Attached files
Table of Contents
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, DC 20549
Form 10-K
| x | Annual report pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 |
| for the fiscal year ended December 31, 2009 |
OR
| ¨ | Transition report pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 |
| for the transition period from to |
Commission File Number 1-7293
TENET HEALTHCARE CORPORATION
(Exact name of Registrant as specified in its charter)
| Nevada | 95-2557091 | |
| (State of Incorporation) | (IRS Employer Identification No.) |
1445 Ross Avenue, Suite 1400
Dallas, TX 75202
(Address of principal executive offices, including zip code)
(469) 893-2200
(Registrant’s telephone number, including area code)
Securities registered pursuant to Section 12(b) of the Act:
| Title of each class |
Name of each exchange on which registered | |
| Common stock | New York Stock Exchange | |
| 6 3/8% Senior Notes due 2011 | New York Stock Exchange | |
| 6 1/2% Senior Notes due 2012 | New York Stock Exchange | |
| 7 3/8% Senior Notes due 2013 | New York Stock Exchange | |
| 9 7/8% Senior Notes due 2014 | New York Stock Exchange | |
| 9 1/4% Senior Notes due 2015 | New York Stock Exchange | |
| 6 7/8% Senior Notes due 2031 | New York Stock Exchange |
Indicate by check mark if the Registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes x No ¨
Indicate by check mark if the Registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. ¨
Indicate by check mark whether the Registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months, and (2) has been subject to such filing requirements for the past 90 days. Yes x No ¨
Indicate by check mark whether the Registrant has submitted electronically and posted on its corporate website every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the Registrant was required to submit and post such files). Yes ¨ No ¨
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of the Registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. ¨
Indicate by check mark whether the Registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer or a smaller reporting company (as defined in Exchange Act Rule 12b-2).
| Large accelerated filer x | Accelerated filer ¨ | Non-accelerated filer ¨ | Smaller reporting company ¨ |
Indicate by check mark whether the Registrant is a shell company (as defined in Exchange Act Rule 12b-2). Yes ¨ No x
As of June 30, 2009, there were 480,816,199 shares of common stock, $0.05 par value, outstanding. The aggregate market value of the shares of common stock held by non-affiliates of the Registrant as of June 30, 2009, based on the closing price of the Registrant’s shares on the New York Stock Exchange on that day, was approximately $1,116,922,242. For the purpose of the foregoing calculation only, all directors and the executive officers who were SEC reporting persons of the Registrant as of June 30, 2009 have been deemed affiliates. As of January 29, 2010, there were 481,148,392 shares of common stock outstanding.
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the Registrant’s definitive proxy statement for the 2010 annual meeting of shareholders are incorporated by reference into Part III of this Form 10-K.
Table of Contents
| Page | ||||
| PART I |
||||
| Item 1. |
1 | |||
| Item 1A. |
15 | |||
| Item 1B. |
19 | |||
| Item 2. |
19 | |||
| Item 3. |
20 | |||
| Item 4. |
21 | |||
| PART II |
||||
| Item 5. |
22 | |||
| Item 6. |
24 | |||
| Item 7. |
Management’s Discussion and Analysis of Financial Condition and Results of Operations |
25 | ||
| Item 7A. |
77 | |||
| Item 8. |
78 | |||
| 81 | ||||
| 86 | ||||
| 118 | ||||
| Item 9. |
Changes in and Disagreements with Accountants on Accounting and Financial Disclosure |
119 | ||
| Item 9A. |
119 | |||
| Item 9B. |
119 | |||
| PART III |
||||
| Item 10. |
120 | |||
| Item 11. |
120 | |||
| Item 12. |
Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
120 | ||
| Item 13. |
Certain Relationships and Related Transactions, and Director Independence |
120 | ||
| Item 14. |
120 | |||
| PART IV |
||||
| Item 15. |
121 | |||
Table of Contents
PART I.
| ITEM 1. | BUSINESS |
DESCRIPTION OF BUSINESS
Tenet Healthcare Corporation is an investor-owned health care services company whose subsidiaries and affiliates principally operate general hospitals and related ancillary health care businesses. All of Tenet’s operations are conducted through its subsidiaries. (Unless the context otherwise requires, Tenet and its subsidiaries are referred to herein as “Tenet,” the “Company,” “we” or “us.”) At December 31, 2009, our subsidiaries operated 50 general hospitals (including one hospital not yet divested at that date that is classified in discontinued operations in our Consolidated Financial Statements) and a critical access hospital, with a combined total of 13,601 licensed beds, serving urban and rural communities in 12 states. Of those general hospitals, 45 were owned by our subsidiaries and five were owned by third parties and leased by our subsidiaries.
At December 31, 2009, our subsidiaries also operated various related health care facilities, including a long-term acute care hospital, outpatient surgery centers, diagnostic imaging centers, occupational and rural health care clinics, and a number of medical office buildings (all of which are located on, or nearby, one of our general hospital campuses). In addition, our subsidiaries operated physician practices and captive insurance companies and owned an interest in a health maintenance organization, all of which comprise a minor portion of our business.
Our hospitals and related health care facilities are committed to providing high quality care to patients in the communities we serve. To accomplish this mission in the complex and competitive health care industry, our operating strategies are to (1) identify best practices in evidence-based medicine and implement those best practices in all of our hospitals, (2) maintain high standards of ethics and compliance, (3) improve operating efficiencies and control operating costs while maintaining or improving the quality of care provided, (4) improve patient, physician and employee satisfaction, (5) improve recruitment and retention of physicians, as well as nurses and other employees, (6) increase collections of accounts receivable and increase cash flow to fund improvements at our hospitals, and (7) build or acquire new, or divest existing, facilities as market conditions, operational goals and other considerations warrant. We adjust these strategies as necessary in response to changes in the economic and regulatory climates in which we operate and the success or failure of our various efforts.
OPERATIONS
Our continuing operations are structured as follows:
| • | Our California region includes all of our hospitals in California, as well as our hospital in Nebraska; |
| • | Our Central region includes all of our hospitals in Missouri, Tennessee and Texas; |
| • | Our Florida region includes all of our hospitals in Florida; |
| • | Our Southern States region includes all of our hospitals in Alabama, Georgia, North Carolina and South Carolina; and |
| • | Our two hospitals in Philadelphia, Pennsylvania are part of a separate market. |
Each of the regions and the market described above report directly to our chief operating officer. Major decisions, including capital resource allocations, are made at the corporate level, not at the regional or hospital level.
We seek to operate our hospitals in a manner that positions them to compete effectively in an evolving health care environment. To that end, we sometimes decide to sell, consolidate or close certain facilities in order to eliminate duplicate services or excess capacity, or because of changing market conditions. Of the three general hospitals and one cancer hospital that were classified as “held for sale” at December 31, 2008, we completed the sale of USC University Hospital and USC Kenneth Norris Jr. Cancer Hospital on March 31, 2009. In addition, we closed Irvine Regional Hospital and Medical Center in January 2009 before the expiration of our lease in February 2009, and we closed Community Hospital of Los Gatos and terminated our lease in April 2009. In May 2009, we announced that we would not renew our operating lease agreement for NorthShore Regional Medical Center, located in Slidell, Louisiana, which lease expires in May 2010. Accordingly, the hospital was reclassified into discontinued operations in the three months ended June 30, 2009. In January 2010, we entered into a definitive agreement to sell certain of our owned assets associated with NorthShore and transition the operation of the hospital to a new hospital operator. We anticipate that the transaction will close effective April 1, 2010, at which time we will terminate our lease of the hospital.
Table of Contents
From time to time, we build new hospitals, make strategic acquisitions of hospitals and other health care facilities, and enter into partnerships or affiliations with related health care businesses. Our newly constructed 140-bed replacement hospital for East Cooper Regional Medical Center in Mt. Pleasant, South Carolina is expected to open in April 2010. In addition, we are seeking to open a new acute care hospital in Fort Mill, South Carolina. Our application for a certificate of need to build the hospital was approved in May 2006, but that approval was appealed by the other applicants and, in December 2009, an administrative law judge ruled that South Carolina regulators must reconsider all of the certificate of need proposals again. We are appealing that decision; however, we are unable to predict the outcome or timing of this process. Once construction begins, the hospital is expected to take up to an additional two years to complete.
Our general hospitals in continuing operations generated in excess of 97% of our net operating revenues for all periods presented in our Consolidated Financial Statements. Factors that affect patient volumes and, thereby, our results of operations at our hospitals and related health care facilities include, but are not limited to: (1) the business environments, economic conditions and demographics of local communities; (2) the number of uninsured and underinsured individuals in local communities treated at our hospitals; (3) seasonal cycles of illness; (4) climate and weather conditions; (5) physician recruitment, retention and attrition; (6) advances in technology and treatments that reduce length of stay; (7) local health care competitors; (8) managed care contract negotiations or terminations; (9) any unfavorable publicity about us, which impacts our relationships with physicians and patients; and (10) the timing of elective procedures.
Each of our general hospitals offers acute care services, operating and recovery rooms, radiology services, respiratory therapy services, clinical laboratories and pharmacies; in addition, most offer intensive care, critical care and/or coronary care units, physical therapy, and orthopedic, oncology and outpatient services. A number of the hospitals also offer tertiary care services such as open-heart surgery, neonatal intensive care and neuroscience. Three of our hospitals—St. Louis University Hospital, Hahnemann University Hospital and St. Christopher’s Hospital for Children—offer quaternary care in areas such as heart, liver, kidney and bone marrow transplants. Sierra Medical Center and Good Samaritan Medical Center also offer gamma-knife brain surgery; and St. Louis University Hospital offers cyberknife surgery for tumors and lesions in the brain, lung, neck and spine that may have been previously considered inoperable or inaccessible by radiation therapy. In addition, our hospitals will continue their efforts to deliver and develop those outpatient services that can be provided on a quality, cost-effective basis and that we believe will meet the needs of the communities served by the facilities.
With the exception of our 25-bed Sylvan Grove Hospital located in Georgia, which is designated by the Centers for Medicare and Medicaid Services (“CMS”) as a critical access hospital and which has not sought to be accredited, each of our facilities that is eligible for accreditation is accredited by the Joint Commission (formerly, the Joint Commission on Accreditation of Healthcare Organizations), the American Osteopathic Association (in the case of one hospital) or another appropriate accreditation agency. With such accreditation, our hospitals are deemed to meet the Medicare Conditions of Participation and are, therefore, eligible to participate in government-sponsored provider programs, such as the Medicare and Medicaid programs. The critical access hospital that is not accredited also participates in the Medicare and Medicaid programs by otherwise meeting the Medicare Conditions of Participation.
2
Table of Contents
The following table lists, by state, the general hospitals owned or leased and operated by our subsidiaries as of December 31, 2009:
| Hospital |
Location |
Licensed Beds |
Status | |||
| Alabama |
||||||
| Brookwood Medical Center |
Birmingham | 602 | Owned | |||
| California |
||||||
| Desert Regional Medical Center(1) |
Palm Springs | 367 | Leased | |||
| Doctors Hospital of Manteca |
Manteca | 73 | Owned | |||
| Doctors Medical Center |
Modesto | 465 | Owned | |||
| Fountain Valley Regional Hospital & Medical Center |
Fountain Valley | 400 | Owned | |||
| John F. Kennedy Memorial Hospital |
Indio | 156 | Owned | |||
| Lakewood Regional Medical Center |
Lakewood | 172 | Owned | |||
| Los Alamitos Medical Center |
Los Alamitos | 167 | Owned | |||
| Placentia Linda Hospital |
Placentia | 114 | Owned | |||
| San Ramon Regional Medical Center |
San Ramon | 123 | Owned | |||
| Sierra Vista Regional Medical Center |
San Luis Obispo | 164 | Owned | |||
| Twin Cities Community Hospital |
Templeton | 114 | Owned | |||
| Florida |
||||||
| Coral Gables Hospital |
Coral Gables | 247 | Owned | |||
| Delray Medical Center |
Delray Beach | 493 | Owned | |||
| Good Samaritan Medical Center |
West Palm Beach | 333 | Owned | |||
| Hialeah Hospital |
Hialeah | 378 | Owned | |||
| North Shore Medical Center |
Miami | 357 | Owned | |||
| North Shore Medical Center – FMC Campus |
Lauderdale Lakes | 459 | Owned | |||
| Palm Beach Gardens Medical Center(2) |
Palm Beach Gardens | 199 | Leased | |||
| Palmetto General Hospital |
Hialeah | 360 | Owned | |||
| Saint Mary’s Medical Center |
West Palm Beach | 463 | Owned | |||
| West Boca Medical Center |
West Boca Raton | 195 | Owned | |||
| Georgia |
||||||
| Atlanta Medical Center |
Atlanta | 460 | Owned | |||
| North Fulton Regional Hospital(2) |
Roswell | 202 | Leased | |||
| South Fulton Medical Center |
East Point | 338 | Owned | |||
| Spalding Regional Hospital |
Griffin | 160 | Owned | |||
| Sylvan Grove Hospital(3) |
Jackson | 25 | Leased | |||
| Louisiana |
||||||
| NorthShore Regional Medical Center(4) |
Slidell | 165 | Leased | |||
| Missouri |
||||||
| Des Peres Hospital |
St. Louis | 167 | Owned | |||
| St. Louis University Hospital |
St. Louis | 356 | Owned | |||
| Nebraska |
||||||
| Creighton University Medical Center(5) |
Omaha | 334 | Owned | |||
| North Carolina |
||||||
| Central Carolina Hospital |
Sanford | 137 | Owned | |||
| Frye Regional Medical Center(2) |
Hickory | 355 | Leased | |||
| Pennsylvania |
||||||
| Hahnemann University Hospital |
Philadelphia | 540 | Owned | |||
| St. Christopher’s Hospital for Children |
Philadelphia | 189 | Owned | |||
3
Table of Contents
| Hospital |
Location | Licensed Beds |
Status | |||
| South Carolina |
||||||
| Coastal Carolina Hospital |
Hardeeville | 41 | Owned | |||
| East Cooper Regional Medical Center |
Mt. Pleasant | 106 | Owned | |||
| Hilton Head Hospital |
Hilton Head | 93 | Owned | |||
| Piedmont Medical Center |
Rock Hill | 288 | Owned | |||
| Tennessee |
||||||
| Saint Francis Hospital |
Memphis | 519 | Owned | |||
| Saint Francis Hospital – Bartlett |
Bartlett | 100 | Owned | |||
| Texas |
||||||
| Centennial Medical Center |
Frisco | 118 | Owned | |||
| Cypress Fairbanks Medical Center |
Houston | 181 | Owned | |||
| Doctors Hospital at White Rock Lake |
Dallas | 218 | Owned | |||
| Houston Northwest Medical Center(6) |
Houston | 430 | Owned | |||
| Lake Pointe Medical Center(7) |
Rowlett | 112 | Owned | |||
| Nacogdoches Medical Center |
Nacogdoches | 153 | Owned | |||
| Park Plaza Hospital |
Houston | 444 | Owned | |||
| Providence Memorial Hospital |
El Paso | 508 | Owned | |||
| Sierra Medical Center |
El Paso | 351 | Owned | |||
| Sierra Providence East Medical Center |
El Paso | 110 | Owned | |||
| (1) | Lease expires in 2027. |
| (2) | The current lease terms for Palm Beach Gardens Medical Center, North Fulton Regional Hospital and Frye Regional Medical Center expire in February 2014, but may be renewed through at least February 2039, in each case subject to certain conditions contained in the respective leases. |
| (3) | Designated by CMS as a critical access hospital. The current lease term for this facility expires in December 2011, but may be renewed through December 2046, subject to certain conditions contained in the lease. |
| (4) | Reclassified into discontinued operations in the three months ended June 30, 2009. In January 2010, we entered into a definitive agreement to sell certain of our owned assets associated with NorthShore and transition the operation of the hospital to a new hospital operator. We anticipate that the transaction will close effective April 1, 2010, at which time we will terminate our lease of the hospital. |
| (5) | Owned by a limited liability company in which a Tenet subsidiary owned a 74.06% interest at December 31, 2009 and is the managing member. |
| (6) | Owned by a limited liability company in which a Tenet subsidiary owned an 87.62% interest at December 31, 2009 and is the managing member. |
| (7) | Owned by a limited liability company in which a Tenet subsidiary owned a 94.63% interest at December 31, 2009 and is the managing member. |
As of December 31, 2009, the largest concentrations of licensed beds in our general hospitals were in Florida (25.6%), Texas (19.3%) and California (17.0%). Strong concentrations of hospital beds within market areas help us contract more successfully with managed care payers, reduce management, marketing and other expenses, and more efficiently utilize resources. However, these concentrations increase the risk that, should any adverse economic, regulatory, environmental or other developments occur in these areas, our business, financial condition, results of operations or cash flows could be materially adversely affected. Only one of our individual hospitals represented more than 5% (approximately 5.1%) of our net operating revenues for the year ended December 31, 2009, and one represented more than 5% (approximately 5.5%) of our total assets, excluding goodwill and intercompany receivables, at December 31, 2009.
The following table shows certain information about the hospitals operated by our subsidiaries at December 31, 2009, 2008 and 2007.
| December 31, | ||||||
| 2009 | 2008 | 2007 | ||||
| Total number of facilities(1) |
51 | 54 | 58 | |||
| Total number of licensed beds(2) |
13,601 | 14,352 | 15,244 | |||
| (1) | Includes all general hospitals and critical access facilities, as well as one facility at December 31, 2009, four facilities at December 31, 2008 and nine facilities at December 31, 2007, respectively, that are classified in discontinued operations for financial reporting purposes as of December 31, 2009. |
| (2) | Information regarding utilization of licensed beds and other operating statistics can be found in Part II, Item 7, Management’s Discussion and Analysis of Financial Condition and Results of Operations. |
4
Table of Contents
PROPERTIES
Description of Real Property. The locations of our hospitals and the number of licensed beds at each hospital at December 31, 2009 are set forth in the table beginning on page 3. At December 31, 2009, our subsidiaries also owned or leased and operated 66 medical office buildings, most of which are adjacent to our general hospitals. We are currently seeking to sell up to 30 of these medical office buildings, totaling approximately 2.25 million square feet of rental space.
Our corporate headquarters are located in Dallas, Texas. We have other corporate administrative offices in Anaheim, California; Coral Springs, Florida; and Philadelphia, Pennsylvania. One of our subsidiaries leases our corporate headquarters space under an operating lease agreement that expires in December 2019. Other subsidiaries lease the space for our offices in Anaheim, Coral Springs and Philadelphia under operating lease agreements. We believe that all of our properties, including the administrative and medical office buildings described above, are suitable for their intended purposes.
Obligations Relating to Real Property. As of December 31, 2009, we had approximately $5 million of outstanding loans secured by property and equipment, and we had approximately $2 million of capital lease obligations. In addition, from time to time, we lease real property to third-party developers for the construction of medical office buildings. Under our current practice, the financing necessary to construct the medical office buildings encumbers only the leasehold and not our fee interest in the real estate. In years past, however, we have at times subordinated our fee interest and allowed our property to be pledged as collateral for third-party loans. We have no contractual obligation to make payments on these third-party loans, but our property could be subject to loss in the case of default by the lessee.
Regulations Affecting Real Property. We are subject to a number of laws and regulations affecting our use of, and purchase and sale of, real property. Among these are California’s seismic standards, the Americans with Disabilities Act (“ADA”), and various environmental laws and regulations.
The State of California has established standards intended to ensure that all hospitals in the state withstand earthquakes and other seismic activity without collapsing or posing the threat of significant loss of life. In general, we are required to meet these standards by December 31, 2012, subject to a two-year extension for hospital projects that are underway in advance of that date. In November 2007, the California Building Standards Commission adopted regulations permitting the use of a new computerized evaluation tool for determining how at risk hospital buildings are of collapse in an earthquake, and the use of this new tool has resulted in fewer hospitals requiring retrofitting by the 2012 deadline. We currently estimate spending a total of approximately $80 million to comply with the requirements under California’s seismic regulations, of which approximately $24 million was spent prior to January 1, 2010. Our current estimated seismic costs are considerably lower than certain previous estimates because a number of our hospitals have been evaluated as having reduced risk using the new evaluation tool. There may be further reductions to our estimated seismic costs as the State of California has recently enacted new regulations relating to the seismic evaluation tool and the new state building code; we are currently evaluating these new regulations to determine what impact they will have on our cost estimate. Our total estimated seismic expenditure amount has not been adjusted for future inflation. In addition to safety standards, over time, hospitals must also meet performance standards meant to ensure that they are generally capable of providing medical services to the public after an earthquake or other disaster. Ultimately, all general acute care hospitals in California must meet seismic performance standards by 2030 to remain open. To date, we have conducted engineering studies and developed compliance plans for all of our California facilities. At this time, all of our general acute care hospitals in California are in compliance with all current seismic requirements.
The Americans with Disabilities Act generally requires that public accommodations, including hospitals and other health care facilities, be made accessible to disabled persons. Certain of our facilities are subject to a negotiated consent decree involving disability access as a result of a class action lawsuit. In accordance with the terms of the consent decree, our facilities have agreed to implement disability access improvements, but have not admitted that they have engaged in any wrongful action or inaction. To date, we have spent approximately $19 million on corrective work at our facilities, and we expect to spend a total of approximately $111 million on such improvements over the next six years.
Our properties are also subject to various federal, state and local environmental laws, rules and regulations, including with respect to asbestos abatement and the treatment of underground storage tanks, among other matters. We believe it is unlikely that the cost of complying with such laws, rules and regulations will have a material effect on our future capital expenditures, results of operations or competitive position.
5
Table of Contents
MEDICAL STAFF AND EMPLOYEES
General. Our hospitals are staffed by licensed physicians who have been admitted to the medical staffs of individual hospitals. Under state laws and other licensing standards, hospital medical staffs are generally self-governing organizations subject to ultimate oversight by the hospital’s local governing board. Members of the medical staffs of our hospitals also often serve on the medical staffs of hospitals not owned by us. Members of our medical staffs are free to terminate their affiliation with our hospitals or admit their patients to competing hospitals at any time. Although we operate some physician practices and, where permitted by law, employ some physicians, the overwhelming majority of the physicians who practice at our hospitals are not our employees. However, nurses, therapists, lab technicians, facility maintenance workers and the administrative staffs of hospitals normally are our employees. We are subject to federal minimum wage and hour laws and various state labor laws, and maintain a number of different employee benefit plans.
Our operations depend on the efforts, abilities and experience of the physicians on the medical staffs of our hospitals, most of whom have no contractual relationship with us. It is essential to our ongoing business that we attract and retain an appropriate number of quality physicians in all specialties on our medical staffs. Although we had a net overall gain in physicians added to our medical staffs in each of the last three years, in some of our markets, physician recruitment and retention are still affected by a shortage of physicians in certain sought-after specialties and the difficulties that physicians experience in obtaining affordable malpractice insurance or finding insurers willing to provide such insurance. Other issues facing physicians, such as proposed decreases in Medicare payments, are forcing them to consider alternatives, including relocating their practices or retiring sooner than expected.
We continue to take steps to successfully attract and retain key employees, qualified physicians and other health care professionals. One of our initiatives is our Physician Relationship Program, which is centered on understanding the needs of physicians who admit patients both to our hospitals and to our competitors’ hospitals and responding to those needs with changes and improvements in our hospitals and operations. In general, the loss of some or all of our key employees or the inability to attract or retain sufficient numbers of qualified physicians and other health care professionals could have a material adverse effect on patient volumes and, thereby, our business, financial condition, results of operations or cash flows.
At December 31, 2009, the approximate number of our employees (of which approximately 25% were part-time employees) was as follows:
| General hospitals and related health care facilities(1) |
56,948 | |
| Administrative offices |
665 | |
| Total |
57,613 | |
| (1) | Includes employees whose employment related to the operations of our general hospitals, critical access facility, long-term acute care hospital, outpatient surgery centers, diagnostic imaging centers, occupational and rural health care clinics, physician practices, in-house collection agency and other health care operations in both continuing and discontinued operations. |
At December 31, 2009, the largest concentrations of our employees (excluding those in our administrative offices, but including those at our general hospitals and related health care facilities in both continuing and discontinued operations) were in those states where we had the largest concentrations of licensed hospital beds:
| % of employees | % of licensed beds | |||
| California |
20.7% | 17.0.% | ||
| Florida |
19.8% | 25.6% | ||
| Texas |
16.7% | 19.3% |
Union Activity and Labor Relations. At December 31, 2009, approximately 19% of the employees at our hospitals and related health care facilities in both continuing and discontinued operations were represented by labor unions. Labor relations at our facilities generally have been satisfactory. We, and the hospital industry in general, are continuing to see an increase in the amount of union activity across the country. We expect this trend to be even more pronounced in 2010, as we renegotiate our existing labor contracts, all of which are scheduled to expire in the next 14 months. As union activity increases, our operating expenses may increase more rapidly than our net operating revenues.
In addition, legislation has been introduced in Congress that could significantly change both union organizing and bargaining over initial labor contracts in a way that is likely to increase union membership, at least in the short term. We are unable to predict what action Congress or the President might take with respect to this or any other labor-related legislation or the impact such legislation might ultimately have on our relations with employees and unions.
We currently have labor contracts and collective bargaining agreements with the California Nurses Association (“CNA”), the Service Employees International Union (“SEIU”), the United Nurses Associations of California (“UNAC”) and the American Federation of State, County and Municipal Employees that cover registered nurses, service and maintenance workers, and other employees at 10 of our general hospitals in California, three of our general hospitals in Florida and one of our general hospitals in Philadelphia. All of these union agreements set stable and competitive wage increases within our budgeted expectations through various dates in 2010 and early 2011. In January 2010, we commenced the process of renegotiating these contracts, beginning with our collective bargaining agreements with UNAC at two of our hospitals in California.
6
Table of Contents
We also have separate “peace accords” with both the CNA and the SEIU that provide each union with limited access to attempt to organize certain of our employees and establish specific guidelines for the parties to follow with respect to organizing activities. Both peace accords expire in December 2011. Such agreements have become more common as employers attempt to balance the disruption caused by traditional union organizing with the rights of employees to determine for themselves whether to seek union representation.
The CNA and the SEIU have engaged in union organizing activities at several of our hospitals in Houston, Memphis and Philadelphia pursuant to the terms of the peace accords. Registered nurses at two of these facilities have participated in elections concerning CNA representation, but – to date – union organizing has been successful at only Cypress Fairbanks Medical Center (“CyFair”). After extended collective bargaining negotiations over an initial contract for CyFair, the CNA triggered an agreed-to interest arbitration process, which began in June 2009, that provides for a neutral third party to mediate unresolved contract terms. If the mediation is unsuccessful, those unresolved terms will be decided by binding arbitration.
We are also defending various allegations that we are in violation of federal labor laws or the terms of our collective bargaining agreements and peace accords, and we expect to continue to be subject to such claims from time to time in the normal course of business.
Shortage of Experienced Nurses and Mandatory Nurse-Staffing Ratios. In addition to union activity, factors that adversely affect our labor costs include the nationwide shortage of experienced nurses and the enactment of state laws regarding nurse-staffing ratios. Like others in the health care industry, we continue to experience a shortage of experienced nurses in certain key specialties and geographic areas. In addition, state-mandated nurse-staffing ratios in California affect not only our labor costs, but, if we are unable to hire the necessary number of experienced nurses to meet the required ratios, they may also cause us to limit patient admissions with a corresponding adverse effect on our net operating revenues. We continually monitor our nurse-staffing ratios in California in an effort to achieve full compliance with the state-mandated nurse-staffing ratios there. Nurse-staffing ratio legislation has been proposed in, but not yet enacted by, Congress and other states besides California in which we operate hospitals, including Florida and Pennsylvania. In 2009, Texas passed the Hospital Safe Staffing Law, which mandates the creation of nurse staffing committees at Texas hospitals and outlines each hospital’s responsibility to adopt, implement and enforce an official nurse staffing plan, but does not mandate staffing ratios. Also in 2009, the Missouri Department of Health and Senior Services published amendments to the state’s hospital nursing services regulations, which became effective on June 30, 2009, that are similar to the new Texas requirements with respect to nurse staffing.
We cannot predict the degree to which we will be affected by the future availability or cost of nursing personnel, but we expect to continue to experience salary, wage and benefit pressures created by the shortage of experienced nurses throughout the country and state-mandated nurse-staffing ratios, particularly in California. In response, we have increased our efforts to recruit and retain experienced nurses and also to address workforce development with local schools of nursing. We expect that 30 of our hospitals will participate in the VersantTM RN Residency Program in 2010 by providing an 18- to 22-week residency program for new nursing school graduates to help ease the transition from student to professional practicing nurse, give nurses evidence-based experience and skills needed to increase their competency and confidence, reduce first-year nurse turnover and decrease the use of contract labor.
COMPETITION
In general, competition among health care providers occurs primarily at the local level. A hospital’s position within the geographic area in which it operates is affected by a number of competitive factors, including, but not limited to (1) the scope, breadth and quality of services a hospital offers to its patients and physicians, (2) the number, quality and specialties of the physicians who admit and refer patients to the hospital, (3) nurses and other health care professionals employed by the hospital or on the hospital’s staff, (4) the hospital’s reputation, (5) its managed care contracting relationships, (6) its location, (7) the location and number of competitive facilities and other health care alternatives, (8) the physical condition of its buildings and improvements, (9) the quality, age and state-of-the-art of its medical equipment, (10) its parking or proximity to public transportation, (11) the length of time it has been a part of the community, and (12) the charges for its services. In addition, tax-exempt competitors may have certain financial advantages not available to our facilities, such as endowments, charitable contributions, tax-exempt financing, and exemptions from sales, property and income taxes. We also face increasing competition from physician-owned specialty hospitals and freestanding diagnostic and imaging centers for market share in high margin services and for quality physicians and personnel.
7
Table of Contents
Overall, our general hospitals and other health care businesses operate in highly competitive environments. Although we have seen some improvements in recent quarters, we have experienced declines in patient volumes over the last several years. We believe these declines can be attributed, in part, to increased competition for physicians and patients. We continue to take steps to address competition and increase patient volumes; however, due to the concentration of our hospitals in California, Florida and Texas, we may not be able to mitigate some factors that contribute to volume declines. Broadly speaking, we attract physicians by striving to equip our hospitals with technologically advanced equipment and quality physical plant, properly maintaining the equipment and physical plant, providing high-quality care to our patients and otherwise creating an environment within which physicians prefer to practice. One of our specific initiatives is our Physician Relationship Program, which is centered on understanding the needs of physicians who admit patients both to our hospitals and to our competitors’ hospitals and responding to those needs with changes and improvements in our hospitals and operations. We have targeted capital spending in order to address specific needs or growth opportunities of our hospitals, which is expected to have a positive impact on their volumes. We have also sought to include all of our hospitals and an increased number of our affiliated physicians in the affected geographic area or nationally when negotiating new managed care contracts, which should result in additional volumes at facilities that were not previously a part of such managed care networks. In addition, we have completed clinical service line market demand analyses and profitability assessments to determine which services are highly valued that can be emphasized and marketed to improve our operating results. This Targeted Growth Initiative has resulted in some reductions in unprofitable service lines in several locations, which have had a slightly negative impact on our volumes. However, the elimination of these unprofitable service lines will allow us to focus more resources on services that are in higher demand and are more profitable.
Our Commitment to Quality initiative is further helping position us to competitively meet the volume challenge. We continue to work with physicians to implement the most current evidence-based medicine techniques to improve the way we provide care. As a result of these efforts, our hospitals have improved substantially in quality metrics reported by the government and have been recognized by several managed care companies for their quality of care. In our continuing efforts to improve our clinical outcomes and drive down our costs of care, we launched our Medicare Performance Initiative in 2009. This initiative is focused on the identification and reduction of costs associated with variations in physician and hospital practices. The project includes the dissemination of best practices based on evidence-based medicine, which we expect will promote the most effective and efficient utilization of resources and result in shorter lengths of stay, as well as reductions in redundant ancillary services and readmissions for hospitalized patients. We believe that quality of care improvements will continue to have the effect of increasing physician and patient satisfaction, potentially improving our volumes.
Further, each hospital has a local governing board, consisting primarily of community members and physicians, that develops short-term and long-term plans for the hospital to foster a desirable medical environment for physicians. Each local governing board also reviews and approves, as appropriate, actions of the medical staff, including staff appointments, credentialing, peer review and quality assurance. While physicians may terminate their association with our hospitals at any time, we believe that by striving to maintain and improve the quality of care at our hospitals and by maintaining ethical and professional standards, we will attract and retain qualified physicians with a variety of specialties.
HEALTH CARE REGULATION AND LICENSING
CERTAIN BACKGROUND INFORMATION
Health care, as one of the largest industries in the United States, continues to attract much legislative interest and public attention. Changes in the Medicare and Medicaid programs and other government health care programs, hospital cost-containment initiatives by public and private payers, proposals to limit payments and health care spending, and industry-wide competitive factors greatly impact the health care industry. The industry is also subject to extensive federal, state and local regulation relating to licensure, conduct of operations, ownership of facilities, physician relationships, addition of facilities and services, and reimbursement rates for services. The laws, rules and regulations governing the health care industry are extremely complex, and, in certain areas, the industry has little or no regulatory or judicial interpretation for guidance. Although we have extensive policies and procedures in place to facilitate compliance in all material respects with such laws, rules and regulations, if a determination is made that we were in material violation of such laws, rules or regulations, our business, financial condition, results of operations or cash flows could be materially adversely affected. In addition, we are unable to predict the future course of federal, state and local regulation or legislation, including Medicare and Medicaid statutes and regulations. Further changes in the regulatory framework affecting health care providers could have a material adverse effect on our business, financial condition, results of operations or cash flows.
8
Table of Contents
Both federal and state government agencies continue heightened and coordinated civil and criminal enforcement efforts against the health care industry. Under the authority of the Inspector General Act of 1978, the Office of Inspector General (“OIG”) of the U.S. Department of Health and Human Services (“HHS”) on an annual basis conducts a comprehensive work-planning process to identify the areas most worthy of attention in the coming year. In recent years, the OIG has allocated approximately 80% of its resources to reviews and investigations of the Medicare and Medicaid programs and 20% to HHS’ public health and human services programs. In its fiscal year 2010 Work Plan, the OIG set forth detailed information about, among other things, its ongoing and planned work examining the integrity of Medicare and Medicaid payments and services, including payments made to and services provided by hospitals. An online version of the 2010 Work Plan is available at http://oig.hhs.gov/publications/docs/workplan/2010/Work_Plan_FY_2010.pdf. We believe that we, and the health care industry in general, will continue to be subject to increased government scrutiny and investigations, which could have a material adverse effect on our business, financial condition, results of operations or cash flows.
Health care providers are also subject to qui tam lawsuits under the federal False Claims Act. Qui tam or “whistleblower” actions can also be filed under certain state false claims laws if the fraud involves Medicaid funds or funding from state and local agencies. Federal and state false claims laws allow private individuals to bring actions on behalf of the government, alleging that a hospital or health care provider has defrauded a federal or state government program, such as Medicare or Medicaid. If the government intervenes in the action and prevails, the defendant may be required to pay three times the actual damages sustained by the government, plus mandatory civil penalties for each false claim submitted to the government. As part of the resolution of a qui tam case, the party filing the initial complaint may share in a portion of any settlement or judgment. If the government does not intervene in the action, the qui tam plaintiff may continue to pursue the action independently. Although companies in the health care industry in general, and us in particular, have been and may continue to be subject to qui tam actions, we are unable to predict the future impact of such actions on our business, financial condition, results of operations or cash flows.
ANTI-KICKBACK AND SELF-REFERRAL REGULATIONS
Medicare and Medicaid anti-kickback and anti-fraud and abuse amendments codified under Section 1128B(b) of the Social Security Act (the “Anti-kickback Statute”) prohibit certain business practices and relationships that might affect the provision and cost of health care services payable under the Medicare and Medicaid programs and other government programs, including the payment or receipt of remuneration for the referral of patients whose care will be paid for by such programs. Sanctions for violating the Anti-kickback Statute include criminal and civil penalties, as well as fines and possible exclusion from government programs, such as Medicare and Medicaid. Many states have statutes similar to the federal Anti-kickback Statute, except that the state statutes usually apply to referrals for services reimbursed by all third-party payers, not just federal programs. In addition, it is a violation of the federal Civil Monetary Penalties Law to offer or transfer anything of value to Medicare or Medicaid beneficiaries that is likely to influence their decision to obtain covered goods or services from one provider or service over another.
The federal government has also issued regulations that describe some of the conduct and business relationships that are permissible under the Anti-kickback Statute. These regulations are often referred to as the “Safe Harbor” regulations. The fact that certain conduct or a given business arrangement does not meet a Safe Harbor does not necessarily render the conduct or business arrangement illegal under the Anti-kickback Statute. Rather, such conduct and business arrangements may be subject to increased scrutiny by government enforcement authorities and should be reviewed on a case-by-case basis.
In addition to addressing other matters, as discussed below, the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) also amended Title XI (42 U.S.C. Section 1301 et seq.) to broaden the scope of fraud and abuse laws to include all health plans, whether or not payments under such health plans are made pursuant to a federal program.
Section 1877 of the Social Security Act (commonly referred to as the “Stark” law) generally restricts referrals by physicians of Medicare or Medicaid patients to entities with which the physician or an immediate family member has a financial relationship, unless one of several exceptions applies. The referral prohibition applies to a number of statutorily defined “designated health services,” such as clinical laboratory, physical therapy, radiology, and inpatient and outpatient hospital services. The exceptions to the referral prohibition cover a broad range of common financial relationships. These statutory, and the subsequent regulatory, exceptions are available to protect certain permitted employment relationships, leases, group practice arrangements, medical directorships, and other common relationships between physicians and providers of designated health services, such as hospitals. A violation of the Stark law may result in a denial of payment, required refunds to patients and the Medicare program, civil monetary penalties of up to $15,000 for each violation, civil monetary penalties of up to $100,000 for “sham” arrangements, civil monetary penalties of up to $10,000 for each day that an entity fails to report required information, and exclusion from participation in the Medicare and Medicaid programs and other federal programs. Many states have adopted or are considering similar self-referral statutes, some of which extend beyond the related state Medicaid program to prohibit the payment or receipt of remuneration for the referral of patients and physician self-referrals regardless of the source of the payment for the care. Our participation in and development of joint ventures and other financial relationships with physicians could be adversely affected by these amendments and similar state enactments.
9
Table of Contents
In accordance with our compliance program and our corporate integrity agreement with the federal government, which are described in detail under “—Compliance Program” below, we have policies and procedures in place concerning compliance with the Anti-kickback Statute and the Stark law, among others. In addition, our compliance, law and audit services departments systematically review a substantial number of our arrangements with referral sources to determine the extent to which they comply with our policies and procedures and with the Anti-kickback Statute, the Stark law and similar state statutes.
HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT
Title II, Subtitle F of the Health Insurance Portability and Accountability Act mandates the adoption of specific standards for electronic transactions and code sets that are used to transmit certain types of health information. HIPAA’s objective is to encourage efficiency and reduce the cost of operations within the health care industry. To protect the information transmitted using the mandated standards and the patient information used in the daily operations of a covered entity, HIPAA also sets forth federal rules protecting the privacy and security of protected health information. The privacy and security regulations address the use and disclosure of individually identifiable health information and the rights of patients to understand and control how their information is used and disclosed. The law provides both criminal and civil fines and penalties for covered entities that fail to comply with HIPAA.
To receive reimbursement from CMS for electronic claims, health care providers must use HIPAA’s electronic data transmission (transaction and code set) standards when transmitting certain health care information electronically. Our electronic data transmissions are compliant with current standards.
All covered entities, including those we operate, are also required to comply with the privacy and security requirements of HIPAA. We are in material compliance with the privacy and security regulations, and we will continue to update training and procedures to address any compliance issues that develop. Further, all covered entities, including those we operate, have been assigned unique 10-digit numeric identifiers and otherwise currently comply with the National Provider Identifier requirements of HIPAA.
We have developed a comprehensive set of policies and procedures in our efforts to comply with HIPAA, and similar state privacy laws, under the guidance of our compliance department. Hospital compliance officers and information security officers are responsible for implementing and monitoring compliance with our HIPAA privacy and security policies and procedures at our hospitals. We have also created an internal web-based HIPAA training program, which is mandatory for all employees. Based on existing and currently proposed regulations, as well as our experience with HIPAA to this point, we continue to believe that the ongoing costs of complying with HIPAA will not have a material adverse effect on our business, financial condition, results of operations or cash flows.
HEALTH CARE FACILITY LICENSING REQUIREMENTS
In order to maintain their operating licenses, health care facilities must comply with strict governmental standards concerning medical care, equipment and cleanliness. Various licenses and permits also are required in order to dispense narcotics, operate pharmacies, handle radioactive materials and operate certain equipment. Our health care facilities hold all required governmental approvals, licenses and permits material to the operation of their business.
UTILIZATION REVIEW COMPLIANCE AND HOSPITAL GOVERNANCE
In addition to certain statutory coverage limits and exclusions, federal laws and regulations, specifically the Medicare Conditions of Participation, generally require health care providers, including hospitals that furnish or order health care services that may be paid for under the Medicare program or state health care programs, to assure that claims for reimbursement are for services or items that are (1) provided economically and only when, and to the extent, they are medically reasonable and necessary, (2) of a quality that meets professionally recognized standards of health care, and (3) supported by appropriate evidence of medical necessity and quality. The Social Security Act established the Utilization and Quality Control Peer Review Organization program, now known as the Quality Improvement Organization (“QIO”) program, to promote the effectiveness, efficiency, economy and quality of services delivered to Medicare beneficiaries and to ensure that those services are reasonable and necessary. CMS administers the QIO program through a network of QIOs that work with consumers, physicians, hospitals and other caregivers to refine care delivery systems to assure patients receive the appropriate care at the appropriate time, particularly among underserved populations. The QIO program also safeguards the integrity of the Medicare trust fund by reviewing Medicare patient admissions, treatments and discharges, and ensuring payment is made only for medically necessary services, and investigates beneficiary complaints about quality of care. The QIOs have the authority to deny payment for services provided and recommend to HHS that a provider that is in substantial noncompliance with certain standards be excluded from participating in the Medicare program.
10
Table of Contents
Medical and surgical services and practices are extensively supervised by committees of staff doctors at each of our health care facilities, are overseen by each facility’s local governing board, the members of which primarily are community members and physicians, and are reviewed by our clinical quality personnel. The local hospital governing board also helps maintain standards for quality care, develop short-term and long-range plans, and establish, review and enforce practices and procedures, as well as approves the credentials and disciplining of medical staff members.
CERTIFICATE OF NEED REQUIREMENTS
Some states require state approval for construction, expansion and closure of health care facilities, including findings of need for additional or expanded health care facilities or services. Certificates of need, which are issued by governmental agencies with jurisdiction over health care facilities, are at times required for capital expenditures exceeding a prescribed amount, changes in bed capacity or services, and certain other matters. As of December 31, 2009, we operated hospitals in eight states that require a form of state approval under certificate of need programs applicable to those hospitals. We are unable to predict whether we will be required or able to obtain any additional certificates of need in any jurisdiction where they are required, or if any jurisdiction will eliminate or alter its certificate of need requirements in a manner that will increase competition and, thereby, affect our competitive position.
ENVIRONMENTAL MATTERS
Our health care operations are subject to a number of federal, state and local environmental laws, rules and regulations that govern, among other things, our disposal of solid waste, as well as our use, storage, transportation and disposal of hazardous and toxic materials (including radiological materials). Our operations also generate medical waste that must be disposed of in compliance with laws and regulations that vary from state to state. In addition, although we are not engaged in manufacturing or other activities that produce meaningful levels of greenhouse gas emissions, our operating expenses could be adversely affected if legal and regulatory developments related to climate change or other initiatives result in increased energy or other costs. We could also be affected by climate change and other environmental issues to the extent such issues adversely affect the general economy or result in severe weather or climate change events affecting our facilities in coastal regions. At this time, based on current climate conditions and our assessment of existing and pending environmental rules and regulations, as well as treaties and international accords relating to climate change, we do not believe that the costs of complying with environmental laws and regulations, including regulations relating to climate change issues, will have a material adverse effect on our future capital expenditures, results of operations or cash flows.
Consistent with our commitment to meet the highest standards of corporate responsibility, we have formed a corporate committee to regularly evaluate our environmental policies and to share best practices among our hospitals by identifying opportunities to reduce waste, use safer chemicals and consume less energy while at the same time managing costs prudently. These efforts, among other things, have resulted in the substantial elimination of the use of mercury at our health care facilities and the adoption of corporate-wide recycling and other programs. We also seek to implement these objectives through our procurement practices by contracting with health care product suppliers and other organizations that endorse environmental and safety goals consistent with our corporate philosophy.
COMPLIANCE PROGRAM
General. We maintain a multi-faceted corporate and hospital-based compliance program that is designed to assist our corporate and hospital staff to meet or exceed applicable standards established by federal and state laws and regulations and industry practice. We established an independent compliance department in 2003 to manage compliance-related functions previously managed by our law department. To ensure the independence of the compliance department, the following measures were implemented:
| • | the compliance department has its own operating budget; |
| • | the compliance department has the authority to hire outside counsel, access any Tenet document and interview any of our personnel; and |
| • | our chief compliance officer reports directly to the quality, compliance and ethics committee of our board of directors. |
11
Table of Contents
In May 2008, the quality, compliance and ethics committee of our board of directors approved an updated ethics and compliance program charter that furthers our goal of fostering and maintaining the highest ethical standards, and valuing our compliance with all state and federal laws and regulations as a foundation of our corporate philosophy. The primary focus of the program is compliance with the requirements of the Medicare and Medicaid programs and other government healthcare programs. Pursuant to the terms of the charter, the compliance department is responsible for the following activities: (1) drafting company policies and procedures related to ethics and compliance issues; (2) developing and providing compliance-related education and training to all of our employees and, as appropriate, directors, contractors, agents and staff physicians; (3) creating and disseminating our Standards of Conduct; (4) monitoring, responding to and resolving all ethics and compliance-related issues; (5) ensuring that we take appropriate corrective and disciplinary action when noncompliant or improper conduct is identified; and (6) measuring compliance with our policies and legal and regulatory requirements related to federal health care programs and our corporate integrity agreement described below.
Each of our hospitals has a compliance officer on site. These hospital-based compliance officers report to regional compliance directors who report directly to our chief compliance officer.
Corporate Integrity Agreement. In June 2006, we entered into a broad civil settlement agreement with the U.S. Department of Justice (“DOJ”) and other federal agencies that concluded several previously disclosed governmental investigations, including inquiries into our receipt of certain Medicare outlier payments before 2003, physician financial arrangements and Medicare coding issues. In accordance with the terms of the settlement, we entered into a five-year corporate integrity agreement (“CIA”) in September 2006 with the OIG. The CIA establishes annual training requirements and compliance reviews by independent review organizations in specific areas. In particular, the CIA requires, among other things, that we:
| • | maintain our existing company-wide quality initiatives in the areas of evidence-based medicine, standards of clinical excellence and quality measurements; |
| • | maintain our existing company-wide compliance program and code of conduct; |
| • | formalize in writing our policies and procedures in the areas of billing and reimbursement, compliance with the Anti-kickback Statute and the Stark law, and clinical quality, almost all of which were already in place when we entered into the CIA and the remainder of which were put into place by January 2007; |
| • | provide a variety of general and specialized compliance training to our employees, contractors and physicians we employ or who serve as medical directors and/or serve on our hospitals’ governing boards; and |
| • | engage independent outside entities to provide reviews of compliance and effectiveness in five areas – Medicare outlier payments, diagnosis-related group claims, unallowable costs, physician financial arrangements and clinical quality systems. |
Further, the CIA requires us to maintain or establish performance standards and incentives that link compensation and incentive awards directly to clinical quality measures and compliance program effectiveness measures. The CIA also establishes a number of specific requirements for the quality, compliance and ethics committee of our board of directors. Notably, the committee must (1) retain an independent compliance expert, and (2) assess our compliance program, including arranging for the performance of a review of the effectiveness of the program. Based on this work, the committee must then adopt a resolution for each reporting period of the CIA regarding its conclusions as to whether we have implemented an effective compliance program.
The CIA has the effect of increasing the amount of information we provide the federal government regarding our health care practices and our compliance with federal regulations. The reports we provide could result in greater scrutiny by regulatory authorities. In addition, any determination that we have breached our CIA or violated applicable health care laws or regulations could subject us to repayment obligations, civil and monetary penalties, exclusion from participation in the Medicare, Medicaid and other federal and state health care programs and, for violations of certain laws and regulations, criminal penalties. We have taken, and continue to take, all necessary steps to promote compliance with the terms of the CIA.
ETHICS PROGRAM
We maintain a values-based ethics program that is designed to monitor and raise awareness of ethical issues among employees and to stress the importance of understanding and complying with our Standards of Conduct.
All of our employees, including our chief executive officer, chief financial officer and principal accounting officer, are required to abide by our Standards of Conduct to ensure that our business is conducted in a legal and ethical manner. The members of our board of directors and many of our contractors are also required to abide by our Standards of Conduct. The standards reflect our basic values and form the foundation of a comprehensive process that includes compliance with all corporate policies, procedures and practices. Our standards cover such areas as quality patient care, compliance with all applicable laws and regulations, appropriate use of our assets, protection of patient information and avoidance of conflicts of interest.
12
Table of Contents
As part of the program, we provide annual ethics and compliance training sessions to every employee, as well as our board of directors and certain physicians and contractors. All employees are required to report incidents that they believe in good faith may be in violation of the Standards of Conduct, and are encouraged to contact our 24-hour toll-free Ethics Action Line when they have questions about the standards or any ethics concerns. Incidents of alleged financial improprieties reported to the Ethics Action Line or the compliance department are communicated to the audit committee of our board of directors. All reports to the Ethics Action Line are kept confidential to the extent allowed by law, and employees have the option to remain anonymous. In cases reported to the Ethics Action Line that involve a possible violation of the law or regulatory policies and procedures, the matter is referred to the compliance department for investigation. Retaliation against employees in connection with reporting ethical concerns is considered a serious violation of our Standards of Conduct, and, if it occurs, it will result in discipline, up to and including termination of employment.
The full text of our Standards of Conduct, and a number of our ethics and compliance policies and procedures, are published on our website, at www.tenethealth.com, under the “Ethics and Compliance” caption in the “About” section. A copy of our Standards of Conduct is also available upon written request to our corporate secretary.
PROPERTY AND PROFESSIONAL AND GENERAL LIABILITY INSURANCE
Property Insurance. We have property, business interruption and related insurance coverage to mitigate the financial impact of catastrophic events or perils that is subject to deductible provisions based on the terms of the policies. These policies are on an occurrence basis. For the policy periods April 1, 2009 through March 31, 2010 and April 1, 2008 through March 31, 2009, we have coverage totaling $600 million per occurrence, after deductibles and exclusions, with annual aggregate sub-limits of $100 million each for floods and earthquakes and a per-occurrence sub-limit of $100 million for windstorms with no annual aggregate. With respect to fires and other perils, excluding floods, earthquakes and windstorms, the total $600 million limit of coverage per occurrence applies. Deductibles are 5% of insured values up to a maximum of $25 million for floods, California earthquakes and wind-related claims, and 2% of insured values for New Madrid fault earthquakes, with a maximum per claim deductible of $25 million. Other covered losses, including fires and other perils, have a minimum deductible of $1 million.
Professional and General Liability Insurance. As is typical in the health care industry, we are subject to claims and lawsuits in the ordinary course of business. The health care industry has seen significant increases in the cost of professional liability insurance due to increased litigation. In response, we formed and maintain captive insurance companies to self-insure a substantial portion of our professional and general liability risk. Claims in excess of our self-insurance retentions are insured with commercial insurance companies.
For the policy period June 1, 2009 through May 31, 2010, our hospitals generally have a self-insurance retention of $5 million per occurrence for all claims incurred. Our captive insurance company, The Healthcare Insurance Corporation (“THINC”), retains $10 million per occurrence above our hospitals’ $5 million self-insurance retention level. The next $10 million of claims in excess of these aggregate self-insurance retentions of $15 million per occurrence are 65% reinsured by THINC with independent reinsurance companies, with THINC retaining 35% or a maximum of $3.5 million. Claims in excess of $25 million are covered by our excess professional and general liability insurance policies with major independent insurance companies, on a claims-made basis, subject to an aggregate limit of $175 million, with Tenet retaining 20% of the initial $50 million layer in excess of $25 million per claim or a maximum of $10 million.
For the policy period June 1, 2008 through May 31, 2009, our hospitals generally have a self-insurance retention of $5 million per occurrence for all claims incurred. THINC retains $10 million per occurrence above our hospitals’ $5 million self-insurance retention level. Claims in excess of these aggregate self-insurance retentions of $15 million per occurrence are substantially reinsured up to $25 million, with THINC retaining 30% of the next $10 million for each claim that exceeds $15 million or a maximum of $3 million. Claims in excess of $25 million are covered by our excess professional and general liability insurance policies with major independent insurance companies, on a claims-made basis, subject to an aggregate limit of $275 million.
If the aggregate limit of any of our excess professional and general liability policies is exhausted, in whole or in part, it could deplete or reduce the excess limits available to pay any other material claims applicable to that policy period. Any losses not covered by or in excess of the amounts maintained under insurance policies will be funded from our working capital.
In addition to the reserves recorded by our captive insurance subsidiaries, we maintain reserves, including reserves for incurred but not reported claims, for our self-insured professional liability retentions and claims in excess of the policies’ aggregate limits, based on actuarial estimates of losses and related expenses. Also, we provide letters of credit to certain of our insurers, which can be drawn upon under certain circumstances, to collateralize the deductible and self-insured retentions under a selected number of our professional and general liability insurance programs.
13
Table of Contents
EXECUTIVE OFFICERS
The names, positions and ages of our executive officers, as of February 12, 2010, are:
| Position |
Age | |||
| Trevor Fetter | President and Chief Executive Officer | 50 | ||
| Stephen L. Newman, M.D. | Chief Operating Officer | 59 | ||
| Biggs C. Porter | Chief Financial Officer | 56 | ||
| Gary Ruff | Senior Vice President, General Counsel and Secretary | 50 | ||
| Cathy Fraser | Senior Vice President, Human Resources | 45 |
Mr. Fetter was named Tenet’s president in November 2002 and was appointed chief executive officer and a director in September 2003. From March 2000 to November 2002, Mr. Fetter was chairman and chief executive officer of Broadlane, Inc. From October 1995 to February 2000, he served in several senior management positions at Tenet, including chief financial officer. Mr. Fetter began his career with Merrill Lynch Capital Markets, where he concentrated on corporate finance and advisory services for the entertainment and health care industries. In 1988, he joined Metro-Goldwyn-Mayer, Inc., where he had a broad range of corporate and operating responsibilities, rising to executive vice president and chief financial officer. Mr. Fetter holds an M.B.A. from Harvard Business School and a bachelor’s degree in economics from Stanford University. Mr. Fetter is a member of the board of directors of The Hartford Financial Services Group, Inc. He will complete his one-year term as the chairman of the board of directors of the Federation of American Hospitals on March 1, 2010, but will remain a director.
Dr. Newman was appointed chief operating officer in January 2007. From March 2003 through December 2006, he served as chief executive officer of our California region. He joined Tenet in February 1999 as vice president, operations, of our former three-state Gulf States region and, in June 2000, he was promoted to senior vice president, operations, of that region. From April 1997 until he came to Tenet, Dr. Newman served in various executive positions at Columbia/HCA Inc., most recently as president of that company’s three-hospital Louisville Healthcare Network. From August 1990 to March 1997, he was senior vice president and chief medical officer of Touro Infirmary in New Orleans. Prior to 1990, Dr. Newman was both associate professor of pediatrics and medicine at Wright State University School of Medicine in Dayton, Ohio, and director of gastroenterology and nutrition support at Children’s Medical Center, also in Dayton. Dr. Newman holds a medical degree from the University of Tennessee, an M.B.A. from Tulane University and a bachelor’s degree from Rutgers University. He completed his internship, residency and fellowship at Emory University School of Medicine. He also completed the Advanced Management Program at the University of Pennsylvania’s Wharton School of Business. Dr. Newman is a member of the board of directors of the Federation of American Hospitals.
Mr. Porter joined Tenet as chief financial officer in June 2006. From May 2003 until June 2006, he served as vice president and corporate controller of Raytheon Company. In addition, Mr. Porter served as acting chief financial officer for Raytheon from April 2005 to March 2006. From December 2000 to May 2003, he was senior vice president and corporate controller of TXU Corp. and, from August 1994 to December 2000, he was chief financial officer of Northrop Grumman Corporation’s integrated systems sector and its commercial aircraft division. Mr. Porter has also served as vice president, controller and assistant treasurer of Vought Aircraft Company, corporate manager of external financial reporting for LTV Corporation, and audit principal at Arthur Young & Co. He is a certified public accountant. Mr. Porter holds a master’s degree in accounting from the University of Texas/Austin and a bachelor’s degree in accounting from Duke University.
Mr. Ruff was appointed senior vice president and general counsel in July 2008. From 2003 until his promotion, he served as vice president and assistant general counsel for hospital operations. In addition, Mr. Ruff acted as the company’s interim general counsel from March 2008 to July 2008. Mr. Ruff joined Tenet in 1992 as associate counsel of the company’s former Gulf States region, which included 12 hospitals. Before joining Tenet, he was a tax manager for Deloitte & Touche LLP. Mr. Ruff received his master’s degree in management from Northwestern University’s Kellogg School of Management, his master of laws degree in taxation from Georgetown University, his J.D. from Pepperdine University and his bachelor’s degree in accounting from Gonzaga University.
Ms. Fraser joined Tenet as senior vice president, human resources, in September 2006. From June 2000 to September 2006, she served as a management consultant with McKinsey & Co. Inc., the international consulting firm. In that role, Ms. Fraser counseled senior executives at a number of large companies on organizational design, talent management and retention strategies, recruiting and related human resources topics. Prior to her work with McKinsey, Ms. Fraser served as a vice president of Sabre Holdings Inc., a major provider of travel product distribution and technology solutions for the travel industry, from 1994 to 2000. She has also worked for American Airlines and General Motors Acceptance Corp. Ms. Fraser holds an M.B.A. from the University of Michigan, and a bachelor’s degree in business administration from the University of Washington in Seattle. She is a board member of Workforce Solutions of Greater Dallas and the JKU Foundation, a family non-profit foundation.
14
Table of Contents
COMPANY INFORMATION
We file annual, quarterly and current reports, proxy statements and other documents with the Securities and Exchange Commission under the Securities Exchange Act of 1934 (the “Exchange Act”). Our reports, proxy statements and other documents filed electronically with the SEC are available at the website maintained by the SEC at www.sec.gov.
Our website, www.tenethealth.com, also offers, free of charge, access to our annual, quarterly and current reports (and amendments to such reports) and other filings made with, or furnished to, the SEC. The information found on our website is not part of this or any other report we file with or furnish to the SEC.
FORWARD-LOOKING STATEMENTS
The information in this report includes “forward-looking statements” within the meaning of Section 27A of the Securities Act of 1933 and Section 21E of the Exchange Act. All statements, other than statements of historical or present facts, that address activities, events, outcomes, business strategies and other matters that we plan, expect, intend, assume, believe, budget, predict, forecast, project, estimate or anticipate (and other similar expressions) will, should or may occur in the future are forward-looking statements. These forward-looking statements represent management’s current belief, based on currently available information, as to the outcome and timing of future events. They involve known and unknown risks, uncertainties and other factors—many of which we are unable to predict or control—that may cause our actual results, performance or achievements, or health care industry results, to be materially different from those expressed or implied by forward-looking statements. Such factors include, but are not limited to, the risks described in Item 1A of this report and the following:
| • | Our ability to identify and execute on measures designed to save or control costs or streamline operations; |
| • | The availability and terms of debt and equity financing sources to fund the requirements of our business; |
| • | Changes in our business strategies or development plans; |
| • | The impact of natural disasters, including our ability to operate facilities affected by such disasters; |
| • | The ultimate resolution of claims, lawsuits and investigations; |
| • | Technological and pharmaceutical improvements that increase the cost of providing, or reduce the demand for, health care services; |
| • | Various factors that may increase supply costs; |
| • | The soundness of our investments in marketable securities and other instruments; |
| • | The creditworthiness of counterparties to our business transactions; |
| • | Adverse fluctuations in interest rates and other risks related to interest rate swaps or any other hedging activities we undertake; |
| • | National, regional and local economic and business conditions; |
| • | Demographic changes; and |
| • | Other factors and risk factors referenced in this report and our other public filings. |
When considering forward-looking statements, a reader should keep in mind the risk factors and other cautionary statements in this report. Should one or more of the risks and uncertainties described above, in Item 1A, Risk Factors, below or elsewhere in this report occur, or should underlying assumptions prove incorrect, our actual results and plans could differ materially from those expressed in any forward-looking statements. We specifically disclaim any obligation to update any information contained in a forward-looking statement or any forward-looking statement in its entirety and, therefore, disclaim any resulting liability for potentially related damages.
All forward-looking statements attributable to us are expressly qualified in their entirety by this cautionary statement.
| ITEM 1A. | RISK FACTORS |
Our business is subject to a number of risks and uncertainties—many of which are beyond our control—that may cause our actual operating results or financial performance to be materially different from our expectations. If one or more of the events discussed in the following risks were to occur, actual outcomes could differ materially from those expressed in or implied by any forward-looking statements we make in this report or our other filings with the SEC, and our business, financial condition, results of operations or liquidity could be materially adversely affected. Additional risks and uncertainties not presently known, or that we currently deem immaterial, may also negatively affect our business and operations. In either case, the trading price of our common stock could decline and shareholders could lose all or part of their investment.
15
Table of Contents
If we are unable to enter into managed care provider arrangements on acceptable terms, or if we have difficulty collecting from managed care payers, our results of operations could be adversely affected.
We currently have thousands of managed care contracts with various health maintenance organizations and preferred provider organizations. The amount of our managed care net patient revenues from our continuing general hospitals during the year ended December 31, 2009 was $4.9 billion, which represented approximately 56.1% of our total net patient revenues from continuing general hospitals. In addition, approximately 62% of our managed care net patient revenues for the year ended December 31, 2009 was derived from our top ten managed care payers. Furthermore, in the year ended December 31, 2009, our commercial managed care net inpatient revenue per admission from our continuing acute care hospitals was approximately 58% higher than our aggregate yield on a per admission basis from government payers, including managed Medicare and Medicaid insurance plans. At December 31, 2009, approximately 57% of our net accounts receivable related to continuing operations were due from managed care payers.
It would harm our business if we were unable to enter into managed care provider arrangements on acceptable terms. Any material reductions in the payments that we receive for our services, coupled with any difficulties in collecting receivables from managed care payers, could have a material adverse effect on our financial condition, results of operations or cash flows.
Changes in the Medicare and Medicaid programs or other government health care programs could have an adverse effect on our business.
For the year ended December 31, 2009, approximately 25.1% of our same-hospital net patient revenues were received from the Medicare program, and approximately 8.1% of our same-hospital net patient revenues were received from various state Medicaid programs, in each case excluding Medicare and Medicaid managed care programs. The Medicare and Medicaid programs are subject to: statutory and regulatory changes, administrative rulings, interpretations and determinations concerning patient eligibility requirements, funding levels and the method of calculating payments or reimbursements, among other things; requirements for utilization review; and federal and state funding restrictions, all of which could materially increase or decrease payments from these government programs in the future, as well as affect the cost of providing services to our patients and the timing of payments to our facilities.
Several states in which we operate have recently faced budgetary challenges that resulted in reduced Medicaid funding levels to hospitals and other providers. Most states began a new fiscal year on July 1, and although most addressed projected shortfalls in their final budgets, some states may face mid-year budget gaps and many are already projecting shortfalls for state fiscal year 2011, which could result in additional reductions to Medicaid payments, coverage and eligibility or additional taxes on hospitals.
In general, we are unable to predict the effect of future government health care funding policy changes on our operations. If the rates paid by governmental payers are reduced, if the scope of services covered by governmental payers is limited or if we, or one or more of our subsidiaries’ hospitals, are excluded from participation in the Medicare or Medicaid program or any other government health care program, there could be a material adverse effect on our business, financial condition, results of operations or cash flows.
Our business continues to be adversely affected by a high volume of uninsured and underinsured patients, as well as declines in commercial managed care patients.
Like other organizations in the health care industry, we continue to provide services to a high volume of uninsured patients and more patients than in prior years with an increased burden of co-payments and deductibles as a result of changes in their health care plans. As a result, we continue to experience a high level of uncollectible accounts, and, unless our business mix shifts toward a greater number of insured patients or the trend of higher co-payments and deductibles reverses, we anticipate this high level of uncollectible accounts to continue or increase.
At the same time, we continue to experience declines in our commercial managed care volumes, which in the aggregate generate substantially higher yields than Medicare and Medicaid volumes. In the year ended December 31, 2009, same-hospital commercial managed care admissions declined 4.7% and same-hospital commercial managed care outpatient visits declined 1.2%, in each case compared to the year ended December 31, 2008. The declines in our commercial managed care volumes are due, in part, to the related effects of higher unemployment and reductions in commercial managed care enrollment. Going forward, our commercial managed care volumes may also be adversely impacted by the expiration of federal subsidies for those unemployed individuals and their family members who have been receiving subsidized continued health insurance coverage under their former employers’ health plans. Without these subsidies, health insurance coverage could become unaffordable for these people, which could result in lower commercial managed care volumes – especially with respect to elective procedures – at our hospitals.
16
Table of Contents
We operate in a highly competitive industry, and competition is one reason for declines we may experience in patient volumes.
A number of factors affect patient volumes and, thereby, our results of operations at our hospitals and related health care facilities, including the influence of local health care competitors. Generally, other hospitals in the local communities we serve provide services similar to those offered by our hospitals. Some of the hospitals that compete with our hospitals are owned by government agencies or not-for-profit organizations. These tax-exempt competitors may have certain financial advantages not available to our facilities, such as endowments, charitable contributions, tax-exempt financing, and exemptions from sales, property and income taxes. We also face increasing competition from physician-owned specialty hospitals and freestanding surgery, diagnostic and imaging centers for market share in high margin services and for quality physicians and personnel. If competing health care providers are better able to attract more patients, recruit and retain physicians, expand services or obtain favorable managed care contracts at their facilities, our patient volume levels may suffer.
Our business and financial condition could be harmed if we are not able to attract and retain employees, physicians and other health care professionals, and our labor costs continue to be adversely affected by union activity and the shortage of experienced nurses.
Our operations depend on the efforts, abilities and experience of our employees and the physicians on the medical staffs of our hospitals, most of whom have no contractual relationship with us. It is essential to our ongoing business that we attract and retain skilled employees and an appropriate number of quality physicians and other health care professionals in all specialties on our medical staffs. In some of our markets, physician recruitment and retention are affected by a shortage of physicians in certain sought-after specialties and the difficulties that physicians experience in obtaining affordable malpractice insurance or finding insurers willing to provide such insurance. Other issues facing physicians, such as proposed decreases in Medicare payments, are forcing them to consider alternatives, including relocating their practices or retiring sooner than expected. In general, the loss of some or all of our key employees or the inability to attract or retain sufficient numbers of qualified physicians and other health care professionals could have a material adverse effect on patient volumes and, thereby, our business, financial condition, results of operations or cash flows.
Factors that adversely affect our labor costs include union activity, the nationwide shortage of experienced nurses and the enactment of state laws regarding nurse-staffing ratios. At December 31, 2009, approximately 19% of the employees at our hospitals and related health care facilities in both continuing and discontinued operations were represented by labor unions, and we (and the hospital industry in general) are continuing to see an increase in the amount of union activity across the country. We expect this trend to be even more pronounced in 2010, as we renegotiate our existing labor contracts, all of which are scheduled to expire in the next 14 months. Furthermore, like others in the health care industry, we continue to experience a shortage of experienced nurses in certain key specialties and geographic areas. In addition, state-mandated nurse-staffing ratios in California affect not only our labor costs, but, if we are unable to hire the necessary number of experienced nurses to meet the required ratios, they may also cause us to limit patient admissions with a corresponding adverse effect on our net operating revenues. We cannot predict the degree to which we will be affected by future union activity or the future availability or cost of nursing personnel, but we expect to continue to experience salary, wage and benefit pressures.
Our licensed hospital beds are heavily concentrated in certain market areas in Florida, Texas and California, which makes us sensitive to economic, regulatory, environmental and other developments in those areas.
As of December 31, 2009, the largest concentrations of licensed beds in our general hospitals were in Florida (25.6%), Texas (19.3%) and California (17.0%). These concentrations increase the risk that, should any adverse economic, regulatory, environmental or other developments occur in these areas, our business, financial condition, results of operations or cash flows could be materially adversely affected.
Specifically, a natural disaster or other catastrophic event could affect us more significantly than other companies with less geographic concentration. In the recent past, hurricanes have had a disruptive effect on the operations of our hospitals in Florida and Texas, as well as in Louisiana, and the patient populations in those states. Our California operations could be adversely affected by a major earthquake or wildfires in that state. Moreover, we currently expect to spend a total of approximately $80 million (unadjusted for inflation) to comply with the requirements of California’s seismic regulations for hospitals, of which approximately $24 million was spent prior to January 1, 2010.
17
Table of Contents
Our business and financial results could be harmed by violations of existing regulations or compliance with new or changed regulations.
Our business is subject to extensive federal, state and local regulation relating to, among other things, licensure, conduct of operations, ownership of facilities, physician relationships, addition of facilities and services, and reimbursement rates for services. The laws, rules and regulations governing the health care industry are extremely complex, and, in certain areas, the industry has little or no regulatory or judicial interpretation for guidance. If a determination is made that we were in material violation of such laws, rules or regulations, we could be subject to penalties or liabilities or required to make significant changes to our operations. In addition, health care, as one of the largest industries in the United States, continues to attract much legislative interest and public attention. We are unable to predict the future course of federal, state and local regulation or legislation, including Medicare and Medicaid statutes and regulations. Further changes in the regulatory framework affecting health care providers could have a material adverse effect on our business, financial condition, results of operations or cash flows.
We are also required to comply with various federal and state labor laws, rules and regulations governing a variety of workplace wage and hour issues. From time to time, we have been and expect to continue to be subject to regulatory proceedings and private litigation concerning our application of such laws, rules and regulations.
We cannot predict the effect that health care reform, if any, and other changes in government programs may have on our business, financial condition, results of operations or cash flows.
National health care reform is a focus at the federal level, and Congress is currently considering a number of proposals that may significantly impact the health care industry. Among other things, these proposals intend to decrease the number of uninsured legal U.S. residents and reduce health care costs. Various mechanisms to fund health care reform legislation are being considered, including proposals that could reduce hospital reimbursement or otherwise adversely affect our revenues, and various mechanisms to control health care costs are being considered, including proposals that could impose new information technology requirements on our hospitals or otherwise increase our operating costs. Several states are also considering health care reform measures. We cannot predict what form health care reform will take, or if significant health care reform in the near term will take place at all. While federal or state health care reform could adversely affect our business, financial condition, results of operations or cash flows, a decision by Congress not to enact significant health care reform in the near term could also have a negative impact on investor sentiment about companies in the health care industry and, therefore, adversely affect the trading price of our common stock.
The focus on health care reform may also increase the likelihood of material changes to existing government health care programs. A significant portion of both our patient volumes and, as a result, our revenues is derived from government health care programs, principally Medicare and Medicaid. In recent years, legislative and regulatory changes have resulted in limitations on and, in some cases, reductions in levels of payments to health care providers for certain services under these government programs. Possible future changes in Medicare, Medicaid and other health care programs may reduce reimbursements to health care providers and insurers and may also increase our operating costs, which could have an adverse effect on our business, financial condition, results of operations or cash flows.
Our operations have not been profitable for most of the last several years, and, if industry trends or general economic conditions worsen, our business operations and financial results may continue to be adversely affected.
We reported losses from continuing operations for the years ended December 31, 2003 through 2007, a period during which we restructured our business to focus on a smaller group of general hospitals. Although our results of operations have recently improved, we continue to be impacted by a number of industry-wide and company-specific challenges, including declines in patient volumes over the last several years and high bad debt levels. Furthermore, we believe factors associated with the current economic downturn – including higher levels of unemployment, reductions in commercial managed care enrollment, tightened credit markets, and instability in the banking and financial institution industries – have had some impact on our volumes and have affected our ability to collect outstanding receivables. If industry trends or general economic conditions worsen, we may not be able to achieve or sustain future profitability, and our liquidity and ability to repay our outstanding debt may be harmed.
Trends affecting our actual or anticipated results may lead to charges that would adversely affect our results of operations.
As a result of factors that have affected our industry generally and our business specifically, we have been required to record various charges in our results of operations. Our impairment tests presume stable, improving or, in some cases, declining results in our hospitals, which are based on programs and initiatives being implemented that are designed to achieve the hospital’s most recent projections. If these projections are not met, or if in the future negative trends occur that impact our future outlook, further impairments of long-lived assets and goodwill may occur, and we may incur additional restructuring charges. Future restructuring of our operating structure that changes our goodwill reporting units could also result in further impairments of our goodwill. Any such charges could adversely affect our results of operations.
18
Table of Contents
The recent worldwide financial and credit crisis could have a material adverse effect on our business, financial condition and results of operations.
The recent worldwide financial and credit crisis has reduced the availability of liquidity and credit to fund the continuation and expansion of many business operations worldwide. This shortage of liquidity and credit, combined with substantial losses in worldwide equity markets, could lead to an extended worldwide economic recession and result in a material adverse effect on our business, financial condition, results of operations or cash flows. Our ability to access the capital markets may be severely restricted at a time when we would like, or need, to access those markets, which could have a negative impact on our growth plans, our flexibility to react to changing economic and business conditions, and our ability to refinance existing debt. The financial and credit crisis also could have an impact on the lenders under our credit facilities, causing them to fail to meet their obligations to us.
Our substantial leverage could have a material adverse effect on our operations.
We are a highly leveraged company. As of December 31, 2009, we had approximately $4.3 billion of total long-term debt, as well as approximately $185 million in letters of credit outstanding under our senior secured revolving credit facility, which is collateralized by patient accounts receivable at our acute care and specialty hospitals. From time to time, we expect to engage in additional capital markets, bank credit and other financing activities depending on our needs and financing alternatives available at that time.
Our leverage and debt service obligations could have important consequences to an investor, including the following:
| • | Our credit agreement and the indentures governing our outstanding senior notes contain, and any future debt obligations may contain, covenants that, among other things, restrict our ability to pay dividends, incur additional debt and sell assets. Our credit agreement also requires us to maintain certain financial ratios. The indentures governing our outstanding senior secured notes contain covenants that, among other things, restrict our ability and the ability of our subsidiaries to incur liens, consummate asset sales, enter into sale and lease-back transactions or consolidate, merge or sell all or substantially all of our or their assets. If we do not comply with these obligations, it may cause an event of default, which, if not cured or waived, could require us to repay the indebtedness immediately. |
| • | We may be more vulnerable in the event of a deterioration in our business, in the health care industry, in the economy generally or if federal or state governments set further limitations on reimbursement under the Medicare or Medicaid programs. |
| • | We may have difficulty obtaining additional financing at economically acceptable interest rates and other terms to meet our requirements for working capital, capital expenditures, the payment of judgments or settlements, or general corporate purposes. |
| • | We may be required to dedicate a substantial portion of our cash flow to the payment of principal and interest on our indebtedness, which could reduce the amount of funds available for our operations or capital expenditures. |
| ITEM 1B. | UNRESOLVED STAFF COMMENTS |
None.
| ITEM 2. | PROPERTIES |
Note: The disclosure required under this Item is included in Item 1.
19
Table of Contents
| ITEM 3. | LEGAL PROCEEDINGS |
Because we provide health care services in a highly regulated industry, we have been and expect to continue to be subject to various lawsuits, claims and regulatory proceedings from time to time. The ultimate resolution of these matters, individually or in the aggregate, whether as a result of litigation or settlement, could have a material adverse effect on our business (both in the near and long term), financial condition, results of operations or cash flows. We are currently a party to a number of legal and regulatory proceedings, including those described below.
GOVERNMENTAL REVIEWS
Pursuant to the five-year corporate integrity agreement we entered into with the Office of Inspector General in September 2006, we notified the OIG in October 2007 that we had completed a preliminary review of admissions to our inpatient rehabilitation unit at South Fulton Medical Center in East Point, Georgia that suggested further review was necessary to determine whether South Fulton had received Medicare overpayments reportable under our CIA. In January 2008, we submitted this matter into the OIG’s voluntary self-disclosure protocol. The OIG subsequently accepted our submission. In February 2009, we received a letter from the Department of Justice, which is participating in this matter with the OIG, requesting additional information regarding the basis for our self-disclosure, as well as information related to admissions at our other active and divested inpatient rehabilitation hospitals and units for the period 2000 to the date of the letter. The government has since limited the scope of its review to the period May 2005 through December 31, 2007. In addition, the government asked to examine a limited sample of patient files at two inpatient rehabilitation facilities besides South Fulton Medical Center before it determines if its review should extend to our other inpatient rehabilitation units. That examination has been completed, and we are continuing to work with the DOJ and the OIG regarding their review. We are unable to predict the timing and outcome of this matter at this time.
Separately, in 2009, the DOJ, through the U.S. Attorney’s Office in the Western District of New York, and the OIG contacted a number of hospitals, including one Tenet hospital, requesting information regarding their billing practices for kyphoplasty procedures. Kyphoplasty is a surgical procedure used to treat pain and related conditions associated with certain vertebrae injuries. The DOJ and the OIG requested the information in connection with their review of the appropriateness of Medicare patients receiving kyphoplasty procedures on an inpatient basis as opposed to an outpatient basis. To date, the request has been limited to only one of our hospitals. We are fully cooperating with the DOJ and the OIG, and have provided the requested information on a voluntary basis. We are unable to predict the timing and outcome of the investigation, which is still in its preliminary stages at this time. However, based on the total number of inpatient kyphoplasty procedures conducted during the review period at the hospital subject to the information request, we do not believe the outcome of this review will have a material adverse impact on us.
In addition, in February 2009, the fiscal intermediary for our Florida Medical Center began a probe review of the group billing practices of that facility’s partial hospitalization program, a psychiatric treatment program that had the capacity to treat 15 patients on an outpatient basis. We also examined the records reviewed by the fiscal intermediary and independently determined that patients had multiple outpatient admissions with lengths of stay longer than expected for this program. As a result of our review of this matter, we closed the program and, pursuant to our CIA, notified the OIG about our findings. We have since engaged an external physician expert to assess the medical necessity and length of stay of the admissions in question. We are working to complete our assessment, but are unable to predict the timing and outcome of this matter at this time.
WAGE AND HOUR ACTIONS
In September 2004, the court granted our petition to coordinate two pending proposed class action lawsuits, McDonough, et al. v. Tenet Healthcare Corporation and Tien, et al. v. Tenet Healthcare Corporation, in Los Angeles Superior Court. The McDonough case was originally filed in June 2003 in San Diego Superior Court, and the Tien case was originally filed in May 2004 in Los Angeles Superior Court. Plaintiffs in both cases allege that our hospitals violated certain provisions of the California Labor Code and applicable California Industrial Welfare Commission Wage Orders with respect to meal breaks, rest periods and the payment of one hour’s compensation for meal breaks or rest periods not taken. The complaint in the Tien case also alleges that we have improperly “rounded off” time entries on timekeeping records and that our pay stubs do not include all information required by California law. Plaintiffs in both cases are seeking back pay, statutory penalties, interest and attorneys’ fees.
The plaintiffs in the McDonough and Tien cases filed motions, which we opposed, to certify these actions on behalf of virtually all nonexempt employees of our California subsidiaries, as separated into four classes (and one subclass) based on the specific claims at issue. The court issued an initial ruling on the plaintiffs’ motions in June 2008. In that ruling, the court denied the plaintiffs’ request for class certification on the claim that employees missed rest periods. However, the court granted the plaintiffs’ request for class certification on the claims that employees’ pay stubs did not contain all information required by California law and hourly employees did not receive appropriate wages due at the time of their termination. The court also certified a subclass of 12-hour shift employees who received missed meal penalties at a reduced rate, but stated that this subclass should be handled in connection with the Pagaduan v. Fountain Valley Regional Medical Center action that was pending in the same court, which case we subsequently settled
20
Table of Contents
in May 2009. Lastly, the court conditionally certified a class of all current or former hourly employees who were allegedly not provided meal periods, for the purpose of determining certain limited preliminary factual issues. We filed a motion for reconsideration of the court’s class certification ruling and, in November 2008, the court issued a reconsidered ruling denying class certification with respect to all of the plaintiffs’ claims, except the subclass involving 12-hour shift employees. In December 2008, the plaintiffs dismissed the claims of that subclass, which left only the claims of the individual plaintiffs. The plaintiffs subsequently filed a notice of appeal of the court’s decision in February 2009. We continue to believe the court’s November 2008 ruling was correct and are defending that ruling on appeal.
CLASS ACTION LAWSUITS RESULTING FROM HURRICANE KATRINA
When Hurricane Katrina hit the Gulf Coast region in August 2005, we owned five hospitals and a number of imaging centers in the New Orleans area. As previously reported, three lawsuits were filed as purported class actions in late 2005 by and on behalf of patients, their family members and others who were present and allegedly injured at two of those hospitals – Memorial Medical Center and Lindy Boggs Medical Center (each of which we have since divested) – during the storm and its aftermath. The plaintiffs allege that the hospitals were negligent in failing to properly prepare for the storm, failing to evacuate patients ahead of the storm, and failing to have a properly configured emergency generator system, among other allegations of general negligence. The plaintiffs are seeking damages in various and unspecified amounts for the alleged wrongful death of some patients, aggravation of pre-existing illnesses or injuries to patients who survived and were successfully evacuated, and the inability of patients and others to evacuate the hospitals for several days under conditions of extreme heat.
In September 2008, class certification was granted in two of the suits – Preston, et al. v. Tenet HealthSystem Memorial Medical Center, Inc., et al. and Husband et al. v. Tenet HealthSystem Memorial Medical Center, Inc., et al. In her order, the judge certified a class of all persons at Memorial between August 29 and September 2, 2005, excluding employees, who sustained injuries or died, as well as family members who themselves sustained injury as a result of such injuries or deaths to any person at Memorial, excluding employees, during that time. Our appeals of the class certification ruling were exhausted in December 2009 when the Supreme Court of Louisiana denied our writ of certiorari. The Civil District Court for the Parish of Orleans will administer the class proceedings. The class certification hearing in the remaining case – Dunn, et al. v. Tenet Mid-City Medical, L.L.C. (formerly d/b/a Lindy Boggs Medical Center), et al., which was also filed in the Civil District Court for the Parish of Orleans – has been scheduled for late October 2010. We are unable to predict the ultimate resolution of these lawsuits, but we intend to continue to vigorously defend the hospitals in these matters.
INTERNAL REVENUE SERVICE DISPUTES
From time to time, we are engaged in disputes with the Internal Revenue Service regarding our federal tax returns. Refer to Note 14 to our Consolidated Financial Statements for further information.
MEDICAL MALPRACTICE AND OTHER ORDINARY COURSE MATTERS
In addition to the matters described above, our hospitals are subject to investigations, claims and lawsuits in the ordinary course of our business. Most of these matters involve allegations of medical malpractice or other injuries suffered at our hospitals.
| ITEM 4. | SUBMISSION OF MATTERS TO A VOTE OF SECURITY HOLDERS |
None.
21
Table of Contents
PART II.
| ITEM 5. | MARKET FOR REGISTRANT’S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES |
Common Stock. Our common stock is listed on the New York Stock Exchange under the symbol “THC.” The following table sets forth, for the periods indicated, the high and low sales prices per share of our common stock on the NYSE.
| High | Low | |||||
| Year Ended December 31, 2009 |
||||||
| First Quarter |
$ | 1.48 | $ | 0.78 | ||
| Second Quarter |
4.08 | 1.04 | ||||
| Third Quarter |
6.07 | 2.57 | ||||
| Fourth Quarter |
6.39 | 4.52 | ||||
| Year Ended December 31, 2008 |
||||||
| First Quarter |
$ | 5.76 | $ | 4.04 | ||
| Second Quarter |
6.88 | 5.16 | ||||
| Third Quarter |
6.70 | 5.19 | ||||
| Fourth Quarter |
5.43 | 0.99 | ||||
On February 12, 2010, the last reported sales price of our common stock on the NYSE composite tape was $5.21 per share. As of that date, there were approximately 9,047 holders of record of our common stock. Our transfer agent and registrar is The Bank of New York Mellon. Shareholders with questions regarding their stock certificates, including inquiries related to exchanging or replacing certificates or changing an address, should contact the transfer agent at (800) 524-4458.
Dividends. We have not paid cash dividends on our common stock since the first quarter of fiscal 1994, and we do not intend to pay cash dividends on our common stock in the foreseeable future. We currently intend to retain earnings, if any, for the future operation and development of our business. In addition, our senior secured revolving credit agreement contains provisions that limit or prohibit the payment of cash dividends on our common stock.
Equity Compensation. Refer to Part III, Item 12, Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters, for information regarding securities authorized for issuance under our equity compensation plans.
Stock Performance Graph. The following graph shows the cumulative, five-year total return for our common stock compared to three indices, each of which includes us. The Standard & Poor’s 500 Stock Index includes 500 companies representing all major industries. The Standard & Poor’s Health Care Composite Index is a group of 52 companies involved in a variety of healthcare-related businesses. Because the Standard & Poor’s Health Care Composite Index is heavily weighted by pharmaceutical and medical device companies, we believe that at times it may be less useful than the Hospital Management Peer Group Index included below. We compiled this Peer Group Index by selecting publicly traded companies that have as their primary business the management of acute care hospitals and that have been in business for all five of the years shown. These companies are: Community Health Systems, Inc. (CYH), Health Management Associates, Inc. (HMA), Tenet Healthcare Corporation (THC) and Universal Health Services, Inc. (UHS).
22
Table of Contents
Performance data assumes that $100.00 was invested on December 31, 2004 in our common stock and each of the indices. The data assumes the reinvestment of all cash dividends and the cash value of other distributions. Stock price performance shown in the graph is not necessarily indicative of future stock price performance.
COMPARISON OF FIVE YEAR CUMULATIVE TOTAL RETURN
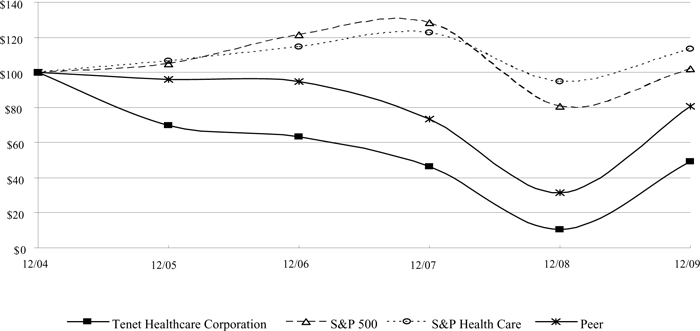
| 12/04 | 12/05 | 12/06 | 12/07 | 12/08 | 12/09 | |||||||||||||
| Tenet Healthcare Corporation |
$ | 100.00 | $ | 69.76 | $ | 63.48 | $ | 46.27 | $ | 10.47 | $ | 49.09 | ||||||
| S&P 500 |
$ | 100.00 | $ | 104.91 | $ | 121.48 | $ | 128.16 | $ | 80.74 | $ | 102.11 | ||||||
| S&P Health Care |
$ | 100.00 | $ | 106.46 | $ | 114.48 | $ | 122.67 | $ | 94.69 | $ | 113.34 | ||||||
| Peer Group |
$ | 100.00 | $ | 95.87 | $ | 94.76 | $ | 73.40 | $ | 31.48 | $ | 80.78 | ||||||
23
Table of Contents
| ITEM 6. | SELECTED FINANCIAL DATA |
OPERATING RESULTS
The following tables present selected audited consolidated financial data for Tenet Healthcare Corporation and its wholly owned and majority-owned subsidiaries for the years ended December 31, 2005 through 2009.
| Years Ended December 31, | ||||||||||||||||||||
| 2009 | 2008 | 2007 | 2006 | 2005 | ||||||||||||||||
| (In Millions, Except Per-Share Amounts) | ||||||||||||||||||||
| Net operating revenues |
$ | 9,014 | $ | 8,585 | $ | 8,083 | $ | 7,676 | $ | 7,557 | ||||||||||
| Operating expenses: |
||||||||||||||||||||
| Salaries, wages and benefits |
3,857 | 3,779 | 3,617 | 3,440 | 3,468 | |||||||||||||||
| Supplies |
1,569 | 1,511 | 1,401 | 1,357 | 1,339 | |||||||||||||||
| Provision for doubtful accounts |
697 | 628 | 555 | 487 | 544 | |||||||||||||||
| Other operating expenses, net |
1,909 | 1,928 | 1,852 | 1,761 | 1,663 | |||||||||||||||
| Depreciation and amortization |
386 | 371 | 336 | 314 | 303 | |||||||||||||||
| Impairment of long-lived assets and goodwill, and restructuring charges, net of insurance recoveries |
27 | 16 | 36 | 312 | 29 | |||||||||||||||
| Hurricane insurance recoveries, net of costs |
— | — | (3 | ) | (14 | ) | 7 | |||||||||||||
| Litigation and investigation costs, net of insurance recoveries |
31 | 41 | 13 | 766 | 212 | |||||||||||||||
| Operating income (loss) |
538 | 311 | 276 | (747 | ) | (8 | ) | |||||||||||||
| Interest expense |
(445 | ) | (418 | ) | (419 | ) | (408 | ) | (403 | ) | ||||||||||
| Gain (loss) from early extinguishment of debt |
97 | — | — | — | (15 | ) | ||||||||||||||
| Investment earnings |
— | 22 | 47 | 62 | 59 | |||||||||||||||
| Net gain on sales of investments |
15 | 139 | — | 5 | 4 | |||||||||||||||
| Income (loss) from continuing operations, before income taxes |
205 | 54 | (96 | ) | (1,088 | ) | (363 | ) | ||||||||||||
| Income tax benefit |
23 | 25 | 61 | 258 | 82 | |||||||||||||||
| Income (loss) from continuing operations, before discontinued operations and cumulative effect of changes in accounting principle |
$ | 228 | $ | 79 | $ | (35 | ) | $ | (830 | ) | $ | (281 | ) | |||||||
| Basic earnings (loss) per share attributable to Tenet Healthcare Corporation common shareholders from continuing operations |
$ | 0.44 | $ | 0.15 | $ | (0.08 | ) | $ | (1.76 | ) | $ | (0.60 | ) | |||||||
| Diluted earnings (loss) per share attributable to Tenet Healthcare Corporation common shareholders from continuing operations |
$ | 0.43 | $ | 0.15 | $ | (0.08 | ) | $ | (1.76 | ) | $ | (0.60 | ) | |||||||
The operating results data presented above are not necessarily indicative of our future results of operations. Reasons for this include, but are not limited to: overall revenue and cost trends, particularly trends in patient accounts receivable collectability and associated provisions for doubtful accounts; the timing and magnitude of price changes; fluctuations in contractual allowances and cost report settlements and valuation allowances; managed care contract negotiations or terminations and payer consolidations; changes in Medicare regulations; Medicaid and other funding levels set by the states in which we operate; fluctuations in interest rates; levels of malpractice insurance expense and settlement trends; impairment of long-lived assets and goodwill; restructuring charges; losses, costs and insurance recoveries related to natural disasters; litigation and investigation costs; acquisitions and dispositions of facilities and other assets; income tax rates and valuation allowances; the timing and amounts of stock option and restricted stock unit grants to employees and directors; and changes in occupancy levels and patient volumes. Factors that affect patient volumes and, thereby, our results of operations at our hospitals and related health care facilities include, but are not limited to: the business environments, economic conditions and demographics of local communities; the number of uninsured and underinsured individuals in local communities treated at our hospitals; seasonal cycles of illness; climate and weather conditions; physician recruitment, retention and attrition; advances in technology and treatments that reduce length of stay; local health care competitors; managed care contract negotiations or terminations; any unfavorable publicity about us, which impacts our relationships with physicians and patients; and the timing of elective procedures. These considerations apply to year-to-year comparisons as well.
24
Table of Contents
BALANCE SHEET DATA
| December 31, | |||||||||||||||
| 2009 | 2008 | 2007 | 2006 | 2005 | |||||||||||
| (In Millions) | |||||||||||||||
| Working capital (current assets minus current liabilities) |
$ | 689 | $ | 760 | $ | 512 | $ | 1,100 | $ | 1,216 | |||||
| Total assets |
7,953 | 8,174 | 8,393 | 8,539 | 9,812 | ||||||||||
| Long-term debt, net of current portion |
4,272 | 4,778 | 4,771 | 4,760 | 4,784 | ||||||||||
| Total equity |
697 | 147 | 88 | 298 | 1,086 | ||||||||||
CASH FLOW DATA
| Years Ended December 31, | ||||||||||||||||||||
| 2009 | 2008 | 2007 | 2006 | 2005 | ||||||||||||||||
| (In Millions) | ||||||||||||||||||||
| Net cash provided by (used in) operating activities |
$ | 425 | $ | 208 | $ | 326 | $ | (462 | ) | $ | 763 | |||||||||
| Net cash used in investing activities |
(125 | ) | (274 | ) | (520 | ) | (379 | ) | (392 | ) | ||||||||||
| Net cash provided by (used in) financing activities |
(117 | ) | 1 | (18 | ) | 252 | 348 | |||||||||||||
| ITEM 7. | MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS |
INTRODUCTION TO MANAGEMENT’S DISCUSSION AND ANALYSIS
The purpose of this section, Management’s Discussion and Analysis of Financial Condition and Results of Operations, is to provide a narrative explanation of our financial statements that enables investors to better understand our business, to enhance our overall financial disclosures, to provide the context within which our financial information may be analyzed, and to provide information about the quality of, and potential variability of, our financial condition, results of operations and cash flows. Unless otherwise indicated, all financial and statistical information included herein relates to our continuing operations, with dollar amounts expressed in millions (except per-share, per admission, per patient day and per visit amounts). This information should be read in conjunction with the accompanying Consolidated Financial Statements. It includes the following sections:
| • | Executive Overview |
| • | Sources of Revenue |
| • | Results of Operations |
| • | Liquidity and Capital Resources |
| • | Off-Balance Sheet Arrangements |
| • | Recently Issued Accounting Standards |
| • | Critical Accounting Estimates |
EXECUTIVE OVERVIEW
We continue to focus on the execution of our operating and financing strategies. While we have seen certain areas of improvement, we are still facing several industry-wide and company-specific challenges that continue to negatively affect our progress. We are dedicated to improving our patients’, shareholders’ and other stakeholders’ confidence in us. We believe we will accomplish that by providing quality care and generating positive volume growth and earnings at our hospitals.
KEY DEVELOPMENTS
Recent key developments include the following:
NorthShore Regional Medical Center Lease Not Renewed—In January 2010, we entered into a definitive agreement to sell certain of our owned assets and transition the operation of NorthShore Regional Medical Center in Slidell, Louisiana to a new hospital operator. We had previously announced in May 2009 that we would not renew the lease for this hospital. We anticipate that the transaction will close effective April 1, 2010.
Repurchases of Outstanding Senior Notes—In December and November 2009, we completed open market repurchases of $3 million aggregate principal amount of our 9 1/4% senior notes due 2015 and $2 million aggregate principal amount of our 63/8% senior notes due 2011 for cash of approximately $5 million. In September 2009, we repurchased approximately $8 million aggregate principal amount of our 91/4% senior notes due 2015 for cash of approximately $8 million. In July 2009, we completed open market repurchases of approximately $68 million aggregate principal amount of our 6 3/8 % senior notes due 2011, our 6 1/2% senior notes due 2012, our 9 7/8 % senior notes due 2014, and our 6 7/8 % senior notes due 2031 for cash of approximately $60 million. As a result of our July note repurchases, we recorded a gain from early extinguishment of debt of approximately $6 million in the three months ended September 30, 2009.
25
Table of Contents
Interest Rate Swap—In November 2009, we terminated an interest rate swap agreement we had entered into effective May 1, 2009 with respect to our 7 3/8 % senior notes due 2013. We realized approximately $8 million in net savings in interest payments during the term of the interest rate swap agreement. For additional information, refer to Note 6 to the Consolidated Financial Statements included in this report.
Quality Designations—In November 2009, we announced that 42 of our hospitals received 257 quality designations through CIGNA HealthCare. These quality designations are based on outcomes for treatment of 29 surgical procedures and medical conditions. In addition, 26 of our hospitals received 76 Centers of Excellence designations for 2009 from CIGNA. These designations recognize hospitals meeting CIGNA’s standards for quality and efficiency. In August 2009, we announced that 29 of our hospitals received 73 UnitedHealth Premium Specialty Center designations for cardiac care, cardiac surgery and heart rhythm disorders. To receive these designations, hospitals must meet or exceed UnitedHealthcare’s quality criteria based on nationally recognized medical standards.
Sale of Mandatory Convertible Preferred Stock and Repurchase of Outstanding Senior Notes with Sales Proceeds—In September 2009, we sold 345,000 shares of 7% mandatory convertible preferred stock for net proceeds of approximately $334 million. We used $315 million of the net proceeds to repurchase $300 million aggregate principal amount of our outstanding 91/4% senior notes due 2015 in September 2009.
Private Offering of Senior Secured Notes—In June 2009, we sold $925 million aggregate principal amount of 8 7/8% senior secured notes due 2019. We will pay interest on the senior secured notes semi-annually in arrears on January 1 and July 1 of each year, commencing January 1, 2010. The senior secured notes rank equally with our 9% senior secured notes due 2015 and 10% senior secured notes due 2018, which we issued in May and March 2009, as described below. All of our senior secured notes are guaranteed by and secured by a first-priority pledge of the capital stock and other ownership interests of certain of our subsidiaries.
Tender Offer to Purchase Senior Notes—In June 2009, we purchased in a cash tender offer approximately $900 million of the $1 billion aggregate principal amount outstanding of our 9 7/8% senior notes due 2014 for total consideration of approximately $941 million, representing approximately $900 million in principal payments and approximately $41 million in accrued and unpaid interest through the dates of purchase. We purchased the 9 7/8% senior notes with the net proceeds of approximately $881 million from the offering of the 8 7/8% senior secured notes due 2019 and cash on hand. In connection with the purchases of our 97/8% senior notes, we recorded a loss from early extinguishment of debt of approximately $24 million in the three months ended June 30, 2009.
New Joint Venture Created—In May 2009, we announced the creation of MED3000 Practice Resources, LLC, a joint venture between MED3000, Inc., an unaffiliated third party, and one of our subsidiaries, which is a 20% minority owner. The new joint venture will initially focus on providing services to physician practices in the 12 states where we currently operate. In addition, the joint venture will provide health information technology (including practice management systems, electronic health records and personal health records) and management services (including revenue cycle management, group purchasing and comprehensive practice and data management).
Sale of Peoples Health Network—In May 2009, we completed the sale of our 50% membership interest in Peoples Health Network (“PHN”), the company that administered the operations of Tenet Choices, Inc. (“TCI”), our wholly owned Medicare Advantage health maintenance organization insurance subsidiary in Louisiana. As part of the transaction, we transferred substantially all of the insurance assets and liabilities of TCI to a PHN subsidiary. The transaction resulted in a pretax gain in continuing operations of approximately $15 million.
Note Exchanges—In May and March 2009, we exchanged approximately $918 million aggregate principal amount of our outstanding 6 3/8% senior notes due 2011 and $510 million aggregate principal amount of our outstanding 6 1/2% senior notes due 2012 for approximately $714 million aggregate principal amount of new 9% senior secured notes due 2015 and approximately $714 million aggregate principal amount of new 10% senior secured notes due 2018, plus additional consideration described in Note 6 to the Consolidated Financial Statements.
Sale of USC University Hospital and USC Kenneth Norris Jr. Cancer Hospital—On March 31, 2009, we completed the previously disclosed sale of USC University Hospital and USC Kenneth Norris Jr. Cancer Hospital to the University of Southern California. The transaction generated cash proceeds of approximately $275 million from the sale of property and equipment. Approximately $30 million from these proceeds was deferred and placed in an escrow account, where they will remain for up to four years. We retained substantially all of the hospitals’ working capital, which is expected to result in approximately $30 million of incremental cash proceeds. The total net proceeds will be used for general corporate purposes.
26
Table of Contents
National Agreement with Aetna—In March 2009, we announced that Tenet Physicians Inc., one of our subsidiaries, had entered into a national agreement with Aetna that covers 400 employed physicians and facilitates the participation of those physicians in Aetna’s provider networks. The agreement also includes provisions promoting a joint, collaborative effort to enhance the credentialing process for the employed physicians.
SIGNIFICANT CHALLENGES
As stated above, there are a number of significant industry-wide and company-specific challenges that have been impacting our operating performance, including those summarized below.
Volumes—Although we have seen some improvements in recent quarters, we have experienced declines in patient volumes over the last several years. We believe the reasons for these declines include, but are not limited to, factors that have affected many hospital companies, including decreases in the demand for invasive cardiac procedures, increased competition and utilization pressure by managed care organizations. Given our geographic concentration, we are also affected by population trends, which have been a particular concern in Florida. In addition, we believe the industry-wide challenges associated with physician recruitment, retention and attrition have also been significant contributors to our past volume declines. Our operations depend on the efforts, abilities and experience of the physicians on the medical staffs of our hospitals, most of whom have no contractual relationship with us. It is essential to our ongoing business that we attract and retain an appropriate number of quality physicians in all specialties on our medical staffs. Although we had a net overall gain in physicians added to our medical staffs in each of the last three years, in some of our markets, physician recruitment and retention are still affected by a shortage of physicians in certain sought-after specialties and the difficulties that physicians experience in obtaining affordable malpractice insurance or finding insurers willing to provide such insurance. Other issues facing physicians, such as proposed decreases in Medicare payments, are forcing them to consider alternatives, including relocating their practices or retiring sooner than expected.
We continue to take steps to increase patient volumes; however, due to the concentration of our hospitals in California, Florida and Texas, we may not be able to mitigate some factors that contribute to volume declines. One of our initiatives is our Physician Relationship Program, which is centered on understanding the needs of physicians who admit patients both to our hospitals and to our competitors’ hospitals and responding to those needs with changes and improvements in our hospitals and operations. We have targeted capital spending in order to address specific needs or growth opportunities of our hospitals, which is expected to have a positive impact on their volumes. We have also sought to include all of our hospitals and an increased number of our affiliated physicians in the affected geographic area or nationally when negotiating new managed care contracts, which should result in additional volumes at facilities that were not previously a part of such managed care networks. In addition, we have completed clinical service line market demand analyses and profitability assessments to determine which services are highly valued that can be emphasized and marketed to improve our operating results. This Targeted Growth Initiative has resulted in some reductions in unprofitable service lines in several locations, which have had a slightly negative impact on our volumes. However, the elimination of these unprofitable service lines will allow us to focus more resources on services that are in higher demand and are more profitable.
Our Commitment to Quality initiative is further helping position us to competitively meet the volume challenge. We continue to work with physicians to implement the most current evidence-based medicine techniques to improve the way we provide care. As a result of these efforts, our hospitals have improved substantially in quality metrics reported by the government and have been recognized by several managed care companies for their quality of care. In our continuing efforts to improve our clinical outcomes and drive down our costs of care, we launched our Medicare Performance Initiative in 2009. This initiative is focused on the identification and reduction of costs associated with variations in physician and hospital practices. The project includes the dissemination of best practices based on evidence-based medicine, which we expect will promote the most effective and efficient utilization of resources and result in shorter lengths of stay, as well as reductions in redundant ancillary services and readmissions for hospitalized patients. We believe that quality of care improvements will continue to have the effect of increasing physician and patient satisfaction, potentially improving our volumes.
Bad Debt—Like other organizations in the health care industry, we continue to provide services to a high volume of uninsured patients and more patients than in prior years with an increased burden of co-payments and deductibles as a result of changes in their health care plans. The discounting components of our Compact with Uninsured Patients (“Compact”) have reduced our provision for doubtful accounts recorded in our Consolidated Financial Statements, but they do not mitigate the net economic effects of treating uninsured or underinsured patients. We continue to experience a high level of uncollectible accounts, and we continue to focus, where applicable, on placement of patients in various government programs, such as Medicaid. However, unless our business mix shifts toward a greater number of insured patients or the trend of higher co-payments and deductibles reverses, we anticipate this high level of uncollectible accounts to continue or increase.
27
Table of Contents
Cost Pressures—Labor and supply expenses remain significant cost pressures for us as well as the industry in general. Controlling labor costs in an environment of fluctuating patient volumes and increased labor union activity will continue to be a challenge. Also, inflation and technology improvements are driving supply costs higher, and our efforts to control supply costs through product standardization, bulk purchases and improved utilization are constantly challenged.
General Economic Conditions—We believe the current economic downturn, tight credit markets, and instability in the banking and financial institution industries has had some impact on our volumes and has affected our ability to collect outstanding receivables. A significant amount of our admissions comes through our emergency rooms and, therefore, is not usually materially impacted by broad economic factors. However, our levels of elective procedures and our ability to collect accounts receivable, due to the related effects of higher unemployment and reductions in commercial managed care enrollment, may be materially impacted if the current economic environment continues. We could also be negatively affected if California, Florida or other states reduce funding of Medicaid and other state health care programs.
RESULTS OF OPERATIONS—OVERVIEW
Our results of operations have been and continue to be influenced by industry-wide and company-specific challenges, including fluctuating volumes, decreased demand for inpatient cardiac procedures and high levels of bad debt, that have negatively affected our revenue growth and operating expenses. We believe our future profitability will be achieved through volume growth, appropriate reimbursement levels and cost control across our portfolio of hospitals. We also believe our results of operations for our most recent fiscal quarter best reflect recent trends we are experiencing with respect to volumes, revenues and expenses; therefore, we have provided below detailed information about these metrics for the three months ended December 31, 2009 and 2008. In order to disclose trends using data comparable to the prior-year period, operating statistics in this section and throughout Management’s Discussion and Analysis are presented on a same-hospital basis, where noted, and exclude the results of our Sierra Providence East Medical Center, which opened in May 2008, and NorthShore Regional Medical Center, which was reclassified to discontinued operations in the three months ended June 30, 2009.
| Same-Hospital Continuing Operations |
|||||||||
| Three Months Ended December 31, | |||||||||
| Admissions, Patient Days and Surgeries |
2009 | 2008 | Increase (Decrease) |
||||||
| Commercial managed care admissions |
32,617 | 34,431 | (5.3 | )% | |||||
| Governmental managed care admissions |
29,347 | 28,150 | 4.3 | % | |||||
| Medicare admissions |
38,166 | 39,312 | (2.9 | )% | |||||
| Medicaid admissions |
16,412 | 15,821 | 3.7 | % | |||||
| Uninsured admissions |
5,742 | 5,956 | (3.6 | )% | |||||
| Charity care admissions |
2,487 | 2,254 | 10.3 | % | |||||
| Other admissions |
3,257 | 3,311 | (1.6 | )% | |||||
| Total admissions |
128,028 | 129,235 | (0.9 | )% | |||||
| Paying admissions (excludes charity and uninsured) |
119,799 | 121,025 | (1.0 | )% | |||||
| Total government program admissions |
83,925 | 83,283 | 0.8 | % | |||||
| Charity admissions and uninsured admissions |
8,229 | 8,210 | 0.2 | % | |||||
| Admissions through emergency department |
73,806 | 73,000 | 1.1 | % | |||||
| Commercial managed care admissions as a percentage of total admissions |
25.5 | % | 26.6 | % | (1.1 | )%(1) | |||
| Emergency department admissions as a percentage of total admissions |
57.6 | % | 56.5 | % | 1.1 | % (1) | |||
| Uninsured admissions as a percentage of total admissions |
4.5 | % | 4.6 | % | (0.1 | )%(1) | |||
| Charity admissions as a percentage of total admissions |
1.9 | % | 1.7 | % | 0.2 | % (1) | |||
| Surgeries – inpatient |
37,663 | 38,296 | (1.7 | )% | |||||
| Surgeries – outpatient |
52,092 | 51,448 | 1.3 | % | |||||
| Total surgeries |
89,755 | 89,744 | — | % | |||||
| Patient days – total |
622,475 | 630,821 | (1.3 | )% | |||||
| Adjusted patient days(2) |
920,652 | 918,560 | 0.2 | % | |||||
| Patient days – commercial managed care |
130,289 | 136,976 | (4.9 | )% | |||||
| Average length of stay (days) |
4.9 | 4.9 | — | (1) | |||||
| Adjusted patient admissions(2) |
190,619 | 189,357 | 0.7 | % | |||||
| (1) | The change is the difference between the amounts shown for the three months ended December 31, 2009 as compared to the three months ended December 31, 2008. |
| (2) | Adjusted patient days/admissions represents actual patient days/admissions adjusted to include outpatient services by multiplying actual patient days/admissions by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
28
Table of Contents
Total same-hospital admissions declined by 1,207, or 0.9%, in the three months ended December 31, 2009 as compared to the same period in 2008. Our California region and our Philadelphia market each reported positive total admissions growth, while our other regions reported admissions declines, in the three months ended December 31, 2009 as compared to the three months ended December 31, 2008. Commercial managed care admissions declined by 5.3% in the three months ended December 31, 2009 as compared to the same period in 2008. Admissions through all government programs, including both traditional and managed government programs, achieved positive growth of 0.8% in the three months ended December 31, 2009 as compared to the three months ended December 31, 2008. Uninsured and charity admissions grew by 0.2% in the three months ended December 31, 2009 as compared to the same period in 2008. There were 666 flu-related admissions in the three months ended December 31, 2009.
| Same-Hospital Continuing Operations |
|||||||||
| Three Months Ended December 31, | |||||||||
| Outpatient Visits |
2009 | 2008 | Increase (Decrease) |
||||||
| Commercial managed care visits |
339,890 | 353,586 | (3.9 | )% | |||||
| Governmental managed care visits |
185,949 | 158,507 | 17.3 | % | |||||
| Medicare visits |
207,878 | 202,539 | 2.6 | % | |||||
| Medicaid visits |
75,648 | 66,419 | 13.9 | % | |||||
| Uninsured visits |
90,257 | 92,825 | (2.8 | )% | |||||
| Charity care visits |
7,032 | 6,051 | 16.2 | % | |||||
| Other visits |
49,214 | 43,390 | 13.4 | % | |||||
| Total visits |
955,868 | 923,317 | 3.5 | % | |||||
| Paying visits (excludes charity and uninsured) |
858,579 | 824,441 | 4.1 | % | |||||
| Total government program visits |
469,475 | 427,465 | 9.8 | % | |||||
| Surgery visits |
52,092 | 51,448 | 1.3 | % | |||||
| Emergency department visits |
353,031 | 322,394 | 9.5 | % | |||||
| Charity visits and uninsured visits |
97,289 | 98,876 | (1.6 | )% | |||||
| Charity visits and uninsured visits as a percentage of total visits |
10.2 | % | 10.7 | % | (0.5 | )%(1) | |||
| Paying visits as a percentage of total visits |
89.8 | % | 89.3 | % | 0.5 | % (1) | |||
| Commercial visits as a percentage of total visits |
35.6 | % | 38.3 | % | (2.7 | )%(1) | |||
| (1) | The change is the difference between the amounts shown for the three months ended December 31, 2009 as compared to the three months ended December 31, 2008. |
We had growth of 32,551 total same-hospital outpatient visits, or 3.5%, in the three months ended December 31, 2009 as compared to the three months ended December 31, 2008. All of our regions reported growth in outpatient visits in the three months ended December 31, 2009, with the strongest growth occurring in our Philadelphia market, which achieved double-digit growth. The outpatient growth in our Philadelphia market was impacted by an increase in flu-related visits at St. Christopher’s Hospital for Children. In addition, our Central region achieved outpatient visit growth of 5.2%. There were 10,391 flu-related outpatient visits in the three months ended December 31, 2009. Newly opened or acquired facilities contributed 967 visits, net of the loss of visits from a center in which our ownership was converted to a minority interest in 2009. Excluding these 967 visits, organic growth in outpatient visits was an increase of 31,584 visits, or 3.4%, in the three months ended December 31, 2009 as compared to the same period in 2008.
29
Table of Contents
Outpatient surgery visits grew by 1.3% in the three months ended December 31, 2009 as compared to the same period in 2008. Outpatient imaging experienced a decline in visits of 1.4% in the three months ended December 31, 2009 as compared to the three months ended December 31, 2008. Emergency department outpatient visits increased 30,637 visits, or 9.5%, in the three months ended December 31, 2009 compared to the same period in 2008. This increase in emergency department outpatient visits contributed 94.1% of the increase in total outpatient visits in the three months ended December 31, 2009 as compared to the same period in 2008. Charity and uninsured outpatient visits decreased by 1.6% in the three months ended December 31, 2009 as compared to the three months ended December 31, 2008.
| Same-Hospital Continuing Operations |
|||||||||
| Three Months Ended December 31, | |||||||||
| Revenues |
2009 | 2008 | Increase (Decrease) |
||||||
| Net operating revenues |
$ | 2,235 | $ | 2,160 | 3.5 | % | |||
| Net patient revenues from commercial managed care |
$ | 892 | $ | 868 | 2.8 | % | |||
| Revenues from the uninsured |
$ | 149 | $ | 148 | 0.7 | % | |||
| Net inpatient revenues(1) |
$ | 1,468 | $ | 1,431 | 2.6 | % | |||
| Net outpatient revenues(1) |
$ | 679 | $ | 641 | 5.9 | % | |||
| (1) | Net inpatient revenues and net outpatient revenues are components of net operating revenues. Net inpatient revenues include self-pay revenues of $60 million and $63 million for the three months ended December 31, 2009 and 2008, respectively. Net outpatient revenues include self-pay revenues of $89 million and $85 million for the three months ended December 31, 2009 and 2008, respectively. |
Net operating revenues increased approximately $75 million, or 3.5%, on a same-hospital basis in the three months ended December 31, 2009 as compared to the same period in 2008. Favorable prior-year cost report adjustments contributed approximately $6 million to net operating revenues in the three months ended December 31, 2009 as compared to a contribution of $2 million in the three months ended December 31, 2008. Also, in the three months ended December 31, 2008, net operating revenues included $8 million related to a Medicare medical education reimbursement issue. Excluding prior-year cost report adjustments and the $8 million medical education reimbursement revenue from the three months ended December 31, 2008, same-hospital net operating revenues would have shown an increase of 3.7% in the three months ended December 31, 2009 as compared to the same period in 2008.
Commercial managed care revenues increased by 2.8% on a same-hospital basis despite the 5.3% decline in commercial managed care admissions and the decline of 3.9% in commercial managed care outpatient visits in the three months ended December 31, 2009 as compared to the same period in 2008.
| Same-Hospital Continuing Operations |
|||||||||
| Three Months Ended December 31, | |||||||||
| Revenues on a Per Admission, Per Patient Day and Per Visit Basis |
2009 | 2008 | Increase (Decrease) |
||||||
| Net inpatient revenue per admission |
$ | 11,466 | $ | 11,073 | 3.5 | % | |||
| Net inpatient revenue per patient day |
$ | 2,358 | $ | 2,268 | 4.0 | % | |||
| Net outpatient revenue per visit |
$ | 710 | $ | 694 | 2.3 | % | |||
| Net patient revenue per adjusted patient admission(1) |
$ | 11,263 | $ | 10,942 | 2.9 | % | |||
| Net patient revenue per adjusted patient day(1) |
$ | 2,332 | $ | 2,256 | 3.4 | % | |||
| Managed care: net inpatient revenue per admission |
$ | 12,364 | $ | 11,821 | 4.6 | % | |||
| Managed care: net outpatient revenue per visit |
$ | 832 | $ | 813 | 2.3 | % | |||
| (1) | Adjusted patient days/admissions represents actual patient days/admissions adjusted to include outpatient services by multiplying actual patient days/admissions by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
Unit revenue improvement was evident across all key metrics, primarily reflecting the improved terms of our commercial managed care contracts. The growth in net inpatient revenue per admission of 3.5% was adversely impacted by a shift in payer mix, including a decline in commercial managed care admissions as a percentage of total admissions to 25.5% in the three months ended December 31, 2009 as compared to 26.6% in the three months ended December 31, 2008.
The outpatient revenue per visit increase of 2.3% was also constrained by an adverse mix shift, including a decline in commercial managed care outpatient visits as a percentage of total outpatient visits to 35.6% in the three months ended December 31, 2009 as compared to 38.3% in the three months ended December 31, 2008.
30
Table of Contents
| Same-Hospital Continuing Operations |
|||||||||
| Three Months Ended December 31, | |||||||||
| Selected Operating Expenses |
2009 | 2008 | Increase (Decrease) |
||||||
| Salaries, wages and benefits |
$ | 981 | $ | 951 | 3.2 | % | |||
| Supplies |
390 | 382 | 2.1 | % | |||||
| Other operating expenses |
474 | 463 | 2.4 | % | |||||
| Total |
$ | 1,845 | $ | 1,796 | 2.7 | % | |||
| Rent/lease expense(1) |
$ | 37 | $ | 34 | 8.8 | % | |||
| Salaries, wages and benefits per adjusted patient day(2) |
$ | 1,065 | $ | 1,035 | 2.9 | % | |||
| Supplies per adjusted patient day(2) |
424 | 416 | 1.9 | % | |||||
| Other operating expenses per adjusted patient day(2) |
515 | 504 | 2.2 | % | |||||
| Total per adjusted patient day |
$ | 2,004 | $ | 1,955 | 2.5 | % | |||
| (1) | Included in other operating expenses. |
| (2) | Adjusted patient days represent actual patient days adjusted to include outpatient services by multiplying actual patient days by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
Total selected operating expenses, which is defined as salaries, wages and benefits, supplies, and other operating expenses, increased by 2.5% on a per adjusted patient day basis in the three months ended December 31, 2009 compared to the three months ended December 31, 2008. Excluding the $16 million discretionary contribution expense for our 401(k) plan discussed below, the percentage increase is 1.6%.
Salaries, wages and benefits per adjusted patient day increased by approximately 2.9% in the three months ended December 31, 2009 as compared to the same period in 2008. This increase is primarily due to merit increases for our employees, increased accruals for annual incentive compensation and our $16 million discretionary contribution to the 401(k) plan accounts of employees who are not eligible for incentive compensation awards, partially offset by reduced contract labor expense and a decline in full-time employee headcount. Excluding the discretionary contribution expense for our 401(k) plan, the percentage increase is 1.3%
Supplies expense per adjusted patient day increased by 1.9% in the three months ended December 31, 2009 compared to the three months ended December 31, 2008. The increase in supplies expense is primarily due to increased utilization of high-cost pharmaceuticals and biologics, as well as implantable devices.
Other operating expenses per adjusted patient day increased by 2.2% in the three months ended December 31, 2009 as compared to the same period in 2008. The increase is primarily due to higher state provider taxes, increases in costs of contracted services, and a reduction in information systems and business office costs allocable to discontinued operations. The increase was offset by a $4 million, or 22.2%, decline in total hospital malpractice expense to $14 million in the three months ended December 31, 2009 compared to $18 million in the three months ended December 31, 2008. This decrease is primarily attributable to improved claims experience.
| Same-Hospital Continuing Operations |
|||||||||||
| Three Months Ended December 31, | |||||||||||
| Provision for Doubtful Accounts |
2009 | 2008 | Increase (Decrease) |
||||||||
| Provision for doubtful accounts |
$ | 176 | $ | 164 | 7.3 | % | |||||
| Provision for doubtful accounts as a percentage of net operating revenues |
7.9 | % | 7.6 | % | 0.3 | %(1) | |||||
| Collection rate on self-pay accounts(2) |
30.1 | % | 32.5 | % | (2.4 | )%(1) | |||||
| Collection rate from managed care payers |
98.0 | % | 97.8 | % | 0.2 | %(1) | |||||
| (1) | The change is the difference between the amounts shown for the three months ended December 31, 2009 as compared to the three months ended December 31, 2008. |
| (2) | Self-pay accounts receivable are comprised of both uninsured and balance-after insurance receivables. |
Provision for doubtful accounts increased by $12 million, or 7.3%, in the three months ended December 31, 2009 as compared to the same period in 2008. The increase in provision for doubtful accounts was related to higher pricing and the 240 basis point decline in our collection rate on self-pay accounts. These items were partially offset by a decline in uninsured volumes, improved collection rates from managed care payers and improved managed care accounts receivable aging categories.
31
Table of Contents
The self-pay collection rate, which is the blended collection rate for uninsured and balance-after insurance accounts receivable, declined to approximately 30.1% in the three months ended December 31, 2009, compared to 32.5% in the three months ended December 31, 2008.
The estimated direct and allocated costs (based on selected operating expenses, which include salaries, wages and benefits, supplies and other operating expenses) of caring for uninsured patients were $93 million for both of the three months ended December 31, 2009 and 2008.
The table below shows the pretax and after-tax impact on continuing operations for the three months and years ended December 31, 2009 and 2008 of the following items:
| Three Months Ended December 31, |
Years Ended December 31, |
|||||||||||||||
| 2009 | 2008 | 2009 | 2008 | |||||||||||||
| (Expense) Income | ||||||||||||||||
| Impairment of long-lived assets and goodwill, and restructuring charges |
$ | (14 | ) | $ | (12 | ) | $ | (27 | ) | $ | (16 | ) | ||||
| Litigation and investigation benefit (costs) |
(18 | ) | 4 | (31 | ) | (41 | ) | |||||||||
| Gain from early extinguishment of debt |
— | — | 97 | — | ||||||||||||
| Net gain (loss) on sales of investments |
— | (1 | ) | 15 | 139 | |||||||||||
| Pretax impact |
$ | (32 | ) | $ | (9 | ) | 54 | $ | 82 | |||||||
| Deferred tax asset valuation allowance and other tax adjustments |
$ | 33 | $ | 9 | $ | 110 | $ | 56 | ||||||||
| Total after-tax impact |
$ | 12 | $ | 6 | $ | 144 | $ | 109 | ||||||||
| Diluted per-share impact of above items |
$ | 0.03 | $ | 0.01 | $ | 0.28 | $ | 0.22 | ||||||||
| Diluted earnings (loss) per share, including above items |
$ | 0.03 | $ | (0.01 | ) | $ | 0.43 | $ | 0.15 | |||||||
LIQUIDITY AND CAPITAL RESOURCES OVERVIEW
Cash and cash equivalents were $690 million at December 31, 2009, a decrease of $41 million from $731 million at September 30, 2009.
Significant cash flow items in the three months ended December 31, 2009 included:
| • | $21 million we received under our interest rate swap agreement; |
| • | Cash distributions of $1 million we received related to our investment in the Reserve Yield Plus Fund, which are classified as investing activity cash flows; |
| • | Capital expenditures of $192 million; |
| • | $23 million in principal payments classified as operating cash outflows from continuing operations related to our 2006 civil settlement with the federal government; |
| • | Interest payments of $99 million; and |
| • | Income tax payments of $58 million, including $60 million in settlement of Internal Revenue Service (“IRS”) audit disputes in order to forestall future interest accruals as described in Note 14 to our Consolidated Financial Statements. |
Net cash provided by operating activities was $425 million in the year ended December 31, 2009 compared to $208 million in the year ended December 31, 2008. Key negative and positive factors contributing to the change between the 2009 and 2008 periods include the following:
| • | Additional interest payments of $48 million, primarily due to monthly interest payments under our interest rate swap agreement, higher interest rate debt issued during the year and interest payments that were accelerated and paid in 2009 as a result of our various long-term debt transactions discussed in Note 6 to the Consolidated Financial Statements; |
| • | $39 million we received under our interest rate swap agreement; |
32
Table of Contents
| • | Increased operating income from continuing operations of $243 million, excluding litigation and investigation costs, impairment and restructuring charges, and depreciation and amortization in the year ended December 31, 2009 compared to the year ended December 31, 2008; |
| • | $81 million in payments related to our 2009 settlement of wage and hour actions; |
| • | Increased income tax payments of $39 million, including $60 million in settlement of IRS audit disputes as discussed above; |
| • | $60 million of insurance recoveries received in the year ended December 31, 2008 related to our December 2004 Redding Medical Center litigation settlement (based on the components of the recoveries, $39 million was classified as discontinued operations cash flows from operations and $21 million was classified as continuing operations cash flows from operations); |
| • | $61 million of additional cash flows related to divested hospitals classified as discontinued operations primarily due to the liquidation of accounts receivable and other working capital balances (such amount excludes the $39 million of insurance recoveries received in 2008 related to Redding Medical Center discussed above); |
| • | Additional cash flows as a result of enhanced management of account payable ($39 million) and accounts receivable ($70 million); |
| • | Lease termination payments of $9 million in the year ended December 31, 2008 associated with the divestiture of the Tarzana campus of Encino-Tarzana Regional Medical Center; |
| • | Additional aggregate annual 401(k) matching contributions and annual incentive compensation payments of $7 million ($123 million in the year ended December 31, 2009 compared to $116 million in 2008); and |
| • | Lower cash investment earnings of approximately $5 million in the year ended December 31, 2009 compared to the same period in 2008. |
SOURCES OF REVENUE
We receive revenues for patient services from a variety of sources, primarily managed care payers and the federal Medicare program, as well as state Medicaid programs, indemnity-based health insurance companies and self-pay patients (i.e., patients who do not have health insurance and are not covered by some other form of third-party arrangement).
The table below shows the sources of net patient revenues on a same-hospital basis, expressed as percentages of net patient revenues from all sources:
| Years Ended December 31, | |||||||||
| Net Patient Revenues from: |
2009 | 2008 | 2007 | ||||||
| Medicare |
25.1 | % | 25.5 | % | 25.9 | % | |||
| Medicaid |
8.1 | % | 8.4 | % | 8.7 | % | |||
| Managed care – governmental |
14.7 | % | 13.3 | % | 12.0 | % | |||
| Managed care – commercial |
41.3 | % | 41.4 | % | 41.1 | % | |||
| Indemnity, self-pay and other |
10.8 | % | 11.4 | % | 12.3 | % | |||
Our payer mix on a same-hospital admissions basis, expressed as a percentage of total admissions from all sources, is shown below:
| Years Ended December 31, | |||||||||
| Admissions from: |
2009 | 2008 | 2007 | ||||||
| Medicare |
30.1 | % | 30.8 | % | 31.8 | % | |||
| Medicaid |
12.4 | % | 12.3 | % | 12.4 | % | |||
| Managed care – governmental |
22.7 | % | 21.0 | % | 18.8 | % | |||
| Managed care – commercial |
25.7 | % | 26.8 | % | 28.0 | % | |||
| Indemnity, self-pay and other |
9.1 | % | 9.1 | % | 9.0 | % | |||
The increase in managed care – governmental admissions is primarily due to a shift from traditional government programs to managed government programs.
33
Table of Contents
GOVERNMENT PROGRAMS
The Medicare program, the nation’s largest health insurance program, is administered by the Centers for Medicare and Medicaid Services (“CMS”) of the U.S. Department of Health and Human Services (“HHS”). Medicare is a health insurance program primarily for individuals 65 years of age and older, certain younger people with disabilities, and people with end-stage renal disease, and is provided without regard to income or assets. Medicaid is a program that pays for medical assistance for certain individuals and families with low incomes and resources, and is jointly funded by the federal government and state governments. Medicaid is the largest source of funding for medical and health-related services for the nation’s poor and most vulnerable individuals.
The Medicare and Medicaid programs are subject to statutory and regulatory changes, administrative rulings, interpretations and determinations, requirements for utilization review, and federal and state funding restrictions, all of which could materially increase or decrease payments from these government programs in the future, as well as affect the cost of providing services to our patients and the timing of payments to our facilities. We are unable to predict the effect of future government health care funding policy changes on our operations. If the rates paid by governmental payers are reduced, if the scope of services covered by governmental payers is limited, or if we or one or more of our subsidiaries’ hospitals are excluded from participation in the Medicare or Medicaid program or any other government health care program, there could be a material adverse effect on our business, financial condition, results of operations or cash flows.
Medicare
Medicare offers its beneficiaries different ways to obtain their medical benefits. One option, the Original Medicare Plan, is a fee-for-service payment system. The other option, called Medicare Advantage, includes health maintenance organizations, preferred provider organizations, private fee-for-service Medicare special needs plans and Medicare medical savings account plans. The major components of our net patient revenues for services provided to patients enrolled in the Original Medicare Plan for the years ended December 31, 2009, 2008 and 2007 are set forth in the table below:
| Years Ended December 31, | |||||||||
| Revenue Descriptions |
2009 | 2008 | 2007 | ||||||
| Diagnosis-related group – operating |
$ | 1,191 | $ | 1,170 | $ | 1,132 | |||
| Diagnosis-related group – capital |
109 | 109 | 111 | ||||||
| Outlier |
68 | 66 | 63 | ||||||
| Outpatient |
421 | 378 | 339 | ||||||
| Disproportionate share |
219 | 211 | 199 | ||||||
| Direct Graduate and Indirect Medical Education(1) |
111 | 110 | 103 | ||||||
| Other(2) |
76 | 92 | 63 | ||||||
| Adjustments for prior-year cost reports and related valuation allowances |
10 | 4 | 43 | ||||||
| Total Medicare net patient revenues |
$ | 2,205 | $ | 2,140 | $ | 2,053 | |||
| (1) | Includes Indirect Medical Education (“IME”) revenue earned by our children’s hospital under the Children’s Hospitals Graduate Medical Education Payment Program administered by the Health Resources and Services Administration of HHS. |
| (2) | The other revenue category includes one skilled nursing facility (which we sold in the three months ended June 30, 2009), inpatient psychiatric units, one inpatient rehabilitation hospital (which we closed in the three months ended March 31, 2009), inpatient rehabilitation units, one long-term acute care hospital, other revenue adjustments, and adjustments related to the estimates for current-year cost reports and related valuation allowances. |
A general description of the types of payments we receive for services provided to patients enrolled in the Original Medicare Plan is provided below. Recent regulatory and legislative updates to the terms of these payment systems and their estimated effect on our revenues can be found under “—Regulatory and Legislative Changes.”
Acute Care Hospital Inpatient Prospective Payment System
Medicare Severity-Adjusted Diagnosis-Related Group Payments—Sections 1886(d) and 1886(g) of the Social Security Act (the “Act”) set forth a system of payments for the operating and capital costs of inpatient acute care hospital admissions based on a prospective payment system (“PPS”). Under the inpatient prospective payment system (“IPPS”), Medicare payments for hospital inpatient operating services are made at predetermined rates for each hospital discharge. Discharges are classified according to a system of Medicare severity-adjusted diagnosis-related groups (“MS-DRGs”), which categorize patients with similar clinical characteristics that are expected to require similar amounts of hospital resources. CMS assigns to each MS-DRG a relative weight that represents the average resources required to treat cases in that particular MS-DRG, relative to the average resources used to treat cases in all MS-DRGs.
34
Table of Contents
The base payment amount for the operating component of the MS-DRG payment is comprised of an average standardized amount that is divided into a labor-related share and a nonlabor-related share. Both the labor-related share of operating base payments and the base payment amount for capital costs are adjusted for geographic variations in labor and capital costs, respectively. Using diagnosis and procedure information submitted by the hospital, CMS assigns each discharge to a MS-DRG, and the base payments are multiplied by the relative weight of the MS-DRG assigned. The MS-DRG operating and capital base rates, relative weights and geographic adjustment factors are updated annually, with consideration given to: the increased cost of goods and services purchased by hospitals; the relative costs associated with each MS-DRG; and changes in labor data by geographic area. Although these payments are adjusted for area labor and capital cost differentials, the adjustments do not take into consideration an individual hospital’s operating and capital costs.
Outlier Payments—Outlier payments are additional payments made to hospitals on individual claims for treating Medicare patients whose medical conditions are costlier to treat than those of the average patient in the same MS-DRG. To qualify for a cost outlier payment, a hospital’s billed charges, adjusted to cost, must exceed the payment rate for the MS-DRG by a fixed threshold established annually by CMS. A Medicare administrative contractor (“MAC”) (formerly known as a Medicare fiscal intermediary) calculates the cost of a claim by multiplying the billed charges by a cost-to-charge ratio that is typically based on the hospital’s most recently filed cost report. Generally, if the computed cost exceeds the sum of the MS-DRG payment plus the fixed threshold, the hospital receives 80% of the difference as an outlier payment.
Under the Act, CMS must project aggregate annual outlier payments to all prospective payment system (“PPS”) hospitals to be not less than 5% nor more than 6% of total MS-DRG payments (“Outlier Percentage”). The Outlier Percentage is determined by dividing total outlier payments by the sum of MS-DRG and outlier payments. CMS annually adjusts the fixed threshold to bring projected outlier payments within the mandated limit. A change to the fixed threshold affects total outlier payments by changing: (1) the number of cases that qualify for outlier payments; and (2) the dollar amount hospitals receive for those cases that still qualify for outlier payments.
Disproportionate Share Hospital Payments—In addition to making payments for services provided directly to beneficiaries, Medicare makes additional payments to hospitals that treat a disproportionately high share of low-income patients. Disproportionate share hospital (“DSH”) payments are determined annually based on certain statistical information defined by CMS and are calculated as a percentage add-on to the MS-DRG payments. During 2009, 41 of our hospitals in continuing operations qualified for DSH payments. The primary method for a hospital to qualify for DSH payments is based on a complex statutory formula that results in a DSH percentage that is applied to payments based on MS-DRGs. The hospital-specific DSH percentage is equal to the sum of the percentage of Medicare inpatient days attributable to patients eligible for both the Traditional Medicare Plan (“Part A”) and Supplemental Security Income (“SSI”) percentage, and the percentage of total inpatient days attributable to patients eligible for Medicaid but not Medicare Part A. Hospitals receive interim DSH payments that are reconciled in the annual cost report. CMS develops and distributes the hospital-specific SSI percentages, typically one year after the close of the federal fiscal year (“FFY”); however, the release of the SSI percentages has been delayed in recent years as CMS continues to examine and refine the data. Historically, the SSI percentage included only patient days paid under Part A. In June 2009, CMS released the FFY 2007 SSI percentages, which reflect a policy change to include the Medicare Advantage (“Part C”) days in the ratio. The 2007 SSI percentages will be used to settle our 2007 cost reports, and we estimate they will have an unfavorable impact on our Medicare net revenue of approximately $9 million. CMS has not released the 2008 and 2009 SSI percentages; however, using the 2007 SSI percentages to approximate the 2008 and 2009 SSI percentages, we estimate they will have an unfavorable impact on our Medicare net revenue for our 2008 and 2009 cost reporting periods through June 30, 2009 of approximately $14 million. Accordingly, we recorded an unfavorable adjustment of $23 million ($16 million related to prior years and $7 million related to the current year) in the three months ended June 30, 2009. In 2009, CMS instructed hospitals to submit information related to Part C for FFY 2006 and, according to the CMS website, the 2006 SSI data is under review. While we believe it is likely that CMS will revise the 2006 SSI percentages in the future, we cannot predict what those changes will be or how they might impact our Medicare net revenue. During the three months ended September 30, 2009, we learned that CMS had instructed the MACs to suspend the settlement of all cost reports (including ours) in which the 2007 SSI percentages would be used. However, the MACs are authorized to use the 2007 SSI percentages for current DSH interim payments and tentative settlements for post-2007 cost reporting periods pending the release of the 2008 SSI percentages. The cost report settlement suspension is still in effect, and we cannot predict when the suspension will be lifted. The SSI percentage is subject to administrative and judicial review through the cost report appeal process, and we have filed a request for a hearing before the Medicare Provider Reimbursement Review Board (“PRRB”) on the inclusion of Part C days in the SSI percentage; however, cost report appeals can take many years to resolve. We cannot predict the outcome of our appeal before the PRRB or any action CMS might take with respect to the SSI percentages.
Direct Graduate and Indirect Medical Education—The Medicare program provides additional reimbursement to approved teaching hospitals for additional expenses incurred by such institutions. This additional reimbursement, which is subject to certain limits, including intern and resident full-time equivalent (“FTE”) limits established in 1996, is made in the form of Direct Graduate Medical Education (“DGME”) and Indirect Medical Education payments. During 2009, 13 of our hospitals in continuing operations were affiliated with academic institutions and were eligible to receive such payments. Medicare rules permit teaching hospitals to enter into Medicare Graduate Medical Education Affiliation Agreements for the purpose of applying the FTE limits on an aggregate basis, and some of our teaching hospitals have entered into such agreements.
35
Table of Contents
We were previously contacted by CMS in connection with DGME FTE limits and related reimbursement at Doctors Medical Center in Modesto, California as a result of our 1997 transaction with a county-owned hospital in Modesto and the IME and DGME residency program sponsored by the county. We have annually collected approximately $2.5 million of DGME reimbursement at the hospital. We replied to CMS that, based on our analysis of the transaction and the applicable CMS rules, we believe that the DGME FTE limits and related reimbursement reported on the hospital’s cost reports were substantially correct. In January 2008, CMS preliminarily advised us that they disagree with our analysis. During the three months ended June 30, 2008, we submitted additional information to CMS regarding the original transaction. CMS subsequently contacted us and stated that: (1) they continue to disagree with our analysis; and (2) they instructed our MAC to reopen settled cost reports to recover IME and DGME payments made to the hospital. During the three months ended September 30, 2008, we submitted additional information for CMS’ consideration. Also during the three months ended September 30, 2008, we received notices from our MAC of its intent to reopen certain cost reports in connection with this matter. We have since received settlement notices for the hospital’s 2001 through 2007 cost reporting periods that reflect a disallowance of all of the hospital’s IME and DGME payments, and the hospital’s 2008 cost report was filed consistent with the MAC’s disallowance on the prior-year cost reports. Additionally, the MAC ceased making IME and DGME interim payments to the hospital for current and future services. Although we have taken steps necessary to protect our rights to formally challenge CMS’ decision to disallow the IME and DGME funding for prior periods, it could take several years to resolve this issue and the outcome is uncertain at this time. As a result, in the three months ended June 30, 2008, we recorded an unfavorable adjustment of $17 million ($16 million related to 2007 and prior years and $1 million related to the year ended December 31, 2008), and we have not subsequently recorded any IME or DGME revenue for this hospital. During the three months ended December 31, 2008, Stanislaus County confirmed its obligation with respect to a residency program funding grant agreement between Doctors Medical Center and the county; as a result, we recorded an $8 million receivable for that additional grant funding, which we received during 2009. CMS recently revised certain of its policies regarding the eligibility of teaching programs for Medicare IME and DGME reimbursement. In January 2010, the program sponsored by the county, Doctors Medical Center and other hospitals obtained accreditation and other approvals effective for the academic year beginning July 1, 2010 for a residency program that we believe will satisfy CMS’ requirements for reimbursement. However, the aforementioned CMS policy changes are not retroactive.
Hospital Outpatient Prospective Payment System
Under the outpatient prospective payment system, hospital outpatient services, except for certain services that are reimbursed on a separate fee schedule, are classified into groups called ambulatory payment classifications (“APCs”). Services in each APC are similar clinically and in terms of the resources they require, and a payment rate is established for each APC. Depending on the services provided, hospitals may be paid for more than one APC for an encounter. CMS periodically updates the APCs and annually adjusts the rates paid for each APC.
Inpatient Psychiatric Facility Prospective Payment System
The inpatient psychiatric facility prospective payment system (“IPF-PPS”) applies to psychiatric hospitals and psychiatric units located within acute care hospitals that have been designated as exempt from the hospital inpatient prospective payment system. The IPF-PPS is based on prospectively determined per-diem rates and includes an outlier policy that authorizes additional payments for extraordinarily costly cases.
Inpatient Rehabilitation Prospective Payment System
Rehabilitation hospitals and rehabilitation units in acute care hospitals meeting certain criteria established by CMS are eligible to be paid as an inpatient rehabilitation facility (“IRF”) under the IRF prospective payment system (“IRF-PPS”). Payments under the IRF-PPS are made on a per-discharge basis. A patient classification system is used to assign patients in IRFs into case-mix groups. The IRF-PPS uses federal prospective payment rates across distinct case-mix groups.
To be paid under the IRF-PPS, each hospital or unit must demonstrate on an annual basis that at least 60% of its total population had either a principal or secondary diagnosis that fell within one or more of the qualifying conditions designated in the Medicare regulations governing IRFs. As of December 31, 2009, all of our rehabilitation units were in compliance with the required 60% threshold.
36
Table of Contents
Cost Reports
The final determination of certain Medicare payments to our hospitals, such as DSH, DGME, IME and bad debt expense, are retrospectively determined based on our hospitals’ cost reports. The final determination of these payments often takes many years to resolve because of audits by the program representatives, providers’ rights of appeal, and the application of numerous technical reimbursement provisions.
For filed cost reports, we adjust the accrual for estimated cost report settlements based on those cost reports and subsequent activity, and record a valuation allowance against those cost reports based on historical settlement trends. The accrual for estimated cost report settlements for periods for which a cost report is yet to be filed is recorded based on estimates of what we expect to report on the filed cost reports and a corresponding valuation allowance is recorded as previously described. Cost reports must generally be filed within five months after the end of the annual cost report reporting period. After the cost report is filed, the accrual and corresponding valuation allowance may need to be adjusted.
Medicaid
Medicaid programs and the corresponding reimbursement methodologies are administered by the states and vary from state to state and from year to year.
Estimated payments under various state Medicaid programs, excluding state-funded managed care Medicaid programs, constituted approximately 8.1%, 8.4% and 8.7% of net patient revenues at our continuing general hospitals for the years ended December 31, 2009, 2008 and 2007, respectively. We also receive DSH payments under various state Medicaid programs. For the years ended December 31, 2009, 2008 and 2007, our revenue attributable to DSH payments and other state-funded subsidy payments was approximately $171 million, $153 million and $162 million, respectively.
Medicaid patient revenues of our continuing general hospitals by state for the years ended December 31, 2009 and 2008 are set forth in the table below:
| Years Ended December 31, | ||||||
| 2009 | 2008 | |||||
| Florida |
$ | 182 | $ | 167 | ||
| California |
125 | 133 | ||||
| Missouri |
75 | 73 | ||||
| Georgia |
73 | 83 | ||||
| Texas |
67 | 52 | ||||
| Pennsylvania |
53 | 56 | ||||
| South Carolina |
52 | 49 | ||||
| North Carolina |
27 | 25 | ||||
| Nebraska |
23 | 25 | ||||
| Alabama |
14 | 23 | ||||
| Tennessee |
9 | 8 | ||||
| $ | 700 | $ | 694 | |||
Several states in which we operate have recently faced budgetary challenges that resulted in reduced Medicaid funding levels to hospitals and other providers. Most states began a new fiscal year on July 1, and although most addressed projected shortfalls in their final budgets, some states may face mid-year budget gaps and many are already projecting shortfalls for state fiscal year 2011, which could result in additional reductions to Medicaid payments, coverage and eligibility or additional taxes on hospitals. Other states have proposed or enacted measures that are designed to preserve or restore Medicaid funding. Provided below is information regarding recent significant state proposals and actions that are likely to affect our hospitals.
California
The State of California has taken numerous actions over the past year to address severe budget shortfalls, including actions that affect revenues for our hospitals in the state. On February 20, 2009, a new budget plan for California was released to address budget deficits in the 2008-2009 state fiscal year, as well as the new state fiscal year beginning July 1, 2009. The new plan included eliminating some benefits and further reductions in coverage. Legal challenges to these reductions have been filed, and temporary injunctive relief on certain elements of the reductions was granted in March 2009. We cannot predict the final outcome of the litigation or the impact it might have on our results of operations, net revenues or cash flows. Additional cuts to the February 2009 budget, including approximately $2 billion in cuts to health programs allocated between disproportionate share hospitals, the Distressed Hospital Fund, hospital-based skilled nursing facilities and other areas, were approved July 28, 2009. The budget agreement approved in July 2009 also included substantial cuts to funding for prison health care, which would have an estimated annual impact on revenues of certain of our California hospitals of approximately $17 million.
37
Table of Contents
According to recent state estimates, California faces a combined fiscal year 2009-2010 and fiscal year 2010-2011 deficit of approximately $20 billion. To address this shortfall, in January 2010, the Governor of California proposed nearly $3 billion in cuts to health and human services programs, including a plan to reduce Medi-Cal spending by limiting services, implementing an additional delay of payments to providers, eliminating Medi-Cal coverage for certain immigrants and cutting other areas of the program. Further savings are proposed that could result in a $64 million reduction in the Healthy Families program and an $811 million reduction in funding for prison health care. The proposed cuts require legislative action and some may require approval by CMS. We cannot predict the final outcome of the proposed reductions or the impact it might have on our results of operations, net revenues or cash flows.
Separately, in October 2009, the Governor of California signed legislation supported by the hospital industry to impose an annual provider fee on general acute care hospitals that, combined with federal matching funds, will be used to provide supplemental Medi-Cal payments to hospitals, as well as provide the state with $320 million annually for children’s health care coverage. The provider supplemental payment plan created by this legislation proposes to provide these payments for up to 21 months retroactive to April 2009 and expiring on December 31, 2010. The state has submitted the plan to CMS for a required review and approval process and is awaiting a final determination. Based on modeling prepared as part of the legislative process, we estimate that, if the legislation is implemented as approved by the state, revenues, net of provider taxes, for our California hospitals could increase by approximately $106 million for the full 21-month period of the plan. Legislation to extend the supplemental payment plan has been introduced and, if approved, would allow the state to extend the provider fee for the length of any Federal Medicaid Assistance Percentage (“FMAP”) extension passed by Congress. We are unable to predict what action the State of California or CMS might take with respect to the provider fees and, because of the uncertainty regarding the final implementation and administration of the legislation, we cannot provide any assurances regarding the estimated impact.
Florida
Florida’s legislature held a special session in January 2009 to address that state’s mid-year budget deficit and proposed several changes for consideration in the full legislative session that commenced February 1, 2009. The changes passed in the special session resulted in a 4% across-the-board reduction in Medicaid rates effective March 1, 2009. The impact of these changes on our Florida hospitals’ revenues was a reduction of approximately $5 million in 2009. The fiscal year 2010 budget adopted in May 2009 did not include additional reductions to Medicaid hospital payments. Recently, the Governor of Florida issued a proposed budget for the state fiscal year 2010-2011 that includes a request for an additional $2.7 billion in Medicaid funding to cover costs associated with increased enrollment and utilization of Medicaid health care services. We cannot predict what action the legislature will take with regard to Medicaid funding in its final budget.
In January 2010, CMS approved an amendment to an existing state Medicaid waiver that preserves $300 million in federal funding tied to the Low Income Pool program. We estimate that, without approval of this amendment, Low Income Pool payments to our hospitals would have been reduced by as much as $5 million in 2010.
Georgia
The Indigent Care Trust Fund (“ICTF”), or DSH program, for private hospitals is funded with state funds that are subject to an annual legislative appropriation. In 2009, we received approximately $8 million in ICTF funds. The availability and amount of future ICTF funds for our hospitals is not guaranteed. As in past years, the fiscal year 2010-2011 budget submitted by the Georgia Department of Community Health provided funding for private hospitals, for which some, but not all, of our Georgia hospitals would be eligible. Also, as in past years, the state legislature is considering extending eligibility for ICTF funds to additional private hospitals. We cannot predict what action the Georgia legislature might take with regard to this legislation.
The Governor’s recent fiscal year 2010-2011 budget request includes a proposed provider tax on hospitals of 1.6% of net patient revenues and a managed care provider fee of 1.6% of premium revenues to balance the state’s Medicaid budget. In the absence of these fees, the Department of Community Health estimates it will need to reduce Medicaid provider payments by 16.5%. We cannot predict what action the Governor or the legislature might take with regard to the implementation of a provider tax or cuts to Medicaid provider payments.
Missouri
The Governor of Missouri is proposing $253 million in general revenue reductions for the state fiscal year 2010-2011, including $121 million to be cut from the state’s Medicaid program. Proposed reductions include cuts to the outpatient reimbursement methodology, placing a ceiling on inpatient unit costs for hospitals contracting with managed care plans, and re-pricing of services for dual eligible individuals. Additionally, pending legislation would trade the state’s current income tax for a tax on goods and services (including health care) of approximately 6%. If passed by the General Assembly and signed by the Governor, this proposal would also require approval by voters in November 2010. We cannot predict what action the Governor or the legislature might take with regard to the implementation of tax changes or cuts to Medicaid provider payments in Missouri.
38
Table of Contents
Pennsylvania
In October 2009, the Pennsylvania legislature passed and the Governor approved a commonwealth fiscal year 2009-2010 budget that cut $1.45 billion in spending compared to the previous fiscal year. Hospital Medicaid supplemental payments were cut an aggregate 11%. We estimate that these cuts will reduce our payments from Pennsylvania by approximately $4 million in the commonwealth’s fiscal year ending June 30, 2010. In January 2010, the commonwealth announced that revenues for the fiscal year were running $120 million below estimates, leading to a projected fiscal year 2009-2010 budget gap of $500 million to $1 billion. As a result, the Governor has proposed additional cuts to inpatient and outpatient DSH payments, medical education and certain supplemental payments. Based on limited details available at this time, we are unable to estimate the impact of the proposed reductions on the revenues of our hospitals in Pennsylvania. In addition, the commonwealth has indicated its intention to delay certain payments to providers.
North Carolina
The North Carolina legislature enacted a $76 million Medicaid reduction in provider rates effective October 1, 2009. This resulted in a 6.3% reduction of inpatient Medicaid rates to hospitals. Hospital outpatient rates were exempted from the cuts. We estimate that the aforementioned 6.3% reduction will reduce our annual Medicaid net revenues in North Carolina by approximately $1 million.
Tennessee
It is anticipated that the 9% reductions the TennCare Bureau outlined over the past several months will be included in the Governor’s budget recommendations. These cuts would reduce projected state payments to hospitals by $230 million and would include an annual $10,000 cap on inpatient hospital reimbursement and a limit of eight non-emergency hospital outpatient procedures per year for non-pregnant adults, as well as a reimbursement ceiling for hospitals at 100% of Medicare rates. These changes are in addition to the fiscal year 2009-2010 cuts scheduled to take effect on July 1, 2010 that are projected to reduce state hospital payments by $296 million and would reduce our annual Medicaid net revenues in Tennessee by approximately $4 million. Approval by CMS will be required for some of the cuts to be implemented. Recently, the member hospitals of the Tennessee Hospital Association voted to support the creation of a provider tax as an alternative to the proposed cuts. This proposal, which would require approval by CMS, could mitigate most, if not all, of the proposed and scheduled reductions. We cannot predict what action the state or CMS might take with respect to the proposed reductions or provider tax.
Texas
To address a projected budget shortfall in Texas of approximately $11 billion, the Governor and legislative leaders recently mandated that each agency submit plans for achieving a 5% reduction in state spending. In February 2010, the Texas Health and Human Services Commission presented options for achieving $304 million in savings from state health programs, including a 1% rate reduction for Medicaid and Children’s Health Insurance Program providers, a $13 million reduction applied to provider rates under Medicaid managed care plans, and a $10 million reduction in emergency services and trauma funds allocated for hospitals to cover indigent care. Legislative approval is not required and some, if not all, of the recommendations could be implemented effective September 1, 2010. We cannot estimate at this time which proposals might be implemented or the impact on our results of operations, net revenues or cash flows.
Pressures on state budgets are expected to continue in the future. The increased FMAP adopted by Congress in the American Recovery and Reinvestment Act of 2009 (“ARRA”) will expire at the end of December 2010. In addition, health care reform legislation, if enacted, will likely include an expansion of Medicaid eligibility. We cannot predict what action Congress might take to extend the increased FMAP or expand Medicaid eligibility or the impact those actions might have on state budgets or Medicaid payments to our hospitals.
Moratorium on Medicaid Regulations
In May 2007, CMS issued a final rule, “Medicaid Program; Cost Limit for Providers Operated by Units of Government and Provisions to Ensure the Integrity of the Federal-State Financial Partnership,” that places limits and restrictions on Medicaid reimbursement to safety-net hospitals. A one-year moratorium on implementation of the final rule was included in the FFY 2007 Supplemental Appropriations Act, which meant that the rule could not take effect before May 25, 2008. On May 21, 2008, CMS announced that it was voluntarily extending the moratorium for an additional 60 days; then in June 2008 the moratorium was extended through March 31, 2009 as part of the FFY 2008 Supplemental Appropriations Act.
39
Table of Contents
Also in May 2007, CMS issued a proposed rule clarifying that the agency would no longer provide federal Medicaid matching funds for graduate medical education purposes; however, the FFY 2007 Supplemental Appropriations Act contained language that placed a one-year moratorium on any such restriction. The moratorium was scheduled to expire on May 23, 2008. On May 21, 2008, CMS announced that it was voluntarily extending the moratorium for an additional 60 days; then in June 2008 the moratorium was extended through March 31, 2009 as part of the FFY 2008 Supplemental Appropriations Act. Annual Medicaid graduate medical education payments to our hospitals are approximately $35 million.
The ARRA did not extend the moratoria on these regulations; however, it did note that Congress believes that the Secretary of HHS should not promulgate the proposed regulations relating to cost limits on public providers and Medicaid graduate medical education payments as final. CMS has not taken further action on these rules, and we cannot predict what further action, if any, Congress or CMS will take on these issues.
Regulatory and Legislative Changes
Recent regulatory and legislative updates to the Medicare and Medicaid payment systems are provided below.
Payment and Policy Changes to the Medicare Inpatient Prospective Payment System
Under Medicare law, CMS is required annually to update certain rules governing the inpatient prospective payment system. The updates generally become effective October 1, the beginning of the federal fiscal year. On July 31, 2009, CMS issued the Changes to the Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and Fiscal Year 2010 Rates (“Final Rule”). The Final Rule includes the following payment and policy changes:
| • | A market basket increase currently estimated at 2.1% for MS-DRG operating payments for hospitals reporting specified quality measure data (hospitals that do not report specified quality measure data would receive an increase of 0.1%); |
| • | An increase in the cost outlier threshold from $20,045 to $23,140; |
| • | A reduction of 0.5% for projected outlier payments and the expiration of Section 508 hospital wage area reclassifications; |
| • | A 1.4% increase in the capital federal MS-DRG rate; and |
| • | Restoration of 100% of capital IME payments for teaching hospitals. |
The Transitional Medical Assistance, Abstinence Education, and Qualifying Individuals Programs Extension Act of 2007 (“TMA Act”) specifies that, to the extent the documentation and coding adjustments applied in FFY 2008 and FFY 2009 result in overpayments relative to the actual amount of documentation and coding-related increases in connection with the transition to the MS-DRG system from the prior classification system, CMS shall correct the overpayments and underpayments in FFYs 2010-2012. In the Proposed Changes to the Hospital Inpatient Prospective Payment Systems and FFY 2010 Rates (“Proposed Rule”) issued on May 1, 2009, CMS estimated the adjustments required to recover estimated coding and documentation overpayments made in FFYs 2008 and 2009 and prevent future coding and documentation overpayments required under the TMA Act to be 5.2% and 3.3%, respectively. Also in the Proposed Rule, CMS proposed to
reduce FFY 2010 rates by 1.9%, the adjustment required to remove the FFY 2008 estimated overpayment from the current rates in order to prevent future coding and documentation overpayments related to FFY 2008 rates. In the Final Rule, CMS confirmed its earlier estimates of the aforementioned adjustments required under the TMA Act; however, instead of imposing the 1.9% reduction to FFY 2010 rates as proposed, in the Final Rule CMS stated its intent not to impose any coding and documentation adjustments to the FFY 2010 IPPS rates pending its complete review of the FFY 2008 and 2009 data. Also in the Final Rule, CMS stated that it will defer the recovery of the FFY 2008 and 2009 estimated coding and documentation adjustments and consider phasing in future coding and documentation adjustments over an extended period beginning in FFY 2011 as permitted under the TMA Act. Refer to “—MedPAC 2011 Recommendations” below for additional information regarding the coding and documentation adjustments.
CMS projects that the combined impact of the payment and policy changes included in the Final Rule will yield an average 1.7% increase in payments for hospitals in large urban areas (populations over 1 million). Using the impact percentages in the Final Rule as applied to our Medicare IPPS payments for the 12 months ended September 30, 2009, the estimated annual impact for all changes in the Final Rule on our hospitals is an increase in our Medicare inpatient revenues of approximately $23 million. Because of the uncertainty regarding other factors that may influence our future IPPS payments by individual hospital, including admission volumes, length of stay and case mix, we cannot provide any assurances regarding this estimate.
40
Table of Contents
Payment Changes to the Medicare Inpatient Psychiatric Facility Prospective Payment System
On April 30, 2009, CMS issued a Notice of the Medicare Inpatient Psychiatric Facility Prospective Payment System Update for the rate year beginning July 1, 2009 (“IPF-PPS Notice”). The IPF-PPS Notice includes the following payment changes:
| • | An update to the IPF payment equal to the market basket of 2.1%; and |
| • | An increase in the fixed dollar loss threshold amount for outlier payments from $6,113 to $6,565. |
At December 31, 2009, 14 of our general hospitals in continuing operations operated inpatient psychiatric units. CMS projects that the combined impact of the payment changes will yield an average 2.0% increase in payments for all IPFs (including psychiatric units in acute care hospitals), and an average 1.8% increase in payments for psychiatric units of acute care hospitals located in urban areas. Using the urban psychiatric unit impact percentage as applied to our Medicare IPF payments for the 12 months ended June 30, 2009, the annual impact of the payment changes included in the IPF-PPS Notice on our psychiatric units may result in an estimated increase in our Medicare revenues of approximately $1 million. Because of the uncertainty of the factors that may influence our future IPF payments, including future legislation, admission volumes, length of stay and case mix, we cannot provide any assurances regarding our estimate of the impact of these changes.
Payment and Policy Changes to the Medicare Inpatient Rehabilitation Facility Prospective Payment System
On July 31, 2009, CMS issued the Final Rule for the Medicare Inpatient Rehabilitation Facility Prospective Payment System for FFY 2010 (“IRF-PPS Final Rule”). The IRF-PPS Final Rule includes the following payment and policy changes, which, except as noted, were effective for discharges on or after October 1, 2009:
| • | A market basket update to the IRF PPS payment rate equal to 2.5%; |
| • | An increase in the outlier threshold for high cost outlier cases from $10,250 to $10,652; |
| • | An update to the case-mix group relative weights and average length of stay values using FFY 2008 data; and |
| • | A new regulatory framework that clarifies the coverage criteria (including provisions regarding patient selection and care) that became effective January 1, 2010. |
At December 31, 2009, 10 of our general hospitals in continuing operations operated inpatient rehabilitation units. CMS projects that the payment and policy changes in the IRF-PPS Final Rule will result in an estimated total increase in aggregate IRF payments of $145 million or 2.5% of total IRF PPS payments. This estimated increase includes an average 2.5% increase for rehabilitation units in urban areas for FFY 2010. Using the urban rehabilitation unit impact percentage as applied to our Medicare IRF payments for the 12 months ended September 30, 2009, the annual impact of all payment and policy changes in the IRF-PPS Final Rule on our rehabilitation units may result in an estimated increase in our Medicare revenues of approximately $1 million. Because of the uncertainty of the factors that may influence our future IRF payments, including legislative action, admission volumes, length of stay and case mix, and the impact of compliance with the IRF admission criteria, we cannot provide any assurances regarding our estimate of the impact of these changes.
Payment and Policy Changes to the Medicare Hospital Outpatient Prospective Payment System
On October 30, 2009, CMS issued the Changes to the Hospital Outpatient Prospective Payment System (“OPPS”) and Calendar Year (“CY”) 2010 Payment Rates (“OPPS Rule”). The OPPS Rule includes the following payment and policy changes:
| • | An update to OPPS payments equal to the estimated market basket of 2.1%; hospitals that did not take part in the Hospital Outpatient Quality Data Reporting Program (“HOP QDRP”) or that did not successfully report their quality measures will have their update reduced by two percentage points; |
| • | The continuing requirement that hospitals taking part in the HOP QDRP report seven existing chart-abstracted emergency department and perioperative measures, along with four claims-based imaging efficiency measures for payment determination for CY 2011 payments; and |
41
Table of Contents
| • | The implementation of provisions of the Medicare Improvements for Patients and Providers Act of 2008 that extend Medicare coverage to important rehabilitative and educational services intended to improve the health of patients diagnosed with certain respiratory, cardiac and renal diseases. Beginning January 1, 2010, hospitals are able to bill Medicare for new pulmonary and intensive cardiac rehabilitation services furnished in hospital outpatient departments to Medicare beneficiaries. |
CMS projects that the combined impact of the payment and policy changes in the OPPS Rule will yield an average 1.9% increase in payments for all hospitals and an average 2.1% increase in payments for hospitals in large urban areas (populations over 1 million). According to CMS’ estimates, the projected annual impact of the payment and policy changes in the OPPS Rule on our hospitals is $8 million, an increase of approximately 2.3% over projected CY 2009 OPPS payments. Because of the uncertainty regarding other factors that may influence our future OPPS payments, including volumes, case mix and additional costs associated with the physician supervision requirements described below, we cannot provide any assurances regarding this estimate.
In the preamble to the Medicare CY 2009 OPPS final rule, CMS provided a “restatement and clarification” of its requirements originally set forth in the April 2000 OPPS final rule for physician supervision of therapeutic services provided to Medicare patients in a hospital setting. In the OPPS Rule, CMS made several important changes to its outpatient physician supervision policy including the following:
| • | In CY 2010, CMS will allow certain nonphysician practitioners – specifically physician assistants, nurse practitioners, clinical nurse specialists, certified nurse-midwives and licensed clinical social workers – to provide direct supervision for all hospital outpatient therapeutic services that they are authorized to personally perform according to their state scope of practice rules and hospital-granted privileges. Under prior policy, generally only physicians could provide the direct supervision of these services. |
| • | For purposes of on-campus hospital outpatient therapeutic services, CMS is defining “direct supervision” to mean that the physician or nonphysician practitioner must be present anywhere on the hospital campus and immediately available to furnish assistance and direction throughout the performance of the procedure. For services furnished in an off-campus provider-based department, “direct supervision” would continue to mean that the physician or nonphysician practitioner must be present in the off-campus provider-based department and immediately available to furnish assistance and direction throughout the performance of the procedure. |
| • | CMS also will require that all hospital outpatient diagnostic services furnished directly or under arrangement, whether provided in the hospital, in a provider-based department or at a non-hospital location, follow the Medicare Physician Fee Schedule physician supervision requirements for individual tests. |
We have completed our evaluation of our provider-based on-campus and off-campus outpatient departments to address the physician supervision requirements set forth in the OPPS Rule. Changes were made in a small number of off-campus departments to meet the new requirements, including location changes and new contracts for required physician coverage. These changes are not expected to have a material impact on our results of operations or cash flows. In the OPPS Rule, CMS has indicated that in the case of outpatient therapeutic services furnished on a hospital’s campus from 2000 through 2008, CMS will exercise its discretion and decline to enforce in situations involving claims where a hospital’s noncompliance with CMS’ direct physician supervision policy resulted from error or mistake.
The American Recovery and Reinvestment Act of 2009
On February 17, 2009, the President signed the ARRA into law. The ARRA includes $31 billion in new spending on health information technology (“HIT”), most of which is for incentive Medicare and Medicaid payments to physicians and hospitals. The legislation requires that hospitals and physicians become “meaningful users” of electronic health records (“EHR”) and submit quality data as a condition of receiving the incentive payments beginning in 2011. If we are able to achieve full compliance at all of our hospitals by 2013, we could receive approximately $350 million in total estimated combined Medicare and Medicaid hospital incentive payments. However, based on the timeframe we anticipate it will take for us to achieve full compliance with the HIT requirements, it is unlikely that we will be able to realize the maximum amount of incentive payments of $350 million. We will be required to make investments in HIT through 2014 of approximately $620 million ($60 million of which has already been incurred) compared to approximately $320 million of Medicare and Medicaid incentive payments that we will likely be able to begin recognizing no later than 2012 based on our anticipated HIT implementation timeframe. The Medicare incentive payments to individual hospitals would be made over a four-year, front-weighted transition period. The Medicaid incentive payments, although 100% federally funded, will be administered by the states and are subject to more flexible payment and compliance standards. Hospitals that achieve compliance between 2014 and 2015 will receive reduced incentive payments during the transition period. We anticipate that, in addition to the expenditures we will incur to qualify for these incentive payments, our operating expenses will increase in the future as a result of these information system investments. Much or all of these expenditures may have been made by us as a part of our clinical systems enhancements, but would not have been incurred in the timeline to comply with the incentive payment requirements of the ARRA. However, we anticipate there will be other operational benefits that we can realize as a result of these HIT enhancements that are not included in the above amounts. Hospitals that fail to become meaningful users of EHR or fail to submit quality data by 2015 will be subject to penalties in the form of a reduction to Medicare payments. This reduction, which will be based on the market basket update, will be phased in over three years and will continue until a hospital achieves compliance. Using an estimated market basket of 2% and our annual Medicare inpatient net revenues for the year ended December 31, 2009, should all of our hospitals fail to become meaningful users of EHR and fail to submit quality data, the penalties would result in reductions to our annual Medicare traditional inpatient net revenues of approximately $15 million, $23 million and $30 million in 2015, 2016, and 2017 and subsequent years, respectively.
42
Table of Contents
On December 30, 2009, CMS released a proposed rule defining the “meaningful use” of EHR and describing the provisions of the incentive programs that encourage the adoption and use of EHRs. A related interim final rule also issued on December 30, 2009 by the Office of the National Coordinator for Health IT sets initial standards, implementation specifications, and certification criteria for EHR technology. Both rules are open to public comment for 60 days from the date of issuance. The interim final rule for EHR certification will take effect 30 days after publication. We are currently evaluating what changes will be required to our information systems, the cost of those changes, and the time and resources required in order for our hospitals to become meaningful users of HIT. The complexity of the changes required to our hospitals’ systems and the time required to complete the changes will likely result in some or all of our hospitals not being fully compliant in time to be eligible for the maximum HIT funding permitted under the ARRA. Because of the uncertainties regarding the implementation of HIT, including CMS’ future implementation regulations, the ability of our hospitals to achieve compliance and the associated costs, we cannot provide any assurances regarding the aforementioned estimates.
Medicare Payments to Physicians
In the final rule updating the Medicare Physician Fee Schedule (“MPFS”) for CY 2010, CMS adopted an update of negative 21.2% that was scheduled to take effect on January 1, 2010. MPFS rates are updated annually based on a formula that includes the sustainable growth rate (“SGR”) formula. The SGR formula has resulted in negative updates since 2002; however, CMS has taken action or Congress has enacted legislation each year to avoid the negative updates. On December 21, 2009, the President signed the Department of Defense Appropriations Act, 2010 into law. Among other things, that act delays the scheduled 21.2% Medicare payment reduction for physician services until March 1, 2010. Congress is now considering several proposals to delay the payment cut further, as well as proposals that would replace the sustainable growth rate formula with another methodology for setting Medicare physician payment rates. We cannot predict what actions, if any, Congress or CMS may take with respect to the MPFS update. Refer to “—MedPAC 2011 Recommendations” below for additional information regarding the MPFS update.
Health Care Reform
On November 7, 2009, the U.S. House of Representatives passed The Affordable Health Care for America Act and, on December 24, 2009, the U.S. Senate passed The Patient Protection and Affordable Care Act, both of which would make significant changes to the U.S. health care system by requiring most individuals to have health insurance coverage. To fund the expansion of insurance coverage, both bills contain measures designed to promote quality and cost efficiency in health care delivery and to generate budgetary savings in the Medicare program. In addition to proposals relating to Medicare Advantage payments, bundling acute and post-acute care, readmissions and value-based purchasing, Congress is considering:
| • | Negative adjustments to the annual market basket updates for Medicare inpatient, outpatient, long-term acute hospital and inpatient rehabilitation payment systems; |
| • | Reductions to Medicare and Medicaid DSH payments; and |
| • | Adjustments to address variations in Medicare reimbursements among geographic regions and individual providers. |
To reduce the number of uninsured Americans, Congress is also considering expanding Medicaid eligibility to additional populations and creating a new insurance exchange.
On February 22, 2010, the President outlined a proposal to bridge the gap between the aforementioned House and Senate bills. The President’s proposal includes the following provisions:
| • | Improving insurance protections for consumers and creating a new federal authority to provide assistance and oversight to the states in monitoring and potentially denying unreasonable rate increases and other unfair practices of insurance companies; |
| • | Requiring most Americans to carry health insurance coverage, with federal subsidies to help many afford the premiums (insurance companies would be barred from denying coverage to people with medical problems or charging them more); |
| • | Strengthening the provisions to fight fraud, waste and abuse in Medicare and Medicaid; |
| • | Increasing the threshold for the excise tax on the most expensive health plans from $23,000 for a family plan to $27,500 and starting the excise tax in 2018 for all plans; and |
| • | Eliminating the favorable Nebraska FMAP provision in the Senate bill and providing additional funding to all states for the expansion of Medicaid. |
We are unable to predict what action Congress or the President might take with respect to final legislation affecting health care or the impact such legislation might have on our revenues, results of operations or cash flows.
43
Table of Contents
FFY 2011 Budget Proposal
On February 1, 2010, the President released a $3.8 trillion FFY 2011 budget proposal. The budget request assumes enactment of health care reform legislation, but does not propose additional cuts to Medicare and Medicaid hospital payments for FFY 2011. The key provisions of the budget proposal affecting hospitals include:
| • | An extension of the FMAP increase contained in the ARRA for an additional six months through June 30, 2011; |
| • | An extension of the period during which an individual may qualify for Consolidated Omnibus Budget Reconciliation Act premium assistance provided in the ARRA through December 31, 2010; |
| • | A proposal to allocate $371 billion over 10 years to eliminate the sustainable growth rate cut and freeze Medicare physician payments; and |
| • | A $250 million increase in discretionary funding for federal Health Care Fraud and Abuse Control activities. |
Legislation to approve these proposals must be enacted by Congress for them to become effective. We cannot predict what action Congress or the President might take with respect to such legislation or the impact the legislation might have on our revenues, results of operations or cash flows.
The budget proposal also states that the President intends to create a bipartisan commission to make recommendations for balancing the federal budget and reducing the deficit starting in 2015. Those recommendations could include cuts to Medicare and Medicaid spending. We cannot predict at this time what recommendations might be made by such a commission or the potential impact of those recommendations on our revenues, results of operations or cash flows.
Medicare Recovery Audit Contractor (“RAC”) Initiative
Section 306 of the Medicare Prescription Drug Improvement and Modernization Act of 2003 directed the Secretary of HHS to demonstrate the use of RACs under CMS’ Medicare Integrity Program in identifying underpayments and overpayments under the Medicare program, and recouping those overpayments. RACs are third-party organizations under contract with CMS, and the law provides that compensation paid to each RAC be based on a percentage of overpayment recoveries identified by the RAC. The RAC demonstration was slated to end in March 2008; however, Section 302 of the Tax Relief and Health Care Act of 2006 (“TRHCA”) made the RAC program permanent and instructed CMS to use RACs to identify Medicare underpayments and overpayments by 2010. The TRHCA also included several provisions that give Medicare providers certain protections and rights. For example, overpayments identified by the RACs are subject to reconsideration and appeal through several forums. We intend to pursue the reversal of adverse determinations where appropriate; however, we cannot predict the outcome of any such appeals. In addition to any overpayments identified by the RACs that are not reversed, we will incur additional costs to respond to requests for records and pursue the reversal of payment denials. We have established protocols to respond to RAC requests and payment denials, if any. Several of our hospitals recently received RAC requests and are in the process of responding to those requests. We cannot predict the impact of the RAC reviews on our results of operations or cash flows at this time.
MedPAC 2011 Recommendations
The Medicare Payment Advisory Commission (“MedPAC”) is an independent Congressional agency established by the Balanced Budget Act of 1997 to advise Congress on issues affecting the Medicare program. The MedPAC’s statutory mandate is quite broad; in addition to advising Congress on payments to private health plans participating in Medicare Advantage and providers in the Original Medicare Plan, MedPAC is also tasked with analyzing access to care, quality of care and other issues affecting Medicare.
On January 14, 2010, MedPAC voted on final recommendations for their March 2010 Report to Congress. Recommendations affecting Medicare payments include the following:
| • | Congress should increase payment rates for the acute inpatient and outpatient prospective payment systems in 2011 by the projected rate of increase in the hospital market basket index, concurrent with implementation of a quality incentive payment program. |
| • | To restore budget neutrality, Congress should require the Secretary of HHS to fully offset increases in inpatient payments due to hospitals’ documentation and coding improvements. To accomplish this, HHS must reduce payment rates in the inpatient prospective payment system by the same percentage (not to exceed 2%) each year in 2011, 2012 and 2013. The lower rates would remain in place until overpayments are fully recovered. |
44
Table of Contents
| • | The update to the payment rates for inpatient rehabilitation services should be eliminated for FFY 2011. |
| • | Congress should update payments for physician services in 2011 by 1.0%. |
PRIVATE INSURANCE
Managed Care
We currently have thousands of managed care contracts with various health maintenance organizations (“HMOs”) and preferred provider organizations (“PPOs”). HMOs generally maintain a full-service health care delivery network comprised of physician, hospital, pharmacy and ancillary service providers that HMO members must access through an assigned “primary care” physician. The member’s care is then managed by his or her primary care physician and other network providers in accordance with the HMO’s quality assurance and utilization review guidelines so that appropriate health care can be efficiently delivered in the most cost-effective manner. HMOs typically provide reduced benefits or reimbursement to their members who use non-contracted health care providers for non-emergency care or none at all.
PPOs generally offer limited benefits to members who use non-contracted health care providers. PPO members who use contracted health care providers receive a preferred benefit, typically in the form of lower co-payments, co-insurance or deductibles. As employers and employees have demanded more choice, managed care plans have developed hybrid products that combine elements of both HMO and PPO plans.
The amount of our managed care net patient revenues during the years ended December 31, 2009, 2008 and 2007 was $4.9 billion, $4.5 billion and $4.1 billion, respectively. Approximately 62% of our managed care net patient revenues for the year ended December 31, 2009 was derived from our top ten managed care payers. National payers generate approximately 44% of our total net managed care revenues. The remainder comes from regional or local payers. At December 31, 2009 and 2008, approximately 57% and 55%, respectively, of our net accounts receivable related to continuing operations were due from managed care payers.
Revenues under managed care plans are based primarily on payment terms involving predetermined rates per diagnosis, per-diem rates, discounted fee-for-service rates and other similar contractual arrangements. These revenues are also subject to review and possible audit by the payers. The payers are billed for patient services on an individual patient basis. An individual patient’s bill is subject to adjustment on a patient-by-patient basis in the ordinary course of business by the payers following their review and adjudication of each particular bill. We estimate the discounts for contractual allowances at the individual hospital level utilizing billing data on an individual patient basis. At the end of each month, on an individual hospital basis, we estimate our expected reimbursement for patients of managed care plans based on the applicable contract terms. We believe it is reasonably likely for there to be an approximately 3% increase or decrease in the estimated contractual allowances related to managed care plans. A 3% increase or decrease in the estimated contractual allowance would impact the estimated reserves by $8 million. Some of the factors that can contribute to changes in the contractual allowance estimates include: (1) changes in reimbursement levels for procedures, supplies and drugs when threshold levels are triggered; (2) changes in reimbursement levels when stop-loss or outlier limits are reached; (3) changes in the admission status of a patient due to physician orders subsequent to initial diagnosis or testing; (4) final coding of in-house and discharged-not-final-billed patients that change reimbursement levels; (5) secondary benefits determined after primary insurance payments; and (6) reclassification of patients among insurance plans with different coverage levels. Contractual allowance estimates are periodically reviewed for accuracy by taking into consideration known contract terms, as well as payment history. Although we do not separately accumulate and disclose the aggregate amount of adjustments to the estimated reimbursement for every patient bill, we believe our estimation and review process enables us to identify instances on a timely basis where such estimates need to be revised. We do not believe there were any adjustments to estimates of individual patient bills that were material to our revenues. In addition, on a corporate-wide basis, we do not record any general provision for adjustments to estimated contractual allowances for managed care plans.
We expect managed care governmental admissions to continue to increase as a percentage of total managed care admissions over the near term. However, the managed Medicare and Medicaid insurance plans typically generate lower yields than commercial managed care plans, which have been experiencing an improved pricing trend. Although we have had eighteen consecutive quarters of improved year-over-year managed care pricing, we expect some moderation in the pricing percentage increases in the future.
In the year ended December 31, 2009, our commercial managed care net inpatient revenue per admission from our acute care hospitals was approximately 58% higher than our aggregate yield on a per admission basis from government payers, including managed Medicare and Medicaid insurance plans.
45
Table of Contents
The U.S. House of Representatives and Senate are currently considering legislation that would make significant changes to the U.S. health care system, including changes designed to expand insurance coverage to many of the estimated 47 million Americans who are uninsured. Proposals include a mandate on individuals to purchase insurance, a mandate on businesses to provide insurance or pay into a government insurance fund, and income-based subsidies for individuals and families to purchase private or public insurance coverage through a government-run “health insurance exchange.” The legislation as proposed would also establish new criteria for health insurance coverage in the individual and small group markets, including guaranteed issue and renewal requirements, restrictions on premium rating and rescissions, and limits on beneficiary cost sharing and annual and lifetime benefit caps. As part of reform legislation, Congress is also considering the President’s proposal to cut as much as $176 billion over ten years from payments to Medicare Advantage health plans, and the imposition of an excise tax on high-cost insurance plans or insurance companies directly. We are unable to predict what action Congress or the President might take with respect to final legislation or the impact such legislation ultimately might have on our managed care business.
Indemnity
An indemnity-based agreement generally requires the insurer to reimburse an insured patient for health care expenses after those expenses have been incurred by the patient, subject to an increasing number of policy conditions and exclusions. Unlike an HMO member, a patient with indemnity insurance is free to control his or her utilization of health care and selection of health care providers.
SELF-PAY PATIENTS
Self-pay patients are patients who do not qualify for government programs payments, such as Medicare and Medicaid, and who do not have some form of private insurance and, therefore, are responsible for their own medical bills. A significant portion of our self-pay patients is being admitted through our hospitals’ emergency departments and often requires high-acuity treatment that is more costly to provide and, therefore, results in higher billings, which are the least collectible of all accounts. We believe our level of self-pay patients has been higher in the last several years than previous periods due to a combination of broad economic factors, including increased unemployment rates, reductions in state Medicaid budgets, increasing numbers of individuals and employers who choose not to purchase insurance, and an increased burden of co-payments and deductibles to be made by patients instead of insurers.
Self-pay accounts pose significant collectability problems. At December 31, 2009 and 2008, approximately 7% and 8%, respectively, of our net accounts receivable related to continuing operations were due from self-pay patients. Further, a significant portion of our provision for doubtful accounts relates to self-pay patients, as well as co-payments and deductibles owed to us by patients with insurance. We have performed systematic analyses to focus our attention on drivers of bad debt for each hospital. While emergency department use is the primary contributor to our provision for doubtful accounts in the aggregate, this is not the case at all hospitals. As a result, we are increasing our focus on targeted initiatives that concentrate on non-emergency department patients. These initiatives are intended to promote process efficiencies in working self-pay accounts, as well as co-payment and deductible amounts owed to us by patients with insurance, that we deem highly collectible. We are dedicated to modifying and refining our processes as needed, enhancing our technology and improving staff training throughout the revenue cycle in an effort to increase collections and reduce accounts receivable.
Over the longer term, several other initiatives we have previously announced should also help address this challenge. For example, our Compact is designed to offer managed care-style discounts to most uninsured patients, which enables us to offer lower rates to those patients who historically have been charged standard gross charges. A significant portion of those charges had previously been written down in our provision for doubtful accounts. Under the Compact, the discount offered to uninsured patients is recognized as a contractual allowance, which reduces net operating revenues at the time the self-pay accounts are recorded. The uninsured patient accounts, net of contractual allowances recorded, are further reduced to their net realizable value through provision for doubtful accounts based on historical collection trends for self-pay accounts and other factors that affect the estimation process.
The estimated costs (based on selected operating expenses, which include salaries, wages and benefits, supplies and other operating expenses) of caring for our self-pay patients for the years ended December 31, 2009, 2008 and 2007 were approximately $365 million, $359 million and $342 million, respectively. We also provide charity care to patients who are financially unable to pay for the health care services they receive. Most patients who qualify for charity care are charged a per-diem amount for services received, subject to a cap. Except for the per-diem amounts, our policy is not to pursue collection of amounts determined to qualify as charity care; therefore, we do not report these amounts in net operating revenues or in provision for doubtful accounts. Most states include an estimate of the cost of charity care in the determination of a hospital’s eligibility for Medicaid DSH payments. The estimated costs (based on the selected operating expenses described above) of caring for charity care patients for the years ended December 31, 2009, 2008 and 2007 were approximately $118 million, $113 million and $121 million, respectively.
46
Table of Contents
The U.S. House of Representatives and Senate are currently working on legislation that would make significant changes to the U.S. health care system, including changes designed to expand insurance coverage to many of the estimated 47 million Americans who are uninsured. A reduction in the number of self-pay patients likely would favorably impact our revenues and provision for doubtful accounts; however, with final legislation still pending, we are unable to predict what impact such legislation ultimately might have on our business, financial condition, results of operations or cash flows.
RESULTS OF OPERATIONS FOR THE YEAR ENDED DECEMBER 31, 2009 COMPARED TO THE YEAR ENDED DECEMBER 31, 2008
The following two tables summarize our net operating revenues, operating expenses and operating income from continuing operations, both in dollar amounts and as percentages of net operating revenues, for the years ended December 31, 2009 and 2008:
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | Increase (Decrease) |
||||||||||
| Net operating revenues: |
||||||||||||
| General hospitals |
$ | 8,808 | $ | 8,412 | $ | 396 | ||||||
| Other operations |
206 | 173 | 33 | |||||||||
| Net operating revenues |
9,014 | 8,585 | 429 | |||||||||
| Operating expenses: |
||||||||||||
| Salaries, wages and benefits |
3,857 | 3,779 | 78 | |||||||||
| Supplies |
1,569 | 1,511 | 58 | |||||||||
| Provision for doubtful accounts |
697 | 628 | 69 | |||||||||
| Other operating expenses, net |
1,909 | 1,928 | (19 | ) | ||||||||
| Depreciation and amortization |
386 | 371 | 15 | |||||||||
| Impairment of long-lived assets and goodwill, and restructuring charges |
27 | 16 | 11 | |||||||||
| Litigation and investigation costs, net of insurance recoveries |
31 | 41 | (10 | ) | ||||||||
| Operating income |
$ | 538 | $ | 311 | $ | 227 | ||||||
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | Increase (Decrease) |
||||||||||
| Net operating revenues: |
||||||||||||
| General hospitals |
97.7 | % | 98.0 | % | (0.3 | )% | ||||||
| Other operations |
2.3 | % | 2.0 | % | 0.3 | % | ||||||
| Net operating revenues |
100.0 | % | 100.0 | % | — | % | ||||||
| Operating expenses: |
||||||||||||
| Salaries, wages and benefits |
42.8 | % | 44.0 | % | (1.2 | )% | ||||||
| Supplies |
17.4 | % | 17.6 | % | (0.2 | )% | ||||||
| Provision for doubtful accounts |
7.7 | % | 7.3 | % | 0.4 | % | ||||||
| Other operating expenses, net |
21.2 | % | 22.5 | % | (1.3 | )% | ||||||
| Depreciation and amortization |
4.3 | % | 4.3 | % | — | % | ||||||
| Impairment of long-lived assets and goodwill, and restructuring charges |
0.3 | % | 0.2 | % | 0.1 | % | ||||||
| Litigation and investigation costs, net of insurance recoveries |
0.3 | % | 0.5 | % | (0.2 | )% | ||||||
| Operating income |
6.0 | % | 3.6 | % | 2.4 | % | ||||||
Net operating revenues of our continuing general hospitals include inpatient and outpatient revenues, as well as nonpatient revenues (primarily rental income, management fee revenue and income from services such as cafeterias, gift shops and parking) and other miscellaneous revenue. Net operating revenues of other operations primarily consist of revenues from (1) physician practices, (2) a rehabilitation hospital, which we closed during the three months ended March 31, 2009, and (3) a long-term acute care hospital. Only one of our individual hospitals represented more than 5% (approximately 5.1%) of our net operating revenues for the year ended December 31, 2009, and one represented more than 5% (approximately 5.5%) of our total assets, excluding goodwill and intercompany receivables, at December 31, 2009.
Net operating revenues from our other operations were $206 million and $173 million in the years ended December 31, 2009 and 2008, respectively. The increase in net operating revenues from other operations during 2009 primarily relates to our additional owned physician practices. Equity earnings for unconsolidated affiliates, included in our net operating revenues from other operations, were $6 million and $13 million for the years ended December 31, 2009 and 2008, respectively.
47
Table of Contents
The tables below show certain selected historical operating statistics of our continuing hospitals on a same-hospital basis. We have excluded two of our hospitals from the same-hospital statistics for the years ended December 31, 2009 and 2008. The hospitals excluded are Sierra Providence East Medical Center, which opened in May 2008, and NorthShore Regional Medical Center, which was reclassified to discontinued operations during the three months ended June 30, 2009.
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Admissions, Patient Days and Surgeries |
2009 | 2008 | Increase (Decrease) |
||||||
| Commercial managed care admissions |
133,511 | 140,030 | (4.7 | )% | |||||
| Governmental managed care admissions |
118,129 | 109,450 | 7.9 | % | |||||
| Medicare admissions |
156,104 | 161,493 | (3.3 | )% | |||||
| Medicaid admissions |
64,405 | 64,411 | — | % | |||||
| Uninsured admissions |
23,205 | 24,039 | (3.5 | )% | |||||
| Charity care admissions |
10,435 | 9,284 | 12.4 | % | |||||
| Other admissions |
13,601 | 13,906 | (2.2 | )% | |||||
| Total admissions |
519,390 | 522,613 | (0.6 | )% | |||||
| Paying admissions (excludes charity and uninsured) |
485,750 | 489,290 | (0.7 | )% | |||||
| Total government program admissions |
338,638 | 335,354 | 1.0 | % | |||||
| Charity admissions and uninsured admissions |
33,640 | 33,323 | 1.0 | % | |||||
| Admissions through emergency department |
297,911 | 293,350 | 1.6 | % | |||||
| Commercial managed care admissions as a percentage of total admissions |
25.7 | % | 26.8 | % | (1.1 | )%(1) | |||
| Emergency department admissions as a percentage of total admissions |
57.4 | % | 56.1 | % | 1.3 | %(1) | |||
| Uninsured admissions as a percentage of total admissions |
4.5 | % | 4.6 | % | (0.1 | )%(1) | |||
| Charity admissions as a percentage of total admissions |
2.0 | % | 1.8 | % | 0.2 | %(1) | |||
| Surgeries – inpatient |
152,846 | 154,268 | (0.9 | )% | |||||
| Surgeries – outpatient |
209,294 | 202,195 | 3.5 | % | |||||
| Total surgeries |
362,140 | 356,463 | 1.6 | % | |||||
| Patient days – total |
2,530,528 | 2,586,187 | (2.2 | )% | |||||
| Adjusted patient days(2) |
3,748,764 | 3,734,085 | 0.4 | % | |||||
| Patient days – commercial managed care |
535,345 | 563,018 | (4.9 | )% | |||||
| Average length of stay (days) |
4.9 | 4.9 | — | (1) | |||||
| Adjusted patient admissions(2) |
774,630 | 759,976 | 1.9 | % | |||||
| Number of general hospitals (at end of period) |
48 | 48 | — | (1) | |||||
| Licensed beds (at end of period) |
13,326 | 13,287 | 0.3 | % | |||||
| Average licensed beds |
13,309 | 13,274 | 0.3 | % | |||||
| Utilization of licensed beds(3) |
52.1 | % | 53.2 | % | (1.1 | )%(1) | |||
| (1) | The change is the difference between the 2009 and 2008 amounts shown. |
| (2) | Adjusted patient days/admissions represents actual patient days/admissions adjusted to include outpatient services by multiplying actual patient days/admissions by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
| (3) | Utilization of licensed beds represents patient days divided by number of days in the period divided by average licensed beds. |
48
Table of Contents
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Outpatient Visits |
2009 | 2008 | Increase (Decrease) |
||||||
| Commercial managed care visits |
1,388,668 | 1,405,088 | (1.2 | )% | |||||
| Governmental managed care visits |
737,827 | 619,284 | 19.1 | % | |||||
| Medicare visits |
850,057 | 840,943 | 1.1 | % | |||||
| Medicaid visits |
299,269 | 272,402 | 9.9 | % | |||||
| Uninsured visits |
371,390 | 395,418 | (6.1 | )% | |||||
| Charity care visits |
29,026 | 21,940 | 32.3 | % | |||||
| Other visits |
204,316 | 197,948 | 3.2 | % | |||||
| Total visits |
3,880,553 | 3,753,023 | 3.4 | % | |||||
| Paying visits (excludes charity and uninsured) |
3,480,137 | 3,335,665 | 4.3 | % | |||||
| Total government program visits |
1,887,153 | 1,732,629 | 8.9 | % | |||||
| Surgery visits |
209,294 | 202,195 | 3.5 | % | |||||
| Emergency department visits |
1,410,081 | 1,318,455 | 6.9 | % | |||||
| Charity visits and uninsured visits |
400,416 | 417,358 | (4.1 | )% | |||||
| Charity visits and uninsured visits as a percentage of total visits |
10.3 | % | 11.1 | % | (0.8 | )%(1) | |||
| Paying visits as a percentage of total visits |
89.7 | % | 88.9 | % | 0.8 | %(1) | |||
| Commercial visits as a percentage of total visits |
35.8 | % | 37.4 | % | (1.6 | )%(1) | |||
| (1) | The change is the difference between the 2009 and 2008 amounts shown. |
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Revenues |
2009 | 2008 | Increase (Decrease) |
||||||
| Net operating revenues |
$ | 8,918 | $ | 8,553 | 4.3 | % | |||
| Net patient revenues from commercial managed care |
$ | 3,541 | $ | 3,409 | 3.9 | % | |||
| Revenues from the uninsured |
$ | 610 | $ | 614 | (0.7 | )% | |||
| Net inpatient revenues(1) |
$ | 5,848 | $ | 5,685 | 2.9 | % | |||
| Net outpatient revenues(1) |
$ | 2,729 | $ | 2,555 | 6.8 | % | |||
| (1) | Net inpatient revenues and net outpatient revenues are components of net operating revenues. Net inpatient revenues include self-pay revenues of $253 million and $262 million for the years ended December 31, 2009 and 2008, respectively. Net outpatient revenues include self-pay revenues of $357 million and $352 million for years ended December 31, 2009 and 2008, respectively. |
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Revenues on a Per Admission, Per Patient Day and Per Visit Basis |
2009 | 2008 | Increase (Decrease) |
||||||
| Net inpatient revenue per admission |
$ | 11,259 | $ | 10,878 | 3.5 | % | |||
| Net inpatient revenue per patient day |
$ | 2,311 | $ | 2,198 | 5.1 | % | |||
| Net outpatient revenue per visit |
$ | 703 | $ | 681 | 3.2 | % | |||
| Net patient revenue per adjusted patient admission(1) |
$ | 11,072 | $ | 10,842 | 2.1 | % | |||
| Net patient revenue per adjusted patient day(1) |
$ | 2,288 | $ | 2,207 | 3.7 | % | |||
| Managed care: net inpatient revenue per admission |
$ | 12,143 | $ | 11,581 | 4.9 | % | |||
| Managed care: net outpatient revenue per visit |
$ | 822 | $ | 800 | 2.8 | % | |||
| (1) | Adjusted patient days/admissions represents actual patient days/admissions adjusted to include outpatient services by multiplying actual patient days/admissions by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
49
Table of Contents
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Selected Operating Expenses |
2009 | 2008 | Increase (Decrease) |
||||||
| Salaries, wages and benefits |
$ | 3,827 | $ | 3,761 | 1.8 | % | |||
| Supplies |
1,555 | 1,507 | 3.2 | % | |||||
| Other operating expenses |
1,888 | 1,913 | (1.3 | )% | |||||
| Total |
$ | 7,270 | $ | 7,181 | 1.2 | % | |||
| Rent/lease expense(1) |
$ | 142 | $ | 135 | 5.2 | % | |||
| Salaries, wages and benefits per adjusted patient day(2) |
$ | 1,020 | $ | 1,007 | 1.3 | % | |||
| Supplies per adjusted patient day(2) |
415 | 404 | 2.7 | % | |||||
| Other operating expenses per adjusted patient day(2) |
504 | 512 | (1.6 | )% | |||||
| Total per adjusted patient day |
$ | 1,939 | $ | 1,923 | 0.8 | % | |||
| (1) | Included in other operating expenses. |
| (2) | Adjusted patient days represent actual patient days adjusted to include outpatient services by multiplying actual patient days by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
| Same-Hospital Continuing Operations |
|||||||||||
| Years Ended December 31, | |||||||||||
| Provision for Doubtful Accounts |
2009 | 2008 | Increase (Decrease) |
||||||||
| Provision for doubtful accounts |
$ | 682 | $ | 623 | 9.5 | % | |||||
| Provision for doubtful accounts as a percentage of net operating revenues |
7.6 | % | 7.3 | % | 0.3 | %(1) | |||||
| Collection rate on self-pay accounts(2) |
30.1 | % | 32.5 | % | (2.4 | )%(1) | |||||
| Collection rate from managed care payers |
98.0 | % | 97.8 | % | 0.2 | %(1) | |||||
| (1) | The change is the difference between the 2009 and 2008 amounts shown. |
| (2) | “Self-pay” accounts receivable are comprised of both uninsured and balance-after insurance receivables. |
REVENUES
During the year ended December 31, 2009, net operating revenues from continuing operations increased 5.0% compared to the year ended December 31, 2008.
Our same-hospital net inpatient revenues for the year ended December 31, 2009 increased by 2.9% compared to the year ended December 31, 2008. There were various positive and negative factors impacting our net inpatient revenues.
Key positive factors include:
| • | Improved managed care pricing as a result of renegotiated contracts; |
| • | Favorable adjustments for prior-year cost reports and related valuation allowances of $15 million in the year ended December 31, 2009 compared to $3 million in the year ended December 31, 2008; and |
| • | DSH payments and other state-funded subsidy payments of $171 million for the year ended December 31, 2009 compared to $153 million in the year ended December 31, 2008. |
Key negative factors include:
| • | A decrease in same-hospital commercial managed care admissions of 4.7%. |
Same-hospital net outpatient revenues during the year ended December 31, 2009 increased 6.8% compared to the year ended December 31, 2008. The primary reasons for this increase are improved managed care pricing and increased volume levels. Total same-hospital outpatient visits and outpatient surgery visits for 2009 increased by 3.4% and 3.5%, respectively, compared to 2008. Commercial managed care outpatient visits declined 1.2% in the year ended December 31, 2009 compared to the year ended December 31, 2008.
50
Table of Contents
SALARIES, WAGES AND BENEFITS
Salaries, wages and benefits expense as a percentage of net operating revenues decreased 1.2% for the year ended December 31, 2009 compared to the year ended December 31, 2008. Same-hospital salaries, wages and benefits per adjusted patient day increased by approximately 1.3% in 2009 as compared to 2008. This increase is primarily due to merit increases for our employees, an increase in the number of employed physicians and higher incentive compensation and health benefits costs, partially offset by a decline in full-time employee headcount, reduced contract labor expense, lower stock-based compensation expense, and lower overtime costs. Contract labor expense, which is included in salaries, wages and benefits, was $81 million in the year ended December 31, 2009, a decrease of $63 million, or 43.8%, as compared to the year ended December 31, 2008.
At December 31, 2009, approximately 19% of the employees at our hospitals and related health care facilities in both continuing and discontinued operations were represented by labor unions. Labor relations at our facilities generally have been satisfactory. We and the hospital industry in general, are continuing to see an increase in the amount of union activity across the country. We expect this trend to be even more pronounced in 2010, as we renegotiate our existing labor contracts, all of which are scheduled to expire in the next 14 months. As union activity increases, our operating expenses may increase more rapidly than our net operating revenues.
In addition, legislation has been introduced in Congress that could significantly change both union organizing and bargaining over initial labor contracts in a way that is likely to increase union membership, at least in the short term. We are unable to predict what action Congress or the President might take with respect to this or any other labor-related legislation or the impact such legislation might ultimately have on our relations with employees and unions.
We currently have labor contracts and collective bargaining agreements with the California Nurses Association (“CNA”), the Service Employees International Union (“SEIU”), the United Nurses Associations of California (“UNAC”) and the American Federation of State, County and Municipal Employees that cover registered nurses, service and maintenance workers, and other employees at 10 of our general hospitals in California, three of our general hospitals in Florida and one of our general hospitals in Philadelphia. All of these union agreements set stable and competitive wage increases within our budgeted expectations through various dates in 2010 and early 2011. In January 2010, we commenced the process of renegotiating these contracts, beginning with our collective bargaining agreements with UNAC at two of our hospitals in California.
We also have separate “peace accords” with both the CNA and the SEIU that provide each union with limited access to attempt to organize certain of our employees and establish specific guidelines for the parties to follow with respect to organizing activities. Both peace accords expire in December 2011. The CNA and the SEIU have engaged in union organizing activities at several of our hospitals in Houston, Memphis and Philadelphia pursuant to the terms of the peace accords. Registered nurses at two of these facilities have participated in elections concerning CNA representation, but – to date – union organizing has been successful at only Cypress Fairbanks Medical Center (“CyFair”). After extended collective bargaining negotiations over an initial contract for CyFair, the CNA triggered an agreed-to interest arbitration process, which began in June 2009, that provides for a neutral third party to mediate unresolved contract terms. If the mediation is unsuccessful, those unresolved terms will be decided by binding arbitration.
We also are defending various allegations that we are in violation of federal labor laws or the terms of our collective bargaining agreements and peace accords, and we expect to continue to be subject to such claims from time to time in the normal course of business.
SUPPLIES
Supplies expense as a percentage of net operating revenues was 17.4% for the year ended December 31, 2009 compared to 17.6% for the year ended December 31, 2008; supplies expense per adjusted patient day on a same-hospital basis increased by 2.7% in 2009 compared to 2008. The increase in supplies expense is primarily due to the increase in the number of surgeries, which grew by 1.6%, and increased utilization of high cost implants, high-cost pharmaceuticals and increased orthopedic costs. A portion of the increase in supplies expense was offset by revenue growth related to payments we receive from certain payers.
We strive to control supplies expense through product standardization, bulk purchases, contract compliance, improved utilization and operational improvements that should minimize waste. The items of current cost reduction focus continue to be cardiac stents and pacemakers, orthopedics and implants, and high-cost pharmaceuticals. We also utilize the group-purchasing strategies and supplies-management services of Broadlane, Inc., a company that offers group-purchasing procurement strategy, outsourcing and e-commerce services to the health care industry.
51
Table of Contents
As part of health care reform legislation, Congress is considering imposing an annual tax on manufacturers of certain medical devices and pharmaceuticals, as well as other provisions that could affect hospital group purchasing organizations. We are unable to predict what action Congress or the President might take with respect to the legislation or the impact those provisions ultimately might have on our supplies expense, if enacted.
PROVISION FOR DOUBTFUL ACCOUNTS
The provision for doubtful accounts as a percentage of net operating revenues on a same-hospital basis was 7.6% for the year ended December 31, 2009 compared to 7.3% for the year ended December 31, 2008. The increase in the provision for doubtful accounts was related to decreased collection rates on self-pay accounts, higher pricing and higher patient insurance deductibles, partially offset by the decline in uninsured revenues and improved managed care accounts receivable aging categories. Our self-pay collection rate, which is the blended collection rate for uninsured and balance-after insurance accounts receivable, declined to approximately 30.1% in the year ended December 31, 2009 from 32.5% in the prior year.
The table below shows the net accounts receivable and allowance for doubtful accounts by payer at December 31, 2009 and December 31, 2008:
| December 31, 2009 | December 31, 2008 | |||||||||||||||||||||
| Accounts Receivable Before Allowance for Doubtful Accounts |
Allowance for Doubtful Accounts |
Net | Accounts Receivable Before Allowance for Doubtful Accounts |
Allowance for Doubtful Accounts |
Net | |||||||||||||||||
| Medicare |
$ | 162 | $ | — | $ | 162 | $ | 156 | $ | — | $ | 156 | ||||||||||
| Medicaid |
106 | — | 106 | 121 | — | 121 | ||||||||||||||||
| Net cost report settlements payable and valuation allowances |
(24 | ) | — | (24 | ) | (20 | ) | — | (20 | ) | ||||||||||||
| Commercial managed care |
527 | 62 | 465 | 549 | 71 | 478 | ||||||||||||||||
| Governmental managed care |
185 | — | 185 | 175 | — | 175 | ||||||||||||||||
| Self-pay uninsured |
204 | 175 | 29 | 190 | 161 | 29 | ||||||||||||||||
| Self-pay balance after insurance |
118 | 62 | 56 | 139 | 71 | 68 | ||||||||||||||||
| Estimated future recoveries from accounts assigned to collection agencies |
35 | — | 35 | 40 | — | 40 | ||||||||||||||||
| Other payers |
164 | 42 | 122 | 176 | 40 | 136 | ||||||||||||||||
| Total continuing operations |
1,477 | 341 | 1,136 | 1,526 | 343 | 1,183 | ||||||||||||||||
| Total discontinued operations |
50 | 28 | 22 | 207 | 53 | 154 | ||||||||||||||||
| $ | 1,527 | $ | 369 | $ | 1,158 | $ | 1,733 | $ | 396 | $ | 1,337 | |||||||||||
A significant portion of our provision for doubtful accounts relates to self-pay patients, as well as co-payments and deductibles owed to us by patients with insurance. Collection of accounts receivable has been a key area of focus, particularly over the past several years, as we have experienced adverse changes in our business mix. At December 31, 2009, our collection rate on self-pay accounts was approximately 30.1%, including collections from point-of-service through collections by our in-house collection agency. During 2008 and 2009, we experienced a downward trend in our self-pay collection rate as follows: 35.0% at March 31, 2008; 34.0% at June 30, 2008; 33.3% at September 30, 2008; 32.5% at December 31, 2008; 31.4% at March 31, 2009; 30.8% at June 30, 2009 and 30.3% at September 30, 2009. These self-pay collection rates include payments made by patients, including co-payments and deductibles paid by patients with insurance, prior to an account being classified and assigned to our in-house self-pay collection group. Based on our accounts receivable from self-pay patients and co-payments and deductibles owed to us by patients with insurance at December 31, 2009, a hypothetical 10% decline in our self-pay collection rate, or approximately 3.0%, would result in an unfavorable adjustment to provision for doubtful accounts of approximately $6 million.
We have performed systematic analyses to focus our attention on drivers of bad debt for each hospital. While emergency department use is the primary contributor to our provision for doubtful accounts in the aggregate, this is not the case at all hospitals. As a result, we are increasing our focus on targeted initiatives that concentrate on non-emergency department patients. These initiatives are intended to promote process efficiencies in working self-pay accounts we deem highly collectible. We are dedicated to modifying and refining our processes as needed, enhancing our technology and improving staff training throughout the revenue cycle in an effort to increase collections and reduce accounts receivable.
52
Table of Contents
Payment pressure from managed care payers also affects our provision for doubtful accounts. We typically experience ongoing managed care payment delays and disputes; however, we continue to work with these payers to obtain adequate and timely reimbursement for our services. Our estimated collection rate from managed care payers was approximately 98.0% at December 31, 2009 and 97.8% at December 31, 2008, which includes collections from point-of-service through collections by our in-house collection agency.
We continue to focus on revenue cycle initiatives to improve cash flow. One specific initiative is our Center for Patient Access Services (“CPAS”), which was completed during 2009 at the hospitals scheduled to participate in the program. CPAS is a centralized, dedicated operation that performs financial clearance, including completing insurance eligibility checks, documenting verification of benefits, providing required notifications to managed care payers, obtaining pre-authorizations when necessary and contacting the patient to offer pre-service financial counseling. Although we continue to improve our methodology for evaluating the collectability of our accounts receivable, we may incur future charges if there are unfavorable changes in the trends affecting the net realizable value of our accounts receivable.
We manage our provision for doubtful accounts using hospital-specific goals and benchmarks such as (1) total cash collections, (2) point-of-service cash collections, (3) accounts receivable days outstanding (“AR Days”), and (4) accounts receivable by aging category. The following tables present the approximate aging by payer of our net accounts receivable from continuing operations of $1.160 billion and $1.203 billion at December 31, 2009 and 2008, respectively, excluding cost report settlements payable and valuation allowances of $24 million and $20 million at December 31, 2009 and 2008, respectively:
| December 31, 2009 | |||||||||||||||
| Medicare | Medicaid | Managed Care |
Indemnity, Self-Pay and Other |
Total | |||||||||||
| 0-60 days |
94 | % | 63 | % | 78 | % | 26 | % | 69 | % | |||||
| 61-120 days |
3 | % | 24 | % | 12 | % | 27 | % | 15 | % | |||||
| 121-180 days |
3 | % | 11 | % | 5 | % | 13 | % | 6 | % | |||||
| Over 180 days |
— | % | 2 | % | 5 | % | 34 | % | 10 | % | |||||
| Total |
100 | % | 100 | % | 100 | % | 100 | % | 100 | % | |||||
| December 31, 2008 | |||||||||||||||
| Medicare | Medicaid | Managed Care |
Indemnity, Self-Pay and Other |
Total | |||||||||||
| 0-60 days |
99 | % | 64 | % | 77 | % | 33 | % | 69 | % | |||||
| 61-120 days |
1 | % | 24 | % | 14 | % | 24 | % | 15 | % | |||||
| 121-180 days |
— | % | 12 | % | 5 | % | 11 | % | 7 | % | |||||
| Over 180 days |
— | % | — | % | 4 | % | 32 | % | 9 | % | |||||
| Total |
100 | % | 100 | % | 100 | % | 100 | % | 100 | % | |||||
Our AR Days from continuing operations were 46 days at December 31, 2009 and 50 days at December 31, 2008. AR Days at December 31, 2009 and 2008 were within our targets of less than 50 and 55 days, respectively. AR Days are calculated as our accounts receivable from continuing operations on the last date in the quarter divided by our revenue from continuing operations for the quarter ended on that date divided by the number of days in the quarter.
As of December 31, 2009, we had a cumulative total of patient account assignments dating back at least three years or older of approximately $4.3 billion related to our continuing operations being pursued by our in-house collection agency. These accounts have already been written off and are not included in our receivables or in the allowance for doubtful accounts; however, an estimate of future recoveries from all the accounts at collection agencies is determined based on our historical experience and recorded in accounts receivable.
Patient advocates from our Medical Eligibility Program (“MEP”) screen patients in the hospital to determine whether those patients meet eligibility requirements for financial assistance programs. They also expedite the process of applying for these government programs. Receivables from patients who are potentially eligible for Medicaid are classified as Medicaid pending, under our MEP, with appropriate contractual allowances recorded. Based on recent trends, approximately 91% of all accounts in our MEP are ultimately approved for benefits under a government program such as Medicaid.
53
Table of Contents
The following table shows the approximate amount of net accounts receivable in our MEP still awaiting determination of eligibility under a government program at December 31, 2009 and 2008 by aging category:
| December 31, | ||||||
| 2009 | 2008 | |||||
| 0-60 days |
$ | 66 | $ | 87 | ||
| 61-120 days |
18 | 25 | ||||
| 121-180 days |
5 | 6 | ||||
| Over 180 days(1) |
— | — | ||||
| Total |
$ | 89 | $ | 118 | ||
| (1) | Includes accounts receivable of $10 million at both December 31, 2009 and 2008 that are fully reserved. |
OTHER OPERATING EXPENSES, NET
Other operating expenses as a percentage of net operating revenues decreased by 1.3% in the year ended December 31, 2009 compared to the year ended December 31, 2008. Other operating expenses per adjusted patient day on a same-hospital basis decreased by approximately 1.6% in 2009 as compared to 2008. Contributing to this decrease was a $37 million, or 29.4%, decline in total hospital malpractice expense to $89 million in the year ended December 31, 2009 compared to $126 million in the year ended December 31, 2008. The decrease in malpractice expense is principally due to a 6% reduction in the number of expected claims, partially offset by a 63 basis point decline in the interest rate used to estimate the discounted present value of projected future liabilities. Declines in consulting costs, utility costs, reimbursable business expenses, recruiting-related costs and systems implementations costs also had a favorable impact on other operating expenses. These declines were partially offset by increases in other items, including higher physician fees relating to increased emergency department on-call payments and higher costs for contracted services, as well as a reduction in information systems and business office costs allocable to discontinued operations.
IMPAIRMENT OF LONG-LIVED ASSETS AND GOODWILL, AND RESTRUCTURING CHARGES
During the year ended December 31, 2009, we recorded net impairment and restructuring charges of $27 million. We recorded a $7 million net impairment charge for the write-down of buildings, equipment and other long-lived assets, primarily capitalized software costs classified in other intangible assets, of one hospital to their estimated fair values, primarily due to a decline in the fair value of real estate in the market in which the hospital operates. Material adverse trends in our most recent estimates of future undiscounted cash flows of the hospital, consistent with our prior estimates during 2008 when impairment charges were recorded at this hospital, indicated the carrying value of the hospital’s long-lived assets was not recoverable from the estimated future cash flows. We believe the most significant factors contributing to the continuing adverse financial trends include reductions in volumes of insured patients due to competition, shifts in payer mix from commercial to governmental payers combined with reductions in reimbursement rates from governmental payers, and high levels of uninsured patients. As a result, we updated the estimate of the fair values of the hospital’s long-lived assets and compared the fair value estimate to the carrying values of the hospital’s long-lived assets. Because the fair value estimate was lower than the carrying values of the hospital’s long-lived assets, an impairment charge was recorded for the difference in the amounts. Unless the anticipated future financial trends of this hospital improve to the extent that the estimated future undiscounted cash flows exceed the carrying values of the long-lived assets, this hospital is at risk of future impairments, particularly if we spend significant amounts of capital at the hospital without generating a corresponding increase in the hospital’s fair value or if the fair value of the hospital’s real estate continues to decline. We also recorded a $10 million net impairment charge for the write-down of land and buildings at the current campus of one hospital that is scheduled to move to a new, replacement campus during 2010. Our estimates of the future undiscounted cash flows from use of the current campus for several months during 2010 and from estimated disposition proceeds were less than the carrying values of the land and buildings at the current campus. We compared the estimated fair values to the carrying values and, because the fair value estimate was lower than the carrying values of the assets, an impairment charge was recorded for the difference in the amounts. The remaining net impairment and restructuring charges for the year ended December 31, 2009 include $4 million of employee severance and other related costs, a $3 million impairment charge for the write-down of a note receivable due from a buyer of one of our previously divested hospitals as a result of the buyer filing for bankruptcy, and a $3 million impairment charge for the write-down of other assets primarily related to an option to purchase certain real property near one of our hospitals that no longer has value due to the financial condition of the owner of the real property.
During the year ended December 31, 2008, net impairment and restructuring charges of $16 million included an $8 million net impairment charge for the write-down of buildings and equipment and other long-lived assets, primarily capitalized software costs classified in other intangible assets, of two hospitals to their estimated fair values due to adverse current and anticipated future financial trends based on their most recent projections at that time. We believe the most significant factors contributing to the adverse financial trends include shifts in payer mix from commercial to governmental payers combined with reductions in reimbursement rates from governmental payers and high levels of uninsured patients. The remaining net impairment and restructuring charges for the year ended December 31, 2008 include $6 million of employee severance and other related costs, $1 million for the acceleration of stock-based compensation expense and $6 million in impairment charges for the write-down of other assets primarily due to the write-down of costs associated with an expansion project at one of our hospitals that we decided not to pursue based on unfavorable economics forecasted for the project, partially offset by a $5 million reduction in reserves recorded in prior periods.
54
Table of Contents
Our impairment tests presume stable, improving or, in some cases, declining results of our hospitals, which are based on programs and initiatives being implemented that are designed to achieve the hospital’s most recent projections. If these projections are not met, or if in the future negative trends occur that impact our future outlook, further impairments of long-lived assets and goodwill may occur, and we may incur additional restructuring charges. Future restructuring of our regions that changes our goodwill reporting units could also result in further impairments of our goodwill.
LITIGATION AND INVESTIGATION COSTS, NET OF INSURANCE RECOVERIES
Litigation and investigation costs in continuing operations for the year ended December 31, 2009 were $31 million compared to $41 million for the year ended December 31, 2008. The 2009 costs primarily relate to reserves established in connection with certain governmental reviews further described in Note 13 to the Consolidated Financial Statements. The 2009 costs also include amounts paid to indemnify a former officer of the Company in a matter to which the Company was not a party and costs to defend the Company in various matters. The 2008 costs primarily relate to changes in our estimated liability for now-settled wage and hour actions further described in Note 13 to the Consolidated Financial Statements. The 2008 costs were partially offset by $6 million of insurance proceeds that were recorded as a recovery of litigation and investigation costs in continuing operations for costs we previously incurred related to our December 2004 Redding Medical Center litigation settlement.
INTEREST EXPENSE
During the year ended December 31, 2009, we recorded interest expense of $445 million compared to $418 million for the year ended December 31, 2008. The increase in interest expense primarily relates to higher interest rates on the senior secured notes issued in 2009, partially offset by the impact of interest rate swap and London Interbank Offered Rate (“LIBOR”) cap agreements, all as further described in Note 6 to the Consolidated Financial Statements.
GAIN (LOSS) FROM EARLY EXTINGUISHMENT OF DEBT
During the three months ended March 31, 2009, we recorded a gain from early extinguishment of debt of approximately $134 million relating to the estimated fair values of our new senior secured notes due in 2015 and 2018 issued in a note exchange at less than their par values, net of the write-off of unamortized note discounts, issuance costs and unrecognized interest rate hedge settlements associated with the senior notes tendered. In the three months ended June 30, 2009, we recorded a loss from early extinguishment of debt of approximately $24 million in connection with the purchases of our senior notes due 2014 related to the write-off of unamortized note discounts and issuance costs. Also during the three months ended June 30, 2009, we recorded a gain from early extinguishment of debt of approximately $3 million for cash we received relating to the difference in the fair values of tendered senior notes due in 2011 and 2012 as compared to the fair values of the senior secured notes due 2015 and 2018 issued in connection with an exchange, net of the write-off of unamortized note discounts, issuance costs and unrecognized interest rate hedge settlements associated with the senior notes tendered. During the three months ended September 30, 2009, we recorded a loss from early extinguishment of debt of approximately $22 million related to the difference between the purchase prices and the par values of the $308 million aggregate principal amount of senior notes due 2015 that we repurchased during the period, as well as the write-off of unamortized note discounts and issuance costs associated with the notes. We also completed open market repurchases of approximately $68 million aggregate principal amount of our senior notes due in 2011, 2012, 2014 and 2031 for cash of approximately $60 million. We recorded a gain from early extinguishment of debt of approximately $6 million related to the difference between the purchase prices and the par values of the purchased notes, partially offset by the write-off of unamortized note discounts, issuance costs and unrecognized interest rate hedge settlements associated with the notes. See Note 6 to the Consolidated Financial Statements for additional details about our recent debt transactions.
55
Table of Contents
INVESTMENT EARNINGS
During the year ended December 31, 2009, we recorded no net investment earnings compared to investment earnings of $22 million for the year ended December 31, 2008. In 2009, investment earnings were offset a $7 million loss related to an agreement reached during June 2009 for the early redemption of our $56 million investment in hospital authority bonds related to previously divested hospitals in the Dallas, Texas area for $49 million of cash that we received in June 2009. In the year ended December 31, 2008, $10 million was recorded in investment earnings related to the Redding Medical Center litigation settlement.
NET GAIN ON SALES OF INVESTMENTS
During the year ended December 31, 2009, we recorded a gain on sale of investments of approximately $15 million related to the sale of our 50% membership interest in Peoples Health Network. During the year ended December 31, 2008, we recorded net gains of $125 million from the sale of our entire interest in Broadlane, Inc. and $14 million on the sale of our interest in a joint venture with a real estate investment trust.
INCOME TAX BENEFIT
During the year ended December 31, 2009, we recorded an income tax benefit of $23 million compared to $25 million during the year ended December 31, 2008. See Note 14 to the Consolidated Financial Statements for additional detail about income taxes.
ADDITIONAL SUPPLEMENTAL NON-GAAP DISCLOSURES
The financial information provided throughout this report, including in our Consolidated Financial Statements and the notes thereto, has been prepared in conformity with accounting principles generally accepted in the United States of America (“GAAP”). However, we use certain non-GAAP financial measures defined below in communications with investors, analysts, rating agencies, banks and others to assist such parties in understanding the impact of various items on our financial statements, some of which are recurring or involve cash payments. In addition, we from time to time use these measures to define certain performance targets under our compensation programs.
“Adjusted EBITDA” is a non-GAAP measure that we use in our analysis of the performance of our business, which we define as net income attributable to our common shareholders before: (1) the cumulative effect of changes in accounting principle, net of tax; (2) net income attributable to noncontrolling interests; (3) preferred stock dividends; (4) income (loss) from discontinued operations, net of tax; (5) income tax (expense) benefit; (6) net gain (loss) on sales of investments; (7) investment earnings (loss); (8) gain (loss) from early extinguishment of debt; (9) interest expense; (10) litigation and investigation (costs) benefit, net of insurance recoveries; (11) hurricane insurance recoveries, net of costs; (12) impairment of long-lived assets and goodwill, and restructuring charges, net of insurance recoveries; (13) amortization; and (14) depreciation. As is the case with all non-GAAP measures, investors should consider the limitations associated with this metric, including the potential lack of comparability of this measure from one company to another, and should recognize that Adjusted EBITDA does not provide a complete measure of our operating performance because it excludes many items that are included in our financial statements. Accordingly, investors are encouraged to use GAAP measures when evaluating our financial performance.
56
Table of Contents
The table below shows the reconciliation of Adjusted EBITDA to net income attributable to our common shareholders (the most comparable GAAP term) for the years ended December 31, 2009 and 2008:
| Years Ended December 31, | ||||||||
| 2009 | 2008 | |||||||
| Net income attributable to Tenet Healthcare Corporation common shareholders |
$ | 181 | $ | 25 | ||||
| Less: Net income attributable to noncontrolling interests |
(10 | ) | (7 | ) | ||||
| Preferred stock dividends |
(6 | ) | — | |||||
| Loss from discontinued operations, net of tax |
(31 | ) | (47 | ) | ||||
| Income from continuing operations |
228 | 79 | ||||||
| Income tax benefit |
23 | 25 | ||||||
| Investment earnings |
— | 22 | ||||||
| Gain from early extinguishment of debt |
97 | — | ||||||
| Net gain on sales of investments |
15 | 139 | ||||||
| Interest expense |
(445 | ) | (418 | ) | ||||
| Operating income |
538 | 311 | ||||||
| Litigation and investigation costs, net of insurance recoveries |
(31 | ) | (41 | ) | ||||
| Impairment of long-lived assets and goodwill, and restructuring charges |
(27 | ) | (16 | ) | ||||
| Amortization |
(44 | ) | (38 | ) | ||||
| Depreciation |
(342 | ) | (333 | ) | ||||
| Adjusted EBITDA |
982 | $ | 739 | |||||
| Less: Adjusted EBITDA of hospital without a full calendar year of operating results in 2008 |
16 | (10 | ) | |||||
| Same-hospital Adjusted EBITDA |
$ | 966 | $ | 749 | ||||
| Net operating revenues |
$ | 9,014 | $ | 8,585 | ||||
| Less: Revenues of hospital without full calendar year of operating results in 2008 |
96 | 32 | ||||||
| Same-hospital net operating revenues |
$ | 8,918 | $ | 8,553 | ||||
| Adjusted EBITDA as % of net operating revenues (Adjusted EBITDA margin) |
10.9 | % | 8.6 | % | ||||
| Adjusted same-hospital EBITDA as % of same-hospital net operating revenues (Adjusted same-hospital EBITDA margin) |
10.8 | % | 8.8 | % | ||||
“Adjusted Free Cash Flow” is a non-GAAP term that we define as cash provided by (used in) operating activities less income tax refunds (payments), payments against reserves for restructuring charges and litigation costs and settlements, operating cash flows from discontinued operations, capital expenditures in continuing operations, and new hospital construction expenditures. Adjusted Free Cash Flow is a measure of liquidity that we use in our business as an alternative to net cash provided by (used in) operating activities. We provide this financial measure as a supplement to GAAP information to assist ourselves and investors in understanding the impact of various items on our cash flows, some of which are recurring. Because Adjusted Free Cash Flow excludes many items that are included in our financial statements, it does not provide a complete measure of our liquidity. Accordingly, investors are encouraged to use GAAP measures when evaluating our liquidity.
The following table shows the reconciliation of Adjusted Free Cash Flow to net cash provided by operating activities (the most comparable GAAP term) for the years ended December 31, 2009 and 2008:
| Years Ended December 31, | ||||||||
| 2009 | 2008 | |||||||
| Net cash provided by operating activities |
$ | 425 | $ | 208 | ||||
| Less: |
||||||||
| Income tax payments, net |
(43 | ) | (4 | ) | ||||
| Payments against reserves for restructuring charges and litigation costs and settlements |
(192 | ) | (100 | ) | ||||
| Net cash provided by operating activities from discontinued operations |
40 | 18 | ||||||
| Adjusted net cash provided by operating activities – continuing operations |
620 | 294 | ||||||
| Purchases of property and equipment – continuing operations |
(397 | ) | (452 | ) | ||||
| Construction of new and replacement hospitals |
(58 | ) | (75 | ) | ||||
| Adjusted Free Cash Flow – continuing operations |
$ | 165 | $ | (233 | ) | |||
57
Table of Contents
RESULTS OF OPERATIONS FOR THE YEAR ENDED DECEMBER 31, 2008 COMPARED TO THE YEAR ENDED DECEMBER 31, 2007
The following two tables summarize our net operating revenues, operating expenses and operating income from continuing operations, both in dollar amounts and as percentages of net operating revenues, for the years ended December 31, 2008 and 2007:
| Years Ended December 31, | ||||||||||||
| 2008 | 2007 | Increase (Decrease) |
||||||||||
| Net operating revenues: |
||||||||||||
| General hospitals |
$ | 8,412 | $ | 7,926 | $ | 486 | ||||||
| Other operations |
173 | 157 | 16 | |||||||||
| Net operating revenues |
8,585 | 8,083 | 502 | |||||||||
| Operating expenses: |
||||||||||||
| Salaries, wages and benefits |
3,779 | 3,617 | 162 | |||||||||
| Supplies |
1,511 | 1,401 | 110 | |||||||||
| Provision for doubtful accounts |
628 | 555 | 73 | |||||||||
| Other operating expenses, net |
1,928 | 1,852 | 76 | |||||||||
| Depreciation and amortization |
371 | 336 | 35 | |||||||||
| Impairment of long-lived assets and goodwill, and restructuring charges, net of insurance recoveries |
16 | 36 | (20 | ) | ||||||||
| Hurricane insurance recoveries, net of costs |
— | (3 | ) | 3 | ||||||||
| Litigation and investigation costs, net of insurance recoveries |
41 | 13 | 28 | |||||||||
| Operating income |
$ | 311 | $ | 276 | $ | 35 | ||||||
| Years Ended December 31, | ||||||||||||
| 2008 | 2007 | Increase (Decrease) |
||||||||||
| Net operating revenues: |
||||||||||||
| General hospitals |
98.0 | % | 98.1 | % | (0.1 | )% | ||||||
| Other operations |
2.0 | % | 1.9 | % | 0.1 | % | ||||||
| Net operating revenues |
100.0 | % | 100.0 | % | — | % | ||||||
| Operating expenses: |
||||||||||||
| Salaries, wages and benefits |
44.0 | % | 44.7 | % | (0.7 | )% | ||||||
| Supplies |
17.6 | % | 17.3 | % | 0.3 | % | ||||||
| Provision for doubtful accounts |
7.3 | % | 6.9 | % | 0.4 | % | ||||||
| Other operating expenses, net |
22.5 | % | 22.9 | % | (0.4 | )% | ||||||
| Depreciation and amortization |
4.3 | % | 4.2 | % | 0.1 | % | ||||||
| Impairment of long-lived assets and goodwill, and restructuring charges, net of insurance recoveries |
0.2 | % | 0.4 | % | (0.2 | )% | ||||||
| Hurricane insurance recoveries, net of costs |
— | % | — | % | — | % | ||||||
| Litigation and investigation costs, net of insurance recoveries |
0.5 | % | 0.2 | % | 0.3 | % | ||||||
| Operating income |
3.6 | % | 3.4 | % | 0.2 | % | ||||||
Only one of our individual hospitals represented more than 5% (approximately 5.2%) of our net operating revenues for the year ended December 31, 2008, and none represented more than 5% of our total assets, excluding goodwill and intercompany receivables, at December 31, 2008.
Net operating revenues from our other operations were $173 million and $157 million in the years ended December 31, 2008 and 2007, respectively. Equity earnings for unconsolidated affiliates, included in our net operating revenues from other operations, were $13 million and $20 million for the years ended December 31, 2008 and 2007, respectively.
The tables below show certain selected historical operating statistics for our continuing general hospitals on a same-hospital basis. We have excluded two of our hospitals from the same-hospital statistics for the years ended December 31, 2008 and 2007. The hospitals excluded are Coastal Carolina Medical Center, which we acquired in June 2007, and Sierra Providence East Medical Center, which opened in May 2008.
58
Table of Contents
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Admissions, Patient Days and Surgeries |
2008 | 2007 | Increase (Decrease) |
||||||
| Commercial managed care admission |
139,862 | 144,021 | (2.9 | )% | |||||
| Governmental managed care admissions |
109,357 | 96,564 | 13.2 | % | |||||
| Medicare admissions |
160,840 | 163,530 | (1.6 | )% | |||||
| Medicaid admissions |
64,339 | 63,763 | 0.9 | % | |||||
| Uninsured admissions |
23,901 | 23,429 | 2.0 | % | |||||
| Charity care admissions |
9,276 | 10,153 | (8.6 | )% | |||||
| Other admissions |
13,811 | 13,118 | 5.3 | % | |||||
| Total admissions |
521,386 | 514,578 | 1.3 | % | |||||
| Paying admissions (excludes charity and uninsured) |
488,209 | 480,996 | 1.5 | % | |||||
| Total government program admissions |
334,536 | 323,857 | 33.0 | % | |||||
| Charity admissions and uninsured admissions |
33,177 | 33,582 | (1.2 | )% | |||||
| Admissions through emergency department |
292,432 | 284,417 | 2.8 | % | |||||
| Commercial managed care admissions as a percentage of total admissions |
26.8 | % | 28.0 | % | (1.2 | )%(1) | |||
| Emergency department admissions as a percentage of total admissions |
56.1 | % | 55.3 | % | 0.8 | %(1) | |||
| Uninsured admissions as a percentage of total admissions |
4.6 | % | 4.6 | % | — | %(1) | |||
| Charity admissions as a percentage of total admissions |
1.8 | % | 2.0 | % | (0.2 | )%(1) | |||
| Surgeries – inpatient |
154,117 | 153,052 | 0.7 | % | |||||
| Surgeries – outpatient |
201,598 | 198,009 | 1.8 | % | |||||
| Total surgeries |
355,715 | 351,061 | 1.3 | % | |||||
| Patient days – total |
2,580,612 | 2,567,878 | 0.5 | % | |||||
| Adjusted patient days(2) |
3,717,171 | 3,650,471 | 1.8 | % | |||||
| Patient days – commercial managed care |
562,413 | 586,500 | (4.1 | )% | |||||
| Average length of stay (days) |
4.9 | 5.0 | (0.1 | )%(1) | |||||
| Adjusted patient admissions(2) |
756,253 | 736,720 | 2.7 | % | |||||
| Number of general hospitals (at end of period) |
47 | 47 | — | %(1) | |||||
| Licensed beds (at end of period) |
13,246 | 13,289 | (0.3 | )% | |||||
| Average licensed beds |
13,233 | 13,266 | (0.2 | )% | |||||
| Utilization of licensed beds(3) |
53.3 | % | 53.0 | % | 0.3 | %(1) | |||
| (1) | The change is the difference between the 2008 and 2007 amounts shown. |
| (2) | Adjusted patient days/admissions represents actual patient days/admissions adjusted to include outpatient services by multiplying actual patient days/admissions by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
| (3) | Utilization of licensed beds represents patient days divided by number of days in the period divided by average licensed beds. |
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Outpatient Visits |
2008 | 2007 | Increase (Decrease) |
||||||
| Commercial managed care visits |
1,396,709 | 1,411,546 | (1.1 | )% | |||||
| Governmental managed care visits |
617,384 | 549,506 | 12.4 | % | |||||
| Medicare visits |
827,156 | 852,423 | (3.0 | )% | |||||
| Medicaid visits |
269,563 | 274,428 | (1.8 | )% | |||||
| Uninsured visits |
390,473 | 413,894 | (5.7 | )% | |||||
| Charity care visits |
21,929 | 25,354 | (13.5 | )% | |||||
| Other visits |
194,552 | 193,087 | 0.8 | % | |||||
| Total visits |
3,717,766 | 3,720,238 | (0.1 | )% | |||||
| Paying visits (excludes charity and uninsured) |
3,305,364 | 3,280,990 | 0.7 | % | |||||
| Total government program visits |
1,714,103 | 1,676,357 | 2.3 | % | |||||
| Surgery visits |
201,598 | 198,009 | 1.8 | % | |||||
| Emergency department visits |
1,304,417 | 1,291,936 | 1.0 | % | |||||
| Charity visits and uninsured visits |
412,402 | 439,248 | (6.1 | )% | |||||
| Charity visits and uninsured visits as a percentage of total visits |
11.1 | % | 11.8 | % | (0.7 | )%(1) | |||
| Paying visits as a percentage of total visits |
88.9 | % | 88.2 | % | 0.7 | %(1) | |||
| Commercial visits as a percentage of total visits |
37.6 | % | 37.9 | % | (0.3 | )%(1) | |||
| (1) | The change is the difference between the 2008 and 2007 amounts shown. |
59
Table of Contents
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Revenues |
2008 | 2007 | Increase (Decrease) |
||||||
| Net operating revenues |
$ | 8,529 | $ | 8,068 | 5.7 | % | |||
| Net patient revenues from commercial managed care |
$ | 3,403 | $ | 3,200 | 6.3 | % | |||
| Revenues from the uninsured |
$ | 608 | $ | 603 | 0.8 | % | |||
| Net inpatient revenues(1) |
$ | 5,675 | $ | 5,434 | 4.4 | % | |||
| Net outpatient revenues(1) |
$ | 2,541 | $ | 2,349 | 8.2 | % | |||
| (1) | Net inpatient revenues and net outpatient revenues are components of net operating revenues. Net inpatient revenues include self-pay revenues of $261 million and $272 million for the years ended December 31, 2008 and 2007, respectively. Net outpatient revenues include self-pay revenues of $347 million and $331million for years ended December 31, 2008 and 2007, respectively. |
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Revenues on a Per Admission, Per Patient Day and Per Visit Basis |
2008 | 2007 | Increase (Decrease) |
||||||
| Net inpatient revenue per admission |
$ | 10,884 | $ | 10,560 | 3.1 | % | |||
| Net inpatient revenue per patient day |
$ | 2,199 | $ | 2,116 | 3.9 | % | |||
| Net outpatient revenue per visit |
$ | 683 | $ | 631 | 8.2 | % | |||
| Net patient revenue per adjusted patient admission(1) |
$ | 10,864 | $ | 10,564 | 2.8 | % | |||
| Net patient revenue per adjusted patient day(1) |
$ | 2,210 | $ | 2,132 | 3.7 | % | |||
| Managed care: net inpatient revenue per admission |
$ | 11,587 | $ | 11,105 | 4.3 | % | |||
| Managed care: net outpatient revenue per visit |
$ | 802 | $ | 746 | 7.5 | % | |||
| (1) | Adjusted patient days/admissions represents actual patient days/admissions adjusted to include outpatient services by multiplying actual patient days/admissions by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
| Same-Hospital Continuing Operations |
|||||||||
| Years Ended December 31, | |||||||||
| Selected Operating Expenses |
2008 | 2007 | Increase (Decrease) |
||||||
| Salaries, wages and benefits |
$ | 3,748 | $ | 3,610 | 3.8 | % | |||
| Supplies |
1,504 | 1,399 | 7.5 | % | |||||
| Other operating expenses |
1,901 | 1,845 | 3.0 | % | |||||
| Total |
$ | 7,153 | $ | 6,854 | 4.4 | % | |||
| Rent/lease expense(1) |
$ | 135 | $ | 130 | 3.8 | % | |||
| Salaries, wages and benefits per adjusted patient day(2) |
$ | 1,008 | $ | 989 | 1.9 | % | |||
| Supplies per adjusted patient day(2) |
405 | 383 | 5.7 | % | |||||
| Other operating expenses per adjusted patient day(2) |
511 | 505 | 1.2 | % | |||||
| Total per adjusted patient day |
$ | 1,924 | $ | 1,877 | 2.5 | % | |||
| (1) | Included in other operating expenses. |
| (2) | Adjusted patient days represents actual patient days adjusted to include outpatient services by multiplying actual patient days by the sum of gross inpatient revenues and outpatient revenues and dividing the results by gross inpatient revenues. |
| Same-Hospital Continuing Operations |
|||||||||||
| Years Ended December 31, | |||||||||||
| Provision for Doubtful Accounts |
2008 | 2007 | Increase (Decrease) |
||||||||
| Provision for doubtful accounts |
$ | 619 | $ | 552 | 12.1 | % | |||||
| Provision for doubtful accounts as a percentage of net operating revenues |
7.3 | % | 6.8 | % | 0.5 | %(1) | |||||
| Collection rate on self-pay accounts(2) |
32.5 | % | 34.8 | % | (2.3 | )%(1) | |||||
| Collection rate from managed care payers |
97.8 | % | 97.9 | % | (0.1 | )%(1) | |||||
| (1) | The change is the difference between the 2008 and 2007 amounts shown. |
| (2) | “Self-pay” accounts receivable are comprised of both uninsured and balance-after insurance receivables. |
60
Table of Contents
REVENUES
During the year ended December 31, 2008, net operating revenues from continuing operations increased 6.2% compared to the year ended December 31, 2007.
Our same-hospital net inpatient revenues for the year ended December 31, 2008 increased by 4.4% compared to the year ended December 31, 2007. There were various positive and negative factors impacting our net inpatient revenues.
Key positive factors include:
| • | Improved managed care pricing as a result of renegotiated contracts, partially offset by a reduction in stop-loss payments to $239 million in 2008 from $278 million in 2007; and |
| • | An increase in total admissions and patient days. |
Key negative factors include:
| • | A decrease in commercial managed care admissions; |
| • | A decrease in DSH payments under various states’ Medicaid programs to $153 million in 2008 from $162 million in 2007; and |
| • | Favorable adjustments for prior-year cost reports and related valuation allowances of $3 million in 2008 compared to $45 million in 2007. |
Same-hospital admissions for the year ended December 31, 2008 increased by 1.3% compared to the year ended December 31, 2007 primarily due to net volume increases in many of the service lines emphasized by our Targeted Growth Initiative, psychiatric volumes at a facility we acquired in Modesto, California in November 2007, and a net growth in physicians resulting from our general focus on recruitment efforts and our targeted physician recruitment strategies at various hospitals for specific service lines, partially offset by lower invasive cardiac procedures.
Same-hospital net outpatient revenues during the year ended December 31, 2008 increased 8.2% compared to the year ended December 31, 2007, while outpatient visits declined by 0.1% for the same periods. The primary reason for the revenue increase is improved managed care pricing.
SALARIES, WAGES AND BENEFITS
Salaries, wages and benefits expense as a percentage of net operating revenues decreased 0.7% for the year ended December 31, 2008 compared to the year ended December 31, 2007. Same hospital salaries, wages and benefits per adjusted patient day increased approximately 1.9% in 2008 compared to 2007. The increase is primarily due to merit increases for our employees, an increase in the number of employed physicians, increased health benefits and retirement plans costs, increased annual incentive compensation costs, and hurricane-related labor costs, partially offset by a decline in full-time employee headcount, a decline in contract labor expenses and stock-compensation expense, and improved workers’ compensation loss experience.
Included in salaries, wages and benefits expense in the year ended December 31, 2008 is $33 million of stock-based compensation expense compared to $40 million in 2007. The decrease is primarily due to the vesting of higher grant-date fair value awards from prior years and the issuance of new awards at lower grant-date fair values primarily due to our lower stock price.
SUPPLIES
Supplies expense as a percentage of net operating revenues increased by 0.3% for the year ended December 31, 2008 compared to the year ended December 31, 2007; supplies expense per adjusted patient day on a same-hospital basis increased approximately 5.7% in 2008 compared to 2007. This increase in supplies expense per adjusted patient day reflects higher costs for orthopedics, pharmaceuticals and implants due to increased volumes, inflation and technology improvements, and higher surgical supply costs due to an increase in surgeries, partially offset by lower cardiovascular supply costs, which resulted from a decrease in cardiovascular procedures.
61
Table of Contents
PROVISION FOR DOUBTFUL ACCOUNTS
The provision for doubtful accounts as a percentage of net operating revenues on a same-hospital basis was 7.3% for the year ended December 31, 2008 compared to 6.8% for the year ended December 31, 2007. The negative impact on bad debts as a result of the growth in self-pay accounts assigned to our collection agencies, a slight decline in self-pay collection trends since the first half of 2008, pricing increases and improved charge capture in our emergency departments were partially mitigated by improved point-of-service collections and improved managed care accounts receivable balances by aging category.
The table below shows the net accounts receivable and allowance for doubtful accounts by payer at December 31, 2008 and December 31, 2007:
| December 31, 2008 | December 31, 2007 | |||||||||||||||||||||
| Accounts Receivable Before Allowance for Doubtful Accounts |
Allowance for Doubtful Accounts |
Net | Accounts Receivable Before Allowance for Doubtful Accounts |
Allowance for Doubtful Accounts |
Net | |||||||||||||||||
| (In Millions) | ||||||||||||||||||||||
| Medicare |
$ | 156 | $ | — | $ | 156 | $ | 163 | $ | — | $ | 163 | ||||||||||
| Medicaid |
121 | — | 121 | 134 | — | 134 | ||||||||||||||||
| Net cost report settlements payable and valuation allowances |
(20 | ) | — | (20 | ) | (16 | ) | — | (16 | ) | ||||||||||||
| Commercial managed care |
549 | 71 | 478 | 525 | 77 | 448 | ||||||||||||||||
| Governmental managed care |
175 | — | 175 | 167 | — | 167 | ||||||||||||||||
| Self-pay uninsured |
190 | 161 | 29 | 190 | 150 | 40 | ||||||||||||||||
| Self-pay balance after insurance |
139 | 71 | 68 | 127 | 66 | 61 | ||||||||||||||||
| Estimated future recoveries from accounts assigned to collection agencies |
40 | — | 40 | 32 | — | 32 | ||||||||||||||||
| Other payers |
176 | 40 | 136 | 204 | 66 | 138 | ||||||||||||||||
| Total continuing operations |
1,526 | 343 | 1,183 | 1,526 | 359 | 1,167 | ||||||||||||||||
| Total discontinued operations |
207 | 53 | 154 | 300 | 82 | 218 | ||||||||||||||||
| $ | 1,733 | $ | 396 | $ | 1,337 | $ | 1,826 | $ | 441 | $ | 1,385 | |||||||||||
At December 31, 2008, our collection rate on self-pay accounts was approximately 32.5%, including collections from point-of-service through collections by our in-house collection agency or external collection vendors. During 2008, we experienced a downward trend in our self-pay collection rate as follows: 35.0% at March 31, 2008; 34.0% at June 30, 2008; and 33.3% at September 30, 2008. These self-pay collection rates include payments made by patients, including co-payments and deductibles paid by patients with insurance, prior to an account being classified and assigned to our in-house self-pay collection agency. The comparable self-pay collection percentage as of December 31, 2007, adjusted for the reclassification of certain hospitals to discontinued operations, was approximately 35.0%. Our provision for doubtful accounts in the three months ended December 31, 2008 includes a $4 million unfavorable adjustment in the estimate of necessary bad debt reserve levels at year-end compared to a favorable adjustment of $16 million in the three months ended December 31, 2007. The change in anticipated collections as of December 31, 2008 was based on a look-back period of 18 months of collections.
Our estimated collection rate from managed care payers was approximately 98.0% at both December 31, 2008 and December 31, 2007, adjusted for hospitals reclassified to discontinued operations, which includes collections from point-of-service through collections by our in-house collection agency or external collection vendors.
The following tables present the approximate aging by payer of our continuing operations’ net accounts receivable of $1.203 billion and $1.183 billion, excluding cost report settlements payable and valuation allowances of $20 million and $16 million, at December 31, 2008 and December 31, 2007, respectively:
| December 31, 2008 | |||||||||||||||
| Medicare | Medicaid | Managed Care |
Indemnity, Self-Pay and Other |
Total | |||||||||||
| 0-60 days |
99 | % | 64 | % | 77 | % | 33 | % | 69 | % | |||||
| 61-120 days |
1 | % | 24 | % | 14 | % | 24 | % | 15 | % | |||||
| 121-180 days |
— | % | 12 | % | 5 | % | 11 | % | 7 | % | |||||
| Over 180 days |
— | % | — | % | 4 | % | 32 | % | 9 | % | |||||
| Total |
100 | % | 100 | % | 100 | % | 100 | % | 100 | % | |||||
62
Table of Contents
| December 31, 2007 | |||||||||||||||
| Medicare | Medicaid | Managed Care |
Indemnity, Self-Pay and Other |
Total | |||||||||||
| 0-60 days |
96 | % | 63 | % | 76 | % | 34 | % | 69 | % | |||||
| 61-120 days |
3 | % | 25 | % | 15 | % | 25 | % | 16 | % | |||||
| 121-180 days |
1 | % | 12 | % | 5 | % | 12 | % | 7 | % | |||||
| Over 180 days |
— | % | — | % | 4 | % | 29 | % | 8 | % | |||||
| Total |
100 | % | 100 | % | 100 | % | 100 | % | 100 | % | |||||
Our AR Days from continuing operations were 50 days at December 31, 2008 and 52 days at December 31, 2007. AR Days at December 31, 2008 and 2007 were within our target at that time of less than 55 days.
As of December 31, 2008, we had a cumulative total of patient account assignments dating back at least three years or older of approximately $4.4 billion related to our continuing operations being pursued by our in-house and outside collection agencies or vendors. These accounts have already been written off and are not included in our receivables or in the allowance for doubtful accounts; however, an estimate of future recoveries from all the accounts at collection agencies is determined based on our historical experience and recorded in accounts receivable.
The following table shows the approximate amount of net accounts receivable in our MEP, still awaiting determination of eligibility under a government program at December 31, 2008 and 2007 by aging category:
| December 31, | ||||||
| 2008 | 2007 | |||||
| 0-60 days |
$ | 87 | $ | 58 | ||
| 61-120 days |
25 | 15 | ||||
| 121-180 days |
6 | 6 | ||||
| Over 180 days(1) |
— | — | ||||
| Total |
$ | 118 | $ | 79 | ||
| (1) | Includes accounts receivable of $10 million at both December 31, 2008 and 2007 that are fully reserved. |
OTHER OPERATING EXPENSES, NET
Other operating expenses as a percentage of net operating revenues decreased by 0.4% in the year ended December 31, 2008 compared to the year ended December 31, 2007. Other operating expenses per adjusted patient day on a same-hospital basis increased by approximately 1.2% in 2008 as compared to 2007 primarily due to higher physician fees, contracted services, repair and maintenance costs, utility costs and an $8 million gain on a sale of a medical office building in Florida in 2007, which reduced 2007 other operating expenses, partially offset by lower information systems implementation costs, consulting costs and malpractice expense. Malpractice expense was $126 million for the year ended December 31, 2008 compared to $162 million for the year ended December 31, 2007. The decrease in malpractice expense is principally due to a 5% reduction in the number of expected claims, partially offset by a 118 basis point decline in the interest rate used to estimate the discounted present value of projected future liabilities.
IMPAIRMENT OF LONG-LIVED ASSETS AND GOODWILL, AND RESTRUCTURING CHARGES, NET OF INSURANCE RECOVERIES
During the year ended December 31, 2008, we recorded net impairment and restructuring charges of $16 million. We recorded an $8 million net impairment charge for the write-down of buildings and equipment and other long-lived assets, primarily capitalized software costs classified in other intangible assets, of two hospitals to their estimated fair values due to adverse current and anticipated future financial trends based on their most recent projections at that time. We believe the most significant factors contributing to the adverse financial trends include shifts in payer mix from commercial to governmental payers combined with reductions in reimbursement rates from governmental payers and high levels of uninsured patients. The remaining net impairment and restructuring charges for the year ended December 31, 2008 include $6 million of employee severance and other related costs, $1 million for the acceleration of stock-based compensation expense and $6 million in impairment charges for the write-down of other assets primarily due to the write-down of costs associated with an expansion project at one of our hospitals that we decided not to pursue based on unfavorable economics forecasted for the project, partially offset by a $5 million reduction in reserves recorded in prior periods.
63
Table of Contents
During the year ended December 31, 2007, net impairment and restructuring charges of $36 million included a $14 million net impairment charge primarily for the write-down of buildings and equipment and other long-lived assets, primarily capitalized software costs classified in other intangible assets, of one hospital to its estimated fair value due to adverse current and anticipated future financial trends based on its most recent projections at that time. We believe the most significant factors contributing to the adverse financial trends included reductions in volume from insured patients due to competition and shifts in payer mix, increased uninsured patients, adverse trends in provision for doubtful accounts and reductions in reimbursement rates from governmental payers. The remaining net impairment and restructuring charges for the year ended December 31, 2007 include $18 million of employee severance and other related costs, $7 million in lease costs, $1 million for the acceleration of stock-based compensation expense and $3 million in impairment charges for the write-down of other assets, partially offset by $5 million of insurance proceeds for property damage from Hurricane Wilma and a $2 million reduction of reserves recorded in prior periods.
LITIGATION AND INVESTIGATION COSTS, NET OF INSURANCE RECOVERIES
Litigation and investigation costs in continuing operations for the year ended December 31, 2008 were $41 million compared to $13 million for the year ended December 31, 2007. The 2008 costs primarily relate to changes in our estimated liability for now-settled wage and hour actions further described in Note 13 to the Consolidated Financial Statements. The 2008 costs were partially offset by $6 million of insurance proceeds that were recorded as a recovery of litigation and investigation costs in continuing operations for costs we previously incurred related to our December 2004 Redding Medical Center litigation settlement.
NET GAIN ON SALES OF INVESMENTS
During the year ended December 31, 2008, we recorded net gains of $125 million from the sale of our entire interest in Broadlane, Inc. and $14 million on the sale of our interest in a joint venture with a real estate investment trust.
INCOME TAX BENEFIT
Income taxes in the year ended December 31, 2008 included an income tax benefit of $27 million to reduce our estimated liabilities for uncertain tax positions, including related interest, and an income tax benefit of $29 million to decrease the valuation allowance for our deferred tax assets and for other tax adjustments. Income taxes in the year ended December 31, 2007 included an income tax benefit of $82 million to reduce our estimated liabilities for uncertain tax positions, including related interest, and income tax expense of $41 million to increase the valuation allowance for our deferred tax assets and for other tax adjustments. See Note 14 to the Consolidated Financial Statements for additional detail about income taxes.
LIQUIDITY AND CAPITAL RESOURCES
CASH REQUIREMENTS
Our obligations to make future cash payments under contracts, such as debt and lease agreements, and under contingent commitments, such as standby letters of credit and minimum revenue guarantees, are summarized in the table below, all as of December 31, 2009:
| Years Ending December 31, | Later | ||||||||||||||||||||
| Total | 2010 | 2011 | 2012 | 2013 | 2014 | Years | |||||||||||||||
| (In Millions) | |||||||||||||||||||||
| Long-term debt(1) |
$ | 7,507 | $ | 390 | $ | 451 | $ | 436 | $ | 1,340 | $ | 402 | $ | 4,488 | |||||||
| Global civil settlement payable(1) |
73 | 73 | — | — | — | — | |||||||||||||||
| Capital lease obligations(1) |
2 | — | — | — | — | — | 2 | ||||||||||||||
| Long-term non-cancelable operating leases |
400 | 99 | 82 | 70 | 60 | 26 | 63 | ||||||||||||||
| Standby letters of credit |
185 | 183 | 2 | — | — | — | — | ||||||||||||||
| Guarantees(2) |
118 | 80 | 24 | 5 | 3 | 2 | 4 | ||||||||||||||
| Asset retirement obligations |
155 | — | — | — | — | — | 155 | ||||||||||||||
| Academic affiliation agreements(3) |
247 | 34 | 33 | 18 | 17 | 17 | 128 | ||||||||||||||
| Tax liabilities |
77 | 28 | — | — | — | — | 49 | ||||||||||||||
| Supplemental executive retirement plan obligations |
514 | 18 | 19 | 19 | 19 | 19 | 420 | ||||||||||||||
| Information technology contract services |
863 | 119 | 138 | 140 | 133 | 108 | 225 | ||||||||||||||
| Purchase orders |
188 | 188 | — | — | — | — | — | ||||||||||||||
| Total |
$ | 10,329 | $ | 1,212 | $ | 749 | $ | 688 | $ | 1,572 | $ | 574 | $ | 5,534 | |||||||
| (1) | Includes interest through maturity date/lease termination. |
| (2) | Includes minimum revenue guarantees, primarily related to physicians under relocation agreements and physician groups that provide services at our hospitals, and operating lease guarantees. |
| (3) | These agreements contain various rights and termination provisions. |
64
Table of Contents
The standby letters of credit are required principally by our insurers and various states to collateralize our workers’ compensation programs pursuant to statutory requirements and as security to collateralize the deductible and self-insured retentions under certain of our professional and general liability insurance programs. The amount of collateral required is principally dependent upon the level of claims activity and our creditworthiness. The insurers require the collateral in case we are unable to meet our obligations to claimants within the deductible or self-insured retention layers. The standby letters of credit are issued under our revolving credit facility.
In 2009, we refinanced approximately $2.3 billion aggregate principal amount of outstanding debt through tender offers and exchange offers. We also repurchased approximately $381 million aggregate principal amount of our outstanding debt through privately negotiated transactions and open market repurchases. These transactions, which were financed with the issuances of new debt securities, the issuance of mandatory convertible preferred stock and cash on hand, are part of our long-term objective to manage the risks associated with our high levels of debt. We may from time to time seek to retire, purchase, redeem or refinance additional amounts of our outstanding debt subject to prevailing market conditions, our liquidity requirements, contractual restrictions and other factors. These actions are part of our strategy to manage our leverage over time, which is dependent on our total amount of debt, our cash and our operating results, with a long-term target to maintain our ratio of total long-term debt, net of cash and cash equivalent balances, to Adjusted EBITDA (as defined above) at 4.0x or below. At December 31, 2009, using the last 12 months of Adjusted EBITDA, this ratio was 3.7x. We anticipate this ratio will fluctuate from quarter to quarter based on earnings performance and other factors. We intend to pursue our objectives by following our business plan, managing our cost structure and through other changes in our capital structure, including, if appropriate, the issuance of equity or convertible securities. Our ability to achieve these long-term objectives is subject to numerous risks and uncertainties, many of which are described in Part I, Item 1A, Risk Factors, of this report.
Our capital expenditures primarily relate to the expansion and renovation of existing facilities, including amounts to comply with applicable laws and regulations, equipment and information systems additions and replacements, introduction of new medical technologies, design and construction of new buildings, and various other capital improvements.
Capital expenditures were $456 million, $547 million and $743 million in the years ended December 31, 2009, 2008 and 2007, respectively. We anticipate that our capital expenditures for the year ending December 31, 2010 will total approximately $475 million to $525 million, including $66 million that was accrued at December 31, 2009, but not paid until 2010. Our anticipated 2010 capital expenditures include approximately $4 million to meet seismic requirements for our California facilities. We currently estimate spending a total of approximately $80 million to comply with the requirements under California’s seismic regulations, of which approximately $24 million was spent prior to January 1, 2010. Our current estimated seismic costs are considerably lower than certain previous estimates because a number of our hospitals have been evaluated as having reduced risk using a new seismic evaluation tool. There may be further reductions to our estimated seismic costs as the State of California has recently enacted new regulations relating to the seismic evaluation tool and the new state building code; we are currently evaluating these new regulations to determine what impact they will have on our cost estimate. Our total estimated seismic expenditure amount has not been adjusted for future inflation. Our budgeted capital expenditures for the year ending December 31, 2010 also include approximately $12 million to improve disability access at certain of our facilities as a result of a consent decree in a class action lawsuit. We expect to spend a total of approximately $111 million on such improvements over the next six years.
Interest payments, net of capitalized interest, were $439 million, $391 million and $395 million in the years ended December 31, 2009, 2008 and 2007, respectively. The increase is primarily due to monthly interest payments under our interest rate swap agreement, higher interest rate debt issued during the year and interest payments that were accelerated and paid in the year ended December 31, 2009 as a result of our various long-term debt transactions discussed in Note 6 to the Consolidated Financial Statements.
We entered into an interest rate swap agreement, which became effective May 1, 2009, for an aggregate notional amount of $1 billion. The interest rate swap agreement was designated as a fair value hedge and was used to manage our exposure to future changes in interest rates. It had the effect of converting our 7 3/8% senior notes due 2013 from a fixed interest rate paid semi-annually to a variable interest rate paid monthly based on the one-month LIBOR plus a floating rate spread of approximately 5.46%. During the term of the interest rate swap agreement, changes in the fair value of the interest rate swap agreement and changes in the fair value of the 7 3/8% senior notes, which substantially offset each other, were recorded in interest expense. To mitigate risks related to potential significant increases in the one-month LIBOR, we also entered into a separate agreement that limited the maximum one-month LIBOR to 8% under the interest rate swap agreement. In November 2009, we terminated the interest rate swap agreement. We realized approximately $8 million in net savings in interest payments during the term of the interest rate swap agreement. Depending on then-existing market conditions, we may elect to enter into similar interest rate swap agreements in the future.
65
Table of Contents
Income tax payments, net of tax refunds, were approximately $43 million in the year ended December 31, 2009 compared to approximately $4 million during the year ended December 31, 2008. At December 31, 2009, our carryforwards available to offset future taxable income consisted of (1) federal net operating loss (“NOL”) carryforwards of approximately $2.0 billion pretax expiring in 2024 to 2029, (2) approximately $25 million in alternative minimum tax credits with no expiration, and (3) general business credit carryforwards of approximately $13 million expiring in 2023 to 2029. Periodic examinations of our tax returns by the IRS or other taxing authorities could result in the payment of additional taxes. Our tax returns for the years ended December 31, 2006 and December 31, 2007 are currently under examination by the IRS. These returns include deductions for amounts paid in connection with our 2006 civil settlement with the federal government and upon which taxes had been paid by us in previous taxable years. We filed tax refund claims to recover such previously paid taxes, and we received tax refunds of approximately $200 million as of December 31, 2009. The tax treatment of the civil settlement payments is being considered as part of the IRS’ examination. We presently cannot predict the ultimate resolution of this IRS examination, which could have a material adverse effect on our financial condition, results of operations or cash flows. Furthermore, our ability to utilize NOL carryforwards to reduce future taxable income may be limited under Section 382 of the Internal Revenue Code if certain ownership changes in our company occur during a rolling three-year period. These ownership changes include the offering of stock by us, the purchase or sale of our stock by 5% shareholders, as defined in the Treasury regulations, or the issuance or exercise of rights to acquire our stock. If such ownership changes by 5% shareholders result in aggregate increases that exceed 50 percentage points during the three-year period, then Section 382 imposes an annual limitation on the amount of our taxable income that may be offset by the NOL carryforwards.
SOURCES AND USES OF CASH
Our liquidity for the year ended December 31, 2009 was primarily derived from cash on hand, net cash provided by operating activities, and proceeds from the sale of USC University Hospital and USC Kenneth Norris Jr. Cancer Hospital.
Our primary source of operating cash is the collection of accounts receivable. As we experience changes in our business mix and as admissions of uninsured and underinsured patients grow, our operating cash flow is negatively impacted due to lower levels of cash collections and higher levels of bad debt.
Net cash provided by operating activities was $425 million in the year ended December 31, 2009 compared to $208 million in the year ended December 31, 2008. Key negative and positive factors contributing to the change between the 2009 and 2008 periods include the following:
| • | Additional interest payments of $48 million, primarily due to monthly interest payments under our interest rate swap agreement, higher interest rate debt issued during the year and interest payments that were accelerated and paid in 2009 as a result of our various long-term debt transactions discussed in Note 6 to the Consolidated Financial Statements; |
| • | $39 million we received under our interest rate swap agreement; |
| • | Increased operating income from continuing operations of $243 million, excluding litigation and investigation costs, impairment and restructuring charges, and depreciation and amortization in the year ended December 31, 2009 compared to the year ended December 31, 2008; |
| • | $81 million in payments related to our 2009 settlement of wage and hour actions; |
| • | Increased income tax payments of $39 million, including $60 million in settlement of IRS audit disputes as discussed above; |
| • | $60 million of insurance recoveries received in the year ended December 31, 2008 related to our December 2004 Redding Medical Center litigation settlement (based on the components of the recoveries, $39 million was classified as discontinued operations cash flows from operations and $21 million was classified as continuing operations cash flows from operations); |
| • | $61 million of additional cash flows related to divested hospitals classified as discontinued operations primarily due to the liquidation of accounts receivable and other working capital balances (such amount excludes the $39 million of insurance recoveries received in 2008 related to Redding Medical Center discussed above); |
| • | Additional cash flows as a result of enhanced management of account payable ($39 million) and accounts receivable ($70 million); |
66
Table of Contents
| • | Lease termination payments of $9 million in the year ended December 31, 2008 associated with the divestiture of the Tarzana campus of Encino-Tarzana Regional Medical Center; |
| • | Additional aggregate annual 401(k) matching contributions and annual incentive compensation payments of $7 million ($123 million in the year ended December 31, 2009 compared to $116 million in 2008); and |
| • | Lower cash investment earnings of approximately $5 million in the year ended December 31, 2009 compared to 2008. |
During the year ended December 31, 2009, we received net cash proceeds of $221 million from the sale of facilities and other assets related to discontinued operations, primarily from the sale of USC University Hospital and USC Kenneth Norris Jr. Cancer Hospital. Excluding the simultaneous purchase and sale of the Tarzana campus of Encino-Tarzana Regional Medical Center for $89 million, during the year ended December 31, 2008, we received proceeds of $71 million from the sales of facilities and other assets related to discontinued operations, primarily from the sales of North Ridge Medical Center, the Encino campus of Encino-Tarzana Regional Medical Center, Garden Grove Hospital and Medical Center, and San Dimas Community Hospital. We received proceeds, which are classified as investing activities, of $49 million and $8 million from our investment in hospital authority bonds related to previously divested hospitals in the Dallas, Texas area during the years ended December 31, 2009 and 2008, respectively. We also received proceeds, which are classified as investing activities, of $18 million during the year ended December 31, 2009 related to the sale of our 50% interest in People’s Health Network and, during the year ended December 31, 2008, of $144 million from the sale of our entire interest in Broadlane, Inc. and $25 million from the sale of our interest in a joint venture with a real estate investment trust.
We continue to seek further initiatives to increase the efficiency of our balance sheet by generating incremental cash. These initiatives include the sale of our medical office buildings and excess land, buildings or other underutilized or inefficient assets. We are currently seeking to sell up to 30 of our 47 owned medical office buildings. However, there is no assurance that we will consummate a sale of these buildings.
Capital expenditures were $456 million and $547 million for the years ended December 31, 2009 and 2008, respectively, including approximately $58 million and $75 million in the same respective years for construction of Sierra Providence East Medical Center, our new hospital in El Paso, Texas, and a replacement hospital for East Cooper Regional Medical Center in Mt. Pleasant, South Carolina.
We use fair market value to record our investments that are available-for-sale. As shown in Note 16 to the Consolidated Financial Statements, the majority of our investments are valued based on quoted market prices or other observable inputs. However, at December 31, 2009, one of our captive insurance subsidiaries held $1 million (principal value) of auction rate securities, classified as investments, whose auctions have failed due to sell orders exceeding buy orders. In addition, we held $2 million of investments in the Reserve Yield Plus Fund and have reclassified the balance out of cash equivalents as the fund has experienced liquidity issues and temporarily suspended distributions. The fund is currently in the process of liquidating its investments and distributing cash to its investors. We expect the fund to liquidate all of its investments; however, the ultimate timing is uncertain. We will continue to closely monitor our investments, but do not anticipate any future decrease in value of either the auction rate securities or the Reserve Yield Plus Fund to have a material impact on our financial condition, results of operations or cash flows. We have no other investments that we expect will be negatively affected by the current economic crisis that will materially impact our financial condition, results of operations or cash flows.
DEBT INSTRUMENTS, GUARANTEES AND RELATED COVENANTS
Credit Agreement
We have a five-year, $800 million senior secured revolving credit facility, which matures on November 16, 2011, that is collateralized by patient accounts receivable at our acute care and specialty hospitals, and bears interest at our option based on LIBOR plus 150 basis points or Citigroup’s base rate, as defined in the credit agreement, plus 50 basis points. The revolving credit agreement contains standard covenants and also includes a provision, which we believe is customary in receivables-backed credit facilities, that gives our banks the right to require that proceeds of collections of substantially all of our consolidated accounts receivable be applied directly to repay outstanding loans and other amounts that are due and payable under the revolving credit facility at any time that unused borrowing availability under the revolving credit facility is less than $100 million or if an event of default has occurred and is continuing thereunder. In that event, we would seek to re-borrow under the revolving credit facility to satisfy our operating cash requirements. Our ability to borrow under the revolving credit facility is subject to conditions that we believe are customary in such facilities, including that no events of default then exist. For additional information, refer to Note 6 to the Consolidated Financial Statements.
67
Table of Contents
We are currently in compliance with all covenants and conditions in our revolving credit agreement. Our borrowing capacity under the revolving credit facility, based on our eligible receivables, was $448 million at December 31, 2009.
At December 31, 2009, there were no cash borrowings outstanding under the revolving credit facility, and we had approximately $185 million of letters of credit outstanding. We also had approximately $690 million of cash and cash equivalents on hand at December 31, 2009 to fund our operations and capital expenditures.
Senior Notes
In December 2009, we completed open market repurchases of $2 million aggregate principal amount outstanding of our 6 3/8 % senior notes due 2011 and approximately $1 million aggregate principal amount outstanding of our 9 1/4 % senior notes due 2015 for cash of approximately $3 million. In November 2009, we completed open market repurchases of $2 million aggregate principal amount outstanding of our 9 1/ 4% senior notes due 2015 for cash of approximately $2 million. In September 2009, we repurchased approximately $8 million of additional aggregate principal amount outstanding of our 9 1/4% senior notes due 2015 for cash of approximately $8 million.
Also in September 2009, we purchased $300 million of the $800 million aggregate principal amount then outstanding of our 9 1/4% senior notes due 2015 for $315 million. The purchase was funded with the net proceeds from our September 2009 sale of 7% mandatory convertible preferred stock as described in Note 2 to the Consolidated Financial Statements. In connection with the repurchase, we paid approximately $4 million in accrued and unpaid interest. This transaction resulted in a loss from early extinguishment of debt of approximately $22 million related to the difference between the purchase prices and the par values of the purchased notes, as well as the write-off of unamortized note discounts and issuance costs associated with the notes.
In July 2009, we purchased approximately $15 million aggregate principal amount of our 6 3/8% senior notes due 2011, $32.5 million aggregate principal amount of our 6 1/2% senior notes due 2012, $0.3 million aggregate principal amount of our 9 7/8% senior notes due 2014, and $20.5 million aggregate principal amount of our 6 7/8% senior notes due 2031 for approximately $60 million. We recorded a gain from early extinguishment of debt of approximately $6 million related to the difference between the purchase prices and the par values of the purchased notes, partially offset by the write-off of unamortized note discounts, issuance costs and unrecognized interest rate hedge settlements associated with the notes.
In June 2009, we purchased approximately $900 million of the $1 billion aggregate principal amount then outstanding of our 9 7/8% senior notes due 2014 for approximately $941 million, representing approximately $900 million in principal payments and approximately $41 million in accrued and unpaid interest through the dates of purchase. We purchased the 9 7/8% senior notes with the net proceeds of approximately $881 million from our sale of new 8 7/8% senior secured notes, as described below, and cash on hand.
In May and March 2009, we exchanged approximately $918 million aggregate principal amount of our outstanding 6 3/8% senior notes due 2011 and approximately $510 million aggregate principal amount of our outstanding 6 1 /2% senior notes due 2012 for new 9% senior secured notes due 2015 and 10% senior secured notes due 2018, as described below.
For additional information regarding our senior notes, see Note 6 to the Consolidated Financial Statements.
Senior Secured Notes
In June 2009, we sold $925 million aggregate principal amount of 8 7/8% senior secured notes due 2019. We will pay interest on the notes semi-annually in arrears on January 1 and July 1 of each year, commencing January 1, 2010. The 8 7/8% senior secured notes rank equally with our 9% senior secured notes due 2015 and 10% senior secured notes due 2018, which we issued in May and March 2009, as described below.
In May 2009, we exchanged approximately $3 million aggregate principal amount of our outstanding 6 3 /8% senior notes due 2011 and approximately $25 million aggregate principal amount of our outstanding 6 1/2% senior notes due 2012 for approximately $14 million aggregate principal amount of 9% senior secured notes due 2015 and approximately $14 million aggregate principal amount of 10% senior secured notes due 2018. In addition, we received approximately $6 million in cash, which represented the difference in the fair values of the tendered notes as compared to the fair values of the 9% senior secured notes and 10% senior secured notes and compensation to us for increased interest expense.
In March 2009, we exchanged approximately $915 million aggregate principal amount of our outstanding 6 3/8% senior notes due 2011 and approximately $485 million aggregate principal amount of our outstanding 6 1/2% senior notes due 2012 for approximately $700 million aggregate principal amount of 9% senior secured notes due 2015 and approximately $700 million aggregate principal amount of 10% senior secured notes due 2018. Interest on these notes is payable semi-annually in arrears on May 1 and November 1 of each year, commencing on May 1, 2009. The 9% and 10% senior secured notes rank equally with our 8 7/8% senior secured notes.
68
Table of Contents
For additional information regarding our senior secured notes, refer to Note 6 to the Consolidated Financial Statements.
Interest Rate Swap Agreement
We entered into an interest rate swap agreement, which became effective May 1, 2009, for an aggregate notional amount of $1 billion. The interest rate swap agreement was designated as a fair value hedge and was used to manage our exposure to future changes in interest rates. It had the effect of converting our 7 3/8% senior notes due 2013 from a fixed interest rate paid semi-annually to a variable interest rate paid monthly based on the one-month LIBOR plus a floating rate spread of approximately 5.46%. During the term of the interest rate swap agreement, changes in the fair value of the interest rate swap agreement and changes in the fair value of the 7 3/8% senior notes, which substantially offset each other, were recorded in interest expense. To mitigate risks related to potential significant increases in the one-month LIBOR, we also entered into a LIBOR cap agreement that limited the maximum one-month LIBOR to 8% under the interest rate swap agreement. We paid approximately $2 million for this limitation on interest rate exposure under the interest rate swap agreement. In November 2009, we terminated the interest rate swap agreement. We realized approximately $8 million in net savings in interest payments during the term of the interest rate swap agreement. Depending on then-existing market conditions, we may elect to enter into similar interest rate swap agreements in the future.
LIQUIDITY
From time to time, we expect to engage in additional capital markets, bank credit and other financing activities depending on our needs and financing alternatives available at that time. We believe our existing agreements provide significant flexibility for future secured or unsecured borrowings.
We believe that existing cash and cash equivalents on hand, availability under our revolving credit facility, anticipated future cash provided by operating activities, anticipated proceeds from the sales of assets held for sale, and our investments in marketable securities of our captive insurance companies classified as noncurrent investments on our balance sheet should be adequate to meet our current cash needs. These sources of liquidity should also be adequate to finance planned capital expenditures, payments on the current portion of our long-term debt and other presently known operating needs. Long-term liquidity for debt service will be dependent on improved cash provided by operating activities, results of balance sheet initiatives previously discussed and, given favorable market conditions, future borrowings or refinancings. However, our cash requirements could be materially affected by a deterioration in our results of operations, as well as the various uncertainties discussed in this and other sections, which could require us to pursue any number of financing options, including, but not limited to, additional borrowings, debt refinancing, asset sales or other financing alternatives. With the current tight credit markets, the level, if any, of these financing sources cannot be assured, and the ability of our counterparties to close asset sales as previously anticipated could also be affected.
We continue to aggressively identify and implement further actions to control costs and enhance our operating performance, including cash flow. Among the areas being addressed are volume growth, managed care payer contracting, procurement efficiencies, cost standardization, bad debt expense reduction initiatives, underperforming hospitals, and certain hospital and overhead costs not related to patient care. Although these initiatives may result in improved performance, that performance may remain somewhat below our hospital management peers because of geographic and other differences in hospital portfolios.
OFF-BALANCE SHEET ARRANGEMENTS
Excluding the hospitals whose operating results are included in discontinued operations, our consolidated operating results for the years ended December 31, 2009, 2008 and 2007 include $923 million, $923 million and $888 million, respectively, of net operating revenues and $99 million, $89 million and $101 million, respectively, of income from operations generated from four general hospitals operated by us under lease arrangements. In accordance with generally accepted accounting principles, the applicable buildings and the future lease obligations under these arrangements are not recorded on our consolidated balance sheet as they are considered operating leases. The current terms of these leases expire between 2010 and 2027, not including lease extensions that we have options to exercise. If these leases expire, we would no longer generate revenue or expenses from these hospitals.
69
Table of Contents
We have no other off-balance sheet arrangements that may have a current or future material effect on our financial condition, revenues or expenses, results of operations, liquidity, capital expenditures or capital resources, except for $303 million of standby letters of credit outstanding and guarantees as of December 31, 2009.
RECENTLY ISSUED ACCOUNTING STANDARDS
See Note 18 to our Consolidated Financial Statements included in this report for a discussion of recently issued accounting standards.
CRITICAL ACCOUNTING ESTIMATES
In preparing our Consolidated Financial Statements in conformity with GAAP, we must use estimates and assumptions that affect the amounts reported in our Consolidated Financial Statements and accompanying notes. We regularly evaluate the accounting policies and estimates we use. In general, we base the estimates on historical experience and on assumptions that we believe to be reasonable, given the particular circumstances in which we operate. Actual results may vary from those estimates.
We consider our critical accounting estimates to be those that (1) involve significant judgments and uncertainties, (2) require estimates that are more difficult for management to determine, and (3) may produce materially different outcomes under different conditions or when using different assumptions.
Our critical accounting estimates cover the following areas:
| • | Recognition of net operating revenues, including contractual allowances; |
| • | Provisions for doubtful accounts; |
| • | Accruals for general and professional liability risks; |
| • | Accruals for supplemental executive retirement plans; |
| • | Accruals for litigation losses; |
| • | Impairment of long-lived assets and goodwill; |
| • | Accounting for income taxes; and |
| • | Accounting for stock-based compensation. |
REVENUE RECOGNITION
We recognize net operating revenues in the period in which services are performed. Net operating revenues primarily consist of net patient service revenues that are recorded based on established billing rates (i.e., gross charges), less estimated discounts for contractual and other allowances, principally for patients covered by Medicare, Medicaid, and managed care and other health plans, as well as uninsured patients under the Compact.
Revenues under the traditional fee-for-service Medicare and Medicaid programs are based primarily on prospective payment systems. Discounts for retrospectively cost-based revenues, which were more prevalent in earlier periods, and certain other payments, such as DSH, DGME, IME and bad debt expense, which are based on our hospitals’ cost reports, are estimated using historical trends and current factors. Cost report settlements under these programs are subject to audit by Medicare and Medicaid auditors and administrative and judicial review, and it can take several years until final settlement of such matters is determined and completely resolved. Because the laws, regulations, instructions and rule interpretations governing Medicare and Medicaid reimbursement are complex and change frequently, the estimates recorded by us could change by material amounts.
We have a system and estimation process for recording Medicare net patient revenue and estimated cost report settlements. This results in us recording accruals to reflect the expected final settlements on our cost reports. For filed cost reports, we record the accrual based on those cost reports and subsequent activity, and record a valuation allowance against those cost reports based on historical settlement trends. The accrual for periods for which a cost report is yet to be filed is recorded based on estimates of what we expect to report on the filed cost reports, and a corresponding valuation allowance is recorded as previously described. Cost reports must generally be filed within five months after the end of the annual cost report reporting period. After the cost report is filed, the accrual and corresponding valuation allowance may need to be adjusted.
70
Table of Contents
Revenues under managed care plans are based primarily on payment terms involving predetermined rates per diagnosis, per-diem rates, discounted fee-for-service rates and/or other similar contractual arrangements. These revenues are also subject to review and possible audit by the payers. The payers are billed for patient services on an individual patient basis. An individual patient’s bill is subject to adjustment on a patient-by-patient basis in the ordinary course of business by the payers following their review and adjudication of each particular bill. We estimate the discounts for contractual allowances at the individual hospital level utilizing billing data on an individual patient basis. At the end of each month, on an individual hospital basis, we estimate our expected reimbursement for patients of managed care plans based on the applicable contract terms. We believe it is reasonably likely for there to be an approximately 3% increase or decrease in the estimated contractual allowances related to managed care plans. A 3% increase or decrease in the estimated contractual allowances would impact the estimated reserves by $8 million. Some of the factors that can contribute to changes in the contractual allowance estimates include: (1) changes in reimbursement levels for procedures, supplies and drugs when threshold levels are triggered; (2) changes in reimbursement levels when stop loss or outlier limits are reached; (3) changes in the admission status of a patient due to physician orders subsequent to initial diagnosis or testing; (4) final coding of in-house and discharged-not-final-billed patients that change reimbursement levels; (5) secondary benefits determined after primary insurance payments; and (6) reclassification of patients among insurance plans with different coverage levels. Contractual allowance estimates are periodically reviewed for accuracy by taking into consideration known contract terms as well as payment history. Although we do not separately accumulate and disclose the aggregate amount of adjustments to the estimated reimbursement for every patient bill, we believe our estimation and review process enables us to identify instances on a timely basis where such estimates need to be revised. We do not believe there were any adjustments to estimates of individual patient bills that were material to our revenues. In addition, on a corporate-wide basis, we do not record any general provision for adjustments to estimated contractual allowances for managed care plans.
Revenues related to self-pay patients may qualify for a discount under the Compact, whereby the gross charges based on established billing rates would be reduced by an estimated discount for contractual allowance.
We believe that adequate provision has been made for any adjustments that may result from final determination of amounts earned under all the above arrangements. We know of no material claims, disputes or unsettled matters with any payers that would affect our revenues for which we have not adequately provided for in our Consolidated Financial Statements.
PROVISIONS FOR DOUBTFUL ACCOUNTS
Although outcomes vary, our policy is to attempt to collect amounts due from patients, including co-payments and deductibles due from patients with insurance, at the time of service while complying with all federal and state laws and regulations, including, but not limited to, the Emergency Medical Treatment and Active Labor Act (“EMTALA”). Generally, as required by EMTALA, patients may not be denied emergency treatment due to inability to pay. Therefore, services, including the legally required medical screening examination and stabilization of the patient, are performed without delaying to obtain insurance information. In non-emergency circumstances or for elective procedures and services, it is our policy to verify insurance prior to a patient being treated; however, there are various exceptions that can occur. Such exceptions can include, for example, instances where (1) we are unable to obtain verification because the patient’s insurance company was unable to be reached or contacted, (2) a determination is made that a patient may be eligible for benefits under various government programs, such as Medicaid or Victims of Crime, and it takes several days or weeks before qualification for such benefits is confirmed or denied, and (3) under physician orders we provide services to patients that require immediate treatment.
We provide for an allowance against accounts receivable that could become uncollectible by establishing an allowance to reduce the carrying value of such receivables to their estimated net realizable value. We estimate this allowance based on the aging of our accounts receivable by hospital, our historical collection experience by hospital and for each type of payer over an 18-month look-back period, and other relevant factors. Based on our accounts receivable from self-pay patients and co-payments and deductibles owed to us by patients with insurance at December 31, 2009, a hypothetical 10% decline in our self-pay collection rate, or approximately 3.0%, would result in an unfavorable adjustment to provision for doubtful accounts of approximately $6 million. There are various factors that can impact collection trends, such as changes in the economy, which in turn have an impact on unemployment rates and the number of uninsured and underinsured patients, the volume of patients through the emergency department, the increased burden of co-payments and deductibles to be made by patients with insurance, and business practices related to collection efforts. These factors continuously change and can have an impact on collection trends and our estimation process.
Our practice is to reduce the net carrying value of self-pay accounts receivable, including accounts related to the co-payments and deductibles due from patients with insurance, to their estimated net realizable value at the time of billing. Generally, uncollected balances are assigned to our in-house collection agency between 90 to 180 days, once patient responsibility has been identified. When accounts are assigned to the collection agency by the hospital, the accounts are completely written off the hospital’s books through the provision for doubtful accounts, and an estimated future recovery amount is calculated and recorded as a receivable on the hospital’s books at the same time. The estimated future recovery amount is adjusted based on the aging of the accounts and changes to actual recovery rates. The estimated future recovery amount for self-pay accounts is gradually written down whereby it is fully reserved if the amount is not paid within two years after the account is assigned to our in-house collection agency.
71
Table of Contents
Managed care accounts are collected through our regional business offices, whereby the account balances remain in the hospital’s patient accounting system and on the hospital’s books, and are adjusted based on an analysis of the net realizable value as they age. Managed care accounts collected through our regional business offices are gradually written down whereby they are fully reserved if the accounts are not paid within two years.
Changes in the collectability of aged managed care accounts receivable are ongoing and impact our provision for doubtful accounts. We continue to experience payment pressure from managed care companies concerning amounts of past billings. We aggressively pursue collection of these accounts receivable using all means at our disposal, including arbitration and litigation, but we may not be successful.
ACCRUALS FOR GENERAL AND PROFESSIONAL LIABILITY RISKS
We accrue for estimated professional and general liability claims, to the extent not covered by insurance, when they are probable and can be reasonably estimated. We maintain reserves, which are based on actuarial estimates for the portion of our professional liability risks, including incurred but not reported claims, to the extent we do not have insurance coverage. Our liability consists of estimates established based upon discounted actuarial calculations using several factors, including the number of expected claims, estimates of losses for these claims based on recent and historical settlement amounts, estimates of incurred but not reported claims based on historical experience, the timing of historical payments, and risk free discount rates used to determine the present value of projected payments. We consider the number of expected claims, average cost per claim and discount rate to be the most significant assumptions in estimating accruals for general and professional liabilities. Our liabilities are adjusted for new claims information in the period such information becomes known. Malpractice expense is recorded within other operating expenses in the accompanying Consolidated Statement of Operations.
Our estimated reserves for professional and general liability claims will change significantly if future claims differ from expected trends. We believe it is reasonably likely for there to be a 5% increase or decrease in the number of expected claims or average cost per claim. A 5% increase in the number of expected claims would increase the estimated reserves by $37 million, and a 5% decrease in the number of expected claims would decrease the estimated reserves by $37 million. A 5% increase in the average cost per claim would increase the estimated reserves by $37 million, and a 5% decrease in the average cost per claim would decrease the estimated reserves by $37 million. Because our estimated reserves for future claim payments are discounted to present value, a change in our discount rate assumption could also have a significant impact on our estimated reserves. A 100 basis point increase in the discount rate would decrease the estimated reserves by $15 million. In addition, because of the complexity of the claims, the extended period of time to settle the claims and the wide range of potential outcomes, our ultimate liability for professional and general liability claims could change materially from our current estimates.
The table below shows the case reserves and incurred but not reported claims reserves as of December 31, 2009, 2008 and 2007.
| December 31, | |||||||||
| 2009 | 2008 | 2007 | |||||||
| Case reserves |
$ | 167 | $ | 185 | $ | 190 | |||
| Incurred but not reported reserves |
483 | 550 | 614 | ||||||
| Total undiscounted reserves |
$ | 650 | $ | 735 | $ | 804 | |||
Several actuarial methods, including incurred, paid loss development and Bornhuetter-Ferguson methods, are applied to our historical loss data to produce estimates of ultimate expected losses and the resulting incurred but not reported reserves. These methods use our specific historical claims data related to paid losses and loss adjustment expenses, historical and current case reserves, reported and closed claim counts, and a variety of hospital census information. Based on these analyses, we determine our estimate of the professional liability claims, including the incurred but not reported reserve estimate. The determination of our estimates involves subjective judgment and could result in material changes to our estimates in future periods if our actual experience is materially different than our assumptions.
Malpractice claims generally take 4 to 5 years to settle from the time of the initial reporting of the occurrence to the settlement payment. Accordingly, the percentage of reserves as of December 31, 2009 representing unsettled claims is approximately 99% compared to 98% as of December 31, 2008.
72
Table of Contents
The following table presents the amount of our accruals for professional liability claims and the corresponding activity therein for each of the respective years presented below.
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Accrual for professional liability claims, beginning of the year |
$ | 663 | $ | 716 | $ | 731 | ||||||
| Expense (income) related to: |
||||||||||||
| Current accident year |
121 | 130 | 168 | |||||||||
| Prior accident years |
(74 | ) | (39 | ) | (5 | ) | ||||||
| Expense (income) from discounting |
9 | 24 | 4 | |||||||||
| Total incurred loss and loss expense |
56 | 115 | 167 | |||||||||
| Paid claims and expenses related to: |
||||||||||||
| Current accident year |
(1 | ) | (3 | ) | (1 | ) | ||||||
| Prior accident years |
(146 | ) | (165 | ) | (181 | ) | ||||||
| Total paid claims and expenses |
(147 | ) | (168 | ) | (182 | ) | ||||||
| Accrual for professional liability claims, end of year |
$ | 572 | $ | 663 | $ | 716 | ||||||
ACCRUALS FOR SUPPLEMENTAL EXECUTIVE RETIREMENT PLANS
Our supplemental executive retirement plan benefit obligations and related costs are calculated using actuarial concepts. The discount rate is a critical assumption in determining the elements of expense and liability measurement. We evaluate this critical assumption annually. Other assumptions include employee demographic factors such as retirement patterns, mortality, turnover and rate of compensation increase.
The discount rate enables us to state expected future cash payments for benefits as a present value on the measurement date. The guideline for setting this rate is a high-quality long-term corporate bond rate. A lower discount rate increases the present value of benefit obligations and increases pension expense. Our discount rate for both 2009 and 2008 was 5.75%. The assumed discount rate for pension plans reflects the market rates for high-quality corporate bonds currently available. A one hundred basis point decrease in the assumed discount rate would increase total net periodic pension expense for 2010 by $1.1 million and would increase the projected benefit obligation at December 31, 2009 by $25.9 million. A one hundred basis point increase in the assumed discount rate would increase net periodic pension expense for 2010 by $0.4 million and decrease the projected benefit obligation at December 31, 2009 by $21.9 million.
ACCRUALS FOR LITIGATION LOSSES
We record reserves for litigation losses if a loss is probable and can be reasonably estimated. We record probable loss contingencies based on the best estimate of the loss. If a range of loss can be reasonably estimated, but no single amount within the range appears to be a better estimate than any other amount within the range, the minimum amount in the range is accrued. These estimates are often initially developed earlier than when the ultimate loss is known, and the estimates are adjusted if additional information becomes known.
IMPAIRMENT OF LONG-LIVED ASSETS
We evaluate our long-lived assets for possible impairment annually or whenever events or changes in circumstances indicate that the carrying amount of the asset, or related group of assets, may not be recoverable from estimated future undiscounted cash flows. We calculate the amount of an impairment if the carrying value of the long-lived assets exceeds the fair value of the assets. The fair value of the assets is estimated based on appraisals, established market values of comparable assets or internal estimates of future net cash flows expected to result from the use and ultimate disposition of the asset. The estimates of these future cash flows are based on assumptions and projections we believe to be reasonable and supportable. They require our subjective judgments and take into account assumptions about revenue and expense growth rates. These assumptions may vary by type of facility and presume stable, improving or, in some cases, declining results at our hospitals, depending on their circumstances. If the presumed level of performance does not occur as expected, impairment may result.
We report long-lived assets to be disposed of at the lower of their carrying amounts or fair values less costs to sell. In such circumstances, our estimates of fair value are based on appraisals, established market prices for comparable assets or internal estimates of future net cash flows.
73
Table of Contents
These fair value estimates can change by material amounts in subsequent periods. Many factors and assumptions can impact the estimates, including the following risks:
| • | future financial results of our hospitals, which can be impacted by volumes of insured patients and declines in commercial managed care patients, terms of managed care payer arrangements, our ability to collect accounts due from uninsured and managed care payers, loss of volumes as a result of competition, and our ability to manage costs such as labor costs, which can be adversely impacted by union activity and the shortage of experienced nurses; |
| • | changes in payments from governmental health care programs and in government regulations such as reductions to Medicare and Medicaid payment rates resulting from government legislation or rule-making or from budgetary challenges of states in which we operate; |
| • | how the hospitals are operated in the future; and |
| • | the nature of the ultimate disposition of the assets. |
We recorded a net impairment charge of $7 million for one hospital during 2009 for the write-down of buildings, equipment and other long-lived assets, primarily capitalized software costs classified in other intangible assets, to their estimated fair values, primarily due to a decline in the fair value of real estate in the market in which the hospital operates. Material adverse trends in our most recent estimates of future undiscounted cash flows of the hospital, consistent with our prior estimates during 2008 when impairment charges were recorded at this hospital, indicated the carrying value of the hospital’s long-lived assets was not recoverable from the estimated future cash flows. We believe the most significant factors contributing to the continuing adverse financial trends include reductions in volumes of insured patients due to competition, shifts in payer mix from commercial to governmental payers combined with reductions in reimbursement rates from governmental payers, and high levels of uninsured patients. As a result, we updated the estimate of the fair values of the hospital’s long-lived assets and compared the fair value estimate to the carrying values of the hospital’s long-lived assets. Because the fair value estimate was lower than the carrying values of the hospital’s long-lived assets, an impairment charge was recorded for the difference in the amounts. Unless the anticipated future financial trends of this hospital improve to the extent that the estimated future undiscounted cash flows exceed the carrying values of the long-lived assets, this hospital is at risk of future impairments, particularly if we spend significant amounts of capital at the hospital without generating a corresponding increase in the hospital’s fair value or if the fair value of the hospital’s real estate continues to decline. We also recorded a $10 million net impairment charge for the write-down of land and buildings at the current campus of one hospital that is scheduled to move to a new, replacement campus during 2010. Our estimates of the future undiscounted cash flows from use of the current campus for several months during 2010 and from estimated disposition proceeds were less than the carrying values of the land and buildings at the current campus. We compared the estimated fair values to the carrying values and, because the fair value estimate was lower than the carrying values of the assets, an impairment charge was recorded for the difference in the amounts. Additionally, in our most recent impairment analysis as of December 31, 2009, we had two hospitals with an aggregate carrying value of long-lived assets of approximately $164 million whose estimated future undiscounted cash flows exceeded the carrying value of long-lived assets by an aggregate amount of approximately $340 million. These two hospitals had the smallest excess of future estimated undiscounted cash flows over carrying value. Changes in the assumptions underlying these estimates of future undiscounted cash flows could result in the estimated cash flows being less than the carrying value of the assets, which would require a fair value assessment of the long-lived assets, and if the fair value amount is less than the carrying value of the assets, impairment charges would occur and could be material.
IMPAIRMENT OF GOODWILL
Goodwill represents the excess of costs over the fair value of assets of businesses acquired. Goodwill and other intangible assets acquired in purchase business combinations and determined to have indefinite useful lives are not amortized, but instead are subject to impairment tests performed at least annually. For goodwill, we perform the test at the reporting unit level, as defined by applicable accounting standards, when events occur that require an evaluation to be performed or at least annually. If we determine the carrying value of goodwill is impaired, or if the carrying value of a business that is to be sold or otherwise disposed of exceeds its fair value, then we reduce the carrying value, including any allocated goodwill, to fair value. Estimates of fair value are based on appraisals, established market prices for comparative assets or internal estimates of future net cash flows and presume stable, improving or, in some cases, declining results at our hospitals, depending on their circumstances. If the presumed level of performance does not occur as expected, impairment may result.
74
Table of Contents
Our continuing operations are structured as follows:
| • | Our California region includes all of our hospitals in California and Nebraska; |
| • | Our Central region includes all of our hospitals in Missouri, Tennessee and Texas; |
| • | Our Florida region includes all of our hospitals in Florida; |
| • | Our Southern States region includes all of our hospitals in Alabama, Georgia, North Carolina and South Carolina; and |
| • | Our two hospitals in Philadelphia, Pennsylvania are part of a separate market. |
These regions and market are reporting units used to perform our goodwill impairment analysis and are one level below our operating segment level. Future restructuring of our regions or markets that changes our goodwill reporting units could also result in further impairments of our goodwill.
Our goodwill balance is primarily related to our Southern States region, which totals approximately $287 million, and our Central region, which totals approximately $310 million. In our latest impairment analysis as of December 31, 2009, the estimated fair value of these regions exceeded the carrying value of long-lived assets, including goodwill, by approximately 17% and 53%, respectively.
ACCOUNTING FOR INCOME TAXES
We account for income taxes using the asset and liability method. This approach requires the recognition of deferred tax assets and liabilities for the expected future tax consequences of temporary differences between the carrying amounts and the tax bases of assets and liabilities. Income tax receivables and liabilities and deferred tax assets and liabilities are recognized based on the amounts that more likely than not will be sustained upon ultimate settlement with taxing authorities.
Developing our provision for income taxes and analysis of uncertain tax positions items requires significant judgment and knowledge of federal and state income tax laws, regulations and strategies, including the determination of deferred tax assets and liabilities and, if necessary, any valuation allowances that may be required for deferred tax assets.
We assess the realization of our deferred tax assets to determine whether an income tax valuation allowance is required. Based on all available evidence, both positive and negative, and the weight of that evidence to the extent such evidence can be objectively verified, we determine whether it is more likely than not that all or a portion of the deferred tax assets will be realized. The main factors that we consider include:
| • | Cumulative losses in recent years, adjusted for certain nonrecurring items; |
| • | Income/losses expected in future years; |
| • | Unsettled circumstances that, if unfavorably resolved, would adversely affect future operations and profit levels; |
| • | The availability, or lack thereof, of taxable income in prior carryback periods that would limit realization of tax benefits; |
| • | The carryforward period associated with the deferred tax assets and liabilities; and |
| • | Prudent and feasible tax-planning strategies. |
During the year ended December 31, 2009, the income tax valuation allowance decreased by $138 million primarily as a result of current year net income against which deferred tax assets were realized and the write-off of deferred tax assets related to stock-based compensation that would otherwise have been charged against additional paid-in capital. As of December 31, 2009, we concluded that a valuation allowance of approximately $1.1 billion was required primarily as a result of negative evidence represented by cumulative losses during the three year period ended December 31, 2009. In 2009, our operating results improved considerably and, if our operating results continue to improve in 2010, we may no longer have cumulative losses for purposes of this analysis. In that case, our judgment about the need for a valuation allowance may change in the near term and, if so, some or all of the valuation allowance may be reduced and recorded as a benefit in income tax expense from continuing operations. We cannot predict at this time when or if the valuation allowance will be reduced.
We consider many factors when evaluating our uncertain tax positions, and such judgments are subject to periodic review. Tax benefits associated with uncertain tax positions are recognized in the period in which one of the following conditions is satisfied: (1) the more likely than not recognition threshold is satisfied; (2) the position is ultimately settled through negotiation or litigation; or (3) the statute of limitations for the taxing authority to examine and challenge the position has expired. Tax benefits associated with an uncertain tax position are derecognized in the period in which the more likely than not recognition threshold is no longer satisfied.
75
Table of Contents
While we believe we have adequately provided for our income tax receivables or liabilities and our deferred tax assets or liabilities, adverse determinations by taxing authorities or changes in tax laws and regulations could have a material adverse effect on our consolidated financial position, results of operations or cash flows.
ACCOUNTING FOR STOCK-BASED COMPENSATION
We account for the cost of stock-based compensation using the fair-value method, under which the cost of stock option grants and other incentive awards to employees, directors, advisors and consultants is measured by the fair value of the awards on their grant dates and is recognized over the requisite service periods of the awards, whether or not the awards had any intrinsic value during the period. We estimate the fair value of stock option grants as of the date of each grant, using a binomial lattice model. The key assumptions of the binomial lattice model include:
| • | Expected volatility; |
| • | Expected dividend yield; |
| • | Expected life; |
| • | Expected forfeiture rate; |
| • | Risk-free interest rate range; |
| • | Early exercise threshold; and |
| • | Early exercise rate. |
The expected volatility used in the binomial lattice model incorporates historical and implied share-price volatility and is based on an analysis of historical prices of our stock and open market exchanged options. The expected volatility reflects the historical volatility for a duration consistent with the contractual life of the options, and the volatility implied by the trading of options to purchase our stock on open-market exchanges. The historical share-price volatility excludes the movements in our stock price during the period October 1, 2002 through December 31, 2002 due to unique events occurring during that time, which caused extreme volatility of our stock price. The expected life of options granted is derived from the output of the binomial lattice model and represents the period of time that the options are expected to be outstanding. This model incorporates an early exercise assumption in the event of a significant increase in stock price. The risk-free interest rates are based on zero-coupon United States Treasury yields in effect at the date of grant consistent with the expected exercise timeframes.
The most critical of the above assumptions in our calculations of fair value is the expected life of an option, because it, in turn, is a principal part of our calculations of expected volatility and interest rates. Accordingly, we reevaluate our estimate of expected life at each major grant date. Our reevaluation is based on recent exercise patterns.
76
Table of Contents
| ITEM 7A. | QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK |
The table below presents information about certain of our market-sensitive financial instruments as of December 31, 2009. The fair values were determined based on quoted market prices for the same or similar instruments. At December 31, 2009, we had no borrowings with variable interest rates.
| Maturity Date, Years Ending December 31, |
|||||||||||||||||||||||||||||||
| 2010 | 2011 | 2012 | 2013 | 2014 | Thereafter | Total | Fair Value | ||||||||||||||||||||||||
| (Dollars in Millions) | |||||||||||||||||||||||||||||||
| Fixed rate long-term debt |
$ | 2 | $ | 67 | $ | 58 | $ | 1,001 | $ | 100 | $ | 3,273 | $ | 4,501 | $ | 4,645 | |||||||||||||||
| Average effective interest rates |
8.9 | % | 6.8 | % | 6.8 | % | 7.8 | % | 10.3 | % | 10.5 | % | 9.8 | % | |||||||||||||||||
At December 31, 2009, we had long-term, market-sensitive investments held by our captive insurance subsidiaries. Our market risk associated with our investments in debt securities classified as non-current assets is substantially mitigated by the long-term nature and type of the investments in the portfolio. At December 31, 2009, the net accumulated unrealized losses related to our captive insurance companies’ investment portfolios were approximately $1 million.
We have no affiliation with partnerships, trusts or other entities (sometimes referred to as “special-purpose” or “variable-interest” entities) whose purpose is to facilitate off-balance sheet financial transactions or similar arrangements by us. Thus, we have no exposure to the financing, liquidity, market or credit risks associated with such entities.
We do not hold or issue derivative instruments for trading purposes and are not a party to any instruments with leverage or prepayment features.
77
Table of Contents
| ITEM 8. | FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA |
MANAGEMENT’S REPORT ON INTERNAL CONTROL OVER FINANCIAL REPORTING
To Our Shareholders:
Management is responsible for establishing and maintaining adequate internal control over financial reporting, as such term is defined in Rule 13a-15(f) under the Securities Exchange Act of 1934, as amended. Management assessed the effectiveness of Tenet’s internal control over financial reporting as of December 31, 2009. This assessment was performed under the supervision of and with the participation of management, including the chief executive officer and chief financial officer.
In making this assessment, management used criteria based on the framework in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (“COSO”). Based on the assessment using the COSO framework, management concluded that Tenet’s internal control over financial reporting was effective as of December 31, 2009.
Tenet’s internal control over financial reporting as of December 31, 2009 has been audited by Deloitte & Touche LLP, an independent registered public accounting firm, as stated in their report, which is included herein. Deloitte & Touche LLP has also audited Tenet’s Consolidated Financial Statements as of and for the year ended December 31, 2009, and that firm’s audit report on such Consolidated Financial Statements is also included herein.
Internal control over financial reporting cannot provide absolute assurance of achieving financial reporting objectives because of its inherent limitations. Internal control over financial reporting is a process that involves human diligence and compliance and is subject to lapses in judgment and breakdowns resulting from human failures. Internal control over financial reporting also can be circumvented by collusion or improper management override. Because of such limitations, there is a risk that material misstatements may not be prevented or detected on a timely basis by internal control over financial reporting. However, these inherent limitations are known features of the financial reporting process. Therefore, it is possible to design into the process safeguards to reduce, though not eliminate, this risk.
| Trevor Fetter | Biggs C. Porter | |
| President and Chief Executive Officer | Chief Financial Officer | |
| February 22, 2010 | February 22, 2010 |
78
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Board of Directors and Shareholders of
Tenet Healthcare Corporation
Dallas, Texas
We have audited the internal control over financial reporting of Tenet Healthcare Corporation and subsidiaries (the “Company”) as of December 31, 2009, based on criteria established in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission. The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting, included in the accompanying Management’s Report on Internal Control Over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company’s internal control over financial reporting is a process designed by, or under the supervision of, the company’s principal executive and principal financial officers, or persons performing similar functions, and effected by the company’s board of directors, management, and other personnel to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of the inherent limitations of internal control over financial reporting, including the possibility of collusion or improper management override of controls, material misstatements due to error or fraud may not be prevented or detected on a timely basis. Also, projections of any evaluation of the effectiveness of the internal control over financial reporting to future periods are subject to the risk that the controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
In our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2009, based on the criteria established in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission.
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated financial statements and financial statement schedule as of and for the year ended December 31, 2009, of the Company and our report dated February 22, 2010 expressed an unqualified opinion on those financial statements and financial statement schedule and included an explanatory paragraph regarding the Company’s adoption of provisions of accounting guidance related to noncontrolling interests in subsidiaries, effective January 1, 2009.
DELOITTE & TOUCHE LLP
Dallas, Texas
February 22, 2010
79
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Board of Directors and Shareholders of
Tenet Healthcare Corporation
Dallas, Texas
We have audited the accompanying consolidated balance sheets of Tenet Healthcare Corporation and subsidiaries (the “Company”) as of December 31, 2009 and 2008, and the related consolidated statements of operations, other comprehensive income (loss), changes in equity, and cash flows for each of the three years in the period ended December 31, 2009. Our audits also included the financial statement schedule listed in the Index at Item 15. These financial statements and financial statement schedule are the responsibility of the Company’s management. Our responsibility is to express an opinion on the financial statements and financial statement schedule based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, such consolidated financial statements present fairly, in all material respects, the financial position of Tenet Healthcare Corporation and subsidiaries at December 31, 2009 and 2008, and the results of their operations and their cash flows for each of the three years in the period ended December 31, 2009, in conformity with accounting principles generally accepted in the United States of America. Also, in our opinion, such financial statement schedule, when considered in relation to the basic consolidated financial statements taken as a whole, presents fairly, in all material respects, the information set forth therein.
As discussed in Note 1 to the consolidated financial statements, the Company adopted provisions of accounting guidance related to noncontrolling interests in subsidiaries, effective January 1, 2009.
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the Company’s internal control over financial reporting as of December 31, 2009, based on the criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission and our report dated February 22, 2010 expressed an unqualified opinion on the Company’s internal control over financial reporting.
DELOITTE & TOUCHE LLP
Dallas, Texas
February 22, 2010
80
Table of Contents
Dollars in Millions
| December 31, 2009 |
December 31, 2008 |
|||||||
| ASSETS | ||||||||
| Current assets: |
||||||||
| Cash and cash equivalents |
$ | 690 | $ | 507 | ||||
| Investments in Reserve Yield Plus Fund |
2 | 14 | ||||||
| Investments in marketable securities |
11 | 2 | ||||||
| Accounts receivable, less allowance for doubtful accounts ($369 at December 31, 2009 and $396 at December 31, 2008) |
1,158 | 1,337 | ||||||
| Inventories of supplies, at cost |
153 | 161 | ||||||
| Income tax receivable |
35 | 6 | ||||||
| Deferred income taxes |
108 | 82 | ||||||
| Assets held for sale |
29 | 310 | ||||||
| Other current assets |
286 | 290 | ||||||
| Total current assets |
2,472 | 2,709 | ||||||
| Investments and other assets |
182 | 242 | ||||||
| Property and equipment, at cost, less accumulated depreciation and amortization ($2,970 at December 31, 2009 and $2,795 at December 31, 2008) |
4,313 | 4,291 | ||||||
| Goodwill |
607 | 609 | ||||||
| Other intangible assets, at cost, less accumulated amortization ($257 at December 31, 2009 and $216 at December 31, 2008) |
379 | 323 | ||||||
| Total assets |
$ | 7,953 | $ | 8,174 | ||||
| LIABILITIES AND EQUITY | ||||||||
| Current liabilities: |
||||||||
| Current portion of long-term debt |
$ | 2 | $ | 2 | ||||
| Accounts payable |
739 | 686 | ||||||
| Accrued compensation and benefits |
370 | 414 | ||||||
| Professional and general liability reserves |
106 | 127 | ||||||
| Accrued interest payable |
127 | 125 | ||||||
| Accrued legal settlement costs |
76 | 168 | ||||||
| Other current liabilities |
363 | 427 | ||||||
| Total current liabilities |
1,783 | 1,949 | ||||||
| Long-term debt, net of current portion |
4,272 | 4,778 | ||||||
| Professional and general liability reserves |
466 | 536 | ||||||
| Accrued legal settlement costs |
19 | 72 | ||||||
| Other long-term liabilities |
568 | 591 | ||||||
| Deferred income taxes |
148 | 101 | ||||||
| Total liabilities |
7,256 | 8,027 | ||||||
| Commitments and contingencies |
||||||||
| Equity: |
||||||||
| Shareholders’ equity: |
||||||||
| Preferred stock, $0.15 par value; authorized 2,500,000 shares; 345,000 of 7% mandatory convertible shares with a liquidation preference of $1,000 per share issued at December 31, 2009 and 0 shares issued at December 31, 2008 |
334 | — | ||||||
| Common stock, $0.05 par value; authorized 1,050,000,000 shares; 538,610,856 shares issued at December 31, 2009 and 532,890,116 shares issued at December 31, 2008 |
27 | 26 | ||||||
| Additional paid-in capital |
4,461 | 4,445 | ||||||
| Accumulated other comprehensive loss |
(32 | ) | (37 | ) | ||||
| Accumulated deficit |
(2,665 | ) | (2,852 | ) | ||||
| Less common stock in treasury, at cost, 57,475,602 shares at December 31, 2009 and 55,716,859 shares at December 31, 2008 |
(1,479 | ) | (1,479 | ) | ||||
| Total shareholders’ equity |
646 | 103 | ||||||
| Noncontrolling interests |
51 | 44 | ||||||
| Total equity |
697 | 147 | ||||||
| Total liabilities and equity |
$ | 7,953 | $ | 8,174 | ||||
See accompanying Notes to Consolidated Financial Statements.
81
Table of Contents
CONSOLIDATED STATEMENTS OF OPERATIONS
Dollars in Millions, Except Per-Share Amounts
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Net operating revenues |
$ | 9,014 | $ | 8,585 | $ | 8,083 | ||||||
| Operating expenses: |
||||||||||||
| Salaries, wages and benefits |
3,857 | 3,779 | 3,617 | |||||||||
| Supplies |
1,569 | 1,511 | 1,401 | |||||||||
| Provision for doubtful accounts |
697 | 628 | 555 | |||||||||
| Other operating expenses, net |
1,909 | 1,928 | 1,852 | |||||||||
| Depreciation and amortization |
386 | 371 | 336 | |||||||||
| Impairment of long-lived assets and goodwill, and restructuring charges, net of insurance recoveries |
27 | 16 | 36 | |||||||||
| Hurricane insurance recoveries, net of costs |
— | — | (3 | ) | ||||||||
| Litigation and investigation costs, net of insurance recoveries |
31 | 41 | 13 | |||||||||
| Operating income |
538 | 311 | 276 | |||||||||
| Interest expense |
(445 | ) | (418 | ) | (419 | ) | ||||||
| Gain from early extinguishment of debt |
97 | — | — | |||||||||
| Investment earnings |
— | 22 | 47 | |||||||||
| Net gain on sales of investments |
15 | 139 | — | |||||||||
| Income (loss) from continuing operations, before income taxes |
205 | 54 | (96 | ) | ||||||||
| Income tax benefit |
23 | 25 | 61 | |||||||||
| Income (loss) from continuing operations, before discontinued operations |
228 | 79 | (35 | ) | ||||||||
| Discontinued operations: |
||||||||||||
| Loss from operations |
(10 | ) | (2 | ) | (5 | ) | ||||||
| Impairment of long-lived assets and goodwill, and restructuring charges, net of insurance recoveries |
(12 | ) | (95 | ) | (53 | ) | ||||||
| Litigation settlements, net of insurance recoveries |
— | 39 | — | |||||||||
| Net gains (losses) on sales of facilities |
(1 | ) | 6 | (8 | ) | |||||||
| Income tax (expense) benefit |
(8 | ) | 5 | 17 | ||||||||
| Loss from discontinued operations |
(31 | ) | (47 | ) | (49 | ) | ||||||
| Net income (loss) |
197 | 32 | (84 | ) | ||||||||
| Less: Preferred stock dividends |
6 | — | — | |||||||||
| Less: Net income attributable to noncontrolling interests |
10 | 7 | 5 | |||||||||
| Net income (loss) attributable to Tenet Healthcare Corporation common shareholders |
$ | 181 | $ | 25 | $ | (89 | ) | |||||
| Amounts attributable to Tenet Healthcare Corporation common shareholders |
||||||||||||
| Income (loss) from continuing operations, net of tax |
$ | 212 | $ | 73 | (38 | ) | ||||||
| Loss from discontinued operations, net of tax |
(31 | ) | (48 | ) | (51 | ) | ||||||
| Net income (loss) attributable to Tenet Healthcare Corporation common shareholders |
$ | 181 | $ | 25 | $ | (89 | ) | |||||
| Earnings (loss) per share attributable to Tenet Healthcare Corporation common shareholders |
||||||||||||
| Basic |
||||||||||||
| Continuing operations |
$ | 0.44 | $ | 0.15 | $ | (0.08 | ) | |||||
| Discontinued operations |
(0.06 | ) | (0.10 | ) | (0.11 | ) | ||||||
| $ | 0.38 | $ | 0.05 | $ | (0.19 | ) | ||||||
| Diluted |
||||||||||||
| Continuing operations |
$ | 0.43 | $ | 0.15 | $ | (0.08 | ) | |||||
| Discontinued operations |
(0.06 | ) | (0.10 | ) | (0.11 | ) | ||||||
| $ | 0.37 | $ | 0.05 | $ | (0.19 | ) | ||||||
| Weighted average shares and dilutive securities outstanding (in thousands): |
||||||||||||
| Basic |
480,240 | 476,349 | 473,405 | |||||||||
| Diluted |
507,277 | 478,606 | 473,405 | |||||||||
See accompanying Notes to Consolidated Financial Statements.
82
Table of Contents
CONSOLIDATED STATEMENTS OF OTHER COMPREHENSIVE INCOME (LOSS)
Dollars in Millions
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Net income (loss) |
$ | 197 | $ | 32 | $ | (84 | ) | |||||
| Other comprehensive income (loss): |
||||||||||||
| Adjustments for supplemental executive retirement plans |
(3 | ) | (9 | ) | 17 | |||||||
| Foreign currency translation adjustments |
— | — | (2 | ) | ||||||||
| Unrealized gain (losses) on securities held as available-for-sale |
3 | (3 | ) | — | ||||||||
| Reclassification adjustments for realized losses included in net income (loss) |
7 | 3 | 2 | |||||||||
| Other comprehensive income (loss) before income taxes |
7 | (9 | ) | 17 | ||||||||
| Income tax (expense) benefit related to items of other comprehensive income (loss) |
(2 | ) | — | — | ||||||||
| Total other comprehensive income (loss), net of tax |
5 | (9 | ) | 17 | ||||||||
| Comprehensive income (loss) |
202 | 23 | (67 | ) | ||||||||
| Less: Preferred stock dividends |
6 | — | — | |||||||||
| Less: Comprehensive income attributable to noncontrolling interests |
10 | 7 | 5 | |||||||||
| Comprehensive income (loss) attributable to Tenet Healthcare Corporation common shareholders |
$ | 186 | $ | 16 | $ | (72 | ) | |||||
See accompanying Notes to Consolidated Financial Statements.
83
Table of Contents
CONSOLIDATED STATEMENTS OF CHANGES IN EQUITY
Dollars in Millions,
Share Amounts in Thousands
| Tenet Healthcare Corporation Shareholders’ Equity | ||||||||||||||||||||||||||||||||||
| Preferred Stock | Common Stock | |||||||||||||||||||||||||||||||||
| Shares Outstanding |
Issued Amount |
Shares Outstanding |
Issued Par Amount |
Additional Paid-in Capital |
Accumulated Other Comprehensive Loss |
Accumulated Deficit |
Treasury Stock |
Noncontrolling Interests |
Total Equity |
|||||||||||||||||||||||||
| Balances at December 31, 2006 |
— | $ | — | 471,585 | $ | 26 | $ | 4,372 | $ | (45 | ) | $ | (2,610 | ) | $ | (1,479 | ) | $ | 34 | $ | 298 | |||||||||||||
| Cumulative effect of adopting ASC 740-10-25 |
— | — | — | — | — | — | (178 | ) | — | — | (178 | ) | ||||||||||||||||||||||
| Net income (loss) |
— | — | — | — | — | — | (89 | ) | — | 5 | (84 | ) | ||||||||||||||||||||||
| Distributions paid to noncontrolling interests |
— | — | — | — | — | — | — | — | (5 | ) | (5 | ) | ||||||||||||||||||||||
| Other comprehensive income |
— | — | — | — | — | 17 | — | — | — | 17 | ||||||||||||||||||||||||
| Stock-based compensation expense and issuance of common stock |
— | — | 2,794 | — | 40 | — | — | — | — | 40 | ||||||||||||||||||||||||
| Balances at December 31, 2007 |
— | $ | — | 474,379 | $ | 26 | $ | 4,412 | $ | (28 | ) | $ | (2,877 | ) | $ | (1,479 | ) | $ | 34 | $ | 88 | |||||||||||||
| Net income |
— | — | — | — | — | — | 25 | — | 7 | 32 | ||||||||||||||||||||||||
| Distributions paid to noncontrolling interests |
— | — | — | — | — | — | — | — | (3 | ) | (3 | ) | ||||||||||||||||||||||
| Contributions from noncontrolling interests |
— | — | — | — | — | — | — | — | 6 | 6 | ||||||||||||||||||||||||
| Other comprehensive loss |
— | — | — | — | — | (9 | ) | — | — | — | (9 | ) | ||||||||||||||||||||||
| Stock-based compensation expense and issuance of common stock |
— | — | 2,794 | — | 33 | — | — | — | — | 33 | ||||||||||||||||||||||||
| Balances at December 31, 2008 |
— | $ | — | 477,173 | $ | 26 | $ | 4,445 | $ | (37 | ) | $ | (2,852 | ) | $ | (1,479 | ) | $ | 44 | $ | 147 | |||||||||||||
| Net income |
— | — | — | — | — | — | 187 | — | 10 | 197 | ||||||||||||||||||||||||
| Distributions paid to noncontrolling interests |
— | — | — | — | — | — | — | — | (7 | ) | (7 | ) | ||||||||||||||||||||||
| Contributions from noncontrolling interests |
— | — | — | — | — | — | — | — | 4 | 4 | ||||||||||||||||||||||||
| Other comprehensive income |
— | — | — | — | — | 5 | — | — | — | 5 | ||||||||||||||||||||||||
| Issuance of mandatory convertible preferred stock |
345,000 | 334 | — | — | — | — | — | — | — | 334 | ||||||||||||||||||||||||
| Preferred stock dividend |
— | — | — | — | (6 | ) | — | — | — | — | (6 | ) | ||||||||||||||||||||||
| Stock-based compensation expense and issuance of common stock |
— | — | 3,962 | 1 | 22 | — | — | — | — | 23 | ||||||||||||||||||||||||
| Balances at December 31, 2009 |
345,000 | $ | 334 | 481,135 | $ | 27 | $ | 4,461 | $ | (32 | ) | $ | (2,665 | ) | $ | (1,479 | ) | $ | 51 | $ | 697 | |||||||||||||
See accompanying Notes to Consolidated Financial Statements.
84
Table of Contents
CONSOLIDATED STATEMENTS OF CASH FLOWS
Dollars in Millions
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Net income (loss) |
$ | 197 | $ | 32 | $ | (84 | ) | |||||
| Adjustments to reconcile net income (loss) to net cash provided by operating activities: |
||||||||||||
| Depreciation and amortization |
386 | 371 | 336 | |||||||||
| Provision for doubtful accounts |
697 | 628 | 555 | |||||||||
| Net gain on sales of investments |
(15 | ) | (139 | ) | — | |||||||
| Deferred income tax expense (benefit) |
20 | (14 | ) | 2 | ||||||||
| Stock-based compensation expense |
23 | 33 | 40 | |||||||||
| Impairment of long-lived assets and goodwill, and restructuring charges, net of insurance recoveries |
27 | 16 | 36 | |||||||||
| Litigation and investigation costs, net of insurance recoveries |
31 | 41 | 13 | |||||||||
| Net gain from early extinguishment of debt |
(97 | ) | — | — | ||||||||
| Fair market value adjustments related to interest rate swap and LIBOR cap agreements |
(1 | ) | — | — | ||||||||
| Proceeds from interest rate swap agreement |
39 | — | — | |||||||||
| Pretax loss from discontinued operations |
23 | 52 | 66 | |||||||||
| Other items, net |
(6 | ) | 4 | (15 | ) | |||||||
| Changes in cash from operating assets and liabilities: |
||||||||||||
| Accounts receivable |
(646 | ) | (647 | ) | (623 | ) | ||||||
| Inventories and other current assets |
(22 | ) | (1 | ) | (28 | ) | ||||||
| Income taxes |
(78 | ) | (20 | ) | 83 | |||||||
| Accounts payable, accrued expenses and other current liabilities |
12 | (29 | ) | (99 | ) | |||||||
| Other long-term liabilities |
(13 | ) | (37 | ) | 39 | |||||||
| Payments against reserves for restructuring charges and litigation costs and settlements |
(192 | ) | (100 | ) | (70 | ) | ||||||
| Net cash provided by operating activities from discontinued operations, excluding income taxes |
40 | 18 | 75 | |||||||||
| Net cash provided by operating activities |
425 | 208 | 326 | |||||||||
| Cash flows from investing activities: |
||||||||||||
| Purchases of property and equipment — continuing operations |
(397 | ) | (452 | ) | (608 | ) | ||||||
| Construction of new and replacement hospitals |
(58 | ) | (75 | ) | (67 | ) | ||||||
| Purchases of property and equipment — discontinued operations |
(1 | ) | (20 | ) | (68 | ) | ||||||
| Purchase of business or joint venture interest |
— | (92 | ) | (36 | ) | |||||||
| Proceeds from sales of facilities and other assets — discontinued operations |
221 | 160 | 91 | |||||||||
| Proceeds from sales of marketable securities, long-term investments and other assets |
67 | 224 | 706 | |||||||||
| Purchases of marketable securities |
(17 | ) | (26 | ) | (652 | ) | ||||||
| Distributions received from (reclassification of) investments in Reserve Yield Plus Fund |
12 | (14 | ) | — | ||||||||
| Proceeds from hospital authority bonds |
49 | 8 | 31 | |||||||||
| Proceeds from cash surrender value or basis reduction of insurance policies |
— | 11 | 82 | |||||||||
| Insurance recoveries for property damage |
— | 1 | 6 | |||||||||
| Other items, net |
(1 | ) | 1 | (5 | ) | |||||||
| Net cash used in investing activities |
(125 | ) | (274 | ) | (520 | ) | ||||||
| Cash flows from financing activities: |
||||||||||||
| Repayments of borrowings |
(1,291 | ) | (2 | ) | (22 | ) | ||||||
| Proceeds from borrowings |
885 | 1 | — | |||||||||
| Deferred debt issuance costs |
(46 | ) | (3 | ) | — | |||||||
| Proceeds from issuance of mandatory convertible preferred stock |
334 | — | — | |||||||||
| Cash dividends on preferred stock |
— | — | — | |||||||||
| Contributions from noncontrolling interests |
4 | 6 | — | |||||||||
| Distributions paid to noncontrolling interests |
(7 | ) | (3 | ) | (5 | ) | ||||||
| Other items, net |
4 | 2 | 9 | |||||||||
| Net cash provided by (used in) financing activities |
(117 | ) | 1 | (18 | ) | |||||||
| Net increase (decrease) in cash and cash equivalents |
183 | (65 | ) | (212 | ) | |||||||
| Cash and cash equivalents at beginning of period |
507 | 572 | 784 | |||||||||
| Cash and cash equivalents at end of period |
$ | 690 | $ | 507 | $ | 572 | ||||||
| Supplemental disclosures: |
||||||||||||
| Interest paid, net of capitalized interest |
$ | (439 | ) | $ | (391 | ) | $ | (395 | ) | |||
| Income tax (payments) refunds, net |
$ | (43 | ) | $ | (4 | ) | $ | 162 | ||||
See accompanying Notes to Consolidated Financial Statements.
85
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
NOTE 1. SIGNIFICANT ACCOUNTING POLICIES
Description of Business
Tenet Healthcare Corporation (together with our subsidiaries, referred to as “Tenet,” the “Company,” “we” or “us”) is an investor-owned health care services company whose subsidiaries and affiliates principally operate general hospitals and related health care facilities. At December 31, 2009, our subsidiaries operated 50 general hospitals (including one hospital not yet divested at that date that is classified in discontinued operations) and a critical access hospital, with a combined total of 13,601 licensed beds, serving urban and rural communities in 12 states. We also own an interest in a health maintenance organization (“HMO”) and operate: various related health care facilities, including a long-term acute care hospital and a number of medical office buildings (all of which are located on, or nearby, one of our general hospital campuses); physician practices; captive insurance companies; and other ancillary health care businesses (including outpatient surgery centers, diagnostic imaging centers, and occupational and rural health care clinics).
Basis of Presentation
Our Consolidated Financial Statements include the accounts of Tenet and its wholly owned and majority-owned subsidiaries. We eliminate intercompany accounts and transactions in consolidation, and we include the results of operations of businesses that are newly acquired in purchase transactions from their dates of acquisition. We account for significant investments in other affiliated companies using the equity method. Unless otherwise indicated, all financial and statistical data included in these notes to the Consolidated Financial Statements relate to our continuing operations, with dollar amounts expressed in millions (except per-share amounts). Certain balances in the accompanying Consolidated Financial Statements and these notes have been reclassified to give retrospective presentation to the discontinued operations described in Note 4. In addition, certain prior-year balances have been reclassified to conform to current-year presentation.
Changes in Accounting Principle
In June 2009, the Financial Accounting Standards Board (“FASB”) issued Statement of Financial Accounting Standards (“SFAS”) No. 168, “The FASB Accounting Standards Codification and the Hierarchy of Generally Accepted Accounting Principles, a replacement of FASB Statement No. 162.” This statement modifies the hierarchy of accounting principles generally accepted in the United States of America (“GAAP”) by establishing only two levels of GAAP, authoritative and nonauthoritative accounting literature. Effective July 2009, the FASB Accounting Standards Codification (“ASC”) is considered the single authoritative source of GAAP used by nongovernmental entities in the preparation of financial statements, except for rules and interpretive releases of the Securities and Exchange Commission (“SEC”) under authority of federal securities laws, which are sources of authoritative accounting guidance for SEC registrants. The ASC is meant to simplify user access to all authoritative accounting guidance by reorganizing GAAP pronouncements into accounting topics within a consistent structure; its purpose is not to create new accounting and reporting guidance. This statement was effective for us beginning in the three months ended September 30, 2009. All accounting references in this report have been updated and SFAS references have been replaced with ASC references unless not yet codified by the FASB. SFAS No. 168 did not impact our financial condition, results of operations or cash flows.
Effective January 1, 2009, we adopted ASC 810-10-45-16 relating to non-controlling interests in consolidated financial statements. The adoption had no impact on our financial condition, results of operations or cash flows. However, we now reflect noncontrolling interests in subsidiaries as a separate component of equity in our Consolidated Financial Statements. We have reclassified certain prior-year amounts to conform to the current-year presentation required by this ASC topic.
Effective January 1, 2009, we adopted the provisions of ASC 820-10-05 relating to fair value measurements and disclosures with respect to our non-financial assets and liabilities that are not permitted or required to be measured at fair value on a recurring basis. The adoption had no impact on our financial condition, results of operations or cash flows. Effective January 1, 2008, we adopted the provisions of this ASC topic as they relate to our financial assets and liabilities that are re-measured and reported at fair value each reporting period. There was no material impact on our Consolidated Financial Statements as a result of adopting this ASC topic. See Note 16 for the disclosure of the fair values of qualifying investments, derivative contracts, long-lived assets held for sale and long-lived assets held and used required by this ASC topic.
Effective January 1, 2007, we adopted ASC 740-10-25-9 relating to uncertainty in income taxes, and we recorded a cumulative effect adjustment that increased the 2007 beginning of year accumulated deficit by $178 million. See Note 14 for additional information.
86
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Use of Estimates
The preparation of financial statements, in conformity with GAAP, requires us to make estimates and assumptions that affect the amounts reported in the Consolidated Financial Statements and these accompanying notes. We regularly evaluate the accounting policies and estimates we use. In general, we base the estimates on historical experience and on assumptions that we believe to be reasonable given the particular circumstances in which we operate. Although we believe all adjustments considered necessary for fair presentation have been included, actual results may vary from those estimates. We have evaluated all material events occurring subsequent to the balance sheet date through February 22, 2010 for events requiring disclosure or recognition in the Consolidated Financial Statements and related notes. Financial and statistical information we report to other regulatory agencies may be prepared on a basis other than GAAP or using different assumptions or reporting periods and, therefore, may vary from amounts presented herein. Although we make every effort to ensure that the information we report to those agencies is accurate, complete and consistent with applicable reporting guidelines, we cannot be responsible for the accuracy of the information they make available to the public.
Net Operating Revenues
We recognize net operating revenues in the period in which services are performed. Net operating revenues primarily consist of net patient service revenues that are recorded based on established billing rates (i.e., gross charges), less estimated discounts for contractual and other allowances, principally for patients covered by Medicare, Medicaid, managed care and other health plans, as well as uninsured patients under our Compact with Uninsured Patients (“Compact”).
Gross charges are retail charges. They are not the same as actual pricing, and they generally do not reflect what a hospital is ultimately paid and, therefore, are not displayed in our Consolidated Statements of Operations. Hospitals are typically paid amounts that are negotiated with insurance companies or are set by the government. Gross charges are used to calculate Medicare outlier payments and to determine certain elements of payment under managed care contracts (such as stop-loss payments). Because Medicare requires that a hospital’s gross charges be the same for all patients (regardless of payer category), gross charges are also what hospitals charge all other patients prior to the application of discounts and allowances.
Revenues under the traditional fee-for-service Medicare and Medicaid programs are based primarily on prospective payment systems. Discounts for retrospective cost-based revenues, which were more prevalent in earlier periods, and certain other payments, such as Indirect Medical Education, Direct Graduate Medical Education, disproportionate share hospital and bad debt expense, which are based on our hospitals’ cost reports, are estimated using historical trends and current factors. Cost report settlements under these programs are subject to audit by Medicare and Medicaid auditors and administrative and judicial review, and it can take several years until final settlement of such matters is determined and completely resolved. Because the laws, regulations, instructions and rule interpretations governing Medicare and Medicaid reimbursement are complex and change frequently, the estimates recorded by us could change by material amounts.
We have a system and estimation process for recording Medicare net patient revenue and estimated cost report settlements. This results in us recording accruals to reflect the expected final settlements on our cost reports. For filed cost reports, we record the accrual based on those cost reports and subsequent activity, and record a valuation allowance against those cost reports based on historical settlement trends. The accrual for periods for which a cost report is yet to be filed is recorded based on estimates of what we expect to report on the filed cost reports, and a corresponding valuation allowance is recorded as previously described. Cost reports generally must be filed within five months after the end of the annual cost reporting period. After the cost report is filed, the accrual and corresponding valuation allowance may need to be adjusted. Adjustments for prior-year cost reports and related valuation allowances, principally related to Medicare and Medicaid, increased revenues in the years ended December 31, 2009, 2008 and 2007 by $16 million, $3 million and $45 million, respectively. Estimated cost report settlements and valuation allowances are deducted from accounts receivable in the accompanying Consolidated Balance Sheets (see Note 3). We believe that we have made adequate provision for any adjustments that may result from final determination of amounts earned under all the above arrangements with Medicare and Medicaid.
Revenues under managed care plans are based primarily on payment terms involving predetermined rates per diagnosis, per-diem rates, discounted fee-for-service rates and/or other similar contractual arrangements. These revenues are also subject to review and possible audit by the payers. The payers are billed for patient services on an individual patient basis. An individual patient’s bill is subject to adjustment on a patient-by-patient basis in the ordinary course of business by the payers following their review and adjudication of each particular bill. We estimate the discounts for contractual allowances at the individual hospital level utilizing billing data on an individual patient basis. At the end of each month, on an individual hospital basis, we estimate our expected reimbursement for patients of managed care plans based on the applicable contract terms. Contractual allowance estimates are periodically reviewed for accuracy by taking into consideration known contract terms as well as payment history. Although we do not separately accumulate and disclose the aggregate amount of adjustments to the estimated reimbursement for every patient bill, we believe our estimation and review process enables us to identify instances on a timely basis where such estimates need to be revised. We do not believe there were any adjustments to estimates of individual patient bills that were material to our revenues. In addition, on a corporate-wide basis, we do not record any general provision for adjustments to estimated contractual allowances for managed care plans.
87
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
We know of no material claims, disputes or unsettled matters with any payers that would affect our revenues for which we have not adequately provided for in the accompanying Consolidated Financial Statements.
Under our Compact, the discount offered to uninsured patients is recognized as a contractual allowance, which reduces net operating revenues at the time the self-pay accounts are recorded. The uninsured patient accounts, net of contractual allowances recorded, are further reduced to their net realizable value through provision for doubtful accounts based on historical collection trends for self-pay accounts and other factors that affect the estimation process.
We also provide charity care to patients who are financially unable to pay for the health care services they receive. Most patients who qualify for charity care are charged a per-diem amount for services received, subject to a cap. Except for the per-diem amounts, our policy is not to pursue collection of amounts determined to qualify as charity care; therefore, we do not report these amounts in net operating revenues or in provision for doubtful accounts. Patient advocates from our Medical Eligibility Program screen patients in the hospital to determine whether those patients meet eligibility requirements for financial assistance programs. They also expedite the process of applying for these government programs.
Cash Equivalents
We treat highly liquid investments with original maturities of three months or less as cash equivalents. Cash and cash equivalents were approximately $690 million and $507 million at December 31, 2009 and 2008, respectively. As of December 31, 2009 and 2008, our book overdrafts were approximately $255 million and $187 million, respectively, which were classified as accounts payable.
In May 2009, we completed the sale of our 50% membership interest in Peoples Health Network, the company that administered the operations of Tenet Choices, Inc., our wholly owned Medicare Advantage HMO insurance subsidiary in Louisiana. The cash and cash equivalent balances of this insurance subsidiary were $53 million at December 31, 2008. The transaction resulted in a pretax gain in continuing operations of approximately $15 million during the year ended December 31, 2009 (see Note 17).
In addition, see Note 16 for disclosure of our investments in the Reserve Yield Plus Fund that were reclassified out of cash and cash equivalents due to liquidity issues of the fund.
Investments in Debt and Equity Securities
We classify investments in debt and equity securities as either available-for-sale, held-to-maturity or as part of a trading portfolio. At December 31, 2009 and 2008, we had no significant investments in securities classified as either held-to-maturity or trading. We carry securities classified as available-for-sale at fair value if unrestricted. We report their unrealized gains and losses, net of taxes, as accumulated other comprehensive income (loss) unless we determine that a loss is other-than-temporary, at which point we would record a loss in the Consolidated Statement of Operations. We include realized gains or losses in the Consolidated Statement of Operations based on the specific identification method.
Provision for Doubtful Accounts
Although outcomes vary, our policy is to attempt to collect amounts due from patients, including co-payments and deductibles due from patients with insurance, at the time of service while complying with all federal and state laws and regulations, including, but not limited to, the Emergency Medical Treatment and Active Labor Act (“EMTALA”). Generally, as required by EMTALA, patients may not be denied emergency treatment due to inability to pay. Therefore, services, including the legally required medical screening examination and stabilization of the patient, are performed without delaying to obtain insurance information. In non-emergency circumstances or for elective procedures and services, it is our policy to verify insurance prior to a patient being treated; however, there are various exceptions that can occur. Such exceptions can include, for example, instances where (1) we are unable to obtain verification because the patient’s insurance company was unable to be reached or contacted, (2) a determination is made that a patient may be eligible for benefits under various government programs, such as Medicaid or Victims of Crime, and it takes several days or weeks before qualification for such benefits is confirmed or denied, and (3) under physician orders we provide services to patients that require immediate treatment.
88
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
We provide for an allowance against accounts receivable that could become uncollectible by establishing an allowance to reduce the carrying value of such receivables to their estimated net realizable value. We estimate this allowance based on the aging of our accounts receivable by hospital, our historical collection experience by hospital and for each type of payer over an 18-month look-back period, and other relevant factors. There are various factors that can impact collection trends, such as changes in the economy, which in turn have an impact on unemployment rates and the number of uninsured and underinsured patients, the volume of patients through the emergency department, the increased burden of co-payments and deductibles to be made by patients with insurance, and business practices related to collection efforts. These factors continuously change and can have an impact on collection trends and our estimation process.
Property and Equipment
Additions and improvements to property and equipment costing $500 or more with a useful life greater than one year are capitalized at cost. Expenditures for maintenance and repairs are charged to expense as incurred. We use the straight-line method of depreciation for buildings, building improvements and equipment. The estimated useful life for buildings and improvements is primarily 25 to 40 years and, for equipment, three to 15 years. We record capital leases at the beginning of the lease term as assets and liabilities. The value recorded is the lower of either the present value of the minimum lease payments or the fair value of the asset. Such assets, including improvements, are amortized over the shorter of either the lease term or their estimated useful life. Interest costs related to construction projects are capitalized. In the years ended December 31, 2009, 2008 and 2007, capitalized interest was $9 million, $10 million and $11 million, respectively.
We evaluate our long-lived assets for possible impairment annually or whenever events or changes in circumstances indicate that the carrying amount of the asset, or related group of assets, may not be recoverable from estimated future undiscounted cash flows. We calculate the amount of an impairment if the carrying value of the long-lived assets exceeds the fair value of the assets. The fair value of the assets is estimated based on appraisals, established market values of comparable assets or internal estimates of future net cash flows expected to result from the use and ultimate disposition of the asset. The estimates of these future cash flows are based on assumptions and projections we believe to be reasonable and supportable. They require our subjective judgments and take into account assumptions about revenue and expense growth rates. These assumptions may vary by type of facility and presume stable, improving or, in some cases, declining results at our hospitals, depending on their circumstances.
We report long-lived assets to be disposed of at the lower of their carrying amounts or fair values less costs to sell. In such circumstances, our estimates of fair value are based on appraisals, established market prices for comparable assets or internal estimates of future net cash flows.
Asset Retirement Obligations
We recognize the fair value of a liability for legal obligations associated with asset retirements, primarily related to asbestos abatement and costs associated with underground storage tanks, in the period in which it is incurred if a reasonable estimate of the fair value of the obligation can be made. When the liability is initially recorded, we capitalize the cost of the asset retirement obligation by increasing the carrying amount of the related long-lived asset. Over time, the liability is accreted to its present value each period, and the capitalized cost associated with the retirement obligation is depreciated over the useful life of the related asset. Upon settlement of the obligation, any difference between the cost to settle the asset retirement obligation and the liability recorded is recognized as a gain or loss in the Consolidated Statement of Operations.
Goodwill and Other Intangible Assets
Goodwill represents the excess of costs over the fair value of assets of businesses acquired. Goodwill and other intangible assets acquired in purchase business combinations and determined to have indefinite useful lives are not amortized, but instead are subject to impairment tests performed at least annually. For goodwill, we perform the test at the reporting unit level when events occur that require an evaluation to be performed or at least annually. If we determine the carrying value of goodwill is impaired, or if the carrying value of a business that is to be sold or otherwise disposed of exceeds its fair value, then we reduce the carrying value, including any allocated goodwill, to fair value. Estimates of fair value are based on appraisals, established market prices for comparative assets or internal estimates of future net cash flows and presume stable, improving or, in some cases, declining results at our hospitals, depending on their circumstances.
Other intangible assets primarily consist of capitalized software costs, which are amortized on a straight-line basis over the estimated useful life of the software, which ranges from three to 15 years. Also included in intangible assets are costs associated with the issuance of our long-term debt, which are being amortized primarily under the straight-line method based on the terms of the specific notes, which is not materially different from the effective interest method.
89
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Accruals for General and Professional Liability Risks
We accrue for estimated professional and general liability claims, to the extent not covered by insurance, when they are probable and can be reasonably estimated. The accrual, which includes an estimate for incurred but not reported claims, is updated each quarter based on an actuarial calculation of projected payments using case-specific facts and circumstances and our historical loss reporting, development and settlement patterns and is discounted to its net present value using a risk-free discount rate (2.69% at December 31, 2009 and 3.32% at December 31, 2008). To the extent that subsequent claims information varies from our estimates, the liability is adjusted in the period such information becomes available. Malpractice liability expense is presented within other operating expenses in the accompanying Consolidated Statement of Operations.
Income Taxes
We account for income taxes using the asset and liability method. This approach requires the recognition of deferred tax assets and liabilities for the expected future tax consequences of temporary differences between the carrying amounts and the tax bases of assets and liabilities. Income tax receivables and liabilities and deferred tax assets and liabilities are recognized based on the amounts that more likely than not will be sustained upon ultimate settlement with taxing authorities.
Developing our provision for income taxes and analysis of uncertain tax positions items requires significant judgment and knowledge of federal and state income tax laws, regulations and strategies, including the determination of deferred tax assets and liabilities and, if necessary, any valuation allowances that may be required for deferred tax assets.
We assess the realization of our deferred tax assets to determine whether an income tax valuation allowance is required. Based on all available evidence, both positive and negative, and the weight of that evidence to the extent such evidence can be objectively verified, we determine whether it is more likely than not that all or a portion of the deferred tax assets will be realized. The main factors that we consider include:
| • | Cumulative losses in recent years; |
| • | Income/losses expected in future years; |
| • | Unsettled circumstances that, if unfavorably resolved, would adversely affect future operations and profit levels; |
| • | The availability, or lack thereof, of taxable income in prior carryback periods that would limit realization of tax benefits; |
| • | The carryforward period associated with the deferred tax assets and liabilities; and |
| • | Prudent and feasible tax-planning strategies. |
We consider many factors when evaluating our uncertain tax positions, and such judgments are subject to periodic review. Tax benefits associated with uncertain tax positions are recognized in the period in which one of the following conditions is satisfied: (1) the more likely than not recognition threshold is satisfied; (2) the position is ultimately settled through negotiation or litigation; or (3) the statute of limitations for the taxing authority to examine and challenge the position has expired. Tax benefits associated with an uncertain tax position are derecognized in the period in which the more likely than not recognition threshold is no longer satisfied.
While we believe we have adequately provided for our income tax receivables or liabilities and our deferred tax assets or liabilities in accordance with FASB income tax guidance, adverse determinations by taxing authorities or changes in tax laws and regulations could have a material adverse effect on our consolidated financial condition, results of operations or cash flows.
Segment Reporting
We operate in one line of business—the provision of health care services through the operation of general hospitals and related health care facilities. Our general hospitals generated 97.7%, 98.0% and 98.1% of our net operating revenues in the years ended December 31, 2009, 2008 and 2007, respectively. Each of our operating regions and our Philadelphia market report directly to our chief operating officer. Major decisions, including capital resource allocations, are made at the consolidated level, not at the region level.
Costs Associated With Exit or Disposal Activities
We recognize costs associated with exit (including restructuring) or disposal activities when they are incurred and can be measured at fair value, rather than at the date of a commitment to an exit or disposal plan.
90
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
NOTE 2. EQUITY
In September 2009, we sold 345,000 shares of 7% mandatory convertible preferred stock for net proceeds of approximately $334 million. Each share of mandatory convertible preferred stock will automatically convert on October 1, 2012 into between 142.4501 and 170.9402 shares of our common stock, subject to anti-dilution adjustments, depending on the average of the closing prices per share of our common stock on each of the 20 consecutive trading days ending on the third trading day immediately preceding the mandatory conversion date, subject to certain conditions. At any time prior to October 1, 2012, holders may elect to convert shares of the mandatory convertible preferred stock at the minimum conversion rate of 142.4501 shares of our common stock, subject to anti-dilution adjustments. If holders elect to convert shares of the mandatory convertible preferred stock during a specified period in connection with a make-whole event, as defined in the certificate of designation relating to the mandatory convertible preferred stock, the conversion rate will be adjusted under certain circumstances and holders will also be entitled to receive a make-whole amount in cash, common stock or a combination thereof as elected by us.
Quarterly dividends on each share of the mandatory convertible preferred stock will accrue at a rate of 7% per year on the liquidation preference of $1,000 per share. Dividends will accrue and accumulate from September 25, 2009, and, to the extent that we declare a dividend payable, we will pay dividends on January 1, April 1, July 1 and October 1 of each year through, and including, October 1, 2012. We accrued dividends for the period September 25, 2009 through December 31, 2009 of approximately $6 million, or $18.67 per share, and paid the dividends in January 2010.
Upon any voluntary or involuntary liquidation, dissolution or winding up of us resulting in a distribution of assets to the holders of any class or series of our capital stock, each holder of the mandatory convertible preferred stock will be entitled to receive the liquidation preference of $1,000 per share, plus an amount equal to accrued, accumulated and unpaid dividends.
NOTE 3. ACCOUNTS RECEIVABLE AND ALLOWANCE FOR DOUBTFUL ACCOUNTS
The principal components of accounts receivable are shown in the table below:
| December 31, | ||||||||
| 2009 | 2008 | |||||||
| Continuing operations: |
||||||||
| Patient accounts receivable |
$ | 1,466 | $ | 1,506 | ||||
| Allowance for doubtful accounts |
(341 | ) | (343 | ) | ||||
| Estimated future recoveries from accounts assigned to collection agencies |
35 | 40 | ||||||
| Net cost report settlements payable and valuation allowances |
(24 | ) | (20 | ) | ||||
| 1,136 | 1,183 | |||||||
| Discontinued operations: |
||||||||
| Patient accounts receivable |
44 | 205 | ||||||
| Allowance for doubtful accounts |
(28 | ) | (53 | ) | ||||
| Estimated future recoveries from accounts assigned to collection agencies |
3 | 3 | ||||||
| Net cost report settlements receivable (payable) and valuation allowances |
3 | (1 | ) | |||||
| 22 | 154 | |||||||
| Accounts receivable, net |
$ | 1,158 | $ | 1,337 | ||||
As of December 31, 2009, our estimated collection rates on managed care accounts and self-pay accounts were approximately 98.0% and 30.1%, respectively, which included collections from point-of-service through collections by our in-house collection agency. The comparable managed care and self-pay collection rates for the same continuing hospitals as of December 31, 2008 were approximately 97.8% and 32.5%, respectively.
Accounts that are pursued for collection through our regional business offices are maintained on our hospitals’ books and reflected in patient accounts receivable with an allowance for doubtful accounts established to reduce the carrying value of such receivables to their estimated net realizable value. We estimate this allowance based on the aging of our accounts receivable by hospital, our historical collection experience by hospital and for each type of payer over an 18-month look-back period, and other relevant factors. Changes in these factors related to self-pay accounts and self-pay balance after insurance accounts from a change in the estimated collection rates could have a material impact on our results of operations.
Accounts assigned to our in-house collection agency are written off and excluded from patient accounts receivable and allowance for doubtful accounts; however, an estimate of future recoveries from all accounts at the collection agency is determined based on historical experience and recorded on our hospitals’ books as a component of accounts receivable in the Consolidated Balance Sheets.
91
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The estimated costs (based on selected operating expenses, which include salaries, wages and benefits, supplies and other operating expenses) of caring for our self-pay patients for the years ended December 31, 2009, 2008 and 2007 were approximately $365 million, $359 million and $342 million, respectively. We also provide charity care to patients who are financially unable to pay for the health care services they receive. Most patients who qualify for charity care are charged a per-diem amount for services received, subject to a cap. Except for the per-diem amounts, our policy is not to pursue collection of amounts determined to qualify as charity care; therefore, we do not report these amounts in net operating revenues or in provision for doubtful accounts. Most states include an estimate of the cost of charity care in the determination of a hospital’s eligibility for Medicaid DSH payments. The estimated costs (based on the selected operating expenses described above) of caring for charity care patients for the years ended December 31, 2009, 2008 and 2007 were approximately $118 million, $113 million and $121 million, respectively.
NOTE 4. DISCONTINUED OPERATIONS
In May 2009, we announced that we would not renew our operating lease agreement for NorthShore Regional Medical Center, located in Slidell, Louisiana, which lease expires in May 2010. Accordingly, the hospital was reclassified into discontinued operations in the three months ended June 30, 2009. In January 2010, we entered into a definitive agreement to sell certain of our owned assets associated with NorthShore and transition the operation of the hospital to a new hospital operator. We anticipate that the transaction will close effective April 1, 2010, at which time we will terminate our lease of the hospital.
Of the three general hospitals and one cancer hospital that were classified as “assets held for sale” at December 31, 2008, we completed the sale of USC University Hospital and USC Kenneth Norris Jr. Cancer Hospital on March 31, 2009. In addition, we closed Irvine Regional Hospital and Medical Center in January 2009 before the expiration of our lease in February 2009, and we closed Community Hospital of Los Gatos and terminated our lease in April 2009.
We classified $17 million and $300 million of assets of the hospitals included in discontinued operations as “assets held for sale” in current assets in the accompanying Consolidated Balance Sheets at December 31, 2009 and December 31, 2008, respectively. These assets primarily consist of property and equipment and were recorded at the lower of the assets’ carrying amount or their fair value less estimated costs to sell. The fair value estimates were derived from appraisals, established market values of comparable assets, or internal estimates of future net cash flows. These fair value estimates can change by material amounts in subsequent periods. Many factors and assumptions can impact the estimates, including the future financial results of these hospitals and how they are operated by us until they are divested, changes in health care industry trends and regulations until the hospitals are divested, and whether we ultimately divest the hospital assets to buyers who will continue to operate the assets as general hospitals or utilize the assets for other purposes. In certain cases, these fair value estimates assume the highest and best use of the assets in the future, to a market place participant, is other than as a hospital. In these cases, the estimates are based on the fair value of the real property and equipment if utilized other than as a hospital. These fair value estimates do not include the costs of closing these hospitals or other future operating costs, which could be substantial. Accordingly, the ultimate net cash realized from the sale of the hospital assets could be significantly less than the fair value estimates. Because we do not intend to sell the accounts receivable of these hospitals, the receivables are included in our consolidated net accounts receivable in the accompanying Consolidated Balance Sheets. See Note 16 for the disclosure of the fair values of long-lived assets held for sale.
Net operating revenues and loss before income taxes reported in discontinued operations are as follows:
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Net operating revenues |
$ | 201 | $ | 909 | $ | 1,278 | ||||||
| Loss before income taxes |
(23 | ) | (52 | ) | (66 | ) | ||||||
We recorded $12 million of net impairment and restructuring charges in discontinued operations during the year ended December 31, 2009, consisting of $3 million for the write-down of long-lived assets to their estimated fair values, less estimated costs to sell, $2 million of goodwill related to NorthShore Regional Medical Center, and $7 million in employee severance, lease termination and other exit costs.
We recorded $95 million of net impairment and restructuring charges in discontinued operations during the year ended December 31, 2008, consisting of $79 million for the write-down of long-lived assets to their estimated fair values, less estimated costs to sell, $7 million in severance costs and $9 million in lease terminations costs.
We recorded $53 million of net impairment and restructuring charges in discontinued operations during the year ended December 31, 2007, consisting of $37 million for the write-down of long-lived assets to their estimated fair values, less estimated costs to sell, $10 million of employee severance and retention costs, $4 million for exit costs of a residency program, and $4 million for impairment of other assets, offset by a $2 million credit to reduce an estimated asset retirement obligation related to asbestos.
92
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
As we move forward with our previously announced divestiture plans, or should we dispose of additional hospitals or other assets in the future, we may incur additional asset impairment and restructuring charges in future periods.
In September 2008, we entered into an agreement to settle our claims against one of the carriers under our excess professional and general liability insurance policies related to our December 2004 Redding Medical Center litigation settlement for approximately $9 million, which was recorded as a recovery in litigation settlements, net of insurance recoveries, in discontinued operations during the three months ended September 30, 2008. Also during the three months ended September 30, 2008, we were awarded $36 million in insurance recoveries from another excess carrier by an independent arbitration panel. With interest, we received approximately $46 million from the excess carrier, of which $30 million was recorded as a recovery in litigation settlements, net of insurance recoveries, in discontinued operations, $6 million was recorded as a recovery of litigation and investigation costs in continuing operations for litigation costs we previously incurred and $10 million of interest income was recorded in continuing operations.
In November 2006, we sold accounts receivable related to discontinued hospitals, which had previously been written down to approximately $1 million, to a third party and received proceeds of $16 million. Effective December 2007, the sale agreement was amended and the transaction qualified as a sale under the accounting guidance related to transfers of financial assets applicable at the time. Accordingly, the proceeds of approximately $15 million in excess of the carrying value of the accounts receivable were recognized as a gain in discontinued operations in the three months ended December 31, 2007. Also in the three months ended December 31, 2007, we reserved approximately $4 million in escrowed funds related to our discontinued operations in Spain, as related bankruptcy proceedings were not likely to be resolved in the required time for us to recover these funds. In 2008, we subsequently received approximately $9 million of escrowed funds related to our previously divested hospital in Spain, which were recognized as a gain in discontinued operations.
NOTE 5. IMPAIRMENT AND RESTRUCTURING CHARGES
We recognized impairment charges on long-lived assets in 2009, 2008 and 2007 because the fair values of those assets or groups of assets indicated that the carrying amount was not recoverable. The fair value estimates were derived from appraisals, established market values of comparable assets, or internal estimates of future net cash flows. These fair value estimates can change by material amounts in subsequent periods. Many factors and assumptions can impact the estimates, including the future financial results of the hospitals, how the hospitals are operated in the future, changes in health care industry trends and regulations, and the nature of the ultimate disposition of the assets. In certain cases, these fair value estimates assume the highest and best use of hospital assets in the future to a market place participant is other than as a hospital. In these cases, the estimates are based on the fair value of the real property and equipment if utilized other than as a hospital. The impairment recognized does not include the costs of closing the hospitals or other future operating costs, which could be substantial. Accordingly, the ultimate net cash realized from the hospitals, should we choose to sell them, could be significantly less than their impaired value.
Our impairment tests presume stable, improving or, in some cases, declining results in our hospitals, which are based on programs and initiatives being implemented that are designed to achieve the hospital’s most recent projections. If these projections are not met, or if in the future negative trends occur that impact our future outlook, further impairments of long-lived assets and goodwill may occur, and we may incur additional restructuring charges.
Our continuing operations are structured as follows:
| • | Our California region includes all of our hospitals in California and Nebraska; |
| • | Our Central region includes all of our hospitals in Missouri, Tennessee and Texas; |
| • | Our Florida region includes all of our hospitals in Florida; |
| • | Our Southern States region includes all of our hospitals in Alabama, Georgia, North Carolina and South Carolina; and |
| • | Our two hospitals in Philadelphia, Pennsylvania are part of a separate market. |
These regions and market are reporting units used to perform our goodwill impairment analysis and are one level below our operating segment level. Future restructuring of our regions or markets that changes our goodwill reporting units could also result in further impairments of our goodwill.
93
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Year Ended December 31, 2009
During the year ended December 31, 2009, we recorded net impairment and restructuring charges of $27 million. We recorded a $7 million net impairment charge for the write-down of buildings, equipment and other long-lived assets, primarily capitalized software costs classified in other intangible assets, of one hospital to their estimated fair values, primarily due to a decline in the fair value of real estate in the market in which the hospital operates. Material adverse trends in our most recent estimates of future undiscounted cash flows of the hospital, consistent with our prior estimates during 2008 when impairment charges were recorded at this hospital, indicated the carrying value of the hospital’s long-lived assets was not recoverable from the estimated future cash flows. We believe the most significant factors contributing to the continuing adverse financial trends include reductions in volumes of insured patients due to competition, shifts in payer mix from commercial to governmental payers combined with reductions in reimbursement rates from governmental payers, and high levels of uninsured patients. As a result, we updated the estimate of the fair values of the hospital’s long-lived assets and compared the fair value estimate to the carrying values of the hospital’s long-lived assets. Because the fair value estimate was lower than the carrying values of the hospital’s long-lived assets, an impairment charge was recorded for the difference in the amounts. Unless the anticipated future financial trends of this hospital improve to the extent that the estimated future undiscounted cash flows exceed the carrying values of the long-lived assets, this hospital is at risk of future impairments, particularly if we spend significant amounts of capital at the hospital without generating a corresponding increase in the hospital’s fair value or if the fair value of the hospital’s real estate continues to decline. We also recorded a $10 million net impairment charge for the write-down of land and buildings at the current campus of one hospital that is scheduled to move to a new, replacement campus during 2010. Our estimates of the future undiscounted cash flows from use of the current campus for several months during 2010 and from estimated disposition proceeds were less than the carrying values of the land and buildings at the current campus. We compared the estimated fair values to the carrying values and, because the fair value estimate was lower than the carrying values of the assets, an impairment charge was recorded for the difference in the amounts. The remaining net impairment and restructuring charges for the year ended December 31, 2009 include $4 million of employee severance and other related costs, a $3 million impairment charge for the write-down of a note receivable due from a buyer of one of our previously divested hospitals as a result of the buyer filing for bankruptcy, and a $3 million impairment charge for the write-down of other assets primarily related to an option to purchase certain real property near one of our hospitals that no longer has value due to the financial condition of the owner of the real property.
Year Ended December 31, 2008
During the year ended December 31, 2008, we recorded net impairment and restructuring charges of $16 million. We recorded an $8 million net impairment charge for the write-down of buildings and equipment and other long-lived assets, primarily capitalized software costs classified in other intangible assets, of two hospitals to their estimated fair values due to adverse current and anticipated future financial trends based on their most recent projections at that time. We believe the most significant factors contributing to the adverse financial trends include shifts in payer mix from commercial to governmental payers combined with reductions in reimbursement rates from governmental payers and high levels of uninsured patients. The remaining net impairment and restructuring charges for the year ended December 31, 2008 include $6 million of employee severance and other related costs, $1 million for the acceleration of stock-based compensation expense and $6 million in impairment charges for the write-down of other assets primarily due to the write-down of costs associated with an expansion project at one of our hospitals that we decided not to pursue based on unfavorable economics forecasted for the project, partially offset by a $5 million reduction in reserves recorded in prior periods.
Year Ended December 31, 2007
During the year ended December 31, 2007, net impairment and restructuring charges of $36 million included a $14 million net impairment charge primarily for the write-down of buildings and equipment and other long-lived assets, primarily capitalized software costs classified in other intangible assets, of one hospital to its estimated fair value due to adverse current and anticipated future financial trends based on its most recent projections at that time. We believe the most significant factors contributing to the adverse financial trends included reductions in volume from insured patients due to competition and shifts in payer mix, increased uninsured patients, adverse trends in provision for doubtful accounts and reductions in reimbursement rates from governmental payers. The remaining net impairment and restructuring charges for the year ended December 31, 2007 include $18 million of employee severance and other related costs, $7 million in lease costs, $1 million for the acceleration of stock-based compensation expense and $3 million in impairment charges for the write-down of other assets, partially offset by $5 million of insurance proceeds for property damage from Hurricane Wilma and a reduction of $2 million in reserves recorded in prior periods.
94
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Accrued Restructuring Charges
The tables below are reconciliations of beginning and ending liability balances in connection with restructuring charges recorded during the years ended December 31, 2009, 2008 and 2007 in continuing and discontinued operations:
| Balances at Beginning of Period |
Restructuring Charges, Net |
Cash Payments |
Other | Balances at End of Period | |||||||||||||
| Year Ended December 31, 2009 |
|||||||||||||||||
| Continuing operations: |
|||||||||||||||||
| Lease and other costs, and employee severance-related costs in connection with hospital cost-control programs and general overhead-reduction plans |
$ | 12 | $ | 4 | $ | (9 | ) | $ | (1 | ) | $ | 6 | |||||
| Discontinued operations: |
|||||||||||||||||
| Employee severance-related costs, and other estimated costs associated with the sale or closure of hospitals and other facilities |
15 | 7 | (14 | ) | — | 8 | |||||||||||
| $ | 27 | $ | 11 | $ | (23 | ) | $ | (1 | ) | $ | 14 | ||||||
| Year Ended December 31, 2008 |
|||||||||||||||||
| Continuing operations: |
|||||||||||||||||
| Lease and other costs, and employee severance-related costs in connection with hospital cost-control programs and general overhead-reduction plans |
$ | 24 | $ | 2 | $ | (15 | ) | $ | 1 | $ | 12 | ||||||
| Discontinued operations: |
|||||||||||||||||
| Employee severance-related costs, and other estimated costs associated with the sale or closure of hospitals and other facilities |
20 | 16 | (21 | ) | — | 15 | |||||||||||
| $ | 44 | $ | 18 | $ | (36 | ) | $ | 1 | $ | 27 | |||||||
| Year Ended December 31, 2007 |
|||||||||||||||||
| Continuing operations: |
|||||||||||||||||
| Lease and other costs, and employee severance-related costs in connection with hospital cost-control programs and general overhead-reduction plans |
$ | 23 | $ | 24 | $ | (18 | ) | $ | (5 | ) | $ | 24 | |||||
| Discontinued operations: |
|||||||||||||||||
| Employee severance-related costs, and other estimated costs associated with the sale or closure of hospitals and other facilities |
16 | 14 | (10 | ) | — | 20 | |||||||||||
| $ | 39 | $ | 38 | $ | (28 | ) | $ | (5 | ) | $ | 44 | ||||||
The above liability balances at December 31, 2009 and 2008 are included in other current liabilities and other long-term liabilities in the accompanying Consolidated Balance Sheets. Cash payments to be applied against these accruals at December 31, 2009 are expected to be approximately $5 million in 2010 and $9 million thereafter. The column labeled “Other” above represents charges recorded in restructuring expense that are not recorded in the liability account, such as the acceleration of stock-based compensation expense related to severance agreements.
95
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
NOTE 6. LONG-TERM DEBT, LEASE OBLIGATIONS AND GUARANTEES
The table below shows our long-term debt as of December 31, 2009 and 2008:
| December 31, | ||||||||
| 2009 | 2008 | |||||||
| Senior notes: |
||||||||
| 6 3/ 8%, due 2011 |
$ | 65 | $ | 1,000 | ||||
| 6 1/2%, due 2012 |
57 | 600 | ||||||
| 7 3/8%, due 2013 |
1,000 | 1,000 | ||||||
| 9 7/8%, due 2014 |
100 | 1,000 | ||||||
| 9 1/4%, due 2015 |
489 | 800 | ||||||
| 6 7/8%, due 2031 |
430 | 450 | ||||||
| Senior secured notes: |
||||||||
| 9%, due 2015 |
714 | — | ||||||
| 10%, due 2018 |
714 | — | ||||||
| 8 7/8%, due 2019 |
925 | — | ||||||
| Capital leases and mortgage notes |
7 | 10 | ||||||
| Unamortized note discounts |
(227 | ) | (80 | ) | ||||
| Total long-term debt |
4,274 | 4,780 | ||||||
| Less current portion |
2 | 2 | ||||||
| Long-term debt, net of current portion |
$ | 4,272 | $ | 4,778 | ||||
Credit Agreement
We have a five-year, $800 million senior secured revolving credit facility, which matures on November 16, 2011, that is collateralized by patient accounts receivable at our acute care and specialty hospitals, and bears interest at our option based on the London Interbank Offered Rate (“LIBOR”) plus 150 basis points or Citigroup’s base rate, as defined in the credit agreement, plus 50 basis points. At December 31, 2009, there were no cash borrowings outstanding under the revolving credit facility, and we had approximately $185 million of letters of credit outstanding. Based on our eligible receivables, the borrowing capacity under the revolving credit facility was $448 million at December 31, 2009.
We are permitted under our credit agreement to grant certain liens and issue preferred stock, convertible debt and other unsecured debt subject to the terms and conditions set forth in the credit agreement, as amended. We are also permitted to incur secured refinancing debt (as defined under the credit agreement) if either (i) the aggregate amount of secured refinancing debt would not exceed $3.2 billion or (ii) the secured leverage ratio (as defined) would be less than 4.0 to 1.0 for each of the most recently ended four consecutive fiscal quarters. The credit agreement terms restricting the incurrence of secured refinancing debt are substantially similar to limitations in the indentures relating to the senior secured notes we issued in 2009, as described below.
Senior Notes
In December 2009, we completed open market repurchases of $2 million aggregate principal amount outstanding of our 63/8% senior notes due 2011 and approximately $1 million aggregate principal amount outstanding of our 91/4% senior notes due 2015 for cash of approximately $3 million. In November 2009, we completed open market repurchases of $2 million aggregate principal amount outstanding of our 91/4% senior notes due 2015 for cash of approximately $2 million. In September 2009, we repurchased approximately $8 million of additional aggregate principal amount outstanding of our 91/4% senior notes for cash of approximately $8 million. These transactions resulted in no gain or loss from early extinguishment of debt.
Also in September 2009, we purchased $300 million of the $800 million aggregate principal amount then outstanding of our 91/ 4% senior notes due 2015 for $315 million. The purchase was funded with the net proceeds from our September 2009 sale of 7% mandatory convertible preferred stock as described in Note 2. In connection with the repurchase, we paid approximately $4 million in accrued and unpaid interest. This transaction resulted in a loss from early extinguishment of debt of approximately $22 million related to the difference between the purchase prices and the par values of the purchased notes, as well as the write-off of unamortized note discounts and issuance costs associated with the notes.
In July 2009, we purchased approximately $15 million aggregate principal amount of our 6 3/8% senior notes due 2011, $32.5 million aggregate principal amount of our 6 1/2% senior notes due 2012, $0.3 million aggregate principal amount of our 9 7/8% senior notes due 2014, and $20.5 million aggregate principal amount of our 6 7/8% senior notes due 2031 for approximately $60 million. We recorded a gain from early extinguishment of debt of approximately $6 million related to the difference between the purchase prices and the par values of the purchased notes, partially offset by the write-off of unamortized note discounts, issuance costs and unrecognized interest rate hedge settlements associated with the notes.
96
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
In June 2009, we purchased approximately $900 million of the $1 billion aggregate principal amount then outstanding of our 9 7/8% senior notes due 2014 for approximately $941 million, representing approximately $900 million in principal payments and approximately $41 million in accrued and unpaid interest through the dates of purchase. We purchased the 9 7/8% senior notes with the net proceeds of approximately $881 million from our sale of new 8 7/8% senior secured notes due 2019, as described below, and cash on hand. In connection with the purchases of our 9 7/8% senior notes, we recorded a loss from early extinguishment of debt of approximately $24 million related to the write-off of unamortized note discounts and issuance costs.
In May and March 2009, we exchanged approximately $918 million aggregate principal amount of our outstanding 6 3/8% senior notes due 2011 and approximately $510 million aggregate principal amount of our outstanding 6 1/2% senior notes due 2012 for new 9% senior secured notes due 2015 and 10% senior secured notes due 2018, as described below.
All of our senior notes are general unsecured senior debt obligations that rank equally in right of payment with all of our other unsecured senior indebtedness, but are effectively subordinated to our new senior secured notes described below, the obligations of our subsidiaries and any obligations under our revolving credit facility to the extent of the collateral. We may redeem any series of our senior notes, in whole or in part, at any time at a redemption price equal to 100% of the principal amount of the notes redeemed, plus a make-whole premium specified in the applicable indenture, together with accrued and unpaid interest to the redemption date.
Senior Secured Notes
In June 2009, we sold $925 million aggregate principal amount of 8 7/8% senior secured notes due 2019. The notes will mature on July 1, 2019. We will pay interest on the 8 7/8% senior secured notes semi-annually in arrears on January 1 and July 1 of each year, commencing January 1, 2010. The notes rank equally with our 9% senior secured notes due 2015 and 10% senior secured notes due 2018, which we issued in May and March 2009, as described below.
In May 2009, we exchanged approximately $3 million aggregate principal amount of our outstanding 6 3/8% senior notes due 2011 and approximately $25 million aggregate principal amount of our outstanding 6 1/2% senior notes due 2012 for approximately $14 million aggregate principal amount of 9% senior secured notes due 2015 and approximately $14 million aggregate principal amount of 10% senior secured notes due 2018. In addition, we received approximately $6 million in cash, which represented the difference in the fair values of the tendered notes as compared to the fair values of the 9% senior secured notes and 10% senior secured notes and compensation to us for increased interest expense. In connection with the exchange, we recorded a gain from early extinguishment of debt of approximately $3 million for cash we received relating to the difference in the fair values of the tendered notes as compared to the fair values of the 9% and 10% senior secured notes, net of the write-off of unamortized note discounts, issuance costs and unrecognized interest rate hedge settlements associated with the senior notes tendered. The remaining $3 million of cash received will be amortized as a reduction of interest expense over the life of the 9% and 10% senior secured notes. The note exchange was completed with eligible holders who did not tender their notes in the March 2009 exchange offer described below.
In March 2009, we exchanged approximately $915 million aggregate principal amount of our outstanding 6 3/8% senior notes due 2011 and approximately $485 million aggregate principal amount of our outstanding 6 1 /2% senior notes due 2012 for approximately $700 million aggregate principal amount of 9% senior secured notes due 2015 and approximately $700 million aggregate principal amount of 10% senior secured notes due 2018. In connection with the exchange, we recorded a gain from early extinguishment of debt of approximately $134 million relating to the estimated fair values of the 9% and 10% senior secured notes issued at less than their par values, net of the write-off of unamortized note discounts, issuance costs and unrecognized interest rate hedge settlements associated with the senior notes tendered.
The 9% senior secured notes will mature on May 1, 2015, and the 10% senior secured notes will mature on May 1, 2018. Interest on these notes is payable semi-annually in arrears on May 1 and November 1 of each year, commencing on May 1, 2009. The 9% and 10% senior secured notes rank equally with our 8 7/8% senior secured notes due 2019.
All of our senior secured notes are guaranteed by and secured by a first-priority pledge of the capital stock and other ownership interests of certain of our subsidiaries. All of our senior secured notes and the related subsidiary guarantees are our and the subsidiary guarantors’ senior secured obligations. Our senior secured notes rank senior to any subordinated indebtedness that we or such subsidiary guarantors may incur; they are effectively senior to our and such subsidiary guarantors’ existing and future unsecured indebtedness and other liabilities to the extent of the value of the collateral securing the notes and the subsidiary guarantees; they are effectively subordinated to our and such subsidiary guarantors’ obligations under our revolving credit facility to the extent of the value of the collateral securing borrowings thereunder; and they are structurally subordinated to all obligations of our non-guarantor subsidiaries.
97
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The indentures setting forth the terms of our senior secured notes contain provisions limiting our ability to redeem the notes and the terms by which we may do so. At any time or from time to time prior to the date specified in the applicable indenture – July 1, 2014 in the case of the 8 7/8% senior secured notes and May 1, 2012 in the case of the 9% and 10% senior secured notes – we, at our option, may redeem up to 35% of the aggregate principal amount of any of these series of senior secured notes with the net cash proceeds of one or more qualified equity offerings (as defined in the applicable indenture) at a redemption price equal to a specified percentage – 108.875% in the case of the 8 7/ 8% senior secured notes, 109% in the case of the 9% senior secured notes and 110% in the case of the 10% senior secured notes – of the principal amount of the notes to be redeemed, plus accrued and unpaid interest thereon, if any, to the date of redemption. In addition, we, at our option, may redeem any series of our senior secured notes, in whole or in part, at any time on or prior to the date specified in the applicable indenture – July 1, 2014 in the case of the 8 7/8% senior secured notes, May 1, 2012 in the case of the 9% senior secured notes and May 1, 2014 in the case of the 10% senior secured notes – at a redemption price equal to 100% of the principal amount of the notes redeemed plus the applicable make-whole premium set forth in the applicable indenture, together with accrued and unpaid interest thereon, if any, to the redemption date. At any time or from time to time after July 1, 2014 in the case of the 8 7/8% senior secured notes, May 1, 2012 in the case of the 9% senior secured notes and May 1, 2014 in the case of the 10% senior secured notes, we, at our option, may redeem the notes, in whole or in part, at the redemption prices set forth in the applicable indenture, together with accrued and unpaid interest thereon, if any, to the redemption date.
In addition, we may be required to purchase for cash all or any part of each series of our senior secured notes upon the occurrence of a change of control (as defined in the applicable indentures) for a cash purchase price of 101% of the aggregate principal amount of the notes, plus accrued and unpaid interest
Covenants
Our revolving credit agreement contains customary covenants for an asset-backed facility, including a minimum fixed charge coverage ratio to be met when the available credit under the facility falls below $100 million, as well as limits on debt, asset sales and prepayments of senior debt. The revolving credit agreement also includes a provision, which we believe is customary in receivables-backed credit facilities, that gives our banks the right to require that proceeds of collections of substantially all of our consolidated accounts receivable be applied directly to repay outstanding loans and other amounts that are due and payable under the revolving credit facility at any time that unused borrowing availability under the revolving credit facility is less than $100 million or if an event of default has occurred and is continuing thereunder. In that event, we would seek to re-borrow under the revolving credit facility to satisfy our operating cash requirements. Our ability to borrow under the revolving credit facility is subject to conditions that we believe are customary in such facilities, including that no events of default then exist.
The indentures governing our senior notes contain covenants and conditions that have, among other requirements, limitations on (1) liens on principal properties and (2) sale and lease-back transactions with respect to principal properties. A principal property is defined in the indentures as a hospital that has an asset value on our books in excess of 5% of our consolidated net tangible assets, as defined. The above limitations do not apply, however, to (1) debt that is not secured by principal properties or (2) debt that is secured by principal properties if the aggregate of such secured debt does not exceed 15% of our consolidated net tangible assets, as further described in the indentures. The indentures also prohibit the consolidation, merger or sale of all or substantially all assets unless no event of default would result after giving effect to such transaction.
The indentures governing our senior secured notes contain covenants that, among other things, restrict our ability and the ability of our subsidiaries to incur liens, consummate asset sales, enter into sale and lease-back transactions or consolidate, merge or sell all or substantially all of our or their assets, other than in certain transactions between one or more of our wholly owned subsidiaries. These restrictions, however, are subject to a number of important exceptions and qualifications. In particular, there are no restrictions on our ability or the ability of our subsidiaries to incur additional indebtedness, make restricted payments, pay dividends or make distributions in respect of capital stock, purchase or redeem capital stock, enter into transactions with affiliates or make advances to, or invest in, other entities (including unaffiliated entities). In addition, the indentures governing our senior secured notes contain a covenant that neither we nor any of our subsidiaries will incur secured debt, unless at the time of and after giving effect to the incurrence of such debt, the aggregate amount of all such secured debt (including the aggregate principal amount of senior secured notes outstanding at such time) does not exceed the greater of (i) $3.2 billion or (ii) the amount that would cause the secured debt ratio (as defined in the indentures) to exceed 4.0 to 1.0; provided that the aggregate amount of all such debt secured by a lien on par to the lien securing the senior secured notes may not exceed the greater of (a) $2.6 billion or (b) the amount that would cause the secured debt ratio to exceed 3.0 to 1.0.
98
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Interest Rate Swap Agreement
We entered into an interest rate swap agreement, which became effective May 1, 2009, for an aggregate notional amount of $1 billion. The interest rate swap agreement was designated as a fair value hedge and was used to manage our exposure to future changes in interest rates. It had the effect of converting our 7 3/8% senior notes due 2013 from a fixed interest rate paid semi-annually to a variable interest rate paid monthly based on the one-month LIBOR plus a floating rate spread of approximately 5.46%. During the term of the interest rate swap agreement, changes in the fair value of the interest rate swap agreement and changes in the fair value of the 7 3/8% senior notes, which substantially offset each other, were recorded in interest expense. To mitigate risks related to potential significant increases in the one-month LIBOR, we also entered into a LIBOR cap agreement that limited the maximum one-month LIBOR to 8% under the interest rate swap agreement. We paid approximately $2 million for this limitation on interest rate exposure under the interest rate swap agreement. In November 2009, we terminated the interest rate swap agreement. We realized approximately $8 million in net savings in interest payments during the term of the interest rate swap agreement.
The fair value of the LIBOR cap agreement included in investments and other assets in the accompanying Consolidated Balance Sheets approximated $3 million at December 31, 2009. During the year ended December 31, 2009, approximately $1 million in gains from mark-to-market adjustments of the LIBOR cap agreement were included as a reduction of interest expense in the accompanying Consolidated Statements of Operations. See Note 16 for the disclosure of the fair value of the LIBOR cap agreement.
Future Maturities
Future long-term debt maturities and minimum operating lease payments as of December 31, 2009 are as follows:
| Total | Years Ending December 31, | Later Years | |||||||||||||||||||
| 2010 | 2011 | 2012 | 2013 | 2014 | |||||||||||||||||
| Long-term debt, including capital lease obligations |
$ | 4,501 | $ | 2 | $ | 67 | $ | 58 | $ | 1,001 | $ | 100 | $ | 3,273 | |||||||
| Long-term non-cancelable operating leases |
$ | 400 | $ | 99 | $ | 82 | $ | 70 | $ | 60 | $ | 26 | $ | 63 | |||||||
Rental expense under operating leases, including short-term leases, was $143 million, $136 million and $130 million in the years ended December 31, 2009, 2008 and 2007, respectively. Included in rental expense for these periods was sublease income of $17 million, $18 million and $19 million, respectively, which was recorded as a reduction to rental expense.
Physician Relocation Agreements and Other Minimum Revenue Guarantees
Consistent with our policy on physician relocation and recruitment, we provide income guarantee agreements to certain physicians who agree to relocate to our communities to fill a community need in a hospital’s service area and commit to remain in practice there for a specified period of time. Under such agreements, we are required to make payments to the physicians in excess of the amounts they earn in their practices up to the amount of the income guarantee. The income guarantee periods are typically 12 months. Such payments are recoverable from the physicians on a prorated basis if they do not fulfill their commitment period to the community, which is typically three years subsequent to the guarantee period. We also provide revenue collection guarantees to hospital-based physician groups providing certain services at our hospitals with terms generally ranging from one to three years.
At December 31, 2009, the maximum potential amount of future payments under our income and revenue collection guarantees was $95 million. We had a liability of $77 million recorded for the fair value of these guarantees included in other current liabilities at December 31, 2009.
At December 31, 2009, we also guaranteed minimum rent revenue to certain landlords who built medical office buildings on or near our hospital campuses. The maximum potential amount of future payments under these guarantees was $11 million. We had a liability of $5 million recorded for the fair value of these guarantees, of which $1 million was included in other current liabilities and $4 million was included in other long-term liabilities at December 31, 2009.
99
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
NOTE 7. EMPLOYEE BENEFIT PLANS
Share-Based Compensation Plans
We currently grant stock-based awards to our directors and key employees pursuant to our 2008 Stock Incentive Plan, which was approved by our shareholders at their 2008 annual meeting. Under that plan, 35 million shares of common stock were approved for stock-based awards. At December 31, 2009, there were approximately 12 million shares of common stock available under our 2008 Stock Incentive Plan for future stock option grants and other incentive awards, including restricted stock units. Options have an exercise price equal to the fair market value of the shares on the date of grant and generally expire 10 years from the date of grant. A restricted stock unit is a contractual right to receive one share of our common stock in the future. Options and restricted stock units typically vest one-third on each of the first three anniversary dates of the grant.
Our income from continuing operations for the years ended December 31, 2009, 2008 and 2007 includes $23 million, $34 million and $41 million, respectively, of pretax compensation costs related to our stock-based compensation arrangements ($14 million, $22 million and $27 million, respectively, after-tax, excluding the impact of the deferred tax valuation allowance). The 2008 and 2007 pretax expense includes $1 million for stock option modification costs related to terminated employees, which are recorded in restructuring charges. The table below shows the stock option and restricted stock unit grants and other awards that comprise the $23 million of stock-based compensation expense recorded in salaries, wages and benefits in the year ended December 31, 2009. Compensation cost is measured by the fair value of the awards on their grant dates and is recognized over the requisite service period of the awards, whether or not the awards had any intrinsic value during the period.
| Grant Date |
Awards | Exercise Price Per Share |
Fair Value Per Share at Grant Date |
Stock-Based Compensation Expense for Year Ended December 31, 2009 | |||||||
| (In Thousands) | (In Millions) | ||||||||||
| Stock Options: |
|||||||||||
| February 26, 2009 |
10,930 | $ | 1.14 | $ | 0.71 | $ | 2 | ||||
| February 26, 2009 |
8,824 | 1.14 | 0.61 | 1 | |||||||
| March 6, 2008 |
3,018 | 4.94 | 2.43 | 3 | |||||||
| March 1, 2007 |
1,357 | 6.60 | 2.77 | 1 | |||||||
| Other grants |
2 | ||||||||||
| Restricted Stock Units: |
|||||||||||
| May 7, 2009 |
522 | 2.24 | 1 | ||||||||
| March 6, 2008 |
3,115 | 4.94 | 5 | ||||||||
| March 1, 2007 |
2,371 | 6.60 | 4 | ||||||||
| March 1, 2007 |
1,339 | 4.71 | 2 | ||||||||
| February 22, 2006 |
3,185 | 7.93 | 1 | ||||||||
| Other grants |
1 | ||||||||||
| $ | 23 | ||||||||||
Prior to our shareholders approving the 2008 Stock Incentive Plan, we granted stock-based awards to our directors and employees pursuant to other plans. Stock options remain outstanding under those other plans, but no additional stock-based awards will be granted under them.
Pursuant to the terms of our stock-based compensation plans, awards granted under the plans vest and may be exercised as determined by the compensation committee of our board of directors. In the event of a change in control, the compensation committee may, at its sole discretion without obtaining shareholder approval, accelerate the vesting or performance periods of the awards.
100
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Stock Options
The following table summarizes stock option activity during the years ended December 31, 2009, 2008 and 2007:
| Options | Weighted Average Exercise Price Per Share |
Aggregate Intrinsic Value |
Weighted Average Remaining Life | ||||||||
| (In Millions) | |||||||||||
| Outstanding as of December 31, 2006 |
38,690,973 | $ | 20.41 | ||||||||
| Granted |
1,418,000 | 6.60 | |||||||||
| Exercised |
(5,100 | ) | 6.25 | ||||||||
| Forfeited/Expired |
(4,142,187 | ) | 16.74 | ||||||||
| Outstanding as of December 31, 2007 |
35,961,686 | 20.28 | |||||||||
| Granted |
3,192,000 | 4.97 | |||||||||
| Exercised |
(16,666 | ) | 5.81 | ||||||||
| Forfeited/Expired |
(7,231,594 | ) | 21.50 | ||||||||
| Outstanding as of December 31, 2008 |
31,905,426 | 18.48 | |||||||||
| Granted |
22,146,180 | 1.17 | |||||||||
| Exercised |
— | — | |||||||||
| Forfeited/Expired |
(5,734,351 | ) | $ | 18.21 | |||||||
| Outstanding as of December 31, 2009 |
48,317,255 | $ | 10.58 | $ | 93 | 6.3 years | |||||
| Vested and expected to vest at December 31, 2009 |
45,549,507 | $ | 11.15 | $ | 81 | 6.1 years | |||||
| Exercisable as of December 31, 2009 |
24,154,402 | $ | 19.57 | $ | — | 3.5 years | |||||
There were no stock options exercised during the year ended December 31, 2009 and 16,666 options exercised during the year ended December 31, 2008 with a minimal aggregate intrinsic value.
As of December 31, 2009 and 2008, there were $13 million and $7 million, respectively, of total unrecognized compensation costs related to stock options. These costs are expected to be recognized over a weighted average period of 1.9 years.
The weighted average estimated fair values of stock options we granted during the year ended December 31, 2009 and 2008 were $0.67 per share and $2.44 per share, respectively. These fair values were calculated based on each grant date, using a binomial lattice model with the following assumptions:
| Years Ended December 31, | |||||||||
| 2009 | 2008 | ||||||||
| Top Eleven Employees |
All Other Employees |
All Employees | |||||||
| Expected volatility |
60 | % | 57% - 61 | % | 47 | % | |||
| Expected dividend yield |
0 | % | 0 | % | 0 | % | |||
| Expected life |
7.00 years | 5.00 years | 5.75 years | ||||||
| Expected forfeiture rate |
4 | % | 20 | % | 7 | % | |||
| Risk-free interest rate |
3.25 | % | 2.34% - 2.81 | % | 4.05% - 4.39 | % | |||
| Early exercise threshold |
75% gain | 50% gain | 100% gain | ||||||
| Early exercise rate |
20% per year | 45% per year | 20% per year | ||||||
The expected volatility used in the binomial lattice model incorporated historical and implied share-price volatility and was based on an analysis of historical prices of our stock and open-market exchanged options. The expected volatility reflects the historical volatility for a duration consistent with the contractual life of the options, and the volatility implied by the trading of options to purchase our stock on open-market exchanges. The historical share-price volatility excludes the movements in our stock price during the period October 1, 2002 through December 31, 2002 due to unique events occurring during that time, which caused extreme volatility in our stock price. The expected life of options granted is derived from the output of the binomial lattice model and represents the period of time that the options are expected to be outstanding. This model incorporates an early exercise assumption in the event of a significant increase in stock price. The risk-free interest rates are based on zero-coupon United States Treasury yields in effect at the date of grant consistent with the expected exercise timeframes.
101
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The following table summarizes information about our outstanding stock options at December 31, 2009:
| Options Outstanding | Options Exercisable | |||||||||||
| Range of Exercise Prices |
Number of Options |
Weighted Average |
Weighted Average Exercise Price |
Number of Options |
Weighted Average Exercise Price | |||||||
| $0.00 to $10.639 |
31,893,120 | 8.3 years | $ | 3.26 | 7,730,267 | $ | 8.46 | |||||
| $10.64 to $13.959 |
3,179,442 | 3.9 years | 12.15 | 3,179,442 | 12.15 | |||||||
| $13.96 to $17.589 |
3,976,324 | 2.8 years | 17.11 | 3,976,324 | 17.11 | |||||||
| $17.59 to $28.759 |
2,777,825 | 1.3 years | 27.32 | 2,777,825 | 27.32 | |||||||
| $28.76 and over |
6,490,544 | 1.6 years | 34.63 | 6,490,544 | 34.63 | |||||||
| 48,317,255 | 6.3 years | $ | 10.58 | 24,154,402 | $ | 19.57 | ||||||
As of December 31, 2009, approximately 70.4% of our outstanding options were held by current employees and approximately 29.6% were held by former employees. Approximately 51.1% of our outstanding options were in-the-money, that is, they had an exercise price less than the $5.39 market price of our common stock on December 31, 2009, and approximately 48.9% were out-of-the-money, that is, they had an exercise price of more than $5.39 as shown in the table below:
| In-the-Money Options | Out-of-the-Money Options | All Options | ||||||||||||||||
| Outstanding | % of Total | Outstanding | % of Total | Outstanding | % of Total | |||||||||||||
| Current employees |
24,704,180 | 100.0 | % | 9,328,456 | 39.5 | % | 34,032,636 | 70.4 | % | |||||||||
| Former employees |
— | — | % | 14,284,619 | 60.5 | % | 14,284,619 | 29.6 | % | |||||||||
| Totals |
24,704,180 | 100.0 | % | 23,613,075 | 100.0 | % | 48,317,255 | 100.0 | % | |||||||||
| % of all outstanding options |
51.1 | % | 48.9 | % | 100.0 | % | ||||||||||||
Restricted Stock Units
The following table summarizes restricted stock unit activity during the years ended December 31, 2009, 2008 and 2007:
| Restricted Stock Units |
Weighted Average Grant Date Fair Value Per Unit | |||||
| Unvested as of December 31, 2006 |
7,101,474 | $ | 9.31 | |||
| Granted |
5,821,924 | 6.58 | ||||
| Vested |
(3,191,794 | ) | 9.66 | |||
| Forfeited |
(1,067,790 | ) | 8.22 | |||
| Unvested as of December 31, 2007 |
8,663,814 | 7.47 | ||||
| Granted |
3,961,628 | 4.98 | ||||
| Vested |
(3,381,784 | ) | 8.39 | |||
| Forfeited |
(573,340 | ) | 6.39 | |||
| Unvested as of December 31, 2008 |
8,670,318 | 6.04 | ||||
| Granted |
542,324 | 2.35 | ||||
| Vested |
(4,069,831 | ) | 5.84 | |||
| Forfeited |
(336,370 | ) | 5.59 | |||
| Unvested as of December 31, 2009 |
4,806,441 | $ | 5.82 | |||
We granted 522,324 restricted stock units to our directors in the year ended December 31, 2009 pursuant to our director compensation program; these units vested immediately on their grant date and will be settled in shares of our common stock on the third anniversary of the date of grant or upon termination of service to the board, unless settlement has been deferred. We also granted 20,000 restricted stock units that vest ratably over three years under our 2008 Stock Incentive Plan in the year ended December 31, 2009. The fair value of all of the restricted stock units granted in 2009 was based on our share price on the grant date.
102
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The total unvested restricted stock units at December 31, 2009 includes 1,120,000 units that include cliff vesting conditions, based on the average closing price of our shares on the last 40 trading days of 2009 (a market condition grant). These units were granted in the three months ended March 31, 2007 to certain of our executives. The fair value of all of the restricted stock units that include cliff vesting conditions is $4.71 per share, which was estimated based on a Monte Carlo valuation model.
Vesting is on the third anniversary of the grant, based on the following share price criteria and is calculated on a straight-line basis for share prices between the following benchmarks:
| Average Share Price |
Vesting % | ||
| $10.25 or above |
100 | % | |
| $8.50 or above, but less than $10.25 |
66.66% -99.99 | % | |
| $6.75 or above, but less than $8.50 |
33.33% -66.66 | % | |
| Less than $6.75 |
33.33 | % |
Based on the average closing price of our shares on the last 40 trading days of 2009 of less than $6.75, 33.33% of these restricted stock units will vest during the three months ended March 31, 2010.
One exception to the above vesting criteria is that up to 700,000 restricted stock units granted to our chief executive officer vest on the third anniversary of the grant based on the average closing price of our shares on the last 40 trading days of 2009 as follows: 100,000 restricted stock units vest if the average closing price of our common stock is $6.75 or less, 400,000 restricted stock units vest if the average closing price of our common stock is at least $8.50, and 700,000 restricted stock units vest if the average closing price of our common stock is $10.25 or more. Based on the average closing price of our shares on the last 40 trading days of 2009 of less than $6.75, 100,000 restricted stock units will vest during the three months ended March 31, 2010.
The unvested restricted stock units at December 31, 2009 also include 700,000 units granted in March 2007 to a group of employees for retention purposes. The fair value of these restricted stock units was based on our share price on the grant date. These units vest 25% on each of the third, fifth, seventh and tenth anniversary dates of the grant.
As of December 31, 2009 and 2008, there were $9 million and $23 million, respectively, of total unrecognized compensation costs related to restricted stock units. These costs are expected to be recognized over a weighted average period of three years.
Restricted Stock
In January 2003, we issued 200,000 shares of restricted stock to our chief executive officer. The stock vested on the second, third and fourth anniversary dates of the grant. The following table summarizes restricted stock activity during the year ended December 31, 2007:
| Shares | Weighted Average Grant Date Fair Value Per Share | |||||
| Unvested as of December 31, 2006 |
66,667 | $ | 18.64 | |||
| Granted |
— | — | ||||
| Vested |
(66,667 | ) | 18.64 | |||
| Forfeited |
— | — | ||||
| Unvested as of December 31, 2007 |
— | $ | — | |||
Employee Stock Purchase Plan
We have an employee stock purchase plan under which we are currently authorized to issue up to 16,250,000 shares of common stock to our eligible employees. In August 2009, our board of directors amended the plan to increase the number of shares authorized to 20,250,000 subject to shareholder approval. As of December 31, 2009, there were approximately 9,509 shares available for issuance under our employee stock purchase plan. Under the terms of the plan, eligible employees may elect to have between 1% and 10% of their base earnings withheld each quarter to purchase shares of our common stock. Shares are purchased at a price equal to 95% of the closing price on the last day of the quarter. The plan requires a one-year holding period for all shares issued. The holding period does not apply upon termination of employment. Under the plan, no individual may purchase, in any year, shares with a fair market value in excess of $25,000. The plan is currently not considered to be compensatory.
103
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
We sold the following numbers of shares under our employee stock purchase plan in the years ended December 31, 2009, 2008 and 2007:
| Years Ended December 31, | |||||||||
| 2009 | 2008 | 2007 | |||||||
| Number of shares |
1,715,591 | 672,872 | 798,380 | ||||||
| Weighted average price |
$ | 1.34 | $ | 5.19 | $ | 5.15 | |||
Employee Retirement Plans
Substantially all of our employees, upon qualification, are eligible to participate in a defined contribution 401(k) plan. Under the plan, employees may contribute 1% to 75% of their eligible compensation, and we match such contributions annually up to a maximum percentage for participants actively employed as of December 31. As of January 1, 2009, the employer match was made discretionary, employees must work 1,000 hours or more during the plan year to be eligible to receive any match and the matching percentage was reduced from 3% to 1.5%. However, based on our improved profitability in 2009, we recorded, in the three months ended December 31, 2009, a $16 million discretionary contribution expense for our 401(k) plan to reward employees who are not eligible to participate in our incentive compensation plan. Plan expenses, primarily related to our contributions to the plan, were approximately $44 million, $52 million and $43 million for the years ended December 31, 2009, 2008 and 2007, respectively. Such amounts are reflected in salaries, wages and benefits in the Consolidated Statements of Operations.
We maintain one active and two frozen non-qualified defined benefit pension plans (“SERPs”) that provide supplemental retirement benefits to certain of our current and former executives. The plans are not funded, and plan obligations are paid from our working capital. Pension benefits are generally based on years of service and compensation. The following tables summarize the balance sheet impact, as well as the benefit obligations, funded status and rate assumptions associated with the SERPs based on actuarial valuations prepared as of December 31, 2009 and 2008:
| December 31, | ||||||||
| 2009 | 2008 | |||||||
| Reconciliation of funded status of plans and the amounts included in the Consolidated Balance Sheets: |
||||||||
| Projected benefit obligations(1) |
||||||||
| Beginning obligations |
$ | (245 | ) | $ | (235 | ) | ||
| Service cost |
(1 | ) | (2 | ) | ||||
| Interest cost |
(14 | ) | (14 | ) | ||||
| Actuarial loss |
(7 | ) | (12 | ) | ||||
| Benefits paid |
18 | 18 | ||||||
| Ending obligations |
(249 | ) | (245 | ) | ||||
| Fair value of plans’ assets |
— | — | ||||||
| Funded status of plans |
$ | (249 | ) | $ | (245 | ) | ||
| Amounts recognized in the Consolidated Balance Sheets consist of: |
||||||||
| Other current liability |
$ | (18 | ) | $ | (18 | ) | ||
| Other long-term liability |
(231 | ) | (227 | ) | ||||
| Accumulated other comprehensive loss |
29 | 26 | ||||||
| $ | (220 | ) | $ | (219 | ) | |||
| Assumptions: |
||||||||
| Discount rate |
5.75 | % | 5.75 | % | ||||
| Compensation increase rate |
3.00 | % | 4.00 | % | ||||
| Measurement date |
December 31, 2009 | December 31, 2008 | ||||||
| (1) | The accumulated benefit obligation at December 31, 2009 and 2008 was approximately $246 million and $242 million, respectively. |
104
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The components of net periodic benefit costs and related assumptions are as follows:
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Service costs |
$ | 1 | $ | 2 | $ | 2 | ||||||
| Interest costs |
14 | 14 | 14 | |||||||||
| Amortization of prior-year service costs |
3 | 3 | 3 | |||||||||
| Amortization of net actuarial loss |
1 | — | — | |||||||||
| Net periodic benefit cost |
$ | 19 | $ | 19 | $ | 19 | ||||||
| Assumptions: |
||||||||||||
| Discount rate |
5.75 | % | 6.25 | % | 5.75 | % | ||||||
| Long-term rate of return on assets |
n/a | n/a | n/a | |||||||||
| Compensation increase rate |
4.00 | % | 4.00 | % | 4.00 | % | ||||||
| Measurement date |
January 1, 2009 | January 1, 2008 | January 1, 2007 | |||||||||
| Census date |
January 1, 2009 | January 1, 2008 | January 1, 2007 | |||||||||
Net periodic benefit costs for the current year are based on assumptions determined at the valuation date of the prior year.
We recorded a $3 million loss adjustment, a $9 million loss adjustment and $17 million gain adjustment in other comprehensive income (loss) in the three months ended December 31, 2009, 2008 and 2007, respectively, to recognize changes in the funded status of our SERPs. Changes in the funded status are recorded as a direct increase or decrease to shareholders’ equity through accumulated other comprehensive loss. Net actuarial gains (losses) of $(7) million, $(12) million and $14 million during the years ended December 31, 2009, 2008 and 2007, respectively, and the amortization of net prior service costs of $3 million for each of the years ended December 31, 2009, 2008 and 2007 were recognized in other comprehensive income (loss). Cumulative net actuarial losses of $29 million, $23 million and $11 million and unrecognized prior service costs of $0, $3 million and $6 million as of December 31, 2009, 2008 and 2007, respectively, have not yet been recognized as components of net periodic benefit costs. During the year ending December 31, 2010, no net prior service costs are expected to be recognized as components of net periodic benefit costs.
The following table presents our estimated future benefit payments for the next five years and in the aggregate for the five years thereafter:
| Total | Years Ending December 31, | Five Years Thereafter | |||||||||||||||||||
| 2010 | 2011 | 2012 | 2013 | 2014 | |||||||||||||||||
| SERP benefit payments |
$ | 188 | $ | 18 | $ | 19 | $ | 19 | $ | 19 | $ | 19 | $ | 94 | |||||||
The SERP obligations of $249 million at December 31, 2009 are classified on the Consolidated Balance Sheet as an other current liability ($18 million) and an other noncurrent liability ($231 million) based on an estimate of the expected payment patterns.
NOTE 8. SELECTED BALANCE SHEET DETAILS
The principal components of other current assets are shown in the table below:
| December 31, | ||||||
| 2009 | 2008 | |||||
| Prepaid expenses |
$ | 70 | $ | 84 | ||
| Physician receivables and relocation agreements |
58 | 38 | ||||
| Physician and group coverage guarantees |
77 | 84 | ||||
| Disproportionate share revenue receivables |
42 | 32 | ||||
| Vendor and other nonpatient receivables |
22 | 23 | ||||
| Grant receivable related to medical residency program |
2 | 11 | ||||
| Sublease receivables |
2 | 6 | ||||
| Notes receivable from asset sales |
4 | 7 | ||||
| Other, net |
9 | 5 | ||||
| Other current assets |
$ | 286 | $ | 290 | ||
105
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Of the total amounts in other current assets, $30 million and $24 million was past due more than 90 days as of December 31, 2009 and 2008, respectively, primarily related to disproportionate share revenue receivables and vendor and other nonpatient receivables.
The principal components of property and equipment are shown in the table below:
| December 31, | ||||||||
| 2009 | 2008 | |||||||
| Land |
$ | 341 | $ | 341 | ||||
| Buildings and improvements |
3,883 | 3,805 | ||||||
| Construction in progress |
264 | 172 | ||||||
| Equipment |
2,795 | 2,768 | ||||||
| 7,283 | 7,086 | |||||||
| Accumulated depreciation and amortization |
(2,970 | ) | (2,795 | ) | ||||
| Net property and equipment |
$ | 4,313 | $ | 4,291 | ||||
Property and equipment is stated at cost, less accumulated depreciation and amortization and impairment write-downs related to assets held and used. At December 31, 2009 and 2008, we had $66 million and $59 million, respectively, of property and equipment purchases accrued for items received but not yet paid. Of these amounts, $61 million and $56 million, respectively, were included in accounts payable.
NOTE 9. GOODWILL AND OTHER INTANGIBLE ASSETS
The following table provides information on changes in the carrying amount of goodwill, which is included in the Consolidated Balance Sheets as of December 31, 2009 and 2008:
| 2009 | 2008 | |||||||
| As of January 1: |
||||||||
| Goodwill |
$ | 3,033 | $ | 3,031 | ||||
| Accumulated impairment losses |
(2,424 | ) | (2,424 | ) | ||||
| Total |
609 | 607 | ||||||
| Goodwill acquired during the year |
— | 2 | ||||||
| Goodwill allocated to assets held for sale |
(2 | ) | — | |||||
| As of December 31: |
||||||||
| Goodwill |
$ | 3,031 | 3,033 | |||||
| Accumulated impairment losses |
(2,424 | ) | (2,424 | ) | ||||
| Total |
$ | 607 | $ | 609 | ||||
The following table provides information regarding other intangible assets, which are included in the Consolidated Balance Sheets as of December 31, 2009 and 2008:
| Gross Carrying Amount |
Accumulated Amortization |
Net Book Value | ||||||||
| As of December 31, 2009: |
||||||||||
| Capitalized software costs |
$ | 563 | $ | (239 | ) | $ | 324 | |||
| Long-term debt issue costs |
72 | (17 | ) | 55 | ||||||
| Other |
1 | (1 | ) | — | ||||||
| Total |
$ | 636 | $ | (257 | ) | $ | 379 | |||
| As of December 31, 2008 |
||||||||||
| Capitalized software costs |
$ | 481 | $ | (193 | ) | $ | 288 | |||
| Long-term debt issue costs |
54 | (23 | ) | 31 | ||||||
| Other |
4 | — | 4 | |||||||
| Total |
$ | 539 | $ | (216 | ) | $ | 323 | |||
106
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Estimated future amortization of intangibles with finite useful lives as of December 31, 2009 is as follows:
| Total | Years Ending December 31, | Later Years | |||||||||||||||||||
| 2010 | 2011 | 2012 | 2013 | 2014 | |||||||||||||||||
| Amortization of intangible assets |
$ | 379 | $ | 50 | $ | 44 | $ | 36 | $ | 34 | $ | 34 | $ | 181 | |||||||
NOTE 10. INVESTMENTS AND OTHER ASSETS
The principal components of investments and other assets in our Consolidated Balance Sheets are as follows:
| December 31, | ||||||
| 2009 | 2008 | |||||
| Collateralized bonds(1) |
$ | — | $ | 56 | ||
| Marketable debt securities |
30 | 59 | ||||
| Equity investments in unconsolidated health care entities(2) |
26 | 25 | ||||
| Other |
1 | — | ||||
| Total investments |
57 | 140 | ||||
| Cash surrender value of life insurance policies |
15 | 13 | ||||
| Long-term deposits |
68 | 51 | ||||
| Land held for expansion, long-term receivables and other assets |
42 | 38 | ||||
| Investments and other assets |
$ | 182 | $ | 242 | ||
| (1) | The collateralized bonds were issued by a local hospital authority from which we leased and operated two hospitals in Dallas, Texas until August 2007. The bonds were redeemed in 2009 before their scheduled maturity, and we received $49 million of proceeds, which resulted in us recognizing a $7 million investment loss. |
| (2) | Equity earnings of unconsolidated affiliates are included in net operating revenues in the Consolidated Statements of Operations and were $6 million and $13 million in the years ended December 31, 2009 and 2008, respectively. |
Our policy is to classify investments that may be needed for cash requirements as “available-for-sale.” In doing so, the carrying values of the shares and debt instruments are adjusted at the end of each accounting period to their market values through a credit or charge to other comprehensive income (loss), net of taxes. At December 31, 2009 and 2008, there were $1 million and $4 million, respectively, of accumulated unrealized losses on these investments.
NOTE 11. ACCUMULATED OTHER COMPREHENSIVE LOSS
Our accumulated other comprehensive loss is comprised of the following:
| December 31, | ||||||||
| 2009 | 2008 | |||||||
| Unamortized realized losses from interest rate lock derivatives |
$ | (2 | ) | $ | (7 | ) | ||
| Adjustments for supplemental executive retirement plans |
(29 | ) | (26 | ) | ||||
| Unrealized losses on securities held as available-for-sale |
(1 | ) | (4 | ) | ||||
| Accumulated other comprehensive loss |
$ | (32 | ) | $ | (37 | ) | ||
There is no tax effect allocated to each component of accumulated other comprehensive loss for the years ended December 31, 2009 and 2008 due to the recording of a deferred tax asset valuation allowance since the fourth quarter of 2004.
NOTE 12. PROPERTY AND PROFESSIONAL AND GENERAL LIABILITY INSURANCE
Property Insurance
We have property, business interruption and related insurance coverage to mitigate the financial impact of catastrophic events or perils that is subject to deductible provisions based on the terms of the policies. These policies are on an occurrence basis. For the policy periods April 1, 2009 through March 31, 2010 and April 1, 2008 through March 31, 2009, we have coverage totaling $600 million per occurrence, after deductibles and exclusions, with annual aggregate sub-limits of $100 million each for floods and earthquakes and a per-occurrence sub-limit of $100 million for windstorms with no annual aggregate. With respect to fires and other perils, excluding floods, earthquakes and windstorms, the total $600 million limit of coverage per occurrence applies. Deductibles are 5% of insured values up to a maximum of $25 million for floods, California earthquakes and wind-related claims, and 2% of insured values for New Madrid fault earthquakes, with a maximum per claim deductible of $25 million. Other covered losses, including fires and other perils, have a minimum deductible of $1 million.
107
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
For the policy period April 1, 2007 through March 31, 2008, we have coverage totaling $600 million per occurrence, after deductibles and exclusions, with annual aggregate sub-limits of $100 million each for floods and earthquakes and a per-occurrence sub-limit of $100 million for windstorms with no annual aggregate. With respect to fires and other perils, excluding floods, earthquakes and windstorms, the total $600 million limit of coverage per occurrence applies. Deductibles are 5% of insured values for floods, California earthquakes and wind-related claims, and 2% of insured values for New Madrid fault earthquakes. Other covered losses, including fires and other perils, have a minimum deductible of $1 million.
Under the policies in effect for the period April 1, 2006 through March 31, 2007, we have coverage totaling $600 million per occurrence, after deductibles and exclusions, with annual aggregate sub-limits of $100 million each for windstorms, floods and earthquakes. With respect to fires and other perils, excluding windstorms, floods and earthquakes, the total $600 million limit of coverage per occurrence applies. Deductibles are 5% of insured values for wind-related claims, floods and California earthquakes, 2% of insured values for New Madrid fault earthquakes, and $1 million for fires and other perils.
Professional and General Liability Insurance
At December 31, 2009 and 2008, the aggregate current and long-term professional and general liability reserves on our Consolidated Balance Sheets were approximately $572 million and $663 million, respectively. These reserves include the reserves recorded by our captive insurance subsidiaries and our self-insured retention reserves recorded based on actuarial estimates for the portion of our professional and general liability risks, including incurred but not reported claims, for which we do not have insurance coverage. We estimated the reserves for losses and related expenses using expected loss-reporting patterns discounted to their present value under a risk-free rate approach using a Federal Reserve seven-year maturity rate of 2.69% and 3.32% at December 31, 2009 and 2008, respectively.
Self-insured retentions are determined for each claim period based on the following insurance policies in effect:
| • | Policy period June 1, 2009 through May 31, 2010—Our hospitals generally have a self-insurance retention of $5 million per occurrence for all claims incurred. Our captive insurance company, The Healthcare Insurance Corporation (“THINC”), retains $10 million per occurrence above our hospitals’ $5 million self-insurance retention level. The next $10 million of claims in excess of these aggregate self-insurance retentions of $15 million per occurrence are 65% reinsured by THINC with independent reinsurance companies, with THINC retaining 35% or a maximum of $3.5 million. Claims in excess of $25 million are covered by our excess professional and general liability insurance policies with major independent insurance companies, on a claims-made basis, subject to an aggregate limit of $175 million, with Tenet retaining 20% of the initial $50 million layer in excess of $25 million per claim or a maximum of $10 million. |
| • | Policy period June 1, 2008 through May 31, 2009—Our hospitals generally have a self-insurance retention of $5 million per occurrence for all claims incurred. THINC retains $10 million per occurrence above our hospitals’ $5 million self-insurance retention level. Claims in excess of these aggregate self-insurance retentions of $15 million per occurrence are substantially reinsured up to $25 million, with THINC retaining 30% of the next $10 million for each claim that exceeds $15 million or a maximum of $3 million. Claims in excess of $25 million are covered by our excess professional and general liability insurance policies with major independent insurance companies, on a claims-made basis, subject to an aggregate limit of $275 million. |
| • | Policy period June 1, 2007 through May 31, 2008—As of January 1, 2008 and retroactive back to June 1, 2002, our hospitals generally have a self-insurance retention per occurrence of $5 million for claims incurred during this policy period. Our captive insurance company, THINC, has a self-insured retention of $10 million per occurrence above our hospitals’ $5 million self-insurance retention level. Prior to January 1, 2008, our hospitals generally had a self-insured retention of $2 million per occurrence, with THINC retaining the next $13 million per occurrence. In each case, the next $10 million of claims in excess of $15 million are 100% reinsured by THINC with independent reinsurance companies. Claims in excess of $25 million are covered by our excess professional and general liability insurance policies from major independent insurance companies, on a claims-made basis, subject to an aggregate limit of $275 million. |
| • | Policy period June 1, 2006 through May 31, 2007—Our hospitals generally have a self-insurance retention per occurrence of $5 million for claims incurred during this policy period. THINC has a self-insured retention of $10 million per occurrence above our hospitals’ $5 million self-insurance retention level. Prior to January 1, 2008, our hospitals generally had a self-insured retention of $2 million per occurrence, with THINC retaining the next $13 million per occurrence. In each case, the next $10 million of claims in excess of $15 million are 100% reinsured by THINC with independent reinsurance companies. Claims in excess of $25 million are covered by our excess professional and general liability insurance policies from major independent insurance companies, on a claims-made basis, subject to an aggregate limit of $275 million. |
108
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
If the aggregate limit of any of our excess professional and general liability policies is exhausted, in whole or in part, it could deplete or reduce the excess limits available to pay any other material claims applicable to that policy period.
Included in other operating expenses, net, in the accompanying Consolidated Statements of Operations is malpractice expense of $89 million, $126 million and $162 million for the years ended December 31, 2009, 2008 and 2007, respectively.
NOTE 13. CLAIMS AND LAWSUITS
Because we provide health care services in a highly regulated industry, we have been and expect to continue to be subject to various lawsuits, claims and regulatory proceedings from time to time. The ultimate resolution of these matters, individually or in the aggregate, whether as a result of litigation or settlement, could have a material adverse effect on our business (both in the near and long term), financial condition, results of operations or cash flows. We are currently a party to, or have recently resolved, various legal proceedings, including those noted below. Where specific amounts are sought in any pending matter, those amounts are disclosed. For all other matters, where a loss is reasonably possible and estimable, an estimate of the loss or a range of loss is provided. Where no estimate is provided, a loss is not reasonably possible or an amount of loss is not reasonably estimable at this time.
| 1. | Governmental Reviews—Pursuant to the five-year corporate integrity agreement (“CIA”) we entered into with the Office of Inspector General (“OIG”) of the U.S. Department of Health and Human Services in September 2006, we notified the OIG in October 2007 that we had completed a preliminary review of admissions to our inpatient rehabilitation unit at South Fulton Medical Center in East Point, Georgia that suggested further review was necessary to determine whether South Fulton had received Medicare overpayments reportable under our CIA. In January 2008, we submitted this matter into the OIG’s voluntary self-disclosure protocol. The OIG subsequently accepted our submission. In February 2009, we received a letter from the U.S. Department of Justice (“DOJ”), which is participating in this matter with the OIG, requesting additional information regarding the basis for our self-disclosure, as well as information related to admissions at our other active and divested inpatient rehabilitation hospitals and units for the period 2000 to the date of the letter. The government has since limited the scope of its review to the period May 2005 through December 31, 2007. In addition, the government asked to examine a limited sample of patient files at two inpatient rehabilitation facilities besides South Fulton Medical Center before it determines if its review should extend to our other inpatient rehabilitation units. That examination has been completed, and we are continuing to work with the DOJ and the OIG regarding their review. |
Separately, in 2009, the DOJ, through the U.S. Attorney’s Office in the Western District of New York, and the OIG contacted a number of hospitals, including one Tenet hospital, requesting information regarding their billing practices for kyphoplasty procedures. Kyphoplasty is a surgical procedure used to treat pain and related conditions associated with certain vertebrae injuries. The DOJ and the OIG requested the information in connection with their review of the appropriateness of Medicare patients receiving kyphoplasty procedures on an inpatient basis as opposed to an outpatient basis. To date, the request has been limited to only one of our hospitals. We are fully cooperating with the DOJ and the OIG, and have provided the requested information on a voluntary basis. We are unable to predict the timing and outcome of the investigation, which is still in its preliminary stages at this time. However, based on the total number of inpatient kyphoplasty procedures conducted during the review period at the hospital subject to the information request, we do not believe the outcome of this review will have a material adverse impact on us.
In addition, in February 2009, the fiscal intermediary for our Florida Medical Center began a probe review of the group billing practices of that facility’s partial hospitalization program, a psychiatric treatment program that had the capacity to treat 15 patients on an outpatient basis. We also examined the records reviewed by the fiscal intermediary and independently determined that patients had multiple outpatient admissions with lengths of stay longer than expected for this program. As a result of our review of this matter, we closed the program and, pursuant to our CIA, notified the OIG about our findings. We have since engaged an external physician expert to assess the medical necessity and length of stay of the admissions in question.
We are unable to predict the timing and outcome of these pending governmental reviews at this time. However, based on the status of these matters to date, we have recorded reserves of approximately $24 million as of December 31, 2009. (We recorded $5 million as of December 31, 2008 and $19 million in the year ended December 31, 2009.)
109
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
| 2. | Pending Wage and Hour Actions—We have been defending two coordinated lawsuits in Los Angeles Superior Court alleging that our hospitals violated certain provisions of California’s labor laws and applicable wage and hour regulations. The cases are: McDonough, et al. v. Tenet Healthcare Corporation and Tien, et al. v. Tenet Healthcare Corporation. The plaintiffs in both cases have sought back pay, statutory penalties, interest and attorneys’ fees. In June 2008, motions for class certification in the McDonough and Tien cases, which we opposed, were initially granted in part and denied in part. We filed a motion for reconsideration of the court’s class certification ruling and, in November 2008, the court issued a reconsidered ruling denying class certification with respect to all of the plaintiffs’ claims, except with respect to one subclass later dismissed by the plaintiffs. In February 2009, the plaintiffs filed a notice of appeal of the court’s decision. We continue to believe the court’s November 2008 ruling was correct and are defending that ruling on appeal. |
| 3. | Class Action Lawsuits Resulting from Hurricane Katrina—We are presently defending three lawsuits filed as purported class actions in late 2005 by and on behalf of patients, their family members and others who were present and allegedly injured at two of our New Orleans area hospitals – Memorial Medical Center and Lindy Boggs Medical Center (each of which we have since divested) – during Hurricane Katrina and its aftermath. The plaintiffs allege that the hospitals were negligent in failing to properly prepare for the storm, failing to evacuate patients ahead of the storm, and failing to have a properly configured emergency generator system, among other allegations of general negligence. The plaintiffs are seeking damages in various and unspecified amounts for the alleged wrongful death of some patients, aggravation of pre-existing illnesses or injuries to patients who survived and were successfully evacuated, and the inability of patients and others to evacuate the hospitals for several days under conditions of extreme heat. In September 2008, class certification was granted in two of the suits. In her order, the judge certified a class of all persons at Memorial between August 29 and September 2, 2005, excluding employees, who sustained injuries or died, as well as family members who themselves sustained injury as a result of such injuries or deaths to any person at Memorial, excluding employees, during that time. Our appeals of the class certification ruling were exhausted in December 2009. The Civil District Court for the Parish of Orleans will administer the class proceedings. The class certification hearing in the remaining case, which was also filed in the Civil District Court for the Parish of Orleans, has been scheduled for late October 2010. We are unable to predict the ultimate resolution of these lawsuits, but we intend to continue to vigorously defend the hospitals in these matters. |
| 4. | Tax Disputes—See Note 14 for information concerning disputes with the Internal Revenue Service (“IRS”) regarding our federal tax returns. Our hospitals are also routinely subject to sales and use tax audits and personal property tax audits by the state and local government jurisdictions in which they do business. The results of the audits are frequently disputed, and such disputes are ordinarily resolved by administrative appeals or litigation. |
| 5. | Ordinary Course Matters—In addition to the matters described above, our hospitals are subject to investigations, claims and lawsuits in the ordinary course of our business. Most of these matters involve allegations of medical malpractice or other injuries suffered at our hospitals. |
| 6. | Matters Resolved in 2009—In September 2009, the U.S. Court of Appeals for the Eleventh Circuit upheld a lower court’s decision to dismiss a civil action, which was originally filed in the federal district court in Miami in March 2005, that principally alleged that Tenet’s past pricing policies and receipt of Medicare outlier payments violated the federal Racketeer Influenced and Corrupt Organizations Act. |
In May 2009, we received final approval of a settlement in two wage and hour matters – Pagaduan v. Fountain Valley Regional Medical Center, which was pending in Los Angeles Superior Court, and Falck v. Tenet Healthcare Corporation, which was pending in the U.S. District Court for the Central District of California. These lawsuits, which were certified as class actions in February 2008, specifically involved allegations regarding unpaid overtime. Although we believed our California hospitals’ overtime payments complied with state and federal law, we entered into the settlement in late 2008, though we did not admit any wrongdoing. Under the terms of the settlement and based on claims received and approved, our total liability (including the employer’s share of taxes on claims paid) was approximately $81 million, and we recorded an accrual of that amount as an estimated liability for these actions. (We recorded $6 million in the three months ended June 30, 2009, $47 million in the three months ended March 31, 2008, $10 million in the three months ended December 31, 2007 and $18 million in prior years.) We paid the settlement in full in the three months ended September 30, 2009.
In March 2009, we completed the sale of USC University Hospital and USC Kenneth Norris Jr. Cancer Hospital. That sale resolved the pending lawsuit filed by the University of Southern California in August 2006 against a Tenet subsidiary seeking to terminate a ground lease and a development and operating agreement between the University and our subsidiary, which built, owned and operated USC University Hospital.
110
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
New claims or inquiries may be initiated against us from time to time. These matters could (1) require us to pay substantial damages or amounts in judgments or settlements, which individually or in the aggregate could exceed amounts, if any, that may be recovered under our insurance policies where coverage applies and is available, (2) cause us to incur substantial expenses, (3) require significant time and attention from our management, and (4) cause us to close or sell hospitals or otherwise modify the way we conduct business.
We record reserves for claims and lawsuits when they are probable and can be reasonably estimated. For matters where the likelihood or extent of a loss is not probable or cannot be reasonably estimated, we have not recognized the potential liabilities that may result in the accompanying Consolidated Financial Statements.
The table below presents reconciliations of the beginning and ending liability balances in connection with legal settlements and other costs recorded during the years ended December 31, 2009, 2008 and 2007:
| Balances at Beginning of Period |
Litigation and Investigation Costs (Benefit) |
Cash (Payments) Receipts |
Other | Balances at End of Period | ||||||||||||||
| Year Ended December 31, 2009 |
||||||||||||||||||
| Continuing operations |
$ | 240 | $ | 31 | $ | (181 | ) | $ | 5 | $ | 95 | |||||||
| Discontinued operations |
— | — | — | — | — | |||||||||||||
| $ | 240 | $ | 31 | $ | (181 | ) | $ | 5 | $ | 95 | ||||||||
| Year Ended December 31, 2008 |
||||||||||||||||||
| Continuing operations |
$ | 282 | $ | 41 | $ | (83 | ) | $ | — | $ | 240 | |||||||
| Discontinued operations |
— | (39 | ) | 39 | — | — | ||||||||||||
| $ | 282 | $ | 2 | $ | (44 | ) | $ | — | $ | 240 | ||||||||
| Year Ended December 31, 2007 |
||||||||||||||||||
| Continuing operations |
$ | 321 | $ | 13 | $ | (51 | ) | $ | (1 | ) | $ | 282 | ||||||
| Discontinued operations |
1 | — | (1 | ) | — | — | ||||||||||||
| $ | 322 | $ | 13 | $ | (52 | ) | $ | (1 | ) | $ | 282 | |||||||
For the years ended December 31, 2009, 2008 and 2007, we recorded net costs of $31 million, $2 million and $13 million, respectively, in connection with significant legal proceedings and investigations. The 2009 costs primarily relate to reserves established in connection with the governmental reviews described above. The 2009 costs also include amounts paid to indemnify a former officer of the Company in a matter to which the Company was not a party and costs to defend the Company in various matters. The 2008 costs primarily relate to changes in our estimated liability for the now-settled wage and hour actions described above. The 2008 costs were partially offset by $6 million that was recorded as a recovery of litigation and investigation costs in continuing operations for costs we previously incurred related to our December 2004 Redding Medical Center litigation settlement. The 2009 payments primarily relate to the wage and hour settlement discussed above and payments related to our 2006 civil settlement with the federal government. The 2008 payments primarily relate to our 2006 civil settlement with the federal government, and the 2008 receipts relate to insurance recoveries associated with our December 2004 Redding Medical Center litigation settlement. The 2007 costs represent $10 million to defend ourselves in various lawsuits and investigations, and an $11 million increase in the estimated minimum liability for pending cases (primarily the now-settled wage and hour cases), offset by an $8 million reduction of reserves recorded in prior periods that were no longer considered necessary based on updated loss estimates. The 2007 payments include $24 million as part of our 2006 civil settlement with the federal government, $10 million for our settlement of an SEC investigation, $5 million of other settlement payments, and $13 million in legal and other costs to defend ourselves in other lawsuits and investigations
111
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
NOTE 14. INCOME TAXES
The provision for income taxes for continuing operations for the years ended December 31, 2009, 2008 and 2007 consists of the following:
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Current tax expense (benefit): |
||||||||||||
| Federal |
$ | (53 | ) | $ | (1 | ) | $ | (78 | ) | |||
| State |
11 | (9 | ) | 13 | ||||||||
| (42 | ) | (10 | ) | (65 | ) | |||||||
| Deferred tax expense (benefit): |
||||||||||||
| Federal |
17 | (1 | ) | 20 | ||||||||
| State |
2 | (14 | ) | (16 | ) | |||||||
| 19 | (15 | ) | 4 | |||||||||
| $ | (23 | ) | $ | (25 | ) | $ | (61 | ) | ||||
A reconciliation between the amount of reported income tax expense (benefit) and the amount computed by multiplying income (loss) from continuing operations before income taxes by the statutory federal income tax rate is shown below:
| Years Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Tax expense (benefit) at statutory federal rate of 35% |
$ | 72 | $ | 19 | $ | (34 | ) | |||||
| State income taxes, net of federal income tax expense (benefit) |
10 | 4 | (4 | ) | ||||||||
| Other changes in valuation allowance |
(118 | ) | (43 | ) | 44 | |||||||
| Change in tax contingency reserves, including interest |
(24 | ) | (11 | ) | (70 | ) | ||||||
| Termination of company-owned life insurance policies |
37 | — | — | |||||||||
| Prior-year provision to return adjustment and other changes in deferred taxes, net of valuation allowance |
(1 | ) | 6 | 3 | ||||||||
| Other items |
1 | — | — | |||||||||
| $ | (23 | ) | $ | (25 | ) | $ | (61 | ) | ||||
Deferred income taxes reflect the tax effects of temporary differences between the carrying amount of assets and liabilities for financial reporting purposes and the amount used for income tax purposes. The following table discloses those significant components of our deferred tax assets and liabilities, including any valuation allowance:
| December 31, 2009 | December 31, 2008 | |||||||||||||
| Assets | Liabilities | Assets | Liabilities | |||||||||||
| Depreciation and fixed-asset differences |
$ | — | $ | 420 | $ | — | $ | 437 | ||||||
| Reserves related to discontinued operations and restructuring charges |
6 | — | 8 | — | ||||||||||
| Receivables (doubtful accounts and adjustments) |
132 | — | 98 | — | ||||||||||
| Deferred gain on debt exchanges |
— | 53 | — | — | ||||||||||
| Accruals for retained insurance risks |
256 | — | 291 | — | ||||||||||
| Intangible assets |
— | 68 | — | 44 | ||||||||||
| Other long-term liabilities |
51 | — | 75 | — | ||||||||||
| Benefit plans |
179 | — | 142 | — | ||||||||||
| Other accrued liabilities |
39 | — | 93 | — | ||||||||||
| Investments and other assets |
14 | — | 11 | — | ||||||||||
| Net operating loss carryforwards |
804 | — | 844 | — | ||||||||||
| Stock-based compensation |
98 | — | 117 | — | ||||||||||
| Other items |
49 | — | 48 | — | ||||||||||
| 1,628 | 541 | 1,727 | 481 | |||||||||||
| Valuation allowance |
(1,127 | ) | — | (1,265 | ) | — | ||||||||
| $ | 501 | $ | 541 | $ | 462 | $ | 481 | |||||||
Effective January 1, 2007, we adopted ASC 740-10-25, which prescribes a comprehensive model for the financial statement recognition, measurement, presentation and disclosure of uncertain tax positions taken or expected to be taken in income tax returns. The cumulative effect of adopting the guidance was a $178 million increase to accumulated deficit as of January 1, 2007, $142 million of which was related to an increase in the valuation allowance for deferred tax assets.
112
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The table below summarizes the total changes in unrecognized tax benefits during the years ended December 31, 2009, 2008 and 2007. The lines for additions and reductions for tax positions in 2009 and 2008 include the impact of items for which the ultimate deductibility is highly certain, but for which there is uncertainty about the timing of such deductions. Such amounts include unrecognized tax benefits that have impacted deferred tax assets and liabilities at December 31, 2009, 2008 and 2007.
| Continuing Operations |
Discontinued Operations |
Total | ||||||||||
| Balance at January 1, 2007 |
$ | 119 | $ | 80 | $ | 199 | ||||||
| Additions for prior-year tax positions |
2 | — | 2 | |||||||||
| Reductions for tax positions of prior years |
(66 | ) | (11 | ) | (77 | ) | ||||||
| Additions for current-year tax positions |
6 | — | 6 | |||||||||
| Reductions for current-year tax positions |
— | — | — | |||||||||
| Reductions due to settlements with taxing authorities |
(3 | ) | — | (3 | ) | |||||||
| Reductions due to a lapse of statute of limitations |
— | — | — | |||||||||
| Balance at December 31, 2007 |
58 | 69 | 127 | |||||||||
| Additions for prior-year tax positions |
22 | 1 | 23 | |||||||||
| Reductions for tax positions of prior years |
(20 | ) | (51 | ) | (71 | ) | ||||||
| Additions for current-year tax positions |
— | — | — | |||||||||
| Reductions for current-year tax positions |
— | — | — | |||||||||
| Additions (reductions) due to settlements with taxing authorities |
1 | (2 | ) | (1 | ) | |||||||
| Reductions due to a lapse of statute of limitations |
— | — | — | |||||||||
| Balance at December 31, 2008 |
$ | 61 | $ | 17 | $ | 78 | ||||||
| Additions for prior-year tax positions |
— | — | — | |||||||||
| Reductions for tax positions of prior years |
(16 | ) | (4 | ) | (20 | ) | ||||||
| Additions for current-year tax positions |
2 | — | 2 | |||||||||
| Reductions for current-year tax positions |
— | — | — | |||||||||
| Reductions due to settlements with taxing authorities |
(11 | ) | (1 | ) | (12 | ) | ||||||
| Reductions due to a lapse of statute of limitations |
(2 | ) | — | (2 | ) | |||||||
| Balance at December 31, 2009 |
$ | 34 | $ | 12 | $ | 46 | ||||||
The total amount of unrecognized tax benefits as of the date of adoption was $199 million ($119 million related to continuing operations and $80 million related to discontinued operations), all of which, if recognized, would affect our effective tax rate and income tax expense (benefit) from continuing and discontinued operations. Total accrued interest and penalties on unrecognized tax benefits as of the date of adoption were $92 million. Included in the balance of unrecognized tax benefits at January 1, 2007 is $172 million related to tax positions for which it is reasonably possible that the total amounts could significantly change during the next 12 months. This amount represents unrecognized tax benefits related to issues in dispute with the IRS and state income tax authorities and other uncertain tax positions. As a result of actions we took during the three months ended March 31, 2007, we reduced our estimated liabilities for uncertain tax positions as of January 1, 2007 by approximately $107 million, which amount included $36 million of accrued interest. This resulted in an income tax benefit of $107 million being recognized as a credit to income tax expense in the Consolidated Statements of Operations during the three months ended March 31, 2007 ($89 million of which was recognized in continuing operations and $18 million in discontinued operations). The actions to reduce our liability for uncertain tax positions could not be taken into consideration in our estimate of the liability and our assessment of the recoverability of deferred tax assets as of January 1, 2007. Accordingly, although the initial impact of establishing the $107 million estimated liability was charged directly to accumulated deficit in total equity effective January 1, 2007 and was included in the $178 million cumulative effect adjustment discussed above, the reduction of the liability was recorded as a tax benefit in the Consolidated Statement of Operations because we took the actions to reduce the estimated exposure related to the uncertain tax positions subsequent to January 1, 2007. The total amount of unrecognized tax benefits as of December 31, 2008 was $78 million ($61 million related to continuing operations and $17 million related to discontinued operations), which, if recognized, would affect our effective tax rate and income tax expense (benefit) from continuing and discontinued operations primarily by reducing our valuation allowance for deferred tax assets.
113
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
During the year ended December 31, 2009, we reduced our estimated liabilities for uncertain tax positions by $32 million ($35 million reduction related to continuing operations and $3 million increase related to discontinued operations), primarily as a result of audit settlements and the expiration of statutes of limitation. The total amount of unrecognized tax benefits as of December 31, 2009 was $46 million ($34 million related to continuing operations and $12 million related to discontinued operations), which, if recognized, would impact our effective tax rate and income tax expense (benefit) from continuing and discontinued operations, primarily by reducing our valuation allowance for deferred tax assets.
Our practice is to recognize interest and/or penalties related to income tax matters in income tax expense in our Consolidated Statements of Operations. Approximately $13 million of interest and penalties related to accrued liabilities for uncertain tax positions ($8 million related to continuing operations and $5 million related to discontinued operations) are included in our Consolidated Statement of Operations in the year ended December 31, 2009. Total accrued interest and penalties on unrecognized tax benefits as of December 31, 2009 were $50 million ($15 million related to continuing operations and $35 million related to discontinued operations).
Income tax expense in the year ended December 31, 2009 included the following: (1) an income tax benefit of $35 million in continuing operations to reduce our estimated liabilities for uncertain tax positions; (2) income tax expense of $37 million in continuing operations for termination of company-owned life insurance policies; (3) an income tax benefit of $112 million in continuing operations to decrease the valuation allowance for our deferred tax assets and for other tax adjustments; (4) income tax expense of $3 million in discontinued operations to increase our estimated liabilities for uncertain tax positions; and (5) income tax expense of $11 million in discontinued operations to increase the valuation allowance and for other tax adjustments.
Income tax benefit in the year ended December 31, 2008 included the following: (1) an income tax benefit of $27 million in continuing operations to reduce our estimated liabilities for uncertain tax positions; (2) an income tax benefit of $29 million in continuing operations to decrease the valuation allowance for our deferred tax assets and for other tax adjustments; (3) an income tax benefit of $3 million in discontinued operations to reduce our estimated liabilities for uncertain tax positions; and (4) income tax expense of $15 million in discontinued operations to increase the valuation allowance and for other tax adjustments.
In connection with an audit of our tax returns for the fiscal years ended May 31, 1998 through the transition period ended December 31, 2002, the IRS issued a statutory notice of tax deficiency asserting an aggregate tax deficiency of $204 million plus interest. This amount does not include an advance tax payment of $85 million we made in December 2006, an overpayment by us of $20 million for one of the years in the audit period, and the impact of our net operating losses from 2004, which would reduce the tax deficiency by $31 million. We have reached a settlement with IRS counsel of all disputed issues in this case. The settlement is subject to approval by the Tax Court and resulted in a payment of approximately $60 million in December 2009 to satisfy accrued taxes and interest.
The IRS has completed its audit of our tax returns for calendar years 2003 through 2005. In connection with that audit, we received a refund of approximately $7 million of tax and interest in 2009 for calendar year 2003 to adjust the impact of loss carrybacks from 2004. Principal issues remaining in dispute include the deductibility of a portion of a civil settlement we paid to the federal government and depreciation expense with respect to certain capital expenditures. The ultimate resolution of the disputed issues in this audit is not expected to result in any material future tax payments due to the net operating loss in 2004.
Our tax returns for the years ended December 31, 2006 and December 31, 2007 are currently under examination by the IRS. These returns include deductions for amounts paid in connection with our 2006 civil settlement with the federal government and upon which taxes had been paid by us in previous taxable years. We filed tax refund claims to recover such previously paid taxes, and we received tax refunds of approximately $200 million as of December 31, 2009. The tax treatment of the civil settlement payments is being considered as part of the IRS’ examination. We presently cannot predict the ultimate resolution of this IRS examination, which could have a material adverse effect on our financial condition, results of operations or cash flows.
We believe we have adequately provided for all probable tax matters presented in these tax disputes, including interest. We presently cannot determine the ultimate resolution of the disputed issues.
As of December 31 2009, approximately $17 million of unrecognized federal and state tax benefits, as well as reserves for interest and penalties, may decrease in the next 12 months as a result of the settlement of audits, the filing of amended tax returns or the expiration of statutes of limitations.
114
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
At December 31, 2009, our carryforwards available to offset future taxable income consisted of (1) federal net operating loss (“NOL”) carryforwards of approximately $2.0 billion pretax expiring in 2024 to 2029, (2) approximately $25 million in alternative minimum tax credits with no expiration, and (3) general business credit carryforwards of approximately $13 million expiring in 2023 to 2029. Our ability to utilize NOL carryforwards to reduce future taxable income may be limited under Section 382 of the Internal Revenue Code if certain ownership changes in our company occur during a rolling three-year period. These ownership changes include the offering of stock by us, the purchase or sale of our stock by 5% shareholders, as defined in the Treasury regulations, or the issuance or exercise of rights to acquire our stock. If such ownership changes by 5% shareholders result in aggregate increases that exceed 50 percentage points during the three-year period, then Section 382 imposes an annual limitation on the amount of our taxable income that may be offset by the NOL carryforwards.
NOTE 15. EARNINGS PER COMMON SHARE
The table below is a reconciliation of the numerators and denominators of our basic and diluted earnings (loss) per common share calculations for income (loss) from continuing operations for the years ended December 31, 2009, 2008 and 2007. Income (loss) is expressed in millions and weighted average shares are expressed in thousands.
| Income (Loss) (Numerator) |
Weighted Average Shares (Denominator) |
Per-Share Amount |
||||||||
| Year Ended December 31, 2009 |
||||||||||
| Income available to Tenet Healthcare Corporation common shareholders for basic earnings per share |
$ | 212 | 480,240 | $ | 0.44 | |||||
| Effect of dilutive stock options, restricted stock units and mandatory convertible preferred stock |
6 | 27,037 | (0.01 | ) | ||||||
| Income available to Tenet Healthcare Corporation common shareholders for diluted earnings per share |
$ | 218 | 507,277 | $ | 0.43 | |||||
| Year ended December 31, 2008 |
||||||||||
| Income available to Tenet Healthcare Corporation common shareholders for basic earnings per share |
$ | 73 | 476,349 | $ | 0.15 | |||||
| Effect of dilutive stock options and restricted stock units |
— | 2,257 | — | |||||||
| Income available to Tenet Healthcare Corporation common shareholders for diluted earnings per share |
$ | 73 | 478,606 | $ | 0.15 | |||||
| Year ended December 31, 2007 |
||||||||||
| Loss to Tenet Healthcare Corporation common shareholders for basic earnings per share |
$ | (38 | ) | 473,405 | $ | (0.08 | ) | |||
| Effect of dilutive stock options and restricted stock units |
— | — | — | |||||||
| Loss to Tenet Healthcare Corporation common shareholders for diluted earnings per share |
$ | (38 | ) | 473,405 | $ | (0.08 | ) | |||
Stock options (in thousands) whose exercise price exceeded the average market price of our common stock and, therefore, were not included in the computation of diluted shares for the years ended December 31, 2009 and 2008 were 26,843 and 31,905 shares, respectively.
All potentially dilutive securities were excluded from the calculation of diluted loss per share for year ended December 31, 2007 because we did not report income from continuing operations. In circumstances where we do not have income from continuing operations, the effect of stock options and other potentially dilutive securities is anti-dilutive, that is, a loss from continuing operations has the effect of making the diluted loss per share less than the basic loss per share. Had we generated income from continuing operations in 2007, the effect (in thousands) of employee stock options, restricted stock units and deferred compensation units on the diluted shares calculation would have been an increase of 1,246 shares. Stock options (in thousands) whose exercise price exceeded the average market price of our common stock and, therefore, would not have been included in the computation of diluted shares if we had income from continuing operations in the year ended December 31, 2007 were 35,962 shares.
115
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
NOTE 16. FAIR VALUE MEASUREMENTS
Our financial assets and liabilities recorded at fair value on a recurring basis primarily relate to investments in available-for-sale securities held by our captive insurance subsidiaries and our derivative contracts. The following tables present information about our assets and liabilities that are measured at fair value on a recurring basis as of December 31, 2009 and 2008. The following tables also indicate the fair value hierarchy of the valuation techniques we utilized to determine such fair value. In general, fair values determined by Level 1 inputs utilize quoted prices (unadjusted) in active markets for identical assets or liabilities. We consider a security that trades at least weekly to have an active market. Fair values determined by Level 2 inputs utilize data points that are observable, such as quoted prices, interest rates and yield curves. Fair values determined by Level 3 inputs are unobservable data points for the asset or liability, and include situations where there is little, if any, market activity for the asset or liability.
| December 31, 2009 |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) | |||||||||
| Investments: |
||||||||||||
| Marketable securities—current |
$ | 11 | $ | 11 | $ | — | $ | — | ||||
| Investments in Reserve Yield Plus Fund |
2 | — | 2 | — | ||||||||
| Marketable debt securities—noncurrent |
30 | 7 | 22 | 1 | ||||||||
| $ | 43 | $ | 18 | $ | 24 | $ | 1 | |||||
| Derivative Contracts (see Note 6): |
||||||||||||
| LIBOR cap agreement asset |
$ | 3 | $ | — | $ | 3 | $ | — | ||||
| December 31, 2008 |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) | |||||||||
| Investments: |
||||||||||||
| Marketable debt securities—current |
$ | 2 | $ | 2 | $ | — | $ | — | ||||
| Investments in Reserve Yield Plus Fund |
14 | — | 14 | — | ||||||||
| Marketable debt securities—noncurrent |
59 | 33 | 25 | 1 | ||||||||
| $ | 75 | $ | 35 | $ | 39 | $ | 1 | |||||
The change in the fair value of our auction rate securities valued using significant unobservable inputs is shown below:
| Fair value recorded at December 31, 2008 |
$ | 1 | ||
| Adjustment to record reduction in estimated fair value of auction rate securities |
— | |||
| Fair value recorded at December 31, 2009 |
$ | 1 | ||
| Fair value recorded at December 31, 2007 |
$ | 2 | ||
| Adjustment to record reduction in estimated fair value of auction rate securities |
(1 | ) | ||
| Fair value recorded at December 31, 2008 |
$ | 1 | ||
At December 31, 2009, one of our captive insurance subsidiaries held $1 million of preferred stock and other securities that were distributed from auction rate securities whose auctions have failed due to sell orders exceeding buy orders. We were not required to record an other-than-temporary impairment of these securities during the year ended December 31, 2009. However, as a result of downgraded ratings on certain of our auction rate securities and an illiquid market for these securities, we recorded a realized loss of $1 million in investment earnings on our Consolidated Statement of Operations during the year ended December 31, 2008 as an other-than-temporary impairment of investments. Fair values using significant other observable inputs were determined using a combination, where applicable, of trading levels of the related operating or holding companies’ credit default swaps, other subordinated and senior securities of the issuers, expected discounted cash flows using LIBOR plus 150 to 200 basis points and a discount from par based on the issuers’ credit ratings.
At December 31, 2009, the fair value of our investments in the Reserve Yield Plus Fund was $2 million. The cost of our investment was $3 million. In mid-September 2008, the net asset value of the fund decreased below $1 per share as a result of a valuation of certain investments at zero that the fund held in a company that filed for bankruptcy. Therefore, we recorded a $1 million loss related to our then $49 million investment in the fund to recognize our pro rata share of the estimated loss in this investment. We requested the redemption of our investments in the fund and, in the year ended December 31, 2009 and three months ended December 31, 2008, we received $12 million and $34 million, respectively, of cash distributions from the fund. While we expect to receive substantially all of our remaining holdings in the fund, we cannot predict the ultimate timing of when we will receive the funds. Accordingly, we have classified our holdings as investments in the Reserve Yield Plus Fund, rather than as cash and cash equivalents, on our Consolidated Balance Sheets as of December 31, 2009 and 2008.
116
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
We adopted the provisions of ASC 820-10-05 as of January 1, 2009 for our non-financial assets and liabilities that are not permitted or required to be measured at fair value on a recurring basis. Our non-financial assets and liabilities not permitted or required to be measured at fair value on a recurring basis typically relate to long-lived assets held and used, long-lived assets held for sale and goodwill. We are now required to provide additional disclosures about fair value measurements as part of our financial statements for each major category of assets and liabilities measured at fair value on a non-recurring basis. The following table presents this information as of December 31, 2009 and indicates the fair value hierarchy of the valuation techniques we utilized to determine such fair values. In general, fair values determined by Level 1 inputs utilize quoted prices (unadjusted) in active markets for identical assets or liabilities, which generally are not applicable to non-financial assets and liabilities. Fair values determined by Level 2 inputs utilize data points that are observable, such as appraisals or established market values of comparable assets. Fair values determined by Level 3 inputs are unobservable data points for the asset or liability and include situations where there is little, if any, market activity for the asset or liability, such as internal estimates of future cash flows.
| December 31, 2009 |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) | |||||||||
| Long-lived assets held for sale |
$ | 16 | $ | — | $ | 16 | $ | — | ||||
| Long-lived assets held and used |
$ | 36 | $ | — | $ | 36 | $ | — | ||||
As described in Note 4, we recorded impairment charges in discontinued operations in the year ended December 31, 2009 of $5 million, consisting of $2 million for the write-down of long-lived assets to their estimated fair values, less estimated costs to sell, and $3 million of goodwill related to NorthShore Regional Medical Center to adjust the carrying values of assets held for sale.
As described in Note 5, we recorded impairment charges in continuing operations in the year ended December 31, 2009 of $17 million, consisting of $7 million to adjust the carrying values of buildings, equipment and other long-lived assets of one hospital to their estimated fair values and $10 million to adjust the carrying value of land and buildings at the current campus of one hospital that is scheduled to move to a new, replacement campus during 2010.
The fair value of our long-term debt is based on quoted market prices. At December 31, 2009 and 2008, the estimated fair value of our long-term debt was approximately 103.2% and 73.3%, respectively, of the carrying value of the debt.
NOTE 17. SALES OF INVESTMENTS
During the year ended December 31, 2009, we recorded a gain on sale of investment of approximately $15 million in continuing operations related to the sale of our 50% membership interest in Peoples Health Network, the company that administered the operations of Tenet Choices, Inc., our wholly owned Medicare Advantage HMO insurance subsidiary in Louisiana.
During the year ended December 31, 2008, we recorded gains on sales of investments in continuing operations of $125 million from the sale of our entire interest in Broadlane, Inc. and $14 million from the sale of our interest in a joint venture with a real estate investment trust.
NOTE 18. RECENTLY ISSUED ACCOUNTING STANDARDS
The following summarizes noteworthy recently issued accounting standards:
| • | In August 2009, the FASB issued Accounting Standards Update (“ASU”) 2009-05, an amendment to ASC 820-10, “Fair Value Measurements and Disclosures—Overall,” for the fair value measurement of liabilities. ASU 2009-05 provides clarification that in circumstances in which a quoted price in an active market for the identical liability is not available, a reporting entity is required to measure fair value using certain other valuation techniques. The guidance provided in this ASU is effective for the first reporting period (including interim periods) beginning after issuance. This ASU had no impact on our financial condition, results of operations or cash flows. |
| • | In June 2009, the FASB issued ASU 2009-17, an amendment to ASC 810, “Consolidation,” which is intended to improve financial reporting by enterprises involved with variable interest entities and to provide more relevant and reliable information to users of financial statements. We are currently evaluating the potential impact of this guidance, which will be effective for us beginning January 1, 2010, but we do not expect it to have a material impact on our financial condition, results of operations or cash flows. |
117
Table of Contents
SUPPLEMENTAL FINANCIAL INFORMATION
SELECTED QUARTERLY FINANCIAL DATA
(UNAUDITED)
| Year Ended December 31, 2009 | ||||||||||||||||
| First | Second | Third | Fourth | |||||||||||||
| Net operating revenues |
$ | 2,262 | $ | 2,229 | $ | 2,262 | $ | 2,261 | ||||||||
| Net income (loss) attributable to Tenet Healthcare Corporation common shareholders |
$ | 178 | $ | (15 | ) | $ | (3 | ) | $ | 21 | ||||||
| Earnings (loss) per share attributable to Tenet Healthcare Corporation common shareholders: |
||||||||||||||||
| Basic |
$ | 0.38 | $ | (0.03 | ) | $ | (0.01 | ) | $ | 0.04 | ||||||
| Diluted |
$ | 0.37 | $ | (0.03 | ) | $ | (0.01 | ) | $ | 0.04 | ||||||
| Year Ended December 31, 2008 | ||||||||||||||||
| First | Second | Third | Fourth | |||||||||||||
| Net operating revenues |
$ | 2,156 | $ | 2,112 | $ | 2,140 | $ | 2,177 | ||||||||
| Net income (loss) attributable to Tenet Healthcare Corporation common shareholders |
$ | (31 | ) | $ | (15 | ) | $ | 104 | $ | (33 | ) | |||||
| Earnings (loss) per share attributable to Tenet Healthcare Corporation common shareholders: |
||||||||||||||||
| Basic |
$ | (0.06 | ) | $ | (0.03 | ) | $ | 0.22 | $ | (0.07 | ) | |||||
| Diluted |
$ | (0.06 | ) | $ | (0.03 | ) | $ | 0.22 | $ | (0.07 | ) | |||||
Quarterly operating results are not necessarily indicative of the results that may be expected for the full year. Reasons for this include, but are not limited to: overall revenue and cost trends, particularly trends in patient accounts receivable collectability and associated provisions for doubtful accounts; the timing and magnitude of price changes; fluctuations in contractual allowances and cost report settlements and valuation allowances; managed care contract negotiations or terminations and payer consolidations; changes in Medicare regulations; Medicaid and other funding levels set by the states in which we operate; fluctuations in interest rates; levels of malpractice insurance expense and settlement trends; impairment of long-lived assets and goodwill; restructuring charges; losses, costs and insurance recoveries related to natural disasters; litigation and investigation costs; acquisitions and dispositions of facilities and other assets; income tax rates and valuation allowances; the timing and amounts of stock option and restricted stock unit grants to employees and directors; and changes in occupancy levels and patient volumes. Factors that affect patient volumes and, thereby, our results of operations at our hospitals and related health care facilities include, but are not limited to: the business environments, economic conditions and demographics of local communities; the number of uninsured and underinsured individuals in local communities treated at our hospitals; seasonal cycles of illness; climate and weather conditions; physician recruitment, retention and attrition; advances in technology and treatments that reduce length of stay; local health care competitors; managed care contract negotiations or terminations; any unfavorable publicity about us, which impacts our relationships with physicians and patients; and the timing of elective procedures. These considerations apply to year-to-year comparisons as well. Salaries, wages and benefits expense in the fourth quarter of 2009 includes a $16 million discretionary contribution expense for our 401(k) plan.
118
Table of Contents
| ITEM 9. | CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE |
None.
| ITEM 9A. | CONTROLS AND PROCEDURES |
We carried out an evaluation of the effectiveness of the design and operation of our disclosure controls and procedures as defined by Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934, as amended. The evaluation was performed under the supervision and with the participation of management, including our chief executive officer and chief financial officer. Based upon that evaluation, the chief executive officer and chief financial officer concluded that, as of the end of the period covered by this report, our disclosure controls and procedures are effective in accumulating and communicating, in a timely manner, the material information related to the Company (including its consolidated subsidiaries) required to be included in our periodic Securities and Exchange Commission filings.
Management’s report on internal control over financial reporting is set forth on page 78 and is incorporated herein by reference. The independent registered public accounting firm that audited the financial statements included in this report has issued an attestation report on our internal control over financial reporting as set forth on page 79 herein.
During the fourth quarter of 2009, there were no changes to our internal control over financial reporting, or in other factors, that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
| ITEM 9B. | OTHER INFORMATION |
None.
119
Table of Contents
PART III.
| ITEM 10. | DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE |
Certain information regarding our directors and our corporate governance will be included in our definitive proxy statement to be filed with the Securities and Exchange Commission not later than 120 days after the end of the fiscal year covered by this Form 10-K, and such information is incorporated herein by reference to the definitive proxy statement. Information concerning our executive officers appears under Part I of this report on Form 10-K under the caption “Business—Executive Officers.”
| ITEM 11. | EXECUTIVE COMPENSATION |
Certain information regarding compensation of our executive officers will be included in our definitive proxy statement to be filed with the Securities and Exchange Commission not later than 120 days after the end of the fiscal year covered by this report on Form 10-K, and such information is incorporated herein by reference to the definitive proxy statement.
| ITEM 12. | SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS |
Certain information regarding (1) security ownership of certain beneficial owners and management, (2) securities authorized for issuance under equity compensation plans and (3) related stockholder matters will be included in our definitive proxy statement to be filed with the Securities and Exchange Commission not later than 120 days after the end of the fiscal year covered by this report on Form 10-K, and such information is incorporated herein by reference to the definitive proxy statement.
| ITEM 13. | CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE |
Certain information on related party transactions and director independence will be included in our definitive proxy statement to be filed with the Securities and Exchange Commission not later than 120 days after the end of the fiscal year covered by this report on Form 10-K, and such information is incorporated herein by reference to the definitive proxy statement.
| ITEM 14. | PRINCIPAL ACCOUNTING FEES AND SERVICES |
Certain information regarding accounting fees and services will be included in our definitive proxy statement to be filed with the Securities and Exchange Commission not later than 120 days after the end of the fiscal year covered by this report on Form 10-K, and such information is incorporated herein by reference to the definitive proxy statement.
120
Table of Contents
PART IV.
| ITEM 15. | EXHIBITS AND FINANCIAL STATEMENT SCHEDULES |
FINANCIAL STATEMENTS
The Consolidated Financial Statements and notes thereto can be found on pages 81 through 117.
FINANCIAL STATEMENT SCHEDULES
Schedule II—Valuation and Qualifying Accounts (included on page 128).
All other schedules and financial statements of the Registrant are omitted because they are not applicable or not required or because the required information is included in the Consolidated Financial Statements or notes thereto.
EXHIBITS
| (3) | Articles of Incorporation and Bylaws |
| (a) | Amended and Restated Articles of Incorporation of the Registrant, as amended and restated May 8, 2008 (Incorporated by reference to Exhibit 3(a) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2008, filed August 5, 2008) |
| (b) | Certificate of Designation for 7.00% Mandatory Convertible Preferred Stock, par value $0.15 per share, dated September 24, 2009 (Incorporated by reference to Exhibit 4.1 to Registrant’s Current Report on Form 8-K, dated September 22, 2009 and filed September 25, 2009) |
| (c) | Restated Bylaws of the Registrant, as amended and restated effective January 12, 2009 (Incorporated by reference to Exhibit 3(a) to Registrant’s Current Report on Form 8-K, dated January 21, 2009 and filed January 23, 2009) |
| (4) | Instruments Defining the Rights of Security Holders, Including Indentures |
| (a) | Indenture, dated as of November 6, 2001, between the Registrant and The Bank of New York, as trustee (Incorporated by reference to Exhibit 4.1 to Registrant’s Current Report on Form 8-K, dated November 6, 2001 and filed November 9, 2001) |
| (b) | Second Supplemental Indenture, dated as of November 6, 2001, between the Registrant and The Bank of New York, as trustee, relating to 6 3/8% Senior Notes due 2011 (Incorporated by reference to Exhibit 4.3 to Registrant’s Current Report on Form 8-K, dated November 6, 2001 and filed November 9, 2001) |
| (c) | Third Supplemental Indenture, dated as of November 6, 2001, between the Registrant and The Bank of New York, as trustee, relating to 6 7/8% Senior Notes due 2031 (Incorporated by reference to Exhibit 4.4 to Registrant’s Current Report on Form 8-K, dated November 6, 2001 and filed November 9, 2001) |
| (d) | Fourth Supplemental Indenture, dated as of March 7, 2002, between the Registrant and The Bank of New York, as trustee, relating to 6 1/2% Senior Notes due 2012 (Incorporated by reference to Exhibit 4.3 to Registrant’s Current Report on Form 8-K, dated and filed March 7, 2002) |
| (e) | Sixth Supplemental Indenture, dated as of January 28, 2003, between the Registrant and The Bank of New York, as trustee, relating to 7 3/8% Senior Notes due 2013 (Incorporated by reference to Exhibit 4.3 to Registrant’s Current Report on Form 8-K, dated January 28, 2003 and filed January 31, 2003) |
| (f) | Seventh Supplemental Indenture, dated as of June 18, 2004, between the Registrant and The Bank of New York, as trustee, relating to 9 7/8% Senior Notes due 2014 (Incorporated by reference to Exhibit 4(a) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2004, filed August 3, 2004) |
| (g) | Eighth Supplemental Indenture, dated as of January 28, 2005, between the Registrant and The Bank of New York, as trustee, relating to 9 1/4% Senior Notes due 2015 (Incorporated by reference to Exhibit 4(g) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2004, filed March 8, 2005) |
121
Table of Contents
| (h) | Ninth Supplemental Indenture, dated as of March 3, 2009, by and among the Registrant, The Bank of New York Mellon Trust Company, N.A., as successor trustee to The Bank of New York, and the guarantors party thereto, relating to 9% senior secured notes due 2015 (Incorporated by reference to Exhibit 4.1 to Registrant’s Current Report on Form 8-K, dated March 3, 2009 and filed March 5, 2009) |
| (i) | Tenth Supplemental Indenture, dated as of March 3, 2009, by and among the Registrant, The Bank of New York Mellon Trust Company, N.A., as successor trustee to The Bank of New York, and the guarantors party thereto, relating to 10% senior secured notes due 2018 (Incorporated by reference to Exhibit 4.2 to Registrant’s Current Report on Form 8-K, dated March 3, 2009 and filed March 5, 2009) |
| (j) | Eleventh Supplemental Indenture, dated as of June 15, 2009, by and among the Registrant, The Bank of New York Mellon Trust Company, N.A., as successor trustee to The Bank of New York, and the guarantors party thereto, relating to 8 7/8% senior secured notes due 2019 (Incorporated by reference to Exhibit 4.1 to Registrant’s Current Report on Form 8-K, dated June 15, 2009 and filed June 16, 2009) |
| (10) | Material Contracts |
| (a) | Credit Agreement, dated as of November 16, 2006, among the Registrant, the lenders and issuers party thereto, Citicorp USA, Inc. as administrative agent, Bank of America, N.A. as syndication agent, Citigroup Global Markets Inc. and Banc of America Securities LLC as joint lead arrangers and joint lead book runners, and General Electric Capital Corporation and The Bank of Nova Scotia as co-documentation agents (Incorporated by reference to Exhibit 10(a) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2006, filed February 27, 2007) |
| (b) | Amendment No. 1 to Credit Agreement, dated as of June 27, 2008, among the Registrant and Citicorp USA, Inc., as administrative agent on behalf of each lender executing an acknowledgement and consent thereto (Incorporated by reference to Exhibit 10(a) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2008, filed August 5, 2008) |
| (c) | Amendment No. 2 to Credit Agreement, dated as of May 15, 2009, among the Registrant and Citicorp USA, Inc., as administrative agent on behalf of each lender executing an acknowledgement and consent thereto (Incorporated by reference to Exhibit 10(a) to Registrant’s Current Report on Form 8-K, dated May 15, 2009 and filed May 21, 2009) |
| (d) | Stock Pledge Agreement, dated as of March 3, 2009, by and among the Registrant, as pledgor, The Bank of New York Mellon Trust Company, N.A., as collateral trustee, and the other pledgors party thereto (Incorporated by reference to Exhibit 10.1 to Registrant’s Current Report on Form 8-K, dated March 3, 2009 and filed March 5, 2009) |
| (e) | Second Amendment to Stock Pledge Agreement, dated as of June 15, 2009, by and among the Registrant, as pledgor, The Bank of New York Mellon Trust Company, N.A., as collateral trustee, and the other pledgors party thereto (Incorporated by reference to Exhibit 10.1 to Registrant’s Current Report on Form 8-K, dated June 15, 2009 and filed June 16, 2009) |
| (f) | Collateral Trust Agreement, dated as of March 3, 2009, by and among the Registrant, as pledgor, The Bank of New York Mellon Trust Company, N.A., as collateral trustee, and the other pledgors party thereto (Incorporated by reference to Exhibit 10.2 to Registrant’s Current Report on Form 8-K, dated March 3, 2009 and filed March 5, 2009) |
| (g) | Exchange and Registration Rights Agreement, dated as of March 3, 2009, by and among the Registrant, Citigroup Global Markets Inc., Bank of America Securities LLC, Goldman, Sachs & Co. and Scotia Capital (USA) Inc., and the guarantors party thereto (Incorporated by reference to Exhibit 10.3 to Registrant’s Current Report on Form 8-K, dated March 3, 2009 and filed March 5, 2009) |
| (h) | Exchange and Registration Rights Agreement, dated as of June 15, 2009, by and among the Registrant, Banc of America Securities LLC, Goldman, Sachs & Co., Citigroup Global Markets Inc., Scotia Capital (USA) Inc., Barclays Capital Inc., Credit Suisse Securities (USA) LLC and Wachovia Capital Markets, LLC and the guarantors party thereto (Incorporated by reference to Exhibit 10.2 to Registrant’s Current Report on Form 8-K, dated June 15, 2009 and filed June 16, 2009) |
122
Table of Contents
| (i) | Civil Settlement Agreement, dated June 28, 2006, among the Registrant, Tenet HealthSystem HealthCorp., Tenet HealthSystem Holdings, Inc., Tenet HealthSystem Medical, Inc., OrNda Hospital Corp., the hospitals named therein and the United States of America (Incorporated by reference to Exhibit 10(b) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2007, filed February 26, 2008) |
| (j) | Corporate Integrity Agreement, dated September 27, 2006, between the Registrant and the Office of Inspector General of the U.S. Department of Health and Human Services (Incorporated by reference to Exhibit 10(a) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2006, filed November 7, 2006) |
| (k) | Second Amended and Restated Information Technology and Management Agreement, dated as of November 16, 2006, between the Registrant and Perot Systems Corporation (Incorporated by reference to Exhibit 10(d) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2006, filed February 27, 2007)• |
| (l) | Letter from the Registrant to Trevor Fetter, dated November 7, 2002 (Incorporated by reference to Exhibit 10(k) to Registrant’s Transition Report on Form 10-K for the seven-month transition period ended December 31, 2002, filed May 15, 2003)* |
| (m) | Letter from the Registrant to Trevor Fetter dated September 15, 2003 (Incorporated by reference to Exhibit 10(l) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2003, filed November 10, 2003)* |
| (n) | Letter from the Registrant to Stephen L. Newman, dated November 27, 2006 (Incorporated by reference to Exhibit 10(h) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2006, filed February 27, 2007)* |
| (o) | Letter from the Registrant to Biggs C. Porter, accepted May 22, 2006 (Incorporated by reference to Exhibit 10(a) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2006, filed August 9, 2006)* |
| (p) | Letter from the Registrant to Gary K. Ruff, accepted August 1, 2008 (Incorporated by reference to Exhibit 10(k) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
| (q) | Letter from the Registrant to Cathy Fraser, dated August 29, 2006 (Incorporated by reference to Exhibit 10(k) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2007, filed February 26, 2008)* |
| (r) | Tenet First Amended and Restated Executive Severance Plan, as amended and restated effective December 31, 2008 (Incorporated by reference to Exhibit 10(o) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
| (s) | Board of Directors Retirement Plan, effective January 1, 1985, as amended August 18, 1993, April 25, 1994 and July 30, 1997 (Incorporated by reference to Exhibit 10(q) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2003, filed on November 10, 2003)* |
| (t) | Tenet Healthcare Corporation Sixth Amended and Restated Supplemental Executive Retirement Plan, as amended and restated effective December 31, 2008 (Incorporated by reference to Exhibit 10(q) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
| (u) | Eighth Amended and Restated Tenet 2001 Deferred Compensation Plan, as amended and restated effective December 31, 2008 (Incorporated by reference to Exhibit 10(r) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
123
Table of Contents
| (v) | First Amended and Restated Tenet 2006 Deferred Compensation Plan, as amended and restated effective December 31, 2008 (Incorporated by reference to Exhibit 10(s) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
| (w) | Tenet Healthcare Corporation Second Amended and Restated 1994 Directors Stock Option Plan (Incorporated by reference to Exhibit 10(u) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2006, filed February 27, 2007)* |
| (x) | First Amended and Restated 1991 Stock Incentive Plan (Incorporated by reference to Exhibit 10(v) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2006, filed February 27, 2007)* |
| (y) | Second Amended and Restated 1995 Stock Incentive Plan (Incorporated by reference to Exhibit 10(w) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2006, filed February 27, 2007)* |
| (z) | Second Amended and Restated Tenet Healthcare Corporation 1999 Broad-Based Stock Incentive Plan (Incorporated by reference to Exhibit 10(x) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2006, filed February 27, 2007)* |
| (aa) | Fourth Amended and Restated Tenet Healthcare Corporation 2001 Stock Incentive Plan, as amended and restated effective December 31, 2008 (Incorporated by reference to Exhibit 10(x) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
| (bb) | Form of Stock Award used to evidence grants of stock options and/or restricted units under the Fourth Amended and Restated Tenet Healthcare Corporation 2001 Stock Incentive Plan (Incorporated by reference to Exhibit 10.3 to Registrant’s Current Report on Form 8-K, dated February 14, 2006 and filed February 17, 2006)* |
| (cc) | First Amended and Restated Tenet Healthcare 2008 Stock Incentive Plan, as amended and restated effective December 31, 2008 (Incorporated by reference to Exhibit 10(z) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
| (dd) | Forms of Award used to evidence (i) initial grants of restricted stock units to directors, (ii) annual grants of restricted stock units to directors, (iii) grants of stock options to executives, and (iv) grants of restricted stock units to executives, all under the First Amended and Restated Tenet Healthcare 2008 Stock Incentive Plan (Incorporated by reference to Exhibit 10(aa) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
| (ee) | Form of Award used to evidence grants of performance cash awards under the Fourth Amended and Restated Tenet Healthcare Corporation 2001 Stock Incentive Plan and the First Amended and Restated Tenet Healthcare 2008 Stock Incentive Plan† |
| (ff) | Tenet Special RSU Deferral Plan (Incorporated by reference to Exhibit 10(d) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2009, filed May 5, 2009)* |
| (gg) | First Amended Tenet Healthcare Corporation Annual Incentive Plan, as amended and restated effective December 31, 2008 (Incorporated by reference to Exhibit 10(bb) to Registrant’s Annual Report on Form 10-K for the year ended December 31, 2008, filed February 24, 2009)* |
| (hh) | Form of Indemnification Agreement entered into with each of the Registrant’s directors (Incorporated by reference to Exhibit 10(a) to Registrant’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2005, filed on November 1, 2005) |
| (21) | Subsidiaries of the Registrant† |
| (23) | Consent of Deloitte & Touche LLP† |
| (31) | Rule 13a-14(a)/15d-14(a) Certifications |
| (a) | Certification of Trevor Fetter, President and Chief Executive Officer† |
| (b) | Certification of Biggs C. Porter, Chief Financial Officer† |
124
Table of Contents
| (32) | Section 1350 Certifications of Trevor Fetter, President and Chief Executive Officer, and Biggs C. Porter, Chief Financial Officer† |
| • | Portions of this exhibit have been omitted pursuant to a request for confidential treatment submitted to the Securities and Exchange Commission. |
| * | Management contract or compensatory plan or arrangement. |
| † | Filed herewith. |
125
Table of Contents
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| TENET HEALTHCARE CORPORATION | ||||
| Date: February 22, 2010 | By: | /S/ BIGGS C. PORTER | ||
| Biggs C. Porter Chief Financial Officer (Principal Financial Officer) | ||||
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the Registrant and in the capacities and on the dates indicated.
| Date: February 22, 2010 | By: | /S/ TREVOR FETTER | ||
| Trevor Fetter President, Chief Executive Officer and Director (Principal Executive Officer) | ||||
| Date: February 22, 2010 | By: | /S/ BIGGS C. PORTER | ||
| Biggs C. Porter Chief Financial Officer (Principal Financial Officer) | ||||
| Date: February 22, 2010 | By: | /S/ DANIEL J. CANCELMI | ||
| Daniel J. Cancelmi Senior Vice President and Controller (Principal Accounting Officer) | ||||
| Date: February 22, 2010 | By: | /S/ JOHN ELLIS BUSH | ||
| John Ellis Bush Director | ||||
| Date: February 22, 2010 | By: | /S/ BRENDA J. GAINES | ||
| Brenda J. Gaines Director | ||||
| Date: February 22, 2010 | By: | /S/ KAREN M. GARRISON | ||
| Karen M. Garrison Director | ||||
126
Table of Contents
| Date: February 22, 2010 | By: | /S/ EDWARD A. KANGAS | ||
| Edward A. Kangas Director | ||||
| Date: February 22, 2010 | By: | /S/ J. ROBERT KERREY | ||
| J. Robert Kerrey Director | ||||
| Date: February 22, 2010 | By: | /S/ FLOYD D. LOOP | ||
| Floyd D. Loop, M.D. Director | ||||
| Date: February 22, 2010 | By: | /S/ RICHARD R. PETTINGILL | ||
| Richard R. Pettingill Director | ||||
| Date: February 22, 2010 | By: | /S/ JAMES A. UNRUH | ||
| James A. Unruh Director | ||||
| Date: February 22, 2010 | By: | /S/ J. MCDONALD WILLIAMS | ||
| J. McDonald Williams Director | ||||
127
Table of Contents
SCHEDULE II—VALUATION AND QUALIFYING ACCOUNTS
(In Millions)
| Balance at Beginning of Period |
Additions Charged To: | Deductions(3) | Other Items(4) |
Balance at End of Period | ||||||||||||||||
| Costs and Expenses(1)(2) |
Other Accounts(5) |
|||||||||||||||||||
| Allowance for doubtful accounts: |
||||||||||||||||||||
| Year ended December 31, 2009 |
$ | 396 | $ | 696 | $ | — | $ | (723 | ) | $ | — | $ | 369 | |||||||
| Year ended December 31, 2008 |
$ | 441 | $ | 644 | $ | — | $ | (689 | ) | $ | — | $ | 396 | |||||||
| Year ended December 31, 2007 |
$ | 498 | $ | 583 | $ | — | $ | (641 | ) | $ | 1 | $ | 441 | |||||||
| Valuation allowance for deferred tax assets |
||||||||||||||||||||
| Year ended December 31, 2009 |
$ | 1,265 | $ | (139 | ) | $ | 1 | $ | — | $ | — | $ | 1,127 | |||||||
| Year ended December 31, 2008 |
$ | 1,310 | $ | (47 | ) | $ | 2 | $ | — | $ | — | $ | 1,265 | |||||||
| Year ended December 31, 2007 |
$ | 1,224 | $ | (49 | ) | $ | 135 | $ | — | $ | — | $ | 1,310 | |||||||
| (1) | Includes amounts charged to discontinued operations. |
| (2) | Before considering recoveries on accounts or notes previously written off. |
| (3) | Accounts written off. |
| (4) | Primarily balances of businesses sold. |
| (5) | Primarily relates to the adoption of ASC 740-10-25 effective January 1, 2007. |
128
