Attached files
| file | filename |
|---|---|
| EX-32.2 - RHB 10K2009 EXHIBIT 32.2 - REHABCARE GROUP INC | tenk2009ex322.htm |
| EX-31.2 - RHB 10K2009 EXHIBIT 31.2 - REHABCARE GROUP INC | tenk2009ex312.htm |
| EX-21.1 - RHB 10K2009 EXHIBIT 21.1 - REHABCARE GROUP INC | tenk2009ex211.htm |
| EX-23.1 - RHB 10K2009 EXHIBIT 23.1 - REHABCARE GROUP INC | tenk2009ex231.htm |
| EX-32.1 - RHB 10K2009 EXHIBIT 32.1 - REHABCARE GROUP INC | tenk2009ex321.htm |
| EX-31.1 - RHB 10K2009 EXHIBIT 31.1 - REHABCARE GROUP INC | tenk2009ex311.htm |
UNITED
STATES
SECURITIES
AND EXCHANGE COMMISSION
Washington,
D.C. 20549
FORM
10-K
Annual
Report Pursuant to Section 13 or 15(d) of the Securities Exchange Act of
1934
for the fiscal year ended December 31,
2009
Commission
file number 001-14655
RehabCare Group,
Inc.
(Exact name of registrant as specified
in its charter)
|
Delaware
|
51-0265872
|
||
|
(State
of Incorporation)
|
(I.R.S.
Employer Identification No.)
|
7733
Forsyth Boulevard, 23rd Floor, St. Louis, Missouri 63105
(Address
of principal executive offices and zip code)
Registrant’s
telephone number, including area code: (800)
677-1238
|
Securities
registered pursuant to Section 12(b) of the Act:
|
Name
of exchange on which registered:
|
|
|
Common
Stock, par value $.01 per share
|
New
York Stock Exchange
|
|
|
Preferred
Stock Purchase Rights
|
New
York Stock Exchange
|
Indicate
by check mark whether the registrant is a well-known seasoned issuer, as defined
in Rule 405 of the Securities Act. Yes o No x
Indicate
by check mark if the registrant is not required to file reports pursuant to
Section 13 or Section 15(d) of the Act.
Yes o No x
Indicate
by check mark whether the registrant (1) has filed all reports required to
be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934
during the preceding 12 months, and (2) has been subject to such
filing requirements for the past
90 days. Yes x No o
Indicate
by check mark whether the registrant has submitted electronically and posted on
its corporate Web site every Interactive Data File required to be submitted and
posted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or
for such shorter period that the registrant was required to submit and post such
files). Yes o No o
Indicate
by check mark if disclosure of delinquent filers pursuant to Item 405 of
Regulation S-K is not contained herein, and will not be contained, to the best
of registrant’s knowledge, in definitive proxy or information statements
incorporated by reference in Part III of this Form 10-K or any amendment to this
Form 10-K.
x
Indicate
by a check mark whether the registrant is a large accelerated filer, an
accelerated filer, a non-accelerated filer, or a smaller reporting company (as
defined in Rule 12b-2 of the Exchange Act).
Large accelerated
filer o Accelerated
filer x
Non-accelerated
filer o Smaller
reporting company o
Indicate
by check mark whether the registrant is a shell company (as defined in
Rule 12b-2 of the Act). Yes o No
x
The
aggregate market value of the common stock held by non-affiliates of the
registrant at June 30, 2009 was approximately $427 million based on the closing
price of the stock on that day. At February 28, 2010, the
registrant had 24,635,959 shares of Common Stock outstanding, including unvested
restricted stock.
DOCUMENTS
INCORPORATED BY REFERENCE
Portions
of the registrant’s Proxy Statement for the 2010 annual meeting of stockholders
are incorporated by reference in Part III of this Annual Report.
- 1
-
TABLE
OF CONTENTS
|
PART
I
|
|
|
Item
1.
|
Business
|
|
Item
1A.
|
Risk
Factors
|
|
Item
1B.
|
Unresolved
Staff Comments
|
|
Item
2.
|
Properties
|
|
Item
3.
|
Legal
Proceedings
|
|
Item
4.
|
Submission
of Matters to a Vote of Security Holders
|
|
PART
II
|
|
|
Item
5.
|
Market
for Registrant’s Common Stock, Related Stockholder Matters and Issuer
Purchases of Equity Securities
|
|
Item
6.
|
Selected
Financial Data
|
|
Item
7.
|
Management’s
Discussion and Analysis of Financial Condition and Results of
Operations
|
|
Item
7A.
|
Quantitative
and Qualitative Disclosures About Market Risk
|
|
Item
8.
|
Financial
Statements and Supplementary Data
|
|
Item
9.
|
Changes
in and Disagreements with Accountants on Accounting and Financial
Disclosure
|
|
Item
9A.
|
Controls
and Procedures
|
|
Item
9B.
|
Other
Information
|
|
PART
III
|
|
|
Item
10.
|
Directors,
Executive Officers and Corporate Governance
|
|
Item
11.
|
Executive
Compensation
|
|
Item
12.
|
Security
Ownership of Certain Beneficial Owners and Management and Related
Stockholder Matters
|
|
Item
13.
|
Certain
Relationships and Related Transactions, and Director
Independence
|
|
Item
14.
|
Principal
Accounting Fees and Services
|
|
PART
IV
|
|
|
Item
15.
|
Exhibits
and Financial Statement Schedules
|
- 2
-
PART
I
ITEM
1. BUSINESS
The terms
“RehabCare,” “our company,” “we” and “our” as used herein refer to RehabCare
Group, Inc. and its subsidiaries.
Overview
of Our Company
RehabCare
Group, Inc., a Delaware corporation, headquartered in St. Louis, Missouri, is a
leading provider of rehabilitation program management services in more than
1,200 hospitals, skilled nursing facilities, outpatient facilities and other
long-term care facilities located in 41 states. We also own and
operate 28 long-term acute care hospitals (“LTACHs”) and 6 rehabilitation
hospitals. These hospitals provide total medical care to patients
with medically complex diagnoses and to patients in need of
rehabilitation.
Established
in 1982, we have more than 25 years of experience helping healthcare providers
grow and become more efficient while effectively and compassionately delivering
rehabilitation services to patients. In partnership with healthcare
providers, we provide post-acute program management, medical direction, physical
therapy rehabilitation, quality assurance, compliance review, specialty programs
and census development services. We believe our clients place a high
value on our extensive experience in assisting them to implement clinical best
practices, to address competition for patient services, and to navigate the
complexities inherent in managed care contracting and government reimbursement
systems. Over the years, we have diversified our program management services to
include management services for inpatient rehabilitation facilities within
hospitals, skilled nursing units, outpatient rehabilitation programs, home
health, and skilled nursing, long-term care and assisted living
facilities.
Effective
November 24, 2009, we acquired all of the outstanding common stock of Triumph
HealthCare Holdings, Inc. (“Triumph”) for a purchase price of approximately
$538.5 million. On the acquisition date, Triumph operated 20 LTACHs
in seven states. In 2009, we also acquired LTACHs in Dallas, Texas
and Philadelphia, Pennsylvania and opened a majority-owned LTACH in Peoria,
Illinois. These activities expanded the number of LTACHs we own and
operate to 28, making us the third largest LTACH provider in the United
States.
Effective
June 1, 2009, we completed the sale of our Phase 2 Consulting, Inc. (“Phase 2”)
business. Phase 2 provides management and economic consulting
services to the healthcare industry and had been a subsidiary of the Company
since it was acquired in 2004. The sale of Phase 2 will allow the
Company to focus on its core businesses: program management services
and hospitals.
For the
year ended December 31, 2009, we had consolidated operating revenues of
$869.4 million, operating earnings of $44.5 million, net earnings attributable
to RehabCare of $23.0 million and diluted earnings per share attributable to
RehabCare of $1.22.
Industry
Overview
As a
provider of program management services and an operator of hospitals, our
revenues and growth are affected by trends and developments in healthcare
spending. According to the Centers for Medicare and Medicaid Services (“CMS”),
total healthcare expenditures in the United States grew by 4.4% to approximately
$2.3 trillion in 2008 or 16.2% of the United States gross domestic
product.
- 3
-
CMS
further projects that total healthcare spending in the United States will
continue to grow an average of 6.1% annually from 2009 through
2019. According to these estimates, healthcare expenditures will
account for approximately $4.5 trillion, or 19.3%, of the United States gross
domestic product by 2019.
Demographic
considerations affect long-term growth projections for healthcare spending.
While we deliver therapy to adults of all ages, most of our services are
delivered to persons 65 and older. According to the U.S. Census Bureau’s latest
projections, there are approximately 40 million U.S. residents aged 65 or older,
comprising approximately 13.0% of the total United States
population. The number of U.S. residents aged 65 or older is expected
to climb to approximately 55 million by 2020 and to approximately 72 million by
2030. By 2040, the number of U.S. residents 65 and older is estimated
to reach approximately 81 million, or 20.0%, of the total
population. Due to the increasing life expectancy of U.S. residents,
the number of people aged 85 years or older is also expected to increase from
5.8 million in 2010 to 14.2 million in 2040.
We
believe healthcare expenditures and longer life expectancy of the general
population will place increased pressure on healthcare providers to find
innovative, efficient means of delivering healthcare services. In particular,
many of the health conditions associated with aging — such as stroke and heart
attack, neurological disorders and diseases and injuries to the muscles, bones
and joints — will increase the demand for rehabilitative therapy and long-term
acute care. These trends, combined with the need for acute care hospitals to
move their patients into the appropriate level of care on a timely basis, will
encourage healthcare providers to efficiently direct patients to long-term acute
care hospitals, inpatient rehabilitation facilities, outpatient therapy, home
health, skilled nursing therapy and other post-acute programs.
The
growth of managed care and its focus on cost control has encouraged healthcare
providers to deliver quality care at the lowest cost
possible. Medicare and Medicaid incentives also have driven declines
in average inpatient days per admission. In many cases, patients are treated
initially in a higher cost, acute-care hospital setting. After their condition
has stabilized, they are either moved to a lower cost setting, such as a skilled
nursing facility or subacute nursing facility, or are moved to another
post-acute institution, such as an inpatient rehabilitation facility or a
long-term acute care hospital. Alternatively, patients are discharged
to their home and treated on a home health or outpatient basis. Thus, while
hospital inpatient admissions have continued to grow, the number of average
inpatient days per admission has declined.
There are
approximately 5,000 general acute-care hospitals in the United States, including
an estimated 1,000 hospitals with inpatient rehabilitation facilities
(“IRFs”). We currently provide acute rehabilitation program
management services to 106 hospitals that operate inpatient rehabilitation
facilities.
There are
approximately 15,700 Medicare-certified skilled nursing facilities in the United
States, including an estimated 5,000 facilities that are the most likely
prospects for our contract therapy services. We currently provide
services to 1,118 of those facilities. In addition to skilled nursing
facilities, we have expanded our service offerings to deliver therapy management
services in additional settings such as long-term care, home health, assisted
living facilities and continuing care retirement communities.
Overview
of Our Business Units
We
currently operate in two business segments: program management
services, which consists of two business units — hospital rehabilitation
services and skilled nursing rehabilitation services — and
hospitals. The following table describes the services we offer within
each segment.
- 4
-
|
Business Segments
|
Description of Service
|
Benefits to Client
|
|
Program Management
Services:
|
||
|
Hospital
Rehabilitation Services:
|
||
|
Inpatient
Inpatient
Rehabilitation Facilities:
Skilled
Nursing Units (Subacute Rehabilitation):
|
High
acuity rehabilitation for conditions such as stroke, orthopedic conditions
and head injuries.
Lower
acuity rehabilitation for conditions such as stroke, cancer, heart
failure, burns and wounds.
|
Affords
the client opportunities to retain and expand market share in the
post-acute market by offering specialized clinical rehabilitation services
to patients who might otherwise be discharged to a setting outside the
client’s facility.
|
|
Outpatient
|
Outpatient
therapy programs for hospital-based and satellite programs (primarily
sports and work-related injuries).
|
Helps
bring patients into the client’s facility by providing specialized
clinical programs and helps the client compete with freestanding
clinics.
|
|
Skilled
Nursing Rehabilitation Services:
|
||
|
Contract
Therapy
|
Rehabilitation
services in freestanding
skilled nursing, long-term
care and assisted living
facilities for neurological, orthopedic and other medical
conditions.
|
Affords
the client the ability to fulfill the continuing need for therapists on a
full-time or part-time basis. Offers the client a better opportunity to
improve the quality of their programs.
|
|
Other
|
Resident-centered
consulting services and therapist and nurse staffing services for
healthcare providers.
|
Provides
management advisory services and solutions to healthcare
providers.
|
|
Hospitals:
|
||
|
Long-Term
Acute Care Hospitals (LTACHs)
|
Provide
high-level therapeutic and clinical care to patients with medically
complex diagnoses requiring an average length of stay of 25 days or
more.
|
|
| Rehabilitation Hospitals | Provide intense interdisciplinary rehabilitation services to patients on an inpatient and outpatient basis. | |
- 5
-
Financial
information about each of our business segments is contained in Note 19,
“Industry Segment Information,” to our consolidated financial
statements.
The
following table summarizes, by geographic region in the United States, our
program management and hospital locations as of December 31, 2009.
|
Program
Management Services
|
||||||||
|
Inpatient
|
||||||||
|
Rehabilitation/
|
Outpatient
|
Contract
|
||||||
|
Skilled
Nursing
|
Therapy
|
Therapy
|
||||||
|
Geographic Region
|
Units
|
Programs
|
Programs
|
Hospitals
|
||||
|
Mountain
Region
|
1/1
|
1
|
66
|
1
|
||||
|
North
Central Region
|
35/1
|
10
|
327
|
7
|
||||
|
Northeast
Region
|
16/1
|
5
|
121
|
2
|
||||
|
South
Central Region
|
32/0
|
6
|
403
|
22
|
||||
|
Southeast
Region
|
14/2
|
7
|
148
|
2
|
||||
|
Western
Region
|
8/4
|
1
|
53
|
0
|
||||
|
Total
|
106/9
|
30
|
1,118
|
34
|
||||
Program
Management Services
Many
healthcare providers partner with companies, like RehabCare, that manage either
a single service line or a broad range of service lines. Partnering allows
healthcare providers to take advantage of the specialized expertise of contract
management companies, enabling them to concentrate on the businesses they know
best, such as facility and acute-care management. Continued managed care and
Medicare reimbursement controls for acute care services have driven healthcare
providers to look for additional sources of revenue. As constraints on overhead
and operating costs have increased and staffing has been reduced, partnering
with providers of ancillary and post-acute services has become more important in
order to increase patient volumes and provide services at a lower cost while
maintaining high quality standards.
By
partnering with contract management companies like RehabCare, healthcare
facilities may be able to:
|
|
·
|
Improve Clinical
Quality. Program managers focused on rehabilitation are able to
develop and employ best practices, which benefit client facilities and
their patients.
|
|
|
·
|
Increase Volumes.
Through the addition of specialty services such as IRFs within
acute-care hospitals, patients who were being discharged to other venues
for treatment can now remain in the hospital setting. This allows
hospitals to capture revenues that would otherwise be realized by another
provider. Upon discharge, patients can return for outpatient care,
creating added revenues for the provider. New services also help hospitals
attract new patients. The addition of a managed rehabilitation program
helps skilled nursing facilities attract residents by broadening their
scope of services.
|
|
|
·
|
Optimize Utilization of Space.
Inpatient services help hospitals optimize physical plant space to
treat patients who have specific diagnoses within the particular
hospital’s targeted service lines.
|
|
|
·
|
Increase Cost Control.
Because of their extensive experience in the service line, contract
management companies can offer pricing structures that effectively control
a healthcare provider’s financial risk related to the service provided.
For hospitals and other providers that utilize program managers, the
result is often lower average cost than that of self-managed programs. As
a result, the facility is able to increase its revenues without having to
increase administrative staff or incur other fixed
costs.
|
- 6
-
|
|
·
|
Establish Agreements with
Managed Care Organizations. Program managers often have the ability
to improve clinical care by capturing and analyzing patient information
from a large number of inpatient rehabilitation and skilled nursing units,
which an individual hospital could not do on its own without a substantial
investment in specialized systems. Becoming part of a managed care network
helps the hospital attract physicians, and in turn, attract more patients
to the hospital.
|
|
|
·
|
Provide Access to
Capital. Contract management companies, particularly
those which have access to public markets, can in certain circumstances
make capital available to their clients for adding programs and services
like physical rehabilitative services or expanding existing programs when
community needs dictate.
|
|
|
·
|
Obtain Reimbursement Advice.
Contract management companies, like RehabCare, employ reimbursement
specialists who are available to assist client facilities in interpreting
complicated regulations within a given specialty — a highly valued service
in the changing healthcare
environment.
|
|
|
·
|
Obtain Clinical Resources and
Expertise. Rehabilitation service providers have the ability to
develop and implement clinical training and development programs that can
provide best practices for clients.
|
|
|
·
|
Ensure Appropriate Levels of
Staffing for Rehabilitation Professionals. Therapy staffing in both
hospitals and skilled nursing settings presents unique challenges that can
be better managed by a provider with a national recruiting presence.
Program managers have the ability to more sharply focus on staffing levels
in order to address the fluctuating clinical needs of the host
facility.
|
Our
program management services segment consists of two business units — hospital
rehabilitation services (which includes inpatient acute and subacute
rehabilitation programs and outpatient therapy programs) and skilled nursing
rehabilitation services.
Inpatient
We have
developed an effective business model in the prospective payment environment,
and we are instrumental in helping our clients achieve favorable outcomes in
their inpatient rehabilitation settings.
Inpatient Rehabilitation.
Since 1982, our inpatient division has been a leader in operating
inpatient rehabilitation facilities (“IRFs”) in acute-care hospitals on a
contract basis. As of December 31, 2009, we managed inpatient rehabilitation
facilities in 106 hospitals for patients with various diagnoses including
stroke, orthopedic conditions, arthritis, spinal cord and traumatic brain
injuries.
We
establish IRFs in acute-care hospitals that have vacant space and unmet
rehabilitation needs in their markets. We also work with hospitals that
currently operate IRFs to determine the projected level of cost savings we can
deliver to them by implementing our scheduling, clinical protocol and outcome
systems, as well as through productivity training for existing staff. In the
case of hospitals that do not operate inpatient rehabilitation facilities, we
review their historical and existing hospital population, as well as the
demographics of the geographic region, to determine the optimal size of the
proposed IRF and the potential of the new facility under our management to
attract patients and generate revenues sufficient to cover anticipated
expenses.
- 7
-
In the
inpatient division, our relationships with hospitals are in the form of
contracts for management services which are typically three to five years in
duration. We are generally paid by our clients on the basis of a
negotiated fee per month or fee per discharge.
An IRF
within an acute-care hospital affords the hospital the ability to offer
rehabilitation services to patients who might otherwise be discharged to a
setting outside the hospital. An IRF within an acute-care hospital typically
consists of 20 beds and is staffed with a program director, a physician or
medical director, and clinical staff, which may include a psychologist, physical
and occupational therapists, a speech/language pathologist, a social worker, a
case manager and other appropriate support personnel.
Subacute Rehabilitation. In
1994, the inpatient division added a skilled nursing service line in response to
client requests for management services and our strategic decision to broaden
our inpatient services. As of December 31, 2009, we managed 9
inpatient skilled nursing units. The hospital-based skilled nursing unit enables
patients to remain in a hospital setting where emergency needs can be met
quickly as opposed to being sent to a freestanding skilled nursing facility.
These types of units are located within the acute-care hospital and are
separately licensed.
We are
paid by our skilled nursing clients either based on a flat monthly fee or a
negotiated fee per patient day pursuant to contracts that are typically for
terms of three to five years. The hospital benefits by retaining patients who
otherwise would be discharged to another setting, capturing additional revenue
and utilizing idle space. A skilled nursing unit treats patients who require
less intensive levels of rehabilitative care. Patients’ diagnoses
typically require long-term care and cover approximately 60 clinical conditions,
including stroke, post-surgical conditions, pulmonary disease, cancer,
congestive heart failure, burns and wounds.
Outpatient
In 1993,
we began managing outpatient therapy programs that provide therapy services to
patients with work-related and sports-related illnesses and injuries. As of
December 31, 2009, we managed 30 hospital-based and satellite outpatient therapy
programs. An outpatient therapy program complements the hospital’s occupational
medicine initiatives and allows therapy to be continued for patients discharged
from inpatient rehabilitation facilities and medical/surgical beds. An
outpatient therapy program also attracts patients into the hospital and is
operated either on the client hospital’s campus or in satellite locations
controlled by the hospital.
We
believe our management of outpatient therapy programs delivers increased
productivity through our scheduling, clinical protocol and outcome systems, as
well as through productivity training for existing staff. We also provide our
clients with expertise in compliance and quality assurance. Typically, the
program is staffed with a facility director, four to six therapists, and two to
four administrative and clerical staff. We are typically paid by our clients on
the basis of a negotiated fee per unit of service.
Skilled
Nursing Rehabilitation Services
In 1997,
we added therapy management for freestanding skilled nursing facilities to our
service offerings. This program affords the client the opportunity to fulfill
its continuing need for therapists on a full-time or part-time basis without the
need to hire and retain full-time staff. As of December 31, 2009, we managed
1,118 contract therapy programs.
- 8
-
Our
typical contract therapy client has a 120 bed skilled nursing facility. We
manage therapy services, including physical and occupational therapy and
speech/language pathology for the skilled nursing facility and in other settings
that provide services to the senior population. Our broad base of staffing
service offerings — full-time and part-time — can be adjusted at each location
according to the facility’s and its patients’ needs. We also provide
our clients improved scheduling, clinical protocols, patient outcomes,
compliance with Medicare requirements and therapist productivity through the use
of handheld point of service devices by our therapists.
We are
generally paid by our clients on the basis of a negotiated patient per diem rate
or a negotiated fee schedule based on the type of service rendered. Typically,
our contract therapy programs are led by a full-time program director who is
also a therapist, and two to four full-time professionals trained in physical,
occupational or speech/language therapy.
Hospitals
We
entered the rehabilitation and long-term acute care hospital market in 2005 when
we acquired substantially all of the operating assets of MeadowBrook Healthcare,
Inc. (“MeadowBrook”), an operator of two rehabilitation hospitals and two
LTACHs. These facilities treat patients who require intensive
inpatient rehabilitative care and patients with medically complex
diagnoses. Patient care is provided by nursing and therapy staff as
directed by a physician order. Effective November 24, 2009, we
acquired all of the outstanding stock of Triumph HealthCare Holdings, Inc.,
which operated 20 LTACHs at the time of acquisition, more than doubling the size
of our hospital segment. As of December 31, 2009, we operated 28
LTACHs and 6 rehabilitation hospitals. We are the sole owner of 20 of
these hospitals. We retain a 51% to 87% ownership in the remaining 14 jointly
owned hospitals. Our hospitals are located in Texas, Oklahoma,
Louisiana, Florida, Georgia, Missouri, Illinois, Ohio, Indiana, Pennsylvania,
Michigan, North Dakota and Colorado. Except for two Company-owned
facilities, all of these facilities are located in property leased by us under
long-term leases. Our facilities range in size from 20 to 115
licensed beds. We also own a 40% equity interest in a freestanding
rehabilitation hospital in Kokomo, Indiana.
LTACHs
serve highly complex, but relatively stable, patients. Typical diagnoses include
respiratory failure, neuromuscular disorders, traumatic brain and spinal cord
injuries, stroke, cardiac disorders, non-healing wounds, renal disorders and
cancer. Most LTACH patients are transferred from inpatient acute
medical/surgical beds. In order to remain certified as an LTACH,
average length of stay for Medicare patients must be at least 25
days.
The
clinical services we provide in LTACHs include: nursing care, rehabilitation
therapies, pulmonology, respiratory care, cardiac and hemodynamic monitoring,
ventilator weaning, dialysis services, IV antibiotic therapy, total parenteral
nutrition, wound care, vacuum assisted closure, pain management and diabetes
management. The majority of our LTACH patients are covered by
Medicare.
Our
rehabilitation hospitals provide services to patients who require intensive
inpatient rehabilitative care. Inpatient rehabilitation patients typically
experience significant physical disabilities due to various conditions, such as
head injury, spinal cord injury, stroke, certain orthopedic problems, and
neuromuscular disease. Our rehabilitation hospitals provide the medical,
nursing, therapy, and ancillary services required to comply with local, state,
and federal regulations, as well as accreditation standards of the Joint
Commission. The outpatient services offered by our hospital division assist us
in managing patients through their post-acute continuum of care. The
majority of our inpatient rehabilitation facility patients are covered by
Medicare.
- 9
-
In the
hospital segment, we are developing joint venture relationships with acute care
hospitals and physician practices whereby the joint venture owns and/or operates
the LTACH or rehabilitation facility, and we provide management services to the
facility, which include billing, collection, and other facility management
services. This joint venture management business model provides the
potential for additional profitability and significantly longer partnerships,
but requires additional capital compared to our traditional contract management
business.
Strategy
Our
operations are guided by a defined strategy aimed at advancing the profitability
and growth of our company and the delivery of high quality healthcare services
to patients. The focal point of that strategy is the development of
clinically integrated post acute continuums of care in geographic regions
throughout the United States where we provide services in a full spectrum of
post acute patient settings. We plan to execute this strategy over
the long-term through acquisitions, joint ownership arrangements with market
leading healthcare providers and by aggressively pursuing additional program
management opportunities.
Competition
Competition
in our program management business is highly fragmented and
intense. We compete with large national companies and smaller
regional companies that offer one or more of the same services. The fundamental
challenge in this line of business is convincing our potential clients,
primarily hospitals and skilled nursing facilities, that we can provide quality
rehabilitation services more efficiently than they can themselves. Among our
principal competitive advantages are our scale, reputation for quality, cost
effectiveness, an outcomes management system, innovation, price and technology
systems.
Our
hospitals compete primarily with LTACHs, IRFs and skilled nursing units within
acute care hospitals located in our respective markets. In addition,
we face competition from other large publicly held companies such as HealthSouth
Corporation, Select Medical Corporation and Kindred Healthcare,
Inc.
We rely
on our ability to attract, develop and retain therapists and program management
personnel. We compete for these professionals with other healthcare
companies, including current and potential clients, which seek to fill positions
with either regular or temporary employees.
Government
Regulation
Overview. The
healthcare industry is required to comply with many federal, state and local
laws and is subject to regulation by a number of federal, state and local
governmental agencies, including those that administer the Medicare and Medicaid
programs, those responsible for the licensure of healthcare providers and
facilities, and those responsible for administering and approving health
facility construction, new services and equipment purchasing. The healthcare
industry is also affected by federal, state and local policies developed to
regulate the manner in which healthcare is provided, administered and paid for
nationally and locally. While Congress attempted to pass major
legislation on healthcare reform in 2009, it is not known when or if such
legislation will occur.
Regulations
in the healthcare industry are extremely complex and, in many instances, the
industry does not have the benefit of significant regulatory or judicial
interpretation. As a result, the healthcare industry is exposed to
legislative and regulatory changes; reductions and limitations in healthcare
spending by government agencies; and changes in employer healthcare policies.
Moreover, our business is impacted not only by those regulations that are
directly applicable to our hospitals, but also by those regulations that are
applicable to our clients’ facilities.
- 10
-
If we
fail to comply with the regulations applicable to our business, we could suffer
civil damages or penalties, criminal penalties, and/or be excluded from
contracting with providers participating
in Medicare, Medicaid and other federal and state healthcare programs. Likewise,
if our hospital, skilled nursing facility, or other clients fail to comply with
the regulations applicable to their businesses, they also could suffer civil
damages or penalties, criminal penalties and/or be excluded from participating
in Medicare, Medicaid and other federal and state healthcare programs. In either
event, such consequences could either directly or indirectly have an adverse
impact on our business.
Facility Licensure, Medicare
Certification, and Certificate of Need. Our clients and our hospitals are
required to comply with state facility licensure, federal Medicare
certification, and certificate of need laws in certain states that are not
generally applicable to our program management business.
Generally,
facility licensure and Medicare certification follow specific standards and
requirements. Compliance is monitored by various mechanisms, including periodic
written reports and on-site inspections by representatives of relevant
government agencies. Loss of licensure or Medicare certification by a healthcare
facility with which we have a contract would likely result in termination of our
contract with that facility. Loss of licensure or Medicare
certification in any of our hospitals would result in a material adverse impact
on the revenues and profitability of the affected unit until such time as the
re-certification process is completed.
A few
states require that healthcare facilities obtain state permission prior to
entering into contracts for the management of their services. Some states also
require that healthcare facilities obtain state permission in the form of a
certificate of need prior to constructing or modifying their space, purchasing
high-cost medical equipment, or adding new healthcare services. If a certificate
of need is required, the process may take up to 12 months or more, depending on
the state. The certificate of need application may be denied if contested by a
competitor or if the new facility or service is deemed unnecessary by the state
reviewing agency. A certificate of need is usually issued for a specified
maximum expenditure and requires implementation of the proposed improvement or
new service within a specified period of time. If we or our clients
are unable to obtain a certificate of need, we may not be able to implement a
contract to provide therapy services or open a new hospital.
Professional Licensure and Corporate
Practice. Many of the healthcare professionals employed or independently
engaged by us are required to be individually licensed or certified under
applicable state laws. We take reasonable steps to ensure that such healthcare
professionals possess all necessary licenses and certifications, and we believe
that our employees and independent contractors comply with all applicable
laws.
In some
states, for profit corporations are restricted from practicing rehabilitation
therapy through the direct employment of therapists. To comply with the
restrictions in such states, we contract to obtain therapist services from
entities permitted to employ therapists.
Reimbursement. Federal and
state regulations establish payment methodologies for healthcare services
covered by Medicare, Medicaid and other government healthcare
programs.
Medicare
pays acute-care hospitals for most inpatient hospital services under a payment
system known as the prospective payment system (“PPS”). Under this system,
acute-care hospitals are paid a fixed amount per discharge based on the
diagnosis-related group (“DRG”) to which each Medicare patient is assigned,
regardless of the amount of services provided to the patient or the length of
the patient’s hospital stay. The amount of reimbursement assigned to
each DRG is established prospectively by the Centers for Medicare and Medicaid
Services (“CMS”), an agency of the Department of Health and Human
Services.
Under
Medicare’s acute-care prospective payment system, a hospital may keep the
difference between its DRG payment and its operating costs incurred in
furnishing inpatient services, but the hospital is generally at risk for any
operating costs that exceed the applicable DRG payment rate. For
certain Medicare beneficiaries who have unusually costly hospital stays, CMS
will provide additional payments above those specified for the diagnosis-related
group.
- 11
-
The
prospective payment system for inpatient rehabilitation facilities (“IRFs”) is
similar to the DRG payment system used for acute-care hospital services but uses
a case-mix group (“CMG”) rather than a diagnosis-related group. Each patient is
assigned to a CMG based on clinical characteristics and expected resource needs
as a result of information reported on a patient assessment instrument which is
completed upon patient admission and discharge. Under the prospective payment
system, an IRF may keep the difference between its CMG payment and its operating
costs incurred in furnishing patient services, but it is at risk for operating
costs that exceed the applicable CMG payment.
We
believe that the PPS for IRFs favors low-cost, efficient providers, and that our
efficiencies gained through economies of scale and our focus on cost management
in the rehabilitation field are attractive to operators in the hospital
sector.
To
qualify for the PPS for IRFs, operators must satisfy what was previously known
as the 75% Rule and is now known as the 60% Rule. The 2007 Medicare,
Medicaid and SCHIP Extension Act (“the 2007 SCHIP Extension Act”), enacted in
December 2007, permanently set the compliance threshold at 60%. The
rule requires that 60% of patients fall within thirteen specific diagnostic
categories. We continue to monitor the regulatory environment for any new rules
that could affect this statute.
The
Medicare program is administered by contractors and fiscal intermediaries. Under
the authority granted by CMS, certain fiscal intermediaries have issued local
coverage determinations that are intended to clarify the clinical criteria under
which Medicare reimbursement is available. Certain local coverage determinations
attempt to require evidence of a greater level of medical necessity for
inpatient rehabilitation facility patients. Those local coverage
determinations have been used by fiscal intermediaries to deny admission or
reimbursement for some patients in our hospital rehabilitation services and
hospital divisions. Where appropriate, we and our clients appeal such
denials and many times are successful in overturning the original decision of
the fiscal intermediary.
The
Medicare Modernization Act of 2003 directed CMS to create a program using
independent recovery audit contractors (“RACs”) to collect improper Medicare
overpayments. The RAC program, which began with a demonstration pilot
in three states and is scheduled to be expanded to all 50 states by 2010, has
been very controversial because the RACs are paid a percentage of claims that
are ultimately disallowed. On October 6, 2008, CMS awarded contracts
to four permanent RACs beginning in March 2009. We will continue to challenge
and appeal any claims that we believe have been inappropriately
denied.
Medicare
reimbursement for outpatient rehabilitation services is based on the lesser of
the provider’s actual charge for such services or the applicable Medicare
physician fee schedule amount established by CMS. This reimbursement system
applies regardless of whether the therapy services are furnished in a hospital
outpatient department, a skilled nursing facility, an assisted living facility,
a physician’s office, or the office of a therapist in private
practice. The physician fee schedule is subject to change from year
to year. The Medicare Improvements for Patients and Providers Act of
2008 provided a 0.5% increase in the fee schedule for 2008 and an additional
1.1% increase beginning January 1, 2009. In December 2009, Congress
passed a short extension of the current fee schedule which expired on March 1,
2010. On March 2, 2010, the President signed HR 4961, a short term
extension for a number of expiring provisions. Contained in this bill
is an extension of the current physician fee schedule through March 31,
2010.
- 12
-
On May 1,
2007, CMS released a rule extending the so-called 25% Rule to all LTACHs,
including those LTACHs that have previously operated under a statutory
grandfathering exemption. The 25% Rule limits LTACH prospective
payment system paid admissions from a single referral source to
25%. Admissions beyond the 25% threshold would be paid using lower
inpatient PPS rates. Our LTACH in New Orleans, Louisiana had been
grandfathered and statutorily exempt from that rule. Such exemption
provided greater operational flexibility and fewer restrictions on the types of
patients that could be admitted to that facility. Under the May 1,
2007 rule, implementation of the 25% threshold was to occur over a three year
transition period. As more fully discussed in Note 7 to our
consolidated financial statements, we recognized a $4.9 million impairment loss
in the second quarter of 2007 to reduce the carrying value of the New Orleans
LTACH’s statutory exemption intangible asset to its revised estimate of fair
value based on the impact of the change in regulations.
LTACHs
are currently reimbursed under a prospective payment system (“LTACH-PPS”)
pursuant to which Medicare classifies patients into distinct diagnostic related
groups based upon specific clinical characteristics and expected resource
needs. The 2007 SCHIP Extension Act provided regulatory relief for a
three year period to LTACHs to ensure continued access to current long-term
acute care hospital services. Specifically, the legislation prevented
CMS from implementing a new payment provision for short stay outlier cases and
provided that the 25% Rule will not be applied to freestanding LTACHs and
grandfathered LTACHs such as the one we operate in New Orleans until
after cost reporting periods beginning on or after July 1, 2010.
The 2007
SCHIP Extension Act also established a three-year moratorium, which is scheduled
to end on December 31, 2010, on the establishment or classification of any new
LTACH facilities, any satellite facilities and increases in bed capacity at
existing LTACHs. The most recent extension of SCHIP, which was
enacted in February 2009, did not alter any Medicare reimbursement policies that
would significantly impact our business.
Skilled
nursing facilities are also subject to a prospective payment system based on
resource utilization group classifications. On July 31, 2009, CMS
issued its final payment rule for skilled nursing facilities for federal fiscal
year 2010 which includes provisions that would take effect in federal fiscal
year 2011. The final rule included a net payment rate reduction of
1.1% for skilled nursing facilities (“SNFs”) beginning on October 1, 2009 and
two provisions that begin on October 1, 2010: a move from the current payment
system of resource utilization groups (“RUGs III”) to RUGs IV and changes to the
reimbursement rules for concurrent therapy. Concurrent therapy occurs
when two or more patients are treated at the same time with different
regimens. In the past, CMS considered the total time of the
concurrent session to be assigned to each patient. The final rule now
requires the total time to be allocated amongst each patient.
As of
January 1, 2006, certain limits or caps on the amount of reimbursement for
therapy services provided to Medicare Part B patients came into
effect. The annual therapy caps are currently $1,860 for occupational
therapy and a combined cap of $1,860 for physical and speech
therapy. Prior to January 1, 2010, most of our Medicare Part B
patients qualified for an automatic exception to these caps due to their
clinical complexities. However, the therapy cap exception process
expired on January 1, 2010. On March 2, 2010, the President signed HR
4961, a short term extension for a number of expiring
provisions. Contained in this bill is a retro-active extension of the
Medicare Part B therapy cap exception process from January 1, 2010 through March
31, 2010. Congress is considering additional legislation to further
extend the exception process.
Health Information Practices.
The Health Insurance Portability and Accountability Act of 1996, as
amended, commonly known as HIPAA, was enacted to improve the efficiency and
effectiveness of the healthcare system through the establishment of standards
and requirements for the electronic transmission of certain health
information. HIPAA regulates, among other things, the use of (i)
protected health information; (ii) electronic transactions and code sets in the
healthcare field; (iii) unique identifiers for patients, healthcare providers,
health insurance plans, and employers; and (iv) electronic signatures. We and
our program management clients are generally subject to the requirements of
HIPAA. HIPAA is a very complex law that has required the careful
implementation of a considerable number of policies, systems, and safeguards to
better ensure our compliance with its requirements.
- 13
-
Fraud and
Abuse. Various federal and state laws prohibit the knowing and
willful submission of false or fraudulent claims for reimbursement, including
claims to obtain payment under Medicare, Medicaid and other government
healthcare programs. The federal anti-kickback statute also prohibits
individuals and entities from knowingly and willfully paying, offering,
receiving or soliciting money or anything else of value in order to induce the
referral of patients, or to induce a person to purchase, lease, order, arrange
for or recommend services or goods covered by Medicare, Medicaid, or other
government healthcare programs.
The
federal anti-kickback statute is susceptible to broad interpretation and
potentially covers many otherwise legitimate business arrangements. Violations
of the statute are punishable by criminal and civil penalties, including fines
of up to $25,000 per violation, civil monetary penalties of up to $50,000 per
violation, assessments of up to three times the amount of the prohibited
remuneration, imprisonment, or exclusion from participation in Medicare,
Medicaid, and other government healthcare programs. The Office of the Inspector
General of the Department of Health and Human Services (“OIG”) has published
guidelines outlining certain safe harbor arrangements that do not violate the
prohibitions of the statute.
A number
of states also have statutes that prohibit the same general types of conduct as
that prohibited by the federal anti-kickback statute. Some states’ antifraud and
anti-kickback laws apply only to goods and services covered by Medicaid. Other
states’ antifraud and anti-kickback laws apply to all healthcare goods and
services, regardless of whether the source of payment is governmental or
private.
In recent
years, federal and state government agencies have increased the level of
enforcement resources and activities targeted at the healthcare industry. In
addition, federal law allows individuals to bring lawsuits on behalf of the
government in what are known as qui tam or “whistleblower” actions, alleging
false or fraudulent Medicare or Medicaid claims and certain other violations of
federal law. The use of these private enforcement actions against healthcare
providers and their business is increasing, in part, because the individual
filing the initial complaint is entitled to share in a portion of any settlement
or judgment if successful.
Anti-Referral
Laws. The federal law generally known as the Stark law
provides that, if a physician or a member of a physician’s immediate family has
a financial relationship with a designated healthcare service entity, the
physician may not make referrals to that entity for the furnishing of designated
health services covered under Medicare or Medicaid unless one of several
specific exceptions applies. For purposes of the Stark law, a financial
relationship with a healthcare entity includes an ownership or investment
interest in that entity or a compensation relationship with that entity.
Designated health services include physical and occupational therapy services,
durable medical equipment, home health services, and inpatient and outpatient
hospital services. CMS has promulgated regulations interpreting the Stark law
and, in instances where the Stark law applies to our activities, we have
instituted policies which set standards intended to prevent violations of the
Stark law.
The
federal government will make no payment for designated health services provided
in violation of the Stark law. In addition, sanctions for violating the Stark
law include civil monetary penalties of up to $15,000 per prohibited service
provided and exclusion from any federal, state, or other government healthcare
programs.
A number
of states have statutes that prohibit the same general types of conduct as that
prohibited by the federal Stark law. Some states’ Stark laws apply only to goods
and services covered by Medicaid. Other states’ Stark laws apply to certain
designated healthcare goods and services, regardless of whether the source of
payment is a governmental or private payor.
- 14
-
Corporate Compliance Program.
In recognition of the importance of achieving and maintaining regulatory
compliance and establishing a culture of ethical conduct, we have a corporate
compliance program that defines standards of conduct and procedures that are
intended to promote compliance with applicable laws and promote proper
behavior. The Office of Inspector General has published guidelines
for corporate compliance programs for certain types of healthcare
organizations. Those guidelines encourage the following seven
elements in any compliance program: (1) implementation of written standards of
conduct; (2) designation of a Chief Compliance Officer with the responsibility
and necessary authority to implement and enforce the compliance program, (3)
regular employee education and training; (4) effective reporting lines of
communication such as a “hotline;” (5) use of audits or other risk evaluation
techniques; (6) disciplinary systems that consistently enforce the program
standards; and (7) response and remediation systems. Our compliance
program has been designed and operates to serve those seven
elements.
In the
recognition of the importance of compliance in our business environment, we have
created a separate Compliance Committee comprised of three independent members
of our board of directors. Our Chief Compliance Officer, who reports
to the Compliance Committee as well as to the Chief Executive Officer, is
responsible for overseeing the design, ongoing enhancement, and implementation
of our compliance program. We believe these safeguards help us to
conduct our operations in compliance with all applicable laws, rules,
regulations, and internal company standards.
Employees
As of
December 31, 2009, we had approximately 18,200 employees, approximately 9,200 of
whom were full-time employees, including approximately 5,300 employees in our
program management business, 3,400 employees in our hospitals and 500 employees
in our corporate offices. The physicians who are the medical
directors in our managed IRFs and hospitals are independent contractors and not
our employees. None of our employees are subject to a collective bargaining
agreement.
Non-Audit
Services Performed by Independent Accountants
Pursuant
to Section 10A(i)(2) of the Securities Exchange Act of 1934 and Section 202 of
the Sarbanes-Oxley Act of 2002, we are responsible for disclosing to investors
the non-audit services approved by our audit committee to be performed by KPMG
LLP, our independent registered public accounting firm. Non-audit services are
defined as services other than those provided in connection with an audit or a
review of our financial statements. During the year ended December 31, 2009, we
did not receive any non-audit services performed by KPMG.
Web
Site Access to Reports
Our Form
10-K, Form 10-Qs, definitive proxy statements, Form 8-Ks, and any amendments to
those reports are made available free of charge on our web site at
www.rehabcare.com as soon as reasonably practicable after such reports are filed
with the Securities and Exchange Commission.
| ITEM 1A. | RISK FACTORS |
Our
business involves a number of risks, some of which are beyond our
control. The risks and uncertainties described below are not the only
ones we face. Additional risks and uncertainties that we do not
currently know about, or that we currently believe to be immaterial, may also
adversely affect our business.
- 15
-
Our
operations may deteriorate if we are unable to attract, develop and retain our
operational personnel.
Our
success is dependent on attracting, developing and retaining operational
personnel, especially those individuals who are responsible for operating the
inpatient units, outpatient programs and contract therapy locations in our
program management business and our hospitals. In particular, we rely
significantly on our ability to attract, develop and retain qualified
recruiters, area managers, program managers, regional managers and hospital
administrators. The available pool of individuals who meet our qualifications
for these positions is limited and the competition for labor in the healthcare
industry is intense. We may not be able to continue to attract and develop
qualified people to fill these essential positions and we may not be able to
retain them once they are employed.
Shortages
of qualified therapists, nurses and other healthcare personnel could increase
our operating costs and negatively impact our business.
Our
operations are dependent on the efforts, abilities and experience of our
management and medical support personnel, such as therapists and other allied
healthcare professionals. We rely significantly on our ability to attract,
develop and retain therapists, nurses and other healthcare personnel who possess
the skills, experience and, as required, the licensure necessary to meet the
specified requirements of our business. In some markets, the availability of
therapists and other medical support personnel has become a significant
operating issue to healthcare providers. Current and future shortages of such
skilled labor may require us to continue to enhance wages and benefits in order
to recruit and retain qualified personnel, or it may require us to hire more
costly temporary personnel. We must continually evaluate, train and upgrade our
employees to keep pace with clients’ and patients’ needs. If we are unable to
attract and retain qualified healthcare personnel, the quality of our services
may decline and we may lose customers.
Unionization
activities could adversely affect the profitability of our
businesses.
None of
our employees are subject to a collective bargaining agreement, and we are not
aware of any current activities to organize our employees. We believe our
relationship with our employees is good. If our employees were to unionize, we
could experience an increase in labor and other costs. Furthermore, we could
experience a disruption of our operations and/or higher ongoing labor costs if
our employees were to engage in a strike or other work stoppage.
Fluctuations
in census levels and patient visits may adversely affect the revenues and
profitability of our businesses.
The
profitability of our program management business is directly affected by the
census levels, or the number of patients per unit, in the inpatient programs
that we manage and the number of visits in the outpatient programs that we
manage. The profitability of our hospitals business is also directly affected by
the census levels at each of our hospitals. Reduction in census levels or
patient visits within facilities, units or programs that we own or manage may
negatively affect our revenues and profitability.
If
there are changes in the rates or methods of government reimbursements of our
clients for the rehabilitation services managed by us, our rehabilitation
program management services clients could attempt to renegotiate our contracts
with them, which may reduce our revenues and profitability.
- 16
-
Most of
the patients cared for in our facilities are beneficiaries of government
sponsored programs such as the Medicare and Medicaid programs. In an effort to
control the expanding costs of the Medicare program, CMS and Congress
periodically change benefits and reimbursement levels. Changes in the rates of
or conditions for government reimbursement, including policies related to
Medicare and Medicaid, could reduce the amounts reimbursed to our clients for
rehabilitation services performed in the programs managed by us and, in turn,
our clients may attempt to renegotiate the terms of our contracts.
Medicaid
reimbursement is a significant revenue source for skilled nursing facilities and
other long-term care facilities where contract therapy services are provided.
Reductions in Medicaid reimbursement could negatively impact skilled nursing
facilities and long-term care facilities which, in turn, could adversely affect
the revenues and profitability of our contract therapy business.
If
we do not manage admissions in the IRFs that we manage or own in compliance with
the 60% Rule, reimbursement for services rendered by us in those IRF settings
will be based on less favorable rates.
IRFs are
subject to the 60% Rule which now requires that 60% or more of the patients
admitted to the facilities have one or more of 13 specific conditions in order
to qualify for the IRF prospective payment system (“PPS”). If that compliance
threshold is not maintained, the IRF will be reimbursed at the lower PPS
applicable to acute care hospitals. That may lead to reduced revenue in our
owned IRFs and may also lead our IRF clients to attempt to renegotiate the terms
of our contracts or terminate our contracts, in either case adversely affecting
our revenues and profitability.
If
there are changes in the rate or methods of government reimbursement for
services provided by our hospitals, the revenue and profitability of those
hospitals may be adversely affected.
In our
hospitals business, we are directly reimbursed for a significant number of the
patients we treat in those facilities through government reimbursement programs,
such as Medicare. Changes in the rates of or conditions for government
reimbursement could reduce the amounts reimbursed to our facilities and in turn
could adversely affect the revenues and profitability of our hospitals
business.
We
conduct business in a heavily regulated healthcare industry and changes in
regulations or violations of regulations may result in increased costs or
sanctions that reduce our revenue and profitability.
The
healthcare industry is subject to extensive federal and state regulation
relating to, among other things:
|
·
|
facility
and professional licensure;
|
|
·
|
conduct
of operations;
|
|
·
|
certain
clinical procedures;
|
|
·
|
addition
of facilities and services, including certificates of
need;
|
|
·
|
coding
and billing for services; and
|
|
·
|
payment
for services.
|
Both
federal and state government agencies have increased coordinated civil and
criminal enforcement efforts related to the healthcare industry. Regulations
related to the healthcare industry are extremely complex and, in many instances,
the industry does not have the benefit of significant regulatory or judicial
interpretation of those laws. Medicare and Medicaid anti-fraud and abuse laws
prohibit certain business practices and relationships related to items or
services reimbursable under Medicare, Medicaid and other government healthcare
programs, including the payment or receipt of remuneration to induce or arrange
for referral of patients or recommendation for the provision of items or
services covered by Medicare or Medicaid or any other federal or state
healthcare program. Federal and state laws prohibit the submission of false or
fraudulent claims, including claims to obtain reimbursement under Medicare and
Medicaid. Although we have implemented a compliance program to help assure
compliance with these regulations as they become effective, different
interpretations or enforcement of these laws and regulations in the future could
subject our current practices to allegations of impropriety or illegality or
could require us to make changes in our facilities, equipment, personnel,
services or the manner in which we conduct our business. If we fail to comply
with government regulations, we or our clients could lose reimbursements or
suffer civil or criminal penalties, which could result in cancellation of our
contracts and a decrease in revenues.
- 17
-
Congress
is currently considering various healthcare reform measures. We are unable to
predict the impact, if any, that new legislation or any other healthcare reform
measures being considered by Congress would have on our business if
adopted.
Beyond
these healthcare industry-specific regulatory risks, we are also subject to all
of the same federal, state and local rules and regulations that apply to other
publicly traded companies and large employers. We are subject to a myriad of
federal, state and local laws regulating, for example, the issuance of
securities, employee rights and benefits, workers compensation and safety, and
many other activities attendant with our business. Failure to comply with such
regulations, even if unintentional, could materially impact our financial
results.
If
our LTACHs fail to maintain their certification as long-term acute care
hospitals, then our profitability may decline.
As of
December 31, 2009, 27 of our 28 long-term acute care hospitals were certified by
Medicare as LTACHs, with one hospital pending LTACH certification. If
our LTACHs fail to meet or maintain the standards for certification as long-term
acute care hospitals, such as average minimum length of patient stay, they will
receive payments under the PPS applicable to general acute care hospitals rather
than payment under the system applicable to long-term acute care hospitals.
Payments at rates applicable to general acute care hospitals would result in our
LTACHs receiving less Medicare reimbursement than they currently receive for
their patient services and our profit margins would likely
decrease.
Expiration
of the moratorium imposed on certain federal regulations otherwise applicable to
LTACHs operated as freestanding or grandfathered “hospital in a hospital”
(“HIH”) or grandfathered “satellites” may have an adverse effect on our future
net operating revenues and profitability.
Medicare
payments to our LTACHs are made pursuant to PPS applicable to LTACHs
(“LTACH-PPS”). In addition, some LTACHs are subject to the so-called
25% Rule which requires that 25% or fewer of the patients admitted to the
facility are referred from the same source. Admissions beyond the 25%
threshold are paid using lower inpatient PPS rates. On May 1, 2007,
CMS released a final rule extending the 25% Rule to all LTACHs, including those
LTACHs that have previously operated under a statutory grandfathering
exemption. We refer to such final rule as “the May 2007 final
rule.”
Prior to
the May 2007 final rule, the 25% admissions threshold was applicable only to
Medicare HIH admissions from hospitals co-located with an LTACH or LTACH
satellite. Under the May 2007 final rule, HIHs that admit Medicare patients from
non-co-located hospitals, freestanding LTACHs and grandfathered LTACH HIHs are
subject to the Medicare admission thresholds. To the extent that any LTACH’s or
LTACH satellite facility’s discharges that are admitted from an individual
hospital (regardless of whether the referring hospital is co-located with the
LTACH or LTACH satellite) exceed the applicable percentage threshold during a
particular cost reporting period, the payment rate for those discharges would be
subject to a downward payment adjustment. Cases admitted in excess of the
applicable threshold would be reimbursed at inpatient PPS rates which are
generally lower than LTACH-PPS rates. Outlier status cases do not count toward
the threshold and would be paid under LTACH-PPS.
- 18
-
The
2007 SCHIP Extension Act provided regulatory relief for a three year period to
LTACHs to ensure continued access to current long-term acute care hospital
services. Specifically, the legislation prevented CMS from
implementing a new payment provision for short stay outlier cases and provided
that the 25% Rule will not be applied to freestanding LTACHs and grandfathered
LTACHs such as the one we operate in New Orleans until after cost reporting
periods beginning on or after July 1, 2010.
When the
three-year moratorium period expires on December 31, 2010, the May 2007 final
rule will be applied as it was originally written unless the moratorium is
extended through new legislation. When the moratorium expires, it
could have an adverse financial impact on our net operating revenues and
profitability.
The
moratorium on the Medicare certification of new LTACHs and beds in existing
LTACHs could limit our ability to increase LTACH bed capacity, expand into new
geographic regions, or increase services in existing areas we
serve.
The 2007
SCHIP Extension Act imposed a three-year moratorium, beginning on December 29,
2007, on the establishment and classification of new LTACHs, LTACH satellite
facilities and LTACH beds in existing LTACH or satellite facilities. The
moratorium does not apply to LTACHs that, before December 29, 2007, (i) began
the qualifying period for payment under the LTACH-PPS, (ii) had a written
agreement with an unrelated party for the construction, renovation, lease or
demolition for a LTACH and had expended at least 10% of the estimated cost of
the project or $2,500,000, or (iii) had obtained an approved certificate of
need. The moratorium also does not apply to an increase in beds in an existing
hospital or satellite facility if the LTACH is located in a state where there is
only one other LTACH and the LTACH requests an increase in beds following the
closure or the decrease in the number of beds of the other LTACH. We may acquire
LTACHs that were in existence prior to December 29, 2007, and would not expect
this moratorium to materially impact our strategy to expand by acquiring
additional LTACHs if such LTACHs can be acquired at attractive valuations. This
moratorium could, however, otherwise adversely affect our ability to increase
LTACH bed capacity, expand into new geographic regions, or increase bed capacity
in existing areas we serve.
Changes
in federal or state law limiting or prohibiting certain physician referrals may
preclude physicians from investing in our hospitals or referring to hospitals in
which they already own an interest.
The
federal self referral law, or “Stark Law,” prohibits a physician who has a
financial relationship with an entity from referring his or her Medicare or
Medicaid patients to that entity for certain designated health services,
including inpatient and outpatient hospital services. Under current law,
physicians who have a direct or indirect ownership interest in a hospital will
not be prohibited from referring to the hospital because of the applicability of
the “whole hospital exception” to the Stark Law. Various healthcare reform bills
introduced in Congress have included provisions that further restrict physician
ownership in hospitals to which the physician refers patients. These provisions
would typically limit the Stark Law’s “whole hospital exception” to existing
hospitals with physician ownership. Physicians with ownership in “new” hospitals
would be prohibited from referring to that hospital. Certain requirements and
limitations would also be placed on existing hospitals with physician ownership,
such as limiting the expansion of any such hospital and limiting the amount and
terms of physician investment. Furthermore, initiatives are underway in some
states to restrict physician referrals to physician-owned hospitals. There can
be no assurance that new legislation or regulation prohibiting or limiting
physician referrals to physician-owned hospitals will not be successfully
enacted in the future. If such federal or state laws are adopted, among other
outcomes, physicians who have invested in, or considered investing in, our
hospitals could be precluded from referring to, investing in or continuing to be
physician owners of a hospital. In addition, expansion of our physician-owned
hospitals may be limited, and the revenues, profitability and overall financial
performance of our hospitals may be negatively affected.
- 19
-
Our
hospitals may be unable to reduce costs to offset completely any decreases in
our revenues.
As of
December 31, 2009, we owned and operated 28 LTACHs and six IRFs operating in 13
states. Reduced levels of occupancy in our facilities and reductions in
reimbursements from Medicare, Medicaid or other payors would adversely impact
our revenues and liquidity. We may be unable to put in place corresponding
reductions in costs in response to declines in census or other revenue
shortfalls. The inability to timely adjust our operations to address a decrease
in our revenues could have a material adverse effect on our business, financial
condition, results of operations and liquidity.
Our
program management business operates in a highly competitive and fragmented
market, and our success in that business depends on our ability to demonstrate
that we can provide rehabilitation services more efficiently than our potential
clients.
Competition
for our program management business is highly fragmented and intense. Hospitals,
skilled nursing facilities and other long-term care facilities that do not
choose to outsource the management of their physical rehabilitation services are
the primary competitors of our program management business. The fundamental
challenge in our program management business is demonstrating to potential
clients, primarily hospitals, skilled nursing facilities and other long-term
care facilities, that we can provide rehabilitation services more efficiently
than they can themselves. The programs we manage are in highly competitive
markets and compete for patients with hospitals, skilled nursing facilities and
long-term care facilities, as well as other larger companies such as HealthSouth
Corporation, Kindred Healthcare, Inc. and Select Medical Corporation. Some of
these competitors may be better capitalized, have greater name recognition,
longer operating histories and their managers may have stronger relationships
with physicians in the communities that they serve. All of these factors could
give our competitors an advantage over us.
Competition
may restrict our future growth by limiting our ability to make acquisitions or
enter into joint ownership agreements at reasonable valuations.
We have
historically faced competition in acquiring companies or entering into joint
ownership agreements with partners in facilities complementary to our lines of
business. Our competitors may acquire or seek to acquire many of the companies
that would be suitable candidates for acquisition by us or enter into or seek to
enter into joint ownership agreements with entities that would be suitable
partners for us. This could limit our ability to grow by either acquisitions or
joint ownership agreements, or make the cost of acquisitions or joint ownership
arrangements higher and less attractive to us.
We
may face difficulties integrating acquisitions into our operations, and our
acquisitions may be unsuccessful, involve significant cash expenditures or
expose us to unforeseen liabilities. Our joint ownership arrangements may be
subject to similar difficulties, require significant cash expenditures or expose
us to unforeseen liabilities.
- 20
-
We expect
to continue pursuing acquisitions and joint ownership arrangements, each of
which involve numerous risks, including:
|
·
|
difficulties
integrating acquired personnel and distinct cultures into our
business;
|
|
·
|
disagreements
with our joint ownership partners;
|
|
·
|
incomplete
due diligence or misunderstanding as to the target company’s future
prospects;
|
|
·
|
diversion
of management attention and capital resources from existing
operations;
|
|
·
|
short-term
(or longer lasting) dilution in the value of our
shares;
|
|
·
|
over-paying
for an acquired company or joint ownership entity due to incorrect
analysis or because of competition from other companies for the same
target;
|
|
·
|
inability
to achieve forecasted revenues, cost savings or other
synergies;
|
|
·
|
potential
loss of key employees, customers or relationships;
and
|
|
·
|
assumption
of liabilities and exposure to unforeseen liabilities of acquired or joint
ownership companies, including liabilities for failure to comply with
healthcare regulations.
|
These
acquisitions and joint ownership arrangements may also result in significant
cash expenditures, incurrence of debt, impairment of goodwill and other
intangible assets, and other expenses that could have a material adverse effect
on our financial condition and results of operations.
Significant
legal actions could subject us to substantial uninsured
liabilities.
In recent
years, healthcare providers have become subject to an increasing number of legal
actions alleging malpractice, product liability, fraud, labor violations or
related legal theories. Many of these actions involve complex claims that can be
extraordinarily broad given the scope of our operations. They may also entail
significant defense costs. To protect us from the cost of these claims, we
maintain professional malpractice liability insurance, general liability
insurance and employment practices liability coverage in amounts and with
deductibles that we believe are appropriate for our operations. However, our
insurance coverage may not cover all claims against us or continue to be
available to us at a reasonable cost. If we are unable to maintain adequate
insurance coverage, we may be exposed to substantial liabilities.
Our
success depends on retention of our key officers.
Our
future success depends in significant part on the continued service of our key
officers. Competition for these individuals is intense and there can be no
assurance that we will retain our key officers or that we can attract or retain
other highly qualified executives in the future. The loss of any of our key
officers could have a material adverse effect on our business, financial
condition, results of operations and/or prospects.
We
may have future capital needs and any future issuances of equity securities may
result in dilution of the value of our common stock.
We
anticipate that the amounts generated internally, together with amounts
available under our credit facility, will be sufficient to implement our
business plan for the foreseeable future, subject to additional needs that may
arise if unexpected events occur or if a substantial acquisition or other growth
opportunity becomes available. We may obtain additional capital through the
public or private sale of debt or equity securities. If we sell equity
securities, the value of our common stock could experience dilution.
Furthermore, these securities could have rights, preferences and privileges more
favorable than those of the common stock. We cannot be assured that additional
capital will be available, or available on terms favorable to us. If
capital is not available, we may not be able to fund internal or external
business expansion or respond to competitive pressures.
- 21
-
We
incurred substantial indebtedness to consummate the acquisition of Triumph and
we may be unable to service or refinance this debt, which could have negative
consequences on our business in the future and may place us at a competitive
disadvantage in our industry.
As of
December 31, 2009, we had total outstanding indebtedness of $464.2 million and
total consolidated stockholders’ equity of $437.3 million. This high
level of debt could have negative consequences. For example, it
could:
|
·
|
result
in our inability to comply with the financial and other restrictive
covenants in our credit facilities;
|
|
·
|
increase
our vulnerability to adverse industry and general economic
conditions;
|
|
·
|
require
us to dedicate a substantial portion of our cash flow from operations to
make payments on our debt, thereby reducing the availability of our cash
flow for working capital, capital investments and other business
activities;
|
|
·
|
limit
our ability to obtain additional financing to fund future working capital,
capital investments and other business
activities;
|
|
·
|
limit
our ability to refinance our indebtedness on terms that are commercially
reasonable, or at all;
|
|
·
|
expose
us to the risk of interest rate fluctuations to the extent we pay interest
at variable rates on the debt;
|
|
·
|
limit
our flexibility to plan for, and react to, changes in our business and our
industry; and
|
|
·
|
place
us at a competitive disadvantage relative to our less leveraged
competitors.
|
Our
senior credit facilities contain restrictions that may limit our ability to
pursue our business strategies.
Our
senior credit facilities contain a number of covenants that impose significant
operating and financial restrictions on us and may limit our ability to engage
in acts that may be in our long-term best interests. These covenants restrict,
among other things, our ability to:
|
·
|
incur
or guarantee additional debt or issue certain preferred
stock;
|
|
·
|
pay
dividends or make distributions on our capital stock or certain
subordinated debt or redeem, repurchase or retire our capital stock or
certain subordinated debt;
|
|
·
|
make
certain investments;
|
|
·
|
create
liens on our or our subsidiaries’
assets;
|
|
·
|
make
distributions from our joint
ventures;
|
|
·
|
enter
into transactions with affiliates;
|
|
·
|
merge
or consolidate with another person or sell or otherwise dispose of all or
substantially all of our assets;
|
|
·
|
enter
into sales leaseback transactions;
|
|
·
|
sell
assets, including capital stock of our
subsidiaries;
|
|
·
|
alter
the business that we conduct; and
|
|
·
|
change
our fiscal year.
|
In
addition, we are required to maintain a total leverage ratio, a senior leverage
ratio and a fixed charge coverage ratio which become more restrictive over time.
A breach of any covenant contained in the senior credit facilities could result
in a default under those agreements. If any such default occurs, the lenders
under the senior credit facilities may elect (after the expiration of any
applicable notice or grace periods) to declare all outstanding borrowings,
together with accrued and unpaid interest and other amounts payable thereunder,
to be immediately due and payable. The lenders under the senior credit
facilities will also have the right upon an event of default thereunder to
terminate any commitments they have to provide further borrowings. If the debt
under the senior credit facilities were to be accelerated, our assets may not be
sufficient to repay in full that debt or any other debt that may become due as a
result of that acceleration.
- 22
-
Uncertainty
in the financial markets could limit the availability and terms of debt
financing sources to fund the capital and liquidity requirements of our
business.
One of
the primary risks relating to current market conditions is the possibility that
the lenders under our credit agreement will be unable to provide liquidity when
needed. While we are not aware of any specific risks involving our
counterparties, there can be no assurance that all of the lenders to our credit
agreement will fulfill their commitments if we need to make additional draws
against our revolving credit facility. In addition, a rapid increase in interest
rates and/or a decline in our operating performance could impair our ability to
comply with the financial covenants contained in our credit facility. A default
due to the violation of these covenants could require us to immediately repay
all amounts then outstanding under the credit facility. If we anticipate a
potential covenant violation, we would seek relief from our lenders; however,
such relief might not be granted or might be granted on terms less favorable
than those in our existing credit agreement. As of December 31, 2009,
we were in compliance with all debt covenants.
We
depend on the proper functioning and availability of our information
systems.
We are
dependent on the proper functioning and availability of our information systems
in operating our business. Our information systems are protected through
physical and software safeguards. However, they are still vulnerable to facility
infrastructure failure, fire, storm, flood, power loss, telecommunications
failures, physical or software break-ins and similar events. Our business
interruption insurance may be inadequate to protect us in the event of a
catastrophe. We also retain confidential patient information in our database. It
is critical that our facilities and infrastructure remain secure and are
perceived by clients as secure. A material security breach could damage our
reputation or result in liability to us. Despite the implementation of security
measures, we may be vulnerable to losses associated with the improper
functioning or unavailability of our information systems. From time to time, we
may also modify our information systems to take advantage of new technologies.
Such modifications may cause temporary disruptions to the operations of our
business, which could have a material adverse effect on our results from
operations in the periods affected.
Natural
disasters, pandemics and other unexpected events, including earthquakes,
hurricanes, fires and floods, could severely damage or interrupt our systems and
operations and result in a material adverse effect on our business, financial
condition and/or results of operations.
Natural
disasters such as fire, flood, earthquake, hurricane and tornado and other
events such as pandemic, power loss, computer virus, telecommunications failure,
break-in or similar event could severely damage or interrupt our systems and
operations, result in loss of data and/or delay or impair our ability to service
our clients and patients. We have in place a disaster recovery plan that is
intended to provide us with the ability to restore critical information systems;
however, we do not have full redundancy for all of our information systems in
the event of a natural disaster. There can be no assurance that our disaster
recovery plan will prevent damage or interruption of our systems and operations
if a natural disaster were to occur. Any such disaster or similar event could
have a material adverse effect on our business, financial condition and/or
results of operations.
- 23
-
Changes
in federal and state income tax laws and regulations or adverse decisions by
regulatory taxing authorities could cause a material adverse effect on our
results of operations.
United
States generally accepted accounting principles require financial statement
recognition of a tax position taken or expected to be taken in a tax return, if
that position is more likely than not of being sustained upon examination, based
on the technical merits of the position. Management believes its
estimates and judgments related to its uncertain tax positions are
reasonable. Nevertheless, the ultimate resolution of our tax matters
could differ from management’s estimates and such differences could be
material. See Note 14 to our accompanying consolidated financial
statements for additional information regarding our uncertain tax
positions.
We
are exposed to the credit risk of our payors which in the future may cause us to
make larger allowances for doubtful accounts or incur bad debt
write-offs.
Due to
deteriorating economic conditions or other factors, commercial payors and
customers may default on their payments to us and individual patients may
default on co-payments and deductibles for which they are responsible under the
terms of either commercial insurance programs or Medicare. Although we review
the credit risk of our commercial payors and customers regularly, such risks
will nevertheless arise from events or circumstances that are difficult to
anticipate or control, such as a general economic downturn. If our payors
default on their payments to us in the future, we may have to make larger
allowances for doubtful accounts or incur bad debt write-offs, both of which may
have an adverse impact on our profitability and cash flow.
Different
interpretations of accounting principles could result in material changes to our
reported results and financial condition.
U. S.
generally accepted accounting principles (“GAAP”) are complex, continually
evolving and may be subject to varied interpretation by third parties, including
the SEC. Such varied interpretations could result from differing views related
to specific facts and circumstances. Differences in interpretation of GAAP could
result in material changes to our reported results and financial
condition.
If
we are found to have violated laws protecting the confidentiality of patient
health information, we could be subject to civil or criminal penalties, which
could increase our liabilities and harm our reputation or our
business.
There are
a number of federal and state laws protecting the confidentiality of certain
patient health information, including patient records, and restricting the use
and disclosure of that protected information. In particular, the U.S. Department
of Health and Human Services promulgated patient privacy rules under the Health
Insurance Portability and Accountability Act of 1996, as amended, or HIPAA.
These privacy rules protect medical records and other personal health
information by limiting their use and disclosure, giving individuals the right
to access, amend and seek accounting of their own health information and
limiting most use and disclosures of health information to the minimum amount
reasonably necessary to accomplish the intended purpose. If we are found to be
in violation of the privacy rules under HIPAA, we could be subject to civil or
criminal penalties, which could increase our liabilities, harm our reputation
and have a material adverse effect on our business, financial condition and
results of operations.
| ITEM 1B. | UNRESOLVED STAFF COMMENTS |
None.
- 24
-
| ITEM 2. | PROPERTIES |
We
currently lease approximately 71,000 square feet of executive office space in
St. Louis, Missouri under a long-term lease which expires in September 2017 and
includes options for us to renew the lease for an additional ten year period
beyond the expiration date. In addition to the monthly rental cost,
we are also responsible for a share of certain other facility charges and
specified increases in operating costs.
We
continue to operate Triumph’s headquarters, which are located in an 86,000
square foot medical office building in Houston, Texas. We own a
controlling interest in the building and approximately 45,000 square feet of
office space is leased out to physicians and other healthcare service
providers.
Our
hospitals generally lease the facilities that support their operations typically
under long-term non-cancellable operating leases and our hospital facility
leases represent the largest portion of our rent expense. As of
December 31, 2009, 32 of our hospitals leased the facilities that support their
operations and two hospitals owned their facilities. Our hospital
leases generally have initial terms of 12 to 20 years, and most of our leases
contain one or more options to extend the lease term for up to five additional
years for each option. Our hospitals are generally responsible for
property taxes, property and casualty insurance and routine maintenance
expenses. Other than our principal executive offices, none of our other
properties are considered materially important.
Our
principal executive offices, hospitals, and other properties are suitable for
their respective uses and are, in general, adequate for our present needs. Our
properties are subject to various federal, state, and local statutes and
ordinances regulating their operation. Management does not believe compliance
with such statutes and ordinances will materially affect our business, financial
position, results of operations, or cash flows.
| ITEM 3. | LEGAL PROCEEDINGS |
At the
current time, we are not a party to any pending legal proceedings which we
believe are material.
In the
ordinary course of our business, we are a party to a number of claims and
lawsuits, as both plaintiff and defendant, which we regard as
immaterial. From time to time, and depending upon the particular
facts and circumstances, we may be subject to indemnification obligations under
our various contracts. We do not believe that any liability resulting
from such matters, after taking into consideration our insurance coverage and
amounts already provided for, will have a material effect on our consolidated
financial position or overall liquidity; however, such matters, or the expense
of prosecuting or defending them, could have a material effect on cash flows and
results of operations in a particular quarter or fiscal year as they develop or
as new issues are identified.
| ITEM 4. | SUBMISSION OF MATTERS TO A VOTE OF SECURITY HOLDERS |
Not
applicable.
- 25
-
PART
II
|
|
ITEM
5.
|
MARKET
FOR THE REGISTRANT’S COMMON STOCK, RELATED STOCKHOLDER MATTERS AND ISSUER
PURCHASES OF EQUITY SECURITIES
|
Our
common stock is listed and traded on the New York Stock Exchange under the
symbol “RHB.” The following graph compares the cumulative total
stockholder returns, assuming the reinvestment of dividends, of our common stock
on an indexed basis with the Dow Jones U.S. Health Care Providers Index and the
New York Stock Exchange (“NYSE”) Market Index for the five year period ended
December 31, 2009. The graph assumes an investment of $100 made in
our common stock and each index on January 1, 2005. We did not pay any dividends
during the period reflected in the graph. The Company does not
anticipate paying cash dividends in the foreseeable future. Our
common stock price performance shown below should not be viewed as being
indicative of future performance.
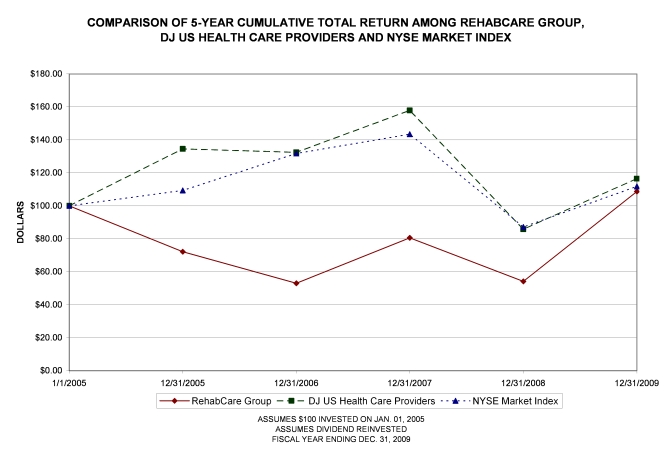
|
1/1/2005
|
12/31/2005
|
12/31/2006
|
12/31/2007
|
12/31/2008
|
12/31/2009
|
||||||
|
RehabCare
Group
|
$100.00
|
$72.17
|
$53.05
|
$80.60
|
$54.16
|
$108.72
|
|||||
|
Health
Care Providers
|
$100.00
|
$134.55
|
$132.44
|
$157.86
|
$85.76
|
$116.49
|
|||||
|
NYSE
Market Index
|
$100.00
|
$109.36
|
$131.75
|
$143.43
|
$87.12
|
$111.76
|
- 26
-
As of
February 26, 2010, there were 529 shareholders of record of the Company’s common
stock and an estimated 7,900 persons or entities holding common stock in nominee
name. The following table sets forth the high and low sales price per
share of our common stock, as reported on the New York Stock Exchange, for the
periods indicated. The stock price information is based on published
financial sources.
|
Calendar
Quarter
|
1st
|
2nd
|
3rd
|
4th
|
|
|
2009
|
High
|
$18.75
|
$23.93
|
$25.65
|
$31.29
|
|
Low
|
12.45
|
16.04
|
20.63
|
18.75
|
|
|
2008
|
High
|
$26.07
|
$17.41
|
$20.23
|
$18.09
|
|
Low
|
14.00
|
13.75
|
14.99
|
10.45
|
|
We did
not purchase any of our equity securities during 2008 or 2009.
See Part
III, Item 12, “Security Ownership of Certain Beneficial Owners and Management
and Related Stockholder Matters,” for information regarding common stock
authorized for issuance under equity compensation plans
| ITEM 6. | SELECTED FINANCIAL DATA |
The
following table presents selected financial data for the periods indicated for
our continuing operations only. See Item 7, “Management’s Discussion
and Analysis of Financial Condition and Results of Operations,” and the notes to
our accompanying consolidated financial statements for additional information
regarding the financial data presented under this item.
- 27
-
|
SIX-YEAR
FINANCIAL SUMMARY
|
|||||||||||||||||||||||
|
Dollars
in thousands, except per share data
|
|||||||||||||||||||||||
|
(Year
ended December 31,)
|
2009
|
2008
|
2007
|
2006
|
2005
|
2004
|
|||||||||||||||||
|
Consolidated
statement of earnings data:
|
|||||||||||||||||||||||
|
Operating
revenues
|
$
|
869,427
|
$
|
735,412
|
$
|
693,013
|
$
|
601,807
|
$
|
443,731
|
$
|
378,797
|
|||||||||||
|
Operating
earnings
|
44,474
|
32,907
|
27,530
|
21,551
|
32,610
|
41,311
|
|||||||||||||||||
|
Amounts
attributable to RehabCare: (2)
|
|||||||||||||||||||||||
|
Earnings (loss) from continuing
operations
|
$
|
23,794
|
$
|
19,568
|
$
|
13,041
|
$
|
7,594
|
$
|
(17,373)
|
$
|
22,893
|
|||||||||||
|
Basic EPS from continuing
operations
|
$
|
1.29
|
$
|
1.11
|
$
|
0.76
|
$
|
0.45
|
$
|
(1.04)
|
$
|
1.41
|
|||||||||||
|
Diluted EPS from continuing
operations
|
$
|
1.26
|
$
|
1.10
|
$
|
0.75
|
$
|
0.44
|
$
|
(1.04)
|
$
|
1.36
|
|||||||||||
|
Weighted
average shares outstanding (000s):
|
|||||||||||||||||||||||
|
Basic
|
18,481
|
17,583
|
17,226
|
17,008
|
16,751
|
16,292
|
|||||||||||||||||
|
Diluted
|
18,862
|
17,798
|
17,459
|
17,243
|
16,751
|
16,835
|
|||||||||||||||||
|
Consolidated
balance sheet data:
|
|||||||||||||||||||||||
|
Working
capital
|
$
|
113,296
|
$
|
97,284
|
$
|
80,285
|
$
|
85,982
|
$
|
60,664
|
$
|
76,451
|
|||||||||||
|
Total
assets
|
1,109,980
|
438,406
|
408,560
|
428,296
|
272,925
|
277,666
|
|||||||||||||||||
|
Total
liabilities
|
650,360
|
160,606
|
163,271
|
217,431
|
74,677
|
70,638
|
|||||||||||||||||
|
Total
equity
|
459,620
|
277,800
|
245,289
|
210,865
|
198,248
|
207,028
|
|||||||||||||||||
|
Financial
statistics:
|
|||||||||||||||||||||||
|
Operating
margin
|
5.1%
|
4.5%
|
4.0%
|
3.6%
|
7.3%
|
10.9%
|
|||||||||||||||||
|
Net
margin (2)
|
2.7%
|
2.7%
|
1.9%
|
1.3%
|
(3.9)%
|
6.0%
|
|||||||||||||||||
|
Current
ratio
|
1.7:1
|
2.1:1
|
1.9:1
|
1.9:1
|
1.9:1
|
2.3:1
|
|||||||||||||||||
|
Diluted
EPS growth rate (2)
|
14.5%
|
46.7%
|
70.5%
|
142.3%
|
(176.5)%
|
258.1%
|
|||||||||||||||||
|
Return
on equity (1)
(2)
|
6.5%
|
7.5%
|
5.7%
|
3.7%
|
(8.6)%
|
11.9%
|
|||||||||||||||||
|
Operating
statistics:
|
|||||||||||||||||||||||
|
Hospitals:
|
|||||||||||||||||||||||
|
Number of hospitals at end of
year (3)
|
34
|
11
|
8
|
7
|
5
|
N/A
|
|||||||||||||||||
|
Number of patient discharges
(3)
|
8,369
|
6,019
|
5,070
|
3,595
|
1,110
|
N/A
|
|||||||||||||||||
|
Program
management:
|
|||||||||||||||||||||||
|
Inpatient
units:
|
|||||||||||||||||||||||
|
Average number of
programs
|
121
|
122
|
127
|
137
|
145
|
142
|
|||||||||||||||||
|
Average admissions per
program
|
393
|
377
|
363
|
360
|
372
|
383
|
|||||||||||||||||
|
Outpatient
programs:
|
|||||||||||||||||||||||
|
Average number of
locations
|
35
|
33
|
35
|
41
|
42
|
42
|
|||||||||||||||||
|
Patient visits
(000s)
|
1,264
|
983
|
1,006
|
1,130
|
1,146
|
1,133
|
|||||||||||||||||
|
Contract
therapy:
|
|||||||||||||||||||||||
|
Average number of locations
(4)
|
1,088
|
1,066
|
1,125
|
1,018
|
749
|
588
|
|
(1)
|
Based
on average of beginning and ending
equity.
|
|
(2)
|
The
results for 2005 include after tax losses on our equity investment in
InteliStaf Holdings, Inc. of $36.5 million or $2.18 per diluted
share.
|
|
(3)
|
We
entered the freestanding hospitals business on August 1, 2005 with the
acquisition of substantially all of the operating assets of MeadowBrook
Healthcare, Inc. Effective November 24, 2009, we acquired
Triumph HealthCare Holdings, Inc., which added 20 long-term acute care
hospitals to our portfolio of
hospitals.
|
|
(4)
|
Effective
July 1, 2006, we acquired Symphony Health Services, LLC and its RehabWorks
business, which added 470 contract therapy
locations.
|
- 28
-
|
|
ITEM
7.
|
MANAGEMENT’S
DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF
OPERATIONS
|
Overview
In the
first quarter of 2009, we made certain changes to the structure of our internal
organization. These changes primarily consisted of making our skilled
nursing rehabilitation services division responsible for oversight of our
businesses that provide resident-centered management consulting services and
staffing services for therapists and nurses. Following these
structural changes and the June 2009 sale of Phase 2 Consulting, Inc. (“Phase
2”), we now operate in the following two business segments, which are managed
separately based on fundamental differences in operations: program management
services and hospitals. Program management services include hospital
rehabilitation services (including inpatient acute and subacute rehabilitation
and outpatient therapy programs) and skilled nursing rehabilitation services
(including contract therapy in skilled nursing facilities, resident-centered
management consulting services and staffing services for therapists and
nurses). Our hospitals segment owns and operates 28 long-term acute
care hospitals (LTACHs) and 6 inpatient rehabilitation hospitals.
|
Year
Ended December 31,
|
|||||||||
|
2009
|
2008
|
2007
|
|||||||
|
(in
thousands)
|
|||||||||
|
Revenues:
|
|||||||||
|
Program
management:
|
|||||||||
|
Skilled
nursing rehabilitation services
|
$
|
496,250
|
$
|
457,229
|
$
|
432,910
|
|||
|
Hospital
rehabilitation services
|
178,168
|
165,658
|
164,102
|
||||||
|
Program
management total
|
674,418
|
622,887
|
597,012
|
||||||
|
Hospitals
|
195,009
|
112,525
|
96,001
|
||||||
|
Total
|
$
|
869,427
|
$
|
735,412
|
$
|
693,013
|
|||
|
Operating
Earnings (Loss):
|
|||||||||
|
Program
management:
|
|||||||||
|
Skilled
nursing rehabilitation services
|
$
|
37,753
|
$
|
25,544
|
$
|
7,249
|
|||
|
Hospital
rehabilitation services
|
29,487
|
21,997
|
22,893
|
||||||
|
Program management
total
|
67,240
|
47,541
|
30,142
|
||||||
|
Hospitals
(1)
|
(22,512
|
)
|
(13,903
|
)
|
(1,972
|
)
|
|||
|
Unallocated
corporate expenses (2)
|
(254
|
)
|
(731
|
)
|
(640
|
)
|
|||
|
Total
|
$
|
44,474
|
$
|
32,907
|
$
|
27,530
|
|||
|
|
(1)
|
The
2009 operating earnings of hospitals include $7.2 million of
acquisition-related expenses for costs directly related to the acquisition
of Triumph including fees for legal, accounting, advisory and other
outside services. The 2007 operating earnings of hospitals
include a $4.9 million impairment loss on a separately identifiable
intangible asset. See Note 7 to the consolidated financial
statements for additional
information.
|
|
|
(2)
|
Represents
general corporate overhead costs associated with Phase 2 Consulting, Inc.,
which was sold on June 1, 2009.
|
Effective
November 24, 2009, we acquired all of the outstanding common stock of Triumph
HealthCare Holdings, Inc. (“Triumph”) for a purchase price of approximately
$538.5 million. On the acquisition date, Triumph operated 20 LTACHs
in seven states. Triumph’s results of operations have been included
in the Company’s financial statements prospectively beginning after the date of
acquisition. In 2009, we also acquired LTACHs in Dallas, Texas and
Philadelphia, Pennsylvania and opened a majority-owned LTACH in Peoria,
Illinois. These activities expanded the number of LTACHs we own and
operate to 28, making us the third largest LTACH provider in the United
States.
- 29
-
Effective
June 1, 2009, the Company completed the sale of all the outstanding common stock
of Phase 2 Consulting, Inc. (“Phase 2”) to Premier, Inc. for approximately $5.5
million. Phase 2 provides management and economic consulting services
to the healthcare industry and had been a subsidiary of the Company since it was
acquired in 2004. This transaction allows the Company’s management to
focus on its core businesses. Phase 2 has been classified as a
discontinued operation pursuant to U.S. generally accepted accounting principles
(“GAAP”). Prior year comparative amounts throughout Management’s
Discussion and Analysis of Financial Condition and Results of Operations have
been adjusted to reflect the treatment of Phase 2 as a discontinued
operation.
Sources
of Revenue
In our
program management segment, we derive the majority of our revenues from fees
paid directly by healthcare providers rather than through payment or
reimbursement by government or other third-party payors. A portion of
our revenues in this segment are derived from our direct bill contract therapy
rehab agencies. Our inpatient and outpatient therapy programs are
typically provided through agreements with hospital clients with three to
five-year terms. Our contract therapy services are typically provided
under one to two year agreements primarily with skilled nursing
facilities.
In our
hospital segment, we derive nearly all of our revenues from fees for patient
care services, which are usually paid for or reimbursed by Medicare, Medicaid or
third party managed care programs. Our hospital segment accounted for
22.4% of our consolidated operating revenues in 2009. We expect that
percentage will increase to approximately 50% in 2010 as a result of the
acquisition of Triumph. The following table identifies the sources
and relative mix of our hospital segment’s net operating revenues for the
periods stated:
|
Year
Ended December 31,
|
|||||||||
|
2009
|
2008
|
2007
|
|||||||
|
Medicare
|
68.8
|
%
|
74.2
|
%
|
77.8
|
%
|
|||
|
Medicaid
|
2.0
|
0.8
|
0.6
|
||||||
|
Other
third party payors
|
27.4
|
22.5
|
19.1
|
||||||
|
Self-pay
|
0.1
|
0.4
|
0.5
|
||||||
|
Total
net patient revenue
|
98.3
|
97.9
|
98.0
|
||||||
|
Other
revenue
|
1.7
|
2.1
|
2.0
|
||||||
|
100.0
|
%
|
100.0
|
%
|
100.0
|
%
|
||||
The
decrease in the percent of net revenues attributable to Medicare reflects an
increase in managed Medicare and private fee-for-service plans that are included
in “other third party payor” category in the table above. As part of
the Balanced Budget Act of 1997, Congress created a program of private, managed
healthcare coverage for Medicare beneficiaries. This program has been referred
to as Medicare Part C, Medicare+Choice or Medicare Advantage. While
we expect our payor mix will remain heavily weighted towards traditional
Medicare, we expect this shift of traditional Medicare patients into managed
Medicare and private fee-for-service plans will continue.
- 30
-
Results
of Operations
The
following table sets forth the percentage that selected items in the
consolidated statements of earnings bear to operating revenues for the years
ended December 31, 2009, 2008 and 2007:
|
Year
Ended December 31,
|
|||||||||
|
2009
|
2008
|
2007
|
|||||||
|
Operating
revenues
|
100.0
|
%
|
100.0
|
%
|
100.0
|
%
|
|||
|
Cost
and expenses:
|
|||||||||
|
Operating
|
81.0
|
81.3
|
81.0
|
||||||
|
Selling,
general and administrative
|
12.0
|
12.2
|
11.9
|
||||||
|
Impairment
of assets
|
—
|
—
|
0.7
|
||||||
|
Depreciation
and amortization
|
1.9
|
2.0
|
2.4
|
||||||
|
Operating
earnings
|
5.1
|
4.5
|
4.0
|
||||||
|
Interest
income
|
—
|
—
|
0.1
|
||||||
|
Interest
expense
|
(0.6
|
)
|
(0.5
|
)
|
(1.2
|
)
|
|||
|
Equity
in net income of affiliate
|
—
|
—
|
—
|
||||||
|
Earnings
from continuing operations before income taxes
|
4.5
|
4.0
|
2.9
|
||||||
|
Income
taxes
|
2.0
|
1.6
|
1.1
|
||||||
|
Earnings
from continuing operations, net of tax
|
2.5
|
2.4
|
1.8
|
||||||
|
Loss
from discontinued operations, net of tax
|
(0.1
|
)
|
(0.1
|
)
|
—
|
||||
|
Net
earnings
|
2.4
|
2.3
|
1.8
|
||||||
|
Net
loss attributable to noncontrolling interests
|
0.2
|
0.2
|
—
|
||||||
|
Net
earnings attributable to RehabCare
|
2.6
|
%
|
2.5
|
%
|
1.8
|
%
|
|||
Twelve
Months Ended December 31, 2009 Compared to Twelve Months Ended December 31,
2008
|
Revenues
|
|||||||||
|
2009
|
2008
|
%
Change
|
|||||||
|
(dollars
in thousands)
|
|||||||||
|
Skilled
nursing rehabilitation services
|
$
|
496,250
|
$
|
457,229
|
8.5
|
%
|
|||
|
Hospital
rehabilitation services
|
178,168
|
165,658
|
7.6
|
||||||
|
Hospitals
|
195,009
|
112,525
|
73.3
|
||||||
|
Consolidated
revenues
|
$
|
869,427
|
$
|
735,412
|
18.2
|
%
|
|||
Consolidated
operating revenues increased from $735.4 million in 2008 to $869.4 million in
2009 due to growth in each of our business units.
Skilled Nursing Rehabilitation
Services (SRS). SRS operating revenues increased $39.0 million
or 8.5% from 2008 to 2009. Same store contract therapy revenues grew
8.8% reflecting a 5.7% increase in same store minutes of
service. Higher average daily census, improved therapist productivity
and a market basket adjustment for skilled nursing facilities which became
effective October 1, 2008 contributed to the growth in same store
revenues. The average number of contract therapy locations operated
during 2009 grew 2.1% compared to 2008. SRS operated in 1,118
contract therapy locations as of December 31, 2009.
- 31
-
Hospital Rehabilitation Services
(HRS). HRS operating revenues increased 7.6% in 2009 as
inpatient revenue increased 6.6% and outpatient revenue increased
10.4%. Inpatient average revenue per program increased 7.7% in 2009
reflecting a favorable change in the division’s contract mix which included a
2.7% increase in the average number of inpatient rehabilitation facility
programs operated in 2009. In addition, same store revenues for
inpatient rehabilitation facilities grew 2.4% and same store discharges
increased 1.2% compared to 2008. The increase in outpatient revenue
in 2009 reflects a 6.7% increase in the average number of units operated and a
7.4% increase in same store revenues.
Hospitals. Hospitals
segment revenues increased $82.5 million or 73.3% from 2008 to
2009. The acquisition of Triumph contributed incremental revenues of
$39.7 million in 2009. The increase in revenues in 2009 also reflects
the June 2009 acquisition of an LTACH in Dallas, the June 2008 acquisition of
The Specialty Hospital in Rome, Georgia, the November 2008 opening of a
rehabilitation hospital in St. Louis, Missouri and the December 2008
certification of an LTACH in Kansas City, Missouri. Same store
revenues increased by $8.8 million or 8.5% in 2009 as compared to
2008. One LTACH hospital contributed $5.4 million to the same store
revenue growth primarily as a result of an increase in patient
census.
|
Cost
and Expenses
|
||||||||||||||
|
%
of
|
%
of
|
|||||||||||||
|
2009
|
Revenue
|
2008
|
Revenue
|
|||||||||||
|
(dollars
in thousands)
|
||||||||||||||
|
Consolidated
costs and expenses:
|
||||||||||||||
|
Operating
expenses
|
$
|
704,394
|
81.0
|
%
|
$
|
597,879
|
81.3
|
%
|
||||||
|
Selling,
general and administrative
|
104,060
|
12.0
|
90,056
|
12.2
|
||||||||||
|
Depreciation
and amortization
|
16,499
|
1.9
|
14,570
|
2.0
|
||||||||||
|
Total
costs and expenses
|
$
|
824,953
|
94.9
|
%
|
$
|
702,505
|
95.5
|
%
|
||||||
Operating
expenses as a percentage of revenues decreased primarily due to improved
operating performances by our skilled nursing rehabilitation services and
hospital rehabilitation services businesses. The decrease in selling,
general and administrative expenses as a percentage of revenues reflects the
increase in revenues combined with the cost savings achieved by eliminating
approximately 60 corporate and division support positions in the second half of
2008. These cost savings were more than offset by, an increase in
both long-term and short-term management incentives, reflecting the improved
overall performance of the Company, and an increase in selling, general and
administrative expenses incurred by our hospital segment including approximately
$7.2 million of external costs associated with the Triumph
acquisition.
The
Company’s provision for doubtful accounts is included in operating
expenses. On a consolidated basis, the provision for doubtful
accounts decreased by $1.0 million from $8.7 million in 2008 to $7.7 million in
2009. Our hospital rehabilitation services (“HRS”) business decreased
its provision by $1.2 million in 2009. HRS recorded a $1.2 million
specific provision in 2008 related to the Company’s trade and note receivables
due from Signature Healthcare Foundation. This specific provision was
a result of Signature’s deteriorating financial condition during
2008. In February 2009, the Company terminated its staffing agreement
with Signature and took possession of Signature’s operating assets in full
satisfaction of the Company’s receivables from Signature. At December
31, 2008, the Company’s receivables from Signature had a remaining carrying
value of $580,000 which approximates the estimated fair value of the assets
received from Signature.
- 32
-
|
%
of
|
%
of
|
|||||||||||||
|
Unit
|
Unit
|
|||||||||||||
|
2009
|
Revenue
|
2008
|
Revenue
|
|||||||||||
|
(dollars
in thousands)
|
||||||||||||||
|
Skilled
Nursing Rehabilitation Services:
|
||||||||||||||
|
Operating
expenses
|
$
|
402,461
|
81.1
|
%
|
$
|
373,939
|
81.8
|
%
|
||||||
|
Selling,
general and administrative
|
49,753
|
10.0
|
50,911
|
11.1
|
||||||||||
|
Depreciation
and amortization
|
6,283
|
1.3
|
6,835
|
1.5
|
||||||||||
|
Total
costs and expenses
|
$
|
458,497
|
92.4
|
%
|
$
|
431,685
|
94.4
|
%
|
||||||
|
Hospital
Rehabilitation Services:
|
||||||||||||||
|
Operating
expenses
|
$
|
124,758
|
70.0
|
%
|
$
|
118,291
|
71.4
|
%
|
||||||
|
Selling,
general and administrative
|
21,500
|
12.1
|
22,729
|
13.7
|
||||||||||
|
Depreciation
and amortization
|
2,423
|
1.3
|
2,641
|
1.6
|
||||||||||
|
Total
costs and expenses
|
$
|
148,681
|
83.4
|
%
|
$
|
143,661
|
86.7
|
%
|
||||||
|
Hospitals:
|
||||||||||||||
|
Operating
expenses
|
$
|
177,175
|
90.8
|
%
|
$
|
105,649
|
93.9
|
%
|
||||||
|
Selling,
general and administrative
|
32,553
|
16.7
|
15,685
|
13.9
|
||||||||||
|
Depreciation
and amortization
|
7,793
|
4.0
|
5,094
|
4.6
|
||||||||||
|
Total
costs and expenses
|
$
|
217,521
|
111.5
|
%
|
$
|
126,428
|
112.4
|
%
|
||||||
Skilled Nursing Rehabilitation
Services (SRS). Total skilled nursing rehabilitation services
(“SRS”) costs and expenses as a percentage of unit revenue decreased in 2009
compared to 2008 primarily due to an increase in therapist productivity and a
decrease in selling, general and administrative expenses. Operating
expenses declined as a percentage of unit revenue primarily due to a reduction
in labor and benefit costs as a percentage of revenue. This was
driven by therapist productivity improvements and lower contract labor usage in
2009 which more than offset the impact of wage rate and benefit cost
increases. Improved therapist retention and a reduction in the time
to fill permanent positions may have contributed to the decreased use of
contract labor. Selling, general and administrative expenses
decreased primarily due to the cost savings achieved from the division and
corporate realignment activities that were completed in the second half of
2008. Depreciation and amortization expense decreased primarily due
to lower depreciation associated with capitalized software which became fully
depreciated in 2008. As a result of these factors combined with
higher revenues, SRS’s operating earnings increased by approximately $12.3
million from $25.5 million in 2008 to $37.8 million in 2009.
Hospital Rehabilitation Services
(HRS). Total HRS costs and expenses as a percentage of unit
revenue decreased in 2009 compared to 2008 primarily due to improved operating
performance and a decrease in selling, general and administrative
expenses. Operating expenses decreased as a percentage of unit
revenue in 2009 reflecting a favorable change in the division’s contract mix,
which included an additional 2.9 inpatient rehabilitation facility (“IRF”)
programs on average in 2009 as compared to 2008 as well as a lower provision for
doubtful accounts primarily due the charge taken in 2008 for receivables from
Signature. While the average number of IRF programs increased from
2008 to 2009, the actual number of IRF programs declined from 113 at the
beginning of 2009 to 106 as of December 31, 2009. Selling, general
and administrative expenses decreased primarily as a result of corporate and
division realignment activities during late 2008 and early 2009,
respectively. Depreciation and amortization expense decreased
primarily due to lower depreciation associated with capitalized software which
became fully depreciated in 2008. HRS’s operating earnings increased
from $22.0 million in 2008 to $29.5 million in 2009.
- 33
-
Hospitals. Total
hospital segment costs and expenses as a percentage of unit revenue decreased
slightly from 2008 to 2009. Operating expenses decreased as a
percentage of unit revenue in 2009 primarily as a result of improved operating
performance by our legacy LTACHs in 2009. In addition, Triumph’s
hospitals provided operating profit of $3.7 million or 9.3% of revenue during
the 37 days we owned Triumph in 2009. Combined start-up and ramp-up
losses declined from $5.8 million in 2008 to $4.8 million in
2009. The 2009 losses relate primarily to the start-up of our LTACH
in Peoria, Illinois and the ramp-up of our LTACH in Kansas City. We
define the ramp-up phase for an LTACH as the period during which the hospital
attempts to build its patient census following the receipt of its LTACH Medicare
provider number. Selling, general and administrative expenses
increased from the prior year largely due to costs incurred for acquisition and
joint venture development activities and an investment in back office resources
to support the recent growth of the business. In 2009, we incurred
$7.2 million of acquisition-related expenses for outside costs directly related
to the acquisition of Triumph and another $3.5 million of expenses for outside
services related to other acquisition-related activities. In 2008, we
incurred $1.8 million of expense related to outside services for canceled
acquisitions and joint venture development projects. On January 1,
2009, we adopted a new accounting standard for business combinations which
requires us to expense all acquisition-related costs. Prior to
January 1, 2009, outside service costs incurred for consummated transactions
were capitalized as a component of the acquisition cost and only costs related
to canceled transactions were expensed. Depreciation and amortization
expense increased from 2008 to 2009 primarily due to depreciation and
amortization associated with Triumph and our other new facilities. As
a result of these factors, the hospital segment incurred operating losses of
$22.5 million in 2009 and $13.9 million in 2008.
Non-operating
Items
Interest
expense increased from $3.9 million in 2008 to $5.5 million in 2009 primarily
due to the net increase in borrowings which occurred in connection with funding
the November 24, 2009 acquisition of Triumph. The balances
outstanding on all forms of indebtedness were $464.2 million and $57.0 million
at December 31, 2009 and 2008, respectively. Interest expense
includes interest incurred on all our borrowings, amortization of deferred loan
origination fees, amortization of original issue discounts, commitment fees paid
on the unused portion of our line of credit and fees paid on outstanding letters
of credit.
Earnings
from continuing operations before income taxes increased to $39.5 million in
2009 from $29.6 million in 2008. The provision for income taxes was
$17.6 million in 2009 compared to $12.1 million in 2008, reflecting effective
income tax rates of 44.7% and 40.7%, respectively. The increase in
the effective tax rate in 2009 reflects the fact that certain
acquisition-related expenses incurred in connection with the Triumph transaction
are not deductible for tax purposes.
The
Company incurred losses from discontinued operations, net of tax, of $0.8
million and $0.9 million during the years ended December 31, 2009 and 2008,
respectively. Such losses relate to Phase 2, which was sold in the
second quarter of 2009, and RehabCare Rehabilitation Hospital – Permian Basin, a
38-bed inpatient rehabilitation hospital located in Midland, Texas (the “Midland
hospital”), which was sold in the third quarter of 2008. The Company
incurred an after tax loss of approximately $0.7 million on the sale of Phase
2.
Net
losses attributable to noncontrolling interests in consolidated subsidiaries
were $2.0 million in both 2009 and 2008. The 2009 losses primarily
relate to our hospitals in Peoria, Dallas and Kansas City while the 2008 losses
primarily relate to our hospitals in Kansas City and St. Louis.
Net
earnings attributable to RehabCare were $23.0 million in 2009 compared to $18.7
million in 2008. Diluted earnings per share attributable to RehabCare
were $1.22 in 2009 compared to $1.05 in 2008.
- 34
-
Twelve
Months Ended December 31, 2008 Compared to Twelve Months Ended December 31,
2007
|
Revenues
|
|||||||||
|
2008
|
2007
|
%
Change
|
|||||||
|
(dollars
in thousands)
|
|||||||||
|
Skilled
nursing rehabilitation services
|
$
|
457,229
|
$
|
432,910
|
5.6
|
%
|
|||
|
Hospital
rehabilitation services
|
165,658
|
164,102
|
0.9
|
||||||
|
Hospitals
|
112,525
|
96,001
|
17.2
|
||||||
|
Consolidated
revenues
|
$
|
735,412
|
$
|
693,013
|
6.1
|
%
|
|||
Consolidated
operating revenues increased from 2007 to 2008 primarily due to the growth in
our skilled nursing rehabilitation services and hospital
businesses.
Skilled Nursing Rehabilitation
Services (SRS). SRS operating revenues increased $24.3 million
from 2007 to 2008. Same store contract therapy revenues increased by
$39.7 million or 12.4% reflecting a 10.3% increase in same store minutes of
service. The same store revenue growth more than offset the impact of
a 5.3% decline in the average number of contract therapy locations operated
during 2008. Higher average daily census and improved
productivity contributed to the growth in same store revenues and same store
minutes of service.
Hospital Rehabilitation Services
(HRS). HRS operating revenues increased 0.9% in 2008 as
inpatient revenue increased 1.4% and outpatient revenue declined
0.4%. The increase in inpatient revenue reflects a 5.3% increase in
average revenue per program, partially offset by a 3.7% decline in the average
number of units operated. Same store inpatient rehabilitation
facility discharges increased 1.9% in 2008 as the division’s units were able to
increase patient volumes in 2008 following the January 1, 2008 effective date of
the freeze in the 60% Rule’s compliance threshold. The decline in
outpatient revenue reflects a 4.2% decline in the average number of units
operated, partially offset by a 3.9% increase in average revenue per
program. Outpatient same store revenues grew 4.9% in
2008.
Hospitals. Hospital
segment revenues increased $16.5 million from 2007 to 2008. The
increase in revenues reflects the acquisition of The Specialty Hospital in Rome,
Georgia effective June 1, 2008 and a full year of operations of our inpatient
rehabilitation hospital in Austin, Texas, which received its Medicare provider
number in November 2007. The hospital segment also opened an LTACH in
Kansas City, Missouri in April 2008 and a rehabilitation hospital in St. Louis,
Missouri in November 2008. Same store revenues increased by $1.5
million or 1.6% in 2008 as compared to 2007. Our inpatient
rehabilitation hospital in Amarillo, Texas, which was in its ramp-up phase in
the first quarter of 2007, contributed $1.2 million to the same store revenue
growth. We define the ramp-up phase as the period during which a
recently opened hospital builds its patient census following the receipt of its
Medicare provider number.
- 35
-
|
Cost
and Expenses
|
||||||||||||||
|
%
of
|
%
of
|
|||||||||||||
|
2008
|
Revenue
|
2007
|
Revenue
|
|||||||||||
|
(dollars
in thousands)
|
||||||||||||||
|
Consolidated
costs and expenses:
|
||||||||||||||
|
Operating
expenses
|
$
|
597,879
|
81.3
|
%
|
$
|
561,233
|
81.0
|
%
|
||||||
|
Selling,
general and administrative
|
90,056
|
12.2
|
82,806
|
11.9
|
||||||||||
|
Impairment
of assets
|
—
|
—
|
4,906
|
0.7
|
||||||||||
|
Depreciation
and amortization
|
14,570
|
2.0
|
16,538
|
2.4
|
||||||||||
|
Total
costs and expenses
|
$
|
702,505
|
95.5
|
%
|
$
|
665,483
|
96.0
|
%
|
||||||
Operating
expenses increased slightly as a percentage of revenues as a decline in earnings
realized by our hospital segment was mostly offset by improved operating
performance from our skilled nursing rehabilitation services
division. Both variances are discussed further below. The
increase in selling, general and administrative expenses reflects the costs of
severance benefits incurred in 2008, an increase in share-based compensation and
other management incentive costs and an investment in back office resources to
support the current year and expected future growth of our hospital
segment. These cost increases were partially offset by the cost
savings achieved from closing Symphony’s corporate office in Hunt Valley,
Maryland at the end of June 2007. The hospital segment incurred a
$4.9 million impairment charge in 2007 as discussed in more detail
below. Depreciation and amortization expense decreased primarily due
to lower amortization associated with capitalized software and intangible assets
which became fully amortized in 2007 and 2008.
The
Company’s provision for doubtful accounts is included in operating
expenses. On a consolidated basis, the provision for doubtful
accounts decreased by $0.4 million from $9.1 million in 2007 to $8.7 million in
2008. The provision recorded by our skilled nursing rehabilitation
services business decreased by $1.7 million in 2008. This decrease
reflects the results of a concerted focus on collection activities and our
efforts over the past two years to improve the quality of the division’s
portfolio of accounts receivable. The decreased provision for our
skilled nursing rehabilitation services business was partially offset by a $0.9
million increase for our hospital rehabilitation services (“HRS”)
business. The increased provision for HRS is primarily related to the
Company’s trade and note receivables due from Signature Healthcare Foundation as
a result of Signature’s deteriorating financial condition during
2008.
- 36
-
|
%
of
|
%
of
|
|||||||||||||
|
Unit
|
Unit
|
|||||||||||||
|
2008
|
Revenue
|
2007
|
Revenue
|
|||||||||||
|
(dollars
in thousands)
|
||||||||||||||
|
Skilled
Nursing Rehabilitation Services:
|
||||||||||||||
|
Operating
expenses
|
$
|
373,939
|
81.8
|
%
|
$
|
363,909
|
84.1
|
%
|
||||||
|
Selling,
general and administrative
|
50,911
|
11.1
|
52,975
|
12.2
|
||||||||||
|
Depreciation
and amortization
|
6,835
|
1.5
|
8,777
|
2.0
|
||||||||||
|
Total
costs and expenses
|
$
|
431,685
|
94.4
|
%
|
$
|
425,661
|
98.3
|
%
|
||||||
|
Hospital
Rehabilitation Services:
|
||||||||||||||
|
Operating
expenses
|
$
|
118,291
|
71.4
|
%
|
$
|
115,706
|
70.5
|
%
|
||||||
|
Selling,
general and administrative
|
22,729
|
13.7
|
21,399
|
13.0
|
||||||||||
|
Depreciation
and amortization
|
2,641
|
1.6
|
4,104
|
2.5
|
||||||||||
|
Total
costs and expenses
|
$
|
143,661
|
86.7
|
%
|
$
|
141,209
|
86.0
|
%
|
||||||
|
Hospitals:
|
||||||||||||||
|
Operating
expenses
|
$
|
105,649
|
93.9
|
%
|
$
|
81,618
|
85.0
|
%
|
||||||
|
Selling,
general and administrative
|
15,685
|
13.9
|
7,792
|
8.1
|
||||||||||
|
Impairment
of intangible assets
|
—
|
—
|
4,906
|
5.1
|
||||||||||
|
Depreciation
and amortization
|
5,094
|
4.6
|
3,657
|
3.9
|
||||||||||
|
Total
costs and expenses
|
$
|
126,428
|
112.4
|
%
|
$
|
97,973
|
102.1
|
%
|
||||||
Skilled Nursing Rehabilitation
Services (SRS). Total SRS costs and expenses as a percentage
of unit revenue decreased in 2008 primarily due to operational efficiencies and
cost savings achieved from completing the integration of Symphony and closing
Symphony’s corporate office in Hunt Valley, Maryland at the end of June
2007. Operating expenses declined as a percentage of unit revenue
reflecting the combined impact of continued efficiencies realized from the
integration of the former RehabWorks’ units and improved therapist productivity
throughout the division. Contract therapy labor and benefit costs per
minute of service declined by 0.5% in 2008 as therapist productivity
improvements during 2008 more than offset the impact of wage rate
increases. Selling, general and administrative expenses decreased as
a percentage of unit revenue primarily due to synergies achieved from the
integration of the Symphony business. Depreciation and amortization
expense decreased primarily because capitalized software assets associated with
the Symphony acquisition became fully depreciated in the fourth quarter of
2007. SRS’s operating earnings were $25.5 million in 2008 compared to
$7.2 million in 2007.
Hospital Rehabilitation Services
(HRS). Total HRS costs and expenses as a percentage of unit
revenue increased in 2008 primarily due to an increase in operating
expenses. Operating expenses increased as a percentage of unit
revenue reflecting an increase in professional liability expense due to
favorable reserve adjustments recognized in 2007 and the increase in the
provision for doubtful accounts explained above. Selling, general and
administrative expenses increased reflecting increases in legal expense,
share-based compensation expense and other management incentive
costs. The increased legal expense in 2008 primarily related to the
proposed settlement of a wage and hour lawsuit in
California. Depreciation and amortization expense decreased primarily
due to lower depreciation and amortization associated with capitalized software
and other fixed assets which became fully depreciated. Total hospital
rehabilitation services operating earnings were $22.0 million in 2008 compared
to $22.9 million in 2007.
- 37
-
Hospitals. Total
hospital segment costs and expenses increased as a percentage of unit revenue in
2008 despite the recognition of a $4.9 million impairment loss in
2007. This impairment loss reduced the carrying value of an
intangible asset to its revised estimate of fair value based on the impact of a
change in LTACH regulations issued by CMS on May 1, 2007. Operating
expenses increased as a percentage of unit revenue in 2008 primarily due to
increased start-up and ramp-up losses and a decline in earnings from our mature
hospitals, including our Clear Lake, Texas hospital which was significantly
impacted by Hurricane Ike. The division incurred start-up losses of
$5.0 million in 2008 primarily related to the development of an LTACH in Kansas
City. Start-up losses were $1.6 million in 2007. Selling,
general and administrative expenses increased from the prior year period
reflecting an investment in back office resources to support the growth in the
business expected in 2009 and a $1.2 million charge to expense in 2008 of
previously deferred direct acquisition costs related to our decision to
discontinue efforts to acquire a controlling interest in an inpatient
rehabilitation hospital in Rhode Island. Depreciation and
amortization expense increased in 2008 primarily due to depreciation and
amortization associated with our newest facilities. As a result of
these factors, the hospitals segment incurred operating losses of $13.9 million
in 2008 and $2.0 million in 2007.
Non-operating
Items
Interest
income decreased from $0.8 million in 2007 to $0.1 million in 2008 primarily due
to the recognition of $0.7 million of interest income in 2007 related to a
federal income tax refund claim.
Interest
expense decreased from $8.4 million in 2007 to $3.9 million in 2008 primarily
due to both a reduction in interest rates and a reduction in average total debt
outstanding. The balance outstanding on our revolving credit facility
was $57.0 million and $68.5 million at December 31, 2008 and 2007,
respectively. Interest expense includes interest incurred on all our
borrowings, amortization of deferred loan origination fees, amortization of
original issue discounts, commitment fees paid on the unused portion of our line
of credit, and fees paid on outstanding letters of credit.
Earnings
from continuing operations before income taxes increased to $29.6 million in
2008 from $20.3 million in 2007. The provision for income taxes was
$12.1 million in 2008 compared to $7.7 million in 2007, reflecting effective
income tax rates of 40.7% and 37.7%, respectively. The increase in
the effective tax rate reflects the increase in net losses attributable to
noncontrolling interests from which we do not derive a related tax
benefit.
The
Company incurred losses from discontinued operations, net of tax, of $0.9
million and $0.4 million during the years ended December 31, 2008 and 2007,
respectively. The losses in 2008 primarily relate to the operations
of the Midland hospital partially offset by a net gain of $0.3 million
recognized on the sale of that hospital effective August 30,
2008. The loss in 2007 reflects a loss from the operations of the
Midland hospital, partially offset by a gain from the operations of Phase 2
Consulting, Inc.
Net
losses attributable to noncontrolling interests in consolidated subsidiaries
increased to $2.0 million in 2008 from $0.4 million in 2007. This
increase is primarily due to the recognition of the noncontrolling interests’
share of the losses incurred by our LTACH in Kansas City.
Net
earnings attributable to RehabCare were $18.7 million in 2008 compared to $12.7
million in 2007. Diluted earnings per share attributable to RehabCare
were $1.05 in 2008 compared to $0.73 in 2007.
Liquidity
and Capital Resources
As of
December 31, 2009, we had $24.7 million in cash and cash equivalents, and a
current ratio, the amount of current assets divided by current liabilities, of
1.7 to 1. Net working capital increased by $16.0 million to $113.3
million at December 31, 2009 as compared to $97.3 million at December 31, 2008
primarily due to the acquisition of Triumph’s net working
capital. Net accounts receivable were $199.4 million at December 31,
2009, compared to $139.2 million at December 31, 2008. The number of
days sales outstanding (“DSO”) in net receivables was 59.8, 66.0 and 71.8 at
December 31, 2009, 2008 and 2007, respectively. DSO of 59.8 at
December 31, 2009 does not include the impact of Triumph
receivables. The increase in outstanding accounts receivable reflects
the acquisition of Triumph in 2009. The improvement in DSO, excluding
Triumph receivables, occurred primarily in our skilled nursing rehabilitation
services division and reflects the results of a concerted focus on collection
activities and our efforts over the past three years to improve the quality of
the division’s portfolio of accounts receivable.
- 38
-
We
generated cash from operations of $48.1 million, $48.7 million and $52.0 million
in the years ended December 31, 2009, 2008 and 2007,
respectively. Capital expenditures were $13.2 million, $18.5
million and $10.0 million in the years ended December 31, 2009, 2008 and 2007,
respectively. Our capital expenditures primarily relate to the
construction of new hospitals, investments in information technology systems,
equipment additions and replacements and various other capital
improvements. Over the next few years, we plan to continue to invest
in information technology systems and the development and renovation of
hospitals.
The
Company has historically financed its operations with funds generated from
operating activities and borrowings under credit facilities and long-term debt
instruments. We believe our cash on hand, cash generated from
operations and availability under our credit facility will be sufficient to meet
our future working capital, capital expenditures, internal and external business
expansion, and debt service requirements.
On
November 24, 2009, we entered into a Credit Agreement (as defined in Note 9 to
our accompanying consolidated financial statements). The Credit
Agreement provides for a five-year revolving credit facility of $125 million and
a swingline subfacility of up to $25 million. At December 31, 2009,
there were no borrowings outstanding under the revolving credit
facility. As of December 31, 2009, we had $11.3 million in letters of
credit issued to insurance carriers as collateral for reimbursement of
claims. The letters of credit reduce the amount we may borrow under
the revolving credit facility. As of December 31, 2009, after
consideration of the effects of restrictive covenants, the available borrowing
capacity under the line of credit was approximately $113.7 million.
The
Credit Agreement also provided for a six-year $450 million term loan
facility. At December 31, 2009, the balance outstanding under the
term loan was $450 million. The term loan facility requires quarterly
installments of $1,125,000 with the balance payable upon the final
maturity. In addition, we are required to make mandatory principal
prepayments equal to a portion of our consolidated excess cash flow (as defined
in the Credit Agreement) when our consolidated leverage ratio reaches certain
levels.
The
Credit Agreement contains certain restrictive covenants that, among other
things, limit the incurrence of additional indebtedness, investments, dividends,
transactions with affiliates, asset sales, acquisitions, mergers and
consolidations, liens and encumbrances and other matters customarily restricted
in similar credit facilities. In addition, we are required to
maintain on a consolidated basis a maximum ratio of total funded debt to
earnings before interest, taxes, depreciation and amortization ((“EBITDA”) as
defined in the Credit Agreement), a maximum ratio of senior funded debt to
EBITDA and a minimum ratio of adjusted earnings before interest, taxes,
depreciation, amortization, rent and operating lease expense ((“Adjusted
EBITDAR”) as defined in the Credit Agreement) to fixed charges. As of
December 31, 2009, we were in compliance with all debt covenants. If
we anticipate a potential covenant violation, we would seek relief from our
lenders; however, such relief might not be granted or might be granted on terms
less favorable than those in our existing Credit Agreement.
In
November 2009, we issued 6,210,000 shares of our common stock in a public equity
offering which resulted in net proceeds, after underwriting fees and other
direct costs, of approximately $140.2 million. We used the net
proceeds from the public equity offering along with the proceeds from our term
loan facility to pay for the majority of the consideration used to acquire
Triumph.
- 39
-
Inflation
Although
inflation has abated during the last several years, the rate of inflation in
healthcare related services continued to exceed the rate experienced by the
economy as a whole. Our management contracts often provide for an
annual increase in the fees paid to us by our clients based on increases in
various inflation indices.
Effect
of Recent Accounting Pronouncements
See Note
1 to the consolidated financial statements in Item 8 for a full description of
recent accounting pronouncements, including the expected dates of adoption and
estimated effects on results of operations and financial condition, which is
incorporated herein by reference.
Commitments
and Contractual Obligations
The
following table summarizes our scheduled contractual commitments as of December
31, 2009 (in thousands):
|
Less
than
|
2-3
|
4-5
|
More
than
|
|||||||||||||||
|
Total
|
1
year
|
years
|
years
|
5
years
|
Other
|
|||||||||||||
|
Operating
leases (1)
|
$
|
426,603
|
$
|
31,611
|
$
|
65,823
|
$
|
66,458
|
$
|
262,711
|
$
|
—
|
||||||
|
Purchase
obligations (2)
|
14,583
|
13,730
|
853
|
—
|
—
|
—
|
||||||||||||
|
Long-term
debt including capital lease obligations (3)
|
464,159
|
7,507
|
19,499
|
9,653
|
427,500
|
—
|
||||||||||||
|
Interest
on long-term debt (4)
|
159,222
|
27,954
|
53,802
|
51,918
|
25,548
|
—
|
||||||||||||
|
Unrecognized
tax benefits (5)
|
1,647
|
—
|
—
|
—
|
—
|
1,647
|
||||||||||||
|
Other
long-term liabilities (6)
|
3,352
|
—
|
—
|
—
|
—
|
3,352
|
||||||||||||
|
Total
|
$
|
1,069,566
|
$
|
80,802
|
$
|
139,977
|
$
|
128,029
|
$
|
715,759
|
$
|
4,999
|
||||||
|
(1)
|
We
lease many of our facilities under non-cancelable operating leases in the
normal course of business. Some lease agreements provide us
with the option to renew the lease. Our future operating lease obligations
would change if we exercised these renewal options and if we entered into
additional operating lease agreements. For more information, see Note 13
to our accompanying consolidated financial
statements.
|
|
(2)
|
Purchase
obligations include agreements to purchase goods or services that are
enforceable and legally binding on us and that specify all significant
terms. Purchase obligations exclude agreements that are cancelable without
penalty.
|
|
(3)
|
The
amount of long-term debt reported on our consolidated balance sheet at
December 31, 2009 includes unamortized original issue discounts of
approximately $8,892,000.
|
|
(4)
|
Interest
on our variable rate debt is estimated using the rate in effect as of
December 31, 2009. This line also includes interest related to
capital lease obligations, but excludes the amortization of original issue
discounts and the amortization of deferred loan
fees.
|
|
(5)
|
Represents
our total liability for unrecognized tax benefits based on the guidance in
the Financial Accounting Standards Board’s Accounting Standards
Codification Topic 740, “Income Taxes.” There is a high degree
of uncertainty regarding the timing of future cash outflows associated
with these liabilities, which involve various taxing
authorities. As a result, we are unable to predict the timing
of payments against this
obligation.
|
- 40
-
|
(6)
|
We
maintain a nonqualified deferred compensation plan for certain employees.
Under the plan, participants may defer up to 70% of their salary and cash
incentive compensation. The amounts are held in trust in investments
designated by participants but remain our property until distribution.
Because most distributions of funds are tied to the termination of
employment or retirement of participants, we are not able to predict the
timing of payments against this obligation. At December 31,
2009, we owned trust assets with a value approximately equal to the total
amount of this obligation.
|
Critical
Accounting Policies and Estimates
The
preparation of our consolidated financial statements in conformity with
accounting principles generally accepted in the United States of America
requires us to make estimates and assumptions that affect the reported amounts
of assets and liabilities and disclosure of contingent assets and liabilities at
the date of the financial statements and the reported amounts of revenues and
expenses during the reporting period. Our estimates, judgments and assumptions
are continually evaluated based on available information and experience. Because
of the use of estimates inherent in the financial reporting process, actual
results could differ from those estimates. Management has discussed and will
continue to discuss its critical accounting policies with the audit committee of
our board of directors.
Certain
of our accounting policies require higher degrees of judgment than others in
their application. These include accounting for business combinations,
estimating the allowance for doubtful accounts, estimating contractual
allowances, impairment of goodwill and other intangible assets, and establishing
accruals for known and incurred but not reported health, workers compensation
and professional liability claims. In addition, Note 1 to the
consolidated financial statements includes further discussion of our significant
accounting policies.
Management
believes the following critical accounting policies affect our more significant
judgments and estimates used in the preparation of our consolidated financial
statements.
Business
Combinations. We allocate the purchase price of acquired
companies to the tangible assets acquired, intangible assets acquired and
liabilities assumed based on their estimated fair values. The excess
of the purchase price over these fair values is recorded as
goodwill. We engage independent third-party appraisal firms to assist
us in determining the fair values of assets acquired and liabilities assumed.
Such valuations require management to make significant estimates and
assumptions, especially with respect to intangible assets. The
significant purchased intangible assets recorded by RehabCare include customer
contracts, trade names and Medicare provider numbers. Critical
estimates in valuing these intangible assets include but are not limited to
discount rates, the asset’s remaining economic life and future expected cash
flows from customer contracts, trade names and Medicare provider
numbers. Management's estimates of fair value are based upon
assumptions believed to be reasonable, but which are inherently uncertain and
unpredictable and, as a result, actual results may differ from
estimates.
Allowance for Doubtful
Accounts. We make estimates of the collectability of our
accounts receivable balances. We determine an allowance for doubtful
accounts based upon an analysis of the collectability of specific accounts,
historical experience and the aging of the accounts receivable. We
specifically analyze customers with historical poor payment history and customer
creditworthiness when evaluating the adequacy of the allowance for doubtful
accounts. In our hospitals segment, the primary collection risks relate to the
amounts for which the patient is responsible (deductibles and
co-payments). Our accounts receivable balance as of December 31, 2009
was $199.4 million, net of allowance for doubtful accounts of $24.7
million. Our estimates of collectability require significant
judgment. If our customers’ ability to make payments to us were to
deteriorate beyond the levels estimated, additional allowances may be
required. We continually evaluate the adequacy of our allowance for
doubtful accounts and make adjustments in the periods any excess or shortfall is
identified.
- 41
-
Contractual
Allowances. Our hospitals recognize net patient revenue in
the reporting period in which the services are performed based on our current
billing rates, less actual adjustments and estimated discounts for contractual
allowances. An individual patient’s bill is subject to adjustment on
a patient-by-patient basis in the ordinary course of business by the payors
following their review of each particular bill. We estimate the
discounts for contractual allowances using the balance sheet approach on an
individual hospital basis. Patient accounts receivable detail is analyzed to
determine expected reimbursement for each patient. Expected
reimbursement is summarized by payor classification and reconciled to the
balance sheet. A secondary review is completed at the consolidated
hospitals level to validate calculations. Estimates are regularly
reviewed for accuracy by taking into consideration Medicare reimbursement rules
and known changes to contract terms, laws and regulations and payment
history. If such information indicates that our allowances are
overstated or understated, we reduce or provide for additional allowances as
appropriate in the period in which we make such a determination.
Laws and
regulations governing Medicare and Medicaid programs are complex and subject to
interpretation. As a result, there is at least a reasonable
possibility that recorded estimates will change by a material
amount. The estimated reimbursement amounts are adjusted in
subsequent periods as cost reports are prepared and filed and as final
settlements are determined. In 2007, our hospitals recorded favorable
net settlements of prior year Medicare and Medicaid cost reports aggregating
$1.4 million. We did not record any significant adjustments for prior
year cost reports in 2008 or 2009. We are not aware of any material
claims, disputes, or unsettled matters with third-party payors.
Goodwill and Other Intangible
Assets. The
cost of acquired companies is allocated first to their identifiable assets, both
tangible and intangible, based on estimated fair values. Costs
allocated to identifiable intangible assets with finite lives are generally
amortized on a straight-line basis over the remaining estimated useful lives of
the assets. The excess of the purchase price over the fair value of
identifiable assets acquired, net of liabilities assumed, is recorded as
goodwill.
Under
GAAP, goodwill and identifiable intangible assets with indefinite lives are not
amortized but must be reviewed at least annually for impairment. If
the impairment test indicates that the carrying value of an intangible asset
exceeds its fair value, then an impairment loss should be recognized in the
consolidated statement of earnings in an amount equal to the excess carrying
value. In 2007, we recognized an impairment loss of $4.9 million to
reduce the carrying value of an intangible asset to its revised estimate of fair
value based on the impact of a change in LTACH regulations issued by CMS on May
1, 2007. See Note 7 to our accompanying consolidated financial
statements for additional information regarding this impairment
loss. No other impairments of identifiable intangible assets
with indefinite-lives were identified during the three years ended December 31,
2009.
As
required by GAAP, we evaluate goodwill for impairment annually and whenever
events or changes in circumstances indicate the carrying value of the goodwill
may not be recoverable. Goodwill impairment is determined using a
two-step process. The first step is to identify if a potential
impairment exists by comparing the fair value of each reporting unit to its
carrying amount. If the fair value of a reporting unit exceeds its
carrying amount, goodwill of that reporting unit is not considered to have a
potential impairment and the second step of the impairment test is not
necessary. However, if the carrying amount of a reporting unit
exceeds its fair value, the second step is performed to determine the implied
fair value of a reporting unit’s goodwill, by comparing the reporting unit’s
fair value to the allocated fair values of all assets and liabilities, including
any unrecognized intangible assets, as if the reporting unit had been acquired
in a business combination. If the carrying amount of goodwill exceeds
its implied fair value, an impairment is recognized in an amount equal to that
excess.
- 42
-
Reporting
units are defined as an operating segment or one level below an operating
segment. Our primary reporting units are our skilled nursing
rehabilitation services, hospital rehabilitation services and hospital
businesses. We calculated the fair value of each reporting unit based
on a discounted cash flow analysis which requires us to make assumptions and
estimates about future cash flows and discount rates. These
assumptions are often subjective and can be affected by a variety of factors,
including external factors such as economic trends and government regulations,
and internal factors such as changes in our forecasts or in our business
strategies. We believe the assumptions used in our impairment
analysis are reasonable and appropriate; however, different assumptions and
estimates could affect the results of our impairment analysis and in turn result
in an impairment charge. We could be required to evaluate the
recoverability of goodwill prior to the annual assessment if we experience
disruptions to the business, unexpected significant declines in operating
results, a divestiture of a significant component of our business, significant
declines in market capitalization or other triggering events. In
addition, as our business or the way we manage our business changes, our
reporting units may also change. These types of events and the
resulting analyses could result in goodwill impairment charges in the future
which could materially impact our reported earnings in the periods such charges
occur.
At
December 31, 2009, unamortized goodwill related to our skilled nursing
rehabilitation services, hospital rehabilitation services and hospitals
businesses was $79.4 million, $39.7 million and $446.9 million,
respectively. We have not recorded any goodwill impairments during
the three years ended December 31, 2009. Our most recent impairment
test was as of December 31, 2009. A 20% decrease in the calculated
fair value of each of our reporting units as of December 31, 2009 would not have
resulted in a potential goodwill impairment.
Health, Workers Compensation, and
Professional Liability Insurance Accruals. We maintain an
accrual for our health, workers compensation and professional liability claim
costs that are partially self-insured and are classified in accrued salaries and
wages (health insurance) and accrued expenses (workers compensation and
professional liability) in our consolidated balance sheets. At
December 31, 2009, the combined amount of these accruals was approximately $21.1
million. We determine the adequacy of these accruals by periodically evaluating
our historical experience and trends related to health, workers compensation,
and professional liability claims and payments, based on actuarial computations
and industry experience and trends. In analyzing the accruals, we
also consider the nature and severity of the claims, analyses provided by third
party claims administrators, as well as current legal, economic and regulatory
factors. If such information indicates that our accruals are
overstated or understated, we reduce or provide for additional accruals as
appropriate in the period in which we make such a determination. The
ultimate cost of these claims may be greater than or less than the established
accruals. While we believe that the recorded amounts are appropriate,
there can be no assurances that changes to management’s estimates will not occur
due to limitations inherent in the estimation process.
We are
subject to various claims and legal actions in the ordinary course of our
business. Some of these matters include professional liability and
employee-related matters. Our hospital and healthcare facility
clients may also become subject to claims, governmental inquiries and
investigations and legal actions to which we may become a party relating to
services provided by our professionals. From time to time, and
depending upon the particular facts and circumstances, we may be subject to
indemnification obligations under our contracts with our hospital and healthcare
facility clients relating to these matters. Although we are currently
not aware of any such pending or threatened litigation that we believe is
reasonably likely to have a material adverse effect on us, if we become aware of
such claims against us, we will evaluate the probability of an adverse outcome
and provide accruals for such contingencies as necessary.
- 43
-
Forward-Looking
Statements
This
annual report contains historical information, as well as forward-looking
statements that involve known and unknown risks and relate to future events, our
future financial performance or our projected business results. In
some cases, forward-looking statements can be identified by terminology such as
“may,” “will,” “should,” “expects,” “plans,” “anticipates,” “believes,”
“estimates,” “predicts,” “targets,” “potential,” or “continue” or the negative
of these terms or other comparable terminology. These statements are
made on the basis of our views and assumptions as of the time the statements are
made and we undertake no obligation to update these statements. We
caution investors that any such forward-looking statements we make are not
guarantees of future performance and that actual results may differ materially
from anticipated results or expectations expressed in our forward-looking
statements as a result of a variety of factors. While it is
impossible to identify all such factors, some of the factors that could impact
our business and cause actual results to differ materially from forward-looking
statements are discussed in Item 1A, “Risk Factors.”
| ITEM 7A. | QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK |
The
Company’s primary market risk exposure consists of changes in interest rates on
certain borrowings that bear interest at floating rates. Interest
rate changes on variable rate debt impact our interest expense and cash flows,
but do not impact the fair value of the underlying debt instruments. Borrowings
under our revolving credit facility bear interest at our option at either a base
rate or the London Interbank Offering Rate (“LIBOR”) for one, two, three or six
month interest periods, or a nine or twelve month period if available, plus an
applicable margin percentage. The base rate is the greater of the
federal funds rate plus one-half of 1%, Bank of America N.A.’s prime rate or one
month LIBOR plus 1%. The applicable margin percentage is based upon
our consolidated total leverage ratio. Borrowings under our term loan
facility bear interest at our option at either the base rate plus 300 basis
points or LIBOR plus 400 basis points with a LIBOR floor of 200 basis
points. Adverse changes in short-term interest rates could affect our
overall borrowing rate when the contracts are renewed. As of December
31, 2009, there were no borrowings outstanding under the revolving credit
facility and the balance outstanding against the term loan facility was $450
million. At December 31, 2009, the term loan facility was subject to
a one-month LIBOR contract and the one-month LIBOR rate was 0.23% resulting in
an all-in interest rate of 6.0% due to the 2.0% LIBOR floor and the 400 basis
point margin. Based on the $450 million of variable rate debt
outstanding at December 31, 2009, a 100 basis point increase in the one-month
LIBOR rate would result in no additional interest expense (as a result of the
LIBOR floor). A 200 basis point increase in the LIBOR rate would
result in additional interest expense of approximately $1.0 million on an
annualized basis. At December 31, 2009, we were not a party to any
derivative financial instruments.
- 44
-
|
|
ITEM
8.
|
FINANCIAL
STATEMENTS AND SUPPLEMENTARY DATA
|
|
Report
of Independent Registered Public Accounting Firm
|
46
|
|
Consolidated
Balance Sheets as of December 31, 2009 and 2008
|
48
|
|
Consolidated
Statements of Earnings for the years
|
|
|
ended December 31, 2009, 2008 and
2007
|
49
|
|
Consolidated
Statements of Comprehensive Income for the years
|
|
|
ended December 31, 2009, 2008 and
2007
|
50
|
|
Consolidated
Statements of Changes in Equity for the years
|
|
|
ended December 31, 2009, 2008
and 2007
|
51
|
|
Consolidated
Statements of Cash Flows for the years
|
|
|
ended December 31, 2009, 2008 and
2007
|
52
|
|
Notes
to the Consolidated Financial Statements
|
53
|
- 45
-
Report
of Independent Registered Public Accounting Firm
The Board
of Directors and Stockholders
RehabCare
Group, Inc.:
We have
audited the accompanying consolidated balance sheets of RehabCare Group, Inc.
(the Company) as of December 31, 2009 and 2008, and the related
consolidated statements of earnings, comprehensive income, changes in equity,
and cash flows for each of the years in the three-year period ended
December 31, 2009. We also have audited the Company’s internal
control over financial reporting as of December 31, 2009, based on criteria
established in Internal
Control – Integrated Framework issued by the Committee of Sponsoring
Organizations of the Treadway Commission (COSO). The Company’s
management is responsible for these consolidated financial statements, for
maintaining effective internal control over financial reporting, and for its
assessment of the effectiveness of internal control over financial reporting,
included in the accompanying “Management’s Report on Internal Control over
Financial Reporting.” Our responsibility is to express an opinion on
these consolidated financial statements and an opinion on the Company’s internal
control over financial reporting based on our audits.
We
conducted our audits in accordance with the standards of the Public Company
Accounting Oversight Board (United States). Those standards require
that we plan and perform the audits to obtain reasonable assurance about whether
the financial statements are free of material misstatement and whether effective
internal control over financial reporting was maintained in all material
respects. Our audits of the consolidated financial statements
included examining, on a test basis, evidence supporting the amounts and
disclosures in the financial statements, assessing the accounting principles
used and significant estimates made by management, and evaluating the overall
financial statement presentation. Our audit of internal control over
financial reporting included obtaining an understanding of internal control over
financial reporting, assessing the risk that a material weakness exists, and
testing and evaluating the design and operating effectiveness of internal
control based on the assessed risk. Our audits also included
performing such other procedures as we considered necessary in the
circumstances. We believe that our audits provide a reasonable basis
for our opinions.
A
company’s internal control over financial reporting is a process designed to
provide reasonable assurance regarding the reliability of financial reporting
and the preparation of financial statements for external purposes in accordance
with generally accepted accounting principles. A company’s internal
control over financial reporting includes those policies and procedures that
(1) pertain to the maintenance of records that, in reasonable detail,
accurately and fairly reflect the transactions and dispositions of the assets of
the company; (2) provide reasonable assurance that transactions are
recorded as necessary to permit preparation of financial statements in
accordance with generally accepted accounting principles, and that receipts and
expenditures of the company are being made only in accordance with
authorizations of management and directors of the company; and (3) provide
reasonable assurance regarding prevention or timely detection of unauthorized
acquisition, use, or disposition of the company’s assets that could have a
material effect on the financial statements.
Because
of its inherent limitations, internal control over financial reporting may not
prevent or detect misstatements. Also, projections of any evaluation of
effectiveness to future periods are subject to the risk that controls may become
inadequate because of changes in conditions, or that the degree of compliance
with the policies or procedures may deteriorate.
- 46
-
The
Company acquired Triumph HealthCare Holdings, Inc. (Triumph) on November 24,
2009, and management excluded from its assessment of the effectiveness of the
Company's internal control over financial reporting as of December 31, 2009,
Triumph's internal control over financial reporting associated with total assets
of $648.8 million and total revenues of $39.7 million included in the
consolidated financial statements of the Company as of and for the year ended
December 31, 2009. Our audit of internal control over financial
reporting of the Company also excluded an evaluation of the internal control
over financial reporting of Triumph.
In our
opinion, the consolidated financial statements referred to above present fairly,
in all material respects, the consolidated financial position of RehabCare
Group, Inc. as of December 31, 2009 and 2008, and the results of its
operations and its cash flows for each of the years in the three-year period
ended December 31, 2009, in conformity with U.S. generally accepted
accounting principles. Also in our opinion, RehabCare Group, Inc. maintained, in
all material respects, effective internal control over financial reporting as of
December 31, 2009, based on criteria established in Internal Control – Integrated
Framework issued by the COSO.
As
discussed in Note 14 to the consolidated financial statements, the Company
adopted Financial Accounting Standards Board (FASB) Interpretation No. 48, Accounting for Uncertainty in Income
Taxes (included in FASB ASC Topic 740, Income Taxes), as of January
1, 2007.
As
discussed in Note 1 to the consolidated financial statements, the Company
adopted FASB Financial Accounting Standard No. 160, Noncontrolling Interests in
Consolidated Financial Statements – an amendment of ARB No. 51 (included
in FASB ASC Topic 810-10-45, Noncontrolling Interests in a
Subsidiary), as of January 1, 2009.
As
discussed in Note 6 to the consolidated financial statements, the Company
adopted FASB Financial Accounting Standard No. 141(R), Business Combinations
(included in FASB ASC Topic 805, Business Combinations), as of
January 1, 2009.

St.
Louis, Missouri
March 8,
2010
- 47
-
REHABCARE
GROUP, INC.
Consolidated
Balance Sheets
(dollars
in thousands, except per share data)
|
December
31,
|
|||||||
|
Assets
|
2009
|
2008
|
|||||
|
Current
assets:
|
|||||||
|
Cash
and cash equivalents
|
$
|
24,690
|
$
|
27,373
|
|||
|
Accounts
receivable, net of allowance for doubtful accounts of $24,729 and $19,480,
respectively
|
199,447
|
139,197
|
|||||
|
Deferred
tax assets
|
21,249
|
14,876
|
|||||
|
Other
current assets
|
19,530
|
7,165
|
|||||
|
Total
current assets
|
264,916
|
188,611
|
|||||
|
Marketable
securities, trading
|
3,314
|
2,810
|
|||||
|
Property
and equipment, net
|
111,814
|
37,851
|
|||||
|
Goodwill
|
566,078
|
171,365
|
|||||
|
Intangible
assets, net
|
135,406
|
28,944
|
|||||
|
Investment
in unconsolidated affiliate
|
4,761
|
4,772
|
|||||
|
Other
|
23,691
|
4,053
|
|||||
|
Total
assets
|
$
|
1,109,980
|
$
|
438,406
|
|||
|
Liabilities and Equity
|
|||||||
|
Current
liabilities:
|
|||||||
|
Current
portion of long-term debt
|
$
|
7,507
|
$
|
—
|
|||
|
Accounts
payable
|
18,293
|
8,330
|
|||||
|
Accrued
salaries and wages
|
80,138
|
55,188
|
|||||
|
Income
taxes payable
|
97
|
776
|
|||||
|
Accrued
expenses
|
45,585
|
27,033
|
|||||
|
Total
current liabilities
|
151,620
|
91,327
|
|||||
|
Long-term
debt, less current portion
|
447,760
|
57,000
|
|||||
|
Deferred
compensation
|
3,352
|
2,833
|
|||||
|
Deferred
tax liabilities
|
45,605
|
8,306
|
|||||
|
Other
|
2,023
|
1,140
|
|||||
|
Total
liabilities
|
650,360
|
160,606
|
|||||
|
Stockholders’
equity:
|
|||||||
|
Preferred
stock, $.10 par value; authorized 10,000,000 shares, none issued and
outstanding
|
—
|
—
|
|||||
|
Common
stock, $.01 par value; authorized 60,000,000 shares, issued 28,036,014
shares and 21,657,544 shares as of December 31, 2009 and 2008,
respectively
|
280
|
217
|
|||||
|
Additional
paid-in capital
|
291,771
|
145,647
|
|||||
|
Retained
earnings
|
199,991
|
177,036
|
|||||
|
Accumulated
other comprehensive loss
|
—
|
(424
|
)
|
||||
|
Less
common stock held in treasury at cost; 4,002,898 shares as of December 31,
2009 and 2008
|
(54,704
|
)
|
(54,704
|
)
|
|||
|
Total
stockholders’ equity
|
437,338
|
267,772
|
|||||
|
Noncontrolling
interests
|
22,282
|
10,028
|
|||||
|
Total
equity
|
459,620
|
277,800
|
|||||
|
Total
liabilities and equity
|
$
|
1,109,980
|
$
|
438,406
|
|||
See
accompanying notes to consolidated financial statements.
- 48
-
REHABCARE
GROUP, INC.
Consolidated
Statements of Earnings
(in
thousands, except per share data)
|
Year
Ended December 31,
|
||||||||||||
|
2009
|
2008
|
2007
|
||||||||||
|
Operating
revenues
|
$
|
869,427
|
$
|
735,412
|
$
|
693,013
|
||||||
|
Costs
and expenses:
|
||||||||||||
|
Operating
|
704,394
|
597,879
|
561,233
|
|||||||||
|
Selling,
general and administrative
|
104,060
|
90,056
|
82,806
|
|||||||||
|
Impairment
of assets
|
—
|
—
|
4,906
|
|||||||||
|
Depreciation
and amortization
|
16,499
|
14,570
|
16,538
|
|||||||||
|
Total
costs and expenses
|
824,953
|
702,505
|
665,483
|
|||||||||
|
Operating
earnings
|
44,474
|
32,907
|
27,530
|
|||||||||
|
Interest
income
|
98
|
143
|
830
|
|||||||||
|
Interest
expense
|
(5,546
|
)
|
(3,897
|
)
|
(8,362
|
)
|
||||||
|
Other
income
|
12
|
21
|
37
|
|||||||||
|
Equity
in net income of affiliate
|
431
|
471
|
287
|
|||||||||
|
Earnings
from continuing operations before income taxes
|
39,469
|
29,645
|
20,322
|
|||||||||
|
Income
taxes
|
17,641
|
12,063
|
7,658
|
|||||||||
|
Earnings
from continuing operations, net of tax
|
21,828
|
17,582
|
12,664
|
|||||||||
|
Loss
from discontinued operations, net of tax
|
(839
|
)
|
(863
|
)
|
(382
|
)
|
||||||
|
Net
earnings
|
20,989
|
16,719
|
12,282
|
|||||||||
|
Net
loss attributable to noncontrolling interests
|
1,966
|
1,986
|
377
|
|||||||||
|
Net
earnings attributable to RehabCare
|
$
|
22,955
|
$
|
18,705
|
$
|
12,659
|
||||||
|
Amounts
attributable to RehabCare stockholders:
|
||||||||||||
|
Earnings
from continuing operations, net of tax
|
$
|
23,794
|
$
|
19,568
|
$
|
13,041
|
||||||
|
Loss
from discontinued operations, net of tax
|
(839
|
)
|
(863
|
)
|
(382
|
)
|
||||||
|
Net
earnings
|
$
|
22,955
|
$
|
18,705
|
$
|
12,659
|
||||||
|
Basic
earnings per share attributable to RehabCare:
|
||||||||||||
|
Earnings
from continuing operations, net of tax
|
$
|
1.29
|
$
|
1.11
|
$
|
0.76
|
||||||
|
Loss
from discontinued operations, net of tax
|
(0.05
|
)
|
(0.05
|
)
|
(0.03
|
)
|
||||||
|
Net
earnings
|
$
|
1.24
|
$
|
1.06
|
$
|
0.73
|
||||||
|
Diluted
earnings per share attributable to RehabCare:
|
||||||||||||
|
Earnings
from continuing operations, net of tax
|
$
|
1.26
|
$
|
1.10
|
$
|
0.75
|
||||||
|
Loss
from discontinued operations, net of tax
|
(0.04
|
)
|
(0.05
|
)
|
(0.02
|
)
|
||||||
|
Net
earnings
|
$
|
1.22
|
$
|
1.05
|
$
|
0.73
|
||||||
See
accompanying notes to consolidated financial statements.
- 49
-
REHABCARE
GROUP, INC.
Consolidated
Statements of Comprehensive Income
(in
thousands)
|
Year
Ended December 31,
|
||||||||||
|
2009
|
2008
|
2007
|
||||||||
|
Net
earnings
|
$
|
20,989
|
$
|
16,719
|
$
|
12,282
|
||||
|
Other
comprehensive income (loss), net of tax:
|
||||||||||
|
Changes
in the fair value of derivative designated as a cash flow hedge, net of
income tax expense (benefit) of $267, $(226) and $(41),
respectively
|
424
|
(358
|
)
|
(66
|
)
|
|||||
|
Total
other comprehensive loss, net of tax
|
424
|
(358
|
)
|
(66
|
)
|
|||||
|
Comprehensive
income
|
21,413
|
16,361
|
12,216
|
|||||||
|
Comprehensive
loss attributable to noncontrolling interests
|
1,966
|
1,986
|
377
|
|||||||
|
Comprehensive
income attributable to RehabCare
|
$
|
23,379
|
$
|
18,347
|
$
|
12,593
|
||||
See
accompanying notes to consolidated financial statements.
- 50
-
REHABCARE
GROUP, INC.
Consolidated
Statements of Changes in Equity
(in
thousands)
|
Amounts
Attributable to RehabCare Stockholders
|
|||||||||||||||||||||
|
Accumulated
|
|||||||||||||||||||||
|
Additional
|
other
|
Non-
|
|||||||||||||||||||
|
Common
|
paid-in
|
Retained
|
Treasury
|
comprehensive
|
controlling
|
Total
|
|||||||||||||||
|
stock
|
capital
|
earnings
|
stock
|
earnings
(loss)
|
interests
|
equity
|
|||||||||||||||
|
Balance,
December 31, 2006
|
$
|
211
|
$
|
134,040
|
$
|
131,232
|
$
|
(54,704
|
)
|
$
|
—
|
$
|
86
|
$
|
210,865
|
||||||
|
Net
earnings (loss)
|
—
|
—
|
12,659
|
—
|
—
|
(377
|
)
|
12,282
|
|||||||||||||
|
Changes
in the fair value of derivative, net of tax
|
—
|
—
|
—
|
—
|
(66
|
)
|
—
|
(66
|
)
|
||||||||||||
|
Adjustment
to initially apply FIN 48
|
—
|
—
|
14,440
|
—
|
—
|
—
|
14,440
|
||||||||||||||
|
Stock-based
compensation
|
—
|
1,726
|
—
|
—
|
—
|
—
|
1,726
|
||||||||||||||
|
Activity
under stock plans
|
4
|
4,480
|
—
|
—
|
—
|
—
|
4,484
|
||||||||||||||
|
Contributions
made by noncontrolling interests
|
—
|
—
|
—
|
—
|
—
|
1,558
|
1,558
|
||||||||||||||
|
Balance,
December 31, 2007
|
215
|
140,246
|
158,331
|
(54,704
|
)
|
(66
|
)
|
1,267
|
245,289
|
||||||||||||
|
Net
earnings (loss)
|
—
|
—
|
18,705
|
—
|
—
|
(1,986
|
)
|
16,719
|
|||||||||||||
|
Changes
in the fair value of derivative, net of tax
|
—
|
—
|
—
|
—
|
(358
|
)
|
—
|
(358
|
)
|
||||||||||||
|
Stock-based
compensation
|
—
|
3,195
|
—
|
—
|
—
|
—
|
3,195
|
||||||||||||||
|
Activity
under stock plans
|
2
|
2,206
|
—
|
—
|
—
|
—
|
2,208
|
||||||||||||||
|
Contributions
made by noncontrolling interests
|
—
|
—
|
—
|
—
|
—
|
10,747
|
10,747
|
||||||||||||||
|
Balance,
December 31, 2008
|
217
|
145,647
|
177,036
|
(54,704
|
)
|
(424
|
)
|
10,028
|
277,800
|
||||||||||||
|
Net
earnings (loss)
|
—
|
—
|
22,955
|
—
|
—
|
(1,966
|
)
|
20,989
|
|||||||||||||
|
Changes
in the fair value of derivative, net of tax
|
—
|
—
|
—
|
—
|
424
|
—
|
424
|
||||||||||||||
|
Sale
of common stock
|
62
|
140,187
|
—
|
—
|
—
|
—
|
140,249
|
||||||||||||||
|
Stock-based
compensation
|
—
|
4,662
|
—
|
—
|
—
|
—
|
4,662
|
||||||||||||||
|
Activity
under stock plans
|
1
|
1,275
|
—
|
—
|
—
|
—
|
1,276
|
||||||||||||||
|
Business
combinations
|
—
|
—
|
—
|
—
|
—
|
11,591
|
11,591
|
||||||||||||||
|
Contributions
made by noncontrolling interests
|
—
|
—
|
—
|
—
|
—
|
4,423
|
4,423
|
||||||||||||||
|
Distributions
to noncontrolling interests
|
—
|
—
|
—
|
—
|
—
|
(1,794
|
)
|
(1,794
|
)
|
||||||||||||
|
Balance,
December 31, 2009
|
$
|
280
|
$
|
291,771
|
$
|
199,991
|
$
|
(54,704
|
)
|
$
|
—
|
$
|
22,282
|
$
|
459,620
|
||||||
See
accompanying notes to consolidated financial statements.
- 51
-
REHABCARE
GROUP, INC.
Consolidated
Statements of Cash Flows
(in
thousands)
|
Year
Ended December 31,
|
|||||||||||||
|
2009
|
2008
|
2007
|
|||||||||||
|
Cash
flows from operating activities:
|
|||||||||||||
|
Net
earnings
|
$
|
20,989
|
$
|
16,719
|
$
|
12,282
|
|||||||
|
Reconciliation
to net cash provided by operating activities:
|
|||||||||||||
|
Depreciation
and amortization
|
16,522
|
14,886
|
17,021
|
||||||||||
|
Provision
for doubtful accounts
|
7,794
|
10,178
|
9,194
|
||||||||||
|
Equity
in net income of affiliate
|
(431
|
)
|
(471
|
)
|
(287
|
)
|
|||||||
|
Impairment
of assets
|
—
|
—
|
4,906
|
||||||||||
|
Stock-based
compensation
|
4,662
|
3,195
|
1,726
|
||||||||||
|
Income
tax benefit related to stock options exercised
|
916
|
812
|
1,122
|
||||||||||
|
Excess
tax benefit related to stock options exercised
|
(405
|
)
|
(564
|
)
|
(973
|
)
|
|||||||
|
Loss
(gain) on disposal of discontinued operation
|
1,188
|
(321
|
)
|
—
|
|||||||||
|
Gain
on disposal of property and equipment
|
(12
|
)
|
(21
|
)
|
(37
|
)
|
|||||||
|
Changes
in assets and liabilities:
|
|||||||||||||
|
Accounts
receivable, net
|
(5,837
|
)
|
(11,318
|
)
|
7,883
|
||||||||
|
Other
current assets
|
(6,821
|
)
|
846
|
925
|
|||||||||
|
Accounts
payable
|
(3,478
|
)
|
2,328
|
(3,895
|
)
|
||||||||
|
Accrued
salaries and wages
|
5,715
|
4,952
|
(523
|
)
|
|||||||||
|
Income
taxes payable and deferred taxes
|
477
|
4,456
|
5,871
|
||||||||||
|
Accrued
expenses
|
6,212
|
2,629
|
(2,486
|
)
|
|||||||||
|
Other
assets and other liabilities
|
599
|
352
|
(720
|
)
|
|||||||||
|
Net
cash provided by operating activities
|
48,090
|
48,658
|
52,009
|
||||||||||
|
Cash
flows from investing activities:
|
|||||||||||||
|
Additions
to property and equipment
|
(13,215
|
)
|
(18,502
|
)
|
(9,989
|
)
|
|||||||
|
Purchase
of marketable securities
|
(476
|
)
|
(509
|
)
|
(354
|
)
|
|||||||
|
Proceeds
from sale/maturities of marketable securities
|
607
|
546
|
1,390
|
||||||||||
|
Investment
in unconsolidated affiliate
|
—
|
—
|
(1,119
|
)
|
|||||||||
|
Proceeds
from disposition of business
|
5,043
|
7,193
|
—
|
||||||||||
|
Purchase
of businesses, net of cash acquired
|
(549,783
|
)
|
(8,408
|
)
|
(1
|
)
|
|||||||
|
Other,
net
|
(27
|
)
|
(406
|
)
|
(871
|
)
|
|||||||
|
Net
cash used in investing activities
|
(557,851
|
)
|
(20,086
|
)
|
(10,944
|
)
|
|||||||
|
Cash
flows from financing activities:
|
|||||||||||||
|
Net
change in revolving credit facility
|
(57,000
|
)
|
(11,500
|
)
|
(45,000
|
)
|
|||||||
|
Proceeds
from the issuance of long-term debt
|
450,000
|
—
|
—
|
||||||||||
|
Debt
issuance costs
|
(28,448
|
)
|
—
|
—
|
|||||||||
|
Principal
payments on long-term debt
|
(1,749
|
)
|
(6,000
|
)
|
(1,059
|
)
|
|||||||
|
Net
proceeds from the sale of common stock
|
140,249
|
—
|
—
|
||||||||||
|
Cash
contributed by noncontrolling interests
|
4,423
|
3,663
|
1,373
|
||||||||||
|
Cash
distributed to noncontrolling interests
|
(1,794
|
)
|
—
|
—
|
|||||||||
|
Activity
under stock plans
|
992
|
1,809
|
3,483
|
||||||||||
|
Excess
tax benefit related to stock options exercised
|
405
|
564
|
973
|
||||||||||
|
Net
cash provided by (used in) financing activities
|
507,078
|
(11,464
|
)
|
(40,230
|
)
|
||||||||
|
Net
(decrease) increase in cash and cash equivalents
|
(2,683
|
)
|
17,108
|
835
|
|||||||||
|
Cash
and cash equivalents at beginning of year
|
27,373
|
10,265
|
9,430
|
||||||||||
|
Cash
and cash equivalents at end of year
|
$
|
24,690
|
$
|
27,373
|
$
|
10,265
|
|||||||
See
accompanying notes to consolidated financial statements.
- 52
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements
December
31, 2009, 2008 and 2007
| (1) | Overview of Company and Summary of Significant Accounting Policies |
Overview
of Company
RehabCare
Group, Inc. (“the Company”) is a leading provider of program management services
for inpatient rehabilitation and skilled nursing units, outpatient therapy
programs and contract therapy services in conjunction with more than 1,200
hospitals, skilled nursing facilities, outpatient facilities and other long-term
care facilities throughout the United States. RehabCare also
operates six rehabilitation hospitals and 28 long term acute care
hospitals, which provide specialized acute care for medically complex
patients.
Effective
November 24, 2009, the Company acquired all of the outstanding common stock of
Triumph HealthCare Holdings, Inc. (“Triumph”). On the acquisition
date, Triumph operated 20 LTACHs in seven states. Triumph’s results
of operations have been included in the Company’s financial statements
prospectively beginning after the date of acquisition. As a result of
the acquisition of Triumph, the Company believes it is now the third largest
LTACH provider in the United States.
Basis
of Presentation and Principles of Consolidation
The
accompanying consolidated financial statements of the Company and its
subsidiaries were prepared in accordance with generally accepted accounting
principles in the United States of America (“GAAP”) and include the accounts of
the Company and all of its wholly owned subsidiaries, majority-owned
subsidiaries over which the Company exercises control and, when applicable,
entities for which the Company has a controlling financial
interest. All significant intercompany balances and transactions have
been eliminated in consolidation.
The
Company uses the equity method to account for its investments in entities that
the Company does not control but has the ability to exercise significant
influence over the entity’s operating and financial policies.
Certain
prior year amounts have been reclassified to conform to current year
presentation. Such reclassifications primarily relate to the June
2009 sale of Phase 2 Consulting, Inc. (“Phase 2”). The Company
reclassified its consolidated statements of earnings for the years ended
December 31, 2008 and 2007 to show the results of operations for Phase 2 as
discontinued operations. In addition, the Company’s adoption of
Financial Accounting Standards Board’s (“FASB’s”) Statement of Financial
Accounting Standards No. 160, “Noncontrolling Interests in Consolidated
Financial Statements” (now codified in the FASB’s Accounting Standards
Codification Topic 810-10-45, “Noncontrolling Interest in a Subsidiary,”), in
the first quarter of 2009 resulted in changes to the presentation of
noncontrolling interests within the Company’s consolidated financial
statements.
Cash
Equivalents and Marketable Securities
Cash in
excess of daily requirements is invested in short-term investments with original
maturities of three months or less. Such investments are deemed to be
cash equivalents for purposes of the consolidated statements of cash
flows.
The
Company classifies its debt and equity securities into one of three
categories: held-to-maturity, trading, or available-for-sale.
Management determines the appropriate classification of its investments at the
time of purchase and reevaluates such determination at each balance sheet
date. Investments at December 31, 2009 and 2008 consist of noncurrent
marketable equity and debt securities. All noncurrent marketable
securities are classified as trading, with all investment income, including
unrealized gains or losses recognized in the consolidated statements of
earnings. Noncurrent marketable securities include assets held in
trust for the Company’s deferred compensation plan that are not available for
operating purposes.
- 53
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
Accounts
Receivable and Credit Risk
The
Company’s program management services segment provides services to a
geographically diverse clientele of healthcare providers throughout the United
States. The Company performs ongoing credit evaluations of its
clientele and does not require collateral. The Company’s hospital
segment is reimbursed for its services primarily by Medicare and other third
party payors. As such, the hospital segment’s primary collection
risks relate to the amounts for which the patient is responsible (such as
deductibles and co-payments).
An
allowance for doubtful accounts is maintained at a level which management
believes is sufficient to cover anticipated credit losses. The
Company determines its allowance for doubtful accounts based upon an analysis of
the collectability of specific accounts, historical experience and the aging of
the accounts receivable. The Company specifically analyzes customers
with historical poor payment history and customer creditworthiness when
evaluating the adequacy of the allowance for doubtful accounts. The Company
continually evaluates the adequacy of its allowance for doubtful accounts and
makes adjustments in the periods any excess or shortfall is
identified. Accounts are written off after all collection efforts
(internal and external) have been exhausted.
As a
result of the acquisition of Triumph, the Company’s hospital segment now
accounts for a larger percentage of the Company’s receivables than in previous
years. At December 31, 2009, the hospital segment accounted for $86.5
million or 43% of the Company’s total net accounts receivable and $9.1 million
or 37% of the Company’s total allowance for doubtful accounts. A
significant portion of Triumph’s business is concentrated in Houston,
Texas. Because the hospital segment is primarily reimbursed by
Medicare and other third party payors, the Company believes concentrations by
type of payor are more meaningful than geographic concentrations. The
following table identifies the sources and relative mix of the hospital
segment’s net accounts receivable as of the dates stated:
|
As
of December 31,
|
||||||
|
Hospital segment
|
2009
|
2008
|
||||
|
Medicare
|
58.7
|
%
|
64.7
|
%
|
||
|
Medicaid
|
2.8
|
2.3
|
||||
|
Other
third party payors
|
36.8
|
32.1
|
||||
|
Self-pay
|
1.6
|
0.9
|
||||
|
Total
net patient accounts receivable
|
99.9
|
100.0
|
||||
|
Other
receivables
|
0.1
|
—
|
||||
|
Total
net accounts receivable
|
100.0
|
%
|
100.0
|
%
|
||
During
the years ended December 31, 2009, 2008, and 2007, approximately 68.8%, 74.2%,
and 77.8%, respectively, of the hospital segment’s net operating revenues
related to patients participating in the Medicare program. Because
Medicare traditionally pays claims faster than other third-party payors, the
hospital segment’s percentage of accounts receivable from Medicare is less than
its percentage of net operating revenues from Medicare. While revenues and
accounts receivable from the Medicare program are significant to the Company’s
operations, the Company does not believe there are significant credit risks
associated with these receivables.
- 54
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
Derivative
Instruments and Hedging Activities
GAAP
requires that every derivative instrument be recorded in the balance sheet as
either an asset or a liability measured at its fair value. In
December 2007, the Company entered into an interest rate swap agreement to
reduce the Company’s exposure to changes in interest rates on certain borrowings
that bear interest at floating rates. The swap agreement expired in
December 2009. This swap agreement was designated as a cash flow
hedge. Therefore, the unrealized gains and losses resulting from the
change in fair value of the swap contract were reflected in other comprehensive
income. Realized gains and losses were reclassified to interest
expense in the period in which the related interest payments being hedged were
made. The Company formally documented its hedging relationships,
including identification of the hedging instruments and hedged items, as well as
the Company’s risk management objectives and strategies for undertaking each
hedge transaction.
Property
and Equipment
Property
and equipment are initially recorded at cost. Depreciation and
amortization of property and equipment are computed using the straight-line
method over the estimated useful lives of the related assets, principally:
equipment – three to seven years; buildings – 39 years; and leasehold
improvements – life of asset or life of lease, whichever is less. Upon
retirement or disposition, the cost and related accumulated depreciation are
removed from the accounts and any gain or loss is included in the results of
operations. Repairs and maintenance are expensed as incurred.
Goodwill
and Other Intangible Assets
Under
GAAP, the cost of acquired companies is allocated first to their identifiable
assets, both tangible and intangible, based on estimated fair
values. The excess of the purchase price over the fair value of
identifiable assets acquired, net of liabilities assumed, is recorded as
goodwill. Goodwill and intangible assets with indefinite lives are
not amortized to expense, but instead tested for impairment at least annually
and any related losses recognized in earnings when identified. See
Note 7, “Goodwill and Other Intangible Assets,” for further
discussion. Other identifiable intangible assets with a finite life
are amortized on a straight-line basis over their estimated lives.
Long-Lived
Assets
The
Company reviews identified intangible and other long-lived assets for impairment
whenever events or changes in circumstances indicate that the carrying value of
the asset may not be recoverable. If such events or changes in
circumstances are present, an impairment loss would be recognized if the sum of
the expected future net cash flows was less than the carrying amount of the
asset.
Disclosure
About Fair Value of Financial Instruments
At
December 31, 2009, the Company’s financial instruments consist of cash
equivalents, accounts receivable, marketable securities, accounts payable and
long-term debt. The carrying values of cash equivalents, accounts
receivable and accounts payable approximate fair value due to their relatively
short-term nature. The carrying values of long-term debt were
$455.3 million and $57.0 million at December 31, 2009 and 2008,
respectively. The fair values of long-term debt were $464.2 million
and $57.0 million at December 31, 2009 and 2008, respectively, and are based on
the interest rates offered for borrowings with comparable
maturities. The Company’s marketable securities (which had carrying
values of $3.3 million and $2.8 million at December 31, 2009 and 2008,
respectively) are recorded at fair value. See Note 18, “Fair Value
Measurements,” for additional information.
- 55
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
Revenue
Recognition
In the
Company’s program management services segment, the Company derives a significant
majority of its revenues from fees paid directly by healthcare providers (i.e.,
acute care hospitals and skilled nursing facilities) rather than through payment
or reimbursement by government or other third-party payors. Revenues
are generally recognized as services are provided to patients based on the
contractually agreed upon rate per unit of service, rate per patient discharge,
a negotiated patient per diem rate, or a negotiated fee schedule based on the
type of service rendered. The Company’s inpatient business also
accrues revenues at the end of each period for services provided to patients
that have not been discharged by the period end based on the number of patient
days completed as a percentage of the average length of stay for the facility
under contract.
The
Company’s hospitals segment derives substantially all of its revenues from fees
for patient care services, which are usually reimbursed by Medicare, Medicaid or
third party managed care programs. The Company’s hospitals
recognize net patient revenues in the reporting period in which the services are
performed based on our current gross billing rates, less actual adjustments and
estimated discounts for contractual allowances. These allowances are
principally required for patients covered by Medicare, Medicaid, managed care
health plans and other third-party payors. Laws governing the
Medicare and Medicaid programs are complex and subject to
interpretation. All healthcare providers participating in the
Medicare and Medicaid programs are required to meet certain financial reporting
requirements. Federal regulations require submission of annual cost reports
covering medical costs and expenses associated with the services provided by
each facility to program beneficiaries. Annual cost reports required
under the Medicare and Medicaid programs are subject to routine audits, which
may result in adjustments to the amounts ultimately determined to be due to the
Company under these reimbursement programs.
In
estimating the discounts for contractual allowances, the Company reduces its
gross patient receivables to the estimated amount that will be recovered for the
service rendered based upon previously agreed to rates with the
payor. These estimates are regularly reviewed for accuracy by taking
into consideration Medicare reimbursement rules and known changes to payor
contract terms, laws and regulations and payment history. If such
information indicates that the Company’s allowances are overstated or
understated, the Company reduces or provides for additional allowances as
appropriate in the period in which such a determination is made.
In 2007,
the Company recorded favorable net settlements of prior year Medicare and
Medicaid cost reports which resulted in an aggregate increase in revenues of
$1.4 million. The Company did not record any material revenue
adjustments for prior year cost reports in 2008 or 2009.
Health,
Workers Compensation and Professional Liability Insurance Accruals
The
Company maintains an accrual for health, workers compensation and professional
liability claim costs that are partially self-insured and are classified in
accrued salaries and wages (health insurance) and accrued expenses (workers
compensation and professional liability). The Company determines the
adequacy of these accruals by periodically evaluating historical experience and
trends related to claims and payments based on actuarial computations and
industry experiences and trends. At December 31, 2009, the balances
for accrued health, workers compensation and professional liability were $8.0
million, $5.3 million and $7.8 million, respectively. At December 31,
2008, the balances for accrued health, workers compensation and professional
liability were $5.4 million, $4.6 million and $6.2 million,
respectively.
- 56
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
Income
Taxes
Deferred
tax assets and liabilities are recognized for temporary differences between the
financial statement carrying amounts of existing assets and liabilities and
their respective tax bases and operating loss and tax credit
carryforwards. Deferred tax assets and liabilities are measured using
enacted tax rates in effect for the year in which those differences are expected
to be recovered or settled.
Treasury
Stock
The
purchase of the Company’s common stock is recorded at cost. Upon
subsequent reissuance, the treasury stock account is reduced by the average cost
basis of such stock.
Use
of Estimates
The
preparation of financial statements in conformity with GAAP requires management
to make estimates and assumptions that affect the reported amounts of assets and
liabilities and disclosure of contingent assets and liabilities at the date of
the consolidated financial statements. Estimates also affect the
reported amounts of revenues and expenses during the period. Actual
results may differ from those estimates.
Recently
Issued Accounting Pronouncements
During
the third quarter of 2009, the FASB Accounting Standards Codification (“ASC” or
“Codification”) became the Company’s single official source of authoritative
GAAP (other than guidance issued by the Securities and Exchange Commission),
superseding existing FASB, American Institute of Certified Public Accountants
(AICPA), Emerging Issues Task Force (EITF) and related
literature. All other non-grandfathered, non-SEC accounting
literature not included in the Codification is now considered
non-authoritative. The FASB will not issue new standards in the form
of Statements or FASB Staff Positions. Instead, it will issue
Accounting Standards Updates (“ASUs”).
In
October 2009, the FASB issued ASU 2009-13, “Multiple-Deliverable Revenue
Arrangements” (“ASU 2009-13”). ASU 2009-13 requires entities to
allocate revenue in an arrangement using estimated selling prices of the
delivered goods and services based on a selling price hierarchy. The
amendments eliminate the residual method of revenue allocation and require
revenue to be allocated using the relative selling price method. ASU
2009-13 should be applied on a prospective basis for revenue arrangements
entered into or materially modified in fiscal years beginning on or after June
15, 2010, with early adoption permitted. The Company does not expect
adoption of ASU 2009-13 to have a material impact on the Company’s consolidated
financial position or results of operations.
- 57
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
In
December 2009, the FASB issued ASU 2009-17, “Improvements to Financial Reporting
by Enterprises Involved with Variable Interest Entities” which amends the
related subsections of the Codification to require ongoing reassessments of
whether an enterprise is the primary beneficiary of a variable interest
entity. In addition, the new standard amends the pre-existing
guidance for determining whether an entity is a variable interest entity and for
identifying the primary beneficiary of a variable interest
entity. ASU 2009-17 is effective as of the beginning of an entity’s
first annual reporting period that begins after November 15,
2009. The Company believes the adoption of ASU 2009-17 will not have
a material impact on the Company’s financial position or results of
operations.
In May
2009, the FASB issued a new standard now codified as ASC Topic 855, “Subsequent
Events,” which establishes the accounting for and disclosure of events that
occur after the balance sheet date but before financial statements are issued or
are available to be issued. The Company adopted the provisions of ASC
Topic 855 during the second quarter of 2009. The Company’s adoption
of the new standard had no material impact on the Company’s financial position
or results of operations.
In
December 2007, the FASB issued a new standard now codified in ASC Topic
810-10-45, “Noncontrolling Interest in a Subsidiary,” which requires
noncontrolling interests (previously referred to as minority interests) to be
reported as a component of equity. The Company adopted the new
standard effective January 1, 2009. The Company’s adoption of the new
standard resulted in changes to the presentation of noncontrolling interests
within the Company’s consolidated financial statements.
| (2) | Stock-Based Compensation |
GAAP
requires the recognition of compensation expense for all share-based
compensation awarded to employees, net of estimated forfeitures, using a
fair-value-based method. The grant-date fair value of each award is
amortized to expense over the award’s vesting period. Compensation
expense associated with share-based awards is included in corporate selling,
general and administrative expense in the accompanying consolidated statements
of earnings. Total pre-tax compensation expense and its related
income tax benefit were as follows (in thousands of dollars):
|
Year
Ended December 31,
|
|||||||||
|
2009
|
2008
|
2007
|
|||||||
|
Share-based
compensation expense
|
$
|
4,662
|
$
|
3,195
|
$
|
1,726
|
|||
|
Income
tax benefit
|
1,802
|
1,235
|
667
|
||||||
The
Company has various incentive plans that provide long-term incentive and
retention awards. These awards include stock options and restricted
stock awards. At December 31, 2009, a total of 274,903 shares were
available for future issuance under the plans. The Company generally
issues new shares of common stock to satisfy stock option exercises and
restricted stock award vestings.
Stock
Options
Stock
options may be granted for a term not to exceed 10 years and must be granted
within 5 years from the adoption of the current equity incentive
plan. All of the unvested stock options currently outstanding become
fully exercisable after four years from date of grant. The fair value
of each option award is estimated on the date of grant using a
Black-Scholes-Merton option valuation model. Estimates of fair value
may not equal the value ultimately realized by those who receive equity
awards. No options were granted in 2009, 2008 or 2007.
- 58
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
The
following table provides a summary of stock options outstanding as of December
31, 2009 and changes during the year then ended:
|
Weighted-
|
Weighted-Average
|
Aggregate
|
||||||
|
Average
|
Remaining
|
Intrinsic
|
||||||
|
Exercise
|
Contractual
|
Value
|
||||||
|
Stock Options
|
Shares
|
Price
|
Life
(yrs)
|
(millions)
|
||||
|
Outstanding
at January 1, 2009
|
974,739
|
$24.10
|
||||||
|
Granted
|
—
|
—
|
||||||
|
Exercised
|
(93,910
|
)
|
14.11
|
|||||
|
Forfeited
or expired
|
(10,000
|
)
|
30.08
|
|||||
|
Outstanding
at December 31, 2009
|
870,829
|
$25.11
|
3.5
|
$5.7
|
||||
|
Exercisable
at December 31, 2009
|
863,329
|
$25.16
|
3.5
|
$5.6
|
The total
intrinsic values of options exercised during the years ended December 31, 2009,
2008 and 2007 were approximately $0.9 million, $1.4 million and $2.5 million,
respectively.
A summary
of the status of the Company’s nonvested stock options as of December 31, 2009
and changes during the year ended December 31, 2009 is presented
below:
|
Weighted-
|
|||||
|
Average
|
|||||
|
Grant-Date
|
|||||
|
Nonvested Stock Options
|
Shares
|
Fair
Value
|
|||
|
Nonvested
at January 1, 2009
|
15,000
|
$7.78
|
|||
|
Granted
|
—
|
—
|
|||
|
Vested
|
(7,500
|
)
|
7.78
|
||
|
Forfeited
|
—
|
—
|
|||
|
Nonvested
at December 31, 2009
|
7,500
|
$7.78
|
As of
December 31, 2009, there was approximately $14,000 of unrecognized compensation
cost related to nonvested options.
Restricted
Stock Awards
In 2006,
the Company began issuing restricted stock awards to attract and retain key
Company executives. At the end of a three-year restriction period,
the awards will vest and be transferred to the participant provided that the
participant has been an employee of the Company continuously throughout the
restriction period. In the first quarter of 2007, the Company also
began issuing restricted stock awards to its nonemployee
directors. One-fourth of such awards generally vest each quarter over
the first four quarters following the date of grant.
- 59
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
The
Company’s restricted stock awards have been classified as equity awards under
Statement 123R. The fair value of each award is the market price of
the Company’s common stock on the date of grant and is amortized to expense
ratably over the vesting period. In general, the Company will receive
a tax deduction for each restricted stock award on the vesting date equal to the
fair market value of the restricted stock on the vesting date.
The
following table provides a summary of the status of the Company’s nonvested
restricted stock awards as of December 31, 2009 and the changes during the year
ended December 31, 2009:
|
Weighted-
|
|||||
|
Average
|
|||||
|
Grant-Date
|
|||||
|
Nonvested Restricted Stock
Awards
|
Shares
|
Fair
Value
|
|||
|
Nonvested
at January 1, 2009
|
398,742
|
$18.90
|
|||
|
Granted
|
382,016
|
14.80
|
|||
|
Vested
|
(92,595
|
)
|
17.91
|
||
|
Forfeited
|
(58,430
|
)
|
16.18
|
||
|
Nonvested
at December 31, 2009
|
629,733
|
$16.81
|
|||
The
weighted-average grant-date fair value of restricted stock granted during the
years ended December 31, 2009, 2008 and 2007 was $14.80, $21.71 and $15.20,
respectively. As of December 31, 2009, there was approximately
$3.1 million of unrecognized compensation cost related to nonvested restricted
stock awards. Such cost is expected to be recognized over a
weighted-average period of approximately 2.0 years.
| (3) | Marketable Securities |
Noncurrent
marketable securities at December 31, 2009 and 2008 consist primarily of
marketable equity securities ($1.9 million and $1.2 million at December 31, 2009
and 2008, respectively), corporate and government bonds ($0.8 million and $1.0
million at December 31, 2009 and 2008, respectively) and money market securities
($0.6 million at December 31, 2009 and 2008) held in trust under the Company’s
deferred compensation plan.
| (4) | Allowance for Doubtful Accounts |
Accounts
receivable is reported net of the allowance for doubtful
accounts. Activity in the allowance for doubtful accounts is as
follows (in thousands):
|
Year
Ended December 31,
|
||||||||||
|
2009
|
2008
|
2007
|
||||||||
|
Balance
at beginning of year
|
$
|
19,480
|
$
|
16,266
|
$
|
14,355
|
||||
|
Provisions
for doubtful accounts
|
7,794
|
9,643
|
9,194
|
|||||||
|
Acquisitions
|
8,201
|
17
|
1,472
|
|||||||
|
Disposition
|
(41
|
)
|
—
|
—
|
||||||
|
Accounts
written off, net of recoveries
|
(10,705
|
)
|
(6,446
|
)
|
(8,755
|
)
|
||||
|
Balance
at end of year
|
$
|
24,729
|
$
|
19,480
|
$
|
16,266
|
||||
- 60
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
In 2008,
the Company also recorded a $535,000 provision for doubtful accounts related to
its note receivable from Signature Healthcare Foundation
(“Signature”). This charge reduced the carrying value of a note
receivable from Signature to $580,000 as of December 31, 2008. In
February 2009, the Company terminated its staffing agreement with Signature and
took possession of Signature’s operating assets in full satisfaction of the
Company’s receivables from Signature. The $580,000 carrying value of
the note receivable at December 31, 2008 approximated the estimated fair value
of the assets received from Signature.
| (5) | Property and Equipment |
Property
and equipment, at cost, consist of the following (in thousands):
|
December
31,
|
|||||||
|
2009
|
2008
|
||||||
|
Equipment
|
$
|
88,808
|
$
|
58,163
|
|||
|
Land
|
6,043
|
1,010
|
|||||
|
Buildings
and leasehold improvements
|
60,328
|
27,599
|
|||||
|
Buildings
and equipment under capital lease obligations
|
11,243
|
—
|
|||||
|
166,422
|
86,772
|
||||||
|
Less
accumulated depreciation
|
54,608
|
48,921
|
|||||
|
$
|
111,814
|
$
|
37,851
|
||||
Depreciation
expense incurred by continuing operations was approximately $11.4 million, $10.2
million and $12.1 million for the years ended December 31, 2009, 2008 and 2007,
respectively. These amounts include amortization of assets recorded
under capital leases.
| (6) | Business Combinations |
The
Company adopted FASB Financial Accounting Standards No. 141(R), “Business
Combinations” (now codified in ASC Topic 805, “Business Combinations”),
effective January 1, 2009. The new standard replaces Financial
Accounting Standards No. 141 which required the acquirer to include
acquisition-related costs (such as finder’s fees and legal fees) in the cost of
the acquisition. The new standard requires acquisition-related costs
to be expensed in the periods incurred.
Effective
November 24, 2009, the Company acquired all of the outstanding common stock of
Triumph HealthCare Holdings, Inc. (“Triumph”) for a total purchase price of
approximately $538.5 million, which includes an estimated adjustment based on
acquired working capital levels as defined in the stock purchase
agreement. All purchase price adjustments are expected to be
finalized in the first half of 2010. The total purchase price was
allocated to the estimated fair value of the assets acquired and liabilities
assumed as presented below. At the acquisition date, Triumph operated
20 LTACHs in seven states. The Triumph acquisition has expanded the
number of LTACHs owned and operated by the Company to 28 as of December 31,
2009. In connection with this transaction, the Company recorded
acquisition-related expenses of approximately $7.2 million in the year ended
December 31, 2009. Acquisition-related expenses are included in
selling, general and administrative expenses in the Company’s consolidated
statements of earnings.
- 61
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
The
following table presents the amounts recognized by the Company as of the
acquisition date for each major class of assets acquired and liabilities assumed
in the Triumph transaction. Amounts are in thousands of
dollars.
|
Cash
|
$
|
—
|
||
|
Accounts
receivable
|
60,636
|
|||
|
Other
current assets
|
13,357
|
|||
|
Property
and equipment
|
67,777
|
|||
|
Identifiable
intangible assets, principally Medicare licenses, trade name and
certificates of need
|
108,960
|
|||
|
Other
assets
|
1,747
|
|||
|
Current
portion of long-term debt
|
(2,536
|
)
|
||
|
Accounts
payable and other current liabilities
|
(45,649
|
)
|
||
|
Noncurrent
portion of long-term debt
|
(10,217
|
)
|
||
|
Other
liabilities
|
(36,455
|
)
|
||
|
Total
identifiable net assets
|
157,620
|
|||
|
Noncontrolling
interests in Triumph
|
(10,000
|
)
|
||
|
Goodwill
|
390,920
|
|||
|
Fair
value of total consideration transferred
|
$
|
538,540
|
The fair
value of the accounts receivable acquired of approximately $60.6 million is net
of an estimated $41.9 million discount for contractual allowances and an
estimated $6.5 million that is expected to be uncollectible. The
total goodwill arising from the acquisition of approximately $390.9 million
consists primarily of Triumph’s assembled workforce and the synergies that are
expected to result from combining the operations of the Company and
Triumph. All of the goodwill was assigned to the Company’s hospitals
segment. None of the goodwill is expected to be deductible for tax
purposes.
The fair
value at the acquisition date of the noncontrolling interests in Triumph was
estimated to be approximately $10.0 million and was based a review of the
control, transferability and other terms of Triumph’s partnership
agreements. This fair value measurement is based on significant
inputs that are not observable in the market and thus represents a Level 3
measurement as defined in GAAP.
Triumph’s
results of operations have been included in the Company’s financial statements
prospectively beginning after the date of acquisition. The Company’s
statement of earnings for 2009 includes operating revenues and operating
earnings of approximately $39.7 million and $3.7 million, respectively, related
to Triumph’s hospitals. The following pro forma information assumes the Triumph
acquisition had occurred at the beginning of each period
presented. Such results have been prepared by adjusting the
historical Company results to include Triumph’s results of operations,
amortization of acquired finite-lived intangibles and incremental interest
related to acquisition debt. The pro forma results do not include any
cost savings that may result from the combination of the Company’s and Triumph’s
operations. The pro forma results may not necessarily reflect the
consolidated operations that would have existed had the acquisition been
completed at the beginning of such periods nor are they necessarily indicative
of future results. Amounts are in thousands of dollars.
- 62
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
|
Year
ended
|
Year
ended
|
||||||||||||||||
|
December
31, 2009
|
December
31, 2008
|
||||||||||||||||
|
As
Reported
|
Pro
Forma
|
As
Reported
|
Pro
Forma
|
||||||||||||||
|
Operating
revenues
|
$
|
869,427
|
$
|
1,260,775
|
$
|
735,412
|
$
|
1,159,138
|
|||||||||
|
Net
earnings from continuing operations attributable to
RehabCare
|
$
|
23,794
|
$
|
45,724
|
$
|
19,568
|
$
|
35,144
|
|||||||||
|
Diluted
earnings per share from continuing operations attributable to
RehabCare
|
$
|
1.26
|
$
|
1.88
|
$
|
1.10
|
$
|
1.46
|
|||||||||
Effective
June 30, 2009, the Company and a group of Dallas area physicians formed a new
jointly-owned entity, Dallas LTACH, LLC. On that same date, Dallas
LTACH, LLC acquired certain assets and assumed certain liabilities of Gulf
States LTAC of Dallas. The physician group is also a member of Gulf
States LTAC of Dallas. In connection with the acquisition, the
Company paid cash consideration of approximately $6.4 million and received an
80% interest in the new entity. The physician group owns the
remaining 20% interest. The assets acquired include a 60-bed
long-term acute care hospital located inside a freestanding facility in Dallas,
Texas (the “Dallas LTACH”). The hospital is leasing the facility
under a 20-year operating lease which expires in September 2027. In
connection with this transaction, the Company recorded acquisition-related
expenses of approximately $0.6 million in the year ended December 31,
2009.
Approximately
$6.1 million of the purchase price in the Dallas LTACH transaction was assigned
to goodwill and consists primarily of the aforementioned physician
relationships, the Dallas LTACH’s assembled workforce and the synergies that are
expected to result from combining the operations of the Company and the Dallas
LTACH. All of the goodwill was assigned to the Company’s hospitals
segment. The Dallas LTACH’s results of operations have been included
in the Company’s financial statements prospectively beginning after the date of
acquisition. The Company’s statement of earnings for 2009 includes
operating revenues and operating losses of approximately $7.5 million and $3.5
million, respectively, related to the Dallas LTACH. The Company has
not presented the pro forma results of operations of the Dallas LTACH because
the presentation of such information is considered impracticable. The
Company believes such disclosures are impracticable because the hospital’s
historical financial statements were not audited and are not considered
reliable. The Company made a reasonable effort, but is unable to
obtain reliable historical financial statements for the Dallas
LTACH.
Effective
December 16, 2009, the Company acquired an LTACH in Philadelphia, Pennsylvania
for a purchase price of approximately $5.1 million in cash. The
results of operations of the Philadelphia LTACH have been included in the
Company’s financial statements prospectively beginning after the date of
acquisition. Approximately $1.7 million of the purchase price was
assigned to goodwill. The remaining purchase price allocation and
other information related to the acquisition of the Philadelphia LTACH have not
been included herein as the impact of the acquisition was not material to the
Company’s financial condition or results of operations.
| (7) | Goodwill and Other Intangible Assets |
In
accordance with GAAP, the Company performs an annual test of impairment for
goodwill and other indefinite lived intangible assets. The impairment
analysis is performed more frequently if events or changes in circumstances
indicate that the carrying amount of such assets may exceed fair
value.
- 63
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
Intangible
assets with indefinite lives are not amortized but must be reviewed for
impairment annually and whenever events or changes in circumstances indicate
that the asset might be impaired. If the impairment test indicates
that the carrying value of an intangible asset exceeds its fair value, then an
impairment loss should be recognized in the consolidated statement of earnings
in an amount equal to the excess carrying value. The Company
performed a test for impairment for goodwill and other indefinite lived
intangible assets as of December 31, 2009, 2008 and 2007. Based upon
the results of the tests performed, no impairment of goodwill or other
intangible assets with indefinite useful lives was identified in 2009 or 2008;
however, in 2007, the Company recognized an impairment loss of $4.9 million to
reduce the carrying value of the Medicare exemption it acquired in the June 1,
2006 acquisition of the assets of Louisiana Specialty Hospital, the Company’s
LTACH in New Orleans, Louisiana. This hospital had been grandfathered
and statutorily exempt from the so-called 25% Rule. The 25% Rule
limits LTACH prospective payment system (“PPS”) paid admissions from a single
referral source to 25%. Admissions beyond the 25% threshold would be
paid using lower inpatient PPS rates. On May 1, 2007, the Centers for
Medicare and Medicaid Services (“CMS”) released a rule extending the 25% Rule to
all LTACHs, including those LTACHs that had previously operated under a
statutory exemption.
As part
of the purchase price allocation for Louisiana Specialty Hospital, the Company
initially recorded the value of the statutory exemption as an indefinite-lived
intangible asset at its estimated acquisition date fair value of $5.4
million. The Company determined that the issuance of the May 1, 2007
rule by CMS resulted in a triggering event during the second quarter of 2007
that required the useful life of the statutory exemption intangible asset to be
reassessed as finite-lived and a corresponding impairment analysis to be
performed. Based on that analysis, the Company recognized an
impairment loss of $4.9 million in the second quarter of 2007 in the hospitals
segment to reduce the carrying value of this intangible asset to its revised
estimate of fair value based on the impact of the change in
regulations. This reduced carrying value represents the asset’s new
cost basis for financial reporting purposes. The Company computed the
fair value of the statutory exemption intangible asset using a present value
technique and the Company’s projections of cash flow expected to be generated
over the intangible asset’s remaining estimated useful life. Starting
on May 1, 2007, the Company began amortizing the remaining $0.5 million carrying
value of the intangible asset on a straight-line basis over the asset’s
remaining estimated useful life. As of December 31, 2009, the
statutory exemption intangible asset had a remaining carrying value of
approximately $0.1 million.
On
December 29, 2007, the 2007 Medicare, Medicaid and SCHIP Extension Act was
signed into law. The Act provides that the 25% Rule will not be
applied to grandfathered LTACHs, such as the Company’s LTACH in New Orleans,
through at least December 31, 2010. GAAP prohibits the reversal of
the Company’s previously recognized $4.9 million impairment loss.
In March
2007, the Company and St. Luke’s Episcopal-Presbyterian Hospitals (“St. Luke’s
Hospitals”) formed a jointly-owned entity, St. Luke’s Rehabilitation Hospital,
LLC, which began developing a new 35-bed rehabilitation hospital facility in St.
Louis, Missouri. In December 2008, St. Luke’s Rehabilitation Hospital
completed construction of the new facility and acquired the assets of St. Luke’s
Hospitals’ existing 16-bed inpatient rehabilitation facility (“IRF”) in exchange
for St. Luke’s Hospitals’ minority interest in the new entity. The
operations of the existing IRF were relocated to the new 35-bed hospital
facility. The Company maintains a controlling ownership interest in
St. Luke’s Rehabilitation Hospital, LLC. This transaction did not
qualify as the purchase of a “business” based on the guidance in
GAAP. As a result, the cost of the assets acquired from St. Luke’s
Hospitals were allocated to the individual assets acquired based on their
relative fair values and no goodwill arose from the transaction.
- 64
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
At
December 31, 2009 and 2008, the Company had the following intangible asset
balances (in thousands of dollars):
|
December 31, 2009
|
December 31, 2008
|
||||||||||||||||
|
Gross
|
Gross
|
||||||||||||||||
|
Carrying
|
Accumulated
|
Carrying
|
Accumulated
|
||||||||||||||
|
Amount
|
Amortization
|
Amount
|
Amortization
|
||||||||||||||
|
Amortizing
Intangible Assets:
|
|||||||||||||||||
|
Noncompete
agreements
|
$
|
4,710
|
$
|
(1,566
|
)
|
$
|
1,850
|
$
|
(1,261
|
)
|
|||||||
|
Customer
contracts and relationships
|
23,096
|
(12,577
|
)
|
23,096
|
(10,042
|
)
|
|||||||||||
|
Trade
names
|
40,083
|
(2,792
|
)
|
9,683
|
(1,929
|
)
|
|||||||||||
|
Medicare
exemption
|
454
|
(340
|
)
|
454
|
(227
|
)
|
|||||||||||
|
Market
access assets
|
5,720
|
(310
|
)
|
5,720
|
(24
|
)
|
|||||||||||
|
Certificates
of need
|
9,442
|
(152
|
)
|
142
|
(28
|
)
|
|||||||||||
|
Lease
arrangements
|
1,305
|
(297
|
)
|
905
|
(205
|
)
|
|||||||||||
|
Total
|
$
|
84,810
|
$
|
(18,034
|
)
|
$
|
41,850
|
$
|
(13,716
|
)
|
|||||||
|
Non-amortizing
Intangible Assets:
|
|||||||||||||||||
|
Trade
names
|
$
|
410
|
$
|
810
|
|||||||||||||
|
Medicare
provider numbers
|
68,220
|
—
|
|||||||||||||||
| $ |
68,630
|
$ |
810
|
||||||||||||||
The
market access assets were acquired in the transaction with St. Luke’s Hospitals
noted above. The assets were valued using a discounted cash flows
analysis under the income approach. The estimated value of the market
access assets is attributable to the Company’s ability to gain access to and
penetrate the former facility’s historical patient market.
Certain
customer contracts and lease arrangements have contractual provisions that
enable renewal or extension of the asset's contractual life. Costs
incurred to renew or extend the term of a recognized intangible asset are
expensed in the period incurred.
Amortizing
intangible assets have the following weighted average useful lives as of
December 31, 2009: noncompete agreements – 4.8 years; contractual
customer relationships – 6.1 years; amortizing trade names – 14.8 years;
Medicare exemption – 1.0 year; market access assets – 18.9 years; certificates
of need – 9.8 years; and lease arrangements – 6.2 years.
Amortization
expense incurred by continuing operations was approximately $4.3 million, $3.7
million and $3.7 million for the years ended December 31, 2009, 2008 and 2007,
respectively. Estimated annual amortization expense for the next 5
years is: 2010 – $8.2 million; 2011 – $6.5 million; 2012 – $5.6 million; 2013 –
$5.4 million and 2014 – $5.4 million.
The
changes in the carrying amount of goodwill for the years ended December 31, 2009
and 2008 are as follows (in thousands):
- 65
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
|
Healthcare
Management
|
|||||||||||||||||||
|
SRS
(a)
|
HRS
(b)
|
Hospitals
|
Consulting
(c)
|
Total
|
|||||||||||||||
|
Balance
at December 31, 2007
|
$ |
79,419
|
$ |
39,715
|
$ |
45,239
|
$ |
4,144
|
$ |
168,517
|
|||||||||
|
Acquisitions
|
—
|
—
|
6,414
|
—
|
6,414
|
||||||||||||||
|
Dispositions
|
—
|
—
|
(3,566
|
)
|
—
|
(3,566
|
)
|
||||||||||||
|
Balance
at December 31, 2008
|
79,419
|
|
39,715
|
|
48,087
|
|
4,144
|
|
171,365
|
||||||||||
|
Acquisitions
|
—
|
—
|
398,857
|
—
|
398,857
|
||||||||||||||
|
Dispositions
|
—
|
—
|
—
|
(4,144
|
)
|
(4,144
|
)
|
||||||||||||
|
Balance
at December 31, 2009
|
$
|
79,419
|
$
|
39,715
|
$
|
446,944
|
$
|
—
|
$
|
566,078
|
|||||||||
|
|
(a)
|
Skilled
Nursing Rehabilitation Services
(SRS).
|
|
|
(b)
|
Hospital
Rehabilitation Services (HRS).
|
|
|
(c)
|
The
healthcare management consulting segment consists of Phase 2 Consulting,
Inc., which was sold effective June 1,
2009.
|
| (8) | Dispositions and Discontinued Operations |
Effective
June 1, 2009, the Company completed the sale of all the outstanding common stock
of Phase 2 Consulting, Inc. (“Phase 2”) to Premier, Inc. for approximately $5.5
million. This transaction allows the Company’s management to focus on
its core businesses. In connection with this transaction, the Company
recognized a pre-tax loss related to the disposal of the Phase 2 business of
approximately $1.2 million in 2009.
Phase 2
provides management and economic consulting services to the healthcare industry
and had been a subsidiary of the Company since it was acquired in
2004. Summarized below are the carrying amounts of the assets and
liabilities of Phase 2 that were sold effective June 1, 2009 (in
thousands):
|
Assets:
|
||||
|
Accounts
receivable
|
$
|
2,202
|
||
|
Other
current assets
|
23
|
|||
|
Property
and equipment, net
|
115
|
|||
|
Goodwill
|
4,144
|
|||
|
Intangible
assets
|
400
|
|||
|
Other
assets
|
13
|
|||
|
Total
assets
|
$
|
6,897
|
||
|
Liabilities:
|
||||
|
Accounts
payable and accrued expenses
|
$
|
209
|
||
|
Total
liabilities
|
$
|
209
|
||
The
Company guaranteed the collection of all but $45,000 of Phase 2’s accounts
receivable. All accounts receivable were subsequently collected by
Premier, Inc. The time available to Premier, Inc. to make a claim
against this guarantee has now lapsed. Accordingly, no liability has
been recognized at December 31, 2009 for this guarantee.
- 66
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
Phase 2
has been classified as a discontinued operation pursuant to GAAP. The
operating results for this discontinued operation are shown in the following
table (in thousands). No interest expense has been
allocated.
|
2009
|
2008
|
2007
|
|||||||||||
|
Operating
revenues
|
$
|
2,833
|
$
|
9,563
|
$
|
12,480
|
|||||||
|
Costs
and expenses
|
3,064
|
9,789
|
11,375
|
||||||||||
|
Operating
gain (loss) from discontinued operations
|
(231
|
)
|
(226
|
)
|
1,105
|
||||||||
|
Loss
on disposal of assets of discontinued operations
|
(1,188
|
)
|
—
|
—
|
|||||||||
|
Income
tax benefit (expense)
|
553
|
88
|
(440
|
)
|
|||||||||
|
Gain
(loss) from discontinued operations
|
$
|
(866
|
)
|
$
|
(138
|
)
|
$
|
665
|
|||||
Effective
August 30, 2008, the Company completed the sale of equipment, goodwill, other
intangible assets and certain related assets associated with its 38-bed
inpatient rehabilitation hospital located in Midland, Texas (the “Midland
hospital”) to HealthSouth Corporation for $7.2 million less direct selling
costs. This transaction was the result of a strategic review of the
Midland-Odessa market. Simultaneous with the sale, the Midland
hospital transferred its operations and remaining patients to HealthSouth’s
rehabilitation hospital also located in the Midland-Odessa area. In
connection with this transaction, the Company recognized a pre-tax gain related
to the disposal of the Midland hospital assets of approximately $0.3 million in
2008.
The
Midland hospital had been a component of the Hospital reporting unit since
mid-2006, and its operations were integrated into the Hospital reporting
unit. Accordingly, the Company determined an appropriate allocation
of goodwill for the Midland hospital based on its fair value relative to the
overall fair value of the Hospital reporting unit. The Company used a
discounted cash flow technique to determine fair value, which resulted in
approximately $3.6 million of goodwill being allocated to the Midland
hospital. Summarized below are the carrying amounts of the assets and
liabilities of the Midland hospital that were sold effective August 30, 2008 (in
thousands):
|
Assets:
|
||||
|
Property
and equipment, net
|
$
|
18
|
||
|
Goodwill
|
3,566
|
|||
|
Intangible
assets, net
|
2,154
|
|||
|
Total
assets
|
$
|
5,738
|
||
|
Liabilities:
|
||||
|
Accrued
salaries and wages
|
$
|
7
|
||
|
Total
liabilities
|
$
|
7
|
The
Midland hospital has been classified as a discontinued operation pursuant to
GAAP. The operating results for this discontinued operation are shown
in the following table (in thousands). No interest expense has been
allocated.
- 67
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
|
2009
|
2008
|
2007
|
|||||||||||
|
Operating
revenues
|
$
|
—
|
$
|
3,962
|
$
|
7,125
|
|||||||
|
Costs
and expenses
|
(44
|
)
|
5,471
|
8,791
|
|||||||||
|
Operating
gain (loss) from discontinued operations
|
44
|
(1,509
|
)
|
(1,666
|
)
|
||||||||
|
Loss
on disposal of assets of discontinued operations
|
—
|
321
|
—
|
||||||||||
|
Income
tax benefit (expense)
|
(17
|
)
|
463
|
619
|
|||||||||
|
Gain
(loss) from discontinued operations
|
$
|
27
|
$
|
(725
|
)
|
$
|
(1,047
|
)
|
|||||
| (9) | Long-Term Debt |
On
November 24, 2009, the Company entered into an Amended and Restated Credit
Agreement (the “Credit Agreement”) with Bank of America, N.A., as administrative
agent and collateral agent, and Banc of America Securities LLC, RBC Capital
Markets and BNP Paribas Securities Corp., as joint lead
arrangers. The Credit Agreement amends and restates the Company’s
former $175 million amended and restated credit agreement, dated June 16, 2006,
and provides for a six-year $450 million term loan facility, a five-year
revolving credit facility of $125 million and a swingline subfacility of up to
$25 million. The Company used the proceeds of the term loan facility and
approximately $22 million in borrowings under the revolving credit facility to
pay a portion of the consideration for its acquisition of Triumph.
The
Credit Agreement contains certain restrictive covenants that, among other
things, limit the incurrence of additional indebtedness, investments, dividends,
transactions with affiliates, asset sales, acquisitions, mergers and
consolidations, liens and encumbrances and other matters customarily restricted
in similar credit facilities. In addition, the Company is required to maintain a
maximum ratio of total funded debt to earnings before interest, taxes,
depreciation and amortization ((“EBITDA”) as defined in the Credit Agreement), a
maximum ratio of senior funded debt to EBITDA and a minimum ratio of adjusted
earnings before interest, taxes, depreciation, amortization, rent and operating
leases ((“Adjusted EBITDAR) as defined in the Credit Agreement) to fixed
charges. As of December 31, 2009, the Company was in compliance with
all debt covenants. The annual commitment fees, letter of credit fees
and interest rates to be charged on the outstanding principal balances in
connection with the revolving credit facility are variable based upon the
Company’s consolidated leverage ratios.
The term loan facility requires
quarterly installments of $1,125,000 with the balance payable upon the final
maturity. In addition, the Company is required to make mandatory
principal prepayments equal to a portion of its consolidated excess cash flow
(as defined in the Credit Agreement) when its consolidated leverage ratio
reaches certain levels. At December 31, 2009, the balance outstanding
under the term loan was $450 million. There were no borrowings
outstanding under the revolving credit facility at December 31,
2009.
As of
December 31, 2009, the Company had approximately $11.3 million in letters of
credit outstanding to its insurance carriers as collateral for reimbursement of
claims. The letters of credit reduce the amount the Company may
borrow under its revolving credit facility. As of December 31, 2009,
after consideration of the effects of restrictive covenants, the available
borrowing capacity under the revolving credit facility was approximately $113.7
million.
- 68
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
As of
December 31, 2009 and 2008, long-term borrowings, including the current portion
of long-term debt, were as follows (dollars in thousands unless otherwise
noted):
|
December
31,
|
|||||||
|
2009
|
2008
|
||||||
|
Borrowings
under $175 million revolving credit facility
|
$
|
—
|
$
|
57,000
|
|||
|
Borrowings
under $125 million revolving credit facility; maturity date of November
24, 2014
|
|
—
|
|
—
|
|||
|
Term
loan facility; payable in quarterly installments of $1.1 million with
remaining balance due on November 24, 2015; net of unamortized original
issue discount of $8,892
|
441,108
|
—
|
|||||
|
Note
payable to bank; bearing interest at prime plus 1%, but not less than 5%
nor greater than 7.5%; payable in monthly installments through January
2011 and $4.2 million due in February 2011
|
4,528
|
—
|
|||||
|
Capital
lease obligations
|
9,631
|
—
|
|||||
|
455,267
|
57,000
|
||||||
|
Less: current
portion
|
(7,507
|
)
|
—
|
||||
|
$
|
447,760
|
$
|
57,000
|
||||
The
Credit Agreement is collateralized by substantially all of the Company’s
assets. Borrowings under the $125 million revolving credit facility
bear interest at the Company’s option at either a base rate or the London
Interbank Offering Rate (“LIBOR”) for one, two, three or six month interest
periods, or a nine or twelve month period if available, plus an applicable
margin percentage. The base rate is the greater of the federal funds
rate plus one-half of 1%, Bank of America N.A.’s prime rate and one month LIBOR
plus 1%. There were no borrowings outstanding under the revolving
credit facility at December 31, 2009. Borrowings under the term loan
facility bear interest at either the base rate plus 300 basis points or LIBOR
plus 400 basis points with a LIBOR floor of 200 basis points. The
interest rate under the term loan facility was 6% at December 31,
2009.
Certain
of the Company’s leases that meet the lease capitalization criteria in
accordance with FASB ASC 840-30 have been recorded as an asset and liability at
the lower of fair value or the net present value of the aggregate future minimum
lease payments at the inception of the lease. Interest rates used in
computing the net present value of the lease payments ranged from 6.5% to 10.7%
and were generally based on the lessee’s incremental borrowing rate at the
inception of the lease.
- 69
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
The
Company’s long-term debt is scheduled to mature as follows. The
maturities below exclude the impact of the term loan’s unamortized original
issue discount of $8,892,000 at December 31, 2009. Amounts are in
thousands.
|
2010
|
$
|
7,507
|
||
|
2011
|
11,708
|
|||
|
2012
|
7,791
|
|||
|
2013
|
5,148
|
|||
|
2014
|
4,505
|
|||
|
Thereafter
|
427,500
|
|||
|
Total
|
$
|
464,159
|
Interest
paid for 2009, 2008 and 2007 was $4.8 million, $4.4 million and $7.6 million,
respectively. Included in the interest paid amounts are commitment fees on the
unused portion of the revolving credit facility of $0.3 million, $0.3 million
and $0.2 million for 2009, 2008 and 2007, respectively.
| (10) | Stockholders’ Equity |
In
November 2009, the Company issued 6,210,000 shares of common stock, par value of
$0.01 in a public equity offering which resulted in net proceeds, after
underwriting fees and other direct costs, of approximately $140.2
million. The net proceeds from the public equity offering were used
in the acquisition of Triumph HealthCare.
The
Company has a stockholder rights plan pursuant to which preferred stock purchase
rights were distributed as a dividend on each share of the Company’s outstanding
common stock. Each right, when exercisable, will entitle the holders
to purchase one one-hundredth of a share of series B junior participating
preferred stock of the Company at an initial exercise price of $150.00 per one
one-hundredth of a share.
The
rights are not exercisable or transferable until a person or affiliated group
acquires beneficial ownership of 20% or more of the Company’s common stock or
commences a tender or exchange offer for 20% or more of the stock, without the
approval of the board of directors. In the event that a person or group actually
acquires 20% or more of the Company’s stock, each holder of rights (other than
the person consummating the transaction) will have the right to receive upon
exercise of the rights shares of the Company’s common stock at one-half of the
then-current market price per share of the
stock. In addition, in the event that the Company consolidates or
merges with another entity or the Company sells or otherwise transfers 50% or
more of its consolidated assets or earnings power, each holder of rights (other
than the person consummating the transaction) will have the right to receive
upon exercise of the rights shares of the surviving or purchasing entity’s
common stock at one-half of the then-current market price of the
stock.
The
series B preferred stock is non-redeemable and junior of any other series of
preferred stock that the Company may issue in the future. Each share of series B
preferred stock, upon issuance, will have a preferential dividend in the amount
equal to the greater of $1.00 per share or 100 times the dividend declared per
share on the Company’s common stock. In the event of a liquidation of the
Company, the series B preferred stock will receive a preferred liquidation
payment equal to the greater of $100 or 100 times the payment made on each share
of the Company’s common stock. Each one one-hundredth of a share of series B
preferred stock will have one vote on all matters submitted to the stockholders
and will vote together as a single class with the Company’s common
stock.
- 70
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
| (11) | Earnings per Share |
Basic
earnings per share excludes dilution and is computed by dividing income
available to common stockholders by the weighted average common shares
outstanding for the period. Diluted earnings per share reflects the
potential dilution that could occur if securities or other contracts to issue
common stock were exercised and converted into common stock or resulted in the
issuance of common stock that then shared in the earnings of the entity (as
calculated utilizing the treasury stock method). These potential
shares include dilutive stock options and unvested restricted stock
awards.
The
following table sets forth the computation of basic and diluted earnings (loss)
per share attributable to RehabCare stockholders (in thousands, except per share
data). The net earnings amounts presented below exclude income and
losses attributable to noncontrolling interests in consolidated
subsidiaries.
|
Year
Ended December 31,
|
||||||||||||
|
2009
|
2008
|
2007
|
||||||||||
|
Numerator:
|
||||||||||||
|
Earnings
from continuing operations, net of tax
|
$
|
23,794
|
$
|
19,568
|
$
|
13,041
|
||||||
|
Loss
from discontinued operations, net of tax
|
(839
|
)
|
(863
|
)
|
(382
|
)
|
||||||
|
Net
earnings
|
$
|
22,955
|
$
|
18,705
|
$
|
12,659
|
||||||
|
Denominator:
|
||||||||||||
|
Basic
weighted average common shares outstanding
|
18,481
|
17,583
|
17,226
|
|||||||||
|
Effect
of dilutive securities:
|
||||||||||||
|
stock
options and restricted stock awards
|
381
|
215
|
233
|
|||||||||
|
Diluted
weighted average common shares outstanding
|
18,862
|
17,798
|
17,459
|
|||||||||
|
Basic
earnings per common share:
|
||||||||||||
|
Earnings
from continuing operations, net of tax
|
$
|
1.29
|
$
|
1.11
|
$
|
0.76
|
||||||
|
Loss
from discontinued operations, net of tax
|
(0.05
|
)
|
(0.05
|
)
|
(0.03
|
)
|
||||||
|
Net
earnings
|
$
|
1.24
|
$
|
1.06
|
$
|
0.73
|
||||||
|
Diluted
earnings per common share:
|
||||||||||||
|
Earnings
from continuing operations, net of tax
|
$
|
1.26
|
$
|
1.10
|
$
|
0.75
|
||||||
|
Loss
from discontinued operations, net of tax
|
(0.04
|
)
|
(0.05
|
)
|
(0.02
|
)
|
||||||
|
Net
earnings
|
$
|
1.22
|
$
|
1.05
|
$
|
0.73
|
||||||
For
fiscal 2009, 2008 and 2007, outstanding stock options totaling approximately 0.7
million, 0.9 million and 1.3 million potential shares, respectively, were
excluded from the calculation of diluted earnings per share because their effect
would have been anti-dilutive.
| (12) | Employee Benefits |
The
Company has an Employee Savings Plan, which is a defined contribution plan
qualified under Section 401(k) of the Internal Revenue Code, for the benefit of
its eligible employees. All employees who are at least 21 years of
age are immediately eligible to participate in the plan. Each
participant may contribute from 2% to 20% of his or her annual compensation to
the plan subject to limitations on the highly compensated employees to ensure
the plan is nondiscriminatory. Contributions made by the Company to
the Employee Savings Plan are at rates of up to 50% of the first 4% of employee
contributions. Expense in connection with the Employee Savings Plan
for 2009, 2008 and 2007 totaled $4.0 million, $4.0 million and $3.9 million,
respectively.
- 71
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
In
connection with the acquisition of Triumph on November 24, 2009, the Company
added the Triumph 401(k) Plan to its portfolio of employee benefit
plans. Substantially all full-time Triumph employees are eligible to
participate in the plan. Matching contributions under the plan are
equal to 25% of the participant contributions up to 6% of their
salary. The Company’s matching contributions in connection with the
Triumph 401(k) Plan were approximately $62,000 in 2009.
The
Company maintains nonqualified deferred compensation plans for certain
employees. Due to changes in the Internal Revenue Code impacting
deferred compensation arrangements, the Company froze its plan, which became
ineligible to receive future deferrals, on December 31, 2004. To
ensure compliance with Internal Revenue Code section 409A, a new plan was
developed and implemented on July 1, 2005. Under the 2005 plan,
participants may defer up to 70% of their base salary and up to 70% of their
cash incentive compensation. Amounts for both plans are held by a
trust in investments that are designated by participants but remain the property
of the Company until distribution. At December 31, 2009 and 2008,
approximately $3.4 million and $2.8 million, respectively, were payable under
the nonqualified deferred compensation plans and approximated the value of the
trust assets owned by the Company.
| (13) | Commitments |
The
Company is obligated under non-cancelable operating leases for the facilities
that support the Company’s hospitals, the Company’s administrative functions and
other operations. The Company’s hospital facility leases represent
the largest portion of rent expense and such leases generally have initial terms
of 12 to 20 years with one or more renewal options. Contingent rents
are included in rent expense in the year incurred. Future minimum
lease payments at December 31, 2009 for those operating leases having an initial
or remaining non-cancelable lease term in excess of one year are as follows
(amounts in thousands):
|
2010
|
$
|
31,611
|
|||
|
2011
|
32,893
|
||||
|
2012
|
32,930
|
||||
|
2013
|
32,987
|
||||
|
2014
|
33,471
|
||||
|
Thereafter
|
262,711
|
||||
|
Total
|
$
|
426,603
|
Rent
expense for 2009, 2008 and 2007 was approximately $20.3 million, $12.9 million
and $12.2 million, respectively. As of December 31, 2009, the
Company expected to receive future minimum rentals of approximately $1.8 million
under noncancelable subleases having a remaining term in excess of one
year.
Triumph’s
headquarters are located in a medical office building in Houston,
Texas. Triumph owns a controlling interest in the building and leases
out the remaining office space to physicians and other healthcare service
providers. As of December 31, 2009, the building had a carrying value
of approximately $6.8 million and the Company expected to receive future minimum
rentals under noncancelable leases of approximately $1.7 million.
- 72
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
Certain
of the Company’s hospitals lease facilities and/or equipment under leases that
are classified as capital leases. Lease commitments under capital
leases at December 31, 2009 are as follows (amounts in thousands):
|
2010
|
$
|
3,533
|
|||
|
2011
|
3,532
|
||||
|
2012
|
3,532
|
||||
|
2013
|
658
|
||||
|
2014
|
5
|
||||
|
Thereafter
|
—
|
||||
|
Total
minimum lease payments
|
11,260
|
||||
|
Less:
interest portion
|
(1,629
|
)
|
|||
|
Total
obligations under capital leases
|
$
|
9,631
|
|||
The
Company was not a party to any material open construction contracts as of
December 31, 2009.
| (14) | Income Taxes |
The
components of income tax expense (benefit), excluding discontinued operations,
are as follows (in thousands):
|
Year
Ended December 31,
|
|||||||||||
|
2009
|
2008
|
2007
|
|||||||||
|
Federal
– current
|
$
|
13,051
|
$
|
7,282
|
$
|
1,196
|
|||||
|
Federal
– deferred
|
2,183
|
3,229
|
6,392
|
||||||||
|
State
|
2,407
|
1,552
|
70
|
||||||||
|
$
|
17,641
|
$
|
12,063
|
$
|
7,658
|
||||||
A
reconciliation between expected income taxes, computed by applying the statutory
Federal income tax rate of 35% to earnings from continuing operations before
income taxes, and actual income tax is as follows (in thousands):
|
Year
Ended December 31,
|
|||||||||||
|
2009
|
2008
|
2007
|
|||||||||
|
Expected
income taxes
|
$
|
13,814
|
$
|
10,376
|
$
|
7,113
|
|||||
|
Tax
effect of interest income from municipal bond obligations exempt from
federal taxation
|
(2
|
)
|
(1
|
)
|
(8
|
)
|
|||||
|
State
income taxes, net of federal income tax benefit
|
1,634
|
982
|
120
|
||||||||
|
Tax
effect of losses attributable to noncontrolling interests not deductible
by the Company
|
688
|
695
|
132
|
||||||||
|
Tax
effect on nondeductible acquisition-related expenses
|
1,347
|
—
|
—
|
||||||||
|
Other,
net
|
160
|
11
|
301
|
||||||||
|
$
|
17,641
|
$
|
12,063
|
$
|
7,658
|
||||||
- 73
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
The tax
effects of temporary differences that give rise to the deferred tax assets and
liabilities are as follows (in thousands):
|
December
31,
|
|||||||
|
2009
|
2008
|
||||||
|
Deferred
tax assets:
|
|||||||
|
Allowance
for doubtful accounts
|
$
|
7,588
|
$
|
5,439
|
|||
|
Accrued
insurance, vacation, bonus and deferred compensation
|
12,563
|
8,348
|
|||||
|
Net
operating loss carryforward/capital loss carryforward
|
1,697
|
184
|
|||||
|
Stock
based compensation
|
3,081
|
1,993
|
|||||
|
Other
|
6,516
|
4,717
|
|||||
|
Total
gross deferred tax assets
|
31,445
|
20,681
|
|||||
|
Valuation
allowance
|
(74
|
)
|
(75
|
)
|
|||
|
Net
deferred tax assets
|
31,371
|
20,606
|
|||||
|
Deferred
tax liabilities:
|
|||||||
|
Acquired
goodwill and intangibles
|
47,402
|
10,500
|
|||||
|
Depreciation
and amortization
|
5,229
|
1,913
|
|||||
|
Other
|
3,096
|
1,623
|
|||||
|
Total
deferred tax liabilities
|
55,727
|
14,036
|
|||||
|
$
|
(24,356
|
)
|
$
|
6,570
|
|||
In
connection with the acquisition of Triumph, as more fully discussed in note 6,
the Company acquired gross net operating loss carryforwards of approximately
$6.6 million. Section 382 of the Internal Revenue Code restricts the
utilization of net operating losses and other carryover tax attributes upon the
occurrence of an ownership change such as the Company’s acquisition of
Triumph. Accordingly, utilization of the acquired Triumph net
operating loss carryforwards will be limited to approximately $0.7 million per
tax year. Based on this limitation and the expiration of the
carryforwards in 2016, the Company estimates approximately $2.2 million of the
acquired net operating loss carryforwards will expire unused. At the
date of acquisition, the Company recorded the acquired net operating loss
carryforwards at their estimated net realizable value, net of the section 382
limitation. At December 31, 2009, the remaining unused net operating
loss carryforwards were approximately $4.3 million and the tax effect of these
carryforwards was approximately $1.5 million.
At
December 31, 2009, the Company also had state net operating loss carryforwards
and federal capital loss carryforwards which resulted in a deferred tax asset of
approximately $0.2 million. These carryforwards expire on various
dates between 2010 and 2026.
The
Company is required to establish a valuation allowance for deferred tax assets
if, based on the weight of available evidence, it is more likely than not that
some portion or all of the deferred tax assets will not be realized. The
ultimate realization of deferred tax assets is dependent upon the generation of
future taxable income during the periods in which those temporary differences
become deductible. Management considers the scheduled reversal of
deferred tax liabilities, projected future taxable income and tax planning
strategies in making this assessment. After consideration of all evidence, both
positive and negative, management concluded that it was more likely than not
that the Company will not realize a portion of its deferred tax assets and that
a valuation allowance of approximately $0.1 million was necessary as of December
31, 2009 and 2008. For the years ended December 31, 2009, 2008, and
2007, the net increases (decreases) in the valuation allowance were $0.0
million, $0.3 million, and $(15.5) million, respectively. The valuation
allowance decrease in 2007 primarily relates to the Company’s adoption of the
accounting standard known at the time as FASB Interpretation No. 48,
“Accounting for Uncertainty in Income Taxes” (“FIN 48”), and now codified in ASC
Topic 740, “Income Taxes.”
- 74
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
The
Company adopted the provisions of FIN 48 on January 1, 2007. This
Interpretation requires financial statement recognition of a tax position taken
or expected to be taken in a tax return, if that position is more likely than
not of being sustained upon examination, based on the technical merits of the
position. Based on the accounting standards that existed prior to FIN
48, the Company had not recognized a $14.4 million potential tax benefit in its
financial statements at December 31, 2006 for the losses incurred in connection
with the Company’s former investment in InteliStaf. In accordance
with the provisions of FIN 48, the Company evaluated the technical merits of its
uncertain tax positions. At that time, the Company believed it would
more likely than not obtain a tax deduction for the full amount of the losses
incurred on its investment in InteliStaf. Based on that evaluation,
the Company recorded a $14.4 million reduction in its liability for unrecognized
tax benefits and a $14.4 million increase to its January 1, 2007 balance of
retained earnings to recognize the cumulative effect of applying FIN
48. This cumulative-effect adjustment represents the difference
between the net amount of assets and liabilities recognized in the statement of
financial position prior to the application of FIN 48 and the net amount of
assets and liabilities recognized as a result of applying FIN 48.
The
following table provides a reconciliation of the beginning and ending amount of
unrecognized tax benefits for the years ended December 31, 2009 and 2008 (in
thousands):
|
2009
|
2008
|
|||||||
|
Balance
at beginning of year
|
$
|
448
|
$
|
308
|
||||
|
Liability
assumed in acquisition of Triumph
|
133
|
—
|
||||||
|
Increase
as a result of tax positions taken in prior years
|
510
|
7
|
||||||
|
Increase
as a result of tax positions taken in the current year
|
710
|
212
|
||||||
|
Lapse
of applicable statute of limitations
|
(154
|
)
|
(79
|
)
|
||||
|
Balance
at end of year
|
$
|
1,647
|
$
|
448
|
As of
December 31, 2009, the Company had approximately $1.6 million of unrecognized
tax benefits that, if recognized, would favorably affect the Company’s effective
income tax rate. The Company currently does not expect any
significant changes to unrecognized tax positions within the next twelve
months.
The
Company’s practice is to recognize interest related to unrecognized tax benefits
as a component of interest expense and penalties related to unrecognized tax
benefits as a component of selling, general and administrative
expenses.
RehabCare
and its subsidiaries file income tax returns for U.S. federal income taxes and
various state income taxes. The Company is no longer subject to U.S.
federal income tax examination for years prior to 2007. The IRS
completed its examination of the Company’s 2006 federal income tax return in
2009.
Income
taxes paid by the Company for 2009, 2008 and 2007 were $15.8 million, $6.7
million and $0.5 million, respectively.
- 75
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements
December
31, 2009, 2008 and 2007
| (15) | Investment in Unconsolidated Affiliate |
In
January 2005, the Company paid $3.6 million for a 40% equity interest in Howard
Regional Specialty Care, LLC (“HRSC”), which operates a freestanding
rehabilitation hospital in Kokomo, Indiana. The Company uses the
equity method to account for its investment in HRSC. The value of the
Company’s investment in HRSC at the transaction date exceeded its share of the
book value of HRSC’s stockholders’ equity by approximately $3.5
million. This excess is being accounted for as equity method
goodwill. In February 2007, the Company invested an additional $1.1
million of cash in HRSC, and the majority owner invested an additional $1.7
million. HRSC used these funds to meet its working capital needs and
to acquire an outpatient rehabilitation business in Kokomo. The
carrying value of the Company’s investment in HRSC was approximately $4.8
million at both December 31, 2009 and 2008.
| (16) | Severance and Restructuring Costs |
In the
fourth quarter of 2009, the Company eliminated 13 corporate positions in an
effort to reduce corporate overhead and eliminate redundancies created by the
acquisition of Triumph. In connection with these efforts, the Company
recognized a pre-tax charge of approximately $0.9 million for employee severance
costs including costs incurred under pre-existing severance
plans. This charge is reflected on the selling, general and
administrative expense line of the Company’s consolidated statement of earnings
for 2009. The following table provides a roll-forward of the
liability for accrued severance costs from January 1, 2009 through December 31,
2009 (amounts in thousands):
|
Balance,
January 1, 2009
|
$
|
—
|
||
|
Accrual
for severance costs
|
862
|
|||
|
Payments
|
(105
|
)
|
||
|
Balance,
December 31, 2009
|
$
|
757
|
||
In the
second half of 2008, the Company eliminated approximately 60 corporate and
division support positions in an effort to better align the Company’s support
functions and reduce corporate and division overhead. In
connection with these efforts, the Company recognized a pre-tax charge of
approximately $2.3 million for employee severance costs including costs incurred
under pre-existing severance plans. This charge is reflected on the
selling, general and administrative expense line of the Company’s consolidated
statement of earnings for 2008. The following table provides a
roll-forward of the liability for accrued severance costs from January 1, 2008
through December 31, 2009 (amounts in thousands):
|
Balance,
January 1, 2008
|
$
|
—
|
||
|
Accrual
for severance costs
|
2,263
|
|||
|
Payments
|
(910
|
)
|
||
|
Balance,
December 31, 2008
|
$
|
1,353
|
||
|
Payments
|
(1,353
|
)
|
||
|
Balance,
December 31, 2009
|
$
|
—
|
||
- 76
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements
December
31, 2009, 2008 and 2007
| (17) | Related Party Transactions |
The
Company’s hospital rehabilitation services division recognized operating
revenues for services provided to HRSC, the Company’s 40% owned equity method
investment, of approximately $0.4 million for the year ended December 31,
2007. In March 2007, the Company canceled its existing management
services contract with HRSC as part of a plan to improve HRSC’s
profitability.
The
Company purchased air transportation services from 55JS Limited, Co. at an
approximate cost of $735,000, $510,000 and $457,000 for the years ended December
31, 2009, 2008 and 2007, respectively. 55JS Limited, Co. is owned by
the Company’s President and Chief Executive Officer, John Short. The
air transportation services are billed to the Company for hourly usage of 55JS’s
plane for Company business.
| (18) | Fair Value Measurements |
GAAP
defines fair value as the price that would be received to sell an asset or paid
to transfer a liability in an orderly transaction between market participants at
the measurement date. The following disclosures provide information
about the extent to which fair value is used to measure recognized assets and
liabilities, the inputs used to develop the measurements and the effect of
certain of the measurements on earnings for the period.
The
Company uses a three-level fair value hierarchy that categorizes assets and
liabilities measured at fair value based on the observability of the inputs
utilized in the valuation: Level 1 - inputs are quoted prices in active markets
for the identical assets or liabilities; Level 2 - inputs other than quoted
prices that are directly or indirectly observable through market-corroborated
inputs; and Level 3 - inputs are unobservable, or observable but cannot be
market-corroborated, requiring the Company to make assumptions about pricing by
market participants. The following tables set forth information for
the Company’s financial assets and liabilities that are measured at fair value
on a recurring basis (amounts in thousands):
|
December
31, 2009
|
||||||||||||||||
|
Carrying
|
Fair
Value Measurements
|
|||||||||||||||
|
Value
|
Level
1
|
Level
2
|
Level
3
|
|||||||||||||
|
Trading
securities
|
$
|
3,314
|
$
|
3,314
|
$
|
—
|
$
|
—
|
||||||||
|
December
31, 2008
|
||||||||||||||||
|
Carrying
|
Fair
Value Measurements
|
|||||||||||||||
|
Value
|
Level
1
|
Level
2
|
Level
3
|
|||||||||||||
|
Trading
securities
|
$
|
2,810
|
$
|
2,810
|
$
|
—
|
$
|
—
|
||||||||
|
Interest
rate swap
|
(692
|
)
|
—
|
(692
|
)
|
—
|
||||||||||
|
Total
net financial assets (liabilities)
|
$
|
2,118
|
$
|
2,810
|
$
|
(692
|
)
|
$
|
—
|
|||||||
The
Company used an income approach to value its liability for the interest rate
swap outstanding as of December 31, 2008. The fair value of the swap
was estimated using a discounted cash flow model that takes into account
observable inputs including contractual terms of the swap and current market
information as of the reporting date such as prevailing interest
rates.
- 77
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
The
Company adopted new accounting guidance effective January 1, 2009 with respect
to fair value measurements of its nonfinancial assets and liabilities including
property and equipment, goodwill and other intangible assets. These
assets are not measured at fair value on a recurring basis; however, they are
subject to fair value adjustments in certain circumstances, such as when there
is evidence that impairment may exist. No impairment related to these
assets was identified in 2009.
| (19) | Industry Segment Information |
In the
first quarter of 2009, the Company made certain changes to the structure of its
internal organization. These changes primarily consisted of making
the Company’s skilled nursing rehabilitation services division responsible for
oversight of the Company’s businesses that provide resident-centered management
consulting services and staffing services for therapists and
nurses. Following these structural changes and the sale of Phase 2,
the Company now operates in the following two business segments, which are
managed separately based on fundamental differences in operations: program
management services and hospitals. Program management services
include hospital rehabilitation services (including inpatient acute and subacute
rehabilitation and outpatient therapy programs) and skilled nursing
rehabilitation services (including contract therapy in skilled nursing
facilities, resident-centered management consulting services and staffing
services for therapists and nurses). The Company’s hospitals segment
owns and operates 28 long-term acute care hospitals and six inpatient
rehabilitation hospitals.
Virtually
all of the Company’s services are provided in the United
States. Summarized information about the Company’s operations in each
industry segment is as follows (in thousands). The following
information and relevant financial information in other footnotes herein have
been restated to reflect the operational oversight changes as noted
above.
|
Operating
Revenues
|
Operating
Earnings (Loss)
|
||||||||||||||||||
|
2009
|
2008
|
2007
|
2009
|
2008
|
2007
|
||||||||||||||
|
Program
management:
|
|||||||||||||||||||
|
Skilled
nursing rehabilitation services
|
$
|
496,250
|
$
|
457,229
|
$
|
432,910
|
$
|
37,753
|
$
|
25,544
|
$
|
7,249
|
|||||||
|
Hospital
rehabilitation services
|
178,168
|
165,658
|
164,102
|
29,487
|
21,997
|
22,893
|
|||||||||||||
|
Program
management total
|
674,418
|
622,887
|
597,012
|
67,240
|
47,541
|
30,142
|
|||||||||||||
|
Hospitals
|
195,009
|
112,525
|
96,001
|
(22,512
|
)
|
(13,903
|
)
|
(1,972
|
)
|
||||||||||
|
Unallocated
corporate expenses (1)
|
N/A
|
N/A
|
N/A
|
(254
|
)
|
(731
|
)
|
(640
|
)
|
||||||||||
|
Total
|
$
|
869,427
|
$
|
735,412
|
$
|
693,013
|
$
|
44,474
|
$
|
32,907
|
$
|
27,530
|
|||||||
- 78
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
|
Depreciation
and Amortization
|
Capital
Expenditures
|
||||||||||||||||||
|
2009
|
2008
|
2007
|
2009
|
2008
|
2007
|
||||||||||||||
|
Program
management:
|
|||||||||||||||||||
|
Skilled
nursing rehabilitation services
|
$
|
6,283
|
$
|
6,835
|
$
|
8,777
|
$
|
2,422
|
$
|
3,824
|
$
|
2,530
|
|||||||
|
Hospital
rehabilitation services
|
2,423
|
2,641
|
4,104
|
1,328
|
1,032
|
442
|
|||||||||||||
|
Program
management total
|
8,706
|
9,476
|
12,881
|
3,750
|
4,856
|
2,972
|
|||||||||||||
|
Hospitals
|
7,793
|
5,094
|
3,657
|
9,465
|
13,604
|
6,824
|
|||||||||||||
|
Healthcare
management consulting (2)
|
N/A
|
N/A
|
N/A
|
—
|
42
|
193
|
|||||||||||||
|
Total
|
$
|
16,499
|
$
|
14,570
|
$
|
16,538
|
$
|
13,215
|
$
|
18,502
|
$
|
9,989
|
|||||||
|
Total
Assets
|
|||||||||||
|
as
of December 31,
|
|||||||||||
|
2009
|
2008
|
2007
|
|||||||||
|
Program
management:
|
|||||||||||
|
Skilled
nursing rehabilitation services
|
$
|
187,744
|
$
|
198,236
|
$
|
201,482
|
|||||
|
Hospital
rehabilitation services
|
127,212
|
115,044
|
105,292
|
||||||||
|
Program
management total
|
314,956
|
313,280
|
306,774
|
||||||||
|
Hospitals
(3)
|
795,024
|
118,267
|
93,659
|
||||||||
|
Healthcare
management consulting
|
—
|
6,859
|
8,127
|
||||||||
|
Total
|
$
|
1,109,980
|
$
|
438,406
|
$
|
408,560
|
|||||
|
|
(1)
|
Represents
general corporate overhead expenses associated with Phase 2 Consulting,
Inc., which was sold effective June 1, 2009. All other costs
and expenses associated with Phase 2 have been reported in discontinued
operations.
|
|
|
(2)
|
The
healthcare management consulting segment consists of Phase 2 Consulting,
Inc., which was sold effective June 1, 2009. Depreciation and
amortization expense associated with Phase 2 has been reported in
discontinued operations.
|
|
|
(3)
|
Hospitals
segment total assets include the carrying value of the Company’s
investment in HRSC.
|
| (20) | Quarterly Financial Information (Unaudited) |
The
following tables present the Company’s quarterly financial
data. Consistent with Note 1, the Company reclassified certain prior
year amounts to conform to the current year presentation. In
addition, certain amounts from the quarter ended March 31, 2009 have been
reclassified to present the results of operations for Phase 2 as discontinued
operations.
- 79
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
|
Quarter
Ended
|
||||||||||||||||
|
2009
|
December
31
|
September
30
|
June
30
|
March
31
|
||||||||||||
|
(in
thousands, except per share data)
|
||||||||||||||||
|
Operating
revenues
|
$
|
254,692
|
$
|
208,040
|
$
|
205,164
|
$
|
201,531
|
||||||||
|
Operating
earnings (1)
|
6,872
|
10,480
|
12,832
|
14,290
|
||||||||||||
|
Earnings
from continuing operations, net of tax
|
295
|
5,706
|
7,430
|
8,397
|
||||||||||||
|
Gain
(loss) from discontinued operations, net of tax
|
8
|
(16
|
)
|
(882
|
)
|
51
|
||||||||||
|
Net
earnings
|
303
|
5,690
|
6,548
|
8,448
|
||||||||||||
|
Net
earnings attributable to RehabCare
|
655
|
6,757
|
6,883
|
8,660
|
||||||||||||
|
Net
earnings per share attributable to RehabCare:
|
||||||||||||||||
|
Basic
|
0.03
|
0.38
|
0.39
|
0.49
|
||||||||||||
|
Diluted
|
0.03
|
0.37
|
0.38
|
0.48
|
||||||||||||
|
Quarter
Ended
|
||||||||||||||||
|
2008
|
December
31
|
September
30
|
June
30
|
March
31
|
||||||||||||
|
(in
thousands, except per share data)
|
||||||||||||||||
|
Operating
revenues
|
$
|
192,059
|
$
|
181,350
|
$
|
181,899
|
$
|
180,104
|
||||||||
|
Operating
earnings
|
9,511
|
7,080
|
7,786
|
8,530
|
||||||||||||
|
Earnings
from continuing operations, net of tax
|
5,408
|
3,666
|
4,008
|
4,500
|
||||||||||||
|
Loss
from discontinued operations, net of tax
|
(352
|
)
|
(280
|
)
|
(159
|
)
|
(72
|
)
|
||||||||
|
Net
earnings
|
5,056
|
3,386
|
3,849
|
4,428
|
||||||||||||
|
Net
earnings attributable to RehabCare
|
5,703
|
3,998
|
4,496
|
4,508
|
||||||||||||
|
Net
earnings per share attributable to RehabCare:
|
||||||||||||||||
|
Basic
|
0.32
|
0.23
|
0.26
|
0.26
|
||||||||||||
|
Diluted
|
0.32
|
0.22
|
0.25
|
0.25
|
||||||||||||
(1)
Operating earnings for the quarter ended December 31, 2009 include $7.2
million of acquisition-related expenses for costs directly related to the
acquisition of Triumph including fees for legal, accounting, advisory and other
outside services.
- 80
-
REHABCARE
GROUP, INC.
Notes to
Consolidated Financial Statements (Continued)
December
31, 2009, 2008 and 2007
| (21) | Contingencies |
The
Company is currently not a party to any material pending legal
proceedings.
In the
ordinary course of our business, the Company is a party to a number of claims
and lawsuits, as both plaintiff and defendant, which the Company regards as
immaterial. From time to time, and depending upon the particular
facts and circumstances, the Company may be subject to indemnification
obligations under its various contracts. The Company does not believe
that any liability resulting from such matters, after taking into consideration
the Company’s insurance coverage and amounts already provided for, will have a
material effect on the Company’s consolidated financial position or overall
liquidity; however, such matters, or the expense of prosecuting or defending
them, could have a material effect on cash flows and results of operations in a
particular quarter or fiscal year as they develop or as new issues are
identified.
- 81
-
| ITEM 9. | CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS |
| ON ACCOUNTING AND FINANCIAL DISCLOSURE |
Not
applicable.
| ITEM 9A. | CONTROLS AND PROCEDURES |
Evaluation
of Controls and Procedures
Under the
supervision and with the participation of our management, including the Chief
Executive Officer and Chief Financial Officer, we conducted an evaluation of the
effectiveness of the Company’s disclosure controls and procedures, as defined in
Rules 13a-15(e) and 15d-15(e) of the Securities and Exchange Act of
1934. Based on that evaluation, the Chief Executive Officer and Chief
Financial Officer have concluded that the Company’s disclosure controls and
procedures as of December 31, 2009 were effective to ensure that information
required to be disclosed by the Company in reports that it files or submits
under the Securities Exchange Act of 1934 is recorded, processed, summarized and
reported within the time periods specified in Securities and Exchange
Commission’s rules and forms.
There
have been no changes in the Company’s internal control over financial reporting
during the fourth quarter of 2009 that have materially affected, or are
reasonably likely to materially affect, the Company’s internal control over
financial reporting.
Management’s
Report on Internal Control Over Financial Reporting
Our
management is responsible for establishing and maintaining adequate internal
control over financial reporting, as defined in Rule 13a-15(f) under the
Securities Exchange Act of 1934. Under the supervision and with the
participation of our management, including the Chief Executive Officer and the
Chief Financial Officer, we conducted an evaluation of the effectiveness of our
internal control over financial reporting as of December 31,
2009. All internal control systems have inherent limitations,
including the possibility of circumvention and overriding the
control. Accordingly, even effective internal control can provide
only reasonable assurance as to the reliability of financial statement
preparation and presentation. Further, because of changes in
conditions, the effectiveness of internal control may vary over
time.
In making
its evaluation, our management used the criteria set forth by the Committee of
Sponsoring Organizations of the Treadway Commission (“COSO”) in Internal Control-Integrated
Framework. Based upon this evaluation, our management has
concluded that our internal control over financial reporting as of December 31,
2009 is effective.
We
acquired Triumph HealthCare Holdings, Inc. (“Triumph”) on November 24, 2009 and
began the process of integrating Triumph into our
operations. Management has excluded Triumph from its assessment of
the effectiveness of our internal control over financial reporting as of
December 31, 2009, as it concluded there was insufficient time between the
acquisition date and the end of 2009 to properly plan, document, test and
remediate, if necessary, the controls of Triumph. Triumph’s total
assets of $648.8 million and total revenues of $39.7 million have been included
in our consolidated financial statements as of and for the year ended December
31, 2009.
Our
independent registered public accounting firm, KPMG LLP, has audited the
effectiveness of our internal control over financial reporting, as stated in its
report which is included herein.
- 82
-
| ITEM 9B. | OTHER INFORMATION |
Not
applicable.
PART
III
| ITEM 10. | DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE |
The
following information is included in our Notice of Annual Meeting of
Stockholders and Proxy Statement to be filed within 120 days after the Company’s
fiscal year end of December 31, 2009 (the "Proxy Statement") and is incorporated
herein by reference:
|
|
·
|
Information
regarding directors who are standing for reelection and any persons
nominated to become directors is set forth under the caption "Election of
Directors."
|
|
|
·
|
Information
regarding the Company’s audit committee and designated "audit committee
financial experts" is set forth under the caption "Audit
Committee."
|
|
|
·
|
Information
regarding Section 16(a) beneficial ownership reporting compliance is set
forth under the caption "Section 16(a) Beneficial Ownership Reporting
Compliance."
|
The
Company has adopted a Code of Ethics that applies to its principal executive
officer, principal financial officer, principal accounting officer or
controller, or persons performing similar functions. The Code of Ethics is
available through the Company’s web site at www.rehabcare.com.
The
following table sets forth the name, age and position of each of our executive
officers as of December 31, 2009. There is no family relationship
between any of the following individuals.
|
Name
|
Age
|
Position
|
||
|
John
H. Short, Ph.D.
|
65
|
President
and Chief Executive Officer
|
||
|
Jay
W. Shreiner
|
59
|
Executive
Vice President, Chief Financial Officer
|
||
|
Patricia
S. Williams
|
42
|
Senior
Vice President, General Counsel and Secretary
|
||
|
Patricia
M. Henry
|
57
|
Executive
Vice President, Operations
|
||
|
Mary
Pat Welc
|
55
|
Senior
Vice President, Operations
|
||
|
Kevin
J. Gross
|
54
|
Senior
Vice President, Operations
|
||
|
James
F. Martin
|
59
|
Senior
Vice President, Chief Human Resources Officer
|
||
|
Jeff
A. Zadoks
|
44
|
Senior
Vice President, Chief Accounting Officer
|
||
|
Samuel
W. Duggan II
|
46
|
Vice
President, Treasurer
|
The
following paragraphs contain biographical information about our executive
officers.
John H. Short, Ph.D. has been
President and Chief Executive Officer since May 2004, having served as Interim
President and Chief Executive Officer since June 2003 and a director of the
company since 1991. Prior to May 2004, Dr. Short was the managing
partner of Phase 2 Consulting, Inc., a healthcare management consulting firm,
for more than 18 years.
Jay W. Shreiner has been
Chief Financial Officer of the Company since joining the Company in March
2006. Prior to joining the Company, Mr. Shreiner was Chief Financial
Officer for several private companies within Austin Ventures’ portfolio of
companies.
- 83
-
Patricia S. Williams has been
Senior Vice President, General Counsel and Secretary since joining the Company
in November 2007. Prior to joining the Company, Ms. Williams was Vice
President, General Counsel and Corporate Secretary for Thermadyne Holdings
Corporation, a multi-national, publicly-traded company engaged in the design,
manufacture, and sale of cutting and welding equipment.
Patricia M. Henry has been
Executive Vice President, Operations since September 2004, having served most
recently as President of our contract therapy division since November
2001. Ms. Henry joined the Company in October 1998.
Mary Pat Welc has been Senior
Vice President, Operations since 2003. Prior to that, Ms. Welc served
as Regional Vice President of Operations. Ms. Welc joined the Company
in 1996.
Kevin J. Gross has been
Senior Vice President, Operations since July 1, 2008. Prior to
joining the Company, Mr. Gross served as Senior Vice President and President of
the Acute Care Division of Universal Health Systems, Inc. from February 2006 to
May 2007. He also served as President of Ardent Health Services’
Oklahoma Division from 2004 to 2006. In the years preceding, he held
various management roles for several hospitals and healthcare systems in Texas,
Kansas and Colorado.
James F. Martin has been
Senior Vice President, Chief Human Resources Officer since December 2007, having
served most recently as the Vice President, Human Resources since joining the
Company in March 2005. Prior to joining the Company, Mr. Martin
was Vice-President, Human Resources at Bankers Life & Casualty Company, a
division of Conseco.
Jeff A. Zadoks has been
Senior Vice President and Chief Accounting Officer since February
2010. Mr. Zadoks has also served as Vice President and Corporate
Controller since joining the Company in December 2003. Prior to
joining the Company, Mr. Zadoks was Corporate Controller of MEMC Electronic
Materials, Inc.
Samuel W. Duggan II has been
Vice President and Treasurer since joining the Company in January
2009. Prior to joining the Company, Mr. Duggan was Vice President,
Investor Relations and Treasurer for Kellwood Company from June 2007 to December
2008. He also served as Kellwood’s Vice President, Treasury Services
and Vice President, Shared Services from 2005 to 2007.
Section
303A.12(a) of the NYSE Listed Company Manual requires the chief executive
officer (“CEO”) of each listed company to certify to the NYSE each year that he
or she is not aware of any violation by the listed company of any of the NYSE’s
corporate governance rules. The CEO of RehabCare submitted the
required certification without qualification to the NYSE on April 29,
2009.
|
ITEM
11.
|
EXECUTIVE
COMPENSATION
|
Information
regarding executive compensation is included in our Proxy Statement under the
caption “Discussion of 2009 Executive Compensation Program” and is incorporated
herein by reference.
| ITEM 12. | SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND |
| MANAGEMENT AND RELATED STOCKHOLDER MATTERS |
Information
regarding security ownership of certain beneficial owners and management is
included in our Proxy Statement under the captions “Voting Securities and
Principal Holders Thereof” and “Security Ownership by Directors and Executive
Officers” and is incorporated herein by reference.
- 84
-
The
following table provides information as of fiscal year ended December 31, 2009
with respect to the shares of common stock that may be issued under our existing
equity compensation plans:
|
Plan
category
|
Number
of
securities
to
be
issued
upon
exercise
of
outstanding
options,
warrants
and
rights
(a)
|
Weighted-average
exercise
price of
outstanding
options,
warrants
and
rights
(b)
|
Number
of securities
remaining
available
for
future issuance
under
equity
compensation
plans
(excluding
securities
reflected
in column (a))
(c)
|
|
|
Equity
compensation plans approved by security holders
|
870,829
|
$25.11
|
274,903
|
(1)
|
|
Equity
compensation plans not approved by security holders
|
-
|
-
|
-
|
|
|
Total
|
870,829
|
$25.11
|
274,903
|
|
|
|
(1)
|
Represents
the number of shares of common stock available for future issuance under
the Company’s 2006 Equity Incentive Plan. Permissible awards
under the Company’s plan include stock options, stock appreciation rights,
restricted stock, stock units and other equity-based
awards.
|
|
ITEM 13.
|
CERTAIN
RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR
INDEPENDENCE
|
Information
regarding certain relationships and related transactions is included in our
Proxy Statement under the caption “Certain Relationships and Related
Transactions” and is incorporated herein by reference.
| ITEM 14. | PRINCIPAL ACCOUNTANT FEES AND SERVICES |
Information
regarding principal accountant fees and services is included in our Proxy
Statement under the caption “Ratification of Appointment of Independent
Registered Public Accounting Firm” and is incorporated herein by
reference.
- 85
-
PART
IV
|
ITEM
15.
|
EXHIBITS
AND FINANCIAL STATEMENT SCHEDULES
|
|
(a)
|
The
following documents are filed as part of this Annual Report on Form
10-K:
|
||
|
(1)
|
Financial
Statements:
|
||
|
Report
of Independent Registered Public Accounting Firm
|
|||
|
Consolidated
Balance Sheets as of December 31, 2009 and 2008
|
|||
|
Consolidated
Statements of Earnings for the years ended December 31, 2009, 2008 and
2007
|
|||
|
Consolidated
Statements of Comprehensive Income for the years ended December 31, 2009,
2008 and 2007
|
|||
|
Consolidated
Statements of Changes in Equity for the years ended December 31, 2009,
2008 and 2007
|
|||
|
Consolidated
Statements of Cash Flows for the years ended December 31, 2009, 2008 and
2007
|
|||
|
Notes
to Consolidated Financial Statements
|
|||
|
(2)
|
Financial
Statement Schedules:
|
||
|
None
|
|||
|
(3)
|
Exhibits:
|
||
|
See
Exhibit Index on page 88 of this Annual Report on Form
10-K.
|
|||
- 86
-
|
|
SIGNATURES
|
Pursuant to the requirements of
Section 13 of the Securities Exchange Act of 1934, the Registrant has duly
caused this report to be signed on its behalf by the undersigned, thereunto duly
authorized.
Dated:
March 8, 2010
|
REHABCARE
GROUP, INC.
|
|
| (Registrant) | |
|
By
:
|
/s/
John H.
Short
|
|
John
H. Short
|
|
|
President
and Chief Executive Officer
|
Pursuant
to the requirements of the Securities Exchange Act of 1934, this report has been
signed below by the following persons on behalf of the Registrant and in the
capacities and on the date indicated.
|
Signature
|
Title
|
Dated
|
||
|
/s/
John H.
Short
|
President,
Chief Executive
|
March
8, 2010
|
||
|
John
H. Short
|
Officer
and Director
|
|||
|
(Principal
Executive Officer)
|
||||
|
/s/
Jay W.
Shreiner
|
Executive
Vice President and
|
March
8, 2010
|
||
|
Jay
W. Shreiner
|
Chief
Financial Officer
|
|||
|
(Principal
Financial Officer)
|
||||
|
/s/
Jeff A.
Zadoks
|
Senior
Vice President and
|
March
8, 2010
|
||
|
Jeff
A. Zadoks
|
Chief
Accounting Officer
|
|||
|
(Principal
Accounting Officer)
|
||||
|
/s/
Colleen
Conway-Welch
|
Director
|
March
8, 2010
|
||
|
Colleen
Conway-Welch
|
||||
|
/s/
Christopher T.
Hjelm
|
Director
|
March
8, 2010
|
||
|
Christopher
T. Hjelm
|
||||
|
/s/
Anthony S.
Piszel
|
Director
|
March
8, 2010
|
||
|
Anthony
S. Piszel
|
||||
|
/s/
Suzan L.
Rayner
|
Director
|
March
8, 2010
|
||
|
Suzan
L. Rayner
|
||||
|
/s/
Harry E.
Rich
|
Director
|
March
8, 2010
|
||
|
Harry
E. Rich
|
||||
|
/s/
Larry
Warren
|
Director
|
March
8, 2010
|
||
|
Larry
Warren
|
||||
|
/s/
Theodore M.
Wight
|
Director
|
March
8, 2010
|
||
|
Theodore
M. Wight
|
||||
- 87
-
EXHIBIT
INDEX
|
2.1
|
Agreement
and Plan of Merger, dated November 3, 2009, between the Registrant,
RehabCare Group East, Inc., RehabCare Hospital Holdings, L.L.C., RehabCare
Merger Sub Corporation, Triumph HealthCare Holdings, Inc. and TA
Associates, Inc. (filed as Exhibit 99.2 to the Registrant’s Current Report
on Form 8-K dated November 3, 2009 and incorporated herein by
reference)
|
|
3.1
|
Restated
Certificate of Incorporation (filed as Exhibit 3.1 to the Registrant’s
Registration Statement on Form S-1, dated May 9, 1991 [Registration No.
33-40467], and incorporated herein by
reference)
|
|
3.2
|
Certificate
of Amendment of Certificate of Incorporation (filed as Exhibit 3.1 to the
Registrant’s Quarterly Report on Form 10-Q for the quarter ended May 31,
1995 and incorporated herein by
reference)
|
|
3.3
|
Amended
and Restated Bylaws, dated October 30, 2007 (filed as Exhibit 3.1 to the
Registrant’s Current Report on Form 8-K dated October 31, 2007 and
incorporated herein by reference)
|
|
4.1
|
Rights
Agreement, dated August 28, 2002, by and between the Registrant and
Computershare Trust Company, Inc. (filed as Exhibit 1 to the Registrant’s
Registration Statement on Form 8-A filed September 5, 2002 and
incorporated herein by reference)
|
|
10.1
|
1987
Incentive Stock Option and 1987 Nonstatutory Stock Option Plans (filed as
Exhibit 10.1 to the Registrant’s Registration Statement on Form S-1, dated
May 9, 1991 [Registration No. 33-40467] and incorporated herein by
reference) *
|
|
10.2
|
Form
of Stock Option Agreement for 1987 Incentive Stock Option and 1987
Nonstatutory Stock Option Plans (filed as Exhibit 10.2 to the Registrant’s
Registration Statement on Form S-1, dated May 9, 1991 [Registration No.
33-40467] and incorporated herein by reference) *
|
|
10.3
|
Termination
Compensation Agreement, dated December 11, 2007 by and between RehabCare
Group, Inc. and John H. Short, Ph.D. (filed as Exhibit 10.1 to
Registrant’s Annual Report on Form 8-K dated December 12, 2007 and
incorporated herein by reference) *
|
|
10.4
|
Amendment
to Termination Compensation Agreement, dated December 11, 2007 by and
between RehabCare Group, Inc. and John H. Short, Ph.D. (filed as Exhibit
10.1 to Registrant’s Current Report on Form 8-K dated December 12, 2008
and incorporated herein by reference)
*
|
|
10.5
|
Termination
Compensation Agreement dated December 8, 2008 by and between RehabCare
Group, Inc. and Jay W. Shreiner (filed as Exhibit 10.2 to Registrant’s
Current Report on Form 8-K dated December 12, 2008 and incorporated herein
by reference) *
|
- 88
-
|
10.6
|
Termination
Compensation Agreement dated December 8, 2008 by and between RehabCare
Group, Inc. and Patricia M. Henry (filed as Exhibit 10.3 to Registrant’s
Current Report on Form 8-K dated December 12, 2008 and incorporated herein
by reference) *
|
|
10.7
|
Form
of Change in Control Termination Agreement dated December 8, 2008 by and
between RehabCare Group, Inc. and Mary Patricia Welc (filed as Exhibit
10.4 to Registrant’s Current Report on Form 8-K dated December 12, 2008
and incorporated herein by reference)
*
|
|
10.8
|
Change
in Control Termination Agreement dated November 12, 2007 by and between
RehabCare Group, Inc. and Patricia S. Williams (filed as Exhibit 10.6 to
Registrant’s Annual Report on Form 10-K for the year ended December 31,
2007 and incorporated herein by reference)
*
|
|
10.9
|
Form
of Termination Compensation Agreement dated March 10, 2006 by and between
RehabCare Group, Inc. and other executive officers who are not named
executive officers in the Registrant’s proxy statement for the 2006 annual
meeting of stockholders (filed as Exhibit 10.5 to Registrant’s Annual
Report on Form 10-K for the year ended December 31, 2005 and incorporated
herein by reference) *
|
|
10.10
|
RehabCare
Severance Plan for Company Senior Vice Presidents effective January 1,
2009 (filed as Exhibit 10.5 to Registrant’s Current Report on Form 8-K
dated December 12, 2008 and incorporated herein by reference)
*
|
|
10.11
|
RehabCare
Severance Plan for Company Vice Presidents effective January 1, 2009
(filed as Exhibit 10.6 to Registrant’s Current Report on Form 8-K dated
December 12, 2008 and incorporated herein by reference)
*
|
|
10.12
|
RehabCare
Executive Deferred Compensation Plan (filed as Exhibit 10.12 to the
Registrant’s Report on Form 10-K, dated May 27, 1994 and incorporated
herein by reference) *
|
|
10.13
|
RehabCare
Executive Deferred Compensation Plan as amended and restated effective
January 1, 2009 (filed as Exhibit 10.7 to Registrant’s Current Report on
Form 8-K dated December 12, 2008 and incorporated herein by reference)
*
|
|
10.14
|
RehabCare
Directors’ Stock Option Plan (filed as Appendix A to Registrant’s
definitive Proxy Statement for the 1994 Annual Meeting of Stockholders and
incorporated herein by reference) *
|
|
10.15
|
Second
Amended and Restated 1996 Long-Term Performance Plan (filed as Appendix B
to Registrant’s definitive Proxy Statement for the 2004 Annual Meeting of
Stockholders and incorporated herein by reference) *
|
|
10.16
|
Form
of Stock Option Agreement for the Second Amended and Restated 1996
Long-Term Performance Plan (filed as Exhibit 10.10 to the Registrant’s
Annual Report on Form 10-K for the year ended December 31, 2005 and
incorporated herein by reference) *
|
- 89
-
|
10.17
|
Form
of Restricted Stock Agreement for the Second Amended and Restated 1996
Long-Term Performance Plan (filed as Exhibit 10.11 to the Registrant’s
Annual Report on Form 10-K for the year ended December 31, 2005 and
incorporated herein by reference) *
|
|
10.18
|
RehabCare
Group, Inc. 2006 Equity Incentive Plan (filed as Appendix A to the
Registrant’s Definitive Proxy Statement for the 2006 Annual Meeting of
Shareholders and incorporated herein by reference)
*
|
|
10.19
|
Amended
and Restated Credit Agreement, dated November 24, 2009, by and among
RehabCare Group, Inc., as borrower, certain subsidiaries and affiliates of
the borrower, as guarantors, and Bank of America, N.A., as administrative
agent and collateral agent, and Banc of America Securities LLC, RBC
Capital Markets and BNP Paribas Securities Corp., as joint lead arrangers
(filed as Exhibit 10.1 to the Registrant’s Current Report on Form 8-K
dated November 24, 2009 and incorporated herein by
reference)
|
|
10.20
|
Pledge
Agreement, dated as of November 24, 2009, by and among RehabCare Group,
Inc. and subsidiaries, as pledgors, and Bank of America, N.A., as
collateral agent (filed as Exhibit 10.1 to the Registrant’s Current Report
on Form 8-K dated November 24, 2009 and incorporated herein by
reference)
|
|
10.21
|
Security
Agreement, dated as of November 24, 2009, by and among RehabCare Group,
Inc. and subsidiaries, as grantors, and Bank of America, N.A., as
collateral agent (filed as Exhibit 10.1 to the Registrant’s Current Report
on Form 8-K dated November 24, 2009 and incorporated herein by
reference)
|
|
10.22
|
Non-Continuous
Aircraft Dry Lease Agreement by and between 55JS Limited, Co. and
RehabCare Group, Inc. (filed as Exhibit 10.1 to Registrant’s Current
Report on Form 8-K dated September 7, 2006 and incorporated herein by
reference)
|
|
10.23
|
Asset
Purchase Agreement dated June 8, 2005 by and among RehabCare Group East,
Inc., a wholly owned subsidiary of Registrant, MeadowBrook HealthCare,
Inc., MeadowBrook Specialty Hospital of Tulsa LLC, Lafayette Rehab
Associate Limited Partnership, Clear Lake Rehabilitation Hospital, Inc.
and South Dade Rehab Associates Limited Partnership (filed as Exhibit 10.1
to Registrant’s Current Report on Form 8-K dated August 4, 2005 and
incorporated herein by reference)
|
|
10.24
|
Purchase
and Sale Agreement, dated May 3, 2006, by and among LUK-Symphony
Management, LLC, Symphony Health Services, LLC and RehabCare Group, Inc.
(filed as exhibit 10.1 to the Registrant’s Current Report on Form 8-K
dated May 8, 2006 and incorporated herein by
reference)
|
|
10.25
|
Termination
Compensation Agreement dated July 1, 2008 by and between RehabCare Group,
Inc. and Kevin Gross (filed as Exhibit 10.2 to Registrant’s Current Report
on Form 8-K dated July 7, 2008 and incorporated herein by reference)
*
|
|
21.1
|
Subsidiaries
of the Registrant (filed herewith)
|
|
23.1
|
Consent
of KPMG LLP (filed herewith)
|
- 90
-
|
31.1
|
Certification
by Chief Executive Officer in accordance with Rule 13a-14(a) under the
Securities Exchange Act of 1934, as adopted pursuant to Section 302 of the
Sarbanes-Oxley Act of 2002 (filed
herewith)
|
|
31.2
|
Certification
by Chief Financial Officer in accordance with Rule 13a-14(a) under the
Securities Exchange Act of 1934, as adopted pursuant to Section 302 of the
Sarbanes-Oxley Act of 2002 (filed
herewith)
|
|
32.1
|
Certification
by Chief Executive Officer in accordance with 18 U.S.C. Section 1350, as
adopted pursuant to Section 906 of the Sarbanes-Oxley Act of 2002 (filed
herewith)
|
|
32.2
|
Certification
by Chief Financial Officer in accordance with 18 U.S.C. Section 1350, as
adopted pursuant to Section 906 of the Sarbanes-Oxley Act of 2002 (filed
herewith)
|
_________________________
* Management
contract or compensatory plan or arrangement.
- 91
-
