Attached files
Table of Contents
As filed with the Securities and Exchange Commission on November 17, 2009
Registration No. 333-162347
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Amendment No. 2
to
FORM S-1
REGISTRATION STATEMENT
UNDER
THE SECURITIES ACT OF 1933
Team Health Holdings, L.L.C.
(to be converted into Team Health Holdings, Inc.)
(Exact Name of Registrant as Specified in its Charter)
| Delaware | 8099 | 36-4276525 | ||
| (State or Other Jurisdiction of Incorporation or Organization) |
(Primary Standard Industrial Classification Code Number) |
(I.R.S. Employer Identification No.) |
1900 Winston Road
Suite 300
Knoxville, Tennessee 37919
(865) 693-1000
(Address, Including Zip Code, and Telephone Number, Including Area Code, of Registrant’s Principal Executive Offices)
c/o David Jones
Chief Financial Officer
1900 Winston Road, Suite 300
Knoxville, Tennessee 37919
(865) 693-1000
(Name, Address, Including Zip Code, and Telephone Number, Including Area Code, of Agent for Service)
With Copies To:
| Edward P. Tolley III, Esq. Simpson Thacher & Bartlett LLP 425 Lexington Avenue New York, New York 10017-3954 Tel: (212) 455-2000 Fax: (212) 455-2502 |
Stephen L. Burns, Esq. Cravath, Swaine & Moore LLP Worldwide Plaza 825 Eighth Avenue New York, New York 10019-7475 Tel: (212) 474-1000 Fax: (212) 474-3700 |
Approximate date of commencement of proposed sale to the public: As soon as practicable after this Registration Statement becomes effective.
If any of the securities being registered on this form are to be offered on a delayed or continuous basis pursuant to Rule 415 under the Securities Act of 1933, check the following box. ¨
If this form is filed to register additional securities for an offering pursuant to Rule 462(b) under the Securities Act of 1933, please check the following box and list the Securities Act of 1933 registration statement number of the earlier effective registration statement for the same offering. ¨
If this form is a post-effective amendment filed pursuant to Rule 462(c) under the Securities Act of 1933, check the following box and list the Securities Act of 1933 registration statement number of the earlier effective registration statement for the same offering. ¨
If this form is a post-effective amendment filed pursuant to Rule 462(d) under the Securities Act of 1933, check the following box and list the Securities Act of 1933 registration statement number of the earlier effective registration statement for the same offering. ¨
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer or a smaller reporting company. See the definitions of “large accelerated filer,” “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Securities Exchange Act of 1934.
| Large accelerated filer | ¨ | Accelerated filer | ¨ | |||
| Non-accelerated filer | x (Do not check if a smaller reporting company) | Smaller reporting company | ¨ | |||
CALCULATION OF REGISTRATION FEE
| Title of Each Class of Securities to be Registered |
Proposed Maximum Aggregate Offering Price(1)(2) |
Amount of Registration Fee(3) | ||||
| Common Stock, par value $0.01 per share |
$ | 100,000,000 | $ | 5,580 | ||
| (1) | Includes shares of common stock that the underwriters have an option to purchase. |
| (2) | This amount represents the proposed maximum aggregate offering price of the securities registered hereunder to be sold by the Registrant and the selling shareholder. These figures are estimated solely for the purpose of calculating the registration fee pursuant to Rule 457(o) under the Securities Act of 1933, as amended. |
| (3) | This fee was previously paid on October 2, 2009. |
The Registrant hereby amends this Registration Statement on such date or dates as may be necessary to delay its effective date until the registrant shall file a further amendment which specifically states that this Registration Statement shall thereafter become effective in accordance with Section 8(a) of the Securities Act of 1933 or until this Registration Statement shall become effective on such date as the Securities and Exchange Commission, acting pursuant to Section 8(a), may determine.
Table of Contents
The information in this prospectus is not complete and may be changed. We and the selling shareholder may not sell these securities until the registration statement filed with the Securities and Exchange Commission is effective. This prospectus is not an offer to sell and it is not soliciting an offer to buy these securities in any state where the offer or sale is not permitted.
Subject to Completion. Dated November 17, 2009.
P R O S P E C T U S
Shares

Team Health Holdings, Inc.
Common Stock
This is the initial public offering of Team Health Holdings, Inc. We are offering shares of common stock. The selling shareholder identified in this prospectus is offering shares of common stock. We will not receive any of the proceeds from the sale of shares being sold by the selling shareholder.
No public market currently exists for our common stock. We estimate the initial public offering price of our common stock to be between $ and $ per share. We have applied for the listing of our common stock on The New York Stock Exchange under the symbol “TMH.”
We intend to use the net proceeds received by us from this offering principally for the repayment of indebtedness.
Investing in our common stock involves risks. See “Risk Factors” beginning on page 12 of this prospectus.
| Per Share |
Total | |||||
| Initial public offering price |
$ | $ | ||||
| Underwriting discounts and commissions |
$ | $ | ||||
| Proceeds, before expenses, to us |
$ | $ | ||||
| Proceeds, before expenses, to the selling shareholder |
$ | $ | ||||
To the extent that the underwriters sell more than shares of common stock, the underwriters have the option to purchase up to an additional shares from the selling shareholder at the initial offering price less underwriting discounts and commissions.
Neither the Securities and Exchange Commission nor any state securities commission has approved or disapproved of these securities or determined if this prospectus is truthful or complete. Any representation to the contrary is a criminal offense.
The underwriters expect to deliver the shares of common stock against payment in New York, New York on or about , 2009.
Joint Book-Running Managers
| BofA Merrill Lynch | Goldman, Sachs & Co. | Barclays Capital | Citi |
| Credit Suisse | Deutsche Bank Securities | UBS Investment Bank |
Prospectus dated , 2009
Table of Contents
You should rely only on the information contained in this prospectus or in any free writing prospectus that we authorize to be delivered to you. Neither we nor the underwriters have authorized anyone to provide you with additional or different information. If anyone provides you with additional, different or inconsistent information, you should not rely on it. We, the selling shareholder and the underwriters are not making an offer to sell these securities in any jurisdiction where an offer or sale is not permitted. You should assume that the information in this prospectus is accurate only as of the date on the cover page, regardless of the time of delivery of this prospectus or of any sale of our common stock. Our business, prospects, financial condition and results of operations may have changed since that date.
| Page | ||
| ii | ||
| ii | ||
| 1 | ||
| 12 | ||
| 36 | ||
| 38 | ||
| 39 | ||
| 40 | ||
| 41 | ||
| 42 | ||
| 45 | ||
| Management’s Discussion and Analysis of Financial Condition and Results of Operations |
47 | |
| 76 | ||
| 99 | ||
| 126 | ||
| 128 | ||
| 133 | ||
| 137 | ||
| 143 | ||
| Certain United States Federal Income and Estate Tax Consequences to Non-U.S. Holders |
145 | |
| 148 | ||
| 153 | ||
| 153 | ||
| 153 | ||
| F-1 |
Dealer Prospectus Delivery Obligation
Until , 2010 (the 25th day after the date of this prospectus), all dealers that effect transactions in these securities, whether or not participating in this offering, may be required to deliver a prospectus. This is in addition to the dealer’s obligation to deliver a prospectus when acting as an underwriter and with respect to unsold allotments or subscriptions.
i
Table of Contents
TRADEMARKS, TRADE NAMES AND SERVICE MARKS
Team Health is a registered trademark of Team Health, Inc. All other service marks, trademarks and trade names referred to in this prospectus are the property of their respective owners. Solely for convenience, our trademarks referred to in this prospectus may appear without the ® symbol, but such references are not intended to indicate, in any way, that we will not assert, to the fullest extent under applicable law, our rights or the right of the applicable licensor to these trademarks.
The market data and other statistical information used throughout this prospectus are based on independent industry publications, government publications, reports by market research firms and other published independent sources. Some data are also based on our good faith estimates, which are derived from our review of internal surveys, as well as the independent sources listed above. Although we believe these sources are reliable, we have not independently verified the information.
ii
Table of Contents
This summary highlights the information contained elsewhere in this prospectus. Because this is only a summary, it does not contain all of the information that may be important to you. We encourage you to read this entire prospectus, including “Risk Factors” and the financial statements and the notes thereto, before making an investment decision.
Unless the context otherwise requires, references in this prospectus to “TeamHealth,” “we,” “our,” “us” and the “Company” refer to Team Health Holdings, L.L.C. (“Team Health Holdings”) prior to the Corporate Conversion (as defined below) described in this prospectus, and Team Health Holdings, Inc. after the Corporate Conversion, and its consolidated subsidiaries and affiliated medical groups. The term “Team Health physicians or providers” or “affiliated providers” includes physicians and/or other healthcare providers who contract with Team Health’s affiliated entities. References to “Team Finance” refer to Team Finance LLC, a wholly-owned subsidiary of Team Health Holdings, which owns all of our businesses and operations. The historical financial statements and financial data included in this prospectus are those of Team Health Holdings and its consolidated subsidiaries.
Our Company
We believe we are one of the largest suppliers of outsourced healthcare professional staffing and administrative services to hospitals and other healthcare providers in the United States, based upon revenues and patient visits. We serve approximately 550 hospital clients and their affiliated clinics in 46 states with a team of approximately 6,100 healthcare professionals, including physicians, physician assistants and nurse practitioners. We recruit and contract with healthcare professionals who then provide professional services within third-party healthcare facilities. We are a physician-founded organization with physician leadership throughout our business and since our inception in 1979, we have provided outsourced services in hospital emergency departments, or EDs. We also provide comprehensive programs for hospital medicine (hospitalist), radiology, pediatrics and other healthcare services. For the year ended December 31, 2008, we generated net revenues less provision for uncollectibles of $1.33 billion and net earnings of $44.7 million. EDs and hospital medicine (hospitalist) represented approximately 79% of our 2008 net revenues less provision for uncollectibles, with locum tenens, radiology, pediatrics, military and other healthcare services representing approximately the remaining 21%.
EDs are a significant source of hospital inpatient admissions with a majority of admissions for key medical service lines starting in EDs, making successful management of this department critical to a hospital’s patient satisfaction rates and overall success. This dynamic, combined with the challenges involved in billing and collections and physician recruiting and retention, is a primary driver for hospitals to outsource their clinical staffing and management services to companies such as ours. For the year ended December 31, 2008, we provided services to over 7.6 million patients within our EDs. Our net revenues less provision for uncollectibles from ED contracts increased by approximately 42% from 2004 to 2008, or at a compound annual growth rate of approximately 9%. We have long-term relationships with customers under exclusive ED contracts with an approximate 98% renewal rate and 95% physician retention rate as of September 30, 2009 (calculated on a preceding 12 months basis), respectively. The EDs that we staff are generally located in larger hospitals. We believe our experience and expertise in managing the complexities of these high-volume EDs enable our hospital clients to provide higher quality and more efficient physician and administrative services. In this type of setting, we can establish stable long-term relationships, recruit and retain high quality physicians and other providers and staff, and obtain attractive payer mixes and reasonable margins.
The range of physician and non-physician staffing and administrative services that we provide to our clients includes the following:
| • | recruiting, scheduling and credential coordination for clinical and non-clinical medical professionals; |
1
Table of Contents
| • | coding, billing and collection of fees for services provided by medical professionals; |
| • | provision of experienced medical directors; |
| • | administrative support services, such as payroll, professional liability insurance coverage, continuing medical education services and management training; |
| • | risk and claims management services; and |
| • | standardized procedures. |
Industry Overview
We estimate the size of the domestic outsourced healthcare professional staffing market to be approximately $50 billion. With the increasing complexity of clinical, regulatory, managed care and reimbursement matters in today’s healthcare environment, healthcare facilities are under significant pressure from the government and private payers both to improve the quality and reduce the cost of care. Healthcare facilities seek third-party physician staffing and administrative service providers that not only can improve department quality, productivity and patient satisfaction while reducing overall costs, but also offer a breadth of staffing and management services, billing and reimbursement expertise, a reputation for regulatory compliance, financial stability and a demonstrated ability to recruit and retain qualified physicians, technicians and nurses. For example, many healthcare facilities are not oriented towards collecting large volumes of smaller dollar payments that are typical in the emergency and other specialty departments.
Since EDs represent a majority of admissions for key medical service lines, the operation of an ED has significant implications for hospitals in terms of revenue, cost, quality and the ability to grow market share. We believe the number of patient visits per ED is increasing while the number of EDs is decreasing. According to the American Hospital Association, ED visits increased at a compound annual growth rate of approximately 3%, from 92.8 million in 1997 to 120.8 million in 2007, and the average number of patient visits per ED grew at a compound annual growth rate of approximately 4%, from approximately 19,300 to approximately 27,000 over the same period. As the baby boomers and older generations above 55 years represent a larger percentage of the population (approximately 23% in 2008 and projected to be approximately 29% in 2020, according to the U.S. Census Bureau), the demand for ED services is likely to increase.
Competitive Strengths
Leading Market Position. We believe we are one of the largest providers of ED staffing and management services in the United States, based upon patient visits and revenue. We are among the top providers of hospital medicine (hospitalist) services in the country and we are a significant provider of contracted staffing of healthcare professionals for military facilities under the U.S. government’s military healthcare system.
Regional Operating Model Supported by a Centralized National Infrastructure. We are a national company serving approximately 550 hospital clients in 46 states from 12 regionally located operating units, which we believe results in responsive service and high physician retention rates. Our regional operating units are supported by our centralized national infrastructure, which we believe enables us to efficiently manage the operations and billing and collections processes and other administrative support functions. We believe our regional operating model supported by our centralized national infrastructure not only improves productivity and quality of care while reducing the cost of care, but also offers operating leverage to drive economies of scale as we continue to grow.
2
Table of Contents
High Quality Relationships with Clients and Physicians. Our local presence gives us the knowledge to optimally match physicians with our hospitals and their affiliated clinics while our national presence and centralized infrastructure enable us to provide physicians with a variety of attractive client locations, operating flexibility, advanced information and reimbursement systems and standardized procedures. This operating flexibility, combined with fewer administrative burdens on physicians and clients, has resulted in our strong physician and client retention rates of approximately 95% and 98% (each, as of September 30, 2009 calculated on a preceding 12 months basis), respectively, for our ED and hospital medicine operations which we believe to be among the highest in the industry.
Long-Term Relationships Generating Recurring Contractual Revenue. We have long-term relationships with customers under exclusive contracts. Within ED and hospital medicine, we have an approximate 98% annual renewal rate as of September 30, 2009 (calculated on a preceding 12 months basis). For ED and hospital medicine customers, the average tenure for our customers is approximately nine years, and our top 50 customers by net revenues have an average tenure with us of 13 years.
Strong and Stable Financial Profile. We believe our historically strong financial performance provides us with a competitive advantage in winning new contracts, renewing existing contracts and establishing and maintaining relationships with physicians and hospitals. Our existing customer relationships have generated a diversified revenue stream, with no one customer representing more than 2.1% of our net revenues less provision for uncollectibles for the nine months ended September 30, 2009.
Significant Investment in Proprietary Information Systems and Procedures. We have developed and maintained proprietary integrated, advanced systems that allow us to monitor and improve hospital performance, which we believe increases quality of care and patient satisfaction. As a result of these investments and the company-wide application of best practices policies, we believe our average cost per patient billed and average recruiting cost per physician and other healthcare professional are among the lowest in the industry.
Comprehensive and Effective Risk and Claims Management Programs. We have comprehensive risk and claims management programs designed to prevent or minimize medical errors and professional liability claims. Excluding the favorable effects of adjustments related to prior period reserves, professional liability costs as a percentage of net revenues less provision for uncollectibles have declined every year since our self-insurance program was implemented in 2003, from 6.6% in 2003 to 3.7% in 2008.
Experienced Management Team. Our senior management team has extensive experience in the outsourced physician staffing and administrative services industry and as a group has an average of more than 20 years of experience in the healthcare industry. In addition, our senior corporate and regional management team reflects a mix of both physician and non-physician leaders with an average of more than 25 years in the healthcare industry and 13 years of experience with us.
Our Growth Strategies
We intend to utilize our competitive strengths to capitalize on favorable industry trends, including increasing patient volumes, an aging population and increased ED visits, to grow our market share, net revenues, profitability and cash flow by:
Capitalizing on Outsourcing Opportunities to Win New Contracts. We believe we are well-positioned to capitalize on the growth in emergency medicine and our other target outsourcing markets by replacing competitors at hospitals that currently outsource their services, obtaining new contracts from healthcare facilities that do not currently outsource and expanding our present base of military facilities by successfully competing for new staffing contracts.
3
Table of Contents
Increasing Revenues from Existing Customers. We have a strong record of achieving growth in revenues from our existing customer base. We plan to continue to increase revenues from these customers by, among other things, capitalizing on increasing patient volumes, enhancing the services that we provide, improving documentation, billing and collection for services provided, cross-selling additional services to our existing customers and negotiating and implementing fee schedule increases, where appropriate.
Pursuing Selective Acquisitions. We believe our fragmented industry provides a number of attractive opportunities for acquisitions, as we estimate that approximately 75% of the ED outsourcing market is currently served by local and regional groups. We intend to continue to selectively acquire businesses that would enhance both our strategic and competitive positions and believe we are well-positioned to take advantage of, and integrate, acquisition opportunities.
Enhancing Profitability Through Our Operational Focus. Our regional operating units supported by our centralized national infrastructure is designed to continually drive operating leverage, improve efficiencies and align employee incentives to drive our growth. Furthermore, we believe our consolidated revenue platform and standardized processes related to managed care contracting, billing, coding, collection and compliance have driven a track record of strong revenue cycle management. We also believe our innovative patient safety and risk management initiatives and robust claims management processes have delivered favorable loss trends.
Increasing Revenues from Additional Clinical Areas. We believe we are well-positioned to increase our market share in the hospital medicine (hospitalist), radiology, temporary staffing or “locum tenens,” anesthesia, pediatrics and medical call center service areas due to our ability to leverage our infrastructure and existing client relationships as well as our recruiting and risk management expertise. We intend to grow our presence in these sectors by adding new clients with whom we do not currently have a relationship and cross-selling these services to our existing clients.
Risks Related to Our Business
Investing in our common stock involves substantial risk. You should carefully consider all of the information in this prospectus prior to investing in our common stock. There are several risks related to our business that are described under “Risk Factors” elsewhere in this prospectus. Among these important risks are the following:
| • | The current U.S. and global economic conditions could materially adversely affect our results of operations and business condition. |
| • | The current U.S. and state health reform legislative initiatives could adversely affect our operations and business condition. |
| • | Laws and regulations that regulate payments for medical services made by government sponsored healthcare programs could cause our revenues to decrease. |
| • | If governmental authorities determine that we violate Medicare, Medicaid or other government payer reimbursement laws or regulations, our revenues may decrease and we may have to restructure our method of billing and collecting Medicare, Medicaid or other government program payments, respectively. |
| • | We could be subject to professional liability lawsuits, some of which we may not be fully insured against or reserved for, which could adversely affect our financial condition and results of operations. |
4
Table of Contents
Our Sponsor
Investment funds associated with or designated by The Blackstone Group (the “Sponsor”) currently own, through Ensemble Parent LLC, approximately 92% of our voting membership interests. Ensemble Parent LLC is the selling shareholder in this offering. After giving effect to this offering, including the Corporate Conversion, our Sponsor, through Ensemble Parent LLC, will beneficially own approximately % of our issued and outstanding common stock (assuming no exercise of the underwriters’ option to purchase additional shares) and % of our issued and outstanding common stock (assuming full exercise of the underwriters’ option to purchase additional shares). Upon completion of this offering, the Sponsor will receive a lump sum payment of approximately $ million in the aggregate, of which the members of management who previously held Class A common units prior to the Corporate Conversion (as defined below) would receive approximately $ million in the aggregate from the Sponsor, in each case based on the mid-point of the price range set forth on the cover page of this prospectus and current interest rates. Certain of our executive officers will receive a portion of the lump sum payment from the Sponsor as follows: Dr. Massingale approximately $ , Mr. Roth approximately $ , Mr. Jones approximately $ , Mr. Sherlin approximately $ , Ms. Allen approximately $ and other members of management approximately $ in the aggregate, in each case based on the mid-point of the price range set forth on the cover page of this prospectus and current interest rates. See “Certain Relationships and Related Party Transactions.”
Team Health Holdings, L.L.C., which will be converted into Team Health Holdings, Inc. in connection with the Corporate Conversion, is a Delaware limited liability company organized on December 15, 1998. See “Corporate Conversion.” Our principal executive offices are located at 1900 Winston Road, Knoxville, Tennessee 37919, and our telephone number at that address is (865) 693-1000. Our website address is www.teamhealth.com. The information on our website is not part of this prospectus.
Corporate Conversion
In connection with this offering, Team Health Holdings, L.L.C. will convert from a Delaware limited liability company to a corporation organized under the laws of the State of Delaware (the “Corporate Conversion”). In connection with the Corporate Conversion, each class of limited liability company interests of Team Health Holdings, L.L.C. will be converted into shares of common stock of Team Health Holdings, Inc. See “Corporate Conversion” for further information regarding the Corporate Conversion.
5
Table of Contents
THE OFFERING
| Common stock we are offering |
shares |
| Common stock the selling shareholder is offering |
shares |
| Selling shareholder |
Ensemble Parent LLC, an affiliate of The Blackstone Group |
| Common stock to be outstanding immediately after this offering |
shares |
| Over-allotment option |
shares |
| Use of proceeds |
We estimate that the net proceeds to us from this offering, after deducting underwriting discounts and commissions and estimated offering expenses payable by us, will be approximately $ million. |
We will use the net proceeds from this offering received by us principally for the repayment of indebtedness.
We will not receive any proceeds from the sale of shares of common stock offered by the selling shareholder, including upon the sale of shares if the underwriters exercise their option to purchase additional shares from the selling shareholder in this offering. The selling shareholder will distribute all of the net proceeds it receives to investment funds affiliated with the Sponsor in accordance with the Ensemble Parent LLC limited liability company agreement. See “Use of Proceeds.”
| Dividend policy |
We currently expect to retain future earnings, if any, for use in the operation and expansion of our business and do not anticipate paying any cash dividends in the foreseeable future. Our ability to pay dividends on our common stock is limited by the covenants of our senior secured credit facilities as well as our 11.25% senior subordinated notes due 2013 (the “senior subordinated notes”) and may be further restricted by the terms of any future debt or preferred securities. See “Dividend Policy” and “Description of Certain Indebtedness.” |
| Risk factors |
See “Risk Factors” beginning on page 12 and other information included in this prospectus for a discussion of factors you should carefully consider before deciding to invest in our common stock. |
| Proposed NYSE symbol |
“TMH” |
Unless we indicate otherwise, all information in this prospectus assumes:
| • | no exercise by the underwriters of their option to purchase additional shares; |
6
Table of Contents
| • | an initial public offering price of $ per share, the mid-point of the price range set forth on the cover page of this prospectus; and |
| • | a conversion of all of our existing limited liability company interests into an aggregate shares of common stock prior to the consummation of this offering as described under “Corporate Conversion.” |
The number of shares of common stock to be outstanding immediately after this offering does not reflect:
| • | shares of common stock issuable upon exercise of options to be granted to our management in connection with the conversion of our limited liability company interests into shares of common stock; and |
| • | additional shares of common stock authorized and reserved for future issuance under the new stock incentive plan. See “Management—Compensation Discussion and Analysis—2009 Stock Plan.” |
7
Table of Contents
SUMMARY CONSOLIDATED FINANCIAL DATA
Team Health Holdings, Inc. (to be converted from Team Health Holdings, L.L.C. in connection with this offering) is a holding company that conducts no operations and its only material assets are the membership interests of Team Finance LLC, which in turn owns all of our businesses through its wholly owned subsidiary, Team Health, Inc. The historical financial statements and information presented in this prospectus are of Team Health Holdings and its consolidated subsidiaries.
The summary historical financial data for the fiscal years ended December 31, 2006, 2007 and 2008 have been derived from our audited historical consolidated financial statements and the notes thereto included elsewhere in this prospectus. The summary historical financial data as of and for the nine months ended September 30, 2008 and 2009 have been derived from our unaudited historical consolidated financial statements and the notes thereto included elsewhere in this prospectus. In the opinion of management, the interim financial data set forth below include all adjustments, consisting of normal recurring accruals, necessary to present fairly our financial position. Operating results for the nine months ended September 30, 2008 and 2009 are not necessarily indicative of the results that may be expected for the entire fiscal year.
The summary unaudited as adjusted balance sheet information as of September 30, 2009 has been prepared to give effect to this offering and the application of the proceeds received by us therefrom as if they had occurred on September 30, 2009. The summary unaudited as adjusted balance sheet information is for informational purposes only and does not purport to indicate balance sheet information as of any future date.
Because the data in this table is only a summary and does not provide all of the data contained in our financial statements, the information should be read in conjunction with “Selected Consolidated Financial Data,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the financial statements and the notes thereto included elsewhere in this prospectus.
| Year Ended December 31, | Nine Months Ended September 30, | ||||||||||||||||
| 2006 | 2007 | 2008 | 2008 | 2009 | |||||||||||||
| (Dollars in thousands, except per share data) | |||||||||||||||||
| Statement of Operations Data: |
|||||||||||||||||
| Net revenue less provision for uncollectibles |
$ | 1,095,387 | $ | 1,232,065 | $ | 1,331,317 | $ | 999,807 | $ | 1,074,657 | |||||||
| Cost of services rendered (exclusive of depreciation and amortization shown separately below): |
|||||||||||||||||
| Professional services expenses |
831,826 | 950,872 | 1,046,806 | 779,426 | 828,268 | ||||||||||||
| Professional liability costs |
37,642 | 21,057 | 15,247 | (2,986 | ) | 19,145 | |||||||||||
| General and administrative expenses |
103,744 | 114,476 | 116,942 | 88,277 | 93,182 | ||||||||||||
| Management fee and other expenses |
3,748 | 4,054 | 3,602 | 2,745 | 2,324 | ||||||||||||
| Impairment of intangibles |
— | — | 9,134 | — | — | ||||||||||||
| Depreciation and amortization |
23,308 | 14,823 | 17,281 | 12,559 | 14,028 | ||||||||||||
| Interest expense, net(1) |
57,813 | 55,234 | 45,849 | 34,033 | 27,671 | ||||||||||||
| Gain on extinguishment of debt |
— | — | (1,640 | ) | — | — | |||||||||||
| Transaction costs |
— | — | 2,386 | 1,805 | 578 | ||||||||||||
| Earnings from continuing operations before income taxes |
37,306 | 71,549 | 75,710 | 83,948 | 89,461 | ||||||||||||
| Provision for income taxes |
13,792 | 27,703 | 31,044 | 33,885 | 34,230 | ||||||||||||
| Earnings from continuing operations |
23,514 | 43,846 | 44,666 | 50,063 | 55,231 | ||||||||||||
8
Table of Contents
| Year Ended December 31, | Nine Months Ended September 30, |
|||||||||||||||||||
| 2006 | 2007 | 2008 | 2008 | 2009 | ||||||||||||||||
| (Dollars in thousands, except per share data) | ||||||||||||||||||||
| Loss from discontinued operations, net of taxes |
(7,049 | ) | (576 | ) | — | — | — | |||||||||||||
| Net earnings |
$ | 16,465 | $ | 43,270 | $ | 44,666 | $ | 50,063 | $ | 55,231 | ||||||||||
| Per Share Data:(2) |
||||||||||||||||||||
| Unaudited pro forma basic net earnings per share(2) |
||||||||||||||||||||
| Net earnings per share |
$ | $ | $ | $ | $ | |||||||||||||||
| Weighted average shares outstanding (in millions) |
||||||||||||||||||||
| Unaudited pro forma diluted net earnings per share |
||||||||||||||||||||
| Net earnings per share |
$ | $ | $ | $ | $ | |||||||||||||||
| Weighted average shares outstanding (in millions) |
||||||||||||||||||||
| Unaudited supplemental pro forma basic net earnings per share(3) |
||||||||||||||||||||
| Net earnings per share |
— | — | $ | — | $ | |||||||||||||||
| Weighted average shares outstanding (in millions) |
— | — | — | |||||||||||||||||
| Unaudited supplemental pro forma diluted net earnings per share(3) |
||||||||||||||||||||
| Net earnings per share |
— | — | $ | — | $ | |||||||||||||||
| Weighted average shares outstanding (in millions) |
— | — | — | |||||||||||||||||
| Cash Flows Data: |
||||||||||||||||||||
| Net cash provided by operating activities |
$ | 49,553 | $ | 70,054 | $ | 61,971 | $ | 62,869 | $ | 84,621 | ||||||||||
| Net cash used in investing activities |
(50,109 | ) | (31,256 | ) | (29,772 | ) | (21,156 | ) | (13,102 | ) | ||||||||||
| Net cash used in financing activities |
(6,089 | ) | (12,507 | ) | (16,091 | ) | (4,986 | ) | (4,923 | ) | ||||||||||
| Other Financial Data: |
||||||||||||||||||||
| EBITDA(4) |
$ | 118,427 | $ | 141,606 | $ | 138,840 | $ | 130,540 | $ | 131,160 | ||||||||||
| Favorable professional liability loss reserve adjustments associated with prior years |
12,068 | 32,089 | 34,927 | 40,364 | 18,824 | |||||||||||||||
| Capital expenditures(5) |
11,271 | 12,680 | 12,141 | 7,341 | 5,244 | |||||||||||||||
| Change in investments at insurance subsidiary(6) |
18,262 | 15,156 | 10,131 | 6,302 | 5,080 | |||||||||||||||
9
Table of Contents
| As of September 30, 2009 | ||||||
| Actual | As Adjusted | |||||
| (In thousands) | ||||||
| Balance Sheet Data: |
||||||
| Cash and cash equivalents |
$ | 112,994 | ||||
| Working capital(7) |
128,427 | |||||
| Total assets |
800,449 | |||||
| Total debt |
612,088 | |||||
| Total members’ deficit |
(228,327 | ) | ||||
| (1) | Interest expense, net for the year ended December 31, 2008 and the nine months ended September 30, 2009 as adjusted to give effect to this offering and the application of the net proceeds received by us therefrom would have been $ and , respectively. |
| (2) | Per share data will be computed based upon the number of shares of common stock outstanding immediately after the Corporate Conversion applied to our historical net income amounts and will give retroactive effect to the conversion of our limited liability company interests into shares of common stock. |
| (3) | The unaudited supplemental pro forma basic and diluted net earnings per share for the year ended December 31, 2008 and the nine months ended September 30, 2009 gives effect to the portion of the offering proceeds to be used for the repayment of indebtedness. See “Use of Proceeds.” |
| (4) | “EBITDA” is defined as net earnings before interest expense, taxes and depreciation and amortization. Other companies may define EBITDA differently and, as a result, our measure of EBITDA may not be directly comparable to EBITDA of other companies. The following table sets forth a reconciliation of EBITDA to net earnings: |
| Year Ended December 31, | Nine Months Ended September 30, | ||||||||||||||
| 2006 | 2007 | 2008 | 2008 | 2009 | |||||||||||
| (In thousands) | |||||||||||||||
| Net earnings |
$ | 16,465 | $ | 43,270 | $ | 44,666 | $ | 50,063 | $ | 55,231 | |||||
| Interest expense, net |
57,813 | 55,234 | 45,849 | 34,033 | 27,671 | ||||||||||
| Provision for income taxes |
13,792 | 27,703 | 31,044 | 33,885 | 34,230 | ||||||||||
| Depreciation and amortization |
23,308 | 14,823 | 17,281 | 12,559 | 14,028 | ||||||||||
| EBITDA |
$ | 111,378 | $ | 141,030 | $ | 138,840 | $ | 130,540 | $ | 131,160 | |||||
The following table sets forth a reconciliation of net earnings to Adjusted EBITDA. Adjusted EBITDA under the indenture governing the senior subordinated notes is defined as net earnings before interest expense, taxes, depreciation and amortization, as further adjusted to exclude unusual items, non-cash items and the other adjustments shown in the table below. We believe that the disclosure of the calculation of Adjusted EBITDA provides information that is useful to an investor’s understanding of our financial flexibility under our indenture covenants. Adjusted EBITDA is not a measurement of financial performance or liquidity under generally accepted accounting principles. It should not be considered in isolation or as a substitute for net income, operating income, cash flows from operating, investing or financing activities, or any other measure calculated in accordance with generally accepted accounting principles.
10
Table of Contents
| Year Ended December 31, | Nine Months Ended September 30, | |||||||||||||||
| 2006 | 2007 | 2008 | 2008 | 2009 | ||||||||||||
| (In thousands) | ||||||||||||||||
| Net earnings |
$ | 16,465 | $ | 43,270 | $ | 44,666 | $ | 50,063 | $ | 55,231 | ||||||
| Interest expense, net |
57,813 | 55,234 | 45,849 | 34,033 | 27,671 | |||||||||||
| Provision for income taxes |
13,792 | 27,703 | 31,044 | 33,885 | 34,230 | |||||||||||
| Depreciation and amortization |
23,308 | 14,823 | 17,281 | 12,559 | 14,028 | |||||||||||
| Loss from discontinued operations, net of taxes |
7,049 | 576 | — | — | — | |||||||||||
| Impairment of intangibles(a) |
— | — | 9,134 | — | — | |||||||||||
| Management fee and other expenses(b) |
3,748 | 4,054 | 3,602 | 2,745 | 2,324 | |||||||||||
| Gain on extinguishment of debt(c) |
— | — | (1,640 | ) | — | — | ||||||||||
| Transaction costs(d) |
— | — | 2,386 | 1,805 | 578 | |||||||||||
| Restricted unit expense(e) |
617 | 560 | 625 | 439 | 558 | |||||||||||
| Insurance subsidiary interest income |
2,024 | 2,867 | 3,341 | 3,040 | 2,138 | |||||||||||
| Severance and other charges |
1,164 | 3,693 | 1,549 | 1,340 | 301 | |||||||||||
| Adjusted EBITDA* |
$ | 125,980 | $ | 152,780 | $ | 157,837 | $ | 139,909 | $ | 137,059 | ||||||
| * | Adjusted EBITDA totals are not adjusted for the favorable effects of professional liability loss reserve adjustments associated with prior years of $12,068, $32,089, $34,927, $40,364 and $18,824 for the years ended December 31, 2006, 2007 and 2008, and the nine months ended September 30, 2008 and 2009, respectively. See “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources.” Adjusting for the effects of professional liability loss reserve adjustments associated with prior years, Adjusted EBITDA would have been reduced to $113,912, $120,691, $122,910, $99,545 and $118,235 for the years ended December 31, 2006, 2007 and 2008, and the nine months ended September 30, 2008 and 2009, respectively. |
| (a) | Includes impairment of goodwill. |
| (b) | Reflects management sponsor fees, loss on disposal of assets and realized gain on investments. |
| (c) | Reflects the gain on the retirement of a portion of the senior subordinated notes, net of write-off of deferred financing costs. |
| (d) | Reflects expenses associated with acquisition transaction fees. |
| (e) | Reflects costs related to the recognition of expense in connection with the issuance of restricted units under the Team Health, Inc. 2005 Unit Plan. |
| (5) | Reflects expenditures for property and equipment used in our business. |
| (6) | Reflects the net funding of cash for investments held by our captive insurance subsidiary as reported in our statements of cash flows by netting purchases of investments at insurance subsidiary and proceeds from investments at insurance subsidiary. |
| (7) | Working capital means current assets minus current liabilities. |
11
Table of Contents
An investment in our common stock involves risks. Before investing in our common stock, you should carefully consider the following information about these risks, together with the other information contained in this prospectus, including “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the financial statements and the notes thereto included elsewhere in this prospectus. If any of the following risks actually occurs, our business, financial condition, operating results and prospects could be adversely affected, which in turn could adversely affect the value of our common stock.
Risks Related to Our Business
The current U.S. and global economic conditions could materially adversely affect our results of operations and business condition.
Our operations and performance depend significantly on economic conditions. If the current economic situation continues or deteriorates further, our business could be negatively impacted by reduced demand for our services or third-party disruptions resulting from higher levels of unemployment, government budget deficits and other adverse economic conditions. For example, loss of jobs and lack of health insurance as a result of the deterioration of the economy could depress demand for healthcare services generally. Patient volume trends in our hospital EDs could be adversely affected as individuals potentially defer or forego seeking care in such departments due to the loss or reduction of coverage previously available to such individuals under commercial insurance or government healthcare programs. In addition, the continuation of the current economic downturn may adversely impact our ability to collect for the services we provide as higher unemployment and reductions in commercial managed care enrollment may increase the number of uninsured and underinsured patients seeking healthcare at one of our staffed EDs. We could also be negatively affected if the federal government or the states reduce funding of Medicare, Medicaid and other federal and state healthcare programs in response to increasing deficits in their budgets. Additionally, private third-party payers may take cost-containment measures, including lowering reimbursement rates or increasing patient co-payments and deductibles, which could adversely affect our business. Any of these risks, among other economic factors, could have a material adverse effect on our financial condition and operating results, and the risks could become more pronounced if the problems in the U.S. and global economies continue or become worse.
The current U.S. and state health reform legislative initiatives could adversely affect our operations and business condition.
The Obama Administration and Congress are considering federal legislation to reform the U.S. healthcare system. The current proposed federal health reform legislation includes various bills with various Congressional sponsors. A common issue addressed in the proposed federal health reform initiatives is increasing access to health benefits for the uninsured or underinsured populations. Some of the current proposed federal health reform legislation includes Medicare payment reforms and reductions that could reduce physician payments in the future. Some states also have pending health reform legislative initiatives. At this time, we are unable determine the ultimate content or timing of any health reform legislation. We will not be able to determine the effect that any such legislation may have on our operations and business condition until such legislation is enacted, but such legislation may adversely affect our operations and business condition.
Laws and regulations that regulate payments for medical services made by government sponsored healthcare programs could cause our revenues to decrease.
Our affiliated physician groups derive a significant portion of their net revenues less provision for uncollectibles from payments made by government sponsored healthcare programs such as Medicare and state reimbursed programs. There are public and private sector pressures to restrain healthcare costs and to restrict reimbursement rates for medical services. Any change in reimbursement policies, practices, interpretations,
12
Table of Contents
regulations or legislation that places limitations on reimbursement amounts or practices could significantly affect hospitals, and consequently affect our operations unless we are able to renegotiate satisfactory contractual arrangements with our hospital clients and contracted physicians.
Under Medicare law, Centers for Medicare & Medicaid Services, or CMS, is required to adjust the Medicare Physician Fee Schedule, or MPFS, payment rates annually based on an update formula which includes application of the sustainable growth rate, or SGR, that was adopted in the Balanced Budget Act of 1997. This formula has yielded negative updates every year beginning in 2002, although CMS was able to take administrative steps to avert a reduction in 2003 and Congress has taken a series of legislative actions to prevent reductions from 2004 to 2009.
On October 30, 2008, CMS released its final 2009 MPFS covering the period from January 1, 2009 through December 31, 2009. As a result of a 1.1% statutory increase in the 2009 MPFS and an increase in the physician work values associated with certain emergency services, we estimate that the 2009 MPFS effectively provides for an average 4.0% increase in the 2009 payment amount over the 2008 payment amount for services most commonly provided by emergency physicians. We estimate these payment updates will increase our revenues from Medicare and other revenue sources whose rates are linked to the Medicare fee schedule by an estimated $9.0 million in 2009. Additionally, the 2009 MPFS extends the Physician Quality Reporting Initiative, or PQRI, payment incentive for physicians who successfully report measures under PQRI for 2009 and 2010. The payments under the PQRI extension increased from 1.5% in 2008 to 2.0% in 2009.
On October 30, 2009, CMS released its final 2010 MPFS payment changes covering the period from January 1, 2010 through December 30, 2010. The final rule includes a 21.2% rate reduction in the MPFS for 2010 as a result of the application of the SGR. The PQRI payment incentives for physicians who successfully report measures under PQRI will remain at 2.0% for 2010. Although there are current legislative proposals that call for a delay in the application of the SGR until 2011 and increase physician payments by 0.5% for 2010, such proposals have not yet been enacted. Absent regulatory changes or further Congressional action with respect to the application of the SGR, Medicare physician services would be subject to significant reductions beginning on January 1, 2010.
Any future reductions in amounts paid by government programs for physician services or changes in methods or regulations governing payment amounts or practices could cause our revenues to decline and we may not be able to offset reduced operating margins through cost reductions, increased volume or otherwise.
If governmental authorities determine that we violate Medicare, Medicaid or other government payer reimbursement laws or regulations, our revenues may decrease and we may have to restructure our method of billing and collecting Medicare, Medicaid or other government program payments, respectively.
The Medicare Prescription Drug Improvement and Modernization Act of 2003 amended the Medicare reassignment statute as of December 8, 2003 to permit our independent contractor physicians to reassign their right to receive Medicare payments to us. We have restructured our method of billing and collecting Medicare payments in light of this statutory reassignment exception. In addition, state Medicaid programs have similar reassignment rules. While we seek to comply substantially with applicable Medicaid reassignment regulations, government authorities may find that we do not comply in all respects with these regulations.
We utilize physician assistants and nurse practitioners, sometimes referred to collectively as mid-level practitioners, to provide care under the supervision of our physicians. State and federal laws require that such supervision be performed and documented using specific procedures. We believe our billing and documentation practices related to our use of mid-level practitioners substantially comply with applicable state and federal laws, but enforcement authorities may find that our practices violate such laws.
13
Table of Contents
When our services are covered by multiple third-party payers, such as a primary and a secondary payer, financial responsibility must be allocated among the multiple payers in a process known as “coordination of benefits,” or COB. The rules governing COB are complex, particularly when one of the payers is Medicare or another government program. Although we believe we currently have procedures in place to assure that we comply with applicable COB rules and that we process refunds appropriately when we receive overpayments or overprovisions, payers or enforcement agencies may determine that we have violated these requirements.
Reimbursement to us is typically conditioned on our providing the correct procedure and diagnosis codes and properly documenting both the service itself and the medical necessity of the service. Despite our measures to ensure coding accuracy, third-party payers may disallow, in whole or in part, requests for reimbursement based on determinations that certain amounts are not reimbursable, that the service was not medically necessary, that there was a lack of sufficient supporting documentation, or for other reasons. Incorrect or incomplete documentation and billing information, or the incorrect selection of codes, could result in nonpayment, recoupment or allegations of billing fraud.
Management is not aware of any inquiry, investigation or notice from any governmental entity indicating that we are in violation of any of the Medicare, Medicaid or other government payer reimbursement laws and regulations. However, such laws and related regulations and regulatory guidance may be ambiguous or contradictory, and may be interpreted or applied by prosecutorial, regulatory or judicial authorities in ways that we cannot predict. Accordingly, our arrangements and business practices may be the subject of government scrutiny or be found to violate applicable laws.
We may incur substantial costs defending our interpretations of federal and state government regulations and if we lose, the government could force us to restructure our operations and subject us to fines, monetary penalties and exclusion from participation in government-sponsored programs such as Medicare and Medicaid.
Our operations, including our billing and other arrangements with healthcare providers, are subject to extensive federal and state government regulation. Such regulations include numerous laws directed at payment for services, conduct of operations, preventing fraud and abuse, laws prohibiting general business corporations, such as us, from practicing medicine, controlling physicians’ medical decisions or engaging in some practices such as splitting fees with physicians, and laws regulating billing and collection of reimbursement from government programs, such as Medicare and Medicaid, and from private payers. Those laws may have related rules and regulations that are subject to interpretation and may not provide definitive guidance as to their application to our operations, including our arrangements with hospitals, physicians and professional corporations. See “Business—Regulatory Matters.”
We believe we are in substantial compliance with these laws, rules and regulations based upon what we believe are reasonable and defensible interpretations of these laws, rules and regulations. However, federal and state laws are broadly worded and may be interpreted or applied by prosecutorial, regulatory or judicial authorities in ways that we cannot predict. Accordingly, our arrangements and business practices may be the subject of government scrutiny or be found to violate applicable laws. If federal or state government officials challenge our operations or arrangements with third parties that we have structured based upon our interpretation of these laws, rules and regulations, the challenge could potentially disrupt our business operations and we may incur substantial defense costs, even if we successfully defend our interpretation of these laws, rules and regulations. In addition, if the government successfully challenges our interpretation as to the applicability of these laws, rules and regulations as they relate to our operations and arrangements with third parties, that may have a material adverse effect on our business, financial condition and results of operations.
In the event regulatory action were to limit or prohibit us from carrying on our business as we presently conduct it or from expanding our operations to certain jurisdictions, we may need to make structural, operational and organizational modifications to our company and/or our contractual arrangements with third party payers,
14
Table of Contents
physicians, professional corporations and hospitals. Our operating costs could increase significantly as a result. We could also lose contracts or our revenues could decrease under existing contracts. Moreover, our financing agreements may also prohibit modifications to our current structure and consequently require us to obtain the consent of the holders of such indebtedness or require the refinancing of such indebtedness. Any restructuring would also negatively impact our operations because our management’s time and attention would be diverted from running our business in the ordinary course.
For example, while we believe that our operations and arrangements comply substantially with existing applicable laws relating to the corporate practice of medicine and fee splitting, we cannot assure you that our existing contractual arrangements, including non-competition agreements with physicians, professional corporations and hospitals, will not be successfully challenged in certain states as unenforceable or as constituting the unlicensed practice of medicine or prohibited fee splitting. In this event, we could be subject to adverse judicial or administrative interpretations or to civil or criminal penalties, our contracts could be found to be legally invalid and unenforceable or we could be required to restructure our contractual arrangements with our affiliated physician groups.
We are subject to billing investigations by federal and state authorities that could have a material adverse effect on our business, financial conditions and results of operations.
State and federal statutes impose substantial penalties, including civil and criminal fines, exclusion from participation in government healthcare programs and imprisonment, on entities or individuals (including any individual corporate officers or physicians deemed responsible) that fraudulently or wrongfully bill governmental or other third-party payers for healthcare services. In addition, federal and certain state laws allow a private person to bring a civil action in the name of the U.S. government for false billing violations or other types of false claims. We believe that additional audits, inquiries and investigations from government agencies will continue to occur from time to time in the ordinary course of our business, which could result in substantial defense costs to us and a diversion of management’s time and attention. Such pending or future audits, inquiries or investigations, or the public disclosure of such matters, may have a material adverse effect on our business, financial condition and results of operations.
We are subject to complex rules and regulations that govern our licensing and certification, and the failure to comply with these rules can result in delays in, or loss of, reimbursement for our services or civil or criminal sanctions.
We, our affiliated physicians and the facilities in which we operate are subject to various federal, state and local licensing and certification laws and regulations and accreditation standards and other laws relating to, among other things, the adequacy of medical care, equipment, personnel and operating policies and procedures. We are also subject to periodic inspection by governmental and other authorities to assure continued compliance with the various standards necessary for licensing and accreditations.
In certain jurisdictions, changes in our ownership structure require pre- or post-notification to governmental licensing and certification agencies. Relevant laws and regulations may also require re-application and approval to maintain or renew our operating authorities or require formal application and approval to continue providing services under certain government contracts.
The relevant laws and regulations are complex and may be unclear or subject to interpretation. We are pursuing the steps we believe we must take to retain or obtain all requisite operating authorities. While we have made reasonable efforts to substantially comply with federal, state and local licensing and certification laws and regulations and accreditation standards based upon what we believe are reasonable and defensible interpretations of these laws, regulations and standards, agencies that administer these programs may find that we have failed to comply in some material respects. Failure to comply with these licensing, certification and accreditation laws, regulations and standards could result in our services being found non-reimbursable or prior payments being subject to recoupment, and can give rise to civil or, in extreme cases, criminal penalties.
15
Table of Contents
In order to receive payment from Medicare, Medicaid and certain other government programs, healthcare providers are required to enroll in these programs by completing complex enrollment applications. Certain government programs, including Medicare and Medicaid programs, require notice or re-enrollment when certain ownership changes occur. Generally, in jurisdictions where we are required to obtain a new licensing authority, we may also be required to re-enroll in that jurisdiction’s government payer program. If the payer requires us to complete the re-enrollment process prior to submitting reimbursement requests, we may be delayed in payment, receive refund requests or be subject to recoupment for services we provide in the interim.
Compliance with these change in ownership requirements is complicated by the fact that they differ from jurisdiction to jurisdiction, and in some cases are not uniformly applied or interpreted even within the same jurisdiction. Failure to comply with these enrollment and reporting requirements could lead not only to delays in payment and refund requests, but in extreme cases could give rise to civil (including refunding of payments for services rendered) or criminal penalties in connection with prior changes in our operations and ownership structure. While we made reasonable efforts to substantially comply with these requirements in connection with prior changes in our operations and ownership structure, the agencies that administer these programs may find that we have failed to comply in some material respects.
We could be subject to professional liability lawsuits, some of which we may not be fully insured against or reserved for, which could adversely affect our financial condition and results of operations.
In recent years, physicians, hospitals and other participants in the healthcare industry have become subject to an increasing number of lawsuits alleging medical malpractice and related legal theories such as negligent hiring, supervision and credentialing, and vicarious liability for acts of their employees or independent contractors. Many of these lawsuits involve large claims and substantial defense costs. Although we do not engage in the practice of medicine or provide medical services nor do we control the practice of medicine by our affiliated physicians or affiliated medical groups or the compliance with regulatory requirements applicable to such physicians and physician groups, we have been and are involved in this type of litigation, and we may become so involved in the future. In addition, through our management of hospital departments and provision of non-physician healthcare personnel, patients who receive care from physicians or other healthcare providers affiliated with medical organizations and physician groups with whom we have a contractual relationship could sue us.
Effective March 12, 2003, we began insuring our professional liability risks principally through a program of self-insurance reserves, commercial insurance and a captive insurance company arrangement. Under our current professional liability insurance program, our exposure for claim losses under professional liability insurance policies provided to affiliated physicians and other healthcare practitioners is limited to the amounts of individual policy coverage limits but there is no limit for claim losses that exceed aggregate losses incurred under all insurance provided to affiliated physicians and other healthcare practitioners or for individual or aggregate professional liability losses incurred by us or other corporate entities that exceed aggregate losses incurred under such insurance. Further, we may be exposed to individual claim losses in excess of limits of coverage under existing or historical insurance programs. While our provisions for professional liability claims and expenses are determined through actuarial estimates, such actuarial estimates may be exceeded by actual losses and related expenses in the future. Claims, regardless of their merit or outcome, may also adversely affect our reputation and ability to expand our business.
We could also be liable for claims against our affiliated physicians for incidents that occurred but were not reported during periods for which claims-made insurance covered the related risk. Under generally accepted accounting principles, the cost of professional liability claims, which includes costs associated with litigating or settling claims, is accrued when the incidents that give rise to the claims occur. The accrual includes an estimate of the losses that will result from incidents, which occurred during the claims-made period, but were not reported during that period. These claims are referred to as incurred-but-not-reported claims, or IBNR claims. With respect to those physicians for whom we provide coverage for claims that occurred during periods prior to March 12, 2003, we have acquired extended reporting period coverage, or tail coverage, for IBNR claims from a commercial
16
Table of Contents
insurance company. Claim losses for periods prior to March 12, 2003 may exceed the limits of available insurance coverage or reserves established by us for any losses in excess of such insurance coverage limits.
Furthermore, for those portions of our professional liability losses that are insured through commercial insurance companies, we are subject to the credit risk of those insurance companies. While we believe our commercial insurance company providers are currently creditworthy, such insurance companies may not remain so in the future.
The reserves that we have established for our professional liability losses are subject to inherent uncertainties and any deficiency may lead to a reduction in our net earnings.
We have established reserves for losses and related expenses that represent estimates at a given point in time involving actuarial and statistical projections of our expectations of the ultimate resolution and administration of costs of losses incurred for professional liability risks for the period on and after March 12, 2003. We have also established a reserve for potential losses in excess of commercial insurance aggregate coverage limits for the period prior to March 12, 2003. Insurance reserves are inherently subject to uncertainty. Our reserves are based on historical claims, demographic factors, industry trends, severity and exposure factors and other actuarial assumptions. Studies of projected ultimate professional liability losses are performed at least annually. We use the actuarial estimates to establish reserves. Our reserves could be significantly affected should current and future occurrences differ from historical claim trends and expectations. While claims are monitored closely when estimating reserves, the complexity of the claims and the wide range of potential outcomes often hampers timely adjustments to the assumptions used in these estimates. Actual losses and related expenses may deviate, perhaps substantially, from the reserve estimates reflected in our financial statements. If our estimated reserves are determined to be inadequate, we will be required to increase reserves at the time of such determination, which would result in a corresponding reduction in our net earnings in the period in which such deficiency is determined. See “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Critical Accounting Policies and Estimates—Insurance Reserves,” Note 14 to the audited consolidated financial statements and Note 11 to the unaudited consolidated financial statements included in this prospectus.
We depend on reimbursements by third-party payers, as well as payments by individuals, which could lead to delays and uncertainties in the reimbursement process.
We receive a substantial portion of our payments for healthcare services on a fee for service basis from third-party payers, including Medicare, Medicaid, the U.S. government’s military healthcare system and other governmental programs, private insurers and managed care organizations. We received approximately 57% of our net revenues less provision for uncollectibles from such third-party payers during 2008 and 2007. Such amounts included approximately 24% from Medicare and Medicaid, collectively, in 2008 and 2007.
The reimbursement process is complex and can involve lengthy delays. Third-party payers continue their efforts to control expenditures for healthcare, including proposals to revise reimbursement policies. While we recognize revenue when healthcare services are provided, there can be delays before we receive payment. In addition, third-party payers may disallow, in whole or in part, requests for reimbursement based on determinations that certain amounts are not reimbursable under plan coverage, that services provided were not medically necessary, that services rendered in an ED did not require ED level care or that additional supporting documentation is necessary. Retroactive adjustments may change amounts realized from third-party payers. We are subject to governmental audits of our reimbursement claims under Medicare, Medicaid, the U.S. government’s military healthcare system and other governmental programs and may be required to repay these agencies if a finding is made that we were incorrectly reimbursed. Delays and uncertainties in the reimbursement process may adversely affect accounts receivable, increase the overall costs of collection and cause us to incur additional borrowing costs.
17
Table of Contents
We also may not be paid with respect to co-payments and deductibles that are the patient’s financial responsibility, or in those instances when physicians provide healthcare services to uninsured and underinsured individuals. Amounts not covered by third-party payers are the obligations of individual patients for which we may not receive whole or partial payment. We may not receive whole or partial payments from uninsured and underinsured individuals. As a result of government laws and regulations requiring hospitals to screen and treat patients who have an emergency medical condition regardless of their ability to pay and our obligation to provide such screening or treatment, a substantial increase in self-pay patients could result in increased costs associated with physician services for which sufficient net revenues less provision for uncollectibles are not realized to offset such additional physician service costs. In such an event, our earnings and cash flow would be adversely affected, potentially affecting our ability to maintain our restrictive debt covenant ratios and meet our financial obligations.
In summary, the risks associated with third-party payers, co-payments and deductibles and uninsured individuals and the inability to monitor and manage accounts receivable successfully could have a material adverse effect on our business, financial condition and results of operations. Furthermore, our collection policies or our provisions for allowances for Medicare, Medicaid and contractual discounts and doubtful accounts receivable may not be adequate.
We are subject to the financial risks associated with our fee for service contracts which could decrease our revenues, including changes in patient volume, mix of insured and uninsured patients and patients covered by government sponsored healthcare programs and third party reimbursement rates.
We derive our revenues primarily through two types of arrangements. If we have a flat fee contract with a hospital, the hospital bills and collects fees for physician services and remits a negotiated amount to us monthly. If we have a fee for service contract with a hospital, either we or our affiliated physicians collect the fees for physician services. Consequently, under fee for service contracts, we assume the financial risks related to changes in the mix of insured, uninsured and underinsured patients and patients covered by government sponsored healthcare programs, third party reimbursement rates and changes in patient volume. We are subject to these risks because under our fee for service contracts, our fees decrease if a smaller number of patients receive physician services or if the patients who do receive services do not pay their bills for services rendered or we are not fully reimbursed for services rendered. Our fee for service contractual arrangements also involve a credit risk related to services provided to uninsured and underinsured individuals. This risk is exacerbated in the hospital ED physician-staffing context because federal law requires hospital EDs to evaluate all patients regardless of the severity of illness or injury. We believe that uninsured and underinsured patients are more likely to seek care at hospital EDs because they frequently do not have a primary care physician with whom to consult. We also collect a relatively smaller portion of our fees for services rendered to uninsured and underinsured patients than for services rendered to insured patients. In addition, fee for service contracts also have less favorable cash flow characteristics in the start-up phase than traditional flat-rate contracts due to longer collection periods. Our revenues could also be reduced if third-party payers successfully negotiate lower reimbursement rates for our physician services.
Failure to timely or accurately bill for our services could have a negative impact on our net revenues, bad debt expense and cash flow.
Billing for ED visits in a hospital setting and other physician-related services is complex. The practice of providing medical services in advance of payment or, in many cases, prior to assessment of ability to pay for such services, may have a significant negative impact on our net revenues, bad debt expense and cash flow. We bill numerous and varied payers, including self-pay patients, various forms of commercial insurance companies and Medicare, Medicaid, the U.S. government’s military healthcare system and other government programs. These different payers typically have differing forms of billing requirements that must be met prior to receiving payment for services rendered. Reimbursement to us is typically conditioned on our providing the proper procedure and diagnosis codes. Incorrect or incomplete documentation and billing information could result in non-payment for services rendered.
18
Table of Contents
Additional factors that could complicate our billing include:
| • | disputes between payers as to which party is responsible for payment; |
| • | variation in coverage for similar services among various payers; |
| • | the difficulty of adherence to specific compliance requirements, coding and various other procedures mandated by responsible parties; |
| • | failure to obtain proper physician enrollment and documentation in order to bill various commercial and governmental payers; |
| • | failure to identify and obtain the proper insurance coverage for the patient; and |
| • | failure to properly code for services rendered. |
To the extent that the complexity associated with billing for our services causes delays in our cash collections, we assume the financial risk of increased carrying costs associated with the aging of our accounts receivable as well as the increased potential for bad debts.
In addition, the majority of the patient visits for which we bill payers are processed in one of three regional billing centers. A disruption of services at any one of these locations could result in a delay in billing and thus cash flows to us, as well as potential additional costs to process billings in alternative settings or locations. In 2008, our billing centers processed approximately 99% of our patient visit billings using a common automated billing system. While we employ what we believe are adequate back-up alternatives in the event of a main computer site disaster, failure to execute our back-up plan successfully or timely may cause a significant disruption to our cash flows and temporarily increase our billing costs. In the event that we do not timely or accurately bill for our services, our net revenues may be subject to a significant negative impact.
If we are unable to timely enroll our healthcare professionals in the Medicare program, our collections and revenues will be harmed.
In the 2009 MPFS, CMS substantially reduced the time within which physicians and other healthcare professionals can retrospectively bill Medicare for services provided by such providers from 27 months prior to the effective date of the enrollment to 30 days prior to the effective date of the enrollment. In addition, the new enrollment rules set forth in the 2009 MPFS also provide that the effective date of the enrollment will be the later of the date on which the enrollment was filed and approved by the Medicare contractor and the date on which the healthcare professional began providing services. If we are unable to properly enroll our physicians and other healthcare professionals within the 30 days after such provider begins providing services, we will be precluded from billing Medicare for any services which were provided to a Medicare beneficiary more than thirty days prior to the effective date of the enrollment. Such failure to timely enroll healthcare professionals could have a material adverse effect on our business, financial condition and results of operations.
A reclassification of our independent contractor physicians by tax authorities could require us to pay retroactive taxes and penalties, which could have a material adverse effect on us.
As of September 30, 2009, we contracted with approximately 2,800 affiliated physicians as independent contractors to fulfill our contractual obligations to clients. Because we consider many of the physicians with whom we contract to be independent contractors, as opposed to employees, we do not withhold federal or state income or other employment related taxes, make federal or state unemployment tax or Federal Insurance Contributions Act payments, or provide workers’ compensation insurance with respect to such affiliated physicians. Our contracts with our independent contractor physicians obligate these physicians to pay these taxes.
19
Table of Contents
The classification of physicians as independent contractors depends on the facts and circumstances of the relationship. In the event of a determination by federal or state taxing authorities that the physicians engaged as independent contractors are employees, we may be adversely affected and subject to retroactive taxes and penalties. Under current federal tax law, a safe harbor from reclassification, and consequently retroactive taxes and penalties, is available if our current treatment is consistent with a long-standing practice of a significant segment of our industry and if we meet certain other requirements. If challenged, we may not prevail in demonstrating the applicability of the safe harbor to our operations. Further, interested persons have recently proposed to eliminate the safe harbor and may do so again in the future.
Our practices with respect to the classification of our independent contractors have periodically been reviewed by the Internal Revenue Service, or IRS, with no adjustments or changes to our practices required as a result of such review. The IRS completed the most recent review of affiliated entities in 2007 with no changes proposed. The IRS relied on the results of prior reviews in 2000 and 2001 and our adherence to the conditions of the safe harbor provisions. Nonetheless, the tax authorities may decide to reclassify our independent contractor physicians as employees or require us to pay retroactive taxes and penalties, which could have a material adverse effect on us.
A significant number of our programs are concentrated in certain states, particularly Florida and Tennessee, which makes us particularly sensitive to regulatory, economic and other conditions in those states.
During the year ended December 31, 2008, Florida and Tennessee accounted for approximately 16% and 17%, respectively, of our net revenues less provision for uncollectibles. If our programs in these states are adversely affected by changes in regulatory, economic and other conditions in such states, our revenues and profitability may decline.
We derive a portion of our net revenues from services provided to the U.S. Department of Defense within the Military Health System Program, or MHS Program. These revenues are derived from contracts subject to a competitive bidding process.
We are a provider of healthcare professionals that serve military personnel and their dependents in military treatment facilities nationwide. Our net revenues derived from military healthcare staffing totaled $160.8 million in 2008, $142.7 million in 2007 and $157.8 million in 2006.
Most of our contracts within the MHS Program have terms of one year. Under a number of these contracts, the government has the option to renew the contract each year for an additional one-year term, subject to a specified maximum number of renewal terms (anywhere from one to four renewal terms). Those contracts without any renewal option are subject to an automatic rebidding and award process at the end of the one-year term. Each contract with a renewal option will become subject to the automatic rebidding and award process upon the earlier of (i) the government electing not to exercise its annual renewal option for such contract or (ii) the expiration of the final renewal term for such contract. In addition, all contracts, including contracts with renewal options, can be terminated by the government at any time without notice. The outcome of any rebidding and award process is uncertain and we may not be awarded new contracts. Our contracts with renewal options may not be so renewed and the government may exercise its rights to terminate the contracts.
In addition, we provide services within the MHS Program pursuant to subcontracting arrangements where we serve as a subcontractor to a primary contractor, generally a small business, that has entered into a direct contract with the government. Subcontracting arrangements pose unique risks to us because our ability to generate revenue under the subcontract is contingent upon the continued existence of the primary contract, which is beyond our control. If the primary contract is terminated, whether for non-performance by the primary contractor, the loss of the primary contractor’s small business status or otherwise, then our subcontract will similarly terminate. Any loss of or failure to renew contracts within the MHS Program may have a material adverse effect on our business, financial condition and results of operations.
20
Table of Contents
We may become involved in litigation that could harm the value of our business.
In the normal course of our business, we are involved in lawsuits, claims, audits and investigations, including those arising out of services provided, personal injury claims, professional liability claims, our billing and marketing practices, employment disputes and contractual claims. The outcome of these matters could have a material adverse effect on our financial position or results of operations. We do not believe that any such claims that have been asserted are likely to have such an effect. However, we may become subject to future lawsuits, claims, audits and investigations that could result in substantial costs and divert our attention and resources. In addition, since our current growth strategy includes acquisitions, among other things, we may become exposed to legal claims arising out of the activities of an acquired business prior to the time of any acquisition.
Our quarterly operating results may fluctuate significantly and may cause the value of our common stock to decline, which could affect our ability to raise new capital for our business.
Our quarterly operating results may vary significantly in the future depending on many factors that may include, but are not limited to, the following:
| • | the overall patient demand for our healthcare services; |
| • | our ability to accurately receive and process on a timely basis billing related information and other demographic factors that in turn can affect our fee for service revenue estimates; |
| • | the relative proportion of revenues we derive from various services; |
| • | increased competition in our local markets; |
| • | changes in our operating expenses; |
| • | our ability to recruit and train new physicians in new or existing local markets; |
| • | changes in our business strategy; and |
| • | economic and political conditions, including fluctuations in interest rates and tax increases. |
Fluctuations in our quarterly operating results could affect our ability to raise new capital for our business.
Our revenues could be adversely affected by a net loss of contracts.
A significant portion of our growth has historically resulted from increases in the number of patient visits and fees for services provided under existing contracts and the addition and acquisition of new contracts. Our contracts with hospitals generally have terms of three years and include automatic renewal options under similar terms and conditions, unless either party gives notice of an intent not to renew. Most of our contracts are terminable by either of the parties upon notice of as little as 90 days. These contracts may not be renewed or, if renewed, may contain terms that are not as favorable to us as our current contracts. In most cases, the termination of a contract is principally due to either an award of the contract to another source of provider staffing or termination of the contract by us due to a lack of an acceptable profit margin. Additionally, to a much lesser extent, contracts may be terminated due to such conditions as a hospital facility closing because of facility mergers or a hospital attempting to provide themselves the service being provided by us. Our current military contracts, which are in the form of direct contracts with military treatment facilities, generally have terms of one year and in many cases grant renewal options to the military. Such renewal options typically are for one to four years. We may experience a net loss of contracts in the future and any such net loss may have a material adverse effect on our operating results and financial condition.
21
Table of Contents
Our failure to accurately assess the costs we will incur under new contracts could have a material adverse effect on our business, financial condition and results of operations.
Our new contracts increasingly involve a competitive bidding process. When we obtain new contracts, we must accurately assess the costs we will incur in providing services in order to realize adequate profit margins and otherwise meet our financial and strategic objectives. Increasing pressures from healthcare payers to restrict or reduce reimbursement rates at a time when the costs of providing medical services continue to increase make assessing the costs associated with the pricing of new contracts, as well as maintenance of existing contracts, more difficult. In addition, integrating new contracts, particularly those in new geographic locations, could prove more costly, and could require more management time than we anticipate. Our failure to accurately predict costs or to negotiate an adequate profit margin could have a material adverse effect on our business, financial condition and results of operations.
If we are not able to find suitable acquisition candidates or successfully integrate completed acquisitions into our current operations, we may not be able to profitably operate our consolidated company.
Between 2005 and 2008, acquisitions have contributed 7.5% toward overall growth in net revenues less provision for uncollectibles during this period. We expect to continue to seek opportunities to grow through attractive acquisitions. However, our acquisition strategy could present some challenges. Some of the difficulties we could encounter include: problems identifying all service and contractual commitments of the acquired entity, evaluating the stability of the acquired entity’s hospital contracts, integrating financial and operational software, accurately projecting physician and employee costs, and evaluating their regulatory compliance. Our acquisition strategy is also subject to the risk that, in the future, we may not be able to identify suitable acquisition candidates, be successful in expanding into new lines of business, obtain acceptable financing or consummate desired acquisitions, any of which could inhibit our growth. In addition, in connection with acquisitions, we may need to obtain the consent of third parties who have contracts with the entity to be acquired, such as managed care companies or hospitals contracting with the entity. We may be unable to obtain these consents. If we fail to integrate acquired operations, fail to manage the cost of providing our services or fail to price our services appropriately, our operating results may decline.
Furthermore, the diversion of management’s attention and any delays or difficulties encountered in connection with the integration of businesses we acquire could negatively impact our business and results of operations. Finally, as a result of our acquisitions of other healthcare businesses, we may be subject to the risk of unanticipated business uncertainties or legal liabilities relating to such acquired businesses for which we may not be indemnified by the sellers of the acquired businesses.
If we fail to implement our business strategy, our business, financial condition and results of operations could be materially and adversely affected.
Our future financial performance and success are dependent in large part upon our ability to implement our business strategy successfully. Our business strategy envisions several initiatives, including increasing revenues from existing customers, capitalizing on outsourcing opportunities to win new contracts, focusing on risk management and pursuing selected acquisitions. We may not be able to implement our business strategy successfully or achieve the anticipated benefits of our business plan. If we are unable to do so, our long-term growth and profitability may be adversely affected. Even if we are able to implement some or all of the initiatives of our business plan successfully, our operating results may not improve to the extent we anticipate, or at all.
If we do not manage our growth effectively, our financial condition may be adversely affected.
Even if we are successful in obtaining new business, failure to manage our growth could adversely affect our financial condition. We may experience extended periods of very rapid growth. If we are not able to manage our growth effectively, our business and financial condition could materially suffer. Our growth may
22
Table of Contents
significantly strain our managerial, operational and financial resources and systems. To manage our growth effectively, we will have to continue to implement and improve our operational, financial and management controls, reporting systems and procedures. In addition, we must effectively expand, train and manage our employees. We will be unable to manage our businesses effectively if we are unable to alleviate the strain on resources caused by growth in a timely and successful manner. We may not be able to manage our growth and our failure to do so could have a material adverse effect on our business.
We may be required to seek additional financing to meet our future capital needs and our failure to raise capital when needed could harm our competitive position, business, financial condition and results of operations.
Continued expansion of our business may require additional capital. In the future, it is possible that we will be required to raise additional funds through public or private financings, collaborative relationships or other arrangements. Global credit markets and the financial services industry have been experiencing a period of unprecedented turmoil, characterized by the bankruptcy, failure or sale of various financial institutions and an unprecedented level of intervention from the U.S. and other governments. These events have lead to unparalleled levels of volatility and disruption to the capital and credit markets and have significantly adversely impacted global economic conditions, resulting in additional, significant recessionary pressures and further declines in investor confidence and economic growth. Despite significant government intervention, global investor confidence remains low and credit remains relatively scarce. These disruptions in the financial markets, including the bankruptcy and restructuring of certain financial institutions, may adversely impact the current availability of credit and the availability and cost of credit in the future. Accordingly, if we need to seek additional funding, we may be significantly reduced in our ability to attract public or private financings or financial partners or relationships as a source of additional capital. In addition, this additional funding, if needed, may not be available on terms attractive to us, if at all. Furthermore, any additional debt financing, if available, may involve restrictive covenants that could restrict our ability to raise additional capital or operate our business. Our failure to raise capital when needed could harm our competitive position, business, financial condition and results of operations.
If we are not able to successfully recruit and retain qualified physicians and nurses to serve as our independent contractors or employees, our net revenues could be adversely affected.
Our affiliated medical groups provide facility-based services in virtually all types of settings. These include urban and suburban hospitals as well as rural and remote facilities. Our ability to recruit and retain affiliated physicians and qualified personnel for such settings can significantly affect our performance at such facilities. Certain of these locations present difficulties in recruiting providers due to limits on compensation, facility and equipment availability, reduced back-up by other specialists and personal and family lifestyle preferences. In addition, a number of our client hospitals increasingly demand a greater degree of specialized skills, training and experience in the physicians who staff their contracts. This decreases the number of physicians who are qualified to staff potential and existing contracts.
In general, recruiting physicians to staff contracts in regions of the country for economically disadvantaged hospitals is challenging. Occasionally, the recruiting of providers may not occur quickly enough to fill all openings with permanent staff. In these situations, clinical shifts are often filled temporarily by existing employees or independent contractors from other areas of our company. If such assistance is not available for any reason, we utilize staffing from our locum tenens company to fill the staffing need until a permanent candidate is identified. Finally, if the aforementioned alternatives are unsuccessful, we contract with one of the many third-party locum tenens companies that exist to provide these services to healthcare facilities or companies such as ours.
Our ability to attract and retain physicians and providers depends on several factors, including our ability to provide competitive benefits and wages. If we do not increase benefits and wages in response to increases by our competitors, we could face difficulties attracting and retaining qualified healthcare personnel. In
23
Table of Contents
addition, if we raise wages in response to our competitors’ wage increases and are unable to pass such increases on to our clients, our margins could decline, which could adversely affect our business, financial condition and results of operations.
Our non-competition and non-solicitation contractual arrangements with some affiliated physicians and professional corporations may be successfully challenged in certain states as unenforceable, which could have a material adverse effect on us.
We have contracts with physicians in many states. State laws governing non-competition and non-solicitation agreements vary from state to state. Some states prohibit non-competition and non-solicitation contractual arrangements with physicians or are otherwise reluctant to strictly enforce such agreements. In such event, we would be unable to prevent former affiliated physicians and professional corporations from soliciting our contracts or otherwise competing with us, potentially resulting in the loss of some of our hospital contracts and other business which could adversely impact our business, financial condition and results of operations.
The high level of competition in our industry could adversely affect our contract and revenue base.
The provision of outsourced physician staffing and administrative services to hospitals and clinics is characterized by a high degree of competition. Competition for outsourced physician and other healthcare staffing and administrative service contracts is based primarily on:
| • | the ability to improve department productivity and patient satisfaction while reducing overall costs; |
| • | the breadth of staffing and management services offered; |
| • | the ability to recruit and retain qualified physicians, technicians and nurses; |
| • | billing and reimbursement expertise; |
| • | a reputation for compliance with state and federal regulations; and |
| • | financial stability, demonstrating an ability to pay providers in a timely manner and provide professional liability insurance. |
Such competition could adversely affect our ability to obtain new contracts, retain existing contracts and increase our profit margins. We compete with national, regional and local enterprises. In addition, some of these firms may have greater access than we do to physicians and potential clients. All of these competitors provide healthcare services that are similar in scope to the services we provide. Although we and our competitors operate on a national or regional basis, the majority of the targeted hospital community for our services engages local physician practice groups to provide services similar to the services we provide. We therefore also compete against local physician groups and self-operated hospital EDs for satisfying staffing and scheduling needs.
The military has changed its approach toward providing most of its outsourced healthcare staffing needs through direct provider contracting on a competitive bid basis. As a result, competition for such outsourced military staffing contracts may be affected by such factors as:
| • | the lowest bid price; |
| • | the ability to meet technical government bid specifications; |
| • | the ability to recruit and retain qualified healthcare providers; and |
24
Table of Contents
| • | restrictions on the ability to competitively bid based on restrictive government bid lists or bid specifications designed to award government contracts to targeted business ownership forms, such as those determined to meet small business or minority ownership qualifications. |
Such services and quality screening considerations may not result in the lowest competitive bid price and thus a failure to win contracts where the decision is based strictly on pricing considerations.
Our business depends on numerous complex information systems, some of which are licensed from third parties, and any failure to successfully maintain these systems or implement new systems could materially harm our operations.
Our business depends on complex, integrated information systems and standardized procedures for operational, financial and billing operations. We may not be able to enhance existing information systems or implement new information systems where necessary. Additionally, we license certain of our information systems, and these licenses may be terminated, or may no longer be available at all or on terms that are acceptable to us. Furthermore, we may experience unanticipated delays, complications and expenses in implementing, integrating and operating our systems. In addition, our information systems may require modifications, improvements or replacements that may require substantial expenditures and may require interruptions in operations during periods of implementation. Implementation of these systems is further subject to the availability of information technology and skilled personnel to assist us in creating and implementing the systems.
There are evolving standards in the healthcare industry relating to electronic medical records and e-prescribing. On October 11, 2005, the Office of Inspector General of the Department of Health and Human Services, or OIG, issued a proposed safe harbor to the federal anti-kickback statute for certain e-prescribing arrangements, and CMS concurrently issued companion proposed exceptions to the federal physician self-referral statute, or the Stark Law, for certain e-prescribing and electronic medical record arrangements. In 2006, both the OIG and CMS issued final versions of each proposed regulation. The exceptions and safe harbors establish the conditions under which entities may donate to physicians (and certain other recipients under the safe harbor) interoperable electronic health records software, information technology and training services. Additionally, the rules permit hospitals and certain other entities to provide physicians (and certain other recipients under the safe harbor) with hardware, software, or information technology and training services necessary and used solely for electronic prescribing. Both rules are permissive, meaning that if requirements are met, they permit the offering or furnishing of free or discounted technology to referral sources. However, the government has signaled its interest in making certain universal e-prescribing and electronic health records mandatory. New legislation enacted under the Health Information Technology for Economic and Clinical Health Act, or HITECH Act, of the American Recovery and Reinvestment At of 2009, or ARRA, requires the government to work to adopt standards-based electronic health records. Depending on the outcome of this regulatory activity, we could be required to make significant expenditures to facilitate connectivity to hospital systems or otherwise develop e-prescribing and electronic medical record capabilities. The failure to successfully implement and maintain operational, financial and billing information systems could have a material adverse effect on our business, financial condition and results of operations.
If we are unable to protect our proprietary technology and services, which form the basis of our complex information systems, our competitive position could be adversely affected.
Our success depends in part on our ability to protect our proprietary technology and services. To do so, we rely upon a combination of trade secret, copyright, trade and service mark, and patent law, as well as confidentiality and other contractual restrictions. These legal means, however, afford only limited protection and may not adequately protect our rights or permit us to gain or keep any competitive advantage. Despite our efforts to protect our proprietary technology and services, unauthorized persons may be able to copy, reverse engineer or otherwise use some of our technology or services. It is also possible that others will develop and market similar
25
Table of Contents
or better technology or services to compete with us. For these reasons, we may have difficulty protecting our proprietary technology and services. Any of these events could have a material adverse effect on our competitive position. Furthermore, litigation may be necessary to protect our proprietary technology and services, which is often costly, time-consuming and a diversion of management’s attention from our business.
Loss of key personnel and/or failure to attract and retain highly qualified personnel could make it more difficult for us to generate cash flow from operations and service our debt.
Our success depends to a significant extent on the continued services of our core senior management team of H. Lynn Massingale, M.D., Executive Chairman; Greg Roth, President and Chief Executive Officer; David Jones, Chief Financial Officer; Heidi Allen, Senior Vice President, General Counsel; Stephen Sherlin, Chief Compliance Officer; Jonathan Grimes, President, Emergency and Hospital Medicine; and Joseph Carman, Chief Administrative Officer as well as the leaders of major components of our company. If one or more of these individuals were unable or unwilling to continue in his present position, our business would be disrupted and we might not be able to find replacements on a timely basis or with the same level of skill and experience. Mr. Sherlin has indicated that he intends to retire effective May 1, 2010. Finding and hiring any such replacements could be costly and might require us to grant significant incentive compensation, which could adversely impact our financial results.
We are exposed to risks relating to the management’s evaluation and auditor’s opinion on the effectiveness of our internal control over financial reporting as required by Section 404 of the Sarbanes-Oxley Act of 2002 and increased costs associated with corporate governance compliance.
The Sarbanes-Oxley Act of 2002, or Sarbanes-Oxley Act, has required changes in some of our corporate governance and compliance practices. Our subsidiary, Team Finance LLC, has evaluated, tested and implemented internal control over financial reporting to enable management to report on such internal control as required by Section 404 of the Sarbanes-Oxley Act. While we believe we are compliant with the management’s evaluation requirements of Section 404, we cannot be certain as to the timing of the completion of our independent registered public accounting firm’s opinion on the effectiveness of our internal control over financial reporting, which is required to be included in Team Finance’s annual report on Form 10-K for the fiscal year ending December 31, 2009, or the impact of the same on our operations. If we are not able to implement all of the requirements of Section 404 in a timely manner or with adequate compliance, we may be subject to investigation and sanctions by regulatory authorities, such as the Securities and Exchange Commission, or SEC. As a result, there could be a negative reaction in the financial markets due to a loss of confidence in the reliability of our financial statements. In addition, we may be required to incur costs in improving our internal control over financial reporting and hiring additional personnel. Any such actions could negatively affect our results of operations.
We may be subject to criminal or civil sanctions if we fail to comply with privacy regulations regarding the use and disclosure of patient information.
Numerous state, federal and international laws and regulations govern the collection, dissemination, use, privacy, confidentiality, security, availability and integrity of patient health information, including the Health Insurance Portability and Accountability Act of 1996, or HIPAA. In the provision of services to our customers, we may collect, use, maintain and transmit patient health information in ways that are subject to many of these laws and regulations. The three rules that were promulgated pursuant to HIPAA that could most significantly affect our business are the Standards for Electronic Transactions, or Transactions Rule; the Standards for Privacy of Individually Identifiable Health Information, or Privacy Rule; and the Security Standards for the Protection of Electronic Protected Health Information, or Security Rule. The respective compliance dates for these rules for most entities were October 16, 2003, April 14, 2003 and April 21, 2005. In addition, the Standard for Unique Health Identifiers for Healthcare Providers, or National Provider Identifier Rule, which was effective May 23, 2007, affects our business. We completed the process of obtaining the necessary national provider identifiers, or NPIs, for our existing providers in 2007, and continue to seek NPIs for new providers, as necessary.
26
Table of Contents
HIPAA applies to covered entities, which include our professional corporations and lay corporations that employ physicians to furnish professional medical services, and most healthcare facilities and health plans that contract with us for our services. Other federal and state laws restricting the use and protecting the privacy of patient health information also apply to us directly by law or indirectly through contractual obligations to our customers that are directly subject to the laws.
The Transactions Rule establishes format and data content standards for eight of the most common healthcare transactions. When we perform billing and collection services on behalf of our customers, we may be engaging in one or more of these standard transactions and are required to conduct those transactions in compliance with the required standards. The Privacy Rule restricts the use and disclosure of patient information, requires entities to safeguard that information and to provide certain rights to individuals with respect to that information. The Security Rule establishes elaborate requirements for safeguarding patient health information transmitted or stored electronically.
The Privacy Rule and Security Rule require the development and implementation of detailed policies, procedures, contracts and forms to assure compliance. We have implemented such compliance measures and made, and may be required to make, additional costly system purchases and modifications to comply with evolving HIPAA rules and our failure to comply may result in liability and adversely affect our business.
The National Provider Identifier Rule establishes the standard for a unique health identifier for healthcare providers for use in the healthcare system along with implementation specifications for obtaining and using the identifier. In general, this rule requires a covered healthcare provider and any subpart of the covered entity that would be a covered healthcare provider if it were a separate legal entity, to apply for a provider identifier and use it in the standard transactions.
The HIPAA rules also require covered entities to contractually obligate certain of their contractors who may receive protected health information during the course of rendering services on behalf of that entity, to abide by certain burdensome business associate contract requirements. We enter into these contracts as business associates of our customers who contract for the use of our protocols and services and with vendors who perform services on our behalf.
ARRA and regulations that are being promulgated under ARRA include additional requirements related to the privacy and security of patient health information. As part of these additional requirements, ARRA extends compliance with the Privacy Rule and Security Rule to business associates, requires, in certain instances, the reporting of incidents to individuals, the Secretary of HHS and, in some circumstances, the media, where the security of patient health information has been compromised, and provides state attorneys general with enforcement authority for the Privacy Rule and Security Rule. We face potential administrative, civil and criminal sanctions if we do not comply with the existing or new laws and regulations, as well as possible harm to our reputation. Imposition of these sanctions could have a material adverse effect on our operations.
Federal and state consumer laws are being applied increasingly by the Federal Trade Commission, or FTC, and state attorneys general to regulate the collection, use and disclosure of personal or patient health information, through web sites or otherwise, and to regulate the presentation of web site content. Courts may also adopt the standards for fair information practices promulgated by the FTC that concern consumer notice, choice, security and access.
Numerous other federal and state laws protect the confidentiality, privacy, availability, integrity and security of patient information. These laws in many cases are more restrictive than, and not preempted by, the HIPAA rules and may be subject to varying interpretations by courts and government agencies, creating complex compliance issues for us and our customers and potentially exposing us to additional expense, adverse publicity and liability. We may not remain in compliance with the diverse privacy requirements in all of the jurisdictions in which we do business.
27
Table of Contents
New health information standards, whether implemented pursuant to HIPAA, congressional action or otherwise, could have a significant effect on the manner in which we must handle healthcare related data, and the cost of complying with standards could be significant. If we do not properly comply with existing or new laws and regulations related to patient health information, we could be subject to criminal or civil sanctions. See “Business—Regulatory Matters.”
We will be required to comply with the FTC’s Red Flag Rules, which could increase our cost of doing business and could subject us to financial penalties if we fail to comply with these regulations.
The FTC has put into effect “Red Flag Rules” which require “creditors” to develop warning signs or “red flags” that indicate potential identity theft (including medical identity theft). The FTC maintains that heath care providers that regularly permit patients to pay for services after the services are rendered, including paying the balance due after third-party payments are made, are “creditors” for Red Flag Rules purposes. Although the effective date for compliance with the Red Flag Rules was originally November 1, 2008, the FTC has postponed compliance several times, with the latest postponement until June 1, 2010. We will be required to implement a fraud prevention program to (i) identify and respond to red flags or warning signs that could indicate identity theft; (ii) explain our process for detecting red flags; (iii) describe how we would respond to red flags to prevent and mitigate identity theft; and (iv) specify how we will keep our program current. The FTC may seek civil monetary penalties and injunctive relief for violations of Red Flag Rules. The maximum fine is $3,500 per violation.
If we fail to comply with federal or state anti-kickback laws, we could be subject to criminal and civil penalties, loss of licenses and exclusion from Medicare, Medicaid and other federal and state healthcare programs, which could have a material adverse effect on our business, financial condition and results of operations.
Section 1128B(b) of the Social Security Act, or SSA, commonly referred to as the Anti-Kickback Statute, prohibits the offer, payment, solicitation or receipt of any form of remuneration in return for referring, ordering, leasing, purchasing or arranging for or recommending the ordering, purchasing or leasing of items or services payable by the Medicare and Medicaid programs or any other federally funded healthcare program. The Anti-Kickback Statute is very broad in scope, and many of its provisions have not been uniformly or definitively interpreted by courts or regulations.
In the operation of our business, we pay various healthcare providers or other referral sources for items or services they provide to us, and healthcare providers or other referral sources pay us for items or services we provide to them. In addition, we have non-financial relationships with referral sources. All of our financial relationships with healthcare providers and other referral sources, and with referral recipients (such as service agreements, equipment leases and space leases potentially implicate the Anti-Kickback Statute, and some of our non-financial relationships may implicate the Anti-Kickback Statute. In addition, most of the states in which we operate also have adopted laws similar to the Anti-Kickback Statute, although some of them are broader and apply regardless of the source of payment for the item or service provided.
Violations of the Anti-Kickback Statute and similar state laws may result in significant fines, imprisonment and exclusion from the Medicare, Medicaid and other federal or state healthcare programs. Such fines and exclusion could have a material adverse effect on our business, financial condition and results of operations. While we believe that our arrangements with healthcare providers and other referral sources and recipients fall within applicable safe harbors or otherwise do not violate the law, there can be no assurance that federal or state regulatory authorities will not challenge these arrangements under anti-kickback laws. See “Business—Regulatory Matters.”
If the OIG, the Department of Justice or other federal regulators determine that certain of our management services arrangements with hospitals where we are compensated based upon a percentage of charges generated by the physician services rendered to patients at the hospital violate the Anti-Kickback Statute, we could be subject to criminal and civil penalties, loss of licenses and exclusion from Medicare, Medicaid and other federal and state healthcare programs, which could have a material adverse effect on our business, financial condition and results of operations.
In the operation of our business, we provide outsourced physician staffing and administrative services to hospitals and other healthcare providers through contractual arrangements with physicians and hospitals. In some
28
Table of Contents
instances, we may enter into contractual arrangements that provide that, as compensation for staffing a hospital department, we will receive a percentage of charges generated by the physician services rendered to patients seeking treatment in the department.
In 1988, the OIG issued an advisory opinion in which it concluded that a proposed management services contract between a medical practice management company and a physician practice, which provided that the management company would be reimbursed for the fair market value of its operating services and its costs and paid a percentage of net practice revenues, may constitute illegal remuneration under the federal Anti-Kickback Statute. The OIG’s analysis focused on the marketing activities conducted by the management company and concluded that the management services arrangement described in the advisory opinion included financial incentives to increase patient referrals, contained no safeguards against overutilization and included financial incentives that increased the risk of abusive billing practices.
While we believe that the nature of our business and our contractual relationships with hospitals and physicians are distinguishable from the arrangement described in this advisory opinion with regard to both the types of services provided and the risk factors identified by the OIG, regulatory authorities may challenge these arrangements under the Anti-Kickback Statute. Violations of the Anti-Kickback Statute may result in significant fines, imprisonment and exclusion from the Medicare, Medicaid and other federal or state healthcare programs. Such fines and exclusion could have a material adverse effect on our business, financial condition and results of operations.
If changes in laws or regulations affect our operations, including our arrangements with physicians, professional corporations, hospitals and other facilities, and third party payers, we may incur additional costs, lose contracts and suffer a reduction in revenue under existing contracts and we may need to refinance our debt or obtain debt holder consent.
Legislators have introduced and may introduce in the future numerous proposals in the U.S. Congress and state legislatures relating to various healthcare issues. We do not know the ultimate content, timing or effect of any healthcare legislation, nor is it possible at this time to estimate the impact of potential legislation. Further, although we exercise care in structuring our arrangements with physicians, professional corporations, hospitals and other facilities to comply in all significant respects with applicable law: (1) government officials charged with responsibility for enforcing those laws may assert that we, or arrangements into which we have entered, violate those laws or (2) governmental entities or courts may not ultimately interpret those laws in a manner consistent with our interpretation.
In addition to the regulations referred to above, aspects of our operations are also subject to state and federal statutes and regulations governing workplace health and safety and, to a small extent, the disposal of medical waste.
Changes in ethical guidelines and operating standards of professional and trade associations and private accreditation commissions such as the American Medical Association and the Joint Commission on Accreditation of Healthcare Organizations may also affect our operations.
Accordingly, changes in existing laws and regulations, adverse judicial or administrative interpretations of these laws and regulations or enactment of new legislation could adversely affect our operations. If restructuring our relationships becomes necessary, this could cause our operating costs to increase significantly. A restructuring could also result in a loss of contracts or a reduction in revenues under existing contracts. Moreover, if these laws require us to modify our structure and organization to comply with these laws, our financing agreements may prohibit such modifications and require us to obtain the consent of the holders of such indebtedness or require the refinancing of such indebtedness.
29
Table of Contents
If we fail to comply with federal and state physician self-referral laws and regulations as they are currently interpreted or may be interpreted in the future, or if other legislative restrictions are issued, we could incur a significant loss of reimbursement revenue and be subject to significant monetary penalties, which could have a material adverse effect on our business, financial condition and results of operations.
We are subject to federal and state laws and regulations that limit the circumstances under which physicians who have a financial relationship with entities that furnish certain specified healthcare services may refer to such entities for the provision of such services, including inpatient and outpatient hospital services, clinical laboratory services, home health services, physical therapy services, occupational and physical therapy services, radiology and other imaging services and certain other diagnostic services. These laws and regulations also prohibit such entities from billing for services provided in violation of the laws and regulations.
We have financial relationships with physicians and hospitals in the form of compensation arrangements for services rendered. In addition, we have financial relationships with physicians to the extent they own an equity interest in us. While we believe our compensation arrangements with physicians and hospitals are in material compliance with applicable laws and regulations, government authorities might take a contrary position or prohibited referrals may occur. Further, because we cannot be certain that we will have knowledge of all physicians who may hold an indirect ownership interest, referrals from any such physicians may cause us to violate these laws and regulations.
Violation of these laws and regulations may result in the prohibition of payment for services rendered, significant fines and penalties, and exclusion from Medicare, Medicaid and other federal and state healthcare programs, any of which could have a material adverse effect on our business, financial condition and results of operations. In addition, expansion of our operations to new jurisdictions, new interpretations of laws in our existing jurisdictions or new physician self-referral laws could require structural and organizational modifications of our relationships with physicians to comply with those jurisdictions’ laws. Such structural and organizational modifications could result in lower profitability and failure to achieve our growth objectives. See “Business—Regulatory Matters.”
We could experience a loss of contracts with our physicians or be required to sever relationships with our affiliated professional corporations in order to comply with antitrust laws.
Our contracts with physicians include contracts with physicians organized as separate legal professional entities (e.g., professional medical corporations) and as individuals. As such, the antitrust laws deem each such physician/practice to be separate, both from us and from each other and, accordingly, each such physician/practice is subject to a wide range of laws that prohibit anti-competitive conduct among separate legal entities or individuals. A review or action by regulatory authorities or the courts that is negative in nature as to the relationship between us and the physicians/practices with which we contract, could force us to terminate our contractual relationships with physicians and affiliated professional corporations. Since we derive a significant portion of our revenues from these relationships, our revenues could substantially decrease. Moreover, if any review or action by regulatory authorities required us to modify our structure and organization to comply with such action or review, our debt covenants may not permit such modifications, thereby requiring us to obtain the consent of the holders of such indebtedness or requiring the refinancing of such indebtedness.
Risks Related to Our Indebtedness
Our substantial indebtedness could adversely affect our financial condition, our ability to operate our business, react to changes in the economy or our industry and pay our debts and could divert our cash flow from operations for debt payments.
We have a significant amount of indebtedness. As of September 30, 2009, our total indebtedness was $612.1 million, excluding $110.0 million of availability under our senior secured revolving credit facility (without giving effect to $7.5 million of undrawn letters of credit which reduces availability and before any potential reduction associated with the CIT Group, Inc. and CIT Group Funding Company of Delaware LLC, or collectively, CIT, bankruptcy). See “Management’s Discussion and Analysis of Financial Condition and
30
Table of Contents
Results of Operations—Liquidity and Capital Resources.” A 0.25% increase in the expected rate of interest under our senior secured credit facilities would increase our annual interest expense by approximately $1.0 million.
Our substantial debt could have important consequences, including the following:
| • | it may be difficult for us to satisfy our obligations, including debt service requirements under our outstanding debt and the senior subordinated notes; |
| • | our ability to obtain additional financing for working capital, capital expenditures, debt service requirements or other general corporate purposes may be impaired; |
| • | requiring a substantial portion of cash flow from operations to be dedicated to the payment of principal and interest on our indebtedness, therefore reducing our ability to use our cash flow to fund our operations, capital expenditures, future business opportunities and other purposes; |
| • | we are more vulnerable to economic downturns and adverse industry conditions and our flexibility to plan for, or react to, changes in our business or industry is more limited; |
| • | our ability to capitalize on business opportunities and to react to competitive pressures, as compared to our competitors, may be compromised due to our high level of debt and the restrictive covenants in some of our debt agreements; |
| • | our ability to borrow additional funds or to refinance debt may be limited; and |
| • | it may cause potential or existing customers or physicians to not contract with us due to concerns over our ability to meet our financial obligations, such as the payment of physicians or insuring against our professional liability risks, under such contracts. |
Furthermore, all of our debt under our senior secured credit facilities bears interest at variable rates and we are subject to an increase in rates under our revolving credit facility in the event our leverage ratio increases and an increase in rates under our term loan facility in the event of a downgrade in the corporate family rating of us by either Moody’s Investors Service, Inc. or Standard and Poor’s Ratings Services. If these rates were to increase significantly, the risks related to our substantial debt would intensify.
Despite current indebtedness levels, we and our subsidiaries may still be able to incur substantially more debt, which could further exacerbate the risks associated with our substantial leverage.
We and our subsidiaries may be able to incur substantial additional indebtedness in the future. Although the agreements governing our debt instruments contain restrictions on the incurrence of additional indebtedness, these restrictions are subject to a number of qualifications and exceptions, and the indebtedness incurred in compliance with these restrictions could be substantial. If we incur additional debt above the levels currently in effect, the risks associated with our leverage, including those described above, would increase. The senior secured revolving credit facility provides aggregate availability of up to $110.0 million, of which no amount is currently drawn (excluding $7.5 million in undrawn outstanding letters of credit as of September 30, 2009 which reduces availability and before any potential reduction associated with the CIT bankruptcy).
Servicing our debt will require a significant amount of cash. Our ability to generate sufficient cash depends on numerous factors beyond our control, and we may be unable to generate sufficient cash flow to service our debt obligations.
Our business may not generate sufficient cash flow from operating activities to service our debt obligations. Our ability to make payments on and to refinance our debt and to fund planned capital expenditures will depend on our ability to generate cash in the future. To some extent, this is subject to general economic, financial, competitive, legislative, regulatory and other factors and reimbursement actions of governmental and commercial payers, all of which are beyond our control. Lower net revenues, or higher provision for uncollectibles, generally will reduce our cash flow.
31
Table of Contents
If we are unable to generate sufficient cash flow to service our debt and meet our other commitments, we may need to refinance all or a portion of our debt, sell material assets or operations or raise additional debt or equity capital. We may not be able to effect any of these actions on a timely basis, on commercially reasonable terms or at all, and these actions may not be sufficient to meet our capital requirements. In addition, the terms of our existing or future debt agreements may restrict us from effecting any of these alternatives.
Restrictive covenants in our senior secured credit facilities and the indenture governing our senior subordinated notes may restrict our ability to pursue our business strategies, and failure to comply with any of these restrictions could result in acceleration of our debt.
The operating and financial restrictions and covenants in our senior secured credit facilities and the indenture governing the senior subordinated notes may adversely affect our ability to finance future operations or capital needs or to engage in other business activities. The senior secured credit facilities and/or the indenture governing our senior subordinated notes limit our ability, among other things, to:
| • | incur additional debt or issue certain preferred shares; |
| • | pay dividends on or make distributions in respect of our common stock or make other restricted payments; |
| • | make certain investments; |
| • | sell certain assets; |
| • | create liens on certain assets; |
| • | consolidate, merge, sell or otherwise dispose of all or substantially all of our assets; |
| • | enter into certain transactions with our affiliates; and |
| • | designate our subsidiaries as unrestricted subsidiaries. |
In addition, the senior secured credit facilities require us to maintain certain financial ratios (including a minimum fixed charge coverage ratio) and satisfy other financial condition tests. Our ability to meet those financial ratios and tests can be affected by events beyond our control, and we may not be able to meet those ratios and tests. A breach of any of these covenants could result in a default under the senior secured credit facilities. Upon the occurrence of an event of default under the senior secured credit agreement, the lenders could elect to declare all amounts outstanding under the senior secured credit agreement to be immediately due and payable and terminate all commitments to extend further credit. If we were unable to repay those amounts, the lenders under the senior secured credit agreement could proceed against the collateral granted to them to secure that indebtedness. We have pledged a significant portion of our assets as collateral under the senior secured credit agreement. Our future operating results may not be sufficient to enable compliance with the covenants in the senior secured credit agreement, the indenture governing the senior subordinated notes or any other indebtedness and we may not have sufficient assets to repay the senior secured credit agreement as well as our unsecured indebtedness. In addition, in the event of an acceleration, we may not have or be able to obtain sufficient funds to make any accelerated payments.
A decline in our operating results or available cash could cause us to experience difficulties in complying with covenants contained in more than one agreement, which could result in our bankruptcy or liquidation.
If we were to sustain a decline in our operating results or available cash, we could experience difficulties in complying with the financial covenants contained in the senior secured credit agreement. For example, the loss of a significant portion of our existing military staffing business that is subject to the re-bidding process or a failure to mitigate such loss by winning new business as it is submitted for bid to the military may
32
Table of Contents
cause us difficulty in complying with such covenants. The failure to comply with such covenants could result in an event of default under the senior secured credit agreement and by reason of cross-acceleration or cross-default provisions, the senior subordinated notes and any other indebtedness may then become immediately due and payable. In addition, should an event of default occur, the lenders under our senior secured credit agreement could elect to terminate their commitments thereunder, cease making loans and institute foreclosure proceedings against our assets, and we could be forced into bankruptcy or liquidation. If our operating performance declines, we may in the future need to obtain waivers from the required lenders under our senior secured credit agreement to avoid being in default. If we breach our covenants under our senior secured credit agreement and seek a waiver, we may not be able to obtain a waiver from the required lenders. If this occurs, we would be in default under our senior secured credit agreement, the lenders could exercise their rights, as described above, and we could be forced into bankruptcy or liquidation.
Risks Related to This Offering
Since our common stock has never been publicly traded, a trading market may not develop for our common stock, and you may not be able to sell your stock.
There has never been a public market for our common stock. A liquid trading market for our common stock may not develop. The initial public offering price will be determined in negotiations among representatives of the underwriters, the selling shareholder and us and may not be indicative of prices that will prevail in the trading market after this offering.
You will experience immediate and substantial dilution in the net tangible book value of the shares you purchase in this offering.
The price you pay for shares of our common stock sold in this offering is substantially higher than the per share value of our net assets, after giving effect to this offering. Assuming an initial public offering price for our common stock of $ per share, the mid-point of the initial public offering price range indicated on the cover page of this prospectus, you will incur immediate dilution in net tangible book value per share of $ . Additionally, new investors in this offering will have contributed % of our total equity as of September 30, 2009, but will own only % of our outstanding shares upon completion of this offering.
If securities analysts do not publish research or reports about our business or if they downgrade our stock or our sector, the price of our stock could decline.
The trading market for our common stock will rely in part on the research and reports that industry or financial analysts publish about us or our business. We do not control these analysts. Furthermore, if one or more of the analysts who do cover us downgrades our stock or our industry, or the stock of any of our competitors, the price of our stock could decline. If one or more of these analysts ceases coverage of our company, we could lose visibility in the market, which in turn could cause our stock price to decline.
Future sales of our common stock or the possibility or perception of such future sales may depress our stock price.
After this offering, we will have shares of common stock outstanding. Sales of a substantial number of shares of common stock in the public market following this offering, or the perception that these sales could occur, could substantially decrease the market price of our common stock. All the shares sold in this offering will be freely tradable. Substantially all of the remaining shares of our common stock are available for resale in the public market, subject to the restrictions on sale or transfer during the 180-day lockup period after the date of this prospectus that is described in “Shares Eligible for Future Sale.” Registration of the sale of these shares of our common stock would permit their sale into the market immediately. As restrictions on resale end or upon registration of any of these shares for resale, the market price of our common stock could drop significantly if the holders of these shares sell them or are perceived by the market as intending to sell them.
33
Table of Contents
In addition, following the expiration of the lock-up period, the selling shareholder will have the right, subject to certain conditions, to require us to register the sale of its remaining shares of our common stock under the Securities Act. By exercising its registration rights and selling a large number of shares, the selling shareholder could cause the prevailing market price of our common stock to decline.
Our stock price may change significantly following the offering, and you could lose all or part of your investment as a result.
We, the selling shareholder and the representatives of the underwriters will negotiate to determine the initial public offering price. You may not be able to resell your shares at or above the initial public offering price due to a number of factors such as those listed in “—Risks Related to Our Business” and the following, some of which are beyond our control:
| • | quarterly variations in our results of operations; |
| • | results of operations that vary from the expectations of securities analysts and investors; |
| • | results of operations that vary from those of our competitors; |
| • | changes in expectations as to our future financial performance, including financial estimates by securities analysts and investors; |
| • | announcements by third parties of significant claims or proceedings against us; |
| • | future sales of our common stock; and |
| • | general U.S. and global economic conditions. |
Furthermore, the stock market recently has experienced extreme volatility that in some cases has been unrelated or disproportionate to the operating performance of particular companies. These broad market and industry fluctuations may adversely affect the market price of our common stock, regardless of our actual operating performance.
In the past, following periods of market volatility, stockholders have instituted securities class action litigation. If we were involved in securities litigation, it could have a substantial cost and divert resources and the attention of our senior management team from our business regardless of the outcome of such litigation.
The interests of our Sponsor may be in conflict with your interests.
Immediately following the completion of this offering, investment funds associated with or designated by the Sponsor will beneficially own, through Ensemble Parent LLC, % of our outstanding common stock and voting power, or % if the underwriters exercise their option to purchase additional shares in full. As a result, the Sponsor will have the ability to elect all of the members of our board of directors and thereby control our policies and operations, including the appointment of management, future issuances of our common stock or other securities, the payments of dividends, if any, on our common stock, the incurrence of debt by us, amendments to our certificate of incorporation and bylaws and the entering into of extraordinary transactions, and their interests may not in all cases be aligned with your interests. In addition, the Sponsor may have an interest in pursuing acquisitions, divestitures and other transactions that, in their judgment, could enhance their equity investment, even though such transactions might involve risks to you. For example, the Sponsor could cause us to make acquisitions that increase our indebtedness or to sell revenue-generating assets. See “Management,” “Principal and Selling Shareholder” and “Certain Relationships and Related Party Transactions.”
Additionally, the Sponsor is in the business of making investments in companies and may from time to time acquire and hold interests in businesses that compete directly or indirectly with us. The Sponsor may also pursue acquisition opportunities that may be complementary to our business and, as a result, those acquisition
34
Table of Contents
opportunities may not be available to us. So long as investment funds associated with or designated by the Sponsor continue to indirectly own a significant amount of our common stock and voting power through Ensemble Parent LLC, even if such amount is less than 50%, the Sponsor will continue to be able to strongly influence or effectively control our decisions. In addition, the Sponsor will be able to determine the outcome of all matters requiring stockholder approval and will be able to cause or prevent a change of control of our company or a change in the composition of our board of directors and could preclude any unsolicited acquisition of our company. The concentration of ownership could deprive you of an opportunity to receive a premium for your common stock as part of a sale of our company and might ultimately affect the market price of your common stock.
We are a “controlled company” within the meaning of The New York Stock Exchange listing standards and, as a result, will qualify for, and intend to rely on, exemptions from certain corporate governance requirements.
Upon the completion of this offering, investment funds associated with or designated by the Sponsor will beneficially own, through Ensemble Parent LLC, approximately % of our outstanding common stock and voting power, or % if the underwriters exercise their option to purchase additional shares in full. Because affiliates of the Sponsor will own more than 50% of the voting power of the issuer after giving effect to this offering, we will be considered a “controlled company” for the purposes of The New York Stock Exchange, or NYSE, listing requirements. As such, we may elect not to comply with certain NYSE corporate governance requirements that: (1) a majority of the board of directors consist of independent directors, (2) we have a compensation committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities and (3) we have a nominating and corporate governance committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities. Following this offering, we intend to utilize these exemptions. As a result, we will not have a majority of independent directors, and we will not have a compensation committee and a nominating and corporate governance committee consisting entirely of independent directors. See “Management—Controlled Company Exception.” Accordingly, you will not have the same protections afforded to stockholders of companies that are subject to all of the corporate governance requirements of the NYSE.
Anti-takeover provisions in our certificate of incorporation and by-laws and Delaware law could delay or prevent a change in control.
Our certificate of incorporation and by-laws may delay or prevent a merger or acquisition that a stockholder may consider favorable by, among other things, establishing a classified board of directors, permitting our board of directors to issue one or more series of preferred stock, requiring advance notice for stockholder proposals and nominations and placing limitations on convening stockholder meetings. In addition, we are subject to provisions of the Delaware General Corporation Law, or DGCL, that restrict certain business combinations with interested stockholders. These provisions may also discourage acquisition proposals or delay or prevent a change in control, which could harm our stock price. See “Description of Capital Stock.”
We do not intend to pay cash dividends in the foreseeable future.
We do not intend to pay cash dividends on our common stock. We currently expect to retain future earnings, if any, for use in the operation and expansion of our business and do not anticipate paying any cash dividends in the foreseeable future. Our ability to pay dividends on our common stock is currently limited by the covenants of our senior secured credit facilities as well as the indenture governing our senior subordinated notes and may be further restricted by the terms of any future debt or preferred securities. Payments of future dividends, if any, will be at the discretion of our board of directors after taking into account various factors, including our business, operating results and financial condition, current and anticipated cash needs, plans for expansion and any legal or contractual limitations on our ability to pay dividends. As a result, capital appreciation, if any, of our common stock will be your sole source of potential gain for the foreseeable future.
35
Table of Contents
Statements made in the prospectus that are not historical facts and that reflect our current view about future events and financial performance are hereby identified as “forward-looking statements.” Some of these statements can be identified by terms and phrases such as “anticipate,” “believe,” “intend,” “estimate,” “expect,” “continue,” “could,” “should” “may,” “plan,” “project,” “predict” and similar expressions and include references to assumptions that we believe are reasonable and relate to our future prospects, developments and business strategies. We caution investors that such “forward-looking statements,” including, without limitation, those relating to our future business prospects, revenues, working capital, professional liability expense, liquidity, capital needs, interest costs and income, wherever they occur in this prospectus, are necessarily estimates reflecting the judgment of our senior management and involve a number of risks and uncertainties that could cause actual results to differ materially from those suggested by the “forward-looking statements.” Factors that could cause our actual results to differ materially from those expressed or implied in such forward-looking statements, include, but are not limited to:
| • | the effect and interpretation of current or future government regulation of the healthcare industry, and our ability to comply with these regulations; |
| • | our exposure to professional liability lawsuits and governmental agency investigations; |
| • | the adequacy of our insurance coverage and insurance reserves; |
| • | our reliance on third-party payers; |
| • | the general level of ED patient volumes at our clients’ facilities; |
| • | our ability to enter into and retain contracts with hospitals, military treatment facilities and other healthcare facilities on attractive terms; |
| • | changes in rates or methods of government payments for our services; |
| • | our ability to successfully integrate strategic acquisitions; |
| • | the control of our company by our sponsor may be in conflict with our interests; |
| • | our future capital needs and ability to obtain future financing; |
| • | our ability to carry out our business strategy; |
| • | our ability to continue to recruit and retain qualified healthcare professionals and our ability to attract and retain operational personnel; |
| • | competition in our market; |
| • | our ability to maintain or implement complex information systems; |
| • | our substantial indebtedness; |
| • | our ability to generate cash flow to service our debt obligations; |
| • | certain covenants in our debt documents described in this prospectus; |
36
Table of Contents
| • | general economic conditions; and |
| • | other factors detailed from time to time in our filings with the SEC. |
Our forward-looking statements speak only as of the date of this prospectus or as of the date they are made. We disclaim any intent or obligation to update “forward-looking statements” made in this prospectus to reflect changed assumptions, the occurrence of unanticipated events or changes to future operating results over time.
37
Table of Contents
We estimate that we will receive net proceeds of approximately $ million from the sale of shares of our common stock in this offering, assuming an initial public offering price of $ per share, the mid-point of the estimated price range set forth on the cover page of this prospectus, and after deducting the underwriting discounts and commissions and estimated offering expenses payable by us. We will not receive any proceeds from the sale of shares of our common stock by the selling shareholder.
We intend to use the net proceeds from this offering principally for the repayment of indebtedness. We intend to apply approximately $ million of net proceeds (including estimated premiums and accrued interest) to repurchase $ million of our existing 11.25% senior subordinated notes due 2013 (the “senior subordinated notes”).
An increase of 1,000,000 shares from the expected number of shares to be sold by us in this offering, assuming no change in the assumed initial public offering price per share, would increase our net proceeds from this offering by $ million. A $1.00 increase (decrease) in the assumed initial public offering price of $ per share, based on the mid-point of the estimated price range set forth on the cover page of this prospectus, would increase (decrease) the net proceeds to us from this offering by $ million, assuming the number of shares offered by us, as set forth on the cover page of this prospectus, remains the same and after deducting the underwriting discounts and commissions and estimated offering expenses payable by us.
In the event of any such increase in net proceeds to us, we would apply such additional net proceeds to further reduce our existing senior subordinated notes. Any excess over the total cost to repay all the senior subordinated notes would be used for general corporate purposes. We may also use a portion of our existing cash to reduce our senior subordinated notes to the extent permitted by our senior secured credit facilities. See “Description of Certain Indebtedness—Senior Secured Credit Facilities.”
38
Table of Contents
We currently expect to retain future earnings, if any, for use in the operation and expansion of our business and do not anticipate paying any cash dividends in the foreseeable future. Our ability to pay dividends on our common stock is currently limited by the covenants of our senior secured credit facilities as well as our senior subordinated notes and may be further restricted by the terms of any future debt or preferred securities. Payments of future dividends, if any, will be at the discretion of our board of directors after taking into account various factors, including our business, operating results and financial condition, current and anticipated cash needs, plans for expansion and any legal or contractual limitations on our ability to pay dividends. See “Description of Certain Indebtedness” for a description of the restrictions on our ability to pay dividends.
39
Table of Contents
The following table sets forth our actual consolidated cash and cash equivalents and capitalization as of September 30, 2009 and our consolidated cash and cash equivalents and capitalization as of September 30, 2009 on an as adjusted basis to give effect to (1) the issuance of shares of common stock by us in this offering, after deducting underwriting discounts and estimated offering expenses, (2) the application of the estimated net proceeds to us as described in “Use of Proceeds” and (3) the use of existing cash to make a lump-sum termination payment to an affiliate of The Blackstone Group pursuant to our transaction and monitoring fee agreement with such affiliate. Certain members of our management will also receive a portion of such payment. See “Certain Relationships and Related Party Transactions.”
The information in this table should be read in conjunction with “Use of Proceeds,” “Selected Consolidated Financial Data,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the consolidated financial statements and the notes thereto included elsewhere in this prospectus.
| As of September 30, 2009 | ||||||||
| Actual | As Adjusted(1) |
|||||||
| (In thousands) |
||||||||
| Cash and cash equivalents |
$ | 112,994 | $ | (2) | ||||
| Long-term debt, including current maturities of long-term debt: |
||||||||
| Term loan facility |
$ | 409,063 | $ | |||||
| Revolving line of credit(3) |
— | |||||||
| 11.25% senior subordinated notes due 2013 |
203,025 | |||||||
| Total debt |
612,088 | |||||||
| Total members’ deficit |
(228,327 | ) | ||||||
| Stockholders’ equity: |
||||||||
| Common stock, $0.01 par value: No shares authorized, issued or outstanding, actual; 100,000,000 shares authorized and shares issued and outstanding, as adjusted |
— | |||||||
| Additional paid-in capital |
— | |||||||
| Retained earnings |
— | |||||||
| Total stockholders’ equity |
— | |||||||
| Total capitalization |
$ | 383,761 | $ | |||||
| (1) | To the extent we change the number of shares of common stock sold by us in this offering from the shares we expect to sell or we change the initial public offering price from the $ per share assumed initial public offering price, representing the mid-point of the estimated price range set forth on the cover page of this prospectus, or any combination of these events occurs, the net proceeds to us from this offering and each of total stockholders’ equity and total capitalization may increase or decrease. A $1.00 increase (decrease) in the assumed initial public offering price per share of the common stock, assuming no change in the number of shares of common stock to be sold, would increase (decrease) the net proceeds that we receive in this offering and each of total stockholders’ equity and total capitalization by approximately $ million. An increase (decrease) of 1,000,000 shares in the expected number of shares to be sold in the offering, assuming no change in the assumed initial offering price per share, would increase (decrease) our net proceeds from this offering and our total stockholders’ equity and total capitalization by approximately $ million. See “Use of Proceeds.” |
| (2) | Based on current interest rates and the mid-point of the price range set forth on the cover page of this prospectus, the lump-sum payment will be $ million. The actual amount is subject to change based on the interest rates in effect at the consummation of this offering. See “Certain Relationships and Related Party Transactions.” |
| (3) | This amount does not include $7.5 million of outstanding letters of credit as of September 30, 2009. As of September 30, 2009, the revolving line of credit was not drawn. |
40
Table of Contents
Dilution is the amount by which the portion of the offering price paid by the purchasers of the common stock to be sold in this offering exceeds the net tangible book value or deficiency per share of our common stock after the offering. Net tangible book value or deficiency per share of our common stock is determined at any date by subtracting our total liabilities from our total assets less our intangible assets and dividing the difference by the number of shares of common stock deemed to be outstanding at that date.
Our net tangible book value as of September 30, 2009 (after giving effect to the Corporate Conversion) was approximately $ million, or $ per share of common stock. After giving effect to our receipt and intended use of approximately $ million of estimated net proceeds (after deducting underwriting discounts and commissions and estimated offering expenses payable by us) from our sale of common stock in this offering based on an assumed initial public offering price of $ per share of common stock, the mid-point of the range set forth on the cover page of this prospectus, our adjusted net tangible book value as of September 30, 2009 would have been approximately $ million, or $ per share of common stock. This amount represents an immediate increase in net tangible book value of $ per share of our common stock to existing stockholders and an immediate dilution of $ per share of our common stock to new investors purchasing shares of common stock in this offering at the assumed initial public offering price.
The following table illustrates this dilution on a per share basis:
| Assumed initial public offering price per share |
$ | ||
| Net tangible book value per share as of September 30, 2009 (after giving effect to the Corporate Conversion) |
|||
| Increase per share attributable to cash payments made by investors in this offering |
|||
| Adjusted net tangible book value per share after this offering |
|||
| Dilution per share to new investors |
$ | ||
If the underwriters exercise their over-allotment option in full, the adjusted tangible book value per share after giving effect to the offering would be $ per share. This represents an increase in adjusted net tangible book value of $ per share to existing stockholders and dilution in adjusted net tangible book value of $ per share to new investors.
A $1.00 increase (decrease) in the assumed initial public offering of $ per share would increase (decrease) our adjusted net tangible book value per share after this offering and dilution to new investors by $ , assuming the number of shares offered by us, as set forth on the cover page of this prospectus, remains the same and after deducting the underwriting discounts and commissions and estimated offering expenses payable by us.
The following table summarizes, on an as adjusted basis as of September 30, 2009, the differences between the number of shares purchased from us, the total consideration paid to us, and the average price per share paid by existing stockholders and by new investors in this offering. As the table shows, new investors purchasing shares in this offering will pay an average price per share substantially higher than our existing stockholders paid. The table below assumes an initial public offering price of $ per share for shares purchased in this offering and excludes underwriting discounts and commissions and estimated offering expenses payable by us:
| Shares Purchased | Total Consideration | Average Price Per Share | ||||||||||||
| Number | Percent | Amount | Percent | |||||||||||
| Existing stockholders |
% | $ | % | $ | ||||||||||
| New investors |
||||||||||||||
| Total |
100.0 | % | $ | 100.0 | % | $ | ||||||||
To the extent that we grant options to our employees in the future and those options are exercised or other issuances of common stock are made, there will be further dilution to new investors.
41
Table of Contents
In connection with this offering, our board of representatives will elect to convert the Company from a Delaware limited liability company to a corporation organized under the laws of the State of Delaware. In order to consummate such a conversion, a certificate of conversion will be filed with the Secretary of State of the State of Delaware prior to the closing of this offering.
Prior to giving effect to the Corporation Conversion, we had three classes of limited liability company interests: Class A, or common units (referred to herein as the Class A units), and Class B and Class C management equity incentive units (referred to herein as the Class B units and Class C units, respectively). In connection with the Corporate Conversion, the Class A units, Class B units and Class C units will be automatically converted into an aggregate shares of common stock. The number of shares and the percentage of our common stock being sold to the public in the primary portion of this offering will be fixed and the initial public offering price will be used to derive the equity value of the Company at the time of this offering. Such equity value will be represented by a fixed number of shares of our common stock, which will be allocated in the Corporate Conversion amongst the former holders of the Class A units, Class B units and Class C units based on the distribution provisions contained in our current limited liability company agreement. The higher the initial public offering price, the greater the percentage of the equity value of the Company would be allocated to the former holders of the Class B units and Class C units. At relatively higher initial public offering prices, the former holders of the Class C units would receive a greater proportion of the shares of our common stock issued in the Corporate Conversion than the former holders of the Class B units and the Class A units, and the former holders of the Class B units would receive a greater proportion of the shares our common stock issued in the Corporate Conversion than the former holders of the Class A units.
42
Table of Contents
Organizational Structure
The diagram below depicts our organizational structure immediately following the Corporate Conversion.
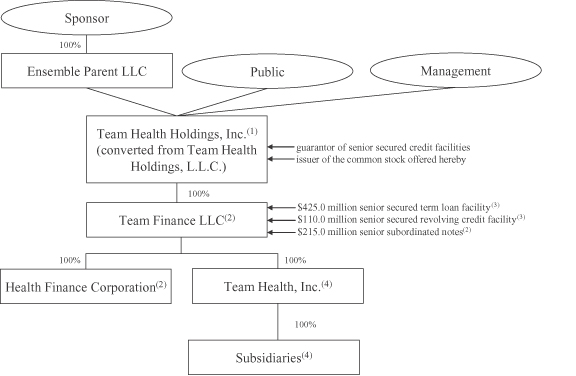
| (1) | In connection with this offering, Team Health Holdings, L.L.C. will convert from a Delaware limited liability company into a corporation. See “Corporate Conversion.” |
| (2) | Team Finance LLC and Health Finance Corporation are co-issuers of the senior subordinated notes. Team Finance LLC has no operations or assets or revenues other than those acquired in the Recapitalization Merger described elsewhere in this prospectus. Health Finance Corporation is a wholly-owned subsidiary of Team Finance LLC and was formed for the sole purpose of serving as corporate co-issuer of the senior subordinated notes. Health Finance Corporation does not have any operations or assets and does not generate any revenues. |
| (3) | As of September 30, 2009, we had approximately $409.1 million of borrowings outstanding under the senior secured term loan facility and no borrowings outstanding under the senior secured revolving credit facility, with an additional $110.0 million of borrowing capacity (without giving effect to $7.5 million of undrawn letters of credit which reduces availability and before any potential reduction associated with the CIT bankruptcy). |
| (4) | Only wholly-owned domestic subsidiaries of Team Finance LLC (other than Health Finance Corporation) currently guarantee the senior secured credit facilities and the senior subordinated notes. All subsidiaries of Team Finance LLC are wholly-owned domestic subsidiaries, other than a subsidiary incorporated in the Cayman Islands for the sole purpose of providing insurance to certain subsidiaries of Team Finance LLC and our physicians with whom we employ or independently contract. Certain of our domestic subsidiaries have ownership interests in joint ventures which currently do not provide us with a significant amount of net revenues. |
43
Table of Contents
The 2005 Transactions
On November 23, 2005, affiliates of the Sponsor, by merging with us, acquired a 91.1% interest in Team Health Holdings, L.L.C. (referred to herein as the Recapitalization Merger). Team Health Holdings, L.L.C. became the parent of Team Finance LLC. In addition, pursuant to the Merger Agreement dated October 11, 2005, Team MergerSub Inc., a Tennessee Corporation and wholly-owned subsidiary of Team Finance LLC merged with and into Team Health, Inc. (referred to herein as the Reorganization Merger). The remaining 8.9% ownership in Team Health Holdings, L.L.C. was held by members of our management at the time of the mergers. The Recapitalization Merger and the Reorganization Merger are referred to as the “2005 Transactions” in this prospectus.
The Recapitalization Merger was accounted for as a recapitalization. The historical information for Team Health, Inc. has been restated to reflect this recapitalization. The Reorganization Merger was accounted for as an acquisition of minority interest, whereby the common shares of Team Health, Inc. that were not owned by Team Health Holdings at November 23, 2005 were recorded at fair value resulting in an adjustment to the carrying value of the pro rata portion of assets and liabilities deemed to have been acquired or assumed in the Reorganization Merger. Pursuant to the Reorganization Merger, all the existing outstanding minority equity interests in Team Health, Inc. were acquired by Team Health Holdings, resulting in Team Health Holdings owning 100% of the outstanding equity interests in Team Health, Inc. In 1999, our former controlling stockholders acquired their controlling interest in Team Health, Inc. in a transaction that was also accounted for as a recapitalization. The acquisition by Team Health Holdings of the existing minority interests in Team Health, Inc. pursuant to the Reorganization Merger requires the “push down” of the accounting basis established in the 1999 Recapitalization as well as the basis created through the acquisition of minority interest from Team Health Holdings to Team Health, Inc.
44
Table of Contents
SELECTED CONSOLIDATED FINANCIAL DATA
The following table sets forth our selected historical financial data as of the dates and for the periods indicated. The selected historical financial data as of December 31, 2007 and 2008 and for each of the three years in the period ended December 31, 2008 have been derived from our audited consolidated financial statements included elsewhere in this prospectus. We derived the selected historical financial data as of December 31, 2006 from our audited consolidated financial statements that are not included in this prospectus. We derived the selected historical financial data as of December 31, 2004 and 2005 and for each of the two years in the period ended December 31, 2005 from our unaudited consolidated financial statements that are not included in this prospectus. We derived the following selected historical financial data as of and for the nine months ended September 30, 2008 and 2009 from our unaudited historical consolidated financial statements and the notes thereto included elsewhere in this prospectus. In the opinion of management, the interim financial data set forth below include all adjustments, consisting of normal recurring accruals, necessary to present fairly our financial position. Operating results for the nine months ended September 30, 2009 are not necessarily indicative of the results that may be expected for the entire fiscal year.
You should read the data presented below together with, and qualified by reference to, our consolidated financial statements and the notes thereto and “Management’s Discussion and Analysis of Financial Condition and Results of Operations,” each of which is included elsewhere in this prospectus.
| Year Ended December 31, | Nine Months Ended September 30, | |||||||||||||||||||||||||
| 2004 | 2005 | 2006 | 2007 | 2008 | 2008 | 2009 | ||||||||||||||||||||
| (Dollars in thousands, except per share data) | ||||||||||||||||||||||||||
| Statement of Operations Data: |
||||||||||||||||||||||||||
| Net revenue less provision for uncollectibles |
$ | 996,408 | $ | 1,001,725 | $ | 1,095,387 | $ | 1,232,065 | $ | 1,331,317 | $ | 999,807 | $ | 1,074,657 | ||||||||||||
| Cost of services rendered (exclusive of depreciation and amortization shown separately below): |
||||||||||||||||||||||||||
| Professional service expenses |
752,041 | 750,632 | 831,826 | 950,872 | 1,046,806 | 779,426 | 828,268 | |||||||||||||||||||
| Professional liability costs |
59,839 | 40,383 | 37,642 | 21,057 | 15,247 | (2,986 | ) | 19,145 | ||||||||||||||||||
| General and administrative expenses |
92,599 | 101,381 | 103,744 | 114,476 | 116,942 | 88,277 | 93,182 | |||||||||||||||||||
| Management fee and other expenses |
1,387 | 1,901 | 3,748 | 4,054 | 3,602 | 2,745 | 2,324 | |||||||||||||||||||
| Impairment of intangibles |
73,177 | — | — | — | 9,134 | — | — | |||||||||||||||||||
| Depreciation and amortization |
26,604 | 24,813 | 23,308 | 14,823 | 17,281 | 12,559 | 14,028 | |||||||||||||||||||
| Interest expense, net |
28,941 | 30,009 | 57,813 | 55,234 | 45,849 | 34,033 | 27,671 | |||||||||||||||||||
| Loss (gain) on extinguishment of debt |
14,731 | 25,340 | — | — | (1,640 | ) | — | — | ||||||||||||||||||
| Transaction costs |
— | 18,223 | — | — | 2,386 | 1,805 | 578 | |||||||||||||||||||
| Earnings (loss) from continuing operations before income taxes |
(52,911 | ) | 9,043 | 37,306 | 71,549 | 75,710 | 83,948 | 89,461 | ||||||||||||||||||
| Provision for income taxes |
5,568 | 8,190 | 13,792 | 27,703 | 31,044 | 33,885 | 34,230 | |||||||||||||||||||
| Earnings (loss) from continuing operations |
(58,479 | ) | 853 | 23,514 | 43,846 | 44,666 | 50,063 | 55,231 | ||||||||||||||||||
| Earnings (loss) from discontinued operations, net of taxes |
536 | 858 | (7,049 | ) | (576 | ) | — | — | — | |||||||||||||||||
| Net earnings (loss) |
(57,943 | ) | 1,711 | 16,465 | 43,270 | 44,666 | 50,063 | 55,231 | ||||||||||||||||||
| Dividends on preferred shares |
3,602 | — | — | — | — | — | — | |||||||||||||||||||
| Net earnings (loss) attributable to common stockholders/members |
$ | (61,545 | ) | $ | 1,711 | $ | 16,465 | $ | 43,270 | $ | 44,666 | $ | 50,063 | $ | 55,231 | |||||||||||
| Per Share Data:(1) |
||||||||||||||||||||||||||
| Unaudited pro forma basic net earnings per share(1) |
||||||||||||||||||||||||||
| Net earnings per share |
$ | $ | $ | $ | $ | $ | $ | |||||||||||||||||||
| Weighted average shares outstanding (in millions) |
||||||||||||||||||||||||||
45
Table of Contents
| Year Ended December 31, | Nine Months Ended September 30, |
|||||||||||||||||||||||||||
| 2004 | 2005 | 2006 | 2007 | 2008 | 2008 | 2009 | ||||||||||||||||||||||
| (Dollars in thousands, except per share data) | ||||||||||||||||||||||||||||
| Unaudited pro forma diluted net earnings per share |
||||||||||||||||||||||||||||
| Net earnings per share |
$ | $ | $ | $ | $ | $ | $ | |||||||||||||||||||||
| Weighted average shares outstanding (in millions) |
||||||||||||||||||||||||||||
| Unaudited supplemental pro forma basic net earnings per share(2) |
||||||||||||||||||||||||||||
| Net earnings per share |
|
$ | — | $ | ||||||||||||||||||||||||
| Weighted average shares outstanding (in millions) |
|
— | ||||||||||||||||||||||||||
| Unaudited supplemental pro forma diluted net earnings per share(2) |
||||||||||||||||||||||||||||
| Net earnings per share |
|
$ | — | $ | ||||||||||||||||||||||||
| Weighted average shares outstanding (in millions) |
|
— | ||||||||||||||||||||||||||
| Cash Flows and Other Financial Data: |
||||||||||||||||||||||||||||
| Net cash provided by operating activities |
$ | 64,585 | $ | 56,843 | $ | 49,553 | $ | 70,054 | $ | 61,971 | $ | 62,869 | $ | 84,621 | ||||||||||||||
| Net cash provided by (used in) investing activities |
(75,795 | ) | 29,286 | (50,109 | ) | (31,256 | ) | (29,772 | ) | (21,156 | ) | (13,102 | ) | |||||||||||||||
| Net cash used in financing activities |
(71,823 | ) | (93,416 | ) | (6,089 | ) | (12,507 | ) | (16,091 | ) | (4,986 | ) | (4,923 | ) | ||||||||||||||
| Capital expenditures (3) |
6,713 | 10,917 | 11,271 | 12,680 | 12,141 | 7,341 | 5,244 | |||||||||||||||||||||
| Balance Sheet Data (at period end): |
||||||||||||||||||||||||||||
| Cash and cash equivalents |
$ | 82,582 | $ | 10,644 | $ | 3,999 | $ | 30,290 | $ | 46,398 | $ | 67,017 | $ | 112,994 | ||||||||||||||
| Working capital(4) |
96,717 | 39,312 | 49,577 | 69,931 | 85,746 | 97,434 | 128,427 | |||||||||||||||||||||
| Total assets |
618,738 | 646,501 | 654,560 | 699,173 | 726,781 | 735,881 | 800,449 | |||||||||||||||||||||
| Total debt |
428,125 | 645,300 | 642,550 | 631,500 | 615,275 | 628,312 | 612,088 | |||||||||||||||||||||
| Total stockholders’ deficit |
(193,188 | ) | — | — | — | — | — | — | ||||||||||||||||||||
| Total members’ deficit |
$ | — | $ | (383,521 | ) | $ | (366,690 | ) | $ | (324,535 | ) | $ | (283,674 | ) | $ | (274,143 | ) | $ | (228,327 | ) | ||||||||
| (1) | Per share data will be computed based upon the number of shares of common stock outstanding immediately after the Corporate Conversion applied to historical net income amounts and will give retroactive effect to the conversion of our limited liability company interests into shares of common stock. |
| (2) | The unaudited supplemental pro forma basic and diluted net earnings per share for the year ended December 31, 2008 and the nine months ended September 30, 2009 gives effect to the portion of the offering proceeds to be used for the repayment of indebtedness. See “Use of Proceeds.” |
| (3) | Reflects expenditures for property and equipment used in our business. |
| (4) | Working capital means current assets minus current liabilities. |
46
Table of Contents
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION
AND RESULTS OF OPERATIONS
The following discussion and analysis of our financial condition and results of operations should be read in conjunction with “Selected Consolidated Financial Data,” and the audited and unaudited interim historical consolidated financial statements and notes thereto included elsewhere in this prospectus. The following discussion contains forward-looking statements and involves numerous risks and uncertainties including, but not limited to, those discussed in “Risk Factors.” Actual results may differ materially from those contained in any forward-looking statements. You should read “Forward-Looking Statements” and “Risk Factors” included elsewhere in this prospectus.
Introduction
We believe we are one of the largest suppliers of outsourced healthcare professional staffing and administrative services to hospitals and other healthcare providers in the United States, based upon revenues and patient visits. Our regional operating models also include comprehensive programs for inpatient care, radiology, pediatrics and other healthcare services, principally within hospital departments and other healthcare treatment facilities. We have focused, however, primarily on providing outsourced services to hospital EDs, which accounts for the majority of our net revenues.
Factors and Trends that Affect Our Results of Operations
In reading our financial statements, you should be aware of the following factors and trends that we believe are important in understanding our financial performance.
General Economic Conditions
The continuation of the current economic downturn may adversely impact our ability to collect for the services we provide as higher unemployment and reductions in commercial managed care and governmental healthcare program enrollment may increase the number of uninsured and underinsured patients seeking healthcare at one of our staffed EDs. We could also be negatively affected if the federal government or the states reduce funding of Medicare, Medicaid and other federal and state healthcare programs in response to increasing deficits in their budgets. Also, patient volume trends in our hospital EDs could be adversely affected as individuals potentially defer or forego seeking care in such departments due to the loss or reduction of coverage previously available to such individuals under commercial insurance or governmental healthcare programs.
Additionally, on November 1, 2009, it was reported that CIT filed for protection under Chapter 11 of the federal Bankruptcy Code in the United States Bankruptcy Court in the Southern District of New York. We have an aggregate revolving credit facility commitment of $110 million with a large consortium of banks, including CIT Lending Services Corporation, or CIT Lending Services, a subsidiary of CIT. As of November 1, 2009, CIT Lending Services’ was not a party to the above-referenced Chapter 11 filing and their total commitment within this existing credit facility was $10 million. As of September 30, 2009, we had no outstanding borrowings under the senior secured revolving credit facility and $7.5 million of outstanding letters of credit. We do not believe any potential reduction in available capacity under this revolving credit facility will have a significant impact on our liquidity. We believe our cash balances, operating cash flows and funds available under our senior secured credit facilities provide adequate resources to fund ongoing operating requirements, future expansion opportunities and capital expenditures in the foreseeable future. Neither Team Finance nor any of our subsidiaries is a counterparty with CIT or any of its subsidiaries under our existing interest rate swap contracts.
The Corporate Conversion
We will convert from a limited liability company to a corporation in connection with this offering. See “Corporate Conversion.” In addition to converting Class A units, Class B units and Class C units into common
47
Table of Contents
stock, each holder of Class B units and Class C units will also be issued vested and unvested options to acquire shares of our common stock in substitution for part of the economic benefits of their outstanding Class B units or Class C units not reflected in the conversion of the units into shares of common stock, with the exercise price of these options equal to the initial public offering price or such higher price as may be necessary to accurately reflect the terms of the Class B units or Class C units to which they relate. The common stock received in the conversion associated with unvested Class B units and Class C units and the unvested options will be subject to the same vesting schedule that was previously applied to the Class B units or Class C units to which they relate. We expect to record pre-tax non-cash stock-based compensation expense in connection with a portion of these option grants. Based on an initial public offering price of $ per share, the mid-point of the estimated price range set forth on the cover page of this prospectus, such expense would be approximately $ million. A portion of this expense would be amortized over the vesting period of the applicable common stock and options and approximately $ million of the expense will be recognized in the fourth quarter of 2009. In the event of a higher initial public offering price, the former holders of Class B or Class C units would receive a greater number of shares of common stock issued in the Corporate Conversion and a reduced number of stock options, which in turn would result in a change in the compensation expense recorded in connection with these option grants. For example, based on an initial public offering price of $ per share, such expense would be approximately $ million.
2009 and 2010 Medicare Fee Schedule Changes
On October 30, 2008, CMS released its final 2009 MPFS covering the period from January 1, 2009 through December 31, 2009. As a result of a 1.1% statutory increase in the 2009 MPFS and in the increase in the physician work values associated with certain emergency services, we estimate that the 2009 MPFS effectively provides for an average 4.0% increase in the 2009 payment amount over the 2008 payment amount for services most commonly provided by emergency physicians. We estimate this increase in rates will increase our revenues from Medicare and other revenue sources whose rates are linked to the Medicare fee schedule by an estimated $9.0 million in 2009. The new legislation also extends the PQRI through 2010, increasing the reporting bonus when certain quality indicators are reported for such Medicare services from 1.5% in 2008 to 2.0% of Medicare reimbursement in 2009 and 2010.
On October 30, 2009, CMS released its final 2010 MPFS payment changes covering the period from January 1, 2010 through December 30, 2010. The final rule includes a 21.2% rate reduction in the MPFS for 2010 as a result of the application of the SGR that was adopted in the Balanced Budget Act of 1997. This formula has yielded negative updates every year beginning in 2002, although CMS was able to take administrative steps to avert a reduction in 2003 and Congress has taken a series of legislative actions to prevent reductions from 2004 to 2009. The PQRI payment incentives for physicians who successfully report measures under PQRI will remain at 2.0% for 2010. Although there are current legislative proposals that call for a delay in the application of the SGR until 2011 and an increase in physician payments by 0.5% for 2010, such proposals have not yet been enacted. Absent regulatory changes or further Congressional action with respect to the application of the SGR, Medicare physician services would be subject to significant reductions beginning on January 1, 2010.
Coding and Billing Changes
We are subject to various coding and billing criteria related to how certain ED physician services can be billed. The way we are able to bill for these services may be modified or changed from time to time eliminating or reducing our reimbursement for these services. During 2008, we experienced a negative revenue impact of changes in billing and coding associated with intravenous infusion of medications, rehydration treatment services and other procedures in hospital ED settings, which was estimated to be approximately $10 million. We sought to counter the adverse impact of the reimbursement reductions in 2008 as well as any future reimbursement reductions through a variety of initiatives, including improved provider productivity, increases in the efficiency and effectiveness of our revenue cycle process, and the reduction or deferral of certain operating costs.
48
Table of Contents
Military Healthcare Staffing
We are a provider of healthcare professionals that serve military personnel and their dependents in military treatment facilities nationwide administered by the U.S. Department of Defense. Our revenues derived from military healthcare staffing totaled $121.0 million and $123.5 million for the nine months ended September 30, 2008 and 2009, respectively. These revenues are derived from contracts that are subject to a competitive bidding process.
Approximately $104.5 million of the estimated annual revenue won by us as part of the military’s contract bidding process in 2008, was awarded to us on a one-year contract basis and was subject to re-bid and award on or about October 1, 2009. Approximately $72.2 million of estimated annual revenue won during the bidding process in 2008 was awarded to us on a two to five option year contract basis which gives the government the option to exercise available option years each October 1. The government also reserves a portion of its contracts for award to small businesses. We participate in these small business awards to the extent we can serve as a sub-contractor to small businesses that win such bids. Approximately 18.6% of our military staffing revenue for the nine months ended September 30, 2009 was derived through a subcontracting agreement with a small business prime contractor, compared to 23.3% for the same period in 2008.
We were successful in retaining existing business or winning new bid following the completion of the bidding process as of October 1, 2009 in the estimated annualized amount of $157.5 million. The estimated annualized amount of $157.5 million included $92.5 million awarded under one-year contracts.
Anesthesiology Related Services
In January 2007, we completed a strategic review of our anesthesia management services business, and based upon our review concluded that the existing business model of providing management services to independent physician groups was not a viable long-term strategy and could not consistently meet our internal growth targets. As a result of this review, we elected to exit this non-core business line. In conjunction with this decision, we recorded an additional impairment loss of $0.7 million in the fourth quarter of 2006 in order to reduce the carrying value of the remaining intangible assets of the anesthesia operations. The total impairment loss in 2006 associated with these operations was $10.2 million. The anesthesia operating segment contributed $2.4 million and $11.1 million of revenue less provision for uncollectibles to our consolidated results during 2007 and 2006, respectively. We recognized approximately $1.0 million related to severance and other exit costs in connection with the transition, which was completed in the third quarter of 2007. Accordingly, under the provisions of Accounting Standards Codification, or ASC, Topic 205-20, “Discontinued Operations,” we have reported the results of the anesthesia operations as discontinued operations for 2007 and 2006.
Critical Accounting Policies and Estimates
The following discussion provides an assessment of our results of operations, liquidity and capital resources and should be read in conjunction with our consolidated financial statements and notes thereto included elsewhere in this prospectus.
Our consolidated financial statements are prepared in accordance with accounting principles generally accepted in the United States, which requires us to make estimates and assumptions. Management believes the following critical accounting policies, among others, affect its more significant judgments and estimates used in the preparation of our consolidated financial statements.
There have been no changes to these critical accounting policies or their application during the nine months ended September 30, 2009.
49
Table of Contents
Revenue Recognition
Net Revenue. Net revenue consists of fee for service revenue, contract revenue and other revenue. Net revenue is recorded in the period services are rendered. Our net revenue is principally derived from the provision of healthcare staffing services to patients within healthcare facilities. The form of billing and related risk of collection for such services may vary by customer. The following is a summary of the principal forms of our billing arrangements and how net revenue is recognized for each.
A significant portion (approximately 81% of our net revenue in the nine months ended September 30, 2009 and 80% for the year ended December 31, 2008) resulted from fee for service patient visits. Fee for service revenue represents revenue earned under contracts in which we bill and collect the professional component of charges for medical services rendered by our contracted and employed physicians. Under the fee for service arrangements, we bill patients for services provided and receive payment from patients or their third-party payers. Fee for service revenue is reported net of contractual allowances and policy discounts. All services provided are expected to result in cash flows and are therefore reflected as net revenue in the financial statements. Fee for service revenue is recognized in the period that the services are rendered to specific patients and reduced immediately for the estimated impact of contractual allowances in the case of those patients having third-party payer coverage. The recognition of net revenue (gross charges less contractual allowances) from such visits is dependent on such factors as proper completion of medical charts following a patient visit, the forwarding of such charts to one of our billing centers for medical coding and entering into our billing systems and the verification of each patient’s submission or representation at the time services are rendered as to the payer(s) responsible for payment of such services. Net revenue is recorded based on the information known at the time of entering such information into our billing systems as well as an estimate of the net revenue associated with medical charts for a given service period that have not been processed yet into our billing systems. The above factors and estimates are subject to change. For example, patient payer information may change following an initial attempt to bill for services due to a change in payer status. Such changes in payer status have an impact on recorded net revenue due to differing payers being subject to different contractual allowance amounts. Such changes in net revenue are recognized in the period that such changes in payer become known. Similarly, the actual volume of medical charts not processed into our billing systems may be different from the amounts estimated. Such differences in net revenue are adjusted in the following month based on actual chart volumes processed.
Contract revenue represents revenue generated under contracts in which we provide physician and other healthcare staffing and administrative services in return for a contractually negotiated fee. Contract revenue consists primarily of billings based on hours of healthcare staffing provided at agreed upon hourly rates. Revenue in such cases is recognized as the hours worked by our staff and contractors. Additionally, contract revenue also includes supplemental revenue from hospitals where we may have a fee for service contract arrangement. Contract revenue for the supplemental billing in such cases is recognized based on the terms of each individual contract. Such contract terms generally either provide for a fixed monthly dollar amount or a variable amount based upon measurable monthly activity, such as hours staffed, patient visits or collections per visit compared to a minimum activity threshold. Such supplemental revenues based on variable arrangements are usually contractually fixed on a monthly, quarterly or annual calculation basis considering the variable factors negotiated in each such arrangement. Such supplemental revenues are recognized as revenue in the period when such amounts are determined to be fixed and therefore contractually obligated as payable by the customer under the terms of the respective agreement.
Other revenue consists primarily of revenue from management and billing services provided to outside parties. Revenue is recognized for such services pursuant to the terms of the contracts with customers. Generally, such contracts consist of fixed monthly amounts with revenue recognized in the month services are rendered or as hourly consulting fees recognized as revenue as hours worked in accordance with such arrangements. Additionally, we derive a portion of our revenues from providing billing services that are contingent upon the collection of third-party physician billings by us on behalf of such customers. Revenues are not considered earned and therefore not recognized as revenue until actual cash collections are achieved in accordance with the contractual arrangements for such services.
50
Table of Contents
Net Revenue Less Provision for Uncollectibles. Net revenue less provision for uncollectibles reflects management’s estimate of billed amounts to ultimately be collected. Management, in estimating the amounts to be collected resulting from over seven million annual fee for service patient visits and procedures, considers such factors as prior contract collection experience, current period changes in payer mix and patient acuity indicators, reimbursement rate trends in governmental and private sector insurance programs, resolution of overprovision account balances, the estimated impact of billing system effectiveness improvement initiatives, and trends in collections from self-pay patients and external collection agencies. In developing our estimate of collections per visit or procedure, we consider the amount of outstanding gross accounts receivable by period of service, but do not use an accounts receivable aging schedule to establish estimated collection valuations. Individual estimates of net revenue less provision by contractual location are monitored and refreshed each month as cash receipts are applied to existing accounts receivable and other current trends that have an impact upon the estimated collections per visit are observed. Such estimates are substantially formulaic in nature. In the ordinary course of business we experience changes in our initial estimates of net revenues less provision for uncollectibles during the year following commencement of services. Such provisions and any subsequent changes in estimates may result in adjustments to our operating results with a corresponding adjustment to our accounts receivable allowance for uncollectibles on our balance sheet. Differences between amounts ultimately realized and the initial estimates of net revenue less provision have historically not been material.
Net revenue less provision for uncollectibles for the years ended December 31, 2006, 2007 and 2008 and the nine months ended September 30, 2008 and 2009, respectively, consisted of the following:
| Year Ended December 31, | Nine Months Ended September 30, | ||||||||||||||
| 2006 | 2007 | 2008 | 2008 | 2009 | |||||||||||
| (In thousands) | |||||||||||||||
| Gross fee for service charges |
$ | 2,873,565 | $ | 3,507,454 | $ | 3,876,032 | $ | 2,906,374 | $ | 3,288,471 | |||||
| Unbilled revenue |
4,007 | 6,149 | 753 | 1,114 | 5,186 | ||||||||||
| Less: contractual adjustments |
1,450,823 | 1,834,499 | 2,049,178 | 1,534,248 | 1,785,157 | ||||||||||
| Fee for service revenue |
1,426,749 | 1,679,104 | 1,827,607 | 1,373,240 | 1,508,500 | ||||||||||
| Contract revenue |
378,658 | 403,086 | 441,050 | 329,914 | 339,928 | ||||||||||
| Other revenue |
23,646 | 23,962 | 23,155 | 17,621 | 19,574 | ||||||||||
| Net revenue |
1,829,053 | 2,106,152 | 2,291,812 | 1,720,775 | 1,868,002 | ||||||||||
| Less: provision for uncollectibles |
733,666 | 874,087 | 960,495 | 720,968 | 793,345 | ||||||||||
| Net revenue less provision for uncollectibles |
$ | 1,095,387 | $ | 1,232,065 | $ | 1,331,317 | $ | 999,807 | $ | 1,074,657 | |||||
Contractual adjustments represent our estimate of discounts and other adjustments to be recognized from gross fee for service charges under contractual payment arrangements, primarily with commercial, managed care and governmental payment plans such as Medicare and Medicaid when affiliated providers participate in such plans. The increase in contractual adjustments noted above is due to the overall increase in gross fee for service charges resulting from annual increases in our gross billing fee schedules and increases in patient visits and procedures between periods. Contractual adjustments increased at a faster pace than the increase in gross fee for service charges as the annual reimbursement increases under contracts with managed care plans and government payers that are subject to contractual adjustments tend to be less than the overall annual increase in our gross billing fee schedules.
51
Table of Contents
The table below summarizes our approximate payer mix as a percentage of fee for service patient volume for the periods indicated:
| Year Ended December 31, | Nine Months Ended September 30, | ||||||||||||||
| 2006 | 2007 | 2008 | 2008 | 2009 | |||||||||||
| Payer: |
|||||||||||||||
| Medicare |
21.2 | % | 21.2 | % | 21.8 | % | 21.7 | % | 21.7 | % | |||||
| Medicaid |
24.9 | 24.0 | 23.8 | 23.7 | 25.4 | ||||||||||
| Commercial and managed care |
29.9 | 29.3 | 29.6 | 29.8 | 28.8 | ||||||||||
| Self pay |
21.6 | 22.7 | 22.3 | 22.3 | 21.9 | ||||||||||
| Other |
2.4 | 2.8 | 2.5 | 2.5 | 2.2 | ||||||||||
| Total |
100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | |||||
Accounts Receivable. As described above and below, we determine the estimated value of our accounts receivable based on estimated cash collection run rates of estimated future collections, by facility contract, for patient visits under our fee for service contract revenue. Accordingly, we are unable to report the payer mix composition on a dollar basis of our outstanding net accounts receivable. However, a 1% change in the estimated carrying value of our net fee for service patient accounts receivable before consideration of the allowance for uncollectible accounts at September 30, 2009 could have an after tax effect of approximately $2.1 million on our financial position and results of operations. Our days of revenue outstanding at September 30, 2009 and at December 31, 2008, were 61.0 days and 66.7 days, respectively. The number of days outstanding will fluctuate over time due to a number of factors. The decrease in average days outstanding of approximately 5.7 days includes a decrease of 5.6 days resulting from an increase in average revenue per day and a decrease of 3.0 days associated with a reduction in the estimated value of contract accounts receivable. These decreases were partially offset by an increase of 3.0 days related to the increase in estimated value of fee for service accounts receivable. The increase in average revenue per day is primarily attributable to an increase in gross charges, increased pricing with managed care plans and increases in Medicare reimbursements. The decrease of 3.0 days associated with the reduction of contract accounts receivable and the increase of 3.0 days related to fee for service accounts receivable are due primarily to timing of cash collections and valuation adjustments recorded in the period. Our allowance for doubtful accounts totaled $192.2 million as of September 30, 2009.
Approximately 98% of our allowance for doubtful accounts is related to gross fees for fee for service patient visits. Our principal exposure for uncollectible fee for service visits is centered in self-pay patients and, to a lesser extent, for co-payments and deductibles from patients with insurance. While we do not specifically allocate the allowance for doubtful accounts to individual accounts or specific payer classifications, the portion of the allowance associated with fee for service charges as of September 30, 2009 was equal to approximately 92% of outstanding self-pay fee for service patient accounts.
The majority of our fee for service patient visits are for the provision of emergency care in hospital settings. Due to federal government regulations governing the provision of such care, we are obligated to provide emergency care regardless of the patient’s ability to pay or whether or not the patient has insurance or other third-party coverage for the cost of the services rendered. While we attempt to obtain all relevant billing information at the time emergency care services are rendered, there are numerous patient encounters where such information is not available at time of discharge. In such cases where detailed billing information relative to insurance or other third-party coverage is not available at discharge, we attempt to obtain such information from the patient or client hospital billing record information subsequent to discharge to facilitate the collections process. Collections at the time of rendering such services (emergency room discharge) are not significant. Primary responsibility for collection of fee for service accounts receivable resides within our internal billing operations. Once a claim has been submitted to a payer or an individual patient, employees within our billing operations have responsibility for the follow up collection efforts. The protocol for follow up differs by payer classification. For self-pay patients, our billing system will automatically send a series of dunning letters on a
52
Table of Contents
prescribed time frame requesting payment or the provision of information reflecting that the balance due is covered by another payer, such as Medicare or a third-party insurance plan. Generally, the dunning cycle on a self pay account will run from 90 to 120 days. At the end of this period, if no collections or additional information is obtained from the patient, the account is no longer considered an active account and is transferred to a collection agency. Upon transfer to a collection agency, the patient account is written off as a bad debt. Any subsequent cash receipts on accounts previously written off are recorded as a recovery. For non-self pay accounts, billing personnel will follow up and respond to any communication from payers such as requests for additional information or denials until collection of the account is obtained or other resolution has occurred. At the completion of our active collection cycle, we factor on a non-recourse basis selected patient accounts to external collection agencies on a non-recourse basis while other selected accounts may be transferred to external collection agencies under a contingent collection basis. The projected value of future factoring and contingent collection proceeds are considered in the estimation of our overall accounts receivable valuation. For contract accounts receivable, invoices for services are prepared in our various operating areas and mailed to our customers, generally on a monthly basis. Contract terms under such arrangements generally require payment within 30 days of receipt of the invoice. Outstanding invoices are periodically reviewed and operations personnel with responsibility for the customer relationship will contact the customer to follow up on any delinquent invoices. Contract accounts receivable will be considered as bad debt and written-off based upon the individual circumstances of the customer situation after all collection efforts have been exhausted, including legal action if warranted, and it is the judgment of management that the account is not expected to be collected.
Methodology for Computing Allowance for Doubtful Accounts. We employ several methodologies for determining our allowance for doubtful accounts depending on the nature of the net revenue recognized. We initially determine gross revenue for our fee for service patient visits based upon established fee schedule prices. Such gross revenue is reduced for estimated contractual allowances for those patient visits covered by contractual insurance arrangements to result in net revenue. Net revenue is then reduced for our estimate of uncollectible amounts. Fee for service net revenue less provision for uncollectibles represents our estimated cash to be collected from such patient visits and is net of our estimate of account balances estimated to be uncollectible. The provision for uncollectible fee for service patient visits is based on historical experience resulting from over seven million annual fee for service patient visits. The significant volume of patient visits and the terms of thousands of commercial and managed care contracts and the various reimbursement policies relating to governmental healthcare programs do not make it feasible to evaluate fee for service accounts receivable on a specific account basis. Fee for service accounts receivable collection estimates are reviewed on a quarterly basis for each of our fee for service contracts by period of accounts receivable origination. Such reviews include the use of historical cash collection percentages by contract adjusted for the lapse of time since the date of the patient visit. In addition, when actual collection percentages differ from expected results, on a contract by contract basis, supplemental detailed reviews of the outstanding accounts receivable balances may be performed by our billing operations to determine whether there are facts and circumstances existing that may cause a different conclusion as to the estimate of the collectibility of that contract’s accounts receivable from the estimate resulting from using the historical collection experience. Contract-related net revenue is billed based on the terms of the contract at amounts expected to be collected. Such billings are typically submitted on a monthly basis and aged trial balances prepared. Allowances for estimated uncollectible amounts related to such contract billings are made based upon specific accounts and invoice periodic reviews once it is concluded that such amounts are not likely to be collected. The methodologies employed to compute allowances for doubtful accounts were unchanged between 2009 and 2008.
Insurance Reserves
The nature of our business is such that it is subject to professional liability claims and lawsuits. Historically, to mitigate a portion of this risk, we have maintained insurance for individual professional liability claims with per incident and annual aggregate limits per physician for all incidents. Prior to March 12, 2003, we obtained such insurance coverage from commercial insurance providers. Subsequent to March 11, 2003, we have provided for a significant portion of our professional liability loss exposures through the use of a captive
53
Table of Contents
insurance company and through greater utilization of self-insurance reserves. Since March 12, 2003, the most significant cost element within our professional liability program has consisted of the actuarial estimates of losses by occurrence period. In addition to the estimated actuarial losses, other costs that are considered by management in the estimation of professional liability costs include program costs such as brokerage fees, claims management expenses, program premiums and taxes, and other administrative costs of operating the program, such as the costs to operate the captive insurance subsidiary. Net costs in any period reflect our estimate of net losses to be incurred in that period as well as any changes to our estimates of the reserves established for net losses of prior periods.
Our commercial insurance policy for professional liability losses for the period March 12, 1999 through March 11, 2003 included insured limits applicable to such coverage in the period. Effective April 2006, we executed an agreement with the commercial insurance provider that issued the policy that ended March 11, 2003 to increase the existing $130.0 million aggregate limit of coverage. Under the terms of the agreement, we will make periodic premium payments to the commercial insurance company and the total aggregate limit of coverage under the policy will be increased by a portion of the premiums paid. We have committed to fund premiums such that the total aggregate limit of coverage under the program remains greater than the paid losses at any point in time. During fiscal year 2008, we funded a total of $2.7 million under this agreement. For the nine months ended September 30, 2009, we funded a total of $4.2 million and have agreed to fund additional payments which will be based upon the level of incurred losses relative to the aggregate limit of coverage at that time.
As of September 30, 2009, the current aggregate limit of coverage under this policy is $155.9 million and the estimated loss reserve for claim losses and expenses in excess of the current aggregate limit we recorded was $9.8 million.
The accounts of the captive insurance company are fully consolidated with those of our other operations in the accompanying financial statements.
The estimation of medical professional liability losses is inherently complex. Medical professional liability claims are typically resolved over an extended period of time, often as long as ten years or more. The combination of changing conditions and the extended time required for claim resolution results in a loss estimation process that requires actuarial skill and the application of judgment, and such estimates require periodic revision. A report of actuarial loss estimates is prepared at least semi-annually. Management’s estimate of our professional liability costs resulting from such actuarial studies is significantly influenced by assumptions and assessments regarding expectations of several factors. These factors include, but are not limited to: historical paid and incurred loss development trends; hours of exposure as measured by hours of physician and related professional staff services; trends in the frequency and severity of claims, which can differ significantly by jurisdiction due to the legislative and judicial climate in such jurisdictions; coverage limits of third-party insurance; the effectiveness of our claims management process; and the outcome of litigation. As a result of the variety of factors that must be considered by management, there is a risk that actual incurred losses may develop differently from estimates.
The underlying information that serves as the foundational basis for making our actuarial estimates of professional liability losses is our internal database of incurred professional liability losses. We have captured extensive professional liability loss data going back, in some cases, over twenty years, that is maintained and updated on an ongoing basis by our internal claims management personnel. Our database contains comprehensive incurred loss information for our existing operations as far back as fiscal 1997 (reflecting the initial timeframe in which we migrated to a consolidated professional liability program concurrent with the consummation of several significant acquisitions) and, in addition, we possess additional loss data that predates 1997 dates of occurrence for certain of our operations. Loss information reflects both paid and reserved losses incurred when we were covered by outside commercial insurance programs as well as paid and reserved losses incurred under our self insurance program. Because of the comprehensive nature of the loss data and our comfort with the completeness and reliability of the loss data, this is the information that is used in the development of our actuarial loss
54
Table of Contents
estimates. We believe this database is one of the largest repositories of physician professional liability loss information available in our industry and provides us and our actuarial consultants with sufficient data to develop reasonable estimates of the ultimate losses under our self insurance program. In addition to the estimated losses, as part of the actuarial process, we obtain revised payment pattern assumptions that are based upon our historical loss and related claims payment experience. Such payment patterns reflect estimated cash outflows for aggregate incurred losses by period based upon the occurrence date of the loss as well as the report date of the loss. Although variances have been observed in the actuarial estimate of ultimate losses by occurrence period between actuarial studies, the estimated payment patterns have shown much more limited variability. We use these payment patterns to develop our estimate of the discounted reserve amounts. The relative consistency of the payment pattern estimates provides us with a foundation in which to develop a reasonable estimate of the discount value of the professional liability reserves based upon the most current estimate of ultimate losses to be paid and the reasonable likelihood of the related cash flows over the payment period. As of September 30, 2009 and December 31, 2008, our estimated loss reserves were discounted at 3.3% and 2.2%, respectively, which was the current ten year U.S. Treasury rate at those dates, and which reflects the risk free interest rate over the expected period of claims payments.
In establishing our initial reserves for a given loss period, management considers the results of the actuarial loss estimates for such periods as well as assumptions regarding loss retention levels and other program costs to be incurred. On a semi-annual basis, we will review our professional liability reserves considering not only the reserves and loss estimates associated with the current period but also the reserves established in prior periods based upon revised actuarial loss estimates. The actuarial estimation process employed utilizes a frequency severity simulation model to estimate the ultimate cost of claims for each loss period. The results of the simulation model are then validated by a comparison to the results from several different actuarial methods (paid loss development, incurred loss development, incurred Bornhuetter-Ferguson method, paid Bornhuetter-Ferguson method) for reasonableness. Each method contains assumptions regarding the underlying claims process. Actuarial loss estimates at various confidence levels capture the variability in the loss estimates for process risk but assume that the underlying model and assumptions are correct. Adjustments to professional liability loss reserves will be made as needed to reflect revised assumptions and emerging trends and data. Any adjustments to reserves are reflected in the current operations. Due to the size of our reserve for professional liability losses, even a small percentage adjustment to these estimates can have a material effect on the results of operations for the period in which the adjustment is made. Given the number of factors considered in establishing the reserves for professional liability losses, it is neither practical nor meaningful to isolate a particular assumption or parameter of the process and calculate the impact of changing that single item. The actuarial reports provide a variety of loss estimates based upon statistical confidence levels reflecting the inherent uncertainty of the medical professional liability claims environment in which we operate. Initial year loss estimates are generally recorded using the actuarial expected loss estimate, but aggregate professional liability loss reserves may be carried at amounts in excess of the expected loss estimates provided by the actuarial reports due to the relatively short time period in which we have provided for our losses on a self insured basis and the expectation that we believe additional adjustments to prior year estimates may occur as our reporting history and loss portfolio matures. In addition, we are subject to the risk of claims in excess of insured limits as well as unlimited aggregate risk of loss in certain loss periods. As our self insurance program continues to mature and additional stability is noted in the loss development trends in the initial years of the program, we expect to continue to review and evaluate the carried level of reserves and make adjustments as needed.
Based on the results of the actuarial study completed in April 2009, we recorded a reduction in professional liability reserves associated with prior year loss estimates in the amount of $18.8 million during the three months ended March 31, 2009. Of the total reserve reduction, $18.3 million was associated with loss estimates established in prior years for the self insurance program covering the loss occurrence periods from March 12, 2003 through December 31, 2008. The remaining reserve reduction of $0.5 million was associated with the estimated losses in excess of the aggregate limit of coverage under the commercial insurance program that ended March 12, 2003.
55
Table of Contents
The second semi-annual report of actuarial loss estimates was completed in October 2009. Based on these results, management determined no additional change was necessary in our consolidated reserves for professional liability losses as of September 30, 2009 related to prior year loss estimates.
It is not possible to quantify the amount of the change in our estimate of prior year losses by individual fiscal period due to the nature of the professional liability loss estimates that are provided to us on an occurrence period basis and the nature of the coverage that is obtained in the commercial insurance market which is generally underwritten on a claims made or report period basis. Even though we are self insured for a significant portion of our risk, due to customer contracting requirements and state insurance regulations, we still, at times, must place coverage on a claims made or report period basis with commercial insurance carriers. When evaluating the appropriate carrying level of our self insured professional liability reserves, management considers the current estimates of occurrence period loss estimates as well as how such loss estimates and related future claims will interact with previous or current commercial insurance programs when projecting future cash flows. However, the complexity that is associated with multiple occurrence periods interacting with multiple report periods that contain risks and related reserves retained by us, as well as transferred to commercial insurance carriers, makes it impossible to allocate the change in prior year loss estimates to individual occurrence periods. Instead, we evaluate the future expected cash flows for all historical loss periods in the aggregate and compare such estimates to the current carrying value of our professional liability reserves. This process provides the basis for us to conclude that our reserves for professional liability losses are reasonable and properly stated. Management considers the results of actuarial studies when estimating the appropriate level of professional liability reserves and no adjustments to prior year loss estimates were made in periods where updated actuarial loss estimates were not available. Contributing to the reduction in professional liability reserves associated with prior years recognized in the first quarter of 2009 were improvements in the estimate of ultimate losses by occurrence periods contained in the actuarial report received in April 2009. The April 2009 actuarial report reflected a reduction in the estimated ultimate undiscounted losses by occurrence period of between 11.3% and 11.5% (at various confidence factors) for the self insured loss period from March 12, 2003 through December 31, 2008. The April 2009 actuarial report also reflected a reduction in the estimated undiscounted losses of between 0.3% and 0.9% (at various confidence factors) for our exposure in excess of the aggregate limit of coverage in place on the commercial insurance program that ended March 12, 2003.
Due to the complexity of the actuarial estimation process, there are many factors, trends, and assumptions that must be considered in the development of the actuarial loss estimates and we are not able to quantify and disclose which specific elements are primarily contributing to the overall favorable development in the revised loss estimates of historical occurrence periods. However, we believe that our internal investments in enhanced risk management and claims management resources and initiatives, such as the employment of additional claims and litigation management personnel and practices and an expansion of programs such as root cause loss analysis, early claim evaluation, and litigation support for insured providers, as well as the improved legal environment resulting from professional liability tort reform efforts in certain key jurisdictions such as Florida and Texas have contributed to the favorable trend in loss development estimates noted during the prior year occurrence periods.
Impairment of Intangible Assets
In assessing the recoverability of our intangibles, we must make assumptions regarding estimated future cash flows and other factors to determine the fair value of the respective assets. Specifically, in estimating the fair value of a reporting unit, we use valuation techniques based on the historical and expected future performance of the specific reporting units and the current valuation multiples of entities that have comparable operations and economic characteristics. If these estimates or their related assumptions change in the future, we may be required to record impairment charges for these assets.
In December 2008, we recorded an impairment loss of $9.1 million related to $8.8 million of goodwill for our After Hours Pediatric and $0.3 million of goodwill for our Radiology reporting units. The goodwill impairment charge was based upon a combination of current market valuations and management’s assessment of
56
Table of Contents
the projected operating performance of the operations. Following the impairment charge, there was no remaining recorded goodwill associated with these reporting units. The remaining reporting units that have recorded goodwill, based on the results of our annual impairment test, are not considered to be at risk as of December 31, 2008. The results of step one of the annual impairment test completed as of December 31, 2008, and as prescribed by the provisions of ASC Topic 350 “Intangibles—Goodwill and Other,” which is used to identify potential impairment by comparing the fair value of a reporting unit with its carrying amount, including goodwill, indicated that the fair value of each reporting unit that has remaining recorded goodwill exceeded its carrying value by more than 10%.
Results of Operations
The following discussion provides an analysis of our results of operations and should be read in conjunction with our unaudited consolidated financial statements. The operating results of the periods presented were not significantly affected by general inflation in the U.S. economy. Net revenue less the provision for uncollectibles is an estimate of future cash collections and as such it is a key measurement by which management evaluates performance of individual contracts as well as us as a whole. The following table sets forth the components of net earnings as a percentage of net revenue less provision for uncollectibles for the periods indicated:
| Year Ended December 31, | Nine Months Ended September 30, | ||||||||||||||
| 2006 | 2007 | 2008 | 2008 | 2009 | |||||||||||
| Net revenue less provision for uncollectibles |
100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | |||||
| Professional services expenses |
75.9 | 77.2 | 78.6 | 78.0 | 77.1 | ||||||||||
| Professional liability costs |
3.4 | 1.7 | 1.2 | (0.3 | ) | 1.8 | |||||||||
| General and administrative expenses |
9.5 | 9.3 | 8.8 | 8.8 | 8.7 | ||||||||||
| Management fee and other expenses |
0.3 | 0.3 | 0.3 | 0.3 | 0.2 | ||||||||||
| Impairment of intangibles |
— | — | 0.7 | — | — | ||||||||||
| Depreciation and amortization |
2.1 | 1.2 | 1.3 | 1.3 | 1.3 | ||||||||||
| Interest expense, net |
5.3 | 4.5 | 3.4 | 3.4 | 2.6 | ||||||||||
| Gain on extinguishment of debt |
— | — | (0.1 | ) | — | — | |||||||||
| Transaction costs |
— | — | 0.2 | 0.2 | 0.1 | ||||||||||
| Earnings from continuing operations before income taxes |
3.4 | 5.8 | 5.7 | 8.4 | 8.3 | ||||||||||
| Provision for income taxes |
1.3 | 2.2 | 2.3 | 3.4 | 3.2 | ||||||||||
| Earnings from continuing operations |
2.1 | 3.6 | 3.4 | 5.0 | 5.1 | ||||||||||
| Loss from discontinued operations, net of taxes |
(0.6 | ) | (0.1 | ) | — | — | — | ||||||||
| Net earnings |
1.5 | % | 3.5 | % | 3.4 | % | 5.0 | % | 5.1 | % | |||||
Nine Months Ended September 30, 2009 Compared to the Nine Months Ended September 30, 2008
Net Revenue. Net revenue in the nine months ended September 30, 2009 increased $147.2 million, or 8.6%, to $1.9 billion from $1.7 billion in the nine months ended September 30, 2008. The increase in net revenue resulted primarily from increases in fee for service revenue of $135.3 million, contract revenue of $10.0 million and other revenue of $2.0 million. The increase in fee for service revenue was a result of a 5.6% increase in total fee for service visits and procedures as well as increases in estimated collections per billed visit. Contributing to the 5.6% increase in fee for service visits and procedures were approximately 231,000 visits and procedures on a same contract basis and approximately 82,000 visits and procedures from new and acquired contracts, net of terminations. Same contract visits and procedures for the nine months ended September 30, 2009 increased 4.6% compared to the prior period. While period over period volume growth was flat to negative in the early part of
57
Table of Contents
the year, beginning in the second quarter, we experienced volume growth that is in excess of recent historical growth levels. We believe that a portion of such elevated volume growth was a result of an increase in reported cases of flu attributed to the H1N1 virus, although we cannot quantify the exact impact of this condition on our volume growth. We anticipate continued volume growth trends through the remainder of 2009; however, as reported cases of the H1N1 virus subside in future periods, we would anticipate that same contract volume growth would revert back to more normalized levels as observed in historical period over period growth rates. Estimated collections per visit increased due to annual increases in gross charges and managed care pricing improvements in addition to improved Medicare pricing and other valuation adjustments between periods. We anticipate that such trends and factors contributing to growth in estimated collections per visit will continue at similar levels for the remainder of fiscal 2009. However, in regard to payments under the Medicare Physician Fee Schedule, effective January 1, 2010, such payments are scheduled to decline by 21.2% in the absence of any administrative or legislative actions to reverse such declines. See “—2009 and 2010 Medicare Fee Schedule Changes.” The increase in contract revenue was due primarily to growth from existing and net new contracts within our ED and hospital medicine and military staffing operations partially offset by declines in our locums tenens and radiology operations associated with reductions in temporary staffing and teleradiology volumes, respectively. Other revenue increased due primarily to an increase in external billing and management fees. In the nine months ended September 30, 2009, fee for service revenue was 80.8% of net revenue compared to 79.8% in 2008, contract revenue was 18.2% of net revenue in 2009 compared to 19.2% in 2008 and other revenue was 1.0% in both 2009 and 2008.
Provision for Uncollectibles. The provision for uncollectibles was $793.3 million in the nine months ended September 30, 2009 compared to $721.0 million in the corresponding period in 2008, an increase of $72.4 million, or 10.0%. The provision for uncollectibles as a percentage of net revenue was 42.5% in 2009 compared with 41.9% in 2008. The provision for uncollectibles was primarily related to revenue generated under fee for service contracts that is not expected to be fully collected. The period over period increase in the provision was due to annual increases in gross fee schedules and increases in patient volume and procedures. For the nine months ended September 30, 2009, self pay fee for service visits were approximately 21.9% of the total fee for service visits compared to approximately 22.3% in the same period of 2008.
Net Revenue Less Provision for Uncollectibles. Net revenue less provision for uncollectibles in the nine months ended September 30, 2009 increased $74.8 million, or 7.5%, to $1.1 billion from $999.8 million in the nine months ended September 30, 2008. Same contract revenue, which consists of contracts under management in both periods, increased $51.2 million, or 5.7%, to $946.3 million in 2009 compared to $895.1 million in 2008. For the nine months ended September 30, 2009, growth in same contract revenue less provision benefited 3.2% from increases in billed patient volume while estimated collections per billing unit contributed 2.1% of the growth between periods. The increase in the estimated collections per billing unit was attributable to annual increases in gross charges and managed care pricing improvements in addition to improved Medicare pricing and other valuation adjustments between periods. Contract and other revenue also contributed 0.5% to the increase in same contract revenue between periods. Growth in contract and other revenue between periods was constrained due to decreases in our locums tenens and radiology operations. The remainder of the increase in revenue less provision for uncollectibles between periods was due to new contracts obtained through internal sales of $74.4 million, partially offset by $58.7 million of revenue derived from contracts that terminated during the periods. Acquisitions contributed $8.0 million of growth between periods. We typically gain new contracts by replacing competitors at hospitals that currently outsource such services, obtaining new contracts from facilities that do not currently outsource and responding to contracting opportunities within the military healthcare system. Factors influencing new contracting opportunities include the depth and breath of our service offerings, our reputation and experience, our ability to recruit and retain qualified clinicians, and pricing considerations when a subsidy or contract payment is required. Contracts are typically terminated due to economic considerations, a change in hospital administration or ownership, dissatisfaction with our service offerings or, primarily relating to our military staffing arrangements, at the end of the contract term.
58
Table of Contents
The components of net revenue less provision for uncollectibles includes revenue from contracts that have been in effect for prior periods (same contracts) and from new and acquired contracts during the periods, as set forth in the table below:
| Nine Months Ended September 30, | ||||||
| 2008 | 2009 | |||||
| (In thousands) | ||||||
| Same contracts: |
||||||
| Fee for service revenue |
$ | 595,505 | $ | 641,786 | ||
| Contract and other revenue |
299,604 | 304,530 | ||||
| Total same contracts |
895,109 | 946,316 | ||||
| New contracts, net of terminations: |
||||||
| Fee for service revenue |
56,017 | 63,941 | ||||
| Contract and other revenue |
46,426 | 54,131 | ||||
| Total new contracts, net of terminations |
102,443 | 118,072 | ||||
| Acquired contracts: |
||||||
| Fee for service revenue |
2,247 | 10,251 | ||||
| Contract and other revenue |
8 | 18 | ||||
| Total acquired contracts |
2,255 | 10,269 | ||||
| Consolidated: |
||||||
| Fee for service revenue |
653,769 | 715,978 | ||||
| Contract and other revenue |
346,038 | 358,679 | ||||
| Total net revenue less provision for uncollectibles |
$ | 999,807 | $ | 1,074,657 | ||
The following table reflects the visits and procedures included within fee for service revenues described in the table above:
| Nine Months Ended September 30, | ||||
| 2008 | 2009 | |||
| (In thousands) | ||||
| Fee for service visits and procedures: |
||||
| Same contract |
5,000 | 5,231 | ||
| New and acquired contracts, net of terminations |
563 | 645 | ||
| Total fee for service visits and procedures |
5,563 | 5,876 | ||
Professional Service Expenses. Professional service expenses, which include physician and provider costs, billing and collection expenses, and other professional expenses, totaled $828.3 million in the nine months ended September 30, 2009 compared to $779.4 million in the nine months ended September 30, 2008, an increase of $48.8 million, or 6.3%. The higher cost between periods included an increase of approximately $31.6 million associated with increases in the number of provider hours staffed and the average rates paid per hour of provider service and an increase in billing costs on a same contract basis. Increases in provider hours staffed on a same contract basis are due to the need to provide additional coverage and resources associated with increasing volumes or an expansion of services. Increases in average rates paid reflect period over period wage and benefit increases associated with the provision of clinical services. Billing cost increases reflect normal annual increases in baseline costs as well as increases associated with growth in the volume of charts processed between periods. Also contributing to the increase in expense was $10.9 million related to new sales, net of terminated contract, and $6.3 million related to our acquisitions. Professional service expenses as a percentage of net revenue less provision for uncollectibles declined to 77.1% in the nine months ended September 30, 2009 compared to 78.0% in the nine months ended September 30, 2008.
Professional Liability Costs. Professional liability costs were $19.1 million in the nine months ended September 30, 2009 compared to a benefit of $3.0 million in the nine months ended September 30, 2008.
59
Table of Contents
Professional liability costs for the nine months ended September 30, 2009 and 2008 included reductions in professional liability reserves related to prior years of $18.8 million in 2009 and $40.3 million in 2008 resulting from actuarial studies completed during the respective periods. Factors contributing to the change in prior year loss estimates included favorable loss development on historical periods between actuarial studies as well as favorable trends in the frequency and severity of claims reported compared to historical trends. We believe that both internal initiatives in the areas of patient safety, risk management and claims management, as well as external factors such as tort reform in certain key states, continue to contribute to these favorable trends in prior year loss estimates. Excluding the favorable actuarial adjustments in both periods, professional liability costs increased $0.6 million, or 1.6%, between periods. The increase was primarily attributable to an increase in provider hours due to growth and increased provider hours staffed on a same contract basis. Excluding the benefit of prior year reserve adjustments in each period, professional liability costs as a percentage of net revenue less provisions for uncollectibles declined to 3.5% in 2009 from 3.7% in 2008.
General and Administrative Expenses. General and administrative expenses increased $4.9 million, or 5.6%, to $93.2 million for the nine months ended September 30, 2009 from $88.3 million in the nine months ended September 30, 2008. General and administrative expenses as a percentage of net revenue less provision for uncollectibles decreased to 8.7% in 2009 from 8.8% in 2008. The increase in general and administrative expenses was primarily due to increased incentive and deferred compensation plan costs, offset by declines in other administrative expenses between periods.
Management Fee and Other Expenses. Management fee and other expenses were $2.3 million in the nine months ended September 30, 2009 and $2.7 million in the same period in 2008.
Depreciation and Amortization. Depreciation and amortization expense was $14.0 million in the nine months ended September 30, 2009 compared to $12.6 million for the nine months ended September 30, 2008. The increase of $1.5 million between periods was primarily due to increased amortization expense associated with acquisitions completed in 2008 and 2009 and higher depreciation expense related to growth in capital expenditures.
Interest Expense, Net. Net interest expense decreased $6.4 million to $27.7 million in the nine months ended September 30, 2009, compared to $34.0 million in the corresponding period in 2008, primarily due to reduced levels of outstanding debt as well as lower borrowing rates on our term loan facilities between periods.
Transaction Costs. Transaction costs were $0.6 million for the nine months ended September 30, 2009 compared to $1.8 million for the nine months ended September 30, 2008. These costs relate to advisory, legal, accounting and other fees incurred related to acquisition activity during the period. The reduction in costs between periods was due to a terminated acquisition effort during 2008.
Earnings Before Income Taxes. Earnings before income taxes in the nine months ended September 30, 2009 were $89.5 million compared to $83.9 million in the corresponding period in 2008.
Provision for Income Taxes. The provision for income taxes was $34.2 million in the nine months ended September 30, 2009 compared to $33.9 million in the corresponding period in 2008.
Net Earnings. Net earnings were $55.2 million in the nine months ended September 30, 2009 compared to $50.1 million in the nine months ended September 30, 2008.
Year Ended December 31, 2008 Compared to the Year Ended December 31, 2007
Net Revenue. Net revenue in 2008 increased $185.7 million, or 8.8%, to $2.29 billion from $2.11 billion in 2007. The increase in net revenue of $185.7 million included an increase of $148.5 million in fee for service revenue and an increase of $38.0 million in contract revenue. These increases in net revenue were slightly offset by a $0.9 million decrease in other revenue. The increase in fee for service revenue was a result of a 4.8%
60
Table of Contents
increase in total fee for service visits and procedures as well as increases in estimated collections per billed visit. Contributing to the 4.8% increase in fee for service visits and procedures were approximately 170,000 visits and procedures on a same contract basis and approximately 169,000 visits and procedures from new and acquired contracts, net of terminations. Same contract visits and procedures for the year ended December 31, 2008 increased 2.9% compared to the prior period. Estimated collections per visit increased due to annual increases in gross charges and managed care pricing improvements between periods. During 2008, growth in estimated collections per visit, compared to 2007, was negatively impacted by declines in certain Medicare reimbursement to physicians and the elimination of the ability to bill for certain services in hospital EDs. The increase in contract revenue was due primarily to growth at existing and net new contracts within our ED and hospital medicine, military and locums tenens operations, between periods. Other revenue declined due primarily to settlements received in 2007. Fee for service revenue was 79.7% of net revenue in 2008 and 2007, contract revenue was 19.2% of net revenue in 2008 compared to 19.1% in 2007 and other revenue was 1.0% of net revenue in 2008 compared to 1.1% in 2007.
Provision for Uncollectibles. The provision for uncollectibles was $960.5 million in 2008 compared to $874.1 million in 2007, an increase of $86.4 million, or 9.9%. As a percentage of net revenue, the provision for uncollectibles was 41.9% in 2008 compared to 41.5% in 2007. The provision for uncollectibles was primarily related to revenue generated under fee for service contracts that is not expected to be fully collected. The year over year increase in the provision was due to a combination of increases in total billed patient volume and annual increases in gross fee schedules. For the year ended December 31, 2008, self pay fee for service patient visits declined to 22.3% of the total fee for service patient visits compared to approximately 22.7% in 2007.
Net Revenue less Provision for Uncollectibles. Net revenue less provision for uncollectibles in 2008 increased $99.3 million, or 8.1%, to $1.33 billion from $1.23 billion in 2007. Same contract revenue less provision for uncollectibles, which consists of contracts under management in both periods, increased $47.5 million, or 4.5%, to $1.09 billion in 2008 from $1.05 billion in 2007. The year over year growth in same contract revenue was primarily due to a 2.3% increase in contract and other revenue and increases in billed patient volume which contributed 1.9% of growth. Increases in estimated collections per visit, net of valuation adjustments, contributed the remainder of same contract revenue growth. During 2008, the growth in estimated collections per visit, compared to 2007, was negatively impacted by declines in Medicare reimbursements to ED physicians and the elimination of the ability to bill for certain services in hospital EDs. Also, growth in estimated collections per visit was adversely impacted by valuation adjustments recorded in 2008 primarily associated with self pay and collection accounts. The remainder of the increase in revenue less provision for uncollectibles between periods is due to new contracts obtained through internal sales of $124.0 million, partially offset by $79.0 million of revenue derived from contracts that terminated during the periods. Acquisitions contributed $6.8 million of growth between periods. We typically gain new contracts by replacing competitors at hospitals that currently outsource such services, obtaining new contracts from facilities that do not currently outsource and responding to contracting opportunities within the military healthcare system. Factors influencing new contracting opportunities include the depth and breadth of our service offerings, our reputation and experience, our ability to recruit and retain qualified clinicians, and pricing considerations when a subsidy or contract payment is required. Contracts are typically terminated due to economic considerations, a change in hospital administration or ownership, dissatisfaction with our service offerings or, primarily relating to our military staffing arrangements, at the end of the contract term.
61
Table of Contents
The components of net revenue less provision for uncollectibles includes revenues from contracts that have been in effect for prior periods (same contracts) and from new and acquired contracts during the periods, as set forth in the table below:
| Year Ended December 31, | ||||||
| 2007 | 2008 | |||||
| (In thousands) | ||||||
| Same contracts: |
||||||
| Fee for service revenue |
$ | 692,487 | $ | 715,671 | ||
| Contract and other revenue |
353,099 | 377,416 | ||||
| Total same contracts |
1,045,586 | 1,093,087 | ||||
| New contracts, net of terminations: |
||||||
| Fee for service revenue |
112,908 | 145,341 | ||||
| Contract and other revenue |
72,151 | 84,690 | ||||
| Total new contracts, net of terminations |
185,059 | 230,031 | ||||
| Acquired contracts: |
||||||
| Fee for service revenue |
1,420 | 8,185 | ||||
| Contract and other revenue |
— | 14 | ||||
| Total acquired contracts |
1,420 | 8,199 | ||||
| Consolidated: |
||||||
| Fee for service revenue |
806,815 | 869,197 | ||||
| Contract and other revenue |
425,250 | 462,120 | ||||
| Total net revenue less provision |
$ | 1,232,065 | $ | 1,331,317 | ||
The following table reflects the visits and procedures included within fee for service revenues described in the table above:
| Year Ended December 31, | ||||
| 2007 | 2008 | |||
| (In thousands) | ||||
| Fee for service visits and procedures: |
||||
| Same contract |
5,868 | 6,038 | ||
| New and acquired contracts, net of terminations |
1,167 | 1,336 | ||
| Total fee for service visits and procedures |
7,035 | 7,374 | ||
Professional Service Expenses. Professional service expenses, which include physician and other provider costs, billing and collection expenses and other professional expenses, totaled $1.05 billion in 2008 compared to $950.9 million in 2007, an increase of $95.9 million, or 10.1%. The increase included an increase of approximately $53.0 million on a same contract basis. Also contributing to the increase was $38.9 million related to new sales net of terminated contracts and $4.1 million related to acquisitions. Professional service expense as a percentage of net revenue less provision for uncollectibles was 78.6% in 2008 compared to 77.2% in 2007. The year over year increase in the cost as a percentage of net revenue less provision for uncollectibles is due primarily to margin compression on a same contract basis as increases in provider compensation costs outpaced increases in same contract revenue growth during the year. Growth in provider compensation costs was due primarily to increases in staffed hours and average rates paid. Increases in provider hours staffed on a same contract basis were due to the need to provide additional coverage and resources associated with increasing volumes or an expansion of services. Increases in average rates paid reflect period over period wage and benefit increases associated with the provision of clinical services. Increases in these cost components resulted in growth in same contract provider costs exceeding the 4.5% increase in same contract revenue less provision between periods.
62
Table of Contents
Professional Liability Costs. Professional liability costs were $15.2 million in 2008 compared with $21.1 million in 2007 reflecting a decrease of $5.8 million. Professional liability costs include reductions in professional liability reserves relating to prior years resulting from actuarial studies completed in April and October of each year of $34.9 million in 2008 and $32.1 million in 2007. The reduction in prior year professional liability reserves is due primarily to favorable changes in prior year loss estimates. Factors contributing to the change in prior year loss estimates included favorable loss development on historical periods between actuarial studies as well as continued favorable trends in the frequency of claims reported compared to historical trends. We believe that both internal initiatives in the areas of patient safety, risk management, and claims management as well as external factors such as tort reform in certain key states are contributing to these favorable trends in prior year loss estimates. Excluding the favorable actuarial adjustments, professional liability costs decreased $3.0 million between periods. Professional liability costs excluding prior year reserve adjustments declined to 3.8% of net revenue less provision for uncollectibles in 2008 compared to 4.3% in 2007. The lower cost between periods is primarily attributable to a decrease in the actuarial estimate of current period losses under our self insurance program partially offset by costs associated with an increase in provider hours due to net growth and increased provider hours staffed on a same contract basis.
General and Administrative Expenses. General and administrative expenses increased $2.5 million in 2008 to $116.9 million from $114.5 million in 2007. General and administrative expenses as a percentage of net revenue less provision for uncollectibles declined to 8.8% in 2008 compared to 9.3% in 2007. The increase in general and administrative expenses is primarily due to inflationary growth in salaries and an increase in the number of employees as well as recruiting expenses and higher travel costs.
Management Fee and Other Expenses. Management fee and other operating expenses totaled $3.6 million in 2008 and $4.1 million in 2007.
Impairment of Intangibles. In December 2008, we recorded an impairment loss of $9.1 million related to $8.8 million of goodwill for our After Hours Pediatric and $0.3 million of goodwill for our Radiology business lines. The goodwill impairment charge was based upon a combination of current market valuations and management’s assessment of the projected operating performance of the operations. Following the impairment charge, there is no remaining recorded goodwill associated with these operations.
Depreciation and Amortization. Depreciation and amortization was $17.3 million in 2008 and $14.8 million in 2007. The increase of $2.5 million between periods was due to the addition of new assets in 2007 and 2008, as well as higher amortization expense related to an increase in contract intangibles from our acquisitions in 2007 and 2008.
Interest Expense, Net. Net interest expense decreased $9.4 million to $45.8 million in 2008 compared to $55.2 million in 2007. The decrease is primarily due to lower borrowing rates on our term loan facilities, as well as reduced debt levels between years.
Transaction Costs. Transaction costs of $2.4 million were recognized during 2008 associated with advisory, legal, accounting, and other fees of $1.8 million incurred related to acquisition discussions that terminated during the year as well as $0.6 million of costs related to ongoing potential transactions. Costs associated with potential transactions are required to be expensed as incurred under the new provisions of Statement of Financial Accounting Standards No. 141 (revised), “Business Combinations,” which will become effective in the first quarter of 2009.
Gain on Extinguishment of Debt. A gain on the extinguishment of debt was recognized in December 2008 associated with the retirement of $12.0 million of our senior subordinated notes which were repurchased in the open market for $10.0 million plus accrued interest. Included in the calculation of the gain on the extinguishment of debt was the write off of deferred financing costs in the amount of $0.3 million.
Earnings from Continuing Operations Before Income Taxes. Earnings from continuing operations before income taxes in 2008 were $75.7 million compared to $71.5 million in 2007.
63
Table of Contents
Provision for Income Taxes. Provision for income taxes in 2008 was $31.0 million compared to $27.7 million in 2007.
Earnings from Continuing Operations. Earnings from continuing operations were $44.7 million in 2008 compared to $43.8 million in 2007.
Loss from Discontinued Operations, Net of Taxes. Loss from discontinued operations, net of taxes was $0.6 million in 2007. Contributing to the loss in 2007 were $1.0 million of severance and other exit costs related to the disposal of the anesthesia business unit.
Net Earnings. For the foregoing reasons, net earnings for 2008 were $44.7 million compared to $43.3 million in 2007.
Year Ended December 31, 2007 Compared to the Year Ended December 31, 2006
Net Revenue. Net revenue in 2007 increased $277.1 million, or 15.1%, to $2.1 billion from $1.8 billion in 2006. The increase in net revenue of $277.1 million included an increase of $252.4 million in fee for service revenue, an increase of $24.4 million in contract revenue and $0.3 million in other revenue. The increase in fee for service revenue was a result of a 10.5% increase in total fee for service visits and procedures as well as increases in estimated collections per billed visit. Contributing to the 10.5% increase in fee for service visits and procedures were approximately 181,000 visits and procedures on a same contract basis and approximately 487,000 visits and procedures from new and acquired contracts, net of terminations. Same contract visits and procedures for the year ended December 31, 2007 increased 3.4% compared to the prior period. Estimated collections per visit increased due to annual increases in gross charges, Medicare and managed care pricing improvements, and increased patient acuity between periods. The increase in contract revenue was due primarily to growth from existing and net new and acquired contracts within our ED and hospital medicine operations offset by declines in our military staffing operations associated with contracting changes between periods within the military healthcare program. In 2007, fee for service revenue was 79.7% of net revenue compared to 78.0% in 2006, contract revenue was 19.1% of net revenue compared to 20.7% in 2006 and other revenue was 1.2% of net revenue in 2007 compared to 1.3% in 2006.
Provision for Uncollectibles. The provision for uncollectibles was $874.1 million in 2007 compared to $733.7 million in 2006, an increase of $140.4 million, or 19.1%. As a percentage of net revenue, the provision for uncollectibles was 41.5% in 2007 compared to 40.1% in 2006. The provision for uncollectibles was primarily related to revenue generated under fee for service contracts that is not expected to be fully collected. The year over year increase in the provision was due to a combination of increases in total billed patient volume, annual increases in gross fee schedules and an increase in self pay gross accounts receivable relative to other payer types. For the year ended December 31, 2007, self pay fee for service patient visits were approximately 22.7% of the total fee for service patient visits compared to approximately 21.6% in 2006.
Net Revenue less Provision for Uncollectibles. Net revenue less provision for uncollectibles in 2007 increased $136.7 million, or 12.5%, to $1.2 billion from $1.1 billion in 2006. Same contract revenue less provision for uncollectibles, which consists of contracts under management in both periods, increased $52.9 million, or 5.9%, to $948.2 million in 2007 from $895.3 million in 2006. The increase in same contract revenue of 5.9% benefited 2.3% from an increase in billed patient volume between periods and 3.2% from increases in estimated net revenue per billing unit. The increase in estimated collections per billing unit was associated primarily with annual increases in gross charges, Medicare and managed care pricing improvements, and increased patient acuity offset by an unfavorable shift in payer mix reflecting an increase in the percentage of self pay volume during the year. Contract revenue and other revenue contributed approximately 0.7% of the increase while year over year changes in prior year revenue estimates and managed care settlements reduced same contract revenue by 0.3%. The remainder of the increase in revenue less provision for uncollectibles between periods was due to new contracts obtained through internal sales of $124.9 million, partially offset by $72.9
64
Table of Contents
million of revenue derived from contracts that terminated during the periods. Acquisitions contributed $31.7 million of growth between periods. We typically gain new contracts by replacing competitors at hospitals that currently outsource such services, obtaining new contracts from facilities that do not currently outsource and responding to contracting opportunities within the military healthcare system. Factors influencing new contracting opportunities include the depth and breadth of our service offerings, our reputation and experience, our ability to recruit and retain qualified clinicians, and pricing considerations when a subsidy or contract payment is required. Contracts are typically terminated due to economic considerations, a change in hospital administration or ownership, dissatisfaction with our service offerings or, primarily relating to our military staffing arrangements, at the end of the contract term.
The components of net revenue less provision for uncollectibles includes revenues from contracts that have been in effect for prior periods (same contracts) and from new and acquired contracts during the periods, as set forth in the table below:
| Year Ended December 31, | ||||||
| 2006 | 2007 | |||||
| (In thousands) | ||||||
| Same contracts: |
||||||
| Fee for service revenue |
$ | 598,567 | $ | 644,967 | ||
| Contract and other revenue |
296,720 | 303,261 | ||||
| Total same contracts |
895,287 | 948,228 | ||||
| New contracts, net of terminations: |
||||||
| Fee for service revenue |
81,094 | 133,839 | ||||
| Contract and other revenue |
84,392 | 83,691 | ||||
| Total new contracts, net of terminations |
165,486 | 217,530 | ||||
| Acquired contracts: |
||||||
| Fee for service revenue |
14,810 | 28,008 | ||||
| Contract and other revenue |
19,804 | 38,299 | ||||
| Total acquired contracts |
34,614 | 66,307 | ||||
| Consolidated: |
||||||
| Fee for service revenue |
694,471 | 806,814 | ||||
| Contract and other revenue |
400,916 | 425,251 | ||||
| Total net revenue less provision |
$ | 1,095,387 | $ | 1,232,065 | ||
The following table reflects the visits and procedures included within fee for service revenues described in the table above:
| Year Ended December 31, | ||||
| 2006 | 2007 | |||
| (In thousands) | ||||
| Fee for service visits and procedures: |
||||
| Same contract |
5,319 | 5,500 | ||
| New and acquired contracts, net of terminations |
1,048 | 1,535 | ||
| Total fee for service visits and procedures |
6,367 | 7,035 | ||
Professional Service Expenses. Professional service expenses, which includes physician costs, billing and collection expenses and other professional expenses, totaled $950.9 million in 2007 compared to $831.8 million in 2006, an increase of $119.1 million, or 14.3%. Contributing to the increase was $49.6 million related to new sales net of terminated contracts and $22.9 million related to acquisitions. The remaining increase in professional service expense was due primarily to increased physician and other practitioner hours staffed along with increased average rates paid per hour of provider service on a same contract basis. Increases in provider
65
Table of Contents
hours staffed on a same contract basis are due to the need to provide additional coverage and resources associated with increasing volumes or an expansion of services. Increases in average rates paid reflect period over period wage and benefit increases associated with the provision of clinical services.
Professional Liability Costs. Professional liability costs were $21.1 million in 2007 compared with $37.6 million in 2006 for a decrease of $16.6 million, or 44.1%. Professional liability costs include reductions in professional liability reserves relating to prior years resulting from actuarial studies completed in April and November of each year of $32.1 million in 2007 and $12.1 million in 2006. Excluding the favorable actuarial adjustments, professional liability costs increased $3.4 million between periods, primarily due to an increase in provider hours in 2007. The increase in provider hours was predominantly a result of our net growth and acquisitions and to a lesser extent increased provider hours staffed on a same contract basis. Partially offsetting the increase in cost associated with increased provider hours was a decrease in the actuarial estimate of current period losses under our self insurance program. The reduction in prior year professional liability reserves was due to favorable trends in loss estimates primarily associated with improvements in the overall frequency of claims reported and favorable changes in loss development assumptions.
General and Administrative Expenses. General and administrative expenses increased $10.7 million in 2007 to $114.5 million from $103.7 million in 2006. General and administrative expenses as a percentage of net revenue less provision for uncollectibles were 9.3% in 2007 compared to 9.5% in 2006. Acquisitions and growth contributed $3.9 million of the increase in general and administrative expenses. The remaining increase in general and administrative expenses between years was due principally to new positions and inflationary growth in salaries and benefits, and increases in incentive plan and commission costs.
Management Fee and Other Expenses. Management fee and other operating expenses were $4.1 million in 2007 and $3.7 million in 2006 for an increase of $0.4 million.
Depreciation and Amortization. Depreciation and amortization was $14.8 million in 2007 and $23.3 million in 2006. Depreciation and amortization expense decreased $8.5 million between periods due principally to a decrease in amortization expense of $9.9 million. The decline in amortization expense was due primarily to the contract intangibles recognized in connection with the Recapitalization Merger being fully amortized during 2006 offset by an increase in contract intangibles resulting from our 2007 and 2006 acquisitions.
Interest Expense, Net. Net interest expense decreased $2.6 million to $55.2 million in 2007 compared to $57.8 million in 2006. The decrease was primarily due to the reduction of our interest rate on our term loan as a result of the second quarter 2007 amendment to our senior secured credit agreement, reduced levels of revolver usage between years and an increase in interest income due to increased cash and investments with our insurance subsidiary.
Earnings from Continuing Operations Before Income Taxes. Earnings from continuing operations before income taxes in 2007 were $71.5 million compared to $37.3 million in 2006.
Provision for Income Taxes. Provision for income taxes in 2007 was $27.7 million compared to $13.8 million in 2006.
Earnings from Continuing Operations. Earnings from continued operations were $43.8 million in 2007 compared to $23.5 million in 2006.
Loss from Discontinued Operations, Net of Taxes. Loss from discontinued operations, net of taxes was $0.6 million in 2007 compared to $7.0 million in 2006. Contributing to the loss in 2007 were $1.0 million of severance and other exit costs related to the disposal of the anesthesia business unit. The loss in 2006 includes an impairment loss of $10.2 million ($7.7 million, net of $2.5 million tax benefit).
Net Earnings. For the foregoing reasons, net earnings for 2007 were $43.3 million compared to $16.5 million in 2006.
66
Table of Contents
Liquidity and Capital Resources
Our principal ongoing uses of cash are to meet working capital requirements, fund debt obligations and to finance our capital expenditures and acquisitions. We believe that our cash needs, other than for significant acquisitions, will continue to be met through the use of existing available cash, cash flows derived from future operating results and cash generated from borrowings under our senior secured revolving credit facility.
Cash provided by operating activities in the nine months ended September 30, 2009 was $84.6 million compared to $62.9 million in the corresponding period in 2008. The $21.8 million increase in cash provided by operating activities was principally due to an improvement in profitability, a lower level of accounts receivable funding and a reduction in interest payments during the first nine months of 2009 compared to the same period in 2008. Cash used in investing activities in the nine months ended September 30, 2009 was $13.1 million compared to $21.2 million in the same period of 2008. The $8.1 million decrease in cash used in investing activities was principally due to a decrease in cash payments made related to acquisitions, a decrease in capital expenditures and a decrease in net purchases of investments between periods at the captive insurance subsidiary. Cash used in financing activities in the nine months ended September 30, 2009 was $4.9 million compared to $5.0 million in the nine months ended September 30, 2008.
Cash provided by operating activities in the year ended December 31, 2008 was $62.0 million compared to $70.1 million in 2007. The $8.1 million decrease in cash provided by operating activities was principally due to an increase in cash taxes paid in 2008 and an increase in working capital between periods in 2008 compared to a decrease in working capital between periods in 2007, offset by a reduction in cash interest payments in 2008. Cash used in investing activities in the year ended December 31, 2008, was $29.8 million compared to $31.3 million in 2007. The $1.5 million decrease in cash used in investing activities was principally due to a decrease in net captive investment purchases between years and a decrease in capital expenditures partially offset by an increase in cash payments for acquisitions. Cash used in financing activities in the year ended December 31, 2008 and 2007 was $16.1 million and $12.5 million, respectively. The $3.6 million increase in cash used in 2008 in financing activities was principally due to the $10.0 million cash payment for retirement of a portion of our 11.25% senior subordinated notes, offset by net reduction in outstanding amounts under the revolving credit facility in 2007.
We spent $5.2 million in the first nine months of 2009 and $7.3 million in the first nine months of 2008 for capital expenditures. These expenditures were primarily for billing and information technology investments and related development projects along with projects in support of operational initiatives. The $2.1 million decrease between periods is mainly attributable to higher expenditures in the prior period related to certain capital projects completed during 2008.
We are highly leveraged. As of September 30, 2009, we had $612.1 million in aggregate indebtedness, consisting of $409.1 million of our term loan and $203.0 million of the senior subordinated notes with an additional $110.0 million of borrowing capacity available under our senior secured revolving credit facility (without giving effect to $7.5 million of undrawn letters of credit and before any potential reduction associated with the CIT bankruptcy).
On November 23, 2005, we issued senior subordinated notes in the amount of $215.0 million due December 1, 2013. The Notes are subordinated in right of payment to all of our senior debt and are senior in right of payment to all of our existing and future subordinated indebtedness. Interest on the Notes accrues at the rate of 11.25% per annum, payable semi-annually in arrears on June 1 and December 1 of each year. Beginning on December 1, 2009, we may redeem some or all of the Notes at any time at various redemption prices. In December 2008, we retired $12.0 million of the Notes in an open market purchase. The Notes are guaranteed jointly and severally by all of our domestic wholly-owned operating subsidiaries as required by the indenture governing the Notes.
67
Table of Contents
Borrowings outstanding under the senior credit facility mature in various years with a final maturity date of November 23, 2012. The senior credit facility agreement and the indenture governing the Notes contain both affirmative and negative covenants, including limitations on our ability to incur additional indebtedness, sell material assets, retire, redeem or otherwise reacquire our capital stock, acquire the capital stock or assets of another business, pay dividends, and require us to comply with certain coverage and leverage ratios. The senior credit agreement also includes a provision for the prepayment of a portion of the outstanding term loan amounts at any year-end if we generate “excess cash flow,” as defined in the agreement.
We entered into three separate forward interest rate swap agreements during 2008. The objective of these agreements is to eliminate the variability of the cash flows in interest payments for $200.0 million of the variable-rate senior secured term loan facility for a three year period. The agreements are contracts to exchange, on a quarterly basis, floating interest rate payments based on the Eurocurrency rate, for fixed interest payments over the life of the agreements. We have determined that the interest rate swaps are highly effective and qualify for hedge accounting; therefore in the nine months ended September 30, 2009 and the year ended December 31, 2008, we have recorded the increase in the fair value of the interest rate swaps, net of tax, of approximately $0.1 million as a component of other comprehensive earnings and the decrease in fair value of the interest rate swaps, net of tax, of approximately $3.4 million as a component of other comprehensive earnings, respectively.
These agreements expose us to credit losses in the event of non-performance by the counterparty to the financial instruments. The counterparty is a creditworthy financial institution, and we believe the counterparty will be able to fully satisfy its obligations under the contracts.
Subject to any contractual restrictions, we and our subsidiaries, affiliates or significant stockholders (including the Sponsor and its affiliates) may from time to time, in their sole discretion, purchase, repay, redeem or retire any of our outstanding debt or equity securities (including any publicly issued debt or equity securities), in privately negotiated or open market transactions, by tender offer or otherwise.
As of September 30, 2009, we had total cash and cash equivalents of approximately $113 million. There are no known liquidity restrictions or impairments on our cash and cash equivalents as of September 30, 2009. Our ongoing cash needs for the nine months ended September 30, 2009 were substantially met from internally generated operating sources. As of September 30, 2009, there were no amounts outstanding under the revolving credit facility. In connection with this offering, we intend to use a portion of our existing cash to pay a lump-sum termination payment to an affiliate of our Sponsor. See “Capitalization” and “Certain Relationships and Related Party Transactions.”
We have historically been an acquirer of other physician staffing businesses and interests. In June 2008, we acquired the operations of an emergency medicine staffing business for $7.5 million in cash. We may have to pay up to $6.7 million in deferred payments. In August 2007, we acquired the operations of an emergency medicine medical practice for $2.4 million in cash. In addition, we may have to pay up to $2.2 million in future contingent payments.
Effective May 1, 2006, we acquired the operations of an emergency medicine medical practice for $3.0 million in cash and the assumption of up to a $1.0 million liability related to medical professional liability insurance.
Effective July 1, 2006, we acquired the operations of a hospital medicine and inpatient services business for $17.9 million in cash. In addition, we paid $7.5 million of contingent consideration related to this acquisition on October 1, 2009. No additional amounts are due under the acquisition agreement. The initial cash payment in 2006 was funded through a borrowing under our senior secured revolving credit facility. The October 1, 2009 payment was funded with available cash.
68
Table of Contents
During the nine months ended September 30, 2009, $2.8 million in payments were made related to our current year acquisition and no contingent consideration was paid on prior year acquisitions. For the same period in 2008, $7.5 million in payments were made related to acquisitions or contingent consideration paid on a prior year acquisition. Future contingent payment obligations are estimated to be $18.3 million (without giving effect to a $7.5 million contingent payment made on October 1, 2009) as of September 30, 2009.
We are currently a party to several letters of intent to acquire certain physician staffing businesses. Such letters are non-binding and subject to conditions such as completion of our due diligence. However, if we do ultimately consummate these potential acquisitions, we would expect to fund such acquisitions using our existing cash. If we were to complete all such potential acquisitions that are currently subject to a letter of intent, we would expect the purchase prices to be approximately $100 million in the aggregate, with an approximate $84 million to be paid at closing. In addition to these potential transactions, we are in preliminary discussions with other parties that have not reached the phase in negotiations where a non-binding letter of intent would be executed.
Effective March 12, 2003, we began providing for professional liability risks in part through a captive insurance company. Prior to such date we insured such risks principally through the commercial insurance market. The change in the professional liability insurance program initially resulted in increased cash flow due to the retention of cash formerly paid out in the form of insurance premiums to a commercial insurance company coupled with a long period (typically 2-4 years or longer on average) before cash payout of such losses occurs. A portion of such cash retained is retained within our captive insurance company and therefore not immediately available for general corporate purposes. As of September 30, 2009, the current value of cash or cash equivalents and related investments held within the captive insurance company totaled $95.6 million. Investments of captive insurance are carried at fair market value and as of September 30, 2009, reflected $3.7 million of net unrealized gains. Effective June 1, 2009, we renewed our fronting carrier program with a commercial insurance carrier through May 31, 2010. In connection with this renewal, we have paid cash premiums of $11.5 million to the commercial insurance carrier. We also expect to pay premiums to the captive insurance subsidiary of $7.9 million through December 31, 2009. For the nine months ended September 30, 2009, we also funded a total of $4.2 million to a commercial insurance provider in order to meet our obligation for incurred costs in excess of the aggregate limits of coverage in place on the commercial insurance policy that ended March 11, 2003. We will fund additional payments which will be based upon the level of incurred losses relative to the aggregate limit of the coverage at that time as additional claims are processed.
Senior Secured Credit Facilities
Our senior secured credit facilities consist of a $425.0 million senior secured term loan facility ($409.1 million outstanding at September 30, 2009), and a $110.0 million senior secured revolving credit facility, of which no amount was drawn at September 30, 2009, but availability as of that date was $102.5 million as a result of $7.5 million of undrawn letters of credit outstanding and before any potential reduction associated with the CIT bankruptcy. Team Finance LLC is the borrower under the senior secured credit facilities, and Team Health Holdings, L.L.C. and the wholly-owned domestic subsidiaries of Team Finance LLC guarantee these borrowings. The senior secured revolving credit facility includes the capacity for issuance of letters of credit and for borrowings on same-day notice, referred to as swingline loans.
Borrowings under the senior secured credit facilities bear interest at a rate equal to an applicable margin plus, at our option, either (a) a base rate determined by reference to the higher of (1) the prime rate of JPMorgan Chase Bank, N.A. and (2) the federal funds rate plus 1/2 of 1% or (b) a LIBOR rate determined by reference to the costs of funds for deposits in the currency of such borrowing for the interest period relevant to such borrowing adjusted for certain additional costs. The current interest rate for term loan borrowings is LIBOR plus a margin of 2.0%. The current interest rate for revolving credit borrowings is LIBOR plus a margin of 2.0% based on our leverage ratio as of September 30, 2009 of 3.39 to 1.0. The applicable margin for borrowings under the senior secured revolving credit facility may be increased if our leverage ratio increases. In addition, the
69
Table of Contents
interest rate under the senior secured term loan facility may be increased in the event of a downgrade in our corporate family rating by either Moody’s Investors Service, Inc. or Standard and Poor’s Ratings Group.
In addition to paying interest on outstanding principal under the senior secured credit facilities, we pay a commitment fee to the lenders under the senior secured revolving credit facility in respect of the unutilized commitments thereunder. The commitment fee rate is 0.50% per annum. We also pay customary letter of credit fees. The senior secured credit agreement also includes a provision for the prepayment of a portion of the outstanding term loan amounts at any year end if we generate “excess cash flow,” as defined in the agreement.
We are required to repay installments on the loans under the senior secured term loan facility in quarterly principal amounts equal to 0.25% of the aggregate principal amount of the term loans outstanding (as such amount may be reduced by any prepayments) through September 30, 2012, with the remaining amount payable on November 23, 2012.
Principal amounts outstanding under the senior secured revolving credit facility are due and payable in full at maturity on November 23, 2011.
The senior secured credit agreement contains a number of covenants that, among other things, restrict, subject to certain exceptions, our ability to:
| • | incur additional indebtedness or issue certain preferred shares; |
| • | create liens on assets; |
| • | enter into sale and leaseback transactions; |
| • | engage in mergers or consolidations; |
| • | sell or otherwise dispose of assets; |
| • | pay dividends and distributions or repurchase our membership interests; |
| • | make investments, loans or advances; |
| • | repay subordinated indebtedness (including the senior subordinated notes); |
| • | make certain acquisitions; |
| • | engage in certain transactions with affiliates; |
| • | amend material agreements governing our subordinated indebtedness (including the senior subordinated notes); |
| • | change our lines of business; and |
| • | change the status of Team Health Holdings, L.L.C. as a passive holding company or the status of Health Finance Corporation as a passive corporate co-issuer of the senior subordinated notes. |
In addition, the senior secured credit agreement requires us to comply with the following financial covenants: a maximum leverage ratio, a minimum interest coverage ratio and a maximum capital expenditures amount. The maximum leverage ratio for the four fiscal quarters ending September 30, 2009 was 6.25x, the minimum interest coverage ratio for the four fiscal quarters ending September 30, 2009 was 1.75x, and the
70
Table of Contents
maximum capital expenditure amount for fiscal year 2008 was $22.0 million and for fiscal year 2009 is $23.0 million. For the four fiscal quarters ended September 30, 2009, our leverage ratio was 3.39x and our interest coverage ratio was 4.09x. For fiscal year 2008, our capital expenditures were $12.1 million and for the nine months ended September 30, 2009 our capital expenditures were $5.2 million. The breach of these maintenance covenants in the senior secured credit agreement could result in a default under the senior secured credit agreement and the required lenders could elect to declare all amounts borrowed due and payable. Any such acceleration would also result in a default under the indenture governing the senior subordinated notes.
Additionally, on November 1, 2009, it was reported that CIT filed for protection under Chapter 11 of the federal Bankruptcy Code in the United States Bankruptcy Court in the Southern District of New York. We have an aggregate revolving credit facility commitment of $110 million with a large consortium of banks, including CIT Lending Services, a subsidiary of CIT. As of November 1, 2009, CIT Lending Services’ was not a party to the above referenced Chapter 11 filing and their total commitment within this existing credit facility was $10 million. As of September 30, 2009, we had no outstanding borrowings under the revolving credit facility and $7.5 million of outstanding letters of credit. We do not believe any potential reduction in available capacity under this revolving credit facility will have a significant impact on our liquidity. We believe our cash balances, operating cash flows and funds available under our credit agreement provide adequate resources to fund ongoing operating requirements, future expansion opportunities and capital expenditures in the foreseeable future. Neither Team Finance nor any of our subsidiaries is a counterparty with CIT or any of its subsidiaries under our existing interest rate swap contracts.
Senior Subordinated Notes
Our subsidiaries, Team Finance LLC and Health Finance Corporation, issued $215.0 million aggregate principal amount of 11.25% senior subordinated notes due 2013 on November 23, 2005 in a private offering not subject to registration under the Securities Act. Subsequently, these senior subordinated notes were exchanged for registered notes in an offering effective May 16, 2006. In December 2008, we retired $12.0 million of our senior subordinated notes in an open market purchase for $10.0 million plus accrued interest. The senior subordinated notes are guaranteed by certain of our subsidiaries as required by the indenture governing the senior subordinated notes. The indenture governing the senior subordinated notes limits the issuers’ (and most or all of their subsidiaries’) ability to:
| • | incur additional debt or issue certain preferred shares; |
| • | pay dividends on or make distributions in respect of their membership units or make other restricted payments; |
| • | make certain investments; |
| • | sell certain assets; |
| • | create liens on certain assets to secure debt; |
| • | consolidate, merge, sell or otherwise dispose of all or substantially all of their assets; |
| • | enter into certain transactions with their affiliates; and |
| • | designate their subsidiaries as unrestricted subsidiaries. |
Under the indenture governing the senior subordinated notes, our ability to engage in certain activities such as incurring certain additional indebtedness, making certain investments and paying certain dividends is tied to ratios based on Adjusted EBITDA (which is defined as “EBITDA” in the indenture). For example, for the four quarters ended December 31, 2008, the minimum Adjusted EBITDA to fixed charge ratio required in order to
71
Table of Contents
incur additional debt pursuant to the ratio provision in the indenture or to make certain investments and restricted payments under the indenture was 2.25x. For the four quarters ended December 31, 2008, our Adjusted EBITDA to fixed charge coverage ratio was 3.40x and for the four quarters ended September 30, 2009, our Adjusted EBITDA to fixed charge coverage ratio was 3.90x. If we were unable to meet the required Adjusted EBITDA to fixed charge coverage ratio, we would be unable to incur indebtedness in excess of certain specified amounts and would be unable to pay dividends or make investments in excess of certain specified amounts. The breach of such covenants could result in a default under the indenture and the required holders could elect to declare all amounts outstanding due and payable. Any such acceleration would also result in a default under our senior secured credit agreement.
Adjusted EBITDA under the indenture is defined as net earnings before interest expense, taxes, depreciation and amortization, as further adjusted to exclude unusual items, non-cash items and the other adjustments shown in the table below. We believe that the disclosure of the calculation of Adjusted EBITDA provides information that is useful to an investor’s understanding of our financial flexibility under our indenture covenants. Adjusted EBITDA is not a measurement of financial performance or liquidity under generally accepted accounting principles. It should not be considered in isolation or as a substitute for net income, operating income, cash flows from operating, investing or financing activities, or any other measure calculated in accordance with generally accepted accounting principles. Adjusted EBITDA, as calculated under the indenture for the senior subordinated notes, is as follows:
| Year Ended December 31, | Nine Months Ended September 30, | |||||||||||||||
| 2006 | 2007 | 2008 | 2008 | 2009 | ||||||||||||
| (In thousands) | ||||||||||||||||
| Net earnings |
$ | 16,465 | $ | 43,270 | $ | 44,666 | $ | 50,063 | $ | 55,231 | ||||||
| Interest expense, net |
57,813 | 55,234 | 45,849 | 34,033 | 27,671 | |||||||||||
| Provision for income taxes |
13,792 | 27,703 | 31,044 | 33,885 | 34,230 | |||||||||||
| Depreciation and amortization |
23,308 | 14,823 | 17,281 | 12,559 | 14,028 | |||||||||||
| Loss from discontinued operations, net of taxes |
7,049 | 576 | — | — | — | |||||||||||
| Impairment of intangibles(a) |
— | — | 9,134 | — | — | |||||||||||
| Management fee and other expenses(b) |
3,748 | 4,054 | 3,602 | 2,745 | 2,324 | |||||||||||
| Gain on extinguishment of debt(c) |
— | — | (1,640 | ) | — | — | ||||||||||
| Transaction costs(d) |
— | — | 2,386 | 1,805 | 578 | |||||||||||
| Restricted unit expense(e) |
617 | 560 | 625 | 439 | 558 | |||||||||||
| Insurance subsidiary interest income |
2,024 | 2,867 | 3,341 | 3,040 | 2,138 | |||||||||||
| Severance and other charges |
1,164 | 3,693 | 1,549 | 1,340 | 301 | |||||||||||
| Adjusted EBITDA* |
$ | 125,980 | $ | 152,780 | $ | 157,837 | $ | 139,909 | $ | 137,059 | ||||||
| * | Adjusted EBITDA totals are not adjusted for the favorable effects of professional liability loss reserve adjustments associated with prior years of $12,068, $32,089, $34,927, $40,364 and $18,824 for the years ended December 31, 2006, 2007 and 2008, and the nine months ended September 30, 2008 and September 30, 2009, respectively. Adjusting for the effects of professional liability loss reserve adjustments associated with prior years, Adjusted EBITDA would have been reduced to $113,912, $120,691, $122,910, $99,545 and $118,235 for the years ended December 31, 2006, 2007 and 2008, and the nine months ended September 30, 2008 and 2009, respectively. |
| (a) | Includes impairment of goodwill. |
| (b) | Reflects management sponsor fees, loss on disposal of assets and realized gains on investments. |
| (c) | Reflects the gain on the retirement of a portion of the senior subordinated notes, net of write-off of deferred financing costs. |
| (d) | Reflects expenses associated with acquisition transaction fees. |
| (e) | Reflects costs related to the recognition of expense in connection with the issuance of restricted units under the Team Health Inc. 2005 Unit Plan. |
72
Table of Contents
Contractual Obligations and Commitments
The following tables reflect a summary of obligations and commitments outstanding as of December 31, 2008:
| Payments Due by Period | |||||||||||||||
| Less than 1 year |
1-3 years | 4-5 years | After 5 years |
Total | |||||||||||
| (In thousands) | |||||||||||||||
| Contractual cash obligations: |
|||||||||||||||
| Long-term debt |
$ | 4,250 | $ | 8,500 | $ | 602,525 | $ | — | $ | 615,275 | |||||
| Operating leases |
8,288 | 14,269 | 8,689 | 9,689 | 40,935 | ||||||||||
| Interest payments |
40,567 | 78,111 | 56,124 | — | 174,802 | ||||||||||
| Sponsor fee |
3,500 | 7,000 | 7,000 | 6,630 | 24,130 | ||||||||||
| Subtotal |
56,605 | 107,880 | 674,338 | 16,319 | 855,142 | ||||||||||
| Amount of Commitment Expiration Per Period | |||||||||||||||
| Less than 1 year |
1-3 years | 4-5 years | After 5 years |
Total | |||||||||||
| (In thousands) | |||||||||||||||
| Other commitments: |
|||||||||||||||
| Standby letters of credit |
$ | 8,733 | $ | — | $ | — | $ | — | $ | 8,733 | |||||
| Contingent acquisition payments |
7,500 | 8,886 | — | — | 16,386 | ||||||||||
| Subtotal |
16,233 | 8,886 | — | — | 25,119 | ||||||||||
| Total obligations and commitments |
$ | 72,838 | $ | 116,766 | $ | 674,338 | $ | 16,319 | $ | 880,261 | |||||
Inflation
We do not believe that general inflation in the U.S. economy has had a material impact on our financial position or results of operations.
Seasonality
Historically, our revenues and operating results have reflected minimal seasonal variation due to the significance of revenues derived from patient visits to EDs, which are generally open on a 365/366 day basis, and also due to our geographic diversification. Revenue from our non-ED staffing lines is dependent on a healthcare facility being open during selected time periods. Revenue in such instances will fluctuate depending upon such factors as the number of holidays in the period.
Recently Issued Accounting Standards
In April 2008, the Financial Accounting Standards Board, or FASB, issued FASB Staff Position, or FSP, No. FAS 142-3, “Determination of the Useful Life of Intangible Assets”, which was primarily codified into Topic 350 “Intangibles—Goodwill and Other” in the Accounting Standards Codification, or ASC. This guidance amends the factors that should be considered in developing renewal or extension assumptions used to determine the useful life of a recognized intangible asset and requires enhanced related disclosures. This guidance must be applied prospectively to all intangible assets acquired as of and subsequent to fiscal years beginning after December 15, 2008. Our adoption of the provisions of this guidance, as of January 1, 2009, did not have a material impact on our consolidated financial statements.
In April 2009, the FASB issued an accounting standard update (formerly FSP FAS 157-4, “Determining Fair Value When the Volume and Level of Activity for the Asset or Liability Have Significantly Decreased and
73
Table of Contents
Identifying Transactions That Are Not Orderly) to ASC Topic 820, “Fair Value Measurements and Disclosures” (formerly Statement of Financial Accounting Standards No. 157, “Fair Value Measurements”). This accounting standard update provides additional guidance for estimating fair value in accordance with when the volume and level of activity for the asset or liability have significantly decreased. This update also includes guidance on identifying circumstances that indicate a transaction is not orderly and it emphasizes that even if there has been a significant decrease in the volume and level of activity for the asset or liability and regardless of the valuation technique(s) used, the objective of a fair value measurement remains the same. Fair value is the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction (that is, not a forced liquidation or distressed sale) between market participants at the measurement date under current market conditions. The provisions of this accounting standard update were effective for interim and annual reporting periods ending after June 15, 2009, and were applied prospectively. The implementation of this standard did not have a material impact on our consolidated financial statements.
In April 2009, the FASB issued an accounting standard update (formerly FSP FAS 107-1 and APB 28-1, “Interim Disclosures about Fair Value of Financial Instruments”) to ASC Topic 825, “Financial Instruments.” This accounting standard update requires disclosures about fair value of financial instruments for interim reporting periods of publicly traded companies as well as in annual financial statements. The update was effective for interim and annual reporting periods ending after June 15, 2009. The implementation of the requirements of this update did not have a material impact on our consolidated financial statements.
In April 2009, the FASB issued an accounting standard update (formerly FSP SFAS 115-2 and SFAS 124-2, “Recognition and Presentation of Other-Than-Temporary Impairments”) to ASC Topic 320, “Investments – Debt and Equity Securities,” to amend the other-than-temporary impairment guidance in debt securities to be based on intent and not more likely than not that we would be required to sell the security before recovery and to improve the presentation and disclosure of other-than-temporary impairments on debt and equity securities in the financial statements. The adoption did not have a material effect on our consolidated financial statements.
In May 2009, the FASB issued ASC Topic 855 (formerly SFAS No. 165), “Subsequent Events,” to establish general standards of accounting for and disclosure of events that occur after the balance sheet date but before financial statements are issued. We adopted this pronouncement for the quarter ended June 30, 2009. The adoption did not have an effect on subsequent events that we report, either through recognition or disclosure, in our consolidated financial statements.
In June 2009, the FASB issued ASC Topic 105 (formerly SFAS No. 168), “The FASB Accounting Standards Codification and the Hierarchy of Generally Accepted Accounting Principles,” (ASC Topic 105-10). ASC Topic 105-10 establishes the FASB Accounting Standards Codification (the Codification) as the single source of authoritative, nongovernmental U.S. GAAP. The Codification did not change U.S. GAAP. All existing accounting standard documents were superseded and all other accounting literature not included in the Codification is considered non-authoritative. ASC Topic 105 is effective for interim and annual periods ending after September 15, 2009. Therefore, we adopted ASC Topic 105 for the reporting in our 2009 third quarter. The adoption did not have a significant impact of the reporting of our financial position, results of operations or cash flows.
Quantitative and Qualitative Disclosures About Market Risk
We are exposed to market risk related to changes in interest rates. We do not use derivative financial instruments for speculative or trading purposes.
Our earnings are affected by changes in short-term interest rates as a result of borrowings under our senior secured credit facilities. Interest rate swap agreements are used to manage a portion of our interest rate exposure.
74
Table of Contents
At September 30, 2009, the fair value of our total debt, which has a carrying value of $612.1 million, was $602.3 million. We had $409.1 million of variable debt outstanding at September 30, 2009. If the market interest rates for our variable rate borrowings had averaged 1% more subsequent to December 31, 2008, our interest expense (excluding the impact of our interest rate swap agreements) would have increased, and earnings before income taxes would have decreased, by approximately $3.1 million for the nine months ended September 30, 2009. This analysis does not consider the effects of the reduced level of overall economic activity that could exist in such an environment. Further, in the event of a change of such magnitude, management could take actions in an attempt to further mitigate its exposure to the change. However, due to the uncertainty of the specific actions that would be taken and their possible effects, the sensitivity analysis assumes no changes in our financial structure.
75
Table of Contents
Our Company
We believe we are one of the largest suppliers of outsourced healthcare professional staffing and administrative services to hospitals and other healthcare providers in the United States, based upon revenues and patient visits. We serve approximately 550 hospital clients and their affiliated clinics in 46 states with a team of approximately 6,100 healthcare professionals, including physicians, physician assistants and nurse practitioners. We recruit and contract with healthcare professionals who then provide professional services within third-party healthcare facilities. We are a physician-founded organization with physician leadership throughout our business and since our inception in 1979, we have provided outsourced services in EDs. We also provide comprehensive programs for hospital medicine (hospitalist), radiology, pediatrics and other healthcare services, by providing permanent staffing that enables the management teams of hospitals and other healthcare facilities to outsource certain management, recruiting, hiring, payroll, billing and collection and benefits functions.
EDs are a significant source of hospital inpatient admissions with a majority of admissions for key medical service lines starting in EDs, making successful management of this department critical to a hospital’s patient satisfaction rates and overall success. This dynamic, combined with the challenges involved in billing and collections and physician recruiting and retention, is a primary driver for hospitals to outsource their clinical staffing and management services to companies such as ours. For the year ended December 31, 2008, we provided services to over 7.6 million patients within our EDs. Our net revenues less provision for uncollectibles from ED contracts increased by approximately 42% from 2004 to 2008, or at a compound annual growth rate of approximately 9%. We have long-term relationships with customers under exclusive ED contracts with an approximate 98% renewal rate and a 95% physician retention rate as of September 30, 2009 (calculated on a preceding 12 months basis), respectively. The EDs that we staff are generally located in larger hospitals. We believe our experience and expertise in managing the complexities of these high-volume EDs enable our hospital clients to provide higher quality and more efficient physician and administrative services. In this type of setting, we can establish stable long-term relationships, recruit and retain high quality physicians and other providers and staff, and obtain attractive payer mixes and reasonable margins.
The range of physician and non-physician staffing and administrative services that we provide to our clients includes the following:
| • | recruiting, scheduling and credential coordination for clinical and non-clinical medical professionals; |
| • | coding, billing and collection of fees for services provided by medical professionals; |
| • | provision of experienced medical directors; |
| • | administrative support services, such as payroll, professional liability insurance coverage, continuing medical education services and management training; |
| • | claims and risk management services; and |
| • | standardized procedures. |
We are a national company delivering our services through 12 regional operating units located in key geographic markets. This operating model enables us to provide a localized presence combined with the benefits of scale in centralized administrative and other back office functions that accrue to a larger, national company. The teams in our regional offices are responsible for managing our customer and physician relationships and providing administrative healthcare services.
76
Table of Contents
Industry Overview
We estimate the size of the domestic outsourced healthcare professional staffing market to be approximately $50 billion. With the increasing complexity of clinical, regulatory, managed care and reimbursement matters in today’s healthcare environment, healthcare facilities are under significant pressure from the government and private payers both to improve the quality and reduce the cost of care. Furthermore, many healthcare facilities are not oriented towards collecting large volumes of smaller dollar payments that are typical in the emergency and other specialty departments. They may also choose to focus on other challenges such as nurse staffing, payer relationships and competition with outpatient facilities or may lack the infrastructure and personnel necessary to effectively recruit physicians and other providers in those same specialty areas. In response to these factors, healthcare facilities have increasingly outsourced the staffing and management of multiple clinical areas to companies with specialized skills, standardized models and information technology to improve service, increase the overall quality of care and reduce administrative costs.
We target certain clinical areas within healthcare facilities, including emergency medicine, hospital medicine, radiology and pediatrics, as well as civilian medical staffing within military treatment facilities. Each of these clinical areas currently faces severe physician shortages, and many healthcare facilities lack the resources necessary to identify and attract specialized, career-oriented physicians. Moreover, physician shortages are exacerbated by the growing demand for services in these clinical areas.
The market for outsourced services in each of these areas tends to be highly fragmented. We estimate that 75% of the outsourcing market is currently serviced by local and regional groups. However, local providers often lack the operating capital, experience, breadth of services and sophisticated information systems necessary to meet the increasingly complex needs of hospitals. As a result, healthcare facilities seek third-party physician staffing and administrative service providers that not only can improve department quality, productivity and patient satisfaction while reducing overall costs, but also offer a breadth of staffing and management services, billing and reimbursement expertise, a reputation for regulatory compliance, financial stability and a demonstrated ability to recruit and retain qualified physicians, technicians and nurses. In particular, EDs face significant challenges with respect to capturing patient billing data and billing and collecting a high volume of relatively small dollar amounts. As a result, EDs seek third-party providers with the billing expertise, information technology infrastructure and systems necessary to reduce their administrative burden and complexity.
Emergency Medicine. According to the American Hospital Association (AHA Hospital Statistics, 2009 edition), there were approximately 4,900 total community hospitals in the United States in 2007 and approximately 4,500 of those hospitals operated EDs. In 2007, hospitals treated more than 120.8 million patients in their EDs, which represents a compound annual growth rate of approximately 3% from 92.8 million in 1997, while more than 160 EDs closed during that same time period. This convergence has resulted in the average number of patient visits per ED to grow from approximately 19,300 to approximately 27,000 over the same period. Since EDs represent a majority of admissions for key medical service lines, the operation of an ED has significant implications for hospitals in terms of revenue, cost, quality, and the ability to grow market share.
With its origins dating back to the early 1970s, the ED is the most established service line for clinical outsourcing. We estimate that, of all hospitals that operate an ED, only 33% employ their emergency physicians and manage the function in-house, while the remaining 67% choose to outsource. The market for outsourced ED staffing and management services is highly fragmented. Depending on how one classifies a national company, this group covers approximately 25% of the outsourced ED market, with the balance being served by smaller local and regional physician groups. These local providers often lack the depth of experience and administrative and systems infrastructure necessary to compete with national providers in the increasingly complex healthcare business and regulatory environment.
77
Table of Contents
Hospital Medicine (Hospitalist). A hospitalist is a physician whose primary focus is the medical care of hospitalized patients. A hospitalist’s patient mix typically includes hospitalized patients admitted from the ED who have no primary care physician as well as the hospitalized patients of community physicians who refer their patients to the hospital medicine program.
First appearing in the early 1990s, hospitalists today are significant providers of acute inpatient care and are increasingly assuming physician leadership roles on their hospitals’ medical staffs. According to the Society of Hospital Medicine, or SHM, over half of U.S. community hospitals have a hospitalist program, and for hospitals with 200 beds or more, over 80% have hospitalist programs. The SHM also reports that approximately 23,000 physicians consider themselves “hospitalist.”
Unlike the fee for service structure of other hospital-based programs, approximately 91% of hospital medicine groups surveyed receive financial support, of which a significant amount is provided by hospitals, according to SHM. The fact that hospitals are willing to support the programs financially demonstrates a growing recognition of the value hospitalists provide. Although hospital medicine is considered the fastest-growing specialty, it is still a relatively untapped market. There are several factors that portend its continued growth, including ongoing cost pressures on hospitals, a national focus on patient safety, growing transparency of quality indicators, increased acuity of hospitalized patients, and the growing preference of primary care physicians not to have a hospital practice.
Radiology. According to the Radiological Society of North America, or RSNA, several indicators are pointing toward some relief in the shortage of radiologists. Many sources are citing increased productivity levels and enhanced technology as helping to abate the shortage, although it is still significant. However, there remains an enhanced ongoing shortage in rural communities and specific subspecialties, such as academic radiology, pediatric radiology, vascular/interventional radiology, and women’s imaging. Industry leaders are also concerned by the continuing growth of radiology procedures, which has steadily increased by approximately 6% annually. The aging of the U.S. population poses an additional issue, as individuals over the age of 65 receive four times the number of imaging tests as other individuals.
The rapid changes in the radiology market present an advantage to companies that have the resources to effectively recruit radiologists and provide the infrastructure necessary to increase productivity for radiology groups and hospitals. The changing market for radiology services has led us to shift from the traditional fee for service compensation arrangement to an increase in cost-plus arrangements with hospitals. These arrangements reduce our economic risk for such services in a time of escalating professional compensation for radiologists in general. The market for outsourced radiology services is highly fragmented and served by a large number of small local and, to a lesser extent, regional radiology groups. Smaller radiology groups are often at a competitive disadvantage since they often lack the recruitment strength, capital, range of medical equipment, teleradiology backup support and information systems required to meet the increasingly complex needs of hospitals.
The digitalization of imaging modalities has fostered the growth of teleradiology—the process of sending radiologic images from one point to another through digital, computer-assisted transmission, typically over standard telephone lines, wide area network, or WAN, or over a local area network, or LAN. Through teleradiology, images can be sent to another part of the hospital, or around the world. This capability provides numerous benefits to hospitals and radiology groups. As radiologists experience a decrease in reimbursement for services, teleradiology allows them to use their time more efficiently, thus increasing volume without substantially increasing costs. Teleradiology enables rural hospitals—which make up approximately 60% of all hospitals in the United States—to have real-time access to radiology consultations 24 hours a day, 7 days a week. It also benefits hospitals that do not have full-time radiologists on staff, as well as those that require specialized radiology services, such as pediatric. Teleradiology can also save money by preventing unnecessary patient transfers as well as the costs associated with film, storage and retrieval of images.
78
Table of Contents
Pediatrics. According to the American College of Emergency Physicians, emergency physicians and nurses treat more than 30 million sick and injured children in U.S. EDs annually. Many of these cases are classified as nonemergent, indicating the growing need for alternative sites for pediatric urgent care. Changing demographics and lifestyles indicate a growing trend in the ability to receive medical care outside of traditional physician office hours. We believe all of these indicators result in a growing demand for freestanding clinics or practice settings which provide after hours care to pediatric patients.
Military Staffing. Demand for healthcare services among military personnel has increased commensurately with the growth in the number of military retirees and the use of services by active duty personnel and their dependents. Military treatment facilities today make extensive use of permanent civilian staffing due to an inability to recruit and retain sufficient numbers of physicians, nurses and other healthcare professionals and a desire to reduce the instances of military personnel seeking off-base civilian medical care that results in higher costs. Industry sources project the military permanent medical staffing market to increase from approximately $873 million to approximately $1 billion over the next five years, representing an approximate 5% compounded annual growth rate.
Competitive Strengths
Leading Market Position. We believe we are one of the largest providers of ED staffing and management services in the United States, based upon patient visits and revenue. We are among the top providers of hospital medicine (hospitalist) services in the country and we are a significant provider of contracted staffing of healthcare professionals for military facilities under the U.S. government’s military healthcare system. We believe our ability to spread the cost of our corporate infrastructure over a broad national contract and revenue base generates significant cost efficiencies that are generally not available to smaller competitors. As a full-service provider with a comprehensive understanding of changing healthcare regulations and policies and the management information systems that provide support to manage these changes, we believe we are well positioned to maintain and grow our market share.
Regional Operating Model Supported by a Centralized National Infrastructure. We are a national company serving approximately 550 hospital clients in 46 states from 12 regionally located operating units. We believe this unique structure allows us to deliver locally focused service combined with the resources and sophistication of a national organization. Our local presence helps us foster community-based relationships with healthcare facilities, which we believe results in responsive service and high physician retention rates. Our strong relationships in local markets enable us to effectively market our services to both local hospital and military treatment facility administrators, who generally are involved in making decisions regarding contract awards and renewals. Our regional operating units are supported by our centralized national infrastructure, which includes integrated information systems and standardized procedures that we believe enable us to efficiently manage the operations and billing and collections processes. We also provide each of our regional operational sites with centralized staffing support, purchasing economies of scale, payroll administration, coordinated marketing efforts, and risk management. We believe our regional operating model supported by our centralized national infrastructure not only improves productivity and quality of care while reducing the cost of care, but also offers operating leverage to drive economies of scale as we continue to grow.
High Quality Relationships with Clients and Physicians. A key to our success has been our ability to recruit and retain high quality physicians to service our contracts. Our local presence gives us the knowledge to optimally match physicians with our hospitals and their affiliated clinics while our national presence and centralized infrastructure enable us to provide physicians with a variety of attractive client locations, operating flexibility, advanced information and reimbursement systems and standardized procedures. Furthermore, we offer physicians substantial flexibility in terms of geographic location, type of facility, scheduling of work hours, benefit packages and opportunities for relocation and career development. This operating flexibility, combined with fewer administrative burdens on physicians and clients, has resulted in our strong physician and client
79
Table of Contents
retention rates of approximately 95% and 98% (each as of September 30, 2009 calculated on a preceding 12 months basis), respectively, for our ED and hospital medicine operations, which we believe to be among the highest in the industry.
Long-Term Relationships Generating Recurring Contractual Revenue. We have long-term relationships with customers under exclusive contracts. Within ED and hospital medicine, we have an approximate 98% annual renewal rate as of September 30, 2009 (calculated on a preceding 12 months basis). While our contracts are exclusive in nature with each client facility, they are not contractually long-term (typically three years with rights of termination and extension). We earn our high renewal rate based on our high quality of service and differentiated value proposition to our clients, and as a result, the average tenure for our ED and hospital medicine customers is approximately nine years and our top 50 customers by revenue have an average tenure with us of 13 years. We continue to retain our first two clients who we began serving at the time of our inception in 1979. These long-term relationships have allowed us to generate a recurring revenue stream.
Strong and Stable Financial Profile. One of the important factors that our potential customers evaluate is financial stability. We believe our historically strong financial performance provides us with a competitive advantage in winning new contracts, renewing existing contracts and establishing and maintaining relationships with physicians and hospitals. Our existing customer relationships have generated a diversified revenue stream, with no one customer representing more than 2.1% of our net revenues less provision for uncollectibles for the nine months ended September 30, 2009. Our operations have generated strong operating cash flow, which provides us with significant financial resources after meeting our capital expenditure needs.
Significant Investment in Proprietary Information Systems and Procedures. Our proprietary information systems link our billing, collections, recruiting, scheduling, credentials coordination and payroll functions among our regional operational sites, allowing our best practices and procedures to be delivered and implemented nationally while retaining the familiarity and flexibility of a regionally-based service provider. We have developed and maintained proprietary integrated, advanced systems that allow us to monitor and improve hospital performance, which we believe increases quality and patient satisfaction. These systems include our Lawson and Hyperion financial accounting and reporting systems, GE Centricity (formerly IDX) Billing System, and our TeamWorks physician database and software package. As a result of these investments and the company-wide application of best practices policies, we believe our average cost per patient billed and average recruiting cost per physician and other healthcare professionals are among the lowest in the industry. The strength of our information systems has enhanced our ability to properly collect patient payments and reimbursements in an orderly and timely fashion and has increased our billing and collections productivity.
Comprehensive and Effective Risk and Claims Management Programs. We have comprehensive risk and claims management programs designed to prevent or minimize medical errors and professional liability claims. These programs include incident reporting and tracking systems, pre-hire testing and screening procedures, staff education, service and review programs, procedures for early intervention in professional liability claims and a risk management quality assurance program. The breadth and depth of our efforts in this area are a critical component of our business strategy and our ability to meet our client retention and acquisition goals. Excluding the favorable effects of adjustments related to prior period reserves, professional liability costs as a percentage of net revenues less provision for uncollectibles have declined every year since our self-insurance program was implemented in 2003, from 6.6% in 2003 to 3.7% in 2008.
Experienced Management Team. Our senior management team has extensive experience in the outsourced physician staffing and administrative services industry and as a group has an average of more than 20 years of experience in the healthcare industry. Our Executive Chairman, H. Lynn Massingale, M.D., co-founded TeamHealth’s predecessor entity in 1979 and has been with TeamHealth ever since. In addition, our senior corporate and regional management team reflects a mix of both physician and non-physician leaders with an average of more than 25 years in the healthcare industry and 13 years of experience with us.
80
Table of Contents
Our Growth Strategies
We intend to utilize our competitive strengths to capitalize on favorable industry trends, including increasing patient volumes, an aging population and increased ED visits, to grow our market share, net revenues, profitability and cash flow by:
Capitalizing on Outsourcing Opportunities to Win New Contracts. As hospitals and other healthcare providers continue to experience pressure from managed care companies and other payers to reduce costs while maintaining or improving their quality of service, we believe hospitals and other contracting parties will increasingly turn to a single source with an established track record of success for outsourced physician staffing and administrative services. We believe we are well-positioned to capitalize on the growth in emergency medicine and our other target outsourcing markets due to our:
| • | demonstrated ability to improve productivity, patient satisfaction and quality of care while reducing overall cost to the healthcare facility; |
| • | successful record of recruiting and retaining high quality physicians and other healthcare professionals; |
| • | national presence; |
| • | sophisticated information systems and standardized procedures that enable us to efficiently manage our core staffing and administrative services as well as the complexities of the billing and collections process; and |
| • | financial strength and resources. |
Furthermore, we seek to obtain new contracts that meet our financial targets by:
| • | replacing competitors at hospitals that currently outsource their services; |
| • | obtaining new contracts from healthcare facilities that do not currently outsource; and |
| • | expanding our present base of military treatment facility contracts by successfully competing for new staffing contracts. |
Increasing Revenues from Existing Customers. We have a strong record of achieving growth in revenues from our existing customer base. In 2008 and 2007, our net revenues less provision for uncollectibles from existing contracts, which consist of contracts under management from the beginning of a period through the end of the subsequent period, grew by approximately 4.5% and 5.9% on a year-over-year basis in 2008 and 2007, respectively. We plan to continue to increase revenues from existing customers by:
| • | capitalizing on increasing patient volumes; |
| • | implementing enhanced point of service capture of non-clinical patient data, resulting in improved billing and collection for services rendered; |
| • | continuing to improve documentation of clinical care delivered, thereby capturing appropriate reimbursement for services provided; |
| • | negotiating and implementing fee schedule increases, where appropriate; |
81
Table of Contents
| • | cross-selling additional services within contracted healthcare facilities; and |
| • | increasing staffing levels and expanding services at current military sites of service to retain patients who might otherwise receive services off-base. |
Pursuing Selective Acquisitions. We believe our fragmented industry provides a number of attractive opportunities for acquisitions, as we estimate that approximately 75% of the ED outsourcing market is currently serviced by local and regional groups. Although we believe we are one of the largest providers of outsourced physician staffing and administrative services in the United States, based on revenues and patient visits, our current ED and hospital medicine market shares are less than 10%. We intend to continue to selectively acquire businesses that would enhance both our strategic and competitive positions and believe we are well-positioned to take advantage of, and integrate, acquisition opportunities.
Enhancing Profitability Through Our Operational Focus. Our regional operating units supported by our centralized national infrastructure is designed to continually drive operating leverage, improve efficiencies and align employee incentives to drive our growth. Our information systems and economy of scale allow us to enhance profitability with revenue growth without compromising the quality of operations or clinical care. Furthermore, we believe our consolidated revenue platform and standardized processes related to managed care contracting, billing, coding, collection and compliance have driven a track record of strong revenue cycle management. We also believe our innovative patient safety and risk management initiatives and robust claims management processes have delivered favorable loss trends.
Increasing Revenues From Additional Clinical Areas. We believe we are well-positioned to increase our market share in hospital medicine (hospitalist), radiology, locum tenens, anesthesia, pediatrics and medical call center areas due to our ability to leverage our infrastructure and existing client relationships as well as our recruiting and risk management expertise. We intend to grow our presence in these sectors by adding new clients with whom we do not currently have a relationship and cross-selling these services to our existing clients.
Service Lines
We provide a full range of outsourced physician staffing and administrative services in emergency medicine, inpatient services, radiology, pediatrics and other hospital-based functions. We also provide a full range of healthcare management services to military treatment facilities. In addition to physician-related services within a military treatment facility setting, we also provide non-physician staffing services to military treatment facilities, including such services as para-professional providers, nursing, specialty technicians and administrative staffing.
Emergency Department. We believe we are one of the largest providers of outsourced physician staffing and administrative services for EDs in the United States, based upon revenues and patient visits. We contract with hospitals to provide qualified emergency physicians, physician assistants and nurse practitioners for their EDs. In addition to the core services of contract management, recruiting, credentials coordination, staffing and scheduling, we provide our client hospitals with enhanced services designed to improve the efficiency and effectiveness of the ED. We have specific programs that apply proven process improvement methodologies to departmental operations. By providing these enhanced services, we believe we increase the value of services we provide to our clients and improve client relations. Additionally, we believe these enhanced services also differentiate us from our competitors in sales situations and improve our chances of being selected in a competitive bidding process. As of September 30, 2009, we independently contracted with approximately 2,400 and employed more than 600 hospital-based emergency physicians.
Inpatient Services (Hospitalist). We provide physician staffing and administrative functions for inpatient services, which include hospital medicine, intensivist and house coverage services. Our inpatient
82
Table of Contents
contracts with hospitals are generally on a cost-plus or flat rate basis. We also contract directly with health plans. As of September 30, 2009, we independently contracted with or employed approximately 245 inpatient physicians.
Radiology. We provide outsourced radiology physician staffing and administrative services in the United States, both on a fee for service basis and a cost-plus basis. We contract directly with radiology groups and hospitals to provide physician staffing and administrative services. A typical radiology management team consists of clinical professionals, board-certified radiologists that are trained in all modalities, and non-clinical professionals and support staff that are responsible for the scheduling, purchasing, billing and collections functions. A component of our radiology business is teleradiology support services. The customers for these services are typically hospitals, radiologists or radiology groups. The business provides support to our customers from a centralized reading location. As of September 30, 2009, we independently contracted with or employed approximately 30 radiologists. In April 2009, TeamHealth Teleradiology was awarded its second consecutive Gold Seal of ApprovalTM from the Joint Commission.
Pediatrics. We provide outsourced pediatric physician staffing and administrative services for general and pediatric hospitals on a fee for service basis. These services include pediatric emergency medicine and radiology, neonatal intensive care, pediatric intensive care, urgent care centers, primary care centers, observation units and inpatient services. We also operate twelve after-hours pediatric urgent care centers in Florida. We have experienced growth of our contracts and centers and net revenues less provision for uncollectibles in our outsourced pediatric physician staffing and administrative services business due primarily to new contract sales and acquisitions, the establishment of new centers, and, to a lesser extent, rate increases on existing contracts.
Temporary Staffing. We provide temporary staffing (locum tenens) of physicians and paraprofessionals to hospitals and other healthcare organizations through our subsidiary Daniel and Yeager, Inc., or D&Y. Specialties placed through D&Y include anesthesiology, radiology and primary care, among others. Revenues from these services are generally derived from a standard contract rate based upon the type of service provided. D&Y’s customers include hospitals, military treatment facilities and medical groups.
Primary Care Clinics and Occupational Medicine. We provide primary care staffing and administrative services in stand-alone primary care clinics and in clinics located on the work-site of industrial clients. While such clinics are not a primary focus of our business, they are complementary to our hospital clients’ interests. We generally contract with hospitals or industrial employers to provide cost-effective, high quality primary care physician staffing and administrative services.
Other Non-Physician Staffing Services. Other non-physician staffing services, including such services as nursing, specialty technician and administrative staffing, are provided primarily in military treatment facilities. These services are currently provided on an hourly contract basis. Net revenues less provision for uncollectibles derived from such non-physician staffing services were approximately 8% of our revenues less provision for uncollectibles in both 2008 and 2007.
Medical Call Center Services. Through our subsidiary, TeamHealth Medical Call Center, we provide medical call center services to hospitals, physician groups and managed care organizations. Our 24-hour medical call center is staffed by registered nurses and specially trained telephone representatives with back-up support from practicing physicians.
The services provided by TeamHealth Medical Call Center include:
| • | physician after-hours call coverage; |
| • | community nurse lines; |
83
Table of Contents
| • | ED advice calls; |
| • | physician referral; |
| • | class scheduling; |
| • | appointment scheduling; and |
| • | web response. |
In addition, the TeamHealth Medical Call Center can provide our ED clients with outbound follow-up calls to patients who have been discharged from an ED. We believe this service results in increased patient satisfaction and decreased liability for the hospital.
The TeamHealth Medical Call Center is one of the few call centers nationwide that is accredited by the Utilization Review Accreditation Committee, an independent nonprofit organization that provides accreditation and certification programs for call centers.
Contractual Arrangements
We earn revenues from both fee for service arrangements and from flat-rate or hourly contracts. Neither form of contract requires any significant financial outlay, investment obligation or equipment purchase by us other than the professional expenses and administrative support costs associated with obtaining and staffing the contracts and the associated cost of working capital for such investments.
Our contracts with hospitals generally have terms of three years. Our present contracts with military treatment facilities are generally for one year. Both types of contracts often include automatic renewal options under similar terms and conditions unless either party gives notice to the other of an intent not to renew. Despite the fact that most contracts are terminable by either party upon notice of as little as 90 days, the average tenure of our existing ED and hospital medicine contracts is approximately nine years. The termination of a contract is usually due to either an award of the contract to another staffing provider as a result of a competitive bidding process or the termination of the contract by us due to a lack of an acceptable profit margin on fee for service patient volumes coupled with inadequate contract subsidies. Less frequently, contracts may be terminated as a result of a hospital facility closing due to facility mergers or a hospital attempting to insource the services being provided by us.
Hospitals. We provide outsourced physician staffing and administrative services to hospitals under fee for service contracts, flat-rate contracts and cost-plus contracts. Hospitals entering into fee for service contracts agree, in exchange for granting exclusivity to us for such services, to authorize us to bill and collect the professional component of the charges for such professional services. Under the fee for service arrangements, we bill patients and third-party payers for services rendered. Depending on the underlying economics of the services provided to the hospital, including its payer mix, we may also receive supplemental revenue from the hospital. In a fee for service arrangement, we accept responsibility for billing and collections.
Under flat-rate contracts, the hospital usually performs the billing and collection services of the professional component and assumes the risk of collectibility. In return for providing the physician staffing and administrative services, the hospital pays us a contractually negotiated fee, often on an hourly basis. Under cost-plus contracts, the hospital typically reimburses us the amount of our total costs incurred in providing physicians and mid-level practitioners to perform the professional services, plus an agreed upon administrative management fee, less our billings and collections of the professional component of the charges for such professional services.
84
Table of Contents
Military Treatment Facilities. Our present contracts to provide staffing for military treatment facilities generally provide such staffing on an hourly or fee basis.
Physicians. We contract with physicians as independent contractors or employees to provide the professional services necessary to fulfill our contractual obligations to our hospital clients. We typically pay physicians: (1) an hourly rate for each hour of coverage provided at rates comparable to the market in which they work; (2) a productivity-based payment such as a relative value unit, or RVU, based payment or (3) a combination of both a fixed rate and a productivity-based payment. The hourly rate varies depending on whether the physician is independently contracted or an employee. Independently contracted physicians are required to pay a self-employment tax, social security, and workers’ compensation insurance premiums. In contrast, we pay these taxes and expenses for employed physicians. See “Risk Factors—Risks Related to Our Business—A reclassification of our independent contractor physicians by tax authorities could require us to pay retroactive taxes and penalties which could have a material adverse effect on us.”
Our contracts with physicians generally have automatic renewal provisions and can be terminated at any time under certain circumstances by either party without cause, typically upon 90 to 180 days notice. Our physician contracts may also be terminated immediately for cause by us under certain circumstances. In addition, we have generally required physicians to sign non-competition and non-solicitation agreements. Although the terms of our non-competition and non-solicitation agreements vary from physician to physician, they generally restrict the physician for 2 years after termination from divulging confidential information, soliciting or hiring our employees and physicians, inducing termination of our agreements, competing for and/or soliciting our clients and, in limited cases, providing services in a particular geographic region. As of September 30, 2009, we had working relationships with more than 3,600 physicians, of which approximately 2,800 were independently contracted. See “Risk Factors—Risks Related to Our Business—If we are not able to successfully recruit and retain qualified physicians and nurses to serve as our independent contractors or employees, our net revenues could be adversely affected.”
Other Healthcare Professionals. We provide para-professionals, nurses, specialty technicians and administrative support staff on a long-term contractual basis to military treatment facilities. These healthcare professionals under our current military staffing contracts are compensated on an hourly or fee basis. As of September 30, 2009, we employed or contracted with approximately 2,500 other healthcare professionals.
Services
We provide a full range of outsourced physician and non-physician healthcare professional staffing and administrative services, including the following:
Contract Management. Our delivery of services for a clinical area of a healthcare facility is led by an experienced contract management team of clinical and other healthcare professionals. The team usually includes a regional medical director, an on-site medical director and a client services manager. The on-site medical director is a physician with the primary responsibility of coordinating the physician component of a clinical area of the facility. The medical director works with the team, in conjunction with the nursing staff and private medical staff, to improve clinical quality and operational effectiveness. Additionally, the medical director works closely with the regional operating unit’s operations staff to meet the client’s ongoing recruiting and staffing needs.
Staffing. We provide a full range of staffing services to meet the unique needs of each healthcare facility. Our dedicated clinical teams include qualified, career-oriented physicians and other healthcare professionals responsible for the delivery of high quality, cost-effective care. These teams also rely on managerial personnel, many of whom have clinical experience, who oversee the administration and operations of the clinical area. As a result of our staffing services, healthcare facilities can focus their efforts on improving
85
Table of Contents
their core business of providing healthcare services for their communities as opposed to recruiting and managing physician staffing. We also provide temporary staffing services of physicians and other healthcare professionals to healthcare facilities on a national basis.
Recruiting. Many healthcare facilities lack the resources necessary to identify and attract specialized, career-oriented physicians. We have a staff of more than 80 professionals dedicated to the recruitment of qualified physicians and other clinicians. These professionals are regionally located and focus on matching qualified, career-oriented physicians with healthcare facilities. Common recruiting methods include the use of our proprietary national physician database, attendance at trade shows, the placement of website and professional journal advertisements, telemarketing efforts, and referrals from our existing providers.
We have committed significant infrastructure and personnel to the development of a proprietary national physician database to be shared among our regional operating units. This database is utilized at all of our operating units. Recruiters contact prospects through telemarketing, direct mail, conventions, journal advertising and our Internet site to confirm and update physicians’ information. Prospects expressing interest in one of our practice opportunities then provide more extensive background on their training, experience, and references, all of which are added to our database. Our goal is to ensure that the practitioner is a good match with both the facility and the community before proceeding with an interview.
Credentials Coordination. We gather primary source information regarding physicians to facilitate the review and evaluation of physicians’ credentials by the healthcare facility.
Scheduling. Our scheduling department assists the on-site medical directors in scheduling physicians and other healthcare professionals within the clinical area on a monthly basis.
Payroll Administration and Benefits. We provide payroll administration services for the physicians and other healthcare professionals with whom we contract. Our clinical employees benefit significantly from our ability to aggregate physicians and other healthcare professionals to negotiate more favorable employee benefit packages and to provide professional liability coverage at lower rates than many hospitals or physicians could negotiate individually. Additionally, healthcare facilities benefit from the elimination of the overhead costs associated with the administration of payroll and, where applicable, employee benefits.
Information Systems. We have invested in advanced information systems and proprietary software packages designed to assist hospitals in lowering administrative costs while improving the efficiency and productivity of a clinical area. These systems include TeamWorks, our national physician database and software package that facilitates the recruitment and retention of physicians and supports our contract requisition, credentials coordination, automated application generation, scheduling and payroll operations.
The strength of our electronic billing system and other information systems has enhanced our ability to properly collect patient payments and reimbursements in an orderly and timely fashion and has increased our billing and collections productivity. As a result of our investments in information systems and the company-wide application of operational best practices policies, we believe our average cost per patient billed and average recruiting cost per physician and other healthcare professionals are among the lowest in the industry.
Billing and Collections. Our billing and collection services are a critical component of our business. Our fee for service billing and collections operations are conducted at one of three billing locations and operate on a uniform billing system using a state of the art billing and accounts receivable software package with comprehensive reporting capabilities. We are able to maintain fee schedules that vary for the level of care rendered and to apply contractually agreed upon allowances (in the case of commercial and managed care insurance payers) and reimbursement policy parameters (in the case of governmental payers) to allow us to process payer reimbursements at levels that are less than the gross charges resulting from our fee schedules. Our billing system calculates the contractual allowances at the time of processing of third-party payer remittances.
86
Table of Contents
The contractual allowance calculation is used principally to determine the propriety of subsequent third-party payer payments. The nature of emergency care services and the requirement to treat all patients in need of such care and often times under circumstances where complete and accurate billing information is not readily available at the time of discharge, precludes the use of our billing system to accurately determine contractual allowances for financial reporting purposes. As a result, management estimates net revenues less provision for uncollectibles, which is our revenue estimated to be collected after considering our contractual allowance obligations and our estimates of doubtful accounts, as further discussed in detail in “Management’s Discussion and Analysis of Financial Condition and Results of Operations.”
We have interfaced a number of other software systems with our billing system to further improve productivity and efficiency. Foremost among these is an electronic registration interface that has the capability to gather registration information directly from a hospital’s management information system. Additionally, we have invested in electronic submission of claims and remittance posting, as well as electronic chart capture, workflow, and online coding. These programs have resulted in lower labor and postage expenses. At the present time, approximately 99% of our over seven million fee for service annual patient visits are processed by one of our three billing locations.
We also operate an internal collection agency. Substantially all collection placements generated from our billing locations are sent to the agency. Comparative analysis has shown that the internal collection agency is more cost effective than the use of outside agencies and has improved the collectibility of existing placements. Our advanced comprehensive billing and collection systems allow us to have full control of accounts receivable at each step of the process.
Risk Management. Through our risk management staff, quality assurance staff and our medical directors, we conduct an aggressive risk management program for loss prevention and early intervention. We are proactive in promoting early reporting, evaluation and resolution of serious incidents that may evolve into claims or suits. Our risk management function is designed to prevent or minimize medical professional liability claims and includes:
| • | incident reporting systems through which we monitor errors that may potentially become claims; |
| • | tracking/trending the cause of errors and claims looking for preventable sources of erroneous medical treatment or decision-making; |
| • | risk management quality improvement programs; |
| • | physician education and service programs, including peer review and monitoring and the provision of more than 78,000 hours of continuing medical education in 2008; |
| • | collection of loss prevention information enabling providers to review current topics in medical care at their convenience; and |
| • | early intervention in potential professional liability claims. |
In addition, during 2007, we completed the conversion of our risk management database over to one of the most comprehensive risk management information systems on the market. We use this information system to enhance our physician risk management assessments, malpractice claims/litigation management and the analysis of claims data to identify loss patterns/trends. The collection and analysis of claims data enables us to evaluate losses and target risk management intervention to proactively address potential liability exposures.
Continuing Medical Education Services. The TeamHealth Institute for Education and Patient Safety is fully accredited by the Accreditation Council for Continuing Medical Education. This allows us to grant our
87
Table of Contents
physicians and nurses continuing medical education credits for both externally and internally developed educational programs at a lower cost than if such credits were earned through external programs. In addition to providing life support certification courses, we have designed a series of client support seminars entitled Successful Customer Relations and Beyond Clinical Competence for physicians, nurses and other personnel to learn specific techniques for becoming effective communicators and delivering top-quality customer service. These seminars help the clinical team sharpen its customer service skills, further develop communication skills and provide techniques to help deal with people in many critical situations.
Patient Safety Organization. We have established a federally qualified Patient Safety Organization, or PSO, whose mission is to improve patient care by conducting quality and safety analyses. Through federal protections of legal privilege and confidentiality, which are authorized by the Patient Safety and Quality Improvement Act of 2005, the TeamHealth PSO creates a secure environment that enables professional analyses of clinical issues so that best practices can be developed and shared in a confidential environment that fosters a culture of continuous quality improvement in patient care and safety.
Consulting Services. We have a long history of providing outsourced physician staffing and administrative services to healthcare facilities and, as a result, have developed an extensive knowledge of the operations of certain areas of the facilities we service. As such, we provide consulting services to our client healthcare facilities to improve the productivity, quality and cost of care delivered by them. These services include:
| • | Process improvement. We have developed a number of utilization review programs designed to track patient flow and identify operating inefficiencies. To rectify such inefficiencies, we have developed patient throughput and other processes to expedite patient care in the hospital ED and urgent care center by separating patients who can be treated in a short period of time from patients who have more serious or time-consuming problems. These patients, once identified through appropriate triage categorization, are examined and treated in a separate area of the hospital ED or urgent care center known as the Fast Track, controlled by its own staff and operational system. We have substantial experience in all phases of development and management of patient throughput programs, including planning, equipping, policy and procedure development and staffing. |
| • | Quality improvement. We provide a quality improvement program designed to assist healthcare facilities in maintaining a consistent level of high quality care. We periodically measure the performance of our services at the healthcare facilities, based on a variety of benchmarks, including patient volume, quality indicators and patient satisfaction. This program is typically integrated into our process improvement program to ensure seamless delivery of high quality, cost-effective care. |
| • | Managed care contracting. We have developed extensive knowledge of the treatment protocols and related documentation requirements of a variety of managed care payers. As a result, we often participate in the negotiation of managed care contracts to make those managed care relationships effective for patients, payers, physicians and hospitals. We provide managed care services in the areas of contracting, negotiating, reimbursement analysis/projections, payer/hospital relations, communications and marketing. We have existing managed care agreements with health maintenance organizations, preferred provider organizations and integrated delivery systems for commercial, Medicaid and Medicare products. While the majority of our agreements with payers continue to be traditional fee for service contracts, we are experienced in providing managed, prepaid healthcare to enrollees of managed care plans. |
| • | Nursing services. We maintain highly regarded, experienced nurse consultants on our client support staff. These nurse consultants provide assistance to nurse managers and medical directors of the client healthcare facility on a variety of issues, including risk management and overall performance improvement. In addition, the nurse consultants are available to make site visits to client facilities on request to assess overall operations, utilization of personnel and patient flow. |
88
Table of Contents
Sales and Marketing
Contracts for outsourced physician staffing and administrative services are generally obtained either through direct selling efforts or requests for proposals. We have a team of sales professionals located throughout the country. Each sales professional is responsible for developing sales opportunities for the operating unit in their territory. In addition to direct selling, the sales professionals are responsible for working in concert with the regional operating unit president and corporate development personnel to respond to requests for proposals or to take other steps to develop new business relationships.
Although practices vary, healthcare facilities generally issue a request for proposal with demographic information of the facility department, a list of services to be performed, the length of the contract, the minimum qualifications of bidders, the selection criteria and the format to be followed in the bid. Supporting the sales professionals is a fully integrated marketing campaign comprised of a telemarketing program, an internet website, journal advertising and a direct mail and lead referral program.
Operations
We currently have six principal service lines located at 12 regional sites. Our regional sites are listed in the table below. The ED units are managed by senior physician and business leaders with profit and loss accountability and the responsibility for pricing new contracts, recruiting and coordinating the schedules of physicians and other healthcare professionals, marketing locally and conducting day-to-day operations. The management of corporate functions such as accounting, payroll, billing and collection, capital spending, information systems and legal are centralized.
| Name |
Location |
Principal Services | ||
| After Hours Pediatrics |
Tampa, FL | Pediatrics | ||
| Daniel and Yeager |
Huntsville, AL | Locum Tenens | ||
| Emergency Coverage Corporation of TeamHealth |
Knoxville, TN | ED | ||
| TeamHealth East |
Woodbury, NJ | ED | ||
| TeamHealth Midwest |
Middleburg Heights, OH | ED | ||
| Health Care Financial Services of TeamHealth |
Knoxville, TN | Billing | ||
| TeamHealth Southeast |
Plantation, FL | ED | ||
| Northwest Emergency Physicians of TeamHealth |
Seattle, WA | ED | ||
| Spectrum Healthcare Resources |
St. Louis, MO | Military Staffing | ||
| TeamHealth Midsouth |
Knoxville, TN | ED | ||
| TeamHealth West |
Pleasanton, CA | ED | ||
| TeamHealth Radiology |
Knoxville, TN | Radiology |
We require the physicians with whom we contract to obtain professional liability insurance coverage. For our independently contracted physicians, we typically arrange for, and for our employed providers, we typically provide for, claims-made coverage with per incident and annual aggregate per physician limits and per incident and annual aggregate limits for various corporate entities. These limits are deemed appropriate by management based upon historical claims, the nature and risks of the business and standard industry practice.
Beginning in 2003, we began providing for a significant portion of our professional liability loss exposures through the use of a captive insurance company and through greater utilization of self-insurance reserves. We base a substantial portion of our provision for professional liability losses on periodic actuarial estimates of such losses.
We are usually obligated to arrange for the provision of tail coverage for claims against our clinicians for incidents that are incurred but not reported during periods for which the related risk was covered by claims- made insurance. With respect to those clinicians for whom we are obligated to provide tail coverage, we accrue professional insurance expenses based on estimates of the cost of procuring tail coverage.
89
Table of Contents
We also maintain general liability, vicarious liability, automobile liability, property, directors and officers and other customary coverages in amounts deemed appropriate by management based upon historical claims and the nature and risks of the business.
Employees and Independent Contractors
As of September 30, 2009, we had more than 6,000 employees, of which approximately 3,000 worked in billing and collections, operations and administrative support functions, more than 700 were physicians and approximately 2,300 were other healthcare providers. In addition, we had agreements with approximately 3,000 independent contractors, of whom approximately 2,800 were physicians.
Competition
The market for outsourced ED staffing and management services is highly fragmented. There are approximately 4,500 community hospitals with EDs in the United States. We believe that approximately 33% of hospitals with EDs choose to employ the emergency physician group. The remaining approximate 67% outsource to a national, regional or local emergency physician group. Of these hospitals that outsource, we believe approximately 52% contract with a local provider, approximately 23% contract with a regional provider and approximately 25% contract with a national provider.
We believe Emergency Medical Services Corporation has one of the largest shares of the ED services market based upon revenues. There are several smaller companies that provide outsourced ED services and that operate in multiple states.
Regulatory Matters
General. As a participant in the healthcare industry, our operations and relationships with healthcare providers such as hospitals are subject to extensive and increasing regulations by numerous federal and state governmental entities as well as local governmental entities. The management services provided by us under contracts with hospitals and other clients include:
| • | the identification and recruitment of physicians and other healthcare professionals for the performance of emergency medicine, radiology and other services at hospitals, outpatient imaging facilities and other facilities; |
| • | utilization review of services and administrative overhead; |
| • | scheduling of staff physicians and other healthcare professionals who provide clinical coverage in designated areas of healthcare facilities; and |
| • | administrative services such as billing and collection of fees for professional services. |
All of the above services are potentially subject to scrutiny and review by federal, state and local governmental entities and are subject to the rules and regulations promulgated by these governmental entities. Specifically, but without limitation, the following laws and regulations may affect our operations and contractual relationships:
Laws Regarding Licensing and Certification. We and our affiliated physicians are subject to various federal, state and local licensing and certification laws and regulations and accreditation standards and other laws relating to, among other things, the adequacy of medical care, equipment, personnel and operating policies and procedures. We are also subject to periodic inspection by governmental and other authorities to assure continued compliance with the various standards necessary for licensing and accreditations. We are pursuing the steps we believe we must take to retain or obtain all requisite operating authorities.
90
Table of Contents
State Laws Regarding Prohibition of Corporate Practice of Medicine and Fee Splitting Arrangements. The laws and regulations relating to our operations in 46 states vary from state to state and many states prohibit general business corporations, as we are, from practicing medicine, controlling physicians’ medical decisions or engaging in some practices such as splitting professional fees with physicians. We believe that we are in substantial compliance with state laws prohibiting the corporate practice of medicine and fee-splitting. We currently employ or contract with providers or physician-owned professional corporations to provide outsourced staffing and administrative services to healthcare facilities in the 46 states in which we provide services. Other parties may assert that, despite the way we are structured, TeamHealth could be engaged in the corporate practice of medicine or unlawful fee-splitting. Were such allegations to be asserted successfully before the appropriate judicial or administrative forums, we could be subject to adverse judicial or administrative penalties, certain contracts could be determined to be unenforceable and we may be required to restructure our contractual arrangements. The laws of other states, including Florida, where we derived approximately 16% of our net revenues less provision for uncollectibles in 2008, do not prohibit non-physician entities from employing physicians to practice medicine but may retain a ban on some types of fee-splitting arrangements.
Debt Collection Regulation. Some of our operations are subject to compliance with the Fair Debt Collection Practices Act and comparable statutes and licensure in many states. Under the Fair Debt Collection Practices Act, a third-party collection company is restricted in the methods it uses in contacting consumer debtors and eliciting payments with respect to placed accounts. Requirements under state collection agency statutes vary; however, most require compliance similar to that required under the federal Fair Debt Collection Practices Act. We believe that we are in substantial compliance with the federal Fair Debt Collection Practices Act and comparable state statutes.
Anti-Kickback Statutes. We are subject to the federal healthcare fraud and abuse laws including the Anti-Kickback Statute. The Anti-Kickback Statute under section 1128B(b) of the SSA prohibits the knowing and willful offer, payment, solicitation or receipt of any bribe, kickback, rebate or other remuneration in return for referring an individual or to induce the referral of an individual to a person for the furnishing (or arranging for the furnishing) of any item or service, or in return for the purchasing, leasing, ordering, or arranging for or recommending the purchasing, leasing, or ordering of any good, facility, service, or item for which payment may be made, in whole or in part, by a federal healthcare program. These fraud and abuse laws define federal healthcare programs to include plans and programs that provide health benefits, whether directly, through insurance, or otherwise, that are funded directly by the United States government or any state healthcare program other than the Federal Employee Health Plan. These programs include Medicare and Medicaid and the U.S. government’s military healthcare system, among others. Violations of the Anti-Kickback Statute may result in civil and criminal penalties and exclusion from participation in federal and state healthcare programs.
As authorized by Congress, the OIG has issued safe harbor regulations that immunize from prosecution certain business arrangements under the Anti-Kickback Statute. The fact that a given business arrangement does not fall within one of these safe harbor provisions does not render the arrangement illegal, but business arrangements of healthcare service providers that fail to satisfy the applicable safe harbor criteria are reviewed based upon a facts and circumstances analysis to determine whether a violation may have occurred. Some of the financial arrangements that we may maintain may not meet all of the requirements for safe harbor protection. The authorities that enforce the Anti-Kickback Statute may in the future determine that one or more of these financial arrangements violate the Anti-Kickback Statute or other federal or state laws. A determination that a financial arrangement violates the Anti-Kickback Statute could subject us to liability under the Social Security Act, including criminal and civil penalties, as well as exclusion from participation in government programs such as Medicare and Medicaid or other federal healthcare programs. In addition, an increasing number of states in which we operate have laws that prohibit some direct or indirect payments, similar to the Anti-Kickback Statute, if those payments are designed to induce or encourage the referral of patients to a particular provider. Possible sanctions for violation of these restrictions include exclusion from state-funded healthcare programs, loss of licensure, and civil and criminal penalties. Statutes vary from state to state, are often vague, and may not have been interpreted by courts or regulatory agencies.
91
Table of Contents
In order to obtain additional clarification on the federal Anti-Kickback Statute, a provider can obtain written interpretative advisory opinions from the OIG regarding existing or contemplated transactions. Advisory opinions are binding as to the Department of Health and Human Services, or HHS, but only with respect to the requesting party or parties. The advisory opinions are not binding as to other governmental agencies (e.g., the Department of Justice) and certain matters (e.g., whether certain payments made in conjunction with conduct seeking to meet certain safe harbor protections are at fair market value) are not within the purview of an advisory opinion.
In 1998, the OIG issued an advisory opinion in which it concluded that a proposed management services contract between a medical practice management company and a physician practice, which provided that the management company would be reimbursed for the fair market value of its operating services and its costs and paid a percentage of net practice revenues, may constitute illegal remuneration under the federal Anti-Kickback Statute. The OIG’s analysis focused on the marketing activities conducted by the management company and concluded that the management services arrangement described in the advisory opinion included financial incentives to increase patient referrals, contained no safeguards against over utilization, and included financial incentives that increased the risk of abusive billing practices. We believe that our contractual relationships with hospitals and physicians are distinguishable from the arrangement described in this advisory opinion with regard to both the types of services provided and the risk factors identified by the OIG. We provide outsourced physician staffing and administrative services to hospitals and other healthcare providers through contractual arrangements with physicians and hospitals. In some instances, we may enter into a contractual arrangement that provides that, as compensation for staffing a hospital department, we will receive a percentage of charges generated by the physician services rendered to patients seeking treatment in that department. However, the nature of our business distinguishes us from the management company in the advisory opinion. We do not perform marketing or any other management services for the hospital or the physicians by which we can influence the number of patients who seek treatment at the hospital department and thereby increase the compensation received by us from the hospital or paid by us to physicians. Additionally, in any percentage compensation arrangement we have with a hospital, the compensation paid to us by that hospital takes into account only the professional services rendered by our physicians and does not contain financial incentives to increase the referrals of patients by our physicians to the hospital for hospital services. Nevertheless, we cannot assure you that OIG, the Department of Justice or other federal regulators will not be able to successfully challenge our arrangements under the federal Anti-Kickback Statute in the future.
Additionally, we are subject to state statutes and regulations that prohibit, among other things, payments for referral of patients. Violations of these state laws may result in prohibition of payments for services rendered, loss of licenses, fines and criminal penalties. We cannot assure you that state regulators will not successfully challenge our arrangements under state anti-kickback statutes.
Physician Self-Referral Laws. Our contractual arrangements with physicians and hospitals may implicate the federal physician self-referral statute commonly known as the Stark Law. The Stark Law prohibits the referral of Medicare and Medicaid “designated health services” to an entity if the physician or a member of such physician’s immediate family has a “financial relationship” with the entity, unless an exception applies.
The Stark Law provides that the entity that renders the “designated health services” may not present or cause to be presented a claim for “designated health services” furnished pursuant to a prohibited referral. A person who engages in a scheme to circumvent the Stark Law’s prohibitions may be fined up to $100,000 for each applicable arrangement or scheme. In addition, anyone who presents or causes to be presented a claim in violation of the Stark Law is subject to payment denials, mandatory refunds, monetary penalties of up to $15,000 per service, an assessment of up to three times the amount claimed, and possible exclusion from participation in federal healthcare programs.
The term “designated health services” includes services commonly performed or supplied by hospitals (including inpatient and outpatient hospital services and diagnostic radiology and radiation therapy services and
92
Table of Contents
supplies) or medical clinics for which we provide physician staffing. In addition, the term “financial relationship” is broadly defined to include any direct or indirect ownership or investment interest or compensation arrangement. There are a number of exceptions to the self-referral prohibition, including exceptions for many of the customary financial arrangements between physicians and providers, such as employment contracts, leases, professional services agreements, non-cash gifts having a value less than $300 and recruitment agreements. On January 4, 2001, CMS issued a final rule, subject to a comment period, intended to clarify parts of the Stark Law and some of the exceptions to it. The majority of the regulations contained in this rule became effective on or before January 4, 2002. On March 26, 2004, CMS issued an interim final rule intended to clarify certain portions of the Stark Law. These rules, known as “phase two” of the Stark Law, became effective July 26, 2004. Subsequently, on September 7, 2007, CMS issued “phase three” of the Stark Law to finalize and clarify “phase two” regulations. The “phase three” regulations became effective on December 4, 2007.
Phase two and phase three regulations clarified certain requirements of the Stark Law. Since the phase three regulations became effective, a number of additional proposed modifications were issued separately from the Stark Law regulations in the 2009 MPFS, and 2009 Inpatient Prospective Payment System regulations, or 2009 IPPS. The 2009 MPFS included provisions related to the anti-markup rule (related to purchased interpretations) that became effective on January 1, 2009. In addition, CMS elected to adopt a number of clarifications and changes in the 2009 IPPS regulations, which include eliminating the unit of service arrangements for leases of office space and equipment, further restricting percentage-based compensation and “under arrangement” services, and modifying signature requirements with respect to physician lease and service contracting. Additionally, CMS contemplates future rulemaking and further clarification. This evolving body of regulations, or the adoption of new federal or state laws or regulations, could affect many of the arrangements entered into by each of the hospitals with which we contract. In addition, courts, Congress, and law enforcement authorities, including the OIG, are increasing the scrutiny of arrangements between healthcare providers and potential referral sources to ensure that the arrangements are not designed as a mechanism to improperly pay for patient referrals and/or other business.
In addition, a number of the states in which we operate have similar prohibitions on physicians’ self-referrals. These state prohibitions may differ from the Stark Law’s prohibitions and exceptions. Violations of these state laws may result in prohibition of payment for services rendered, loss of licenses, fines, and criminal penalties. State statutes and regulations also may require physicians or other healthcare professionals to disclose to patients any financial relationship the physicians or healthcare professionals have with a healthcare provider that is recommended to the patients. These laws and regulations vary significantly from state to state, are often vague and, in many cases, have not been interpreted by courts or regulatory agencies. Exclusions and penalties, if applied to us, could result in significant loss of reimbursement to us, thereby significantly affecting our financial condition.
Other Healthcare Fraud and Abuse Laws. Our arrangements and operations may implicate other healthcare fraud and abuse laws, including federal and certain state laws related to false claims. For example, section 1128B of SSA, commonly referred to as the Federal False Claims Act, imposes criminal liability on individuals who or entities that knowingly and willfully make or cause to be made any false statement of material fact in any application for any payment, or for use in determining rights to such payment, under a federal healthcare program. The statute also sets forth other specific activities that constitute the submission of false statements or representations. A violation of such section by a healthcare provider is a felony, and may result in fines up to $25,000 and exclusion from participation in federal healthcare programs.
The Federal False Claims Act imposes civil liability on individuals and entities that submit or cause to be submitted false or fraudulent claims for payment to the government. On May 20, 2009, the Fraud Enforcement and Recovery Act, or FERA, an act designated to overhaul the False Claims Act, was enacted. FERA greatly expanded the reach of the False Claims Act by eliminating the prior requirement that a false claim be presented to a federal official, or that that such a claim directly involve federal funds. The new law clarifies that liability attaches whenever an individual or entity makes a false claim to obtain money or property, any part of which is
93
Table of Contents
provided by the government, without regard to whether the individual or entity makes such claim directly to the federal government. Consequently, under FERA, liability attaches when such false claim is submitted to an agent acting on the government’s behalf or with a third party contractor, grantee or other recipient of such federal money or property. Additionally, under FERA, individuals and entities violate the Federal False Claims Act by knowingly retaining historic improper payments even if the individual or entity did not make claim for such payments. Violations of the Federal False Claims Act may include treble damages and penalties of up to $11,000 per false or fraudulent claim.
In addition to actions being brought under the Federal False Claims Act by government officials, the Federal False Claims Act also allows a private individual with direct knowledge of fraud to bring a whistleblower or qui tam lawsuit on behalf of the government for violations of the Federal False Claims Act. In that event, the whistleblower is responsible for initiating a lawsuit that sets in motion a chain of events that may eventually lead to the recovery of money by the government. The Federal False Claims Act and FERA extend broad protections to whistleblowers that prohibit entities from demoting, harassing, terminating or otherwise retaliating against whistleblowers for making Federal False Claims Act allegations.
After the whistleblower has initiated the lawsuit, the government must decide whether to intervene in the lawsuit and to become the primary prosecutor and the whistleblower will receive up to 25% of the government’s award in a successful lawsuit or settlement. In the event the government declines to join the lawsuit, the whistleblower plaintiff may choose to pursue the case alone, in which case the whistleblower will have primary control over the prosecution, although the government must be kept apprised of the progress of the lawsuit and will still receive at least 70% of any recovered amounts. In return for bringing a whistleblower lawsuit on the government’s behalf, the whistleblower plaintiff receives a statutory amount of up to 30% of the recovered amount from the government’s litigation proceeds if the litigation is successful or if the case is successfully settled. Violations of the Federal Anti-Kickback Statute and the Stark Law have also been used by prosecutors as a basis for Federal False Claims Act liability.
In addition to the Federal False Claims Act, several states and the District of Columbia have enacted false claims laws that allow the recovery of money that was fraudulently obtained by a healthcare provider from the state, such as Medicaid funds provided by the state, or, in some cases, from private payers, and assess other fines and penalties.
In addition to the Federal False Claims Act, under the Health Insurance Portability and Accountability Act of 1996, or HIPAA, there are five additional federal criminal statutes: “healthcare fraud,” “false statements relating to healthcare matters,” “theft or embezzlement in connection with healthcare,” “obstruction of criminal investigations of healthcare offenses,” and “laundering of monetary instruments.” These HIPAA criminal statutes encompass fraud against private payers. Violations of these statutes constitute felonies and may result in fines, imprisonment, and/or exclusion from government-sponsored programs. The “healthcare fraud” provisions of HIPAA prohibit knowingly and willfully executing a scheme or artifice to defraud any healthcare benefit program, including private payers. The “false statements” provisions of HIPAA prohibit knowingly and willfully falsifying, concealing or covering up a material fact by any trick, scheme or device or making any materially false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services.
In addition to criminal and civil monetary penalties, healthcare providers that are found to have defrauded the federal or state healthcare programs may be excluded from participation in government healthcare programs. Providers that are excluded are not entitled to receive payment under Medicare, or other federal and state healthcare programs for items or services provided to program beneficiaries. Exclusion for a minimum of five years is mandatory for a conviction with respect to the delivery of a healthcare item or service. The presence of aggravating circumstances in a case can lead to a longer period of exclusion. The OIG also has the discretion to exclude providers for certain conduct even absent a criminal conviction. Such conduct includes participation in a fraud scheme, the payment or receipt of kickbacks, and failing to provide services of a quality that meets professionally recognized standards.
94
Table of Contents
The federal government has made a policy decision to significantly increase the financial resources allocated to enforcing the general fraud and abuse laws. In addition, private insurers and various state enforcement agencies have increased their level of scrutiny of healthcare claims in an effort to identify and prosecute fraudulent and abusive practices in the healthcare area. We are subject to these increased enforcement activities and may be subject to specific subpoenas and requests for information.
Administrative Simplification and the Transactions, Privacy and Security Rules. HIPAA mandates the adoption of standards for the exchange of electronic health information in an effort to encourage overall administrative simplification and enhance the effectiveness and efficiency of the healthcare industry. Ensuring privacy and security of patient information was one of the key factors behind the legislation.
In August 2000, HHS issued final regulations establishing electronic transaction standards that healthcare providers must use when submitting or receiving certain healthcare data electronically. Most affected entities, including us, were required to comply with these regulations by October 16, 2002 or request an extension to comply with these regulations by October 16, 2003 from CMS. We received confirmation from CMS of CMS’s receipt of our request and were therefore required to comply with these regulations by October 16, 2003. On October 16, 2003, CMS implemented a HIPAA contingency plan to permit providers to temporarily submit electronic Medicare claims in a non-standard format. CMS terminated the contingency plan effective October 1, 2005. We have completed the necessary actions to comply with the new standards and transmit data in the standardized format to health plans that are able to accept the format.
In December 2000, HHS issued final regulations concerning the privacy of healthcare information that were subsequently clarified in August 2002. These regulations regulate the use and disclosure of individuals’ healthcare information, whether communicated electronically, on paper or verbally. Most affected entities, including us, were required to comply with these regulations by April 2003. The regulations also provide patients with significant new rights related to understanding and controlling how their health information is used or disclosed. We adopted privacy policies for our covered entity activities and entered into business associate agreements with affiliated providers, including physicians, hospitals and other covered entities and our vendors. We believe we are in substantial compliance with the final regulations concerning the privacy of healthcare information.
In February 2003, CMS issued final regulations concerning the security of electronic protected healthcare information. These regulations mandate the use of certain administrative, physical and technical safeguards to protect the confidentiality, integrity, and availability of electronic protected healthcare information. Most affected entities, including us, were required to comply with these regulations by April 21, 2005. We evaluated our systems, procedures and policies relative to the security of electronic protected healthcare information and modified them as necessary to comply with the security regulations. We believe we are currently in substantial compliance with the regulations.
In January 2004, CMS issued final regulations concerning the national unique health identifier for healthcare providers. These regulations establish the standard for a unique national identifier for healthcare providers for use in the healthcare system and the adoption of the NPI. In general, this rule requires any part of our business that would be a covered healthcare provider if it were a separate legal entity, to apply for a NPI and to use the identifier when submitting claims and conducting certain other electronic transactions. The regulations required compliance by May 23, 2007. However, subsequently, CMS announced that it would not penalize for another year those covered entities that have implemented contingency plans for providers who have not yet obtained their NPIs. While the guidance surrounding this “extension” is directed toward covered entity health plans, it suggests that such plans may continue to pay providers who do not have an NPI. We completed the process of obtaining the necessary NPIs for its existing providers in 2007 and continue to seek NPIs for new providers as necessary.
ARRA and the regulations that are being promulgated under ARRA include additional requirements related to the privacy and security of patient information. As part of these additional requirements, ARRA
95
Table of Contents
extends compliance with the Privacy Rule and Security Rule to business associates; requires, in certain instances, the reporting of incidents where the security of patient information has been compromised; and provides state attorneys general with enforcement authority over the Privacy Rule and Security Rule.
The HIPAA statute includes penalties for violations of the HIPAA regulations. The Secretary of HHS is permitted to impose civil penalties for violations of HIPAA requirements of $100 per violation (with a maximum of $25,000 in penalties per calendar year for the same type of violation). The United States Justice Department has the authority to enforce criminal violations of HIPAA that include fines of between $50,000 and $250,000, and 10 years’ imprisonment, or both. Criminal offenses including knowingly (i) using or causing to be used a unique health identifier in violation of the privacy standards, (ii) obtaining individually identifiable health information relating to an individual in violation of the privacy standards, or (iii) disclosing individually identifiable health information to another person in violation of the privacy standards. Other bases for criminal prosecution, for example, include committing an offense with the intent to use individually identifiable health information for commercial advantage, personal gain, or malicious harm.
In February 2006, HHS issued final regulations relating to the enforcement and imposition of penalties on entities that violate a HIPAA standard. These regulations set forth procedural and substantive requirements for the enforcement and imposition of civil penalties under HIPAA. We have established a plan and engaged the resources necessary to comply with the HIPAA administrative simplification requirements. At this time, we believe our operations are currently conducted in substantial compliance with these HIPAA requirements.
Amendments to HIPAA in the ARRA significantly increased the penalties for HIPAA violations and extended the reach of these penalties to business associates, such as the Company. There is a tiered system of penalties ranging from $100 to $50,000 per violation, with an annual maximum of $25,000 to $1,500,000. State attorneys general are empowered to bring suit on behalf of residents of their state for injunctions, statutory damages, and attorneys’ fees. The increased penalties and the authorization of state attorneys general for enforcement became effective on February 17, 2009. In addition, ARRA provisions provide that in the event of a breach of “unsecured” patient information, disclosure must be made to the patient , the Secretary of HHS, and in some cases the media. Electronic patient information is “unsecured” if it is not encrypted in accordance with standards required by HHS. Based on the existing and proposed administrative simplification of HIPAA regulations, we believe the cost of our compliance with HIPAA will not have a material adverse effect on our business, financial condition or results of operations.
There are other federal and state laws relating to privacy, security and confidentiality of patient healthcare information. In addition to federal privacy regulations, there are a number of state laws governing confidentiality of health information that are applicable to our operations. New laws governing privacy may be adopted in the future as well. We have taken steps to comply with health information privacy requirements to which we are aware that we are subject. However, we can provide no assurance that we are or will remain in compliance with the diverse privacy requirements in all of the jurisdictions in which we do business. Failure to comply with privacy requirements could result in civil or criminal penalties, which could have a materially adverse impact on our business.
Related Laws and Guidelines. Because we perform services at hospitals, outpatient facilities and other types of healthcare facilities, we and our affiliated providers may be subject to laws which are applicable to those entities. For example, our operations are impacted by the Emergency Medical Treatment and Labor Act, or EMTALA, that prohibits “patient dumping” by requiring Medicare-participating hospitals and hospital ED physicians or hospital urgent care center physicians to provide a medical screening examination to any patient presented to the hospital’s ED or urgent care center, regardless of the patient’s ability to pay, legal status or citizenship. In addition, if it is determined that the individual has an emergency medical condition, the facility must provide stabilizing treatment within its capabilities or provide for an appropriate transfer of the individual. Many states in which we operate have similar state law provisions concerning patient dumping.
96
Table of Contents
In addition to the EMTALA and its state law equivalents, significant aspects of our operations are subject to state and federal statutes and regulations governing workplace health and safety, dispensing of controlled substances and the disposal of medical waste. Changes in ethical guidelines and operating standards of professional and trade associations and private accreditation commissions such as the American Medical Association and the Joint Commission on Accreditation of Healthcare Organizations may also affect our operations. We believe our operations as currently conducted are in substantial compliance with these laws and guidelines.
Corporate Compliance Program. We have developed a corporate compliance program in an effort to monitor compliance with federal and state laws and regulations applicable to healthcare entities and to implement policies and procedures so that employees act in compliance with all applicable laws, regulations and company policies.
The OIG has issued a series of compliance program guidance documents in which the OIG has set out the elements of an effective compliance program. Our compliance program has been structured to include these elements and we believe we have taken reasonable steps to implement them. The primary compliance program components recommended by the OIG, all of which we have attempted to implement, include:
| • | formal policies and written procedures; |
| • | designation of a compliance officer; |
| • | education and training programs; |
| • | internal monitoring and reviews; |
| • | responding appropriately to detected misconduct; |
| • | open lines of communication; and |
| • | discipline and accountability. |
We audit compliance with our compliance program on a randomized sample basis; for example, we do not audit 100% of our submitted claims. Although such an approach reflects a reasonable and accepted approach in the industry, we cannot assure you that our program will detect and rectify all compliance issues in all markets and for all time periods. If we fail to detect such issues, depending on the nature and scope of the issue, this could result in future claims for recoupment of overpayments, civil fines and penalties, or other material adverse consequences.
Properties
We currently lease approximately 38,000 square feet at 1900 Winston Road, Knoxville, Tennessee for our corporate headquarters. We have executed a new lease of approximately 58,000 square feet at Brookview Town Centre, Knoxville, Tennessee for our corporate headquarters, which we expect to occupy beginning in 2010. We also lease or sublease other facilities for our corporate functions as well as for the operations of our clinics, billing centers and certain regional operations. We believe our current and future facilities will be adequate to meet our current and projected needs. The leases and subleases have various terms primarily ranging from one to seven years and monthly rents ranging from approximately $1,000 to $83,000. Our monthly lease payments total approximately $700,000. We expect to be able to renew each of our leases or to lease comparable facilities on terms commercially acceptable to us.
97
Table of Contents
Legal Proceedings
We are currently a party to various legal proceedings. While we currently believe that the ultimate outcome of such proceedings, individually and in the aggregate, will not have a material adverse effect on our financial position or overall trends in results of operations, litigation is subject to inherent uncertainties. If an unfavorable ruling were to occur, there exists the possibility of a material adverse impact on our net earnings in the period in which the ruling occurs. The estimate of the potential impact from such legal proceedings on our financial position or overall results of operations could change in the future.
98
Table of Contents
Representatives and Executive Officers
The following table sets forth information with respect to the members of our board of representatives and executive officers. After the Corporate Conversion, our board of representatives will constitute our board of directors. We use the term Board to refer to the board of representatives prior to the Corporate Conversion and to the board of directors following the Corporate Conversion.
| Name |
Age* | Position | ||
| H. Lynn Massingale, M.D. |
56 | Executive Chairman and Representative | ||
| Greg Roth |
52 | President, Chief Executive Officer and Representative | ||
| David P. Jones |
41 | Chief Financial Officer | ||
| Stephen Sherlin |
63 | Chief Compliance Officer | ||
| Heidi S. Allen |
55 | Senior Vice President, General Counsel | ||
| Neil P. Simpkins |
42 | Representative | ||
| Michael A. Dal Bello |
38 | Representative | ||
| Alan Muney, M.D. |
56 | Representative | ||
| Earl P. Holland |
63 | Representative | ||
| Glenn A. Davenport |
56 | Representative |
| * | As of September 30, 2009 |
H. Lynn Massingale, M.D. became a member of our Board following the 2005 Transactions in November 2005 and was named Executive Chairman in May 2008. Prior to May 2008, Dr. Massingale had been Chief Executive Officer and director of Team Health, Inc. since 1994 and also held the title of President until October 2004. Dr. Massingale previously served as President and Chief Executive Officer of Southeastern Emergency Physicians, a provider of emergency physician services to hospitals in the Southeast and the predecessor of Team Health, Inc., which Dr. Massingale co-founded in 1979. Dr. Massingale served as the director of Emergency Services for the state of Tennessee from 1989 to 1993. Dr. Massingale is a graduate of the University of Tennessee Medical Center for Health Services.
Greg Roth joined TeamHealth, Inc. in November 2004 as President and Chief Operating Officer. In May 2008, Mr. Roth was promoted to President and Chief Executive Officer and became a member of our Board. Prior to joining TeamHealth, Mr. Roth was employed by HCA—The Healthcare Company, a provider of healthcare services, since January 1995. Beginning in July 1998, Mr. Roth served as President of HCA, Ambulatory Surgery Division. Prior to his appointment as President, Mr. Roth served in the capacity of Senior Vice President of Operations, Western Region from May 1997 to July 1998 and the Division’s Chief Financial Officer from January 1995 to May 1997. Prior to these positions, Mr. Roth held various positions in the healthcare industry. Mr. Roth received a B.S. from Ohio State University and a M.H.A. from Xavier University.
David P. Jones has been our Chief Financial Officer since May 1996. From 1994 to 1996, Mr. Jones was our Controller. Prior to that, Mr. Jones worked at Pershing, Yoakley and Associates, a regional healthcare audit and consulting firm, as a Supervisor. Before joining Pershing, Yoakley and Associates, Mr. Jones worked at KPMG Peat Marwick as an Audit Senior. Mr. Jones received a B.S. in Business Administration from the University of Tennessee.
Stephen Sherlin was named Chief Compliance Officer effective July 1, 2004. Mr. Sherlin previously served as Executive Vice President, Healthcare Financial Services since February 2000. Mr. Sherlin joined Team Health, Inc. in January 1997 as Senior Vice President, Finance and Administration, and was promoted to Executive Vice President, Finance and Administration in July 1998. From 1993 until 1996, Mr. Sherlin served as Vice President and Chief Financial Officer of the Tennessee Division of Columbia/HCA. Mr. Sherlin has also
99
Table of Contents
served as Chief Financial Officer for the Athens Community Hospital in Athens, Tennessee; Park West Medical Center in Knoxville, Tennessee; and Doctors Hospital in Little Rock, Arkansas. Mr. Sherlin is a graduate of Indiana University.
Heidi S. Allen was named Senior Vice President and General Counsel of TeamHealth, Inc. effective June 23, 2008. From February 2003 to June 2008, Ms. Allen was Associate General Counsel, U.S. Litigation and Investigations, for Sanofi-Aventis, a major global pharmaceutical company. Admitted to practice law in and a member in good standing of the state bars of Tennessee, South Carolina and New Jersey, Ms. Allen has more than 15 years of experience advising corporations on healthcare law, including a position as Associate General Counsel, Head of Litigation, for Blue Cross Blue Shield of New Jersey. She also served as an Assistant United States Attorney for 11 years. Ms. Allen received a B.A. from the University of Pennsylvania and a J.D. from Rutgers School of Law.
Neil P. Simpkins became a member of our Board following the 2005 Transactions in November 2005. Mr. Simpkins has served as a Senior Managing Director of the Sponsor, Blackstone, an investment and advisory firm, since December 1999. From 1993 until the time he joined Blackstone, Mr. Simpkins was a principal at Bain Capital. Prior to joining Bain Capital, Mr. Simpkins was a consultant at Bain & Company in London and the Asia Pacific region. He currently serves as Chairman of the board of directors of TRW Automotive Inc. and is a director of Vanguard Health Systems and Apria Healthcare Group.
Michael A. Dal Bello became a member of our Board following the 2005 Transactions in November 2005. Mr. Dal Bello is a Managing Director in the Private Equity Group of the Sponsor, Blackstone, an investment and advisory firm, and has been at the firm since 2002 and is actively involved in Blackstone’s healthcare investment activities. Prior to joining Blackstone, Mr. Dal Bello received an M.B.A. from Harvard Business School in 2002. Mr. Dal Bello worked at Hellman & Friedman LLC from 1998 to 2000 and prior thereto at Bain & Company. He currently serves as a director of Vanguard Health Systems, Biomet, Catalent, Sithe Global, Apria Healthcare Group and Alliant.
Alan Muney, M.D. became a member of our Board in 2008. Since 2007, Dr. Muney has been an Executive Director in the Corporate Private Equity group and the CEO of Equity Healthcare, the proprietary healthcare services group purchasing organization of the Sponsor, Blackstone. Dr. Muney is involved in portfolio management and monitoring of healthcare benefits. Before joining Blackstone, Dr. Muney was the executive vice president and chief medical officer of Oxford Health Plans and chief medical officer of United Healthcare of the Northeast region, both managed healthcare companies, from 1998 to 2007. Prior to that, he was senior vice president and chief medical officer for Avanti Health systems, a division of NYLCare health plans. He was also regional medical director for Mullikin Medical Centers, a large multi-specialty medical group in California. Dr. Muney received his B.S. in Biology and his Doctor of Medicine degrees from Brown University, and a Masters in Health Administration from the University of La Verne. He currently serves as a director of Vanguard Health Systems.
Earl P. Holland became a member of our Board in 2001. Mr. Holland has over 32 years of experience working in the healthcare industry. Prior to his retirement in January 2001, Mr. Holland held several positions with Health Management Associates, an operator of acute care hospitals, including the positions of Vice Chairman and Chief Operating Officer at the time of his retirement. Mr. Holland also serves on the board of directors of several other companies engaged in the business of providing healthcare services as well as other business services, including Rural/Metro Corporation. Mr. Holland graduated from Southeast Missouri State University with a B.S. degree in business administration.
Glenn A. Davenport became a member of our Board in 2001. From March 2007 to February 2009, Mr. Davenport was President of Horizon Software International, LLC, a company specializing in food service technology. Until his retirement in August 2006, Mr. Davenport served as Chairman and Chief Executive Officer
100
Table of Contents
of Morrison Management Specialists, a member of Compass Group. Prior thereto, he served in various management capacities with Morrison Restaurants, Inc. since 1973. Mr. Davenport also serves on the board of directors of several other organizations.
Controlled Company Exception
Our Board currently consists of seven representatives, two of whom are independent. Earl P. Holland and Glenn A. Davenport qualify as independent directors under the corporate governance standards of the NYSE and the independence requirements of Rule 10A-3 of the Securities Exchange Act of 1934, as amended, or Exchange Act. Following the completion of this offering, we expect our Board to consist of seven directors, two of whom will be independent. We will have a classified Board, with two directors in Class I (expected to be Messrs. and ), two directors in Class II (expected to be Messrs. and ) and three directors in Class III (expected to be Messrs. , and ). See “Description of Capital Stock—Anti-Takeover Effects of Certain Provisions of Our Certificate of Incorporation and Bylaws—Classified Board.”
After the completion of this offering, investment funds associated with or designated by the Sponsor will continue to beneficially own, through Ensemble Parent LLC, more than 50% of our common stock and voting power. As a result, (x) under the terms of the Stockholders’ Agreement, our Sponsor, through Ensemble Parent LLC, will be entitled to nominate four of the seven members of our Board (see “Certain Relationships and Related Party Transactions—Stockholders’ Agreement”) and (y) we will be a “controlled company” within the meaning of the NYSE corporate governance standards. Under the NYSE corporate governance standards, a company of which more than 50% of the voting power is held by an individual, group or another company is a “controlled company” and may elect not to comply with certain corporate governance standards, including (1) the requirement that a majority of the board of directors consist of independent directors, (2) the requirement that we have a compensation committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities and (3) the requirement that we have a nominating and corporate governance committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities. In the event that we cease to be a controlled company, we will be required to comply with these provisions within the transition periods specified in the NYSE corporate governance rules.
Board Committees
Audit Committee
Upon the completion of this offering, we expect to have an audit committee, consisting of Messrs. Holland, Davenport and Dal Bello. Messrs. Holland and Davenport qualify as independent directors under the corporate governance standards of the NYSE and the independence requirements of Rule 10A-3 of the Exchange Act. We expect a third new independent member to replace Mr. Dal Bello within one year of the completion of this offering so that all of our audit committee members will be independent as such term is defined in Rule 10A-3(b)(i) under the Exchange Act and under the NYSE Rule 303(A). Following this offering, our Board will determine which member of our audit committee qualifies as an “audit committee financial expert” as such term is defined in Item 407(d)(5) of Regulation S-K.
The purpose of the audit committee will be to assist our Board in overseeing and monitoring (1) the quality and integrity of our financial statements, (2) our compliance with legal and regulatory requirements, (3) our independent registered public accounting firm’s qualifications and independence, (4) the performance of our internal audit function and (5) the performance of our independent registered public accounting firm.
Our Board will adopt a written charter for the audit committee which will be available on our website upon the completion of this offering.
101
Table of Contents
Compensation Committee
Upon the completion of this offering, we expect to have a compensation committee, consisting of Messrs. Simpkins, Davenport and Dal Bello. The purpose of the compensation committee will be to assist our Board in discharging its responsibilities relating to (1) setting our compensation program and compensation of our executive officers and directors, (2) monitoring our incentive and equity-based compensation plans and (3) preparing the compensation committee report required to be included in our proxy statement under the rules and regulations of the SEC.
Our Board will adopt a written charter for the compensation committee which will be available on our website upon the completion of this offering.
Nominating Committee
Upon the completion of this offering, we expect to have a nominating committee, consisting of Dr. Massingale and Mr. Simpkins. The purpose of our nominating committee will be to assist our Board in discharging its responsibilities relating to (1) developing and recommending criteria for selecting new directors and (2) screening and recommending to the Board individuals qualified to become executive officers.
Our Board will adopt a written charter for the nominating committee which will be available on our website upon completion of this offering.
Compensation Committee Interlocks and Insider Participation
We do not anticipate any interlocking relationships between any member of our compensation committee and any of our executive officers that would require disclosure under the applicable rules promulgated under the federal securities laws.
Compensation Discussion and Analysis
Philosophy of Executive Compensation Programs
Our Board has historically been responsible for the administration and oversight of our executive compensation programs. Following this offering, we will have a compensation committee to whom this responsibility will be delegated.
Our overall executive compensation objective is to provide a comprehensive plan that encourages our executive officers to focus on our strategic business initiatives, financial performance objectives and the creation and maintenance of equity value. The following are the principal objectives of our executive compensation program:
| • | attract, retain, and motivate superior management talent critical to our long-term success with compensation that is competitive within the marketplace; |
| • | ensure compensation levels reflect our internal value and future potential of each executive and the achievement of outstanding individual results; |
| • | link executive compensation to the creation and maintenance of our long-term equity value; |
| • | promote equity ownership by executives in order to align their interests with the interests of our equity holders; and |
| • | ensure that incentive compensation is linked to the achievement of specific financial and strategic objectives, which are established in advance and approved by the Board. |
102
Table of Contents
Compensation Determination Process
Our Board has historically made all determinations regarding the compensation for our executive officers. Following this offering, we will have a compensation committee that will be responsible for making all such determinations.
In the past, our Board took into account a number of variables, both quantitative and qualitative, in making its determinations regarding the appropriate level of compensation. Generally, the named executive officers’ compensation was determined based on the Board’s assessment of our overall performance and the individual performance of the named executive officer, as well as the Board’s experience and general market knowledge regarding the competitiveness of compensation and the employment agreements of the executive officers. During 2008, the Board did not retain the services of any external compensation consultant.
Dr. Massingale, our Executive Chairman and Representative, and Mr. Roth, our President, Chief Executive Officer and Representative, as members of the Board, participated in discussions and deliberations of the Board regarding executive compensation. Other named executive officers also attended the Board meetings and participated as required. Any discussion by the Board regarding specific compensation for Dr. Massingale, Mr. Roth or other named executive officers was conducted by the Board in executive session without such persons in attendance.
Following the completion of this offering, we intend to make annual awards of equity-based incentives to our employees, including our named executive officers, under the 2009 Stock Plan. We have reserved an aggregate of shares of common stock under our 2009 Stock Plan of which an aggregate of shares of common stock will remain available for future awards after giving effect to the conversion of Class B units and Class C units into options and shares in connection with the Corporate Conversion. See “—2009 Stock Plan.” We also intend to review, and may engage a compensation consultant to assist us in evaluating, the elements and levels of our executive compensation, including base salaries, bonus payments and annual equity-based incentives for our named executive officers.
Compensation Elements
We provide different elements of compensation to our named executive officers in a way that the Board believes best promotes our compensation objectives. Consistent with the philosophy that compensation to the executive officers should be aligned closely with our short and long-term financial performance, a portion of executive compensation is “at risk” and is tied to the attainment of previously established financial goals. However, the Board also believes that it is prudent to provide competitive base salaries and other benefits to attract and retain the appropriate management talent in order to achieve our strategic objectives. Accordingly, we provide compensation to our named executive officers through a combination of the following:
| • | base salary; |
| • | annual cash incentive opportunities; |
| • | long-term equity based incentives; and |
| • | benefits and executive perquisites. |
Additional detail regarding each of these elements is discussed below.
103
Table of Contents
Base Salaries
Annual base salaries reflect the compensation for an executive’s ongoing contribution to the performance of his or her functional area of responsibility with us. We believe that base salaries must be competitive based upon the executive officers’ scope of responsibilities and market compensation of similarly situated executives. Other factors such as internal consistency and comparability are also considered when establishing a base salary for a given executive. The Board utilized the experience, market knowledge and insight of its members in evaluating the competitiveness of current salary levels. Our Human Resources Department is also a resource for such information as needed.
Generally, base salaries are adjusted effective April 1 of each year based upon the Board’s assessment of each executive officer’s individual performance and our overall budgetary guidelines. In addition, base salaries may be adjusted at other times during the year in connection with promotions or increased responsibilities or to maintain competitiveness within the market. In 2008, the annual base salaries of all of our named executive officers (other than Ms. Allen, who joined us in June 2008) were increased by 3.8% effective April 1, 2008. In addition, effective May 1, 2008, Mr. Roth’s annual base salary was increased to $600,000, which represented an additional 30.3% increase, in connection with his appointment as our President, Chief Executive Officer and Representative. Ms. Allen’s annual base salary for 2008 was $315,000 and is set forth in her employment agreement. As a result of these increases, the annual base salaries of our named executive officers (other than Ms. Allen) as of April 1, 2008 (or May 1, 2008 in the case of Mr. Roth) were as follows: Dr. Massingale—$595,565; Mr. Roth—$600,000; Mr. Jones—$361,378; Mr. Sherlin—$143,717; and Mr. Joyner—$339,140.
Annual Cash Incentive Compensation
Annual cash incentive awards are available to our named executive officers, as well as to other members of our executive management team, under the Team Health Holdings, Inc. Annual Management Incentive Plan, or Bonus Plan, which will be amended and restated in connection with this offering as further described below. The Bonus Plan is designed to reward management for the achievement of annual financial targets and other operational goals, which are linked to the creation of long-term equity value of our company.
Under the Bonus Plan, as it operates with respect to performance years 2008 and 2009, each participant has a potential bonus pool that is based on a certain percentage of his or her base salary. For the named executive officers and other corporate and administrative managers, a portion of each of their respective potential bonus pools is tied to the achievement of the overall consolidated Bonus Plan EBITDA results (defined as earnings before interest, taxes, depreciation and amortization and further adjusted to exclude other non-recurring or non-operating items such as acquisitions, restructured or discontinued operations or other extraordinary or unusual events occurring during the year), or Financial Performance Component, and a portion is tied to the achievement of specific objectives as defined by management and our Board and to senior management’s assessment of our and the individual executive officer’s performance, or Discretionary Component. Our Board establishes a Bonus Plan EBITDA target at the beginning of each year. In addition, while the Financial Performance Component generally makes up a substantial portion of the potential bonus pool, the exact allocation between the Financial Performance Component and the Discretionary Component can vary from year to year. Our Board evaluates the allocation between the two components on an annual basis and has the flexibility to adjust the allocation percentages as needed in order to better align the incentives under the Bonus Plan.
The Financial Performance Component under the Bonus Plan contains threshold, target and maximum achievement levels which can increase or decrease the potential payments under the bonus pools. The threshold level of achievement reflects Bonus Plan EBITDA results equal to 95% of the Bonus Plan EBITDA target, and the maximum level of achievement reflects Bonus Plan EBITDA results equal to or above 110% of the Bonus Plan EBITDA target. No payment is made under the Financial Performance Component if the threshold level of
104
Table of Contents
achievement is not achieved, and no additional amount will be paid under the Financial Performance Component if greater than the maximum level of achievement is achieved. At the threshold level of achievement, a participant’s bonus payment is equal to 50% of his or her potential bonus pool allocated to the Financial Performance Component, and at the maximum level of achievement, a participant’s bonus payment is equal to 200% of his or her bonus pool allocated to the Financial Performance Component. Bonus payments for actual results that fall between the threshold and maximum are adjusted on a linear basis.
The determination of the bonus payment amounts under the Discretionary Component of the Bonus Plan is subject to the discretion of our Board after considering the individual executive officer’s achievement of specific operational objectives as defined by management, as well as our Board’s and senior management’s assessment of our past and future performance, including, but not limited to, subjective assessments of our operational performance during the performance year and the position of our company for the achievement of acceptable earnings growth in the subsequent year. The specific objectives defined by management vary from year to year and from one executive officer to another, but they generally relate to operational improvements that are within the individual executive officer’s area of responsibility, our strategic goals and enhancement of leadership and management skills. These objectives are typically qualitative objectives, and the Board applies its business judgement in assessing the extent to which the individual executive officers met their objectives. For 2008, these individual objectives included leadership in regard to our physician relations and key issues, leadership in our mergers and acquisitions process, development of our operational strategies, oversight with respect to our compliance with the requirements under Section 404 of Sarbanes-Oxley Act and completing our regulatory compliance goals.
The following table sets forth some of the detailed individual objectives for our named executive officers in fiscal 2008:
| Name |
Objectives | |
| Dr. Massingale | • Lead mergers and acquisitions process • Support sales growth • Guide and advise in key physician matters | |
| Mr. Roth | • Achieve sales growth target, contract retention goal and revenue cycle performance goals • Formulate development strategies for specialty services and hospital medicine | |
| Mr. Jones | • Support mergers and acquisitions process • Enhance working relationships with key operations personnel and monitor conformity to approved budgets • Ensure Sarbanes-Oxley Act compliance and oversight • Improve long-range financial planning | |
| Mr. Sherlin | • Complete audits and monitoring to ensure compliance and reporting • Implement training and education programs | |
| Ms. Allen | • Develop familiarity with the Company and its regulatory environment and pertinent legal issues | |
| Mr. Joyner | • No objectives were specified in light of Mr. Joyner’s pending retirement | |
In subjectively assessing our performance and our position for earnings growth in the subsequent year, the Board considers a number of factors, including our Bonus Plan EBITDA results during the performance year, our expectations regarding subsequent year’s Bonus Plan EBITDA results, the quality of our revenue and sales growth during the performance year and our expectations regarding our revenue and sales growth in the subsequent year. The Board does not use any specific formula in determining the bonus payments under the Discretionary Component of the Bonus Plan or assign any particular relative weightings to the various factors it
105
Table of Contents
considers in determining the payments but generally makes its determination by first considering the extent of the executive officers’ achievement of their individual objectives and then by taking into account the various factors related to the assessment of our performance described above. Our Board may decide to award nothing or more than the full amount allocated to the Discretionary Component under the potential bonus pool of any given named executive officer.
For 2008, the potential bonus pool of each of Dr. Massingale and Mr. Roth was 65% of his respective annual base salary in effect as of December 31, 2008. The potential bonus pool of each of the other named executive officers was 50% of his or her respective annual base salary in effect as of December 31, 2008. The Board allocated 80% of the bonus pool for each of the named executive officers and administrative managers to the Financial Performance Component and 20% to the Discretionary Component. Additionally, the Board set a Bonus Plan EBITDA target of $125.6 million for 2008 for our named executive officers. The actual Bonus Plan EBITDA result for 2008 was approximately $134.9 million, or 107.3% of the Bonus Plan EBITDA target set for the year. This actual Bonus Plan EBITDA result was calculated by adjusting net income as set forth in the table below and by further excluding 50% of the 2008 professional liability loss reserve adjustment related to prior years.
Bonus Plan EBITDA Calculation
| Year Ended December 31, 2008 |
||||
| (in thousands) | ||||
| Net earnings |
$ | 44,666 | ||
| Less: Gain on extinguishment of debt |
(1,640 | ) | ||
| 50% of prior year professional liability adjustment |
(17,463 | ) | ||
| Plus: Provision for income taxes |
31,044 | |||
| Transaction costs |
2,386 | |||
| Interest expense, net |
45,849 | |||
| Depreciation and amortization |
17,281 | |||
| Impairment of intangibles |
9,134 | |||
| Management fee and other expenses |
3,602 | |||
| Bonus Plan EBITDA |
$ | 134,859 | ||
Based upon the actual Bonus Plan EBITDA results, the Board determined to pay 150.0% of the Financial Performance Component of each named executive officer’s bonus pool to each such named executive officer. The Board also determined that each of Dr. Massingale and Mr. Roth partially achieved their respective objectives, and that each of the other named executive officers achieved all of their respective objectives. Since earnings growth during the year from acquisitions fell short of expectations, the Board reduced Dr. Massingale’s payment associated with this objective by approximately 75%. Because certain aspects of our specialty services and hospital medicine operations fell short of operational and financial objectives for current and future periods, the Board reduced Mr. Roth’s payments associated with these objectives by approximately 33%. Based upon this assessment, the Board determined to pay the following approximate percentages of the Discretionary Component to each named executive officer: Dr. Massingale—53%; Mr. Roth—62%; Mr. Jones—72%; Mr. Sherlin—72%; Ms. Allen—72%; and Mr. Joyner—72%. The determination regarding the payment under the Discretionary Component reflects the Board’s subjective assessment, in its business judgment, regarding the appropriate amount of total bonus payment for each named executive officer based on the executive officer’s achievement of all or many of the objectives defined for himself or herself and in light of our overall performance during 2008 and the position of our company for the achievement of earnings growth in 2009. The specific awards under the Bonus Plan for 2008 were reviewed and approved by the Board in February 2009 and paid in March 2009.
The following table illustrates the operation of the Bonus Plan for fiscal 2008. As explained above, for fiscal 2008, the Board allocated 80% of the bonus pool to the Financial Performance Component and 20% of the
106
Table of Contents
Bonus Pool to the Discretionary Component and determined to pay 150% of the Financial Performance Component of each named executive officer’s bonus pool based on the Company exceeding the Bonus Plan EBITDA target.
| Name |
Percentage of Base Salary Allocated to Bonus Pool |
Bonus Pool |
Financial Performance Component of Bonus Pool |
Amount Awarded under Financial Performance Component of Bonus Pool |
Discretionary Component of Bonus Pool |
Amount Awarded under Discretionary Component of Bonus Pool |
Total Amount Awarded under Bonus Plan for Fiscal 2008 | ||||||||||||||
| Dr. Massingale |
65 | % | $ | 387,117 | $ | 309,694 | $ | 464,541 | $ | 77,423 | $ | 41,275 | $ | 505,815 | |||||||
| Mr. Roth |
65 | % | $ | 390,000 | $ | 312,000 | $ | 468,000 | $ | 78,000 | $ | 48,578 | $ | 516,578 | |||||||
| Mr. Jones |
50 | % | $ | 180,689 | $ | 144,551 | $ | 216,827 | $ | 36,138 | $ | 25,929 | $ | 242,756 | |||||||
| Mr. Sherlin |
50 | % | $ | 71,859 | $ | 57,487 | $ | 86,230 | $ | 14,372 | $ | 10,312 | $ | 96,542 | |||||||
| Ms. Allen |
50 | % | $ | 85,438 | $ | 68,351 | $ | 102,526 | $ | 17,088 | $ | 12,260 | $ | 114,786 | |||||||
| Mr. Joyner | 50 | % | $ | 84,088 | $ | 67,271 | $ | 100,906 | $ | 16,818 | $ | 12,067 | $ | 112,972 | |||||||
In connection with the Corporate Conversion and this offering, we will amend and restate the Bonus Plan to provide the maximum bonus amount that may be payable to any participant with respect to a fiscal year and to provide the Board with greater flexibility in determining performance goals with respect to subsequent fiscal years in a manner intended to comply with the transition period exception under Section 162(m) of the Internal Revenue Code and the regulations promulgated thereunder available with respect to compensation plans or agreements that existed prior to the initial public offering and the terms of which are disclosed in the initial public offering prospectus. Under the amended and restated Bonus Plan, the maximum annual payments that may become payable with respect to any fiscal year to any individual under the Bonus Plan will be $2,000,000. For our 2010 fiscal year and for each fiscal year thereafter, the Bonus Plan will be amended to (1) provide greater flexibility as to the performance goals that may be used for purposes of any individual’s Financial Performance Component under the Bonus Plan, which may but need not be tied to the achievement of our overall consolidated Bonus Plan EBITDA results and (2) provide that the Bonus Plan will be administered by the administrator, which shall be either the Board, the compensation committee of the Board or any other committee of the Board as our Board may designate, and that the administrator shall, in its sole discretion, be authorized to waive any applicable performance goals for any participant or group of participants under the Bonus Plan and pay the amount that would have become payable had the applicable performance goals been achieved.
Long-Term Equity Incentive Compensation
In the past, the Board provided equity incentive awards to executive officers from time to time in order to directly align their interests with the long-term interests of the equity holders of Team Health Holdings.
Prior to giving effect to the Corporate Conversion, our total equity consisted of three classes of membership units: Class A units (or common units) and Class B and Class C units (or management equity incentive units). There is no vesting element associated with the Class A units, but the Class B and C units generally vest daily on a pro rata basis over a five year period from the date of issuance. Upon a change of control of the company, all outstanding Class B and Class C units will automatically vest. In conjunction with the 2005 Transactions in November 2005, members of our management reinvested a portion of their individual proceeds from the 2005 Transactions in the Class A units of Holdings. As a result, some of the named executive officers have various levels of ownership in the Class A units. Under our existing Amended and Restated Limited Liability Company Agreement, the timing and amount of any distribution of available cash, when made, are to be made in the order and priority among the different classes of units as specified therein. Generally, distributions of available cash are to be made to the holders of Class A units first before any distributions are made to the holders
107
Table of Contents
of Class B or Class C units and to the holders of Class A units and Class B units before any distributions are made to the holders of Class C units. No distributions on any of the Class B units or Class C units were made during 2008. The equity participation schedule and the vesting schedule for the Class A, Class B and Class C units described above were designed to motivate the executives and other members of management to enhance our financial and operational performance and equity value over the long-term as well as to enhance executive retention.
As of December 31, 2008, our Board had granted 329,951 Class B units and 461,931 Class C units as equity incentive awards under the existing Ensemble Acquisition (now known as Team Health Holdings, L.L.C.) 2005 Unit Plan, or the 2005 Unit Plan, to members of our management, including our named executive officers. See “Narrative Supplement to the Summary Compensation Table and 2008 Grants of Plan-Based Awards—Terms of Restricted Equity Awards” for further information regarding the terms of the restricted equity incentive awards. During 2008, the Board granted 6,250 Class B units and 8,750 Class C Units to Mr. Roth in connection with his promotion to the position of President and Chief Executive Officer and appointment as a member of the Board and, concurrent with such grants to Mr. Roth, granted the same number of Class B units and Class C units to Mr. Jones. The grants to Mr. Roth and Mr. Jones were in recognition of their respective roles and contributions to us as the Chief Executive Officer and the Chief Financial Officer and were made in order to further align their interests with the long-term interests of the equity unit holders of Team Health Holdings. Furthermore, Ms. Allen was granted 8,333 Class B units and 11,667 Class C Units as a sign-on equity award in connection with the commencement of her employment in June 2008. The Board’s determination of the amount of the Class B and Class C units granted to certain of our named executive officers in 2008 was informal and was aimed at further effectuating the objective of using equity incentive awards to motivate our management to enhance our long-term performance and executive retention.
In connection with the Corporate Conversion, each outstanding Class A unit, Class B unit and Class C unit will be automatically converted into a number of shares of our common stock calculated based upon the valuation of the company derived from the initial public offering price and the number of shares sold by the selling shareholder. The allocation of such shares of common stock among the former holders of the Class A units, Class B units and Class C units will be determined based upon such valuation. The common stock received in the conversion and shares of common stock that will be issued in respect of any Class B units or Class C units that remain unvested at the time of the Corporate Conversion will be restricted and, accordingly, will be subject to the same vesting schedule that previously applied to the corresponding Class B units or Class C units. In addition, any unvested restricted shares received in the Corporate Conversion will be generally forfeited by a holder without consideration as a result of his or her termination of employment; provided, however, that unless the holder’s employment is terminated for cause, the holder will be entitled to reimbursement by us for any U.S. federal or state income taxes paid by the holder with respect to the fair market value of the corresponding Class B units or Class C units from which such forfeited shares were converted in connection with the Corporate Conversion as of the grant date of such corresponding Class B units or Class C units as reported by the holder pursuant to his or her election under Section 83 of the Internal Revenue Code.
Each holder of Class B units or Class C units will also be issued vested and unvested options to acquire shares of our common stock in substitution for part of the economic benefits of their outstanding Class B units or Class C units not reflected in the conversion of the units into shares of common stock, with the exercise price per share of these options equal to the initial public offering price per share or such higher price per share as may be necessary to accurately reflect the terms of the Class B units or Class C units to which they relate. The unvested options will be subject to the same vesting schedule that previously applied to the Class B units or Class C units to which they relate.
In connection with the Corporate Conversion, we plan to terminate our existing 2005 Unit Plan and adopt and have our stockholders approve the Team Heath Holdings, Inc. 2009 Stock Incentive Plan, or 2009 Stock Plan, so that we can continue to provide our named executive officers and other key service providers with equity-based long-term incentives. At the time of the consummation of this offering, we also intend to grant additional fully vested options to acquire shares of our common stock under the 2009 Stock Plan to members of
108
Table of Contents
our management, including our named executive officers. These fully vested stock options will generally remain exercisable for a period of up to ten years from the date of grant, subject to the recipient’s continued employment with us (with limited post-termination exercise periods varying based upon the circumstances of termination), and the exercise price per share of these options will be equal to or higher than the initial public offering price per share. We expect to grant our named executive officers these fully vested stock options to acquire the following number of shares: Dr. Massingale shares; Mr. Roth shares; Mr. Jones shares; Mr. Sherlin shares; and Ms. Allen shares. See “—2009 Stock Plan.”
Benefits and Executive Perquisites
We also provide certain other benefits described below to our employees, including the named executive officers, which are not tied to any performance criteria and are intended to be part of a competitive compensation program. These benefits are intended to support our compensation objectives related to the attraction and retention of superior management talent and to ensure that our executives remain appropriately focused on their job responsibilities without unnecessary distraction.
Retirement Benefits
Substantially all of the salaried employees, including our named executive officers, are eligible to participate in the Team Health, Inc. 401(k) savings plan. Employees are permitted to defer a portion of their income under the 401(k) plan. At the discretion of the Board, we may make a matching contribution of up to 50%, subject to annual limits established under the Internal Revenue Code, of the first 6% of employees’ contributions under this 401(k) plan as determined each year. The Board authorized such maximum discretionary amount as a match on employees’ 401(k) Plan contributions for 2008, including the named executive officers. Employee and company matching contributions are fully vested immediately. Participants may receive distribution of their 401(k) accounts any time after their service with us ceases.
In addition, the named executive officers and other senior employees are eligible to participate in the Team Health, Inc. non-qualified Supplemental Executive Retirement Plan, or SERP. Currently, all active participants are permitted to defer a portion of their income under the SERP. In its sole discretion, we may make contributions to the accounts of any of the active participants in the SERP, and the participants will always be vested in all amounts credited to their accounts. None of the named executive officers that participate in the SERP received a contribution from us for 2008.
We maintain no defined benefit plans.
Other Benefits
All executive officers, including the named executive officers, are eligible for other benefits from us including: medical, dental, life insurance and short-term disability insurance. In addition, we provide long-term disability insurance coverage on behalf of the named executive officers at an amount equal to 60% of current base salary. The named executive officers also participate in our Personal Time Off program which provides paid leave during the year at various amounts based upon the executive’s position within the Company and length of service.
Perquisites
Each of the named executive officers receives an annual automobile allowance of $9,000 ($12,000 in the case of Dr. Massingale and Mr. Roth) for personal and business use. We also provide an annual allowance of $600 ($800 in the case of Dr. Massingale and Mr. Roth) for personal financial planning assistance. In addition, Dr. Massingale (and other senior executives upon approval of the Chairman and CEO) may have limited use of our plane for personal purposes.
These benefits and perquisites are reflected in the All Other Compensation column of the Summary Compensation Table and the accompanying footnotes in accordance with the SEC rules.
109
Table of Contents
Severance Arrangements
The Board believes that severance arrangements are necessary to attract and retain the talent necessary for our long-term success. Accordingly, our named executive officers are entitled, under their employment agreements with us, to cash and certain other benefits in the event their employment is terminated under certain circumstances. See the description of these arrangements under “Potential Payments Upon Termination or Change-In-Control—Summary of Severance Arrangements.”
Summary Compensation Table
The following table summarizes all compensation awarded to, earned by, or paid to, our named executive officers for fiscal years 2008, 2007 and 2006 for services rendered to us.
| Name and Principal Position |
Year | Salary ($) |
Bonus ($) |
Stock Awards(1) ($) |
Option Awards ($) |
Non-Equity Incentive Plan Compensation(2) ($) |
Change in Pension Value and Nonqualified Deferred Compensation Earnings(3) ($) |
All Other Compensation(4) ($) |
Total ($) | |||||||||||||||
| H. Lynn Massingale, M.D. |
2008 | $ | 589,595 | — | $ | 49,372 | — | $ | 505,815 | — | $ | 54,335 | $ | 1,199,117 | ||||||||||
| Executive Chairman and |
2007 | 568,538 | — | 49,372 | — | 531,447 | — | 65,360 | 1,214,717 | |||||||||||||||
| Representative |
2006 | 549,312 | — | 54,433 | — | 396,629 | — | 445,653 | 1,446,027 | |||||||||||||||
| Greg Roth |
2008 | 545,507 | — | 66,410 | — | 516,578 | — | 25,117 | 1,153,612 | |||||||||||||||
| President, Chief Executive |
2007 | 439,449 | — | 49,372 | — | 315,984 | — | 22,702 | 827,507 | |||||||||||||||
| Officer and Representative |
2006 | 424,589 | — | 54,433 | — | 235,826 | — | 16,131 | 730,979 | |||||||||||||||
| David P. Jones |
2008 | 357,816 | — | 31,591 | — | 242,756 | — | 25,626 | 657,789 | |||||||||||||||
| Chief Financial Officer |
2007 | 344,979 | — | 14,553 | — | 248,055 | — | 24,392 | 631,979 | |||||||||||||||
| 2006 | 331,630 | — | 16,045 | — | 185,129 | — | 23,018 | 555,822 | ||||||||||||||||
| Stephen Sherlin |
2008 | 142,301 | — | 3,664 | — | 96,542 | — | 12,655 | 255,162 | |||||||||||||||
| Chief Compliance Officer |
2007 | 137,196 | — | 3,664 | — | 98,650 | — | 12,655 | 252,165 | |||||||||||||||
| 2006 | 132,589 | — | 4,040 | — | 73,624 | — | 11,357 | 221,610 | ||||||||||||||||
| Heidi S. Allen(5) |
2008 | 157,500 | 20,000 | 22,718 | — | 114,786 | — | 282,781 | 597,785 | |||||||||||||||
| Senior Vice President, |
||||||||||||||||||||||||
| General Counsel |
||||||||||||||||||||||||
| Robert C. Joyner(6) |
2008 | 204,054 | — | 7,259 | — | 112,972 | — | 23,255 | 347,540 | |||||||||||||||
| Former Executive Vice |
2007 | 323,750 | — | 14,553 | — | 232,791 | — | 20,133 | 591,227 | |||||||||||||||
| President, General Counsel |
2006 | 311,880 | — | 16,045 | — | 173,736 | — | 16,824 | 518,485 | |||||||||||||||
| (1) | These amounts represent the compensation expense recognized by us for financial statement reporting purposes during the applicable fiscal year under ASC Topic 718, “Compensation—Stock Compensation” (excluding estimates of forfeitures) associated with our Class B and Class C units that were granted under the 2005 Unit Plan. The compensation expense for the stock awards differs from the grant date fair values for these awards as shown in the “2008 Grants of Plan Based Awards” table because the compensation expense for the stock awards is recognized over the requisite vesting period. See footnote 16 to the audited financial statements included in this prospectus to review assumptions made in the valuation of such grants under ASC Topic 718. |
| (2) | Reflects bonus amounts earned in 2008 under the Bonus Plan. Such bonus amounts were paid in March 2009. |
| (3) | We maintain no defined benefit plans, and there were no above-market or preferential earnings during the year on the Team Health, Inc. Non-Qualified Supplemental Executive Retirement Plan, a non-qualified deferred compensation plan. |
110
Table of Contents
| (4) | All Other Compensation for Dr. Massingale for 2008 included the following: |
| Personal use of company plane |
$ | 25,288 | |
| Automobile allowance |
12,000 | ||
| 401(k) matching contribution |
6,900 | ||
| Health and dental insurance premiums |
4,752 | ||
| Long-term disability insurance premiums |
4,431 | ||
| Life insurance premiums |
964 |
All Other Compensation for Mr. Roth for 2008 included the following:
| Automobile allowance |
$ | 12,000 | |
| 401(k) matching contribution |
6,900 | ||
| Long-term disability insurance premiums |
4,373 | ||
| Life insurance premiums |
1,044 | ||
| Financial planning |
800 |
All Other Compensation for Mr. Jones for 2008 included the following:
| Automobile allowance |
$ | 9,000 | |
| 401(k) matching contribution |
6,900 | ||
| Health and dental insurance premiums |
6,112 | ||
| Long-term disability insurance premiums |
2,298 | ||
| Personal use of Company plane |
872 | ||
| Life insurance premiums |
444 |
All Other Compensation for Mr. Sherlin for 2008 included the following:
| Automobile allowance |
$ | 9,000 | |
| 401(k) matching contribution |
3,655 |
All Other Compensation for Ms. Allen for 2008 included the following:
| Relocation assistance |
$ | 235,919 | |
| Gross-up of taxable relocation assistance |
42,183 | ||
| Automobile allowance |
4,500 | ||
| Life insurance premiums |
179 |
All Other Compensation for Mr. Joyner for 2008 included the following:
| Tax reimbursement relating to Internal Revenue Code Section 83 election |
$ | 8,727 | |
| Automobile allowance |
5,538 | ||
| Health and dental insurance premiums |
5,818 | ||
| Long-term disability insurance premiums |
2,033 | ||
| Personal use of company plane |
872 | ||
| Life insurance premiums |
237 |
Perquisites and other personal benefits included in All Other Compensation reflect the incremental cost to us and are valued based upon the actual costs of such services. The aggregate incremental cost to us of Dr. Massingale’s, Mr. Jones’, and Mr. Joyner’s personal use of our plane is based upon the standard hourly operating costs of the aircraft.
| (5) | Ms. Allen was appointed our Senior Vice President and General Counsel effective June 19, 2008. The amount reflected under the Bonus column for Ms. Allen reflects a sign-on bonus she received in connection with the commencement of her employment with us. |
| (6) | Mr. Joyner retired from his position as our Executive Vice President, General Counsel effective July 31, 2008. The table excludes all amounts paid to Mr. Joyner for the repurchase of his Class A, Class B and Class C common units. We paid the following amounts to Mr. Joyner in connection with such repurchases: Class A units —$902,379; vested Class B units—$60,619; and vested Class C units—$32,246. |
111
Table of Contents
2008 Grants of Plan-Based Awards
| Estimated Future Payouts Under Non-Equity Incentive Plan Awards |
Estimated Future Payouts Under Equity Incentive Plan Awards |
All Other Stock Awards: Number of Shares of Stock Units(3) (#) |
All Other Option Awards: Number of Securities Underlying Options (#) |
Exercise or Base Price of Option Awards ($/Sh) |
Grant Date Fair Value of Stock Awards(4) ($) | ||||||||||||||||||||||||
| Name |
Grant Date |
Threshold ($) |
Target ($) |
Maximum ($) |
Threshold (#) |
Target (#) |
Maximum (#) |
||||||||||||||||||||||
| H. Lynn Massingale, M.D. |
$ | 158,847 | (1) | $ | 309,694 | (1) | $ | 619,388 | (1) | ||||||||||||||||||||
| N/A | 77,423 | (2) | N/A | ||||||||||||||||||||||||||
| Greg Roth |
156,000 | (1) | 312,000 | (1) | 624,000 | (1) | |||||||||||||||||||||||
| N/A | 78,000 | (2) | N/A | ||||||||||||||||||||||||||
| Class B units |
5/19/08 | — | — | — | 6,250 | — | — | $ | 89,813 | ||||||||||||||||||||
| Class C units |
5/19/08 | — | — | — | 8,750 | — | — | 47,775 | |||||||||||||||||||||
| David P. Jones |
72,276 | (1) | 144,551 | (1) | 289,102 | (1) | |||||||||||||||||||||||
| N/A | 36,138 | (2) | N/A | ||||||||||||||||||||||||||
| Class B units |
5/19/08 | — | — | — | 6,250 | — | — | 89,813 | |||||||||||||||||||||
| Class C units |
5/19/08 | — | — | — | 8,750 | — | — | 47,775 | |||||||||||||||||||||
| Stephen Sherlin |
28,744 | (1) | 57,487 | (1) | 114,974 | (1) | |||||||||||||||||||||||
| N/A | 14,372 | (2) | N/A | ||||||||||||||||||||||||||
| Heidi S. Allen(5) |
34,175 | (1) | 68,350 | (1) | 136,701 | (1) | |||||||||||||||||||||||
| N/A | 17,088 | (2) | N/A | ||||||||||||||||||||||||||
| Class B units |
7/23/08 | — | — | — | 8,333 | — | — | 119,745 | |||||||||||||||||||||
| Class C units |
7/23/08 | — | — | — | 11,667 | — | — | 63,702 | |||||||||||||||||||||
| Robert C. Joyner(6) |
33,635 | (1) | 62,270 | (1) | 134,541 | (1) | |||||||||||||||||||||||
| N/A | 16,818 | (2) | N/A | ||||||||||||||||||||||||||
| (1) | Reflects possible payouts under the Financial Performance Component of the Bonus Plan for the 2008 performance year. Threshold represents the amount payable if actual Bonus Plan EBITDA was equal to 95% of the Bonus Plan EBITDA target, Target represents the amount payable if actual Bonus Plan EBITDA was equal to 100% of the EBITDA target, and Maximum represents the amount payable if actual Bonus Plan EBITDA was equal to or greater than 110% of the Bonus Plan EBITDA target. The actual bonuses paid to our named executive officers under the Bonus Plan, which includes payouts under both the Financial Performance Component and the Discretionary Component, are disclosed in the Summary Compensation Table under the Non-Equity Incentive Plan Compensation column. |
| (2) | Reflects possible target payouts under the Discretionary Component of the Bonus Plan for the 2008 performance year, which is equal to 20% of the named executive officer’s bonus pool. See “Compensation Discussion and Analysis—Compensation Elements—Annual Cash Incentive Compensation” for further information regarding the Discretionary Component of the Bonus Plan. |
| (3) | Reflects the Class B and Class C units granted to Mr. Roth, Mr. Jones and Ms. Allen in 2008 under the 2005 Unit Plan. See “Compensation Discussion and Analysis—Compensation Elements—Long Term Incentive Compensation.” |
| (4) | Reflects the grant date fair value computed in accordance with ASC Topic 718 for the Class B and Class C units that were granted in 2008 |
| (5) | Ms. Allen joined us effective June 19, 2008. Therefore, the amounts shown for Ms. Allen under “Estimated Future Payouts Under Non-Equity Incentive Plan Awards” reflect possible payouts to her under the Bonus Plan during the time she was with us in 2008. |
| (6) | Mr. Joyner retired from us effective July 31, 2008. Therefore, the amounts shown for Mr. Joyner under “Estimated Future Payouts Under Non-Equity Incentive Plan Awards” reflect possible payouts to him under the Bonus Plan for the first seven months of the year he was with us. |
112
Table of Contents
Narrative Supplement to the Summary Compensation Table and
2008 Grants of Plan-Based Awards
Employment Agreements
We entered into a new employment agreement with Dr. Massingale on November 23, 2005, pursuant to which Dr. Massingale initially continued to serve as our Chief Executive Officer and pursuant to which he still serves as the Chairman of our Board. Effective May 1, 2008, Dr. Massingale’s employment agreement was amended to reflect that he shall serve as Executive Chairman, instead of our Chief Executive Officer, and that he will continue to serve as the Chairman of our Board during the term of his agreement. We also maintain employment agreements with each of our other named executive officers (other than Mr. Joyner, who retired during 2008). The agreements for all of our named executive officers were amended and restated on November , 2009 to comply with the requirements of Section 409A of the Code and, where applicable, to make other changes to their employment terms, which are reflected herein.
Each agreement has an initial five-year term that commenced on June 1, 2006 (November 23, 2005 in the case of Dr. Massingale and June 19, 2008 in the case of Ms. Allen), and each provides for automatic one-year renewal periods upon the expiration of the initial term or any subsequent term, unless either party provides a notice of non-renewal at least 180 days prior to the end of the then current term.
Each employment agreement provides for the payment of an annual base salary, subject to annual review and adjustment, as well as the opportunity to earn an annual bonus having a target amount. Currently, the target amount is equal to 50% of the named executive officer’s base salary (or 65% of base salary in the cases of Dr. Massingale and Mr. Roth). However, the maximum annual bonus that can be earned by any of these executive officers with respect to a fiscal year may be adjusted pursuant to the terms of the Bonus Plan. See “Compensation Discussion and Analysis—Compensation Elements—Annual Cash Incentive Compensation.”
Pursuant to each employment agreement, we have agreed to provide the executive officer with all standard benefits that we normally provide to other similarly situated executive officers. Pursuant to the employment agreements with Dr. Massingale and Mr. Roth, we have also agreed to cover the cost of standard medical and dental benefits for the executive officer and his eligible dependents, and pursuant to the employment agreement with Mr. Jones, we have agreed to cover the cost of standard medical and dental benefits for his eligible dependents. Each employment agreement also requires us to maintain a life insurance policy in a face amount that is equivalent to two times the executive officer’s base salary (or three times in the case of Dr. Massingale and Mr. Roth), as adjusted from time to time. Dr. Massingale is also entitled to other benefits and perquisites under his employment agreement, including, but not limited to, paid vacation, the right to an unpaid three week sabbatical after each consecutive five years of service, disability benefits, a monthly automobile allowance (of $1,000 per month) and reasonable use of our aircraft (for personal travel) for up to forty hours per year (with unused hours forfeited at the end of each applicable year). The other named executive officers are also entitled to other benefits and perquisites under their respective employment agreements, including but not limited to, paid vacation, certain disability benefits and a monthly automobile allowance.
In connection with the commencement of Ms. Allen’s employment, we agreed to grant her 8,333 Class B Common units and 11,667 Class C Common units, and we also provided her with certain relocation benefits, including, but not limited to, a signing bonus to cover miscellaneous relocation costs of $20,000, as well as reimbursement for certain losses she incurs resulting from the sale of her residence in New Jersey, up to a maximum reimbursement of $200,000.
Each employment agreement also provides for certain payments and benefits in the event the executive officer’s employment is terminated under specified circumstances or in the event of a change of control. See “Potential Payments upon Termination or Change-in-Control—Summary of Severance Arrangements” for a summary description of these provisions.
113
Table of Contents
Retirement Agreement with Mr. Joyner
On March 12, 2008, we entered into a retirement agreement with Robert Joyner, pursuant to which he retired from his position as our Executive Vice President, General Counsel, effective as of July 31, 2008. According to the terms of the retirement agreement, we agreed to pay Mr. Joyner a pro-rated annual bonus for 2008 and to subsidize his and his spouse’s premiums for health and dental continuation coverage under COBRA for six months following the date of his termination. We also agreed to repurchase the Class A Common units that he owned, as well as his Class B Common units and Class C Common units that became vested through June 30, 2008. The retirement agreement also provides that the restrictions on activities that were previously set forth in Mr. Joyner’s employment agreement will remain in full force and effect for a period of two years from the date of his termination and that the confidentiality of information provisions set forth in his employment agreement will remain in full force and effect for their applicable periods. Pursuant to the terms of the retirement agreement, Mr. Joyner also agreed to be available to provide us with consulting services for up to 5 days per month during the one-year period following the date of his termination, at a rate of $1,366 per day. We did not use his consulting services during 2008.
Terms of Restricted Equity Awards
To date, an aggregate of 73,275 Class B units and 102,585 Class C units were granted to our named executive officers in 2006, and an additional 20,833 Class B units and 29,167 Class C units were granted to our named executive officers during 2008 under the 2005 Unit Plan.
Vesting Schedule
There is no vesting associated with Class A units. Class B and Class C units vest daily on a pro rata basis over a five-year period from the date of issuance. The five-year vesting period for the Class B and Class C units that were granted on January 23, 2006 is deemed to commence on November 23, 2005.
Forfeiture and Post-Employment Treatment
Any unvested Class B and Class C units are generally forfeited without consideration upon the holder’s termination of employment; provided, however, that unless the holder’s employment is terminated for cause, the holder is entitled to be reimbursed by us for any U.S. federal or state income taxes paid by the holder with respect to the fair market value of such unvested units as of the grant date as reported by the holder pursuant to his or her election under Section 83 of the Internal Revenue Code.
114
Table of Contents
Outstanding Equity Awards at 2008 Fiscal-Year End
The following table provides information with respect to holdings of equity-based awards held by the named executive officers at 2008 fiscal-year end:
| Option Awards | Stock Awards | ||||||||||||||||||||
| Name |
Grant Date |
Number of Securities Underlying Unexercised Options (#) Exercisable |
Number of Securities Underlying Unexercised Options (#) Unexercisable |
Equity Incentive Plan Awards: Number of Securities Underlying Unexercised Unearned Options (#) |
Option Exercise Price ($) |
Option Expiration Date |
Number of Shares or Units of Stock That Have Not Vested(1) (#) |
Market Value of Shares or Units of Stock That Have Not Vested(2) ($) |
Equity Incentive Plan Awards: Number of Unearned Shares, Units or Other Rights That Have Not Vested (#) |
Equity Incentive Plan Awards: Market or Payout Value of Unearned Shares, Units or Other Rights That Have Not Vested ($) | |||||||||||
| H. Lynn Massingale, M.D., |
|||||||||||||||||||||
| Class B units |
1/23/06 | — | — | — | — | — | 10,439 | $ | 203,045 | — | — | ||||||||||
| Class C units |
1/23/06 | — | — | — | — | — | 14,615 | 135,190 | — | — | |||||||||||
| Greg Roth, |
|||||||||||||||||||||
| Class B units |
1/23/06 | — | — | — | — | — | 10,439 | 203,039 | — | — | |||||||||||
| Class C units |
6/19/08 | — | — | — | — | — | 14,615 | 135,189 | — | — | |||||||||||
| 1/23/06 | — | — | — | — | — | 5,476 | 106,508 | — | — | ||||||||||||
| 5/19/08 | — | — | — | — | — | 7,666 | 70,911 | — | — | ||||||||||||
| David P. Jones, |
|||||||||||||||||||||
| Class B units |
1/23/06 | — | — | — | — | — | 3,078 | 59,849 | — | — | |||||||||||
| Class C units |
5/19/08 | — | — | — | — | — | 4,308 | 39,848 | — | — | |||||||||||
| 1/23/06 | — | — | — | — | — | 5,476 | 106,509 | — | — | ||||||||||||
| 5/19/08 | — | — | — | — | — | 7,666 | 70,915 | — | — | ||||||||||||
| Stephen Sherlin, |
|||||||||||||||||||||
| Class B units |
1/23/06 | — | — | — | — | — | 775 | 15,070 | — | — | |||||||||||
| Class C units |
1/23/06 | — | — | — | — | — | 1,085 | 10,034 | — | — | |||||||||||
| Heidi S. Allen |
|||||||||||||||||||||
| Class B units |
7/23/08 | — | — | — | — | — | 7,301 | 142,006 | — | — | |||||||||||
| Class C units |
7/23/08 | — | — | — | — | — | 10,222 | 94,555 | — | — | |||||||||||
| Robert C. Joyner(3) |
— | — | — | — | — | — | — | — | — | ||||||||||||
| (1) | The Class B and Class C units vest daily on a pro rata basis over a five-year period. |
| (2) | The Board has determined a fair market value of $19.45 and $9.25 per unit for Class B and Class C equity units, respectively, as of December 31, 2008. |
| (3) | We repurchased all of Mr. Joyner’s vested Class B units and Class C units in 2008, and he forfeited all of his unvested units, in conjunction with his retirement. Therefore, he did not have any outstanding equity awards at December 31, 2008. |
115
Table of Contents
Option Exercises and Units Vested in 2008
The following restricted equity units in Team Health Holdings vested for the named executive officers during fiscal year 2008.
| Option Awards | Stock Awards | ||||||||
| Name |
Number of Shares Acquired on Exercise (#) |
Value Realized on Exercise ($) |
Number of Shares Acquired on Vesting (#) |
Value Realized on Vesting(1) ($) | |||||
| H. Lynn Massingale, M.D. |
|||||||||
| Class B units |
— | — | 5,502 | $ | 107,007 | ||||
| Class C units |
— | — | 7,702 | 71,247 | |||||
| Greg Roth |
|||||||||
| Class B units |
— | — | 6,276 | 122,061 | |||||
| Class C units |
— | — | 8,786 | 81,270 | |||||
| David P. Jones |
|||||||||
| Class B units |
— | — | 2,396 | 46,595 | |||||
| Class C units |
— | — | 3,354 | 31,024 | |||||
| Stephen Sherlin |
|||||||||
| Class B units |
— | — | 408 | 7,942 | |||||
| Class C units |
— | — | 572 | 5,288 | |||||
| Heidi S. Allen |
|||||||||
| Class B units |
— | — | 1,032 | 20,071 | |||||
| Class C units |
— | — | 1,445 | 13,364 | |||||
| Robert C. Joyner |
|||||||||
| Class B units |
— | — | 809 | 15,733 | |||||
| Class C units |
— | — | 1,132 | 10,475 | |||||
| (1) | The Board has determined a fair market value of $19.45 and $9.25 per unit for Class B and Class C units, respectively, as of December 31, 2008. |
Nonqualified Deferred Compensation for 2008
The following table reflects activity in the SERP plan for the named executive officers during fiscal year 2008.
| Name |
Executive Contributions in Last FY(2) ($) |
Registrant Contributions in Last FY ($) |
Aggregate Earnings in Last FY ($) |
Aggregate Withdrawals/ Distributions ($) |
Aggregate Balance at Last FYE(3) ($) | ||||||||||
| H. Lynn Massingale, M.D., |
— | — | — | — | — | ||||||||||
| Greg Roth, |
— | — | — | — | — | ||||||||||
| David P. Jones(1) |
$ | 14,423 | — | $ | (28,611 | ) | $ | 47 | $ | 54,886 | |||||
| Stephen Sherlin, |
— | — | — | — | — | ||||||||||
| Heidi S. Allen, |
— | — | — | — | — | ||||||||||
| Robert C. Joyner(1) |
1,731 | — | (1,669 | ) | 18,017 | — | |||||||||
| (1) | Mr. Jones and Mr. Joyner were the only named executive officers that elected to participate in the SERP plan in 2008. Mr. Joyner received the remaining balance of his SERP account upon his retirement in July 2008. |
| (2) | The amount represents salary deferrals to the SERP Plan and is included in the Salary column of the Summary Compensation Table. |
| (3) | All of the amount shown under the Aggregate Balance at Last FYE column was previously reported in the Summary Compensation Table. |
116
Table of Contents
In addition to the amount a SERP participant elects to defer to his or her account, a participant’s SERP account is credited (or charged) with an amount equal to the performance of certain hypothetical investment vehicles. These hypothetical investment vehicles are generally available to our employees participating in the 401(k) Plan.
Potential Payments upon Termination or Change-in-Control
The following tables describe the potential payments and benefits under our compensation and benefit plans and contractual agreements to which the named executive officers would be entitled upon termination of employment on December 31, 2008.
| Name |
Involuntary Termination without Cause or Voluntary Termination for Good Reason |
Voluntary Termination without Good Reason |
Voluntary Termination without Good Reason Following a Change of Control |
Voluntary Termination without Good Reason |
Death | Disability | Change of Control |
Additional Value if Termination (other than for Cause) Following a Change of Control | ||||||||||||||||
| H. Lynn Massingale, M.D. |
||||||||||||||||||||||||
| Cash Severance Payment(1) |
$ | 3,342,588 | $ | — | $ | 2,228,392 | $ | — | $ | 440,392 | $ | 1,321,432 | $ | — | $ | — | ||||||||
| Continuing Medical Benefits |
34,041 | — | 22,694 | — | 22,694 | 22,694 | — | — | ||||||||||||||||
| Acceleration of Equity Awards |
— | — | 338,235 | — | — | — | $ | 338,235 | — | |||||||||||||||
| Tax Reimbursement Relating to IRC Section 83 Election(2) |
23,388 | 23,388 | 23,388 | 23,388 | 23,388 | 23,388 | — | — | ||||||||||||||||
| Excise Tax Gross-up(3) |
— | — | — | — | — | — | — | — | ||||||||||||||||
| Total Termination Benefits |
$ | 3,400,017 | $ | 23,388 | $ | 2,612,709 | $ | 23,388 | $ | 486,474 | $ | 1,367,514 | $ | 338,235 | $ | — | ||||||||
| (1) | Represents (1) the sum of an amount equal to three times his base salary and an amount equal to three times his annual bonus in the event of involuntary termination without cause or voluntary termination for good reason, (2) the sum of an amount equal to two times his base salary, an amount equal to two times his annual bonus in the event of voluntary termination without good reason within one year following a change of control and (3) the sum of an amount equal to two times his base salary and an amount equal to two times his annual bonus less the amount of estimated life or disability insurance proceeds, as applicable, in the event of termination as a result of death or disability (in each case, as further described under the “Summary of Severance Arrangements” below). |
| (2) | Represents the reimbursement payable by us for any U.S. federal or state income taxes paid by Dr. Massingale with respect to the fair market value of the unvested units as of the grant date as reported by Dr. Massingale pursuant to his election under Section 83 of the Internal Revenue Code. See “Summary of Severance Arrangements—Restricted Unit Award Agreement” below. |
| (3) | Dr. Massingale’s employment agreement also provides that in the event his employment is terminated for any reason (other than by us for cause) during the one-year period following a change of control, we will indemnify him against any excise taxes that may be imposed under Section 4999 of the Internal Revenue Code on any payments or benefits to be received by him from us so that he will be in the same position as if no such taxes had been imposed. See “Summary of Severance Arrangements—Dr. Massingale’s Employment Agreement.” This amount represents the tax indemnity we would be required to pay under the terms of Dr. Massingale’s employment agreement. No such excise taxes would have been due assuming Dr. Massingale’s employment was terminated on December 31, 2008. |
117
Table of Contents
| Name |
Involuntary Termination without Cause or Voluntary Termination for Good Reason |
Voluntary Termination without Good Reason |
Involuntary Termination for Cause Following a Change of Control |
Involuntary Termination without Cause Following a Change of Control |
Change of Control | ||||||||||
| Greg Roth |
|||||||||||||||
| Cash Severance Payment(1) |
$ | 2,032,562 | $ | — | $ | 2,032,562 | $ | 2,032,562 | $ | — | |||||
| Continuing Medical Benefits |
7,880 | — | 7,880 | 7,880 | — | ||||||||||
| Acceleration of Equity Awards |
— | — | 515,658 | 515,658 | 515,658 | ||||||||||
| Tax Reimbursement Relating to IRC Section 83 Election(2) |
53,528 | 53,528 | — | 53,528 | — | ||||||||||
| Total Termination Benefits |
$ | 2,093,970 | $ | 53,528 | $ | 2,556,100 | $ | 2,609,628 | $ | 515,658 | |||||
| David P. Jones |
|||||||||||||||
| Cash Severance Payment(1) |
$ | 1,213,567 | $ | — | $ | 1,213,567 | $ | 1,213,567 | $ | — | |||||
| Continuing Medical Benefits |
30,125 | — | 30,125 | 30,125 | — | ||||||||||
| Acceleration of Equity Awards |
— | — | 277,121 | 277,121 | 277,121 | ||||||||||
| Tax Reimbursement Relating to IRC Section 83 Election(2) |
37,034 | 37,034 | — | 37,034 | — | ||||||||||
| Total Termination Benefits |
$ | 1,280,726 | $ | 37,034 | $ | 1,520,813 | $ | 1,557,847 | $ | 277,121 | |||||
| Stephen Sherlin |
|||||||||||||||
| Cash Severance Payment(1) |
$ | 482,626 | $ | — | $ | 482,626 | $ | 482,626 | $ | — | |||||
| Continuing Medical Benefits |
12,819 | — | 12,819 | 12,819 | — | ||||||||||
| Acceleration of Equity Awards |
— | — | 25,104 | 25,104 | 25,104 | ||||||||||
| Tax Reimbursement Relating to IRC Section 83 Election(2) |
1,736 | 1,736 | — | 1,736 | — | ||||||||||
| Total Termination Benefits |
$ | 497,181 | $ | 1,736 | $ | 520,549 | $ | 522,285 | $ | 25,104 | |||||
| Heidi S. Allen |
|||||||||||||||
| Cash Severance Payment(1) |
$ | 744,786 | $ | — | $ | 744,786 | $ | 744,786 | $ | — | |||||
| Continuing Medical Benefits |
8,026 | — | 8,026 | 8,026 | — | ||||||||||
| Acceleration of Equity Awards |
— | — | 236,561 | 236,561 | 236,561 | ||||||||||
| Tax Reimbursement Relating to IRC Section 83 Election(2) |
40,802 | 40,802 | — | 40,802 | — | ||||||||||
| Total Termination Benefits |
$ | 793,614 | $ | 40,802 | $ | 989,373 | $ | 1,030,175 | $ | 236,561 | |||||
| (1) | Represents the sum of an amount equal to two times the executive officer’s base salary and an amount equal to two times the executive officer’s annual bonus (as further described under the “Summary of Severance Arrangements” below). |
| (2) | Represents the reimbursement payable by us for any U.S. federal or state income taxes paid by the executive officer with respect to the fair market value of the unvested units as of the grant date as reported by the executive officer pursuant to his or her election under Section 83 of the Internal Revenue Code. See “Summary of Severance Arrangements—Restricted Unit Award Agreement” below. |
Summary of Severance Arrangements
As discussed above, each of our named executive officers has an employment agreement. The following is a summary of certain payments and benefits that would be provided to the named executive officers upon certain terminations of employment or, as applicable, following a change of control of the Company.
118
Table of Contents
Dr. Massingale’s Employment Agreement
Involuntary Termination without Cause or Voluntary Termination for Good Reason. In the event Dr. Massingale’s employment is terminated by us without “cause” or he resigns for “good reason” (as such terms are defined in his employment agreement and summarized below), in each case subject to continued compliance with the restrictive covenants described below, we will provide him with:
| • | a pro-rata portion of his annual bonus for the current bonus period calculated through the date of termination; |
| • | an amount equal to three times his base salary plus an amount equal to three times his annual bonus (based on the average bonus that he received during the two most recently completed bonus periods, provided that the pro-rata bonus payable upon his termination will be used to calculate the average bonus if it is greater than either of the bonuses he received during the two most recently completed bonus periods) paid in twelve equal monthly installments beginning on the date of termination; and |
| • | an amount equal to the aggregate premiums that would be necessary to continue group medical benefits provided to Dr. Massingale and his applicable family members for 36 months, paid in 36 equal monthly installments, beginning on the date of termination. |
Termination as a Result of Death or Disability or Voluntary Termination without Good Reason following a Change of Control. In the event Dr. Massingale’s employment is terminated due to his death or by us as a result of his “disability” (as such term is defined in his employment agreement), or if he resigns without good reason within one year following a change of control, in each case, subject to continued compliance with the restrictive covenants described below, we will provide him with:
| • | a pro-rata portion of his annual bonus for the current bonus period calculated through the date of termination; |
| • | an amount equal to two times his base salary plus an amount equal to two times his annual bonus (based on the average bonus that he received during the two most recently completed bonus periods, provided that the pro-rata bonus payable upon his termination will be used to calculate the average bonus if it is greater than either of the bonuses he received during the two most recently completed bonus periods) paid in 12 equal monthly installments (or, in the case of his death, 24 equal monthly installments) beginning on the date of termination; and |
| • | an amount equal to the aggregate premiums that would be necessary to continue group medical benefits provided to Dr. Massingale and his applicable family members for twenty-four months, paid in 36 equal monthly installments (or, in the case of his death, 24 equal monthly installments), beginning on the date of termination. |
These payments, however, will be reduced by the amount of any life or disability proceeds that are paid to Dr. Massingale (or his estate) from any life insurance or disability insurance policy that we maintain for his benefit.
Termination for Any Reason following a Change of Control. In the event Dr. Massingale’s employment is terminated for any reason (other than by us for cause) during the one-year period following a change of control, we will indemnify him against any excise taxes that may be imposed under Section 4999 of the Internal Revenue Code on any payments or benefits to be received by him from us so that he will be in the same position as if no such taxes had been imposed. In addition, if, within the one-year period following a change of control, any payments due to Dr. Massingale, as a result of the termination of his employment, are required to be delayed
119
Table of Contents
for six months in order to comply with the requirements of Section 409A of the Internal Revenue Code, then we will contribute an amount equal to the payments into a rabbi trust and the amounts contributed to the trust will be required to be delivered to Dr. Massingale on the date that is six months and one day after his separation of service with us.
Accelerated Vesting upon a Change of Control. Upon the occurrence of a change of control, Dr. Massingale’s outstanding equity awards will become fully vested.
Restrictive Covenants. As a result of the restrictive covenants contained in his employment agreement, Dr. Massingale agreed not to disclose our confidential information at any time, and, for the period during which he provides services to us and for the two-year period thereafter (or, if he is terminated by us without cause or if he resigns for good reason, for the one-year period thereafter), he has also agreed not to solicit our employees or contractors, compete with us or interfere with our business.
Mr. Roth’s Employment Agreement
Involuntary Termination without Cause, Voluntary Termination for Good Reason. In the event Mr. Roth’s employment is terminated by us without “cause” or he resigns for “good reason” (as such terms are defined in his employment agreement and summarized below), in each case, subject to continued compliance with the restrictive covenants described below, we will provide Mr. Roth with:
| • | an amount equal to three times his base salary plus an amount equal to three times his annual bonus (based on the average bonus that he received during the two most recently completed bonus periods) paid in 12 equal monthly installments beginning on the date of termination; and |
| • | an amount equal to the aggregate premiums that would be necessary to continue group medical benefits provided to Mr. Roth and his applicable family members for 36 months, paid in 36 equal monthly installments, beginning on the date of termination. |
In addition, if, within the one-year period following a change of control, any payments due to Mr. Roth as a result of the termination of his employment by us without cause or by him for good reason, are required to be delayed for six months in order to comply with the requirements of Section 409A of the Internal Revenue Code, then we will contribute an amount equal to the payments into a rabbi trust and the amounts contributed to the trust will be required to be delivered to Mr. Roth on the date that is six months and one day after his separation from us. Furthermore, in the event such termination occurs during the one-year period following a change of control, we will indemnify him against any excise taxes that may be imposed under Section 4999 of the Internal Revenue Code on any payments or benefits to be received by him from us so that he will be in the same position as if no such taxes had been imposed.
Involuntary Termination by us following a Change of Control. In the event Mr. Roth’s employment is terminated by us for any reason (other than by us without Cause, or as a result of his death or disability) during the one-year period following a change of control, in each case, subject to continued compliance with the restrictive covenants described below, we will provide Mr. Roth with:
| • | an amount equal to two times his base salary plus an amount equal to two times his annual bonus (based on the average bonus that he received during the two most recently completed bonus periods) paid in 12 equal monthly installments beginning on the date of termination; and |
| • | an amount equal to the aggregate premiums that would be necessary to continue group medical benefits provided to Mr. Roth and his applicable family members for 24 months, paid in 36 equal monthly installments, beginning on the date of termination. |
Accelerated Vesting upon a Change of Control. In addition, under the applicable award agreements, upon the occurrence of a change of control, Mr. Roth’s outstanding equity awards will become fully vested.
120
Table of Contents
Restrictive Covenants. As a result of the restrictive covenants contained in his employment agreement, Mr. Roth has agreed not to disclose our confidential information at any time, and, for the period during which he provides services to us and for the two-year period thereafter, Mr. Roth has also agreed not to solicit our employees or contractors, compete with us or interfere with our business.
Employment Agreements for Messrs. Jones, Sherlin and Ms. Allen
Involuntary Termination without Cause, Voluntary Termination for Good Reason or Involuntary Termination by us following a Change of Control. In the event one of the above-named named executive officer’s employment is terminated by us without “cause” or the executive resigns for “good reason” (as such terms are defined in the executive’s employment agreement and summarized below), or the executive’s employment is terminated by us for any reason (other than death or disability) during the one-year period following a change of control, in each case, subject to continued compliance with the restrictive covenants described below, we will provide the executive with:
| • | an amount equal to two times the executive’s base salary plus an amount equal to two times the executive’s annual bonus (based on the average bonus that the executive received during the two most recently completed bonus periods) paid in 24 equal monthly installments beginning on the date of termination; and |
| • | an amount equal to the aggregate premiums due that would be necessary to continue group medical benefits provided to the executive and the executive’s applicable family members for twenty-four months, paid in 24 equal monthly installments, beginning on the date of termination. |
Accelerated Vesting upon a Change of Control. In addition, under the applicable award agreements, upon the occurrence of a change of control, each of the above-named executive officer’s outstanding equity awards will become fully vested.
Restrictive Covenants. As a result of the restrictive covenants contained in the employment agreements with the above-named executive officers, each such executive officer has agreed not to disclose our confidential information at any time, and, for the period during which the executive officer provides services to us and for the two-year period thereafter, the executive officer has also agreed not to solicit our employees or contractors, compete with us or interfere with our business.
The term “good reason” is generally defined in all of our employment agreements with our named executive officers to mean (1) a substantial adverse change to the executive’s primary responsibilities (which, in the case of Dr. Massingale and Messrs. Roth and Jones, would also include an adverse change in the executive’s authority), (2) reduction of the executive’s base salary or our failure to make bonus payments in accordance with the terms of the executive’s employment agreement, (3) relocation of the executive to a place of business more than 50 miles away from the executive’s current place of business, (4) any other material breach by us of the executive’s employment agreement or (5) in the case of Dr. Massingale only, if we deliver a notice of non-renewal of the employment term. Notwithstanding the foregoing, upon receiving notice from an executive that an occurrence constituting good reason has occurred, we will have twenty days (or, in the case of Dr. Massingale, ten days) following receipt of such notice to cure such event.
The term “cause” is generally defined in all of our employment agreements with our named executive officers to mean (1) the executive’s conviction of or the entering into a guilty plea or plea of no contest with respect to a felony, or any other crime involving fraud, dishonesty, or moral turpitude and which is materially detrimental to us or materially affects the executive’s ability to perform his duties, (2) the executive’s intentional neglect of or material inattention to executive’s duties and which neglect remains uncorrected for more than ten days following notice from us, (3) the commission of an intentional and material act to defraud us or embezzlement or dishonesty against us or (4) the executive willfully impedes or endeavors to influence, obstruct or impede or fails to materially cooperate with an investigation authorized by us, a self-regulatory organization or a governmental department or agency.
121
Table of Contents
Mr. Sherlin has indicated that he intends to retire effective May 1, 2010.
Retirement Agreement with Mr. Joyner
As discussed above under “Narrative Supplement to the Summary Compensation Table and 2008 Grants of Plan-Based Awards,” we entered into a retirement agreement with Mr. Joyner on March 12, 2008 pursuant to which he retired from our company effective July 31, 2008. In accordance with Mr. Joyner’s retirement agreement, we paid him a pro-rated annual bonus for 2008 of $112,972 and subsidized his and his spouse’s premiums for health and dental continuation coverage under COBRA for six months following Mr. Joyner’s retirement at a cost to us of $3,141. We also reimbursed Mr. Joyner for taxes in respect of unvested Class B Common units and Class C Common units that were forfeited upon his retirement in the amount of $8,727. This reimbursement related to U.S. federal or state income taxes paid by Mr. Joyner with respect to the fair market value of the unvested units as of the grant date as reported by Mr. Joyner pursuant to his election under Section 83 of the Internal Revenue Code. Finally, we repurchased at fair market value Mr. Joyner’s Class A Common units and the Class B Common units and Class C Common units that became vested through June 30, 2008. We paid the following amounts to Mr. Joyner in connection with such repurchases: Class A units—$902,379; vested Class B units—$60,619; and vested Class C units—$32,246. As described above, Mr. Joyner is subject to the non-competition and confidentiality restrictions specified in his employment agreement.
Restricted Unit Award Agreement
As discussed under the “Compensation Discussion and Analysis—Long Term Incentive Compensation,” in the past we have granted restricted units as equity incentive awards to each of our named executive officers. Pursuant to the restricted unit award agreement governing the terms of such awards, if the executive officer’s employment with us is terminated, the restricted units will, to the extent not then vested, be forfeited by the executive officer without consideration. Any executive officer terminated for any reason other than for cause will receive reimbursements for any U.S. federal or state income taxes paid by the executive officer with respect to the fair market value of such forfeited restricted units as of the grant date as reported by the executive officer pursuant to his or her election under Section 83 of the Internal Revenue Code.
Compensation of Directors
We have historically paid an annual cash retainer of $40,000 to our non-employee representatives (other than Sponsor-affiliated representatives). We also granted 2,042 Class B units and 2,858 Class C units to each of these representatives in 2006. We have not paid any director compensation to our employee representatives and Sponsor-affiliated representatives. Following the completion of this offering, we intend to continue to pay a cash retainer to our independent directors for serving as directors and an additional cash payment for serving as a committee chair, and we expect to grant equity-based awards to our independent directors under the 2009 Stock Plan.
122
Table of Contents
The following table summarizes all compensation for our non-employee representatives (other than Sponsor-affiliated representatives) for fiscal year 2008. The employee representatives and Sponsor-affiliated representatives receive no additional compensation for serving on the Board or its committees and, as a result, are not listed in the table below.
| Name |
Fees Earned or Paid in Cash(1) ($) |
Stock Awards(2)(3) ($) |
Option Awards ($) |
Non-Equity Incentive Plan Compensation ($) |
Change in Pension Value and Nonqualified Deferred Compensation Earnings |
All Other Compensation ($) |
Total ($) | ||||||||||
| Earl P. Holland |
$ | 40,000 | $ | 3,664 | — | — | — | — | $ | 43,664 | |||||||
| Glenn A. Davenport |
40,000 | 3,664 | — | — | — | — | 43,664 | ||||||||||
| (1) | The director compensation in the above table reflects an annual retainer paid to each independent, non-employee representative of $40,000. |
| (2) | The amounts represent the compensation expense recognized by us for financial statement reporting purposes for fiscal year 2008 under ASC Topic 718 associated with our Class B and Class C units that were granted in 2006 under the 2005 Unit Plan. The compensation expense for the stock awards differs from the 2006 grant date fair values for these awards because the compensation expense for the stock awards is recognized over the requisite vesting period. See footnote 16 to the audited financial statements included in this prospectus to review assumptions made in the valuation of such grants under ASC Topic 718. |
| (3) | 2,042 Class B units and 2,858 Class C units were granted to each of Mr. Holland and Mr. Davenport in 2006 under the 2005 Unit Plan. Of those units, they each held 774 unvested Class B units and 1,084 unvested Class C units as of December 31, 2008. |
2009 Stock Plan
Our Board expects to adopt, and our stockholders expect to approve, the Team Health Holdings, Inc. 2009 Stock Incentive Plan, or 2009 Stock Plan prior to the completion of this offering. The following description of the 2009 Stock Plan is not complete and is qualified by reference to the full text of the 2009 Stock Plan, which has been filed as an exhibit to the registration statement of which this prospectus forms a part.
Purpose. The purpose of the 2009 Stock Plan is to aid us and our affiliates in recruiting and retaining key employees, directors, consultants, and other service providers of outstanding ability and to motivate those employees, directors, consultants, and other service providers to exert their best efforts on our behalf and the behalf of our affiliates by providing incentives through the granting of options, stock appreciation rights and other stock-based awards.
Shares Subject to the Plan. The 2009 Stock Plan provides that the total number of shares of common stock that may be issued under the 2009 Stock Plan is , and the maximum number of shares for which incentive stock options may be granted is . Shares of our common stock covered by awards that terminate or lapse without the payment of consideration may be granted again under the 2009 Stock Plan.
Administration. The 2009 Stock Plan will be administered by the compensation committee of our Board or such other committee of our Board to which it has delegated power, or Committee. The Committee is authorized to interpret the 2009 Stock Plan, to establish, amend and rescind any rules and regulations relating to the 2009 Stock Plan and to make any other determinations that it deems necessary or advisable for the administration of the 2009 Stock Plan. The Committee may correct any defect or supply any omission or reconcile any inconsistency in the 2009 Stock Plan in the manner and to the extent the Committee deems necessary or advisable. The Committee shall have the full power and authority to establish the terms and conditions of any award consistent with the provisions of the 2009 Stock Plan and to waive any such terms and conditions at any time (including, without limitation, accelerating or waiving any vesting conditions). Determinations made by the Committee need not be uniform and may be made selectively among participants in the 2009 Stock Plan.
123
Table of Contents
Limitations. No award may be granted under the 2009 Stock Plan after the tenth anniversary of the effective date (as defined therein), but awards theretofore granted may extend beyond that date.
Options. The Committee may grant non-qualified stock options and incentive stock options, which shall be subject to the terms and conditions as set forth in the 2009 Stock Plan, the related award agreement and any other terms, not inconsistent therewith, as determined by the Committee; provided that all stock options granted under the 2009 Stock Plan are required to have a per share exercise price that is not less than 100% of the fair market value of our common stock underlying such stock options on the date an option is granted (other than in the case of options granted in substitution of previously granted awards), and all stock options that are intended to qualify as incentive stock options will be subject to the terms and conditions that comply with the rules as may be prescribed by Section 422 of the Code. The maximum term for stock options granted under the 2009 Plan will be ten years from the initial date of grant. The purchase price for the shares as to which a stock option is exercised shall be paid to us, to the extent permitted by law (i) in cash or its equivalent at the time the stock option is exercised, (ii) in shares having a fair market value equal to the aggregate exercise price for the shares being purchased and satisfying any requirements that may be imposed by the Committee, so long as the shares shall have been held for no less than six months (or such other period established by the Committee in order to avoid adverse accounting treatment), (iii) partly in cash and partly in shares (as described above), (iv) if there is a public market for the shares at such time, through the delivery of irrevocable instructions to a broker to sell the shares being acquired upon the exercise of the stock option and to deliver to us the amount of the proceeds of such sale equal to the aggregate exercise price for the shares being purchased, or (v) to the extent the Committee shall provide in the award agreement or otherwise, through net settlement in shares.
Stock Appreciation Rights. The Committee may grant stock appreciation rights independent of or in connection with a stock option. The exercise price per share of a stock appreciation right shall be an amount determined by the Committee but in no event shall such amount be less than the fair market value of a share on the date the stock appreciation right is granted (other than in the case of stock appreciation rights granted in substitution of previously granted awards). Generally, each stock appreciation right shall entitle the participant upon exercise to an amount equal to the product of (i) the excess of (A) the fair market value on the exercise date of one share of common stock, over (B) the exercise price per share, times (ii) the numbers of shares of common stock covered by the stock appreciation right.
Other Stock-Based Awards. In addition to stock options and stock appreciation rights, the Committee may grant or sell awards of shares, restricted shares and awards that are valued in whole or in part by reference to, or otherwise based on the fair market value of shares, including performance-based awards. Prior to the payment of any performance-based award, the Committee, or its delegate, will certify that the applicable performance goals have been met. In connection with such certification, the Committee, or its delegate, may decide to pay amounts, which are less than the award otherwise payable for achievement of the applicable performance goals; provided that the Committee shall have the authority to waive any applicable performance goal. In the event the applicable performance goals are not waived by the Committee, payment of an award to a participant will occur only after certification and will be made as determined by our Committee in its sole discretion after the end of the applicable performance period.
Effect of Certain Events on 2009 Plan and Awards. In the event of any change in the outstanding shares of our common stock by reason of any stock dividend or split, reorganization, recapitalization, merger, consolidation, spin-off, combination or exchange of shares or other corporate exchange or change in capital structure, any distribution to stockholders of common stock other than regular cash dividends or any similar event, the Committee without liability to any person shall make such substitution or adjustment, if any, as it deems to be equitable, as to the number or kind of common stock or other securities that may be issued as set forth in the 2009 Stock Plan or pursuant to outstanding awards; provided that the Committee shall determine in its sole discretion the manner in which such substitution or adjustment shall be made. Except as otherwise provided in an award agreement or otherwise determined by the Committee, in the event of a Change of Control (as defined below) or similar corporate transaction (whether or not involving a permitted holder), with respect to
124
Table of Contents
any outstanding awards then held by participants which are unexercisable or otherwise unvested or subject to lapse restrictions, the Committee may, but shall not be obligated to, in a manner intended to comply with the requirements of Section 409A of the Code, (i) accelerate, vest, or cause the restrictions to lapse with all or any portion of an award, (ii) cancel awards for fair value (as determined in the sole discretion of the Committee), which, in the case of stock options and stock appreciation rights, may equal the excess, if any, of the value of the consideration to be paid in the Change of Control transaction to holders of the same number of shares subject to such stock options or stock appreciation rights over the aggregate exercise price of such stock options or stock appreciation rights, (iii) provide for the issuance of substitute awards or (iv) provide that the stock options shall be exercisable for all shares subject thereto for a period of at least 10 days prior to the Change of Control and that upon the occurrence of the Change of Control, the stock options shall terminate and be of no further force or effect. For the avoidance of doubt, the Committee may cancel stock options and stock appreciation rights for no consideration if the fair market value of the shares subject to such options or stock appreciation rights is less than or equal to the aggregate exercise price of such stock options or stock appreciation rights.
For purposes of the 2009 Stock Plan, a Change of Control shall generally mean the occurrence of any of the following events (i) the sale or disposition of all or substantially all of the assets of the Company, (ii) any person or group (other than certain permitted holders) is or becomes the holder of more than 50% of the total voting power of the voting stock of the Company, (iii) a reorganization, recapitalization, merger or consolidation involving the Company, unless securities representing more than 50% or more of the combined voting power of the Company are held in substantially the proportion as prior to such corporate transaction or (iv) the individuals comprising our board at the beginning of any two-year period together with any new directors whose election or nomination was approved by such individuals no longer constitute a majority of the board in office at the end of the two-year period.
Nontransferability of Awards. Unless otherwise determined by the Committee, an award will not be transferable or assignable by a participant otherwise than by will or by the laws of descent and distribution.
Amendment and Termination. The Committee may amend, alter or discontinue the 2009 Stock Plan, but no amendment, alteration or discontinuation shall be made which, (i) without the approval of our stockholders, would (except as provided in the 2009 Plan in connection with adjustments in certain corporate events), increase the total number of shares of our common stock reserved for the purposes of the 2009 Stock Plan or change the maximum number of shares of common stock for which awards may be granted to any participant, or (ii) without the consent of a participant, would materially adversely impair any of the rights or obligations under any award theretofore granted to the participant under the 2009 Stock Plan; provided, however, that the Committee may amend the 2009 Stock Plan in such manner as it deems necessary to permit the granting of awards meeting the requirements of the Code or other applicable laws, including, without limitation, to avoid adverse tax consequences to us or any participant.
125
Table of Contents
PRINCIPAL AND SELLING SHAREHOLDER
The following table and accompanying footnotes set forth information regarding the beneficial ownership of our common stock as of September 30, 2009 by: (i) each person known by us to own beneficially more than 5% of our common stock, (ii) each of the named executive officers, (iii) each of our representatives and (iv) all of our representatives and executive officers as a group.
The amounts and percentages of shares beneficially owned are reported on the basis of SEC regulations governing the determination of beneficial ownership of securities. Under SEC rules, a person is deemed to be a “beneficial owner” of a security if that person has or shares voting power or investment power, which includes the power to dispose of or to direct the disposition of such security. A person is also deemed to be a beneficial owner of any securities of which that person has a right to acquire beneficial ownership within 60 days. Securities that can be so acquired are deemed to be outstanding for purposes of computing such person’s ownership percentage, but not for purposes of computing any other person’s percentage. Under these rules, more than one person may be deemed to be a beneficial owner of the same securities and a person may be deemed to be a beneficial owner of securities as to which such person has no economic interest.
The number of shares and percentages of beneficial ownership prior to this offering set forth below are based on the number of shares of our common stock to be issued and outstanding immediately prior to the consummation of this offering after giving effect to the Corporate Conversion. The number of shares and percentages of beneficial ownership after this offering set forth below are based on the number of shares of our common stock to be issued and outstanding immediately after the consummation of this offering.
Except as otherwise indicated in the footnotes below, each of the beneficial owners has, to our knowledge, sole voting and investment power with respect to the indicated shares of common stock. Unless otherwise noted, the address of each beneficial owner is 1900 Winston Road, Suite 300, Knoxville, Tennessee 37919.
| After this Offering | ||||||||||||||
| Prior to this Offering | Assuming the Underwriters’ Option is Not Exercised |
Assuming the Underwriters’ Option is Exercised in Full | ||||||||||||
| Name of beneficial owner |
Shares of Common Stock |
Percent of Common Stock |
Shares of Common Stock Being Offered |
Shares of Common Stock |
Percent of Common Stock |
Shares of Common Stock |
Percent of Common Stock | |||||||
| Principal and Selling Shareholder | ||||||||||||||
| Ensemble Parent LLC(1) c/o The Blackstone |
||||||||||||||
| Representatives and Executive Officers* |
||||||||||||||
| H. Lynn Massingale, M.D(2) |
||||||||||||||
| Greg Roth |
||||||||||||||
| David P. Jones |
||||||||||||||
| Stephen Sherlin |
||||||||||||||
| Heidi S. Allen |
||||||||||||||
| Earl P. Holland |
||||||||||||||
| Glenn A. Davenport |
||||||||||||||
| Neil P. Simpkins(1) |
||||||||||||||
| Michael A. Dal Bello(1) |
||||||||||||||
| Alan Muney, M.D(1). |
||||||||||||||
| All representatives and executive officers as a |
||||||||||||||
| * | The number of shares of common stock to be held by each individual after this offering will be based on an allocation of shares of common stock among the former holders of Class A units, Class B units and Class C units as determined based upon the distribution provisions in our existing limited liability company agreement and the value of the Company based on the actual initial public offering price and the number of shares sold by the selling shareholder. Since each individual held a different number of Class A units, Class B |
126
Table of Contents
| units and Class C units prior to the Corporate Conversion, there is no precise formula or sensitivity analysis that can be applied to determine what each individual will actually receive in advance of determining the actual initial public offering price. However, we can illustrate the number of shares a particular individual would have received based on different initial public offering prices. For example, for purposes of the table above, the share ownership amounts have been estimated based on the mid-point of the price range set forth on the cover page of this prospectus. If the value of the Company were to be based on the low-point of the price range set forth on the cover page of this prospectus, then the number of shares held for such individuals would have been as follows: Dr. Massingale shares; Mr. Roth shares; Mr. Jones shares; Mr. Sherlin shares; Ms. Allen shares; Mr. Holland shares; Mr. Davenport shares; and all representatives and executive officers as a group (excluding beneficial ownership disclaimed by the Blackstone directors) shares. If the value of the Company were to be based on the high-point of the price range set forth on the cover page of this prospectus, then the number of shares held for such individuals would have been as follows: Dr. Massingale shares; Mr. Roth shares; Mr. Jones shares; Mr. Sherlin shares; Ms. Allen shares; Mr. Holland shares; Mr. Davenport shares; and all representatives and executive officers as a group (excluding beneficial ownership disclaimed by the Blackstone directors) shares. |
| (1) | Ensemble Parent LLC directly holds the shares of common stock shown as beneficially owned by it in the table above. All of the membership units of Ensemble Parent LLC are held by Blackstone Capital Partners IV L.P., Blackstone Capital Partners IV-A L.P., Blackstone Family Investment Partnership IV-A L.P., and Blackstone Participation Partnership IV, L.P. (the “Blackstone Funds”). Blackstone Management Associates IV L.L.C. (“BMA”) is the general partner having voting and investment power over membership interests held or controlled by each of the Blackstone Funds. Mr. Simpkins is a member of BMA and Mr. Dal Bello and Dr. Muney are employees of BMA. Each of the Blackstone Funds, BMA and Messrs. Simpkins and Dal Bello and Dr. Muney disclaim beneficial ownership of any shares of our common stock beneficially owned by Ensemble Parent LLC. |
| (2) | Includes directly held shares of common stock. Also includes shares of common stock held by a family member and shares of common stock held in various trusts as to which Dr. Massingale disclaims beneficial ownership. |
| (3) | Excludes beneficial ownership disclaimed by the Blackstone directors for purposes of this calculation. |
127
Table of Contents
DESCRIPTION OF CERTAIN INDEBTEDNESS
Senior Secured Credit Facilities
Overview
In connection with the 2005 Transactions, we entered into a senior secured credit agreement with J.P. Morgan Securities Inc., Lehman Brothers Inc. and Merrill Lynch, Pierce, Fenner & Smith Incorporated, as co-lead arrangers and joint bookrunners, JPMorgan Chase Bank, N.A. as administrative agent and collateral agent and Lehman Brothers Inc. and Merrill Lynch, Pierce, Fenner & Smith Incorporated, as co-syndication agents. This senior secured credit agreement was subsequently amended on April 5, 2007. The following description is only a summary of certain material provisions of the senior secured credit facilities, does not purport to be complete and is qualified in its entirety by reference to the provisions of that agreement.
The senior secured credit facilities provide senior secured financing of $535.0 million, consisting of:
| • | a $425.0 million term loan facility; and |
| • | a $110.0 million revolving credit facility (before any potential reduction associated with the CIT bankruptcy). |
Team Finance LLC is the borrower under the senior secured credit facilities. The senior secured revolving credit facility includes capacity for issuance of letters of credit and for borrowings on same-day notice referred to as the swingline loans.
Interest Rates and Fees
Borrowings under the senior secured credit facilities bear interest at a rate equal to an applicable margin plus, at our option, either (a) a base rate determined by reference to the higher of (1) the prime rate of JPMorgan Chase Bank, N.A. and (2) the federal funds rate plus 1/2 of 1% or (b) a LIBOR rate determined by reference to the costs of funds for deposits in the currency of such borrowing for the interest period relevant to such borrowing adjusted for certain additional costs. The current interest rate for term loan borrowings is LIBOR plus a margin of 2.0%. The current interest rate for revolving credit borrowings is LIBOR plus a margin of 2.0% based on our leverage ratio at September 30, 2009 of 3.39 to 1.0. The applicable margin for borrowings under the senior secured revolving credit facility may be increased if our leverage ratio increases. In addition, the applicable margin for borrowings under the term loan facility may be increased in the event of a downgrade in the corporate family rating of us by either Moody’s Investors Service, Inc. or Standard and Poor’s Ratings Services.
In addition to paying interest on outstanding principal under the senior secured credit facilities, we pay a commitment fee to the lenders under the senior secured revolving credit facility in respect of the unutilized commitments thereunder. The commitment fee rate is 0.50% per annum. We also pay customary letter of credit fees.
Prepayments
The senior secured credit agreement requires us to prepay outstanding term loans, subject to certain exceptions, with:
| • | 50% (which percentage will be reduced to 25% and 0% if our total leverage ratio is less than certain ratios) of our annual excess cash flow; |
| • | 100% of the net cash proceeds of all nonordinary course asset sales or other dispositions of property by us and our subsidiaries (including insurance and condemnation proceeds), subject to certain |
128
Table of Contents
| exceptions, if we do not (i) reinvest those proceeds within 15 months in assets to be used in our business or to make certain other permitted investments or (ii) enter into a legally binding commitment within 15 months to reinvest those proceeds in assets to be used in our business or to make certain other permitted investments as long as such reinvestment is completed within 180 days of the date of such legally binding commitment; and |
| • | 100% of the net cash proceeds of any incurrence of debt, other than debt permitted under the senior secured credit agreement. |
The foregoing mandatory prepayments will be applied to installments of the senior secured term loan facility in direct order of maturity.
We may voluntarily repay outstanding loans under the senior secured credit facilities at any time without premium or penalty, other than customary “breakage” costs with respect to LIBOR loans.
Amortization
We are required to repay installments on the loans under the senior secured term loan facility in quarterly principal amounts of 0.25% of the aggregate principal amount of the term loans outstanding (as such amount may be reduced by any prepayments) through September 30, 2012, with the remaining amount payable on November 23, 2012.
Principal amounts outstanding under the senior secured revolving credit facility are due and payable in full at maturity on November 23, 2011.
Guarantees and Security
All obligations under the senior secured credit facilities are unconditionally guaranteed by Team Health Holdings and, subject to certain exceptions, each of Team Finance LLC’s existing and future domestic wholly-owned subsidiaries, referred to in this section, collectively as “Guarantors.”
All obligations under the senior secured credit facilities, and the guarantees of those obligations, are secured by the following assets of Team Health Holdings, Team Finance LLC and each Guarantor, subject to certain exceptions:
| • | a first-priority pledge of 100% of the capital stock of Team Finance LLC, 100% of the capital stock of our wholly-owned domestic subsidiaries that are directly owned by Team Finance LLC or one of the Guarantors and 65% of the capital stock of each of our wholly-owned foreign subsidiaries that are directly owned by Team Finance LLC or one of the Guarantors; and |
| • | a security interest in, and mortgages on, substantially all tangible and intangible assets of Team Health Holdings, Team Finance LLC and each Guarantor. |
Certain Covenants and Events of Default
The senior secured credit agreement contains a number of covenants that, among other things, restrict, subject to certain exceptions, our ability to:
| • | incur additional indebtedness or issue certain preferred stock; |
| • | create liens on assets; |
129
Table of Contents
| • | enter into sale and leaseback transactions; |
| • | engage in mergers or consolidations; |
| • | sell or otherwise dispose of assets; |
| • | pay dividends and distributions or repurchase our membership units; |
| • | make investments, loans or advances; |
| • | repay subordinated indebtedness (including the senior subordinated notes); |
| • | make certain acquisitions; |
| • | engage in certain transactions with affiliates; |
| • | amend material agreements governing our subordinated indebtedness (including the senior subordinated notes); |
| • | change our lines of business; and |
| • | change the status of Team Health Holdings as a passive holding company or the status of Health Finance Corporation as a passive corporate co-issuer of the senior subordinated notes. |
In addition, the senior secured credit agreement requires us to comply with the following financial covenants:
| • | a maximum leverage ratio; |
| • | a minimum interest coverage ratio; and |
| • | a maximum capital expenditures amount. |
The senior secured credit agreement also contains certain customary affirmative covenants and events of default.
Senior Subordinated Notes
Overview
In November 2005, our subsidiary, Team Finance LLC, issued $215,000,000 aggregate principal amount of 11 1/4% Senior Subordinated Notes due 2013 under an indenture dated November 23, 2005 among Team Finance LLC, Health Finance Corporation, each of the existing and future domestic wholly-owned subsidiaries of Team Finance LLC, as guarantors, and The Bank of New York Trust Company, N.A., as trustee.
Ranking
The payment of the principal of, premium, if any, and interest on the senior subordinated notes and the payment of any guarantee are subordinate in right of payment to the prior payment in cash in full of all senior indebtedness of Team Finance LLC, Health Finance Corporation or the relevant guarantor, as the case may be, including the obligations of Team Finance LLC, Health Finance Corporation and such guarantor under the senior secured credit facilities.
130
Table of Contents
The senior subordinated notes are subordinated in right of payment to all of the existing and future senior indebtedness of Team Finance LLC, Health Finance Corporation and the guarantors and effectively subordinated to all of the existing and future secured indebtedness of Team Finance LLC, Health Finance Corporation and the guarantors to the extent of the value of the assets securing such indebtedness.
Optional Redemption
At any time prior to December 1, 2009, Team Finance LLC and Health Finance Corporation may redeem all or a part of the senior subordinated notes at a redemption price equal to 100% of the principal amount of senior subordinated notes redeemed plus the greater of (1) 1.0% of the principal amount of such note; and (2) the excess, if any, of (a) the present value at such redemption date of (i) the redemption price of such note at December 1, 2009 (such redemption price being set forth in the table below), plus (ii) all required interest payments due on such note through December 1, 2009 (excluding accrued but unpaid interest to the redemption date), computed using a discount rate equal to the applicable treasury rate plus 50 basis points; over (b) the principal amount of such note, as of, and accrued and unpaid interest and additional interest, if any, to the redemption date.
On and after December 1, 2009, Team Finance LLC and Health Finance Corporation may redeem the senior subordinated notes, in whole or in part, at the redemption prices (expressed as percentages of the principal amount of the senior subordinated notes to be redeemed) set forth below, plus accrued and unpaid interest thereon and additional interest, if any, to the applicable redemption date:
| Year |
Percentage | ||
| 2009 |
107.000 | % | |
| 2010 |
102.813 | % | |
| 2011 and thereafter |
100.000 | % |
Change of Control
Upon the occurrence of a change of control, which is defined in the indenture governing the senior subordinated notes, each holder of the senior subordinated notes has the right to require Team Finance LLC and Health Finance Corporation to repurchase some or all of such holder’s senior subordinated notes at a purchase price in cash equal to 101% of the aggregate principal amount thereof plus accrued and unpaid interest and additional interest, if any, to the date of purchase.
Covenants
The indenture governing the senior subordinated notes contains covenants limiting, among other things, the issuers’ (and most or all of their subsidiaries’) ability to:
| • | incur additional debt or issue certain preferred shares; |
| • | pay dividends on or make other distributions in respect of their membership units or make other restricted payments; |
| • | make certain investments; |
| • | sell certain assets; |
| • | create liens on certain assets to secure debt; |
| • | consolidate, merge, sell or otherwise dispose of all or substantially all of their assets; |
| • | enter into certain transactions with their affiliates; and |
| • | designate their subsidiaries as unrestricted subsidiaries. |
131
Table of Contents
Events of Default
The indenture governing the senior subordinated notes also provides for events of default which, if any of them occurs, would permit or require the principal of and accrued interest on such senior subordinated notes to become or to be declared due and payable.
As of September 30, 2009, Team Finance LLC, Health Finance Corporation and the guarantors were in compliance in all material respects with all covenants and provisions contained under the indenture governing the senior subordinated notes.
Team Health Holdings
The indenture governing the senior subordinated notes permits the reports, information and other documents required to be filed or furnished to holders of the senior subordinated notes to be filed by, and be those of, Team Health Holdings if we become a guarantor of the senior subordinated notes, meet certain other conditions and comply with the requirements of Rule 3-10 of Regulation S-X promulgated by the SEC. Accordingly, subsequent to this offering we may guarantee the senior subordinated notes in order to simplify our reporting requirements going forward.
132
Table of Contents
CERTAIN RELATIONSHIPS AND RELATED PARTY TRANSACTIONS
Stockholders’ Agreement
In connection with this offering, we will enter into a stockholders’ agreement. This agreement will grant the Sponsor, through Ensemble Parent LLC (and its permitted assigns), the right to designate representatives to our Board as follows: (i) at least a majority of the total number of directors comprising our Board at such time as long as the Sponsor and its affiliates and/or permitted assigns, directly or indirectly, collectively beneficially owns 50% or more of the voting power of all shares of our capital stock entitled to vote generally in the election of our directors; (ii) 40% of the total number of directors comprising our Board at such time as long as the Sponsor and its affiliates and/or permitted assigns, directly or indirectly, collectively beneficially owns 40% or more of the voting power of all shares of our capital stock entitled to vote generally in the election of our directors; (iii) 30% of the total number of directors comprising our Board at such time as long as the Sponsor and its affiliates and/or permitted assigns, directly or indirectly, collectively beneficially owns 30% or more of the voting power of all shares of our capital stock entitled to vote generally in the election of our directors; (iv) 20% of the total number of directors comprising our Board at such time as long as the Sponsor and its affiliates and/or permitted assigns, directly or indirectly, collectively beneficially owns 20% or more of the voting power of all shares of our capital stock entitled to vote generally in the election of our directors; and (v) 10% of the total number of directors comprising our Board at such time as long as the Sponsor and its affiliates and/or permitted assigns, directly or indirectly, collectively beneficially owns 5% or more of the voting power of all shares of our capital stock entitled to vote generally in the election of our directors. For purposes of calculating the number of directors that Ensemble Parent LLC and its affiliates and/or permitted assigns are entitled to designate pursuant to the formula outlined above, any fractional amounts would be rounded up to the nearest whole number and the calculation would be made on a pro forma basis, taking into account any increase in the size of our Board (e.g., one and one quarter (1 1/4) directors shall equate to two (2) directors). In addition, the Sponsor, through Ensemble Parent LLC, shall have the right to remove and replace its director-designees at any time and for any reason and to designate any individual(s) to fill any such vacancies.
Registration Rights Agreement
In connection with this offering, we will enter into a registration rights agreement with Ensemble Parent LLC and the members of management who previously owned Class A units. Pursuant to this registration rights agreement, our Sponsor, through Ensemble Parent LLC, will have an unlimited number of demand registration rights, which, when and if exercised, will require us to register the shares of common stock beneficially owned by them with the SEC for sale by them to the public. We are not obligated to file a registration statement relating to any request to register shares pursuant to such demand registration rights within a period of 180 days after the effective date of any other registration statement we file pursuant to such demand registration rights (including the registration statement of which this prospectus is a part). In addition, in the event that we are registering additional shares of common stock for sale to the public in connection with any such demand registration, we are required to give notice of such registration to all members of management who received shares of common stock in exchange for the Class A units formerly held by them in the Corporation Conversion, and such persons have piggyback registration rights providing them the right to have us include the shares of common stock owned by them in any such registration. In each such event, we are required to pay the registration expenses.
Amended and Restated Transaction and Monitoring Fee Agreement
An affiliate of the Sponsor (which we refer to herein as the “Advisor”) has entered into an amended and restated transaction and monitoring fee agreement with us relating to certain monitoring, advisory and consulting services that the Advisor will provide to us until such time as (i) the Advisor provides notice of termination to us at any time following the Advisor’s receipt of the lump sum payment described below, (ii) we and the Advisor agree to terminate such agreement or (iii) the Sponsor’s and its affiliates’ direct and indirect ownership of us falls below 10%. These monitoring services include, among other things, (i) advice regarding the structure, terms, conditions and other provisions, distribution and timing of debt and equity offerings and advice regarding
133
Table of Contents
relationships with our and our subsidiaries’ lenders and bankers, (ii) advice regarding dispositions and/or acquisitions and (iii) such other advice directly or indirectly related to the financial advisory services described above as we may reasonably request. The annual monitoring fee under this agreement is $3.5 million. Additionally, we have agreed to reimburse the Advisor and each of its affiliates for their out-of-pocket expenses in connection with the monitoring services rendered under this agreement and the ownership and subsequent transfer by the Sponsor of equity interests in the Company. Under the agreement, we paid a $10.0 million transaction and advisory fee to such entity upon the completion of the 2005 Transactions and approximately $38,000 in related out-of-pocket expenses. We paid a monitoring fee of $3.5 million for each of 2006, 2007 and 2008.
The transaction and monitoring fee agreement also provides for a right of first refusal to the Advisor to provide us with services as a financial advisor, consultant, investment banker or any similar advisor in connection with any merger, acquisition, disposition, recapitalization, issuance of securities, financing or any similar transaction.
In connection with the initial public offering of our stock, a sale of all or substantially all of our assets or a change of control, the Advisor is entitled to elect to receive, in lieu of payment of the ongoing monitoring fee, a lump sum payment equal to the present value (using a discount rate equal to the yield to maturity on the date of notice of such election of the class of outstanding U.S. government bonds having a final maturity closest to the tenth anniversary of such notice of election) of all then-current and future monitoring fees payable under the agreement (assuming that the agreement terminates on the tenth anniversary of the notice of election). Upon the payment of that lump sum amount, the Advisor would no longer be obligated to provide monitoring services and we would no longer be obligated to pay the monitoring fees. In connection with this offering, it is expected that the Advisor will elect to receive a lump sum payment, and thus the monitoring portion of such agreement would be terminated as described above.
Under the transaction and monitoring fee agreement, we have agreed to indemnify the Advisor and its affiliates and their respective partners, members, officers, directors, employees, agents and representatives for any and all losses relating to the services contemplated by the transaction and monitoring fee agreement and the engagement of the Advisor pursuant to, and the performance by the Advisor of the services contemplated by, the transaction and monitoring fee agreement.
Upon completion of this offering, the Sponsor will receive a lump sum payment of approximately $ million in the aggregate, of which the members of management who previously held Class A common units prior to the Corporate Conversion would receive approximately $ million in the aggregate from the Sponsor, in each case based on the mid-point of the price range set forth on the cover page of this prospectus and current interest rates. The payment to the members of management is to be made to each such person on a pro rata basis based on the shares of our common stock owned by such person after the Corporate Conversion and immediately prior to the consummation of this offering. At current interest rates, the portion of the lump sum payment to management from the Sponsor would be $ in the aggregate at the low point of the price range set forth on the cover page of this prospectus and $ in the aggregate at the high point of the price range set forth on the cover page of this prospectus. Certain of our executive officers will receive a portion of the lump sum payment as follows: Dr. Massingale approximately $ , Mr. Roth approximately $ , Mr. Jones approximately $ , Mr. Sherlin approximately $ , Ms. Allen approximately $ and other members of management approximately $ in the aggregate. At current interest rates and assuming the high point of the price range set forth on the cover page of this prospectus the amounts would be as follows: Dr. Massingale approximately $ , Mr. Roth approximately $ , Mr. Jones approximately $ , Mr. Sherlin approximately $ , Ms. Allen approximately $ and other members of management approximately $ in the aggregate.
134
Table of Contents
Continuing Arrangements
We lease office space for our corporate headquarters from Winston Road Properties, an entity that is owned by seven individuals, including Dr. H. Lynn Massingale, our executive chairman and one of our representatives who has a 10% ownership stake in Winston Road Properties. We paid $0.7 million in each of 2006 and 2007 and $0.8 million in 2008 to Winston Road Properties in connection with the lease agreement. In addition, Park Med Properties owns a building which houses a medical clinic that is operated by our consolidated affiliate. In each of 2006, 2007 and 2008, the consolidated affiliate paid $0.1 million to Park Med Properties in connection with the lease agreement.
Related Person Transaction Approval Policy
Prior to the completion of this offering, our Board will adopt a written statement of policy for the review, approval and monitoring of transactions involving us and “related persons.” For the purposes of the policy, “related persons” will include executive officers, directors and director nominees or their immediate family members, or stockholders owning five percent or more of our outstanding common stock.
Our related person transaction approval policy will require:
| • | that any transaction in which a related person has a material direct or indirect interest and which exceeds $120,000, such transaction referred to as a “related person transaction,” and any material amendment or modification to a related person transaction, be reviewed and approved or ratified by any committee of the Board composed solely of independent directors who are disinterested or by the disinterested members of the Board; and |
| • | that any employment relationship or transaction involving an executive officer and any related compensation must be approved by the compensation committee of the Board or recommended by the compensation committee to the Board for its approval. |
In connection with the review and approval or ratification of a related person transaction:
| • | management must disclose to the committee or disinterested directors, as applicable, the material terms of the related person transaction, including the approximate dollar value of the amount involved in the transaction, and all the material facts as to the related person’s direct or indirect interest in, or relationship to, the related person transaction; |
| • | management must advise the committee or disinterested directors, as applicable, as to whether the related person transaction complies with the terms of our agreements governing our material outstanding indebtedness that limit or restrict our ability to enter into a related person transaction; |
| • | management must advise the committee or disinterested directors, as applicable, as to whether the related person transaction will be required to be disclosed in our SEC filings. To the extent it is required to be disclosed, management must ensure that the related person transaction is disclosed in accordance with SEC rules; and |
| • | management must advise the committee or disinterested directors, as applicable, as to whether the related person transaction constitutes a “personal loan” for purposes of Section 402 of the Sarbanes-Oxley Act. |
In addition, the related person transaction policy provides that the Committee, in connection with any approval or ratification of a related person transaction involving a non-employee director or director nominee, should consider whether such transaction would compromise the director or director nominee’s status as an “independent,” “outside,” or “non-employee” director, as applicable, under the rules and regulations of the SEC, NYSE and Internal Revenue Code.
135
Table of Contents
Core Trust Purchasing Group Participation Agreement
On November 27, 2006, we entered into a three-year participation agreement (“participation agreement”) with Core Trust Purchasing Group (“CPG”) designating CPG as exclusive agent for the purchase of certain indirect products and services. CPG is a “group purchasing organization” which secures from vendors pricing terms for goods and services that are believed to be more favorable than participants could obtain for themselves on an individual basis. Under the participation agreement we must purchase 80% of the requirements of our participating locations for core categories of specified products and services, through CPG or CPG may terminate the contract. In connection with purchases by its participants (including us), CPG receives a commission from the vendor in respect of purchases. Although CPG is not affiliated with Blackstone, in consideration for Blackstone’s facilitating participation generally by its portfolio companies with CPG and monitoring the services CPG provides to such portfolio companies, CPG generally remits a portion of the commissions received from vendors in respect of such purchases to an affiliate of Blackstone. However, since we are a supplier of outsourced services healthcare, our purchases made under the participation agreement do not result in any commissions being paid to Blackstone.
136
Table of Contents
The following is a description of the material terms that will be in our certificate of incorporation and by-laws, as each will be in effect as of the date of this prospectus. We refer you to our certificate of incorporation and by-laws, copies of which will be filed as exhibits to the registration statement of which this prospectus forms a part.
Authorized Capitalization
Our authorized capital stock consists of 100,000,000 shares of common stock, par value $0.01 per share, of which shares were issued and outstanding immediately prior to this offering, and 10,000,000 shares of preferred stock, par value $0.01 per share, of which no shares are currently issued and outstanding. Immediately following the completion of this offering, we will have shares of common stock outstanding and no shares of preferred stock outstanding.
Common Stock
Voting Rights. Holders of common stock are entitled to one vote per share on all matters to be voted upon by the stockholders. The holders of common stock do not have cumulative voting rights in the election of directors.
Dividend Rights. Holders of common stock are entitled to receive dividends ratably if, as and when dividends are declared from time to time by our Board out of funds legally available for that purpose, after payment of dividends required to be paid on outstanding preferred stock, as described below, if any. The amounts available to us to pay cash dividends will be restricted by our subsidiaries’ debt agreements. Our credit facilities and the indenture impose restrictions on our ability to declare dividends with respect to our common stock. Any decision to declare and pay dividends in the future will be made at the discretion of our Board and will depend on, among other things, our results of operations, cash requirements, financial condition, contractual restrictions and other factors that our Board may deem relevant.
Liquidation Rights. Upon liquidation, dissolution or winding up, the holders of common stock are entitled to receive ratably the assets available for distribution to the stockholders after payment of liabilities and liquidation preferences on any outstanding preferred stock.
Other Matters. The common stock has no preemptive or conversion rights and is not subject to further calls or assessment by us. There are no redemption or sinking fund provisions applicable to the common stock. All shares of our common stock that will be outstanding at the time of the completion of the offering will be fully paid and non-assessable.
Preferred Stock
Our certificate of incorporation authorizes our Board to establish one or more series of preferred stock and to determine, with respect to any series of preferred stock, the terms and rights of that series, including:
| • | the designation of the series; |
| • | the number of shares of the series, which our board may, except where otherwise provided in the preferred stock designation, increase (but not above the total number of authorized shares of the class) or decrease (but not below the number of shares then outstanding); |
| • | whether dividends, if any, will be cumulative or non-cumulative and the dividend rate of the series; |
| • | the dates at which dividends, if any, will be payable; |
137
Table of Contents
| • | the redemption rights and price or prices, if any, for shares of the series; |
| • | the terms and amounts of any sinking fund provided for the purchase or redemption of shares of the series; |
| • | the amounts payable on shares of the series in the event of any voluntary or involuntary liquidation, dissolution or winding-up of the affairs of our company; |
| • | whether the shares of the series will be convertible into shares of any other class or series, or any other security, of our company or any other corporation, and, if so, the specification of the other class or series or other security, the conversion price or prices or rate or rates, any rate adjustments, the date or dates as of which the shares will be convertible and all other terms and conditions upon which the conversion may be made; |
| • | restrictions on the issuance of shares of the same series or of any other class or series; and |
| • | the voting rights, if any, of the holders of the series. |
Anti-Takeover Effects of Certain Provisions of Our Certificate of Incorporation and Bylaws
Certain provisions of our certificate of incorporation and bylaws, which are summarized in the following paragraphs, may have an anti-takeover effect and may delay, defer or prevent a tender offer or takeover attempt that a stockholder might consider in its best interest, including those attempts that might result in a premium over the market price for the shares held by stockholders.
Classified Board
Our certificate of incorporation provides that our Board will be divided into three classes of directors, with the classes to be as nearly equal in number as possible. Prior to consummation of this offering, our Board will assign each of the current members to their respective class as the Board shall determine in its sole discretion, subject to the foregoing requirement that the classes be nearly equal in size. We will have a classified Board, with two directors in Class I (expected to be Messrs. and ), two directors in Class II (expected to be Messrs. and ) and three directors in Class III (expected to be Messrs. , and ). The members of each class serve for a term expiring at the third succeeding annual meeting of stockholders. As a result, approximately one-third of our Board will be elected each year. A replacement director shall serve in the same class as the former director he or she is replacing. The classification of our Board will have the effect of making it more difficult for stockholders to change the composition of our Board. Our certificate of incorporation and the bylaws provide that the number of directors will be fixed from time to time pursuant to a resolution adopted by the Board, but must consist of not less than six or more than 15 directors.
Business Combinations
We have opted out of Section 203 of the DGCL; however, our certificate of incorporation contains similar provisions providing that we may not engage in certain “business combinations” with any “interested stockholder” for a three-year period following the time that the stockholder became an interested stockholder, unless:
| • | prior to such time, our Board approved either the business combination or the transaction which resulted in the stockholder becoming an interested stockholder; |
| • | upon consummation of the transaction which resulted in the stockholder becoming an interested stockholder, the interested stockholder owned at least 85% of our voting stock outstanding at the time the transaction commenced, excluding certain shares; or |
138
Table of Contents
| • | at or subsequent to that time, the business combination is approved by our Board and by the affirmative vote of holders of at least 66 2/3% of the outstanding voting stock that is not owned by the interested stockholder. |
Generally, a “business combination” includes a merger, asset or stock sale or other transaction resulting in a financial benefit to the interested stockholder. Subject to certain exceptions, an “interested stockholder” is a person who, together with that person’s affiliates and associates, owns, or within the previous three years owned, 15% or more of our voting stock.
Under certain circumstances, this provision will make it more difficult for a person who would be an “interested stockholder” to effect various business combinations with a corporation for a three-year period. This provision may encourage companies interested in acquiring our company to negotiate in advance with our Board because the stockholder approval requirement would be avoided if our Board approves either the business combination or the transaction which results in the stockholder becoming an interested stockholder. These provisions also may have the effect of preventing changes in our Board and may make it more difficult to accomplish transactions which stockholders may otherwise deem to be in their best interests.
Our certificate of incorporation provides that the Sponsor and its affiliates, and any of their respective direct or indirect transferees and any group as to which such persons are a party or will not constitute “interested stockholders” for purposes of this provision.
Conflicts of Interest
Delaware law permits corporations to adopt provisions renouncing any interest or expectancy in certain opportunities that are presented to the corporation or its officers, directors or stockholders. Our certificate of incorporation will renounce any interest or expectancy that we have in, or right to be offered an opportunity to participate in, specified business opportunities. Our certificate of incorporation will provide that none of the Sponsor, Ensemble Parent, LLC or any of their respective affiliates or any director who is not employed by us (including any non-employee director who serves as one of our officers in both his director and officer capacities) or his or her affiliates will have any duty to refrain from (i) engaging in a corporate opportunity in the same or similar lines of business in which we or our affiliates now engage or propose to engage or (ii) otherwise competing with us. In addition, in the event that Ensemble Parent, LLC, the Sponsor or any non-employee director acquires knowledge of a potential transaction or other business opportunity which may be a corporate opportunity for itself or himself or its or his affiliates or for us or our affiliates, such person will have no duty to communicate or offer such transaction or business opportunity to us and they may take any such opportunity for themselves or offer it to another person or entity. Our certificate of incorporation will not renounce our interest in any business opportunity that is expressly offered to a non-employee director solely in his or her capacity as a director or officer of the company. No business opportunity offered to any non-employee director will be deemed to be a potential corporate opportunity for us unless we would be permitted to undertake the opportunity under our certificate of incorporation, we have sufficient financial resources to undertake the opportunity and the opportunity would be in line with our business.
Removal of Directors; Vacancies
Our certificate of incorporation and bylaws provide that (i) prior to the date on which the Sponsor and its affiliates beneficially own, in the aggregate, less than a majority in voting power of all outstanding shares of our stock entitled to vote generally in the election of directors, directors may be removed with or without cause upon the affirmative vote of holders of at least a majority of the voting power of all the then outstanding shares of stock entitled to vote generally in the election of directors, voting together as a single class and (ii) on and after the date the Sponsor and its affiliates beneficially own, in the aggregate, less than a majority in voting power of all outstanding shares of our stock entitled to vote generally in the election of directors, directors may be removed only for cause and only upon the affirmative vote of holders of at least 75% of the voting power of all the then outstanding shares of stock entitled to vote generally in the election of directors, voting together as a
139
Table of Contents
single class. In addition, our amended and restated bylaws also provide that, except as set forth in the stockholders agreement, any vacancies on our Board will be filled only by the affirmative vote of a majority of the remaining directors, although less than a quorum, or by a sole remaining director.
No Cumulative Voting
The DGCL provides that stockholders are not entitled to the right to cumulate votes in the election of directors unless our certificate of incorporation provides otherwise. Our certificate of incorporation does not provide for cumulative voting.
Calling of Special Meetings of Stockholders
Our certificate of incorporation provides that special meetings of our stockholders may be called at any time by the holders of a majority in voting power of all outstanding shares of our stock entitled to vote generally in the election of directors; provided, however, at any time when the Sponsor and its affiliates beneficially own, in the aggregate, less than a majority in voting power of all outstanding shares of our stock entitled to vote generally in the election of directors, special meetings of our stockholders may be called at any time only by or at the direction of the chairman of the Board, the Board or a committee of the Board which has been designated by the Board.
Stockholder Action by Written Consent
The DGCL permits stockholder action by written consent unless otherwise provided by our certificate of incorporation. Our certificate of incorporation precludes stockholder action by written consent at any time when the Sponsor and its affiliates beneficially own, in the aggregate, less than a majority in voting power of all outstanding shares of our stock entitled to vote generally in the election of directors.
Advance Notice Requirements for Stockholder Proposals and Director Nominations
Our bylaws provide that stockholders seeking to nominate candidates for election as directors or to bring business before an annual meeting of stockholders must provide timely notice of their proposal in writing to the corporate secretary.
Generally, to be timely, a stockholder’s notice must be received at our principal executive offices not less than 90 days nor more than 120 days prior to the first anniversary of the preceding year’s annual meeting. Our bylaws also specify requirements as to the form and content of a stockholder’s notice. These provisions, which do not apply to the Sponsor and its affiliates, may impede stockholders’ ability to bring matters before an annual meeting of stockholders or make nominations for directors at an annual meeting of stockholders.
Supermajority Provisions
The DGCL provides generally that the affirmative vote of a majority of the outstanding shares of stock entitled to vote is required to amend a corporation’s certificate of incorporation or bylaws, unless the certificate of incorporation requires a greater percentage. Our certificate of incorporation provides that at any time when the Sponsor and its affiliates beneficially own, in the aggregate, less than a majority in voting power of all outstanding shares of our stock entitled to vote generally in the election of directors, the following provisions in the certificate of incorporation and bylaws may be amended only by a vote of at least 75% of the voting power of all of the outstanding shares of our common stock entitled to vote in the election of directors, voting together as a single class:
| • | classified board (the election and term of our directors); |
| • | the resignation and removal of directors; |
140
Table of Contents
| • | the provisions regarding competition and corporate opportunities; |
| • | the provisions regarding entering into business combinations with interested stockholders; |
| • | the provisions regarding stockholder action by written consent; |
| • | the provisions regarding calling special meetings of stockholders; |
| • | filling vacancies on our board and newly created directorships; |
| • | the advance notice requirements for stockholder proposals and director nominations; |
| • | the indemnification provisions; and |
| • | the amendment provision requiring that the above provisions be amended only with a 75% supermajority vote. |
In addition, our certificate of incorporation grants our Board the authority to amend and repeal our bylaws without a stockholder vote in any manner not inconsistent with the laws of the State of Delaware or our certificate of incorporation.
Limitations on Liability and Indemnification of Officers and Directors
The DGCL authorizes corporations to limit or eliminate the personal liability of directors to corporations and their stockholders for monetary damages for breaches of directors’ fiduciary duties. Our certificate of incorporation includes a provision that eliminates the personal liability of directors for monetary damages for actions taken as a director, except for liability:
| • | for breach of the duty of loyalty; |
| • | for acts or omissions not in good faith or involving intentional misconduct or knowing violation of law; |
| • | under Section 174 of the DGCL (unlawful dividends or stock repurchases); or |
| • | for transactions from which the director derived improper personal benefit. |
Our certificate of incorporation and bylaws provide that we must indemnify our directors and officers to the fullest extent authorized by the DGCL. We are also expressly obligated to advance certain expenses (including attorneys’ fees and disbursements and court costs) and carry directors’ and officers’ insurance providing indemnification for our directors, officers and certain employees for some liabilities. We believe that these indemnification provisions and insurance are useful to attract and retain qualified directors and executive officers.
The limitation of liability and indemnification provisions in our certificate of incorporation and bylaws may discourage stockholders from bringing a lawsuit against directors for breach of their fiduciary duty. These provisions may also have the effect of reducing the likelihood of derivative litigation against directors and officers, even though such an action, if successful, might otherwise benefit us and our stockholders. In addition, your investment may be adversely affected to the extent we pay the costs of settlement and damage awards against directors and officers pursuant to these indemnification provisions.
There is currently no pending material litigation or proceeding involving any of our directors, officers or employees for which indemnification is sought.
141
Table of Contents
Transfer Agent and Registrar
The transfer agent and registrar for our common stock will be American Stock Transfer & Trust Company.
Listing
We have applied for listing on The New York Stock Exchange under the symbol “TMH.”
142
Table of Contents
SHARES ELIGIBLE FOR FUTURE SALE
Future sales or the availability for sale of substantial amounts of our common stock in the public market could adversely affect prevailing market prices and could impair our ability to raise capital through future sales of our securities. Upon completion of this offering, shares of our common stock will be outstanding. The shares of common stock sold in this offering will be freely tradable without restriction or further registration under the Securities Act. The remaining shares of common stock outstanding, including the shares owned by our existing equity investors, will be restricted securities within the meaning of Rule 144 under the Securities Act but will be eligible for resale subject to applicable volume, manner of sale, holding period and other requirements of Rule 144. Upon completion of this offering, our existing equity investors will own shares of common stock representing an aggregate % ownership interest in us after the offering (or shares of common stock representing a % aggregate ownership interest in us, assuming the underwriters exercise their over-allotment option in full).
We may issue shares of common stock from time to time as consideration for future acquisitions, investments or other corporate purposes. In the event that any such acquisition, investment or other transaction is significant, the number of shares of common stock that we may issue may in turn be significant. In addition, we may also grant registration rights covering those shares of common stock issued in connection with any such acquisitions and investments.
Stock Options
Upon completion of this offering, we intend to file a registration statement on Form S-8 under the Securities Act to register the shares of common stock reserved for issuance under the 2009 Stock Plan and, as a result, all shares of common stock acquired upon exercise of stock options will also be freely tradable under the Securities Act unless such common stock is held by our affiliates.
Lock-Up Arrangements
We, Ensemble Parent LLC, our executive officers and our directors have agreed, with specified exceptions, not to sell or transfer any of our common stock for 180 days after the date of this prospectus without first obtaining the written consent of each of the representatives, on behalf of the underwriters. Specifically, we and these other entities and individuals have agreed not to directly or indirectly:
| • | offer, pledge, sell, contract to sell, sell any option or contract to purchase, purchase any option or contract to sell, grant any option, right or warrant to purchase, or otherwise transfer or dispose of, directly or indirectly, any shares of our common stock, or any securities convertible into or exercisable or exchangeable for any shares of our common stock or any right to acquire shares of our common stock; or |
| • | enter into any swap or other arrangement that transfers to another, in whole or in part, any of the economic consequences of ownership of the common stock, whether any such transaction described above is to be settled by delivery of common stock or such other securities, in cash or otherwise. |
Rule 144
In general, under Rule 144 as in effect on the date of this prospectus, a person who is not one of our affiliates at any time during the three months preceding a sale, and who has beneficially owned shares of our common stock for at least six months, would be entitled to sell an unlimited number of shares of our common stock provided current public information about us is available and, after owning such shares for at least one year, would be entitled to sell an unlimited number of shares of our common stock without restriction. Our
143
Table of Contents
affiliates who have beneficially owned shares of our common stock for at least six months are entitled to sell within any three-month period a number of shares that does not exceed the greater of:
| • | 1% of the number of shares of our common stock then outstanding; or |
| • | the average weekly trading volume of our common stock on The New York Stock Exchange during the four calendar weeks preceding the filing of a notice on Form 144 with respect to the sale. |
Sales under Rule 144 by our affiliates are also subject to manner of sale provisions, notice requirements and the availability of current public information about us.
Registration Rights
In connection with this offering, we will enter into a registration rights agreement with Ensemble Parent LLC and members of management who own our shares of common stock. See “Certain Relationships and Related Party Transactions—Registration Rights Agreement.”
144
Table of Contents
CERTAIN UNITED STATES FEDERAL INCOME AND ESTATE TAX CONSEQUENCES
TO NON-U.S. HOLDERS
The following is a summary of certain United States federal income and estate tax consequences of the purchase, ownership and disposition of our common stock as of the date hereof. Except where noted, this summary deals only with common stock that is held as a capital asset by a non-U.S. holder.
A “non-U.S. holder” means a person (other than a partnership) that is not for United States federal income tax purposes any of the following:
| • | an individual citizen or resident of the United States; |
| • | a corporation (or any other entity treated as a corporation for United States federal income tax purposes) created or organized in or under the laws of the United States, any state thereof or the District of Columbia; |
| • | an estate the income of which is subject to United States federal income taxation regardless of its source; or |
| • | a trust if it (1) is subject to the primary supervision of a court within the United States and one or more United States persons have the authority to control all substantial decisions of the trust or (2) has a valid election in effect under applicable United States Treasury regulations to be treated as a United States person. |
This summary is based upon provisions of the Internal Revenue Code of 1986, as amended, or the Code, and regulations, rulings and judicial decisions as of the date hereof. Those authorities may be changed, perhaps retroactively, so as to result in United States federal income and estate tax consequences different from those summarized below. This summary does not address all aspects of United States federal income and estate taxes and does not deal with foreign, state, local or other tax considerations that may be relevant to non-U.S. holders in light of their personal circumstances. In addition, it does not represent a detailed description of the United States federal income tax consequences applicable to you if you are subject to special treatment under the United States federal income tax laws (including if you are a United States expatriate, “controlled foreign corporation,” “passive foreign investment company” or a partnership or other pass-through entity for United States federal income tax purposes). We cannot assure you that a change in law will not alter significantly the tax considerations that we describe in this summary.
If a partnership holds our common stock, the tax treatment of a partner will generally depend upon the status of the partner and the activities of the partnership. If you are a partner of a partnership holding our common stock, you should consult your tax advisors.
If you are considering the purchase of our common stock, you should consult your own tax advisors concerning the particular United States federal income and estate tax consequences to you of the ownership of the common stock, as well as the consequences to you arising under the laws of any other taxing jurisdiction.
Dividends
Dividends paid to a non-U.S. holder of our common stock generally will be subject to withholding of United States federal income tax at a 30% rate or such lower rate as may be specified by an applicable income tax treaty. However, dividends that are effectively connected with the conduct of a trade or business by the non-U.S. holder within the United States (and, if required by an applicable income tax treaty, are attributable to a United States permanent establishment) are not subject to the withholding tax, provided certain certification and
145
Table of Contents
disclosure requirements are satisfied. Instead, such dividends are subject to United States federal income tax on a net income basis in the same manner as if the non-U.S. holder were a United States person as defined under the Code. Any such effectively connected dividends received by a foreign corporation may be subject to an additional “branch profits tax” at a 30% rate or such lower rate as may be specified by an applicable income tax treaty.
A non-U.S. holder of our common stock who wishes to claim the benefit of an applicable treaty rate and avoid backup withholding, as discussed below, for dividends will be required (a) to complete Internal Revenue Service Form W-8BEN (or other applicable form) and certify under penalty of perjury that such holder is not a United States person as defined under the Code and is eligible for treaty benefits or (b) if our common stock is held through certain foreign intermediaries, to satisfy the relevant certification requirements of applicable United States Treasury regulations. Special certification and other requirements apply to certain non-U.S. holders that are pass-through entities rather than corporations or individuals.
A non-U.S. holder of our common stock eligible for a reduced rate of United States withholding tax pursuant to an income tax treaty may obtain a refund of any excess amounts withheld by filing an appropriate claim for refund with the Internal Revenue Service.
Gain on Disposition of Common Stock
Any gain realized on the disposition of our common stock generally will not be subject to United States federal income tax unless:
| • | the gain is effectively connected with a trade or business of the non-U.S. holder in the United States (and, if required by an applicable income tax treaty, is attributable to a United States permanent establishment of the non-U.S. holder); |
| • | the non-U.S. holder is an individual who is present in the United States for 183 days or more in the taxable year of that disposition, and certain other conditions are met; or |
| • | we are or have been a “United States real property holding corporation” for United States federal income tax purposes and the non-U.S. holder holds or has held, directly or indirectly, at any time within the five-year period ending on the date of disposition of our common stock, more than 5% of our common stock. |
An individual non-U.S. holder described in the first bullet point immediately above will be subject to tax on the net gain derived from the sale under regular graduated United States federal income tax rates. An individual non-U.S. holder described in the second bullet point immediately above will be subject to a flat 30% tax on the gain derived from the sale, which may be offset by United States source capital losses, even though the individual is not considered a resident of the United States. If a non-U.S. holder that is a foreign corporation falls under the first bullet point immediately above, it will be subject to tax on its net gain in the same manner as if it were a United States person as defined under the Code and, in addition, may be subject to the branch profits tax equal to 30% of its effectively connected earnings and profits or at such lower rate as may be specified by an applicable income tax treaty.
We believe we are not, have not at any time during the five-year period ending as of the date of this offering, and do not anticipate becoming a “United States real property holding corporation” for United States federal income tax purposes.
146
Table of Contents
Federal Estate Tax
Common stock held by an individual non-U.S. holder at the time of death will be included in such holder’s gross estate for United States federal estate tax purposes, unless an applicable estate tax treaty provides otherwise.
Information Reporting and Backup Withholding
We must report annually to the Internal Revenue Service and to each non-U.S. holder the amount of dividends paid to such holder and the tax withheld with respect to such dividends, regardless of whether withholding was required. Copies of the information returns reporting such dividends and withholding may also be made available to the tax authorities in the country in which the non-U.S. holder resides under the provisions of an applicable income tax treaty.
A non-U.S. holder will be subject to backup withholding for dividends paid to such holder unless such holder certifies under penalty of perjury that it is a non-U.S. holder (and the payor does not have actual knowledge or reason to know that such holder is a United States person as defined under the Code), or such holder otherwise establishes an exemption.
Information reporting and, depending on the circumstances, backup withholding will apply to the proceeds of a sale of our common stock within the United States or conducted through certain United States-related financial intermediaries, unless the beneficial owner certifies under penalty of perjury that it is a non-U.S. holder (and the payor does not have actual knowledge or reason to know that the beneficial owner is a United States person as defined under the Code), or such owner otherwise establishes an exemption.
Any amounts withheld under the backup withholding rules may be allowed as a refund or a credit against a non-U.S. holder’s United States federal income tax liability provided the required information is furnished to the Internal Revenue Service.
147
Table of Contents
Merrill Lynch, Pierce, Fenner & Smith Incorporated, Goldman, Sachs & Co., Barclays Capital Inc. and Citigroup Global Markets Inc. are acting as representatives of each of the underwriters named below. Subject to the terms and conditions set forth in an underwriting agreement among us, the selling shareholder and the underwriters, we and the selling shareholder have agreed to sell to the underwriters, and each of the underwriters has agreed, severally and not jointly, to purchase from us and the selling shareholder, the number of shares of common stock set forth opposite its name below.
| Underwriters | Number of Shares | |
| Merrill Lynch, Pierce, Fenner & Smith |
||
| Goldman, Sachs & Co. |
||
| Barclays Capital Inc. |
||
| Citigroup Global Markets Inc. |
||
| Credit Suisse Securities (USA) LLC |
||
| Deutsche Bank Securities Inc. |
||
| UBS Securities LLC |
||
| Total |
||
Subject to the terms and conditions set forth in the underwriting agreement, the underwriters have agreed, severally and not jointly, to purchase all of the shares of common stock sold under the underwriting agreement if any of these shares are purchased. If an underwriter defaults, the underwriting agreement provides that the purchase commitments of the nondefaulting underwriters may be increased or the underwriting agreement may be terminated.
We and the selling shareholder have agreed to indemnify the several underwriters against certain liabilities, including liabilities under the Securities Act, or to contribute to payments the underwriters may be required to make in respect of those liabilities.
The underwriters are offering the shares, subject to prior sale, when, as and if issued to and accepted by them, subject to approval of legal matters by their counsel, including the validity of the shares, and other conditions contained in the underwriting agreement, such as the receipt by the underwriters of officer’s certificates and legal opinions. The underwriters reserve the right to withdraw, cancel or modify offers to the public and to reject orders in whole or in part.
Commissions and Discounts
The representatives have advised us and the selling shareholder that the underwriters propose initially to offer the shares of common stock to the public at the public offering price set forth on the cover page of this prospectus and to dealers at that price less a concession not in excess of $ per share. The underwriters may allow, and the dealers may reallow, a discount not in excess of $ per share to other dealers. After the initial offering, the public offering price, concession or any other term of the offering may be changed.
148
Table of Contents
The following table shows the public offering price, underwriting discounts and commissions and proceeds before expenses to us and the selling shareholder. Such amounts are shown assuming both no exercise and full exercise of the underwriters’ option to purchase additional shares.
| Per Share | Without Over- allotment Option |
With Over- allotment Option | ||||
| Public offering price |
||||||
| Underwriting discounts and commissions |
||||||
| Proceeds, before expenses, to us |
||||||
| Proceeds, before expenses, to the selling shareholder |
The expenses of the offering that are payable by us and the selling shareholder, excluding underwriting discounts and commissions, are estimated to be approximately $ . We have agreed to pay expenses incurred by the selling shareholder in connection with the offering, other than the underwriting discounts and commissions.
Option to Purchase Additional Shares
The selling shareholder has granted an option to the underwriters to purchase up to additional shares at the public offering price, less underwriting discounts and commissions. The underwriters may exercise this option for 30 days from the date of this prospectus. If the underwriters exercise this option, each will be obligated, subject to certain conditions contained in the underwriting agreement, to purchase a number of additional shares proportionate to that underwriter’s initial amount reflected in the table above.
No Sales of Similar Securities
We, all of our directors and executive officers and the selling shareholder have agreed that, subject to specified exceptions, without the prior written consent of each of the representatives on behalf of the underwriters, we and they will not directly or indirectly, offer, pledge, announce the intention to sell, sell, contract to sell, sell an option or contract to purchase, purchase any option or contract to sell, grant any option, right or warrant to purchase, or otherwise transfer or dispose of any common stock or any securities that may be converted into or exchanged for any common stock, enter into any swap or other agreement that transfers, in whole or in part, any of the economic consequences of ownership of the common stock, make any demand for or exercise any right or file or cause to be filed a registration statement with respect to the registration of any shares of common stock or securities convertible, exercisable or exchangeable into common stock or any of our other securities or publicly disclose the intention to do any of the foregoing for a period of 180 days from the date of this prospectus other than permitted transfers; provided that the selling shareholder may make a demand under our registration rights agreement so long as the applicable registration statement is not filed during such period.
Reserved Share Program
At our request, the underwriters have reserved for sale, at the initial public offering price, up to shares offered by this prospectus for sale to certain members of management and members of physician leadership, including facility medical directors. If these persons purchase reserved shares, this will reduce the number of shares available for sale to the general public. Any reserved shares that are not so purchased will be offered by the underwriters to the general public on the same terms as the other shares offered by this prospectus.
Offering Price Determination
Before this offering, there has been no public market for our common stock. The initial public offering price will be determined through negotiations among us, the selling shareholder and the representatives. In addition to prevailing market conditions, the factors to be considered in determining the initial public offering price are:
| • | the valuation multiples of publicly traded companies that the representatives believe to be comparable to us; |
149
Table of Contents
| • | our financial information; |
| • | the history of, and prospects for, our company and the industry in which we compete; |
| • | an assessment of our management, its past and present operations, and the prospects for and timing of, our future revenues; |
| • | the present state of our development; and |
| • | the above factors in relation to market values and various measures of other companies engaged in activities similar to ours. |
An active trading market for the shares may not develop. It is also possible that after the offering the shares will not trade in the public market at or above the initial public offering price.
The underwriters do not expect to sell more than 5% of the shares in the aggregate to accounts over which they exercise discretionary authority.
New York Stock Exchange Listing
We have applied for listing on The New York Stock Exchange under the symbol “TMH.” In order to meet the requirements for listing on that exchange, the underwriters have undertaken to sell a minimum number of shares to a minimum number of beneficial owners as required by that exchange.
Price Stabilization, Short Positions and Penalty Bids
Until the distribution of the shares is completed, SEC rules may limit underwriters and selling group members from bidding for and purchasing our common stock. However, the representatives may engage in transactions that stabilize the price of our common stock, such as bids or purchases to peg, fix or maintain that price.
In connection with the offering, the underwriters may purchase and sell shares of our common stock in the open market. These transactions may include short sales, stabilizing transactions and purchases to cover positions created by short sales. Short sales involve the sale by the underwriters of a greater number of shares than they are required to purchase in the offering. “Covered” short sales are sales made in an amount not greater than the underwriters’ option to purchase additional shares from the selling shareholder in the offering. The underwriters may close out any covered short position by either exercising their option to purchase additional shares or purchasing shares in the open market. In determining the source of shares to close out the covered short position, the underwriters will consider, among other things, the price of shares available for purchase in the open market as compared to the price at which they may purchase additional shares pursuant to the option granted to them. “Naked” short sales are any sales in excess of such option. The underwriters must close out any naked short position by purchasing shares in the open market. A naked short position is more likely to be created if the underwriters are concerned that there may be downward pressure on the price of our common stock in the open market after pricing that could adversely affect investors who purchase in the offering. Stabilizing transactions consist of various bids for or purchases of common stock made by the underwriters in the open market prior to the completion of the offering.
The underwriters may also impose a penalty bid. This occurs when a particular underwriter repays to the underwriters a portion of the underwriting discount received by it because the representatives have repurchased shares sold by or for the account of such underwriter in stabilizing or short covering transactions.
Purchases to cover a short position and stabilizing transactions, as well as other purchases by the underwriters for their own accounts, may have the effect of preventing or retarding a decline in the market price of our common stock, and together with the imposition of the penalty bid, may stabilize, maintain or otherwise affect the market price of our common stock. As a result, the price of our common stock may be higher than the price that otherwise might exist in the open market.
150
Table of Contents
Neither we nor any of the underwriters make any representation or prediction as to the direction or magnitude of any effect that the transactions described above may have on the price of our common stock. In addition, neither we nor any of the underwriters represent that the representatives will engage in these stabilizing transactions or that any transaction, once commenced, will not be discontinued without notice.
Notice to Prospective Investors in the European Economic Area and the United Kingdom
In relation to each Member State of the European Economic Area which has implemented the Prospectus Directive, each, a Relevant Member State, an offer to the public of any shares which are the subject of the offering contemplated by this prospectus, or Shares, may not be made in that Relevant Member State except that an offer to the public in that Relevant Member State of any Shares may be made at any time under the following exemptions under the Prospectus Directive, if they have been implemented in that Relevant Member State:
(a) to legal entities which are authorised or regulated to operate in the financial markets or, if not so authorised or regulated, whose corporate purpose is solely to invest in securities;
(b) to any legal entity which has two or more of (1) an average of at least 250 employees during the last financial year; (2) a total balance sheet of more than €43,000,000 and (3) an annual net turnover of more than €50,000,000, as shown in its last annual or consolidated accounts;
(c) by the underwriters to fewer than 100 natural or legal persons (other than “qualified investors” as defined in the Prospectus Directive) subject to obtaining the prior consent of the representatives for any such offer; or
(d) in any other circumstances falling within Article 3(2) of the Prospectus Directive, provided that no such offer of Shares shall result in a requirement for the publication by the Company or any underwriter of a prospectus pursuant to Article 3 of the Prospectus Directive.
Any person making or intending to make any offer within the European Economic Area of Shares which are the subject of the offering contemplated in this Prospectus should only do so in circumstances in which no obligation arises for the Company or any of the underwriters to produce a prospectus for such offer. Neither the Company nor the underwriters have authorised, nor do they authorise, the making of any offer of Shares through any financial intermediary, other than offers made by the underwriters which constitute the final offering of Shares contemplated in this Prospectus.
For the purposes of this provision, and the buyer’s representation below, the expression an “offer to the public” in relation to any Shares in any Relevant Member State means the communication in any form and by any means of sufficient information on the terms of the offer and any Shares to be offered so as to enable an investor to decide to purchase any Shares, as the same may be varied in that Relevant Member State by any measure implementing the Prospectus Directive in that Relevant Member State and the expression “Prospectus Directive” means Directive 2003/71/EC and includes any relevant implementing measure in each Relevant Member State.
Each person in a Relevant Member State who receives any communication in respect of, or who acquires any Shares under, the offers contemplated in this Prospectus will be deemed to have represented, warranted and agreed to and with each underwriter and the Company that:
(a) it is a qualified investor within the meaning of the law in that Relevant Member State implementing Article 2(1)(e) of the Prospectus Directive; and
(b) in the case of any Shares acquired by it as a financial intermediary, as that term is used in Article 3(2) of the Prospectus Directive, (i) the Shares acquired by it in the offering have not been acquired on behalf of, nor have they been acquired with a view to their offer or resale to, persons in any Relevant Member State other
151
Table of Contents
than “qualified investors” as defined in the Prospectus Directive, or in circumstances in which the prior consent of the representatives has been given to the offer or resale or (ii) where Shares have been acquired by it on behalf of persons in any Relevant Member State other than qualified investors, the offer of those Shares to it is not treated under the Prospectus Directive as having been made to such persons.
Notice to Prospective Investors in Switzerland
This document as well as any other material relating to the shares of common stock which are the subject of the offering contemplated by this prospectus do not constitute an issue prospectus pursuant to Article 652a and/or 1156 of the Swiss Code of Obligations. The shares of common stock will not be listed on the SIX Swiss Exchange and, therefore, the documents relating to the shares of common stock, including, but not limited to, this document, do not claim to comply with the disclosure standards of the listing rules of SIX Swiss Exchange and corresponding prospectus schemes annexed to the listing rules of the SIX Swiss Exchange.
The shares of common stock are being offered in Switzerland by way of a private placement (i.e., to a small number of selected investors only, without any public offer and only to investors who do not purchase the shares of common stock with the intention to distribute them to the public). The investors will be individually approached by us from time to time.
This document as well as any other material relating to the shares of common stock is personal and confidential and do not constitute an offer to any other person. This document may only be used by those investors to whom it has been handed out in connection with the offering described herein and may neither directly nor indirectly be distributed or made available to other persons without our express consent. It may not be used in connection with any other offer and shall in particular not be copied and/or distributed to the public in (or from) Switzerland.
Notice to Prospective Investors in the Dubai International Financial Centre
This document relates to an exempt offer in accordance with the Offered Securities Rules of the Dubai Financial Services Authority. This document is intended for distribution only to persons of a type specified in those rules. It must not be delivered to, or relied on by, any other person. The Dubai Financial Services Authority has no responsibility for reviewing or verifying any documents in connection with exempt offers. The Dubai Financial Services Authority has not approved this document nor taken steps to verify the information set out in it, and has no responsibility for it. The Shares may be illiquid and/or subject to restrictions on their resale. Prospective purchasers of the Shares offered should conduct their own due diligence on the Shares. If you do not understand the contents of this document you should consult an authorised financial adviser.
Other Relationships
Certain of the underwriters and their respective affiliates have engaged in, and may in the future engage in, investment banking and other commercial dealings in the ordinary course of business with us and/or our affiliates. In particular, certain of the underwriters or their affiliates are lenders under our senior secured credit facilities. They have received, or may in the future receive, customary fees and commissions for these transactions.
Electronic Distribution
In connection with the offering, certain of the underwriters or securities dealers may distribute prospectuses by electronic means, such as e-mail. In addition, certain of the underwriters may facilitate Internet distribution for this offering to certain of its Internet subscription customers. These underwriters may allocate a limited number of shares for sale to its online brokerage customers. An electronic prospectus supplement may be made available on the Internet web site maintained by certain underwriters. Other than any prospectus in electronic format, the information on an underwriter’s Internet web site is not part of this prospectus.
152
Table of Contents
The validity of our common stock offered by this prospectus will be passed upon for us by Simpson Thacher & Bartlett LLP, New York, New York. Certain legal matters in connection with this offering will be passed upon for the underwriters by Cravath, Swaine & Moore LLP.
The consolidated financial statements of Team Health Holdings, Inc. at December 31, 2007 and 2008, and for each of the three years in the period ended December 31, 2008, appearing in this prospectus and Registration Statement have been audited by Ernst & Young LLP, independent registered public accounting firm, as set forth in their report thereon appearing elsewhere herein, and are included in reliance upon such report given on the authority of such firm as experts in accounting and auditing.
We have filed with the SEC a registration statement on Form S-1 under the Securities Act with respect to the common stock offered by this prospectus. This prospectus is a part of the registration statement and does not contain all of the information set forth in the registration statement. For further information about us and our common stock, you should refer to the registration statement. This prospectus summarizes material provisions of contracts and other documents to which we refer you. Since the prospectus may not contain all of the information that you may find important, you should review the full text of these contracts and other documents. We have included or incorporated by reference copies of these documents as exhibits to our registration statement.
Our wholly-owned subsidiary, Team Finance LLC, files annual, quarterly and current reports and other information with the SEC and upon completion of this offering, we will file annual, quarterly and current reports and other information with the SEC. Our filings with the SEC are available to the public on the SEC’s website at http://www.sec.gov. Those filings are also available to the public on our corporate web site at http://www.teamhealth.com. The information we file with the SEC or contained on our corporate web site or any other web site that we may maintain is not part of this prospectus or the registration statement of which this prospectus is a part. You may also read and copy, at SEC prescribed rates, any document we file with the SEC, including the registration statement (and its exhibits) of which this prospectus is a part, at the SEC’s Public Reference Room located at 100 F Street, N.E., Washington D.C. 20549. You can call the SEC at 1-800-SEC-0330 to obtain information on the operation of the Public Reference Room.
153
Table of Contents
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
| Index to Consolidated Financial Statements |
||
| F-2 | ||
| F-3 | ||
| Consolidated Statements of Operations for the Years Ended December 31, 2006, 2007 and 2008 |
F-4 | |
| F-5 | ||
| Consolidated Statements of Cash Flows for the Years Ended December 31, 2006, 2007 and 2008 |
F-6 | |
| F-7 | ||
| Index to Consolidated Financial Statements (unaudited) |
||
| Consolidated Balance Sheets at December 31, 2008 and September 30, 2009 |
F-32 | |
| Consolidated Statements of Operations for the Nine Months Ended September 30, 2008 and 2009 |
F-33 | |
| Consolidated Statements of Cash Flows for the Nine Months Ended September 30, 2008 and 2009 |
F-34 | |
| F-35 | ||
F-1
Table of Contents
Report of Independent Registered Public Accounting Firm
The Board of Directors and Stockholders
Team Health Holdings, Inc.
We have audited the accompanying consolidated balance sheets of Team Health Holdings, Inc. (the Company) as of December 31, 2007 and 2008, and the related consolidated statements of operations, member’s equity (deficit) and comprehensive earnings (loss) and cash flows for each of the three years in the period ended December 31, 2008. Our audits also included the financial statement schedule listed in Item 16(b). These financial statements and schedule are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements and schedule based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. We were not engaged to perform an audit of the Company’s internal control over financial reporting. Our audits included consideration of internal control over financial reporting as a basis for designing audit procedures that are appropriate in the circumstances, but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion. An audit also includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, and evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated financial position of Team Health Holdings, Inc. at December 31, 2007 and 2008, and the consolidated results of its operations and its cash flows for each of the three years in the period ended December 31, 2008, in conformity with U.S. generally accepted accounting principles. Also, in our opinion, the related financial statement schedule referred to above, when considered in relation to the basic financial statements taken as a whole, presents fairly in all material respects the information set forth therein.
As discussed in Note 18 to the consolidated financial statements, the Company adopted FASB Interpretation No. 48, “Accounting for Uncertainty in Income Taxes,” which was codified into ASC Topic 740, “Income Taxes”, effective January 1, 2007.
Nashville, Tennessee
, 2009
The foregoing report is in the form that will be signed upon the completion of the reorganization described in Note 1 to the consolidated financial statements.
/s/ Ernst & Young LLP
Nashville, Tennessee
November 17, 2009
F-2
Table of Contents
Consolidated Balance Sheets
| December 31, | Unaudited Pro forma as of December 31, 2008 |
|||||||||||
| 2007 | 2008 | |||||||||||
| (In thousands) | ||||||||||||
| Assets |
||||||||||||
| Current Assets: |
||||||||||||
| Cash and cash equivalents |
$ | 30,290 | $ | 46,398 | $ | 46,398 | ||||||
| Accounts receivable, less allowance for uncollectibles of $165,226 and $158,685 in 2007 and 2008, respectively |
222,603 | 237,790 | 237,790 | |||||||||
| Prepaid expenses and other current assets |
13,242 | 15,467 | 15,467 | |||||||||
| Receivables under insured programs |
34,118 | 27,145 | 27,145 | |||||||||
| Income tax receivable |
— | 3,446 | 3,446 | |||||||||
| Total current assets |
300,253 | 330,246 | 330,246 | |||||||||
| Investments of insurance subsidiary |
76,057 | 87,413 | 87,413 | |||||||||
| Property and equipment, net |
25,276 | 27,477 | 27,477 | |||||||||
| Other intangibles, net |
27,247 | 32,438 | 32,438 | |||||||||
| Goodwill |
158,898 | 149,763 | 149,763 | |||||||||
| Deferred income taxes |
60,104 | 47,915 | 47,915 | |||||||||
| Receivables under insured programs |
23,896 | 20,589 | 20,589 | |||||||||
| Other |
27,442 | 30,940 | 30,940 | |||||||||
| $ | 699,173 | $ | 726,781 | $ | 726,781 | |||||||
| Liabilities and members’ equity (deficit) |
||||||||||||
| Current liabilities: |
||||||||||||
| Accounts payable |
$ | 12,177 | $ | 13,451 | $ | 13,451 | ||||||
| Accrued compensation and physician payable |
101,421 | 111,556 | 111,556 | |||||||||
| Other accrued liabilities |
83,854 | 82,012 | 82,012 | |||||||||
| Income tax payable |
985 | — | — | |||||||||
| Current maturities of long-term debt |
4,250 | 4,250 | 4,250 | |||||||||
| Deferred income taxes |
27,635 | 33,231 | 33,231 | |||||||||
| Total current liabilities |
230,322 | 244,500 | 244,500 | |||||||||
| Long-term debt, less current maturities |
627,250 | 611,025 | 611,025 | |||||||||
| Other non-current liabilities |
166,136 | 154,930 | 154,930 | |||||||||
| Members’ equity (deficit): |
||||||||||||
| Class A equity units |
339,418 | 339,070 | — | |||||||||
| Class B equity units |
719 | 1,028 | — | |||||||||
| Class C equity units |
436 | 616 | — | |||||||||
| Common stock, shares authorized and shares issued and outstanding at December 31, 2008 |
— | — | — | |||||||||
| Additional paid-in capital |
— | — | 340,714 | |||||||||
| Accumulated deficit |
(665,542 | ) | (622,234 | ) | (622,234 | ) | ||||||
| Accumulated other comprehensive earnings (loss) |
434 | (2,154 | ) | (2,154 | ) | |||||||
| Total members’ deficit |
(324,535 | ) | (283,674 | ) | (283,674 | ) | ||||||
| $ | 699,173 | $ | 726,781 | $ | 726,781 | |||||||
See accompanying notes to the consolidated financial statements.
F-3
Table of Contents
Consolidated Statements of Operations
| Year Ended December 31, | ||||||||||||
| 2006 | 2007 | 2008 | ||||||||||
| (In thousands, except per share data) |
||||||||||||
| Net revenues |
$ | 1,829,053 | $ | 2,106,152 | $ | 2,291,812 | ||||||
| Provision for uncollectibles |
733,666 | 874,087 | 960,495 | |||||||||
| Net revenues less provision for uncollectibles |
1,095,387 | 1,232,065 | 1,331,317 | |||||||||
| Cost of services rendered (exclusive of depreciation and amortization shown separately below) |
||||||||||||
| Professional service expenses |
831,826 | 950,872 | 1,046,806 | |||||||||
| Professional liability costs |
37,642 | 21,057 | 15,247 | |||||||||
| General and administrative expenses |
103,744 | 114,476 | 116,942 | |||||||||
| Management fee and other expenses |
3,748 | 4,054 | 3,602 | |||||||||
| Impairment of intangibles |
— | — | 9,134 | |||||||||
| Depreciation and amortization |
23,308 | 14,823 | 17,281 | |||||||||
| Interest expense, net |
57,813 | 55,234 | 45,849 | |||||||||
| Gain on extinguishment of debt |
— | — | (1,640 | ) | ||||||||
| Transaction costs |
— | — | 2,386 | |||||||||
| Earnings from continuing operations before income taxes |
37,306 | 71,549 | 75,710 | |||||||||
| Provision for income taxes |
13,792 | 27,703 | 31,044 | |||||||||
| Earnings from continuing operations |
23,514 | 43,846 | 44,666 | |||||||||
| Loss from discontinued operations, net of taxes |
(7,049 | ) | (576 | ) | — | |||||||
| Net earnings |
$ | 16,465 | $ | 43,270 | $ | 44,666 | ||||||
| Unaudited pro forma net earnings per share |
||||||||||||
| Basic |
$ | $ | $ | |||||||||
| Diluted |
$ | $ | $ | |||||||||
| Unaudited pro forma weighted average shares outstanding |
||||||||||||
| Basic |
||||||||||||
| Diluted |
||||||||||||
| Unaudited supplemental pro forma net earnings per share |
||||||||||||
| Basic |
$ | |||||||||||
| Diluted |
$ | |||||||||||
| Unaudited supplemental weighted average shares outstanding |
||||||||||||
| Basic |
||||||||||||
| Diluted |
||||||||||||
See accompanying notes to the consolidated financial statements.
F-4
Table of Contents
Consolidated Statements of
Members’ Equity (Deficit) and Comprehensive Earnings (Loss)
| Class A Equity Units |
Class B Equity Units |
Class C Equity Units |
Members’ Equity (Deficit) |
Accumulated Other Comprehensive Earnings (Loss) |
Total | |||||||||||||||||||
| (In thousands) | ||||||||||||||||||||||||
| Balance at December 31, 2005 |
$ | 339,813 | $ | — | $ | — | $ | (722,996 | ) | $ | (338 | ) | $ | (383,521 | ) | |||||||||
| Net earnings |
— | — | — | 16,465 | — | 16,465 | ||||||||||||||||||
| Other comprehensive income, net of tax: |
||||||||||||||||||||||||
| Net change in fair value of investments, net of tax of $33 |
— | — | — | — | 62 | 62 | ||||||||||||||||||
| Total comprehensive earnings |
— | — | — | — | — | 16,527 | ||||||||||||||||||
| Equity based compensation |
— | 384 | 233 | — | — | 617 | ||||||||||||||||||
| Redemption of equity units |
(410 | ) | (1 | ) | — | (17 | ) | — | (428 | ) | ||||||||||||||
| Proceeds from sale of equity units |
115 | — | — | — | — | 115 | ||||||||||||||||||
| Balance at December 31, 2006 |
$ | 339,518 | $ | 383 | $ | 233 | $ | (706,548 | ) | $ | (276 | ) | $ | (366,690 | ) | |||||||||
| Net earnings |
— | — | — | 43,270 | — | 43,270 | ||||||||||||||||||
| Other comprehensive income, net of tax: |
||||||||||||||||||||||||
| Net change in fair value of investments, net of tax of $382 |
— | — | — | — | 710 | 710 | ||||||||||||||||||
| Total comprehensive earnings |
— | — | — | — | — | 43,980 | ||||||||||||||||||
| Adjustment to initially apply FIN No. 48 |
— | — | — | (1,428 | ) | — | (1,428 | ) | ||||||||||||||||
| Equity based compensation |
— | 349 | 211 | — | — | 560 | ||||||||||||||||||
| Redemption of equity units |
(150 | ) | (13 | ) | (8 | ) | (836 | ) | — | (1,007 | ) | |||||||||||||
| Proceeds from sale of equity units |
50 | — | — | — | — | 50 | ||||||||||||||||||
| Balance at December 31, 2007 |
$ | 339,418 | $ | 719 | $ | 436 | $ | (665,542 | ) | $ | 434 | $ | (324,535 | ) | ||||||||||
| Net earnings |
— | — | — | 44,666 | — | 44,666 | ||||||||||||||||||
| Other comprehensive income, net of tax: |
||||||||||||||||||||||||
| Net change in fair value of investments, net of tax of $429 |
— | — | — | — | 795 | 795 | ||||||||||||||||||
| Net change in fair value of swaps, net of tax of ($2,164) |
— | — | — | — | (3,383 | ) | (3,383 | ) | ||||||||||||||||
| Total comprehensive earnings |
— | — | — | — | — | 42,078 | ||||||||||||||||||
| Equity based compensation |
— | 394 | 231 | — | — | 625 | ||||||||||||||||||
| Redemption of equity units |
(348 | ) | (85 | ) | (51 | ) | (1,358 | ) | — | (1,842 | ) | |||||||||||||
| Balance at December 31, 2008 |
$ | 339,070 | $ | 1,028 | $ | 616 | $ | (622,234 | ) | $ | (2,154 | ) | $ | (283,674 | ) | |||||||||
See accompanying notes to the consolidated financial statements.
F-5
Table of Contents
Consolidated Statements of Cash Flows
| Year Ended December 31, | ||||||||||||
| 2006 | 2007 | 2008 | ||||||||||
| (In thousands) | ||||||||||||
| Operating activities |
||||||||||||
| Net earnings |
$ | 16,465 | $ | 43,270 | $ | 44,666 | ||||||
| Adjustments to reconcile net earnings: |
||||||||||||
| Depreciation and amortization |
23,987 | 14,872 | 17,281 | |||||||||
| Amortization of deferred financing costs |
2,426 | 2,138 | 2,082 | |||||||||
| Employee equity based compensation expense |
617 | 560 | 625 | |||||||||
| Provision for uncollectibles |
733,666 | 874,087 | 960,495 | |||||||||
| Impairment of intangibles |
10,198 | — | 9,134 | |||||||||
| Deferred income taxes |
4,518 | 22,788 | 19,519 | |||||||||
| Gain on extinguishment of debt |
— | — | (1,640 | ) | ||||||||
| Loss on disposal of equipment |
128 | 553 | 78 | |||||||||
| Equity in joint venture (income) loss |
(274 | ) | 51 | 64 | ||||||||
| Changes in operating assets and liabilities, net of acquisitions: |
||||||||||||
| Accounts receivable |
(760,290 | ) | (889,659 | ) | (975,682 | ) | ||||||
| Prepaids and other assets |
(8,530 | ) | (7,761 | ) | (8,250 | ) | ||||||
| Income tax accounts |
14,777 | 1,802 | (4,709 | ) | ||||||||
| Accounts payable |
(4,979 | ) | (1,557 | ) | 1,254 | |||||||
| Accrued compensation and physician payable |
6,760 | 16,712 | 9,389 | |||||||||
| Other accrued liabilities |
(1,743 | ) | (194 | ) | (2,999 | ) | ||||||
| Professional liability reserves |
11,827 | (7,608 | ) | (9,336 | ) | |||||||
| Net cash provided by operating activities |
49,553 | 70,054 | 61,971 | |||||||||
| Investing activities |
||||||||||||
| Purchases of property and equipment |
(11,271 | ) | (12,680 | ) | (12,141 | ) | ||||||
| Cash paid for acquisitions, net |
(20,898 | ) | (3,545 | ) | (7,513 | ) | ||||||
| Purchases of investments at insurance subsidiary |
(96,337 | ) | (181,233 | ) | (180,578 | ) | ||||||
| Proceeds from investments at insurance subsidiary |
78,075 | 166,077 | 170,447 | |||||||||
| Other investing activities |
322 | 125 | 13 | |||||||||
| Net cash used in investing activities |
(50,109 | ) | (31,256 | ) | (29,772 | ) | ||||||
| Financing activities |
||||||||||||
| Payments on notes payable |
(4,250 | ) | (4,250 | ) | (4,250 | ) | ||||||
| Payments on 11.25% senior subordinated notes |
— | — | (9,999 | ) | ||||||||
| Proceeds from revolving credit facility |
265,400 | 83,000 | — | |||||||||
| Payments on revolving credit facility |
(263,900 | ) | (89,800 | ) | — | |||||||
| Transaction payments in connection with recapitalization |
(56 | ) | — | — | ||||||||
| Payments of deferred financing costs |
(825 | ) | (500 | ) | — | |||||||
| Purchase of treasury shares |
(2,570 | ) | — | — | ||||||||
| Proceeds from sale of common units |
115 | 50 | — | |||||||||
| Redemptions of common units |
(3 | ) | (1,007 | ) | (1,842 | ) | ||||||
| Net cash used in financing activities |
(6,089 | ) | (12,507 | ) | (16,091 | ) | ||||||
| Increase (decrease) in cash and cash equivalents |
(6,645 | ) | 26,291 | 16,108 | ||||||||
| Cash and cash equivalents, beginning of year |
10,644 | 3,999 | 30,290 | |||||||||
| Cash and cash equivalents, end of year |
$ | 3,999 | $ | 30,290 | $ | 46,398 | ||||||
| Supplemental cash flow information: |
||||||||||||
| Interest paid |
$ | 57,997 | $ | 57,881 | $ | 48,550 | ||||||
| Taxes paid |
$ | 5,766 | $ | 3,600 | $ | 16,392 | ||||||
See accompanying notes to the consolidated financial statements.
F-6
Table of Contents
Notes to the Consolidated Financial Statements
December 31, 2008
1. Organization and Basis of Presentation
The Company, as used herein, refers to Team Health Holdings, LLC (See Corporate Reorganization below) and its consolidated subsidiaries. The Company is the largest provider of outsourced physician staffing and administrative services to hospitals and other healthcare providers in the United States, based upon revenues and patient visits. We serve approximately 550 hospital clients and their affiliated clinics and surgical centers in 46 states with a team of approximately 6,200 healthcare professionals including physicians, mid-level practitioners and nurses. Since our inception in 1979, we have focused primarily on providing outsourced services to hospital emergency departments, which accounted for 70% of our net revenues less provision for uncollectibles in 2008. We also provide comprehensive programs for inpatient care (hospitalist), radiology, pediatrics and other healthcare services, principally within hospitals and other healthcare facilities.
Corporate Reorganization
On the Company converted from a limited liability company to a Delaware corporation, Team Health Holdings, Inc. (“Holdings”), so that its existing investors will own common stock rather than equity interests in a limited liability company. The Company refers to this event as its corporate reorganization.
As a result of the corporate reorganization, Team Health Holdings, LLC’s Class A shares were converted to shares of Holdings’ common stock. In addition, outstanding Class B and C shares that had vested on or prior to (the date of our corporate reorganization) were converted to shares of Holdings’ common stock.
Unaudited Pro forma Financial Information
The unaudited pro forma balance sheet gives effect to the change in capitalization on resulting from the conversion of Class A, B, and C shares for Holdings’ common stock. The pro forma balance sheet does not reflect any initial public offering proceeds.
The accompanying consolidated statements of operations discloses unaudited pro forma earnings per share for the years ended December 31, 2006 and 2007, and 2008 giving affect to the exchange of Class A, B and C shares for Holdings’ common stock.
Unaudited Supplemental Pro Forma Financial Information
The accompanying consolidated statements of operations discloses unaudited supplemental pro forma earnings per share for the year ended December 31, 2008 giving effect to the portion of the offering proceeds to be used for the repayment of the Company’s indebtedness.
2. Significant Accounting Policies
Principles of Consolidation
The consolidated financial statements include the accounts of the Company and its wholly-owned subsidiaries and have been prepared in accordance with accounting principles generally accepted in the United States. All intercompany and inter-affiliate accounts and transactions have been eliminated.
F-7
Table of Contents
The Company consolidates its subsidiaries in accordance with the nominee shareholder model of Accounting Standards Codification (“ASC”) Topic 810-10-15 (formerly Emerging Issues Task Force (EITF) No. 97-2 “Application of FASB No. 94 and APB Opinion No. 16 to Physician Practice Entities and Certain Other Entities with Contractual Management Arrangements”). The Company’s arrangements with associated professional corporations (“PC”) are captive in nature as a majority of the outstanding voting equity instruments of the different PCs are owned by a nominee shareholder appointed at the sole discretion of the Company. The Company has a contractual right to transfer the ownership of the PC at any time to any person it designates as the nominee shareholder. This transfer can occur without cause and any cost incurred as a result of the transfer is minimal. There would be no significant impact on the PC or the Company as a result of the transfer of ownership. The Company provides staffing services to its client hospitals through management services agreements between subsidiaries of the Company and the PCs.
Cash and Cash Equivalents
Cash consists primarily of funds on deposit in commercial banks. Cash equivalents are highly liquid investments with maturities of three months or less when acquired.
Marketable Securities
In accordance with ASC Topic 320, “Debt and Equity Securities” (formerly Statement of Financial Accounting Standards (SFAS) No. 115 “Accounting for Certain Investments in Debt and Equity Securities,”) management determines the appropriate classification of the Company’s investments at the time of purchase and reevaluates such determination at each balance sheet date. As of December 31, 2008 and 2007, the Company has classified all marketable debt securities as available-for-sale. Available-for-sale securities are carried at fair value, with the unrealized gains and losses, net of tax, reported in other comprehensive earnings. Realized gains and losses and declines in value judged to be other-than-temporary on available for sale securities are recognized in earnings.
Accounts Receivable
Accounts receivable are primarily due from hospitals and clinics, third-party payers, such as insurance companies, government-sponsored healthcare programs, including Medicare and Medicaid, and self-insured employers and patients. Accounts receivable are stated net of reserves for amounts estimated by management to not be collectible. Concentration of credit risk relating to accounts receivable is somewhat limited by the diversity and number of hospitals, patients, payers and by the geographic dispersion of the Company’s operations. In addition, a portion of the Company’s military staffing business is conducted on a sub-contract basis with a third-party direct contractor to the military. The amount owed by such direct contractor represents approximately 5.2% of the Company’s consolidated accounts receivable as of December 31, 2008.
Property and Equipment
Property and equipment are stated at cost. Depreciation is computed using the straight-line method over estimated useful lives, which generally range from 3 to 10 years for furniture and equipment, from 3 to 5 years for software and from 10 to 40 years for buildings and leasehold improvements. Property under capital lease is amortized using the straight-line method over the life of the respective lease and such amortization is included in depreciation expense.
Intangible Assets
The Company’s intangible assets include goodwill and other intangibles that consist primarily of the fair value of service contracts acquired. Goodwill represents the excess of purchase price over the fair value of net assets acquired.
F-8
Table of Contents
In accordance with the provisions of ASC Topic 350, “Intangibles—Goodwill and other” (formerly SFAS No. 142, Goodwill and Other Intangible Assets) goodwill and intangible assets deemed to have indefinite lives are not amortized. The cost of service contracts and other intangibles acquired is amortized using the straight-line method over their estimated lives.
Goodwill is evaluated for possible impairment on an annual basis or more frequently if events and circumstances occur that may indicate the potential for impairment. Goodwill assigned to a reporting unit is evaluated for potential impairment following a two-step procedure. The fair value of the reporting unit is initially determined and compared to its carrying value. If the carrying value exceeds the fair value of the applicable reporting unit, the implied fair value of the goodwill of the reporting unit is then determined. If it is determined that the implied fair value of the goodwill of the reporting unit is less than the carrying value of goodwill, an impairment loss is recorded equal to such difference.
The carrying value of other intangibles is evaluated when indicators are present to determine whether such intangibles may be impaired with respect to their recorded values. If this review indicates that certain intangibles will not be recoverable, as determined based on the undiscounted cash flows derived from the assets acquired over the remaining estimated asset life, the carrying value of the intangibles is reduced by the estimated shortfall of discounted cash flows.
Deferred Financing Costs
Deferred financing costs, which are included in other noncurrent assets and are amortized over the term of the related debt using the effective interest method, consisted of the following as of December 31 (in thousands):
| 2007 | 2008 | |||||||
| Deferred financing costs |
$ | 19,696 | $ | 19,246 | ||||
| Less accumulated amortization |
(4,814 | ) | (6,782 | ) | ||||
| $ | 14,882 | $ | 12,464 | |||||
Risk Management
Although the Company does not principally engage in the practice of medicine or provide medical services, it does require the physicians with whom it contracts to obtain professional liability insurance coverage and makes this insurance available to these physicians. The Company typically provides claims-made coverage on a per incident and annual aggregate limit per physician to affiliated physicians and other healthcare practitioners. In addition, the Company has claims-made coverage on a per incident and annual aggregate limit for all corporate entities.
Effective March 12, 2003, the Company began providing for its professional liability losses principally under a program of self-insurance, including the use of a wholly owned captive insurance company. The Company’s estimated losses under the self-insurance program are determined using periodic actuarial estimates of losses and related expenses, adjusted on an interim basis for actual provider hours worked and loss development trends. Any differences between amounts previously recorded and the results of updated actuarial studies of prior periods are recorded in the period when such differences are known.
Professional liability insurance expense consists of premium costs, an accrual to establish reserves for future payments under the self-insured retention component, an accrual to establish a reserve for future claims incurred but not reported, and other administrative costs of operating the insurance program.
F-9
Table of Contents
Derivatives
The Company at times may utilize derivative financial instruments to reduce interest rate risks. The Company does not hold or issue derivative financial instruments for trading purposes. The Company recognizes all derivatives as either assets or liabilities in the balance sheet and measures those instruments at fair value. Changes in the fair value of these instruments are reported in earnings or other comprehensive income depending on the use of the derivative and whether it qualifies for hedge accounting. The accounting for gains and losses associated with changes in the fair value of the derivative and the effect on the consolidated financial statements depends on its hedge designation and whether the hedge is highly effective in achieving offsetting changes in the fair value of cash flows of the asset or liability hedged. There were no outstanding agreements during 2006 or 2007. During 2008, the Company entered into three separate forward interest rate swap agreements. The objective of the agreements is to eliminate the variability of the cash flows in interest payments for $200.0 million of the variable-rate term loan for a three-year period. The agreements are contracts to exchange, on a quarterly basis, floating interest rate payments based on the Eurocurrency rate, for fixed interest payments over the life of the agreements. The Company has determined the interest rate swaps are highly effective and qualify for hedge accounting.
Revenue Recognition
Net revenues consist of fee for service revenue, contract revenue and other revenue. Net revenues are recorded in the period services are rendered.
Net revenues are principally derived from the provision of healthcare staffing services to patients within healthcare facilities. The form of billing and related risk of collection for such services may vary by customer. The following is a summary of the principal forms of the Company’s billing arrangements and how net revenue is recognized for each. A significant portion (80% of the Company’s net revenue in 2007 and 2008) resulted from fee for service patient visits. Fee for service revenue represents revenue earned under contracts in which the Company bills and collects the professional component of charges for medical services rendered by the Company’s contracted and employed physicians. Under the fee for service arrangements, the Company bills patients for services provided and receives payment from patients or their third-party payers. Fee for service revenue is reported net of contractual allowances and policy discounts. All services provided are expected to result in cash flows and are therefore, reflected as net revenues in the financial statements. Fee for service revenue is recognized in the period that the services are rendered to specific patients and reduced immediately for the estimated impact of contractual allowances in the case of those patients having third-party payer coverage. The recognition of net revenue (gross charges less contractual allowances) from such visits is dependent on such factors as proper completion of medical charts following a patient visit, the forwarding of such charts to one of the Company’s billing centers for medical coding and entering into the Company’s billing systems and the verification of each patient’s submission or representation at the time services are rendered as to the payer(s) responsible for payment of such services. Net revenues are recorded based on the information known at the time of entering of such information into the Company’s billing systems as well as an estimate of the net revenues associated with medical charts for a given service period that have not been processed yet into the Company’s billing systems. The above factors and estimates are subject to change. For example, patient payer information may change following an initial attempt to bill for services due to a change in payer status. Such changes in payer status have an impact on recorded net revenue due to differing payers being subject to different contractual allowance amounts. Such changes in net revenue are recognized in the period that such changes in payer become known. Similarly, the actual volume of medical charts not processed into the billing systems may be different from the amounts estimated. Such differences in net revenue are adjusted in the following month based on actual chart volumes processed.
Contract revenue represents revenue generated under contracts in which the Company provides physician and other healthcare staffing and administrative services in return for a contractually negotiated fee. Contract revenue consists primarily of billings based on hours of healthcare staffing provided at agreed to hourly
F-10
Table of Contents
rates. Revenue in such cases is recognized as the hours are worked by the Company’s staff. Additionally, contract revenue also includes supplemental revenue from hospitals where the Company may have a fee for service contract arrangement. Contract revenue for the supplemental billing in such cases is recognized based on the terms of each individual contract. Such contract terms generally either provide for a fixed monthly dollar amount or a variable amount based upon measurable monthly activity, such as hours staffed, patient visits or collections per visit compared to a minimum activity threshold. Such supplemental revenues based on variable arrangements are usually contractually fixed on a monthly, quarterly or annual calculation basis considering the variable factors negotiated in each such arrangement. Such supplemental revenues are recognized as revenue in the period when such amounts are determined to be fixed and therefore, contractually obligated as payable by the customer under the terms of the respective agreement.
Other revenue consists primarily of revenue from management and billing services provided to outside parties. Revenue is recognized for such services pursuant to the terms of the contracts with customers. Generally, such contracts consist of fixed monthly amounts with revenue recognized in the month services are rendered or as hourly consulting fees recognized as revenue as hours are worked in accordance with such arrangements. Additionally, the Company derives a small percentage of revenue from providing administrative and billing services that are contingent upon the collection of third-party physician billings, either by us on their behalf or other third-party billing companies. Such revenues are not considered earned and therefore, not recognized as revenue until actual cash collections are achieved in accordance with the contractual arrangements for such services.
Net revenues are reduced for management’s estimates of amounts that will not be collected. The resulting net revenue less provision for uncollectibles reflects net cash collections for services rendered in the period, plus management’s estimate of the remaining collections to be realized for services rendered in the period. Such estimates of amounts to be collected are subject to adjustment as actual experience is realized. If subsequent collections experience indicates that an adjustment to previously recorded collection estimates is necessary, such change of estimate adjustment is recorded in the current period in which such assessment is made.
Management in estimating the amounts to be collected resulting from its over seven million annual fee for service patient visits and procedures considers such factors as prior contract collection experience, current period changes in payer mix and patient acuity indicators, reimbursement rate trends in governmental and private sector insurance programs, resolution of overprovision account balances, the estimated impact of billing system effectiveness improvement initiatives and trends in collections from self-pay patients and external credit agencies. The complexity of the estimation process associated with the Company’s fee for service volumes and diverse payer mix, along with the difficulty of assessing such factors as changes in the economy impacting the number of healthcare insured versus uninsured patients and other socio-economic trends that can have an impact on collection rates, could result in subsequent material adjustments to previously reported revenues.
The Company derives a significant portion of its net revenues less provision for uncollectibles from government sponsored healthcare programs. Net revenue less provision for uncollectibles derived from the Medicare and Medicaid programs was approximately 24% of total net revenue less provision for uncollectibles in years 2006, 2007 and 2008. In addition, net revenues less provision for uncollectibles derived from within the Military Health System (“MHS”), which is the U.S. military’s dependent healthcare program, was approximately 14% in 2006 and 12% in 2007 and 2008.
Segment Reporting
The Company provides its services through four operating segments which are aggregated into two reportable segments, Healthcare Services and Billing Services. The Healthcare Services segment, which is an aggregation of healthcare staffing, clinics, and occupation health, provides comprehensive healthcare service programs to users and providers of healthcare services on a fee for service as well as a cost plus basis. The Billing Services segment provides a range of external billing, collection and consulting services on a fee basis to outside third-party customers.
F-11
Table of Contents
Unaudited Pro Forma Basic and Diluted Net Earnings Per Share
Pro forma basic and diluted net earnings per share is calculated in accordance with ASC Topic 260, “Earning Per Share” (formerly SFAS No. 128, Earnings Per Share). Pro forma basic and diluted net earnings per share (“EPS”) is calculated using the weighted-average common shares outstanding in each period.
The shares used to calculate pro forma basic and dilutive EPS represent the weighted-average common shares outstanding.
| Year ended December 31, | |||||||||
| 2006 | 2007 | 2008 | |||||||
| Numerator for basic and diluted net earnings per share: |
|||||||||
| Earnings from continuing operations |
$ | $ | $ | ||||||
| Earnings from discontinued operations |
|||||||||
| Net earnings |
|||||||||
| Denominator: |
|||||||||
| Denominator for basic earnings per share-weighted average shares |
|||||||||
| Effect of dilutive securities |
|||||||||
| Denominator for diluted net earnings per share-weighted average shares |
|||||||||
| Basic net earnings per share: |
|||||||||
| Basic earnings from continuing operations |
$ | $ | $ | ||||||
| Basic earnings from discontinued operations |
|||||||||
| Basic net earnings |
|||||||||
| Diluted net earnings per share: |
|||||||||
| Diluted earnings from continuing operations |
$ | $ | $ | ||||||
| Diluted earnings from discontinued operations |
|||||||||
| Diluted net earnings |
|||||||||
Unaudited Supplemental Pro Forma Basic and Diluted Earnings per Share
Unaudited supplemental pro forma basic and diluted net earnings per share for the year ended December 31, 2008 gives effect to the portion of the offering proceeds to be used for the repayment of the Company’s indebtedness.
| Year ended December 31, 2008 | |||||||||||
| Unaudited Pro forma |
Supplemental Pro Forma Adjustments |
Notes | Unaudited Supplemental Pro forma | ||||||||
| Numerator for basic and diluted net earning per share: |
|||||||||||
| Net earnings |
$ | $ | $ | ||||||||
| Denominator: |
|||||||||||
| Denominator for basic earnings per share–weighted average shares |
|||||||||||
| Effect of dilutive securities |
|||||||||||
| Denominator for diluted net earnings per share–weighted average shares outstanding |
|||||||||||
| Basic net earnings per share: |
|||||||||||
| Basic net earnings |
$ | $ | $ | ||||||||
| Diluted net earnings per share: |
|||||||||||
| Diluted net earnings |
$ | $ | $ | ||||||||
F-12
Table of Contents
Implementation of New Accounting Standards
In June 2009, the Financial Accounting Standards Board (“FASB”) issued ASC Topic 105 (formerly SFAS No. 168), “The FASB Accounting Standards Codification and the Hierarchy of Generally Accepted Accounting Principles”. ASC Topic 105 establishes the FASB Accounting Standards Codification (the “Codification”) as the single source of authoritative, nongovernmental U.S. GAAP. The Codification did not change U.S. GAAP. All existing accounting standard documents were superseded and all other accounting literature not included in the Codification is considered non-authoritative. ASC Topic 105 is effective for interim and annual periods ending after September 15, 2009. Therefore, the Company adopted ASC Topic 105 for the reporting in its 2009 third quarter. The adoption did not have a significant impact on the reporting of its financial position, results of operations or cash flows.
In April 2008, the FASB issued FASB Staff Position (“FSP”) No. FAS 142-3, “Determination of the Useful Life of Intangible Assets”, which was primarily codified into Topic 350 “Intangibles—Goodwill and Other” in the Accounting Standards Codification (“ASC”). This guidance amends the factors that should be considered in developing renewal or extension assumptions used to determine the useful life of a recognized intangible asset and requires enhanced related disclosures. This guidance must be applied prospectively to all intangible assets acquired as of and subsequent to fiscal years beginning after December 15, 2008. The adoption of FSP 142-3 did not have a material impact on the Company’s financial position, results of operations or cash flows.
In March 2008, the FASB issued and accounting update to ASC 815 “Derivatives and Hedging” (formerly SFAS No. 161, “Disclosures about Derivative Instruments and Hedging Activities-an amendment of FASB Statement No. 133”). ASC Topic 815 now requires enhanced disclosure related to derivatives and hedging activities and thereby seeks to improve the transparency of financial reporting. Under ASC Topic 815, entities are required to provide enhanced disclosures relating to: (a) how and why an entity uses derivative instruments; (b) how derivative instruments and related hedge items are accounted for under ASC Topic 815 , and its related interpretations; and (c) how derivative instruments and related hedged items affect an entity’s financial position, financial performance, and cash flows. The provisions of this update must be applied prospectively to all derivative instruments and non-derivative instruments that are designated and qualify as hedging instruments and related hedged items accounted for under ASC Topic 815 for all financial statements issued for fiscal years and interim periods beginning after November 15, 2008, which for the Company begins with its 2009 fiscal year. The adoption did not have a material impact on the reporting of its financial position, results of operations or cash flows.
In December 2007, the FASB issued ASC Topic 805 “Business Combinations” (formerly SFAS No. 141 (Revised 2007), “Business Combinations”). ASC Topic 805 continues to require the purchase method of accounting to be applied to all business combinations, but it significantly changes the accounting for certain aspects of business combinations. Under ASC Topic 805, an acquiring entity will be required to recognize all the assets acquired and liabilities assumed in a transaction at the acquisition-date fair value with limited exceptions. ASC TOPIC 805 will change the accounting treatment for certain specific acquisition related items including: (1) expensing acquisition related costs as incurred; (2) valuing noncontrolling interests at fair value at the acquisition date; and (3) recognizing contingent consideration arrangements on the acquisition date at fair value. ASC TOPIC 805 also includes a substantial number of new disclosure requirements. ASC TOPIC 805 is to be applied prospectively to business combinations for which the acquisition date is on or after January 1, 2009. As further discussed in Note 4, the Company recognized $0.6 million of direct transaction fees associated with ongoing discussions related to potential transactions that did not close before the effective date of ASC TOPIC 805. The Company expects ASC TOPIC 805 will have an impact on its accounting for future business combinations once adopted but the effect is dependent upon the acquisitions that are made in such periods.
In December 2007, the FASB released an accounting update to ASC Topic 810 “Consolidation” (formerly SFAS No. 160, “Noncontrolling Interests in Consolidated Financial Statements—an amendment of ARB No. 51”). The provisions of this update are effective for fiscal years, and interim periods within those fiscal
F-13
Table of Contents
years, beginning on or after December 15, 2008, which for the Company is the year ending December 31, 2009 and the interim periods within that fiscal year. The objective of this update is to improve the relevance, comparability, and transparency of the financial information that a reporting entity provides in its consolidated financial statements. This accounting update currently does not impact the Company as it has full controlling interest of all of its subsidiaries.
In February 2007, the FASB issued SFAS No. 159, “The Fair Value Option for Financial Assets and Financial Liabilities” (“SFAS 159”) which was codified into ASC Topic 825 “Financial Instruments”. The provisions within ASC Topic 825 allows entities to voluntarily choose to measure certain financial assets and liabilities at fair value (“fair value option”). The fair value option may be elected on an instrument-by-instrument basis and is irrevocable, unless a new election date occurs. If the fair value option is elected for an instrument, ASC Topic 825 specifies that unrealized gains and losses for that instrument be reported in earnings at each subsequent reporting date. The provisions of ASC Topic 825 were effective for the Company on January 1, 2008. The implementation of these provisions did not have an impact on the Company’s results of operations, financial position or cash flows as the Company did not elect to measure any eligible items at fair value other than instruments such as investments or interest rate swaps that are currently required to be measured at fair value.
In April 2009, the FASB issued an accounting standard update (formerly FSP FAS 157-4, “Determining Fair Value When the Volume and Level of Activity for the Asset or Liability Have Significantly Decreased and Identifying Transactions That Are Not Orderly) to ASC Topic 820, “Fair Value Measurements and Disclosures” (formerly Statement of Financial Accounting Standards No. 157, “Fair Value Measurements”). This accounting standard update provides additional guidance for estimating fair value in accordance with when the volume and level of activity for the asset or liability have significantly decreased. This update also includes guidance on identifying circumstances that indicate a transaction is not orderly and it emphasizes that even if there has been a significant decrease in the volume and level of activity for the asset or liability and regardless of the valuation technique(s) used, the objective of a fair value measurement remains the same. Fair value is the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction (that is, not a forced liquidation or distressed sale) between market participants at the measurement date under current market conditions. The provisions of this accounting standard update were effective for interim and annual reporting periods ending after June 15, 2009, and were applied prospectively. The implementation of this standard did not to have a material impact on the Company’s consolidated financial statements.
In April 2009, the FASB issued an accounting standard update (formerly FSP FAS 107-1 and APB 28-1, “Interim Disclosures about Fair Value of Financial Instruments”) to ASC Topic 825, “Financial Instruments”. This accounting standard update requires disclosures about fair value of financial instruments for interim reporting periods of publicly traded companies as well as in annual financial statements. The update was effective for interim and annual reporting periods ending after June 15, 2009. The implementation of the requirements of this update did not have a material impact on the Company’s consolidated financial statements.
In April 2009, the FASB issued an accounting standard update (formerly FSP SFAS 115-2 and SFAS 124-2, “Recognition and Presentation of Other-Than-Temporary Impairments”) to ASC Topic 320, “Investments—Debt and Equity Securities”, to amend the other-than-temporary impairment guidance in debt securities to be based on intent and not more likely than not that the Company would be required to sell the security before recovery and to improve the presentation and disclosure of other-than-temporary impairments on debt and equity securities in the financial statements. The adoption did not have a material effect on the Company’s consolidated financial statements.
In May 2009, the FASB issued ASC Topic 855 (formerly SFAS No. 165), “Subsequent Events”, to establish general standards of accounting for and disclosure of events that occur after the balance sheet date but before financial statements are issued. The provisions of ASC Topic 855 are effective for the quarter ended June 30, 2009.
F-14
Table of Contents
Use of Estimates
The preparation of financial statements in conformity with United States generally accepted accounting principles requires management to make estimates and assumptions that affect the amounts reported in the financial statements and accompanying notes. Actual results could differ from those estimates.
3. Discontinued Operations
In January 2007, the Company completed a strategic review of Team Health Anesthesiology Management Services (“THAMS”), and based upon the review, concluded that the existing business model of providing management services to independent physician groups was not a viable long term strategy and could not consistently meet internal growth targets. As a result of this review, the Company elected to exit this non-core business line. The final phase of this business line disposal was substantially completed during the third quarter of 2007, therefore in accordance with the provisions of ASC Topic 205-20, “Discontinued operations”. (formerly SFAS No. 144, Accounting for the Impairment or Disposal of Long-Lived Assets), the operating results of THAMS are presented in the accompanying consolidated statements of operations as a discontinued operation for all periods presented.
The financial results of THAMS included in discontinued operations as of December 31, were as follows (in thousands):
| 2006 | 2007 | 2008 | |||||||||
| Net revenue |
$ | 11,124 | $ | 2,368 | $ | — | |||||
| Total cost of services |
2,687 | 399 | — | ||||||||
| Loss before income taxes |
(9,524 | ) | (939 | ) | — | ||||||
| Benefit from income taxes |
(2,475 | ) | (363 | ) | — | ||||||
| Loss from discontinued operations |
$ | (7,049 | ) | $ | (576 | ) | $ | — | |||
The loss from discontinued operations in the year ended December 31, 2007 includes approximately $1.0 million of severance and other exit costs related to the disposal of this business unit.
The loss from discontinued operations in the year ended December 31, 2006 consists of an impairment loss of $10.2 million ($7.7 million, net of $2.5 million tax benefit). In April 2006, THAMS received notification from its largest anesthesia practice client of its intent to terminate its contract in accordance with the terms of the agreement. Management concluded that THAMS’ existing revenues and operating income would be materially adversely affected as a result of this contract termination. The above noted facts and circumstances were concluded by management to require a test for recoverability of the existing contract intangibles under the provisions of ASC Topic 360 “Property, Plant and Equipment” (formerly SFAS No. 144 “Accounting for the Impairment or Disposal of Long-Lived Assets”) and a “triggering event” under the provisions of ASC Topic 350 “Intangibles—Goodwill and other.” Consequently the Company recorded a charge of $2.0 million in the results of operations in the first quarter of 2006. The charge reduced the book value of the contract intangibles within the management services reporting segment to its fair value estimated to be $0.7 million, as determined by using a discounted cash flow model. In conjunction with management’s decision to exit this business line, the Company recorded an additional impairment loss of $0.7 million in the fourth quarter of 2006 in order to reduce the carrying value of the remaining intangible assets of THAMS.
Additionally, the Company recorded a goodwill impairment loss of $7.5 million in the first quarter of 2006. The estimated impairment was determined following the provisions of ASC Topic 350. Accordingly, the Company initially estimated the fair value of THAMS. The fair value of the business was determined using a multiple of projected cash flows on remaining contracts. The carrying value of the business exceeded its fair
F-15
Table of Contents
market value. The estimated fair value was allocated to the underlying net assets of the business following generally accepted accounting principles for allocating purchase prices. This included an allocation of value to the components of working capital, contract intangibles (based on discounting of future cash flows estimated to be derived from such contracts) with the remainder of such fair value assigned to goodwill. The estimate of the implied goodwill resulting from the aforementioned application of the principles outlined in ASC Topic 350 was less than the recorded goodwill related to THAMS.
For the year ended December 31, 2008, THAMS had no operating use of cash, and for the years ended December 31, 2007 and 2006, had uses of cash of $1.6 million and $0.9 million, respectively.
4. Acquisitions and Transaction Costs
Effective March 14, 2009, the Company acquired the operations of a physician staffing business that provides hospital emergency department services under three contracts for locations in Kentucky. The purchase price for the acquired company was $2.9 million which was paid in cash on the date of the closing. In addition, the Company may have to pay up to $1.3 million in future contingent payments based on the financial performance of the acquired company. The purchase agreement also provides for the payment of additional purchase price based on the twelve month results of operations of one of the contracts. The purchase price was allocated to, in accordance with the provisions of ASC Topic 805, to net assets acquired, including contract intangibles and accounts receivable, and goodwill based on management’s estimates. The results of operations of the acquired business are included in the Company’s consolidated financial statements beginning on the acquisition date.
Effective June 1, 2008, the Company completed the acquisition of certain assets and related business operations of an emergency medicine staffing business located in New Jersey. An officer of an affiliated corporation of the Company held an ownership interest in the selling party. The purchase price for the acquired business was $7.5 million which was paid in cash on the date of the closing. In addition, the Company may have to pay up to $6.7 million in deferred payments if future financial targets are achieved and certain contract terms are modified. In connection with the transaction the Company has recorded a $12.6 million contract intangible, which is the estimated fair value of the assets acquired at the date of the acquisition. The excess of fair value of the assets acquired compared to the amount paid as of the acquisition date has been reflected as “estimated amount due seller” in accordance with ASC Topic 805. Any contingent consideration payable in the future will be first applied to reduce the amount recorded as “estimated amount due seller”, and thereafter recorded to goodwill.
Effective August 24, 2007, the Company completed the acquisition of certain assets and related business operations of an emergency medicine staffing business located in Florida. The purchase price for the acquired business was $2.4 million which was paid in cash on the date of the closing. In addition, the Company may have to pay up to $2.2 million in future contingent payments. In connection with the transaction the Company has recorded a $4.3 million contract intangible, which is the estimated fair value of the assets acquired at the date of the acquisition. The excess of fair value of the assets acquired compared to the amount paid as of the acquisition date has been reflected as “estimated amount due seller” in accordance with ASC Topic 805. Any contingent consideration payable in the future will be first applied to reduce the amount recorded as “estimated amount due seller,” and thereafter to goodwill.
Effective May 1, 2006, the Company acquired the operations of two businesses. The acquired companies provide hospital emergency department and hospital physician staffing services under eleven contracts for locations in Ohio. The purchase price for the acquired companies was $4.0 million of which $3.0 million was paid in cash at May 1, 2006 and $1.0 million in assumed liabilities. The purchase price was allocated to contract intangibles based on the estimated fair value of the contracts obtained on the acquisition date.
Effective July 1, 2006, the Company completed the acquisition of certain assets and related business operations of a hospital medicine and inpatient services business located in Florida. The purchase price for the acquired business was $17.9 million which was paid in cash on the date of the closing. In addition, the Company
F-16
Table of Contents
paid $7.5 million of contingent consideration related to this acquisition on October 1, 2009. Following the payment no additional amounts are due under the acquisition agreement. Of the total purchase price, $6.6 million was allocated to contract intangibles based on the estimated fair value of the contracts obtained on the acquisition date. The remaining $18.8 million was recorded as goodwill.
During 2008 the Company made no payments related to previous acquisitions and in 2007 and 2006 the Company made payments of approximately $1.1 million and $0.1 million, respectfully, with respect to contingent payments established as a result of certain previous acquisitions. The $1.1 million payment made in 2007 had previously been recorded as a liability. The 2006 amount represents payments of additional purchase price for such acquisitions and have been recorded as goodwill.
Also, the Company recognized $2.4 million of transaction costs associated with terminated transactions in 2008 as well as costs associated with ongoing potential transactions. Costs associated with potential transactions are required to be expensed as incurred under the new accounting provisions of ASC Topic 805 which became effective for the Company January 1, 2009, and the Company elected to expense these costs during 2008 since the potential transactions did not close before the effective date for the new rules.
5. Impairment
The Company recorded an impairment loss of $9.1 million in 2008 related to $8.8 million of goodwill for its After Hours Pediatric and $0.3 million of goodwill for its Radiology business lines. The impairments were determined following the provisions of ASC Topic 350. Accordingly, the Company initially estimated the individual fair value of its After Hours Pediatric and Radiology reporting units. The fair value of the business lines was based upon a combination of current market valuations and the Company’s assessment of the projected operating performance and cash flows of these operations. The carrying value of these operations exceeded their estimated fair value. The estimated fair values were allocated to the underlying net assets of these operations following generally accepted accounting principles for allocation of purchase prices. This included an allocation of value to the components of working capital and fixed assets of these operations. After completion of the allocation of the estimated fair value to the existing assets and liabilities of these operations, there was no implied goodwill; therefore, the total recorded goodwill associated with these operations was considered impaired.
6. Fair Value Measurements
In September 2006, the FASB issued ASC Topic 820 “Fair Value Measurements and Disclosures” SFAS No. 157, Fair Value Measurements (“SFAS 157”). ASC Topic 820 defines fair value and applies to other accounting pronouncements that require or permit fair value measurements and expands disclosures about fair value measurements. ASC Topic 820 was effective for financial assets and liabilities in fiscal years beginning after November 15, 2007. In February 2008, the FASB issued an accounting standard update (formerly FASB Staff Position (“FSP”) FAS 157-1, Application of FASB Statement No. 157 to FASB Statement No. 13 and Other Accounting Pronouncements That Address Fair Value Measurements for Purposes of Lease Classification or Measurement under Statement 13), which states that ASC Topic 820 does not address fair value measurements for purposes of lease classification or measurement. This update does not apply to assets acquired and liabilities assumed in a business combination that are required to be measured at fair value under ASC Topic 805, regardless of whether those assets and liabilities are related to leases. In February 2008, the FASB also issued an accounting standards update (formerly FSP FAS 157-2, Effective Date of FASB Statement No. 157), which delayed the effective date of ASC Topic 820 to fiscal years beginning after November 15, 2008, for nonfinancial assets and liabilities, except for items that are recognized or disclosed at fair value in the financial statements on a recurring basis. In October 2008, the FASB also issued an accounting standards update (formerly FSP FAS 157-3, Determining the Fair Value of a Financial Asset When the Market for That Asset Is Not Active), which clarifies the application of ASC Topic 820 in a market that is not active.
The Company’s adoption of the provisions of ASC Topic 820 on January 1, 2008, with respect to financial assets and liabilities measured at fair value, did not have a material impact on our fair value measurements or our financial statements for the year ended December 31, 2008.
F-17
Table of Contents
ASC Topic 820 prioritizes the inputs used in measuring fair value into the following hierarchy:
| Level 1 | Quoted prices (unadjusted) in active markets for identical assets or liabilities; |
| Level 2 | Inputs other than quoted prices included within Level 1 that are either directly or indirectly observable; |
| Level 3 | Unobservable inputs in which little or no market activity exists, therefore requiring an entity to develop its own assumptions about the assumptions that market participants would use in pricing. |
The following table provides information on those assets and liabilities the Company measures at fair value on a recurring basis (in thousands):
| Carrying Amount In Consolidated Balance Sheet December 31, 2008 |
Fair Value December 31, 2008 |
Fair Value Level 1 |
Fair Value Level 2 |
Fair Value Level 3 | |||||||||||
| Investments of insurance subsidiary |
$ | 87,413 | $ | 87,413 | $ | 87,413 | $ | — | $ | — | |||||
| Interest rate swap liability |
5,547 | 5,547 | — | 5,547 | — | ||||||||||
The fair value of the Company’s investments of insurance subsidiary are based on quoted prices. As of December 31, 2008, the fair value of these investments reflected net unrealized gains of $0.8 million. The fair value of the Company’s interest rate swaps were determined by the Company’s counterparty using inputs that are available in the public swap markets for similarly termed instruments and then making adjustments for terms specific to the Company’s instruments. See Note 13 for more information regarding our interest rate swap agreements.
In addition to the preceding disclosures prescribed by the provisions of ASC Topic 820, ASC Topic 825 “Financial Instruments” (formerly SFAS No. 107 “Disclosures About Fair Value of Financial Instruments”) requires the disclosure of the estimated fair value of financial instruments. The Company’s short term financial instruments include cash and cash equivalents, accounts receivable, and accounts payable. The carrying value of the short term financial instruments approximates the fair value due to their short term nature. These financial instruments have no stated maturities or the financial instruments have short term maturities that approximate market.
The fair value of the Company’s debt is estimated using quoted market prices when available. When quoted market prices are not available, fair value is estimated based on current market interest rates for debt with similar maturities. The fair value of the Company’s debt was $621.5 million and $439.7 million at December 31, 2007 and 2008, respectively. The financial statement carrying value was $631.5 million and $615.3 million at December 31, 2007 and 2008, respectively.
F-18
Table of Contents
7. Other Intangible Assets
The following is a summary of other intangible assets and related amortization as of December 31, 2007 and 2008 for intangibles that are subject to amortization (in thousands):
| Gross Carrying Amount |
Accumulated Amortization | |||||
| As of December 31, 2007: |
||||||
| Contracts |
$ | 40,020 | $ | 12,864 | ||
| Other |
448 | 357 | ||||
| Total |
$ | 40,468 | $ | 13,221 | ||
| As of December 31, 2008: |
||||||
| Contracts |
$ | 52,632 | $ | 20,241 | ||
| Other |
448 | 401 | ||||
| Total |
$ | 53,080 | $ | 20,642 | ||
Total amortization expense for other intangibles was $15.9 million, $6.1 million and $7.4 million for the years 2006, 2007 and 2008, respectively.
The estimated annual amortization expense for intangibles for the next five years is as follows (in thousands):
| 2009 |
$ | 8,105 | |
| 2010 |
7,674 | ||
| 2011 |
5,955 | ||
| 2012 |
5,523 | ||
| 2013 |
3,909 |
Contract intangibles are amortized over their estimated life which is approximately four to seven years.
8. Property and Equipment
Property and equipment consists of the following at December 31 (in thousands):
| 2007 | 2008 | |||||||
| Land |
$ | 370 | $ | 370 | ||||
| Buildings and leasehold improvements |
10,652 | 10,747 | ||||||
| Furniture and equipment |
29,427 | 25,230 | ||||||
| Software |
9,502 | 10,528 | ||||||
| 49,951 | 46,875 | |||||||
| Less accumulated depreciation |
(24,675 | ) | (19,398 | ) | ||||
| $ | 25,276 | $ | 27,477 | |||||
Depreciation expense was $7.4 million in 2006, $8.8 million in 2007 and $9.9 million in 2008.
9. Receivables Under Insured Programs
Receivables under insured programs represent the portion of the Company’s reserves for professional liability losses estimated to be reimbursable under commercial insurance company policies. The entities providing professional liability coverage to the Company are creditworthy commercial insurance companies and the Company believes such receivables are probable of being collected and these companies will be able to fully satisfy their obligations under the insurance contracts.
F-19
Table of Contents
10. Other Assets
Other assets consist of the following as of December 31 (in thousands):
| 2007 | 2008 | |||||
| Deferred financing costs |
$ | 14,882 | $ | 12,464 | ||
| Other |
12,560 | 18,476 | ||||
| $ | 27,442 | $ | 30,940 | |||
11. Investments
Long term investments represent securities held by the captive insurance subsidiary. At December 31, the amortized cost basis and aggregate fair value of the Company’s available-for-sale securities by investment type were as follows (in thousands):
| 2007 | 2008 | |||||||||||
| Cost Basis | Fair Value | Cost Basis | Fair Value | |||||||||
| Money market funds |
$ | 34,184 | $ | 34,184 | $ | 17,780 | $ | 17,780 | ||||
| Treasury |
5,957 | 5,995 | 1,977 | 2,024 | ||||||||
| Municipal bonds |
— | — | 32,893 | 33,382 | ||||||||
| Agency notes |
23,553 | 24,179 | 23,909 | 25,263 | ||||||||
| Certificates of deposit |
11,699 | 11,699 | 8,964 | 8,964 | ||||||||
| $ | 75,393 | $ | 76,057 | $ | 85,523 | $ | 87,413 | |||||
At December 31, the amortized cost basis and aggregate fair value of the Company’s available-for-sale securities by contractual maturities were as follows (in thousands):
| 2007 | 2008 | |||||||||||
| Cost Basis | Fair Value | Cost Basis | Fair Value | |||||||||
| Due in less than one year |
$ | 36,838 | $ | 36,838 | $ | 20,857 | $ | 20,896 | ||||
| Due after one year through five years |
38,555 | 39,219 | 43,523 | 44,859 | ||||||||
| Due after five years through ten years |
— | — | 19,520 | 19,956 | ||||||||
| Due after ten years |
— | — | 1,623 | 1,702 | ||||||||
| $ | 75,393 | $ | 76,057 | $ | 85,523 | $ | 87,413 | |||||
As of December 31, 2007, there were $0.7 million of unrealized gains and no unrealized losses on investments. There were no realized gains or losses on investments during 2007. As of December 31, 2008, there were $2.2 million of unrealized gains and $0.3 million of unrealized losses on investments. There were $40,000 of realized gains and no realized losses on investments during 2008.
12. Other Accrued Liabilities
The Company’s other accrued liabilities consist of the following as of December 31 (in thousands):
| 2007 | 2008 | |||||
| Professional liability loss reserves |
$ | 67,666 | $ | 67,874 | ||
| Other |
16,188 | 14,138 | ||||
| $ | 83,854 | $ | 82,012 | |||
F-20
Table of Contents
13. Long-Term Debt
Long-term debt consists of the following as of December 31 (in thousands):
| 2007 | 2008 | |||||||
| Term Loan Facilities |
$ | 416,500 | $ | 412,250 | ||||
| 11.25% Senior Subordinated Notes |
215,000 | 203,025 | ||||||
| Revolving line of credit |
— | — | ||||||
| 631,500 | 615,275 | |||||||
| Less current portion |
(4,250 | ) | (4,250 | ) | ||||
| $ | 627,250 | $ | 611,025 | |||||
The interest rate for any revolving credit facility borrowings is based on a grid that is based on the consolidated ratio of total funded debt less unrestricted cash on the balance sheet to earnings before interest, taxes, depreciation and amortization, all as set forth in the credit agreement. As of December 31, 2008, the interest rate for borrowings under the revolving credit facility was equal to the euro dollar rate plus 2.0% or the agent bank’s base rate plus 1.0%. In addition, the Company pays a commitment fee for the revolving credit facility which is equal to 0.5% of the commitment at December 31, 2008.
The interest rate at December 31, 2008 was 4.0% for amounts outstanding under the term loan facility. Effective April 5, 2007, the Company amended its senior credit agreement. The amendment reduced the interest rate on any term loans outstanding equal to the euro dollar rate plus 2.0% or the agent bank’s base rate plus 1.0%. Previously, the interest rate on term loan borrowings was equal to the euro dollar rate plus 2.50% or the agent bank’s base rate plus 1.50%. The Company is subject to an increase in the term loan interest rate in the amount of 0.25% in the event of a downgrade in the corporate family rating of the Company by either Moody’s or Standard and Poor’s rating agencies. Other significant terms and conditions of the credit agreement, including the maturity date of November 23, 2012, did not change under the amendment.
During 2008, the Company entered into three separate forward interest rate swap agreements. The objective of the agreements is to eliminate the variability of the cash flows in interest payments for $200.0 million of the variable-rate term loan for a three-year period. The agreements are contracts to exchange, on a quarterly basis, floating interest rate payments based on the Eurocurrency rate, for fixed interest payments over the life of the agreements. The Company has determined the interest rate swaps are highly effective and qualify for hedge accounting, therefore in 2008, the Company has recorded the decrease in fair value of the interest rate swaps, net of tax, of approximately $3.4 million as a component of other comprehensive earnings. As of December 31, 2008 the Company had a $5.5 million liability recorded related to the swaps.
These agreements expose the Company to credit losses in the event of non-performance by the counterparty to the financial instruments. The counterparty is a creditworthy financial institution and the Company believes the counterparty will be able to fully satisfy its obligations under the contracts.
No borrowings under the $125.0 million revolving credit facility were outstanding as of December 31, 2008, and the Company had $8.7 million of standby letters of credit outstanding against the revolving credit facility commitment. Of the $125.0 million revolving credit facility, $15.0 million was held by Lehman Brothers Commercial Paper, Inc., a subsidiary of Lehman Brothers Holdings, Inc. which filed for bankruptcy on September 15, 2008. The Lehman Brothers Holdings, Inc. bankruptcy effectively reduced our borrowing capacity under the revolving credit facility by $15 million. The Company does not believe the potential reduction in available capacity under the revolving credit facility will have a material impact on its liquidity or the liquidity of its subsidiaries.
F-21
Table of Contents
The Company issued on November 23, 2005, 11.25% Senior Subordinated Notes (“Notes”) in the amount of $215.0 million due December 1, 2013. The Notes are subordinated in right of payment to all senior debt of the Company and are senior in right of payment to all existing and future subordinated indebtedness of the Company. Interest on the Notes accrues at the rate of 11.25% per annum, payable semi-annually in arrears on June 1 and December 1 of each year. Beginning on December 1, 2009, the Company may redeem some or all of the Notes at any time at various redemption prices. During 2008 the Company retired $12.0 million of the Notes in an open market purchase for $10.0 million plus accrued interest resulting in a net gain of $1.6 million. Included in the calculation of the gain on the extinguishment of debt was the write off of deferred financing costs of approximately $0.3 million.
The Notes are guaranteed jointly and severally on a full and unconditional basis by all of the Company’s domestic wholly-owned operating subsidiaries (“Subsidiary Guarantors”) as required by the Indenture Agreement.
Both the Notes and the senior secured credit facilities contain both affirmative and negative covenants, including limitations on the Company’s ability to incur additional indebtedness, sell material assets, retire, redeem or otherwise reacquire its capital stock, acquire the capital stock or assets of another business, pay dividends, and require the Company to comply with certain coverage and leverage ratios.
Aggregate annual maturities of long-term debt as of December 31, 2008 are as follows (in thousands):
| 2009 |
$ | 4,250 | |
| 2010 |
4,250 | ||
| 2011 |
4,250 | ||
| 2012 |
399,500 | ||
| 2013 |
203,025 | ||
| Thereafter |
— |
14. Other Noncurrent Liabilities
Other noncurrent liabilities consist of the following as of December 31 (in thousands):
| 2007 | 2008 | |||||
| Professional liability loss reserves |
$ | 153,252 | $ | 133,428 | ||
| Other |
12,884 | 21,502 | ||||
| $ | 166,136 | $ | 154,930 | |||
The Company’s professional liability loss reserves consist of the following as of December 31 (in thousands):
| 2007 | 2008 | |||||
| Estimated losses under self-insured programs |
$ | 162,904 | $ | 153,567 | ||
| Estimated losses under commercial insurance programs |
58,014 | 47,735 | ||||
| 220,918 | 201,302 | |||||
| Less—estimated amount payable within one year |
67,666 | 67,874 | ||||
| $ | 153,252 | $ | 133,428 | |||
F-22
Table of Contents
The changes to the Company’s estimated losses under self-insured programs for 2007 and 2008 are as follows (in thousands):
| 2007 | 2008 | |||||||
| Balance, December 31 |
$ | 170,512 | $ | 162,904 | ||||
| Reserves related to current period |
39,329 | 39,826 | ||||||
| Changes related to prior period reserves |
(32,089 | ) | (34,927 | ) | ||||
| Payments for current period reserves |
(16 | ) | (43 | ) | ||||
| Payment for prior period reserves |
(14,832 | ) | (14,193 | ) | ||||
| Balance, December 31 |
$ | 162,904 | $ | 153,567 | ||||
The Company provides for its estimated professional liability losses through a combination of self-insurance and commercial insurance programs. During the period March 12, 1999 through March 11, 2003, the primary source of the Company’s coverage for such risks was a professional liability insurance policy provided through one insurance carrier. The commercial insurance carrier policy included an insured loss limit of $130.0 million. In April 2006, the Company amended the policy with the commercial insurance carrier to provide for an increase in the aggregate limit of coverage based upon certain premium funding levels. As of December 31, 2008, the insured loss limit under the policy was $151.9 million. Losses in excess of the limit of coverage remain as a self-insured obligation of the Company. Beginning March 12, 2003, professional liability loss risks are principally being provided for through self-insurance with a portion of such risks (“claims-made” basis) transferred to and funded into a captive insurance company. The accounts of the captive insurance company are fully consolidated with those of the other operations of the Company in the accompanying financial statements.
The self insurance components of our risk management program include reserves for future claims incurred but not reported (“IBNR”). As of December 31, 2008, of the $153.6 million of estimated losses under self-insured programs, approximately $85.6 million represents an estimate of IBNR claims and expenses and additional loss development, with the remaining $68.0 million representing specific case reserves. Of the existing case reserves as of December 31, 2008, $0.9 million represent case reserves that have settled but not yet funded, and $67.1 million reflect unsettled case reserves.
At December 31, 2007, of the $162.9 million of estimated losses under self-insured programs, approximately $103.0 million represents an estimate of IBNR claims and expenses and additional loss development, with the remaining $59.9 million representing specific case reserves. Of the existing case reserves as of December 31, 2007, $1.0 million represent case reserves that have been settled but not yet funded, and $58.9 million reflect unsettled case reserves.
The Company’s provisions for losses under its self-insurance components are estimated using the results of periodic actuarial studies. Such actuarial studies include numerous underlying estimates and assumptions, including assumptions as to future claim losses, the severity and frequency of such projected losses, loss development factors and others. The Company’s provisions for losses under its self-insured components are subject to subsequent adjustment should future actuarial projected results for such periods indicate projected losses greater or less than previously projected. The Company’s estimated loss reserves under such programs are discounted at 4.0% and 2.2% at December 31, 2007 and 2008, respectively, which was the current ten year U.S. Treasury rate at those dates, which reflects the risk free interest rate over the expected period of claims payments.
The amounts at December 31, 2007 and 2008 reflected above as estimated losses under commercial insurance programs are expected to be paid by the underlying commercial insurance carriers to which applicable insurance premiums have previously been paid. Such amounts are, accordingly, offset by identical insurance receivable amounts in the accompanying balance sheets of the Company.
F-23
Table of Contents
Included in the consolidated statements of operations for the year ended December 31, 2007 and 2008 are reductions of professional liability reserves related to prior years of $32.1 million and $34.9 million, respectively, resulting from the Company’s receipt of revised actuarial loss estimates for these periods during the first and third quarters of each year.
15. Members’ Equity
Prior to our reorganization described in Note 1, Holdings total equity comprised of three classes of membership units: Class A Common Units, Class B Common Units, and Class C Common Units. The Company was authorized to issue 10,000,000 Class A Common Units, 400,000 Class B Common Units and 600,000 Class C Common Units. There is no vesting element associated with the Class A Common Units, but the Class B and C Common Units generally vest daily on a pro rata basis over a five year period from the date of issuance. Upon a change of control of the Company, all outstanding Class B and C Common Units automatically vest. Under the Company’s previous Amended and Restated Limited Liability Company Agreement, the timing and amount of any distribution of available cash, when made, are to be made in the order and priority among the different classes of units as specified in the Agreement. Generally, distributions of available cash could be made to the holders of Class A Common Units first before any distributions could be made to the holders of Class B or Class C Common Units and to the holders of Class A and Class B Common Units before any distributions could be made to the holders of Class C Common Units.
Class A membership units of Holdings
The Company purchased $1.0 million and $1.5 million of Class A Common Units from members of management in 2007 and 2008, respectively. Also, during 2007 the Company received proceeds of $0.1 million related to the issuance of Class A Common Units.
Equity incentive membership units of Holdings
Prior to the reorganization, Holdings adopted the 2005 unit plan on November 23, 2005 in connection with, and automatically upon the consummation of, the transactions contemplated by the Reorganization Merger. The plan provided for grants, sales or other issuances of Class A Common Units, Class B Common Units and Class C Common Units. The Company’s representatives, officers and other employees and persons who engaged in services for the Company and its affiliates were eligible for awards under the plan. The purpose of the plan was to provide these individuals with incentives to maximize shareholder value and otherwise contribute to the Company’s success and to enable it to attract, retain and reward the best available persons for positions of responsibility.
A total of 600,000 Class A Common Units had been authorized for issuance under the plan, subject to adjustment in the event of a reorganization, stock split, merger or similar change in our corporate structure or the outstanding Units. In addition, 400,000 Class B Common Units and 600,000 Class C Common Units had also been authorized for issuance under the plan. Holdings’ compensation committee administered the plan. Holdings’ board also had the authority to administer the plan and to take all actions that the compensation committee is otherwise authorized to take under the plan. The terms and conditions of each award made under the plan, including vesting requirements, was set forth consistent with the plan in a written agreement with the grantee.
Common units. Under the plan, the compensation committee could award or sell Class A Common Units, Class B Common Units, and Class C Common Units subject to such conditions (including vesting, performance conditions or otherwise), if any, as determined in the discretion of the compensation committee.
Amendment and termination of the plan. The board of representatives of Holdings could amend or terminate the plan in its discretion, except that no amendment could become effective without prior approval of
F-24
Table of Contents
the shareholders if such approval was necessary to satisfy any applicable tax or regulatory requirement. If not previously terminated by the board, the plan would terminate on the tenth anniversary of its adoption.
Compensation of representatives
None of our officers or those of Holdings receive any compensation for serving as a representative or as a member or chair of a committee of the board of representatives.
16. Share-based Compensation
In January 2006, Holdings adopted the 2005 Unit Plan. A total of 600,000 Class A Common Units, 400,000 Class B Common Units, and 600,000 Class C Common Units were authorized for issuance to executives and other key employees under the 2005 Unit Plan. No Class A Common Units were issued under the 2005 Unit Plan. Restricted Class B and Class C Common Unit activity under the 2005 Unit Plan during 2006, 2007 and 2008 was as follows (units in thousands):
| Class B Units | Class C Units | |||||
| Outstanding at December 31, 2005 |
— | — | ||||
| Granted |
318 | 445 | ||||
| Cancelled |
(5 | ) | (8 | ) | ||
| Outstanding at December 31, 2006 |
313 | 437 | ||||
| Granted |
4 | 6 | ||||
| Cancelled |
(11 | ) | (15 | ) | ||
| Outstanding at December 31, 2008 |
306 | 428 | ||||
| Granted |
55 | 77 | ||||
| Cancelled |
(31 | ) | (43 | ) | ||
| Outstanding at December 31, 2008 |
330 | 462 | ||||
| Vested units at December 31, 2006 |
68 | 95 | ||||
| Vested units at December 31, 2007 |
130 | 181 | ||||
| Vested units at December 31, 2008 |
193 | 270 |
The outstanding units vest ratably over five years from the date of grant and the Company is recognizing the related compensation expense over the five year period. Compensation expense for the employee equity based awards granted is based on the grant date fair value as calculated by the Black-Scholes option pricing formula with the following assumptions: risk-free interest rate of 4.3%, 4.7% and 3.1% in 2006, 2007 and 2008, respectively; implied volatility of 41.2%, 45.0% and 40% in 2006, 2007 and 2008, respectively; and an expected life of the units of four years in 2006, three years in 2007 and 2008. The average grant date fair value for Class B Units granted in 2006, 2007 and 2008 was $5.60, $12.27 and $14.37, respectively. The average grant date fair value for Class C Units granted in 2006, 2007 and 2008 was $2.41, $4.44 and $5.46, respectively. The Company recognized $0.6 million of employee equity based compensation expense in 2006, 2007 and 2008. As of December 31, 2007 and 2008, there was $1.6 million and $2.0 million, respectively of unrecognized compensation expense related to unvested restricted unit awards, which will be recognized over the remaining requisite service period. Forfeitures of employee equity based awards have been historically immaterial to the Company.
Also, in connection with the issuance of the restricted units, the Company recognized a tax benefit of approximately $1.0 million in 2006, $30,000 in 2007 and $0.5 million in 2008.
F-25
Table of Contents
17. Net Revenues
Net revenues in the following periods consisted of the following (in thousands):
| Year Ended December | |||||||||
| 2006 | 2007 | 2008 | |||||||
| Fee for service revenue |
$ | 1,426,749 | $ | 1,679,104 | $ | 1,827,607 | |||
| Contract revenue |
378,658 | 403,086 | 441,050 | ||||||
| Other revenue |
23,646 | 23,962 | 23,155 | ||||||
| $ | 1,829,053 | $ | 2,106,152 | $ | 2,291,812 | ||||
18. Income Taxes
The provision for income taxes from continuing operations consists of the following (in thousands):
| Year Ended December 31, | |||||||||
| 2006 | 2007 | 2008 | |||||||
| Current: |
|||||||||
| Federal |
$ | 1,238 | $ | 4,630 | $ | 10,411 | |||
| State |
986 | 2,644 | 3,150 | ||||||
| 2,224 | 7,274 | 13,561 | |||||||
| Deferred: |
|||||||||
| Federal |
10,966 | 20,205 | 16,514 | ||||||
| State |
602 | 224 | 969 | ||||||
| 11,568 | 20,429 | 17,483 | |||||||
| $ | 13,792 | $ | 27,703 | $ | 31,044 | ||||
The reconciliation of the provision for income taxes computed at the federal statutory tax rate to the provision for income taxes is as follows:
| Year Ended December 31, | |||||||||
| 2006 | 2007 | 2008 | |||||||
| Tax at statutory rate |
35.0 | % | 35.0 | % | 35.0 | % | |||
| State income tax (net of federal tax benefit) |
4.2 | 2.7 | 4.1 | ||||||
| Change in valuation allowance |
— | 2.4 | 0.7 | ||||||
| Adjustments to state net operating losses |
— | (1.1 | ) | 0.6 | |||||
| Resolution of tax issue |
(2.8 | ) | (0.5 | ) | — | ||||
| Permanent items and other |
0.6 | 0.2 | 0.3 | ||||||
| Nondeductible transaction related costs |
— | — | 0.3 | ||||||
| 37.0 | % | 38.7 | % | 41.0 | % | ||||
The effective income tax rates for 2006, 2007 and 2008 vary from the federal statutory tax rate due to state income taxes and the changes to state net operating losses and valuation allowances, in addition to the non-deductibility for tax purposes of transaction related costs in 2008.
F-26
Table of Contents
Deferred income taxes reflect the net tax effects of temporary differences between the carrying amounts of assets and liabilities for financial reporting purposes and the amounts used for income tax purposes. The components of the Company’s deferred tax assets and liabilities are as follows at December 31 (in thousands):
| 2007 | 2008 | |||||||
| Current deferred income tax assets: |
||||||||
| Accounts receivable |
$ | 14,376 | $ | 3,834 | ||||
| Accrued compensation and other |
3,186 | 3,034 | ||||||
| Professional liability reserves |
3,409 | 3,552 | ||||||
| Total current deferred income tax assets |
20,971 | 10,420 | ||||||
| Current deferred income tax liabilities: |
||||||||
| Affiliate deferred revenue |
(48,606 | ) | (43,651 | ) | ||||
| Total current deferred income tax liabilities |
(48,606 | ) | (43,651 | ) | ||||
| Net current deferred income tax liabilities |
$ | (27,635 | ) | $ | (33,231 | ) | ||
| Long term deferred income tax assets: |
||||||||
| Accrued compensation and other |
$ | 282 | $ | 2,340 | ||||
| Amortization and depreciation |
13,634 | 10,502 | ||||||
| Professional liability reserves |
41,673 | 30,303 | ||||||
| Net operating losses |
8,627 | 9,414 | ||||||
| Total long term deferred income tax assets |
64,216 | 52,559 | ||||||
| Valuation allowance |
(4,112 | ) | (4,644 | ) | ||||
| Net long-term deferred income tax assets |
$ | 60,104 | $ | 47,915 | ||||
| Total deferred income tax assets |
$ | 85,187 | $ | 62,979 | ||||
| Total deferred income tax liabilities |
(48,606 | ) | (43,651 | ) | ||||
| Valuation allowance |
(4,112 | ) | (4,644 | ) | ||||
| Net deferred income tax assets |
$ | 32,469 | $ | 14,684 | ||||
The Company recognizes valuation allowances on deferred tax assets reported, if based on the weight of evidence, it believes that it is more likely than not that some or not all of the deferred tax assets will be realized. As of December 31, 2007 and 2008, the Company had a valuation allowance of $4.1 million and $4.6 million, respectively. The net increase in the valuation allowance was due to an increase in state net operating losses incurred by subsidiaries that continue to report tax losses.
The Company, as of December 31, 2008, had net operating loss carryforwards in various states that expire at various times depending on the year generated and jurisdiction, the earliest expiration year being 2014.
The Company files income tax returns in the U.S. and in various states for its subsidiaries and remains subject to examination of its U.S. federal income tax returns for 2005 through 2007. In addition, the Company generally remains subject to examination of its various state returns for a period of three or four years from the date the returns were filed.
The Company adopted the provisions of FASB Interpretations (FIN) No. 48, “Accounting for Uncertainty in Income Taxes,” (FIN 48), which was codified into ASC Topic 740 “Income Taxes”, effective January 1, 2007. Because of the implementation of this update, the Company recognized a $1.4 million charge to members’ equity and an increase in the liability for unrecognized tax benefits of approximately $0.4 million.
F-27
Table of Contents
A reconciliation of the beginning and ending amount of unrecognized tax benefit (excluding interest and penalties) is as follows (in thousands):
| 2007 | 2008 | |||||||
| Balance at January 1 |
$ | 1,631 | $ | 2,612 | ||||
| Additions based on tax positions related to the current year |
1,088 | 397 | ||||||
| Reductions for tax positions of prior years |
— | (630 | ) | |||||
| Lapse of statutes of limitations |
(107 | ) | (166 | ) | ||||
| Balance at December 31 |
$ | 2,612 | $ | 2,213 | ||||
Operations of all operating subsidiaries are included in the consolidated federal income tax return of the Company for the three years in the period ended December 31, 2008. The Company is organized for tax purposes as a federal and state tax paying entity. The Company files tax returns in the U.S. and numerous state jurisdictions. A number of years may pass before an uncertain tax position, for which we have unrecognized benefits, is audited and resolved. It is difficult to predict the outcome for resolution; however, management believes that the unrecognized tax benefits recorded reflect the most likely outcome.
The total unrecognized tax benefits that, if recognized, would affect the effective rate is the entire balance of $2.2 million as it relates to uncertainties that are permanent deductions. It is reasonably possible that the amount of unrecognized tax benefits will decrease in 2009 as the result of a state audit, but the amount is not expected to be material.
The Company recognizes accrued interest and penalties, if applicable, associated with uncertain tax positions in the respective accounts in operating expenses. During the year ended December 31, 2008, the Company reported $0.1 million in interest expense related to the uncertain tax positions and no penalties.
19. Employee Savings Plans
The Company sponsors various employee savings plans that are primarily defined contribution plans. The Company recognized expense of approximately $3.1 million in 2006, $2.9 million in 2007 and $3.3 million in 2008 related to these plans.
The Company maintains a retirement savings plan for its employees. The plan is a defined contribution plan in accordance with the provisions of Section 401(k) of the Internal Revenue Code. The plan provides for a discretionary match by the Company up to a maximum of 50% of the first 6% of compensation contributed by employees. The Company’s provisions in the periods comprising 2006, 2007 and 2008 reflect the maximum discretionary provisions provided for under the plan.
The Company also maintains non-qualified deferred compensation plans for certain of its employees. Total deferred compensation payable as of December 31, 2007 and 2008 was approximately $11.5 million and $10.8 million, respectively.
F-28
Table of Contents
20. Commitments and Contingencies
Leases
The Company leases office space for terms of primarily one to ten years with options to renew for additional periods. Future minimum payments due on these non cancellable operating leases at December 31, 2008 are as follows (in thousands):
| 2009 |
$ | 8,288 | |
| 2010 |
8,066 | ||
| 2011 |
6,202 | ||
| 2012 |
5,065 | ||
| 2013 |
3,623 | ||
| Thereafter |
9,690 |
Operating lease costs were approximately $8.4 million, $10.6 million and $10.2 million for the years ended December 31, 2006, 2007 and 2008, respectively.
Litigation
We are currently a party to various legal proceedings. While we currently believe that the ultimate outcome of such proceedings, individually and in the aggregate, will not have a material adverse effect on our financial position or overall trends in results of operations, litigation is subject to inherent uncertainties. If an unfavorable ruling were to occur, there exists the possibility of a material adverse impact on our net earnings in the period in which a ruling occurs. The estimate of the potential impact from such legal proceedings on our financial position or overall results of operations could change in the future.
Healthcare Regulatory Matters
Laws and regulations governing the Medicare and Medicaid programs are complex and subject to interpretation. Compliance with such laws and regulations can be subject to future governmental review and interpretation as well as significant regulatory action. From time to time, governmental regulatory agencies will conduct inquiries and audits of the Company’s practices. It is the Company’s current practice and future intent to cooperate fully with such inquiries.
In addition to laws and regulations governing the Medicare and Medicaid programs, there are a number of federal and state laws and regulations governing such matters as the corporate practice of medicine and fee splitting arrangements, anti-kickback statutes, physician self-referral laws, false or fraudulent claims filing and patient privacy requirements. The failure to comply with any of such laws or regulations could have an adverse impact on our operations and financial results. It is management’s belief that the Company is in substantial compliance in all material respects with such laws and regulations.
Contingent Acquisition Payments
As of December 31, 2008, the Company may have to pay up to $16.5 million in future contingent payments as additional consideration for acquisitions made prior to December 31, 2008. Should the acquired operations achieve the financial targets contracted in the respective agreements related to their acquisition, any future payments made will first be applied to reduce the $5.8 million existing contingent payment liabilities recorded as “estimated amount due seller”, and the remaining $10.7 million will be recorded as goodwill.
F-29
Table of Contents
21. Related Party Transactions
The Company leases office space from several partnerships that are partially or entirely owned by certain employees of the Company. The leases were assumed by the Company as part of the merger or purchase transactions. Total related party lease costs were approximately $1.0 million in 2007 and $1.2 million in 2008 and 2006.
Effective with the merger on November 23, 2005, the Company is obligated under the terms of a 10-year agreement with Blackstone to pay an annual monitoring fee in the amount of $3.5 million. Furthermore, in the event of a change of control of the Company, as defined in the agreement, the Company is obligated to pay Blackstone on a discounted basis any remaining portion of the monitoring fee under the 10-year commitment that has not previously been paid prior to the date of the change of control event. In such event, an additional payment to management equity holders is payable by the Company on a pro rata basis equal to the amount of such discounted payment to Blackstone. Management services paid under this arrangement were $3.5 million in 2006, 2007 and 2008.
22. Segment Reporting
After consideration of the discontinued operations of its anesthesia management services business (Note 3), the Company provides services through four operating segments which are aggregated into two reportable segments, Healthcare Services and Billing Services. The Healthcare Services segment, which is an aggregation of healthcare staffing, clinics and occupational health, provides comprehensive healthcare service programs to users and providers of healthcare services on a fee for service as well as a cost plus basis. The Billing Services segment provides a range of external billing, collection and consulting services on a fee basis to outside third-party customers.
The accounting policies of the segments are the same as those described in the summary of significant accounting policies. Segment amounts disclosed are prior to any elimination entries made in consolidation, except in the case of net revenue, where intercompany charges have been eliminated. Certain expenses are not allocated to the segments. These unallocated expenses are corporate expenses, net interest expense, depreciation and amortization, transaction costs and income taxes. The Company evaluates segment performance based on profit and loss before the aforementioned expenses.
F-30
Table of Contents
The following table presents financial information for each reportable segment. Depreciation, amortization, impairment of intangibles, management fee and other expenses separately identified in the consolidated statements of operations are included as a reduction to the respective segments’ operating earnings for each year below (in thousands):
| Year ended December 31, | ||||||||||||
| 2006 | 2007 | 2008 | ||||||||||
| Net Revenues less Provision for Uncollectibles: |
||||||||||||
| Healthcare Services |
$ | 1,083,904 | $ | 1,220,173 | $ | 1,319,025 | ||||||
| Billing Services |
11,483 | 11,892 | 12,292 | |||||||||
| $ | 1,095,387 | $ | 1,232,065 | $ | 1,331,317 | |||||||
| Operating Earnings: |
||||||||||||
| Healthcare Services |
$ | 135,976 | $ | 173,851 | $ | 169,155 | ||||||
| Billing Services |
3,182 | 1,916 | 2,415 | |||||||||
| General Corporate |
(44,039 | ) | (48,984 | ) | (50,011 | ) | ||||||
| $ | 95,119 | $ | 126,783 | $ | 121,559 | |||||||
| Reconciliation of Operating Earnings to Net Earnings: |
||||||||||||
| Operating earnings |
$ | 95,119 | $ | 126,783 | $ | 121,559 | ||||||
| Interest expense, net |
57,813 | 55,234 | 45,849 | |||||||||
| Provision for income taxes |
13,792 | 27,703 | 31,044 | |||||||||
| Loss from discontinued operations, net of taxes |
7,049 | 576 | — | |||||||||
| Net earnings |
$ | 16,465 | $ | 43,270 | $ | 44,666 | ||||||
| Capital Expenditures: |
||||||||||||
| Healthcare Services |
$ | 2,920 | $ | 3,798 | $ | 2,328 | ||||||
| Billing Services |
758 | 2,786 | 2,696 | |||||||||
| General Corporate |
7,593 | 6,096 | 7,117 | |||||||||
| $ | 11,271 | $ | 12,680 | $ | 12,141 | |||||||
| Total Assets: |
||||||||||||
| Healthcare Services |
$ | 503,604 | $ | 526,075 | $ | 569,603 | ||||||
| Billing Services |
11,705 | 12,682 | 14,366 | |||||||||
| General Corporate |
139,251 | 160,416 | 142,812 | |||||||||
| $ | 654,560 | $ | 699,173 | $ | 726,781 | |||||||
F-31
Table of Contents
CONSOLIDATED BALANCE SHEETS
| December 31, 2008 |
September 30, 2009 |
Unaudited Pro forma as of September 30, 2009 |
||||||||||
| (Unaudited) (In thousands, except per share data) |
||||||||||||
| ASSETS |
||||||||||||
| Current assets: |
||||||||||||
| Cash and cash equivalents |
$ | 46,398 | $ | 112,994 | $ | 112,994 | ||||||
| Accounts receivable, less allowance for uncollectibles of $158,685 and $192,154 in 2008 and 2009, respectively |
237,790 | 237,563 | 237,563 | |||||||||
| Prepaid expenses and other current assets |
15,467 | 19,784 | 19,784 | |||||||||
| Income tax receivable |
3,446 | — | — | |||||||||
| Receivables under insured programs |
27,145 | 13,452 | 13,452 | |||||||||
| Total current assets |
330,246 | 383,793 | 383,793 | |||||||||
| Investments of insurance subsidiary |
87,413 | 95,591 | 95,591 | |||||||||
| Property and equipment, net |
27,477 | 24,841 | 24,841 | |||||||||
| Other intangibles, net |
32,438 | 27,938 | 27,938 | |||||||||
| Goodwill |
149,763 | 160,256 | 160,256 | |||||||||
| Deferred income taxes |
47,915 | 40,845 | 40,845 | |||||||||
| Receivables under insured programs |
20,589 | 30,298 | 30,298 | |||||||||
| Other |
30,940 | 36,887 | 36,887 | |||||||||
| $ | 726,781 | $ | 800,449 | $ | 800,449 | |||||||
| LIABILITIES AND MEMBERS’ EQUITY (DEFICIT) |
||||||||||||
| Current liabilities: |
||||||||||||
| Accounts payable |
$ | 13,451 | $ | 17,071 | $ | 17,071 | ||||||
| Accrued compensation and physician payable |
111,556 | 122,287 | 122,287 | |||||||||
| Other accrued liabilities |
82,012 | 68,681 | 68,681 | |||||||||
| Income tax payable |
— | 12,400 | 12,400 | |||||||||
| Current maturities of long-term debt |
4,250 | 4,250 | 4,250 | |||||||||
| Deferred income taxes |
33,231 | 30,677 | 30,677 | |||||||||
| Total current liabilities |
244,500 | 255,366 | 255,366 | |||||||||
| Long-term debt, less current maturities |
611,025 | 607,838 | 607,838 | |||||||||
| Other non-current liabilities |
154,930 | 165,572 | 165,572 | |||||||||
| Members’ equity (deficit): |
||||||||||||
| Class A equity units |
339,070 | 338,756 | — | |||||||||
| Class B equity units |
1,028 | 1,350 | — | |||||||||
| Class C equity units |
616 | 801 | — | |||||||||
| Common stock, shares authorized and shares issues and outstanding at September 30, 2009 |
— | — | ||||||||||
| Additional paid in capital |
— | — | 340,907 | |||||||||
| Accumulated deficit |
(622,234 | ) | (568,374 | ) | (568,374 | ) | ||||||
| Accumulated other comprehensive loss |
(2,154 | ) | (860 | ) | (860 | ) | ||||||
| Total members’ deficit |
(283,674 | ) | (228,327 | ) | (228,327 | ) | ||||||
| $ | 726,781 | $ | 800,449 | $ | 800,449 | |||||||
See accompanying notes to consolidated financial statements.
F-32
Table of Contents
CONSOLIDATED STATEMENTS OF OPERATIONS
| Nine Months Ended September 30, | |||||||
| 2008 | 2009 | ||||||
| (Unaudited) (In thousands, except per share data) | |||||||
| Net revenue |
$ | 1,720,775 | $ | 1,868,002 | |||
| Provision for uncollectibles |
720,968 | 793,345 | |||||
| Net revenue less provision for uncollectibles |
999,807 | 1,074,657 | |||||
| Cost of services rendered (exclusive of depreciation and amortization shown separately below) |
|||||||
| Professional service expenses |
779,426 | 828,268 | |||||
| Professional liability costs |
(2,986 | ) | 19,145 | ||||
| General and administrative expenses |
88,277 | 93,182 | |||||
| Management fee and other expenses |
2,745 | 2,324 | |||||
| Depreciation and amortization |
12,559 | 14,028 | |||||
| Interest expense, net |
34,033 | 27,671 | |||||
| Transaction costs |
1,805 | 578 | |||||
| Earnings before income taxes |
83,948 | 89,461 | |||||
| Provision for income taxes |
33,885 | 34,230 | |||||
| Net earnings |
$ | 50,063 | $ | 55,231 | |||
| Unaudited pro forma net earnings per share |
|||||||
| Basic |
$ | $ | |||||
| Diluted |
$ | $ | |||||
| Unaudited pro forma weighted average shares outstanding |
|||||||
| Basic |
|||||||
| Diluted |
|||||||
| Unaudited supplemental pro forma net earnings per share |
|||||||
| Basic |
$ | ||||||
| Diluted |
$ | ||||||
| Unaudited supplemental weighted average shares outstanding |
|||||||
| Basic |
$ | ||||||
| Diluted |
$ | ||||||
See accompanying notes to consolidated financial statements.
F-33
Table of Contents
CONSOLIDATED STATEMENTS OF CASH FLOWS
| Nine Months Ended September 30, |
||||||||
| 2008 | 2009 | |||||||
| (Unaudited) (In thousands) |
||||||||
| Operating Activities |
||||||||
| Net earnings |
$ | 50,063 | $ | 55,231 | ||||
| Adjustments to reconcile net earnings: |
||||||||
| Depreciation and amortization |
12,559 | 14,028 | ||||||
| Amortization of deferred financing costs |
1,561 | 1,554 | ||||||
| Employee equity based compensation expense |
439 | 558 | ||||||
| Provision for uncollectibles |
720,968 | 793,345 | ||||||
| Deferred income taxes |
19,864 | 2,782 | ||||||
| Loss on disposal of equipment |
63 | 75 | ||||||
| Equity in joint venture income |
(974 | ) | (1,473 | ) | ||||
| Changes in operating assets and liabilities, net of acquisitions: |
||||||||
| Accounts receivable |
(724,432 | ) | (792,051 | ) | ||||
| Prepaids and other assets |
(12,465 | ) | (11,658 | ) | ||||
| Income tax accounts |
3,327 | 16,051 | ||||||
| Accounts payable |
(2,194 | ) | 3,582 | |||||
| Accrued compensation and physician payable |
8,517 | 14,019 | ||||||
| Other accrued liabilities |
3,924 | (1,465 | ) | |||||
| Professional liability reserves |
(18,351 | ) | (9,957 | ) | ||||
| Net cash provided by operating activities |
62,869 | 84,621 | ||||||
| Investing Activities |
||||||||
| Purchases of property and equipment |
(7,341 | ) | (5,244 | ) | ||||
| Cash paid for acquisitions, net |
(7,513 | ) | (2,787 | ) | ||||
| Purchases of investments at insurance subsidiary |
(148,893 | ) | (92,962 | ) | ||||
| Proceeds from investments at insurance subsidiary |
142,591 | 87,882 | ||||||
| Other investing activities |
— | 9 | ||||||
| Net cash used in investing activities |
(21,156 | ) | (13,102 | ) | ||||
| Financing Activities |
||||||||
| Payments on notes payable |
(3,188 | ) | (3,187 | ) | ||||
| Redemption of common units |
(1,798 | ) | (1,736 | ) | ||||
| Net cash used in financing activities |
(4,986 | ) | (4,923 | ) | ||||
| Net increase in cash |
36,727 | 66,596 | ||||||
| Cash and cash equivalents, beginning of period |
30,290 | 46,398 | ||||||
| Cash and cash equivalents, end of period |
$ | 67,017 | $ | 112,994 | ||||
| Interest paid |
$ | 31,086 | $ | 22,426 | ||||
| Taxes paid |
$ | 10,158 | $ | 15,360 | ||||
See accompanying notes to consolidated financial statements.
F-34
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
(Unaudited)
Note 1. Organization and Basis of Presentation
The accompanying unaudited consolidated financial statements include the accounts of Team Health Holdings, Inc. (“Holdings” or the Company) and its wholly owned subsidiaries and have been prepared in accordance with accounting principles generally accepted in the United States for interim financial reporting and with the instructions to Form 10-Q and Article 10 of Regulation S-X. Accordingly, they do not include all of the information and notes required by accounting principles generally accepted in the United States for complete financial statements.
In the opinion of management, the accompanying unaudited consolidated financial statements contain all adjustments (consisting of normal recurring items) necessary for a fair presentation of results for the interim periods presented. The results of operations for any interim period are not necessarily indicative of results for the full year. Subsequent events have been evaluated through November 17, 2009. The consolidated balance sheet of the Company at December 31, 2008 has been derived from the audited financial statements at that date, but does not include all of the information and disclosures required by accounting principles generally accepted in the United States for complete financial statements. These financial statements and footnote disclosures should be read in conjunction with the December 31, 2008 audited consolidated financial statements and the notes thereto.
The preparation of the financial statements in conformity with accounting principles generally accepted in the United States requires management to make estimates and assumptions that affect the amounts reported in the accompanying consolidated financial statements and notes. Actual results could differ from those estimates.
Corporate Reorganization
On the Company converted from a limited liability company to a Delaware corporation, Team Health Holdings, Inc. (“Holdings”), so that its existing investors will own common stock rather than equity interests in a limited liability company. The Company refers to this event as its corporate reorganization.
As a result of the corporate reorganization, Team Health Holdings, LLC’s Class A shares were converted for shares of Holdings’ common stock. In addition, outstanding Class B and C shares that had vested on or prior to (the date of our corporate reorganization) were converted for shares of Holdings’ common stock.
Unaudited Pro forma Financial Information
The unaudited pro forma balance sheet gives effect to the change in capitalization on resulting from the exchange of Class A, B, and C shares for Holdings’ common stock. The pro forma balance sheet does not reflect any initial public offering proceeds.
The accompanying consolidated statement of operations discloses unaudited pro forma earnings per share for the nine months ended September 30, 2008 and 2009 giving affect to the exchange of Class A, B and C shares for Holdings common stock.
Unaudited Supplemental Pro Forma Financial Information
The accompanying consolidated statements of operations discloses unaudited supplemental pro forma earnings per share for the nine months ended September 30, 2009 giving effect to the portion of the offering proceeds to be used for the repayment of the Company’s indebtedness.
F-35
Table of Contents
Note 2. Unaudited Pro Forma and Supplemental Pro Forma Basic and Diluted Net Earnings Per Share
Pro forma basic and diluted earnings per share is calculated in accordance with ASC Topic 260 “Earnings Per Share” (formerly SFAS No. 128, Earnings Per Share). Pro forma basic and diluted earnings per share (“EPS”) is calculated using the weighted-average common shares outstanding in each period.
The shares used to calculate pro forma basic and dilutive EPS represent the weighted-average common shares outstanding.
| Nine months ended September 30, | ||||||
| 2008 | 2009 | |||||
| Numerator for basic and diluted net earnings per share: |
||||||
| Net earnings |
$ | $ | ||||
| Denominator: |
||||||
| Denominator for basic earnings per share-weighted average shares outstanding |
||||||
| Effect of dilutive securities |
||||||
| Denominator for diluted net earnings per share-weighted average shares |
||||||
| Basic net earnings per share: |
||||||
| Basic net earnings |
$ | $ | ||||
| Diluted net earnings per share: |
||||||
| Diluted net earnings |
$ | $ | ||||
Unaudited supplemental pro forma basic and diluted net earnings per share for the nine months ended September 30, 2009 gives effect to the portion of the offering proceeds to be used for the repayment of the Company’s indebtedness.
| Nine Months ended September 30, 2009 | |||||||||||
| Unaudited Pro forma |
Supplemental pro forma adjustments |
Notes | Unaudited Supplemental Pro forma | ||||||||
| Numerator for basic and dilute net earning per share: |
|||||||||||
| Net earnings |
$ | $ | $ | ||||||||
| Denominator: |
|||||||||||
| Denominator for basic earnings per share – weighted average shares. |
|||||||||||
| Effect of dilutive securities |
|||||||||||
| Denominator for diluted net earnings per share – weighted average shares outstanding |
|||||||||||
| Basic net earnings per share: |
|||||||||||
| Basic net earnings |
$ | $ | $ | ||||||||
| Diluted net earnings per share: |
|||||||||||
| Diluted net earnings |
$ | $ | $ | ||||||||
Note 3. New Accounting Standards
In June 2009, the Financial Accounting Standards Board (“FASB”) issued ASC Topic 105 (formerly SFAS No. 168), “The FASB Accounting Standards Codification and the Hierarchy of Generally Accepted Accounting Principles”. ASC Topic 105 establishes the FASB Accounting Standards Codification (the “Codification”) as the single source of authoritative, nongovernmental U.S. GAAP. The Codification did not change U.S. GAAP. All existing accounting standard documents were superseded and all other accounting
F-36
Table of Contents
literature not included in the Codification is considered non-authoritative. ASC Topic 105 is effective for interim and annual periods ending after September 15, 2009. Therefore, the Company adopted ASC Topic 105 for the reporting in its 2009 third quarter. The adoption did not have a significant impact on the reporting of its financial position, results of operations or cash flows.
In April 2008, the FASB issued FASB Staff Position (“FSP”) No. FAS 142-3, Determination of the Useful Life of Intangible Assets which was primarily codified into Topic 350 “Intangibles—Goodwill and Other” in Accounting Standards Codification (“ASC”). This guidance amends the factors that should be considered in developing renewal or extension assumptions used to determine the useful life of a recognized intangible asset and requires enhanced related disclosures. This guidance must be applied prospectively to all intangible assets acquired as of and subsequent to fiscal years beginning after December 15, 2008. The Company’s adoption of the provisions of this guidance did not have a material impact on its consolidated financial statements.
In April 2009, the FASB issued an accounting standard update (formerly FSP FAS 157-4, Determining Fair Value When the Volume and Level of Activity for the Asset or Liability Have Significantly Decreased and Identifying Transactions That Are Not Orderly) to ASC Topic 820, “Fair Value Measurements and Disclosures”. This accounting standard update provides additional guidance for estimating fair value in accordance with the volume and level of activity for the asset or liability have significantly decreased. This update also includes guidance on identifying circumstances that indicate a transaction is not orderly and it emphasizes that even if there has been a significant decrease in the volume and level of activity for the asset or liability and regardless of the valuation technique(s) used, the objective of a fair value measurement remains the same. Fair value is the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction (that is, not a forced liquidation or distressed sale) between market participants at the measurement date under current market conditions. The provisions of this accounting standard update were effective for interim and annual reporting periods ending after June 15, 2009, and is applied prospectively. The implementation of this standard did not have a material impact on the Company’s consolidated financial statements.
In April 2009, the FASB issued an accounting standard update (formerly FSP FAS 107-1 and APB 28-1, Interim Disclosures about Fair Value of Financial Instruments) to ASC Topic 825 “Financial Instruments”, this accounting standard update requires disclosures about fair value of financial instruments for interim reporting periods of publicly traded companies as well as in annual financial statements. The update was effective for interim and annual reporting periods ending after June 15, 2009. The implementation of the requirements of this update did not have a material impact on the Company’s consolidated financial statements.
In April 2009, the FASB issued an accounting standard update (formerly FSP SFAS 115-2 and SFAS 124-2, “Recognition and Presentation of Other-Than-Temporary Impairments”) to ASC Topic 320, “Investments—Debt and Equity Securities, to amend the other-than-temporary impairment guidance in debt securities to be based on intent and not more likely than not that the Company would be required to sell the security before recovery and to improve the presentation and disclosure of other-than-temporary impairments on debt and equity securities in the financial statements. The adoption did not have a material effect on the Company’s consolidated financial statements.
In May 2009, the FASB issued ASC Topic 855 (formerly) SFAS No. 165, “Subsequent Events”, to establish general standards of accounting for and disclosure of events that occur after the balance sheet date but before financial statements are issued. The Company adopted this pronouncement for the quarter ended June 30, 2009.
Note 4. Acquisitions
Effective March 14, 2009, the Company acquired the operations of a physician staffing business that provides hospital emergency department services under three contracts for locations in Kentucky for approximately $4.6 million, net of cash received. The purchase price included an initial cash payment of $2.7 million with the remaining $1.9 million to be paid based on the financial performance of the acquired company.
F-37
Table of Contents
The purchase price was allocated, in accordance with the provisions of ASC Topic 805, “Business Combinations”, to net assets acquired, including contract intangibles and accounts receivables, and goodwill based on management’s estimates. The total goodwill recognized was $3.0 million. The results of operations of the acquired business are included in the Company’s consolidated financial statements beginning on the acquisition date.
During the nine months ended September 30, 2008 and 2009 the Company made no payments related to previous acquisitions, however the Company paid $7.5 million of contingent consideration on October 1, 2009 related to an acquisition completed in 2006. The liability for this payment was recognized as of September 30, 2009. The payment represents additional purchase price and has been recorded as goodwill.
Note 5. Fair Value Measurements
The Company applies the provisions of FASB ASC Topic 820, “Fair Value Measurements and Disclosures,” in determining the fair value of its financial assets and liabilities. This standard defines fair value, provides guidance for measuring fair value and requires certain disclosures. This standard does not require any new fair value measurements, but rather applies to all other accounting pronouncements that require or permit fair value measurements.
FASB ASC Topic 820, prioritizes the inputs used in measuring fair value into the following hierarchy:
| Level 1 | Quoted prices (unadjusted) in active markets for identical assets or liabilities; | |
| Level 2 | Inputs other than quoted prices included within Level 1 that are either directly or indirectly observable; | |
| Level 3 | Unobservable inputs in which little or no market activity exists, therefore requiring an entity to develop its own assumptions about the assumptions that market participants would use in pricing. | |
The following table provides information on those assets and liabilities the Company measures at fair value on a recurring basis (in thousands):
| Carrying Amount In Consolidated Balance Sheet September 30, 2009 |
Fair Value September 30, 2009 |
Fair Value Level 1 |
Fair Value Level 2 |
Fair Value Level 3 | |||||||||||
| Investments of insurance subsidiary |
$ | 95,591 | $ | 95,591 | $ | 95,591 | $ | — | $ | — | |||||
| Interest rate swap liability |
5,334 | 5,334 | — | 5,334 | — | ||||||||||
The fair value of the Company’s investments of insurance subsidiary is based on quoted prices. As of September 30, 2009, the fair value of these investments reflected unrealized gains of $3.9 million and $0.2 million of unrealized losses on investments. The fair value of the Company’s interest rate swaps were determined using inputs that are available in the public swap markets for similarly termed instruments and then making adjustments for terms specific to the Company’s instruments and the Company’s and counterparty’s implied credit risk. See Note 6 for more information regarding our interest rate swap agreements. The fair value of our other financial instruments approximates their carrying values.
Note 6. Financial Derivative Instruments
During the nine months ended September 30, 2008, the Company entered into three separate forward interest rate swap agreements. The objective of the agreements is to eliminate the variability of the cash flows in interest payments for $200.0 million of the variable-rate term loan for a three-year period. The agreements are contracts to exchange, on a quarterly basis, floating interest rate payments based on the Eurocurrency rate, for fixed interest payments over the life of the agreements. The Company has determined the interest rate swaps are
F-38
Table of Contents
highly effective and qualify for hedge accounting, therefore the changes in fair value of the interest rate swaps, net of tax, are recorded as a component of other comprehensive earnings. At September 30, 2009, the Company does not expect to reclassify any net gains or losses on its interest rate swap agreements from accumulated other comprehensive income to earnings during the next twelve months.
These agreements expose the Company to credit losses in the event of non-performance by the counterparty to the financial instruments. The counterparty is a creditworthy financial institution and the Company believes the counterparty will be able to fully satisfy its obligations under the contracts.
The following table presents the location of the liabilities associated with the Company’s interest rate swap agreements within the accompanying consolidated Balance Sheets (in thousands):
| Asset Derivatives | Liability Derivatives | |||||||||||||
| Balance Sheet Location |
Fair Value at December 31, 2008 |
Fair Value at September 30, 2009 |
Fair Value at December 31, 2008 |
Fair Value at September 30, 2009 | ||||||||||
| Derivatives designated as hedging: |
||||||||||||||
| Interest rate swap contracts |
Other non-current liabilities | $ | — | $ | — | $ | 5,547 | $ | 5,334 | |||||
The following table presents the impact of the Company’s interest rate swap agreements and their location within the accompanying consolidated Statements of Operations (in thousands):
| Amount of (Gain) Loss Recognized in Other Comprehensive Income on Derivative (Effective Portion) |
Amount of (Gain) Loss Reclassified from Other Comprehensive Income into Income (Effective Portion) |
Amount of (Gain) Loss Recognized in Income on Derivative (Ineffective Portion) | ||||||||||||||||||
| Nine Months Ended September 30, |
Nine Months Ended September 30, |
Nine Months Ended September 30, | ||||||||||||||||||
| 2008 | 2009 | 2008 | 2009 | 2008 | 2009 | |||||||||||||||
| Interest rate swap contracts |
$ | (1,951 | )(a) | $ | (130 | )(a) | $ | — | $ | — | $ | — | $ | — | ||||||
| (a) | Net of tax |
Note 7. Investments
Long term investments represent securities held by the Company’s captive insurance subsidiary. At December 31, 2008 and September 30, 2009 amortized cost basis and aggregate fair value of the Company’s available-for-sale securities by investment type were as follows (in thousands):
| Cost Basis |
Gross Unrealized Gains |
Gross Unrealized Losses |
Fair Value | ||||||||||
| December 31, 2008 |
|||||||||||||
| Money market funds |
$ | 17,780 | $ | — | $ | — | $ | 17,780 | |||||
| Treasury |
1,977 | 47 | — | 2,024 | |||||||||
| Municipal bonds |
32,893 | 789 | (300 | ) | 33,382 | ||||||||
| Agency notes |
23,909 | 1,354 | — | 25,263 | |||||||||
| Certificates of deposit |
8,964 | — | — | 8,964 | |||||||||
| $ | 85,523 | $ | 2,190 | $ | (300 | ) | $ | 87,413 | |||||
| September 30, 2009 |
|||||||||||||
| Money market funds |
$ | 11,665 | $ | — | $ | — | $ | 11,665 | |||||
| Treasury |
12,697 | 113 | (202 | ) | 12,608 | ||||||||
| Municipal bonds |
44,646 | 2,879 | (1 | ) | 47,524 | ||||||||
| Agency notes |
22,902 | 892 | — | 23,794 | |||||||||
| $ | 91,910 | $ | 3,884 | $ | (203 | ) | $ | 95,591 | |||||
F-39
Table of Contents
At December 31, 2008 and September 30, 2009, the amortized cost basis and aggregate fair value of the Company’s available-for-sale securities by contractual maturities were as follows (in thousands):
| Cost Basis |
Gross Unrealized Gains |
Gross Unrealized Losses |
Fair Value | ||||||||||
| December 31, 2008 |
|||||||||||||
| Due in less than one year |
$ | 20,857 | $ | 47 | $ | (8 | ) | $ | 20,896 | ||||
| Due after one year through five years |
43,523 | 1,387 | (51 | ) | 44,859 | ||||||||
| Due after five years through ten years |
19,520 | 677 | (241 | ) | 19,956 | ||||||||
| Due after ten years |
1,623 | 79 | — | 1,702 | |||||||||
| Total |
$ | 85,523 | $ | 2,190 | $ | (300 | ) | $ | 87,413 | ||||
| September 30, 2009 |
|||||||||||||
| Due in less than one year |
$ | 23,937 | $ | 299 | $ | — | $ | 24,236 | |||||
| Due after one year through five years |
26,987 | 1,139 | — | 28,126 | |||||||||
| Due after five years through ten years |
40,641 | 2,434 | (203 | ) | 42,872 | ||||||||
| Due after ten years |
345 | 12 | — | 357 | |||||||||
| Total |
$ | 91,910 | $ | 3,884 | $ | (203 | ) | $ | 95,591 | ||||
A summary of the Company’s temporarily impaired investment securities available-for-sale as of September 30, 2009 follows (in thousands):
| Less than 12 months |
Impaired Over 12 months |
Total | ||||||||||||||||||
| Fair Value |
Unrealized Losses |
Fair Value |
Unrealized Losses |
Fair Value |
Unrealized Losses |
|||||||||||||||
| September 30, 2009 |
||||||||||||||||||||
| Money market funds |
$ | — | $ | — | $ | — | $ | — | $ | — | $ | — | ||||||||
| Treasury |
2,847 | (202 | ) | — | — | 2,847 | (202 | ) | ||||||||||||
| Municipal bonds |
402 | (1 | ) | — | — | 402 | (1 | ) | ||||||||||||
| Agency notes |
— | — | — | — | — | — | ||||||||||||||
| Total investment |
$ | 3,249 | $ | (203 | ) | $ | — | $ | — | $ | 3,249 | $ | (203 | ) | ||||||
The unrealized losses resulted from changes in market interest rates and liquidity, not from changes in the probability of contractual cash flows. Because the Company has the ability and intent to hold the investments until a recovery of carrying value and full collection of the amounts due according to the contractual terms of the investments is expected, the Company does not consider these investments to be other-than-temporarily impaired at September 30, 2009.
During the nine months ended September 30, 2009, the Company recorded a gain on the sale of investments of approximately $0.4 million.
F-40
Table of Contents
Note 8. Net Revenue
Net revenue for the nine months ended September 30, 2008 and 2009 consisted of the following (in thousands):
| Nine Months Ended September 30, | ||||||
| 2008 | 2009 | |||||
| Fee for service revenue |
$ | 1,373,240 | $ | 1,508,500 | ||
| Contract revenue |
329,914 | 339,928 | ||||
| Other revenue |
17,621 | 19,574 | ||||
| $ | 1,720,775 | $ | 1,868,002 | |||
Note 9. Other Intangible Assets
The following is a summary of intangible assets and related amortization as of December 31, 2008 and September 30, 2009 (in thousands):
| Gross Carrying Amount |
Accumulated Amortization | |||||
| As of December 31, 2008: |
||||||
| Contracts |
$ | 52,632 | $ | 20,241 | ||
| Other |
448 | 401 | ||||
| Total |
$ | 53,080 | $ | 20,642 | ||
| As of September 30, 2009: |
||||||
| Contracts |
$ | 50,424 | $ | 22,498 | ||
| Other |
448 | 436 | ||||
| Total |
$ | 50,872 | $ | 22,934 | ||
| Aggregate amortization expense: |
||||||
| For the nine months ended September 30, 2009 |
$ | 6,342 | ||||
| Estimated amortization expense: |
||||||
| For the remainder of the year ended December 31, 2009 |
$ | 2,007 | ||||
| For the year ended December 31, 2010 |
7,981 | |||||
| For the year ended December 31, 2011 |
6,262 | |||||
| For the year ended December 31, 2012 |
5,830 | |||||
| For the year ended December 31, 2013 |
4,216 | |||||
Note 10. Long-Term Debt
Long-term debt as of September 30, 2009 consisted of the following (in thousands):
| Term Loan Facility |
$ | 409,063 | ||
| 11.25% Senior Subordinated Notes |
203,025 | |||
| Revolving line of credit |
— | |||
| 612,088 | ||||
| Less current portion |
(4,250 | ) | ||
| $ | 607,838 | |||
F-41
Table of Contents
The interest rate for any revolving credit facility borrowings is based on a grid which is based on the consolidated ratio of total funded debt to earnings before interest, taxes, depreciation and amortization, all as set forth in the credit agreement. As of September 30, 2009, the interest rate for borrowings under the revolving credit facility was equal to the euro dollar rate plus 2.0% or the agent bank’s base rate plus 1.0%. In addition, the Company pays a commitment fee for the revolving credit facility which is equal to 0.5% of the commitment at September 30, 2009. No borrowings under the $110.0 million revolving credit facility were outstanding as of September 30, 2009, and the Company had $7.5 million of standby letters of credit outstanding against the revolving credit facility commitment. Of the $110.0 million revolving credit facility, $10.0 million is held by CIT Lending Services Corporation (“CIT Lending Services”), a subsidiary of CIT Group, Inc. CIT Group, Inc and CIT Group Funding Company of Delaware LLC filed for Chapter 11 bankruptcy protection on November 1, 2009. Although CIT Lending Services is not currently a party to this filing, at this time it is not certain if this portion of the revolving credit facility will be available to the Company. The Company does not believe any potential reduction in available capacity under the revolving credit facility will have a material impact on its liquidity or the liquidity of its subsidiaries.
The interest rate at September 30, 2009 was 2.4% for amounts outstanding under the term loan facility. In accordance with the terms of the Company’s loan agreement, as amended, it is subject to an increase in the term loan interest rate in the amount of 0.25% in the event of a downgrade in the corporate family rating of the Company by either Moody’s or Standard and Poor’s rating agencies.
The Company issued on November 23, 2005, 11.25% Senior Subordinated Notes (the “Notes”) in the amount of $215.0 million due December 1, 2013. The Notes are subordinated in right of payment to all senior debt of the Company and are senior in right of payment to all existing and future subordinated indebtedness of the Company. Interest on the Notes accrues at the rate of 11.25% per annum, payable semi-annually in arrears on June 1 and December 1 of each year. Beginning on December 1, 2009, the Company may redeem some or all of the Notes at any time at various redemption prices. In December 2008, the Company retired $12.0 million of the Notes in an open market purchase.
The Notes are guaranteed jointly and severally on a full and unconditional basis by all of the Company’s domestic wholly-owned operating subsidiaries (the “Subsidiary Guarantors”) as required by the indenture governing the Notes.
Each of the Notes, the revolving credit facilities and the current term loan facility contain both affirmative and negative covenants, including limitations on the Company’s ability to incur additional indebtedness, sell material assets, retire, redeem or otherwise reacquire its capital stock, acquire the capital stock or assets of another business, pay dividends, and require the Company to comply with certain coverage and leverage ratios.
Aggregate annual maturities of long-term debt as of September 30, 2009 are as follows (in thousands):
| 2009 |
$ | 4,250 | |
| 2010 |
4,250 | ||
| 2011 |
4,250 | ||
| 2012 |
396,313 | ||
| 2013 |
203,025 | ||
| Thereafter |
— |
The fair value of the Company’s debt is estimated using quoted market prices when available. When quoted market prices are not available, fair value is estimated based on current market interest rates for debt with similar maturities.
The fair value of the Company’s debt was $439.7 million and $602.3 million at December 31, 2008 and September 30, 2009, respectively. The financial statement carrying value was $615.3 million and $612.1 million at December 31, 2008 and September 30, 2009, respectively.
F-42
Table of Contents
Note 11. Professional Liability Insurance
The Company’s professional liability loss reserves consisted of the following (in thousands):
| December 31, 2008 |
September 30, 2009 | |||||
| Estimated losses under self-insured programs |
$ | 153,567 | $ | 143,611 | ||
| Estimated losses under commercial insurance programs |
47,735 | 43,750 | ||||
| 201,302 | 187,361 | |||||
| Less estimated payable within one year |
67,874 | 48,346 | ||||
| $ | 133,428 | $ | 139,015 | |||
The changes to the Company’s estimated losses under self-insured programs as of September 30, 2009 were as follows (in thousands):
| Balance, December 31, 2008 |
$ | 153,567 | ||
| Reserves related to current period |
24,938 | |||
| Changes related to prior period reserves |
(18,824 | ) | ||
| Payments for current period reserves |
(95 | ) | ||
| Payments for prior period reserves |
(15,975 | ) | ||
| Balance, September 30, 2009 |
$ | 143,611 | ||
The Company provides for its estimated professional liability losses through a combination of self-insurance and commercial insurance programs. During the period March 12, 1999 through March 11, 2003, the primary source of the Company’s coverage for such risks was a professional liability insurance policy provided through one insurance carrier. The commercial insurance carrier policy initially included an insured loss limit of $130.0 million. In April 2006, the Company amended the policy with its commercial insurance carrier to provide for an increase in the aggregate limit of coverage based upon certain premium funding levels. As of September 30, 2009, the insured loss limit under the policy was $155.9 million. Losses in excess of the limit of coverage remain as a self-insured obligation of the Company. Beginning March 12, 2003, professional liability loss risks are principally being provided for through self-insurance with a portion of such risks (“claims-made” basis) transferred to and funded into a captive insurance company. The accounts of the captive insurance company are fully consolidated with those of the other operations of the Company in the accompanying consolidated financial statements.
The self-insurance components of our risk management program include reserves for future claims incurred but not reported (“IBNR”). As of December 31, 2008, of the $153.6 million of estimated losses under self-insured programs, approximately $85.6 million represents an estimate of IBNR claims and expenses and additional loss development, with the remaining $68.0 million representing specific case reserves. Of the existing case reserves as of December 31, 2008, $0.9 million represent case reserves that have settled but not yet funded, and $67.1 million reflect unsettled case reserves.
As of September 30, 2009, of the $143.6 million of estimated losses under self insurance programs, approximately $76.6 million represents an estimate of IBNR claims and expenses and additional loss development with the remaining $67.0 million representing specific case reserves. Of the existing case reserves as of September 30, 2009, $1.2 million represent case reserves that have been settled but not yet funded, and $65.8 million reflect unsettled case reserves.
The Company’s provisions for losses under its self-insurance components are estimated using the results of periodic actuarial studies. Such actuarial studies include numerous underlying estimates and assumptions, including
F-43
Table of Contents
assumptions as to future claim losses, the severity and frequency of such projected losses, loss development factors and others. The Company’s provisions for losses under its self-insured components are subject to subsequent adjustment should future actuarial projected results for such periods indicate projected losses greater or less than previously projected. The Company’s estimated loss reserves under such programs are discounted at 2.2% and 3.3% at December 31, 2008 and September 30, 2009, respectively, which was the current ten year U. S. Treasury rate at that date, which reflects the risk free interest rate over the expected period of claims payments.
The Company’s most recent actuarial valuation was completed in October 2009. As a result of such actuarial valuation, the Company determined no change was necessary in its reserves for professional liability losses as of September 30, 2009 related to prior year loss estimates. During the first quarter of 2009, the Company realized an $18.8 million reduction in its reserves for professional liability losses associated with prior year loss estimates. For the nine months ended September 30, 2008, the Company realized a reduction of $40.3 million in its reserves for professional liability losses related to prior year loss estimates resulting from favorable trends in actuarial loss estimates. Actuarial reports received in 2009 reflect favorable trends in the development of previous loss estimates necessitating the revaluation of prior year loss reserves during the nine months ended September 30, 2009. Factors contributing to the change in prior year loss estimates included favorable loss development on historical periods between actuarial studies as well as continued favorable trends in the frequency and severity of claims reported compared to historical trends.
Note 12. Share-based Compensation
In November 2005, the Company adopted the 2005 Unit Plan. A total of 400,000 Class B Common Units of Holdings and 600,000 Class C Common Units of Holdings are authorized for issuance to executives and other key employees under the 2005 Unit Plan. As of September 30, 2009, there were 329,594 restricted Class B Common Units and 461,430 Class C Common Units outstanding. The outstanding units vest ratably over five years and the Company is recognizing the related compensation expense over the five year period. Compensation expense for the employee equity based awards granted is based on the grant date fair value in accordance with the provisions of ASC Topic 718, “Compensation—Stock Compensation”. For the nine months ended September 30, 2008 and 2009, the Company recognized $0.4 million and $0.6 million, respectively, of employee equity based compensation expense. As of September 30, 2009, there was approximately $1.7 million of unrecognized compensation expense related to nonvested restricted unit awards, which will be recognized over the remaining requisite service period. Forfeitures of employee equity based awards have been historically immaterial to the Company.
Note 13. Contingencies
Litigation
We are currently a party to various legal proceedings. While we currently believe that the ultimate outcome of such proceedings, individually and in the aggregate, will not have a material adverse effect on our financial position or overall trends in results of operations, litigation is subject to inherent uncertainties. If an unfavorable ruling were to occur, there exists the possibility of a material adverse impact on our net earnings in the period in which a ruling occurs. The estimate of the potential impact from such legal proceedings on our financial position or overall results of operations could change in the future.
Healthcare Regulatory Matters
Laws and regulations governing the Medicare and Medicaid programs are complex and subject to interpretation. Compliance with such laws and regulations can be subject to future governmental review and interpretation as well as significant regulatory action. From time to time, governmental regulatory agencies will conduct inquiries and audits of the Company’s practices. It is the Company’s current practice and future intent to cooperate fully with such inquiries.
F-44
Table of Contents
In addition to laws and regulations governing the Medicare and Medicaid programs, there are a number of federal and state laws and regulations governing such matters as the corporate practice of medicine and fee splitting arrangements, anti-kickback statutes, physician self-referral laws, false or fraudulent claims filing and patient privacy requirements. The failure to comply with any of such laws or regulations could have an adverse impact on our operations and financial results. It is management’s belief that the Company is in substantial compliance in all material respects with such laws and regulations.
Acquisition Payments
As of September 30, 2009, the Company may have to pay up to $18.3 million in future contingent payments (excluding the effect of the $7.5 million contingent consideration payment made on October 1, 2009) additional consideration for acquisitions made prior to September 30, 2009. These payments will be made and recorded as additional purchase price or will reduce existing liabilities should the acquired operations achieve the financial targets or certain contract terms are modified as agreed to in the respective acquisition agreements. No payments were made related to previous acquisitions in the nine months ended September 30, 2008 or 2009.
Note 14. Comprehensive Earnings
The components of comprehensive earnings, net of related taxes, are as follows (in thousands):
| Nine Months Ended September 30, | |||||||
| 2008 | 2009 | ||||||
| Net earnings |
$ | 50,063 | $ | 55,231 | |||
| Net change in fair market value of investments |
(260 | ) | 1,164 | ||||
| Net change in fair market value of interest rate swap |
1,951 | 130 | |||||
| Comprehensive earnings |
$ | 51,754 | $ | 56,525 | |||
Note 15. Segment Reporting
The Company provides services through four operating segments which are aggregated into two reportable segments, Healthcare Services and Billing Services. The Healthcare Services segment, which is an aggregation of healthcare staffing, clinics and occupational health, provides comprehensive healthcare service programs to users and providers of healthcare services on a fee for service as well as a cost plus basis. The Billing Services segment provides a range of external billing, collection and consulting services on a fee basis to outside third-party customers.
Segment amounts disclosed are prior to any elimination entries made in consolidation, except in the case of net revenue, where intercompany charges have been eliminated. Certain expenses are not allocated to the segments. These unallocated expenses are corporate expenses, net interest expense, depreciation and amortization, transaction costs and income taxes. The Company evaluates segment performance based on profit and loss before the aforementioned expenses.
F-45
Table of Contents
The following table presents financial information for each reportable segment. Depreciation, amortization, management fee and other expenses separately identified in the consolidated statements of operations are included as a reduction to the operating earnings of each segment in each period below (in thousands):
| Nine Months Ended September 30, |
||||||||
| 2008 | 2009 | |||||||
| Net Revenue less provision for uncollectibles: |
||||||||
| Healthcare Services |
$ | 990,593 | $ | 1,064,070 | ||||
| Billing Services |
9,214 | 10,587 | ||||||
| $ | 999,807 | $ | 1,074,657 | |||||
| Operating earnings: |
||||||||
| Healthcare Services |
$ | 154,703 | $ | 153,478 | ||||
| Billing Services |
1,795 | 2,597 | ||||||
| General Corporate |
(38,517 | ) | (38,943 | ) | ||||
| $ | 117,981 | $ | 117,132 | |||||
| Reconciliation of operating earnings to net earnings: |
||||||||
| Operating earnings |
$ | 117,981 | $ | 117,132 | ||||
| Interest expense, net |
34,033 | 27,671 | ||||||
| Provision for income taxes |
33,885 | 34,230 | ||||||
| Net earnings |
$ | 50,063 | $ | 55,231 | ||||
F-46
Table of Contents
Shares

Team Health Holdings, Inc.
Common Stock
PROSPECTUS
BofA Merrill Lynch
Goldman, Sachs & Co.
Barclays Capital
Citi
Credit Suisse
Deutsche Bank Securities
UBS Investment Bank
, 2009
Table of Contents
PART II
INFORMATION NOT REQUIRED IN PROSPECTUS
ITEM 13. OTHER EXPENSES OF ISSUANCE AND DISTRIBUTION.
The following table sets forth the expenses payable by the Registrant in connection with the issuance and distribution of the common stock being registered hereby. All of such expenses are estimates, other than the filing and listing fees payable to the SEC and the Financial Industry Regulatory Authority, Inc., or FINRA.
| SEC Registration Fee |
$ | 5,580 | |
| FINRA filing fee |
10,500 | ||
| NYSE listing fee |
* | ||
| Legal Fees and Expenses |
* | ||
| Accounting Fees and Expenses |
* | ||
| Printing Expenses |
* | ||
| Fees and Expenses of Accountants |
* | ||
| Transfer Agent Fees and Expenses |
* | ||
| Miscellaneous Expenses |
* | ||
| Total |
$ | * | |
| * | To be provided by amendment. |
ITEM 14. INDEMNIFICATION OF DIRECTORS AND OFFICERS.
Section 102 of the DGCL, as amended, allows a corporation to eliminate or limit the personal liability of a director to the corporation or its stockholders for monetary damages for a breach of fiduciary duty as a director, except where the director breached his duty of loyalty, failed to act in good faith, engaged in intentional misconduct or knowingly violated a law, authorized the payment of a dividend or approved a stock repurchase in violation of Delaware law or obtained an improper personal benefit. Our certificate of incorporation and our by-laws provide for such limitations.
Section 145 of the DGCL provides, among other things, that a corporation may indemnify any person who was or is a party, or is threatened to be made a party, to any threatened, pending or completed action, suit or proceeding (other than an action by or in the right of the corporation) by reason of the fact that the person is or was a director, officer, agent or employee of the corporation or is or was serving at the corporation’s request as a director, officer, agent or employee of another corporation, partnership, joint venture, trust or other enterprise, against expenses (including attorneys’ fees) judgments, fines and amounts paid in settlement actually and reasonably incurred by the person in connection with such action, suit or proceeding. The power to indemnify applies if such person acted in good faith and in a manner he reasonably believed to be in the best interests, or not opposed to the best interests, of the corporation, and with respect to any criminal action or proceeding, had no reasonable cause to believe his conduct was unlawful. The power to indemnify applies to actions brought by or in the right of the corporation as well, but only to the extent of defense expenses (including attorneys’ fees but excluding amounts paid in settlement) actually and reasonably incurred and not to any satisfaction of judgment or settlement of the claim itself, and with the further limitation that in such actions no indemnification shall be made in the event of any adjudication of negligence or misconduct in the performance of duties to the corporation, unless the Delaware Court of Chancery or the court in which such action was brought believes that in light of all the circumstances indemnification should apply. Our certificate of incorporation and our by-laws provide for such limitations.
Section 174 of the DGCL provides, among other things, that a director, who willfully or negligently approves of an unlawful payment of dividends or an unlawful stock purchase or redemption, may be held liable
II-1
Table of Contents
for such actions. A director who was either absent when the unlawful actions were approved or dissented at the time may avoid liability by causing his or her dissent to such actions to be entered in the books containing the minutes of the meetings of the board of directors at the time such action occurred or immediately after such absent director receives notice of the unlawful acts.
We will enter into indemnification agreements with each of our directors and officers providing for additional indemnification protection beyond that provided by the directors and officers liability insurance policy. In the indemnification agreements, we will agree subject to certain exceptions, to indemnify and hold harmless the director or officer to the maximum extent then authorized or permitted by the provisions of the certificate of incorporation, the DGCL, or by any amendment(s) thereto.
The underwriting agreement provides for indemnification by the underwriters of us and our officers and directors, and by us of the underwriters, for certain liabilities arising under the Securities Act or otherwise in connection with this offering.
ITEM 15. RECENT SALES OF UNREGISTERED SECURITIES.
None.
ITEM 16. EXHIBITS AND FINANCIAL STATEMENT SCHEDULES.
(a) Exhibits
| 1.1 | Form of Underwriting Agreement (1) | |
| 3.1 | Form of Certificate of Incorporation of Team Health Holdings, Inc. (1) | |
| 3.2 | Form of By-laws of Team Health Holdings, Inc. (1) | |
| 4.1 | Form of certificate of Team Health Holdings, Inc. common stock (1) | |
| 4.2 | Indenture, dated as of November 23, 2005, among Team Finance LLC, Health Finance Corporation, the Guarantors named on the signature pages thereto and The Bank of New York Trust Company, N.A., as Trustee (incorporated by reference to Exhibit 4.1 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 4.3 | First Supplemental Indenture, dated as of June 30, 2006, to the Indenture, dated as of November 23, 2005, among Florida Hospital Medicine Services, Inc., a subsidiary of Team Finance LLC, and The Bank of New York Trust Company, N.A., as Trustee (incorporated by reference to Exhibit 4.3 of Team Finance LLC’s Quarterly Report on Form 10-Q (File No. 333-132495) for the quarterly period ended June 30, 2006) | |
| 4.4 | Second Supplemental Indenture, dated as of June 30, 2007, to the Indenture, dated as of November 23, 2005, by and among THW Emergency Management of Houston, Inc., a subsidiary of Team Finance LLC, and The Bank of New York Trust Company, N.A., as Trustee (incorporated by reference to Exhibit 4.4 of Team Finance LLC’s Quarterly Report on Form 10-Q (File No. 333-132495) for the quarterly period ended June 30, 2008) | |
| 4.5 | Third Supplemental Indenture, dated as of April 30, 2008, to the Indenture, dated as of November 23, 2005, among EPA of Woodbury, Inc., a subsidiary of Team Finance LLC, and The Bank of New York Trust Company, N.A., as Trustee (incorporated by reference to Exhibit 4.5 of Team Finance LLC’s Quarterly Report on Form 10-Q (File No. 333-132495) for the quarterly period ended June 30, 2008) | |
| 5.1 | Form of Opinion of Simpson Thacher & Bartlett LLP | |
| 10.1 | Credit Agreement, dated as of November 23, 2005, by and among Team Finance LLC, Team Health Holdings, LLC, JPMorgan Chase Bank, N.A., each Lender from time to time party thereto and Lehman Brothers, Inc. and Merrill Lynch, Pierce, Fenner & Smith Incorporated (incorporated by reference to Exhibit 10.1 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.2 | Amendment No. 1, dated as of April 5, 2007, to the Credit Agreement, dated as of November 23, 2005 by and among Team Finance LLC, Team Health Holdings, LLC, JPMorgan Chase Bank, N.A. and each Lender from time to time party thereto (incorporated by reference to Exhibit 10.14 of Team Finance LLC’s Quarterly Report on Form 10-Q (File No. 333-132495) for the quarterly period ended March 31, 2007) | |
II-2
Table of Contents
| 10.3 | Trust Agreement, dated as of December 3, 2004, by and among Team Health, Inc. and The Trust Company of Knoxville (incorporated by reference to Exhibit 10.3 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.4 | Lease Agreement dated August 27, 1992 between Med: Assure Systems and Winston Road Properties (incorporated by reference to Exhibit 10.6 of the Registration Statement on Form S-4
(File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.5 | Lease Agreement dated August 27, 1999 between Americare Medical Services, Inc. and Winston Road Properties for space located at 1900 Winston Road, Knoxville, TN (incorporated by reference to Exhibit 10.7 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.6 | Amended and Restated Transaction and Monitoring Fee agreement between Team Health Holdings, LLC and Blackstone Management Partners IV LLC, dated March 7, 2006 (incorporated by reference to Exhibit 10.12 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.7 | Team Health, Inc. Non-Qualified Supplemental Executive Retirement Plan dated as of January 1, 2004 (incorporated by reference to Exhibit 10.9 of the Registration Statement on Form
S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006)* (2) | |
| 10.8 | Ensemble Acquisition LLC 2005 Unit Plan (incorporated by reference to Exhibit 10.10 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006)* | |
| 10.9 | Form of Restricted Unit Award Agreement* (2) | |
| 10.10 | Team Health Holdings, Inc. 2009 Stock Incentive Plan* (1) | |
| 10.11 | Amended and Restated Team Health Holdings, Inc. Annual Management Incentive Program* (1) | |
| 10.12 | Employment Agreement, dated November 23, 2005, between Team Health, Inc. and Dr. Massingale (incorporated by reference to Exhibit 10.13 of the Registration Statement on Form S-4
(File No. 333-132495) filed by Team Finance LLC on March 16, 2006)* (2) | |
| 10.13 | First Amendment to Employment Agreement, dated May 1, 2008, between Team Health, Inc. and Dr. Massingale* (2) | |
| 10.14 | Employment Agreement, dated June 1, 2006, between Team Health, Inc. and Gregory S. Roth* (2) | |
| 10.15 | Employment Agreement, dated as of June 1, 2006, between Team Health, Inc. and David P. Jones* (2) | |
| 10.16 | Employment Agreement, dated as of June 1, 2008, between Team Health, Inc. and Heidi Solomon Allen* (2) | |
| 10.17 | Employment Agreement, dated as of June 1, 2006, between Team Health, Inc. and Stephen Sherlin* (2) | |
| 10.18 | Retirement Agreement, dated March 12, 2008, between Team Health, Inc. and Robert C. Joyner* (2) | |
| 10.19 | Form of Stockholders Agreement (1) | |
| 10.20 | Form of Registration Rights Agreement (1) | |
| 10.21 | Participation Agreement, dated as of November 27, 2006 between Team Health, Inc. and Core Trust Purchasing Group | |
| 21.1 | List of Subsidiaries (1) | |
| 23.1 | Consent of Ernst & Young LLP | |
| 23.2 | Consent of Simpson Thacher & Bartlett LLP (included as part of Exhibit 5.1) | |
| 24.1 | Power of Attorney | |
| (1) | To be filed by amendment. |
| (2) | Previously filed. |
| * | Management contracts or compensatory plans or arrangements. |
II-3
Table of Contents
(b) Schedules
Schedule II—Valuation and Qualifying Accounts of Team Health Holdings, Inc.
Team Health Holdings, Inc.
Schedule II—Valuation and Qualifying Accounts
For the Years Ended December 31,
(In thousands)
| Allowance for uncollectibles |
Balance at Beginning of Period |
Costs and Expenses |
Other | Deductions | Balance at End of Period | ||||||||||
| 2006 |
$ | 127,740 | $ | 733,666 | $ | — | $ | 692,990 | $ | 168,416 | |||||
| 2007 |
$ | 168,416 | $ | 874,087 | $ | — | $ | 877,277 | $ | 165,226 | |||||
| 2008 |
$ | 165,226 | $ | 960,495 | $ | — | $ | 967,036 | $ | 158,685 | |||||
The following schedules are omitted as not applicable or not required under the rules of Regulation S-X: I, III, IV and V.
ITEM 17. UNDERTAKINGS
(a) The undersigned Registrant hereby undertakes to provide to the underwriters at the closing specified in the underwriting agreement certificates in such denominations and registered in such names as required by the underwriter to permit prompt delivery to each purchaser.
(b) Insofar as indemnification for liabilities arising under the Securities Act of 1933 may be permitted to directors, officers and controlling persons of the Registrant pursuant to the foregoing provisions, or otherwise, the Registrant has been advised that in the opinion of the Securities and Exchange Commission such indemnification is against public policy as expressed in the Securities Act of 1933 and is, therefore, unenforceable. In the event that a claim for indemnification against such liabilities (other than the payment by the Registrant of expenses incurred or paid by a director, officer or controlling person of the Registrant in the successful defense of any action, suit or proceeding) is asserted by such director, officer or controlling person in connection with the securities being registered, the Registrant will, unless in the opinion of its counsel the matter has been settled by controlling precedent, submit to a court of appropriate jurisdiction the question whether such indemnification by it is against public policy as expressed in the Securities Act of 1933 and will be governed by the final adjudication of such issue.
(c) The undersigned Registrant hereby undertakes that:
(1) For purposes of determining any liability under the Securities Act of 1933, the information omitted from the form of prospectus filed as part of this registration statement in reliance upon Rule 430A and contained in a form of prospectus filed by the Registrant pursuant to Rule 424(b)(1) or (4) or 497(h) under the Securities Act shall be deemed to be part of this registration statement as of the time it was declared effective.
(2) For the purpose of determining any liability under the Securities Act of 1933, each post-effective amendment that contains a form of prospectus shall be deemed to be a new registration statement relating to the securities offered therein, and the offering of such securities at that time shall be deemed to be the initial bona fide offering thereof.
II-4
Table of Contents
SIGNATURES
Pursuant to the requirements of the Securities Act of 1933, as amended, Team Health Holdings, L.L.C. has duly caused this amendment to the Registration Statement to be signed on its behalf by the undersigned, thereunto duly authorized, in the City of Knoxville, State of Tennessee, on November 17, 2009.
| TEAM HEALTH HOLDINGS, L.L.C. | ||
| By: | /S/ DAVID P. JONES | |
| Name: Title: |
David P. Jones Chief Financial Officer | |
Pursuant to the requirements of the Securities Act of 1933, this amendment to the Registration Statement has been signed by the following persons in the capacities indicated on November 17, 2009.
| Signature |
Capacity | |
| * Greg Roth |
President, Chief Executive Officer and Representative (Principal Executive Officer) | |
| /s/ DAVID P. JONES David P. Jones |
Chief Financial Officer (Principal Financial Officer and Principal Accounting Officer) | |
| * H. Lynn Massingale, M.D. |
Executive Chairman and Representative | |
| * Neil P. Simpkins |
Representative | |
| * Michael A. Dal Bello |
Representative | |
| * Earl P. Holland |
Representative | |
| * Glenn A. Davenport |
Representative | |
| * Alan Muney, M.D. |
Representative | |
| By: | /S/ DAVID P. JONES | |||
| David P. Jones Attorney-in-fact |
||||
II-5
Table of Contents
EXHIBIT INDEX
| 1.1 | Form of Underwriting Agreement (1) | |
| 3.1 | Form of Certificate of Incorporation of Team Health Holdings, Inc. (1) | |
| 3.2 | Form of By-laws of Team Health Holdings, Inc. (1) | |
| 4.1 | Form of certificate of Team Health Holdings, Inc. common stock(1) | |
| 4.2 | Indenture, dated as of November 23, 2005, among Team Finance LLC, Health Finance Corporation, the Guarantors named on the signature pages thereto and The Bank of New York Trust Company, N.A., as Trustee (incorporated by reference to Exhibit 4.1 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 4.3 | First Supplemental Indenture, dated as of June 30, 2006, to the Indenture, dated as of November 23, 2005, among Florida Hospital Medicine Services, Inc., a subsidiary of Team Finance LLC, and The Bank of New York Trust Company, N.A., as Trustee (incorporated by reference to Exhibit 4.3 of Team Finance LLC’s Quarterly Report on Form 10-Q (File No. 333-132495) for the quarterly period ended June 30, 2006) | |
| 4.4 | Second Supplemental Indenture, dated as of June 30, 2007, to the Indenture, dated as of November 23, 2005, by and among THW Emergency Management of Houston, Inc., a subsidiary of Team Finance LLC, and The Bank of New York Trust Company, N.A., as Trustee (incorporated by reference to Exhibit 4.4 of Team Finance LLC’s Quarterly Report on Form 10-Q (File No. 333-132495) for the quarterly period ended June 30, 2008) | |
| 4.5 | Third Supplemental Indenture, dated as of April 30, 2008, to the Indenture, dated as of November 23, 2005, among EPA of Woodbury, Inc., a subsidiary of Team Finance LLC, and The Bank of New York Trust Company, N.A., as Trustee (incorporated by reference to Exhibit 4.5 of Team Finance LLC’s Quarterly Report on Form 10-Q (File No. 333-132495) for the quarterly period ended June 30, 2008) | |
| 5.1 | Form of Opinion of Simpson Thacher & Bartlett LLP | |
| 10.1 | Credit Agreement, dated as of November 23, 2005, by and among Team Finance LLC, Team Health Holdings, LLC, JPMorgan Chase Bank, N.A., each Lender from time to time party thereto and Lehman Brothers, Inc. and Merrill Lynch, Pierce, Fenner & Smith Incorporated (incorporated by reference to Exhibit 10.1 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.2 | Amendment No. 1, dated as of April 5, 2007, to the Credit Agreement, dated as of November 23, 2005 by and among Team Finance LLC, Team Health Holdings, LLC, JPMorgan Chase Bank, N.A. and each Lender from time to time party thereto (incorporated by reference to Exhibit 10.14 of Team Finance LLC’s Quarterly Report on Form 10-Q (File No. 333-132495) for the quarterly period ended March 31, 2007) | |
| 10.3 | Trust Agreement, dated as of December 3, 2004, by and among Team Health, Inc. and The Trust Company of Knoxville (incorporated by reference to Exhibit 10.3 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.4 | Lease Agreement dated August 27, 1992 between Med: Assure Systems and Winston Road Properties (incorporated by reference to Exhibit 10.6 of the Registration Statement on Form S-4
(File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.5 | Lease Agreement dated August 27, 1999 between Americare Medical Services, Inc. and Winston Road Properties for space located at 1900 Winston Road, Knoxville, TN (incorporated by reference to Exhibit 10.7 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
| 10.6 | Amended and Restated Transaction and Monitoring Fee agreement between Team Health Holdings, LLC and Blackstone Management Partners IV LLC, dated March 7, 2006 (incorporated by reference to Exhibit 10.12 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006) | |
Table of Contents
| 10.7 | Team Health, Inc. Non-Qualified Supplemental Executive Retirement Plan dated as of January 1, 2004 (incorporated by reference to Exhibit 10.9 of the Registration Statement on Form
S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006)* (2) | |
| 10.8 | Ensemble Acquisition LLC 2005 Unit Plan (incorporated by reference to Exhibit 10.10 of the Registration Statement on Form S-4 (File No. 333-132495) filed by Team Finance LLC on March 16, 2006)* | |
| 10.9 | Form of Restricted Unit Award Agreement* (2) | |
| 10.10 | Team Health Holdings, Inc. 2009 Stock Incentive Plan* (1) | |
| 10.11 | Amended and Restated Team Health Holdings, Inc. Annual Management Incentive Program* (1) | |
| 10.12 | Employment Agreement, dated November 23, 2005, between Team Health, Inc. and Dr. Massingale (incorporated by reference to Exhibit 10.13 of the Registration Statement on Form S-4
(File No. 333-132495) filed by Team Finance LLC on March 16, 2006)* (2) | |
| 10.13 | First Amendment to Employment Agreement, dated May 1, 2008, between Team Health, Inc. and Dr. Massingale* (2) | |
| 10.14 | Employment Agreement, dated June 1, 2006, between Team Health, Inc. and Gregory S. Roth* (2) | |
| 10.15 | Employment Agreement, dated as of June 1, 2006, between Team Health, Inc. and David P. Jones* (2) | |
| 10.16 | Employment Agreement, dated as of June 1, 2008, between Team Health, Inc. and Heidi Solomon Allen* (2) | |
| 10.17 | Employment Agreement, dated as of June 1, 2006, between Team Health, Inc. and Stephen Sherlin* (2) | |
| 10.18 | Retirement Agreement, dated March 12, 2008, between Team Health, Inc. and Robert C. Joyner* (2) | |
| 10.19 | Form of Stockholders Agreement (1) | |
| 10.20 | Form of Registration Rights Agreement (1) | |
| 10.21 | Participation Agreement, dated as of November 27, 2006 between Team Health, Inc. and Core Trust Purchasing Group. | |
| 21.1 | List of Subsidiaries (1) | |
| 23.1 | Consent of Ernst & Young LLP | |
| 23.2 | Consent of Simpson Thacher & Bartlett LLP (included as part of Exhibit 5.1) | |
| 24.1 | Power of Attorney. | |
| (1) | To be filed by amendment. |
| (2) | Previously filed. |
| * | Management contracts or compensatory plans or arrangements. |
