Attached files
| file | filename |
|---|---|
| EXCEL - IDEA: XBRL DOCUMENT - Option Care Health, Inc. | Financial_Report.xls |
| EX-31.1 - 302 CERTIFICATION OF CEO - Option Care Health, Inc. | ceo302cert.htm |
| EX-32.2 - 906 CERTIFICATION OF CFO - Option Care Health, Inc. | cfo906cert.htm |
| EX-31.2 - 302 CERTIFICATION OF CFO - Option Care Health, Inc. | cfo302cert.htm |
| EX-32.1 - 906 CERTIFICATION OF CEO - Option Care Health, Inc. | ceo906cert.htm |
| EX-21.1 - LIST OF SUBSIDIARIES - Option Care Health, Inc. | subsidiaries.htm |
| EX-23.1 - CONSENT OF ERNST & YOUNG LLP - Option Care Health, Inc. | auditorconsent.htm |
UNITED
STATES
SECURITIES
AND EXCHANGE COMMISSION
Washington, D.C.
20549
Form 10-K
|
(Mark
One)
|
|
|
þ
|
ANNUAL
REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT
OF 1934
|
|
For
the fiscal year ended December 31, 2009
|
|
|
OR
|
|
|
o
|
PERIODIC
REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT
OF 1934
|
|
For
the transition period from
to
|
|
Commission
file number: 0-28740

BioScrip,
Inc.
(Exact
name of registrant as specified in its charter)
|
Delaware
|
05-0489664
|
|
(State
of incorporation)
|
(I.R.S.
Employer
Identification
No.)
|
|
100
Clearbrook Road, Elmsford NY
|
10523
|
|
(Address
of principal executive offices)
|
(Zip
Code)
|
Registrant’s
telephone number, including area code:
914-460-1600
Securities
registered pursuant to Section 12(b) of the Act:
None
Securities
registered pursuant to section 12(g) of the Act:
Common
Stock, $.0001 par value
Indicate
by check mark if the registrant is a well-known seasoned issuer, as defined in
Rule 405 of the Securities Act. Yes o No þ
Indicate
by check mark if the registrant is not required to file reports pursuant to
Section 13 or Section 15(d) of the Act Yes o No þ
Indicate
by check mark whether the registrant (1) has filed all reports required to
be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934
during the preceding 12 months (or for such shorter period that the
registrant was required to file such reports), and (2) has been subject to
such filing requirements for the past 90 days. Yes þ No o
Indicate
by check mark whether the registrant has submitted electronically and posted to
its corporate Web site, if any, every Interactive Data File required to be
submitted and posted pursuant to Rule 405 of Regulation S-T (§ 232.405 of this
chapter) during the preceding 12 months (or for such shorter period that the
registrant was required to submit and post such files). Yes £ No £
Indicate
by check mark if disclosure of delinquent filers pursuant to Item 405 of
Regulation S-K (§ 229.405 of this chapter) is not contained herein, and will not
be contained, to the best of registrant’s knowledge, in definitive proxy or
information statements incorporated by reference in Part III of this Form 1-K or
any amendment to this Form 10-K. £
Indicate
by check mark whether the registrant is a large accelerated filer, an
accelerated filer, or a non-accelerated filer. See definition of “large
accelerated filer”, “accelerated filer” and “smaller reporting company” in
Rule 12b-2 of the Exchange Act.
Large
accelerated filer o Accelerated
filer þ Non-accelerated
filer o Smaller
reporting company o
Indicate
by check mark whether the registrant is a shell company (as defined in
Rule 12b-2 of the Exchange Act). Yes o No þ
The
aggregate market value of the registrant’s Common Stock held by non-affiliates
of the registrant as of June 30, 2009, the last business day of the
registrant’s most recently completed second fiscal quarter, was approximately
$125,041,731
based on the closing price of the Common Stock on the Nasdaq Global Market on
such date.
On
February 24, 2010 there were outstanding 39,794,757 shares of the
registrant’s Common Stock.
DOCUMENTS
INCORPORATED BY REFERENCE
Portions
of the registrant’s definitive proxy statement for its 2010 Annual Meeting of
Stockholders to be filed with the SEC within 120 days after the close of
the registrant’s fiscal year are incorporated by reference into Part III of
this Annual Report.
|
Page
|
||
|
Number
|
||
|
PART
I
|
||
| 3 | ||
| 15 | ||
| 21 | ||
| 21 | ||
| 22 | ||
| 22 | ||
|
PART
II
|
||
| 22 | ||
| 24 | ||
| 25 | ||
| 34 | ||
| 35 | ||
| 57 | ||
| 57 | ||
| 59 | ||
|
PART
III
|
||
| 59 | ||
| 59 | ||
| 59 | ||
| 59 | ||
| 59 | ||
|
PART
IV
|
||
| 59 | ||
| 63 | ||
| 64 | ||
| EXHIBIT INDEX | 65 | |
2
PART I
This
Annual Report contains “forward-looking statements” within the meaning of the
Private Securities Litigation Reform Act of 1995. Forward-looking statements
relate to expectations, beliefs, future plans and strategies, anticipated events
or trends concerning matters that are not historical facts or that necessarily
depend upon future events. In some cases, you can identify forward-looking
statements by terms such as “may,” “will,” “should,” “could,” “would,” “expect,”
“plan,” “anticipate,” “believe,” “estimate,” “project,” “predict,” “potential,”
and similar expressions. Specifically, this Annual Report contains, among
others, forward-looking statements about:
|
|
·
|
our
expectations regarding financial condition or results of operations for
periods after December 31,
2009;
|
|
|
·
|
our
future sources of, and needs for, liquidity and capital
resources;
|
|
|
·
|
our
expectations regarding general economic and business
conditions;
|
|
|
·
|
our
critical accounting policies;
|
|
|
·
|
our
expectations regarding the size and growth of the market for our products
and services;
|
|
|
·
|
our
business strategies and our ability to grow our
business;
|
|
|
·
|
the
implementation or interpretation of current or future regulations and
legislation, particularly governmental oversight of our
business;
|
|
|
·
|
our
ability to maintain contracts and relationships with our customers;
and
|
|
|
·
|
our
ability to successfully complete the acquisition of Critical Homecare
Solutions Holdings, Inc. (“CHS”), and if completed, successfully integrate
CHS and realize the anticipated synergies of the
acquisition.
|
The
forward-looking statements contained in this Annual Report reflect our current
views about future events, are based on assumptions, and are subject to known
and unknown risks and uncertainties. Many important factors could cause actual
results or achievements to differ materially from any future results or
achievements expressed in or implied by our forward-looking statements. Many of
the factors that will determine future events or achievements are beyond our
ability to control or predict. Certain of these are important factors that could
cause actual results or achievements to differ materially from the results or
achievements reflected in our forward-looking statements.
The
forward-looking statements contained in this Annual Report reflect our views and
assumptions only as of the date this Annual Report is signed. The reader should
not place undue reliance on forward-looking statements. Except as required by
law, we assume no responsibility for updating any forward-looking
statements.
We
qualify all of our forward-looking statements by these cautionary statements. In
addition, with respect to all of our forward-looking statements, we claim the
protection of the safe harbor for forward-looking statements contained in the
Private Securities Litigation Reform Act of 1995.
Overview
We are a
specialty pharmaceutical healthcare organization that partners with patients,
physicians, healthcare payors and pharmaceutical manufacturers to provide access
to medications and management solutions to optimize outcomes for chronic and
other complex healthcare conditions.
Our
business is reported under two operating segments: (i) Specialty Pharmacy
Services, and (ii) Traditional Pharmacy Services. Our Specialty
Pharmacy Services segment includes comprehensive support, dispensing and
distribution, patient care management, data reporting, as well as a range of
other complex therapy management services for certain chronic and acute health
conditions. The medications we dispense include oral, injectable and
infusible
medications which are used to treat patients living with chronic and other
complex health conditions. Our Traditional Pharmacy Services segment
consists mainly of traditional mail service pharmacy fulfillment, and to a
lesser extent, prescription discount card programs and fully funded pharmacy
benefit management (“PBM”) services.
In the
quarter ended September 30, 2009, we renamed the reportable segment formerly
known as “PBM Services” to “Traditional Pharmacy Services”. Our
decision to rename this segment reflects a shift in the nature of the business
included within this segment away from fully funded pharmacy benefit management
services and more towards traditional mail services and prescription discount
card programs.
Revenues
from Specialty Pharmacy Services and Traditional Pharmacy Services are derived
from our relationships with healthcare payors including managed care
organizations, government-funded and/or operated programs, third party
administrators (“TPAs”) and self-funded employer groups (collectively, “Plan
Sponsors”), as well as from our relationships with pharmaceutical manufacturers,
patients and physicians.
Our
Specialty Pharmacy Services are marketed and/or sold to Plan Sponsors,
pharmaceutical manufacturers, physicians, and patients, and target certain
specialty medications that are used to treat patients living with chronic and
other complex health conditions. These services include the distribution of
biotech and other high cost injectable, oral and infusible prescription
medications and the provision of therapy management services.
Our
Traditional Pharmacy Services are marketed and/or sold to Plan Sponsors and are
designed to promote a broad range of cost-effective, clinically appropriate
pharmacy services through our own mail service distribution facility and
national pharmacy retail network. We also administer prescription discount card
programs on behalf of commercial Plan Sponsors, most typically TPAs. Under such
programs we derive revenue on a per claim basis from the dispensing network
pharmacy.
Specialty
Pharmacy Services
Our
Specialty Pharmacy Services business consists of our comprehensive specialty
pharmacy distribution and therapy management services. Specialty
Pharmacy Services distribution occurs locally through our BioScrip community
pharmacies, centrally through our mail order facilities and through our infusion
pharmacies for patients requiring infused medications either in the home or at a
variety of sites including the Company’s ambulatory treatment
centers. All Specialty Pharmacy Services target certain specialty
medications that are used to treat patients living with chronic and other
complex healthcare conditions.
We own
and operate 43 specialty pharmacies comprised of community pharmacies, located
in major metropolitan areas across the United States; mail order pharmacies; and
infusion pharmacies. While all of our locations are full-service pharmacies that
carry both traditional and specialty medications and are able to treat people
with a variety of diseases and medical conditions, we primarily focus on serving
patient populations with chronic health conditions, including:
|
|
·
|
Dermatology
|
|
|
·
|
Psoriasis
|
|
|
·
|
Endocrinology
|
|
|
·
|
Growth
Hormones, Thyroid Cancer
|
|
|
·
|
Hematology
|
|
|
·
|
Sickle
Cell Anemia/Thalassemia, Myelodysplastic Syndromes, Bleeding
Disorders/Hemophilia
|
|
|
·
|
Neurology
|
|
|
·
|
Multiple
Sclerosis, Neuropathies
|
|
|
·
|
Oncology
|
|
|
·
|
In
office infusions, Oral Oncolytics, supportive
medications
|
|
|
·
|
Rheumatology/Orthopedic
|
|
|
·
|
Rheumatoid
Arthritis, Osteoarthritis,
Osteoporosis
|
|
|
|
|
·
|
Transplant
|
|
|
·
|
Solid
Organ, Bone Marrow Transplant
|
|
|
·
|
Virology
|
The
patients we service typically have prescription or medical drug coverage through
commercial insurance, Medicare, Medicaid and/or other governmental programs, and
we are primarily reimbursed by the patient’s insurer at a contracted rate or our
“usual and customary” rate for the specific drug and/or service provided to the
customer. Our Specialty Pharmacy Services programs are designed to optimize the
therapeutic outcomes for patients while achieving Plan Sponsors’ and/or
pharmaceutical manufacturer’s program goals. These goals include
appropriate utilization of therapies, improved patient compliance and adherence
rates, reduced expenditures through discounted drug rates and utilization
reporting. Our software and data management tools permit Plan Sponsors,
pharmaceutical manufacturers and physicians to: (i) access utilization data
to manage better healthcare outcomes; and (ii) measure cost,
utilization, prescribing and other pharmacy trends.
Medication
Dispensing and Distribution
We carry
a full range of prescription medications and are able to dispense nearly all
prescription medications for acute and chronic diseases and conditions. As a
specialty pharmacy provider our mail and community pharmacy locations also carry
hard to find and hard to handle medications that are generally more expensive or
more complex than medications carried by retail or traditional
pharmacies.
Special
shipping and handling techniques in compliance with a manufacturer’s specific
requirements are employed, including refrigeration and shipping with dry-ice
packs. When necessary, we provide the drug product along with
supplies and equipment needed for administration.
Our
pharmacies also deliver medications to physicians’ offices for in-office
administration. The majority of our business is patient-specific dispensing,
whereby we receive a prescription for a medication and bill the appropriate
party or parties for reimbursement of the drug, which may include Plan Sponsors,
manufacturers and/or the patient. In some instances we deliver drugs
on a wholesale basis directly to qualified healthcare professionals or
institutions, including physicians and in some cases other specialty pharmacy
providers or wholesalers.
Billing
and Coordination of Benefits
Our
pharmacies offer comprehensive billing, patient reimbursement and coordination
of benefits (“COB”) services under both a patient’s pharmacy and medical
benefits. Our pharmacy locations are contracted with nearly all Federal and
state governmental benefit programs including Medicare, Medicaid, and state
benefit programs such as AIDS Drug Assistance Programs (“ADAPs”) as well as
other Ryan White-funded programs. In addition, our pharmacies participate in
most of the pharmacy networks; as well as with managed care organizations
directly.
Our
comprehensive COB services help patients with multiple sources of insurance
and/or government assistance handle complex insurance billing and reimbursement
challenges. Retail pharmacies and many of our competitors in the specialty
pharmacy arena do not typically provide COB services; we believe providing these
services differentiates us from our competitors. We facilitate
comprehensive assistance to patients through third party sources in order to
identify financial assistance programs and obtain funding for patients who are
unable to afford their out-of-pocket expenditures, including co-payments. We
work with a variety of assistance organizations and pharmaceutical manufacturers
to obtain this type of funding on behalf of our patients. Co-payments
and coinsurance payments are diligently pursued for collection as required
unless approved financial hardship exemptions are in effect.
Specialty
Therapy Management
We design
and administer clinical programs to maximize the benefits of pharmaceutical
utilization as a tool in achieving pharmaceutical therapy goals for certain
targeted disease states. Our programs focus on preventing high-risk adverse
events through the appropriate use of pharmaceuticals while eliminating
unnecessary or duplicate therapies. Key components of these programs include
patient education and training, integration of care between pharmacy and medical
health disciplines, monitoring of patient
compliance,
measurement of the care process and quality, and providing feedback for
continuous improvement in achieving therapy goals. The goal of these services is
to improve patient outcomes and lower overall healthcare costs.
Our bioscripcare™
patient care programs are designed to address the changing nature of chronic
patient care. We believe that our bioscripcare™
patient care programs address chronic patient needs by providing the optimal
structure of patient care through consistent assessment and intervention,
ongoing education and patient support, and adherence and persistence management
which results in improved patient quality of life and outcomes. Also, as part of
our normal business operations for refill management, we initiate monthly
telephonic interactions with patients. During the course of these calls,
important demographic, therapy and compliance data are gathered. Modifying the
existing refill call process by including additional scripted survey questions
specific to targeted disease states results in a significantly more robust data
gathering process that leads to important health outcome measures.
Our
programs incorporate Healthcare Effectiveness Data and Information Set (“HEDIS”)
guidelines, National Committee for Quality Assurance (“NCQA”) measures and
Disease Management Association of America (“DMAA”): The Care Continuum Alliance
guidelines. Measurement, analysis, as well as improvement and
repetition are key components of our regular program reviews. Our programs
remain dynamic through our focus on continual improvement. Some of
the components of the programs are described below:
|
|
·
|
Professional
Intervention
|
Most of
the disease states and conditions for which we dispense medications require
complex, multi-drug regimens for treatment, many of which have potential adverse
side effects and drug interactions. Our pharmacists review prescriptions
presented for a patient against that patient’s medical history, his or her past
and current medication usage, and clinical references known to us in order to
insure that the therapy selected is clinically appropriate. If our pharmacists
find a potential or actual problem they contact the prescriber or patient to
discuss that patient’s case and alternative medications. Our
pharmacists and clinical staff stay informed about new medications and changing
treatment protocols which are utilized in our target disease states and
conditions.
|
|
·
|
Patient
Education
|
Due to
the complexity of the regimens associated with the medications we dispense and
the need to educate patients on the importance of compliance and proper dosing
and administration, we make great efforts to help our patients, including their
caregivers, understand how their drug regimen may affect their health status and
lifestyle. We routinely consult with each patient when they receive a
prescription from us. We consult on what each medication is for, how it works,
and what adverse side effects are most likely to occur, as well as potential
interactions between or among multiple medications. Our goal is to fully inform
each patient in order to prevent missed doses, delayed starts, and loss of other
healthcare treatment options in some cases. We also provide patients with
information concerning how medications might influence their lifestyle and give
them recommendations on how to fit drug therapies into alternative schedules and
travel plans.
Many of
the specialty medications we dispense are given by injection. We teach patients
how to prepare their medications for administration, how to inject themselves,
and how to deal with any reactions that may occur. We often have the patient
administer their first dose in the pharmacy so they feel comfortable with taking
the medications when they get home. Our pharmacists are always available by
telephone for patient questions.
Our
pharmacies also provide physicians, patients and their caregivers with a broad
range of written educational materials. We create some of those materials and
receive others from pharmaceutical manufacturers and not-for-profit
organizations. We promote local and national disease-related
events.
|
|
·
|
Adherence and Persistence
Management
|
“Adherence”
is defined as taking medications on a timely basis, as and when
prescribed — for example, twice daily. “Persistence” is defined
as taking a regimen of medications for the length of time
prescribed. People with the diseases and conditions we treat often
struggle with both of these self-management issues, since their medications are
often difficult to take and require months or years of use.
Adherence
and persistence are key factors in achieving optimal medication effectiveness
and our pharmacists and professional staffs are active with patients, caregivers
and physicians in an effort to ensure the highest success rates. From
the start of therapy and throughout the treatment cycle we stress the importance
of adherence and persistence through initial teaching sessions and ongoing
communications with each medication refill.
We
provide refill reminders to alert people when a prescription refill is due or to
take their daily medication regimen. We proactively contact patients in
instances of missed refills and alert physicians and other healthcare providers
when the patient cannot be located. We reinforce these activities with
nurse-based adherence management and therapy optimization programs for select
conditions that carry a higher risk of complications or treatment failures. The
management methodology applied to each specific therapy constantly evolves to
reflect such things as new available treatments, revised treatment guidelines,
and other market developments. Since the inception of these programs, we have
observed results that indicate the achievement of higher compliance rates as
compared to industry averages and other documented and available
metrics.
Traditional
Pharmacy Services
Our
Traditional Pharmacy Services business consists mainly of traditional mail order
pharmacy fulfillment and, to a lesser extent, prescription discount card
programs and integrated PBM services. These services are designed to
offer Plan Sponsors cost-effective delivery of pharmacy benefit plans including
the low cost distribution of mail services for plan members who receive
traditional maintenance medications. Traditional Pharmacy Services
available to our customers include the following:
Mail Order Pharmacy
Dispensing
Our
traditional mail service pharmacy, located in Columbus, Ohio, provides patients
with medications, primarily via home delivery from a state-of-the-art
pharmaceutical management facility. Customers may order prescriptions
by mail, phone or Internet, while ensuring accuracy. For our
partners, using mail service provides enhanced formulary compliance capabilities
as well as the ability to utilize appropriate generic medications, all designed
to help save money for Plan Sponsors and patients while maintaining high levels
of patient satisfaction.
Clinical Services, Formulary
and Benefit Design
We work
closely with our Plan Sponsors to offer formularies and benefit plan designs
that meet their specific program requirements. Formulary design assists in
controlling program costs to the extent consistent with accepted medical and
pharmacy practices and applicable law, primarily through three principal
techniques: (i) tiered co-pay or percentage coinsurance designs, which provide
lower co-pays for formulary preferred medications and higher co-pays for
non-preferred medications, or charge a percentage of the prescription price to
the member at different percentages based on the preferred or non-preferred
status of a drug; (ii) generic substitution, which involves the selection
of a generic drug as a cost-effective alternative to its bio-equivalent brand
name drug; and/or (iii) therapeutic interchange, which involves the
selection of a lower cost brand name drug as an alternative to a higher priced
brand name drug within a therapeutic class. Formulary rebates on brand name
drugs are negotiated with drug manufacturers based on the drug’s preferred
status and are typically shared with Plan Sponsors. We do not manage
a rebate program on our own. Rather, our rebates are managed and
administered by a third party vendor.
Many
commercial Plan Sponsors do not restrict coverage to a specific list of
pharmaceuticals and are said to have no formulary or an “open” formulary that
generally covers all drugs approved by the United States Food and Drug
Administration (the “FDA”) except for certain classes of excluded
pharmaceuticals, such as certain vitamins and cosmetics, experimental,
investigative or over-the-counter drugs. Other Plan Sponsors utilize
a “restricted” or “closed” formulary. We actively involve our
clinical staff with a Plan Sponsor’s Pharmacy and Therapeutics Committee
(“P&T Committee”) to assist with the design of clinically appropriate
formularies in order to control pharmacy costs. Typically, the P&T Committee
consists of a Plan Sponsor’s physicians, pharmacists and others, including
independent healthcare professionals. The ultimate composition and approval of
the formulary resides with the Plan Sponsor. The primary method for assuring
formulary compliance on behalf of a Plan Sponsor is by managing pharmacy
reimbursement to ensure that non-formulary drugs are not dispensed, or dispensed
with higher co-payments, subject to certain limited
exceptions. Closed formularies typically identify a limited number of
drugs for preferred status within each therapeutic class to be the preferred
drug agent in order to treat most medical conditions appropriately. Provision is
also made for coverage of non-formulary or non-preferred drugs, other than
certain excluded products, when documented to be clinically appropriate for a
particular member. Since non-formulary drugs are rejected for coverage by the
real-time POS system, we employ procedures to override restrictions on
non-formulary medications for a particular member and period of treatment when
necessary.
Drug Usage
Evaluation
Drug
usage is evaluated on a concurrent, prospective and/or retrospective basis
utilizing the real-time POS system and information systems for multiple drug
interactions, duplication of therapy, step therapy protocol enforcement,
minimum/maximum dose range edits, compliance with prescribed utilization levels
and early refill notification. In addition, we maintain a drug utilization
review program through which select medication therapies are
reviewed
and data is collected, analyzed and reported for management
applications. At the request of Plan Sponsors our clinical pharmacy
team also provides clinical reviews of a patient’s prescription history and
medical condition, and our clinical pharmacist provides analysis and
recommendations for the patient’s future treatment.
Pharmacy Data
Services
Our
proprietary software and data management tools permit Plan Sponsors to access
key industry measures, which are updated daily and delivered through secure
internet-based access. Plan Sponsors often monitor these key measures associated
with their members in order to review the effectiveness and success of our
Traditional Pharmacy Services programs. In addition we also build
custom reporting systems to support specific customer projects.
Discount Prescription Card
Programs
In
addition to the managed pharmacy benefit services described above, we administer
numerous cash card or discount card programs on behalf of consumer marketing
organizations and to a lesser extent other Plan Sponsors. Those cards may be
“stand-alone” pharmacy discount programs or bundled with other healthcare or
other discount arrangements. Under those discount programs,
individuals who present a discount card at one of our participating network
pharmacies or who order medications through one of our mail service pharmacies
receive prescription medications at a discounted price off of the retail or
“cash” price.
Supply
Agreement
Effective August 25, 2009, we entered into a prime vendor agreement with
AmerisourceBergen Drug Corporation (“ABDC”), pursuant to which we purchase from
ABDC substantially all of our prescription products, subject to certain minimum
periodic purchase levels and excluding purchases of therapeutic plasma
products. Under the prime vendor agreement, we participate in ABDC’s
PRxO Generics™ Program and purchase from ABDC a specified percentage of our
requirements for generic pharmaceuticals. Pricing of pharmaceutical
products under the agreement is generally based on published Wholesale
Acquisition Costs (“WAC”), less certain discounts, rebates and other adjustments
that vary with the type of products being purchased.
Sales
and Marketing
Our sales
and marketing efforts are focused on payors, manufacturers, patients and
physicians, and are driven by dedicated managed markets, pharmaceutical
relations and physician sales teams. Contracts with healthcare
payors, including managed care organizations, are an integral component for
sales success. Additionally, contracting with pharmaceutical manufacturers for
distribution and management services for newly approved and/or marketed
specialty medications continues to contribute to our revenue
growth.
Competition
We face
substantial competition within the pharmaceutical healthcare services industry
and the past year has seen even more consolidation among PBMs, specialty
pharmacy providers and pharmaceutical wholesalers. We expect to see this trend
continue in the coming year and it is uncertain what effect, if any, these
consolidations will have on us or the industry as a whole. The industry also
includes a number of large, well-capitalized companies with nationwide
operations and capabilities in the specialty services and PBM services arenas,
such as CVS Caremark, Express Scripts, Medco Health Solutions, Walgreens,
MedImpact Healthcare Systems and many smaller organizations that typically
operate on a local or regional basis. In the Specialty Pharmacy Services
segment, we compete with several national and regional specialty pharmaceutical
distribution companies that have substantial financial resources and which also
provide products and services to the chronically ill such as CVS Caremark,
Express Scripts and Medco Health Solutions and Walgreens.
Some of
our Specialty Pharmacy Services competitors are under common control with, or
are owned by, pharmaceutical wholesalers and distributors or retail pharmacy
chains and may be better positioned with respect to the cost-effective
distribution of pharmaceuticals. Some of our primary competitors, such as US
Bioservices, an AmerisourceBergen Specialty Group company, may have a
substantially larger market share in many of our specialty disease therapies
than our existing market share. Moreover, some of our competitors may have
secured long-term supply or distribution arrangements for prescription
pharmaceuticals necessary to treat certain chronic disease states on price terms
substantially more favorable than the terms currently available to us. As a
result of such advantageous pricing, we may be less price competitive than some
of these competitors with respect to certain pharmaceutical products. However,
we do not believe that we compete strictly on the selling price of particular
products or services in either business segment; rather, we offer customers the
opportunity to lower overall pharmaceutical and medical costs through therapy
management while receiving high quality care.
Information
Technology
Over the
last three years our investment in information technology has increased each
year as we continue to upgrade our core infrastructure and
systems. In 2009 we continued our focus on the migration to a new
integrated pharmacy dispensing, clinical management and accounts receivable
management system. We believe that this new system will yield
increased efficiencies and improved controls when dispensing or transferring
prescriptions and provide improved data reporting and management. The
new system, in conjunction with other information technology infrastructure
improvements, will enhance our product and service offerings to payors,
physicians and pharmaceutical companies.
In 2010
we will continue to focus on migrating to our new platform, as well as
leveraging new technology solutions to transform how we interface with our
patients, referral sources and valued partners.
Financial
Information about Segments
The
following table presents revenue and income from operations by segment.
Operating segment financial information is provided in Note 3 of Notes to
Consolidated Financial Statements (in thousands).
Segment
Financial Information (1)
|
2009
|
2008
|
2007
|
|||||||
|
Revenue:
|
|||||||||
|
Specialty
Pharmacy Services
|
$ | 1,113,305 | $ | 1,196,587 | $ | 974,571 | |||
|
Traditional
Pharmacy Services
|
216,220 | 205,324 | 223,161 | ||||||
|
Total
|
$ | 1,329,525 | $ | 1,401,911 | $ | 1,197,732 | |||
|
Income
(loss) from operations (2):
|
|||||||||
|
Specialty
Pharmacy Services (3)
|
$ | (1,320 | ) | $ | (93,120 | ) | $ | (2,453 | ) |
|
Traditional
Pharmacy Services
|
16,786 | 9,603 | 11,304 | ||||||
|
Total
|
$ | 15,466 | $ | (83,517 | ) | $ | 8,851 | ||
__________________________
|
(1)
|
Certain
prior period amounts have been reclassified to conform to the current year
presentation. Such reclassifications had no material effect on the
Company’s previously reported consolidated financial position, results of
operations or cash flows.
|
|
(2)
|
Certain
corporate expenses have been allocated between the two segments for
reporting purposes.
|
|
(3)
|
The
year ended December 31, 2008 includes $93.9 million of goodwill and
intangible asset impairment in the Specialty Pharmacy Services
segment.
|
Government
Regulation
As a
participant in the healthcare industry our operations and relationships are
subject to Federal and state laws and regulations and enforcement by Federal and
state governmental agencies. Various Federal and state laws and regulations
govern the purchase, dispensing or distribution, and management of prescription
drugs and related services we provide and may affect us. We believe that we are
in substantial compliance with all legal requirements material to our
operations.
We
conduct ongoing educational programs to inform employees regarding compliance
with relevant laws and regulations and maintain a formal reporting procedure to
disclose possible violations of these laws and regulations to the Office of
Inspector General (“OIG”) of the U.S. Department of Health and Human
Services.
Among the
various Federal and state laws and regulations which may govern or impact our
current and planned operations are the following:
Mail Service Pharmacy
Regulation. Many of the states into which we deliver
pharmaceuticals have laws and regulations that require out-of-state mail service
pharmacies to register with, or be licensed by, the boards of pharmacy or
similar regulatory bodies in those states. These states generally permit the
dispensing pharmacy to follow the laws of the state within which the dispensing
pharmacy is located.
However,
various state pharmacy boards have enacted laws and/or adopted rules or
regulations directed at restricting or prohibiting the operation of out-of-state
pharmacies by, among other things, requiring compliance with all laws of the
states into which the out-of-state pharmacy dispenses medications, whether or
not those laws conflict with the laws of the state in which the pharmacy is
located, or requiring the pharmacist-in-charge to be licensed in that state. To
the extent that such laws or regulations are found to be applicable to our
operations, we comply with them. To the extent that any of the
foregoing laws or regulations prohibit or restrict the operation of mail service
pharmacies and are found to be applicable to us, they could have an adverse
effect on our prescription mail service operations. A number of state Medicaid
programs prohibit the participation in those states by out-of-state retail or
mail service pharmacies, whether in-state or out-of-state.
There are
other statutes and regulations which may also affect our mail service
operations. The Federal Trade Commission requires mail order sellers of goods
generally to engage in truthful advertising, to stock a reasonable supply of the
products to be sold, to fill mail orders within 30 days, and to provide
clients with refunds when appropriate.
Professional Licensure.
Nurses, pharmacists and certain other health care professionals employed
by us are required to be individually licensed or certified under applicable
state law. We perform criminal and other background checks on employees and are
required under state licensure to ensure that our employees possess all
necessary licenses and certifications. We believe that our employees comply in
all material respects with applicable licensure laws.
State
laws require that each of our pharmacy locations be licensed as an in-state
pharmacy to dispense pharmaceuticals in that state. State controlled substance
laws require registration and compliance with state pharmacy licensure,
registration or permit standards promulgated by the state’s pharmacy licensing
authority. Such standards often address the qualification of an applicant’s
personnel, the adequacy of its prescription fulfillment and inventory control
practices and the adequacy of its facilities. In general, pharmacy licenses are
renewed annually. We believe that our pharmacy locations comply with all state
licensing laws applicable to these businesses. If our pharmacy locations become
subject to additional licensure requirements, are unable to maintain their
required licenses or if states place burdensome restrictions or limitations on
pharmacies, our ability to operate in some states would be limited, which could
have an adverse impact on its business.
Licensure
Laws. Many states have licensure or registration laws
governing certain types of ancillary healthcare organizations, including
preferred provider organizations, TPAs, discount cash card prescription drug
programs and companies that provide utilization review services. The scope of
these laws differs significantly from state to state, and the application of
such laws to the activities of pharmacy benefit managers often is unclear. We
have registered under such laws in those states in which we have concluded that
such registration or licensure is required.
We
dispense prescription drugs pursuant to orders received through our BioScrip.com
web site, as well as other affiliated private label web sites. Accordingly, we
may be subject to laws affecting on-line pharmacies. Several states have
proposed laws to regulate on-line pharmacies and require on-line pharmacies to
obtain state pharmacy licenses. Additionally, Federal regulation by the FDA, or
another Federal agency, of on-line pharmacies that dispense prescription drugs
has been proposed. To the extent that such state or Federal regulation could
apply to our operations, certain of our operations could be adversely affected
by such licensure legislation. Management does not believe that the adoption of
any of these internet related laws would have a material adverse effect on our
business or operations.
Other Laws Affecting Pharmacy
Operations. We are subject to Federal and state statutes and
regulations governing the operation of pharmacies, repackaging of drug products,
wholesale distribution, dispensing of controlled substances, medical waste
disposal, and clinical trials. Federal statutes and regulations govern the
labeling, packaging, advertising and adulteration of prescription drugs and the
dispensing of controlled substances. Federal controlled substance laws require
us to register our pharmacies and repackaging facilities with the United States
Drug Enforcement Administration and to comply with security, recordkeeping,
inventory control and labeling standards in order to dispense controlled
substances.
FDA
Regulation. The FDA generally has authority to regulate drug
promotional information and materials that are disseminated by a drug
manufacturer or by other persons on behalf of a drug manufacturer. In January
1998, the FDA issued Draft Guidance regarding its intent to regulate certain
drug promotion and switching activities of pharmaceutical manufacturers that
control, directly or indirectly, a PBM. The FDA effectively withdrew the
Draft Guidance
and has
indicated that it would not issue new draft guidance. However, there can be no
assurance that the FDA will not assert jurisdiction over certain aspects of our
PBM business, including the internet sale of prescription drugs.
Food, Drug and Cosmetic
Act. Certain
provisions of the Federal Food, Drug and Cosmetic Act govern the handling and
distribution of pharmaceutical products. This law exempts many pharmaceuticals
and medical devices from federal labeling and packaging requirements as long as
they are not adulterated or misbranded and are dispensed in accordance with, and
pursuant to, a valid prescription. We believe that we comply in all material
respects with all applicable requirements.
Network Access
Legislation. A majority of states now have some form of
legislation affecting our ability to limit access to a pharmacy provider network
or remove network providers from our PBM pharmacy network. Subject to various
geographic, managed care or other exceptions, such legislation (“any willing
provider” legislation) may require us or our clients to admit any retail
pharmacy willing to meet the plan’s price and other terms for network
participation, or may prohibit the removal of a provider from a network except
in compliance with certain procedures (“due process” legislation) or may
prohibit days’ supply limitations or co-payment differentials between mail and
retail pharmacy providers. Many states with any willing provider statutes also
permit a member suspected of substance abuse or who otherwise needs oversight by
a pharmacist to be “locked into” one particular pharmacy for the purchase of his
or her prescription medicine. Many states have exceptions to the applicability
of these statutes for managed care arrangements or other government benefit
programs. As a dispensing pharmacy, however, such legislation benefits us by
ensuring us access to all networks in those states. Additionally, as a specialty
provider, these any willing provider regulations enable us to participate in
other PBM’s networks, restricting their ability to lock our pharmacies out of
their networks.
Legislation Imposing Plan Design
Mandates. Some states have enacted legislation that prohibits
Plan Sponsors from implementing certain restrictions on design features, and
many states have introduced legislation to regulate various aspects of managed
care plans including legislation that prohibits or restricts therapeutic
substitution, requires coverage of all drugs approved by the FDA, or prohibits
denial of coverage for non-FDA approved uses. For example, some states provide
that members may not be required to use network providers, but that they must
instead be provided with benefits even if they choose to use non-network
providers (“freedom of choice” legislation), or provide that a member may sue
his or her health plan if care is denied. Some states have enacted, and other
states have introduced, legislation regarding plan design mandates. Some states
mandate coverage of certain benefits or conditions. Such legislation does not
generally apply to our business, but it may apply to certain of our customers
(generally, HMOs and health insurers). If any such legislation were to become
widespread and broad in scope, it could have the effect of limiting the economic
benefits achievable through pharmacy benefit management. To the extent that such
legislation is applicable and is not preempted by the Employee Retirement Income
Security Act of 1974, as amended (“ERISA”) (as to plans governed by ERISA),
certain of our operations could be adversely affected. The Federal
government, as well as a number of states, have re-enacted legislation
purporting to prohibit health plans from requiring or offering members financial
incentives for use of mail order pharmacies.
Anti-Kickback
Laws. Subject to certain statutory and regulatory exceptions
(including exceptions relating to certain managed care, discount, bona fide
employment arrangements, group purchasing and personal services arrangements),
the Federal “anti-kickback” law prohibits the knowing and willful offer or
payment of any remuneration to induce the referral of an individual or the
purchase, lease or order (or the arranging for or recommending of the purchase,
lease or order) of healthcare items or services paid for in whole or in part by
Medicare, Medicaid or other government-funded healthcare programs (including
both traditional Medicaid fee-for-service programs as well as Medicaid managed
care programs). Violation of the Federal anti-kickback statute could
subject us to criminal and/or civil penalties including suspension or exclusion
from Medicare and Medicaid programs and other government-funded healthcare
programs. A number of states also have enacted anti-kickback laws
that sometimes apply not only to state-sponsored healthcare programs but also to
items or services that are paid for by private insurance and self-pay
patients. State anti-kickback laws can vary considerably in their
applicability and scope and sometimes have fewer statutory and regulatory
exceptions than does the federal law. Management carefully considers
the importance of such anti-kickback laws when structuring our operations, and
believes that we are in compliance therewith.
The
Federal anti-kickback law has been interpreted broadly by courts, the OIG and
other administrative bodies. Because of the broad scope of those statutes,
Federal regulations establish certain safe harbors from liability. Safe harbors
exist for certain properly reported discounts received from vendors, certain
investment interests held by a person or entity, and certain properly disclosed
payments made by vendors to group purchasing organizations, as well as for other
transactions or relationships. Nonetheless, a practice that does not fall within
a safe harbor is not necessarily unlawful, but may be subject to scrutiny and
challenge. In the absence of an applicable exception or safe harbor, a violation
of the statute may occur even if only one purpose of a payment arrangement is to
induce patient referrals or purchases. Among the practices that have been
identified by the OIG as potentially improper under the
statute
are certain “product conversion” or “switching” programs in which benefits are
given by drug manufacturers to pharmacists or physicians for changing a
prescription (or recommending or requesting such a change) from one drug to
another. Anti-kickback laws have been cited as a partial basis, along with state
consumer protection laws discussed below, for investigations and multi-state
settlements relating to financial incentives provided by drug manufacturers to
retail pharmacies in connection with such programs.
Certain
governmental entities have commenced investigations of PBM companies and other
companies having dealings with the PBM industry and have identified issues
concerning selection of drug formularies, therapeutic substitution programs and
discounts or rebates from prescription drug manufacturers and whether best
pricing requirements are being complied with. Additionally, at least one state
has filed a lawsuit concerning similar issues against a health plan.
Governmental entities have also commenced investigations against specialty
pharmaceutical distribution companies having dealings with pharmaceutical
manufacturers concerning retail distribution and sales and marketing practices
of certain products and therapies. There can be no assurance that we will not
receive subpoenas or be requested to produce documents in pending investigations
or litigation from time to time. As well, we may be the target or subject of one
or more such investigations or named parties in corresponding
actions.
We
believe that we are in compliance with the legal requirements imposed by the
anti-kickback laws and regulations, and we believe that there are material and
substantial differences between drug switching programs that have been
challenged under these laws and the generic substitution and therapeutic
interchange practices and formulary management programs offered by us to our
Plan Sponsors, since no remuneration or other incentives are provided to
patients, pharmacists or others. However, there can be no assurance that we will
not be subject to scrutiny or challenge under such laws or regulations, or that
any such challenge would not have a material adverse effect on us.
On
April 18, 2003, the OIG released Compliance Program Guidance for
Pharmaceutical Manufacturers (the “Guidance”) which is designed to provide
voluntary, nonbinding guidance in devising effective compliance programs to
assist companies that develop, manufacture, market and sell pharmaceutical
products or biological products in devising effective compliance programs. The
Guidance provides the OIG’s view of the fundamental elements of a pharmaceutical
manufacturer’s compliance program and principles that should be considered when
creating and implementing an effective compliance program, or as a benchmark for
companies with existing compliance programs. We currently maintain a compliance
program that includes the key compliance program elements described in the
Guidance. We believe that the fundamental elements of our compliance program are
consistent with the principles, policies and intent of the
Guidance.
The Stark
Laws. The Federal self-referral law, commonly known as the
“Stark Law”, prohibits physicians from referring Medicare patients for
“designated health services” (which include, among other things, outpatient
prescription drugs, durable medical equipment and supplies and home health
services) to an entity with which the physician, or an immediate family member
of the physician, has a direct or indirect financial relationship, unless the
financial relationship is structured to meet an applicable exception. Possible
penalties for violation of the Stark Law include denial of payment, refund of
amounts collected in violation of the statute, civil monetary penalties and
program exclusion. Management carefully considers the Stark Law and its
accompanying regulations in structuring our financial relationships with
physicians and believes that we are in compliance therewith.
State Self-Referral
Laws. We are subject to state statutes and regulations that
prohibit payments for the referral of patients and referrals by physicians to
healthcare providers with whom the physicians have a financial relationship.
Some state statutes and regulations apply to services reimbursed by governmental
as well as private payors. Violation of these laws may result in prohibition of
payment for services rendered, loss of pharmacy or health provider licenses,
fines and criminal penalties. The laws and exceptions or safe harbors may vary
from the Federal Stark Law and vary significantly from state to state. Certain
of these state statutes mirror the Federal Stark Law while others may be more
restrictive. The laws are often vague, and in many cases, have not been widely
interpreted by courts or regulatory agencies; however, we believe we are in
compliance with such laws.
Statutes Prohibiting False Claims
and Fraudulent Billing Activities. A range of Federal civil
and criminal laws target false claims and fraudulent billing activities. One of
the most significant is the Federal False Claims Act (the “False Claims Act”),
which imposes civil penalties for knowingly making or causing to be made false
claims in order to secure a reimbursement from government-sponsored programs,
such as Medicare and Medicaid. Investigations or actions commenced under the
False Claims Act may be brought either by the government or by private
individuals on behalf of the government, through a “whistleblower” or “qui tam”
action. The False Claims Act authorizes the payment of a portion of any recovery
to the individual bringing suit. Such actions are initially required to be filed
under seal pending their review by the Department of Justice. If the government
intervenes in the lawsuit and prevails, the whistleblower (or plaintiff filing
the initial complaint) may share with the Federal government in any settlement
or judgment. If the government does not intervene in the lawsuit, the
whistleblower plaintiff may pursue the action independently. The False Claims
Act generally provides for the imposition of civil penalties and for treble
damages, resulting in the possibility of substantial financial penalties for
small billing errors tht are replicated in a large number of claims, as each
individual claim could be deemed to be a separate violation of the False Claims
Act.
Some
states also have enacted statutes similar to the False Claims Act which may
include criminal penalties, substantial fines, and treble damages. In recent
years, Federal and state governments have launched several initiatives aimed at
uncovering practices that violate false claims or fraudulent billing laws. Under
Section 1909 of the Social Security Act, which became effective
January 1, 2007, if a state false claim act meets certain requirements as
determined by the OIG in consultation with the U.S. Attorney General the
state is entitled to an increase of ten percentage points in the state medical
assistance percentage with respect to any amounts recovered under a state action
brought under such a law. Some of the larger states in terms of population that
have had the OIG review such laws include: California, Florida, Illinois,
Indiana, Massachusetts, Michigan, Nevada, Tennessee and Texas. We operate in all
nine of these states and submit claims for Medicaid reimbursement to the
respective state Medicaid agencies. We expect the list of states that
enact qualifying false claims act to continue to grow. This
legislation has led to increased auditing activities by state healthcare
regulators. As such, we have been the subject of an increased number
of audits. While we believe that we are in compliance with Medicaid
and Medicare billing rules and requirements, there can be no assurance that
regulators would agree with the methodology employed by us in billing for our
products and services and a material disagreement between us and these
governmental agencies on the manner in which we provide products or services
could have a material adverse effect on our business and operations, our
financial position and our results of operations.
The False
Claims Act also has been used by the Federal government and private
whistleblowers to bring enforcement actions under so-called “fraud and abuse”
laws like the Federal anti-kickback statute and the Stark Law. Such
actions are not based on a contention that an entity has submitted claims that
are facially invalid. Instead, such actions are based on the theory
that when an entity submits a claim, it either expressly or impliedly certifies
that it has provided the underlying services in compliance with applicable laws,
and therefore that services provided and billed for during an anti-kickback
statute or Stark Law violation result in false claims, even if such claims are
billed accurately for appropriate and medically necessary
services. The availability of the False Claims Act to enforce alleged
fraud and abuse violations has increased the potential for such actions to be
brought, and which often are costly and time-consuming to defend.
Reimbursement. Approximately
25% of our revenues are derived directly from Medicare, Medicaid or other
government-sponsored healthcare programs. Also, we indirectly provide benefits
to managed care entities that provide services to beneficiaries of Medicare,
Medicaid and other government-sponsored healthcare programs. Should there be
material changes to Federal or state reimbursement methodologies, regulations or
policies, our direct reimbursements from government-sponsored healthcare
programs, as well as services fees that relate indirectly to such
reimbursements, could be adversely affected. In addition, certain state Medicaid
programs only allow for reimbursement to pharmacies residing in the state or in
a border state. While we believe that we can service our current Medicaid
patients through existing pharmacies, there can be no assurance that additional
states will not enact in-state dispensing requirements for their Medicaid
programs. To the extent such requirements are enacted, certain therapeutic
pharmaceutical reimbursements could be adversely affected.
Legislation and Other Matters
Affecting Drug Prices. Some states have adopted legislation
providing that a pharmacy participating in the state Medicaid program must give
the state the best price that the pharmacy makes available to any third party
plan (“most favored nation” legislation). Such legislation may adversely affect
our ability to negotiate discounts in the future from network pharmacies. At
least one state has enacted “unitary pricing” legislation, which mandates that
all wholesale purchasers of drugs within the state be given access to the same
discounts and incentives. Such legislation has not yet been enacted in the
states where our mail service pharmacies are located. Such legislation, if
enacted in other states, could adversely affect our ability to negotiate
discounts on our purchase of prescription drugs to be dispensed by the mail
service pharmacies.
Effective
September 26, 2009, First DataBank and Medi-Span reduced the mark-up factor
applied to WAC, on which the average wholesale price (“AWP”) is based, from
1.25 to 1.20 for approximately 18,000 national drug codes. These AWP publishers
also have indicated that, within the next two years, they will discontinue
publication of AWP information. The impact of this reduction in AWP was to
reduce our gross margins beginning in the fourth quarter of 2009. See
“Risk Factors - Changes in industry pricing benchmarks could adversely affect
our financial performance.”
Confidentiality, Privacy and
HIPAA. Most of our activities involve the receipt, use and
disclosure of confidential medical, pharmacy or other health-related information
concerning individual members, including the disclosure of the confidential
information to the member’s health benefit plan. In addition, we use aggregated
and blinded (anonymous) data for research and analysis purposes.
On
April 14, 2003 the final regulations issued by United States Department of
Health and Human Services (“HHS”), regarding the privacy of
individually identifiable health information (the “Privacy Regulations”)
pursuant to the Health Insurance Portability and Accountability Act of 1996
(“HIPAA”) took effect. The Privacy Regulations are designed to protect the
medical information of a healthcare patient or health plan enrollee that could
be used to identify the individual. We refer to this information as protected
health information (“PHI”). The Privacy Regulations apply directly to certain
entities known as “covered entities,” which include Plan Sponsors and most
healthcare providers. In addition, the Privacy Regulations require covered
entities to enter into contracts requiring their “business associates” to agree
to certain restrictions regarding the use and disclosure of PHI. The Privacy
Regulations apply to PHI maintained in any format, including both electronic and
paper records, and impose extensive restrictions on the way in which covered
entities (and indirectly their business associates) may use and disclose PHI. In
addition, the Privacy Regulations also give patients significant rights to
understand and control how their PHI is used and disclosed. Often, use and
disclosure of PHI must be limited to the minimum amount necessary to achieve the
purpose of the use or disclosure. Certain of our businesses are covered entities
directly subject to the Privacy Regulations, and other of our businesses are
“business associates” of covered entities, such as Plan Sponsors.
Since
October 16, 2003 we have been subject to compliance with the rules
governing transaction standards and code sets issued by HHS pursuant to HIPAA
(the “Transactions Standards”). The Transactions Standards establish uniform
standards to be utilized by covered entities in the electronic transmission of
health information in connection with certain common healthcare financing
transactions, such as healthcare claims. Under the new Transactions Standards,
any party transmitting or receiving health transactions electronically must send
and receive data in a single format, rather than the large number of different
data formats currently used. The Transactions Standards apply to us in
connection with submitting and processing healthcare claims. The Transactions
Standards also applies to many of our payors and to our relationships with those
payors.
In
addition, in February 2003, HHS issued final regulations governing the security
of PHI pursuant to HIPAA (the “Security Standards”). The Security Standards
impose substantial requirements on covered entities and their business
associates regarding the storage, utilization of, access to and transmission of
electronic PHI.
The
requirements imposed by the Privacy Regulations, the Transactions Standards, and
the Security Standards are extensive and have required substantial cost and
effort to assess and implement. We have taken and will continue to take steps
that we believe are reasonable to ensure that our policies and procedures are in
compliance with the Privacy Regulations, the Transactions Standards and
the
Security Standards. The requirements imposed by HIPAA have increased our burden
and costs of regulatory compliance (including our health improvement programs
and other information-based products), altered our reporting to Plan Sponsors
and reduced the amount of information we can use or disclose if members do not
authorize such uses or disclosures.
Most
states also have enacted health information privacy laws which restrict the use
and disclosure of patient health information. In addition, several
states recently have enacted pharmacy-related privacy legislation that applies
not only to patient records but that also prohibits the transfer or use for
commercial purposes of pharmacy data that identifies prescribers. In
response to concerns about identity theft, many states also have adopted
so-called “security breach” notification laws that may impose requirements
regarding the safeguarding of personal information such as social security
numbers and bank and credit card account numbers, and that impose an obligation
to notify persons when their personal information has or may have been accessed
by an unauthorized person. Many of these laws apply to our business
and have and will continue to increase our burden and costs of privacy and
security related regulatory compliance.
On
February 17, 2009, the American Recovery and Reinvestment Act of 2009 (“ARRA”)
was enacted, and included Title XIII, the Health Information Technology for
Economic and Clinical Health Act (the “HITECH Act”). The HITECH Act modified
certain provisions of the HIPAA Privacy Regulations and Security Standards, and
included additional requirements meant to protect the privacy and security of
health information, including, but not limited to, a new federal breach
notification obligation applicable to HIPAA covered entities and their business
associates. HHS, as required by the HITECH Act, has issued a regulation setting
forth the breach notification obligations applicable to covered entities and
their business associates (the “HHS Breach Notification Rule”). The various
requirements of the HITECH Act and the HHS Breach Notification Rule have
different compliance dates, some of which have passed and some of which will
occur in the future. With respect to those requirements whose compliance dates
have passed, we believe that we are in compliance with these provisions. With
respect to those requirements whose compliance dates are in the future, we are
in the process of implementing these new requirements or have done so already,
and believe that we will be in compliance with these requirements on or before
the applicable compliance date.
Consumer Protection
Laws. Most states have consumer protection laws that have been
the basis for investigations and multi-state settlements relating to financial
incentives provided by drug manufacturers to pharmacies in connection with drug
switching programs. No assurance can be given that we will not be subject to
scrutiny or challenge under one or more of these laws.
Disease Management Services
Regulation. All states regulate the practice of medicine. To
our knowledge, no PBM has been found to be engaging in the practice of medicine
by reason of its disease management services. However, there can be no assurance
that a Federal or state regulatory authority will not assert that such services
constitute the practice of medicine, thereby subjecting such services to Federal
and state laws and regulations applicable to the practice of
medicine.
Comprehensive PBM
Regulation. Although no state has passed legislation
regulating PBM activities in a comprehensive manner, such legislation has been
introduced in the past in several states. Since we do not derive significant PBM
revenues from business in any particular state, such legislation, if currently
enacted in a state, would not have a material adverse impact on our
operations.
Antitrust
Laws. Numerous lawsuits have been filed throughout the United
States by retail pharmacies against drug manufacturers challenging certain brand
drug pricing practices under various state and Federal antitrust laws. A
settlement in one such suit would require defendant drug manufacturers to
provide the same types of discounts on pharmaceuticals to retail pharmacies and
buying groups as are provided to managed care entities to the extent that their
respective abilities to affect market share are comparable, a practice which, if
generally followed in the industry, could increase competition from pharmacy
chains and buying groups and reduce or eliminate the availability to us of
certain discounts, rebates and fees currently received in connection with our
drug purchasing and formulary administration programs. In addition, to the
extent that we, or an associated business, appear to have actual or potential
market power in a relevant market, business arrangements and practices may be
subject to heightened scrutiny from an anti-competitive perspective and possible
challenge by state or Federal regulators or private parties.
While
management believes that we are in substantial compliance with all of the
existing laws and regulations stated above, such laws and regulations are
subject to rapid change and often are uncertain in their application. As
controversies continue to arise in the healthcare industry, Federal and state
regulation and enforcement priorities in this area may increase, the impact of
which cannot be predicted. There can be no assurance that we will not be subject
to scrutiny or challenge under one or more of these laws or that any such
challenge would not be successful. Any such challenge, whether or not
successful, could have a material adverse effect upon our business and results
of operations.
Employees
At
February 24, 2010, we had 885 full-time, 34 part-time and 423 per
diem employees, including 199 licensed pharmacists. Per diem employees are
defined as those available on an as-needed basis. None of our employees are
represented by any union and, in our opinion, relations with our employees are
satisfactory.
Available
Information
We
maintain a website at www.bioscrip.com. We make available,
free of charge, through our web site our reports on Forms 10-K, 10-Q, and
8-K, and amendments to those reports, as soon as reasonably practicable after
they are filed with or furnished to the SEC.
We have
adopted a code of business conduct and ethics for our Company, including our
directors, officers and employees. Our code of conduct policy, our corporate
governance guidelines and the charters of the audit, compensation and nominating
and corporate governance committees of our board of directors are available on
our website at www.bioscrip.com.
The
continuing pressure on the global credit and financial markets could materially
and adversely affect our business and results of operations.
The
ongoing global financial crisis continues to result in severely diminished
liquidity and credit availability, volatility in consumer confidence, declines
in economic growth, increases in unemployment rates and an on-going uncertainty
about market stability. The effect of these actions could reduce
enrollment in governmental programs or benefits available to be
enrolled.
Limited
or expensive access to credit could also reduce the ability of the patients we
serve to pay deductibles and co-insurance. Higher unemployment rates
and significant employment layoffs and downsizings may lead to lower numbers of
patients enrolled in employer-provided plans. The adverse economic
conditions could also cause employers to stop offering, or limit, certain health
care coverage, or the program designs associated with the
coverage,
as an
employee benefit or cause them to offer this coverage on a voluntary,
employee-funded basis as a means to reduce their operating costs, leaving the
patient’s ability to pay in question and increasing the likelihood that
compliance to drug therapies will be interrupted.
During an
economic downturn, Federal and state budgets could be adversely affected,
resulting in reduced reimbursements or payments by our Federal and state
government health care coverage programs in which we participate, including
Medicare, Medicaid and other Federal or state assistance plans. Also,
a reduction in state Medicaid reimbursement rates could be implemented to
agreements already negotiated with the government and could adversely affect our
revenues and financial results. Government programs could also slow
or temporarily suspend payments on Medicaid obligations, negatively impacting
our cash flow and increase our working capital needs and interest
payments.
Availability
of financing sources may be restricted in the future.
The
economic crisis caused contraction in the credit markets and the availability of
credit continues to remain restricted. While we believe our existing financing
relationship is good and our credit facility is adequate to cover our needs,
this agreement has historically been our largest source of funding and expires
in the fourth quarter of 2010. There can be no assurances that this
agreement will continue beyond its current maturity. In addition, if
extreme market conditions continue or if our primary financing source were to
fail, we can provide no assurance that any financing sources would be available
or favorably priced. Also, future growth may be limited by our
ability to gain access to additional capital.
Existing
and new government legislative and regulatory action could adversely affect our
business and financial results.
Our Specialty Pharmacy Services and Traditional Pharmacy Services segments are
subject to numerous Federal, state and local laws and
regulations. See “Business – Government
Regulation.” Changes in these regulations may require extensive
changes to our systems and operations that may be difficult to
implement. Untimely compliance or noncompliance with applicable laws
and regulations could adversely affect the continued operation of our business,
including, but not limited to: imposition of civil or criminal penalties;
suspension of payments from government programs; loss of required government
certifications or approvals; loss of authorizations to participate in or
exclusion from government reimbursement programs, such as the Medicare and
Medicaid programs; or loss of licensure. The regulations to which we are subject
include, but are not limited to, Anti-Kickback laws; Federal and state
self-referral laws; HIPAA; regulations of the FDA, U.S. Federal Trade
Commission, and the U.S. Drug Enforcement Administration, and regulations of
various state regulatory authorities. In that regard, our business,
financial position and results of operations could be affected by one or more of
the following:
|
|
·
|
Federal
and state laws and regulations governing the purchase, distribution,
management, dispensing and reimbursement of prescription drugs and related
services, whether at retail or mail, and applicable licensing
requirements;
|
|
|
·
|
impact
of limited distribution drugs;
|
|
|
·
|
the
frequency and rate of approvals by the FDA of new brand named and generic
drugs, or of over-the-counter status for brand name
drugs;
|
|
|
·
|
FDA
regulation affecting the retail or PBM
industry;
|
|
|
·
|
rules
and regulations issued pursuant to HIPAA and HITECH; and other federal and
state laws affecting the use, disclosure and transmission of health
information, such as state security breach laws and state laws limiting
the use and disclosure of prescriber
information;
|
|
|
·
|
administration
of the Medicare Drug Benefit, including legislative changes and/or CMS
rulemaking and interpretation;
|
|
|
·
|
government
regulation of the development, administration, review and updating of
formularies and drug lists;
|
|
|
·
|
state
laws and regulations establishing or changing prompt payment requirements
for payments to retail pharmacies;
|
|
|
·
|
managed
care reform and plan design legislation;
and
|
|
|
·
|
direct
regulation of pharmacies or PBMs by regulatory and quasi-regulatory
bodies.
|
Competition in the pharmaceutical
healthcare services industry could reduce profit margins.
The
pharmaceutical healthcare services industry is very competitive. Our competitors
include large and well-established companies that may have greater financial,
marketing and technological resources than we do.
The
specialty pharmacy industry is highly competitive. Some of our competitors are
under common control with, or ownership by, pharmaceutical wholesalers and
distributors, managed care organizations, pharmacy benefit managers or retail
pharmacy chains and may be better positioned with respect to the cost-effective
distribution of pharmaceuticals. In addition, some of our competitors may have
secured long-term supply or distribution arrangements for prescription
pharmaceuticals necessary to treat certain chronic disease states on price terms
substantially more favorable than the terms currently available to us. As a
result of such advantageous pricing, we may be less price competitive than some
of these competitors with respect to certain pharmaceutical products. Our
competitive position could also be adversely affected by any inability to obtain
access to new biotech pharmaceutical products.
Changes
in industry pricing benchmarks could adversely affect our financial
performance.
Contracts
with our Traditional Pharmacy Services and Specialty Pharmacy Services clients
generally use certain published benchmarks to establish pricing for the
reimbursement of prescription medications dispensed by us. These benchmarks
include AWP, WAC and average manufacturer price. Most of our contracts utilize
the AWP benchmark.
As a
result of the settlement of class-action lawsuits brought against First DataBank
and Medi-Span, effective September 26, 2009, First DataBank and Medi-Span agreed
to reduce the mark-up factor applied to WAC, on which AWP is based, from 1.25 to
1.20 for the approximately 1,400 drug codes that were the subject of the
lawsuits. These AWP publishers also similarly reduced the mark-up factor on all
other national drug codes on which they had marked up AWP. This voluntary
reduction affected approximately 18,000 national drug codes. First DataBank and
Medi-Span also have indicated that, within the next two years, they will
discontinue publication of AWP information. In response to this change, a number
of pharmacy benefit managers and third-party payors made adjustments to existing
contracts with network pharmacy providers in order to preserve the economic
structure of those agreements. The majority of the state Medicaid agencies did
not make any such adjustments, the consequence of which is lowered reimbursement
levels. The impact of the AWP settlement was to reduce our gross margins
beginning in the fourth quarter of 2009. Based on revenue from all
sources on a year-to-date basis, we estimated the impact of this change to be
approximately $5.0 million on an annual basis. In 2010, we expect this margin
impact will be offset by overall organic growth as well as an emphasis on higher
margin business mix.
Client
demands for enhanced service levels or possible loss or unfavorable modification
of contracts with clients or providers could pressure margins.
As our
clients face the continued rapid growth in prescription drug costs, they may
demand additional services and enhanced service levels to help mitigate the
increase in spending. We operate in a very competitive environment, and we may
not be able to increase our fees to compensate for these increased services,
which could put pressure on our margins.
Our
contracts with clients generally do not have terms longer than three years and,
in some cases, may be terminated by the client on relatively short notice. Our
clients generally seek bids from other PBM or specialty providers in advance of
the expiration of their contracts. If several of these clients elect not to
extend their relationship with us, and we are not successful in generating sales
to replace the lost business, our future business and operating results could be
materially and adversely affected. In addition, we believe the managed care
industry is undergoing substantial consolidation, and another party that is not
our client could acquire some of our managed care clients. In such case, the
likelihood such client would renew its contract with us could be
reduced.
There are
approximately 56,000 retail pharmacies in the United States. All major
retail chain pharmacies and a vast majority of independent pharmacies
participate in our pharmacy network. The top ten retail pharmacy chains
represent approximately 65% of the total number of stores and over 80% of
prescriptions filled in our network. Our contracts with retail pharmacies, which
are non-exclusive, are generally terminable on relatively short notice. If one
or more of the top pharmacy chains elects to terminate its relationship with us,
our members’ access to retail pharmacies and our business could be materially
adversely affected. In addition, many large pharmacy chains either own PBMs
today, or could attempt to acquire a PBM in the future. Ownership of PBMs by
retail pharmacy chains could have material adverse effects on our relationships
with such pharmacy chains and on our consolidated results of operations,
consolidated financial position and/or consolidated cash flow from
operations. Pending and future litigation could subject us to
significant monetary damages and/or require us to change our business
practices.
We are
subject to risks relating to litigation and other proceedings in connection with
our operations, including the dispensing of pharmaceutical products by our mail
service, infusion services and community pharmacies. See Item 3 –
Legal Proceedings for a list of material proceedings pending against
us. While we believe that these suits are without merit and intend to
contest them vigorously, we can give no assurance that an adverse outcome in one
or more of these suits would not have a material adverse effect on our
consolidated results of operations, consolidated financial position and/or
consolidated cash flow from operations, or would not require us to make material
changes to our business practices. We are presently responding to several
subpoenas and requests for information from governmental agencies. We confirmed
that we are not a target or a potential subject of those investigations and
requests. We cannot predict with certainty what the outcome of any of the
foregoing might be. In addition to potential monetary liability arising from
these suits and proceedings, we are incurring costs in the defense of the suits
and in providing documents to government agencies. Many of the current pending
claims and associated costs are covered by our insurance, but certain other
costs are not insured, such as deductibles on each claim. While these costs are
not currently material to our financial performances and there can be no
assurance that such costs will not increase and/or become in the
future.
We
may be subject to liability claims for damages and other expenses that are not
covered by insurance.
A
successful product or professional liability claim in excess of our insurance
coverage could harm our financial condition and results of operations. Various
aspects of our business may subject us to litigation and liability for damages,
including the provision of PBM services and the operation of our pharmacies. For
example, a prescription drug dispensing error could result in a patient
receiving the wrong or incorrect amount of medication, leading to personal
injury or death. Our business, financial condition and results of operations
could suffer if we pay damages or defense costs in connection with a claim that
is outside the scope of any applicable contractual indemnity or insurance
coverage.
Loss
of relationships with one or more pharmaceutical manufacturers and changes in
payments made by pharmaceutical manufacturers could adversely affect our
business and financial results.
We have
contractual relationships with pharmaceutical manufacturers that provide
discounts on drugs dispensed from our mail service and community pharmacies, and
pay service fees for other programs and services that we provide. Our business
and financial results could be adversely affected if: (i) we were to lose
relationships with one or more key pharmaceutical manufacturers; (ii)
discounts decline due to changes in utilization of specified pharmaceutical
products by health Plan Sponsors and other clients; (iii) legal
restrictions are imposed on the ability of pharmaceutical manufacturers to offer
rebates, administrative fees or other discounts or to purchase our programs or
services; or (iv) pharmaceutical manufacturers choose not to offer rebates,
administrative fees or other discounts or to purchase our programs or
services.
We
purchase substantially all of our pharmaceutical products from one vendor and a
disruption in our purchasing arrangements could adversely impact our
business.
We purchase substantially all of our prescription products, subject to certain
minimum periodic purchase levels and excluding purchases of therapeutic plasma
products, from a single wholesaler, ADBC, pursuant to a prime vendor agreement.
The term of this agreement extends until August 2012, subject to extension for
up to two additional years. Any significant disruption in our relationship with
ABDC, or in ABDC's supply of products to us, would make it difficult and
possibly more costly for us to continue to operate our business until we are
able to execute a replacement wholesaler agreement. There can be no assurance
that we would be able to find a replacement wholesaler on a timely basis or that
such wholesaler would be able to fulfill our demands on similar financial terms.
If we are unable to identify a replacement on substantially similar financial
terms, our results of operations, financial condition and cash flows may be
materially adverse affected.
Failure
to develop new products, services and delivery channels may adversely affect our
business.
We
operate in a highly competitive environment. We develop new products and
services from time to time to assist our clients. If we are unsuccessful in
developing innovative products and services, our ability to attract new clients
and retain existing clients may suffer.
Technology
is also an important component of our business as we continue to utilize new and
better channels to communicate and interact with our clients, members and
business partners. If our competitors are more successful than us in employing
this technology, our ability to attract new clients, retain existing clients and
operate efficiently may suffer.
The
success of our business depends on maintaining a well-secured business and
technology infrastructure.
We are
dependent on our infrastructure, including our information systems, for many
aspects of our business operations. A fundamental requirement for our business
is the secure storage and transmission of personal health information and other
confidential data. Our business and operations may be harmed if we do not
maintain our business processes and information systems in a secure manner, and
maintain and improve continually the integrity of our confidential information.
Although we have developed systems and processes that are designed to protect
information against security breaches, failure to protect such information or
mitigate any such breaches may adversely affect our operating results.
Malfunctions in our business processes, breaches of our information systems or
the failure to maintain effective and up-to-date information systems could
disrupt our business operations, result in customer and member disputes, damage
our reputation, expose us to risk of loss or litigation, result in regulatory
violations, increase administrative
expenses
or lead to other adverse consequences.
Problems
in the implementation and conversion of our new pharmacy system could result in
additional expense.
The
Company has committed significant financial and other resources to migrate to a
new pharmacy dispensing, clinical management and accounts receivable management
system designed to streamline our business processes, provide improved data
reporting, data management, scalability and cash posting and billing and
collections. Delays in the implementation of this system
could result in higher operating costs, additional charges for system design
changes or delays in the execution of our strategic plan due to our inability to
scale our current operating systems.
Our
failure to maintain controls and processes over billing and collecting could
have a significant negative impact on our results of operations and financial
condition.
The
collection of accounts receivable is a significant challenge and requires
constant focus and involvement by management and ongoing enhancements to
information systems and billing center operating procedures. If we are unable to
properly bill and collect our accounts receivable, our results could be
materially and adversely affected. While management believes that controls and
processes are satisfactory there can be no assurance that accounts receivable
collectability will remain at current levels.
Efforts
to reduce healthcare costs and alter health care financing practices could
adversely affect our business.
During
the past several years, the U.S. healthcare industry has been subject to
increased governmental regulation at both the Federal and state levels. Certain
proposals have been made at the Federal and state government levels in an effort
to control healthcare costs, including proposing to lower reimbursement under
Medicaid and Medicare programs. These proposals include “single payor”
government funded healthcare and price controls on prescription drugs. If these
or similar efforts are successful, our business and operations could be
materially adversely affected. In addition, changing political, economic and
regulatory influences may affect healthcare financing and reimbursement
practices. If the current healthcare financing and reimbursement system changes
significantly, our business could be materially adversely affected. Congress
periodically considers proposals to reform the U.S. healthcare system. Both
the U.S. Senate and House of Representatives approved reform legislation in late
2009 and the Obama administration has submitted a 2010 Federal budget that
emphasizes maintaining patient choice, reducing inefficiencies and costs,
increasing prevention programs, improving coverage portability and universality,
and improving quality of care. These proposals may also increase
government involvement in healthcare providers reimbursement under Medicare and
Medicaid, or otherwise change the way in which our clients do business. Plan
Sponsors may react to these proposals and the uncertainty surrounding them by
reducing or delaying purchases of clinical services, cost control mechanisms and
other related services that we provide. We cannot predict what effect, if any,
these proposals may have on our business. Other legislative or market-driven
changes in the healthcare system that we cannot anticipate could also materially
adversely affect our consolidated results of operations, consolidated financial
position and/or consolidated cash flow from operations.
Prescription
volumes may decline, and our net revenues and profitability may be negatively
impacted, when products are withdrawn from the market or when increased safety
risk profiles of specific drugs result in utilization decreases.
We
process significant volumes of pharmacy claims for brand-name and generic drugs
from our mail service and community pharmacies and through our network of retail
pharmacies. These volumes are the basis for our net revenues and profitability.
When products are withdrawn by manufacturers, or when increased safety risk
profiles of specific drugs or classes of drugs result in utilization decreases,
physicians may cease writing or reduce the numbers of prescriptions written for
these higher-risk drugs. Additionally, negative media reports regarding drugs
with higher safety risk profiles may result in reduced consumer demand for such
drugs. In cases where there are no acceptable prescription drug equivalents or
alternatives for these prescription drugs, our prescription volumes, net
revenues, profitability and cash flows may decline.
The
loss of a relationship with one or more Plan Sponsors could negatively impact
our business.
Where we
do not have preferred or exclusive arrangements with Plan Sponsors, our
contracts for reimbursement with Plan Sponsors are often on a perpetual or
“evergreen” basis. These evergreen contracts are subject to
termination by a Plan Sponsor’s written notice. The required notice
varies by contract and is typically 30 to 90 days. Depending on the
amount of revenues generated by any single Plan Sponsor or more than one Plan
Sponsor in the aggregate, one or more terminations could have a material and
adverse effect on our results of operations and financial
performance. We are unaware of any intention by a Plan Sponsor to
terminate or not renew an agreement with us.
Network lock-outs by health insurers and PBMs could adversely affect our
financial results.
Many Plan
Sponsors and PBMs continue to create exclusive specialty networks which limit a
member’s access to a mail service facility or network of preferred pharmacies.
To the extent our pharmacies are excluded from these networks, we are unable to
dispense medications to those members and bill for prescriptions to those
member’s insurance carriers. If these specialty networks continue to expand and
we are locked out from dispensing specialty medications to members of exclusive
networks, our revenues, financial condition and results of operations could be
adversely affected.
Failure
to complete the acquisition of CHS could negatively impact the stock price and
the future business and financial results of BioScrip.
As
previously announced, on January 24, 2010, we entered into an agreement to
acquire CHS, a privately held company that is a leading provider of home
infusion and home nursing services and products. See Item 7 –
Management’s Discussion and Analysis of Financial Condition and Results of
Operations for more information.
Although
we have agreed to use our reasonable efforts to obtain stockholder approval of
the issuance of shares of our common stock necessary to complete the acquisition
of CHS, there is no assurance that the acquisition will be approved. If the
share issuance is not approved, and as a result the acquisition is not
completed, we will have expended substantial sums, including a possible
termination fee of $1.0 million payable to CHS, which may adversely affect our
financial condition and results of operations.
Although
we expect that the merger with CHS will result in benefits to BioScrip, we may
not realize those benefits because of integration difficulties.
We may
not be able to successfully integrate CHS with BioScrip. The
inability to achieve the full extent of, or any of the anticipated synergies of,
the acquisition of CHS, including anticipated cost savings and additional
revenue opportunities, could have an adverse effect on our business, financial
position and results of operations.
Realizing
the benefits of the merger will depend in part on the integration of information
technology, operations and personnel. These integration activities
are complex and time-consuming and we may encounter unexpected difficulties or
incur unexpected costs.
We may
not successfully integrate the operations of the businesses of CHS in a timely
manner, and we may not realize the anticipated net reductions in costs and
expenses and other benefits and synergies of the merger with CHS to the extent,
or in the timeframe, anticipated. In addition to the integration
risks discussed above, our ability to realize these net reductions in costs and
expenses and other benefits and synergies could be adversely impacted by
practical or legal constraints on our ability to combine
operations.
We
anticipate that the significant indebtedness that will be incurred if we
complete the merger with CHS will impose operating and financial restrictions on
us which, together with the resulting debt service obligations, may
significantly limit our ability to execute our business strategy and increase
the risk of default under our debt obligations.
We intend
to borrow an aggregate of approximately $325.0 million (not including up to
$50.0 million that would also be available under our new revolving credit
facility) in connection with the merger. We expect that the terms of
our new credit facilities that we will enter into in connection with the merger
will require us to comply with certain financial covenants, including a maximum
total leverage ratio and a minimum fixed charge coverage ratio. In
addition, the proposed terms of our new indebtedness also include certain
covenants restricting or limiting our ability to, among other
things:
|
|
·
|
incur
indebtedness or liens;
|
|
|
·
|
make
investments or capital expenditures;
|
|
|
·
|
engage
in mergers, acquisitions or asset sales;
|
|
|
·
|
declare
dividends or redeem or repurchase capital stock;
|
|
|
·
|
enter
into transactions with affiliates;
|
|
|
·
|
modify
our organizational documents; and
|
|
|
·
|
change
our fiscal year.
|
Our
significant indebtedness could have important consequences, including: making it
more difficult for us to satisfy our obligations; limiting our ability to borrow
additional amounts to fund working capital and other purposes; requiring us to
dedicate a substantial portion of our cash flow from operations to pay interest
on our debt; making us more vulnerable to adverse changes in general economic,
industry and government regulations; placing us at a competitive disadvantage
compared with those of our competitors with less debt; and exposing us to risks
in inherent interest rate fluctuations because some of our borrowings are at
variable rates. In addition, we may not be able to generate
sufficient cash flow from our operations to repay our indebtedness when it
becomes due and to meet our other cash needs. If this happens and we
are not able to refinance our debt, sell additional debt or equity securities or
our assets on favorable terms, if at all, it may negatively affect our ability
to generate revenues.
None.
Our
executive offices are located in Elmsford, New York, and our business offices
are located in Eden Prairie, Minnesota. Our mail operations are located in
Columbus, Ohio; Lake Success, New York and Burbank, California. Our pharmacies
are located in major metropolitan locations across the United
States. Some of our properties are licensed to operate as dual
purpose properties. We currently lease all of our properties from
third parties under various lease terms expiring over periods extending to 2019.
Property locations are as follows:
|
Corporate
Offices
|
Community
and Infusion Pharmacies (2)
|
||||||
|
Elmsford,
NY
|
California
|
Minnesota
|
|||||
|
Eden
Prairie, MN
|
Burbank
(Infusion)
|
Minneapolis
|
|||||
|
San
Diego
|
Missouri
|
||||||
|
San
Francisco (Community & Infusion)
|
Kansas
City
|
||||||
|
Sherman
Oaks
|
St.
Louis
|
||||||
|
Mail
Operations
|
West
Hollywood
|
Nevada
|
|||||
|
Columbus,
OH (1)
|
District
of Columbia
|
Las
Vegas (Community & Infusion)
|
|||||
|
Burbank,
CA (2)
|
Washington,
D.C.
|
New
Jersey
|
|||||
|
Lake
Success, NY (2)
|
Florida
|
Morris
Plains (Infusion)
|
|||||
|
Ft.
Lauderdale
|
New
York
|
||||||
|
Miami
Beach
|
Lake
Success (Infusion)
|
||||||
|
Orlando
|
Hawthorne
|
||||||
|
Pompano
Beach (Infusion)
|
Bronx
|
||||||
|
St.
Petersburg
|
New
York
|
||||||
|
Tampa
Bay
|
Pennsylvania
|
||||||
|
West
Palm Beach
|
Philadelphia
|
||||||
|
Georgia
|
King
of Prussia (Infusion)
|
||||||
|
Atlanta
|
Tennessee
|
||||||
|
Illinois
|
Memphis
(Community & Infusion)
|
||||||
|
Chicago
|
Texas
|
||||||
|
Indiana
|
Dallas
(two locations)
|
||||||
|
Indianapolis
(two locations)
|
Houston
|
||||||
|
Maryland
|
Washington
|
||||||
|
Baltimore
|
Seattle
(Community & Infusion)
|
||||||
|
Massachusetts
|
Wisconsin
|
||||||
|
Boston
|
Milwaukee
|
||||||
__________________________
|
(1)
|
Facility
houses operations for both Specialty Pharmacy Services and Traditional
Pharmacy Services operations.
|
|
(2)
|
Facility
houses operations for Specialty Pharmacy Services
operations.
|
On
February 14, 2005, a complaint was filed in the Alabama Circuit Court for
Barbour County, captioned Eufaula Drugs, Inc. v.
ScriptSolutions [sic], one of approximately fourteen substantially
identical complaints commenced in Alabama courts against various unrelated
pharmacy benefit management companies. On April 8, 2005, the plaintiff
filed an amended complaint substituting our BioScrip PBM Services f/k/a
ScripSolutions (“PBM Services”) as the defendant, seeking unspecified money
damages and injunctive relief, and alleging breach of contract and related tort
and equitable claims on behalf of a putative nationwide class of pharmacies
alleging insufficient reimbursement for prescriptions dispensed by
ScripSolutions, principally on the theory that PBM Services was obligated to
update its prescription pricing files on a daily rather than weekly basis.
Following preliminary proceedings and class discovery, the parties reached a
settlement agreement on August 6, 2009, in which we continued to deny liability,
with a class of pharmacies which was certified solely for settlement purposes,
and class members were entitled to receive $0.065 for each branded prescription
filled during the settlement class period. The court approved the
settlement on November 4, 2009 and a final judgment dismissing the action has
been entered in the action, the time to appeal which has expired. The
costs of the settlement are covered by insurance.
The
sellers of a company, Northland Pharmacy, to Chronimed Holdings, Inc., (now
known as BioScrip Pharmacy, Inc.) one of our subsidiaries, are claiming a right
to additional purchase price of at least $5.64 million in connection with an
earn out provision in the stock purchase agreement regarding the
acquisition. The sellers, named DiCello, first sued in federal court
in Ohio in July 2007, but the court stayed the case and directed arbitration of
the disagreement by the accounting firm KPMG, LLP, as the stock purchase
agreement provides. We deny owing the sellers any additional purchase
price. The parties have made extensive filings as directed by the
arbitrator and are waiting for either the arbitrator’s decision or instructions
as to further proceedings in the matter. We are confident in our
position and do not believe an adverse ruling is likely; however, there can be
no assurance that an adverse ruling will not be rendered. If the
arbitrator rules in favor of DiCello, such ruling could have a material adverse
effect on our business, operations, or financial position.
Our
common stock, par value $0.0001 per share (“Common Stock”), is traded on
the Nasdaq Global Market under the symbol “BIOS.” The following table represents
the range of high and low sale prices for our Common Stock for the last eight
quarters. Such prices reflect interdealer prices, without retail mark-up,
mark-down or commission and may not necessarily represent actual
transactions.
|
High
|
Low
|
|||||||
|
2008
|
First
Quarter
|
$ | 8.47 | $ | 5.65 | |||
|
Second
Quarter
|
$ | 7.06 | $ | 2.55 | ||||
|
Third
Quarter
|
$ | 5.07 | $ | 1.94 | ||||
|
Fourth
Quarter
|
$ | 5.00 | $ | 1.26 | ||||
|
2009
|
First
Quarter
|
$ | 2.84 | $ | 1.35 | |||
|
Second
Quarter
|
$ | 5.99 | $ | 1.95 | ||||
|
Third
Quarter
|
$ | 7.29 | $ | 5.26 | ||||
|
Fourth
Quarter
|
$ | 9.05 | $ | 6.25 | ||||
As of
February 24, 2010, there were 284 stockholders of record in addition to
approximately 7,100 stockholders whose shares were held in nominee name. On
February 24, 2010 the closing sale price of our Common Stock on Nasdaq was
$7.14.
We have
never paid cash dividends on our Common Stock and do not anticipate doing so in
the foreseeable future.
Between
January 1, 2009 and December 31, 2009, we did not issue any shares of common
stock without registration under the Securities Act of 1933, as amended (the
“Securities Act”).
Information
regarding securities authorized for issuance under our equity compensation plans
required by this Item 5 is included in our definitive proxy statement to be
filed with the SEC on or before April 30, 2010 in connection with our 2010
Annual Meeting of Stockholders and is hereby incorporated by
reference.
The graph
set forth below compares, for the five-year period commencing December 31,
2004 and ending December 31, 2009, the total cumulative return to holders
of our Common Stock with the cumulative total return of the Nasdaq Composite
Index and the Nasdaq Health Services Index.
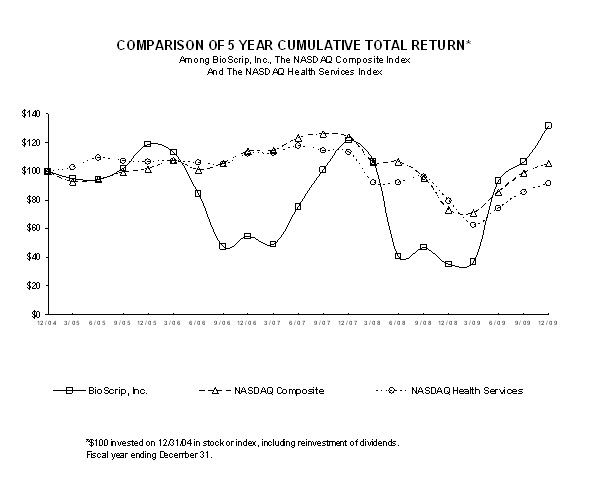
The
selected consolidated financial data presented below should be read in
conjunction with, and is qualified in its entirety by reference to, Management’s
Discussion and Analysis and our Consolidated Financial Statements and the Notes
thereto appearing elsewhere in this Annual Report. Acquisitions during the
periods below include: Chronimed, Inc. (“Chronimed”) beginning March, 2005, JPD,
Inc., d/b/a Northland Medical Pharmacy beginning October, 2005, and BioScrip
Infusion Services, Inc., (“Infusion West”) beginning March, 2006.
|
December
31,
|
||||||||||||||||
|
Balance
Sheet Data
|
2009
|
2008
|
2007
|
2006
|
2005
|
|||||||||||
|
(in
thousands)
|
||||||||||||||||
|
Working
capital
|
$ | 91,078 | $ | 58,844 | $ | 49,213 | $ | 37,023 | $ | 67,488 | ||||||
|
Line
of Credit
|
$ | 30,389 | $ | 50,411 | $ | 33,778 | $ | 52,895 | $ | 7,427 | ||||||
|
Total
assets (3)
|
$ | 287,220 | $ | 246,957 | $ | 296,822 | $ | 305,456 | $ | 298,629 | ||||||
|
Stockholders'
equity (3)
|
$ | 155,793 | $ | 95,537 | $ | 166,203 | $ | 161,833 | $ | 195,765 | ||||||
|
Year
Ended December 31,
|
||||||||||||||||
|
Statement
of Operations Data
|
2009
|
2008
|
2007
|
2006
|
2005
|
|||||||||||
|
(in
thousands, except per share amounts)
|
||||||||||||||||
|
Revenue
(1)
|
$ | 1,329,525 | $ | 1,401,911 | $ | 1,197,732 | $ | 1,151,940 | $ | 1,072,895 | ||||||
|
Gross
profit
|
$ | 157,822 | $ | 142,170 | $ | 137,015 | $ | 118,056 | $ | 116,376 | ||||||
|
Merger
related expenses (2)
|
$ | 1,774 | $ | - | $ | - | $ | 58 | $ | 4,575 | ||||||
|
Goodwill
and intangible impairment (3)
|
$ | - | $ | 93,882 | $ | - | $ | - | $ | 25,165 | ||||||
|
Net
income (loss) (4, 5)
|
$ | 54,099 | $ | (74,032 | ) | $ | 3,317 | $ | (38,289 | ) | $ | (23,847 | ) | |||
|
Net
income (loss) per basic share
|
$ | 1.39 | $ | (1.93 | ) | $ | 0.09 | $ | (1.03 | ) | $ | (0.70 | ) | |||
|
Net
income (loss) per diluted share (6)
|
$ | 1.36 | $ | (1.93 | ) | $ | 0.09 | $ | (1.03 | ) | $ | (0.70 | ) | |||
|
Weighted
average shares outstanding used in computing:
|
||||||||||||||||
|
basic
income (loss) per share
|
38,985 | 38,417 | 37,647 | 37,304 | 34,129 | |||||||||||
|
diluted
income (loss) per share
|
39,737 | 38,417 | 38,491 | 37,304 | 34,129 | |||||||||||
__________________________
|
(1)
|
Revenues
in 2008 include Competitive Acquisition Program (“CAP”) revenues of $71.2
million. The CAP program ended December 31,
2008. Revenues in 2008 also included United Healthcare (“UHC”)
HIV/AIDS and solid organ transplant service revenues of $116.6 million
from contracts which ended in the first quarter of 2009. 2009
revenues included $23.3 million related to these UHC HIV/AIDS
contracts. Certain PBM customer contracts ended in 2007 and
prior. Revenue related to these contracts were $15.0 million,
$76.8 million and $154.8 million in the years 2007, 2006 and 2005,
respectively.
|
|
(2)
|
Expenses
in 2009 reflect expenses related to our proposed acquisition of
CHS. Expenses in 2005 and 2006 reflect merger, integration and
re-branding expenses related to the acquisition of Chronimed on
March 12, 2005.
|
|
(3)
|
2008
includes a $90.0 million charge related to impairment of goodwill, and a
$3.9 million charge related to write-off of remaining intangible
assets. 2005 includes a $6.6 million charge related to
write-off of non-compete agreements, trade names and customer lists due to
our rebranding strategy in the Specialty Pharmacy Services segment, and an
$18.6 million charge related to goodwill impairment in the
Traditional Pharmacy Services segment.
|
|
(4)
|
Net
loss in 2005 includes a $4.3 million charge, net of tax, to reflect
an increase in the allowance for doubtful accounts receivable created by
lower than expected collections during the merger integration
period.
|
|
(5)
|
Net
income in 2009 includes a $40.6 million tax benefit, primarily relating to
the reversal of the valuation allowance on deferred tax assets. Net
loss in 2006 includes a $25.7 million income tax charge for the
establishment of a valuation allowance recorded against deferred tax
assets.
|
|
(6)
|
The
2008, 2006 and 2005 net loss per diluted share excludes the effect of
common stock equivalents, as their inclusion would be
anti-dilutive.
|
The
following Management’s Discussion and Analysis of Financial Condition and
Results of Operations (“MD&A”) is designed to assist the reader in
understanding our Consolidated Financial Statements, the changes in certain key
items in those financial statements from year to year and the primary factors
that accounted for those changes, as well as how certain accounting principles
affect our Consolidated Financial Statements. The discussion also provides
information about the financial results of the various segments of our business
to provide a better understanding of how those segments and their results affect
our financial condition and results of operations as a whole. This discussion
should be read in conjunction with our Consolidated Financial Statements,
including the Notes thereto, and the information discussed in
Item 1A — Risk Factors.
“Safe
Harbor” Statement Under the Private Securities Litigation Reform Act of
1995
This
report contains statements not purely historical and which may be considered
forward-looking statements within the meaning of Section 27A of the
Securities Act, and Section 21E of the Securities Exchange Act of 1934, as
amended (the “Exchange Act”), including statements regarding our expectations,
hopes, beliefs, intentions or strategies regarding the future. These forward
looking statements may include statements relating to our business development
activities, sales and marketing efforts, the status of material contractual
arrangements, including the negotiation or re-negotiation of such arrangements,
future capital expenditures, the effects of regulation and competition on our
business, future operating performance and the results, benefits and risks
associated with integration of acquired companies. Investors are cautioned that
any such forward-looking statements are not guarantees of future performance and
involve risks and uncertainties; that actual results may differ materially from
those possible results discussed in the forward-looking statements as a result
of various risks, uncertainties and other factors. You should not place undue
reliance on such forward-looking statements as they speak only as of the date
they are made, and we assume no obligation to publicly update or revise any
forward-looking statement even if experience or future changes make it clear
that any projected results expressed or implied therein will not be
realized.
These
factors include, among other things, risks associated with increased government
regulation related to the healthcare and insurance industries in general and
more specifically, pharmacy benefit management and specialty pharmaceutical
distribution organizations, changes in reimbursement rates from government and
private payors, the existence of complex laws and regulations relating to our
business, increased competition from our competitors, including competitors with
greater financial, technical, marketing and other resources. This report
contains information regarding important factors that could cause such
differences.
Business
Overview
We are a
specialty pharmaceutical healthcare organization that partners with patients,
physicians, healthcare payors and pharmaceutical manufacturers to provide access
to medications and management solutions to optimize outcomes for chronic and
other complex healthcare conditions.
Our
business is reported under two operating segments: (i) Specialty Pharmacy
Services, and (ii) Traditional Pharmacy Services. Our Specialty
Pharmacy Services segment includes comprehensive support, dispensing and
distribution, patient care management, data reporting, as well as a range of
other complex therapy management services for certain chronic health
conditions. The medications we dispense include oral, injectable and
infusible medications used to treat patients living with chronic, acute and
other complex health conditions and are provided to patients and
physicians. Our Traditional Pharmacy Services segment consists mainly
of traditional mail service pharmacy fulfillment, and to a lesser extent,
prescription discount card programs and fully funded pharmacy benefit management
services.
In the
quarter ended September 30, 2009, we renamed the reportable segment formerly
known as “PBM Services” to “Traditional Pharmacy Services”. Our
decision to rename this segment reflects a shift in the nature of the business
included within this segment away from fully funded pharmacy benefit management
services and more towards traditional mail services and prescription discount
card programs.
Revenues
from Specialty Pharmacy Services and Traditional Pharmacy Services are derived
from our relationships with healthcare payors including Plan Sponsors, as well
as from our relationship with pharmaceutical manufacturers, patients and
physicians.
Our
Specialty Pharmacy Services are marketed and/or sold to Plan Sponsors,
pharmaceutical manufacturers, physicians, and patients, and target certain
specialty medications that are used to treat patients living with chronic, acute
and other complex health conditions. These services include the
distribution of biotech and other high cost injectable, oral and infusible
prescription medications and the provision of therapy management
services.
We
experienced a reduction in revenue in 2009 due to the termination of the Centers
for Medicare and Medicaid Services’ (“CMS”) Competitive Acquisition Program
(“CAP”), and certain United Healthcare (“UHC”) contracts. As
expected, our gross profit as a percentage of revenue increased as a result of
these contract terminations, as they operated at margin rates below the average
for Specialty Pharmacy Services.
Effective
September 26, 2009, First DataBank and Medi-Span reduced the mark-up factor
applied to WAC, on which AWP is based, from 1.25 to 1.20 for approximately
18,000 national drug codes. These AWP publishers also have indicated that,
within the next two years, they will discontinue publication of AWP information.
The impact of this reduction in AWP was to reduce our gross margins beginning in
the fourth quarter of 2009. See “Risk Factors - Changes in industry
pricing benchmarks could adversely affect our financial
performance.”
Our
Traditional Pharmacy Services are marketed to Plan Sponsors and are designed to
promote a broad range of cost-effective, clinically appropriate pharmacy
services through our own mail service distribution facilities and national
pharmacy retail network. We also administer prescription discount card programs
on behalf of commercial Plan Sponsors, most typically TPAs, as well as PBM
services. Under such programs we derive revenue on a per claim basis from the
dispensing network pharmacy.
Pending
Acquisition
On
January 24, 2010, we entered into an Agreement and Plan of Merger to acquire
CHS. CHS is a privately held company that is a leading provider of
home infusion and home nursing services and products to patients suffering from
chronic and acute medical conditions. Completion of the acquisition
is subject to stockholder approval of the issuance of additional shares of our
common stock to CHS stockholders and satisfaction of certain other customary
conditions. The acquisition is expected to close on or about March
31, 2010.
If the
merger is completed, we will:
|
|
·
|
Repay
the net indebtedness of CHS, which is approximately $132.0 million at
December 31, 2009, and enter into a new credit
facility;
|
|
|
·
|
Pay
cash consideration of $110.0 million, subject to
adjustment;
|
|
|
·
|
Issue
up to approximately 12.9 million shares of our Common Stock, subject to
adjustment, of which 2,696,516 shares initially will be held in escrow to
fund indemnification payments, if any;
and
|
|
|
·
|
Issue
warrants to acquire approximately 3.4 million shares of our Common Stock,
exercisable at $10.00 per share and having a five-year
term.
|
In order
to fund the payment of the cash consideration required to be paid for the
acquisition of CHS, refinance our existing indebtedness and repay the existing
indebtedness of CHS, we have entered into a commitment letter with Jefferies
Finance LLC (“Jefferies”), pursuant to which Jefferies has committed to provide
us with $375.0 million in debt financing, comprised of $150.0 million senior
credit facilities and $225.0 million in other indebtedness. We
project that the acquisition of CHS will cause dilution of earnings per share in
year one and will be accretive thereafter.
Critical
Accounting Estimates
Our
Consolidated Financial Statements have been prepared in accordance with
U.S. generally accepted accounting principles (“GAAP”). In preparing our
financial statements, we are required to make estimates and assumptions that
affect the reported amounts of assets and liabilities, the disclosure of
contingent assets and liabilities at the date of the financial statements and
the reported amounts of revenues and expenses during the reporting period. We
evaluate our estimates and judgments on an ongoing basis. We base our estimates
and judgments on historical experience and on various other factors that we
believe to be reasonable under the circumstances, the results of which form the
basis for making judgments about the carrying values of assets and liabilities
that may not be readily apparent from other sources. Our actual results
may differ from these estimates, and different assumptions or
conditions
may yield
different estimates. The following discussion highlights what we believe to be
the critical accounting estimates and judgments made in the preparation of our
Consolidated Financial Statements.
The
following discussion is not intended to be a comprehensive list of all the
accounting estimates or judgments made in the preparation of our financial
statements and in many cases the accounting treatment of a particular
transaction is specifically dictated by GAAP, with no need for management’s
judgment in its application. See our audited Consolidated Financial Statements
and notes thereto appearing elsewhere in this Annual Report, which contain a
description of our accounting policies and other disclosures required by
GAAP.
Revenue
Recognition
We
generate revenue principally through the sale of prescription drugs, which are
dispensed either through a pharmacy participating in our pharmacy network or a
pharmacy owned by us. Revenue is generally derived under fee-for-service
agreements; however, an immaterial amount of revenue is derived from capitated
agreements where the fee is based on a per patient basis. Fee-for-service
agreements include: (i) specialty and mail service agreements, where we
dispense prescription medications through our pharmacy facilities and
(ii) PBM agreements, where prescription medications are dispensed through
pharmacies participating in our retail pharmacy network as well as through our
traditional mail service facility.
Financial
Accounting Standards Board (“FASB”) Accounting Standards Codification (“ASC”)
Subtopic 605-25, Revenue
Recognition: Multiple-Element Arrangements (“ASC 605-25”), addresses
situations in which there are multiple deliverables under one revenue
arrangement with a customer and provides guidance in determining whether
multiple deliverables should be recognized separately or in
combination. We provide a variety of therapies to
patients. For infusion related therapies we frequently provide the
multiple deliverables of drug delivery and related nursing
services. After applying the criteria from ASC 605-25, we concluded
that separate units of accounting exist in revenue arrangements where we provide
multiple deliverables.
Under
fee-for-service agreements in the Specialty Pharmacy Services segment, drug
revenue is recognized at the time the drug is shipped, and nursing revenue is
recognized on the date of service. At that point, the earnings process is
considered complete and we have substantially accomplished the terms of our
transaction. In the Traditional Pharmacy Services segment, revenue is
recognized when the pharmacy services are reported to us through the point
of sale (“POS”) claims processing system and the drug is dispensed to the
member.
Revenue
generated under PBM agreements is classified as either gross or net by us based
on whether we are acting as a principal or an agent in the fulfillment of
prescriptions through our retail pharmacy network. When we independently have a
contractual obligation to pay a network pharmacy provider for benefits provided
to its Plan Sponsors’ members, and therefore are the “primary obligor” as
defined in ASC Topic 605, Revenue Recognition (“ASC
605”), we include
payments (which include the drug ingredient cost) from these Plan Sponsors as
revenue and payments to the network pharmacy providers as cost of revenue. These
transactions require us to pay network pharmacy providers, assume credit risk of
Plan Sponsors and act as a principal. If we merely act as an agent, and
consequently administer Plan Sponsors’ network pharmacy contracts, we do not
have the primary obligation to pay the network pharmacy and assume credit risk
and as such record only the administrative fees (and not the drug ingredient
cost) as revenue.
Allowance
for Doubtful Accounts
Allowances
for doubtful accounts are based on estimates of losses related to customer
receivable balances. The procedure for estimating the allowance for doubtful
accounts requires significant judgment. The risk of collection varies based upon
the product, the payor (commercial health insurance, government, physician), the
patient’s ability to pay the amounts not reimbursed by the payor and point of
distribution (retail, mail service and infusion). We estimate the allowance for
doubtful accounts based upon a variety of factors including the age of the
outstanding receivables and our historical experience of collections, adjusting
for current economic conditions and, in some cases, evaluating specific customer
accounts for risk of loss. We periodically review the estimation process and
make changes to the estimates as necessary. When it is deemed that a customer
account is uncollectible, that balance is written off against the existing
allowance.
Allowance
for Contractual Discounts
We are
reimbursed by Plan Sponsors for the medications and services we sell. Revenues
and related accounts receivable are recorded net of payor contractual discounts
to reflect the estimated net billable amounts for the products and services
delivered. We estimate the allowance for contractual discounts, based on
historical experience and in certain cases on a customer-specific basis, given
our interpretation of the contract term or applicable
regulations.
However, reimbursement rates are often subject to interpretation that could
result in payments that differ from our estimates. Additionally, updated
regulations and contract negotiations occur frequently, necessitating our
continual review and assessment of the estimation process.
Rebates
Manufacturers’
rebates are primarily part of the Company’s Specialty Pharmacy Services
segment. Rebates are generally volume-based incentives that are
earned and recorded upon dispense. Volume-based rebates are recorded
as a reduction of both inventory and cost of goods sold.
The
Traditional Pharmacy Services segment also includes rebates earned on the PBM
portion of the business. Rebates are recorded on historical PBM
results and trends and are revised on a regular basis depending on our latest
forecasts, as well as information received from rebate
sources. Should actual results differ, adjustments will be recorded
in future earnings when the adjustment becomes known. In some
instances, rebate payments are shared with our Plan Sponsors. PBM
rebates earned by us are recorded as a reduction of cost of goods
sold. PBM rebates shared with clients are recorded as a reduction of
revenue consistent with the sales incentive provisions of ASC 605.
Payables
to Plan Sponsors
Payables
to Plan Sponsors primarily represent payments made to us by Plan Sponsors in the
Specialty Pharmacy Services segment in excess of the contractually required
reimbursement. These amounts are refunded to Plan Sponsors. These
payables also include the sharing of manufacturers’ rebates with Plan Sponsors
in the Traditional Pharmacy Services segment.
Income
Taxes
As part
of the process of preparing our Consolidated Financial Statements, management is
required to estimate income taxes in each of the jurisdictions in which we
operate. We account for income taxes under ASC Topic 740, Income Taxes (“ASC
740”). ASC 740 requires the use of the asset and liability method of
accounting for income taxes. Under this method, deferred taxes are determined by
calculating the future tax consequences attributable to differences between the
financial accounting and tax bases of existing assets and liabilities. A
valuation allowance is recorded against deferred tax assets when, in the opinion
of management, it is more likely than not that we will not be able to realize
the benefit from our deferred tax assets.
We file
income tax returns, including returns for our subsidiaries, as prescribed by
Federal tax laws and the tax laws of the state and local jurisdictions in which
we operate. Our uncertain tax positions are related to tax years that
remain subject to examination and are recognized in the financial statements
when the recognition threshold and measurement attributes of ASC 740 are
met. Interest and penalties related to unrecognized tax benefits are
recorded as income tax expense.
Goodwill
In
accordance with ASC Topic 350, Intangibles – Goodwill and
Other (“ASC 350”), we evaluate goodwill for impairment on an annual basis
and whenever events or circumstances exist that indicate that the carrying value
of goodwill may no longer be recoverable. The impairment evaluation
is based on a two-step process. The first step compares the fair
value of a reporting unit with its carrying amount, including
goodwill. If the first step indicates that the fair value of the
reporting unit is less than its carrying amount, the second step must be
performed which determines the implied fair value of reporting unit
goodwill. The measurement of possible impairment is based upon the
comparison of the implied fair value of reporting unit to its carrying
value.
We have
two reporting units: Specialty Pharmacy Services and Traditional Pharmacy
Services. The goodwill associated with the Specialty Pharmacy Services segment
was evaluated and no impairment was recorded at December 31, 2009. In
the 2008 evaluation an impairment was identified and recorded at
December 31, 2008. There is no goodwill associated with the
Traditional Pharmacy Services segment.
Impairment
of Long Lived Assets
We
evaluate whether events and circumstances have occurred that indicate that the
remaining estimated useful life of long-lived assets, including intangible
assets, may warrant revision or that the remaining balance of an asset may not
be recoverable in accordance with the provisions of ASC Topic 360, Property, Plant and Equipment ("ASC
360"). The measurement of possible impairment is based on the ability to
recover the balance of assets from
expected
future operating cash flows on an undiscounted basis. Impairment losses, if any,
would be determined based on the present value of the cash flows using discount
rates that reflect the inherent risk of the underlying business. As a result of
the analysis performed at December 31, 2008, we wrote off all intangible
assets. In 2009 there was no impairment of remaining long lived
assets.
Accounting
for Stock-Based Compensation
Compensation
cost for all share-based payments are based on the grant-date fair value
estimated in accordance with the provisions of ASC Topic 718, Compensation – Stock
Compensation (“ASC 718”). The fair value of each option award
is estimated on the date of grant using a binomial option-pricing model that
uses the following assumptions: (i) expected volatility is based on the
historical volatility of our stock, (ii) the risk-free interest rate for
periods within the contractual life of the option is based on the
U.S. Treasury yield curve in effect at the time of the grant, and
(iii) the expected life of options granted is derived from previous history
of stock exercises from the grant date and represents the period of time that
options granted are expected to be outstanding. We use historical data to
estimate option exercise and employee termination assumptions under the
valuation model. The fair value of the award is amortized to expense
on a straight line basis over the requisite service period. We
expense restricted stock awards based on vesting requirements, including time
elapsed, market conditions, and/or performance conditions. Because of
these requirements, the weighted average period for which the expense is
recognized varies.
Off-Balance
Sheet Arrangements
We do not
participate in transactions that generate relationships with unconsolidated
entities or financial partnerships, such as special purpose entities or variable
interest entities, which would have been established for the purpose of
facilitating off-balance sheet arrangements or other limited purposes. As of
December 31, 2009, we are not involved in any unconsolidated special
purpose entities or variable interest entities.
Reclassifications
Certain
prior period amounts have been reclassified to conform to the current year
presentation. Such reclassifications had no material effect on our previously
reported consolidated financial position, results of operations or cash
flows.
Results
of Operations
CONSOLIDATED
RESULTS
Year
ended December 31, 2009 vs. December 31, 2008
|
Year
Ended December 31,
|
||||||||||
|
2009
|
2008
|
|||||||||
| (dollars in thousands) | ||||||||||
|
Revenue
|
$ | 1,329,525 | 100.0 | % | $ | 1,401,911 | 100.0 | % | ||
|
Gross
profit
|
157,822 | 11.9 | % | 142,170 | 10.1 | % | ||||
|
Income
(loss) from operations
|
15,466 | 1.2 | % | (83,517 | ) | -6.0 | % | |||
|
Interest
expense, net
|
1,920 | 0.1 | % | 2,711 | 0.2 | % | ||||
|
Income
(loss) before income taxes
|
13,546 | 1.0 | % | (86,228 | ) | -6.2 | % | |||
|
Tax
(benefit) provision
|
(40,553 | ) | -3.1 | % | (12,196 | ) | -0.9 | % | ||
|
Net
income (loss)
|
54,099 | 4.1 | % | (74,032 | ) | -5.3 | % | |||
Revenue. Total
reported revenue for the year ended December 31, 2009 decreased $72.4
million, or 5.2%, to $1,329.5 million from $1,401.9 million for the same
period in 2008.
Specialty
Pharmacy Services revenue for the year ended December 31, 2009 was $1,113.3
million compared to $1,196.6 million for the same period in 2008, an $83.3
million, or 7.0%, decrease. This decrease was primarily due to
the
termination
of the CAP and certain UHC contracts and the impact of the industry-wide AWP
settlement, partially offset by revenue generated under new contracts and drug
inflation. We also experienced revenue growth in our various
specialty disease state management programs such as Oncology, Multiple
Sclerosis, Iron Overload, and from our infusion business.
Traditional
Pharmacy Services revenue for the year ended December 31, 2009 was $216.2
million compared to $205.3 million for the same period in 2008, a $10.9
million, or 5.3%, increase. The increase in revenue was primarily due to the
growth in our discount cash card program.
Cost of Revenue and Gross
Profit. Cost of revenue for the year ended December 31, 2009
was $1,171.7 million as compared to $1,259.7 million for the year ended December
31, 2008. Gross margin dollars were $157.8 million for the year ended
December 31, 2009 as compared to $142.2 million for the year ended December 31,
2008, an increase of $15.6 million, or 11.0%. Gross margin as a
percentage of revenue increased to 11.9% in 2009 from 10.1% in
2008. The increase in gross margin percentage was primarily the
result of the termination of the CAP and certain UHC contracts which, as
expected, reduced volumes and increased Specialty Pharmacy Services’ overall
margin percentage to 10.6% for the year ended December 31, 2009 from 9.5% for
the year ended December 31, 2008. In addition to a more favorable
business mix, our supply chain management programs and reduced shipping costs
also contributed to the increase of gross margin percentage and
dollars.
Selling, General and Administrative
Expenses. For the year ended December 31, 2009, selling,
general and administrative expenses (“SG&A”) increased to $133.7 million, or
10.1% of total revenue, from $125.2 million, or 8.9% of total revenue, for
the same period in 2008. The year-over-year increase in SG&A is
due to several offsetting factors including the accrual of $4.3 million of
management bonus expense as a result of meeting specified criteria for the year,
an increase in variable broker costs of $3.1 million related to the marketing of
discount card programs as well as additional professional fees and costs of
approximately $1.8 million relating to the pending acquisition of
CHS. These additional costs were partially offset by continued cost
control measures in our operating units and reduction in corporate overhead
costs such as employee benefits.
Goodwill and Intangible
Impairment. There were no goodwill or other impairment charges
in 2009. Goodwill and other impairment charges in 2008 consisted of
$90.0 million related to our Specialty Pharmacy Services segment and $3.9
million related to intangible assets, such as customer lists and non-compete
agreements. The 2008 goodwill and other impairment charges related
primarily to certain acquisitions in the years 2000 through 2006.
Bad Debt
Expense. For the year ended December 31, 2009 we recorded
bad debt expense of $8.6 million, or 0.6% of total revenue, an increase of $3.9
million, compared to $4.7 million, or 0.3% of total revenue in 2008. The
increase in bad debt expense is primarily a result of a reduction in 2009
recoveries of previously reserved amounts as compared to the rate of bad debt
recovery experienced in 2008, and an additional provision related to uncollected
CAP receivables. Our overall methodology used for determining our
provision for bad debt remains essentially unchanged.
Net Interest
Expense. Net interest expense was $1.9 million, or 0.1% of
total revenue, for the year ended December 31, 2009 compared to
$2.7 million, or 0.2% of total revenue, for the year ended
December 31, 2008. The decrease in interest expense was the result of lower
weighted average interest which is tied to LIBOR (defined below) and a lower
average daily debt balance.
Benefit From Income
Taxes. We reported an income tax benefit of $40.6 million for
2009 compared to an income tax benefit of $12.2 million for 2008. The
benefit in 2009 was due to the reversal of the valuation allowance on deferred
tax assets. The benefit in 2008 was due to goodwill impairment which
reduced the deferred tax liability associated with goodwill, which was partially
offset by the increase in the valuation allowance on deferred tax
assets. At December 31, 2009, we had Federal net operating loss
carryforwards available to us of approximately $18.0 million, of which $3.2
million is subject to an annual limitation, all of which will begin expiring in
2012 and later.
Net Income (Loss) and Earnings Per
Share. We reported net income of $54.1 million, or $1.36 per
diluted share, for the year ended December 31, 2009, compared to a net loss
of $74.0 million, or $1.93 per diluted share, for the same period a
year ago. The number of weighted average basic and diluted shares at
December 31, 2009 was 38,984,797 and 39,728,653, respectively, compared to
38,416,644 for both basic and diluted shares at December 31,
2008.
Year
ended December 31, 2008 vs. December 31, 2007
|
Year
Ended December 31,
|
||||||||||
|
2008
|
2007
|
|||||||||
| (dollars in thousands) | ||||||||||
|
Revenue
|
$ | 1,401,911 | 100.0 | % | $ | 1,197,732 | 100.0 | % | ||
|
Gross
profit
|
142,170 | 10.1 | % | 137,015 | 11.4 | % | ||||
|
Income
(loss) from operations
|
(83,517 | ) | -6.0 | % | 8,851 | 0.7 | % | |||
|
Interest
expense, net
|
2,711 | 0.2 | % | 3,270 | 0.3 | % | ||||
|
Income
(loss) before income taxes
|
(86,228 | ) | -6.2 | % | 5,581 | 0.5 | % | |||
|
Tax
(benefit) provision
|
(12,196 | ) | -0.9 | % | 2,264 | 0.2 | % | |||
|
Net
income (loss)
|
(74,032 | ) | -5.3 | % | 3,317 | 0.3 | % | |||
Revenue. Total
reported revenue for the year ended December 31, 2008 increased $204.2
million, or 17.0%, to $1,401.9 million from $1,197.7 million for the same
period in 2007.
Specialty
Pharmacy Services revenue for the year ended December 31, 2008 was $1,196.6
million compared to $974.6 million for the same period in 2007, a
$222.0 million, or 22.8%, increase. The increase was primarily due to
additional revenues associated with sales from Specialty Pharmacy Services payor
contracts, including an agreement with UHC for the HIV/AIDS and solid organ
transplant programs and the CAP agreement, as well as growth in the sale of
oncology drugs and the increase associated with drug cost
inflation.
Traditional
Pharmacy Services revenue for the year ended December 31, 2008 was $205.3
million compared to $223.2 million for the same period in 2007, a $17.9
million, or 8.0%, decrease. The decline in revenue was due primarily to the loss
of a PBM customer during 2007.
Cost of Revenue and Gross
Profit. Reported cost of revenue for the year ended
December 31, 2008 was $1,259.7 million compared to $1,060.7 million
for the same period in 2007. The increase in cost of revenue was primarily the
result of increased sales in our Specialty Pharmacy Services segment, which came
in at lower than historical margins, offset by lower Traditional Pharmacy
Services segment cost of revenue which is a result of lower
revenue. The decline in gross profit percentage was primarily the
result of the planned addition of higher revenue, lower margin business
including the UHC Agreement. The reduced profitability of the CAP
business also contributed to the overall decline. Additionally, in
the first quarter of 2008, the gross profit percentage was also impacted by
timing delays in obtaining increases in reimbursement rates after drug
acquisition cost increases were implemented by manufacturers of specialty
drugs. Drug acquisition cost increases typically occur in the first
quarter of each year along with a corresponding increase in reimbursement rates,
however, there was a longer than usual delay in updating the industry price
lists used by us and our peers to charge customers for
reimbursement. As a result of all these factors, the total gross
profit as a percentage of revenue for the year ended December 31, 2008 was
10.1%, compared to 11.4% for the same period in 2007.
Selling, General and Administrative
Expenses. For the year ended December 31, 2008, SG&A
increased to $125.2 million, or 8.9% of total revenue, from $120.1 million,
or 10.0% of total revenue, for the same period in 2007. The
year-over-year increase in SG&A was primarily the result of increased salary
and medical benefits, higher brokers’ fees due to the growth in our cash card
business and a settlement with the OIG of the U.S. Department of Health and
Human Services during the third quarter of 2008. These increases were
partially offset by the elimination of bonus expense as no management bonuses
were earned in 2008.
Bad Debt
Expense. For the year ended December 31, 2008 we recorded
bad debt expense of $4.7 million, a decrease of $0.4 million, compared to
$5.1 million in 2007. The decrease in bad debt expense was primarily the
result of improved billing, cash collection and posting practices as well as a
large bad debt recovery related to a prior year PBM customer bankruptcy
claim. Our overall methodology used for determining our provision for
bad debt remains essentially unchanged.
Amortization of
Intangibles. For the year ended December 31, 2008 we
recorded amortization expense of intangibles of $1.9 million compared to
amortization expense of intangibles of $2.9 million in 2007. The
decrease was due to certain intangible assets becoming fully amortized in the
first quarter of 2007. Also we recorded a write-off of intangibles
under ASC 360 discussed further below. In addition, amortization of
intangibles expense was reduced by $1.9 million annually as a result of the
write-off.
Net Interest
Expense. Net interest expense was $2.7 million for the year
ended December 31, 2008 compared to $3.3 million for the year ended
December 31, 2007. The decrease in interest expense was the result of lower
weighted average interest which is tied to LIBOR partially offset by an increase
in the average daily balance required to fund the growth of the Specialty
Pharmacy Services segment.
Goodwill and Intangible
Impairment. Goodwill and other impairment charges in 2008
consisted of $90.0 million related to our Specialty Pharmacy Services segment
and $3.9 million related to intangible assets, such as customer lists and
non-compete agreements. The goodwill charge relates primarily to
certain acquisitions in the years 2000 through 2006.
We
evaluated goodwill based upon the two-step process required by ASC
350. As part of step one, we noted the significant decline in our
market capitalization below book value, which was sustained through the fourth
quarter of 2008. We had also previously announced changes in the
status of long-term Specialty Pharmacy Services contracts which were expected to
reduce 2009 revenues. Those contract changes were (a) the decision by
UHC to internalize services for HIV/AIDS and solid organ transplant drugs
starting in the first quarter of 2009, and (b) the expiration of CAP with CMS
effective December 31, 2008. The expiration of these contracts, our
reduced market capitalization, and the reduced market capitalization of our
peers in the healthcare industry were considered to be potential indicators of
impairment in contemplation of our annual impairment analysis.
Based on
our annual assessment, we determined that the fair value of the Specialty
Pharmacy Services segment was less than the carrying value of its net
assets. We then determined the fair value of the Specialty Pharmacy
Services segment using a combination of an income approach using the discounted
cash flow method and a market approach using the guideline public company
method. We completed step two of the impairment analysis and
concluded that the carrying value of the goodwill associated with the Specialty
Pharmacy Services segment was impaired, resulting in a fourth quarter non-cash
impairment charge of $90.0 million. The non-cash impairment charge
does not change management’s view of the Specialty Pharmacy Services segment
reporting unit as our strategic business unit and will not affect liquidity,
cash flows from operating activities, debt covenants or our ability to borrow
under our existing credit facility.
As part
of the annual assessment and in consideration of the impairment indicators, we
also evaluated the recoverability of our property and equipment and
definite-lived intangible assets in accordance with ASC 350. As a
result, we determined that $3.9 million of definitive-lived intangible assets,
consisting of $3.5 million of customer lists and $0.4 million of non-compete
agreements, were impaired, and an impairment charge for this amount was recorded
in the fourth quarter of 2008. These impairment tests were performed
and the related impairment charges were recorded prior to completing the
goodwill impairment analysis.
Benefit From/Provision For Income
Taxes. We reported an income tax benefit of $12.2 million for
2008 compared to an income tax expense $2.3 million for 2007. The benefit
in 2008 was due to the goodwill impairment which reduced the deferred tax
liability associated with goodwill, partially offset by the increase in the
valuation allowance on deferred tax assets. At December 31,
2008, we had Federal net operating loss carryforwards available to us of
approximately $29.0 million, of which $5.9 million is subject to an
annual limitation, all of which will begin expiring in 2017 and
later.
Net (Loss) Income and Earnings Per
Share. We reported a net loss of $74.0 million, or $1.93 per
diluted share, for the year ended December 31, 2008, compared to net income
of $3.3 million, or $0.09 per diluted share, for the same period in
2007. The number of weighted average shares for both the basic and diluted
shares at December 31, 2008 was 38,416,644, compared to basic and diluted
shares of 37,647,270 and 38,491,009, respectively, at December 31,
2007.
Liquidity
and Capital Resources
We
utilize both funds generated from operations and available credit under our
Facility (as defined below) for general working capital needs, capital
expenditures and acquisitions.
Net cash
provided by operating activities totaled $22.7 million for the year ended
December 31, 2009, as compared to $8.7 million of cash used in operating
activities for the year ended December 31, 2008. The increase in cash
provided by operating activities was primarily the result of net income of $54.1
million of which $40.5 million was the non-cash effect of deferred taxes due
primarily to the reversal of the valuation allowance on deferred tax
assets. Other charges which reduced net income but had no impact on
cash from operations were: bad debt of $8.6 million, depreciation
expense of $5.0 million, option expense of $3.4 million, and an increase in our
accrued expenses of $4.8 million relating primarily to the 2009 bonus
accrual. Operating uses of cash during the year ended December 31,
2009 include an increase in inventory of $6.0 million relating to various supply
chain initiatives and a decrease in accounts payable of $2.4 million due to
timing of vendor payments.
Net cash
used in investing activities in 2009 was $5.7 million compared to net cash used
in investing activities of $7.5 million in 2008. The change was
driven primarily by the continued investment in our information technology
infrastructure.
Net cash
used in financing activities in 2009 was $17.0 million compared to $16.2 million
net cash provided by financing activities in 2008. The cash used in
financing activities to pay down the line of credit was generated from higher
net income and lower working capital requirements. We also received
$2.8 million from the exercise of employee stock compensation plans in
2009.
At
December 31, 2009, there was $30.4 million in outstanding borrowings under our
revolving credit facility (the “Facility”) with an affiliate of Healthcare
Finance Group, Inc. (“HFG”), as compared to $50.4 million at December 31,
2008. The Facility provides for borrowing up to $85.0 million at the
London Inter-Bank Offered Rate (“LIBOR”) or a pre-determined minimum rate plus
the applicable margin and other associated fees, provided a sufficient level of
receivable assets are available as collateral. The term of the
Facility runs through November 1, 2010. Under the terms of the
Facility, we may request to increase the amount available for borrowing up to
$100.0 million, and convert a portion of any outstanding borrowings from a
Revolving Loan into a Term Loan. The borrowing base utilizes
receivable balances and proceeds thereof as security under the
Facility. At December 31, 2009 we had $54.6 million of credit
available on a borrowing basis of $85.0 million under the
Facility. We have received a financing commitment as part of the CHS
acquisition described above under the heading “Pending Acquisition” which we
believe will be sufficient to meet our on-going liquidity needs. If
the acquisition does not close, we believe we will be able to renew and extend
the Facility.
The
weighted average interest rate on the line of credit was 4.4% during 2009
compared to 5.0% for 2008. At February 24, 2010, we had $74.4 million of credit
available under the Facility.
The
Facility contains various covenants that, among other things, require us to
maintain certain financial ratios as defined in the agreements governing the
Facility. In December 2009, we entered an agreement with HFG to amend
the terms of the Facility to revise certain calculations required by the
covenants. We were in compliance with all the covenants contained in the
agreements as of December 31, 2009.
As part
of the anticipated acquisition of CHS, we have received a financing commitment
from Jefferies to provide a five year senior credit facility in the amount of
$150.0 million, including a $50.0 million revolver, and a $225.0 million bridge
loan facility. The bridge loan facility will be drawn on only if
$225.0 million in senior unsecured notes are not sold prior to the closing date
of the acquisition. We plan to use $100.0 million of the senior term
loan and the proceeds from the senior unsecured notes offering to finance, in
part, the acquisition of CHS, to refinance our existing indebtedness and repay
CHS’s existing indebtedness, for general corporate purposes and to pay related
fees and expenses. The $50.0 million revolver is expected to be
undrawn at closing. The specific interest rates of the senior term
loan and notes is subject to final pricing and we expect the interest to reflect
market rates relative to our credit ratings.
At
December 31, 2009, we had working capital of $91.1 million compared to $58.8
million at December 31, 2008. We made substantial information
technology (“IT”) systems investments throughout both years to improve
efficiencies, internal controls, and data reporting. We believe that
our cash on hand, together with funds available under the Facility and cash
expected to be generated from operating activities, will be sufficient to fund
our anticipated working capital, IT systems investments and other cash needs for
at least the next twelve months.
We may
also pursue joint venture arrangements, business acquisitions and other
transactions designed to expand our business, which we would expect to fund from
borrowings under the Facility, other future indebtedness or, if appropriate, the
private and/or public sale or exchange of our debt or equity
securities.
At
December 31, 2009, we had Federal net operating loss (“NOL”) carryforwards
of approximately $18.0 million, of which $3.2 million is subject to an
annual limitation, all of which will begin expiring in 2012 and
later. We have post apportioned state NOL carryforwards remaining of
approximately $8.1 million, the majority of which will begin expiring in
2017 and later.
Under the
terms of the prime vendor agreement with AmerisourceBergen Drug Company
(“ABDC”), we granted ABDC a secured, first priority lien in all of our inventory
as well as the proceeds thereof. In the ordinary course of business,
we obtained certain letters of credit (“LC”) from commercial banks in favor of
various parties. At December 31, 2009 there was $1.1 million on
deposit as collateral for these LCs.
The
following table sets forth our contractual obligations affecting cash in the
future:
|
Payments
Due in Period
|
||||||||||||||||
|
(in
thousands)
|
||||||||||||||||
|
Contractual
Obligations
|
Total
|
Less
Than 1 Year
|
1-3
Years
|
4-5
Years
|
After
5 Years
|
|||||||||||
|
Line
of credit (1)
|
$ | 30,389 | $ | 30,389 | $ | - | $ | - | $ | - | ||||||
|
Operating
leases
|
19,148 | 4,738 | 8,500 | 3,221 | 2,689 | |||||||||||
|
Purchase
commitment
|
17,673 | 17,673 | - | - | - | |||||||||||
|
Total
Contractual Cash
|
||||||||||||||||
|
Obligations
|
$ | 67,210 | $ | 52,800 | $ | 8,500 | $ | 3,221 | $ | 2,689 | ||||||
__________________________
|
(1)
|
Interest
on the line of credit is payable monthly. For additional information
regarding the line of credit see information
above.
|
Exposure
to market risk for changes in interest rates relates to our outstanding debt. At
December 31, 2009 we did not have any long-term debt. We are exposed to
interest rate risk primarily through our borrowing activities under the Facility
discussed in Item 7 of this Annual Report. A one percent increase in
interest rates would result in an increase in annual interest expense of
approximately $0.4 million, pre-tax, based upon the average daily balance
during 2009. We do not use financial instruments for trading or other
speculative purposes and are not a party to any derivative financial
instruments.
At
December 31, 2009, the carrying values of cash and cash equivalents,
accounts receivable, accounts payable, claims payable, payables to Plan Sponsors
and others, debt and line of credit approximate fair value due to their
short-term nature.
Because
management does not believe that our exposure to interest rate market risk is
material at this time, we have not developed or implemented a strategy to manage
this market risk through the use of derivative financial instruments or
otherwise. We will assess the significance of interest rate market risk from
time to time and will develop and implement strategies to manage that market
risk as appropriate.
The Board
of Directors and Stockholders
BioScrip,
Inc.
We have
audited the accompanying consolidated balance sheets of BioScrip, Inc. and
subsidiaries as of December 31, 2009 and 2008, and the related consolidated
statements of operations, stockholders’ equity, and cash flows for each of the
three years in the period ended December 31, 2009. Our audits also included the
financial statement schedule listed in the Index at Item 15. These financial
statements and schedule are the responsibility of the Company’s management. Our
responsibility is to express an opinion on these financial statements and
schedule based on our audits.
We
conducted our audits in accordance with the standards of the Public Company
Accounting Oversight Board (United States). Those standards require that we plan
and perform the audit to obtain reasonable assurance about whether the financial
statements are free of material misstatement. An audit includes examining, on a
test basis, evidence supporting the amounts and disclosures in the financial
statements. An audit also includes assessing the accounting principles used and
significant estimates made by management, as well as evaluating the overall
financial statement presentation. We believe that our audits provide a
reasonable basis for our opinion.
In our
opinion, the financial statements referred to above present fairly, in all
material respects, the consolidated financial position of BioScrip, Inc. and
subsidiaries at December 31, 2009 and 2008, and the consolidated results of
their operations and their cash flows for each of the three years in the period
ended December 31, 2009, in conformity with U.S. generally accepted accounting
principles. Also, in our opinion, the related financial statement schedule, when
considered in relation to the basic financial statements taken as a whole,
presents fairly in all material respects the information set forth
therein.
We have
also audited, in accordance with the standards of the Public Company Accounting
Oversight Board (United States), BioScrip, Inc.’s internal control over
financial reporting as of December 31, 2009, based on criteria established in
Internal Control-Integrated
Framework issued by the Committee of Sponsoring Organizations of the
Treadway Commission and our report dated March 2, 2010, expressed an unqualified
opinion thereon.
|
Minneapolis,
Minnesota
|
/s/
Ernst & Young LLP
|
|
March
2, 2010
|
BIOSCRIP,
INC. AND SUBSIDIARIES
December
31,
(in
thousands, except for share amounts)
|
2009
|
2008
|
||||||
|
ASSETS
|
|||||||
|
Current
assets
|
|||||||
|
Cash
and cash equivalents
|
$ | - | $ | - | |||
|
Receivables,
less allowance for doubtful accounts of $11,504 and $11,629 at
December 31, 2009 and 2008, respectively
|
151,113 | 158,649 | |||||
|
Inventory
|
51,256 | 45,227 | |||||
|
Short
term deferred taxes
|
12,913 | - | |||||
|
Prepaid
expenses and other current assets
|
3,999 | 2,766 | |||||
|
Total
current assets
|
219,281 | 206,642 | |||||
|
Property
and equipment, net
|
15,454 | 14,748 | |||||
|
Long
term deferred taxes
|
26,793 | - | |||||
|
Goodwill
|
24,498 | 24,498 | |||||
|
Other
non-current assets
|
1,194 | 1,069 | |||||
|
Total
assets
|
$ | 287,220 | $ | 246,957 | |||
|
LIABILITIES
AND STOCKHOLDERS' EQUITY
|
|||||||
|
Current
liabilities
|
|||||||
|
Line
of credit
|
$ | 30,389 | $ | 50,411 | |||
|
Accounts
payable
|
74,535 | 76,936 | |||||
|
Claims
payable
|
4,068 | 5,230 | |||||
|
Amounts
due to plan sponsors
|
4,938 | 5,646 | |||||
|
Accrued
expenses and other current liabilities
|
14,273 | 9,575 | |||||
|
Total
current liabilities
|
128,203 | 147,798 | |||||
|
Deferred
taxes
|
- | 533 | |||||
|
Income
taxes payable
|
2,437 | 2,764 | |||||
|
Other
non-current liabilities
|
787 | 325 | |||||
|
Total
liabilities
|
131,427 | 151,420 | |||||
|
Commitments
and Contingencies
|
|||||||
|
Stockholders'
equity
|
|||||||
|
Preferred
stock, $.0001 par value; 5,000,000 shares authorized; no shares issued or
outstanding
|
- | - | |||||
|
Common
stock, $.0001 par value; 75,000,000 shares authorized; shares
issued: 42,766,478, and 41,622,629, respectively; shares outstanding;
39,675,865 and
|
|||||||
|
38,691,356,
respectively
|
4 | 4 | |||||
|
Treasury stock, shares at cost: 2,647,613 and 2,624,186,
respectively
|
(10,367 | ) | (10,288 | ) | |||
|
Additional paid-in capital
|
254,677 | 248,441 | |||||
|
Accumulated deficit
|
(88,521 | ) | (142,620 | ) | |||
|
Total
stockholders' equity
|
155,793 | 95,537 | |||||
|
Total
liabilities and stockholders' equity
|
$ | 287,220 | $ | 246,957 | |||
The
accompanying notes are an integral part of these Consolidated Financial
Statements.
BIOSCRIP,
INC. AND SUBSIDIARIES
Years
Ended December 31,
(in
thousands, except per share amounts)
|
2009
|
2008
|
2007
|
||||||||
|
Revenue
|
$ | 1,329,525 | $ | 1,401,911 | $ | 1,197,732 | ||||
|
Cost
of revenue
|
1,171,703 | 1,259,741 | 1,060,717 | |||||||
|
Gross
profit
|
157,822 | 142,170 | 137,015 | |||||||
|
Selling,
general and administrative expenses
|
133,720 | 125,202 | 120,147 | |||||||
|
Bad
debt expense
|
8,636 | 4,667 | 5,119 | |||||||
|
Amortization
of intangibles
|
- | 1,936 | 2,898 | |||||||
|
Goodwill
and intangible impairment
|
- | 93,882 | - | |||||||
|
Income
(loss) from operations
|
15,466 | (83,517 | ) | 8,851 | ||||||
|
Interest
expense, net
|
1,920 | 2,711 | 3,270 | |||||||
|
Income
(loss) before income taxes
|
13,546 | (86,228 | ) | 5,581 | ||||||
|
Tax
(benefit) provision
|
(40,553 | ) | (12,196 | ) | 2,264 | |||||
|
Net
income (loss)
|
$ | 54,099 | $ | (74,032 | ) | $ | 3,317 | |||
|
Net
income per common share
|
||||||||||
|
Basic
|
$ | 1.39 | $ | (1.93 | ) | $ | 0.09 | |||
|
Diluted
|
$ | 1.36 | $ | (1.93 | ) | $ | 0.09 | |||
|
Weighted
average common shares outstanding
|
||||||||||
|
Basic
|
38,985 | 38,417 | 37,647 | |||||||
|
Diluted
|
39,737 | 38,417 | 38,491 | |||||||
The
accompanying notes are an integral part of these Consolidated Financial
Statements.
BIOSCRIP,
INC. AND SUBSIDIARIES
(in
thousands)
|
Additional
|
Total
|
|||||||||||||||
|
Common
|
Treasury
|
Paid-in
|
Accumulated
|
Stockholders'
|
||||||||||||
|
Stock
|
Stock
|
Capital
|
Deficit
|
Equity
|
||||||||||||
|
Balance
December 31, 2006
|
$ | 4 | $ | (8,002 | ) | $ | 239,315 | $ | (69,484 | ) | $ | 161,833 | ||||
|
Exercise
of stock options
|
- | - | 1,867 | - | 1,867 | |||||||||||
|
Surrender
of stock to satisfy minimum tax withholding
|
- | (1,397 | ) | - | - | (1,397 | ) | |||||||||
|
Compensation
under employee stock compensation plans
|
- | - | 3,004 | - | 3,004 | |||||||||||
|
Cumulative
effect of accounting pronouncement adoption
|
- | - | - | (2,421 | ) | (2,421 | ) | |||||||||
|
Net
income
|
- | - | - | 3,317 | 3,317 | |||||||||||
|
Balance
December 31, 2007
|
4 | (9,399 | ) | 244,186 | (68,588 | ) | 166,203 | |||||||||
|
Exercise
of stock options
|
- | - | 465 | - | 465 | |||||||||||
|
Surrender of
stock to satisfy minimum tax withholding
|
- | (889 | ) | - | - | (889 | ) | |||||||||
|
Compensation
under employee stock compensation plans
|
- | - | 3,790 | - | 3,790 | |||||||||||
|
Net
loss
|
- | - | - | (74,032 | ) | (74,032 | ) | |||||||||
|
Balance
December 31, 2008
|
4 | (10,288 | ) | 248,441 | (142,620 | ) | 95,537 | |||||||||
|
Exercise
of stock options
|
- | - | 3,015 | - | 3,015 | |||||||||||
|
Income
tax shortfall from stock option plan
|
- | - | (158 | ) | - | (158 | ) | |||||||||
|
Surrender
of stock to satisfy minimum tax withholding
|
- | (119 | ) | - | - | (119 | ) | |||||||||
|
Issuance
of treasury stock for restricted stock vesting
|
- | 40 | (40 | ) | - | - | ||||||||||
|
Compensation
under employee stock compensation plans
|
- | - | 3,419 | - | 3,419 | |||||||||||
|
Net
income
|
- | - | - | 54,099 | 54,099 | |||||||||||
|
Balance
December 31, 2009
|
$ | 4 | $ | (10,367 | ) | $ | 254,677 | $ | (88,521 | ) | $ | 155,793 | ||||
The
accompanying notes are an integral part of these Consolidated Financial
Statements.
BIOSCRIP,
INC. AND SUBSIDIARIES
Years
Ended December 31,
(in
thousands)
|
2009
|
2008
|
2007
|
||||||||
|
Cash
flows from operating activities:
|
||||||||||
|
Net
income (loss)
|
$ | 54,099 | $ | (74,032 | ) | $ | 3,317 | |||
|
Adjustments
to reconcile net income (loss) to net cash provided by (used in) operating
activities:
|
||||||||||
|
Depreciation
|
5,033 | 4,457 | 4,192 | |||||||
|
Amortization
|
- | 1,936 | 2,898 | |||||||
|
Goodwill
and intangible impairment
|
- | 93,882 | - | |||||||
|
Change
in net deferred income taxes
|
(40,517 | ) | (12,221 | ) | 2,808 | |||||
|
Excess
tax benefits relating to employee stock compensation
|
(120 | ) | - | - | ||||||
|
Compensation
under stock-based compensation plans
|
3,419 | 3,790 | 3,004 | |||||||
|
Bad
debt expense
|
8,636 | 4,667 | 5,119 | |||||||
|
Changes
in assets and liabilities
|
||||||||||
|
Receivables,
net of bad debt expense
|
(1,100 | ) | (34,347 | ) | 1,050 | |||||
|
Inventory
|
(6,029 | ) | (11,629 | ) | (127 | ) | ||||
|
Prepaid
expenses and other assets
|
(1,237 | ) | (1,923 | ) | 859 | |||||
|
Accounts
payable
|
(2,401 | ) | 19,594 | 5,618 | ||||||
|
Claims
payable
|
(1,162 | ) | 66 | (4,384 | ) | |||||
|
Amounts
due to plan sponsors
|
(708 | ) | 1,078 | (5,712 | ) | |||||
|
Accrued
expenses and other liabilities
|
4,832 | (4,064 | ) | 5,545 | ||||||
|
Net
cash provided by (used in) operating activities
|
22,745 | (8,746 | ) | 24,187 | ||||||
|
Cash
flows from investing activities:
|
||||||||||
|
Purchases
of property and equipment, net of disposals
|
(5,739 | ) | (7,463 | ) | (5,526 | ) | ||||
|
Net
cash used in investing activities
|
(5,739 | ) | (7,463 | ) | (5,526 | ) | ||||
|
Cash
flows from financing activities:
|
||||||||||
|
Borrowings
on line of credit
|
1,331,000 | 1,409,003 | 1,200,760 | |||||||
|
Repayments
on line of credit
|
(1,351,022 | ) | (1,392,370 | ) | (1,219,891 | ) | ||||
|
Excess
tax benefits relating to employee stock compensation
|
120 | - | - | |||||||
|
Surrender
of stock to satisfy minimum tax withholding
|
(119 | ) | (889 | ) | (1,397 | ) | ||||
|
Proceeds
from exercise of employee stock compensation plans
|
3,015 | 465 | 1,867 | |||||||
|
Net
cash (used in) provided by financing activities
|
(17,006 | ) | 16,209 | (18,661 | ) | |||||
|
Net
change in cash and cash equivalents
|
- | - | - | |||||||
|
Cash
and cash equivalents - beginning of period
|
- | - | - | |||||||
|
Cash
and cash equivalents - end of period
|
$ | - | $ | - | $ | - | ||||
|
DISCLOSURE
OF CASH FLOW INFORMATION:
|
||||||||||
|
Cash
paid during the period for interest
|
$ | 1,918 | $ | 4,011 | $ | 3,471 | ||||
|
Cash
paid during the period for income taxes
|
$ | 741 | $ | 382 | $ | 1,599 | ||||
The
accompanying notes are an integral part of these Consolidated Financial
Statements
BIOSCRIP,
INC. AND SUBSIDIARIES
NOTE 1 — NATURE
OF BUSINESS
Corporate
Organization and Business
BioScrip,
Inc. and subsidiaries (the “Company” or “BioScrip”) is a specialty
pharmaceutical healthcare organization that partners with patients, physicians,
healthcare payors and pharmaceutical manufacturers to provide access to
medications and management solutions to optimize outcomes for chronic and other
complex healthcare conditions.
BioScrip’s
business is reported under two operating segments: (i) Specialty Pharmacy
Services, and (ii) Traditional Pharmacy Services. The Specialty
Pharmacy Services segment includes comprehensive support, dispensing and
distribution, patient care management, data reporting, as well as a range of
other complex therapy management services for certain chronic and acute health
conditions. The medications we dispense include oral, injectable and
infusible medications which are used to treat patients living with chronic and
other complex health conditions. The Traditional Pharmacy Services
segment consists mainly of traditional mail service pharmacy fulfillment, and to
a lesser extent, prescription discount card programs and fully funded pharmacy
benefit management (“PBM”) services.
The
Company distributes high-cost pharmaceuticals and provides clinically focused
case and disease management programs to healthcare payors including managed care
organizations, government-funded and/or operated programs, third party
administrators (“TPAs”) and self-funded employer groups (collectively, “Plan
Sponsors”), enrollees afflicted with chronic and other complex health
conditions. The disease states or conditions for which the Company has such
programs include Psoriasis, Growth Hormone Deficiency, Thyroid Cancer, Sickle
Cell/Thalassemia, Hemophilia, Multiple Sclerosis, Rheumatoid Arthritis,
Osteoarthritis, Osteoporosis, Solid Organ Transplants, HIV/AIDS, Hepatitis
C&B and RSV. The specialty drugs distributed through the BioScrip programs
are dispensed and serviced from the Company’s 43 specialty pharmacy locations
across the United States.
Basis
of Presentation
The
Company’s Consolidated Financial Statements have been prepared in accordance
with U.S. generally accepted accounting principles (“GAAP”).
Reclassification
Certain
prior period amounts have been reclassified to conform to the current year
presentation. Such reclassifications had no material effect on the Company’s
previously reported consolidated financial position, results of operations or
cash flows.
Subsequent
Events
The
Company has evaluated events that occurred during the period subsequent to the
balance sheet date. With the exception of the pending acquisition
(See Note 14 – Subsequent Events), there were no subsequent events that require
recognition or disclosure in the financial statements.
NOTE 2 — SUMMARY
OF SIGNIFICANT ACCOUNTING POLICIES
Consolidation
The
Consolidated Financial Statements include the accounts of the Company and its
wholly-owned subsidiaries. All significant intercompany accounts and
transactions have been eliminated in consolidation.
Use
of Estimates
The
preparation of financial statements in conformity with GAAP requires management
to make certain estimates and assumptions. These estimates and assumptions
affect the reported amounts of assets and liabilities and disclosure of
contingent assets and liabilities at the date of the financial statements and
the reported amounts of revenues and expenses during the reporting period.
Actual results could differ from those estimates.
Receivables
Receivables
include amounts due from certain third party payors and patient co-payments for
pharmacies owned by the Company, amounts due from Plan Sponsors under the
Company’s PBM agreements, amounts due from pharmaceutical manufacturers for
rebates, and service fees resulting from the distribution of certain drugs
through retail pharmacies.
Allowance
for Doubtful Accounts
Allowances
for doubtful accounts are based on estimates of losses related to customer
receivable balances. The procedure for estimating the allowance for doubtful
accounts requires significant judgment and assumptions. The risk of collection
varies based upon the product, the payor (commercial health insurance,
government, and physician), the patient’s ability to pay the amounts not
reimbursed by the payor and the point of distribution (retail, national mail).
The Company estimates the allowance for doubtful accounts based upon a variety
of factors including the age of the outstanding receivables and the historical
experience of collections, adjusting for current economic conditions and, in
certain cases, evaluating specific customer accounts for risk of loss. The
Company periodically reviews the estimation process and makes changes to the
estimates as necessary. When it is deemed that a customer account is
uncollectible, that balance is written off against the existing
allowance.
Allowance
for Contractual Discounts
The
Company is reimbursed for the medications and services it sells by Plan
Sponsors. Revenues and related accounts receivable are recorded net of payor
contractual discounts to reflect the estimated net billable amounts for the
products and services delivered. The Company estimates the allowance for
contractual discounts, based on historical experience and in certain cases on a
customer-specific basis, given its interpretation of the contract terms or
applicable regulations. However, the reimbursement rates are often subject to
interpretation that could result in payments that differ from estimates.
Additionally, updated regulations and contract negotiations occur frequently,
necessitating the continual review and assessment of the estimation
process.
Inventory
Inventory
is recorded at the lower of cost or market. Cost is determined using the
first-in, first-out method. Inventory consists principally of purchased
prescription drugs for the Company’s traditional mail and specialty distribution
operations. Included in inventory is a reserve for expired
inventory.
Property
and Equipment
Property
and equipment is stated at cost less accumulated depreciation and amortization.
Depreciation is calculated using the straight-line method over the estimated
useful lives of assets. The estimated useful lives of the Company’s assets are
as follows:
|
Asset
|
Useful Life
|
|
|
Computer
hardware and software
|
3-5
years
|
|
|
Office
equipment
|
3-5
years
|
|
|
Furniture
and fixtures
|
5-7
years
|
Leasehold
improvements and leased assets are amortized using a straight-line basis over
the related lease term or estimated useful life of the assets, whichever is
less. The cost and related accumulated depreciation of assets sold or
retired are removed from the accounts with the gain or loss, if applicable,
recorded in the statement of operations. Maintenance and repair costs
are expensed as incurred.
Costs
relating to the development of software for internal purposes are charged to
expense until technological feasibility is established in accordance with
Accounting Standards Codification (“ASC”) Topic 350, Intangibles – Goodwill and
Other (“ASC 350”). Thereafter, the remaining software production costs up
to the date placed into production are capitalized and included as Property and
Equipment. Amortization of the capitalized amounts commences on the
date the asset is ready for its intended use and is calculated using the
straight-line method over the estimated useful life of the
software.
Amounts due to Plan Sponsors
Amounts
due to Plan Sponsors primarily represent overpayments that will be paid back to
Plan Sponsors in Specialty Pharmacy Services. In addition, these payables
include the sharing of manufacturer’s rebates with Plan Sponsors in the
Traditional Pharmacy Services segment.
Rebates
Manufacturers’
rebates are primarily part of the Company’s Specialty Pharmacy Services
segment. Rebates are generally volume-based incentives that are
earned and recorded upon dispense. Volume-based rebates are recorded
as a reduction of both inventory and cost of goods sold.
The
Traditional Pharmacy Services segment also includes rebates earned on the PBM
portion of the business. Rebates are recorded on historical PBM
results and trends and are revised on a regular basis depending on the Company’s
latest forecasts, as well as information received from rebate
sources. Should actual results differ, adjustments will be recorded
in future earnings when the adjustment becomes known. In some
instances, rebate payments are shared with the Company’s Plan
Sponsors. PBM rebates earned by the Company are recorded as a
reduction of cost of goods sold. PBM rebates shared with clients are
recorded as a reduction of revenue consistent with the sales incentive
provisions of ASC Topic 605, Revenue Recognition (“ASC
605”).
Revenue
Recognition
The
Company generates revenue principally through the sale of prescription drugs,
which are dispensed either through a pharmacy participating in its pharmacy
network or a pharmacy owned by the Company. Revenue is generally derived under
fee-for-service agreements. Fee-for-service agreements include:
(i) specialty and mail service agreements, where the Company dispenses
prescription medications through its pharmacy facilities and (ii) PBM
agreements, where prescription medications are dispensed through pharmacies
participating in the Company’s retail pharmacy network as well as through its
traditional mail service facility.
Accounting
Standards Codification (“ASC”) Subtopic 605-25, Revenue Recognition:
Multiple-Element Arrangements (“ASC 605-25”), addresses situations in
which there are multiple deliverables under one revenue arrangement with a
customer and provides guidance in determining whether multiple deliverables
should be recognized separately or in combination. The Company
provides a variety of therapies to patients. For infusion related
therapies the Company frequently provides the multiple deliverables of drug
delivery and related nursing services. After applying the criteria
from ASC 605-25, the Company concluded that separate units of accounting exist
in revenue arrangements where we provide multiple deliverables.
Under
fee-for-service agreements in the Specialty Pharmacy Services segment, drug
revenue is recognized at the time the drug is shipped, and nursing revenue is
recognized on the date of service. At that point, the earnings process is
considered complete and the Company has substantially accomplished the terms of
its transaction. In the Traditional Pharmacy Services segment,
revenue is recognized when the pharmacy services are reported to the
Company through the point of sale (“POS”) claims processing system and the drug
is dispensed to the member.
Revenue
generated under PBM agreements is classified as either gross or net by the
Company based on whether it is acting as a principal or an agent in the
fulfillment of prescriptions through its retail pharmacy network. When the
Company independently has a contractual obligation to pay a network pharmacy
provider for benefits provided to its Plan Sponsors’ members, and therefore is
the “primary obligor” as defined in ASC Topic 605, Revenue Recognition, the
Company includes payments (which include the drug ingredient cost) from these
Plan Sponsors as revenue and payments to the network pharmacy providers as cost
of revenue. These transactions require the Company to pay network pharmacy
providers, assume credit risk of Plan Sponsors and act as a principal. If the
Company merely acts as an agent, and consequently administers Plan Sponsors’
network pharmacy contracts, it does not have the primary obligation to pay the
network pharmacy and assume credit risk and as such records only the
administrative fees (and not the drug ingredient cost) as revenue.
Cost
of Revenue
Cost of
revenue includes the costs of prescription medications, pharmacy claims, fees
paid to pharmacies, shipping and other direct and indirect costs associated with
pharmacy management and administration, claims processing operations, mail order
services and nursing services, offset by volume and prompt pay discounts
received from pharmaceutical manufacturers and distributors and total
manufacturer rebates.
Impairment
of Long Lived Assets
The
Company evaluates whether events and circumstances have occurred that indicate
the remaining estimated useful life of long lived assets, including intangible
assets, may warrant revision or that the remaining balance of an asset may not
be recoverable. The measurement of possible impairment is based on the ability
to recover the balance of assets from expected future operating cash flows on an
undiscounted basis. Impairment losses, if any, are determined based on the
present value of the cash flows using discount rates that reflect the inherent
risk of the underlying business.
Goodwill
In
accordance with ASC 350, the Company evaluates goodwill for impairment on an
annual basis and whenever events or circumstances exist that indicate that the
carrying value of goodwill may no longer be recoverable. The
impairment evaluation is based on a two-step process. The first step
compares the fair value of a reporting unit with its carrying amount, including
goodwill. If the first step indicates that the fair value of the
reporting unit is less than its carrying amount, the second step must be
performed which determines the implied fair value of reporting unit goodwill.
The measurement of possible impairment is based upon the comparison of the
implied fair value of reporting unit to its carrying value.
Lease
Accounting
The
Company accounts for leasing transactions by recording rent expense on a
straight-line basis over the expected life of the lease, starting on the date it
gains possession of leased property. Lease terms are generally five years, with
many containing options to extend for periods ranging from one to five years.
The Company includes tenant improvement allowances and rent holidays received
from landlords and the effect of any rent escalation clauses as adjustments to
straight-line rent expense over the expected life of the lease. The
Company does not enter into capital lease obligations due to certain covenant
requirements in our credit facility.
Income
Taxes
As part
of the process of preparing the Company’s Consolidated Financial Statements,
management is required to estimate income taxes in each of the jurisdictions in
which it operates. The Company accounts for income taxes under ASC Topic 740,
Income Taxes (“ASC
740”). ASC 740 requires the use of the asset and liability method of accounting
for income taxes. Under this method, deferred taxes are determined by
calculating the future tax consequences attributable to differences between the
financial accounting and tax bases of existing assets and liabilities. A
valuation allowance is recorded against deferred tax assets when, in the opinion
of management, it is more likely than not that the Company will not be able to
realize the benefit from its deferred tax assets.
The
Company files income tax returns, including returns for its subsidiaries, as
prescribed by Federal tax laws and the tax laws of the state and local
jurisdictions in which it operates. The Company’s uncertain tax
positions are related to tax years that remain subject to examination and are
recognized in the Consolidated Financial Statements when the recognition
threshold and measurement attributes of ASC 740 are met. Interest and
penalties related to unrecognized tax benefits are recorded as income tax
expense.
Disclosure
of Fair Value of Financial Instruments
The
Company’s financial instruments consist mainly of cash and cash equivalents and
its line of credit. The carrying amounts of cash, cash equivalents and the line
of credit approximate fair value due to their fully liquid or short-term
nature.
Accounting
for Stock-Based Compensation
The
Company accounts for stock-based employee compensation expense under the
provisions of ASC Topic 718, Compensation – Stock
Compensation (“ASC 718”). At December 31, 2009, the
Company has one stock-based employee compensation plan (the “Plan”) pursuant to
which incentive stock options (“ISOs”), non-qualified stock options (“NQSOs”),
restricted stock, performance units and performance share awards may be granted
to employees and non-employee directors. Option and stock awards are typically
settled by issuing authorized but unissued shares of the Company.
The
Company estimates the fair value of each stock option award on the measurement
date using a binomial option-pricing model. The fair value of the
award is amortized to expense on a straight line basis over the requisite
service period. The Company expenses restricted stock awards based on vesting
requirements, including time elapsed, market conditions and/or performance
conditions. Because of these requirements, the weighted average
period for which the expense is recognized varies.
Income
(Loss) Per Share
Basic
income (loss) per common share is based on the weighted average number of shares
outstanding. Diluted income per share is based on the weighted average number of
shares outstanding, including common stock equivalents, and diluted (loss) per
share is based on the weighted average number of shares outstanding because the
impact of common stock equivalents would be anti-dilutive (in thousands except
per share data):
|
2009
|
2008
|
2007
|
||||||||
|
Numerator:
|
||||||||||
|
Net
income (loss):
|
$ | 54,099 | $ | (74,032 | ) | $ | 3,317 | |||
|
Denominator
- Basic:
|
||||||||||
|
Weighted
average number of common shares outstanding
|
38,985 | 38,417 | 37,647 | |||||||
|
Basic
income (loss) per common share
|
$ | 1.39 | $ | (1.93 | ) | $ | 0.09 | |||
|
Denominator
- Diluted:
|
||||||||||
|
Weighted
average number of common shares outstanding
|
38,985 | 38,417 | 37,647 | |||||||
|
Common
share equivalents of outstanding stock options and restricted
awards
|
752 | - | 844 | |||||||
|
Total
diluted shares outstanding
|
39,737 | 38,417 | 38,491 | |||||||
|
Diluted
income (loss) per common share
|
$ | 1.36 | $ | (1.93 | ) | $ | 0.09 | |||
Employee
stock options and restricted stock awards of 3,681,109, 3,996,523 and 3,259,893
for 2009, 2008 and 2007, respectively, were excluded from the diluted net income
per share calculation because their effect would be anti-dilutive.
Recent
Accounting Pronouncements
In June
2009, FASB issued Accounting Standards Update No. 2009-01, Generally Accepted Accounting
Principles (“ASC Topic 105”) which established the FASB Accounting
Standards Codification (the “Codification”) as the official single source of
authoritative GAAP. All previously existing accounting standards were
superseded at that date. All other accounting guidance not included
in the Codification will be considered non-authoritative. The
Codification also includes relevant SEC guidance organized using the same
topical structure in separate sections within the Codification.
Following
the Codification, FASB has stated that it will not issue new standards in the
form of Statements, FASB Staff Positions or Emerging Issues Task Force
Abstracts. Instead, it will issue Accounting Standards Updates
(“ASU”) that will serve to update the Codification, provide background
information about the guidance and provide the basis for conclusions on the
changes to the Codification.
The
Codification is not intended to change GAAP, but will change the way GAAP is
organized and presented. The Codification was effective for the
Company’s third quarter 2009 financial statements and the principal impact is
limited to disclosures as all future references to authoritative accounting
literature will be referenced in accordance with the Codification.
In
September 2009, FASB issued ASU 2009-13, Multiple Element Arrangements
(“ASU 2009-13”), which is effective for fiscal years beginning on or
after June 15, 2010. Early adoption is permitted. If early
adoption is elected and the period of adoption is not the beginning of the
entity’s fiscal year, the entity will be required to apply the amendments of
this ASU retrospectively from the beginning of the entity’s fiscal
year. An entity may elect, but will not be required, to adopt the
amendments in this ASU retrospectively for all prior periods. However, an entity
cannot apply the amendments in this ASU retrospectively to a period if it is
impracticable for it to report the change through retrospective application to
that prior period.
ASU
2009-13 addresses the determination of when the individual deliverables included
in a multiple arrangement may be treated as separate units of accounting. ASU
2009-13 also eliminates the residual method of allocation and requires that
arrangement consideration be allocated at the inception of the arrangement to
all deliverables using the relative selling price method. This standard must be
adopted by the Company no later than January 1, 2011. The Company is
currently evaluating the impact, if any, that this standard update will have on
its results of operations, financial position or cash flows.
In
2009, the Company adopted the provisions of ASC Topic 855, Subsequent Events (“ASC
855”), which was effective for interim and annual periods after June 15, 2009
and amended on February 24, 2010. This Statement incorporates
guidance into accounting literature that was previously addressed only in
auditing standards. The statement refers to subsequent events that provide
additional evidence about conditions that existed at the balance-sheet date as
“recognized subsequent events”. Subsequent events which provide
evidence about conditions that arose after an issuer’s most recent balance-sheet
date but prior to the issuance of its most recent financial statements are
referred to as “non-recognized subsequent events”. It also requires
companies to evaluate subsequent events through the date the financial
statements were issued.
NOTE 3 —
OPERATING SEGMENTS
In
accordance with ASC Topic 280, Segment Reporting (“ASC
280”), and based on the nature of the Company’s services, the Company has two
operating and reportable segments: Specialty Pharmacy Services and Traditional
Pharmacy Services. ASC 280 requires an enterprise to report segment
information in the same way that management internally organizes its business
for assessing performance and making decisions regarding allocation of
resources. The Company evaluates the performance of operating
segments and allocates resources based on income from operations.
Revenues
from Specialty Pharmacy Services and Traditional Pharmacy Services are derived
from the Company’s relationships with healthcare payors including Plan Sponsors
as well as from our relationship with pharmaceutical manufacturers, patients and
physicians.
The
Specialty Pharmacy Services segment consists of the Company’s specialty pharmacy
distribution and therapy management services. Specialty Pharmacy
Services distribution occurs locally through community pharmacies, centrally
through mail order facilities and through our infusion pharmacies for patients
requiring infused medications in the home or infused at a variety of sites
including the Company’s ambulatory infusion sites. All Specialty
Pharmacy Services target certain specialty medications that are used to treat
patients living with chronic and other complex healthcare
conditions.
The
Traditional Pharmacy Services segment consists mainly of traditional mail order
pharmacy fulfillment, and to a lesser extent, prescription discount card
programs and integrated PBM services. These Traditional Pharmacy
Services are designed to offer Plan Sponsors cost-effective delivery of pharmacy
benefit plans including the low cost distribution of mail services for plan
members who receive traditional maintenance medications.
In the
quarter ended September 30, 2009, the Company renamed the reportable segment
formerly known as “PBM Services” to “Traditional Pharmacy
Services”. The decision to rename this segment reflects a shift in
the nature of the business included within this segment away from fully funded
pharmacy benefit management services and more towards traditional mail services
and prescription discount card programs.
The
accounting policies applied to the business segments are the same as those
described in Note 2 - Summary of Significant Accounting Policies.
Certain prior period amounts have been reclassified to conform to the current
year presentation. Such reclassifications are deemed immaterial to segment data
presented below. There is no effect on previously reported net income
(loss) from operations.
Segment
Reporting Information
(in
thousands)
|
Years
Ended December 31,
|
||||||||||
|
2009
|
2008
|
2007
|
||||||||
|
Revenue:
|
||||||||||
|
Specialty
Pharmacy Services
|
$ | 1,113,305 | $ | 1,196,587 | $ | 974,571 | ||||
|
Traditional
Pharmacy Services
|
216,220 | 205,324 | 223,161 | |||||||
|
Total
|
$ | 1,329,525 | $ | 1,401,911 | $ | 1,197,732 | ||||
|
Income
(loss) from operations:
|
||||||||||
|
Specialty
Pharmacy Services
|
$ | (1,320 | ) | $ | (93,120 | ) | $ | (2,453 | ) | |
|
Traditional
Pharmacy Services
|
16,786 | 9,603 | 11,304 | |||||||
|
Total
|
15,466 | (83,517 | ) | 8,851 | ||||||
|
Interest
expense, net
|
1,920 | 2,711 | 3,270 | |||||||
|
Income
tax (benefit) provision
|
(40,553 | ) | (12,196 | ) | 2,264 | |||||
|
Net
income (loss):
|
$ | 54,099 | $ | (74,032 | ) | $ | 3,317 | |||
|
Capital
expenditures:
|
||||||||||
|
Specialty
Pharmacy Services
|
$ | 5,074 | $ | 6,280 | $ | 4,843 | ||||
|
Traditional
Pharmacy Services
|
665 | 1,183 | 683 | |||||||
|
Total
|
$ | 5,739 | $ | 7,463 | $ | 5,526 | ||||
|
Depreciation
Expense:
|
||||||||||
|
Specialty
Pharmacy Services
|
$ | 4,206 | $ | 3,919 | $ | 3,691 | ||||
|
Traditional
Pharmacy Services
|
827 | 538 | 501 | |||||||
|
Total
|
$ | 5,033 | $ | 4,457 | $ | 4,192 | ||||
|
Total
Assets
|
||||||||||
|
Specialty
Pharmacy Services
|
$ | 208,521 | $ | 180,237 | $ | 232,823 | ||||
|
Traditional
Pharmacy Services
|
78,699 | 66,720 | 63,999 | |||||||
|
Total
|
$ | 287,220 | $ | 246,957 | $ | 296,822 | ||||
NOTE 4 —
CONCENTRATION OF CREDIT RISK
The
Company provides trade credit to its customers in the normal course of
business. The following table outlines one pharmacy network agreement
under which various Plan Sponsors are served and which Plan Sponsors account
for, in the aggregate, revenues and receivables that exceeded 10% of the
Company’s total revenues and accounts receivables during the applicable time
period:
| Plan Sponsors Aggregated | |||
|
Year
ended December 31, 2007
|
|||
|
%
of total revenue
|
12 | % | |
|
%
of total accounts receivable at period end
|
19 | % | |
|
Year
ended December 31, 2008
|
|||
|
%
of total revenue
|
13 | % | |
|
%
of total accounts receivable at period end
|
19 | % | |
|
Year
ended December 31, 2009
|
|||
|
%
of total revenue
|
14 | % | |
|
%
of total accounts receivable at period end
|
17 | % | |
Plan
Sponsor revenue and accounts receivable is primarily in the Traditional Pharmacy
Services segment with a lesser amount in the Specialty Pharmacy Services
segment.
NOTE 5 —
GOODWILL AND INTANGIBLES
The
Company follows ASC 350 in accounting and reporting for its goodwill and
intangible assets. ASC 350 states that goodwill is no longer subject to
amortization over its estimated useful life. Goodwill is subject to at least an
annual assessment for impairment by applying a fair-value based
test. Management assesses impairment in the fourth quarter of each
year or whenever there is an impairment indicator. The Company
has two reporting units: Specialty Pharmacy Services and Traditional Pharmacy
Services. As of December 31, 2009 and 2008, all goodwill is
associated with the Specialty Pharmacy Services reporting
unit. Portions of goodwill are expected to be deductible for income
tax purposes.
Based on
its annual assessment for the year ended December 31, 2009, management
determined that the fair value of the Company’s Specialty Pharmacy Services
reporting unit was greater than the carrying value of its net assets, and as
such, no impairment was incurred for fiscal year 2009.
In 2008,
the Company experienced a significant decline in its market capitalization below
book value, which was sustained through the fourth quarter of
2008. The Company also previously announced changes in the status of
long-term Specialty Pharmacy Services contracts. Those contract
changes included (a) the decision by United Healthcare (“UHC”) to internalize
services for HIV/AIDS and solid organ transplant drugs starting in the first
quarter of 2009, and (b) the expiration of the Competitive Acquisition Program
(“CAP”) with the Centers for Medicare and Medicaid Services effective December
31, 2008. The expiration or termination of these contracts, the
reduced market capitalization of the Company and the reduced market
capitalization of the Company’s peers in the healthcare industry were considered
to be potential indicators of impairment in contemplation of the Company’s
annual impairment analysis.
Based on
its 2008 annual assessment, management determined that the fair value of the
Company’s Specialty Pharmacy Services segment was less than the carrying value
of its net assets. The Company determined the fair value of the
Specialty Pharmacy Services segment using a combination of an income approach
using the discounted cash flow method and a market approach using the guideline
public company method. The Company completed step two of the
impairment analysis and concluded that the carrying value of the goodwill
associated with the Specialty Pharmacy Services segment was impaired, resulting
in a fourth quarter non-cash impairment charge of $90.0 million.
The
following table provides a reconciliation of goodwill (in
thousands):
|
Total
|
||||
|
Balance
as of December 31, 2007
|
$ | 114,824 | ||
|
Goodwill
acquired
|
- | |||
|
Goodwill
adjustments
|
(286 | ) | ||
|
Goodwill
impairment
|
(90,040 | ) | ||
|
Balance
as of December 31, 2008
|
24,498 | |||
|
Goodwill
acquired
|
- | |||
|
Goodwill
adjustments
|
- | |||
|
Balance
as of December 31, 2009
|
$ | 24,498 | ||
As part
of the 2008 annual assessment and in consideration of the impairment indicators,
the Company also evaluated the recoverability of its property and equipment and
definite-lived intangible assets in accordance with ASC 350. As a
result, the Company determined that $3.9 million of definitive-lived intangible
assets, consisting of $3.5 million of customer lists and $0.4 million of
non-compete agreements, were impaired, and an impairment charge for this amount
was recorded in the fourth quarter of 2008. These impairment tests
were performed and the related impairment charges were recorded prior to
completing the goodwill impairment analysis.
NOTE 6 —
PROPERTY AND EQUIPMENT
Property
and equipment, at cost, consists of the following at December 31 (in
thousands):
|
2009
|
2008
|
||||||
|
Computer
and office equipment, including equipment acquired under capital
leases
|
$ | 23,067 | $ | 13,534 | |||
|
Work
in progress
|
971 | 7,161 | |||||
|
Furniture
and fixtures
|
2,998 | 2,760 | |||||
|
Leasehold
improvements
|
9,818 | 8,418 | |||||
| 36,854 | 31,873 | ||||||
|
Less:
Accumulated depreciation
|
(21,400 | ) | (17,125 | ) | |||
|
Property
and equipment, net
|
$ | 15,454 | $ | 14,748 | |||
Work in
progress for 2009 and 2008 includes $0.7 million and $5.7 million, respectively,
of costs capitalized for internal use software.
Depreciation
expense for the years ended December 31, 2009, 2008 and 2007 was
$5.0 million, $4.5 million and $4.2 million,
respectively. In 2009, $0.9 million of depreciation expense related
to capitalized computer software costs for internal use was
recorded. Previous to 2009 no significant cost of software developed
for internal use was recorded to depreciation expense.
NOTE
7 — LINE OF CREDIT
At
December 31, 2009, there was $30.4 million in outstanding borrowings under our
revolving credit facility (the “Facility”) with an affiliate of Healthcare
Finance Group, Inc. (“HFG”), as compared to $50.4 million at December 31,
2008. The Facility provides for borrowing up to $85.0 million at the
London Inter-Bank Offered Rate (“LIBOR”) or a pre-determined minimum rate plus
the applicable margin and other associated fees, provided a sufficient level of
receivable assets are available as collateral. The term of the
Facility runs through November 1, 2010. Under the terms of the
Facility, the Company may request to increase the amount available for borrowing
up to $100.0 million, and convert a portion of any outstanding borrowings from a
Revolving Loan into a Term Loan. The borrowing base utilizes
receivable balances and proceeds thereof as security under the
Facility. At December 31, 2009 the Company had $54.6 million of
credit available on a borrowing basis of $85.0 million under the
Facility.
The
weighted average interest rate on the line of credit was 4.4% during 2009
compared to 5.0% for 2008.
The
Facility contains various covenants that, among other things, require the
Company to maintain certain financial ratios as defined in the agreements
governing the Facility. In December 2009, the Company and HFG agreed
to amend the terms of the Facility to revise certain calculations required by
the covenants. The Company was in compliance with all the covenants contained in
the agreements as of December 31, 2009.
As part
of the anticipated acquisition of CHS, the Company has received a financing
commitment from Jefferies Finance LLC (“Jefferies”) to provide a five year
senior credit facility in the amount of $150.0 million, including a $50.0
million revolver, and a $225.0 million bridge loan facility. The
bridge loan facility will be drawn on only if the $225.0 million, five and a
half year unsecured notes are not sold prior to the closing date of the
acquisition. The Company plans to use $100.0 million of the senior
term loan and the proceeds from the senior unsecured notes offering to finance,
in part, the acquisition of CHS, to refinance its existing indebtedness and
repay CHS’s existing indebtedness, for general corporate purposes and to pay
related fees and expenses. The $50.0 million revolver is expected to
be undrawn at closing. The specific interest rates of the senior term
loan and notes is subject to final pricing and the Company expects the
interest to reflect market rates relative to its credit ratings. See
Note 14 – Subsequent Events for additional information about the proposed
acquisition of CHS.
NOTE 8 —
COMMITMENTS AND CONTINGENCIES
Legal
Proceedings
On
February 14, 2005, a complaint was filed in the Alabama Circuit Court for
Barbour County, captioned Eufaula Drugs, Inc. v.
ScriptSolutions [sic], one of approximately fourteen substantially
identical complaints commenced in Alabama courts against various unrelated
pharmacy benefit management companies. On April 8, 2005, the plaintiff
filed an amended complaint substituting BioScrip PBM Services f/k/a
ScripSolutions (“PBM Services”) as the defendant, seeking unspecified money
damages and injunctive relief, and alleging breach of contract and related tort
and equitable claims on behalf of a putative nationwide class of pharmacies
alleging insufficient reimbursement for prescriptions dispensed by
ScripSolutions, principally on the theory that PBM Services was obligated to
update its prescription pricing files on a daily rather than weekly basis.
Following preliminary proceedings and class discovery, the parties reached a
settlement agreement on August 6, 2009, in which the Company continues to deny
liability, with a class of pharmacies which was certified solely for settlement
purposes, and class members were entitled to receive $0.065 for each branded
prescription filled during the settlement class period. The court
approved the settlement on November 4, 2009 and a final judgment dismissing the
action has been entered in the action, the time to appeal which has
expired. The costs of the settlement are covered by
insurance.
The
sellers of a company, Northland Pharmacy, to Chronimed Holdings, Inc., (now
known as BioScrip Pharmacy, Inc.) one of BioScrip’s subsidiaries, are claiming a
right to additional purchase price of at least $5.64 million in connection with
an earn out provision in the stock purchase agreement regarding the
acquisition. The sellers, named DiCello, first sued in federal court
in Ohio in July 2007, but the court stayed the case and directed arbitration of
the disagreement by the accounting firm KPMG, LLP, as the stock purchase
agreement provides. BioScrip Pharmacy denies owing the sellers any
additional purchase price. The parties have made extensive filings as
directed by the arbitrator and are waiting for either the arbitrator’s decision
or instructions as to further proceedings in the matter. The Company
is confident in its position and does not believe an adverse ruling is likely;
however, there can be no assurance that an adverse ruling will not be
rendered. If the arbitrator rules in favor of DiCello, such ruling
could have a material adverse effect on the Company’s business, operations, or
financial position.
Government
Regulation
Various
Federal and state laws and regulations affecting the healthcare industry do or
may impact the Company’s current and planned operations, including, without
limitation, Federal and state laws prohibiting kickbacks in government health
programs, Federal and state antitrust and drug distribution laws, and a wide
variety of consumer protection, insurance and other state laws and regulations.
While management believes that the Company is in substantial compliance with all
existing laws and regulations material to the operation of its business, such
laws and regulations are subject to rapid change and often are uncertain in
their application. As controversies continue to arise in the healthcare industry
(for example, regarding the efforts of Plan Sponsors and pharmacy benefit
managers to limit formularies, alter drug choice and establish limited networks
of participating pharmacies), Federal and state regulation and enforcement
priorities in this area can be expected to increase, the impact of which on the
Company cannot be predicted. There can be no assurance that the Company will not
be subject to scrutiny or challenge under one or more of these laws or that any
such challenge would not be successful. Any such challenge, whether or not
successful, could have a material adverse effect upon the Company’s financial
position, results of operations and cash flows. Violation of the Federal
anti-kickback statute, for example, may result in substantial criminal
penalties, as well as suspension or exclusion from the Medicare and Medicaid
programs. Further, there can be no assurance that the Company will be able to
obtain or maintain any of the regulatory approvals that may be required to
operate its business, and the failure to do so could have a material adverse
effect on the Company’s financial position, results of operations and cash
flows.
Operating
Leases
The
Company leases its facilities and certain equipment under various operating
leases with third parties. Facility lease terms are generally five years, the
majority containing options to extend for periods ranging from one to five
years. Approximately 80% of these leases contain escalation clauses that
increase base rent payments based upon either the Consumer Price Index or an
agreed upon schedule. Equipment leases are generally for periods of three to
five years.
The
future minimum lease payments under operating leases at December 31 are as
follows (in thousands):
|
2010
|
$ | 4,738 | ||
|
2011
|
3,489 | |||
|
2012
|
2,784 | |||
|
2013
|
2,227 | |||
|
2014
|
1,897 | |||
|
Thereafter
|
4,013 | |||
| $ | 19,148 |
Rent
expense for leased facilities and equipment was approximately $5.1 million,
$4.6 million and $4.4 million for the years ended December 31,
2009, 2008 and 2007, respectively.
Security
Interest and Letters of Credit
Under the
terms of the prime vendor agreement with AmerisourceBergen Drug Company
(“ABDC”), the Company granted ABDC a secured, first priority lien in all of its
inventory as well as the proceeds thereof. In the ordinary course of
business, the Company obtained certain letters of credit (“LC”) from commercial
banks in favor of various parties. At December 31, 2009 there was
$1.1 million on deposit as collateral for these LCs.
Purchase
Commitments
As of
December 31, 2009, the Company had commitments to purchase prescription drugs
from drug manufacturers of approximately $17.7 million in 2010. These
purchase commitments are made at levels expected to be used in the normal course
of business.
NOTE 9 —
INCOME TAXES
The
Company’s Federal and state income tax provision (benefit) is summarized in the
following table (in thousands):
|
For
the Years Ended December 31,
|
||||||||||||
|
2009
|
2008
|
2007
|
||||||||||
|
Current
|
||||||||||||
|
Federal
|
$ | (319 | ) | $ | (18 | ) | $ | (501 | ) | |||
|
State
|
283 | 43 | (43 | ) | ||||||||
|
Total
Current
|
(36 | ) | 25 | (544 | ) | |||||||
|
Deferred
|
||||||||||||
|
Federal
|
(36,764 | ) | (10,660 | ) | 2,448 | |||||||
|
State
|
(3,753 | ) | (1,561 | ) | 360 | |||||||
|
Total
Deferred
|
(40,517 | ) | (12,221 | ) | 2,808 | |||||||
|
Total
(Benefit from) Provision for Income Taxes
|
$ | (40,553 | ) | $ | (12,196 | ) | $ | 2,264 | ||||
The
effect of temporary differences that give rise to a significant portion of
deferred taxes is as follows (in thousands):
|
December
31,
|
|||||||
|
2009
|
2008
|
||||||
|
Deferred
tax assets:
|
|||||||
|
Reserves
not currently deductible
|
$ | 7,131 | $ | 6,533 | |||
|
Net
operating loss carryforwards
|
3,595 | 8,455 | |||||
|
Intangibles
|
4,817 | 5,310 | |||||
|
Goodwill
(tax deductible)
|
14,794 | 17,720 | |||||
|
Accrued
expenses
|
2,117 | 1,091 | |||||
|
Stock
based compensation
|
3,342 | 2,653 | |||||
|
Property
basis differences
|
2,025 | 1,666 | |||||
|
Other
|
1,885 | 1,411 | |||||
|
Subtotal
deferred tax assets
|
39,706 | 44,839 | |||||
|
Deferred
tax liabilities:
|
|||||||
|
Goodwill
(tax deductible)
|
- | (533 | ) | ||||
|
Less:
valuation allowance
|
- | (44,839 | ) | ||||
|
Net
deferred tax asset (liability)
|
$ | 39,706 | $ | (533 | ) | ||
The
Company continually assesses the ability to realize the benefit of its deferred
tax assets. In the fourth quarter of 2006 a valuation allowance on
deferred tax assets was recorded. During the fourth quarter of 2009,
based upon an evaluation of the positive and negative evidence, the Company
concluded that the valuation allowance in the amount of $44.8 million was no
longer required. As part of its analysis, the Company evaluated,
among other factors, its recent history of generating taxable income, the
underlying factors which resulted in the goodwill impairment charge that was
incurred during the fourth quarter of 2008, and its near-term forecasts of
future taxable income. After considering these factors, the Company
concluded that a reversal of the valuation allowance was
appropriate. Accordingly, the Company recognized a tax benefit of
$44.8 million during the 2009 fourth quarter.
At
December 31, 2009, the Company had Federal net operating loss (“NOL”)
carryforwards of approximately $18.0 million, of which $3.2 million is
subject to an annual limitation, all of which will begin expiring in 2012 and
later. Of the Company’s $18.0 million Federal NOLs, $8.5 million will
be recorded in additional paid-in capital when realized. These NOLs
are related to the exercise of non-qualified stock options. The
Company has post apportioned state NOL carryforwards remaining of approximately
$8.1 million, the majority of which will begin expiring in 2017 and
later.
The
Company’s reconciliation of the statutory rate to the effective income tax rate
is as follows (in thousands):
|
2009
|
2008
|
2007
|
||||||||
|
Tax
(benefit) provision at statutory rate
|
$ | 4,566 | $ | (29,310 | ) | $ | 1,897 | |||
|
State
tax (benefit) provision, net of Federal taxes
|
633 | (2,616 | ) | 366 | ||||||
|
Non-deductible
goodwill
|
- | 1,687 | - | |||||||
|
Change
in tax contingencies
|
(216 | ) | (360 | ) | (1,165 | ) | ||||
|
Valuation
allowance changes affecting income tax expense
|
(44,839 | ) | 18,245 | 930 | ||||||
|
Change
in deferred tax rate
|
(992 | ) | - | - | ||||||
|
Other
|
295 | 158 | 236 | |||||||
|
Provision
for income taxes
|
$ | (40,553 | ) | $ | (12,196 | ) | $ | 2,264 | ||
As of
December 31, 2009 the Company had $1.9 million of total gross unrecognized tax
benefits, all of which, if recognized, would favorably affect its effective
income tax rate in future periods. A reconciliation of the beginning
and ending amount of gross unrecognized tax benefits is as follows (in
thousands):
|
2009
|
2008
|
2007
|
||||||||
|
Unrecognized
tax benefits balance at January 1,
|
$ | 2,287 | $ | 2,940 | $ | 4,137 | ||||
|
Gross
increases for tax positions of prior years
|
- | - | 284 | |||||||
|
Gross
decreases for tax positions of prior years
|
- | (239 | ) | (380 | ) | |||||
|
Gross
increases for tax positions taken in current year
|
- | - | 6 | |||||||
|
Settlements
with taxing authorities
|
- | (46 | ) | (114 | ) | |||||
|
Lapse
of statute of limitations
|
(339 | ) | (368 | ) | (993 | ) | ||||
|
Unrecognized
tax benefits balance at December 31,
|
$ | 1,948 | $ | 2,287 | $ | 2,940 | ||||
The
Company's policy for recording interest and penalties associated with uncertain
tax positions is to record such items as a component of income tax expense in
the statement of operations. As of December 31, 2009 and December 31,
2008, the Company had approximately $0.5 million and $0.5 million of
accrued interest related to uncertain tax positions, respectively.
The
Company files income tax returns, including returns for its subsidiaries, with
Federal, state and local jurisdictions. The Company's uncertain tax
positions are related to tax years that remain subject to
examination. As of December 31, 2009, U.S. tax returns for 2006,
2007, 2008 and 2009 remain subject to examination by Federal tax
authorities. Tax returns for the years 2005 through 2009 remain
subject to examination by state and local tax authorities for a majority of the
Company's state and local filings.
During
January 2008, the Company settled certain controversies with taxing
authorities. The settlement called for payment of $63,000 of tax and
interest. The remaining amount of $0.3 million of unrecognized tax
benefits and interest for this tax position was reversed during first quarter
2008 through goodwill.
NOTE 10 —
TREASURY STOCK
On
February 27, 2003, the Executive Committee of the Board of Directors (the
“Board”) approved a stock repurchase program authorizing the Company to
repurchase up to an aggregate of $10.0 million of its common stock in open
market or private transactions. No stock was repurchased during 2009, 2008 or
2007; however, during 2009, 2008 and 2007, 33,552; 187,544 and 189,492 shares,
respectively, were surrendered to satisfy tax withholding obligations on the
vesting of restricted stock awards. As of December 31, 2009, approximately
$4.9 million of the $10.0 million authorized remains available for
additional share repurchases. The Company holds a total of 2,647,613 shares
of treasury stock acquired under current and prior repurchase programs as well
as forfeitures to satisfy tax obligations in the vesting of restricted stock
awards.
NOTE 11 —
STOCK-BASED COMPENSATION
Under the
Company’s 2008 Equity Incentive Plan (the “2008 Plan”) the Company may issue,
among other things, incentive stock options (“ISOs”), non-qualified stock
options (“NQSOs”), stock appreciation rights, restricted stock, and performance
units to employees and directors. Under the 2008 Plan, 3,580,000
shares were authorized for issuance (subject to adjustment for grants made under
the Company’s 2001 Incentive Stock Plan (the “2001 Plan”) after January 1, 2008,
as well as for forfeitures, expirations or awards that under the 2001 Plan
otherwise settled in cash after the adoption thereof). As of December
31, 2009 209,253 shares remained available for grant under the 2008
Plan. Upon effectiveness of the 2008 Plan in April 2008, the Company
ceased making grants under the 2001 Plan. The 2008 Plan and the 2001
Plan are administered by the Company’s Management Development and Compensation
Committee (the “Compensation Committee”), a standing committee of the
Board.
Under the
terms of the 2008 Plan and the 2001 Plan, plan participants may use shares to
cover tax withholding on income earned as a result of appreciation of
equity-based instruments upon exercise, vesting and/or lapsing of restrictions
thereon. Upon the exercise of stock options and the vesting of other
equity awards granted under the Plans, participants will generally have taxable
income subject to statutory withholding requirements. The number of
shares that may be issued to participants upon the exercise of stock options and
the vesting of equity awards may be reduced by the number of shares having a
market value equal to the amount of tax required to be withheld by the Company
to satisfy Federal, state and local tax obligations as a result of such exercise
or vesting.
Stock
Options
Options
granted under the plans: (a) typically vest over a three-year period and, in
certain instances, fully vest upon a change in control of the Company, (b) have
an exercise price that may not be less than 100% of its fair market value on the
date of grant (110% for ISOs granted to a stockholder who holds more than 10% of
the outstanding stock of the Company), and (c) are generally exercisable for ten
years (five years for ISOs granted to a stockholder
holding
more than 10% of the outstanding stock of the Company) after the date of grant,
subject to earlier termination in certain circumstances.
The
Company recognized compensation expense related to stock options of $2.2
million, $2.1 million and $1.9 million for the years ended December 31, 2009,
2008 and 2007, respectively.
The fair
value of each stock option award on the date of the grant was calculated using a
binomial option-pricing model. Option expense is amortized on a
straight-line basis over the requisite service period and was calculated with
the following weighted average assumptions:
|
2009
|
2008
|
2007
|
||||||||
|
Expected
volatility
|
66.4 | % | 51.4 | % | 54.4 | % | ||||
|
Risk-free
interest rate
|
2.99 | % | 3.86 | % | 4.70 | % | ||||
|
Expected
life of options
|
5.6
years
|
5.7
years
|
5.2
years
|
|||||||
|
Dividend
rate
|
- | - | - | |||||||
|
Fair
value of options
|
$ | 1.70 | $ | 3.46 | $ | 2.29 | ||||
Stock
option activity through December 31, 2009 is as follows:
|
Weighted
|
Aggregate
|
Weighted
Average
|
|||||||||
|
Average
|
Intrinsic
Value
|
Remaining
|
|||||||||
|
Options
|
Exercise
Price
|
(thousands)
|
Contractual
Life
|
||||||||
|
Balance,
December 31, 2008
|
5,784,371 | $ | 6.53 | $ | 27.5 |
5.6
years
|
|||||
|
Granted
|
1,918,600 | 2.84 | |||||||||
|
Exercised
|
(889,606 | ) | 3.39 | ||||||||
|
Forfeited
|
(182,974 | ) | 4.86 | ||||||||
|
Expired
|
(580,334 | ) | 7.01 | ||||||||
|
Balance,
December 31, 2009
|
6,050,057 | $ | 5.83 | $ | 19,014.1 |
6.2
years
|
|||||
|
Outstanding
options less expected
|
|||||||||||
|
forfeitures
at December 31, 2009
|
5,430,876 | $ | 6.09 | $ | 16,023.4 |
5.9
years
|
|||||
|
Exercisable
at December 31, 2009
|
3,589,751 | $ | 7.32 | $ | 7,437.5 |
4.6
years
|
|||||
The
weighted-average, grant-date fair value of options granted during the years
ending December 31, 2009, 2008 and 2007 was $1.70, $3.46 and $2.29
respectively. The total intrinsic value of options exercised during the years
December 31, 2009, 2008, and 2007, was $3.0 million,
$0.1 million, and $1.3 million, respectively.
Cash
received from option exercises under share-based payment arrangements for the
years ended December 31, 2009, 2008, and 2007, was $3.0 million, $0.2
million and $1.9 million, respectively.
The
maximum term of stock options under these plans is ten years. Options
outstanding as of December 31, 2009 expire on various dates ranging from
August 2010 through October 2019. The following table outlines our outstanding
and exercisable stock options as of December 31, 2009:
|
Options
Outstanding
|
Options
Exercisable
|
||||||||||||||
|
Weighted
|
Weighted
|
||||||||||||||
|
Average
|
Weighted
Average
|
Average
|
|||||||||||||
|
Outstanding
|
Exercise
|
Remaining
|
Options
|
Exercise
|
|||||||||||
|
Range
of Option Exercise Price
|
Options
|
Price
|
Contractual
Life
|
Exercisable
|
Price
|
||||||||||
| $1.50 - $4.69 | 2,584,801 | $ | 2.65 |
7.96
years
|
806,141 | $ | 2.80 | ||||||||
| $5.29 - $7.03 | 1,811,021 | 6.35 |
5.68
years
|
1,196,707 | 6.35 | ||||||||||
| $7.16 - $9.56 | 1,062,648 | 7.87 |
5.20
years
|
995,316 | 7.90 | ||||||||||
| $9.77 - $12.20 | 344,920 | 12.01 |
1.93
years
|
344,920 | 12.01 | ||||||||||
| $16.50 - $20.25 | 246,667 | 17.92 |
2.04
years
|
246,667 | 17.92 | ||||||||||
| 6,050,057 | $ | 5.83 |
6.21
years
|
3,589,751 | $ | 7.32 | |||||||||
As of
December 31, 2008 and 2007, the exercisable portion of outstanding options
was approximately 4.2 million shares and approximately 3.7 million
shares, respectively.
Stock
option activity for non-vested shares through December 31, 2009 is as
follows:
|
Weighted
|
|||||||
|
Average
|
|||||||
|
Grant
Date
|
|||||||
|
Options
|
Fair
Value
|
||||||
|
Balance,
December 31, 2008
|
1,614,718 | $ | 2.70 | ||||
|
Granted
|
1,918,600 | 1.71 | |||||
|
Vested
|
(640,973 | ) | 2.56 | ||||
|
Exercised
|
(203,204 | ) | 1.85 | ||||
|
Forfeited
and expired
|
(228,835 | ) | 2.31 | ||||
|
Balance,
December 31, 2009
|
2,460,306 | $ | 2.07 | ||||
As of
December 31, 2009 there was $3.1 million of unrecognized compensation expense
related to unvested option grants. That expense is expected to be
recognized over a weighted-average period of 2.0 years.
As
compensation expense for options granted is recorded over the requisite service
period of options, future stock-based compensation expense may be greater as
additional options are granted.
Restricted
Stock
Under the
2008 Plan, stock grants subject solely to an employee’s or director’s continued
service with the Company will not become fully vested less than (a) three years
from the date of grant to employees and, in certain instances, may fully vest
upon a change in control of the Company, and (b) one year from the date of grant
for directors. Stock grants subject to the achievement of performance
conditions will not vest less than one year from the date of grant where the
vesting of stock grants is subject to performance measures. Such
performance shares may vest after one year from grant. No such time
restrictions applied to stock grants made under the Company’s prior equity
compensation plans.
The
Company recognized compensation expense related to restricted stock awards of
$1.2 million, $1.7 million and $1.1 million for the years ended December 31,
2009, 2008 and 2007, respectively.
Since the
Company records compensation expense for restricted stock awards based on the
vesting requirements, which generally includes time elapsed, market conditions
and/or performance conditions, the weighted average period over which the
expense is recognized varies. Also, future equity-based compensation expense may
be greater if additional restricted stock awards are made.
Restricted
stock award activity through December 31, 2009 is as follows:
|
Weighted
Average
|
Weighted
Average
|
|||||||
|
Restricted
|
Award
|
Remaining
|
||||||
|
Stock
|
Date
Fair Value
|
Recognition
Period
|
||||||
|
Balance
December 31, 2008
|
713,637 | $ | 4.24 |
1.5
years
|
||||
|
Granted
|
257,860 | $ | 1.76 | |||||
|
Awards
Vested
|
(132,455 | ) | $ | 4.32 | ||||
|
Canceled
|
(93,282 | ) | $ | 5.28 | ||||
|
Balance
December 31, 2009
|
745,760 | $ | 3.24 |
1.1
years
|
||||
As of
December 31, 2009, there was $0.6 million of unrecognized compensation
expense related to unvested restricted stock awards. That expense is
expected to be recognized over a weighted average period of 1.1 years. The
total grant date fair market value of awards vested during the years ended
December 31, 2009, 2008 and 2007 was $0.6 million, $1.1 million
and $0.6 million, respectively. The total intrinsic value of
restricted stock awards vested during the years December 31, 2009, 2008 and 2007
was $0.5 million, $2.3 million and $3.9 million, respectively.
Performance
Units
Under the
2008 Plan, the Compensation Committee may grant performance units to key
employees. The Compensation Committee will establish the terms and conditions of
any performance units granted, including the performance goals, the performance
period and the value for each performance unit. If the performance goals are
satisfied, the Company would pay the key employee an amount in cash equal to the
value of each performance unit at the time of payment. In no event may a key
employee receive an amount in excess of $1.0 million with respect to performance
units for any given year. To date, no performance units have been granted under
the 2008 Plan.
NOTE 12 —
DEFERRED COMPENSATION PLANS
The
Company maintains a deferred compensation plan under Section 401(k) of the
Internal Revenue Code. Under the Plan, employees may elect to defer up to 50% of
their salary, subject to Internal Revenue Service limits. The Company may make a
discretionary matching contribution. The Company recorded matching contributions
in selling, general and administrative expenses of $1.1 million,
$0.9 million and $1.0 million in the years ended December 31,
2009, 2008, and 2007, respectively.
In 2008
the Company entered into a deferred compensation agreement with its Chief
Executive Officer to provide certain retirement benefits. These
benefits are earned over the period of his employment contract. The
Company recorded $0.5 million and $0.3 million of compensation expense for the
years ended December 31, 2009 and 2008, respectively.
NOTE 13 —
SELECTED QUARTERLY FINANCIAL DATA (UNAUDITED)
A summary
of quarterly financial information for fiscal 2009 and 2008 is as follows (in
thousands except per share data):
|
First
Quarter
|
Second
Quarter
|
Third
Quarter
|
Fourth
Quarter
|
||||||||||
|
2009:
|
|||||||||||||
|
Revenue
|
$ | 325,749 | $ | 328,749 | $ | 333,476 | $ | 341,551 | |||||
|
Gross
profit
|
$ | 35,990 | $ | 38,388 | $ | 41,496 | $ | 41,948 | |||||
|
Net
income (1)
|
$ | 3,285 | $ | 4,377 | $ | 5,747 | $ | 40,690 | |||||
|
Basic
income per share
|
$ | 0.08 | $ | 0.11 | $ | 0.15 | $ | 1.03 | |||||
|
Diluted
income per share
|
$ | 0.08 | $ | 0.11 | $ | 0.14 | $ | 0.99 | |||||
|
2008:
|
|||||||||||||
|
Revenue
|
$ | 327,471 | $ | 348,440 | $ | 359,427 | $ | 366,573 | |||||
|
Gross
profit
|
$ | 32,372 | $ | 35,726 | $ | 36,081 | $ | 37,991 | |||||
|
Net
(loss) income (2)
|
$ | (477 | ) | $ | 1,619 | $ | 1,410 | $ | (76,584 | ) | |||
|
Basic
(loss) income per share
|
$ | (0.01 | ) | $ | 0.04 | $ | 0.04 | $ | (1.98 | ) | |||
|
Diluted
(loss) income per share
|
$ | (0.01 | ) | $ | 0.04 | $ | 0.04 | $ | (1.98 | ) | |||
__________________________
|
(1)
|
The
fourth quarter of 2009 includes $41.8 million tax benefit due
primarily to the reversal of the valuation allowance on deferred tax
assets, the expiration of statute of limitation on certain state
liabilities and an NOL carry back claim.
|
|
(2)
|
The
fourth quarter of 2008 includes $93.9 million goodwill and intangible
impairment.
|
NOTE 14 —
SUBSEQUENT EVENTS
Pending
Acquisition
On
January 24, 2010, the Company entered into an Agreement and Plan of Merger to
acquire Critical Homecare Solutions Holdings, Inc. (“CHS”). CHS is a
privately held company that is a leading provider of home infusion and home
nursing services and products to patients suffering from chronic and acute
medical conditions. Completion of the acquisition is subject to
stockholders approval of the issuance of additional shares of the Company’s
common stock to CHS stockholders and satisfaction of certain other customary
conditions. The acquisition is expected to close on or about March
31, 2010.
If the
merger is completed, the Company will:
|
|
·
|
Repay
the net indebtedness of CHS, which is approximately $132.0 million at
December 31, 2009, and enter into a new credit
facility;
|
|
|
·
|
Pay
cash consideration of $110.0 million, subject to
adjustment;
|
|
|
·
|
Issue
up to approximately 12.9 million shares of BioScrip common stock, subject
to adjustment, of which 2,696,516 shares initially will be held in escrow
to fund indemnification payments, if any;
and
|
|
|
·
|
Issue
warrants to acquire approximately 3.4 million shares of BioScrip common
stock, exercisable at $10.00 per share and having a five-year
term.
|
In order
to fund the payment of the cash consideration required to be paid for the
acquisition of CHS, refinance the Company's existing indebtedness and
repay the existing indebtedness of CHS, the Company has entered into a
commitment letter with Jefferies, pursuant to which Jefferies has committed to
provide BioScrip with $375.0 million in debt financing, comprised of $150.0
million senior credit facilities and $225.0 million in other
indebtedness.
None.
Evaluation
of Disclosure Controls and Procedures
As of the
end of the period covered by this Annual Report, we evaluated the effectiveness
of the design and operation of our disclosure controls. This evaluation was
performed under the supervision and with the participation of management
including our Chief Executive Officer (“CEO”) and Chief Financial Officer
(“CFO”). Disclosure controls are controls and procedures (as defined in the
Exchange Act Rules 13d-15(e) and 15d-15(e)) designed to reasonably assure
that information required to be disclosed in our reports filed under the
Exchange Act, such as this Annual Report, is recorded, processed, summarized and
reported within the time periods specified in the SEC’s rules and forms.
Disclosure controls are also designed to reasonably assure that such information
is accumulated and communicated to our management, including the CEO and CFO, as
appropriate, to allow timely decisions regarding required
disclosure.
The
evaluation of our disclosure controls included a review of the controls
objectives and design, our implementation of the controls and the effect of the
controls on the information generated for use in this Annual Report. Based upon
the controls evaluation, our CEO and CFO have concluded that our disclosure
controls as of December 31, 2009 were effective.
Management
Report on Internal Control over Financial Reporting
Our
management is responsible for establishing and maintaining adequate internal
control over financial reporting. Internal control over financial reporting is a
process designed by, or under the supervision of, our CEO and CFO, and effected
by our Board, management, and other personnel, to provide reasonable assurance
regarding the reliability of financial reporting and the preparation of
financial statements for external purposes in accordance with generally accepted
accounting principles and includes those policies and procedures
that:
|
|
•
|
Pertain
to the maintenance of records that in reasonable detail accurately and
fairly reflect the Company’s financial
transactions;
|
|
|
•
|
Provide
reasonable assurance that transactions are recorded as necessary to permit
preparation of financial statements in accordance with generally accepted
accounting principles, and that our revenues and expenditures are being
made only in accordance with authorizations of our management and
directors; and
|
|
|
•
|
Provide
reasonable assurance regarding the prevention or timely detection of
unauthorized acquisition, use or disposition of our assets that could have
a material effect on our financial
statements.
|
Management
assessed our internal control over financial reporting as of December 31,
2009, the end of our fiscal year. Management based its assessment on criteria
established in Internal Control — Integrated Framework issued by the
Committee of Sponsoring Organizations of the Treadway Commission. Management’s
assessment included an evaluation of such elements as the design and operating
effectiveness of key financial reporting controls, process documentation,
accounting policies, and our overall control environment.
Based on
management’s assessment of internal control over financial reporting our
management believes that as of December 31, 2009, our internal control over
financial reporting was effective. Our independent registered public
accounting firm, Ernst & Young LLP, has issued an attestation report on
the Company’s internal control over financial reporting which is included
herein.
Inherent
Limitations on Control Systems
Because
of the inherent limitations in all control systems, no evaluation of controls
can provide absolute assurance that all control issues and instances of fraud,
if any, will be or have been detected. These inherent limitations include the
realities that judgments in decision-making can be faulty, and that breakdowns
can occur because of simple error or mistake. Additionally, controls can be
circumvented by the individual acts of some persons, by collusion of two or more
people, or by management override of the control. The design of any system of
controls also is based in part upon certain assumptions about the likelihood of
future events, and there can be no assurance that any design will succeed in
achieving its stated goals under all potential future conditions; over time,
control may become
inadequate because of changes in conditions, or the degree of compliance with
the policies or procedures may deteriorate.
Changes
in Internal Control over Financial Reporting
During
the fiscal year ended December 31, 2009, there was no change in our internal
control over financial reporting that has materially affected, or is reasonably
likely to materially affect, our internal control over financial
reporting.
Report
of Independent Registered Public Accounting Firm
The Board
of Directors and Stockholders
BioScrip,
Inc.
We have
audited BioScrip, Inc.’s internal control over financial reporting as of
December 31, 2009, based on criteria established in Internal Control—Integrated
Framework issued by the Committee of Sponsoring Organizations of the
Treadway Commission (the COSO criteria). BioScrip, Inc.’s management is
responsible for maintaining effective internal control over financial reporting
and for its assessment of the effectiveness of internal control over financial
reporting included in the accompanying Management Report on Internal Control
Over Financial Reporting. Our responsibility is to express an opinion on the
Company’s internal control over financial reporting based on our
audit.
We
conducted our audit in accordance with the standards of the Public Company
Accounting Oversight Board (United States). Those standards require that we plan
and perform the audit to obtain reasonable assurance about whether effective
internal control over financial reporting was maintained in all material
respects. Our audit included obtaining an understanding of internal control over
financial reporting, assessing the risk that a material weakness exists, testing
and evaluating the design and operating effectiveness of internal control based
on the assessed risk, and performing such other procedures as we considered
necessary in the circumstances. We believe that our audit provides a reasonable
basis for our opinion.
A
company’s internal control over financial reporting is a process designed to
provide reasonable assurance regarding the reliability of financial reporting
and the preparation of financial statements for external purposes in accordance
with generally accepted accounting principles. A company’s internal control over
financial reporting includes those policies and procedures that (1) pertain to
the maintenance of records that, in reasonable detail, accurately and fairly
reflect the transactions and dispositions of the assets of the company; (2)
provide reasonable assurance that transactions are recorded as necessary to
permit preparation of financial statements in accordance with generally accepted
accounting principles and that receipts and expenditures of the company are
being made only in accordance with authorizations of management and directors of
the company; and (3) provide reasonable assurance regarding prevention or timely
detection of unauthorized acquisition, use or disposition of the company’s
assets that could have a material effect on the financial
statements.
Because
of its inherent limitations, internal control over financial reporting may not
prevent or detect misstatements. Also, projections of any evaluation
of effectiveness to future periods are subject to the risk that controls may
become inadequate because of changes in conditions, or that the degree of
compliance with the policies or procedures may deteriorate.
In our
opinion, BioScrip, Inc. maintained, in all material respects, effective internal
control over financial reporting as of December 31, 2009, based on the COSO criteria.
We also
have audited, in accordance with the standards of the Public Company Accounting
Oversight Board (United States), the consolidated balance sheets of BioScrip,
Inc. and subsidiaries as of December 31, 2009 and 2008, and the related
consolidated statements of operations, stockholders’ equity, and cash flows for
each of the three years in the period ended December 31, 2009 of BioScrip, Inc.
and our report dated March 2, 2010, expressed an unqualified opinion
thereon.
|
Minneapolis,
Minnesota
|
/s/
Ernst & Young LLP
|
|
March
2, 2010
|
None.
|
Directors,
Executive Officers and Corporate
Governance
|
The information required by this item is incorporated by
reference from the information contained in our definitive proxy statement to be
filed with the SEC on or before April 30, 2010 in connection with our 2010
Annual Meeting of Stockholders.
|
Executive
Compensation
|
The information required by this item is incorporated by
reference from the information contained in our definitive proxy statement to be
filed with the SEC on or before April 30, 2010 in connection with our 2010
Annual Meeting of Stockholders.
|
Security
Ownership of Certain Beneficial Owners and Management and Related
Stockholder Matters
|
The information required by this item is incorporated by
reference from the information contained in our definitive proxy statement to be
filed with the SEC on or before April 30, 2010 in connection with our 2010
Annual Meeting of Stockholders.
|
Certain
Relationships and Related Transactions, and Director
Independence
|
The information required by this item is incorporated by
reference from the information contained in our definitive proxy statement to be
filed with the SEC on or before April 30, 2010 in connection with our 2010
Annual Meeting of Stockholders.
| Item 14. | Principal Accountant Fees and Services |
The information required by this item is incorporated by
reference from the information contained in our definitive proxy statement to be
filed with the SEC on or before April 30, 2010 in connection with our 2010
Annual Meeting of Stockholders.
| Item 15. | Exhibits, Financial Statement Schedules and Reports on Form 8-K |
All other
schedules not listed above have been omitted since they are not applicable or
are not required.
|
Exhibit
Number
|
Description
|
|
Location
|
|
|
2.1
|
Agreement
and Plan of Merger, dated as of August 9, 2004, among MIM
Corporation, Chronimed Acquisition Corp. and Chronimed
Inc.
|
|
(1)
(Exhibit 99.2)
|
|
|
2.2
|
Amendment
No. 1 dated January 3, 2005 to Agreement and Plan of Merger
dated August 9, 2004 by and among MIM Corporation, Chronimed
Acquisition Corp. and Chronimed Inc.
|
|
(2) (Exhibit 10.1) | |
|
2.3
|
Agreement
and Plan of Merger, dated as of January 24, 2010, by and among
BioScrip, Inc., Camelot Acquisition Corp., Critical Homecare Solutions
Holdings, Inc., Kohlberg Investors V, L.P., Kohlberg Partners V, L.P.,
Kohlberg Offshore Investors V, L.P., Kohlberg TE Investors V, L.P., KOCO
Investors V, L.P., Robert Cucuel, Mary Jane Graves, Nitin Patel, Joey
Ryan, Blackstone Mezzanine Partners II L.P., Blackstone Mezzanine Holdings
II L.P., and S.A.C. Domestic Capital Funding, Ltd.
|
|
(3) (Exhibit 2.1) | |
|
3.1
|
Second
Amended and Restated Certificate of Incorporation.
|
|
(4) (Exhibit 4.1) | |
|
3.2
|
Amended
and Restated By-Laws.
|
|
(5)
(Exhibit 3.1)
|
|
|
4.1
|
Specimen
Common Stock Certificate.
|
|
(6)
(Exhibit 4.1)
|
|
|
4.2
|
Amended
and Restated Rights Agreement, dated as of December 3, 2002 between
the Company and American Stock Transfer and Trust Company, as Rights
Agent.
|
|
(7)
(Exhibit 4.2)
|
|
|
4.3
|
First
Amendment, dated December 13, 2006, to the Amended and Restated
Rights Agreement, dated as of December 3, 2002 (the “Rights
Agreement”), between the Company and American Stock Transfer &
Trust Company, as Rights Agent.
|
|
(8)
(Exhibit 4.3)
|
|
|
4.4
|
Second
Amendment, dated March 4, 2009, to the Rights Agreement, as amended on
December 13, 2006, between the Company and American Stock Transfer &
Trust Company, as Rights Agent.
|
|
(9)
(Exhibit 4.4)
|
|
|
4.5
|
Third
Amendment, dated as of January 24, 2010, to the Rights Agreement, as
amended on December 13, 2006 and March 4, 2009, between the Company and
American Stock Transfer & Trust Company LLC, as Rights Agent, as
amended on December 13, 2006 and March 4, 2009.
|
|
(3)
(Exhibit 4.1)
|
|
|
10.1
|
Amended
and Restated 1996 Incentive Stock Plan**
|
|
(10)
|
|
|
10.2
|
Amended
and Restated 1996 Non-Employee Director’s Stock Incentive
Plan**
|
|
(11) | |
|
10.3
|
Amended
and Restated 2001 Incentive Stock Plan**
|
|
(12) | |
|
10.4
|
2008
Equity Incentive Plan**
|
|
(13) | |
|
10.5
|
Employment
Letter, dated October 15, 2001, between the Company and
Russell J. Corvese**
|
|
(13)
(Exhibit 10.51)
|
|
|
10.6
|
Amendment,
dated September 19, 2003, to Employment Letter Agreement between the
Company and Russel J. Corvese**
|
|
(14)
(Exhibit 10.46)
|
|
|
10.7
|
Amendment,
dated December 1, 2004, to Employment Letter Agreement between the
Company and Russel J. Corvese**
|
|
(15)
(Exhibit 10.1)
|
|
|
10.8
|
Separation
Agreement between BioScrip, Inc. and Henry F.
Blissenbach**
|
|
(16)
(Exhibit 99.1)
|
|
|
10.9
|
Severance
Letter Agreement, dated August 17, 2006, between the Company and Brian
Reagan**
|
|
(17)
(Exhibit 10.1)
|
|
|
10.10
|
Severance
Agreement, dated August 24, 2006, between BioScrip, Inc. and
Barry A. Posner**
|
|
(18)
(Exhibit 10.1)
|
| 10.11 | Severance Agreement, dated August 2, 2007 between BioScrip, Inc. and Stanley G. Rosenbaum** | (19) (Exhibit 10.1) | ||
|
10.12
|
Amended
and Restated Loan and Security Agreement, dated as of September 26, 2007,
among MIM Funding, LLC, BioScrip Pharmacy Services, Inc., BioScrip
Infusion Services, Inc., BioScrip Pharmacy (NY), Inc., BioScrip PBM
Services, LLC, BioScrip Pharmacy, Inc., Natural Living, Inc., and BioScrip
Infusion Services, LLC as Borrowers, and HFG Healthco-4 LLC, as
Lender
|
(20)
(Exhibit 10.15)
|
||
|
10.13
|
Amended
and Restated Pledge Agreement, dated as of November 1, 2007 among
BioScrip, Inc., Chronimed Inc., MIM Funding, LLC, BioScrip Pharmacy
Services, Inc., BioScrip Infusion Services, Inc., BioScrip Pharmacy (NY),
Inc., BioScrip PBM Services, LLC, BioScrip Pharmacy, Inc., Natural Living,
Inc., and BioScrip Infusion Services, LLC, and HFG Healthco-4
LLC,
|
(21)
(Exhibit 10.16)
|
||
|
10.14
|
Amended
and Restated Guaranty, effective as of October 1, 2007, by BioScrip, Inc.
and Chronimed, Inc. in favor of HFG Healthco-4 LLC
|
(21)
(Exhibit 10.17)
|
||
|
10.15
|
Refinancing
Arrangements Agreement among BioScrip Pharmacy Services, Inc., BioScrip
Infusion Services, Inc., BioScrip Pharmacy (NY), Inc., BioScrip PBM
Services, LLC, BioScrip Pharmacy, Inc., Natural Living, Inc., BioScrip
Infusion Services, LLC and MIM Funding, LLC
|
(21)
(Exhibit 10.18)
|
||
|
10.16
|
First
Amendment to the Amended and Restated Loan and Security Agreement, dated
as of September 26, 2007, among, MIM Funding, LLC, BioScrip Pharmacy
Services, Inc., BioScrip Infusion Services, Inc., BioScrip Pharmacy (NY),
Inc., BioScrip PBM Services, LLC, BioScrip Pharmacy, Inc., Natural Living,
Inc., and BioScrip Infusion Services, LLC as Borrowers, and HFG Healthco-4
LLC, as Lender.
|
(22)
(Exhibit 10.1)
|
||
|
10.17
|
Second
Amendment to the Amended and Restated Loan and Security Agreement, dated
as of September 26, 2007, among, MIM Funding, LLC, BioScrip Pharmacy
Services, Inc., BioScrip Infusion Services, Inc., BioScrip Pharmacy (NY),
Inc., BioScrip PBM Services, LLC, BioScrip Pharmacy, Inc., Natural Living,
Inc., and BioScrip Infusion Services, LLC as Borrowers, and HFG Healthco-4
LLC, as Lender.
|
(23)
(Exhibit 10.1)
|
||
|
10.18
|
Third
Amendment to the Amended and Restated Loan and Security Agreement, dated
as of September 26, 2007, among, MIM Funding, LLC, BioScrip Pharmacy
Services, Inc., BioScrip Infusion Services, Inc., BioScrip Pharmacy (NY),
Inc., BioScrip PBM Services, LLC, BioScrip Pharmacy, Inc., Natural Living,
Inc., and BioScrip Infusion Services, LLC as Borrowers, and HFG Healthco-4
LLC, as Lender.
|
(24)
(Exhibit 10.1)
|
||
|
10.19
|
Employment
Agreement dated May 30, 2008, by and between BioScrip, Inc. and
Richard H. Friedman.**
|
(25)
(Exhibit 10.1)
|
||
|
10.20
|
Employment
Letter Agreement dated November 13, 2008 between BioScrip, Inc. and
Richard M. Smith.**
|
(26)
(Exhibit 10.1)
|
||
|
10.21
|
Severance
Agreement dated November 13, 2008 between BioScrip, Inc. and Richard M.
Smith.**
|
(26)
(Exhibit 10.2)
|
||
|
10.22
|
Amendment
No. 1 to Severance Agreement between BioScrip, Inc. and Stanley G.
Rosenbaum.**
|
(27)
|
||
|
10.23
|
Amendment
No. 1 to Severance Agreement between BioScrip, Inc. and Barry A.
Posner.**
|
(27)
|
||
|
10.24
|
(28)
(Exhibit 10.1)
|
|||
|
10.25
|
Cash
Collateral Agreement dated July 8, 2009.
|
(28)
(Exhibit 10.2)
|
||
|
10.26
|
Employment
Letter Agreement, dated August 21, 2003, between MIM Corporation (now
BioScrip, Inc.) and Scott Friedman.**
|
(29)
(Exhibit 10.1)
|
||
|
10.27
|
Amendment,
dated October 14, 2004, to Employment Letter Agreement between MIM
Corporation (now BioScrip, Inc.) and Scott Friedman.**
|
(29)
(Exhibit 10.2)
|
||
|
10.28
|
Prime
Vendor Agreement dated as of July 1, 2009 between AmerisourceBergen Drug
Corporation and the Company.
|
(30)
(Exhibit 10.1)
|
||
|
10.29
|
Fourth
Amendment to the Amended and Restated Loan and Security Agreement, dated
as of September 26, 2007, among, MIM Funding, LLC, BioScrip Pharmacy
Services, Inc., BioScrip Infusion Services, Inc., BioScrip Pharmacy (NY),
Inc., BioScrip PBM Services, LLC, BioScrip Pharmacy, Inc., Natural Living,
Inc., and BioScrip Infusion Services, LLC as Borrowers, and HFG Healthco-4
LLC, as Lender.
|
(31)
(Exhibit 10.1)
|
||
|
10.30
|
Stockholders’
Agreement, dated as of January 24, 2010, by and among BioScrip, Inc.,
Kohlberg Investors V, L.P., Kohlberg Partners V, L.P., Kohlberg Offshore
Investors V, L.P., Kohlberg TE Investors V, L.P., KOCO Investors V, L.P.,
Robert Cucuel, Mary Jane Graves, Nitin Patel, Joey Ryan, Colleen Lederer,
Blackstone Mezzanine Partners II L.P., Blackstone Mezzanine Holdings II
L.P., and S.A.C. Domestic Capital Funding, Ltd.
|
(3)
(Exhibit 10.1)
|
||
|
21.1
|
List
of Subsidiaries.
|
*
|
||
|
23.1
|
Consent
of Ernst and Young LLP.
|
*
|
||
|
31.1
|
Certification
of Richard H. Friedman pursuant to 18 U.S.C. Section 1350, as
adopted pursuant to Section 302 of the Sarbanes-Oxley Act of
2002.
|
*
|
||
|
31.2
|
Certification
of Stanley G. Rosenbaum pursuant to 18 U.S.C. Section 1350, as
adopted pursuant to Section 302 of the Sarbanes-Oxley Act of
2002.
|
*
|
||
|
32.1
|
Certification
of Richard H. Friedman pursuant to 18 U.S. C. Section 1350, as
adopted pursuant to Section 906 of the Sarbanes-Oxley Act of
2002.
|
*
|
||
|
32.2
|
Certification
of Stanley G. Rosenbaum pursuant to 18 U.S. C. Section 1350, as
adopted pursuant to Section 906 of the Sarbanes-Oxley Act of
2002.
|
*
|
|
(1)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on August 9, 2004., SEC Accession No.
0001089355-04-000197.
|
|
(2)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on January 5, 2005, SEC Accession No.
0001014739-05-000007.
|
|
(3)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on January 27, 2010, SEC Accession No.
0000950123-10-005446.
|
|
(4)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on March 17, 2005, SEC Accession No.
0000950123-05-003294.
|
|
(5)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on July 30, 2009, SEC Accession no.
0001014739-09-000029.
|
|
(6)
|
Incorporated
by reference to the indicated exhibit to the Company’s Annual Report on
Form 10-K for the fiscal year ended December 31, 2005 filed with
the SEC on March 31, 2006, SEC Accession no.
0000950123-06-004022.
|
|
(7)
|
Incorporated
by reference to Post-Effective Amendment No. 3 to the Company’s form 8-A/A
dated December 4, 2002.
|
|
(8)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on December 14, 2006, SEC Accession No.
0000950123-06-0155184.
|
|
(9)
|
Incorporated
by reference to Exhibit 10.1 to the Company’s Current Report on Form 8-K
filed with the SEC on March 4, 2009, Accession No.
0001014739-09-000006.
|
|
(10)
|
Incorporated
by reference from the Company’s definitive proxy statement for its 1999
annual meeting of stockholders filed with the Commission July 7,
1999.
|
|
(11)
|
Incorporated
by reference from the Company’s definitive proxy statement for its 2002
annual meeting of stockholders filed with the Commission April 30,
2002.
|
|
(12)
|
Incorporated
by reference from the Company’s definitive proxy statement for its 2003
annual meeting of stockholders filed with the Commission April 30,
2003.
|
|
(13)
|
Incorporated
by reference from the Company’s definitive proxy statement for its 2008
annual meeting of stockholders filed with the Commission March 21,
2008.
|
|
(14)
|
Incorporated
by reference to the indicated exhibit to the Company’s Annual Report on
Form 10-K for the fiscal year ended December 31, 2001, SEC
Accession No. 0001089355-02-000248.
|
|
(14)
|
Incorporated
by reference to the indicated exhibit to the Company’s
Annual Report on Form 10-K filed on for the fiscal year
ended December 31, 2003, filed March 15, 2004, SEC Accession No.
001014739-04-000021.
|
|
(16)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on December 1, 2004, SEC Accession No.
0001014739-04-000082.
|
|
(17)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on March 1, 2006, SEC Accession No.
0000950123-06-002440.
|
|
(18)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on August 21, 2006, SEC Accession No.
0000950123-06-010723.
|
|
(19)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on August 25, 2006, SEC Accession No.
0000950123-06-010904.
|
|
(20)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on August 3, 2007, SEC Accession No.
0000950123-07-010803.
|
|
(21)
|
Incorporated
by reference to the indicated exhibit to the Company’s
Annual Report on Form 10-K filed on for the fiscal year
ended December 31, 2008, filed March 7, 2008, SEC Accession No.
0000950123-08-002707.
|
|
(22)
|
Incorporated
by reference to the indicated exhibit to the Company’s Quarterly Report on
Form 10-Q for the quarter ended March 31, 2008, SEC Accession No.
0000950123-08-005203.
|
|
(23)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on September 4, 2008, SEC Accession No.
0000950123-08-010551.
|
|
(24)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on August 14, 2008, SEC Accession No.
0000950123-08-009594.
|
|
(25)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on June 3, 2008, SEC Accession No.
0000950123-08-006507.
|
|
(26)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on November 24, 2008 SEC Accession No.
0000950123-08-016150.
|
|
(27)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on January 20, 2009 SEC Accession No.
0000950123-09-000854.
|
|
(28)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on July 9, 2009 SEC Accession No.
0001014739-09-000023.
|
|
(29)
|
Incorporated
by reference to the indicated exhibit to the Company’s Quarterly Report on
Form 10-Q for the quarter ended June 30, 2009, SEC Accession No.
0001014739-09-000031.
|
|
(30)
|
Incorporated
by reference to the indicated exhibit to the Company’s Amended Quarterly
Report on Form 10-Q/A for the quarter ended September 30, 2009,
SEC Accession No.
0001014739-09-000048.
|
|
(31)
|
Incorporated
by reference to the indicated exhibit to the Company’s Current Report on
Form 8-K filed on December 31, 2009 SEC Accession No.
0001014739-09-000050.
|
* Filed
with this Annual Report on Form 10-K.
** Designate
the Company’s management contracts or compensatory plan or arrangement to be
filed herewith.
Pursuant
to the requirements of Section 13 or 15(d) of the Securities Exchange Act
of 1934, the registrant has duly caused this report to be signed on its behalf
by the undersigned, thereunto duly authorized, on March 2,
2010.
| BIOSCRIP INC. | |
| /s/ Stanley G. Rosenbaum | |
|
Chief
Financial Officer and Treasurer,
|
|
| Principal Accounting Officer and | |
|
Principal
Financial Officer
|
Pursuant
to the requirements of the Securities Exchange Act of 1934, this report has been
signed below by the following persons on behalf of the registrant and in the
capacities and on the dates indicated.
|
Signature
|
Title(s)
|
Date
|
|
/s/
Richard H.
Friedman
Richard
H. Friedman
|
Chairman
of the Board and Chief Executive Officer (Principal Executive
Officer)
|
March 2,
2010
|
|
/s/ Stanley G.
Rosenbaum
Stanley
G. Rosenbaum
|
Chief
Financial Officer and Treasurer
(Principal
Financial Officer and Principal Accounting Officer)
|
March 2,
2010
|
|
/s/ Richard M.
Smith
Richard
M. Smith
|
President
and Chief Operating Officer
Director
|
March 2,
2010
|
|
/s/ Charlotte W.
Collins
Charlotte
W. Collins
|
Director
|
March 2,
2010
|
|
/s/ Louis T.
DiFazio
Louis
T. DiFazio, Ph.D.
|
Director
|
March 2,
2010
|
|
/s/ Myron Z.
Holubiak
Myron
Z. Holubiak
|
Director
|
March 2,
2010
|
|
/s/ David R.
Hubers
David
R. Hubers
|
Director
|
March 2,
2010
|
|
/s/ Richard L.
Robbins
Richard
L. Robbins
|
Director
|
March 2,
2010
|
|
/s/ Stuart A.
Samuels
Stuart
A. Samuels
|
Director
|
March 2,
2010
|
Bioscrip,
Inc. and Subsidiaries
(in
thousands)
|
Balance
at
|
Write-Off
|
Charged
to
|
|||||||||||
|
Beginning
of
|
of
|
Costs
|
Balance
at
|
||||||||||
|
Period
|
Receivables
|
and
Expenses
|
End
of Period
|
||||||||||
|
Year
ended December 31, 2007
|
|||||||||||||
|
Accounts
receivable
|
$ | 13,774 | $ | (6,810 | ) | $ | 5,119 | $ | 12,083 | ||||
|
Year
ended December 31, 2008
|
|||||||||||||
|
Accounts
receivable
|
$ | 12,083 | $ | (5,121 | ) | $ | 4,667 | $ | 11,629 | ||||
|
Year
ended December 31, 2009
|
|||||||||||||
|
Accounts
receivable
|
$ | 11,629 | $ | (8,761 | ) | $ | 8,636 | $ | 11,504 | ||||
EXHIBIT INDEX
(Exhibits being filed with this Annual Report on
Form 10-K)
