | |||
| 10.5 | Loan Agreement between Health Plan Intermediaries, LLC and SunTrust Bank. Incorporated by reference to Exhibit 10.7 of the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121193612) filed November 9, 2012. | |||
| 10.6 | Master Service Agreement between Health Plan Intermediaries, LLC and BimSym eBusiness Solutions, Inc. Incorporated by reference to Exhibit 10.8 of the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121193612) filed November 9, 2012. | |||
| 10.7 | Software Assignment Agreement between Health Plan Intermediaries, LLC and BimSym eBusiness Solutions, Inc. Incorporated by reference to Exhibit 10.9 of the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121193612) filed November 9, 2012. | |||
| 10.8† | General Manager’s Agreement between Health Plan Intermediaries, LLC and Companion Life Insurance Company. Incorporated by reference to Exhibit 10.10 of the Second Submission to the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121245775) filed December 6, 2012. | |||
| 10.9† | Agency Agreement between Health Plan Intermediaries, LLC and Starr Indemnity & Liability Company. Incorporated by reference to Exhibit 10.11 of the Second Submission to the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film. No. 121245775) filed December 6, 2012. | |||
| 10.10 | Administrative Services Agreement among Health Plan Insurance Innovations, LLC, United States Fire Insurance Company and The North River Insurance Company. Incorporated by reference to Exhibit 10.12 of the Second Submission to the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121245775) filed December 6, 2012. | |||
| 10.11 | Marketing/Billing Agreement between Med-Sense Guaranteed Association and Health Insurance Innovations. Incorporated by reference to Exhibit 10.13 of the Second Submission to the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121245775) filed December 6, 2012. | |||
| 10.12# | Employment Agreement between Michael W. Kosloske and Health Insurance Innovations, Inc. Incorporated by reference to Exhibit 10.6 of Form 8-K filed February 13, 2013. | |||
| 10.13# | Employment and Non-Compete Agreement between Gary Raeckers and Health Plan Intermediaries, LLC. Incorporated by reference to Exhibit 10.16 of the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121193612) filed November 9, 2012. | |||
| 10.14# | Employment and Non-Compete Agreement between Scott Lingle and Health Plan Intermediaries, LLC. Incorporated by reference to Exhibit 10.17 of the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121193612) filed November 9, 2012. | |||
| 10.15# | Employment Agreement between Lori Kosloske and Health Insurance Innovations, Inc. Incorporated by reference to Exhibit 10.8 of Form 8-K filed February 13, 2013. | |||
Table of Contents
| Exhibit No. |
Description | |||
| 10.16# | Employment and Non-Compete Agreement between Bryan Krul and Health Plan Intermediaries, LLC. Incorporated by reference to Exhibit 10.19 of the Draft Registration Statement on Form S-1 (File No. 377-00034 / Film No. 121193612) filed November 9, 2012. | |||
| 10.17# | Health Insurance Innovations, Inc. Long Term Incentive Plan. Incorporated by reference to Exhibit 10.4 of Form 8-K filed February 13, 2013. | |||
| 10.18# | Health Insurance Innovations, Inc. Restricted Stock Award Agreement pursuant to the Health Insurance Innovations, Inc. Long Term Incentive Plan between Health Insurance Innovations, Inc. and Michael D. Hershberger. Incorporated by reference to Exhibit 10.5 of Form 8-K filed February 13, 2013. | |||
| 10.19 | Office Lease Agreement between Health Plan Intermediaries, LLC and Magdalene Center of Tampa, LLC. Incorporated by reference to Exhibit 10.22 of the Registration Statement on Form S-1 (File No. 333-185596 / Film No. 121278087) filed December 20, 2012. | |||
| 10.20 | Commitment Letter between Health Plan Intermediaries, LLC and SunTrust Bank. Incorporated by reference to Exhibit 10.23 of Amendment No. 2 to the Registration Statement on Form S-1 (File No. 333-185596 / Film No. 13547034) filed January 25, 2013. | |||
| 10.21 | Employment Agreement between Michael D. Hershberger and Health Insurance Innovations, Inc. Incorporated by reference to Exhibit 10.7 of Form 8-K filed February 13, 2013. | |||
| 10.22 | Asset Purchase Agreement dated March 14, 2013, by and among the Company, TSG Agency, LLC, and Ivan Spinner. Incorporated by reference to Exhibit 10.1 of the Form 8-K filed March 14, 2013. | |||
| 10.23 | Employment Agreement by and between Health Plan Intermediaries Holdings, LLC and Ivan Spinner. Incorporated by reference to Exhibit 10.2 of the Form 8-K filed March 14, 2013. | |||
| 21* | List of subsidiaries. | |||
| 23.1* | Consent of Independent Registered Public Accounting Firm. | |||
| 31.1* | Certification of Principal Executive Officer pursuant to Rule 13a-14(a). | |||
| 31.2* | Certification of Principal Financial Officer pursuant to Rule 13a-14(a). | |||
| 32* | Section 1350 Certifications. | |||
| * | Document is filed with this Form 10-K. |
| # | Indicates a management contract or compensatory plan or arrangement contemplated by Item 15(a)(3) of Form 10-K. |
| † | The Registrant has received confidential treatment with respect to portions of this exhibit. Those portions have been omitted and filed separately with the Securities and Exchange Commission pursuant to a confidential treatment request. |
