Attached files
| file | filename |
|---|---|
| 8-K - FORM 8-K - TRIPLE-S MANAGEMENT CORP | d245101d8k.htm |
| EX-99.1 - EX-99.1 - TRIPLE-S MANAGEMENT CORP | d245101dex991.htm |
Exhibit 10.1
CONTRACT BETWEEN
ADMINISTRACIÓN DE SEGUROS DE SALUD DE PUERTO RICO
(ASES)
and
TRIPLE-S SALUD, INC.
(Contractor)
to
ADMINISTER THE PROVISION OF THE PHYSICAL HEALTH
COMPONENT OF THE MISALUD PROGRAM
IN DESIGNATED SERVICE REGIONS
Contract No.:
| Service Regions: | Metro North, North, San Juan, Northeast, West and Virtual Regions |
TABLE OF CONTENTS
| ARTICLE 1 |
GENERAL PROVISIONS | 5 | ||||
| 1.2 BACKGROUND |
6 | |||||
| 1.3 GROUPS ELIGIBLE FOR SERVICES UNDER MISALUD |
8 | |||||
| 1.4 SERVICE REGIONS |
12 | |||||
| 1.5 DELEGATION OF AUTHORITY |
12 | |||||
| 1.6 AVAILABILITY OF FUNDS |
13 | |||||
| ARTICLE 2 |
DEFINITIONS | 13 | ||||
| ARTICLE 3 |
ACRONYMS | 49 | ||||
| ARTICLE 4 |
ASES RESPONSIBILITIES | 55 | ||||
| 4.1 GENERAL PROVISION |
55 | |||||
| 4.2 LEGAL COMPLIANCE |
55 | |||||
| 4.3 ELIGIBILITY |
55 | |||||
| 4.4 ENROLLMENT RESPONSIBILITIES OF ASES |
58 | |||||
| 4.5 DISENROLLMENT RESPONSIBILITIES OF ASES |
63 | |||||
| 4.6 ENROLLEE SERVICES AND MARKETING |
67 | |||||
| 4.7 COVERED SERVICES |
68 | |||||
| 4.8 Provider Network |
69 | |||||
| 4.9 QUALITY MONITORING |
70 | |||||
| 4.10 COORDINATION WITH CONTRACTOR’S KEY STAFF |
72 | |||||
| 4.11 INFORMATION SYSTEMS AND REPORTING |
72 | |||||
| 4.12 READINESS REVIEW |
75 | |||||
| ARTICLE 5 |
CONTRACTOR RESPONSIBILITIES | 77 | ||||
| 5.1 GENERAL PROVISIONS |
77 | |||||
| 5.2 ENROLLMENT RESPONSIBILITIES OF THE CONTRACTOR |
78 | |||||
| 5.3 SELECTION AND CHANGE OF A PRIMARY MEDICAL GROUP (“PMG”) AND PRIMARY CARE PHYSICIAN (“PCP”) |
89 | |||||
Page i
| 5.4 DISENROLLMENT RESPONSIBILITIES OF THE CONTRACTOR |
93 | |||||
| 5.5 CONVERSION CLAUSE |
102 | |||||
| ARTICLE 6 |
ENROLLEE SERVICES | 106 | ||||
| 6.1 GENERAL PROVISIONS |
106 | |||||
| 6.2 ASES APPROVAL OF ALL WRITTEN MATERIALS |
108 | |||||
| 6.3 REQUIREMENTS FOR WRITTEN MATERIALS |
109 | |||||
| 6.4 ENROLLEE HANDBOOK REQUIREMENTS |
111 | |||||
| 6.5 ENROLLEE RIGHTS AND RESPONSIBILITIES |
121 | |||||
| 6.6 PROVIDER DIRECTORY |
123 | |||||
| 6.7 ENROLLEE IDENTIFICATION (ID) CARD |
125 | |||||
| 6.8 TELE MISALUD (TOLL FREE TELEPHONE SERVICE) |
129 | |||||
| 6.9 INTERNET PRESENCE / WEB SITE |
138 | |||||
| 6.10 CULTURAL COMPETENCY |
139 | |||||
| 6.11 INTERPRETER SERVICES |
140 | |||||
| 6.12 ENROLLMENT OUTREACH FOR THE HOMELESS POPULATION |
141 | |||||
| 6.13 SPECIAL ENROLLEE INFORMATION REQUIREMENTS FOR DUAL ELIGIBLE BENEFICIARIES |
141 | |||||
| 6.14 MARKETING |
142 | |||||
| ARTICLE 7 |
COVERED SERVICES AND BENEFITS | 147 | ||||
| 7.1 REQUIREMENT TO MAKE AVAILABLE COVERED SERVICES |
147 | |||||
| 7.2 MEDICAL NECESSITY |
149 | |||||
| 7.3 EXPERIMENTAL OR COSMETIC PROCEDURES |
150 | |||||
| 7.4 COVERED SERVICES AND ADMINISTRATIVE SERVICES |
150 | |||||
| 7.5 BASIC COVERAGE |
150 | |||||
| 7.6 DENTAL SERVICES |
207 | |||||
| 7.7 SPECIAL COVERAGE |
209 | |||||
| 7.8 CASE AND DISEASE MANAGEMENT |
220 | |||||
Page ii
| 7.9 EARLY AND PERIODIC SCREENING, DIAGNOSIS AND TREATMENT REQUIREMENTS (“EPSDT”) |
227 | |||||
| 7.10 ADVANCE DIRECTIVES |
235 | |||||
| 7.11 ENROLLEE COST-SHARING |
237 | |||||
| 7.12 DUAL ELIGIBLE BENEFICIARIES |
239 | |||||
| 7.13 MORAL OR RELIGIOUS OBJECTIONS |
241 | |||||
| ARTICLE 8 |
INTEGRATION OF PHYSICAL AND BEHAVIORAL HEALTH SERVICES | 242 | ||||
| 8.1 GENERAL PROVISIONS |
242 | |||||
| 8.2 CO-LOCATION OF STAFF |
243 | |||||
| 8.3 REFERRALS |
244 | |||||
| 8.4 INFORMATION SHARING |
245 | |||||
| 8.5 STAFF EDUCATION |
246 | |||||
| 8.6 COOPERATION WITH PUERTO RICO AND FEDERAL GOVERNMENT AGENCIES |
247 | |||||
| 8.7 CONTRACTOR AND MBHO COVERAGE OF HOSPITALIZATION SERVICES |
247 | |||||
| 8.8 INTEGRATION PLAN |
247 | |||||
| ARTICLE 9 |
PROVIDER NETWORK | 248 | ||||
| 9.1 GENERAL PROVISIONS |
248 | |||||
| 9.2 NETWORK CRITERIA |
250 | |||||
| 9.3 PROVIDER QUALIFICATIONS |
252 | |||||
| 9.4 PROVIDER CREDENTIALING |
256 | |||||
| 9.5 PROVIDER RATIOS |
261 | |||||
| 9.6 NETWORK PROVIDERS |
263 | |||||
|
9.7 OUT-OF-NETWORK PROVIDERS |
267 | |||||
| 9.8 MINIMUM REQUIREMENTS FOR ACCESS TO PROVIDERS |
268 | |||||
| 9.9 REFERRALS |
269 | |||||
| 9.10 TIMELINESS OF PRIOR AUTHORIZATION |
271 | |||||
| 9.11 BEHAVIORAL HEALTH SERVICES |
272 | |||||
Page iii
| 9.12 HOURS OF SERVICE |
273 | |||||
| 9.13 PROHIBITED ACTIONS |
274 | |||||
| 9.14 ACCESS TO SERVICES FOR ENROLLEES WITH SPECIAL HEALTH NEEDS |
274 | |||||
| 9.15 PREFERENTIAL TURNS |
275 | |||||
| 9.16 CONTRACTING WITH GOVERNMENT FACILITIES |
275 | |||||
| 9.17 CONTRACTING WITH OTHER PROVIDERS |
276 | |||||
| 9.18 PMG ADDITIONS OR MERGERS |
277 | |||||
| 9.19 EXTENDED SCHEDULE OF PMGS |
277 | |||||
| 9.20 DIRECT RELATIONSHIP |
278 | |||||
| 9.21 ADDITIONAL PPN STANDARDS |
279 | |||||
| 9.22 CONTRACTOR DOCUMENTATION OF ADEQUATE CAPACITY AND SERVICES |
280 | |||||
| ARTICLE 10 |
PROVIDER CONTRACTING | 281 | ||||
| 10.1 GENERAL PROVISIONS |
281 | |||||
| 10.2 PROVIDER TRAINING |
284 | |||||
| 10.3 REQUIRED PROVISIONS IN PROVIDER CONTRACTS |
287 | |||||
| 10.4 TERMINATION OF PROVIDER CONTRACTS |
298 | |||||
| 10.5 PROVIDER PAYMENT |
301 | |||||
| 10.6 ACCEPTABLE RISK ARRANGEMENTS |
309 | |||||
| 10.7 PHYSICIAN INCENTIVE PLAN |
310 | |||||
| 10.8 REQUIRED INFORMATION REGARDING PROVIDERS |
314 | |||||
| ARTICLE 11 |
UTILIZATION MANAGEMENT | 317 | ||||
| 11.1 UTILIZATION MANAGEMENT POLICIES AND PROCEDURES |
317 | |||||
| 11.2 UTILIZATION MANAGEMENT GUIDANCE TO ENROLLEES |
319 | |||||
| 11.3 PRIOR AUTHORIZATION AND REFERRAL POLICIES |
319 | |||||
| 11.4 USE OF TECHNOLOGY TO PROMOTE UTILIZATION MANAGEMENT |
324 | |||||
| 11.5 COURT-ORDERED EVALUATIONS AND SERVICES |
325 | |||||
| 11.6 SECOND OPINIONS |
325 | |||||
Page iv
| 11.7 UTILIZATION REPORTING PROGRAM |
326 | |||||
| ARTICLE 12 |
QUALITY IMPROVEMENT AND PERFORMANCE PROGRAM | 329 | ||||
| 12.1 GENERAL PROVISIONS |
329 | |||||
| 12.2 QUALITY ASSESSMENT PERFORMANCE IMPROVEMENT (QAPI) PROGRAM |
329 | |||||
| 12.3 PERFORMANCE IMPROVEMENT PROJECTS |
332 | |||||
| 12.4 ER QUALITY INITIATIVE PROGRAM |
335 | |||||
| 12.5 QUALITY INCENTIVE PROGRAM |
337 | |||||
| 12.6 PERFORMANCE MEASURES |
343 | |||||
| 12.7 PROVIDER AND ENROLLEE SATISFACTION SURVEYS |
346 | |||||
| 12.8 EXTERNAL QUALITY REVIEW |
347 | |||||
| ARTICLE 13 |
FRAUD AND ABUSE | 349 | ||||
| 13.1 GENERAL PROVISIONS |
349 | |||||
| 13.2 COMPLIANCE PLAN |
350 | |||||
| 13.3 PROGRAM INTEGRITY PLAN |
353 | |||||
| 13.4 PROHIBITED AFFILIATIONS WITH INDIVIDUALS DEBARRED BY FEDERAL AGENCIES |
355 | |||||
| 13.5 REPORTING AND INVESTIGATIONS |
356 | |||||
| ARTICLE 14 |
GRIEVANCE SYSTEM | 358 | ||||
| 14.1 GENERAL REQUIREMENTS |
358 | |||||
| 14.2 COMPLAINT |
366 | |||||
| 14.3 GRIEVANCE PROCESS |
367 | |||||
| 14.4 ACTION |
369 | |||||
| 14.5 APPEAL PROCESS |
373 | |||||
| 14.6 ADMINISTRATIVE LAW HEARING |
378 | |||||
| 14.7 CONTINUATION OF BENEFITS WHILE THE CONTRACTOR APPEAL AND ADMINISTRATIVE LAW HEARING ARE PENDING |
380 | |||||
| 14.8 REPORTING REQUIREMENTS |
382 | |||||
| 14.9 REMEDY FOR CONTRACTOR NON-COMPLIANCE WITH ADVANCE DIRECTIVE REQUIREMENTS |
383 | |||||
Page v
| ARTICLE 15 |
ADMINISTRATION AND MANAGEMENT |
383 | ||||
| 15.1 GENERAL PROVISIONS |
383 | |||||
| 15.2 PLACE OF BUSINESS AND HOURS OF OPERATION |
384 | |||||
| 15.3 TRAINING AND STAFFING |
386 | |||||
| 15.4 DATA CERTIFICATION |
386 | |||||
| 15.5 IMPLEMENTATION PLAN AND SUBMISSION OF INITIAL DELIVERABLES |
387 | |||||
| ARTICLE 16 |
PROVIDER PAYMENT MANAGEMENT |
388 | ||||
| 16.1 GENERAL PROVISIONS |
388 | |||||
| 16.2 [INTENTIONALLY LEFT BLANK] |
391 | |||||
| 16.3 [INTENTIONALLY LEFT BLANK] |
391 | |||||
| 16.4 [INTENTIONALLY LEFT BLANK] |
391 | |||||
| 16.5 PAYMENT SCHEDULE |
391 | |||||
| 16.6 CONTRACTOR ADMINISTRATION RESPONSIBILITIES –FOR VIEQUES AND GUAYNABO |
392 | |||||
| 16.7 REQUIRED CLAIMS PROCESSING REPORTS |
393 | |||||
| 16.8 SUBMISSION OF ENCOUNTER DATA |
394 | |||||
| 16.9 RELATIONSHIP WITH PHARMACY BENEFIT MANAGER (PBM) |
395 | |||||
| 16.10TIMELY PAYMENT OF CLAIMS |
396 | |||||
| 16.11CONTRACTOR DENIAL OF CLAIMS AND RESOLUTION OF CONTRACTUAL AND CLAIMS DISPUTES |
400 | |||||
| 16.12CONTRACTOR RECOVERY FROM PROVIDERS |
408 | |||||
| ARTICLE 17 |
INFORMATION MANAGEMENT AND SYSTEMS |
409 | ||||
| 17.1 GENERAL PROVISIONS |
409 | |||||
| 17.2 GLOBAL SYSTEM ARCHITECTURE AND DESIGN REQUIREMENTS |
412 | |||||
| 17.3 SYSTEM AND DATA INTEGRATION REQUIREMENTS |
416 | |||||
| 17.4 SYSTEM ACCESS MANAGEMENT AND INFORMATION ACCESSIBILITY REQUIREMENTS |
417 | |||||
| 17.5 SYSTEMS AVAILABILITY AND PERFORMANCE REQUIREMENTS |
418 | |||||
| 17.6 SYSTEM TESTING AND CHANGE MANAGEMENT REQUIREMENTS |
424 | |||||
Page vi
| 17.7 SYSTEM SECURITY AND INFORMATION CONFIDENTIALITY AND PRIVACY REQUIREMENTS |
426 | |||||
| 17.8 INFORMATION MANAGEMENT PROCESS AND INFORMATION SYSTEMS DOCUMENTATION REQUIREMENTS |
428 | |||||
| 17.9 REPORTING FUNCTIONALITY REQUIREMENTS |
428 | |||||
| 17.10COMMUNITY HEALTH RECORD AND HEALTH INFORMATION EXCHANGE (HIE) REQUIREMENTS |
429 | |||||
| ARTICLE 18 |
REPORTING |
430 | ||||
| 18.1 GENERAL REQUIREMENTS |
430 | |||||
| 18.2 SPECIFIC REQUIREMENTS |
433 | |||||
| ARTICLE 19 |
ENFORCEMENT AND LIQUIDATED DAMAGES |
443 | ||||
| 19.1 GENERAL PROVISIONS |
443 | |||||
| 19.2 CATEGORY 1 |
445 | |||||
| 19.3 CATEGORY 2 |
445 | |||||
| 19.4 CATEGORY 3 |
447 | |||||
| 19.5 CATEGORY 4 |
450 | |||||
| 19.6 OTHER REMEDIES |
453 | |||||
| 19.7 NOTICE OF REMEDIES |
454 | |||||
| ARTICLE 20 |
TERM OF CONTRACT |
457 | ||||
| ARTICLE 21 |
PAYMENT FOR SERVICES |
458 | ||||
| 21.1 GENERAL PROVISIONS |
458 | |||||
| 21.2 ADMINISTRATIVE FEE |
459 | |||||
| 21.3 CLAIMS PAYMENT |
463 | |||||
| 21.4 CLAIMS INCURRED BUT NOT REPORTED |
464 | |||||
| 21.5 CONTRACTOR OBJECTIONS TO PAYMENT |
466 | |||||
| 21.6 RETENTION FUND FOR QUALITY INCENTIVE PROGRAM |
467 | |||||
| 21.7 FINANCIAL PERFORMANCE INCENTIVE |
467 | |||||
| ARTICLE 22 |
FINANCIAL MANAGEMENT |
468 | ||||
| 22.1 GENERAL PROVISIONS |
468 | |||||
Page vii
| 22.2 SOLVENCY AND FINANCIAL REQUIREMENTS |
471 | |||||
| 22.3 REINSURANCE AND STOP LOSS |
472 | |||||
| 22.4 THIRD PARTY LIABILITY AND COST AVOIDANCE |
473 | |||||
| 22.5 MISALUD AS SECONDARY PAYER TO MEDICARE |
482 | |||||
| 22.6 [INTENTIONALLY LEFT BLANK] |
484 | |||||
| 22.7 REPORTING REQUIREMENTS |
484 | |||||
| ARTICLE 23 |
PAYMENT OF TAXES |
489 | ||||
| ARTICLE 24 |
RELATIONSHIP OF PARTIES |
490 | ||||
| ARTICLE 25 |
INSPECTION OF WORK |
490 | ||||
| ARTICLE 26 |
GOVERNMENT PROPERTY |
491 | ||||
| ARTICLE 27 |
OWNERSHIP AND USE OF DATA AND SOFTWARE |
492 | ||||
| 27.1 OWNERSHIP AND USE OF DATA |
492 | |||||
| 27.2 RESPONSIBILITY FOR INFORMATION TECHNOLOGY INVESTMENTS |
493 | |||||
| ARTICLE 28 |
CRIMINAL BACKGROUND CHECKS |
494 | ||||
| ARTICLE 29 |
SUBCONTRACTS |
496 | ||||
| 29.1 USE OF SUBCONTRACTORS |
496 | |||||
| 29.2 COST OR PRICING BY SUBCONTRACTORS |
499 | |||||
| ARTICLE 30 |
REQUIREMENT OF INSURANCE LICENSE |
499 | ||||
| ARTICLE 31 |
CERTIFICATIONS |
500 | ||||
| ARTICLE 32 |
RECORDS REQUIREMENTS |
503 | ||||
| 32.1 GENERAL PROVISIONS |
503 | |||||
| 32.2 RECORDS RETENTION AND AUDIT REQUIREMENTS |
504 | |||||
| 32.3 MEDICAL RECORD REQUESTS |
507 | |||||
| ARTICLE 33 |
CONFIDENTIALITY |
508 | ||||
| 33.1 GENERAL CONFIDENTIALITY REQUIREMENTS |
508 | |||||
| 33.2 HIPAA COMPLIANCE |
510 | |||||
Page viii
| ARTICLE 34 |
TERMINATION OF CONTRACT |
511 | ||||
| 34.1 TERMINATION BY ASES |
511 | |||||
| 34.2 TERMINATION BY THE CONTRACTOR |
513 | |||||
| 34.3 GENERAL PROCEDURES |
515 | |||||
| 34.4 TERMINATION PROCEDURES |
517 | |||||
| ARTICLE 35 |
PHASE IN, PHASE-OUT AND COOPERATION WITH OTHER CONTRACTORS |
523 | ||||
| 35.1 [INTENTIONALLY LEFT BLANK] |
523 | |||||
| 35.5 PHASE OUT TRANSITION PERIOD |
525 | |||||
| 35.6 PHASE-IN TRANSITION REPORTS AND MEETINGS |
533 | |||||
| 35.7 ASES OBLIGATIONS |
535 | |||||
| 35.8 CONTRACTOR OBJECTIONS TO PAYMENT |
535 | |||||
| 35.9 RUNOFF PERIOD |
536 | |||||
| ARTICLE 36 |
INSURANCE |
538 | ||||
| ARTICLE 37 |
COMPLIANCE WITH ALL LAWS |
540 | ||||
| 37.1 NONDISCRIMINATION |
540 | |||||
| 37.2 COMPLIANCE WITH ALL LAWS |
541 | |||||
Page ix
| ARTICLE 38 |
CONFLICT OF INTEREST AND CONTRACTOR INDEPENDENCE |
543 | ||||
| ARTICLE 39 |
CHOICE OF LAW OR VENUE |
545 | ||||
| ARTICLE 40 |
THIRD-PARTY BENEFICIARIES |
545 | ||||
| ARTICLE 41 |
SURVIVABILITY |
546 | ||||
| ARTICLE 42 |
PROHIBITED AFFILIATIONS WITH INDIVIDUALS DEBARRED AND SUSPENDED |
546 | ||||
| ARTICLE 43 |
WAIVER |
547 | ||||
| ARTICLE 44 |
FORCE MAJEURE |
547 | ||||
| ARTICLE 45 |
BINDING |
547 | ||||
| ARTICLE 46 |
TIME IS OF THE ESSENCE |
548 | ||||
| ARTICLE 47 |
AUTHORITY |
548 | ||||
| ARTICLE 48 |
ETHICS IN PUBLIC CONTRACTING |
548 | ||||
| ARTICLE 49 |
DISPUTE RESOLUTION |
549 | ||||
| 49.2 INFORMAL DISPUTE RESOLUTION PROCEDURES |
549 | |||||
| 49.3 ARBITRATION |
550 | |||||
| 49.4 COURT ACTION |
552 | |||||
Page x
| ARTICLE 50 |
SECTION TITLES NOT CONTROLLING |
552 | ||||
| ARTICLE 51 |
HOLD HARMLESS |
552 | ||||
| ARTICLE 52 |
COOPERATION WITH AUDITS |
553 | ||||
| ARTICLE 53 |
OWNERSHIP AND FINANCIAL DISCLOSURE |
554 | ||||
| ARTICLE 54 |
AMENDMENT IN WRITING |
554 | ||||
| ARTICLE 55 |
CONTRACT ASSIGNMENT |
555 | ||||
| ARTICLE 56 |
SEVERABILITY |
555 | ||||
| ARTICLE 57 |
ENTIRE AGREEMENT |
555 | ||||
| ARTICLE 58 |
NOTICES |
556 | ||||
| ARTICLE 59 |
OFFICE OF THE COMPTROLLER |
559 | ||||
Page xi
THIS CONTRACT is made and entered into as of the Effective Date (defined below) by and between the Puerto Rico Health Insurance Administration (Administración de Seguros de Salud de Puerto Rico, hereinafter referred to as “ASES” or “the Administration”), a public corporation in the Government of Puerto Rico, and TRIPLE-S SALUD, INC. (“the Contractor”), an insurance company duly organized and authorized to do business under the laws of the Government of Puerto Rico, with employer identification number 66-0555677.
WHEREAS, pursuant to Title XIX of the federal Social Security Act, codified as 42 USC 1396 et seq. (“the Social Security Act”), and Act No. 72 of September 7, 1993 of the Laws of the Government of Puerto Rico, as amended, (“Act 72”), a comprehensive program of medical assistance for needy persons exists in the Commonwealth of Puerto Rico;
WHEREAS, under Act 72 and other sources of law of the Government of Puerto Rico designated in Attachment 1 ASES is responsible for health care policy, purchasing, planning, and regulation of health insurance plans, and pursuant to these statutory provisions, ASES has established a managed care program under the medical assistance program, known as “MiSalud,” or “the MiSalud Program”;
WHEREAS, the Puerto Rico Health Department (“the Health Department”) is the single State agency designated to administer medical assistance in Puerto Rico under Title XIX of the Social Security Act of 1935, as amended, and is charged with ensuring the appropriate delivery of
Page 1
health care services under Medicaid and the Children’s Health Insurance Program (“CHIP”) in Puerto Rico, and ASES manages these programs pursuant to a 1993 interagency collaborative agreement;
WHEREAS, MiSalud serves a mixed population including not only the Medicaid and CHIP populations, but also other eligible individuals as established under Act 72;
WHEREAS, ASES seeks to comply with the public policy objective of the Government of Puerto Rico (“the Government” or “Puerto Rico”) of creating MiSalud, an integrated system of physical and behavioral health services, with an emphasis on preventative services and access to quality care;
WHEREAS, in connection with the implementation of this public policy ASES caused a Request for Proposals for Physical Health Services to be issued on May 3, 2010, subsequently amended on June 17, 2010, (as amended, “the RFP”);
WHEREAS, ASES accepted the proposal submitted under the RFP by MCS Health Management Options, Inc. (“MCS”) to provide Physical Health Services in the Service Regions (as hereinafter defined);
Page 2
WHEREAS, on October 14, 2010, ASES and MCS executed a contract for the Provision of Physical Health Services under the MiSalud Program in six service regions (hereinafter referred to as the “Original Contract”). These service regions were the WEST, NORTH, METRO NORTH, SAN JUAN, NORTHEAST, and VIRTUAL Regions (hereinafter collectively referred to as the “Service Regions”);
WHEREAS, on June 9, 2011, ASES and MCS executed a restated contract (the Original Contract, as amended and restated is hereinafter referred to as the “Restated Contract”);
WHEREAS, the Restated Contract granted MCS a Limited Right of Non-Renewal and a Limited Right of Termination, in the event that MCS and ASES failed to agree on the Per Member Per Month Payment rates for the succeeding Fiscal Year, to be exercised on a specified period of time before the last day of the then current year under the Restated Contract;
WHEREAS, MCS and ASES were unable to agree on new Per Member Per Month Payment rates for each Service Region to be applicable for the Fiscal Year commencing on July 1, 2011 and therefore, MCS provided notice of non-renewal, which notice of non-renewal constituted notice of termination under the Restated Contract;
WHEREAS, MCS did not rescinded its notice of termination for which reason MCS and ASES agreed to proceed with the transition of the Service Regions to a new physical health services
Page 3
provider or providers to be designated by ASES for the MiSalud Program, as provided in the Restated Contract;
WHEREAS, in connection with the transition to a new physical health service provider or providers, ASES requested from all the participants in the RFP procurement process proposals for the provision of Physical Health Services in the Service Regions;
WHEREAS, the Contractor agreed to submit to ASES a proposal to administer the provision of physical health services in the Service Regions previously serviced by MCS as a third party administrator for a fee;
WHEREAS, after considering the different proposals submitted by the other proponents under the RFP, ASES selected the Contractor to administer the provision of physical health services in the Service Regions;
WHEREAS, the Contractor has agreed to administer and arrange for the provision of physical health services by Network Providers in the Service Regions as a third party administrator under the terms and conditions specified in this Contract.
NOW, THEREFORE, FOR AND IN CONSIDERATION of the mutual promises, covenants and agreements contained herein, and other good and valuable consideration, the receipt
Page 4
and sufficiency of which are hereby acknowledged, ASES and the Contractor (each individually a “Party” and collectively the “Parties”) hereby agree as follows:
ARTICLE 1 GENERAL PROVISIONS
The Government of Puerto Rico implemented certain reforms to its government health program, which serves Medicaid and CHIP recipients, as well as foster care children, certain individuals and families eligible based on income, and certain Government employees, pensioners, and veterans. The reforms produced an integrated model of physical and behavioral health services, with an emphasis on prevention and on facilitating prompt access to needed primary and specialty services. The Parties acknowledge that the Contractor shall not be financially responsible or otherwise at risk for the provision of Covered Services and Benefits to Enrollees in the MiSalud Program.
| 1.1 | The Contractor shall assist the Government of Puerto Rico by arranging for and administering the delivery of certain services under MiSalud through the described tasks, obligations, and responsibilities specified in, and subject to the terms of, this Contract. |
| 1.1.1 | All references in this document to the defined term “Contract” shall be deemed to mean this Contract, and the contractual relationship between the Parties shall now be governed and controlled by this Contract. |
Page 5
| 1.1.2 | All references herein to the Contractor’s compliance with federal or Puerto Rico laws, regulations or rules, including but not limited to 42 CFR Part 438, shall apply to the Contractor and/or Contractor’s provision of Administrative Services only to the extent any such laws, regulations or rules apply to a PIHP when such an entity is arranging for the provision of medical services or inpatient hospital or institutional services or providing administrative services. For the avoidance of doubt, the Parties agree that the Contractor is not providing medical services under this Contract and shall not be regulated as such. The foregoing notwithstanding, this will not be considered a limitation on the Contractor’s ability to render the Administrative Services. |
| 1.2 | Background |
| 1.2.1 | Effective October 1, 2010, the government health program previously referred to as La Reforma has been known as MiSalud. MiSalud continues the services offered under La Reforma, but also embodies new policy objectives. |
| 1.2.2 | MiSalud has the following objectives: |
| 1.2.2.1 | To transform Puerto Rico’s health system through an integrated vision of physical and behavioral health. |
Page 6
| 1.2.2.2 | To encourage the Contractor and other selected health plans to work together with Managed Behavioral Health Organizations (“MBHOs”) in each of nine service regions of Puerto Rico to provide integrated physical and behavioral health services. |
| 1.2.2.3 | To establish Primary Medical Groups (“PMGs”), which shall enter agreements with the Contractor, and shall act as the monitors for medical care. PMGs shall provide, manage, and direct health services, including coordination with behavioral health personnel and specialist services, in a timely manner. |
| 1.2.2.4 | To develop within each of the nine service regions a Preferred Provider Network (“PPN”), which shall be composed of physician specialists, laboratories, radiology facilities, hospitals, and Ancillary Service Providers that shall render Covered Services to persons enrolled in MiSalud (“Enrollees”). |
| 1.2.2.5 | To facilitate access to quality primary care and specialty services within the PPN by providing all services without the requirement of a referral, and not requiring cost-sharing for services within the PPN. |
Page 7
| 1.2.2.6 | To ensure that, other than through appropriate utilization control measures, services to Enrollees in MiSalud are not refused, restricted, or reduced, including by reason of pre-existing conditions or waiting periods. |
| 1.2.2.7 | To support the Puerto Rico Health Department and the Puerto Rico Mental Health and Against Addiction Services Administration (Administración de Servicios de Salud Mental y Contra la Adicción, hereinafter “ASSMCA”) in health education efforts focusing on lifestyles, HIV/AIDS prevention, the prevention of drug and substance abuse, and maternal and child health. |
| 1.3 | Groups Eligible for Services Under MiSalud |
| 1.3.1 | The following groups served under MiSalud are hereinafter referred to collectively as “Eligible Persons.” |
| 1.3.1.1 | Medicaid. These groups shall be referred to hereinafter as “Medicaid Eligible Persons.” All Medicaid eligibility categories, including the following, are eligible to enroll in MiSalud: |
| 1.3.1.1.1 | Categorically needy, as defined in 42 CFR Part 436, refers to families and children; aged, blind, or disabled individuals; and pregnant women, who are eligible for Medicaid. These groups are mandatory |
Page 8
| eligibility groups who, generally, are receiving or deemed to be receiving cash assistance. |
| 1.3.1.1.2 | Families and children refers to eligible members of families with children who are financially eligible under AFDC (Aid to Families with Dependent Children) or medically needy rules and who are deprived of parental support or care as defined under the AFDC program (see 45 CFR 233.90, 233.100). In addition, this group includes individuals under age 21 who are not deprived of parental support or care but are financially eligible under AFDC rules or medically needy rules. |
| 1.3.1.1.3 | Medically needy refers to families, children, aged, blind or disabled individuals, and pregnant women who are not listed as categorically needy but who may be eligible for Medicaid because their income and resources are within limits set by the Government of Puerto Rico under its Medicaid Plan (including persons whose income and resources fall within these limits after their incurred expenses for medical or remedial care are deducted). |
| 1.3.1.1.4 | Dual eligible beneficiaries refers to persons eligible for both Medicaid and Medicare (either Part A only, or Parts A and B). |
Page 9
| 1.3.1.1.5 | Foster care children in the custody of the Family and Children Administration (Administración de Familias y Niños, hereinafter “ADFAN”), provided that they otherwise meet Medicaid eligibility criteria; and |
| 1.3.1.1.6 | Survivors of domestic violence referred by the Office of the Women’s Advocate (Oficina de la Procuradora de las Mujeres), provided that they otherwise meet Medicaid eligibility criteria. |
| 1.3.1.2 | Children’s Health Insurance Program (CHIP). This group, comprised of children whose family income does not exceed two hundred percent (200%) of the Puerto Rico poverty level, will be referred to hereinafter as “CHIP Eligible Persons.” The CHIP population may include foster care children in the custody of ADFAN, provided that they otherwise meet CHIP eligibility criteria. |
| 1.3.1.3 | Other Groups (Non-Medicaid/CHIP). The following groups, which receive services under MiSalud without any federal participation, will be referred to hereinafter as “Other Eligible Persons.” |
| 1.3.1.3.1 | The “Commonwealth Population,” comprised of the following groups: |
Page 10
| 1.3.1.3.1.1 | Certain persons whose family income does not exceed two hundred percent (200%) of the Puerto Rico poverty level, who are between twenty-one (21) and sixty-four (64) years of age, and who do not qualify for either Medicaid or CHIP; |
| 1.3.1.3.1.2 | Police officers of the Government of Puerto Rico, and their Dependents; |
| 1.3.1.3.1.3 | Surviving Spouses of deceased police officers; |
| 1.3.1.3.1.4 | Survivors of domestic violence referred by the Office of the Women’s Advocate; |
| 1.3.1.3.1.5 | Veterans; and |
| 1.3.1.3.1.6 | Any other group of Eligible Persons that may be added during the Term of this Contract as a result of a change in laws or regulations. |
| 1.3.1.3.2 | Government Employees and Pensioners, whose eligibility for MiSalud is not based on income. |
Page 11
| 1.3.1.4 | Throughout the term of this Contract, ASES may amend the definition of the eligibility groups to be consistent with any amendments made to the Medicaid State plan. |
| 1.4 | Service Regions |
| 1.4.1 | The Contractor shall perform Administrative Services under this Contract in the Service Regions. |
| 1.4.2 | For the delivery of services under MiSalud, ASES has divided Puerto Rico into nine regions: eight geographical service regions and one “Virtual Region.” See Attachment 2 for a map of the geographical service regions. |
| 1.4.3 | The “Virtual Region” encompasses services provided throughout Puerto Rico to two groups of Enrollees: children who are under the custody of ADFAN; and certain survivors of domestic violence referred by the Office of the Women’s Advocate, who enroll in the MiSalud program. |
| 1.5 | Delegation of Authority |
Federal law and Puerto Rico law limit the capacity of ASES to delegate decisions to the Contractor. All decisions relating to public policy and to the administration of the Medicaid,
Page 12
CHIP, and the Puerto Rico government health assistance program included in MiSalud rest with the Puerto Rico Medicaid Program and ASES.
| 1.6 | Availability of Funds |
This Contract is subject to the availability of funds on the part of ASES, which in turn is subject to the transfer of federal, Puerto Rico, and municipal funds. If available funds are insufficient to meet its contractual obligations, ASES reserves the right to terminate this Contract, pursuant to Sections 34.1 and 34.6 of this Contract.
ARTICLE 2 DEFINITIONS
Whenever capitalized in this Contract, the following terms have the respective meaning set forth below, unless the context clearly requires otherwise.
Act 72: The law of the Government of Puerto Rico, adopted on September 7, 1993, and subsequently amended, which created the Puerto Rico Health Insurance Administration (ASES) and empowered ASES to administer certain government health programs.
Abandoned Call: A call initiated to a Call Center that is ended by the caller before any conversation occurs or before a caller is permitted access to a caller-selected option.
Page 13
Abuse: Provider practices that are inconsistent with sound fiscal, business, or medical practices, and result in unnecessary cost to the MiSalud Program, or in reimbursement for services that are not Medically Necessary or that fail to meet professionally recognized standards for Health Care. It also includes Enrollee practices that result in unnecessary cost to the Medicaid program.
Access: Adequate availability of Benefits to fulfill the needs of Enrollees.
Action: The denial or limited authorization of a requested service, including the type or level of service; the reduction, suspension, or termination of a previously authorized service; the denial, in whole or part, of payment for a service (including in circumstances in which an Enrollee is forced to pay for a service; the failure to provide services in a timely manner (within the timeframes established by this Contract or otherwise established by ASES); or the failure of the Contractor to act within the timeframes provided in 42 CFR 438.408(b).
ADFAN: Families and Children Administration (Administración de Familias y Niños), which is responsible for foster care children in the custody of the Government of Puerto Rico.
Administrative Fee: The monthly amount that ASES will pay to the Contractor for performing the Administrative Services which shall be determined by multiplying the number of Enrollees by the Per Member Per Month Administrative Fee. This payment is made, without any deduction or
Page 14
Withhold unless otherwise specified in this Contract, regardless of whether Enrollees receive Covered Services or Benefits during the period covered by the payment.
Administrative Services: The Contractual obligations of the Contractor to perform administrative services with respect to the provision of Covered Services as set forth in this Contract, including Case Management, Disease Management, Utilization Management, Credentialing Network Providers, Network management, quality improvement, Marketing, Enrollment, Enrollee services, Claims administration, Information Systems, financial management and reporting, and other administrative services to be performed by the Contractor as specified in this Contract or as may be mutually agreed by the Parties in writing by amending this Contract.
Administrative Law Hearing: The appeal process administered by the Government of Puerto Rico and as required by federal law, available to Enrollees and Providers after they exhaust the applicable grievance system and complaint process.
Administrative Referral: A Referral of an Enrollee by the Contractor to a Provider or facility located outside the PPN, when the Enrollee’s PCP or other PMG physician does not provide a Referral in the required time period.
Advance Directive: A written instruction, such as a living will or durable power of attorney for Health Care, as defined in 42 CFR 489.100, and as recognized under Puerto Rico law under Act 160
Page 15
of November 17, 2001, as amended, relating to the provision of health care when the individual is incapacitated.
Agent: An entity that contracts with ASES to perform administrative services, including but not limited to: fiscal agent activities; outreach, eligibility, and Enrollment activities; and Information Systems and technical support.
Ancillary Services: Professional services, including laboratory, radiology, physical therapy, and respiratory therapy, which are provided in conjunction with other medical or hospital care.
Appeal: An Enrollee request for a review of an Action.
ASES: Administración de Seguros de Salud de Puerto Rico (the Puerto Rico Health Insurance Administration), the entity in the Government of Puerto Rico responsible for oversight and administration of the MiSalud Program, or its Agent.
ASES Data: All data created from information, documents, messages (verbal or electronic), Reports, or meetings involving or arising out of this Contract, except for the Contractor Proprietary Information.
Page 16
ASSMCA: Administración de Servicios de Salud Mental y Contra la Addiccion (the Puerto Rico Mental Health and Against Addiction Services Administration), the government agency responsible for the planning and establishment of mental health and substance abuse policies and procedures and for the coordination, development, and monitoring of all behavioral health services rendered to Enrollees in MiSalud.
Authorized Representative: A person authorized by an Enrollee in writing to make health-related decisions on behalf of an Enrollee, including, but not limited to, Enrollment and Disenrollment decisions, filing Complaints, Grievances, and Appeals, and choice of a PCP or PMG.
Authorized Signatory: An individual designated by the Contractor who is either the Contractor’s Chief Executive Officer, the Contractor’s Chief Financial Officer, or an individual who has delegated authority to sign for, and who reports directly to, the Contractor’s Chief Executive Officer or Chief Financial Officer.
Automatic Assignment (or Auto-Assignment): The assignment of an Enrollee to a Primary Medical Group and a Primary Care Physician by the Contractor, normally at the time that ASES or the Contractor Auto-Enrolls the person in the MiSalud Program.
Page 17
Auto-Enrollment: The Enrollment of an individual who is certified eligible for Medicaid or CHIP and the Commonwealth Population, in a MiSalud Plan by the Contractor without any action by the individual, as provided in Articles 4 and 5 of this Contract.
Basic Coverage: The MiSalud Covered Services listed in Section 7.5 of this Contract, which are available to all Enrollees.
Benefits: The services set forth in this Contract, including Basic Coverage, Dental Services and Special Coverage for which the Contractor has agreed to provide Administrative Services.
Blocked Call: A call that cannot be connected immediately because no circuit is available at the time the call arrives or the telephone system is programmed to block calls from entering the queue when the queue backs up beyond a defined threshold.
Business Days: Traditional workdays, including Monday, Tuesday, Wednesday, Thursday, and Friday. Puerto Rico holidays are excluded.
Calendar Days: All seven days of the week.
Call Center: A telephone service facility equipped to handle a large number of inbound and outbound calls.
Page 18
Capitation: A method of risk sharing reimbursement contained in a written agreement through which a Provider agrees to provide specified health care services to Enrollees for a fixed amount per month.
Case Management: An Administrative Service comprised of a set of Enrollee-centered steps to ensure that an Enrollee with intensive needs, including catastrophic or high-risk conditions, receives needed services in a supportive, effective, efficient, timely, and cost-effective manner.
Centers for Medicare and Medicaid Services: The agency within the U.S. Department of Health and Human Services with responsibility for the Medicare, Medicaid and the Children’s Health Insurance Programs.
Center for the Collection of Municipal Revenues: The tax collection agency of the Government of Puerto Rico.
Central Access Units: Clinics that serve as points of entry for Enrollees seeking to access Behavioral Health Services, which are staffed by an interdisciplinary team responsible for referring Enrollees to the required level of treatment, and for tracking and monitoring quality in the delivery of Behavioral Health Services.
Page 19
Certification: As provided in Section 4.3.3 of this Contract, a decision by the Puerto Rico Medicaid Program that a person is eligible for services under the MiSalud Program because the person is Medicaid Eligible, CHIP Eligible, or a member of the Commonwealth Population. Some public employees and pensioners may enroll in MiSalud without first receiving a Certification.
Children’s Health Insurance Program (“CHIP”): The Government of Puerto Rico’s Children’s Health Insurance Program established pursuant to Title XXI of the Social Security Act.
CHIP Eligible Person: A child eligible to enroll in the MiSalud Program because he or she is eligible for CHIP.
Chronic Condition: An ongoing physical, behavioral, or cognitive disorder, with duration of at least twelve (12) months with resulting functional limitations, reliance on compensatory mechanisms (medications, special diet, assistive devices, etc.) and service use or need beyond that which is normally considered routine.
Claim: Whether submitted manually or electronically, a bill for Covered Services, a line item of Covered Services, or all Covered Services for one Enrollee within a bill.
Claims Payment: The amount that ASES pays the Contractor for Claims submitted by Providers for Covered Services provided to Enrollees under this Contract.
Page 20
Claims Payment Report: The report required to be submitted each fifteenth (15th) and (30th) day of each calendar month by the Contractor with detailed claims information and check request numbers consistent with Article 16.
Clean Claim: A Claim received by the Contractor for adjudication, which can be processed without obtaining additional information from the Provider of the service or from a Third Party, as provided in Section 22.4.5.1 of this Contract. It includes a claim with errors originating in the Contractor’s claims system. It does not include a claim from a Provider who is under investigation for Fraud or Abuse, or a claim under review for Medical Necessity.
Cold-Call Marketing: Any unsolicited personal contact by the Contractor with an Eligible Person, for the purposes of marketing.
Commonwealth Population: A group eligible for participation in MiSalud as Other Eligible Persons, with no federal participation in the cost of their coverage, which is comprised of low-income persons and other groups listed in Section 1.3.1.3.1 of this Contract.
Complaint: The procedure for addressing Enrollee complaints, defined as expressions of dissatisfaction about any matter other than an Action that are resolved at the point of contact rather than through filing a formal grievance.
Page 21
Comprehensive Care Centers (“CCuSaI”): Integrated care centers focused on prevention, offering additional services in the areas of health promotion, healthy lifestyles, and preventing chronic diseases.
Contract: The written agreement between ASES and the Contractor; comprised of the Contract, any addenda, appendices, attachments, or amendments thereto.
Contract Term: The duration of time that this Contract is in effect (including any Transition Period), as defined in Article 20 of this Contract.
Contractor: Triple-S Salud, Inc., a corporation licensed as an insurer by the PRICO, which contracts hereunder with ASES for the provision of Administrative Functions.
Contractor Proprietary Information: As defined in Section 27.1.2 of this Contract.
Conversion Clause: The provision in Section 5.5 of this Contract giving the Enrollee the right to apply for a direct pay insurance policy from the Contractor upon the Effective Date of Disenrollment from the Plan.
Page 22
Co-Payment: A cost-sharing requirement which is a fixed monetary amount paid by the Enrollee to a Provider for certain Covered Services as specified by ASES.
Corrective Action Plan: The detailed written plan required by ASES from the Contractor to correct or resolve a deficiency which may include a remedy as provided in Article 19 of this Contract.
Cost Avoidance: A method of paying Claims in which the Provider is not reimbursed until the Provider has demonstrated that all available health insurance, and other sources of Third Party Liability, have been exhausted.
Countersignature: An authorization provided by the Enrollee’s PCP, or another Provider within the Enrollee’s PMG, for a prescription written by another Provider to be dispensed.
Covered Services: Those Medically Necessary physical health care services (listed in Article 7 of this Contract) provided to Enrollees by Providers, the payment or indemnification of which is covered under this Contract.
Credentialing: The Contractor’s determination as to the qualifications of a specific Provider to render specific health care services.
Page 23
Cultural Competency: A set of interpersonal skills that allow individuals to increase their understanding, appreciation, acceptance, and respect for cultural differences and similarities within, among and between groups and the sensitivity to know how these differences influence relationships with Enrollees. This requires a willingness and ability to draw on community-based values, traditions and customs, to devise strategies to better meet culturally diverse Enrollee needs, and to work with knowledgeable persons of and from the community in developing focused interactions, communications, and other supports.
Cultural Competency Plan: Shall have the meaning ascribed to such term in Section 6.10.1 of this Contract.
Daily Basis: Each Business Day.
Deductible: In the context of Medicare, the dollar amount of covered services that must be incurred before Medicare will pay for all or part of the remaining covered services.
Dental Services: The dental services provided under MiSalud, listed in Section 7.6 of this Contract.
Dependent: A person who is enrolled in MiSalud as the spouse or child of the principal Enrollee.
Page 24
Deliverable: A document, manual or report submitted to ASES by the Contractor to fulfill requirements of this Contract.
Disease Management: An Administrative Service comprised of a set of Enrollee-centered steps to provide coordinated care to Enrollees suffering from diseases listed in Section 7.8.3 of this Contract.
Disenrollment: The termination of a person’s Enrollment in the MiSalud Plan.
Dual Eligible Beneficiary: An Enrollee eligible for both Medicaid and Medicare.
Durable Medical Equipment: Equipment, including assistive technology, which: a) can withstand repeated use; b) is used to service a health or functional purpose; c) is ordered by a Health Care Professional to address an illness, injury or disability; and d) is appropriate for use in the home, work place, or school.
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) Program: A Medicaid-mandated program that covers screening and diagnostic services to determine physical and mental deficiencies in Enrollees less than twenty-one (21) years of age, and health care, prevention, treatment, and other measures to correct or ameliorate any deficiencies and chronic conditions discovered.
Page 25
Effective Date of the Contract: The first day of the Term of this Contract, which shall be the date upon which the Contract is fully executed as specified on the signature page of this Contract, but in no event later than the Implementation Date.
Effective Date of Disenrollment: The date, as defined in Section 4.5.3 of this Contract, on which an Enrollee ceases to be covered under the MiSalud Plan.
Effective Date of Enrollment: The date, as defined in Section 4.4.1 of this Contract, on which an Eligible Person becomes an Enrollee and acquires coverage under the MiSalud Plan.
EHR system: An electronic health record as provided in Section 4.11.4 of this Contract.
Eligible Person: A person eligible to enroll in the MiSalud Program, as provided in Section 1.3.1 of this Contract, by virtue of being Medicaid Eligible, CHIP Eligible, or an Other Eligible Person.
Emergency Medical Condition or Medical Emergency: A medical or mental health condition, regardless of diagnosis or symptoms, manifesting itself by acute symptoms of sufficient severity (including severe pain) that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect to result in the following, in the absence of immediate medical attention: (i) placing the physical or mental health of the individual (or, with respect to a pregnant
Page 26
woman, the health of the woman or her unborn child) in serious jeopardy; (ii) seriously impairing bodily functions; or (iii) causing serious dysfunction of any bodily organ or part.
Emergency Services: Covered Services (as described in Section 7.5.9 of this Contract) furnished by a qualified Provider in an emergency room that are needed to evaluate or stabilize an Emergency Medical Condition as defined above.
Encounter: A distinct set of services provided to an Enrollee in a face-to-face setting on the dates that the services were delivered, regardless of whether the Provider is paid on a Fee-for-Service or Capitated basis. Encounters with more than one Health Care Professional, and multiple Encounters with the same Health Care Professional, that take place on the same day in the same location will constitute a single Encounter, except when the Enrollee, after the first Encounter, suffers an illness or injury requiring an additional diagnosis or treatment.
Encounter Data: (i) All data captured during the course of a single Encounter that specify the diagnoses, comorbidities, procedures (therapeutic, rehabilitative, maintenance, or palliative), pharmaceuticals, medical devices and equipment associated with the Enrollee receiving services during the Encounter; (ii) The identification of the Enrollee receiving and the Provider(s) delivering the health care services during the single Encounter; and, (iii) A unique, i.e. unduplicated, identifier for the single Encounter.
Page 27
Enrollee: A person who is currently enrolled in the Plan, as provided in this Contract, and who, by virtue of relevant federal and Puerto Rico laws and regulations, is an Eligible Person listed in Section 1.3.1 of this Contract.
Enrollment: The process by which an Eligible Person becomes a member of the MiSalud Plan.
EPSDT Checkups: Shall have the meaning ascribed to such term in Section 7.9.3.1 of this Contract.
EPSDT Eligible Children: Shall have the meaning ascribed to such term in Section 7.9.1 of this Contract.
EPSDT Plan: Shall have the meaning ascribed to such term in Section 7.9.1.1 of this Contract.
External Quality Review Organization (“EQRO”): An organization that meets the competence and independence requirements set forth in 42 CFR 438.354 and performs analysis and evaluation on the quality, timeliness, and access to Covered Services and Benefits to Enrollees with respect to which the Contractor provides Administrative Services under this Contract.
Federally Qualified Health Center (“FQHC”) Services: An entity that provides outpatient health programs pursuant to Section 1905(l)(2)(B) of the Social Security Act.
Page 28
Federally Qualified Health Center (“FQHC”) Services: Services furnished to an individual as an outpatient of an FQHC.
Fee-for-Service: A method of reimbursement based on payment for specific Covered Services rendered to an Enrollee.
Final Report: Shall have the meaning ascribed to such term in Section 34.8.4 of this Contract.
Fiscal Year: The period from July 1 of one calendar year through June 30 of the following calendar year.
Fraud: An intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit or financial gain to him/herself or some other person, and it includes any act that constitutes Fraud under applicable federal or Puerto Rico law.
General Network: The group of Providers under contract with the Contractor that are not members of the Contractor’s Preferred Provider Networks.
Grievance: An expression of dissatisfaction about any matter other than an Action.
Page 29
Grievance System: The overall system that includes Complaints, Grievances, and Appeals at the Contractor level, as well as access to the Administrative Law Hearing process.
Health Care Professional: A physician or other health care professional, including but not limited to podiatrists, optometrists, chiropractors, psychologists, dentists, physician’s assistants, physical or occupational therapists and therapists assistants, speech-language pathologists, audiologists, registered or licensed practical nurses (including nurse practitioners, clinical nurse specialist, certified registered nurse anesthetists, and certified nurse midwives), licensed certified social workers, registered respiratory therapists, and certified respiratory therapy technicians.
Health Certificate: Certificate issued by a physician after an examination that includes Venereal Disease Research Laboratory (“VRDL”) and tuberculosis (“TB”) tests if the individual suffers from a contagious disease that could incapacitate him or her or prevent him or her from doing his or her job, and does not represent a danger to public health.
Healthy Child Care: The battery of screenings (listed in Section 7.5.3.1 of this Contract) provided to children under age two (2) who are Medicaid- or CHIP Eligible as part of Puerto Rico’s Early and Periodic Screening, Diagnostic and Treatment Program.
HEDIS: The Healthcare Effectiveness Data and Information Set, a set of performance measures for managed care developed by the National Committee for Quality Assurance (“NCQA”).
Page 30
Health Insurance Portability and Accountability Act (“HIPAA”): A law enacted in 1996 by the Congress of the United States. When referenced in this Contract it includes all related rules, regulations and procedures.
Immediately or Immediate: Within twenty-four (24) hours, unless otherwise provided in this Contract.
Implementation Date of the Contract: The date on which the Contractor shall first be entitled to compensation for providing Administrative Services and arranging for the provision of Covered Services and Benefits under this Contract, which is November 1, 2011.
Incurred-But-Not-Reported (IBNR): Estimate of unpaid Claims liability, including received but unpaid Claims.
Indian: Indian means an individual, defined at title 25 of the U.S.C. sections 1603(c), 1603(f), 1603(f) or who has been determined eligible, as an Indian, pursuant to 42 C.F.R. 136.12 or Title V of the Indian Health Care Improvement Act, to receive health care services from Indian health care providers (HIS, an Indian Tribe, Tribal Organization, or Urban Indian Organization-I/T/U) or through referral under Contract Health Services.
Page 31
Information Service: The component of Tele MiSalud, a Call Center operated by the Contractor (described in Section 6.8 of this Contract), intended to assist Enrollees with routine inquiries which shall be fully staffed between the hours of 7:00 a.m. and, 7:00 p.m., Monday through Friday, excluding Puerto Rico holidays.
Information System(s): A combination of computing and communications hardware and software that is used in: (a) the capture, storage, manipulation, movement, control, display, interchange and/or transmission of information, i.e. structured data (which may include digitized audio and video) and documents; and/or (b) the processing of such information for the purposes of enabling and/or facilitating a business process or related transaction.
Insolvent: Unable to meet or discharge financial liabilities.
Integration Model: The service delivery model under the MiSalud Program, providing physical and behavioral health services in close coordination, to ensure optimum detection, prevention, and treatment of physical and behavioral health conditions.
MA-10: Form issued by the Puerto Rico Medicaid Program, entitled “Notice of Action Taken,” containing the Certification decision (whether a person was determined eligible or ineligible for Medicaid, CHIP, or the Commonwealth Population).
Page 32
Managed Behavioral Health Organization (“MBHO”): An entity that contracts with ASES for the provision of the behavioral health component of the MiSalud program.
Managed Care Organization (“MCO”): An entity that is organized for the purpose of providing health care and is licensed as an insurer by the PRICO, which contracts with ASES for the provision of Covered Services and Benefits, except for Behavioral Health Services, in designated Service Regions, under the MiSalud program. For the avoidance of doubt, the Parties agree that Contractor is not an MCO for purposes of this Contract.
Marketing: Any communication from the Contractor to any Eligible Person regarding the MiSalud Program that can reasonably be interpreted as intended to influence the individual to enroll in the MiSalud Plan, or not to enroll in another plan, or to disenroll from another plan.
Marketing Materials: Materials that are produced in any medium, by or on behalf of the Contractor, that can reasonably be interpreted as intended to market to individuals the MiSalud Program.
Master Formulary: The list of pharmaceutical products set forth on Attachment 5 to this Contract.
Medicaid: The joint federal/state program of medical assistance established by Title XIX of the Social Security Act.
Page 33
Medicaid Eligible Person: An individual eligible to receive services under Medicaid, who is eligible, on this basis, to enroll in the MiSalud Program.
Medicaid Management Information System (MMIS): Computerized system used for the processing, collecting, analysis and reporting of Information needed to support Medicaid and CHIP functions. The MMIS consists of all required subsystems as specified in the State Medicaid Manual.
Medical Advice Service: The twenty-four (24) hour emergency medical advice toll-free phone line operated by the Contractor through its Tele MiSalud service, described in Section 6.8 of this Contract.
Medical Record: The complete, comprehensive record of an Enrollee including, but not limited to, x-rays, laboratory tests, results, examinations and notes, accessible at the site of the Enrollee’s Network Primary Care Physician or Provider, that documents all health care services received by the Enrollee, including inpatient, outpatient, ancillary, and emergency care, prepared in accordance with all applicable federal and Puerto Rico rules and regulations, and signed by the Provider rendering the services.
Medical Necessity or Medically Necessary: Shall have the meaning ascribed to such terms in Section 7.2 of this Contract.
Page 34
Medicare: The federal program of medical assistance for persons over age 65 and certain disabled persons under Title XVIII of the Social Security Act.
Medicare Part A: The part of the Medicare program that covers inpatient hospital stays and skilled nursing facility, home health, and hospice care.
Medicare Part B: The part of the Medicare program that covers physician, outpatient, home health, and preventive services.
Medicare Part C: The part of the Medicare program that permits Medicare recipients to select coverage among various private insurance plans.
Medicare Platino: A program administered by ASES for Dual Eligible Beneficiaries, in which managed care organizations or other insurers under contract with ASES function as Part C plans to provide services covered by Medicare, and also to provide a “wraparound” benefit of Covered Services and Benefits under MiSalud.
MiSalud (or “the MiSalud Program”): The government health services program (formerly referred to as “La Reforma”) offered by the Government of Puerto Rico, and administered by ASES,
Page 35
which serves a mixed population of Medicaid Eligible, CHIP Eligible, and Other Eligible Persons, and emphasizes integrated delivery of physical and behavioral health services.
MiSalud Plan or Plan: The physical health component of the MiSalud Program offered to Eligible Persons in the Service Regions covered by this Contract, and with respect to which the Contractor shall provide Administrative Services under this Contract.
MiSalud Policies and Procedures: Shall have the meaning ascribed to such term in Section 4.7.3 of this Contract.
National Provider Identifier: The unique identifying number system for Providers created by the Centers for Medicare & Medicaid Services (CMS), through the National Plan and Provider Enumeration System.
Negative Redetermination Decision: A decision by the Puerto Rico Medicaid Program that a person is no longer eligible for services under the MiSalud Program (because the person no longer meets the eligibility standards for Medicaid, CHIP, or Puerto Rico’s government health assistance program).
Network: The entire group of Providers under contract with the Contractor, including those that are members of the General Network and those that are members of the PPN.
Page 36
Network Provider: A Provider that has a contract with the Contractor under the MiSalud Program. This term includes Providers in the General Network and Providers in the PPN.
Non-Emergency Medical Transportation (“NEMT”): Transportation for a non-emergency service.
Notice of Action: The notice described in Section 14.4.3 of this Contract, in which the Contractor notifies both the Enrollee and the Provider of an Action.
Notice of Disposition: The notice in which the Contractor explains in writing to the Enrollee and the Provider of the results and date of resolution of a Complaint, Grievance, or Appeal.
Office of the Patient Advocate: An office of the Government of Puerto Rico created by Law 11 of April 11, 2001, which is tasked with protecting the patient rights and protections contained in the Patient’s Bill of Rights Act.
Office of the Women’s Advocate: An office of the Government of Puerto Rico which is tasked, among other responsibilities, with protecting victims of domestic violence.
Page 37
Other Eligible Person: A person eligible to enroll in the MiSalud Program under Section 1.3.1.3 of this Contract, who is not Medicaid- or CHIP Eligible; this group is comprised of the Commonwealth Population and certain public employees and pensioners.
Out-of-Network Provider: A Provider that does not have a contract with the Contractor under MiSalud; i.e., the Provider is not in either the General Network or the PPN.
Patient’s Bill of Rights Act: Law 194 of August 25, 2000, as amended, a law of the Government of Puerto Rico relating to patient rights and protection.
Per Member Per Month Administrative Fee: The monthly amount that ASES will pay to the Contractor per member per month (PMPM) in accordance with Attachment 11 of this Contract, in consideration of the Administrative Services.
Pharmacy Benefit Manager (PBM): An entity under contract with ASES under the MiSalud Program, responsible for the administration of pharmacy Claims processing, formulary management, drug utilization review, pharmacy network management, and Enrollee information services relating to Pharmacy Services.
Page 38
Pharmacy Program Administrator (PPA): An entity, under contract with ASES, responsible for implementing and offering support to ASES and the contracted PBMs in the negotiation of rebates and development of the Maximum Allowable Cost (“MAC”) List.
Physician Incentive Plan: Any compensation arrangement between the Contractor and a physician or physician group that is intended to advance Utilization Management.
Plan: See definition of the MiSalud Plan.
Post-Stabilization Services: Covered Services, relating to an Emergency Medical Condition, that are provided after an Enrollee is stabilized, in order to maintain the stabilized condition, or to improve or resolve the Enrollee’s condition.
Potential Enrollee: A person who has been Certified by the Puerto Rico Medicaid Program as eligible to enroll in MiSalud (whether on the basis of Medicaid eligibility, CHIP eligibility, or eligibility as a member of the Commonwealth Population), but who was not enrolled in the MiSalud Plan prior to July 1, 2011.
PR Prompt Payment Law: collectively, Chapter 30 of the Puerto Rico Insurance Code and Rule Number 73 promulgated thereunder by the PRICO.
Page 39
Preferential Turns: The policy of requiring Network Providers to give priority in treating Enrollees from the island municipalities of Vieques and Culebra, so that they may be seen by a Provider within a reasonable time after arriving in the Provider’s office. This priority treatment is necessary because of the remote locations of these municipalities, and the greater travel time required for their residents to seek medical attention.
Preferred Drug List (“PDL”): A published subset of pharmaceutical products used for the treatment of physical and behavioral health conditions developed by the PPA from the Master Formulary after clinical and financial review.
Preferred Provider Network: A group of Network Providers that MiSalud Enrollees may access without any requirement of a Referral or Prior Authorization; provides services to MiSalud Enrollees without imposing any Co-Payments; and meets the Network requirements described in Article 9 of this Contract.
Prepaid Inpatient Health Plan (“PIHP”): An entity that: (a) provides medical services to Enrollees under a contract with ASES with prepaid Capitation or other payment arrangements that do not use State plan payment plans; (b) provides, arranges for, or otherwise has responsibility for the provision of any inpatient hospital or institutional services for its Enrollees; and (c) does not have a comprehensive risk contract.
Page 40
Preventive Services: Health care services provided by a physician or other Health Care Professional within the scope of his or her practice under Puerto Rico law to prevent disease, disability, or other health conditions; and to promote physical and mental health and efficiency.
Primary Care: All health care services, including periodic examinations, preventive health care services and counseling, immunizations, diagnosis and treatment of illness or injury, coordination of overall medical care, record maintenance, and initiation of Referrals to specialty Providers described in this Contract and for maintaining continuity of patient care.
Primary Care Physician (“PCP”): A licensed medical doctor (MD) who is a Provider and who, within the scope of practice and in accordance with Puerto Rico certification and licensure requirements, is responsible for providing all required Primary Care to Enrollees. The PCP is responsible for determining services required by Enrollees, provides continuity of care, and provides Referrals for Enrollees when Medically Necessary. A PCP may be a general practitioner, family physician, internal medicine physician, obstetrician/gynecologist, or pediatrician.
Primary Medical Group (“PMG”): A grouping of associated Primary Care Physicians and other Providers for the delivery of services to MiSalud Enrollees using a coordinated care model. PMGs may be organized as Provider care organizations, or as another group of Providers who have contractually agreed to offer a coordinated care model to MiSalud Enrollees under the terms of this Contract.
Page 41
Prior Authorization: Authorization granted by the Contractor in advance of the rendering of a Covered Service, which, in some instances, is made a condition for receiving the Covered Service.
Provider: Any physician, hospital, facility, or other Health Care Professional who is licensed or otherwise authorized to provide health care services in the jurisdiction in which they are furnished.
Provider Contract: Any written contract between the Contractor and a Provider setting forth the terms and conditions under which the Provider will provide Covered Services to Enrollees under this Contract.
Psychiatric Emergency: A psychiatric condition manifesting itself in acute symptoms of sufficient severity (including severe pain) that a prudent layperson, who possesses an average knowledge of health and medicine could reasonably expect the absence of immediate medical attention to result in placing the health of the individual (or, with respect to a pregnant woman, the health of the woman or her unborn child) in serious jeopardy, or in causing serious impairments of bodily functions, or serious dysfunction of any bodily organ or part. A Psychiatric Emergency shall not be defined on the basis of lists of diagnoses or symptoms.
Page 42
Puerto Rico Health Department (“Health Department”): The Single State Agency charged with administration of the Medicaid Program of the Government of Puerto Rico, which (through the Puerto Rico Medicaid Program) is responsible for Medicaid and CHIP eligibility determinations.
Puerto Rico Insurance Commissioner’s Office (“PRICO”): The Puerto Rico Government agency responsible for regulating, monitoring, and licensing insurance business.
Puerto Rico Medicaid Program: The subdivision of the Puerto Rico Health Department that conducts eligibility determinations for Medicaid, CHIP, and the Commonwealth Population.
Quality Assessment and Performance Improvement Program (QAPI): A set of programs aiming to increase the likelihood of desired health outcomes of Enrollees through the provision of health services that are consistent with current professional knowledge; the QAPI Program includes incentives to comply with HEDIS standards, to provide adequate preventive service, and to reduce the unnecessary use of Emergency Services.
Quality Incentive Program: Shall have the meaning ascribed to such term in Article 12 of the Contract.
Reasonable Efforts: means the taking of those steps in the power of the relevant Party that are capable of producing the desired result, being steps which a reasonable person desiring to achieve
Page 43
such result would take; provided that, subject to the relevant Party’s other express obligations under this Agreement, the relevant Party shall not be required to expend any funds other than those funds (A) necessary to meet the reasonable costs reasonably incidental or ancillary to the steps to be taken by the relevant Party and (B) the expenditure of which is not the obligation of the other Party hereunder.
Recertification: A determination by the Puerto Rico Medicaid Program that a person previously enrolled in MiSalud subsequently received a Negative Redetermination Decision, is again eligible for services under the MiSalud Program.
Redetermination: The periodic redetermination of eligibility for Medicaid, CHIP, or the Commonwealth Population, conducted by the Puerto Rico Medicaid Program.
Referral: A request by a PCP or other Provider in the PMG for an Enrollee to be evaluated and/or treated by a different Provider, usually a specialist.
Reinsurance: An agreement whereby ASES transfers risk or liability for losses, in whole or in part, sustained under this Contract. A reinsurance agreement may also exist at the Provider level through a stop-loss arrangement as provided in Section 22.3 of this Contract.
Page 44
Remedy: ASES’s means to enforce the terms of the Contract through liquidated damages and other sanctions.
Reports: Shall have the meaning ascribed to such term in Section 18.2 of this Contract.
Retention Fund: Shall have the meaning ascribed to such term in Section 12.5.2 of this Contract.
Runoff Period: A period not to exceed ten (10) consecutive months, commencing on the Calendar Day immediately following the Termination Date.
Rural Health Clinic (“RHC”): A clinic that is located in an area that has a health-care Provider shortage. An RHC provides primary health care and related diagnostic services and may provide optometric, podiatry, chiropractic and mental health services. An RHC employs, contracts or obtains volunteer services from Providers to provide services.
Service Authorization Request: An Enrollee’s request for the provision of a Covered Service.
Service Region: A geographic area comprised of those municipalities where the Contractor is responsible for providing services under the MiSalud Program which for purposes of this Contract shall include the Virtual Region and the following geographic service regions: Metro North, North, San Juan, Northeast and West regions.
Page 45
Span of Control: Information systems and telecommunications capabilities that the Contractor operates or for which it is otherwise legally responsible according to the terms and conditions of this Contract. The Contractor’s Span of Control also includes Systems and telecommunications capabilities outsourced by the Contractor.
Special Coverage: A component of Covered Services, described in Section 7.7 of this Contract, which are more extensive than the Basic Coverage services, and for which Enrollees are eligible only by “registering”; registration for Special Coverage is based on intensive medical needs occasioned by serious illness.
Subcontract: Any written contract between the Contractor and a third party, including a Provider, to perform a specified part of the Contractor’s obligations under this Contract.
Subcontractor(s): A third party to a written contract with the Contractor to perform a specified part of the Contractor’s obligations under this Contract.
Systems Unavailability: As measured within the Contractor’s information systems Span of Control, when a system user does not get the complete, correct full-screen response to an input command within three (3) minutes after depressing the “Enter” or other function key.
Page 46
Telecommunication Device for the Deaf (“TDD”): Special telephone devices with keyboard attachments for use by individuals with hearing impairments who are unable to use conventional phones.
Tele MiSalud: The Enrollee support Call Center that the Contractor shall operate as described in Section 6.8 of this Contract, containing two components: the Information Service and the Medical Advice Service.
Tele MiSalud Outreach Program: Shall have the meaning ascribed to such term in Section 6.8.12 of this Contract.
Terminal Condition: A condition caused by injury, illness, or disease, from which, to a reasonable degree of certainty, will lead to the patient’s death in a period of, at most, six (6) months.
Termination Date of Contract or Termination Date: The final date upon which the Contractor is required to provide Administrative Services hereunder including any services rendered during the Transition Period, but excluding the Runoff Period, as described in Articles 34 and 35 of this Contract.
Page 47
Third Party: Any person, institution, corporation, insurance company, public, private or governmental entity who is or may be liable in Contract, tort, or otherwise by law or equity to pay all or part of the medical cost of injury, disease or disability of an Enrollee.
Third Party Liability: Legal responsibility of any Third Party to pay for health care services.
Transition Report: Any Report that is not otherwise required to be prepared by the Contractor during the Contract Term, except upon ASES’s reasonable request during the Transition Period regarding the Contractor’s operations with respect to the MiSalud Program under this Contract during the Transition Period or the Runoff Period.
Urgency: Shall have the meaning ascribed to such term in the Patient’s Bill of Rights Act.
Utilization: The rate patterns of service usage or types of service occurring within a specified time.
Utilization Management (“UM”): A service performed by the Contractor which seeks to ensure that Covered Services provided to Enrollees are in accordance with, and appropriate under, the standards and requirements established by this Contract, or a similar program developed, established or administered by ASES.
Page 48
Virtual Region: The Service Region for the MiSalud Program that is comprised of children who are in the custody of ADFAN, as well as certain survivors of domestic violence referred by the Office of the Women’s Advocate, who enroll in the MiSalud Program. The Virtual Region encompasses services for these Enrollees throughout Puerto Rico.
Week: The traditional seven-day week, Sunday through Saturday.
Withhold: A percentage of payments or set dollar amounts that ASES deducts from its payment to the Contractor, or that the Contractor deducts from its payment to a Network Provider, depending on specific predetermined factors.
ARTICLE 3 ACRONYMS
The acronyms included in this Contract stand for the following terms.
| ACH - | Automated Clearinghouse | |
| ADFAN - | Puerto Rico Administración de Familias y Niños, or Families and Children Administration | |
| AICPA - | American Institute of Certified Public Accountants | |
Page 49
| ARRA - | American Recovery and Reinvestment Act of 2009 | |
| ASES - | Administración de Seguros de Salud, or Puerto Rico Health Insurance Administration | |
| ASSMCA - | The Mental Health and Against Addiction Services Administration or Administración de Servicios de Salud Mental y Contra la Addicción | |
| ASUME - | Minor Children Support Administration | |
| BC-DR - | Business Continuity and Disaster Recovery | |
| CCuSAI - | Comprehensive Health Center | |
| CFR - | Code of Federal Regulations | |
| CHIP - | Children’s Health Insurance Program | |
| CLIA - | Clinical Laboratory Improvement Amendment | |
| CMS - | Centers for Medicare & Medicaid Services | |
Page 50
| DME - | Durable Medical Equipment | |
| ECM - | Electronic Claims Management | |
| EDI - | Electronic Data Interchange | |
| EFT - | Electronic Funds Transfer | |
| EHR - | Electronic Health Record | |
| EIN - | Employer Identification Number | |
| EMTALA - | Emergency Medical Treatment and Labor Act | |
| EPSDT - | Early and Periodic Screening, Diagnostic, and Treatment | |
| EQR - | External Quality Review | |
| EQRO - | External Quality Review Organization | |
Page 51
| ER - | Emergency Room | |
| FQHC - | Federally Qualified Health Center | |
| PMG - | Primary Medical Group | |
| HEDIS - | The Healthcare Effectiveness Data and Information Set | |
| HHS - | U.S. Department of Health & Human Services | |
| HIE - | Health Information Exchange | |
| HIPAA - | Health Insurance Portability and Accountability Act of 1996 | |
| IBNR - | Incurred-But-Not-Reported | |
| MAC - | Maximum Allowable Cost | |
| MBHO - | Managed Behavioral Health Organization | |
| MMIS - | Medicaid Management Information System | |
Page 52
| NEMT - | Non-Emergency Medical Transportation | |
| NPI - | National Provider Identifier | |
| OIG - | Office of the Inspector General of the U.S. Department of Health and Human Services | |
| PBM - | Pharmacy Benefits Manager | |
| PCP - | Primary Care Physician | |
| PDL - | Preferred Drug List | |
| PIHP - | Prepaid Inpatient Health Plan | |
| PIP - | Performance Improvement Projects | |
| PMG - | Primary Medical Group | |
| PPA - | Pharmacy Program Administrator | |
Page 53
| PPN - | Preferred Provider Network | |
| QAPI - | Quality Assessment Performance Improvement Program | |
| RFP - | Request for Proposals | |
| RHC - | Rural Health Center | |
| SAS - | Statements on Auditing Standards | |
| SSN - | Social Security Number | |
| TDD - | Telecommunication Device for the Deaf | |
| TPL - | Third-Party Liability | |
| UCF - | Uniform Central Formulary | |
| UM - | Utilization Management | |
Page 54
ARTICLE 4 ASES RESPONSIBILITIES
| 4.1 | General Provision |
ASES will be responsible for administering the MiSalud government health plan. ASES will administer contracts, monitor the Contractor’s performance, and provide oversight of all aspects of the Contractor’s operations. Specifically, ASES will perform the activities as specified in Article 4.
| 4.2 | Legal Compliance |
ASES will comply with, and will monitor the Contractor’s compliance with, all federal and Puerto Rico laws, rules, regulations, statutes, policies or procedures that may govern the Contract, including but not limited to those listed in Attachment 1, to the extent applicable.
| 4.3 | Eligibility |
| 4.3.1 | The Government of Puerto Rico has sole authority to determine eligibility for MiSalud, as provided in federal law and Puerto Rico’s State Plan, with respect to the Medicaid and CHIP eligibility groups listed in Sections 1. 3.1.1-1.3.1.2 of this Contract; and, with respect to the Other Eligible Persons listed in Section 1.3.1.3 of this Contract, as provided in Article VI, Section 5 of Act 72 and other Puerto Rico |
Page 55
| law and Regulation 7758 – Regulation Number 138 of the Puerto Rico Health Department. |
| 4.3.2 | The Puerto Rico Medicaid Program will determine eligibility for the eligibility categories listed in Sections 1.3.1.1, 1.3.1.2, and 1.3.1.3.1 above (Medicaid - and CHIP Eligible Persons and the Commonwealth Population). |
| 4.3.3 | The Medicaid Program determination that a person is eligible for MiSalud is contained on Form MA-10, titled “Notification of Action Taken on Request and/or Re-Evaluation,” and shall be referred to hereinafter as “Certification.” A person who has received a Certification after July 1, 2011 shall be referred to hereinafter as “Enrollee.” |
| 4.3.4 | Effective Date of Eligibility. ASES shall observe the following rules with respect to the Effective Date of Eligibility for services under MiSalud. |
| 4.3.4.1 | Effective Date of Eligibility for Medicaid - and CHIP Eligible Persons and Commonwealth Population. Medicaid - and CHIP Eligible Persons and members of the Commonwealth Population (see Sections 1.3.1.1, 1.3.1.2, 1.3.1.3.1 of this Contract) shall be eligible to enroll in MiSalud as of the eligibility effective date specified on the MA-10. |
Page 56
| 4.3.4.2 | Effective Date of Eligibility for Public Employees and Pensioners. Public employees and pensioners (see Section 1.3.1.3.2 of this Contract) shall be eligible to enroll in MiSalud according to policies determined by the Government of Puerto Rico. The Puerto Rico Medicaid Program does not play a role in determining their eligibility. |
| 4.3.5 | Termination of Eligibility |
| 4.3.5.1 | An Enrollee who is determined ineligible for MiSalud after a Redetermination conducted by the Puerto Rico Medicaid Program shall remain eligible for services under MiSalud until the date specified in a Negative Redetermination Decision issued by the Medicaid Program. |
| 4.3.5.2 | An Enrollee who is a public employee or pensioner (see Section 1.3.1.3.2 of this Contract) shall remain eligible until disenrolled from MiSalud. |
| 4.3.6 | ASES Notice to Contractor |
| 4.3.6.1 | ASES shall notify the Contractor of Certifications and Negative Redetermination Decisions referenced in Sections 4.3.3 and 4.3.5 of this Contract. |
Page 57
| 4.3.6.2 | ASES will receive a file with Certification and Negative Redetermination Decision data from the Puerto Rico Medicaid Program on a daily basis, and shall notify the Contractor of a Certification or Negative Redetermination Decision within one (1) Business Day of receiving notice of it via said file. ASES shall forward these data to the Contractor in an electronic format agreed to between the Parties (the “Daily Update / Carrier Eligibility File Format”). |
| 4.4 | Enrollment Responsibilities of ASES |
| 4.4.1 | Effective Date of Enrollment |
| 4.4.1.1 | General Provision. Except as provided below, Enrollment will be effective (hereinafter referred to as the “Effective Date of Enrollment”) as of the eligibility certification date shown on the MA-10. The effective date on the MA-10 is the day the application process is complete. |
| 4.4.1.2 | Enrollment of Persons who Access Emergency Services Before Completing the Certification Process. When an Eligible Person who is a Medicaid or CHIP Eligible Person (see Sections 1.3.1.1, 1.3.1.2 of this Contract and 1.3.1.3.1) receives Emergency Services before the date indicated in Section 4.4.1.1 above, the Effective Date of Enrollment shall |
Page 58
| be deemed to be the date of the first Emergency Service covered by the Contractor or by the MBHO, regardless of whether the Medicaid or CHIP Eligible Person had submitted an Enrollment application to the Puerto Rico Medicaid Program as of that date, provided that ASES provides written notification to the Contractor from the Health Care Reform Eligibility (HCRE) System of (1) the Certification of eligibility for the Eligible Person, and (2) the fact that the Potential Enrollee has accessed Emergency Services. The Contractor shall promptly, per Section 5.2.3 of this Contract, enroll the individual in the Plan. |
| 4.4.1.3 | Effective Date of Re-Enrollment for Enrollees Who Lose Eligibility. If an Enrollee who is a Medicaid- or CHIP Eligible Person or member of the Commonwealth Population loses eligibility for MiSalud for not more than two (2) months, Enrollment in the MiSalud Plan shall be reinstated. Upon notification from ASES of the Recertification, the Contractor shall Auto-Enroll the person, with Enrollment effective as of the new Effective Date of Eligibility. |
| 4.4.1.4 | Effective Date of Enrollment for Newborns |
Page 59
| 4.4.1.4.1 | A newborn shall be Auto-Enrolled, with an Effective Date of Enrollment of the date of his or her birth, provided that the Contractor meets the notification requirements in Section 5.2.5 of this Contract. |
| 4.4.1.4.2 | ASES shall require the Contractor to provide notification to ASES when it learns about any Enrollee that a Network Provider encounters who is an expectant mother, per Section 5.2.5 of this Contract. |
| 4.4.1.4.3 | ASES shall require the Contractor to Auto-Enroll the newborn as provided in Section 5.2.5 of this Contract. |
| 4.4.1.5 | Re-Enrollment Policy and Effective Date of Re-Enrollment for Mothers Who are Minor Dependents. In the event that a female Enrollee who is included in a family group for coverage under MiSalud as a Dependent child becomes pregnant, the Enrollee shall be referred to the Puerto Rico Medicaid Program. She will be considered to be a new family and will become the head of household of the new family. The Effective Date of Enrollment of the new family will be the date of the first diagnosis of the pregnancy, and the Enrollee shall be Auto-Enrolled, effective as of this date. The mother shall be Auto-Assigned to the PMG and PCP to which she was assigned before the Re-Enrollment. |
Page 60
| 4.4.2 | Term of Enrollment. The Term of Enrollment shall be a period of twelve (12) consecutive months for all MiSalud Enrollees, except that in cases in which the Puerto Rico Medicaid Program has designated an eligibility redetermination period shorter than twelve months for an Enrollee who is a Medicaid or CHIP Eligible Person or a member of the Commonwealth Population, that same period shall also be considered the Enrollee’s Term of Enrollment. Such a shortened eligibility redetermination period may apply, in the discretion of the Puerto Rico Medicaid Program, when an Enrollee is pregnant, is homeless, or anticipates a change in status (such as receipt of unemployment benefits) or in family composition. Notwithstanding this Section, Section 4.5 of this Contract controls the Effective Date of Disenrollment. |
| 4.4.3 | General Auto-Enrollment. Effective July 1, 2011, ASES implemented an Auto-Enrollment process for MiSalud for Medicaid and CHIP Eligible Persons and members of the Commonwealth Population. |
| 4.4.3.1 | The Contractor shall Auto-Enroll each Enrollee in the MiSalud Plan covering the Service Region where the Enrollee lives or, for an Enrollee who is a foster child in the custody of ADFAN or a survivor of domestic violence referred by the Women’s Advocate, in the MiSalud Plan covering the Virtual Region. |
Page 61
| 4.4.3.2 | Puerto Rico Medicaid Program will ensure that each Enrollee receives an MA-10 and welcome letter upon certification. The welcome letter shall explain to the Enrollee how to use the MA-10 until the membership card is received, to obtain services immediately. |
| 4.4.3.3 | The Auto-Enrollment process will include Auto-Assignment of a PMG and PCP. A new Enrollee who is a dependent of a current MiSalud Enrollee shall be automatically assigned to the same PMG as his or her parent or spouse who is a current MiSalud Enrollee. |
| 4.4.3.4 | The Contractor shall notify the Enrollee in writing of the right to request a change in assigned PMG and/or PCP for up to ninety (90) days after the Auto-Assignment, without cause. |
| 4.4.3.5 | The Contractor’s notice to the Enrollee and to ASES of the Enrollment shall be carried out as provided in Sections 5.2.3 through 5.2.9 of this Contract. |
| 4.4.3.6 | The Effective Date of Enrollment for those Auto-Enrolled will be governed by the rules stated in Section 4.4.1 of this Contract. The Contractor’s notice of Auto-Enrollment, required by Section 5.2.4 of this |
Page 62
| Contract, shall serve as the notice of Enrollment referenced in Section 4.4.1.1 of this Contract. |
| 4.4.4 | Except as otherwise provided in this Section 4.4 of this Contract, and notwithstanding the Term of Enrollment provided in Section 4.4.2 of this Contract, Enrollees shall remain enrolled in the MiSalud Plan until the occurrence of an event listed in Section 4.5 of this Contract (Disenrollment Responsibilities of ASES). |
| 4.5 | Disenrollment Responsibilities of ASES |
| 4.5.1 | Disenrollment occurs only when ASES or the Medicaid Program determines that an Enrollee is no longer eligible for MiSalud; or when Disenrollment is requested by the Contractor or Enrollee, and approved by ASES, as provided in Section 5.4.3-5.4.4 of this Contract. |
| 4.5.2 | Disenrollment will be effected by ASES, and ASES will issue notification to the Contractor. Such notice shall be delivered via file transfer to the Contractor on a daily basis simultaneously with information on Enrollees within five (5) Calendar Days of making a final determination on Disenrollment. ASES’s notice to the Contractor concerning Disenrollment will be conveyed by ASES simultaneously with information on Enrollees (see Section 4.3.6.1 of this Contract). |
Page 63
| 4.5.3 | Disenrollment shall occur according to the following timeframes (the “Effective Date of Disenrollment”). Upon the Effective Date of Disenrollment, the Conversion Clause in Section 5.5 of this Contract shall be triggered. |
| 4.5.3.1 | Except as otherwise provided in this Section 4.5, Disenrollment will take effect as of the Disenrollment date specified in ASES’s notice to the Contractor that an Enrollee is no longer eligible. If ASES notifies the Contractor of Disenrollment on or before the last working day of the month in which eligibility ends, the Disenrollment will be effective on the first day of the following month. |
| 4.5.3.2 | When Disenrollment is effected at the Contractor’s or the Enrollee’s request, as provided in Sections 4.5.4, 4.5.5, and 5.4 of this Contract, Disenrollment shall take effect no later than the first day of the second month following the month that the Contractor or Enrollee requested the Disenrollment. If ASES fails to make a decision on the Contractor’s or Enrollee’s request before this date, the Disenrollment will be deemed granted. If the Enrollee requests reconsideration of a Disenrollment through the Contractor’s Grievance System, as provided in Article 14, the Grievance process shall be completed in time to permit the Disenrollment (if approved) to take effect in accordance with this timeframe. |
Page 64
| 4.5.3.3 | If what would otherwise be the Effective Date of Disenrollment under this subsection 4.5.3 falls: |
| 4.5.3.3.1 | When the Enrollee is an inpatient at a hospital, ASES shall postpone the Effective Date of Disenrollment so that it occurs on the last day of the month in which the Enrollee is discharged from the hospital, or the last day of the month following the month in which Disenrollment would otherwise be effective, whichever occurs earlier; |
| 4.5.3.3.2 | During a month in which the Enrollee is in the second or third trimester of pregnancy, ASES shall postpone the Effective Date of Disenrollment so that it occurs on the date of delivery; or |
| 4.5.3.3.3 | During a month in which an Enrollee is diagnosed with a Terminal Condition, ASES shall postpone the Effective Date of Disenrollment so that it occurs on the last day of the following month. |
| 4.5.3.4 | For the public employees and pensioners who are Other Eligible Persons referred to in Section 1.3.1.3.2 of this Contract, Disenrollment shall occur according to the timeframes set for in Normative Letter 10-10-06, issued by ASES on October 6, 2010 (Attachment 13 to this Contract). |
Page 65
| 4.5.4 | ASES will initiate Disenrollment at the request of the Contractor only under the circumstances set forth in Section 5.4.4 of this Contract. ASES will approve a Disenrollment request by the Contractor, in ASES’s discretion, only if ASES determines: |
| 4.5.4.1 | That it is impossible for the Contractor to continue to provide services to the Enrollee without endangering the Enrollee or other MiSalud Enrollees; and |
| 4.5.4.2 | That an action short of Disenrollment, such as transferring the Enrollee to a different PCP or PMG, will not resolve the problem. |
| 4.5.5 | ASES will initiate Disenrollment at the request of an Enrollee only under the circumstances set forth in Section 5.4.3 of this Contract. ASES may approve or disapprove the request based on the reasons specified in the Enrollee’s request, or upon any relevant information provided to ASES by the Contractor about the Disenrollment request. |
| 4.5.6 | Upon the Effective Date of Disenrollment, the Conversion Clause in Section 5.5 of this Contract shall apply. |
Page 66
| 4.5.7 | ASES shall ensure, through the obligations of the Contractor under this Contract that Enrollees receive the notices contained in Section 5.2.6 (Re-Enrollment Procedures). While these notices shall be issued by the Contractor, per Section 5.4.2 of this Contract, ASES shall provide the Contractor with the information on Certification and Negative Redetermination Decision (see Section 4.3.6.1 of this Contract) needed for the Contractor to carry out this responsibility. |
| 4.6 | Enrollee Services and Marketing |
| 4.6.1 | ASES will provide to the Contractor a document entitled MiSalud Universal Beneficiary Guidelines (Attachment 3 to this Contract) for the purpose of providing uniform information in the Contractor’s Enrollee Handbook for MiSalud, as required by 42 CFR 438.10, and according to the requirements set forth in Section 6.4 of this Contract. |
| 4.6.2 | ASES shall have sole authority to review and approve all informational and Marketing Materials disseminated to Enrollees of the MiSalud Plan, including, but not limited to, the following: |
| 4.6.2.1 | ASES shall have sole authority to review and approve the Enrollee Handbook before it is printed and distributed, and will review and approve any amendment to the Enrollee Handbook before it is printed and |
Page 67
| distributed. The Handbook, and any subsequent substantive changes to it, shall be final only upon ASES’s written confirmation of approval, as required in Sections 6.2.2 and 6.4.5 of this Contract. |
| 4.6.2.2 | ASES shall have sole authority to review and approve the format and content of the Enrollee ID Card that the Contractor intends to issue in accordance with CMS requirements and the guidelines set forth in Section 6.7 of this Contract. |
| 4.7 | Covered Services |
| 4.7.1 | Given the objective of MiSalud to promote an integrated approach to physical and behavioral health, and to improve Access to quality primary and specialty care services, ASES shall utilize all mechanisms set forth in this Contract (including, but not limited to, the Quality Improvement and Reporting provisions set forth in Articles 12 and 18) to ensure that the Contractor performs the services and tasks assigned to advance the program goals of MiSalud. |
| 4.7.2 | [Intentionally left blank]. |
| 4.7.3 | ASES shall provide to the Contractor before the Implementation Date of this Contract, and on an ongoing basis, updated information on the operational policies, |
Page 68
| procedures, and regulations of MiSalud that affect the scope of the Administrative Services to be provided by the Contractor and Covered Services under this Contract or otherwise affect this Contract (collectively, the “MiSalud Policies and Procedures”). Accordingly, the Contractor will be included in any mailing list for the purpose of providing such information, and in any advisory committee or general meetings convened by ASES, the Pharmacy Benefits Manager, or any other organization whose objectives are to instruct MiSalud contractors on modifications to policies or benefits coverage. |
| 4.8 | Provider Network |
| 4.8.1 | ASES will provide the Contractor with timely updates to Puerto Rico’s list of excluded Providers, and also, if applicable, any such list issued by CMS or the U.S. Department of Health and Human Services, as well as any additional information that will affect who may be included in the Contractor’s Provider Network. ASES will provide the Puerto Rico Provider Credentialing policies to the Contractor prior to the Implementation Date of this Contract. The Puerto Rico Provider Credentialing policies shall be considered to be part of the MiSalud Policies and Procedures. |
Page 69
| 4.9 | Quality Monitoring |
| 4.9.1 | ASES, in strict compliance with applicable provisions of 42 CFR 438.204 and other federal and Puerto Rico regulations, shall evaluate the delivery of health care by the Contractor’s Provider Network. Such quality monitoring shall include monitoring of all the Contractor’s Quality Improvement programs described in Article 12 of this Contract. ASES shall monitor the following items, among others: |
| 4.9.1.1 | The availability of Covered Services; |
| 4.9.1.2 | The adequacy of the Contractor’s Provider Network; |
| 4.9.1.3 | The Contractor’s coordination and continuity of care for Enrollees; |
| 4.9.1.4 | The coverage and authorization of Covered Services and Benefits; |
| 4.9.1.5 | The Contractor’s policies and procedures for selection and retention of Providers; |
| 4.9.1.6 | The Contractor’s compliance with Enrollee information requirements in accordance with 42 CFR 438.10; |
Page 70
| 4.9.1.7 | The Contractor’s compliance with Puerto Rico and federal privacy laws and regulations relative to confidentiality of Enrollee information; |
| 4.9.1.8 | The Contractor’s compliance with Enrollment and Disenrollment requirements and limitations; |
| 4.9.1.9 | The Contractor’s Grievance System; |
| 4.9.1.10 | The Contractor’s oversight of all Subcontractor relationships and delegations; |
| 4.9.1.11 | The Contractor’s adoption of practice guidelines, including the dissemination of the guidelines to Providers and, upon request, to Enrollees, and Providers’ application of the Guidelines; |
| 4.9.1.12 | The Contractor’s quality assessment and performance improvement program; and |
| 4.9.1.13 | The Contractor’s Information Systems to ensure it supports initial and ongoing review of Puerto Rico’s quality strategy. |
Page 71
| 4.10 | Coordination with Contractor’s Key Staff |
| 4.10.1 | ASES will make diligent, good-faith efforts to facilitate effective and continuous communication and coordination with the Contractor in all areas of MiSalud operations. |
| 4.10.2 | Specifically, ASES will designate individuals within ASES who will serve as liaisons to the corresponding individuals on the Contractor’s staff, including: |
| 4.10.2.1 | A program integrity staff member; |
| 4.10.2.2 | A quality oversight staff member; |
| 4.10.2.3 | A Grievance System staff member; and |
| 4.10.2.4 | An information systems coordinator. |
| 4.11 | Information Systems and Reporting |
| 4.11.1 | ASES reserves the right to modify, expand, or delete the requirements contained in Articles 16 and 17 with respect to the data that the Contractor is required to submit to ASES, or to issue new requirements, subject to consultation with the Contractor. If |
Page 72
| the change in requirements imposes material additional costs or expenses on the Contractor, or otherwise reduces such costs and expenses materially, the Parties shall negotiate and implement an adjustment in the Administative Fee prior to any change in the data requirements set forth in Articles 16 and 17. Unless otherwise mutually agreed upon by the Parties, the Contractor shall have no less than thirty (30) Calendar Days and no more than ninety (90) Calendar Days from the day on which ASES issues notice of a required modification, addition, or deletion, to comply with the modification, addition, or deletion. Any payment made by ASES that is based on data submitted by the Contractor is contingent upon the Contractor’s compliance with the certification requirements contained in 42 CFR 438.606. |
| 4.11.2 | ASES will make available a secure FTP server, accessible via the Internet, for receipt of electronic files and reports from the Contractor. The Contractor shall provide a similar system for ASES to transmit files and reports deliverable by ASES to the Contractor. When such systems are not operational, ASES and the Contractor shall agree mutually on alternate methods for the exchange of files. |
| 4.11.3 | ASES will deliver data to the Contractor, according to the layouts defined by ASES, with the following information, according to the following timeframes: |
| 4.11.3.1 | On a Daily basis: Certifications and Negative Redetermination Decisions; Enrollment rejections and errors; |
Page 73
| 4.11.3.2 | On a Daily and Monthly Basis: Enrollment data (including Certification and Negative Redetermination Decision); |
| 4.11.3.3 | On a Monthly Basis: Error return files and processing summary reports for monthly files submitted by the Contractor. |
| 4.11.4 | In an effort to improve the efficiency and quality of services to Enrollees and to help prevent Fraud and Abuse in the MiSalud Program, ASES shall require that all PCPs and PPN physician specialists maintain Enrollees’ Medical Records through an EHR system. Any such EHR system, whether maintained as a complete or component system, must be ONC and CCHIT certified and shall meet the specifications set forth in Attachment 15. The PCPs and PPN physician specialists shall have an operational EHR system in place on or before July 1, 2012 or such later date as set forth in his/her Provider Contract. Upon request, the Contractor shall assist the PCPs and PPN physician specialists in the acquisition and installation of such an appropriate EHR system at the Contractor’s expense. The Contractor shall also provide each such Provider with information on (i) the benefits of the EHR system and (ii) the costs of maintaining the EHR system. |
Page 74
| 4.12 | Readiness Review |
| 4.12.1 | ASES will conduct a readiness review of Contractor’s operations related to this Contract that will include, at a minimum, one (1) on-site review to provide assurances that the Contractor is able and prepared to perform all Administrative Services. |
| 4.12.2 | ASES’s review will document the status of the Contractor’s compliance with the MiSalud Program standards set forth in this Contract. A multidisciplinary team appointed by ASES will conduct the readiness review. The scope of the readiness review will include, but not be limited to, review and/or verification of: |
| 4.12.2.1 | Provider Network composition and Access; |
| 4.12.2.2 | Staff; |
| 4.12.2.3 | Marketing materials; |
| 4.12.2.4 | Content of Provider contracts; |
| 4.12.2.5 | EPSDT Plan; |
| 4.12.2.6 | Enrollee services capability; |
Page 75
| 4.12.2.7 | Comprehensiveness of quality and Utilization Management strategies; |
| 4.12.2.8 | Policies and procedures for the Grievance System; |
| 4.12.2.9 | Financial solvency; |
| 4.12.2.10 | Contractor litigation history, current litigation, audits and other government investigations both in Puerto Rico and in other jurisdictions; |
| 4.12.2.11 | Information Systems performance and interfacing capabilities; and |
| 4.12.2.12 | All other matters ASES may deem reasonable in order to determine the Contractor’s compliance with the requirements of this Contract. |
| 4.12.3 | The readiness review may assess the Contractor’s ability to meet any requirements set forth in this Contract and the documents referenced herein. |
| 4.12.4 | Eligible Persons may not be enrolled in the MiSalud Program until ASES has determined that the Contractor is capable of meeting these standards. The Contractor’s failure to pass the readiness review may result in the application of a Corrective Action Plan for any areas where the Contractor fails to pass the readiness review. |
Page 76
| 4.12.5 | ASES will provide the Contractor with a summary of findings from the readiness review, as well as areas requiring remedial action. |
ARTICLE 5 CONTRACTOR RESPONSIBILITIES
| 5.1 | General Provisions |
| 5.1.1 | The Contractor shall complete the following actions, tasks, obligations, and responsibilities: |
| 5.1.2 | The Contractor must maintain the staff, organizational, and administrative capacity and capabilities necessary to carry out all the duties and responsibilities under this Contract. |
| 5.1.3 | The Contractor shall notify ASES within five (5) Business Days of a change in the following: |
| 5.1.3.1 | Its business address, telephone number, facsimile number, and e-mail address; |
| 5.1.3.2 | Its corporate status; |
Page 77
| 5.1.3.3 | Its solvency (as a result of a non-operational event); |
| 5.1.3.4 | Its corporate officers or executive employees involved in providing the Administrative Services contemplated in this Contract; |
| 5.1.3.5 | Its federal employee identification number or federal tax identification number; or |
| 5.1.3.6 | Its owner’s business address, telephone number, facsimile number, and e-mail address. |
| 5.2 | Enrollment Responsibilities of the Contractor |
| 5.2.1 | General Provisions |
| 5.2.1.1 | The Contractor shall coordinate with ASES as necessary for all Enrollment and Disenrollment functions. |
| 5.2.1.2 | The Contractor shall enroll in the Plan all certified Eligible Persons within the Service Regions upon receipt of notice from ASES that the individual is eligible, as provided in this Contract. |
Page 78
| 5.2.1.3 | The Contractor shall recognize Enrollees as enrolled as provided in, and effective according to the timeframes specified in Section 4.4 of this Contract. |
| 5.2.1.4 | The Contractor shall accept all certified Eligible Persons into the Plan without restrictions. The Contractor shall not discriminate against individuals on the basis of religion, gender, race, color, national origin, or sexual preference, and will not use any policy or practice that has the effect of discriminating on the basis of religion, gender, race, color, or national origin or on the basis of health, health status, pre-existing condition, or need for health care services. |
| 5.2.2 | General Enrollment Procedures for Certified Eligible Persons |
| 5.2.2.1 | The Contractor shall maintain adequate capacity in the Service Regions, to ensure prompt and voluntary Enrollment of all Enrollees, on a daily basis and in the order in which they apply. |
| 5.2.2.2 | The Contractor shall provide Enrollees with specific information allowing for prompt, voluntary, and reliable Enrollment. |
Page 79
| 5.2.2.3 | The Contractor shall use its Reasonable Efforts to maintain the functionality and reliability of all systems necessary for Enrollment and Disenrollment as provided in Article 17 of this Contract. |
| 5.2.3 | Enrollment Procedures with Respect to Potential Enrollees |
| 5.2.3.1 | ASES will initiate the Auto-Enrollment of all Potential Enrollees in the following manner: (1) Group One will include all Potential Enrollees who became Certified between April 1, 2011 and June 30, 2011; (2) Group Two will include all Potential Enrollees who became Certified between January 1, 2011 and March 31, 2011; (3) Group Three will include all Potential Enrollees who became Certified between October 1, 2010 and December 31, 2010. |
| 5.2.3.2 | The Effective Date of Enrollment for each Potential Enrollee group is as follows: (1) Group One Effective Date of Enrollment is November 1, 2011; (2) Group Two Effective Date of Enrollment is December 1, 2011; (3) Group Three Effective Date of Enrollment is January 1, 2012. Any Potential Enrollee may initiate the manual enrollment process prior to the assigned Auto-Enrollment date by contacting the Contractor directly. If the Potential Enrollee visits the Contractor’s office to enroll, the Contractor shall request that the Potential Enrollee select a PMG and PCP. |
Page 80
| During the visit, the Contractor shall issue to the new Enrollee an Enrollee ID Card, a notice of Enrollment, an Enrollee Handbook, and a Provider Directory; or, such notice, ID Card, Handbook, and Provider Directory may be sent to the Enrollee via surface mail within five (5) Business Days of the Enrollee’s visit to the Contractor’s office to enroll. |
| 5.2.3.3 | The notice of Enrollment that the Contractor issues pursuant to Section 5.2.3.2 of this Contract will clearly state the Effective Date of Enrollment. The notice of Enrollment will explain that the Enrollee is entitled to both physical health services through the MiSalud Plan and behavioral services through the MBHO. The notice will inform the Enrollee of his or her limited right to disenroll, per Section 5.4.3 of this Contract, and will explain that the Enrollee has separate Disenrollment rights with respect to the physical health services in the Plan and with respect to the behavioral services in the MiSalud Program. The notice of Enrollment shall inform the Enrollee that exercising the right to disenroll means losing access to services under MiSalud. The notice shall advise the Enrollee of the Enrollee’s right to select a different PCP or to change PMGs, as described in Section 5.3 of this Contract, and will encourage the Enrollee to pursue this option, rather than Disenrollment, if he or she is dissatisfied with care or services. |
Page 81
| For Eligible Persons who access Emergency Services before completing the Certification process, the Contractor shall notify the Eligible Person that he/she must visit the Medicaid office to obtain Certification. |
| 5.2.4 | Procedures with Respect to Auto-Enrollment of Enrollees Other Than Newborns |
| 5.2.4.1 | Upon receipt from ASES of Certification of persons listed in Section 4.4.1.3 of this Contract (Enrollees who lose and regain eligibility within two months) and 4.4.1.5 of this Contract (mothers who are minor dependents and re-apply for MiSalud), the Contractor shall send the person, via surface mail, a notice that he or she has been Auto-Enrolled; that he or she shall be Auto-Assigned to the same PMG or PCP that he or she had during his or her previous Term of Enrollment; that he or she shall have ninety (90) Calendar Days from the Effective Date of Enrollment to disenroll from the Plan or the MBHO or to change PMG without cause; and that he or she has the right to disenroll for cause, as provided in Section 5.4.3.2 of this Contract. The notice of Enrollment will clearly state the Effective Date of Enrollment. Such notice shall be issued within five (5) Business Days of receipt of this information from ASES. |
| 5.2.4.2 | With the notice of Auto-Enrollment, the Contractor shall deliver the Enrollee ID Card, Enrollee Handbook, and Provider Directory; or, if it is |
Page 82
| impracticable to send these items in the same mailing, they shall be sent to the Enrollee via surface mail within two (2) Business Days of the date of mailing of the notice of Auto-Enrollment. |
| 5.2.5 | Procedures for Auto-Enrollment of Newborns |
| 5.2.5.1 | The Contractor shall notify ASES of any Enrollees who are expectant mothers, promptly upon its being informed about the diagnosis of the pregnancy by a Network Provider. |
| 5.2.5.2 | The Contractor shall promptly, upon learning that an Enrollee is an expectant mother, mail a newborn Enrollment packet to the expectant mother (1) instructing her to register the newborn with the Puerto Rico Medicaid Program within ninety (90) Calendar Days of the newborn’s birth by providing the newborn’s birth certificate; (2) notifying her that the newborn will be Auto-Enrolled in the MiSalud Plan; (3) informing her that unless she visits the Contractor’s office to select a PMG and PCP, the child will be Auto-Assigned to the mother’s PMG and to a PCP who is a pediatrician; and (4) informing her that she will have ninety (90) days after the child’s birth to disenroll the child from the Plan or the MBHO or to change the child’s PMG and PCP, without cause. |
Page 83
| 5.2.5.3 | The Contractor shall provide assistance to any expectant mother who contacts the Contractor wishing to make a PCP and PMG selection for her newborn, per Section 5.3 of this Contract, and record that selection. |
| 5.2.5.4 | If the mother has not made a PCP and PMG selection at the time of the child’s birth, the Contractor shall, within five (5) Business Days of becoming aware of the birth, Auto-Assign the newborn to a PCP who is a pediatrician and to the mother’s PMG. |
| 5.2.5.5 | Within seventy-two (72) hours of becoming aware of the birth of a child to an Enrollee, the Contractor shall submit a newborn notification to ASES and to the Puerto Rico Medicaid Program, using a standard form to be provided by ASES,. |
| 5.2.5.6 | If the mother has made a PCP and PMG selection on behalf of the newborn, per Section 5.3.1.3 of this Contract, this information shall be included in the newborn notification form. |
| 5.2.5.7 | The Contractor shall participate in any meeting, working group, or other mechanism requested by ASES in order to ensure coordination among the Contractor, ASES, and the Puerto Rico Medicaid Program in order to implement newborn Auto-Enrollment. |
Page 84
| 5.2.6 | Re-Enrollment Procedures |
| 5.2.6.1 | The Contractor shall inform Enrollees who are Medicaid- and CHIP Eligible Persons and members of the Commonwealth Population of an impending Redetermination. Such notice shall be provided ninety (90) Calendar Days, sixty (60) Calendar Days, and thirty (30) Calendar Days before the scheduled date of the Redetermination. The notice shall inform the Enrollee that, if he or she is Recertified, his or her term of Enrollment in the Plan will automatically renew; but that, effective as of the date of Recertification, he or she will have a ninety- (90) day period in which he or she may disenroll from the Plan or from the MBHO without cause or to change his or her PMG selection without cause. The notice shall advise Enrollees that Disenrollment will terminate the Enrollee’s access to health services under the MiSalud Plan. |
| 5.2.6.2 | The Contractor shall provide Enrollees with sixty (60) Calendar Days written notice before the start of each Term of Enrollment, as specified in Section 5.4.3.1 of this Contract, of the right to disenroll or to change PMG or PCP during the first ninety (90) Calendar Days of the new Term of Enrollment. The notice shall specify that the right of Disenrollment applies separately to the Contractor and to the MBHO. |
Page 85
| 5.2.6.3 | Upon written request of ASES, the Contractor shall provide a report for a specific period of time containing documentation that the Contractor has furnished the notices required in this subsection 5.2.6 of this Contract. |
| 5.2.6.4 | The form letters used for the notices in Sections 5.2.6.1and 5.2.6.2 of this Contract fall within the requirement in Section 6.2.1 of this Contract that the Contractor seek advance written approval from ASES of certain documents |
| 5.2.7 | Specific Contractor Responsibilities Regarding Dual Eligible Beneficiaries. At the time of Enrollment, the Contractor shall provide Enrollees who are Medicaid-eligible and are also eligible for Medicare Part A or Part A and Part B (“Dual Eligible Beneficiaries”) with the information about their Covered Services and Co-Payments that is listed in Section 6.13 of this Contract. In determining whether an Enrollee is a Dual Eligible Beneficiary, the Contractor must, in compliance with the ASES Normative Letter issued June 28, 2010, review the MA-10 to determine whether the Enrollee is Medicaid-Eligible (see Section 1.3.1 of this Contract). Members of the Commonwealth Population (see Section 1.3.1.3.1 of this Contract) who are Medicare-eligible shall not be considered Dual Eligible Beneficiaries. |
| 5.2.8 | Enrollment Database |
Page 86
| 5.2.8.1 | The Contractor shall maintain an Enrollment database that includes all Enrollees in its knowledge, and contains, for each Enrollee, the information specified in the carrier billing file/carrier eligibility file format agreed to by the Parties. |
| 5.2.8.2 | The Contractor shall notify ASES within one (1) Business Day when the Enrollment Database is updated to reflect a change in the place of residence of an Enrollee. |
| 5.2.8.3 | The Contractor shall secure any authorization required from Enrollees under the laws of Puerto Rico in order to allow the U.S. Department of Health and Human Services, and ASES and its Agents to review Enrollee medical records, in order to evaluate determine quality, appropriateness, timeliness and cost of services performed under this Contract; provided that such authorization shall be limited by the Contractor’s obligation to observe the confidentiality of Enrollee patient information, as provided in Article 33. |
| 5.2.9 | Notification to ASES, the MBHO, and the PBM of New Enrollees and of Completed Disenrollments |
Page 87
| 5.2.9.1 | ASES shall notify Contractor, the MBHO, and the Pharmacy Benefits Manager (“PBM”) of new Enrollees and of completed Disenrollments on a routine daily basis. Such notification will be made through electronic transmissions. |
| 5.2.9.2 | The notification will include all new Enrollees as of the Business Day before the notification is issued, and will be sent no later than the following Business Day after the Enrollment process has been completed (as signified by issuance of the Enrollee ID Card, either in person or by surface mail) or the Disenrollment process has been complete (as signified by the issuance of a Disenrollment notice). |
| 5.2.9.3 | In the event that the Contractor must update information previously submitted to ASES about a new Enrollment, or that the Contractor must add a new Enrollee who was previously omitted from the daily report, such update must occur the next Business Day after the information is updated or a new Enrollee is added. ASES reserves the authority not to accept any new additions or corrections to Enrollment data after sixty (60) Calendar Days past the Effective Date of Enrollment stated in the Contractor’s notification to ASES. |
Page 88
| 5.2.10 | Collaboration with MBHO. Within the limits set by federal and Puerto Rico law, the Contractor shall provide to the MBHO any information relating to new Enrollees that will assist the MBHO in its operations. |
| 5.3 | Selection and Change of a Primary Medical Group (“PMG”) and Primary Care Physician (“PCP”) |
| 5.3.1 | Selection of a PMG and PCP |
| 5.3.1.1 | The Contractor shall, at the time of Auto-Enrollment as described in Sections 4.4.3.3, 5.2.3 and 5.2.4 of this Contract, Auto-Assign the Enrollee to a PCP and PMG, bearing in mind the Enrollee’s needs as described in Section 5.3.1.2 of this Contract. |
| 5.3.1.2 | When Auto-Assigning the Enrollee to a PCP, the Contractor shall choose a physician other than, or in addition to, a general practice physician as their PCP, as follows: |
| 5.3.1.2.1 | Women Enrollees will be recommended to choose an obstetrician / gynecologist as a PCP. |
Page 89
| 5.3.1.2.2 | Enrollees under 21 years of age will be recommended to choose a pediatrician as a PCP. |
| 5.3.1.2.3 | Enrollees with chronic health conditions including heart failure, kidney failure, or diabetes will be recommended to choose an internist as a PCP. |
| 5.3.1.3 | Per Section 5.2.5 of this Contract, following the Contractor’s notice to an expectant mother of her child’s upcoming Auto-Enrollment in the MiSalud Plan, the Contractor shall record any notice it receives from the mother concerning the selection of a PCP or PMG for the child. The Contractor shall ensure that such selections take effect as of the date of the child’s birth. |
| 5.3.1.4 | Enrollee PCP and PMG selections shall take effect on the Effective Date of Enrollment. |
| 5.3.1.5 | The Contractor shall provide the Enrollee with information related to PCPs and PMGs in its MiSalud Plan (in accordance with Section 6.6 of this Contract) to ensure that the Enrollee is informed that he or she can change its PCP and/or PMG pursuant to Section 5.3.2 of this Contract. |
Page 90
| 5.3.2 | Change of PMG or PCP |
| 5.3.2.1 | The Contractor shall permit Enrollees to change their PMG or PCP at any time for cause. The following shall constitute cause for change of PMG. |
| 5.3.2.1.1 | The Enrollee’s religious or moral convictions conflict with the services offered by Providers in the PMG; |
| 5.3.2.1.2 | The Enrollee needs related services to be provided concurrently; not all services are available within the Preferred Provider Network associated with a PMG; and the Enrollee’s PCP or any other Provider has determined that receiving the services separately could expose the Enrollee to an unnecessary risk; or |
| 5.3.2.1.3 | Other reasons, including poor quality of care, inaccessibility to Covered Services, inaccessibility to Providers with the experience to take care of the health care needs of the Enrollee. |
| 5.3.2.2 | The Contractor shall permit Enrollees to change their PMG or PCP for any reason, within certain timeframes: |
Page 91
| 5.3.2.2.1 | During the ninety (90) Calendar days following the Effective Date of Enrollment; |
| 5.3.2.2.2 | At least every twelve (12) months, following the ninety (90) Calendar days after the Effective Date of Enrollment; |
| 5.3.2.2.3 | At any time, during time periods in which the Contractor is subject to intermediate sanctions, as defined in 42 CFR 438.702(a)(3). |
| 5.3.2.2.4 | If a request to change PMGs is submitted to the Contractor on or before the fifth day of a month, the change will become effective on the first day of the following month. If a change is filed after the fifth day of the month, the change will be effective on the first day of the second succeeding month. |
| 5.3.2.3 | A Contractor may change an Enrollee’s PMG at the request of the PCP or other Provider within that PMG, in limited situations, as follows: |
| 5.3.2.3.1 | The Enrollee’s continued participation in the PMG seriously impairs the PMG’s ability to furnish services to either this particular Enrollee or other Enrollees; |
Page 92
| 5.3.2.3.2 | The Enrollee demonstrates a pattern of disruptive or abusive behavior that could be construed as non-compliant and is not caused by a presenting illness; or |
| 5.3.2.3.3 | The Enrollee’s use of services constitutes Fraud or Abuse (for example, the Enrollee has loaned his or her Enrollee ID Card to other persons to seek services). |
| 5.4 | Disenrollment Responsibilities of the Contractor |
| 5.4.1 | Disenrollment occurs only (1) when ASES determines that an Enrollee is no longer eligible for MiSalud; or (2) for any of the reasons listed in this Section 5.4 of this Contract. |
| 5.4.2 | Notice to Enrollee of Disenrollment |
| 5.4.2.1 | Disenrollment decisions are the responsibility of ASES; however, notice to Enrollees of Disenrollment shall be issued by the Contractor. The Contractor shall issue such notice in person or via surface mail to the Enrollee within five (5) Business Days of its receipt of a final Disenrollment decision from ASES, as provided in Sections 5.4.3 and 5.4.4 of this Contract. |
Page 93
| 5.4.2.2 | Each notice of Disenrollment shall include information concerning: |
| 5.4.2.2.1 | the Effective Date of Disenrollment; |
| 5.4.2.2.2 | the reason for the Disenrollment; |
| 5.4.2.2.3 | the Enrollee’s appeal rights, including the availability of the Grievance System and of ASES’s Administrative Law Hearing process, as provided by Act 72 of September 7, 1993; |
| 5.4.2.2.4 | the right to re-enroll in MiSalud upon receiving a Recertification from the Puerto Rico Medicaid Program, if applicable; and |
| 5.4.2.2.5 | the Enrollee’s right, under the Conversion Clause in Section 5.5 of this Contract, to apply for a direct payment policy from the Contractor. |
| 5.4.2.3 | The Contractor shall be responsible for processing any Disenrollment from the MBHO that is distinct from a Disenrollment from the MiSalud Plan. If an Enrollee requests Disenrollment from the MBHO, as provided in 42 CFR 438.56(c), or if the MBHO wishes to request the Disenrollment of an Enrollee, as provided in 42 CFR 438.56(b), the MBHO shall convey the request to the Contractor, which shall forward the request to ASES, |
Page 94
| within ten (10) Business Days of receipt of the request, with a recommendation of the action to be taken (except that Disenrollments without cause from the MBHO, during specific timeframes established at 42 CFR 438.56(c)(2), shall be granted without any recommendation from the MiSalud Plan). |
| 5.4.3 | Disenrollment at Enrollee Request |
| 5.4.3.1 | ASES shall make the final decision on Enrollee requests for Disenrollment. An Enrollee wishing to request Disenrollment must submit an oral or written request to ASES or to the Contractor. If the request is made to the Contractor, the Contractor shall forward the request to ASES, within ten (10) Business Days of receipt of the request, with a recommendation of the action to be taken. |
| 5.4.3.2 | An Enrollee may request Disenrollment from the Plan without cause during the ninety (90) Calendar Days following the Effective Date of Enrollment with the Plan or the date that the Contractor sends the Enrollee notice of the Enrollment, whichever is later. An Enrollee may request Disenrollment without cause every twelve (12) months thereafter. In addition, an Enrollee may request Disenrollment without cause in the event that ASES notifies the Enrollee that Puerto Rico has imposed or |
Page 95
| intends to impose on the Contractor that sanction pursuant to the applicable intermediate sanctions set forth in 42 CFR 438.702(a)(3). |
| 5.4.3.3 | An Enrollee may request Disenrollment from the MiSalud Plan for cause at any time. The following constitute cause for Disenrollment by the Enrollee: |
| 5.4.3.3.1 | The Enrollee moves to a Service Region not administered by the Contractor, or outside of Puerto Rico; |
| 5.4.3.3.2 | The Enrollee needs related services to be performed at the same time, and not all related services are available within the General Network. The Enrollee’s PCP or another Provider in the Preferred Provider Network have determined that receiving service separately would subject the Enrollee to unnecessary risk; and |
| 5.4.3.3.3 | Other acceptable reasons for Disenrollment at Enrollee request, per 42 CFR 438.56(d)(2), including, but not limited to, poor quality of care, lack of Access to Covered Services, or lack of Providers experienced in dealing with the Enrollee’s health care needs. ASES shall determine whether the reason constitutes cause. |
Page 96
| 5.4.3.4 | If the Contractor fails to refer a Disenrollment request within the timeframe specified in Section 5.4.3.1 of this Contract, or if ASES fails to make a Disenrollment determination so that the Enrollee may be disenrolled by the first day of the second month following the month when the Disenrollment request was made, per Section 4.5.3 of this Contract, the Disenrollment shall be deemed approved at that time. |
| 5.4.3.5 | If the Enrollee’s request for Disenrollment under this Section is denied, the Contractor shall provide the Enrollee with a notice of the decision. The notice shall include the grounds for the denial and shall inform the Enrollee of his or her right to use the Grievance System as provided in Article 14, and to have access to an Administrative Law Hearing. |
| 5.4.4 | Disenrollment Initiated by the Contractor |
| 5.4.4.1 | The Contractor shall complete all paperwork required by ASES for the Disenrollment of Enrollees it is seeking to disenroll. |
| 5.4.4.2 | ASES reserves authority to make all Disenrollment decisions; nonetheless, the Contractor shall issue the notice of Disenrollment to the Enrollee (see Section 5.4.2 of this Contract). |
Page 97
| 5.4.4.3 | The Contractor has a limited right to request that an Enrollee be disenrolled without the Enrollee’s consent. The Contractor shall notify ASES upon identification of an Enrollee who it knows or believes meets the criteria for Disenrollment. |
| 5.4.4.4 | When requesting Disenrollment of an Enrollee for reasons described in Section 5.4.4.7 of this Contract, the Contractor shall document at least three (3) interventions over a period of ninety (90) Calendar Days that occurred through treatment, case management, and care coordination to resolve any difficulty leading to the request. The Contractor shall also provide evidence of having given at least one (1) written warning to the Enrollee, certified return receipt requested, regarding implications of his or her actions. |
| 5.4.4.5 | If the Enrollee has demonstrated abusive or threatening behavior as defined by ASES, only one (1) Contractor intervention, and a subsequent written attempt to resolve the difficulty, are required. |
| 5.4.4.6 | The Contractor shall submit Disenrollment requests to ASES, and the Contractor shall honor all Disenrollment determinations made by ASES. ASES’s decision on the matter shall be final, conclusive and not subject to appeal by the Contractor. |
Page 98
| 5.4.4.7 | The following are acceptable reasons for the Contractor to request Disenrollment: |
| 5.4.4.7.1 | The Enrollee’s continued Enrollment in the MiSalud Plan seriously impairs the ability to furnish services to either this particular Enrollee or other Enrollees; |
| 5.4.4.7.2 | The Enrollee demonstrates a pattern of disruptive or abusive behavior that could be construed as non-compliant and is not caused by a presenting illness; |
| 5.4.4.7.3 | The Enrollee’s use of services constitutes Fraud or Abuse (for example, the Enrollee has loaned his or her Enrollee ID Card to other persons to seek services); |
| 5.4.4.7.4 | The Enrollee has moved out of Puerto Rico or out of the Contractor’s Service Regions; |
| 5.4.4.7.5 | The Enrollee is placed in a long-term care nursing facility or intermediate care facility for the mentally retarded; |
Page 99
| 5.4.4.7.6 | The Enrollee’s Medicaid or CHIP eligibility category changes to a category ineligible for MiSalud; or |
| 5.4.4.7.7 | The Enrollee has died or has been incarcerated, thereby making him or her ineligible for Medicaid or CHIP or otherwise ineligible for MiSalud. |
| 5.4.4.8 | The Contractor may not request Disenrollment for any discriminatory reason, including but not limited to the following: |
| 5.4.4.8.1 | Adverse changes in an Enrollee’s health status; |
| 5.4.4.8.2 | Missed appointments; |
| 5.4.4.8.3 | Utilization of medical services; |
| 5.4.4.8.4 | Diminished mental capacity; |
| 5.4.4.8.5 | Pre-existing medical condition; |
| 5.4.4.8.6 | The Enrollee’s attempt to exercise his or her rights under the Grievance System; or |
Page 100
| 5.4.4.8.7 | Uncooperative or disruptive behavior resulting from the Enrollee’s special needs (except when his or her continued enrollment in the MiSalud Plan seriously impairs the entity’s ability to furnish services to either such Enrollee or other Enrollees). |
| 5.4.4.9 | The request of one PMG to have an Enrollee assigned to a different PMG, per Section 5.3.2.3 of this Contract, shall not be sufficient cause for the Contractor to request that the Enrollee be disenrolled from the Plan. Rather, the Contractor shall, if possible, assign the Enrollee to a different and available PMG within the Plan. |
| 5.4.4.10 | In the event that the Contractor seeks Disenrollment of an Enrollee, the Contractor must notify the Enrollee of the availability of the Grievance System and of ASES’s Administrative Law Hearing process, as provided by Act 72 of September 7, 1993, as amended. |
| 5.4.4.11 | The Contractor shall maintain policies and procedures to comply with the Puerto Rico Patient’s Bill of Rights Act and with the Medicaid Regulations at 42 CFR 438.100, to ensure that Enrollee’s exercise of Grievance rights does not adversely affect the services provided to the Enrollee by the Contractor or by ASES. |
Page 101
| 5.4.5 | Use of the Contractor’s Grievance System. ASES may at its option require that the Enrollee seek redress through the Contractor’s Grievance System before ASES makes a determination on the Enrollee’s request for Disenrollment. The Contractor shall within two (2) Business Days inform ASES of the outcome of the grievance process. ASES may take this information into account in making a determination on the request for Disenrollment. The Grievance process must be completed in time to permit the Disenrollment (if approved) to be effective in accordance with the timeframe specified in Section 4.5.3 of this Contract; if the process is not completed by that time, then the Disenrollment will be deemed approved by ASES. |
| 5.4.6 | Disenrollment during Termination Hearing Process. If ASES notifies the Contractor of its intention to terminate the Contract as provided in Article 34, ASES may allow Enrollees to disenroll immediately without cause. In the event of such termination, ASES must provide Enrollees with the notice required by 42 CFR 438.10, listing their options for receiving services following the Termination Date of the Contract. |
| 5.5 | Conversion Clause |
| 5.5.1 | If during the term of this Contract, an Enrollee is disenrolled from the MiSalud Plan, the Enrollee shall have the right to subscribe to a direct payment policy from the Contractor pursuant to the Contractor’s standard policies and procedures. The Contractor’s obligation to provide such a policy is limited as provided in this Section |
Page 102
| 5.5. The direct payment policy shall be issued by the Contractor without imposing pre-existing condition bars or waiting periods. The Enrollee must request the subscription to a direct payment policy in writing, and submit the first premium to the Contractor, on or before thirty-one (31) Calendar Days after the Effective Date of Disenrollment, bearing in mind that: |
| 5.5.1.1 | Enrollment in the direct payment policy shall be at the option of the former Enrollee. |
| 5.5.1.2 | The premium for the direct payment policy will be in accordance with the Contractor’s rate then in effect, applicable to the form and benefits of the direct payment policy, in accordance with the risk category applicable to the former Enrollee, and the age reached on the Effective Date of Disenrollment from the direct payment policy. |
| 5.5.1.3 | The direct payment policy shall also provide for coverage to any Dependent of the former Enrollee, if such Dependent was considered an Eligible Person for MiSalud as of the Effective Date of Disenrollment. At the option by the Contractor, separate direct payment policies may be issued to cover family members who were formerly MiSalud Enrollees, rather than enrolling such family members in one policy. |
Page 103
| 5.5.2 | If the Enrollee requests a direct payment policy in the timeframe provided in this Section, the policy will be effective upon the Effective Date of Disenrollment from MiSalud. |
| 5.5.3 | The Contractor will not be obligated to issue a direct payment policy covering a person who has the right to receive similar services provided by any insurance coverage or under the Medicare Program, if such benefits, jointly provided with the direct payment policy, result in an excess of coverage (over insurance), according to the standards of the Contractor. |
| 5.5.4 | [Intentionally left blank]. |
| 5.5.5 | Subject to the conditions and limitations in this Section, a conversion to a direct payment policy shall be granted only: |
| 5.5.5.1 | To Enrollees who are Disenrolled because they receive a Negative Redetermination Decision from the Puerto Rico Medicaid Program; and |
| 5.5.5.2 | To Enrollees who are Disenrolled because they are no longer Eligible Persons as defined in Section 1.3.1 of this Contract, regardless of whether their family members who are MiSalud Enrollees remain eligible and continue to be enrolled. |
Page 104
| 5.5.6 | If a former Enrollee under this Contract receives health services that are covered services under the direct payment policy described in this Section, and such services are rendered during the period when the former Enrollee is already eligible to receive the direct payment policy pursuant to this Section but before the policy is in effect, the benefits which he or she would have a right to collect under such direct payment policy will be paid as a claim under the direct payment policy, so long as the former Enrollee has requested the direct payment policy as of the date such services are rendered and has paid the first premium. |
| 5.5.7 | If any Enrollee under this Contract subsequently acquires the right to obtain a direct payment policy, as provided in this Section 5.5 and is not notified of the existence of this right at least fifteen (15) Calendar Days prior to the expiration of the period in which the Enrollee may request the subscription to a direct payment policy and pay its corresponding first premium, as provided in Section 5.5.1, such Enrollee will be granted an additional period during which time the Enrollee may request to be subscribed to a direct payment policy. This additional period does not imply the continuation of the Enrollee’s Enrollment under this Contract. The additional period specified in this Section 5.5.7 will expire fifteen (15) Calendar Days after the Enrollee is notified, but in no case will it be extended beyond sixty (60) Calendar Days after the Disenrollment or event of termination specified in sections 5.5.5 and 5.5.8 of this Contract, respectively. The notification of the additional period specified |
Page 105
| herein shall be made in writing and handed to the Enrollee or mailed to the last known address of the Enrollee. If the Enrollee is granted an additional period, as provided herein, and if during such additional period the Enrollee submits the written request and makes the first premium payment, the effective date of the direct payment policy will be the termination of the health insurance coverage under this Contract. |
| 5.5.8 | Subject to the other conditions stated in this Section 5.5, Enrollees will have the right to conversion, up to the following dates: |
| 5.5.8.1 | The Enrollee’s Effective Date of Disenrollment; |
| 5.5.8.2 | The Termination Date of this Contract; or |
| 5.5.8.3 | The date of amendment of this Contract, if such an amendment eliminates the Enrollee’s eligibility. |
ARTICLE 6 ENROLLEE SERVICES
| 6.1 | General Provisions |
| 6.1.1 | The Contractor shall ensure that Enrollees are aware of their rights and responsibilities; how to obtain care; what to do in an emergency or urgent medical |
Page 106
| situation; how to request a Grievance, Appeal, or Administrative Law Hearing; and how to report suspected Fraud and Abuse. |
| 6.1.2 | The Contractor’s informational materials must convey to Enrollees the important changes in the delivery of Covered Services reflected in the introduction of the MiSalud Program, including the integration of physical and behavioral health services and the concepts of Primary Medical Groups and Preferred Provider Networks. |
| 6.1.3 | The information conveyed in the Contractor’s written materials shall conform with ASES’s Universal Beneficiary Guidelines, included as Attachment 3 to this Contract. |
| 6.1.4 | The Contractor shall convey information to Enrollees via written materials and via telephone, internet, and face-to-face communications and shall allow Enrollees to submit questions and to receive responses from the Contractor. |
| 6.1.5 | In developing informational materials on MiSalud, the Contractor shall remain cognizant that MiSalud includes a mixed population of Enrollees. In advising an individual Enrollee about Enrollment, the scope of services, and cost-sharing, Contractor shall provide information applicable to that Enrollee’s eligibility category. The Contractor shall ensure that the informational materials disseminated to all MiSalud Enrollees accurately identify differences among the categories of Eligible Persons. |
Page 107
| 6.1.6 | The Contractor shall provide Enrollees with at least thirty (30) Calendar Days written notice of any significant change in policies concerning Enrollees’ Disenrollment rights (see Section 5.4.3 of this Contract), right to change PMGs or PCPs (see Section 5.3 of this Contract), or any significant change to any of the items listed in Enrollee Rights and Responsibilities (Section 6.5 of this Contract), regardless of whether ASES or the Contractor caused the change to take place. This Section 6.1.6 shall not be construed as giving the Contractor the right to change its policies and procedures related to its services under this Contract without prior written approval from ASES. |
| 6.2 | ASES Approval of All Written Materials |
| 6.2.1 | Except as otherwise provided below, written materials described in this Article 6 must be submitted to ASES for review at least thirty (30) Calendar days before their printing and distribution, as required by Act 194 of August 2000. This requirement applies to: |
| 6.2.1.1 | The materials described in this Article 6 distributed to all Enrollees, including the Enrollee Handbook; |
| 6.2.1.2 | Policy letters, coverage policy statements, or other communications about Covered Services under MiSalud distributed to Enrollees; and |
Page 108
| 6.2.1.3 | Standard letters and notifications, such as the notice of Enrollment required in Section 5.2.3.2 of this Contract, the notice of Redetermination required in Section 5.2.6.1 of this Contract, and the notice of Disenrollment required in Section 5.4.2 of this Contract. |
| 6.2.2 | The Contractor shall provide ASES with advance notice of any changes made to written materials that will be distributed to all Enrollees. Notice shall be provided to ASES at least thirty (30) Calendar Days before the effective date of the change. Within five (5) Business Days of receipt of the materials, ASES will respond to the Contractor’s submission with either an approval of the materials, recommended modifications, or a notification that more review time is required. If the Contractor receives no response from ASES within ten (10) Business Days of ASES’s receipt of the materials, the materials shall be deemed approved. Except as otherwise provided in this Section, the Contractor may distribute the revised written materials only upon written approval of the changes from ASES. |
| 6.3 | Requirements for Written Materials |
| 6.3.1 | The Contractor shall make all written materials available in alternative formats and in a manner that takes into consideration the Enrollee’s special needs, including Enrollees who are visually impaired or have limited reading proficiency. The |
Page 109
| Contractor shall notify all Enrollees that information is available in alternative formats, and shall instruct them how to access those formats. |
| 6.3.2 | Except as provided in Section 6.4 of this Contract (Enrollee Handbook), the Contractor shall make all written information available in Spanish, with a language block in English, explaining (1) that the Enrollee may access an English translation of the information if needed; and (2) that the Contractor will provide oral interpretation services into any language other than Spanish or English, if needed. Such translation or interpretation shall be provided by the Contractor at no cost to the Enrollee. The language block shall comply with 42 CFR 438.10(c)(2). |
| 6.3.3 | If oral interpretation services are required in order to explain the Benefits covered under MiSalud to an Enrollee or Potential Enrollee who does not speak either English or Spanish, the Contractor must, at its own cost, make such services available in a third language, in compliance with 42 CFR 438.10(c)(4). |
| 6.3.4 | All written materials shall be worded such that they are understandable to a person who reads at the fourth (4th) grade level. |
| 6.3.5 | Within ninety (90) Calendar Days of a notification from ASES that ASES has identified a prevalent language other than Spanish or English (with “prevalent language” defined as a language that is the primary language of more than five |
Page 110
| percent (5%) of the population of Puerto Rico), all vital Contractor documents shall be translated into and made available in such language. |
| 6.4 | Enrollee Handbook Requirements |
| 6.4.1 | The Contractor shall produce at its sole cost, and shall mail to all new Enrollees, an Enrollee Handbook including information on both physical and behavioral health services offered under MiSalud. The Contractor shall collect from the MBHO the information on behavioral health services needed to compile the Enrollee Handbook. The Contractor shall distribute the Handbook either simultaneously with the notice of Enrollment referenced in Section 5.2.3.2 of this Contract or within five (5) Calendar Days of sending the notice of Enrollment via surface mail. |
| 6.4.2 | The Contractor shall either: |
| 6.4.2.1 | Mail to all Enrollees an Enrollee Handbook at least annually on July 1, after the initial distribution of the Handbook; or |
| 6.4.2.2 | At least annually as required by 42 CFR 438.10(i), on July 1 mail to all Enrollees a Handbook supplement that includes information on the following: |
Page 111
| 6.4.2.2.1 | The Contractor’s service area; |
| 6.4.2.2.2 | Benefits covered under MiSalud in the Service Regions; |
| 6.4.2.2.3 | Any cost-sharing imposed by ASES; and |
| 6.4.2.2.4 | To the extent available, quality and performance indicators, including Enrollee satisfaction. |
| 6.4.3 | The Contractor shall use the Universal Beneficiary Guide, provided by ASES and included as Attachment 3 to this Contract, as a model for its Handbook; however, the Contractor shall ensure that its Handbook meets all the requirements listed in this Section 6.4. |
| 6.4.4 | Pursuant to the requirements set forth in 42 CFR 438.10, the Enrollee Handbook shall include, at a minimum, the following: |
| 6.4.4.1 | A table of contents; |
| 6.4.4.2 | An explanation of the purpose of the Enrollee ID Card and a warning that transfer of the card to another person constitutes Fraud; |
Page 112
| 6.4.4.3 | Information about the role of the PCP and how to choose a PCP; |
| 6.4.4.4 | Information about the PMG, how to choose a PMG, and which Benefits may be accessed through the PMG; |
| 6.4.4.5 | Information about the Preferred Provider Network associated with the Enrollee’s PMG, and the benefits of seeking services within the PPN; |
| 6.4.4.6 | Information about the circumstances under which Enrollees may change to a different PMG; |
| 6.4.4.7 | Information about what to do when family size changes, including the responsibility of new mothers who are Medicaid Eligible to register their newborn with the Puerto Rico Medicaid Program and to apply for Enrollment of the newborn; |
| 6.4.4.8 | Appointment procedures; |
| 6.4.4.9 | Information on Benefits and Covered Services, including how the scope of Benefits and Covered Services differs between Medicaid- and CHIP Eligible Persons and Other Eligible Persons; |
Page 113
| 6.4.4.10 | An explanation of the integration of physical and behavioral health services under MiSalud, and the availability of behavioral health Providers within the PPN; |
| 6.4.4.11 | Information on how to access local resources for Non-Emergency Medical Transportation (NEMT); |
| 6.4.4.12 | An explanation of any service limitations or exclusions from coverage; |
| 6.4.4.13 | Information on where and how Enrollees may access benefits not available from or not covered by the MiSalud Plan; |
| 6.4.4.14 | The Medical Necessity definition used in determining whether services will be covered (see Section 7.2 of this Contract); |
| 6.4.4.15 | A description of all pre-certification, Prior Authorization or other requirements for treatments and services; |
| 6.4.4.16 | The policy on Referrals for specialty care and for other Covered Services not furnished by the Enrollee’s PCP; |
Page 114
| 6.4.4.17 | Information on how to obtain services when the Enrollee is outside the Contractor’s Service Regions; |
| 6.4.4.18 | Information on how to obtain after-hours coverage; |
| 6.4.4.19 | An explanation of cost-sharing, including |
| 6.4.4.19.1 | the differences in cost-sharing responsibilities between Medicaid- and CHIP Eligible Persons and Other Eligible Persons, and |
| 6.4.4.19.2 | the cost-sharing responsibilities of Dual Eligible Beneficiaries, as well as the other information for Dual Eligible Beneficiaries listed in Section 6.13 of this Contract; |
| 6.4.4.20 | The geographic boundaries of the Service Regions; |
| 6.4.4.21 | Notice of all appropriate mailing addresses and telephone numbers to be utilized by Enrollees seeking information or authorization, including the Contractor’s toll-free telephone line and Web site address; |
| 6.4.4.22 | A description of Utilization Management policies and procedures used by the Contractor; |
Page 115
| 6.4.4.23 | A description of Enrollee rights and responsibilities as described in Section 6.5 of this Contract; |
| 6.4.4.24 | The policies and procedures for Disenrollment, including when Disenrollment may be requested without Enrollee consent by the Contractor and information about Enrollee’s right to request Disenrollment, and including notice of the fact that the Enrollee will lose access to services under MiSalud if he or she chooses to disenroll; |
| 6.4.4.25 | Information on Advance Directives, including the right of Enrollees to file directly with ASES or with the Puerto Rico Office of the Patient Advocate, complaints concerning Advance Directive requirements listed in Section 7.10 of this Contract; |
| 6.4.4.26 | A statement that additional information, including the Provider guidelines and information on the structure and operation of the MiSalud Plan and the Physician Incentive Plan, shall be made available to Enrollees upon request; |
| 6.4.4.27 | Information on the extent to which, and how, after-hours and emergency coverage are provided, including the following: |
Page 116
| 6.4.4.27.1 | What constitutes an Emergency Medical Condition; |
| 6.4.4.27.2 | The fact that Prior Authorization is not required for Emergency Services; |
| 6.4.4.27.3 | Notice that |
| 6.4.4.27.3.1 | For Medicaid and CHIP Eligible Persons, |
| 6.4.4.27.3.1.1 | No Co-Payments shall be charged for the treatment of an Emergency Medical Condition; |
| 6.4.4.27.3.1.2 | No Co-Payments shall be charged for CHIP children under eighteen years of age under any circumstances; |
| 6.4.4.27.3.1.3 | No Co-Payments will be charged for Indians; and |
| 6.4.4.27.3.1.4 | Co-Payments apply to emergency room services outside the Enrollee’s PPN to treat a condition that does not meet the definition of Emergency Medical Condition set forth in this Contract, but by using the |
Page 117
| Tele MiSalud service (see Section 6.8 of this Contract), the Enrollee may avoid a Co-Payment for such services; and |
| 6.4.4.27.3.2 | For Other Eligible Persons, Co-Payments apply to Emergency Services outside the Enrollee’s PPN, but the Enrollee may avoid a Co-Payment by using the Tele MiSalud service (see Section 6.8 of this Contract). |
| 6.4.4.27.4 | The process and procedures for obtaining Emergency Services, including the use of the 911 telephone systems or its local equivalent; |
| 6.4.4.27.5 | The scope of Post-Stabilization Services offered under the Plan; |
| 6.4.4.27.6 | The locations of emergency rooms and other locations at which Providers and hospitals furnish Emergency Services and Post-Stabilization Services covered herein; and |
| 6.4.4.27.7 | The fact that an Enrollee has a right to use any hospital or other setting for Emergency Services; |
| 6.4.4.28 | An explanation of the Redetermination process, including |
Page 118
| 6.4.4.28.1 | Disenrollment as a consequence of a Negative Redetermination Decision, and |
| 6.4.4.28.2 | The Re-Enrollment period that follows a new Certification; and |
| 6.4.4.29 | Information on the Contractor’s Grievance Systems policies and procedures, as described in Article 14 of this Contract. This description must include the following: |
| 6.4.4.29.1 | The right to file a Grievance and Appeal with the Contractor; |
| 6.4.4.29.2 | The requirements and timeframes for filing a Grievance or Appeal with the Contractor; |
| 6.4.4.29.3 | The availability of assistance in filing a Grievance or Appeal with the Contractor; |
| 6.4.4.29.4 | The toll-free numbers that the Enrollee can use to file a Grievance or an Appeal with the Contractor by phone; |
| 6.4.4.29.5 | The right to an Administrative Law Hearing, the method for obtaining a hearing, and the rules that govern representation at the hearing; |
Page 119
| 6.4.4.29.6 | Notice that if the Enrollee files an Appeal or a request for an Administrative Law Hearing and requests continuation of services, the Enrollee may be required to pay the cost of services furnished while the Appeal is pending, if the final decision is adverse to the Enrollee; |
| 6.4.4.29.7 | Any Appeal rights that Puerto Rico chooses to make available to Providers to challenge the failure of the Contractor to cover a service; |
| 6.4.4.29.8 | Instructions on how an Enrollee can report suspected Fraud on the part of a Provider, and protections that are available for whistleblowers; and |
| 6.4.4.29.9 | Information on the family planning services provided by the Puerto Rico Health Department. |
| 6.4.5 | The Enrollee Handbook shall be submitted to ASES for review and prior written approval. Submission of the Handbook by the Contractor shall be in accordance with the timeframes specified in Attachment 12 to this Contract (Initial Deliverable Due Dates). |
| 6.4.6 | The Contractor shall be responsible for producing the Enrollee Handbook in both English and Spanish. |
Page 120
| 6.5 | Enrollee Rights and Responsibilities |
The Contractor shall have written policies and procedures regarding the rights of Enrollees and shall comply with any applicable federal and Puerto Rico laws and regulations that pertain to Enrollee rights, including those set forth in 42 CFR 438.100 and in the Puerto Rico Patient’s Bill of Rights Act 194 of August 25, 2000; the Puerto Rico Mental Health Law of October 2, 2000, as amended and implemented; and Law 11 of April 11, 2001, creating the Office of the Patient Advocate. These rights shall be included in the Enrollee Handbook. At a minimum, the policies and procedures shall specify the Enrollee’s right to:
| 6.5.1 | Receive information pursuant to 42 CFR 438.10; |
| 6.5.2 | Be treated with respect and with due consideration for the Enrollee’s dignity and privacy; |
| 6.5.3 | Have all records and medical and personal information remain confidential, except to the extent it may be or must be disclosed by law. |
| 6.5.4 | Receive information on available treatment options and alternatives, presented in a manner appropriate to the Enrollee’s condition and ability to understand; |
Page 121
| 6.5.5 | Participate in decisions regarding his or her health care, including the right to refuse treatment; |
| 6.5.6 | Be free from any form of restraint or seclusion as a means of coercion, discipline, convenience or retaliation, as specified in 42 CFR 482.13(e) and other federal regulations on the use of restraints and seclusion; |
| 6.5.7 | Request and receive a copy of his or her Medical Records pursuant to 45 CFR Parts 160 and 164, subparts A and E, and request to amend or correct the record, as specified in 45 CFR 164.524 and 164.526, respectively; |
| 6.5.8 | Be furnished health care services in accordance with 42 CFR 438.206 through 438.210; |
| 6.5.9 | Freely exercise his or her rights, including those related to filing a Grievance or Appeal, and that the exercise of these rights will not adversely affect the way the Enrollee is treated; |
| 6.5.10 | Not be held liable for the Contractor’s debts in the event of insolvency; not be held liable for the Covered Services provided to the Enrollee for which ASES does not pay the Contractor; not be held liable for Covered Services provided to the Enrollee for which ASES or the MiSalud Plan does not pay the Provider that furnishes the |
Page 122
| services; and not be held liable for payments of Covered Services furnished under a contract, Referral, or other arrangement to the extent that those payments are in excess of amount the Enrollee would owe if the Provider provided the services directly; and |
| 6.5.11 | Only be responsible for cost-sharing in accordance with 42 CFR 447.50 through 42 CFR 447.59. |
| 6.6 | Provider Directory |
| 6.6.1 | The Contractor shall produce and shall mail to all new Enrollees a Provider Directory that includes information on both physical and behavioral health service Providers under MiSalud. The Contractor shall collect from the MBHO the information on behavioral health Providers needed in order to compile the Provider Directory. The Contractor shall distribute the Provider Directory by delivering it at the time of Certification in person, or, if this is impractical, by sending it via surface mail, within five (5) Calendar Days of sending the notice of Enrollment referenced in Section 5.2.3.2 of this Contract. |
| 6.6.2 | The Contractor shall produce and distribute annual updates of the Provider Directory to all Enrollees. |
Page 123
| 6.6.3 | The Contractor shall make the Provider Directory available on its Web site. |
| 6.6.4 | The Provider Directory shall include names, locations, office hours, and telephone numbers of current Network Providers. This includes, at a minimum, information, sorted by Service Region, on PCPs, specialists, dentists, FQHCs and RHCs, behavioral health and substance abuse Providers affiliated with the MBHO in each Service Region, and hospitals. The Provider Directory shall also identify providers that are not accepting new patients. |
| 6.6.5 | The Provider Directory shall group Providers according to the PMG Preferred Provider Network with which they are affiliated. |
| 6.6.6 | The Contractor shall submit the Provider Directory to ASES for review and prior approval in the timeframe specified in Attachment 12 to this Contract. |
| 6.6.7 | The Contractor shall update and amend the Provider Directory on its Web site within five (5) Business Days of any changes. |
| 6.6.8 | On a monthly basis, the Contractor shall submit to ASES any changes and edits to the Provider Directory, including any changes supplied to the Contractor by the MBHO. Such changes shall be submitted electronically in the format specified by ASES. |
Page 124
| 6.7 | Enrollee Identification (ID) Card |
| 6.7.1 | The Contractor shall furnish to all new Enrollees an Enrollee ID Card. The card shall be made of durable plastic material and shall be delivered at the time of Enrollment in person, or, if this is impractical, by sending the Enrollee ID Card sent to the Enrollee via surface mail within two (2) Calendar Days of sending the notice of Enrollment referenced in Section 5.2.3.2 of this Contract. |
| 6.7.2 | The Enrollee ID Card must, at a minimum, include the following information: |
| 6.7.2.1 | The “MiSalud” logo; |
| 6.7.2.2 | The Enrollee’s name; |
| 6.7.2.3 | A designation of the Enrollee as a Medicaid Eligible, CHIP Eligible, or Other Eligible Person; |
| 6.7.2.4 | The Enrollee’s Medicaid identification number, or CHIP identification number; |
| 6.7.2.5 | The Enrollee’s Plan group number; |
Page 125
| 6.7.2.6 | If the Enrollee is eligible for MiSalud as a Dependent, the Enrollee’s relationship to the principal Enrollee; |
| 6.7.2.7 | The Effective Date of Enrollment in MiSalud; |
| 6.7.2.8 | The master patient index; |
| 6.7.2.9 | The applicable Co-Payment levels for various services outside the Enrollee’s PPN, and the assurance that no Co-Payment will be charged for the treatment of an Emergency Medical Condition for a Medicaid Eligible Person and for CHIP children under eighteen (18) years of age, no co-payments will be charged under any circumstances; |
| 6.7.2.10 | The PCP’s and the PMG’s names; |
| 6.7.2.11 | The name and telephone number(s) of the Contractor; |
| 6.7.2.12 | The twenty-four (24) hour, seven (7) day a week toll-free Tele MiSalud Medical Advice Service phone number; |
| 6.7.2.13 | A notice that the Enrollee ID Card may under no circumstances be used by a person other than the identified Enrollee; and |
Page 126
| 6.7.2.14 | Instructions for emergencies. |
| 6.7.3 | The Contractor shall reissue the Enrollee ID Card in the following situations and timeframes: |
| 6.7.3.1 | within ten (10) Calendar Days of notice if an Enrollee reports a lost, stolen or damaged ID Card and requests a replacement; |
| 6.7.3.2 | within ten (10) Calendar Days of notice if an Enrollee reports a name change; |
| 6.7.3.3 | within twenty (20) Calendar Days of the effective date of a change of PMG or change or addition of PCP, as provided in Section 5.3.2 of this Contract. |
| 6.7.4 | The Contractor may charge a fee of $5 to replace lost, damaged, or stolen Enrollee ID Cards; provided, however, that the Contractor may not charge a replacement fee because of a name change or change of PMG or PCP, and that the Contractor may not charge a replacement fee in any circumstance for Medicaid and CHIP Eligible Persons. |
Page 127
| 6.7.5 | The Contractor shall submit a front and back sample Enrollee ID Card to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to Enrollee ID Card must be previously approved in writing by ASES. |
| 6.7.6 | The Contractor must require an Enrollee to surrender his or her ID Card in each of the following events: |
| 6.7.6.1 | the Enrollee is disenrolled; |
| 6.7.6.2 | the Enrollee requests a change to his or her PCP or PMG, and is therefore issued a new Enrollee ID Card; or |
| 6.7.6.3 | the Enrollee requests a new ID Card because his or her existing card is damaged. |
| 6.7.7 | In the event ASES requires that the Contractor issue new Enrollee ID Cards to all or part of the Enrollee population as a result of a change in the Enrollees’ MBHO or PBM at any time during the Contract Term, ASES shall cover all costs related to the production and delivery of such cards. |
Page 128
| 6.8 | Tele MiSalud (Toll Free Telephone Service) |
| 6.8.1 | The Contractor shall operate a toll-free telephone number, “Tele MiSalud,” equipped with caller identification and automatic call distribution equipment capable of handling the expected volume of calls. Tele MiSalud shall have two components: |
| 6.8.1.1 | An Information Service to respond to questions, concerns, inquiries, and complaints regarding MiSalud from the Enrollee or the Enrollee’s family; and |
| 6.8.1.2 | A Medical Advice Service to advise Enrollees about how to resolve medical or behavioral health concerns. |
| 6.8.2 | The Contractor shall establish, operate, monitor and support an automated call distribution system for Tele MiSalud that supports, at a minimum: |
| 6.8.2.1 | Capacity to handle the call volume; |
| 6.8.2.2 | A daily analysis of the quantity, length, and types of calls received; |
| 6.8.2.3 | A daily analysis of the amount of time it takes to answer the call, Blocked Calls, and Abandoned Calls; |
Page 129
| 6.8.2.4 | The ability to measure average waiting time; and |
| 6.8.2.5 | The ability to monitor calls from a location by a third party, including ASES. |
| 6.8.3 | Hours of Operation. Each service shall be made available as follows: |
| 6.8.3.1 | The Information Service shall be fully staffed between the hours of 7:00 a.m. and 7:00 p.m., Monday through Friday, excluding Puerto Rico holidays. The Contractor shall have an automated system available between the hours of 7:00 p.m. and 7:00 a.m. Puerto Rico time Monday through Friday and at all hours on weekends and holidays. This automated system must provide callers with operating instructions on what to do in case of an emergency and shall include, at a minimum, a voice mailbox for callers to leave messages. The Contractor shall ensure that the voice mailbox has the required capacity to receive all messages. A Contractor’s representative shall reply to one hundred percent (100%) of messages by the next Business Day. |
| 6.8.3.2 | The Medical Advice Service shall be fully staffed and available to Enrollees twenty-four (24) hours per day, seven (7) days per week. |
Page 130
| 6.8.4 | Staffing |
| 6.8.4.1 | The Contractor shall be responsible for the required staffing of Tele MiSalud with individuals who are able to communicate effectively with MiSalud Enrollees. |
| 6.8.4.2 | The Contractor shall make key staff responsible for operating Tele MiSalud available to meet with ASES staff on a regular basis, as requested by ASES, to review reports and all other obligations under the Contract relating to Tele MiSalud. |
| 6.8.4.3 | The Contractor shall hire and train adequate staff by the Implementation Date of the Contract. The training program shall include, but is not limited to, systems, policies and procedures, and telephone scripts. |
| 6.8.4.4 | For the Information Service, the Contractor shall ensure that call center attendants have the necessary training to respond to Enrollee questions, concerns, inquiries, and complaints from the Enrollee or the Enrollee’s family relating to this Contract, including but not limited to Covered Services, Grievances and Appeals, the Provider Network, and Enrollment and Disenrollment. |
Page 131
| 6.8.4.5 | For the Medical Advice Service, the Contractor shall ensure that call center attendants are registered nurses with the necessary training to advise Enrollees about appropriate steps they should take to resolve a medical or behavioral health complaint or concern. |
| 6.8.4.6 | The Contractor shall ensure that Tele MiSalud call center staff are trained to identify behavioral health concerns and, where appropriate, to transfer Enrollee callers to the MBHO’s Call Center for assistance. Tele MiSalud shall be equipped with the capacity to effect a “warm transfer” to the MBHO’s Call Center for behavioral health advice. |
| 6.8.4.7 | The Contractor shall ensure that Tele MiSalud call center staff is trained to identify situations in which an Enrollee may need services that are offered through the Puerto Rico Health Department rather than through MiSalud, and Tele MiSalud staff shall provide the Enrollee with information on where to access these services. |
| 6.8.4.8 | The Contractor shall ensure that Tele MiSalud call center staff is trained to provide to Medicaid and CHIP Eligible Enrollees information on how to access any local NEMT resources, to enable an Enrollee without available transportation to receive Medically Necessary services. |
Page 132
| 6.8.4.9 | The Contractor shall ensure that Tele MiSalud call center staff are trained to process and fulfill requests by Enrollees to receive, by surface mail, the Enrollee Handbook, the Provider Directory, or the Provider guidelines. The Contractor shall fulfill such requests by mailing the requested document within five (5) Business Days of the request. |
| 6.8.5 | The Contractor may provide the Information Service and the Medical Advice Service as separate phone lines with a “warm transfer” capability, or as separate dialing options within one phone line. “Warm transfer” refers to the process of an agent connecting a caller to a third-party contact. Once the third-party contact has answered, the agent introduces himself to the contact and provides the caller’s necessary information. The agent stays on the line to confirm that the third-party contact and the caller have connected before the agent disconnects. |
| 6.8.6 | The Contractor shall have the capability of making out-bound calls. |
| 6.8.7 | Tele MiSalud shall be equipped to handle calls in Spanish and English, as well as, through a telecommunication device for the deaf (TDD), calls from Enrollees who are hearing-impaired. For callers who do not speak either English or Spanish, the Contractor shall provide interpreter services free of charge to Enrollees. The Contractor shall not permit Enrollees’ family members, especially minor children, or |
Page 133
| friends to provide oral interpreter services, unless specifically requested by the Enrollee. |
| 6.8.8 | The Contractor shall (i) record calls on a random basis following its standard call center protocols, and (ii) document all calls, identifying the date and time, the type of call, the reason for the call and the resolution of the call. |
| 6.8.9 | The Contractor shall generate a call identification number for each phone call made by an Enrollee to the Medical Advice Service. Enrollees who use this service to seek advice on their health condition before visiting the emergency room will not be responsible for any Co-Payment otherwise imposed for emergency room visits (as provided under Section 7.11.4 of this Contract) outside the Enrollee’s PPN, provided that the Enrollee presents his or her Tele MiSalud call identification number at the emergency room. No Co-Payment shall be imposed on a Medicaid or CHIP Eligible Enrollee for the treatment of an Emergency Medical Condition (regardless of whether the Enrollee uses the Medical Advice Service). The Medical Advice Service does not apply to services outside of Puerto Rico. |
| 6.8.10 | The Contractor shall develop Tele MiSalud policies and procedures, including staffing, training, hours of operation, access and response standards, transfers/referrals, monitoring of calls via recording and other means, and compliance with other performance standards. |
Page 134
| 6.8.11 | The Contractor shall develop Tele MiSalud Quality Criteria and Protocols. These protocols shall, at a minimum, |
| 6.8.11.1 | Measure and monitor the accuracy of responses and phone etiquette in Tele MiSalud (including through recording of phone calls) and take corrective action as necessary to ensure the accuracy of responses and appropriate phone etiquette by staff; |
| 6.8.11.2 | Provide for quality calibration sessions between the Contractor’s staff and ASES; |
| 6.8.11.3 | Require that, on a monthly basis, the Average Speed of Answer is at least eighty percent (80%) of calls answered within thirty (30) seconds; |
| 6.8.11.4 | Require that, on a monthly basis, the Blocked Call rate does not exceed three percent (3%) of all calls from or relating to Enrollees or Potential Enrollees; and |
| 6.8.11.5 | Require that, on a monthly basis, the rate of Abandoned Calls does not exceed five percent (5%) of all calls from or relating to Enrollees or Potential Enrollees. |
Page 135
These standards serve as a minimum for each Tele MiSalud service. The Contractor may elect to establish more rigorous performance standards. The Contractor may elect to establish different quality criteria for the Medical Advice Service than for the Information Service; provided, however, that in that event, the standards governing the Medical Advice Service must be stricter than the standards for the Information Service.
| 6.8.12 | The Contractor must develop and implement a Tele MiSalud outreach program to educate Enrollees about the Tele MiSalud service and to encourage its use (the “Tele MiSalud Outreach Program”). The Tele MiSalud Outreach Program shall include, at a minimum, the following components: |
| 6.8.12.1 | A section on Tele MiSalud in the Enrollee Handbook; |
| 6.8.12.2 | Contact information for Tele MiSalud on the Enrollee ID Card and on the Contractor’s Web site; and |
| 6.8.12.3 | Informational flyers on Tele MiSalud to be placed in the offices of the Contractor and the Network Providers. |
Each document or communication included in this Tele MiSalud Outreach Program must explain that (1) by using the Medical Advice Service before visiting the
Page 136
emergency room, and presenting their call identification number at the emergency room, Enrollees can avoid any emergency room Co-Payments otherwise applicable under Section 7.11.4 of this Contract for services outside the PPN; and (2) no Co-Payment shall be imposed for the treatment of an Emergency Medical Condition for a Medicaid or CHIP Eligible Person. All written materials included in the Tele MiSalud Outreach Program must be written at a fourth- (4th) grade reading level and must be available in Spanish and English.
| 6.8.13 | The Contractor shall prepare scripts addressing the questions expected to arise most often for both the Information Service and the Medical Advice Service. The Contractor shall submit these scripts to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. It is the responsibility of the Contractor to maintain and update these scripts and to ensure that they are developed at the fourth (4th) grade reading level. The Contractor shall submit revisions to the script to ASES for approval prior to use, pursuant to Section 6.2 of this Contract. |
| 6.8.14 | The Contractor shall submit the following written materials referred to in this Section 6.8 to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract and any subsequent changes to the following must be previously approved in writing by ASES, which approval shall not be unreasonably withheld, conditioned or delayed: |
Page 137
| 6.8.14.1 | Tele MiSalud policies and procedures; |
| 6.8.14.2 | Tele MiSalud quality criteria and protocols; |
| 6.8.14.3 | Tele MiSalud Outreach Program; and |
| 6.8.14.4 | Training materials for Tele MiSalud call center employees. |
| 6.9 | Internet Presence / Web Site |
| 6.9.1 | The Contractor shall provide on its Web site general and up-to-date information about MiSalud and about the MiSalud Plan, including the Provider Network, customer services, Tele MiSalud, and its Grievance System. The Enrollee Handbook and the Provider Directory shall be available on the Web site. |
| 6.9.2 | The Contractor shall maintain an Enrollee portal that allows Enrollees to access a searchable Provider Directory that shall be updated within five (5) Business Days to reflect any change to the Provider Network. |
| 6.9.3 | The Web site must have the capability for Enrollees to submit questions and comments to the Contractor and receive responses. The Contractor shall reply to Enrollee questions within two (2) Business Days. |
Page 138
| 6.9.4 | The Web site must comply with the marketing policies and procedures and with requirements for written materials described in Sections 6.2 and 6.3 of this Contract and must be consistent with applicable Puerto Rico and federal laws. |
| 6.9.5 | The Contractor shall submit Web site screenshots to ASES for review and approval of information on the website relating to the MiSalud Program according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to Contractor’s Web site relating to the MiSalud Program must be previously approved in writing by ASES, which approval shall not be unreasonably withheld, conditioned or delayed. |
| 6.9.6 | The Contractor’s Web site shall provide secured online access to the Enrollee’s historical and current information. |
| 6.9.7 | The Contractor’s Web site shall prominently feature a link to the MiSalud Web site of ASES, www.misaludpuertorico.com; and to the ASES Web site, www.asespr.org. |
| 6.10 | Cultural Competency |
| 6.10.1 | In accordance with 42 CFR 438.206, the Contractor shall have a comprehensive written cultural competency plan describing how the Contractor will ensure that services are provided in a culturally competent manner to all Enrollees (the “Cultural |
Page 139
| Competency Plan”). The Cultural Competency Plan must describe how the Providers, individuals and systems within the Contractor’s Plan will effectively provide services to people of all cultures, races, ethnic backgrounds and religions in a manner that recognizes, values, affirms and respects the worth of the individual Enrollees and protects and preserves the dignity of each. |
| 6.10.2 | The Contractor shall submit the Cultural Competency Plan to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to the Cultural Competency Plan must be previously approved in writing by ASES. |
| 6.10.3 | The Contractor may distribute a summary of the Cultural Competency Plan, rather than the entire document, to Providers if the summary includes information on how the Provider may access the full Cultural Competency Plan on the Contractor’s Web site. This summary shall also detail how the Provider can request a hard copy from the Contractor at no charge to the Provider. |
| 6.11 | Interpreter Services |
| 6.11.1 | The Contractor shall provide oral interpreter services to any Enrollee who speaks any language other than English or Spanish as his or her primary language, regardless of whether the Enrollee speaks a language that meets the threshold of a Prevalent Non- |
Page 140
| English Language. The Contractor is required to notify its Enrollees of the availability of oral interpretation services and to inform them of how to access oral interpretation services. There shall be no charge to an Enrollee for interpreter services. |
| 6.12 | Enrollment Outreach for the Homeless Population |
The Contractor shall, upon prior written notice, participate in at least four (4) public events per year held by government agencies in different locations in each Service Region, to allow homeless individuals to complete the Enrollment process pursuant to the terms of this Contract.
| 6.13 | Special Enrollee Information Requirements for Dual Eligible Beneficiaries |
The Contractor shall inform an Enrollee who is a Dual Eligible Beneficiary:
| 6.13.1 | That the Dual Eligible Beneficiary is eligible for services under MiSalud with the limits stated in Section 7.12 of this Contract; |
| 6.13.2 | That the MiSalud Plan will cover Medicare Part B deductibles and co-insurance, but not Medicare Part A deductibles; |
Page 141
| 6.13.3 | That the Dual Eligible Beneficiary may not be simultaneously enrolled in MiSalud and in a Medicare Platino plan, for the reason that the Platino plan already includes MiSalud Benefits; and |
| 6.13.4 | That as an Enrollee in the Plan, the Dual Eligible Beneficiary may access Covered Services only through the PMG, not through the Medicare provider list. |
| 6.14 | Marketing |
| 6.14.1 | Prohibited Marketing Activities. The Contractor is prohibited from engaging in the following activities: |
| 6.14.1.1 | Directly or indirectly engaging in door-to-door, telephone, or other Cold-Call Marketing activities to Enrollees or Eligible Individuals; |
| 6.14.1.2 | Offering any favors, inducements or gifts, promotions, or other insurance products that are designed to induce Enrollment in the MiSalud Plan; |
| 6.14.1.3 | Distributing plans and materials that contain statements that ASES determines are inaccurate, false, or misleading. Statements considered false or misleading include, but are not limited to, any assertion or statement (whether written or oral) that the MiSalud Plan is endorsed by |
Page 142
| the federal government or Government of Puerto Rico, or similar entity; and |
| 6.14.1.4 | Distributing materials that, according to ASES, mislead or falsely describe the Contractor’s Provider network, the participation or availability of Network Providers, the qualifications and skills of Network Providers (including their bilingual skills); or the hours and location of network services. |
| 6.14.2 | Allowable Marketing Activities. The Contractor shall be permitted to perform the following Marketing activities: |
| 6.14.2.1 | Distribute general information through mass media (i.e. newspapers, magazines and other periodicals, radio, television, the Internet, public transportation advertising, and other media outlets); |
| 6.14.2.2 | Make telephone calls, mailings and home visits only to Enrollees currently enrolled in the MiSalud Plan, for the sole purpose of educating them about services offered by or available through the Contractor; |
| 6.14.2.3 | Distribute brochures and display posters at Provider offices that inform patients that the Provider is part of MiSalud Provider Network; and |
Page 143
| 6.14.2.4 | Attend activities that benefit the entire community, such as health fairs or other health education and promotion activities. |
| 6.14.3 | If the Contractor performs an allowable activity in a Service Region, the Contractor shall conduct that activity in all other Service Regions covered by this Contract. |
| 6.14.4 | All Marketing Materials shall be in compliance with the information requirements in 42 CFR 438.10. |
| 6.14.5 | ASES Approval of Marketing Materials |
| 6.14.5.1 | The Contractor shall submit a detailed description of its Marketing Plan and copies of all Marketing Materials (written and oral) that it or its Subcontractors plan to distribute to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. This requirement includes, but is not limited to posters, brochures, Web sites, and any materials that contain statements regarding the benefit package and Provider network-related materials. Neither the Contractor nor its Subcontractors shall distribute any Marketing Materials without the prior written approval from ASES pursuant to Section 6.2. |
Page 144
| 6.14.5.2 | The Contractor shall submit any changes to previously approved marketing materials and receive the approval from ASES of the changes before distribution pursuant to Section 6.2. |
| 6.14.5.3 | The Advisory Committee of the Puerto Rico Medicaid Program, which advises the Puerto Rico Medicaid Program and ASES about government health programs, will assist ASES in the evaluation and review of any marketing materials submitted by the Contractor for approval. |
| 6.14.6 | Provider Marketing Materials |
| 6.14.6.1 | The Contractor is responsible for ensuring that not only its Marketing activities, but also the marketing activities of its Subcontractors and Providers, meet the requirements of this Section 6.14. |
| 6.14.6.2 | The Contractor shall collect from its Providers any Marketing Materials they intend to distribute and submit these to ASES for review and approval prior to distribution. |
| 6.14.6.3 | The Contractor shall provide for equitable distribution of all Marketing Materials without bias toward or against any group. |
Page 145
| 6.14.7 | The Parties acknowledge and agree that nothing herein shall require the Contractor to engage in the Marketing of the MiSalud Program to: (a) Other Eligible Persons who are public employees or pensioners as described in Section 1.4.1.3.2 of this Contract; or (b) small or medium businesses located in the Service Regions. The Parties further agree that nothing herein is intended to limit the Contractor’s right to market its other insurance or managed care products to Other Eligible Persons who are public employees or pensioners as described in Section 1.4.1.3.2 of this Contract or any other Eligible Person. |
| 6.14.8 | Assistance with Network Provider EHR Systems |
| 6.14.8.1 | The Contractor shall assist the PCPs and PPN physician specialists, upon their request, in the acquisition and installation of such an appropriate EHR system, at its expense, consisting of the hardware, software and related materials specified in Attachment 15. Any such EHR system, whether maintained as a complete or component system, must be ONC and CCHIT certified, and shall meet the specifications set forth in Attachment 15. |
| 6.14.8.2 | The Contractor shall ensure that all the PCPs and PPN physician specialists shall have an operational EHR system in place on or before July 1, 2012 or such later date as set forth in his/her Provider Contract. |
Page 146
| 6.14.8.3 | The Contractor shall also provide each such Provider with information on (i) the benefits of the EHR system and (ii) the costs of maintaining the EHR system. |
ARTICLE 7 COVERED SERVICES AND BENEFITS
| 7.1 | Requirement to Make Available Covered Services |
| 7.1.1 | The Contractor shall, at a minimum, make available through its Network Providers Covered Services, and other Benefits set forth in this Article, as of the Effective Date of Enrollment (including the period specified in Section 4.4.1.2 of this Contract) pursuant to the program requirements of MiSalud, and the Puerto Rico Medicaid State Plan and CHIP Plan. The Contractor may not impose any other exclusions, limitations, or restrictions, and may not arbitrarily deny or reduce the amount, duration or scope of a required service solely because of the diagnosis, type of illness, or condition. |
| 7.1.2 | The Contractor may not deny Covered Services based on pre-existing conditions or waiting periods. |
Page 147
| 7.1.3 | The Contractor shall not be required to pay a Claim for a service that would otherwise be a Covered Service, but for the fact that the recipient of the service is not an Eligible Person. |
| 7.1.4 | The Contractor shall not be required to pay a Claim for a service already provided, which would be a Covered Service but for the fact that: |
| 7.1.4.1 | The Enrollee paid the Provider for the service (except when, in an extenuating circumstance, a Medicaid or CHIP Eligible Enrollee incurs out-of-pocket expenses for Emergency Services provided in the United States; these expenses shall be reimbursed under MiSalud); or |
| 7.1.4.2 | The service was provided by a person or entity that does not meet the definition of a Network Provider (with the exception of Medical Emergencies and cases where the service was Prior Authorized by the Contractor). |
| 7.1.5 | Notwithstanding the provisions of this Section 7.1, the Contractor shall comply with Section 9.7 of this Contract. |
Page 148
| 7.2 | Medical Necessity |
Based upon generally accepted medical practices in light of conditions at the time of treatment, Medically Necessary services are those that relate to the prevention, diagnosis, and treatment of health impairments, or to the ability to achieve age-appropriate growth and development and the ability to attain, maintain, or regain functional capacity, and are:
| 7.2.1 | Appropriate and consistent with the diagnosis of the treating Provider and the omission of which could adversely affect the eligible Enrollee’s medical condition; |
| 7.2.2 | Compatible with the standards of acceptable medical practice in the community; |
| 7.2.3 | Provided in a safe, appropriate, and cost-effective setting given the nature of the diagnosis and the severity of the symptoms; |
| 7.2.4 | Not provided solely for the convenience of the Enrollee or the convenience of the Provider; and |
| 7.2.5 | Not primarily custodial care (for example, foster care). |
Page 149
| 7.3 | Experimental or Cosmetic Procedures |
In no instance shall the Contractor be required to pay Claims for experimental or cosmetic procedures, except as required by the Puerto Rico Patient’s Bill of Rights Act or any other federal or Puerto Rico law or regulation. As provided in Section 7.5.6.2 of this Contract, breast reconstruction after a mastectomy and surgical procedures that are determined to be Medically Necessary to treat morbid obesity shall not be regarded as cosmetic procedures.
| 7.4 | Covered Services and Administrative Services |
| 7.4.1 | Benefits under MiSalud are comprised of four categories: (1) Basic Coverage, (2) Dental Services, (3) Special Coverage, and (4) Administrative Services. The scope of items (1) – (3) is described in Section 7.5 of this Contract. |
| 7.5 | Basic Coverage |
| 7.5.1 | Basic Coverage is available to all MiSalud Enrollees, except as provided in the table below. Basic Coverage includes the following categories: |
| BASIC COVERAGE SERVICES |
MISALUD ELIGIBILITY GROUPS COVERED | |
| Preventive Services |
All |
Page 150
| BASIC COVERAGE SERVICES |
MISALUD ELIGIBILITY GROUPS COVERED | |
| Diagnostic Test Services |
All | |
| Outpatient Rehabilitation Services |
All | |
| Medical and Surgical Services |
All | |
| Emergency Transportation Services |
All | |
| Maternity and Pre-Natal Services |
All | |
| Emergency Services |
All (Services outside Puerto Rico available only for Medicaid and CHIP Eligible Persons) | |
| Hospitalization Services |
All | |
| Behavioral Health Services |
All (Note: Services provided by MBHO; not covered under this Contract.) | |
| Pharmacy Services |
All (Note: Claims processing and adjudication Services provided by PBM; not covered under this Contract.) |
Page 151
| 7.5.2 | Exclusions from Basic Coverage |
| 7.5.2.1 | The following services are excluded from all Basic Coverage. In addition, exclusions specific to each category of Covered Services are noted in subsections 7.5.3 – 7.5.12 below. |
| 7.5.2.1.1 | Expenses for personal comfort material or services, such as, telephone, television, toiletries; |
| 7.5.2.1.2 | Services rendered by close family relatives (parents, children, siblings, grandparents, grandchildren, spouses); |
| 7.5.2.1.3 | Weight control treatment (obesity or weight gain) for aesthetic reasons, provided, however, that procedures determined Medically Necessary to address morbid obesity shall not be excluded; |
| 7.5.2.1.4 | Sports medicine, music therapy, and natural medicine; |
| 7.5.2.1.5 | Services, diagnostic testing or treatment ordered or rendered by naturopaths, naturists, chiropractors, iridologists, or osteopaths; |
Page 152
| 7.5.2.1.6 | Health certificates, except as provided in Section 7.6.3.2.10 of this Contract (Preventive Services); |
| 7.5.2.1.7 | Epidural anesthesia services; |
| 7.5.2.1.8 | Chronic pain treatment, if it is determined that the pain has a psychological or psychosomatic origin; |
| 7.5.2.1.9 | Smoking cessation treatment, except as provided in Section 7.5.8.3.7 of this Contract for pregnant women (smoking cessation in general is covered by the MBHO); |
| 7.5.2.1.10 | Educational tests or services; |
| 7.5.2.1.11 | Peritoneal dialysis or hemodialysis services (covered under Special Coverage, not Basic Coverage); |
| 7.5.2.1.12 | Hospice care; |
| 7.5.2.1.13 | Services received outside the territorial limits of Puerto Rico, except as provided in Sections 7.5.7.10 (Emergency Transportation) and 7.5.9.3 (Emergency Services) of this Contract; |
Page 153
| 7.5.2.1.14 | Expenses incurred for the treatment of conditions resulting from services not covered under MiSalud; |
| 7.5.2.1.15 | Judicially ordered evaluations for legal purposes; |
| 7.5.2.1.16 | Psychological/ psychometric and psychiatric tests and evaluations to obtain employment or insurance, or for purposes of litigation; |
| 7.5.2.1.17 | Travel expenses, even when ordered by the primary care physician; |
| 7.5.2.1.18 | Eyeglasses, contact lenses and hearing aids; |
| 7.5.2.1.19 | Acupuncture services; |
| 7.5.2.1.20 | Rent or purchase of durable medical equipment, wheelchair or any other transportation method for the handicapped, either manual or electric, and any expense for the repair or alteration of said equipment, except when the patient’s life depends on this service; and |
| 7.5.2.1.21 | Sex change procedures. |
| 7.5.3 | Preventive Services |
Page 154
| 7.5.3.1 | Healthy Child Care. The Contractor shall make available through its Network Providers the following Preventive Services under the Healthy Child Care Program, which serves Enrollees under age two: |
| 7.5.3.1.1 | An annual comprehensive evaluation (1) by a certified health professional, which complements other services for children and young adults provided pursuant to the periodicity scheme of the American Academy of Pediatrics; and |
| 7.5.3.1.2 | Other services, as needed, during the first two years of the child’s life. |
| 7.5.3.2 | Other Preventive Services. The following are required Preventive Services for all MiSalud Enrollees: |
| 7.5.3.2.1 | Vaccines (the vaccines themselves are provided and paid for by the Puerto Rico Health Department; the Contractor shall cover the administration of the vaccines); |
| 7.5.3.2.2 | Eye exam; |
| 7.5.3.2.3 | Hearing exam, including hearing screening for newborns; |
Page 155
| 7.5.3.2.4 | Evaluation and nutritional screening; |
| 7.5.3.2.5 | Medically Necessary laboratory exams and diagnostic tests, appropriate to the Enrollee’s age, sex, and health condition, including, but not limited to: |
| 7.5.3.2.5.1 | Prostate and gynecological cancer screening according to accepted medical practice, including Pap smears (for Enrollees over age 18), mammograms (for Enrollees age 40 and over), and P.S.A. tests when Medically Necessary; and |
| 7.5.3.2.5.2 | Sigmoidoscopy and colonoscopy for colon cancer detection in adults 50 years and over, classified in risk groups according to accepted medical practice; |
| 7.5.3.2.6 | Nutritional, oral and physical health education; |
| 7.5.3.2.7 | Reproductive health counseling and family planning (The Contractor shall make available through its Network Providers and pay Claims for the following family planning services: counseling, pregnancy testing, diagnosis and treatment of sexually transmitted diseases, infertility |
Page 156
| assessment, and oral contraceptive medications that are used for the purpose of treating menstrual dysfunction and other hormonal conditions. Contraceptive methods prescribed for family planning purposes, however, are not covered under MiSalud, but shall be provided by the Puerto Rico Health Department); |
| 7.5.3.2.8 | Syringes for home medicine administration; |
| 7.5.3.2.9 | Annual physical exam and follow-up for diabetic patients according to the diabetic patient treatment guide and Puerto Rico Health Department protocols; and |
| 7.5.3.2.10 | Health Certificates covered under MiSalud; provided that Co-Payments applicable for necessary procedures and laboratory testing related to generating a Health Certificate will be the Enrollee’s responsibility. Such certificates shall include |
| 7.5.3.2.10.1 | Venereal Disease Research Laboratory (VDRL) tests; |
| 7.5.3.2.10.2 | Tuberculosis (TB) tests; and |
Page 157
| 7.5.3.2.10.3 | Any certification for MiSalud Enrollees related to eligibility for the Medicaid Program (provided at no charge). |
| 7.5.3.3 | Except where Medically Necessary to treat a health condition, weight control measures are not a covered Preventive Service. |
| 7.5.3.4 | Wellness Plan |
| 7.5.3.4.1 | In order to advance the goals of strengthening preventive services and providing integrated physical, behavioral health, and dental services to all Eligible Persons, the Contractor shall develop a Wellness Plan. |
| 7.5.3.4.2 | The Wellness Plan shall include a strategy for coordination with government agencies of the Government of Puerto Rico integral to disease prevention efforts, including the Puerto Rico Health Department, the Department of the Family, and the Department of Education. |
| 7.5.3.4.3 | The Wellness Plan shall present strategies for encouraging Enrollees to: |
Page 158
| 7.5.3.4.3.1 | Seek an annual health checkup; |
| 7.5.3.4.3.2 | Appropriately use the services of MiSalud, including Tele MiSalud; |
| 7.5.3.4.3.3 | Seek women’s health screenings including mammograms, Pap smears, cervical screenings, and tests for sexually transmitted diseases; |
| 7.5.3.4.3.4 | Maintain a healthy body weight, through good nutrition and exercise; |
| 7.5.3.4.3.5 | Seek an annual dental exam; and |
| 7.5.3.4.3.6 | Attend to the medical and developmental needs of children and adolescents, including vaccinations. |
| 7.5.3.4.4 | The Contractor shall, according to the timeframe specified in Attachment 12 to this Contract, present its Wellness Plan containing the strategies described above, to ASES for review and approval, which approval will not be unreasonably withheld, conditioned or |
Page 159
| delayed. Any subsequent changes to the Wellness Plan must be previously approved in writing by ASES. |
| 7.5.4 | Diagnostic Test Services |
| 7.5.4.1 | The Contractor shall make available through its Network Providers the following Diagnostic Test Services: |
| 7.5.4.1.1 | Diagnostic and testing services for Enrollees under age 21 required by EPSDT, as defined in section 1905(r) of the Social Security Act; |
| 7.5.4.1.2 | Clinical labs, including any laboratory order for disease diagnostic purposes, even if the final diagnosis is a condition or disease whose treatment is not a Covered Service; |
| 7.5.4.1.3 | X-Rays; |
| 7.5.4.1.4 | Electrocardiograms; |
| 7.5.4.1.5 | Radiation Therapy (Prior Authorization required); |
| 7.5.4.1.6 | Pathology; |
Page 160
| 7.5.4.1.7 | Arterial gases and pulmonary function test; |
| 7.5.4.1.8 | Electroencephalograms; and |
| 7.5.4.1.9 | Diagnostic services for Enrollees who present learning disorder symptoms. |
| 7.5.4.2 | The following shall not be considered Diagnostic Test Services covered under MiSalud: |
| 7.5.4.2.1 | Polysomnography Study; and |
| 7.5.4.2.2 | Clinical labs processed outside of Puerto Rico. |
| 7.5.5 | Outpatient Rehabilitation Services |
| 7.5.5.1 | The Contractor shall make available through its Network Providers the following Outpatient Rehabilitation Services: |
| 7.5.5.1.1 | Medically Necessary outpatient rehabilitation services for Enrollees under age 21, as required by EPSDT, section 1905(r) of the Social Security Act; |
Page 161
| 7.5.5.1.2 | Physical therapy (minimum fifteen sessions per Enrollee condition per year, when indicated by an orthopedist or physiatrist); |
| 7.5.5.1.3 | Occupational therapy, without limitations; and |
| 7.5.5.1.4 | Speech therapy, without limitations. |
| 7.5.6 | Medical and Surgical Services |
| 7.5.6.1 | The Contractor shall make available through its Network Providers the following Medical and Surgical Services: |
| 7.5.6.1.1 | Early and Periodic Screening, Diagnostic and Treatment (EPSDT) services, as defined in section 1905(r) of the Social Security Act; |
| 7.5.6.1.2 | Primary care physician visits, including nursing services; |
| 7.5.6.1.3 | Specialist treatment; |
| 7.5.6.1.4 | Sub-specialist treatment; |
| 7.5.6.1.5 | Physician home visits when Medically Necessary; |
Page 162
| 7.5.6.1.6 | Respiratory therapy, without limitations; |
| 7.5.6.1.7 | Anesthesia services (except for epidural anesthesia); |
| 7.5.6.1.8 | Radiology services; |
| 7.5.6.1.9 | Pathology services; |
| 7.5.6.1.10 | Surgery; |
| 7.5.6.1.11 | Outpatient surgery facility services; |
| 7.5.6.1.12 | Practical nurse services; |
| 7.5.6.1.13 | Voluntary sterilization of men and women of legal age and sound mind, provided that they have been previously informed about the medical procedure implications, and that there is evidence of Enrollee’s written consent; |
| 7.5.6.1.14 | Public health nursing services; |
Page 163
| 7.5.6.1.15 | Prosthetics, including supply of all body extremities including therapeutic ocular prosthetics, segmental instrument tray and spine fusion in scoliosis and vertebral surgery; |
| 7.5.6.1.16 | Ostomy equipment for outpatient level ostomized patients; |
| 7.5.6.1.17 | Blood and blood plasma, without limitations, including |
| 7.5.6.1.17.1 | authologal and irradiated blood; |
| 7.5.6.1.17.2 | monoclonal factor IX with a certified hematologist Referral; |
| 7.5.6.1.17.3 | intermediate purity concentrated ant hemophilic factor (Factor VIII); |
| 7.5.6.1.17.4 | monoclonal type antihemophilic factor with a certified hematologist’s authorization; and |
| 7.5.6.1.17.5 | activated protrombine complex (Autoflex and Feiba) with a certified hematologist’s authorization; and |
Page 164
| 7.5.6.1.18 | Services to patients with chronic renal disease in Levels 1 and 2 (Levels 3 to 5 are included in Special Coverage). |
| 7.5.6.1.18.1 | Renal disease levels 1 and 2 are defined as follows: |
| 7.5.6.1.18.1.1 | Level 1- GFR (Glomerular Filtration – ml/min. per 1.73m² per corporal area surface) over 90; slight damage when protein is present in the urine. |
| 7.5.6.1.18.1.2 | Level 2- GFR between 60 and 89, a slight decrease in kidney function. |
| 7.5.6.1.18.2 | When GFR decreases to under 60 ml/min per 1.73 m², the Enrollee must be referred to a nephrologist for proper management. The Enrollee will be registered for Special Coverage. |
| 7.5.6.2 | While cosmetic procedures shall be excluded from Basic Coverage, breast reconstruction after a mastectomy and surgical procedures Medically Necessary to treat morbid obesity shall not be considered to be cosmetic procedures. |
Page 165
| 7.5.6.3 | To the extent possible, medical and surgical services, as furnished through PCPs, PMGs, and other Providers, must be made available to Enrollees twenty-four (24) hours per day, seven (7) days per week. |
| 7.5.7 | Emergency Transportation Services |
| 7.5.7.1 | The Contractor shall arrange for the provision of Emergency Transportation Services, including maritime and ground transportation, in emergency situations. |
| 7.5.7.2 | Emergency Transportation Services shall be available twenty-four (24) hours a day, seven (7) days per week, in each municipality in each of the Contractor’s Service Regions, and throughout Puerto Rico. |
| 7.5.7.3 | Emergency Transportation Services do not require Prior Authorization. |
| 7.5.7.4 | The Contractor shall ensure that adequate Emergency Transportation is available to transport Enrollees with Emergency Medical Conditions, or whose conditions require Emergency Transportation because of their geographical location. |
| 7.5.7.5 | [Intentionally left blank]. |
Page 166
| 7.5.7.6 | Aerial Emergency Transportation Services are not included in this Contract. ASES will provide aerial Emergency Transportation Services directly (without any role of the Contractor); provided, that the Contractor agrees to cooperate with any Provider subcontracted by ASES to render such services in the Service Regions. |
| 7.5.7.7 | The Contractor shall pay Claims for Emergency Transportation and shall adhere to Puerto Rico laws and regulations concerning Emergency Transportation, including fees. Fees paid by the Contractor for type 3 ambulances shall be $100 for the initial use, plus $1.50 for each mile traveled. The Contractor shall negotiate fees for the remaining categories. |
| 7.5.7.8 | The Contractor may not retroactively deny a Claim for Emergency Transportation Services because the Enrollee’s condition, which at the time of service appeared to be an Emergency Medical Condition under the prudent layperson standard, was ultimately determined to be non-emergency. |
| 7.5.7.9 | In any case in which an Enrollee is transported by ambulance to a facility that is not a Network Provider, and, after being stabilized, is transported by ambulance to a facility that is a Network Provider, all Emergency Transportation Claims, provided that they are justified by the definition of |
Page 167
| Emergency Services in this Contract prudent layperson standards, shall be paid by the Contractor. |
| 7.5.7.10 | The Contractor shall be responsible for timely payment for Claims for Emergency Transportation Services in the United States for Enrollees who are Medicaid or CHIP Eligible Persons, if the emergency transportation is associated with an Emergency Service in the United States covered under Section 7.5.9.3.1.2 of this Contract. If, in an extenuating circumstance, a Medicaid or CHIP Eligible Enrollee incurs out-of-pocket expenses for Emergency Transportation Services provided in the United States, the Contractor shall reimburse the Enrollee for such expenses within 30 days of receipt of such expenses, and the reimbursement shall be considered a Covered Service. |
| 7.5.7.11 | Emergency Transportation Services will be subject to periodic reviews by applicable governmental agencies to ensure quality of services. |
| 7.5.8 | Maternity and Pre-Natal Services |
| 7.5.8.1 | The Contractor shall make available through its Network Providers the following Maternity and Pre-Natal Services: |
Page 168
| 7.5.8.1.1 | Pregnancy testing; |
| 7.5.8.1.2 | Medical services during pregnancy and post-partum; |
| 7.5.8.1.3 | Physician and nurse obstetrical services during vaginal delivery and caesarean section, and services to address any complication that arises during delivery; |
| 7.5.8.1.4 | Treatment of conditions secondary to pregnancy or delivery, when medically recommended; |
| 7.5.8.1.5 | Hospitalization for a period of at least forty-eight (48) hours in cases of vaginal delivery, and at least ninety-six hours (96) in cases of caesarean section; |
| 7.5.8.1.6 | Anesthesia, excluding epidural; |
| 7.5.8.1.7 | Incubator use; |
| 7.5.8.1.8 | Fetal monitoring services, during hospitalization only; |
| 7.5.8.1.9 | Nursery room routine care for newborns; |
Page 169
| 7.5.8.1.10 | Circumcision and dilatation services for newborns; |
| 7.5.8.1.11 | Transportation of newborns to tertiary facilities newborn when necessary; |
| 7.5.8.1.12 | Pediatrician assistance during delivery; and |
| 7.5.8.1.13 | Delivery services provided in free-standing birth centers. |
| 7.5.8.2 | The following are excluded from Maternity and Pre-Natal Services: |
| 7.5.8.2.1 | Outpatient use of fetal monitor; |
| 7.5.8.2.2 | Treatment services for infertility and/or related to conception by artificial means; and |
| 7.5.8.2.3 | Services, treatments or hospitalizations as a result of a provoked non-therapeutic abortion or its complications; the following are considered to be provoked abortions: |
| 7.5.8.2.3.1 | Dilatation and curettage (Code 59840); |
Page 170
| 7.5.8.2.3.2 | Dilatation and expulsion (Code 59841); |
| 7.5.8.2.3.3 | Intra-amniotic injection (Codes 59850, 59851, 59852); |
| 7.5.8.2.3.4 | One or more vaginal suppositories (e.g., Prostaglandin) with or without cervical dilatation (e.g., Laminar), including hospital admission and visits, fetus birth and secundines (Code 59855); |
| 7.5.8.2.3.5 | One or more vaginal suppositories (e.g., prostaglandin) with dilatation and curettage/or evacuation (Code 59856); |
| 7.5.8.2.3.6 | One or more vaginal suppositories (e.g., prostaglandin) with hysterectomy (omitted medical expulsion) (Code 59857); and |
| 7.5.8.2.3.7 | Epidural anesthesia services. |
| 7.5.8.3 | The Contractor shall implement a Pre-Natal and Maternal Wellness Plan, aimed at preventing complications during and after pregnancy, and |
Page 171
| advancing the objective of lowering the incidence of low birth weight and premature deliveries. |
| 7.5.8.3.1 | The Plan shall include, at a minimum, the following components: |
| 7.5.8.3.2 | A Pre-Natal Care Card, ensuring access to services; |
| 7.5.8.3.3 | Counseling regarding HIV testing; |
| 7.5.8.3.4 | Pregnancy testing; |
| 7.5.8.3.5 | A RhoGAM injection for all pregnant women who have a negative RH factor according to the established protocol; |
| 7.5.8.3.6 | Alcohol screening of pregnant women with the TWEAK instrument or CAGE Test; |
| 7.5.8.3.7 | Smoking cessation counseling and treatment (to be provided by the MBHO, which will collaborate with the Contractor in providing services under the Maternal and Pre-Natal Wellness Plan); |
Page 172
| 7.5.8.3.8 | Post-partum depression screening using the Edinburgh post-natal depression scale; |
| 7.5.8.3.9 | Post-partum counseling and referral to the WIC program; |
| 7.5.8.3.10 | Dental evaluation during the second trimester of gestation; and |
| 7.5.8.3.11 | Educational workshops regarding prenatal care topics (importance of pre-natal medical visits and post-partum care), breast-feeding, stages of childbirth, oral and mental health, family planning, newborn care, among others. |
| 7.5.8.3.12 | The Contractor shall prepare Marketing Materials regarding services under the Pre-Natal and Maternal Wellness Plan, and contractually require that PCP Providers inform pregnant Enrollees either directly or through such Marketing Materials of such services. The Contractor shall submit its Pre-Natal and Maternal Wellness Plan to ASES according to the timeframe specified in Attachment 12 to this Contract, and shall submit reports quarterly concerning the usage of services under this program. ASES will monitor the performance of such plan on a quarterly basis. Any subsequent changes to the Pre- |
Page 173
| Natal and Maternal Wellness Plan must be previously approved in writing by ASES. |
| 7.5.8.4 | The Contractor shall make available through its Network Providers reproductive health and family planning counseling. Such services shall be provided voluntarily and confidentially, including where the Enrollee is under age eighteen (18). Family Planning Services will include, at a minimum, the following: |
| 7.5.8.4.1 | Education and counseling necessary to make informed choices and understand contraceptive methods; |
| 7.5.8.4.2 | Pregnancy testing; |
| 7.5.8.4.3 | Diagnosis and treatment of sexually transmitted diseases; |
| 7.5.8.4.4 | Infertility assessment; |
| 7.5.8.4.5 | Oral contraceptive medications, but only when prescribed for the purpose of treating menstrual dysfunction and other hormonal conditions; and |
Page 174
| 7.5.8.4.6 | Information on the family planning services available through the Department of Health. |
| 7.5.9 | Emergency Services |
| 7.5.9.1 | The Contractor shall pay Claims for Emergency Services where necessary to treat an Emergency Medical Condition. The Contractor shall ensure that Emergency Services are available twenty-four (24) hours a day, seven (7) days per week. No Prior Authorization will be required for Emergency Services. |
| 7.5.9.2 | Emergency Services shall include the following: |
| 7.5.9.2.1 | Emergency room visits, including medical attention and routine and necessary services; |
| 7.5.9.2.2 | Trauma services; |
| 7.5.9.2.3 | Operating room use; |
| 7.5.9.2.4 | Respiratory therapy; |
Page 175
| 7.5.9.2.5 | Specialist and sub-specialist treatment when required by the emergency room physician; |
| 7.5.9.2.6 | Anesthesia; |
| 7.5.9.2.7 | Surgical material; |
| 7.5.9.2.8 | Laboratory tests and X-Rays; |
| 7.5.9.2.9 | Post-Stabilization Services, as provided in Section 7.5.9.5 below; |
| 7.5.9.2.10 | Drugs, medicine and intravenous solutions used in the emergency room; and |
| 7.5.9.2.11 | Blood and blood plasma, without limitations, including |
| 7.5.9.2.11.1 | authologal and irradiated blood; |
| 7.5.9.2.11.2 | monoclonal factor IX with a certified hematologist Referral; |
Page 176
| 7.5.9.2.11.3 | intermediate purity concentrated ant hemophilic factor (Factor VIII); |
| 7.5.9.2.11.4 | monoclonal type antihemophilic factor with a certified hematologist’s authorization; and |
| 7.5.9.2.11.5 | activated protrombine complex (Autoflex and Feiba) with a certified hematologist’s authorization. |
| 7.5.9.3 | Emergency Services Within and Outside Puerto Rico |
| 7.5.9.3.1 | The Contractor shall arrange for Emergency Services to be available: |
| 7.5.9.3.1.1 | For all Enrollees, throughout Puerto Rico, including outside the Contractor’s Service Regions, and notwithstanding whether the emergency room is a Network Provider; and |
| 7.5.9.3.1.2 | For Medicaid and CHIP Eligible Persons, in Puerto Rico or in the United States, when the services are Medically Necessary and could not be anticipated, notwithstanding that emergency rooms outside of |
Page 177
| Puerto Rico are not Network Providers. Subject to Sections 16.10.2.3 and 21.3 of this Contract, the Contractor shall be responsible for timely payment of Claims for Emergency Services rendered to Enrollees in the United States. If, in an extenuating circumstance, a Medicaid or CHIP Eligible Enrollee incurs out-of-pocket expenses for Emergency Services provided in the United States, ASES shall reimburse the Enrollee for such expenses within thirty (30) days of receipt of such expenses, and the reimbursement shall be considered a Covered Service. |
| 7.5.9.3.2 | In covering Emergency Services provided by Puerto Rico Providers outside the Contractor’s Network, or by Providers in the United States, the Contractor shall pay Claims for such Emergency Services to such out-of-Network or United States based Providers equal to at least the average rate paid to Network Providers in Puerto Rico. |
| 7.5.9.4 | Emergency Room Overuse |
| 7.5.9.4.1 | The Contractor shall establish mechanisms for measuring and counteracting misuse of Emergency Services. Excessively frequent |
Page 178
| visits to emergency rooms and seeking treatment in emergency rooms for non-emergent conditions will be considered misuse. |
| 7.5.9.4.2 | The Contractor shall have the capacity to: |
| 7.5.9.4.2.1 | Identify Enrollees who misuse Emergency Services; |
| 7.5.9.4.2.2 | Contact Enrollees by mail or telephone to learn the reasons for their behavior; and |
| 7.5.9.4.2.3 | Inform PCPs about the Enrollee’s behavior so that between the two entities, they can attend to complaints by Enrollees and curb overuse of Emergency Services. |
| 7.5.9.4.3 | The Contractor shall include a clause in Hospital and Emergency Room contracts that prohibits the Provider from refusing to admit MiSalud Enrollees to its Emergency Room, and instead referring them to other Emergency Room facilities. |
| 7.5.9.5 | Post-Stabilization Services |
Page 179
| 7.5.9.5.1 | The Contractor shall pay Claims for Post-Stabilization Services rendered by any Provider in accordance with applicable federal regulations. The attending emergency room physician or other treating Provider shall be responsible for determining whether the Enrollee is sufficiently stabilized for transfer or discharge, and that determination is binding on the Contractor with respect to its responsibility for coverage and payment. |
| 7.5.9.5.2 | An Enrollee who has been treated for an Emergency Condition shall not be held liable for any subsequent screening or treatment necessary to stabilize the Enrollee. |
| 7.5.9.5.3 | Any Post-Stabilization Service that requires Prior Authorization shall be processed and granted by the Contractor within one (1) hour of the Service Authorization Request. |
| 7.5.9.5.4 | Any Post-Stabilization Service that requires Prior Authorization shall be deemed authorized if, within one (1) hour of the Service Authorization Request, (i) the Prior Authorization is not granted, or (ii) the Contractor and the treating physician cannot reach an agreement concerning the Enrollee’s care and a Network Provider is not available for consultation. For the avoidance of doubt, the Contractor must give |
Page 180
| the treating physician the opportunity to consult with a Network Provider, and the treating physician may continue with care of the Enrollee until a Network Provider is reached. |
| 7.5.9.5.5 | For every Prior Authorization granted pursuant to Section 7.5.9.5.4 above, the Contractor shall (i) review the Service Authorization Request after the corresponding Post-Stabilization Service has been rendered to determine whether the service was Medically Necessary, (ii) document its determination, and (iii) if it has determined that the service was Medically Necessary, submit the Claim to ASES in its next Claims Payment Report, in accordance with Sections 11.1.1.4 and 16.7 of this Contract. Notwithstanding the above, if the Contractor submits a Claim to ASES for a Post-Stabilization Service and later determines that the service was not Medically Necessary, the Contractor shall recoup any payment made with respect to such Claim from the Provider and return such amount to ASES. |
| 7.5.9.5.6 | ASES or the PMG shall be financially responsible for all Post-Stabilization Services, except that the Contractor shall be financially responsible for any Post-Stabilization Service that requires Prior Authorization with respect to which the Contractor does not follow the procedure established in Section 7.5.9.5.5 above and which is |
Page 181
| determined not to be Medically Necessary. |
| 7.5.9.5.7 | The Contractor shall not be financially responsible for Post-Stabilization Services that it has not Prior Authorized with respect to any Enrollee for any period after: |
| 7.5.9.5.7.1 | A Network Provider with privileges at the treating hospital assumes responsibility for the Enrollee’s care; |
| 7.5.9.5.7.2 | A Network Provider assumes responsibility for the Enrollee’s care through transfer; |
| 7.5.9.5.7.3 | A Contractor representative and the treating physician reach an agreement concerning the Enrollee’s care; or |
| 7.5.9.5.7.4 | The Enrollee is discharged. |
| 7.5.9.6 | Responsibility of Payment for Emergency Services |
| 7.5.9.6.1 | When an Enrollee (or, as provided in Section 4.4.1.2 of this Contract, an Eligible Person) accesses any hospital emergency room, the |
Page 182
| responsible party for the payment of services rendered in this facility shall be as follows: |
| 7.5.9.6.1.1 | When a physician has concluded, after a medical evaluation (including physical or mental evaluation), that the patient has a behavioral health diagnosis, the MBHO shall be responsible for the totality of the payment of all services. |
| 7.5.9.6.1.2 | When a physician has concluded after a medical evaluation (including physical or mental evaluation) that the patient has a physical health diagnosis, the Contractor shall be responsible for the payment of the Claim for the services rendered. |
| 7.5.9.6.1.3 | In both cases, the physicians from the emergency room must include in the patient’s Medical Record the final diagnosis. The payment shall be based on the final diagnosis. |
| 7.5.9.6.1.4 | If the diagnosis includes both mental and physical health diagnoses or conditions, the hospital must |
Page 183
| include a detailed invoice, by item, which will be used to determine which entity is responsible for the services and for payment. Both parties, the MBHO and the Contractor, shall be responsible for payment according to the diagnosis listed on the invoice submitted by the hospital. |
| 7.5.9.7 | Coverage of Services Ultimately Determined to be Non-Emergencies. The Contractor shall not retroactively deny a Claim for an emergency screening examination because the Condition, which appeared to be an Emergency Medical Condition, turned out to be non-emergency in nature. |
| 7.5.9.8 | Enrollee Use of Tele MiSalud. The Contractor shall train Emergency Services Providers concerning the Tele MiSalud Medical Advice Service, and shall make Providers aware that: |
| 7.5.9.8.1 | An Enrollee who consults this service before visiting the emergency room shall not be responsible for any Co-Payment, provided that he or she presents his or her Tele MiSalud call identification number when he or she arrives at the emergency room; |
Page 184
| 7.5.9.8.2 | No Co-Payments shall be charged for CHIP children under eighteen years of age under any circumstances; and |
| 7.5.9.8.3 | No Co-Payment shall be imposed for the treatment of an Emergency Medical Condition for a Medicaid or CHIP Eligible Person. However, a Co-Payment shall be imposed when a Medicaid Eligible Person seeks care in an emergency room outside the Enrollee’s PPN to treat a condition that does not meet the definition of Emergency Medical Condition as set forth in this Contract; and |
| 7.5.9.8.4 | The Contractor shall not deny a Claim for Emergency Services when the Enrollee seeks Emergency Services at the instruction of the Contractor or its Agent (including a Tele MiSalud representative). |
| 7.5.9.9 | Coverage of Services Provided to an Eligible Person Who Has Not Completed Enrollment. When an Eligible Person who is a Medicaid-or CHIP Eligible Person (see Sections 1.3.1.1, 1.3.1.2, and 1.3.1.3.1 of this Contract) receives Emergency Services before the date indicated in Section 4.4.1.1 above, the Effective Date of Enrollment shall be deemed to be the date of the first Emergency Service covered by the Contractor or by the MBHO, regardless of whether the Medicaid or CHIP Eligible Person had submitted an Enrollment application to the Puerto Rico Medicaid |
Page 185
| Program as of that date, provided that ASES provides written notification to the Contractor from the Health Care Reform Eligibility (HCRE) System of (1) the Certification of eligibility for the Eligible Person, and (2) the fact that the Potential Enrollee has accessed Emergency Services. The Contractor shall promptly, per Section 5.2.3 of this Contract, enroll the person in the MiSalud Plan. The Contractor shall pay for Claims for such Emergency Services, whether provided within or outside the Service Regions. |
| 7.5.9.10 | Coverage of All Emergency Medical Conditions. |
| 7.5.9.10.1 | The Contractor shall not deny Claims for treatment of an Emergency Medical Condition, including in cases in which the absence of immediate medical attention would not have resulted in the outcomes specified in the definition of Emergency Medical Condition in this Contract and in 42 CFR 438.114(a). |
| 7.5.9.10.2 | The Contractor shall not refuse to pay a Claim for an Emergency Medical Condition on the ground that the emergency room Provider, hospital, or fiscal agent did not notify the Enrollee’s PCP or the Contractor of the Enrollee’s screening or treatment following the Enrollee’s presentation for Emergency Services. |
Page 186
| 7.5.10 | Hospitalization Services |
| 7.5.10.1 | The Contractor shall make available through its Network Providers hospitalization services, including the following: |
| 7.5.10.1.1 | Nursery; |
| 7.5.10.1.2 | Semi-private room (bed available 24 hours a day, every day of the year); |
| 7.5.10.1.3 | Isolation room for medical reasons; |
| 7.5.10.1.4 | Food, including specialized nutrition services; |
| 7.5.10.1.5 | Regular nursing services; |
| 7.5.10.1.6 | Specialized room use, such as operation, surgical, recovery, treatment and maternity without limitations; |
| 7.5.10.1.7 | Drugs, medicine and contrast agents, without limitations; |
Page 187
| 7.5.10.1.8 | Materials such as bandages, gauze, plaster or any other therapeutic or healing material; |
| 7.5.10.1.9 | Therapeutic and maintenance care services, including the use of the necessary equipment to offer the service; |
| 7.5.10.1.10 | Specialized diagnostic tests, such as electrocardiograms, electroencephalograms, arterial gases and other specialized tests that are available at the hospital and necessary during Enrollee’s hospitalization; |
| 7.5.10.1.11 | Supply of oxygen, anesthetics and other gases including administration; |
| 7.5.10.1.12 | Respiratory therapy, without limitations; |
| 7.5.10.1.13 | Rehabilitation services while patient is hospitalized, including physical, occupational and speech therapy; |
| 7.5.10.1.14 | Outpatient surgery facility use; and |
| 7.5.10.1.15 | Blood and blood plasma, without limitations, including |
Page 188
| 7.5.10.1.15.1 | authologal and irradiated blood; |
| 7.5.10.1.15.2 | monoclonal factor IX with a certified hematologist Referral; |
| 7.5.10.1.15.3 | intermediate purity concentrated ant hemophilic factor (Factor VIII); |
| 7.5.10.1.15.4 | monoclonal type antihemophilic factor with a certified hematologist’s authorization; and |
| 7.5.10.1.15.5 | activated protrombine complex (Autoflex and Feiba) with a certified hematologist’s authorization. |
| 7.5.10.2 | Hospitalization for services that would normally be considered outpatient services, or for diagnostic purposes only, is not a Covered Service under MiSalud. |
| 7.5.11 | Behavioral Health Services |
| 7.5.11.1 | Behavioral Health Services shall be included in MiSalud, but shall be primarily the responsibility of the MBHO. The Contractor shall pursue |
Page 189
| close cooperation with the MBHO, as detailed in Article 8, to facilitate a service delivery model that integrates physical and behavioral health services and that effectively combats substance abuse and addiction. |
| 7.5.11.2 | Covered Behavioral Health Services include the following: |
| 7.5.11.2.1 | Evaluation, screening and treatment to individuals, couples, families and groups; |
| 7.5.11.2.2 | Outpatient services with psychiatrists, psychologists and social workers; |
| 7.5.11.2.3 | Hospital or outpatient services for substance and alcohol abuse disorders; |
| 7.5.11.2.4 | Intensive outpatient services; |
| 7.5.11.2.5 | Immediate access to Emergency Services or services in events of Urgency twenty-four (24) hours a day, seven days a week; |
Page 190
| 7.5.11.2.6 | Detoxification services for Enrollees intoxicated with illegal substances, whether as a result of substance abuse, a suicide attempt, or accidental poisoning; |
| 7.5.11.2.7 | Long lasting injected medicine clinics; |
| 7.5.11.2.8 | Escort/professional assistance and ambulance services when needed; |
| 7.5.11.2.9 | Prevention and secondary education services; |
| 7.5.11.2.10 | Pharmacy coverage and access to medicine for a maximum of twenty-four (24) hours, in compliance with Act No. 408; |
| 7.5.11.2.11 | Medically Necessary laboratories; and |
| 7.5.11.2.12 | Treatment for Enrollees diagnosed with attention deficit disorder (with or without hyperactivity). |
| 7.5.11.3 | While substance abuse treatment for alcoholism and illegal drugs is considered a Covered Service, smoking cessation treatment is not, except where included in the Pre-Natal and Maternal Wellness Plan set forth in Section 7.5.8.3.7 of this Contract. |
Page 191
| 7.5.11.4 | The Contractor shall, in addition to the cooperation with the MBHO required by Article 8 of this Contract, establish and strengthen relationships (if needed, through memoranda of understanding) with ASSMCA, ADFAN, the Office of the Women’s Advocate, and other government or nonprofit entities, to improve the delivery of Behavioral Health Services. |
| 7.5.12 | Pharmacy Services |
| 7.5.12.1 | The Contractor shall make available the following pharmacy services: |
| 7.5.12.1.1 | All costs related to prescribed medications for Enrollees, excluding the Enrollee’s Co-Payment where applicable; |
| 7.5.12.1.2 | Drugs in the Preferred Drug List (PDL); |
| 7.5.12.1.3 | Drugs included in the Master Formulary described in Attachment 5 of this Contract, but not in the PDL (through the exceptions process); and |
| 7.5.12.1.4 | In some instances, through the exceptions process, drugs that are not included in either the PDL or the Master Formulary. |
Page 192
| 7.5.12.2 | The Contractor may not impose restrictions on available prescription drugs beyond those stated in the PDL, Master Formulary, or any other drug formulary approved by ASES. |
| 7.5.12.3 | The following drugs are excluded from the pharmacy services benefit: |
| 7.5.12.3.1 | Rebetron (to be provided by the Puerto Rico Health Department, upon referral to the Puerto Rico Health Department by a Network Provider; this medication not provided through MiSalud); and |
| 7.5.12.3.2 | Medications delivered directly to Enrollees by a Provider that does not have a pharmacy license, with the exception of medications that are traditionally administered in a doctor’s office, such as injections. |
| 7.5.12.4 | Prescriptions ordered under the pharmacy services benefit are subject to the following utilization controls: |
| 7.5.12.4.1 | Certain prescription drugs may be subject to Prior Authorization, which shall be implemented and managed by the PBM or the Contractor, according to policies and procedures established by the ASES Pharmacy and Therapeutic (“P&T”) Committee and decided in consultation with the Contractor when applicable. |
Page 193
| 7.5.12.4.2 | The Contractor shall ensure that Prior Authorization for pharmacy services is provided for the Enrollee in the following timeframes, including outside of business hours. |
| 7.5.12.4.2.1 | The decision whether to grant a Prior Authorization of a prescription must not exceed seventy-two (72) hours from the time of the Enrollee’s Service Authorization Request for any Covered Service; except that, where the Contractor or the Enrollee’s Provider determines that an Urgency exists, Prior Authorization must be provided no later than within twenty-four (24) hours of the Service Authorization Request. |
| 7.5.12.4.2.2 | ASES may, in its discretion, grant an extension of the time allowed for Prior Authorization decisions, where: |
| 7.5.12.4.2.2.1 | The Enrollee, or the Provider, requests the extension; or |
| 7.5.12.4.2.2.2 | The Contractor justifies to ASES a need for the extension in order to collect additional information, |
Page 194
| such that the extension is in the Enrollee’s best interest. |
| 7.5.12.4.3 | Prescriptions written by a Provider who is outside the PPN may be filled only upon a Countersignature from the Enrollee’s PCP, or another assigned PCP from the PMG in case of absence or unavailability of the Enrollee’s PCP unless ASES issues a normative letter eliminating this requirement in which case a Countersignature would not be required. A Countersignature request made to the PCP shall be acted upon within three (3) Calendar Days of the request of the prescribing Provider, or, in the event of an Urgency, within twenty-four (24) hours. |
| 7.5.12.4.4 | Prescriptions written by a Provider within the PPN shall require no PCP Countersignature. |
| 7.5.12.5 | The Contractor shall advise its prescribing Providers to use bioequivalent drugs approved by the Food and Drug Administration (FDA), provided they are classified as “AB” and authorized by regulations, unless the Provider notes a contraindication in the prescription. Nonetheless, the Contractor shall not deny Claims for a drug solely because the bioequivalent drug is unavailable; nor shall the Contractor impose an |
Page 195
| additional payment by the Enrollee because the bioequivalent is unavailable. |
| 7.5.12.6 | The Contractor shall observe the following timeframe limits with respect to prescribed drugs: |
| 7.5.12.6.1 | Medication for critical conditions will cover a maximum of thirty (30) days; and additional time, where Medically Necessary. |
| 7.5.12.6.2 | Medication for chronic conditions will cover a maximum of thirty (30) days, except at the beginning of therapy where, upon a Provider’s recommendation, a minimum of fifteen (15) days shall be prescribed in order to reevaluate compliance and tolerance. Under a doctor’s orders, a prescription may be refilled up to five (5) times. |
| 7.5.12.6.3 | For maintenance drugs that require Prior Authorization, the Prior Authorization will be effective for six (6) months, unless there are contraindications or side effects. |
| 7.5.12.6.4 | The prescribing Provider shall reevaluate pharmacotherapy as to compliance, tolerance, and dosage within ninety (90) days of having prescribed a maintenance drug. Dosage changes will not require Prior |
Page 196
| Authorization. Changes in the drug used may require Prior Authorization. |
| 7.5.12.7 | Special considerations, including cooperation with Puerto Rico governmental entities other than ASES, govern coverage of medications for the following conditions. |
| 7.5.12.7.1 | Medications for Treatment of HIV / AIDS |
| 7.5.12.7.1.1 | The following HIV/AIDS medications are excluded from the ASES PDL: Viread, Emtriva, Truvada, Fuzeon, Atripla, Epzicom, Selzentry, Intelence, and Isentress. |
| 7.5.12.7.1.2 | Because of an agreement between the Health Department and ASES, Enrollees diagnosed with HIV/AIDS may access the medications listed above through Health Department clinics. |
| 7.5.12.7.1.3 | The Contractor shall inform Providers of the ASES/Health Department agreement described in Section 7.5.12.7.1.2 of this Contract, and shall require |
Page 197
| Providers to refer Enrollees for whom these medications are Medically Necessary to CPTET Centers (Centros de Prevencion y Tratamiento de Enfermedades Transmisibles) or community-based organizations, where the Enrollee may be screened to determine whether the Enrollee is eligible for ADAP. |
| 7.5.12.7.1.4 | A list of CPTET Centers and community-based organizations that administer these medications is included as Attachment 4 to this Contract. |
| 7.5.12.7.2 | Contraceptive Medications. Contraceptive medications shall be provided by the Contractor’s Providers under MiSalud, but only for the treatment of menstrual dysfunction and other hormonal conditions. Contraceptives prescribed for family planning purposes are not included in this Contract and shall be provided separately by the Health Department. |
| 7.5.12.7.3 | Medications for Chronic Conditions for Children with Special Health Needs. Directions in prescriptions for chronic use drugs for Children with Special Health Needs shall cover therapy for thirty (30) days, and if necessary up to five (5) refills of the original prescription, according |
Page 198
| to medical opinion. When Medically Necessary, additional prescriptions will be covered. |
| 7.5.12.7.4 | Medications for Enrollees with Opiate Addictions. It is the responsibility of the MBHO to cover Buprenorphine medication and associated services and follow-up visits required to treat substance abuse disorders. |
| 7.5.12.8 | Except as provided in Section 7.5.12.3.2 of this Contract, all prescriptions must be dispensed by a pharmacy under contract with the PBM that is duly authorized under the laws of the Government of Puerto Rico, and is freely selected by the Enrollee. The PBM shall maintain responsibility for ensuring that the Pharmacy Services Network complies with the terms specified by ASES. |
| 7.5.12.9 | Prescribed drugs must be dispensed at the time and date, as established by the Puerto Rico Pharmacy Law, when the Enrollee submits the prescription for dispensation. |
| 7.5.12.10 | Use of PDL Medications. The Contractor shall ensure that its Providers prescribe drugs on the PDL whenever possible. |
Page 199
| 7.5.12.10.1 | In the following two categories of exceptional cases, however, the Contractor shall pay Claims for drugs not included on the PDL, upon submission of acceptable written documentation from the Provider of the medical justification for the drug. |
| 7.5.12.10.1.1 | The Contractor shall pay Claims for drugs included on the Master Formulary (Attachment 5 to this Contract) in lieu of a PDL drug, only as a part of an exceptions process, upon a showing that no drug in the PDL is clinically effective for the Enrollee. |
| 7.5.12.10.1.2 | The Contractor shall pay Claims for a drug that is not included in either the PDL or the Master Formulary, provided that the drug is not in an experimental stage and that the drug has been approved by the FDA for the treatment of the condition. |
| 7.5.12.10.2 | In addition to demonstrating that the drug prescribed has FDA approval and is not considered experimental, a Provider prescribing a drug not on the PDL must demonstrate to the Contractor’s reasonable satisfaction that: |
Page 200
| 7.5.12.10.2.1 | The drug does not have any bioequivalent on the market; and |
| 7.5.12.10.2.2 | The drug is clinically indicated because of: |
| 7.5.12.10.2.2.1 | Contraindication with some drugs that are in the PDL that the Enrollee is already taking, and scientific literature indicates serious adverse health effects related; |
| 7.5.12.10.2.2.2 | History of adverse reaction by the Enrollee to some drugs that are in the PDL; |
| 7.5.12.10.2.2.3 | Therapeutic failure of all available alternatives in the PDL; or |
| 7.5.12.10.2.2.4 | Other special circumstances. |
| 7.5.12.11 | Role of Pharmacy Benefit Manager |
| 7.5.12.11.1 | Pharmacy services are administered primarily by a Pharmacy Benefit Manager (“PBM”) under contract with ASES. The Contractor shall |
Page 201
| work with the PBM as well as the Pharmacy Program Administrator (“PPA”) selected by ASES as needed, and as provided in this Section, in order to ensure a successful pharmacy services benefit. |
| 7.5.12.11.2 | The Contractor shall be obligated to accept the terms and conditions of the contract that ASES awards to a PBM. The Contractor shall use the procedures, guidelines, and other instructions implemented by ASES through the PBM. Notwithstanding the foregoing, to the extent of any conflict between the terms of this Contract, on the one hand, and the terms of the PBM agreement or any procedure, guideline or instruction of the PBM on the other hand, the terms of this Contract shall govern and control. |
| 7.5.12.11.3 | Among other measures, to enhance cooperation with the PBM, the Contractor shall: |
| 7.5.12.11.3.1 | Work with the PBM to improve information flow and to develop protocols for information-sharing; |
| 7.5.12.11.3.2 | Establish, in consultation with the PBM, the procedures to deposit funds for the payment of claims to the |
Page 202
| pharmacy network according to the payments cycle specified by the PBM; |
| 7.5.12.11.3.3 | Coordinate with the PBM to establish customer service protocols concerning Pharmacy Services; and |
| 7.5.12.11.3.4 | Collaborate with ASES to facilitate the transition between any current PBM, PPA or rebate provider and any successors in the event ASES replaces any of them during the Term of this Contract. |
| 7.5.12.12 | Claims Processing and Administrative Services for Pharmacy. The Contractor shall: |
| 7.5.12.12.1 | Assume the cost of implementing and maintaining online connection with the PBM; |
| 7.5.12.12.2 | Cover all of its own costs of implementation, including but not limited to payment processes, utilization review and approval processes, connection and line charges, and other costs incurred to implement the payment arrangements for pharmacy claims; |
Page 203
| 7.5.12.12.3 | Review Claims payments summary reports for each payment cycle and transfer funds required for payment to pharmacies; |
| 7.5.12.12.4 | Review denials and rejections of Claims; |
| 7.5.12.12.5 | Maintain a phone line to provide for Prior Authorization of drugs, according to the established policies and the PDL and Master Formulary; and |
| 7.5.12.12.6 | Electronically submit daily to the PBM a list of all Contractor’s Network Providers and a list of Enrollees. |
| 7.5.12.13 | Fraud Investigations. The Contractor shall develop tracking mechanisms for Fraud and Abuse issues, and shall forward Fraud and Abuse complaints regarding pharmacy services from Enrollees to the PBM and to ASES. |
| 7.5.12.14 | Formulary Management Program |
| 7.5.12.14.1 | The Contractor shall select two (2) members of its staff to serve on a cross-functional committee, the Pharmacy Benefit Financial Committee, tasked with rebate maximization. The Committee will |
Page 204
| evaluate recommendations on the PDL, from the P&T Committee and the PPA, and will ultimately develop and review the PDL from time to time under the direction of ASES and the PPA. |
| 7.5.12.14.2 | The Contractor shall select a member of its staff to serve on a cross-functional subcommittee tasked with rebate maximization. The subcommittee will take recommendations on the PDL from the P&T Committee and will ultimately create and manage the PDL. |
| 7.5.12.15 | Utilization Management and Reports. The Contractor shall: |
| 7.5.12.15.1 | Perform drug utilization review that meets the standards established by both ASES and federal authorities; and |
| 7.5.12.15.2 | Develop and distribute protocols, to be subject to ASES approval, when necessary. |
| 7.5.12.16 | Communication with Providers. The Contractor shall ensure the following communications with Providers: |
| 7.5.12.16.1 | The Contractor shall advise Providers of the use of the PDL as a first option at the moment of prescribing; and of the need to observe the |
Page 205
| exceptions process when filling a prescription for a drug not on the PDL. |
| 7.5.12.16.2 | The Contractor shall advise Providers that they may not outright deny medication because it is not included on ASES’s PDL. A medication not on the PDL may be provided through the exceptions process described in Section 7.5.12.10 of this Contract. |
| 7.5.12.16.3 | The Contractor shall advise Providers on the use of brand-name drugs, and the availability of the bio-equivalent version, if any. |
| 7.5.12.17 | Cooperation with the Pharmacy Program Administrator (“PPA”) |
| 7.5.12.17.1 | The Contractor shall receive from the PPA updates to the PDL. The Contractor shall adhere to these updates. |
| 7.5.12.17.2 | Any rebates shall be negotiated by the PPA and retained in their entirety by ASES. The Contractor shall neither negotiate, collect, nor retain, any pharmacy rebate for the utilization by Enrollees of brand drugs included in the ASES PDL. |
Page 206
| 7.6 | Dental Services |
| 7.6.1 | Dental Services shall include the following: |
| 7.6.1.1 | All preventative and corrective services for children under age 21 mandated by the EPSDT requirement; |
| 7.6.1.2 | Pediatric Pulp Therapy (Pulpotomy) for children under age 21; |
| 7.6.1.3 | Stainless Steel Crowns for use in primary teeth following a Pediatric Pulpotomy; |
| 7.6.1.4 | Preventive dental services for adults; |
| 7.6.1.5 | Restorative dental services for adults; |
| 7.6.1.6 | One comprehensive oral exam; |
| 7.6.1.7 | One periodical exam every six months; |
| 7.6.1.8 | One defined problem-limited oral exam; |
Page 207
| 7.6.1.9 | One full series of intra-oral radiographies, including bite, every three years; |
| 7.6.1.10 | One initial periapical intra-oral radiography; |
| 7.6.1.11 | Up to five additional periapical/intra-oral radiographies per year; |
| 7.6.1.12 | One single film-bite radiography per year; |
| 7.6.1.13 | One two-film bite radiography per year; |
| 7.6.1.14 | One panoramic radiography every three years; |
| 7.6.1.15 | One adult cleanse every six months; |
| 7.6.1.16 | One child cleanse every six months; |
| 7.6.1.17 | One topical fluoride application every six month for Enrollees under 19 years old; |
Page 208
| 7.6.1.18 | Fissure sealants for life for Enrollees up to 14 years old (including decidual molars up to 8 years old when Medically Necessary because of cavity tendencies); |
| 7.6.1.19 | Amalgam restoration; |
| 7.6.1.20 | Resin restorations; |
| 7.6.1.21 | Root canal; |
| 7.6.1.22 | Palliative treatment; and |
| 7.6.1.23 | Oral surgery. |
| 7.7 | Special Coverage |
| 7.7.1 | The Special Coverage benefit is designed to provide services for Enrollees with special health care needs caused by serious illness. |
| 7.7.2 | The Contractor shall provide to ASES the strategy implemented for the identification of populations with special health care needs in order to identify any ongoing special |
Page 209
| conditions of Enrollees that require a treatment plan and regular care monitoring by appropriate health care professionals. |
| 7.7.3 | The Contractor shall implement a system for screening Enrollees for Special Coverage and registering Enrollees who qualify. The Contractor shall design a form to be used by Providers in submitting a registration for Special Coverage. |
| 7.7.4 | The registration system for Special Coverage shall emphasize speedy processing of the registration. |
| 7.7.5 | Once a Provider supplies all the required information for the Contractor to process a registration, Special Coverage shall take effect retroactively as of the date the Provider reaches a diagnosis, including documentation of test results, for any condition included in Special Coverage. In case information is submitted to Contractor after diagnosis was reached, coverage can be made retroactive up to sixty (60) Calendar Days before the date on which Provider submitted the registration request. |
| 7.7.6 | According to the timeframes specified in Attachment 12 to this Contract, the Contractor shall submit to ASES for approval proposed protocols to be established for Special Coverage and any subsequent changes to the proposed protocols for Special |
Page 210
| Coverage must be previously approved in writing by ASES. The proposed protocols must be established for, at a minimum, the following: |
| 7.7.6.1 | Registration procedures; |
| 7.7.6.2 | Formats established for registration forms; |
| 7.7.6.3 | Forms of notices to be issued to the Enrollee and to the Provider to inform them of the Contractor’s decision concerning Special Coverage; |
| 7.7.6.4 | Protocols for the development of treatment plan; |
| 7.7.6.5 | Provisions for ensuring that Enrollees with Special Coverage have timely access to specialists appropriate for the Enrollee’s condition and identified needs; and |
| 7.7.6.6 | A summary of the Contractor’s strategy for the identification of populations with special health care needs. |
| 7.7.7 | The protocols shall emphasize both the need for a speedy determination and the need for screening evaluations to be conducted by competent Health Care Professionals with appropriate expertise. |
Page 211
| 7.7.8 | The Contractor shall complete, monitor, and routinely update a treatment plan for each Enrollee who is registered for Special Coverage. |
| 7.7.8.1 | The treatment plan shall be developed by the Enrollee’s PCP, with the Enrollee’s participation, and in consultation with any specialists caring for the Enrollee. The Contractor shall require, in its Provider Contracts with PCPs, that Special Registration treatment plans be submitted to the Contractor for review and approval in a timely manner. |
| 7.7.8.2 | The Contractor shall coordinate with the MBHO in development of the treatment plan, and shall consider any impact treatment provided by the MBHO may have on the treatment plan. |
| 7.7.9 | Autism |
| 7.7.9.1 | The physical health services that the autism population need to access through specialists as gastroenterologists, neurologists, allergists, and dentists, will be offered through Special Coverage. The Uniform Guide for Special Coverage (Attachment 7 to this Contract) includes the procedures to follow for this condition. The MBHO will cover all Behavioral Health Services relating to autism, including collaboration and integration with any treatment plan developed by the Contractor. The |
Page 212
| Contractor shall submit, according to the timeframes set forth in Attachment 12 to this Contract, a plan for coordination with the MBHO to meet the integration requirement. |
| 7.7.9.2 | The Contractor shall require in its Provider Contracts with PCPs that the PCP carry out the M-CHAT screen to detect Autism in Enrollees under age eighteen (18) months, or in any other age range established by the Department of Health. Once the PCP diagnoses autism, the PCP will refer the patient to the mental health Provider. The M-CHAT test may be accessed through the Internet, and does not entail any cost, nor does it infringe any copyright. |
| 7.7.9.3 | The Contractor shall also require, through its Provider Contracts, that PCPs administer the Ages and Stages Questionnaire (ASQ) to the parents of child Enrollees. This questionnaire must be completed when the child is nine (9), eighteen (18), and thirty (30) months old, or at any other age established by the Department of Health. ASES acquired the license for the exclusive use child Enrollees in MiSalud and will provide the questionnaires to the Contract, which shall transmit the questionnaire to PCPs and mentor them in its use. |
Page 213
| 7.7.9.4 | The Contractor shall audit PCPs’ use of the M-CHAT and ASQ as part of its Physician Incentive Plan. |
| 7.7.10 | Services provided under Special Coverage shall be subject to Prior Authorization by the Contractor as specified in Section 7.7.11 of this Contract. |
| 7.7.11 | Special Coverage shall include in its scope the following services; provided, however, that an Enrollee shall be entitled only to those services Medically Necessary to treat the condition that qualified the Enrollee for Special Coverage: |
| 7.7.11.1 | Coronary and intensive care services, without limit; |
| 7.7.11.2 | Maxillary surgery; |
| 7.7.11.3 | Neurosurgical and cardiovascular procedures, including pacemakers, valves and any other instrument or artificial devices (Prior Authorization required); |
| 7.7.11.4 | Peritoneal dialysis, hemodialysis and related services; |
| 7.7.11.5 | Pathological and clinical laboratory tests that are required to be sent outside Puerto Rico for processing (Prior Authorization required); |
Page 214
| 7.7.11.6 | Neonatal intensive care unit services, without limit; |
| 7.7.11.7 | Radioisotope, chemotherapy, radiotherapy and cobalt treatments; |
| 7.7.11.8 | Treatment of gastrointestinal conditions and allergies and nutritional services in autism patients; |
| 7.7.11.9 | The following procedures and diagnostic tests, when Medically Necessary (Prior Authorization required): |
| 7.7.11.9.1 | Computerized Tomography; |
| 7.7.11.9.2 | Magnetic resonance test; |
| 7.7.11.9.3 | Cardiac catheters; |
| 7.7.11.9.4 | Holter test; |
| 7.7.11.9.5 | Doppler test; |
| 7.7.11.9.6 | Stress tests; |
| 7.7.11.9.7 | Lithotripsy; |
Page 215
| 7.7.11.9.8 | Electromyography; |
| 7.7.11.9.9 | SPECT test; |
| 7.7.11.9.10 | OPG test; and |
| 7.7.11.9.11 | Impedance Plesthymography; |
| 7.7.11.10 | Other neurological, cerebrovascular and cardiovascular procedures, invasive and noninvasive; |
| 7.7.11.11 | Nuclear medicine imaging; |
| 7.7.11.12 | Diagnostic endoscopies; |
| 7.7.11.13 | Genetic studies; |
| 7.7.11.14 | Up to fifteen (15) additional (beyond the services provided under Basic Coverage) physical therapy treatments per Enrollee condition per year when indicated by an orthopedist or physiatrist after Contractor Prior Authorization; |
Page 216
| 7.7.11.15 | General anesthesia, including for dental treatment of special needs children; |
| 7.7.11.16 | Hyperbaric Chamber; |
| 7.7.11.17 | Immunosuppressive medicine and laboratories required for maintenance treatment of post-surgical patients or transplant patients, to ensure the stability of the Enrollee’s health, and for emergencies that may occur after said surgery; and |
| 7.7.11.18 | Treatment for the following conditions after confirmed laboratory results and established diagnosis: |
| 7.7.11.18.1 | HIV Positive factor and/or Acquired Immunodeficiency Syndrome (AIDS) (Outpatient and hospitalization services are included; no Referral or Prior Authorization is required for Enrollee visits and treatment at the Health Department’s Regional Immunology Clinics and other qualified Providers); |
| 7.7.11.18.2 | Tuberculosis; |
| 7.7.11.18.3 | Leprosy; |
Page 217
| 7.7.11.18.4 | Lupus; |
| 7.7.11.18.5 | Cystic Fibrosis; |
| 7.7.11.18.6 | Cancer; |
| 7.7.11.18.7 | Hemophilia; and |
| 7.7.11.18.8 | Special conditions of children, including the prescribed conditions in the Special Needs Children Codes (see Attachment 13), except: |
| 7.7.11.18.8.1 | Asthma and diabetes, which are included in the Disease Management program; |
| 7.7.11.18.8.2 | Mental Disorders; and |
| 7.7.11.18.8.3 | Mental Retardation (Behavioral manifestations shall be managed by behavioral health Providers within the Basic Coverage, with the exception of situations of catastrophic disease); |
| 7.7.11.18.9 | Scleroderma; |
Page 218
| 7.7.11.18.10 | Multiple Sclerosis; |
| 7.7.11.18.11 | Conditions resulting from self-inflicted damage or as a result of a felony by an Enrollee or negligence; and |
| 7.7.11.18.12 | Chronic renal disease in levels three (3), four (4) and five (5) (Levels 1 and 2 are included in the Basic Coverage); these levels of renal disease are defined as follows: |
| 7.7.11.18.12.1 | Level 3 – GFR (Glomerular Filtration – ml/min. per 1.73m² per corporal surface area) between 30 and 59, a moderate decrease in kidney function; |
| 7.7.11.18.12.2 | Level 4 – GFR between 15 and 29, a severe decrease in kidney function; and |
| 7.7.11.18.12.3 | Level 5 – GFR under 15, renal failure that will probably require either dialysis or a kidney transplant. |
| 7.7.11.19 | Required medication for the outpatient treatment of Tuberculosis and Leprosy is included under Special Coverage. Medication for the outpatient treatment or hospitalization for AIDS-diagnosed Enrollees or |
Page 219
| HIV-positive Enrollees is also included, with the exception of Protease inhibitors which will be provided by CPTET Centers. |
| 7.7.12 | An Enrollee may register for Special Coverage based on one of the conditions listed in Attachment 7 to this Contract (Uniform Guide to Special Coverage). The Contractor must seek ASES authorization for any other special condition not listed in Attachment 7, which the Enrollee, PCP, or PMG requests to be the basis of Special Coverage for an Enrollee. The request must include sufficient documentation of Enrollee(s) need for services and the cost-effectiveness of the care option. ASES will consult with the Health Department and issue a decision which will be binding between the parties. |
| 7.7.13 | Except as expressly noted in this Section 7.7, the exclusions applied to Basic Coverage apply to Special Coverage. |
| 7.8 | Case and Disease Management |
| 7.8.1 | Benefits under MiSalud include Case Management and Disease Management, which are intended to coordinate care for Enrollees with intense health service needs. |
| 7.8.2 | Case Management |
Page 220
| 7.8.2.1 | The Contractor shall be responsible for the Case Management of Enrollees who have the greatest need, including those who have catastrophic, high-cost, or high-risk conditions. |
| 7.8.2.2 | The Contractor’s case management system shall emphasize prevention, continuity of care, and coordination of care. The system will advocate for, and link Enrollees to, services as necessary across Providers and settings. Case Management functions include: |
| 7.8.2.2.1 | Early identification of Enrollees who have or may have special needs, including through use of the screening tools M-CHAT and ASQ-SE; |
| 7.8.2.2.2 | Assessment of an Enrollee’s risk factors including identification of any behavioral health needs; |
| 7.8.2.2.3 | Development of a plan of care; |
| 7.8.2.2.4 | Coordination and assistance to ensure timely Access to Providers; |
| 7.8.2.2.5 | Coordination of care actively linking the Enrollee to Providers, medical services, residential, social and other support services where needed; |
Page 221
| 7.8.2.2.6 | Monitoring; |
| 7.8.2.2.7 | Continuity of care; |
| 7.8.2.2.8 | Follow-up and documentation; and |
| 7.8.2.2.9 | Coordination with the MBHO for any Enrollee with behavioral health needs, including autism, attention deficit disorders, and substance or alcohol abuse disorders. |
| 7.8.2.3 | The Contractor shall develop policies and procedures for Case Management that include, at a minimum, the following elements: |
| 7.8.2.3.1 | The provision of an individual needs assessment and diagnostic assessment; |
| 7.8.2.3.2 | The development of an individual treatment plan, as necessary, based on the needs assessment; |
| 7.8.2.3.3 | The establishment of treatment objectives; |
| 7.8.2.3.4 | The monitoring of outcomes; |
Page 222
| 7.8.2.3.5 | A process to ensure that treatment plans are revised as necessary; |
| 7.8.2.3.6 | A strategy to ensure that all Enrollees or Authorized Representatives, as well as any specialists caring for the Enrollee, are involved in a treatment planning process coordinated by the PCP; |
| 7.8.2.3.7 | Procedures and criteria for making Referrals to specialists and subspecialists; |
| 7.8.2.3.8 | Procedures and criteria for maintaining care plans and Referral services when the Enrollee changes PCPs; |
| 7.8.2.3.9 | Capacity to implement, when indicated, case management functions such as individual needs assessment, including establishing treatment objectives, treatment follow-up, monitoring of outcomes, or revision of treatment plan; and |
| 7.8.2.3.10 | Process for referring Enrollees into Disease Management. |
| 7.8.2.4 | These procedures must be designed to include consultation and coordination with the MBHO and any behavioral health Providers when |
Page 223
| the Enrollee is receiving behavioral health services or is identified to require behavioral health services. |
| 7.8.2.5 | As part of its Case Management Program, the Contractor shall maintain statistical reports in the following areas: |
| 7.8.2.5.1 | Number of Enrollees receiving intensive one-on-one counseling interventions by case managers; |
| 7.8.2.5.2 | Number of Prior Authorizations and denials of Prior Authorization for the conditions included in Special Coverage; |
| 7.8.2.5.3 | Number of Enrollees screened for depression using the PHQ-9 (Patient Health Questionnaire-9) in adults and the ASQ-SE (Ages and Stages Questionnaire Socio-Emotional) in children; and |
| 7.8.2.5.4 | The number of Enrollees with chronic behavioral health conditions. |
| 7.8.2.6 | The Contractor shall submit its Case Management policies and procedures to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to Case |
Page 224
| Management policies and procedures must be previously approved in writing by ASES. |
| 7.8.3 | Disease Management |
| 7.8.3.1 | The Contractor shall develop a Disease Management program for individuals with Chronic Conditions, including the following: |
| 7.8.3.1.1 | Asthma; |
| 7.8.3.1.2 | Depression (to be handled by the MBHO in its Disease Management Program); |
| 7.8.3.1.3 | Diabetes Type 1 or 2; |
| 7.8.3.1.4 | Congestive heart failure and other cardiovascular disease; |
| 7.8.3.1.5 | Hypertension; |
| 7.8.3.1.6 | Obesity; and |
Page 225
| 7.8.3.1.7 | Chronic renal disease, levels 1 and 2 (see definition at Section 7.5.6.1.18.1 of this Contract). |
| 7.8.3.2 | The Contractor shall identify and categorize Enrollees using clinical protocols of the Health Department and protocols developed by the Committee for Management of Conditions established by ASES. |
| 7.8.3.3 | The Contractor shall report quarterly on the number of Enrollees diagnosed with each of these conditions. |
| 7.8.3.4 | The Contractor shall develop Disease Management policies and procedures detailing its program, including how Enrollees are identified for and referred to Disease Management, Disease Management program descriptions, and monitoring and evaluation activities. |
| 7.8.3.5 | The Contractor shall submit its Disease Management policies and procedures to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to Disease Management policies and procedures must be previously approved in writing by ASES. |
Page 226
| 7.8.3.6 | The Contractor shall require in its policies and procedures that an individualized treatment plan be developed for each Enrollee who receives Disease Management services. The policies and procedures shall include a strategy to ensure that all Enrollees or Authorized Representatives, as well as any specialists caring for the Enrollee, are involved in a treatment planning process coordinated by the PCP. |
| 7.9 | Early and Periodic Screening, Diagnosis and Treatment Requirements (“EPSDT”) |
| 7.9.1 | The Contractor shall arrange with the Network Providers for the provision of EPSDT Program services to Enrollees who are less than twenty-one (21) years of age (“EPSDT Eligible Children”), as specified below. |
| 7.9.1.1 | The Contractor and ASES shall develop an EPSDT plan that sets forth those Administrative Services that the Contractor shall perform in connection with EPSDT (the “EPSDT Plan”), pursuant to applicable provisions of section 1902(a)(43) of the Social Security Act. The EPSDT Plan shall address the following: |
| 7.9.1.1.1 | EPSDT screening standards and guidelines; |
Page 227
| 7.9.1.1.2 | Education programs for Network Providers regarding the requirements to (i) track gaps in care, (ii) promote follow-up to ensure that Network Providers comply with the Healthy Child Care periodicity schedules, and (iii) provide the information necessary for ASES to produce its CMS 416 reports; and |
| 7.9.1.1.3 | Outreach and education programs for parents. |
| 7.9.1.2 | The EPSDT Plan shall emphasize outreach and compliance monitoring for children and adolescents (young adults), taking into account the multi-lingual, multi-cultural nature of the population, as well as other unique characteristics of this population. |
| 7.9.1.3 | The EPSDT Plan shall include procedures for tracking gaps in care and follow up for annual dental examinations and visits. The Contractor shall submit its EPSDT Plan for review and approval according to the timeframe specified in Attachment 12 to this Contract. |
| 7.9.1.4 | The EPSDT Plan shall require that quarterly reports compiled by the Contractor on EPSDT screening, based on Claims data submitted by Network Providers for EPSDT Eligible Children, will be submitted in |
Page 228
| accordance with the requirements of the CMS 416 reports to be prepared by ASES. |
| 7.9.2 | Outreach and Education |
| 7.9.2.1 | The Contractor’s EPSDT outreach and education process for EPSDT Eligible Children and their families shall include: |
| 7.9.2.1.1 | The importance of preventive care; |
| 7.9.2.1.2 | The periodicity schedule and the depth and breadth of services; |
| 7.9.2.1.3 | How and where to access services; and |
| 7.9.2.1.4 | A statement that services are provided without cost. |
| 7.9.2.2 | The Contractor shall inform its newly enrolled families with EPSDT Eligible Children about the EPSDT program upon Enrollment with the MiSalud Plan. This requirement includes inform pregnant women and new mothers, either before or within fourteen (14) Calendar Days after the birth of their children, that EPSDT services are available. |
Page 229
| 7.9.2.3 | The Contractor will coordinate through its clinical programs necessary covered preventive services upon member request. |
| 7.9.2.4 | [Intentionally left blank] |
| 7.9.2.5 | The Contractor shall provide to each PCP, at least three (February, June and October) times per year, a list of the PCP’s EPSDT Eligible Children who are not in compliance with the EPSDT periodicity schedule. |
| 7.9.2.6 | The Contractor will ensure that the PCP receives a Gaps in Care analysis for at least eighty percent (80%) of his or her EPSDT Eligible Children. For purposes of this Contract, “Gaps in Care analysis” shall mean the comparison of the actual provision of preventive services for EPSDT Eligible Children with the recommended preventive services according to evidence-based clinical practice guidelines. |
| 7.9.2.7 | Outreach and education shall include a combination of written and oral (on the telephone, face-to-face, or films/tapes) methods, and may be done by Contractor personnel or by Providers. All outreach and education shall be documented and shall be conducted in non-technical language at or below a fourth (4th) grade reading level. The Contractor shall use accepted |
Page 230
| methods for informing persons who are blind or deaf, or cannot read or understand the Spanish language. |
| 7.9.3 | Screening |
| 7.9.3.1 | The Contractor will promote periodic screens (“EPSDT Checkups”) in accordance with the Puerto Rico Medicaid Program’s periodicity schedule and the American Academy of Pediatrics EPSDT periodicity schedule. Such EPSDT Checkups shall include, but not be limited to, the Healthy Child Care checkups described in Section 7.5.3.1 of this Contract. |
| 7.9.3.2 | The Contractor shall arrange for the provision of an initial health and screening visit to all newly enrolled EPSDT Eligible Children for all newborns within twenty-four (24) hours of birth. |
| 7.9.3.3 | The Contractor shall advise the EPSDT Enrollee and his or her parents, or his or her legal guardian, of his or her right to have an EPSDT Checkup as well will provide a written notification of preventive care according to the EPSDT protocols. |
| 7.9.3.4 | EPSDT Checkups must include all of the following: |
Page 231
| 7.9.3.4.1 | A comprehensive health and developmental history; |
| 7.9.3.4.2 | Developmental assessment, including mental, emotional, and behavioral health development; |
| 7.9.3.4.3 | Measurements (including head circumference for infants); |
| 7.9.3.4.4 | An assessment of nutritional status; |
| 7.9.3.4.5 | A comprehensive unclothed physical exam; |
| 7.9.3.4.6 | Immunizations according to the guidance issued by the Advisory Committee on Immunization Practices (ACIP) (the vaccines themselves are paid for by the Department of Health; the Contractor shall cover Providers’ administration of the vaccines, under the fee schedule established by the Department of Health); |
| 7.9.3.4.7 | Certain laboratory tests; |
| 7.9.3.4.8 | Anticipatory guidance and health education; |
| 7.9.3.4.9 | Vision screening; |
Page 232
| 7.9.3.4.10 | Tuberculosis; as applicable |
| 7.9.3.4.11 | Hearing screening; |
| 7.9.3.4.12 | Dental and oral health assessment; and |
| 7.9.3.4.13 | Lead Screening. |
| 7.9.3.5 | The Contractor shall promote and inform providers of the requirements for the appropriate screening of lead toxicity. Regardless of health risk, the Contractor shall require in its Provider Contracts that Network Providers arrange for a blood lead screening test for all EPSDT Eligible children at twelve (12) and twenty-four (24) months of age. Children between twenty-four (24) and seventy-two (72) months of age should receive a blood lead screening test if there is no record of a previous test. |
| 7.9.3.6 | The Contractor shall have procedures that ensure appropriate access to care of EPSDT Eligible Children in need of further diagnostic and/or treatment services to correct or ameliorate defects, and physical and mental illnesses and conditions discovered by the EPSDT Checkup. Referral and follow up may be made from the Provider conducting the screening or to another Provider, as appropriate. |
Page 233
| 7.9.3.7 | The Contractor will include EPSDT level of compliance of the population assigned to every PCP as one of the qualifying criteria for the Physician Incentive Program. |
| 7.9.3.8 | The Contractor shall monitor Providers’ compliance with EPSDT guidelines according with CMS objectives and report on such compliance every quarter pursuant to its EPSDT Plan. |
| 7.9.4 | Tracking |
| 7.9.4.1 | The Contractor shall establish a tracking system using the Gaps in Care analysis that provides information on compliance with the following EPSDT requirements: |
| 7.9.4.1.1 | Preventive diagnostic services; and |
| 7.9.4.1.2 | Immunizations and dental services. |
| 7.9.4.1.3 | [Intentionally left blank] |
Page 234
| 7.9.4.2 | All information generated and maintained in the tracking system shall be consistent with Encounter Data requirements as specified in Section 16.8 of this Contract. |
| 7.9.5 | Diagnostic and Treatment Services |
| 7.9.5.1 | If a suspected problem is detected by a screening EPSDT Checkup, the child shall be evaluated as necessary for further diagnosis. This diagnosis is used to determine treatment needs. |
| 7.9.5.2 | The MiSalud Plan will provide access for all follow-up diagnostic and treatment services under this coverage deemed Medically Necessary to ameliorate or correct a problem discovered during the Checkup. The Contractor shall arrange for the provision of Medically Necessary Covered Services through its Network Providers. |
| 7.10 | Advance Directives |
| 7.10.1 | In compliance with 42 CFR 438.6 (i) (1)-(2), and with Law No. 160 of November 17, 2001, and with 42 CFR 489.100, the Contractor shall maintain written policies and procedures for Advance Directives. The Contractor shall require Network Providers to: (i) include Advance Directives in each Enrollee’s Medical Record, (ii) provide |
Page 235
| these policies and procedures to all Enrollees eighteen (18) years of age and older and (iii) advise Enrollees of: |
| 7.10.1.1 | Their rights under the law of Puerto Rico, including the right to accept or refuse medical or surgical treatment and the right to formulate Advance Directives; |
| 7.10.1.2 | The Contractor’s written policies respecting the implementation of those rights, including a statement of any limitation regarding the implementation of Advance Directives as a matter of conscience; and |
| 7.10.1.3 | The Enrollee’s right to file complaints concerning the Advance Directive requirements directly with ASES or with the Puerto Rico Office of the Patient Advocate. |
| 7.10.2 | The information must include a description of Puerto Rico law and must reflect changes in laws as soon as possible, but no later than ninety (90) Calendar Days after the effective change. |
| 7.10.3 | The Contractor shall contractually require its Network Providers to educate their staff about its policies and procedures on Advance Directives, situations in which Advance |
Page 236
| Directives may be of benefit to Enrollees, and their responsibility to educate Enrollees about this tool and assist them to make use of it. |
| 7.10.4 | The Contractor shall educate Enrollees about their ability to direct their care using Advance Directives and shall specifically designate which staff members or Network Providers are responsible for providing this education. |
| 7.11 | Enrollee Cost-Sharing |
| 7.11.1 | The Contractor shall ensure that Network Providers collect Enrollee cost-sharing only as specified in Attachment 8 to this Contract. |
| 7.11.2 | The Contractor shall ensure that it accurately differentiates the categories of MiSalud Enrollees in its Marketing Materials and communications, to clarify the cost-sharing rules that are applied to each group. The Contractor shall ensure that the Enrollee’s eligibility category appears on the Enrollee ID Card, so that cost-sharing is correctly determined. |
| 7.11.3 | The Contractor shall ensure that, in keeping with the Co-Payment policies included in Attachment 8, Medicaid and CHIP Eligible Persons bear no cost-sharing responsibility under MiSalud for services provided within the Contractor’s PPN or for the treatment of an Emergency Medical Condition. |
Page 237
| 7.11.4 | As provided in Attachment 8 to this Contract, the Contractor shall impose Co-Payments for services provided in an emergency room outside the Enrollee’s PPN, but only in limited circumstances. |
| 7.11.4.1 | For Medicaid and CHIP Eligible Persons, the Contractor shall not impose any Co-Payment for the treatment of an Emergency Medical Condition. The Contractor shall, however, as provided in Attachment 8 to this Contract, impose Co-Payments for services provided in an emergency room to treat a condition that does not meet the definition of Emergency Medical Condition as set forth in this Contract. |
| 7.11.4.2 | No Co-Payments shall be charged for CHIP children under eighteen years of age under any circumstances; and |
| 7.11.4.3 | For Other Eligible Persons, the Contractor shall impose a Co-Payment for any emergency room visit outside the Enrollee’s PPN, if the Enrollee does not consult the Tele MiSalud Medical Advice Line before visiting the emergency room, and provide his or her call identification number at the emergency room. If the Enrollee presents the call identification number, no Co-Payment may be imposed. |
Page 238
| 7.11.5 | As provided in 42 CFR 447.53(e), if a Medicaid or CHIP Eligible Person expresses his or her inability to pay the established Co-Payment at the time of service, the Contractor (through its contracted Providers) shall not deny the service. |
| 7.11.6 | An Indian as defined in Article 2, is exempt from all Co-Payments. |
| 7.12 | Dual Eligible Beneficiaries |
| 7.12.1 | Dual Eligible Beneficiaries enrolled in MiSalud are eligible, with the limitations provided below, for the Covered Services described in this Article, in addition to some coverage of Medicare cost-sharing. |
| 7.12.1.1 | Dual Eligible Beneficiaries Who Receive Medicare Part A Only |
| 7.12.1.1.1 | The Contractor shall arrange for the provision of Basic Coverage as provided in this Article 7, excluding services covered under Medicare Part A (hospitalization); except that MiSalud shall cover hospitalization services after the Medicare Part A coverage limit has been reached. |
| 7.12.1.1.2 | The Contractor shall not cover the Medicare Part A premium or deductible. |
Page 239
| 7.12.1.2 | Dual Eligible Beneficiaries Who Receive Medicare Part A and Part B |
| 7.12.1.2.1 | The Contractor shall arrange for the provision of the following Basic Coverage services only: Dental Services, Pharmacy Services, and Hospitalization Services (after the Medicare Part A coverage limit has been reached). |
| 7.12.1.2.2 | The Contractor shall not pay Claims for the Medicare Part A premium or deductible. |
| 7.12.1.2.3 | The Contractor shall pay Claims for Medicare Part B deductibles and co-insurance. |
| 7.12.1.3 | Dual Eligible Beneficiaries Enrolled in a Medicare Part C Plan |
| 7.12.1.3.1 | Medicare Platino is a Medicare Part C Plan that includes a supplementary package of MiSalud benefits for Dual Eligible Beneficiaries. A Dual Eligible Beneficiary enrolled in a Platino plan is eligible for the Benefits listed in Sections 7.12.1.1 and 7.12.1.2 above. |
Page 240
| 7.12.1.3.2 | An Enrollee who is independently enrolled in a private Medicare Advantage plan is also eligible for the Benefits listed in Sections 7.12.1 and 7.12.2 above. |
| 7.12.2 | Any MiSalud cost-sharing for Dual Eligible Beneficiaries shall be determined according to Section 7.11 and Attachment 8 of this Contract. |
| 7.13 | Moral or Religious Objections |
| 7.13.1 | If, during the course of the Contract period, pursuant to 42 CFR 438.102, the Contractor elects not to arrange for the provision of, not to reimburse for, or not to provide a Referral or Prior Authorization for a service that is a Covered Service, because of an objection on moral or religious grounds, the Contractor shall notify: |
| 7.13.1.1 | ASES within one hundred and twenty (120) Calendar Days before adopting the policy with respect to any service; |
| 7.13.1.2 | Enrollees within ninety (90) Calendar Days after adopting the policy with respect to any service; and |
| 7.13.1.3 | Enrollees before and during Enrollment. |
Page 241
| 7.13.2 | The Contractor acknowledges that such objection will be grounds for recalculation of rates paid to the Contractor. |
ARTICLE 8 INTEGRATION OF PHYSICAL AND BEHAVIORAL HEALTH SERVICES
| 8.1 | General Provisions |
| 8.1.1 | The “integration model” of MiSalud refers to the program goal of ensuring that physical and behavioral health services are closely interconnected, to ensure optimal detection, prevention, and treatment of physical and mental illness. |
| 8.1.2 | The Contractor (through contracted PCPs and PMGs, and other Network Providers) shall be jointly responsible, along with the MBHO, for identifying Enrollees’ needs and coordinating proper Access to both physical and behavioral health services. |
| 8.1.3 | In implementing an integrated model of service delivery, the Contractor shall strive to observe all the protections of the Mental Health Code (Act 408) and the Puerto Rico Patient’s Bill of Rights Act, as well as other applicable federal and Government of Puerto Rico legislation. |
Page 242
| 8.1.4 | The Contractor shall ensure a collaborative relationship with the MBHO and shall develop protocols that define the relationship and include, at a minimum, the process for making referrals to the MBHO and providing the appropriate supporting documentation, the process for receiving referrals from the MBHO and requesting the appropriate supporting documentation, and the process for monitoring Enrollees referred to the MBHO. |
| 8.2 | Co-Location of Staff |
| 8.2.1 | The Contractor shall coordinate with the MBHO to facilitate the placement of a psychologist or other behavioral health Provider in each PMG setting. The behavioral health Provider shall be present, to the extent feasible, between the hours of 8:00 a.m. and 5:00 p.m. each Business Day and one Saturday per month; but at a minimum, between 8:00 a.m. and 5:00 p.m. two Business Days per week. |
| 8.2.2 | The Contractor shall ensure that the PMG provides adequate space and resources for the behavioral health Provider to provide care and consultations in a confidential setting. |
| 8.2.3 | The salary costs for the behavioral health Provider within the PMG shall be borne by the MBHO; however, the Contractor and the MBHO shall negotiate the associated administrative costs. |
Page 243
| 8.2.4 | The behavioral health Provider housed within the PMG shall conduct screening evaluations, crisis intervention, and limited psychotherapy (between four (4) and six (6) sessions, according to the needs of the Enrollee). |
| 8.2.5 | The Contractor shall share with the MBHO Behavioral Health Provider stationed within the PMG, the screening instruments for intervention and early detection of mental health conditions. |
| 8.3 | Referrals |
| 8.3.1 | MiSalud Enrollees with chronic or severe mental health conditions, which require more intensive or continuous care than can be provided within the PMG environment as set forth in Section 8.2 of this Contract, shall be referred to the MBHO for services. |
| 8.3.2 | An Enrollee may access behavioral health services through the MBHO through the following means: |
| 8.3.2.1 | A Referral from the PCP or other PMG physician; |
| 8.3.2.2 | Self-referral (walk-in); |
Page 244
| 8.3.2.3 | Visiting a Comprehensive Health Center (“CCuSAI”); |
| 8.3.2.4 | Visiting Central Access Units; |
| 8.3.2.5 | The Tele MiSalud Service; |
| 8.3.2.6 | The telephone Call Center provided by ASSMCA, known as “Linea Pas”; |
| 8.3.2.7 | MBHO clinics; |
| 8.3.2.8 | Hospitals; and |
| 8.3.2.9 | Emergency rooms. |
| 8.4 | Information Sharing |
| 8.4.1 | The Contractor and the MBHO shall share documents in the possession of each (including agreements, processes, guidelines and clinical protocols), in order for each to understand the other’s operations to ensure optimal cooperation. |
| 8.4.2 | The Contractor and the MBHO shall jointly develop forms to facilitate electronic communications, such as: |
Page 245
| 8.4.2.1 | Information sheet for Enrollees on HIPAA requirements; |
| 8.4.2.2 | Referral sheet; and |
| 8.4.2.3 | Informed consent form. |
| 8.4.3 | The Contractor shall establish a process for monitoring exchange of information, documenting receipt of information and following up on information not submitted in a timely manner. |
| 8.4.4 | The Contractor shall require PMG staff to follow up with MBHO staff concerning the care of Enrollees referred by the PMG to the MBHO. |
| 8.5 | Staff Education |
| 8.5.1 | The Contractor shall train PMG staff on the goals and operational details of the integrated model of care, and, as appropriate, identification of behavioral health issues and conditions. |
| 8.5.2 | The Contractor shall require PMGs to Immediately refer Enrollees to the Behavioral Health Professional located within the PMG (or, if the professional is not available, to the Emergency Room) when an Enrollee manifests suicidal behavior. |
Page 246
| 8.6 | Cooperation With Puerto Rico and Federal Government Agencies |
The Contractor shall ensure that government entities including ASSMCA and SAMHSA shall be consulted where appropriate and shall acknowledge that these entities participate, as appropriate, in the regulation of Behavioral Health Services under MiSalud.
| 8.7 | Contractor and MBHO Coverage of Hospitalization Services |
In the event of any dispute between the Contractor and the MBHO concerning whether a Covered Service provided in a hospital or other inpatient facility falls within the scope of Behavioral Health Services covered by the MBHO, or within the scope of other Basic and Special Coverage covered by the Contractor, the terms of ASES Normative Letter 04-0130, dated February 13, 2004 (Attachment 13 to this Contract), shall govern.
| 8.8 | Integration Plan |
The Contractor shall submit to ASES, for its review and approval, an Integration Plan incorporating the elements in this Article 8, according to the timeframe specified in Attachment 12 to this Contract.
Page 247
ARTICLE 9 PROVIDER NETWORK
| 9.1 | General Provisions |
| 9.1.1 | The Contractor shall have an adequate network of available Providers, in accordance with the timeframe specified in Attachment 12, meeting all Contract requirements in order: 1) to ensure timely Access to Covered Services (including complying with all federal and Puerto Rico requirements concerning timeliness, amount, duration, and scope of services); and 2) to provide sufficient Network Providers to satisfy the demand of Covered Services with adequate capacity and quality service delivery. |
| 9.1.2 | The Contractor shall ensure that its General Network of Providers is adequate to assure Access to all Covered Services, and that all Providers are appropriately Credentialed, maintain current licenses, and have appropriate locations to provide the Covered Services. |
| 9.1.3 | The Contractor shall also develop, as a subset of its General Network of Providers, a Preferred Provider Network (“PPN”). The objectives of the PPN model are to increase Access to Providers and needed services, improve availability of Covered Services on a timely basis, improve the quality of Enrollee care, enhance continuity of care, and facilitate effective exchange of health information between Providers and the Contractor. |
Page 248
| 9.1.3.1 | The Contractor’s PPN shall include a sufficient number of PMGs, PCPs, specialists, hospitals, surgery centers, clinical laboratories and other Providers to adequately address the needs of Enrollees. |
| 9.1.3.2 | At a minimum, except as indicated below, the General Network standards will also apply to the PPN. |
| 9.1.3.3 | The PPN does not include Dental and Pharmacy Services. |
| 9.1.4 | The Contractor shall collaborate with the MBHO to provide integrated MiSalud mental and physical health services in order to achieve a proper management of both services. |
| 9.1.5 | The Contractor’s Network shall not include a Provider if the Provider, or any person or entity that has an ownership or control interest in the Provider, or is an agent or managing employee of the Provider, has been excluded from participation in Medicaid, Medicare, or CHIP by HHS, the HHS Office of Inspector General, or who are on the EPLS or on Puerto Rico’s list of excluded Providers. The Contractor is responsible for checking the exclusions list and providing notice of any exclusions pursuant to Section 9.4.9 of this Contract. |
Page 249
| 9.1.6 | The Contractor shall require that each Provider have a unique National Provider Identifier (“NPI”). |
| 9.1.7 | With respect to Dental Services, the Contractor shall include in its Network any Provider that is qualified, per the requirements in this Article 9, and willing to participate. |
| 9.2 | Network Criteria |
| 9.2.1 | When establishing and maintaining an adequate network of Providers the Contractor shall consider and comply with each of the following criteria, in accordance with 42 CFR 438.206(b)(1): |
| 9.2.1.1 | Estimated eligible population and number of Enrollees; |
| 9.2.1.2 | Estimated use of services, considering the specific characteristics of the population and special needs for health care; |
| 9.2.1.3 | Number and type of Providers required to offer services, taking experience, training and specialties into account; |
| 9.2.1.4 | Maximum number of patients per Provider; |
Page 250
| 9.2.1.5 | Number of Providers in the PPN and General Network that are not accepting new patients; and |
| 9.2.1.6 | Geographic location of Providers and Enrollees, taking into account distance as permitted by law, the duration of trip, the means of transportation commonly used by Enrollees, and whether the facilities provide physical access for Enrollees with physical disabilities or special needs. |
| 9.2.2 | These provisions shall not be construed to: |
| 9.2.2.1 | Require the Contractor to contract with Providers beyond the number necessary to meet the needs of its Enrollees; or |
| 9.2.2.2 | Preclude the Contractor from establishing measures that are designed to maintain quality of services and control costs and are consistent with its responsibilities to Enrollees. |
| 9.2.3 | If the Contractor declines to include a Provider or group of Providers that have requested inclusion in its Network, the Contractor shall give the affected Provider(s) written notice of the reason for its decision. |
Page 251
| 9.2.4 | The Contractor will use Reasonable Efforts to negotiate health services using state facilities, academic medical centers, municipal health services and facilities. The Contractor will keep ASES informed about the status of such negotiations and ASES will cooperate with the Contractor’s efforts. |
| 9.3 | Provider Qualifications |
| 9.3.1 | The following requirements apply to specific Providers in the Contractor’s Network: |
| FQHC
Federal Qualified Health Centers |
A Federally Qualified Health Center is an entity that provides outpatient care under Section 330 of the Public Health Service Act (42 USC 254b) and complies with the standards and regulations established by the federal government and is an eligible Provider enrolled in the Medicaid Program. | |
| PHYSICIAN |
A person with a license to practice medicine as an M.D. or a D.O. in Puerto Rico, whether as a PCP or in the area of specialty under which he or she will provide medical services through a contract with the | |
Page 252
| Contractor; and that it is a Provider enrolled in the Puerto Rico Medicaid Program; and has a valid registration number from the Drug Enforcement Agency and the Certificate of Controlled Substances of Puerto Rico, if required in his or her practice. | ||
| HOSPITAL |
An institution licensed as a general or special hospital by the Puerto Rico Health Department under Chapter 241 of the Health and Safety Code or Private Psychiatric Hospitals under Chapter 577 of the Health and Safety Code (or who is a Provider which is a component part of the Puerto Rico or local government entity which does not require a license under the laws of the Government of Puerto Rico) which is enrolled as a Provider in the Puerto Rico Medicaid Program. | |
Page 253
| NON-MEDICAL PRACTICING PROVIDER | A person who possesses a license issued by the licensing agency of the Government of Puerto Rico enrolled in the Puerto Rico Medicaid Program or a properly trained person who practices under the direct supervision of a licensed professional offering support in health services. | |
| CLINICAL LABORATORY | An entity that has a valid certificate issued by the Clinical Laboratory Improvement Act (CLIA) and which has a license issued by the Health Department, licensing agency of the Government of Puerto Rico. | |
| RURAL HEALTH CLINIC (RHC) | A health facility that the Secretary of Health and Human Services has determined meets the requirements of Section 1861(aa)(2) of the Social Security Act; and that has entered into an agreement with the Secretary to provide services in Rural Health Clinics or Centers under Medicare and in accordance with 42 CFR 405.2402. | |
Page 254
| LOCAL HEALTH DEPARTMENT | Local Health Department established under Act 81 from March 14, 1912. | |
| NON-HOSPITAL PROVIDING FACILITY | A health care service Provider which is duly licensed and credentialed to provide services and enroll in the Puerto Rico Medicaid program. | |
| SCHOOLS OF MEDICINE | Clinics located in the medicine campus that provide primary and preventive care to children and adolescents. | |
| 9.3.2 | The Contractor shall require the Network Providers to comply with any additional Provider qualifications as prescribed by ASES. |
Page 255
| 9.4 | Provider Credentialing |
The Contractor shall be responsible for Credentialing and re-Credentialing its Providers.
| 9.4.1 | The Contractor shall ensure that all Network Providers are appropriately Credentialed and qualified to provide services per the terms of this Contract. |
| 9.4.2 | The Contractor shall contract with all available private Providers that meet its Credentialing process (based on the Contractor’s evaluation of the materials listed in Section 9.4.3 of this Contract) and agree to its contractual terms, in order to ensure sufficient Network Providers to address Enrollee needs. |
| 9.4.3 | At a minimum, the file documenting the Contractor’s Credentialing process shall include, as applicable, but shall not be limited to copies of: |
| 9.4.3.1 | The accredited medical school diploma; |
| 9.4.3.2 | The license issued by the Medical Examining Board of Puerto Rico or applicable state professional licensing authority; |
| 9.4.3.3 | Certificate of specialty (good standing); |
Page 256
| 9.4.3.4 | Residency certificate; |
| 9.4.3.5 | A certificate of the corresponding Board according to specialty; |
| 9.4.3.6 | Board certification; |
| 9.4.3.7 | A continuing education certificate; |
| 9.4.3.8 | Licensing certificate; |
| 9.4.3.9 | The Puerto Rico license to prescribe medications (ASSMCA); |
| 9.4.3.10 | The Federal license to prescribe medications (DEA); |
| 9.4.3.11 | Evidence of Hospital privileges; |
| 9.4.3.12 | Medical Malpractice Policy; |
| 9.4.3.13 | Retention Document of the Internal Revenue Service (Department of Treasury); |
| 9.4.3.14 | Incorporation Document; |
Page 257
| 9.4.3.15 | National Provider Identification (NPI) Certification; |
| 9.4.3.16 | Studies report; diplomas; boards; eligibility; sanctions; limitations from an authorized entity, such as: Medicare, Network NPDB (National Practitioner data Bank); OIG (Office of the Inspector General); EPLS (Excluded Parties List System of GSA-General Service Administration); |
| 9.4.3.17 | The Provider Contract; |
| 9.4.3.18 | Related communications with the Credentialing process, selection and cancellation; |
| 9.4.3.19 | Disclosure of the information concerning the Provider and fiscal agents about participation and control including: name, address, participation percentage, familial relationships and others (as required by 42 CFR Part 455.104); |
| 9.4.3.20 | Provider’s disclosure of the information related to business transactions, in compliance with the 42 CFR Part 455.105; |
| 9.4.3.21 | Disclosure of the information about criminal convictions of the Provider or a person or entity with an ownership or control interest in the Provider, |
Page 258
| or who is an agent or managing employee of the Provider, in compliance with 42 CFR Part 455.106; |
| 9.4.3.22 | Completed application (all parts); |
| 9.4.3.23 | Certificate of conduct issued by the Puerto Rico Police Department; |
| 9.4.3.24 | Inspection report of medical facilities in which the Provider’s services are offered; |
| 9.4.3.25 | Disclosure of malpractice suits, if any, filed against the Provider; |
| 9.4.3.26 | Provider’s Curriculum Vitae (if Provider is an individual); and |
| 9.4.3.27 | Other necessary and available documents. |
| 9.4.4 | Credentialing of health care facilities shall be governed by, but not limited to, Law 101 of June 26, 1965, as amended, known as “Law of Facilities of Puerto Rico.” |
| 9.4.5 | The Contractor shall re-Credential its Network Providers every three (3) years. |
Page 259
| 9.4.6 | The re-Credentialing process shall include, at a minimum, verification and/or updating of Sections 9.4.3.1 – 9.4.3.27 of this Contract, as appropriate, in order to ensure continued adequacy of the Network. |
| 9.4.7 | The Contractor shall maintain a Provider file for all Network Providers. The Provider file shall be updated annually and shall consist of, at a minimum, the following documents: annual state review, DEA license, malpractice insurance and ASSMCA license. Corroboration data will also be required quarterly as provided by the National Practitioner Data Bank, HHS OIG (Office of Inspector General), EPLS (Excluded Parties List System). |
| 9.4.8 | The Contractor shall ensure, and be able to demonstrate at the request of ASES, that: (a) Out-of-Network Providers are duly licensed to provide the Covered Services for which they submit Claims; and (b) the Contractor’s internal Credentialing and re-Credentialing processes are in accordance with 42 CFR 438.214 (Provider Selection). |
| 9.4.9 | If the Contractor determines, through the Credentialing or re-Credentialing process, or otherwise, that a Provider could be excluded pursuant to 42 CFR 1001.1001, or if the Contractor determines that the Provider has failed to make full and accurate disclosures as required in Sections 9.4.3.19–9.4.3.21 above, the Contractor shall deny the Provider’s request to participate in the Network, or, for a current Network Provider, as provided in Section 10.4.1.2.2 of this Contract, terminate the Provider |
Page 260
| Contract. The Contractor shall notify ASES of such a decision, and shall provide documentation of the bar on the Provider’s Network participation, within twenty (20) Business Days of communicating the decision to the Provider. The Contractor shall screen its employees, Network Providers, and other subcontractors under this Contract as required by law to determine whether any of them has been excluded from participation in Medicare, Medicaid, CHIP, or any other Federal health care program (as defined in Section 1128B(f) of the Social Security Act). ASES or the Puerto Rico Medicaid Program shall, upon receiving notification from the Contractor that the Contractor has denied Credentialing, notify the HHS Office of the Inspector General of the denial with twenty (20) Business Days of the date it receives the information, in conformance with 42 CFR 1002.3. |
| 9.5 | Provider Ratios |
| 9.5.1 | The Contractor shall comply with the following minimum Provider ratios. |
| 9.5.1.1 | One PCP per 1,700 Enrollees (1:1,700) (ratio applicable to both General Network and PPN) (only those gynecologists-obstetricians selected as an Enrollee’s PCP may be included in the ratios set forth in this subsection); |
| 9.5.1.2 | One specialty for each 2,200 Enrollees (1:2,200) (ratio applicable only to General Network) (only those gynecologists-obstetricians selected as an |
Page 261
| Enrollee’s PCP may be included in the ratios set forth in this subsection); and |
| 9.5.1.3 | One dentist for each 1,350 Enrollees (1:1,350) (ratio applicable only to the General Network). |
| 9.5.1.4 | The Parties acknowledge that there are shortages of certain specialists in the Service Regions. The Contractor will work with the Provider community to address Enrollee access to specialists to the extent possible. The Contractor will then develop policies and procedures to ensure Enrollees have access to specialty services as necessary. |
| 9.5.2 | The Contractor shall also ensure that the PPN, in addition to meeting the requirements set forth above, adheres to the following minimum Provider ratios: |
| 9.5.2.1 | One X-ray facility per 10,000 Enrollees (1:10,000) in each Service Region; |
| 9.5.2.2 | One (1) clinical laboratory per 5,000 Enrollees (1:5,000) in each Service Region; and |
| 9.5.2.3 | Two (2) hospitals in each Service Region. |
Page 262
Subject to Section 10.5.5 of this Contract, the aforementioned ratios must be maintained for Enrollees, regardless of whether the PMG offers treatment to other private patients.
| 9.6 | Network Providers |
| 9.6.1 | PCPs |
| 9.6.1.1 | The Contractor shall establish a system of coordinated care in which the Primary Care Physician (PCP), will be part of a Primary Medical Group (PMG). PCPs will be responsible for providing, managing and coordinating all the services of the Enrollee, including the coordination with behavioral health personnel, in a timely manner, and in accordance with the guidelines, protocols and practices generally accepted in medicine. |
| 9.6.1.2 | The PCP is responsible for maintaining each Enrollee’s Medical Record, which includes documentation of all services provided by the PCP as well as any specialty services, which may be maintained through a certified EHR system meeting the specifications set forth in Attachment 15 to this Contract. |
Page 263
| 9.6.1.3 | The following shall be considered PCPs for purposes of contracting with a PMG: |
| 9.6.1.3.1 | General practitioners; |
| 9.6.1.3.2 | Internists; |
| 9.6.1.3.3 | Family doctors; |
| 9.6.1.3.4 | Pediatricians (optional for minors under the age of 21); and |
| 9.6.1.3.5 | Gynecologists-obstetricians (obligatory when the woman is pregnant or of reproductive age; this Provider will also be selected for usual gynecological visits). |
| 9.6.1.4 | The Contractor shall promote the selection, by women who are pregnant, of a gynecologist-obstetrician as their PCP. Additionally, the Contractor will permit female Enrollees to select a gynecologist-obstetrician for their routine gynecological visits at initial Enrollment. |
Page 264
| 9.6.1.5 | The PCP shall be available to attend to the health needs of the Enrollee twenty-four (24) hours a day, seven (7) days a week. On-call or telephone answering services will suffice to meet this requirement. |
| 9.6.1.6 | The Contractor shall offer its Enrollees freedom of choice in selecting a PCP. The Contractor shall have policies and procedures describing how Enrollees select their PCP. The Contractor shall submit these policies and procedures to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. |
| 9.6.1.7 | No PCP may own any financial control or have a direct or indirect economic interest (as defined in Act 101 of July 26, 1965) in any Ancillary Services facility or any other Provider (including laboratories, pharmacies, etc.) under contract with the PMG. |
| 9.6.1.8 | Nurse practitioners and physician’s assistants may not be PCPs. |
| 9.6.2 | Specialists and Other Providers |
| 9.6.2.1 | For both the General Network and the PPN (except as specifically indicated below), the Contractor shall have available and under contract within each Service Region the following types of Network Providers: |
Page 265
| 9.6.2.1.1 | Podiatrists; |
| 9.6.2.1.2 | Optometrists; |
| 9.6.2.1.3 | Ophthalmologists; |
| 9.6.2.1.4 | Radiologists; |
| 9.6.2.1.5 | Clinical Laboratories (the Contractor shall ensure that all of the laboratories under contract have a registration certificate (Clinical Laboratory Improvement Amendment, CLIA) and the registration number (CLIA) or a waiver certificate); |
| 9.6.2.1.6 | X-Ray Facilities; |
| 9.6.2.1.7 | Hospitals; |
| 9.6.2.1.8 | Other Health Care Professionals, provided they are duly licensed as required by ASES; |
| 9.6.2.1.9 | Specialized Service Providers; |
Page 266
| 9.6.2.1.10 | Urgent care centers and emergency rooms; and |
| 9.6.2.1.11 | Any other Providers needed to offer services under Basic Coverage (except that Pharmacy Services are not included within the PPN) and Special Coverage, considering the specific health needs of the Service Region. |
| 9.6.2.2 | The Contractor shall offer its Enrollees freedom of choice in selecting a dentist. |
| 9.7 | Out-of-Network Providers |
| 9.7.1 | If the Contractor’s network is unable to provide Medically Necessary Covered Services or FQHC Services to an Enrollee, the Contractor shall adequately and timely cover these services using Providers outside of its Network. |
| 9.7.2 | Except as provided with respect to Emergency Services (see Section 7.5.9.3.1.2 of this Contract) and FQHC Services, if the Contractor offers the service through a Provider in the Network but the Enrollee chooses to access the service from an Out-of-Network Provider, the Contractor is not responsible for payment of such Claims. |
Page 267
| 9.7.3 | The Contractor must ensure that Out-of-Network Providers are duly licensed to provide the Covered Services for which they submit Claims. |
| 9.7.4 | ASES shall ensure, in setting Co-Payments, that in the event that a Co-Payment is imposed on Enrollees for an Out-of-Network service, the Co-Payment shall not exceed the Co-Payment that would apply if services were provided by a Provider in the General Network. |
| 9.8 | Minimum Requirements for Access to Providers |
| 9.8.1 | The Contractor shall provide Access to Covered Services in accordance with the following terms: |
| 9.8.1.1 | Emergency Services shall be provided within twenty-four (24) hours of the moment service is requested. |
| 9.8.1.2 | Specialist services shall be provided within thirty (30) Calendar Days of the Enrollee’s original request for the service. |
| 9.8.1.3 | Routine physical exams shall be provided for adults within ten (10) weeks of the Enrollee’s request for the service, taking into account the medical need and condition. For minors under 21 years of age, routine physical |
Page 268
| exams shall be provided within the timeframes specified in Section 7.9.3 of this Contract. |
| 9.8.1.4 | Covered Services, other than those listed in Sections 9.8.1.1 – 9.8.1.3 of this Contract, shall be provided within fourteen (14) Calendar Days following the request for service. |
| 9.8.1.5 | FQHC Services. FQHC Services shall be provided in an FQHC. The Contractor shall adequately and timely cover these services out-of-network at no cost to Enrollees for as long as the FQHC Services are unavailable in the Contractor’s Network. All Out-of-Network services require a Referral from the Enrollee’s PCP. |
| 9.9 | Referrals |
| 9.9.1 | The Contractor shall not require a Referral from a PCP when an Enrollee seeks care from a Provider in the Contractor’s PPN. |
| 9.9.2 | A written Referral from the PCP shall be required: |
| 9.9.2.1 | for the Enrollee to access specialty care and services within the Contractor’s General Network but outside the PPN; and |
Page 269
| 9.9.2.2 | For the Enrollee to access any service outside of the Provider Network (with the exception of Emergency Services). |
| 9.9.3 | A Referral for either General Network services or Out-of-Network services will be provided within five (5) Calendar Days of the Enrollee’s request; except that if the Enrollee’s life or health could be endangered by a delay in accessing services, the Referral shall be provided within three (3) Calendar Days of the request. |
| 9.9.4 | Neither the Contractor nor any Provider may impose a requirement that Referrals be submitted for the approval of Committees, Boards, Medical Directors, etc. The Contractor shall strictly enforce this directive and shall issue Administrative Referrals (see Section 11.3 of this Contract) whenever it deems Medically Necessary. |
| 9.9.5 | If the Provider Access requirements of Section 9.8.1.2 of this Contract cannot be met within the PPN within thirty (30) Calendar Days of the Enrollee’s request for the Service, the PMG shall refer the Enrollee to a specialist within the General Network, without the imposition of Co-Payments. However, the Enrollee shall return to the PPN specialist once the PPN specialist is available to treat the Enrollee. |
| 9.9.6 | The Contractor shall ensure that PMGs comply with the rules stated in this Section concerning Referrals, so that Enrollees are not forced to change PMGs in order to obtain needed Referrals. |
Page 270
| 9.9.7 | The Contractor shall be responsible for the development and implementation of written policies and procedures that ensure a system of Referrals to Providers outside of the Network and the processing of authorizations for requested services. These policies will be included in the Provider guidelines (see Section 10.2.1 of this Contract). |
| 9.9.8 | If the Referral system that is developed by the Contractor requires the use of electronic media, such equipment shall be installed in PMG offices at the Contractor’s expense. |
| 9.10 | Timeliness of Prior Authorization |
| 9.10.1 | The Contractor shall ensure that Prior Authorization is provided for the Enrollee in the following timeframes, including on holidays and outside of business hours. |
| 9.10.1.1 | The decision to grant or deny a Prior Authorization must not exceed seventy-two (72) hours from the time of the Enrollee’s Service Authorization Request for any Covered Service; except that, where the Contractor or the Enrollee’s Provider determines that the Enrollee’s life or health could be endangered by a delay in accessing services, Prior Authorization must be provided as expeditiously as the Enrollee’s health |
Page 271
| requires, and no later than within twenty-four (24) hours of the Service Authorization Request. |
| 9.10.1.2 | ASES may, in its discretion, grant an extension of the time allowed for Prior Authorization decisions, where: |
| 9.10.1.2.1 | the Enrollee, or the Provider, requests the extension; or |
| 9.10.1.2.2 | the Contractor justifies to ASES a need for the extension in order to collect additional information, such that the extension is in the Enrollee’s best interest. |
| 9.10.2 | For services that require Prior Authorization by the Contractor, the Service Authorization Request shall be submitted promptly by the PCP for the Contractor’s approval, so that Prior Authorization may be provided in compliance within the timeframe set forth in Section 9.10.1 of this Contract. |
| 9.11 | Behavioral Health Services |
| 9.11.1 | The Contractor shall implement procedures in conjunction with the MBHO to ensure that each Enrollee has Access to outpatient and inpatient Behavioral Health Services. |
Page 272
| 9.11.2 | The Contractor shall develop policies and procedures that ensure timely Access to Behavioral Health Services and integration of care. |
| 9.11.3 | The Contractor shall submit its policies and procedures to ASES for prior approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to the policies and procedures must be previously approved in writing by ASES. |
| 9.11.4 | Notwithstanding that the MiSalud Program is an integrated mental and physical health services program, the Parties acknowledge that to the extent of any conflict between the terms of this Contract and the terms of any MBHO policy or procedure, the terms of this Contract shall govern and control. |
| 9.12 | Hours of Service |
| 9.12.1 | The Contractor shall prohibit its Network Providers from having different hours and schedules for Enrollees than what is offered to patients with commercial coverage. |
| 9.12.2 | The Contractor shall prohibit its Providers from establishing specific days for the delivery of Referrals and requests for Prior Authorization for MiSalud Enrollees, and the Contractor shall monitor compliance with this rule. |
Page 273
| 9.13 | Prohibited Actions |
Any denial, unreasonable delay, or rationing of Medically Necessary Services to Enrollees is expressly prohibited. The Contractor shall monitor compliance with this prohibition by Network Providers related to their provision of Covered Services to Enrollees.
| 9.14 | Access to Services for Enrollees with Special Health Needs |
| 9.14.1 | The Contractor shall require that its Network Providers evaluate any progressive condition of an Enrollee with special health needs that requires a course of regular monitored care or treatment. This evaluation will include the use of Health Care Professionals for each identified case. |
| 9.14.2 | The Contractor shall establish a protocol to screen Enrollees for Special Coverage and for the Case Management and Disease Management benefits, in order to facilitate direct Access to specialists. The Contractor shall submit its operational protocol to ASES for prior approval according to the timeframe specified in Attachment 12 to this Contract. |
Page 274
| 9.15 | Preferential Turns |
The Contractor shall agree to establish a system of Preferential Turns for residents of the island municipalities of Vieques and Culebra. Preferential Turns refers to a policy of requiring Providers to give priority in treating Enrollees from these island municipalities, so that they may be seen by a physician within a reasonable time after arriving in the Provider’s office. This priority treatment is necessary because of the remote locations of these municipalities, and the greater travel time required for their residents to seek medical attention. This requirement was established in Laws No. 86 enacted on August 16, 1997 (Arts. 1 through 4) and Law No. 200 enacted on August 5, 2004 (Arts. 1 through 5). The Contractor shall include this requirement in the Provider guidelines (see Section 10.2.1 of this Contract).
| 9.16 | Contracting with Government Facilities |
| 9.16.1 | The Contractor shall contract, as a first option, with the following government health facilities: |
| 9.16.1.1 | State Facilities; |
| 9.16.1.2 | CCuSaI Centers; |
Page 275
| 9.16.1.3 | Municipal Centers; |
| 9.16.1.4 | Federally Qualified Health Centers (FQHC); |
| 9.16.1.5 | Schools of Medicine; |
| 9.16.1.6 | Puerto Rico Medical Center; and |
| 9.16.1.7 | Public Health Corporations of the Government of Puerto Rico. |
| 9.16.2 | These health facilities shall be contracted under the same conditions as any other Provider, in the same level of service and shall have to comply with all applicable requirements. |
| 9.17 | Contracting with Other Providers |
The Contractor shall comply with Capitated contract rules established by PRICO, in accordance with Normative Letter CA-I-2-1232-91 (Attachment 13 to this Contract), which provides that every contract based on a Capitated payment arrangement prohibits the Provider from in turn subcontracting on a Capitated basis.
Page 276
| 9.18 | PMG Additions or Mergers |
| 9.18.1 | In order to ensure the reasonableness of the risk allocation, the Contractor shall not be bound to contract with new PMGs unless ASES so requires after an actuarial analysis, and as long as it does not place other PMGs in a position of harm. |
| 9.18.2 | The creation, cancellation, fusion, and merger of PMGs are administrative matters. ASES is not responsible for these processes, except in specific conditions to guarantee that the continuity of services to Enrollees is not affected. These mergers may not under any circumstances exceed the established Provider requirements regarding ratios, or create Committees or Boards for the approval of Referrals to services outside of the Network. Issuing Referrals outside of the PPN shall be the sole and exclusive responsibility of the PCP. The Contractor shall be the only entity authorized to issue administrative referrals when these are medically required. |
| 9.19 | Extended Schedule of PMGs |
| 9.19.1 | PMGs shall provide primary care services seven (7) days a week, from 8:00 a.m. to 6:00 p.m. |
Page 277
| 9.19.2 | In addition, each PMG shall have sufficient personnel to offer urgent care services during extended periods Monday through Friday from 6:00 p.m. to 9:00 p.m., in order to provide Enrollees greater Access to their PCPs and to urgent care services. |
| 9.19.3 | PMGs may collaborate with each other to establish extended office hours at one facility. |
| 9.19.4 | The Contractor shall submit to ASES its policies and procedures for how it will determine the adequacy and appropriateness of such arrangements, approve such arrangements and monitor their operation. The policies and procedures shall be submitted for prior approval according to the timeframe specified in Attachment 12 to this Contract. |
| 9.20 | Direct Relationship |
| 9.20.1 | The Contractor shall ensure that all Network Providers have knowingly and willingly agreed to participate in the Contractor’s Network. |
| 9.20.2 | The Contractor shall be prohibited from acquiring established networks without contacting each individual Provider to ensure knowledge of the requirements of this Contract and the Provider’s complete understanding and agreement to fulfill all terms of the Provider Contract. |
Page 278
| 9.20.3 | ASES reserves the right to confirm and validate, through collection of information, documentation from the Contractor and on-site visits to Network Providers, the existence of a direct relationship between the Contractor and the Network Providers. |
| 9.21 | Additional PPN Standards |
| 9.21.1 | In addition to the Provider Network requirements prescribed in this Section, the Contractor shall adhere to additional standards for the PPN. |
| 9.21.2 | The Contractor shall establish policies and procedures that, at a minimum, include: |
| 9.21.2.1 | Criteria for participating in the PPN versus the General Network; |
| 9.21.2.2 | Standards for monitoring Provider performance; |
| 9.21.2.3 | Methodologies for measuring Access to care; |
| 9.21.2.4 | Methodologies for identifying issues; and |
| 9.21.2.5 | Measures to address identified issues. |
Page 279
| 9.21.3 | The Contractor shall submit its policies and procedures to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to the policies and procedures must be previously approved in writing by ASES. |
| 9.22 | Contractor Documentation of Adequate Capacity and Services |
| 9.22.1 | Before the Implementation Date of this Contract, as well as on the occasions listed in Section 9.22.2 of this Contract, the Contractor shall provide documentation demonstrating that: |
| 9.22.1.1 | The Network Providers offer an appropriate range of preventive, primary care, and specialty services that is adequate for the anticipated number of Enrollees in each of the Contractor’s Service Regions; and |
| 9.22.1.2 | It maintains a Provider Network that is sufficient in number, mix, and geographic distribution to meet the needs of the anticipated number of Enrollees in each of the Contractor’s Service Regions. |
Page 280
| 9.22.2 | The Contractor shall provide documentation of the Network adequacy conditions stated in this Section, at any time that there has been a significant change in the Contractor’s operations that would affect adequate capacity and services, including |
| 9.22.2.1 | When there is a change in Benefits, geographic Service Regions, or payments; or |
| 9.22.2.2 | Upon the Enrollment of a new eligibility group in the MiSalud Plan. |
ARTICLE 10 PROVIDER CONTRACTING
| 10.1 | General Provisions |
| 10.1.1 | The Contractor shall establish a coordinated care model in which the PCP, located within a PMG, directs the Enrollee’s care. |
| 10.1.2 | The PCP shall provide, manage and coordinate services to the Enrollee, including coordination with behavioral health personnel, in a timely manner, and in accordance with the guidelines, protocols, and practices generally accepted in medicine. |
Page 281
| 10.1.3 | The Contractor and each of its Network Providers shall work to ensure that physical and behavioral health services are delivered in a coordinated manner, and each shall cooperate with the MBHO to achieve effective integration of physical and behavioral health services, as provided in Article 8. |
| 10.1.4 | The Contractor shall contract with enough PMGs to serve the Enrollees in each of its Service Regions. As a precondition to executing any Provider Contract, the Contractor shall comply with the requirements stated in Section 10.1.6 of this Contract regarding submitting model Provider Contracts to ASES. |
| 10.1.5 | The Contractor shall not contract with any Provider without ascertaining that the Provider meets all of the credentialing requirements specified in Article 9 of this Contract. |
| 10.1.6 | Model Provider Contracts |
| 10.1.6.1 | The Contractor shall submit to ASES for review and approval a model for each type of Provider Contract, according to the timeframe specified in Attachment 12 to this Contract. The Contractor shall include in such submission, at a minimum, model contracts for PMGs, PCPs, Ancillary Service Providers, Hospitals, Emergency Rooms, and Ambulance Services. The Contractor shall deliver to ASES an electronic copy of each |
Page 282
| finalized Provider Contract within thirty (30) Calendar Days of the effective date of such contract. |
| 10.1.6.2 | ASES shall review each executed Provider Contract against the approved model Provider Contracts. ASES reserves the right to cancel Provider Contracts or to impose sanctions against the Contractor for the omission of clauses required in the contracts with Providers. |
| 10.1.6.3 | On an ongoing basis, any material modifications to model Provider Contracts shall be submitted to ASES for review and approval, before the amendment may be executed. Similarly, any amendments to Provider Contracts shall be submitted to ASES for review and prior approval. |
| 10.1.7 | The Contractor shall not discriminate against a Provider that is acting within the scope of its license or certification under applicable Puerto Rico law, in decisions concerning contracting, solely on the basis of that license or certification. This subsection shall not be construed as precluding the Contractor from using different payment amounts for different specialties, or for different Providers in the same specialty. |
| 10.1.8 | To comply with Section 9.22.1 of this Contract, the Contractor may comply with Section 10.1.6.1 of this Contract by submitting to ASES, for its review and approval, |
Page 283
| the Contractor’s current contracts with Providers, including any amendments thereto, containing the provisions required under Sections 10.3 and 10.4 of this Contract. |
| 10.2 | Provider Training |
| 10.2.1 | Provider guidelines |
| 10.2.1.1 | The Contractor shall prepare Provider guidelines, to be distributed to all Network (General Network and PPN), summarizing the MiSalud Program. The Provider guidelines shall, in accordance with 42 CFR 438.236, (1) be based on valid and reliable clinical evidence or a consensus of health care professionals in the particular field; (2) consider the needs of the Contractor’s Enrollees; (3) be adopted in consultation with Providers; and (4) be reviewed and updated periodically, as appropriate. |
| 10.2.1.2 | The Provider guidelines shall describe the procedures to be used to comply with the Provider’s duties and obligations pursuant to this Contract, and under the Provider Contract. |
| 10.2.1.3 | The Contractor shall submit the Provider guidelines to ASES for review and approval according to the timeframe specified in Attachment 12 |
Page 284
| to this Contract. Any subsequent changes to the Provider guidelines must be previously approved in writing by ASES. |
| 10.2.1.4 | The content of the Provider guidelines will include, without being limited to, the following topics: the duty to verify eligibility; selection of Providers by the Enrollee; Covered Services; procedures for Access to and provision of services; Preferential Turns; coordination of Access to Behavioral Health Services; required service schedule; Medically Necessary services available 24 hours (see Section 9.6.1.5 of this Contract); Report requirements; Medical Record maintenance requirements; Complaint, Grievance, and Appeal procedures (see Article 14); Co-Payments; HIPAA requirements; the prohibition on denial of Medically Necessary services; and sanctions or fines applicable in cases of non-compliance. |
| 10.2.1.5 | The Provider guidelines shall be delivered to each Provider as part of the Provider contracting process, and shall be made available to Enrollees and to Potential Enrollees upon request. The Contractor shall provide evidence of having delivered the guidelines to all of its Providers within fifteen (15) Calendar Days of award of the Provider Contract. The evidence of receipt shall include the legible name of the Provider, Provider number, date of delivery, and signature of the Provider. |
Page 285
| 10.2.1.6 | The Contractor shall have a process in place (including both updates to the Provider guidelines and other communications) to inform its Provider Network, in a timely manner, of programmatic changes such as changes to drug formularies, Covered Services, and protocols. |
| 10.2.2 | Provider Education Program |
| 10.2.2.1 | The Contractor shall develop a continuing education curriculum of twenty (20) hours per year divided into five (5) hours per quarter. The curriculum shall be submitted to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to the curriculum must be previously approved in writing by ASES. |
| 10.2.2.2 | The Contractor shall coordinate topics with the PBM’s Academic Detailing Program to develop educational activities addressing: |
| 10.2.2.2.1 | Management and implications of polypharmacy; |
| 10.2.2.2.2 | Condition management; |
| 10.2.2.2.3 | Management of prescriptions; and |
Page 286
| 10.2.2.2.4 | Working with patients with conditions of special concern, including autism, ADHD, depression, and diabetes among others. |
| 10.2.2.3 | The Contractor shall use various forms of delivery for Providers’ training sessions, including web-based sessions, group workshops, and face-to-face individualized education. |
| 10.2.2.4 | The Contractor shall make available to Providers dates and locations of sessions, as soon as possible, but no later than five (5) Business Days prior to the event. |
| 10.2.2.5 | The Contractor shall have a process to document Provider participation in continuing education. |
| 10.3 | Required Provisions in Provider Contracts |
| 10.3.1 | All Provider Contracts shall be labeled with the Provider’s NPI, if applicable. In general, the Contractor’s Provider Contracts shall: |
| 10.3.1.1 | Include a section summarizing the Contractor’s obligations under this Contract, as they affect the delivery of Health Care services under |
Page 287
| MiSalud, and describing Covered Services and populations (or, include the Provider guidelines as an attachment); |
| 10.3.1.2 | Require that the Provider cooperate and collaborate with the MBHO in serving Enrollees, and work to advance the integrated model of physical and behavioral health services; |
| 10.3.1.3 | Require that the Provider comply with the federal and Puerto Rico laws, rules, regulations, statutes, policies or procedures, including but not limited to those listed in Attachment 1 to this Contract, to the extent applicable, and with all CMS requirements; |
| 10.3.1.4 | Require that the Provider verify the Enrollee’s Eligibility before providing services or making a Referral; |
| 10.3.1.5 | Prohibit any unreasonable denial, delay, or rationing of Covered Services to Enrollees, and provide that any violation of this prohibition shall be subject to the provisions of Article VI, Section 6 of Act 72 and of 42 CFR Part 438, Subpart I (Sanctions); |
| 10.3.1.6 | Prohibit the Provider from claiming for any non-allowed administrative expenses, as listed in Article 21; |
Page 288
| 10.3.1.7 | Prohibit the unauthorized sharing or transfer of ASES Data, as defined in Section 27.1 of this Contract; |
| 10.3.1.8 | Notify the Provider that the terms of the contract for services under the MiSalud Program are subject to subsequent changes in legal requirements that are outside of the control of ASES; |
| 10.3.1.9 | Require the Provider to comply with all reporting requirements contained in Article 18 of this Contract, and particularly with the requirements to submit Encounter Data for all services provided, and to report all instances of suspected Fraud or Abuse; |
| 10.3.1.10 | Require the Provider to acknowledge that ASES Data (as defined in Section 27.1.1 of this Contract) belongs exclusively to ASES, and that the Provider may not give access to, assign, or sell such data to third parties, without prior authorization from ASES. The Contractor shall include penalty clauses in its Provider Contracts to prohibit this practice, and require that the fines be paid to ASES; |
| 10.3.1.11 | Prohibit the Provider from seeking payment from the Enrollee for any Covered Services provided to the Enrollee within the terms of the Contract, and require the Provider to look solely to the Contractor for |
Page 289
| compensation for services rendered to Enrollees, with the exception of any nominal cost-sharing, as provided in Section 7.11 of this Contract; |
| 10.3.1.12 | Require the Provider to cooperate with the Contractor’s quality improvement and Utilization Management activities; |
| 10.3.1.13 | Not prohibit a Provider from acting within the lawful scope of practice, from advising or advocating on behalf of an Enrollee for the Enrollee’s health status, medical care, or treatment or non-treatment options; |
| 10.3.1.14 | Not prohibit a Provider from advocating on behalf of the Enrollee in any Grievance System or Utilization Management process, or individual authorization process to obtain necessary health care services; |
| 10.3.1.15 | Require Providers to meet the timeframes for Access to services pursuant to Sections 9.8 and 9.9 of this Contract; |
| 10.3.1.16 | Provide for continuity of treatment in the event that a Provider’s participation in the Contractor’s Network terminates during the course of an Enrollee’s treatment by that Provider; |
Page 290
| 10.3.1.17 | Require Providers to monitor Enrollee patients to determine whether they have a Medical Condition that suggests Case Management or Disease Management services are warranted; |
| 10.3.1.18 | Prohibit Provider discrimination against high-risk populations or Enrollees requiring costly treatments; |
| 10.3.1.19 | Prohibit Providers who do not have a pharmacy license from directly dispensing medications, as required by the Puerto Rico Pharmacy Act (with the exception noted in Section 7.5.12.3.2 of this Contract); |
| 10.3.1.20 | Specify that HHS and its sub-agencies and ASES shall have the right to inspect, evaluate, and audit any pertinent books, financial records, documents, papers, and records of any Provider involving financial transactions related to the MiSalud Program; |
| 10.3.1.21 | Include the definition and standards for Medical Necessity, pursuant to the definition in Section 7.2.1 of this Contract; |
| 10.3.1.22 | Require that the Provider attend promptly to requests for Prior Authorizations and Referrals, when Medically Necessary, in compliance |
Page 291
| with the timeframes set forth in Section 9.10 of this Contract and in 42 CFR 438.210 and the Puerto Rico Patient’s Bill of Rights; |
| 10.3.1.23 | Prohibit the Provider from establishing specific days for the delivery of Referrals or requests for Prior Authorization; |
| 10.3.1.24 | Notify the Provider that, in order to participate in the Medicare Platino Program, the Provider must accept MiSalud Enrollees; |
| 10.3.1.25 | Specify rates of payment, as detailed in Section 10.5 of this Contract, and require that Providers accept such payment as payment in full for Covered Services provided to Enrollees, less any applicable Enrollee Co-Payments pursuant to Section 7.11 of this Contract; |
| 10.3.1.26 | Specify acceptable billing and coding requirements; |
| 10.3.1.27 | Require that the Provider comply with the Contractor’s Cultural Competency plan; |
| 10.3.1.28 | Require that any marketing materials developed and distributed by the Provider be submitted to the Contractor to submit to ASES for prior approval; |
Page 292
| 10.3.1.29 | Specify that the Contractor shall be responsible for any payment owed to Providers for services rendered after the Effective Date of Enrollment, as provided in Section 4.4.1 of this Contract, including during the period described in Section 4.4.1.2; |
| 10.3.1.30 | Require Providers to collect Enrollee Co-Payments as specified in Attachment 8; |
| 10.3.1.31 | Require that Providers not employ or subcontract with individuals on the Puerto Rico or Federal Exclusions list, or with any entity that could be excluded from the Medicaid program under 42 CFR 1001.1001 (ownership or control in sanctioned entities) and 1001.1051 (entities owned or controlled by a sanctioned person); |
| 10.3.1.32 | Require that Medically Necessary services shall be available twenty-four (24) hours per day, seven (7) days per week, to the extent feasible; |
| 10.3.1.33 | Prohibit the Provider from operating on a different schedule for MiSalud Enrollees than for other patients, and from in any other way discriminating in an adverse manner between MiSalud Enrollees and other patients; |
Page 293
| 10.3.1.34 | Not require that Providers sign exclusive Provider Contracts with the Contractor if the Provider is an FQHC or RHC; |
| 10.3.1.35 | Provide notice that the Contractor’s negotiated rates with Providers shall be adjusted in the event that the Executive Director of ASES directs the Contractor to make such adjustments in order to reflect budgetary changes to the Medical Assistance program; |
| 10.3.1.36 | Impose fees or penalties if the Provider breaches the contract or violates federal or Puerto Rico laws or regulations; |
| 10.3.1.37 | Require that the Provider make every effort to cost-avoid claims and identify and communicate to the Contractor available Third Party resources, as required in Section 22.4 of this Contract, and require that the Contractor cover no health services that are the responsibility of the Medicare program; |
| 10.3.1.38 | Provide that the Contractor shall not pay claims for services covered under the Medicare Program, and that the Provider may not bill both MiSalud and the Medicare Program for a single service to a Dual Eligible Beneficiary; |
Page 294
| 10.3.1.39 | Require the Provider to sign a release giving ASES access to the Provider’s Medicare billing data for MiSalud Enrollees who are Dual Eligible Beneficiaries, provided that such access is authorized by CMS, and subject to compliance with all HIPAA requirements; |
| 10.3.1.40 | Set forth the Provider’s obligations under the Physician Incentive Plan outlined in Section 10.7 of this Contract; |
| 10.3.1.41 | Require the Provider to notify the Contractor Immediately if or whether the Provider falls within the prohibition stated in Sections 28.1, 28.2 or 28.6 of this Contract or has been excluded from the Medicare, Medicaid, or Title XX Services Programs; |
| 10.3.1.42 | Include a penalty clause to require the return of public funds paid to a Provider that falls within the prohibition stated in Sections 28.1, 28.2 or 28.6 of this Contract; |
| 10.3.1.43 | Require that all reports submitted by the Provider to the Contractor be labeled with the Provider’s NPI, if applicable; and |
| 10.3.1.44 | Require the Provider to furnish complete Encounter Data to the Contractor on a monthly basis. |
Page 295
| 10.3.2 | In addition to the required provisions in Section 10.3.1 of this Contract, the following requirements apply to specific categories of Provider Contracts. |
| 10.3.2.1 | The Contractor’s contracts with PMGs shall: |
| 10.3.2.1.1 | Require that the PMG provide services on a regular time schedule, seven days a week, from 8:00 a.m. to 6:00 p.m.; |
| 10.3.2.1.2 | Require that the PMG employ enough personnel to offer urgent care services between 6:00 and 9:00 p.m., Monday through Friday; |
| 10.3.2.1.3 | Require that the PMG coordinate with MBHO personnel to ensure integrated physical and behavioral health services, as provided in Article 8; |
| 10.3.2.1.4 | Require the PMG to work, to the extent possible, within the Contractor’s established PPN, in directing care for Enrollees and coordinating services; |
| 10.3.2.1.5 | Authorize the Contractor to adjudicate disputes between the PMG and its Network Providers about the validity of claims by any Network Provider; |
Page 296
| 10.3.2.1.6 | Require PMGs to provide assurances that the Encounter Data submitted by the PMG to the Contractor encompass all services provided to MiSalud Enrollees, including laboratories; and |
| 10.3.2.1.7 | Include the provisions set forth in Sections 7.5.8.3.12, 7.10.1, 10.5.4, 10.5.5, 10.5.7, 16.10.2, 16.10.3, 16.10.5, and 22.1.8 of this Contract. |
| 10.3.2.2 | The Contractor’s contracts with PCPs shall require the PCP to inform and distribute information to Enrollee patients about instructions on Advance Directives, and shall require the PCP to notify Enrollees of any changes in federal or Puerto Rico law relating to Advance Directives, no more than ninety (90) Calendar Days after the effective date of such change. |
| 10.3.2.3 | The Contractor’s contract with a Provider who is a member of the PPN shall prohibit the Provider from collecting cost-sharing payments from MiSalud Enrollees, subject only to the exceptions established in Article 9 of this Contract and the Attachment 8 to this Contract (Co-Payment Chart). |
| 10.3.2.4 | The Contractor’s contracts with Hospitals and Emergency Rooms shall prohibit the Hospital or Emergency Room from placing a lower priority on MiSalud Enrollees than on other patients, and from referring MiSalud |
Page 297
| Enrollees to other facilities for reasons of economic convenience. Such contracts must include sanctions penalizing this practice. |
| 10.3.2.5 | The Contractor’s contracts with PCPs and PPN physician specialists shall require such Providers to maintain Enrollees’ Medical Records through an EHR system that is ONC and CCHIT certified and meets the specifications set forth in Attachment 15. The contracts shall provide that the EHR system be operational on or before July 1, 2012 or such later date as set forth in his/her Provider Contract. The contracts shall require the Contractor to assist the PCPs and PPN physician specialists in the acquisition and installation of an appropriate EHR system, at the Contractor’s expense. The Contractor’s contracts with such Providers shall also specify that the Contractor shall provide each such Provider with information on the benefits of the EHR system and the costs of maintaining the EHR system. |
| 10.4 | Termination of Provider Contracts |
| 10.4.1 | The Contractor shall comply with all Puerto Rico and federal laws regarding Provider termination. The Provider Contracts shall: |
Page 298
| 10.4.1.1 | Contain provisions allowing immediate termination of the contract by the Contractor “for cause.” Cause for termination includes gross negligence in complying with the contractual considerations or obligations; insufficiency of funds of ASES or the Contractor, which prevents them from continuing to pay for their obligations; termination of this Contract for any reason; and changes in federal law. |
| 10.4.1.2 | Specify that in addition to any other right to terminate the Provider Contract, and notwithstanding any other provision of this Contract, ASES may demand Provider termination Immediately, or the Contractor may Immediately terminate on its own, a Provider’s participation under the Provider Contract if: |
| 10.4.1.2.1 | A Provider fails to abide by the terms and conditions of the Provider Contract, as determined by ASES, or, in the sole discretion of ASES, if the Provider fails to come into compliance within fifteen (15) Calendar Days after a receipt of notice from the Contractor specifying such failure and requesting such Provider to abide by the terms and conditions hereof; or |
| 10.4.1.2.2 | The Contractor or ASES learns that the Provider: |
Page 299
| 10.4.1.2.2.1 | Falls within the prohibition stated in Sections 28.1 or 28.2 of this Contract, or has a criminal conviction as provided in Section 28.6 of this Contract; |
| 10.4.1.2.2.2 | Has been or could be excluded from participation in the Medicare, Medicaid, or CHIP Programs; or |
| 10.4.1.2.2.3 | Could be excluded from the Medicaid program under 42 CFR 1001.1001 (ownership or control in sanctioned entities) and 1001.1051 (entities owned or controlled by a sanctioned person). |
| 10.4.1.3 | Specify that any Provider whose participation is terminated under the Provider Contract for any reason shall utilize the applicable appeals procedures outlined in the Provider Contract. No additional or separate right of appeal to ASES or the Contractor is created as a result of the Contractor’s act of terminating, or decision to terminate any Provider under this Contract. Notwithstanding the termination of the Provider Contract with respect to any particular Provider, this Contract shall remain in full force and effect with respect to all other Providers. |
Page 300
| 10.4.2 | The Contractor shall notify ASES at least forty-five (45) Calendar Days prior to the effective date of the suspension, termination, or withdrawal of a Provider from participation in the Network. If the termination was for cause, the Contractor shall provide to ASES the reasons for termination. |
| 10.4.3 | The Contractor shall, within fifteen (15) Calendar Days of issuance of a notice of termination to a Provider, notify Enrollees of the termination, and shall assist the Enrollee as needed in finding a new Provider. |
| 10.5 | Provider Payment |
| 10.5.1 | General Provisions |
| 10.5.1.1 | ASES guarantees payment for all Medically Necessary services rendered by Providers after a person’s Effective Date of Enrollment, including during the period described in Section 4.4.1.2 of this Contract. |
| 10.5.1.2 | The insolvency, liquidation, bankruptcy, or breach of contract of any Provider will not release ASES from its obligation to pay for all services rendered as authorized under this Contract. |
Page 301
| 10.5.1.3 | ASES shall provide to the Contractor maximum rates for certain Covered Service on or before the Implementation Date of this Contract. The Contractor shall negotiate rates with Providers, which rates shall be specified in the corresponding Provider Contracts, utilizing as a reference the rate information established by ASES’s actuaries and contained in Attachment 10 to this Contract. If such rates adversely affect the Provider ratios required to be maintained under Section 9.5 of this Contract, the Parties agree to negotiate in good faith to make such adjustments to the rates as required to comply with Section 9.5 of this Contract. Further, such rates shall be subject to Section 10.5.5 of this Contract. Payment arrangements may take any form allowed under federal law and the law of Puerto Rico, including capitation payments, fee-for-service payment, and salary, subject to Section 10.6 of this Contract concerning permitted risk arrangements. The Contractor shall inform ASES in writing when it enters any Provider payment arrangement other than fee-for-service. Payment arrangements other than fee-for-service shall be prohibited for Dental Services. |
| 10.5.1.4 | All capitation payment arrangements in Provider Contracts must comply with Normative Letter CA-1-2-1232-91 of the Puerto Rico Office of the Insurance Commissioner (Attachment 13 to this Contract). |
Page 302
| 10.5.1.5 | Any capitation payment made by the Contractor to Providers shall be based on sound actuarial methods. The Contractor shall establish its Capitation methodology utilizing the information provided by ASES in Attachment 10 to this Contract as a reference to develop its capitated rates. The Contractor shall provide its Capitation methodology to ASES for approval in the timeframe allotted in Attachment 12. All Provider payments by the Contractor shall be reasonable, and the amount paid shall not jeopardize or infringe upon the quality of the services provided. |
| 10.5.1.6 | Even if the Contractor does not enter into a Capitated payment arrangement with a Provider, the Provider shall nonetheless be required to submit to the Contractor detailed Encounter Data. |
| 10.5.1.7 | The Contractor shall be responsible for issuing to the Providers the forms required by the Department of the Treasury, in accordance with all Puerto Rico laws, regulations and guidelines. In addition, the Contractor, in accordance with all Puerto Rico laws, regulations, and guidelines, must also Withhold taxes when appropriate and shall remit such taxes to the Department of Treasury. |
Page 303
| 10.5.1.8 | The Contractor shall submit its provider fee schedule to ASES for approval in the timeframe set forth in Attachment 12. Any subsequent changes must be previously approved in writing by ASES. |
| 10.5.2 | Payments to FQHCs, RHCs, and CCuSaI. When the Contractor negotiates a contract with an FQHC and/or an RHC, as defined in Section 1905(a)(2)(B) and 1905(a)(2)(C) of the Social Security Act, or with a Comprehensive Health Care Center (“CCuSaI”), the Contractor shall pay to the FQHC, RHC, or CCuSaI rates that are comparable to rates paid to other similar Providers providing similar services. If an FQHC is not included in the Contractor’s Network and the Enrollee requests FQHC Services, the Contractor shall make these out-of-network services available to the Enrollee through a referral from his or her PCP, and the FQHC shall be paid as an out-of-network Provider for FQHC Services (as defined in Article 2 of this Contract). The Contractor shall cooperate with ASES and the Health Department in ensuring that payments to FQHCs and RHCs are consistent with Sections 1902(a)(15) and 1902(bb)(5) of the Social Security Act. Pursuant to 42 U.S.C. 1396a(bb)(5), the Puerto Rico Health Department shall pay the FQHCs applicable wrap-around payments to make up the difference, if any, between the Capitation Contractor pays to the FQHC under this Contract, and the amounts Puerto Rico Health Department pays to the FHQCs under the prospective payment system formula. |
Page 304
| 10.5.3 | Requirement To Verify Eligibility. The Contractor will require that all of its Network Providers verify the eligibility of Enrollees before the Provider provides Covered Services. This verification of eligibility is a condition of receiving payment from the Contractor for Covered Services. |
| 10.5.4 | Payments to Providers Owing Funds to the Government. ASES and the Contractor will agree to a process to recoup money owed by Providers to the Government. All of the Contractor’s Provider Contracts shall contain a provision giving notice of the agreed to procedures, such that the Provider’s execution of the Contract shall constitute agreement with the agreed to procedures. |
| 10.5.5 | Payment Rates Subject to Change. The Contractor shall adjust its negotiated rates with Providers to reflect budgetary changes, as directed by the Executive Director of ASES, to the extent that such adjustments can be made within funds appropriated to ASES and available for payment to the Contractor; provided, however, that if such rates adversely affect the Provider ratios required to be maintained under Section 9.5 of this Contract, the Parties agree to negotiate in good faith to make such adjustment to the rates as required to comply with such Section 9.5 of this Contract. The Contractor’s Provider contracts shall contain a provision giving notice to the Provider that its rates are subject to adjustment, such that the Provider’s execution of the Contract shall constitute agreement with the Contractor’s obligation to ASES. |
Page 305
| 10.5.6 | Payments for Hospitalization Services or Services Extending for More than Thirty (30) Days. In the event of hospitalization or extended services that exceed thirty (30) Calendar Days, the Provider may bill and collect at least once per month for services rendered to the Enrollee. These services shall be paid according to the procedures specified in this Article 10. The Contractor shall implement Medicare hospital readmission payment policies and shall require all hospital Providers to implement the Medicare hospital readmission guidelines. |
| 10.5.7 | Payments for Services to Dual Eligible Beneficiaries. The Contractor shall include in its Provider Contracts a notice that the Contractor shall not pay claims for services covered under the Medicare Program. No Provider may bill both MiSalud and the Medicare Program for a single service to a Dual Eligible Beneficiary. |
| 10.5.8 | Payment for Pharmacy Services. The Contractor shall abide by and comply with following payment process hereby established: |
| 10.5.8.1 | Except as provided in Section 7.5.12 of this Contract, the PMG shall accept the financial risk of ingredient cost and dispensing fees for pharmacy services relating to Basic Coverage. ASES shall accept the financial risk of ingredient cost and dispending fees for pharmacy services relating to Special Coverage. |
Page 306
| 10.5.8.2 | In covering Pharmacy Services, the Contractor shall adhere to the Retail Pharmacy Reimbursement Levels established in Attachment 6 to this Contract. |
| 10.5.8.3 | On a semi-monthly payment cycle to be set by the PBM, the PBM will provide the Contractor with the proposed claims listing. The Contractor shall promptly review the payment listing and submit it to ASES within five (5) Business Days with a certification from the Authorized Signatory. |
| 10.5.8.4 | ASES shall transmit funds to the Contractor on account of the PBM Claims no later than five (5) Business Days after receipt of the proposed claims listing. The Contractor shall then submit funds for claims payment to the PBM’s zero-balance account. The Contractor shall provide funds or wire transfers to a bank account established for the payment of the claims, or otherwise submit payment, within two (2) Business Days of the date that the prescription was filled. |
| 10.5.8.5 | The Contractor, ASES, and the PBM shall cooperate to identify additional savings opportunities, including special purchasing opportunities, changes in network fees, etc. |
Page 307
| 10.5.9 | Payments to State Health Facilities. ASES will establish a payment system to improve cash flow to health facilities administered or operated by the Central Government, State Academic Medical Centers, and certain facilities in the San Juan Municipality that participate in the Network. To that end, at the request of ASES, the Contractor shall make advance payments directly (based on historical payments, not on billings) to health facilities. The Contractor shall submit a reconciliation report on a quarterly basis that is certified by the Authorized Signatory pursuant to the terms of this Contract. The following health facilities may participate, subject to reaching agreement with the Contractor under contracts to be approved by ASES: |
| 10.5.9.1 | Cardiovascular Hospital; |
| 10.5.9.2 | Pediatric Hospital; |
| 10.5.9.3 | University Hospital; |
| 10.5.9.4 | Medical Center Trauma Room; |
| 10.5.9.5 | Mayagüez Center Trauma Room; |
| 10.5.9.6 | Dr. Ramón Ruiz-Arnau University Hospital (HURRA, acronym in Spanish); |
Page 308
| 10.5.9.7 | Dr. Federico Trilla UPR Hospital; and |
| 10.5.9.8 | San Juan Municipal Hospital. |
| 10.5.10 | Payments to Providers Outside the PPN. The Contractor shall provide for adequate payment in its contracts with Providers outside the PPN. |
| 10.6 | Acceptable Risk Arrangements |
| 10.6.1 | The Contractor’s Provider Contracts with PMGs shall comply with the following guidelines concerning the apportionment of financial risk between ASES and the PMG for MiSalud services. Any sharing of risk between ASES and PMGs other than as expressly provided in this 10.6 shall require prior written approval by ASES. |
| 10.6.2 | The distribution of risks for Covered Services between and ASES and the PMGs shall be in accordance with Attachment 16 of this Contract. Any proposed arrangement between the Contractor and a PMG that changes such risk distribution shall require prior written approval from ASES. |
| 10.6.3 | The risk associated with Emergency Services related to Basic Coverage Services shall be borne by the PMG. The risk associated with Emergency Services related to Special Coverage Services shall be borne by ASES. The risk associated with |
Page 309
| Emergency Services received outside of Puerto Rico that are covered under this Contract shall be borne by ASES. |
| 10.6.4 | The risk associated with Basic Coverage services, including Diagnostic Test Services in Special Coverage which are not related to high risk registered members and excluding those services mentioned in Sections 10.6.2 and 10.6.3 of this Contract, shall be borne in full by the PMG. |
| 10.6.5 | Notwithstanding Sections 10.6.2-10.6.4 of this Contract, ASES shall assume full risk for services provided in the Virtual Region. |
| 10.7 | Physician Incentive Plan |
| 10.7.1 | The Contractor will design and implement a plan that evaluates the quality of care delivered by PCPs and provides financial incentives to promote PCPs’ commitment to Preventive Services (the “Physician Incentive Plan”). The Contractor will submit such plan to ASES for approval at on or before December 1, 2011, and ASES shall approve it no later than thirty (30) Calendar Days after its submission. The Provider Incentive Plan will include, at a minimum, the following components: |
| 10.7.1.1 | The Contractor shall allocate three cents ($0.03) PMPM of the Per Member Per Month Administrative Fee received from ASES to the |
Page 310
| Provider Incentive Plan (the “Provider Incentive Pool”). |
| 10.7.1.2 | Each PCP who reaches the minimum target, which shall be mutually established between ASES and the Contractor, for each of the criteria set forth below (the “Qualification Criteria”) shall receive a pro-rata portion of the Provider Incentive Pool. |
| 10.7.1.3 | The Contractor will review the Medical Records at the PMG or PCP level to ascertain and evidence the Preventive Services provided by the PCPs to Enrollees. ASES requires through this review that the PCPs comply with the documentation requirements established by the Health Department and EPSDT guidelines. |
| 10.7.2 | The Qualification Criteria shall be based, to the extent applicable, on certain HEDIS measures to be mutually agreed by the Parties and may include, without limitation, the following additional criteria: |
| 10.7.2.1 | That the PCP performs preventive screening to its population according to evidence based on clinical practice guidelines. |
| 10.7.2.2 | That the PCP provides early detection of population with neuro-developmental disorders and autism. |
Page 311
| 10.7.2.3 | That the PCP adopts an EHR system that meets the specifications contained in Attachment 15 to this Contract. |
| 10.7.2.4 | That the PCP complies with the EPSDT screening and parent education requirements. |
| 10.7.2.5 | That the PCP complies with the requirements of a mental and physical health integration program to be mutually agreed between the Parties. |
| 10.7.3 | The Contractor will provide a quarterly report on the Physician Incentive Plan to ASES, which report shall contain, with respect to each Provider: |
| 10.7.3.1 | Service Region |
| 10.7.3.2 | PMG Name |
| 10.7.3.3 | PMG Number |
| 10.7.3.4 | Provider ID |
| 10.7.3.5 | Provider Name |
Page 312
| 10.7.3.6 | Preventive Services Compliance Percentage |
| 10.7.3.7 | Provider’s Education Contact Hours |
| 10.7.3.8 | Provider’s percentage of Compliance with Qualification Criteria |
| 10.7.4 | The Contractor will provide the incentive based on a mathematically sound formula, which shall have the prior written approval of ASES, which approval shall not be unreasonably withheld, conditioned or delayed. |
| 10.7.5 | The Contractor will grant the incentive to those PCPs that comply with the preceding requirements, based on a twelve month natural year measuring period, or as otherwise provided in the Physician Incentive Plan with respect to any partial natural year, plus a three month Claims run out period and a three month period for incentive calculation and analysis. |
| 10.7.6 | The Physician Incentive Plan shall comply with federal and Puerto Rico regulations, including 42 CFR 422.208, 42 CFR 422.210, and 42 CFR 438.6(h). |
Page 313
| 10.8 | Required Information Regarding Providers |
| 10.8.1 | The Contractor shall provide to ASES, according to the timeframe specified in Attachment 12 to this Contract, an electronic file and a list of all of the Network Providers, listed by municipality, indicating the capacity of each Provider, as well as the specialty or subspecialty of physicians. This file must be updated in accordance with Section 18.2 of this Contract. |
| 10.8.2 | Electronic files shall be provided on compact discs (CD) in Microsoft Excel format (.XLS or .XLSX) without column titles. Two hard copies will be included in the same submission. |
| 10.8.3 | List of Doctors and Providers Who Are Individuals. This list will include all available doctors and other Health Care Professionals who are individuals, such as optometrists, podiatrists, psychologists, social workers, health educators, physical therapists, speech therapists, occupational therapists, respiratory therapists, dietitians, nutritionists, and any other health service Provider who is an individual, as applicable. The information file shall include all of the following information: |
| 10.8.3.1 | EIN or SSN; |
Page 314
| 10.8.3.2 | Whether the Provider is a member of the PPN (list “Y” for yes or “N” for no); |
| 10.8.3.3 | Last name; |
| 10.8.3.4 | Mother’s maiden name; |
| 10.8.3.5 | First name; |
| 10.8.3.6 | Municipality (The Provider’s municipality is the place where his or her office is located. If the Provider maintains more than one office, he or she will have to appear more than once in the list and file. Similarly, a physician or Provider with more than one specialty has to be listed for each specialty.); |
| 10.8.3.7 | Specialty Code (see Attachment 9 for a list of Specialty Codes); |
| 10.8.3.8 | Provider license number; and |
| 10.8.3.9 | Provider’s National Provider ID (“NPI”), if applicable. |
Page 315
| 10.8.4 | List of Providers That Are Not Individuals. In another separate list, the Contractor shall include a list of all Providers that are not individuals, such as PMGs, Clinics, Hospitals (identified as private or government), laboratories, x-ray facilities, dialysis facilities, blood banks, and others, using the following format. |
| 10.8.4.1 | EIN; |
| 10.8.4.2 | Name of Entity; |
| 10.8.4.3 | Municipality Code; |
| 10.8.4.4 | Provider Type Code; and |
| 10.8.4.5 | Provider’s National Provider ID (“NPI”), if applicable. |
| 10.8.5 | With these two (2) files, the Contractor shall submit a control sheet that includes (1) a general description of the content of each file, and (2) the total number of records in each file, i.e. “control totals.” The Contractor shall submit all information required in this paragraph to ASES according to the timeframe specified in Attachment 12 to this Contract. |
Page 316
ARTICLE 11 UTILIZATION MANAGEMENT
| 11.1 | Utilization Management Policies and Procedures |
| 11.1.1 | The Contractor shall provide assistance to Enrollees and Providers to ensure the appropriate utilization of resources. The Contractor shall have written Utilization Management Policies and Procedures that: |
| 11.1.1.1 | Include protocols and criteria for evaluating Medical Necessity, authorizing services, and detecting and addressing over-Utilization and under-Utilization. Such protocols and criteria shall comply with federal and Puerto Rico laws and regulations. |
| 11.1.1.2 | Address which services require PCP Referral, which services require Prior Authorization and how requests for initial and continuing services are processed, and which services will be subject to concurrent, retrospective or prospective review. |
| 11.1.1.3 | Describe mechanisms in place that ensure consistent application of review criteria for Prior Authorization decisions. |
Page 317
| 11.1.1.4 | Provide that all Medical Necessity determinations made by the Contractor be made in accordance with ASES’s Medical Necessity definition as stated in Section 7.2 of this Contract. |
| 11.1.2 | The Contractor shall submit its Utilization Management Policies and Procedures to ASES for review and prior approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to Utilization Management Policies and Procedures must be previously approved in writing by ASES, which approval shall not be unreasonably withheld, conditioned, or delayed. |
| 11.1.3 | Providers may participate in Utilization Management activities in their own Service Region to the extent that there is not a conflict of interest. The Utilization Management Policies and Procedures shall define when such a conflict may exist and shall describe the remedy. |
| 11.1.4 | The Contractor, and any delegated Utilization Management agent, shall not permit or provide compensation or anything of value to its employees, agents, or contractors based on: |
| 11.1.4.1 | Either a percentage of the amount by which a Claim is reduced for payment or the number of Claims or the cost of services for which the person has denied authorization or payment; or |
Page 318
| 11.1.4.2 | Any other method that encourages a decision to deny or limit a service. |
| 11.2 | Utilization Management Guidance to Enrollees. |
As provided in Section 6.4.4.22 of this Contract, the Contractor shall provide clear guidance in its Enrollee Handbook on Utilization Management policies.
| 11.3 | Prior Authorization and Referral Policies |
| 11.3.1 | Prior Authorization is authorization granted by the Contractor, including based on an Enrollee’s Service Authorization Request, in advance of the rendering of a service after review to determine whether the service is Medically Necessary. |
| 11.3.2 | A Referral is a request by a PCP or other Provider in the PMG for an Enrollee to be evaluated or treated by a different Provider, usually a specialist. Referrals shall be required only for services outside the Contractor’s PPN. |
| 11.3.3 | In situations, as set forth below in this Section 11.3 of this Contract, where a Provider Referral is permitted or required: |
| 11.3.3.1 | The Contractor shall not impose any requirement of Contractor review of the Provider’s Referral decision; and |
Page 319
| 11.3.3.2 | The Contractor shall ensure that a Referral shall be either made or refused by the PCP or other Provider in the PMG within five (5) Calendar Days of the Enrollee’s request for the Referral. Referrals shall be made expeditiously in the event that a Provider perceives that an Enrollee’s life or health could be endangered by a delay in accessing services; in such situations, a Referral must be made, at a maximum, three (3) Calendar Days from the Enrollee’s request for the Referral (in compliance with 42 CFR 438.210, and a higher standard than that regulation, which refers to working days). |
| 11.3.4 | In situations, as set forth in this Section 11.3 of this Contract, in which Prior Authorization is required, the Contractor shall ensure that Prior Authorization is provided for the Enrollee in the following timeframes, including on holidays and outside of business hours. |
| 11.3.4.1 | The decision whether to grant a Prior Authorization must not exceed seventy-two (72) hours from the time of the Enrollee’s Service Authorization Request for any Covered Service; except that, where the Contractor or the Enrollee’s Provider determines that the Enrollee’s life or health could be endangered by a delay in accessing services, Prior Authorization must be provided as expeditiously as the Enrollee’s health |
Page 320
| requires, and no later than within twenty-four (24) hours of the Service Authorization Request. |
| 11.3.4.2 | ASES may, in its discretion, grant an extension of the time allowed for Prior Authorization decisions, where: |
| 11.3.4.2.1 | the Enrollee, or the Provider, requests the extension; or |
| 11.3.4.2.2 | the Contractor justifies to ASES a need for the extension in order to collect additional information, such that the extension is in the Enrollee’s best interest. |
| 11.3.5 | The Contractor shall use appropriately licensed professionals to supervise all Prior Authorization decisions, and shall in its policies and procedures specify the type of personnel responsible for each type of Prior Authorization. Any decision to deny a Service Authorization Request or to authorize a service in an amount, duration, or scope that is less than requested shall be made by a Health Care Professional who has appropriate clinical expertise in treating the Enrollee’s condition, and for Service Authorization Requests for Dental Services, only licensed dentists may make such decisions. |
| 11.3.6 | Emergency Services |
Page 321
| 11.3.6.1 | Neither a Referral nor Prior Authorization shall be required for any Emergency Service, no matter whether the Provider is within the PPN, and notwithstanding whether there is ultimately a determination that the condition for which the Enrollee sought treatment in the emergency room was not an Emergency Medical Condition. |
| 11.3.7 | Basic Coverage and Dental Services |
| 11.3.7.1 | No Referral shall be required for any service category of Basic Coverage other than Pharmacy and Behavioral Health Services; or for Dental Services, so long as the service is provided within the PPN. |
| 11.3.7.2 | The Contractor shall require a Referral for the services listed in this subsection 11.3.7, where the Enrollee seeks such services outside of the PPN. Such Referral shall be provided by the PCP or other PMG Provider. The Referral shall serve as a determination that the service for which the Referral is being made is Medically Necessary. |
| 11.3.7.3 | Where a Provider does not make in the required timeframe specified, or refuses to make a Referral, the Contractor may issue an Administrative Referral. |
Page 322
| 11.3.8 | Pharmacy Services |
| 11.3.8.1 | The Contractor shall require Prior Authorization for filling a drug prescription for certain drugs specified on the PDL, as provided in Section 7.5.12.10 of this Contract. |
| 11.3.8.2 | The Contractor shall require a Countersignature of the Enrollee’s PCP in order to fill a prescription written by a Provider who is not in the PPN. |
| 11.3.8.3 | Any required Prior Authorization or Countersignature for Pharmacy Services shall be conducted within the timeframes provided in Sections 11.3.4 and 7.5.12.4.2 of this Contract. |
Page 323
| 11.3.9 | Special Coverage |
| 11.3.9.1 | In order to obtain services under Special Coverage, an Enrollee must register, as provided in Section 7.7.6 of this Contract. Registration is a form of utilization control, to determine whether the Enrollee’s health condition warrants Access to the expanded services included in Special Coverage. |
| 11.3.9.2 | In addition, as noted in Section 7.7.12 of this Contract, some individual Special Coverage services require Prior Authorization for an Enrollee who has registered under Special Coverage. |
| 11.3.10 | Behavioral Health Services. Referrals shall be required for Behavioral Health Services as provided in Section 8.3 of this Contract. |
| 11.4 | Use of Technology to Promote Utilization Management |
| 11.4.1 | ASES strongly encourages the Contractor to develop electronic, web-based Referral processes and systems. In the event that a Referral is made via the telephone, the Contractor shall ensure that Referral data are maintained in a data file that can be accessed electronically by the Contractor, the Provider and ASES. |
Page 324
| 11.4.2 | In conjunction with its other Utilization Management policies, the Contractor shall submit the Referral processes to ASES for review and approval. |
| 11.5 | Court-Ordered Evaluations and Services |
| 11.5.1 | In the event that an Enrollee requires Medicaid-covered services ordered by a court, the Contractor shall fully comply with all court orders while maintaining appropriate Utilization Management practices. |
| 11.6 | Second Opinions |
| 11.6.1 | The Contractor shall adopt procedures to obtain a second opinion in any situation when there is a question concerning a diagnosis or the options for surgery or other treatment of a health Condition when requested by any Enrollee, or by a parent, guardian, or other person exercising a custodial responsibility over the Enrollee. |
| 11.6.2 | The second opinion must be provided by a qualified Network Provider, or, if a Network Provider is unavailable, the Contractor shall arrange for the Enrollee to obtain a second opinion from an Out-of-Network Provider. |
| 11.6.3 | The second opinion shall be provided at no cost to the Enrollee. |
Page 325
| 11.7 | Utilization Reporting Program. |
| 11.7.1 | The Contractor shall submit to ASES on a monthly basis by Service Region health care data reports that should include, among other things: |
| 11.7.1.1 | Useful data of Claim experience broken down by diagnosis and health care providers; |
| 11.7.1.2 | Claim experience by Enrollee and by coverage (basic, special, dental and pharmacy); |
| 11.7.1.3 | Claim cost and benefit utilization levels; |
| 11.7.1.4 | Benefits utilization levels or indicators, as well as comparative data such as: (i) hospital inpatient days per year per 1,000 Enrollees, (ii) hospital admission rate per 1,000 Enrollees, (iii) average length of inpatient stays, (iv) number of inpatient and outpatient surgeries, (v) number of outpatient visits per year per Enrollee, and (vi) emergency room visits per 1,000 Enrollee; |
Page 326
| 11.7.1.5 | Cost measures, such as (i) average annual cost per Enrollee, (ii) total hospital inpatient payments, (iii) total surgical payments and (iv) total out of hospital payments; and |
| 11.7.1.6 | Demographics of the population of the Service Region. |
| 11.7.2 | The Contractor shall assist ASES in analyzing the utilization report data to determine trends, necessary plan design modifications, effectiveness of educations programs for both Enrollees and Providers, the impact of cost-control measures and the appropriateness of cost-management programs. |
| 11.7.3 | As part of this program, and in conformance with 42 CFR 438.240(2)(b)(3), the Contractor shall submit to ASES, on a quarterly basis, utilization statistical reports. ASES requires the following reports, with data to be submitted according to specifications determined by ASES: |
| 11.7.3.1 | Provider Credentialing Report; |
| 11.7.3.2 | Network Providers and Out-of-Network Providers; |
| 11.7.3.3 | Ratio of Enrollees to PCPs; |
Page 327
| 11.7.3.4 | Utilization of Diabetes Disease Management; |
| 11.7.3.5 | Utilization of Asthma Disease Management; |
| 11.7.3.6 | Utilization of Hypertension Disease Management; |
| 11.7.3.7 | EPSDT Utilization; |
| 11.7.3.8 | Tele MiSalud Utilization; |
| 11.7.3.9 | Preventive Services Utilization; |
| 11.7.3.10 | Pharmacy Services Utilization; |
| 11.7.3.11 | Dental Services Utilization; |
| 11.7.3.12 | ER Utilization by Region and by PMG; |
| 11.7.3.13 | Prenatal Care; and |
| 11.7.3.14 | Covered Population by Municipality, Group, Age, and Gender. |
Page 328
ARTICLE 12 QUALITY IMPROVEMENT AND PERFORMANCE PROGRAM
| 12.1 | General Provisions |
| 12.1.1 | The Contractor shall provide for the delivery of quality care to all Enrollees with the primary goal of improving health status or, in instances where the Enrollee’s health is not amenable to improvement, maintaining the Enrollee’s current health status by implementing measures to prevent any further deterioration of health status. |
| 12.1.2 | The Contractor shall seek input from, and work with, Enrollees, Providers and community resources and agencies to actively improve the quality of care provided to Enrollees. |
| 12.1.3 | The Contractor shall ensure that its Quality Improvement and Performance Program effectively monitors the program elements listed in 42 CFR 438.66. |
| 12.2 | Quality Assessment Performance Improvement (QAPI) Program |
| 12.2.1 | The Contractor shall have in place a quality assessment and performance improvement program (QAPI) that specifies the Contractor’s quality measurement and performance improvement activities. |
Page 329
| 12.2.2 | For Medicaid and CHIP Eligible Persons, the QAPI program shall be in compliance with federal requirements specified at 42 CFR 438.240. |
| 12.2.3 | The Contractor’s QAPI program shall be based on the latest available research in the area of quality assurance and at a minimum shall include: |
| 12.2.3.1 | A method of monitoring, analyzing, evaluating and improving the delivery, quality and appropriateness of health care furnished to all Enrollees (including under and over utilization of services), including those with special health care needs; |
| 12.2.3.2 | Written policies and procedures for quality assessment, utilization management and continuous quality improvement that are periodically assessed for efficacy; |
| 12.2.3.3 | A health information system sufficient to support the collection, integration, tracking, analysis and reporting of data, in compliance with 42 CFR 438.242; |
| 12.2.3.4 | Designated staff with expertise in quality assessment, Utilization Management and continuous quality improvement; |
Page 330
| 12.2.3.5 | Reports that are evaluated, indicated recommendations that are implemented, and feedback provided to Providers and Enrollees; |
| 12.2.3.6 | A methodology and process for conducting Provider profiling, Credentialing and re-Credentialing; |
| 12.2.3.7 | Procedures for validating completeness and quality of Encounter Data; |
| 12.2.3.8 | Annual performance improvement projects (PIPs) as provided in Section 12.3 below; |
| 12.2.3.9 | Development of an emergency room (ER) quality initiative program (see Section 12.4 of this Contract); |
| 12.2.3.10 | Development of a quality incentive program (see Section 12.5 of this Contract); |
| 12.2.3.11 | Reporting on specified performance measures, including specified HEDIS measures (see Section 12.6 of this Contract); |
| 12.2.3.12 | Conducting Provider and Enrollee surveys (see Section 12.7 of this Contract); |
Page 331
| 12.2.3.13 | Quarterly reports on program results, conclusions, recommendations and implemented system changes, as specified by ASES; and |
| 12.2.3.14 | Process for evaluating the impact of the Contractor’s QAPI program. |
| 12.2.4 | The Contractor’s QAPI program shall be submitted to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to the QAPI program must be previously approved in writing by ASES, which approval shall not be unreasonably withheld, conditioned, or delayed. |
| 12.2.5 | The Contractor shall submit any changes to its QAPI program to ASES for review and approval sixty (60) Calendar Days prior to implementation of the change. |
| 12.2.6 | Upon the request of ASES, the Contractor shall provide any information and documents related to the implementation of the QAPI program. |
| 12.3 | Performance Improvement Projects |
| 12.3.1 | As part of its QAPI program the Contractor shall conduct performance improvement projects (PIPs) in accordance with ASES and, as applicable, federal protocols. |
Page 332
| 12.3.2 | The Contractor shall perform the following required PIPs ongoing for the duration of this Contract Term: |
| 12.3.2.1 | One (1) in the area of diabetes; |
| 12.3.2.2 | One (1) in the area of kidney disease; |
| 12.3.2.3 | One (1) in the area of asthma; and |
| 12.3.2.4 | One (1) in the area of cardiovascular conditions. |
| 12.3.2.5 | The Contractor shall conduct such additional PIPs as mutually agreed by the Parties. |
| 12.3.3 | In designing its PIPs, the Contractor shall: |
| 12.3.3.1 | Show that the selected area of study is based on a demonstration of need and is expected to achieve measurable benefit to Enrollee (rationale); |
| 12.3.3.2 | Establish clear, defined and measurable goals and objectives that the Contractor shall achieve in each year of the project; |
Page 333
| 12.3.3.3 | Measure performance using quality indicators that are objective, measurable, clearly defined and that allow tracking of performance and improvement over time; |
| 12.3.3.4 | Implement interventions designed to achieve quality improvements; |
| 12.3.3.5 | Evaluate the effectiveness of the interventions; |
| 12.3.3.6 | Establish standardized performance measures (such as HEDIS or another similarly standardized product); |
| 12.3.3.7 | Plan and initiate activities for increasing or sustaining improvement; and |
| 12.3.3.8 | Document the data collection methodology used (including sources) and steps taken to assure data is valid and reliable. |
| 12.3.4 | The Contractor shall submit all descriptions of PIPs and program details to ASES as part of the QAPI program. |
| 12.3.5 | Each performance improvement project shall be completed in a time period to be specified by ASES to allow information on the success of the project in the aggregate to produce new information on quality of care each year. |
Page 334
| 12.3.6 | When requested, the Contractor shall submit data to ASES for standardized PIPs, within specified timelines and according to the established procedures data collection and reporting. The Contractor shall collect valid and reliable data, using qualified staff and personnel to collect the data. Failure of the Contractor to follow data collection and reporting requirements may result in sanctions under this Contract. |
| 12.4 | ER Quality Initiative Program |
| 12.4.1 | The Contractor shall develop an Emergency Room (ER) Quality Initiative Program, implementing efficient and timely monitoring of Enrollees’ use of the emergency room, including whether such use was justified by a legitimate Medical Emergency. |
| 12.4.2 | The ER Quality Initiative Program shall be designed to identify high users of Emergency Services for non-emergency situations and to allow for early interventions in order to ensure appropriate utilization of services and resources. |
| 12.4.3 | The ER Quality Initiative Program shall specify all strategies to be used by the Contractor to address high users of inappropriate Emergency Services and include, at a minimum, the following components: |
| 12.4.3.1 | Description of system(s) for tracking, monitoring and reporting high users of ER services for non-emergency situations; |
Page 335
| 12.4.3.2 | Criteria for defining non-emergency situations; |
| 12.4.3.3 | Educational component to inform: (1) Enrollees about the proper use of ER services and how to access ER services; and (2) PCPs about identifying high users or potential high users of ER services and reporting to the Contractor; |
| 12.4.3.4 | Protocols for identifying high users of inappropriate ER services and referring them to Case Management for needs assessment and identification of other more appropriate services and resources; |
| 12.4.3.5 | Process for coordinating with and referring to MBHO upon identification of the need for behavioral health services and interventions based upon a needs assessment. |
| 12.4.3.6 | Quarterly reporting on ER services utilization; and |
| 12.4.3.7 | Process for monitoring and evaluating program effectiveness, identifying issues and modifying the ER Quality Initiative Program as necessary to improve service utilization. |
Page 336
| 12.4.4 | The Contractor shall submit its ER Quality Initiative Program to ASES as part of its QAPI program. |
| 12.5 | Quality Incentive Program |
| 12.5.1 | The Contractor shall establish and implement a Quality Incentive Program as a mechanism to improve the quality of services provided to Enrollees. The Quality Incentive Program shall be based on a work plan to be submitted to ASES by the Contractor as part of its QAPI program, pursuant to Attachment 12 of this Contract. The Contractor shall implement the Quality Incentive Program within thirty (30) Calendar Days of its approval by ASES. |
| 12.5.2 | The Quality Incentive Program shall consist of three (3) categories of performance indicators: performance measures, preventive clinical program measures and ER Utilization measures. ASES will Withhold a total of five percent (5%) of the amount budgeted within the Contractor’s Administrative Fee for the administration of the Quality Incentive Program (hereinafter the “Retention Fund”), which budgeted amount is specified in Attachment 11 of this Contract, and will reimburse the Contractor according to compliance with each of the categories of performance indicators in this Section 12.5. |
Page 337
| 12.5.3 | The Contractor shall, within thirty (30) Calendar Days after the end of each calendar quarter, submit a quarterly report for each of the performance indicators to be evaluated by ASES. For each measure, ASES shall, within thirty (30) Calendar Days after receipt of the Contractor’s quarterly report, make a determination whether the Contractor has met the applicable performance objectives for the quarter. In addition, the Contractor shall submit an annual report within thirty (30) Calendar Days after the end of the year for which the performance is measured. If the Contractor is then in compliance with the applicable performance targets or portions thereof for said period, ASES shall then release to the Contractor, no later than thirty (30) Calendar Days after ASES determines compliance with the performance objectives, the portion of the Retention Fund associated with each measure for such period, or the portion corresponding to the percentage of compliance with each such indicator, as the case may be. |
| 12.5.4 | The following is a description of each of the three categories of performance indicators and the associated reimbursement level for each. |
| 12.5.4.1 | Performance Measures |
| 12.5.4.1.1 | The Contractor shall demonstrate a three percent (3%) annual increase in performance measures (measured by ASES reporting protocol and HEDIS coding for each measure) using base line measures to be |
Page 338
| provided by ASES within fifteen (15) Calendar Days of the Effective Date of the Contract, which measures shall be based on actual and verifiable information for the following HEDIS measures of effectiveness for medical care and Access: |
| 12.5.4.1.1.1 | Effectiveness of medical care; |
| 12.5.4.1.1.1.1 | Prevention and screening metrics; |
| 12.5.4.1.1.1.2 | Respiratory condition metrics; |
| 12.5.4.1.1.1.3 | Cardiovascular conditions; and |
| 12.5.4.1.1.1.4 | Comprehensive Diabetes Care (with all its components). |
| 12.5.4.1.1.2 | Access; |
| 12.5.4.1.1.2.1 | Metrics for availability of health services. |
| 12.5.4.1.2 | The Contractor shall demonstrate a five percent (5%) annual increase in EPSDT screenings (measured by ASES reporting protocol and |
Page 339
| HEDIS coding for each measure) using baseline measures to be provided by ASES within fifteen (15) Calendar Days of the Effective Date of the Contract, which measures shall be based on actual and verifiable information. |
| 12.5.4.1.3 | ASES shall release to the Contractor, in accordance with Section 12.5.3 above, forty percent (40%) of the Retention Fund for compliance with the above quality performance measures of this Contract. |
| 12.5.4.1.4 | The foregoing notwithstanding, the Contractor shall comply with the HEDIS measures as required by CMS. The Contractor shall prepare (i) the HEDIS activity for 2012 measure year 2011 provided that ASES delivers on a timely basis the data required to accurately complete such report and (ii) the HEDIS activity for 2013 measure year 2012. The Contractor shall continue to collect HEDIS measures throughout the term of the Contract. |
| 12.5.4.2 | Preventive Clinical Programs |
Page 340
| 12.5.4.2.1 | The Contractor shall comply with objectives to be established by mutual agreement of the Parties for each of the following preventive clinical programs: |
| 12.5.4.2.1.1 | Case Management; |
| 12.5.4.2.1.2 | Disease Management; |
| 12.5.4.2.1.3 | Pre-Natal and Maternal Wellness Program; and |
| 12.5.4.2.1.4 | Provider Education Program, including EPSDT and Provider and Enrollee based education. |
| 12.5.4.2.2 | ASES shall release to the Contractor, in accordance with Section 12.5.3, twenty percent (20%) of the retained Retention Fund for compliance with these objectives. |
| 12.5.4.3 | Emergency Room Use Indicators |
| 12.5.4.3.1 | As described in Section 12.4 above, the Contractor shall develop an ER Quality Initiative Program to reduce the inappropriate use of ER services for non-emergency situations. ASES will provide the |
Page 341
| Contractor with the related baseline measures within fifteen (15) Calendar Days of the Effective Date of the Contract, which measures shall be based on actual and verifiable information. |
| 12.5.4.3.2 | [Intentionally left blank]. |
| 12.5.4.3.3 | ASES shall release to the Contractor, in accordance with Section 12.5.3, forty percent (40%) of the retained Retention Fund for compliance with this objective. |
| 12.5.4.4 | The Contractor shall submit its Quality Incentive Program as part of its QAPI program. The program description shall include, at a minimum: |
| 12.5.4.4.1 | How the Contractor will educate Providers regarding the program requirements; and |
| 12.5.4.4.2 | Strategies for ensuring and monitoring program compliance. |
| 12.5.4.5 | During the Contract Term ASES may issue from time to time normative or policy letters setting forth the terms and conditions it may deem necessary or convenient for the purpose of implementing the Quality Incentive Program described in this Article 12. |
Page 342
| 12.6 | Performance Measures |
| 12.6.1 | The Contractor shall report, annually, on the following HEDIS measures in the format specified by ASES. |
| 12.6.1.1 | Effectiveness of Care: Prevention and Screening Measures |
| 12.6.1.1.1 | Childhood immunization; |
| 12.6.1.1.2 | Breast cancer screening; |
| 12.6.1.1.3 | Cervical cancer screening; |
| 12.6.1.1.4 | Chlamydia screening; |
| 12.6.1.1.5 | Adult BMI assessment; and |
| 12.6.1.1.6 | Weight assessment and counseling for nutrition and physical activities for children and adolescents. |
| 12.6.1.2 | Effectiveness of Care: Respiratory Condition Measures |
| 12.6.1.2.1 | Use of appropriate medication for people with asthma. |
Page 343
| 12.6.1.2.2 | Appropriate treatment for children with upper respiratory conditions. |
| 12.6.1.3 | Effectiveness of Care: Cardiovascular Conditions |
| 12.6.1.3.1 | Cholesterol management for people with cardiovascular conditions; |
| 12.6.1.3.2 | Controlling high blood pressure; and |
| 12.6.1.3.3 | Comprehensive diabetes care (with all its components). |
| 12.6.1.4 | Access/Availability of Care Measures |
| 12.6.1.4.1 | Adult Access to preventive/outpatient health services; |
| 12.6.1.4.2 | Annual dentist visit; |
| 12.6.1.4.3 | Children and adolescent Access to PCPs; |
| 12.6.1.4.4 | Prenatal and postpartum care; |
| 12.6.1.4.5 | Frequency of ongoing prenatal care; |
| 12.6.1.4.6 | Well Child visits in the first 15 months of life; and |
Page 344
| 12.6.1.4.7 | Adolescent well care visits. |
| 12.6.1.5 | ASES may add, change, or remove reporting requirements with sixty (60) Calendar Days notice in advance of the effective date of the addition, change, or removal. |
| 12.6.1.6 | The Contractor shall contract with an NCQA certified HEDIS auditor to validate the processes of the Contractor in accordance with NCQA requirements. For Medicaid and CHIP Eligible Persons, the validation procedures shall be consistent with federal requirements specified at 42 CFR 438.358(b)(2). |
| 12.6.1.7 | When requested, the Contractor shall submit data to ASES for standardized performance measures, within specified timelines and according to the established procedures for data collection and reporting. The Contractor shall collect valid and reliable data, using qualified staff and personnel to collect the data. Failure of the Contractor to follow data collection and reporting requirements may result in sanctions under this Contract. |
Page 345
| 12.7 | Provider and Enrollee Satisfaction Surveys |
| 12.7.1 | During the Contract Term, the Contractor shall perform at least two (2) satisfaction surveys of Providers and Enrollees. The first such survey will be performed not later than April 30, 2012 and the second, not later than March 1, 2013. The survey for Enrollees shall use the CAHPS survey instrument. |
| 12.7.2 | The sample size for both surveys shall equal the number of respondents needed for a statistical confidence level of ninety-five percent (95%) with a margin of error not more than five percent (5%) and shall not have a response rate less than fifty percent (50%). |
| 12.7.3 | The results of the surveys shall be submitted to ASES and to the Puerto Rico Medicaid Program. |
| 12.7.4 | The Contractor shall have a process for notifying Providers and Enrollees about the availability of survey findings and making survey findings available upon request. |
| 12.7.5 | The Contractor shall have a process for utilizing the results of the Provider and Enrollee surveys for monitoring service delivery and quality of services and for making program enhancements. |
Page 346
| 12.8 | External Quality Review |
| 12.8.1 | In compliance with federal requirements at 42 CFR 438.358(b)(3), ASES will contract with an External Quality Review Organization (EQRO) to conduct annual, external, independent reviews of the quality outcomes, timeliness of, and Access to, the services covered in this Contract. The Contractor shall collaborate with ASES’s EQRO to develop studies, surveys and other analytic activities to assess the Quality of care and services provided to Enrollees and to identify opportunities for program improvement. To facilitate this process the Contractor shall supply data, including but not limited to claims data and medical records, to the EQRO. Upon the request of ASES, the Contractor shall provide its protocols for providing information, participating in review activities, and using the results of the reviews to improve the quality of the services and programs provided to Enrollees. |
| 12.8.2 | The EQRO will evaluate the following program components: |
| 12.8.2.1 | Enrollee rights and protection; |
| 12.8.2.2 | Availability of services; |
| 12.8.2.3 | Coordination and continuity of care; |
Page 347
| 12.8.2.4 | Coverage and authorization of services; |
| 12.8.2.5 | Provider selection; |
| 12.8.2.6 | Enrollee information; |
| 12.8.2.7 | Confidentiality; |
| 12.8.2.8 | Enrollment and Disenrollment; |
| 12.8.2.9 | Grievance System; |
| 12.8.2.10 | Subcontracts; |
| 12.8.2.11 | Provider guidelines; and |
| 12.8.2.12 | Health Information Systems. |
Page 348
ARTICLE 13 FRAUD AND ABUSE
| 13.1 | General Provisions |
| 13.1.1 | The Contractor shall have internal controls and policies and procedures in place designed to prevent, detect, and report known or suspected Fraud and Abuse. |
| 13.1.2 | For Medicaid and CHIP Eligible Persons, the Contractor’s internal controls, policies and procedures shall comply with all federal requirements regarding Fraud and Abuse and program integrity, including but not limited to Sections 1128, 1156, and 1902(a)(68) of the Social Security Act and 42 CFR 438.606. The Contractor shall exercise diligent efforts to ensure that no payments are made to any person or entity that has been excluded from participation in Federal health care programs. (See State Medicaid Director Letter #09-001, January 16, 2009.) |
| 13.1.3 | The Contractor shall submit its Fraud and Abuse policies and procedures, its proposed compliance plan, and its Program Integrity Plan to ASES for approval according to the timeframe specified in Attachment 12 to this Contract. |
| 13.1.4 | Any changes to the Contractor’s Fraud and Abuse policies and procedures must be submitted to ASES for approval within fifteen (15) Calendar Days of the date the |
Page 349
| Contractor plans to implement the changes; and the changes shall not go into effect until ASES gives written approval. |
| 13.2 | Compliance Plan |
| 13.2.1 | The Contractor shall have a written Fraud and Abuse compliance plan with stated program goals and objectives, program scope and methodology to evaluate program performance. |
| 13.2.2 | At a minimum, the Contractor’s Fraud and Abuse compliance plan shall: |
| 13.2.2.1 | Ensure that all of its officers, directors, managers and employees know and understand the provisions of the Contractor’s Fraud and Abuse compliance plan; |
| 13.2.2.2 | Require the designation of a compliance officer and a compliance committee that are accountable to senior management; |
| 13.2.2.3 | Ensure and describe effective training and education for the compliance officer and the organization’s employees; |
Page 350
| 13.2.2.4 | Ensure that Providers and Enrollees are educated about Fraud and Abuse identification and reporting in Provider and Enrollee materials; |
| 13.2.2.5 | Ensure effective lines of communication between the Contractor’s compliance officer and the Contractor’s employees; |
| 13.2.2.6 | Ensure enforcement of standards through well-publicized disiplinary guidelines; |
| 13.2.2.7 | Ensure internal monitoring and auditing with provisions for prompt response to potential offenses, and for the development of corrective action initiatives relating to the Contractor’s Fraud and Abuse efforts; |
| 13.2.2.8 | Describe standards of conduct that articulate the Contractor’s commitment to comply with all applicable Puerto Rico and federal requirements and standards; |
| 13.2.2.9 | Ensure that no individual who reports Provider violations or suspected Fraud and Abuse is retaliated against; and |
Page 351
| 13.2.2.10 | Include a monitoring program that is designed to prevent and detect potential or suspected Fraud and Abuse. This monitoring program shall include but not be limited to: |
| 13.2.2.10.1 | Monitoring the Claims of its Providers to ensure Enrollees receive services for which the Contractor is administering Claims and ASES is required to pay under this Contract; |
| 13.2.2.10.2 | Requiring the investigation of all reports of suspected Fraud and over billings; |
| 13.2.2.10.3 | Reviewing Providers for over or under-utilization; |
| 13.2.2.10.4 | Verifying with Enrollees the delivery of services as claimed; and |
| 13.2.2.10.5 | Reviewing and trending Enrollee complaints regarding Providers. |
| 13.2.2.11 | The Contractor shall include in any employee handbook a specific discussion of its Fraud and Abuse policies and procedures, the rights of whistleblowers, and the Contractor’s procedures for detecting and preventing Fraud and Abuse. |
Page 352
| 13.2.2.12 | The Contractor shall include in the Enrollee Handbook instructions on how to report Fraud and Abuse and the protections for whistleblowers. |
| 13.3 | Program Integrity Plan |
| 13.3.1 | The Contractor shall develop a Program Integrity Plan that at a minimum: |
| 13.3.1.1 | Defines Fraud, waste and Abuse; |
| 13.3.1.2 | Specifies methods to detect Fraud, waste and Abuse, |
| 13.3.1.3 | Describes a process to perform investigations on each suspected case of Fraud, waste and Abuse; |
| 13.3.1.4 | Describes persons responsible for conducting these investigations; |
| 13.3.1.5 | Includes a variety of methods for identifying, investigating and referring suspected cases to appropriate entities; |
| 13.3.1.6 | Includes a systematic approach to data analysis; |
Page 353
| 13.3.1.7 | Defines mechanisms to monitor frequency of Encounters and services rendered to Enrollees billed by Providers; and |
| 13.3.1.8 | Identifies requirements to complete the preliminary investigation of Providers and Enrollees. |
| 13.3.2 | The Contractor’s Program Integrity Plan shall comply in all respects with the ASES Guidelines for the Development of Program Integrity Plan, included as Attachment 14 to this Contract. Upon review of the Contractor’s Program Integrity Plan (see Section 13.1.3 of this Contract), ASES will promptly (within twenty (20) Business Days) notify the Contractor of any needed revisions in order for the Program Integrity Plan to comply with the Guidelines for the Development of Program Integrity Plan (Attachment 14) and with federal law. The Contractor, in turn, shall promptly (within twenty (20) Business Days of receipt of the ASES comments) re-submit its Plan for ASES review and approval. |
| 13.3.3 | The Contractor shall notify ASES within twenty (20) Business Days of any initiated investigation of a suspected case of Fraud, waste, or Abuse. The Contractor shall subsequently report preliminary results of such investigations activities to ASES and other appropriate Puerto Rico and federal entities. ASES will provide the Contractor with guidance during the pendency of the investigation and will refer the matter to the U.S. Department of Justice. |
Page 354
| 13.4 | Prohibited Affiliations with Individuals Debarred by Federal Agencies |
| 13.4.1 | The Contractor shall not knowingly have a relationship with the following: |
| 13.4.1.1 | An individual who is debarred, suspended, or otherwise excluded from participating in procurement activities under the Federal Acquisition Regulation or from participating in non-procurement activities under Executive Order No. 12549. |
| 13.4.1.2 | An individual who is an affiliate, as defined in the Federal Acquisition Regulation, of a person described in Section 13.4.1.1 of this Contract. The relationship is defined as follows: |
| 13.4.1.2.1 | A director, officer, or partner of the Contractor; |
| 13.4.1.2.2 | A person with beneficial ownership of five percent of more of the Contractor’s equity; or |
| 13.4.1.2.3 | A person with an employment, consulting or other arrangement with the Contractor for the provision of items or services that are significant and material the Contractor’s obligations under this Contract. |
Page 355
| 13.5 | Reporting and Investigations |
| 13.5.1 | On quarterly basis, the Contractor shall report all instances of suspected Provider Fraud, Abuse, or waste, or Enrollee Abuse of the services covered under this Contract, using a format and data elements prescribed by ASES. |
| 13.5.1.1 | At a minimum, the Contractor shall include in each report, with respect to individual investigations of Fraud, Abuse, or waste: |
| 13.5.1.1.1 | Enrollee name and ID number; |
| 13.5.1.1.2 | Provider name and NPI; |
| 13.5.1.1.3 | Source of complaint; |
| 13.5.1.1.4 | Type of provider; |
| 13.5.1.1.5 | Nature of complaint, including alleged persons or entities involved, category of services, factual explanation of the allegation, and dates of the conduct; |
Page 356
| 13.5.1.1.6 | All communication between the Contractor and the Provider about the complaint; |
| 13.5.1.1.7 | Date of the complaint; |
| 13.5.1.1.8 | Approximate dollars involved or amount paid to the Provider during the past three years, whichever is greater; |
| 13.5.1.1.9 | Disciplinary measures imposed, if any; |
| 13.5.1.1.10 | Contact information for a Contractor staff person with relevant knowledge of the matter; and |
| 13.5.1.1.11 | Legal and administrative disposition of the case. |
| 13.5.1.2 | The Contractor shall also include in the report a summary (not specific to an individual case) of |
| 13.5.1.2.1 | Investigative activities, corrective actions, prevention efforts, and results; and |
Page 357
| 13.5.1.2.2 | Trending and analysis of Utilization Management and Provider payment management. |
| 13.5.2 | The Contractor shall report to ASES, within (1) one Business Day of obtaining knowledge with respect to the identity of any Provider or other person who, in violation of 42 CFR 438.610 (a) and (b), is debarred, suspended, or otherwise prohibited from participating in procurement activities. ASES shall promptly notify the Secretary of HHS of the noncompliance, as required by 42 CFR 438.610(c). |
| 13.5.3 | The Contractor and all Subcontractors shall cooperate fully with federal and Puerto Rico agencies in Fraud and Abuse investigations and subsequent legal actions. Such cooperation shall include providing, upon request, information, access to records, and access to interview employees and consultants, including but not limited to those with expertise in the administration of the program and/or medical or pharmaceutical questions or in any matter related to an investigation. |
ARTICLE 14 GRIEVANCE SYSTEM
| 14.1 | General Requirements |
| 14.1.1 | The Contractor shall have a Grievance System in place to address Enrollee concerns and Appeals of service decisions. The Grievance System shall consist of the |
Page 358
| following four (4) components: 1) Complaint process, 2) Grievance process, 3) Appeal process, and 4) access to the Administrative Law Hearing process. |
| 14.1.2 | The Contractor shall designate, in writing, an officer who shall have primary responsibility for ensuring that Complaints, Grievances, and Appeals are resolved pursuant to this Contract and for signing all Notices of Action. |
| 14.1.3 | The Contractor shall develop written Grievance System policies and procedures that detail the operation of the Grievance System. The Grievance System policies and procedures shall be submitted to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. In the event that changes are made to the existing approved Grievance System policies and procedures, a copy of the proposed changes shall be made available to ASES for approval according to the timeframe specified in Attachment 12 to this Contract. |
| 14.1.4 | At a minimum, the Contractor’s Grievance System Policies and Procedures shall include the following: |
| 14.1.4.1 | Process for filing a Complaint, Grievance, or Appeal, or seeking an Administrative Law Hearing; |
Page 359
| 14.1.4.2 | Process for receiving, recording, tracking, reviewing, reporting and resolving Grievances filed verbally, in writing, or in-person; |
| 14.1.4.3 | Process for receiving, recording, tracking, reviewing, reporting and resolving Appeals filed verbally or in writing; |
| 14.1.4.4 | Process for requesting an expedited review of an Appeal; |
| 14.1.4.5 | Process for notifying Enrollees of their right to file a Complaint, Grievance or Appeal with the Patient Advocate Office and how to contact the Patient Advocate Office; |
| 14.1.4.6 | Procedures for the exchange of information regarding Complaints, Grievances and Appeals; |
| 14.1.4.7 | Process and timeframes for notifying Enrollees in writing regarding receipt of Complaints, Grievances or Appeals, resolution, action, delay of review, and denial of request for expedited review. |
| 14.1.5 | The Contractor’s Grievance System shall fully comply with the Patient’s Bill of Rights Act and with Act No. 11 of April 11, 2001 (known as the Organic Law of the |
Page 360
| Office of the Patient Advocate), to the extent that such provisions do not conflict with, or pose an obstacle to, federal regulations. |
| 14.1.6 | For Medicaid and CHIP Eligible Persons, the Contractor’s Grievance System shall be in compliance with federal requirements at 42 CFR 438.400 – 438.424 and 42 CFR 431.200 – 431.250. |
| 14.1.7 | The Contractor shall process each Complaint, Grievance, or Appeal in accordance with applicable Puerto Rico and federal statutory and regulatory requirements, this Contract, and the Contractor’s written policies and procedures. Pertinent facts from all parties must be collected during the process. |
| 14.1.8 | The Contractor shall include in the Enrollee Handbook educational information regarding the Contractor’s Grievance System which at a minimum includes: |
| 14.1.8.1 | A description of the Contractor’s Grievance System; |
| 14.1.8.2 | Instructions on how to file Complaints, Grievances and Appeals including the timeframes for filing; |
| 14.1.8.3 | The Contractor’s toll-free telephone number and office hours; |
Page 361
| 14.1.8.4 | Information regarding an Enrollee’s right to file a Complaint, Grievance or Appeal with the Patient Advocate Office and how to file a Complaint, Grievance or Appeal with the Patient Advocate Office; |
| 14.1.8.5 | Information describing the Administrative Law Hearing process and governing rules; and |
| 14.1.8.6 | Timelines and limitations associated with filing Grievances or Appeals. |
| 14.1.9 | The Contractor shall give Enrollees reasonable assistance in completing forms and taking other procedural steps for Complaints, Grievances and Appeals. This includes, but is not limited to, providing interpreter services and toll-free numbers that have adequate TDD and interpreter capability. |
| 14.1.10 | The Contractor shall include information regarding the Grievance System in the Provider guidelines and upon joining the Contractor’s Network, all Providers shall receive education regarding the Contractor’s Grievance System, which includes but is not limited to: |
| 14.1.10.1 | The Enrollee’s right to file Complaints, Grievances and Appeals and the requirements and timeframes for filing; |
Page 362
| 14.1.10.2 | The Enrollee’s right to file a Complaint, Grievance or Appeal with the Patient Advocate Office; |
| 14.1.10.3 | The Enrollee’s right to an Administrative Law Hearing, how to obtain an Administrative Law Hearing, and representation rules at a Administrative Law Hearing; |
| 14.1.10.4 | The availability of assistance in filing a Complaint, Grievance, or Appeal; |
| 14.1.10.5 | The toll-free numbers to file oral Complaints, Grievances and Appeals; |
| 14.1.10.6 | The Enrollee’s right to request continuation of Benefits during an Appeal, or an Administrative Law Hearing filing, and that if the Contractor’s action is upheld in a Administrative Law Hearing, the Enrollee may be liable for the cost of any continued Benefits; and |
| 14.1.10.7 | Any Puerto Rico-determined Provider Appeal rights to challenge the failure of the Contractor to cover a service. |
| 14.1.11 | The Contractor shall acknowledge receipt of each filed Grievance and Appeal in writing within ten (10) Business Days of receipt. |
Page 363
| 14.1.12 | The Contractor shall have procedures in place to notify all Enrollees in their primary language of Complaint, Grievance and Appeal dispositions. |
| 14.1.13 | All Complaints, Grievances and Appeals files and forms shall be made available to ASES for auditing. All Complaint, Grievance, and Appeal documents and related information shall be considered as containing protected health information and shall be treated in accordance with HIPAA regulations and other applicable laws of Puerto Rico. |
| 14.1.14 | The Contractor shall develop Grievance System forms to be submitted for approval by ASES according to the timeframe specified in Attachment 12 to this Contract. The approved forms shall be made available to all Enrollees, shall meet all requirements listed in Sections 6.2 and 6.3 of this Contract for written materials, and shall, at a minimum: |
| 14.1.14.1 | Instruct the Enrollee or Enrollee’s Authorized Representative that documentary evidence should be included, if available; and |
| 14.1.14.2 | Include instructions for completion and submission. |
| 14.1.15 | The Contractor shall ensure that the individuals who make decisions on Grievances and Appeals were not involved in any previous level of review or decision-making; |
Page 364
| and are Health Care Professionals who have the appropriate clinical expertise, as determined by ASES, in treating the Enrollee’s condition or disease if deciding any of the following: |
| 14.1.15.1 | An Appeal of a denial that is based on lack of Medical Necessity; |
| 14.1.15.2 | A Grievance regarding denial of expedited resolutions of Appeal; and |
| 14.1.15.3 | Any Grievance or Appeal that involves clinical issues. |
| 14.1.16 | The Contractor shall have a system in place to collect, analyze and integrate data regarding Complaints, Grievances and Appeals. At a minimum, the following information shall be recorded: |
| 14.1.16.1 | Date Complaint, Grievance or Appeal was filed; |
| 14.1.16.2 | Enrollee’s name; |
| 14.1.16.3 | Enrollee’s Medicaid ID number, if applicable; |
| 14.1.16.4 | Name of the individual filing the Complaint, Grievance or Appeal on behalf of the Enrollee; |
Page 365
| 14.1.16.5 | Date acknowledgement of receipt of Grievance/Appeal was mailed to the Enrollee; |
| 14.1.16.6 | Summary of Complaint, Grievance or Appeal; |
| 14.1.16.7 | Date Notice of Disposition or Notice of Adverse Action was mailed to the Enrollee; |
| 14.1.16.8 | Corrective action required; and |
| 14.1.16.9 | Date of resolution. |
| 14.2 | Complaint |
| 14.2.1 | The Complaint process is the procedure for addressing Enrollee Complaints, defined as expressions of dissatisfaction about any matter other than an Action that are resolved at the point of contact rather than through filing a formal Grievance. |
| 14.2.2 | An Enrollee or Enrollee’s Authorized Representative may file a Complaint either orally or in writing. The Enrollee or Enrollee’s Authorized Representative may follow up an oral request with a written request, however, the timeframe for resolution begins with the date the Contractor receives the oral request. |
Page 366
| 14.2.3 | An Enrollee or Enrollee’s Authorized Representative shall file a Complaint within fifteen (15) Calendar Days after the date of occurrence that initiated the Complaint. |
| 14.2.4 | The Contractor shall have procedures in place to notify all Enrollees in their primary language of Complaint dispositions. |
| 14.2.5 | The Contractor shall resolve each Complaint within seventy-two (72) hours of the time the Contractor received the initial Complaint, whether orally or in writing. If the Complaint is not resolved within this timeframe, the Complaint shall be treated as a Grievance. |
| 14.2.6 | The Notice of Disposition shall include the results and date of the resolution of the Complaint and shall include notice of the right to file a Grievance or Appeal and information necessary to allow the Enrollee to request an Administrative Law Hearing, if appropriate, including contact information necessary to pursue an Administrative Law Hearing. |
| 14.3 | Grievance Process |
| 14.3.1 | The Grievance process is the procedure for filing an expression of dissatisfaction about any matter other than an Action (see Section 14.4 of this Contract for definition of Action). |
Page 367
| 14.3.2 | Any written or verbal communication from an Enrollee or Network Provider, which expresses dissatisfaction about any matter other than an Action shall be promptly and properly handled and resolved by the Contractor. |
| 14.3.3 | An Enrollee or Enrollee’s Authorized Representative may file a Grievance with the Contractor or with the Office of the Patient’s Advocate of Puerto Rico either orally or in writing. A Provider cannot file a Grievance on behalf of an Enrollee unless written consent is granted by the Enrollee. |
| 14.3.4 | The Contractor shall provide written notice of the disposition of the Grievance as expeditiously as the Enrollee’s health condition requires, but in any event, within ninety (90) Calendar Days of the filing date. The notice shall include the resolution and the basis for the resolution. However, if the Contractor resolved the Grievance and verbally informed the Enrollee of the resolution within five (5) Business Days of receipt of the Grievance, the Contractor shall not be required to provide written notice of resolution, but the Grievance shall be included in the Contractor’s Grievance and Appeals report as described in Section 14.8 of this Contract. |
| 14.3.5 | The Contractor may extend the timeframe for disposition of a Grievance for up to fourteen (14) Calendar Days if the Enrollee requests the extension or the Contractor demonstrates (to the satisfaction of ASES, upon its request) that there is a need for additional information and how the delay is in the Enrollee’s interest. If the |
Page 368
| Contractor extends the timeframe, it shall, for any extension not requested by the Enrollee, give the Enrollee written notice of the reason for the delay prior to the delay. |
| 14.4 | Action |
| 14.4.1 | As defined in 42 CFR §438.400(b), an Action means: |
| 14.4.1.1 | The denial or limited authorization of a requested service, including the type or level of service; |
| 14.4.1.2 | The reduction, suspension, or termination of a previously authorized service; |
| 14.4.1.3 | The denial, in whole or in part, of payment for a service; |
| 14.4.1.4 | The failure to provide services in a timely manner, as defined by this Contract; |
| 14.4.1.5 | The failure of the Contractor to act within the timeframes provided in 42 CFR 438.408(b); or |
Page 369
| 14.4.1.6 | For a resident of a rural area, the denial of an Enrollee’s request to exercise his or her right, under 42 CFR 438.52(b)(2)(ii), to obtain services outside the General Network. |
| 14.4.2 | In the event of an Action, the Contractor shall notify the Enrollee in writing. The Contractor shall also provide written notice of an Action to the Provider. This notice shall meet the language and format requirements in accordance with Sections 6.2 and 6.3 of this Contract and be sent in accordance with the timeframes described in Section 14.4.4 of this Contract. |
| 14.4.3 | The Notice of Action shall contain the following: |
| 14.4.3.1 | The Action the Contractor has taken or intends to take; |
| 14.4.3.2 | The reasons for the Action; |
| 14.4.3.3 | The Enrollee’s right to file an Appeal through the Contractor’s internal Grievance System and the procedure for filing an Appeal; |
| 14.4.3.4 | The Provider’s right to dispute an ASES determination as described in Section 16.11 of this Contract; |
Page 370
| 14.4.3.5 | The Enrollee’s right to request an Administrative Law Hearing; |
| 14.4.3.6 | The Enrollee’s right to allow a Provider to act on behalf of the Enrollee, upon written consent; |
| 14.4.3.7 | The circumstances under which expedited review is available and how to request it; and |
| 14.4.3.8 | The Enrollee’s right to have Benefits continue pending resolution of the Appeal with the Contractor or during the Administrative Law Hearing, how to request that Benefits be continued, and the circumstances under which the Enrollee may be required to pay the costs of these services. |
| 14.4.4 | The Contractor shall mail the Notice of Action within the following timeframes: |
| 14.4.4.1 | For termination, suspension, or reduction of previously authorized Covered Services at least ten (10) Calendar Days before the date of Action or not later than the date of Action in the event of one of the following exceptions: |
| 14.4.4.1.1 | The Contractor has factual information confirming the death of an Enrollee. |
Page 371
| 14.4.4.1.2 | The Contractor receives a clear written statement signed by the Enrollee that he or she no longer wishes services or gives information that requires termination or reduction of services and indicates that he or she understands that this must be the result of supplying that information. |
| 14.4.4.1.3 | The Enrollee’s whereabouts are unknown and the post office returns Contractor mail directed to the Enrollee indicating no forwarding address (refer to 42 CFR 431.231(d) for procedures if the Enrollee’s whereabouts become known). |
| 14.4.4.1.4 | The Enrollee’s Provider prescribes a change in the level of medical care. |
| 14.4.4.1.5 | The date of action will occur in less than ten (10) Calendar Days in accordance with 42 CFR 483.12(a)(5)(ii). |
| 14.4.4.1.6 | The Contractor may shorten the period of advance notice to five (5) Calendar Days before the date of Action if the Contractor has facts indicating that Action should be taken because of probable Enrollee Fraud and the facts have been verified, if possible, through secondary sources. |
Page 372
| 14.4.4.2 | For denial of payment, at the time of any Action affecting the Claim. |
| 14.4.4.3 | For standard authorization decisions that deny or limit Covered Services, within the timeframes required in Section 11.3 of this Contract. |
| 14.4.4.4 | If the Contractor extends the timeframe for the authorization decision and issuance of Notice of Action according to Section 14.4.3 of this Contract, the Contractor shall give the Enrollee written notice of the reasons for the decision to extend if he or she did not request the extension. The Contractor shall issue and carry out its determination as expeditiously as the Enrollee’s health requires and no later than the date the extension expires. |
| 14.4.4.5 | For authorization decisions not reached within the timeframes required in Section 11.3.4 of this Contract for either standard or expedited authorizations, the Notice of Action shall be mailed on the date the timeframe expires, as this constitutes a denial and is thus an Action. |
| 14.5 | Appeal Process |
| 14.5.1 | An Appeal is the request for review of an “Action.” It is a formal petition by an Enrollee, an Enrollee’s Authorized Representative, or the Enrollee’s Provider, acting |
Page 373
| on behalf of the Enrollee with the Enrollee’s written consent, to reconsider a decision where the Enrollee or Provider does not agree with an Action taken. |
| 14.5.2 | The Enrollee, the Enrollee’s Authorized Representative, or the Provider may file an Appeal either orally or in writing. Unless the Enrollee requests expedited review, the Enrollee, the Enrollee’s Authorized Representative, or the Provider acting on behalf of the Enrollee with the Enrollee’s written consent, must follow an oral filing with a written, signed, request for Appeal. |
| 14.5.3 | Oral inquiries seeking to Appeal an action are treated as Appeals (to establish the earliest possible filing date for the Appeal), but Enrollees must confirm oral requests for Appeals in writing, unless the Enrollee requests expedited resolution. |
| 14.5.4 | The requirements of the Appeal process shall be binding for all types of Appeals, including expedited Appeals, unless otherwise established for expedited Appeals. |
| 14.5.5 | The Enrollee, the Enrollee’s Authorized Representative, or the Provider acting on behalf of the Enrollee with the Enrollee’s written consent, may file an Appeal to the Contractor during a period no less than twenty (20) Calendar Days and not to exceed ninety (90) Calendar Days from the date on the Contractor’s Notice of Action or Notice of Adverse Action. |
Page 374
| 14.5.6 | Appeals shall be filed directly with the Contractor, or its delegated representatives. The Contractor may delegate this authority to an Appeal committee, but the delegation shall be in writing. |
| 14.5.7 | The Appeals process shall provide the Enrollee, the Enrollee’s Authorized Representative, or the Provider acting on behalf of the Enrollee with the Enrollee’s written consent, a reasonable opportunity to present evidence and allegations of fact or law, in person, as well as in writing. The Contractor shall inform the Enrollee of the limited time available to provide this in case of expedited review. |
| 14.5.8 | The Appeals process shall provide the Enrollee, the Enrollee’s Authorized Representative, or the Provider acting on behalf of the Enrollee with the Enrollee’s written consent, opportunity, before and during the Appeals process, to examine the Enrollee’s case file, including Medical Records, and any other documents and records considered during the Appeals process. |
| 14.5.9 | The Appeals process shall include as parties to the Appeal the Enrollee, the Enrollee’s Authorized Representative, the Provider acting on behalf of the Enrollee with the Enrollee’s written consent, or the legal representative of a deceased Enrollee’s estate. |
| 14.5.10 | The Contractor shall establish and maintain an expedited review process for Appeals when the Contractor determines (based on a request from the Enrollee) or the |
Page 375
| Provider indicates (in making the request on the Enrollee’s behalf) that taking the time for a standard resolution could seriously jeopardize the Enrollee’s life or health or ability to attain, maintain, or regain maximum function. The Enrollee, the Enrollee’s Authorized Representative, or the Provider acting on behalf of the Enrollee with the Enrollee’s written consent, may file an expedited Appeal either orally or in writing. The Contractor shall ensure that punitive action is not taken against either a Provider who requests an expedited resolution, or a Provider that supports an Enrollee’s Appeal. |
| 14.5.11 | The Contractor shall resolve each expedited Appeal and provide a notice of disposition, as expeditiously as the Enrollee’s health condition requires, within the Government-established timeframes not to exceed three (3) Business Days after the Contractor receives the Appeal. |
| 14.5.12 | The Contractor shall resolve each Appeal and provide written notice of the disposition, as expeditiously as the Enrollee’s health condition requires but shall not exceed forty-five (45) Calendar Days from the date the Contractor receives the Appeal. For expedited reviews of an Appeal and notice to affected parties, the Contractor has no longer than seventy-two (72) hours or as expeditiously as the Enrollee’s physical or mental health condition requires. If the Contractor denies an Enrollee’s request for expedited review, it shall transfer the Appeal to the timeframe for standard appeal specified herein and shall make reasonable efforts to give the |
Page 376
| Enrollee prompt oral notice of the denial, and follow up within two (2) Calendar Days with a written notice. The Contractor shall also make reasonable efforts to provide oral notice for resolution of an expedited review of an Appeal. |
| 14.5.13 | The Contractor may extend the timeframe for standard or expedited resolution of the Appeal by up to fourteen (14) Calendar Days if the Enrollee, Enrollee’s Authorized Representative, or the Provider acting on behalf of the Enrollee with the Enrollee’s written consent, requests the extension or the Contractor demonstrates (to the satisfaction of ASES, upon its request) that there is need for additional information and how the delay is in the Enrollee’s interest. If the Contractor extends the timeframe, it shall, for any extension not requested by the Enrollee, give the Enrollee written notice of the reason for the delay. The Contractor shall inform the Enrollee of the right to file a grievance if the Enrollee disagrees with the decision to extend the timeframe. |
| 14.5.14 | The Contractor shall provide written notice of disposition. The written notice shall include: |
| 14.5.14.1 | The results of the Appeal resolution; and |
| 14.5.14.2 | For decisions not wholly in the Enrollee’s favor: |
Page 377
| 14.5.14.2.1 | The right to request an Administrative Law Hearing; |
| 14.5.14.2.2 | How to request an Administrative Law Hearing; |
| 14.5.14.2.3 | The right to continue to receive benefits pending an Administrative Law Hearing; |
| 14.5.14.2.4 | How to request the continuation of Benefits; and |
| 14.5.14.2.5 | Notification that if the Contractor’s action is upheld in a hearing, the Enrollee may liable for the cost of any continued benefits. |
| 14.6 | Administrative Law Hearing |
| 14.6.1 | The Contractor is responsible for explaining the Enrollee’s right to and the procedures for an Administrative Law Hearing. |
| 14.6.2 | The parties to the Administrative Law Hearing include ASES, the Contractor as well as the Enrollee or his or her representative, or the representative of a deceased Enrollee’s estate. |
Page 378
| 14.6.3 | If the Contractor takes an Action and the Enrollee requests an Administrative Law Hearing, ASES shall grant the Enrollee such hearing. The right to such fair hearing, how to obtain it, and the rules concerning who may represent the Enrollee at such hearing shall be explained to the Enrollee and by the Contractor. |
| 14.6.4 | ASES shall permit the Enrollee to request an Administrative Law Hearing before it within a reasonable time period, as follows: |
| 14.6.4.1 | In the event that the Enrollee first files an appeal with the Contractor, per Section 14.5 of this Contract, not less than twenty (20) Calendar Days or more than ninety (90) Calendar Days from receipt of Contractor’s Notice of Action; or |
| 14.6.4.2 | In the event that the Enrollee seeks an Administrative Law Hearing without recourse to the Contractor’s appeal process, as expeditiously as the Enrollee’s health condition requires; but no later than three (3) Business Days after ASES receives, directly from the Enrollee, a hearing request on a decision to deny a service, when ASES determines that taking the time for a standard resolution could seriously jeopardize the Enrollee’s life or health or ability to attain, maintain, or regain maximum function. |
Page 379
| 14.6.5 | The Contractor shall make available any records and any witnesses at its own expense in conjunction with a request pursuant to an Administrative Law Hearing. |
| 14.6.6 | The decision issued as a result of the Administrative Law Hearing is subject to review before the Court of Appeals of the Commonwealth of Puerto Rico. |
| 14.7 | Continuation of Benefits while the Contractor Appeal and Administrative Law Hearing are Pending |
| 14.7.1 | As used in this Section, “timely” filing means filing on or before the later of the following: |
| 14.7.1.1 | Within ten (10) Calendar Days of the Contractor mailing the Notice of Adverse Action; or |
| 14.7.1.2 | The intended effective date of the Contractor’s Action. |
| 14.7.2 | The Contractor shall continue the Enrollee’s Benefits if the Enrollee or the Enrollee’s Authorized Representative files the Appeal timely; the Appeal involves the termination, suspension, or reduction of a previously authorized course of treatment; the services were ordered by a Provider; the period covered by the original authorization has not expired; and the Enrollee requests extension of the Benefits. |
Page 380
| 14.7.3 | If, at the Enrollee’s request, the Contractor continues or reinstates the Enrollee’s Benefits while the Appeal or Administrative Law Hearing is pending, the Benefits shall be continued until one of the following occurs: |
| 14.7.3.1 | The Enrollee withdraws the Appeal or request for the Administrative Law Hearing. |
| 14.7.3.2 | Ten (10) Calendar Day pass after the Contractor mails the Notice of Adverse Action, unless the Enrollee, within the ten (10) Calendar Day timeframe, has requested an Administrative Law Hearing with continuation of Benefits until an Administrative Law Hearing decision is reached. |
| 14.7.3.3 | An Administrative Law Judge issues an Administrative Law Hearing decision adverse to the Enrollee. |
| 14.7.3.4 | The time period or service limits of a previously authorized service has been met. |
| 14.7.4 | If the final resolution of Appeal or Administrative Law Hearing is adverse to the Enrollee, that is, upholds the Contractor action, the Contractor (on behalf of ASES) may recover from the Enrollee the cost of the services furnished to the Enrollee while |
Page 381
| the Appeal / Administrative Law Hearing was pending, to the extent that they were furnished solely because of the requirements of this Section. After recoupment of the cost of the service from the Enrollee (either in full or in part), the Contractor shall submit such funds to ASES. |
| 14.7.5 | If the Contractor or ASES reverses a decision to deny, limit, or delay services that were not furnished while the Appeal / Administrative Law Hearing was pending, the Contractor shall authorize or provide this disputed services promptly and as expeditiously as the Enrollee’s health condition requires. |
| 14.7.6 | If the Contractor or ASES reverses a decision to deny authorization of services, and the Enrollee received the disputed services while the Appeal / Administrative Law Hearing was pending, those services shall be paid for in accordance with Article 16 this Contract. |
| 14.8 | Reporting Requirements |
| 14.8.1 | The Contractor shall log and track all Complaints, Grievances, Notices of Action, Appeals and Administrative Law Hearing requests (see Section 14.1.16 of this Contract for details regarding information collected). |
Page 382
| 14.8.2 | ASES may publicly disclose summary information regarding the nature of Complaints, Grievances and Appeals and related dispositions or resolutions in consumer information materials. |
| 14.8.3 | The Contractor shall submit quarterly Grievance System Reports to ASES using a format prescribed by ASES. |
| 14.9 | Remedy for Contractor Non-Compliance with Advance Directive Requirements. |
In addition to the Complaint, Grievance, and Appeal rights described in this Article, an Enrollee may lodge with ASES a complaint concerning the Contractor’s non-compliance with the Advance Directive requirements stated in Section 7.10 of this Contract.
ARTICLE 15 ADMINISTRATION AND MANAGEMENT
| 15.1 | General Provisions |
| 15.1.1 | The Contractor shall be responsible for the administration and management of all requirements of this Contract, and consistent with the Medicaid managed care regulations at 42 CFR Part 438. |
Page 383
| 15.1.2 | All costs and expenses related to the administration and management of this Contract shall be the responsibility of the Contractor. |
| 15.2 | Place of Business and Hours of Operation |
| 15.2.1 | Given that Enrollment occurs chiefly on site in the Contractor’s administrative offices, the Contractor shall ensure that its administrative offices are physically accessible to all Enrollees and fully equipped to perform all functions related to carrying out this Contract. |
| 15.2.2 | The Contractor shall maintain administrative offices in each Service Region. |
| 15.2.3 | The Contractor shall accommodate any request by ASES to visit the Contractor’s administrative offices to ensure that the offices are compliant with Americans with Disabilities Act (“ADA”) requirements for public buildings, and with all other applicable federal and Puerto Rico rules and regulations. |
| 15.2.4 | The Contractor must maintain one (1) central administrative office and an additional administrative office in each Service Region covered under this Contract. |
| 15.2.5 | The Contractor’s office shall be centrally located and in a location accessible by foot and vehicle traffic. The Contractor may establish more than one (1) administrative |
Page 384
| office within each of its Service Regions, but must designate one (1) of the offices as the central administrative office. |
| 15.2.6 | All of the Contractor’s written communications to Enrollees must contain the address of the location identified as the legal, duly licensed, central administrative office. This administrative office must be open at least between the hours of 9:00 a.m. and 5:00 p.m. Puerto Rico Time, Monday through Friday; in addition, pursuant to the Contractor’s Enrollment Outreach Plan (see Section 6.12.2 of this Contract), the Contractor’s administrative office must have extended opening hours (until 7:00 p.m.) one Business Day per week; and must be open (to the extent necessary to permit Enrollment activities) one Saturday per month, from 9:00 a.m. to 5:00 p.m. |
| 15.2.7 | The Contractor shall ensure that the office(s) are adequately staffed, throughout the Term of this Contract, to ensure that Enrollees may visit the office to enroll at any time during Contractor’s hours of operation; and to ensure that Enrollees and Providers receive prompt and accurate responses to inquiries. |
| 15.2.8 | The Contractor shall provide access to information to Enrollees through Tele MiSalud, during the hours provided in Section 6.8.3 of this Contract. |
| 15.2.9 | The Contractor shall provide access twenty-four (24) hours a day, seven (7) days per week to its Web site. |
Page 385
| 15.3 | Training and Staffing |
| 15.3.1 | The Contractor shall conduct ongoing training for all of its staff involved in Contractor’s performance of its obligations under this Contract, in all departments, to ensure appropriate functioning in all such areas and to ensure that such staff: |
| 15.3.1.1 | Understand the MiSalud program and the Medicaid managed care requirements; |
| 15.3.1.2 | Are aware of all programmatic changes; and |
| 15.3.1.3 | Are trained in the Contractor’s Cultural Competency Plan. |
| 15.3.2 | The Contractor shall submit a Staff Training Plan and a current organizational chart to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to the Staff Training Plan must be previously approved in writing by ASES. |
| 15.4 | Data Certification |
| 15.4.1 | The Contractor shall certify all data that (i) is the basis of ASES payments under this Contract pursuant to 42 CFR 438.604 and 42 CFR 438.606 or (ii) that is otherwise |
Page 386
| required to be certified by ASES. The data that must be certified include, but are not limited to, Enrollment information, Encounter Data, Claims Reports, reconciliation reports and other information reasonably required on a timely basis by ASES as a basis for payment. The data must be certified by the Authorized Signatory. The certification must attest, based on best knowledge, information, and belief, as follows: |
| 15.4.1.1 | To the accuracy, completeness and truthfulness of the data; and |
| 15.4.1.2 | To the accuracy, completeness, and truthfulness of the documents specified by ASES. |
| 15.4.2 | The Contractor shall submit the certification concurrently with the certified data. |
| 15.5 | Implementation Plan and Submission of Initial Deliverables |
| 15.5.1 | The Contractor shall develop an Implementation Plan that verifies that the Contractor will submit the Deliverables listed in the chart in Attachment 12 to this Contract, and that details any additional procedures and activities that will be accomplished during the period between the Effective Date of this Contract and the Implementation Date of this Contract. The Implementation Plan shall include coordination and cooperation with ASES and its representatives during all phases. The continued effectiveness of |
Page 387
| this Contract shall be contingent upon the Contractor’s submission and ASES’s approval of any Deliverables that, as provided in Attachment 12, were due before the Implementation Date of this Contract, and provided that ASES’s approval shall not be unreasonably withheld, conditioned or delayed. |
| 15.5.2 | The Contractor shall submit its Implementation Plan to ASES for ASES’s review and approval according to the timeframe specified in Attachment 12 to this Contract. Implementation of the Contract shall not commence prior to ASES approval. |
| 15.5.2.1 | The Contractor will not receive any additional payment to cover start up or implementation costs. |
ARTICLE 16 PROVIDER PAYMENT MANAGEMENT
| 16.1 | General Provisions |
| 16.1.1 | ASES expressly guarantees payment for all Medically Necessary Covered Services rendered to Enrollees by any Network Providers and all Providers. So long as ASES is making the Claims Payments, the Contractor shall pay Claims to Providers in the manner described in this Contract, and shall monitor the implemented compensation systems to prevent the compromise of access to services or their quality. The Contractor shall administer an effective, accurate and efficient Provider payment |
Page 388
| management function that (a) under this Contract’s arrangement adjudicates and settles Provider Claims for Covered Services that are filed within the timeframes specified by this Article and in compliance with all applicable Puerto Rico and federal laws, rules, and regulations; (b) processes Claims Payments to applicable Providers within the timeframes specified by this Article; and (c) performs third-party administration functions. |
| 16.1.2 | The Contractor shall maintain a Claims management system that can identify the date of receipt (the date the Contractor receives the Claim as indicated by the date-stamp), real-time-accurate history of actions taken on each Provider Claim (i.e. paid, denied, suspended, appealed, etc.), and the date of payment (the date of the check or other form of payment). |
| 16.1.3 | To the extent feasible, the Contractor shall implement an Automated Clearinghouse (“ACH”) mechanism that allows Providers to request and receive electronic funds transfer (“EFT”) of Claims payments. The Contractor shall encourage its Providers, as an alternative to the filing of paper-based Claims, to submit and receive Claims information through electronic data interchange (“EDI”), i.e., electronic Claims. Electronic Claims must be processed in adherence to information exchange and data management requirements specified in Article 17. As part of this Electronic Claims Management (“ECM”) function, the Contractor shall also provide on-line and phone-based capabilities to obtain Claims processing status information. |
Page 389
| 16.1.4 | If the Contractor does not make payments through an ACH system, the Contractor shall either provide a central address to which Providers must submit Claims; or provide to each Network Provider a complete list, including names, addresses, and phone number, of entities to which the Providers must submit Claims. |
| 16.1.5 | The Contractor shall notify Providers in writing of any changes in the Claims filing list at least thirty (30) Calendar Days before the effective date of the change. If the Contractor is unable to provide 30 Calendar Days of notice, it must (i) give Providers a thirty- (30) Calendar Day extension on their Claims filing deadline to ensure Claims are routed to the correct processing center and (ii) provide written notification to ASES within one (1) Business Day. |
| 16.1.6 | All Claims submitted for payment, in order to be processed, shall comply with the Clean Claim standards as established by federal regulation (42 CFR 447.45), and as described in Section 16.10.2 of this Contract. |
| 16.1.7 | The Contractor shall generate explanations of benefits and remittance advices in accordance with ASES standards for formatting, content, and timeliness. |
| 16.1.8 | The Contractor shall not pay any Claim submitted by a Provider who is excluded or suspended from the Medicare, Medicaid or CHIP programs for Fraud, Abuse or waste or otherwise included on HHS Office of the Inspector General exclusions list, or |
Page 390
| employs someone on this list. The Contractor shall not pay any Claim submitted by a Provider that is on payment hold under the authority of ASES (see Section 10.5.4 of this Contract). The Contractor shall only pay Claims that have been submitted by the Provider within ninety (90) Calendar Days of providing such service. |
| 16.2 | [Intentionally left blank]. |
| 16.3 | [Intentionally left blank]. |
| 16.4 | [Intentionally left blank]. |
| 16.5 | Payment Schedule |
| 16.5.1 | At a minimum, the Contractor shall run two (two) Provider payment cycles per month, on the same day each week, as determined by the Contractor. The Contractor shall develop a payment schedule to be submitted to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. |
| 16.5.2 | Other than for cause explicitly stated in the Provider Contract, payment to Providers made in the form of a Capitation payment shall be issued no later than the fifteenth (15th) Calendar Day of the month in which ASES issues its Claims Payment to the Contractor. Any Provider Capitation payment retained by the Contractor past this |
Page 391
| date in a given month shall accrue interest at the prevailing legal interest rate for personal loans as such rate is determined by the Board of the Office of the Commissioner of Financial Institutions, and interest shall be paid along with the Capitation payment to the Provider for that month. |
| 16.6 | Contractor Administration Responsibilities – for Vieques and Guaynabo. |
| 16.6.1 | ASES will set up a separate account from which the Contractor shall draw the necessary funding to process payments for services rendered in the Centro de Diagnostico y Tratamiento de Vieques (“Vieques CDT”); these draws shall be in accordance with ASES specifications. All draws against this account shall be substantiated through the submission of Encounter Data as prescribed in 16.8.1 and reconciled to these data on a monthly basis on a schedule to be agreed upon between ASES and the Contractor. |
| 16.6.2 | The Contractor shall coordinate with the applicable appropriate personnel of the Vieques CDT and the Grupo Medico de Guaynabo to ensure proper incorporation of the service management and reimbursement terms associated with such Provider into the Contractor’s business operations and information systems. |
Page 392
| 16.7 | Required Claims Processing Reports |
| 16.7.1 | The Contractor shall provide to ASES each fifteenth (15th) and (30th) day of each calendar month a Claims Payment Report listing all Claims submitted by Providers that are pending and have not been paid. The Claims Payment Report shall be certified by the Authorized Signatory in accordance with Sections 15.4 and 22 of this Contract. The report shall include a pre-check register with proposed payments to be made by the Contractor to the Providers. The Claims Payment Report shall not include requests for the payment of Claims that are determined not to be Medically Necessary. The format of the report shall be provided by ASES. |
| 16.7.2 | The Contractor shall provide an additional report listing all paid and denied Claims each fifteenth (15th) and (30th) day of each calendar month. The format of the report shall be provided by ASES and shall detail payments made to all Providers. |
| 16.7.2.1 | The report shall list, by Provider, Claims from the preceding month that were paid, and those that have not been made by reason of administrative delay or the Contractor’s decision to deny the Claim. |
| 16.7.3 | In the event that Providers associated with a PMG consent to the disbursement of payment directly to the PMG, the Contractor shall so specify in its report. |
Page 393
| 16.7.4 | The Contractor shall provide to ASES, each fifteenth (15th) and (30th) day of each calendar month, records or financial data related to Claims submitted but not paid by reason of accounting or by reason of Contractor decision to deny the Claim. Such data shall be submitted in a format acceptable to ASES. |
| 16.7.5 | The Contractor shall provide to PMGs, on a monthly basis, and through an electronic or machine readable media format, a detailed report classified by Enrollee, by Provider, by diagnosis, by procedure, by date of service and by real cost, of all payments made by the Contractor to the PMG. The Contractor shall provide this report to ASES at the same time the report is provided to the PMGs. |
| 16.8 | Submission of Encounter Data |
| 16.8.1 | The Contractor shall establish an efficient information system to maintain all data pertaining to Enrollee Encounters, Claims processing and rapid transmission of all the information required by ASES. |
| 16.8.2 | The PMGs must report on a quarterly basis each Encounter to the Contractor, classified by each participating Provider within the PMG, as well as the health services of each Encounter. The data shall be submitted regardless of the payment arrangement, Capitated or otherwise, agreed upon between the Contractor and the Provider. The Contractor must submit to ASES the Capitation distribution, if |
Page 394
| applicable, within each PMG as established in the formats required by ASES actuarial reports. |
| 16.8.3 | To assure that all Enrollees Encounters are registered and recorded, the Contractor shall conduct audits of Encounter data submitted by Providers. Any violations with respect to Encounter reporting shall be subject to corrective measures. The Contractor shall provide quarterly reports to ASES of all the findings and corrective measures taken with respect to the Encounter Data reporting requirements. |
| 16.8.4 | Providers shall furnish complete Encounter Data to the Contractor on a monthly basis. |
| 16.9 | Relationship With Pharmacy Benefit Manager (PBM) |
| 16.9.1 | The Contractor shall work with the PBM selected by ASES to facilitate the processing of Pharmacy Services Claims submitted by the PBM, as provided in Section 7.5.12.11 of this Contract. ASES is responsible for the funding of pharmacy claims, and the Contractor is responsible to execute the payment of the Claims to be paid to the PBMs on behalf of the network of pharmacies in accordance with the PBM contract. |
Page 395
| 16.9.2 | The Contractor acknowledges its obligation with respect to the validation and payment of Pharmacy Claims, and timely notification, and certification to ASES with respect to the process and payment of those Claims. The Contractor shall submit Pharmacy Services Claims reports in accordance with Section 18.2 of this Contract in a format approved by ASES. |
| 16.9.3 | PBMs’ switching and transaction fees are to be paid by ASES with corresponding validation by the Contractor. |
| 16.9.4 | ASES acknowledges that the Contractor is undertaking the process of validation and payment of those claims on behalf of ASES and the Contractor is not responsible in any manner for the liability and/or risk of pharmacy coverage within the Contractor responsibilities, other than for reasons solely attributable to Contractor, its employees and agents. |
| 16.9.5 | In order to facilitate Claims processing, the Contractor shall send to the PBM, on a daily basis, the Enrollee data described in Section 5.2.9 of this Contract. |
| 16.10 | Timely Payment of Claims |
| 16.10.1 | The Contractor shall comply with the timely processing of claims standards contained in section 1902(a)(37) of the Social Security Act, Section 5001(f)(2) of the American |
Page 396
| Recovery and Reinvestment Act of 2009 (ARRA) and in implementing Federal Medicaid regulations at 42 CFR 447.45(d). |
| 16.10.2 | Provider Contracts shall include the following provisions for timely payment of Clean Claims. |
| 16.10.2.1 | A Clean Claim, as defined in 42 CFR 447.45, is a Claim received by the Contractor for adjudication, which can be processed without obtaining additional information from the Provider of the service or from a Third Party, as provided in Section 22.4.5.1 of this Contract. It includes a Claim with errors originating in the Contractor’s claims system. It does not include a Claim from a Provider who is under investigation for Fraud or Abuse, or a Claim under review for Medical Necessity. |
| 16.10.2.2 | Provider Contracts shall provide that ninety-five percent (95%) of all Clean Claims must be paid by the Contractor not later than thirty (30) Calendar Days from the date of receipt of the Claim (including Claims billed by paper and electronically), and one hundred percent (100%) of all Clean Claims must be paid by the Contractor not later than fifty (50) Calendar Days from the date of receipt of the Claim. |
Page 397
| 16.10.2.3 | Any Clean Claim not paid within thirty (30) Calendar Days shall bear interest in favor of Provider on the total unpaid amount of such Claim, according to the prevailing legal interest rate fixed by the Puerto Rico Commissioner of Financial Institutions. Such interest shall be considered payable on the day following the terms of this Section 16.10, and interest shall be paid together with the Claim. If the delay in payment to a Provider is the result of the actions or omissions by the Contractor, the Contractor shall be responsible (i) for payment of any interest due to the Provider under this Section and (ii) compliance with the applicable requirements of the PR Prompt Payment Law. If the delay in payment to a Provider is the result of ASES’s failure to make timely and complete Claims Payments to the Contractor when due, ASES (and not the Contractor) shall be responsible to (i) pay any such interest due to the Provider and (ii) compliance with the applicable requirements of the PR Prompt Payment Law. |
| 16.10.3 | An Unclean Claim is any Claim that falls outside the definition of Clean Claim in Section 16.10.2.1 of this Contract. The Contractor shall include the following provisions in its Provider Contracts for timely resolution of Unclean Claims. |
| 16.10.3.1 | Ninety percent (90%) of Unclean Claims must be resolved and processed with payment by the Contractor, if applicable, not later than thirty (30) |
Page 398
| Calendar Days from the date of initial receipt of the Claim. This includes Claims billed on paper or electronically. |
| 16.10.3.2 | Of the remaining ten percent (10%) of total Unclean Claims that may remain outstanding after thirty (30) Calendar Days. |
| 16.10.3.2.1 | Nine percent (9%) of the Unclean Claims must be resolved and processed with payment by the Contractor, if applicable, not later than ninety (90) Calendar Days from the date of initial receipt (including Claims billed on paper and those billed electronically); and |
| 16.10.3.2.2 | One percent (1%) of the Unclean Claims must be resolved and processed with payment by the Contractor, if applicable, not later than one year (12 months) from the date of initial receipt of the Claim (including Claims billed on paper and those billed electronically). |
| 16.10.3.2.3 | The Contractor shall submit an Unclean Claims Report each fifteenth (15th) and (30th) day of each calendar month in a format to be provided by ASES. The Contractor shall continue to submit an Unclean Claims Report until all such Claims have been resolved or through the Runoff Period, whichever is longer. |
Page 399
| 16.10.4 | The Contractor shall not establish any administrative procedures, such as administrative audits, authorization number, or other formalities under the control of the Contractor, which could prevent the Provider from submitting a Clean Claim. |
| 16.10.5 | The foregoing timely payment standards are more stringent than those required in the federal regulations, at 42 CFR 447.45(d). The Contractor shall include the foregoing standards in each Provider Contract and ASES will submit proof of this alternative payment agreement to CMS. |
| 16.10.6 | The Contractor shall deliver to Providers, within fifteen (15) Calendar Days of award of the Provider Contract (along with the Provider guidelines described in Section 10.2.1 of this Contract), Claims coding and processing guidelines for the applicable Provider type, and the definition of a Clean Claim to be applied. |
| 16.10.7 | The Contractor shall give Providers ninety (90) Calendar Days notice in advance of the effective date of any change in Claims coding and processing deadlines. |
| 16.11 | Contractor Denial of Claims and Resolution of Contractual and Claims Disputes |
| 16.11.1 | Not later than the fifth (5th) Business Day after the receipt of a Provider Claim that the Contractor has deemed not to meet the Clean Claim requirements, the Contractor |
Page 400
| shall suspend the Claim and request in writing (notification via e-mail, the Contractor’s Web site, or an interim remittance advice satisfies this requirement) all outstanding information such that the Claim can be deemed clean. Upon receipt of all the requested information from the Provider, the Contractor shall complete processing of the Claim in accordance with the standards outlined in Section 16.10 of this Contract. |
| 16.11.2 | Claims suspended for additional information must be closed (paid or denied) such that compliance with the timely payment rules outlined in Section 16.10 of this Contract is achieved. |
| 16.11.3 | The Contractor must process, and finalize, all appealed Claims to a paid or denied status within thirty (30) Calendar Days of receipt of the Appealed Claim; for Claims for which the Contractor has requested further information, per Section 16.11.1 of this Contract, the Contractor shall pay or deny the Claim within thirty (30) Calendar Days of receipt of the requested information. |
| 16.11.4 | The Contractor shall send Providers written notice (notification via e-mail, surface mail, the Contractor’s Web site, or a remittance advice satisfies this requirement) for each Claim that is denied, including the reason(s) for the denial, the date the Contractor received the Claim, and a reiteration of the outstanding information required from the Provider to adjudicate the Claim. |
Page 401
| 16.11.5 | In situations in which the Contractor denies a Provider’s Claim for services, and the Provider disputes the denial, as provided in Section 16.11.6 of this Contract, the Contractor shall not Withhold payment pending final resolution of the dispute, but instead shall pay the Claim within thirty (30) Calendar Days of the Contractor’s receipt of the Provider’s written complaint and request for mediation (see Section 16.11.6.2.1 of this Contract). The Contractor shall seek recoupment of the paid Claim only in the event that the dispute is resolved, at the level of the mediation described in Section 16.11.6.2.1 of this Contract, in the Contractor’s favor. |
| 16.11.6 | Provider Dispute Resolution System |
| 16.11.6.1 | The Contractor shall establish and use a procedure to resolve billing, payment, and other administrative disputes between Providers and the Contractor arising under Provider Contracts including: |
| 16.11.6.1.1 | A mediation system for resolution of Provider disputes of denied Claims; and |
| 16.11.6.1.2 | A Provider complaint resolution process implemented by the Contractor to address, among others, lost or incomplete Claims forms or electronic submissions; Contractor requests for additional |
Page 402
| explanation as to services or treatment rendered by a Provider; and inappropriate or unapproved Referrals issued by Providers. |
| 16.11.6.1.3 | This dispute resolution system shall exclude Grievances filed by Providers on behalf of Enrollees pursuant to Section 14.3 of this Contract. |
| 16.11.6.2 | Provider Complaints Concerning Denied Claims |
| 16.11.6.2.1 | If there is no agreement between the Contractor and the Provider on a denied Claim, a third party, external to the Contractor and the Provider and chosen by mutual agreement, shall be appointed to adjudicate the denial, upon the Provider’s submission of a written complaint and request for mediation. The third party shall render his or her decision no more than thirty (30) Calendar Days from the date of the Provider’s request for third-party mediation. If there is no agreement on the third party’s selection, he or she shall be appointed by ASES, and, subject to the appeal rights described in this Section, the parties will comply with the third party’s decision. The party adversely affected shall pay for the third party’s service fees. If both the Provider and the Contractor have caused an error, the third party shall determine the percentage |
Page 403
| attributable to each party, and payment to the third party shall be in accordance with percentage of responsibility. |
| 16.11.6.2.2 | The party adversely affected by the mediator’s decision may pursue an Administrative Law Hearing. The parties to the Administrative Law Hearing shall be the Contractor and the Provider. ASES shall grant a Provider or Contractor request for an Administrative Law Hearing, provided that the Provider or Contractor, as the case may be, submits a written appeal, accompanied by supporting documentation, not more than thirty (30) Calendar Days following the Provider’s or Contractor’s receipt of the mediator’s written decision. ASES, at its sole expense, shall contract with an independent party to serve as the examining officer in any such Administrative Law Hearing. |
| 16.11.6.3 | Other Disputes Arising Under the Provider Contract |
| 16.11.6.3.1 | For any dispute between the Provider and Contractor arising under the Provider Contract, other than a disputed denial of a Claim, the Contractor shall implement an internal dispute resolution system, which shall include the opportunity for an aggrieved Provider to submit a timely written complaint to the Contractor. The Contractor shall issue a written decision on the Provider’s complaint within |
Page 404
| fifteen (15) Calendar Days of receipt of the Provider’s written complaint. A Contractor written decision that is in any way adverse to the Provider shall include an explanation of the grounds for the decision and a notice of the Provider’s right to and procedures for an Administrative Law Hearing within ASES. |
| 16.11.6.3.2 | If the Provider is not satisfied with the decision on its complaint within the Contractor’s dispute resolution system, the Provider may pursue an Administrative Law Hearing. The parties to the Administrative Law Hearing shall be the Contractor and the Provider. ASES shall grant a Provider request for an Administrative Law Hearing, provided that the Provider submits a written appeal, accompanied by supporting documentation, not more than thirty (30) Calendar Days following the Provider’s receipt of the Contractor’s written decision. ASES, at its sole expense, shall contract with an independent party to serve as the examining officer in any such Administrative Law Hearing. |
| 16.11.6.4 | Judicial Review. A decision issued as a result of the Administrative Law Hearing provided for in Section 16.11.6.2.2 or 16.11.6.3.2 of this Contract shall be subject to review before the Court of Appeals of the Commonwealth of Puerto Rico. |
Page 405
| 16.11.7 | [Intentionally left blank]. |
| 16.11.8 | ASES Guarantee of Payment |
| 16.11.8.1 | ASES expressly guarantees payment for all Covered Services and Benefits rendered to Enrollees by any Provider pursuant to the terms of this Contract. Subject to Section 16.11.8.10 of this Contract, the Contractor shall use such ASES Claims Payments to compensate Providers for all Covered Services and Benefits, and its compensation systems will not compromise access to services or their quality. |
| 16.11.8.2 | The insolvency, liquidation, bankruptcy or breach of contract by ASES, the Contractor, a PMG or Provider shall not release said party from its corresponding obligation to pay for Covered Services rendered as authorized herein. |
| 16.11.8.3 | ASES’s obligation to guarantee payment to all PMGs, Providers or Subcontractors for services rendered by them in connection with this Contract is subject to compliance with established claim proceedings and requisites set forth in this Contract. |
Page 406
| 16.11.8.4 | If Providers or Subcontractors claim direct substitute payments due from the Contractor or PMG to ASES in accordance with this Section, then ASES shall deduct any amounts payable to Providers or Subcontractors from amounts due to a PMG as Claims Payments. |
| 16.11.8.5 | ASES agrees to pay direct substitute payments to the PMGs and/or Providers according to the payment schedule agreed in their respective contracts. |
| 16.11.8.6 | ASES shall Immediately notify the Contractor in writing in the event sufficient funds are not available to satisfy ASES’s payment obligations under this Contract when due. |
| 16.11.8.7 | [Intentionally left blank]. |
| 16.11.8.8 | [Intentionally left blank]. |
| 16.11.8.9 | [Intentionally left blank]. |
| 16.11.8.10 | The Contractor shall have no obligation to pay Claims to Providers for Covered Services to the extent that ASES has failed to make timely and complete payments of the Claims Payment as required under Section 21 of |
Page 407
| this Contract and shall not be subject to any prompt payment law penalties (including the PR Prompt Payment Law) for such non-payment or any interest to Providers. ASES agrees to guaranty any interest due to the Providers and penalties under any prompt payment laws (including the PR Prompt Payment Law) as a result of such non-payment. |
| 16.12 | Contractor Recovery from Providers |
| 16.12.1 | When ASES or the Contractor determines after the fact that it has paid a Claim incorrectly, or when ASES or the Contractor, per Section 16.11.5 of this Contract, is entitled to seek recoupment after a mediation concerning a denied Claim has been resolved in the Contractor’s favor, ASES or the Contractor (on behalf of ASES) may request applicable reimbursement from the Provider through written notice, stating the basis for the request. The notice shall list the Claims and the amounts to be recovered. |
| 16.12.2 | The Provider will have a period of ninety (90) Calendar Days to make the requested payment, to agree to ASES or the Contractor’s retention of said payment (on behalf of ASES), or to dispute the recovery action following the process described in Section 16.11 of this Contract. To the extent the Provider requests additional time to make the requested payment, the Contractor may agree to a payment plan; however, the |
Page 408
| Contractor shall not accept any payment plan in excess of one (1) year, unless the Contractor receives advance written authorization from ASES. |
| 16.12.3 | To the extent the Contractor recoups amounts on behalf of ASES, the Contractor shall remit such amounts to ASES within fourteen (14) Business Days. The Contractor shall not be authorized to reduce any amount, unless the Contractor receives advance written authorization from ASES. For the avoidance of doubt, the Contractor shall not retain any amount of the recouped funds for such administrative service. |
ARTICLE 17 INFORMATION MANAGEMENT AND SYSTEMS
| 17.1 | General Provisions |
| 17.1.1 | The Contractor shall have Information management processes and Information Systems (hereafter referred to as Systems) that enable it to meet MiSalud requirements, ASES and federal reporting requirements, all other Contract requirements, and any other applicable Puerto Rico and federal laws, rules and regulations including but not limited to the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and associated regulations and 42 CFR 438.242. |
Page 409
| 17.1.2 | The Contractor’s Systems shall possess capacity sufficient to handle the workload projected for the start of the program and will be scalable and flexible so they can be adapted as needed, within negotiated timeframes, in response to program or Enrollment changes. |
| 17.1.3 | The Contractor’s Systems shall have the capability of adapting to any future changes necessary as a result of modifications to the service delivery system and its requirements, including data collection, records and reporting based upon unique Enrollee and Provider identifiers to track services and expenditures across funding streams. The Systems shall be scalable and flexible so they can be adapted as needed, within negotiated timeframes, in response to changes in Contract requirements, increases in enrollment estimates, etc. The System architecture shall facilitate rapid application of the more common changes that can occur in the Contractor’s operation, including but not limited to: |
| 17.1.3.1 | Changes in pricing methodology; |
| 17.1.3.2 | Rate changes; |
| 17.1.3.3 | Changes in utilization management criteria; |
| 17.1.3.4 | Additions and deletions of Provider types; and |
Page 410
| 17.1.3.5 | Additions and deletions of procedure, diagnosis and other service codes. |
| 17.1.4 | The Contractor shall provide secure, online access to select system functionality to at least three (3) ASES personnel to facilitate resolution of Enrollee inquiries and to research Enrollee-related issues as needed. |
| 17.1.5 | The Contractor shall participate in Systems Work Groups organized by ASES. The Systems Work Groups will meet on a designated schedule as agreed to by ASES and the MiSalud Plans and the MBHO. |
| 17.1.6 | The Contractor shall provide a continuously available electronic mail communication link (E-mail system) with ASES. This system shall be: |
| 17.1.6.1 | Available from the workstations of the designated Contractor contacts; and |
| 17.1.6.2 | Capable of attaching and sending documents created using software products other than Contractor systems, including the Government of Puerto Rico’s currently installed version of Microsoft Office and any subsequent upgrades as adopted. |
Page 411
| 17.2 | Global System Architecture and Design Requirements |
| 17.2.1 | The Contractor shall comply with federal and Puerto Rico policies, standards and regulations in the design, development and/or modification of the Systems it will employ to meet the aforementioned requirements and in the management of Information contained in those Systems. Additionally, the Contractor shall adhere to ASES and Puerto Rico-specific system and data architecture standards and/or guidelines. |
| 17.2.2 | The Contractor’s Systems shall: |
| 17.2.2.1 | Be (i) SQL and ODBC compliant and/or have the connectivity required to for proper system communication with ASES’s system, and (ii) capable of storing in relational databases all Enrollee-related information as required by ASES; |
| 17.2.2.2 | Adhere to Internet Engineering Task Force/Internet Engineering Standards Group standards for data communications, including TCP and IP for data transport; |
| 17.2.2.3 | Conform to HIPAA standards for data and document management; |
Page 412
| 17.2.2.4 | Contain controls to maintain information integrity. These controls shall be in place at all appropriate points of processing. The controls shall be tested in periodic and spot audits following a methodology to be developed jointly by and mutually agreed upon by the Contractor and ASES; and |
| 17.2.2.5 | Partner with ASES in the development of transaction/event code set, data exchange and reporting standards not specific to HIPAA or other federal effort and will conform to such standards as stipulated in the plan to implement the standards. |
| 17.2.3 | Where Web services are used in the engineering of applications, the Contractor’s Systems shall conform to World Wide Web Consortium (W3C) standards such as XML, UDDI, WSDL and SOAP so as to facilitate integration of these Systems with ASES and other State systems that adhere to a service-oriented architecture. |
| 17.2.4 | Audit trails shall be incorporated into all Systems to allow information on source data files and documents to be traced through the processing stages to the point where the Information is finally recorded. The audit trails shall: |
Page 413
| 17.2.4.1 | Contain a unique log-on or terminal ID, the date, and time of any create/modify/delete action and, if applicable, the ID of the system job that effected the action; |
| 17.2.4.2 | Have the date and identification “stamp” displayed on any on-line inquiry; |
| 17.2.4.3 | Have the ability to trace data from the final place of recording back to its source data file and/or document shall also exist; |
| 17.2.4.4 | Be supported by listings, transaction Reports, update Reports, transaction logs, or error logs; |
| 17.2.4.5 | Facilitate auditing of individual Claim records as well as batch audits; and |
| 17.2.4.6 | Be maintained for seven (7) years in either live and/or archival systems. The duration of the retention period may be extended at the discretion of and as indicated to the Contractor by ASES as needed for ongoing audits or other purposes, subject to and in accordance with Section 32 of this Contract. |
| 17.2.5 | The Contractor shall house indexed images of documents used by Enrollees and Providers to transact with the Contractor in the appropriate database(s) and document |
Page 414
| management systems so as to maintain the logical relationships between certain documents and certain data. The Contractor shall follow all applicable requirements for the management of data in the management of documents. |
| 17.2.6 | The Contractor shall institute processes to insure the validity and completeness of the data it submits to ASES. At its discretion, ASES will conduct general data validity and completeness audits using industry-accepted statistical sampling methods. Data elements that will be audited include but are not limited to: Enrollee ID, date of service, Provider ID, category and sub category (if applicable) of service, diagnosis codes, procedure codes, revenue codes, date of Claim processing, and date of Claim payment. |
| 17.2.7 | Where a System is herein required to, or otherwise supports, the applicable batch or on-line transaction type, the system shall comply with HIPAA-standard transaction code sets. |
| 17.2.8 | The Contractor shall assure that all Contractor staff is trained in all HIPAA requirements, as applicable. |
| 17.2.9 | The layout and other applicable characteristics of the pages of Contractor Web sites shall be compliant with Federal “section 508 standards” and Web Content Accessibility Guidelines developed and published by the Web Accessibility Initiative. |
Page 415
| 17.3 | System and Data Integration Requirements |
| 17.3.1 | The Contractor’s applications shall be able to interface with ASES’s systems for purposes of data exchange and will conform to standards and specifications set by ASES. These standards and specifications are detailed in Attachment 9. |
| 17.3.2 | The Contractor’s System(s) shall be able to transmit and receive transaction data to and from ASES’s systems as required for the appropriate processing of Claims. |
| 17.3.3 | Each month the Contractor shall generate Encounter Data files from its claims management system(s) and/or other sources. The files will contain settled Claims and Claim adjustments and Encounter Data from Providers for the most recent month for which all such transactions were completed. The Contractor shall provide these files electronically to ASES and/or its Agent in adherence to the procedure, content standards and format indicated in Attachment 9. The Contractor shall make changes or corrections to any systems, processes or data transmission formats as needed to comply with Encounter Data quality standards as originally defined or subsequently amended. |
| 17.3.4 | The Contractor’s System(s) shall be capable of generating files in the prescribed formats for upload into ASES Systems used specifically for program integrity and compliance purposes. |
Page 416
| 17.3.5 | The Contractor’s System(s) shall possess mailing address standardization functionality in accordance with US Postal Service conventions. |
| 17.4 | System Access Management and Information Accessibility Requirements |
| 17.4.1 | The Contractor’s System shall employ an access management function that restricts access to varying hierarchical levels of system functionality and Information. The access management function shall: |
| 17.4.1.1 | Restrict access to Information on a “need to know” basis, e.g. users permitted inquiry privileges only will not be permitted to modify information; |
| 17.4.1.2 | Restrict access to specific system functions and information based on an individual user profile, including inquiry only capabilities; global access to all functions will be restricted to specified staff jointly agreed to by ASES and the Contractor; and |
| 17.4.1.3 | Restrict attempts to access system functions to three (3), with a system function that automatically prevents further access attempts and records these occurrences. |
Page 417
| 17.4.2 | The Contractor shall make System Information available to duly Authorized Representatives of ASES and other Puerto Rico and federal agencies to evaluate, through inspections or other means, the quality, appropriateness and timeliness of services performed. |
| 17.4.3 | The Contractor shall have procedures to provide for prompt transfer of System Information upon request to other Network or Out-of-Network Providers for the medical management of the Enrollee in adherence to HIPAA and other applicable requirements. |
| 17.4.4 | All Information, whether data or documents, and reports that contain or make references to said Information, involving or arising out of this Contract are owned by ASES except as provided in Section 27.1.2 of this Contract. The Contractor is expressly prohibited from sharing or publishing ASES Data without the prior written consent of ASES. In the event of a dispute regarding the sharing or publishing of ASES Data, ASES’s decision on the matter shall be final and not subject to appeal. |
| 17.5 | Systems Availability and Performance Requirements |
| 17.5.1 | The Contractor shall ensure that Enrollee and Provider portal and/or phone-based functions and information, such as confirmation of Contractor Enrollment (CCE) and electronic claims management (ECM), Enrollee services and Provider services, are |
Page 418
available to the applicable System users twenty-four (24) hours a day, seven (7) Days a week, except during periods of scheduled System Unavailability agreed upon by ASES and the Contractor. Unavailability caused by events outside of a Contractor’s Span of Control is outside of the scope of this requirement.
| 17.5.2 | The Contractor shall ensure that at a minimum all other System functions and Information are available to the applicable system users between the hours of 7:00 a.m. and 7:00 p.m. Monday through Friday. |
| 17.5.3 | The Contractor shall develop an automated method of monitoring the CCE and ECM functions on at least a thirty (30) minute basis twenty-four (24) hours a day, seven (7) days per week. |
| 17.5.4 | Upon discovery of any problem within its Span of Control that may jeopardize System availability and performance as defined in this Section of the Contract, the Contractor shall notify the applicable ASES staff in person, via phone, electronic mail and/or surface mail. |
| 17.5.5 | The Contractor shall deliver notification as soon as possible but no later than 7:00 pm if the problem occurs during the business day and no later than 9:00 am the following business day if the problem occurs after 7:00 pm. |
Page 419
| 17.5.6 | Where the operational problem results in delays in report distribution or problems in on-line access during the business day, the Contractor shall notify the applicable ASES staff within fifteen (15) minutes of discovery of the problem, in order for the applicable work activities to be rescheduled or be handled based on System Unavailability protocols. |
| 17.5.7 | The Contractor shall provide to appropriate ASES staff information on System Unavailability events, as well as status updates on problem resolution. These up-dates shall be provided on an hourly basis and made available via electronic mail, telephone and, if applicable, the Contractor’s Web site. |
| 17.5.8 | The following rules govern Unscheduled System Unavailability for CCE functions, ECM functions, and all other functions. |
| 17.5.8.1 | CCE Functions |
| 17.5.8.1.1 | Unscheduled System Unavailability of CCE functions caused by the failure of systems and telecommunications technologies within the Contractor’s Span of Control will be resolved, and the restoration of services implemented, within thirty (30) minutes of the official declaration of System Unavailability. |
Page 420
| 17.5.8.1.2 | From the Effective Date of the Contract through December 31, 2011, Unscheduled System Unavailability for CCE functions shall be remedied within sixty (60) minutes of the official declaration of System Unavailability, if unavailability occurs during normal business hours; or within sixty (60) minutes of the start of the next Business Day, if unavailability occurs outside business hours. |
| 17.5.8.1.3 | Throughout the Contract Term, the Contractor shall have in place a method to validate eligibility manually twenty-four (24) hours per day, seven (7) days a week as a contingency to any Unscheduled Systems Unavailability for CCE functions. |
| 17.5.8.2 | ECM Functions. Unscheduled System Unavailability of ECM functions caused by the failure of systems and technologies within the Contractor’s Span of Control will be resolved, and the restoration of services implemented, within sixty (60) minutes of the official declaration of System Unavailability, if unavailability occurs during normal business hours; or within sixty (60) minutes of the start of the next Business Day, if unavailability occurs outside business hours. |
| 17.5.8.3 | All Other Contractor System Functions. Unscheduled System Unavailability of all other Contractor System functions caused by systems |
Page 421
| and telecommunications technologies within the Contractor’s Span of Control shall be resolved, and the restoration of services implemented, |
| 17.5.8.3.1 | within four (4) hours of the official declaration of Unscheduled System Unavailability, when unavailability occurs during business hours, and |
| 17.5.8.3.2 | within two (2) hours of the start of the next Business Day, when unavailability occurs during non-business hours. |
| 17.5.9 | [Intentionally left blank]. |
| 17.5.10 | Cumulative System Unavailability caused by systems and telecommunications technologies within the Contractor’s Span of Control shall not exceed one (1) hour during any continuous five (5) day period for functions that affect MiSalud Enrollees and services. For functions that do not affect MiSalud Enrollees, Cumulative System Unavailability caused by systems and telecommunications technologies within the Contractor’s Span of Control shall not exceed four (4) hours during any continuous five (5) Business Day period. |
| 17.5.11 | The Contractor shall not be responsible for the availability and performance of systems and telecommunications technologies outside of the Contractor’s Span of Control. |
Page 422
| 17.5.12 | Full written documentation that includes a Corrective Action Plan, describing how the problem will be prevented from occurring again, shall be delivered within five (5) Business Days of the problem’s occurrence. |
| 17.5.13 | Regardless of the architecture of its Systems, the Contractor shall develop and be continually ready to invoke a Business Continuity and Disaster Recovery (BC-DR) plan that at a minimum addresses the following scenarios: (a) the central computer installation and resident software are destroyed or damaged, (b) System interruption or failure resulting from network, operating hardware, software, or operational errors that compromises the integrity of transactions that are active in a live system at the time of the outage, (c) System interruption or failure resulting from network, operating hardware, software or operational errors that compromises the integrity of data maintained in a live or archival system, (d) System interruption or failure resulting from network, operating hardware, software or operational errors that does not compromise the integrity of transactions or data maintained in a live or archival system but does prevent access to the System, i.e. causes unscheduled System Unavailability. |
| 17.5.14 | The Contractor shall on an annual basis test its BC-DR plan through simulated disasters and lower level failures in order to demonstrate to ASES that it can restore System functions per the standards outlined elsewhere in this Section 17.5 of the |
Page 423
| Contract. The results of these tests shall be reported to ASES within thirty (30) Calendar Days of completion of said tests. |
| 17.5.15 | In the event that the Contractor fails to demonstrate in the tests of its BC-DR plan that it can restore system functions per the standards outlined in this Contract, the Contractor shall be required to submit to ASES a Corrective Action Plan that describes how the failure will be resolved. The Corrective Action Plan will be delivered within five (5) Business Days of the conclusion of the test. |
| 17.5.16 | The Contractor shall submit a monthly Systems Availability and Performance Report to ASES. |
| 17.6 | System Testing and Change Management Requirements |
| 17.6.1 | The Contractor shall absorb the cost of routine maintenance, inclusive of defect correction, System changes required to effect changes in Puerto Rico and federal statute and regulations, and production control activities, of all Systems within its Span of control. |
| 17.6.2 | The Contractor shall respond to ASES reports of System problems not resulting in System Unavailability according to the following timeframes: |
Page 424
| 17.6.2.1 | Within five (5) Calendar Days of receipt the Contractor shall respond in writing to notices of system problems. |
| 17.6.2.2 | Within fifteen (15) Calendar Days, the correction will be made or a Requirements Analysis and Specifications document will be due. |
| 17.6.3 | The Contractor shall correct the deficiency by an effective date to be determined by ASES. |
| 17.6.4 | Contractor systems will have a system-inherent mechanism for recording any change to a software module or subsystem. |
| 17.6.5 | The Contractor shall put in place procedures and measures for safeguarding ASES from unauthorized modifications to Contractor Systems. |
| 17.6.6 | Unless otherwise agreed to in advance by ASES, scheduled System Unavailability to perform System maintenance, repair and/or upgrade activities to Contractor’s CCE systems shall take place between 11 p.m. on a Saturday and 6 a.m. on the following Sunday. |
| 17.6.7 | The Contractor shall work with ASES pertaining to any testing initiative as required by ASES. |
Page 425
| 17.6.8 | The Contractor shall provide sufficient system access to allow verification of system functionality, availability and performance by ASES during the times required by ASES prior to the Implementation Date and as subsequently required during the term of the Contract. |
| 17.7 | System Security and Information Confidentiality and Privacy Requirements |
| 17.7.1 | The Contractor shall provide for the physical safeguarding of its data processing facilities and the systems and information housed therein. The Contractor shall provide ASES with access to data facilities upon ASES’s request. The physical security provisions shall be in effect for the life of this Contract. |
| 17.7.2 | The Contractor shall restrict perimeter access to equipment sites, processing areas, and storage areas through a card key or other comparable system, as well as provide accountability control to record access attempts, including attempts of unauthorized access. |
| 17.7.3 | The Contractor shall include physical security features designed to safeguard processor site(s) through required provision of fire retardant capabilities, as well as smoke and electrical alarms, monitored by security personnel. |
Page 426
| 17.7.4 | The Contractor shall ensure that the operation of all of its systems is performed in accordance with Puerto Rico and federal regulations and guidelines related to security and confidentiality and meet all privacy and security requirements of HIPAA regulations. |
| 17.7.5 | The Contractor will put in place procedures, measures and technical security to prohibit unauthorized access to the regions of the data communications network inside of a Contractor’s Span of Control. |
| 17.7.6 | The Contractor shall ensure compliance with: |
| 17.7.6.1 | 42 CFR Part 431 Subpart F (confidentiality of information concerning applicants and Enrollees of public medical assistance programs); |
| 17.7.6.2 | 42 CFR Part 2 (confidentiality of alcohol and drug abuse records); and |
| 17.7.6.3 | Special confidentiality provisions in Puerto Rico or federal law related to people with HIV/AIDS and mental illness. |
| 17.7.7 | The Contractor shall provide its Enrollees with a privacy notice as required by HIPAA. The Contractor shall provide ASES with a copy of its Privacy Notice for its filing. |
Page 427
| 17.8 | Information Management Process and Information Systems Documentation Requirements |
| 17.8.1 | The Contractor shall ensure that written System Process and Procedure Manuals document and describe all manual and automated system procedures for its information management processes and information systems. |
| 17.8.2 | The System User Manuals shall contain information about, and instructions for, using applicable System functions and accessing applicable system data. |
| 17.8.3 | When a System change that would alter the conditions and services agreed upon in this Contract is subject to ASES sign off, the Contractor shall draft revisions to the appropriate manuals prior to ASES sign off of the change. |
| 17.8.4 | Updates to the electronic version of these manuals shall occur in real time; updates to the printed version of these manuals shall occur within ten (10) Business Days of the update taking effect. |
| 17.9 | Reporting Functionality Requirements |
| 17.9.1 | The Contractor’s Systems shall have the capability of producing a wide variety of reports that support program management, policymaking, quality improvement, |
Page 428
| program evaluation, analysis of fund sources and uses, funding decisions and assessment of compliance with federal and Puerto Rico requirements. |
| 17.9.2 | The Contractor shall support a mechanism for obtaining service and expenditure reports by funding source, Provider, Provider Type or other characteristic; and Enrollee, Enrollee Group/Category or other characteristic. |
| 17.9.3 | The Contractor shall extend access to this mechanism to select ASES personnel in a secure manner to access data, including program and fiscal information regarding Enrollees served, services rendered, etc. and the ability for said personnel to develop and/or retrieve reports. This requirement could be met by the provision of access to a decision support system/data warehouse. The Contractor shall provide training in and documentation on the use of this mechanism. |
| 17.10 | Community Health Record and Health Information Exchange (HIE) Requirements |
| 17.10.1 | The Contractor shall participate in any community health record and HIE efforts designed to tie multiple data elements and service, Enrollee and Provider records into a data warehouse and/or HIE solution that shall include, but not be limited to, claims/encounter information, formulary information, Medically Necessary service |
Page 429
| information, and a listing of Providers by specialty. At such time that ASES requires, the Contractor shall participate and cooperate with this effort. |
| 17.10.2 | The record format and the design of the mechanism for accessing the community health record and/or HIE solution shall comply with HIPAA, other federal and all Puerto Rico privacy and confidentiality regulations. |
| 17.10.3 | The Contractor shall work with Network Providers and staff to encourage use of these solutions. |
ARTICLE 18 REPORTING
| 18.1 | General Requirements |
| 18.1.1 | The Contractor shall comply with all the reporting requirements established by ASES in this Article 18. ASES has provided the Contractor with the appropriate reporting formats, data elements, instructions, and/or submission timetables in this Article 18. The Parties may upon mutual agreement, change the content, format or frequency of such reports. |
| 18.1.2 | ASES may, at its discretion, require the Contractor to submit additional reports not otherwise included in Section 18.2 of this Contract, both ad hoc and recurring |
Page 430
(collectively, the “Additional Reports”). If ASES requests any revisions or corrections to the reports already submitted, the Contractor shall make the changes and re-submit the reports, according to the time period and format specified by ASES in Section 18.1.4 below.
| 18.1.3 | All reports containing information about a Provider must include the Provider’s NPI, if applicable. |
| 18.1.4 | The Contractor shall submit all reports to ASES, unless indicated otherwise in this Contract, according to the schedule below: |
| DELIVERABLES |
DUE DATE | |
| Weekly Reports | Friday of the following week | |
| Each fifteenth (15th) and (30th) day of each calendar month Reports | The fifteenth (15th) and (30th) day of each calendar month | |
| Monthly Reports | 5th Calendar Day of the following month | |
| Quarterly Reports | 30th Calendar Day of the following month | |
| Annual Reports | Ninety (90) Calendar Days after the end of the calendar year | |
| Additional Reports | Within ten (10) Business Days of the date of the request (or such shorter period if circumstances so require subject to agreement by the Parties) | |
Page 431
| 18.1.5 | The Contractor shall submit all reports to ASES in the manner and format prescribed by ASES. |
| 18.1.6 | The Contractor shall transmit to and receive from ASES all transactions and code sets in the appropriate standard formats as specified under HIPAA and as directed by ASES, so long as ASES’s direction does not conflict with federal law. |
Page 432
| 18.2 | Specific Requirements |
The following is an overview of the Contract reporting requirements by Section. This list constitutes all reports required for the Contractor (collectively, the “Reports”). . ASES has the discretion to add Additional Reports pursuant to Section 18.1.2 of this Contract as deemed appropriate.
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Contractor Responsibilities – Enrollment (Article 5) | Daily
Within One Business Day of change |
Report on new Enrollments
Enrollment Database: notify ASES when Database is updated to reflect a change in the place of residence of an Enrollee |
Page 433
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Covered Services (Article 7) |
Quarterly
Quarterly |
Report on EPSDT screening
Report on the case management services received by Enrollees with specific chronic conditions and associated outcomes | ||
| Quarterly |
Report on number of Enrollees diagnosed with predicate conditions for disease management services | |||
| Quarterly |
Report on the Maternal and Pre-Natal Wellness Plan | |||
Page 434
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Provider Contracting (Article 10) |
Quarterly | Reconciliation report of advance payments made to State Health Facilities | ||
| Quarterly | Report on Physician Incentive Plan | |||
| Utilization Management (Article 11) |
Monthly | Health Care Data Reports | ||
| Quarterly |
Reports on:
Provider Credentialing
Network and Out-of Network Providers
Ratio of Enrollees to PCPs
Utilization of Diabetes Disease Management | |||
Page 435
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Utilization of Asthma Disease Management
Utilization of Hypertension Disease Management
EPSDT Utilization
Tele MiSalud Utilization
Preventive Services Utilization
Pharmacy Services Utilization
Dental Services Utilization
ER Utilization by Region and by PMG |
Page 436
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Prenatal Care Utilization
Covered Population by Municipality, Group, Age, and Gender | ||||
| Quality Improvement (Article 12) |
Quarterly | Various HEDIS medical care and Access measures listed in Section 12.5.3 of this Contract; Preventive Clinical Programs; Emergency Room Use Indicators | ||
| Annually |
Report on HEDIS Measures in the areas of Prevention and Screening, Respiratory Conditions, Cardiovascular Conditions, and Access / Availability of Care | |||
Page 437
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Fraud and Abuse (Article 13) |
Quarterly | Report on preliminary investigations of Fraud and Abuse | ||
| Within one Business Day of obtaining knowledge | Disclosure of persons debarred, suspended, or excluded from participation in the Medicaid, Medicare or CHIP Programs | |||
| Grievance System (Article 14) |
Quarterly | Report on Enrollee complaints, Grievances, Notices of Action, Appeals, and Administrative Law Hearing Requests | ||
| Provider Payment Management (Article 16) |
Each fifteenth (15th) and (30th) day of each calendar month | Claims Payment Report | ||
Page 438
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Each fifteenth (15th) and (30th) day of each calendar month | Report listing all paid and denied Claims | |||
| Monthly | Encounter Data | |||
| Quarterly | Findings and corrective measures taken with respect to encounter registration and reporting | |||
| Each fifteenth (15th) and (30th) day of each calendar month | Pharmacy Claims report | |||
Page 439
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Each fifteenth (15th) and (30th) day of each calendar month | Unclean Claims Report | |||
| Information Systems (Article 17) | Monthly | Systems Availability and Performance Report | ||
| Payment for Services (Article 21) | Quarterly | Actuarial Report | ||
| Monthly | IBNR report | |||
| Monthly | Administrative Fee Disbursement Report | |||
| Quarterly | PMG IBNR report | |||
| Financial Management (Article 22) | Quarterly | Contractor’s findings regarding routine audits of Providers to evaluate cost-avoidance performance | ||
Page 440
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Quarterly | Contractor’s unaudited quarterly financial statement | |||
| Monthly | Report listing Enrollees who have new health insurance coverage, casualty insurance coverage, or a change in health or casualty insurance coverage | |||
| Monthly | Report on Provider stop loss limits | |||
| Annually | Audited financial statement | |||
| Annually | Report to the Puerto Rico Insurance Commissioner’s Office | |||
Page 441
| CONTRACT ARTICLE |
FREQUENCY |
GENERAL DESCRIPTION | ||
| Annually | Corporate annual report | |||
| Annually | Report on Controls Placed in Operation and Tests of Operating Effectiveness | |||
| Annually |
Disclosure of Information on Annual Business Transactions | |||
| Termination of Contract (Article 34) | Upon reasonable request during the Transition Period | Any Transition Report (not otherwise listed above) | ||
| Transition of Contract (Article 35) | Once, on the Termination Date | Final Report | ||
Page 442
ARTICLE 19 ENFORCEMENT AND LIQUIDATED DAMAGES
| 19.1 | General Provisions |
| 19.1.1 | In the event the Contractor is in default as to any applicable term, condition, or requirement of this Contract, and in accordance with any applicable provision of 42 CFR 438.700 and Section 4707 of the Balanced Budget Act of 1997, at any time on or after one hundred twenty (120) Calendar Days following the Effective Date, the Contractor agrees that, in addition to the terms of Section 34.1.1 of this Contract, ASES may assess liquidated damages against the Contractor for any such default, in accordance with this Article 19; provided, however, that ASES may not impose liquidated damages with respect to a specific event of default of Contractor if ASES has not complied with its obligations with respect to, or giving rise to, the same event. The Parties further acknowledge and agree that the specified liquidated damages are reasonable and the result of a good faith effort by the Parties to estimate the actual harm caused by the Contractor’s breach and are in lieu of any other financial remedies to which ASES may otherwise have been entitled. The Contractor’s failure to meet the requirements in this Contract is divided into four (4) categories of events. |
| 19.1.2 | Notwithstanding any sanction, including liquidated damages, imposed upon the Contractor, other than Contract termination, the Contractor shall continue to provide |
Page 443
| Administrative Services and make available through its Network Providers all Covered Services and other Benefits under this Contract. |
| 19.1.3 | The Contractor shall not be subject to the assessment of liquidated damages under more than one category for the same event, or arising from the same occurrence of non-compliance with this Contract; provided, that ASES may, in its discretion, impose the highest of any applicable category to such event. |
| 19.1.4 | In the event corrective action is taken by the Contractor within four (4) Business Days of ASES’s approval of a Corrective Action Plan, liquidated damages shall not be imposed, notwithstanding any provision of this Contract to the contrary, unless the corresponding violation remains uncured upon expiration of the term provided for remediation in such Corrective Action Plan. |
| 19.1.5 | Except as specified in sections 10.1.6.2, 12.3.6, 12.6.1.7 and 31.2 of this Contract, the Contractor shall not be subject to any liquidated damages, penalties, fines, financial sanctions, reimbursement obligations or other financial assessments by ASES except as provided in this Article 19. |
Page 444
| 19.2 | Category 1 |
| 19.2.1 | Liquidated damages up to $100,000 per violation may be imposed for Category 1 events. For Category 1 events, the Contractor shall submit a written Corrective Action Plan to ASES for review and approval prior to implementing the corrective action. ASES shall review such Corrective Action Plan within ten (10) Business Days of submission. The following constitute Category 1 events: |
| 19.2.1.1 | Acts that discriminate among Enrollees on the basis of their health status or need for health care services; or |
| 19.2.1.2 | Misrepresentation of actions or falsification of information furnished to CMS or ASES. |
| 19.3 | Category 2 |
| 19.3.1 | Liquidated damages up to $25,000 per violation may be imposed for Category 2 events. For Category 2 events, the Contractor shall submit a written Corrective Action Plan to ASES for review and approval prior to implementing the corrective action. ASES shall review such Corrective Action Plan within ten (10) Business Days of submission. The following constitute Category 2 events: |
Page 445
| 19.3.1.1 | Subject to ASES compliance with its obligations under Article 21 of this Contract, repeated noncompliance by the Contractor with any material obligation that adversely affects the services that the Contractor is required to provide under Article 7 of this Contract; |
| 19.3.1.2 | Misrepresentation or falsification of information furnished to Enrollees or Providers; |
| 19.3.1.3 | Failure to comply with the requirements for the Physician Incentive Plan, as set forth in 42 CFR 422.208 and 422.210; |
| 19.3.1.4 | Distribution directly, or indirectly, or through any independent contractor, marketing materials that have not been approved by ASES or that contain false or materially misleading information; |
| 19.3.1.5 | Violation of any other applicable requirements of the Social Security Act and any implementing regulations that may, in either case, have a material impact on the Administrative Services provided under this Contract; |
| 19.3.1.6 | Failure of the Contractor to assume its material duties under this Contract in accordance with the transition timeframes specified herein; |
Page 446
| 19.3.1.7 | Failure to terminate a Provider that imposes Co-Payments or other cost-sharing on Enrollees that are in excess of the premiums permitted by ASES, as listed on Attachment 8 (ASES will deduct the amount of the overcharge and return it to the affected Enrollees); |
| 19.3.1.8 | Failure to address Enrollees’ Complaints, Appeals, and Grievances, and Provider disputes, within the timeframes specified in this Contract; |
| 19.3.1.9 | Failure to comply with the confidentiality provisions in accordance with 45 CFR 160 and 164; |
| 19.3.1.10 | Failure to enroll any Potential Enrollee because of any discriminatory practice; and |
| 19.3.1.11 | Violation of a subcontracting requirement in the Contract. |
| 19.4 | Category 3 |
| 19.4.1 | Liquidated damages up to $5,000 per day may be imposed for Category 3 events. For Category 3 events, the Contractor shall submit a written Corrective Action Plan to ASES for review and approval prior to implementing the corrective action. ASES |
Page 447
| shall review such Corrective Action Plan within ten (10) Business Days of submission. The following constitute Category 3 events: |
| 19.4.1.1 | Failure to submit required Reports in the timeframes prescribed in Article 18; |
| 19.4.1.2 | Submission of incorrect or deficient Deliverables or Reports in accordance with Article 18 of this Contract; |
| 19.4.1.3 | Failure to comply with the Claims processing standards as follows: |
| 19.4.1.3.1 | Failure to process and finalize to a paid or denied status ninety-five percent (95%) of all Clean Claims within thirty (30) Calendar Days of receipt; |
| 19.4.1.3.2 | Failure to process and finalize to a paid or denied status one hundred percent (100%) of all Clean Claims within fifty (50) Calendar Days of receipt; and |
| 19.4.1.3.3 | Failure to process Unclean Claims as specified in Section 16.9.3 of this Contract; |
Page 448
| 19.4.1.4 | Failure to pay Providers interest at the rate identified in and otherwise in accordance with Section 16.10.2.3 of this Contract when a Clean Claim is not adjudicated within the claims processing deadlines; |
| 19.4.1.5 | Failure to comply with the quarterly submission of EPSDT reports to ASES. |
| 19.4.1.6 | Failure to notify PCPs of the Gaps in Care analysis in accordance with the EPSDT guidelines specified in Section 7.9 of this Contract; |
| 19.4.1.7 | Failure to comply with any Corrective Action Plan as required by ASES; |
| 19.4.1.8 | Failure to provide the Claims Payment Disbursement Illustration and Actuarial Report information required in Sections 21.1.14 and 21.1.15 of this Contract; |
| 19.4.1.9 | Failure to seek, collect and/or report Third Party Liability information as provided in Section 22.4 of this Contract; and |
| 19.4.1.10 | Failure of Contractor to issue written notice to Enrollees upon Provider’s termination as a Provider in the Plan as described in Section 10.4.3 of this Contract. |
Page 449
| 19.5 | Category 4 |
| 19.5.1 | Liquidated damages as specified below may be imposed for Category 4 events. For Category 4 events, the Contractor shall submit a written Corrective Action Plan to ASES for review and approval prior to implementing the corrective action. ASES shall review such Corrective Action Plan within ten (10) Business Days of submission. The following constitute Category 4 events: |
| 19.5.1.1 | Failure to implement the business continuity-disaster recovery (BC-DR) plan as follows: |
| 19.5.1.1.1 | Implementation of the (BC-DR) plan exceeds the proposed time by two (2) or less Calendar Days: five thousand dollars ($5,000) per day up to day 2; |
| 19.5.1.1.2 | Implementation of the (BC-DR) plan exceeds the proposed time by more than (2) and up to five (5) Calendar Days: ten thousand dollars ($10,000) per each day beginning with Day 3 and up to Day 5; |
| 19.5.1.1.3 | Implementation of the (BC-DR) plan exceeds the proposed time by more than five (5) and up to ten (10) Calendar Days, twenty-five |
Page 450
| thousand dollars ($25,000) per day beginning with Day 6 and up to Day 10; and |
| 19.5.1.1.4 | Implementation of the (BC-DR) plan exceeds the proposed time by more than ten (10) Calendar Days: fifty thousand dollars ($50,000) per each day beginning with Day 11. |
| 19.5.1.2 | Unscheduled System Unavailability in violation of Article 17, in ASES’s discretion, two hundred fifty dollars ($250) for each thirty (30) minutes or portions thereof. |
| 19.5.1.3 | Failure to make available to ASES or its Agent, valid extracts of Encounter Information for a specific month within fifteen (15) Calendar Days of the close of the month: five hundred dollars ($500) per day. After thirty (30) Calendar Days of the close of the month: two thousand dollars ($2000) per day. |
| 19.5.1.4 | Failure to correct a system problem not resulting in System Unavailability within the allowed timeframe, where failure to complete was not due to the action or inaction on the part of ASES as documented in writing by the Contractor: |
Page 451
| 19.5.1.4.1 | One (1) to fifteen (15) Calendar Days late: two hundred and fifty dollars ($250) per Calendar Day for Days 1 through 15; |
| 19.5.1.4.2 | Sixteen (16) to thirty (30) Calendar Days late: five hundred dollars ($500) per Calendar Day for Days 16 through 30; and |
| 19.5.1.4.3 | More than thirty (30) Calendar Days late: one thousand dollars ($1,000) per Calendar Day for Days 31 and beyond. |
| 19.5.1.5 | Failure to meet the Tele MiSalud performance standards: |
| 19.5.1.5.1 | $1,000 for each percentage point that is below the target answer rate of eighty percent (80%) in thirty (30) seconds; |
| 19.5.1.5.2 | $1,000 for each percentage point that is above the target of a three percent (3%) Blocked Call rate; and |
| 19.5.1.5.3 | $1,000 for each percentage point that is above the target of a five percent (5%) Abandoned Call rate. |
Page 452
| 19.6 | Other Remedies |
| 19.6.1 | In addition to the other liquidated damages described above for Category 1-4 events, ASES may impose the following other remedies: |
| 19.6.1.1 | [Intentionally left blank]. |
| 19.6.1.2 | Granting Enrollees the right to terminate Enrollment without cause and notifying the affected Enrollees of their right to disenroll; |
| 19.6.1.3 | Suspension of all new Enrollment, including Auto-Enrollment, after the effective date of remedies; |
| 19.6.1.4 | Additional remedies allowed under Puerto Rico law or regulations that address areas of non-compliance specified in 42 CFR 438.700. |
| 19.6.2 | Subject to Article 34 of this Contract, in lieu of imposing a remedy allowed under this Article 19, ASES may terminate this Contract, without any liability whatsoever (but subject to making any payments due under this Contract through any such date of termination), in the event of any failure specified in Category 1 or Category 2, if the terms of the Corrective Action Plan are not implemented to ASES’s reasonable |
Page 453
| satisfaction or if such failure continues or is not corrected, to ASES’s sole reasonable satisfaction. |
| 19.6.3 | In the event of noncompliance by the Contractor with Article 18 or Sections 21.3.2 or 21.3.3 of this Contract, ASES shall have the right to Withhold, with respect to Article 18, a sum not to exceed ten percent (10%)—and with respect to Sections 21.3.2 or 21.3.3 of this Contract, a sum not to exceed thirty percent (30%)—of the Administrative Fee for the following month and for continuous consecutive months thereafter until such noncompliance is cured and corrected, in lieu of imposing any liquidated damages, penalties or sanctions against the Contractor hereunder. ASES shall release the Withhold of the Administrative Fee to the Contractor within two (2) Business Days after the corresponding event of noncompliance is cured to ASES’s sole but reasonable satisfaction. |
| 19.7 | Notice of Remedies |
| 19.7.1 | Prior to the imposition of either sanctions or other remedies, ASES will issue a written notice of remedies that will include the following: |
| 19.7.1.1 | A citation to the law, regulation or Contract provision that has been violated; |
Page 454
| 19.7.1.2 | The remedies to be applied and the date the remedies will be imposed; |
| 19.7.1.3 | The basis for ASES’s determination that the remedies should be imposed; |
| 19.7.1.4 | Request for a Corrective Action Plan, if applicable; and |
| 19.7.1.5 | The timeframe and procedure for the Contractor to dispute ASES’s determination. Liquidated damages shall only be imposed and payable after the Parties have completed the procedure for the imposition of sanctions pursuant to Section 19.7.2 of this Contract. |
| 19.7.2 | Procedure for the Imposition of Sanctions |
| 19.7.2.1 | The Contractor has the right, within fifteen (15) Calendar Days of receipt from ASES of a notice of remedies, to appeal in writing any such remedy. If any such appeal is filed by the Contractor, ASES may take any of the following actions: |
| 19.7.2.1.1 | Confirm the remedy; |
| 19.7.2.1.2 | Modify or amend the remedy; or |
Page 455
| 19.7.2.1.3 | Eliminate the remedy, provided Contractor has taken all the necessary actions to correct any such deficiency or cure the failure that caused the remedy. |
| 19.7.2.2 | If the sanctions are confirmed or otherwise modified, the Contractor has the right to appeal ASES’s decision as provided in Act 72 or under other applicable law. |
| 19.7.2.3 | [Intentionally Left Blank]. |
Page 456
ARTICLE 20 TERM OF CONTRACT
| 20.1 | The term of this Contract (“Contract Term”) shall begin at 12:01 a.m., Puerto Rico time, on the date in which this Contract is duly executed as specified on the signature page of this Contract (also referred to as the “Effective Date of the Contract”), and shall continue until 11:59 p.m., Puerto Rico time, on June 30, 2013. |
| 20.2 | Notwithstanding Section 20.1 above, the arrangement for the provision of Covered Services and Benefits to Enrollees by the Contractor under this Contract shall begin on the Implementation Date of the Contract. |
| 20.3 | The Administrative Fee shall remain the same for the Contract Term unless modified pursuant to the terms of this Contract. |
| 20.4 | The Contract shall expire at the close of the Contract Term unless earlier terminated in accordance with Article 34. |
| 20.5 | Ninety (90) Calendar Days prior to June 30, 2013, the Parties may elect to commence negotiations to renew the Contract Term. If the Parties elect to engage in these negotiations, they agree to negotiate in good faith any such renewal under terms and conditions to be mutually agreed. |
Page 457
ARTICLE 21 PAYMENT FOR SERVICES
| 21.1 | General Provisions |
| 21.1.1 | ASES’s obligations under this Contract to make Claims Payments and Administrative Fee payments to the Contractor shall commence on the Implementation Date of the Contract. |
| 21.1.2 | The Parties acknowledge and agree that any change in the scope or extent of the services to be performed by the Contractor hereunder that materially affects the basis upon which the Administrative Fee was originally calculated will be grounds for recalculation of the Administrative Fee paid hereunder. |
| 21.1.3 | [Intentionally left blank]. |
| 21.1.4 | ASES acknowledges that the Claims Payments agreed to under the terms of this Contract in addition to any applicable cost-sharing as provided in Attachment 8 may not constitute full payment for Covered Services and Benefits under MiSalud. The Contractor will have no responsibility for payment for Covered Services and Benefits in excess of the Claims Payments unless the Contractor has obtained prior written approval, in the form of a Contract amendment, authorizing an increase in the total payment and the payments for Covered Services are increased by an amount |
Page 458
| sufficient to cover any such increase by an amount which is actuarially sound, as certified by ASES actuaries. |
| 21.1.5 | The Contractor shall maintain all the utilization and financial data related to this Contract duly segregated from its commercial and Platino business accounting system including, but not limited to, the general ledger. In addition, the Contractor shall maintain separate utilization and financial data for each Service Region covered under this Contract. |
| 21.1.6 | [Intentionally left blank]. |
| 21.1.7 | Fee-for-service amounts paid by the Contractor for Claims, or Capitation payments made by the Contractor derived or otherwise based on Encounter Data submitted by Providers, resulting from services determined not to be Medically Necessary by the Contractor, will not be considered in the MiSalud Program experience for any purposes or for the incentive plans contemplated under this Contract. |
| 21.2 | Administrative Fee |
| 21.2.1 | The Administrative Fee shall be calculated by multiplying the actual number of Enrollees as of the last day of the month preceding the month in which payment is made by the Per Member Per Month Administrative Fee agreed to between the |
Page 459
| Contractor and ASES for each Service Region covered by this Contract. The Per Member Per Month Administrative Fee for each Service Region is specified in Attachment 11. The Administrative Fee shall be due to the Contractor on the fifth (5th) day of each month; however, ASES shall have the right to make partial payments throughout the month, provided that payment in full of the corresponding monthly Administrative Fee in each Service Region is made on or before the last day of the same month. |
| 21.2.2 | The Per Member Per Month Administrative Fee shall only be paid for Enrollees for whom ASES has received adequate notification of Enrollment from the Contractor as of the date specified by ASES, under Section 5.2.3 of this Contract; provided, however, that the Contractor shall receive the applicable fee once it cures, to ASES’s reasonable satisfaction, any deficiency in the notification of Enrollment. |
| 21.2.3 | The Per Member Per Month Administrative Fee for Enrollees not enrolled in MiSalud for the entire month shall be determined on a pro rata basis by the following calculation: (i) the Per Member Per Month Administrative Fee shall be divided by the number of days in the month, (ii) such amount shall be multiplied by the number of days in the month the Enrollee was enrolled in MiSalud, including the Effective Date of Enrollment and the period referred to in Section 4.4.1.2 of this Contract. |
Page 460
| 21.2.4 | Any Administrative Fee invoice to be submitted by the Contractor shall be certified as provided in this Contract and any Federal requirement. The certification must attest, based on best knowledge, information, and belief, as to the accuracy, completeness and truthfulness of the enrollment data, encounter data, and any other financial data as ASES may reasonably request under the terms of this Contract. The monthly Administrative Fee invoice that the Contractor must submit to ASES shall include the following certification: |
“Bajo pena de nulidad absoluta certifico que ningún servidor público de ASES es parte o tiene algún interés en las ganancias o beneficios producto del contrato objeto de esta factura y, de ser parte o tener interés en las ganancias o beneficios productos del contrato, ha mediado una dispensa previa. La única consideración para suministrar los bienes o servicios objeto del contrato han sido el pago acordado con el representante autorizado de ASES. El importe de esta factura es justo y correcto. Los trabajos han sido realizados, los productos y servicios han sido entregados y/o prestados y no han sido pagados.”
Under penalty of absolute nullity, I certify that no employee of ASES is a party to or has any interest in the payments or benefits arising from the Contract that underlies this invoice or, alternatively, that if an employee thereof is a party to or has an interest
Page 461
in the payments or benefits arising of said Contract, that the necessary waiver was obtained in connection hereto. The payment agreed upon with the appropriate, duly authorized representative of ASES constitutes the sole consideration for providing the services called for in the Contract. The amount billed in this invoice is just and correct. The services billed for in this invoice have been performed according to the Contract’s terms and have not been paid.”
| 21.2.5 | [Intentionally left blank]. |
| 21.2.6 | If ASES makes payment in excess of the Administrative Fee or Claims Payment, ASES may, upon five (5) Business Days prior written notice to the Contractor, Withhold any future payment of the Administrative Fee or Claims Payment, as applicable, to offset any such excess payment. |
| 21.2.7 | Administrative expenses to be included in determining the experience of the MiSalud Program are those related to this Contract in accordance with Section 22.1.8 of this Contract. Separate allocations of expenses from any other of the Contractor’s business or insurance plans other than expenses under this Contract related to the MiSalud Program, from the Contractor’s subsidiaries or affiliated companies, from the Contractor’s parent company, or from other entities will not be reflected or commingled with the financial data of the MiSalud Program. Any cost-shifting, |
Page 462
| financial consolidation or the implementation of other combined financial measures is expressly forbidden. |
| 21.2.8 | [Intentionally left blank.] |
| 21.3 | Claims Payment |
| 21.3.1 | The Claims Payment Report shall be certified as provided in this Contract and any Federal requirement. The certification must attest, based on best knowledge, information, and belief, as to the accuracy, completeness and truthfulness of the enrollment data, encounter data, and any other data required in this Contract. |
| 21.3.2 | After receipt of the Claims Payment Report, ASES shall have five (5) Business Days to review the Claims Payment Report and transfer funds into a zero-balance account. To the extent ASES determines that a request for payment of a Claim is unwarranted under the terms of this Contract, ASES shall provide notice to the Contractor of such determination and the corresponding explanation before deducting any such amount(s) from the total amount requested in the Claims Payment Report. The Contractor shall have two (2) Business Days to remit payment to Providers after such payment by ASES. |
Page 463
| 21.3.3 | After receipt of the Pharmacy Claims Payment Report, ASES shall have five (5) Business Days to review the Pharmacy Claims Payment Report and transfer funds into a zero-balance account. In compliance with Section 10.5.8.4 of this Contract after such payment by ASES, the Contractor shall have two (2) Business Days to remit payment into the zero-balance account for the PBM after such payment by ASES. |
| 21.3.4 | ASES shall provide written instructions to the Contractor on or before the Implementation Date with respect to the management and operation of all zero balance accounts to be established under this Contract. |
| 21.4 | Claims Incurred But Not Reported |
| 21.4.1 | As part of its Administrative Services and in accordance with the Insurance Code of Puerto Rico, the Contractor shall perform, on a monthly basis, an actuarially sound process to estimate and track potential liability associated with Claims incurred but not reported (“IBNR”) for each Service Region and for each PMG. In addition, as part of its Administrative Services, the Contractor shall conduct annual reviews to its IBNR methodology and make adjustments as necessary or otherwise as reasonably required by ASES. |
| 21.4.1.1 | IBNR Claims at the Contractor |
Page 464
| 21.4.1.1.1 | Every thirty (30) Calendar Days, the Contractor shall submit an estimated amount of Claims incurred but not reported (“IBNR”). |
| 21.4.1.2 | IBNR Claims at the PMG |
| 21.4.1.2.1 | ASES shall establish a reserve fund for IBNR for Capitation payments to PMGs based on actuarial estimates to be provided by the Contractor. If such reserve fund were to exceed twenty percent (20%) of Per Member Per Month Capitation payments to PMGs for the first Fiscal Year of the Contract (i.e., the period from the Effective Date of the Contract through June 30, 2012); or ten percent (10%) of Per Member Per Month Capitation payments to PMGs for the second Fiscal Year (i.e., the period from July 1, 2012 to June 30, 2013), the Contractor shall inform ASES so that ASES may determine, in its discretion, any change in the reserve fund under this section 21.4.1.2. |
| 21.4.1.2.2 | The reserve shall be reconciled and adjusted every ninety (90) Calendar Days. The Contractor shall submit quarterly reconciliation reports to ASES. ASES shall have five (5) Business Days to review the IBNR reconciliation reports and, if necessary, any excess will be liquidated in the following twenty five (25) Business Days. Once the PMG has the reserve necessary as determined by the Contractor, the |
Page 465
| monthly retention may not exceed three percent (3%) of Per Member Per Month Capitation payments to PMGs; provided, that if at any time the reserve falls below the amount determined as adequate by the Contractor’s actuaries, the Contractor shall inform ASES so that ASES may determine, in its discretion, any change in the retention amount to ensure the adequacy of the reserve fund. Any increase must be justified in information from the PMG file. |
| 21.4.1.2.3 | The Contractor shall continue to submit quarterly IBNR reconciliation reports to ASES until three hundred and sixty-five (365) Calendar Days after the end of the Contract Term. Any remainder of the IBNR funds shall be returned to the PMGs in an unextendable period of sixty (60) Calendar Days from the date that ASES approves in writing the Contractor’s final quarterly reconciliation report. |
| 21.5 | Contractor Objections to Payment |
| 21.5.1 | If the Contractor wishes to contest the amount of payments (including but not limited to the Administrative Fee) made by ASES in accordance with the terms outlined in this Article for services provided under the terms of this Contract, the Contractor shall submit to ASES all relevant documentation supporting the Contractor’s objection no |
Page 466
| later than ninety (90) Calendar Days after payment is made. Once this term has ended, the Contralor forfeits its rights to object payments made by ASES hereunder. |
| 21.5.2 | After the Contractor’s submission of all relevant information, the Contractor and ASES will meet to discuss any objections to payment and the relevant data and information. If after discussing the matter and analyzing all relevant data it is subsequently determined that an error in payment was made, the Contractor and ASES will develop a plan to remedy the situation, which would include a timeframe for resolution agreed to by both Parties, within a time period mutually agreed upon by both Parties. |
| 21.6 | Retention Fund for Quality Incentive Program |
ASES will Withhold and release the Retention Fund for the Quality Incentive Program in accordance with Section 12.5 of this Contract.
| 21.7 | Financial Performance Incentive |
| 21.7.1 | A financial performance incentive has been agreed to between ASES and the Contractor. If the member-weighted average of the cost of actual Claims incurred per member per month for all Service Regions is more than one and a half percent (1.5%) below the member-weighted average of ASES’s projected Claims cost per member |
Page 467
| per month for all Service Regions, excluding the Virtual Region (the “Threshold Amount”) as per Attachment 10 of this Contract, the Contractor shall be entitled to fifty percent of the difference between the aggregate Threshold Amount and the actual incurred Claims for such regions. The calculation methodology for the Claims cost is included in Attachment 10A to this Contract. |
| 21.7.2 | Calculation of the actual Claims incurred will be made on June 30, 2014 (after the end of the Runoff Period), following a reconciliation process to be agreed upon by the Parties. No later than July 31, 2014, the agreed amount of the Contractor’s share of the savings below the Threshold Amount, if any, will be paid to the Contractor. |
ARTICLE 22 FINANCIAL MANAGEMENT
| 22.1 | General Provisions |
| 22.1.1 | Subject to ASES timely payment of all Claims Payment for each Service Region under the terms of this Contract, the Contractor shall be responsible for the sound financial management of the MiSalud Program. |
| 22.1.2 | The Contractor shall notify ASES of any loans or other special financial arrangements made between the Contractor and any PMG or other Network Provider. Any such |
Page 468
| loans shall strictly conform to the legal requirements of federal and Puerto Rico anti-fraud and anti-kickback laws and regulations. |
| 22.1.3 | The Contractor shall provide ASES with copies of its audited financial statements following Generally Accepted Accounting Principles (“GAAP”) in the United States, at its own cost and charge, for the duration of the Contract, and as of the end of each the Contractor’s fiscal year during the Contract Term, regarding the financial operations related to the MiSalud Program. The statements shall provide (1) a separate accounting of activities relating to each Service Region, and (2) a consolidated section accounting for all MiSalud Program activities. These reports shall be submitted to ASES no later than ninety (90) days after the close of each Fiscal Year during the term of this Contract. |
| 22.1.4 | The Contractor shall provide to ASES a copy of its Annual Report to the Office of the Insurance Commissioner, as applicable, in the format agreed upon by the National Association of Insurance Commissioners (NAIC), for the year ended on December 31, 2010, and subsequently thereafter, if the Contract is renewed, not later than March 31 of each year. |
| 22.1.5 | The Contractor shall provide to ASES unaudited financial statements for each quarter during the Contract Term, not later thirty (30) Calendar Days after the closing of each quarter. The Contractor shall submit (1) a separate accounting of activities relating to |
Page 469
| each Service Region, and (2) a consolidated section accounting for all MiSalud Program activities. |
| 22.1.6 | The Contractor shall provide to ASES a copy of its annual corporate report at the close of the calendar year. |
| 22.1.7 | The Contractor shall maintain adequate procedures and controls to ensure that any payments pursuant to this Contract are properly made. The Contractor shall submit such proposed procedures and controls to ASES for review and approval according to the timeframe specified in Attachment 12 to this Contract. Any subsequent changes to these procedures and controls must be previously approved in writing by ASES. In establishing and maintaining such procedures, the Contractor will provide for separation of the functions of certification and disbursement. |
| 22.1.8 | The Contractor acknowledges, and shall incorporate in contracts with Providers, Subcontractors, and other persons engaged by the Contractor in connection with this Contract, that the MiSalud Program is a government-funded program. As such, administrative costs shall be in accordance with cost principles permissible, and with applicable federal and Puerto Rico guidelines, including applicable Office of Management and Budget Circulars, primarily recognizing that: (1) a cost shall be reasonable if it is of the type generally recognized as ordinary and necessary, and if in its nature and amount, and taking into consideration the purpose for which it was |
Page 470
| disbursed, it does not exceed that which would be incurred by a prudent person in the ordinary course of business under the circumstances prevailing at the time the decision was made to incur the cost; and (2) a cost shall be reasonable if it is allocable to or related to the cost objective that compels cost association. |
| 22.1.9 | The Contractor shall maintain an accounting system for MiSalud separate from the rest of its commercial activities. This system will only include only MiSalud data. The data contained in any report required to be provided by the Contractor to ASES hereunder will be provided by Service Region unless otherwise agreed to in writing by the Parties. |
| 22.1.10 | The Contractor shall provide, throughout the Contract Term, any other necessary and related information that is deemed necessary by ASES in order to evaluate the Contractor’s financial capacity and stability. |
| 22.2 | Solvency and Financial Requirements |
| 22.2.1 | The Contractor shall establish and maintain adequate net worth, working capital, and financial reserves to carry out its obligations under this Contract. |
| 22.2.2 | The Contractor shall comply with the Puerto Rico Insurance Code with respect to insolvency protection. |
Page 471
| 22.3 | Reinsurance and Stop Loss |
| 22.3.1 | ASES may enter, in its discretion, into a Reinsurance program at any time. The Contractor shall provide any information requested by ASES in a timely manner as may be required for ASES to enter into a Reinsurance program. |
| 22.3.2 | For the First Fiscal Year of the Contract Term (November 1, 2011 to June 30, 2012), ASES shall establish a stop-loss limit of six thousand five hundred dollars ($6,500) per Enrollee per Fiscal Year for Primary Medical Groups. For the Second Fiscal Year July 1, 2012 to June 30, 2013 of the Contract Term, ASES shall establish a stop-loss limit of ten thousand dollars ($10,000) per Enrollee per Fiscal Year for Primary Medical Groups. Stop-loss coverage shall comply with the limits specified in 42 CFR 422.208(f). The limit shall be activated when the expense of providing Covered Services to an Enrollee, including all outpatient and inpatient expenses, reaches this sum. The Contractor shall have mechanisms in place to identify the stop loss once it is reached for an Enrollee, and shall establish monthly reports to inform ASES and the PMGs of Enrollees who have reached the stop-loss limit. ASES shall assume all losses exceeding the limit. |
| 22.3.3 | The stop-loss responsibility shall not be transferred to a PMG unless the PMG and the Contractor expressly agree to the PMG’s assuming this risk and the associated risk distribution arrangement has been previously approved in writing by ASES. |
Page 472
| 22.4 | Third Party Liability and Cost Avoidance |
| 22.4.1 | General Provisions |
| 22.4.1.1 | The MiSalud program shall be the payer of last resort for all Covered Services rendered on behalf of Medicaid and CHIP Enrollees in accordance with federal regulations; ASES intends to enforce this rule with respect to all MiSalud Enrollees. ASES and the Contractor shall agree to develop protocols and procedures for the coordination of benefits in the event any other source of payment or health insurance with respect to the Covered Services. |
| 22.4.1.2 | The Contractor shall exercise full assignment rights as applicable and shall be responsible for making every reasonable effort to determine the legal liability of Third Parties to pay for services rendered to Enrollees under this Contract and to cost avoid or recover any such liability from the Third Party. “Third Party,” for purposes of this Section, shall mean any person or entity that is or may be liable to pay for the care and services rendered to a MiSalud Enrollee. Examples of a Third Party include an Enrollee’s health insurer, casualty insurer, a managed care organization, and Medicare. |
Page 473
| 22.4.1.3 | The Contractor hereby agrees to utilize, and cause its Providers to utilize, available public or private sources of payment for services rendered to Enrollees in the MiSalud Plan for claims cost avoidance purposes, within thirty (30) Calendar Days of becoming aware of such sources. If Third Party Liability (TPL) exists for part or all of the Covered Services provided directly by the Contractor to an Enrollee, the Contractor shall make Reasonable Efforts to recover from TPL sources the value of Covered Services rendered. If TPL exists for part or all of the Covered Services provided to an Enrollee by a Subcontractor or a Provider, and the Third Party will make payment within a reasonable time, the Contractor may pay the Subcontractor or Provider only the amount, if any, by which the Subcontractor’s or Provider’s allowable claim exceeds the amount of TPL. |
| 22.4.1.4 | The Contractor shall deny payment on a Claim that has been denied by a Third Party payer when the reason for denial is the Provider’s failure to follow prescribed procedures, including, but not limited to, failure to obtain Prior Authorization, failure to file Claims timely, etc. |
| 22.4.1.5 | The Contractor shall, within five (5) Business Days of issuing a denial of any claim based on TPL, provide TPL data to the Provider. |
Page 474
| 22.4.1.6 | The Contractor shall treat funds recovered from Third Parties as offsets to Claims payments. The Contractor shall report all cost avoidance values to ASES in accordance with federal guidelines and as described subsequently in this Section. |
| 22.4.1.7 | The Contractor shall post all Third Party payments or recoveries to Claim-level detail by Enrollee. |
| 22.4.1.8 | If the Contractor operates or administers a non-MiSalud health plan, the Contractor shall, to the extent permitted by law, assist ASES with the identification of Enrollees with access to other insurance to coordinate benefits for such Enrollees. |
| 22.4.1.9 | The Contractor shall audit and review its Providers’ claims, using monthly the reports submitted pursuant to Section 16.7 of this Contract or other pertinent data, to ensure that Providers are not receiving duplicate payment for services billable to third parties, in particular the Medicare program. The Contractor shall report to ASES on a quarterly basis its findings regarding claims, invoices, or duplicate or inappropriate payments. According to the timeframe specified in Attachment 12 to this Contract, the Contractor shall submit to ASES for its review and approval |
Page 475
| a plan for such routine audits. Any subsequent changes to the plan for routine audits must be previously approved in writing by ASES. |
| 22.4.1.10 | The Contractor shall make a reasonable effort (in accordance with reasonable industry standards and practices), including through collaboration with Providers, to collect and report Third Party recoveries. Third Party recoveries shall be remitted to ASES promptly upon receipt by the Contractor. |
| 22.4.1.11 | The Contractor shall comply with the applicable provisions of 42 CFR 433 Subpart D – Third Party Liability and 42 CFR 447.20 Provider Restrictions: State Plan Requirements, or work cooperatively with ASES to assure compliance with the requirements therein, as it relates to the Medicaid and CHIP populations served by the MiSalud Plan and its Third Party Liability and cost avoidance responsibilities. |
| 22.4.2 | Legal Causes of Action for Damages. ASES (or another agency of the Government of Puerto Rico) will have the sole and exclusive right to pursue and collect payments made by the Contractor when a legal cause of action for damages is instituted on behalf of a MiSalud Enrollee against a Third Party, or when ASES receives notices that legal counsel has been retained by or on behalf of any Enrollee. The Contractor |
Page 476
| shall cooperate with ASES in all collection efforts, and shall also direct its Providers to cooperate with ASES in these efforts. |
| 22.4.3 | Estate Recoveries. ASES (or another agency of the Government of Puerto Rico) will have the sole and exclusive right to pursue and recover correctly paid benefits from the estate of a deceased MiSalud Enrollee who was Medicaid Eligible in accordance with federal and Puerto Rico law. Such recoveries will be retained by ASES. |
| 22.4.4 | Subrogation |
| 22.4.4.1 | Third Party resources shall include subrogation recoveries. The Contractor shall be required to seek subrogation amounts regardless of the amount believed to be available as required by federal Medicaid guidelines and Puerto Rico law. |
| 22.4.4.2 | The amount of any subrogation recoveries collected by the Contractor outside of the Claims processing system shall be treated by the Contractor as offsets to medical expenses for the purposes of reporting. |
| 22.4.4.3 | The Contractor shall conduct diagnosis and trauma code editing to identify potential subrogation claims. This editing should, at minimum, identify |
Page 477
| claims with a diagnosis of 900.00 through 999.99 (excluding 994.6) or claims submitted with an accident trauma indicator of ‘Y.’ |
| 22.4.5 | Cost Avoidance |
| 22.4.5.1 | When the Contractor is aware of health or casualty insurance coverage before paying for a Covered Service, the Contractor shall avoid payment by promptly (within fifteen (15) Business Days of receipt) rejecting the Provider’s claim and directing that the Claim be submitted first to the appropriate Third Party. |
| 22.4.5.2 | Exceptions to the Cost-Avoidance Rule. In the following situations, the Contractor shall first pay its Providers and then coordinate with the liable Third Party, unless prior approval to take other action is obtained from ASES: |
| 22.4.5.2.1 | The coverage is derived from a parent whose obligation to pay support is being enforced by a government agency. |
| 22.4.5.2.2 | The claim is for Maternal and Prenatal Services to a pregnant woman or for EPSDT services that are covered by the Medicaid program. |
Page 478
| 22.4.5.2.3 | The claim is for labor, delivery, and post-partum care and does not involve hospital costs associated with an inpatient stay. |
| 22.4.5.2.4 | The claim is for a child who is in the custody of ADFAN. |
| 22.4.5.2.5 | The claim involves coverage or services mentioned in this subsection in combination with another service. |
| 22.4.5.3 | If the Contractor knows that the Third Party will neither pay for nor provide the Covered Service, and the service is Medically Necessary, the Contractor shall neither deny payment for the service nor require a written denial from the Third Party. |
| 22.4.5.4 | If the Contractor does not know whether a particular service is covered by the Third Party, and the service is Medically Necessary, the Contractor shall promptly (within ten (10) Business Days of receipt of the Claim) contact the Third Party and determine whether or not such service is covered rather than requiring the Enrollee to do so. Further, the Contractor shall require the Provider to bill the Third Party if coverage is available. |
| 22.4.6 | Sharing of TPL Information by ASES |
Page 479
By the fifth (5th) Calendar Day after the close of the month during which ASES learns of such information, ASES will provide the Contractor with a list of all known health insurance information on Enrollees for the purpose of updating the Contractor’s files.
| 22.4.6.1 | Additionally, by the fifteenth (15th) Calendar Day after the close of the calendar quarter, ASES will provide to the Contractor a copy of a document containing all of the health insurers licensed by the Government of Puerto Rico as of the close of the previous quarter, and any other related information that is needed in order to file TPL claims. |
| 22.4.7 | Sharing of TPL Information by the Contractor |
The Contractor shall submit a monthly report to ASES (following ASES file content, format and transmission specifications) by the fifth (5th) Calendar Day after the close of the month during which the Contractor learns that an Enrollee has new health insurance coverage, or casualty insurance coverage, or of any change in an Enrollee’s health insurance coverage. The Contractor shall impose a corresponding requirement on its Providers to notify the Contractor of any newly discovered coverage.
Page 480
| 22.4.7.1 | When the Contractor becomes aware that an Enrollee has retained counsel, who either may institute or has instituted a legal cause of action for damages against a Third Party, the Contractor shall notify ASES in writing, including the Enrollee’s name and MiSalud Enrollee Identification number, the date of the accident / incident, the nature of the injury, the name and address of Enrollee’s legal representative, copies of the pleadings, and any other documents related to the action in the Contractor’s possession or control. This shall include, but not be limited to, the name of the Provider, the Enrollee’s diagnosis, the Covered Service provided to the Enrollee, and the amount paid to the Provider for each service. |
| 22.4.7.2 | The Contractor shall notify ASES within thirty (30) Calendar Days of the date it becomes aware of the death of one of its Medicaid Eligible Enrollees age fifty-five (55) or older, giving the Enrollee’s full name, Social Security number, and date of death. ASES will then determine whether it can recover correctly paid Medicaid benefits from the Enrollee’s estate. |
| 22.4.7.3 | The Contractor agrees to share with ASES instances of Enrollee non-cooperation with the Contractor’s and with Network Providers’ efforts to determine sources of Third Party Liability. |
Page 481
| 22.4.8 | Historic cost avoidance due to the existence of liable Third Parties is embedded in the cost of health services delivery and is reflected in the rates upon which ASES will base Claims Payments to the Contractor. The Claims Payment does not include any reductions due to tort recoveries. |
| 22.5 | MiSalud as Secondary Payer to Medicare |
| 22.5.1 | In general, as provided in Section 7.12 of this Contract, save for services offered by Medicare Platino plans which operate independently of this Contract, MiSalud does not duplicate coverage provided by Medicare to Dual Eligible Beneficiaries and the Contractor shall not be a secondary payer for services for which Medicare is liable. |
| 22.5.1.1 | However, in a situation in which a Covered Service is covered in whole or part by both Medicare and MiSalud (for example, hospitalization services for a Dual Eligible Beneficiary who is enrolled in Medicare Part A only and whose hospitalization costs exceed the Medicare limit, per Section 7.12.1.1.1 of this Contract), the Contractor shall determine liability as a secondary payer as follows: |
| 22.5.1.1.1 | If the total amount of Medicare’s established liability for the services (Medicare paid amount) is equal to or greater than the negotiated contract rate between the Contractor and the Provider for the services, |
Page 482
minus any MiSalud cost-sharing requirements, then the Provider is not entitled to, and the Contractor shall not pay, any additional amounts for the services.
| 22.5.1.1.2 | If the total amount of Medicare’s established liability (Medicare paid amount) is less than the negotiated contract rate between the Contractor and the Provider for the services, minus any MiSalud cost-sharing requirements, the Provider is entitled to, and the Contractor shall pay, the lesser of: |
| 22.5.1.1.2.1 | The Medicaid cost-sharing (deductibles and coinsurance) payment amount for which the Dual Eligible Beneficiary is responsible under Medicare, and |
| 22.5.1.1.2.2 | An amount which represents the difference between (1) the negotiated contract rate between the Contractor and the Provider for the service minus any MiSalud cost-sharing requirements, and (2) the established Medicare liability for the services. |
| 22.5.2 | Enrollment Exclusions and Contractor Liability for the Cost of Care. Any Dual Eligible Beneficiary who is already enrolled in a Medicare Platino Plan may not be |
Page 483
enrolled by the Contractor. However, if the Contractor operates its own Medicare Platino Plan, the Contractor may enroll a Dual Eligible Beneficiary in the Platino Plan, which furnishes MiSalud benefits, per separate contract with ASES.
| 22.5.3 | Protections for Medicaid Enrollees |
| 22.5.3.1 | The Contractor shall neither impose, nor allow Network Providers to impose, any cost-sharing charges of any kind upon Medicaid Eligible Persons enrolled in MiSalud, other than as authorized in this Contract. |
| 22.5.3.2 | Unless otherwise permitted by federal or Puerto Rico law, Covered Services may not be denied to a Medicaid Enrollee because of a Third Party’s potential liability to pay for the services, and the Contractor shall ensure that its cost avoidance efforts do not prevent Enrollees from receiving Medically Necessary services. |
| 22.6 | [Intentionally left blank]. |
| 22.7 | Reporting Requirements |
| 22.7.1 | The Contractor shall submit to ASES all of the reports as indicated in Section 18.2 of this Contract. |
Page 484
| 22.7.2 | Failure to submit the reports within the established timeframes, or failure to submit complete, accurate reports, may result in the imposition of liquidated damages pursuant to Article 19 of this Contract or Withhold of the Administrative Fee as outlined in Section 19.6.3 of this Contract. |
| 22.7.3 | The Contractor, at its sole expense, shall submit by May 15 (or a later date if approved by ASES) of each year a “Report on Controls Placed in Operation and Tests of Operating Effectiveness,” meeting all standards and requirements of the AICPA’s SAS 70, for the Contractor’s operations performed for ASES under the MiSalud Contract. |
| 22.7.3.1 | The audit shall be conducted by an independent auditing firm, which has prior SAS 70 audit experience. The auditor must meet all AICPA standards for independence. The selection of, and contract with the independent auditor shall be subject to the prior written approval of ASES. ASES reserves the right to, at the Contractor’s expense, designate other auditors or reviewers to examine the Contractor’s operations and records for monitoring and/or stewardship purposes. |
| 22.7.3.2 | The independent auditing firm shall simultaneously deliver identical reports of its findings and recommendations to the Contractor and ASES within forty-five (45) Calendar Days after the close of each review period. |
Page 485
The audit shall be conducted and the report shall be prepared in accordance with generally accepted auditing standards for such audits as defined in the publications of the AICPA, entitled “Statements on Auditing Standards” (SAS). In particular, both the “Statements on Auditing Standards Number 70-Reports on the Processing of Transactions by Service Organizations” and the AICPA Audit Guide, “Audit Guide of Service-Center-Produced Records” are to be used.
| 22.7.3.3 | The Contractor shall respond to the audit findings and recommendations within thirty (30) Calendar Days of receipt of the audit and shall submit an acceptable proposed corrective action to ASES. The Contractor shall implement the Corrective Action Plan within forty (40) Calendar Days of its approval by ASES. |
| 22.7.4 | The Contractor shall submit to ASES a “Disclosure of Information on Annual Business Transactions.” This Report must include: |
| 22.7.4.1 | Definition of A Party in Interest – As defined in Section 1318(b) of the Public Health Service Act, a party in interest is: |
| 22.7.4.1.1 | Any director, officer, partner, or employee responsible for management or administration of the Contractor; any person who is |
Page 486
directly or indirectly the beneficial owner of more than five percent (5%) of the equity of the Contractor; any person who is the beneficial owner of a mortgage, deed of trust, note, or other interest secured by, and valuing more than five percent (5%) of the Contractor; or, in the case of a Contractor organized as a nonprofit corporation, an incorporator or Enrollee of such corporation under applicable State corporation law;
| 22.7.4.1.2 | Any organization in which a person described in Section 22.7.4.1.1 above is director, officer or partner; has directly or indirectly a beneficial interest of more than five percent (5%) of the equity of the Contractor; or has a mortgage, deed of trust, note, or other interest valuing more than five percent (5%) of the assets of the Contractor; |
| 22.7.4.1.3 | Any person directly or indirectly controlling, controlled by, or under common control with the Contractor; or |
| 22.7.4.1.4 | Any spouse, child, or parent of an individual described in Sections 22.7.4.1.1-22.7.4.1.3 of this Contract. |
| 22.7.4.2 | Types of Transactions Which Must Be Disclosed. Business transactions which must be disclosed include: |
Page 487
| 22.7.4.2.1 | Any sale, exchange or lease of any property between the Contractor and a party in interest; |
| 22.7.4.2.2 | Any lending of money or other extension of credit between the Contractor and a party in interest; and |
| 22.7.4.2.3 | Any furnishing for consideration of goods, services (including management services) or facilities between the Contractor and the party in interest. This does not include salaries paid to employees for services provided in the normal course of their employment. |
| 22.7.4.3 | The information which must be disclosed in the transactions listed in this Section 22.7.4 between the Contractor and a party of interest includes: |
| 22.7.4.3.1 | The name of the party in interest for each transaction; |
| 22.7.4.3.2 | A description of each transaction and the quantity or units involved; |
| 22.7.4.3.3 | The accrued dollar value of each transaction during the Fiscal Year; and |
| 22.7.4.3.4 | Justification of the reasonableness of each transaction. |
Page 488
ARTICLE 23 PAYMENT OF TAXES
| 23.1 | The Contractor certifies and guarantees that at the time of execution of this Contract: |
| 23.1.1 | It is a corporation duly authorized to conduct business in Puerto Rico and has filed income tax returns for the previous five (5) years; |
| 23.1.2 | It complied with and paid unemployment insurance tax, disability insurance tax (Law 139), social security for drivers (“seguro social choferil”), if applicable; |
| 23.1.3 | It filed any required corporation reports with the State Department for the five (5) previous years; and |
| 23.1.4 | It does not owe any kind of taxes to the Commonwealth of Puerto Rico, its instrumentalities, dependencies, corporations or municipalities. |
| 23.2 | The Contractor will forthwith pay all taxes lawfully imposed upon it with respect to this Contract or any product delivered in accordance herewith. ASES makes no representation whatsoever as to the liability or exemption from liability of Contractor to any tax imposed by any governmental entity. |
Page 489
ARTICLE 24 RELATIONSHIP OF PARTIES
| 24.1 | Neither Party is an agent, employee, or servant of the other. It is expressly agreed that the Contractor and any Subcontractors and agents, officers, and employees of the Contractor or any Subcontractor in the performance of this Contract shall act as independent contractors and not as officers or employees of ASES. The Parties acknowledge, and agree, that the Contractor, its agent, employees, and servants shall in no way hold themselves out as Agent, employees, or servants of ASES. It is further expressly agreed that this Contract shall not be construed as a partnership or joint venture between the Contractor or any Subcontractor and ASES. |
ARTICLE 25 INSPECTION OF WORK
| 25.1 | ASES, the Puerto Rico Medicaid Program, other agencies of the Government of Puerto Rico, the Department of Health and Human Services, the General Accounting Office, the Comptroller General of the United States, the Comptroller General of the Government of Puerto Rico, if applicable, or their Authorized Representatives, shall have the right to enter into the premises of the Contractor or all Subcontractors, or such other places where duties under this Contract are being performed for ASES, to inspect, monitor or otherwise evaluate the services or any work performed pursuant to this Contract. All inspections and evaluations of work being performed shall be conducted with reasonable prior notice and during normal business hours. All inspections and |
Page 490
evaluations shall be performed in such a manner as will not unduly impact or delay the Contractor’s business operations.
ARTICLE 26 GOVERNMENT PROPERTY
| 26.1 | The Contractor agrees that any papers, materials and other documents that are produced or that result, directly or indirectly, from or in connection with the Contractor’s provision of the services under this Contract shall be the property of ASES upon creation of such documents, for whatever use that ASES deems appropriate, and the Contractor further agrees to prepare any and all documents, including the Deliverables listed in Attachment 12 to this Contract, or to take any additional actions that may be necessary in the future to effectuate this provision fully. In particular, if the work product or services include the taking of photographs or videotapes of individuals, the Contractor shall obtain the consent from such individuals authorizing the use by ASES of such photographs, videotapes, and names in conjunction with such use. Contractor shall also obtain necessary releases from such individuals, releasing ASES from any and all claims or demands arising from such use. |
| 26.2 | The Contractor shall be responsible for the proper custody and care of any ASES-owned property furnished for the Contractor’s use in connection with the performance of this Contract. The Contractor will reimburse ASES for its loss or |
Page 491
damage, normal wear and tear excepted, while such property is in the Contractor’s custody or use.
ARTICLE 27 OWNERSHIP AND USE OF DATA AND SOFTWARE
| 27.1 | Ownership and Use of Data |
| 27.1.1 | All data created from information, documents, messages (verbal or electronic), Reports, or meetings involving or arising out of this Contract are owned by ASES (the information will be hereinafter referred to as “ASES Data”). The Contractor shall make all ASES Data available to ASES, which will also provide such ASES Data to CMS or other pertinent government agencies and authorities upon request. The Contractor is expressly prohibited from sharing or publishing ASES Data without the prior written consent of ASES, except as required by law. In the event of a dispute regarding what constitutes ASES Data, the Parties shall resolve any such dispute under the provisions of Article 49 of this Contract. |
| 27.1.2 | ASES acknowledges that before executing this Contract and in contemplation of the same, the Contractor has developed and designed certain programs and systems such as standard operating procedures, programs, business plans, policies and procedures, which ASES acknowledges are the exclusive property of the Contractor (the “Contractor Proprietary Information”). Nevertheless, in case of default by the |
Page 492
Contractor or termination pursuant to the terms of this Contract, ASES is hereby authorized to use to the extent allowable by any applicable commercial software and hardware licensing that exists at that moment or with which agreement can be reached at that moment with the vendor to modify such licensing to permit its use by ASES, at no cost to ASES, such Contractor properties for a period of one hundred and twenty (120) Calendar Days to effect an orderly transition to any new contractor or service provider for the Service Regions. In any cases where the use of such systems from an operational perspective would also impact other lines of Contractor’s business or where licensing restrictions cannot be remedied, Contractor shall operate such systems on behalf of ASES. Such operation by Contractor on behalf of ASES can occur at ASES’ reasonable discretion under the full supervision of their employees or appointed third party personnel. Under such a scenario, ASES’ access to data will be restricted through the most efficient means possible.
| 27.2 | Responsibility for Information Technology Investments |
The Parties understand and agree that the cost of any newly acquired or developed software programs or upgrades or enhancements to existing software programs, hardware, or other related information technology equipment or infrastructure component, made in order to comply with the requirements of this Contract shall be borne in its entirety by the Contractor.
Page 493
ARTICLE 28 CRIMINAL BACKGROUND CHECKS
| 28.1 | ASES is prohibited by law from entering into contracts with any entity that has been, or whose president, vice president, director, executive director, member of the board of directors or a person performing equivalent functions been convicted of, or entered a guilty plea, in Puerto Rico, the United States of America, or any other jurisdiction, for any crime involving corruption, fraud, embezzlement, or unlawful appropriation of public funds, pursuant to Act 458, as amended, and Act 84 of 2002. |
| 28.2 | Before the Implementation Date of this Contract, and as a condition for the continued effectiveness of the Contract, the Contractor shall provide to ASES a certification that neither the Contractor nor the persons listed in Section 28.1 of this Contract, fall under the prohibition stated in Section 28.1 of this Contract. As an essential and indispensable condition for the execution and delivery of this Contract, the Contractor must deliver concurrently with the execution of the Contract, the sworn statements required to comply with Act 458 of December 29, 2000, as amended. |
| 28.3 | ASES may terminate this Contract if ASES determines that the Contractor, or any of the natural persons listed in Section 28.1 of this Contract, falls within the prohibition stated in Section 28.1 of this Contract, or failed to provide an accurate certification as required in Section 28.2 of this Contract. In addition, the Contractor shall terminate a Provider Contract if it learns that a Provider, or any of the natural |
Page 494
| persons listed in Section 28.1 of this Contract related to the Provider, falls within the prohibition stated in Section 28.1 of this Contract. |
| 28.4 | During the Contract Term, the Contractor shall promptly (within twenty (20) Business Days of the date it receives the information) provide to ASES any material information it obtains regarding any of the claims referred to in Section 28.1 and attributed to the persons listed in Section 28.1. |
| 28.5 | In cases in which none of the events listed in Section 28.1 of this Contract has occurred, but statements or admissions of crimes have been made by or against the Contractor, or one of its shareholders, partners, officers, principals, subsidiaries, or parent companies, ASES shall provide all pertinent information about the matter, within twenty (20) Business Days from the date it receives the information, to the Secretary of Justice of Puerto Rico, who will make the pertinent findings and recommendations concerning the Contract. |
| 28.6 | In addition, as provided in 42 CFR 455.106(c), ASES may refuse to enter into or renew an agreement with any entity if any person who has an ownership or control interest in the entity, or is an agent or managing employee of the entity, has been convicted of a criminal offense related to the person’s involvement in any program established under Medicare, Medicaid, or the Title XX services programs. Before the Implementation Date of this Contract, pursuant to 42 CFR 455.106(a), the Contractor |
Page 495
shall disclose to ASES the identity of any person who has an ownership or control interest in the Contractor, or is an agent or managing employee of the such entity who has been convicted of a criminal offense related to the Medicare, Medicaid, or Title XX services programs. The Contractor shall collect the same information on criminal conviction for Providers during the Credentialing process, as provided in Section 9.4.3.21 of this Contract, and shall, immediately upon receipt of such information relating to a Provider, disclose the information to ASES. ASES will notify the HHS Inspector General of any disclosures related to criminal convictions within twenty (20) Business Days from the date that ASES receives the information, as required by 42 CFR 455.106.
ARTICLE 29 SUBCONTRACTS
| 29.1 | Use of Subcontractors |
| 29.1.1 | The Contractor shall not subcontract or permit anyone other than Contractor personnel to perform any of the work, services, or other performances required of the Contractor under this Contract relating to the Administrative Services associated with the provision of Covered Services and Benefits to Enrollees or assign any of its rights or obligations hereunder, without the prior written consent of ASES. Prior to hiring or entering into an agreement with any Subcontractor, any and all Subcontractors shall be approved by ASES; provided, that such approval shall not be unreasonably |
Page 496
withheld, conditioned or delayed; and further provided, that the subcontracts included in Attachment 17 to this Contract are expressly approved by ASES as of the Effective Date of this Contract. ASES reserves the right to inspect all subcontract agreements at any time during the Contract period. Upon request from ASES the Contractor shall provide in writing the names of all proposed or actual Subcontractors. The Contractor is solely accountable for all functions and responsibilities contemplated and required by this Contract, whether the Contractor performs the work directly or through a Subcontractor.
| 29.1.2 | All contracts between the Contractor and Subcontractors must be in writing and must specify the activities and responsibilities delegated to the Subcontractor containing terms and conditions consistent with this Contract. The contracts must also include provisions for revoking delegation or imposing other sanctions if the Subcontractor’s performance is inadequate. |
| 29.1.3 | All contracts must ensure that the Contractor evaluates the prospective Subcontractor’s ability to perform the activities to be delegated; monitors the Subcontractor’s performance on an ongoing basis and subjects it to formal review according to a periodic schedule established by ASES and consistent with industry standards or Puerto Rico laws and regulations; and identifies deficiencies or areas for improvement, ensuring that corrective action is taken as appropriate. |
Page 497
| 29.1.4 | The Contractor shall give ASES prompt notice in writing by registered mail or certified mail of any action or suit filed by any Subcontractor and prompt notice of any Claim made against the Contractor by any Subcontractor or vendor that, in the opinion of Contractor, may result in litigation related in any way to this Contract. |
| 29.1.5 | All Subcontractors must fulfill the requirements of applicable law, including 42 CFR 438 as appropriate. |
| 29.1.6 | All Provider Contracts shall be in compliance with the requirements and provisions as set forth in Section 10.3 of this Contract. |
| 29.1.7 | The Contractor shall be held directly accountable and liable for all of the contractual provisions in this Contract regardless of whether the Contractor chooses to subcontract their responsibilities to a third party. No subcontract shall operate to terminate the legal responsibility of the Contractor to assure that all activities carried out by the subcontractor conform to the provisions of the Contract. Subcontracts shall not terminate the legal liability of the Contractor under this Contract. |
| 29.1.8 | Notwithstanding Section 29.2.1 of this Contract, ASES agrees that the Contractor will be allowed to assign or subcontract all or part of its obligations under the Contract to its sister company Triple-C, Inc., provided that notwithstanding such assignment or |
Page 498
| subcontract the Contractor shall remain obligated to ASES under the terms of this Contract. |
| 29.2 | Cost or Pricing by Subcontractors |
| 29.2.1 | The Contractor shall submit, and shall require any Subcontractors hereunder to submit, cost or pricing data for any subcontract to this Contract prior to award. The Contractor shall also certify that the information submitted by the Subcontractor is, to the best of the Contractor’s knowledge and belief, accurate, complete and current as of the date of agreement, or the date of the negotiated price of the subcontract or amendment to the Contract. The Contractor shall insert the substance of this Section in each subcontract hereunder. |
| 29.2.2 | If ASES determines that any price, including profit or fee negotiated in connection with this Contract, or any cost reimbursable under this Contract was increased by any significant sum because of the inaccurate cost or pricing data, then such price and cost shall be reduced accordingly and this Contract and the subcontract shall be modified in writing to reflect such reduction. |
ARTICLE 30 REQUIREMENT OF INSURANCE LICENSE
Page 499
| 30.1 | In order for this Contract to take effect, the Contractor must be licensed to underwrite health insurance by the Puerto Rico Insurance Commissioner. The Contractor must submit a copy of its insurance license according to the timeframe specified in Attachment 12 to this Contract. |
| 30.2 | The Contractor shall renew the license as required, and shall submit evidence of the renewal to ASES within thirty (30) Calendar Days of the expiration date of the license. |
ARTICLE 31 CERTIFICATIONS
| 31.1 | As essential and indispensable condition for the execution and delivery of the Contract, the Contractor must deliver concurrently with the execution of the Contract the sworn statement required by Article 28 of the Contract to comply with act 458 of December 29, 2000, as amended. |
| 31.2 | The Contractor shall provide to ASES within fifteen (15) Calendar Days of the execution of this Contract, and thereafter by January 10 of each calendar year, the certifications and other documents set forth below, according to the timeframe specified below. If any certification, document, acknowledgment, or other representation or assurance on the Contractor’s part under this Article, or elsewhere in this Contract, is determined to be false or misleading, ASES shall have cause for termination of this |
Page 500
| Contract pursuant to Article 34 of this Contract. In the event that the Contract is terminated based upon this Article, the Contractor shall reimburse ASES all Administrative Fees received by the Contractor under the Contract. |
| 31.3 | The Contractor shall submit the following certifications: |
| 31.3.1 | Certification issued by the Treasury Department of Puerto Rico (Model SC-2888) evidencing that Contractor has filed income tax returns in the past five years, or evidence of Contractor’s non-profit status; |
| 31.3.2 | Certification from the Treasury Department of Puerto Rico that Contractor has no outstanding debt with the Department or, if such a debt exists, it is subject to a payment plan or pending administrative review under applicable law or regulation (Model SC-3537); |
| 31.3.3 | Certification from the Center for the Collection of Municipal Revenues (“CRIM”, its Spanish acronym) certifying that there is no outstanding debt or, if a debt exists, that such debt is subject to payment plan or pending administrative review under applicable law or regulations; |
Page 501
| 31.3.4 | Certification from the Department of Labor and Human Resources certifying compliance with unemployment insurance, temporary disability insurance and/or chauffeur’s social security, if applicable; |
| 31.3.5 | Evidence of Incorporation and of Good Standing issued by the Department of State of Puerto Rico; |
| 31.3.6 | Certification of current municipal license tax (“Patentes Municipales”), if applicable; and |
| 31.3.7 | Certification issued by the Minor Children Support Administration (“ASUME”, by its Spanish acronym) of no outstanding alimony or child support debts, if applicable. |
| 31.4 | The Contractor shall, in addition, provide the following documents: |
| 31.4.1 | A list of all contracts Contractor has with government agencies, public corporations or municipalities, including those contracts in the process of being executed; |
| 31.4.2 | A letter indicating if any of its directors serves as member of any governmental board of directors or commission; |
Page 502
| 31.4.3 | A certificate of the Corporate Resolution authorizing the person signing this Contract to appear on behalf of the Contractor; |
| 31.4.4 | Evidence of compliance with the Compensation System for Work-Related Accidents Act (“Fondo del Seguro del Estado de Puerto Rico”); and |
| 31.4.5 | A copy of the Insurance Coverage Certificate as required in Article 36. |
| 31.5 | If the Contractor fails to meet the obligations of Sections 31.2 and 31.3 of this Contract within the required timeframe, ASES shall cease payment to the Contractor until the documents have been delivered to the ASES’s satisfaction, or adequate evidence is provided to ASES that reasonable efforts have been made to obtain the documents. |
ARTICLE 32 RECORDS REQUIREMENTS
| 32.1 | General Provisions |
| 32.1.1 | The Contractor shall preserve and make available all of its records pertaining to the performance under this Contract for inspection or audit, as provided below, throughout the Term of this Contract, for a period of seven (7) years from the date of final payment under this Contract, and for such period, if any, as is required by |
Page 503
| applicable statute or by any other Section of this Contract. If the Contract is completely or partially terminated, the records relating to the work terminated shall be preserved and made available for period of seven (7) years from the date of termination or of any resulting final settlement. Records that relate to Appeals, litigation, or the settlements of Claims arising out of the performance of this Contract, or costs and expenses of any such agreements as to which exception has been taken by the Contractor or any of its duly Authorized Representatives, shall be retained by Contractor until such Appeals, litigation, Claims or exceptions have been disposed of. |
| 32.2 | Records Retention and Audit Requirements |
| 32.2.1 | Since funds from the Puerto Rico Plans under Title XIX and Title XXI of the Social Security Act Medical Assistance Programs (Medicaid and CHIP) are used to finance this project in part, the Contractor shall agree to comply with the requirements and conditions of the Centers for Medicare and Medicaid Services (CMS), the Comptroller General of the United States, the Comptroller of Puerto Rico and ASES, as to the maintenance of records related to this Contract. |
| 32.2.2 | Puerto Rico and federal standards for audits of ASES agents, contractors, and programs are applicable to this Section and are incorporated by reference into this Contract as though fully set out herein. |
Page 504
| 32.2.3 | Pursuant to the requirements of 42 CFR 434.6(a)(5) and 42 CFR 434.40, the Contractor shall make all of its books, documents, papers, Provider records, Medical Records, financial records, data, surveys and computer databases available for examination and audit by ASES, HSS and its sub-agencies, the Comptroller of Puerto Rico, the Comptroller General of the United States of America and/or their authorized representatives. Any records requested hereunder shall be produced for on-site review by ASES or sent to the requesting authority by mail within fourteen (14) Calendar Days following a request. All records shall be provided at the sole cost and expense of the Contractor. ASES shall have unlimited rights to use, disclose, and duplicate all information and data in any way relating to this Contract in accordance with applicable Puerto Rico and federal laws and regulations but subject to any proprietary rights of the Contractor over such information and data. |
| 32.2.4 | In certain circumstances, as follows, the authorities listed in Section 32.2.3 of this Contract shall have the right to inspect and audit records in a timeframe that exceeds the timeframe set forth in Section 32.1.1 of this Contract. |
| 32.2.4.1 | ASES determines that there is a special need to retain a particular record or group of records for a longer period and notifies the Contractor at least thirty (30) Calendar Days before the expiration of the timeframe set forth in Section 32.1.1 of this Contract. |
Page 505
| 32.2.4.2 | There has been a Contract termination, dispute, Fraud, or similar fault by the Contractor, resulting in a final judgment or settlement against the Contractor, in which case the retention may be extended to three (3) years from the date of the final judgment or settlement. |
| 32.2.4.3 | ASES determines that there is a reasonable possibility of Fraud, and gives the Contractor notice, before the expiration of the timeframe set forth in Section 32.1.1 of this Contract, that it wishes to extend the time period for retention of records. |
| 32.2.4.4 | There has been, during the time period set forth in Section 32.1.1, an audit initiated by CMS, the Comptroller of Puerto Rico, the Comptroller General of the United States, or ASES, in which case the timeframe for retention of records shall extend until the conclusion of the audit and publication of the final report. |
| 32.2.5 | All records retention requirements set forth in this Article or in any other Article shall be subject at all times and to the extent mandated by law and regulation, to the HIPAA regulations described elsewhere in this Contract. |
| 32.2.6 | Subject to Article 52 of this Contract, the Contractor shall be subject to Claims audits once every six months commencing on the Implementation Date. The Contractor |
Page 506
| shall maintain accurate records at all times. Upon five (5) Business Days notice, the Contractor shall provide ASES reasonable access to Claims’ records to verify conformance with the terms of the Contract. If any such audit is an on-site audit, it shall be conducted during the Contractor’s normal business hours, and shall not be disruptive to the normal operations of the Contractor. ASES shall be permitted to conduct audits in accordance with this Section with any or all of its own internal resources or by securing the services of a third party accounting or auditing firm, solely at ASES’s election and expense. |
| 32.2.7 | Every six months commencing on the Implementation Date, ASES shall have the right to perform MIS audits. |
| 32.3 | Medical Record Requests |
| 32.3.1 | The Contractor shall require that the Network Providers agree that a copy of each Enrollee’s Medical Record be made available, without charge, upon the written request of the Enrollee or Authorized Representative within fourteen (14) Calendar Days of the receipt of the written request. |
| 32.3.2 | The Contractor shall require that the Network Providers agree that Medical Records be furnished at no cost to a new PCP, a PMG, an Out-of-Network Provider or other |
Page 507
| specialist, upon the Enrollee’s written request, no later than fourteen (14) Calendar Days following the written request. |
| 32.3.3 | Notwithstanding the foregoing, the Contractor must comply with the Puerto Rico Patient Bill of Rights which states that every provider, medical-hospital institution, and every insurer shall provide every patient a speedy access to their files and records. A patient is entitled to receive a copy of his/her medical record within a term which shall not exceed five (5) Calendar Days. |
ARTICLE 33 CONFIDENTIALITY
| 33.1 | General Confidentiality Requirements |
| 33.1.1 | The Contractor shall treat all information, including Medical Records and any other health and Enrollment information that identifies a particular Enrollee or that is obtained or viewed by it or through its staff and Subcontractors’ performance under this Contract as confidential information, consistent with the confidentiality requirements of 45 CFR parts 160 and 164 and the terms of that certain Business Associate Agreement dated as of September 19, 2011 by and between the Contractor and ASES (the “Business Associate Agreement”). The Contractor shall not use or disclose any information so obtained in any manner, except as may be necessary for |
Page 508
| the proper discharge of its obligations under this Contract and permitted under the Business Associate Agreement. |
| 33.1.2 | Employees or authorized Subcontractors of the Contractor who have a reasonable need to know such Enrollee information for purposes of performing their duties under this Contract shall use personal or patient information, provided such employees or Subcontractors are covered by a non-disclosure agreement that has been approved by ASES; provided, however, that the Business Associate Agreement shall be considered pre-approved by ASES. The Contractor shall remove any person from performance of services hereunder upon notice that ASES reasonably believes that such person has failed to comply with the confidentiality obligations of this Contract. The Contractor shall replace such removed personnel in accordance with the staffing requirements of this Contract. |
| 33.1.3 | ASES, the Government of Puerto Rico, federal officials as authorized by federal law or regulations, or the Authorized Representatives of these parties shall have access to all confidential information in accordance with the requirements of Puerto Rico and federal laws and regulations. |
| 33.1.4 | The confidentiality provisions contained in this Contract survive the termination of this Contract and shall bind the Contractor, and its PMGs and Network Providers, so |
Page 509
| long as they maintain any “protected health information” relating to Enrollees, as such term is defined by 45 CFR Parts 160 and 164. |
| 33.2 | HIPAA Compliance |
| 33.2.1 | The Contractor shall assist ASES in its efforts to comply with the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) and its amendments, rules, procedures, and regulations. To that end, the Contractor shall cooperate with and abide by any requirements mandated by HIPAA and any other applicable laws. The Contractor and ASES are bound by the terms and conditions of the Business Associate Agreement for HIPAA compliance purposes. In addition, the Contractor is required to sign a business associate agreement with the PBM and the MBHO. The Parties shall cooperate on these matters and sign all documents required to be HIPAA compliant including but not limited to the Business Associate Agreement. |
| 33.2.2 | The Contractor must inform ASES in writing within two (2) Business Days of any HIPAA compliance issues as a result of any breach or threatened breach of this Article 33. |
Page 510
ARTICLE 34 TERMINATION OF CONTRACT
| 34.1 | Termination by ASES |
| 34.1.1 | In addition to any other non-financial remedy set forth in this Contract or available by law, or in lieu of any financial remedy contained in Article 19 of this Contract or available by law, and subject to compliance with the termination procedures set forth in Section 34.4 below, ASES may terminate this Contract: |
| 34.1.1.1 | Termination Due to the Contractor’s Default. Upon thirty (30) Calendar Days notice to the Contractor in the event the Contractor has failed to carry out the material terms of this Contract, unless ASES, in its reasonable discretion, determines that the Contractor has cured the default to ASES’s reasonable satisfaction within the notice period. For purposes of this Section a default shall not include any delay or non-performance of the Contractor’s obligations that is caused by ASES’s failure to timely fulfill its obligations hereunder, including but not limited to payments of the Claims Payment under Section 21 of this Contract. |
| 34.1.1.2 | Termination Due to the Contractor’s Insolvency or Bankruptcy. Immediately, upon ASES providing written notice to the Contractor, in the event of the Contractor is Insolvent or the Contractor files a petition in |
Page 511
| bankruptcy. |
| 34.1.1.2.1 | In the event of the filing of a petition in bankruptcy, the Contractor shall advise ASES within one (1) Business Day. If ASES reasonably determines that the Contractor’s financial condition is not sufficient to allow the Contractor to perform its Administrative Functions as described herein in the manner reasonably required by ASES, ASES may terminate this Contract in whole or in part, Immediately or in stages. |
| 34.1.1.2.2 | In the event that this Contract is terminated the Contractor is Insolvent, the Contractor shall guarantee that Enrollees shall not be liable for: |
| 34.1.1.2.2.1 | the Contractor’s debts; or |
| 34.1.1.2.3 | the Covered Services provided to the Enrollees for which ASES does not pay the Contractor or its Network Providers. |
| 34.1.1.3 | Termination Due to Insufficient Funding. Immediately, upon ASES providing the Contractor written notice pursuant to Section 16.11.8.6 that appropriated federal and/or Puerto Rico funds become unavailable or that such funds will be insufficient for the payment of ASES’s obligations |
Page 512
| under this Contract when due, unless both Parties agree, through a written Amendment, to a modification of the obligations under this Contract. |
| 34.1.1.4 | Termination Due to the Contractor’s Breach of Article 28. Immediately, upon ASES providing written notice to the Contractor, in the event that the Contractor or any of the persons listed in Section 28.1 of this Contract fall under the prohibition stated in Section 28.1 or 28.6 of this Contract; or, subject to Section 34.3 of this Contract, upon the occurrence of any of the events specified in Section 28.3 of this Contract, as required under Act 458 and Act 458 and Act 84. |
| 34.1.1.5 | Termination Due to Change In Law Adversely Affecting Finances. Immediately, upon prior written notice, upon the occurrence of any circumstance described in Section 37.2.6 or any amendment of this Contract pursuant to Section 54.2 that would adversely affect the economic circumstances of ASES, in its reasonable determination. |
| 34.2 | Termination by the Contractor |
| 34.2.1 | In addition to any other remedy set forth in this Contract or available by law, and subject to compliance with the termination procedures set forth in Section 34.4 below, the Contractor may terminate this Contract: |
Page 513
| 34.2.1.1 | Termination Due to ASES’s Financial Breach. Upon fifteen (15) Calendar Days written notice, in the event ASES is in arrears more than ninety (90) Calendar Days with respect to the full payment of a monthly Administrative Fee, or defaults in making full payment of three (3) consecutive monthly payments of the Administrative Fee or in making full payment of two (2) consecutive monthly payments of Claims Payments, and fails to cure such breach within the notice period. For purposes of this Section, a default in making full payment does not include instances where ASES has made any Withhold payments of the Administrative Fee pursuant to the terms of this Contract, provided that ASES has given the Contractor advance written notice of any such Withhold of the Administrative Fee. |
| 34.2.1.2 | Termination Due to ASES’s General Breach. Upon thirty (30) Calendar Days written notice to ASES, in the event ASES has failed to carry out the material terms of this Contract unless the Contractor, in its reasonable discretion, determines that ASES has cured the default to the Contractor’s reasonable satisfaction within the notice period. For purposes of this Section, a default does not include the delay or failure in making payment of the Administrative Fee or Claims Payments due under this Contract. |
| 34.2.1.3 | Termination Due to Insufficient Funding. Immediately, upon receipt from |
Page 514
| ASES of a written notice pursuant to Section 16.11.8.6 that appropriated federal and/or Puerto Rico funds become unavailable or that such funds will be insufficient for the payment of ASES’s obligation under this Contract when due, unless both Parties agree, through a written Amendment, to a modification of the obligations under this Contract. |
| 34.2.1.4 | Termination Due to Change In Law Adversely Affecting Finances. Immediately, upon prior written notice, upon the occurrence of any circumstance described in Section 37.2.6 or any amendment of this Contract pursuant to Section 54.2 that would adversely affect the economic circumstances of the Contractor, in its reasonable determination. |
| 34.3 | General Procedures |
| 34.3.1 | Opportunity to Cure. Each Party shall have the opportunity to cure any default alleged in a termination notice sent pursuant to this Article 34, upon receiving a written termination notice the other Party. With respect to termination by ASES, the Contractor shall have the right to submit to ASES a written Corrective Action Plan containing terms and conditions acceptable to ASES to cure such default or an explanation of non-default in the thirty (30) Calendar Day period from the date of receipt of ASES’ written termination notice and such plan or explanation of non-default is accepted by ASES, in ASES’ sole discretion, which acceptance shall not be |
Page 515
| unreasonably withheld, conditioned or delayed. With respect to termination by the Contractor, ASES shall have the right to submit to the Contractor a written Corrective Action Plan containing terms and conditions acceptable to the Contractor to cure such default or an explanation of non-default in the thirty (30) Calendar Day period from the date of receipt of the Contractor’s written termination notice and such plan or explanation of non-default is accepted by the Contractor, in the Contractor’s sole discretion, which acceptance shall not be unreasonably withheld, conditioned or delayed. Failure to respond to a termination notice or to invoke the Party’s right to resolve the matter through the dispute resolution procedure under Article 49 of this Contract within such thirty (30) Calendar Day notice period, shall constitute the Party’s waiver of its right to contest the termination notice. |
| 34.3.2 | Continuing Obligations of the Contractor. Notwithstanding the termination of this Contract pursuant to this Article 34 for any reason, the Contractor shall remain obligated to provide the Administrative Functions as described in Article 35, including but not limited to the payment of Claims for Covered Services provided to Enrollees prior to the Termination Date and as specified in the Patient’s Bill of Rights Act through the Runoff Period. |
| 34.3.3 | Continuing Obligations of ASES. Notwithstanding the termination of this Contract for pursuant to this Article 34 for any reason, ASES shall remain obligated to pay to the Contractor the Administrative Fee through the Termination Date (inclusive of the |
Page 516
| Transition Period) and the Claims Payments through the end of the Runoff Period. |
| 34.3.4 | Termination Procedures to be Strictly Followed. No termination of this Contract shall be effective unless the termination procedures under Section 34.4 of this Contract have been strictly followed or waived by the Parties. |
| 34.4 | Termination Procedures |
| 34.4.1 | Provision of Termination Notice. ASES or the Contractor shall issue a written termination notice pursuant to this Article 34 by certified mail, return receipt requested, or in person with proof of delivery. Any such termination notice shall cite the provision of this Contract giving the right to terminate, the circumstances giving rise to termination, and the Termination Date. Notwithstanding such termination notice (including any Immediate termination), the Parties agree that this Contract shall remain in full force and effect during a period not to exceed one-hundred twenty (120) Calendar Days commencing on the date: (i) of the termination notice if such notice is not challenged by the non-moving Party or the breach giving rise to the notice of termination is not cured in accordance with Section 34.3.1of this Contract; (ii) of disposition of the matter pursuant to Article 49 of this Contract; or (iii) as the Parties otherwise mutually agree in writing (such period to be referred to as the “Transition Period”, as further described under Article 35 of this Contract). Termination of this Contract shall be effective at 11:59 p.m. Puerto Rico time on the |
Page 517
| last day of the Transition Period, which shall be known as the Termination Date. |
| 34.4.2 | Termination Procedure. The Parties agree that the following actions must occur to effectuate the termination of this Contract: |
| 34.4.2.1 | The moving Party shall provide the written termination notice to the non-moving Party pursuant to Section 34.4.1 of this Contract, stating the reason for the termination and the Termination Date (inclusive of the Transition Period), which shall become effective unless the non-moving Party responds to the termination notice in a timely manner pursuant to Section 34.4.2 B below; |
| 34.4.2.2 | The non-moving Party shall provide to the moving Party a Corrective Action Plan to address the alleged breach stated in the termination notice or a written explanation of non-breach, or the non terminating Party submits the matter for disposition under the dispute resolution procedure contained in Article 49 of this Contract, within thirty (30) Calendar Days following receipt of such termination notice; |
| 34.4.2.3 | The moving Party shall provide written notice to the other Party of its determination as to whether the breach described in the termination notice has been waived or cured to its reasonable satisfaction within the thirty |
Page 518
| (30) Calendar Days period; |
| 34.4.2.4 | The non-moving Party shall have a right to appeal the moving Party’s unfavorable determination through the dispute resolution procedure under Article 49 within ten (10) Calendar Days following receipt of the unfavorable determination; and |
| 34.4.2.5 | ASES, upon any termination, including any determination affirmed through the dispute resolution procedure under Article 49, shall give Enrollees notice of the termination and information consistent with 42 CFR 438.10 on their options for receiving Covered Services and Benefits following the Termination Date. |
| 34.4.3 | Termination Procedures During Transition Period. As provided in the Transition Plan required under Section 35.4 of this Contract, the Contractor shall, during the Transition Period leading up to the Termination Date: |
| 34.4.3.1 | Stop work under the Contract on the date and to the extent specified in the notice of termination; |
| 34.4.3.2 | Place no further orders or subcontract for materials, services, or facilities, except as may be necessary for completion of such portion of the work |
Page 519
| under the Contract as is not terminated; |
| 34.4.3.3 | Terminate all orders and subcontracts to the extent that they relate to the performance of work terminated by the notice of termination; |
| 34.4.3.4 | Assign to ASES, in the manner and to the extent directed by ASES, all of the right, title, and interest of Contractor under the orders or subcontracts so terminated, in which case ASES will have the right, at its discretion, to settle or pay any or all claims arising out of the termination of such orders and subcontracts; |
| 34.4.3.5 | With the approval of ASES, settle all outstanding liabilities and all claims arising out of such termination or orders and subcontracts, the cost of which would be reimbursable in whole or in part, in accordance with the provisions of the Contract; |
| 34.4.3.6 | Complete the performance of such part of the work as shall not have been terminated by the notice of termination; |
| 34.4.3.7 | Take such action as may be necessary, or as ASES may direct, for the protection and preservation of any and all property or information related to the Contract that is in the possession of Contractor and in which ASES |
Page 520
| has or may acquire an interest; |
| 34.4.3.8 | Promptly make available to ASES, or to another MCO or third party administrator acting on behalf of ASES, any and all records, whether medical or financial, related to the Contractor’s activities undertaken pursuant to this Contract and the Transition Plan. Such records shall be provided at no expense to ASES; |
| 34.4.3.9 | Promptly supply all information necessary to ASES, or a managed care plan or third party administrator acting on behalf of ASES, for payment of any outstanding Claims at the time of termination subject to the terms of this Contract; and |
| 34.4.3.10 | Submit a Transition Plan to ASES for review and approval, which approval shall not be unreasonably withheld, conditioned or delayed. Such plan shall include commitments to carry out the following obligations: |
| 34.4.3.10.1 | Maintain Claims processing functions during the Transition Period and the Runoff Period, as necessary, in order to complete adjudication of all Claims. No Administrative Fee will be paid during the Runoff Period; |
Page 521
| 34.4.3.10.2 | Comply with all duties and/or obligations incurred prior to the Termination Date of the Contract, including but not limited to, any pending Appeal process as described in Section 14.5 of this Contract; |
| 34.4.3.10.3 | File all Reports require to Article 18 of this Contract during the Term of the Contract (including the Transition Period) in the manner described in this Contract; |
| 34.4.3.10.4 | Ensure the efficient and orderly transition of Enrollees from coverage under this Contract to coverage under any new arrangement developed or agreed to by ASES, including diligent cooperation with another contractor, upon the terms set forth in Article 35; |
| 34.4.3.10.5 | Maintain the financial requirements and insurance set forth in this Contract until the Termination Date; |
| 34.4.3.10.6 | Meet with ASES personnel, as requested, to ensure satisfactory completion of all obligations under the Transition Plan; and |
| 34.4.3.10.7 | Submit Reports to ASES as directed, but no less frequently than every thirty (30) Calendar Days, detailing the Contractor’s progress in completing its obligations under this Contract during the Transition |
Page 522
| Period, unless otherwise established in Article 18 of this Contract. |
| 34.4.4 | Final Report. On the Termination Date, the Contractor shall submit a final report to ASES describing how the Contractor has completed its obligations under this Contract as of the Termination Date (the “Final Report”). ASES will advise, within twenty (20) Calendar Days of receipt of the Final Report, if all of the Contractor’s obligations are discharged. If ASES finds that the Final Report does not evidence that the Contractor has fulfilled its continuing obligations, then ASES will require the Contractor to submit a revised Final Report to ASES for approval, and take any other action necessary to discharge all of its duties under this Contract, as directed by ASES. ASES acknowledges that it shall not unreasonably withhold, condition or delay its approval of the Final Report or revised Final Report, as applicable. |
| 34.5 | Except as provided in this Article 34, a notification from a Party that it intends to terminate this Contract shall not release the other Party from its obligations under this Contract. |
ARTICLE 35 PHASE IN, PHASE-OUT AND COOPERATION WITH OTHER CONTRACTORS
| 35.1 | [Intentionally left blank]. |
Page 523
| 35.2 | If in the best interest of Enrollees of MiSalud, ASES develops and implements new projects that impact the scope of services in the Service Regions, the Contractor shall assist in the implementation process after receiving at least ninety (90) Calendar Days written notice from ASES of such change, and pursuant to written Amendment of the Contract. The Per Member Per Month Administrative Fee shall be adjusted accordingly and documented in the Amendment. |
| 35.3 | In the event that ASES has entered into, or enters into, agreements with other contractors for additional work related to the Covered Services and Benefits made available by the Contractor hereunder, the Contractor agrees to cooperate fully with such other contractors. The Contractor shall not commit any act or omission that will interfere with the performance of work by any other contractor, or actions taken by ASES to facilitate the work. |
| 35.4 | If either Party exercises its right of termination under Article 34, the Contractor agrees that it will not engage in any behavior or inaction that prevents or hinders the work of another contractor or ASES, as the case may be. The Contractor shall continue to comply with the terms of this Contract until the Termination Date, subject to compliance by ASES with its obligations under this Contract including those set forth in Article 21. Upon receiving ASES’s notice that it intends to terminate the Contract or upon Contractor exercising its limited termination rights, the Parties shall formulate and agree on a written transition plan (the “Transition Plan”) within thirty (30) Calendar |
Page 524
| Days of receiving or giving the notice, as the case may be. The Transition Plan shall include all the elements listed in Section 34.8 of this Contract. The Parties agree that the Contractor will not have successfully met its obligation under this Section until ASES accepts the Contractor’s Transition Plan, which acceptance shall not be unreasonably withheld, conditioned or delayed. |
| 35.5 | Phase Out Transition Period |
| 35.5.1 | The Transition Period shall allow a new physical health care services plan designated by ASES under the MiSalud Program to take over for the Contractor in the Service Regions. During the Transition Period, this Contract shall remain in full force and effect. |
| 35.5.2 | The Transition Period shall always be deemed to end on the last day of a month, and shall never be of a term of more than one hundred twenty (120) Calendar Days from the date specified under the applicable circumstances in Section 34.8. Upon termination of the Transition Period, the Contractor shall not be obligated to continue to provide Administrative Services and arrange for Covered Services except as required under the Patient’s Bill of Rights Act. The Contractor shall continue all reporting requirements in accordance with the Contract. |
Page 525
| 35.5.3 | The Contractor will comply with any clarifications, amendments or supplements made to this Contract during the Transition Period as required by applicable federal law or CMS regulations; provided, that the Contractor may contact CMS directly to clarify any doubts regarding to the applicability of any such clarifications, amendments or supplements to this Contract. |
| 35.5.4 | The Parties agree that during the Transition Period and, if applicable, the Runoff Period, the terms and conditions of the Contract shall remain in full force and effect, including but not limited to ASES’ ongoing obligation to pay the Administrative Fee during the Transition Period and Claims Payments during the Transition Period and Runoff Period. |
| 35.5.5 | Continuation and Access of Care |
| 35.5.5.1 | During the Transition Period, the Contractor shall arrange for the continuation of care and access to Covered Services and Benefits for Enrollees as provided and contemplated under the Contract. To assure continuation of care and access of Covered Services and Benefits during the Transition Period, the Contractor shall comply with the requirements of Section 9.5 and 9.6 of the Contract. Any proposed change, modification, or reduction in the Provider ratio requirements in Section 9.5 of this Contract or the Network Provider ratio requirements in Section 9.6 |
Page 526
| of this Contract during the Transition Period must be previously approved in writing by ASES. If a Provider leaves the Network, the Contractor shall notify Enrollees pursuant to Sections 6.6 of this Contract. |
| 35.5.5.2 | Following the Transition Period, the Contractor shall have no obligation to arrange for the continuation of care and access to Covered Services and Benefits for any Enrollee, except as required under the Patient’s Bill of Right Act. |
| 35.5.6 | Providers’ Claims Payment |
| 35.5.6.1 | The Contractor shall pay Providers’ Claims for Covered Services furnished prior to and during the Transition Period provided ASES has complied with its obligations under this Contract including those set forth in Article 21 of this Contract. |
| 35.5.6.2 | ASES or its designee shall have the right to audit and monitor payments made to Providers during the Transition Period and the Runoff Period. |
| 35.5.6.3 | ASES or its designee may verify the payment process once completed and the verification process may proceed as follows: |
Page 527
| 35.5.6.3.1 | Final check register for each payment cycle will be provided to ASES or its designee and will be used as the master document for the validation of payments being produced and delivered to Providers. |
| 35.5.6.3.2 | Confirmation to ASES or its designee of the production of checks or electronic wire payments to the Providers, as per the final check registers. ASES or its designee will confirm the production of the checks by being present at the Contractor’s facility when the Contractor is issuing the checks and at the time the processing of the electronic wire transfers is taking place. |
| 35.5.6.3.3 | Upon notification by the Contractor to ASES or its designee that the production of the checks or the wire transfer will take place, ASES or its designee agree to be present at the Contractor’s facilities as soon as practicable. |
| 35.5.6.3.4 | Confirmation to ASES or its designee of the delivery of payments to Providers either by checks or electronic wire transfer. The confirmation to ASES may include the examination of the delivery of such payments by ASES or its designee. |
Page 528
| 35.5.6.3.5 | Certification issued by the Contractor that the checks to Providers reflected in the final check registers were duly issued and mailed to Providers. |
| 35.5.6.3.6 | ASES retains the ability to reasonably request and receive pertinent documents from the Contractor with respect to confirmation of payments made by the Contractor to Providers. This may include, at ASES’s discretion, but pursuant to and as provided in the Contract, without limitation the actual examination of pertinent documents, other than checks, as they are processed through the payment cycle. |
| 35.5.6.3.7 | The monitoring process may include the verification by ASES or its designee of the delivery of the corresponding payments made by the Contractor to the corresponding Providers, including the presence of ASES or its designee at the time of actual delivery of the checks to the Providers. In the case such delivery consists in payment by mail, ASES retains the ability to monitor the delivery of such payments to the US Post Office, either by the Contractor or by any Subcontractor retained by the Contractor to perform such delivery. |
Page 529
| 35.5.6.3.8 | ASES or its designee may reasonably request information regarding advances of future payment of Claims made by the Contractor to its Providers. |
| 35.5.6.3.9 | The activities of ASES or its designee shall in no manner unduly or unreasonably delay, disrupt or interfere with the Contractor’s customary process for Claims payment to Providers. |
| 35.5.6.3.10 | ASES acknowledges that in order for the Contractor to process the cycle of payments to Providers as hereby contemplated during the Contract Term (inclusive of the Transition Period) and the Runoff Period, it must receive the Claims Payment in accordance with the Contract. |
| 35.5.6.4 | The Contractor shall process all Claims for Covered Services provided during the Contract Term (inclusive of the Transition Period) and the Runoff Period, provided ASES has complied with its obligations under this Contract including those set forth in Article 21. |
| 35.5.6.5 | During the Transition Period and Runoff Period, the Contractor shall continue to comply with all Claims reporting requirements in this Contract. |
Page 530
| 35.5.7 | Grievance System |
| 35.5.7.1 | The Contractor shall comply with all duties and/or obligations incurred under the Contract during the Transition Period, with respect to the Grievance System process established in Article 14 of the Contract. |
| 35.5.8 | Phase-Out Transition Reports and Meetings |
| 35.5.8.1 | The Contractor shall file, on a timely basis, all necessary Reports concerning the operations of the Contractor pursuant to the Contract, including the Transition Period and the Runoff Period as required by applicable law and as otherwise required pursuant to this Contract. The Contractor shall also deliver Reports concerning the operations of the Contractor with respect to the MiSalud Program reasonably requested by ASES throughout the duration of the Transition Period or the Runoff Period, as the case may be (collectively “Transition Reports”). Unless otherwise specifically indicated, the Contractor shall use Reasonable Efforts to submit to ASES any Transition Reports requested by ASES at least three (3) Calendar Days prior to the due date of any such Report, provided the request is made during normal business hours Monday through Thursday, excluding Friday and holidays, unless otherwise a |
Page 531
| shorter period is reasonably warranted under the then existing circumstances. |
| 35.5.8.2 | ASES shall provide Transition Report templates. ASES will provide training on the Transition Report templates. |
| 35.5.8.2.1 | Transition Reports may include the following: (i) Grievances and Appeals (Enrollee complaints, grievances, notices of Action, Appeals, and Administrative Law Hearing requests); (ii) Enrollee and Provider Mailings (ID cards mailed to Enrollees, Enrollee and Provider notices mailed and date mailed, Enrollee notices returned to the Contractor); (iii) Provider Network (network report by Provider type including Providers leaving the Contractor Provider network (General or PPN) to ensure network adequacy as defined in the Contract during the Transition Period); (iv) Financial Management and Claims Payment (financial records, encounter data, paid, pending, and denied Claims); (v) Call Center Operations, and (vi) PMG Services and Payments. |
| 35.5.8.3 | ASES and the Contractor shall meet with each other’s personnel, as reasonably requested, to ensure satisfactory completion of all obligations under the Contract, the Transition Period or Runoff Period, including, but |
Page 532
| not limited to weekly meetings and designating a transition team and a team leader. |
| 35.6 | Phase-In Transition Reports and Meetings |
| 35.6.1 | Upon request by ASES, the Contractor shall assist and diligently cooperate with other contractors that ASES enters into agreement with during the Transition Period. |
| 35.6.1.1 | The Contractor cooperation and assistance includes, but is not limited to, submission of data and reports as reasonably required by ASES to protect the Enrollees and to promote continuity of care. |
| 35.6.2 | External Quality Review |
| 35.6.2.1 | The Contractor shall be available to participate in the EQRO’s onsite evaluation process during the Transition Period. The Contractor shall assist the EQRO with all reasonable requests including, but not limited to, providing samples of Grievances for the period covered by the Contract Term, by Service Region. |
| 35.6.2.2 | The HEDIS activity for calendar year 2013 shall be prepared by the new physical health service provider or providers. The Contractor shall |
Page 533
| provide all HEDIS data to the new physical health service provider or providers, as of the Termination Date of the Contract. |
| 35.6.3 | Notices and Communications to Enrollees and Providers |
| 35.6.3.1 | The Contractor shall make all necessary notices to Enrollees and Providers as may be legally required under the Contract, or otherwise required under applicable law during the Transition Period. Such notices shall be previously approved in writing by ASES. |
| 35.6.4 | Call Centers |
| 35.6.4.1 | The call center scripts used during the Transition Period shall be previously approved in writing by ASES. |
| 35.6.5 | Records Retention |
| 35.6.5.1 | The Contractor shall abide by the record retention schedule provided by ASES in compliance with the Contract. Records must be provided and made available to ASES for inspection and audit for a period of seven (7) years from the date of final payment under the Contract, the Transition Period or the Runoff Period, as applicable. The Contractor shall provide |
Page 534
| ASES during normal business hours, the right to inspect these records during the seven (7) year period specified in the Contract. |
| 35.7 | ASES Obligations |
| 35.7.1 | ASES shall continue to pay the Contractor its Administrative Fee pursuant to the terms of the Contract until the Termination Date of the Contract, inclusive of the Transition Period. |
| 35.7.2 | ASES shall process the Per Member Per Month Administrative Fee corresponding to Enrollees that were enrolled during the last month of the Transition Period to calculate the Administrative Fee. This Administrative Fee will be due on the next month following the termination of the Transition Period. |
| 35.7.3 | During the Transition Period, ASES will continue submitting to the Contractor the eligibility files, including new eligible, cancellations, rejections and full files. |
| 35.8 | Contractor Objections to Payment |
| 35.8.1 | The Contractor shall present to ASES, in accordance with the provisions of the Contract, any objections to payment of Claims Payment or the Administrative Fee |
Page 535
| payment due or other amounts due by ASES to the Contractor under the Contract, as the case may be. |
| 35.8.2 | Once ASES submits to the Contractor the payment file corresponding to the last month of the Transition Period, the Contractor will have ninety (90) Calendar Days from the date the Contractor receives the detailed payment file to reconcile the Administrative Fee and submit the enrollment discrepancies and corrections to ASES for processing. |
| 35.9 | Runoff Period |
| 35.9.1 | During the Runoff Period the Contractor shall: |
| 35.9.1.1 | Arrange for the continuation of care and access to Covered Services and Benefits for those certain Enrollees specified, and under the circumstances described, in Section 35.5.5.2 of this Contract; provided, that ASES shall be responsible for the payment of such services in accordance with Article 21 of this Contract; |
| 35.9.1.2 | Pay Providers’ Claims for Covered Services furnished to Enrollees prior to and during the Transition Period provided ASES has complied with its |
Page 536
| obligations under this Contract including those set forth in Article 21 of this Contract; |
| 35.9.1.3 | Provide to ASES upon its reasonable request Transition Reports regarding the operations of the Contractor with respect to the MiSalud Program during the Runoff Period; and |
| 35.9.1.4 | Cooperate and meet with representatives of ASES at mutually agreed upon times to review and facilitate the Contractor’s provision of its limited Administrative Services described in this Section 35.9.1 of this Contract during the Runoff Period. |
| 35.9.2 | During the Runoff Period ASES shall: |
| 35.9.2.1 | Make Claims Payments to the Contractor pursuant to Article 21 of this Contract to enable the Contractor to pay Providers’ Claims for Covered Services furnished to Enrollees prior to and during the Transition Period; |
| 35.9.1.3 | Provide to the Contractor upon its reasonable request such information, including but not limited to information described in Article 4 of this Contract, reasonably necessary for the Contractor to render its limited |
Page 537
| Administrative Services as described in Section 35.9.1 of this Contract during the Runoff Period; and |
| 35.9.1.4 | Cooperate and meet with representatives of the Contractor at mutually agreed upon times to review and facilitate the Contractor’s provision of its limited Administrative Services described in this Section 35.9.1 of this Contract during the Runoff Period. |
ARTICLE 36 INSURANCE
| 36.1 | The Contractor shall, at a minimum, prior to the commencement of work, procure the insurance policies identified below at the Contractor’s own cost and expense and shall furnish ASES with proof of coverage at least in the amounts indicated. It shall be the responsibility of the Contractor to require any Subcontractor to secure the same insurance coverage as prescribed herein for the Contractor, and to obtain a certificate evidencing that such insurance is in effect. In the event that any such insurance is proposed to be reduced, terminated or cancelled for any reason, the Contractor shall provide to ASES at least thirty (30) Calendar Days prior written notice. Prior to the reduction, expiration and/or cancellation of any insurance policy required hereunder, the Contractor shall secure replacement coverage upon the same terms and provisions to ensure no lapse in coverage, and shall furnish, at the request of ASES, a |
Page 538
| certificate of insurance indicating the required coverage. The provisions of this Section shall survive the expiration or termination of this Contract for any reason. The Contractor shall maintain insurance coverage sufficient to insure against claims arising at any time during the term of the Contract, consisting of the following: |
| 36.1.1 | Workers’ Compensation Insurance, the policy(ies) to insure the statutory limits established by law of the Government of Puerto Rico. The Workers’ Compensation Policy must include Coverage B – Employer’s Liability Limits of: |
| 36.1.1.1 | Bodily injury by accident: five hundred thousand dollars ($500,000) each accident; |
| 36.1.1.2 | Bodily Injury by Disease: five hundred thousand dollars ($500,000) each employee; and |
| 36.1.1.3 | One million dollars ($1,000,000) policy limits. |
| 36.1.2 | The Contractor shall require all Subcontractors performing work under this Contract to obtain an insurance certificate showing proof of Worker’s Compensation Coverage. |
| 36.1.3 | The Contractor shall have commercial general liability policy(ies) as follows: |
Page 539
| 36.1.3.1 | Combined single limits of one million dollars ($1,000,000) per person and three million dollars ($3,000,000) per occurrence; |
| 36.1.3.2 | On an “occurrence” basis; and |
| 36.1.3.3 | Liability for property damage in the amount of three million dollars ($3,000,000) including contents coverage for all records maintained pursuant to this Contract. |
ARTICLE 37 COMPLIANCE WITH ALL LAWS
| 37.1 | Nondiscrimination |
| 37.1.1 | The Contractor shall comply with applicable federal and Puerto Rico laws, rules, and regulations, and the Puerto Rico policy relative to nondiscrimination in employment practices because of political affiliation, religion, race, color, sex, physical handicap, age, or national origin. Applicable federal nondiscrimination law includes, but is not limited to, Title VI of the Civil Rights Act of 1964, as amended; Title IX of the Education Amendments of 1972, as amended; the Age Discrimination Act of 1975, as amended; Equal Employment Opportunity and its implementing regulations (45 CFR 74 Appendix A (1), Executive Order 11246 and 11375); the Rehabilitation Act of 1973; and the Americans with Disabilities Act of 1993 and its implementing |
Page 540
| regulations (including but not limited to 28 CFR § 35.101 et seq.). Nondiscrimination in employment practices is applicable to employees for employment, promotions, dismissal and other elements affecting employment. |
| 37.1.2 | The Contractor shall comply with all applicable provisions of the Puerto Rico Patient’s Bill of Rights and its implementing regulation, which prohibit discrimination against any patient. |
| 37.2 | Compliance with All Laws |
| 37.2.1 | Each Party agrees that it will comply fully with and abide by all federal and Puerto Rico laws, rules, regulations, statutes, policies, or procedures that may govern the Contract, including but not limited to those listed in Attachment 1, to the extent applicable. |
| 37.2.2 | Subject to Sections 34.1.1.5, 34.1.3.4, 37.26 and 54.2 of this Contract, all Puerto Rico and federal laws, rules, and regulations, consent decrees, court orders, policy letters and normative letters, and policies and procedures, including but not limited to those described in Attachment 1, are hereby incorporated by reference into this Contract to the extent applicable. |
Page 541
| 37.2.3 | To the extent that applicable laws, rules, regulations, statutes, policies, or procedures require the Contractor to take action or inaction, any costs, expenses, or fees associated with that action or inaction shall be borne and paid by the Contractor solely. Such compliance-associated costs include, but are not limited to, attorneys’ fees, accounting fees, research costs, or consultant costs, where these costs are related to, arise from, or are caused by compliance with any and all laws. |
| 37.2.4 | The Contractor shall include notice of grantor agency requirements and regulations pertaining to reporting and patient rights under any contracts involving research, developmental, experimental or demonstration work with respect to any discovery or invention which arises or is developed in the course of or under such contract, and of grantor agency requirements and regulations pertaining to copyrights and rights in data. |
| 37.2.5 | The Contractor certifies and warrants to ASES that at the time of execution of this Contract: (i) it is a corporation duly authorized to conduct business in Puerto Rico, and has filed all the required income tax returns for the preceding five years; and (ii) it filed its report due with the Office of the Commissioner of Insurance during the five (5) years preceding the Effective Date of this Contract. |
| 37.2.6 | Notwithstanding any other provision of this Contract to the contrary, if, as a result of (i) any change in or adoption of any Puerto Rico and/or federal laws, rules, |
Page 542
| regulations, policies, or procedures, or the interpretation of such laws, rules, regulations, policies, or procedures, including without limitation, those from CMS or any change to the Medicaid State plan, (ii) any amendment of this Contact pursuant to Section 54.2, (iii) any change required pursuant to Section 57.3 due to changes, clarifications, or supplementations as a result of CMS requirements, or (iv) any change in an adoption of any MiSalud Policies and Procedures, either Party is adversely affected by such change, it may so notify the other Party. The Parties shall use good faith efforts to promptly renegotiate, in a term not to exceed thirty (30) Business Days, the Administrative Fee and amend the Contract to reflect the additional cost and expenses to the Contractor as a result of such change or amendment. In the event that the Parties cannot agree on the adjustment to the Administrative Fee, the matter shall be resolved pursuant to the dispute resolution provisions set forth in Article 49 of this Contract, subject to the Contractor’s rights under Section 34.1.3.4 of this Contract and ASES’s rights under Section 34.1.1.5 of this Contract. |
ARTICLE 38 CONFLICT OF INTEREST AND CONTRACTOR INDEPENDENCE
| 38.1 | The duty to provide information about interests and conflicting relations is continuous and extends throughout the Contract Term. |
Page 543
| 38.2 | The Contractor covenants that it presently has no interest and shall not acquire any interest, direct or indirect, that would conflict in any material manner or degree with, or have a material adverse effect on the performance of its services hereunder. The Contractor further covenants that in the performance of the Contract no person having any such interest shall be employed. The Contractor shall submit a conflict of interest form, attesting to these same facts, by January 10 of each calendar year; and at any time, within fifteen (15) Calendar Days of request by ASES. |
| 38.3 | It shall be the responsibility of the Contractor to maintain independence and to establish necessary policies and procedures to assist the Contractor in determining if the actual Contractors performing work under this Contract have any impairment to their independence. |
| 38.4 | The Contractor further agrees to take all necessary actions to eliminate threats to impartiality and independence, including but not limited to reassigning, removing, or terminating Providers or Subcontractors. |
| 38.5 | ASES acknowledges that it has no objections to the Contractor during the Term of this Contract acquiring and operating, through an affiliated HMO organized under Chapter 19 of the Puerto Rico Insurance Code, health facilities that may provide Covered Services to Enrollees in the MiSalud Program. Upon the request of the Contractor, ASES shall request the opinion of the Puerto Rico Department of Justice |
Page 544
| confirming that any such action by the Contractor and its affiliated HMO would not adversely affect the Contractor’s ability to comply with applicable Puerto Rico law. |
| 38.6 | ASES acknowledges that: (i) the Contractor has disclosed to ASES that the Contractor holds a minority ownership interest in NeoDeck Holdings, Inc., a software development company that offers a certified EHR system that meets the specifications in Attachment 15 of this Contract; and (ii) Network Providers may select the NeoDeck EHR system, from among other EHR Systems produced by other software developers with which the Contractor has no affiliation, to meet their obligations to implement and maintain an EHR system in accordance with the specifications set forth in Attachment 15 of this Contract. The Contractor acknowledges that it will not require the use of NeoDeck Holdings, Inc.’s EHR system to satisfy such Provider obligation. |
ARTICLE 39 CHOICE OF LAW OR VENUE
| 39.1 | This Contract shall be governed in all respects by the laws of Puerto Rico. Any lawsuit or other action brought against ASES or the Government of Puerto Rico based upon or arising from this Contract shall be brought in a court or other forum of competent jurisdiction in Puerto Rico. |
ARTICLE 40 THIRD-PARTY BENEFICIARIES
Page 545
| 40.1 | Except as expressly provided herein, no term or provision hereof shall be construed in any way to grant, convey or create any rights or interest to or in any person or entity not a Party to this Contract, except with respect to payments to Providers that have rendered Covered Services and Benefits to Enrollees in the MiSalud Plan as set forth in this Contract. |
ARTICLE 41 SURVIVABILITY
| 41.1 | The representations and warranties made by the Parties in this Contract shall survive the delivery or provision of all services hereunder. |
ARTICLE 42 PROHIBITED AFFILIATIONS WITH INDIVIDUALS DEBARRED AND SUSPENDED
| 42.1 | The Contractor certifies that it is not presently debarred, suspended, proposed for debarment or declared ineligible for award of contracts by any federal or Puerto Rico agency, as provided in Section 13.4 of this Contract. In addition, the Contractor certifies that, to the best of its knowledge based on its compliance with the procedures established in Section 9.4.9 of this Contract, it does not presently employ or subcontract with any person or entity that could be excluded from participation in the Medicaid Program under 42 CFR 1001.1001 (exclusion of entities owned or controlled by a sanctioned person) or 1001.1051 (exclusion of individuals with ownership or control |
Page 546
| interest in sanctioned entities). Any violation of this Article shall be grounds for termination pursuant to Article 34 of this Contract. |
ARTICLE 43 WAIVER
| 43.1 | The waiver by either Party of any breach of any provision contained in this Contract by the other Party shall not be deemed to be a waiver of such provision on any subsequent breach of the same or any other provision contained in this Contract and shall not establish a course of performance between the Parties contradictory to the terms hereof. |
ARTICLE 44 FORCE MAJEURE
| 44.1 | Neither Party to this Contract shall be responsible for delays or failures in performance resulting from acts beyond the control of such Party. Such acts shall include, but not be limited to, acts of God, strikes, riots, lockouts, acts of war, epidemics, fire, earthquakes, or other disasters. |
ARTICLE 45 BINDING
Page 547
| 45.1 | This Contract and all of its terms, conditions, requirements, and amendments shall be binding on ASES and the Contractor and their respective successors and permitted assigns. |
ARTICLE 46 TIME IS OF THE ESSENCE
| 46.1 | Time is of the essence in this Contract. Any reference to “Days” shall be deemed Calendar Days unless otherwise specifically stated. |
ARTICLE 47 AUTHORITY
| 47.1 | ASES has full power and authority to enter into this Contract, and the person signing on behalf of ASES has been properly authorized and empowered to enter into this Contract on behalf of ASES and to bind ASES to the terms of this Contract. The Contractor has full power and authority to enter into this Contract, and the person signing on behalf of the Contractor has been properly authorized and empowered to enter into this Contract on behalf of the Contractor and to bind the Contractor to the terms of this Contract. Each Party further acknowledges that it has had the opportunity to consult with and/or retain legal counsel of its choice, read this Contract. Each party acknowledges that it understands this Contract and agrees to be bound by it. |
ARTICLE 48 ETHICS IN PUBLIC CONTRACTING
Page 548
| 48.1 | The Contractor understands, states, and certifies that it made its Proposal without collusion or fraud and that it did not offer or receive any kickbacks or other inducements from any other contractor, supplier, manufacturer, or Subcontractor in connection with its Proposal. |
ARTICLE 49 DISPUTE RESOLUTION
| 49.1 | Any dispute between the Parties arising out of, relating to, or in connection with this Contract, including any question regarding its existence, validity or termination or any question as to whether such dispute is subject to the provisions contained in this Article 49, shall be resolved as set forth in this Article 49. |
| 49.2 | Informal Dispute Resolution Procedures |
The Parties agree that, at all times, they will attempt in good faith to resolve all disputes that may arise under this Contract. The Parties further agree that, upon receipt of written notice of a dispute from a Party, the Parties shall refer the dispute to the designated person of each Party. The designated persons shall negotiate in good faith to resolve the dispute, conferring as often as they deem reasonably necessary, and shall gather and in good faith furnish to each other the information pertinent to the dispute. Statements made by representatives of the Parties during the dispute resolution mechanisms set forth in this Article 49 and documents specifically created for such
Page 549
dispute resolution mechanisms shall be considered part of settlement negotiations and shall not be admissible in evidence in any proceeding without the mutual written consent of the Parties.
| 49.3 | Arbitration. |
| 49.3.1 | If the procedures described in Sections 49.2 do not result in resolution of a dispute arising under this Contract within thirty (30) Calendar Days after the notice referring the dispute to the designated person of each Party as provided in Section 49.2, the dispute shall be exclusively and finally settled by arbitration in accordance with the Commercial Arbitration Rules for the AAA then in effect (the “AAA Commercial Rules”). Either Party may initiate the arbitration, as provided in the AAA Commercial Rules. The place of arbitration shall be San Juan, Puerto Rico, unless the Parties otherwise agree. Pursuant to Section 39 of this Contract, the arbitration panel shall determine the rights and obligations of the Parties in accordance with the substantive laws of Puerto Rico and without regard to the conflict of laws principles thereof. Except as agreed by the Parties, the arbitration panel shall have no power to alter or modify any terms or provisions of this Agreement or to render any award that, by its terms or effects, would alter or modify any term or provision of this Agreement. The arbitration panel shall be composed of three arbitrators, one to be selected by ASES, one to be selected by the Contractor and the third to be selected by the two previously-selected arbitrators. If the two previously-selected arbitrators |
Page 550
| cannot agree on the selection of the third arbitrator, within thirty (30) Calendar Days from their appointment by the Parties, either Party may file an action in the Puerto Rico Court of First Instance in San Juan, Puerto Rico, and request that said Court appoint the third arbitrator. Once the arbitration panel has been composed, the arbitrators shall act as neutrals and not as party arbitrators, and no Party shall engage in any ex parte communication with any member of the arbitration panel. Each Party shall bear equally the costs of the arbitration panel and attorneys’ fees as determined by the arbitration panel. The award shall include interest from the date of any breach or violation of this Agreement or the incurring of any obligation as determined in the arbitration award until paid in full. The award shall be in writing and state the reasons upon which it is based. The award shall be final and binding on the Parties. Judgment on the award may be entered by any court of competent jurisdiction. |
| 49.3.2. | Disputes Regarding Arbitration Any dispute between the Parties as to whether a dispute shall be submitted to arbitration under Sections 49.2 shall be resolved by initiation of an action in the Commonwealth Court of First Instance, San Juan Part (the “Commonwealth Court”). |
Page 551
| 49.4 | Court Action Each Party to this Contract agrees that it may not initiate a civil action in Commonwealth Court other than provisional remedies sought on an expedited basis. |
ARTICLE 50 SECTION TITLES NOT CONTROLLING
| 50.1 | The Section and Article titles used in this Contract are for reference purposes only and shall not be deemed a part of this Contract. |
ARTICLE 51 HOLD HARMLESS
| 51.1 | The Contractor shall indemnify and hold ASES, and its officers and directors harmless from and against all losses, damages, claims, demands, fines, costs, penalties, liabilities and expenses of every kind, including but not limited to reasonable attorneys’ fees (collectively, “Losses”) to which they may be subjected based on or arising from (i) the acts or omissions of the Contractor, or its employees and permitted assigns in the conduct, performance, or execution of any obligation of the Contractor under this Contract; or (ii) any breach by the Contractor of any of its representations or warranties contained in this Contract. The Parties acknowledge that the Contractor shall not be liable for any such Losses to the extent that such Losses are caused by or arise from the negligence or willful misconduct of ASES. |
Page 552
| 51.2 | ASES shall indemnify and hold the Contractor, Triple-C, Inc., and their respective officers and directors harmless from and against all Losses to which they may be subjected: (i) based on or arising from the acts or omissions of the ASES or its employees, and permitted assigns in the conduct, performance, or execution of any obligation of ASES under this Contract; (ii) based on or arising from any breach by ASES of any of its representations or warranties contained in this Contract; (iii) by any FQHC with respect to any dispute regarding payment for any FQHC Service provided outside the scope of this Contract; or (iv) by any Provider, PMG or Enrollee on account of the conduct, performance, execution, decisions, and representations of MCS during its tenure and administration of the MiSalud Program in the Service Regions. ASES further agrees that the Contractor shall not be liable for the financial condition of any PMG or Provider who served an Enrollee in the Service Regions during such tenure and administration or for monies owed or that may be owed by MCS to such PMG or Provider. The Parties acknowledge that ASES shall not be liable for any such Losses to the extent that such Losses are caused by or arise from the negligence or willful misconduct of the Contractor. |
ARTICLE 52 COOPERATION WITH AUDITS
| 52.1 | The Contractor agrees to assist and cooperate with ASES in any and all matters and activities related to or arising out of any audit or review, whether federal or internal in nature. |
Page 553
| 52.2 | The Parties also agree that each Party shall be solely responsible for any costs it incurs for any audit related inquiries or matters. Moreover, neither party may charge or collect any fees or compensation from the other party for any matter, activity, or inquiry related to, arising out of, or based on an audit or review. |
ARTICLE 53 OWNERSHIP AND FINANCIAL DISCLOSURE
| 53.1 | The Contractor shall disclose financial statements for each person or corporation with a direct ownership or control interest of five percent (5%) or more in the Contractor’s entity. |
ARTICLE 54 AMENDMENT IN WRITING
| 54.1 | No amendment, waiver, termination or discharge of this Contract, or any of the terms or provisions hereof, shall be binding upon either party unless confirmed in writing. Additionally, CMS approval shall be required before any such amendment is effective. Any agreement of the Parties to amend, modify, eliminate, or otherwise change any part of this Contract shall not affect any other part of this Contract, and the remainder of this Contract shall continue to be of full force and effect as set out herein. |
| 54.2 | ASES reserves the authority to seek an amendment of this Contract at any time if such amendment is necessary in order for the terms of this Contract to comply with |
Page 554
| federal law or a CMS requirement, and the Contractor shall consent to any such amendment, subject to its renegotiation rights under Section 37.2.6 of this Contract and its termination rights under Section 34.1.3.4 of this Contract. |
ARTICLE 55 CONTRACT ASSIGNMENT
| 55.1 | Contractor shall not assign this Contract, in whole or in part, without the prior written consent of ASES, and any attempted assignment not in accordance herewith shall be null and void and of no force or effect. Notwithstanding the foregoing, the Contractor shall have a right to delegate any obligation arising hereunder or to assign this Contract to Triple-C, Inc., its corporate affiliate, upon prior written notice to ASES. |
ARTICLE 56 SEVERABILITY
| 56.1 | Any section, subsection, paragraph, term, condition, provision, or other part of this Contract that is judged, held, found or declared to be voidable, void, invalid, illegal or otherwise not fully enforceable shall not affect any other part of this Contract, and the remainder of this Contract shall continue to be of full force and effect as set out herein. |
ARTICLE 57 ENTIRE AGREEMENT
Page 555
| 57.1 | This Contract constitutes the entire agreement between the parties with respect to the subject matter hereof and supersedes all prior negotiations, representations or contracts. No written or oral agreements, representatives, statements, negotiations, understandings, or discussions that are not set out, referenced, or specifically incorporated in this Contract shall in any way be binding or of effect between the parties. |
| 57.2 | All applicable laws as in effect on the Effective Date of the Contract are incorporated by reference into this Contract, as provided in Article 37. |
| 57.3 | Subject to Section 37.2.6 of this Contract, the Contractor acknowledges that it may be necessary or convenient during the Term of this Contract to clarify or supplement certain terms and conditions of this Contract to conform it to or otherwise to incorporate CMS requirements. In any of these events, the Contractor agrees that ASES shall have the right to issue from time to time normative letters which shall be then incorporated into the Contract. Such normative letters are advisory in nature, and shall not, absent an amendment to the Contract, change the Contractor’s obligations under this Contract. |
ARTICLE 58 NOTICES
Page 556
| 58.1 | All notices, consents, approvals and requests required or permitted shall be given in writing and shall be effective for all purposes if hand delivered or sent by (a) personal delivery, (b) expedited prepaid delivery service, either commercial or United States Postal Service, with proof of attempted delivery, or (c) telecopier or (d) electronic mail (in each case of (c) and (d), with answer back acknowledged, addressed as follows: |
| 58.1.1 | If to ASES at: |
| Mailing Address: |
Physical Address: | |
| Administración de Seguros de Salud |
Urb. Caribe 1552 | |
| P.O. Box 195661 |
Ave. Ponce de León, Sec. El Cinco | |
| San Juan, PR 00919-5661 |
San Juan, PR 00926-2706 | |
| Attention: Executive Director | ||
| 58.1.2 | If to Contractor at: |
Page 557
| Mailing Address: |
Physical Address: | |
| Triple-S Salud, Inc. |
Triple-S Salud, Inc. | |
| P.O. Box 363628 |
1441 Ave. Roosevelt, 6th Floor | |
| San Juan, PR 00936-3628 |
San Juan, PR 00920 | |
| Attention: President | ||
| 58.1.3 | All notices, elections, requests and demands under this Contract shall be effective and deemed received upon the earliest of (i) the actual receipt of the same by personal delivery or otherwise, (ii) two (2) Business Days after being deposited with a nationally recognized overnight courier service as required above, (iii) three (3) Business Days after being deposited in the United States mail as required above or (iv) on the day sent if sent by facsimile with voice confirmation on or before 4:00 p.m. Puerto Rico time on any Business Day or on the next Business Day if so delivered after 4:00 p.m. Puerto Rico time or on any day other than a Business Day. Rejection or other refusal to accept or the inability to deliver because of changed address of which no notice was given as herein required shall be deemed to be receipt of the notice, election, request, or demand sent. |
Page 558
ARTICLE 59 OFFICE OF THE COMPTROLLER
| 59.1 | ASES will file this Contract before the Office of the Comptroller of Puerto Rico within fifteen (15) days from its execution. |
(Signatures on following page)
Page 559
SIGNATURE PAGE
IN WITNESS WHEREOF, the parties state and affirm that they are duly authorized to bind the respected entities designated below as of the day of October, 2011 (the “Execution Date”).
ADMINISTRACIÓN DE SEGUROS DE SALUD DE PUERTO RICO (ASES)
| Frank Diaz Gines | Date | |||
| Executive Director |
Page 560
| TRIPLE-S SALUD, INC. | ||||
| Socorro Rivas Rodríguez | Date | |||
| President and Chief Executive Officer | ||||
Page 561
Puerto Rico MiSalud Model TPA Contract
Relevant Puerto Rico and Federal Laws and Regulations
(Attachment 1)
Applicable Puerto Rico laws and regulations:
| • | Act 72 of September 7, 1993, as amended (Puerto Rico Health Insurance Administration Law) |
| • | Puerto Rico Insurance Code and its applicable regulations. |
| • | Act 81 of May 14,1912 (Organic Law of the Puerto Rico Health Department) |
| • | Act 194 of August 25, 2000, as amended (the Puerto Rico Patient’s Bill of Rights Act) |
| • | Act 408 of October 2, 2000, as amended (Puerto Rico Mental Health Code) |
| • | Reorganization Plan of Advocates Offices, Number 1 from 2010 (Office of Health Advocate) |
| • | Act 247 of September 3, 2004, as amended (Puerto Rico Pharmacy Law) |
| • | Act 139 of August 1, 2008, as amended, known as (Law of the Medical Licensing and Discipline Board) |
| • | Act 109 of June 28, 1974, as amended (Law of the Puerto Rico Public Service Commission) |
| • | Act 225 of July 23, 1974, as amended (Law of Ambulance Services) |
| • | The Public Service Commission’s regulations for ambulance services in Puerto Rico, Regulation Num. 6737 of December 1, 2003. |
| • | Act 86 of August 16, 1997 (Law of Residents of Culebra and Vieques) |
| • | Act 27 of August 12, 1999 (Law of the Implementation of the Public Policy on Suicide Prevention) |
| • | Act 243 of November 10, 2006, known as (Law to Establish the Public Policy Concerning the Use of the Social Security Number for Identification and the Protection of Its Confidentiality) |
| • | Act 84 of June 18, 2002 (Code of Ethics for Contractors, Suppliers and Applicants for Economic Incentives from the Executive Agencies of the Commonwealth) |
| • | Act 12 of July 24, 1985, as amended (Government Ethics Law) |
| • | Act 458 of December 29, 2000, as amended, (Law to Prohibit the Adjudication of Auctions to convicts of Fraud, Embezzlement or Illegal Misappropriation of Public Funds) |
| • | Act 70 of August 12, 1988, as amended (Puerto Rico Uniform Administrative Proceedings Law) |
Applicable federal laws and regulations:
| • | Puerto Rico Health Department’s State Plans (Medicaid State Plan and CHIP State Plan) |
| • | Title XIX of the Medical Assistance Program (Grants to States for Medical Assistance Programs) |
| • | Title XXI of the Social Security Act, governing the Children’s Health Insurance Program (CHIP) |
| • | Federal Rules and Regulations as established by the Center for Medicare & Medicaid Services (“CMS”) contained in 42 CFR Subchapters C (Medical Assistance Programs) and D (Children’s Health Insurance Programs), including, but not limited to: 42 CFR 422.208 and |
| 210 (physician incentive plans); 422.560 -422.626; 42 CFR 438 (managed care) including subsections 56, 60, 66, 206(b), 214, 242; 42 CFR 431 (fair hearings and appeals); 42 CFR 455 (fraud and abuse reporting); 42 CFR 447 (timely claims payment); 45 CFR 74.53 (retention requirements for records); 42 CFR 433 Subpart D, 42 CFR 447.20 and 42 CFR 434 (third party liability); 42 CFR 435.911 and 435.914; 42 CFR 431.52-53 (ambulance services); 42 CFR 405.2402; 42 CFR Part 455.104; 42 CFR Part 455.106; 42 CFR 447.20 and 42 CFR 434.6(a)(9); and each regulation cited in the CMS Checklist for Managed Care Contract Approval |
| • | Federal rules and regulations as established by the United States Department of Labor in Title XXIX of the Code of Federal Regulations as applicable |
| • | Davis-Bacon Act, 40 U.S.C. 276a, et seq. |
| • | Social Security Act Titles VI and VII |
| • | Copeland Anti-Kickback Act, 40 U.S.C 276c |
| • | Fair Labor Standards Act of 1938, 29 U.S.C 201 et seq. |
| • | Clean Air Act, 42 U.S.C. 7401 et seq. |
| • | Federal Water Pollution Control Act as Amended, 33 U.S.C. 1251 et seq. |
| • | Federal Rehabilitation Act of 1973 |
| • | Byrd Anti-Lobbying Amendment, 31 U.S.C 1352 |
| • | The Clinical Laboratory Improvement Amendments of 1988 |
| • | The Health Insurance Portability and Accountability Act of 1996 (HIPAA) |
| • | Omnibus Budget Reconciliation Act of 1981, P.L. 97-3 8 |
| • | Debarment and Supsension, 45 CFR 74 Appendix A (8) and Executive Orders 12549 and 12689 |
| • | Americans with Disabilities Act, 42 USC 12101 et seq. |
| • | Medicare Modernization Act of 2003, Pub. L. No. 108-173 |
| • | Mental Health Parity and Addiction Equity Act of 2008, Pub. L. No. 110-343 |
| • | Children Health Insurance Program Reauthorization Act of 2009, Pub. L. No. 111-3 |
| • | American Recovery and Reinvestment Act of 2009, Pub. L. No. 111-5 |
| • | Patient Protection and Affordable Care Act of 2010, Pub. L. No. 111 -148 |
(Attachment 2)
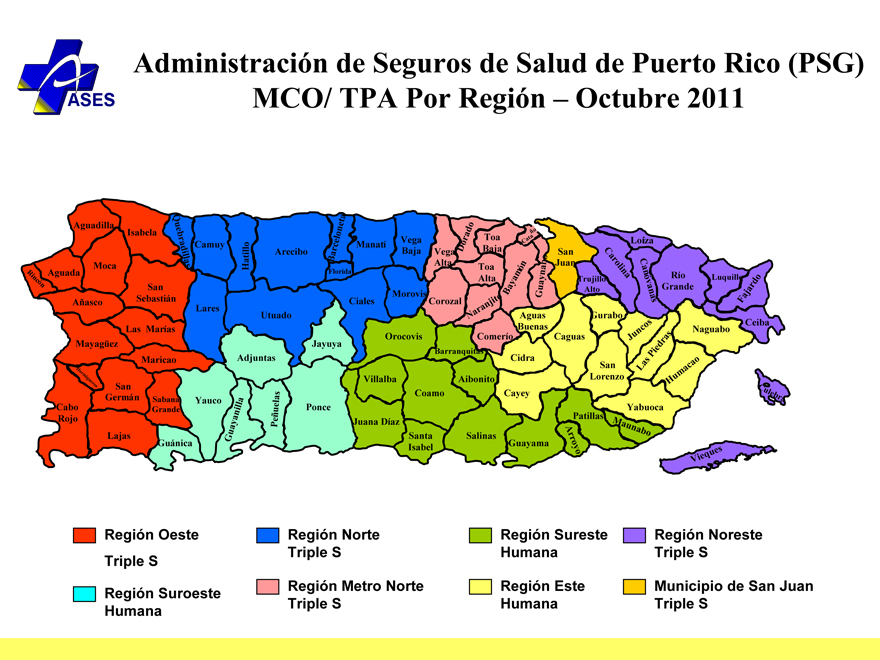
Administración de Seguros de Salud de Puerto Rico (PSG) MCO/ TPA Por Región – Octubre 2011
Aguadilla
Rincón
Aguada
Moca
Isabela
Añasco
San Sebastián
Quebradillas
Camuy
Lares
Mayagüez
Las Marías
Maricao
Hatillo
Arecibo
Utuado
Adjuntas
Hormigueros
Cabo Rojo
San Germán
Lajas
Sabana Grande
Yauco
Guánica
Guayanilla
Peñuelas
Ponce
Jayuya
Barceloneta
Florida
Manatí
Vega Baja
Ciales
Morovis
Vega Alta
Dorado
Corozal
Orocovis
Villalba
Juana Díaz
Coamo
Santa Isabel
Salinas
Guayama
Aibonito
Cayey
Comerío Barranquitas Cidra
Toa Baja Toa Alta
Naranjito
Bayamón
Cataño
Guaynabo
Aguas Buenas
Gurabo
Caguas
Arroyo
Patillas
Yabuoca
Maunabo
San Lorenzo
Juncos
Las Piedras
Humacao
Ceiba Naguabo
San Juan
Trujillo Alto
Carolina
Loíza
Canóvanas
Río Grande
Luquillo
Fajardo
Culebra
Vieques
Región Oeste Triple S
Región Norte Triple S
Región Sureste Humana
Región Noreste Triple S
Región Suroeste Humana
Región Metro Norte Triple S
Región Este Humana
Municipio de San Juan Triple S
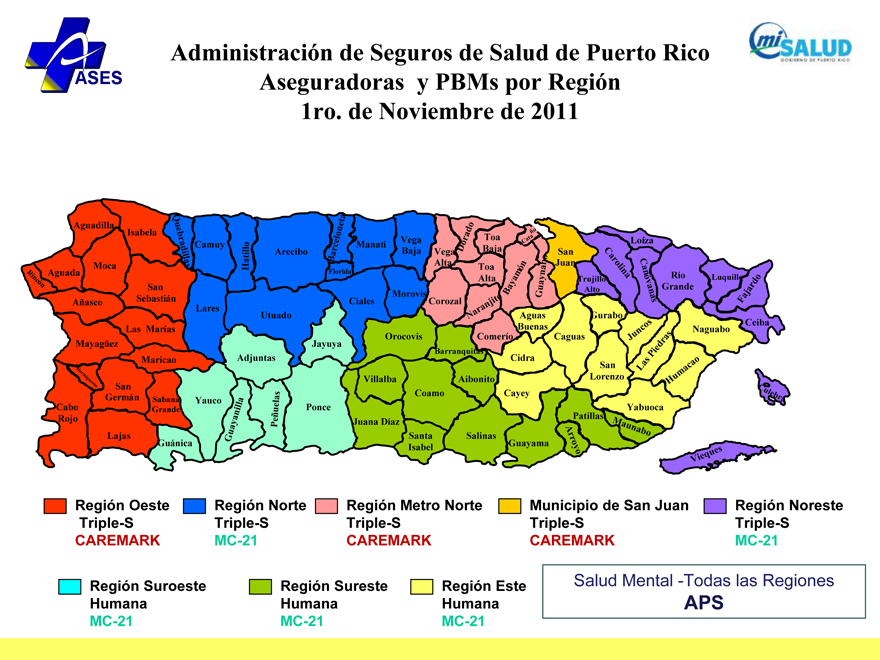
Administración de Seguros de Salud de Puerto Rico Aseguradoras y PBMs por Región 1ro. de Noviembre de 2011
Aguadilla
Rincón
Aguada
Moca
Isabela
Añasco
San Sebastián
Quebradillas
Camuy
Lares
Mayagüez
Las Marías
Maricao
Hatillo
Arecibo
Utuado
Adjuntas
Hormigueros
Cabo Rojo
San Germán
Lajas
Sabana Grande
Yauco
Guánica
Guayanilla
Peñuelas
Ponce
Jayuya
Barceloneta
Florida
Manatí
Vega Baja
Ciales
Morovis
Vega Alta
Dorado
Corozal
Orocovis
Villalba
Juana Díaz
Coamo
Santa Isabel
Salinas
Guayama
Aibonito
Cayey
Comerío Barranquitas Cidra
Toa Baja Toa Alta
Naranjito
Bayamón
Cataño
Guaynabo
Aguas Buenas
Gurabo
Caguas
Arroyo
Patillas
Yabuoca
Maunabo
San Lorenzo
Juncos
Las Piedras
Humacao
Ceiba Naguabo
San Juan
Trujillo Alto
Carolina
Loíza
Canóvanas
Río Grande
Luquillo
Fajardo
Culebra
Vieques
Región Oeste Triple-S CAREMARK
Región Norte Triple-S MC-21
Región Metro Norte Triple-S
CAREMARK
Municipio de San Juan Triple-S
CAREMARK
Región Noreste Triple-S MC-21
Región Suroeste Humana MC-21
Región Sureste Humana MC-21
Región Este Humana MC-21
Salud Mental -Todas las Regiones APS
Attachment 4
Centers for Prevention and Treatment of Transmissible Diseases (CPTET, by its Spanish acronym)
Updated August 2010
| REGION |
COORDINATOR |
TELEPHONE/FAX |
ADDRESS | |||
| ARECIBO | Dra. Evelyn Reyes García Internist |
(787) 878-7895 (787) 881-5773 (787) 879-3388 |
Antiguo Hosp. Distrito Carr. 129 hacia Lares Box 897 Arecibo, PR 00618 | |||
| Contracted pharmacy | Farmacia Garcia (Hatillo) Daniel Mahiques |
(787) 898-3975 (787) 820-9048 fax |
121 Calle Vidal Feliz Hatillo, PR | |||
| CPTET BAYAMON | Dra. Aileen Romero (Administration) Doctors: Dr. Francisco R. Bellaflores (Internist) Dra. Verónica Pérez (GP) |
(787) 787-5151 Ext. 2224 /2435 (787) 787-5154 (d) (787) 787-4211 (787) 778-1209 fax |
Hosp. Regional Bayamón Dr. Ramón Ruiz Arnau Ave. Laurel Santa Juanita Bayamón, PR 00956 | |||
| Other contracted pharmacy | (See enclosed list Pharmacy by Network: HIV) | |||||
| CPTET CAGUAS | Dra. Gloria Morales | Ext. 11142, 11150 (787) 744-8645 (787) 746-2898 fax |
Hosp. San Juan Bautista Apartado 5729 Caguas, PR | |||
| Contracted pharmacy Caguas |
Farmacia Arleen Roberto Peirats |
(787) 746-5952 (787) 744-3397 |
Urb. Villa del Rey Caguas, PR | |||
| Satellite Clinic Humacao | (787) 640-0980 | Humacao Shopping Center Ave. Font Martelo 100 Humacao, PR | ||||
| Contracted | Farmacia Central | (787) 852-0520 | #11 Calle Nolla y Hernández | |||
| pharmacy Humacao | Julio Garriga | (787) 850-5500 | Humacao, PR | |||
| CPTET CAROLINA |
Dr. Milton Garland Internist |
(787) 757-1800 Ext. 454, 459 (787) 257-3615 (d) (787) 257-3615 fax |
Hosp. Universitario de Carolina P.O. Box 8969 Carolina, PR 00984-3869 | |||
| CLETS (Centro Médico, Rio Piedras) |
Dr. Hermes García Internist |
(787) 754-8118 (c) (787) 754-8128 (d) (787) 754-8127 (787) 754-8199 fax |
P.O. Box 71423 Correo General San Juan, PR 00936-8523 | |||
| FAJARDO | Dr. Arturo Hernández GP Dr. Jorge Ruiz Infectious Disease Physician |
(787) 801-1992 (787) 801-1995 (787) 801-6767 (787) 863-5487 fax |
Calle Rafael #55 Fajardo, PR | |||
| Contracted pharmacy | Farmacia Denirka Gil Nieves |
(787) 863-7788 (787) 863-1422 |
305 Ave. General Valero Fajardo, PR 00738 | |||
| CPTET MAYAGUEZ |
Dr. Ramón Ramírez Ronda Infectious Disease Physician |
(787) 884-2110 (787) 884-2115 (787) 884-2118 Ext. 4634 (787) 881-4495 fax |
Centro Médico Mayagüez Hosp. Ramón Emeterio Betances, Suite 6, Ave. Hostos # 40 Mayagüez, PR 00680 | |||
| CPTET PONCE | Sra. Ineabelle Alameda ETS Clínic
Dra. Gladys Sepúlveda CIR Coordinator Infectious Disease Physician |
787) 848-2000 (787) 848-5574 (d) (787) 844-2080 Ext. 1516 (787) 842-1948 fax (787) 259-4731 (787) 259-4046 (787) 842-8626 (787) 259-8998 fax |
Antiguo Hosp. Distrito-Ponce Dr. José Gándara, ahora Hosp. San Lucas II Carr. Estatal, Bo. Machuelo 14 Ponce, PR 00731 | |||
| CENTRAL LEVEL | Dr. Hermes Garcia Director Prevention and Treatment Division of Transmissible Diseases |
(787) 274-5504 (787) 274-5505 (787) 274-5501 (787) 274-5502 (787) 274-5508 fax |
Antiguo Hosp. Psiquiatría Pabellón 1, Primer Piso Centro Médico Río Piedras, P.O. Box 70184 San Juan, PR 00936 | |||
2
Pharmacies By Network: HIV
Privates or CBO
| ID |
NAME | ADDRESS1 | ST | Zip | Type | Chain | Municipality | Region | NPI | Phone | Fax | |||||||||||
| 4015548 |
Farmacia Arleen |
Urbanización Villa Del Rey |
PR | 00726 | COMUNIDAD | Independent | Caguas | Este | 1154308716 | 787-746-5952 | 787-744-3397 | |||||||||||
| 4020183 |
Farmacia Camuy Health Services, Inc. |
53 Avenida Muñoz Rivera |
PR | 00627 | CDT’S PRIVADOS |
Independent | Camuy | Norte | 1104995968 | 787-898-2660 | 787-262-4822 | |||||||||||
| 4018188 |
Farmacia Caridad 4 |
Carretera 862 KM 1.9 |
PR | 00959 | COMUNIDAD | Independent | Bayamon | MetroNorte | 1437214244 | 787-269-3140 | 787-269-0022 | |||||||||||
| 4023064 |
Farmacia CDT Programa SIDA |
1306 Avenida Fernández Juncos |
PR | 00908 | CDT’S PÚBLICOS |
Independent | San Juan | San Juan | 1376665174 | 787-723-2424 | 787-724-5104 | |||||||||||
| 4020222 |
Farmacia CDT Quebradillas |
Calle Muñoz Rivera |
PR | 00678 | CDT’S PRIVADOS |
Independent | Quebradillas | Norte | 1235179532 | 787-895-2670 | 787-895-1540 | |||||||||||
| 4000028 |
Farmacia Central |
11 Calle Noya y Hernández |
PR | 00791 | COMUNIDAD | Independent | Humacao | Este | 1124185566 | 787-852-0520 | 787-850-5500 | |||||||||||
| 4026349 |
Farmacia Centro de Prevención y Tratamiento de ETS |
PR-2 KM 157.0 Antigua Casa Salud |
PR | 00682 | CDT’S PÚBLICOS |
Independent | Mayaguez | Oeste | 1366600207 | 787-834-2115 | 787-834-6488 | |||||||||||
| 4020210 |
Farmacia Centro de Salud de Lares, Inc. |
Carretera 111 KM 1 HM 9 |
PR | 00669 | CDT’S PRIVADOS |
Independent | Lares | Norte | 1417907502 | 787-897-3610 | 787-897-2725 | |||||||||||
| 4020121 |
Farmacia Centro de Salud Familiar de Patillas |
99 Calle Guillermo Riefkhol |
PR | 00723 | CDT’S PRIVADOS |
Independent | Patillas | SurEste | 1639207681 | 787-839-4320 | 787-271-0004 | |||||||||||
| 4024458 |
Farmacia Centro de Salud Familiar Dr. Julio Palmie |
Calle Morse Esquina Valentina |
PR | 00714 | CDT’S PRIVADOS |
Independent | Arroyo | SurEste | 1548373293 | 787-839-4150 | 787-839-3989 | |||||||||||
| 4020727 |
Farmacia Centro de Salud Integral en Barranquitas |
Calle Barceló Salida A Comerio |
PR | 00794 | CDT’S PRIVADOS |
Independent | Barranquitas | SurEste | 1336282417 | 787-857-5923 | 787-857-1730 | |||||||||||
| 4020739 |
Farmacia Centro de Salud Integral en Comerío |
18 Calle Georgetti |
PR | 00782 | CDT’S PRIVADOS |
Independent | Comerio | MetroNorte | 1174667257 | 787-875-3375 | 787-875-4230 | |||||||||||
| 4020741 |
Farmacia Centro de Salud Integral en Corozal |
Calle Nueva Final |
PR | 00783 | CDT’S PRIVADOS |
Independent | Corozal | MetroNorte | 1831233667 | 787-859-2560 | 787-859-5390 | |||||||||||
| 4020753 |
Farmacia Centro de Salud Integral en Naranjito |
Barrio Achiote Sector Desvío |
PR | 00719 | CDT’S PRIVADOS |
Independent | Naranjito | MetroNorte | 1740324573 | 787-869-1290 | 787-869-1800 | |||||||||||
| 4020765 |
Farmacia Centro de Salud Integral en Orocovis |
Carretera 155 Salida Desvío |
PR | 00720 | CDT’S PRIVADOS |
Independent | Orocovis | SurEste | 1457495285 | 787-867-6010 | 787-867-6008 | |||||||||||
| 4020323 |
Farmacia Ciales Primary Health Care Services, Inc. |
Carretera 149 KM 12.3 |
PR | 00638 | CDT’S PRIVADOS |
Independent | Ciales | Norte | 1649362195 | 787-871-0601 | 787-871-3960 | |||||||||||
| 4026008 |
Farmacia CLETS Centro Médico |
Paseo José C. Barbosa |
PR | 00936 | CDT’S PÚBLICOS |
Independent | San Juan | San Juan | 1528279262 | 787-754-8118 | 787-754-8127 | |||||||||||
| 4009280 |
Farmacia Concilio de Salud Integral |
Carretera 187 INT 188 |
PR | 00772 | CDT’S PÚBLICOS |
Independent | Loiza | NorEste | 1396758686 | 787-876-2042 | 787-876-2005 | |||||||||||
| 4025955 |
Farmacia COSSMA |
50 Calle Ulises Martínez Norte |
PR | 00791 | CDT’S PRIVADOS |
Independent | Humacao | Este | 1225210297 | 787-852-2551 | 787-937-0062 | |||||||||||
| 4026123 |
Farmacia COSSMA |
186 Calle Muñoz Rivera |
PR | 00754 | CDT’S PRIVADOS |
Independent | San Lorenzo | Este | 1568634483 | 787-937-0058 | 787-937-0064 | |||||||||||
| 4019849 |
Farmacia COSSMA |
Carretera 172 Avenida El Jíbaro |
PR | 00739 | CDT’S PRIVADOS |
Independent | Cidra | Este | 1760530760 | 787-739-8182 | 787-714-1444 | |||||||||||
| 4013544 |
Farmacia Denirka |
305 Avenida General Valero |
PR | 00738 | COMUNIDAD | Independent | Fajardo | NorEste | 1891836623 | 787-863-7788 | 787-863-1422 | |||||||||||
| 4012960 |
Farmacia El Apotecario |
Urbanización La Rambla |
PR | 00716 | COMUNIDAD | Independent | Ponce | SurOeste | 1558307355 | 787-844-2135 | 787-284-2135 | |||||||||||
| 4016906 |
Farmacia El Tuque |
553 Ernesto Ramos Antonini |
PR | 00732 | COMUNIDAD | Independent | Ponce | SurOeste | 1932185824 | 787-844-2805 | 787-841-5551 | |||||||||||
| 4000903 |
Farmacia García |
121 Calle Vidal Feliz |
PR | 00659 | COMUNIDAD | Independent | Hatillo | Norte | 1588600407 | 787-898-3975 | 787-820-9048 | |||||||||||
| 4022303 | Farmacia Gurabo Community |
Carretera 941 Salida Barrio |
PR | 00778 | CDT’S PRIVADOS |
Independent | Gurabo | Este | 1316068026 | 787-737-2311 | 787-737-1242 | |||||||||||
| Health Center |
Jaguas | |||||||||||||||||||||
3
| 4020157 | Farmacia Hospital General Castañer |
Carretera 135 KM 64.2 Castañer |
PR | 00631 | HOSPITALES PRIVADOS |
Independent | Adjuntas | SurOeste | 1336341379 | 787-829-5010 | 787-829-2913 | |||||||||||
| 4004026 | Farmacia Hospital Ryder Memorial |
Avenida Font Martelo |
PR | 00792 | LONG TERM CARE PHARMACY |
Independent | Humacao | Este | 1770697757 | 787-852-0768 | 787-850-1444 | |||||||||||
| 4014801 | Farmacia Hospital Universitario Dr. Federico Trill |
Carretera 3 KM 8.3 |
PR | 00984 | HOSPITALES PRIVADOS |
Independent | Carolina | NorEste | 1023107182 | 787-757-1800 | 787-750-4214 | |||||||||||
| 4021553 | Farmacia MedCentro Consejo de Salud de Puerto Rico |
1034 Avendia Hostos |
PR | 00716 | CDT’S PRIVADOS |
Independent | Ponce | SurOeste | 1467518340 | 787-843-9370 | 787-843-9395 | |||||||||||
| 4021046 | Farmacia Migrant Health Center |
Carretera 1 KM 7.1 |
PR | 00681 | CDT’S PRIVADOS |
Independent | Mayaguez | Oeste | 1336286400 | 787-805-2920 | 787-805-4707 | |||||||||||
| 4022175 | Farmacia Migrant Health Center |
23 Calle Montalva |
PR | 00658 | CDT’S PRIVADOS |
Independent | Guanica | SurOeste | 1619013067 | 787-821-4511 | 787-821-4511 | |||||||||||
| 4020690 | Farmacia Migrant Health Center Western |
Carretera 119 KM 35.2 |
PR | 00685 | CDT’S PRIVADOS |
Independent | San Sebastian |
Oeste | 1114064102 | 787-896-1665 | 787-896-1690 | |||||||||||
| 4002236 | Farmacia Plaza 3 |
57 Calle Barbosa |
PR | 00961 | CADENA | Farmacias Plaza |
Bayamon | MetroNorte | 1801941919 | 787-785-0000 | 787-785-2387 | |||||||||||
| 4020880 | Farmacia Rincón Health Center |
28 Calle Muñoz Rivera |
PR | 00677 | CDT’S PRIVADOS |
Independent | Rincon | Oeste | 1093743023 | 787-823-5555 | 787-823-2990 | |||||||||||
| 4013013 | Farmacia San Miguel |
127 Avenida Dr. Susoni |
PR | 00659 | COMUNIDAD | Independent | Hatillo | Norte | 1659406015 | 787-898-5764 | 787-262-3984 | |||||||||||
| 4000484 | Farmacia San Rafael |
851 Calle Laffayette |
PR | 00909 | FARMACIAS ESPECIALIZADA |
Independent | San Juan | San Juan | 1952446825 | 787-724-3307 | 787-721-4165 | |||||||||||
| 4026010 | Farmacia Sección de Prevención de ETS |
Antiguo Hospital Regional San Lucas 2 |
PR | 00733 | CDT’S PÚBLICOS |
Independent | Ponce | SurOeste | 1245416684 | 787-843-2188 | 787-840-7427 | |||||||||||
| 4020549 | Farmacia Sonia |
61 Calle Comercio |
PR | 00795 | COMUNIDAD | Independent | Juana Diaz |
SurEste | 1154497477 | 787-837-2666 | 787-837-4602 | |||||||||||
4
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
ARECIBO REGION
| Clinic |
Pharmacy | |
| CPTET Arecibo / Clinic de Immunology Tel. (787) 817-2677 / 878-7895 Fax. (787) 881-5773 Physical Address: Antiguo Hospital de Distrito, Carr. 129 Hacia Lares Postal Address: PO Box 397 Arecibo, PR 00613 Medical Director: Dra. Evelyn Reyes MC: Lourdes Castro |
Pharmacy García Tel. (787) 898-3975 / 820-5158 Fax. (787) 820-9048 Physical Address: Calle Vidal Félix #121 Hatillo, P.R. 00659 Postal Address: PO Box 67 Hatillo PR 00659 Pharmacist: Daniel Mahíques Nieves | |
| Centro de Salud de Lares, Inc. Ryan White Part C Tel. (787) 897-2727 / 2155 /1720 /1730 Fax. (787) 897-2155 / 2725 Physical Address: Carr. 111 KM 1.9 Ave. Los Patriotas Postal Address: PO Box 379 Lares, P.R. 00669 Director: Sr. Gonzálo Maldonado R.N. MC: Elsie Camacho MC: Zulma Román |
In House Pharmacy Tel. (787) 897-3610 / 897-3023 Tel. (787) 897-2727 / 2155 / 1720 Cel. (787) 414-1304 Fax: (787) 897-2725 Physical Address: Carr. 111 KM 1.9 Ave. Los Patriotas Postal Address: PO Box 379 Lares, P.R. 00669 Pharmacist: Lic. Mayra Vélez E mail: rw_csl@hotmail.com Contact: Domingo Carrero | |
| *Branches attached to Lares Health Center, Inc. | ||
| *Centro de Salud de Quebradillas Tel. (787) 895-2660 / 2670 Physical Address: Calle Muñoz Rivera Esq. San Justo #114 Quebradillas, PR 00678 Postal Address: Apartado 1551 Quebradillas, PR 00678 Administrador: Sr. Daniel González Rivera MC: Marilyn Acevedo E mail: cdtquebradillas@hotmail.com |
In House Pharmacy Tel. (787) 895-2512 Fax. (787) 895-2512 Physical Address: Calle Muñoz Rivera Esq. San Justo #114 Quebradillas, PR 00678 Postal Address: Apartado 1551 Quebradillas, PR 00678 Contact: Vanessa Pérez Pharmacist: Hilda Torres | |
| pog |
1 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
ARECIBO REGION
| Clinics |
Pharmacys | |
| *Camuy Health Services, Inc. Tel. (787) 898-2290 / 262-6603 Fax. (787) 262-1210 / 3789 Physical Address: Ave. Muñoz Rivera #63, Camuy PR 00627 Postal Address: PO Box 660 Camuy, PR 00627-0660 Director: Lcdo. Eddie Pérez MC: Zaida González |
In House Pharmacy Tel. (787) 898-2660 Ext. 227 Fax. (787) 262-4822 Physical Address: Ave. Muñoz Rivera #63, Camuy PR 00627 Postal Address: PO Box 660 Camuy, PR 00627-0660 Pharmacist: Lcda. Luz del Alba Ramírez E mail: camuy660@coqui.net | |
| *Corporación de Servicios Médicos Primarios y Prevención de Hatillo Tel. (787) 898-3935 / 4190 Fax. (787) 262-3984 Physical Address: Ave. Dr. Susoni #121 Hatillo Postal Address: PO Box 907 Hatillo, PR 00659 Director: Armando Legarreta MC: Wanda León |
In House Pharmacy Tel. (787) 898-5764 Fax. (787) 262-3984 Physical Address: Ave. Dr. Susoni #121 Hatillo Postal Address: PO Box 907 Hatillo, PR 00659 Contact: Leticia Reyes Pharmacist: Carmelo Nistal E mail: hatipa19@libertypr.net | |
| *Ciales Primary Health Care Services Tel. (787) 871-0601 / 0602 / 0603 Fax. (787) 871-3960 Physical Address: Carr. 149 k.m. 12.3 Ciales Postal Address: PO Box 1427 Ciales, PR 00638 Medical Director: Gladys Rivera Estela MC: Iraida Marero Contact: Carmen Sandoval Santiago |
In House Pharmacy Tel. (787) 871-0601 Ext. 210 Fax: (787) 871-3960 Physical Address: Carr. 149 k.m. 12.3 Ciales PR 00638 Postal Address: PO Box 1427 Ciales, PR 00638 Contact: Janet Maldonado Villalobos Pharmacist: Aixa Bou E mail: cphcsinc@yahoo.com | |
| *Hospital General de Castañer Tel. (787) 829-5010 / 2055 / 7500 / 5600 Fax. (787) 829-2913 / 2166 / 4668 Physical Address: Carr. 135 k.m. 64.2 Castañer Postal Address: PO Box 1003 Castañer, PR 00631 Contact: Doris Bengoechea |
In House Pharmacy Tel. (787) 829-5010 Ext. 233 / 289 Fax. (787) 829-1479 Physical Address: Carr. 135 k.m. 64.2 Castañer Postal Address: PO Box 1003 Castañer, PR 00631 Pharmacist: Yivet Aquino E mail: hospitalcastaner@hotmail.com | |
| pog |
2 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
BAYAMÓN REGION
| Clinic |
Pharmacy | |
| Salud Integral en la Montaña, Inc. (SIM) Central Office Tel. (787) 869-5900 / 5960 / 5950 x. 225, 251 Fax: 1 (787) 869-6120 Physical Address: Carr. 152 Naranjito a Barranquitas Postal Address: PO Box 515 Naranjito, PR 00719 Directora: Sandra V. García Gerente Servicios Clínicos: Nelly Vargas MC: Maritza Rolón Madeline Figueroa E mail: mfigueroa@sim.pr.com |
Central Office Tel. (787) 869-5900 Ext. 252 Contact: Sra. Lourdes Chevere * Pharmacy Director, including 5 clinics Pharmacist: Sandra V. García E mail: sgarcia@sim.pr.com | |
| *Centro de Salud Integral de Naranjito Tel. (787) 869-1290 Ext. 2203, 2237, 2204 Fax: (787) 869-1800 Physical Address: Carr. 164 Sector el Desvío, Barrio Achiote, Naranjito PR 00719 Postal Address: PO Box 525 Naranjito PR 00719 Directora: Maritza Ortíz Berríos MC: Maritza Rolón Nieves MC: Judith Rosa |
In House Pharmacy Tel. (787) 869-1290 Ext. 2208, 2238 Fax: (787) 869-1800 Physical Address: Carr. 164 Sector el Desvío, Barrio Achiote, Naranjito PR 00719 Postal Address: PO Box 525 Naranjito PR 00719 Pharmacist: Marienilda La Santa | |
| *Centro de Salud Integral de Barranquitas Tel. (787) 857-2688 Fax: (787) 857-1730 / 3440 Physical Address: Calle Barceló #3, Barranquitas, PR 00794 Postal Address: PO Box 728 Barranquitas, PR 00794 Directora: Lourdes MC: Carmen Carro |
In House Pharmacy Tel. (787) 857-2688 Ext. 225 Fax. (787) 857-1730 Physical Address: Calle Barceló #3, Barranquitas, PR 00794 Postal Address: PO Box 728 Barranquitas, PR 00794 Pharmacist: Lcda. Lourdes Chéverez | |
| pog |
3 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
BAYAMÓN REGION
| Clinic |
Pharmacy | |
| *Centro de Salud Integral de Comerío Tel. (787) 875-3375 / 2750 Fax: (787) 875-4230 / 2769 Physical Address: Calle Georgetti, Carr. 167 Postal Address: PO Box 418 Comerío PR 00782 Director: Angel robles Medical Director: Fernando Roura Contact: Jannette Gailé |
In House Pharmacy Tel. (787) 875-3375 Fax. (787) 875-4230 Physical Address: Calle Georgetti, Carr. 167 Postal Address: PO Box 418 Comerío PR 00782 Pharmacist: Helen Feshold | |
| *Centro de Salud Integral de Corozal Tel. (787) 859-2560 / 2470 Fax: (787) 859-5390 Physical Address: Carr. 159 Sector El Desvio, Corozal PR 00783 Postal Address: PO Box 739 Corozal PR 00783 Medical Director: Michael Fusile Nelson MC: Daysi Alvino Martínez MC: Leidy Rivera Santiago |
In House Pharmacy Tel. (787) 859-2560 / 215 Fax. (787) 859-5390 Physical Address: Carr. 159 Sector El Desvio, Corozal PR 00783 Postal Address: PO Box 739 Corozal PR 00783 Contact: Hairilys Vázquez | |
| *Centro de Salud Integral de Orocovis Tel. (787) 867-6010 Fax. (787) 867-5210 Physical Address: Ave. Luis Muñoz Marín, Carr. 155, Orocovis PR 00720 Postal Address: PO Box 2105 Orocovis PR 00720 Directora: Maritza Rolón Nieves Medical Director: Ada L. Santos Santos MC: Elba Miranda |
In House Pharmacy Tel. (787) 867-6010 Fax. (787) 867-6008 Physical Address: Ave. Luis Muñoz Marín, Carr. 155, Orocovis PR 00720 Postal Address: PO Box 2105 Orocovis PR 00720 Pharmacist: Lcda. Brenda Ortíz | |
| pog |
4 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
BAYAMÓN REGION
| Clinic |
Pharmacy | |
| CPTET Bayamón Immunology Clinic Tel. (787) 798-1580 / 5154 Tel. (787) 780-6690 Hospital Switchboard Tel. (787) 787-5151 Ext. 2112,2224,2534,2510 Fax. (787) 269-7740 ETS. (787) 786-4211 Pediatric: (787) 786-6940 Contact:(787) 313-2573 Zuley Huguet E mail: zhuguet@salud.gov.pr Physical Address: Hospital Universitario Dr. Ramón Ruiz Arnau, Ave. Laurel, Santa Juanita Bayamón, P.R. 00956 Postal Address: University Hospital Dr. Ramón Ruiz Arnau, Ave. Laurel, Santa Juanita Bayamón, P.R. 00956 Coordinador: Dr. Calos León Valiente |
Caridad Pharmacy Tel. (787) 785-3055 / 269-3140 Fax: (787) 740-5445 Fax. (787) 269-0022 Physical Address: Barrio Hato Tejas Carr. 862 Km 1.9 Bayamón, PR 00954 Postal Address: PO Box 4218 Bayamón, PR 00954 Pharmacist: Linnette Rivera E mail: lynnettepr@hotmail.com | |
| Centro de Epidemiología de Bayamón Tel. (787) 787-9831 Fax. (787) 269-5230 / (787) 785-2387 Physical Address: Calle Isabel 2da Esq. Degetau Sotano, Antiguo CDT Bay. Pueblo Postal Address: PO Box 1588 BAyamón, P.R. 00961 Directora: Deborath Medina, Marisel Cruz MC: Alma Ortíz, Rocío Román, David Ayala |
Plaza III Pharmacy Tel. (787) 785-0000 Fax: (787) 785-2387 Physical Address: Calle Barbosa # 57 Bayamón PR 00961 Postal Address: Calle Barbosa # 57 Bayamón PR 00961 Contact: Lcda. Mayda Rodríguez | |
| Casa Joven del Caribe Tel. (787) 870-1911 Cel. (787) 630-3571 Fax. (787) 796-2832 870-1911 Physical Address: Carr. # 820 Bo. Marzán Sector Río Lajas, Toa Alta Postal Address: PO Box 694, Dorado, P.R. 00646 Director: Rev. Samuel Agosto López MC: Felicita Santiago, Betzaida Rivera |
Plaza III Pharmacy Tel. (787) 785-0000 Fax: (787) 785-2387 Physical Address: Calle Barbosa # 57 Bayamón PR 00961 Postal Address: Calle Barbosa #57 Bayamón, PR 00961 Contact: Lcda. Mayda Rodríguez | |
| pog |
5 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
CAGUAS REGION
| Clinics |
Pharmacy | |
| CPTET Caguas Immunology Clinic Tel. (787) 744-3141 Ext.1142 ETS. (787) 744-8645 Fax. (787) 746-2898 Postal Address: San Juan Bautista Medical Center PO Box 5729 Caguas, P.R. 00726 Contacts: Norma Sánchez, Nancy del Valle Coordinador: Dr. Milton Garland Pediátrico Tel. (787) 744-3141 Ext.1158 / 1563 Tel. (787) 282-6300 / 8509 Tel. (787) 649-3930 Case Manager: Ivette Peña Nurse: Juanita Gómez Ext. 1153 Infectious: Armando Torres Nieves |
Arleen Pharmacy Tel. (787) 746-5952 / 745-2838 Fax. (787) 744-3397 Physical Address: Carr 172 tercera sección de Villa del Rey Caguas, PR 00725 Postal Address: PO Box 5986 Caguas, PR 00726 Contact: Sra. Adria Pharmacist: Lic. Roberto Peirats Cel. (787) 379-0116 Pharmacist: Arleen Hernández E-mail: Pharmacyarleen@gmail.com | |
| Humacao Satellite Clinic Tel. (787) 640-0980 Physical Address: Centro Comercial de Humacao Ave. Font Martelo # 100 Humacao, P.R. 00792 |
Central Pharmacy Tel. (787) 852-0520 Fax. (787) 850-5500 Physical Address: Calle Noya Hernández # 12 Este, Humacao PR 00791 Postal Address: PO Box 669 Humacao 00792 Contact: Lic. Julio Garriga E-mail: julioegarriga@hotmail.com | |
| Gurabo Community Health Center/Gurabo Family Medicine Center SIVIF Program Tel. (787) 737-1131/ 630-5564 Fax. (787) 737-2365 Tel. (787) 737-2377 SIVIF Fax. (787) 737-2377 Physical Address: Ramal 941 Sección Oscar Dávila, Gurabo PR Postal Address: Apartado 1277 Gurabo, PR 00778 Contact: Denisse Figueroa E mail: dfigueroa@sivif.com |
In House Pharmacy Tel. (787) 737-4449 Fax: (787) 737-1242 Physical Address: Carr 941 Salida Barrio Jaguas Gurabo, PR Postal Address: Apartado 1277 Gurabo, PR 00778 Pharmacist: Noemí Rivera | |
| pog |
6 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
CAGUAS REGION
| Clinic |
Pharmacy | |
| Project CIS Hospital Ryder Memorial Ryan White Part C Tel. (787) 852-0768 Ext. 4716, 4717, 4609, 4276 Fax. (787) 656-0735 850-1444 Physical Address:
Ave. Font Martello #355 Postal Address: PO Box 859 Humacao, P.R. 00792 Contacts: Carmelo Rivera Awilda, Felicita de Jesús |
In House Pharmacy Tel. (787) 852-0768 Ext. 4730, 4724, 4466, 4467, 4718 Fax: (787) 850-1444 Physical Address: Ave. Font Martello #355 Postal Address: PO Box 859 Humacao, P.R. 00792 Contacts: Carmen Ortíz Cristina Marrero Lilliam Sepúlveda María Carradero | |
| *Corporación de Servicios de Salud y Medicina Avanzada (COSSMA) Humacao Tel. (787) 852-2551 / 2595 Fax: (787) 850-1218 Physical Address: Ulises Martínez St. # 50 Humacao, PR 00791 Contact: Bárbara Rodríguez |
In House Pharmacy Tel. (787) 852-2551 Fax. (787) 937-0062 Physical Address: Calle Ulises Martínez # 50 Postal Address: PO Box 1330, Cidra, P.R. 00739 Pharmacist: María de L. García | |
| *Corporación de Servicios de Salud y Medicina Avanzada (COSSMA) San Lorenzo Tel. (787) 736-3655 / 3646 Fax: (787) 937-0059 Physical Address: Calle
Muñoz Rivera #186, Postal Address: Calle Muñoz Rivera #186, Contact: Wanda Nieves |
In House Pharmacy Tel. (787) 736-3655 Ext.1115 Fax: (787) 937-0064 Physical Address: Calle Muñoz Rivera # 186, San Lorenzo, P.R. 00754 Postal Address: PO Box 1330, Cidra, P.R. 00739 Pharmacist: Dra. Ilia Huertas | |
| pog |
7 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
CAGUAS REGION
| Clinic |
Pharmacy | |
| *Corporación de Servicios de Salud y Medicina Avanzada (COSSMA) Cidra Tel. (787) 739-8182 / 8183 Physical Address: Ave. Industrial El Jíbaro Lote #2 Carr. 172 Km. 13.5 Postal Address: Apartado 1330 Cidra, PR 00739 Contact: Yesenia Velázquez E mail: cossma@cossmapr.org Internet page: www.cossmapr.org Sra. Isolina Miranda: imiranda@cossmapr.com |
In House Pharmacy Tel. (787) 739-8182 Ext. 1228 Fax: (787) 714-1444 Physical Address: Ave. Industrial El Jíbaro Lote #2 Carr. 172 Km. 13.5 Postal Address: Apartado 1330 Cidra, PR 00739 Pharmacist: Lidian Rosario | |
| *Corporación de Servicios de Salud y Medicina Avanzada (COSSMA) Yabucoa Tel. (787) 893-3060 / 3055 Fax: (787) 266-6292 Physical Address: Calle Muñoz Rivera #15 Yabucoa, PR Contact: Diana Mulero |
Pharmacy Not applicable | |
| pog |
8 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
FAJARDO REGION
| Clinic |
Pharmacy | |
| CPTET Fajardo Immunology Clinic Tel. (787) 801-1992 / 1995 Tel. (787) 863-5437 Fax. (787) 801-6767 Physical Address: Urb. Monte Brisa Calle Rafael #55 Fajardo, P.R. 00738 Coordinador: Dr. Arturo Hernández Estrella Contact: Rafaela Díaz |
Denirka Pharmacy Tel. (787) 863-7788 / 860-7788 Fax. (787) 863-1422 Physical Address: Avenida General Valero # 305 Fajardo, PR 00738 Postal Address: PO Box 850 Fajardo, PR 00738 Contact: Vanessa Hernández Contact: Gil Nieves E-mail: gilnieves@hotmail.com | |
| pog |
9 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
MAYAGÜEZ REGION
| Clinic |
Pharmacy | |
| CPTET Mayagüez Immunology Clinic Tel. (787) 834-2115 / 2118 Fax. (787) 265-2850 / 834-2370 Physical Address: Centro Médico al lado de Salud Mental, Carr. #2 Postal Address: PO Box 400 Mayagüez, P.R. 00680 Contact: Damariz Ruiz, Marianita Torres Coordinador: Ramón Ramírez Ronda |
In House Pharmacy Tel. (787) 834-2116 / 2115 / 2118 Cel. (787) 546-5527 Sonia Cel. (787) 644-3277 Janette Torres Cel. (787) 233-8080 Sandra Physical Address: Centro Médico al lado de Salud Mental, Carr. #2 Postal Address: PO Box 400 Mayagüez, P.R. 00680 Pharmacist: Lic. Janette Torres Contacts: Sonia Vargas, Sandra Rivera | |
| Centro de Salud de Migrantes West REGION SSIMA Program Serv. Salud Integrado Ryan White Part C Tel. (787) 805-2900 / 805-2920 Ext. 294 Fax. (787) 805-4750 Clinic: (787) 834-1470 ADM: (787) 834-1924 Fax.(787) 805-4750 Physical Address: Calle Ramón E. Betánces #392 Sur Mayagüez, PR 00680 Postal Address: PO Box 7128 Mayagüez, PR 00681-7128 Contact: Wanda Acosta Director: Reynaldo Serrano |
In House Pharmacy Tel. (787) 805-2900 / 920 Ext. 237 Fax: (787) 265-4245 Physical Address: Calle Ramón E. Betánces #392 Sur Mayagüez, PR 00680 Postal Address: PO Box 190 Mayagüez PR 00681-7128 Contact: Lcda. Juliana Torres Contact: Lcda. Lilliam Torres
Pharmacy Clinic Satélite de San Sebastián Tel. (787) 896-1665 Tel. (787) 896-6975 Fax. (787) 896-4570 Physical Address: Carr. 119 k.m. 35.2 Bo. Piedras Blancas San Sebastián PR Contact: Lcda. Grisel A. Cabá
Pharmacy Clinic Satélite de Guánica Tel. (787) 821-4511 / 821-3377 / 821-2144 Fax. (787) 821-4511 Physical Address: Calle Montalva #23 Ensenada Guánica, PR 00647 Postal Address: Calle Montalva #23 Ensenada Guánica, PR 00647 Pharmacist: Lcda. Wanda Torres | |
| pog Rev. 06.09 |
10 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
PONCE REGION
| Clinic |
Pharmacy | |
| Ararat Center Tel. (787) 284-5884 / 5887 Fax. (787) 284-5874 Physical Address: 8169 Condominio San Vicente, Suite 204, Ponce, P.R. Postal Address: PO Box 7793 Ponce, P.R. 00732 Contact: Juan Rivera, Madeline Torres E mail: jrivera@centroararat.org Administrator: Iván Meléndez Rivera |
El Apotecario Pharmacy Tel. (787) 844-2135 / 290-4654 Fax. (787) 844-2135 Physical Address: Tito Castro Ave #625 Carr. 14 Front to Pharmacy El Amal La Rambla, Ponce Postal Address: PMB 381 Ave. Tito Castro #609, Ponce, PR 00716 Contact: Lcdo. Ricardo Cintrón | |
| Centro de Salud Fam. Dr. Julio Palmieri Ryan White Part C Program Tel. (787) 271-3779 / (787) 839-4150 Fax. (787) 271-3779 MC: Ilka Santiago Physical Address: Valentina Corner Morse St., Arroyo Postal Address: PO Box 450 Arroyo, P.R. 00714 Contact: Dra. Antonia Márquez |
In House Pharmacy Tel. (787) 839-4150 Ext. 234 Fax: (787) 839-3989 Physical Address: Valentina Corner –Morse St. , Arroyo, PR 00714 Postal Address: PO Box 450 Arroyo, P.R. 00714 Farmacéutoco: Lcda. Doris Porrata | |
| Consejo de Salud de la Comunidad CDT Playa de Ponce Ryan White Part C Program Tel. (787) 843-9393 Ext. 258, 262 Fax. (787) 843-0899 / 841-0077 Physical Address: Ave. Hostos 1034 Ponce, P.R. 00716 Postal Address: PO Box 220 Ponce, P.R. 00715 - 0220 Contact: Dra. Awilda García |
In House Pharmacy Tel. (787) 843-9370 Fax. (787) 843-9395 Physical Address: Ave. Hostos 1034 Ponce, P.R. 00716 Postal Address: PO Box 220 Ponce, P.R. 00715 - 0220 Contact: Hilda Torres | |
| CPTET Ponce Immunology Clinic Tel. (787) 259-4046 / 259-4731 ETS. (787) 848-2000 Fax. (787) 259-3998 / 842-1943 Physical Address: Antiguo Hospital de Distrito de Ponce Carretera Estatal Bo. Machuelo #14 Ponce, P.R. 00717 Coordinadora: Dra. Gladys Sepúlveda |
In House Pharmacy Tel. (787) 843-2188 Fax. (787) 842-1943 Physical Address: Antiguo Hospital de Distrito de Ponce Carretera Estatal Bo. Machuelo #14 Ponce, P.R. 00717 Pharmacist: Jorge López Vega | |
| pog Rev. 06.09 |
11 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
PONCE REGION
| Clinic |
Pharmacy | |
| Especial de la Salud Clinic Tel. (787) 260-9446 Cuadro: (787) 837-2185 Ext. 2296, 2297, 2298 Fax. (787) 260-2943 Physical Address: Calle Hostos #23 Juana Díaz Postal Address: Apartado 1409 Juana Díaz, P.R. 00795 Director: Carlos Ortíz Torres |
Sonia Pharmacy Tel. (787) 837-2666 Fax: (787) 837-4602 Physical Address: Comercio St. #61 Juana Díaz, PR 00795 Postal Address: Comercio St. #61 Juana Díaz, PR 00795 Pharmacist: Sonia Muñoz De Toro | |
| Centro de Ambulantes Cristo Pobre Inc. Tel. (787) 841-7149 Fax. (787) 844-5656 Physical Address: Calle Guadalupe Esq. Unión #100 Ponce, P.R. Postal Address: PO Box 334651 Ponce, P.R. 00733-4651 Contact: Irma Valentín Administrador: Juan de Dios Videau |
El Apotecario Pharmacy Tel. (787) 844-2135 / 290-4654 Fax. (787) 844-2135 Physical Address: Ave.Tito Castro #625 Carr. 14 Frente a Pharmacy El Amal La Rambla, Ponce Postal Address: PMB 381 Ave. Tito Castro #609, Ponce, PR 00716 Contact: Ricardo Cintrón | |
| Centro de Servicios de Salud de Patillas Tel. (787) 839-4320 / 839-4360 Fax. (787) 271-0004 Physical Address: Calle Riefhkol # 99 Patillas, PR 00723 Postal Address: PO Box 697 Patillas, PR 00723 Contact: Sra. Carmen Carro |
In House Pharmacy Tel. (787) 839-4320 Ext. 241 / 247 Fax. (787) 839-4337 Physical Address: Calle Riefhkol # 99 Patillas, PR 00723 Postal Address: PO Box 697 Contact: Anette Alvarado E mail: pphsc_inc.com | |
| Amor que Sana, Inc. Project Administrative Offices Tel. (787) 844-8081 Fax. (787) 844-8117 Tel./Fax. (787) 259-2882 Manejo de Caso Physical Address: Traditional Plaza 7033 Méndez Vigo y Aurora Ponce, PR 00717-1250 Postal Address: Traditional Plaza 7033 Méndez Vigo y Aurora Ponce, PR 00717-1250 Contact: Héctor Torres Director: Juan A. Panelli |
El Apotecario Pharmacy Tel. (787) 844-2135 / 290-4654 Fax. (787) 844-8117 Physical Address: Ave. Tito Castro #625 Carr. 14 (Front of El Amal Pharmacy) La Rambla, Ponce, PR 00716 Postal Address: PMB 381 Ave. Tito Castro #609 Ponce, PR 00716 Contact: Ricardo Cintrón | |
| pog Rev. 06.09 |
12 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
SAN JUAN REGION
| Clinic |
Pharmacy | |
| Centro Latinoamericano de Enfermedades Transmisibles (CLETS) Tel. (787) 754-8123 / 8118 Fax. (787) 754-8127 Physical Address: Barrio Monacillos Paseo Celso Barbosa Centro Médico San Juan, P.R. 00936 Postal Address: PO Box 70184 San Juan PR 00936 Director: Dr. Hermes García |
In House Pharmacy Tel. (787) 754-8118 Fax: (787) 754-8127 Physical Address: Barrio Monacillos Paseo Celso Barbosa Centro Médico San Juan, P.R. 00936 Postal Address: PO Box 70184 San Juan PR 00936 Pharmacist: Lourdes Fornés | |
| Concilio de Salud Integral de Loíza Tel. (787) 876-3130 / 2042 Ext. 261 Fax. (787) 256-1900 Physical Address: Carr. 188 Intersección # 187 Loíza Postal Address: PO Box 509, Loíza P.R. 00772 Contact: Juan C. Castellanos |
In House Pharmacy Tel. (787) 876-2005 Fax. (787) 876-6613 / 1120 / 1900 Physical Address: Carr. 188 Intersección # 187 Loíza Postal Address: Apartado 509, Loíza P.R. 00772 Contact: Irma Alvárez | |
| CPTET Carolina Immunology Clinic Tel. (787) 757-1800 Fax. (787) 257-3615 Physical Address: Ave. 65 de Infantería KM 8.4 next to Plaza Carolina Postal Address: Hospital Universitario de Carolina, PO Box 6021, Carolina P.R. 00984-6021 Coordinadora: Dra. Adiana Zayas |
Hospital UPR Pharmacy Tel. (787) 757-1800 Ext. 227 Fax: (787) 750-4214 Physical Address: Ave. 65 de Infabntería KM 8.4 al lado de Plaza Carolina Postal Address: Hospital Universitario de Carolina, PO Box 6021, Carolina P.R. 00984-6021 Pharmacist: Juan Villegas | |
| Community Initiative Tel. (787) 250-8629 / 8680 / 8690 Fax. (787) 753-4454 Physical Address: Calle Quisqueya #61 Esq. Chile, Hato Rey P.R. 00918 Postal Address: PO Box 366535 San Juan, P.R. 00936-366535 Contact: Jonathan Fernández Director: Dr. José Vargas Vidot E mail: iniciator@hotmail.com |
San Rafael Pharmacy Tel. (787) 724-3307 Fax: (787) 721-4165 Physical Address: 851 Lafayette Esq. San Rafael, Urb. Hipódromo Pda. 20 Santurce PR Postal Address: 851 Lafayette Esq. San Rafael, Urb. Hipódromo Pda. 20 Santurce PR 00909 Contact: Rafael Díaz | |
| pog Rev. 06.09 |
13 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
SAN JUAN REGION
| Clinic |
Pharmacy | |
| San Juan Municipality Programa Más Salud: Sida con Salud Tel. (787) 723-2424 Ext. 239 / 243 /294 Fax. (787) 724-5104 Physical Address: Ave. Fernández Juncos 1306 Pda. 19 Santurce, P.R. 00908 Postal Address: PO Box 13694 San Juan, P.R. 00908 Contact: Dr. Luis Martínez Manager: Sonia Collazo |
In House Pharmacy Tel. (787) 723-2424 Ext. 4071 Fax: (787) 721-7596 Physical Address: Ave. Fernández Juncos 1306 Pda. 19 Santurce, P.R. 00908 Postal Address: PO Box 13694 San Juan, P.R. 00908 Contact: Laura Del Carmen Rivera | |
| New Puerto Rico CoNCRA Ryan White Part C Program Tel. (787) 753-9443 / 9463 Ext. 32 Fax. (787) 753-2894 / 9463 Physical Address; Urb. García Ubarry Brunbaugh St. #162 San Juan, PR 00925 Postal Address: PO Box 20850 San Juan, P.R. 00928-9463 Contact: Manuel Quiñones, Magaly Nieves Director: Rosaura López Medical Director: Ext. 11 |
García Pharmacy Tel. (787) 898-3975 / 820-5158 Fax. (787) 820-9048 Physical Address: Vidal Félix St. #121 Hatillo, P.R. 00659 Postal Address: PO Box 67 Hatillo PR 00659 Pharmacist: Daniel Mahíques Nieves | |
| Project CEMI Tel. (787) 766-0025 / 0030 Tel. (787) 771-4740 / 753-5913 Pediatric AIDS Tel. (787) 274-5762 Physical Address: Recinto de Ciencias Médicas Biomedical II Building Floor I, Río Piedras, PR 00935 Contact: Janice Pérez |
||
| ACTU Project Tel. (787) 767-9192/9193/9194/9195 Fax. (787) 754-8002 Physical Address: Recinto de Ciencias Médicas UPR Biomedical II Bldg. next to nuclear medicine, Río Piedras, PR 00935 Contact: Silvia Dávila / sdavila@rcm.upr.edu |
||
| pog |
14 | |
| Rev. 06.09 |
Commonwealth of Puerto Rico
Health Department
Assistant Secretary for Family Health, Integrated Services and Health Promotion
Central Office for AIDS Affairs and Transmissible Diseases
Division of HIV/AIDS Services: Preventive Care and Health
Ryan White Part B Program
SAN JUAN REGION
| Clinic |
Pharmacy | |
| GAMMA Project Tel. (787) 759-9595 Fax: (787) 767-4798 Physical Address: Centro Cardiovascular de PR Project GAMMA, Piso 8 Oficina 814 San Juan Postal Address: Universidad de Puerto Rico RCM Project GAMMA, PO Box 365067 San Juan PR 00936-5067 Contact: Dra. Irma L. Febo, Contact: Iraida Salabarria |
| pog |
15 | |
| Rev. 06.09 |
(Attachment 6)
| PUERTO RICO HEALTH INSURANCE ADMINISTRATION Retail Pharmacy Reimbursement Level Effective date: November 1, 2006 until the expiration date of the contract. |
||||||||
| Pharmacy Type | Ingredient Cost (AWP Discounts) |
Dispensive Fee | ||||||
|
Independent: |
||||||||
|
Brand |
11% | $2.50 | ||||||
|
Bioequivalent Generics |
ASES’ MAC List | $2.50 | ||||||
| Non *MAC Generics |
11% | $2.50 | ||||||
| Local Pharmacy Chains: |
||||||||
|
Brand |
11% | $2.50 | ||||||
|
Bioequivalent Generics |
ASES’ MAC List | $2.50 | ||||||
| Non MAC Generics |
11% | $2.50 | ||||||
| National Pharmacy Chain: |
||||||||
|
Brand |
15% | $1.75 | ||||||
|
Generics |
ASES’ MAC List | $2.50 | ||||||
| Non-MAC Generics |
15% | $2.00 | ||||||
|
*Walgreens |
Not Contracted | |||||||
|
Diagnostic and Treatment Centers |
||||||||
|
Brand |
12% | $2.50 | ||||||
|
Generics |
ASES’ MAC List | $2.50 | ||||||
| Non-MAC Generics |
12% | $2.50 | ||||||
|
*MAC=Maximum Allowable Cost |
||||||||
(Attachment 8)
| CO-PAYS & CO-INSURANCE - effective on November 1st, 2011
| ||||||||||||||||
| Federal
|
CHIPs | Commonwealth Population | *ELA | |||||||||||||
| SERVICES | 100 | 110 | 230 | 300 | 310 | 320 | 330 | 400 | ||||||||
| HOSPITAL
|
HOSPITAL | HOSPITAL | HOSPITAL | HOSPITAL | ||||||||||||
| Admissions | $0 | $3 | $0 | $3 | $5 | $6 | $20 | $50 | ||||||||
| Nursery | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||||||||
| EMERGENCY ROOM (ER)
|
EMERGENCY ROOM (ER) | EMERGENCY ROOM (ER) | EMERGENCY ROOM (ER) | EMERGENCY ROOM (ER) | ||||||||||||
| Emergency Room (ER) Visit | $0 | $0 | $0 | $1 | $5 | $10 | $15 | $20 | ||||||||
| Non-emergency visit to a hospital emergency room. | $5 | $5 | $0 | $15 | $15 | $15 | $15 | $20 | ||||||||
| Trauma | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||||||||
|
AMBULATORY VISITS TO
|
AMBULATORY VISITS TO | AMBULATORY VISITS TO | AMBULATORY VISITS TO | AMBULATORY VISITS TO | ||||||||||||
| Primary Care Physician (PCP) | $0 | $1 | $0 | $0 | $1 | $2 | $2 | $3 | ||||||||
| Specialist | $0 | $1 | $0 | $1 | $1 | $3 | $4 | $7 | ||||||||
| Sub-Specialist | $0 | $1 | $0 | $1 | $1 | $3 | $5 | $10 | ||||||||
| Pre-natal services | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||||||||
| OTHER SERVICES
|
OTHER SERVICES | OTHER SERVICES | OTHER SERVICES | OTHER SERVICES | ||||||||||||
| High-Tech Laboratories** | $0 | 50¢ | $0 | $1 | $1 | $2 | $3 | 20% | ||||||||
| Clinical Laboratories** | $0 | 50¢ | $0 | $1 | $1 | $2 | $3 | 20% | ||||||||
| X-Rays** | $0 | 50¢ | $0 | $1 | $1 | $2 | $3 | 20% | ||||||||
| Special Diagnostic Tests** | $0 | $1 | $0 | $1 | $2 | $2 | $6 | 40% | ||||||||
| Therapy – Physical | $0 | $1 | $0 | $1 | $2 | $2 | $3 | $5 | ||||||||
| Therapy – Respiratory | $0 | $1 | $0 | $1 | $2 | $2 | $3 | $5 | ||||||||
| Therapy – Occupational | $0 | $1 | $0 | $1 | $2 | $2 | $3 | $5 | ||||||||
| Vaccines | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||||||||
| Healthy Child Care | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||||||||
| DENTAL
|
DENTAL | DENTAL | DENTAL | DENTAL | ||||||||||||
| Preventive (Child) | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | ||||||||
| Preventive (Adult) | $0 | $1 | $0 | $0 | $1 | $2 | $3 | $3 | ||||||||
| Restorative | $0 | $1 | $0 | $0 | $1 | $5 | $6 | $10 | ||||||||
| PHARMACY***
|
PHARMACY | PHARMACY | PHARMACY | PHARMACY | ||||||||||||
| Generic (Children 0-21) | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $5 | ||||||||
| Generic (Adult)**** | $1 | $1 | N/A | $1 | $2 | $3 | $5 | $5 | ||||||||
| Brand (Children 0-21) | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $10 | ||||||||
| Brand (Adult)**** | $3 | $3 | N/A | $3 | $4 | $5 | $7 | $10 | ||||||||
| Federal | CHIPs | Commonwealth Population | ELA | |||||||||||||
| SERVICES | 100 | 110 | 230 | 300 | 310 | 320 | 330 | 400 | ||||||||
*Code 400 in ELA column means the copayments that will applied for the population suscribes as public employees of the Puerto Rico Government.
** Apply for diagnostic tests only, copays will not applied in those tests when they are required as part of a preventive service.
***Copays will apply for each drug included in the same prescription pad. Exceptions shown on Pharmacy (children 0-21) does not apply for 400 ELA employees.
****Co-pays for children 0-21 years of age are not applicable for Medicaid, Commonwealth medically indigent eligible, and for children under the CHIP Program in group ages 0-18.
Co-pays may apply to children ages over twenty one (21) as well as to adults. Limit to 6 scripts per month (except for anti-psychotic and antivirals). 90 days dispensing for some chronic conditions. Polypharmacy program.
As established in 42 CFR 447.53(b) the following exceptions will be applicable for federal population under code 110:
(b) Exclusions from cost sharing. The plan may not provide for impositions of a deductible, coinsurance, copayment, or similar charge upon categorically or medically needy individuals for the following:
(1) (Children. Services furnished to individuals under 18 years of age (and, at the option of the State, individuals under 21, 20, or 19 years of age, or any reasonable category of individuals 18 years of age or over but under 21) are excluded from cost sharing.
| (2) Pregnant women. Services furnished to pregnant women if such services related to the pregnancy, or to any other medical condition which may complicate the pregnancy are excluded from cost sharing obligations. These services include routine prenatal care, labor and delivery, routine post-partum care, family planning services, complications of pregnancy or delivery likely to affect the pregnancy, such as hypertension, diabetes, urinary tract infection, and services furnished during the postpartum period for conditions or complications related to the pregnancy. The postpartum period is the immediate postpartum period which begins on the last day of pregnancy and extends through the end of the month in which the 60-day period following termination of pregnancy ends. States may further exclude from cost sharing all services furnished to pregnant women if they desire.
(3) Institutionalized individuals. Services furnished to any individual who is an inpatient in a hospital, long-term care facility, or other medical institution if the individual is required {pursuant to §435.725, §435,733, §435.832, or §436.832), as a condition of receiving services in the institution, to spend all but a minimal amount of his income required for personal needs, for medical care costs are excluded from cost sharing.
(4) Emergency services. Services as defined at section 1932(b)(2) of the Act and §438.114(a). (5) Family planning. Family planning services and supplies furnished to individuals of child-bearing age are excluded from cost sharing. (6) American Indians. Items and services furnished to an American Indian directly by an American Indian health care provider or through referral under contract health services. |
(Attachment 10)
Projected Medical Costs by Region: November 1, 2011 - June 30, 2012
| West | Metro North | North | San Juan | Northeast | ||||||||||||||||
|
With Plan Changes |
With Plan Changes |
With Plan Changes |
With Plan Changes |
With Plan Changes |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
||||||||||||
| Facility |
$ | 35.19 | $ | 45.75 | $ | 37.55 | $ | 52.65 | $ | 37.24 | ||||||||||
| Professional |
$ | 31.25 | $ | 39.70 | $ | 28.05 | $ | 49.54 | $ | 45.01 | ||||||||||
| Dental |
$ | 3.00 | $ | 4.07 | $ | 3.85 | $ | 4.53 | $ | 4.31 | ||||||||||
| Drugs |
$ | 11.74 | $ | 14.97 | $ | 12.66 | $ | 21.78 | $ | 15.99 | ||||||||||
| Other |
$ | 6.31 | $ | 7.08 | $ | 5.94 | $ | 9.59 | $ | 7.65 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| $ | 87.49 | $ | 111.57 | $ | 88.05 | $ | 138.09 | $ | 110.20 | |||||||||||
Developed by ASES’ actuaries
Attachment # 10
H:\Projected Medical Costs TPA SSS contract Nov, 2011-June 2012
Sheet1
| TJW | MILLIMAN | 1 of 1 |
ATTACHMENT 10A
Calculation of Threshold Per Member Per Month (PMPM)
November 2011 - June 2012
| West |
Metro North |
North |
San Juan |
Northeast |
Threshold* |
|||||||||||||||||||
| Projected Medical Cost PMPM |
$ | 87.49 | $ | 111.57 | $ | 88.05 | $ | 138.09 | $ | 110.20 | $ | 102.25 | ||||||||||||
| June 2011 Membership |
225,038 | 196,267 | 200,616 | 92,198 | 130,114 | |||||||||||||||||||
*Threshold is calculated as weighted average projected medical PMPM cost. The threshold will be recalculated based on actual membership for November 2011 - June 2012 at the end of the contract period.
Rev. 10.17.2011
ATTACHMENT 11
ADMINISTRATIVE FEES PER MEMBER PER MONTH
&
QUALITY INCENTIVE PROGRAM RETENTION FUND
| Region | Per Member Per Month Administrative Fee | |
|
North |
$7.80 | |
| Metro North |
$8.17 | |
| San Juan |
$11.42 | |
|
Northeast |
$8.64 | |
|
West |
$7.15 | |
|
Virtual |
Included above | |
|
Retention Fund |
$0.03 | |
| 5% withhold amount |
$0.002 |
Rev. 10.15.2011
Administración de Seguros de Salud de Puerto Rico (ASES)
TPA Contract
Attachment 12
Deliverables
|
Section
|
Deliverable
|
Contractor delivery date
| ||
|
6.4.5
|
Enrollee Handbook - (Universal Guide) |
November 1, 2011 | ||
|
6.6.6
|
Provider Directory |
December 1, 2011 | ||
|
6.7.5 |
Front and back sample of Enrollee ID Card
|
October 20, 2011 | ||
|
6.8.13 |
Scripts addressing the questions expected to arise most often for both the Information Service and the Medical Advice Service
|
October 20, 2011 | ||
|
6.8.14 |
Tele Mi Salud Policies and Procedures, Quality Criteria and Protocols, Outreach Program, Scripts and Training materials for Tele MI Salud Call Center Employees
|
October 20, 2011 | ||
|
6.9.5 |
Website screenshots
|
December 1, 2011 | ||
|
6.10.2 |
Cultural Competency Plan
|
December 1, 2011 | ||
|
6.14.5.1 |
Marketing Plan and copies of all Marketing Materials (written and oral)
|
December 1, 2011 | ||
|
7.5.3.4.5 |
Wellness Plan
|
December 1, 2011 | ||
|
7.5.8.3.12 |
Pre-Natal and Maternal Wellness Plan
|
December 1, 2011 | ||
|
7.7.6.6 |
Summary of the Strategy for the identification of populations with special health care needs
|
November 15, 2011 | ||
|
7.7.6 & 9.14.2
|
Protocols for screening and registering Enrollees for Special Coverage |
November 1, 2011 | ||
|
7.7.9.1 |
Coordination Plan with the MBHO to meet the integration requirements for autism.
|
October 17, 2011 | ||
|
7.8.2.6 |
Case Management Policies and Procedures
|
October 17, 2011 | ||
|
7.8.3.5 |
Disease Management Policies and Procedures
|
December 1, 2011 | ||
|
7.9.1.4 |
EPSDT Plan including procedures for follow-up of missed appointments, including missed Referral appointments for
|
October 17, 2011 |
|
1 |
Administración de Seguros de Salud de Puerto Rico (ASES)
TPA Contract
Attachment 12
Deliverables
|
problems identified through EPSDT screens and exams
|
||||
|
8.8 |
Integration Plan incorporating the elements in Article 8, to ensure cooperation between TPA and MBHO
|
October 17, 2011 | ||
|
9.6.1.6 |
Policies and procedures for Enrollee selection of PCP
|
October 17, 2011 | ||
|
9.11.3 |
MBHO Policies and Procedures that ensure timely Access to Behavioral Services and integration of Care.
|
November 1, 2011 | ||
|
9.14.2 |
Protocols for screening Enrollees for participation in Case Management and Disease Management Programs
|
October 17, 2011 | ||
|
9.19.4 |
Policies and procedures for determining the adequacy of Providers’ available hours
|
December 1, 2011 | ||
|
9.21.3 |
Policies and procedures for monitoring (PPN) Provider performance, measuring access to care, and identifying Provider compliance issues
|
December 1, 2011 | ||
|
9.1.1; 9.22.1
|
Assurances concerning adequacy of Provider Network |
TBD - Certifications Due Upon Request | ||
|
10.1.6.1 |
Model for each type of Provider Contract
|
Upon Execution | ||
|
10.1.6.1 |
Compact disk with copies of provider contract templates
|
Upon Execution | ||
|
10.2.1.3 |
Provider Guidelines
|
October 17, 2011 | ||
|
10.2.2.1 |
Continuing Education Curriculum for Providers
|
December 1, 2011 | ||
|
10.5.1.5 |
Capitation methodology
|
October 28, 2011 | ||
|
10.8.1 |
Electronic file and a list of all participating providers, listed by municipality, indicating the capacity of each Provider, as well as the specialty or subspecialty of physicians |
File Submission Weekly based on Contract Execution Date
| ||
|
10.8.5 |
Control sheet of provider files |
File Submission Weekly based on Contract Execution Date
| ||
|
11.1.2 |
Utilization Management Policies and Procedures
|
October 17, 2011 |
|
2 |
Administración de Seguros de Salud de Puerto Rico (ASES)
TPA Contract
Attachment 12
Deliverables
|
12.2.4; 12.5.1
|
QAPI Program |
December 1, 2011 | ||
|
13.1.3 |
Fraud and Abuse Policies and Procedures, proposed compliance plan, and Program Integrity Plan
|
December 1, 2011 | ||
|
14.1.3 |
Grievance System Policies and Procedures
|
October 24, 2011 | ||
|
14.1.14 |
Grievance System Forms
|
October 24, 2011 | ||
|
15.3.2 |
Staff Training Plan and a current organizational chart
|
October 17, 2011 | ||
|
15.5.1-2 |
Implementation Plan
|
October 17, 2011 | ||
|
10.5.1.8; 16.5.1
|
Provider Payment Schedule |
October 17, 2011 | ||
|
22.1.7
|
Payment procedures and controls
|
December 1, 2011 | ||
|
22.4.1.9 |
Plan for Routine Audits to prevent duplicate payments for third party billable services
|
December 1, 2011 | ||
|
28.2 |
Certification that the Contractor does not contract with entities that have been under investigation for, accused of, convicted of, or sentenced to imprisonment, in Puerto Rico, the United States of America, or any other country, for any crime involving corruption, fraud, embezzlement, or unlawful appropriation of public funds, pursuant to Act 458, as amended, and Act 84 of 2002
|
October 17, 2011 | ||
|
30.1 |
Insurance license issued by PRICO
|
October 17, 2011 | ||
|
31.1 |
Certifications from government agencies, a list of Contractor’s contracts with government agencies, and other documents relating to Contractor’s compliance with federal and Puerto Rico law.
|
Within 15 days of execution of contract. | ||
|
38.2 |
Conflict of Interest Disclosure Form
|
October 17, 2011 |
|
3 |
(Attachment 14)
Commonwealth of Puerto Rico
Puerto Rico Medicaid Program/Puerto Rico Department of Health
Puerto Rico Health Insurance Administration
Guidelines for the
Development of Program
Integrity Plan
2011 – 2013
(This document is to be used by all contracted companies participating in the
Commonwealth of Puerto Rico “Mi Salud”. The purpose of sharing information
with contracted companies is to provide them guidelines with minimum
requirements to formulate their own Plan Integrity Program for the Health Care
Delivery System sponsored by the Commonwealth of Puerto Rico)
The Insurer shall comply with the following Medicaid Integrity requirements:
| A. | 60 days after the dated of the agreement the Company must submit to ASES Compliance Office copy of the policies and procedures for identifying and tracking potential provider fraud cases, for conducting preliminary and full investigation and for referring cases of suspected fraud to an appropriate law enforcement agency. The Compliance Plan should be developed in accordance with 42 CFR 438.608. |
| B. | Each company must submit to the Administration’s Compliance Office on a quarterly basis a report with the following information: preliminary and full investigations, audits performed, administrative actions against providers, overpayments identified and providers referred to the Department of Justice (if not submit a certification signed by the Compliance Director and the President or CEO). |
| C. | Each company must submit to the Compliance Office on a quarterly basis a report with the following information: fraud investigations pending, fraud investigations in process, fraud investigations finished and referrals to the Department of Justice or U.S. Attorney’s Field Office (if there were no investigations, submit a certifications signed by the Compliance Director and the President or CEO). |
| D. | Each Company has five (5) days to notify ASES about the referrals made to the US Attorney’s Field Office and HHS-OIG. |
| E. | Each company must submit to the Compliance Office a certification signed by the Compliance Director and the President or CEO indicating that all full investigations were made in accordance with 42 CFR 455.15. |
| F. | Each Company has five (5) days to notify ASES about any adverse or negative action that the MCO has taken on provider application (upon initial application or application renewal) or actions which limit the ability of providers to participate in the program. |
| G. | Each Company must review the credentialing forms of all providers and any fiscal agents they may use to ensure that they are in accordance with federal regulation 42 CFR 455.104. |
| H. | Each Company must require providers to fill out a complete ownership and control disclosures form. The Company is responsible to ensure compliance with regulation. |
2
| I. | Each Company must review providers agreement to incorporate appropriate business transaction language to ensure accordance with federal regulation 42 CFR 455.105. |
| J. | Each Company must request providers to fulfill a business transactions form and verify compliance with regulation. |
| K. | Each Company must establish a method to capture criminal conviction information on owners, persons with control interest, agents, and managing employees of providers to ensure that is in accordance with federal regulation 42 CFR 455.106. |
| L. | Each Company must review the enrollment packages for all provider types to request criminal conviction information as stated before. |
| M. | Each Company should develop and implement procedures to report to HHS-OIG and ASES within 20 working days any criminal conviction disclosures made during the MCO credentialing process. Copy of the policies should be submitted to ASES Compliance Office. |
| N. | Each Company must submit to the Compliance Office a certification signed by the Compliance Director and the President or CEO stating compliance with 42 CFR 455.106. |
| 0. | Each Company must comply with requirement in 42 CFR 455.20 and must document in a quarterly report compliance with regulation. |
| P. | Each Company must comply with requirement in 42 CFR 455.101. |
| Q. | Each Company must review the enrollment form and credentialing packages for all provider types to capture the identity of agents and managing employees. |
3
TABLE OF CONTENTS
Integrity Program Basis and Scope
Definitions
Other applicable regulations
Guidelines for Sub-Parts A, B
Sub-Part A: Fraud Detection and Investigation Program
PI A001: State plan requirement. § 455.12
PI A002: Methods for identification, investigation, and referral. § 455.13
PI A003: Preliminary investigation. § 455.14
PI A004: Full investigation. § 455.15
PI A005: Resolution of full investigation. § 455.16
PI A006: Reporting requirements. § 455.17
PI A007: Provider’s statements on claims forms. § 455.18
PI A008: Provider’s statement on check. § 455.19
PI A009: Recipient verification procedure. § 455.20
PI A010: Cooperation with State Medicaid fraud control units. § 455.21
PI A011: Withholding of payments in cases of fraud or willful misrepresentation (§ 455.23)
Sub-Part B: Disclosure of Information by Providers and Fiscal Agents
PI B001: Purpose § 455.100
PI B002; Definitions.§ 455.101
PI B003: Determination of ownership or control percentages.§ 455.102
PI B004: State Plan requirements § 455.103
PI B005: Disclosure by providers and agents: Information on ownership and control. § 455.104
PI B006: Disclosure by providers: Information related to business transactions. § 455.105
PI B007: Disclosure by providers: Information on persons convicted of crimes. § 455.106
4
Introduction
Under the authority of Sec. 1102 of the Social Security Act (42 U.S.C. 1302); as detailed in the 43 FR 45262, Sept. 29, 1978, the Medicaid Program must have a program to detect and investigate fraud, waste and abuse.
The Commonwealth of Puerto Rico Department of Health and its Office for the Medically Indigent, acting as the single state agency are responsible for the management of the Medicaid and SCHIP grant funds. These funds are transferred to the Puerto Rico Health Insurance Administration (ASES), to be combined with state funds to provide health benefit coverage to the medically indigent population under a managed care fully capitated health plan. Acting as a sub-grantee to the Office for the Medically Indigent Medicaid program, ASES establishes contracts with insurance companies and other organizations to facilitate the beneficiaries’ access to the benefit coverage through out their provider’s networks.
Integrity Program Basis and Scope
This document sets forth guidelines with minimum criteria for the compliance with Program Integrity Policies and Procedures that each organization (grantee, sub-grantee, insurance companies) must have for the administration of the Commonwealth of Puerto Rico’s Medicaid and State Health Plans. This document includes guidelines for the elaboration of the 3 main sections in the organizations Program Integrity Plan (PIP):
| 1. | Fraud Detection and Investigation |
| 2. | Providers and Fiscal Agents Disclosure of Information on Ownership and Control |
| 3. | Integrity Program |
Regulation Citation
Sections 1902(a)(4) [42 USC 1396(a)(4)1, (61)2, (64)3}; 1903(i)(2) [42 USC 1396(b)(i)(2)]4 1936[42 USC 1396u-6]5) and regulations at 42 CFR Parts 438,455,1001 and 1002
Overall Requirement
All providers/contractors are required to comply with the CMS Medicaid Integrity Group State Medicaid Director Letters #08-003 and #09-001, which explain what all states and contractors should do in terms of checking for excluded parties. The letters provide guidance on where to check for excluded individuals as well as the consequences of contracting with individuals and entities that have been excluded from participating in federally funded programs.
5
Companies are also required to notify to the Department of Health and Human Services-Office of Inspector General (HHS-OIG) of any action it takes to limit the ability of an individual or entity to participate in its program as stated in 42 CFR 1002.3.
Each contracted company must report actions it takes when it denies a provider enrollment based on program integrity concerns. Companies should report on each provider whom it has disenrolled, suspended, terminated or otherwise restricted from participation in the Medicaid program based on program integrity concerns. Companies are required to report affected providers directly to HHS-OIG while copying ASES.
6
Definitions
Abuse means provider practices that are inconsistent with sound fiscal, business, or medical practices, and result in an unnecessary cost to the Medicaid program, or in reimbursement for services that are not medically necessary or that fail to meet professionally recognized standards for health care. It also includes recipient practices that result in unnecessary cost to the Medicaid program.
Agent means any person who has been delegated the authority to obligate or act on behalf of a provider
Conviction or Convicted means that a judgment of conviction has been entered by a Federal, State, or local court, regardless of whether an appeal from that judgment is pending.
Disclosing Entity means a Medicaid provider (other than an individual practitioner or group of practitioners) or a fiscal agent
Exclusion means that items or services furnished by a specific provider who has defrauded or abused the Medicaid program will not be reimbursed under Medicaid.
Fiscal agent means a contractor that processes or pays vendor claims on behalf of the Medicaid agency.
Fraud means an intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit for him/her or some other person. It includes any act that constitutes fraud under applicable Federal or State law.
Furnished refers to items and services provided directly by, or under the direct supervision of, or ordered by, a practitioner or other individual (either as an employee or in his or her own capacity), a provider, or other supplier of services. (For purposes of denial of reimbursement within this part, it does not refer to services ordered by one party but billed for and provided by or under the supervision of another.)
Group of practitioners means two or more health care practitioners who practice their profession at a common location (whether or not they share common facilities, common supporting staff, or common equipment).
Health insuring organization (HIO) has the meaning specified in §438.2.
Indirect ownership interest means an ownership interest in an entity that has an ownership interest in the disclosing entity. This term includes an ownership interest in any entity that has an indirect ownership interest in the disclosing entity.
7
Managing employee means a general manager, business manager, administrator, director, or other individual who exercises operational or managerial control over, or who directly or indirectly conducts the day-to-day operation of an institution, organization, or agency.
Other disclosing entity means any other Medicaid disclosing entity and any entity that does not participate in Medicaid, but is required to disclose certain ownership and control information because of participation in any of the programs established under title V, XVIII, or XX of the Act. This includes:
(a) Any hospital, skilled nursing facility, home health agency, independent clinical laboratory, renal disease facility, rural health clinic, or health maintenance organization that participates in Medicare (title XVIII);
(b) Any Medicare intermediary or carrier; and
(c) Any entity (other than an individual practitioner or group of practitioners) that furnishes, or arranges for the furnishing of, health-related services for which it claims payment under any plan or program established under title V or title XX of the Act.
Person with an ownership or control interest means a person or corporation that—
(a) Has an ownership interest totaling 5 percent or more in a disclosing entity;
(b) Has an indirect ownership interest equal to 5 percent or more in a disclosing entity;
(c) Has a combination of direct and indirect ownership interests equal to 5 percent or more in a disclosing entity;
(d) Owns an interest of 5 percent or more in any mortgage, deed of trust, note, or other obligation secured by the disclosing entity if that interest equals at least 5 percent of the value of the property or assets of the disclosing entity;
(e) Is an officer or director of a disclosing entity that is organized as a corporation; or
(f) Is a partner in a disclosing entity that is organized as a partnership.
Practitioner means a physician or other individual licensed under State law to practice his or her profession.
Program Integrity Plan (PIP) means the program, process or policy that each contracted company has to comply with integrity requirements. The plan should be developed in accordance with federal regulation.
8
Significant business transaction means any business transaction or series of transactions that, during any one fiscal year, exceed the lesser of $25,000 and 5 percent of a provider’s total operating expenses.
Subcontractor means—
(a) An individual, agency, or organization to which a disclosing entity has contracted or delegated some of its management functions or responsibilities of providing medical care to its patients; or
(b) An individual, agency, or organization with which a fiscal agent has entered into a contract, agreement, purchase order, or lease (or leases of real property) to obtain space, supplies, equipment, or services provided under the Medicaid agreement.
Supplier means an individual, agency, or organization from which a provider purchases goods and services used in carrying out its responsibilities under Medicaid (e.g., a commercial laundry, a manufacturer of hospital beds, or a pharmaceutical firm).
Stakeholder means the single state agency, the sub-grantee and all organizations contracted to provide health care management and services to Medicaid beneficiaries
Suspension means that items or services furnished by a specified provider who has been convicted of a program-related offense in a Federal, State, or local court will not be reimbursed under Medicaid.
Termination means—
(1) For a—
(i) Medicaid or CHIP provider, a State Medicaid program or CHIP has taken an action to revoke the provider’s billing privileges, and the provider has exhausted all applicable appeal rights or the timeline for appeal has expired; and
(ii) Medicare provider, supplier or eligible professional, the Medicare program has revoked the provider or supplier’s billing privileges, and the provider has exhausted all applicable appeal rights or the timeline for appeal has expired.
(2)(i) In all three programs, there is no expectation on the part of the provider or supplier or the State or Medicare program that the revocation is temporary.
(ii) The provider, supplier, or eligible professional will be required to reenroll with the applicable program if they wish billing privileges to be reinstated.
(3) The requirement for termination applies in cases where providers, suppliers, or eligible professionals were terminated or had their billing privileges revoked for cause which may include, but is not limited to—
9
(i) Fraud;
(ii) Integrity; or
(iii) Quality.
Wholly owned supplier means a supplier whose total ownership interest is held by a provider or by a person, persons, or other entity with an ownership or control interest in a provider
10
Section A
Fraud Detection and Investigation sub part represents each one of the elements that must be included as part of the integrity program activities, although they are not necessarily the only elements that come into play.
All contracted plans must have an integrity program with their own structure, policies and procedures. Among other areas, they should have written policies and procedures on methods for the identification, investigation and referral of suspected cases; procedure to perform preliminary investigations as well as full investigations; procedures to address resolution of full investigations; procedures to comply with reporting requirements; provider’s statements on claims form (if applicable); provider’s statement on checks; cooperation with the Commonwealth of Puerto Rico Office for the Medically Indigent fraud control unit and procedure to withhold payments in case of fraud or willful misrepresentation. Contracted companies are required to submit to ASES Compliance Office copy of their integrity programs for evaluation. The plan should be developed in accordance with 42 CFR 438.608.
Each one of the Guidelines under section A includes the name or title of the guideline, scope, purpose, process and general information to identify the creation date, creator, and revisions or updates. This document will be attached to the contract each organization holds with the Puerto Rico Insurance Administration; while each one of the contracted organization should have at least a minimum set of policies and procedures to address the guidelines included.
The Program Integrity Plan (PIP) of each organization is to be monitored by the sub-grantee on periodic basis. An annual report will be issued reporting data and findings.
11
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA1.1 | State Plan Requirements | |
| Scope | Applies to Single State Agency and Sub-Grantee | |
| Purpose | This guideline describes the commitment of the single state agency and the sub-grantee in adhering to the statue rules and regulations and the implementation of a Program Integrity Plan for the Medicaid Program | |
| General | The grantee and the sub-grantee will abide bye the following guidelines on how to manage the integrity program activities in the whole service delivery system. | |
| Guidelines | 1. The single state agency and sub-grantee acknowledge the need to adhere to a Medicaid Integrity Program as defined in the state plan. 2. The grantee and sub-grantee agree to establish a structure to manage Program Integrity Plan (PIP) activities. 3. The organization structure to perform above mentioned activities is furnished with a Program Integrity Plan (PIP) of members representing the single state agency, the sub-grantee and each contracted organization. 4. The PIP leads the efforts toward achieving compliance with state plan requirements regulation by establishing the minimum criteria of required PI program policies and procedures. 5. The PIP monitors contracted companies plan compliance on regular basis. 6. The PIP chairman develops the meeting calendar each year, develops the committee agenda, and keeps minutes of all meetings and call for meetings. 7. Sub-grantee facilitates the development and update of the Program Integrity Plan guidelines, reports and notification to guarantees its distribution and final acceptance among contracted companies and regulatory agencies. 8. Sub-grantee review performance of each organization, level of adherence to policies and recommend corrective action plan development for areas that must be improved. 9. Sub-grantee develops an annual report that is to be submitted to the Medicaid Program Integrity Group and to the CMS region 2. The report will include the areas and companies reviewed during the period and the findings of each company, if any. 10. The PIP provides guidance and guarantees that each contracted companies develop and implement policies and procedures in their organizations. 11. The PIP guidelines are integrated into each contracted organization Program Integrity Plan Policies and Procedures; and are assumed as a standard operating procedure to prevent fraud, waste and abuse in the management of Medicaid funds and health plan benefit coverage for the indigent population. |
12
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA02.1 | Methods for identification, investigation, and referral | |
| Scope | Grantee, Sub-grantee and Contracted Organizations | |
| Purpose | This guide describes what the organization must include in their PIP to guarantee the use of methods for the identification, investigation, and referral of suspected fraud and abuse cases. | |
| General | The organization must establish methods for the identification, investigation and referral of suspected cases, that guarantees the use of a consistent and objective approach to address fraud, waste and abuse when performing PIP activities. | |
| Guidelines | The PIP must include an explicit definition of methods to perform identification of cases suspected of fraud, waste and abuse a. what is fraud, waste and abuse b. how is detected fraud, waste and abuse c. who performs the identification d. when preliminary, full investigation and resolutions are done
The PIP must have a detailed process to perform investigations on each suspected case guaranteeing objective methods to identify potential cases and perform investigations a. open and documents the case b. initiate data gathering process c. follow a protocol to verify information d. issue a report of findings e. refer case to next level f. close the case
The PIP must include a variety of methods for the identification, investigation and referral of suspected cases, accepted in the industry and without infringing provider or beneficiary rights. Methods might include a. electronic data exchanges b. data mining c. claims registries / reconciliation d. targeted procedures e. profiling
The PIP must include a systematic approach of data analysis by: a. flagging the case b. identifying cause for flagging (i.e. over-under payment) c. establishing actions and sanctions
The PIP must have procedures in placed for referring suspect fraud cases to law enforcement officials, at a minimum: |
13
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Guidelines | a. an organizational structure to address the reports. b. a due process that includes but is not limited to: case identification, complete record with supporting materials, notification letter to suspect, notification letter to single state agency, documentation of entrance and exit interviews, and if necessary copy of referral letters and case resolution letter to and from legal authorities. c. a flowchart to work in cooperation with the grantee and sub-grantee as well as with the state legal authorities such as: Organization’s Legal Affairs Department, ASES, Single State Agency – Department of Health Legal Department, State Department of Justice, and the Office of Inspector General. d. a follow up process to work with legal authorities each case of fraud, waste and abuse suspicion until final disposition and notification to the single state agency.
|
14
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA03 | Preliminary Investigations | |
| Scope | Grantee, Sub-grantee and Contracted Organizations | |
| Purpose | To provide guidance on how to perform a preliminary investigation when the agency receives a complaint of fraud or abuse from any source or identifies any questionable practices. | |
| General | The organization must conduct a preliminary investigation to determine whether there is sufficient basis to warrant a full investigation. | |
| Guidelines | The PIP defines a standard operating procedure to complete a preliminary investigation of all suspect cases of fraud, waste and abuse.
The PIP identifies the requirements to complete the preliminary investigation when evaluating providers and beneficiaries. It should include at least: a. Source of information b. Identification method (how the case is detected) c. Cause for investigation d. Case documentation e. Analysis of Data and documents f. Report of Findings g. Action Taken (Recommended Action)
The PIP includes a mechanism to keep tracking of all preliminary investigations and results.
The PIP establishes a mechanism to report preliminary investigations activity to the sub-grantee (ASES) which will be in charge of reporting activity to the single state agency (Office for the Medically Indigent). |
15
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA04 | Full Investigations | |
| Scope | Grantee, Sub-grantee and Contracted Organizations | |
| Purpose | To provide guidance and minimum set of elements in the PIP to perform full investigations on incidents of fraud and abuse. | |
| General | If the findings of a preliminary investigation give the agency reason to believe that an incident of fraud or abuse has occur in the Medicaid program, the organization must take the appropriate actions. | |
| Guidelines | The PIP must define the process to conduct a full investigation and specify when a case requires the full investigation. Full investigations must be done in accordance with federal regulation and based in the company written policy. The company must submit copy of the written policies to ASES for review and approval.
The PIP must define the process to refer the cases to the companies fraud liaison (i.e. companies compliance office), the appropriate law enforcement agency / sub-grantee when there is a reason: a. to suspect a provider has engaged in fraud or abuse of the program. b. to suspect a recipient is defrauding the program. c. to suspect a recipient has abused the Medicaid program.
The PIP must have a mechanism to keep tracking of all full investigations performed in progress and closed.
The PIP must have a mechanism to report the sub-grantee (ASES) informed full investigations in progress, conducted and results. |
16
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA05 | Resolution of full investigation | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide guidance on minimum actions that must be taken in order to complete the process of a full investigation. | |
| General | The full investigations must continue until the cases are referred, solved or closed. | |
| Guidelines | The PIP must include the process to guarantee that a full investigation must continue until: a. appropriate legal action is initiated. b. the case is closed or dropped because of insufficient evidence to support the allegations of fraud or abuse. c. the matter is resolved between the organization and the provider or recipient ü the resolution may include but is not limited to: 1) Sending a warning letter to the provider or recipient, giving notice that continuation of the activity in question will result in further action; 2) Suspending or terminating the provider from participation in the Medicaid program; 3) Seeking recovery of payments made to the provider; or 4) Imposing other sanctions provided under the organization PIP plan.
The PIP must guarantee that there is a mechanism to keep tracking of all full investigations until resolution. |
17
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA06 | Reporting Requirements | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide guidance on how to adhere to a minimum set of elements that must be included in the process to report fraud and abuse information to the appropriate organizations officials. | |
| General | The organization must submit a progress report the fraud and abuse information and statistics to the appropriate department / grantee / sub-grantee on quarterly basis. | |
| Guidelines | The PIP must describe the mechanism to report fraud and abuse data to the appropriate fraud liaison, organization structure, sub-grantee (ASES) and grantee (Office for the Medically Indigent).
The PIP progress report must include at least the following information: a. # of complaints on fraud and abuse received. b. # of complaints that warrant preliminary investigation. c. Detailed information for each case of suspected provider fraud and abuse that warrants a full investigation: ü Provider’s name and id number ü Source of the complaint ü Type of the provider ü Nature of the complaint ü Estimate amount of money involved ü Legal and administrative disposition of the case and actions taken by the law enforcement officials to whom the case has been referred.
Suspected fraud cases must be reported immediately in a written format to ASES Compliance Office.
The PIP reports must be submitted in electronic format to facilitate its inclusion in the Commonwealth of Puerto Rico Medicaid Program PI Annual Report. |
18
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA07 | Provider’s statements on claims forms | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide guidance on how to comply with regulation on provider’s statements on claims forms. | |
| General | The organization may print that all provider claims forms be imprinted in boldface type with the following statement, or with alternate wording that is approved by the Regional CMS Administration. | |
| Guidelines | The PIP must include that providers are required to attest in the claim forms that they agree with the following statement: | |
| ü “This is to certify that the foregoing information is true accurate and complete”. | ||
| ü “I understand that payment of this claim will be from federal and state funds and that any falsification or concealment of a material fact maybe prosecutes under federal and state laws”. | ||
| For electronic claims, providers must attest that they agree with the following statements: | ||
| ü “This is to certify the truthfulness of the foregoing information and certify that is true, accurate, complete and that the service was provided”. | ||
| The statements may be printed above the claimant’s signature or, if they are printed on the revenue of the form, a reference to the statements must appear immediately preceding the claimant’s signature.
| ||
19
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA08 | Provider’s statements on check | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide guidance on how to comply with regulation on provider’s statements on check. | |
| General | The organization may print the following wording above the claimant’s endorsement on the reverse of checks or warrants payable to each provider. | |
| Guidelines | The PIP must include that providers are required to attest (in addition to the statements required in providers claims form) that they agree with the following statement either by having it written on checks or temporarily in a legal document as an affidavit:
ü “I understand in endorsing or depositing this check that payment will be from Federal and State funds and that any falsification, or concealment of a material fact, may be prosecuted under Federal and State laws”.
The above attestation must be included in electronic and checks payment.
The PIP must indicate frequency and responsible for conducting spot checks to guarantee the organization complies with the provider’s statements and / or the provider signature appears on a legal document attesting compliance. |
20
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA09 | Recipient verification procedure | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To verify that the services listed on claims forms have been rendered. | |
| General | The organization must have a method for verifying with recipients whether services billed by providers were received. | |
| Guidelines | The PIP must include a description of how the organization performs claims matches with medical records to guarantee adequacy of billing.
The PIP must define the mechanism to monitor frequency of encounters and services rendered to patients billed by providers.
The PIP will provide periodic up dates on reconciliation findings report to the sub-grantee and grantee.
The sub-grantee will select a sample to perform independent reviews to verify that recipient’s services billed by providers (as well as encounters under capitated environment) were indeed rendered. This review will be performed through confirmations to beneficiaries. |
Note: All contracted companies are required to comply with Law 114 which require that the beneficiaries must receive an Evidence of Medical Benefits with a detailed of the services and expenses incurred during a quarter. ASES compliance office will review the compliance with the Law.
21
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA10 | Cooperation with Medicaid Fraud Control Units | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide guidance on how to communicate findings and to cooperate with any Puerto Rico or federal law enforcement agency. To request that all contracted companies must communicate preliminary findings to ASES. | |
| General | The organization must have a mechanism to provide information to the regulatory and legal authorities on cases, investigations, schemes and any other activity where intention to commit fraud, abuse and waste of services occur. | |
| Guidelines | The PIP must demonstrate it has an effective mechanism to cooperate with the Medicaid anti fraud unit as well as with other program divisions in charge of preventing and prosecuting cases related to fraud, waste and abuse of services under the Medicaid program.
The PIP must establish a process to guarantee the organization complies with the following:
ü All cases of suspected provider fraud are referred to the anti fraud / integrity organization’s unit. ü If the anti fraud / integrity unit determines that it may be useful in carrying out the unit’s responsibilities, promptly comply with a request from the unit for -- i. Access to, and free copies of, any records or information kept by the organization or its contractors; ii. Computerized data stored by the organization or its contractors. These data must be supplied without charge and in the form requested by the unit; iii. Access to any information kept by providers to which the organization is authorized access. In using this information, the unit must protect the privacy rights of recipients; ü Communicate to ASES preliminary findings; and ü On referral from the unit, coordinate with ASES or appropriate law enforcement agency before initiating any available administrative or judicial action to recover improper payments to a provider.
The PIP must recommend the organization to have in the provider’s contract a disclaimer that as a contracted provider any data related to services or payments provided must be available for review of the integrity staff. |
22
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA11 | Withholding of payments in cases of fraud or willful misrepresentations | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide guidance on elements to be considered when withholding of payments to providers who committed fraud or willful misrepresentation. | |
| General | The organization should consider withholding payments to providers as a mechanism to prevent wrong disbursement of payments when suspect of fraud. | |
| Guidelines | The PIP will establish a mechanism and adhere to the following recommendations when considering withholding of payments: (a) Basis for withholding. The organization may withhold capitation or claims payments, in whole or in part, to a provider upon receipt of reliable evidence that the circumstances giving rise to the need for a withholding of payments involve fraud or willful misrepresentation under the Medicaid program. The organization may withhold payments without first notifying the provider of its intention to withhold such payments. A provider may request, and must be granted, administrative review where State law so requires. (b) Notice of withholding. The organization must send notice of its withholding of program payments within 5 days of taking such action. The notice must set forth the general allegations as to the nature of the withholding action, but need not disclose any specific information concerning its ongoing investigation. The notice must: ü State that payments are being withheld in accordance with this provision; ü State that the withholding is for a temporary period, and cite the circumstances under which withholding will be terminated; ü Specify, when appropriate, to which type or types of payment (capitation or claims) withholding is effective; and ü Inform the provider of the right to submit written evidence for consideration bye the agency. (c) Duration of withholding. All withholding of payment actions under this section will be temporary and will not continue after: ü The agency or the prosecuting authorities determine that there is insufficient evidence of fraud or willful misrepresentation bye the provider; or ü Legal proceedings related to the provider’s alleged fraud or willful misrepresentations are completed. |
23
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA12 | Disclosure of Information by Providers and Fiscal Agents | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide definition of concepts in order to fully adhere to the regulation on providers control and ownership of facilities. | |
| General | The organization must adhere to standard definitions when dealing with disclosure of information by providers and fiscal agents when establishing mechanism to regulate providers control and ownership of facilities. | |
| Guidelines | The PIP will adhere to the following definitions of concepts to keep consistency with federal regulation and application of law:
Agent means any person who has been delegated the authority to obligate or act on behalf of a provider.
Disclosing entity means a Medicaid provider (other than an individual practitioner or group of practitioners), or a fiscal agent.
Other disclosing entity means any other Medicaid disclosing entity and any entity that does not participate in Medicaid, but is required to disclose certain ownership and control information because of participation in any of the federal programs (Medicaid, SCHIP, FQHC’s). This includes:
(a) Any hospital, skilled nursing facility, home health agency, independent clinical laboratory, renal disease facility, rural health clinic, or health maintenance organization that participates in Medicare (title XVIII); (b) Any Medicare intermediary or carrier; and (c) Any entity (other than an individual practitioner or group of practitioners) that furnishes, or arranges for the furnishing of, health- related services for which it claims payment under any plan or program established under title V or title XX of the Act.
Fiscal agent means a contractor that processes or pays vendor claims on behalf of the Medicaid agency.
Group of practitioners means two or more health care practitioners who practice their profession at a common location (whether or not they share common facilities, common supporting staff, or common equipment).
Indirect ownership interest means an ownership interest in an entity that has an ownership interest in the disclosing entity. This term includes an ownership interest in any entity that has an indirect ownership interest in the disclosing entity. |
24
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Guideline | Managing employee means a general manager, business manager, administrator, director, or other individual who exercises operational or managerial control over, or who directly or indirectly conducts the day-to-day operation of an institution, organization, or agency. | |
| Ownership interest means the possession of equity in the capital, the stock, or the profits of the disclosing entity. | ||
| Person with an ownership or control interest means a person or corporation that – | ||
| (a) Has an ownership interest totaling 5 percent or more in a disclosing entity; | ||
| (b) Has an indirect ownership interest equal to 5 percent or more in a disclosing entity; | ||
| (c) Has a combination of direct and indirect ownership interests equal to 5 percent or more in a disclosing entity; | ||
| (d) Owns an interest of 5 percent or more in any mortgage, deed of trust, note, or other obligation secured bye the disclosing entity if that interest equals at least 5 percent of the value of the property or assets of the disclosing entity; | ||
| (e) Is an officer or director of a disclosing entity that is organized as a corporation; or | ||
| (f) Is a partner in a disclosing entity that is organized as a partnership. | ||
| Significant business transaction means any business transaction or series of transactions that, during any one fiscal year, exceed the lesser of $25,000 and 5 percent of a provider’s total operating expenses. | ||
| Subcontractor means – | ||
| (a) An individual, agency or organization to which a disclosing entity has contracted or delegated some of its management functions or responsibilities of providing medical care to its patients; or | ||
| (b) An individual, agency, or organization with which a fiscal agent has entered into a contract, agreement, purchase order, or lease (or leases of real property) to obtain space, supplies, equipment, or services provided under the Medicaid agreement. | ||
| Supplier means an individual, agency or organization from which a provider purchases goods and services used in carrying out its responsibilities under Medicaid (e.g., a commercial laundry, a manufacturer of hospital beds, or a pharmaceutical firm). | ||
25
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Guideline | Wholly owned supplier means a supplier whose total ownership interest is held by a provider or by a person, persons, or other entity with an ownership or control interest in a provider. |
26
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA13 | Disclosure by disclosing entities: Information on ownership and control. | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide guidelines on what information must be disclosed by entities that have ownership and control over facilities. | |
| General | The organization must have a mechanism to monitor on a timely manner the providers and fiscal agents that owns or control facilities where Medicaid beneficiaries receive services. | |
| Guidelines | The PIP must require each disclosing entity to disclose the following information in a timely manner: | |
| (a) Type of Information that must be disclosed. | ||
| ü The name and address of each person with an ownership or control interest in the disclosing entity or in any subcontractor in which the disclosing entity has direct or indirect ownership of 5 percent or more; | ||
| ü Whether any of the persons named is related to another as spouse, parent, child, or sibling. ü The name of any other disclosing entity in which a person with an ownership or control interest in the disclosing entity also has an ownership or control interest. This requirement applies to the extent that the disclosing entity can obtain this information by requesting it in writing from the person. The disclosing entity must – | ||
| (i) Keep copies of all these requests and the responses to them; | ||
| (ii) Make them available to the Secretary or the Medicaid agency upon request; and | ||
| (iii) Advise the Medicaid agency when there is no response to a request. | ||
| (b) Time and manner of disclosure. | ||
| ü Any disclosing entity that is subject to periodic survey and certification of its compliance with Medicaid standards must supply the information specified to the organization. | ||
| ü Any disclosing entity that is not subject to periodic survey and certification and has not supplied the information specified. | ||
| Updated information must be furnished to the Secretary or the State survey or Medicaid agency at intervals between recertification or contract renewals, within 35 days of a written request. |
27
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Guidelines | (c) Provider agreements and fiscal agent contracts. The organization shall not approve a provider agreement or a contract with a fiscal agent, and must terminate an existing agreement or contract, if the provider or fiscal agent fails to disclose ownership or control information as required by this section. | |
|
The PIP will include the process to provide an annual report to the grantee and sub-grantee on above information and data. |
28
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA14 | Disclosure by providers: Information related to business transactions. | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | The organization must establish a mechanism to facilitate the providers disclose information related to their business transactions when own or control facilities where Medicaid beneficiaries received services. | |
| Guidelines | The PIP must describe the mechanism to allow providers owning or controlling facilities disclose information related to business transactions.
The PIP must attest the organization abide by the following regulation:
(a) Provider agreements. The organization must enter into an agreement with each provider or provider group under which the provider agrees to furnish to it or to the grantee / sub-grantee on request, information related to business transactions. (b) Information that must be submitted. A provider must submit, within 35 days of the date on a request by the organization full and complete information about – ü The ownership of any subcontractor with whom the provider has had business transactions totaling more than $25,000 during the 12-month period ending on the date of the request; and ü Any significant business transactions between the provider and any wholly owned supplier, or between the provider and any subcontractor, during the 5-year period ending on the date of the request.
The PIP must include withholding of payment processes and procedures to enforce above guideline. |
29
Commonwealth of Puerto Rico
Program Integrity Plan 2011 - 2013
| Title SA15 | Disclosure by providers: Information on persons convicted of crimes | |
| Scope | Grantee, Sub-Grantee and Contracted Organizations | |
| Purpose | To provide guidance on type of information providers must report in compliance with integrity program. | |
| General | The organization is obliged to request providers to report any conviction of crimes or any other in the program integrity regulation. | |
| Guidelines | The PIP must include a mechanism to confirm information included below is considered as part of the integrity activities.
(c) Information that must be disclosed. Before the organization enters into or renews a provider agreement, or at any time upon written request by the organization, the provider must disclose to the organization the identity of any person who: (1) Has ownership or control interest in the provider, or is an agent or managing employee of the provider; and (2) Has been convicted of a criminal offense related to that person’s involvement in any program under Medicare, Medicaid, or the title XX services program since the inception of those programs. (b) Notification to Inspector General. (1) The organization must notify the Inspector General of the Department of any disclosures made under paragraph (a) of this section within 20 working days from the date it receives the information. (2) The organization must also promptly notify the Inspector General of the Department of any action it takes on the provider’s application for participation in the program. (c) Denial or termination of provider participation. (1) The organization may refuse to enter into or renew an agreement with a provider if any person who has an ownership or control interest in the provider, or who is an agent or managing employee of the provider, has been convicted of a criminal offense related to that person’s involvement in any program established under Medicare, Medicaid or the title XX Services Program. (2) The organization may refuse to enter into or may terminate a provider agreement if it determines that the provider did not fully and accurately make any disclosure required under paragraph (a) of this section. | |
|
|
| |||
| Miguel Negron Rivera | Frank R. Diaz Gines | |||
| Executive Director of Medicaid Puerto Rico Department of Health |
Executive Director PR Health Insurance Administration |
30
ATTACHMENT 15
ELECTRONIC HEALTH RECORD SPECIFICATIONS
| 1. | Overview: Primary Care Physicians (PCPs) and physician specialists within the Preferred Provider Network (PPN) shall have an operational Electronic Health Record (“EHR”) system in their practice in place on or before July 1, 2012. The EHR system must be certified by (i) an Office of the National Coordinator Authorized Testing and Certification Body (“OCN-ATCB”) and (ii) the Certification Commission for Healthcare Information Technology (“CCHIT”) to participate in the MiSalud Program. The purpose of implementing an EHR is to: (i) become a Meaningful User of Health Information Technology (HIT); (ii) improve quality of care; (iii) maximize cost-efficiency; (iv) connect with a Health Information Exchange (“HIE”) hub; and (v) allow patients to access their personal health information through a mechanism such as a Personal Health Record (PHR). |
| 2. | EHR System Specifications: To comply with technological as well as MiSalud model of care requirements, the EHR system shall: |
| 2.1. | Be certified by an ONC-ATCB |
| 2.2. | Be certified by the CCHIT |
| 2.3. | Be capable to perform SureScripts-certified ePrescribing |
| 2.4. | Be supported by one of the major drug-databases such as: |
2.4.1.1. First DataBank;
2.4.1.2. MediSpan; or
2.4.1.3. Multum.
| 2.5. | Provide for ePrescribing Clinical Decision Support (“CDS”) interaction checks. |
| 2.6. | Meet federal meaningful use objectives and measures in force at any given time. For example, during stage 1, must implement, at minimum, the capacity to detect drug-drug and drug-allergy interactions, as well as drug-formulary checks. |
| 2.7. | Support applicable (according to practice) federally mandated transactions and code-sets standards, as follows: |
2.7.1. Transactions CCD, CDA, HL7, X12, NCPDP, and others.
2.7.2. Code-Sets ICD, CPT, HCPCS, NDC, CDT, LOINC, and SNOMED.
| 2.8. | Be certified by, and connected to, the Puerto Rico Health Information Network (“PRHIN”), the ONC-supported and the state-designated entity or organization for HIE, as its services are made available. The EHR system must also be able to connect to other alternative hubs and be capable of reading and importing CCD files. |
| 2.9. | Support compliance and reporting of CMS quality measures. |
| 2.10. | Provide electronic copy of health information or clinical summaries to patients and other providers. |
| 2.11. | Support electronic submittal of public health and/or reportable-disease/conditions data as these capabilities are made available in Puerto Rico. |
| 2.12. | Be capable of quality monitoring. |
| 2.13. | Be capable of prospective-preventive services management. |
| 2.14. | Have mental and physical health integration capabilities. |
| 2.15. | Have screening capabilities according to age group, gender and risks factors. |
| 2.16. | Have an EPSDT prospective tracking system. |
| 2.17. | Have the capacity to register members on Special Coverage. |
| 2.18. | Have the capacity to generate an electronic referral. |
| 2.19. | Have the capacity to update MiSalud’s drug formulary |
| 2.20. | Provide electronic referral to the Contractor’s clinical programs |
| 2.21. | Document Enrollee’s Advance Directives preferences |
| 2.22. | Document Enrollee’s moral or religious objections |
| 2.23. | Generate a Prior Authorization request to the Contractor |
| 2.24. | Provide access to a Network Provider’s education module |
| 3. | Contractor’s Certification Program: The Contractor will develop and implement a Certification Program for Electronic Medical Records (“EMR”) with technological requirements as well as MiSalud model of care requirements. Compliance with the established requirements will be taken into consideration to determine PCP qualification for the Physician Incentive Plan, as defined in Section 10.7 of the Contract. |
ATTACHMENT 17
LIST OF SUBCONTRACTORS
| 1. | Jaye, Inc. |
| 2. | McKesson Health Solutions |
| 3. | Mercer Oliver Wyman Actuarial Consulting, Inc. |
| 4. | Uticorp |
| 5. | VIPS Healthcare Information Solutions |
| 6. | Telemedik |
Rev. 10.17.2011