Attached files
| file | filename |
|---|---|
| 8-K - FORM 8-K - MOLINA HEALTHCARE, INC. | d410435d8k.htm |
 Investor Day
2012B September 19, 2012
New York, New York
Exhibit 99.1 |
 ©
2012 Molina Healthcare, Inc.
Cautionary Statement
2
Safe
Harbor
Statement
under
the
Private
Securities
Litigation
Reform
Act
of
1995:
This
slide presentation and our accompanying oral remarks contain numerous “forward looking
statements”
regarding our cost control initiatives in Texas and Wisconsin; our expansion into
the dual eligible markets in California, Texas, Michigan, and Ohio; growth in the Medicaid
membership of our health plans as a result of the Affordable Care Act and otherwise;
our planned participation in health insurance exchanges; requests for proposals in
Florida and New
Mexico;
the
rates
paid
to
our
health
plans
and
the
estimated
effect
of
those
rates
on
plan
revenues;
our
capital
needs
and
capital
planning;
and
other
various
matters.
All
of
our
forward-looking
statements
are
subject
to
numerous
risks,
uncertainties,
and
other
factors
that
could
cause
our
actual
results
to
differ
materially.
Anyone
viewing
or
listening
to
this
presentation is urged to read the risk factors and cautionary statements found under Item
1A in our annual report on Form 10-K, as well as the risk factors and cautionary
statements in our quarterly reports and in our other reports and filings with the
Securities and Exchange Commission
and
available
for
viewing
on
its
website
at
www.sec.gov.
Except
to
the
extent
otherwise required by federal securities laws, we do not undertake to address or update
forward-looking
statements
in
future
filings
or
communications
regarding
our
business
or
operating results. |
 ©
2012 Molina Healthcare, Inc.
Agenda
Approx. Time
Topic
Speaker
12:30pm-12:35pm
Opening Remarks
Juan José
Orellana, VP Investor Relations
12:35pm-1:10pm
Operations Review
Terry Bayer, Chief Operating Officer
1:10pm-1:45pm
Business Overview
Dr. J. Mario Molina, Chief Executive Officer
1:45pm-2:00pm
Q&A
2:00pm-2:15pm
Break
2:15pm-2:45pm
Long-Term Growth
John Molina, Chief Financial Officer
Joseph White, Chief Accounting Officer
2:45pm-3:05pm
Q&A
3:05pm-3:50pm
Funding Our Growth
John Molina, Chief Financial Officer
3:50pm-4:30pm
Q&A
4:30pm
End of Program
3 |
 Operations
Review Terry Bayer
Chief Operations Officer
September 19, 2012
New York, New York |
 ©
2012 Molina Healthcare, Inc.
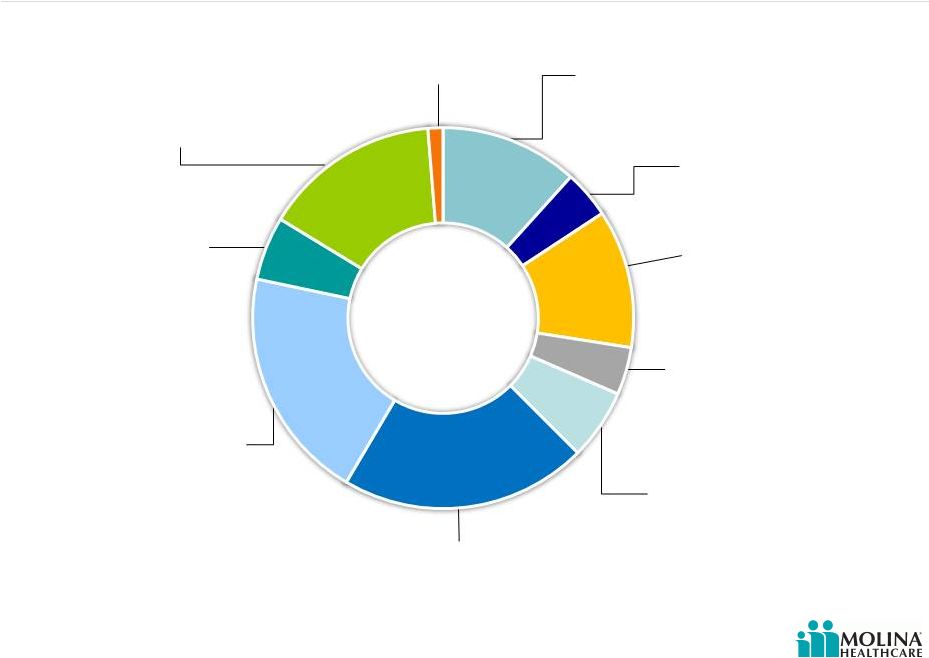
Revenue Contribution by State
5
Washington 15%
Began serving ABD
population 7/1/2012
Utah 5%
RX carve-in effective
1/2013
Texas 20%
Medical management
initiatives implemented
Ohio 21%
Dual eligible contract in 3 regions
effective 2013; statewide
expansion effective 1/2013
Missouri 4%
Contract ended June 30, 2012
Michigan 12%
CSHCS effective 10/1/2012
Florida 4%
Submitted Long-Term Care
contract RFP
California 12%
Dual eligible contract in 4
counties effective 2013
Wisconsin 1%
PDR taken 2Q 2012
Please refer to the Company’s cautionary statements.
New Mexico 6%
RFP effective 1/2014
1H 2012 |
 Texas
Existing Molina
footprint
6
Molina new SDAs
effective 3/1/2012
Effective March 1, 2012, Molina added three new service
delivery areas (SDAs).
Molina New SDAs
(effective 3/1/2012)
El Paso Service Area
STAR & STAR+PLUS
El Paso and Hudspeth
Counties
Hidalgo Service Area
STAR & STAR+PLUS
Cameron, Duval, Hidalgo, Jim Hogg,
Maverick, McMullen, Starr, Webb,
Willacy, and Zapata counties
Jefferson Service Area
CHIP
Chambers, Hardin,
Jasper, Jefferson,
Liberty, Newton, Orange,
Polk, San Jacinto, Tyler
and Walker counties
Texas Health Plan Enrollment
Source: Texas Health and Human Services Commission
301K
155K
94K
40K
31K
2008
2009
2010
2011
1H
2012
©
2012 Molina Healthcare, Inc. |
 ©
2012 Molina Healthcare, Inc.
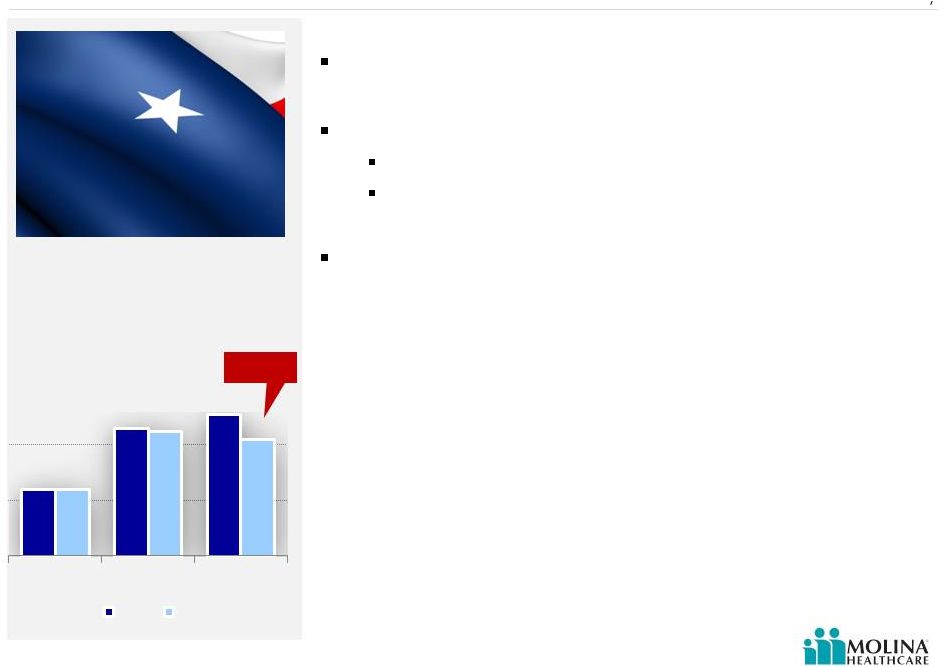
Texas Overview
7
Remediation activities
Blended rate increase of 4% effective 9/1
Provider contract changes
Re-contracted at lower unit costs
Implementation of state required fee schedules
New President & Management Team
Enrollment at September 1
st
was 291,000; ABD declined
8.1% from June 30th
Source: Molina Healthcare, Inc. 2Q 2012 earnings release and company data.
84K
106K
111K
84K
105K
102K
CHIP
TANF
ABD
Jun 30
Sep 1
(8.1%) |
 ©
2012 Molina Healthcare, Inc.
Wisconsin
Premium rates low in relation to benefits
United
Healthcare
exit
regions
1
Remediation activities
Terminated certain high-cost providers
Utilization Management
New leadership
8
(http//www.jsonline.com)
1. Milwaukee Wisconsin Journal Sentinel, “UnitedHealthcare ends
BadgerCare Plus contract with state” August 19, 2012.
|
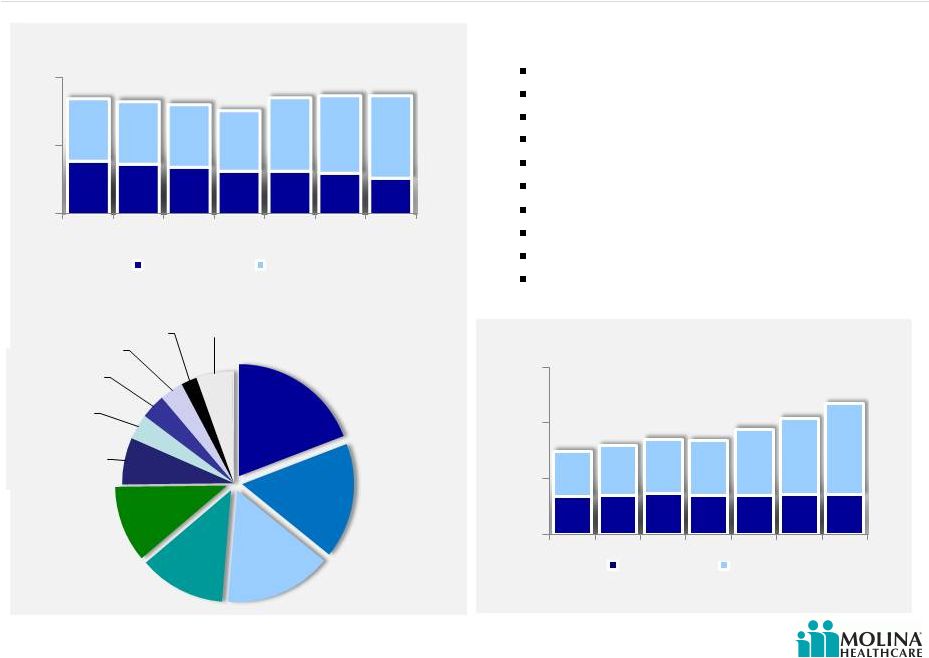
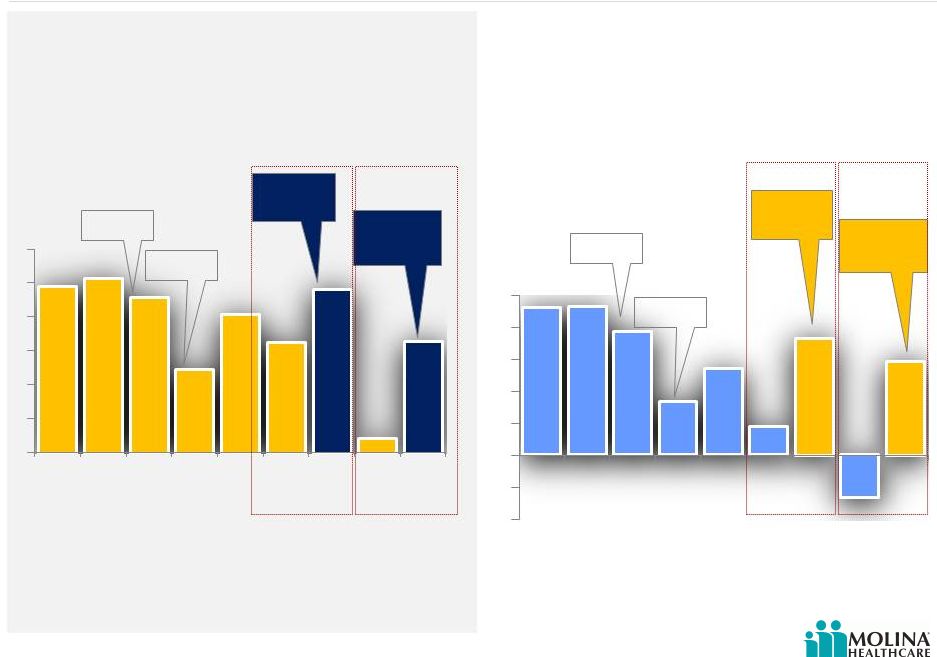
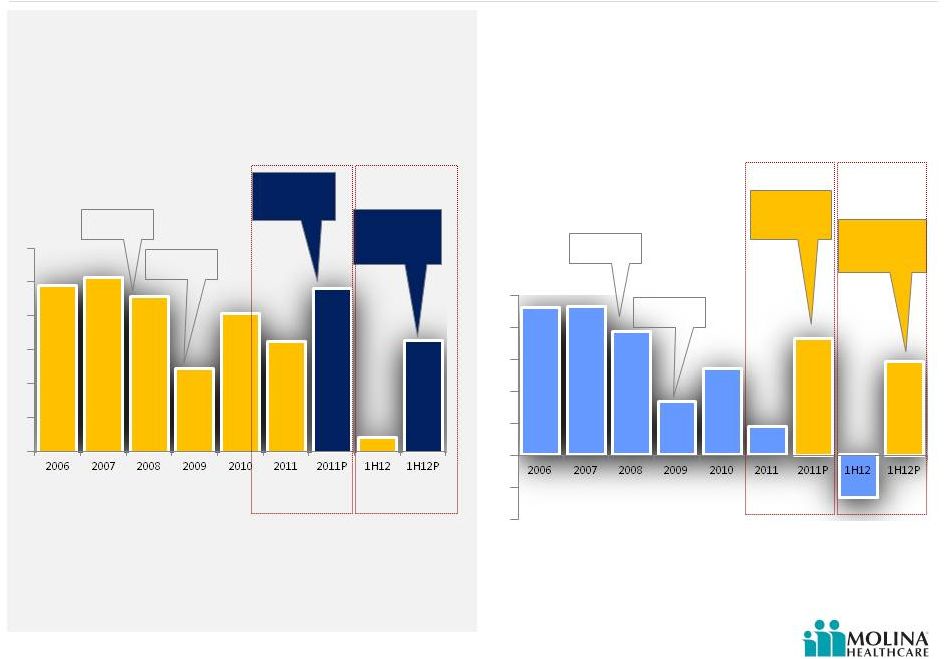 Earnings Margin
2006-1H2012 9
AFTER TAX MARGIN
Please refer to the Company’s cautionary statements.
1. P denotes results excluding Missouri write-down in 2011, and Texas and Missouri
operations in 2012 1
1
H1N1 Flu
Excluding
Texas and
Missouri
Excluding
Missouri
write-down
TX & OH
Startup
H1N1 Flu
Excluding
Texas and
Missouri
Excluding
Missouri
write-down
TX & OH
Startup
EBITDA MARGIN
1
1
©
2012 Molina Healthcare, Inc.
4.9%
5.1%
4.6%
2.5%
4.1%
3.2%
4.6%
0.4%
3.3%
2.3%
2.3%
1.9%
0.8%
1.3%
0.4%
1.7%
-
0.7%
1.5% |
 ©
2012 Molina Healthcare, Inc.
California’s Coordinated Care Initiative (CCI)
Health plans must have an existing Medicaid contract
The CCI will impact Molina Healthcare of California as
follows:
1.
Mandatory managed care enrollment of dual eligibles
for the Medicaid
portion of the benefit
2.
Passive Medicare enrollment with opt-out option
3.
A carve in for the long term support services (LTSS),
which will become the MCOs’
responsibility
»
Long-term nursing facility care
»
Personal care
»
Adult day care
»
Other support services
10
Three Party Agreement between
the health plans, the State, and
CMS, which will provide funding
for Medicare and Long-Term Care
services on the Medicaid side for
California’s dual eligibles. |
 ©
2012 Molina Healthcare, Inc.
California’s Coordinated Care Initiative (CCI)
11
Health Plan Readiness
Membership
Eligible populations
defined for duals
enrollment and
mandatory Medicaid
managed care
enrollment
Passive enrollment with
opt-out (Medicare)
Rolling enrollment
based on birth month
Unknown:
Auto-assignment
methodology
Opt-out rate
Rates
Benefits
Network
Two payments for dual
members with Medicare
and Medicaid portions
determined by CMS and
DHCS, respectively
Some level of risk
adjustment for both
Medicare and Medicaid
payments
Withholds for quality
measures
Unknown:
Specific rate
methodology
All Medicare Parts A, B,
and D
All current Medicaid
managed care benefits
Medicaid LTSS
Nursing facility long
term care
Personal care (IHSS)
Adult day health (CBAS)
Non-medical assistive
services (MSSP)
Case management
Transition management
Coordination with
Medicaid behavioral
health
Leverage current
Medicaid and Medicare
networks
Direct contracts with
LTSS providers (not
delegated and
subcapitated to groups)
Contracts with county
agencies and LTSS
providers
Counties for IHSS
CBAS providers
MSSP providers
Case management
vendors
Legislatively mandated
payment provisions for
certain providers
Expected 6/1/13
Plans begin to enroll
duals into
demonstration
Expected plan rates released
12/15/12
Deadline for
CMS/DHCS/Plan
3-way contracts
Plan readiness
review by CMS
and DHCS
Aug
Sep
Oct
Nov
Dec
Jan
Feb
Mar
Apr
May
Jun |
 ©
2012 Molina Healthcare, Inc.
Utilization Decreases With Length of Enrollment
12
As length of enrollment increases for our ABD populations, utilization decreases.
Admits per K
(manageable)
by enrollment month
Days per K
(manageable)
by enrollment month
Please refer to the Company’s cautionary statements.
Month
Month
Source: Molina CA ABD Length of Enrollment
289
252
276
259
231
261
237
229
225
215
1,239
1,154
1,238
1,044
1,113
1,060
902
939
1,119
926
1
2
3
4
5
6
7
8
9
10
1
2
3
4
5
6
7
8
9
10 |
 ©
2012 Molina Healthcare, Inc.
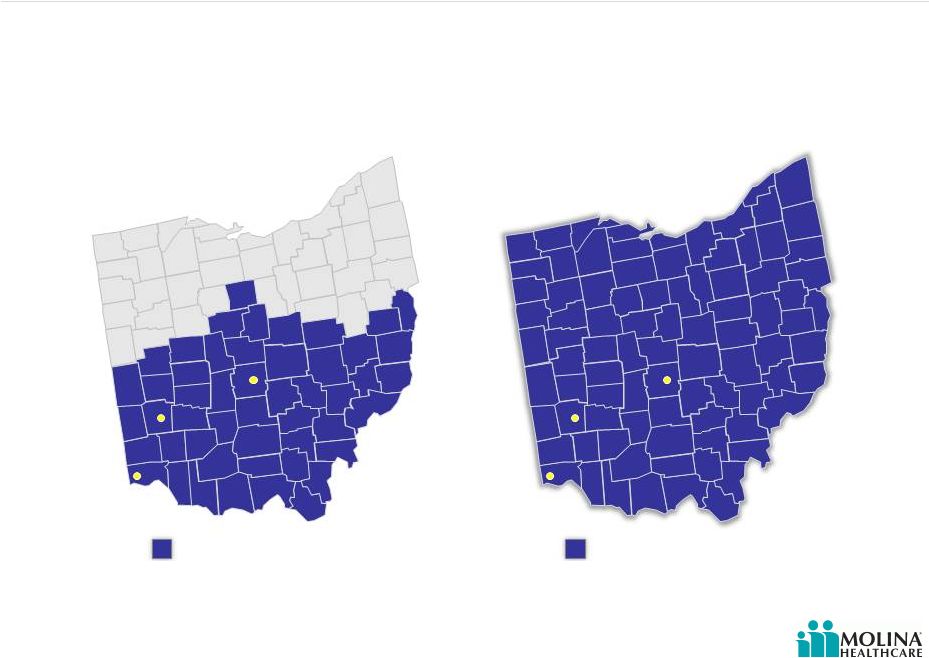
Post-2012 RFA
Ohio Managed Care Regions
1.6M Eligibles
Ohio (TANF & ABD)
Source: Ohio Department of Job and Family Services
http://jfs.ohio.gov/rfp/JFSR1213078019/JFSR1213078019.stm
http://jfs.ohio.gov/ohp/bmhc/documents/reports/December2011_CFC_Penetration-Enrollment.pdf
13
Pre-2012 RFA
Current Molina Service Area
Effective June 1, 2013 Molina Healthcare will expand into 38 new
counties.
Dayton
Cincinnati
Columbus
Dayton
Cincinnati
Columbus
Current Molina service area
New Molina service area |
 ©
2012 Molina Healthcare, Inc.
Molina Selected To Serve Duals in Max Regions Allowed
14
The state of Ohio chose Molina to participate in the 3-year demonstration program in the
Southwest, West Central, and Central regions. Implementation expected to begin
June 1, 2013.
Current Molina Service Area
260,000 members (TANF+ABD)
Molina Integrated Care
Coordination Program Regions
45,000 dual eligibles
Dayton
Cincinnati
Columbus
Dayton
Cincinnati
Columbus
Central Region:
16,000 eligibles
South West Region:
17,000 eligibles
West Central Region:
12,000 eligibles |
 ©
2012 Molina Healthcare, Inc.
Washington
15
Successfully defended
Washington Medicaid
contract in 34 counties and
added one additional county,
effective 7/1/12
On September 1, enrollment was 410,000, including
19,000 ABD members
Established provider relationships
Molina was only health plan in Washington participating
in the Washington Medicaid Integration Program (WMIP)
No Long Term Care benefits for new Aged, Blind, or
Disabled (ABD) members |
 ©
2012 Molina Healthcare, Inc.
New Opportunities in Florida –
Long Term Care Program
Molina has bid in 8 of 11 regions (30 counties) with
90,000 beneficiaries to be shared by awarded MCOs
Molina Florida Experience
Nursing Home Diversion Program in Pinellas and
Hillsborough counties (Tampa area)
Waiver focused on intensive case management and
home and community based services vs. nursing home
placement
Timeline:
8/28/12 Bids Submitted
1/15/13 Anticipated Awards announced
8/1/13 Effective for first region awarded (Region #7);
other regions will “roll in”
each month through 3/2014
16
Florida is gradually moving toward
statewide Medicaid managed
care, Molina is competing for
contracts to provide long term
care for seniors.
The program involves nursing home, hospice, and home and
community-based services in 11 regions. The State of Florida
is expected to select 2-5 plans per region.
1. Regions: Pensacola, Tallahassee, Gainesville, Jacksonville, St.
Petersburg, Tampa, Orlando, Sarasota, Palm Beach, Ft. Lauderdale,
Miami
1 |
 ©
2012 Molina Healthcare, Inc.
New Opportunities in New Mexico –
Centennial Care
Overview:
Integrates medical, behavioral health, and long term care
services
680,000 beneficiaries
Plans must be statewide Special Needs Plan (SNP) or Medicare
Advantage plan
Reduces 7 MCOs to 5
Timeline:
11/20/12 Bids Due
1/7/13 Awards announced
1/1/14 Effective
17
Managed Care Organizations will
provide medical, behavioral
health, and long term care
services
which were previously
procured as separate contracts |
 ©
2012 Molina Healthcare, Inc.
MMS Comes of Age
18
MMS Operating Income by Quarter
Please refer to the Company’s cautionary statements.
The year over year improvement due to CMS certifications in
Idaho and Maine.
Diversifying profit stream
Generating cash flow
Serving 2.5M beneficiaries
($5.5M)
($0.2M)
($8M)
($6M)
($4M)
($2M)
$0M
$2M
$4M
$6M
$8M
$10M
$1.7M
$6.1M
$8.4M
$6.6M
©
2012 Molina Healthcare, Inc. |
 Business
Overview J. Mario Molina, MD
Chief Executive Officer
September 19, 2012
New York, New York |
 ©
2012 Molina Healthcare, Inc.
Business Snapshot
Markets and members served –
2Q 2012
Washington
356,000
California
350,000
New Mexico
89,000
Utah
86,000
Texas
301,000
Michigan
220,000
Ohio
260,000
Florida
2
70,000
Health plan enrollment growth
Health plan membership profile
(in thousands)
Molina Healthcare Health Plans
Molina Medicaid Solutions
Idaho
Maine
Louisiana
West
Virginia
New
Jersey
1.
2.
3.
Virginia
1
Wisconsin
42,000
AGED,
BLIND
OR
DISABLED
MEDICARE 2%
76%
TANF
14%
CHIP
8%
20
Molina Direct Delivery
3
(1 clinic)
(17 clinics)
(2 clinics)
(1 clinic)
(3 clinics)
1,256
1,455
1,613
1,697
1,853
'08
'09
'10
'11
2Q 2012
Note: Map does not include Missouri since the contract ended June 30, 2012. However
the enrollment chart does. Virginia clinics provide Direct Delivery, operated by Molina and owned by Fairfax County. Florida has a managed
care program as well as a Pharmacy Rebate Program.
Company owned and operated primary care clinics. |
 ©
2012 Molina Healthcare, Inc.
Revenue Contribution by State
21
Washington 15%
Began serving ABD
population 7/1/2012
Utah 5%
RX carve-in effective
1/2013
Texas 20%
Medical management
initiatives implemented
Ohio 21%
Dual eligible contract in 3 regions
effective 2013; statewide
expansion effective 1/2013
Missouri 4%
Contract ended June 30, 2012
Michigan 12%
CSHCS effective 10/1/2012
Florida 4%
Submitted Long-Term Care
contract RFP
California 12%
Dual eligible contract in 4
counties effective 2013
Wisconsin 1%
PDR taken 2Q 2012
Please refer to the Company’s cautionary statements.
New Mexico 6%
RFP effective 1/2014
1H 2012 |
 ©
2012 Molina Healthcare, Inc.
Market Dynamics
State Budget Shortfalls
*Reported to Date
Source: Center on Budget and Policy Priorities.
Analysis using data from U.S. Department of Health
and Human Services, U.S. Department of Education,
Congressional Budget Office, and state budget
documents. June 2012.
Budget gaps offset by Recovery
Act and extension
Remaining budget gaps after
Recovery Act and extension
State Budget
Unemployment
ACA
Makes Medicaid
expansion optional for
states
11 million additional
Medicaid beneficiaries
Federal government
incurs 100% of the cost
of expansion for the first
3 years
2012 Elections
Budget shortfalls in billions
Unemployment
Nationwide through July 2012
22
Joblessness and slow
economic recovery
-$110
-$191
-$130
-$107
-$55*
Supreme Court Decision
2012 Elections |
 ©
2012 Molina Healthcare, Inc.
23
A History of Adapting to Constant Change
1980
Opened 3 Primary
Care Clinics
in
California
1997
Established
Utah
operation, the first
venture outside of
California
2006
Launched
Medicare SNP
product
2003
Completed
successful Initial
Public Offering
2010
Acquired
the
Health
Information Management
business from Unisys, now
Molina Medicaid Solutions
2013+
Medicaid
Expansion &
the dual eligible
1994
First
Medicaid
Managed Care
contract
(California)
2000
First
CHIP Managed
Care contract
(California)
C. David Molina, MD
Founder
Molina Healthcare, Founded 1980 |
 ©
2012 Molina Healthcare, Inc.
Long-Term Incremental Growth Drivers
24
Estimated additional revenue by 2015 as a result of duals and Medicaid expansion
4
Estimated 2015 run rate
Duals
1
Current
Health Plan
Business
ACA
2
Total
1.
Duals denote revenue potential for dual eligibles in CA, MI, OH and TX.
2.
ACA denotes revenue potential as a result of Medicaid expansion in CA, MI, OH, NM, UT, WA, WI;
and exchanges in CA, FL, MI, NM, OH, TX, UT, WA, WI. 3.
Other includes FL, MI, NM, TX, UT, WI.
4.
Figures may not add up due to rounding.
Please refer to the Company’s cautionary statements.
2012
2015
~$6B
~$4B
~$12B
CA: $1.2B
OH: $0.5B
TX: $1.5B
MI: $0.9B
OH: $0.5B
WA: $0.3B
CA: $0.3B
Other: $1.0B
3
~$2B |
 ©
2012 Molina Healthcare, Inc.
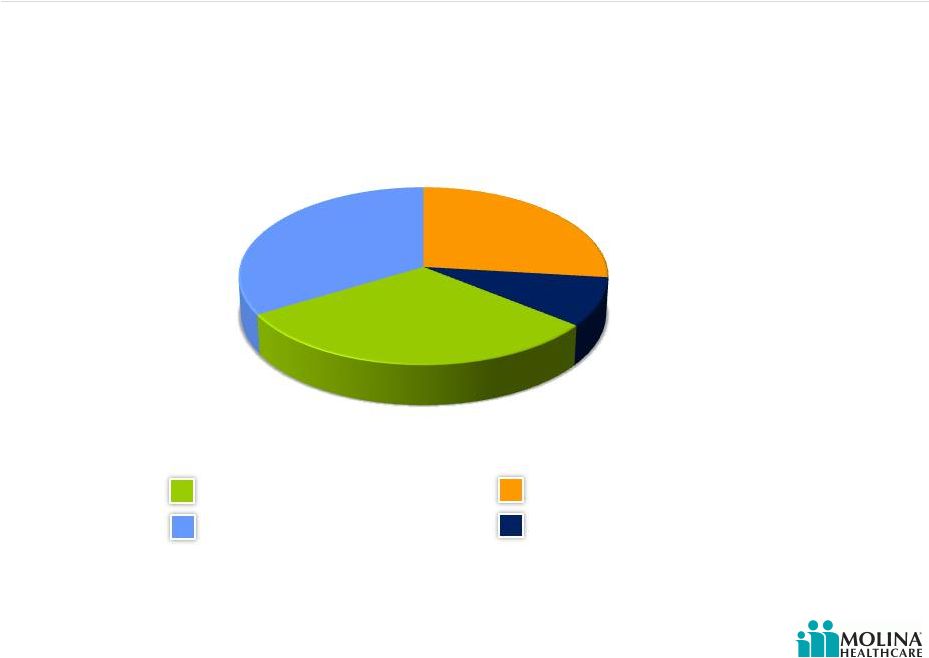
U.S. Medicaid Coverage Estimates Updated for the Supreme Court Decision
25
* Source:
Congressional
Budget
Office,
“Estimates
for
the
Insurance
Coverage
Provisions
of
the
Affordable
Care
Act
Updated
for
the
Recent
Supreme
Court
Decision.”
July
2012.
1.
The change in employment-based coverage is the net result of increases in and losses of
offers of health insurance from employers and changes in enrollment by workers and their families.
2.
Other includes Medicare; the effects of the ACA are almost entirely on nongroup coverage
. Medicaid
& CHIP
Exchanges
Employer
Nongroup
& Other
Uninsured
Estimated Changes in Insurance Coverage by 2022*
1
2
March 2012 Baseline
July 2012 Estimate Incorporating
SCOTUS Decision |
 ©
2012 Molina Healthcare, Inc.
Two Ends of the Continuum
26
Duals
TANF
More continuous eligibility
Chronic illnesses
Behavioral health
More likely to have greater
limitations in activities of
daily living (ADL)
Require more focused care
including home care
More likely to have a usual
source of care and less likely
to delay care due to cost
Breaks in eligibility
Episodic care
Pregnancy
Greater ethnic diversity
Larger support system at
clinic visits
Under
Age 65
38%
Over Age
65
62%
Under
Age 65
75%
Over Age
65
25%
TANF
ABDs
Duals
Demographics
Source: 1. KFF.org
TANF
Duals
1 |
 ©
2012 Molina Healthcare, Inc.
Most Common Diagnoses
27
TANF Diagnoses
ABD Diagnoses
Dual Eligibles Diagnoses
Inpatient Services
Delivery
Affective psychoses
Affective psychoses
Complications of delivery
Septicemia
Septicemia
Other maternal complications
Schizophrenic disorders
Care involving use of rehabilitation
procedures
Prolonged pregnancy
Chronic bronchitis
Pneumonia
Other OB
Pneumonia
Chronic bronchitis
Outpatient Services
Well Child care
Respiratory & other chest
Essential hypertension
Acute upper respiratory infection
Fever and fatigue
Respiratory and other chest
Respiratory & other chest
Diabetes mellitus
Diabetes mellitus
Fever and fatigue
Back disorders
Fever and fatigue
Ear infection
Joint disorders
Joint disorders |
 ©
2012 Molina Healthcare, Inc.
Specific Benefits for Duals
28
Medicaid Benefits*
Medicare Benefits
Hospital Insurance (Part A)
Blood, home health care, hospice care,
hospital inpatient stay, mental health
inpatient stay, skilled nursing facility
stay
Medical Insurance (Part B)
Blood, clinical laboratory services,
home health services, medical and
other services, outpatient mental
health services, outpatient hospital
services, other covered services
Medicare Prescription Drug
Coverage (Part D)
Copayments for Medicare services
Long Term Care
Institutional
HCBS (Home & Community Based
Services)
Personal Care
Adult Day Care
Home modifications
Meals
Paramedical/nursing services
Physical, speech, and occupational
therapies
Behavioral health
*Subject to state carve-outs
Sources: KFF.org, “Proposed Models to Integrate Medicare and Medicaid Benefits for Dual
Eligibles: A Look at the 15 State Design Contracts Funded By CMS” and Medicare.gov,
“Medicare costs at a glance” |
 ©
2012 Molina Healthcare, Inc.
We Currently Manage Many Dual Benefits
Benefits
California
(SPD Duals)
Washington
(WMIP)
Texas
(STAR+PLUS)
Personal Care
X
X
Nursing Home
Adult Day Care
X
X
X
Behavioral Health
X
X
Paramedical/Nursing Services
X
X
Meals
X
X
Physical, Speech, and
Occupational Therapies
X
X
X
Home Modifications
X
X
29 |
 ©
2012 Molina Healthcare, Inc.
CMS
Rate
Setting
Process
Guidance
30
Savings targets may differ among States with low historic
Medicare spending, low utilization of institutional long-
term care services, or a high penetration of Medicaid
managed care.
Sample Aggregate Savings Targets
Under the Demonstrations
Aggregate Savings would be applied to Medicare
A/B and Medicaid components of the rate
Both payers proportionally share in the
contribution to the capitation rate and in the
savings achieved
Savings targets not applied to the Part D
component of the rate
1
1.0%
3.0%
5.0%
Year 1
Year 2
Year 3
1. CMS Joint Rate Setting Process Under the Capitated Financial Alignment Initiative |
 ©
2012 Molina Healthcare, Inc.
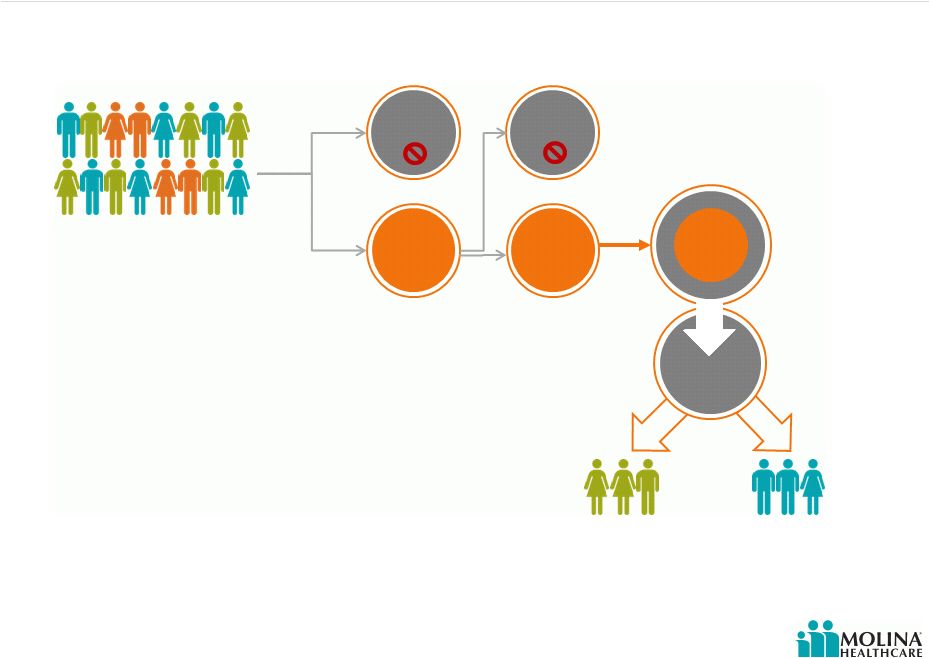
Opt Out Impact On Dual Premium
31
Auto
Assignment
Opt-Out
of Medicare
Managed
Care
?
Medicaid
Benefit Only
Medicaid + Medicare
Integrated Benefits
Yes
State/County/Region
Dual Eligible Population
No
Partial
Dual
Full Dual
D-SNP*
Parts A, B, D
Illustrative Example for California
*Specific to California example |
 ©
2012 Molina Healthcare, Inc.
Strategic Priorities
32
Mission
Priorities
Quality Care
Current Portfolio
Health plan business
MMS
Direct delivery
Growth
Organic growth
Medicaid expansion
Dual eligible population
Acquisitions
RFPs
Margin Expansion
Long-Term EBITDA target: 4% -
5% EBITDA margin
1.5%-2% after tax margin
Our mission is to provide quality
health services to financially
vulnerable families and individuals
covered by government programs. |
 ©
2012 Molina Healthcare, Inc.
Q&A
33 |
 Long-Term
Growth September 19, 2012
New York, New York
John Molina,
Chief Financial Officer
Joseph White,
Chief Accounting Officer |
 ©
2012 Molina Healthcare, Inc.
Long-Term Incremental Growth Drivers
35
Estimated additional revenue by 2015 as a result of duals and Medicaid expansion
4
Estimated 2015 run rate
Duals
Current
Health Plan
Business
~$6B
~$4B
ACA
~$12B
CA: $1.2B
OH: $0.5B
MI: $0.9B
Total
1.
Duals denote revenue potential for dual eligibles in CA, MI, OH and TX.
2.
ACA denotes revenue potential as a result of Medicaid expansion in CA, MI, OH, NM, UT, WA, WI;
and exchanges in CA, FL, MI, NM, OH, TX, UT, WA, WI. 3.
Other includes FL, MI, NM, TX, UT, WI.
4.
Figures may not add due to rounding.
Please refer to the Company’s cautionary statements.
OH: $0.5B
WA: $0.3B
CA: $0.3B
Other: $1.0B
~$2B
2012
2015
1
TX: $1.5B
3
2 |
 ©
2012 Molina Healthcare, Inc.
Estimating Dual Revenue PMPM
36
Two Molina programs could help us estimate dual eligible premiums
Please refer to the Company’s cautionary statements.
1.
2.
Program
Medicaid &
Medicare
LTC
Total
Texas SNP
$1,900
$700
$2,600
WMIP
$1,700
$700
$2,400
Our
expectation
for
Dual
Eligible
premium
(Medicare
&
Medicaid
–
No
opt-out)
$2,500 PMPM
Note:
LTC based on Florida LTC RFP Region 11 Assumes 15% of
Integrated Dual population would be institutionalized LTC
1
2 |
 ©
2012 Molina Healthcare, Inc.
Opt Out Impact On Dual Premiums
37
Auto
Assignment
Opt-Out
of Medicare
Managed
Care
?
Medicaid
Benefit Only
Medicaid + Medicare
Integrated Benefits
Yes
State/County/Region
Dual Eligible Population
No
Partial
Dual
Full Dual
Parts A, B, D
Illustrative Example for California
10%
90%
Substantial
Uncertainty
~50%
10%
80%
Please refer to the Company’s cautionary statements.
*Specific to California example
D-SNP* |
 ©
2012 Molina Healthcare, Inc.
Dual Market Opportunity
State
Estimated Number of
Participating Duals in
Molina markets
Opt-Out Rate
Potential Range
Molina’s
Estimated Dual
Enrollment
Annualized
Premium
Revenues
California
430K
20% -
80%
50K
$0.9B -
$1.4B
Michigan
160K
20% -
80%
40K
$0.7B -
$1.0B
Ohio
50K
20% -
80%
25K
$0.4B –
$0.7B
Texas
215K
20% -
80%
60K
$1.1B -
$1.6B
Total
855K
175K
$3.1B -
$4.7B
38
Source: Company estimates; figures may not add due to rounding.
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
Medicaid Expansion Opportunity
State
Expansion Eligibles
in Medicaid
Managed Care
Molina’s
Estimated
Enrollment
Estimated
Premium
1
PMPM
Annualized
Premium Revenues
California
1M
100K
$100
$120M
Florida
not included
not included
not included
not included
Michigan
500K
100K
$125
$150M
New Mexico
100K
25K
$200
$60M
Ohio
500K
125K
$250
$375M
Texas
not included
not included
not included
not included
Utah
125K
40K
$200
$95M
Washington
250K
125K
$175
$260M
Wisconsin
125K
15K
$125
$20M
Total
2.6M
530K
$ 1.1B
39
Source:
1.
Based on Molina’s current TANF premium
Company estimates, figures may not add due to rounding. |
 ©
2012 Molina Healthcare, Inc.
Exchange Opportunity
State
Number of Exchange
Members in Molina
Markets
Molina’s
Estimated
Exchange
Enrollment
Estimated
Premium
1
PMPM
Annualized
Premium Revenues
California
2.2M
180K
$100
$ 215M
Florida
1.0M
80K
$150
$145M
Michigan
400K
35K
$125
$50M
New Mexico
100K
10K
$200
$25M
Ohio
500K
40K
$250
$120M
Texas
1.6M
125K
$225
$340M
Utah
200K
15K
$200
$40M
Washington
300K
30K
$175
$60M
Wisconsin
300K
20K
$125
$30M
Total
6.6M
535K
$1.0B
40
1.
Source: Company estimates, figures may not add due to rounding.
Based on Molina’s current TANF premium |
 ©
2012 Molina Healthcare, Inc.
Premium Rate Changes
41
1. Denotes announced rate changes.
Please refer to the Company’s cautionary statements.
Health Plan
Effective Date
Revenue Change
California
10/1/2012
unknown
Florida
9/1/2012
unknown
Michigan
10/1/2012
unknown
New Mexico
7/1/2012
(1)
Ohio
1/1/2012
(1)
Texas
9/1/2012
(1)
Utah
7/1/2012
(1)
Washington
7/1/2012
(1)
Wisconsin
1/1/2012
1%
(1)
( 0.5%)
( 2%)
4%
( 2%)
( 2%) |
 Leveraging
Administrative Costs Two types of administrative costs:
Activities that improve healthcare outcomes
General & administrative costs (G&A)
42
Please refer to the Company’s cautionary statements.
©
2012 Molina Healthcare, Inc. |
 ©
2012 Molina Healthcare, Inc.
43
As a % of Total Revenue
Per Member Per Month (PMPM)
Cost by Category –
YTD 2012
2.6%
Please refer to the Company’s cautionary statements.
Activities That Improve Healthcare Outcomes
$5
Utilization
Management
Quality
Mgmt
Medical
Affairs
Service
Coordination
Health Education
Nurse Advice Line
Other
Utilization Management
Quality Management
Coordination of Medical Management
Coordination of Care, CM & DM
Health Education
Nurse Advice Line
Include the following services: |
 Dual Eligibles
– Level of Care
Level IV
Level III
Level II
Level I
% of potential enrollees
10%
20%
30%
40%
At High Risk For
Institutionalization
Critical Event or Diagnosis Requiring
Extensive Medical Care
Medium-Risk Chronic Illness
Episodic Care –
No or Low Risk Factors
44
Please refer to the Company’s cautionary statements.
©
2012 Molina Healthcare, Inc. |
 Dual Eligibles
Level of Care – Financial Impact
Greater portion of duals are categorized as care Level III
and Level IV
Require home visits
Require in-home care manager assessments and visits
Increased medical staffing especially for:
Care Managers (CM) & Nurse Practitioners (NP)
Community Connectors (CC)
Services of Medical Directors and Pharmacy Directors also
required
45
Please refer to the Company’s cautionary statements.
©
2012 Molina Healthcare, Inc. |
 Not All
Activities That Improve Healthcare Outcomes Are Equal 46
Fixed Costs
Variable Costs
Please refer to the Company’s cautionary statements.
Utilization
Management
Quality
Mgmt
Medical
Affairs
Service
Coordination
Nurse Advice Line
Other
©
2012 Molina Healthcare, Inc.
Health Education |
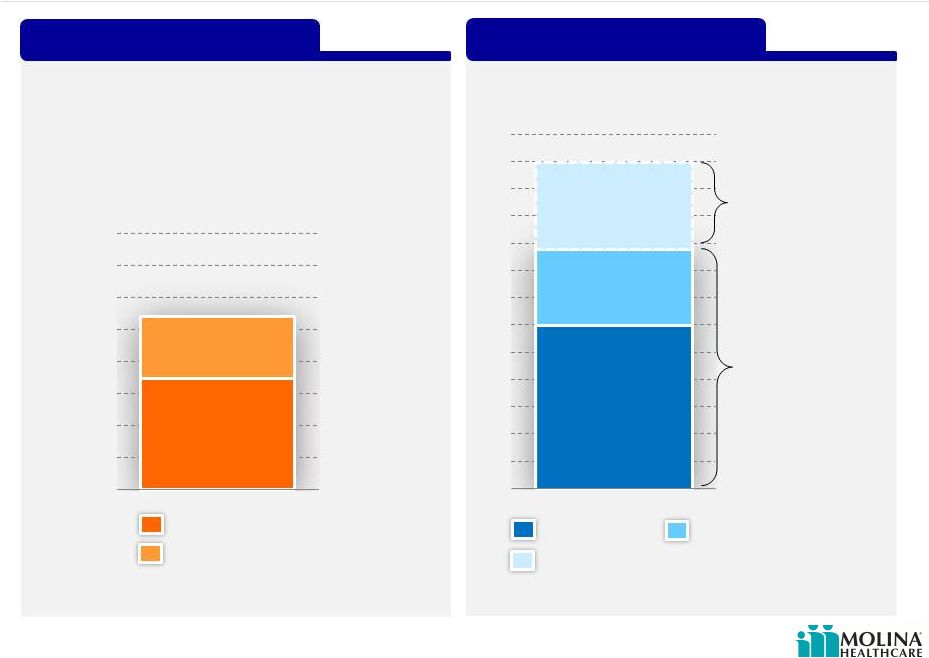
 Estimated Costs
of Activities That Improve Healthcare Outcomes 47
As a % of Premium Revenue
Per Member Per Month
Current Cost
Incremental
Cost of
Dual Eligibles
(Model Care)
@ $2,500 premium
Estimated
@ $260 premium
as of June 30, 2012
Please refer to the Company’s cautionary statements.
$50
$6
2.2%
2.0%
Current
Dual Eligibles
Current
Dual Eligibles
©
2012 Molina Healthcare, Inc. |
 ©
2012 Molina Healthcare, Inc.
General & Administrative Costs
48
As a % of Total Revenue
Include the following:
Per Member Per Month (PMPM)
8.7%
8.6%
Cost
by
Category
–
YTD
2012
Please refer to the Company’s cautionary statements.
$16
$7
IT
Claims
Executive
Finance
Provider
Services
Legal
HR
Marketing
Sales
Other
Operations
2006
2007
2008
2009
2010
2011
Q2-
12
YTD
Health Plans
Corporate
8.4%
8.2%
8.0%
7.5%
8.5%
2006
2007
2008
2009
2010
2011
Q2-
12
YTD
Health Plans
Corporate
$14
$16
$17
$17
$19
$21
$23
Claims
Information Technology
Finance
Operations
Marketing
Provider Services
Legal
HR
Marketing
Medicare Sales |
 Not All General
& Administrative Costs Are Equal 49
Please refer to the Company’s cautionary statements.
IT
Claims
Executive
Finance
Provider
Services
Legal
HR
Marketing
Sales
Other
Operations
Fixed Costs
Variable Costs
©
2012 Molina Healthcare, Inc. |
 ©
2012 Molina Healthcare, Inc.
Long-Term Admin Ratio Goal Below 8%
50
$23
$17
$25
$95
Corporate
Subsidiaries
G&A Ratio
G&A PMPM
Corporate
Subsidiaries
$16
$70
$10
$17
$7
$25
$7
$8
Current
Duals
ACA
Consolidated
6.0%
3.7%
5.8%
5.2%
2.5%
1.3%
4.2%
2.3%
Current
Duals
ACA
Consolidated
8.5%
10.0%
7.5%
5.0% |
 Q&A
51
©
2012 Molina Healthcare, Inc. |
 Funding Our
Growth John Molina
Chief Financial Officer
September 19, 2012
New York, New York |
 ©
2012 Molina Healthcare, Inc.
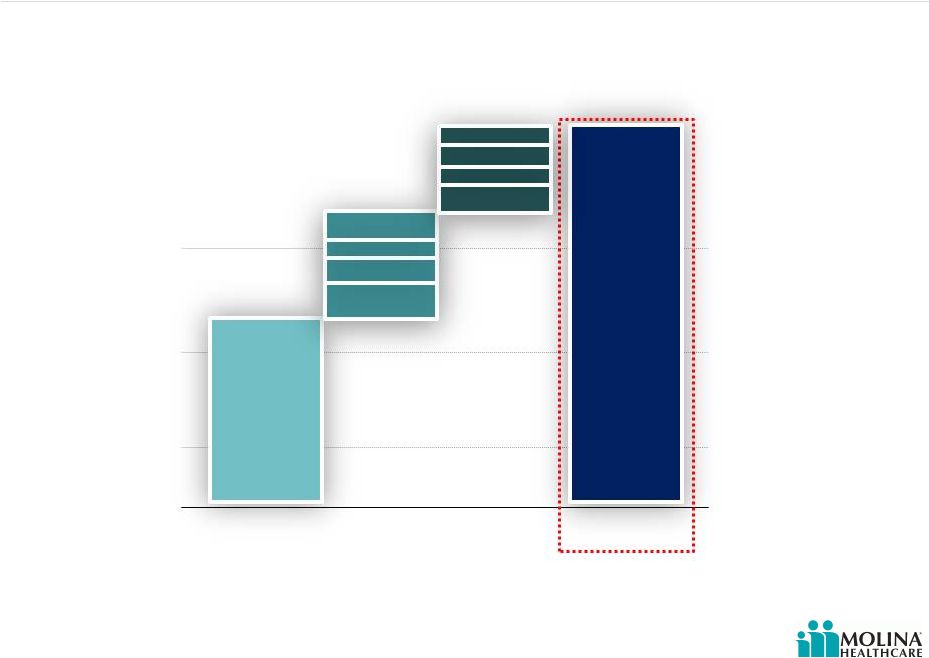
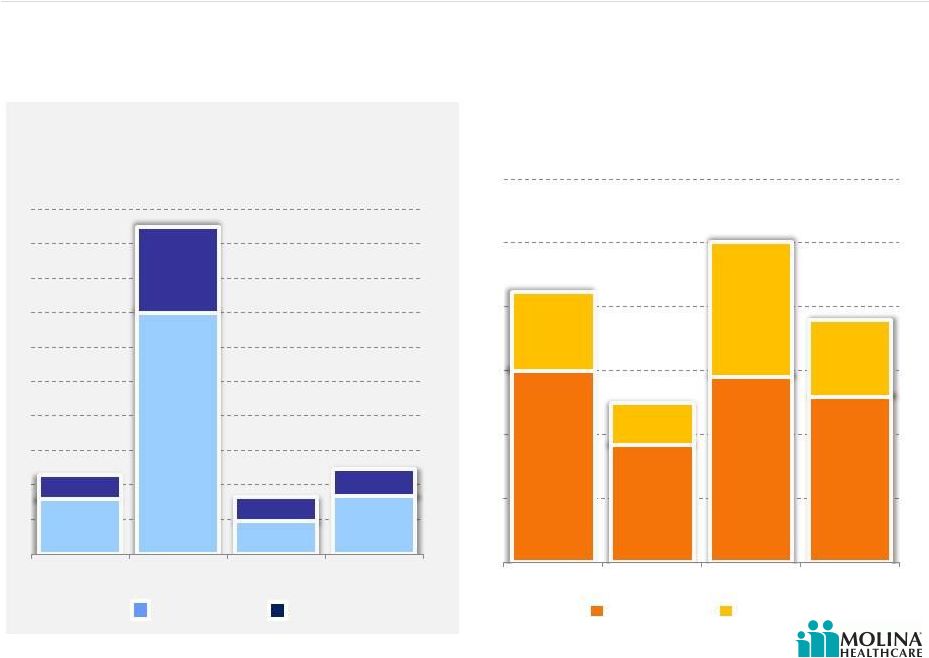
Molina Earnings Have Funded Past Growth
53
Sources of Capital
2006 through 2Q2012
Common Equity
Convertible Debt
Net Income
Source(s): SEC Filings
*CAGR calculated from 2006 to 2012E.
Please refer to the Company’s cautionary statements.
Total Premium Revenue
2006-2011
20%
46%
34%
$12B
$5B
$6B
$4B
$4B
$3B
$2B
$2B |
 ©
2012 Molina Healthcare, Inc.
Molina Has Invested to Grow Its Business
54
Cash Paid for Acquisitions
Contributions to Subsidiaries
Capital Expenditures
Share Repurchases
Source(s): SEC Filings and Company Data
Please refer to the Company’s cautionary statements.
Capital Deployment
2006 through 2Q2012
27%
9%
31%
33% |
 ©
2012 Molina Healthcare, Inc.
Earnings Margin 2006-1H2012
55
EBITDA MARGIN
AFTER TAX MARGIN
Please refer to the Company’s cautionary statements.
1. P denotes results excluding Missouri write-down in 2011, and Texas and Missouri
operations in 2012 1
1
1
1
2.3%
2.3%
1.9%
0.8%
1.3%
0.4%
1.7%
-0.7%
1.5%
Excluding
Missouri
write-down
Excluding
Missouri
write-down
Excluding
Texas and
Missouri
Excluding
Texas and
Missouri
H1N1 Flu
TX & OH
Startup
H1N1 Flu
TX & OH
Startup
4.9%
5.1%
4.6%
2.5%
4.1%
3.2%
4.6%
0.4%
3.3%
2006
2007
2008
2009
2010
2011
2011P
1H12
1H12P
2006
2007
2008
2009
2010
2011
2011P
1H12
1H12P |
 ©
2012 Molina Healthcare, Inc.
Estimated regulatory capital at 12/31/12
approximately $0.5B; compared to a
requirement of approximately $0.3B.
1. Denotes estimated required regulatory capital for 12.31.12
2. Excess assumes actual regulatory capital as of 6.30.2012
Regulatory Capital
Preparing for Growth
$0.3B
Surplus regulatory capital would contribute
to funding growth
Current Revenue
Growth Capacity with Existing
Growth Capacity
$0.2B
Excess
Regulatory
Capital
Required
Regulatory
Capital
$0.5B
Estimated
Revenues
Requiring
additional
Regulatory
Capital
1. Assumes estimated required regulatory capital for 12.31.12 and actual
regulatory capital as of 6.30.2012. Please refer to the Company’s cautionary
statements. $6B
$2.8B
$3.2B
Additional
regulatory capital
($0.2B); to fund up
to $12B of revenue
Existing
regulatory capital
($0.5B); funds up
to $8.8B of
revenue
$12B
56
2
1
1
1
Regulatory
Capital |
 ©
2012 Molina Healthcare, Inc.
57
Potential Capital Needs
Please refer to the Company’s cautionary statements.
Average 7%
Required Equity as % of Premium Revenue
2006 -
2Q2012*
*Denotes estimated required regulatory capital for 12.31.12 as a percentage of annualized
revenue for the six months ended 6.30.12. Source(s): Company Data
2Q2012*
Est. Incremental Capital Sensitivity
Low
Med
High
Base Revenue
$6B
$6B
$6B
Incremental
Revenue
$3B
$4.5B
$6B
Total Revenue
$9B
$10.5B
$12B
After Tax Margin
1.5%
1.5%
1.5%
Avg. Incremental
Cap Requirement
(%)
7.0%
7.0%
7.0%
Incremental Cap
Requirement ($)
($210M)
($315M)
($420M)
Pro-forma Net
Income @ 1.5%
$135M
$158M
$180M
Estimated 2012
Excess Capacity
$200M
$200M
$200M
Capital Need
$0M
$0M
$40M
7.9%
8.1%
6.8%
7.0%
7.0%
5.8%
6.1%
0%
2%
4%
6%
8%
10%
2011
2010
2009
2008
2007
2006 |
 ©
2012 Molina Healthcare, Inc.
Earnings Margin 2006-1H2012
58
EBITDA MARGIN
AFTER TAX MARGIN
Please refer to the Company’s cautionary statements.
1. P denotes results excluding Missouri write-down in 2011, and Texas and Missouri
operations in 2012 |
 Why We Might Want
To Raise Capital? Acquisitions
Convertible debt repayment in 2014
Capital expenditures
Variability in profitability
Timing
New benefits
Growth above expectations
Desire for capital cushion (e.g. debt covenant and rating
agencies)
Excluded duals in WA and potential FL & TX ACA Medicaid
expansion
Regulatory capital in excess of minimum requirements
Regulatory requirements in advance of premium receipts
59
Please refer to the Company’s cautionary statements.
©
2012 Molina Healthcare, Inc. |
 Investment
Highlights 60
Attractive sector growth prospects driven by
government policies and economic conditions
Proven flexible health care services portfolio (risk-
based, fee-based and direct delivery)
Diversified geographic exposure with significant
presence in high growth regions
Focus on government-sponsored health care
programs
Seasoned management team with strong track
record of delivering earnings growth
Over 30 years of experience
Please refer to the Company’s cautionary statements.
©
2012 Molina Healthcare, Inc. |
 Q&A
61
©
2012 Molina Healthcare, Inc. |
